User login
Eruptive Keratoacanthomas After Nivolumab Treatment of Stage III Melanoma
To the Editor:
Programmed cell death protein 1 (PD-1) inhibitors have been widely used in the treatment of various cancers. Programmed cell death-ligand 1 (PD-L1) and programmed cell death-ligand 2 located on cancer cells will bind to PD-1 receptors on T cells and suppress them, which will prevent cancer cell destruction. Programmed cell death protein 1 inhibitors block the binding of PD-L1 to cancer cells, which then prevents T-cell immunosuppression.1 However, cutaneous adverse effects have been associated with PD-1 inhibitors. Dermatitis associated with PD-1 inhibitor therapy occurs more frequently in patients with cutaneous tumors such as melanoma compared to those with head and neck cancers.2 Curry et al1 reported that treatment with an immune checkpoint blockade can lead to immune-related adverse effects, most commonly affecting the gastrointestinal tract, liver, and skin. The same report cited dermatologic toxicity as an adverse effect in approximately 39% of patients treated with anti–PD-1 and approximately 17% of anti–PD-L1.1 The 4 main categories of dermatologic toxicities to immunotherapies in general include inflammatory disorders, immunobullous disorders, alterations of keratinocytes, and alteration of melanocytes. The most common adverse effects from the use of the PD-1 inhibitor nivolumab were skin rashes, not otherwise specified (14%–20%), pruritus (13%–18%), and vitiligo (~8%).1 Of the cutaneous dermatitic reactions to PD-1 and PD-L1 inhibitors that were biopsied, the 2 most common were lichenoid dermatitis and spongiotic dermatitis.2 Seldomly, there have been reports of keratoacanthomas (KAs) in association with anti–PD-1 therapy.3
A KA is a common skin tumor that appears most frequently as a solitary lesion and is thought to arise from the hair follicle.4 It resembles squamous cell carcinoma and commonly regresses within months without intervention. Exposure to UV light is a known risk factor for the development of KAs.
Eruptive KAs have been found in association with 10 cases of various cancers treated with the PD-1 inhibitors pembrolizumab and nivolumab.3 Multiple lesions on photodistributed areas of the body were reported in all 10 cases. Various treatments were used in these 10 cases—doxycycline and niacinamide, electrodesiccation and curettage, clobetasol ointment and/or intralesional triamcinolone, cryotherapy, imiquimod, or no treatment—as well as the cessation of PD-1 inhibitor therapy, with 4 cases continuing therapy and 6 cases discontinuing therapy. Nine cases regressed by 6 months; electrodesiccation and curettage of the lesions was used in the tenth case.3 We report a case of eruptive KA after 1 cycle of nivolumab therapy for metastatic melanoma.
A 79-year-old woman with stage III melanoma presented to her dermatologist after developing generalized pruritic lichenoid eruptions involving the torso, arms, and legs, as well as erosions on the lips, buccal mucosa, and palate 1 month after starting nivolumab therapy. The patient initially presented to dermatology with an irregularly shaped lesion on the left upper back 3 months prior. Biopsy results at that time revealed a diagnosis of malignant melanoma, lentigo maligna type. The lesion was 1.5-mm thick and classified as Clark level IV with a mitotic count of 6 per mm2. Molecular genetic studies showed expression of PD-L1 and no expression of c-KIT. The patient underwent wide local excision, and a sentinel lymph node biopsy was positive. Positron emission tomography did not show any hypermetabolic lesions, and magnetic resonance imaging did not indicate brain metastasis. The patient underwent an axillary dissection, which did not show any residual melanoma. She was started on adjuvant immunotherapy with intravenous nivolumab 480 mg monthly and developed pruritic crusted lesions on the arms, legs, and torso 1 month later, which prompted follow-up to dermatology.
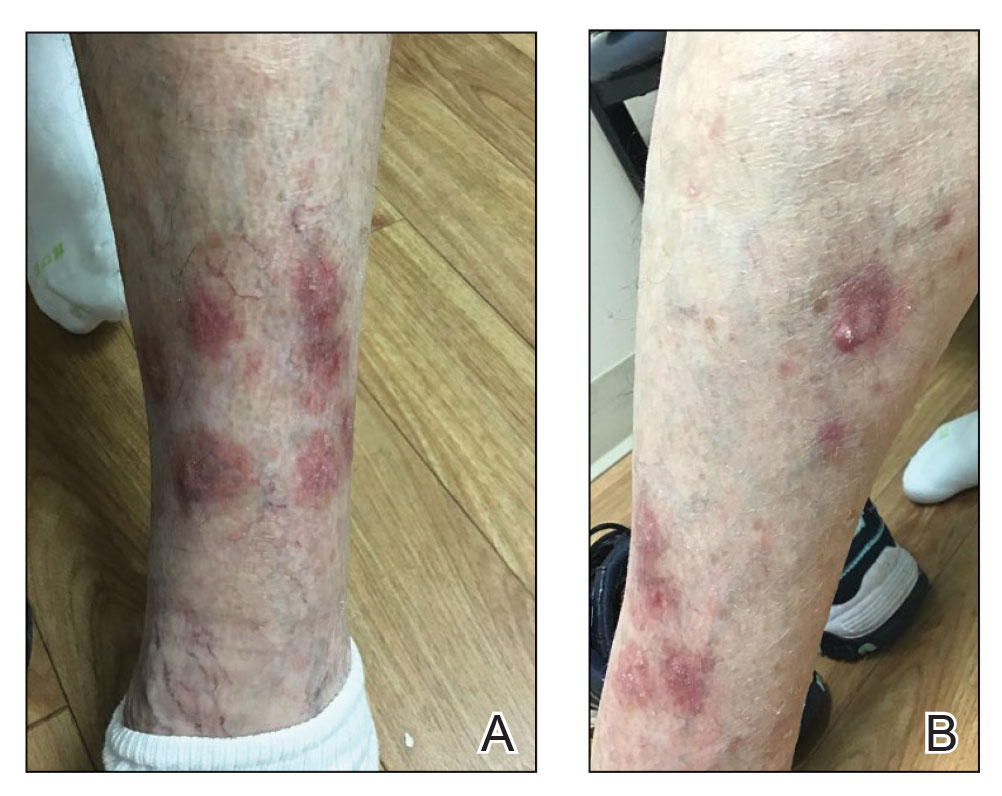
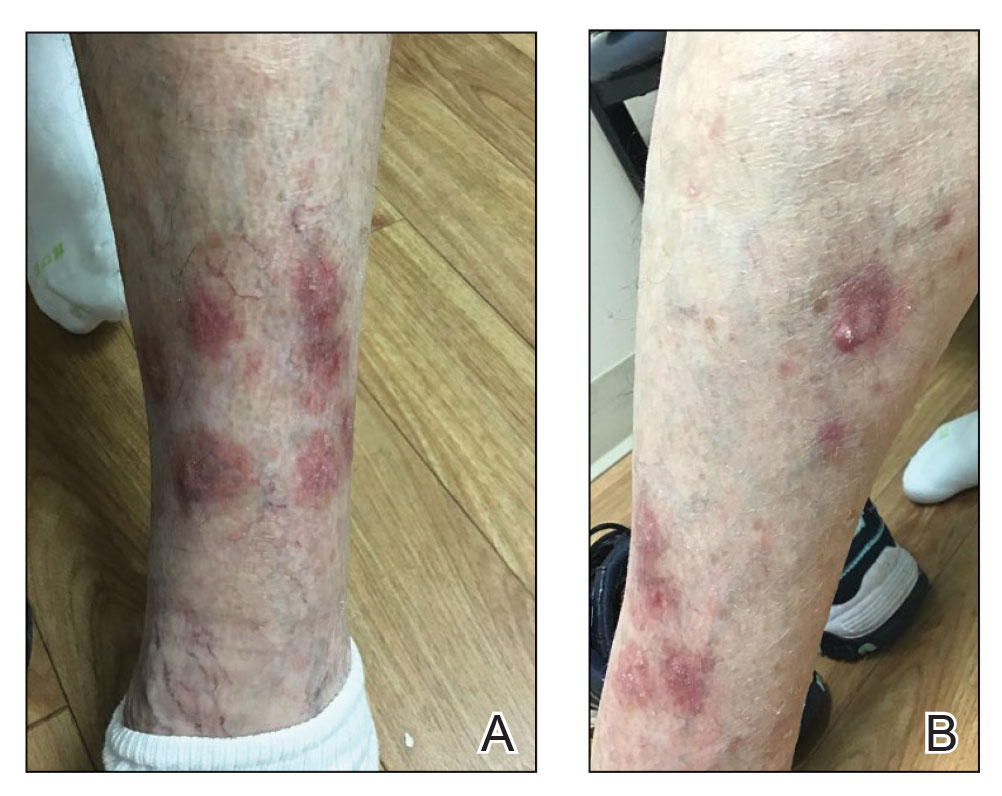
At the current presentation 4 months after the onset of lesions, physical examination revealed lichenoid patches with serous crusting that were concentrated on the torso but also affected the arms and legs. She developed erosions on the upper and lower lips, buccal mucosa, and hard and soft palates, as well as painful, erythematous, dome-shaped papules and nodules on the legs (Figure 1). Her oncologist previously had initiated treatment at the onset of the lesions with clobetasol cream and valacyclovir for the lesions, but the patient showed no improvement.

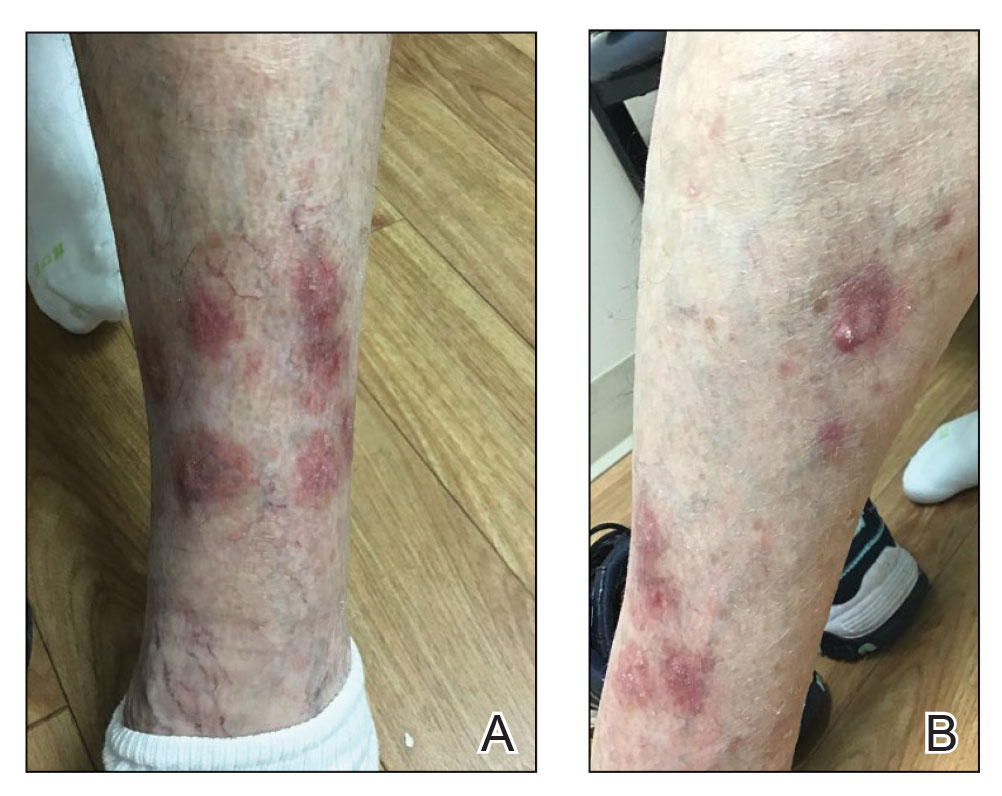
Four months after the onset of the lesions, the patient was re-referred to her dermatologist, and a biopsy was performed on the left lower leg that showed squamous cell carcinoma, KA type. Additionally, flat erythematous patches were seen on the legs that were consistent with a lichenoid drug eruption. Two weeks later, she was started on halobetasol propionate ointment 0.05% for treatment of the KAs. At 2-week follow-up, 5 months after the onset of the lesions, the patient showed no signs of improvement. An oral prednisone taper of 60 mg for 3 days, 40 mg for 3 days, and then 20 mg daily for a total of 4 weeks was started to treat the lichenoid dermatitis and eruptive KAs. At the next follow-up 6.5 months following the first eruptive KAs, she was no longer using topical or oral steroids, she did not have any new eruptive KAs, and old lesions showed regression (Figure 2). The patient still experienced postinflammatory erythema and hyperpigmentation at the location of the KAs but showed improvement of the lichenoid drug eruption.
We describe a case of eruptive KAs after use of a PD-1 inhibitor for treatment of melanoma. Our patient developed eruptive KAs after only 1 nivolumab treatment. Another report described onset of eruptive KAs after 1 month of nivolumab infusions.3 The KAs experienced by our patient took 6.5 months to regress, which is unusual compared to other case reports in which the KAs self-resolved within a few months, though one other case described lesions that persisted for 6 months.3
Our patient was treated with topical steroids and an oral steroid taper for the concomitant lichenoid drug eruption. It is unknown if the steroids affected the course of the KAs or if they spontaneously regressed on their own. Freites-Martinez et al5 described that regression of KAs may be related to an immune response, but corticosteroids are inherently immunosuppressive. They hypothesized that corticosteroids help to temper the heightened immune response of eruptive KAs.5
Our patient had oral ulcers, which may have been indicative of an oral lichenoid drug eruption, as well as skin lesions representative of a cutaneous lichenoid drug eruption. This is a favorable reaction, as lichenoid dermatitis is thought to represent successful PD-1 inhibition and therefore a better response to oncologic therapies.2 Comorbid lichenoid drug eruption lesions and eruptive KAs may be suggestive of increased T-cell activity,2,6,7 though some prior case studies have reported eruptive KAs in isolation.3
Discontinuation of immunotherapy due to development of eruptive KAs presents a challenge in the treatment of underlying malignancies such as melanoma. Immunotherapy was discontinued in 7 of 11 cases due to these cutaneous reactions.3 Similarly, our patient underwent only 1 cycle of immunotherapy before developing eruptive KAs and discontinuing PD-1 inhibitor therapy. If we are better able to treat eruptive KAs, then patients can remain on immunotherapy to treat underlying malignancies. Crow et al8 showed improvement in lesions when 3 patients with eruptive KAs were treated with hydroxychloroquine; the Goeckerman regimen consisting of steroids, UVB phototherapy, and crude coal tar; and Unna boots with zinc oxide and compression stockings. The above may be added to a list of possible treatments to consider for hastening the regression of eruptive KAs.
Our patient’s clinical course was similar to reports on the regressive nature of eruptive KAs within 6 months after initial eruption. Although it is likely that KAs will regress on their own, treatment modalities that speed up recovery are a future source for research.
- Curry JL, Tetzlaff MT, Nagarajan P, et al. Diverse types of dermatologic toxicities from immune checkpoint blockade therapy. J Cutan Pathol. 2017;44:158-176.
- Min Lee CK, Li S, Tran DC, et al. Characterization of dermatitis after PD-1/PD-L1 inhibitor therapy and association with multiple oncologic outcomes: a retrospective case-control study. J Am Acad Dermatol. 2018;79:1047-1052. doi:10.1016/j.jaad.2018.05.035
- Antonov NK, Nair KG, Halasz CL. Transient eruptive keratoacanthomas associated with nivolumab. JAAD Case Rep. 2019;5:342-345. doi:10.1016/j.jdcr.2019.01.025
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74:1220-1233.
- Freites-Martinez A, Kwong BY, Rieger KE, et al. Eruptive keratoacanthomas associated with pembrolizumab therapy. JAMA Dermatol. 2017;153:694-697. doi:10.1001/jamadermatol.2017.0989
- Bednarek R, Marks K, Lin G. Eruptive keratoacanthomas secondary to nivolumab immunotherapy. Int J Dermatol. 2018;57:E28-E29.
- Feldstein SI, Patel F, Kim E, et al. Eruptive keratoacanthomas arising in the setting of lichenoid toxicity after programmed cell death 1 inhibition with nivolumab. J Eur Acad Dermatol Venereol. 2018;32:E58-E59.
- Crow LD, Perkins I, Twigg AR, et al. Treatment of PD-1/PD-L1 inhibitor-induced dermatitis resolves concomitant eruptive keratoacanthomas. JAMA Dermatol. 2020;156:598-600. doi:10.1001/jamadermatol.2020.0176
To the Editor:
Programmed cell death protein 1 (PD-1) inhibitors have been widely used in the treatment of various cancers. Programmed cell death-ligand 1 (PD-L1) and programmed cell death-ligand 2 located on cancer cells will bind to PD-1 receptors on T cells and suppress them, which will prevent cancer cell destruction. Programmed cell death protein 1 inhibitors block the binding of PD-L1 to cancer cells, which then prevents T-cell immunosuppression.1 However, cutaneous adverse effects have been associated with PD-1 inhibitors. Dermatitis associated with PD-1 inhibitor therapy occurs more frequently in patients with cutaneous tumors such as melanoma compared to those with head and neck cancers.2 Curry et al1 reported that treatment with an immune checkpoint blockade can lead to immune-related adverse effects, most commonly affecting the gastrointestinal tract, liver, and skin. The same report cited dermatologic toxicity as an adverse effect in approximately 39% of patients treated with anti–PD-1 and approximately 17% of anti–PD-L1.1 The 4 main categories of dermatologic toxicities to immunotherapies in general include inflammatory disorders, immunobullous disorders, alterations of keratinocytes, and alteration of melanocytes. The most common adverse effects from the use of the PD-1 inhibitor nivolumab were skin rashes, not otherwise specified (14%–20%), pruritus (13%–18%), and vitiligo (~8%).1 Of the cutaneous dermatitic reactions to PD-1 and PD-L1 inhibitors that were biopsied, the 2 most common were lichenoid dermatitis and spongiotic dermatitis.2 Seldomly, there have been reports of keratoacanthomas (KAs) in association with anti–PD-1 therapy.3
A KA is a common skin tumor that appears most frequently as a solitary lesion and is thought to arise from the hair follicle.4 It resembles squamous cell carcinoma and commonly regresses within months without intervention. Exposure to UV light is a known risk factor for the development of KAs.
Eruptive KAs have been found in association with 10 cases of various cancers treated with the PD-1 inhibitors pembrolizumab and nivolumab.3 Multiple lesions on photodistributed areas of the body were reported in all 10 cases. Various treatments were used in these 10 cases—doxycycline and niacinamide, electrodesiccation and curettage, clobetasol ointment and/or intralesional triamcinolone, cryotherapy, imiquimod, or no treatment—as well as the cessation of PD-1 inhibitor therapy, with 4 cases continuing therapy and 6 cases discontinuing therapy. Nine cases regressed by 6 months; electrodesiccation and curettage of the lesions was used in the tenth case.3 We report a case of eruptive KA after 1 cycle of nivolumab therapy for metastatic melanoma.
A 79-year-old woman with stage III melanoma presented to her dermatologist after developing generalized pruritic lichenoid eruptions involving the torso, arms, and legs, as well as erosions on the lips, buccal mucosa, and palate 1 month after starting nivolumab therapy. The patient initially presented to dermatology with an irregularly shaped lesion on the left upper back 3 months prior. Biopsy results at that time revealed a diagnosis of malignant melanoma, lentigo maligna type. The lesion was 1.5-mm thick and classified as Clark level IV with a mitotic count of 6 per mm2. Molecular genetic studies showed expression of PD-L1 and no expression of c-KIT. The patient underwent wide local excision, and a sentinel lymph node biopsy was positive. Positron emission tomography did not show any hypermetabolic lesions, and magnetic resonance imaging did not indicate brain metastasis. The patient underwent an axillary dissection, which did not show any residual melanoma. She was started on adjuvant immunotherapy with intravenous nivolumab 480 mg monthly and developed pruritic crusted lesions on the arms, legs, and torso 1 month later, which prompted follow-up to dermatology.
At the current presentation 4 months after the onset of lesions, physical examination revealed lichenoid patches with serous crusting that were concentrated on the torso but also affected the arms and legs. She developed erosions on the upper and lower lips, buccal mucosa, and hard and soft palates, as well as painful, erythematous, dome-shaped papules and nodules on the legs (Figure 1). Her oncologist previously had initiated treatment at the onset of the lesions with clobetasol cream and valacyclovir for the lesions, but the patient showed no improvement.

