User login
Bullying HURTs! Assessing and managing the bullied child
Technological developments—most notably, the increasing popularity of social networking sites such as Facebook—have led to a resurgence in the prevalence of bullying.1,2 The unlimited reach and anonymity of “cyber” bullying has introduced new challenges for pediatricians and child psychiatrists. Traditional bullying—defined as a specific form of aggression that is intentional, repeated, and involves a disparity of power between the victim and perpetrators—remains more common, with 54% of middle school students reporting verbal bullying, compared with 14% reporting at least 1 episode of electronic bullying over 2 months.2 Compared with students who weren’t bullied, middle and high school students who were bullied were 3 times more likely to report seriously considering suicide, engaging in intentional self-harm, being physically hurt by a family member, and witnessing violence in their families.3
Although bullying occurs frequently and is closely associated with several psychiatric conditions, including attention-deficit/hyperactivity disorder,4 depression,1 and anxiety,1 clinicians often don’t thoroughly assess patients to determine if they’ve been bullied and rarely intervene. The mnemonic HURT may aid in the clinical assessment and management of bullied children.
Help empower the child who is being bullied by encouraging him or her to find appropriate help from teachers, school counselors, or other resources, which may decrease the likelihood of psychological and physical consequences.
Understand the risk factors for being bullied, including less parental support,2 violent family encounters,3 and obesity,3 that may contribute to a child’s emotional experiences or behavior in ways that make him or her an easy target for bullying.2
Recognize a child who is at risk for being bullied and ask about his or her peer relations at school and use of online social networks. At-risk children warrant further evaluation for depression, anxiety, loneliness, and low self-esteem.
Teach the child why others engage in bullying so he or she may avoid actions and words that instigate or provoke a bully, and discuss techniques for dealing with confrontations.
Disclosures
Dr. Madaan is a consultant for The NOW Coalition for Bipolar Disorder and Avanir Pharmaceuticals and has pending research support from Merck and Otsuka.
Ms. Kepple reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
The authors would like to thank Sara Kepple for her assistance with this article.
1. Kowalski RM. Cyber bullying: recognizing and treating victim and aggressor. Psychiatric Times. October 1, 2008.
2. Wang J, Iannotti RJ, Nansel TR. School bullying among adolescents in the United States: physical, verbal, relational, and cyber. J Adolesc Health. 2009;45(4):368-375.
3. Centers for Disease Control and Prevention. Bullying among middle school and high school students—Massachusetts, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(15):465-471.
4. Holmberg K. The association of bullying and health complaints in children with attention-deficit/hyperactivity disorder. Postgrad Med. 2010;122(5):62-68.
Technological developments—most notably, the increasing popularity of social networking sites such as Facebook—have led to a resurgence in the prevalence of bullying.1,2 The unlimited reach and anonymity of “cyber” bullying has introduced new challenges for pediatricians and child psychiatrists. Traditional bullying—defined as a specific form of aggression that is intentional, repeated, and involves a disparity of power between the victim and perpetrators—remains more common, with 54% of middle school students reporting verbal bullying, compared with 14% reporting at least 1 episode of electronic bullying over 2 months.2 Compared with students who weren’t bullied, middle and high school students who were bullied were 3 times more likely to report seriously considering suicide, engaging in intentional self-harm, being physically hurt by a family member, and witnessing violence in their families.3
Although bullying occurs frequently and is closely associated with several psychiatric conditions, including attention-deficit/hyperactivity disorder,4 depression,1 and anxiety,1 clinicians often don’t thoroughly assess patients to determine if they’ve been bullied and rarely intervene. The mnemonic HURT may aid in the clinical assessment and management of bullied children.
Help empower the child who is being bullied by encouraging him or her to find appropriate help from teachers, school counselors, or other resources, which may decrease the likelihood of psychological and physical consequences.
Understand the risk factors for being bullied, including less parental support,2 violent family encounters,3 and obesity,3 that may contribute to a child’s emotional experiences or behavior in ways that make him or her an easy target for bullying.2
Recognize a child who is at risk for being bullied and ask about his or her peer relations at school and use of online social networks. At-risk children warrant further evaluation for depression, anxiety, loneliness, and low self-esteem.
Teach the child why others engage in bullying so he or she may avoid actions and words that instigate or provoke a bully, and discuss techniques for dealing with confrontations.
Disclosures
Dr. Madaan is a consultant for The NOW Coalition for Bipolar Disorder and Avanir Pharmaceuticals and has pending research support from Merck and Otsuka.
Ms. Kepple reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
The authors would like to thank Sara Kepple for her assistance with this article.
Technological developments—most notably, the increasing popularity of social networking sites such as Facebook—have led to a resurgence in the prevalence of bullying.1,2 The unlimited reach and anonymity of “cyber” bullying has introduced new challenges for pediatricians and child psychiatrists. Traditional bullying—defined as a specific form of aggression that is intentional, repeated, and involves a disparity of power between the victim and perpetrators—remains more common, with 54% of middle school students reporting verbal bullying, compared with 14% reporting at least 1 episode of electronic bullying over 2 months.2 Compared with students who weren’t bullied, middle and high school students who were bullied were 3 times more likely to report seriously considering suicide, engaging in intentional self-harm, being physically hurt by a family member, and witnessing violence in their families.3
Although bullying occurs frequently and is closely associated with several psychiatric conditions, including attention-deficit/hyperactivity disorder,4 depression,1 and anxiety,1 clinicians often don’t thoroughly assess patients to determine if they’ve been bullied and rarely intervene. The mnemonic HURT may aid in the clinical assessment and management of bullied children.
Help empower the child who is being bullied by encouraging him or her to find appropriate help from teachers, school counselors, or other resources, which may decrease the likelihood of psychological and physical consequences.
Understand the risk factors for being bullied, including less parental support,2 violent family encounters,3 and obesity,3 that may contribute to a child’s emotional experiences or behavior in ways that make him or her an easy target for bullying.2
Recognize a child who is at risk for being bullied and ask about his or her peer relations at school and use of online social networks. At-risk children warrant further evaluation for depression, anxiety, loneliness, and low self-esteem.
Teach the child why others engage in bullying so he or she may avoid actions and words that instigate or provoke a bully, and discuss techniques for dealing with confrontations.
Disclosures
Dr. Madaan is a consultant for The NOW Coalition for Bipolar Disorder and Avanir Pharmaceuticals and has pending research support from Merck and Otsuka.
Ms. Kepple reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Acknowledgement
The authors would like to thank Sara Kepple for her assistance with this article.
1. Kowalski RM. Cyber bullying: recognizing and treating victim and aggressor. Psychiatric Times. October 1, 2008.
2. Wang J, Iannotti RJ, Nansel TR. School bullying among adolescents in the United States: physical, verbal, relational, and cyber. J Adolesc Health. 2009;45(4):368-375.
3. Centers for Disease Control and Prevention. Bullying among middle school and high school students—Massachusetts, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(15):465-471.
4. Holmberg K. The association of bullying and health complaints in children with attention-deficit/hyperactivity disorder. Postgrad Med. 2010;122(5):62-68.
1. Kowalski RM. Cyber bullying: recognizing and treating victim and aggressor. Psychiatric Times. October 1, 2008.
2. Wang J, Iannotti RJ, Nansel TR. School bullying among adolescents in the United States: physical, verbal, relational, and cyber. J Adolesc Health. 2009;45(4):368-375.
3. Centers for Disease Control and Prevention. Bullying among middle school and high school students—Massachusetts, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(15):465-471.
4. Holmberg K. The association of bullying and health complaints in children with attention-deficit/hyperactivity disorder. Postgrad Med. 2010;122(5):62-68.
Psychotropic-induced dry mouth: Don’t overlook this potentially serious side effect
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
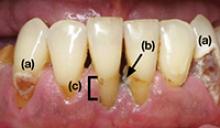
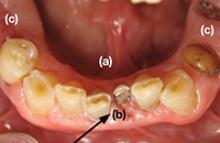
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Xerostomia, commonly known as “dry mouth,” is a reported side effect of >1,800 drugs from >80 classes.1 This condition often goes unrecognized and untreated, but it can significantly affect patients’ quality of life and cause oral and medical health problems.2,3 Although psychotropic medications are not the only offenders, they comprise a large portion of the agents that can cause dry mouth. Antidepressants, anticonvulsants, anxiolytics, antipsychotics, anticholinergics, and alpha agonists can cause xerostomia.4 The risk of salivary hypofunction increases with polypharmacy and may be especially likely when ≥3 drugs are taken per day.5
Among all reported side effects of antidepressants and antipsychotics, dry mouth often is the most prevalent complaint. For example, in a study of 5 antidepressants 35% to 46% of patients reported dry mouth.6 Rates are similar in users of various antipsychotics. Patients with severe, persistent mental illness often cite side effects as the primary reason for psychotropic noncompliance.7-9
Few psychiatrists routinely screen patients for xerostomia, and if a patient reports this side effect, they may be unlikely to address it or understand its implications because of more pressing concerns such as psychosis or risk of suicide. Historically, education in general medical training about the effects of oral health on a patient’s overall health has been limited. It is crucial for psychiatrists to be aware of potential problems related to dry mouth and the impact it can have on their patients. In this article, we:
- describe how dry mouth can impact a patient’s oral, medical, and psychiatric health
- provide psychiatrists with an understanding of pathology related to xerostomia
- explain how psychiatrists can screen for xerostomia
- discuss the benefits patients may receive when psychiatrists collaborate with dental clinicians to manage this condition.
Implications of xerostomia
Saliva provides a protective function. It is an antimicrobial, buffering, and lubricating agent that aids cleansing and removal of food debris within the mouth. It also helps maintain oral mucosa and remineralizing of tooth structure.10
Psychotropics can affect the amount of saliva secreted and may alter the composition of saliva via their receptor affects on the dual sympathetic and parasympathetic innervations of the salivary glands.11 When the protective environment produced by saliva is altered, patients may start to develop oral problems before experiencing dryness. A 50% reduction in saliva flow may occur before they become aware of the problem.12,13
Patients may not taste food properly, experience cracked lips, or have trouble eating, oral pain, or dentures that no longer fit well.14 Additionally, oral diseases such as dental decay and periodontal disease (Photos 1 and 2), inflamed soft tissue, and candidiasis (Photo 3) also may occur.10,15 Patients may begin to notice dry mouth when they wake at night, which could disrupt sleep. Patients with xerostomia can accumulate excessive amounts of plaque on their teeth and the dorsum of the tongue. The increased bacterial count and release of volatile sulfide gases that occur with dry mouth may explain some cases of halitosis.16,17 Patients also may have difficulty swallowing or speaking and be unaware of the oral health destruction occurring as a result of reduced saliva. Some experts report oral bacteria levels can skyrocket as much as 10-fold in people who take medications that cause dry mouth.18
Infections of the mouth can create havoc elsewhere in the body. The evidence base that establishes an association between periodontal disease and other chronic inflammatory conditions such as diabetes, cardiovascular disease, cancer, and rheumatoid arthritis is steadily growing.19-22 Periodontal disease also is a risk factor for preeclampsia and other illnesses that can negatively affect neonatal health.23,24
Failure to recognize xerostomia caused by psychotropic medications may lead to an increase in cavities, periodontal disease, and chronic systemic inflammatory conditions that can shorten a patient’s life span. Recognizing and treating causes of xerostomia is vital because doing so may halt this chain of events.
Photo 1
This patient complained of dry mouth and exhibits decay (a) and evidence of periodontal disease. Plaque and calculus is present (b), along with gingival recession from the loss of attachment and bone (c). This patient was taking venlafaxine, zolpidem, and alprazolam
Photo 2
Dental cavities were restored with tooth-colored restorations (arrows) on this patient, who has xerostomia. Every effort must be made to manage this patient’s dry mouth or the restorations may fail due to recurrent decay
Photo 3
This partial denture wearer, who complained of dry mouth, has evidence of palatal irritation and sores as a result of xerostomia and use of a partial denture. This patient was taking bupropion, esomeprazole, and tolterodine
Psychiatric patients’ oral health
Psychiatric patients’ oral health status often is poor. Several studies found that compared with the general population, patients who have severe, persistent mental illness are at higher risk to be missing teeth, schedule fewer visits to the dentist, and neglect oral hygiene.25-28 Periodontal disease also could be a problem in these patients.29 Although some evidence suggests mental illness may make patients less likely to go to the dentist, psychotropic medications also may contribute to their dental difficulties.
Screening for xerostomia
Simply advising patients of the problems related to xerostomia and asking several questions may help prevent pain and deterioration in function within the oral cavity (Table 1).14,30
You can perform a simple in-office assessment of the oral cavity by visual inspection and by placing a dry tongue blade against the inside of the cheek mucosa. If the blade sticks to the mucosa and a gentle tug is needed to lift it away, xerostomia may be present.30 Conversely, a healthy mouth will have a collection of saliva on the floor of the oral cavity, and pulling a tongue blade away from the inside of the cheek will not require any effort (Photos 4 and 5).
Table 1
Screening questions for xerostomia
| Does the amount of saliva in your mouth seem to have decreased? |
| Do you have any trouble swallowing, speaking, or eating dry foods? |
| Do you sip liquids more often to help you swallow? |
| Do you notice any dryness or cracking of your lips? |
| Do you have mouth sores or a burning feeling in the mouth? |
| When was the last time you saw your dentist? (Patients with xerostomia may need to see their dentist more frequently) |
| Are you aware of any halitosis (ie, mouth odor)? |
| Source: Reference 14 |
Photo 4
The arrow shows the normal appearance of saliva collecting on the floor of the mouth
Photo 5
This patient complained of dry mouth. Note the floor of the mouth is free of saliva (a). Decay is present (b), and the patient is missing posterior teeth (c). This patient was taking clonidine, metoprolol, hydrochlorothiazide, amlodipine, and irbesartan
Treatment options
Patients who have reduced salivary flow as a result of a medication may become so affected by dryness that their drug regimen may need to be changed. However, the greatest concern is for deteriorating oral health among patients who may be unaware xerostomia is occurring.31
Counsel patients who take medications that can affect their salivary function about the importance of seeing a dentist regularly, and provide referrals when appropriate. Depending upon the patient’s oral health, dentists recommend patients with xerostomia have their teeth cleaned/examined 3 or 4 times per year, rather than the 2 times per year allowed by third-party payers (ie, insurance companies). Also advise patients to be diligent in their oral hygiene practices, including flossing and brushing the teeth and tongue, and to avoid foods that are sticky and/or have high sucrose content (Table 2). Recommend using a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate, which could contribute to mouth sores14—and drinking fluoridated water. Explain to patients that their dentist may recommend in-office high-fluoride applications, high-fluoride prescription toothpaste, and/or “mouth trays” that contain high fluoride gel. Tell patients to avoid cigarettes and caffeinated beverages, which can increase dryness. Alcohol use should be minimized and mouth rinses containing alcohol should not be used.
Many over-the-counter products are available to address xerostomia, including toothpastes, mouth rinses, and gels. Salivary substitutes—which are available as sprays, liquids, tablets, and swab sticks—imitate saliva and may provide a temporary reprieve from dryness. Although none of these products will cure dry mouth, they may help manage the condition. Advise patients to eat foods that stimulate saliva production, such as carrots, apples, and celery, and to chew sugarless gum and candies, which also will stimulate salivary flow.
The FDA has approved 2 prescription drugs for treating xerostomia: cevimeline and pilocarpine. Cevimeline is approved for treating dry mouth associated with Sjögren’s syndrome and pilocarpine is approved for treating dry mouth caused by head and neck radiation therapy; however, these medications’ role in treating dry mouth in psychiatric patients has not been investigated. Both agents are contraindicated in patients with narrow-angle glaucoma, uncontrolled asthma, or liver disease, and should be prescribed with caution for patients with cardiovascular disease, chronic respiratory conditions, or kidney disease.32
Acupuncture and electrostimulation are being studied as a treatment for xerostomia. Trials have found acupuncture improves symptoms of xerostomia,33,34 and 1 study found electrostimulation improved xerostomia in patients with Sjögren’s syndrome.35 Both approaches require more study to confirm their effectiveness.33-35
Table 2
Managing dry mouth: What to tell patients
| Oral hygiene. Tell patients to be diligent in their oral hygiene practices, including brushing and flossing. They should use a toothpaste containing fluoride—preferably one free of sodium lauryl sulfate—and schedule regular dental visits, where they can receive high-fluoride applications or be prescribed high-fluoride prescription toothpastes |
| Diet. Advise patients to avoid foods high in sucrose content, rinse their mouth with water soon after eating, and drink fluoridated water regularly. Tell them that they may be able to stimulate saliva flow with sugarless gum, candies, and foods such as celery and carrots |
| Drying agents. Instruct patients to avoid cigarettes, caffeinated beverages, and mouth rinses that contain alcohol. Explain that some patients may benefit from sleeping in a room with a cool air humidifier |
| Over-the-counter products. Suggest patients try salivary substitutes, which are dispensed in spray bottles, rinses, swish bottles, or oral swab sticks. In addition, products such as dry-mouth toothpaste and moisturizing gels also may help relieve their symptoms |
- Persson K, Axtelius B, Söderfeldt B, et al. Monitoring oral health and dental attendance in an outpatient psychiatric population. J Psychiatr Ment Health Nurs. 2009;16(3):263-271.
- Keene JJ Jr, Galasko GT, Land MF. Antidepressant use in psychiatry and medicine: importance for dental practice. J Am Dent Assoc. 2003;134(1):71-79.
Drug Brand Names
- Alprazolam • Xanax
- Amlodipine • Norvasc
- Bupropion • Wellbutrin, Zyban
- Cevimeline • Evoxac
- Clonidine • Catapres, Kapvay, others
- Esomeprazole • Nexium
- Irbesartan • Avapro
- Metoprolol • Lopressor, Toprol
- Pilocarpine • Salagen
- Tolterodine • Detrol
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
1. Drymouth.info. Overview of drugs and dry mouth. http://drymouth.info/practitioner/overview.asp. Accessed September 2, 2011.
2. Stewart CM, Berg KM, Cha S, et al. Salivary dysfunction and quality of life in Sjögren syndrome: a critical oral-systemic connection. J Am Dent Assoc. 2008;139(3):291-299.
3. Friedman PK. Xerostomia: The invisible oral health condition. http://www.dentistryiq.com/index/display/article-display/295922/articles/woman-dentist-journal/health/xerostomia-the-invisible-oral-health-condition.html. Accessed September 6, 2011.
4. Physician Desk Reference. Montvale NJ: PDR Network LLC.; 2011.
5. Bardow A, Lagerlof F, Nauntofte B, et al. The role of saliva. In: Fejerskov O, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford, United Kingdom: Blackwell Munksgaard; 2008:195.
6. Vanderkooy JD, Kennedy SH, Bagby RM. Antidepressant side effects in depression patients treated in a naturalistic setting: a study of bupropion moclobemide, paroxetine, sertraline, and venlafaxine. Can J Psychiatry. 2002;47(2):174-180.
7. Löffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36(3):105-112.
8. Lambert M, Conus P, Eide P, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19(7):415-422.
9. Rettenbacher MA, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211-1218.
10. Bulkacz J, Carranza FA. Defense mechanisms of the gingiva. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:69–70.
11. Szabadi E, Tavernor S. Hypo-and hyper-salivation induced by psychoactive drugs. CNS Drugs. 1999;11(6):449-466.
12. Guggenheimer J, Moore PA. Xerostomia: etiology recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
13. Dawes C. Physiological factors affecting salivary flow rate oral sugar clearance, and the sensation of dry mouth in man. J Dent Res. 1987;66:648-653.
14. Bartels CL. Xerostomia information for dentists. http://www.homesteadschools.com/dental/courses/Xerostomia/Course.htm. Accessed August 15, 2011.
15. Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-267.
16. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
17. Quirynen M, Van den Veide S, Vanderkerckhove B, et al. Oral malodor. In: Newman MG, Takei HH, Klokkevold PR, et al, eds. Carranza’s clinical periodontology. St. Louis, MO: Elsevier Saunders; 2011:333.
18. Papas A. Dry mouth from drugs: more than just an annoying side effect. Tufts University Heath and Nutrition Letter. 2000;3.-
19. American Academy of Periodontology. Gum disease information from the American Academy of Periodontology http://perio.org. Accessed August 12, 2011.
20. Geismar K, Stoltze K, Sigurd B, et al. Periodontal disease and coronary heart disease. J Periodontol. 2006;77(9):1547-1554.
21. Lee HJ, Garcia RI, Janket SJ, et al. The association between cumulative periodontal disease and stroke history in older adults. J Periodontol. 2006;77(10):1744-1754.
22. Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1021-1032.
23. Contreras A, Herrera JA, Soto JE, et al. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77(2):182-188.
24. Dasanayake AP, Li Y, Wiener H, et al. Salivary Actinomyces naeslundii genospecies 2 and Lactobacillus casei levels predict pregnancy outcomes. J Periodontol. 2005;76(2):171-177.
25. McCreadie RG, Stevens H, Henderson J, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004;110(4):306-310.
26. Anttila S, Knuuttila M, Ylöstalo P, et al. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur J Oral Sci. 2006;114(2):109-114.
27. Sjögren R, Nordström G. Oral health status of psychiatric patients. J Clin Nurs. 2000;9(4):632-638.
28. Ramon T, Grinshpoon A, Zusman SP, et al. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101-105.
29. Portilla MI, Mafla AC, Arteaga JJ. Periodontal status in female psychiatric patients. Colomb Med. 2009;40(2):167-176.
30. Navazesh M. ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
31. Mignogna MD, Fedele S, Lo Russo L, et al. Sjögren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;34(1):1-6.
32. Spolarich AE. Managing the side effects of medications. J Dent Hyg. 2000;74(1):57-69.
33. Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 2002;94(4):1151-1156.
34. Garcia MK, Chiang JS, Cohen L, et al. Acupuncture for radiation-induced xerostomia in patients with cancer: a pilot study. Head Neck. 2009;31(10):1360-1368.
35. Strietzel FP, Lafaurie GI, Mendoza GR, et al. Efficacy and safety of an intraoral electrostimulation device for xerostomia relief: a multicenter, randomized trial. Arthritis Rheum. 2011;63(1):180-190.
Practicing psychiatry via Skype: Medicolegal considerations
Dear Dr. Mossman:
I practice in a region with few psychiatrists and very little public transportation. For many patients, coming to my office is inconvenient, expensive, or time-consuming. Sometimes, their emotional problems make it hard for them to travel, and sometimes, bad weather makes travel difficult. I am considering providing remote treatment via Skype. Is this a reasonable idea? What are the risks of using this technology in my practice? — Submitted by “Dr. A”
Diagnosing and treating patients without a face-to-face encounter is not new. Doctors have provided “remote treatment” since shortly after telephones were invented.1 Until recently, however, forensic psychiatrists advised colleagues not to diagnose patients or start treatment based on phone contact alone.2
The Internet has revolutionized our attitudes about many things. Communication technologies that seemed miraculous a generation ago have become commonplace and have transformed standards for ordinary and “acceptable” human contact. A quick Internet search of “telephone psychotherapy” turns up hundreds of mental health professionals who offer remote treatment services to patients via computers and Web cams.
Physicians in many specialties practice telemedicine, often with the support and encouragement of state governments and third-party payers. To decide whether to include telepsychiatry in your psychiatric practice, you should know:
- what “telemedicine” means and includes
- the possible advantages of offering remote health care
- potential risks and ambiguity about legal matters.
Defining telemedicine
Studies of remote, closed-circuit “telediagnosis” extend back more than 4 decades, closely following mid-20th century advancements in audio and video relay technologies that made space broadcasts possible.3 Then as now, “telemedicine” simply means conveying health-related information from 1 site to another for diagnostic or treatment purposes.4 It’s an adaptation of available technology to deliver care more easily, with the goal of improving patients’ access to care and health status.
Telemedicine usage accelerated as the Internet and related technologies developed. Telemedicine programs in the United States increased by 1,500% from 1993 to 1998.4 Telemedicine use has grown 10% annually in recent years and has become a $4 billion per year industry in the United States.5 Recently enacted federal legislation is likely to extend health care coverage to 36 million Americans and require coverage of pre-existing conditions. To make these changes affordable, health care delivery will need to exploit new, efficiency-enhancing technologies.6
Advantages of telemedicine
State governments and some third-party payers have recognized that telemedicine can overcome geographic and cost barriers to health services and patient education.5,7-9 Although closed-circuit video transmission has served this purpose for some time, Skype—free software that allows individuals to make video phone calls over the Internet using their computers—is an option that doctors are using to treat patients.10-12
Research suggests that telepsychiatry may provide huge benefits to medically underserved areas while reducing health care costs.4 Telepsychiatry can reduce travel time and expenses for professionals and patients, and it also may lower wait times and “no-show” rates (Table 1).4 Telepsychiatry lets patients see caregivers when winter weather makes roads unsafe. It may allow geriatric patients who can no longer drive to access psychiatric care and it lowers health care’s “carbon footprint,” making it “eco-friendly.”13
Social media strategies are playing an expanding role in medical education,14,15 and this probably will help practitioners feel more at ease about incorporating the underlying technologies into work with patients. Increased use of laptops and mobile phones lends itself well to telepsychiatry applications,13 and studies have examined the feasibility of psychotherapies delivered via remote communication devices.16 Smartphone apps are being designed to assist mental health professionals17 and consumers.18
Table 1
Potential benefits of telemedicine
| Category | Benefit(s) |
|---|---|
| Access | Patients can see specialists more readily Addresses regional doctor shortages Reduces health care disparities between urban and rural areas |
| Urgent care | Facilitates information transfer for rapid interventions |
| Productivity | Provides a conduit for clinicians to share skills and expertise Facilitates remote monitoring and home care |
| Cost | No travel costs Alternative revenue stream for health care organizations that offer more broadly delivered medical services |
| Patient-centric care | Care is taken to the patient Translator services are more readily available |
| Source: Reference 4 | |
Potential pitfalls and drawbacks
Although convenience, access, cost, and fossil fuel savings may favor video-chat doctor visits, telemedicine has downsides, some of which apply specifically to psychiatry. First, no current technology provides psychiatrists with “the rich multidimensional aspects of a person-to-person encounter,”19 and remote communication may change what patients tell us, how they feel when they tell us things, and how they feel when we respond. Often, an inherent awkwardness affects many forms of Internet communication.20
Also uncertain is whether Skype is compliant with the Health Insurance Portability and Accountability Act and protects doctor-patient privacy well enough to satisfy ethical standards—although it probably is far better than e-mail in this regard. Third-party payers often will not reimburse for telephone calls and may balk at paying for Skype-based therapy, even in states that require insurers to reimburse for telemedicine.
Psychiatrists typically have limited physical contact with patients, but we often check weight and vital signs when we prescribe certain psychotropic medications. Results from home- and drugstore-based blood pressure monitors may not be accurate enough for treatment purposes. Remote communication also reduces the quality of visual information,20 which can be crucial—for example, when good lighting and visual resolution is needed to decide whether a skin rash might be drug-induced.
Telemedicine raises concerns about licensure and meeting adequate standards of care. Medical care usually is deemed to have occurred in the state where the patient is located. For example, only physicians licensed to practice medicine in California are legally permitted to treat patients in California. As is the case with any treatment, care delivered via telemedicine must include appropriate patient examination and diagnosis.21
Help and guidance
Despite these potential drawbacks, many state agencies recognize the promise of telemedicine, and have developed networks to promote it (Table 2).7-9,22,23 These networks have various goals but share a common pattern of establishing infrastructure, policies, and organized results. In the future, states may adopt laws or regulations that address conflicts in malpractice standards and liability coverage, licensing, accreditation, reimbursement, privacy, and data protection policies that now may impede or inhibit use of telepsychiatric services across jurisdictional boundaries. Last year, Ohio produced regulations to guide psychiatrists in prescribing medication remotely without an in-person examination. The University of Hawaii suggested steps that its state legislature might take to help providers predict the potential legal ramifications of telemedicine.6
Further help for telepsychiatry practitioners may be found in practice standards and guidelines developed by the American Telemedicine Association.24,25 These documents gave guidance and support for the practice of telemedicine and for providing appropriate telepsychiatry health services.
Table 2
Telemedicine services available in different states
| State/Network | Description |
|---|---|
