User login
Researchers generate RBCs to treat SCD
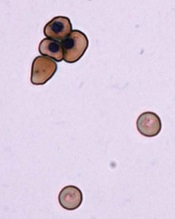
Image by Ying Wang–
Johns Hopkins Medicine
Researchers say they have devised a technique for generating normal, mature red blood cells (RBCs) from patients with sickle cell disease (SCD).
The team hopes that, ultimately, the RBCs could be transfused back into the patients from which they are derived and eliminate the need for donor transfusion in SCD.
Linzhao Cheng, PhD, of the Johns Hopkins School of Medicine in Baltimore, Maryland, and his colleagues described the technique in Stem Cells.
Dr Cheng noted that SCD patients often require RBC transfusions, but over time, their bodies may begin to mount an immune response against the foreign blood.
“Their bodies quickly kill off the blood cells,” Dr Cheng said. “So they have to get transfusions more and more frequently.”
A solution, Dr Cheng and his colleagues thought, would be to generate RBCs for transfusion using a patient’s own cells.
To do this, the researchers first took hematopoietic cells from an SCD patient and generated induced pluripotent stem cells (iPSCs).
Then, the team used the gene-editing technique CRISPR/Cas9 to target the homozygous SCD mutation (nt. 69A>T) in the HBB gene and ensure the RBCs they generated would not be sickled.
Finally, they coaxed the iPSCs into mature RBCs that expressed the corrected HBB gene. The edited iPSCs generated RBCs just as efficiently as iPSCs that hadn’t been subjected to CRISPR/Cas9.
And the level of HBB protein expression in the RBCs derived from edited iPSCs was similar to that of RBCs generated from unedited iPSCs.
Dr Cheng noted that, to become medically useful, this method will have to be made more efficient and scaled up significantly. And the cells would need to be tested for safety.
“[Nevertheless,] this study shows it may be possible in the not-too-distant future to provide patients with sickle cell disease with an exciting new treatment option,” Dr Cheng said.
He and his colleagues believe this method of RBC generation may also be applicable for other blood disorders. And they think it might be possible to edit cells from healthy individuals so they can resist malaria and other infectious agents.
Another research group has reported the ability to correct the SCD mutation using zinc-finger nucleases. ![]()
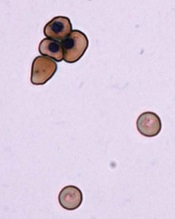
Image by Ying Wang–
Johns Hopkins Medicine
Researchers say they have devised a technique for generating normal, mature red blood cells (RBCs) from patients with sickle cell disease (SCD).
The team hopes that, ultimately, the RBCs could be transfused back into the patients from which they are derived and eliminate the need for donor transfusion in SCD.
Linzhao Cheng, PhD, of the Johns Hopkins School of Medicine in Baltimore, Maryland, and his colleagues described the technique in Stem Cells.
Dr Cheng noted that SCD patients often require RBC transfusions, but over time, their bodies may begin to mount an immune response against the foreign blood.
“Their bodies quickly kill off the blood cells,” Dr Cheng said. “So they have to get transfusions more and more frequently.”
A solution, Dr Cheng and his colleagues thought, would be to generate RBCs for transfusion using a patient’s own cells.
To do this, the researchers first took hematopoietic cells from an SCD patient and generated induced pluripotent stem cells (iPSCs).
Then, the team used the gene-editing technique CRISPR/Cas9 to target the homozygous SCD mutation (nt. 69A>T) in the HBB gene and ensure the RBCs they generated would not be sickled.
Finally, they coaxed the iPSCs into mature RBCs that expressed the corrected HBB gene. The edited iPSCs generated RBCs just as efficiently as iPSCs that hadn’t been subjected to CRISPR/Cas9.
And the level of HBB protein expression in the RBCs derived from edited iPSCs was similar to that of RBCs generated from unedited iPSCs.
Dr Cheng noted that, to become medically useful, this method will have to be made more efficient and scaled up significantly. And the cells would need to be tested for safety.
“[Nevertheless,] this study shows it may be possible in the not-too-distant future to provide patients with sickle cell disease with an exciting new treatment option,” Dr Cheng said.
He and his colleagues believe this method of RBC generation may also be applicable for other blood disorders. And they think it might be possible to edit cells from healthy individuals so they can resist malaria and other infectious agents.
Another research group has reported the ability to correct the SCD mutation using zinc-finger nucleases. ![]()
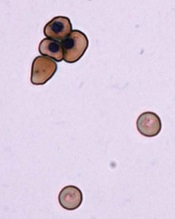
Image by Ying Wang–
Johns Hopkins Medicine
Researchers say they have devised a technique for generating normal, mature red blood cells (RBCs) from patients with sickle cell disease (SCD).
The team hopes that, ultimately, the RBCs could be transfused back into the patients from which they are derived and eliminate the need for donor transfusion in SCD.
Linzhao Cheng, PhD, of the Johns Hopkins School of Medicine in Baltimore, Maryland, and his colleagues described the technique in Stem Cells.
Dr Cheng noted that SCD patients often require RBC transfusions, but over time, their bodies may begin to mount an immune response against the foreign blood.
“Their bodies quickly kill off the blood cells,” Dr Cheng said. “So they have to get transfusions more and more frequently.”
A solution, Dr Cheng and his colleagues thought, would be to generate RBCs for transfusion using a patient’s own cells.
To do this, the researchers first took hematopoietic cells from an SCD patient and generated induced pluripotent stem cells (iPSCs).
Then, the team used the gene-editing technique CRISPR/Cas9 to target the homozygous SCD mutation (nt. 69A>T) in the HBB gene and ensure the RBCs they generated would not be sickled.
Finally, they coaxed the iPSCs into mature RBCs that expressed the corrected HBB gene. The edited iPSCs generated RBCs just as efficiently as iPSCs that hadn’t been subjected to CRISPR/Cas9.
And the level of HBB protein expression in the RBCs derived from edited iPSCs was similar to that of RBCs generated from unedited iPSCs.
Dr Cheng noted that, to become medically useful, this method will have to be made more efficient and scaled up significantly. And the cells would need to be tested for safety.
“[Nevertheless,] this study shows it may be possible in the not-too-distant future to provide patients with sickle cell disease with an exciting new treatment option,” Dr Cheng said.
He and his colleagues believe this method of RBC generation may also be applicable for other blood disorders. And they think it might be possible to edit cells from healthy individuals so they can resist malaria and other infectious agents.
Another research group has reported the ability to correct the SCD mutation using zinc-finger nucleases. ![]()
Automated Sepsis Alert Systems
Sepsis is the most expensive condition treated in the hospital, resulting in an aggregate cost of $20.3 billion or 5.2% of total aggregate cost for all hospitalizations in the United States.[1] Rates of sepsis and sepsis‐related mortality are rising in the United States.[2, 3] Timely treatment of sepsis, including adequate fluid resuscitation and appropriate antibiotic administration, decreases morbidity, mortality, and costs.[4, 5, 6] Consequently, the Surviving Sepsis Campaign recommends timely care with the implementation of sepsis bundles and protocols.[4] Though effective, sepsis protocols require dedicated personnel with specialized training, who must be highly vigilant and constantly monitor a patient's condition for the course of an entire hospitalization.[7, 8] As such, delays in administering evidence‐based therapies are common.[8, 9]
Automated electronic sepsis alerts are being developed and implemented to facilitate the delivery of timely sepsis care. Electronic alert systems synthesize electronic health data routinely collected for clinical purposes in real time or near real time to automatically identify sepsis based on prespecified diagnostic criteria, and immediately alert providers that their patient may meet sepsis criteria via electronic notifications (eg, through electronic health record [EHR], e‐mail, or pager alerts).
However, little data exist to describe whether automated, electronic systems achieve their intended goal of earlier, more effective sepsis care. To examine this question, we performed a systematic review on automated electronic sepsis alerts to assess their suitability for clinical use. Our 2 objectives were: (1) to describe the diagnostic accuracy of alert systems in identifying sepsis using electronic data available in real‐time or near real‐time, and (2) to evaluate the effectiveness of sepsis alert systems on sepsis care process measures and clinical outcomes.
MATERIALS AND METHODS
Data Sources and Search Strategies
We searched PubMed MEDLINE, Embase, The Cochrane Library, and the Cumulative Index to Nursing and Allied Health Literature from database inception through June 27, 2014, for all studies that contained the following 3 concepts: sepsis, electronic systems, and alerts (or identification). All citations were imported into an electronic database (EndNote X5; Thomson‐Reuters Corp., New York, NY) (see Supporting Information, Appendix, in the online version of this article for our complete search strategy).
Study Selection
Two authors (A.N.M. and O.K.N.) reviewed the citation titles, abstracts, and full‐text articles of potentially relevant references identified from the literature search for eligibility. References of selected articles were hand searched to identify additional eligible studies. Inclusion criteria for eligible studies were: (1) adult patients (aged 18 years) receiving care either in the emergency department or hospital, (2) outcomes of interest including diagnostic accuracy in identification of sepsis, and/or effectiveness of sepsis alerts on process measures and clinical outcomes evaluated using empiric data, and (3) sepsis alert systems used real time or near real time electronically available data to enable proactive, timely management. We excluded studies that: (1) tested the effect of other electronic interventions that were not sepsis alerts (ie, computerized order sets) for sepsis management; (2) studies solely focused on detecting and treating central line‐associated bloodstream infections, shock (not otherwise specified), bacteremia, or other device‐related infections; and (3) studies evaluating the effectiveness of sepsis alerts without a control group.
Data Extraction and Quality Assessment
Two reviewers (A.N.M. and O.K.N.) extracted data on the clinical setting, study design, dates of enrollment, definition of sepsis, details of the identification and alert systems, diagnostic accuracy of the alert system, and the incidence of process measures and clinical outcomes using a standardized form. Discrepancies between reviewers were resolved by discussion and consensus. Data discrepancies identified in 1 study were resolved by contacting the corresponding author.[10]
For studies assessing the diagnostic accuracy of sepsis identification, study quality was assessed using the Quality Assessment of Diagnostic Accuracy Studies revised tool.[11] For studies evaluating the effectiveness of sepsis alert systems, studies were considered high quality if a contemporaneous control group was present to account for temporal trends (eg, randomized controlled trial or observational analysis with a concurrent control). Fair‐quality studies were before‐and‐after studies that adjusted for potential confounders between time periods. Low‐quality studies included those that did not account for temporal trends, such as before‐and‐after studies using only historical controls without adjustment. Studies that did not use an intention‐to‐treat analysis were also considered low quality. The strength of the overall body of evidence, including risk of bias, was guided by the Grading of Recommendations Assessment, Development, and Evaluation Working Group Criteria adapted by the Agency of Healthcare Research and Quality.[12]
Data Synthesis
To analyze the diagnostic accuracy of automated sepsis alert systems to identify sepsis and to evaluate the effect on outcomes, we performed a qualitative assessment of all studies. We were unable to perform a meta‐analysis due to significant heterogeneity in study quality, clinical setting, and definition of the sepsis alert. Diagnostic accuracy of sepsis identification was measured by sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio (LR). Effectiveness was assessed by changes in sepsis care process measures (ie, time to antibiotics) and outcomes (length of stay, mortality).
RESULTS
Description of Studies
Of 1293 titles, 183 qualified for abstract review, 84 for full‐text review, and 8 articles met our inclusion criteria (see Supporting Figure in the online version of this article). Five articles evaluated the diagnostic accuracy of sepsis identification,[10, 13, 14, 15, 16] and 5 articles[10, 14, 17, 18, 19] evaluated the effectiveness of automated electronic sepsis alerts on sepsis process measures and patient outcomes. All articles were published between 2009 and 2014 and were single‐site studies conducted at academic medical centers (Tables 1 and 2). The clinical settings in the included studies varied and included the emergency department (ED), hospital wards, and the intensive care unit (ICU).
| Source | Site No./Type | Setting | Alert Threshold | Gold Standard Definition | Gold Standard Measurement | No. | Study Qualitya |
|---|---|---|---|---|---|---|---|
| |||||||
| Hooper et al., 201210 | 1/academic | MICU | 2 SIRS criteriab | Reviewer judgment, not otherwise specified | Chart review | 560 | High |
| Meurer et al., 200913 | 1/academic | ED | 2 SIRS criteria | Reviewer judgment whether diagnosis of infection present in ED plus SIRS criteria | Chart review | 248 | Low |
| Nelson J. et al., 201114 | 1/academic | ED | 2 SIRS criteria and 2 SBP measurements 90 mm Hg | Reviewer judgment whether infection present, requiring hospitalization with at least 1 organ system involved | Chart review | 1,386 | High |
| Nguyen et al., 201415 | 1/academic | ED | 2 SIRS criteria and 1 sign of shock (SBP 90 mm Hg or lactic acid 2.0 mmol/L) | Reviewer judgment to confirm SIRS, shock, and presence of a serious infection | Chart review | 1,095 | Low |
| Thiel et al., 201016 | 1/academic | Wards | Recursive partitioning tree analysis including vitals and laboratory resultsc | Admitted to the hospital wards and subsequently transferred to the ICU for septic shock and treated with vasopressor therapy | ICD‐9 discharge codes for acute infection, acute organ dysfunction, and need for vasopressors within 24 hours of ICU transfer | 27,674 | Low |
| Source | Design | Site No./ Type | Setting | No. | Alert System Type | Alert Threshold | Alert Notificationa | Treatment Recommendation | Study Qualityb |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Berger et al., 201017 | Before‐after (6 months pre and 6 months post) | 1/academic | ED | 5796c | CPOE system | 2 SIRS criteria | CPOE passive alert | Yes: lactate collection | Low |
| Hooper et al., 201210 | RCT | 1/academic | MICU | 443 | EHR | 2 SIRS criteriad | Text page and EHR passive alert | No | High |
| McRee et al., 201418 | Before‐after (6 months pre and 6 months post) | 1/academic | Wards | 171e | EHR | 2 SIRS criteria | Notified nurse, specifics unclear | No, but the nurse completed a sepsis risk evaluation flow sheet | Low |
| Nelson et al., 201114 | Before‐after (3 months pre and 3 months post) | 1/academic | ED | 184f | EHR | 2 SIRS criteria and 2 or more SBP readings 90 mm Hg | Text page and EHR passive alert | Yes: fluid resuscitation, blood culture collection, antibiotic administration, among others | Low |
| Sawyer et al., 201119 | Prospective, nonrandomized (2 intervention and 4 control wards) | 1/academic | Wards | 300 | EHR | Recursive partitioning regression tree algorithm including vitals and lab valuesg | Text page to charge nurse who then assessed patient and informed treating physicianh | No | High |
Among the 8 included studies, there was significant heterogeneity in threshold criteria for sepsis identification and subsequent alert activation. The most commonly defined threshold was the presence of 2 or more systemic inflammatory response syndrome (SIRS) criteria.[10, 13, 17, 18]
Diagnostic Accuracy of Automated Electronic Sepsis Alert Systems
The prevalence of sepsis varied substantially between the studies depending on the gold standard definition of sepsis used and the clinical setting (ED, wards, or ICU) of the study (Table 3). The 2 studies[14, 16] that defined sepsis as requiring evidence of shock had a substantially lower prevalence (0.8%4.7%) compared to the 2 studies[10, 13] that defined sepsis as having only 2 or more SIRS criteria with a presumed diagnosis of an infection (27.8%32.5%).
| Source | Setting | Alert Threshold | Prevalence, % | Sensitivity, % (95% CI) | Specificity, % (95% CI) | PPV, % (95% CI) | NPV, % (95% CI) | LR+, (95% CI) | LR, (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Hooper et al., 201210 | MICU | 2 SIRS criteriaa | 36.3 | 98.9 (95.799.8) | 18.1 (14.222.9) | 40.7 (36.145.5) | 96.7 (87.599.4) | 1.21 (1.14‐1.27) | 0.06 (0.01‐0.25) |
| Meurer et al., 200913 | ED | 2 SIRS criteria | 27.8 | 36.2 (25.348.8) | 79.9 (73.185.3) | 41.0 (28.854.3) | 76.5 (69.682.2) | 1.80 (1.17‐2.76) | 0.80 (0.67‐0.96) |
| Nelson et al., 201114 | ED | 2 SIRS criteria and 2 SBP measurements90 mm Hg | 0.8 | 63.6 (31.687.8) | 99.6 (99.099.8) | 53.8 (26.179.6) | 99.7 (99.299.9) | 145.8 (58.4364.1) | 0.37 (0.17‐0.80) |
| Nguyen et al., 201415 | ED | 2 SIRS criteria and 1 sign of shock (SBP 90 mm Hg or lactic acid 2.0 mmol/L) | Unable to estimateb | Unable to estimateb | Unable to estimateb | 44.7 (41.248.2) | 100.0c (98.8100.0) | Unable to estimateb | Unable to estimateb |
| Thiel et al., 201016 | Wards | Recursive partitioning tree analysis including vitals and laboratory resultsd | 4.7 | 17.1 (15.119.3) | 96.7 (96.596.9) | 20.5 (18.223.0) | 95.9 (95.796.2) | 5.22 (4.56‐5.98) | 0.86 (0.84‐0.88) |
All alert systems had suboptimal PPV (20.5%‐53.8%). The 2 studies that designed the sepsis alert to activate by SIRS criteria alone[10, 13] had a positive predictive value of 41% and a positive LR of 1.21 to 1.80. The ability to exclude the presence of sepsis varied considerably depending on the clinical setting. The study by Hooper et al.[10] that examined the alert among patients in the medical ICU appeared more effective at ruling out sepsis (NPV=96.7%; negative LR=0.06) compared to a similar alert system used by Meurer et al.[13] that studied patients in the ED (NPV=76.5%, negative LR=0.80).
There were also differences in the diagnostic accuracy of the sepsis alert systems depending on how the threshold for activating the sepsis alert was defined and applied in the study. Two studies evaluated a sepsis alert system among patients presenting to the ED at the same academic medical center.[13, 14] The alert system (Nelson et al.) that was triggered by a combination of SIRS criteria and hypotension (PPV=53.8%, LR+=145.8; NPV=99.7%, LR=0.37) outperformed the alert system (Meurer et al.) that was triggered by SIRS criteria alone (PPV=41.0%, LR+=1.80; NPV=76.5%, LR=0.80). Furthermore, the study by Meurer and colleagues evaluated the accuracy of the alert system only among patients who were hospitalized after presenting to the ED, rather than all consecutive patients presenting to the ED. This selection bias likely falsely inflated the diagnostic accuracy of the alert system used by Meurer et al., suggesting the alert system that was triggered by a combination of SIRS criteria and hypotension was comparatively even more accurate.
Two studies evaluating the diagnostic accuracy of the alert system were deemed to be high quality (Table 4). Three studies were considered low quality1 study did not include all patients in their assessment of diagnostic accuracy13; 1 study consecutively selected alert cases but randomly selected nonalert cases, greatly limiting the assessment of diagnostic accuracy15; and the other study applied a gold standard that was unlikely to correctly classify sepsis (septic shock requiring ICU transfer with vasopressor support in the first 24 hours was defined by discharge International Classification of Diseases, Ninth Revision diagnoses without chart review), with a considerable delay from the alert system trigger (alert identification was compared to the discharge diagnosis rather than physician review of real‐time data).[16]
| Study | Patient Selection | Index Test | Reference Standard | Flow and Timing |
|---|---|---|---|---|
| ||||
| Hooper et al., 201210 | +++ | +++ | ++b | +++ |
| Meurer et al., 200913 | +++ | +++ | ++b | +c |
| Nelson et al., 201114 | +++ | +++ | ++b | +++ |
| Nguyen et al., 201415 | +d | +++ | +e | +++ |
| Thiel et al., 201016 | +++ | +++ | +f | +g |
Effectiveness of Automated Electronic Sepsis Alert Systems
Characteristics of the studies evaluating the effectiveness of automated electronic sepsis alert systems are summarized in Table 2. Regarding activation of the sepsis alert, 2 studies notified the provider directly by an automated text page and a passive EHR alert (not requiring the provider to acknowledge the alert or take action),[10, 14] 1 study notified the provider by a passive electronic alert alone,[17] and 1 study only employed an automated text page.[19] Furthermore, if the sepsis alert was activated, 2 studies suggested specific clinical management decisions,[14, 17] 2 studies left clinical management decisions solely to the discretion of the treating provider,[10, 19] and 1 study assisted the diagnosis of sepsis by prompting nurses to complete a second manual sepsis risk evaluation.[18]
Table 5 summarizes the effectiveness of automated electronic sepsis alert systems. Two studies evaluating the effectiveness of the sepsis alert system were considered to be high‐quality studies based on the use of a contemporaneous control group to account for temporal trends and an intention‐to‐treat analysis.[10, 19] The 2 studies evaluating the effectiveness of a sepsis alert system in the ED were considered low quality due to before‐and‐after designs without an intention‐to‐treat analysis.[14, 17]
| Source | Outcomes Evaluated | Key Findings | Quality |
|---|---|---|---|
| |||
| Hooper et al., 201210 | Primary: time to receipt of antibiotic (new or changed) | No difference (6.1 hours for control vs 6.0 hours for intervention, P=0.95) | High |
| Secondary: sepsis‐related process measures and outcomes | No difference in amount of 6 hour IV fluid administration (964 mL vs 1,019 mL, P=0.6), collection of blood cultures (adjusted HR 1.01; 95% CI, 0.76 to 1.35), collection of lactate (adjusted HR 0.84; 95% CI, 0.54 to 1.30), ICU length of stay (3.0 vs 3.0 days, P=0.2), hospital length of stay (4.7 vs 5.7 days, P=0.08), and hospital mortality (10% for control vs 14% for intervention, P=0.3) | ||
| Sawyer et al., 201119 | Primary: sepsis‐related process measures (antibiotic escalation, IV fluids, oxygen therapy, vasopressor initiation, diagnostic testing (blood culture, CXR) within 12 hours of alert | Increases in receiving 1 measure (56% for control vs 71% for intervention, P=0.02), antibiotic escalation (24% vs 36%, P=0.04), IV fluid administration (24% vs 38%, P=0.01), and oxygen therapy (8% vs 20%, P=0.005). There was a nonsignificant increase in obtaining diagnostic tests (40% vs 52%, P=0.06) and vasopressor initiation (3% vs 6%, P=0.4) | High |
| Secondary: ICU transfer, hospital length of stay, hospital length of stay after alert, in‐hospital mortality | Similar rate of ICU transfer (23% for control vs 26% for intervention, P=0.6), hospital length of stay (7 vs 9 days, median, P=0.8), hospital length of stay after alert (5 vs 6 days, median, P=0.7), and in‐hospital mortality (12% vs 10%, P=0.7) | ||
| Berger et al., 201017 | Primary: lactate collection in ED | Increase in lactate collection in the ED (5.2% before vs 12.7% after alert implemented, absolute increase of 7.5%, 95% CI, 6.0% to 9.0%) | Low |
| Secondary: lactate collection among hospitalized patients, proportion of patients with abnormal lactate (4 mmol/L), and in‐hospital mortality among hospitalized patients | Increase in lactate collection among hospitalized patients (15.3% vs 34.2%, absolute increase of 18.9%, 95% CI, 15.0% to 22.8%); decrease in the proportion of abnormal lactate values (21.9% vs 14.8%, absolute decrease of 7.6%, 95% CI, 15.8% to 0.6%), and no significant difference in mortality (5.7% vs 5.2%, absolute decrease of 0.5%, 95% CI, 1.6% to 2.6%, P=0.6) | ||
| McRee et al., 201418 | Stage of sepsis, length of stay, mortality, discharge location | Nonsignificant decrease in stage of sepsis (34.7% with septic shock before vs 21.9% after, P>0.05); no difference in length‐of‐stay (8.5 days before vs 8.7 days after, P>0.05). Decrease in mortality (9.3% before vs 1.0% after, P0.05) and proportion of patients discharged home (25.3% before vs 49.0% after, P0.05) | Low |
| Nelson et al., 201114 | Frequency and time to completion of process measures: lactate, blood culture, CXR, and antibiotic initiation | Increases in blood culture collection (OR 2.9; 95% CI, 1.1 to 7.7) and CXR (OR 3.2; 95% CI, 1.1 to 9.5); nonsignificant increases in lactate collection (OR 1.7; 95% CI, 0.9 to 3.2) and antibiotic administration (OR 2.8; 95% CI, 0.9 to 8.3). Only blood cultures were collected in a more timely manner (median of 86 minutes before vs 81 minutes after alert implementation, P=0.03). | Low |
Neither of the 2 high‐quality studies that included a contemporaneous control found evidence for improving inpatient mortality or hospital and ICU length of stay.[10, 19] The impact of sepsis alert systems on improving process measures for sepsis management depended on the clinical setting. In a randomized controlled trial of patients admitted to a medical ICU, Hooper et al. did not find any benefit of implementing a sepsis alert system on improving intermediate outcome measures such as antibiotic escalation, fluid resuscitation, and collection of blood cultures and lactate.[10] However, in a well‐designed observational study, Sawyer et al. found significant increases in antibiotic escalation, fluid resuscitation, and diagnostic testing in patients admitted to the medical wards.[19] Both studies that evaluated the effectiveness of sepsis alert systems in the ED showed improvements in various process measures,[14, 17] but without improvement in mortality.[17] The single study that showed improvement in clinical outcomes (in‐hospital mortality and disposition location) was of low quality due to the prestudypoststudy design without adjustment for potential confounders and lack of an intention‐to‐treat analysis (only individuals with a discharge diagnosis of sepsis were included, rather than all individuals who triggered the alert).[18] Additionally, the preintervention group had a higher proportion of individuals with septic shock compared to the postintervention group, raising the possibility that the observed improvement was due to difference in severity of illness between the 2 groups rather than due to the intervention.
None of the studies included in this review explicitly reported on the potential harms (eg, excess antimicrobial use or alert fatigue) after implementation of sepsis alerts, but Hooper et al. found a nonsignificant increase in mortality, and Sawyer et al. showed a nonsignificant increase in the length of stay in the intervention group compared to the control group.[10, 19] Berger et al. showed an overall increase in the number of lactate tests performed, but with a decrease in the proportion of abnormal lactate values (21.9% vs 14.8%, absolute decrease of 7.6%, 95% confidence interval, 15.8% to 0.6%), suggesting potential overtesting in patients at low risk for septic shock. In the study by Hooper et al., 88% (442/502) of the patients in the medical intensive care unit triggered an alert, raising the concern for alert fatigue.[10] Furthermore, 3 studies did not perform intention‐to‐treat analyses; rather, they included only patients who triggered the alert and also had provider‐suspected or confirmed sepsis,[14, 17] or had a discharge diagnosis for sepsis.[18]
DISCUSSION
The use of sepsis alert systems derived from electronic health data and targeting hospitalized patients improve a subset of sepsis process of care measures, but at the cost of poor positive predictive value and no clear improvement in mortality or length of stay. There is insufficient evidence for the effectiveness of automated electronic sepsis alert systems in the emergency department.