Four months after the onset of the lesions, the patient was re-referred to her dermatologist, and a biopsy was performed on the left lower leg that showed squamous cell carcinoma, KA type. Additionally, flat erythematous patches were seen on the legs that were consistent with a lichenoid drug eruption. Two weeks later, she was started on halobetasol propionate ointment 0.05% for treatment of the KAs. At 2-week follow-up, 5 months after the onset of the lesions, the patient showed no signs of improvement. An oral prednisone taper of 60 mg for 3 days, 40 mg for 3 days, and then 20 mg daily for a total of 4 weeks was started to treat the lichenoid dermatitis and eruptive KAs. At the next follow-up 6.5 months following the first eruptive KAs, she was no longer using topical or oral steroids, she did not have any new eruptive KAs, and old lesions showed regression (Figure 2). The patient still experienced postinflammatory erythema and hyperpigmentation at the location of the KAs but showed improvement of the lichenoid drug eruption.
We describe a case of eruptive KAs after use of a PD-1 inhibitor for treatment of melanoma. Our patient developed eruptive KAs after only 1 nivolumab treatment. Another report described onset of eruptive KAs after 1 month of nivolumab infusions.3 The KAs experienced by our patient took 6.5 months to regress, which is unusual compared to other case reports in which the KAs self-resolved within a few months, though one other case described lesions that persisted for 6 months.3
Our patient was treated with topical steroids and an oral steroid taper for the concomitant lichenoid drug eruption. It is unknown if the steroids affected the course of the KAs or if they spontaneously regressed on their own. Freites-Martinez et al5 described that regression of KAs may be related to an immune response, but corticosteroids are inherently immunosuppressive. They hypothesized that corticosteroids help to temper the heightened immune response of eruptive KAs.5
Our patient had oral ulcers, which may have been indicative of an oral lichenoid drug eruption, as well as skin lesions representative of a cutaneous lichenoid drug eruption. This is a favorable reaction, as lichenoid dermatitis is thought to represent successful PD-1 inhibition and therefore a better response to oncologic therapies.2 Comorbid lichenoid drug eruption lesions and eruptive KAs may be suggestive of increased T-cell activity,2,6,7 though some prior case studies have reported eruptive KAs in isolation.3
Discontinuation of immunotherapy due to development of eruptive KAs presents a challenge in the treatment of underlying malignancies such as melanoma. Immunotherapy was discontinued in 7 of 11 cases due to these cutaneous reactions.3 Similarly, our patient underwent only 1 cycle of immunotherapy before developing eruptive KAs and discontinuing PD-1 inhibitor therapy. If we are better able to treat eruptive KAs, then patients can remain on immunotherapy to treat underlying malignancies. Crow et al8 showed improvement in lesions when 3 patients with eruptive KAs were treated with hydroxychloroquine; the Goeckerman regimen consisting of steroids, UVB phototherapy, and crude coal tar; and Unna boots with zinc oxide and compression stockings. The above may be added to a list of possible treatments to consider for hastening the regression of eruptive KAs.
Our patient’s clinical course was similar to reports on the regressive nature of eruptive KAs within 6 months after initial eruption. Although it is likely that KAs will regress on their own, treatment modalities that speed up recovery are a future source for research.
To the Editor:
Programmed cell death protein 1 (PD-1) inhibitors have been widely used in the treatment of various cancers. Programmed cell death-ligand 1 (PD-L1) and programmed cell death-ligand 2 located on cancer cells will bind to PD-1 receptors on T cells and suppress them, which will prevent cancer cell destruction. Programmed cell death protein 1 inhibitors block the binding of PD-L1 to cancer cells, which then prevents T-cell immunosuppression.1 However, cutaneous adverse effects have been associated with PD-1 inhibitors. Dermatitis associated with PD-1 inhibitor therapy occurs more frequently in patients with cutaneous tumors such as melanoma compared to those with head and neck cancers.2 Curry et al1 reported that treatment with an immune checkpoint blockade can lead to immune-related adverse effects, most commonly affecting the gastrointestinal tract, liver, and skin. The same report cited dermatologic toxicity as an adverse effect in approximately 39% of patients treated with anti–PD-1 and approximately 17% of anti–PD-L1.1 The 4 main categories of dermatologic toxicities to immunotherapies in general include inflammatory disorders, immunobullous disorders, alterations of keratinocytes, and alteration of melanocytes. The most common adverse effects from the use of the PD-1 inhibitor nivolumab were skin rashes, not otherwise specified (14%–20%), pruritus (13%–18%), and vitiligo (~8%).1 Of the cutaneous dermatitic reactions to PD-1 and PD-L1 inhibitors that were biopsied, the 2 most common were lichenoid dermatitis and spongiotic dermatitis.2 Seldomly, there have been reports of keratoacanthomas (KAs) in association with anti–PD-1 therapy.3
A KA is a common skin tumor that appears most frequently as a solitary lesion and is thought to arise from the hair follicle.4 It resembles squamous cell carcinoma and commonly regresses within months without intervention. Exposure to UV light is a known risk factor for the development of KAs.
Eruptive KAs have been found in association with 10 cases of various cancers treated with the PD-1 inhibitors pembrolizumab and nivolumab.3 Multiple lesions on photodistributed areas of the body were reported in all 10 cases. Various treatments were used in these 10 cases—doxycycline and niacinamide, electrodesiccation and curettage, clobetasol ointment and/or intralesional triamcinolone, cryotherapy, imiquimod, or no treatment—as well as the cessation of PD-1 inhibitor therapy, with 4 cases continuing therapy and 6 cases discontinuing therapy. Nine cases regressed by 6 months; electrodesiccation and curettage of the lesions was used in the tenth case.3 We report a case of eruptive KA after 1 cycle of nivolumab therapy for metastatic melanoma.
A 79-year-old woman with stage III melanoma presented to her dermatologist after developing generalized pruritic lichenoid eruptions involving the torso, arms, and legs, as well as erosions on the lips, buccal mucosa, and palate 1 month after starting nivolumab therapy. The patient initially presented to dermatology with an irregularly shaped lesion on the left upper back 3 months prior. Biopsy results at that time revealed a diagnosis of malignant melanoma, lentigo maligna type. The lesion was 1.5-mm thick and classified as Clark level IV with a mitotic count of 6 per mm2. Molecular genetic studies showed expression of PD-L1 and no expression of c-KIT. The patient underwent wide local excision, and a sentinel lymph node biopsy was positive. Positron emission tomography did not show any hypermetabolic lesions, and magnetic resonance imaging did not indicate brain metastasis. The patient underwent an axillary dissection, which did not show any residual melanoma. She was started on adjuvant immunotherapy with intravenous nivolumab 480 mg monthly and developed pruritic crusted lesions on the arms, legs, and torso 1 month later, which prompted follow-up to dermatology.
At the current presentation 4 months after the onset of lesions, physical examination revealed lichenoid patches with serous crusting that were concentrated on the torso but also affected the arms and legs. She developed erosions on the upper and lower lips, buccal mucosa, and hard and soft palates, as well as painful, erythematous, dome-shaped papules and nodules on the legs (Figure 1). Her oncologist previously had initiated treatment at the onset of the lesions with clobetasol cream and valacyclovir for the lesions, but the patient showed no improvement.

Four months after the onset of the lesions, the patient was re-referred to her dermatologist, and a biopsy was performed on the left lower leg that showed squamous cell carcinoma, KA type. Additionally, flat erythematous patches were seen on the legs that were consistent with a lichenoid drug eruption. Two weeks later, she was started on halobetasol propionate ointment 0.05% for treatment of the KAs. At 2-week follow-up, 5 months after the onset of the lesions, the patient showed no signs of improvement. An oral prednisone taper of 60 mg for 3 days, 40 mg for 3 days, and then 20 mg daily for a total of 4 weeks was started to treat the lichenoid dermatitis and eruptive KAs. At the next follow-up 6.5 months following the first eruptive KAs, she was no longer using topical or oral steroids, she did not have any new eruptive KAs, and old lesions showed regression (Figure 2). The patient still experienced postinflammatory erythema and hyperpigmentation at the location of the KAs but showed improvement of the lichenoid drug eruption.
We describe a case of eruptive KAs after use of a PD-1 inhibitor for treatment of melanoma. Our patient developed eruptive KAs after only 1 nivolumab treatment. Another report described onset of eruptive KAs after 1 month of nivolumab infusions.3 The KAs experienced by our patient took 6.5 months to regress, which is unusual compared to other case reports in which the KAs self-resolved within a few months, though one other case described lesions that persisted for 6 months.3
Our patient was treated with topical steroids and an oral steroid taper for the concomitant lichenoid drug eruption. It is unknown if the steroids affected the course of the KAs or if they spontaneously regressed on their own. Freites-Martinez et al5 described that regression of KAs may be related to an immune response, but corticosteroids are inherently immunosuppressive. They hypothesized that corticosteroids help to temper the heightened immune response of eruptive KAs.5
Our patient had oral ulcers, which may have been indicative of an oral lichenoid drug eruption, as well as skin lesions representative of a cutaneous lichenoid drug eruption. This is a favorable reaction, as lichenoid dermatitis is thought to represent successful PD-1 inhibition and therefore a better response to oncologic therapies.2 Comorbid lichenoid drug eruption lesions and eruptive KAs may be suggestive of increased T-cell activity,2,6,7 though some prior case studies have reported eruptive KAs in isolation.3
Discontinuation of immunotherapy due to development of eruptive KAs presents a challenge in the treatment of underlying malignancies such as melanoma. Immunotherapy was discontinued in 7 of 11 cases due to these cutaneous reactions.3 Similarly, our patient underwent only 1 cycle of immunotherapy before developing eruptive KAs and discontinuing PD-1 inhibitor therapy. If we are better able to treat eruptive KAs, then patients can remain on immunotherapy to treat underlying malignancies. Crow et al8 showed improvement in lesions when 3 patients with eruptive KAs were treated with hydroxychloroquine; the Goeckerman regimen consisting of steroids, UVB phototherapy, and crude coal tar; and Unna boots with zinc oxide and compression stockings. The above may be added to a list of possible treatments to consider for hastening the regression of eruptive KAs.
Our patient’s clinical course was similar to reports on the regressive nature of eruptive KAs within 6 months after initial eruption. Although it is likely that KAs will regress on their own, treatment modalities that speed up recovery are a future source for research.
- Curry JL, Tetzlaff MT, Nagarajan P, et al. Diverse types of dermatologic toxicities from immune checkpoint blockade therapy. J Cutan Pathol. 2017;44:158-176.
- Min Lee CK, Li S, Tran DC, et al. Characterization of dermatitis after PD-1/PD-L1 inhibitor therapy and association with multiple oncologic outcomes: a retrospective case-control study. J Am Acad Dermatol. 2018;79:1047-1052. doi:10.1016/j.jaad.2018.05.035
- Antonov NK, Nair KG, Halasz CL. Transient eruptive keratoacanthomas associated with nivolumab. JAAD Case Rep. 2019;5:342-345. doi:10.1016/j.jdcr.2019.01.025
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74:1220-1233.
- Freites-Martinez A, Kwong BY, Rieger KE, et al. Eruptive keratoacanthomas associated with pembrolizumab therapy. JAMA Dermatol. 2017;153:694-697. doi:10.1001/jamadermatol.2017.0989
- Bednarek R, Marks K, Lin G. Eruptive keratoacanthomas secondary to nivolumab immunotherapy. Int J Dermatol. 2018;57:E28-E29.
- Feldstein SI, Patel F, Kim E, et al. Eruptive keratoacanthomas arising in the setting of lichenoid toxicity after programmed cell death 1 inhibition with nivolumab. J Eur Acad Dermatol Venereol. 2018;32:E58-E59.
- Crow LD, Perkins I, Twigg AR, et al. Treatment of PD-1/PD-L1 inhibitor-induced dermatitis resolves concomitant eruptive keratoacanthomas. JAMA Dermatol. 2020;156:598-600. doi:10.1001/jamadermatol.2020.0176
- Curry JL, Tetzlaff MT, Nagarajan P, et al. Diverse types of dermatologic toxicities from immune checkpoint blockade therapy. J Cutan Pathol. 2017;44:158-176.
- Min Lee CK, Li S, Tran DC, et al. Characterization of dermatitis after PD-1/PD-L1 inhibitor therapy and association with multiple oncologic outcomes: a retrospective case-control study. J Am Acad Dermatol. 2018;79:1047-1052. doi:10.1016/j.jaad.2018.05.035
- Antonov NK, Nair KG, Halasz CL. Transient eruptive keratoacanthomas associated with nivolumab. JAAD Case Rep. 2019;5:342-345. doi:10.1016/j.jdcr.2019.01.025
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74:1220-1233.
- Freites-Martinez A, Kwong BY, Rieger KE, et al. Eruptive keratoacanthomas associated with pembrolizumab therapy. JAMA Dermatol. 2017;153:694-697. doi:10.1001/jamadermatol.2017.0989
- Bednarek R, Marks K, Lin G. Eruptive keratoacanthomas secondary to nivolumab immunotherapy. Int J Dermatol. 2018;57:E28-E29.
- Feldstein SI, Patel F, Kim E, et al. Eruptive keratoacanthomas arising in the setting of lichenoid toxicity after programmed cell death 1 inhibition with nivolumab. J Eur Acad Dermatol Venereol. 2018;32:E58-E59.
- Crow LD, Perkins I, Twigg AR, et al. Treatment of PD-1/PD-L1 inhibitor-induced dermatitis resolves concomitant eruptive keratoacanthomas. JAMA Dermatol. 2020;156:598-600. doi:10.1001/jamadermatol.2020.0176
Practice Points
- Eruptive keratoacanthomas (KAs) are a rare buttransient adverse effect of programmed cell death protein 1 (PD-1) inhibitor therapy.
- Nivolumab, a human monoclonal IgG4 antibody, is used as an antitumor treatment for melanoma by blocking PD-1.
- Possible new treatments may hasten the regression of eruptive KAs, which could allow patients to continue PD-1 inhibitor therapy.
Inpatient Dermatology Consultation Services in Hospital Institutions
Inpatient dermatology consultation services are becoming increasingly prevalent in hospital institutions.1-3 Although often underutilized as a consulting service, dermatology-related admissions cost hundreds of millions of dollars for the health care system.1,2 Misdiagnosis, prolonged hospital stays, and incorrect treatment are common results of lack of involvement by a skin expert.1-3 The importance of consultative inpatient dermatology cannot be understated. Accreditation Council for Graduate Medical Education requirements for proficiency in dermatology residency include exposure to inpatient dermatology, and it is our duty as residents to aid our colleagues in the management and treatment of cutaneous disease.
Although exposure to inpatient dermatology varies across residency programs, nearly every dermatology resident is bound to perform a consultation and be involved in the care of a hospitalized patient. At our program at the University of Utah (Salt Lake City), we have robust inpatient exposure, and after numerous hours spent on the forefront of inpatient dermatology, I have accrued a list of specific tips and techniques that have aided me as a resident clinician.
Pre-Rounding More Thoroughly
When I started as a postgraduate year 2 (PGY-2) on the inpatient dermatology rotation, I found myself perplexed. I had learned how to round in internal medicine but was unaccustomed to the nuances of specialty rounds. My list included calciphylaxis, small vessel vasculitis, cellulitis, stasis dermatitis, toxic epidermal necrolysis, and atypical mycobacterial infection. The first few days of service were undeniably difficult due to the daily consultations, complexity of admitted patients, and need for efficiency. I sometimes overlooked important laboratory test results, medication changes, and interdisciplinary discussions that prolonged rounding. As dermatologists, we are responsible for the largest organ of the body, and it is important to approach patients in a comprehensive manner. Pre-rounding should include reviewing interdisciplinary notes, laboratory values/results, and medications, and performing a focused skin examination with a review of systems during the encounter. Importantly, most electronic medical record systems offer an automated rounding sheet. In Epic (Epic Systems Corporation), I would use the bone marrow transplant rounding sheet, which includes laboratory test results, vitals, and medications. After printing out the rounding sheet, I would note important updates for each patient. Although pre-rounding and chart review requires time and effort, it aided me in providing elevated patient care and becoming more efficient during rounds. Over time I have come to strongly appreciate the term dermatology hospitalist. Cutaneous manifestations of systemic disease require thoughtful consideration and workup.
New Patient Consultations: Must-Ask Questions
Holding the university inpatient pager can be stressful. At the University of Utah, we often carry 5 to 10 patients on our list and receive 3 to 4 new consultations a day, sometimes right before 5
- What is the patient’s name, room number, and medical record number?
- Is this patient getting admitted or admitted currently?
- Is the rash the reason for admission? (This can greatly help with triaging the urgency of evaluation.)
- Is the rash painful?
- Is this patient ill?
- How would you describe the rash?
When evaluating new patients, it is crucial to remember the morphology camps. Formulating a differential diagnosis on a complex patient can be difficult; however, remembering the morphology camps of acneiform, dermal, eczematous, erythematous, subcutaneous, vasculitic, vasculopathic, and vesiculobullous lesions can be extremely helpful. Additionally, it is crucial to perform a thorough and complete skin examination on every patient. When emphasizing the importance of this, I often am reminded of a humbling moment early in my training. Our team was consulted on a patient with cellulitis and stasis dermatitis. It was a busy day, and my examination was quick and focused on the lower and upper extremities, chest, and back. The patient improved from a cutaneous standpoint and was discharged. At follow-up the next week, one of my attending providers biopsied an atypical macule on the retroauricular region, which was found to be consistent with a stage 1A melanoma. Even on the longest and most tiring hospital days, it is important to perform a full-body skin examination on each patient. You may end up saving a life.