| Arizona www.narbha.org7 | The Northern Arizona Regional Behavioral Health Authority manages a comprehensive telemental health network (NARBHAnet) that uses 2-way videoconferencing to connect mental health experts and patients. It has provided >50,000 clinical psychiatric sessions |
| Kansas www.kumc.edu8 | The University of Kansas Medical Center provides specialty services (including telepsychiatry) through 14 clinical sites in rural Kansas. Cost-sharing helps the telepsychiatric application be successful |
| Montana www.emtn.org9 | Eastern Montana Telemedicine Network is a consortium of not-for-profit facilities that link health care providers and their patients in Montana and Wyoming. This telemental health network includes shared sites for all physicians practicing in the network and has yielded large out-of-pocket savings for patients |
| Oregon www.ortelehealth.org22 | The Telehealth Alliance of Oregon, which began in 2001 as a committee of the Oregon Telecommunications Coordinating Council, was created by the legislature and has served as advisors to the governor and the legislature regarding telecommunications in Oregon |
| Texas www.jsahealthmd.com23 | The Burke Center provides services to people in 12 counties in East Texas. It uses telepsychiatry services to conduct emergency evaluations, therefore keeping people in mental health crises out of emergency rooms |
What should Dr. A do?
In answer to Dr. A’s question, many factors favor including telepsychiatry in her practice. Yet we know little about the accuracy and reliability of psychiatric assessments made solely via Skype or other remote video technology in ordinary practice. Legislation and legal rules about acceptable practices are ambiguous, although in the absence of clear guidance, psychiatrists should assume that all usual professional standards and expectations about adequate care apply to treatment via Skype or other remote communication methods.
Related Resources
- Skype. www.skype.com.
- American Telemedicine Association. www.americantelemed.org.
1. Lipman M. The doctor will Skype you now. Consum Rep. 2011;76(8):12.-
2. Simon RI. Clinical psychiatry and the law. 2nd ed. Washington DC: American Psychiatric Press; 1992.
3. Murphy RL, Jr, Bird KT. Telediagnosis: a new community health resource. Observations on the feasibility of telediagnosis based on 1000 patient transactions. Am J Public Health. 1974;64(2):113-119.
4. Hilty DM, Yellowlees PM, Cobb HC, et al. Models of telepsychiatric consultation—liaison service to rural primary care. Psychosomatics. 2006;47(2):152-157.
5. Freudenheim M. The doctor will see you now. Please log on. New York Times. May 29 2010:BU1.
6. University of Hawai’i. Report to the 2009 legislature: preliminary report by the John A. Burns School of Medicine on the current practices of Hawai’i telemedicine system for 2009. http://www.hawaii.edu/offices/eaur/govrel/reports/2009. Published November 2008. Accessed September 27 2011.
7. Northern Arizona Regional Behavioral Health Authority. http://www.narbha.org. Accessed September 27 2011.
8. University of Kansas Medical Center. http://www.kumc.edu. Accessed September 27 2011.
9. Eastern Montana Telemedicine Network. http://www.emtn.org. Accessed September 27 2011.
10. Ciccia AH, Whitford B, Krumm M, et al. Improving the access of young urban children to speech, language and hearing screening via telehealth. J Telemed Telecare. 2011;17(5):240-244.
11. Hori M, Kubota M, Ando K, et al. The effect of videophone communication (with skype and webcam) for elderly patients with dementia and their caregivers [in Japanese]. Gan To Kagaku Ryoho. 2009;36(suppl 1):36-38.
12. Klock C, Gomes Rde P. Web conferencing systems: Skype and MSN in telepathology. Diagn Pathol. 2008;3(suppl 1):S13.-
13. Luo J. VoIP: The right call for your practice? Current Psychiatry. 2005;4(10):24-27.
14. George DR, Dellasega C. Use of social media in graduate-level medical humanities education: two pilot studies from Penn State College of Medicine. Med Teach. 2011;33(8):e429-434.
15. Lillis S, Gibbons V, Lawrenson R. The experience of final year medical students undertaking a general practice run with a distance education component. Rural Remote Health. 2010;10(1):1268.-
16. Bee PE, Bower P, Lovell K, et al. Psychotherapy mediated by remote communication technologies: a meta-analytic review. BMC Psychiatry. 2008;8:60.-
17. Maheu MM. iPhone app reviews for psychologists and mental health professionals. http://telehealth.net/blog/554. Accessed September 27 2011.
18. Maheu MM. iPhone apps reviews for mental health psychology and personal growth consumers. http://telehealth.net/blog/557. Accessed September 27, 2011.
19. Eckardt MH. The use of the telephone to extend our therapeutic availability. J Am Acad Psychoanal Dyn Psychiatry. 2011;39(1):151-153.
20. Hoffman J. When your therapist is only a click away. New York Times. September 23 2011:ST1.
21. Medical Board of California. Practicing medicine through telemedicine technology. http://www.mbc.ca.gov/licensee/telemedicine.html. Accessed September 27 2011.
22. Telehealth Alliance of Oregon. http://www.ortelehealth.org. Accessed October 31 2011.
23. JSA Health Telepsychiatry. http://jsahealthmd.com. Accessed September 27 2011.
24. American Telemedicine Association. Telemental standards and guidelines. http://www.americantelemed.org/i4a/pages/index.cfm?pageID=3311. Accessed September 27 2011.
25. American Telemedicine Association. Evidence-based practice for telemental health. http://www.americantelemed.org/i4a/forms/form.cfm?id=25&pageid=3718&showTitle=1. Accessed September 27 2011.
Dear Dr. Mossman:
I practice in a region with few psychiatrists and very little public transportation. For many patients, coming to my office is inconvenient, expensive, or time-consuming. Sometimes, their emotional problems make it hard for them to travel, and sometimes, bad weather makes travel difficult. I am considering providing remote treatment via Skype. Is this a reasonable idea? What are the risks of using this technology in my practice? — Submitted by “Dr. A”
Diagnosing and treating patients without a face-to-face encounter is not new. Doctors have provided “remote treatment” since shortly after telephones were invented.1 Until recently, however, forensic psychiatrists advised colleagues not to diagnose patients or start treatment based on phone contact alone.2
The Internet has revolutionized our attitudes about many things. Communication technologies that seemed miraculous a generation ago have become commonplace and have transformed standards for ordinary and “acceptable” human contact. A quick Internet search of “telephone psychotherapy” turns up hundreds of mental health professionals who offer remote treatment services to patients via computers and Web cams.
Physicians in many specialties practice telemedicine, often with the support and encouragement of state governments and third-party payers. To decide whether to include telepsychiatry in your psychiatric practice, you should know:
- what “telemedicine” means and includes
- the possible advantages of offering remote health care
- potential risks and ambiguity about legal matters.
Defining telemedicine
Studies of remote, closed-circuit “telediagnosis” extend back more than 4 decades, closely following mid-20th century advancements in audio and video relay technologies that made space broadcasts possible.3 Then as now, “telemedicine” simply means conveying health-related information from 1 site to another for diagnostic or treatment purposes.4 It’s an adaptation of available technology to deliver care more easily, with the goal of improving patients’ access to care and health status.
Telemedicine usage accelerated as the Internet and related technologies developed. Telemedicine programs in the United States increased by 1,500% from 1993 to 1998.4 Telemedicine use has grown 10% annually in recent years and has become a $4 billion per year industry in the United States.5 Recently enacted federal legislation is likely to extend health care coverage to 36 million Americans and require coverage of pre-existing conditions. To make these changes affordable, health care delivery will need to exploit new, efficiency-enhancing technologies.6
Advantages of telemedicine
State governments and some third-party payers have recognized that telemedicine can overcome geographic and cost barriers to health services and patient education.5,7-9 Although closed-circuit video transmission has served this purpose for some time, Skype—free software that allows individuals to make video phone calls over the Internet using their computers—is an option that doctors are using to treat patients.10-12
Research suggests that telepsychiatry may provide huge benefits to medically underserved areas while reducing health care costs.4 Telepsychiatry can reduce travel time and expenses for professionals and patients, and it also may lower wait times and “no-show” rates (Table 1).4 Telepsychiatry lets patients see caregivers when winter weather makes roads unsafe. It may allow geriatric patients who can no longer drive to access psychiatric care and it lowers health care’s “carbon footprint,” making it “eco-friendly.”13
Social media strategies are playing an expanding role in medical education,14,15 and this probably will help practitioners feel more at ease about incorporating the underlying technologies into work with patients. Increased use of laptops and mobile phones lends itself well to telepsychiatry applications,13 and studies have examined the feasibility of psychotherapies delivered via remote communication devices.16 Smartphone apps are being designed to assist mental health professionals17 and consumers.18
Table 1
Potential benefits of telemedicine
| Category | Benefit(s) |
|---|---|
| Access | Patients can see specialists more readily Addresses regional doctor shortages Reduces health care disparities between urban and rural areas |
| Urgent care | Facilitates information transfer for rapid interventions |
| Productivity | Provides a conduit for clinicians to share skills and expertise Facilitates remote monitoring and home care |
| Cost | No travel costs Alternative revenue stream for health care organizations that offer more broadly delivered medical services |
| Patient-centric care | Care is taken to the patient Translator services are more readily available |
| Source: Reference 4 | |
Potential pitfalls and drawbacks
Although convenience, access, cost, and fossil fuel savings may favor video-chat doctor visits, telemedicine has downsides, some of which apply specifically to psychiatry. First, no current technology provides psychiatrists with “the rich multidimensional aspects of a person-to-person encounter,”19 and remote communication may change what patients tell us, how they feel when they tell us things, and how they feel when we respond. Often, an inherent awkwardness affects many forms of Internet communication.20
Also uncertain is whether Skype is compliant with the Health Insurance Portability and Accountability Act and protects doctor-patient privacy well enough to satisfy ethical standards—although it probably is far better than e-mail in this regard. Third-party payers often will not reimburse for telephone calls and may balk at paying for Skype-based therapy, even in states that require insurers to reimburse for telemedicine.
Psychiatrists typically have limited physical contact with patients, but we often check weight and vital signs when we prescribe certain psychotropic medications. Results from home- and drugstore-based blood pressure monitors may not be accurate enough for treatment purposes. Remote communication also reduces the quality of visual information,20 which can be crucial—for example, when good lighting and visual resolution is needed to decide whether a skin rash might be drug-induced.
Telemedicine raises concerns about licensure and meeting adequate standards of care. Medical care usually is deemed to have occurred in the state where the patient is located. For example, only physicians licensed to practice medicine in California are legally permitted to treat patients in California. As is the case with any treatment, care delivered via telemedicine must include appropriate patient examination and diagnosis.21
Help and guidance
Despite these potential drawbacks, many state agencies recognize the promise of telemedicine, and have developed networks to promote it (Table 2).7-9,22,23 These networks have various goals but share a common pattern of establishing infrastructure, policies, and organized results. In the future, states may adopt laws or regulations that address conflicts in malpractice standards and liability coverage, licensing, accreditation, reimbursement, privacy, and data protection policies that now may impede or inhibit use of telepsychiatric services across jurisdictional boundaries. Last year, Ohio produced regulations to guide psychiatrists in prescribing medication remotely without an in-person examination. The University of Hawaii suggested steps that its state legislature might take to help providers predict the potential legal ramifications of telemedicine.6
Further help for telepsychiatry practitioners may be found in practice standards and guidelines developed by the American Telemedicine Association.24,25 These documents gave guidance and support for the practice of telemedicine and for providing appropriate telepsychiatry health services.
Table 2
Telemedicine services available in different states
| State/Network | Description |
|---|---|
| Arizona www.narbha.org7 | The Northern Arizona Regional Behavioral Health Authority manages a comprehensive telemental health network (NARBHAnet) that uses 2-way videoconferencing to connect mental health experts and patients. It has provided >50,000 clinical psychiatric sessions |
| Kansas www.kumc.edu8 | The University of Kansas Medical Center provides specialty services (including telepsychiatry) through 14 clinical sites in rural Kansas. Cost-sharing helps the telepsychiatric application be successful |
| Montana www.emtn.org9 | Eastern Montana Telemedicine Network is a consortium of not-for-profit facilities that link health care providers and their patients in Montana and Wyoming. This telemental health network includes shared sites for all physicians practicing in the network and has yielded large out-of-pocket savings for patients |
| Oregon www.ortelehealth.org22 | The Telehealth Alliance of Oregon, which began in 2001 as a committee of the Oregon Telecommunications Coordinating Council, was created by the legislature and has served as advisors to the governor and the legislature regarding telecommunications in Oregon |
| Texas www.jsahealthmd.com23 | The Burke Center provides services to people in 12 counties in East Texas. It uses telepsychiatry services to conduct emergency evaluations, therefore keeping people in mental health crises out of emergency rooms |
What should Dr. A do?
In answer to Dr. A’s question, many factors favor including telepsychiatry in her practice. Yet we know little about the accuracy and reliability of psychiatric assessments made solely via Skype or other remote video technology in ordinary practice. Legislation and legal rules about acceptable practices are ambiguous, although in the absence of clear guidance, psychiatrists should assume that all usual professional standards and expectations about adequate care apply to treatment via Skype or other remote communication methods.
Related Resources
- Skype. www.skype.com.
- American Telemedicine Association. www.americantelemed.org.
Dear Dr. Mossman:
I practice in a region with few psychiatrists and very little public transportation. For many patients, coming to my office is inconvenient, expensive, or time-consuming. Sometimes, their emotional problems make it hard for them to travel, and sometimes, bad weather makes travel difficult. I am considering providing remote treatment via Skype. Is this a reasonable idea? What are the risks of using this technology in my practice? — Submitted by “Dr. A”
Diagnosing and treating patients without a face-to-face encounter is not new. Doctors have provided “remote treatment” since shortly after telephones were invented.1 Until recently, however, forensic psychiatrists advised colleagues not to diagnose patients or start treatment based on phone contact alone.2
The Internet has revolutionized our attitudes about many things. Communication technologies that seemed miraculous a generation ago have become commonplace and have transformed standards for ordinary and “acceptable” human contact. A quick Internet search of “telephone psychotherapy” turns up hundreds of mental health professionals who offer remote treatment services to patients via computers and Web cams.
Physicians in many specialties practice telemedicine, often with the support and encouragement of state governments and third-party payers. To decide whether to include telepsychiatry in your psychiatric practice, you should know:
- what “telemedicine” means and includes
- the possible advantages of offering remote health care
- potential risks and ambiguity about legal matters.
Defining telemedicine
Studies of remote, closed-circuit “telediagnosis” extend back more than 4 decades, closely following mid-20th century advancements in audio and video relay technologies that made space broadcasts possible.3 Then as now, “telemedicine” simply means conveying health-related information from 1 site to another for diagnostic or treatment purposes.4 It’s an adaptation of available technology to deliver care more easily, with the goal of improving patients’ access to care and health status.
Telemedicine usage accelerated as the Internet and related technologies developed. Telemedicine programs in the United States increased by 1,500% from 1993 to 1998.4 Telemedicine use has grown 10% annually in recent years and has become a $4 billion per year industry in the United States.5 Recently enacted federal legislation is likely to extend health care coverage to 36 million Americans and require coverage of pre-existing conditions. To make these changes affordable, health care delivery will need to exploit new, efficiency-enhancing technologies.6
Advantages of telemedicine
State governments and some third-party payers have recognized that telemedicine can overcome geographic and cost barriers to health services and patient education.5,7-9 Although closed-circuit video transmission has served this purpose for some time, Skype—free software that allows individuals to make video phone calls over the Internet using their computers—is an option that doctors are using to treat patients.10-12
Research suggests that telepsychiatry may provide huge benefits to medically underserved areas while reducing health care costs.4 Telepsychiatry can reduce travel time and expenses for professionals and patients, and it also may lower wait times and “no-show” rates (Table 1).4 Telepsychiatry lets patients see caregivers when winter weather makes roads unsafe. It may allow geriatric patients who can no longer drive to access psychiatric care and it lowers health care’s “carbon footprint,” making it “eco-friendly.”13
Social media strategies are playing an expanding role in medical education,14,15 and this probably will help practitioners feel more at ease about incorporating the underlying technologies into work with patients. Increased use of laptops and mobile phones lends itself well to telepsychiatry applications,13 and studies have examined the feasibility of psychotherapies delivered via remote communication devices.16 Smartphone apps are being designed to assist mental health professionals17 and consumers.18
Table 1
Potential benefits of telemedicine
| Category | Benefit(s) |
|---|---|
| Access | Patients can see specialists more readily Addresses regional doctor shortages Reduces health care disparities between urban and rural areas |
| Urgent care | Facilitates information transfer for rapid interventions |
| Productivity | Provides a conduit for clinicians to share skills and expertise Facilitates remote monitoring and home care |
| Cost | No travel costs Alternative revenue stream for health care organizations that offer more broadly delivered medical services |
| Patient-centric care | Care is taken to the patient Translator services are more readily available |
| Source: Reference 4 | |
Potential pitfalls and drawbacks
Although convenience, access, cost, and fossil fuel savings may favor video-chat doctor visits, telemedicine has downsides, some of which apply specifically to psychiatry. First, no current technology provides psychiatrists with “the rich multidimensional aspects of a person-to-person encounter,”19 and remote communication may change what patients tell us, how they feel when they tell us things, and how they feel when we respond. Often, an inherent awkwardness affects many forms of Internet communication.20
Also uncertain is whether Skype is compliant with the Health Insurance Portability and Accountability Act and protects doctor-patient privacy well enough to satisfy ethical standards—although it probably is far better than e-mail in this regard. Third-party payers often will not reimburse for telephone calls and may balk at paying for Skype-based therapy, even in states that require insurers to reimburse for telemedicine.
Psychiatrists typically have limited physical contact with patients, but we often check weight and vital signs when we prescribe certain psychotropic medications. Results from home- and drugstore-based blood pressure monitors may not be accurate enough for treatment purposes. Remote communication also reduces the quality of visual information,20 which can be crucial—for example, when good lighting and visual resolution is needed to decide whether a skin rash might be drug-induced.
Telemedicine raises concerns about licensure and meeting adequate standards of care. Medical care usually is deemed to have occurred in the state where the patient is located. For example, only physicians licensed to practice medicine in California are legally permitted to treat patients in California. As is the case with any treatment, care delivered via telemedicine must include appropriate patient examination and diagnosis.21
Help and guidance
Despite these potential drawbacks, many state agencies recognize the promise of telemedicine, and have developed networks to promote it (Table 2).7-9,22,23 These networks have various goals but share a common pattern of establishing infrastructure, policies, and organized results. In the future, states may adopt laws or regulations that address conflicts in malpractice standards and liability coverage, licensing, accreditation, reimbursement, privacy, and data protection policies that now may impede or inhibit use of telepsychiatric services across jurisdictional boundaries. Last year, Ohio produced regulations to guide psychiatrists in prescribing medication remotely without an in-person examination. The University of Hawaii suggested steps that its state legislature might take to help providers predict the potential legal ramifications of telemedicine.6
Further help for telepsychiatry practitioners may be found in practice standards and guidelines developed by the American Telemedicine Association.24,25 These documents gave guidance and support for the practice of telemedicine and for providing appropriate telepsychiatry health services.
Table 2
Telemedicine services available in different states
| State/Network | Description |
|---|---|
| Arizona www.narbha.org7 | The Northern Arizona Regional Behavioral Health Authority manages a comprehensive telemental health network (NARBHAnet) that uses 2-way videoconferencing to connect mental health experts and patients. It has provided >50,000 clinical psychiatric sessions |
| Kansas www.kumc.edu8 | The University of Kansas Medical Center provides specialty services (including telepsychiatry) through 14 clinical sites in rural Kansas. Cost-sharing helps the telepsychiatric application be successful |
| Montana www.emtn.org9 | Eastern Montana Telemedicine Network is a consortium of not-for-profit facilities that link health care providers and their patients in Montana and Wyoming. This telemental health network includes shared sites for all physicians practicing in the network and has yielded large out-of-pocket savings for patients |
| Oregon www.ortelehealth.org22 | The Telehealth Alliance of Oregon, which began in 2001 as a committee of the Oregon Telecommunications Coordinating Council, was created by the legislature and has served as advisors to the governor and the legislature regarding telecommunications in Oregon |
| Texas www.jsahealthmd.com23 | The Burke Center provides services to people in 12 counties in East Texas. It uses telepsychiatry services to conduct emergency evaluations, therefore keeping people in mental health crises out of emergency rooms |
What should Dr. A do?
In answer to Dr. A’s question, many factors favor including telepsychiatry in her practice. Yet we know little about the accuracy and reliability of psychiatric assessments made solely via Skype or other remote video technology in ordinary practice. Legislation and legal rules about acceptable practices are ambiguous, although in the absence of clear guidance, psychiatrists should assume that all usual professional standards and expectations about adequate care apply to treatment via Skype or other remote communication methods.
Related Resources
- Skype. www.skype.com.
- American Telemedicine Association. www.americantelemed.org.
1. Lipman M. The doctor will Skype you now. Consum Rep. 2011;76(8):12.-
2. Simon RI. Clinical psychiatry and the law. 2nd ed. Washington DC: American Psychiatric Press; 1992.
3. Murphy RL, Jr, Bird KT. Telediagnosis: a new community health resource. Observations on the feasibility of telediagnosis based on 1000 patient transactions. Am J Public Health. 1974;64(2):113-119.
4. Hilty DM, Yellowlees PM, Cobb HC, et al. Models of telepsychiatric consultation—liaison service to rural primary care. Psychosomatics. 2006;47(2):152-157.
5. Freudenheim M. The doctor will see you now. Please log on. New York Times. May 29 2010:BU1.
6. University of Hawai’i. Report to the 2009 legislature: preliminary report by the John A. Burns School of Medicine on the current practices of Hawai’i telemedicine system for 2009. http://www.hawaii.edu/offices/eaur/govrel/reports/2009. Published November 2008. Accessed September 27 2011.
7. Northern Arizona Regional Behavioral Health Authority. http://www.narbha.org. Accessed September 27 2011.
8. University of Kansas Medical Center. http://www.kumc.edu. Accessed September 27 2011.
9. Eastern Montana Telemedicine Network. http://www.emtn.org. Accessed September 27 2011.
10. Ciccia AH, Whitford B, Krumm M, et al. Improving the access of young urban children to speech, language and hearing screening via telehealth. J Telemed Telecare. 2011;17(5):240-244.
11. Hori M, Kubota M, Ando K, et al. The effect of videophone communication (with skype and webcam) for elderly patients with dementia and their caregivers [in Japanese]. Gan To Kagaku Ryoho. 2009;36(suppl 1):36-38.
12. Klock C, Gomes Rde P. Web conferencing systems: Skype and MSN in telepathology. Diagn Pathol. 2008;3(suppl 1):S13.-
13. Luo J. VoIP: The right call for your practice? Current Psychiatry. 2005;4(10):24-27.
14. George DR, Dellasega C. Use of social media in graduate-level medical humanities education: two pilot studies from Penn State College of Medicine. Med Teach. 2011;33(8):e429-434.
15. Lillis S, Gibbons V, Lawrenson R. The experience of final year medical students undertaking a general practice run with a distance education component. Rural Remote Health. 2010;10(1):1268.-
16. Bee PE, Bower P, Lovell K, et al. Psychotherapy mediated by remote communication technologies: a meta-analytic review. BMC Psychiatry. 2008;8:60.-
17. Maheu MM. iPhone app reviews for psychologists and mental health professionals. http://telehealth.net/blog/554. Accessed September 27 2011.
18. Maheu MM. iPhone apps reviews for mental health psychology and personal growth consumers. http://telehealth.net/blog/557. Accessed September 27, 2011.
19. Eckardt MH. The use of the telephone to extend our therapeutic availability. J Am Acad Psychoanal Dyn Psychiatry. 2011;39(1):151-153.
20. Hoffman J. When your therapist is only a click away. New York Times. September 23 2011:ST1.
21. Medical Board of California. Practicing medicine through telemedicine technology. http://www.mbc.ca.gov/licensee/telemedicine.html. Accessed September 27 2011.
22. Telehealth Alliance of Oregon. http://www.ortelehealth.org. Accessed October 31 2011.
23. JSA Health Telepsychiatry. http://jsahealthmd.com. Accessed September 27 2011.
24. American Telemedicine Association. Telemental standards and guidelines. http://www.americantelemed.org/i4a/pages/index.cfm?pageID=3311. Accessed September 27 2011.
25. American Telemedicine Association. Evidence-based practice for telemental health. http://www.americantelemed.org/i4a/forms/form.cfm?id=25&pageid=3718&showTitle=1. Accessed September 27 2011.
1. Lipman M. The doctor will Skype you now. Consum Rep. 2011;76(8):12.-
2. Simon RI. Clinical psychiatry and the law. 2nd ed. Washington DC: American Psychiatric Press; 1992.
3. Murphy RL, Jr, Bird KT. Telediagnosis: a new community health resource. Observations on the feasibility of telediagnosis based on 1000 patient transactions. Am J Public Health. 1974;64(2):113-119.
4. Hilty DM, Yellowlees PM, Cobb HC, et al. Models of telepsychiatric consultation—liaison service to rural primary care. Psychosomatics. 2006;47(2):152-157.
5. Freudenheim M. The doctor will see you now. Please log on. New York Times. May 29 2010:BU1.
6. University of Hawai’i. Report to the 2009 legislature: preliminary report by the John A. Burns School of Medicine on the current practices of Hawai’i telemedicine system for 2009. http://www.hawaii.edu/offices/eaur/govrel/reports/2009. Published November 2008. Accessed September 27 2011.
7. Northern Arizona Regional Behavioral Health Authority. http://www.narbha.org. Accessed September 27 2011.
8. University of Kansas Medical Center. http://www.kumc.edu. Accessed September 27 2011.
9. Eastern Montana Telemedicine Network. http://www.emtn.org. Accessed September 27 2011.
10. Ciccia AH, Whitford B, Krumm M, et al. Improving the access of young urban children to speech, language and hearing screening via telehealth. J Telemed Telecare. 2011;17(5):240-244.
11. Hori M, Kubota M, Ando K, et al. The effect of videophone communication (with skype and webcam) for elderly patients with dementia and their caregivers [in Japanese]. Gan To Kagaku Ryoho. 2009;36(suppl 1):36-38.
12. Klock C, Gomes Rde P. Web conferencing systems: Skype and MSN in telepathology. Diagn Pathol. 2008;3(suppl 1):S13.-
13. Luo J. VoIP: The right call for your practice? Current Psychiatry. 2005;4(10):24-27.
14. George DR, Dellasega C. Use of social media in graduate-level medical humanities education: two pilot studies from Penn State College of Medicine. Med Teach. 2011;33(8):e429-434.
15. Lillis S, Gibbons V, Lawrenson R. The experience of final year medical students undertaking a general practice run with a distance education component. Rural Remote Health. 2010;10(1):1268.-
16. Bee PE, Bower P, Lovell K, et al. Psychotherapy mediated by remote communication technologies: a meta-analytic review. BMC Psychiatry. 2008;8:60.-
17. Maheu MM. iPhone app reviews for psychologists and mental health professionals. http://telehealth.net/blog/554. Accessed September 27 2011.
18. Maheu MM. iPhone apps reviews for mental health psychology and personal growth consumers. http://telehealth.net/blog/557. Accessed September 27, 2011.
19. Eckardt MH. The use of the telephone to extend our therapeutic availability. J Am Acad Psychoanal Dyn Psychiatry. 2011;39(1):151-153.
20. Hoffman J. When your therapist is only a click away. New York Times. September 23 2011:ST1.
21. Medical Board of California. Practicing medicine through telemedicine technology. http://www.mbc.ca.gov/licensee/telemedicine.html. Accessed September 27 2011.
22. Telehealth Alliance of Oregon. http://www.ortelehealth.org. Accessed October 31 2011.
23. JSA Health Telepsychiatry. http://jsahealthmd.com. Accessed September 27 2011.
24. American Telemedicine Association. Telemental standards and guidelines. http://www.americantelemed.org/i4a/pages/index.cfm?pageID=3311. Accessed September 27 2011.
25. American Telemedicine Association. Evidence-based practice for telemental health. http://www.americantelemed.org/i4a/forms/form.cfm?id=25&pageid=3718&showTitle=1. Accessed September 27 2011.
The Buck Starts Here
Some of the best companies in America started in a garage or a basement with an individual who had a great idea and the ability to grow it into a progressively larger business.
“It takes a leader with different capabilities to take a company to the next level,” says Martin Buser, MPH, FACHE, a partner with Hospitalist Management Resources LLC in San Diego, which has helped more than 350 HM programs nationwide in the past 15 years. “It’s an attitude of never stop learning, an ability to look at issues from 30,000 feet instead of ground zero so you can see the whole picture.”
Similarly, the most important predictor of an HM program’s success is its director, Buser says. If directors know how to communicate, innovate, facilitate, problem-solve, and inspire, they are much more likely to run a high-performing hospitalist program, says David Lee, MD, MBA, FACP, FHM, vice chairman of the Hospital Medicine Department at Ochsner Health System in New Orleans.
If group directors lack the skills and fail to adapt to change, the program’s outlook is far from certain. “We unfortunately get involved with these programs,” Buser says. “It’s painful to see.” Bad behavior is nothing new to the hospital setting, and HM is not immune to poor management. The following are common examples of bad behaviors and how groups can avoid the mishaps.
Scenario No. 1 : Great Clinician, Nice Person, Weak Advocate

