User login
HHS Nominee: Take Two
The so-far fitful process of choosing a U.S. Department of Health and Human Services (HHS) secretary may not delay meaningful healthcare reform—if President Obama remains committed to making the overhaul a top priority, says one of SHM's co-founders.
"On the one hand, he hasn't been able to get anything done in the first 100 days," says Hospitalist Win Whitcomb, MD, vice president of quality improvement at Mercy Medical Center in Springfield, Mass. "That's not as concerning as if he did not prioritize the first year of his presidency. If he doesn't lay the groundwork for meaningful reform in healthcare, that's concerning."
Dr. Whitcomb's comments came as Obama picked Kansas Gov. Kathleen Sebelius as his new HHS secretary nominee. Obama's original choice, former Sen. Tom Daschle, withdrew from consideration amid questions about his taxes. Sebelius, a Democratic governor in a conservative state, could face a contentious Senate confirmation because of her anti-abortion critics. Obama, however, already has filled the other job Daschle was to hold with Nancy-Ann DeParle, a former health policy official during the Clinton administration. She will lead the White House Office on Health Reform; the appointment does not require Senate approval.
What this means for hospitalists is that Obama's goals to expand health insurance coverage, help install electronic record systems, and establish pay for performance in care delivery are receiving significant Oval Office attention. All were discussion topics last week as SHM officials met with congressional leaders on Capitol Hill.
"Any sort of reform that's going to be affecting hospitals, we'll be the key role players in making those changes," Dr. Whitcomb says. "We're in the hospital all the time and [among] the most invested."
For more on Obama's healthcare agenda visit http://www.whitehouse.gov/agenda/health_care.
The so-far fitful process of choosing a U.S. Department of Health and Human Services (HHS) secretary may not delay meaningful healthcare reform—if President Obama remains committed to making the overhaul a top priority, says one of SHM's co-founders.
"On the one hand, he hasn't been able to get anything done in the first 100 days," says Hospitalist Win Whitcomb, MD, vice president of quality improvement at Mercy Medical Center in Springfield, Mass. "That's not as concerning as if he did not prioritize the first year of his presidency. If he doesn't lay the groundwork for meaningful reform in healthcare, that's concerning."
Dr. Whitcomb's comments came as Obama picked Kansas Gov. Kathleen Sebelius as his new HHS secretary nominee. Obama's original choice, former Sen. Tom Daschle, withdrew from consideration amid questions about his taxes. Sebelius, a Democratic governor in a conservative state, could face a contentious Senate confirmation because of her anti-abortion critics. Obama, however, already has filled the other job Daschle was to hold with Nancy-Ann DeParle, a former health policy official during the Clinton administration. She will lead the White House Office on Health Reform; the appointment does not require Senate approval.
What this means for hospitalists is that Obama's goals to expand health insurance coverage, help install electronic record systems, and establish pay for performance in care delivery are receiving significant Oval Office attention. All were discussion topics last week as SHM officials met with congressional leaders on Capitol Hill.
"Any sort of reform that's going to be affecting hospitals, we'll be the key role players in making those changes," Dr. Whitcomb says. "We're in the hospital all the time and [among] the most invested."
For more on Obama's healthcare agenda visit http://www.whitehouse.gov/agenda/health_care.
The so-far fitful process of choosing a U.S. Department of Health and Human Services (HHS) secretary may not delay meaningful healthcare reform—if President Obama remains committed to making the overhaul a top priority, says one of SHM's co-founders.
"On the one hand, he hasn't been able to get anything done in the first 100 days," says Hospitalist Win Whitcomb, MD, vice president of quality improvement at Mercy Medical Center in Springfield, Mass. "That's not as concerning as if he did not prioritize the first year of his presidency. If he doesn't lay the groundwork for meaningful reform in healthcare, that's concerning."
Dr. Whitcomb's comments came as Obama picked Kansas Gov. Kathleen Sebelius as his new HHS secretary nominee. Obama's original choice, former Sen. Tom Daschle, withdrew from consideration amid questions about his taxes. Sebelius, a Democratic governor in a conservative state, could face a contentious Senate confirmation because of her anti-abortion critics. Obama, however, already has filled the other job Daschle was to hold with Nancy-Ann DeParle, a former health policy official during the Clinton administration. She will lead the White House Office on Health Reform; the appointment does not require Senate approval.
What this means for hospitalists is that Obama's goals to expand health insurance coverage, help install electronic record systems, and establish pay for performance in care delivery are receiving significant Oval Office attention. All were discussion topics last week as SHM officials met with congressional leaders on Capitol Hill.
"Any sort of reform that's going to be affecting hospitals, we'll be the key role players in making those changes," Dr. Whitcomb says. "We're in the hospital all the time and [among] the most invested."
For more on Obama's healthcare agenda visit http://www.whitehouse.gov/agenda/health_care.
IV Contrast in Thyrotoxic Patients
Thyrotoxicosis is a relatively common endocrine disorder. An epidemiologic study estimated the prevalence of hyperthyroidism in the United States at 1.3%.1 In our experience newly diagnosed thyrotoxicosis is 1 of the more frequent reasons for inpatient endocrinology specialty consultation. Generally, the diagnosis of thyrotoxicosis is made on clinical and laboratory grounds, and consultation is obtained in order to assist with diagnosing the specific cause and to arrange necessary treatment. A 24‐hour radioactive iodine uptake and scan are useful studies for differentiating the cause of thyrotoxicosis. These tests provide an indication of thyroid pathophysiology based on measurement and imaging of thyroidal uptake of a small dose of orally administered radioiodine. In thyrotoxic patients, the uptake is typically high in those with conditions associated with increased hormone synthesis, such as Graves' disease or autonomously functioning thyroid nodules, and is low in those with conditions associated with decreased hormone synthesis, such as thyroiditis or exogenous thyroid hormone ingestion.
Establishing the correct diagnosis has significant impact on the selection of appropriate therapy for these vastly different etiologies. Radioactive iodine in the form of I‐131 is useful in the treatment of certain thyrotoxic conditions. Radioiodine is the treatment most frequently employed in the United States for Graves' disease,2 and is also the most commonly used treatment of solitary toxic nodules and toxic multinodular goiter. However, it is of no use in treatment of subacute thyroiditis or exogenous ingestion of thyroid hormone. While antithyroid drugs such as methimazole or propylthiouracil can be used to treat conditions associated with increased thyroid hormone synthesis, they also are not effective in treating subacute thyroiditis or thyrotoxicosis factitia; therefore, it is important to establish the diagnosis before using these medications.
Exogenous iodine that has been administered prior to administration of radioiodine can interfere with the uptake of radioiodine by the thyroid, thus rendering the 24‐hour uptake and scan inaccurate as a means of diagnosis, and interfering with the utility of I‐131 as a treatment.3 In our experience, many inpatients with newly diagnosed thyrotoxicosis receive exogenous iodine in the form of intravenous (IV) contrast agents near the time of their presentation, leading to an inability to utilize radioactive iodine to diagnose and potentially treat them. One common reason for the use of iodinated contrast is to enhance computed tomography (CT) scan images. Many symptoms that could presumably lead to the ordering of a CT scan may overlap with symptoms of thyrotoxicosis. Prompt diagnosis of thyrotoxicosis, along with awareness of the interference of IV contrast with use of radioactive iodine and the frequency with which this occurs, may prevent unnecessary CT scans in some patients. Therefore, we undertook this study to quantify the frequency of this occurrence, and the frequency that the IV contrast studies were ultimately useful in the management of these patients.
Methods
The records of inpatient endocrinology consultations over a 48‐month period (January 2003 through January 2007) were reviewed. Consultations requested for thyroid disease were identified, and those which were for thyrotoxicosis were reviewed. Patients with thyrotoxicosis with a cause that had been previously determined, or who had already undergone treatment, were not included in the analysis. The remaining patients with new onset thyrotoxicosis, based on clinical and laboratory findings, in whom radioactive iodine would have been useful for diagnostic and potentially treatment purposes, were included.
Of the patients included, our records were reviewed to determine demographic data, whether intravenous contrast had been administered within 2 weeks of endocrinology consultation, and the type of study that was performed. The results of the contrast studies were reviewed, with attention to findings that potentially could have changed acute or inpatient management of the patients.
Results
A total of 1171 consults were reviewed. Of these, 324 (27.7%) were for thyroid disease. One hundred patients (8.5% of total consults, 30.8% of thyroid disease consults) were identified with previously unevaluated thyrotoxicosis as the primary reason for the consult. Of these patients, 74% were women, and 26% were men. The mean age was 54.6 years (range 18‐93 years).
Forty‐five patients (45%) had been given iodinated contrast within 2 weeks prior to endocrinology evaluation, 43 for CT scanning, and 2 for angiography. There were a total of 50 contrast‐enhanced CT scans done (7 patients had CT scans of multiple anatomic regions). There were 26 chest CT scans, 16 abdominal/pelvic CT scans, and 8 neck CT scans. Indications for the CT scans in these patients are shown in Table 1.
| Indication for CT Scan | Number of Patients |
|---|---|
| Palpitations/shortness of breath | 20 |
| Abdominal pain | 6 |
| Neck swelling | 6 |
| Weight loss | 2 |
| Atrial fibrillation | 1 |
| Loose stool | 1 |
| Question of abdominal mass | 1 |
| Jaundice | 1 |
| Palpable lymphadenopathy | 1 |
| Trauma | 1 |
| Abnormal chest radiograph | 1 |
| Unknown | 2 |
Of the 43 patients who underwent CT scanning, 7 (16%) had a finding that potentially changed their inpatient management (2 with tracheal compression by a goiter, 1 with airway compromise from tonsillar edema, 1 with appendicitis, 1 with pulmonary hypertension, 1 with diffuse lymphoma, and 1 with a rib fracture after trauma). Only 1 of these patients (appendicitis) required emergent treatment of their condition before further diagnostic studies could have been reasonably performed. Among the angiography patients, 1 had undergone cardiac catheterization, which was diagnostic of coronary artery disease, and 1 had undergone angiography of the lower extremities, which revealed an acute arterial clot.
Also of note, in April 2005 at our institution, a new emergency department opened which made it logistically easier to obtain a CT scan. Prior to that time, 16 of 49 patients (33%) evaluated for thyrotoxicosis had received iodinated contrast for a CT scan. After that time, 27 of 51 patients (52%) received a contrast CT study.
Discussion
Indications for contrast‐enhanced CT scans in the acute care setting are numerous. The majority of the CT scans ordered in the above patients were of the chest. CT scans of the chest may be used to evaluate suspected pulmonary emboli or aortic dissection. Coronary CT angiography is also being studied as a method of risk stratification of patients presenting with acute chest pain.4 Common signs and symptoms of the above disorders include chest pain, dyspnea, palpitations, and tachycardia. Many of the most common cardiovascular signs and symptoms associated with thyrotoxicosis overlap with those seen in the above disorders. A recent study of thyrotoxic patients found that on presentation, 73% had palpitations, 60% had dyspnea, 25% had chest pain, and 35% had cough.5 Mean heart rate has been shown to be significantly elevated in thyrotoxic patients compared with normal controls.5, 6 Atrial fibrillation or flutter can occur in about 8% of thyrotoxic patients, especially in males, in older ages, and in those with underlying cardiac disease.7
We also noted that 16 out of the 50 total contrast‐enhanced CT scans performed were of the abdomen and pelvis. While abdominal and gastrointestinal signs and symptoms seem to be less common manifestations of thyrotoxicosis than cardiovascular ones, hyperdefecation with or without diarrhea can be seen in approximately in one‐third of cases. Nausea, vomiting, abdominal pain, and jaundice occur less commonly but can be seen occasionally with severe thyrotoxicosis.3 Weight loss is common, and fever may occur occasionally, which also may trigger evaluation by imaging for malignancy or infection.
Indications for the CT scans ordered for the patients in this study can be seen in Table 1. Some of the studies were ordered for symptoms not likely to be thyroid‐related and may have been unavoidable. However, many of the studies, especially those done for complaints such as palpitations, dyspnea, and weight loss were likely obtained due to symptoms that ultimately turned out to be caused by thyrotoxicosis.
A variety of other factors may uncommonly decrease radioactive iodine uptake, including cardiac decompensation, vomiting after ingestion of the orally dosed radioiodine capsule, and medications, including thioureas. However, exogenous iodine is probably the most common interfering factor.8 Exogenous iodine decreases thyroidal radioiodine uptake both by dilution of the total body iodine pool, and by inhibition of thyroid hormone synthesis via the Wolff‐Chaikoff effect.8 Sources of iodine include diet, medications (amiodarone, which contains approximately 6 mg of inorganic iodine per 200 mg tablet, and potassium iodide), and, most prominently in the hospitalized patient, intravenous contrast material. It has been shown that exposure to as little as 100 g of intravenous iodide can suppress uptake in hyperthyroid patients.9 Both ionic and nonionic intravenous contrast media contain sufficient amounts of inorganic iodide (10 g/ml) to induce this suppression when given in typical doses of 50‐200 ml. This iodide may be derived from deiodination of the contrast media molecule, and also from free iodide contaminants.10 The duration of uptake suppression varies among patients and generally ranges from 4 to 12 weeks, although it may be shorter in hyperthyroid patients.8 This long‐term suppression may be related to the slow deiodination of contrast media remaining in the body.10 Urinary iodine normalization can be used as a means of determining the time when uptake can be measured without interference from exogenous iodine.
Iodine administration can also have deleterious effects on thyroid function apart from its effect on radioiodine uptake. In euthyroid patients, exogenous iodine in large doses inhibits organification of iodide and thyroid hormone synthesis (Wolff‐Chaikoff effect). Normally this effect diminishes after several weeks, but in patients with autoimmune thyroid disease, it may persist, leading to hypothyroidism.11 Iodine ingestion may also lead to hyperthyroidism. In areas of endemic iodine deficiency, this is thought to represent unmasking of thyroid autonomy that had been suppressed by lack of iodine, encompassing such patients as those with Graves' disease or autonomous nodules. In areas of iodine sufficiency such as the United States, the incidence of iodine‐induced thyrotoxicosis is low, and typically occurs in patients with autonomous thyroid nodules or multinodular goiter.11, 12 Cases of thyroid storm have been reported following iodinated contrast administration.13 The elderly may be at greater risk for iodine‐induced thyrotoxicosis,14 which is of concern given their inherent higher likelihood of cardiac disease. It is possible that in some of the patients in our study who had CT scans done for nonthyroid‐related symptoms, iodinated contrast could have precipitated subsequent thyrotoxicosis. In general, caution should be used when administering intravenous contrast agents to patients with known thyroid disease.
CT scanning is being used much more frequently in the acute care setting. One study in the emergency department at a single institution revealed that from the years 2000 to 2005, CT scanning of the chest increased by 226%, and of the abdomen by 72%, despite only a 13% increase in patient volume and a stable level of acuity.15 We refer the reader to this recent review for a discussion of the recent increase in the use of CT scans and the associated risks.16 We have found that a substantial proportion of inpatients with thyrotoxicosis receive intravenous contrast prior to endocrinologic evaluation, thus limiting the ability to use radioactive iodine in diagnosis and treatment. The vast majority of these diagnostic studies are contrast‐enhanced CT scans. Acute findings from these studies in this population that change patient management are uncommon.
The increasing usage of CT scans may exacerbate this problem. Education of physicians that are likely to diagnose thyrotoxicosis prior to subspecialty evaluation (internists, family practitioners, and emergency medicine physicians) regarding the similarity of thyrotoxic symptoms to those typically triggering the request of a CT scan is essential. Clinicians should have an appreciation of the interference of iodinated contrast with the ability to obtain a radioiodine uptake and scan. They should also be aware of the potential effects of iodinated contrast on thyroid function when ordering a contrast‐enhanced CT scan in patients with known thyroid disease or symptoms consistent with the presence of thyrotoxicosis. Under these circumstances consideration of thyroid dysfunction with appropriate blood tests may result in more accurate and timely diagnosis and treatment of underlying thyroid disease and enhance patient outcomes.
- ,,, et al.Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III).J Clin Endo Metab.2002;87:489–499.
- ,,,.Differences and similarities in the diagnosis and treatment of Graves' disease in Europe, Japan, and the United States.Thyroid.1991;1:129–135.
- ,.Thyrotoxicosis. In: Larsen PR, Kronenberg HM, Melmed S, Polonsky KS, eds.Williams Textbook of Endocrinology.10th ed.Philadelphia:Saunders;2003:374–421.
- .Chest pain in the emergency department.JThorac Imaging.2007;22:49–55.
- ,,, et al.Cardiovascular manifestations of hyperthyroidism before and after antithyroid therapy.J Am Coll Cardiol.2007;49:71–81.
- ,.Thyroid hormone and the cardiovascular system.N Engl J Med.2001;344:501–509.
- ,,.Hyperthyroidism and risk of atrial fibrillation or flutter.Arch Intern Med.2004;164:1675–1678.
- .Factors which influence the radioactive iodine thyroidal uptake test.Am J Med.1960;28:397–415.
- ,,, et al.The effect of varying quantities of inorganic iodide (carrier) on the urinary excretion and thyroidal accumulation of radioiodine in exophthalmic goiter.J Clin Invest.1950;29:726–738.
- ,,.Contrast material iodides: potential effects on radioactive iodine thyroid uptake.J Nucl Med.1992;33:237–238.
- ,.Iodine excess and hyperthyroidism.Thyroid.2001;11:493–500.
- ,,.Effect of iodinated contrast media on thyroid function in adults.Eur Radiol.2004;14:902–907.
- ,,,.Thyroidectomy in iodine induced thyrotoxic storm.Exp Clin Endocrinol Diabetes.1999;107:468–472.
- ,.Hyperthyroidism in elderly hospitalized patients.Med J Aust.1996;164:200–203.
- ,.Increasing utilization of computed tomography in the adult emergency department, 2000–2005.Emerg Radiol.2006;13:25–30.
- ,.Computed tomography—an increasing source of radiation exposure.N Engl J Med.2007;357:2277–2284.
Thyrotoxicosis is a relatively common endocrine disorder. An epidemiologic study estimated the prevalence of hyperthyroidism in the United States at 1.3%.1 In our experience newly diagnosed thyrotoxicosis is 1 of the more frequent reasons for inpatient endocrinology specialty consultation. Generally, the diagnosis of thyrotoxicosis is made on clinical and laboratory grounds, and consultation is obtained in order to assist with diagnosing the specific cause and to arrange necessary treatment. A 24‐hour radioactive iodine uptake and scan are useful studies for differentiating the cause of thyrotoxicosis. These tests provide an indication of thyroid pathophysiology based on measurement and imaging of thyroidal uptake of a small dose of orally administered radioiodine. In thyrotoxic patients, the uptake is typically high in those with conditions associated with increased hormone synthesis, such as Graves' disease or autonomously functioning thyroid nodules, and is low in those with conditions associated with decreased hormone synthesis, such as thyroiditis or exogenous thyroid hormone ingestion.
Establishing the correct diagnosis has significant impact on the selection of appropriate therapy for these vastly different etiologies. Radioactive iodine in the form of I‐131 is useful in the treatment of certain thyrotoxic conditions. Radioiodine is the treatment most frequently employed in the United States for Graves' disease,2 and is also the most commonly used treatment of solitary toxic nodules and toxic multinodular goiter. However, it is of no use in treatment of subacute thyroiditis or exogenous ingestion of thyroid hormone. While antithyroid drugs such as methimazole or propylthiouracil can be used to treat conditions associated with increased thyroid hormone synthesis, they also are not effective in treating subacute thyroiditis or thyrotoxicosis factitia; therefore, it is important to establish the diagnosis before using these medications.
Exogenous iodine that has been administered prior to administration of radioiodine can interfere with the uptake of radioiodine by the thyroid, thus rendering the 24‐hour uptake and scan inaccurate as a means of diagnosis, and interfering with the utility of I‐131 as a treatment.3 In our experience, many inpatients with newly diagnosed thyrotoxicosis receive exogenous iodine in the form of intravenous (IV) contrast agents near the time of their presentation, leading to an inability to utilize radioactive iodine to diagnose and potentially treat them. One common reason for the use of iodinated contrast is to enhance computed tomography (CT) scan images. Many symptoms that could presumably lead to the ordering of a CT scan may overlap with symptoms of thyrotoxicosis. Prompt diagnosis of thyrotoxicosis, along with awareness of the interference of IV contrast with use of radioactive iodine and the frequency with which this occurs, may prevent unnecessary CT scans in some patients. Therefore, we undertook this study to quantify the frequency of this occurrence, and the frequency that the IV contrast studies were ultimately useful in the management of these patients.
Methods
The records of inpatient endocrinology consultations over a 48‐month period (January 2003 through January 2007) were reviewed. Consultations requested for thyroid disease were identified, and those which were for thyrotoxicosis were reviewed. Patients with thyrotoxicosis with a cause that had been previously determined, or who had already undergone treatment, were not included in the analysis. The remaining patients with new onset thyrotoxicosis, based on clinical and laboratory findings, in whom radioactive iodine would have been useful for diagnostic and potentially treatment purposes, were included.
Of the patients included, our records were reviewed to determine demographic data, whether intravenous contrast had been administered within 2 weeks of endocrinology consultation, and the type of study that was performed. The results of the contrast studies were reviewed, with attention to findings that potentially could have changed acute or inpatient management of the patients.
Results
A total of 1171 consults were reviewed. Of these, 324 (27.7%) were for thyroid disease. One hundred patients (8.5% of total consults, 30.8% of thyroid disease consults) were identified with previously unevaluated thyrotoxicosis as the primary reason for the consult. Of these patients, 74% were women, and 26% were men. The mean age was 54.6 years (range 18‐93 years).
Forty‐five patients (45%) had been given iodinated contrast within 2 weeks prior to endocrinology evaluation, 43 for CT scanning, and 2 for angiography. There were a total of 50 contrast‐enhanced CT scans done (7 patients had CT scans of multiple anatomic regions). There were 26 chest CT scans, 16 abdominal/pelvic CT scans, and 8 neck CT scans. Indications for the CT scans in these patients are shown in Table 1.
| Indication for CT Scan | Number of Patients |
|---|---|
| Palpitations/shortness of breath | 20 |
| Abdominal pain | 6 |
| Neck swelling | 6 |
| Weight loss | 2 |
| Atrial fibrillation | 1 |
| Loose stool | 1 |
| Question of abdominal mass | 1 |
| Jaundice | 1 |
| Palpable lymphadenopathy | 1 |
| Trauma | 1 |
| Abnormal chest radiograph | 1 |
| Unknown | 2 |
Of the 43 patients who underwent CT scanning, 7 (16%) had a finding that potentially changed their inpatient management (2 with tracheal compression by a goiter, 1 with airway compromise from tonsillar edema, 1 with appendicitis, 1 with pulmonary hypertension, 1 with diffuse lymphoma, and 1 with a rib fracture after trauma). Only 1 of these patients (appendicitis) required emergent treatment of their condition before further diagnostic studies could have been reasonably performed. Among the angiography patients, 1 had undergone cardiac catheterization, which was diagnostic of coronary artery disease, and 1 had undergone angiography of the lower extremities, which revealed an acute arterial clot.
Also of note, in April 2005 at our institution, a new emergency department opened which made it logistically easier to obtain a CT scan. Prior to that time, 16 of 49 patients (33%) evaluated for thyrotoxicosis had received iodinated contrast for a CT scan. After that time, 27 of 51 patients (52%) received a contrast CT study.
Discussion
Indications for contrast‐enhanced CT scans in the acute care setting are numerous. The majority of the CT scans ordered in the above patients were of the chest. CT scans of the chest may be used to evaluate suspected pulmonary emboli or aortic dissection. Coronary CT angiography is also being studied as a method of risk stratification of patients presenting with acute chest pain.4 Common signs and symptoms of the above disorders include chest pain, dyspnea, palpitations, and tachycardia. Many of the most common cardiovascular signs and symptoms associated with thyrotoxicosis overlap with those seen in the above disorders. A recent study of thyrotoxic patients found that on presentation, 73% had palpitations, 60% had dyspnea, 25% had chest pain, and 35% had cough.5 Mean heart rate has been shown to be significantly elevated in thyrotoxic patients compared with normal controls.5, 6 Atrial fibrillation or flutter can occur in about 8% of thyrotoxic patients, especially in males, in older ages, and in those with underlying cardiac disease.7
We also noted that 16 out of the 50 total contrast‐enhanced CT scans performed were of the abdomen and pelvis. While abdominal and gastrointestinal signs and symptoms seem to be less common manifestations of thyrotoxicosis than cardiovascular ones, hyperdefecation with or without diarrhea can be seen in approximately in one‐third of cases. Nausea, vomiting, abdominal pain, and jaundice occur less commonly but can be seen occasionally with severe thyrotoxicosis.3 Weight loss is common, and fever may occur occasionally, which also may trigger evaluation by imaging for malignancy or infection.
Indications for the CT scans ordered for the patients in this study can be seen in Table 1. Some of the studies were ordered for symptoms not likely to be thyroid‐related and may have been unavoidable. However, many of the studies, especially those done for complaints such as palpitations, dyspnea, and weight loss were likely obtained due to symptoms that ultimately turned out to be caused by thyrotoxicosis.
A variety of other factors may uncommonly decrease radioactive iodine uptake, including cardiac decompensation, vomiting after ingestion of the orally dosed radioiodine capsule, and medications, including thioureas. However, exogenous iodine is probably the most common interfering factor.8 Exogenous iodine decreases thyroidal radioiodine uptake both by dilution of the total body iodine pool, and by inhibition of thyroid hormone synthesis via the Wolff‐Chaikoff effect.8 Sources of iodine include diet, medications (amiodarone, which contains approximately 6 mg of inorganic iodine per 200 mg tablet, and potassium iodide), and, most prominently in the hospitalized patient, intravenous contrast material. It has been shown that exposure to as little as 100 g of intravenous iodide can suppress uptake in hyperthyroid patients.9 Both ionic and nonionic intravenous contrast media contain sufficient amounts of inorganic iodide (10 g/ml) to induce this suppression when given in typical doses of 50‐200 ml. This iodide may be derived from deiodination of the contrast media molecule, and also from free iodide contaminants.10 The duration of uptake suppression varies among patients and generally ranges from 4 to 12 weeks, although it may be shorter in hyperthyroid patients.8 This long‐term suppression may be related to the slow deiodination of contrast media remaining in the body.10 Urinary iodine normalization can be used as a means of determining the time when uptake can be measured without interference from exogenous iodine.
Iodine administration can also have deleterious effects on thyroid function apart from its effect on radioiodine uptake. In euthyroid patients, exogenous iodine in large doses inhibits organification of iodide and thyroid hormone synthesis (Wolff‐Chaikoff effect). Normally this effect diminishes after several weeks, but in patients with autoimmune thyroid disease, it may persist, leading to hypothyroidism.11 Iodine ingestion may also lead to hyperthyroidism. In areas of endemic iodine deficiency, this is thought to represent unmasking of thyroid autonomy that had been suppressed by lack of iodine, encompassing such patients as those with Graves' disease or autonomous nodules. In areas of iodine sufficiency such as the United States, the incidence of iodine‐induced thyrotoxicosis is low, and typically occurs in patients with autonomous thyroid nodules or multinodular goiter.11, 12 Cases of thyroid storm have been reported following iodinated contrast administration.13 The elderly may be at greater risk for iodine‐induced thyrotoxicosis,14 which is of concern given their inherent higher likelihood of cardiac disease. It is possible that in some of the patients in our study who had CT scans done for nonthyroid‐related symptoms, iodinated contrast could have precipitated subsequent thyrotoxicosis. In general, caution should be used when administering intravenous contrast agents to patients with known thyroid disease.
CT scanning is being used much more frequently in the acute care setting. One study in the emergency department at a single institution revealed that from the years 2000 to 2005, CT scanning of the chest increased by 226%, and of the abdomen by 72%, despite only a 13% increase in patient volume and a stable level of acuity.15 We refer the reader to this recent review for a discussion of the recent increase in the use of CT scans and the associated risks.16 We have found that a substantial proportion of inpatients with thyrotoxicosis receive intravenous contrast prior to endocrinologic evaluation, thus limiting the ability to use radioactive iodine in diagnosis and treatment. The vast majority of these diagnostic studies are contrast‐enhanced CT scans. Acute findings from these studies in this population that change patient management are uncommon.
The increasing usage of CT scans may exacerbate this problem. Education of physicians that are likely to diagnose thyrotoxicosis prior to subspecialty evaluation (internists, family practitioners, and emergency medicine physicians) regarding the similarity of thyrotoxic symptoms to those typically triggering the request of a CT scan is essential. Clinicians should have an appreciation of the interference of iodinated contrast with the ability to obtain a radioiodine uptake and scan. They should also be aware of the potential effects of iodinated contrast on thyroid function when ordering a contrast‐enhanced CT scan in patients with known thyroid disease or symptoms consistent with the presence of thyrotoxicosis. Under these circumstances consideration of thyroid dysfunction with appropriate blood tests may result in more accurate and timely diagnosis and treatment of underlying thyroid disease and enhance patient outcomes.
Thyrotoxicosis is a relatively common endocrine disorder. An epidemiologic study estimated the prevalence of hyperthyroidism in the United States at 1.3%.1 In our experience newly diagnosed thyrotoxicosis is 1 of the more frequent reasons for inpatient endocrinology specialty consultation. Generally, the diagnosis of thyrotoxicosis is made on clinical and laboratory grounds, and consultation is obtained in order to assist with diagnosing the specific cause and to arrange necessary treatment. A 24‐hour radioactive iodine uptake and scan are useful studies for differentiating the cause of thyrotoxicosis. These tests provide an indication of thyroid pathophysiology based on measurement and imaging of thyroidal uptake of a small dose of orally administered radioiodine. In thyrotoxic patients, the uptake is typically high in those with conditions associated with increased hormone synthesis, such as Graves' disease or autonomously functioning thyroid nodules, and is low in those with conditions associated with decreased hormone synthesis, such as thyroiditis or exogenous thyroid hormone ingestion.
Establishing the correct diagnosis has significant impact on the selection of appropriate therapy for these vastly different etiologies. Radioactive iodine in the form of I‐131 is useful in the treatment of certain thyrotoxic conditions. Radioiodine is the treatment most frequently employed in the United States for Graves' disease,2 and is also the most commonly used treatment of solitary toxic nodules and toxic multinodular goiter. However, it is of no use in treatment of subacute thyroiditis or exogenous ingestion of thyroid hormone. While antithyroid drugs such as methimazole or propylthiouracil can be used to treat conditions associated with increased thyroid hormone synthesis, they also are not effective in treating subacute thyroiditis or thyrotoxicosis factitia; therefore, it is important to establish the diagnosis before using these medications.
Exogenous iodine that has been administered prior to administration of radioiodine can interfere with the uptake of radioiodine by the thyroid, thus rendering the 24‐hour uptake and scan inaccurate as a means of diagnosis, and interfering with the utility of I‐131 as a treatment.3 In our experience, many inpatients with newly diagnosed thyrotoxicosis receive exogenous iodine in the form of intravenous (IV) contrast agents near the time of their presentation, leading to an inability to utilize radioactive iodine to diagnose and potentially treat them. One common reason for the use of iodinated contrast is to enhance computed tomography (CT) scan images. Many symptoms that could presumably lead to the ordering of a CT scan may overlap with symptoms of thyrotoxicosis. Prompt diagnosis of thyrotoxicosis, along with awareness of the interference of IV contrast with use of radioactive iodine and the frequency with which this occurs, may prevent unnecessary CT scans in some patients. Therefore, we undertook this study to quantify the frequency of this occurrence, and the frequency that the IV contrast studies were ultimately useful in the management of these patients.
Methods
The records of inpatient endocrinology consultations over a 48‐month period (January 2003 through January 2007) were reviewed. Consultations requested for thyroid disease were identified, and those which were for thyrotoxicosis were reviewed. Patients with thyrotoxicosis with a cause that had been previously determined, or who had already undergone treatment, were not included in the analysis. The remaining patients with new onset thyrotoxicosis, based on clinical and laboratory findings, in whom radioactive iodine would have been useful for diagnostic and potentially treatment purposes, were included.
Of the patients included, our records were reviewed to determine demographic data, whether intravenous contrast had been administered within 2 weeks of endocrinology consultation, and the type of study that was performed. The results of the contrast studies were reviewed, with attention to findings that potentially could have changed acute or inpatient management of the patients.
Results
A total of 1171 consults were reviewed. Of these, 324 (27.7%) were for thyroid disease. One hundred patients (8.5% of total consults, 30.8% of thyroid disease consults) were identified with previously unevaluated thyrotoxicosis as the primary reason for the consult. Of these patients, 74% were women, and 26% were men. The mean age was 54.6 years (range 18‐93 years).
Forty‐five patients (45%) had been given iodinated contrast within 2 weeks prior to endocrinology evaluation, 43 for CT scanning, and 2 for angiography. There were a total of 50 contrast‐enhanced CT scans done (7 patients had CT scans of multiple anatomic regions). There were 26 chest CT scans, 16 abdominal/pelvic CT scans, and 8 neck CT scans. Indications for the CT scans in these patients are shown in Table 1.
| Indication for CT Scan | Number of Patients |
|---|---|
| Palpitations/shortness of breath | 20 |
| Abdominal pain | 6 |
| Neck swelling | 6 |
| Weight loss | 2 |
| Atrial fibrillation | 1 |
| Loose stool | 1 |
| Question of abdominal mass | 1 |
| Jaundice | 1 |
| Palpable lymphadenopathy | 1 |
| Trauma | 1 |
| Abnormal chest radiograph | 1 |
| Unknown | 2 |
Of the 43 patients who underwent CT scanning, 7 (16%) had a finding that potentially changed their inpatient management (2 with tracheal compression by a goiter, 1 with airway compromise from tonsillar edema, 1 with appendicitis, 1 with pulmonary hypertension, 1 with diffuse lymphoma, and 1 with a rib fracture after trauma). Only 1 of these patients (appendicitis) required emergent treatment of their condition before further diagnostic studies could have been reasonably performed. Among the angiography patients, 1 had undergone cardiac catheterization, which was diagnostic of coronary artery disease, and 1 had undergone angiography of the lower extremities, which revealed an acute arterial clot.
Also of note, in April 2005 at our institution, a new emergency department opened which made it logistically easier to obtain a CT scan. Prior to that time, 16 of 49 patients (33%) evaluated for thyrotoxicosis had received iodinated contrast for a CT scan. After that time, 27 of 51 patients (52%) received a contrast CT study.
