User login
Small EMR tweak makes a big difference
I’m happier doing patient messages these days. That’s because of a little feature that we turned on in EPIC, our electronic medical record. The change doesn’t make me any faster or smarter. It doesn’t make me any more money. It merely adds a sprinkle of meaning to the work I do, and that has made all the difference.
In contrast to the usually glamorous portrayal of physicians’ work, most of our days are mundane. On a typical clinic day I’ll get up to a dozen requests from patients asking for something. Usually it’s just a refill, but several are from patients asking for a earlier appointment, when there are none. Or asking for a stronger treatment, when there aren’t any. Most of these requests are from patients who do not have interesting diagnoses or require sophisticated treatments. They are the itchy, and they remain itchy despite my advice. After a long day of seeing patients, the long list of messages that requires action feels endless, burdensome. Optimizing extenders has made me more efficient, but the work that remains isn’t fulfilling. A subtle change in our EMR has helped, though.
What is different? Our EPIC now includes a photo of each patient. That’s it. Ostensibly, having a photo is a security feature: it allows us to positively identify a patient, thereby reducing the risk that we treat an imposter posing as that patient (a small but real problem with drug seekers).
Why might this matter for physician satisfaction? Because seeing a patient photo brings an actual person to the top of mind. This changes our emotional connection to the work: how we interpret work is all that matters when it comes to job satisfaction. This is why volunteer work is so rewarding, despite having no monetary incentive, and why highly compensated professions, like those of many Wall Street traders, can ultimately fail to be fulfilling.
Tonight, long after the sun has set, I’m still working through messages. The next one, however, is not from any patient with nummular eczema. I see it’s from Mrs. Morales (not her real name), a sweet older woman with a warm smile and rich accent. She teaches water aerobics and she spent 5 minutes describing a typical Puerto Rican dinner (lots of stews) during her last appointment with me. Seeing her smiling face in the top left corner of the chart reminds me that the work I’m doing is for someone I know, someone I care for.
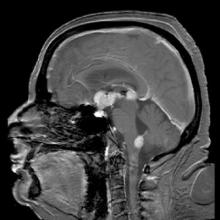
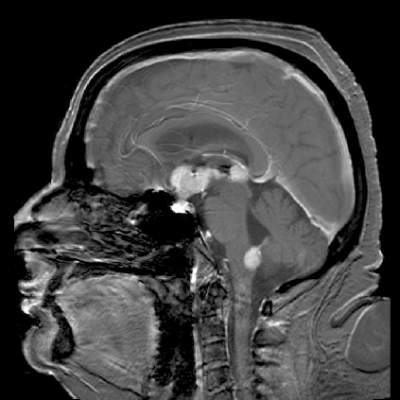
Radiologists have actually studied this phenomenon. Like much of medicine, radiology can be tedious. Researchers devised a simple test to see if making radiology work more human could improve not only the experience for, but also the effectiveness of, doctors. With patients’ consent, they took photos of 300 participants before their films were sent for reading. Radiologists who saw a patient’s photo along with their radiographic studies reported feeling more empathy for their patients. They also reported reading cases with photos more meticulously than those cases without photos. But that’s not all. When the radiologists were later shown the same films but without the patient photos, the doctors were less likely to notice incidental findings in the radiographs. The authors concluded that seeing patient photos made radiologists both more effective and more empathic (ScienceDaily 2008 Dec 14).
So consider adding photos of your patients to your EMR. Then remember to take a second or two to look at them before engaging in the task to be done. You, and your patients, will be better off because of it.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. He is @dermdoc on Twitter. He has no conflicts related to the topic of this column.
I’m happier doing patient messages these days. That’s because of a little feature that we turned on in EPIC, our electronic medical record. The change doesn’t make me any faster or smarter. It doesn’t make me any more money. It merely adds a sprinkle of meaning to the work I do, and that has made all the difference.
In contrast to the usually glamorous portrayal of physicians’ work, most of our days are mundane. On a typical clinic day I’ll get up to a dozen requests from patients asking for something. Usually it’s just a refill, but several are from patients asking for a earlier appointment, when there are none. Or asking for a stronger treatment, when there aren’t any. Most of these requests are from patients who do not have interesting diagnoses or require sophisticated treatments. They are the itchy, and they remain itchy despite my advice. After a long day of seeing patients, the long list of messages that requires action feels endless, burdensome. Optimizing extenders has made me more efficient, but the work that remains isn’t fulfilling. A subtle change in our EMR has helped, though.
What is different? Our EPIC now includes a photo of each patient. That’s it. Ostensibly, having a photo is a security feature: it allows us to positively identify a patient, thereby reducing the risk that we treat an imposter posing as that patient (a small but real problem with drug seekers).
Why might this matter for physician satisfaction? Because seeing a patient photo brings an actual person to the top of mind. This changes our emotional connection to the work: how we interpret work is all that matters when it comes to job satisfaction. This is why volunteer work is so rewarding, despite having no monetary incentive, and why highly compensated professions, like those of many Wall Street traders, can ultimately fail to be fulfilling.
Tonight, long after the sun has set, I’m still working through messages. The next one, however, is not from any patient with nummular eczema. I see it’s from Mrs. Morales (not her real name), a sweet older woman with a warm smile and rich accent. She teaches water aerobics and she spent 5 minutes describing a typical Puerto Rican dinner (lots of stews) during her last appointment with me. Seeing her smiling face in the top left corner of the chart reminds me that the work I’m doing is for someone I know, someone I care for.
Radiologists have actually studied this phenomenon. Like much of medicine, radiology can be tedious. Researchers devised a simple test to see if making radiology work more human could improve not only the experience for, but also the effectiveness of, doctors. With patients’ consent, they took photos of 300 participants before their films were sent for reading. Radiologists who saw a patient’s photo along with their radiographic studies reported feeling more empathy for their patients. They also reported reading cases with photos more meticulously than those cases without photos. But that’s not all. When the radiologists were later shown the same films but without the patient photos, the doctors were less likely to notice incidental findings in the radiographs. The authors concluded that seeing patient photos made radiologists both more effective and more empathic (ScienceDaily 2008 Dec 14).
So consider adding photos of your patients to your EMR. Then remember to take a second or two to look at them before engaging in the task to be done. You, and your patients, will be better off because of it.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. He is @dermdoc on Twitter. He has no conflicts related to the topic of this column.
I’m happier doing patient messages these days. That’s because of a little feature that we turned on in EPIC, our electronic medical record. The change doesn’t make me any faster or smarter. It doesn’t make me any more money. It merely adds a sprinkle of meaning to the work I do, and that has made all the difference.
In contrast to the usually glamorous portrayal of physicians’ work, most of our days are mundane. On a typical clinic day I’ll get up to a dozen requests from patients asking for something. Usually it’s just a refill, but several are from patients asking for a earlier appointment, when there are none. Or asking for a stronger treatment, when there aren’t any. Most of these requests are from patients who do not have interesting diagnoses or require sophisticated treatments. They are the itchy, and they remain itchy despite my advice. After a long day of seeing patients, the long list of messages that requires action feels endless, burdensome. Optimizing extenders has made me more efficient, but the work that remains isn’t fulfilling. A subtle change in our EMR has helped, though.
What is different? Our EPIC now includes a photo of each patient. That’s it. Ostensibly, having a photo is a security feature: it allows us to positively identify a patient, thereby reducing the risk that we treat an imposter posing as that patient (a small but real problem with drug seekers).
Why might this matter for physician satisfaction? Because seeing a patient photo brings an actual person to the top of mind. This changes our emotional connection to the work: how we interpret work is all that matters when it comes to job satisfaction. This is why volunteer work is so rewarding, despite having no monetary incentive, and why highly compensated professions, like those of many Wall Street traders, can ultimately fail to be fulfilling.
Tonight, long after the sun has set, I’m still working through messages. The next one, however, is not from any patient with nummular eczema. I see it’s from Mrs. Morales (not her real name), a sweet older woman with a warm smile and rich accent. She teaches water aerobics and she spent 5 minutes describing a typical Puerto Rican dinner (lots of stews) during her last appointment with me. Seeing her smiling face in the top left corner of the chart reminds me that the work I’m doing is for someone I know, someone I care for.