—Martin Buser, MPH, FACHE, partner, Hospitalist Management Resources LLC, San Diego
The case: Earlier this year, medical center administrators asked the hospitalist program to do more with less, explaining the hospital was having a bad financial year. Administration approached the HM director, an exceptional, gregarious clinician who was named to the position years ago to help the program gain acceptance. The director agreed to indefinitely postpone two much-needed hirings, deciding it was better to share in the sacrifice than protest the cuts to the program’s budget. Hospitalists have since been working more shifts without a pay increase, and burnout symptoms have emerged with no signs of a thaw in the hiring freeze.
Expert advice: Buser says the “weak advocate” is a common issue among hospitalist groups, many of which he says are “going to hell” when he gets a rescue call. When a hospital is facing financial hardship, it is imperative that the HM director stand up for the program by explaining in detail the ramifications of each level of budget cuts. That’s because administrators might not realize the long-term damage that would result from such actions, he says. Being a strong, savvy advocate is even more important now since the financial future of many hospitals is ominous.
“With all of our hospitalist clients, we ask the CFO what is happening in the future…and the numbers are phenomenal,” says Buser. “They are seeing reductions of $10 million to $30 million off their bottom line.”
Administrators’ knee-jerk reaction is to cut costs. But there is another option: Grow the hospital out of its financial difficulties. It is up to the HM director to show administrators how the HM group has strategically gained them market share and how it will continue to do so. Good directors are in near constant contact with administrators, demonstrating the value their hospitalist program brings to the hospital, Buser says.
“You’re having regular meetings with the administrator, you’re producing the dashboard on a regular basis, you’re giving him trends that are going on,” he explains. “Show that you understand the hospital’s issues. Certain things you want to compromise on, but other things you have to say, ‘If we do that, the ramifications are such that it’s just not going to work.’”
Scenario No. 2 : Recruiting Roulette