We found considerable variability in the diagnostic accuracy of automated electronic sepsis alert systems. There was moderate evidence that alert systems designed to identify severe sepsis (eg, SIRS criteria plus measures of shock) had greater diagnostic accuracy than alert systems that detected sepsis based on SIRS criteria alone. Given that SIRS criteria are highly prevalent among hospitalized patients with noninfectious diseases,[20] sepsis alert systems triggered by standard SIRS criteria may have poorer predictive value with an increased risk of alert fatigueexcessive electronic warnings resulting in physicians disregarding clinically useful alerts.[21] The potential for alert fatigue is even greater in critical care settings. A retrospective analysis of physiological alarms in the ICU estimated on average 6 alarms per hour with only 15% of alarms considered to be clinically relevant.[22]
The fact that sepsis alert systems improve intermediate process measures among ward and ED patients but not ICU patients likely reflects differences in both the patients and the clinical settings.[23] First, patients in the ICU may already be prescribed broad spectrum antibiotics, aggressively fluid resuscitated, and have other diagnostic testing performed before the activation of a sepsis alert, so it would be less likely to see an improvement in the rates of process measures assessing initiation or escalation of therapy compared to patients treated on the wards or in the ED. The apparent lack of benefit of these systems in the ICU may merely represent a ceiling effect. Second, nurses and physicians are already vigilantly monitoring patients in the ICU for signs of clinical deterioration, so additional alert systems may be redundant. Third, patients in the ICU are connected to standard bedside monitors that continuously monitor for the presence of abnormal vital signs. An additional sepsis alert system triggered by SIRS criteria alone may be superfluous to the existing infrastructure. Fourth, the majority of patients in the ICU will trigger the sepsis alert system,[10] so there likely is a high noise‐to‐signal ratio with resultant alert fatigue.[21]
In addition to greater emphasis on alert systems of greater diagnostic accuracy and effectiveness, our review notes several important gaps that limit evidence supporting the usefulness of automated sepsis alert systems. First, there are little data to describe the optimal design of sepsis alerts[24, 25] or the frequency with which they are appropriately acted upon or dismissed. In addition, we found little data to support whether effectiveness of alert systems differed based on whether clinical decision support was included with the alert itself (eg, direct prompting with specific clinical management recommendations) or the configuration of the alert (eg, interruptive alert or informational).[24, 25] Most of the studies we reviewed employed alerts primarily targeting physicians; we found little evidence for systems that also alerted other providers (eg, nurses or rapid response teams). Few studies provided data on harms of these systems (eg, excess antimicrobial use, fluid overload due to aggressive fluid resuscitation) or how often these treatments were administered to patients who did not eventually have sepsis. Few studies employed study designs that limited biases (eg, randomized or quasiexperimental designs) or used an intention‐to‐treat approach. Studies that exclude false positive alerts in analyses could bias estimates toward making sepsis alert systems appear more effective than they actually were. Finally, although presumably, deploying automated sepsis alerts in the ED would facilitate more timely recognition and treatment, more rigorously conducted studies are needed to identify whether using these alerts in the ED are of greater value compared to the wards and ICU. Given the limited number of studies included in this review, we were unable to make strong conclusions regarding the clinical benefits and cost‐effectiveness of implementing automated sepsis alerts.
Our review has certain limitations. First, despite our extensive literature search strategy, we may have missed studies published in the grey literature or in non‐English languages. Second, there is potential publication bias given the number of abstracts that we identified addressing 1 of our prespecified research questions compared to the number of peer‐reviewed publications identified by our search strategy.
CONCLUSION
Automated electronic sepsis alert systems have promise in delivering early goal‐directed therapies to patients. However, at present, automated sepsis alerts derived from electronic health data may improve care processes but tend to have poor PPV and have not been shown to improve mortality or length of stay. Future efforts should develop and study methods for sepsis alert systems that avoid the potential for alert fatigue while improving outcomes.
Acknowledgements
The authors thank Gloria Won, MLIS, for her assistance with developing and performing the literature search strategy and wish her a long and joyous retirement.
Disclosures: Part of Dr. Makam's work on this project was completed while he was a primary care research fellow at the University of California, San Francisco, funded by a National Research Service Award (training grant T32HP19025‐07‐00). Dr. Makam is currently supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR001103). Dr. Nguyen was supported by the Agency for Healthcare Research and Quality (R24HS022428‐01). Dr. Auerbach was supported by an NHLBI K24 grant (K24HL098372). Dr. Makam had full access to the data in the study and takes responsibility for the integrity of the date and accuracy of the data analysis. Study concept and design: all authors. Acquisition of data: Makam and Nguyen. Analysis and interpretation of data: all authors. Drafting of the manuscript: Makam. Critical revision of the manuscript: all authors. Statistical analysis: Makam and Nguyen. The authors have no conflicts of interest to disclose.
- , . National inpatient hospital costs: the most expensive conditions by payer, 2011: statistical brief #160. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2013.
- , , , . Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011;(62):1–8.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , , et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
- , , , et al. Early goal‐directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377.
- , , , et al. A randomized trial of protocol‐based care for early septic shock. N Engl J Med. 2014;370(18):1683–1693.
- , . Implementation of early goal‐directed therapy for septic patients in the emergency department: a review of the literature. J Emerg Nurs. 2013;39(1):13–19.
- , , , , , . Factors influencing variability in compliance rates and clinical outcomes among three different severe sepsis bundles. Ann Pharmacother. 2007;41(6):929–936.
- , , , et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299(19):2294–2303.
- , , , et al. Randomized trial of automated, electronic monitoring to facilitate early detection of sepsis in the intensive care unit*. Crit Care Med. 2012;40(7):2096–2101.
- , , , et al. QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536.
- , , , et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health‐care program. J Clin Epidemiol. 2010;63(5):513–523.
- , , , et al. Real‐time identification of serious infection in geriatric patients using clinical information system surveillance. J Am Geriatr Soc. 2009;57(1):40–45.
- , , , . Prospective trial of real‐time electronic surveillance to expedite early care of severe sepsis. Ann Emerg Med. 2011;57(5):500–504.
- , , , et al. Automated electronic medical record sepsis detection in the emergency department. PeerJ. 2014;2:e343.
- , , , , , . Early prediction of septic shock in hospitalized patients. J Hosp Med. 2010;5(1):19–25.
- , , , , . A Computerized alert screening for severe sepsis in emergency department patients increases lactate testing but does not improve inpatient mortality. Appl Clin Inform. 2010;1(4):394–407.
- , , , , . The impact of an electronic medical record surveillance program on outcomes for patients with sepsis. Heart Lung. 2014;43(6):546–549.
- , , , et al. Implementation of a real‐time computerized sepsis alert in nonintensive care unit patients. Crit Care Med. 2011;39(3):469–473.
- . The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26(suppl 1):S64–S74.
- , , , et al. Overrides of medication‐related clinical decision support alerts in outpatients. J Am Med Inform Assoc. 2014;21(3):487–491.
- , , , , , . Intensive care unit alarms–how many do we need? Crit Care Med. 2010;38(2):451–456.
- , . How can we best use electronic data to find and treat the critically ill?*. Crit Care Med. 2012;40(7):2242–2243.
- , , , et al. Identifying best practices for clinical decision support and knowledge management in the field. Stud Health Technol Inform. 2010;160(pt 2):806–810.
- , , , et al. Best practices in clinical decision support: the case of preventive care reminders. Appl Clin Inform. 2010;1(3):331–345.
Sepsis is the most expensive condition treated in the hospital, resulting in an aggregate cost of $20.3 billion or 5.2% of total aggregate cost for all hospitalizations in the United States.[1] Rates of sepsis and sepsis‐related mortality are rising in the United States.[2, 3] Timely treatment of sepsis, including adequate fluid resuscitation and appropriate antibiotic administration, decreases morbidity, mortality, and costs.[4, 5, 6] Consequently, the Surviving Sepsis Campaign recommends timely care with the implementation of sepsis bundles and protocols.[4] Though effective, sepsis protocols require dedicated personnel with specialized training, who must be highly vigilant and constantly monitor a patient's condition for the course of an entire hospitalization.[7, 8] As such, delays in administering evidence‐based therapies are common.[8, 9]
Automated electronic sepsis alerts are being developed and implemented to facilitate the delivery of timely sepsis care. Electronic alert systems synthesize electronic health data routinely collected for clinical purposes in real time or near real time to automatically identify sepsis based on prespecified diagnostic criteria, and immediately alert providers that their patient may meet sepsis criteria via electronic notifications (eg, through electronic health record [EHR], e‐mail, or pager alerts).
However, little data exist to describe whether automated, electronic systems achieve their intended goal of earlier, more effective sepsis care. To examine this question, we performed a systematic review on automated electronic sepsis alerts to assess their suitability for clinical use. Our 2 objectives were: (1) to describe the diagnostic accuracy of alert systems in identifying sepsis using electronic data available in real‐time or near real‐time, and (2) to evaluate the effectiveness of sepsis alert systems on sepsis care process measures and clinical outcomes.
MATERIALS AND METHODS
Data Sources and Search Strategies
We searched PubMed MEDLINE, Embase, The Cochrane Library, and the Cumulative Index to Nursing and Allied Health Literature from database inception through June 27, 2014, for all studies that contained the following 3 concepts: sepsis, electronic systems, and alerts (or identification). All citations were imported into an electronic database (EndNote X5; Thomson‐Reuters Corp., New York, NY) (see Supporting Information, Appendix, in the online version of this article for our complete search strategy).
Study Selection
Two authors (A.N.M. and O.K.N.) reviewed the citation titles, abstracts, and full‐text articles of potentially relevant references identified from the literature search for eligibility. References of selected articles were hand searched to identify additional eligible studies. Inclusion criteria for eligible studies were: (1) adult patients (aged 18 years) receiving care either in the emergency department or hospital, (2) outcomes of interest including diagnostic accuracy in identification of sepsis, and/or effectiveness of sepsis alerts on process measures and clinical outcomes evaluated using empiric data, and (3) sepsis alert systems used real time or near real time electronically available data to enable proactive, timely management. We excluded studies that: (1) tested the effect of other electronic interventions that were not sepsis alerts (ie, computerized order sets) for sepsis management; (2) studies solely focused on detecting and treating central line‐associated bloodstream infections, shock (not otherwise specified), bacteremia, or other device‐related infections; and (3) studies evaluating the effectiveness of sepsis alerts without a control group.
Data Extraction and Quality Assessment
Two reviewers (A.N.M. and O.K.N.) extracted data on the clinical setting, study design, dates of enrollment, definition of sepsis, details of the identification and alert systems, diagnostic accuracy of the alert system, and the incidence of process measures and clinical outcomes using a standardized form. Discrepancies between reviewers were resolved by discussion and consensus. Data discrepancies identified in 1 study were resolved by contacting the corresponding author.[10]
For studies assessing the diagnostic accuracy of sepsis identification, study quality was assessed using the Quality Assessment of Diagnostic Accuracy Studies revised tool.[11] For studies evaluating the effectiveness of sepsis alert systems, studies were considered high quality if a contemporaneous control group was present to account for temporal trends (eg, randomized controlled trial or observational analysis with a concurrent control). Fair‐quality studies were before‐and‐after studies that adjusted for potential confounders between time periods. Low‐quality studies included those that did not account for temporal trends, such as before‐and‐after studies using only historical controls without adjustment. Studies that did not use an intention‐to‐treat analysis were also considered low quality. The strength of the overall body of evidence, including risk of bias, was guided by the Grading of Recommendations Assessment, Development, and Evaluation Working Group Criteria adapted by the Agency of Healthcare Research and Quality.[12]
Data Synthesis
To analyze the diagnostic accuracy of automated sepsis alert systems to identify sepsis and to evaluate the effect on outcomes, we performed a qualitative assessment of all studies. We were unable to perform a meta‐analysis due to significant heterogeneity in study quality, clinical setting, and definition of the sepsis alert. Diagnostic accuracy of sepsis identification was measured by sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio (LR). Effectiveness was assessed by changes in sepsis care process measures (ie, time to antibiotics) and outcomes (length of stay, mortality).
RESULTS
Description of Studies
Of 1293 titles, 183 qualified for abstract review, 84 for full‐text review, and 8 articles met our inclusion criteria (see Supporting Figure in the online version of this article). Five articles evaluated the diagnostic accuracy of sepsis identification,[10, 13, 14, 15, 16] and 5 articles[10, 14, 17, 18, 19] evaluated the effectiveness of automated electronic sepsis alerts on sepsis process measures and patient outcomes. All articles were published between 2009 and 2014 and were single‐site studies conducted at academic medical centers (Tables 1 and 2). The clinical settings in the included studies varied and included the emergency department (ED), hospital wards, and the intensive care unit (ICU).
| Source | Site No./Type | Setting | Alert Threshold | Gold Standard Definition | Gold Standard Measurement | No. | Study Qualitya |
|---|---|---|---|---|---|---|---|
| |||||||
| Hooper et al., 201210 | 1/academic | MICU | 2 SIRS criteriab | Reviewer judgment, not otherwise specified | Chart review | 560 | High |
| Meurer et al., 200913 | 1/academic | ED | 2 SIRS criteria | Reviewer judgment whether diagnosis of infection present in ED plus SIRS criteria | Chart review | 248 | Low |
| Nelson J. et al., 201114 | 1/academic | ED | 2 SIRS criteria and 2 SBP measurements 90 mm Hg | Reviewer judgment whether infection present, requiring hospitalization with at least 1 organ system involved | Chart review | 1,386 | High |
| Nguyen et al., 201415 | 1/academic | ED | 2 SIRS criteria and 1 sign of shock (SBP 90 mm Hg or lactic acid 2.0 mmol/L) | Reviewer judgment to confirm SIRS, shock, and presence of a serious infection | Chart review | 1,095 | Low |
| Thiel et al., 201016 | 1/academic | Wards | Recursive partitioning tree analysis including vitals and laboratory resultsc | Admitted to the hospital wards and subsequently transferred to the ICU for septic shock and treated with vasopressor therapy | ICD‐9 discharge codes for acute infection, acute organ dysfunction, and need for vasopressors within 24 hours of ICU transfer | 27,674 | Low |
| Source | Design | Site No./ Type | Setting | No. | Alert System Type | Alert Threshold | Alert Notificationa | Treatment Recommendation | Study Qualityb |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Berger et al., 201017 | Before‐after (6 months pre and 6 months post) | 1/academic | ED | 5796c | CPOE system | 2 SIRS criteria | CPOE passive alert | Yes: lactate collection | Low |
| Hooper et al., 201210 | RCT | 1/academic | MICU | 443 | EHR | 2 SIRS criteriad | Text page and EHR passive alert | No | High |
| McRee et al., 201418 | Before‐after (6 months pre and 6 months post) | 1/academic | Wards | 171e | EHR | 2 SIRS criteria | Notified nurse, specifics unclear | No, but the nurse completed a sepsis risk evaluation flow sheet | Low |
| Nelson et al., 201114 | Before‐after (3 months pre and 3 months post) | 1/academic | ED | 184f | EHR | 2 SIRS criteria and 2 or more SBP readings 90 mm Hg | Text page and EHR passive alert | Yes: fluid resuscitation, blood culture collection, antibiotic administration, among others | Low |
| Sawyer et al., 201119 | Prospective, nonrandomized (2 intervention and 4 control wards) | 1/academic | Wards | 300 | EHR | Recursive partitioning regression tree algorithm including vitals and lab valuesg | Text page to charge nurse who then assessed patient and informed treating physicianh | No | High |
Among the 8 included studies, there was significant heterogeneity in threshold criteria for sepsis identification and subsequent alert activation. The most commonly defined threshold was the presence of 2 or more systemic inflammatory response syndrome (SIRS) criteria.[10, 13, 17, 18]
Diagnostic Accuracy of Automated Electronic Sepsis Alert Systems
The prevalence of sepsis varied substantially between the studies depending on the gold standard definition of sepsis used and the clinical setting (ED, wards, or ICU) of the study (Table 3). The 2 studies[14, 16] that defined sepsis as requiring evidence of shock had a substantially lower prevalence (0.8%4.7%) compared to the 2 studies[10, 13] that defined sepsis as having only 2 or more SIRS criteria with a presumed diagnosis of an infection (27.8%32.5%).
| Source | Setting | Alert Threshold | Prevalence, % | Sensitivity, % (95% CI) | Specificity, % (95% CI) | PPV, % (95% CI) | NPV, % (95% CI) | LR+, (95% CI) | LR, (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Hooper et al., 201210 | MICU | 2 SIRS criteriaa | 36.3 | 98.9 (95.799.8) | 18.1 (14.222.9) | 40.7 (36.145.5) | 96.7 (87.599.4) | 1.21 (1.14‐1.27) | 0.06 (0.01‐0.25) |
| Meurer et al., 200913 | ED | 2 SIRS criteria | 27.8 | 36.2 (25.348.8) | 79.9 (73.185.3) | 41.0 (28.854.3) | 76.5 (69.682.2) | 1.80 (1.17‐2.76) | 0.80 (0.67‐0.96) |
| Nelson et al., 201114 | ED | 2 SIRS criteria and 2 SBP measurements90 mm Hg | 0.8 | 63.6 (31.687.8) | 99.6 (99.099.8) | 53.8 (26.179.6) | 99.7 (99.299.9) | 145.8 (58.4364.1) | 0.37 (0.17‐0.80) |
| Nguyen et al., 201415 | ED | 2 SIRS criteria and 1 sign of shock (SBP 90 mm Hg or lactic acid 2.0 mmol/L) | Unable to estimateb | Unable to estimateb | Unable to estimateb | 44.7 (41.248.2) | 100.0c (98.8100.0) | Unable to estimateb | Unable to estimateb |
| Thiel et al., 201016 | Wards | Recursive partitioning tree analysis including vitals and laboratory resultsd | 4.7 | 17.1 (15.119.3) | 96.7 (96.596.9) | 20.5 (18.223.0) | 95.9 (95.796.2) | 5.22 (4.56‐5.98) | 0.86 (0.84‐0.88) |
All alert systems had suboptimal PPV (20.5%‐53.8%). The 2 studies that designed the sepsis alert to activate by SIRS criteria alone[10, 13] had a positive predictive value of 41% and a positive LR of 1.21 to 1.80. The ability to exclude the presence of sepsis varied considerably depending on the clinical setting. The study by Hooper et al.[10] that examined the alert among patients in the medical ICU appeared more effective at ruling out sepsis (NPV=96.7%; negative LR=0.06) compared to a similar alert system used by Meurer et al.[13] that studied patients in the ED (NPV=76.5%, negative LR=0.80).
There were also differences in the diagnostic accuracy of the sepsis alert systems depending on how the threshold for activating the sepsis alert was defined and applied in the study. Two studies evaluated a sepsis alert system among patients presenting to the ED at the same academic medical center.[13, 14] The alert system (Nelson et al.) that was triggered by a combination of SIRS criteria and hypotension (PPV=53.8%, LR+=145.8; NPV=99.7%, LR=0.37) outperformed the alert system (Meurer et al.) that was triggered by SIRS criteria alone (PPV=41.0%, LR+=1.80; NPV=76.5%, LR=0.80). Furthermore, the study by Meurer and colleagues evaluated the accuracy of the alert system only among patients who were hospitalized after presenting to the ED, rather than all consecutive patients presenting to the ED. This selection bias likely falsely inflated the diagnostic accuracy of the alert system used by Meurer et al., suggesting the alert system that was triggered by a combination of SIRS criteria and hypotension was comparatively even more accurate.
Two studies evaluating the diagnostic accuracy of the alert system were deemed to be high quality (Table 4). Three studies were considered low quality1 study did not include all patients in their assessment of diagnostic accuracy13; 1 study consecutively selected alert cases but randomly selected nonalert cases, greatly limiting the assessment of diagnostic accuracy15; and the other study applied a gold standard that was unlikely to correctly classify sepsis (septic shock requiring ICU transfer with vasopressor support in the first 24 hours was defined by discharge International Classification of Diseases, Ninth Revision diagnoses without chart review), with a considerable delay from the alert system trigger (alert identification was compared to the discharge diagnosis rather than physician review of real‐time data).[16]
| Study | Patient Selection | Index Test | Reference Standard | Flow and Timing |
|---|---|---|---|---|
| ||||
| Hooper et al., 201210 | +++ | +++ | ++b | +++ |
| Meurer et al., 200913 | +++ | +++ | ++b | +c |
| Nelson et al., 201114 | +++ | +++ | ++b | +++ |
| Nguyen et al., 201415 | +d | +++ | +e | +++ |
| Thiel et al., 201016 | +++ | +++ | +f | +g |
Effectiveness of Automated Electronic Sepsis Alert Systems
Characteristics of the studies evaluating the effectiveness of automated electronic sepsis alert systems are summarized in Table 2. Regarding activation of the sepsis alert, 2 studies notified the provider directly by an automated text page and a passive EHR alert (not requiring the provider to acknowledge the alert or take action),[10, 14] 1 study notified the provider by a passive electronic alert alone,[17] and 1 study only employed an automated text page.[19] Furthermore, if the sepsis alert was activated, 2 studies suggested specific clinical management decisions,[14, 17] 2 studies left clinical management decisions solely to the discretion of the treating provider,[10, 19] and 1 study assisted the diagnosis of sepsis by prompting nurses to complete a second manual sepsis risk evaluation.[18]
Table 5 summarizes the effectiveness of automated electronic sepsis alert systems. Two studies evaluating the effectiveness of the sepsis alert system were considered to be high‐quality studies based on the use of a contemporaneous control group to account for temporal trends and an intention‐to‐treat analysis.[10, 19] The 2 studies evaluating the effectiveness of a sepsis alert system in the ED were considered low quality due to before‐and‐after designs without an intention‐to‐treat analysis.[14, 17]
| Source | Outcomes Evaluated | Key Findings | Quality |
|---|---|---|---|
| |||
| Hooper et al., 201210 | Primary: time to receipt of antibiotic (new or changed) | No difference (6.1 hours for control vs 6.0 hours for intervention, P=0.95) | High |
| Secondary: sepsis‐related process measures and outcomes | No difference in amount of 6 hour IV fluid administration (964 mL vs 1,019 mL, P=0.6), collection of blood cultures (adjusted HR 1.01; 95% CI, 0.76 to 1.35), collection of lactate (adjusted HR 0.84; 95% CI, 0.54 to 1.30), ICU length of stay (3.0 vs 3.0 days, P=0.2), hospital length of stay (4.7 vs 5.7 days, P=0.08), and hospital mortality (10% for control vs 14% for intervention, P=0.3) | ||
| Sawyer et al., 201119 | Primary: sepsis‐related process measures (antibiotic escalation, IV fluids, oxygen therapy, vasopressor initiation, diagnostic testing (blood culture, CXR) within 12 hours of alert | Increases in receiving 1 measure (56% for control vs 71% for intervention, P=0.02), antibiotic escalation (24% vs 36%, P=0.04), IV fluid administration (24% vs 38%, P=0.01), and oxygen therapy (8% vs 20%, P=0.005). There was a nonsignificant increase in obtaining diagnostic tests (40% vs 52%, P=0.06) and vasopressor initiation (3% vs 6%, P=0.4) | High |
| Secondary: ICU transfer, hospital length of stay, hospital length of stay after alert, in‐hospital mortality | Similar rate of ICU transfer (23% for control vs 26% for intervention, P=0.6), hospital length of stay (7 vs 9 days, median, P=0.8), hospital length of stay after alert (5 vs 6 days, median, P=0.7), and in‐hospital mortality (12% vs 10%, P=0.7) | ||
| Berger et al., 201017 | Primary: lactate collection in ED | Increase in lactate collection in the ED (5.2% before vs 12.7% after alert implemented, absolute increase of 7.5%, 95% CI, 6.0% to 9.0%) | Low |
| Secondary: lactate collection among hospitalized patients, proportion of patients with abnormal lactate (4 mmol/L), and in‐hospital mortality among hospitalized patients | Increase in lactate collection among hospitalized patients (15.3% vs 34.2%, absolute increase of 18.9%, 95% CI, 15.0% to 22.8%); decrease in the proportion of abnormal lactate values (21.9% vs 14.8%, absolute decrease of 7.6%, 95% CI, 15.8% to 0.6%), and no significant difference in mortality (5.7% vs 5.2%, absolute decrease of 0.5%, 95% CI, 1.6% to 2.6%, P=0.6) | ||
| McRee et al., 201418 | Stage of sepsis, length of stay, mortality, discharge location | Nonsignificant decrease in stage of sepsis (34.7% with septic shock before vs 21.9% after, P>0.05); no difference in length‐of‐stay (8.5 days before vs 8.7 days after, P>0.05). Decrease in mortality (9.3% before vs 1.0% after, P0.05) and proportion of patients discharged home (25.3% before vs 49.0% after, P0.05) | Low |
| Nelson et al., 201114 | Frequency and time to completion of process measures: lactate, blood culture, CXR, and antibiotic initiation | Increases in blood culture collection (OR 2.9; 95% CI, 1.1 to 7.7) and CXR (OR 3.2; 95% CI, 1.1 to 9.5); nonsignificant increases in lactate collection (OR 1.7; 95% CI, 0.9 to 3.2) and antibiotic administration (OR 2.8; 95% CI, 0.9 to 8.3). Only blood cultures were collected in a more timely manner (median of 86 minutes before vs 81 minutes after alert implementation, P=0.03). | Low |
Neither of the 2 high‐quality studies that included a contemporaneous control found evidence for improving inpatient mortality or hospital and ICU length of stay.[10, 19] The impact of sepsis alert systems on improving process measures for sepsis management depended on the clinical setting. In a randomized controlled trial of patients admitted to a medical ICU, Hooper et al. did not find any benefit of implementing a sepsis alert system on improving intermediate outcome measures such as antibiotic escalation, fluid resuscitation, and collection of blood cultures and lactate.[10] However, in a well‐designed observational study, Sawyer et al. found significant increases in antibiotic escalation, fluid resuscitation, and diagnostic testing in patients admitted to the medical wards.[19] Both studies that evaluated the effectiveness of sepsis alert systems in the ED showed improvements in various process measures,[14, 17] but without improvement in mortality.[17] The single study that showed improvement in clinical outcomes (in‐hospital mortality and disposition location) was of low quality due to the prestudypoststudy design without adjustment for potential confounders and lack of an intention‐to‐treat analysis (only individuals with a discharge diagnosis of sepsis were included, rather than all individuals who triggered the alert).[18] Additionally, the preintervention group had a higher proportion of individuals with septic shock compared to the postintervention group, raising the possibility that the observed improvement was due to difference in severity of illness between the 2 groups rather than due to the intervention.