Radiologists have actually studied this phenomenon. Like much of medicine, radiology can be tedious. Researchers devised a simple test to see if making radiology work more human could improve not only the experience for, but also the effectiveness of, doctors. With patients’ consent, they took photos of 300 participants before their films were sent for reading. Radiologists who saw a patient’s photo along with their radiographic studies reported feeling more empathy for their patients. They also reported reading cases with photos more meticulously than those cases without photos. But that’s not all. When the radiologists were later shown the same films but without the patient photos, the doctors were less likely to notice incidental findings in the radiographs. The authors concluded that seeing patient photos made radiologists both more effective and more empathic (ScienceDaily 2008 Dec 14).
So consider adding photos of your patients to your EMR. Then remember to take a second or two to look at them before engaging in the task to be done. You, and your patients, will be better off because of it.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego, and a volunteer clinical assistant professor at the University of California, San Diego. He is @dermdoc on Twitter. He has no conflicts related to the topic of this column.
Protein plays key role in B-ALL subtype

An RNA binding protein promotes the development of MLL-rearranged B-cell acute lymphoblastic leukemia (B-ALL), according to research published in The Journal of Clinical Investigation.
Researchers found an overabundance of the protein, IGF2BP3, in MLL-rearranged B-ALL.
They also identified genes that are directly regulated by IFG2BP3, and many of them turned out to be oncogenes that have already been implicated in cancers.
The overall effect of IFG2BP3 in MLL-rearranged B-ALL is to promote the proliferation of B cells by shifting the expression of a large number of genes, explained study author Jeremy Sanford, PhD, of the University of California Santa Cruz.
“This protein, IFG2BP3, has been correlated with many types of malignancies and with the worst prognoses,” he noted. “What is exciting about this study is that it goes beyond correlation and shows causation, because we demonstrated, for the first time, that aberrant expression of this protein is sufficient to induce pathology.”
This research began in the lab of Dinesh Rao, PhD, an assistant professor at the University of California Los Angeles who was studying MLL-rearranged B-ALL.
After researchers in Dr Rao’s lab identified IGF2BP3 as one of the top dysregulated genes in this malignancy, they began working with Dr Sanford’s lab to figure out which genes were being directly regulated by IGF2BP3.
Dr Sanford’s lab was among the few using individual nucleotide resolution crosslinking immunoprecipitation (iCLIP), a technique that can capture RNA molecules bound to a particular protein.
iCLIP enabled the researchers to identify IGF2BP3 binding sites in several hundred RNA transcripts in 2 B-ALL cell lines.
The work also revealed that IGF2BP3 enhanced the expression of MYC and other oncogenes in hematopoietic stem cells.
In experiments with mice, the researchers found that overexpression of IGF2BP3 in the bone marrow leads to proliferation of hematopoietic stem cells and B-cell progenitors, reproducing some features of MLL-rearranged B-ALL.
“Understanding its mechanism of action is important for thinking about therapeutics that might interfere with the action of this protein in disease,” Dr Sanford said.
“One possibility is an RNA-based therapeutic that could sequester the protein and keep it from binding to RNA transcripts. That would be a way to influence the expression of many genes involved in the proliferation of cancer cells.” ![]()

An RNA binding protein promotes the development of MLL-rearranged B-cell acute lymphoblastic leukemia (B-ALL), according to research published in The Journal of Clinical Investigation.
Researchers found an overabundance of the protein, IGF2BP3, in MLL-rearranged B-ALL.
They also identified genes that are directly regulated by IFG2BP3, and many of them turned out to be oncogenes that have already been implicated in cancers.
The overall effect of IFG2BP3 in MLL-rearranged B-ALL is to promote the proliferation of B cells by shifting the expression of a large number of genes, explained study author Jeremy Sanford, PhD, of the University of California Santa Cruz.
“This protein, IFG2BP3, has been correlated with many types of malignancies and with the worst prognoses,” he noted. “What is exciting about this study is that it goes beyond correlation and shows causation, because we demonstrated, for the first time, that aberrant expression of this protein is sufficient to induce pathology.”
This research began in the lab of Dinesh Rao, PhD, an assistant professor at the University of California Los Angeles who was studying MLL-rearranged B-ALL.
After researchers in Dr Rao’s lab identified IGF2BP3 as one of the top dysregulated genes in this malignancy, they began working with Dr Sanford’s lab to figure out which genes were being directly regulated by IGF2BP3.
Dr Sanford’s lab was among the few using individual nucleotide resolution crosslinking immunoprecipitation (iCLIP), a technique that can capture RNA molecules bound to a particular protein.
iCLIP enabled the researchers to identify IGF2BP3 binding sites in several hundred RNA transcripts in 2 B-ALL cell lines.
The work also revealed that IGF2BP3 enhanced the expression of MYC and other oncogenes in hematopoietic stem cells.
In experiments with mice, the researchers found that overexpression of IGF2BP3 in the bone marrow leads to proliferation of hematopoietic stem cells and B-cell progenitors, reproducing some features of MLL-rearranged B-ALL.
“Understanding its mechanism of action is important for thinking about therapeutics that might interfere with the action of this protein in disease,” Dr Sanford said.
“One possibility is an RNA-based therapeutic that could sequester the protein and keep it from binding to RNA transcripts. That would be a way to influence the expression of many genes involved in the proliferation of cancer cells.” ![]()

An RNA binding protein promotes the development of MLL-rearranged B-cell acute lymphoblastic leukemia (B-ALL), according to research published in The Journal of Clinical Investigation.
Researchers found an overabundance of the protein, IGF2BP3, in MLL-rearranged B-ALL.
They also identified genes that are directly regulated by IFG2BP3, and many of them turned out to be oncogenes that have already been implicated in cancers.
The overall effect of IFG2BP3 in MLL-rearranged B-ALL is to promote the proliferation of B cells by shifting the expression of a large number of genes, explained study author Jeremy Sanford, PhD, of the University of California Santa Cruz.
“This protein, IFG2BP3, has been correlated with many types of malignancies and with the worst prognoses,” he noted. “What is exciting about this study is that it goes beyond correlation and shows causation, because we demonstrated, for the first time, that aberrant expression of this protein is sufficient to induce pathology.”
This research began in the lab of Dinesh Rao, PhD, an assistant professor at the University of California Los Angeles who was studying MLL-rearranged B-ALL.
After researchers in Dr Rao’s lab identified IGF2BP3 as one of the top dysregulated genes in this malignancy, they began working with Dr Sanford’s lab to figure out which genes were being directly regulated by IGF2BP3.
Dr Sanford’s lab was among the few using individual nucleotide resolution crosslinking immunoprecipitation (iCLIP), a technique that can capture RNA molecules bound to a particular protein.
iCLIP enabled the researchers to identify IGF2BP3 binding sites in several hundred RNA transcripts in 2 B-ALL cell lines.
The work also revealed that IGF2BP3 enhanced the expression of MYC and other oncogenes in hematopoietic stem cells.
In experiments with mice, the researchers found that overexpression of IGF2BP3 in the bone marrow leads to proliferation of hematopoietic stem cells and B-cell progenitors, reproducing some features of MLL-rearranged B-ALL.
“Understanding its mechanism of action is important for thinking about therapeutics that might interfere with the action of this protein in disease,” Dr Sanford said.
“One possibility is an RNA-based therapeutic that could sequester the protein and keep it from binding to RNA transcripts. That would be a way to influence the expression of many genes involved in the proliferation of cancer cells.” ![]()
Start Preparing for the Focused Practice in Hospital Medicine Exam
SHM recently developed the only maintenance of certification (MOC) exam by hospitalists for hospitalists. SHM SPARK is a fantastic complement to MOC tools already on the market and will help hospitalists succeed in the upcoming exam; it delivers access to relevant hospital medicine review content to enhance patient care while at the same time giving you the flexibility to fill your knowledge gaps and study needs at your own pace.
