User login
PE patients with malignancy survived longer if given LMWH instead of oral VKA
Among pulmonary embolism patients with malignancy, post-treatment lengths of survival were higher for those who received long-term low-molecular-weight heparin (LMWH) than for those who received oral vitamin K agonist (VKA), according to a prospective study.
Of the 92 PE patients with malignancy studied, 56 received long-term LMWH and 36 received oral VKA. The long-term LMWH treatment group had a median survival time of 30 months, which was significantly longer than the 12.5-month median survival time of the VKA treatment group, according to Shuai Zhang and colleagues.
The overall mortality rate for patients with malignancy was 48.9%, and the mortality rates of patients with malignancy treated with LMWH and VKA were 44.4% and 55.4%, respectively. Although a higher percentage of the LMWH treatment group survived than the VKA treatment group, the difference between the groups’ overall survival rates was not significant. However, the median survival time was significantly longer in the LMWH group than the VKA group (30 months vs. 12.5 months; P = .041), with the rate of all-cause death in the first 6 months decreased by long-term therapy with LMWH (19.6% vs. 41.7%; P = .022). In the multivariable Cox regression, long-term LMWH was a protective factor for all-cause death in the first 6 months (hazard ratio, 0.399; P = .022).
PE patients with malignancies could more effectively protect their lives and extend their survival time by using LMWH for at least 3 months instead of oral VKA, the investigators said. “In order to evaluate the impact of extended duration of LMWH on mortality, randomized controlled trials with [a] large sample size need to be designed,” they said.
Find the full study in Thrombosis Research (doi.org/10.1016/j.thromres.2014.11.015).
Among pulmonary embolism patients with malignancy, post-treatment lengths of survival were higher for those who received long-term low-molecular-weight heparin (LMWH) than for those who received oral vitamin K agonist (VKA), according to a prospective study.
Of the 92 PE patients with malignancy studied, 56 received long-term LMWH and 36 received oral VKA. The long-term LMWH treatment group had a median survival time of 30 months, which was significantly longer than the 12.5-month median survival time of the VKA treatment group, according to Shuai Zhang and colleagues.
The overall mortality rate for patients with malignancy was 48.9%, and the mortality rates of patients with malignancy treated with LMWH and VKA were 44.4% and 55.4%, respectively. Although a higher percentage of the LMWH treatment group survived than the VKA treatment group, the difference between the groups’ overall survival rates was not significant. However, the median survival time was significantly longer in the LMWH group than the VKA group (30 months vs. 12.5 months; P = .041), with the rate of all-cause death in the first 6 months decreased by long-term therapy with LMWH (19.6% vs. 41.7%; P = .022). In the multivariable Cox regression, long-term LMWH was a protective factor for all-cause death in the first 6 months (hazard ratio, 0.399; P = .022).
PE patients with malignancies could more effectively protect their lives and extend their survival time by using LMWH for at least 3 months instead of oral VKA, the investigators said. “In order to evaluate the impact of extended duration of LMWH on mortality, randomized controlled trials with [a] large sample size need to be designed,” they said.
Find the full study in Thrombosis Research (doi.org/10.1016/j.thromres.2014.11.015).
Among pulmonary embolism patients with malignancy, post-treatment lengths of survival were higher for those who received long-term low-molecular-weight heparin (LMWH) than for those who received oral vitamin K agonist (VKA), according to a prospective study.
Of the 92 PE patients with malignancy studied, 56 received long-term LMWH and 36 received oral VKA. The long-term LMWH treatment group had a median survival time of 30 months, which was significantly longer than the 12.5-month median survival time of the VKA treatment group, according to Shuai Zhang and colleagues.
The overall mortality rate for patients with malignancy was 48.9%, and the mortality rates of patients with malignancy treated with LMWH and VKA were 44.4% and 55.4%, respectively. Although a higher percentage of the LMWH treatment group survived than the VKA treatment group, the difference between the groups’ overall survival rates was not significant. However, the median survival time was significantly longer in the LMWH group than the VKA group (30 months vs. 12.5 months; P = .041), with the rate of all-cause death in the first 6 months decreased by long-term therapy with LMWH (19.6% vs. 41.7%; P = .022). In the multivariable Cox regression, long-term LMWH was a protective factor for all-cause death in the first 6 months (hazard ratio, 0.399; P = .022).
PE patients with malignancies could more effectively protect their lives and extend their survival time by using LMWH for at least 3 months instead of oral VKA, the investigators said. “In order to evaluate the impact of extended duration of LMWH on mortality, randomized controlled trials with [a] large sample size need to be designed,” they said.
Find the full study in Thrombosis Research (doi.org/10.1016/j.thromres.2014.11.015).
New guideline outlines management of hip fractures in elderly patients
The American Academy of Orthopaedic Surgeons’ new guideline on the diagnosis and treatment of hip fractures in elderly patients targets problem areas such as postoperative delirium and pain management.
The clinical practice guideline, “Management of Hip Fractures in the Elderly,” addresses hip fractures in patients age 65 years and older and offers recommendations on issues such as the timing of surgery and the use of vitamin D.
The AAOS also hopes the guideline will expose gaps in the body of research literature that should be addressed in future studies. The guideline has been endorsed by the American Geriatrics Society, the U.S. Bone and Joint Initiative, the Orthopaedic Trauma Association, the American Association of Clinical Endocrinologists, and the Hip Society.
The guideline’s recommendations include:
• Regional analgesia should be used to improve preoperative pain control in patients with hip fracture.
• MRI should be the advanced imaging of choice for diagnosis of presumed hip fracture not apparent on initial radiographs.
• Hip fracture surgery should be performed within 48 hours of admission.
• An interdisciplinary care program should be utilized for patients with mild to moderate dementia who have sustained a hip fracture.
• Supplemental vitamin D and calcium should be given to patients following hip fracture surgery.
• Patients should be evaluated and treated for osteoporosis after sustaining a hip fracture.
To read the entire guideline document, click here: www.aaos.org/research/guidelines/HipFxGuideline.pdf.
The American Academy of Orthopaedic Surgeons’ new guideline on the diagnosis and treatment of hip fractures in elderly patients targets problem areas such as postoperative delirium and pain management.
The clinical practice guideline, “Management of Hip Fractures in the Elderly,” addresses hip fractures in patients age 65 years and older and offers recommendations on issues such as the timing of surgery and the use of vitamin D.
The AAOS also hopes the guideline will expose gaps in the body of research literature that should be addressed in future studies. The guideline has been endorsed by the American Geriatrics Society, the U.S. Bone and Joint Initiative, the Orthopaedic Trauma Association, the American Association of Clinical Endocrinologists, and the Hip Society.
The guideline’s recommendations include:
• Regional analgesia should be used to improve preoperative pain control in patients with hip fracture.
• MRI should be the advanced imaging of choice for diagnosis of presumed hip fracture not apparent on initial radiographs.
• Hip fracture surgery should be performed within 48 hours of admission.
• An interdisciplinary care program should be utilized for patients with mild to moderate dementia who have sustained a hip fracture.
• Supplemental vitamin D and calcium should be given to patients following hip fracture surgery.
• Patients should be evaluated and treated for osteoporosis after sustaining a hip fracture.
To read the entire guideline document, click here: www.aaos.org/research/guidelines/HipFxGuideline.pdf.
The American Academy of Orthopaedic Surgeons’ new guideline on the diagnosis and treatment of hip fractures in elderly patients targets problem areas such as postoperative delirium and pain management.
The clinical practice guideline, “Management of Hip Fractures in the Elderly,” addresses hip fractures in patients age 65 years and older and offers recommendations on issues such as the timing of surgery and the use of vitamin D.
The AAOS also hopes the guideline will expose gaps in the body of research literature that should be addressed in future studies. The guideline has been endorsed by the American Geriatrics Society, the U.S. Bone and Joint Initiative, the Orthopaedic Trauma Association, the American Association of Clinical Endocrinologists, and the Hip Society.
The guideline’s recommendations include:
• Regional analgesia should be used to improve preoperative pain control in patients with hip fracture.
• MRI should be the advanced imaging of choice for diagnosis of presumed hip fracture not apparent on initial radiographs.
• Hip fracture surgery should be performed within 48 hours of admission.
• An interdisciplinary care program should be utilized for patients with mild to moderate dementia who have sustained a hip fracture.
• Supplemental vitamin D and calcium should be given to patients following hip fracture surgery.
• Patients should be evaluated and treated for osteoporosis after sustaining a hip fracture.
To read the entire guideline document, click here: www.aaos.org/research/guidelines/HipFxGuideline.pdf.
Extended anticoagulant therapy reduced risk of VTE recurrence
Apixaban was the safest anticoagulant used for extended treatment of venous thromboembolism (VTE), according to a network meta-analysis of more than 11.000 patients.
While several anticoagulants significantly reduced the risk of VTE recurrence compared to placebo, only apixaban also did not increase bleeding risk significantly more than placebo. In fact, all active therapies except aspirin increased the risk of composite bleeding by 2-4 times compared to apixaban (2.5 mg), according to Diana M. Sobieraj, Pharm.D., of the University of Connecticut, and her colleagues.
In addition to apixaban (2.5 mg and 5 mg), the other anticoagulants that significantly reduced the risk of VTE recurrence compared to placebo were dabigatran, rivaroxaban, idraparinux, and vitamin K antagonists (VKAs). Of these drugs, idraparinux was least effective and VKAs were most effective at reducing the risk of a recurring VTE,
All of the anticoagulants other than idraparinux significantly reduced VTE risk more than aspirin did, ranging from a 73% reduction, with either apixaban (2.5 mg) or rivaroxaban, to an 80% reduced risk with VKAs.
Whether anticoagulation therapy should be extended for patients with VTE beyond 3 months remains a topic of debate, but results of the analysis “provide additional justification for” doing so, “primarily in patients with unprovoked proximal [VTE] with low to moderate bleeding risk,” the researchers reported.
Find the full study in Thrombosis Research (doi.org/10.1016/j.thromres.2015.02.032)
Apixaban was the safest anticoagulant used for extended treatment of venous thromboembolism (VTE), according to a network meta-analysis of more than 11.000 patients.