None of the studies included in this review explicitly reported on the potential harms (eg, excess antimicrobial use or alert fatigue) after implementation of sepsis alerts, but Hooper et al. found a nonsignificant increase in mortality, and Sawyer et al. showed a nonsignificant increase in the length of stay in the intervention group compared to the control group.[10, 19] Berger et al. showed an overall increase in the number of lactate tests performed, but with a decrease in the proportion of abnormal lactate values (21.9% vs 14.8%, absolute decrease of 7.6%, 95% confidence interval, 15.8% to 0.6%), suggesting potential overtesting in patients at low risk for septic shock. In the study by Hooper et al., 88% (442/502) of the patients in the medical intensive care unit triggered an alert, raising the concern for alert fatigue.[10] Furthermore, 3 studies did not perform intention‐to‐treat analyses; rather, they included only patients who triggered the alert and also had provider‐suspected or confirmed sepsis,[14, 17] or had a discharge diagnosis for sepsis.[18]
DISCUSSION
The use of sepsis alert systems derived from electronic health data and targeting hospitalized patients improve a subset of sepsis process of care measures, but at the cost of poor positive predictive value and no clear improvement in mortality or length of stay. There is insufficient evidence for the effectiveness of automated electronic sepsis alert systems in the emergency department.
We found considerable variability in the diagnostic accuracy of automated electronic sepsis alert systems. There was moderate evidence that alert systems designed to identify severe sepsis (eg, SIRS criteria plus measures of shock) had greater diagnostic accuracy than alert systems that detected sepsis based on SIRS criteria alone. Given that SIRS criteria are highly prevalent among hospitalized patients with noninfectious diseases,[20] sepsis alert systems triggered by standard SIRS criteria may have poorer predictive value with an increased risk of alert fatigueexcessive electronic warnings resulting in physicians disregarding clinically useful alerts.[21] The potential for alert fatigue is even greater in critical care settings. A retrospective analysis of physiological alarms in the ICU estimated on average 6 alarms per hour with only 15% of alarms considered to be clinically relevant.[22]
The fact that sepsis alert systems improve intermediate process measures among ward and ED patients but not ICU patients likely reflects differences in both the patients and the clinical settings.[23] First, patients in the ICU may already be prescribed broad spectrum antibiotics, aggressively fluid resuscitated, and have other diagnostic testing performed before the activation of a sepsis alert, so it would be less likely to see an improvement in the rates of process measures assessing initiation or escalation of therapy compared to patients treated on the wards or in the ED. The apparent lack of benefit of these systems in the ICU may merely represent a ceiling effect. Second, nurses and physicians are already vigilantly monitoring patients in the ICU for signs of clinical deterioration, so additional alert systems may be redundant. Third, patients in the ICU are connected to standard bedside monitors that continuously monitor for the presence of abnormal vital signs. An additional sepsis alert system triggered by SIRS criteria alone may be superfluous to the existing infrastructure. Fourth, the majority of patients in the ICU will trigger the sepsis alert system,[10] so there likely is a high noise‐to‐signal ratio with resultant alert fatigue.[21]
In addition to greater emphasis on alert systems of greater diagnostic accuracy and effectiveness, our review notes several important gaps that limit evidence supporting the usefulness of automated sepsis alert systems. First, there are little data to describe the optimal design of sepsis alerts[24, 25] or the frequency with which they are appropriately acted upon or dismissed. In addition, we found little data to support whether effectiveness of alert systems differed based on whether clinical decision support was included with the alert itself (eg, direct prompting with specific clinical management recommendations) or the configuration of the alert (eg, interruptive alert or informational).[24, 25] Most of the studies we reviewed employed alerts primarily targeting physicians; we found little evidence for systems that also alerted other providers (eg, nurses or rapid response teams). Few studies provided data on harms of these systems (eg, excess antimicrobial use, fluid overload due to aggressive fluid resuscitation) or how often these treatments were administered to patients who did not eventually have sepsis. Few studies employed study designs that limited biases (eg, randomized or quasiexperimental designs) or used an intention‐to‐treat approach. Studies that exclude false positive alerts in analyses could bias estimates toward making sepsis alert systems appear more effective than they actually were. Finally, although presumably, deploying automated sepsis alerts in the ED would facilitate more timely recognition and treatment, more rigorously conducted studies are needed to identify whether using these alerts in the ED are of greater value compared to the wards and ICU. Given the limited number of studies included in this review, we were unable to make strong conclusions regarding the clinical benefits and cost‐effectiveness of implementing automated sepsis alerts.
Our review has certain limitations. First, despite our extensive literature search strategy, we may have missed studies published in the grey literature or in non‐English languages. Second, there is potential publication bias given the number of abstracts that we identified addressing 1 of our prespecified research questions compared to the number of peer‐reviewed publications identified by our search strategy.
CONCLUSION
Automated electronic sepsis alert systems have promise in delivering early goal‐directed therapies to patients. However, at present, automated sepsis alerts derived from electronic health data may improve care processes but tend to have poor PPV and have not been shown to improve mortality or length of stay. Future efforts should develop and study methods for sepsis alert systems that avoid the potential for alert fatigue while improving outcomes.
Acknowledgements
The authors thank Gloria Won, MLIS, for her assistance with developing and performing the literature search strategy and wish her a long and joyous retirement.
Disclosures: Part of Dr. Makam's work on this project was completed while he was a primary care research fellow at the University of California, San Francisco, funded by a National Research Service Award (training grant T32HP19025‐07‐00). Dr. Makam is currently supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR001103). Dr. Nguyen was supported by the Agency for Healthcare Research and Quality (R24HS022428‐01). Dr. Auerbach was supported by an NHLBI K24 grant (K24HL098372). Dr. Makam had full access to the data in the study and takes responsibility for the integrity of the date and accuracy of the data analysis. Study concept and design: all authors. Acquisition of data: Makam and Nguyen. Analysis and interpretation of data: all authors. Drafting of the manuscript: Makam. Critical revision of the manuscript: all authors. Statistical analysis: Makam and Nguyen. The authors have no conflicts of interest to disclose.
Sepsis is the most expensive condition treated in the hospital, resulting in an aggregate cost of $20.3 billion or 5.2% of total aggregate cost for all hospitalizations in the United States.[1] Rates of sepsis and sepsis‐related mortality are rising in the United States.[2, 3] Timely treatment of sepsis, including adequate fluid resuscitation and appropriate antibiotic administration, decreases morbidity, mortality, and costs.[4, 5, 6] Consequently, the Surviving Sepsis Campaign recommends timely care with the implementation of sepsis bundles and protocols.[4] Though effective, sepsis protocols require dedicated personnel with specialized training, who must be highly vigilant and constantly monitor a patient's condition for the course of an entire hospitalization.[7, 8] As such, delays in administering evidence‐based therapies are common.[8, 9]
Automated electronic sepsis alerts are being developed and implemented to facilitate the delivery of timely sepsis care. Electronic alert systems synthesize electronic health data routinely collected for clinical purposes in real time or near real time to automatically identify sepsis based on prespecified diagnostic criteria, and immediately alert providers that their patient may meet sepsis criteria via electronic notifications (eg, through electronic health record [EHR], e‐mail, or pager alerts).
However, little data exist to describe whether automated, electronic systems achieve their intended goal of earlier, more effective sepsis care. To examine this question, we performed a systematic review on automated electronic sepsis alerts to assess their suitability for clinical use. Our 2 objectives were: (1) to describe the diagnostic accuracy of alert systems in identifying sepsis using electronic data available in real‐time or near real‐time, and (2) to evaluate the effectiveness of sepsis alert systems on sepsis care process measures and clinical outcomes.
MATERIALS AND METHODS
Data Sources and Search Strategies
We searched PubMed MEDLINE, Embase, The Cochrane Library, and the Cumulative Index to Nursing and Allied Health Literature from database inception through June 27, 2014, for all studies that contained the following 3 concepts: sepsis, electronic systems, and alerts (or identification). All citations were imported into an electronic database (EndNote X5; Thomson‐Reuters Corp., New York, NY) (see Supporting Information, Appendix, in the online version of this article for our complete search strategy).
Study Selection
Two authors (A.N.M. and O.K.N.) reviewed the citation titles, abstracts, and full‐text articles of potentially relevant references identified from the literature search for eligibility. References of selected articles were hand searched to identify additional eligible studies. Inclusion criteria for eligible studies were: (1) adult patients (aged 18 years) receiving care either in the emergency department or hospital, (2) outcomes of interest including diagnostic accuracy in identification of sepsis, and/or effectiveness of sepsis alerts on process measures and clinical outcomes evaluated using empiric data, and (3) sepsis alert systems used real time or near real time electronically available data to enable proactive, timely management. We excluded studies that: (1) tested the effect of other electronic interventions that were not sepsis alerts (ie, computerized order sets) for sepsis management; (2) studies solely focused on detecting and treating central line‐associated bloodstream infections, shock (not otherwise specified), bacteremia, or other device‐related infections; and (3) studies evaluating the effectiveness of sepsis alerts without a control group.
Data Extraction and Quality Assessment
Two reviewers (A.N.M. and O.K.N.) extracted data on the clinical setting, study design, dates of enrollment, definition of sepsis, details of the identification and alert systems, diagnostic accuracy of the alert system, and the incidence of process measures and clinical outcomes using a standardized form. Discrepancies between reviewers were resolved by discussion and consensus. Data discrepancies identified in 1 study were resolved by contacting the corresponding author.[10]
For studies assessing the diagnostic accuracy of sepsis identification, study quality was assessed using the Quality Assessment of Diagnostic Accuracy Studies revised tool.[11] For studies evaluating the effectiveness of sepsis alert systems, studies were considered high quality if a contemporaneous control group was present to account for temporal trends (eg, randomized controlled trial or observational analysis with a concurrent control). Fair‐quality studies were before‐and‐after studies that adjusted for potential confounders between time periods. Low‐quality studies included those that did not account for temporal trends, such as before‐and‐after studies using only historical controls without adjustment. Studies that did not use an intention‐to‐treat analysis were also considered low quality. The strength of the overall body of evidence, including risk of bias, was guided by the Grading of Recommendations Assessment, Development, and Evaluation Working Group Criteria adapted by the Agency of Healthcare Research and Quality.[12]
Data Synthesis
To analyze the diagnostic accuracy of automated sepsis alert systems to identify sepsis and to evaluate the effect on outcomes, we performed a qualitative assessment of all studies. We were unable to perform a meta‐analysis due to significant heterogeneity in study quality, clinical setting, and definition of the sepsis alert. Diagnostic accuracy of sepsis identification was measured by sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio (LR). Effectiveness was assessed by changes in sepsis care process measures (ie, time to antibiotics) and outcomes (length of stay, mortality).
RESULTS
Description of Studies
Of 1293 titles, 183 qualified for abstract review, 84 for full‐text review, and 8 articles met our inclusion criteria (see Supporting Figure in the online version of this article). Five articles evaluated the diagnostic accuracy of sepsis identification,[10, 13, 14, 15, 16] and 5 articles[10, 14, 17, 18, 19] evaluated the effectiveness of automated electronic sepsis alerts on sepsis process measures and patient outcomes. All articles were published between 2009 and 2014 and were single‐site studies conducted at academic medical centers (Tables 1 and 2). The clinical settings in the included studies varied and included the emergency department (ED), hospital wards, and the intensive care unit (ICU).
| Source | Site No./Type | Setting | Alert Threshold | Gold Standard Definition | Gold Standard Measurement | No. | Study Qualitya |
|---|---|---|---|---|---|---|---|
| |||||||
| Hooper et al., 201210 | 1/academic | MICU | 2 SIRS criteriab | Reviewer judgment, not otherwise specified | Chart review | 560 | High |
| Meurer et al., 200913 | 1/academic | ED | 2 SIRS criteria | Reviewer judgment whether diagnosis of infection present in ED plus SIRS criteria | Chart review | 248 | Low |
| Nelson J. et al., 201114 | 1/academic | ED | 2 SIRS criteria and 2 SBP measurements 90 mm Hg | Reviewer judgment whether infection present, requiring hospitalization with at least 1 organ system involved | Chart review | 1,386 | High |
| Nguyen et al., 201415 | 1/academic | ED | 2 SIRS criteria and 1 sign of shock (SBP 90 mm Hg or lactic acid 2.0 mmol/L) | Reviewer judgment to confirm SIRS, shock, and presence of a serious infection | Chart review | 1,095 | Low |
| Thiel et al., 201016 | 1/academic | Wards | Recursive partitioning tree analysis including vitals and laboratory resultsc | Admitted to the hospital wards and subsequently transferred to the ICU for septic shock and treated with vasopressor therapy | ICD‐9 discharge codes for acute infection, acute organ dysfunction, and need for vasopressors within 24 hours of ICU transfer | 27,674 | Low |
| Source | Design | Site No./ Type | Setting | No. | Alert System Type | Alert Threshold | Alert Notificationa | Treatment Recommendation | Study Qualityb |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Berger et al., 201017 | Before‐after (6 months pre and 6 months post) | 1/academic | ED | 5796c | CPOE system | 2 SIRS criteria | CPOE passive alert | Yes: lactate collection | Low |
| Hooper et al., 201210 | RCT | 1/academic | MICU | 443 | EHR | 2 SIRS criteriad | Text page and EHR passive alert | No | High |
| McRee et al., 201418 | Before‐after (6 months pre and 6 months post) | 1/academic | Wards | 171e | EHR | 2 SIRS criteria | Notified nurse, specifics unclear | No, but the nurse completed a sepsis risk evaluation flow sheet | Low |
| Nelson et al., 201114 | Before‐after (3 months pre and 3 months post) | 1/academic | ED | 184f | EHR | 2 SIRS criteria and 2 or more SBP readings 90 mm Hg | Text page and EHR passive alert | Yes: fluid resuscitation, blood culture collection, antibiotic administration, among others | Low |
| Sawyer et al., 201119 | Prospective, nonrandomized (2 intervention and 4 control wards) | 1/academic | Wards | 300 | EHR | Recursive partitioning regression tree algorithm including vitals and lab valuesg | Text page to charge nurse who then assessed patient and informed treating physicianh | No | High |
Among the 8 included studies, there was significant heterogeneity in threshold criteria for sepsis identification and subsequent alert activation. The most commonly defined threshold was the presence of 2 or more systemic inflammatory response syndrome (SIRS) criteria.[10, 13, 17, 18]
Diagnostic Accuracy of Automated Electronic Sepsis Alert Systems
The prevalence of sepsis varied substantially between the studies depending on the gold standard definition of sepsis used and the clinical setting (ED, wards, or ICU) of the study (Table 3). The 2 studies[14, 16] that defined sepsis as requiring evidence of shock had a substantially lower prevalence (0.8%4.7%) compared to the 2 studies[10, 13] that defined sepsis as having only 2 or more SIRS criteria with a presumed diagnosis of an infection (27.8%32.5%).
| Source | Setting | Alert Threshold | Prevalence, % | Sensitivity, % (95% CI) | Specificity, % (95% CI) | PPV, % (95% CI) | NPV, % (95% CI) | LR+, (95% CI) | LR, (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Hooper et al., 201210 | MICU | 2 SIRS criteriaa | 36.3 | 98.9 (95.799.8) | 18.1 (14.222.9) | 40.7 (36.145.5) | 96.7 (87.599.4) | 1.21 (1.14‐1.27) | 0.06 (0.01‐0.25) |
| Meurer et al., 200913 | ED | 2 SIRS criteria | 27.8 | 36.2 (25.348.8) | 79.9 (73.185.3) | 41.0 (28.854.3) | 76.5 (69.682.2) | 1.80 (1.17‐2.76) | 0.80 (0.67‐0.96) |
| Nelson et al., 201114 | ED | 2 SIRS criteria and 2 SBP measurements90 mm Hg | 0.8 | 63.6 (31.687.8) | 99.6 (99.099.8) | 53.8 (26.179.6) | 99.7 (99.299.9) | 145.8 (58.4364.1) | 0.37 (0.17‐0.80) |
| Nguyen et al., 201415 | ED | 2 SIRS criteria and 1 sign of shock (SBP 90 mm Hg or lactic acid 2.0 mmol/L) | Unable to estimateb | Unable to estimateb | Unable to estimateb | 44.7 (41.248.2) | 100.0c (98.8100.0) | Unable to estimateb | Unable to estimateb |
| Thiel et al., 201016 | Wards | Recursive partitioning tree analysis including vitals and laboratory resultsd | 4.7 | 17.1 (15.119.3) | 96.7 (96.596.9) | 20.5 (18.223.0) | 95.9 (95.796.2) | 5.22 (4.56‐5.98) | 0.86 (0.84‐0.88) |
All alert systems had suboptimal PPV (20.5%‐53.8%). The 2 studies that designed the sepsis alert to activate by SIRS criteria alone[10, 13] had a positive predictive value of 41% and a positive LR of 1.21 to 1.80. The ability to exclude the presence of sepsis varied considerably depending on the clinical setting. The study by Hooper et al.[10] that examined the alert among patients in the medical ICU appeared more effective at ruling out sepsis (NPV=96.7%; negative LR=0.06) compared to a similar alert system used by Meurer et al.[13] that studied patients in the ED (NPV=76.5%, negative LR=0.80).
There were also differences in the diagnostic accuracy of the sepsis alert systems depending on how the threshold for activating the sepsis alert was defined and applied in the study. Two studies evaluated a sepsis alert system among patients presenting to the ED at the same academic medical center.[13, 14] The alert system (Nelson et al.) that was triggered by a combination of SIRS criteria and hypotension (PPV=53.8%, LR+=145.8; NPV=99.7%, LR=0.37) outperformed the alert system (Meurer et al.) that was triggered by SIRS criteria alone (PPV=41.0%, LR+=1.80; NPV=76.5%, LR=0.80). Furthermore, the study by Meurer and colleagues evaluated the accuracy of the alert system only among patients who were hospitalized after presenting to the ED, rather than all consecutive patients presenting to the ED. This selection bias likely falsely inflated the diagnostic accuracy of the alert system used by Meurer et al., suggesting the alert system that was triggered by a combination of SIRS criteria and hypotension was comparatively even more accurate.
Two studies evaluating the diagnostic accuracy of the alert system were deemed to be high quality (Table 4). Three studies were considered low quality1 study did not include all patients in their assessment of diagnostic accuracy13; 1 study consecutively selected alert cases but randomly selected nonalert cases, greatly limiting the assessment of diagnostic accuracy15; and the other study applied a gold standard that was unlikely to correctly classify sepsis (septic shock requiring ICU transfer with vasopressor support in the first 24 hours was defined by discharge International Classification of Diseases, Ninth Revision diagnoses without chart review), with a considerable delay from the alert system trigger (alert identification was compared to the discharge diagnosis rather than physician review of real‐time data).[16]
| Study | Patient Selection | Index Test | Reference Standard | Flow and Timing |
|---|---|---|---|---|
| ||||
| Hooper et al., 201210 | +++ | +++ | ++b | +++ |
| Meurer et al., 200913 | +++ | +++ | ++b | +c |
| Nelson et al., 201114 | +++ | +++ | ++b | +++ |
| Nguyen et al., 201415 | +d | +++ | +e | +++ |
| Thiel et al., 201016 | +++ | +++ | +f | +g |
Effectiveness of Automated Electronic Sepsis Alert Systems
Characteristics of the studies evaluating the effectiveness of automated electronic sepsis alert systems are summarized in Table 2. Regarding activation of the sepsis alert, 2 studies notified the provider directly by an automated text page and a passive EHR alert (not requiring the provider to acknowledge the alert or take action),[10, 14] 1 study notified the provider by a passive electronic alert alone,[17] and 1 study only employed an automated text page.[19] Furthermore, if the sepsis alert was activated, 2 studies suggested specific clinical management decisions,[14, 17] 2 studies left clinical management decisions solely to the discretion of the treating provider,[10, 19] and 1 study assisted the diagnosis of sepsis by prompting nurses to complete a second manual sepsis risk evaluation.[18]
Table 5 summarizes the effectiveness of automated electronic sepsis alert systems. Two studies evaluating the effectiveness of the sepsis alert system were considered to be high‐quality studies based on the use of a contemporaneous control group to account for temporal trends and an intention‐to‐treat analysis.[10, 19] The 2 studies evaluating the effectiveness of a sepsis alert system in the ED were considered low quality due to before‐and‐after designs without an intention‐to‐treat analysis.[14, 17]
| Source | Outcomes Evaluated | Key Findings | Quality |
|---|---|---|---|
| |||
| Hooper et al., 201210 | Primary: time to receipt of antibiotic (new or changed) | No difference (6.1 hours for control vs 6.0 hours for intervention, P=0.95) | High |
| Secondary: sepsis‐related process measures and outcomes | No difference in amount of 6 hour IV fluid administration (964 mL vs 1,019 mL, P=0.6), collection of blood cultures (adjusted HR 1.01; 95% CI, 0.76 to 1.35), collection of lactate (adjusted HR 0.84; 95% CI, 0.54 to 1.30), ICU length of stay (3.0 vs 3.0 days, P=0.2), hospital length of stay (4.7 vs 5.7 days, P=0.08), and hospital mortality (10% for control vs 14% for intervention, P=0.3) | ||
| Sawyer et al., 201119 | Primary: sepsis‐related process measures (antibiotic escalation, IV fluids, oxygen therapy, vasopressor initiation, diagnostic testing (blood culture, CXR) within 12 hours of alert | Increases in receiving 1 measure (56% for control vs 71% for intervention, P=0.02), antibiotic escalation (24% vs 36%, P=0.04), IV fluid administration (24% vs 38%, P=0.01), and oxygen therapy (8% vs 20%, P=0.005). There was a nonsignificant increase in obtaining diagnostic tests (40% vs 52%, P=0.06) and vasopressor initiation (3% vs 6%, P=0.4) | High |
| Secondary: ICU transfer, hospital length of stay, hospital length of stay after alert, in‐hospital mortality | Similar rate of ICU transfer (23% for control vs 26% for intervention, P=0.6), hospital length of stay (7 vs 9 days, median, P=0.8), hospital length of stay after alert (5 vs 6 days, median, P=0.7), and in‐hospital mortality (12% vs 10%, P=0.7) | ||
| Berger et al., 201017 | Primary: lactate collection in ED | Increase in lactate collection in the ED (5.2% before vs 12.7% after alert implemented, absolute increase of 7.5%, 95% CI, 6.0% to 9.0%) | Low |
| Secondary: lactate collection among hospitalized patients, proportion of patients with abnormal lactate (4 mmol/L), and in‐hospital mortality among hospitalized patients | Increase in lactate collection among hospitalized patients (15.3% vs 34.2%, absolute increase of 18.9%, 95% CI, 15.0% to 22.8%); decrease in the proportion of abnormal lactate values (21.9% vs 14.8%, absolute decrease of 7.6%, 95% CI, 15.8% to 0.6%), and no significant difference in mortality (5.7% vs 5.2%, absolute decrease of 0.5%, 95% CI, 1.6% to 2.6%, P=0.6) | ||
| McRee et al., 201418 | Stage of sepsis, length of stay, mortality, discharge location | Nonsignificant decrease in stage of sepsis (34.7% with septic shock before vs 21.9% after, P>0.05); no difference in length‐of‐stay (8.5 days before vs 8.7 days after, P>0.05). Decrease in mortality (9.3% before vs 1.0% after, P0.05) and proportion of patients discharged home (25.3% before vs 49.0% after, P0.05) | Low |
| Nelson et al., 201114 | Frequency and time to completion of process measures: lactate, blood culture, CXR, and antibiotic initiation | Increases in blood culture collection (OR 2.9; 95% CI, 1.1 to 7.7) and CXR (OR 3.2; 95% CI, 1.1 to 9.5); nonsignificant increases in lactate collection (OR 1.7; 95% CI, 0.9 to 3.2) and antibiotic administration (OR 2.8; 95% CI, 0.9 to 8.3). Only blood cultures were collected in a more timely manner (median of 86 minutes before vs 81 minutes after alert implementation, P=0.03). | Low |
Neither of the 2 high‐quality studies that included a contemporaneous control found evidence for improving inpatient mortality or hospital and ICU length of stay.[10, 19] The impact of sepsis alert systems on improving process measures for sepsis management depended on the clinical setting. In a randomized controlled trial of patients admitted to a medical ICU, Hooper et al. did not find any benefit of implementing a sepsis alert system on improving intermediate outcome measures such as antibiotic escalation, fluid resuscitation, and collection of blood cultures and lactate.[10] However, in a well‐designed observational study, Sawyer et al. found significant increases in antibiotic escalation, fluid resuscitation, and diagnostic testing in patients admitted to the medical wards.[19] Both studies that evaluated the effectiveness of sepsis alert systems in the ED showed improvements in various process measures,[14, 17] but without improvement in mortality.[17] The single study that showed improvement in clinical outcomes (in‐hospital mortality and disposition location) was of low quality due to the prestudypoststudy design without adjustment for potential confounders and lack of an intention‐to‐treat analysis (only individuals with a discharge diagnosis of sepsis were included, rather than all individuals who triggered the alert).[18] Additionally, the preintervention group had a higher proportion of individuals with septic shock compared to the postintervention group, raising the possibility that the observed improvement was due to difference in severity of illness between the 2 groups rather than due to the intervention.
None of the studies included in this review explicitly reported on the potential harms (eg, excess antimicrobial use or alert fatigue) after implementation of sepsis alerts, but Hooper et al. found a nonsignificant increase in mortality, and Sawyer et al. showed a nonsignificant increase in the length of stay in the intervention group compared to the control group.[10, 19] Berger et al. showed an overall increase in the number of lactate tests performed, but with a decrease in the proportion of abnormal lactate values (21.9% vs 14.8%, absolute decrease of 7.6%, 95% confidence interval, 15.8% to 0.6%), suggesting potential overtesting in patients at low risk for septic shock. In the study by Hooper et al., 88% (442/502) of the patients in the medical intensive care unit triggered an alert, raising the concern for alert fatigue.[10] Furthermore, 3 studies did not perform intention‐to‐treat analyses; rather, they included only patients who triggered the alert and also had provider‐suspected or confirmed sepsis,[14, 17] or had a discharge diagnosis for sepsis.[18]
DISCUSSION
The use of sepsis alert systems derived from electronic health data and targeting hospitalized patients improve a subset of sepsis process of care measures, but at the cost of poor positive predictive value and no clear improvement in mortality or length of stay. There is insufficient evidence for the effectiveness of automated electronic sepsis alert systems in the emergency department.