Discussion
Indications for contrast‐enhanced CT scans in the acute care setting are numerous. The majority of the CT scans ordered in the above patients were of the chest. CT scans of the chest may be used to evaluate suspected pulmonary emboli or aortic dissection. Coronary CT angiography is also being studied as a method of risk stratification of patients presenting with acute chest pain.4 Common signs and symptoms of the above disorders include chest pain, dyspnea, palpitations, and tachycardia. Many of the most common cardiovascular signs and symptoms associated with thyrotoxicosis overlap with those seen in the above disorders. A recent study of thyrotoxic patients found that on presentation, 73% had palpitations, 60% had dyspnea, 25% had chest pain, and 35% had cough.5 Mean heart rate has been shown to be significantly elevated in thyrotoxic patients compared with normal controls.5, 6 Atrial fibrillation or flutter can occur in about 8% of thyrotoxic patients, especially in males, in older ages, and in those with underlying cardiac disease.7
We also noted that 16 out of the 50 total contrast‐enhanced CT scans performed were of the abdomen and pelvis. While abdominal and gastrointestinal signs and symptoms seem to be less common manifestations of thyrotoxicosis than cardiovascular ones, hyperdefecation with or without diarrhea can be seen in approximately in one‐third of cases. Nausea, vomiting, abdominal pain, and jaundice occur less commonly but can be seen occasionally with severe thyrotoxicosis.3 Weight loss is common, and fever may occur occasionally, which also may trigger evaluation by imaging for malignancy or infection.
Indications for the CT scans ordered for the patients in this study can be seen in Table 1. Some of the studies were ordered for symptoms not likely to be thyroid‐related and may have been unavoidable. However, many of the studies, especially those done for complaints such as palpitations, dyspnea, and weight loss were likely obtained due to symptoms that ultimately turned out to be caused by thyrotoxicosis.
A variety of other factors may uncommonly decrease radioactive iodine uptake, including cardiac decompensation, vomiting after ingestion of the orally dosed radioiodine capsule, and medications, including thioureas. However, exogenous iodine is probably the most common interfering factor.8 Exogenous iodine decreases thyroidal radioiodine uptake both by dilution of the total body iodine pool, and by inhibition of thyroid hormone synthesis via the Wolff‐Chaikoff effect.8 Sources of iodine include diet, medications (amiodarone, which contains approximately 6 mg of inorganic iodine per 200 mg tablet, and potassium iodide), and, most prominently in the hospitalized patient, intravenous contrast material. It has been shown that exposure to as little as 100 g of intravenous iodide can suppress uptake in hyperthyroid patients.9 Both ionic and nonionic intravenous contrast media contain sufficient amounts of inorganic iodide (10 g/ml) to induce this suppression when given in typical doses of 50‐200 ml. This iodide may be derived from deiodination of the contrast media molecule, and also from free iodide contaminants.10 The duration of uptake suppression varies among patients and generally ranges from 4 to 12 weeks, although it may be shorter in hyperthyroid patients.8 This long‐term suppression may be related to the slow deiodination of contrast media remaining in the body.10 Urinary iodine normalization can be used as a means of determining the time when uptake can be measured without interference from exogenous iodine.
Iodine administration can also have deleterious effects on thyroid function apart from its effect on radioiodine uptake. In euthyroid patients, exogenous iodine in large doses inhibits organification of iodide and thyroid hormone synthesis (Wolff‐Chaikoff effect). Normally this effect diminishes after several weeks, but in patients with autoimmune thyroid disease, it may persist, leading to hypothyroidism.11 Iodine ingestion may also lead to hyperthyroidism. In areas of endemic iodine deficiency, this is thought to represent unmasking of thyroid autonomy that had been suppressed by lack of iodine, encompassing such patients as those with Graves' disease or autonomous nodules. In areas of iodine sufficiency such as the United States, the incidence of iodine‐induced thyrotoxicosis is low, and typically occurs in patients with autonomous thyroid nodules or multinodular goiter.11, 12 Cases of thyroid storm have been reported following iodinated contrast administration.13 The elderly may be at greater risk for iodine‐induced thyrotoxicosis,14 which is of concern given their inherent higher likelihood of cardiac disease. It is possible that in some of the patients in our study who had CT scans done for nonthyroid‐related symptoms, iodinated contrast could have precipitated subsequent thyrotoxicosis. In general, caution should be used when administering intravenous contrast agents to patients with known thyroid disease.
CT scanning is being used much more frequently in the acute care setting. One study in the emergency department at a single institution revealed that from the years 2000 to 2005, CT scanning of the chest increased by 226%, and of the abdomen by 72%, despite only a 13% increase in patient volume and a stable level of acuity.15 We refer the reader to this recent review for a discussion of the recent increase in the use of CT scans and the associated risks.16 We have found that a substantial proportion of inpatients with thyrotoxicosis receive intravenous contrast prior to endocrinologic evaluation, thus limiting the ability to use radioactive iodine in diagnosis and treatment. The vast majority of these diagnostic studies are contrast‐enhanced CT scans. Acute findings from these studies in this population that change patient management are uncommon.
The increasing usage of CT scans may exacerbate this problem. Education of physicians that are likely to diagnose thyrotoxicosis prior to subspecialty evaluation (internists, family practitioners, and emergency medicine physicians) regarding the similarity of thyrotoxic symptoms to those typically triggering the request of a CT scan is essential. Clinicians should have an appreciation of the interference of iodinated contrast with the ability to obtain a radioiodine uptake and scan. They should also be aware of the potential effects of iodinated contrast on thyroid function when ordering a contrast‐enhanced CT scan in patients with known thyroid disease or symptoms consistent with the presence of thyrotoxicosis. Under these circumstances consideration of thyroid dysfunction with appropriate blood tests may result in more accurate and timely diagnosis and treatment of underlying thyroid disease and enhance patient outcomes.
- ,,, et al.Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III).J Clin Endo Metab.2002;87:489–499.
- ,,,.Differences and similarities in the diagnosis and treatment of Graves' disease in Europe, Japan, and the United States.Thyroid.1991;1:129–135.
- ,.Thyrotoxicosis. In: Larsen PR, Kronenberg HM, Melmed S, Polonsky KS, eds.Williams Textbook of Endocrinology.10th ed.Philadelphia:Saunders;2003:374–421.
- .Chest pain in the emergency department.JThorac Imaging.2007;22:49–55.
- ,,, et al.Cardiovascular manifestations of hyperthyroidism before and after antithyroid therapy.J Am Coll Cardiol.2007;49:71–81.
- ,.Thyroid hormone and the cardiovascular system.N Engl J Med.2001;344:501–509.
- ,,.Hyperthyroidism and risk of atrial fibrillation or flutter.Arch Intern Med.2004;164:1675–1678.
- .Factors which influence the radioactive iodine thyroidal uptake test.Am J Med.1960;28:397–415.
- ,,, et al.The effect of varying quantities of inorganic iodide (carrier) on the urinary excretion and thyroidal accumulation of radioiodine in exophthalmic goiter.J Clin Invest.1950;29:726–738.
- ,,.Contrast material iodides: potential effects on radioactive iodine thyroid uptake.J Nucl Med.1992;33:237–238.
- ,.Iodine excess and hyperthyroidism.Thyroid.2001;11:493–500.
- ,,.Effect of iodinated contrast media on thyroid function in adults.Eur Radiol.2004;14:902–907.
- ,,,.Thyroidectomy in iodine induced thyrotoxic storm.Exp Clin Endocrinol Diabetes.1999;107:468–472.
- ,.Hyperthyroidism in elderly hospitalized patients.Med J Aust.1996;164:200–203.
- ,.Increasing utilization of computed tomography in the adult emergency department, 2000–2005.Emerg Radiol.2006;13:25–30.
- ,.Computed tomography—an increasing source of radiation exposure.N Engl J Med.2007;357:2277–2284.
- ,,, et al.Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III).J Clin Endo Metab.2002;87:489–499.
- ,,,.Differences and similarities in the diagnosis and treatment of Graves' disease in Europe, Japan, and the United States.Thyroid.1991;1:129–135.
- ,.Thyrotoxicosis. In: Larsen PR, Kronenberg HM, Melmed S, Polonsky KS, eds.Williams Textbook of Endocrinology.10th ed.Philadelphia:Saunders;2003:374–421.
- .Chest pain in the emergency department.JThorac Imaging.2007;22:49–55.
- ,,, et al.Cardiovascular manifestations of hyperthyroidism before and after antithyroid therapy.J Am Coll Cardiol.2007;49:71–81.
- ,.Thyroid hormone and the cardiovascular system.N Engl J Med.2001;344:501–509.
- ,,.Hyperthyroidism and risk of atrial fibrillation or flutter.Arch Intern Med.2004;164:1675–1678.
- .Factors which influence the radioactive iodine thyroidal uptake test.Am J Med.1960;28:397–415.
- ,,, et al.The effect of varying quantities of inorganic iodide (carrier) on the urinary excretion and thyroidal accumulation of radioiodine in exophthalmic goiter.J Clin Invest.1950;29:726–738.
- ,,.Contrast material iodides: potential effects on radioactive iodine thyroid uptake.J Nucl Med.1992;33:237–238.
- ,.Iodine excess and hyperthyroidism.Thyroid.2001;11:493–500.
- ,,.Effect of iodinated contrast media on thyroid function in adults.Eur Radiol.2004;14:902–907.
- ,,,.Thyroidectomy in iodine induced thyrotoxic storm.Exp Clin Endocrinol Diabetes.1999;107:468–472.
- ,.Hyperthyroidism in elderly hospitalized patients.Med J Aust.1996;164:200–203.
- ,.Increasing utilization of computed tomography in the adult emergency department, 2000–2005.Emerg Radiol.2006;13:25–30.
- ,.Computed tomography—an increasing source of radiation exposure.N Engl J Med.2007;357:2277–2284.
Copyright © 2009 Society of Hospital Medicine
Hospitalist‐PCP Communication Needs
Hospitalist systems focus on providing acute treatments to patients and expediting hospital discharge, sometimes without regard for the need to work in concert with community providers, leading to fragmentation of care.1 This fragmentation, particularly at the transitions of care, such as when patients move from the outpatient setting to a hospitalist system and then back to their primary care providers (PCPs), can lead to communication breakdowns and delays in care, and may compromise patient outcomes.2 Suboptimal treatments, such as medication errors and the ordering of redundant tests can occur in either setting if prior treatment information is not relayed in a timely and accurate fashion. Landrigan et al.3 described a conceptual model in 2001 that recognized the complexity of the hospitalist‐PCP communication system. Specifically, optimal care of hospitalized children includes PCPs, family members, hospitalists, and support staff while meeting the communication needs of families and PCPs. Additionally, mediating a smooth transition into and out of the hospital needs to be measured carefully.3
Previous adult studies have reported that hospitalist systems sometimes create discontinuity of patient care, which can have a negative impact on the quality of care provided to patients if there is poor communication between hospitalists and PCPs.2, 4, 5 Existing research on hospitalist‐PCP communication focuses mainly on adult hospitalist models with little known about the quality of current pediatric hospitalist‐PCP communication.
The objective of this study was to qualitatively explore issues around communication between pediatric hospitalists and PCPs. Specifically, we sought to explore the quality of communication practices and barriers to optimal communication within the hospitalist‐PCP model at a tertiary care children's hospital. The results are serving as a needs assessment to guide the design of a quality improvement project with the aim of improving pediatric hospitalist‐PCP communication.
METHODS
Study Design
Phone interviews of pediatric hospitalists and PCPs were conducted. The study was approved by the University of Utah and Primary Children's Medical Center (PCMC) Institutional Review Boards.
Setting
PCMC is a 232‐bed, tertiary‐care referral center and community hospital in Salt Lake City, UT, which serves a catchment area of approximately 1,000,000 children in 5 Intermountain West states (Utah, Idaho, Nevada, Montana, and Wyoming). In 2005, there were more than 40,000 emergency department visits and more than 11,000 hospital admissions. At the time of this study, the Division of Pediatric Inpatient Medicine (hospitalist division) included 11 full‐time equivalents. All hospitalists play a teaching role and are on faculty at the University of Utah School of Medicine. In 2005, approximately 45% of medical inpatients at PCMC were cared for by the hospitalist division, with approximately 95% cared for by resident teams.
Participants
Ten University of Utah pediatric hospitalists and 12 PCPs within our catchment area completed interviews. Verbal consent was given before study participants began the phone interview. All hospitalists from the hospitalist division, excluding the first author, completed an interview. PCPs who had referred patients to the hospitalist division in the year preceding this study (2004) were identified through a referring database kept by the hospitalist division. An attempt was made to interview physicians in multiple practice settings and geographic locations.
Inclusion criteria for PCPs included their willingness to complete the interview as well as having had patients cared for by the hospitalist division in the preceding year (2004). There was no preference given to any physicians, including physicians well‐known by the research team or more frequent users of the hospitalist division.
Instrument
To develop our questionnaire, we conducted a detailed literature search to identify issues surrounding hospitalist‐PCP communication in the adult and pediatric hospitalist literature. Search terms included: hospitalists, interprofessional relations, patient discharge, communication, follow‐up care, transitions, and primary care provider using the PubMed database, limited to English language articles from 1990 to 2005. The 6 issues for the final questionnaire were identified from published hospitalist survey questions (in both adult and pediatric literature) and published articles addressing themes regarding hospitalist and PCP attitudes (specifically in regard to the communication process).1, 2, 4, 6 These 6 issues (quality of communication, barriers to communication, methods of information sharing, key data element requirements, critical timing, and perceived benefits) were incorporated into the open‐ended and closed‐ended questionnaire (Table 1). The original draft of the questionnaire was pretested on 2 hospitalists and 3 PCPs by L.H., who has graduate level formal training and experience in the design, refinement, implementation, and evaluation of questionnaires.
| Questions |
|---|
| 1. Do you use the hospitalist system at PCMC? yes/no |
| 1a. If yes: For what % of your patients that are hospitalized do you use the hospitalist system? |
| 2. How would you rate the quality of communications between hospitalists and Primary Care Providers? |
| a: excellent; b: very good; c: good; d: fair; e: poor. |
| 2a. Why did you give it that rating? |
| 3. What barriers, if any, have you experienced in communicating with hospitalists/Primary Care Providers? |
| 4. What communication methods have been effective in the past? What suggestions do you have for improving communication methods? |
| 5. What information would you like to receive from hospitalists/Primary Care Providers regarding your patients' hospital care? |
| 6. At what points in the care process would you like to receive communications from hospitalists/Primary Care Providers? |
| 7. What suggestions do you have for improving overall communications between hospitalists and Primary Care Providers? |
| 8. Do you have access to e‐mail and use it regularly in your practice? |
| 8a. Do you have access to a fax machine and use it regularly in your practice? |
| 8b. Do you have access to a telephone and use it regularly in your practice? |
| 8c. Considering e‐mail, fax, and telephone, which of these methods do you think would be the most effective for communicating with hospitalists/Primary Care Providers? |
| 9. Do you believe that improving communications between hospitalists and Primary Care Providers would improve the quality of patient care? |
| 9a. If yes: How? |
| 9b. If no: Why not? |
| 10. Any other comments/feedback? |
Data Collection/Analysis
After consent, participants were administered the phone questionnaire by L.H. during April, May, and June 2005. Interviews were transcribed verbatim into a Microsoft Word document by a trained transcriptionist. Responses were openly coded and then grouped into the respective main topics of interest. No further interviews were conducted when theoretical saturation was obtained (ie, respondents did not identify any new themes). Themes were compared using qualitative methods.7, 8
RESULTS
Only 1 physician per practice was interviewed. No PCP who was able to be contacted declined an interview, although some did require multiple phone attempts to schedule the interview. PCPs were located in Salt Lake County (n = 6), in other Utah counties (n = 3), and in surrounding Intermountain West states (n = 3). From January 1, 2004 to December 31, 2004, we estimate that the hospitalist division cared for patients from approximately 35 practices (50% in Salt Lake County, 30% in other Utah counties, and 20% in surrounding Intermountain West states).
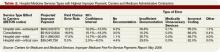
Hospitalists and PCPs agreed that overall quality of communication ranged from poor to very good (Table 2). Both parties acknowledged that significant barriers to optimal communication exist, yet the barriers differed for each group. Hospitalists and PCPs also agreed that optimal communication could improve many aspects of patient care and should take place upon discharge and admission of patients and with major clinical changes. Both hospitalists and PCPs also wanted accurate and timely information. One priority that the participants emphasized is the timely transfer of admission notification and the receipt of accurate and timely discharge summaries by PCPs.
| Hospitalists | Primary Care Providers | |
|---|---|---|
| Quality of communication | ||
| Poor | 0% | 33% |
| Fair | 50% | 17% |
| Good | 40% | 8% |
| Very good | 10% | 42% |
| Excellent | 0% | 0% |
| Barriers to communication | Lack of PCP directory; | Not knowing name and contact information of hospitalist taking care of their patient; |
| Lack of access to patients' medication or problem list; | Teaching hospital with numerous residents and students | |
| Lack of standardized system | ||
| Methods of information sharing | Electronic medical record ideal for sharing information | Electronic medical record ideal for sharing information; |
| Phone calls and faxes effective, especially if pager numbers were included | ||
| Key data elements | Diagnoses; | Diagnoses; |
| Medications; | Medications; | |
| Follow‐up plans | Follow‐up plans | |
| Critical timing | At discharge; | At discharge; |
| After admission; | After admission; | |
| Major clinical changes | Major clinical changes | |
| Perceived benefits | Improved patient satisfaction; | Improved patient satisfaction; |
| Improved follow‐up; | Improved follow‐up; | |
| Decreased medication errors; | Decreased medication errors; | |
| Increased efficiency | Increased efficiency |
Quality of Communication
Overall, both groups rated communication quality from poor to very good (Table 2). Notably, no hospitalists or PCPs rated overall quality as excellent, but 33% of PCPs rated it as poor compared to 0% of the hospitalists. Fifty‐eight percent (7/12) of PCPs used the hospitalists for 80% of their admissions to the hospital.
For hospitalists, lack of communication stemmed from busy schedules, not knowing who the PCP was, or not having the PCP contact information. Similarly, PCPs commented that they often found out their patient was admitted to the hospital only when the patient showed up in their office for a follow‐up visit. Both hospitalists and PCPs felt it was the hospitalist's job to inform and update PCPs on their patient's status while hospitalized. However, if the patient was admitted via the emergency department (ED), hospitalists felt that it was the ED's responsibility to inform the PCPs of their patients' admission.
Barriers to Communication
PCPs and hospitalists noted different barriers to optimal communication. Hospitalists identified the lack of a PCP directory, the lack of access to patients' medication and problem lists, and the lack of a standardized system to communicate with PCPs as major barriers. The delayed receipt of the discharge summary by PCPs was also viewed as a barrier by hospitalists. Pediatric hospitalists found the large variation in PCP availability as well as the variation in PCP preferred methods of communication (phone call, fax, or e‐mail) to be additional barriers. PCPs, on the other hand, struggled with the complexity of the hospital system. The fact that PCMC is a teaching hospital with numerous residents and students assisting in their patients' care, as well as not knowing the names and contact information of the hospitalists taking care of their patients, served as barriers to optimal communication. Additionally, PCPs noted the delay in receiving discharge summaries as a barrier and a source of frustration.
Methods of Information Sharing
All PCPs and hospitalists had access to telephones and faxes and used them regularly in their practices (100% for both groups). A majority of PCPs believed phone calls and faxes were effective means of information sharing, especially if pager numbers of the hospitalists were included. Some PCPs and a larger number of hospitalists thought an electronic medical record was an ideal tool for sharing information. However, PCPs appeared to have a lower rate of e‐mail access and usage compared with hospitalists.
Key Data Elements
There was agreement among PCPs and hospitalists regarding which data elements were important to be relayed among providers. PCPs and hospitalists were most interested in the following data elements upon patient discharge: diagnoses from the hospitalization, medications the patient was to take, and follow‐up plans for the patient. Hospitalists also thought PCPs could help by providing a list of current medications and a detailed past medical and social history upon admission. This information could be easily provided to the accepting hospitalist attending by phone or fax from the PCP.
Critical Timing and Perceived Benefits
Hospitalists and PCPs agreed that the most critical times for optimal hospitalist‐PCP communication were primarily at time of discharge from the hospital, after admission to the hospital, and when major clinical changes occurred. The majority of hospitalists and PCPs thought that improved communication would improve the quality of patient care through: (1) improved patient satisfaction; (2) improved quality and quantity of follow‐up; (3) decreased medication errors; and (4) increased efficiency for the PCPs and hospitalists.
DISCUSSION
Both pediatric hospitalists and PCPs agree on what information is important to transmit (diagnoses, medications, follow‐up needs, and pending laboratory test results) and critical times for communication during the hospitalization (at discharge, admission, and during major clinical changes). However, there was discrepancy in the barriers to optimal communication for each group. Identifying and addressing these barriers can help both hospitalists and PCPs implement targeted interventions aimed at improving communication. As the number of pediatric hospitalist programs increases, the risk for hospitalist‐PCP communication breakdowns, which can have a negative impact on patient care, also increases.
Previous adult studies describe the scope of the problem around poor communication between hospitalists and PCPs.1, 912 Kripalani et al.10 reported recently that delays and omissions in communication are common at hospital discharge among adult hospitalists and that computer‐generated summaries, educational interventions, and standardized formats may facilitate more timely transfer of pertinent information. However, there is limited data on pediatric hospitalist‐PCP communication. Srivastava et al.5 found that 60% of community physicians thought hospitalist systems may impair communication with PCPs when evaluating community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.
PCPs can feel left out when their patients are cared for by hospitalists.13 One PCP in our study commented: Include the referral doc as part of the team. We're the ones who will take care of them after discharge. It seems like an autonomous thing down there and we're excluded from the patient care team. Additionally, patients want their PCPs to remain involved in their care as they transition into and out of the hospital setting.1, 13
The continuity visit model has been proposed by Wachter and Pantilat14 to describe a clinical encounter between the primary physician and hospitalized patient, when the patient has a different physician of record. In this model, the PCP can endorse the hospitalist model and the individual hospitalist, notice subtle findings that differ from the patient's baseline, and help clarify patient preferences regarding difficult situations by drawing on their previous relationship with the patient. This visit may also benefit the PCP by providing insights into the patient's illness, personality, or social support that he or she was unaware of previously. However, in order for the continuity visit to exist, the PCP has to be informed of their patient's admission in the first place. Ethical dilemmas also have been raised regarding who bears primary responsibility for maintaining open lines of communication when patients are hospitalized.15 Lo15 advocates that PCPs can and should be involved in meaningful ways in the inpatient care of their patients even when they are not acting as the treating physicians. Specifically, he suggests that PCPs personally visit particularly ill patients or those with difficult diagnoses and use frequent phone calls to all admitted patients.
Beyond telephone calls and continuity visits, hospitalists and PCPs rely on discharge summaries as a key part of the information transfer about a patient's hospitalization.1, 16, 17 These documents are rendered useless if they are inaccurate, illegible, or not delivered in a timely manner.18 In a study of California family physicians, discharge summaries were thought to be too detailed by 84% of PCPs, and reportedly arrived before the patient's first follow‐up appointment only 33% of the time.1 O'Leary et al.19 found that 41% of the Department of Medicine physicians surveyed believed that at least 1 of their patients hospitalized in the previous 6 months had experienced a preventable adverse event related to poor transfer of information at discharge. In our study, PCPs noted that discharge summaries often arrived in their offices well after the patient had been seen for their follow‐up appointment.
Both hospitalists and PCPs agree that a concise and precise discharge summary should include an overview of the hospitalization with important details highlighted. Similar to the findings of Pantilat et al.,1 in our study PCPs specifically want detailed information with regard to diagnoses, discharge medications, and what to expect when they see the patient in their clinic. Follow‐up phone calls to PCPs to see that they received written information and if they require further details is 1 solution to ensuring good follow‐up, yet this adds to the burden of communication and could be an additional barrier.
The teaching institutions in which physicians train also pose unique obstacles to optimal communication. In academic medical centers, medical students and residents perform a majority of the discharge duties (eg, writing prescriptions, dictating discharge summaries, making follow‐up appointments, and calling PCPs), and teaching these trainees the importance of timely and accurate communication becomes an added challenge. Educators have to find novel ways of providing incentives to residents and medical students to get them to effectively participate in this process. Plauth et al.20 reports that hospitalists feel they needed better training in residency around communicating, noting a meaningful underemphasis during residency training in regard to communication with referring physicians. These skills should be taught in medical school and supported by both hospitalists and PCPs throughout residency training.
Both hospitalists and PCPs also want easy and reliable ways to access their colleagues, which ideally would be automatic. One PCP commented: a weekly or semiweekly phone call would be nice. Another suggested to: fax a short note. One hospitalist acknowledged: a systematic approach would be betterwhether a fax or telephone call and make sure there is a way of checking to make sure the communication has happened. Another hospitalist simply remarked: it needs to be done on every patient.
Thus, it seems an improved communication system should be flexible enough to accommodate unique provider preferences, such as communication via phone, fax, or e‐mail. This is demonstrated by 1 PCP who preferred the phone, but most convenient is the periodic fax updates. I don't have to be taken away from seeing patients.
Lo15 calls for a standard to be established for delivering care within the patient‐PCP‐hospitalist triad. Phone calls and faxes are 2 readily available methods of communication. However, the frequent back‐and‐forth of missed calls, unreturned calls, and days‐off is certainly a factor in determining efficiency and effectiveness of phone calls.
E‐mail, if it is widely used by all participants, may be an effective option for delivery that could provide confirmation of receipt. However, the lack of universal e‐mail usage by all providers remains a barrier. Questions as to which method is more time consuming and for whom, need to be studied further. Patient confidentiality also requires that this protected health information arrive in the proper hands. Personal relationships can also contribute to successful communication. One provider may be more likely to contact another if they know each other through some personal connection, such as medical school, residency, or a social group.
Our study has several limitations. The sample size was small. We obtained responses from a sample of key stakeholders in the hospitalist‐PCP communication process. We were limited by the number of hospitalists at our institution as well as the interest and availability of PCPs to respond. We are unable to determine the total number of patients by respondent PCP practice cared for by the hospitalist division. This could influence the results depending on whether the respondent PCP was a frequent or infrequent utilizer of the hospitalist system. However, we feel reassured that we are not missing important information, because in our methods, a priori, we had intended to stop interviewing PCPs once theoretical saturation had been reached (ie, respondents did not identify any new information). In our study, that occurred with 12 PCPs.
We attempted to interview a single physician in a number of different practice settings in order to gain insight into the perceptions of that individual as well as those of their partners. The views expressed by these individuals may not represent the views of hospitalists and PCPs outside of our practice area. Furthermore, PCMC serves as both a community pediatric hospital and a tertiary‐referral center for a large area, yet the current experience of 1 hospitalist division and 1 cohort of referring PCPs may contain regional variation that contributed bias to the responses.
Selection bias may have been introduced in our study by the inherent nature of phone interviews. We interviewed only providers with previous communication experience with our hospitalist division. These providers may have had a vested interest in the communication process. We did not interview those PCPs who did not have any communication with our hospitalist division or those who may have used the hospitalist division previously and decided to no longer use the division. Interviewing these groups may have provided additional insight into the communication issues mentioned here. Additionally, useful information could have been gleaned from trying to find out more from the 33% of PCPs who felt communication was poor. We anticipate further studies exploring this issue in more depth.
Future Directions
As a result of this study, we have implemented several interventions to improve information sharing between hospitalists and PCPs, including: 1) we updated current contact information (including names of physicians, office addresses, phone numbers, fax numbers, and e‐mail addresses) for all PCPs in our catchment area along with their preferred methods of communication; 2) we worked with the transcription services to automatically add PCP addresses, phone numbers, and fax numbers to dictated notes, eliminating time wasted searching for contact information; and 3) we standardized key data elements in admission history and physicals and discharge notes to increase the efficiency of the communication process.
Furthermore, we have implemented a standardized system to facilitate communication with PCPs. This system includes an automated process to notify PCPs of their patient's hospital admission, including the admission date, preliminary diagnoses, and responsible physician's contact information. We are currently undertaking a quality improvement project aimed at achieving timely transfer of discharge information to PCPs, including medications, follow‐up appointments, and a succinct hospital summary. Finally, establishing an evaluation process to monitor both successes and failures will be paramount to any interventions.
CONCLUSIONS
Hospitalists and PCPs agree that overall quality of communication ranges from poor to very good. Both PCPs and pediatric hospitalists acknowledge that significant barriers to optimal communication exist, yet the barriers differ for each group. They also agree that optimal communication would improve many aspects of patient care and should take place upon discharge and admission of patients and with major clinical changes.
Pediatric hospitalists and PCPs identified issues around optimal communication similar to those noted in the adult hospital medicine literature. Interventions to improve pediatric hospitalist‐PCP communication should at least address these 6 issues: (1) quality of communication; (2) barriers to communication; (3) methods of information sharing; (4) key data element requirements; (5) critical timing; and (6) perceived benefits. Such interventions will likely improve hospitalist‐PCP communication and potentially improve the quality of patient care. However, future studies will need to demonstrate the link between improved hospitalist‐PCP communication and improved patient care and outcomes.
Acknowledgements
The authors are indebted to Flory Nkoy, MD, MPH, MS, for his help in manuscript preparation and critical review.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,,,.Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey.Am J Med.2000;109(8):648–653.
- ,,,,,.Pediatric hospitalists: what do we know, and where do we go from here?Ambul Pediatr.2001;1(6):340–345.
- ,,.Physician views on caring for hospitalized patients and the hospitalist model of inpatient care.J Gen Intern Med.2001;16(2):116–119.
- ,,,,,.Community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.Pediatrics.2005;115(1):34–38.
- ,.The patient provider relationship and the hospitalist movement. Introduction.Dis Mon.2002;48(4):189–190.
- ,.Rigour and qualitative research.BMJ.1995;311(6997):109–112.
- ,.Needs assessment in post graduate medical education: a review.Med Educ Online.2001;7:1–8.
- ,,,.How physicians perceive hospitalist services after implementation: anticipation vs reality.Arch Intern Med.2003;163(19):2330–2336.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- ,,.Generalist‐subspecialist communication for children with chronic conditions: a regional physician survey.Pediatrics.2003;112(6 Pt 1):1314–1320.
- ,,,,,.Communication breakdown in the outpatient referral process.J Gen Intern Med.2000;15(9):626–631.
- ,,.How do patients view the role of the primary care physician in inpatient care?Dis Mon.2002;48(4):230–238.
- ,.The “continuity visit” and the hospitalist model of care.Dis Mon.2002;48(4):267–272.
- .Ethical and policy implications of hospitalist systems.Dis Mon.2002;48(4):281–290.
- ,,, et al.From a paper‐based transmission of discharge summaries to electronic communication in health care regions.Int J Med Inform.2006;75(3‐4):209–215.
- ,,.Tying up loose ends: discharging patients with unresolved medical issues.Arch Intern Med.2007;167(12):1305–1311.
- ,.Improving communication between hospital and community physicians. Feasibility study of a handwritten, faxed hospital discharge summary. Discharge Summary Study Group.Can Fam Physician.1999;45:2893–2899.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
Hospitalist systems focus on providing acute treatments to patients and expediting hospital discharge, sometimes without regard for the need to work in concert with community providers, leading to fragmentation of care.1 This fragmentation, particularly at the transitions of care, such as when patients move from the outpatient setting to a hospitalist system and then back to their primary care providers (PCPs), can lead to communication breakdowns and delays in care, and may compromise patient outcomes.2 Suboptimal treatments, such as medication errors and the ordering of redundant tests can occur in either setting if prior treatment information is not relayed in a timely and accurate fashion. Landrigan et al.3 described a conceptual model in 2001 that recognized the complexity of the hospitalist‐PCP communication system. Specifically, optimal care of hospitalized children includes PCPs, family members, hospitalists, and support staff while meeting the communication needs of families and PCPs. Additionally, mediating a smooth transition into and out of the hospital needs to be measured carefully.3
Previous adult studies have reported that hospitalist systems sometimes create discontinuity of patient care, which can have a negative impact on the quality of care provided to patients if there is poor communication between hospitalists and PCPs.2, 4, 5 Existing research on hospitalist‐PCP communication focuses mainly on adult hospitalist models with little known about the quality of current pediatric hospitalist‐PCP communication.
The objective of this study was to qualitatively explore issues around communication between pediatric hospitalists and PCPs. Specifically, we sought to explore the quality of communication practices and barriers to optimal communication within the hospitalist‐PCP model at a tertiary care children's hospital. The results are serving as a needs assessment to guide the design of a quality improvement project with the aim of improving pediatric hospitalist‐PCP communication.
METHODS
Study Design
Phone interviews of pediatric hospitalists and PCPs were conducted. The study was approved by the University of Utah and Primary Children's Medical Center (PCMC) Institutional Review Boards.
Setting
PCMC is a 232‐bed, tertiary‐care referral center and community hospital in Salt Lake City, UT, which serves a catchment area of approximately 1,000,000 children in 5 Intermountain West states (Utah, Idaho, Nevada, Montana, and Wyoming). In 2005, there were more than 40,000 emergency department visits and more than 11,000 hospital admissions. At the time of this study, the Division of Pediatric Inpatient Medicine (hospitalist division) included 11 full‐time equivalents. All hospitalists play a teaching role and are on faculty at the University of Utah School of Medicine. In 2005, approximately 45% of medical inpatients at PCMC were cared for by the hospitalist division, with approximately 95% cared for by resident teams.
Participants
Ten University of Utah pediatric hospitalists and 12 PCPs within our catchment area completed interviews. Verbal consent was given before study participants began the phone interview. All hospitalists from the hospitalist division, excluding the first author, completed an interview. PCPs who had referred patients to the hospitalist division in the year preceding this study (2004) were identified through a referring database kept by the hospitalist division. An attempt was made to interview physicians in multiple practice settings and geographic locations.
Inclusion criteria for PCPs included their willingness to complete the interview as well as having had patients cared for by the hospitalist division in the preceding year (2004). There was no preference given to any physicians, including physicians well‐known by the research team or more frequent users of the hospitalist division.
Instrument
To develop our questionnaire, we conducted a detailed literature search to identify issues surrounding hospitalist‐PCP communication in the adult and pediatric hospitalist literature. Search terms included: hospitalists, interprofessional relations, patient discharge, communication, follow‐up care, transitions, and primary care provider using the PubMed database, limited to English language articles from 1990 to 2005. The 6 issues for the final questionnaire were identified from published hospitalist survey questions (in both adult and pediatric literature) and published articles addressing themes regarding hospitalist and PCP attitudes (specifically in regard to the communication process).1, 2, 4, 6 These 6 issues (quality of communication, barriers to communication, methods of information sharing, key data element requirements, critical timing, and perceived benefits) were incorporated into the open‐ended and closed‐ended questionnaire (Table 1). The original draft of the questionnaire was pretested on 2 hospitalists and 3 PCPs by L.H., who has graduate level formal training and experience in the design, refinement, implementation, and evaluation of questionnaires.
| Questions |
|---|
| 1. Do you use the hospitalist system at PCMC? yes/no |
| 1a. If yes: For what % of your patients that are hospitalized do you use the hospitalist system? |
| 2. How would you rate the quality of communications between hospitalists and Primary Care Providers? |
| a: excellent; b: very good; c: good; d: fair; e: poor. |
| 2a. Why did you give it that rating? |
| 3. What barriers, if any, have you experienced in communicating with hospitalists/Primary Care Providers? |
| 4. What communication methods have been effective in the past? What suggestions do you have for improving communication methods? |
| 5. What information would you like to receive from hospitalists/Primary Care Providers regarding your patients' hospital care? |
| 6. At what points in the care process would you like to receive communications from hospitalists/Primary Care Providers? |
| 7. What suggestions do you have for improving overall communications between hospitalists and Primary Care Providers? |
| 8. Do you have access to e‐mail and use it regularly in your practice? |
| 8a. Do you have access to a fax machine and use it regularly in your practice? |
| 8b. Do you have access to a telephone and use it regularly in your practice? |
| 8c. Considering e‐mail, fax, and telephone, which of these methods do you think would be the most effective for communicating with hospitalists/Primary Care Providers? |
| 9. Do you believe that improving communications between hospitalists and Primary Care Providers would improve the quality of patient care? |
| 9a. If yes: How? |
| 9b. If no: Why not? |
| 10. Any other comments/feedback? |
Data Collection/Analysis
After consent, participants were administered the phone questionnaire by L.H. during April, May, and June 2005. Interviews were transcribed verbatim into a Microsoft Word document by a trained transcriptionist. Responses were openly coded and then grouped into the respective main topics of interest. No further interviews were conducted when theoretical saturation was obtained (ie, respondents did not identify any new themes). Themes were compared using qualitative methods.7, 8
RESULTS
Only 1 physician per practice was interviewed. No PCP who was able to be contacted declined an interview, although some did require multiple phone attempts to schedule the interview. PCPs were located in Salt Lake County (n = 6), in other Utah counties (n = 3), and in surrounding Intermountain West states (n = 3). From January 1, 2004 to December 31, 2004, we estimate that the hospitalist division cared for patients from approximately 35 practices (50% in Salt Lake County, 30% in other Utah counties, and 20% in surrounding Intermountain West states).