While several anticoagulants significantly reduced the risk of VTE recurrence compared to placebo, only apixaban also did not increase bleeding risk significantly more than placebo. In fact, all active therapies except aspirin increased the risk of composite bleeding by 2-4 times compared to apixaban (2.5 mg), according to Diana M. Sobieraj, Pharm.D., of the University of Connecticut, and her colleagues.
In addition to apixaban (2.5 mg and 5 mg), the other anticoagulants that significantly reduced the risk of VTE recurrence compared to placebo were dabigatran, rivaroxaban, idraparinux, and vitamin K antagonists (VKAs). Of these drugs, idraparinux was least effective and VKAs were most effective at reducing the risk of a recurring VTE,
All of the anticoagulants other than idraparinux significantly reduced VTE risk more than aspirin did, ranging from a 73% reduction, with either apixaban (2.5 mg) or rivaroxaban, to an 80% reduced risk with VKAs.
Whether anticoagulation therapy should be extended for patients with VTE beyond 3 months remains a topic of debate, but results of the analysis “provide additional justification for” doing so, “primarily in patients with unprovoked proximal [VTE] with low to moderate bleeding risk,” the researchers reported.
Find the full study in Thrombosis Research (doi.org/10.1016/j.thromres.2015.02.032)
Apixaban was the safest anticoagulant used for extended treatment of venous thromboembolism (VTE), according to a network meta-analysis of more than 11.000 patients.
While several anticoagulants significantly reduced the risk of VTE recurrence compared to placebo, only apixaban also did not increase bleeding risk significantly more than placebo. In fact, all active therapies except aspirin increased the risk of composite bleeding by 2-4 times compared to apixaban (2.5 mg), according to Diana M. Sobieraj, Pharm.D., of the University of Connecticut, and her colleagues.
In addition to apixaban (2.5 mg and 5 mg), the other anticoagulants that significantly reduced the risk of VTE recurrence compared to placebo were dabigatran, rivaroxaban, idraparinux, and vitamin K antagonists (VKAs). Of these drugs, idraparinux was least effective and VKAs were most effective at reducing the risk of a recurring VTE,
All of the anticoagulants other than idraparinux significantly reduced VTE risk more than aspirin did, ranging from a 73% reduction, with either apixaban (2.5 mg) or rivaroxaban, to an 80% reduced risk with VKAs.
Whether anticoagulation therapy should be extended for patients with VTE beyond 3 months remains a topic of debate, but results of the analysis “provide additional justification for” doing so, “primarily in patients with unprovoked proximal [VTE] with low to moderate bleeding risk,” the researchers reported.
Find the full study in Thrombosis Research (doi.org/10.1016/j.thromres.2015.02.032)
April 2015 Quiz 2
ANSWER: A
Critique
While small bowel biopsies are the gold standard test for the exclusion of celiac disease, HLA typing for DQ2 and DQ8 (A) is very useful as an exclusionary test for celiac disease, as the diagnosis is quite unlikely in their absence. DQ2 and DQ8 haplotyping also are useful when small intestinal biopsies are equivocal. Antigliadin antibodies (B & C) do not have particularly high negative predictive values, and have little value here. Also, gluten challenge testing (E) would be of limited utility in excluding the presence of celiac disease.
Reference
1. Liu E., Rewers M., Eisenbarth G.S. Genetic testing: who should do the testing and what is the role of genetic testing in the setting of celiac disease? Gastroenterology 2005;128(4 Suppl 1):S33-7.
ANSWER: A
Critique
While small bowel biopsies are the gold standard test for the exclusion of celiac disease, HLA typing for DQ2 and DQ8 (A) is very useful as an exclusionary test for celiac disease, as the diagnosis is quite unlikely in their absence. DQ2 and DQ8 haplotyping also are useful when small intestinal biopsies are equivocal. Antigliadin antibodies (B & C) do not have particularly high negative predictive values, and have little value here. Also, gluten challenge testing (E) would be of limited utility in excluding the presence of celiac disease.
Reference
1. Liu E., Rewers M., Eisenbarth G.S. Genetic testing: who should do the testing and what is the role of genetic testing in the setting of celiac disease? Gastroenterology 2005;128(4 Suppl 1):S33-7.
ANSWER: A
Critique
While small bowel biopsies are the gold standard test for the exclusion of celiac disease, HLA typing for DQ2 and DQ8 (A) is very useful as an exclusionary test for celiac disease, as the diagnosis is quite unlikely in their absence. DQ2 and DQ8 haplotyping also are useful when small intestinal biopsies are equivocal. Antigliadin antibodies (B & C) do not have particularly high negative predictive values, and have little value here. Also, gluten challenge testing (E) would be of limited utility in excluding the presence of celiac disease.
Reference
1. Liu E., Rewers M., Eisenbarth G.S. Genetic testing: who should do the testing and what is the role of genetic testing in the setting of celiac disease? Gastroenterology 2005;128(4 Suppl 1):S33-7.
April 2015 Quiz 1
ANSWER: C
Critique
The patient in this clinical presentation has symptoms most consistent with cyclic vomiting syndrome (CVS) and has undergone additional testing to exclude luminal pathology. His gastric emptying study is consistent with rapid gastric emptying, which can be seen in 60% of patients with CVS. There is increasing recognition of hyperemesis in the setting of cannabis use, and this may be contributing to this patient’s symptoms. However, prior to recommending that patients stop using cannabis, appropriate treatment for CVS should be instituted. There are several reports that suggest long-term tricyclic antidepressant (TCA) therapy significantly reduces the frequency and duration of CVS episodes, ED visits, and hospitalizations. Although psychiatric disorders are associated with nonresponse to TCA therapy, an appropriate trial of a TCA is warranted prior to referral to psychiatry in the absence of a clear psychological diagnosis. The clinical picture does not suggest small intestinal bacterial overgrowth.
Reference
1. Hejazi R.A., Reddymasu S.C., Namin F., Lavenbarg T., Foran P., McCallum R.W. Efficacy of tricyclic antidepressant therapy in adults with cyclic vomiting syndrome: a two-year follow-up study. J. Clin. Gastroenterol. 2010;44:18-21.
ANSWER: C
Critique
The patient in this clinical presentation has symptoms most consistent with cyclic vomiting syndrome (CVS) and has undergone additional testing to exclude luminal pathology. His gastric emptying study is consistent with rapid gastric emptying, which can be seen in 60% of patients with CVS. There is increasing recognition of hyperemesis in the setting of cannabis use, and this may be contributing to this patient’s symptoms. However, prior to recommending that patients stop using cannabis, appropriate treatment for CVS should be instituted. There are several reports that suggest long-term tricyclic antidepressant (TCA) therapy significantly reduces the frequency and duration of CVS episodes, ED visits, and hospitalizations. Although psychiatric disorders are associated with nonresponse to TCA therapy, an appropriate trial of a TCA is warranted prior to referral to psychiatry in the absence of a clear psychological diagnosis. The clinical picture does not suggest small intestinal bacterial overgrowth.
Reference
1. Hejazi R.A., Reddymasu S.C., Namin F., Lavenbarg T., Foran P., McCallum R.W. Efficacy of tricyclic antidepressant therapy in adults with cyclic vomiting syndrome: a two-year follow-up study. J. Clin. Gastroenterol. 2010;44:18-21.
ANSWER: C
Critique
The patient in this clinical presentation has symptoms most consistent with cyclic vomiting syndrome (CVS) and has undergone additional testing to exclude luminal pathology. His gastric emptying study is consistent with rapid gastric emptying, which can be seen in 60% of patients with CVS. There is increasing recognition of hyperemesis in the setting of cannabis use, and this may be contributing to this patient’s symptoms. However, prior to recommending that patients stop using cannabis, appropriate treatment for CVS should be instituted. There are several reports that suggest long-term tricyclic antidepressant (TCA) therapy significantly reduces the frequency and duration of CVS episodes, ED visits, and hospitalizations. Although psychiatric disorders are associated with nonresponse to TCA therapy, an appropriate trial of a TCA is warranted prior to referral to psychiatry in the absence of a clear psychological diagnosis. The clinical picture does not suggest small intestinal bacterial overgrowth.
Reference
1. Hejazi R.A., Reddymasu S.C., Namin F., Lavenbarg T., Foran P., McCallum R.W. Efficacy of tricyclic antidepressant therapy in adults with cyclic vomiting syndrome: a two-year follow-up study. J. Clin. Gastroenterol. 2010;44:18-21.
New and Noteworthy Information—April 2015
Gout is inversely associated with the risk of developing Alzheimer’s disease, and uric acid may play a neuroprotective role, according to a study published March 4 in Annals of the Rheumatic Diseases. Researchers conducted a study using data from the Health Improvement Network, an electronic medical record database that is representative of the United Kingdom’s general population. Investigators identified 309 new cases of Alzheimer’s disease among 59,224 patients with gout (average age, 65) and 1,942 cases of Alzheimer’s disease among 238,805 people in the comparison group over a five-year follow up. After accounting for age, sex, BMI, socioeconomic status, lifestyle factors, prior heart conditions, and use of heart drugs, people with a history of gout had a 24% lower risk of developing Alzheimer’s disease.
In patients with ST-segment elevation myocardial infarction who are undergoing primary percutaneous coronary intervention (PCI), routine manual thrombectomy may not reduce the risk of cardiovascular death, compared with PCI alone, according to a study published online ahead of print March 16 in New England Journal of Medicine. In a randomized controlled trial that involved 10,732 patients at 87 hospitals in 20 countries, half of participants received PCI alone and half received PCI with manual thrombectomy. Death from cardiovascular causes, recurrent myocardial infarction, cardiogenic shock, or heart failure occurred within 180 days in 6.9% of the thrombectomy group and 7% of the PCI-alone group. “The message from this study is that thrombectomy should not be used as a routine strategy,” the researchers stated.