We found considerable variability in the diagnostic accuracy of automated electronic sepsis alert systems. There was moderate evidence that alert systems designed to identify severe sepsis (eg, SIRS criteria plus measures of shock) had greater diagnostic accuracy than alert systems that detected sepsis based on SIRS criteria alone. Given that SIRS criteria are highly prevalent among hospitalized patients with noninfectious diseases,[20] sepsis alert systems triggered by standard SIRS criteria may have poorer predictive value with an increased risk of alert fatigueexcessive electronic warnings resulting in physicians disregarding clinically useful alerts.[21] The potential for alert fatigue is even greater in critical care settings. A retrospective analysis of physiological alarms in the ICU estimated on average 6 alarms per hour with only 15% of alarms considered to be clinically relevant.[22]
The fact that sepsis alert systems improve intermediate process measures among ward and ED patients but not ICU patients likely reflects differences in both the patients and the clinical settings.[23] First, patients in the ICU may already be prescribed broad spectrum antibiotics, aggressively fluid resuscitated, and have other diagnostic testing performed before the activation of a sepsis alert, so it would be less likely to see an improvement in the rates of process measures assessing initiation or escalation of therapy compared to patients treated on the wards or in the ED. The apparent lack of benefit of these systems in the ICU may merely represent a ceiling effect. Second, nurses and physicians are already vigilantly monitoring patients in the ICU for signs of clinical deterioration, so additional alert systems may be redundant. Third, patients in the ICU are connected to standard bedside monitors that continuously monitor for the presence of abnormal vital signs. An additional sepsis alert system triggered by SIRS criteria alone may be superfluous to the existing infrastructure. Fourth, the majority of patients in the ICU will trigger the sepsis alert system,[10] so there likely is a high noise‐to‐signal ratio with resultant alert fatigue.[21]
In addition to greater emphasis on alert systems of greater diagnostic accuracy and effectiveness, our review notes several important gaps that limit evidence supporting the usefulness of automated sepsis alert systems. First, there are little data to describe the optimal design of sepsis alerts[24, 25] or the frequency with which they are appropriately acted upon or dismissed. In addition, we found little data to support whether effectiveness of alert systems differed based on whether clinical decision support was included with the alert itself (eg, direct prompting with specific clinical management recommendations) or the configuration of the alert (eg, interruptive alert or informational).[24, 25] Most of the studies we reviewed employed alerts primarily targeting physicians; we found little evidence for systems that also alerted other providers (eg, nurses or rapid response teams). Few studies provided data on harms of these systems (eg, excess antimicrobial use, fluid overload due to aggressive fluid resuscitation) or how often these treatments were administered to patients who did not eventually have sepsis. Few studies employed study designs that limited biases (eg, randomized or quasiexperimental designs) or used an intention‐to‐treat approach. Studies that exclude false positive alerts in analyses could bias estimates toward making sepsis alert systems appear more effective than they actually were. Finally, although presumably, deploying automated sepsis alerts in the ED would facilitate more timely recognition and treatment, more rigorously conducted studies are needed to identify whether using these alerts in the ED are of greater value compared to the wards and ICU. Given the limited number of studies included in this review, we were unable to make strong conclusions regarding the clinical benefits and cost‐effectiveness of implementing automated sepsis alerts.
Our review has certain limitations. First, despite our extensive literature search strategy, we may have missed studies published in the grey literature or in non‐English languages. Second, there is potential publication bias given the number of abstracts that we identified addressing 1 of our prespecified research questions compared to the number of peer‐reviewed publications identified by our search strategy.
CONCLUSION
Automated electronic sepsis alert systems have promise in delivering early goal‐directed therapies to patients. However, at present, automated sepsis alerts derived from electronic health data may improve care processes but tend to have poor PPV and have not been shown to improve mortality or length of stay. Future efforts should develop and study methods for sepsis alert systems that avoid the potential for alert fatigue while improving outcomes.
Acknowledgements
The authors thank Gloria Won, MLIS, for her assistance with developing and performing the literature search strategy and wish her a long and joyous retirement.
Disclosures: Part of Dr. Makam's work on this project was completed while he was a primary care research fellow at the University of California, San Francisco, funded by a National Research Service Award (training grant T32HP19025‐07‐00). Dr. Makam is currently supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (KL2TR001103). Dr. Nguyen was supported by the Agency for Healthcare Research and Quality (R24HS022428‐01). Dr. Auerbach was supported by an NHLBI K24 grant (K24HL098372). Dr. Makam had full access to the data in the study and takes responsibility for the integrity of the date and accuracy of the data analysis. Study concept and design: all authors. Acquisition of data: Makam and Nguyen. Analysis and interpretation of data: all authors. Drafting of the manuscript: Makam. Critical revision of the manuscript: all authors. Statistical analysis: Makam and Nguyen. The authors have no conflicts of interest to disclose.
- , . National inpatient hospital costs: the most expensive conditions by payer, 2011: statistical brief #160. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2013.
- , , , . Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011;(62):1–8.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , , et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
- , , , et al. Early goal‐directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377.
- , , , et al. A randomized trial of protocol‐based care for early septic shock. N Engl J Med. 2014;370(18):1683–1693.
- , . Implementation of early goal‐directed therapy for septic patients in the emergency department: a review of the literature. J Emerg Nurs. 2013;39(1):13–19.
- , , , , , . Factors influencing variability in compliance rates and clinical outcomes among three different severe sepsis bundles. Ann Pharmacother. 2007;41(6):929–936.
- , , , et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299(19):2294–2303.
- , , , et al. Randomized trial of automated, electronic monitoring to facilitate early detection of sepsis in the intensive care unit*. Crit Care Med. 2012;40(7):2096–2101.
- , , , et al. QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536.
- , , , et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health‐care program. J Clin Epidemiol. 2010;63(5):513–523.
- , , , et al. Real‐time identification of serious infection in geriatric patients using clinical information system surveillance. J Am Geriatr Soc. 2009;57(1):40–45.
- , , , . Prospective trial of real‐time electronic surveillance to expedite early care of severe sepsis. Ann Emerg Med. 2011;57(5):500–504.
- , , , et al. Automated electronic medical record sepsis detection in the emergency department. PeerJ. 2014;2:e343.
- , , , , , . Early prediction of septic shock in hospitalized patients. J Hosp Med. 2010;5(1):19–25.
- , , , , . A Computerized alert screening for severe sepsis in emergency department patients increases lactate testing but does not improve inpatient mortality. Appl Clin Inform. 2010;1(4):394–407.
- , , , , . The impact of an electronic medical record surveillance program on outcomes for patients with sepsis. Heart Lung. 2014;43(6):546–549.
- , , , et al. Implementation of a real‐time computerized sepsis alert in nonintensive care unit patients. Crit Care Med. 2011;39(3):469–473.
- . The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26(suppl 1):S64–S74.
- , , , et al. Overrides of medication‐related clinical decision support alerts in outpatients. J Am Med Inform Assoc. 2014;21(3):487–491.
- , , , , , . Intensive care unit alarms–how many do we need? Crit Care Med. 2010;38(2):451–456.
- , . How can we best use electronic data to find and treat the critically ill?*. Crit Care Med. 2012;40(7):2242–2243.
- , , , et al. Identifying best practices for clinical decision support and knowledge management in the field. Stud Health Technol Inform. 2010;160(pt 2):806–810.
- , , , et al. Best practices in clinical decision support: the case of preventive care reminders. Appl Clin Inform. 2010;1(3):331–345.
- , . National inpatient hospital costs: the most expensive conditions by payer, 2011: statistical brief #160. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2013.
- , , , . Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011;(62):1–8.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , , et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
- , , , et al. Early goal‐directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377.
- , , , et al. A randomized trial of protocol‐based care for early septic shock. N Engl J Med. 2014;370(18):1683–1693.
- , . Implementation of early goal‐directed therapy for septic patients in the emergency department: a review of the literature. J Emerg Nurs. 2013;39(1):13–19.
- , , , , , . Factors influencing variability in compliance rates and clinical outcomes among three different severe sepsis bundles. Ann Pharmacother. 2007;41(6):929–936.
- , , , et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299(19):2294–2303.
- , , , et al. Randomized trial of automated, electronic monitoring to facilitate early detection of sepsis in the intensive care unit*. Crit Care Med. 2012;40(7):2096–2101.
- , , , et al. QUADAS‐2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536.
- , , , et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health‐care program. J Clin Epidemiol. 2010;63(5):513–523.
- , , , et al. Real‐time identification of serious infection in geriatric patients using clinical information system surveillance. J Am Geriatr Soc. 2009;57(1):40–45.
- , , , . Prospective trial of real‐time electronic surveillance to expedite early care of severe sepsis. Ann Emerg Med. 2011;57(5):500–504.
- , , , et al. Automated electronic medical record sepsis detection in the emergency department. PeerJ. 2014;2:e343.
- , , , , , . Early prediction of septic shock in hospitalized patients. J Hosp Med. 2010;5(1):19–25.
- , , , , . A Computerized alert screening for severe sepsis in emergency department patients increases lactate testing but does not improve inpatient mortality. Appl Clin Inform. 2010;1(4):394–407.
- , , , , . The impact of an electronic medical record surveillance program on outcomes for patients with sepsis. Heart Lung. 2014;43(6):546–549.
- , , , et al. Implementation of a real‐time computerized sepsis alert in nonintensive care unit patients. Crit Care Med. 2011;39(3):469–473.
- . The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26(suppl 1):S64–S74.
- , , , et al. Overrides of medication‐related clinical decision support alerts in outpatients. J Am Med Inform Assoc. 2014;21(3):487–491.
- , , , , , . Intensive care unit alarms–how many do we need? Crit Care Med. 2010;38(2):451–456.
- , . How can we best use electronic data to find and treat the critically ill?*. Crit Care Med. 2012;40(7):2242–2243.
- , , , et al. Identifying best practices for clinical decision support and knowledge management in the field. Stud Health Technol Inform. 2010;160(pt 2):806–810.
- , , , et al. Best practices in clinical decision support: the case of preventive care reminders. Appl Clin Inform. 2010;1(3):331–345.
Statins for all eligible under new guidelines could save lives
BALTIMORE – If all Americans eligible for statins under new American College of Cardiology/American Heart Association guidelines actually took them, thousands of deaths per year from cardiovascular disease might be prevented but at a cost of increased incidence of diabetes and myopathy.
The 2013 ACC/AHA guidelines expand criteria for the use of statins for primary prevention of CVD to more Americans (Circulation 2015;131:A05). Compliance with those guidelines would save 7,930 lives per year that would have been lost to CVD, according to Quanhe Yang, Ph.D., of the Centers for Disease Control and Prevention’s Division for Heart Disease and Stroke Prevention, and colleagues from the CDC and Emory University, Atlanta. Dr. Yang presented the findings at the American Heart Association Epidemiology and Prevention, Lifestyle and Cardiometabolic Health 2015 Scientific Sessions.
Statins are now indicated for primary prevention of CVD for anyone with an LDL cholesterol level greater than or equal to 190 mg/dL, for individuals aged 40-75 years with diabetes, and for those aged 40-75 years with LDL cholesterol greater than or equal to 70 mg/dL but less than 190 mg/dL who have at least a 7.5% estimated 10-year risk of developing atherosclerotic CVD. This means that an additional 24.2 million Americans are now eligible for statins but are not taking one, according to Dr. Yang and coinvestigators. However, “no study has assessed the potential impact of statin therapy under the new guidelines,” said Dr. Yang.
In order to obtain treatment group-specific atherosclerotic CVD, investigators first estimated hazard ratios for each treatment group by sex from the National Health and Nutrition Examination Survey III (NHANES III)–linked Mortality files. These hazard ratios were then applied to data from NHANES 2005-2010, the 2010 Multiple Cause of Death file, and the 2010 U.S. census to obtain age/race/sex-specific atherosclerotic CVD for each treatment group.
Applying the per-group hazard ratios, Dr. Yang and colleagues calculated that an annual 7,930 atherosclerotic CVD deaths would be prevented with full statin compliance, a reduction of 12.6%. However, modeling predicted an additional 16,400 additional cases of diabetes caused by statin use, he cautioned. More cases of myopathy would also occur, though the estimated number depends on whether the rate is derived from randomized, controlled trials (RCTs) or from population-based reports of myopathy. If the RCT data are used, just 1,510 excess cases of myopathy would be seen, in contrast to the 36,100 cases predicted by population-based data.
The study could model deaths caused by CVD only and not the reduction in disease burden of CVD that would result if all of the additional 24.2 million Americans took a statin, Dr Yang noted. Other limitations of the study included the lack of agreement in incidence of myopathy between RCTs and population-based studies, as well as the likelihood that the risk of diabetes increases with age and higher statin dose – effects not accounted for in the study.
Questioning after the talk focused on sex-specific differences in statin takers. For example, statin-associated diabetes is more common in women than men, another effect not accounted for in the study’s modeling, noted an audience member. Additionally, given that women have been underrepresented in clinical trials in general and in those for CVD in particular, some modeling assumptions in the present study may also lack full generalizability to women at risk for CVD.
BALTIMORE – If all Americans eligible for statins under new American College of Cardiology/American Heart Association guidelines actually took them, thousands of deaths per year from cardiovascular disease might be prevented but at a cost of increased incidence of diabetes and myopathy.
The 2013 ACC/AHA guidelines expand criteria for the use of statins for primary prevention of CVD to more Americans (Circulation 2015;131:A05). Compliance with those guidelines would save 7,930 lives per year that would have been lost to CVD, according to Quanhe Yang, Ph.D., of the Centers for Disease Control and Prevention’s Division for Heart Disease and Stroke Prevention, and colleagues from the CDC and Emory University, Atlanta. Dr. Yang presented the findings at the American Heart Association Epidemiology and Prevention, Lifestyle and Cardiometabolic Health 2015 Scientific Sessions.
Statins are now indicated for primary prevention of CVD for anyone with an LDL cholesterol level greater than or equal to 190 mg/dL, for individuals aged 40-75 years with diabetes, and for those aged 40-75 years with LDL cholesterol greater than or equal to 70 mg/dL but less than 190 mg/dL who have at least a 7.5% estimated 10-year risk of developing atherosclerotic CVD. This means that an additional 24.2 million Americans are now eligible for statins but are not taking one, according to Dr. Yang and coinvestigators. However, “no study has assessed the potential impact of statin therapy under the new guidelines,” said Dr. Yang.
In order to obtain treatment group-specific atherosclerotic CVD, investigators first estimated hazard ratios for each treatment group by sex from the National Health and Nutrition Examination Survey III (NHANES III)–linked Mortality files. These hazard ratios were then applied to data from NHANES 2005-2010, the 2010 Multiple Cause of Death file, and the 2010 U.S. census to obtain age/race/sex-specific atherosclerotic CVD for each treatment group.
Applying the per-group hazard ratios, Dr. Yang and colleagues calculated that an annual 7,930 atherosclerotic CVD deaths would be prevented with full statin compliance, a reduction of 12.6%. However, modeling predicted an additional 16,400 additional cases of diabetes caused by statin use, he cautioned. More cases of myopathy would also occur, though the estimated number depends on whether the rate is derived from randomized, controlled trials (RCTs) or from population-based reports of myopathy. If the RCT data are used, just 1,510 excess cases of myopathy would be seen, in contrast to the 36,100 cases predicted by population-based data.
The study could model deaths caused by CVD only and not the reduction in disease burden of CVD that would result if all of the additional 24.2 million Americans took a statin, Dr Yang noted. Other limitations of the study included the lack of agreement in incidence of myopathy between RCTs and population-based studies, as well as the likelihood that the risk of diabetes increases with age and higher statin dose – effects not accounted for in the study.
Questioning after the talk focused on sex-specific differences in statin takers. For example, statin-associated diabetes is more common in women than men, another effect not accounted for in the study’s modeling, noted an audience member. Additionally, given that women have been underrepresented in clinical trials in general and in those for CVD in particular, some modeling assumptions in the present study may also lack full generalizability to women at risk for CVD.
BALTIMORE – If all Americans eligible for statins under new American College of Cardiology/American Heart Association guidelines actually took them, thousands of deaths per year from cardiovascular disease might be prevented but at a cost of increased incidence of diabetes and myopathy.
The 2013 ACC/AHA guidelines expand criteria for the use of statins for primary prevention of CVD to more Americans (Circulation 2015;131:A05). Compliance with those guidelines would save 7,930 lives per year that would have been lost to CVD, according to Quanhe Yang, Ph.D., of the Centers for Disease Control and Prevention’s Division for Heart Disease and Stroke Prevention, and colleagues from the CDC and Emory University, Atlanta. Dr. Yang presented the findings at the American Heart Association Epidemiology and Prevention, Lifestyle and Cardiometabolic Health 2015 Scientific Sessions.
Statins are now indicated for primary prevention of CVD for anyone with an LDL cholesterol level greater than or equal to 190 mg/dL, for individuals aged 40-75 years with diabetes, and for those aged 40-75 years with LDL cholesterol greater than or equal to 70 mg/dL but less than 190 mg/dL who have at least a 7.5% estimated 10-year risk of developing atherosclerotic CVD. This means that an additional 24.2 million Americans are now eligible for statins but are not taking one, according to Dr. Yang and coinvestigators. However, “no study has assessed the potential impact of statin therapy under the new guidelines,” said Dr. Yang.
In order to obtain treatment group-specific atherosclerotic CVD, investigators first estimated hazard ratios for each treatment group by sex from the National Health and Nutrition Examination Survey III (NHANES III)–linked Mortality files. These hazard ratios were then applied to data from NHANES 2005-2010, the 2010 Multiple Cause of Death file, and the 2010 U.S. census to obtain age/race/sex-specific atherosclerotic CVD for each treatment group.
Applying the per-group hazard ratios, Dr. Yang and colleagues calculated that an annual 7,930 atherosclerotic CVD deaths would be prevented with full statin compliance, a reduction of 12.6%. However, modeling predicted an additional 16,400 additional cases of diabetes caused by statin use, he cautioned. More cases of myopathy would also occur, though the estimated number depends on whether the rate is derived from randomized, controlled trials (RCTs) or from population-based reports of myopathy. If the RCT data are used, just 1,510 excess cases of myopathy would be seen, in contrast to the 36,100 cases predicted by population-based data.
The study could model deaths caused by CVD only and not the reduction in disease burden of CVD that would result if all of the additional 24.2 million Americans took a statin, Dr Yang noted. Other limitations of the study included the lack of agreement in incidence of myopathy between RCTs and population-based studies, as well as the likelihood that the risk of diabetes increases with age and higher statin dose – effects not accounted for in the study.
Questioning after the talk focused on sex-specific differences in statin takers. For example, statin-associated diabetes is more common in women than men, another effect not accounted for in the study’s modeling, noted an audience member. Additionally, given that women have been underrepresented in clinical trials in general and in those for CVD in particular, some modeling assumptions in the present study may also lack full generalizability to women at risk for CVD.
AT AHA EPI/LIFESTYLE 2015MEETING
Key clinical point: New statin guidelines, if followed, could save lives but increase cases of myopathy and diabetes.
Major finding: Up to 12.6% of current deaths from CVD could be prevented if all guideline-eligible Americans took statins; saving of these lives would come at the cost of excess cases of diabetes and myopathy.
Data source: Analysis of U.S. census data and data from the NHANES study, together with meta-analysis of RCTs, used to model outcomes for 100% guideline-eligible statin use.
Disclosures: No authors reported financial disclosures.
Update on Pediatric Psoriasis
Psoriasis affects 2% to 4% of the US population, with approximately one-third of cases beginning in childhood. The understanding of pediatric psoriasis has developed at a far slower pace than adult disease, with limitations in care including few medications that are approved by the US Food and Drug Administration for pediatric and adolescent use. Recently, a stable fixed-combination dose of calcipo-triene 0.005%–betamethasone dipropionate 0.064% topical suspension was approved for treatment of plaque psoriasis of the scalp in patients aged 12 to 17 years, which hopefully will lead a trend in psoriasis medication approval for children and teenagers.1 Based on a PubMed search of articles indexed for MEDLINE using the search terms pediatric psoriasis, psoriasis, and strep that were published from April 2012 to April 2014, this article reviews newer data to address the issues that surround pediatric psoriasis and to provide an update on prior review articles on pediatric psoriasis.2-5 This article reviews some of the newer literature on clinical presentation and comorbidities in pediatric psoriasis.5 Based on these recent findings, additional screenings including review of obesity parameters are recommended for pediatric patients with psoriasis (Table 1).
Update on Disease Manifestations, Associations, and Comorbidities
Disease Manifestations
A 2013 multicenter study delineated the clinical features of pediatric psoriasis.6 The study was conducted at 8 geographically diverse dermatology clinics in the United States to delineate the clinical manifestations of pediatric psoriasis. In an assessment of 181 participants aged 5 to 17 years, the investigators sought to determine the frequency of disease sites, severity, and guttate disease. Over a period of approximately 2 years, 43.1% of participants were determined to have mild disease and 56.9% had severe disease. Family history of psoriasis was present in 51.4% of participants, with first-degree relatives affected in 59.8% of cases. Scalp involvement at some time was noted in 79.0% of participants, and nail disease was noted in 55% of boys and 29% of girls. Guttate psoriasis was noted in 30% of participants, with more cases in the severe range (35.9%) versus the mild range (21.8%). Additionally, 22.1% of participants had a precipitating streptococcal infection, with the association being more common in pediatric patients with guttate psoriasis than plaque psoriasis.6 This study highlighted that pediatric psoriasis has a genetic basis, is frequently guttate in nature, commonly affects the nails, shows a trend toward being classified as severe, and may be triggered by streptococcal infections.
Streptococcal Infection
Pediatric psoriasis may be triggered or flared by Streptococcus pyogenes (group A β-hemolytic streptococci) infections, specifically β-hemolytic streptococci groups A, C, and G that have streptococcal M protein,2,3,7 and this tendency can be associated with HLA-Cw6 or guttate psoriasis. Newer data have elucidated the role of streptococcal throat infections in psoriasis. Given that streptococcal throat infections are most common in school-aged children, these studies suggest a putative mechanism in pediatric psoriasis for triggering streptococcal infections, which would need to be confirmed in future studies, specifically in pediatric psoriasis patients.
It has been shown that T cells in psoriasis patients recognize common streptococcal M proteins and keratin determinants.7 Ferran et al8 recently demonstrated activation of circulating cutaneous lymphocyte–associated antigen (CLA)+ T cells but not CLA- memory T cells in 27 psoriasis patients (ages not specified) when mixed with streptococcal throat extracts, causing production of IL-17, IP-10, IL-22, and IFN-γ; activation was not found in 6 healthy control patients. Antistreptolysin O levels were correlated with the messenger RNA up- regulation for IL-17, IP-10, IL-22, and IFN-γ, and also correlated with psoriasis area and severity index score in psoriasis patients. In this same study, injection of the activated culture supernatant into mouse skin caused epidermal hyperkeratosis and activation of nonlesional epidermal cells from psoriatic patients. This study thereby delineated some of the potential pathways of the streptococcal induction of psoriasis and psoriatic flares in childhood8; however, confirmation is needed through further study of pediatric psoriatic lymphocyte activity.
Differential Diagnosis
Additions to the extensive differential list have been cited in the recent literature. The differential diagnosis of pediatric psoriasis now includes sodium valproate–induced psoriasiform drug eruption9 and allergic contact dermatitis to methylchloroisothiazolinone and methylisothiazolinone, which are present in many sanitizing hand and diaper wipes and has been reported to cause psoriasiform dermatitis in a periorificial or perineal distribution.10 Clinicians should inquire about the use of these wipes, as caregivers rarely suspect this agent to be causative of the eruption.
Psoriatic Arthritis
Previously, psoriasis and psoriatic arthritis have been linked to autoimmune thyroid disease in adults.11 A study of the Childhood Arthritis & Rheumatology Research Alliance (CARRA) registry showed that family history of psoriasis, autoimmune thyroiditis, Crohn disease, and ankylosing spondylitis in a first-degree relative has been linked to juvenile idiopathic arthritis, highlighting that pediatric psoriasis can be genetically linked or associated with multiple autoimmune conditions and vice versa.12
Obesity, Metabolic Syndrome, and Cardiovascular Risks
Obesity is associated with pediatric psoriasis as highlighted in a growing body of recent literature.13 Excess adiposity as manifested by body mass index in the 85th percentile or greater (37.9% of 155 pediatric psoriasis patients vs 20.5% of 42 controls) and excess central adiposity as manifested by excess waist circumference and increased waist-to-height ratios are more common in pediatric patients with psoriasis than in controls.14
Obesity may be a trigger or associated with increased disease activity in pediatric psoriasis patients. Excess overall adiposity correlates with more severe disease. Obesity parameters may correlate with the onset of psoriasis and with disease severity. In fact, the odds of obesity may be higher in childhood than in adults.14,15 A 2011 report of pediatric psoriasis patients aged 10 to 17 years (n=12) and wart controls (n=6)(mean age, 13.2 and 13.5 years, respectively) demonstrated that 4 of 12 patients with psoriasis and 0 of 6 patients with warts met criteria for metabolic syndrome as defined by 3 of the following: (1) triglycerides greater than or equal to 100 mg/dL; (2) high-density lipoprotein cholesterol less than 50 mg/dL in females and less than 5 mg/dL in males; (3) fasting blood glucose levels greater than or equal to 110 mg/dL, (4) waist circumference greater than the 75th percentile for age and sex; and (5) systolic or diastolic blood pressure greater than the 90th percentile for age, sex, and height.16 These studies highlight that obesity and metabolic syndrome are of concern in pediatric psoriasis patients; however, the best management approach using diet and weight interventions has yet to be identified.
Adiposity may precede the onset of psoriasis. A recent cohort of 27 pediatric psoriasis patients reported that the average age at onset of psoriasis was 8.7 years and the average age at onset of obesity was 4.1 years.15 In this study, 93% (25/27) of patients had adiposity preceding their psoriasis by 2 or more years. It is unclear if this is nature or nurture, as 48% (13/27) of patients had a family history of obesity, 41% (11/27) had a family history of psoriasis, and 48% (13/27) had a family history of hyperlipidemia.15 Therefore, obesity may be cultivated in some psoriatic families. The issue of household influences on diet and obesity needs to be addressed if successful weight management is to be achieved in future studies of pediatric psoriasis.
Cardiovascular risks in the pediatric psoriasis population are the subject of ongoing assessment but will likely mimic studies of adult psoriasis patients when reviewed longitudinally.16 Weight loss and healthy lifestyle interventions likely are beneficial to long-term health, but there is a lack of published data addressing dietary modification as a disease modifier for long-term care of pediatric psoriasis.