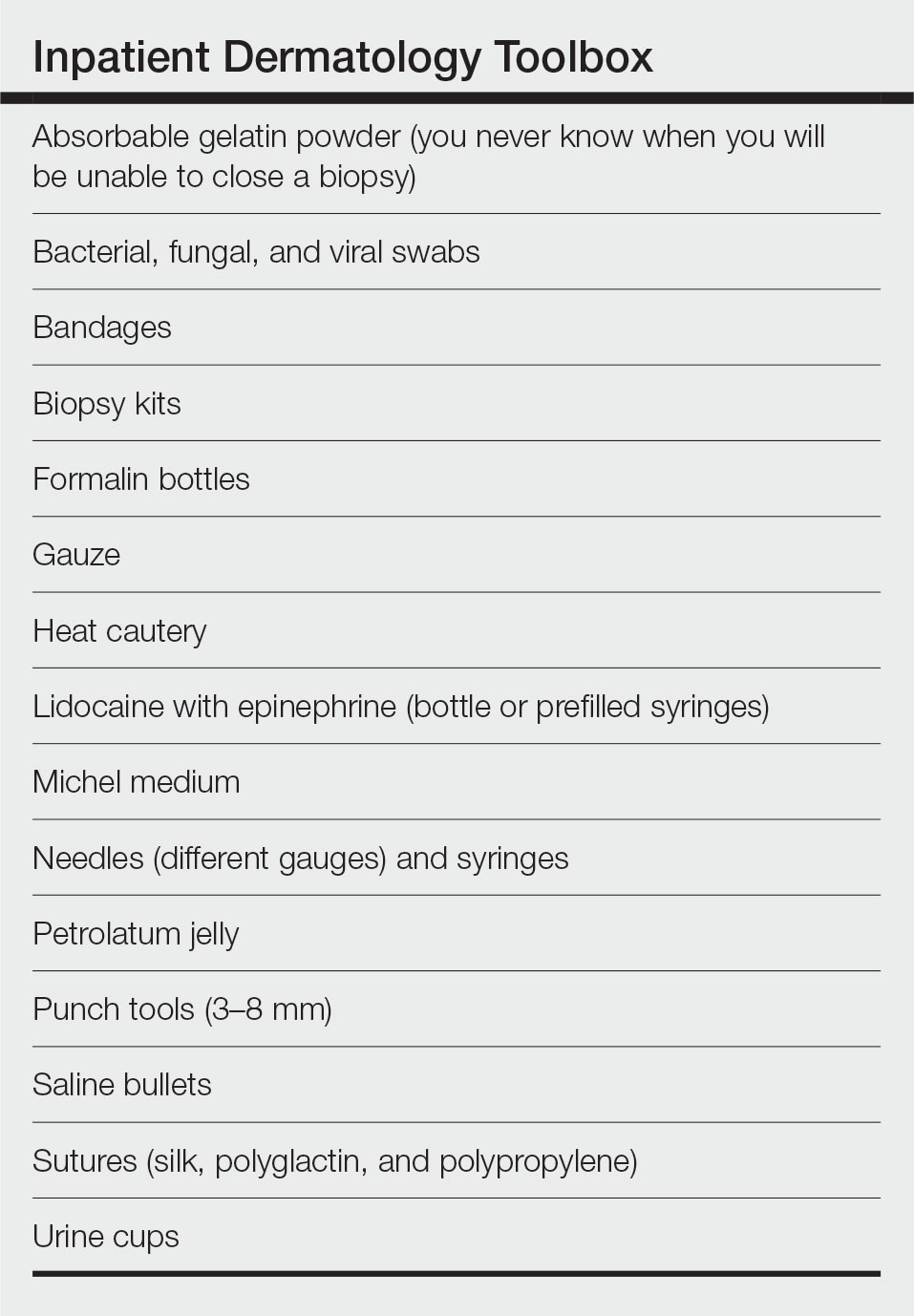
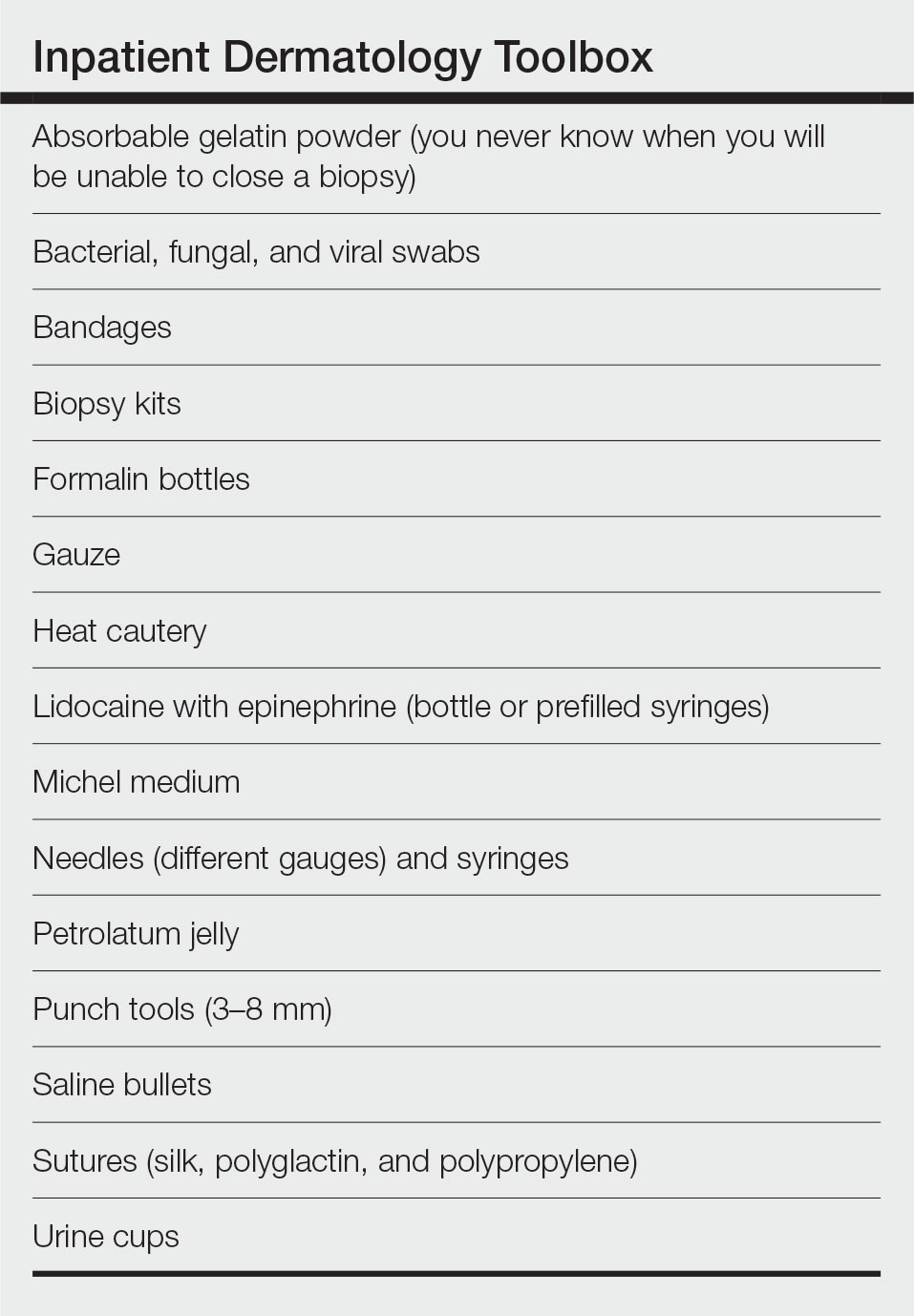
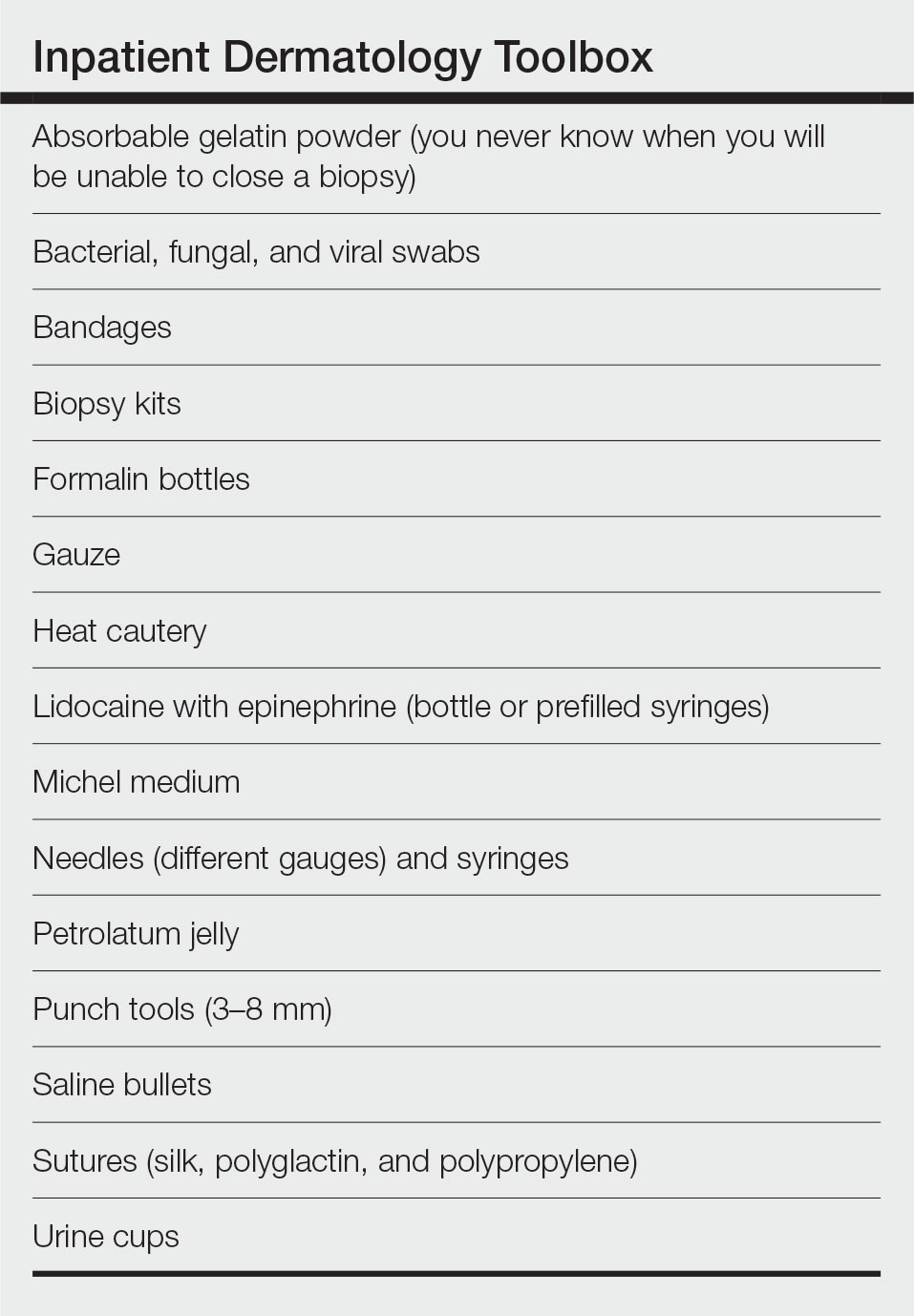
An Organized Toolbox: What to Carry
Similar to our ophthalmology colleagues who are seen carrying around a suitcase in the hospital, I highly recommend some form of a toolbox or bag for performing inpatient biopsies (Table). Carrying around an organized bag, albeit bulky and unfashionable, has saved me numerous trips back to clinic for unexpected complications including fixing leaky vessels, closing stubborn ulcers, and coordinating sedated biopsies in the operating room.
Final Thoughts
As I near the completion of my residency journey, I hope these tips will aid budding and current dermatology residents at excelling as dermatology hospitalists during inpatient rotations. Dermatologists can make a profound impact on a variety of patients, especially when treating hospitalized patients on the clinical forefront. Our role extends beyond the skin, as cutaneous manifestations of internal disease are not uncommon.
- Afifi L, Shinkai K. Optimizing education on the inpatient dermatology consultative service. Semin Cutan Med Surg. 2017;36:28-34. doi:10.12788/j.sder.2017.003
- Biesbroeck LK, Shinohara MM. Inpatient consultative dermatology [published online September 1, 2015]. Med Clin North Am. 2015;99:1349-1364. doi:10.1016/j.mcna.2015.06.004
- Madigan LM, Fox LP. Where are we now with inpatient consultative dermatology? assessing the value and evolution of this subspecialty over the past decade. J Am Acad Dermatol. 2019;80:1804-1808. doi:10.1016/j.jaad.2019.01.031
Inpatient dermatology consultation services are becoming increasingly prevalent in hospital institutions.1-3 Although often underutilized as a consulting service, dermatology-related admissions cost hundreds of millions of dollars for the health care system.1,2 Misdiagnosis, prolonged hospital stays, and incorrect treatment are common results of lack of involvement by a skin expert.1-3 The importance of consultative inpatient dermatology cannot be understated. Accreditation Council for Graduate Medical Education requirements for proficiency in dermatology residency include exposure to inpatient dermatology, and it is our duty as residents to aid our colleagues in the management and treatment of cutaneous disease.
Although exposure to inpatient dermatology varies across residency programs, nearly every dermatology resident is bound to perform a consultation and be involved in the care of a hospitalized patient. At our program at the University of Utah (Salt Lake City), we have robust inpatient exposure, and after numerous hours spent on the forefront of inpatient dermatology, I have accrued a list of specific tips and techniques that have aided me as a resident clinician.
Pre-Rounding More Thoroughly
When I started as a postgraduate year 2 (PGY-2) on the inpatient dermatology rotation, I found myself perplexed. I had learned how to round in internal medicine but was unaccustomed to the nuances of specialty rounds. My list included calciphylaxis, small vessel vasculitis, cellulitis, stasis dermatitis, toxic epidermal necrolysis, and atypical mycobacterial infection. The first few days of service were undeniably difficult due to the daily consultations, complexity of admitted patients, and need for efficiency. I sometimes overlooked important laboratory test results, medication changes, and interdisciplinary discussions that prolonged rounding. As dermatologists, we are responsible for the largest organ of the body, and it is important to approach patients in a comprehensive manner. Pre-rounding should include reviewing interdisciplinary notes, laboratory values/results, and medications, and performing a focused skin examination with a review of systems during the encounter. Importantly, most electronic medical record systems offer an automated rounding sheet. In Epic (Epic Systems Corporation), I would use the bone marrow transplant rounding sheet, which includes laboratory test results, vitals, and medications. After printing out the rounding sheet, I would note important updates for each patient. Although pre-rounding and chart review requires time and effort, it aided me in providing elevated patient care and becoming more efficient during rounds. Over time I have come to strongly appreciate the term dermatology hospitalist. Cutaneous manifestations of systemic disease require thoughtful consideration and workup.
New Patient Consultations: Must-Ask Questions
Holding the university inpatient pager can be stressful. At the University of Utah, we often carry 5 to 10 patients on our list and receive 3 to 4 new consultations a day, sometimes right before 5
- What is the patient’s name, room number, and medical record number?
- Is this patient getting admitted or admitted currently?
- Is the rash the reason for admission? (This can greatly help with triaging the urgency of evaluation.)
- Is the rash painful?
- Is this patient ill?
- How would you describe the rash?
When evaluating new patients, it is crucial to remember the morphology camps. Formulating a differential diagnosis on a complex patient can be difficult; however, remembering the morphology camps of acneiform, dermal, eczematous, erythematous, subcutaneous, vasculitic, vasculopathic, and vesiculobullous lesions can be extremely helpful. Additionally, it is crucial to perform a thorough and complete skin examination on every patient. When emphasizing the importance of this, I often am reminded of a humbling moment early in my training. Our team was consulted on a patient with cellulitis and stasis dermatitis. It was a busy day, and my examination was quick and focused on the lower and upper extremities, chest, and back. The patient improved from a cutaneous standpoint and was discharged. At follow-up the next week, one of my attending providers biopsied an atypical macule on the retroauricular region, which was found to be consistent with a stage 1A melanoma. Even on the longest and most tiring hospital days, it is important to perform a full-body skin examination on each patient. You may end up saving a life.
An Organized Toolbox: What to Carry
Similar to our ophthalmology colleagues who are seen carrying around a suitcase in the hospital, I highly recommend some form of a toolbox or bag for performing inpatient biopsies (Table). Carrying around an organized bag, albeit bulky and unfashionable, has saved me numerous trips back to clinic for unexpected complications including fixing leaky vessels, closing stubborn ulcers, and coordinating sedated biopsies in the operating room.
Final Thoughts
As I near the completion of my residency journey, I hope these tips will aid budding and current dermatology residents at excelling as dermatology hospitalists during inpatient rotations. Dermatologists can make a profound impact on a variety of patients, especially when treating hospitalized patients on the clinical forefront. Our role extends beyond the skin, as cutaneous manifestations of internal disease are not uncommon.
Inpatient dermatology consultation services are becoming increasingly prevalent in hospital institutions.1-3 Although often underutilized as a consulting service, dermatology-related admissions cost hundreds of millions of dollars for the health care system.1,2 Misdiagnosis, prolonged hospital stays, and incorrect treatment are common results of lack of involvement by a skin expert.1-3 The importance of consultative inpatient dermatology cannot be understated. Accreditation Council for Graduate Medical Education requirements for proficiency in dermatology residency include exposure to inpatient dermatology, and it is our duty as residents to aid our colleagues in the management and treatment of cutaneous disease.
Although exposure to inpatient dermatology varies across residency programs, nearly every dermatology resident is bound to perform a consultation and be involved in the care of a hospitalized patient. At our program at the University of Utah (Salt Lake City), we have robust inpatient exposure, and after numerous hours spent on the forefront of inpatient dermatology, I have accrued a list of specific tips and techniques that have aided me as a resident clinician.
Pre-Rounding More Thoroughly
When I started as a postgraduate year 2 (PGY-2) on the inpatient dermatology rotation, I found myself perplexed. I had learned how to round in internal medicine but was unaccustomed to the nuances of specialty rounds. My list included calciphylaxis, small vessel vasculitis, cellulitis, stasis dermatitis, toxic epidermal necrolysis, and atypical mycobacterial infection. The first few days of service were undeniably difficult due to the daily consultations, complexity of admitted patients, and need for efficiency. I sometimes overlooked important laboratory test results, medication changes, and interdisciplinary discussions that prolonged rounding. As dermatologists, we are responsible for the largest organ of the body, and it is important to approach patients in a comprehensive manner. Pre-rounding should include reviewing interdisciplinary notes, laboratory values/results, and medications, and performing a focused skin examination with a review of systems during the encounter. Importantly, most electronic medical record systems offer an automated rounding sheet. In Epic (Epic Systems Corporation), I would use the bone marrow transplant rounding sheet, which includes laboratory test results, vitals, and medications. After printing out the rounding sheet, I would note important updates for each patient. Although pre-rounding and chart review requires time and effort, it aided me in providing elevated patient care and becoming more efficient during rounds. Over time I have come to strongly appreciate the term dermatology hospitalist. Cutaneous manifestations of systemic disease require thoughtful consideration and workup.
New Patient Consultations: Must-Ask Questions
Holding the university inpatient pager can be stressful. At the University of Utah, we often carry 5 to 10 patients on our list and receive 3 to 4 new consultations a day, sometimes right before 5
- What is the patient’s name, room number, and medical record number?
- Is this patient getting admitted or admitted currently?
- Is the rash the reason for admission? (This can greatly help with triaging the urgency of evaluation.)
- Is the rash painful?
- Is this patient ill?
- How would you describe the rash?
When evaluating new patients, it is crucial to remember the morphology camps. Formulating a differential diagnosis on a complex patient can be difficult; however, remembering the morphology camps of acneiform, dermal, eczematous, erythematous, subcutaneous, vasculitic, vasculopathic, and vesiculobullous lesions can be extremely helpful. Additionally, it is crucial to perform a thorough and complete skin examination on every patient. When emphasizing the importance of this, I often am reminded of a humbling moment early in my training. Our team was consulted on a patient with cellulitis and stasis dermatitis. It was a busy day, and my examination was quick and focused on the lower and upper extremities, chest, and back. The patient improved from a cutaneous standpoint and was discharged. At follow-up the next week, one of my attending providers biopsied an atypical macule on the retroauricular region, which was found to be consistent with a stage 1A melanoma. Even on the longest and most tiring hospital days, it is important to perform a full-body skin examination on each patient. You may end up saving a life.
An Organized Toolbox: What to Carry
Similar to our ophthalmology colleagues who are seen carrying around a suitcase in the hospital, I highly recommend some form of a toolbox or bag for performing inpatient biopsies (Table). Carrying around an organized bag, albeit bulky and unfashionable, has saved me numerous trips back to clinic for unexpected complications including fixing leaky vessels, closing stubborn ulcers, and coordinating sedated biopsies in the operating room.
Final Thoughts
As I near the completion of my residency journey, I hope these tips will aid budding and current dermatology residents at excelling as dermatology hospitalists during inpatient rotations. Dermatologists can make a profound impact on a variety of patients, especially when treating hospitalized patients on the clinical forefront. Our role extends beyond the skin, as cutaneous manifestations of internal disease are not uncommon.
- Afifi L, Shinkai K. Optimizing education on the inpatient dermatology consultative service. Semin Cutan Med Surg. 2017;36:28-34. doi:10.12788/j.sder.2017.003
- Biesbroeck LK, Shinohara MM. Inpatient consultative dermatology [published online September 1, 2015]. Med Clin North Am. 2015;99:1349-1364. doi:10.1016/j.mcna.2015.06.004
- Madigan LM, Fox LP. Where are we now with inpatient consultative dermatology? assessing the value and evolution of this subspecialty over the past decade. J Am Acad Dermatol. 2019;80:1804-1808. doi:10.1016/j.jaad.2019.01.031
- Afifi L, Shinkai K. Optimizing education on the inpatient dermatology consultative service. Semin Cutan Med Surg. 2017;36:28-34. doi:10.12788/j.sder.2017.003
- Biesbroeck LK, Shinohara MM. Inpatient consultative dermatology [published online September 1, 2015]. Med Clin North Am. 2015;99:1349-1364. doi:10.1016/j.mcna.2015.06.004
- Madigan LM, Fox LP. Where are we now with inpatient consultative dermatology? assessing the value and evolution of this subspecialty over the past decade. J Am Acad Dermatol. 2019;80:1804-1808. doi:10.1016/j.jaad.2019.01.031
Resident Pearl
- When performing inpatient dermatology consultations, residents should focus on pre-rounding and must-ask questions of requesting providers as well as carrying an organized toolbox.
Brepocitinib shows promise for psoriatic arthritis patients
The investigational drug brepocitinib showed superior symptom reduction in adults with moderate to severe active psoriatic arthritis (PsA), compared with placebo, by meeting primary and secondary endpoints of a phase 2b trial at 16 weeks, which persisted out to 1 year, according to data from 218 individuals.
Brepocitinib, a combination tyrosine kinase 2 and Janus kinase 1 inhibitor, is being studied for the treatment of several immunologic diseases including PsA, wrote Philip Mease, MD, of the Swedish Medical Center/Providence St. Joseph Health and the University of Washington, both in Seattle.
Previous studies in patients with PsA support the use of Janus kinase inhibitors and demonstrate the efficacy of tyrosine kinase 2 inhibitors, but more data are needed in patients with active PsA, the researchers noted.