A broad range of pre-existing mental disorders are associated with the subsequent onset of severe or frequent headaches, according to a study published in the January issue of Journal of Pain. Researchers evaluated data from 19 World Health Organization World Mental Health Surveys completed by more than 50,000 subjects. The investigators looked at the association between pre-existing mood, anxiety, impulse control, and substance use disorders with subsequent onset of frequent or severe headaches. After adjusting for sex, age, and mental disorder comorbidity, the researchers found that mood, anxiety, and impulse control disorders increased the likelihood of developing severe and frequent headaches by 40%. Respondents with early-onset pre-existing mental disorders had a 21% higher risk for developing headaches than people with later-onset mental disorders.
Early symptoms of post-traumatic stress, such as anxiety, emotional numbness, flashbacks, and irritability, are the strongest predictors of later disability, according to a study published online ahead of print March 4 in Brain. The trial included 38 service members diagnosed with blast-related concussive traumatic brain injury and 34 service members without brain injury who volunteered to serve as controls. Early assessments of service members were conducted in Afghanistan during the first week after injury. Follow-up mental health assessments were conducted with standard interviews at six to 12 months afterward. Sixty-three percent of patients with brain injury were classified as moderately disabled, compared with 20% of people in the control group. The remaining 37% of the brain injury group were considered to have a good recovery.
Among teenagers, heavy marijuana use is associated with an abnormally shaped hippocampus and poor performance on long-term memory tasks, according to a study published online ahead of print March 11 in Hippocampus. Researchers examined 97 people, including matched groups of healthy controls, subjects with a marijuana use disorder, people with schizophrenia and no history of substance use disorders, and people with schizophrenia and a marijuana use disorder. Participants had started using marijuana daily between ages 16 and 17 and continued for about three years. Overall, the longer participants used marijuana, the more abnormal the shape of their hippocampus became. Young adults with schizophrenia who abused cannabis as teens also performed about 26% more poorly on memory tests than young adults with schizophrenia who never abused cannabis.
The combination of enalapril and folic acid, compared with enalapril alone, significantly reduces the risk of a first stroke in adults with hypertension, according to a study published online ahead of print March 15 in JAMA. Researchers randomized 20,702 adults with hypertension and no history of stroke or heart attack to daily treatment with a single-pill combination containing 10 mg of enalapril and 0.8 mg of folic acid or to a tablet containing 10 mg of enalapril alone. During a median treatment duration of 4.5 years, first stroke occurred in 282 participants in the enalapril–folic acid group, compared with 355 participants in the enalapril group. Analyses also showed significant reductions in the risk of ischemic stroke and cardiovascular events among participants in the enalapril– folic acid group.
Responsive direct cortical stimulation safely and effectively reduces seizures in adults with medically refractory partial onset seizures, according to a study published February 24 in Neurology. The results are part of an ongoing, seven-year, multicenter, prospective, open-label study to evaluate the long-term efficacy and safety of the RNS System. A total of 256 participants were implanted with the neurostimulator and leads. Seizure frequency decreased in the majority of participants treated with responsive stimulation. The median percent reduction in seizures was 44% at one year and 53% at two years postimplant. The median percent reduction in seizures was 60% at the beginning of year three and 66% at the beginning of year six. The responder rates at the same time points were 58% and 59%, respectively.
Persistent insomnia is associated with increased risk for all-cause and cardiopulmonary mortality and a steeper increase in inflammation, according to a study published March 12 in American Journal of Medicine. Researchers assessed the persistence of insomnia complaints in 1,409 adult participants from the Tucson Epidemiological Study of Airway Obstructive Disease. The study began in 1972 and included multiple follow-up surveys until 1996 and continuous mortality follow-up data until 2011. Using data from the survey from 1972 through 1973 and from the 1990 through 1992 follow-up survey, the researchers found that serum C-reactive protein (CRP) levels increased over time in people with persistent insomnia. In those subjects for whom CRP data were available, persistent insomnia was associated with a 58% increase in mortality risk, after adjustments for confounding factors.
Prolonged sleep is a potentially useful marker to determine increased future stroke risk in a healthy aging population, according to a study published online ahead of print February 25 in Neurology. Researchers followed 9,692 people with a mean age of 62 who had never had a stroke. Participants were asked about their sleeping habits once and then again four years later. The participants were followed for an average of 9.5 years, and 346 people had a stroke. Of the 986 people who slept more than eight hours per night, 52 had a stroke, compared with 211 of the 6,684 people who slept an average amount. The relationship between long sleep and stroke remained the same after researchers accounted for high cholesterol, high blood pressure, physical activity, and BMI.
Higher levels of physical activity may reduce the effects of white matter hyperintensity burden on motor function in healthy older adults, according to a study published online ahead of print March 11 in Neurology. Researchers examined 167 people (average age, 80) who wore movement monitors on their wrists for as long as 11 days to measure exercise and nonexercise activity. Participants also took 11 motor performance tests. For the people in the top 10% of activity, greater amounts of brain damage did not influence scores on the movement tests. However, for people in the less active half of the population, greater amounts of brain damage were associated with lower scores on the movement tests. For all participants, the average score on the movement tests was 1.04.
Patients with Parkinson’s disease have reduced low- and high-contrast visual acuity, compared with controls, according to a study published January 1 in Journal of Parkinson’s Disease. Thirty-two patients with Parkinson’s disease and 71 control subjects underwent a neurologic examination, which included the Unified Parkinson’s Disease Rating Scale and vision testing using the Variable Contrast Acuity Chart displayed on an iPad. The chart was displayed at low and high contrast at distances of 40 cm and 2 m. Based on the number of letters correctly identified, patients with Parkinson’s disease saw about 10% fewer letters than control subjects in the low-contrast tests at either distance and in the high-contrast tests at 2 m. Researchers found no significant difference between Parkinson’s disease and control subjects in the high-contrast testing at 40 cm.
Statins may not lower the risk for Parkinson’s disease, according to a study published online ahead of print January 14 in Movement Disorders. The researchers examined blood cholesterol levels, medications, and Parkinson’s disease status in participants in the ongoing, long-term Atherosclerosis Risk in Communities study. Cholesterol readings were taken at three-year intervals between 1987 and 1998. Statin use before 1998 was associated with significantly higher risk of Parkinson’s disease after 1998. Higher total cholesterol, however, was associated with lower risk for Parkinson’s disease after adjustment for statin use and confounders. Compared with the lowest tertile of average total cholesterol, the odds ratios for Parkinson’s disease were 0.56 for the second tertile and 0.43 for the third tertile. These data are inconsistent with the hypothesis that statins protect against Parkinson’s disease.
—Kimberly Williams
Gout is inversely associated with the risk of developing Alzheimer’s disease, and uric acid may play a neuroprotective role, according to a study published March 4 in Annals of the Rheumatic Diseases. Researchers conducted a study using data from the Health Improvement Network, an electronic medical record database that is representative of the United Kingdom’s general population. Investigators identified 309 new cases of Alzheimer’s disease among 59,224 patients with gout (average age, 65) and 1,942 cases of Alzheimer’s disease among 238,805 people in the comparison group over a five-year follow up. After accounting for age, sex, BMI, socioeconomic status, lifestyle factors, prior heart conditions, and use of heart drugs, people with a history of gout had a 24% lower risk of developing Alzheimer’s disease.
In patients with ST-segment elevation myocardial infarction who are undergoing primary percutaneous coronary intervention (PCI), routine manual thrombectomy may not reduce the risk of cardiovascular death, compared with PCI alone, according to a study published online ahead of print March 16 in New England Journal of Medicine. In a randomized controlled trial that involved 10,732 patients at 87 hospitals in 20 countries, half of participants received PCI alone and half received PCI with manual thrombectomy. Death from cardiovascular causes, recurrent myocardial infarction, cardiogenic shock, or heart failure occurred within 180 days in 6.9% of the thrombectomy group and 7% of the PCI-alone group. “The message from this study is that thrombectomy should not be used as a routine strategy,” the researchers stated.
A broad range of pre-existing mental disorders are associated with the subsequent onset of severe or frequent headaches, according to a study published in the January issue of Journal of Pain. Researchers evaluated data from 19 World Health Organization World Mental Health Surveys completed by more than 50,000 subjects. The investigators looked at the association between pre-existing mood, anxiety, impulse control, and substance use disorders with subsequent onset of frequent or severe headaches. After adjusting for sex, age, and mental disorder comorbidity, the researchers found that mood, anxiety, and impulse control disorders increased the likelihood of developing severe and frequent headaches by 40%. Respondents with early-onset pre-existing mental disorders had a 21% higher risk for developing headaches than people with later-onset mental disorders.
Early symptoms of post-traumatic stress, such as anxiety, emotional numbness, flashbacks, and irritability, are the strongest predictors of later disability, according to a study published online ahead of print March 4 in Brain. The trial included 38 service members diagnosed with blast-related concussive traumatic brain injury and 34 service members without brain injury who volunteered to serve as controls. Early assessments of service members were conducted in Afghanistan during the first week after injury. Follow-up mental health assessments were conducted with standard interviews at six to 12 months afterward. Sixty-three percent of patients with brain injury were classified as moderately disabled, compared with 20% of people in the control group. The remaining 37% of the brain injury group were considered to have a good recovery.
Among teenagers, heavy marijuana use is associated with an abnormally shaped hippocampus and poor performance on long-term memory tasks, according to a study published online ahead of print March 11 in Hippocampus. Researchers examined 97 people, including matched groups of healthy controls, subjects with a marijuana use disorder, people with schizophrenia and no history of substance use disorders, and people with schizophrenia and a marijuana use disorder. Participants had started using marijuana daily between ages 16 and 17 and continued for about three years. Overall, the longer participants used marijuana, the more abnormal the shape of their hippocampus became. Young adults with schizophrenia who abused cannabis as teens also performed about 26% more poorly on memory tests than young adults with schizophrenia who never abused cannabis.
The combination of enalapril and folic acid, compared with enalapril alone, significantly reduces the risk of a first stroke in adults with hypertension, according to a study published online ahead of print March 15 in JAMA. Researchers randomized 20,702 adults with hypertension and no history of stroke or heart attack to daily treatment with a single-pill combination containing 10 mg of enalapril and 0.8 mg of folic acid or to a tablet containing 10 mg of enalapril alone. During a median treatment duration of 4.5 years, first stroke occurred in 282 participants in the enalapril–folic acid group, compared with 355 participants in the enalapril group. Analyses also showed significant reductions in the risk of ischemic stroke and cardiovascular events among participants in the enalapril– folic acid group.
