User login
Vagus nerve stimulator used for epilepsy also improves symptoms of rheumatoid arthritis
An implanted vagus nerve stimulator like that used for epilepsy treatment reduced inflammatory markers and significantly improved symptoms and function in a small cohort of patients with rheumatoid arthritis.
After 42 days, almost 30% of patients had achieved disease remission, Frieda A. Koopman, MD, and her colleagues reported in the July issue of the Proceedings of the National Academy of Science (doi: 10.1073/pnas.1605635113). The improvements disappeared rapidly when the devices were turned off, but were quickly reestablished after stimulation resumed.
“This first-in-class study supports a conceptual framework for further studies of electronic medical devices in diseases currently treated with drugs, an approach termed ‘bioelectronic medicine,’” wrote Dr. Koopman of the University of Amsterdam, and her coauthors.
The team built on evidence of what they termed a “reflex neural circuit” in the vagus that strongly influences the production of inflammatory cytokines. Animal studies showed that electrical stimulation of the vagus nerve encouraged choline acetyltransferase–positive T cells to secrete acetylcholine in the spleen and other tissues. Acetylcholine binds to a class of nicotinic receptors on monocytes, macrophages, and stromal cells, and inhibits their inflammatory response.
“Inflammatory reflex signaling, which is enhanced by electrically stimulating the vagus nerve, significantly reduces cytokine production and attenuates disease severity in experimental models of endotoxemia, sepsis, colitis, and other preclinical animal models of inflammatory syndromes,” the team noted.
The group reported on two human studies, totaling 25 patients. The first comprised seven patients with epilepsy who received the implanted vagus nerve stimulator for medically refractory seizures. None of these patients had a history of RA or any other inflammatory disease. The second group was all patients with active RA.
Each epilepsy patient contributed peripheral blood for study, which was collected before, during and after the implantation surgery. The team studied inflammatory markers by adding endotoxin to the samples. Those collected after the patient had been exposed to a single 30-second stimulation at 20 Hertz showed significantly inhibited production of TNF-alpha, compared with that seen in unexposed blood. Interleukin (IL)-6 and IL-1beta was also inhibited significantly by vagus nerve stimulation.
The next study involved 17 patients who had active RA, but not epilepsy. Of these, seven had failed methotrexate but were naïve to biologics; the rest had failed methotrexate and at least two biologics from different classes. Their average disease duration was 11 years.
The 86-day study gradually titrated the stimulation dose, but even at its highest, stimulation was far less than what is typically employed in epilepsy, “in which current is delivered at 60-second intervals, followed by an off interval of 5-180 minutes, repeated continuously,” the investigators wrote. “Thus, epilepsy patients may receive electrical current delivery for up to 240 minutes daily. Preclinical studies have established that stimulation of the inflammatory reflex for as little as 60 seconds confers significant inhibition of cytokine production for up to 24 hours.”
There was a 14-day post-implantation washout period with no stimulation, followed by 28 days of treatment titration. During that time, stimulation was ramped up from single 60-second stimulation with electric pulses of 250-microseconds duration at 10 Hertz and an output current between 0.25-2.0 milliamps, to the highest amperage tolerated (up to 2.0 milliamps).
That dose was the treatment target, and delivered once daily for 60 seconds in 250-microsecond pulse widths at 10 Hertz. At day 28, patients who had not had good clinical response according to EULAR response criteria, had their stimulation increased to four times daily.
In the group of seven methotrexate-resistant patients, two received electric current pulses four times daily. In the group of 10 methotrexate- and biologic-resistant patients, 6 received the four-dose stimulation.
On day 42, TNF-alpha levels in cultured peripheral blood were significantly reduced from baseline.
At that time, the vagus nerve stimulator was turned off for 14 days. By the end of the silent period, TNF-alpha levels had risen significantly from the day 42 levels. The stimulator was restarted on day 56. By day 84, after 28 more days of stimulation, TNF-alpha levels had again decreased significantly.
Symptoms and function as measured by the Disease Activity Score 28 followed a similar trajectory, improving during the initial treatment, worsening during the period of no stimulation, and improving again when stimulation was restarted. Symptom and function scores correlated positively with change in TNF levels.
The investigators also assessed the response rates according to American College of Rheumatology criteria. At day 42, 71% of those in the methotrexate-resistant group had achieved a 20% response; 57% a 50% response; and 28.6% a 70% response. Response was not as dramatic in the group resistant to both drug classes: rates were 70%, 30%, and 0%.