Featuring a unique online platform, SHM SPARK offers 175 vignette-style multiple-choice questions that bridge the primary knowledge gaps found within existing MOC exam-preparation products today. Other preparation tools are targeted toward the ABIM Internal Medicine exam and cover only roughly 60% of the Focused Practice in Hospital Medicine exam.
SHM SPARK is designed to serve as a supplemental study guide providing targeted study in the remaining roughly 40% of the Focused Practice in Hospital Medicine exam blueprint.
SHM SPARK provides in-depth review on the following systems-based content:
- Palliative care, ethics, and decision making
- Patient safety
- Perioperative care and consultative co-management
- Quality, cost, and clinical reasoning
The tool’s self-study provides detailed learning objectives and discussion points and allows users to define individual areas of strengths and weaknesses. Users will have the option to claim applicable ABIM MOC Part II Medical Knowledge points as they complete each module with a minimum passing score of 80%. After successful completion of all four modules, participants may claim up to 10.5 AMA PRA Category 1 Credits.
Order SPARK today at www.hospitalmedicine.org/SPARK.
SHM recently developed the only maintenance of certification (MOC) exam by hospitalists for hospitalists. SHM SPARK is a fantastic complement to MOC tools already on the market and will help hospitalists succeed in the upcoming exam; it delivers access to relevant hospital medicine review content to enhance patient care while at the same time giving you the flexibility to fill your knowledge gaps and study needs at your own pace.
Featuring a unique online platform, SHM SPARK offers 175 vignette-style multiple-choice questions that bridge the primary knowledge gaps found within existing MOC exam-preparation products today. Other preparation tools are targeted toward the ABIM Internal Medicine exam and cover only roughly 60% of the Focused Practice in Hospital Medicine exam.
SHM SPARK is designed to serve as a supplemental study guide providing targeted study in the remaining roughly 40% of the Focused Practice in Hospital Medicine exam blueprint.
SHM SPARK provides in-depth review on the following systems-based content:
- Palliative care, ethics, and decision making
- Patient safety
- Perioperative care and consultative co-management
- Quality, cost, and clinical reasoning
The tool’s self-study provides detailed learning objectives and discussion points and allows users to define individual areas of strengths and weaknesses. Users will have the option to claim applicable ABIM MOC Part II Medical Knowledge points as they complete each module with a minimum passing score of 80%. After successful completion of all four modules, participants may claim up to 10.5 AMA PRA Category 1 Credits.
Order SPARK today at www.hospitalmedicine.org/SPARK.
SHM recently developed the only maintenance of certification (MOC) exam by hospitalists for hospitalists. SHM SPARK is a fantastic complement to MOC tools already on the market and will help hospitalists succeed in the upcoming exam; it delivers access to relevant hospital medicine review content to enhance patient care while at the same time giving you the flexibility to fill your knowledge gaps and study needs at your own pace.
Featuring a unique online platform, SHM SPARK offers 175 vignette-style multiple-choice questions that bridge the primary knowledge gaps found within existing MOC exam-preparation products today. Other preparation tools are targeted toward the ABIM Internal Medicine exam and cover only roughly 60% of the Focused Practice in Hospital Medicine exam.
SHM SPARK is designed to serve as a supplemental study guide providing targeted study in the remaining roughly 40% of the Focused Practice in Hospital Medicine exam blueprint.
SHM SPARK provides in-depth review on the following systems-based content:
- Palliative care, ethics, and decision making
- Patient safety
- Perioperative care and consultative co-management
- Quality, cost, and clinical reasoning
The tool’s self-study provides detailed learning objectives and discussion points and allows users to define individual areas of strengths and weaknesses. Users will have the option to claim applicable ABIM MOC Part II Medical Knowledge points as they complete each module with a minimum passing score of 80%. After successful completion of all four modules, participants may claim up to 10.5 AMA PRA Category 1 Credits.
Order SPARK today at www.hospitalmedicine.org/SPARK.
Idelalisib trials stopped due to AEs

Photo courtesy of
Gilead Sciences
The US Food and Drug Administration (FDA) has reported that Gilead Sciences, Inc., is stopping 6 clinical trials of idelalisib (Zydelig) due to adverse events (AEs) observed in patients receiving idelalisib in combination with other drugs.
The AEs, which include deaths, were mostly related to infections.
The trials include patients with chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma, and indolent non-Hodgkin lymphomas.
The FDA said it is reviewing the findings of these trials and will communicate new information as necessary.
A few days ago, the European Medicines Agency (EMA) announced its decision to review the safety of idelalisib due to the aforementioned AEs. The EMA said it is reviewing data from 3 idelalisib trials.
While this review is underway, the EMA advised that patients starting or already on treatment with idelalisib be carefully monitored for signs of infection. If the drug is well tolerated, treatment should not be stopped.
The FDA has not made any recommendations about treatment with idelalisib.
About idelalisib
Idelalisib is currently approved by the FDA for use in combination with rituximab to treat patients with relapsed CLL who cannot receive rituximab alone.
Idelalisib also has accelerated approval from the FDA to treat patients with relapsed follicular lymphoma who have received at least 2 prior systemic therapies and patients with relapsed small lymphocytic lymphoma who have received at least 2 prior systemic therapies.
In the European Union, idelalisib is approved for use in combination with rituximab to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment in the presence of 17p deletion or TP53 mutation in CLL patients deemed unsuitable for chemo-immunotherapy.
Idelalisib is also approved in the European Union as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment. ![]()

Photo courtesy of
Gilead Sciences
The US Food and Drug Administration (FDA) has reported that Gilead Sciences, Inc., is stopping 6 clinical trials of idelalisib (Zydelig) due to adverse events (AEs) observed in patients receiving idelalisib in combination with other drugs.
The AEs, which include deaths, were mostly related to infections.
The trials include patients with chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma, and indolent non-Hodgkin lymphomas.
The FDA said it is reviewing the findings of these trials and will communicate new information as necessary.
A few days ago, the European Medicines Agency (EMA) announced its decision to review the safety of idelalisib due to the aforementioned AEs. The EMA said it is reviewing data from 3 idelalisib trials.
While this review is underway, the EMA advised that patients starting or already on treatment with idelalisib be carefully monitored for signs of infection. If the drug is well tolerated, treatment should not be stopped.
The FDA has not made any recommendations about treatment with idelalisib.
About idelalisib
Idelalisib is currently approved by the FDA for use in combination with rituximab to treat patients with relapsed CLL who cannot receive rituximab alone.
Idelalisib also has accelerated approval from the FDA to treat patients with relapsed follicular lymphoma who have received at least 2 prior systemic therapies and patients with relapsed small lymphocytic lymphoma who have received at least 2 prior systemic therapies.
In the European Union, idelalisib is approved for use in combination with rituximab to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment in the presence of 17p deletion or TP53 mutation in CLL patients deemed unsuitable for chemo-immunotherapy.
Idelalisib is also approved in the European Union as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment. ![]()

Photo courtesy of
Gilead Sciences
The US Food and Drug Administration (FDA) has reported that Gilead Sciences, Inc., is stopping 6 clinical trials of idelalisib (Zydelig) due to adverse events (AEs) observed in patients receiving idelalisib in combination with other drugs.
The AEs, which include deaths, were mostly related to infections.
The trials include patients with chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma, and indolent non-Hodgkin lymphomas.
The FDA said it is reviewing the findings of these trials and will communicate new information as necessary.
A few days ago, the European Medicines Agency (EMA) announced its decision to review the safety of idelalisib due to the aforementioned AEs. The EMA said it is reviewing data from 3 idelalisib trials.
While this review is underway, the EMA advised that patients starting or already on treatment with idelalisib be carefully monitored for signs of infection. If the drug is well tolerated, treatment should not be stopped.
The FDA has not made any recommendations about treatment with idelalisib.
About idelalisib
Idelalisib is currently approved by the FDA for use in combination with rituximab to treat patients with relapsed CLL who cannot receive rituximab alone.