Responsive direct cortical stimulation safely and effectively reduces seizures in adults with medically refractory partial onset seizures, according to a study published February 24 in Neurology. The results are part of an ongoing, seven-year, multicenter, prospective, open-label study to evaluate the long-term efficacy and safety of the RNS System. A total of 256 participants were implanted with the neurostimulator and leads. Seizure frequency decreased in the majority of participants treated with responsive stimulation. The median percent reduction in seizures was 44% at one year and 53% at two years postimplant. The median percent reduction in seizures was 60% at the beginning of year three and 66% at the beginning of year six. The responder rates at the same time points were 58% and 59%, respectively.
Persistent insomnia is associated with increased risk for all-cause and cardiopulmonary mortality and a steeper increase in inflammation, according to a study published March 12 in American Journal of Medicine. Researchers assessed the persistence of insomnia complaints in 1,409 adult participants from the Tucson Epidemiological Study of Airway Obstructive Disease. The study began in 1972 and included multiple follow-up surveys until 1996 and continuous mortality follow-up data until 2011. Using data from the survey from 1972 through 1973 and from the 1990 through 1992 follow-up survey, the researchers found that serum C-reactive protein (CRP) levels increased over time in people with persistent insomnia. In those subjects for whom CRP data were available, persistent insomnia was associated with a 58% increase in mortality risk, after adjustments for confounding factors.
Prolonged sleep is a potentially useful marker to determine increased future stroke risk in a healthy aging population, according to a study published online ahead of print February 25 in Neurology. Researchers followed 9,692 people with a mean age of 62 who had never had a stroke. Participants were asked about their sleeping habits once and then again four years later. The participants were followed for an average of 9.5 years, and 346 people had a stroke. Of the 986 people who slept more than eight hours per night, 52 had a stroke, compared with 211 of the 6,684 people who slept an average amount. The relationship between long sleep and stroke remained the same after researchers accounted for high cholesterol, high blood pressure, physical activity, and BMI.
Higher levels of physical activity may reduce the effects of white matter hyperintensity burden on motor function in healthy older adults, according to a study published online ahead of print March 11 in Neurology. Researchers examined 167 people (average age, 80) who wore movement monitors on their wrists for as long as 11 days to measure exercise and nonexercise activity. Participants also took 11 motor performance tests. For the people in the top 10% of activity, greater amounts of brain damage did not influence scores on the movement tests. However, for people in the less active half of the population, greater amounts of brain damage were associated with lower scores on the movement tests. For all participants, the average score on the movement tests was 1.04.
Patients with Parkinson’s disease have reduced low- and high-contrast visual acuity, compared with controls, according to a study published January 1 in Journal of Parkinson’s Disease. Thirty-two patients with Parkinson’s disease and 71 control subjects underwent a neurologic examination, which included the Unified Parkinson’s Disease Rating Scale and vision testing using the Variable Contrast Acuity Chart displayed on an iPad. The chart was displayed at low and high contrast at distances of 40 cm and 2 m. Based on the number of letters correctly identified, patients with Parkinson’s disease saw about 10% fewer letters than control subjects in the low-contrast tests at either distance and in the high-contrast tests at 2 m. Researchers found no significant difference between Parkinson’s disease and control subjects in the high-contrast testing at 40 cm.
Statins may not lower the risk for Parkinson’s disease, according to a study published online ahead of print January 14 in Movement Disorders. The researchers examined blood cholesterol levels, medications, and Parkinson’s disease status in participants in the ongoing, long-term Atherosclerosis Risk in Communities study. Cholesterol readings were taken at three-year intervals between 1987 and 1998. Statin use before 1998 was associated with significantly higher risk of Parkinson’s disease after 1998. Higher total cholesterol, however, was associated with lower risk for Parkinson’s disease after adjustment for statin use and confounders. Compared with the lowest tertile of average total cholesterol, the odds ratios for Parkinson’s disease were 0.56 for the second tertile and 0.43 for the third tertile. These data are inconsistent with the hypothesis that statins protect against Parkinson’s disease.
—Kimberly Williams
Gout is inversely associated with the risk of developing Alzheimer’s disease, and uric acid may play a neuroprotective role, according to a study published March 4 in Annals of the Rheumatic Diseases. Researchers conducted a study using data from the Health Improvement Network, an electronic medical record database that is representative of the United Kingdom’s general population. Investigators identified 309 new cases of Alzheimer’s disease among 59,224 patients with gout (average age, 65) and 1,942 cases of Alzheimer’s disease among 238,805 people in the comparison group over a five-year follow up. After accounting for age, sex, BMI, socioeconomic status, lifestyle factors, prior heart conditions, and use of heart drugs, people with a history of gout had a 24% lower risk of developing Alzheimer’s disease.
In patients with ST-segment elevation myocardial infarction who are undergoing primary percutaneous coronary intervention (PCI), routine manual thrombectomy may not reduce the risk of cardiovascular death, compared with PCI alone, according to a study published online ahead of print March 16 in New England Journal of Medicine. In a randomized controlled trial that involved 10,732 patients at 87 hospitals in 20 countries, half of participants received PCI alone and half received PCI with manual thrombectomy. Death from cardiovascular causes, recurrent myocardial infarction, cardiogenic shock, or heart failure occurred within 180 days in 6.9% of the thrombectomy group and 7% of the PCI-alone group. “The message from this study is that thrombectomy should not be used as a routine strategy,” the researchers stated.
A broad range of pre-existing mental disorders are associated with the subsequent onset of severe or frequent headaches, according to a study published in the January issue of Journal of Pain. Researchers evaluated data from 19 World Health Organization World Mental Health Surveys completed by more than 50,000 subjects. The investigators looked at the association between pre-existing mood, anxiety, impulse control, and substance use disorders with subsequent onset of frequent or severe headaches. After adjusting for sex, age, and mental disorder comorbidity, the researchers found that mood, anxiety, and impulse control disorders increased the likelihood of developing severe and frequent headaches by 40%. Respondents with early-onset pre-existing mental disorders had a 21% higher risk for developing headaches than people with later-onset mental disorders.
Early symptoms of post-traumatic stress, such as anxiety, emotional numbness, flashbacks, and irritability, are the strongest predictors of later disability, according to a study published online ahead of print March 4 in Brain. The trial included 38 service members diagnosed with blast-related concussive traumatic brain injury and 34 service members without brain injury who volunteered to serve as controls. Early assessments of service members were conducted in Afghanistan during the first week after injury. Follow-up mental health assessments were conducted with standard interviews at six to 12 months afterward. Sixty-three percent of patients with brain injury were classified as moderately disabled, compared with 20% of people in the control group. The remaining 37% of the brain injury group were considered to have a good recovery.
Among teenagers, heavy marijuana use is associated with an abnormally shaped hippocampus and poor performance on long-term memory tasks, according to a study published online ahead of print March 11 in Hippocampus. Researchers examined 97 people, including matched groups of healthy controls, subjects with a marijuana use disorder, people with schizophrenia and no history of substance use disorders, and people with schizophrenia and a marijuana use disorder. Participants had started using marijuana daily between ages 16 and 17 and continued for about three years. Overall, the longer participants used marijuana, the more abnormal the shape of their hippocampus became. Young adults with schizophrenia who abused cannabis as teens also performed about 26% more poorly on memory tests than young adults with schizophrenia who never abused cannabis.
The combination of enalapril and folic acid, compared with enalapril alone, significantly reduces the risk of a first stroke in adults with hypertension, according to a study published online ahead of print March 15 in JAMA. Researchers randomized 20,702 adults with hypertension and no history of stroke or heart attack to daily treatment with a single-pill combination containing 10 mg of enalapril and 0.8 mg of folic acid or to a tablet containing 10 mg of enalapril alone. During a median treatment duration of 4.5 years, first stroke occurred in 282 participants in the enalapril–folic acid group, compared with 355 participants in the enalapril group. Analyses also showed significant reductions in the risk of ischemic stroke and cardiovascular events among participants in the enalapril– folic acid group.
Responsive direct cortical stimulation safely and effectively reduces seizures in adults with medically refractory partial onset seizures, according to a study published February 24 in Neurology. The results are part of an ongoing, seven-year, multicenter, prospective, open-label study to evaluate the long-term efficacy and safety of the RNS System. A total of 256 participants were implanted with the neurostimulator and leads. Seizure frequency decreased in the majority of participants treated with responsive stimulation. The median percent reduction in seizures was 44% at one year and 53% at two years postimplant. The median percent reduction in seizures was 60% at the beginning of year three and 66% at the beginning of year six. The responder rates at the same time points were 58% and 59%, respectively.
Persistent insomnia is associated with increased risk for all-cause and cardiopulmonary mortality and a steeper increase in inflammation, according to a study published March 12 in American Journal of Medicine. Researchers assessed the persistence of insomnia complaints in 1,409 adult participants from the Tucson Epidemiological Study of Airway Obstructive Disease. The study began in 1972 and included multiple follow-up surveys until 1996 and continuous mortality follow-up data until 2011. Using data from the survey from 1972 through 1973 and from the 1990 through 1992 follow-up survey, the researchers found that serum C-reactive protein (CRP) levels increased over time in people with persistent insomnia. In those subjects for whom CRP data were available, persistent insomnia was associated with a 58% increase in mortality risk, after adjustments for confounding factors.
Prolonged sleep is a potentially useful marker to determine increased future stroke risk in a healthy aging population, according to a study published online ahead of print February 25 in Neurology. Researchers followed 9,692 people with a mean age of 62 who had never had a stroke. Participants were asked about their sleeping habits once and then again four years later. The participants were followed for an average of 9.5 years, and 346 people had a stroke. Of the 986 people who slept more than eight hours per night, 52 had a stroke, compared with 211 of the 6,684 people who slept an average amount. The relationship between long sleep and stroke remained the same after researchers accounted for high cholesterol, high blood pressure, physical activity, and BMI.