Anxiety and Depression
Anxiety and depression have been noted in adults with chronic skin diseases. A recent study assessed 118 patients and caregivers of pediatric patients with atopic dermatitis (n=50), psoriasis (n=25), or vitiligo (n=43) using the Children’s Dermatology Life Quality Index, the Hamilton Anxiety Scale, and the Beck Depression Inventory.17 Anxiety and depression were found in 36% of caregivers of pediatric psoriasis patients and depression was found in 36% of pediatric psoriasis patients, highlighting the need for interventions on a personal and family level to improve quality of life. As a comparator, anxiety was more prevalent in vitiligo caregivers (42%), but depression was only found in 26% of caregivers in the same group. Extent of disease (25%–75% body surface area affected) correlated with both depression and anxiety in the caregivers of pediatric patients with psoriasis as well as with anxiety in caregivers of pediatric patients with increased visible surface area of vitiligo.17 Parental anxiety has been reported at times to be linked to corticosteroid phobia, or corticophobia, which may interfere with disease therapy, as topical corticosteroids are considered the mainstay of therapy in childhood disease.18 Coordinating care with caregivers and addressing their concerns about the safety of medications should be integral to the pediatric psoriasis visit.
Pustular Psoriasis
Pustular psoriasis can be seen in any age group. Researchers recently have attempted to delineate the features and successful management of this severe subset of pediatric psoriasis patients. Twenty-four pediatric pustular psoriasis cases reviewed by Posso-De Los Rios et al19 revealed that 92% (22/24) had generalized and 8% (2/24) had limited acral disease. The mean (standard deviation) age at onset of pediatric pustular psoriasis was 6.3 (4.9) years. Half of the reported cases required more than one intervention. Treatment with acitretin, cyclosporine, and methotrexate was effective, but the investigators identified that there is a true dearth of evidence-based therapeutics in pediatric pustular psoriasis and much rebound with discontinuation.19 Although the subset of pediatric pustular psoriasis is rare, study of evidence-based intervention is needed.
Therapy
Recent reviews of pediatric and adolescent psoriasis highlight the paucity of therapeutic information for these patient populations. Investigators typically focus on topical therapies as the basis of treatment,20 as well as the addition of phototherapy in mild to moderate plaque or guttate psoriasis and biologic or systemic agents in moderate to severe flares of plaque, erythrodermic, or pustular psoriasis.21 Further studies are needed to identify evidence-based therapeutic paradigms for pediatric psoriasis and to pinpoint therapies associated with the best quality of life in patients and their caregivers.
Tumor Necrosis Factor α Inhibitors
Safety and efficacy of etanercept for juvenile idiopathic arthritis including oligoarthritis, enthesitis-related arthritis, and psoriatic arthritis recently was reviewed by Windschall et al22 using data from the German pediatric Biologika in der Kinderrheumatologie registry. Juvenile Arthritis Disease Activity Score 10 improved from baseline for 127 pediatric patients with psoriatic arthritis in 3 to 24 months (mean [standard deviation], 14.7 [6.4], 5.0 [4.6], 5.3 [6.4] at baseline, 3 months, and 24 months, respectively). Overall side effects were relatively higher in the psoriatic arthritis group; the rate of serious (relative risk, 1.39 [0.95-2.03; P=.08]) and nonserious (relative risk, 1.18 [1.02-1.35; P=.03]) adverse events also was elevated. Uveitis risk was greatest in the psoriatic arthritis group and the number of associated cases of inflammatory bowel disease outnumbered those seen in other forms of arthritis. The investigators concluded that monitoring for extra-articular immunopathies should be conducted in pediatric patients with psoriatic arthritis who are undergoing etanercept therapy.22
Tumor necrosis factor α (TNF-α) inhibitors have been associated with triggering psoriasiform dermatitis in pediatric patients treated for inflammatory bowel disease. A Finnish study of infliximab side effects in pediatric patients with inflammatory bowel disease (n=84; Crohn disease: n=64) demonstrated that almost half (47.6% [40/84]) of the participants presented with chronic skin reactions, 23% of which were severe in nature.23 Psoriasiform lesions of the scalp and ears were most common, followed by the periorificial area, genitals, trunk, and extremities. Rare association with HLA-Cw*0602 genotype was noted. Skin manifestations did not correlate with gut inflammation (as determined by fecal calprotectin levels). Discontinuation of therapy rarely was required.23 Other studies also have highlighted this side effect, suggesting an incidence of 2.7% in adults with colitis treated with TNF-α inhibitors24 and 10.5% in pediatric patients with Crohn disease.25 In a study by Sherlock et al,25 pediatric patients with Crohn disease developing psoriasis following infliximab therapy were more likely to be homozygous for specific polymorphisms in the IL-23R gene (rs10489628, rs10789229, and rs1343151).
Methotrexate
For pediatric patients who are being treated with methotrexate, the polyglutamate assay recently has been reported to be helpful in identifying patients needing a dose escalation.26 Higher numbers on the polyglutamate assay are associated with superior response to methotrexate therapy. Doses can be increased after 12 weeks in patients with low assays.26
IL-23
The safety of IL-23 blockade in pediatric psoriasis patients has not yet been established, but data from adult cases have implicated the IL-17 and IL-23 pathways in psoriasis/psoriatic arthritis, including an association with IL-23R polymorphisms27 and increases in soluble IL-20 and IL-22 associated with disease severity and an association of IL-17 levels with activity on the psoriasis area and severity index scores.28 The data are more limited for pediatric cases. Pediatric patients with inflammatory bowel disease who have an IL-23R polymorphism appear to be susceptible to psoriatic flares while on TNF-α inhibitor therapy,25 which suggests that the IL-23 blockade may be of benefit for some pediatric patients with psoriasis or psoriatic arthritis.
Conclusion
Pediatric psoriasis and psoriatic arthritis have now been identified as being part of the autoimmune spectrum and are associated with metabolic syndrome, including obesity and excess central adiposity, similar to their adult variants. An overview of potential unmet needs in pediatric psoriasis is included in Table 2. These unmet needs include further delineation of diet and weight modification in the care and prevention of psoriasis; expansion of therapeutic trials and US Food and Drug Administration–approved medications for children with psoriasis, especially severe variants such as extensive plaque and pustular disease; and development of guidelines for ongoing monitoring of children with psoriasis. The role of therapeutic interventions and weight management on long-term disease course remains to be shown in extended clinical trials. Despite the great advancements in psoriatic care, knowledge gaps remain in pediatric psoriasis that will need to be addressed in the future.
1. Taclonex Expanded Indication. OptumRx Web site. https://www.optumrx.com/vgnpreview/HCP/Assets/RxNews/Clinical%20Updates_Taclonex_2014-1003.pdf. Published August 29, 2014. Accessed January 28, 2015.
2. Silverberg NB. Update on pediatric psoriasis, part 1: clinical features and demographics. Cutis. 2010;86:118-124.
3. Silverberg NB. Update on pediatric psoriasis, part 2: therapeutic management. Cutis. 2010;86:172-176.
4. Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33(2 suppl 2):S42-S44.
5. Khorsand K, Sidbury R. Recent advances in pediatric dermatology. Arch Dis Child. 2014;99:944-948.
6. Mercy K, Kwasny M, Cordoro KM, et al. Clinical manifestations of pediatric psoriasis: results of a multicenter study in the United States. Pediatr Dermatol. 2013;30:424-428.
7. Gudjonsson JE, Thorarinsson AM, Sigurgeirsson B, et al. Streptococcal throat infections and exacerbation of chronic plaque psoriasis: a prospective study. Br J Dermatol. 2003;149:530-534.
8. Ferran M, Galván AB, Rincón C, et al. Streptococcus induces circulating CLA(+) memory T-cell-dependent epidermal cell activation in psoriasis. J Invest Dermatol. 2013;133:999-1007.
9. Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate [published online ahead of print November 13, 2013]. Case Rep Pediatr. 2013;2013:823469.
10. Chang MW, Nakrani R. Six children with allergic contact dermatitis to methylisothiazolinone in wet wipes (baby wipes). Pediatrics. 2014;133:e434-e438.
11. Gul U, Gonul M, Kaya I, et al. Autoimmune thyroid disorders in patients with psoriasis. Eur J Dermatol. 2009;19:221-223.
12. Prahalad S, McCracken C, Ponder L, et al. A120: Familial autoimmunity in the CARRA registry. Arthritis Rheumatol. 2014;66(suppl 11):S157.
13. Mercy KM, Paller AS. The relationship between obesity and psoriasis in the pediatric population: implications and future directions. Cutis. 2013;92:107-109.
14. Paller AS, Mercy K, Kwasny MJ, et al. Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol. 2013;149:166-176.
15. Becker L, Tom WL, Eshagh K, et al. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014;150:573-574.
16. Volf EM, Levine DE, Michelon MA, et al. Assessor-blinded study of the metabolic syndrome and surrogate markers of increased cardiovascular risk in children with moderate-to-severe psoriasis compared with age-matched population of children with warts. J Drugs Dermatol. 2011;10:900-901.
17. Manzoni AP, Weber MB, Nagatomi AR, et al. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-899.
18. Belloni Fortina A, Neri L. Topical steroids and corticophobia. G Ital Dermatol Venereol. 2013;148:651-654.
19. Posso-De Los Rios CJ, Pope E, Lara-Corrales I. A systematic review of systemic medications for pustular psoriasis in pediatrics. Pediatr Dermatol. 2014;31:430-439.
20. Tollefson MM. Diagnosis and management of psoriasis in children. Pediatr Clin North Am. 2014;61:261-277.
21. Fotiadou C, Lazaridou E, Ioannides D. Management of psoriasis in adolescence. Adolesc Health Med Ther. 2014;5:25-34.
22. Windschall D, Müller T, Becker I, et al. Safety and efficacy of etanercept in children with the JIA categories extended oligoarthritis, enthesitis-related arthritis and psoriasis arthritis [published online ahead of print July 18, 2014]. Clin Rheumatol. 2015;34:61-69.
23. Mälkönen T, Wikström A, Heiskanen K, et al. Skin reactions during anti-TNFa therapy for pediatric inflammatory bowel disease: a 2-year prospective study. Inflamm Bowel Dis. 2014;20:1309-1315.
24. Afzali A, Wheat CL, Hu JK, et al. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8:480-488.
25. Sherlock ME, Walters T, Tabbers MM, et al. Infliximab-induced psoriasis and psoriasiform skin lesions in pediatric Crohn disease and a potential association with IL-23 receptor polymorphisms. J Pediatr Gastroenterol Nutr. 2013;56:512-518.
26. Rahman SI, Siegfried E, Flanagan KH, et al. The methotrexate polyglutamate assay supports the efficacy of methotrexate for severe inflammatory skin disease in children. J Am Acad Dermatol. 2014;70:252-256.
27. Suzuki E, Mellins ED, Gershwin ME, et al. The IL-23/IL-17 axis in psoriatic arthritis. Autoimmun Rev. 2014;13:496-502.
28. Michalak-Stoma A, Bartosi´nska J, Kowal M, et al. Serum levels of selected Th17 and Th22 cytokines in psoriatic patients. Dis Markers. 2013;35:625-631.
Psoriasis affects 2% to 4% of the US population, with approximately one-third of cases beginning in childhood. The understanding of pediatric psoriasis has developed at a far slower pace than adult disease, with limitations in care including few medications that are approved by the US Food and Drug Administration for pediatric and adolescent use. Recently, a stable fixed-combination dose of calcipo-triene 0.005%–betamethasone dipropionate 0.064% topical suspension was approved for treatment of plaque psoriasis of the scalp in patients aged 12 to 17 years, which hopefully will lead a trend in psoriasis medication approval for children and teenagers.1 Based on a PubMed search of articles indexed for MEDLINE using the search terms pediatric psoriasis, psoriasis, and strep that were published from April 2012 to April 2014, this article reviews newer data to address the issues that surround pediatric psoriasis and to provide an update on prior review articles on pediatric psoriasis.2-5 This article reviews some of the newer literature on clinical presentation and comorbidities in pediatric psoriasis.5 Based on these recent findings, additional screenings including review of obesity parameters are recommended for pediatric patients with psoriasis (Table 1).
Update on Disease Manifestations, Associations, and Comorbidities
Disease Manifestations
A 2013 multicenter study delineated the clinical features of pediatric psoriasis.6 The study was conducted at 8 geographically diverse dermatology clinics in the United States to delineate the clinical manifestations of pediatric psoriasis. In an assessment of 181 participants aged 5 to 17 years, the investigators sought to determine the frequency of disease sites, severity, and guttate disease. Over a period of approximately 2 years, 43.1% of participants were determined to have mild disease and 56.9% had severe disease. Family history of psoriasis was present in 51.4% of participants, with first-degree relatives affected in 59.8% of cases. Scalp involvement at some time was noted in 79.0% of participants, and nail disease was noted in 55% of boys and 29% of girls. Guttate psoriasis was noted in 30% of participants, with more cases in the severe range (35.9%) versus the mild range (21.8%). Additionally, 22.1% of participants had a precipitating streptococcal infection, with the association being more common in pediatric patients with guttate psoriasis than plaque psoriasis.6 This study highlighted that pediatric psoriasis has a genetic basis, is frequently guttate in nature, commonly affects the nails, shows a trend toward being classified as severe, and may be triggered by streptococcal infections.
Streptococcal Infection
Pediatric psoriasis may be triggered or flared by Streptococcus pyogenes (group A β-hemolytic streptococci) infections, specifically β-hemolytic streptococci groups A, C, and G that have streptococcal M protein,2,3,7 and this tendency can be associated with HLA-Cw6 or guttate psoriasis. Newer data have elucidated the role of streptococcal throat infections in psoriasis. Given that streptococcal throat infections are most common in school-aged children, these studies suggest a putative mechanism in pediatric psoriasis for triggering streptococcal infections, which would need to be confirmed in future studies, specifically in pediatric psoriasis patients.
It has been shown that T cells in psoriasis patients recognize common streptococcal M proteins and keratin determinants.7 Ferran et al8 recently demonstrated activation of circulating cutaneous lymphocyte–associated antigen (CLA)+ T cells but not CLA- memory T cells in 27 psoriasis patients (ages not specified) when mixed with streptococcal throat extracts, causing production of IL-17, IP-10, IL-22, and IFN-γ; activation was not found in 6 healthy control patients. Antistreptolysin O levels were correlated with the messenger RNA up- regulation for IL-17, IP-10, IL-22, and IFN-γ, and also correlated with psoriasis area and severity index score in psoriasis patients. In this same study, injection of the activated culture supernatant into mouse skin caused epidermal hyperkeratosis and activation of nonlesional epidermal cells from psoriatic patients. This study thereby delineated some of the potential pathways of the streptococcal induction of psoriasis and psoriatic flares in childhood8; however, confirmation is needed through further study of pediatric psoriatic lymphocyte activity.
Differential Diagnosis
Additions to the extensive differential list have been cited in the recent literature. The differential diagnosis of pediatric psoriasis now includes sodium valproate–induced psoriasiform drug eruption9 and allergic contact dermatitis to methylchloroisothiazolinone and methylisothiazolinone, which are present in many sanitizing hand and diaper wipes and has been reported to cause psoriasiform dermatitis in a periorificial or perineal distribution.10 Clinicians should inquire about the use of these wipes, as caregivers rarely suspect this agent to be causative of the eruption.
Psoriatic Arthritis
Previously, psoriasis and psoriatic arthritis have been linked to autoimmune thyroid disease in adults.11 A study of the Childhood Arthritis & Rheumatology Research Alliance (CARRA) registry showed that family history of psoriasis, autoimmune thyroiditis, Crohn disease, and ankylosing spondylitis in a first-degree relative has been linked to juvenile idiopathic arthritis, highlighting that pediatric psoriasis can be genetically linked or associated with multiple autoimmune conditions and vice versa.12
Obesity, Metabolic Syndrome, and Cardiovascular Risks
Obesity is associated with pediatric psoriasis as highlighted in a growing body of recent literature.13 Excess adiposity as manifested by body mass index in the 85th percentile or greater (37.9% of 155 pediatric psoriasis patients vs 20.5% of 42 controls) and excess central adiposity as manifested by excess waist circumference and increased waist-to-height ratios are more common in pediatric patients with psoriasis than in controls.14
Obesity may be a trigger or associated with increased disease activity in pediatric psoriasis patients. Excess overall adiposity correlates with more severe disease. Obesity parameters may correlate with the onset of psoriasis and with disease severity. In fact, the odds of obesity may be higher in childhood than in adults.14,15 A 2011 report of pediatric psoriasis patients aged 10 to 17 years (n=12) and wart controls (n=6)(mean age, 13.2 and 13.5 years, respectively) demonstrated that 4 of 12 patients with psoriasis and 0 of 6 patients with warts met criteria for metabolic syndrome as defined by 3 of the following: (1) triglycerides greater than or equal to 100 mg/dL; (2) high-density lipoprotein cholesterol less than 50 mg/dL in females and less than 5 mg/dL in males; (3) fasting blood glucose levels greater than or equal to 110 mg/dL, (4) waist circumference greater than the 75th percentile for age and sex; and (5) systolic or diastolic blood pressure greater than the 90th percentile for age, sex, and height.16 These studies highlight that obesity and metabolic syndrome are of concern in pediatric psoriasis patients; however, the best management approach using diet and weight interventions has yet to be identified.
Adiposity may precede the onset of psoriasis. A recent cohort of 27 pediatric psoriasis patients reported that the average age at onset of psoriasis was 8.7 years and the average age at onset of obesity was 4.1 years.15 In this study, 93% (25/27) of patients had adiposity preceding their psoriasis by 2 or more years. It is unclear if this is nature or nurture, as 48% (13/27) of patients had a family history of obesity, 41% (11/27) had a family history of psoriasis, and 48% (13/27) had a family history of hyperlipidemia.15 Therefore, obesity may be cultivated in some psoriatic families. The issue of household influences on diet and obesity needs to be addressed if successful weight management is to be achieved in future studies of pediatric psoriasis.
Cardiovascular risks in the pediatric psoriasis population are the subject of ongoing assessment but will likely mimic studies of adult psoriasis patients when reviewed longitudinally.16 Weight loss and healthy lifestyle interventions likely are beneficial to long-term health, but there is a lack of published data addressing dietary modification as a disease modifier for long-term care of pediatric psoriasis.
Anxiety and Depression
Anxiety and depression have been noted in adults with chronic skin diseases. A recent study assessed 118 patients and caregivers of pediatric patients with atopic dermatitis (n=50), psoriasis (n=25), or vitiligo (n=43) using the Children’s Dermatology Life Quality Index, the Hamilton Anxiety Scale, and the Beck Depression Inventory.17 Anxiety and depression were found in 36% of caregivers of pediatric psoriasis patients and depression was found in 36% of pediatric psoriasis patients, highlighting the need for interventions on a personal and family level to improve quality of life. As a comparator, anxiety was more prevalent in vitiligo caregivers (42%), but depression was only found in 26% of caregivers in the same group. Extent of disease (25%–75% body surface area affected) correlated with both depression and anxiety in the caregivers of pediatric patients with psoriasis as well as with anxiety in caregivers of pediatric patients with increased visible surface area of vitiligo.17 Parental anxiety has been reported at times to be linked to corticosteroid phobia, or corticophobia, which may interfere with disease therapy, as topical corticosteroids are considered the mainstay of therapy in childhood disease.18 Coordinating care with caregivers and addressing their concerns about the safety of medications should be integral to the pediatric psoriasis visit.
Pustular Psoriasis
Pustular psoriasis can be seen in any age group. Researchers recently have attempted to delineate the features and successful management of this severe subset of pediatric psoriasis patients. Twenty-four pediatric pustular psoriasis cases reviewed by Posso-De Los Rios et al19 revealed that 92% (22/24) had generalized and 8% (2/24) had limited acral disease. The mean (standard deviation) age at onset of pediatric pustular psoriasis was 6.3 (4.9) years. Half of the reported cases required more than one intervention. Treatment with acitretin, cyclosporine, and methotrexate was effective, but the investigators identified that there is a true dearth of evidence-based therapeutics in pediatric pustular psoriasis and much rebound with discontinuation.19 Although the subset of pediatric pustular psoriasis is rare, study of evidence-based intervention is needed.
Therapy
Recent reviews of pediatric and adolescent psoriasis highlight the paucity of therapeutic information for these patient populations. Investigators typically focus on topical therapies as the basis of treatment,20 as well as the addition of phototherapy in mild to moderate plaque or guttate psoriasis and biologic or systemic agents in moderate to severe flares of plaque, erythrodermic, or pustular psoriasis.21 Further studies are needed to identify evidence-based therapeutic paradigms for pediatric psoriasis and to pinpoint therapies associated with the best quality of life in patients and their caregivers.
Tumor Necrosis Factor α Inhibitors
Safety and efficacy of etanercept for juvenile idiopathic arthritis including oligoarthritis, enthesitis-related arthritis, and psoriatic arthritis recently was reviewed by Windschall et al22 using data from the German pediatric Biologika in der Kinderrheumatologie registry. Juvenile Arthritis Disease Activity Score 10 improved from baseline for 127 pediatric patients with psoriatic arthritis in 3 to 24 months (mean [standard deviation], 14.7 [6.4], 5.0 [4.6], 5.3 [6.4] at baseline, 3 months, and 24 months, respectively). Overall side effects were relatively higher in the psoriatic arthritis group; the rate of serious (relative risk, 1.39 [0.95-2.03; P=.08]) and nonserious (relative risk, 1.18 [1.02-1.35; P=.03]) adverse events also was elevated. Uveitis risk was greatest in the psoriatic arthritis group and the number of associated cases of inflammatory bowel disease outnumbered those seen in other forms of arthritis. The investigators concluded that monitoring for extra-articular immunopathies should be conducted in pediatric patients with psoriatic arthritis who are undergoing etanercept therapy.22
Tumor necrosis factor α (TNF-α) inhibitors have been associated with triggering psoriasiform dermatitis in pediatric patients treated for inflammatory bowel disease. A Finnish study of infliximab side effects in pediatric patients with inflammatory bowel disease (n=84; Crohn disease: n=64) demonstrated that almost half (47.6% [40/84]) of the participants presented with chronic skin reactions, 23% of which were severe in nature.23 Psoriasiform lesions of the scalp and ears were most common, followed by the periorificial area, genitals, trunk, and extremities. Rare association with HLA-Cw*0602 genotype was noted. Skin manifestations did not correlate with gut inflammation (as determined by fecal calprotectin levels). Discontinuation of therapy rarely was required.23 Other studies also have highlighted this side effect, suggesting an incidence of 2.7% in adults with colitis treated with TNF-α inhibitors24 and 10.5% in pediatric patients with Crohn disease.25 In a study by Sherlock et al,25 pediatric patients with Crohn disease developing psoriasis following infliximab therapy were more likely to be homozygous for specific polymorphisms in the IL-23R gene (rs10489628, rs10789229, and rs1343151).
Methotrexate
For pediatric patients who are being treated with methotrexate, the polyglutamate assay recently has been reported to be helpful in identifying patients needing a dose escalation.26 Higher numbers on the polyglutamate assay are associated with superior response to methotrexate therapy. Doses can be increased after 12 weeks in patients with low assays.26
IL-23
The safety of IL-23 blockade in pediatric psoriasis patients has not yet been established, but data from adult cases have implicated the IL-17 and IL-23 pathways in psoriasis/psoriatic arthritis, including an association with IL-23R polymorphisms27 and increases in soluble IL-20 and IL-22 associated with disease severity and an association of IL-17 levels with activity on the psoriasis area and severity index scores.28 The data are more limited for pediatric cases. Pediatric patients with inflammatory bowel disease who have an IL-23R polymorphism appear to be susceptible to psoriatic flares while on TNF-α inhibitor therapy,25 which suggests that the IL-23 blockade may be of benefit for some pediatric patients with psoriasis or psoriatic arthritis.
Conclusion
Pediatric psoriasis and psoriatic arthritis have now been identified as being part of the autoimmune spectrum and are associated with metabolic syndrome, including obesity and excess central adiposity, similar to their adult variants. An overview of potential unmet needs in pediatric psoriasis is included in Table 2. These unmet needs include further delineation of diet and weight modification in the care and prevention of psoriasis; expansion of therapeutic trials and US Food and Drug Administration–approved medications for children with psoriasis, especially severe variants such as extensive plaque and pustular disease; and development of guidelines for ongoing monitoring of children with psoriasis. The role of therapeutic interventions and weight management on long-term disease course remains to be shown in extended clinical trials. Despite the great advancements in psoriatic care, knowledge gaps remain in pediatric psoriasis that will need to be addressed in the future.
Psoriasis affects 2% to 4% of the US population, with approximately one-third of cases beginning in childhood. The understanding of pediatric psoriasis has developed at a far slower pace than adult disease, with limitations in care including few medications that are approved by the US Food and Drug Administration for pediatric and adolescent use. Recently, a stable fixed-combination dose of calcipo-triene 0.005%–betamethasone dipropionate 0.064% topical suspension was approved for treatment of plaque psoriasis of the scalp in patients aged 12 to 17 years, which hopefully will lead a trend in psoriasis medication approval for children and teenagers.1 Based on a PubMed search of articles indexed for MEDLINE using the search terms pediatric psoriasis, psoriasis, and strep that were published from April 2012 to April 2014, this article reviews newer data to address the issues that surround pediatric psoriasis and to provide an update on prior review articles on pediatric psoriasis.2-5 This article reviews some of the newer literature on clinical presentation and comorbidities in pediatric psoriasis.5 Based on these recent findings, additional screenings including review of obesity parameters are recommended for pediatric patients with psoriasis (Table 1).
Update on Disease Manifestations, Associations, and Comorbidities
Disease Manifestations
A 2013 multicenter study delineated the clinical features of pediatric psoriasis.6 The study was conducted at 8 geographically diverse dermatology clinics in the United States to delineate the clinical manifestations of pediatric psoriasis. In an assessment of 181 participants aged 5 to 17 years, the investigators sought to determine the frequency of disease sites, severity, and guttate disease. Over a period of approximately 2 years, 43.1% of participants were determined to have mild disease and 56.9% had severe disease. Family history of psoriasis was present in 51.4% of participants, with first-degree relatives affected in 59.8% of cases. Scalp involvement at some time was noted in 79.0% of participants, and nail disease was noted in 55% of boys and 29% of girls. Guttate psoriasis was noted in 30% of participants, with more cases in the severe range (35.9%) versus the mild range (21.8%). Additionally, 22.1% of participants had a precipitating streptococcal infection, with the association being more common in pediatric patients with guttate psoriasis than plaque psoriasis.6 This study highlighted that pediatric psoriasis has a genetic basis, is frequently guttate in nature, commonly affects the nails, shows a trend toward being classified as severe, and may be triggered by streptococcal infections.
Streptococcal Infection
Pediatric psoriasis may be triggered or flared by Streptococcus pyogenes (group A β-hemolytic streptococci) infections, specifically β-hemolytic streptococci groups A, C, and G that have streptococcal M protein,2,3,7 and this tendency can be associated with HLA-Cw6 or guttate psoriasis. Newer data have elucidated the role of streptococcal throat infections in psoriasis. Given that streptococcal throat infections are most common in school-aged children, these studies suggest a putative mechanism in pediatric psoriasis for triggering streptococcal infections, which would need to be confirmed in future studies, specifically in pediatric psoriasis patients.