Idelalisib also has accelerated approval from the FDA to treat patients with relapsed follicular lymphoma who have received at least 2 prior systemic therapies and patients with relapsed small lymphocytic lymphoma who have received at least 2 prior systemic therapies.
In the European Union, idelalisib is approved for use in combination with rituximab to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment in the presence of 17p deletion or TP53 mutation in CLL patients deemed unsuitable for chemo-immunotherapy.
Idelalisib is also approved in the European Union as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment. ![]()
Drug granted orphan designation for DLBCL

The US Food and Drug Administration (FDA) has granted orphan designation to the oncology drug candidate PNT2258 for the treatment of diffuse large B-cell lymphoma (DLBCL).
The FDA grants orphan designation to drugs intended to treat conditions affecting fewer than 200,000 patients in the US.
The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved.
About PNT2258
PNT2258 is designed to target cancers that overexpress BCL2, and BCL2 overexpression is thought to be a key driver of DLBCL.
PNT2258 consists of a single-stranded, 24-base DNAi oligonucleotide known as PNT100 that is encapsulated in lipid nanoparticles (LNPs).
The DNAi technology platform is based on a discovery that single-stranded DNA oligonucleotides can interact with genomic DNA to interfere with oncogenes. PNT100 DNAi is designed to target a genetic regulatory region associated with BCL2.
The LNPs are designed to provide enhanced serum stability and optimized pharmacokinetic properties to facilitate broad systemic distribution after intravenous infusion. Within the acidic environment found in tumors, the LNPs become positively charged and therefore more amenable to cellular uptake and cytoplasmic release of their payloads.
Trials of PNT2258
PNT2258 is being developed by ProNAi Therapeutics, Inc. The company has completed 2 trials of PNT2258 to date—a phase 1 trial of patients with solid tumors and a phase 2 trial of patients with non-Hodgkin lymphoma.
The phase 1 trial enrolled 22 patients with relapsed or refractory solid tumor malignancies. Results were published in Cancer Chemotherapy and Pharmacology in February 2014.
PNT2258 was deemed well-tolerated in this trial. There was no evidence of a systemic immune response to the LNPs or PNT100. There were no significant changes in immune-stimulatory cytokines or clinical signs of anaphylaxis following PNT2258 administration.
The phase 2 trial enrolled 13 patients with relapsed or refractory non-Hodgkin lymphoma. Results were presented at ASH 2014 (abstract 1716).
Six patients responded to PNT2258—4 with complete responses and 2 with partial responses. Five patients had stable disease, and 2 progressed. All 4 of the DLBCL patients in this trial responded—3 with complete responses and 1 with a partial response.
Adverse events reported in this trial include nausea (n=11), pain (n=9), chills (n=7), diarrhea (n=7), vomiting (n=7), fatigue (n=6), fever (n=6), headache (n=6), dyspnea (n=5), generalized aching (n=4), anorexia (n=4), back pain (n=4), sensory neuropathy (n=4), hypophosphatemia (n=4), anemia (n=3), hypokalemia (n=3), hyperuricemia (n=2), neutropenia (n=2), thrombocytopenia (n=4), and elevated AST/ALT (n=1).
ProNAi Therapeutics is now enrolling patients in “Wolverine,” a phase 2 trial evaluating PNT2258 in patients with relapsed or refractory DLBCL, and in “Brighton,” a phase 2 trial evaluating PNT2258 for the treatment of Richter’s transformation. ![]()

The US Food and Drug Administration (FDA) has granted orphan designation to the oncology drug candidate PNT2258 for the treatment of diffuse large B-cell lymphoma (DLBCL).
The FDA grants orphan designation to drugs intended to treat conditions affecting fewer than 200,000 patients in the US.
The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved.
About PNT2258
PNT2258 is designed to target cancers that overexpress BCL2, and BCL2 overexpression is thought to be a key driver of DLBCL.
PNT2258 consists of a single-stranded, 24-base DNAi oligonucleotide known as PNT100 that is encapsulated in lipid nanoparticles (LNPs).
The DNAi technology platform is based on a discovery that single-stranded DNA oligonucleotides can interact with genomic DNA to interfere with oncogenes. PNT100 DNAi is designed to target a genetic regulatory region associated with BCL2.
The LNPs are designed to provide enhanced serum stability and optimized pharmacokinetic properties to facilitate broad systemic distribution after intravenous infusion. Within the acidic environment found in tumors, the LNPs become positively charged and therefore more amenable to cellular uptake and cytoplasmic release of their payloads.
Trials of PNT2258
PNT2258 is being developed by ProNAi Therapeutics, Inc. The company has completed 2 trials of PNT2258 to date—a phase 1 trial of patients with solid tumors and a phase 2 trial of patients with non-Hodgkin lymphoma.
The phase 1 trial enrolled 22 patients with relapsed or refractory solid tumor malignancies. Results were published in Cancer Chemotherapy and Pharmacology in February 2014.
PNT2258 was deemed well-tolerated in this trial. There was no evidence of a systemic immune response to the LNPs or PNT100. There were no significant changes in immune-stimulatory cytokines or clinical signs of anaphylaxis following PNT2258 administration.
The phase 2 trial enrolled 13 patients with relapsed or refractory non-Hodgkin lymphoma. Results were presented at ASH 2014 (abstract 1716).
Six patients responded to PNT2258—4 with complete responses and 2 with partial responses. Five patients had stable disease, and 2 progressed. All 4 of the DLBCL patients in this trial responded—3 with complete responses and 1 with a partial response.
Adverse events reported in this trial include nausea (n=11), pain (n=9), chills (n=7), diarrhea (n=7), vomiting (n=7), fatigue (n=6), fever (n=6), headache (n=6), dyspnea (n=5), generalized aching (n=4), anorexia (n=4), back pain (n=4), sensory neuropathy (n=4), hypophosphatemia (n=4), anemia (n=3), hypokalemia (n=3), hyperuricemia (n=2), neutropenia (n=2), thrombocytopenia (n=4), and elevated AST/ALT (n=1).
ProNAi Therapeutics is now enrolling patients in “Wolverine,” a phase 2 trial evaluating PNT2258 in patients with relapsed or refractory DLBCL, and in “Brighton,” a phase 2 trial evaluating PNT2258 for the treatment of Richter’s transformation. ![]()

The US Food and Drug Administration (FDA) has granted orphan designation to the oncology drug candidate PNT2258 for the treatment of diffuse large B-cell lymphoma (DLBCL).
The FDA grants orphan designation to drugs intended to treat conditions affecting fewer than 200,000 patients in the US.
The designation provides the drug’s sponsor with various development incentives, including opportunities to apply for research-related tax credits and grant funding, assistance in designing clinical trials, and 7 years of US market exclusivity if the drug is approved.
About PNT2258
PNT2258 is designed to target cancers that overexpress BCL2, and BCL2 overexpression is thought to be a key driver of DLBCL.
PNT2258 consists of a single-stranded, 24-base DNAi oligonucleotide known as PNT100 that is encapsulated in lipid nanoparticles (LNPs).
The DNAi technology platform is based on a discovery that single-stranded DNA oligonucleotides can interact with genomic DNA to interfere with oncogenes. PNT100 DNAi is designed to target a genetic regulatory region associated with BCL2.
The LNPs are designed to provide enhanced serum stability and optimized pharmacokinetic properties to facilitate broad systemic distribution after intravenous infusion. Within the acidic environment found in tumors, the LNPs become positively charged and therefore more amenable to cellular uptake and cytoplasmic release of their payloads.
Trials of PNT2258
PNT2258 is being developed by ProNAi Therapeutics, Inc. The company has completed 2 trials of PNT2258 to date—a phase 1 trial of patients with solid tumors and a phase 2 trial of patients with non-Hodgkin lymphoma.
The phase 1 trial enrolled 22 patients with relapsed or refractory solid tumor malignancies. Results were published in Cancer Chemotherapy and Pharmacology in February 2014.
PNT2258 was deemed well-tolerated in this trial. There was no evidence of a systemic immune response to the LNPs or PNT100. There were no significant changes in immune-stimulatory cytokines or clinical signs of anaphylaxis following PNT2258 administration.