Higher levels of physical activity may reduce the effects of white matter hyperintensity burden on motor function in healthy older adults, according to a study published online ahead of print March 11 in Neurology. Researchers examined 167 people (average age, 80) who wore movement monitors on their wrists for as long as 11 days to measure exercise and nonexercise activity. Participants also took 11 motor performance tests. For the people in the top 10% of activity, greater amounts of brain damage did not influence scores on the movement tests. However, for people in the less active half of the population, greater amounts of brain damage were associated with lower scores on the movement tests. For all participants, the average score on the movement tests was 1.04.
Patients with Parkinson’s disease have reduced low- and high-contrast visual acuity, compared with controls, according to a study published January 1 in Journal of Parkinson’s Disease. Thirty-two patients with Parkinson’s disease and 71 control subjects underwent a neurologic examination, which included the Unified Parkinson’s Disease Rating Scale and vision testing using the Variable Contrast Acuity Chart displayed on an iPad. The chart was displayed at low and high contrast at distances of 40 cm and 2 m. Based on the number of letters correctly identified, patients with Parkinson’s disease saw about 10% fewer letters than control subjects in the low-contrast tests at either distance and in the high-contrast tests at 2 m. Researchers found no significant difference between Parkinson’s disease and control subjects in the high-contrast testing at 40 cm.
Statins may not lower the risk for Parkinson’s disease, according to a study published online ahead of print January 14 in Movement Disorders. The researchers examined blood cholesterol levels, medications, and Parkinson’s disease status in participants in the ongoing, long-term Atherosclerosis Risk in Communities study. Cholesterol readings were taken at three-year intervals between 1987 and 1998. Statin use before 1998 was associated with significantly higher risk of Parkinson’s disease after 1998. Higher total cholesterol, however, was associated with lower risk for Parkinson’s disease after adjustment for statin use and confounders. Compared with the lowest tertile of average total cholesterol, the odds ratios for Parkinson’s disease were 0.56 for the second tertile and 0.43 for the third tertile. These data are inconsistent with the hypothesis that statins protect against Parkinson’s disease.
—Kimberly Williams
Enzyme keeps HSCs functional to prevent anemia
Preclinical research suggests an enzyme found in hematopoietic stem cells (HSCs) is key to maintaining periods of inactivity, thereby decreasing the odds that HSCs will divide too often and acquire mutations or cell damage.
Experiments showed that animals lacking this enzyme, inositol trisphosphate 3-kinase B (Itpkb), experience dangerous HSC activation and ultimately succumb to lethal anemia.
“These HSCs remain active too long and then disappear,” said Karsten Sauer, PhD, of The Scripps Research Institute in La Jolla, California.
“As a consequence, the mice lose their red blood cells and die.”
With this new understanding of Itpkb, Dr Sauer and his colleagues believe they are closer to improving therapies for diseases such as bone marrow failure syndrome, anemia, leukemia, and lymphoma.
The team described their research in Blood.
The group set out to investigate the mechanisms that activate and deactivate HSCs. They focused on Itpkb because it is produced in HSCs, and the enzyme is known to dampen activating signaling in other cells.
“We hypothesized that Itpkb might do the same in HSCs to keep them at rest,” Dr Sauer said. “Moreover, Itpkb is an enzyme whose function can be controlled by small molecules. This might facilitate drug development if our hypothesis were true.”
The researchers started with a strain of mice that lacked the gene to produce Itpkb. As expected, these mice developed hyperactive HSCs. Eventually, the mutant HSCs exhausted themselves and stopped producing progenitor cells, so the mice developed severe anemia and died.
Dr Sauer and his colleagues linked the abnormal behavior of the mutant HSCs to a chain of events at the molecular level.
Itpkb’s job is to attach phosphates to molecules called inositols, which then send messages to other parts of the cell. The researchers found that Itpkb can turn one inositol, IP3, into another inositol known as IP4.
This is significant because IP4 controls cell proliferation, cellular metabolism, and aspects of the immune system. The study showed that IP4 also protects HSCs by dampening PI3K/Akt/mTOR signaling.
To confirm this finding, the researchers treated the animals with the mTOR inhibitor rapamycin. The drug halted the abnormal signaling process and prevented the excessive division of HSCs lacking Itpkb. This supported the notion that Itpkb maintains HSCs’ quiescence by dampening PI3K/Akt/mTOR signaling.
Dr Sauer said future research in his lab will focus on studying whether Itpkb has a similar function in human HSCs.
“A major question is whether we can translate our findings into innovative therapies,” he said. “If we can show that Itpkb also keeps human HSCs healthy, this could open avenues to target Itpkb to improve HSC function in bone marrow failure syndromes and immunodeficiencies or to increase the success rates of HSC transplantation therapies for leukemias and lymphomas.” ![]()
Preclinical research suggests an enzyme found in hematopoietic stem cells (HSCs) is key to maintaining periods of inactivity, thereby decreasing the odds that HSCs will divide too often and acquire mutations or cell damage.
Experiments showed that animals lacking this enzyme, inositol trisphosphate 3-kinase B (Itpkb), experience dangerous HSC activation and ultimately succumb to lethal anemia.
“These HSCs remain active too long and then disappear,” said Karsten Sauer, PhD, of The Scripps Research Institute in La Jolla, California.
“As a consequence, the mice lose their red blood cells and die.”
With this new understanding of Itpkb, Dr Sauer and his colleagues believe they are closer to improving therapies for diseases such as bone marrow failure syndrome, anemia, leukemia, and lymphoma.
The team described their research in Blood.
The group set out to investigate the mechanisms that activate and deactivate HSCs. They focused on Itpkb because it is produced in HSCs, and the enzyme is known to dampen activating signaling in other cells.
“We hypothesized that Itpkb might do the same in HSCs to keep them at rest,” Dr Sauer said. “Moreover, Itpkb is an enzyme whose function can be controlled by small molecules. This might facilitate drug development if our hypothesis were true.”
The researchers started with a strain of mice that lacked the gene to produce Itpkb. As expected, these mice developed hyperactive HSCs. Eventually, the mutant HSCs exhausted themselves and stopped producing progenitor cells, so the mice developed severe anemia and died.
Dr Sauer and his colleagues linked the abnormal behavior of the mutant HSCs to a chain of events at the molecular level.
Itpkb’s job is to attach phosphates to molecules called inositols, which then send messages to other parts of the cell. The researchers found that Itpkb can turn one inositol, IP3, into another inositol known as IP4.
This is significant because IP4 controls cell proliferation, cellular metabolism, and aspects of the immune system. The study showed that IP4 also protects HSCs by dampening PI3K/Akt/mTOR signaling.
To confirm this finding, the researchers treated the animals with the mTOR inhibitor rapamycin. The drug halted the abnormal signaling process and prevented the excessive division of HSCs lacking Itpkb. This supported the notion that Itpkb maintains HSCs’ quiescence by dampening PI3K/Akt/mTOR signaling.
Dr Sauer said future research in his lab will focus on studying whether Itpkb has a similar function in human HSCs.
“A major question is whether we can translate our findings into innovative therapies,” he said. “If we can show that Itpkb also keeps human HSCs healthy, this could open avenues to target Itpkb to improve HSC function in bone marrow failure syndromes and immunodeficiencies or to increase the success rates of HSC transplantation therapies for leukemias and lymphomas.” ![]()
Preclinical research suggests an enzyme found in hematopoietic stem cells (HSCs) is key to maintaining periods of inactivity, thereby decreasing the odds that HSCs will divide too often and acquire mutations or cell damage.
Experiments showed that animals lacking this enzyme, inositol trisphosphate 3-kinase B (Itpkb), experience dangerous HSC activation and ultimately succumb to lethal anemia.
“These HSCs remain active too long and then disappear,” said Karsten Sauer, PhD, of The Scripps Research Institute in La Jolla, California.
“As a consequence, the mice lose their red blood cells and die.”
With this new understanding of Itpkb, Dr Sauer and his colleagues believe they are closer to improving therapies for diseases such as bone marrow failure syndrome, anemia, leukemia, and lymphoma.
The team described their research in Blood.
The group set out to investigate the mechanisms that activate and deactivate HSCs. They focused on Itpkb because it is produced in HSCs, and the enzyme is known to dampen activating signaling in other cells.
“We hypothesized that Itpkb might do the same in HSCs to keep them at rest,” Dr Sauer said. “Moreover, Itpkb is an enzyme whose function can be controlled by small molecules. This might facilitate drug development if our hypothesis were true.”
The researchers started with a strain of mice that lacked the gene to produce Itpkb. As expected, these mice developed hyperactive HSCs. Eventually, the mutant HSCs exhausted themselves and stopped producing progenitor cells, so the mice developed severe anemia and died.
Dr Sauer and his colleagues linked the abnormal behavior of the mutant HSCs to a chain of events at the molecular level.
Itpkb’s job is to attach phosphates to molecules called inositols, which then send messages to other parts of the cell. The researchers found that Itpkb can turn one inositol, IP3, into another inositol known as IP4.
This is significant because IP4 controls cell proliferation, cellular metabolism, and aspects of the immune system. The study showed that IP4 also protects HSCs by dampening PI3K/Akt/mTOR signaling.
To confirm this finding, the researchers treated the animals with the mTOR inhibitor rapamycin. The drug halted the abnormal signaling process and prevented the excessive division of HSCs lacking Itpkb. This supported the notion that Itpkb maintains HSCs’ quiescence by dampening PI3K/Akt/mTOR signaling.
Dr Sauer said future research in his lab will focus on studying whether Itpkb has a similar function in human HSCs.
“A major question is whether we can translate our findings into innovative therapies,” he said. “If we can show that Itpkb also keeps human HSCs healthy, this could open avenues to target Itpkb to improve HSC function in bone marrow failure syndromes and immunodeficiencies or to increase the success rates of HSC transplantation therapies for leukemias and lymphomas.” ![]()
Pesticides may cause NHL, other cancers

Photo by John Messina
The International Agency for Research on Cancer (IARC), the specialized cancer agency of the World Health Organization, has found evidence suggesting that 5 organophosphate pesticides may be carcinogenic.
The IARC classified the herbicide glyphosate and the insecticides malathion and diazinon as “probably carcinogenic” to humans and the insecticides tetrachlorvinphos and parathion as “possibly carcinogenic” to humans.