In a study published in Arthritis & Rheumatology, the researchers randomized adults aged 18-75 years with moderate to severe PsA to once-daily oral doses of brepocitinib at 10 mg, 30 mg, or 60 mg, or a placebo for 16 weeks to assess safety, efficacy, and dose response. Placebo-treated patients were advanced to 30 mg or 60 mg of brepocitinib at week 16. Baseline demographics and disease characteristics were similar among the treatment groups. The mean Psoriatic Arthritis Disease Activity Score (PASDAS) and Disease Activity Index for PsA scores were 5.6 and 38.2, respectively, for the overall study population. Approximately two-thirds (64.7%) had a baseline Psoriasis Area and Severity Index (PASI) score greater than 0 and 3% or more of their body surface area affected by psoriasis.
The primary endpoint was the proportion of patients achieving 20% improvement in American College of Rheumatology response criteria (ACR 20) at week 16. Secondary endpoints included rates of patients meeting ACR 50 and ACR 70 response criteria, the proportion of patients achieving 75% and 90% improvement in PASI scores (PASI 70 and 90), as well as the rates of patients meeting Minimal Disease Activity (MDA) criteria at 16 and 52 weeks.
At week 16, ACR 20 response rates were significantly higher in the brepocitinib 30-mg and 60-mg groups, compared with the placebo group (66.7% and 74.6%, respectively, vs. 43.3%), but not for those who received brepocitinib 10 mg (64.5%).
Response rates for ACR 50, ACR 70, PASI 75, PASI 90, and MDA were similarly higher in the 30-mg and 60-mg brepocitinib groups, compared with placebo, and these responses persisted at week 52. Notably, significant differences in PASI 75 and PASI 90 were observed in patients taking 30 mg and 60 mg brepocitinib, compared with placebo, as early as weeks 4 and 8, respectively, the researchers said.
In addition, disease activity based on PASDAS improved significantly more from baseline to week 16 in all brepocitinib groups, compared with placebo.
The overall safety data were consistent with previous brepocitinib studies, and most of the adverse events were mild or moderate, the researchers said. A total of 12 participants (5.5%) experienced a total of 15 serious adverse events, including 6 infections with brepocitinib 30 mg or 60 mg. No major adverse cardiovascular events or deaths occurred during the study period.
The findings were limited by several factors, including the use of clinics in a limited geographic area (11 countries in Europe), small sample size, and mainly White population, the researchers noted. Other limitations included the large placebo effect and relatively short placebo-controlled period.
The study was supported by Pfizer. Dr. Mease disclosed relationships with Pfizer and other companies including AbbVie, Amgen, Bristol-Myers Squibb, Boehringer Ingelheim, Galapagos, Gilead, GlaxoSmithKline, Inmagene, Janssen, Lilly, Novartis, Sun, and UCB. Many coauthors were employees of Pfizer, and others reported financial relationships with Pfizer and other pharmaceutical companies.
The investigational drug brepocitinib showed superior symptom reduction in adults with moderate to severe active psoriatic arthritis (PsA), compared with placebo, by meeting primary and secondary endpoints of a phase 2b trial at 16 weeks, which persisted out to 1 year, according to data from 218 individuals.
Brepocitinib, a combination tyrosine kinase 2 and Janus kinase 1 inhibitor, is being studied for the treatment of several immunologic diseases including PsA, wrote Philip Mease, MD, of the Swedish Medical Center/Providence St. Joseph Health and the University of Washington, both in Seattle.
Previous studies in patients with PsA support the use of Janus kinase inhibitors and demonstrate the efficacy of tyrosine kinase 2 inhibitors, but more data are needed in patients with active PsA, the researchers noted.
In a study published in Arthritis & Rheumatology, the researchers randomized adults aged 18-75 years with moderate to severe PsA to once-daily oral doses of brepocitinib at 10 mg, 30 mg, or 60 mg, or a placebo for 16 weeks to assess safety, efficacy, and dose response. Placebo-treated patients were advanced to 30 mg or 60 mg of brepocitinib at week 16. Baseline demographics and disease characteristics were similar among the treatment groups. The mean Psoriatic Arthritis Disease Activity Score (PASDAS) and Disease Activity Index for PsA scores were 5.6 and 38.2, respectively, for the overall study population. Approximately two-thirds (64.7%) had a baseline Psoriasis Area and Severity Index (PASI) score greater than 0 and 3% or more of their body surface area affected by psoriasis.
The primary endpoint was the proportion of patients achieving 20% improvement in American College of Rheumatology response criteria (ACR 20) at week 16. Secondary endpoints included rates of patients meeting ACR 50 and ACR 70 response criteria, the proportion of patients achieving 75% and 90% improvement in PASI scores (PASI 70 and 90), as well as the rates of patients meeting Minimal Disease Activity (MDA) criteria at 16 and 52 weeks.
At week 16, ACR 20 response rates were significantly higher in the brepocitinib 30-mg and 60-mg groups, compared with the placebo group (66.7% and 74.6%, respectively, vs. 43.3%), but not for those who received brepocitinib 10 mg (64.5%).
Response rates for ACR 50, ACR 70, PASI 75, PASI 90, and MDA were similarly higher in the 30-mg and 60-mg brepocitinib groups, compared with placebo, and these responses persisted at week 52. Notably, significant differences in PASI 75 and PASI 90 were observed in patients taking 30 mg and 60 mg brepocitinib, compared with placebo, as early as weeks 4 and 8, respectively, the researchers said.
In addition, disease activity based on PASDAS improved significantly more from baseline to week 16 in all brepocitinib groups, compared with placebo.
The overall safety data were consistent with previous brepocitinib studies, and most of the adverse events were mild or moderate, the researchers said. A total of 12 participants (5.5%) experienced a total of 15 serious adverse events, including 6 infections with brepocitinib 30 mg or 60 mg. No major adverse cardiovascular events or deaths occurred during the study period.
The findings were limited by several factors, including the use of clinics in a limited geographic area (11 countries in Europe), small sample size, and mainly White population, the researchers noted. Other limitations included the large placebo effect and relatively short placebo-controlled period.
The study was supported by Pfizer. Dr. Mease disclosed relationships with Pfizer and other companies including AbbVie, Amgen, Bristol-Myers Squibb, Boehringer Ingelheim, Galapagos, Gilead, GlaxoSmithKline, Inmagene, Janssen, Lilly, Novartis, Sun, and UCB. Many coauthors were employees of Pfizer, and others reported financial relationships with Pfizer and other pharmaceutical companies.
The investigational drug brepocitinib showed superior symptom reduction in adults with moderate to severe active psoriatic arthritis (PsA), compared with placebo, by meeting primary and secondary endpoints of a phase 2b trial at 16 weeks, which persisted out to 1 year, according to data from 218 individuals.
Brepocitinib, a combination tyrosine kinase 2 and Janus kinase 1 inhibitor, is being studied for the treatment of several immunologic diseases including PsA, wrote Philip Mease, MD, of the Swedish Medical Center/Providence St. Joseph Health and the University of Washington, both in Seattle.
Previous studies in patients with PsA support the use of Janus kinase inhibitors and demonstrate the efficacy of tyrosine kinase 2 inhibitors, but more data are needed in patients with active PsA, the researchers noted.
In a study published in Arthritis & Rheumatology, the researchers randomized adults aged 18-75 years with moderate to severe PsA to once-daily oral doses of brepocitinib at 10 mg, 30 mg, or 60 mg, or a placebo for 16 weeks to assess safety, efficacy, and dose response. Placebo-treated patients were advanced to 30 mg or 60 mg of brepocitinib at week 16. Baseline demographics and disease characteristics were similar among the treatment groups. The mean Psoriatic Arthritis Disease Activity Score (PASDAS) and Disease Activity Index for PsA scores were 5.6 and 38.2, respectively, for the overall study population. Approximately two-thirds (64.7%) had a baseline Psoriasis Area and Severity Index (PASI) score greater than 0 and 3% or more of their body surface area affected by psoriasis.
The primary endpoint was the proportion of patients achieving 20% improvement in American College of Rheumatology response criteria (ACR 20) at week 16. Secondary endpoints included rates of patients meeting ACR 50 and ACR 70 response criteria, the proportion of patients achieving 75% and 90% improvement in PASI scores (PASI 70 and 90), as well as the rates of patients meeting Minimal Disease Activity (MDA) criteria at 16 and 52 weeks.
At week 16, ACR 20 response rates were significantly higher in the brepocitinib 30-mg and 60-mg groups, compared with the placebo group (66.7% and 74.6%, respectively, vs. 43.3%), but not for those who received brepocitinib 10 mg (64.5%).
Response rates for ACR 50, ACR 70, PASI 75, PASI 90, and MDA were similarly higher in the 30-mg and 60-mg brepocitinib groups, compared with placebo, and these responses persisted at week 52. Notably, significant differences in PASI 75 and PASI 90 were observed in patients taking 30 mg and 60 mg brepocitinib, compared with placebo, as early as weeks 4 and 8, respectively, the researchers said.
In addition, disease activity based on PASDAS improved significantly more from baseline to week 16 in all brepocitinib groups, compared with placebo.
The overall safety data were consistent with previous brepocitinib studies, and most of the adverse events were mild or moderate, the researchers said. A total of 12 participants (5.5%) experienced a total of 15 serious adverse events, including 6 infections with brepocitinib 30 mg or 60 mg. No major adverse cardiovascular events or deaths occurred during the study period.
The findings were limited by several factors, including the use of clinics in a limited geographic area (11 countries in Europe), small sample size, and mainly White population, the researchers noted. Other limitations included the large placebo effect and relatively short placebo-controlled period.
The study was supported by Pfizer. Dr. Mease disclosed relationships with Pfizer and other companies including AbbVie, Amgen, Bristol-Myers Squibb, Boehringer Ingelheim, Galapagos, Gilead, GlaxoSmithKline, Inmagene, Janssen, Lilly, Novartis, Sun, and UCB. Many coauthors were employees of Pfizer, and others reported financial relationships with Pfizer and other pharmaceutical companies.
FROM ARTHRITIS & RHEUMATOLOGY
Analysis: 40% of information about cirrhosis on TikTok is incorrect
CHICAGO –
TikTok’s short video format is increasingly becoming a major source for news and information, especially for adolescents and young adults. In 2022 the technology news website The Verge reported that about 10% of all U.S. adults regularly get news from TikTok, including an estimated 26% of adults under 30.
“Our study highlights the alarming prevalence of misinformation related to liver disease and cirrhosis on the TikTok platform. This misinformation can potentially lead to harm and poor health outcomes for individuals seeking accurate information about their conditions,” wrote the study authors in their abstract.
The study, which was led by Macklin Loveland, MD, an internal medicine resident at the University of Arizona, Tucson, found that, among 2,223 TikTok posts related to liver disease or cirrhosis as of November 2022, 60.3% were found to have accurate medical information, but the remaining 39.7% contained misinformation.
Some of the misinformation offered highly dubious and potentially dangerous advice, such as “Reishi mushrooms can reverse liver damage,” when in fact there is evidence to suggest that reishi mushrooms, especially in powder form, may be toxic to the liver and may even cause fatal fulminant hepatitis.
In an interview, Dr. Loveland said that much of the good information about liver disease on TikTok seems to come from patients with cirrhosis or other liver diseases who post videos chronicling their experiences, whereas bad information seems to come from people who are trying to pitch a product such as “natural” or “alternative” medicine.
“People who have real-life, firsthand experiences with cirrhosis have a really nice platform to talk about their disease process and share information with other people with similar disease processes, and the majority of them are accurate,” he said. “Where the inaccuracies come in are when people are trying to profit off a product or sell a dietary supplement, and then things go by the wayside.”
It’s important for TikTok users to understand the intentions of other users, he said, and expressed the hope that content mediators within TikTok would help to keep misinformation at bay.
Skyler B. Johnson, MD, assistant professor of radiation oncology at the University of Utah Huntsman Cancer Institute, Salt Lake City, has studied misinformation about cancer on social media, and as he and colleagues reported in the Journal of the National Cancer Institute, of 200 articles on cancer posted on social media sites, 32.5% contained misinformation and 30.5% contained harmful information.
In an interview, Dr. Johnson, who was not involved in the study by Dr. Loveland and colleagues, offered advice for colleagues about countering misinformation.
“What we’re trying to do, as part of our research group, is encourage physicians to take an active role in addressing misinformation with their patients and also in their social networking interactions,” he said. “When I see a new patient with a new diagnosis of cancer, I warn them that they’re going to encounter things online that may or may not be true.”
He noted that, often when physicians instruct patients not to go online to research their disease, the first thing the vast majority of patients do after leaving the office is to jump online.
Instead, Dr. Johnson recommended inoculating patients against misinformation – not to discourage them from going online, but to inform them about the myriad good and bad information sources, and steer them toward trustworthy sites such as government agencies (the National Institutes of Health, Centers for Disease Control and Prevention, etc), academic medical center sites, or select nonprofit organizations, foundations, and medical associations.
“But at the end of the day, even those you have to be somewhat vigilant about, because there are some unscrupulous providers who exploit even those sites,” he added.
Study details
Dr. Loveland and colleagues used the TikTok search engine to look for posts containing the terms “cirrhosis” and “liver disease,” and watched all such videos that turned up in the search from beginning to end. They classified each post as either educational in intent or whether it depicted a firsthand experience with liver disease.
They determined whether each post was accurate or erroneous according to guidelines from the American Association for the Study of Liver Disease, American College of Gastroenterology, and American Gastroenterological Association. They also recorded the number of likes, comments, and the number of times that each video was shared.
Accurate posts were viewed and liked significantly more often than inaccurate ones, and accurate posts had significantly more comments that faulty posts.
However, both accurate and inaccurate posts were shared a similar number of times, suggesting that bad-quality information can metastasize just as easily as good information can be disseminated.
Dr. Loveland and colleagues echoed the recommendations of Dr. Johnson, stating that “health care provides should be aware of the potential for misinformation on social media and should strive to provide their patients with accurate and evidence-based information to inform their health care decisions.”
The study was internally funded. Dr. Loveland and Dr. Johnson reported having no conflicts of interest to disclose.
DDW is sponsored by the American Association for the Study of Liver Diseases, the AGA, the American Society for Gastrointestinal Endoscopy, and The Society for Surgery of the Alimentary Tract.
CHICAGO –
TikTok’s short video format is increasingly becoming a major source for news and information, especially for adolescents and young adults. In 2022 the technology news website The Verge reported that about 10% of all U.S. adults regularly get news from TikTok, including an estimated 26% of adults under 30.
“Our study highlights the alarming prevalence of misinformation related to liver disease and cirrhosis on the TikTok platform. This misinformation can potentially lead to harm and poor health outcomes for individuals seeking accurate information about their conditions,” wrote the study authors in their abstract.
The study, which was led by Macklin Loveland, MD, an internal medicine resident at the University of Arizona, Tucson, found that, among 2,223 TikTok posts related to liver disease or cirrhosis as of November 2022, 60.3% were found to have accurate medical information, but the remaining 39.7% contained misinformation.
Some of the misinformation offered highly dubious and potentially dangerous advice, such as “Reishi mushrooms can reverse liver damage,” when in fact there is evidence to suggest that reishi mushrooms, especially in powder form, may be toxic to the liver and may even cause fatal fulminant hepatitis.
In an interview, Dr. Loveland said that much of the good information about liver disease on TikTok seems to come from patients with cirrhosis or other liver diseases who post videos chronicling their experiences, whereas bad information seems to come from people who are trying to pitch a product such as “natural” or “alternative” medicine.
“People who have real-life, firsthand experiences with cirrhosis have a really nice platform to talk about their disease process and share information with other people with similar disease processes, and the majority of them are accurate,” he said. “Where the inaccuracies come in are when people are trying to profit off a product or sell a dietary supplement, and then things go by the wayside.”
It’s important for TikTok users to understand the intentions of other users, he said, and expressed the hope that content mediators within TikTok would help to keep misinformation at bay.
Skyler B. Johnson, MD, assistant professor of radiation oncology at the University of Utah Huntsman Cancer Institute, Salt Lake City, has studied misinformation about cancer on social media, and as he and colleagues reported in the Journal of the National Cancer Institute, of 200 articles on cancer posted on social media sites, 32.5% contained misinformation and 30.5% contained harmful information.
In an interview, Dr. Johnson, who was not involved in the study by Dr. Loveland and colleagues, offered advice for colleagues about countering misinformation.
“What we’re trying to do, as part of our research group, is encourage physicians to take an active role in addressing misinformation with their patients and also in their social networking interactions,” he said. “When I see a new patient with a new diagnosis of cancer, I warn them that they’re going to encounter things online that may or may not be true.”
He noted that, often when physicians instruct patients not to go online to research their disease, the first thing the vast majority of patients do after leaving the office is to jump online.
Instead, Dr. Johnson recommended inoculating patients against misinformation – not to discourage them from going online, but to inform them about the myriad good and bad information sources, and steer them toward trustworthy sites such as government agencies (the National Institutes of Health, Centers for Disease Control and Prevention, etc), academic medical center sites, or select nonprofit organizations, foundations, and medical associations.
“But at the end of the day, even those you have to be somewhat vigilant about, because there are some unscrupulous providers who exploit even those sites,” he added.
Study details
Dr. Loveland and colleagues used the TikTok search engine to look for posts containing the terms “cirrhosis” and “liver disease,” and watched all such videos that turned up in the search from beginning to end. They classified each post as either educational in intent or whether it depicted a firsthand experience with liver disease.
They determined whether each post was accurate or erroneous according to guidelines from the American Association for the Study of Liver Disease, American College of Gastroenterology, and American Gastroenterological Association. They also recorded the number of likes, comments, and the number of times that each video was shared.
Accurate posts were viewed and liked significantly more often than inaccurate ones, and accurate posts had significantly more comments that faulty posts.
However, both accurate and inaccurate posts were shared a similar number of times, suggesting that bad-quality information can metastasize just as easily as good information can be disseminated.
Dr. Loveland and colleagues echoed the recommendations of Dr. Johnson, stating that “health care provides should be aware of the potential for misinformation on social media and should strive to provide their patients with accurate and evidence-based information to inform their health care decisions.”
The study was internally funded. Dr. Loveland and Dr. Johnson reported having no conflicts of interest to disclose.
DDW is sponsored by the American Association for the Study of Liver Diseases, the AGA, the American Society for Gastrointestinal Endoscopy, and The Society for Surgery of the Alimentary Tract.
CHICAGO –
TikTok’s short video format is increasingly becoming a major source for news and information, especially for adolescents and young adults. In 2022 the technology news website The Verge reported that about 10% of all U.S. adults regularly get news from TikTok, including an estimated 26% of adults under 30.
“Our study highlights the alarming prevalence of misinformation related to liver disease and cirrhosis on the TikTok platform. This misinformation can potentially lead to harm and poor health outcomes for individuals seeking accurate information about their conditions,” wrote the study authors in their abstract.
The study, which was led by Macklin Loveland, MD, an internal medicine resident at the University of Arizona, Tucson, found that, among 2,223 TikTok posts related to liver disease or cirrhosis as of November 2022, 60.3% were found to have accurate medical information, but the remaining 39.7% contained misinformation.
Some of the misinformation offered highly dubious and potentially dangerous advice, such as “Reishi mushrooms can reverse liver damage,” when in fact there is evidence to suggest that reishi mushrooms, especially in powder form, may be toxic to the liver and may even cause fatal fulminant hepatitis.
In an interview, Dr. Loveland said that much of the good information about liver disease on TikTok seems to come from patients with cirrhosis or other liver diseases who post videos chronicling their experiences, whereas bad information seems to come from people who are trying to pitch a product such as “natural” or “alternative” medicine.
“People who have real-life, firsthand experiences with cirrhosis have a really nice platform to talk about their disease process and share information with other people with similar disease processes, and the majority of them are accurate,” he said. “Where the inaccuracies come in are when people are trying to profit off a product or sell a dietary supplement, and then things go by the wayside.”
It’s important for TikTok users to understand the intentions of other users, he said, and expressed the hope that content mediators within TikTok would help to keep misinformation at bay.
Skyler B. Johnson, MD, assistant professor of radiation oncology at the University of Utah Huntsman Cancer Institute, Salt Lake City, has studied misinformation about cancer on social media, and as he and colleagues reported in the Journal of the National Cancer Institute, of 200 articles on cancer posted on social media sites, 32.5% contained misinformation and 30.5% contained harmful information.
In an interview, Dr. Johnson, who was not involved in the study by Dr. Loveland and colleagues, offered advice for colleagues about countering misinformation.