The phase 2 trial enrolled 13 patients with relapsed or refractory non-Hodgkin lymphoma. Results were presented at ASH 2014 (abstract 1716).
Six patients responded to PNT2258—4 with complete responses and 2 with partial responses. Five patients had stable disease, and 2 progressed. All 4 of the DLBCL patients in this trial responded—3 with complete responses and 1 with a partial response.
Adverse events reported in this trial include nausea (n=11), pain (n=9), chills (n=7), diarrhea (n=7), vomiting (n=7), fatigue (n=6), fever (n=6), headache (n=6), dyspnea (n=5), generalized aching (n=4), anorexia (n=4), back pain (n=4), sensory neuropathy (n=4), hypophosphatemia (n=4), anemia (n=3), hypokalemia (n=3), hyperuricemia (n=2), neutropenia (n=2), thrombocytopenia (n=4), and elevated AST/ALT (n=1).
ProNAi Therapeutics is now enrolling patients in “Wolverine,” a phase 2 trial evaluating PNT2258 in patients with relapsed or refractory DLBCL, and in “Brighton,” a phase 2 trial evaluating PNT2258 for the treatment of Richter’s transformation. ![]()
Intervention helps parents cope with kids’ HSCT

Photo by Chad McNeeley
A new social-cognitive intervention can reduce stress in parents of children undergoing hematopoietic stem cell transplant (HSCT), according to research published in the Journal of Consulting and Clinical Psychology.
In the short-term, the parent social-cognitive intervention program (P-SCIP) appeared more effective than the current best-practice psychosocial care (BPC) for reducing anxiety, depression, and traumatic distress.
However, there was not much difference between P-SCIP and BPC when it came to long-term results.
Certain subgroups of parents seemed to derive more benefit from P-SCIP than other parents.
“[P]revious research from our team and others has shown that between 20% and 66% of caregivers have elevated depression and/or anxiety prior to their child’s transplant procedure,” said study author Sharon Manne, PhD, of the Rutgers Cancer Institute of New Jersey in New Brunswick.
“It was our aim in this study to develop and test an individual intervention program that targets cognitive and social processing strategies associated with caregiver adjustment and compare that to available best-practice psychosocial care.”
Interventions
This study included 218 biological or foster parents of HSCT recipients under age 19. The parents were assigned to receive P-SCIP or BPC.
P-SCIP required parents to view an interactive CD-ROM for five 60-minute sessions over a 2- to 3-week period following the child’s transplant.
The CD-ROM addressed parents’ worries about their child, coping with solvable concerns related to HSCT, coping with unchangeable problems related to HSCT, and communication and the importance of expressing feelings and needs.
Parents receiving BPC viewed a 1-hour video guide to pediatric HSCT and received a pamphlet covering common caregiver issues. The parents were also given the option of having someone watch their child for up to 5 hours and the use of walkie-talkies so the parents could communicate with their child when they were not in the room.
All participants were asked to complete an in-person survey within a month’s time of their child receiving the transplant and to complete follow-up surveys by phone or mail at 1 month, 6 months, and 1 year post-HSCT.
One hundred and ten parents were randomized to P-SCIP and 108 to BPC. Sixty-six parents completed P-SCIP through the last follow-up, as did 72 parents assigned to BPC.
Results
The researchers found that P-SCIP could reduce anxiety, depression, and—to a marginal degree—traumatic distress more than BPC.
However, the beneficial effects of P-SCIP relative to BPC were only seen at the first follow-up. The overall psychological benefits of P-SCIP were no longer evident at the 6-month or 1-year follow ups.
Still, anxiety, depression, and traumatic distress declined among all the parents over the 1-year follow-up period, which is consistent with other research on caregiver distress after pediatric HSCT.
“Our study suggests that our intervention had an impact when primary caregivers were experiencing high levels of trauma and stress—during the time of the actual transplant and hospitalization—and that the intervention was more beneficial for specific subgroups of caregivers,” Dr Manne said.
P-SCIP had a stronger effect than BPC among parents who began the study reporting higher depression and anxiety and among parents whose children developed graft-versus-host disease.
Similarly, P-SCIP had long-term effects on traumatic distress among parents who reported higher anxiety pre-HSCT and among parents whose children had graft-versus-host disease at HSCT discharge.
“Our findings suggest that screening caregivers for elevations in anxiety and targeting interventions specifically to them may prove beneficial,” Dr Manne said.
She added that a next step for this research might be to examine possible differences between mothers and fathers in the caregiver role, as most of the primary caregivers in this study were mothers.
Additionally, if this intervention is carried into the clinical setting, methods of improving intervention attendance might be considered. Utilizing phone or web-based contact that would allow the parent to remain in the room with the child during hospitalization might help the caregivers more easily access the intervention. ![]()

Photo by Chad McNeeley
A new social-cognitive intervention can reduce stress in parents of children undergoing hematopoietic stem cell transplant (HSCT), according to research published in the Journal of Consulting and Clinical Psychology.
In the short-term, the parent social-cognitive intervention program (P-SCIP) appeared more effective than the current best-practice psychosocial care (BPC) for reducing anxiety, depression, and traumatic distress.
However, there was not much difference between P-SCIP and BPC when it came to long-term results.
Certain subgroups of parents seemed to derive more benefit from P-SCIP than other parents.
“[P]revious research from our team and others has shown that between 20% and 66% of caregivers have elevated depression and/or anxiety prior to their child’s transplant procedure,” said study author Sharon Manne, PhD, of the Rutgers Cancer Institute of New Jersey in New Brunswick.
“It was our aim in this study to develop and test an individual intervention program that targets cognitive and social processing strategies associated with caregiver adjustment and compare that to available best-practice psychosocial care.”
Interventions
This study included 218 biological or foster parents of HSCT recipients under age 19. The parents were assigned to receive P-SCIP or BPC.
P-SCIP required parents to view an interactive CD-ROM for five 60-minute sessions over a 2- to 3-week period following the child’s transplant.
The CD-ROM addressed parents’ worries about their child, coping with solvable concerns related to HSCT, coping with unchangeable problems related to HSCT, and communication and the importance of expressing feelings and needs.
Parents receiving BPC viewed a 1-hour video guide to pediatric HSCT and received a pamphlet covering common caregiver issues. The parents were also given the option of having someone watch their child for up to 5 hours and the use of walkie-talkies so the parents could communicate with their child when they were not in the room.
All participants were asked to complete an in-person survey within a month’s time of their child receiving the transplant and to complete follow-up surveys by phone or mail at 1 month, 6 months, and 1 year post-HSCT.
One hundred and ten parents were randomized to P-SCIP and 108 to BPC. Sixty-six parents completed P-SCIP through the last follow-up, as did 72 parents assigned to BPC.
Results
The researchers found that P-SCIP could reduce anxiety, depression, and—to a marginal degree—traumatic distress more than BPC.
However, the beneficial effects of P-SCIP relative to BPC were only seen at the first follow-up. The overall psychological benefits of P-SCIP were no longer evident at the 6-month or 1-year follow ups.
Still, anxiety, depression, and traumatic distress declined among all the parents over the 1-year follow-up period, which is consistent with other research on caregiver distress after pediatric HSCT.
“Our study suggests that our intervention had an impact when primary caregivers were experiencing high levels of trauma and stress—during the time of the actual transplant and hospitalization—and that the intervention was more beneficial for specific subgroups of caregivers,” Dr Manne said.
P-SCIP had a stronger effect than BPC among parents who began the study reporting higher depression and anxiety and among parents whose children developed graft-versus-host disease.
Similarly, P-SCIP had long-term effects on traumatic distress among parents who reported higher anxiety pre-HSCT and among parents whose children had graft-versus-host disease at HSCT discharge.
“Our findings suggest that screening caregivers for elevations in anxiety and targeting interventions specifically to them may prove beneficial,” Dr Manne said.
She added that a next step for this research might be to examine possible differences between mothers and fathers in the caregiver role, as most of the primary caregivers in this study were mothers.