Hospitalists and PCPs agreed that overall quality of communication ranged from poor to very good (Table 2). Both parties acknowledged that significant barriers to optimal communication exist, yet the barriers differed for each group. Hospitalists and PCPs also agreed that optimal communication could improve many aspects of patient care and should take place upon discharge and admission of patients and with major clinical changes. Both hospitalists and PCPs also wanted accurate and timely information. One priority that the participants emphasized is the timely transfer of admission notification and the receipt of accurate and timely discharge summaries by PCPs.
| Hospitalists | Primary Care Providers | |
|---|---|---|
| Quality of communication | ||
| Poor | 0% | 33% |
| Fair | 50% | 17% |
| Good | 40% | 8% |
| Very good | 10% | 42% |
| Excellent | 0% | 0% |
| Barriers to communication | Lack of PCP directory; | Not knowing name and contact information of hospitalist taking care of their patient; |
| Lack of access to patients' medication or problem list; | Teaching hospital with numerous residents and students | |
| Lack of standardized system | ||
| Methods of information sharing | Electronic medical record ideal for sharing information | Electronic medical record ideal for sharing information; |
| Phone calls and faxes effective, especially if pager numbers were included | ||
| Key data elements | Diagnoses; | Diagnoses; |
| Medications; | Medications; | |
| Follow‐up plans | Follow‐up plans | |
| Critical timing | At discharge; | At discharge; |
| After admission; | After admission; | |
| Major clinical changes | Major clinical changes | |
| Perceived benefits | Improved patient satisfaction; | Improved patient satisfaction; |
| Improved follow‐up; | Improved follow‐up; | |
| Decreased medication errors; | Decreased medication errors; | |
| Increased efficiency | Increased efficiency |
Quality of Communication
Overall, both groups rated communication quality from poor to very good (Table 2). Notably, no hospitalists or PCPs rated overall quality as excellent, but 33% of PCPs rated it as poor compared to 0% of the hospitalists. Fifty‐eight percent (7/12) of PCPs used the hospitalists for 80% of their admissions to the hospital.
For hospitalists, lack of communication stemmed from busy schedules, not knowing who the PCP was, or not having the PCP contact information. Similarly, PCPs commented that they often found out their patient was admitted to the hospital only when the patient showed up in their office for a follow‐up visit. Both hospitalists and PCPs felt it was the hospitalist's job to inform and update PCPs on their patient's status while hospitalized. However, if the patient was admitted via the emergency department (ED), hospitalists felt that it was the ED's responsibility to inform the PCPs of their patients' admission.
Barriers to Communication
PCPs and hospitalists noted different barriers to optimal communication. Hospitalists identified the lack of a PCP directory, the lack of access to patients' medication and problem lists, and the lack of a standardized system to communicate with PCPs as major barriers. The delayed receipt of the discharge summary by PCPs was also viewed as a barrier by hospitalists. Pediatric hospitalists found the large variation in PCP availability as well as the variation in PCP preferred methods of communication (phone call, fax, or e‐mail) to be additional barriers. PCPs, on the other hand, struggled with the complexity of the hospital system. The fact that PCMC is a teaching hospital with numerous residents and students assisting in their patients' care, as well as not knowing the names and contact information of the hospitalists taking care of their patients, served as barriers to optimal communication. Additionally, PCPs noted the delay in receiving discharge summaries as a barrier and a source of frustration.
Methods of Information Sharing
All PCPs and hospitalists had access to telephones and faxes and used them regularly in their practices (100% for both groups). A majority of PCPs believed phone calls and faxes were effective means of information sharing, especially if pager numbers of the hospitalists were included. Some PCPs and a larger number of hospitalists thought an electronic medical record was an ideal tool for sharing information. However, PCPs appeared to have a lower rate of e‐mail access and usage compared with hospitalists.
Key Data Elements
There was agreement among PCPs and hospitalists regarding which data elements were important to be relayed among providers. PCPs and hospitalists were most interested in the following data elements upon patient discharge: diagnoses from the hospitalization, medications the patient was to take, and follow‐up plans for the patient. Hospitalists also thought PCPs could help by providing a list of current medications and a detailed past medical and social history upon admission. This information could be easily provided to the accepting hospitalist attending by phone or fax from the PCP.
Critical Timing and Perceived Benefits
Hospitalists and PCPs agreed that the most critical times for optimal hospitalist‐PCP communication were primarily at time of discharge from the hospital, after admission to the hospital, and when major clinical changes occurred. The majority of hospitalists and PCPs thought that improved communication would improve the quality of patient care through: (1) improved patient satisfaction; (2) improved quality and quantity of follow‐up; (3) decreased medication errors; and (4) increased efficiency for the PCPs and hospitalists.
DISCUSSION
Both pediatric hospitalists and PCPs agree on what information is important to transmit (diagnoses, medications, follow‐up needs, and pending laboratory test results) and critical times for communication during the hospitalization (at discharge, admission, and during major clinical changes). However, there was discrepancy in the barriers to optimal communication for each group. Identifying and addressing these barriers can help both hospitalists and PCPs implement targeted interventions aimed at improving communication. As the number of pediatric hospitalist programs increases, the risk for hospitalist‐PCP communication breakdowns, which can have a negative impact on patient care, also increases.
Previous adult studies describe the scope of the problem around poor communication between hospitalists and PCPs.1, 912 Kripalani et al.10 reported recently that delays and omissions in communication are common at hospital discharge among adult hospitalists and that computer‐generated summaries, educational interventions, and standardized formats may facilitate more timely transfer of pertinent information. However, there is limited data on pediatric hospitalist‐PCP communication. Srivastava et al.5 found that 60% of community physicians thought hospitalist systems may impair communication with PCPs when evaluating community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.
PCPs can feel left out when their patients are cared for by hospitalists.13 One PCP in our study commented: Include the referral doc as part of the team. We're the ones who will take care of them after discharge. It seems like an autonomous thing down there and we're excluded from the patient care team. Additionally, patients want their PCPs to remain involved in their care as they transition into and out of the hospital setting.1, 13
The continuity visit model has been proposed by Wachter and Pantilat14 to describe a clinical encounter between the primary physician and hospitalized patient, when the patient has a different physician of record. In this model, the PCP can endorse the hospitalist model and the individual hospitalist, notice subtle findings that differ from the patient's baseline, and help clarify patient preferences regarding difficult situations by drawing on their previous relationship with the patient. This visit may also benefit the PCP by providing insights into the patient's illness, personality, or social support that he or she was unaware of previously. However, in order for the continuity visit to exist, the PCP has to be informed of their patient's admission in the first place. Ethical dilemmas also have been raised regarding who bears primary responsibility for maintaining open lines of communication when patients are hospitalized.15 Lo15 advocates that PCPs can and should be involved in meaningful ways in the inpatient care of their patients even when they are not acting as the treating physicians. Specifically, he suggests that PCPs personally visit particularly ill patients or those with difficult diagnoses and use frequent phone calls to all admitted patients.
Beyond telephone calls and continuity visits, hospitalists and PCPs rely on discharge summaries as a key part of the information transfer about a patient's hospitalization.1, 16, 17 These documents are rendered useless if they are inaccurate, illegible, or not delivered in a timely manner.18 In a study of California family physicians, discharge summaries were thought to be too detailed by 84% of PCPs, and reportedly arrived before the patient's first follow‐up appointment only 33% of the time.1 O'Leary et al.19 found that 41% of the Department of Medicine physicians surveyed believed that at least 1 of their patients hospitalized in the previous 6 months had experienced a preventable adverse event related to poor transfer of information at discharge. In our study, PCPs noted that discharge summaries often arrived in their offices well after the patient had been seen for their follow‐up appointment.
Both hospitalists and PCPs agree that a concise and precise discharge summary should include an overview of the hospitalization with important details highlighted. Similar to the findings of Pantilat et al.,1 in our study PCPs specifically want detailed information with regard to diagnoses, discharge medications, and what to expect when they see the patient in their clinic. Follow‐up phone calls to PCPs to see that they received written information and if they require further details is 1 solution to ensuring good follow‐up, yet this adds to the burden of communication and could be an additional barrier.
The teaching institutions in which physicians train also pose unique obstacles to optimal communication. In academic medical centers, medical students and residents perform a majority of the discharge duties (eg, writing prescriptions, dictating discharge summaries, making follow‐up appointments, and calling PCPs), and teaching these trainees the importance of timely and accurate communication becomes an added challenge. Educators have to find novel ways of providing incentives to residents and medical students to get them to effectively participate in this process. Plauth et al.20 reports that hospitalists feel they needed better training in residency around communicating, noting a meaningful underemphasis during residency training in regard to communication with referring physicians. These skills should be taught in medical school and supported by both hospitalists and PCPs throughout residency training.
Both hospitalists and PCPs also want easy and reliable ways to access their colleagues, which ideally would be automatic. One PCP commented: a weekly or semiweekly phone call would be nice. Another suggested to: fax a short note. One hospitalist acknowledged: a systematic approach would be betterwhether a fax or telephone call and make sure there is a way of checking to make sure the communication has happened. Another hospitalist simply remarked: it needs to be done on every patient.
Thus, it seems an improved communication system should be flexible enough to accommodate unique provider preferences, such as communication via phone, fax, or e‐mail. This is demonstrated by 1 PCP who preferred the phone, but most convenient is the periodic fax updates. I don't have to be taken away from seeing patients.
Lo15 calls for a standard to be established for delivering care within the patient‐PCP‐hospitalist triad. Phone calls and faxes are 2 readily available methods of communication. However, the frequent back‐and‐forth of missed calls, unreturned calls, and days‐off is certainly a factor in determining efficiency and effectiveness of phone calls.
E‐mail, if it is widely used by all participants, may be an effective option for delivery that could provide confirmation of receipt. However, the lack of universal e‐mail usage by all providers remains a barrier. Questions as to which method is more time consuming and for whom, need to be studied further. Patient confidentiality also requires that this protected health information arrive in the proper hands. Personal relationships can also contribute to successful communication. One provider may be more likely to contact another if they know each other through some personal connection, such as medical school, residency, or a social group.
Our study has several limitations. The sample size was small. We obtained responses from a sample of key stakeholders in the hospitalist‐PCP communication process. We were limited by the number of hospitalists at our institution as well as the interest and availability of PCPs to respond. We are unable to determine the total number of patients by respondent PCP practice cared for by the hospitalist division. This could influence the results depending on whether the respondent PCP was a frequent or infrequent utilizer of the hospitalist system. However, we feel reassured that we are not missing important information, because in our methods, a priori, we had intended to stop interviewing PCPs once theoretical saturation had been reached (ie, respondents did not identify any new information). In our study, that occurred with 12 PCPs.
We attempted to interview a single physician in a number of different practice settings in order to gain insight into the perceptions of that individual as well as those of their partners. The views expressed by these individuals may not represent the views of hospitalists and PCPs outside of our practice area. Furthermore, PCMC serves as both a community pediatric hospital and a tertiary‐referral center for a large area, yet the current experience of 1 hospitalist division and 1 cohort of referring PCPs may contain regional variation that contributed bias to the responses.
Selection bias may have been introduced in our study by the inherent nature of phone interviews. We interviewed only providers with previous communication experience with our hospitalist division. These providers may have had a vested interest in the communication process. We did not interview those PCPs who did not have any communication with our hospitalist division or those who may have used the hospitalist division previously and decided to no longer use the division. Interviewing these groups may have provided additional insight into the communication issues mentioned here. Additionally, useful information could have been gleaned from trying to find out more from the 33% of PCPs who felt communication was poor. We anticipate further studies exploring this issue in more depth.
Future Directions
As a result of this study, we have implemented several interventions to improve information sharing between hospitalists and PCPs, including: 1) we updated current contact information (including names of physicians, office addresses, phone numbers, fax numbers, and e‐mail addresses) for all PCPs in our catchment area along with their preferred methods of communication; 2) we worked with the transcription services to automatically add PCP addresses, phone numbers, and fax numbers to dictated notes, eliminating time wasted searching for contact information; and 3) we standardized key data elements in admission history and physicals and discharge notes to increase the efficiency of the communication process.
Furthermore, we have implemented a standardized system to facilitate communication with PCPs. This system includes an automated process to notify PCPs of their patient's hospital admission, including the admission date, preliminary diagnoses, and responsible physician's contact information. We are currently undertaking a quality improvement project aimed at achieving timely transfer of discharge information to PCPs, including medications, follow‐up appointments, and a succinct hospital summary. Finally, establishing an evaluation process to monitor both successes and failures will be paramount to any interventions.
CONCLUSIONS
Hospitalists and PCPs agree that overall quality of communication ranges from poor to very good. Both PCPs and pediatric hospitalists acknowledge that significant barriers to optimal communication exist, yet the barriers differ for each group. They also agree that optimal communication would improve many aspects of patient care and should take place upon discharge and admission of patients and with major clinical changes.
Pediatric hospitalists and PCPs identified issues around optimal communication similar to those noted in the adult hospital medicine literature. Interventions to improve pediatric hospitalist‐PCP communication should at least address these 6 issues: (1) quality of communication; (2) barriers to communication; (3) methods of information sharing; (4) key data element requirements; (5) critical timing; and (6) perceived benefits. Such interventions will likely improve hospitalist‐PCP communication and potentially improve the quality of patient care. However, future studies will need to demonstrate the link between improved hospitalist‐PCP communication and improved patient care and outcomes.
Acknowledgements
The authors are indebted to Flory Nkoy, MD, MPH, MS, for his help in manuscript preparation and critical review.
Hospitalist systems focus on providing acute treatments to patients and expediting hospital discharge, sometimes without regard for the need to work in concert with community providers, leading to fragmentation of care.1 This fragmentation, particularly at the transitions of care, such as when patients move from the outpatient setting to a hospitalist system and then back to their primary care providers (PCPs), can lead to communication breakdowns and delays in care, and may compromise patient outcomes.2 Suboptimal treatments, such as medication errors and the ordering of redundant tests can occur in either setting if prior treatment information is not relayed in a timely and accurate fashion. Landrigan et al.3 described a conceptual model in 2001 that recognized the complexity of the hospitalist‐PCP communication system. Specifically, optimal care of hospitalized children includes PCPs, family members, hospitalists, and support staff while meeting the communication needs of families and PCPs. Additionally, mediating a smooth transition into and out of the hospital needs to be measured carefully.3
Previous adult studies have reported that hospitalist systems sometimes create discontinuity of patient care, which can have a negative impact on the quality of care provided to patients if there is poor communication between hospitalists and PCPs.2, 4, 5 Existing research on hospitalist‐PCP communication focuses mainly on adult hospitalist models with little known about the quality of current pediatric hospitalist‐PCP communication.
The objective of this study was to qualitatively explore issues around communication between pediatric hospitalists and PCPs. Specifically, we sought to explore the quality of communication practices and barriers to optimal communication within the hospitalist‐PCP model at a tertiary care children's hospital. The results are serving as a needs assessment to guide the design of a quality improvement project with the aim of improving pediatric hospitalist‐PCP communication.
METHODS
Study Design
Phone interviews of pediatric hospitalists and PCPs were conducted. The study was approved by the University of Utah and Primary Children's Medical Center (PCMC) Institutional Review Boards.
Setting
PCMC is a 232‐bed, tertiary‐care referral center and community hospital in Salt Lake City, UT, which serves a catchment area of approximately 1,000,000 children in 5 Intermountain West states (Utah, Idaho, Nevada, Montana, and Wyoming). In 2005, there were more than 40,000 emergency department visits and more than 11,000 hospital admissions. At the time of this study, the Division of Pediatric Inpatient Medicine (hospitalist division) included 11 full‐time equivalents. All hospitalists play a teaching role and are on faculty at the University of Utah School of Medicine. In 2005, approximately 45% of medical inpatients at PCMC were cared for by the hospitalist division, with approximately 95% cared for by resident teams.
Participants
Ten University of Utah pediatric hospitalists and 12 PCPs within our catchment area completed interviews. Verbal consent was given before study participants began the phone interview. All hospitalists from the hospitalist division, excluding the first author, completed an interview. PCPs who had referred patients to the hospitalist division in the year preceding this study (2004) were identified through a referring database kept by the hospitalist division. An attempt was made to interview physicians in multiple practice settings and geographic locations.
Inclusion criteria for PCPs included their willingness to complete the interview as well as having had patients cared for by the hospitalist division in the preceding year (2004). There was no preference given to any physicians, including physicians well‐known by the research team or more frequent users of the hospitalist division.
Instrument
To develop our questionnaire, we conducted a detailed literature search to identify issues surrounding hospitalist‐PCP communication in the adult and pediatric hospitalist literature. Search terms included: hospitalists, interprofessional relations, patient discharge, communication, follow‐up care, transitions, and primary care provider using the PubMed database, limited to English language articles from 1990 to 2005. The 6 issues for the final questionnaire were identified from published hospitalist survey questions (in both adult and pediatric literature) and published articles addressing themes regarding hospitalist and PCP attitudes (specifically in regard to the communication process).1, 2, 4, 6 These 6 issues (quality of communication, barriers to communication, methods of information sharing, key data element requirements, critical timing, and perceived benefits) were incorporated into the open‐ended and closed‐ended questionnaire (Table 1). The original draft of the questionnaire was pretested on 2 hospitalists and 3 PCPs by L.H., who has graduate level formal training and experience in the design, refinement, implementation, and evaluation of questionnaires.
| Questions |
|---|
| 1. Do you use the hospitalist system at PCMC? yes/no |
| 1a. If yes: For what % of your patients that are hospitalized do you use the hospitalist system? |
| 2. How would you rate the quality of communications between hospitalists and Primary Care Providers? |
| a: excellent; b: very good; c: good; d: fair; e: poor. |
| 2a. Why did you give it that rating? |
| 3. What barriers, if any, have you experienced in communicating with hospitalists/Primary Care Providers? |
| 4. What communication methods have been effective in the past? What suggestions do you have for improving communication methods? |
| 5. What information would you like to receive from hospitalists/Primary Care Providers regarding your patients' hospital care? |
| 6. At what points in the care process would you like to receive communications from hospitalists/Primary Care Providers? |
| 7. What suggestions do you have for improving overall communications between hospitalists and Primary Care Providers? |
| 8. Do you have access to e‐mail and use it regularly in your practice? |
| 8a. Do you have access to a fax machine and use it regularly in your practice? |
| 8b. Do you have access to a telephone and use it regularly in your practice? |
| 8c. Considering e‐mail, fax, and telephone, which of these methods do you think would be the most effective for communicating with hospitalists/Primary Care Providers? |
| 9. Do you believe that improving communications between hospitalists and Primary Care Providers would improve the quality of patient care? |
| 9a. If yes: How? |
| 9b. If no: Why not? |
| 10. Any other comments/feedback? |
Data Collection/Analysis
After consent, participants were administered the phone questionnaire by L.H. during April, May, and June 2005. Interviews were transcribed verbatim into a Microsoft Word document by a trained transcriptionist. Responses were openly coded and then grouped into the respective main topics of interest. No further interviews were conducted when theoretical saturation was obtained (ie, respondents did not identify any new themes). Themes were compared using qualitative methods.7, 8
RESULTS
Only 1 physician per practice was interviewed. No PCP who was able to be contacted declined an interview, although some did require multiple phone attempts to schedule the interview. PCPs were located in Salt Lake County (n = 6), in other Utah counties (n = 3), and in surrounding Intermountain West states (n = 3). From January 1, 2004 to December 31, 2004, we estimate that the hospitalist division cared for patients from approximately 35 practices (50% in Salt Lake County, 30% in other Utah counties, and 20% in surrounding Intermountain West states).
Hospitalists and PCPs agreed that overall quality of communication ranged from poor to very good (Table 2). Both parties acknowledged that significant barriers to optimal communication exist, yet the barriers differed for each group. Hospitalists and PCPs also agreed that optimal communication could improve many aspects of patient care and should take place upon discharge and admission of patients and with major clinical changes. Both hospitalists and PCPs also wanted accurate and timely information. One priority that the participants emphasized is the timely transfer of admission notification and the receipt of accurate and timely discharge summaries by PCPs.
| Hospitalists | Primary Care Providers | |
|---|---|---|
| Quality of communication | ||
| Poor | 0% | 33% |
| Fair | 50% | 17% |
| Good | 40% | 8% |
| Very good | 10% | 42% |
| Excellent | 0% | 0% |
| Barriers to communication | Lack of PCP directory; | Not knowing name and contact information of hospitalist taking care of their patient; |
| Lack of access to patients' medication or problem list; | Teaching hospital with numerous residents and students | |
| Lack of standardized system | ||
| Methods of information sharing | Electronic medical record ideal for sharing information | Electronic medical record ideal for sharing information; |
| Phone calls and faxes effective, especially if pager numbers were included | ||
| Key data elements | Diagnoses; | Diagnoses; |
| Medications; | Medications; | |
| Follow‐up plans | Follow‐up plans | |
| Critical timing | At discharge; | At discharge; |
| After admission; | After admission; | |
| Major clinical changes | Major clinical changes | |
| Perceived benefits | Improved patient satisfaction; | Improved patient satisfaction; |
| Improved follow‐up; | Improved follow‐up; | |
| Decreased medication errors; | Decreased medication errors; | |
| Increased efficiency | Increased efficiency |
Quality of Communication
Overall, both groups rated communication quality from poor to very good (Table 2). Notably, no hospitalists or PCPs rated overall quality as excellent, but 33% of PCPs rated it as poor compared to 0% of the hospitalists. Fifty‐eight percent (7/12) of PCPs used the hospitalists for 80% of their admissions to the hospital.
For hospitalists, lack of communication stemmed from busy schedules, not knowing who the PCP was, or not having the PCP contact information. Similarly, PCPs commented that they often found out their patient was admitted to the hospital only when the patient showed up in their office for a follow‐up visit. Both hospitalists and PCPs felt it was the hospitalist's job to inform and update PCPs on their patient's status while hospitalized. However, if the patient was admitted via the emergency department (ED), hospitalists felt that it was the ED's responsibility to inform the PCPs of their patients' admission.
Barriers to Communication
PCPs and hospitalists noted different barriers to optimal communication. Hospitalists identified the lack of a PCP directory, the lack of access to patients' medication and problem lists, and the lack of a standardized system to communicate with PCPs as major barriers. The delayed receipt of the discharge summary by PCPs was also viewed as a barrier by hospitalists. Pediatric hospitalists found the large variation in PCP availability as well as the variation in PCP preferred methods of communication (phone call, fax, or e‐mail) to be additional barriers. PCPs, on the other hand, struggled with the complexity of the hospital system. The fact that PCMC is a teaching hospital with numerous residents and students assisting in their patients' care, as well as not knowing the names and contact information of the hospitalists taking care of their patients, served as barriers to optimal communication. Additionally, PCPs noted the delay in receiving discharge summaries as a barrier and a source of frustration.
Methods of Information Sharing
All PCPs and hospitalists had access to telephones and faxes and used them regularly in their practices (100% for both groups). A majority of PCPs believed phone calls and faxes were effective means of information sharing, especially if pager numbers of the hospitalists were included. Some PCPs and a larger number of hospitalists thought an electronic medical record was an ideal tool for sharing information. However, PCPs appeared to have a lower rate of e‐mail access and usage compared with hospitalists.
Key Data Elements
There was agreement among PCPs and hospitalists regarding which data elements were important to be relayed among providers. PCPs and hospitalists were most interested in the following data elements upon patient discharge: diagnoses from the hospitalization, medications the patient was to take, and follow‐up plans for the patient. Hospitalists also thought PCPs could help by providing a list of current medications and a detailed past medical and social history upon admission. This information could be easily provided to the accepting hospitalist attending by phone or fax from the PCP.
Critical Timing and Perceived Benefits
Hospitalists and PCPs agreed that the most critical times for optimal hospitalist‐PCP communication were primarily at time of discharge from the hospital, after admission to the hospital, and when major clinical changes occurred. The majority of hospitalists and PCPs thought that improved communication would improve the quality of patient care through: (1) improved patient satisfaction; (2) improved quality and quantity of follow‐up; (3) decreased medication errors; and (4) increased efficiency for the PCPs and hospitalists.
DISCUSSION
Both pediatric hospitalists and PCPs agree on what information is important to transmit (diagnoses, medications, follow‐up needs, and pending laboratory test results) and critical times for communication during the hospitalization (at discharge, admission, and during major clinical changes). However, there was discrepancy in the barriers to optimal communication for each group. Identifying and addressing these barriers can help both hospitalists and PCPs implement targeted interventions aimed at improving communication. As the number of pediatric hospitalist programs increases, the risk for hospitalist‐PCP communication breakdowns, which can have a negative impact on patient care, also increases.
Previous adult studies describe the scope of the problem around poor communication between hospitalists and PCPs.1, 912 Kripalani et al.10 reported recently that delays and omissions in communication are common at hospital discharge among adult hospitalists and that computer‐generated summaries, educational interventions, and standardized formats may facilitate more timely transfer of pertinent information. However, there is limited data on pediatric hospitalist‐PCP communication. Srivastava et al.5 found that 60% of community physicians thought hospitalist systems may impair communication with PCPs when evaluating community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.
PCPs can feel left out when their patients are cared for by hospitalists.13 One PCP in our study commented: Include the referral doc as part of the team. We're the ones who will take care of them after discharge. It seems like an autonomous thing down there and we're excluded from the patient care team. Additionally, patients want their PCPs to remain involved in their care as they transition into and out of the hospital setting.1, 13
The continuity visit model has been proposed by Wachter and Pantilat14 to describe a clinical encounter between the primary physician and hospitalized patient, when the patient has a different physician of record. In this model, the PCP can endorse the hospitalist model and the individual hospitalist, notice subtle findings that differ from the patient's baseline, and help clarify patient preferences regarding difficult situations by drawing on their previous relationship with the patient. This visit may also benefit the PCP by providing insights into the patient's illness, personality, or social support that he or she was unaware of previously. However, in order for the continuity visit to exist, the PCP has to be informed of their patient's admission in the first place. Ethical dilemmas also have been raised regarding who bears primary responsibility for maintaining open lines of communication when patients are hospitalized.15 Lo15 advocates that PCPs can and should be involved in meaningful ways in the inpatient care of their patients even when they are not acting as the treating physicians. Specifically, he suggests that PCPs personally visit particularly ill patients or those with difficult diagnoses and use frequent phone calls to all admitted patients.
Beyond telephone calls and continuity visits, hospitalists and PCPs rely on discharge summaries as a key part of the information transfer about a patient's hospitalization.1, 16, 17 These documents are rendered useless if they are inaccurate, illegible, or not delivered in a timely manner.18 In a study of California family physicians, discharge summaries were thought to be too detailed by 84% of PCPs, and reportedly arrived before the patient's first follow‐up appointment only 33% of the time.1 O'Leary et al.19 found that 41% of the Department of Medicine physicians surveyed believed that at least 1 of their patients hospitalized in the previous 6 months had experienced a preventable adverse event related to poor transfer of information at discharge. In our study, PCPs noted that discharge summaries often arrived in their offices well after the patient had been seen for their follow‐up appointment.
Both hospitalists and PCPs agree that a concise and precise discharge summary should include an overview of the hospitalization with important details highlighted. Similar to the findings of Pantilat et al.,1 in our study PCPs specifically want detailed information with regard to diagnoses, discharge medications, and what to expect when they see the patient in their clinic. Follow‐up phone calls to PCPs to see that they received written information and if they require further details is 1 solution to ensuring good follow‐up, yet this adds to the burden of communication and could be an additional barrier.
The teaching institutions in which physicians train also pose unique obstacles to optimal communication. In academic medical centers, medical students and residents perform a majority of the discharge duties (eg, writing prescriptions, dictating discharge summaries, making follow‐up appointments, and calling PCPs), and teaching these trainees the importance of timely and accurate communication becomes an added challenge. Educators have to find novel ways of providing incentives to residents and medical students to get them to effectively participate in this process. Plauth et al.20 reports that hospitalists feel they needed better training in residency around communicating, noting a meaningful underemphasis during residency training in regard to communication with referring physicians. These skills should be taught in medical school and supported by both hospitalists and PCPs throughout residency training.
Both hospitalists and PCPs also want easy and reliable ways to access their colleagues, which ideally would be automatic. One PCP commented: a weekly or semiweekly phone call would be nice. Another suggested to: fax a short note. One hospitalist acknowledged: a systematic approach would be betterwhether a fax or telephone call and make sure there is a way of checking to make sure the communication has happened. Another hospitalist simply remarked: it needs to be done on every patient.
Thus, it seems an improved communication system should be flexible enough to accommodate unique provider preferences, such as communication via phone, fax, or e‐mail. This is demonstrated by 1 PCP who preferred the phone, but most convenient is the periodic fax updates. I don't have to be taken away from seeing patients.
Lo15 calls for a standard to be established for delivering care within the patient‐PCP‐hospitalist triad. Phone calls and faxes are 2 readily available methods of communication. However, the frequent back‐and‐forth of missed calls, unreturned calls, and days‐off is certainly a factor in determining efficiency and effectiveness of phone calls.
E‐mail, if it is widely used by all participants, may be an effective option for delivery that could provide confirmation of receipt. However, the lack of universal e‐mail usage by all providers remains a barrier. Questions as to which method is more time consuming and for whom, need to be studied further. Patient confidentiality also requires that this protected health information arrive in the proper hands. Personal relationships can also contribute to successful communication. One provider may be more likely to contact another if they know each other through some personal connection, such as medical school, residency, or a social group.
Our study has several limitations. The sample size was small. We obtained responses from a sample of key stakeholders in the hospitalist‐PCP communication process. We were limited by the number of hospitalists at our institution as well as the interest and availability of PCPs to respond. We are unable to determine the total number of patients by respondent PCP practice cared for by the hospitalist division. This could influence the results depending on whether the respondent PCP was a frequent or infrequent utilizer of the hospitalist system. However, we feel reassured that we are not missing important information, because in our methods, a priori, we had intended to stop interviewing PCPs once theoretical saturation had been reached (ie, respondents did not identify any new information). In our study, that occurred with 12 PCPs.
We attempted to interview a single physician in a number of different practice settings in order to gain insight into the perceptions of that individual as well as those of their partners. The views expressed by these individuals may not represent the views of hospitalists and PCPs outside of our practice area. Furthermore, PCMC serves as both a community pediatric hospital and a tertiary‐referral center for a large area, yet the current experience of 1 hospitalist division and 1 cohort of referring PCPs may contain regional variation that contributed bias to the responses.
Selection bias may have been introduced in our study by the inherent nature of phone interviews. We interviewed only providers with previous communication experience with our hospitalist division. These providers may have had a vested interest in the communication process. We did not interview those PCPs who did not have any communication with our hospitalist division or those who may have used the hospitalist division previously and decided to no longer use the division. Interviewing these groups may have provided additional insight into the communication issues mentioned here. Additionally, useful information could have been gleaned from trying to find out more from the 33% of PCPs who felt communication was poor. We anticipate further studies exploring this issue in more depth.
Future Directions
As a result of this study, we have implemented several interventions to improve information sharing between hospitalists and PCPs, including: 1) we updated current contact information (including names of physicians, office addresses, phone numbers, fax numbers, and e‐mail addresses) for all PCPs in our catchment area along with their preferred methods of communication; 2) we worked with the transcription services to automatically add PCP addresses, phone numbers, and fax numbers to dictated notes, eliminating time wasted searching for contact information; and 3) we standardized key data elements in admission history and physicals and discharge notes to increase the efficiency of the communication process.
Furthermore, we have implemented a standardized system to facilitate communication with PCPs. This system includes an automated process to notify PCPs of their patient's hospital admission, including the admission date, preliminary diagnoses, and responsible physician's contact information. We are currently undertaking a quality improvement project aimed at achieving timely transfer of discharge information to PCPs, including medications, follow‐up appointments, and a succinct hospital summary. Finally, establishing an evaluation process to monitor both successes and failures will be paramount to any interventions.
CONCLUSIONS
Hospitalists and PCPs agree that overall quality of communication ranges from poor to very good. Both PCPs and pediatric hospitalists acknowledge that significant barriers to optimal communication exist, yet the barriers differ for each group. They also agree that optimal communication would improve many aspects of patient care and should take place upon discharge and admission of patients and with major clinical changes.
Pediatric hospitalists and PCPs identified issues around optimal communication similar to those noted in the adult hospital medicine literature. Interventions to improve pediatric hospitalist‐PCP communication should at least address these 6 issues: (1) quality of communication; (2) barriers to communication; (3) methods of information sharing; (4) key data element requirements; (5) critical timing; and (6) perceived benefits. Such interventions will likely improve hospitalist‐PCP communication and potentially improve the quality of patient care. However, future studies will need to demonstrate the link between improved hospitalist‐PCP communication and improved patient care and outcomes.
Acknowledgements
The authors are indebted to Flory Nkoy, MD, MPH, MS, for his help in manuscript preparation and critical review.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,,,.Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey.Am J Med.2000;109(8):648–653.
- ,,,,,.Pediatric hospitalists: what do we know, and where do we go from here?Ambul Pediatr.2001;1(6):340–345.
- ,,.Physician views on caring for hospitalized patients and the hospitalist model of inpatient care.J Gen Intern Med.2001;16(2):116–119.
- ,,,,,.Community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.Pediatrics.2005;115(1):34–38.
- ,.The patient provider relationship and the hospitalist movement. Introduction.Dis Mon.2002;48(4):189–190.
- ,.Rigour and qualitative research.BMJ.1995;311(6997):109–112.
- ,.Needs assessment in post graduate medical education: a review.Med Educ Online.2001;7:1–8.
- ,,,.How physicians perceive hospitalist services after implementation: anticipation vs reality.Arch Intern Med.2003;163(19):2330–2336.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- ,,.Generalist‐subspecialist communication for children with chronic conditions: a regional physician survey.Pediatrics.2003;112(6 Pt 1):1314–1320.