“What we’re trying to do, as part of our research group, is encourage physicians to take an active role in addressing misinformation with their patients and also in their social networking interactions,” he said. “When I see a new patient with a new diagnosis of cancer, I warn them that they’re going to encounter things online that may or may not be true.”
He noted that, often when physicians instruct patients not to go online to research their disease, the first thing the vast majority of patients do after leaving the office is to jump online.
Instead, Dr. Johnson recommended inoculating patients against misinformation – not to discourage them from going online, but to inform them about the myriad good and bad information sources, and steer them toward trustworthy sites such as government agencies (the National Institutes of Health, Centers for Disease Control and Prevention, etc), academic medical center sites, or select nonprofit organizations, foundations, and medical associations.
“But at the end of the day, even those you have to be somewhat vigilant about, because there are some unscrupulous providers who exploit even those sites,” he added.
Study details
Dr. Loveland and colleagues used the TikTok search engine to look for posts containing the terms “cirrhosis” and “liver disease,” and watched all such videos that turned up in the search from beginning to end. They classified each post as either educational in intent or whether it depicted a firsthand experience with liver disease.
They determined whether each post was accurate or erroneous according to guidelines from the American Association for the Study of Liver Disease, American College of Gastroenterology, and American Gastroenterological Association. They also recorded the number of likes, comments, and the number of times that each video was shared.
Accurate posts were viewed and liked significantly more often than inaccurate ones, and accurate posts had significantly more comments that faulty posts.
However, both accurate and inaccurate posts were shared a similar number of times, suggesting that bad-quality information can metastasize just as easily as good information can be disseminated.
Dr. Loveland and colleagues echoed the recommendations of Dr. Johnson, stating that “health care provides should be aware of the potential for misinformation on social media and should strive to provide their patients with accurate and evidence-based information to inform their health care decisions.”
The study was internally funded. Dr. Loveland and Dr. Johnson reported having no conflicts of interest to disclose.
DDW is sponsored by the American Association for the Study of Liver Diseases, the AGA, the American Society for Gastrointestinal Endoscopy, and The Society for Surgery of the Alimentary Tract.
AT DDW 2023
Misdiagnosis, mismatch still common in pancreatic cystic neoplasms
CHICAGO – , data from a retrospective study show.
An analysis of all pancreatic resections performed for presumed PCN at the Verona Pancreas Institute, Italy, from 2011 through 2020 showed a high degree of discrepancy between the preoperative clinical diagnosis and the final postoperative pathology, with some lesions being misdiagnosed in nearly two-thirds of cases, reported Anna Burelli, MD, of the department of general and pancreatic surgery at the University of Verona.
“Diagnostic errors are still common for resected PCNs. Morphological and clinical information alone still poorly frame actual targets for surgery, and hopefully the development of new reliable biomarkers will represent the next evolution in pancreatic cystic neoplasm management,” she said in an oral abstract session at the annual Digestive Disease Week® (DDW).
Diagnostic errors are significant issues in care of patients with PCN, because clinicians must balance the need for prompt, definitive treatment when necessary with the need for avoiding the significant morbidity of pancreatic resection for patients with lesions that turn out to be nonmalignant.
The investigators define “misdiagnosis” as a discrepancy between the preoperative clinical diagnosis and the postoperative pathology, and “mismatch” as a discrepancy between the preoperative suspicion of malignant or benign disease and the final pathology.
Checkered history
In previous cases series from Massachusetts General Hospital in Boston (2010) and the Verona Pancreas Institute (2012) – both experienced, high-volume centers – PCN misdiagnosis rates were 30% and 21%, respectively, and results from the current study show that things haven’t changed much since then, Dr. Burelli said.
PCNs are divided into neoplastic and nonneoplastic categories, with mucin-producing subtypes considered to be precancerous lesions that require accurate diagnosis and close monitoring.
Examples of neoplastic PCNs are intraductal papillary mucinous neoplasms (IPMNs) of the main pancreatic duct or side branch and mucinous cystadenomas. In contrast, serous cystadenomas, considered nonneoplastic, are mostly benign lesions discovered incidentally during abdominal imaging for another indication. It is very difficult, however, to distinguish between the two PCN subtypes clinically.
For example, Dr. Burelli showed images from a patient who received a preoperative diagnosis of mixed IPMN that was in fact found to be chronic pancreatitis on postoperative pathology.
Dr. Burelli noted that AGA and joint European guidelines for management of PCNs have been updated over the past decade, with the latest AGA iteration in 2015.
A 2017 study evaluating the 2015 AGA guidelines for management of asymptomatic PCNs found that following the guidelines in a large multicenter cohort “would have resulted in 60 % fewer patients being referred for surgical resection, and accurately recommended surveillance in 95% of patients with asymptomatic PCNs.”
Misdiagnosis and mismatch common
In the current study, Dr. Burelli and colleagues reviewed all pancreatic resections performed for PCNs at their center from 2011 through 2020.
Of 601 patients included in the retrospective study, 301 underwent endoscopic ultrasound (EUS).
The investigators identified misdiagnosis in 19% of cases and mismatch in 34%, and there was no significant improvement in diagnostic accuracy among the 50% of patients who underwent EUS.
The most frequently misdiagnosed lesions were cystic neuroendocrine tumors, in 61% of cases. The least misdiagnosed lesions were pseudopapillary tumors, in 6% of cases.
Many of the diagnostic errors were clinically important. For example, seven cases presumed to be serous cystic neoplasms (an almost always benign lesion) were found on final pathology to have a different, malignant histology.
Mismatch examples included 50 IPMNs with high-risk stigmata that were presumed to be malignant before surgery but were nonmalignant on final pathology, and 38 IPMNs without high-risk stigmata which were thought on clinical examination to be benign but turned out to be malignant on final pathology.
“Our results are in line with the current literature,” Dr. Burelli said, citing a recent meta-analysis showing that among 3,292 patients who underwent resection for mucinous cystic neoplasms (MCNs), the pooled rate of malignancy was 16.1%, yet the 2012 International Association of Pancreatology guidelines recommend surgery for all fit patients with MCNs, and joint European evidence-based guidelines from 2018 recommend surgery for MCNs 40 mm or larger, those with mural nodules, and for patients who are symptomatic.
The 16.1% pooled malignancy rate suggests “that there is space for surveillance in most cases of MCNs,” she said.
In addition, morphologic and clinical evaluation for IPMN with high-risk stigmata have been shown to have low specificity and low sensitivity, “so should guideline recommendations be revised?” Dr. Burelli said.
She pointed to a recent multi-institutional study in Gastroenterology showing that real-time next-generation sequencing of pancreatic cyst fluid “is sensitive and specific for various pancreatic cyst types and advanced neoplasia arising from mucinous cysts, but also reveals the diversity of genomic alterations seen in pancreatic cysts and their clinical significance.”
“This is not the future; this is the present,” she concluded.
Invited discussant R. Matthew Walsh, MD, a surgeon specializing in pancreatic and cancer surgery at the Cleveland Clinic, complimented the contributions of her group.
“The patient that you showed with chronic pancreatitis could have very well benefited from the operation regardless of the diagnosis if they were symptomatic,” he said, addressing Dr. Burelli. “So what is the group that is the regrettable surgical patients, and where are you aiming your studies? Is it really the 24% with high-risk features in IPMN that have low-grade dysplasia, or is it the 58% who we’re not sure why they were operated on because they didn’t have high-grade features who had low-grade dysplasia?”
She replied that “the goal here is to avoid surgery for benign entities, and we know that the only true benign entities are serous cystic neoplasms, and all the others have a malignant potential, but we think at Verona Pancreas Institute there is no reason to operate on low-grade dysplasia free patients. This is what we really would like to avoid.”
Dr. Walsh also asked, given their finding that EUS did not appear to offer a benefit to patients or change decision making, which patients should still get EUS.
“I think that only patients in which the diagnosis is uncertain or in which there are some worrisome features or high-risk stigmata should undergo EUS before surgery, and also to continue follow-up,” Dr. Burelli said. “I don’t think that the conclusion is that EUS is not useful, but it’s not useful in all.”
For example, large, microcystic lesions can be readily identified radiographically, but other, more complex cases may still require EUS to help nail down or refine a diagnosis, she said.
The study was internally funded. Dr. Burelli and Dr. Walsh reported having no conflicts of interest.
DDW is sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
CHICAGO – , data from a retrospective study show.
An analysis of all pancreatic resections performed for presumed PCN at the Verona Pancreas Institute, Italy, from 2011 through 2020 showed a high degree of discrepancy between the preoperative clinical diagnosis and the final postoperative pathology, with some lesions being misdiagnosed in nearly two-thirds of cases, reported Anna Burelli, MD, of the department of general and pancreatic surgery at the University of Verona.
“Diagnostic errors are still common for resected PCNs. Morphological and clinical information alone still poorly frame actual targets for surgery, and hopefully the development of new reliable biomarkers will represent the next evolution in pancreatic cystic neoplasm management,” she said in an oral abstract session at the annual Digestive Disease Week® (DDW).
Diagnostic errors are significant issues in care of patients with PCN, because clinicians must balance the need for prompt, definitive treatment when necessary with the need for avoiding the significant morbidity of pancreatic resection for patients with lesions that turn out to be nonmalignant.
The investigators define “misdiagnosis” as a discrepancy between the preoperative clinical diagnosis and the postoperative pathology, and “mismatch” as a discrepancy between the preoperative suspicion of malignant or benign disease and the final pathology.
Checkered history
In previous cases series from Massachusetts General Hospital in Boston (2010) and the Verona Pancreas Institute (2012) – both experienced, high-volume centers – PCN misdiagnosis rates were 30% and 21%, respectively, and results from the current study show that things haven’t changed much since then, Dr. Burelli said.
PCNs are divided into neoplastic and nonneoplastic categories, with mucin-producing subtypes considered to be precancerous lesions that require accurate diagnosis and close monitoring.
Examples of neoplastic PCNs are intraductal papillary mucinous neoplasms (IPMNs) of the main pancreatic duct or side branch and mucinous cystadenomas. In contrast, serous cystadenomas, considered nonneoplastic, are mostly benign lesions discovered incidentally during abdominal imaging for another indication. It is very difficult, however, to distinguish between the two PCN subtypes clinically.
For example, Dr. Burelli showed images from a patient who received a preoperative diagnosis of mixed IPMN that was in fact found to be chronic pancreatitis on postoperative pathology.
Dr. Burelli noted that AGA and joint European guidelines for management of PCNs have been updated over the past decade, with the latest AGA iteration in 2015.
A 2017 study evaluating the 2015 AGA guidelines for management of asymptomatic PCNs found that following the guidelines in a large multicenter cohort “would have resulted in 60 % fewer patients being referred for surgical resection, and accurately recommended surveillance in 95% of patients with asymptomatic PCNs.”
Misdiagnosis and mismatch common
In the current study, Dr. Burelli and colleagues reviewed all pancreatic resections performed for PCNs at their center from 2011 through 2020.
Of 601 patients included in the retrospective study, 301 underwent endoscopic ultrasound (EUS).
The investigators identified misdiagnosis in 19% of cases and mismatch in 34%, and there was no significant improvement in diagnostic accuracy among the 50% of patients who underwent EUS.
The most frequently misdiagnosed lesions were cystic neuroendocrine tumors, in 61% of cases. The least misdiagnosed lesions were pseudopapillary tumors, in 6% of cases.
Many of the diagnostic errors were clinically important. For example, seven cases presumed to be serous cystic neoplasms (an almost always benign lesion) were found on final pathology to have a different, malignant histology.
Mismatch examples included 50 IPMNs with high-risk stigmata that were presumed to be malignant before surgery but were nonmalignant on final pathology, and 38 IPMNs without high-risk stigmata which were thought on clinical examination to be benign but turned out to be malignant on final pathology.
“Our results are in line with the current literature,” Dr. Burelli said, citing a recent meta-analysis showing that among 3,292 patients who underwent resection for mucinous cystic neoplasms (MCNs), the pooled rate of malignancy was 16.1%, yet the 2012 International Association of Pancreatology guidelines recommend surgery for all fit patients with MCNs, and joint European evidence-based guidelines from 2018 recommend surgery for MCNs 40 mm or larger, those with mural nodules, and for patients who are symptomatic.
The 16.1% pooled malignancy rate suggests “that there is space for surveillance in most cases of MCNs,” she said.
In addition, morphologic and clinical evaluation for IPMN with high-risk stigmata have been shown to have low specificity and low sensitivity, “so should guideline recommendations be revised?” Dr. Burelli said.
She pointed to a recent multi-institutional study in Gastroenterology showing that real-time next-generation sequencing of pancreatic cyst fluid “is sensitive and specific for various pancreatic cyst types and advanced neoplasia arising from mucinous cysts, but also reveals the diversity of genomic alterations seen in pancreatic cysts and their clinical significance.”
“This is not the future; this is the present,” she concluded.
Invited discussant R. Matthew Walsh, MD, a surgeon specializing in pancreatic and cancer surgery at the Cleveland Clinic, complimented the contributions of her group.
“The patient that you showed with chronic pancreatitis could have very well benefited from the operation regardless of the diagnosis if they were symptomatic,” he said, addressing Dr. Burelli. “So what is the group that is the regrettable surgical patients, and where are you aiming your studies? Is it really the 24% with high-risk features in IPMN that have low-grade dysplasia, or is it the 58% who we’re not sure why they were operated on because they didn’t have high-grade features who had low-grade dysplasia?”
She replied that “the goal here is to avoid surgery for benign entities, and we know that the only true benign entities are serous cystic neoplasms, and all the others have a malignant potential, but we think at Verona Pancreas Institute there is no reason to operate on low-grade dysplasia free patients. This is what we really would like to avoid.”
Dr. Walsh also asked, given their finding that EUS did not appear to offer a benefit to patients or change decision making, which patients should still get EUS.
“I think that only patients in which the diagnosis is uncertain or in which there are some worrisome features or high-risk stigmata should undergo EUS before surgery, and also to continue follow-up,” Dr. Burelli said. “I don’t think that the conclusion is that EUS is not useful, but it’s not useful in all.”
For example, large, microcystic lesions can be readily identified radiographically, but other, more complex cases may still require EUS to help nail down or refine a diagnosis, she said.
The study was internally funded. Dr. Burelli and Dr. Walsh reported having no conflicts of interest.
DDW is sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
CHICAGO – , data from a retrospective study show.
An analysis of all pancreatic resections performed for presumed PCN at the Verona Pancreas Institute, Italy, from 2011 through 2020 showed a high degree of discrepancy between the preoperative clinical diagnosis and the final postoperative pathology, with some lesions being misdiagnosed in nearly two-thirds of cases, reported Anna Burelli, MD, of the department of general and pancreatic surgery at the University of Verona.
“Diagnostic errors are still common for resected PCNs. Morphological and clinical information alone still poorly frame actual targets for surgery, and hopefully the development of new reliable biomarkers will represent the next evolution in pancreatic cystic neoplasm management,” she said in an oral abstract session at the annual Digestive Disease Week® (DDW).
Diagnostic errors are significant issues in care of patients with PCN, because clinicians must balance the need for prompt, definitive treatment when necessary with the need for avoiding the significant morbidity of pancreatic resection for patients with lesions that turn out to be nonmalignant.
The investigators define “misdiagnosis” as a discrepancy between the preoperative clinical diagnosis and the postoperative pathology, and “mismatch” as a discrepancy between the preoperative suspicion of malignant or benign disease and the final pathology.
Checkered history
In previous cases series from Massachusetts General Hospital in Boston (2010) and the Verona Pancreas Institute (2012) – both experienced, high-volume centers – PCN misdiagnosis rates were 30% and 21%, respectively, and results from the current study show that things haven’t changed much since then, Dr. Burelli said.
PCNs are divided into neoplastic and nonneoplastic categories, with mucin-producing subtypes considered to be precancerous lesions that require accurate diagnosis and close monitoring.
Examples of neoplastic PCNs are intraductal papillary mucinous neoplasms (IPMNs) of the main pancreatic duct or side branch and mucinous cystadenomas. In contrast, serous cystadenomas, considered nonneoplastic, are mostly benign lesions discovered incidentally during abdominal imaging for another indication. It is very difficult, however, to distinguish between the two PCN subtypes clinically.
For example, Dr. Burelli showed images from a patient who received a preoperative diagnosis of mixed IPMN that was in fact found to be chronic pancreatitis on postoperative pathology.
Dr. Burelli noted that AGA and joint European guidelines for management of PCNs have been updated over the past decade, with the latest AGA iteration in 2015.
A 2017 study evaluating the 2015 AGA guidelines for management of asymptomatic PCNs found that following the guidelines in a large multicenter cohort “would have resulted in 60 % fewer patients being referred for surgical resection, and accurately recommended surveillance in 95% of patients with asymptomatic PCNs.”
Misdiagnosis and mismatch common
In the current study, Dr. Burelli and colleagues reviewed all pancreatic resections performed for PCNs at their center from 2011 through 2020.
Of 601 patients included in the retrospective study, 301 underwent endoscopic ultrasound (EUS).
The investigators identified misdiagnosis in 19% of cases and mismatch in 34%, and there was no significant improvement in diagnostic accuracy among the 50% of patients who underwent EUS.
The most frequently misdiagnosed lesions were cystic neuroendocrine tumors, in 61% of cases. The least misdiagnosed lesions were pseudopapillary tumors, in 6% of cases.
Many of the diagnostic errors were clinically important. For example, seven cases presumed to be serous cystic neoplasms (an almost always benign lesion) were found on final pathology to have a different, malignant histology.
Mismatch examples included 50 IPMNs with high-risk stigmata that were presumed to be malignant before surgery but were nonmalignant on final pathology, and 38 IPMNs without high-risk stigmata which were thought on clinical examination to be benign but turned out to be malignant on final pathology.
“Our results are in line with the current literature,” Dr. Burelli said, citing a recent meta-analysis showing that among 3,292 patients who underwent resection for mucinous cystic neoplasms (MCNs), the pooled rate of malignancy was 16.1%, yet the 2012 International Association of Pancreatology guidelines recommend surgery for all fit patients with MCNs, and joint European evidence-based guidelines from 2018 recommend surgery for MCNs 40 mm or larger, those with mural nodules, and for patients who are symptomatic.
The 16.1% pooled malignancy rate suggests “that there is space for surveillance in most cases of MCNs,” she said.
In addition, morphologic and clinical evaluation for IPMN with high-risk stigmata have been shown to have low specificity and low sensitivity, “so should guideline recommendations be revised?” Dr. Burelli said.
She pointed to a recent multi-institutional study in Gastroenterology showing that real-time next-generation sequencing of pancreatic cyst fluid “is sensitive and specific for various pancreatic cyst types and advanced neoplasia arising from mucinous cysts, but also reveals the diversity of genomic alterations seen in pancreatic cysts and their clinical significance.”
“This is not the future; this is the present,” she concluded.
Invited discussant R. Matthew Walsh, MD, a surgeon specializing in pancreatic and cancer surgery at the Cleveland Clinic, complimented the contributions of her group.
“The patient that you showed with chronic pancreatitis could have very well benefited from the operation regardless of the diagnosis if they were symptomatic,” he said, addressing Dr. Burelli. “So what is the group that is the regrettable surgical patients, and where are you aiming your studies? Is it really the 24% with high-risk features in IPMN that have low-grade dysplasia, or is it the 58% who we’re not sure why they were operated on because they didn’t have high-grade features who had low-grade dysplasia?”
She replied that “the goal here is to avoid surgery for benign entities, and we know that the only true benign entities are serous cystic neoplasms, and all the others have a malignant potential, but we think at Verona Pancreas Institute there is no reason to operate on low-grade dysplasia free patients. This is what we really would like to avoid.”
Dr. Walsh also asked, given their finding that EUS did not appear to offer a benefit to patients or change decision making, which patients should still get EUS.
“I think that only patients in which the diagnosis is uncertain or in which there are some worrisome features or high-risk stigmata should undergo EUS before surgery, and also to continue follow-up,” Dr. Burelli said. “I don’t think that the conclusion is that EUS is not useful, but it’s not useful in all.”
For example, large, microcystic lesions can be readily identified radiographically, but other, more complex cases may still require EUS to help nail down or refine a diagnosis, she said.
The study was internally funded. Dr. Burelli and Dr. Walsh reported having no conflicts of interest.
DDW is sponsored by the American Association for the Study of Liver Diseases, the American Gastroenterological Association, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
AT DDW 2023
Emotional eating isn’t all emotional
“Food gives me ‘hugs,’ ” Ms. S* said as her eyes lit up. Finally, after weeks of working together, she could articulate her complex relationship with food. She had been struggling to explain why she continued to eat when she was full or consumed foods she knew wouldn’t help her health.