It has been shown that T cells in psoriasis patients recognize common streptococcal M proteins and keratin determinants.7 Ferran et al8 recently demonstrated activation of circulating cutaneous lymphocyte–associated antigen (CLA)+ T cells but not CLA- memory T cells in 27 psoriasis patients (ages not specified) when mixed with streptococcal throat extracts, causing production of IL-17, IP-10, IL-22, and IFN-γ; activation was not found in 6 healthy control patients. Antistreptolysin O levels were correlated with the messenger RNA up- regulation for IL-17, IP-10, IL-22, and IFN-γ, and also correlated with psoriasis area and severity index score in psoriasis patients. In this same study, injection of the activated culture supernatant into mouse skin caused epidermal hyperkeratosis and activation of nonlesional epidermal cells from psoriatic patients. This study thereby delineated some of the potential pathways of the streptococcal induction of psoriasis and psoriatic flares in childhood8; however, confirmation is needed through further study of pediatric psoriatic lymphocyte activity.
Differential Diagnosis
Additions to the extensive differential list have been cited in the recent literature. The differential diagnosis of pediatric psoriasis now includes sodium valproate–induced psoriasiform drug eruption9 and allergic contact dermatitis to methylchloroisothiazolinone and methylisothiazolinone, which are present in many sanitizing hand and diaper wipes and has been reported to cause psoriasiform dermatitis in a periorificial or perineal distribution.10 Clinicians should inquire about the use of these wipes, as caregivers rarely suspect this agent to be causative of the eruption.
Psoriatic Arthritis
Previously, psoriasis and psoriatic arthritis have been linked to autoimmune thyroid disease in adults.11 A study of the Childhood Arthritis & Rheumatology Research Alliance (CARRA) registry showed that family history of psoriasis, autoimmune thyroiditis, Crohn disease, and ankylosing spondylitis in a first-degree relative has been linked to juvenile idiopathic arthritis, highlighting that pediatric psoriasis can be genetically linked or associated with multiple autoimmune conditions and vice versa.12
Obesity, Metabolic Syndrome, and Cardiovascular Risks
Obesity is associated with pediatric psoriasis as highlighted in a growing body of recent literature.13 Excess adiposity as manifested by body mass index in the 85th percentile or greater (37.9% of 155 pediatric psoriasis patients vs 20.5% of 42 controls) and excess central adiposity as manifested by excess waist circumference and increased waist-to-height ratios are more common in pediatric patients with psoriasis than in controls.14
Obesity may be a trigger or associated with increased disease activity in pediatric psoriasis patients. Excess overall adiposity correlates with more severe disease. Obesity parameters may correlate with the onset of psoriasis and with disease severity. In fact, the odds of obesity may be higher in childhood than in adults.14,15 A 2011 report of pediatric psoriasis patients aged 10 to 17 years (n=12) and wart controls (n=6)(mean age, 13.2 and 13.5 years, respectively) demonstrated that 4 of 12 patients with psoriasis and 0 of 6 patients with warts met criteria for metabolic syndrome as defined by 3 of the following: (1) triglycerides greater than or equal to 100 mg/dL; (2) high-density lipoprotein cholesterol less than 50 mg/dL in females and less than 5 mg/dL in males; (3) fasting blood glucose levels greater than or equal to 110 mg/dL, (4) waist circumference greater than the 75th percentile for age and sex; and (5) systolic or diastolic blood pressure greater than the 90th percentile for age, sex, and height.16 These studies highlight that obesity and metabolic syndrome are of concern in pediatric psoriasis patients; however, the best management approach using diet and weight interventions has yet to be identified.
Adiposity may precede the onset of psoriasis. A recent cohort of 27 pediatric psoriasis patients reported that the average age at onset of psoriasis was 8.7 years and the average age at onset of obesity was 4.1 years.15 In this study, 93% (25/27) of patients had adiposity preceding their psoriasis by 2 or more years. It is unclear if this is nature or nurture, as 48% (13/27) of patients had a family history of obesity, 41% (11/27) had a family history of psoriasis, and 48% (13/27) had a family history of hyperlipidemia.15 Therefore, obesity may be cultivated in some psoriatic families. The issue of household influences on diet and obesity needs to be addressed if successful weight management is to be achieved in future studies of pediatric psoriasis.
Cardiovascular risks in the pediatric psoriasis population are the subject of ongoing assessment but will likely mimic studies of adult psoriasis patients when reviewed longitudinally.16 Weight loss and healthy lifestyle interventions likely are beneficial to long-term health, but there is a lack of published data addressing dietary modification as a disease modifier for long-term care of pediatric psoriasis.
Anxiety and Depression
Anxiety and depression have been noted in adults with chronic skin diseases. A recent study assessed 118 patients and caregivers of pediatric patients with atopic dermatitis (n=50), psoriasis (n=25), or vitiligo (n=43) using the Children’s Dermatology Life Quality Index, the Hamilton Anxiety Scale, and the Beck Depression Inventory.17 Anxiety and depression were found in 36% of caregivers of pediatric psoriasis patients and depression was found in 36% of pediatric psoriasis patients, highlighting the need for interventions on a personal and family level to improve quality of life. As a comparator, anxiety was more prevalent in vitiligo caregivers (42%), but depression was only found in 26% of caregivers in the same group. Extent of disease (25%–75% body surface area affected) correlated with both depression and anxiety in the caregivers of pediatric patients with psoriasis as well as with anxiety in caregivers of pediatric patients with increased visible surface area of vitiligo.17 Parental anxiety has been reported at times to be linked to corticosteroid phobia, or corticophobia, which may interfere with disease therapy, as topical corticosteroids are considered the mainstay of therapy in childhood disease.18 Coordinating care with caregivers and addressing their concerns about the safety of medications should be integral to the pediatric psoriasis visit.
Pustular Psoriasis
Pustular psoriasis can be seen in any age group. Researchers recently have attempted to delineate the features and successful management of this severe subset of pediatric psoriasis patients. Twenty-four pediatric pustular psoriasis cases reviewed by Posso-De Los Rios et al19 revealed that 92% (22/24) had generalized and 8% (2/24) had limited acral disease. The mean (standard deviation) age at onset of pediatric pustular psoriasis was 6.3 (4.9) years. Half of the reported cases required more than one intervention. Treatment with acitretin, cyclosporine, and methotrexate was effective, but the investigators identified that there is a true dearth of evidence-based therapeutics in pediatric pustular psoriasis and much rebound with discontinuation.19 Although the subset of pediatric pustular psoriasis is rare, study of evidence-based intervention is needed.
Therapy
Recent reviews of pediatric and adolescent psoriasis highlight the paucity of therapeutic information for these patient populations. Investigators typically focus on topical therapies as the basis of treatment,20 as well as the addition of phototherapy in mild to moderate plaque or guttate psoriasis and biologic or systemic agents in moderate to severe flares of plaque, erythrodermic, or pustular psoriasis.21 Further studies are needed to identify evidence-based therapeutic paradigms for pediatric psoriasis and to pinpoint therapies associated with the best quality of life in patients and their caregivers.
Tumor Necrosis Factor α Inhibitors
Safety and efficacy of etanercept for juvenile idiopathic arthritis including oligoarthritis, enthesitis-related arthritis, and psoriatic arthritis recently was reviewed by Windschall et al22 using data from the German pediatric Biologika in der Kinderrheumatologie registry. Juvenile Arthritis Disease Activity Score 10 improved from baseline for 127 pediatric patients with psoriatic arthritis in 3 to 24 months (mean [standard deviation], 14.7 [6.4], 5.0 [4.6], 5.3 [6.4] at baseline, 3 months, and 24 months, respectively). Overall side effects were relatively higher in the psoriatic arthritis group; the rate of serious (relative risk, 1.39 [0.95-2.03; P=.08]) and nonserious (relative risk, 1.18 [1.02-1.35; P=.03]) adverse events also was elevated. Uveitis risk was greatest in the psoriatic arthritis group and the number of associated cases of inflammatory bowel disease outnumbered those seen in other forms of arthritis. The investigators concluded that monitoring for extra-articular immunopathies should be conducted in pediatric patients with psoriatic arthritis who are undergoing etanercept therapy.22
Tumor necrosis factor α (TNF-α) inhibitors have been associated with triggering psoriasiform dermatitis in pediatric patients treated for inflammatory bowel disease. A Finnish study of infliximab side effects in pediatric patients with inflammatory bowel disease (n=84; Crohn disease: n=64) demonstrated that almost half (47.6% [40/84]) of the participants presented with chronic skin reactions, 23% of which were severe in nature.23 Psoriasiform lesions of the scalp and ears were most common, followed by the periorificial area, genitals, trunk, and extremities. Rare association with HLA-Cw*0602 genotype was noted. Skin manifestations did not correlate with gut inflammation (as determined by fecal calprotectin levels). Discontinuation of therapy rarely was required.23 Other studies also have highlighted this side effect, suggesting an incidence of 2.7% in adults with colitis treated with TNF-α inhibitors24 and 10.5% in pediatric patients with Crohn disease.25 In a study by Sherlock et al,25 pediatric patients with Crohn disease developing psoriasis following infliximab therapy were more likely to be homozygous for specific polymorphisms in the IL-23R gene (rs10489628, rs10789229, and rs1343151).
Methotrexate
For pediatric patients who are being treated with methotrexate, the polyglutamate assay recently has been reported to be helpful in identifying patients needing a dose escalation.26 Higher numbers on the polyglutamate assay are associated with superior response to methotrexate therapy. Doses can be increased after 12 weeks in patients with low assays.26
IL-23
The safety of IL-23 blockade in pediatric psoriasis patients has not yet been established, but data from adult cases have implicated the IL-17 and IL-23 pathways in psoriasis/psoriatic arthritis, including an association with IL-23R polymorphisms27 and increases in soluble IL-20 and IL-22 associated with disease severity and an association of IL-17 levels with activity on the psoriasis area and severity index scores.28 The data are more limited for pediatric cases. Pediatric patients with inflammatory bowel disease who have an IL-23R polymorphism appear to be susceptible to psoriatic flares while on TNF-α inhibitor therapy,25 which suggests that the IL-23 blockade may be of benefit for some pediatric patients with psoriasis or psoriatic arthritis.
Conclusion
Pediatric psoriasis and psoriatic arthritis have now been identified as being part of the autoimmune spectrum and are associated with metabolic syndrome, including obesity and excess central adiposity, similar to their adult variants. An overview of potential unmet needs in pediatric psoriasis is included in Table 2. These unmet needs include further delineation of diet and weight modification in the care and prevention of psoriasis; expansion of therapeutic trials and US Food and Drug Administration–approved medications for children with psoriasis, especially severe variants such as extensive plaque and pustular disease; and development of guidelines for ongoing monitoring of children with psoriasis. The role of therapeutic interventions and weight management on long-term disease course remains to be shown in extended clinical trials. Despite the great advancements in psoriatic care, knowledge gaps remain in pediatric psoriasis that will need to be addressed in the future.
1. Taclonex Expanded Indication. OptumRx Web site. https://www.optumrx.com/vgnpreview/HCP/Assets/RxNews/Clinical%20Updates_Taclonex_2014-1003.pdf. Published August 29, 2014. Accessed January 28, 2015.
2. Silverberg NB. Update on pediatric psoriasis, part 1: clinical features and demographics. Cutis. 2010;86:118-124.
3. Silverberg NB. Update on pediatric psoriasis, part 2: therapeutic management. Cutis. 2010;86:172-176.
4. Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33(2 suppl 2):S42-S44.
5. Khorsand K, Sidbury R. Recent advances in pediatric dermatology. Arch Dis Child. 2014;99:944-948.
6. Mercy K, Kwasny M, Cordoro KM, et al. Clinical manifestations of pediatric psoriasis: results of a multicenter study in the United States. Pediatr Dermatol. 2013;30:424-428.
7. Gudjonsson JE, Thorarinsson AM, Sigurgeirsson B, et al. Streptococcal throat infections and exacerbation of chronic plaque psoriasis: a prospective study. Br J Dermatol. 2003;149:530-534.
8. Ferran M, Galván AB, Rincón C, et al. Streptococcus induces circulating CLA(+) memory T-cell-dependent epidermal cell activation in psoriasis. J Invest Dermatol. 2013;133:999-1007.
9. Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate [published online ahead of print November 13, 2013]. Case Rep Pediatr. 2013;2013:823469.
10. Chang MW, Nakrani R. Six children with allergic contact dermatitis to methylisothiazolinone in wet wipes (baby wipes). Pediatrics. 2014;133:e434-e438.
11. Gul U, Gonul M, Kaya I, et al. Autoimmune thyroid disorders in patients with psoriasis. Eur J Dermatol. 2009;19:221-223.
12. Prahalad S, McCracken C, Ponder L, et al. A120: Familial autoimmunity in the CARRA registry. Arthritis Rheumatol. 2014;66(suppl 11):S157.
13. Mercy KM, Paller AS. The relationship between obesity and psoriasis in the pediatric population: implications and future directions. Cutis. 2013;92:107-109.
14. Paller AS, Mercy K, Kwasny MJ, et al. Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol. 2013;149:166-176.
15. Becker L, Tom WL, Eshagh K, et al. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014;150:573-574.
16. Volf EM, Levine DE, Michelon MA, et al. Assessor-blinded study of the metabolic syndrome and surrogate markers of increased cardiovascular risk in children with moderate-to-severe psoriasis compared with age-matched population of children with warts. J Drugs Dermatol. 2011;10:900-901.
17. Manzoni AP, Weber MB, Nagatomi AR, et al. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-899.
18. Belloni Fortina A, Neri L. Topical steroids and corticophobia. G Ital Dermatol Venereol. 2013;148:651-654.
19. Posso-De Los Rios CJ, Pope E, Lara-Corrales I. A systematic review of systemic medications for pustular psoriasis in pediatrics. Pediatr Dermatol. 2014;31:430-439.
20. Tollefson MM. Diagnosis and management of psoriasis in children. Pediatr Clin North Am. 2014;61:261-277.
21. Fotiadou C, Lazaridou E, Ioannides D. Management of psoriasis in adolescence. Adolesc Health Med Ther. 2014;5:25-34.
22. Windschall D, Müller T, Becker I, et al. Safety and efficacy of etanercept in children with the JIA categories extended oligoarthritis, enthesitis-related arthritis and psoriasis arthritis [published online ahead of print July 18, 2014]. Clin Rheumatol. 2015;34:61-69.
23. Mälkönen T, Wikström A, Heiskanen K, et al. Skin reactions during anti-TNFa therapy for pediatric inflammatory bowel disease: a 2-year prospective study. Inflamm Bowel Dis. 2014;20:1309-1315.
24. Afzali A, Wheat CL, Hu JK, et al. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8:480-488.
25. Sherlock ME, Walters T, Tabbers MM, et al. Infliximab-induced psoriasis and psoriasiform skin lesions in pediatric Crohn disease and a potential association with IL-23 receptor polymorphisms. J Pediatr Gastroenterol Nutr. 2013;56:512-518.
26. Rahman SI, Siegfried E, Flanagan KH, et al. The methotrexate polyglutamate assay supports the efficacy of methotrexate for severe inflammatory skin disease in children. J Am Acad Dermatol. 2014;70:252-256.
27. Suzuki E, Mellins ED, Gershwin ME, et al. The IL-23/IL-17 axis in psoriatic arthritis. Autoimmun Rev. 2014;13:496-502.
28. Michalak-Stoma A, Bartosi´nska J, Kowal M, et al. Serum levels of selected Th17 and Th22 cytokines in psoriatic patients. Dis Markers. 2013;35:625-631.
1. Taclonex Expanded Indication. OptumRx Web site. https://www.optumrx.com/vgnpreview/HCP/Assets/RxNews/Clinical%20Updates_Taclonex_2014-1003.pdf. Published August 29, 2014. Accessed January 28, 2015.
2. Silverberg NB. Update on pediatric psoriasis, part 1: clinical features and demographics. Cutis. 2010;86:118-124.
3. Silverberg NB. Update on pediatric psoriasis, part 2: therapeutic management. Cutis. 2010;86:172-176.
4. Cather JC. Psoriasis in children and women: addressing some special needs. Semin Cutan Med Surg. 2014;33(2 suppl 2):S42-S44.
5. Khorsand K, Sidbury R. Recent advances in pediatric dermatology. Arch Dis Child. 2014;99:944-948.
6. Mercy K, Kwasny M, Cordoro KM, et al. Clinical manifestations of pediatric psoriasis: results of a multicenter study in the United States. Pediatr Dermatol. 2013;30:424-428.
7. Gudjonsson JE, Thorarinsson AM, Sigurgeirsson B, et al. Streptococcal throat infections and exacerbation of chronic plaque psoriasis: a prospective study. Br J Dermatol. 2003;149:530-534.
8. Ferran M, Galván AB, Rincón C, et al. Streptococcus induces circulating CLA(+) memory T-cell-dependent epidermal cell activation in psoriasis. J Invest Dermatol. 2013;133:999-1007.
9. Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate [published online ahead of print November 13, 2013]. Case Rep Pediatr. 2013;2013:823469.
10. Chang MW, Nakrani R. Six children with allergic contact dermatitis to methylisothiazolinone in wet wipes (baby wipes). Pediatrics. 2014;133:e434-e438.
11. Gul U, Gonul M, Kaya I, et al. Autoimmune thyroid disorders in patients with psoriasis. Eur J Dermatol. 2009;19:221-223.
12. Prahalad S, McCracken C, Ponder L, et al. A120: Familial autoimmunity in the CARRA registry. Arthritis Rheumatol. 2014;66(suppl 11):S157.
13. Mercy KM, Paller AS. The relationship between obesity and psoriasis in the pediatric population: implications and future directions. Cutis. 2013;92:107-109.
14. Paller AS, Mercy K, Kwasny MJ, et al. Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol. 2013;149:166-176.
15. Becker L, Tom WL, Eshagh K, et al. Excess adiposity preceding pediatric psoriasis. JAMA Dermatol. 2014;150:573-574.
16. Volf EM, Levine DE, Michelon MA, et al. Assessor-blinded study of the metabolic syndrome and surrogate markers of increased cardiovascular risk in children with moderate-to-severe psoriasis compared with age-matched population of children with warts. J Drugs Dermatol. 2011;10:900-901.
17. Manzoni AP, Weber MB, Nagatomi AR, et al. Assessing depression and anxiety in the caregivers of pediatric patients with chronic skin disorders. An Bras Dermatol. 2013;88:894-899.
18. Belloni Fortina A, Neri L. Topical steroids and corticophobia. G Ital Dermatol Venereol. 2013;148:651-654.
19. Posso-De Los Rios CJ, Pope E, Lara-Corrales I. A systematic review of systemic medications for pustular psoriasis in pediatrics. Pediatr Dermatol. 2014;31:430-439.
20. Tollefson MM. Diagnosis and management of psoriasis in children. Pediatr Clin North Am. 2014;61:261-277.
21. Fotiadou C, Lazaridou E, Ioannides D. Management of psoriasis in adolescence. Adolesc Health Med Ther. 2014;5:25-34.
22. Windschall D, Müller T, Becker I, et al. Safety and efficacy of etanercept in children with the JIA categories extended oligoarthritis, enthesitis-related arthritis and psoriasis arthritis [published online ahead of print July 18, 2014]. Clin Rheumatol. 2015;34:61-69.
23. Mälkönen T, Wikström A, Heiskanen K, et al. Skin reactions during anti-TNFa therapy for pediatric inflammatory bowel disease: a 2-year prospective study. Inflamm Bowel Dis. 2014;20:1309-1315.
24. Afzali A, Wheat CL, Hu JK, et al. The association of psoriasiform rash with anti-tumor necrosis factor (anti-TNF) therapy in inflammatory bowel disease: a single academic center case series. J Crohns Colitis. 2014;8:480-488.
25. Sherlock ME, Walters T, Tabbers MM, et al. Infliximab-induced psoriasis and psoriasiform skin lesions in pediatric Crohn disease and a potential association with IL-23 receptor polymorphisms. J Pediatr Gastroenterol Nutr. 2013;56:512-518.
26. Rahman SI, Siegfried E, Flanagan KH, et al. The methotrexate polyglutamate assay supports the efficacy of methotrexate for severe inflammatory skin disease in children. J Am Acad Dermatol. 2014;70:252-256.
27. Suzuki E, Mellins ED, Gershwin ME, et al. The IL-23/IL-17 axis in psoriatic arthritis. Autoimmun Rev. 2014;13:496-502.
28. Michalak-Stoma A, Bartosi´nska J, Kowal M, et al. Serum levels of selected Th17 and Th22 cytokines in psoriatic patients. Dis Markers. 2013;35:625-631.
Practice Points
- The majority of children with psoriasis have severe disease, scalp involvement, and a family history.
- Pediatric psoriasis is associated with metabolic syndrome, especially obesity.
- Anxiety and depression may be noted in children with psoriasis as well as their caregivers.
Kinetin and the skin
Kinetin (N6-furfuryladenine or 6-furfurylaminopurine) is a plant cytokinin or phytohormone that promotes cell division, delays senescence in plants, and is reputed to aid in the restoration of skin barrier function and, possibly, in reducing the signs and symptoms of rosacea (Clin. Exp. Dermatol. 2007;32:693-5; Plant Sci. 1999;148:37-45).
Kinetin is believed to develop in cellular DNA as a product of the oxidative, secondary modification of DNA (Plant Sci. 1999;148:37-45). In 1955, it became the first cytokinin isolated from DNA (from herring sperm) as an artifactual rearrangement product of the autoclaving process (J. Cosmet. Dermatol. 2007;6:243-9; Int. J. Biol. Macromol. 2007;40:182-92).
It has since been found to be present in human urine as well as DNA freshly extracted from human cells (Int. J. Biol. Macromol. 2007;40:182-92). The preponderance of amassed experimental evidence suggests that endogenous kinetin acts in vitro and in vivo as a potent antioxidant (Plant Sci. 1999;148:37-45). Currently, it is used as an anti-aging agent in various cosmetic products (J. Cosmet. Dermatol. 2007;6:243-9; J. Cosmet. Dermatol. 2010;9:218-25). Synthetic kinetin is thought to have the capacity to neutralize free radicals as well as limit the damage to DNA and fibroblasts (Photochem. Photobiol. 2012;88:748-52).
In vitro results
Olsen et al. demonstrated in vitro in 1999 that kinetin dose-dependently protected DNA against oxidative damage mediated by the Fenton reaction, and noted that kinetin had previously been linked to anti-aging activity in plants, fruit flies, and human cells in culture (Biochem. Biophys. Res. Commun. 1999;265:499-502). The following year, Verbeke et al. showed in vitro that kinetin potently inhibited damage caused by oxidation and glycoxidation (Biochem. Biophys. Res. Commun. 2000;276:1265-70).
In 2006, Vicanova et al. analyzed the effects of active ingredients from topical and systemic skin care formulations in vitro, finding that kinetin affected the upper dermis by enhancing deposits of fibrillin-1 and elastin fibers as well as their organization perpendicular to the dermal-epidermal junction. In the epidermis, kinetin stimulated keratinocyte production. Further, the investigators noted that the combination of topically applied kinetin with Imedeen Time Perfection ingredients (i.e., BioMarine Complex, grape seed extract, tomato extract, and vitamin C) supplemented systemically into culture medium yielded complementary benefits to dermal and epidermal development (Ann. N.Y. Acad. Sci. 2006;1067:337-42).
It is worth noting that in a study by Tournas et al. published the same month, investigators found that the topical application of a combination of vitamins C and E and ferulic acid yielded photoprotection to pig skin at 5 times the minimal erythema dose (MED) while individual antioxidants to which it was compared (i.e., coenzyme Q10, idebenone, and kinetin) delivered no photoprotective effects (J. Invest. Dermatol. 2006;126:1185-7). Nevertheless, Barciszewski et al. have observed that kinetin is the first stable secondary DNA damage product characterized by well defined cytokinin and anti-aging activity, with data showing that it has delayed human cellular aging in culture (Int. J. Biol. Macromol. 2007;40:182-92).
Rosacea
In 2007, Wu et al. performed a 12-week open-label study in 15 women and 3 men (aged 30-67 years) to ascertain the tolerability and efficacy of kinetin 0.1% lotion in the treatment of mild to moderate facial rosacea. Patients (17 of whom completed the study) applied the lotion twice daily, also daily applying an SPF 30 sunscreen. By week 4, significant improvements were observed in the reduction of skin roughness and mottled hyperpigmentation. Subject assessments at each 4-week interval after baseline and after 12 weeks revealed that kinetin 0.1% was well tolerated and effective for mild to moderate inflammatory rosacea (Clin. Exp. Dermatol. 2007;32:693-5).
Anti-aging
A 2002 study by J.L. McCullough and G.D. Weinstein represented the first evidence of the efficacy of topical kinetin in human beings, with twice-daily application for 24 weeks found to ameliorate skin texture, color, and blotchiness while diminishing rhytides and transepidermal water loss (J. Cosmet. Dermatol. 2002;15:29-32).
Two years later, T. Kimura and K. Doi showed that topical administration of kinetin improved the texture, wrinkling, and pigmentation of aged skin of hairless descendants of Mexican hairless dogs, resulting in notable depigmentation and rejuvenation after 100 days of treatment (Rejuvenation Res. 2004;7:32-9).In 2007, Chiu et al. conducted a randomized, double-blind, placebo-controlled, split-face comparative study in 52 Taiwanese subjects aged 30-60 years (90% of whom were female, all of whom had Fitzpatrick skin types II, III, or IV) to evaluate the clinical anti-aging effects and efficacy differences between kinetin plus niacinamide (kinetin 0.03%, niacinamide 4%) and niacinamide 4% alone versus vehicle placebo.
In the combination group, significant and sustained decreases were observed in counts of spots, pores, wrinkles, and evenness as well as persistent reductions in erythema index at weeks 8 and 12. At week 12, stratum corneum hydration status also was significantly enhanced in this group. In the niacinamide-only group, pore and evenness counts were significantly decreased at week 8, with declines in wrinkle counts emerging at week 12. The investigators concluded that kinetin and niacinamide display synergistic and dynamic anti-aging effects, showing substantial potential as topical anti-aging cosmeceutical agents (J. Cosmet. Dermatol. 2007;6:243-9).
However, Levin et al. noted in 2010 that while the effects of kinetin have been established in plants and its antioxidant properties have been displayed in vitro, the anti-aging effects and clinical efficacy ascribed to kinetin have been based on limited evidence, with no studies extant on the percutaneous absorption of kinetin. They added that research elucidating the mechanisms through which kinetin appears to improve skin barrier function, texture, and pigmentation also are lacking (J. Clin. Aesthet. Dermatol. 2010;3:22-41).