Additionally, if this intervention is carried into the clinical setting, methods of improving intervention attendance might be considered. Utilizing phone or web-based contact that would allow the parent to remain in the room with the child during hospitalization might help the caregivers more easily access the intervention. ![]()

Photo by Chad McNeeley
A new social-cognitive intervention can reduce stress in parents of children undergoing hematopoietic stem cell transplant (HSCT), according to research published in the Journal of Consulting and Clinical Psychology.
In the short-term, the parent social-cognitive intervention program (P-SCIP) appeared more effective than the current best-practice psychosocial care (BPC) for reducing anxiety, depression, and traumatic distress.
However, there was not much difference between P-SCIP and BPC when it came to long-term results.
Certain subgroups of parents seemed to derive more benefit from P-SCIP than other parents.
“[P]revious research from our team and others has shown that between 20% and 66% of caregivers have elevated depression and/or anxiety prior to their child’s transplant procedure,” said study author Sharon Manne, PhD, of the Rutgers Cancer Institute of New Jersey in New Brunswick.
“It was our aim in this study to develop and test an individual intervention program that targets cognitive and social processing strategies associated with caregiver adjustment and compare that to available best-practice psychosocial care.”
Interventions
This study included 218 biological or foster parents of HSCT recipients under age 19. The parents were assigned to receive P-SCIP or BPC.
P-SCIP required parents to view an interactive CD-ROM for five 60-minute sessions over a 2- to 3-week period following the child’s transplant.
The CD-ROM addressed parents’ worries about their child, coping with solvable concerns related to HSCT, coping with unchangeable problems related to HSCT, and communication and the importance of expressing feelings and needs.
Parents receiving BPC viewed a 1-hour video guide to pediatric HSCT and received a pamphlet covering common caregiver issues. The parents were also given the option of having someone watch their child for up to 5 hours and the use of walkie-talkies so the parents could communicate with their child when they were not in the room.
All participants were asked to complete an in-person survey within a month’s time of their child receiving the transplant and to complete follow-up surveys by phone or mail at 1 month, 6 months, and 1 year post-HSCT.
One hundred and ten parents were randomized to P-SCIP and 108 to BPC. Sixty-six parents completed P-SCIP through the last follow-up, as did 72 parents assigned to BPC.
Results
The researchers found that P-SCIP could reduce anxiety, depression, and—to a marginal degree—traumatic distress more than BPC.
However, the beneficial effects of P-SCIP relative to BPC were only seen at the first follow-up. The overall psychological benefits of P-SCIP were no longer evident at the 6-month or 1-year follow ups.
Still, anxiety, depression, and traumatic distress declined among all the parents over the 1-year follow-up period, which is consistent with other research on caregiver distress after pediatric HSCT.
“Our study suggests that our intervention had an impact when primary caregivers were experiencing high levels of trauma and stress—during the time of the actual transplant and hospitalization—and that the intervention was more beneficial for specific subgroups of caregivers,” Dr Manne said.
P-SCIP had a stronger effect than BPC among parents who began the study reporting higher depression and anxiety and among parents whose children developed graft-versus-host disease.
Similarly, P-SCIP had long-term effects on traumatic distress among parents who reported higher anxiety pre-HSCT and among parents whose children had graft-versus-host disease at HSCT discharge.
“Our findings suggest that screening caregivers for elevations in anxiety and targeting interventions specifically to them may prove beneficial,” Dr Manne said.
She added that a next step for this research might be to examine possible differences between mothers and fathers in the caregiver role, as most of the primary caregivers in this study were mothers.
Additionally, if this intervention is carried into the clinical setting, methods of improving intervention attendance might be considered. Utilizing phone or web-based contact that would allow the parent to remain in the room with the child during hospitalization might help the caregivers more easily access the intervention. ![]()
Cold turkey better for smoking cessation
Quitting smoking abruptly rather than gradually leads to higher abstinence rates both at 4 weeks and 6 months, a report published online March 14 shows.
Worldwide guidelines for smoking cessation generally recommend abrupt cessation over a gradual reduction in smoking, based on data from observational studies. However a recent review of 10 randomized trials concluded that quitting “cold turkey” produces only slightly higher quit rates, said Nicola Lindson-Hawley, Ph.D., of the department of primary care health services, University of Oxford (England), and her associates.
They compared the two approaches in a noninferiority trial involving 697 adults treated at 31 primary care practices in England during a 2.5-year period. The study participants smoked at least 15 cigarettes per day and had an end-expiratory carbon monoxide concentration of at least 15 parts per million. The average age was 49 years, and the study population was evenly divided between men and women. Their mean score on the Fagerström Test for Cigarette Dependence was 6, indicating a high degree of dependence.
These participants were randomly assigned either to stop smoking abruptly on a quit date 2 weeks from baseline (355 patients) or to stop gradually, by reducing their cigarette use by half at 1 week from baseline, by half again during the second week, and completely by a quit date 2 weeks from baseline. The latter group was given a choice of three structured reduction programs to follow before the quit date, as well as nicotine patches and a choice of short-acting nicotine replacement products (gum, lozenges, nasal sprays, sublingual tablets, inhalators, or mouth sprays). The abrupt-cessation group received only the nicotine patches just before the quit day. Both groups received identical behavioral counseling, nicotine patches, and nicotine replacement products after the quit date.
The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (relative risk, 0.80). Thus, gradual cessation did not prove to be noninferior to abrupt cessation. The secondary outcome measure of abstinence at 6 months also was superior for the abrupt-cessation group (22%) over the gradual-cessation group (15.5%), Dr. Lindson-Hawley and her associates reported (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M14-2805).
Most of the between-group difference was attributed to the fact that fewer participants in the gradual-cessation group actually attempted to quit on their quit date (61.4% vs. 71.0%). Relapse rates were similar between the two study groups at 4 weeks (36.2% vs. 31.0%) and at 6 months (74.8% vs. 69.1%).
“These results imply that, in clinical practice, we should encourage persons to stop smoking abruptly and not gradually,” Dr. Lindson-Hawley and her associates wrote. “However, gradual cessation programs could still be worthwhile if they increase the number of persons who try to quit or take up support and medication while trying.”
The study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
The trial by Nicola Lindson-Hawley, Ph.D., is well designed and suggests that “setting a quit date and quitting abruptly increases long-term cessation rates in smokers who want to quit,” Dr. Gabriela S. Ferreira and Dr. Michael B. Steinberg wrote in an accompanying editorial. However, a gradual approach to smoking cessation still may be useful for some smokers, so that method shouldn’t be entirely abandoned just yet.
Many smokers try several times to quit abruptly but are not successful. They may not wish to set another abrupt quit date for fear of “failing” yet again. However, they may instead respond well to gradually reducing their smoking, with the eventual goal of reducing it all the way to zero.
These findings raise important questions about how clinicians should approach patients who smoke and are ready to quit, they wrote.
Dr. Ferreira and Dr. Steinberg are at the Robert Wood Johnson Medical School in New Brunswick. Dr. Ferreira reported having no relevant financial disclosures; Dr. Steinberg reported receiving personal fees from Arena Pharmaceuticals, Major League Baseball, and Pfizer outside of this work. Their remarks (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M16-0362) accompanied Dr. Lindson-Hawley’s report.
The trial by Nicola Lindson-Hawley, Ph.D., is well designed and suggests that “setting a quit date and quitting abruptly increases long-term cessation rates in smokers who want to quit,” Dr. Gabriela S. Ferreira and Dr. Michael B. Steinberg wrote in an accompanying editorial. However, a gradual approach to smoking cessation still may be useful for some smokers, so that method shouldn’t be entirely abandoned just yet.
Many smokers try several times to quit abruptly but are not successful. They may not wish to set another abrupt quit date for fear of “failing” yet again. However, they may instead respond well to gradually reducing their smoking, with the eventual goal of reducing it all the way to zero.
These findings raise important questions about how clinicians should approach patients who smoke and are ready to quit, they wrote.