By day 42, nearly 30% of patients overall achieved remission, which was defined as a DAS28 score of less than 2.6. This constituted improvement in all the score components, including tender joint count, swollen joint count, patient’s assessment of pain, patient’s global assessment, physician’s global assessment, and C-reactive protein.
Finally, the investigators noted decreased levels of most serum cytokines. Most, including serum TNF, IL-10, IL-12p70, IL-13, IL-1alpha, IL-1beta, IL-2, IL-4, IL-5, and TNF-a-beta, were below 1 pg/ml.
Adverse events were common (16 patients) but reported as mild-moderate. The included hoarseness (5), hypoesthesia (4), parasthesia (2), dyspnea (2), and bradycardia (1), among others. There were no implantation-related infections. One patient reported postimplantation pain.
SetPoint Medical, of Valencia, Calif., makes the device and conducted the study. Dr. Koopman made no financial disclosures. However, several of the other authors are employees of Set Point, and of GlaxoSmithKline, which holds equity interest in the company.
On Twitter @Alz_Gal
The many different functions and brain regions associated with the vagus nerve have led researchers to test its usefulness in treating several illnesses, including epilepsy, treatment-resistant depression, anxiety disorders, Alzheimer’s disease, migraines, fibromyalgia, obesity, and tinnitus.
The Food and Drug Administration’s approval of a vagus nerve stimulator (VNS) subsequent to a 1997 neurological devices panel meeting has remained controversial. In the only randomized, controlled trial of severe depression, VNS failed to perform any better when turned on than in otherwise similarly implanted patients whose device was not turned on, according to the agency’s summary of the data.

|
| Dr. Maurizio Cutolo |
However, the discovery in 2007 by Kevin J. Tracey that vagus nerve stimulation inhibits inflammation by suppressing pro-inflammatory cytokine production (inflammatory reflex) has led to significant interest in the potential to use this approach for treating inflammatory diseases ranging from arthritis to colitis, ischemia, myocardial infarction, and heart failure (J Clin Invest. 2007;117[2]:289-96).
At present, the study by Dr. Koopman and her colleagues showed that vagus nerve stimulation (up to four times daily) by the implantable VNS in rheumatoid arthritis (RA) patients significantly inhibited tumor necrosis factor (TNF) production for up to 84 days. RA disease severity apparently improved significantly. The results of this investigation seem to confirm the crucial role played by the neuroendocrine immune system network in RA (Nat Rev Rheumatol. 2011;7[9]:500-2).
However, the question now is: Are there issues and limitations about this possible new approach to RA treatment based on previous experiences? An obvious issue is the limited number of adverse events reported by the authors.
In contrast, adverse events have been signaled in all previous studies for VNS use as expected: cardiac arrhythmia during implantation, intermittent decrease in respiratory flow during sleep, posttreatment increase of apnea hypopnea index, and the development of posttreatment mild obstructive sleep apnea in up to one-third of patients, a minority of whom develop severe obstructive sleep apnea clearly related to VNS therapy. Another study has shown alteration of voice in 66%, coughing in 45%, pharyngitis in 35%, and throat pain in 28% (Pediatr Neurol. 2008;38[2]:99-103). Other reports of VNS device adverse events range from hoarseness (very common) to frank laryngeal muscle spasm and upper airway obstruction (rare). Other nonspecific symptoms include headache, nausea, vomiting, dyspepsia, dyspnea, and paresthesia.
At present, the approach of VNS therapy in RA needs further strict investigations, especially regarding the large number of potential adverse events expected. In addition, the target of reducing TNF levels in RA patients is already obtainable with several other noninvasive and established treatments.
Maurizio Cutolo, MD, is professor of rheumatology and internal medicine and director of the research laboratories and academic division of clinical rheumatology in the department of internal medicine at the University of Genova (Italy). He has no relevant disclosures.
The many different functions and brain regions associated with the vagus nerve have led researchers to test its usefulness in treating several illnesses, including epilepsy, treatment-resistant depression, anxiety disorders, Alzheimer’s disease, migraines, fibromyalgia, obesity, and tinnitus.
The Food and Drug Administration’s approval of a vagus nerve stimulator (VNS) subsequent to a 1997 neurological devices panel meeting has remained controversial. In the only randomized, controlled trial of severe depression, VNS failed to perform any better when turned on than in otherwise similarly implanted patients whose device was not turned on, according to the agency’s summary of the data.