A summary of these findings has been published in The Lancet Oncology.
Glyphosate
For the herbicide glyphosate, the IARC found limited evidence of carcinogenicity in humans. Case-control studies of occupational exposure to glyphosate in the US, Canada, and Sweden showed increased risks for non-Hodgkin lymphoma (NHL).
However, the Agricultural Health Study (AHS) showed no significantly increased risk of NHL in subjects exposed to glyphosate.
A study of community residents showed increases in blood markers of chromosomal damage after glyphosate formulations were sprayed nearby. And glyphosate was shown to cause DNA and chromosomal damage in human cells, although bacterial mutagenesis tests were negative.
In studies of male mice, glyphosate increased the incidence of renal tubule carcinoma and hemangiosarcoma. Glyphosate also increased the incidence of pancreatic islet-cell adenoma in male rats, and a glyphosate formulation promoted skin tumors in mice.
The IARC said glyphosate has the highest global production volume of all herbicides. It is used in agriculture, forestry, urban, and home applications.
Glyphosate has been detected in the air during spraying, in water, and in food. The general population is exposed to the chemical primarily by living near sprayed areas, home use, and diet. But the IARC said the level of exposure observed is generally low.
Malathion
The IARC classified malathion as “probably carcinogenic” for humans based on limited evidence linking the insecticide to NHL and prostate cancer. Occupational use of malathion was associated with an increased risk of prostate cancer in a Canadian case-control study and in the AHS.
Studies of occupational exposures in the US, Canada, and Sweden revealed positive associations between malathion and NHL. However, results of the AHS did not show an association between the insecticide and NHL.
Studies showed that malathion induced DNA and chromosomal damage in humans and animals, although bacterial mutagenesis tests were negative. Results also suggested malathion disrupts hormone pathways.
Experiments in mice showed malathion increased the incidence of hepatocellular adenoma or carcinoma (combined). In rats, the insecticide increased the incidence of thyroid carcinoma in males, hepatocellular adenoma or carcinoma (combined) in females, and mammary gland adenocarcinoma after subcutaneous injection in females.
The IARC said malathion is used in “substantial volumes throughout the world” to control insects in agricultural and residential areas.
Workers may be exposed to malathion during the use and production of the product. The general population may be exposed if they live near sprayed areas, use the product at home, or consume food exposed to the chemical.
Diazinon
The IARC classified diazinon as “probably carcinogenic” for humans based on limited evidence linking the insecticide to NHL, leukemia, and lung cancer.
Two multicenter, case-control studies of agricultural exposures suggested a positive association between diazinon and NHL. The AHS showed positive associations with specific subtypes of NHL but no overall increased risk of NHL. The AHS also suggested an increased risk of leukemia and lung cancer in subjects exposed to diazinon.
Evidence suggested that diazinon induced DNA or chromosomal damage in human and mammalian cells in vitro. In vivo, diazinon increased the incidence of hepatocellular carcinoma in mice and leukemia or lymphoma (combined) in rats, but only in males receiving the low dose in each study.
Diazinon has been used to control insects in agricultural and residential areas. The IARC said production volumes have been relatively low and decreased further after 2006 due to restrictions in the US and the European Union (EU). There was limited information on the use of this pesticide in other countries.
Tetrachlorvinphos
The insecticide tetrachlorvinphos was classified as “possibly carcinogenic” to humans based on convincing evidence that the agent causes cancer in lab animals. The IARC said the evidence in humans was inadequate.
However, tetrachlorvinphos was shown to induce hepatocellular tumors (benign or malignant) in mice, renal tubule tumors (benign or malignant) in male mice, and spleen hemangioma in male rats.
Tetrachlorvinphos is banned in the EU. In the US, the insecticide is still used on livestock and pets (in flea collars). The IARC said there was no information available on tetrachlorvinphos use in other countries.
Parathion
The insecticide parathion was classified as “possibly carcinogenic” to humans based on convincing evidence that the agent causes cancer in lab animals.
Researchers have observed associations between the insecticide and cancers in several tissues in occupational studies. But the IARC said the evidence that parathion is carcinogenic in humans remains sparse.
Experiments in mice showed that parathion increased the incidence of bronchioloalveolar adenoma and/or carcinoma in males and lymphoma in females. In rats, parathion induced adrenal cortical adenoma or carcinoma (combined), malignant pancreatic tumors, and thyroid follicular cell adenoma in males, and mammary gland adenocarcinoma (after subcutaneous injection in females).
Parathion use has been severely restricted since the 1980s, and all authorized uses of this chemical were cancelled in the EU and the US by 2003. ![]()

Photo by John Messina
The International Agency for Research on Cancer (IARC), the specialized cancer agency of the World Health Organization, has found evidence suggesting that 5 organophosphate pesticides may be carcinogenic.
The IARC classified the herbicide glyphosate and the insecticides malathion and diazinon as “probably carcinogenic” to humans and the insecticides tetrachlorvinphos and parathion as “possibly carcinogenic” to humans.
A summary of these findings has been published in The Lancet Oncology.
Glyphosate
For the herbicide glyphosate, the IARC found limited evidence of carcinogenicity in humans. Case-control studies of occupational exposure to glyphosate in the US, Canada, and Sweden showed increased risks for non-Hodgkin lymphoma (NHL).
However, the Agricultural Health Study (AHS) showed no significantly increased risk of NHL in subjects exposed to glyphosate.
A study of community residents showed increases in blood markers of chromosomal damage after glyphosate formulations were sprayed nearby. And glyphosate was shown to cause DNA and chromosomal damage in human cells, although bacterial mutagenesis tests were negative.
In studies of male mice, glyphosate increased the incidence of renal tubule carcinoma and hemangiosarcoma. Glyphosate also increased the incidence of pancreatic islet-cell adenoma in male rats, and a glyphosate formulation promoted skin tumors in mice.
The IARC said glyphosate has the highest global production volume of all herbicides. It is used in agriculture, forestry, urban, and home applications.
Glyphosate has been detected in the air during spraying, in water, and in food. The general population is exposed to the chemical primarily by living near sprayed areas, home use, and diet. But the IARC said the level of exposure observed is generally low.
Malathion
The IARC classified malathion as “probably carcinogenic” for humans based on limited evidence linking the insecticide to NHL and prostate cancer. Occupational use of malathion was associated with an increased risk of prostate cancer in a Canadian case-control study and in the AHS.
Studies of occupational exposures in the US, Canada, and Sweden revealed positive associations between malathion and NHL. However, results of the AHS did not show an association between the insecticide and NHL.
Studies showed that malathion induced DNA and chromosomal damage in humans and animals, although bacterial mutagenesis tests were negative. Results also suggested malathion disrupts hormone pathways.
Experiments in mice showed malathion increased the incidence of hepatocellular adenoma or carcinoma (combined). In rats, the insecticide increased the incidence of thyroid carcinoma in males, hepatocellular adenoma or carcinoma (combined) in females, and mammary gland adenocarcinoma after subcutaneous injection in females.
The IARC said malathion is used in “substantial volumes throughout the world” to control insects in agricultural and residential areas.
Workers may be exposed to malathion during the use and production of the product. The general population may be exposed if they live near sprayed areas, use the product at home, or consume food exposed to the chemical.
Diazinon
The IARC classified diazinon as “probably carcinogenic” for humans based on limited evidence linking the insecticide to NHL, leukemia, and lung cancer.
Two multicenter, case-control studies of agricultural exposures suggested a positive association between diazinon and NHL. The AHS showed positive associations with specific subtypes of NHL but no overall increased risk of NHL. The AHS also suggested an increased risk of leukemia and lung cancer in subjects exposed to diazinon.
Evidence suggested that diazinon induced DNA or chromosomal damage in human and mammalian cells in vitro. In vivo, diazinon increased the incidence of hepatocellular carcinoma in mice and leukemia or lymphoma (combined) in rats, but only in males receiving the low dose in each study.
Diazinon has been used to control insects in agricultural and residential areas. The IARC said production volumes have been relatively low and decreased further after 2006 due to restrictions in the US and the European Union (EU). There was limited information on the use of this pesticide in other countries.
Tetrachlorvinphos
The insecticide tetrachlorvinphos was classified as “possibly carcinogenic” to humans based on convincing evidence that the agent causes cancer in lab animals. The IARC said the evidence in humans was inadequate.
However, tetrachlorvinphos was shown to induce hepatocellular tumors (benign or malignant) in mice, renal tubule tumors (benign or malignant) in male mice, and spleen hemangioma in male rats.
Tetrachlorvinphos is banned in the EU. In the US, the insecticide is still used on livestock and pets (in flea collars). The IARC said there was no information available on tetrachlorvinphos use in other countries.
Parathion
The insecticide parathion was classified as “possibly carcinogenic” to humans based on convincing evidence that the agent causes cancer in lab animals.
Researchers have observed associations between the insecticide and cancers in several tissues in occupational studies. But the IARC said the evidence that parathion is carcinogenic in humans remains sparse.
Experiments in mice showed that parathion increased the incidence of bronchioloalveolar adenoma and/or carcinoma in males and lymphoma in females. In rats, parathion induced adrenal cortical adenoma or carcinoma (combined), malignant pancreatic tumors, and thyroid follicular cell adenoma in males, and mammary gland adenocarcinoma (after subcutaneous injection in females).
Parathion use has been severely restricted since the 1980s, and all authorized uses of this chemical were cancelled in the EU and the US by 2003. ![]()

Photo by John Messina
The International Agency for Research on Cancer (IARC), the specialized cancer agency of the World Health Organization, has found evidence suggesting that 5 organophosphate pesticides may be carcinogenic.
The IARC classified the herbicide glyphosate and the insecticides malathion and diazinon as “probably carcinogenic” to humans and the insecticides tetrachlorvinphos and parathion as “possibly carcinogenic” to humans.
A summary of these findings has been published in The Lancet Oncology.
Glyphosate
For the herbicide glyphosate, the IARC found limited evidence of carcinogenicity in humans. Case-control studies of occupational exposure to glyphosate in the US, Canada, and Sweden showed increased risks for non-Hodgkin lymphoma (NHL).