- ,,,,,.Communication breakdown in the outpatient referral process.J Gen Intern Med.2000;15(9):626–631.
- ,,.How do patients view the role of the primary care physician in inpatient care?Dis Mon.2002;48(4):230–238.
- ,.The “continuity visit” and the hospitalist model of care.Dis Mon.2002;48(4):267–272.
- .Ethical and policy implications of hospitalist systems.Dis Mon.2002;48(4):281–290.
- ,,, et al.From a paper‐based transmission of discharge summaries to electronic communication in health care regions.Int J Med Inform.2006;75(3‐4):209–215.
- ,,.Tying up loose ends: discharging patients with unresolved medical issues.Arch Intern Med.2007;167(12):1305–1311.
- ,.Improving communication between hospital and community physicians. Feasibility study of a handwritten, faxed hospital discharge summary. Discharge Summary Study Group.Can Fam Physician.1999;45:2893–2899.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,,,.Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey.Am J Med.2000;109(8):648–653.
- ,,,,,.Pediatric hospitalists: what do we know, and where do we go from here?Ambul Pediatr.2001;1(6):340–345.
- ,,.Physician views on caring for hospitalized patients and the hospitalist model of inpatient care.J Gen Intern Med.2001;16(2):116–119.
- ,,,,,.Community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.Pediatrics.2005;115(1):34–38.
- ,.The patient provider relationship and the hospitalist movement. Introduction.Dis Mon.2002;48(4):189–190.
- ,.Rigour and qualitative research.BMJ.1995;311(6997):109–112.
- ,.Needs assessment in post graduate medical education: a review.Med Educ Online.2001;7:1–8.
- ,,,.How physicians perceive hospitalist services after implementation: anticipation vs reality.Arch Intern Med.2003;163(19):2330–2336.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297(8):831–841.
- ,,.Generalist‐subspecialist communication for children with chronic conditions: a regional physician survey.Pediatrics.2003;112(6 Pt 1):1314–1320.
- ,,,,,.Communication breakdown in the outpatient referral process.J Gen Intern Med.2000;15(9):626–631.
- ,,.How do patients view the role of the primary care physician in inpatient care?Dis Mon.2002;48(4):230–238.
- ,.The “continuity visit” and the hospitalist model of care.Dis Mon.2002;48(4):267–272.
- .Ethical and policy implications of hospitalist systems.Dis Mon.2002;48(4):281–290.
- ,,, et al.From a paper‐based transmission of discharge summaries to electronic communication in health care regions.Int J Med Inform.2006;75(3‐4):209–215.
- ,,.Tying up loose ends: discharging patients with unresolved medical issues.Arch Intern Med.2007;167(12):1305–1311.
- ,.Improving communication between hospital and community physicians. Feasibility study of a handwritten, faxed hospital discharge summary. Discharge Summary Study Group.Can Fam Physician.1999;45:2893–2899.
- ,,,,.Outpatient physicians' satisfaction with discharge summaries and perceived need for an electronic discharge summary.J Hosp Med.2006;1(5):317–320.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111(3):247–254.
Copyright © 2009 Society of Hospital Medicine
Academic Hospital Medicine
The past decade has seen hospital medicine grow from fewer than 1000 hospitalists nationwide to more than 20,000.1 In fact, survey data suggest that hospital medicine is the fastest growing field of internal medicine in the history of the US, and the growth of hospital medicine has produced a net increase in the number of generalists in the US.2
Although few direct estimates exist, academic hospital medicine (AHM) is also growing rapidly.1 Fueled by potential efficiency gains, a need for increased educational oversight of teaching services, and new residency work hour limitations, many academic medical centers and teaching hospitals have developed large hospital medicine programs. Internal medicine residency graduates interested in general medicine are finding hospital medicine an increasingly popular career choice. As a result, AHM groups have many recent residency graduates with an average age that is generally younger than 40.3
Over 85% of hospitalists are generalists and should find natural alliances with the nonhospitalist side of general internal medicine by collaborating in the course of clinical care, by teaching residents and students, or by designing quality improvement or research projects. In many academic centers, hospitalists are part of the division of general internal medicine, whereas in a few centers, hospitalists either have a separate division or lie outside the internal medicine department (employed by their hospitals).
Despite sharing a common training background and generalist mindset, many new academic hospitalists face different challenges than those faced by pure outpatient‐based academic generalists. First, at many centers, the financial arrangements between the AHM group and the hospital discourage hospitalists from traditional academic pursuits and draw them into clinical, operational, or administrative duties (such as responsibility for utilization review) that, although locally valuable, may not count as academic products in themselves or may take time away from more academic activities. Close alignment between hospitals and AHM may result in hospital administrators dictating hospitalists' practice in a way that further impedes academic viability. Reductions in resident training hours and an increasing need to provide 24‐hour coverage have facilitated growth in AHM into roles beyond those of the traditional academic generalist, such as medical comanagement of surgical patients and coverage of nonteaching services.4, 5 The youth of the field may exacerbate these problems. Most academic hospitalist groups have few senior leaders, whether they are clinical‐, education‐, or research‐focused. Young faculty need senior leaders as mentors to buffer them from relentless clinical demands that would compromise their hopes for academic success.
In order to better characterize these concerns and develop a shared work plan for future activities in support of AHM, the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM) convened an AHM consensus conference, a collaborative meeting developed and attended by representatives from SHM, SGIM, the Association of Chiefs of General Internal Medicine (ACGIM), the Association of Professors of Medicine, the Association of Program Directors in Internal Medicine, and the Association of Administrators in Internal Medicine. Using a structured consensus‐building format, we identified key barriers and challenges to AHM, then developed potential solutions.
Consensus Conference Format
Consensus Conference Steering Committee
The consensus conference was developed first by the sponsoring professional societies (SGIM, SHM, and ACGIM) being asked to nominate 2 people to be part of the consensus conference steering committee. The steering committee's main functions were to identify key tasks for the consensus conference, invite consensus conference attendees, ensure adequate representation from all participating organizations, synthesize the results of the consensus conference, and work with the individual professional societies so that results from the consensus conference were acted upon in a coordinated and effective manner.
Consensus Conference Prework
The consensus conference co‐chairs convened a series of conference calls in the spring of 2007, during which the steering committee developed a series of key areas to be explored during the conference. Topic areas were selected on the basis of the group's expertise and referred to past work by AHM taskforces convened by both SGIM/ACGIM and SHM.
The steering committee then invited stakeholders from each invited society so that each professional organization would provide at least 1 representative with expertise appropriate to 1 of the key domains identified:
-
Clinical and financial issues (within which topics such as optimal job descriptions and salary structures would be explored).
-
Teaching and education mission (within which topics such as mentorship for AHM junior faculty might be discussed).
-
Research and promotable activities (within which issues related to the development of promotable activities for AHM would be discussed).
Invitees to the consensus conference were assigned to one working group, given a general description of the potential areas within their domain, and instructed to consider a number of broad questions relevant to the topic area. These questions were as follows:
-
What are the key barriers to AHM in each key domain?
-
What viewpoints or barriers are the most pressing and/or actionable?
-
What solutions could be implemented or initiated in the next 1 to 3 years?
In order to facilitate discussion, consensus conference invitees were provided copies of findings from the SGIM/ACGIM and SHM Academic Hospitalist Task Forces, preliminary results from a survey of AHM leaders, and key literature related to the field.
Consensus Conference Format
The AHM consensus conference followed a modified Delphi consensus‐building format, in which the members of each working group developed findings relevant to their area, presented these viewpoints back to the overall group for feedback, and returned to their working group to refine their initial recommendations or move on to subsequent areas.
We used Day 1 of the meeting to confirm and refine lists of key barriers and opportunities to AHM. On Day 2, we developed actionable solutions and identified barriers with no ready solution but which were felt to be worth highlighting.
Each cycle of feedback (1 on Day 1 and 2 on Day 2) was used to identify additional barriers or opportunities prespecified by the steering committee, prioritize issues/opportunities, clarify uncertainties or point them out when they existed, and identify new areas requiring consensus. Between each cycle, workflow and interim results were summarized by the co‐chairs and a professional meeting coordinator to ensure that the group felt consensus had been achieved and to identify where additional work was required.
Writing Group/Peer Review
After the consensus conference adjourned, minutes were circulated to the group and approved, whereupon a summary of the meeting was reformatted into manuscript form. The manuscript was circulated to the steering committee, consensus conference attendees, and 2 selected peer reviewers as an additional check on the external validity of the study's results.
Consensus Findings 1: Current Challenges in AHM (Table 1)
Clinical and Financial Issues in AHM
The consensus group identified misalignment of the mission of hospitals (which often provide substantial financial support for hospital medicine programs) and the mission of departments of internal medicine (or divisions of general internal medicine) in which adult hospitalists reside as a fundamental barrier in AHM. Misalignment of missions produces challenges to the development of hospitalist groups in that their primary funder, the hospital, focuses on clinical care delivery, productivity, efficiency, and, in some cases, participation in patient safety and quality improvement efforts, whereas academic departments place considerable value on education, research, grants received, dissemination of scholarly work, and the national reputation of its faculty. Further exacerbating this tension is the fact that hospitalists do not always reside within traditional academic divisions (such as divisions of general medicine) and are therefore viewed by the hospital and their peers as hospital employees more than academic faculty.
As yet, few hospital medicine programs have successfully integrated academic and clinical needs. In many AHM programs, clinical demands have trumped academic pursuits and, as a result, produced jobs that have frequent turnover. This occurs most often when hospitalists are hired by academic medical centers primarily to staff nonresident services. Hospitalists who join these academic programs expecting ample opportunity to teach and pursue scholarly work often leave when they realize these jobs differ little from those in community settings (with the exception of less pay and, in most cases, a less efficient clinical delivery system). This turnover contributes to the perception of hospitalists as transient nonacademic faculty. The participants felt that we needed to define the ideal academic hospitalist job description.
| Clinical and Financial Issues | Teaching and Education Mission | Research and Promotable Activities | Cross‐Cutting Issues |
|---|---|---|---|
| |||
| Hospitalists' functions more often explicitly linked to hospital initiatives (clinical care, quality improvement, utilization, and throughput) | Distinguishing jobs that are predominantly clinical (C‐e) from those that are predominantly education‐focused (c‐E), which is important given the high clinical burdens | Lack of a pipeline producing hospitalist clinician investigators | Lack of leadership or negotiation skill training |
| Differing political, financial, and scientific priorities between hospitalists and administrators | Further exacerbation of C‐e/c‐E distinctions by the emergence of uncovered services | Few national funders focusing on inpatient general internal medicine | Little infrastructure for academic functions |
| Little guidance on the best models for each job type | Little recognition of quality improvement as a promotable/testable activity | Rapidly moving/growing field | |
| Decreasing interest in general internal medicine as a career path | |||
Teaching and Education Mission in AHM
Traditionally, faculty in academic medical centers have had prominent roles in resident teaching services, supervising medical residents, interns, and students. Hospitalists fill these roles at some institutions and in many cases have replaced senior faculty who are no longer able (because of competing demands from clinics or labs) or willing (because of an increased need for oversight and availability) to staff the teaching service. The teaching hospitalists start at these positions straight out of residency with little experience, training, or mentoring in how to succeed as a clinician educator. The creation of nonresident hospitalist services to address residency work hour requirements has removed many hospitalists from teaching opportunities as these services often have few if any teaching opportunities. The consensus group identified the lack of teaching opportunities and a lack of any formal preparation for those who do teach as the key challenges for new hospitalist clinician educators.
Research and Promotable Activities in AHM
Numerous challenges to promotion and success in hospital medicine research were identified. Most conference attendees felt that chairs of departments of medicine do not fully understand what the roles of academic hospitalists are, how they fit into the department's mission, or what is needed to better integrate hospitalists into the research and academic activities of the department. In addition, there are few hospital medicine fellowship programs, and those that have been created focus primarily on improving teaching skills or quality improvement rather than on research or the development of academic products. Aspiring academic hospitalists could pursue research fellowship training in existing programs (ie, the Robert Wood Johnson Foundation), but few graduates currently pursue these opportunities, and federally funded fellowships (eg, the National Research Service Awards and Health Resources and Services Administration T32 awards) explicitly exclude physicians who are not focused on primary care research. The group noted that a number of Veterans Administration fellowships (such as the Quality Scholars programs) may provide avenues for the training of hospital medicinefocused researchers, but they have been underused.
For researchers who focus on hospital medicine, federal funding sources are limited for both career development awards (K‐series) and later (R‐series) grants, particularly those funding the quality and safety research that hospitalists often pursue. Agencies of the National Institutes of Health currently do not provide many opportunities for hospital‐based general internal medicine research, and thus academic hospitalist research is undervalued by many promotion committees.
Cross‐Cutting Issues
Challenges in leadership and mentorship were identified as cross‐cutting. Many AHM programs are young, and so are their leaders. As a result, hospital medicine leaders often lack the experience and skills necessary to successfully negotiate for the support that is critical for the ideal program's success. As a young field, hospital medicine lacks faculty who have succeeded in careers as hospitalists, have been promoted in tenure tracks, and can mentor and guide young faculty through the complexities of academic medicine. Absent leadership and mentoring, few hospital medicine programs will succeed in traditional academic pursuits.
Consensus Findings 2: Overcoming Challenges to the Development of AHM (Table 2)
Summit attendees spent considerable time developing and refining solutions to the challenges described previously. Addressing the challenges resulted in a diverse group of proposed products that included educating key stakeholders, designing meetings, courses, or workshops, and gathering and disseminating data. There was considerable overlap among the solutions (Table 2).
| Solutions | Proposed Products | Challenge Domains Addressed* |
|---|---|---|
| ||
| 1. Educate stakeholders | Workshops at professional society meetings (SHM, SGIM, ACGIM, APM, and APDIM) | Addresses all domains |
| Publications highlighting issues | ||
| 2. Define the sustainable job | Data gathering and publication | Clinical/financial |
| 3. Quality improvement portfolio | Development and dissemination of criteria for the QI portfolio | Research/promotion |
| 4. Hospitalist training/mentoring | Academic hospitalist boot camp | Teaching/education |
| Research/promotion | ||
| Cross‐cutting | ||
| 5. Enhance research career pathways | Advocacy for enhanced training programs and funding sources | Research/promotion |
| 6. Improved relationships among general medicine societies | Society collaboration on product development | Addresses all domains |
Outreach to and Education of Stakeholders in Academic Medicine
The focus of the educational and outreach efforts suggested by the consensus group is to help leaders in academic medicine (not just AHM) and academic medical centers understand the challenges facing AHM. More importantly, efforts should reinforce the value of academic hospitalists to their hospital, department, and division. Efforts to engage these critical stakeholders to discuss and potentially address a number of the conference's proposed solutions are needed. Leaders include deans of medical schools, chairs of departments of medicine, division chiefs, and hospital administrative leadership.
Suggested outreach and educational activities included the publication of articles in key journals with the goal of increasing the visibility of AHM in professional societies as well as meetings and workshops focusing on teaching hospitalists and academic leaders methods to overcome challenges. Professional societies with a stake in AHM should better understand the challenges and position themselves to address these issues. The AHM task forces of SHM and SGIM can help give academic hospitalists a voice in having their needs addressed.
Publications
Articles have been commissioned in the following areas: descriptions of challenges and proposed solutions, best practices for nonresident hospitalist services, and metrics for the success of hospital medicine programs.
Meetings/Workshops
Meetings and workshops, sponsored by professional societies with a vested interest in AHM, were thought to be an effective way to address the needs of hospitalists, particularly those pursuing careers as clinician educators. Such workshops would provide skills in teaching and early career survival (eg, how to bill correctly) and in developing an educator's portfolio. Leadership training offerings, perhaps building on examples from SHM and ACGIM, were also thought to be valuable resources and venues that should be directed toward hospitalists, their chiefs, and relevant leaders.
Defining a Sustainable Job Description for Academic Hospitalists
The group strongly endorsed the need for transparent and readily available data aimed at developing sustainable academic hospitalist positions. For example, required information would include how academic jobs are constructed (in terms of months on service per year and the number of nights or weekends of coverage) and what successful programs and their hospitalists have found to be acceptable. Over the longer term, empiric comparisons based on key metrics are needed to not only help guide career development and retention but also facilitate negotiations for programmatic support.
The group pointed out that embedded in delineating an optimal academic hospitalist job description is the longstanding work of general medicine societies in supporting and fostering the development of clinician educators. In many ways, the pressures of academic physicians to be mostly clinician and less educator versus someone who focuses heavily on educational work is similar for hospitalists and outpatient generalists. Academic general internal medicine divisions hired many general internists in the early 1990s to expand the reach of academic medical centers and increase the outpatient base.6 Many university hospitals are now hiring hospitalists to provide the inpatient care for these patients, but residency work hour reductions have added a layer of complexity, creating the need for entirely new roles for academic generalists (such as surgical comanagement of medically complex patients).7, 8 Past experiences in refining and reinforcing education as a key function (
Development of a Quality‐Improvement Portfolio Akin to an Educator's Portfolio
Many hospitalists actively participate in administrative work related to quality improvement activities, and we should develop this additional pathway for promotable academic activities (eg, clinician administrator); however, such a pathway may not be recognized by all promotion committees. The group observed that many aspects of quality improvement are similar to those of education (eg, developing a curriculum, leading a team, evaluating a process, defining generalizability, and disseminating locally proven interventions) and as such would be amenable to the development of a quality improvement portfolio, which candidates could submit to promotion committees. Again, past work in developing the importance and value of the educator's portfolio would facilitate the development of a quality improvement portfolio, which would require endorsement from key stakeholders (eg, the Association of Professors of Medicine, SGIM, and SHM).9 Importantly, this work may also benefit many outpatient‐based generalists who are increasingly focusing their careers on quality and safety improvement.
Developing Mentoring and Training Opportunities for Newly Hired and Junior Hospitalists
We reached a strong consensus about the need to develop a retreat‐format training opportunity by which junior academic hospitalists would be able to gain training in tasks critical to early‐career success. These were envisioned as an initial 2‐ to 3‐day meeting followed by mentorship at a distance and continued collaboration within the class of attendees. Topics would include key functions in AHM, such as becoming an effective attending physician and teacher, leadership, quality improvement, the business of medicine, effective billing, and maintaining a curriculum vitae. A number of professional societies have developed leadership or mentoring retreats, and at the time of this article's preparation, both regional and national efforts were underway to develop these products.
Developing Training and Mentorship Pathways for Hospitalist Researchers
There are few funded hospitalist researchers in the midcareer phase and a small but growing number of academic hospitalists entering the field with a focus on research. Enhancing a pipeline of researchers is a critical need for the field, as cementing AHM as an equal member of the academic medical community will be predicated on the successful development of hospitalist investigators. To this end, academic hospitalist groups should be encouraged to partner with other established research units (particularly general internal medicine) to create mentoring relationships and increase collaborative activities. The emergence of the Clinical and Translational Science Awards consortium sites, with a focus on implementation and effectiveness research, may also provide local opportunities for hospitalists to partner in research important for early‐career grant submission. Furthermore, building the pipeline of academic hospitalist researchers will require a strong focus on identifying students and residents through outreach at individual sites as well as presentations at national meetings (eg, the American College of Physicians).
Two other issues were also thought to be important. First, professional societies should work to encourage funders of primary carefocused general medicine training programs (the National Research Service Awards and the Health Resources and Services Administration) to allow hospitalists to qualify for such critical research training. Second, continuing to advocate for increasing funding for implementation and effectiveness research, via either the Agency for Healthcare Research and Quality or individual agencies of the National Institutes of Health, will be key; the emergence of a medical effectiveness institute would also be a potential boon.
Improving Relationships Between the Professional Homes of Academic Generalists
Relationships between outpatient‐based general medicine and hospital medicine were rocky as the field of AHM first took shape, and some residua of initial tensions persist a decade later. These tensions persist in part because hospitalists remain underdeveloped members of the academic community, and this perhaps gives some license to aver that hospitalists are merely transient faculty in a stage between residency and fellowship hired to improve throughput.
Overcoming this perception will require more engagement between academic generalists of all types, not less. The consensus group felt strongly that there need not be a single professional home for academic hospitalists and that generalists should be willing and even encouraged to self‐identify as hospital‐ or clinic‐focused, much as they might be geriatrics‐focused, informatics‐focused, or women's healthfocused. In fact, in some academic centers, a few generalists have successfully integrated themselves into both clinic‐based and hospitalist roles. In this way, the emergence and growth of AHM should be viewed as a boon to the practice of general medicine, not a challenge.
Resources
Much of what is proposed to enhance AHM will require resources. Academic hospitals have a vested interest in supporting AHM as a way to reduce turnover in a group that is increasingly critical for hospital operations, not to mention key leadership roles. Negotiating for these resources should emphasize that hospitals benefit directly from the revenue and margin that comes from incremental hospital admissions, collect most of the federal graduate medical education dollars, and benefit from improved care processes that are a result of hospitalist quality improvement efforts.
Deans and Departments, a key audience for the conference findings, also have a clear stake in fostering a less transient, more professionally satisfied and academically successful work force, particularly when hospitalists are increasingly the key educators of medical residents. Moreover, schools have a vested interest in the academic accomplishments and national reputation of their hospitalists. The financial arrangements will be unique to each setting and institution, and it is clear that the sources to be tapped will vary from site to site, but these resources are clearly necessary for the field.
Conclusions
AHM is at a crossroads. Unparalleled growth has created a large cadre of hospitalists who are struggling to meet the clinical demands of practice and the requirements for academic promotion; this situation will likely lead to, at a minimum, worsening problems with faculty turnover, and even greater losses of talented and passionate clinicians from the field of academic General Internal Medicine.
The challenges are numerous but not insurmountable, and our process identified issues and potential solutions which address clinical, educational, and research aspects of academic hospitalists' lives. We acknowledge that our findings are most relevant to hospitalists at academic medical centers or large academically oriented community teaching hospitals rather than hospitalists at community hospitals whose work is predominantly clinical with smaller teaching roles. However, we feel the academic hospitalists we targeted are in greater need of assistance. We believe that the most important issues are unsustainable, nonacademic positions, poor job preparation and training, inadequate prioritization of academic roles, and insufficient leadership and mentoring within the field.
It is the hope of all the consensus conference attendees that efforts focusing on academic hospitalists in the short term are not viewed as effort diverted from general internal medicine; in fact, the group felt that while many of the products of the consensus conference were probably most needed by AHM in the short term, these same solutions would likely be useful to outpatient‐based generalists as well. Despite the concerns and challenges outlined, the consensus conference group was also very hopeful that, in the setting where resources and collaboration are appropriately marshaled, that AHM will flourish quickly. In doing so, academic hospitalists will become better role models for residents and students, attracting the next generation of generalists needed to provide care to an increasingly complex patient population, and further advance the mission of General Internal Medicine.
Acknowledgements
The authors thank Dr. Jeff Glasheen and Dr. Robert Wachter for their comments on an earlier version of this article. In addition, the authors thank the following conference participants: Dan Brotman, MD, Johns Hopkins University; Deborah M. DeMarco, MD, President of the Association of Program Directors in Internal Medicine; Jeff Glasheen, MD, University of Colorado; Rusty Holman, MD, President of the Society of Hospital Medicine; Martha A. Hooven, President of the Administrators of Internal Medicine; Peter Kaboli, MD, University of Iowa; David O Meltzer, MD, PhD, University of Chicago; Vikas Parekh, MD, University of Michigan; Russell Phillips, MD MPH, Harvard Medical School; Sanjay Saint, MD, MPH, University of Michigan; Barbara Schuster, MD, President of the Association of Professors of Medicine; Brad Sharpe, MD, University of California San Francisco; Jeff Wiese, MD, Tulane University; David Kushner, Facilitator of the Kushner Companies; Geri Barnes, Support Staff of the Society of Hospital Medicine; and Amy Woodward, Support Staff of the Society of General Internal Medicine.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- ,,,,,.Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21:1079–1085.
- Society of Hospital Medicine. 2006 Hospital Medicine Survey. Available at: http://www.hospitalmedicine.org/content/navigationmenu/media/mediakit/media_kit.htm. Accessed January 2009.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- UCLA rewrites the script for academic networks.Med Netw Strategy Rep.1998;7:1–5.
- ,,,,,.Systematic review: effects of resident work hours on patient safety.Ann Intern Med.2004;141:851–857.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Documentation systems for educators seeking academic promotion in U.S. medical schools.Acad Med.2004;79:783–790.
The past decade has seen hospital medicine grow from fewer than 1000 hospitalists nationwide to more than 20,000.1 In fact, survey data suggest that hospital medicine is the fastest growing field of internal medicine in the history of the US, and the growth of hospital medicine has produced a net increase in the number of generalists in the US.2
Although few direct estimates exist, academic hospital medicine (AHM) is also growing rapidly.1 Fueled by potential efficiency gains, a need for increased educational oversight of teaching services, and new residency work hour limitations, many academic medical centers and teaching hospitals have developed large hospital medicine programs. Internal medicine residency graduates interested in general medicine are finding hospital medicine an increasingly popular career choice. As a result, AHM groups have many recent residency graduates with an average age that is generally younger than 40.3
Over 85% of hospitalists are generalists and should find natural alliances with the nonhospitalist side of general internal medicine by collaborating in the course of clinical care, by teaching residents and students, or by designing quality improvement or research projects. In many academic centers, hospitalists are part of the division of general internal medicine, whereas in a few centers, hospitalists either have a separate division or lie outside the internal medicine department (employed by their hospitals).
Despite sharing a common training background and generalist mindset, many new academic hospitalists face different challenges than those faced by pure outpatient‐based academic generalists. First, at many centers, the financial arrangements between the AHM group and the hospital discourage hospitalists from traditional academic pursuits and draw them into clinical, operational, or administrative duties (such as responsibility for utilization review) that, although locally valuable, may not count as academic products in themselves or may take time away from more academic activities. Close alignment between hospitals and AHM may result in hospital administrators dictating hospitalists' practice in a way that further impedes academic viability. Reductions in resident training hours and an increasing need to provide 24‐hour coverage have facilitated growth in AHM into roles beyond those of the traditional academic generalist, such as medical comanagement of surgical patients and coverage of nonteaching services.4, 5 The youth of the field may exacerbate these problems. Most academic hospitalist groups have few senior leaders, whether they are clinical‐, education‐, or research‐focused. Young faculty need senior leaders as mentors to buffer them from relentless clinical demands that would compromise their hopes for academic success.
In order to better characterize these concerns and develop a shared work plan for future activities in support of AHM, the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM) convened an AHM consensus conference, a collaborative meeting developed and attended by representatives from SHM, SGIM, the Association of Chiefs of General Internal Medicine (ACGIM), the Association of Professors of Medicine, the Association of Program Directors in Internal Medicine, and the Association of Administrators in Internal Medicine. Using a structured consensus‐building format, we identified key barriers and challenges to AHM, then developed potential solutions.
Consensus Conference Format
Consensus Conference Steering Committee
The consensus conference was developed first by the sponsoring professional societies (SGIM, SHM, and ACGIM) being asked to nominate 2 people to be part of the consensus conference steering committee. The steering committee's main functions were to identify key tasks for the consensus conference, invite consensus conference attendees, ensure adequate representation from all participating organizations, synthesize the results of the consensus conference, and work with the individual professional societies so that results from the consensus conference were acted upon in a coordinated and effective manner.
Consensus Conference Prework
The consensus conference co‐chairs convened a series of conference calls in the spring of 2007, during which the steering committee developed a series of key areas to be explored during the conference. Topic areas were selected on the basis of the group's expertise and referred to past work by AHM taskforces convened by both SGIM/ACGIM and SHM.
The steering committee then invited stakeholders from each invited society so that each professional organization would provide at least 1 representative with expertise appropriate to 1 of the key domains identified:
-
Clinical and financial issues (within which topics such as optimal job descriptions and salary structures would be explored).
-
Teaching and education mission (within which topics such as mentorship for AHM junior faculty might be discussed).
-
Research and promotable activities (within which issues related to the development of promotable activities for AHM would be discussed).
Invitees to the consensus conference were assigned to one working group, given a general description of the potential areas within their domain, and instructed to consider a number of broad questions relevant to the topic area. These questions were as follows:
-
What are the key barriers to AHM in each key domain?
-
What viewpoints or barriers are the most pressing and/or actionable?
-
What solutions could be implemented or initiated in the next 1 to 3 years?
In order to facilitate discussion, consensus conference invitees were provided copies of findings from the SGIM/ACGIM and SHM Academic Hospitalist Task Forces, preliminary results from a survey of AHM leaders, and key literature related to the field.
Consensus Conference Format
The AHM consensus conference followed a modified Delphi consensus‐building format, in which the members of each working group developed findings relevant to their area, presented these viewpoints back to the overall group for feedback, and returned to their working group to refine their initial recommendations or move on to subsequent areas.
We used Day 1 of the meeting to confirm and refine lists of key barriers and opportunities to AHM. On Day 2, we developed actionable solutions and identified barriers with no ready solution but which were felt to be worth highlighting.
Each cycle of feedback (1 on Day 1 and 2 on Day 2) was used to identify additional barriers or opportunities prespecified by the steering committee, prioritize issues/opportunities, clarify uncertainties or point them out when they existed, and identify new areas requiring consensus. Between each cycle, workflow and interim results were summarized by the co‐chairs and a professional meeting coordinator to ensure that the group felt consensus had been achieved and to identify where additional work was required.
Writing Group/Peer Review
After the consensus conference adjourned, minutes were circulated to the group and approved, whereupon a summary of the meeting was reformatted into manuscript form. The manuscript was circulated to the steering committee, consensus conference attendees, and 2 selected peer reviewers as an additional check on the external validity of the study's results.
Consensus Findings 1: Current Challenges in AHM (Table 1)
Clinical and Financial Issues in AHM
The consensus group identified misalignment of the mission of hospitals (which often provide substantial financial support for hospital medicine programs) and the mission of departments of internal medicine (or divisions of general internal medicine) in which adult hospitalists reside as a fundamental barrier in AHM. Misalignment of missions produces challenges to the development of hospitalist groups in that their primary funder, the hospital, focuses on clinical care delivery, productivity, efficiency, and, in some cases, participation in patient safety and quality improvement efforts, whereas academic departments place considerable value on education, research, grants received, dissemination of scholarly work, and the national reputation of its faculty. Further exacerbating this tension is the fact that hospitalists do not always reside within traditional academic divisions (such as divisions of general medicine) and are therefore viewed by the hospital and their peers as hospital employees more than academic faculty.
As yet, few hospital medicine programs have successfully integrated academic and clinical needs. In many AHM programs, clinical demands have trumped academic pursuits and, as a result, produced jobs that have frequent turnover. This occurs most often when hospitalists are hired by academic medical centers primarily to staff nonresident services. Hospitalists who join these academic programs expecting ample opportunity to teach and pursue scholarly work often leave when they realize these jobs differ little from those in community settings (with the exception of less pay and, in most cases, a less efficient clinical delivery system). This turnover contributes to the perception of hospitalists as transient nonacademic faculty. The participants felt that we needed to define the ideal academic hospitalist job description.
| Clinical and Financial Issues | Teaching and Education Mission | Research and Promotable Activities | Cross‐Cutting Issues |
|---|---|---|---|
| |||
| Hospitalists' functions more often explicitly linked to hospital initiatives (clinical care, quality improvement, utilization, and throughput) | Distinguishing jobs that are predominantly clinical (C‐e) from those that are predominantly education‐focused (c‐E), which is important given the high clinical burdens | Lack of a pipeline producing hospitalist clinician investigators | Lack of leadership or negotiation skill training |
| Differing political, financial, and scientific priorities between hospitalists and administrators | Further exacerbation of C‐e/c‐E distinctions by the emergence of uncovered services | Few national funders focusing on inpatient general internal medicine | Little infrastructure for academic functions |
| Little guidance on the best models for each job type | Little recognition of quality improvement as a promotable/testable activity | Rapidly moving/growing field | |
| Decreasing interest in general internal medicine as a career path | |||
Teaching and Education Mission in AHM
Traditionally, faculty in academic medical centers have had prominent roles in resident teaching services, supervising medical residents, interns, and students. Hospitalists fill these roles at some institutions and in many cases have replaced senior faculty who are no longer able (because of competing demands from clinics or labs) or willing (because of an increased need for oversight and availability) to staff the teaching service. The teaching hospitalists start at these positions straight out of residency with little experience, training, or mentoring in how to succeed as a clinician educator. The creation of nonresident hospitalist services to address residency work hour requirements has removed many hospitalists from teaching opportunities as these services often have few if any teaching opportunities. The consensus group identified the lack of teaching opportunities and a lack of any formal preparation for those who do teach as the key challenges for new hospitalist clinician educators.
Research and Promotable Activities in AHM
Numerous challenges to promotion and success in hospital medicine research were identified. Most conference attendees felt that chairs of departments of medicine do not fully understand what the roles of academic hospitalists are, how they fit into the department's mission, or what is needed to better integrate hospitalists into the research and academic activities of the department. In addition, there are few hospital medicine fellowship programs, and those that have been created focus primarily on improving teaching skills or quality improvement rather than on research or the development of academic products. Aspiring academic hospitalists could pursue research fellowship training in existing programs (ie, the Robert Wood Johnson Foundation), but few graduates currently pursue these opportunities, and federally funded fellowships (eg, the National Research Service Awards and Health Resources and Services Administration T32 awards) explicitly exclude physicians who are not focused on primary care research. The group noted that a number of Veterans Administration fellowships (such as the Quality Scholars programs) may provide avenues for the training of hospital medicinefocused researchers, but they have been underused.
For researchers who focus on hospital medicine, federal funding sources are limited for both career development awards (K‐series) and later (R‐series) grants, particularly those funding the quality and safety research that hospitalists often pursue. Agencies of the National Institutes of Health currently do not provide many opportunities for hospital‐based general internal medicine research, and thus academic hospitalist research is undervalued by many promotion committees.
Cross‐Cutting Issues
Challenges in leadership and mentorship were identified as cross‐cutting. Many AHM programs are young, and so are their leaders. As a result, hospital medicine leaders often lack the experience and skills necessary to successfully negotiate for the support that is critical for the ideal program's success. As a young field, hospital medicine lacks faculty who have succeeded in careers as hospitalists, have been promoted in tenure tracks, and can mentor and guide young faculty through the complexities of academic medicine. Absent leadership and mentoring, few hospital medicine programs will succeed in traditional academic pursuits.