—David Friar, MD, SFHM, CEO, Hospitalists of Northern Michigan, Traverse City
The case: The HM director felt pressure to hire. The program’s hospitalists were seeing two to three patients a day more than they should have been, and hospital administrators were worried the program was losing ground to the other hospitalist group in the community. Using an outside recruiter, the director hired two adept physicians with stellar CVs after an expedited review process that included a background check, a few phone interviews, and day of in-person interviews with some administrators and a hospitalist on the team. Now, nearly a year later, one of the physicians is about to leave because her family doesn’t like the community, and the other new hire’s abrasive personality has caused considerable damage to the team’s cohesion.
Expert advice: A big part of an HM program’s value is how it practices as a unified team, and directors need to recognize how vital the “team fit” is to hospitalists, says David Friar, MD, SFHM, CEO of Hospitalists of Northern Michigan in Traverse City.
“A bad team fit is often worse than being short-staffed because it can literally destroy the team spirit,” he says.
Directors should have a standardized recruitment process that includes a comprehensive background screening where references are closely checked, a round of interviews by people outside the HM program (nurses and referring physicians), and substantial time spent with hospitalists in the program, says Bryce Gartland, MD, FHM, associate director of the hospital medicine division and medical director of care coordination at Emory Healthcare in Atlanta.
“We put [candidates] with one of our physicians to actually go around the hospital,” he says. “It’s amazing to me the number of things you can pick up by that broader exposure that you may not pick up sitting in a room with a candidate across the table for an hour.”
If a recruitment service is used, the director must describe the HM program in detail to the recruiter and even have them meet hospitalists on the staff, Dr. Friar says.
“Sending them a memo saying ‘We need three new hospitalists ASAP’ isn’t helping them find you the perfect candidate,” he says. “Even the best recruiter can only do a great job for you if they really know your team and what it is you need in a candidate.”
A director also is well served to make recruiting a family event where spouses and even children are part of the interview process.
“By including the entire family and then supporting them after the move, we are much more likely to recruit providers that will stay good members of our team for years to come,” Dr. Friar says.
Scenario No. 3 : Amitte Diem