Like millions of people struggling with their weight or the disease of obesity, Ms. S had tried multiple diets and programs but continued to return to unhelpful eating patterns. Ms. S was an emotional eater, and the pandemic only worsened her emotional eating. As a single professional forced to work from home during the pandemic, she became lonely. She went from working in a busy downtown office, training for half-marathons, and teaching live workout sessions to being alone daily. Her only “real” human interaction was when she ordered daily delivery meals of her favorite comfort foods. As a person with type 2 diabetes, she knew that her delivery habit was wrecking her health, but willpower wasn’t enough to make her stop.
Her psychologist referred her to our virtual integrative obesity practice to help her lose weight and find long-term solutions. Ms. S admitted that she knew what she was doing as an emotional eater. But like many emotional eaters, she didn’t know why or how to switch from emotional eating to eating based on her biological hunger signals. As a trained obesity expert and recovering emotional eater of 8 years, personally and professionally I can appreciate the challenges of emotional eating and how it can sabotage even the best weight loss plan. In this article, I will share facts and feelings that drive emotional eating. I aim to empower clinicians seeking to help patients with emotional eating.
Fact: Emotional eating isn’t all emotional
It’s important not to dismiss emotional eating as all emotion driven. Recall that hunger is hormonally regulated. There are two main hunger pathways: the homeostatic pathway and the hedonic pathway. The homeostatic pathway is our biological hunger pathway and is driven by the need for energy in calories. Conversely, hedonic eating is pleasure-driven and uses emotional stimuli to “bypass” the physical hunger/satisfaction signals.
Emotional eating falls under the hedonic pathway. As clinicians, the first step in helping a patient struggling with emotional eating is empathetically listening, then assessing for any physiologic causes.
Several factors can disrupt physiologic appetite regulation, such as sleep disturbances; high stress levels; and many medical conditions, including but not limited to obesity, diabetes, and polycystic ovarian syndrome. Such factors as insulin resistance and inflammation are a common link in these conditions. Both contribute to the pathophysiology of the changes in appetite and can influence other hormones that lead to reduced satisfaction after eating. Furthermore, mental health conditions may disrupt levels of neurotransmitters such as serotonin and dopamine, which can also cause appetite changes.
These settings of physiologically disrupted appetite can trigger hedonic eating. But the relationship is complex. For example, one way to research hedonic eating is by using the Power of Food Scale. Functional MRI studies show that people with higher Power of Food Scale readings have more brain activity in the visual cortex when they see highly palatable foods. While more studies are needed to better understand the clinical implications of this finding, it’s yet another indicator that “emotional” eating isn’t all emotional. It’s also physiologic.
Feelings: Patterns, personality, places, psychological factors
Physiology only explains part of emotional eating. Like Ms. S, emotional eaters have strong emotional connections to food and behavior patterns. Often, physiologic cues have been coupled with psychological habits.
For example, menses is a common physiologic trigger for stress-eating for many of my patients. Studies have shown that in addition to iron levels changing during menses, calcium, magnesium, and phosphorous levels also change. Emotionally, the discomfort of “that time of the month” can lead to solace in comfort foods such as chocolate in different forms. But this isn’t surprising, as cacao and its derivative, chocolate, are rich in iron and other minerals. The chocolate is actually addressing a physical and emotional need. It can be helpful to point out this association to your patients. Suggest choosing a lower-sugar form of chocolate, such as dark chocolate, or even trying cacao nibs, while addressing any emotions.
But physiologic conditions and patterns aren’t the only emotional eating triggers. Places and psychological conditions can also trigger emotional eating.
Places and people
Celebrations, vacations, proximity to certain restaurants, exposure to food marketing, and major life shifts can lead to increased hedonic eating. Helping patients recognize this connection opens the door to advance preparation for these situations.
Psychological conditions can be connected to emotional eating. It’s important to screen for mental health conditions and past traumas. For example, emotional eating could be a symptom of binge eating disorder, major depression, or generalized anxiety disorder. Childhood trauma is associated with disordered eating. The adverse childhood events quiz can be used clinically.
Emotional eating can lead to feelings of guilt, shame, and negative self-talk. It’s helpful to offer patients reassurance and encourage self-compassion. After all, it’s natural to eat. The goal isn’t to stop eating but to eat on the basis of physiologic needs.
Putting it together: Addressing the facts and feelings of emotional eating
1. Treat biological causes that impact physiologic hunger and trigger emotional eating.
2. Triggers: Address patterns, places/people, psychological events.
3. Transition to non-food rewards; the key to emotional eating is eating. While healthier substitutes can be a short-term solution for improving eating behaviors, ultimately, helping patients find non-food ways to address emotions is invaluable.
4. Stress management: Offer your patients ways to decrease stress levels through mindfulness and other techniques.
5. Professional support: Creating a multidisciplinary team is helpful, given the complexity of emotional eating. In addition to the primary care physician/clinician, other team members may include:
- Psychologist
- Psychiatrist
- coach and/or certified wellness coaches
- Obesity specialist
Back to Ms. S
Ms. S is doing well. We started her on a GLP-1 agonist to address her underlying insulin resistance. Together we’ve found creative ways to satisfy her loneliness, such as volunteering and teaching virtual workout classes. Her emotional eating has decreased by over 60%, and we continue to discover new strategies to address her emotional eating triggers.
Conclusion
Despite being common, the impact of emotional eating is often minimized. With no DSM-5 criteria or ICD-11 code, it’s easy to dismiss emotional eating clinically. However, emotional eating is common and associated with weight gain.
In light of the obesity epidemic, this significance can’t be overlooked. Thankfully we have groundbreaking medications to address the homeostatic hunger pathway and physiologic drivers of emotional eating, but they’re not a substitute for addressing the psychosocial components of emotional eating.
As clinicians, we can have a meaningful impact on our patients’ lives beyond writing a prescription.
*Name/initial changed for privacy.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating.
A version of this article first appeared on Medscape.com.
“Food gives me ‘hugs,’ ” Ms. S* said as her eyes lit up. Finally, after weeks of working together, she could articulate her complex relationship with food. She had been struggling to explain why she continued to eat when she was full or consumed foods she knew wouldn’t help her health.
Like millions of people struggling with their weight or the disease of obesity, Ms. S had tried multiple diets and programs but continued to return to unhelpful eating patterns. Ms. S was an emotional eater, and the pandemic only worsened her emotional eating. As a single professional forced to work from home during the pandemic, she became lonely. She went from working in a busy downtown office, training for half-marathons, and teaching live workout sessions to being alone daily. Her only “real” human interaction was when she ordered daily delivery meals of her favorite comfort foods. As a person with type 2 diabetes, she knew that her delivery habit was wrecking her health, but willpower wasn’t enough to make her stop.
Her psychologist referred her to our virtual integrative obesity practice to help her lose weight and find long-term solutions. Ms. S admitted that she knew what she was doing as an emotional eater. But like many emotional eaters, she didn’t know why or how to switch from emotional eating to eating based on her biological hunger signals. As a trained obesity expert and recovering emotional eater of 8 years, personally and professionally I can appreciate the challenges of emotional eating and how it can sabotage even the best weight loss plan. In this article, I will share facts and feelings that drive emotional eating. I aim to empower clinicians seeking to help patients with emotional eating.
Fact: Emotional eating isn’t all emotional
It’s important not to dismiss emotional eating as all emotion driven. Recall that hunger is hormonally regulated. There are two main hunger pathways: the homeostatic pathway and the hedonic pathway. The homeostatic pathway is our biological hunger pathway and is driven by the need for energy in calories. Conversely, hedonic eating is pleasure-driven and uses emotional stimuli to “bypass” the physical hunger/satisfaction signals.
Emotional eating falls under the hedonic pathway. As clinicians, the first step in helping a patient struggling with emotional eating is empathetically listening, then assessing for any physiologic causes.
Several factors can disrupt physiologic appetite regulation, such as sleep disturbances; high stress levels; and many medical conditions, including but not limited to obesity, diabetes, and polycystic ovarian syndrome. Such factors as insulin resistance and inflammation are a common link in these conditions. Both contribute to the pathophysiology of the changes in appetite and can influence other hormones that lead to reduced satisfaction after eating. Furthermore, mental health conditions may disrupt levels of neurotransmitters such as serotonin and dopamine, which can also cause appetite changes.
These settings of physiologically disrupted appetite can trigger hedonic eating. But the relationship is complex. For example, one way to research hedonic eating is by using the Power of Food Scale. Functional MRI studies show that people with higher Power of Food Scale readings have more brain activity in the visual cortex when they see highly palatable foods. While more studies are needed to better understand the clinical implications of this finding, it’s yet another indicator that “emotional” eating isn’t all emotional. It’s also physiologic.
Feelings: Patterns, personality, places, psychological factors
Physiology only explains part of emotional eating. Like Ms. S, emotional eaters have strong emotional connections to food and behavior patterns. Often, physiologic cues have been coupled with psychological habits.
For example, menses is a common physiologic trigger for stress-eating for many of my patients. Studies have shown that in addition to iron levels changing during menses, calcium, magnesium, and phosphorous levels also change. Emotionally, the discomfort of “that time of the month” can lead to solace in comfort foods such as chocolate in different forms. But this isn’t surprising, as cacao and its derivative, chocolate, are rich in iron and other minerals. The chocolate is actually addressing a physical and emotional need. It can be helpful to point out this association to your patients. Suggest choosing a lower-sugar form of chocolate, such as dark chocolate, or even trying cacao nibs, while addressing any emotions.
But physiologic conditions and patterns aren’t the only emotional eating triggers. Places and psychological conditions can also trigger emotional eating.
Places and people
Celebrations, vacations, proximity to certain restaurants, exposure to food marketing, and major life shifts can lead to increased hedonic eating. Helping patients recognize this connection opens the door to advance preparation for these situations.
Psychological conditions can be connected to emotional eating. It’s important to screen for mental health conditions and past traumas. For example, emotional eating could be a symptom of binge eating disorder, major depression, or generalized anxiety disorder. Childhood trauma is associated with disordered eating. The adverse childhood events quiz can be used clinically.
Emotional eating can lead to feelings of guilt, shame, and negative self-talk. It’s helpful to offer patients reassurance and encourage self-compassion. After all, it’s natural to eat. The goal isn’t to stop eating but to eat on the basis of physiologic needs.
Putting it together: Addressing the facts and feelings of emotional eating
1. Treat biological causes that impact physiologic hunger and trigger emotional eating.
2. Triggers: Address patterns, places/people, psychological events.
3. Transition to non-food rewards; the key to emotional eating is eating. While healthier substitutes can be a short-term solution for improving eating behaviors, ultimately, helping patients find non-food ways to address emotions is invaluable.
4. Stress management: Offer your patients ways to decrease stress levels through mindfulness and other techniques.
5. Professional support: Creating a multidisciplinary team is helpful, given the complexity of emotional eating. In addition to the primary care physician/clinician, other team members may include:
- Psychologist
- Psychiatrist
- coach and/or certified wellness coaches
- Obesity specialist
Back to Ms. S
Ms. S is doing well. We started her on a GLP-1 agonist to address her underlying insulin resistance. Together we’ve found creative ways to satisfy her loneliness, such as volunteering and teaching virtual workout classes. Her emotional eating has decreased by over 60%, and we continue to discover new strategies to address her emotional eating triggers.
Conclusion
Despite being common, the impact of emotional eating is often minimized. With no DSM-5 criteria or ICD-11 code, it’s easy to dismiss emotional eating clinically. However, emotional eating is common and associated with weight gain.
In light of the obesity epidemic, this significance can’t be overlooked. Thankfully we have groundbreaking medications to address the homeostatic hunger pathway and physiologic drivers of emotional eating, but they’re not a substitute for addressing the psychosocial components of emotional eating.
As clinicians, we can have a meaningful impact on our patients’ lives beyond writing a prescription.
*Name/initial changed for privacy.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating.
A version of this article first appeared on Medscape.com.
“Food gives me ‘hugs,’ ” Ms. S* said as her eyes lit up. Finally, after weeks of working together, she could articulate her complex relationship with food. She had been struggling to explain why she continued to eat when she was full or consumed foods she knew wouldn’t help her health.
Like millions of people struggling with their weight or the disease of obesity, Ms. S had tried multiple diets and programs but continued to return to unhelpful eating patterns. Ms. S was an emotional eater, and the pandemic only worsened her emotional eating. As a single professional forced to work from home during the pandemic, she became lonely. She went from working in a busy downtown office, training for half-marathons, and teaching live workout sessions to being alone daily. Her only “real” human interaction was when she ordered daily delivery meals of her favorite comfort foods. As a person with type 2 diabetes, she knew that her delivery habit was wrecking her health, but willpower wasn’t enough to make her stop.
Her psychologist referred her to our virtual integrative obesity practice to help her lose weight and find long-term solutions. Ms. S admitted that she knew what she was doing as an emotional eater. But like many emotional eaters, she didn’t know why or how to switch from emotional eating to eating based on her biological hunger signals. As a trained obesity expert and recovering emotional eater of 8 years, personally and professionally I can appreciate the challenges of emotional eating and how it can sabotage even the best weight loss plan. In this article, I will share facts and feelings that drive emotional eating. I aim to empower clinicians seeking to help patients with emotional eating.
Fact: Emotional eating isn’t all emotional
It’s important not to dismiss emotional eating as all emotion driven. Recall that hunger is hormonally regulated. There are two main hunger pathways: the homeostatic pathway and the hedonic pathway. The homeostatic pathway is our biological hunger pathway and is driven by the need for energy in calories. Conversely, hedonic eating is pleasure-driven and uses emotional stimuli to “bypass” the physical hunger/satisfaction signals.
Emotional eating falls under the hedonic pathway. As clinicians, the first step in helping a patient struggling with emotional eating is empathetically listening, then assessing for any physiologic causes.
Several factors can disrupt physiologic appetite regulation, such as sleep disturbances; high stress levels; and many medical conditions, including but not limited to obesity, diabetes, and polycystic ovarian syndrome. Such factors as insulin resistance and inflammation are a common link in these conditions. Both contribute to the pathophysiology of the changes in appetite and can influence other hormones that lead to reduced satisfaction after eating. Furthermore, mental health conditions may disrupt levels of neurotransmitters such as serotonin and dopamine, which can also cause appetite changes.
These settings of physiologically disrupted appetite can trigger hedonic eating. But the relationship is complex. For example, one way to research hedonic eating is by using the Power of Food Scale. Functional MRI studies show that people with higher Power of Food Scale readings have more brain activity in the visual cortex when they see highly palatable foods. While more studies are needed to better understand the clinical implications of this finding, it’s yet another indicator that “emotional” eating isn’t all emotional. It’s also physiologic.
Feelings: Patterns, personality, places, psychological factors
Physiology only explains part of emotional eating. Like Ms. S, emotional eaters have strong emotional connections to food and behavior patterns. Often, physiologic cues have been coupled with psychological habits.
For example, menses is a common physiologic trigger for stress-eating for many of my patients. Studies have shown that in addition to iron levels changing during menses, calcium, magnesium, and phosphorous levels also change. Emotionally, the discomfort of “that time of the month” can lead to solace in comfort foods such as chocolate in different forms. But this isn’t surprising, as cacao and its derivative, chocolate, are rich in iron and other minerals. The chocolate is actually addressing a physical and emotional need. It can be helpful to point out this association to your patients. Suggest choosing a lower-sugar form of chocolate, such as dark chocolate, or even trying cacao nibs, while addressing any emotions.
But physiologic conditions and patterns aren’t the only emotional eating triggers. Places and psychological conditions can also trigger emotional eating.
Places and people
Celebrations, vacations, proximity to certain restaurants, exposure to food marketing, and major life shifts can lead to increased hedonic eating. Helping patients recognize this connection opens the door to advance preparation for these situations.
Psychological conditions can be connected to emotional eating. It’s important to screen for mental health conditions and past traumas. For example, emotional eating could be a symptom of binge eating disorder, major depression, or generalized anxiety disorder. Childhood trauma is associated with disordered eating. The adverse childhood events quiz can be used clinically.
Emotional eating can lead to feelings of guilt, shame, and negative self-talk. It’s helpful to offer patients reassurance and encourage self-compassion. After all, it’s natural to eat. The goal isn’t to stop eating but to eat on the basis of physiologic needs.
Putting it together: Addressing the facts and feelings of emotional eating
1. Treat biological causes that impact physiologic hunger and trigger emotional eating.
2. Triggers: Address patterns, places/people, psychological events.
3. Transition to non-food rewards; the key to emotional eating is eating. While healthier substitutes can be a short-term solution for improving eating behaviors, ultimately, helping patients find non-food ways to address emotions is invaluable.
4. Stress management: Offer your patients ways to decrease stress levels through mindfulness and other techniques.
5. Professional support: Creating a multidisciplinary team is helpful, given the complexity of emotional eating. In addition to the primary care physician/clinician, other team members may include:
- Psychologist
- Psychiatrist
- coach and/or certified wellness coaches
- Obesity specialist
Back to Ms. S
Ms. S is doing well. We started her on a GLP-1 agonist to address her underlying insulin resistance. Together we’ve found creative ways to satisfy her loneliness, such as volunteering and teaching virtual workout classes. Her emotional eating has decreased by over 60%, and we continue to discover new strategies to address her emotional eating triggers.
Conclusion
Despite being common, the impact of emotional eating is often minimized. With no DSM-5 criteria or ICD-11 code, it’s easy to dismiss emotional eating clinically. However, emotional eating is common and associated with weight gain.
In light of the obesity epidemic, this significance can’t be overlooked. Thankfully we have groundbreaking medications to address the homeostatic hunger pathway and physiologic drivers of emotional eating, but they’re not a substitute for addressing the psychosocial components of emotional eating.
As clinicians, we can have a meaningful impact on our patients’ lives beyond writing a prescription.
*Name/initial changed for privacy.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating.
A version of this article first appeared on Medscape.com.
Meat heavy diets may lead to ulcerative colitis flares
CHICAGO –
The data, which was presented on May 7 in Chicago at the annual Digestive Disease Week® meeting, is based on an analysis of data from the PREdiCCt study (Prognostic Effect of Environmental Factors in Crohn’s and Colitis) in which diets of patients with IBD were tracked over 2-3 months with 2-year follow-ups. While the study itself includes nearly 3,000 patients from the United Kingdom who are in clinical remission, this analysis included 497 patients with Crohn’s disease and 520 with ulcerative colitis.
The highest level of patient-reported meat consumption was associated with doubled risk for hard flares – defined as an increase in symptoms plus elevation in c-reactive protein (CRP) and fecal calprotection (FCAL) plus a change in IBD therapy – in patients with ulcerative colitis, said study author Charlie W Lees, PhD, FRCP(Ed), Western General Hospital and University of Edinburgh.
Investigators also evaluated the occurrence of soft flares, which was defined as a negative response to the question, “Do you think your disease has been well controlled in the past month or since you last logged on to the portal?”
After a median follow-up of 1,481.5 days, hard flares occurred at a rate of 5.6% per year, but it did not differ by IBD subtype. However, soft flares accumulated rapidly. Hard flares with baseline FCAL levels in the 50-250 mcg/g range, as well as FCAL levels above 250 mcg, were associated with flares.
The mean baseline total protein intake was 91.9 g per day of which 35.8 g came from animal sources. The hazard ratio for the highest vs. lowest quartile of meat intake in the ulcerative colitis group was 2.08. They found no associations between hard flares with intake of total dietary fiber, N-6 polyunsaturated acids, or ultraprocessed foods, which Dr. Lees found surprising.
“Perhaps most intriguingly, when we look at ultraprocessed food intake, no difference in Crohn’s disease, and no difference in ulcerative colitis,” Dr. Lees said.
The finding is in contradiction to a study reported at the Crohn’s & Colitis Congress this year that found additives in ultraprocessed foods appear to have deleterious effects on intestinal microbiota, while others may exert their influence through mechanisms, such as endoplasmic stress.
However, the new data are consistent with a previously reported association between meat consumption and ulcerative colitis development, and suggests that reducing meat consumption could help to reduce the risk of flare in patients with ulcerative colitis.
PREdiCCt is designed to examine dietary, environmental, genetic, and microbiotic factors that are associated with disease flares in patients with Crohn’s disease and ulcerative colitis. Investigators are evaluating potential contributions to disease flares from total animal protein intake, dietary fiber, N-6 polyunsaturated fatty acids, dietary emulsifiers, and ultraprocessed foods, and total bacterial gene count in stool samples. They aim to examine data from 2,500 microbiome samples currently being sequenced at the Wellcome Sanger Institute in Hinxton, England, to determine whether the association between meat and ulcerative colitis flares could be related, as they hypothesize, to diet-induced alterations in the gut microbiome.