Consensus Findings 2: Overcoming Challenges to the Development of AHM (Table 2)
Summit attendees spent considerable time developing and refining solutions to the challenges described previously. Addressing the challenges resulted in a diverse group of proposed products that included educating key stakeholders, designing meetings, courses, or workshops, and gathering and disseminating data. There was considerable overlap among the solutions (Table 2).
| Solutions | Proposed Products | Challenge Domains Addressed* |
|---|---|---|
| ||
| 1. Educate stakeholders | Workshops at professional society meetings (SHM, SGIM, ACGIM, APM, and APDIM) | Addresses all domains |
| Publications highlighting issues | ||
| 2. Define the sustainable job | Data gathering and publication | Clinical/financial |
| 3. Quality improvement portfolio | Development and dissemination of criteria for the QI portfolio | Research/promotion |
| 4. Hospitalist training/mentoring | Academic hospitalist boot camp | Teaching/education |
| Research/promotion | ||
| Cross‐cutting | ||
| 5. Enhance research career pathways | Advocacy for enhanced training programs and funding sources | Research/promotion |
| 6. Improved relationships among general medicine societies | Society collaboration on product development | Addresses all domains |
Outreach to and Education of Stakeholders in Academic Medicine
The focus of the educational and outreach efforts suggested by the consensus group is to help leaders in academic medicine (not just AHM) and academic medical centers understand the challenges facing AHM. More importantly, efforts should reinforce the value of academic hospitalists to their hospital, department, and division. Efforts to engage these critical stakeholders to discuss and potentially address a number of the conference's proposed solutions are needed. Leaders include deans of medical schools, chairs of departments of medicine, division chiefs, and hospital administrative leadership.
Suggested outreach and educational activities included the publication of articles in key journals with the goal of increasing the visibility of AHM in professional societies as well as meetings and workshops focusing on teaching hospitalists and academic leaders methods to overcome challenges. Professional societies with a stake in AHM should better understand the challenges and position themselves to address these issues. The AHM task forces of SHM and SGIM can help give academic hospitalists a voice in having their needs addressed.
Publications
Articles have been commissioned in the following areas: descriptions of challenges and proposed solutions, best practices for nonresident hospitalist services, and metrics for the success of hospital medicine programs.
Meetings/Workshops
Meetings and workshops, sponsored by professional societies with a vested interest in AHM, were thought to be an effective way to address the needs of hospitalists, particularly those pursuing careers as clinician educators. Such workshops would provide skills in teaching and early career survival (eg, how to bill correctly) and in developing an educator's portfolio. Leadership training offerings, perhaps building on examples from SHM and ACGIM, were also thought to be valuable resources and venues that should be directed toward hospitalists, their chiefs, and relevant leaders.
Defining a Sustainable Job Description for Academic Hospitalists
The group strongly endorsed the need for transparent and readily available data aimed at developing sustainable academic hospitalist positions. For example, required information would include how academic jobs are constructed (in terms of months on service per year and the number of nights or weekends of coverage) and what successful programs and their hospitalists have found to be acceptable. Over the longer term, empiric comparisons based on key metrics are needed to not only help guide career development and retention but also facilitate negotiations for programmatic support.
The group pointed out that embedded in delineating an optimal academic hospitalist job description is the longstanding work of general medicine societies in supporting and fostering the development of clinician educators. In many ways, the pressures of academic physicians to be mostly clinician and less educator versus someone who focuses heavily on educational work is similar for hospitalists and outpatient generalists. Academic general internal medicine divisions hired many general internists in the early 1990s to expand the reach of academic medical centers and increase the outpatient base.6 Many university hospitals are now hiring hospitalists to provide the inpatient care for these patients, but residency work hour reductions have added a layer of complexity, creating the need for entirely new roles for academic generalists (such as surgical comanagement of medically complex patients).7, 8 Past experiences in refining and reinforcing education as a key function (
Development of a Quality‐Improvement Portfolio Akin to an Educator's Portfolio
Many hospitalists actively participate in administrative work related to quality improvement activities, and we should develop this additional pathway for promotable academic activities (eg, clinician administrator); however, such a pathway may not be recognized by all promotion committees. The group observed that many aspects of quality improvement are similar to those of education (eg, developing a curriculum, leading a team, evaluating a process, defining generalizability, and disseminating locally proven interventions) and as such would be amenable to the development of a quality improvement portfolio, which candidates could submit to promotion committees. Again, past work in developing the importance and value of the educator's portfolio would facilitate the development of a quality improvement portfolio, which would require endorsement from key stakeholders (eg, the Association of Professors of Medicine, SGIM, and SHM).9 Importantly, this work may also benefit many outpatient‐based generalists who are increasingly focusing their careers on quality and safety improvement.
Developing Mentoring and Training Opportunities for Newly Hired and Junior Hospitalists
We reached a strong consensus about the need to develop a retreat‐format training opportunity by which junior academic hospitalists would be able to gain training in tasks critical to early‐career success. These were envisioned as an initial 2‐ to 3‐day meeting followed by mentorship at a distance and continued collaboration within the class of attendees. Topics would include key functions in AHM, such as becoming an effective attending physician and teacher, leadership, quality improvement, the business of medicine, effective billing, and maintaining a curriculum vitae. A number of professional societies have developed leadership or mentoring retreats, and at the time of this article's preparation, both regional and national efforts were underway to develop these products.
Developing Training and Mentorship Pathways for Hospitalist Researchers
There are few funded hospitalist researchers in the midcareer phase and a small but growing number of academic hospitalists entering the field with a focus on research. Enhancing a pipeline of researchers is a critical need for the field, as cementing AHM as an equal member of the academic medical community will be predicated on the successful development of hospitalist investigators. To this end, academic hospitalist groups should be encouraged to partner with other established research units (particularly general internal medicine) to create mentoring relationships and increase collaborative activities. The emergence of the Clinical and Translational Science Awards consortium sites, with a focus on implementation and effectiveness research, may also provide local opportunities for hospitalists to partner in research important for early‐career grant submission. Furthermore, building the pipeline of academic hospitalist researchers will require a strong focus on identifying students and residents through outreach at individual sites as well as presentations at national meetings (eg, the American College of Physicians).
Two other issues were also thought to be important. First, professional societies should work to encourage funders of primary carefocused general medicine training programs (the National Research Service Awards and the Health Resources and Services Administration) to allow hospitalists to qualify for such critical research training. Second, continuing to advocate for increasing funding for implementation and effectiveness research, via either the Agency for Healthcare Research and Quality or individual agencies of the National Institutes of Health, will be key; the emergence of a medical effectiveness institute would also be a potential boon.
Improving Relationships Between the Professional Homes of Academic Generalists
Relationships between outpatient‐based general medicine and hospital medicine were rocky as the field of AHM first took shape, and some residua of initial tensions persist a decade later. These tensions persist in part because hospitalists remain underdeveloped members of the academic community, and this perhaps gives some license to aver that hospitalists are merely transient faculty in a stage between residency and fellowship hired to improve throughput.
Overcoming this perception will require more engagement between academic generalists of all types, not less. The consensus group felt strongly that there need not be a single professional home for academic hospitalists and that generalists should be willing and even encouraged to self‐identify as hospital‐ or clinic‐focused, much as they might be geriatrics‐focused, informatics‐focused, or women's healthfocused. In fact, in some academic centers, a few generalists have successfully integrated themselves into both clinic‐based and hospitalist roles. In this way, the emergence and growth of AHM should be viewed as a boon to the practice of general medicine, not a challenge.
Resources
Much of what is proposed to enhance AHM will require resources. Academic hospitals have a vested interest in supporting AHM as a way to reduce turnover in a group that is increasingly critical for hospital operations, not to mention key leadership roles. Negotiating for these resources should emphasize that hospitals benefit directly from the revenue and margin that comes from incremental hospital admissions, collect most of the federal graduate medical education dollars, and benefit from improved care processes that are a result of hospitalist quality improvement efforts.
Deans and Departments, a key audience for the conference findings, also have a clear stake in fostering a less transient, more professionally satisfied and academically successful work force, particularly when hospitalists are increasingly the key educators of medical residents. Moreover, schools have a vested interest in the academic accomplishments and national reputation of their hospitalists. The financial arrangements will be unique to each setting and institution, and it is clear that the sources to be tapped will vary from site to site, but these resources are clearly necessary for the field.
Conclusions
AHM is at a crossroads. Unparalleled growth has created a large cadre of hospitalists who are struggling to meet the clinical demands of practice and the requirements for academic promotion; this situation will likely lead to, at a minimum, worsening problems with faculty turnover, and even greater losses of talented and passionate clinicians from the field of academic General Internal Medicine.
The challenges are numerous but not insurmountable, and our process identified issues and potential solutions which address clinical, educational, and research aspects of academic hospitalists' lives. We acknowledge that our findings are most relevant to hospitalists at academic medical centers or large academically oriented community teaching hospitals rather than hospitalists at community hospitals whose work is predominantly clinical with smaller teaching roles. However, we feel the academic hospitalists we targeted are in greater need of assistance. We believe that the most important issues are unsustainable, nonacademic positions, poor job preparation and training, inadequate prioritization of academic roles, and insufficient leadership and mentoring within the field.
It is the hope of all the consensus conference attendees that efforts focusing on academic hospitalists in the short term are not viewed as effort diverted from general internal medicine; in fact, the group felt that while many of the products of the consensus conference were probably most needed by AHM in the short term, these same solutions would likely be useful to outpatient‐based generalists as well. Despite the concerns and challenges outlined, the consensus conference group was also very hopeful that, in the setting where resources and collaboration are appropriately marshaled, that AHM will flourish quickly. In doing so, academic hospitalists will become better role models for residents and students, attracting the next generation of generalists needed to provide care to an increasingly complex patient population, and further advance the mission of General Internal Medicine.
Acknowledgements
The authors thank Dr. Jeff Glasheen and Dr. Robert Wachter for their comments on an earlier version of this article. In addition, the authors thank the following conference participants: Dan Brotman, MD, Johns Hopkins University; Deborah M. DeMarco, MD, President of the Association of Program Directors in Internal Medicine; Jeff Glasheen, MD, University of Colorado; Rusty Holman, MD, President of the Society of Hospital Medicine; Martha A. Hooven, President of the Administrators of Internal Medicine; Peter Kaboli, MD, University of Iowa; David O Meltzer, MD, PhD, University of Chicago; Vikas Parekh, MD, University of Michigan; Russell Phillips, MD MPH, Harvard Medical School; Sanjay Saint, MD, MPH, University of Michigan; Barbara Schuster, MD, President of the Association of Professors of Medicine; Brad Sharpe, MD, University of California San Francisco; Jeff Wiese, MD, Tulane University; David Kushner, Facilitator of the Kushner Companies; Geri Barnes, Support Staff of the Society of Hospital Medicine; and Amy Woodward, Support Staff of the Society of General Internal Medicine.
The past decade has seen hospital medicine grow from fewer than 1000 hospitalists nationwide to more than 20,000.1 In fact, survey data suggest that hospital medicine is the fastest growing field of internal medicine in the history of the US, and the growth of hospital medicine has produced a net increase in the number of generalists in the US.2
Although few direct estimates exist, academic hospital medicine (AHM) is also growing rapidly.1 Fueled by potential efficiency gains, a need for increased educational oversight of teaching services, and new residency work hour limitations, many academic medical centers and teaching hospitals have developed large hospital medicine programs. Internal medicine residency graduates interested in general medicine are finding hospital medicine an increasingly popular career choice. As a result, AHM groups have many recent residency graduates with an average age that is generally younger than 40.3
Over 85% of hospitalists are generalists and should find natural alliances with the nonhospitalist side of general internal medicine by collaborating in the course of clinical care, by teaching residents and students, or by designing quality improvement or research projects. In many academic centers, hospitalists are part of the division of general internal medicine, whereas in a few centers, hospitalists either have a separate division or lie outside the internal medicine department (employed by their hospitals).
Despite sharing a common training background and generalist mindset, many new academic hospitalists face different challenges than those faced by pure outpatient‐based academic generalists. First, at many centers, the financial arrangements between the AHM group and the hospital discourage hospitalists from traditional academic pursuits and draw them into clinical, operational, or administrative duties (such as responsibility for utilization review) that, although locally valuable, may not count as academic products in themselves or may take time away from more academic activities. Close alignment between hospitals and AHM may result in hospital administrators dictating hospitalists' practice in a way that further impedes academic viability. Reductions in resident training hours and an increasing need to provide 24‐hour coverage have facilitated growth in AHM into roles beyond those of the traditional academic generalist, such as medical comanagement of surgical patients and coverage of nonteaching services.4, 5 The youth of the field may exacerbate these problems. Most academic hospitalist groups have few senior leaders, whether they are clinical‐, education‐, or research‐focused. Young faculty need senior leaders as mentors to buffer them from relentless clinical demands that would compromise their hopes for academic success.
In order to better characterize these concerns and develop a shared work plan for future activities in support of AHM, the Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM) convened an AHM consensus conference, a collaborative meeting developed and attended by representatives from SHM, SGIM, the Association of Chiefs of General Internal Medicine (ACGIM), the Association of Professors of Medicine, the Association of Program Directors in Internal Medicine, and the Association of Administrators in Internal Medicine. Using a structured consensus‐building format, we identified key barriers and challenges to AHM, then developed potential solutions.
Consensus Conference Format
Consensus Conference Steering Committee
The consensus conference was developed first by the sponsoring professional societies (SGIM, SHM, and ACGIM) being asked to nominate 2 people to be part of the consensus conference steering committee. The steering committee's main functions were to identify key tasks for the consensus conference, invite consensus conference attendees, ensure adequate representation from all participating organizations, synthesize the results of the consensus conference, and work with the individual professional societies so that results from the consensus conference were acted upon in a coordinated and effective manner.
Consensus Conference Prework
The consensus conference co‐chairs convened a series of conference calls in the spring of 2007, during which the steering committee developed a series of key areas to be explored during the conference. Topic areas were selected on the basis of the group's expertise and referred to past work by AHM taskforces convened by both SGIM/ACGIM and SHM.
The steering committee then invited stakeholders from each invited society so that each professional organization would provide at least 1 representative with expertise appropriate to 1 of the key domains identified:
-
Clinical and financial issues (within which topics such as optimal job descriptions and salary structures would be explored).
-
Teaching and education mission (within which topics such as mentorship for AHM junior faculty might be discussed).
-
Research and promotable activities (within which issues related to the development of promotable activities for AHM would be discussed).
Invitees to the consensus conference were assigned to one working group, given a general description of the potential areas within their domain, and instructed to consider a number of broad questions relevant to the topic area. These questions were as follows:
-
What are the key barriers to AHM in each key domain?
-
What viewpoints or barriers are the most pressing and/or actionable?
-
What solutions could be implemented or initiated in the next 1 to 3 years?
In order to facilitate discussion, consensus conference invitees were provided copies of findings from the SGIM/ACGIM and SHM Academic Hospitalist Task Forces, preliminary results from a survey of AHM leaders, and key literature related to the field.
Consensus Conference Format
The AHM consensus conference followed a modified Delphi consensus‐building format, in which the members of each working group developed findings relevant to their area, presented these viewpoints back to the overall group for feedback, and returned to their working group to refine their initial recommendations or move on to subsequent areas.
We used Day 1 of the meeting to confirm and refine lists of key barriers and opportunities to AHM. On Day 2, we developed actionable solutions and identified barriers with no ready solution but which were felt to be worth highlighting.
Each cycle of feedback (1 on Day 1 and 2 on Day 2) was used to identify additional barriers or opportunities prespecified by the steering committee, prioritize issues/opportunities, clarify uncertainties or point them out when they existed, and identify new areas requiring consensus. Between each cycle, workflow and interim results were summarized by the co‐chairs and a professional meeting coordinator to ensure that the group felt consensus had been achieved and to identify where additional work was required.
Writing Group/Peer Review
After the consensus conference adjourned, minutes were circulated to the group and approved, whereupon a summary of the meeting was reformatted into manuscript form. The manuscript was circulated to the steering committee, consensus conference attendees, and 2 selected peer reviewers as an additional check on the external validity of the study's results.
Consensus Findings 1: Current Challenges in AHM (Table 1)
Clinical and Financial Issues in AHM
The consensus group identified misalignment of the mission of hospitals (which often provide substantial financial support for hospital medicine programs) and the mission of departments of internal medicine (or divisions of general internal medicine) in which adult hospitalists reside as a fundamental barrier in AHM. Misalignment of missions produces challenges to the development of hospitalist groups in that their primary funder, the hospital, focuses on clinical care delivery, productivity, efficiency, and, in some cases, participation in patient safety and quality improvement efforts, whereas academic departments place considerable value on education, research, grants received, dissemination of scholarly work, and the national reputation of its faculty. Further exacerbating this tension is the fact that hospitalists do not always reside within traditional academic divisions (such as divisions of general medicine) and are therefore viewed by the hospital and their peers as hospital employees more than academic faculty.
As yet, few hospital medicine programs have successfully integrated academic and clinical needs. In many AHM programs, clinical demands have trumped academic pursuits and, as a result, produced jobs that have frequent turnover. This occurs most often when hospitalists are hired by academic medical centers primarily to staff nonresident services. Hospitalists who join these academic programs expecting ample opportunity to teach and pursue scholarly work often leave when they realize these jobs differ little from those in community settings (with the exception of less pay and, in most cases, a less efficient clinical delivery system). This turnover contributes to the perception of hospitalists as transient nonacademic faculty. The participants felt that we needed to define the ideal academic hospitalist job description.
| Clinical and Financial Issues | Teaching and Education Mission | Research and Promotable Activities | Cross‐Cutting Issues |
|---|---|---|---|
| |||
| Hospitalists' functions more often explicitly linked to hospital initiatives (clinical care, quality improvement, utilization, and throughput) | Distinguishing jobs that are predominantly clinical (C‐e) from those that are predominantly education‐focused (c‐E), which is important given the high clinical burdens | Lack of a pipeline producing hospitalist clinician investigators | Lack of leadership or negotiation skill training |
| Differing political, financial, and scientific priorities between hospitalists and administrators | Further exacerbation of C‐e/c‐E distinctions by the emergence of uncovered services | Few national funders focusing on inpatient general internal medicine | Little infrastructure for academic functions |
| Little guidance on the best models for each job type | Little recognition of quality improvement as a promotable/testable activity | Rapidly moving/growing field | |
| Decreasing interest in general internal medicine as a career path | |||
Teaching and Education Mission in AHM
Traditionally, faculty in academic medical centers have had prominent roles in resident teaching services, supervising medical residents, interns, and students. Hospitalists fill these roles at some institutions and in many cases have replaced senior faculty who are no longer able (because of competing demands from clinics or labs) or willing (because of an increased need for oversight and availability) to staff the teaching service. The teaching hospitalists start at these positions straight out of residency with little experience, training, or mentoring in how to succeed as a clinician educator. The creation of nonresident hospitalist services to address residency work hour requirements has removed many hospitalists from teaching opportunities as these services often have few if any teaching opportunities. The consensus group identified the lack of teaching opportunities and a lack of any formal preparation for those who do teach as the key challenges for new hospitalist clinician educators.
Research and Promotable Activities in AHM
Numerous challenges to promotion and success in hospital medicine research were identified. Most conference attendees felt that chairs of departments of medicine do not fully understand what the roles of academic hospitalists are, how they fit into the department's mission, or what is needed to better integrate hospitalists into the research and academic activities of the department. In addition, there are few hospital medicine fellowship programs, and those that have been created focus primarily on improving teaching skills or quality improvement rather than on research or the development of academic products. Aspiring academic hospitalists could pursue research fellowship training in existing programs (ie, the Robert Wood Johnson Foundation), but few graduates currently pursue these opportunities, and federally funded fellowships (eg, the National Research Service Awards and Health Resources and Services Administration T32 awards) explicitly exclude physicians who are not focused on primary care research. The group noted that a number of Veterans Administration fellowships (such as the Quality Scholars programs) may provide avenues for the training of hospital medicinefocused researchers, but they have been underused.
For researchers who focus on hospital medicine, federal funding sources are limited for both career development awards (K‐series) and later (R‐series) grants, particularly those funding the quality and safety research that hospitalists often pursue. Agencies of the National Institutes of Health currently do not provide many opportunities for hospital‐based general internal medicine research, and thus academic hospitalist research is undervalued by many promotion committees.
Cross‐Cutting Issues
Challenges in leadership and mentorship were identified as cross‐cutting. Many AHM programs are young, and so are their leaders. As a result, hospital medicine leaders often lack the experience and skills necessary to successfully negotiate for the support that is critical for the ideal program's success. As a young field, hospital medicine lacks faculty who have succeeded in careers as hospitalists, have been promoted in tenure tracks, and can mentor and guide young faculty through the complexities of academic medicine. Absent leadership and mentoring, few hospital medicine programs will succeed in traditional academic pursuits.
Consensus Findings 2: Overcoming Challenges to the Development of AHM (Table 2)
Summit attendees spent considerable time developing and refining solutions to the challenges described previously. Addressing the challenges resulted in a diverse group of proposed products that included educating key stakeholders, designing meetings, courses, or workshops, and gathering and disseminating data. There was considerable overlap among the solutions (Table 2).
| Solutions | Proposed Products | Challenge Domains Addressed* |
|---|---|---|
| ||
| 1. Educate stakeholders | Workshops at professional society meetings (SHM, SGIM, ACGIM, APM, and APDIM) | Addresses all domains |
| Publications highlighting issues | ||
| 2. Define the sustainable job | Data gathering and publication | Clinical/financial |
| 3. Quality improvement portfolio | Development and dissemination of criteria for the QI portfolio | Research/promotion |
| 4. Hospitalist training/mentoring | Academic hospitalist boot camp | Teaching/education |
| Research/promotion | ||
| Cross‐cutting | ||
| 5. Enhance research career pathways | Advocacy for enhanced training programs and funding sources | Research/promotion |
| 6. Improved relationships among general medicine societies | Society collaboration on product development | Addresses all domains |
Outreach to and Education of Stakeholders in Academic Medicine
The focus of the educational and outreach efforts suggested by the consensus group is to help leaders in academic medicine (not just AHM) and academic medical centers understand the challenges facing AHM. More importantly, efforts should reinforce the value of academic hospitalists to their hospital, department, and division. Efforts to engage these critical stakeholders to discuss and potentially address a number of the conference's proposed solutions are needed. Leaders include deans of medical schools, chairs of departments of medicine, division chiefs, and hospital administrative leadership.
Suggested outreach and educational activities included the publication of articles in key journals with the goal of increasing the visibility of AHM in professional societies as well as meetings and workshops focusing on teaching hospitalists and academic leaders methods to overcome challenges. Professional societies with a stake in AHM should better understand the challenges and position themselves to address these issues. The AHM task forces of SHM and SGIM can help give academic hospitalists a voice in having their needs addressed.
Publications
Articles have been commissioned in the following areas: descriptions of challenges and proposed solutions, best practices for nonresident hospitalist services, and metrics for the success of hospital medicine programs.
Meetings/Workshops
Meetings and workshops, sponsored by professional societies with a vested interest in AHM, were thought to be an effective way to address the needs of hospitalists, particularly those pursuing careers as clinician educators. Such workshops would provide skills in teaching and early career survival (eg, how to bill correctly) and in developing an educator's portfolio. Leadership training offerings, perhaps building on examples from SHM and ACGIM, were also thought to be valuable resources and venues that should be directed toward hospitalists, their chiefs, and relevant leaders.
Defining a Sustainable Job Description for Academic Hospitalists
The group strongly endorsed the need for transparent and readily available data aimed at developing sustainable academic hospitalist positions. For example, required information would include how academic jobs are constructed (in terms of months on service per year and the number of nights or weekends of coverage) and what successful programs and their hospitalists have found to be acceptable. Over the longer term, empiric comparisons based on key metrics are needed to not only help guide career development and retention but also facilitate negotiations for programmatic support.
The group pointed out that embedded in delineating an optimal academic hospitalist job description is the longstanding work of general medicine societies in supporting and fostering the development of clinician educators. In many ways, the pressures of academic physicians to be mostly clinician and less educator versus someone who focuses heavily on educational work is similar for hospitalists and outpatient generalists. Academic general internal medicine divisions hired many general internists in the early 1990s to expand the reach of academic medical centers and increase the outpatient base.6 Many university hospitals are now hiring hospitalists to provide the inpatient care for these patients, but residency work hour reductions have added a layer of complexity, creating the need for entirely new roles for academic generalists (such as surgical comanagement of medically complex patients).7, 8 Past experiences in refining and reinforcing education as a key function (
Development of a Quality‐Improvement Portfolio Akin to an Educator's Portfolio
Many hospitalists actively participate in administrative work related to quality improvement activities, and we should develop this additional pathway for promotable academic activities (eg, clinician administrator); however, such a pathway may not be recognized by all promotion committees. The group observed that many aspects of quality improvement are similar to those of education (eg, developing a curriculum, leading a team, evaluating a process, defining generalizability, and disseminating locally proven interventions) and as such would be amenable to the development of a quality improvement portfolio, which candidates could submit to promotion committees. Again, past work in developing the importance and value of the educator's portfolio would facilitate the development of a quality improvement portfolio, which would require endorsement from key stakeholders (eg, the Association of Professors of Medicine, SGIM, and SHM).9 Importantly, this work may also benefit many outpatient‐based generalists who are increasingly focusing their careers on quality and safety improvement.
Developing Mentoring and Training Opportunities for Newly Hired and Junior Hospitalists
We reached a strong consensus about the need to develop a retreat‐format training opportunity by which junior academic hospitalists would be able to gain training in tasks critical to early‐career success. These were envisioned as an initial 2‐ to 3‐day meeting followed by mentorship at a distance and continued collaboration within the class of attendees. Topics would include key functions in AHM, such as becoming an effective attending physician and teacher, leadership, quality improvement, the business of medicine, effective billing, and maintaining a curriculum vitae. A number of professional societies have developed leadership or mentoring retreats, and at the time of this article's preparation, both regional and national efforts were underway to develop these products.
Developing Training and Mentorship Pathways for Hospitalist Researchers
There are few funded hospitalist researchers in the midcareer phase and a small but growing number of academic hospitalists entering the field with a focus on research. Enhancing a pipeline of researchers is a critical need for the field, as cementing AHM as an equal member of the academic medical community will be predicated on the successful development of hospitalist investigators. To this end, academic hospitalist groups should be encouraged to partner with other established research units (particularly general internal medicine) to create mentoring relationships and increase collaborative activities. The emergence of the Clinical and Translational Science Awards consortium sites, with a focus on implementation and effectiveness research, may also provide local opportunities for hospitalists to partner in research important for early‐career grant submission. Furthermore, building the pipeline of academic hospitalist researchers will require a strong focus on identifying students and residents through outreach at individual sites as well as presentations at national meetings (eg, the American College of Physicians).
Two other issues were also thought to be important. First, professional societies should work to encourage funders of primary carefocused general medicine training programs (the National Research Service Awards and the Health Resources and Services Administration) to allow hospitalists to qualify for such critical research training. Second, continuing to advocate for increasing funding for implementation and effectiveness research, via either the Agency for Healthcare Research and Quality or individual agencies of the National Institutes of Health, will be key; the emergence of a medical effectiveness institute would also be a potential boon.
Improving Relationships Between the Professional Homes of Academic Generalists
Relationships between outpatient‐based general medicine and hospital medicine were rocky as the field of AHM first took shape, and some residua of initial tensions persist a decade later. These tensions persist in part because hospitalists remain underdeveloped members of the academic community, and this perhaps gives some license to aver that hospitalists are merely transient faculty in a stage between residency and fellowship hired to improve throughput.
Overcoming this perception will require more engagement between academic generalists of all types, not less. The consensus group felt strongly that there need not be a single professional home for academic hospitalists and that generalists should be willing and even encouraged to self‐identify as hospital‐ or clinic‐focused, much as they might be geriatrics‐focused, informatics‐focused, or women's healthfocused. In fact, in some academic centers, a few generalists have successfully integrated themselves into both clinic‐based and hospitalist roles. In this way, the emergence and growth of AHM should be viewed as a boon to the practice of general medicine, not a challenge.
Resources
Much of what is proposed to enhance AHM will require resources. Academic hospitals have a vested interest in supporting AHM as a way to reduce turnover in a group that is increasingly critical for hospital operations, not to mention key leadership roles. Negotiating for these resources should emphasize that hospitals benefit directly from the revenue and margin that comes from incremental hospital admissions, collect most of the federal graduate medical education dollars, and benefit from improved care processes that are a result of hospitalist quality improvement efforts.
Deans and Departments, a key audience for the conference findings, also have a clear stake in fostering a less transient, more professionally satisfied and academically successful work force, particularly when hospitalists are increasingly the key educators of medical residents. Moreover, schools have a vested interest in the academic accomplishments and national reputation of their hospitalists. The financial arrangements will be unique to each setting and institution, and it is clear that the sources to be tapped will vary from site to site, but these resources are clearly necessary for the field.
Conclusions
AHM is at a crossroads. Unparalleled growth has created a large cadre of hospitalists who are struggling to meet the clinical demands of practice and the requirements for academic promotion; this situation will likely lead to, at a minimum, worsening problems with faculty turnover, and even greater losses of talented and passionate clinicians from the field of academic General Internal Medicine.
The challenges are numerous but not insurmountable, and our process identified issues and potential solutions which address clinical, educational, and research aspects of academic hospitalists' lives. We acknowledge that our findings are most relevant to hospitalists at academic medical centers or large academically oriented community teaching hospitals rather than hospitalists at community hospitals whose work is predominantly clinical with smaller teaching roles. However, we feel the academic hospitalists we targeted are in greater need of assistance. We believe that the most important issues are unsustainable, nonacademic positions, poor job preparation and training, inadequate prioritization of academic roles, and insufficient leadership and mentoring within the field.
It is the hope of all the consensus conference attendees that efforts focusing on academic hospitalists in the short term are not viewed as effort diverted from general internal medicine; in fact, the group felt that while many of the products of the consensus conference were probably most needed by AHM in the short term, these same solutions would likely be useful to outpatient‐based generalists as well. Despite the concerns and challenges outlined, the consensus conference group was also very hopeful that, in the setting where resources and collaboration are appropriately marshaled, that AHM will flourish quickly. In doing so, academic hospitalists will become better role models for residents and students, attracting the next generation of generalists needed to provide care to an increasingly complex patient population, and further advance the mission of General Internal Medicine.
Acknowledgements
The authors thank Dr. Jeff Glasheen and Dr. Robert Wachter for their comments on an earlier version of this article. In addition, the authors thank the following conference participants: Dan Brotman, MD, Johns Hopkins University; Deborah M. DeMarco, MD, President of the Association of Program Directors in Internal Medicine; Jeff Glasheen, MD, University of Colorado; Rusty Holman, MD, President of the Society of Hospital Medicine; Martha A. Hooven, President of the Administrators of Internal Medicine; Peter Kaboli, MD, University of Iowa; David O Meltzer, MD, PhD, University of Chicago; Vikas Parekh, MD, University of Michigan; Russell Phillips, MD MPH, Harvard Medical School; Sanjay Saint, MD, MPH, University of Michigan; Barbara Schuster, MD, President of the Association of Professors of Medicine; Brad Sharpe, MD, University of California San Francisco; Jeff Wiese, MD, Tulane University; David Kushner, Facilitator of the Kushner Companies; Geri Barnes, Support Staff of the Society of Hospital Medicine; and Amy Woodward, Support Staff of the Society of General Internal Medicine.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- ,,,,,.Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21:1079–1085.
- Society of Hospital Medicine. 2006 Hospital Medicine Survey. Available at: http://www.hospitalmedicine.org/content/navigationmenu/media/mediakit/media_kit.htm. Accessed January 2009.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- UCLA rewrites the script for academic networks.Med Netw Strategy Rep.1998;7:1–5.
- ,,,,,.Systematic review: effects of resident work hours on patient safety.Ann Intern Med.2004;141:851–857.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Documentation systems for educators seeking academic promotion in U.S. medical schools.Acad Med.2004;79:783–790.
- ,,,.The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- ,,,,,.Trends in market demand for internal medicine 1999 to 2004: an analysis of physician job advertisements.J Gen Intern Med.2006;21:1079–1085.
- Society of Hospital Medicine. 2006 Hospital Medicine Survey. Available at: http://www.hospitalmedicine.org/content/navigationmenu/media/mediakit/media_kit.htm. Accessed January 2009.
- ,,,,,.Effects of work hour reduction on residents' lives: a systematic review.JAMA.2005;294:1088–1100.
- ,.Hospitalists in teaching hospitals: opportunities but not without danger.J Gen Intern Med.2004;19:392–393.
- UCLA rewrites the script for academic networks.Med Netw Strategy Rep.1998;7:1–5.
- ,,,,,.Systematic review: effects of resident work hours on patient safety.Ann Intern Med.2004;141:851–857.
- ,.The expanding role of hospitalists in the United States.Swiss Med Wkly.2006;136:591–596.
- ,,,.Documentation systems for educators seeking academic promotion in U.S. medical schools.Acad Med.2004;79:783–790.
The latest research you need to know
Literature at a Glance
A guide to this month’s studies.
- Score predicts risk of intracerebral hemorrhage after thrombolysis.
- Trigylcerides and stroke-risk predictors.
- PPI use and risk of community-acquired pneumonia.
- Clopidogrel before coronary intervention might improve outcomes.
- High-dose clopidogrel after coronary intervention is beneficial.
- B-type natriuretic peptide level and sepsis.
- Thrombolytic use in pulmonary embolism.
- Hospitalists and ED patient flow.
Simple Clinical Score Predicts Intracerebral Hemorrhage after Thrombolysis
Clinical question: Is there a simple scoring tool that will predict the risk of intracerebral hemorrhage (ICH) following IV tissue-plasminogen activator (t-PA) in ischemic strokes?
Background: The use of t-PA in acute ischemic stroke (AIS) is about 2% to 4%, due in part to fear of conversion of an ischemic event to an ICH. Several studies using t-PA after AIS have identified risk factors for ICH; however, none has looked at the cumulative risk and prognosis for an individual candidate based on these factors.
Study design: Retrospective, observational cohort study.
Setting: The National Institute of Neurological Disorders and Stroke Trials 1 and 2, and consecutive patients treated at Beth Israel Deaconess Medical Center, Boston.
Synopsis: After an extensive literature review, a five-point scale to determine the risk of hemorrhage after t-PA (HAT) was developed using the top four predictive factors based on odds ratios. These included the National Institutes of Health Stroke Scale (NIHSS), presence and extent of hypodensity on initial CT scan, history of diabetes, and high baseline serum glucose. The predictive value of this scale was tested against two independent cohorts of patients with AIS treated with IV t-PA. The HAT scale was able to reasonably predict both the risk of ICH following t-PA and the functional outcome at 90 days. Higher scores on the scale tended to do worse, especially scores of three or more. Its retrospective nature and small number of patients experiencing ICH limit this study.
Bottom line: The HAT score is a quick bedside tool that can help in the counseling of patients and families in conjunction with the risks and benefits of t-PA after ischemic stroke.
Citation: Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71:1417-1423.
Nonfasting Triglycerides Predict Stroke Risk
Clinical question: Is there a correlation between nonfasting triglyceride levels and ischemic stroke?
Background: Most individuals are in a nonfasting state, with the exception of several hours prior to breakfast. Fasting cholesterol levels exclude most remnant lipoproteins, which might play a role in early atherosclerotic disease. Increased levels of triglycerides in a nonfasting state indicate the presence of these remnants.
Study design: Prospective, population-based cohort study.
Setting: The Copenhagen City Heart Study.