In 2012, Campos et al. assessed the effects on hydration, viscoelastic characteristics, and photoprotection of cosmetic preparations containing a dispersion of liposome with magnesium ascorbyl phosphate, alpha-lipoic acid, and kinetin. They observed that the formulation protected hairless mouse skin barrier function against UV harm. After 4 weeks of application on human skin, the combination product was found to have improved moisturization of the stratum corneum, also delivering hydration effects to deeper skin layers. The researchers concluded that the cosmetic formulation containing kinetin shows promise as a cutaneous anti-aging product (Photochem. Photobiol. 2012;88:748-52).
Conclusion
While some experimental and clinical results appear to suggest an anti-aging effect exerted by topically applied kinetin, much more research – particularly randomized controlled and comparison studies – are needed to provide a clearer picture as to the mechanisms and appropriate role of kinetin in the dermatologic armamentarium.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy,Topix Pharmaceuticals, and Unilever.
Kinetin (N6-furfuryladenine or 6-furfurylaminopurine) is a plant cytokinin or phytohormone that promotes cell division, delays senescence in plants, and is reputed to aid in the restoration of skin barrier function and, possibly, in reducing the signs and symptoms of rosacea (Clin. Exp. Dermatol. 2007;32:693-5; Plant Sci. 1999;148:37-45).
Kinetin is believed to develop in cellular DNA as a product of the oxidative, secondary modification of DNA (Plant Sci. 1999;148:37-45). In 1955, it became the first cytokinin isolated from DNA (from herring sperm) as an artifactual rearrangement product of the autoclaving process (J. Cosmet. Dermatol. 2007;6:243-9; Int. J. Biol. Macromol. 2007;40:182-92).
It has since been found to be present in human urine as well as DNA freshly extracted from human cells (Int. J. Biol. Macromol. 2007;40:182-92). The preponderance of amassed experimental evidence suggests that endogenous kinetin acts in vitro and in vivo as a potent antioxidant (Plant Sci. 1999;148:37-45). Currently, it is used as an anti-aging agent in various cosmetic products (J. Cosmet. Dermatol. 2007;6:243-9; J. Cosmet. Dermatol. 2010;9:218-25). Synthetic kinetin is thought to have the capacity to neutralize free radicals as well as limit the damage to DNA and fibroblasts (Photochem. Photobiol. 2012;88:748-52).
In vitro results
Olsen et al. demonstrated in vitro in 1999 that kinetin dose-dependently protected DNA against oxidative damage mediated by the Fenton reaction, and noted that kinetin had previously been linked to anti-aging activity in plants, fruit flies, and human cells in culture (Biochem. Biophys. Res. Commun. 1999;265:499-502). The following year, Verbeke et al. showed in vitro that kinetin potently inhibited damage caused by oxidation and glycoxidation (Biochem. Biophys. Res. Commun. 2000;276:1265-70).
In 2006, Vicanova et al. analyzed the effects of active ingredients from topical and systemic skin care formulations in vitro, finding that kinetin affected the upper dermis by enhancing deposits of fibrillin-1 and elastin fibers as well as their organization perpendicular to the dermal-epidermal junction. In the epidermis, kinetin stimulated keratinocyte production. Further, the investigators noted that the combination of topically applied kinetin with Imedeen Time Perfection ingredients (i.e., BioMarine Complex, grape seed extract, tomato extract, and vitamin C) supplemented systemically into culture medium yielded complementary benefits to dermal and epidermal development (Ann. N.Y. Acad. Sci. 2006;1067:337-42).
It is worth noting that in a study by Tournas et al. published the same month, investigators found that the topical application of a combination of vitamins C and E and ferulic acid yielded photoprotection to pig skin at 5 times the minimal erythema dose (MED) while individual antioxidants to which it was compared (i.e., coenzyme Q10, idebenone, and kinetin) delivered no photoprotective effects (J. Invest. Dermatol. 2006;126:1185-7). Nevertheless, Barciszewski et al. have observed that kinetin is the first stable secondary DNA damage product characterized by well defined cytokinin and anti-aging activity, with data showing that it has delayed human cellular aging in culture (Int. J. Biol. Macromol. 2007;40:182-92).
Rosacea
In 2007, Wu et al. performed a 12-week open-label study in 15 women and 3 men (aged 30-67 years) to ascertain the tolerability and efficacy of kinetin 0.1% lotion in the treatment of mild to moderate facial rosacea. Patients (17 of whom completed the study) applied the lotion twice daily, also daily applying an SPF 30 sunscreen. By week 4, significant improvements were observed in the reduction of skin roughness and mottled hyperpigmentation. Subject assessments at each 4-week interval after baseline and after 12 weeks revealed that kinetin 0.1% was well tolerated and effective for mild to moderate inflammatory rosacea (Clin. Exp. Dermatol. 2007;32:693-5).
Anti-aging
A 2002 study by J.L. McCullough and G.D. Weinstein represented the first evidence of the efficacy of topical kinetin in human beings, with twice-daily application for 24 weeks found to ameliorate skin texture, color, and blotchiness while diminishing rhytides and transepidermal water loss (J. Cosmet. Dermatol. 2002;15:29-32).
Two years later, T. Kimura and K. Doi showed that topical administration of kinetin improved the texture, wrinkling, and pigmentation of aged skin of hairless descendants of Mexican hairless dogs, resulting in notable depigmentation and rejuvenation after 100 days of treatment (Rejuvenation Res. 2004;7:32-9).In 2007, Chiu et al. conducted a randomized, double-blind, placebo-controlled, split-face comparative study in 52 Taiwanese subjects aged 30-60 years (90% of whom were female, all of whom had Fitzpatrick skin types II, III, or IV) to evaluate the clinical anti-aging effects and efficacy differences between kinetin plus niacinamide (kinetin 0.03%, niacinamide 4%) and niacinamide 4% alone versus vehicle placebo.
In the combination group, significant and sustained decreases were observed in counts of spots, pores, wrinkles, and evenness as well as persistent reductions in erythema index at weeks 8 and 12. At week 12, stratum corneum hydration status also was significantly enhanced in this group. In the niacinamide-only group, pore and evenness counts were significantly decreased at week 8, with declines in wrinkle counts emerging at week 12. The investigators concluded that kinetin and niacinamide display synergistic and dynamic anti-aging effects, showing substantial potential as topical anti-aging cosmeceutical agents (J. Cosmet. Dermatol. 2007;6:243-9).
However, Levin et al. noted in 2010 that while the effects of kinetin have been established in plants and its antioxidant properties have been displayed in vitro, the anti-aging effects and clinical efficacy ascribed to kinetin have been based on limited evidence, with no studies extant on the percutaneous absorption of kinetin. They added that research elucidating the mechanisms through which kinetin appears to improve skin barrier function, texture, and pigmentation also are lacking (J. Clin. Aesthet. Dermatol. 2010;3:22-41).
In 2012, Campos et al. assessed the effects on hydration, viscoelastic characteristics, and photoprotection of cosmetic preparations containing a dispersion of liposome with magnesium ascorbyl phosphate, alpha-lipoic acid, and kinetin. They observed that the formulation protected hairless mouse skin barrier function against UV harm. After 4 weeks of application on human skin, the combination product was found to have improved moisturization of the stratum corneum, also delivering hydration effects to deeper skin layers. The researchers concluded that the cosmetic formulation containing kinetin shows promise as a cutaneous anti-aging product (Photochem. Photobiol. 2012;88:748-52).
Conclusion
While some experimental and clinical results appear to suggest an anti-aging effect exerted by topically applied kinetin, much more research – particularly randomized controlled and comparison studies – are needed to provide a clearer picture as to the mechanisms and appropriate role of kinetin in the dermatologic armamentarium.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy,Topix Pharmaceuticals, and Unilever.
Kinetin (N6-furfuryladenine or 6-furfurylaminopurine) is a plant cytokinin or phytohormone that promotes cell division, delays senescence in plants, and is reputed to aid in the restoration of skin barrier function and, possibly, in reducing the signs and symptoms of rosacea (Clin. Exp. Dermatol. 2007;32:693-5; Plant Sci. 1999;148:37-45).
Kinetin is believed to develop in cellular DNA as a product of the oxidative, secondary modification of DNA (Plant Sci. 1999;148:37-45). In 1955, it became the first cytokinin isolated from DNA (from herring sperm) as an artifactual rearrangement product of the autoclaving process (J. Cosmet. Dermatol. 2007;6:243-9; Int. J. Biol. Macromol. 2007;40:182-92).
It has since been found to be present in human urine as well as DNA freshly extracted from human cells (Int. J. Biol. Macromol. 2007;40:182-92). The preponderance of amassed experimental evidence suggests that endogenous kinetin acts in vitro and in vivo as a potent antioxidant (Plant Sci. 1999;148:37-45). Currently, it is used as an anti-aging agent in various cosmetic products (J. Cosmet. Dermatol. 2007;6:243-9; J. Cosmet. Dermatol. 2010;9:218-25). Synthetic kinetin is thought to have the capacity to neutralize free radicals as well as limit the damage to DNA and fibroblasts (Photochem. Photobiol. 2012;88:748-52).
In vitro results
Olsen et al. demonstrated in vitro in 1999 that kinetin dose-dependently protected DNA against oxidative damage mediated by the Fenton reaction, and noted that kinetin had previously been linked to anti-aging activity in plants, fruit flies, and human cells in culture (Biochem. Biophys. Res. Commun. 1999;265:499-502). The following year, Verbeke et al. showed in vitro that kinetin potently inhibited damage caused by oxidation and glycoxidation (Biochem. Biophys. Res. Commun. 2000;276:1265-70).
In 2006, Vicanova et al. analyzed the effects of active ingredients from topical and systemic skin care formulations in vitro, finding that kinetin affected the upper dermis by enhancing deposits of fibrillin-1 and elastin fibers as well as their organization perpendicular to the dermal-epidermal junction. In the epidermis, kinetin stimulated keratinocyte production. Further, the investigators noted that the combination of topically applied kinetin with Imedeen Time Perfection ingredients (i.e., BioMarine Complex, grape seed extract, tomato extract, and vitamin C) supplemented systemically into culture medium yielded complementary benefits to dermal and epidermal development (Ann. N.Y. Acad. Sci. 2006;1067:337-42).
It is worth noting that in a study by Tournas et al. published the same month, investigators found that the topical application of a combination of vitamins C and E and ferulic acid yielded photoprotection to pig skin at 5 times the minimal erythema dose (MED) while individual antioxidants to which it was compared (i.e., coenzyme Q10, idebenone, and kinetin) delivered no photoprotective effects (J. Invest. Dermatol. 2006;126:1185-7). Nevertheless, Barciszewski et al. have observed that kinetin is the first stable secondary DNA damage product characterized by well defined cytokinin and anti-aging activity, with data showing that it has delayed human cellular aging in culture (Int. J. Biol. Macromol. 2007;40:182-92).
Rosacea
In 2007, Wu et al. performed a 12-week open-label study in 15 women and 3 men (aged 30-67 years) to ascertain the tolerability and efficacy of kinetin 0.1% lotion in the treatment of mild to moderate facial rosacea. Patients (17 of whom completed the study) applied the lotion twice daily, also daily applying an SPF 30 sunscreen. By week 4, significant improvements were observed in the reduction of skin roughness and mottled hyperpigmentation. Subject assessments at each 4-week interval after baseline and after 12 weeks revealed that kinetin 0.1% was well tolerated and effective for mild to moderate inflammatory rosacea (Clin. Exp. Dermatol. 2007;32:693-5).
Anti-aging
A 2002 study by J.L. McCullough and G.D. Weinstein represented the first evidence of the efficacy of topical kinetin in human beings, with twice-daily application for 24 weeks found to ameliorate skin texture, color, and blotchiness while diminishing rhytides and transepidermal water loss (J. Cosmet. Dermatol. 2002;15:29-32).
Two years later, T. Kimura and K. Doi showed that topical administration of kinetin improved the texture, wrinkling, and pigmentation of aged skin of hairless descendants of Mexican hairless dogs, resulting in notable depigmentation and rejuvenation after 100 days of treatment (Rejuvenation Res. 2004;7:32-9).In 2007, Chiu et al. conducted a randomized, double-blind, placebo-controlled, split-face comparative study in 52 Taiwanese subjects aged 30-60 years (90% of whom were female, all of whom had Fitzpatrick skin types II, III, or IV) to evaluate the clinical anti-aging effects and efficacy differences between kinetin plus niacinamide (kinetin 0.03%, niacinamide 4%) and niacinamide 4% alone versus vehicle placebo.
In the combination group, significant and sustained decreases were observed in counts of spots, pores, wrinkles, and evenness as well as persistent reductions in erythema index at weeks 8 and 12. At week 12, stratum corneum hydration status also was significantly enhanced in this group. In the niacinamide-only group, pore and evenness counts were significantly decreased at week 8, with declines in wrinkle counts emerging at week 12. The investigators concluded that kinetin and niacinamide display synergistic and dynamic anti-aging effects, showing substantial potential as topical anti-aging cosmeceutical agents (J. Cosmet. Dermatol. 2007;6:243-9).
However, Levin et al. noted in 2010 that while the effects of kinetin have been established in plants and its antioxidant properties have been displayed in vitro, the anti-aging effects and clinical efficacy ascribed to kinetin have been based on limited evidence, with no studies extant on the percutaneous absorption of kinetin. They added that research elucidating the mechanisms through which kinetin appears to improve skin barrier function, texture, and pigmentation also are lacking (J. Clin. Aesthet. Dermatol. 2010;3:22-41).
In 2012, Campos et al. assessed the effects on hydration, viscoelastic characteristics, and photoprotection of cosmetic preparations containing a dispersion of liposome with magnesium ascorbyl phosphate, alpha-lipoic acid, and kinetin. They observed that the formulation protected hairless mouse skin barrier function against UV harm. After 4 weeks of application on human skin, the combination product was found to have improved moisturization of the stratum corneum, also delivering hydration effects to deeper skin layers. The researchers concluded that the cosmetic formulation containing kinetin shows promise as a cutaneous anti-aging product (Photochem. Photobiol. 2012;88:748-52).
Conclusion
While some experimental and clinical results appear to suggest an anti-aging effect exerted by topically applied kinetin, much more research – particularly randomized controlled and comparison studies – are needed to provide a clearer picture as to the mechanisms and appropriate role of kinetin in the dermatologic armamentarium.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). She has contributed to the Cosmeceutical Critique column in Dermatology News since January 2001. Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy,Topix Pharmaceuticals, and Unilever.
‘Perfect storm’ of depression, stress raises risk of MI, death
Patients with coronary heart disease who have both depression and stress are at increased risk of myocardial infarction and death, according to findings from a large, prospective, cohort study.
Of 4,487 adults with CHD who were part of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, 1,337 experienced MI or death during a median of nearly 6 years of follow-up. Those with both high depressive symptoms and high stress at baseline – about 6% of the study population – were at significantly increased risk of such events (adjusted hazard ratio, 1.48) during the first 2.5 years of follow-up, compared with those with low stress and low depressive symptoms. However, the association was not significant beyond the initial 2.5 years (HR, 0.89), Carmela Alcántara, Ph.D., of Columbia University, New York, and her colleagues reported.
Those with low stress and high depressive symptoms, and those with high stress and low depressive symptoms, were not at increased risk (HR, 0.92 and 0.86, respectively) at any point during follow-up (Circ. Cardiovasc. Qual. Outcomes 2015 March 10 [doi:10.1161/IRCOUTCOMES.114.001180]).
The findings provide initial empirical evidence to support a “psychosocial perfect storm conceptual model” based on the idea that it takes an underlying chronic psychosocial vulnerability such as depression along with a more transient state such as psychological stress to precipitate a clinical event. The confluence of these factors may be particularly destructive in the short term, the investigators concluded, noting that the findings could have implications for the development of preventive treatments that focus on depression and stress during this vulnerable period in CHD patients.
The National Institute of Neurological Disorders and Stroke and the National Heart, Lung, and Blood Institute supported the study. Dr. Alcantara reported having no disclosures, but two other authors received salary support from Amgen for research, and one served as a consultant for DiaDexus.
Patients with coronary heart disease who have both depression and stress are at increased risk of myocardial infarction and death, according to findings from a large, prospective, cohort study.
Of 4,487 adults with CHD who were part of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, 1,337 experienced MI or death during a median of nearly 6 years of follow-up. Those with both high depressive symptoms and high stress at baseline – about 6% of the study population – were at significantly increased risk of such events (adjusted hazard ratio, 1.48) during the first 2.5 years of follow-up, compared with those with low stress and low depressive symptoms. However, the association was not significant beyond the initial 2.5 years (HR, 0.89), Carmela Alcántara, Ph.D., of Columbia University, New York, and her colleagues reported.
Those with low stress and high depressive symptoms, and those with high stress and low depressive symptoms, were not at increased risk (HR, 0.92 and 0.86, respectively) at any point during follow-up (Circ. Cardiovasc. Qual. Outcomes 2015 March 10 [doi:10.1161/IRCOUTCOMES.114.001180]).
The findings provide initial empirical evidence to support a “psychosocial perfect storm conceptual model” based on the idea that it takes an underlying chronic psychosocial vulnerability such as depression along with a more transient state such as psychological stress to precipitate a clinical event. The confluence of these factors may be particularly destructive in the short term, the investigators concluded, noting that the findings could have implications for the development of preventive treatments that focus on depression and stress during this vulnerable period in CHD patients.
The National Institute of Neurological Disorders and Stroke and the National Heart, Lung, and Blood Institute supported the study. Dr. Alcantara reported having no disclosures, but two other authors received salary support from Amgen for research, and one served as a consultant for DiaDexus.
Patients with coronary heart disease who have both depression and stress are at increased risk of myocardial infarction and death, according to findings from a large, prospective, cohort study.
Of 4,487 adults with CHD who were part of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, 1,337 experienced MI or death during a median of nearly 6 years of follow-up. Those with both high depressive symptoms and high stress at baseline – about 6% of the study population – were at significantly increased risk of such events (adjusted hazard ratio, 1.48) during the first 2.5 years of follow-up, compared with those with low stress and low depressive symptoms. However, the association was not significant beyond the initial 2.5 years (HR, 0.89), Carmela Alcántara, Ph.D., of Columbia University, New York, and her colleagues reported.
Those with low stress and high depressive symptoms, and those with high stress and low depressive symptoms, were not at increased risk (HR, 0.92 and 0.86, respectively) at any point during follow-up (Circ. Cardiovasc. Qual. Outcomes 2015 March 10 [doi:10.1161/IRCOUTCOMES.114.001180]).
The findings provide initial empirical evidence to support a “psychosocial perfect storm conceptual model” based on the idea that it takes an underlying chronic psychosocial vulnerability such as depression along with a more transient state such as psychological stress to precipitate a clinical event. The confluence of these factors may be particularly destructive in the short term, the investigators concluded, noting that the findings could have implications for the development of preventive treatments that focus on depression and stress during this vulnerable period in CHD patients.
The National Institute of Neurological Disorders and Stroke and the National Heart, Lung, and Blood Institute supported the study. Dr. Alcantara reported having no disclosures, but two other authors received salary support from Amgen for research, and one served as a consultant for DiaDexus.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Concurrent depression and stress in CHD patients may increase the early risk of MI and death.
Major finding: CHD patients with high depressive symptoms and high stress at baseline had an increased risk of MI and death early during follow-up (adjusted HR, 1.48).
Data source: A prospective cohort study of 4,487 adults.
Disclosures: The National Institute of Neurological Disorders and Stroke and the National Heart, Lung, and Blood Institute supported the study. Dr. Alcantara reported having no disclosures; two other authors received salary support from Amgen for research, and one served as a consultant for DiaDexus.
Venous thromboembolism common after heart transplant
For every 1,000 patients who underwent heart transplantation, about 45 had an episode of venous thromboembolism within a year after surgery, according to a retrospective study reported in the February issue of the Journal of Heart and Lung Transplantation.
Furthermore, patients who had a single VTE episode after transplant had a “high” risk of recurrent VTE, said Dr. Rolando Alvarez, a cardiologist at Complejo Hospitalario Universitario A Coruna in A Coruna, Spain, and his associates.
“Our opinion is that long-term oral anticoagulation should be maintained in these patients, especially if other risk factors are present and provided that the bleeding risk is not excessive,” said the researchers.
Venous thromboembolism is a common complication of lung, kidney, and liver transplantation, but less is known about VTE after heart transplant. The researchers found that “classic” risk factors for VTE, such as being older, obese, or having renal dysfunction, also increased the risk of VTE after heart transplant (J. Heart Lung Transplant. 2015;34:167-74).
The study included data from 635 consecutive patients who underwent heart transplantation at a single hospital between 1991 and 2013. During a median of 8.4 years of follow-up, the cumulative incidence of VTE was 8.5%, for an annual incidence rate of 12.7 episodes per year for every 1,000 patients, the researchers reported. The risk of VTE was far higher during the first year after transplant (45.1 episodes per 1,000 patients), but even after excluding these episodes, VTE was six times more common among heart transplant recipients than among the general population. Furthermore, VTE recurred an estimated 30.5 times/1,000 patient-years, and 50.8 times/1,000 patients-years among patients who had stopped anticoagulants.
The cumulative incidence rate of DVT and PE were 8.4 and 8.7 episodes per 1,000 patient-years.
In the multivariate analysis, significant risk factors for VTE at less than 1 year after transplantation included age, obesity, chronic kidney disease, and emergency transplantation, the investigators said. More than a year after transplantation, only use of the mammalian target of rapamycin (mTOR) inhibitors sirolimus and everolimus significantly increased VTE risk.
“The evidence that supports a potential association between mTOR inhibitors and an increased risk of VTE events is still weak, and might be confounded by a high prevalence of comorbid conditions such as chronic renal failure, dyslipidemia, or malignancy in patients taking these kinds of drugs,” the investigators cautioned.
The authors suggested that in view of the high recurrence rate, long-term anticoagulation should be considered in heart transplant patients after their first VTE episode.
The Fundacion BBVA-Carolina funded the study. Four coauthors reported receiving travel support from Novartis Pharma and Astellas Pharma. The other authors reported no relevant conflicts of interest.
For every 1,000 patients who underwent heart transplantation, about 45 had an episode of venous thromboembolism within a year after surgery, according to a retrospective study reported in the February issue of the Journal of Heart and Lung Transplantation.
Furthermore, patients who had a single VTE episode after transplant had a “high” risk of recurrent VTE, said Dr. Rolando Alvarez, a cardiologist at Complejo Hospitalario Universitario A Coruna in A Coruna, Spain, and his associates.
“Our opinion is that long-term oral anticoagulation should be maintained in these patients, especially if other risk factors are present and provided that the bleeding risk is not excessive,” said the researchers.
Venous thromboembolism is a common complication of lung, kidney, and liver transplantation, but less is known about VTE after heart transplant. The researchers found that “classic” risk factors for VTE, such as being older, obese, or having renal dysfunction, also increased the risk of VTE after heart transplant (J. Heart Lung Transplant. 2015;34:167-74).
The study included data from 635 consecutive patients who underwent heart transplantation at a single hospital between 1991 and 2013. During a median of 8.4 years of follow-up, the cumulative incidence of VTE was 8.5%, for an annual incidence rate of 12.7 episodes per year for every 1,000 patients, the researchers reported. The risk of VTE was far higher during the first year after transplant (45.1 episodes per 1,000 patients), but even after excluding these episodes, VTE was six times more common among heart transplant recipients than among the general population. Furthermore, VTE recurred an estimated 30.5 times/1,000 patient-years, and 50.8 times/1,000 patients-years among patients who had stopped anticoagulants.
The cumulative incidence rate of DVT and PE were 8.4 and 8.7 episodes per 1,000 patient-years.
In the multivariate analysis, significant risk factors for VTE at less than 1 year after transplantation included age, obesity, chronic kidney disease, and emergency transplantation, the investigators said. More than a year after transplantation, only use of the mammalian target of rapamycin (mTOR) inhibitors sirolimus and everolimus significantly increased VTE risk.
“The evidence that supports a potential association between mTOR inhibitors and an increased risk of VTE events is still weak, and might be confounded by a high prevalence of comorbid conditions such as chronic renal failure, dyslipidemia, or malignancy in patients taking these kinds of drugs,” the investigators cautioned.
The authors suggested that in view of the high recurrence rate, long-term anticoagulation should be considered in heart transplant patients after their first VTE episode.
The Fundacion BBVA-Carolina funded the study. Four coauthors reported receiving travel support from Novartis Pharma and Astellas Pharma. The other authors reported no relevant conflicts of interest.
For every 1,000 patients who underwent heart transplantation, about 45 had an episode of venous thromboembolism within a year after surgery, according to a retrospective study reported in the February issue of the Journal of Heart and Lung Transplantation.
Furthermore, patients who had a single VTE episode after transplant had a “high” risk of recurrent VTE, said Dr. Rolando Alvarez, a cardiologist at Complejo Hospitalario Universitario A Coruna in A Coruna, Spain, and his associates.
“Our opinion is that long-term oral anticoagulation should be maintained in these patients, especially if other risk factors are present and provided that the bleeding risk is not excessive,” said the researchers.
Venous thromboembolism is a common complication of lung, kidney, and liver transplantation, but less is known about VTE after heart transplant. The researchers found that “classic” risk factors for VTE, such as being older, obese, or having renal dysfunction, also increased the risk of VTE after heart transplant (J. Heart Lung Transplant. 2015;34:167-74).
The study included data from 635 consecutive patients who underwent heart transplantation at a single hospital between 1991 and 2013. During a median of 8.4 years of follow-up, the cumulative incidence of VTE was 8.5%, for an annual incidence rate of 12.7 episodes per year for every 1,000 patients, the researchers reported. The risk of VTE was far higher during the first year after transplant (45.1 episodes per 1,000 patients), but even after excluding these episodes, VTE was six times more common among heart transplant recipients than among the general population. Furthermore, VTE recurred an estimated 30.5 times/1,000 patient-years, and 50.8 times/1,000 patients-years among patients who had stopped anticoagulants.
The cumulative incidence rate of DVT and PE were 8.4 and 8.7 episodes per 1,000 patient-years.
In the multivariate analysis, significant risk factors for VTE at less than 1 year after transplantation included age, obesity, chronic kidney disease, and emergency transplantation, the investigators said. More than a year after transplantation, only use of the mammalian target of rapamycin (mTOR) inhibitors sirolimus and everolimus significantly increased VTE risk.
“The evidence that supports a potential association between mTOR inhibitors and an increased risk of VTE events is still weak, and might be confounded by a high prevalence of comorbid conditions such as chronic renal failure, dyslipidemia, or malignancy in patients taking these kinds of drugs,” the investigators cautioned.
The authors suggested that in view of the high recurrence rate, long-term anticoagulation should be considered in heart transplant patients after their first VTE episode.
The Fundacion BBVA-Carolina funded the study. Four coauthors reported receiving travel support from Novartis Pharma and Astellas Pharma. The other authors reported no relevant conflicts of interest.