—John Bulger, DO, FACP, FHM, chief quality officer, director, hospital medicine service line, Geisinger Health System, Danville, Pa.
The case: For months, the medical center has been receiving an increased number of referrals from outlying hospitals, and no end is in sight. The extra patient load, much of it involving complex cases, has agitated the medical center’s staff, particularly the specialists, and they’ve begun to complain to hospital administrators. Seeking an ally, the specialists reach out to the HM director to present their case. Without doing independent analysis, the HM director sides with the specialists. Hospital administrators, facing growing resistance, work to decrease the referrals and are successful.
Expert advice: Consider working in the opposite direction, one that might turn a referral challenge into a profitable opportunity, Buser says. One of his firm’s clients, after thorough research, established a transfer center and set up an activation fee for the specialists who took the referrals. Hospitalists admitted about 90% of the cases, called consults, and named specialists so they received full fee-for-service at Medicare rates if they saw uninsured patients.
“That hospital is now making about $78 million a year, and the medical staff is saying, ‘How can we grow this?’” Buser says. “Here’s an example of how the hospital medicine director was key to turning the bad into something good.”
Because physicians tend to be reticent to change, it’s critical for hospitalist directors who want to seize an opportunity to thoroughly plan out how the change will occur and to prepare for potential obstacles along the way, says John Bulger, DO, FACP, FHM, chief quality officer and director of the hospital medicine service line for Geisinger Health System in Danville, Pa.
“You really need to be prepared with your rationale of why you’re doing it, if there’s data behind why you’re doing it, what the data is that’s driving it, and really what you hope to do with that change,” he says. “If you don’t get buy in from your staff, the change is doomed to fail from the beginning.”
Directors must embrace being a change agent if they want their HM programs to continue to be successful. In the minds of many hospital administrators, a program is only as good as its last achievement.
“It’s kind of like, ‘What have you done for me lately?’” Buser says. “You want to stay ahead of the curve and be alert to what’s going on and not be caught keeping your eyes off the ball and, as a result, not moving your program forward.”
Scenario No. 4 : Fumbling the Handoff

—Daniel Cusator, MD, MBA, vice president, Camden Group, El Segundo, Calif.
The case: The medical center’s monthly data for the past year has shown that hospitalists are taking care of their patients efficiently and getting them out of the hospital more quickly. However, mixed in with the positive numbers is a stubbornly high 30-day readmission rate. Indeed, some primary care groups and referring geriatricians have begun to grouse to the HM director about the discharge notes, complaining they aren’t as comprehensive as they would like.
Plus, the notes always arrive via office fax, which makes them more likely to get misplaced and harder to receive when doctors are out of the office.
Expert advice: Handoffs from discharge to pickup are where a lot of complications, errors, and safety issues arise, and poor handoffs are one of the largest drivers of readmission rates, especially in the elderly patient population, says Daniel Cusator, MD, MBA, vice president of the Camden Group, a healthcare consulting firm in El Segundo, Calif.
If the hospitalist director doesn’t provide the leadership and resources to help the HM team better coordinate with patients’ regular doctors, handoffs won’t be a priority throughout the group.
The HM director must recognize that the term “discharge note” is a misnomer.
What referring physicians really want is a care plan, which includes information about testing done in the hospital, testing that might be needed in the outpatient setting, medications the patient is on, complications the patient had in the hospital, potential problems to monitor, and any necessary follow-up, says Dr. Cusator, formerly the chief medical officer of clinical integration at Providence Health & Services in Southern California.
PCPs also want the care plan transmitted in their preferred method, whether that is text messaging, HIPAA-compliant email messaging, secure messaging, or fax.
“What I’ve seen some hospitalist groups do is create a menu capability for each of the physicians to choose their preferred method of notification of discharge of their patient,” Dr. Cusator says. Results suggest such a menu leads to improved physician satisfaction and reduced patient complications after discharge, he adds.
With today’s technological innovations, HM directors are unlimited in their ability to improve handoffs between their team and patients’ PCPs and specialists, Dr. Cusator says. Some HM directors, for example, are leading efforts to link electronic medical records systems to hospital-based health information exchange hubs that are accessible to physicians in the community.
“Notes and clinical information are submitted to this health information exchange and made available to any of the physicians who are caring for the patient almost immediately upon dictation and notation,” he says.
Scenario No. 5 : Protect Your Assets

—David Lee, MD, MBA, FACP, FHM, vice chairman, Hospital Medicine Department, Ochsner Health System, New Orleans.
The case: A physician isn’t sure she wants a career in hospital medicine. She finds the specialty rewarding but is looking for a different challenge, something beyond exclusively seeing patients. The HM director notices the physician has an aptitude for finding ways to do tasks more efficiently.
The director privately thinks the physician would be a good fit for a quality improvement project that’s about to start but doesn’t pursue it. The HM team just added a primary care group, and its patient census is quickly rising, requiring the hospitalists to devote their entire shifts to patient care. Within the year, the physician leaves the team for a fellowship program outside hospital medicine.
Expert advice: There are three communities in hospital medicine, Dr. Bulger says: people who want to be hospitalists, people who are passing through on their way to something else, and people who sit somewhere in the middle.
HM directors, he says, should do everything they can to develop not only the career hospitalists but also those on the fence.
“A lot of them you can turn into people who are going to be hospitalists if they are doing something that is rewarding for them,” Dr. Bulger says. “Many times rewarding for them is being involved more in the leadership of the group, being involved in quality improvement projects, really seeing how they can impact the care for populations of patients—and not just the patient who happens to be sitting in front of them.”
It’s incumbent on HM group leaders to link hospitalists with mentors and help them find a niche, Dr. Lee says. It keeps people interested and makes them feel part of a group.
“They need to feel they belong,” he says. “There has to be a cohesiveness in order for your department to excel. You have to protect your assets in the group, which is your physicians.”
Sending hospitalists to professional development training, such as SHM’s Leadership Academy (see “Leadership Academy Adds ‘Women in HM Issues’ to Schedule,” p. 9) or QI-focused webinars offered by SHM or the Institute of Healthcare Improvement, and following up with day-to-day coaching is a solid physician-development strategy, Dr. Gartland says. By virtue of their job, hospitalists are expected to lead and manage people in interactions with the ED, primary care, non-physician providers, nursing staff, and beyond, he says.
Directors also have to stop assuming that competent physicians are competent managers. “A lot of physicians don’t have those core skill sets, and we’ve got to pay conscious attention toward spending time dedicated to developing those,” Dr. Gartland says.
If directors don’t make professional development a priority or provide hospitalists with the flexibility to do non-clinical activities, retention may become an issue, Dr. Bulger says. “They could leave and go somewhere else,” he says, yet perhaps the more significant danger is losing hospitalists to programs and specialties outside hospital medicine.
Lisa Ryan is a freelance writer based in New Jersey.
Some of the best companies in America started in a garage or a basement with an individual who had a great idea and the ability to grow it into a progressively larger business.
“It takes a leader with different capabilities to take a company to the next level,” says Martin Buser, MPH, FACHE, a partner with Hospitalist Management Resources LLC in San Diego, which has helped more than 350 HM programs nationwide in the past 15 years. “It’s an attitude of never stop learning, an ability to look at issues from 30,000 feet instead of ground zero so you can see the whole picture.”
Similarly, the most important predictor of an HM program’s success is its director, Buser says. If directors know how to communicate, innovate, facilitate, problem-solve, and inspire, they are much more likely to run a high-performing hospitalist program, says David Lee, MD, MBA, FACP, FHM, vice chairman of the Hospital Medicine Department at Ochsner Health System in New Orleans.
If group directors lack the skills and fail to adapt to change, the program’s outlook is far from certain. “We unfortunately get involved with these programs,” Buser says. “It’s painful to see.” Bad behavior is nothing new to the hospital setting, and HM is not immune to poor management. The following are common examples of bad behaviors and how groups can avoid the mishaps.
Scenario No. 1 : Great Clinician, Nice Person, Weak Advocate