Synopsis: The study included 13,956 individuals between the ages of 20 and 93 with a follow-up period of up to 31 years. Cholesterol levels were checked during four evaluation periods: 1976-1978, 1981-1983, 1991-1994, and 2001-2003. Eighty-two percent of the participants had eaten a meal within three hours of the blood draw; the other 18% had eaten more than three hours prior to the draw. The study showed an association between increasing nonfasting triglyceride levels and a step-wise increase in the risk of ischemic stroke. The highest risk came in individuals with nonfasting triglyceride levels > 443mg/dl, which was associated with a three- to fourfold greater risk of ischemic stroke. The study was limited in that it evaluated a homogenous group of individuals, which may not reflect other racial or ethnic populations.
Bottom line: Increasing levels of nonfasting triglycerides are associated with an increased risk of ischemic stroke.
Citation: Freiberg J, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300(18):2142-2152.
Proton-Pump Inhibitor (PPI) Use Increases the Risk of Community-Acquired Pneumonia (CAP)
Clinical question: Is there an association between PPI use and CAP?
Background: CAP is associated with significant morbidity, annually accounting for billions of healthcare dollars. Proton-pump inhibitors (PPI) are a mainstay treatment for gastric acid suppression. Previous studies have suggested using PPIs may increase the risk of developing CAP.
Study design: Nested case control study.
Setting: Outpatient general practices, United Kingdom.
Synopsis: The association between PPI use and CAP was evaluated in a cohort of more than 7 million patients using the UK’s general-practice research database. Eligible participants were divided into two groups: case patients and control patients. Initial results indicated an increased risk of CAP with PPI use. After adjusting for confounding variables, the use of a PPI was strongly associated with CAP development when used within 30 days prior of the diagnosis, and most notably within 48 hours of diagnosis. It also was noted that the risk of developing CAP with longer-term PPI use was much lower. This inverse temporal relationship was noted in two previous studies. The limitations of this study were related to presumed adherence and compliance with PPI therapy. There also was no radiographic data to support the diagnosis of pneumonia in these cases, both of which could bias the results.
Bottom line: There appears to be an increased risk of CAP with PPI use. This risk is most notable within 48 hours. However, long-term, chronic PPI use was not associated with an increased risk of CAP.
Citation: Sarkar M, Hennessy S, Yang YX. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008;149:391-398.
Clopidogrel Prior to Percutaneous Intervention (PCI) Might Improve Outcomes in Patients with Acute ST-Elevation Myocardial Infarction (STEMI)
Clinical question: Does pretreatment with clopidogrel prior to PCI in acute STEMI improve outcomes?
Background: Extant guidelines for early utilization of clopidogrel in STEMI patients are based on results of studies of patients with non-ST-elevation acute coronary syndromes or treatment with thrombolytics.
Study design: Systematic review.
Setting: MEDLINE and Cochrane Controlled Trials Register of randomized controlled trials.
Synopsis: The authors selected 38 treatment groups, including 8,429 patients with STEMI who underwent primary PCI. They found a statistically significant difference in initial patency, and further found clopidogrel pretreatment was an independent predictor of early reperfusion and improved clinical outcome. This study suggests a benefit to pretreatment with clopidogrel but likely is not sufficient to establish such pretreatment as the standard of care. The limitations of this study were a retrospective review/meta-analysis, as the ability to limit the influence of confounding variables is reduced.
Bottom line: Pretreatment with clopidogrel in patients with acute STEMI undergoing primary PCI appears beneficial based on the results of this review of available evidence.
Citation: Vlaar PJ, Svilaas T, Damman K, et al. Impact of pretreatment with clopidogrel on initial patency and outcomes in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836.
High-Dose Clopidogrel after PCI Is Beneficial
Clinical question: Does high-dose clopidogrel improve patient outcome following PCI?
Background: Studies have shown antiplatelet resistance after PCI is associated with an increased risk of cardiovascular events, including in-stent thrombosis and death. Other studies have shown the benefit of high-dose clopidogrel by the inhibition of platelet aggregation. Limited information is available regarding the applicability to patients after PCI.
Study design: Retrospective study of 2,954 consecutive patients divided into two groups, low-dose and high-dose clopidogrel use.
Setting: Single hospital in France.
Synopsis: The low-dose study group undergoing PCI was pretreated with 300 mg clopidogrel, followed by ASA 75 mg and clopidogrel 75 mg daily for two months. The second group undergoing PCI was pretreated with 600 mg clopidogrel followed by ASA 75 mg and clopidogrel 150 mg for 15 days, then maintained on ASA 75 mg and clopidogrel 75 mg. Patients received follow-up at two months and were evaluated for in-stent thrombosis, myocardial infarction (MI), death, and hemorrhagic complications. The two groups were matched one-to-one using propensity scoring and the nearest-pair-matching method blinded to patient outcome.
The high-dose clopidogrel group showed a decreased incidence of MI, in-stent thrombosis, and death. This benefit confirms the importance of achieving early and adequate antiplatelet therapy. However, the study authors noted a higher percentage of major bleeding and minor bleeding, although the increase was not statistically significant (2.8% vs. 3.5%, P=0.379, and 7.4% vs. 8.2%, P=0.699, respectively).
Bottom line: High-dose clopidogrel before and within the first 15 days after PCI decreases the risk of MI, in-stent thrombosis, and death, with no statistical increase in bleeding complications. Long-range studies beyond the two-month interval might be beneficial.
Citation: Lemesle G, Delhaye C, Sudre A, et al. Impact of high loading and maintenance dose of clopidogrel within the first 15 days after percutaneous coronary intervention on patient outcome. Am Heart J. 2008;10:1-8.
B-Type Natriuretic Peptide (BNP) Identifies Patients Developing Sepsis-Induced Myocardial Depression
Clinical question: Can plasma BNP be used as a marker to identify patients at risk for sepsis-induced depression of myocardial function?
Background: Previous studies have established BNP levels are increased in patients with septic shock but have not examined the relationship between plasma BNP concentration and left ventricular (LV) systolic dysfunction.
Study design: Prospective cohort.
Setting: Academic medical center.
Synopsis: The authors divided 93 prospectively selected ICU patients with severe sepsis into two groups: one with normal left ventricular (LV) function and a group with LV systolic dysfunction. Comparison of the plasma BNP concentrations between these two groups demonstrated a significant positive correlation between the BNP level and the degree of LV systolic dysfunction, suggesting BNP is a reasonable marker for identification of septic patients with sepsis-induced myocardial depression.
Further, the study’s results suggest BNP measurements early in the course of septic shock might be useful prognostic indicators. However, it is unclear to what extent the knowledge gained from such measurements would alter care management, or how BNP compares to echocardiography in terms of diagnostic and prognostic utility. Thus, these results might not be adequate to justify the routine measurement of BNP in patients with severe sepsis.
Bottom line: Elevated BNP in septic patients is associated with the presence or risk of sepsis-induced myocardial depression, and might be a negative prognostic indicator.
Citation: Post F, Weilemann LS, Messow CM, Sinning C, Munzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–3037.
High Risk of Death with Thrombolytic Use in Low-Risk Pulmonary Embolism (PE)
Clinical question: Is there an advantage to thrombolytic therapy in the treatment of acute PE versus treatment with unfractionated or low-molecular-weight (LMW) heparin?
Background: Given the high mortality linked to PE, consistent indications for thrombolytic therapy in acute PE are needed. An assessment of the prevalence of thrombolytic therapy and mortality, as compared with standard anticoagulation, has been described inconsistently.
Study design: Retrospective cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using a database of ICD-9 codes, 15,116 patients were reviewed. Logistic regression was used to evaluate the association between thrombolytic therapy and 30-day mortality. Poisson regression was used to evaluate the association between thrombolytic therapy and in-hospital mortality. For those receiving thrombolysis and considered unlikely candidates for the therapy based on documentation at presentation (low predicted probability), the in-hospital mortality and overall 30-day mortality rate were higher when compared with those who did not receive thrombolysis. An exception to this was a group of patients with high predicted probability of receiving thrombolysis. In this group, thrombolysis was not associated with increased risk. Limitations to the study include lack of assessment of right ventricular function, changes in condition after presentation, lack of long-term outcomes, and lack of exact cause of death.
Bottom line: Thrombolytic therapy is associated with higher mortality in patients with hemodynamically uncomplicated PE, and therefore not indicated. Thrombolytic therapy in a subgroup of patients with hemodynamic instability or right ventricular dysfunction improves the clinical course and outcome.
Citation: Ibrahim SA, Stone RA, Obrosky S, Geng M, Fine MJ, Aujesky D. Thrombolytic therapy and mortality in patients with acute pulmonary embolism. Arch Intern Med. 2008;168(20):2183-2190.
Hospitalists Improve Patient Flow in the ED
Clinical question: Can active-bed management by hospitalists reduce ED throughput times and diversionary status?
Background: ED overcrowding leads to ambulance diversion, which has been associated with increased mortality. A primary cause of ED crowding is inpatient boarding, which can reduce patient satisfaction and quality of care. Previous studies targeting the ED have had little impact on throughput and ambulance diversion.
Study design: Pre-post case study in a single institution.
Setting: Academic teaching hospital in Baltimore.
Synopsis: ED throughput times and ambulance diversion hours were measured for all adult patients registered in the department from November 2005 to February 2006 (control period) and November 2006 to February 2007 (intervention period). Active-bed management was defined as appointing a hospitalist to assess bed availability in real time and assigning department of medicine admissions to the appropriate clinical setting, as well as the creation of a bed director. Although the ED census was 8.8% higher during the intervention period, throughput time for admitted patients decreased by 98 minutes per patient, to 458 from 360. The time spent under diversionary status for overcrowding or lack of ICU beds decreased by 6% and 27%, respectively. Limitations of this study include the pre-post design and the implementation at a single institution. Additionally, active-bed management is expensive, and in this case required the hiring of three full-time-equivalent faculty. However, this study successfully demonstrates that a quality improvement partnership between hospitalists and the ED can substantially reduce overcrowding.
Bottom line: Active-bed management by hospitalists improves ED throughput by decreasing the length of time admitted patients spend in the ED and reducing ambulance diversion hours.
Citation: Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Int Med. 2008;149(11):804-810.
Literature at a Glance
A guide to this month’s studies.
- Score predicts risk of intracerebral hemorrhage after thrombolysis.
- Trigylcerides and stroke-risk predictors.
- PPI use and risk of community-acquired pneumonia.
- Clopidogrel before coronary intervention might improve outcomes.
- High-dose clopidogrel after coronary intervention is beneficial.
- B-type natriuretic peptide level and sepsis.
- Thrombolytic use in pulmonary embolism.
- Hospitalists and ED patient flow.
Simple Clinical Score Predicts Intracerebral Hemorrhage after Thrombolysis
Clinical question: Is there a simple scoring tool that will predict the risk of intracerebral hemorrhage (ICH) following IV tissue-plasminogen activator (t-PA) in ischemic strokes?
Background: The use of t-PA in acute ischemic stroke (AIS) is about 2% to 4%, due in part to fear of conversion of an ischemic event to an ICH. Several studies using t-PA after AIS have identified risk factors for ICH; however, none has looked at the cumulative risk and prognosis for an individual candidate based on these factors.
Study design: Retrospective, observational cohort study.
Setting: The National Institute of Neurological Disorders and Stroke Trials 1 and 2, and consecutive patients treated at Beth Israel Deaconess Medical Center, Boston.
Synopsis: After an extensive literature review, a five-point scale to determine the risk of hemorrhage after t-PA (HAT) was developed using the top four predictive factors based on odds ratios. These included the National Institutes of Health Stroke Scale (NIHSS), presence and extent of hypodensity on initial CT scan, history of diabetes, and high baseline serum glucose. The predictive value of this scale was tested against two independent cohorts of patients with AIS treated with IV t-PA. The HAT scale was able to reasonably predict both the risk of ICH following t-PA and the functional outcome at 90 days. Higher scores on the scale tended to do worse, especially scores of three or more. Its retrospective nature and small number of patients experiencing ICH limit this study.
Bottom line: The HAT score is a quick bedside tool that can help in the counseling of patients and families in conjunction with the risks and benefits of t-PA after ischemic stroke.
Citation: Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71:1417-1423.
Nonfasting Triglycerides Predict Stroke Risk
Clinical question: Is there a correlation between nonfasting triglyceride levels and ischemic stroke?
Background: Most individuals are in a nonfasting state, with the exception of several hours prior to breakfast. Fasting cholesterol levels exclude most remnant lipoproteins, which might play a role in early atherosclerotic disease. Increased levels of triglycerides in a nonfasting state indicate the presence of these remnants.
Study design: Prospective, population-based cohort study.
Setting: The Copenhagen City Heart Study.
Synopsis: The study included 13,956 individuals between the ages of 20 and 93 with a follow-up period of up to 31 years. Cholesterol levels were checked during four evaluation periods: 1976-1978, 1981-1983, 1991-1994, and 2001-2003. Eighty-two percent of the participants had eaten a meal within three hours of the blood draw; the other 18% had eaten more than three hours prior to the draw. The study showed an association between increasing nonfasting triglyceride levels and a step-wise increase in the risk of ischemic stroke. The highest risk came in individuals with nonfasting triglyceride levels > 443mg/dl, which was associated with a three- to fourfold greater risk of ischemic stroke. The study was limited in that it evaluated a homogenous group of individuals, which may not reflect other racial or ethnic populations.
Bottom line: Increasing levels of nonfasting triglycerides are associated with an increased risk of ischemic stroke.
Citation: Freiberg J, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300(18):2142-2152.
Proton-Pump Inhibitor (PPI) Use Increases the Risk of Community-Acquired Pneumonia (CAP)
Clinical question: Is there an association between PPI use and CAP?
Background: CAP is associated with significant morbidity, annually accounting for billions of healthcare dollars. Proton-pump inhibitors (PPI) are a mainstay treatment for gastric acid suppression. Previous studies have suggested using PPIs may increase the risk of developing CAP.
Study design: Nested case control study.
Setting: Outpatient general practices, United Kingdom.
Synopsis: The association between PPI use and CAP was evaluated in a cohort of more than 7 million patients using the UK’s general-practice research database. Eligible participants were divided into two groups: case patients and control patients. Initial results indicated an increased risk of CAP with PPI use. After adjusting for confounding variables, the use of a PPI was strongly associated with CAP development when used within 30 days prior of the diagnosis, and most notably within 48 hours of diagnosis. It also was noted that the risk of developing CAP with longer-term PPI use was much lower. This inverse temporal relationship was noted in two previous studies. The limitations of this study were related to presumed adherence and compliance with PPI therapy. There also was no radiographic data to support the diagnosis of pneumonia in these cases, both of which could bias the results.
Bottom line: There appears to be an increased risk of CAP with PPI use. This risk is most notable within 48 hours. However, long-term, chronic PPI use was not associated with an increased risk of CAP.
Citation: Sarkar M, Hennessy S, Yang YX. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008;149:391-398.
Clopidogrel Prior to Percutaneous Intervention (PCI) Might Improve Outcomes in Patients with Acute ST-Elevation Myocardial Infarction (STEMI)
Clinical question: Does pretreatment with clopidogrel prior to PCI in acute STEMI improve outcomes?
Background: Extant guidelines for early utilization of clopidogrel in STEMI patients are based on results of studies of patients with non-ST-elevation acute coronary syndromes or treatment with thrombolytics.
Study design: Systematic review.
Setting: MEDLINE and Cochrane Controlled Trials Register of randomized controlled trials.
Synopsis: The authors selected 38 treatment groups, including 8,429 patients with STEMI who underwent primary PCI. They found a statistically significant difference in initial patency, and further found clopidogrel pretreatment was an independent predictor of early reperfusion and improved clinical outcome. This study suggests a benefit to pretreatment with clopidogrel but likely is not sufficient to establish such pretreatment as the standard of care. The limitations of this study were a retrospective review/meta-analysis, as the ability to limit the influence of confounding variables is reduced.
Bottom line: Pretreatment with clopidogrel in patients with acute STEMI undergoing primary PCI appears beneficial based on the results of this review of available evidence.
Citation: Vlaar PJ, Svilaas T, Damman K, et al. Impact of pretreatment with clopidogrel on initial patency and outcomes in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836.
High-Dose Clopidogrel after PCI Is Beneficial
Clinical question: Does high-dose clopidogrel improve patient outcome following PCI?
Background: Studies have shown antiplatelet resistance after PCI is associated with an increased risk of cardiovascular events, including in-stent thrombosis and death. Other studies have shown the benefit of high-dose clopidogrel by the inhibition of platelet aggregation. Limited information is available regarding the applicability to patients after PCI.
Study design: Retrospective study of 2,954 consecutive patients divided into two groups, low-dose and high-dose clopidogrel use.
Setting: Single hospital in France.
Synopsis: The low-dose study group undergoing PCI was pretreated with 300 mg clopidogrel, followed by ASA 75 mg and clopidogrel 75 mg daily for two months. The second group undergoing PCI was pretreated with 600 mg clopidogrel followed by ASA 75 mg and clopidogrel 150 mg for 15 days, then maintained on ASA 75 mg and clopidogrel 75 mg. Patients received follow-up at two months and were evaluated for in-stent thrombosis, myocardial infarction (MI), death, and hemorrhagic complications. The two groups were matched one-to-one using propensity scoring and the nearest-pair-matching method blinded to patient outcome.
The high-dose clopidogrel group showed a decreased incidence of MI, in-stent thrombosis, and death. This benefit confirms the importance of achieving early and adequate antiplatelet therapy. However, the study authors noted a higher percentage of major bleeding and minor bleeding, although the increase was not statistically significant (2.8% vs. 3.5%, P=0.379, and 7.4% vs. 8.2%, P=0.699, respectively).
Bottom line: High-dose clopidogrel before and within the first 15 days after PCI decreases the risk of MI, in-stent thrombosis, and death, with no statistical increase in bleeding complications. Long-range studies beyond the two-month interval might be beneficial.
Citation: Lemesle G, Delhaye C, Sudre A, et al. Impact of high loading and maintenance dose of clopidogrel within the first 15 days after percutaneous coronary intervention on patient outcome. Am Heart J. 2008;10:1-8.
B-Type Natriuretic Peptide (BNP) Identifies Patients Developing Sepsis-Induced Myocardial Depression
Clinical question: Can plasma BNP be used as a marker to identify patients at risk for sepsis-induced depression of myocardial function?
Background: Previous studies have established BNP levels are increased in patients with septic shock but have not examined the relationship between plasma BNP concentration and left ventricular (LV) systolic dysfunction.
Study design: Prospective cohort.
Setting: Academic medical center.
Synopsis: The authors divided 93 prospectively selected ICU patients with severe sepsis into two groups: one with normal left ventricular (LV) function and a group with LV systolic dysfunction. Comparison of the plasma BNP concentrations between these two groups demonstrated a significant positive correlation between the BNP level and the degree of LV systolic dysfunction, suggesting BNP is a reasonable marker for identification of septic patients with sepsis-induced myocardial depression.
Further, the study’s results suggest BNP measurements early in the course of septic shock might be useful prognostic indicators. However, it is unclear to what extent the knowledge gained from such measurements would alter care management, or how BNP compares to echocardiography in terms of diagnostic and prognostic utility. Thus, these results might not be adequate to justify the routine measurement of BNP in patients with severe sepsis.
Bottom line: Elevated BNP in septic patients is associated with the presence or risk of sepsis-induced myocardial depression, and might be a negative prognostic indicator.
Citation: Post F, Weilemann LS, Messow CM, Sinning C, Munzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–3037.
High Risk of Death with Thrombolytic Use in Low-Risk Pulmonary Embolism (PE)
Clinical question: Is there an advantage to thrombolytic therapy in the treatment of acute PE versus treatment with unfractionated or low-molecular-weight (LMW) heparin?
Background: Given the high mortality linked to PE, consistent indications for thrombolytic therapy in acute PE are needed. An assessment of the prevalence of thrombolytic therapy and mortality, as compared with standard anticoagulation, has been described inconsistently.
Study design: Retrospective cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using a database of ICD-9 codes, 15,116 patients were reviewed. Logistic regression was used to evaluate the association between thrombolytic therapy and 30-day mortality. Poisson regression was used to evaluate the association between thrombolytic therapy and in-hospital mortality. For those receiving thrombolysis and considered unlikely candidates for the therapy based on documentation at presentation (low predicted probability), the in-hospital mortality and overall 30-day mortality rate were higher when compared with those who did not receive thrombolysis. An exception to this was a group of patients with high predicted probability of receiving thrombolysis. In this group, thrombolysis was not associated with increased risk. Limitations to the study include lack of assessment of right ventricular function, changes in condition after presentation, lack of long-term outcomes, and lack of exact cause of death.
Bottom line: Thrombolytic therapy is associated with higher mortality in patients with hemodynamically uncomplicated PE, and therefore not indicated. Thrombolytic therapy in a subgroup of patients with hemodynamic instability or right ventricular dysfunction improves the clinical course and outcome.
Citation: Ibrahim SA, Stone RA, Obrosky S, Geng M, Fine MJ, Aujesky D. Thrombolytic therapy and mortality in patients with acute pulmonary embolism. Arch Intern Med. 2008;168(20):2183-2190.
Hospitalists Improve Patient Flow in the ED
Clinical question: Can active-bed management by hospitalists reduce ED throughput times and diversionary status?
Background: ED overcrowding leads to ambulance diversion, which has been associated with increased mortality. A primary cause of ED crowding is inpatient boarding, which can reduce patient satisfaction and quality of care. Previous studies targeting the ED have had little impact on throughput and ambulance diversion.
Study design: Pre-post case study in a single institution.
Setting: Academic teaching hospital in Baltimore.
Synopsis: ED throughput times and ambulance diversion hours were measured for all adult patients registered in the department from November 2005 to February 2006 (control period) and November 2006 to February 2007 (intervention period). Active-bed management was defined as appointing a hospitalist to assess bed availability in real time and assigning department of medicine admissions to the appropriate clinical setting, as well as the creation of a bed director. Although the ED census was 8.8% higher during the intervention period, throughput time for admitted patients decreased by 98 minutes per patient, to 458 from 360. The time spent under diversionary status for overcrowding or lack of ICU beds decreased by 6% and 27%, respectively. Limitations of this study include the pre-post design and the implementation at a single institution. Additionally, active-bed management is expensive, and in this case required the hiring of three full-time-equivalent faculty. However, this study successfully demonstrates that a quality improvement partnership between hospitalists and the ED can substantially reduce overcrowding.
Bottom line: Active-bed management by hospitalists improves ED throughput by decreasing the length of time admitted patients spend in the ED and reducing ambulance diversion hours.
Citation: Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Int Med. 2008;149(11):804-810.
Literature at a Glance
A guide to this month’s studies.
- Score predicts risk of intracerebral hemorrhage after thrombolysis.
- Trigylcerides and stroke-risk predictors.
- PPI use and risk of community-acquired pneumonia.
- Clopidogrel before coronary intervention might improve outcomes.
- High-dose clopidogrel after coronary intervention is beneficial.
- B-type natriuretic peptide level and sepsis.
- Thrombolytic use in pulmonary embolism.
- Hospitalists and ED patient flow.
Simple Clinical Score Predicts Intracerebral Hemorrhage after Thrombolysis
Clinical question: Is there a simple scoring tool that will predict the risk of intracerebral hemorrhage (ICH) following IV tissue-plasminogen activator (t-PA) in ischemic strokes?
Background: The use of t-PA in acute ischemic stroke (AIS) is about 2% to 4%, due in part to fear of conversion of an ischemic event to an ICH. Several studies using t-PA after AIS have identified risk factors for ICH; however, none has looked at the cumulative risk and prognosis for an individual candidate based on these factors.
Study design: Retrospective, observational cohort study.
Setting: The National Institute of Neurological Disorders and Stroke Trials 1 and 2, and consecutive patients treated at Beth Israel Deaconess Medical Center, Boston.
Synopsis: After an extensive literature review, a five-point scale to determine the risk of hemorrhage after t-PA (HAT) was developed using the top four predictive factors based on odds ratios. These included the National Institutes of Health Stroke Scale (NIHSS), presence and extent of hypodensity on initial CT scan, history of diabetes, and high baseline serum glucose. The predictive value of this scale was tested against two independent cohorts of patients with AIS treated with IV t-PA. The HAT scale was able to reasonably predict both the risk of ICH following t-PA and the functional outcome at 90 days. Higher scores on the scale tended to do worse, especially scores of three or more. Its retrospective nature and small number of patients experiencing ICH limit this study.
Bottom line: The HAT score is a quick bedside tool that can help in the counseling of patients and families in conjunction with the risks and benefits of t-PA after ischemic stroke.
Citation: Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology. 2008;71:1417-1423.
Nonfasting Triglycerides Predict Stroke Risk
Clinical question: Is there a correlation between nonfasting triglyceride levels and ischemic stroke?
Background: Most individuals are in a nonfasting state, with the exception of several hours prior to breakfast. Fasting cholesterol levels exclude most remnant lipoproteins, which might play a role in early atherosclerotic disease. Increased levels of triglycerides in a nonfasting state indicate the presence of these remnants.
Study design: Prospective, population-based cohort study.
Setting: The Copenhagen City Heart Study.
Synopsis: The study included 13,956 individuals between the ages of 20 and 93 with a follow-up period of up to 31 years. Cholesterol levels were checked during four evaluation periods: 1976-1978, 1981-1983, 1991-1994, and 2001-2003. Eighty-two percent of the participants had eaten a meal within three hours of the blood draw; the other 18% had eaten more than three hours prior to the draw. The study showed an association between increasing nonfasting triglyceride levels and a step-wise increase in the risk of ischemic stroke. The highest risk came in individuals with nonfasting triglyceride levels > 443mg/dl, which was associated with a three- to fourfold greater risk of ischemic stroke. The study was limited in that it evaluated a homogenous group of individuals, which may not reflect other racial or ethnic populations.
Bottom line: Increasing levels of nonfasting triglycerides are associated with an increased risk of ischemic stroke.
Citation: Freiberg J, Tybjaerg-Hansen A, Jensen JS, Nordestgaard BG. Nonfasting triglycerides and risk of ischemic stroke in the general population. JAMA. 2008;300(18):2142-2152.
Proton-Pump Inhibitor (PPI) Use Increases the Risk of Community-Acquired Pneumonia (CAP)
Clinical question: Is there an association between PPI use and CAP?
Background: CAP is associated with significant morbidity, annually accounting for billions of healthcare dollars. Proton-pump inhibitors (PPI) are a mainstay treatment for gastric acid suppression. Previous studies have suggested using PPIs may increase the risk of developing CAP.
Study design: Nested case control study.
Setting: Outpatient general practices, United Kingdom.
Synopsis: The association between PPI use and CAP was evaluated in a cohort of more than 7 million patients using the UK’s general-practice research database. Eligible participants were divided into two groups: case patients and control patients. Initial results indicated an increased risk of CAP with PPI use. After adjusting for confounding variables, the use of a PPI was strongly associated with CAP development when used within 30 days prior of the diagnosis, and most notably within 48 hours of diagnosis. It also was noted that the risk of developing CAP with longer-term PPI use was much lower. This inverse temporal relationship was noted in two previous studies. The limitations of this study were related to presumed adherence and compliance with PPI therapy. There also was no radiographic data to support the diagnosis of pneumonia in these cases, both of which could bias the results.
Bottom line: There appears to be an increased risk of CAP with PPI use. This risk is most notable within 48 hours. However, long-term, chronic PPI use was not associated with an increased risk of CAP.
Citation: Sarkar M, Hennessy S, Yang YX. Proton-pump inhibitor use and the risk for community-acquired pneumonia. Ann Intern Med. 2008;149:391-398.
Clopidogrel Prior to Percutaneous Intervention (PCI) Might Improve Outcomes in Patients with Acute ST-Elevation Myocardial Infarction (STEMI)
Clinical question: Does pretreatment with clopidogrel prior to PCI in acute STEMI improve outcomes?
Background: Extant guidelines for early utilization of clopidogrel in STEMI patients are based on results of studies of patients with non-ST-elevation acute coronary syndromes or treatment with thrombolytics.
Study design: Systematic review.
Setting: MEDLINE and Cochrane Controlled Trials Register of randomized controlled trials.
Synopsis: The authors selected 38 treatment groups, including 8,429 patients with STEMI who underwent primary PCI. They found a statistically significant difference in initial patency, and further found clopidogrel pretreatment was an independent predictor of early reperfusion and improved clinical outcome. This study suggests a benefit to pretreatment with clopidogrel but likely is not sufficient to establish such pretreatment as the standard of care. The limitations of this study were a retrospective review/meta-analysis, as the ability to limit the influence of confounding variables is reduced.
Bottom line: Pretreatment with clopidogrel in patients with acute STEMI undergoing primary PCI appears beneficial based on the results of this review of available evidence.
Citation: Vlaar PJ, Svilaas T, Damman K, et al. Impact of pretreatment with clopidogrel on initial patency and outcomes in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review. Circulation. 2008;118:1828-1836.
High-Dose Clopidogrel after PCI Is Beneficial
Clinical question: Does high-dose clopidogrel improve patient outcome following PCI?
Background: Studies have shown antiplatelet resistance after PCI is associated with an increased risk of cardiovascular events, including in-stent thrombosis and death. Other studies have shown the benefit of high-dose clopidogrel by the inhibition of platelet aggregation. Limited information is available regarding the applicability to patients after PCI.
Study design: Retrospective study of 2,954 consecutive patients divided into two groups, low-dose and high-dose clopidogrel use.
Setting: Single hospital in France.
Synopsis: The low-dose study group undergoing PCI was pretreated with 300 mg clopidogrel, followed by ASA 75 mg and clopidogrel 75 mg daily for two months. The second group undergoing PCI was pretreated with 600 mg clopidogrel followed by ASA 75 mg and clopidogrel 150 mg for 15 days, then maintained on ASA 75 mg and clopidogrel 75 mg. Patients received follow-up at two months and were evaluated for in-stent thrombosis, myocardial infarction (MI), death, and hemorrhagic complications. The two groups were matched one-to-one using propensity scoring and the nearest-pair-matching method blinded to patient outcome.
The high-dose clopidogrel group showed a decreased incidence of MI, in-stent thrombosis, and death. This benefit confirms the importance of achieving early and adequate antiplatelet therapy. However, the study authors noted a higher percentage of major bleeding and minor bleeding, although the increase was not statistically significant (2.8% vs. 3.5%, P=0.379, and 7.4% vs. 8.2%, P=0.699, respectively).
Bottom line: High-dose clopidogrel before and within the first 15 days after PCI decreases the risk of MI, in-stent thrombosis, and death, with no statistical increase in bleeding complications. Long-range studies beyond the two-month interval might be beneficial.
Citation: Lemesle G, Delhaye C, Sudre A, et al. Impact of high loading and maintenance dose of clopidogrel within the first 15 days after percutaneous coronary intervention on patient outcome. Am Heart J. 2008;10:1-8.
B-Type Natriuretic Peptide (BNP) Identifies Patients Developing Sepsis-Induced Myocardial Depression
Clinical question: Can plasma BNP be used as a marker to identify patients at risk for sepsis-induced depression of myocardial function?
Background: Previous studies have established BNP levels are increased in patients with septic shock but have not examined the relationship between plasma BNP concentration and left ventricular (LV) systolic dysfunction.
Study design: Prospective cohort.
Setting: Academic medical center.
Synopsis: The authors divided 93 prospectively selected ICU patients with severe sepsis into two groups: one with normal left ventricular (LV) function and a group with LV systolic dysfunction. Comparison of the plasma BNP concentrations between these two groups demonstrated a significant positive correlation between the BNP level and the degree of LV systolic dysfunction, suggesting BNP is a reasonable marker for identification of septic patients with sepsis-induced myocardial depression.
Further, the study’s results suggest BNP measurements early in the course of septic shock might be useful prognostic indicators. However, it is unclear to what extent the knowledge gained from such measurements would alter care management, or how BNP compares to echocardiography in terms of diagnostic and prognostic utility. Thus, these results might not be adequate to justify the routine measurement of BNP in patients with severe sepsis.
Bottom line: Elevated BNP in septic patients is associated with the presence or risk of sepsis-induced myocardial depression, and might be a negative prognostic indicator.
Citation: Post F, Weilemann LS, Messow CM, Sinning C, Munzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36:3030–3037.
High Risk of Death with Thrombolytic Use in Low-Risk Pulmonary Embolism (PE)
Clinical question: Is there an advantage to thrombolytic therapy in the treatment of acute PE versus treatment with unfractionated or low-molecular-weight (LMW) heparin?
Background: Given the high mortality linked to PE, consistent indications for thrombolytic therapy in acute PE are needed. An assessment of the prevalence of thrombolytic therapy and mortality, as compared with standard anticoagulation, has been described inconsistently.
Study design: Retrospective cohort study.
Setting: 186 acute-care hospitals in Pennsylvania.
Synopsis: Using a database of ICD-9 codes, 15,116 patients were reviewed. Logistic regression was used to evaluate the association between thrombolytic therapy and 30-day mortality. Poisson regression was used to evaluate the association between thrombolytic therapy and in-hospital mortality. For those receiving thrombolysis and considered unlikely candidates for the therapy based on documentation at presentation (low predicted probability), the in-hospital mortality and overall 30-day mortality rate were higher when compared with those who did not receive thrombolysis. An exception to this was a group of patients with high predicted probability of receiving thrombolysis. In this group, thrombolysis was not associated with increased risk. Limitations to the study include lack of assessment of right ventricular function, changes in condition after presentation, lack of long-term outcomes, and lack of exact cause of death.
Bottom line: Thrombolytic therapy is associated with higher mortality in patients with hemodynamically uncomplicated PE, and therefore not indicated. Thrombolytic therapy in a subgroup of patients with hemodynamic instability or right ventricular dysfunction improves the clinical course and outcome.
Citation: Ibrahim SA, Stone RA, Obrosky S, Geng M, Fine MJ, Aujesky D. Thrombolytic therapy and mortality in patients with acute pulmonary embolism. Arch Intern Med. 2008;168(20):2183-2190.
Hospitalists Improve Patient Flow in the ED
Clinical question: Can active-bed management by hospitalists reduce ED throughput times and diversionary status?
Background: ED overcrowding leads to ambulance diversion, which has been associated with increased mortality. A primary cause of ED crowding is inpatient boarding, which can reduce patient satisfaction and quality of care. Previous studies targeting the ED have had little impact on throughput and ambulance diversion.
Study design: Pre-post case study in a single institution.
Setting: Academic teaching hospital in Baltimore.
Synopsis: ED throughput times and ambulance diversion hours were measured for all adult patients registered in the department from November 2005 to February 2006 (control period) and November 2006 to February 2007 (intervention period). Active-bed management was defined as appointing a hospitalist to assess bed availability in real time and assigning department of medicine admissions to the appropriate clinical setting, as well as the creation of a bed director. Although the ED census was 8.8% higher during the intervention period, throughput time for admitted patients decreased by 98 minutes per patient, to 458 from 360. The time spent under diversionary status for overcrowding or lack of ICU beds decreased by 6% and 27%, respectively. Limitations of this study include the pre-post design and the implementation at a single institution. Additionally, active-bed management is expensive, and in this case required the hiring of three full-time-equivalent faculty. However, this study successfully demonstrates that a quality improvement partnership between hospitalists and the ED can substantially reduce overcrowding.