Dr. Ferreira and Dr. Steinberg are at the Robert Wood Johnson Medical School in New Brunswick. Dr. Ferreira reported having no relevant financial disclosures; Dr. Steinberg reported receiving personal fees from Arena Pharmaceuticals, Major League Baseball, and Pfizer outside of this work. Their remarks (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M16-0362) accompanied Dr. Lindson-Hawley’s report.
The trial by Nicola Lindson-Hawley, Ph.D., is well designed and suggests that “setting a quit date and quitting abruptly increases long-term cessation rates in smokers who want to quit,” Dr. Gabriela S. Ferreira and Dr. Michael B. Steinberg wrote in an accompanying editorial. However, a gradual approach to smoking cessation still may be useful for some smokers, so that method shouldn’t be entirely abandoned just yet.
Many smokers try several times to quit abruptly but are not successful. They may not wish to set another abrupt quit date for fear of “failing” yet again. However, they may instead respond well to gradually reducing their smoking, with the eventual goal of reducing it all the way to zero.
These findings raise important questions about how clinicians should approach patients who smoke and are ready to quit, they wrote.
Dr. Ferreira and Dr. Steinberg are at the Robert Wood Johnson Medical School in New Brunswick. Dr. Ferreira reported having no relevant financial disclosures; Dr. Steinberg reported receiving personal fees from Arena Pharmaceuticals, Major League Baseball, and Pfizer outside of this work. Their remarks (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M16-0362) accompanied Dr. Lindson-Hawley’s report.
Quitting smoking abruptly rather than gradually leads to higher abstinence rates both at 4 weeks and 6 months, a report published online March 14 shows.
Worldwide guidelines for smoking cessation generally recommend abrupt cessation over a gradual reduction in smoking, based on data from observational studies. However a recent review of 10 randomized trials concluded that quitting “cold turkey” produces only slightly higher quit rates, said Nicola Lindson-Hawley, Ph.D., of the department of primary care health services, University of Oxford (England), and her associates.
They compared the two approaches in a noninferiority trial involving 697 adults treated at 31 primary care practices in England during a 2.5-year period. The study participants smoked at least 15 cigarettes per day and had an end-expiratory carbon monoxide concentration of at least 15 parts per million. The average age was 49 years, and the study population was evenly divided between men and women. Their mean score on the Fagerström Test for Cigarette Dependence was 6, indicating a high degree of dependence.
These participants were randomly assigned either to stop smoking abruptly on a quit date 2 weeks from baseline (355 patients) or to stop gradually, by reducing their cigarette use by half at 1 week from baseline, by half again during the second week, and completely by a quit date 2 weeks from baseline. The latter group was given a choice of three structured reduction programs to follow before the quit date, as well as nicotine patches and a choice of short-acting nicotine replacement products (gum, lozenges, nasal sprays, sublingual tablets, inhalators, or mouth sprays). The abrupt-cessation group received only the nicotine patches just before the quit day. Both groups received identical behavioral counseling, nicotine patches, and nicotine replacement products after the quit date.
The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (relative risk, 0.80). Thus, gradual cessation did not prove to be noninferior to abrupt cessation. The secondary outcome measure of abstinence at 6 months also was superior for the abrupt-cessation group (22%) over the gradual-cessation group (15.5%), Dr. Lindson-Hawley and her associates reported (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M14-2805).
Most of the between-group difference was attributed to the fact that fewer participants in the gradual-cessation group actually attempted to quit on their quit date (61.4% vs. 71.0%). Relapse rates were similar between the two study groups at 4 weeks (36.2% vs. 31.0%) and at 6 months (74.8% vs. 69.1%).
“These results imply that, in clinical practice, we should encourage persons to stop smoking abruptly and not gradually,” Dr. Lindson-Hawley and her associates wrote. “However, gradual cessation programs could still be worthwhile if they increase the number of persons who try to quit or take up support and medication while trying.”
The study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
Quitting smoking abruptly rather than gradually leads to higher abstinence rates both at 4 weeks and 6 months, a report published online March 14 shows.
Worldwide guidelines for smoking cessation generally recommend abrupt cessation over a gradual reduction in smoking, based on data from observational studies. However a recent review of 10 randomized trials concluded that quitting “cold turkey” produces only slightly higher quit rates, said Nicola Lindson-Hawley, Ph.D., of the department of primary care health services, University of Oxford (England), and her associates.
They compared the two approaches in a noninferiority trial involving 697 adults treated at 31 primary care practices in England during a 2.5-year period. The study participants smoked at least 15 cigarettes per day and had an end-expiratory carbon monoxide concentration of at least 15 parts per million. The average age was 49 years, and the study population was evenly divided between men and women. Their mean score on the Fagerström Test for Cigarette Dependence was 6, indicating a high degree of dependence.
These participants were randomly assigned either to stop smoking abruptly on a quit date 2 weeks from baseline (355 patients) or to stop gradually, by reducing their cigarette use by half at 1 week from baseline, by half again during the second week, and completely by a quit date 2 weeks from baseline. The latter group was given a choice of three structured reduction programs to follow before the quit date, as well as nicotine patches and a choice of short-acting nicotine replacement products (gum, lozenges, nasal sprays, sublingual tablets, inhalators, or mouth sprays). The abrupt-cessation group received only the nicotine patches just before the quit day. Both groups received identical behavioral counseling, nicotine patches, and nicotine replacement products after the quit date.
The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (relative risk, 0.80). Thus, gradual cessation did not prove to be noninferior to abrupt cessation. The secondary outcome measure of abstinence at 6 months also was superior for the abrupt-cessation group (22%) over the gradual-cessation group (15.5%), Dr. Lindson-Hawley and her associates reported (Ann Intern Med. 2016 Mar 15. doi: 10.7326/M14-2805).
Most of the between-group difference was attributed to the fact that fewer participants in the gradual-cessation group actually attempted to quit on their quit date (61.4% vs. 71.0%). Relapse rates were similar between the two study groups at 4 weeks (36.2% vs. 31.0%) and at 6 months (74.8% vs. 69.1%).
“These results imply that, in clinical practice, we should encourage persons to stop smoking abruptly and not gradually,” Dr. Lindson-Hawley and her associates wrote. “However, gradual cessation programs could still be worthwhile if they increase the number of persons who try to quit or take up support and medication while trying.”
The study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
FROM THE ANNALS OF INTERNAL MEDICINE
Key clinical point: Quitting cigarette smoking abruptly rather than gradually leads to higher abstinence rates in the short and long term.
Major finding: The primary outcome measure, abstinence at 4 weeks, was achieved by 49% of the abrupt-cessation group, compared with only 39.2% of the gradual-cessation group (RR, 0.80).
Data source: A randomized, controlled noninferiority study involving 697 smokers at 31 primary care practices in England.
Disclosures: This study was supported by the British Heart Foundation, Cancer Research United Kingdom, the Economic and Social Research Council, the Medical Research Council, and the National Institute for Health Research. Dr. Lindson-Hawley reported having no relevant financial disclosures; two of her associates reported ties to Pfizer, GlaxoSmithKline, and McNeil.
Flu vaccination found safe in surgical patients
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Immunizing surgical patients against seasonal influenza before they leave the hospital appears safe.
Major finding: Patients received a flu vaccine in only 6,420 hospital stays for surgery, comprising only 15% of the patient hospitalizations that were eligible.
Data source: A retrospective cohort study involving 81,647 surgeries at 14 California hospitals during three consecutive flu seasons.
Disclosures: This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Anti-Remicade antibodies also cross-react with infliximab biosimilar
Antibodies to the innovator infliximab drug Remicade found in rheumatoid arthritis and spondyloarthritis patients also cross-react with the infliximab biosimilar CT-P13, marketed as Remsima or Inflectra, suggesting that switches from the innovator drug to the biosimilar are not advisable in the presence of anti-infliximab antibodies.