The research is preliminary with many unanswered questions, said Russell D. Cohen, MD, director of the inflammatory bowel disease center at the University of Chicago.
“I think he still has to evaluate a lot of the data that he has already collected because, are you talking about meat? Are you talking about poultry? Are you talking about fish? It is interesting, but it still needs to be evaluated further before we make any conclusive decisions,” he said. Dr. Cohen was not involved in the research.
He said the presumed effect of meat consumption on disease exacerbation appeared to take years, “which is a little surprising. If you really thought that IBD was due to something in diet, you would see the response right away, so it doesn’t follow timewise. Why does it takes 5 years? It should be within 5 weeks or 5 days.”
Dr. Lees disclosed relationships with Abbvie, Takeda, Pfizer, Galapagos, and BDD Pharma, among others.
DDW is sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
CHICAGO –
The data, which was presented on May 7 in Chicago at the annual Digestive Disease Week® meeting, is based on an analysis of data from the PREdiCCt study (Prognostic Effect of Environmental Factors in Crohn’s and Colitis) in which diets of patients with IBD were tracked over 2-3 months with 2-year follow-ups. While the study itself includes nearly 3,000 patients from the United Kingdom who are in clinical remission, this analysis included 497 patients with Crohn’s disease and 520 with ulcerative colitis.
The highest level of patient-reported meat consumption was associated with doubled risk for hard flares – defined as an increase in symptoms plus elevation in c-reactive protein (CRP) and fecal calprotection (FCAL) plus a change in IBD therapy – in patients with ulcerative colitis, said study author Charlie W Lees, PhD, FRCP(Ed), Western General Hospital and University of Edinburgh.
Investigators also evaluated the occurrence of soft flares, which was defined as a negative response to the question, “Do you think your disease has been well controlled in the past month or since you last logged on to the portal?”
After a median follow-up of 1,481.5 days, hard flares occurred at a rate of 5.6% per year, but it did not differ by IBD subtype. However, soft flares accumulated rapidly. Hard flares with baseline FCAL levels in the 50-250 mcg/g range, as well as FCAL levels above 250 mcg, were associated with flares.
The mean baseline total protein intake was 91.9 g per day of which 35.8 g came from animal sources. The hazard ratio for the highest vs. lowest quartile of meat intake in the ulcerative colitis group was 2.08. They found no associations between hard flares with intake of total dietary fiber, N-6 polyunsaturated acids, or ultraprocessed foods, which Dr. Lees found surprising.
“Perhaps most intriguingly, when we look at ultraprocessed food intake, no difference in Crohn’s disease, and no difference in ulcerative colitis,” Dr. Lees said.
The finding is in contradiction to a study reported at the Crohn’s & Colitis Congress this year that found additives in ultraprocessed foods appear to have deleterious effects on intestinal microbiota, while others may exert their influence through mechanisms, such as endoplasmic stress.
However, the new data are consistent with a previously reported association between meat consumption and ulcerative colitis development, and suggests that reducing meat consumption could help to reduce the risk of flare in patients with ulcerative colitis.
PREdiCCt is designed to examine dietary, environmental, genetic, and microbiotic factors that are associated with disease flares in patients with Crohn’s disease and ulcerative colitis. Investigators are evaluating potential contributions to disease flares from total animal protein intake, dietary fiber, N-6 polyunsaturated fatty acids, dietary emulsifiers, and ultraprocessed foods, and total bacterial gene count in stool samples. They aim to examine data from 2,500 microbiome samples currently being sequenced at the Wellcome Sanger Institute in Hinxton, England, to determine whether the association between meat and ulcerative colitis flares could be related, as they hypothesize, to diet-induced alterations in the gut microbiome.
The research is preliminary with many unanswered questions, said Russell D. Cohen, MD, director of the inflammatory bowel disease center at the University of Chicago.
“I think he still has to evaluate a lot of the data that he has already collected because, are you talking about meat? Are you talking about poultry? Are you talking about fish? It is interesting, but it still needs to be evaluated further before we make any conclusive decisions,” he said. Dr. Cohen was not involved in the research.
He said the presumed effect of meat consumption on disease exacerbation appeared to take years, “which is a little surprising. If you really thought that IBD was due to something in diet, you would see the response right away, so it doesn’t follow timewise. Why does it takes 5 years? It should be within 5 weeks or 5 days.”
Dr. Lees disclosed relationships with Abbvie, Takeda, Pfizer, Galapagos, and BDD Pharma, among others.
DDW is sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
CHICAGO –
The data, which was presented on May 7 in Chicago at the annual Digestive Disease Week® meeting, is based on an analysis of data from the PREdiCCt study (Prognostic Effect of Environmental Factors in Crohn’s and Colitis) in which diets of patients with IBD were tracked over 2-3 months with 2-year follow-ups. While the study itself includes nearly 3,000 patients from the United Kingdom who are in clinical remission, this analysis included 497 patients with Crohn’s disease and 520 with ulcerative colitis.
The highest level of patient-reported meat consumption was associated with doubled risk for hard flares – defined as an increase in symptoms plus elevation in c-reactive protein (CRP) and fecal calprotection (FCAL) plus a change in IBD therapy – in patients with ulcerative colitis, said study author Charlie W Lees, PhD, FRCP(Ed), Western General Hospital and University of Edinburgh.
Investigators also evaluated the occurrence of soft flares, which was defined as a negative response to the question, “Do you think your disease has been well controlled in the past month or since you last logged on to the portal?”
After a median follow-up of 1,481.5 days, hard flares occurred at a rate of 5.6% per year, but it did not differ by IBD subtype. However, soft flares accumulated rapidly. Hard flares with baseline FCAL levels in the 50-250 mcg/g range, as well as FCAL levels above 250 mcg, were associated with flares.
The mean baseline total protein intake was 91.9 g per day of which 35.8 g came from animal sources. The hazard ratio for the highest vs. lowest quartile of meat intake in the ulcerative colitis group was 2.08. They found no associations between hard flares with intake of total dietary fiber, N-6 polyunsaturated acids, or ultraprocessed foods, which Dr. Lees found surprising.
“Perhaps most intriguingly, when we look at ultraprocessed food intake, no difference in Crohn’s disease, and no difference in ulcerative colitis,” Dr. Lees said.
The finding is in contradiction to a study reported at the Crohn’s & Colitis Congress this year that found additives in ultraprocessed foods appear to have deleterious effects on intestinal microbiota, while others may exert their influence through mechanisms, such as endoplasmic stress.
However, the new data are consistent with a previously reported association between meat consumption and ulcerative colitis development, and suggests that reducing meat consumption could help to reduce the risk of flare in patients with ulcerative colitis.
PREdiCCt is designed to examine dietary, environmental, genetic, and microbiotic factors that are associated with disease flares in patients with Crohn’s disease and ulcerative colitis. Investigators are evaluating potential contributions to disease flares from total animal protein intake, dietary fiber, N-6 polyunsaturated fatty acids, dietary emulsifiers, and ultraprocessed foods, and total bacterial gene count in stool samples. They aim to examine data from 2,500 microbiome samples currently being sequenced at the Wellcome Sanger Institute in Hinxton, England, to determine whether the association between meat and ulcerative colitis flares could be related, as they hypothesize, to diet-induced alterations in the gut microbiome.
The research is preliminary with many unanswered questions, said Russell D. Cohen, MD, director of the inflammatory bowel disease center at the University of Chicago.
“I think he still has to evaluate a lot of the data that he has already collected because, are you talking about meat? Are you talking about poultry? Are you talking about fish? It is interesting, but it still needs to be evaluated further before we make any conclusive decisions,” he said. Dr. Cohen was not involved in the research.
He said the presumed effect of meat consumption on disease exacerbation appeared to take years, “which is a little surprising. If you really thought that IBD was due to something in diet, you would see the response right away, so it doesn’t follow timewise. Why does it takes 5 years? It should be within 5 weeks or 5 days.”
Dr. Lees disclosed relationships with Abbvie, Takeda, Pfizer, Galapagos, and BDD Pharma, among others.
DDW is sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract.
AT DDW 2023
FDA OKs spinal cord stimulation devices for chronic back pain
The Food and Drug Administration has expanded the indication for Abbott Laboratories’ spinal cord stimulation (SCS) devices to include treatment of chronic back pain in patients who have not had, or are not eligible for, back surgery, the company has announced.
The new indication spans all of Abbott’s SCS devices in the United States, which include the recharge-free Proclaim SCS family and the rechargeable Eterna SCS platform.
The devices feature the company’s proprietary, low-energy BurstDR stimulation waveform, a form of stimulation therapy that uses bursts of mild electrical energy without causing an abnormal tingling sensation to help disrupt pain signals before they can reach the brain, the company explained.
The expanded indication was supported by results from the DISTINCT study, which enrolled 270 adults suffering from severe, disabling chronic back pain for an average of more than 12 years and who were not eligible for surgery.
The study showed that significantly more patients who were treated with SCS achieved significant improvements in back pain, function, quality of life, and psychological status than peers treated with conservative medical management.
“To date, we have struggled with how to treat people who weren’t considered a good surgical candidate because we didn’t have clear, data-driven treatment options for non-surgical back pain,” Timothy Deer, MD, president and CEO of the Spine and Nerve Centers of the Virginias in Charleston, W.Va., said in a news release.
“This new indication for Abbott’s SCS devices, together with BurstDR stimulation, allows physicians the ability to identify and treat a new group of people, providing them with relief from chronic back pain,” Dr. Deer said.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has expanded the indication for Abbott Laboratories’ spinal cord stimulation (SCS) devices to include treatment of chronic back pain in patients who have not had, or are not eligible for, back surgery, the company has announced.
The new indication spans all of Abbott’s SCS devices in the United States, which include the recharge-free Proclaim SCS family and the rechargeable Eterna SCS platform.
The devices feature the company’s proprietary, low-energy BurstDR stimulation waveform, a form of stimulation therapy that uses bursts of mild electrical energy without causing an abnormal tingling sensation to help disrupt pain signals before they can reach the brain, the company explained.
The expanded indication was supported by results from the DISTINCT study, which enrolled 270 adults suffering from severe, disabling chronic back pain for an average of more than 12 years and who were not eligible for surgery.
The study showed that significantly more patients who were treated with SCS achieved significant improvements in back pain, function, quality of life, and psychological status than peers treated with conservative medical management.
“To date, we have struggled with how to treat people who weren’t considered a good surgical candidate because we didn’t have clear, data-driven treatment options for non-surgical back pain,” Timothy Deer, MD, president and CEO of the Spine and Nerve Centers of the Virginias in Charleston, W.Va., said in a news release.
“This new indication for Abbott’s SCS devices, together with BurstDR stimulation, allows physicians the ability to identify and treat a new group of people, providing them with relief from chronic back pain,” Dr. Deer said.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has expanded the indication for Abbott Laboratories’ spinal cord stimulation (SCS) devices to include treatment of chronic back pain in patients who have not had, or are not eligible for, back surgery, the company has announced.
The new indication spans all of Abbott’s SCS devices in the United States, which include the recharge-free Proclaim SCS family and the rechargeable Eterna SCS platform.
The devices feature the company’s proprietary, low-energy BurstDR stimulation waveform, a form of stimulation therapy that uses bursts of mild electrical energy without causing an abnormal tingling sensation to help disrupt pain signals before they can reach the brain, the company explained.
The expanded indication was supported by results from the DISTINCT study, which enrolled 270 adults suffering from severe, disabling chronic back pain for an average of more than 12 years and who were not eligible for surgery.
The study showed that significantly more patients who were treated with SCS achieved significant improvements in back pain, function, quality of life, and psychological status than peers treated with conservative medical management.
“To date, we have struggled with how to treat people who weren’t considered a good surgical candidate because we didn’t have clear, data-driven treatment options for non-surgical back pain,” Timothy Deer, MD, president and CEO of the Spine and Nerve Centers of the Virginias in Charleston, W.Va., said in a news release.
“This new indication for Abbott’s SCS devices, together with BurstDR stimulation, allows physicians the ability to identify and treat a new group of people, providing them with relief from chronic back pain,” Dr. Deer said.
A version of this article first appeared on Medscape.com.
TransCon PTH nears U.S. approval for hypoparathyroidism?
SEATTLE –
Findings from 110-week phase 2 data for the once-daily investigational parathyroid hormone (PTH) replacement drug were recently presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Overall, the drug was associated with independence from conventional calcium and active vitamin D therapy in most patients at 110 weeks, with no discontinuations due to adverse effects.
“Patients with hypoparathyroidism have low serum calcium levels and struggle with quality of life and biochemical abnormalities. The data from the TransCon PTH studies seem to show that a lot of these abnormalities can be reversed,” presenter Mishaela R. Rubin, MD, said in an interview.
Other PTH replacement therapies such as Nupara (now discontinued) and teriparatide (off-label) have been used in some patients with hypoparathyroidism.
However, “[TransCon PTH] is delivered in such a way as to have a prolonged half-life, so that’s kind of a special benefit that it has,” added Dr. Rubin of the division of endocrinology and metabolic bone disease, department of medicine, Columbia University, New York.
Asked to comment, session moderator Thanh Hoang, DO, of Walter Reed National Military Medical Center, Silver Spring, Md., said: “I think it’s a very promising medication because right now we don’t have a lot of options ... I think it would help a lot of patients.”
Approval denied, company addressing concerns
On May 1, the Food and Drug Administration issued a complete response letter, signaling denial of approval for the TransCon PTH, citing concerns related to manufacturing control of the product’s drug/device combination product, but not about the product’s safety and efficacy, according to an Ascendis statement.
The company is now working with the FDA to address these issues and is awaiting a European Union decision later this year.
The FDA did not request that the company conduct further clinical trials of TransCon PTH, which now include published 26-week phase 2 and phase 3 data along with the current longer-term phase 2 data presented at AACE.
“The company has said that they’re hopeful the issues will be addressable and that the FDA did not have any concerns about safety,” Dr. Rubin said in an interview.
Calcium normalized, bone turnover improved
Dr. Rubin presented long-term efficacy and safety data from the Phase 2 PaTH Forward trial, which involved 57 of the initial 59 participants who completed week 110 of an open-label extension of the trial.
During the first 4 weeks, patients had been randomized to TransCon PTH at fixed doses of 15 µg/day, 18 µg/day, 21 µg/day, or placebo. After week 4, all patients switched to TransCon PTH titrated to doses of 6-60 µg/day along with conventional therapy, with the goal of maintaining normocalcemia.
Participants were a mean age of 50 years, 81% were women, and 92% were White. Causes of hypoparathyroidism were neck surgery in 80%, autoimmune disease in 2%, and idiopathic disease in 19%. Disease duration was 12 years (range 1-39), and all were taking conventional therapy including calcium and active vitamin D (calcitriol or alfacaldiol).
At 110 weeks, all 57 patients were able to stop taking active vitamin D, and 53 of the 57 (93%) patients achieved independence from conventional therapy, defined as taking 0 µg/day of active vitamin D and no more than 600 mg/day of calcium (the dietary supplement dose). A total of 44 (77%) patients were not taking any calcium or active vitamin D.
“This really establishes the durability up to 2 years of keeping people off conventional therapy,” Dr. Rubin said during her presentation.
There was an initial uptick to 9.4 mg/dL in mean serum calcium, as some participants were still taking active vitamin D, but that dropped to 8.9 mg/dL by week 26. Mean 24-hour urine calcium dropped from 428 mg/day at baseline to 173 mg/day by week 26. Both serum calcium and urine calcium remained in the normal range through week 110 in all patients, at 8.6 mg/dL and 167 mg/day, respectively.
“This is a really important outcome because we know that high urine calcium in these patients sets them at risk for going on to develop nephrocalcinosis, nephrolithiasis, and ultimately, chronic kidney disease,” Dr. Rubin said.
Serum levels of two bone formation markers peaked at 12 weeks after initiation of TransCon PTH. Both trended downward thereafter through week 110 to levels approximating those of age- and sex-matched controls.
“Both markers started off low, consistent with hypoparathyroidism, but with initiation of TransCon PTH we see a robust increase in bone turnover markers, almost as if the bone is ‘waking up,’ if you will. And this is consistent with calcium being mobilized from the skeleton and going into the circulation,” Dr. Rubin explained.
Bone mineral density assessed by dual-energy x-ray absorptiometry normalized, primarily in the first 26 weeks. For lumbar spine L1-L4, mean Z-scores dropped from 1.6 to 1.0 at 26 weeks and down to 0.7 by week 100. For total hip, those values were 1.0, 0.6, and 0.4, respectively. The values approached age- and sex-matched norms, Dr. Rubin noted, to “perhaps where their skeleton would be if they hadn’t had hypoparathyroidism.”
Overall 56 of the 57 (94.9%) patients reported treatment-emergent adverse events, of which 25 (42.4%) were treatment related and none were deemed serious. There were no treatment-emergent adverse events related to hypercalcemia or hypocalcemia leading to health care visits or hospitalization, none leading to discontinuation of study drug, and none to death.
“So overall, a reassuring safety profile,” Dr. Rubin said. “We look forward to presenting the next 2 years’ worth of data to the end of the open-label extension study.”
Dr. Rubin is a paid researcher for Ascendis, which funded the study. Dr. Hoang has reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SEATTLE –
Findings from 110-week phase 2 data for the once-daily investigational parathyroid hormone (PTH) replacement drug were recently presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Overall, the drug was associated with independence from conventional calcium and active vitamin D therapy in most patients at 110 weeks, with no discontinuations due to adverse effects.
“Patients with hypoparathyroidism have low serum calcium levels and struggle with quality of life and biochemical abnormalities. The data from the TransCon PTH studies seem to show that a lot of these abnormalities can be reversed,” presenter Mishaela R. Rubin, MD, said in an interview.
Other PTH replacement therapies such as Nupara (now discontinued) and teriparatide (off-label) have been used in some patients with hypoparathyroidism.
However, “[TransCon PTH] is delivered in such a way as to have a prolonged half-life, so that’s kind of a special benefit that it has,” added Dr. Rubin of the division of endocrinology and metabolic bone disease, department of medicine, Columbia University, New York.
Asked to comment, session moderator Thanh Hoang, DO, of Walter Reed National Military Medical Center, Silver Spring, Md., said: “I think it’s a very promising medication because right now we don’t have a lot of options ... I think it would help a lot of patients.”
Approval denied, company addressing concerns
On May 1, the Food and Drug Administration issued a complete response letter, signaling denial of approval for the TransCon PTH, citing concerns related to manufacturing control of the product’s drug/device combination product, but not about the product’s safety and efficacy, according to an Ascendis statement.
The company is now working with the FDA to address these issues and is awaiting a European Union decision later this year.
The FDA did not request that the company conduct further clinical trials of TransCon PTH, which now include published 26-week phase 2 and phase 3 data along with the current longer-term phase 2 data presented at AACE.
“The company has said that they’re hopeful the issues will be addressable and that the FDA did not have any concerns about safety,” Dr. Rubin said in an interview.
Calcium normalized, bone turnover improved
Dr. Rubin presented long-term efficacy and safety data from the Phase 2 PaTH Forward trial, which involved 57 of the initial 59 participants who completed week 110 of an open-label extension of the trial.
During the first 4 weeks, patients had been randomized to TransCon PTH at fixed doses of 15 µg/day, 18 µg/day, 21 µg/day, or placebo. After week 4, all patients switched to TransCon PTH titrated to doses of 6-60 µg/day along with conventional therapy, with the goal of maintaining normocalcemia.
Participants were a mean age of 50 years, 81% were women, and 92% were White. Causes of hypoparathyroidism were neck surgery in 80%, autoimmune disease in 2%, and idiopathic disease in 19%. Disease duration was 12 years (range 1-39), and all were taking conventional therapy including calcium and active vitamin D (calcitriol or alfacaldiol).
At 110 weeks, all 57 patients were able to stop taking active vitamin D, and 53 of the 57 (93%) patients achieved independence from conventional therapy, defined as taking 0 µg/day of active vitamin D and no more than 600 mg/day of calcium (the dietary supplement dose). A total of 44 (77%) patients were not taking any calcium or active vitamin D.
“This really establishes the durability up to 2 years of keeping people off conventional therapy,” Dr. Rubin said during her presentation.
There was an initial uptick to 9.4 mg/dL in mean serum calcium, as some participants were still taking active vitamin D, but that dropped to 8.9 mg/dL by week 26. Mean 24-hour urine calcium dropped from 428 mg/day at baseline to 173 mg/day by week 26. Both serum calcium and urine calcium remained in the normal range through week 110 in all patients, at 8.6 mg/dL and 167 mg/day, respectively.