Key clinical point: Venous thromboembolism (VTE) was common after heart transplant, especially when patients had relevant risk factors and were not on anticoagulants.
Major finding: Cumulative incidence of VTE was 8.5% during eight years of follow-up and was much higher during the first year after transplant.
Data source: Single-center retrospective cohort study of 635 heart transplant recipients.
Disclosures: The Fundacion BBVA-Carolina funded the study. Four coauthors reported receiving travel support from Novartis Pharma and Astellas Pharma. The other authors reported no relevant conflicts of interest.
Stroke ambulances speed treatment to U.S. patients
NASHVILLE, TENN. – Bringing a CT scanner and thrombolytic treatment directly to stroke patients in the field sped the time to thrombolysis, compared with waiting for the patient to arrive at the hospital.
Some U.S. stroke centers now send out a team that can immediately assess and start treating stroke patients in the community. In 2014, the first two U.S. mobile stroke-treatment units began operating, one in Houston and the second in Cleveland.
Initial reports show both programs were successful in cutting the time to deliver thrombolytic treatment with intravenous tissue plasminogen activator (TPA) to appropriate patients.
In Houston, the active phase of the program started in May 2014, and by October 2014, 47 acute ischemic stroke patients had been treated with TPA. The mobile-unit crews started 43% of eligible patients on thrombolysis within 60 minutes of their symptom onset and another 31% were treated starting 61-80 minutes after symptom onset, said Stephanie A. Parker at the International Stroke Conference.
The unit also treats patients diagnosed with hemorrhagic stroke with intravenous nicardipine for rapid blood pressure reduction, said Ms. Parker, a critical care and emergency medicine–trained registered nurse who is project manager for the Houston mobile unit.
The Cleveland program began in July 2014; of the first 100 stroke patients seen by the mobile unit 16 of 19 eligible patients received tPA, with an average time of 56 minutes from symptom onset to treatment. This compared with an average 94 minutes to tPA onset in patients brought conventionally last year to a Cleveland-area hospital, Dr. M. Shazam Hussain said in a report at the meeting, sponsored by the American Heart Association.
The clinical impact and cost effectiveness of the pilot programs using the mobile units have not yet been assessed from the data, Dr. Hussain and Ms. Parker emphasized. Funding for the Cleveland and Houston vehicles came from local donors; the Houston program also received equipment donations from manufacturers.
The two mobile units are standard 12-foot, box-shaped ambulances outfitted with a CT scanner, a point-of-care lab, and telemedicine components as well as more standard emergency-vehicle equipment. The Houston vehicle contains “all the diagnostic equipment that is in our emergency room,” Ms. Parker said.
The concept behind both the Cleveland unit, operated by the Cleveland Clinic, and the Houston unit, operated by the University of Texas, Houston, is that the mobile stroke unit arrives to a patient with a suspected stroke, the unit is stationary while a CT scan and other diagnostic tests are run, diagnosis occurs with telemedicine assistance. If the patient is cleared for TPA treatment, the infusion starts and the vehicle carries the patient to an appropriate stroke center.
Currently, the Houston unit goes out with a vascular neurologist and a telemedicine physician on board, but plans are in place to test the feasibility of relying entirely on telemedicine when making diagnostic and treatment decisions. The Cleveland mobile unit already operates in this fashion, with no physician on board, and was the first mobile stroke unit in the world to depend completely on telemedicine, according to Dr. Hussain, a neurologist and head of the stroke program at the Cleveland Clinic.
The world’s first mobile stroke unit began operating in Saarland, Germany, in 2008 (Lancet Neurology 2012;11:397-404), and a second unit began running in Berlin after that, Dr. Hussain noted. Because of limited funding, the service he directs in Cleveland has been operating from 8 a.m.-8 p.m., 7 days a week. The program plans to expand to 24-hour coverage. The Houston mobile unit operates 24/7; it averages two runs per day and administers TPA on 1 of every 10 runs, Ms. Parker said. Both the Houston and Cleveland units tie into the local 911 emergency activation systems for their respective regions.
On Twitter @mitchelzoler
NASHVILLE, TENN. – Bringing a CT scanner and thrombolytic treatment directly to stroke patients in the field sped the time to thrombolysis, compared with waiting for the patient to arrive at the hospital.
Some U.S. stroke centers now send out a team that can immediately assess and start treating stroke patients in the community. In 2014, the first two U.S. mobile stroke-treatment units began operating, one in Houston and the second in Cleveland.
Initial reports show both programs were successful in cutting the time to deliver thrombolytic treatment with intravenous tissue plasminogen activator (TPA) to appropriate patients.
In Houston, the active phase of the program started in May 2014, and by October 2014, 47 acute ischemic stroke patients had been treated with TPA. The mobile-unit crews started 43% of eligible patients on thrombolysis within 60 minutes of their symptom onset and another 31% were treated starting 61-80 minutes after symptom onset, said Stephanie A. Parker at the International Stroke Conference.
The unit also treats patients diagnosed with hemorrhagic stroke with intravenous nicardipine for rapid blood pressure reduction, said Ms. Parker, a critical care and emergency medicine–trained registered nurse who is project manager for the Houston mobile unit.
The Cleveland program began in July 2014; of the first 100 stroke patients seen by the mobile unit 16 of 19 eligible patients received tPA, with an average time of 56 minutes from symptom onset to treatment. This compared with an average 94 minutes to tPA onset in patients brought conventionally last year to a Cleveland-area hospital, Dr. M. Shazam Hussain said in a report at the meeting, sponsored by the American Heart Association.
The clinical impact and cost effectiveness of the pilot programs using the mobile units have not yet been assessed from the data, Dr. Hussain and Ms. Parker emphasized. Funding for the Cleveland and Houston vehicles came from local donors; the Houston program also received equipment donations from manufacturers.
The two mobile units are standard 12-foot, box-shaped ambulances outfitted with a CT scanner, a point-of-care lab, and telemedicine components as well as more standard emergency-vehicle equipment. The Houston vehicle contains “all the diagnostic equipment that is in our emergency room,” Ms. Parker said.
The concept behind both the Cleveland unit, operated by the Cleveland Clinic, and the Houston unit, operated by the University of Texas, Houston, is that the mobile stroke unit arrives to a patient with a suspected stroke, the unit is stationary while a CT scan and other diagnostic tests are run, diagnosis occurs with telemedicine assistance. If the patient is cleared for TPA treatment, the infusion starts and the vehicle carries the patient to an appropriate stroke center.
Currently, the Houston unit goes out with a vascular neurologist and a telemedicine physician on board, but plans are in place to test the feasibility of relying entirely on telemedicine when making diagnostic and treatment decisions. The Cleveland mobile unit already operates in this fashion, with no physician on board, and was the first mobile stroke unit in the world to depend completely on telemedicine, according to Dr. Hussain, a neurologist and head of the stroke program at the Cleveland Clinic.
The world’s first mobile stroke unit began operating in Saarland, Germany, in 2008 (Lancet Neurology 2012;11:397-404), and a second unit began running in Berlin after that, Dr. Hussain noted. Because of limited funding, the service he directs in Cleveland has been operating from 8 a.m.-8 p.m., 7 days a week. The program plans to expand to 24-hour coverage. The Houston mobile unit operates 24/7; it averages two runs per day and administers TPA on 1 of every 10 runs, Ms. Parker said. Both the Houston and Cleveland units tie into the local 911 emergency activation systems for their respective regions.
On Twitter @mitchelzoler
NASHVILLE, TENN. – Bringing a CT scanner and thrombolytic treatment directly to stroke patients in the field sped the time to thrombolysis, compared with waiting for the patient to arrive at the hospital.
Some U.S. stroke centers now send out a team that can immediately assess and start treating stroke patients in the community. In 2014, the first two U.S. mobile stroke-treatment units began operating, one in Houston and the second in Cleveland.
Initial reports show both programs were successful in cutting the time to deliver thrombolytic treatment with intravenous tissue plasminogen activator (TPA) to appropriate patients.
In Houston, the active phase of the program started in May 2014, and by October 2014, 47 acute ischemic stroke patients had been treated with TPA. The mobile-unit crews started 43% of eligible patients on thrombolysis within 60 minutes of their symptom onset and another 31% were treated starting 61-80 minutes after symptom onset, said Stephanie A. Parker at the International Stroke Conference.
The unit also treats patients diagnosed with hemorrhagic stroke with intravenous nicardipine for rapid blood pressure reduction, said Ms. Parker, a critical care and emergency medicine–trained registered nurse who is project manager for the Houston mobile unit.
The Cleveland program began in July 2014; of the first 100 stroke patients seen by the mobile unit 16 of 19 eligible patients received tPA, with an average time of 56 minutes from symptom onset to treatment. This compared with an average 94 minutes to tPA onset in patients brought conventionally last year to a Cleveland-area hospital, Dr. M. Shazam Hussain said in a report at the meeting, sponsored by the American Heart Association.
The clinical impact and cost effectiveness of the pilot programs using the mobile units have not yet been assessed from the data, Dr. Hussain and Ms. Parker emphasized. Funding for the Cleveland and Houston vehicles came from local donors; the Houston program also received equipment donations from manufacturers.
The two mobile units are standard 12-foot, box-shaped ambulances outfitted with a CT scanner, a point-of-care lab, and telemedicine components as well as more standard emergency-vehicle equipment. The Houston vehicle contains “all the diagnostic equipment that is in our emergency room,” Ms. Parker said.
The concept behind both the Cleveland unit, operated by the Cleveland Clinic, and the Houston unit, operated by the University of Texas, Houston, is that the mobile stroke unit arrives to a patient with a suspected stroke, the unit is stationary while a CT scan and other diagnostic tests are run, diagnosis occurs with telemedicine assistance. If the patient is cleared for TPA treatment, the infusion starts and the vehicle carries the patient to an appropriate stroke center.
Currently, the Houston unit goes out with a vascular neurologist and a telemedicine physician on board, but plans are in place to test the feasibility of relying entirely on telemedicine when making diagnostic and treatment decisions. The Cleveland mobile unit already operates in this fashion, with no physician on board, and was the first mobile stroke unit in the world to depend completely on telemedicine, according to Dr. Hussain, a neurologist and head of the stroke program at the Cleveland Clinic.
The world’s first mobile stroke unit began operating in Saarland, Germany, in 2008 (Lancet Neurology 2012;11:397-404), and a second unit began running in Berlin after that, Dr. Hussain noted. Because of limited funding, the service he directs in Cleveland has been operating from 8 a.m.-8 p.m., 7 days a week. The program plans to expand to 24-hour coverage. The Houston mobile unit operates 24/7; it averages two runs per day and administers TPA on 1 of every 10 runs, Ms. Parker said. Both the Houston and Cleveland units tie into the local 911 emergency activation systems for their respective regions.
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point: Dedicated stroke ambulances that bring a CT scanner and thrombolytic treatment to patients in the field speed thrombolytic therapy.
Major finding: In Cleveland, stroke patients received thrombolysis an average of 38 minutes sooner from the CT-equipped ambulance, compared with standard protocols.
Data source: Prospectively collected data on time-to-treatment from case series in Houston and in Cleveland.
Disclosures: Dr. Hussain and Ms. Parker had no disclosures.
Women having heart attacks face longer prehospital delay
When heart attack symptoms begin, women wait longer than do men to call for help, and it takes longer for them to arrive at a hospital that can care for them appropriately.
Further, statistical analysis suggests that this prehospital delay is a chief contributor to the higher in-hospital mortality rate for women who have sustained myocardial infarctions. Dr. Raffaele Bugiardini of the University of Bologna and his associates in the ISACS-TC study group examined data from a large international study to clarify gender disparities in heart attacks, and to identify more precisely where time is lost in caring for women.
They examined data from 2,282 women and 5,175 men who experienced ST-segment–elevation myocardial infarction (STEMI). Overall, female participants were older than males and were more likely to have diabetes, to be treated for hypertension, and to have experienced atypical chest pain – or no chest pain at all – during their heart attacks. The men were more likely to be smokers, to have chronic renal failure, and to have a prior history of angina.
The results were released in advance of the researchers’ presentation on March 14 at the annual meeting of the American College of Cardiology in San Diego.
Once symptoms began, women tended to wait significantly longer to call for help, a median 60.0 minutes, compared with 45.5 for men. Time to hospital admission was just a bit longer for women (60 minutes) compared to men (55 minutes). On admission, time to angioplasty or fibrinolysis did not vary significantly between the sexes. The likelihood of receiving appropriate medical treatment (aspirin, clopidogrel, heparin use) was also similar.
In outcome measures, 30% of women achieved hospital admission in 60 minutes or less from leaving home, compared with 70% of men. Dr. Bugiardini explained that the 60-minute admission marker is an important quality standard in the European framework. The odds ratio (OR) for a greater-than 60-minute time from home to hospital admission for women was 2.90 (95% CI, 1.52-5.82).
In-hospital mortality for women was nearly double that for men, at 11.8% compared to 6.3% for men (OR 1.34, 95% CI 1.01-1.77). However, after logistic regression analysis adjusted for the differences in time from home to hospital admission, the disparity in mortality disappeared (OR 0.90, 95% CI 0.31-2.56). Dr. Bugiardini emphasized that his analysis makes clear that delay in treatment is an important contributor to greater in-hospital mortality for women suffering heart attacks.
Though these finding were drawn from a large international study, American College of Cardiology Vice President Richard Chazal affirmed during a media briefing that the results are definitely applicable to the United States and other developed nations. “They are confirmatory,” said Dr. Chazal, “of other studies that have suggested this but have not shown this in such a complete and comprehensive way. This is very important information in this population.”
Heart disease kills more women than do all forms of cancer combined, but the varied presentation of heart attack symptoms in women is still underrecognized, noted Dr. Chazal of Lee Memorial Health System, Fort Myers, Fla. Raising awareness about heart disease risk and heart attack symptoms is critical to addressing the disparities identified in this study. “The delays in getting the patient to the hospital are really crucial in determining what the outcomes are,” he said.
“Time is still lost between contact with the system and arrival to the hospital” for women, he added. “There is less awareness not just by women, but in doctors in underestimating what’s going on with women. We are confused, so we stop and do one more EKG. We are losing time.”
Dr. Marija Vavlukis is on the speakers bureau for KRKA Macedonia. The other authors have no disclosures.
When heart attack symptoms begin, women wait longer than do men to call for help, and it takes longer for them to arrive at a hospital that can care for them appropriately.
Further, statistical analysis suggests that this prehospital delay is a chief contributor to the higher in-hospital mortality rate for women who have sustained myocardial infarctions. Dr. Raffaele Bugiardini of the University of Bologna and his associates in the ISACS-TC study group examined data from a large international study to clarify gender disparities in heart attacks, and to identify more precisely where time is lost in caring for women.
They examined data from 2,282 women and 5,175 men who experienced ST-segment–elevation myocardial infarction (STEMI). Overall, female participants were older than males and were more likely to have diabetes, to be treated for hypertension, and to have experienced atypical chest pain – or no chest pain at all – during their heart attacks. The men were more likely to be smokers, to have chronic renal failure, and to have a prior history of angina.
The results were released in advance of the researchers’ presentation on March 14 at the annual meeting of the American College of Cardiology in San Diego.
Once symptoms began, women tended to wait significantly longer to call for help, a median 60.0 minutes, compared with 45.5 for men. Time to hospital admission was just a bit longer for women (60 minutes) compared to men (55 minutes). On admission, time to angioplasty or fibrinolysis did not vary significantly between the sexes. The likelihood of receiving appropriate medical treatment (aspirin, clopidogrel, heparin use) was also similar.
In outcome measures, 30% of women achieved hospital admission in 60 minutes or less from leaving home, compared with 70% of men. Dr. Bugiardini explained that the 60-minute admission marker is an important quality standard in the European framework. The odds ratio (OR) for a greater-than 60-minute time from home to hospital admission for women was 2.90 (95% CI, 1.52-5.82).
In-hospital mortality for women was nearly double that for men, at 11.8% compared to 6.3% for men (OR 1.34, 95% CI 1.01-1.77). However, after logistic regression analysis adjusted for the differences in time from home to hospital admission, the disparity in mortality disappeared (OR 0.90, 95% CI 0.31-2.56). Dr. Bugiardini emphasized that his analysis makes clear that delay in treatment is an important contributor to greater in-hospital mortality for women suffering heart attacks.
Though these finding were drawn from a large international study, American College of Cardiology Vice President Richard Chazal affirmed during a media briefing that the results are definitely applicable to the United States and other developed nations. “They are confirmatory,” said Dr. Chazal, “of other studies that have suggested this but have not shown this in such a complete and comprehensive way. This is very important information in this population.”
Heart disease kills more women than do all forms of cancer combined, but the varied presentation of heart attack symptoms in women is still underrecognized, noted Dr. Chazal of Lee Memorial Health System, Fort Myers, Fla. Raising awareness about heart disease risk and heart attack symptoms is critical to addressing the disparities identified in this study. “The delays in getting the patient to the hospital are really crucial in determining what the outcomes are,” he said.
“Time is still lost between contact with the system and arrival to the hospital” for women, he added. “There is less awareness not just by women, but in doctors in underestimating what’s going on with women. We are confused, so we stop and do one more EKG. We are losing time.”
Dr. Marija Vavlukis is on the speakers bureau for KRKA Macedonia. The other authors have no disclosures.
When heart attack symptoms begin, women wait longer than do men to call for help, and it takes longer for them to arrive at a hospital that can care for them appropriately.
Further, statistical analysis suggests that this prehospital delay is a chief contributor to the higher in-hospital mortality rate for women who have sustained myocardial infarctions. Dr. Raffaele Bugiardini of the University of Bologna and his associates in the ISACS-TC study group examined data from a large international study to clarify gender disparities in heart attacks, and to identify more precisely where time is lost in caring for women.
They examined data from 2,282 women and 5,175 men who experienced ST-segment–elevation myocardial infarction (STEMI). Overall, female participants were older than males and were more likely to have diabetes, to be treated for hypertension, and to have experienced atypical chest pain – or no chest pain at all – during their heart attacks. The men were more likely to be smokers, to have chronic renal failure, and to have a prior history of angina.
The results were released in advance of the researchers’ presentation on March 14 at the annual meeting of the American College of Cardiology in San Diego.
Once symptoms began, women tended to wait significantly longer to call for help, a median 60.0 minutes, compared with 45.5 for men. Time to hospital admission was just a bit longer for women (60 minutes) compared to men (55 minutes). On admission, time to angioplasty or fibrinolysis did not vary significantly between the sexes. The likelihood of receiving appropriate medical treatment (aspirin, clopidogrel, heparin use) was also similar.
In outcome measures, 30% of women achieved hospital admission in 60 minutes or less from leaving home, compared with 70% of men. Dr. Bugiardini explained that the 60-minute admission marker is an important quality standard in the European framework. The odds ratio (OR) for a greater-than 60-minute time from home to hospital admission for women was 2.90 (95% CI, 1.52-5.82).
In-hospital mortality for women was nearly double that for men, at 11.8% compared to 6.3% for men (OR 1.34, 95% CI 1.01-1.77). However, after logistic regression analysis adjusted for the differences in time from home to hospital admission, the disparity in mortality disappeared (OR 0.90, 95% CI 0.31-2.56). Dr. Bugiardini emphasized that his analysis makes clear that delay in treatment is an important contributor to greater in-hospital mortality for women suffering heart attacks.
Though these finding were drawn from a large international study, American College of Cardiology Vice President Richard Chazal affirmed during a media briefing that the results are definitely applicable to the United States and other developed nations. “They are confirmatory,” said Dr. Chazal, “of other studies that have suggested this but have not shown this in such a complete and comprehensive way. This is very important information in this population.”
Heart disease kills more women than do all forms of cancer combined, but the varied presentation of heart attack symptoms in women is still underrecognized, noted Dr. Chazal of Lee Memorial Health System, Fort Myers, Fla. Raising awareness about heart disease risk and heart attack symptoms is critical to addressing the disparities identified in this study. “The delays in getting the patient to the hospital are really crucial in determining what the outcomes are,” he said.
“Time is still lost between contact with the system and arrival to the hospital” for women, he added. “There is less awareness not just by women, but in doctors in underestimating what’s going on with women. We are confused, so we stop and do one more EKG. We are losing time.”
Dr. Marija Vavlukis is on the speakers bureau for KRKA Macedonia. The other authors have no disclosures.
FROM ACC 15
Key clinical point: Women having heart attacks wait longer to call for help, and it takes longer to get them to a hospital.
Major findings: The median time from onset of symptoms to ambulance call was 45.5 minutes for men vs. 60.0 minutes for women; just 30% of women vs. 70% of men were admitted within 60 minutes of leaving home.
Data source: Multivariate analysis of data from 7,457 patients enrolled in the International Survey of Acute Coronary Syndromes in Transitional Countries (ISACS-TC).
Disclosures: Dr. Marija Vavlukis is on the speakers bureau for KRKA Macedonia. The other authors have no disclosures.
FDA approves first drug for high-risk neuroblastoma
The Food and Drug Administration has approved dinutuximab as part of a multimodality regimen, including surgery, chemotherapy, and radiation therapy, for pediatric patients with high-risk neuroblastoma.
The drug “marks the first approval for a therapy aimed specifically for the treatment of patients with high-risk neuroblastoma,” Dr. Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in the March 10 FDA announcement.
Dinutuximab is a chimeric monoclonal antibody that targets GD2, a glycolipid on the surface of tumor cells, according to the manufacturer, United Therapeutics.
The FDA granted approval based on a clinical trial of 226 pediatric participants with high-risk neuroblastoma whose tumors shrunk or disappeared after treatment with multiple-drug chemotherapy and surgery followed by additional intensive chemotherapy and who subsequently received bone marrow transplantation support and radiation therapy. Three years after being randomly assigned to receive either isotretinoin or dinutuximab in combination with interleukin-2 and granulocyte macrophage colony-stimulating factor, 63% of participants receiving the combination were alive and free of tumor growth or recurrence, compared with 46% of participants treated with isotretinoin alone.
In an updated analysis, 73% of participants who received the combination were alive, compared with 58% of those receiving isotretinoin alone, the FDA said in the announcement.
The most common side effects were severe pain, fever, low platelet counts, infusion reactions, low blood pressure, hyponatremia, elevated liver enzymes, anemia, vomiting, diarrhea, low potassium levels in the blood, capillary leak syndrome, neutropenia and lymphopenia, hives, and low blood calcium levels, the statement said.
The drug carries a boxed warning that the drug can irritate nerve cells, causing severe pain that requires treatment with intravenous narcotics, and can cause nerve damage and life-threatening infusion reactions, including upper airway swelling, difficulty breathing, and low blood pressure, during or shortly following completion of the infusion. Dinutuximab may also cause other serious side effects, including infections, eye problems, electrolyte abnormalities, and bone marrow suppression.
The FDA granted approval of dinutuximab, to be marketed as Unituxin, following a priority review and orphan product designation.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has approved dinutuximab as part of a multimodality regimen, including surgery, chemotherapy, and radiation therapy, for pediatric patients with high-risk neuroblastoma.
The drug “marks the first approval for a therapy aimed specifically for the treatment of patients with high-risk neuroblastoma,” Dr. Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in the March 10 FDA announcement.
Dinutuximab is a chimeric monoclonal antibody that targets GD2, a glycolipid on the surface of tumor cells, according to the manufacturer, United Therapeutics.
The FDA granted approval based on a clinical trial of 226 pediatric participants with high-risk neuroblastoma whose tumors shrunk or disappeared after treatment with multiple-drug chemotherapy and surgery followed by additional intensive chemotherapy and who subsequently received bone marrow transplantation support and radiation therapy. Three years after being randomly assigned to receive either isotretinoin or dinutuximab in combination with interleukin-2 and granulocyte macrophage colony-stimulating factor, 63% of participants receiving the combination were alive and free of tumor growth or recurrence, compared with 46% of participants treated with isotretinoin alone.
In an updated analysis, 73% of participants who received the combination were alive, compared with 58% of those receiving isotretinoin alone, the FDA said in the announcement.
The most common side effects were severe pain, fever, low platelet counts, infusion reactions, low blood pressure, hyponatremia, elevated liver enzymes, anemia, vomiting, diarrhea, low potassium levels in the blood, capillary leak syndrome, neutropenia and lymphopenia, hives, and low blood calcium levels, the statement said.
The drug carries a boxed warning that the drug can irritate nerve cells, causing severe pain that requires treatment with intravenous narcotics, and can cause nerve damage and life-threatening infusion reactions, including upper airway swelling, difficulty breathing, and low blood pressure, during or shortly following completion of the infusion. Dinutuximab may also cause other serious side effects, including infections, eye problems, electrolyte abnormalities, and bone marrow suppression.
The FDA granted approval of dinutuximab, to be marketed as Unituxin, following a priority review and orphan product designation.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has approved dinutuximab as part of a multimodality regimen, including surgery, chemotherapy, and radiation therapy, for pediatric patients with high-risk neuroblastoma.
The drug “marks the first approval for a therapy aimed specifically for the treatment of patients with high-risk neuroblastoma,” Dr. Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in the March 10 FDA announcement.
Dinutuximab is a chimeric monoclonal antibody that targets GD2, a glycolipid on the surface of tumor cells, according to the manufacturer, United Therapeutics.
The FDA granted approval based on a clinical trial of 226 pediatric participants with high-risk neuroblastoma whose tumors shrunk or disappeared after treatment with multiple-drug chemotherapy and surgery followed by additional intensive chemotherapy and who subsequently received bone marrow transplantation support and radiation therapy. Three years after being randomly assigned to receive either isotretinoin or dinutuximab in combination with interleukin-2 and granulocyte macrophage colony-stimulating factor, 63% of participants receiving the combination were alive and free of tumor growth or recurrence, compared with 46% of participants treated with isotretinoin alone.
In an updated analysis, 73% of participants who received the combination were alive, compared with 58% of those receiving isotretinoin alone, the FDA said in the announcement.
The most common side effects were severe pain, fever, low platelet counts, infusion reactions, low blood pressure, hyponatremia, elevated liver enzymes, anemia, vomiting, diarrhea, low potassium levels in the blood, capillary leak syndrome, neutropenia and lymphopenia, hives, and low blood calcium levels, the statement said.
The drug carries a boxed warning that the drug can irritate nerve cells, causing severe pain that requires treatment with intravenous narcotics, and can cause nerve damage and life-threatening infusion reactions, including upper airway swelling, difficulty breathing, and low blood pressure, during or shortly following completion of the infusion. Dinutuximab may also cause other serious side effects, including infections, eye problems, electrolyte abnormalities, and bone marrow suppression.
The FDA granted approval of dinutuximab, to be marketed as Unituxin, following a priority review and orphan product designation.
[email protected]
On Twitter @nikolaideslaura