However, the Agricultural Health Study (AHS) showed no significantly increased risk of NHL in subjects exposed to glyphosate.
A study of community residents showed increases in blood markers of chromosomal damage after glyphosate formulations were sprayed nearby. And glyphosate was shown to cause DNA and chromosomal damage in human cells, although bacterial mutagenesis tests were negative.
In studies of male mice, glyphosate increased the incidence of renal tubule carcinoma and hemangiosarcoma. Glyphosate also increased the incidence of pancreatic islet-cell adenoma in male rats, and a glyphosate formulation promoted skin tumors in mice.
The IARC said glyphosate has the highest global production volume of all herbicides. It is used in agriculture, forestry, urban, and home applications.
Glyphosate has been detected in the air during spraying, in water, and in food. The general population is exposed to the chemical primarily by living near sprayed areas, home use, and diet. But the IARC said the level of exposure observed is generally low.
Malathion
The IARC classified malathion as “probably carcinogenic” for humans based on limited evidence linking the insecticide to NHL and prostate cancer. Occupational use of malathion was associated with an increased risk of prostate cancer in a Canadian case-control study and in the AHS.
Studies of occupational exposures in the US, Canada, and Sweden revealed positive associations between malathion and NHL. However, results of the AHS did not show an association between the insecticide and NHL.
Studies showed that malathion induced DNA and chromosomal damage in humans and animals, although bacterial mutagenesis tests were negative. Results also suggested malathion disrupts hormone pathways.
Experiments in mice showed malathion increased the incidence of hepatocellular adenoma or carcinoma (combined). In rats, the insecticide increased the incidence of thyroid carcinoma in males, hepatocellular adenoma or carcinoma (combined) in females, and mammary gland adenocarcinoma after subcutaneous injection in females.
The IARC said malathion is used in “substantial volumes throughout the world” to control insects in agricultural and residential areas.
Workers may be exposed to malathion during the use and production of the product. The general population may be exposed if they live near sprayed areas, use the product at home, or consume food exposed to the chemical.
Diazinon
The IARC classified diazinon as “probably carcinogenic” for humans based on limited evidence linking the insecticide to NHL, leukemia, and lung cancer.
Two multicenter, case-control studies of agricultural exposures suggested a positive association between diazinon and NHL. The AHS showed positive associations with specific subtypes of NHL but no overall increased risk of NHL. The AHS also suggested an increased risk of leukemia and lung cancer in subjects exposed to diazinon.
Evidence suggested that diazinon induced DNA or chromosomal damage in human and mammalian cells in vitro. In vivo, diazinon increased the incidence of hepatocellular carcinoma in mice and leukemia or lymphoma (combined) in rats, but only in males receiving the low dose in each study.
Diazinon has been used to control insects in agricultural and residential areas. The IARC said production volumes have been relatively low and decreased further after 2006 due to restrictions in the US and the European Union (EU). There was limited information on the use of this pesticide in other countries.
Tetrachlorvinphos
The insecticide tetrachlorvinphos was classified as “possibly carcinogenic” to humans based on convincing evidence that the agent causes cancer in lab animals. The IARC said the evidence in humans was inadequate.
However, tetrachlorvinphos was shown to induce hepatocellular tumors (benign or malignant) in mice, renal tubule tumors (benign or malignant) in male mice, and spleen hemangioma in male rats.
Tetrachlorvinphos is banned in the EU. In the US, the insecticide is still used on livestock and pets (in flea collars). The IARC said there was no information available on tetrachlorvinphos use in other countries.
Parathion
The insecticide parathion was classified as “possibly carcinogenic” to humans based on convincing evidence that the agent causes cancer in lab animals.
Researchers have observed associations between the insecticide and cancers in several tissues in occupational studies. But the IARC said the evidence that parathion is carcinogenic in humans remains sparse.
Experiments in mice showed that parathion increased the incidence of bronchioloalveolar adenoma and/or carcinoma in males and lymphoma in females. In rats, parathion induced adrenal cortical adenoma or carcinoma (combined), malignant pancreatic tumors, and thyroid follicular cell adenoma in males, and mammary gland adenocarcinoma (after subcutaneous injection in females).
Parathion use has been severely restricted since the 1980s, and all authorized uses of this chemical were cancelled in the EU and the US by 2003. ![]()
Studies investigate risk of DVT, infection with PICCs
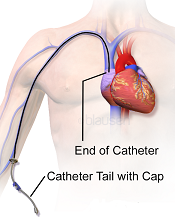
Image courtesy of Blausen
Medical Communications, Inc.
Three recently published papers may help ensure the appropriate use of peripherally inserted central catheters (PICCs).
A case-control study uncovered several factors that appear to affect the risk of deep vein thrombosis (DVT) associated with PICCs.
A retrospective study revealed the “prevalence, patterns, and predictors” of PICC-associated bloodstream infections.
And a literature review informed the creation of a guide to help hospitalists choose the right intravenous device.
“[PICCs] are very popular, but in an under-the-radar way, because they make care more convenient and can be placed relatively easily,” said Vineet Chopra, MD, an author on all 3 articles and a hospitalist at the University of Michigan Health System in Ann Arbor.
“But our new results, and review of research on the topic, show it’s important for physicians to think hard about both the risks and the benefits.”
Case-control study
In the study of PICC-DVT, published in Thrombosis Research, the investigators looked at records from 909 patients who received PICCs at the University of Michigan Health System in 2012 and 2013.
Patients had PICCs placed so they could receive long-term intravenous antibiotic therapy (n=447; 49.1%) or total parenteral nutrition (n=120; 6.7%). They also required PICCs for in-hospital venous access for blood draws or infusion of medications (n=342; 44.2%).
In all, 268 patients developed a DVT associated with their PICC. The median time to DVT development was 12.4 days from PICC placement.
Patients who were already taking aspirin and statins before their PICC was placed had a significantly lower risk of DVT-PICC (odds ratio [OR]=0.31). Patients who received pharmacological DVT prophylaxis had a lower risk of DVT-PICC than patients who were not on prophylaxis, although the difference was not statistically significant (OR=0.72).
Patients had a significantly greater risk of PICC-DVT if they underwent surgery during their hospital stay (OR=2.17) or had a prior history of venous thromboembolism (OR=1.70). And, compared to patients who received 4-Fr PICCs, those who had 5-Fr or 6-Fr PICCs had a significantly greater risk of DVT (ORs=2.74 and 7.40, respectively).
Retrospective study
In The American Journal of Medicine, Dr Chopra and his colleagues described a retrospective study of bloodstream infections associated with PICCs.
The investigators analyzed data from 747 patients who received 966 PICCs for a total of 26,887 catheter days. Patients had PICCs for long-term antibiotic administration (n=503; 52%), venous access (n=201; 21%), total parenteral nutrition (n=155; 16%), and chemotherapy (n=107; 11%).
There were 58 cases (6%) of PICC-bloodstream infection over 1156 catheter days, for an infection rate of 2.16 per 1000 catheter days. The median time to infection was 10 days.
Bivariate analysis revealed several factors associated with PICC-bloodstream infections. These included intensive care unit status (ICU; OR=3.23), mechanical ventilation (OR=4.39), length of stay (hospital, OR=1.04; ICU, OR=1.03), PowerPICCs (OR=2.58), devices placed by interventional radiology (OR=2.57), double lumens (OR=5.21), and triple lumens (OR=10.84).
In multivariable analysis, only some of these factors remained significantly associated with PICC-bloodstream infection. These included hospital length of stay (OR=1.04), ICU status (OR=1.02), double lumens (OR=3.99), and triple lumens (OR=6.34).
Dr Chopra said the results of these 2 studies suggest hospitalists should tread carefully when considering PICCs.
“These are not innocuous devices,” he said. “The time has come to stop thinking of them as a device of convenience and rather one with clear risks and benefits.”
Review and guide
In the Journal of Hospital Medicine, Dr Chopra and his colleagues offered advice on choosing vascular access devices. After reviewing the literature, the investigators designed a flow chart that can help hospitalists decide which device is appropriate for each patient.
For instance, different devices will work best depending on whether access to the bloodstream is needed urgently or less urgently, whether the patient will likely need the device for more or less than a week, what kind of drug or nutrition the doctor will order, and whether the patient’s kidneys are functioning normally. ![]()
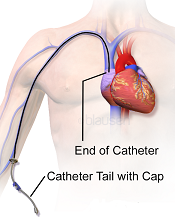
Image courtesy of Blausen
Medical Communications, Inc.
Three recently published papers may help ensure the appropriate use of peripherally inserted central catheters (PICCs).
A case-control study uncovered several factors that appear to affect the risk of deep vein thrombosis (DVT) associated with PICCs.
A retrospective study revealed the “prevalence, patterns, and predictors” of PICC-associated bloodstream infections.
And a literature review informed the creation of a guide to help hospitalists choose the right intravenous device.
“[PICCs] are very popular, but in an under-the-radar way, because they make care more convenient and can be placed relatively easily,” said Vineet Chopra, MD, an author on all 3 articles and a hospitalist at the University of Michigan Health System in Ann Arbor.
“But our new results, and review of research on the topic, show it’s important for physicians to think hard about both the risks and the benefits.”
Case-control study
In the study of PICC-DVT, published in Thrombosis Research, the investigators looked at records from 909 patients who received PICCs at the University of Michigan Health System in 2012 and 2013.
Patients had PICCs placed so they could receive long-term intravenous antibiotic therapy (n=447; 49.1%) or total parenteral nutrition (n=120; 6.7%). They also required PICCs for in-hospital venous access for blood draws or infusion of medications (n=342; 44.2%).
In all, 268 patients developed a DVT associated with their PICC. The median time to DVT development was 12.4 days from PICC placement.
Patients who were already taking aspirin and statins before their PICC was placed had a significantly lower risk of DVT-PICC (odds ratio [OR]=0.31). Patients who received pharmacological DVT prophylaxis had a lower risk of DVT-PICC than patients who were not on prophylaxis, although the difference was not statistically significant (OR=0.72).
Patients had a significantly greater risk of PICC-DVT if they underwent surgery during their hospital stay (OR=2.17) or had a prior history of venous thromboembolism (OR=1.70). And, compared to patients who received 4-Fr PICCs, those who had 5-Fr or 6-Fr PICCs had a significantly greater risk of DVT (ORs=2.74 and 7.40, respectively).