“This is a really important outcome because we know that high urine calcium in these patients sets them at risk for going on to develop nephrocalcinosis, nephrolithiasis, and ultimately, chronic kidney disease,” Dr. Rubin said.
Serum levels of two bone formation markers peaked at 12 weeks after initiation of TransCon PTH. Both trended downward thereafter through week 110 to levels approximating those of age- and sex-matched controls.
“Both markers started off low, consistent with hypoparathyroidism, but with initiation of TransCon PTH we see a robust increase in bone turnover markers, almost as if the bone is ‘waking up,’ if you will. And this is consistent with calcium being mobilized from the skeleton and going into the circulation,” Dr. Rubin explained.
Bone mineral density assessed by dual-energy x-ray absorptiometry normalized, primarily in the first 26 weeks. For lumbar spine L1-L4, mean Z-scores dropped from 1.6 to 1.0 at 26 weeks and down to 0.7 by week 100. For total hip, those values were 1.0, 0.6, and 0.4, respectively. The values approached age- and sex-matched norms, Dr. Rubin noted, to “perhaps where their skeleton would be if they hadn’t had hypoparathyroidism.”
Overall 56 of the 57 (94.9%) patients reported treatment-emergent adverse events, of which 25 (42.4%) were treatment related and none were deemed serious. There were no treatment-emergent adverse events related to hypercalcemia or hypocalcemia leading to health care visits or hospitalization, none leading to discontinuation of study drug, and none to death.
“So overall, a reassuring safety profile,” Dr. Rubin said. “We look forward to presenting the next 2 years’ worth of data to the end of the open-label extension study.”
Dr. Rubin is a paid researcher for Ascendis, which funded the study. Dr. Hoang has reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SEATTLE –
Findings from 110-week phase 2 data for the once-daily investigational parathyroid hormone (PTH) replacement drug were recently presented at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Overall, the drug was associated with independence from conventional calcium and active vitamin D therapy in most patients at 110 weeks, with no discontinuations due to adverse effects.
“Patients with hypoparathyroidism have low serum calcium levels and struggle with quality of life and biochemical abnormalities. The data from the TransCon PTH studies seem to show that a lot of these abnormalities can be reversed,” presenter Mishaela R. Rubin, MD, said in an interview.
Other PTH replacement therapies such as Nupara (now discontinued) and teriparatide (off-label) have been used in some patients with hypoparathyroidism.
However, “[TransCon PTH] is delivered in such a way as to have a prolonged half-life, so that’s kind of a special benefit that it has,” added Dr. Rubin of the division of endocrinology and metabolic bone disease, department of medicine, Columbia University, New York.
Asked to comment, session moderator Thanh Hoang, DO, of Walter Reed National Military Medical Center, Silver Spring, Md., said: “I think it’s a very promising medication because right now we don’t have a lot of options ... I think it would help a lot of patients.”
Approval denied, company addressing concerns
On May 1, the Food and Drug Administration issued a complete response letter, signaling denial of approval for the TransCon PTH, citing concerns related to manufacturing control of the product’s drug/device combination product, but not about the product’s safety and efficacy, according to an Ascendis statement.
The company is now working with the FDA to address these issues and is awaiting a European Union decision later this year.
The FDA did not request that the company conduct further clinical trials of TransCon PTH, which now include published 26-week phase 2 and phase 3 data along with the current longer-term phase 2 data presented at AACE.
“The company has said that they’re hopeful the issues will be addressable and that the FDA did not have any concerns about safety,” Dr. Rubin said in an interview.
Calcium normalized, bone turnover improved
Dr. Rubin presented long-term efficacy and safety data from the Phase 2 PaTH Forward trial, which involved 57 of the initial 59 participants who completed week 110 of an open-label extension of the trial.
During the first 4 weeks, patients had been randomized to TransCon PTH at fixed doses of 15 µg/day, 18 µg/day, 21 µg/day, or placebo. After week 4, all patients switched to TransCon PTH titrated to doses of 6-60 µg/day along with conventional therapy, with the goal of maintaining normocalcemia.
Participants were a mean age of 50 years, 81% were women, and 92% were White. Causes of hypoparathyroidism were neck surgery in 80%, autoimmune disease in 2%, and idiopathic disease in 19%. Disease duration was 12 years (range 1-39), and all were taking conventional therapy including calcium and active vitamin D (calcitriol or alfacaldiol).
At 110 weeks, all 57 patients were able to stop taking active vitamin D, and 53 of the 57 (93%) patients achieved independence from conventional therapy, defined as taking 0 µg/day of active vitamin D and no more than 600 mg/day of calcium (the dietary supplement dose). A total of 44 (77%) patients were not taking any calcium or active vitamin D.
“This really establishes the durability up to 2 years of keeping people off conventional therapy,” Dr. Rubin said during her presentation.
There was an initial uptick to 9.4 mg/dL in mean serum calcium, as some participants were still taking active vitamin D, but that dropped to 8.9 mg/dL by week 26. Mean 24-hour urine calcium dropped from 428 mg/day at baseline to 173 mg/day by week 26. Both serum calcium and urine calcium remained in the normal range through week 110 in all patients, at 8.6 mg/dL and 167 mg/day, respectively.
“This is a really important outcome because we know that high urine calcium in these patients sets them at risk for going on to develop nephrocalcinosis, nephrolithiasis, and ultimately, chronic kidney disease,” Dr. Rubin said.
Serum levels of two bone formation markers peaked at 12 weeks after initiation of TransCon PTH. Both trended downward thereafter through week 110 to levels approximating those of age- and sex-matched controls.
“Both markers started off low, consistent with hypoparathyroidism, but with initiation of TransCon PTH we see a robust increase in bone turnover markers, almost as if the bone is ‘waking up,’ if you will. And this is consistent with calcium being mobilized from the skeleton and going into the circulation,” Dr. Rubin explained.
Bone mineral density assessed by dual-energy x-ray absorptiometry normalized, primarily in the first 26 weeks. For lumbar spine L1-L4, mean Z-scores dropped from 1.6 to 1.0 at 26 weeks and down to 0.7 by week 100. For total hip, those values were 1.0, 0.6, and 0.4, respectively. The values approached age- and sex-matched norms, Dr. Rubin noted, to “perhaps where their skeleton would be if they hadn’t had hypoparathyroidism.”
Overall 56 of the 57 (94.9%) patients reported treatment-emergent adverse events, of which 25 (42.4%) were treatment related and none were deemed serious. There were no treatment-emergent adverse events related to hypercalcemia or hypocalcemia leading to health care visits or hospitalization, none leading to discontinuation of study drug, and none to death.
“So overall, a reassuring safety profile,” Dr. Rubin said. “We look forward to presenting the next 2 years’ worth of data to the end of the open-label extension study.”
Dr. Rubin is a paid researcher for Ascendis, which funded the study. Dr. Hoang has reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT AACE 2023
Redo-TAVR in U.S. database yields good news: Outcomes rival first intervention
Data support redo if needed.
Even after 3 years of follow-up, redo transcatheter aortic valve replacement (TAVR) performs about as well as the first procedure, whether compared for hard endpoints, such as death and stroke, or for softer endpoints, such as function and quality of life, new registry data suggest.
reported Rajendra Makkar, MD, associate director, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles.
The results were presented at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Data for this analysis were drawn from 348,338 TAVR procedures with the Edwards balloon-expandable valves in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Replacement Registry.
Of these, 1,216 were redo procedures. In 475 of the cases, the redo was performed in a patient whose first procedure was with an Edwards device. In the remaining 741 cases, the Edwards device replaced a different prosthetic heart valve. The median time to the redo from the first procedure was 26 months.
For the analysis, the redo-TAVRs were compared with native TAVR patients through 1:1 propensity matching employing 35 covariates, such as age, body mass index (BMI), baseline comorbidities, prior cardiovascular procedures, valve size, and Society of Thoracic Surgeons risk score.
Low death and stroke rates following TAVR redos
The rates of all-cause death or stroke within hospital (4.7% vs. 3.9%; P = .32) and at 30 days (6.1% vs. 5.9%; P = .77) were numerically but not statistically higher in the redo group.
At 1 year, the rates of death (17.3% vs. 17.7%; P = .961) and stroke (3.3% vs. 3.5%; P = .982) were numerically but not significantly lower among those who underwent a redo procedure.
The secondary endpoints told the same story. The one exception was the higher aortic valve reintervention rate (0.61% vs. 0.09%; P = .03) at 30 days in the redo group. This did reach statistical significance, but Dr. Makkar pointed out rates were very low regardless. The rates climbed in both groups by 1 year (1.09% vs. 0.21%; P = .01).
No other secondary endpoints differed significantly at 30 days or at 1 year. Even though some were numerically higher after redo at 1 year, such as major vascular complications (1.25 vs. 1.60; P = .51), others were lower, such as new-start dialysis (1.62 vs. 0.98; P = .26). All-cause readmission rates at 1 year were nearly identical (32.56% vs. 32.23%; P = .82).
Consistent with the comparable outcomes on the hard endpoints, major and similar improvements were seen in both the redo and the propensity-matched native TAVR patients on the Kansas City Cardiomyopathy Questionnaire Overall Summary. The slight advantage for the redo group was not significant at 30 days, but the degree of improvement was greater after the redo than after native TAVR at 1 year (15% vs. 10%; P = .03).
“You bring good news,” said Alain G. Cribier, MD, director of cardiology, Charles Nicolle Hospital, University of Rouen, France. Widely regarded as the father of TAVR for his first-in-human series in 2002, Dr. Cribier said that there are several reassuring take-home messages from this study.
“First, these data tell us that the redo rate is extremely low,” he said, noting that the registry data suggests a risk well below 1%. “Second, we are seeing from this data that there are no more complications [than TAVR in a native valve] if you need to do this.”
Redo patients are generally sicker
The propensity matching was designed to eliminate baseline differences for the outcome comparisons, but Dr. Makkar did point out that redo-TAVR patients were sicker than the native TAVR patients. For example, when compared prior to propensity matching, the STS score was higher (8.3 vs. 5.2; P < .01), more patients had atrial fibrillation (47.9% vs. 36.2%; P < .01), and more patients had a prior stroke (15.0% vs. 10.7%; P < .01).
The registry only has follow-up out to 1 year, but participating patients were matched to a claims database to capture outcomes out to 3 years. Mortality rates at long-term follow-up were not significantly different for redo vs. native TAVR (42.2% vs. 40.3% respectively; P = .98); for the entire dataset or when compared in subgroups defined by Edwards valve redo of an Edwards valve (P = .909) or an Edwards valve redo of a non-Edwards device (P = .871).
Whether an early redo, defined as 12 months after the index TAVR procedure, or a late redo, the rate of mortality ranged from approximately 16% to 18% with no significant difference between redo and native TAVR.
A moderator for the late-breaking trials session where these data were presented, Darren Mylotte, MD, a consultant in cardiology for the Galway University Hospitals, Ireland, challenged Dr. Makkar about the potential for selection bias. He said redo patients might be the ones that interventionalists feel confident about helping, making this comparison unrepresentative.
“I think that the selection bias is likely to cut both ways,” Dr. Makkar replied. For many patients with a failed TAVR, he explained that clinicians might think, “There is nothing to be done for this patient except to try a redo.”
Dr. Makkar reports financial relationships with Abbott, Cordis, Edwards Lifesciences, and Medtronic. Dr. Cribier reports a financial relationship with Edwards Lifesciences. Dr. Mylotte reports no potential conflicts of interest.
Data support redo if needed.
Data support redo if needed.
Even after 3 years of follow-up, redo transcatheter aortic valve replacement (TAVR) performs about as well as the first procedure, whether compared for hard endpoints, such as death and stroke, or for softer endpoints, such as function and quality of life, new registry data suggest.
reported Rajendra Makkar, MD, associate director, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles.
The results were presented at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Data for this analysis were drawn from 348,338 TAVR procedures with the Edwards balloon-expandable valves in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Replacement Registry.
Of these, 1,216 were redo procedures. In 475 of the cases, the redo was performed in a patient whose first procedure was with an Edwards device. In the remaining 741 cases, the Edwards device replaced a different prosthetic heart valve. The median time to the redo from the first procedure was 26 months.
For the analysis, the redo-TAVRs were compared with native TAVR patients through 1:1 propensity matching employing 35 covariates, such as age, body mass index (BMI), baseline comorbidities, prior cardiovascular procedures, valve size, and Society of Thoracic Surgeons risk score.
Low death and stroke rates following TAVR redos
The rates of all-cause death or stroke within hospital (4.7% vs. 3.9%; P = .32) and at 30 days (6.1% vs. 5.9%; P = .77) were numerically but not statistically higher in the redo group.
At 1 year, the rates of death (17.3% vs. 17.7%; P = .961) and stroke (3.3% vs. 3.5%; P = .982) were numerically but not significantly lower among those who underwent a redo procedure.
The secondary endpoints told the same story. The one exception was the higher aortic valve reintervention rate (0.61% vs. 0.09%; P = .03) at 30 days in the redo group. This did reach statistical significance, but Dr. Makkar pointed out rates were very low regardless. The rates climbed in both groups by 1 year (1.09% vs. 0.21%; P = .01).
No other secondary endpoints differed significantly at 30 days or at 1 year. Even though some were numerically higher after redo at 1 year, such as major vascular complications (1.25 vs. 1.60; P = .51), others were lower, such as new-start dialysis (1.62 vs. 0.98; P = .26). All-cause readmission rates at 1 year were nearly identical (32.56% vs. 32.23%; P = .82).
Consistent with the comparable outcomes on the hard endpoints, major and similar improvements were seen in both the redo and the propensity-matched native TAVR patients on the Kansas City Cardiomyopathy Questionnaire Overall Summary. The slight advantage for the redo group was not significant at 30 days, but the degree of improvement was greater after the redo than after native TAVR at 1 year (15% vs. 10%; P = .03).
“You bring good news,” said Alain G. Cribier, MD, director of cardiology, Charles Nicolle Hospital, University of Rouen, France. Widely regarded as the father of TAVR for his first-in-human series in 2002, Dr. Cribier said that there are several reassuring take-home messages from this study.
“First, these data tell us that the redo rate is extremely low,” he said, noting that the registry data suggests a risk well below 1%. “Second, we are seeing from this data that there are no more complications [than TAVR in a native valve] if you need to do this.”
Redo patients are generally sicker
The propensity matching was designed to eliminate baseline differences for the outcome comparisons, but Dr. Makkar did point out that redo-TAVR patients were sicker than the native TAVR patients. For example, when compared prior to propensity matching, the STS score was higher (8.3 vs. 5.2; P < .01), more patients had atrial fibrillation (47.9% vs. 36.2%; P < .01), and more patients had a prior stroke (15.0% vs. 10.7%; P < .01).
The registry only has follow-up out to 1 year, but participating patients were matched to a claims database to capture outcomes out to 3 years. Mortality rates at long-term follow-up were not significantly different for redo vs. native TAVR (42.2% vs. 40.3% respectively; P = .98); for the entire dataset or when compared in subgroups defined by Edwards valve redo of an Edwards valve (P = .909) or an Edwards valve redo of a non-Edwards device (P = .871).
Whether an early redo, defined as 12 months after the index TAVR procedure, or a late redo, the rate of mortality ranged from approximately 16% to 18% with no significant difference between redo and native TAVR.
A moderator for the late-breaking trials session where these data were presented, Darren Mylotte, MD, a consultant in cardiology for the Galway University Hospitals, Ireland, challenged Dr. Makkar about the potential for selection bias. He said redo patients might be the ones that interventionalists feel confident about helping, making this comparison unrepresentative.
“I think that the selection bias is likely to cut both ways,” Dr. Makkar replied. For many patients with a failed TAVR, he explained that clinicians might think, “There is nothing to be done for this patient except to try a redo.”
Dr. Makkar reports financial relationships with Abbott, Cordis, Edwards Lifesciences, and Medtronic. Dr. Cribier reports a financial relationship with Edwards Lifesciences. Dr. Mylotte reports no potential conflicts of interest.
Even after 3 years of follow-up, redo transcatheter aortic valve replacement (TAVR) performs about as well as the first procedure, whether compared for hard endpoints, such as death and stroke, or for softer endpoints, such as function and quality of life, new registry data suggest.
reported Rajendra Makkar, MD, associate director, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles.
The results were presented at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Data for this analysis were drawn from 348,338 TAVR procedures with the Edwards balloon-expandable valves in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Replacement Registry.
Of these, 1,216 were redo procedures. In 475 of the cases, the redo was performed in a patient whose first procedure was with an Edwards device. In the remaining 741 cases, the Edwards device replaced a different prosthetic heart valve. The median time to the redo from the first procedure was 26 months.
For the analysis, the redo-TAVRs were compared with native TAVR patients through 1:1 propensity matching employing 35 covariates, such as age, body mass index (BMI), baseline comorbidities, prior cardiovascular procedures, valve size, and Society of Thoracic Surgeons risk score.
Low death and stroke rates following TAVR redos
The rates of all-cause death or stroke within hospital (4.7% vs. 3.9%; P = .32) and at 30 days (6.1% vs. 5.9%; P = .77) were numerically but not statistically higher in the redo group.
At 1 year, the rates of death (17.3% vs. 17.7%; P = .961) and stroke (3.3% vs. 3.5%; P = .982) were numerically but not significantly lower among those who underwent a redo procedure.
The secondary endpoints told the same story. The one exception was the higher aortic valve reintervention rate (0.61% vs. 0.09%; P = .03) at 30 days in the redo group. This did reach statistical significance, but Dr. Makkar pointed out rates were very low regardless. The rates climbed in both groups by 1 year (1.09% vs. 0.21%; P = .01).
No other secondary endpoints differed significantly at 30 days or at 1 year. Even though some were numerically higher after redo at 1 year, such as major vascular complications (1.25 vs. 1.60; P = .51), others were lower, such as new-start dialysis (1.62 vs. 0.98; P = .26). All-cause readmission rates at 1 year were nearly identical (32.56% vs. 32.23%; P = .82).
Consistent with the comparable outcomes on the hard endpoints, major and similar improvements were seen in both the redo and the propensity-matched native TAVR patients on the Kansas City Cardiomyopathy Questionnaire Overall Summary. The slight advantage for the redo group was not significant at 30 days, but the degree of improvement was greater after the redo than after native TAVR at 1 year (15% vs. 10%; P = .03).
“You bring good news,” said Alain G. Cribier, MD, director of cardiology, Charles Nicolle Hospital, University of Rouen, France. Widely regarded as the father of TAVR for his first-in-human series in 2002, Dr. Cribier said that there are several reassuring take-home messages from this study.
“First, these data tell us that the redo rate is extremely low,” he said, noting that the registry data suggests a risk well below 1%. “Second, we are seeing from this data that there are no more complications [than TAVR in a native valve] if you need to do this.”
Redo patients are generally sicker
The propensity matching was designed to eliminate baseline differences for the outcome comparisons, but Dr. Makkar did point out that redo-TAVR patients were sicker than the native TAVR patients. For example, when compared prior to propensity matching, the STS score was higher (8.3 vs. 5.2; P < .01), more patients had atrial fibrillation (47.9% vs. 36.2%; P < .01), and more patients had a prior stroke (15.0% vs. 10.7%; P < .01).
The registry only has follow-up out to 1 year, but participating patients were matched to a claims database to capture outcomes out to 3 years. Mortality rates at long-term follow-up were not significantly different for redo vs. native TAVR (42.2% vs. 40.3% respectively; P = .98); for the entire dataset or when compared in subgroups defined by Edwards valve redo of an Edwards valve (P = .909) or an Edwards valve redo of a non-Edwards device (P = .871).
Whether an early redo, defined as 12 months after the index TAVR procedure, or a late redo, the rate of mortality ranged from approximately 16% to 18% with no significant difference between redo and native TAVR.
A moderator for the late-breaking trials session where these data were presented, Darren Mylotte, MD, a consultant in cardiology for the Galway University Hospitals, Ireland, challenged Dr. Makkar about the potential for selection bias. He said redo patients might be the ones that interventionalists feel confident about helping, making this comparison unrepresentative.
“I think that the selection bias is likely to cut both ways,” Dr. Makkar replied. For many patients with a failed TAVR, he explained that clinicians might think, “There is nothing to be done for this patient except to try a redo.”
Dr. Makkar reports financial relationships with Abbott, Cordis, Edwards Lifesciences, and Medtronic. Dr. Cribier reports a financial relationship with Edwards Lifesciences. Dr. Mylotte reports no potential conflicts of interest.
FROM EUROPCR 2023