—Martin Buser, MPH, FACHE, partner, Hospitalist Management Resources LLC, San Diego
The case: Earlier this year, medical center administrators asked the hospitalist program to do more with less, explaining the hospital was having a bad financial year. Administration approached the HM director, an exceptional, gregarious clinician who was named to the position years ago to help the program gain acceptance. The director agreed to indefinitely postpone two much-needed hirings, deciding it was better to share in the sacrifice than protest the cuts to the program’s budget. Hospitalists have since been working more shifts without a pay increase, and burnout symptoms have emerged with no signs of a thaw in the hiring freeze.
Expert advice: Buser says the “weak advocate” is a common issue among hospitalist groups, many of which he says are “going to hell” when he gets a rescue call. When a hospital is facing financial hardship, it is imperative that the HM director stand up for the program by explaining in detail the ramifications of each level of budget cuts. That’s because administrators might not realize the long-term damage that would result from such actions, he says. Being a strong, savvy advocate is even more important now since the financial future of many hospitals is ominous.
“With all of our hospitalist clients, we ask the CFO what is happening in the future…and the numbers are phenomenal,” says Buser. “They are seeing reductions of $10 million to $30 million off their bottom line.”
Administrators’ knee-jerk reaction is to cut costs. But there is another option: Grow the hospital out of its financial difficulties. It is up to the HM director to show administrators how the HM group has strategically gained them market share and how it will continue to do so. Good directors are in near constant contact with administrators, demonstrating the value their hospitalist program brings to the hospital, Buser says.
“You’re having regular meetings with the administrator, you’re producing the dashboard on a regular basis, you’re giving him trends that are going on,” he explains. “Show that you understand the hospital’s issues. Certain things you want to compromise on, but other things you have to say, ‘If we do that, the ramifications are such that it’s just not going to work.’”
Scenario No. 2 : Recruiting Roulette

—David Friar, MD, SFHM, CEO, Hospitalists of Northern Michigan, Traverse City
The case: The HM director felt pressure to hire. The program’s hospitalists were seeing two to three patients a day more than they should have been, and hospital administrators were worried the program was losing ground to the other hospitalist group in the community. Using an outside recruiter, the director hired two adept physicians with stellar CVs after an expedited review process that included a background check, a few phone interviews, and day of in-person interviews with some administrators and a hospitalist on the team. Now, nearly a year later, one of the physicians is about to leave because her family doesn’t like the community, and the other new hire’s abrasive personality has caused considerable damage to the team’s cohesion.
Expert advice: A big part of an HM program’s value is how it practices as a unified team, and directors need to recognize how vital the “team fit” is to hospitalists, says David Friar, MD, SFHM, CEO of Hospitalists of Northern Michigan in Traverse City.
“A bad team fit is often worse than being short-staffed because it can literally destroy the team spirit,” he says.
Directors should have a standardized recruitment process that includes a comprehensive background screening where references are closely checked, a round of interviews by people outside the HM program (nurses and referring physicians), and substantial time spent with hospitalists in the program, says Bryce Gartland, MD, FHM, associate director of the hospital medicine division and medical director of care coordination at Emory Healthcare in Atlanta.
“We put [candidates] with one of our physicians to actually go around the hospital,” he says. “It’s amazing to me the number of things you can pick up by that broader exposure that you may not pick up sitting in a room with a candidate across the table for an hour.”
If a recruitment service is used, the director must describe the HM program in detail to the recruiter and even have them meet hospitalists on the staff, Dr. Friar says.
“Sending them a memo saying ‘We need three new hospitalists ASAP’ isn’t helping them find you the perfect candidate,” he says. “Even the best recruiter can only do a great job for you if they really know your team and what it is you need in a candidate.”
A director also is well served to make recruiting a family event where spouses and even children are part of the interview process.
“By including the entire family and then supporting them after the move, we are much more likely to recruit providers that will stay good members of our team for years to come,” Dr. Friar says.
Scenario No. 3 : Amitte Diem

—John Bulger, DO, FACP, FHM, chief quality officer, director, hospital medicine service line, Geisinger Health System, Danville, Pa.
The case: For months, the medical center has been receiving an increased number of referrals from outlying hospitals, and no end is in sight. The extra patient load, much of it involving complex cases, has agitated the medical center’s staff, particularly the specialists, and they’ve begun to complain to hospital administrators. Seeking an ally, the specialists reach out to the HM director to present their case. Without doing independent analysis, the HM director sides with the specialists. Hospital administrators, facing growing resistance, work to decrease the referrals and are successful.
Expert advice: Consider working in the opposite direction, one that might turn a referral challenge into a profitable opportunity, Buser says. One of his firm’s clients, after thorough research, established a transfer center and set up an activation fee for the specialists who took the referrals. Hospitalists admitted about 90% of the cases, called consults, and named specialists so they received full fee-for-service at Medicare rates if they saw uninsured patients.
“That hospital is now making about $78 million a year, and the medical staff is saying, ‘How can we grow this?’” Buser says. “Here’s an example of how the hospital medicine director was key to turning the bad into something good.”
Because physicians tend to be reticent to change, it’s critical for hospitalist directors who want to seize an opportunity to thoroughly plan out how the change will occur and to prepare for potential obstacles along the way, says John Bulger, DO, FACP, FHM, chief quality officer and director of the hospital medicine service line for Geisinger Health System in Danville, Pa.
“You really need to be prepared with your rationale of why you’re doing it, if there’s data behind why you’re doing it, what the data is that’s driving it, and really what you hope to do with that change,” he says. “If you don’t get buy in from your staff, the change is doomed to fail from the beginning.”
Directors must embrace being a change agent if they want their HM programs to continue to be successful. In the minds of many hospital administrators, a program is only as good as its last achievement.
“It’s kind of like, ‘What have you done for me lately?’” Buser says. “You want to stay ahead of the curve and be alert to what’s going on and not be caught keeping your eyes off the ball and, as a result, not moving your program forward.”
Scenario No. 4 : Fumbling the Handoff

—Daniel Cusator, MD, MBA, vice president, Camden Group, El Segundo, Calif.
The case: The medical center’s monthly data for the past year has shown that hospitalists are taking care of their patients efficiently and getting them out of the hospital more quickly. However, mixed in with the positive numbers is a stubbornly high 30-day readmission rate. Indeed, some primary care groups and referring geriatricians have begun to grouse to the HM director about the discharge notes, complaining they aren’t as comprehensive as they would like.
Plus, the notes always arrive via office fax, which makes them more likely to get misplaced and harder to receive when doctors are out of the office.
Expert advice: Handoffs from discharge to pickup are where a lot of complications, errors, and safety issues arise, and poor handoffs are one of the largest drivers of readmission rates, especially in the elderly patient population, says Daniel Cusator, MD, MBA, vice president of the Camden Group, a healthcare consulting firm in El Segundo, Calif.
If the hospitalist director doesn’t provide the leadership and resources to help the HM team better coordinate with patients’ regular doctors, handoffs won’t be a priority throughout the group.
The HM director must recognize that the term “discharge note” is a misnomer.
What referring physicians really want is a care plan, which includes information about testing done in the hospital, testing that might be needed in the outpatient setting, medications the patient is on, complications the patient had in the hospital, potential problems to monitor, and any necessary follow-up, says Dr. Cusator, formerly the chief medical officer of clinical integration at Providence Health & Services in Southern California.
PCPs also want the care plan transmitted in their preferred method, whether that is text messaging, HIPAA-compliant email messaging, secure messaging, or fax.
“What I’ve seen some hospitalist groups do is create a menu capability for each of the physicians to choose their preferred method of notification of discharge of their patient,” Dr. Cusator says. Results suggest such a menu leads to improved physician satisfaction and reduced patient complications after discharge, he adds.
With today’s technological innovations, HM directors are unlimited in their ability to improve handoffs between their team and patients’ PCPs and specialists, Dr. Cusator says. Some HM directors, for example, are leading efforts to link electronic medical records systems to hospital-based health information exchange hubs that are accessible to physicians in the community.
“Notes and clinical information are submitted to this health information exchange and made available to any of the physicians who are caring for the patient almost immediately upon dictation and notation,” he says.
Scenario No. 5 : Protect Your Assets

—David Lee, MD, MBA, FACP, FHM, vice chairman, Hospital Medicine Department, Ochsner Health System, New Orleans.
The case: A physician isn’t sure she wants a career in hospital medicine. She finds the specialty rewarding but is looking for a different challenge, something beyond exclusively seeing patients. The HM director notices the physician has an aptitude for finding ways to do tasks more efficiently.
The director privately thinks the physician would be a good fit for a quality improvement project that’s about to start but doesn’t pursue it. The HM team just added a primary care group, and its patient census is quickly rising, requiring the hospitalists to devote their entire shifts to patient care. Within the year, the physician leaves the team for a fellowship program outside hospital medicine.
Expert advice: There are three communities in hospital medicine, Dr. Bulger says: people who want to be hospitalists, people who are passing through on their way to something else, and people who sit somewhere in the middle.
HM directors, he says, should do everything they can to develop not only the career hospitalists but also those on the fence.
“A lot of them you can turn into people who are going to be hospitalists if they are doing something that is rewarding for them,” Dr. Bulger says. “Many times rewarding for them is being involved more in the leadership of the group, being involved in quality improvement projects, really seeing how they can impact the care for populations of patients—and not just the patient who happens to be sitting in front of them.”
It’s incumbent on HM group leaders to link hospitalists with mentors and help them find a niche, Dr. Lee says. It keeps people interested and makes them feel part of a group.
“They need to feel they belong,” he says. “There has to be a cohesiveness in order for your department to excel. You have to protect your assets in the group, which is your physicians.”
Sending hospitalists to professional development training, such as SHM’s Leadership Academy (see “Leadership Academy Adds ‘Women in HM Issues’ to Schedule,” p. 9) or QI-focused webinars offered by SHM or the Institute of Healthcare Improvement, and following up with day-to-day coaching is a solid physician-development strategy, Dr. Gartland says. By virtue of their job, hospitalists are expected to lead and manage people in interactions with the ED, primary care, non-physician providers, nursing staff, and beyond, he says.
Directors also have to stop assuming that competent physicians are competent managers. “A lot of physicians don’t have those core skill sets, and we’ve got to pay conscious attention toward spending time dedicated to developing those,” Dr. Gartland says.
If directors don’t make professional development a priority or provide hospitalists with the flexibility to do non-clinical activities, retention may become an issue, Dr. Bulger says. “They could leave and go somewhere else,” he says, yet perhaps the more significant danger is losing hospitalists to programs and specialties outside hospital medicine.
Lisa Ryan is a freelance writer based in New Jersey.
Some of the best companies in America started in a garage or a basement with an individual who had a great idea and the ability to grow it into a progressively larger business.
“It takes a leader with different capabilities to take a company to the next level,” says Martin Buser, MPH, FACHE, a partner with Hospitalist Management Resources LLC in San Diego, which has helped more than 350 HM programs nationwide in the past 15 years. “It’s an attitude of never stop learning, an ability to look at issues from 30,000 feet instead of ground zero so you can see the whole picture.”
Similarly, the most important predictor of an HM program’s success is its director, Buser says. If directors know how to communicate, innovate, facilitate, problem-solve, and inspire, they are much more likely to run a high-performing hospitalist program, says David Lee, MD, MBA, FACP, FHM, vice chairman of the Hospital Medicine Department at Ochsner Health System in New Orleans.
If group directors lack the skills and fail to adapt to change, the program’s outlook is far from certain. “We unfortunately get involved with these programs,” Buser says. “It’s painful to see.” Bad behavior is nothing new to the hospital setting, and HM is not immune to poor management. The following are common examples of bad behaviors and how groups can avoid the mishaps.
Scenario No. 1 : Great Clinician, Nice Person, Weak Advocate

—Martin Buser, MPH, FACHE, partner, Hospitalist Management Resources LLC, San Diego
The case: Earlier this year, medical center administrators asked the hospitalist program to do more with less, explaining the hospital was having a bad financial year. Administration approached the HM director, an exceptional, gregarious clinician who was named to the position years ago to help the program gain acceptance. The director agreed to indefinitely postpone two much-needed hirings, deciding it was better to share in the sacrifice than protest the cuts to the program’s budget. Hospitalists have since been working more shifts without a pay increase, and burnout symptoms have emerged with no signs of a thaw in the hiring freeze.
Expert advice: Buser says the “weak advocate” is a common issue among hospitalist groups, many of which he says are “going to hell” when he gets a rescue call. When a hospital is facing financial hardship, it is imperative that the HM director stand up for the program by explaining in detail the ramifications of each level of budget cuts. That’s because administrators might not realize the long-term damage that would result from such actions, he says. Being a strong, savvy advocate is even more important now since the financial future of many hospitals is ominous.
“With all of our hospitalist clients, we ask the CFO what is happening in the future…and the numbers are phenomenal,” says Buser. “They are seeing reductions of $10 million to $30 million off their bottom line.”
Administrators’ knee-jerk reaction is to cut costs. But there is another option: Grow the hospital out of its financial difficulties. It is up to the HM director to show administrators how the HM group has strategically gained them market share and how it will continue to do so. Good directors are in near constant contact with administrators, demonstrating the value their hospitalist program brings to the hospital, Buser says.
“You’re having regular meetings with the administrator, you’re producing the dashboard on a regular basis, you’re giving him trends that are going on,” he explains. “Show that you understand the hospital’s issues. Certain things you want to compromise on, but other things you have to say, ‘If we do that, the ramifications are such that it’s just not going to work.’”
Scenario No. 2 : Recruiting Roulette

—David Friar, MD, SFHM, CEO, Hospitalists of Northern Michigan, Traverse City
The case: The HM director felt pressure to hire. The program’s hospitalists were seeing two to three patients a day more than they should have been, and hospital administrators were worried the program was losing ground to the other hospitalist group in the community. Using an outside recruiter, the director hired two adept physicians with stellar CVs after an expedited review process that included a background check, a few phone interviews, and day of in-person interviews with some administrators and a hospitalist on the team. Now, nearly a year later, one of the physicians is about to leave because her family doesn’t like the community, and the other new hire’s abrasive personality has caused considerable damage to the team’s cohesion.
Expert advice: A big part of an HM program’s value is how it practices as a unified team, and directors need to recognize how vital the “team fit” is to hospitalists, says David Friar, MD, SFHM, CEO of Hospitalists of Northern Michigan in Traverse City.
“A bad team fit is often worse than being short-staffed because it can literally destroy the team spirit,” he says.
Directors should have a standardized recruitment process that includes a comprehensive background screening where references are closely checked, a round of interviews by people outside the HM program (nurses and referring physicians), and substantial time spent with hospitalists in the program, says Bryce Gartland, MD, FHM, associate director of the hospital medicine division and medical director of care coordination at Emory Healthcare in Atlanta.
“We put [candidates] with one of our physicians to actually go around the hospital,” he says. “It’s amazing to me the number of things you can pick up by that broader exposure that you may not pick up sitting in a room with a candidate across the table for an hour.”
If a recruitment service is used, the director must describe the HM program in detail to the recruiter and even have them meet hospitalists on the staff, Dr. Friar says.
“Sending them a memo saying ‘We need three new hospitalists ASAP’ isn’t helping them find you the perfect candidate,” he says. “Even the best recruiter can only do a great job for you if they really know your team and what it is you need in a candidate.”
A director also is well served to make recruiting a family event where spouses and even children are part of the interview process.
“By including the entire family and then supporting them after the move, we are much more likely to recruit providers that will stay good members of our team for years to come,” Dr. Friar says.
Scenario No. 3 : Amitte Diem