Switching an antibody-positive patient from the innovator drug to the biosimilar could mean that existing infliximab antibodies will “interact with the new drug, enhance clearance, and potentially lead to loss of response and infusion-related reactions,” wrote first author M. Begoña Ruiz-Argüello, Ph.D., an employee of the molecular biology testing company Progenika-Grifols in Derio, Spain, and colleagues (Ann Rheum Dis. 2016 Mar 10. doi: 10.1136/annrheumdis-2015-208684).
In the current study, the investigators set out to discover whether anti-Remicade antibodies cross-reacted with the biosimilar CT-P13, which was approved by the European Medicines Agency in 2013 for the same indications as the originator infliximab biologic Remicade.
They retrospectively selected 250 patients with rheumatoid arthritis (RA) or spondyloarthritis (SpA) who were treated with Remicade and 77 control patients who were infliximab naive.
Antibodies to infliximab were measured at the same time using three bridging ELISA assays: one that used Remicade to detect antibodies (Promonitor-ANTI-IFX kit, Progenika-Grifols, Spain); one that used Remsima (Orion Pharma, Norway); and another that used Inflectra (Hospira, United States).
Overall, 126 (50.4%) patients tested positive for antibodies using the Promonitor-ANTI-IFX kit.
These patients also tested positive for antibodies when the Remsima and Inflectra assays were used. Median antibody concentrations between the assays were not statistically different (P greater than .05). No significant differences were observed between patients with RA and SpA (P greater than .05) or in patients on concomitant immunosuppressive treatment, such as methotrexate.
Contrary to previous research, patients who tested negative for antibodies with the Promonitor-ANTI-IFX kit also tested negative with the Remsima and Inflectra assays. “Although additional epitopes may be present in the biosimilar, results suggest that epitopes influencing the immune response to [infliximab] are also present in the biosimilar,” the researchers said.
The investigators said that their findings also supported the use of therapeutic drug monitoring before considering switching patients between drugs.
Although the researchers recommended not switching between Remicade and Remsima or Inflectra, a small subanalysis in their study suggests it would be okay to switch from adalimumab to the infliximab biosimilar. A control population of 19 patients involved in the study who were anti–adalimumab antibody positive tested negative for antibodies to infliximab across the three assays.
Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
Antibodies to the innovator infliximab drug Remicade found in rheumatoid arthritis and spondyloarthritis patients also cross-react with the infliximab biosimilar CT-P13, marketed as Remsima or Inflectra, suggesting that switches from the innovator drug to the biosimilar are not advisable in the presence of anti-infliximab antibodies.
Switching an antibody-positive patient from the innovator drug to the biosimilar could mean that existing infliximab antibodies will “interact with the new drug, enhance clearance, and potentially lead to loss of response and infusion-related reactions,” wrote first author M. Begoña Ruiz-Argüello, Ph.D., an employee of the molecular biology testing company Progenika-Grifols in Derio, Spain, and colleagues (Ann Rheum Dis. 2016 Mar 10. doi: 10.1136/annrheumdis-2015-208684).
In the current study, the investigators set out to discover whether anti-Remicade antibodies cross-reacted with the biosimilar CT-P13, which was approved by the European Medicines Agency in 2013 for the same indications as the originator infliximab biologic Remicade.
They retrospectively selected 250 patients with rheumatoid arthritis (RA) or spondyloarthritis (SpA) who were treated with Remicade and 77 control patients who were infliximab naive.
Antibodies to infliximab were measured at the same time using three bridging ELISA assays: one that used Remicade to detect antibodies (Promonitor-ANTI-IFX kit, Progenika-Grifols, Spain); one that used Remsima (Orion Pharma, Norway); and another that used Inflectra (Hospira, United States).
Overall, 126 (50.4%) patients tested positive for antibodies using the Promonitor-ANTI-IFX kit.
These patients also tested positive for antibodies when the Remsima and Inflectra assays were used. Median antibody concentrations between the assays were not statistically different (P greater than .05). No significant differences were observed between patients with RA and SpA (P greater than .05) or in patients on concomitant immunosuppressive treatment, such as methotrexate.
Contrary to previous research, patients who tested negative for antibodies with the Promonitor-ANTI-IFX kit also tested negative with the Remsima and Inflectra assays. “Although additional epitopes may be present in the biosimilar, results suggest that epitopes influencing the immune response to [infliximab] are also present in the biosimilar,” the researchers said.
The investigators said that their findings also supported the use of therapeutic drug monitoring before considering switching patients between drugs.
Although the researchers recommended not switching between Remicade and Remsima or Inflectra, a small subanalysis in their study suggests it would be okay to switch from adalimumab to the infliximab biosimilar. A control population of 19 patients involved in the study who were anti–adalimumab antibody positive tested negative for antibodies to infliximab across the three assays.
Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
Antibodies to the innovator infliximab drug Remicade found in rheumatoid arthritis and spondyloarthritis patients also cross-react with the infliximab biosimilar CT-P13, marketed as Remsima or Inflectra, suggesting that switches from the innovator drug to the biosimilar are not advisable in the presence of anti-infliximab antibodies.
Switching an antibody-positive patient from the innovator drug to the biosimilar could mean that existing infliximab antibodies will “interact with the new drug, enhance clearance, and potentially lead to loss of response and infusion-related reactions,” wrote first author M. Begoña Ruiz-Argüello, Ph.D., an employee of the molecular biology testing company Progenika-Grifols in Derio, Spain, and colleagues (Ann Rheum Dis. 2016 Mar 10. doi: 10.1136/annrheumdis-2015-208684).
In the current study, the investigators set out to discover whether anti-Remicade antibodies cross-reacted with the biosimilar CT-P13, which was approved by the European Medicines Agency in 2013 for the same indications as the originator infliximab biologic Remicade.
They retrospectively selected 250 patients with rheumatoid arthritis (RA) or spondyloarthritis (SpA) who were treated with Remicade and 77 control patients who were infliximab naive.
Antibodies to infliximab were measured at the same time using three bridging ELISA assays: one that used Remicade to detect antibodies (Promonitor-ANTI-IFX kit, Progenika-Grifols, Spain); one that used Remsima (Orion Pharma, Norway); and another that used Inflectra (Hospira, United States).
Overall, 126 (50.4%) patients tested positive for antibodies using the Promonitor-ANTI-IFX kit.
These patients also tested positive for antibodies when the Remsima and Inflectra assays were used. Median antibody concentrations between the assays were not statistically different (P greater than .05). No significant differences were observed between patients with RA and SpA (P greater than .05) or in patients on concomitant immunosuppressive treatment, such as methotrexate.
Contrary to previous research, patients who tested negative for antibodies with the Promonitor-ANTI-IFX kit also tested negative with the Remsima and Inflectra assays. “Although additional epitopes may be present in the biosimilar, results suggest that epitopes influencing the immune response to [infliximab] are also present in the biosimilar,” the researchers said.
The investigators said that their findings also supported the use of therapeutic drug monitoring before considering switching patients between drugs.
Although the researchers recommended not switching between Remicade and Remsima or Inflectra, a small subanalysis in their study suggests it would be okay to switch from adalimumab to the infliximab biosimilar. A control population of 19 patients involved in the study who were anti–adalimumab antibody positive tested negative for antibodies to infliximab across the three assays.
Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: Rheumatology patients with positive antibodies to Remicade should not be switched to infliximab biosimilar (Remsima, Inflectra).
Major finding: Antibodies to infliximab in Remicade-treated rheumatology patients showed identical reactivity towards the biosimilar CT-P13.
Data source: A retrospective study of 250 consecutive patients with RA and SpA taking Remicade and 77 infliximab-naive controls.
Disclosures: Six of the authors are full-time employees of Progenika Biopharma S.A., maker of the Remicade assay used in the study.
Temsirolimus results in good but short-duration responses in primary CNS lymphoma
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Relapsed/refractory primary CNS lymphoma has a poor prognosis and no standard treatment option.
Major finding: The overall response rate to once-weekly temsirolimus was 54%; most responses were short lived.
Data source: Open-label phase 2 study in 37 adults with relapsed/refractory primary CNS lymphoma.
Disclosures: The study was supported by Pfizer Germany. Dr. Korfel and several colleagues disclosed research support from or consulting/advising for the company.