Bottom line: Active-bed management by hospitalists improves ED throughput by decreasing the length of time admitted patients spend in the ED and reducing ambulance diversion hours.
Citation: Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Int Med. 2008;149(11):804-810.
New Design for Discharge
With hospitalists playing key roles in improving transitions in care, a new study has tested a low-cost process that shows increases in outpatient follow-up and completed workups soon after hospital discharge.
The improvements potentially could lead to better patient outcomes and lower readmission rates, according to Richard B. Balaban, MD, who as the medical director of Cambridge Health Alliance’s (CHA) Somerville, Mass., primary-care center and a hospitalist at CHA’s Cambridge Hospital has a unique, dual perspective on the discharge process.
Dr. Balaban’s team’s discharge-transfer intervention process, tested in one of the few randomized controlled studies on the subject of transitions of care, is intended to improve communication between hospitalists and primary-care providers, as well as promptly connect inpatients to outpatient providers. It’s also designed to better equip patients to participate in their care and to improve accountability within the medical team.
The study, published in the August 2008 issue of the Journal of General Internal Medicine, garnered praise from Mark Williams, MD, FACP, professor and chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago and principal investigator of SHM’s Project BOOST study (see “BOOST Sites Chosen,” August 2008, p. 1), which is examining ways to improve transitions of care.1 “This small but well-done study demonstrates how using interventions similar to components in the Project BOOST toolkit resulted in a significant improvement in outpatient follow-up, and a trend toward a reduction in hospitalizations and emergency room visits,” Dr. Williams says.
The four-part process calls for:
- The patient to receive a comprehensive, “user-friendly” discharge instruction form;
- Electronic transfer of the discharge instruction form to RNs at the patient’s primary-care site;
- A primary-care RN to call the patient by the next business day to monitor his or her condition; and
- The review and modification of the discharge plan by the primary-care provider as needed.
The research team, which included Joel S. Weissman, PhD, of Massachusetts General Hospital, Harvard Medical School, and the Harvard School of Public Health; Peter A. Samuel of Harvard Medical School; and Stephanie Woolhandler, MD, of CHA and Harvard Medical School, thinks the discharge process, a key task for hospitalists, should be treated as vital as the admissions process. “Hospitalists need to improve the level of detail in discharge plans; this form and process supports that,” Dr. Balaban says. By providing this quality information to outpatient providers, collaboration is improved, making hospitalists more effective, he says.
Proof in the Pudding
The process was tested at Somerville Hospital, a 100-bed community hospital and teaching facility affiliated with Harvard Medical School. Approx-imately 25% of Somerville’s patients are non-English-speakers; the process was designed to serve a culturally diverse population.
All patients in the study, conducted between June 2006 and January 2007, had received care from hospitalist-led teams and received outpatient care at CHA facilities. Ninety-six patients were studied; 47 took part in the new discharge process and the rest were discharged according to existing procedures. Outcomes were compared with those of 100 patients who previously had been discharged from the hospital.
The team measured four undesirable outcomes after discharge:
- No outpatient follow-up within 21 days;
- Readmission within 31 days;
- Emergency department visit within 31 days; and
- Failure by the primary-care provider to complete an outpatient workup recommended by hospital doctors.
The study found just 25.5% of the patients who completed the new process had one or more undesirable outcomes, compared with 55.1% of the control group patients and 55% in the historical group. The most significant improvements were in the rates of outpatient follow-up and completed workups (see “Better Process Equals Better Outcomes”).
The process was especially effective among patients discharged on weekends, and had a greater effect on patients who did not speak English, were hospitalized one or two days, and were age 60 and older. The effect of the new process also was evident in outpatient treatment, Dr. Balaban says. At least seven of the 47 patients discharged through the new process had their treatment plan changed by the RNs who made the follow-up phone call. “They weren’t big changes, things like calling in prescriptions and making urgent appointments,” he says, “but they made a difference: for example, providing a pneumonia patient with a thermometer to monitor possible infections, and a scale so that a patient with congestive heart failure could monitor weight gain possibly caused by harmful retention of fluid.”
Dr. Balaban’s team plans to conduct a larger study, though not randomized, at Cambridge Hospital to test the new process on all discharges. “There usually is little collaboration on discharges,” Dr. Balaban says. “This process provides detail, a record of critical information, and creates interchange between care teams. Discharge should be looked at as a continuing, key part of care.” TH
Karla Feuer is a freelance writer based in North Carolina.
Reference
1. Balaban RB, Weissmann JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;8:1228-1233.
With hospitalists playing key roles in improving transitions in care, a new study has tested a low-cost process that shows increases in outpatient follow-up and completed workups soon after hospital discharge.
The improvements potentially could lead to better patient outcomes and lower readmission rates, according to Richard B. Balaban, MD, who as the medical director of Cambridge Health Alliance’s (CHA) Somerville, Mass., primary-care center and a hospitalist at CHA’s Cambridge Hospital has a unique, dual perspective on the discharge process.
Dr. Balaban’s team’s discharge-transfer intervention process, tested in one of the few randomized controlled studies on the subject of transitions of care, is intended to improve communication between hospitalists and primary-care providers, as well as promptly connect inpatients to outpatient providers. It’s also designed to better equip patients to participate in their care and to improve accountability within the medical team.
The study, published in the August 2008 issue of the Journal of General Internal Medicine, garnered praise from Mark Williams, MD, FACP, professor and chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago and principal investigator of SHM’s Project BOOST study (see “BOOST Sites Chosen,” August 2008, p. 1), which is examining ways to improve transitions of care.1 “This small but well-done study demonstrates how using interventions similar to components in the Project BOOST toolkit resulted in a significant improvement in outpatient follow-up, and a trend toward a reduction in hospitalizations and emergency room visits,” Dr. Williams says.
The four-part process calls for:
- The patient to receive a comprehensive, “user-friendly” discharge instruction form;
- Electronic transfer of the discharge instruction form to RNs at the patient’s primary-care site;
- A primary-care RN to call the patient by the next business day to monitor his or her condition; and
- The review and modification of the discharge plan by the primary-care provider as needed.
The research team, which included Joel S. Weissman, PhD, of Massachusetts General Hospital, Harvard Medical School, and the Harvard School of Public Health; Peter A. Samuel of Harvard Medical School; and Stephanie Woolhandler, MD, of CHA and Harvard Medical School, thinks the discharge process, a key task for hospitalists, should be treated as vital as the admissions process. “Hospitalists need to improve the level of detail in discharge plans; this form and process supports that,” Dr. Balaban says. By providing this quality information to outpatient providers, collaboration is improved, making hospitalists more effective, he says.
Proof in the Pudding
The process was tested at Somerville Hospital, a 100-bed community hospital and teaching facility affiliated with Harvard Medical School. Approx-imately 25% of Somerville’s patients are non-English-speakers; the process was designed to serve a culturally diverse population.
All patients in the study, conducted between June 2006 and January 2007, had received care from hospitalist-led teams and received outpatient care at CHA facilities. Ninety-six patients were studied; 47 took part in the new discharge process and the rest were discharged according to existing procedures. Outcomes were compared with those of 100 patients who previously had been discharged from the hospital.
The team measured four undesirable outcomes after discharge:
- No outpatient follow-up within 21 days;
- Readmission within 31 days;
- Emergency department visit within 31 days; and
- Failure by the primary-care provider to complete an outpatient workup recommended by hospital doctors.
The study found just 25.5% of the patients who completed the new process had one or more undesirable outcomes, compared with 55.1% of the control group patients and 55% in the historical group. The most significant improvements were in the rates of outpatient follow-up and completed workups (see “Better Process Equals Better Outcomes”).
The process was especially effective among patients discharged on weekends, and had a greater effect on patients who did not speak English, were hospitalized one or two days, and were age 60 and older. The effect of the new process also was evident in outpatient treatment, Dr. Balaban says. At least seven of the 47 patients discharged through the new process had their treatment plan changed by the RNs who made the follow-up phone call. “They weren’t big changes, things like calling in prescriptions and making urgent appointments,” he says, “but they made a difference: for example, providing a pneumonia patient with a thermometer to monitor possible infections, and a scale so that a patient with congestive heart failure could monitor weight gain possibly caused by harmful retention of fluid.”
Dr. Balaban’s team plans to conduct a larger study, though not randomized, at Cambridge Hospital to test the new process on all discharges. “There usually is little collaboration on discharges,” Dr. Balaban says. “This process provides detail, a record of critical information, and creates interchange between care teams. Discharge should be looked at as a continuing, key part of care.” TH
Karla Feuer is a freelance writer based in North Carolina.
Reference
1. Balaban RB, Weissmann JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;8:1228-1233.
With hospitalists playing key roles in improving transitions in care, a new study has tested a low-cost process that shows increases in outpatient follow-up and completed workups soon after hospital discharge.
The improvements potentially could lead to better patient outcomes and lower readmission rates, according to Richard B. Balaban, MD, who as the medical director of Cambridge Health Alliance’s (CHA) Somerville, Mass., primary-care center and a hospitalist at CHA’s Cambridge Hospital has a unique, dual perspective on the discharge process.
Dr. Balaban’s team’s discharge-transfer intervention process, tested in one of the few randomized controlled studies on the subject of transitions of care, is intended to improve communication between hospitalists and primary-care providers, as well as promptly connect inpatients to outpatient providers. It’s also designed to better equip patients to participate in their care and to improve accountability within the medical team.
The study, published in the August 2008 issue of the Journal of General Internal Medicine, garnered praise from Mark Williams, MD, FACP, professor and chief of the Division of Hospital Medicine at Northwestern University’s Feinberg School of Medicine in Chicago and principal investigator of SHM’s Project BOOST study (see “BOOST Sites Chosen,” August 2008, p. 1), which is examining ways to improve transitions of care.1 “This small but well-done study demonstrates how using interventions similar to components in the Project BOOST toolkit resulted in a significant improvement in outpatient follow-up, and a trend toward a reduction in hospitalizations and emergency room visits,” Dr. Williams says.
The four-part process calls for:
- The patient to receive a comprehensive, “user-friendly” discharge instruction form;
- Electronic transfer of the discharge instruction form to RNs at the patient’s primary-care site;
- A primary-care RN to call the patient by the next business day to monitor his or her condition; and
- The review and modification of the discharge plan by the primary-care provider as needed.
The research team, which included Joel S. Weissman, PhD, of Massachusetts General Hospital, Harvard Medical School, and the Harvard School of Public Health; Peter A. Samuel of Harvard Medical School; and Stephanie Woolhandler, MD, of CHA and Harvard Medical School, thinks the discharge process, a key task for hospitalists, should be treated as vital as the admissions process. “Hospitalists need to improve the level of detail in discharge plans; this form and process supports that,” Dr. Balaban says. By providing this quality information to outpatient providers, collaboration is improved, making hospitalists more effective, he says.
Proof in the Pudding
The process was tested at Somerville Hospital, a 100-bed community hospital and teaching facility affiliated with Harvard Medical School. Approx-imately 25% of Somerville’s patients are non-English-speakers; the process was designed to serve a culturally diverse population.
All patients in the study, conducted between June 2006 and January 2007, had received care from hospitalist-led teams and received outpatient care at CHA facilities. Ninety-six patients were studied; 47 took part in the new discharge process and the rest were discharged according to existing procedures. Outcomes were compared with those of 100 patients who previously had been discharged from the hospital.
The team measured four undesirable outcomes after discharge:
- No outpatient follow-up within 21 days;
- Readmission within 31 days;
- Emergency department visit within 31 days; and
- Failure by the primary-care provider to complete an outpatient workup recommended by hospital doctors.
The study found just 25.5% of the patients who completed the new process had one or more undesirable outcomes, compared with 55.1% of the control group patients and 55% in the historical group. The most significant improvements were in the rates of outpatient follow-up and completed workups (see “Better Process Equals Better Outcomes”).
The process was especially effective among patients discharged on weekends, and had a greater effect on patients who did not speak English, were hospitalized one or two days, and were age 60 and older. The effect of the new process also was evident in outpatient treatment, Dr. Balaban says. At least seven of the 47 patients discharged through the new process had their treatment plan changed by the RNs who made the follow-up phone call. “They weren’t big changes, things like calling in prescriptions and making urgent appointments,” he says, “but they made a difference: for example, providing a pneumonia patient with a thermometer to monitor possible infections, and a scale so that a patient with congestive heart failure could monitor weight gain possibly caused by harmful retention of fluid.”
Dr. Balaban’s team plans to conduct a larger study, though not randomized, at Cambridge Hospital to test the new process on all discharges. “There usually is little collaboration on discharges,” Dr. Balaban says. “This process provides detail, a record of critical information, and creates interchange between care teams. Discharge should be looked at as a continuing, key part of care.” TH
Karla Feuer is a freelance writer based in North Carolina.
Reference
1. Balaban RB, Weissmann JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;8:1228-1233.
Eagle-Eye Your Payors
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Protection of the Medicare program has reached new heights in recent years. One of the most important ways hospitalist groups can protect their Medicare funding is the discovery and recovery of improper contractor payments of Medicare claims.
The Centers for Medicare and Medicaid Services (CMS) reviews various types of contractors—Medicare administrative contractors (MACs), carriers, durable medical equipment regional carriers (DMERCs), fiscal intermediaries (FIs), and quality improvement organizations (QIOs)—through its protection efforts as part of the Comprehensive Error Rate Testing (CERT) program and Hospital Payment Monitoring Program (HPMP). The CERT program’s contractors review physician (i.e., professional) claims processed by MACs and carriers.
The primary goal of a contractor is to “pay it right”—that is, pay the correct amount to the right provider for covered and correctly coded services.1 During the 12-month reporting period ending Sept. 30, 2007, the CERT program sampled 129,875 claims from carriers, DMERCs, FIs, and MACs.
The CERT contractor randomly and electronically selects about 172 claims each month from each type of claims-processing contractor. Since some of these contractors were transitioning to MACs, the target Part B (i.e., professional) sample size for the May 2008 report was approximately 2,000 reviewable claims per MAC cluster. However, this might have varied if a MAC was not processing claims during the entire sampling period.
Document Requests
Physicians need to be mindful of CERT requests for documentation. When possible, every attempt is made to benefit the physician. Initial CERT requests are attempted by way of a letter. If the physician does not respond within 30 days, the CERT contractor attempts one to three more contacts with correspondence and phone calls. If documentation is received after 75 days, it is considered “late.” It then will be reviewed, unless the reporting period has expired.
However, this should not be considered a prudent approach, and timely responses are ideal. If the physician offers no response, and documentation is not received, it is counted as a “no documentation” error.
Physicians often worry about accusations of fraud. The purpose of the CERT program is not to assume or accuse physicians of fraud, although it may serve as a deterrent. It does not, and cannot, label a claim fraudulent.
One scenario of potential fraud the CERT program is able to identify occurs when a CERT documentation contractor is unable to locate a provider or supplier when requesting medical record documentation.2
Outcomes
Individual contractors are notified of improper payments. These include overpayments and underpayments. Unfortunately, contractors do not have to resolve CERT issues involving underpayments, although they are encouraged to do so by CMS.
The CERT program identified overpayments totaling $875,005 during the 12-month reporting period, but collected only $650,418 in overpayments after consideration of appeals that overturned a CERT decision or the provider discontinued business operations. (See Table 1, p. 18, for error rates and Table 2, p. 18, for highest rates of improper payment)
To improve billing compliance and prevent repetitive errors, contractors must implement provider education regarding erroneously paid claims. A contractor may determine the best education method to distribute information about Medicare rules and effectively answer coverage and coding questions.
Some contractors have designed Web-based training modules, Web pages with frequently-asked-questions sections, or local coverage analyses to address contractor-specific errors. Detailed CERT contractor information can be found at www.cms.hhs.gov/ mcd/indexes.asp?from2=indexes.asp&
Due to its successful outcomes, future CMS goals include the continuation of the CERT program. MACs will look more closely at service types based on identified error rates.
Apart from CERT requests, prepayment contractor reviews already exist for most of the services included in Table 2 (p. 18). Timely response is crucial to justify and receive appropriate reimbursement. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is on the faculty of SHM’s inpatient coding course.
References
1. Centers for Medicare and Medicaid Services. Improper Medicare fee-for-service payments report: May 2008. CMS Web site. Available at: www.cms.hhs.gov/apps/er_report/preview_er_report.asp?from=public&which=long&reportID=9. Accessed Dec. 20, 2008.
2. Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association; 2008.
Advancement Opportunities
Sunil Kripalani, MD, MSc, chief of hospital medicine at Vanderbilt University in Nashville, Tenn., was working in the emergency department when a woman arrived with an asthma exacerbation. The woman, who spoke only Spanish, had been hospitalized just five days earlier for asthma, and hospital staff had given her discharge instructions through her husband. Speaking to the patient in Spanish, Dr. Kripalani soon learned something had been lost in translation: The patient had not taken any of the prescribed prednisone tablets, and instead was taking a burst of montelukast. She also was taking a long-acting bronchodilator every two hours instead of every 12, and she was incorrectly using her rescue inhaler.
As the principal investigator of a trial aiming to reduce post-discharge adverse events and emergency room visits, Dr. Kripalani knows well the issues that contributed to the patient’s re-hospitalization.1 Through research, he and his colleagues hope to prevent future cases.
“It’s very rewarding to identify problems in the care of hospitalized patients and then develop and evaluate interventions to solve those problems,” says Dr. Kripalani, a 2001 graduate of the Emory Mentored Clinical Research Scholars Program who also leads Vanderbilt University’s hospital medicine fellowship. “Sharing those solutions with colleagues so they can be applied to patient care at my institution and others brings the research full circle.”
As the field of hospital medicine grows, the number of hospitalists moving into research careers is expanding, says Peter Kaboli, MD, MS, associate professor in the Department of Internal Medicine at the University of Iowa and a 2001 graduate of the Veterans Administration Quality Scholars Fellowship program. Research training programs, or fellowships, put hospitalists on the path to new skills and position them for careers in academic medicine and other leadership positions, Dr. Kaboli says. Training programs also put fellows in contact with mentors who provide valuable guidance.
Although there are dozens of general internal medicine (GIM) fellowships available to hospitalists, few programs are specifically designed to train hospitalists in research. “Hospital medicine is still a relatively new field,” Dr. Kaboli explains. “The field still does not have many research training options that are separate from general internal medicine.”
Still, hospitalists have advanced training choices, and, depending on their interests, can pursue field-specific programs or follow a general internal medicine path.
Career Investment
Many hospitalists receive basic research training from GIM fellowships. Once they have a research foundation, they can take their experience in another direction.
“Some physicians use their clinical interest—hospital medicine—as the platform for their research,” Dr. Kaboli says, using his own resume as an example. “It’s a nice synergy—doing research in a clinical area of interest.”
Physicians interested in fellowships often start looking for opportunities before they complete their residency, or immediately after. The transition makes sense for some; they move from one academic setting to another. Others, however, consider fellowship programs after they have spent some time in practice and get what Dr. Kaboli calls “boots-on-the-ground experience.”
“I think this is an area where there is potential for growth,” Dr. Kaboli says of physicians returning to fellowship programs after years spent in practice. “It’s the equivalent of a businessperson going back to school to get an MBA. They say, ‘Now I understand what this job really means, and I want to do more.’ ”
The caveat is a pay cut. Physicians in fellowship programs generally are paid a stipend of about $50,000 a year, Kaboli says. By comparison, the average hospitalist makes about $193,000 per year, according to SHM’s 2007-2008 Bi-Annual Survey on the State of Hospital Medicine. For two years, fellows devote their lives to training, coursework, and research, and spend only about 25% of their time treating patients, he says.
Road to Research
Hospitalists can choose from a range of general internal medicine fellowships at universities, clinics, and medical centers across the country. Each program offers something different; the fit depends on the candidates’ interests, says Geri Barnes, SHM senior director of education and meetings. For instance, training programs offer advanced study in the areas of biostatistics, epidemiology, and research methodology, to name a few. GIM fellowships (see “To Be or Not to Be a Fellow,” May 2006, p. 26) encourage scholars to develop relationships with mentors to guide them through research projects, she explains. A program’s duration can span one to three years. Some programs give fellows the opportunity to earn an advanced degree in quality improvement, clinical research, public policy, health studies, public health, or clinical epidemiology.
A handful of institutions, including Johns Hopkins Hospital in Baltimore, offer GIM fellowships with a hospital medicine emphasis. The National Institutes of Health (NIH) funds the Johns Hopkins program with training grants, says Daniel J. Brotman, MD, director of the hospitalist program there. GIM leadership is taking a “big tent” approach, promoting the development of hospital medicine tracks within the full program, which is good for the fellowship and for the hospitalist program, Dr. Brotman says.
“Some of the challenges for hospitalists are that they are generally young and don’t have the skills to succeed in academic medicine,” Dr. Brotman says, “and the number of mentors in hospitalist medicine is few and far between. [The fellowship] allows scholars to tap into experienced research mentors who may not be hospitalists themselves but are interested in investigating research questions and promoting academic careers in hospitalist medicine.”
The GIM program at Johns Hopkins draws physicians trained in internal medicine as well as general medicine/pediatrics. Candidates are required to have completed an internal medicine or medicine/pediatrics residency and must provide strong letters of recommendation. Scholars receive training in statistical methods while obtaining a master’s degree in public health or health science at the Johns Hopkins Bloomberg School of Public Health. Fellows commit 80% of their time to research and research training, and 20% of their time to clinical duties; they are expected to form relationships with faculty, which ultimately leads to careers in academia or public health, Dr. Brotman explains.
Minimize Burnout
Physician burnout—so common in the current healthcare system—is an excellent reason to consider a research career. Five years ago, David Meltzer, MD, PhD, an associate professor in the Department of Medicine at the University of Chicago, wanted to increase the number of research-trained hospitalists, so he moved to create a hospitalist training program. Around the same time, the hospital approached Dr. Meltzer and others, asking them to expand the number of clinical physician positions.
“We were afraid the new physicians would burn out rather quickly if their jobs included only clinical work,” Dr. Meltzer says. “We designed positions that had less clinical work but more time for physicians to develop research skills to support sustainable academic careers.”
Hospital leaders agreed, and the university’s Hospitalist Scholars Training Program was born. The two-year curriculum trains hospitalists for a career in academic research, and combines inpatient clinical work, coursework, and mentored training related to an academic project. Scholars typically leave the program with a master’s degree in public policy or health studies.
“Most of our graduates are working in academic research,” Dr. Meltzer says. “The program has been a great source of new faculty for us.”
Short-term programs are available in select topics. For example, the University of Chicago offers a summer program in outcomes research training for hospitalists interested in careers in health research, Dr. Meltzer says. SHM and the Agency for Healthcare Research and Quality have provided funding to expand the program to include as many as six hospitalists from around the country.
Pioneer Program
Applicants from any medical or surgical specialty are eligible to apply for the Robert Wood Johnson (RWJ) Clinical Scholars Program, the nation’s oldest research training program for physicians in health services, research, and leadership.
“The mandate of Robert Wood Johnson is ‘health and healthcare for all Americans,’ ” says Desmond Runyan, MD, DrPH, national program director of the RWJ Clinical Scholars Program. “We give physicians the skills they need to be leaders, and then we push them out the door so they can go out and shape the future of healthcare in this country.”
Applicants must be U.S. citizens and, with the exception of surgeons, must complete their residency training before entering the clinical scholars program. The two-year program offers a master’s degree in graduate-level study and research, and scholars may be considered for a third year of support. Scholars have their choice of four training sites: the University of California at Los Angeles; Yale University in New Haven, Conn.; the University of Pennsylvania in Philadelphia; or the University of Michigan in Ann Arbor.
Programs vary, but each university has a curriculum to teach the basics of healthcare research. It also provides protected time for research; about 20% of time is spent on clinical activities, according to the program’s Web site. Graduates receive leadership, health services, and community-based research training.
The RWJ Foundation spends about $9 million per year on the program, which covers research support, salaries for scholars and program administrators, travel, and other expenses. About half of the program’s graduates go into academic positions; the other half go into public health or other leadership positions. One recent graduate opted for a position in quality control; three other graduates serve as staff in the U.S. House of Representatives and the U.S. Senate, he says. Other graduates work with foundations, state and federal health agencies, or with companies working in the healthcare industry.
“This program looks for people who don’t march to a standard drummer,” Dr. Runyon says. “We are looking for risk-takers who want to make a difference.”
VA Training
The Veterans Administration National Quality Scholars Fellowship Program (VAQS) welcomes physicians from all medical specialties, including pathology, OB/GYN, surgery, and dermatology. This year, the program will begin recruiting nurses.
The program is offered at six academic-affiliated VA medical centers: Iowa City, Iowa; Nashville, Tenn.; Birmingham, Ala.; Cleveland; San Francisco; and White River Junction, Vt. The Iowa City and Nashville programs have a track designed specifically for hospitalists. These tracks focus on clinical research and quality improvement work in the inpatient setting, and provide fellows with training for advancement in academic and private-sector hospitalist careers, says Dr. Kaboli, the Iowa City VAQS Fellowship director.
To qualify, fellowship applicants must have completed an Accreditation Council for Graduate Medical Education residency or fellowship (see “A Pregnant Pause: The necessary evolution of residency training,” January 2007, p. 35), be board-eligible or board-certified, and have an active, unrestricted U.S. license to practice. International graduates must meet visa and Educational Commission for Foreign Medical Graduates requirements.
The two-year VAQS focuses on quality improvement in healthcare, Dr. Kaboli says. The program offers master’s-level training in epidemiology and biostatistics, and trains fellows to design and conduct research and improvement projects. Fellows publish the results of their research in peer-reviewed journals. They also learn how to write grants to gain funding for future projects.
Mentoring is an important element of the VAQS program, Dr. Kaboli says, adding that the value a trainee receives from any fellowship depends on the level of mentoring available through the program. Fellows work with senior faculty members who provide guidance on all aspects of research, Dr. Kaboli says. This includes study design, research methodology, data collection and analyses, and writing.
New experiences and the opportunity to take part in research are among the benefits of completing the VAQS program, Dr. Kaboli says. Some physicians also find a great deal of career satisfaction through research.
“I love seeing patients,” Dr. Kaboli says, “but I also like the challenge of doing research to find new ways to improve patient care.” TH
Gina Gotsill is a freelance medical writer based in California.
Reference
1. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowship: works in progress. Am J Med. 2006;119;72.e1-72.e7.
Sunil Kripalani, MD, MSc, chief of hospital medicine at Vanderbilt University in Nashville, Tenn., was working in the emergency department when a woman arrived with an asthma exacerbation. The woman, who spoke only Spanish, had been hospitalized just five days earlier for asthma, and hospital staff had given her discharge instructions through her husband. Speaking to the patient in Spanish, Dr. Kripalani soon learned something had been lost in translation: The patient had not taken any of the prescribed prednisone tablets, and instead was taking a burst of montelukast. She also was taking a long-acting bronchodilator every two hours instead of every 12, and she was incorrectly using her rescue inhaler.
As the principal investigator of a trial aiming to reduce post-discharge adverse events and emergency room visits, Dr. Kripalani knows well the issues that contributed to the patient’s re-hospitalization.1 Through research, he and his colleagues hope to prevent future cases.
“It’s very rewarding to identify problems in the care of hospitalized patients and then develop and evaluate interventions to solve those problems,” says Dr. Kripalani, a 2001 graduate of the Emory Mentored Clinical Research Scholars Program who also leads Vanderbilt University’s hospital medicine fellowship. “Sharing those solutions with colleagues so they can be applied to patient care at my institution and others brings the research full circle.”
As the field of hospital medicine grows, the number of hospitalists moving into research careers is expanding, says Peter Kaboli, MD, MS, associate professor in the Department of Internal Medicine at the University of Iowa and a 2001 graduate of the Veterans Administration Quality Scholars Fellowship program. Research training programs, or fellowships, put hospitalists on the path to new skills and position them for careers in academic medicine and other leadership positions, Dr. Kaboli says. Training programs also put fellows in contact with mentors who provide valuable guidance.
Although there are dozens of general internal medicine (GIM) fellowships available to hospitalists, few programs are specifically designed to train hospitalists in research. “Hospital medicine is still a relatively new field,” Dr. Kaboli explains. “The field still does not have many research training options that are separate from general internal medicine.”
Still, hospitalists have advanced training choices, and, depending on their interests, can pursue field-specific programs or follow a general internal medicine path.
Career Investment
Many hospitalists receive basic research training from GIM fellowships. Once they have a research foundation, they can take their experience in another direction.
“Some physicians use their clinical interest—hospital medicine—as the platform for their research,” Dr. Kaboli says, using his own resume as an example. “It’s a nice synergy—doing research in a clinical area of interest.”
Physicians interested in fellowships often start looking for opportunities before they complete their residency, or immediately after. The transition makes sense for some; they move from one academic setting to another. Others, however, consider fellowship programs after they have spent some time in practice and get what Dr. Kaboli calls “boots-on-the-ground experience.”
“I think this is an area where there is potential for growth,” Dr. Kaboli says of physicians returning to fellowship programs after years spent in practice. “It’s the equivalent of a businessperson going back to school to get an MBA. They say, ‘Now I understand what this job really means, and I want to do more.’ ”
The caveat is a pay cut. Physicians in fellowship programs generally are paid a stipend of about $50,000 a year, Kaboli says. By comparison, the average hospitalist makes about $193,000 per year, according to SHM’s 2007-2008 Bi-Annual Survey on the State of Hospital Medicine. For two years, fellows devote their lives to training, coursework, and research, and spend only about 25% of their time treating patients, he says.
Road to Research
Hospitalists can choose from a range of general internal medicine fellowships at universities, clinics, and medical centers across the country. Each program offers something different; the fit depends on the candidates’ interests, says Geri Barnes, SHM senior director of education and meetings. For instance, training programs offer advanced study in the areas of biostatistics, epidemiology, and research methodology, to name a few. GIM fellowships (see “To Be or Not to Be a Fellow,” May 2006, p. 26) encourage scholars to develop relationships with mentors to guide them through research projects, she explains. A program’s duration can span one to three years. Some programs give fellows the opportunity to earn an advanced degree in quality improvement, clinical research, public policy, health studies, public health, or clinical epidemiology.
A handful of institutions, including Johns Hopkins Hospital in Baltimore, offer GIM fellowships with a hospital medicine emphasis. The National Institutes of Health (NIH) funds the Johns Hopkins program with training grants, says Daniel J. Brotman, MD, director of the hospitalist program there. GIM leadership is taking a “big tent” approach, promoting the development of hospital medicine tracks within the full program, which is good for the fellowship and for the hospitalist program, Dr. Brotman says.
“Some of the challenges for hospitalists are that they are generally young and don’t have the skills to succeed in academic medicine,” Dr. Brotman says, “and the number of mentors in hospitalist medicine is few and far between. [The fellowship] allows scholars to tap into experienced research mentors who may not be hospitalists themselves but are interested in investigating research questions and promoting academic careers in hospitalist medicine.”
The GIM program at Johns Hopkins draws physicians trained in internal medicine as well as general medicine/pediatrics. Candidates are required to have completed an internal medicine or medicine/pediatrics residency and must provide strong letters of recommendation. Scholars receive training in statistical methods while obtaining a master’s degree in public health or health science at the Johns Hopkins Bloomberg School of Public Health. Fellows commit 80% of their time to research and research training, and 20% of their time to clinical duties; they are expected to form relationships with faculty, which ultimately leads to careers in academia or public health, Dr. Brotman explains.
Minimize Burnout
Physician burnout—so common in the current healthcare system—is an excellent reason to consider a research career. Five years ago, David Meltzer, MD, PhD, an associate professor in the Department of Medicine at the University of Chicago, wanted to increase the number of research-trained hospitalists, so he moved to create a hospitalist training program. Around the same time, the hospital approached Dr. Meltzer and others, asking them to expand the number of clinical physician positions.
“We were afraid the new physicians would burn out rather quickly if their jobs included only clinical work,” Dr. Meltzer says. “We designed positions that had less clinical work but more time for physicians to develop research skills to support sustainable academic careers.”
Hospital leaders agreed, and the university’s Hospitalist Scholars Training Program was born. The two-year curriculum trains hospitalists for a career in academic research, and combines inpatient clinical work, coursework, and mentored training related to an academic project. Scholars typically leave the program with a master’s degree in public policy or health studies.
“Most of our graduates are working in academic research,” Dr. Meltzer says. “The program has been a great source of new faculty for us.”
Short-term programs are available in select topics. For example, the University of Chicago offers a summer program in outcomes research training for hospitalists interested in careers in health research, Dr. Meltzer says. SHM and the Agency for Healthcare Research and Quality have provided funding to expand the program to include as many as six hospitalists from around the country.
Pioneer Program
Applicants from any medical or surgical specialty are eligible to apply for the Robert Wood Johnson (RWJ) Clinical Scholars Program, the nation’s oldest research training program for physicians in health services, research, and leadership.
“The mandate of Robert Wood Johnson is ‘health and healthcare for all Americans,’ ” says Desmond Runyan, MD, DrPH, national program director of the RWJ Clinical Scholars Program. “We give physicians the skills they need to be leaders, and then we push them out the door so they can go out and shape the future of healthcare in this country.”
Applicants must be U.S. citizens and, with the exception of surgeons, must complete their residency training before entering the clinical scholars program. The two-year program offers a master’s degree in graduate-level study and research, and scholars may be considered for a third year of support. Scholars have their choice of four training sites: the University of California at Los Angeles; Yale University in New Haven, Conn.; the University of Pennsylvania in Philadelphia; or the University of Michigan in Ann Arbor.
Programs vary, but each university has a curriculum to teach the basics of healthcare research. It also provides protected time for research; about 20% of time is spent on clinical activities, according to the program’s Web site. Graduates receive leadership, health services, and community-based research training.
The RWJ Foundation spends about $9 million per year on the program, which covers research support, salaries for scholars and program administrators, travel, and other expenses. About half of the program’s graduates go into academic positions; the other half go into public health or other leadership positions. One recent graduate opted for a position in quality control; three other graduates serve as staff in the U.S. House of Representatives and the U.S. Senate, he says. Other graduates work with foundations, state and federal health agencies, or with companies working in the healthcare industry.
“This program looks for people who don’t march to a standard drummer,” Dr. Runyon says. “We are looking for risk-takers who want to make a difference.”
VA Training
The Veterans Administration National Quality Scholars Fellowship Program (VAQS) welcomes physicians from all medical specialties, including pathology, OB/GYN, surgery, and dermatology. This year, the program will begin recruiting nurses.
The program is offered at six academic-affiliated VA medical centers: Iowa City, Iowa; Nashville, Tenn.; Birmingham, Ala.; Cleveland; San Francisco; and White River Junction, Vt. The Iowa City and Nashville programs have a track designed specifically for hospitalists. These tracks focus on clinical research and quality improvement work in the inpatient setting, and provide fellows with training for advancement in academic and private-sector hospitalist careers, says Dr. Kaboli, the Iowa City VAQS Fellowship director.
To qualify, fellowship applicants must have completed an Accreditation Council for Graduate Medical Education residency or fellowship (see “A Pregnant Pause: The necessary evolution of residency training,” January 2007, p. 35), be board-eligible or board-certified, and have an active, unrestricted U.S. license to practice. International graduates must meet visa and Educational Commission for Foreign Medical Graduates requirements.