—John Bulger, DO, FACP, FHM, chief quality officer, director, hospital medicine service line, Geisinger Health System, Danville, Pa.
The case: For months, the medical center has been receiving an increased number of referrals from outlying hospitals, and no end is in sight. The extra patient load, much of it involving complex cases, has agitated the medical center’s staff, particularly the specialists, and they’ve begun to complain to hospital administrators. Seeking an ally, the specialists reach out to the HM director to present their case. Without doing independent analysis, the HM director sides with the specialists. Hospital administrators, facing growing resistance, work to decrease the referrals and are successful.
Expert advice: Consider working in the opposite direction, one that might turn a referral challenge into a profitable opportunity, Buser says. One of his firm’s clients, after thorough research, established a transfer center and set up an activation fee for the specialists who took the referrals. Hospitalists admitted about 90% of the cases, called consults, and named specialists so they received full fee-for-service at Medicare rates if they saw uninsured patients.
“That hospital is now making about $78 million a year, and the medical staff is saying, ‘How can we grow this?’” Buser says. “Here’s an example of how the hospital medicine director was key to turning the bad into something good.”
Because physicians tend to be reticent to change, it’s critical for hospitalist directors who want to seize an opportunity to thoroughly plan out how the change will occur and to prepare for potential obstacles along the way, says John Bulger, DO, FACP, FHM, chief quality officer and director of the hospital medicine service line for Geisinger Health System in Danville, Pa.
“You really need to be prepared with your rationale of why you’re doing it, if there’s data behind why you’re doing it, what the data is that’s driving it, and really what you hope to do with that change,” he says. “If you don’t get buy in from your staff, the change is doomed to fail from the beginning.”
Directors must embrace being a change agent if they want their HM programs to continue to be successful. In the minds of many hospital administrators, a program is only as good as its last achievement.
“It’s kind of like, ‘What have you done for me lately?’” Buser says. “You want to stay ahead of the curve and be alert to what’s going on and not be caught keeping your eyes off the ball and, as a result, not moving your program forward.”
Scenario No. 4 : Fumbling the Handoff

—Daniel Cusator, MD, MBA, vice president, Camden Group, El Segundo, Calif.
The case: The medical center’s monthly data for the past year has shown that hospitalists are taking care of their patients efficiently and getting them out of the hospital more quickly. However, mixed in with the positive numbers is a stubbornly high 30-day readmission rate. Indeed, some primary care groups and referring geriatricians have begun to grouse to the HM director about the discharge notes, complaining they aren’t as comprehensive as they would like.
Plus, the notes always arrive via office fax, which makes them more likely to get misplaced and harder to receive when doctors are out of the office.
Expert advice: Handoffs from discharge to pickup are where a lot of complications, errors, and safety issues arise, and poor handoffs are one of the largest drivers of readmission rates, especially in the elderly patient population, says Daniel Cusator, MD, MBA, vice president of the Camden Group, a healthcare consulting firm in El Segundo, Calif.
If the hospitalist director doesn’t provide the leadership and resources to help the HM team better coordinate with patients’ regular doctors, handoffs won’t be a priority throughout the group.
The HM director must recognize that the term “discharge note” is a misnomer.
What referring physicians really want is a care plan, which includes information about testing done in the hospital, testing that might be needed in the outpatient setting, medications the patient is on, complications the patient had in the hospital, potential problems to monitor, and any necessary follow-up, says Dr. Cusator, formerly the chief medical officer of clinical integration at Providence Health & Services in Southern California.
PCPs also want the care plan transmitted in their preferred method, whether that is text messaging, HIPAA-compliant email messaging, secure messaging, or fax.
“What I’ve seen some hospitalist groups do is create a menu capability for each of the physicians to choose their preferred method of notification of discharge of their patient,” Dr. Cusator says. Results suggest such a menu leads to improved physician satisfaction and reduced patient complications after discharge, he adds.
With today’s technological innovations, HM directors are unlimited in their ability to improve handoffs between their team and patients’ PCPs and specialists, Dr. Cusator says. Some HM directors, for example, are leading efforts to link electronic medical records systems to hospital-based health information exchange hubs that are accessible to physicians in the community.
“Notes and clinical information are submitted to this health information exchange and made available to any of the physicians who are caring for the patient almost immediately upon dictation and notation,” he says.
Scenario No. 5 : Protect Your Assets