|
| Dr. Maurizio Cutolo |
However, the discovery in 2007 by Kevin J. Tracey that vagus nerve stimulation inhibits inflammation by suppressing pro-inflammatory cytokine production (inflammatory reflex) has led to significant interest in the potential to use this approach for treating inflammatory diseases ranging from arthritis to colitis, ischemia, myocardial infarction, and heart failure (J Clin Invest. 2007;117[2]:289-96).
At present, the study by Dr. Koopman and her colleagues showed that vagus nerve stimulation (up to four times daily) by the implantable VNS in rheumatoid arthritis (RA) patients significantly inhibited tumor necrosis factor (TNF) production for up to 84 days. RA disease severity apparently improved significantly. The results of this investigation seem to confirm the crucial role played by the neuroendocrine immune system network in RA (Nat Rev Rheumatol. 2011;7[9]:500-2).
However, the question now is: Are there issues and limitations about this possible new approach to RA treatment based on previous experiences? An obvious issue is the limited number of adverse events reported by the authors.
In contrast, adverse events have been signaled in all previous studies for VNS use as expected: cardiac arrhythmia during implantation, intermittent decrease in respiratory flow during sleep, posttreatment increase of apnea hypopnea index, and the development of posttreatment mild obstructive sleep apnea in up to one-third of patients, a minority of whom develop severe obstructive sleep apnea clearly related to VNS therapy. Another study has shown alteration of voice in 66%, coughing in 45%, pharyngitis in 35%, and throat pain in 28% (Pediatr Neurol. 2008;38[2]:99-103). Other reports of VNS device adverse events range from hoarseness (very common) to frank laryngeal muscle spasm and upper airway obstruction (rare). Other nonspecific symptoms include headache, nausea, vomiting, dyspepsia, dyspnea, and paresthesia.
At present, the approach of VNS therapy in RA needs further strict investigations, especially regarding the large number of potential adverse events expected. In addition, the target of reducing TNF levels in RA patients is already obtainable with several other noninvasive and established treatments.
Maurizio Cutolo, MD, is professor of rheumatology and internal medicine and director of the research laboratories and academic division of clinical rheumatology in the department of internal medicine at the University of Genova (Italy). He has no relevant disclosures.
The many different functions and brain regions associated with the vagus nerve have led researchers to test its usefulness in treating several illnesses, including epilepsy, treatment-resistant depression, anxiety disorders, Alzheimer’s disease, migraines, fibromyalgia, obesity, and tinnitus.
The Food and Drug Administration’s approval of a vagus nerve stimulator (VNS) subsequent to a 1997 neurological devices panel meeting has remained controversial. In the only randomized, controlled trial of severe depression, VNS failed to perform any better when turned on than in otherwise similarly implanted patients whose device was not turned on, according to the agency’s summary of the data.

|
| Dr. Maurizio Cutolo |
However, the discovery in 2007 by Kevin J. Tracey that vagus nerve stimulation inhibits inflammation by suppressing pro-inflammatory cytokine production (inflammatory reflex) has led to significant interest in the potential to use this approach for treating inflammatory diseases ranging from arthritis to colitis, ischemia, myocardial infarction, and heart failure (J Clin Invest. 2007;117[2]:289-96).
At present, the study by Dr. Koopman and her colleagues showed that vagus nerve stimulation (up to four times daily) by the implantable VNS in rheumatoid arthritis (RA) patients significantly inhibited tumor necrosis factor (TNF) production for up to 84 days. RA disease severity apparently improved significantly. The results of this investigation seem to confirm the crucial role played by the neuroendocrine immune system network in RA (Nat Rev Rheumatol. 2011;7[9]:500-2).
However, the question now is: Are there issues and limitations about this possible new approach to RA treatment based on previous experiences? An obvious issue is the limited number of adverse events reported by the authors.
In contrast, adverse events have been signaled in all previous studies for VNS use as expected: cardiac arrhythmia during implantation, intermittent decrease in respiratory flow during sleep, posttreatment increase of apnea hypopnea index, and the development of posttreatment mild obstructive sleep apnea in up to one-third of patients, a minority of whom develop severe obstructive sleep apnea clearly related to VNS therapy. Another study has shown alteration of voice in 66%, coughing in 45%, pharyngitis in 35%, and throat pain in 28% (Pediatr Neurol. 2008;38[2]:99-103). Other reports of VNS device adverse events range from hoarseness (very common) to frank laryngeal muscle spasm and upper airway obstruction (rare). Other nonspecific symptoms include headache, nausea, vomiting, dyspepsia, dyspnea, and paresthesia.