The two-year VAQS focuses on quality improvement in healthcare, Dr. Kaboli says. The program offers master’s-level training in epidemiology and biostatistics, and trains fellows to design and conduct research and improvement projects. Fellows publish the results of their research in peer-reviewed journals. They also learn how to write grants to gain funding for future projects.
Mentoring is an important element of the VAQS program, Dr. Kaboli says, adding that the value a trainee receives from any fellowship depends on the level of mentoring available through the program. Fellows work with senior faculty members who provide guidance on all aspects of research, Dr. Kaboli says. This includes study design, research methodology, data collection and analyses, and writing.
New experiences and the opportunity to take part in research are among the benefits of completing the VAQS program, Dr. Kaboli says. Some physicians also find a great deal of career satisfaction through research.
“I love seeing patients,” Dr. Kaboli says, “but I also like the challenge of doing research to find new ways to improve patient care.” TH
Gina Gotsill is a freelance medical writer based in California.
Reference
1. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowship: works in progress. Am J Med. 2006;119;72.e1-72.e7.
Sunil Kripalani, MD, MSc, chief of hospital medicine at Vanderbilt University in Nashville, Tenn., was working in the emergency department when a woman arrived with an asthma exacerbation. The woman, who spoke only Spanish, had been hospitalized just five days earlier for asthma, and hospital staff had given her discharge instructions through her husband. Speaking to the patient in Spanish, Dr. Kripalani soon learned something had been lost in translation: The patient had not taken any of the prescribed prednisone tablets, and instead was taking a burst of montelukast. She also was taking a long-acting bronchodilator every two hours instead of every 12, and she was incorrectly using her rescue inhaler.
As the principal investigator of a trial aiming to reduce post-discharge adverse events and emergency room visits, Dr. Kripalani knows well the issues that contributed to the patient’s re-hospitalization.1 Through research, he and his colleagues hope to prevent future cases.
“It’s very rewarding to identify problems in the care of hospitalized patients and then develop and evaluate interventions to solve those problems,” says Dr. Kripalani, a 2001 graduate of the Emory Mentored Clinical Research Scholars Program who also leads Vanderbilt University’s hospital medicine fellowship. “Sharing those solutions with colleagues so they can be applied to patient care at my institution and others brings the research full circle.”
As the field of hospital medicine grows, the number of hospitalists moving into research careers is expanding, says Peter Kaboli, MD, MS, associate professor in the Department of Internal Medicine at the University of Iowa and a 2001 graduate of the Veterans Administration Quality Scholars Fellowship program. Research training programs, or fellowships, put hospitalists on the path to new skills and position them for careers in academic medicine and other leadership positions, Dr. Kaboli says. Training programs also put fellows in contact with mentors who provide valuable guidance.
Although there are dozens of general internal medicine (GIM) fellowships available to hospitalists, few programs are specifically designed to train hospitalists in research. “Hospital medicine is still a relatively new field,” Dr. Kaboli explains. “The field still does not have many research training options that are separate from general internal medicine.”
Still, hospitalists have advanced training choices, and, depending on their interests, can pursue field-specific programs or follow a general internal medicine path.
Career Investment
Many hospitalists receive basic research training from GIM fellowships. Once they have a research foundation, they can take their experience in another direction.
“Some physicians use their clinical interest—hospital medicine—as the platform for their research,” Dr. Kaboli says, using his own resume as an example. “It’s a nice synergy—doing research in a clinical area of interest.”
Physicians interested in fellowships often start looking for opportunities before they complete their residency, or immediately after. The transition makes sense for some; they move from one academic setting to another. Others, however, consider fellowship programs after they have spent some time in practice and get what Dr. Kaboli calls “boots-on-the-ground experience.”
“I think this is an area where there is potential for growth,” Dr. Kaboli says of physicians returning to fellowship programs after years spent in practice. “It’s the equivalent of a businessperson going back to school to get an MBA. They say, ‘Now I understand what this job really means, and I want to do more.’ ”
The caveat is a pay cut. Physicians in fellowship programs generally are paid a stipend of about $50,000 a year, Kaboli says. By comparison, the average hospitalist makes about $193,000 per year, according to SHM’s 2007-2008 Bi-Annual Survey on the State of Hospital Medicine. For two years, fellows devote their lives to training, coursework, and research, and spend only about 25% of their time treating patients, he says.
Road to Research
Hospitalists can choose from a range of general internal medicine fellowships at universities, clinics, and medical centers across the country. Each program offers something different; the fit depends on the candidates’ interests, says Geri Barnes, SHM senior director of education and meetings. For instance, training programs offer advanced study in the areas of biostatistics, epidemiology, and research methodology, to name a few. GIM fellowships (see “To Be or Not to Be a Fellow,” May 2006, p. 26) encourage scholars to develop relationships with mentors to guide them through research projects, she explains. A program’s duration can span one to three years. Some programs give fellows the opportunity to earn an advanced degree in quality improvement, clinical research, public policy, health studies, public health, or clinical epidemiology.
A handful of institutions, including Johns Hopkins Hospital in Baltimore, offer GIM fellowships with a hospital medicine emphasis. The National Institutes of Health (NIH) funds the Johns Hopkins program with training grants, says Daniel J. Brotman, MD, director of the hospitalist program there. GIM leadership is taking a “big tent” approach, promoting the development of hospital medicine tracks within the full program, which is good for the fellowship and for the hospitalist program, Dr. Brotman says.
“Some of the challenges for hospitalists are that they are generally young and don’t have the skills to succeed in academic medicine,” Dr. Brotman says, “and the number of mentors in hospitalist medicine is few and far between. [The fellowship] allows scholars to tap into experienced research mentors who may not be hospitalists themselves but are interested in investigating research questions and promoting academic careers in hospitalist medicine.”
The GIM program at Johns Hopkins draws physicians trained in internal medicine as well as general medicine/pediatrics. Candidates are required to have completed an internal medicine or medicine/pediatrics residency and must provide strong letters of recommendation. Scholars receive training in statistical methods while obtaining a master’s degree in public health or health science at the Johns Hopkins Bloomberg School of Public Health. Fellows commit 80% of their time to research and research training, and 20% of their time to clinical duties; they are expected to form relationships with faculty, which ultimately leads to careers in academia or public health, Dr. Brotman explains.
Minimize Burnout
Physician burnout—so common in the current healthcare system—is an excellent reason to consider a research career. Five years ago, David Meltzer, MD, PhD, an associate professor in the Department of Medicine at the University of Chicago, wanted to increase the number of research-trained hospitalists, so he moved to create a hospitalist training program. Around the same time, the hospital approached Dr. Meltzer and others, asking them to expand the number of clinical physician positions.
“We were afraid the new physicians would burn out rather quickly if their jobs included only clinical work,” Dr. Meltzer says. “We designed positions that had less clinical work but more time for physicians to develop research skills to support sustainable academic careers.”
Hospital leaders agreed, and the university’s Hospitalist Scholars Training Program was born. The two-year curriculum trains hospitalists for a career in academic research, and combines inpatient clinical work, coursework, and mentored training related to an academic project. Scholars typically leave the program with a master’s degree in public policy or health studies.
“Most of our graduates are working in academic research,” Dr. Meltzer says. “The program has been a great source of new faculty for us.”
Short-term programs are available in select topics. For example, the University of Chicago offers a summer program in outcomes research training for hospitalists interested in careers in health research, Dr. Meltzer says. SHM and the Agency for Healthcare Research and Quality have provided funding to expand the program to include as many as six hospitalists from around the country.
Pioneer Program
Applicants from any medical or surgical specialty are eligible to apply for the Robert Wood Johnson (RWJ) Clinical Scholars Program, the nation’s oldest research training program for physicians in health services, research, and leadership.
“The mandate of Robert Wood Johnson is ‘health and healthcare for all Americans,’ ” says Desmond Runyan, MD, DrPH, national program director of the RWJ Clinical Scholars Program. “We give physicians the skills they need to be leaders, and then we push them out the door so they can go out and shape the future of healthcare in this country.”
Applicants must be U.S. citizens and, with the exception of surgeons, must complete their residency training before entering the clinical scholars program. The two-year program offers a master’s degree in graduate-level study and research, and scholars may be considered for a third year of support. Scholars have their choice of four training sites: the University of California at Los Angeles; Yale University in New Haven, Conn.; the University of Pennsylvania in Philadelphia; or the University of Michigan in Ann Arbor.
Programs vary, but each university has a curriculum to teach the basics of healthcare research. It also provides protected time for research; about 20% of time is spent on clinical activities, according to the program’s Web site. Graduates receive leadership, health services, and community-based research training.
The RWJ Foundation spends about $9 million per year on the program, which covers research support, salaries for scholars and program administrators, travel, and other expenses. About half of the program’s graduates go into academic positions; the other half go into public health or other leadership positions. One recent graduate opted for a position in quality control; three other graduates serve as staff in the U.S. House of Representatives and the U.S. Senate, he says. Other graduates work with foundations, state and federal health agencies, or with companies working in the healthcare industry.
“This program looks for people who don’t march to a standard drummer,” Dr. Runyon says. “We are looking for risk-takers who want to make a difference.”
VA Training
The Veterans Administration National Quality Scholars Fellowship Program (VAQS) welcomes physicians from all medical specialties, including pathology, OB/GYN, surgery, and dermatology. This year, the program will begin recruiting nurses.
The program is offered at six academic-affiliated VA medical centers: Iowa City, Iowa; Nashville, Tenn.; Birmingham, Ala.; Cleveland; San Francisco; and White River Junction, Vt. The Iowa City and Nashville programs have a track designed specifically for hospitalists. These tracks focus on clinical research and quality improvement work in the inpatient setting, and provide fellows with training for advancement in academic and private-sector hospitalist careers, says Dr. Kaboli, the Iowa City VAQS Fellowship director.
To qualify, fellowship applicants must have completed an Accreditation Council for Graduate Medical Education residency or fellowship (see “A Pregnant Pause: The necessary evolution of residency training,” January 2007, p. 35), be board-eligible or board-certified, and have an active, unrestricted U.S. license to practice. International graduates must meet visa and Educational Commission for Foreign Medical Graduates requirements.
The two-year VAQS focuses on quality improvement in healthcare, Dr. Kaboli says. The program offers master’s-level training in epidemiology and biostatistics, and trains fellows to design and conduct research and improvement projects. Fellows publish the results of their research in peer-reviewed journals. They also learn how to write grants to gain funding for future projects.
Mentoring is an important element of the VAQS program, Dr. Kaboli says, adding that the value a trainee receives from any fellowship depends on the level of mentoring available through the program. Fellows work with senior faculty members who provide guidance on all aspects of research, Dr. Kaboli says. This includes study design, research methodology, data collection and analyses, and writing.
New experiences and the opportunity to take part in research are among the benefits of completing the VAQS program, Dr. Kaboli says. Some physicians also find a great deal of career satisfaction through research.
“I love seeing patients,” Dr. Kaboli says, “but I also like the challenge of doing research to find new ways to improve patient care.” TH
Gina Gotsill is a freelance medical writer based in California.
Reference
1. Ranji SR, Rosenman DJ, Amin AN, Kripalani S. Hospital medicine fellowship: works in progress. Am J Med. 2006;119;72.e1-72.e7.
Your hospital medicine questions answered
The Value of Medicare’s Nursing Home Ratings
Is it true that the government has gone public with ratings of nursing homes? If so, where can I find this information? Is this information useful?
H. Sawyer, Richmond, Va.
Dr. Hospitalist responds: Many healthcare providers are familiar with Medicare’s goal to improve the quality of inpatient care. Medicare reports this data at www.hospitalcompare.hhs.gov. The program has its critics, many of whom question whether checking off a list really represents an improved quality of care.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? E-mail your questions to [email protected].
Analogous to its Web site with information about hospital care, Medicare recently unveiled a site with information about the quality of care that our nation’s nursing homes are delivering to Medicare beneficiaries. You can find this information at www.medicare.gov/nhcompare. Medi-care ranks nursing homes on a system that awards ratings from one to five stars, with five stars being the best. Medicare explains it created this rating system to “help consumers, their families, and caregivers compare nursing homes more easily and help identify areas about which you may want to ask questions.” Medicare utilized information from three sources of data to create this overall rating:
- Staffing;
- Quality measures; and
- Health inspections.
The site provides an individual rating for each piece of data and combines the info to determine a composite rating.
Pros and Cons
Medicare acknowledges the rating system has strengths and weaknesses. The staffing information is adjusted for acuity of illness in a given facility’s resident population. That said, the data is self-reported and gathered annually, so it reflects data from just two weeks out of the year. Medicare notes each facility is judged on 10 quality measures, but again, the data is self-reported, is not adjusted for severity, and represents just a few of the many aspects of care that may be important to residents and their families.
Medicare also notes the health inspections are comprehensive and require onsite visits by trained inspectors. Comparisons are best made between facilities in the same state.
Nursing Home Checklist
Aside from facility ratings, Medicare also provides the public with a “nursing home checklist” and encourages the public to take a printed copy of the checklist, along with other information provided on its Web site, when they visit a nursing home. Medicare encourages the public to “talk with the nursing home staff about the information.”
I found no surprising information on this checklist. It encourages the public to think about basic information, such as:
- Is the home Medicare- and Medicaid-certified?
- Is the facility close to family and friends, clean, free from unpleasant odors, and comfortable for its residents?
- Is there a physician present every day and available when necessary?
- Are licensed nurses available 24 hours a day; is an RN available eight hours per day, seven days per week.
The site says individuals should think about resident rooms and the areas outside the resident rooms. It also encourages the public to think about the food and activities available to residents.
Much like the program for evaluating hospital care, I believe Medicare has taken a reasonable first step in providing information to the public to evaluate the care being provided in our nation’s nursing homes. But you will not find information regarding nursing homes that do not accept Medicare. And this information is only about nursing homes, and does not include other types of residential facilities. TH
The Value of Medicare’s Nursing Home Ratings
Is it true that the government has gone public with ratings of nursing homes? If so, where can I find this information? Is this information useful?
H. Sawyer, Richmond, Va.
Dr. Hospitalist responds: Many healthcare providers are familiar with Medicare’s goal to improve the quality of inpatient care. Medicare reports this data at www.hospitalcompare.hhs.gov. The program has its critics, many of whom question whether checking off a list really represents an improved quality of care.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? E-mail your questions to [email protected].
Analogous to its Web site with information about hospital care, Medicare recently unveiled a site with information about the quality of care that our nation’s nursing homes are delivering to Medicare beneficiaries. You can find this information at www.medicare.gov/nhcompare. Medi-care ranks nursing homes on a system that awards ratings from one to five stars, with five stars being the best. Medicare explains it created this rating system to “help consumers, their families, and caregivers compare nursing homes more easily and help identify areas about which you may want to ask questions.” Medicare utilized information from three sources of data to create this overall rating:
- Staffing;
- Quality measures; and
- Health inspections.
The site provides an individual rating for each piece of data and combines the info to determine a composite rating.
Pros and Cons
Medicare acknowledges the rating system has strengths and weaknesses. The staffing information is adjusted for acuity of illness in a given facility’s resident population. That said, the data is self-reported and gathered annually, so it reflects data from just two weeks out of the year. Medicare notes each facility is judged on 10 quality measures, but again, the data is self-reported, is not adjusted for severity, and represents just a few of the many aspects of care that may be important to residents and their families.
Medicare also notes the health inspections are comprehensive and require onsite visits by trained inspectors. Comparisons are best made between facilities in the same state.
Nursing Home Checklist
Aside from facility ratings, Medicare also provides the public with a “nursing home checklist” and encourages the public to take a printed copy of the checklist, along with other information provided on its Web site, when they visit a nursing home. Medicare encourages the public to “talk with the nursing home staff about the information.”
I found no surprising information on this checklist. It encourages the public to think about basic information, such as:
- Is the home Medicare- and Medicaid-certified?
- Is the facility close to family and friends, clean, free from unpleasant odors, and comfortable for its residents?
- Is there a physician present every day and available when necessary?
- Are licensed nurses available 24 hours a day; is an RN available eight hours per day, seven days per week.
The site says individuals should think about resident rooms and the areas outside the resident rooms. It also encourages the public to think about the food and activities available to residents.
Much like the program for evaluating hospital care, I believe Medicare has taken a reasonable first step in providing information to the public to evaluate the care being provided in our nation’s nursing homes. But you will not find information regarding nursing homes that do not accept Medicare. And this information is only about nursing homes, and does not include other types of residential facilities. TH
The Value of Medicare’s Nursing Home Ratings
Is it true that the government has gone public with ratings of nursing homes? If so, where can I find this information? Is this information useful?
H. Sawyer, Richmond, Va.
Dr. Hospitalist responds: Many healthcare providers are familiar with Medicare’s goal to improve the quality of inpatient care. Medicare reports this data at www.hospitalcompare.hhs.gov. The program has its critics, many of whom question whether checking off a list really represents an improved quality of care.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? E-mail your questions to [email protected].
Analogous to its Web site with information about hospital care, Medicare recently unveiled a site with information about the quality of care that our nation’s nursing homes are delivering to Medicare beneficiaries. You can find this information at www.medicare.gov/nhcompare. Medi-care ranks nursing homes on a system that awards ratings from one to five stars, with five stars being the best. Medicare explains it created this rating system to “help consumers, their families, and caregivers compare nursing homes more easily and help identify areas about which you may want to ask questions.” Medicare utilized information from three sources of data to create this overall rating:
- Staffing;
- Quality measures; and
- Health inspections.
The site provides an individual rating for each piece of data and combines the info to determine a composite rating.
Pros and Cons
Medicare acknowledges the rating system has strengths and weaknesses. The staffing information is adjusted for acuity of illness in a given facility’s resident population. That said, the data is self-reported and gathered annually, so it reflects data from just two weeks out of the year. Medicare notes each facility is judged on 10 quality measures, but again, the data is self-reported, is not adjusted for severity, and represents just a few of the many aspects of care that may be important to residents and their families.
Medicare also notes the health inspections are comprehensive and require onsite visits by trained inspectors. Comparisons are best made between facilities in the same state.
Nursing Home Checklist
Aside from facility ratings, Medicare also provides the public with a “nursing home checklist” and encourages the public to take a printed copy of the checklist, along with other information provided on its Web site, when they visit a nursing home. Medicare encourages the public to “talk with the nursing home staff about the information.”
I found no surprising information on this checklist. It encourages the public to think about basic information, such as:
- Is the home Medicare- and Medicaid-certified?
- Is the facility close to family and friends, clean, free from unpleasant odors, and comfortable for its residents?
- Is there a physician present every day and available when necessary?
- Are licensed nurses available 24 hours a day; is an RN available eight hours per day, seven days per week.
The site says individuals should think about resident rooms and the areas outside the resident rooms. It also encourages the public to think about the food and activities available to residents.
Much like the program for evaluating hospital care, I believe Medicare has taken a reasonable first step in providing information to the public to evaluate the care being provided in our nation’s nursing homes. But you will not find information regarding nursing homes that do not accept Medicare. And this information is only about nursing homes, and does not include other types of residential facilities. TH
Bridge the Attending Divide
I always wear a sport coat and tie when I’m speaking, but I thought I knew the orthopedic psyche well enough to know they would be very casually dressed for their conference on a warm Saturday this past fall. I was stunned to see about 40 of the 60 orthopods in attendance wearing jackets and ties—a very dapper bunch. While I misjudged their fashion sense, I’m still confident I’ll fit in wearing a bow tie (borrowed, since I don’t own one) to a neurology conference or a Mickey Mouse tie to a pediatric conference.
I had been invited to speak at the Washington State Orthopedic Association last fall. (Maybe they spell it “orthopædics,” but that seems a little pretentious to me.) They wanted to hear about the latest trends in how orthopods and hospitalists collaborate in the care of patients, and how this interaction might evolve.
Attending or Consultants?
I told them that, in my experience, determining the best doctor to serve as attending for certain types of patients generates a wide range of sometimes passionately held opinions among hospitalists. In my consulting work with practices around the country, I’ve come across some hospitalists who are insistent that they should never serve as attending for patients whose primary reason for admission is:
- Hip fracture due to osteoporosis and fall from ground level;
- Nonoperative low-speed or low-impact trauma, such as pelvic fracture; and
- Limb infection with potential for compartment syndrome.
Interestingly, I’ve found that hospitalists almost universally admit patients with osteoporotic vertebral compression fractures, even if they strongly believe that they shouldn’t admit patients with pelvic fractures.
My own experience leads me to believe that hospitalists in most settings should plan to serve as attending for all of these patient types, if they aren’t already. For example, a hip fracture is essentially a marker for a sick and frail person with complex medical needs. While it is the marquee event of the hospital stay, surgical repair of the fracture is just one of many important things that need to happen before discharge. Most of these patients need attention for medical comorbidities—such as a urinary infection or decompensated heart failure—which often are the proximate cause of the fracture. The patient might need a discussion of medical directives, which usually is an area in which orthopods usually don’t excel (and I’m being kind to the orthopods).
Let me be clear: Reasonable people can conclude hospitalists should not serve as attending for the diagnoses listed above. SHM does not have a position on this, and I’m not speaking for all hospitalists. But don’t you think hospitalists opposed to admitting these types of patients will find themselves in a small and shrinking minority? It seems to me that the pressure to serve as attending for these patients is similar to surviving a riptide: You shouldn’t try to swim directly against the riptide toward shore, and instead should swim across it or even go with the flow.
Popular Term, No Universal Definition
I went on to talk with the orthopods about the concept of partnering with hospitalists to co-manage patients. Orthopods and hospital executives usually are enthusiastic supporters of the co-management idea, and hospitalists usually are supportive, though sometimes with a little less excitement than the others. In public, all three parties usually express confidence that co-management will be good for patient outcomes and have other benefits, such as improved efficiency. But in private, orthopods sometimes let on that their support of the idea is largely based on their belief that it relieves them of tedious paperwork and late-night phone calls.
A hospital CEO might not know the details of the co-management model, so the CEO’s public support of it often boils down to an analysis along the lines of “Isn’t co-management just a euphemism for hospitalists doing more of the scut work to keep the hospital’s money-making specialists—like orthopods—happy?” Even hospitalists themselves sometimes express public support for the idea, but privately are thinking, “These guys want me to do what?”
My view is that co-management is a broad term and can mean very different things from one institution to the next. The term “co-management” has a connotation of something new and progressive, and might help steer conversations about who does what in a more positive direction than the old vocabulary of who is dumping on whom—you know, the traditional role for the doctors in each specialty.
A terrific entry in “Debates in Hospital Medicine” that runs periodically in the Journal of Hospital Medicine offers two points of view. In the September/October 2008 issue of JHM, Christopher Whinney, MD, and Frank Michota, MD, of Cleveland Clinic took the stance in favor of co-management, and Eric Siegal, MD, SHM’s Public Policy Committee chair (and formerly in private and corporate hospitalist practice), raised concerns about co-management.1 The articles review what little—and in my view inconclusive—research exists on this topic but provide some thoughtful advice and opinions.
Issues to Address
As I have written in the past, I’m convinced hospitalists’ scope of practice will broaden and grow to include patients we don’t commonly admit today.2 But we will need to think carefully about how to mitigate the potential problems created by changes in how doctors divide responsibility for who does what. In the case of hospitalists serving as admitters and attending for hip fracture patients, I have concerns, such as:
- Will there be delays in going to the operating room or confusion regarding which orthopedist is responsible for the patient?
- Will the orthopedist be less available to talk with the patient and family post-op?
- How long before the orthopedist stops making post-op visits?
- Who decides about transfusion and manages post-op and discharge pain control, wound care, and rehab?
- Who gets the nighttime call regarding a laxative or sleeping pill?
- Who handles discharge paperwork?
Your list of concerns probably differs from mine, but you should take the time to write down the issues that concern you any time duties and responsibilities shift from one specialty to another. Keep that list handy the next time you talk with another specialty about co-management or other new ways of dividing the work to ensure good outcomes for patients, doctors (including hospitalists), and the healthcare system as a whole. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospital practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position.
References
1. Whinney C, Michota F, and Siegal EM. Surgical comanagement: a natural evolution of hospitalist practice. Just because you can, doesn’t mean that you should: A call for the rational application of hospitalist comanagement. J Hosp Med. 2008;3(5); 394-402.
2. Nelson J. Hip fractures to head bleeds: The hospitalist’s ever-changing scope of practice. The Hospitalist. 2006; 10(9);77.
I always wear a sport coat and tie when I’m speaking, but I thought I knew the orthopedic psyche well enough to know they would be very casually dressed for their conference on a warm Saturday this past fall. I was stunned to see about 40 of the 60 orthopods in attendance wearing jackets and ties—a very dapper bunch. While I misjudged their fashion sense, I’m still confident I’ll fit in wearing a bow tie (borrowed, since I don’t own one) to a neurology conference or a Mickey Mouse tie to a pediatric conference.
I had been invited to speak at the Washington State Orthopedic Association last fall. (Maybe they spell it “orthopædics,” but that seems a little pretentious to me.) They wanted to hear about the latest trends in how orthopods and hospitalists collaborate in the care of patients, and how this interaction might evolve.
Attending or Consultants?
I told them that, in my experience, determining the best doctor to serve as attending for certain types of patients generates a wide range of sometimes passionately held opinions among hospitalists. In my consulting work with practices around the country, I’ve come across some hospitalists who are insistent that they should never serve as attending for patients whose primary reason for admission is:
- Hip fracture due to osteoporosis and fall from ground level;
- Nonoperative low-speed or low-impact trauma, such as pelvic fracture; and
- Limb infection with potential for compartment syndrome.
Interestingly, I’ve found that hospitalists almost universally admit patients with osteoporotic vertebral compression fractures, even if they strongly believe that they shouldn’t admit patients with pelvic fractures.
My own experience leads me to believe that hospitalists in most settings should plan to serve as attending for all of these patient types, if they aren’t already. For example, a hip fracture is essentially a marker for a sick and frail person with complex medical needs. While it is the marquee event of the hospital stay, surgical repair of the fracture is just one of many important things that need to happen before discharge. Most of these patients need attention for medical comorbidities—such as a urinary infection or decompensated heart failure—which often are the proximate cause of the fracture. The patient might need a discussion of medical directives, which usually is an area in which orthopods usually don’t excel (and I’m being kind to the orthopods).
Let me be clear: Reasonable people can conclude hospitalists should not serve as attending for the diagnoses listed above. SHM does not have a position on this, and I’m not speaking for all hospitalists. But don’t you think hospitalists opposed to admitting these types of patients will find themselves in a small and shrinking minority? It seems to me that the pressure to serve as attending for these patients is similar to surviving a riptide: You shouldn’t try to swim directly against the riptide toward shore, and instead should swim across it or even go with the flow.
Popular Term, No Universal Definition
I went on to talk with the orthopods about the concept of partnering with hospitalists to co-manage patients. Orthopods and hospital executives usually are enthusiastic supporters of the co-management idea, and hospitalists usually are supportive, though sometimes with a little less excitement than the others. In public, all three parties usually express confidence that co-management will be good for patient outcomes and have other benefits, such as improved efficiency. But in private, orthopods sometimes let on that their support of the idea is largely based on their belief that it relieves them of tedious paperwork and late-night phone calls.
A hospital CEO might not know the details of the co-management model, so the CEO’s public support of it often boils down to an analysis along the lines of “Isn’t co-management just a euphemism for hospitalists doing more of the scut work to keep the hospital’s money-making specialists—like orthopods—happy?” Even hospitalists themselves sometimes express public support for the idea, but privately are thinking, “These guys want me to do what?”
My view is that co-management is a broad term and can mean very different things from one institution to the next. The term “co-management” has a connotation of something new and progressive, and might help steer conversations about who does what in a more positive direction than the old vocabulary of who is dumping on whom—you know, the traditional role for the doctors in each specialty.
A terrific entry in “Debates in Hospital Medicine” that runs periodically in the Journal of Hospital Medicine offers two points of view. In the September/October 2008 issue of JHM, Christopher Whinney, MD, and Frank Michota, MD, of Cleveland Clinic took the stance in favor of co-management, and Eric Siegal, MD, SHM’s Public Policy Committee chair (and formerly in private and corporate hospitalist practice), raised concerns about co-management.1 The articles review what little—and in my view inconclusive—research exists on this topic but provide some thoughtful advice and opinions.
Issues to Address
As I have written in the past, I’m convinced hospitalists’ scope of practice will broaden and grow to include patients we don’t commonly admit today.2 But we will need to think carefully about how to mitigate the potential problems created by changes in how doctors divide responsibility for who does what. In the case of hospitalists serving as admitters and attending for hip fracture patients, I have concerns, such as:
- Will there be delays in going to the operating room or confusion regarding which orthopedist is responsible for the patient?
- Will the orthopedist be less available to talk with the patient and family post-op?
- How long before the orthopedist stops making post-op visits?
- Who decides about transfusion and manages post-op and discharge pain control, wound care, and rehab?
- Who gets the nighttime call regarding a laxative or sleeping pill?
- Who handles discharge paperwork?
Your list of concerns probably differs from mine, but you should take the time to write down the issues that concern you any time duties and responsibilities shift from one specialty to another. Keep that list handy the next time you talk with another specialty about co-management or other new ways of dividing the work to ensure good outcomes for patients, doctors (including hospitalists), and the healthcare system as a whole. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospital practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position.
References
1. Whinney C, Michota F, and Siegal EM. Surgical comanagement: a natural evolution of hospitalist practice. Just because you can, doesn’t mean that you should: A call for the rational application of hospitalist comanagement. J Hosp Med. 2008;3(5); 394-402.
2. Nelson J. Hip fractures to head bleeds: The hospitalist’s ever-changing scope of practice. The Hospitalist. 2006; 10(9);77.
I always wear a sport coat and tie when I’m speaking, but I thought I knew the orthopedic psyche well enough to know they would be very casually dressed for their conference on a warm Saturday this past fall. I was stunned to see about 40 of the 60 orthopods in attendance wearing jackets and ties—a very dapper bunch. While I misjudged their fashion sense, I’m still confident I’ll fit in wearing a bow tie (borrowed, since I don’t own one) to a neurology conference or a Mickey Mouse tie to a pediatric conference.
I had been invited to speak at the Washington State Orthopedic Association last fall. (Maybe they spell it “orthopædics,” but that seems a little pretentious to me.) They wanted to hear about the latest trends in how orthopods and hospitalists collaborate in the care of patients, and how this interaction might evolve.
Attending or Consultants?
I told them that, in my experience, determining the best doctor to serve as attending for certain types of patients generates a wide range of sometimes passionately held opinions among hospitalists. In my consulting work with practices around the country, I’ve come across some hospitalists who are insistent that they should never serve as attending for patients whose primary reason for admission is:
- Hip fracture due to osteoporosis and fall from ground level;
- Nonoperative low-speed or low-impact trauma, such as pelvic fracture; and
- Limb infection with potential for compartment syndrome.
Interestingly, I’ve found that hospitalists almost universally admit patients with osteoporotic vertebral compression fractures, even if they strongly believe that they shouldn’t admit patients with pelvic fractures.
My own experience leads me to believe that hospitalists in most settings should plan to serve as attending for all of these patient types, if they aren’t already. For example, a hip fracture is essentially a marker for a sick and frail person with complex medical needs. While it is the marquee event of the hospital stay, surgical repair of the fracture is just one of many important things that need to happen before discharge. Most of these patients need attention for medical comorbidities—such as a urinary infection or decompensated heart failure—which often are the proximate cause of the fracture. The patient might need a discussion of medical directives, which usually is an area in which orthopods usually don’t excel (and I’m being kind to the orthopods).
Let me be clear: Reasonable people can conclude hospitalists should not serve as attending for the diagnoses listed above. SHM does not have a position on this, and I’m not speaking for all hospitalists. But don’t you think hospitalists opposed to admitting these types of patients will find themselves in a small and shrinking minority? It seems to me that the pressure to serve as attending for these patients is similar to surviving a riptide: You shouldn’t try to swim directly against the riptide toward shore, and instead should swim across it or even go with the flow.
Popular Term, No Universal Definition
I went on to talk with the orthopods about the concept of partnering with hospitalists to co-manage patients. Orthopods and hospital executives usually are enthusiastic supporters of the co-management idea, and hospitalists usually are supportive, though sometimes with a little less excitement than the others. In public, all three parties usually express confidence that co-management will be good for patient outcomes and have other benefits, such as improved efficiency. But in private, orthopods sometimes let on that their support of the idea is largely based on their belief that it relieves them of tedious paperwork and late-night phone calls.
A hospital CEO might not know the details of the co-management model, so the CEO’s public support of it often boils down to an analysis along the lines of “Isn’t co-management just a euphemism for hospitalists doing more of the scut work to keep the hospital’s money-making specialists—like orthopods—happy?” Even hospitalists themselves sometimes express public support for the idea, but privately are thinking, “These guys want me to do what?”
My view is that co-management is a broad term and can mean very different things from one institution to the next. The term “co-management” has a connotation of something new and progressive, and might help steer conversations about who does what in a more positive direction than the old vocabulary of who is dumping on whom—you know, the traditional role for the doctors in each specialty.
A terrific entry in “Debates in Hospital Medicine” that runs periodically in the Journal of Hospital Medicine offers two points of view. In the September/October 2008 issue of JHM, Christopher Whinney, MD, and Frank Michota, MD, of Cleveland Clinic took the stance in favor of co-management, and Eric Siegal, MD, SHM’s Public Policy Committee chair (and formerly in private and corporate hospitalist practice), raised concerns about co-management.1 The articles review what little—and in my view inconclusive—research exists on this topic but provide some thoughtful advice and opinions.
Issues to Address
As I have written in the past, I’m convinced hospitalists’ scope of practice will broaden and grow to include patients we don’t commonly admit today.2 But we will need to think carefully about how to mitigate the potential problems created by changes in how doctors divide responsibility for who does what. In the case of hospitalists serving as admitters and attending for hip fracture patients, I have concerns, such as:
- Will there be delays in going to the operating room or confusion regarding which orthopedist is responsible for the patient?
- Will the orthopedist be less available to talk with the patient and family post-op?
- How long before the orthopedist stops making post-op visits?
- Who decides about transfusion and manages post-op and discharge pain control, wound care, and rehab?
- Who gets the nighttime call regarding a laxative or sleeping pill?
- Who handles discharge paperwork?
Your list of concerns probably differs from mine, but you should take the time to write down the issues that concern you any time duties and responsibilities shift from one specialty to another. Keep that list handy the next time you talk with another specialty about co-management or other new ways of dividing the work to ensure good outcomes for patients, doctors (including hospitalists), and the healthcare system as a whole. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospital practice management consulting firm. He is part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official SHM position.
References
1. Whinney C, Michota F, and Siegal EM. Surgical comanagement: a natural evolution of hospitalist practice. Just because you can, doesn’t mean that you should: A call for the rational application of hospitalist comanagement. J Hosp Med. 2008;3(5); 394-402.
2. Nelson J. Hip fractures to head bleeds: The hospitalist’s ever-changing scope of practice. The Hospitalist. 2006; 10(9);77.