—David Lee, MD, MBA, FACP, FHM, vice chairman, Hospital Medicine Department, Ochsner Health System, New Orleans.
The case: A physician isn’t sure she wants a career in hospital medicine. She finds the specialty rewarding but is looking for a different challenge, something beyond exclusively seeing patients. The HM director notices the physician has an aptitude for finding ways to do tasks more efficiently.
The director privately thinks the physician would be a good fit for a quality improvement project that’s about to start but doesn’t pursue it. The HM team just added a primary care group, and its patient census is quickly rising, requiring the hospitalists to devote their entire shifts to patient care. Within the year, the physician leaves the team for a fellowship program outside hospital medicine.
Expert advice: There are three communities in hospital medicine, Dr. Bulger says: people who want to be hospitalists, people who are passing through on their way to something else, and people who sit somewhere in the middle.
HM directors, he says, should do everything they can to develop not only the career hospitalists but also those on the fence.
“A lot of them you can turn into people who are going to be hospitalists if they are doing something that is rewarding for them,” Dr. Bulger says. “Many times rewarding for them is being involved more in the leadership of the group, being involved in quality improvement projects, really seeing how they can impact the care for populations of patients—and not just the patient who happens to be sitting in front of them.”
It’s incumbent on HM group leaders to link hospitalists with mentors and help them find a niche, Dr. Lee says. It keeps people interested and makes them feel part of a group.
“They need to feel they belong,” he says. “There has to be a cohesiveness in order for your department to excel. You have to protect your assets in the group, which is your physicians.”
Sending hospitalists to professional development training, such as SHM’s Leadership Academy (see “Leadership Academy Adds ‘Women in HM Issues’ to Schedule,” p. 9) or QI-focused webinars offered by SHM or the Institute of Healthcare Improvement, and following up with day-to-day coaching is a solid physician-development strategy, Dr. Gartland says. By virtue of their job, hospitalists are expected to lead and manage people in interactions with the ED, primary care, non-physician providers, nursing staff, and beyond, he says.
Directors also have to stop assuming that competent physicians are competent managers. “A lot of physicians don’t have those core skill sets, and we’ve got to pay conscious attention toward spending time dedicated to developing those,” Dr. Gartland says.
If directors don’t make professional development a priority or provide hospitalists with the flexibility to do non-clinical activities, retention may become an issue, Dr. Bulger says. “They could leave and go somewhere else,” he says, yet perhaps the more significant danger is losing hospitalists to programs and specialties outside hospital medicine.
Lisa Ryan is a freelance writer based in New Jersey.
Dr. Shen Responds to Kernicterus Letters
I sincerely appreciate the responses to my review of an article (“Incidence Rates of Kernicterus Remain Unchanged,” The Hospitalist, October 2011, p. 12) that raised questions regarding a “resurgence” of kernicterus in the 1990s. Kernicterus is a devastating illness, and family members bear an unquestionable burden from this disease. Because phototherapy appears to limit the burden of disease, evidence-based guidelines for appropriate treatment of hyperbilirubinemia are paramount to decreasing the incidence of kernicterus. True rates of kernicterus have been difficult to calculate for a variety of reasons, yet we must get a handle on “who” gets kernicterus if we are to appropriately decide which infants receive phototherapy. Thus, I would strongly agree that using the California database is a limitation of the study reviewed.
The mission of the monthly “Pediatric HM” literature review is to regularly summarize articles that might be of interest in the field of pediatric HM. The letters to the editor we received highlight a critical need to delve deeper into the epidemiology of kernicterus, a journey that must begin with accurate reporting of this disease. We appreciate the opportunity to raise awareness of family-centered concerns surrounding the interpretation and analysis of scientific evidence.
As a final note, Mr. Spencer Brown’s letter states that “nearly half of all babies born (44,000 out of every 100,000) have hyperbilirubinemia” based on an incidence of 0.44 per 100,000 mentioned in my review. I would clarify that 0.44 per 100,000 is a rate of kernicterus and is not a percentage. Thus, 0.44 out of 100,000 children (or 4.4 per million) will develop kernicterus, not 44,000 per 100,000.
Mark Shen, MD, FHM, director of hospital medicine, Dell Children’s Medical Center, Austin, Texas, pediatric physician editor, The Hospitalist
I sincerely appreciate the responses to my review of an article (“Incidence Rates of Kernicterus Remain Unchanged,” The Hospitalist, October 2011, p. 12) that raised questions regarding a “resurgence” of kernicterus in the 1990s. Kernicterus is a devastating illness, and family members bear an unquestionable burden from this disease. Because phototherapy appears to limit the burden of disease, evidence-based guidelines for appropriate treatment of hyperbilirubinemia are paramount to decreasing the incidence of kernicterus. True rates of kernicterus have been difficult to calculate for a variety of reasons, yet we must get a handle on “who” gets kernicterus if we are to appropriately decide which infants receive phototherapy. Thus, I would strongly agree that using the California database is a limitation of the study reviewed.
The mission of the monthly “Pediatric HM” literature review is to regularly summarize articles that might be of interest in the field of pediatric HM. The letters to the editor we received highlight a critical need to delve deeper into the epidemiology of kernicterus, a journey that must begin with accurate reporting of this disease. We appreciate the opportunity to raise awareness of family-centered concerns surrounding the interpretation and analysis of scientific evidence.
As a final note, Mr. Spencer Brown’s letter states that “nearly half of all babies born (44,000 out of every 100,000) have hyperbilirubinemia” based on an incidence of 0.44 per 100,000 mentioned in my review. I would clarify that 0.44 per 100,000 is a rate of kernicterus and is not a percentage. Thus, 0.44 out of 100,000 children (or 4.4 per million) will develop kernicterus, not 44,000 per 100,000.
Mark Shen, MD, FHM, director of hospital medicine, Dell Children’s Medical Center, Austin, Texas, pediatric physician editor, The Hospitalist
I sincerely appreciate the responses to my review of an article (“Incidence Rates of Kernicterus Remain Unchanged,” The Hospitalist, October 2011, p. 12) that raised questions regarding a “resurgence” of kernicterus in the 1990s. Kernicterus is a devastating illness, and family members bear an unquestionable burden from this disease. Because phototherapy appears to limit the burden of disease, evidence-based guidelines for appropriate treatment of hyperbilirubinemia are paramount to decreasing the incidence of kernicterus. True rates of kernicterus have been difficult to calculate for a variety of reasons, yet we must get a handle on “who” gets kernicterus if we are to appropriately decide which infants receive phototherapy. Thus, I would strongly agree that using the California database is a limitation of the study reviewed.
The mission of the monthly “Pediatric HM” literature review is to regularly summarize articles that might be of interest in the field of pediatric HM. The letters to the editor we received highlight a critical need to delve deeper into the epidemiology of kernicterus, a journey that must begin with accurate reporting of this disease. We appreciate the opportunity to raise awareness of family-centered concerns surrounding the interpretation and analysis of scientific evidence.
As a final note, Mr. Spencer Brown’s letter states that “nearly half of all babies born (44,000 out of every 100,000) have hyperbilirubinemia” based on an incidence of 0.44 per 100,000 mentioned in my review. I would clarify that 0.44 per 100,000 is a rate of kernicterus and is not a percentage. Thus, 0.44 out of 100,000 children (or 4.4 per million) will develop kernicterus, not 44,000 per 100,000.
Mark Shen, MD, FHM, director of hospital medicine, Dell Children’s Medical Center, Austin, Texas, pediatric physician editor, The Hospitalist
Kernicterus Is Observable, Predictable, Curable
I recently read your article on the rates of kernicterus and found it quite alarming. I am asking for an immediate apology and a retraction of this article.
This article is interesting since it states that only 25 out of 64,346 hyperbilirubinemia patients actually were truly kernicterus kids. That is a very low stat of 0.0003885 of all children diagnosed with hyperbilirubinemia. It is far less when you take into account all live births. Using DDS as a yardstick may be acceptable, but the surprising conclusion was that treatment made little difference.
To say “The time trend of incidence remained stable during the study years at 0.44 per 100,000 live births” means that nearly half of all babies born (44,000 out of every 100,000) have hyperbilirubinemia. If we use the 0.0003885 multiplier, then we can state that approximately 17 out of every 100,000 live births result in kernicterus. It would be interesting to plot those stats against other states, as well as other countries, to see if 0.0003885 times the total amount of kids with diagnosed hyperbilirubinemia represents a stable sum of actual kernicterus kids.
The clinician’s report seems to imply that kernicterus is an event that is statistically predictable, inevitable, and unavoidable; therefore, in spite of medical intervention, a predictable number of newborns will develop the disease. In a morbid sense, mortality rates are also predictable: “Data from a national database of death certificates revealed a similar stable trend in deaths attributed to kernicterus.”
The bottom line “kernicterus rates remained unchanged in the 1990s” conclusion and the bold citation that “there was not a ‘resurgence’ of kernicterus in the 1990s” are offered up in spite of the zero-tolerance policy of many hospitals that claim to know how to prevent the onset of kernicterus. The monitoring of infants, the early detection of hyperbilirubinemia, the effective and timely use of bili-lights, and possible blood transfusion should be adequate to quash kernicterus forever.
Perhaps newborn patients “with hyperbilirubinemia who are at extremely low risk for kernicterus are being overtreated,” but this does not preclude the need for those at high risk to obtain an early assessment and aggressive treatment. Perhaps the reason why there is no observable change in the incidence of kernicterus over the past 20 years is because the policy does not translate into procedures. Doctors seem to take on a lackadaisical, roll-of-the-dice type of approach to the prevention of kernicterus. Since the numbers are so low, they are not providing the vigilant watch and, therefore, allowing newborns to slip from hyperbilirubinemia to actual kernicterus.
The solution is there; the problem is the implementation. And it is not even a matter of insurance costs, since the therapy for prevention and/or intervention is extremely cheap. The needless suffering of a single kernicterus kid flies in the face of the fact that this is an observable, predictable, and curable disease.
The statistics may be right, but the medical approach is wrong. Whether it is 17 in every 100,000 or 1 in every 5,882, it makes a big difference if the 1 belongs to you. The only acceptable number is zero. The question is not about resurgence; it is more about why we are still seeing any incidences of such an easily preventable disease.
Spencer L. Brown, grandfather of a “kernicterus kid”
I recently read your article on the rates of kernicterus and found it quite alarming. I am asking for an immediate apology and a retraction of this article.
This article is interesting since it states that only 25 out of 64,346 hyperbilirubinemia patients actually were truly kernicterus kids. That is a very low stat of 0.0003885 of all children diagnosed with hyperbilirubinemia. It is far less when you take into account all live births. Using DDS as a yardstick may be acceptable, but the surprising conclusion was that treatment made little difference.
To say “The time trend of incidence remained stable during the study years at 0.44 per 100,000 live births” means that nearly half of all babies born (44,000 out of every 100,000) have hyperbilirubinemia. If we use the 0.0003885 multiplier, then we can state that approximately 17 out of every 100,000 live births result in kernicterus. It would be interesting to plot those stats against other states, as well as other countries, to see if 0.0003885 times the total amount of kids with diagnosed hyperbilirubinemia represents a stable sum of actual kernicterus kids.
The clinician’s report seems to imply that kernicterus is an event that is statistically predictable, inevitable, and unavoidable; therefore, in spite of medical intervention, a predictable number of newborns will develop the disease. In a morbid sense, mortality rates are also predictable: “Data from a national database of death certificates revealed a similar stable trend in deaths attributed to kernicterus.”
The bottom line “kernicterus rates remained unchanged in the 1990s” conclusion and the bold citation that “there was not a ‘resurgence’ of kernicterus in the 1990s” are offered up in spite of the zero-tolerance policy of many hospitals that claim to know how to prevent the onset of kernicterus. The monitoring of infants, the early detection of hyperbilirubinemia, the effective and timely use of bili-lights, and possible blood transfusion should be adequate to quash kernicterus forever.
Perhaps newborn patients “with hyperbilirubinemia who are at extremely low risk for kernicterus are being overtreated,” but this does not preclude the need for those at high risk to obtain an early assessment and aggressive treatment. Perhaps the reason why there is no observable change in the incidence of kernicterus over the past 20 years is because the policy does not translate into procedures. Doctors seem to take on a lackadaisical, roll-of-the-dice type of approach to the prevention of kernicterus. Since the numbers are so low, they are not providing the vigilant watch and, therefore, allowing newborns to slip from hyperbilirubinemia to actual kernicterus.
The solution is there; the problem is the implementation. And it is not even a matter of insurance costs, since the therapy for prevention and/or intervention is extremely cheap. The needless suffering of a single kernicterus kid flies in the face of the fact that this is an observable, predictable, and curable disease.
The statistics may be right, but the medical approach is wrong. Whether it is 17 in every 100,000 or 1 in every 5,882, it makes a big difference if the 1 belongs to you. The only acceptable number is zero. The question is not about resurgence; it is more about why we are still seeing any incidences of such an easily preventable disease.
Spencer L. Brown, grandfather of a “kernicterus kid”
I recently read your article on the rates of kernicterus and found it quite alarming. I am asking for an immediate apology and a retraction of this article.
This article is interesting since it states that only 25 out of 64,346 hyperbilirubinemia patients actually were truly kernicterus kids. That is a very low stat of 0.0003885 of all children diagnosed with hyperbilirubinemia. It is far less when you take into account all live births. Using DDS as a yardstick may be acceptable, but the surprising conclusion was that treatment made little difference.
To say “The time trend of incidence remained stable during the study years at 0.44 per 100,000 live births” means that nearly half of all babies born (44,000 out of every 100,000) have hyperbilirubinemia. If we use the 0.0003885 multiplier, then we can state that approximately 17 out of every 100,000 live births result in kernicterus. It would be interesting to plot those stats against other states, as well as other countries, to see if 0.0003885 times the total amount of kids with diagnosed hyperbilirubinemia represents a stable sum of actual kernicterus kids.
The clinician’s report seems to imply that kernicterus is an event that is statistically predictable, inevitable, and unavoidable; therefore, in spite of medical intervention, a predictable number of newborns will develop the disease. In a morbid sense, mortality rates are also predictable: “Data from a national database of death certificates revealed a similar stable trend in deaths attributed to kernicterus.”
The bottom line “kernicterus rates remained unchanged in the 1990s” conclusion and the bold citation that “there was not a ‘resurgence’ of kernicterus in the 1990s” are offered up in spite of the zero-tolerance policy of many hospitals that claim to know how to prevent the onset of kernicterus. The monitoring of infants, the early detection of hyperbilirubinemia, the effective and timely use of bili-lights, and possible blood transfusion should be adequate to quash kernicterus forever.
Perhaps newborn patients “with hyperbilirubinemia who are at extremely low risk for kernicterus are being overtreated,” but this does not preclude the need for those at high risk to obtain an early assessment and aggressive treatment. Perhaps the reason why there is no observable change in the incidence of kernicterus over the past 20 years is because the policy does not translate into procedures. Doctors seem to take on a lackadaisical, roll-of-the-dice type of approach to the prevention of kernicterus. Since the numbers are so low, they are not providing the vigilant watch and, therefore, allowing newborns to slip from hyperbilirubinemia to actual kernicterus.
The solution is there; the problem is the implementation. And it is not even a matter of insurance costs, since the therapy for prevention and/or intervention is extremely cheap. The needless suffering of a single kernicterus kid flies in the face of the fact that this is an observable, predictable, and curable disease.
The statistics may be right, but the medical approach is wrong. Whether it is 17 in every 100,000 or 1 in every 5,882, it makes a big difference if the 1 belongs to you. The only acceptable number is zero. The question is not about resurgence; it is more about why we are still seeing any incidences of such an easily preventable disease.
Spencer L. Brown, grandfather of a “kernicterus kid”
Medical Community Should Take Proactive Approach to Kernicterus Treatment, Reporting
I’m writing in regard to the article “Incidence Rates of Kernicterus Remain Unchanged” (The Hospitalist, October 2011, p. 12) by Mark Shen, MD, FHM. As a mother of a child with kernicterus (born in 2005), I’m very concerned with the cavalier attitude toward hyperbilirubenia treatment and the reliance upon inaccurate statistics. Reasons for the inaccuracy:
- Your data is for California only;
- DDS reports of kernicterus are likely inaccurate. Nothing our son is enrolled in lists his diagnosis as kernicterus. Most institutions don’t have it in their database. Paperwork for my son shows encephalopathy, cerebral palsy, athetoid cerebral palsy, dystonia, or quadraplegia, but rarely kernicterus. As a result, I and other parents of children with kernicterus can attest to a massive under reporting of kernicterus, wherever you look;
- Our parent group, PICK, is constantly growing, with new members every month across the country and across the world;
- Even death certificates are subject to the fear that comes with kernicterus. Physicians know that putting this information on a death certificate will lead to a lawsuit, and thus are more inclined to list respiratory failure or other secondary causes as the cause of death; and
- Many children with kernicterus are never properly diagnosed or given diagnostic tests like an MRI to confirm the damage. They are instead steered away from the diagnosis, even when it is the obvious cause.
Please understand that the “kinder, gentler” approach to hyperbilirubinemia is why my son has kernicterus. He was repeatedly inspected visually, and our concerns were dismissed. At nine days old, they dismissed our concerns and coded us “low priority.” When finally seen, his bilirubin was 45.6, his pulse ox was 69, and he was posturing. His MRI revealed the classic signal intensity in the globus pallidus. He failed the hearing test that he had passed easily the weak before. His life care plan is 69,000,000. He is fed via G-tube and unable to manipulate his limbs of trunk to perform any daily living tasks. He uses a wheelchair, gait trainer, stander, bath chair, lift, cochlear implant—the list goes on and on.
All of this could have been avoided with a little “overtreatment.” I believe the cost of a proactive approach could hardly compare to the costs that these children with kernicterus incur in their lifetimes.
So many are afraid to admit the potential dangers of newborn jaundice. Many say that they wouldn’t want to scare a parent. As a parent, I’d like to say that I am not afraid of something that is treatable and preventable. Educate us and let us help our children avoid serious peril!
Everyone in the medical community needs to take the proactive approach, as well as find a means of reporting kernicterus that is free of the liability concerns, or be willing to face them.
The CDC has created excellent new materials that seem to be getting very little attention but could have saved my son a lifetime of unspeakable struggle. Please take a look at them and consider distributing them at your treatment facilities.
Miriam Iliff, Fayetteville, N.C., past board member, Parents of Infants and Children with Kernicterus (PICK)
I’m writing in regard to the article “Incidence Rates of Kernicterus Remain Unchanged” (The Hospitalist, October 2011, p. 12) by Mark Shen, MD, FHM. As a mother of a child with kernicterus (born in 2005), I’m very concerned with the cavalier attitude toward hyperbilirubenia treatment and the reliance upon inaccurate statistics. Reasons for the inaccuracy:
- Your data is for California only;
- DDS reports of kernicterus are likely inaccurate. Nothing our son is enrolled in lists his diagnosis as kernicterus. Most institutions don’t have it in their database. Paperwork for my son shows encephalopathy, cerebral palsy, athetoid cerebral palsy, dystonia, or quadraplegia, but rarely kernicterus. As a result, I and other parents of children with kernicterus can attest to a massive under reporting of kernicterus, wherever you look;
- Our parent group, PICK, is constantly growing, with new members every month across the country and across the world;
- Even death certificates are subject to the fear that comes with kernicterus. Physicians know that putting this information on a death certificate will lead to a lawsuit, and thus are more inclined to list respiratory failure or other secondary causes as the cause of death; and
- Many children with kernicterus are never properly diagnosed or given diagnostic tests like an MRI to confirm the damage. They are instead steered away from the diagnosis, even when it is the obvious cause.
Please understand that the “kinder, gentler” approach to hyperbilirubinemia is why my son has kernicterus. He was repeatedly inspected visually, and our concerns were dismissed. At nine days old, they dismissed our concerns and coded us “low priority.” When finally seen, his bilirubin was 45.6, his pulse ox was 69, and he was posturing. His MRI revealed the classic signal intensity in the globus pallidus. He failed the hearing test that he had passed easily the weak before. His life care plan is 69,000,000. He is fed via G-tube and unable to manipulate his limbs of trunk to perform any daily living tasks. He uses a wheelchair, gait trainer, stander, bath chair, lift, cochlear implant—the list goes on and on.
All of this could have been avoided with a little “overtreatment.” I believe the cost of a proactive approach could hardly compare to the costs that these children with kernicterus incur in their lifetimes.
So many are afraid to admit the potential dangers of newborn jaundice. Many say that they wouldn’t want to scare a parent. As a parent, I’d like to say that I am not afraid of something that is treatable and preventable. Educate us and let us help our children avoid serious peril!
Everyone in the medical community needs to take the proactive approach, as well as find a means of reporting kernicterus that is free of the liability concerns, or be willing to face them.
The CDC has created excellent new materials that seem to be getting very little attention but could have saved my son a lifetime of unspeakable struggle. Please take a look at them and consider distributing them at your treatment facilities.
Miriam Iliff, Fayetteville, N.C., past board member, Parents of Infants and Children with Kernicterus (PICK)
I’m writing in regard to the article “Incidence Rates of Kernicterus Remain Unchanged” (The Hospitalist, October 2011, p. 12) by Mark Shen, MD, FHM. As a mother of a child with kernicterus (born in 2005), I’m very concerned with the cavalier attitude toward hyperbilirubenia treatment and the reliance upon inaccurate statistics. Reasons for the inaccuracy:
- Your data is for California only;
- DDS reports of kernicterus are likely inaccurate. Nothing our son is enrolled in lists his diagnosis as kernicterus. Most institutions don’t have it in their database. Paperwork for my son shows encephalopathy, cerebral palsy, athetoid cerebral palsy, dystonia, or quadraplegia, but rarely kernicterus. As a result, I and other parents of children with kernicterus can attest to a massive under reporting of kernicterus, wherever you look;
- Our parent group, PICK, is constantly growing, with new members every month across the country and across the world;
- Even death certificates are subject to the fear that comes with kernicterus. Physicians know that putting this information on a death certificate will lead to a lawsuit, and thus are more inclined to list respiratory failure or other secondary causes as the cause of death; and
- Many children with kernicterus are never properly diagnosed or given diagnostic tests like an MRI to confirm the damage. They are instead steered away from the diagnosis, even when it is the obvious cause.
Please understand that the “kinder, gentler” approach to hyperbilirubinemia is why my son has kernicterus. He was repeatedly inspected visually, and our concerns were dismissed. At nine days old, they dismissed our concerns and coded us “low priority.” When finally seen, his bilirubin was 45.6, his pulse ox was 69, and he was posturing. His MRI revealed the classic signal intensity in the globus pallidus. He failed the hearing test that he had passed easily the weak before. His life care plan is 69,000,000. He is fed via G-tube and unable to manipulate his limbs of trunk to perform any daily living tasks. He uses a wheelchair, gait trainer, stander, bath chair, lift, cochlear implant—the list goes on and on.
All of this could have been avoided with a little “overtreatment.” I believe the cost of a proactive approach could hardly compare to the costs that these children with kernicterus incur in their lifetimes.
So many are afraid to admit the potential dangers of newborn jaundice. Many say that they wouldn’t want to scare a parent. As a parent, I’d like to say that I am not afraid of something that is treatable and preventable. Educate us and let us help our children avoid serious peril!
Everyone in the medical community needs to take the proactive approach, as well as find a means of reporting kernicterus that is free of the liability concerns, or be willing to face them.
The CDC has created excellent new materials that seem to be getting very little attention but could have saved my son a lifetime of unspeakable struggle. Please take a look at them and consider distributing them at your treatment facilities.
Miriam Iliff, Fayetteville, N.C., past board member, Parents of Infants and Children with Kernicterus (PICK)
Are You Ready to Care for Obese Patients?
The growing problem of obesity in America could pose a future liability issue for hospitalists and their employers, according to a bariatric surgeon.
Michael Jay Nusbaum, MD, FACS, FASMBS, FACN, says it's all too common for hospitalists and other physicians to "turf that patient out" to larger medical centers, but he cautions those doctors might be opening themselves to liability issues unless they can explain why they sent a patient elsewhere for care. For example, many hospitals lack wheelchairs, stretchers, tables, and gantries to hold morbidly obese patients.
"Is it really because you feel that the hospital lacks the infrastructure or because you just don't feel like taking on the additional liability that you're transferring the patient?" says Dr. Nusbaum, chief of bariatric surgery at Morristown (N.J.) Medical Center. "That's the question."
Dr. Nusbaum says hospitalists who believe their hospitals lack the proper equipment to treat obese patients should be "going out to the administration and saying, 'Look, we've got a liability issue. We don't have the equipment to take care of these patients if they start coming in.'"
He also believes that some physicians try to avoid obese patients for fear that their quality scores will drop. Dr. Nusbaum says that "disincentive" is built into the system, and it is incumbent on HM leaders and other physicians to push for change.
"The healthcare system in general is unprepared for the obesity epidemic," he adds. "And quite a bit of that is due to decreasing reimbursement and the fact that they need to lay out a lot of capital to take care of morbidly obese patients. ... It comes down to money."
The growing problem of obesity in America could pose a future liability issue for hospitalists and their employers, according to a bariatric surgeon.
Michael Jay Nusbaum, MD, FACS, FASMBS, FACN, says it's all too common for hospitalists and other physicians to "turf that patient out" to larger medical centers, but he cautions those doctors might be opening themselves to liability issues unless they can explain why they sent a patient elsewhere for care. For example, many hospitals lack wheelchairs, stretchers, tables, and gantries to hold morbidly obese patients.
"Is it really because you feel that the hospital lacks the infrastructure or because you just don't feel like taking on the additional liability that you're transferring the patient?" says Dr. Nusbaum, chief of bariatric surgery at Morristown (N.J.) Medical Center. "That's the question."
Dr. Nusbaum says hospitalists who believe their hospitals lack the proper equipment to treat obese patients should be "going out to the administration and saying, 'Look, we've got a liability issue. We don't have the equipment to take care of these patients if they start coming in.'"
He also believes that some physicians try to avoid obese patients for fear that their quality scores will drop. Dr. Nusbaum says that "disincentive" is built into the system, and it is incumbent on HM leaders and other physicians to push for change.
"The healthcare system in general is unprepared for the obesity epidemic," he adds. "And quite a bit of that is due to decreasing reimbursement and the fact that they need to lay out a lot of capital to take care of morbidly obese patients. ... It comes down to money."
The growing problem of obesity in America could pose a future liability issue for hospitalists and their employers, according to a bariatric surgeon.
Michael Jay Nusbaum, MD, FACS, FASMBS, FACN, says it's all too common for hospitalists and other physicians to "turf that patient out" to larger medical centers, but he cautions those doctors might be opening themselves to liability issues unless they can explain why they sent a patient elsewhere for care. For example, many hospitals lack wheelchairs, stretchers, tables, and gantries to hold morbidly obese patients.
"Is it really because you feel that the hospital lacks the infrastructure or because you just don't feel like taking on the additional liability that you're transferring the patient?" says Dr. Nusbaum, chief of bariatric surgery at Morristown (N.J.) Medical Center. "That's the question."
Dr. Nusbaum says hospitalists who believe their hospitals lack the proper equipment to treat obese patients should be "going out to the administration and saying, 'Look, we've got a liability issue. We don't have the equipment to take care of these patients if they start coming in.'"
He also believes that some physicians try to avoid obese patients for fear that their quality scores will drop. Dr. Nusbaum says that "disincentive" is built into the system, and it is incumbent on HM leaders and other physicians to push for change.
"The healthcare system in general is unprepared for the obesity epidemic," he adds. "And quite a bit of that is due to decreasing reimbursement and the fact that they need to lay out a lot of capital to take care of morbidly obese patients. ... It comes down to money."
Hospitalist Joins C-Suite Elite
Pediatric hospitalist Jeff Sperring, MD, didn't set out to be a hospital administrator. But earlier this month he became the president and CEO of Riley Hospital for Children at Indiana University Health in Indianapolis.
Dr. Sperring's path to the C-suite started in 2002, when he helped launch Riley's pediatric HM program following four years in community practice. The program eventually grew to a team of 22 physicians at four hospital sites. He was promoted to Riley's associate chief medical officer (CMO) in 2007, and in 2009 became the hospital's CMO.
"Being a hospitalist was critical to that progression," Dr. Sperring says. "You understand what needs to be changed. More than anything else it's just being available, willing, and able to help."
Dr. Sperring spearheaded a quality project to address the hospital's average length of stay (LOS), which was excessive by national benchmarks. The project helped reduce Riley's LOS by two full days.
He also helped develop a health-system-wide call center for patient referrals from physicians across the state. "Leading a project leads to additional roles, and that leads to this," he says.
Other keys to his advancement: drawing upon mentors and coaches, both within and outside of his health system; relying on his team in the HM department; and building effective partnerships with community physicians, he says. He has not pursued a formal business degree, focusing instead on leadership development training opportunities, including the multi-professional Hoosier Fellows Program at Indiana University. He plans to continue working as hospitalist at Riley, "a week here and there" when he can squeeze it into his expanded administrative responsibilities.
SHM President Joseph Ming Wah Li, MD, MBA, SFHM, says he is not aware of other examples of working hospitalists rising to the top of their hospital's organizational charts. "But I would expect we'd see more and more hospitalists becoming hospital CEOs—both pediatric and adult," he says.
Pediatric hospitalist Jeff Sperring, MD, didn't set out to be a hospital administrator. But earlier this month he became the president and CEO of Riley Hospital for Children at Indiana University Health in Indianapolis.
Dr. Sperring's path to the C-suite started in 2002, when he helped launch Riley's pediatric HM program following four years in community practice. The program eventually grew to a team of 22 physicians at four hospital sites. He was promoted to Riley's associate chief medical officer (CMO) in 2007, and in 2009 became the hospital's CMO.
"Being a hospitalist was critical to that progression," Dr. Sperring says. "You understand what needs to be changed. More than anything else it's just being available, willing, and able to help."
Dr. Sperring spearheaded a quality project to address the hospital's average length of stay (LOS), which was excessive by national benchmarks. The project helped reduce Riley's LOS by two full days.
He also helped develop a health-system-wide call center for patient referrals from physicians across the state. "Leading a project leads to additional roles, and that leads to this," he says.
Other keys to his advancement: drawing upon mentors and coaches, both within and outside of his health system; relying on his team in the HM department; and building effective partnerships with community physicians, he says. He has not pursued a formal business degree, focusing instead on leadership development training opportunities, including the multi-professional Hoosier Fellows Program at Indiana University. He plans to continue working as hospitalist at Riley, "a week here and there" when he can squeeze it into his expanded administrative responsibilities.
SHM President Joseph Ming Wah Li, MD, MBA, SFHM, says he is not aware of other examples of working hospitalists rising to the top of their hospital's organizational charts. "But I would expect we'd see more and more hospitalists becoming hospital CEOs—both pediatric and adult," he says.
Pediatric hospitalist Jeff Sperring, MD, didn't set out to be a hospital administrator. But earlier this month he became the president and CEO of Riley Hospital for Children at Indiana University Health in Indianapolis.
Dr. Sperring's path to the C-suite started in 2002, when he helped launch Riley's pediatric HM program following four years in community practice. The program eventually grew to a team of 22 physicians at four hospital sites. He was promoted to Riley's associate chief medical officer (CMO) in 2007, and in 2009 became the hospital's CMO.
"Being a hospitalist was critical to that progression," Dr. Sperring says. "You understand what needs to be changed. More than anything else it's just being available, willing, and able to help."
Dr. Sperring spearheaded a quality project to address the hospital's average length of stay (LOS), which was excessive by national benchmarks. The project helped reduce Riley's LOS by two full days.
He also helped develop a health-system-wide call center for patient referrals from physicians across the state. "Leading a project leads to additional roles, and that leads to this," he says.
Other keys to his advancement: drawing upon mentors and coaches, both within and outside of his health system; relying on his team in the HM department; and building effective partnerships with community physicians, he says. He has not pursued a formal business degree, focusing instead on leadership development training opportunities, including the multi-professional Hoosier Fellows Program at Indiana University. He plans to continue working as hospitalist at Riley, "a week here and there" when he can squeeze it into his expanded administrative responsibilities.
SHM President Joseph Ming Wah Li, MD, MBA, SFHM, says he is not aware of other examples of working hospitalists rising to the top of their hospital's organizational charts. "But I would expect we'd see more and more hospitalists becoming hospital CEOs—both pediatric and adult," he says.
She's Found Her Calling
Kate Goodrich, MD, MHS, was a medical resident at George Washington University (GW) Medical Center in Washington, D.C., in 1997 when a hospitalist service there was launched. A year later, as chief resident, she was able to work as a hospitalist. She enjoyed HM so much that she stayed on at GW in a faculty position and later directed its growing division of hospital medicine.
“I absolutely loved it,” she says.
But other career interests were calling her away from her patients and working the hospital floor. Eventually, she became a key player in the health reform debate and overhaul. “I became more aware of the issues that the country was grappling with because I was seeing them on the front lines—issues such as poor access to primary care,” she says. “I began to wonder: Why does a sector of my patient population keep getting readmitted to the hospital? Why is it so difficult for them to get medications, even when they have insurance? What happens to people who have poor family support or multiple comorbidities?”
Such questions eventually became more important to her than the clinical questions she encountered. And now she is in position to make even more of a difference to patients at GW and across the country. In March 2010, Dr. Goodrich became medical officer for the Office of the Assistant Secretary for Planning and Evaluation (ASPE) in the U.S. Department of Health and Human Services (HHS). And more recently, she became senior technical advisor in the Office of Clinical Standards and Quality at the Centers for Medicare & Medicaid Services (CMS), working closely with another hospitalist leader, Patrick Conway, MD, MSc, SFHM, who recently was appointed CMS’ chief medical officer (see “Hospitalist Takes Charge,” June 2011, p. 20).
“When I started this job, I was gratified to learn that my experience as a hospitalist had unbelievable relevance,” she says. “It surprised me how often I draw upon that experience. My clinical perspective on quality is really valued.”
She retains that connection by working as a hospitalist three or four weeks a year at GW. “I now view the hospitalist world from a different lens,” she says.
Winding Path to Washington
Dr. Goodrich’s path to a health policy career didn’t happen overnight. She originally enrolled in GW’s School of Public Health, taking classes at night, but soon realized that it would take too long to obtain a public health degree that way. In 2008, the Robert Wood Johnson Clinical Scholars Program, based at Yale University, offered her an opportunity to focus more intensively on research questions. “I discovered at Yale that what was more satisfying to me was application of research into action,” she says.
Sian Spurney, MD, director of GW’s hospital medicine division, once shared an office with Dr. Goodrich. She describes Dr. Goodrich as dedicated and committed. “Although I was admittedly very sad when she left GW to pursue her passion for health policy, I was hardly surprised to hear of her successes since completing the RWJ program,” Dr. Spurney says.
During a 2009 summer internship at HHS while she was doing her Yale coursework, Dr. Goodrich worked with Dr. Conway, who was working as the ASPE medical officer at HHS. Dr. Goodrich helped write a report to Congress on the Federal Coordinating Council for Cost-Effectiveness Research (CER), and became immersed in this area of research. She worked on an interagency work group to assemble a spending plan for $400 million in federal CER allocations.
“One of the premises of CER is that it will lead to improved quality of healthcare, which we all know isn’t where it should be—in part because of uncertainty regarding best care,” she says. “We think CER will help us define best treatment in the hospital, as well as outpatient settings.” Examples, she says, would be the treatment of delirium or care for patients with multiple comorbidities. “Hospitalists are well-positioned to disseminate CER within their hospitals and to train others, actively looking for the right evidence, and applying it in practice,” she adds.
Dr. Goodrich refers to Dr. Conway as a mentor and recalls days when they would “talk about the ways the issues we were working on affect hospitalists and how to make them aware of those issues,” she says. “I found myself drawn like a magnet to the policy stuff, especially during the 2008 election. It finally dawned on me that if I love this so much, why not see if I can make it a career?”
Exciting Times for Public Servants
Dr. Goodrich acknowledges the importance of care transitions and hospital readmissions for the national quality agenda. In fact, while at Yale, she researched care transitions for patients with low health literacy.
“I doubt that any hospitalist would disagree that readmissions are bad for patients, but sometimes they feel like everyone’s looking at them when readmissions happen. As a hospitalist, you know it’s a complex problem, by no means within the control of any single hospitalist,” she says. “But we also know that some hospitals have very low readmission rates. So it can be done, and we need to learn from the high performers.”
Given the current focus on healthcare reform, Dr. Goodrich believes now is an exciting time to be working for the government. She suggests ways that other hospitalists can learn about health policy and participate in its development:
- Get involved in local quality initiatives in the hospital and the community;
- Join SHM’s Public Policy Committee;
- Follow health policy blogs, websites, and other resources offered by HHS, SHM, and private groups such as the Commonwealth Fund; and
- Look into health policy fellowships or training opportunities.
Clinical experience is highly valued throughout CMS, Dr. Conway says, noting Dr. Goodrich’s background as a teaching hospitalist with more than a decade of patient care under her belt.
“In all of CMS, there are less than a hundred physicians in total, and not all of them are still in medical practice. So we have to leverage the clinical skills of that small group. As we develop health policies, that experience gives us a greater understanding of what the policies mean—their potential impact on patients,” he says.
Larry Beresford is a freelance writer based in Oakland, Calif.
Kate Goodrich, MD, MHS, was a medical resident at George Washington University (GW) Medical Center in Washington, D.C., in 1997 when a hospitalist service there was launched. A year later, as chief resident, she was able to work as a hospitalist. She enjoyed HM so much that she stayed on at GW in a faculty position and later directed its growing division of hospital medicine.
“I absolutely loved it,” she says.
But other career interests were calling her away from her patients and working the hospital floor. Eventually, she became a key player in the health reform debate and overhaul. “I became more aware of the issues that the country was grappling with because I was seeing them on the front lines—issues such as poor access to primary care,” she says. “I began to wonder: Why does a sector of my patient population keep getting readmitted to the hospital? Why is it so difficult for them to get medications, even when they have insurance? What happens to people who have poor family support or multiple comorbidities?”
Such questions eventually became more important to her than the clinical questions she encountered. And now she is in position to make even more of a difference to patients at GW and across the country. In March 2010, Dr. Goodrich became medical officer for the Office of the Assistant Secretary for Planning and Evaluation (ASPE) in the U.S. Department of Health and Human Services (HHS). And more recently, she became senior technical advisor in the Office of Clinical Standards and Quality at the Centers for Medicare & Medicaid Services (CMS), working closely with another hospitalist leader, Patrick Conway, MD, MSc, SFHM, who recently was appointed CMS’ chief medical officer (see “Hospitalist Takes Charge,” June 2011, p. 20).
“When I started this job, I was gratified to learn that my experience as a hospitalist had unbelievable relevance,” she says. “It surprised me how often I draw upon that experience. My clinical perspective on quality is really valued.”
She retains that connection by working as a hospitalist three or four weeks a year at GW. “I now view the hospitalist world from a different lens,” she says.
Winding Path to Washington
Dr. Goodrich’s path to a health policy career didn’t happen overnight. She originally enrolled in GW’s School of Public Health, taking classes at night, but soon realized that it would take too long to obtain a public health degree that way. In 2008, the Robert Wood Johnson Clinical Scholars Program, based at Yale University, offered her an opportunity to focus more intensively on research questions. “I discovered at Yale that what was more satisfying to me was application of research into action,” she says.
Sian Spurney, MD, director of GW’s hospital medicine division, once shared an office with Dr. Goodrich. She describes Dr. Goodrich as dedicated and committed. “Although I was admittedly very sad when she left GW to pursue her passion for health policy, I was hardly surprised to hear of her successes since completing the RWJ program,” Dr. Spurney says.
During a 2009 summer internship at HHS while she was doing her Yale coursework, Dr. Goodrich worked with Dr. Conway, who was working as the ASPE medical officer at HHS. Dr. Goodrich helped write a report to Congress on the Federal Coordinating Council for Cost-Effectiveness Research (CER), and became immersed in this area of research. She worked on an interagency work group to assemble a spending plan for $400 million in federal CER allocations.
“One of the premises of CER is that it will lead to improved quality of healthcare, which we all know isn’t where it should be—in part because of uncertainty regarding best care,” she says. “We think CER will help us define best treatment in the hospital, as well as outpatient settings.” Examples, she says, would be the treatment of delirium or care for patients with multiple comorbidities. “Hospitalists are well-positioned to disseminate CER within their hospitals and to train others, actively looking for the right evidence, and applying it in practice,” she adds.
Dr. Goodrich refers to Dr. Conway as a mentor and recalls days when they would “talk about the ways the issues we were working on affect hospitalists and how to make them aware of those issues,” she says. “I found myself drawn like a magnet to the policy stuff, especially during the 2008 election. It finally dawned on me that if I love this so much, why not see if I can make it a career?”
Exciting Times for Public Servants
Dr. Goodrich acknowledges the importance of care transitions and hospital readmissions for the national quality agenda. In fact, while at Yale, she researched care transitions for patients with low health literacy.
“I doubt that any hospitalist would disagree that readmissions are bad for patients, but sometimes they feel like everyone’s looking at them when readmissions happen. As a hospitalist, you know it’s a complex problem, by no means within the control of any single hospitalist,” she says. “But we also know that some hospitals have very low readmission rates. So it can be done, and we need to learn from the high performers.”
Given the current focus on healthcare reform, Dr. Goodrich believes now is an exciting time to be working for the government. She suggests ways that other hospitalists can learn about health policy and participate in its development:
- Get involved in local quality initiatives in the hospital and the community;
- Join SHM’s Public Policy Committee;
- Follow health policy blogs, websites, and other resources offered by HHS, SHM, and private groups such as the Commonwealth Fund; and
- Look into health policy fellowships or training opportunities.
Clinical experience is highly valued throughout CMS, Dr. Conway says, noting Dr. Goodrich’s background as a teaching hospitalist with more than a decade of patient care under her belt.
“In all of CMS, there are less than a hundred physicians in total, and not all of them are still in medical practice. So we have to leverage the clinical skills of that small group. As we develop health policies, that experience gives us a greater understanding of what the policies mean—their potential impact on patients,” he says.
Larry Beresford is a freelance writer based in Oakland, Calif.
Kate Goodrich, MD, MHS, was a medical resident at George Washington University (GW) Medical Center in Washington, D.C., in 1997 when a hospitalist service there was launched. A year later, as chief resident, she was able to work as a hospitalist. She enjoyed HM so much that she stayed on at GW in a faculty position and later directed its growing division of hospital medicine.
“I absolutely loved it,” she says.
But other career interests were calling her away from her patients and working the hospital floor. Eventually, she became a key player in the health reform debate and overhaul. “I became more aware of the issues that the country was grappling with because I was seeing them on the front lines—issues such as poor access to primary care,” she says. “I began to wonder: Why does a sector of my patient population keep getting readmitted to the hospital? Why is it so difficult for them to get medications, even when they have insurance? What happens to people who have poor family support or multiple comorbidities?”
Such questions eventually became more important to her than the clinical questions she encountered. And now she is in position to make even more of a difference to patients at GW and across the country. In March 2010, Dr. Goodrich became medical officer for the Office of the Assistant Secretary for Planning and Evaluation (ASPE) in the U.S. Department of Health and Human Services (HHS). And more recently, she became senior technical advisor in the Office of Clinical Standards and Quality at the Centers for Medicare & Medicaid Services (CMS), working closely with another hospitalist leader, Patrick Conway, MD, MSc, SFHM, who recently was appointed CMS’ chief medical officer (see “Hospitalist Takes Charge,” June 2011, p. 20).
“When I started this job, I was gratified to learn that my experience as a hospitalist had unbelievable relevance,” she says. “It surprised me how often I draw upon that experience. My clinical perspective on quality is really valued.”
She retains that connection by working as a hospitalist three or four weeks a year at GW. “I now view the hospitalist world from a different lens,” she says.
Winding Path to Washington
Dr. Goodrich’s path to a health policy career didn’t happen overnight. She originally enrolled in GW’s School of Public Health, taking classes at night, but soon realized that it would take too long to obtain a public health degree that way. In 2008, the Robert Wood Johnson Clinical Scholars Program, based at Yale University, offered her an opportunity to focus more intensively on research questions. “I discovered at Yale that what was more satisfying to me was application of research into action,” she says.
Sian Spurney, MD, director of GW’s hospital medicine division, once shared an office with Dr. Goodrich. She describes Dr. Goodrich as dedicated and committed. “Although I was admittedly very sad when she left GW to pursue her passion for health policy, I was hardly surprised to hear of her successes since completing the RWJ program,” Dr. Spurney says.
During a 2009 summer internship at HHS while she was doing her Yale coursework, Dr. Goodrich worked with Dr. Conway, who was working as the ASPE medical officer at HHS. Dr. Goodrich helped write a report to Congress on the Federal Coordinating Council for Cost-Effectiveness Research (CER), and became immersed in this area of research. She worked on an interagency work group to assemble a spending plan for $400 million in federal CER allocations.
“One of the premises of CER is that it will lead to improved quality of healthcare, which we all know isn’t where it should be—in part because of uncertainty regarding best care,” she says. “We think CER will help us define best treatment in the hospital, as well as outpatient settings.” Examples, she says, would be the treatment of delirium or care for patients with multiple comorbidities. “Hospitalists are well-positioned to disseminate CER within their hospitals and to train others, actively looking for the right evidence, and applying it in practice,” she adds.
Dr. Goodrich refers to Dr. Conway as a mentor and recalls days when they would “talk about the ways the issues we were working on affect hospitalists and how to make them aware of those issues,” she says. “I found myself drawn like a magnet to the policy stuff, especially during the 2008 election. It finally dawned on me that if I love this so much, why not see if I can make it a career?”
Exciting Times for Public Servants
Dr. Goodrich acknowledges the importance of care transitions and hospital readmissions for the national quality agenda. In fact, while at Yale, she researched care transitions for patients with low health literacy.
“I doubt that any hospitalist would disagree that readmissions are bad for patients, but sometimes they feel like everyone’s looking at them when readmissions happen. As a hospitalist, you know it’s a complex problem, by no means within the control of any single hospitalist,” she says. “But we also know that some hospitals have very low readmission rates. So it can be done, and we need to learn from the high performers.”
Given the current focus on healthcare reform, Dr. Goodrich believes now is an exciting time to be working for the government. She suggests ways that other hospitalists can learn about health policy and participate in its development:
- Get involved in local quality initiatives in the hospital and the community;
- Join SHM’s Public Policy Committee;
- Follow health policy blogs, websites, and other resources offered by HHS, SHM, and private groups such as the Commonwealth Fund; and
- Look into health policy fellowships or training opportunities.
Clinical experience is highly valued throughout CMS, Dr. Conway says, noting Dr. Goodrich’s background as a teaching hospitalist with more than a decade of patient care under her belt.
“In all of CMS, there are less than a hundred physicians in total, and not all of them are still in medical practice. So we have to leverage the clinical skills of that small group. As we develop health policies, that experience gives us a greater understanding of what the policies mean—their potential impact on patients,” he says.
Larry Beresford is a freelance writer based in Oakland, Calif.