Retrospective study
In The American Journal of Medicine, Dr Chopra and his colleagues described a retrospective study of bloodstream infections associated with PICCs.
The investigators analyzed data from 747 patients who received 966 PICCs for a total of 26,887 catheter days. Patients had PICCs for long-term antibiotic administration (n=503; 52%), venous access (n=201; 21%), total parenteral nutrition (n=155; 16%), and chemotherapy (n=107; 11%).
There were 58 cases (6%) of PICC-bloodstream infection over 1156 catheter days, for an infection rate of 2.16 per 1000 catheter days. The median time to infection was 10 days.
Bivariate analysis revealed several factors associated with PICC-bloodstream infections. These included intensive care unit status (ICU; OR=3.23), mechanical ventilation (OR=4.39), length of stay (hospital, OR=1.04; ICU, OR=1.03), PowerPICCs (OR=2.58), devices placed by interventional radiology (OR=2.57), double lumens (OR=5.21), and triple lumens (OR=10.84).
In multivariable analysis, only some of these factors remained significantly associated with PICC-bloodstream infection. These included hospital length of stay (OR=1.04), ICU status (OR=1.02), double lumens (OR=3.99), and triple lumens (OR=6.34).
Dr Chopra said the results of these 2 studies suggest hospitalists should tread carefully when considering PICCs.
“These are not innocuous devices,” he said. “The time has come to stop thinking of them as a device of convenience and rather one with clear risks and benefits.”
Review and guide
In the Journal of Hospital Medicine, Dr Chopra and his colleagues offered advice on choosing vascular access devices. After reviewing the literature, the investigators designed a flow chart that can help hospitalists decide which device is appropriate for each patient.
For instance, different devices will work best depending on whether access to the bloodstream is needed urgently or less urgently, whether the patient will likely need the device for more or less than a week, what kind of drug or nutrition the doctor will order, and whether the patient’s kidneys are functioning normally. ![]()
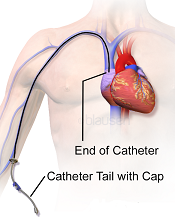
Image courtesy of Blausen
Medical Communications, Inc.
Three recently published papers may help ensure the appropriate use of peripherally inserted central catheters (PICCs).
A case-control study uncovered several factors that appear to affect the risk of deep vein thrombosis (DVT) associated with PICCs.
A retrospective study revealed the “prevalence, patterns, and predictors” of PICC-associated bloodstream infections.
And a literature review informed the creation of a guide to help hospitalists choose the right intravenous device.
“[PICCs] are very popular, but in an under-the-radar way, because they make care more convenient and can be placed relatively easily,” said Vineet Chopra, MD, an author on all 3 articles and a hospitalist at the University of Michigan Health System in Ann Arbor.
“But our new results, and review of research on the topic, show it’s important for physicians to think hard about both the risks and the benefits.”
Case-control study
In the study of PICC-DVT, published in Thrombosis Research, the investigators looked at records from 909 patients who received PICCs at the University of Michigan Health System in 2012 and 2013.
Patients had PICCs placed so they could receive long-term intravenous antibiotic therapy (n=447; 49.1%) or total parenteral nutrition (n=120; 6.7%). They also required PICCs for in-hospital venous access for blood draws or infusion of medications (n=342; 44.2%).
In all, 268 patients developed a DVT associated with their PICC. The median time to DVT development was 12.4 days from PICC placement.
Patients who were already taking aspirin and statins before their PICC was placed had a significantly lower risk of DVT-PICC (odds ratio [OR]=0.31). Patients who received pharmacological DVT prophylaxis had a lower risk of DVT-PICC than patients who were not on prophylaxis, although the difference was not statistically significant (OR=0.72).
Patients had a significantly greater risk of PICC-DVT if they underwent surgery during their hospital stay (OR=2.17) or had a prior history of venous thromboembolism (OR=1.70). And, compared to patients who received 4-Fr PICCs, those who had 5-Fr or 6-Fr PICCs had a significantly greater risk of DVT (ORs=2.74 and 7.40, respectively).
Retrospective study
In The American Journal of Medicine, Dr Chopra and his colleagues described a retrospective study of bloodstream infections associated with PICCs.
The investigators analyzed data from 747 patients who received 966 PICCs for a total of 26,887 catheter days. Patients had PICCs for long-term antibiotic administration (n=503; 52%), venous access (n=201; 21%), total parenteral nutrition (n=155; 16%), and chemotherapy (n=107; 11%).
There were 58 cases (6%) of PICC-bloodstream infection over 1156 catheter days, for an infection rate of 2.16 per 1000 catheter days. The median time to infection was 10 days.
Bivariate analysis revealed several factors associated with PICC-bloodstream infections. These included intensive care unit status (ICU; OR=3.23), mechanical ventilation (OR=4.39), length of stay (hospital, OR=1.04; ICU, OR=1.03), PowerPICCs (OR=2.58), devices placed by interventional radiology (OR=2.57), double lumens (OR=5.21), and triple lumens (OR=10.84).
In multivariable analysis, only some of these factors remained significantly associated with PICC-bloodstream infection. These included hospital length of stay (OR=1.04), ICU status (OR=1.02), double lumens (OR=3.99), and triple lumens (OR=6.34).
Dr Chopra said the results of these 2 studies suggest hospitalists should tread carefully when considering PICCs.
“These are not innocuous devices,” he said. “The time has come to stop thinking of them as a device of convenience and rather one with clear risks and benefits.”
Review and guide
In the Journal of Hospital Medicine, Dr Chopra and his colleagues offered advice on choosing vascular access devices. After reviewing the literature, the investigators designed a flow chart that can help hospitalists decide which device is appropriate for each patient.
For instance, different devices will work best depending on whether access to the bloodstream is needed urgently or less urgently, whether the patient will likely need the device for more or less than a week, what kind of drug or nutrition the doctor will order, and whether the patient’s kidneys are functioning normally. ![]()
Team describes new method to target MM cells

Researchers say they have discovered a new way to target multiple myeloma (MM) and other cancer cells.
The investigators developed human T-cell receptors (TCRs) that have no tolerance toward human cancer antigens and specifically recognize the antigen MAGE-A1, which is present on MM and other cancer cells.
Matthias Obenaus, MD, of the Max-Delbrück-Center for Molecular Medicine in Berlin, Germany, and his colleagues described this work in Nature Biotechnology.
Instead of directly using human-derived TCRs, which do not mediate substantial anti-tumor effects, the researchers took a “detour” by employing a mouse model.
First, they transferred the genetic information for human TCRs into the mice, thereby creating an arsenal of human TCRs.
Then, the investigators isolated the TCRs from the mice and transferred them into human T cells. This “trained” the cells to recognize MM and other cancer cells (eg, melanoma and fibrosarcoma cells) as foreign.
The researchers noted that some people possess T cells that naturally recognize MAGE-A1 on tumor cells, but only in vitro.
In vivo experiments revealed that only the human TCRs derived from mice were effective against tumors. The TCRs derived directly from humans were too weak to recognize the tumor antigens sufficiently.
The investigators said the fact that their mouse-derived human TCRs were more effective is a strong indication that human T cells are tolerant toward MAGE-A1.
Using the TCRs they developed, the researchers are now planning a clinical trial of patients with MAGE-A1 positive MM. ![]()

Researchers say they have discovered a new way to target multiple myeloma (MM) and other cancer cells.
The investigators developed human T-cell receptors (TCRs) that have no tolerance toward human cancer antigens and specifically recognize the antigen MAGE-A1, which is present on MM and other cancer cells.
Matthias Obenaus, MD, of the Max-Delbrück-Center for Molecular Medicine in Berlin, Germany, and his colleagues described this work in Nature Biotechnology.
Instead of directly using human-derived TCRs, which do not mediate substantial anti-tumor effects, the researchers took a “detour” by employing a mouse model.
First, they transferred the genetic information for human TCRs into the mice, thereby creating an arsenal of human TCRs.
Then, the investigators isolated the TCRs from the mice and transferred them into human T cells. This “trained” the cells to recognize MM and other cancer cells (eg, melanoma and fibrosarcoma cells) as foreign.
The researchers noted that some people possess T cells that naturally recognize MAGE-A1 on tumor cells, but only in vitro.
In vivo experiments revealed that only the human TCRs derived from mice were effective against tumors. The TCRs derived directly from humans were too weak to recognize the tumor antigens sufficiently.
The investigators said the fact that their mouse-derived human TCRs were more effective is a strong indication that human T cells are tolerant toward MAGE-A1.
Using the TCRs they developed, the researchers are now planning a clinical trial of patients with MAGE-A1 positive MM. ![]()

Researchers say they have discovered a new way to target multiple myeloma (MM) and other cancer cells.
The investigators developed human T-cell receptors (TCRs) that have no tolerance toward human cancer antigens and specifically recognize the antigen MAGE-A1, which is present on MM and other cancer cells.
Matthias Obenaus, MD, of the Max-Delbrück-Center for Molecular Medicine in Berlin, Germany, and his colleagues described this work in Nature Biotechnology.
Instead of directly using human-derived TCRs, which do not mediate substantial anti-tumor effects, the researchers took a “detour” by employing a mouse model.
First, they transferred the genetic information for human TCRs into the mice, thereby creating an arsenal of human TCRs.
Then, the investigators isolated the TCRs from the mice and transferred them into human T cells. This “trained” the cells to recognize MM and other cancer cells (eg, melanoma and fibrosarcoma cells) as foreign.
The researchers noted that some people possess T cells that naturally recognize MAGE-A1 on tumor cells, but only in vitro.
In vivo experiments revealed that only the human TCRs derived from mice were effective against tumors. The TCRs derived directly from humans were too weak to recognize the tumor antigens sufficiently.
The investigators said the fact that their mouse-derived human TCRs were more effective is a strong indication that human T cells are tolerant toward MAGE-A1.
Using the TCRs they developed, the researchers are now planning a clinical trial of patients with MAGE-A1 positive MM. ![]()