At present, the approach of VNS therapy in RA needs further strict investigations, especially regarding the large number of potential adverse events expected. In addition, the target of reducing TNF levels in RA patients is already obtainable with several other noninvasive and established treatments.
Maurizio Cutolo, MD, is professor of rheumatology and internal medicine and director of the research laboratories and academic division of clinical rheumatology in the department of internal medicine at the University of Genova (Italy). He has no relevant disclosures.
An implanted vagus nerve stimulator like that used for epilepsy treatment reduced inflammatory markers and significantly improved symptoms and function in a small cohort of patients with rheumatoid arthritis.
After 42 days, almost 30% of patients had achieved disease remission, Frieda A. Koopman, MD, and her colleagues reported in the July issue of the Proceedings of the National Academy of Science (doi: 10.1073/pnas.1605635113). The improvements disappeared rapidly when the devices were turned off, but were quickly reestablished after stimulation resumed.
“This first-in-class study supports a conceptual framework for further studies of electronic medical devices in diseases currently treated with drugs, an approach termed ‘bioelectronic medicine,’” wrote Dr. Koopman of the University of Amsterdam, and her coauthors.
The team built on evidence of what they termed a “reflex neural circuit” in the vagus that strongly influences the production of inflammatory cytokines. Animal studies showed that electrical stimulation of the vagus nerve encouraged choline acetyltransferase–positive T cells to secrete acetylcholine in the spleen and other tissues. Acetylcholine binds to a class of nicotinic receptors on monocytes, macrophages, and stromal cells, and inhibits their inflammatory response.
“Inflammatory reflex signaling, which is enhanced by electrically stimulating the vagus nerve, significantly reduces cytokine production and attenuates disease severity in experimental models of endotoxemia, sepsis, colitis, and other preclinical animal models of inflammatory syndromes,” the team noted.
The group reported on two human studies, totaling 25 patients. The first comprised seven patients with epilepsy who received the implanted vagus nerve stimulator for medically refractory seizures. None of these patients had a history of RA or any other inflammatory disease. The second group was all patients with active RA.
Each epilepsy patient contributed peripheral blood for study, which was collected before, during and after the implantation surgery. The team studied inflammatory markers by adding endotoxin to the samples. Those collected after the patient had been exposed to a single 30-second stimulation at 20 Hertz showed significantly inhibited production of TNF-alpha, compared with that seen in unexposed blood. Interleukin (IL)-6 and IL-1beta was also inhibited significantly by vagus nerve stimulation.
The next study involved 17 patients who had active RA, but not epilepsy. Of these, seven had failed methotrexate but were naïve to biologics; the rest had failed methotrexate and at least two biologics from different classes. Their average disease duration was 11 years.
The 86-day study gradually titrated the stimulation dose, but even at its highest, stimulation was far less than what is typically employed in epilepsy, “in which current is delivered at 60-second intervals, followed by an off interval of 5-180 minutes, repeated continuously,” the investigators wrote. “Thus, epilepsy patients may receive electrical current delivery for up to 240 minutes daily. Preclinical studies have established that stimulation of the inflammatory reflex for as little as 60 seconds confers significant inhibition of cytokine production for up to 24 hours.”
There was a 14-day post-implantation washout period with no stimulation, followed by 28 days of treatment titration. During that time, stimulation was ramped up from single 60-second stimulation with electric pulses of 250-microseconds duration at 10 Hertz and an output current between 0.25-2.0 milliamps, to the highest amperage tolerated (up to 2.0 milliamps).
That dose was the treatment target, and delivered once daily for 60 seconds in 250-microsecond pulse widths at 10 Hertz. At day 28, patients who had not had good clinical response according to EULAR response criteria, had their stimulation increased to four times daily.
In the group of seven methotrexate-resistant patients, two received electric current pulses four times daily. In the group of 10 methotrexate- and biologic-resistant patients, 6 received the four-dose stimulation.
On day 42, TNF-alpha levels in cultured peripheral blood were significantly reduced from baseline.
At that time, the vagus nerve stimulator was turned off for 14 days. By the end of the silent period, TNF-alpha levels had risen significantly from the day 42 levels. The stimulator was restarted on day 56. By day 84, after 28 more days of stimulation, TNF-alpha levels had again decreased significantly.
Symptoms and function as measured by the Disease Activity Score 28 followed a similar trajectory, improving during the initial treatment, worsening during the period of no stimulation, and improving again when stimulation was restarted. Symptom and function scores correlated positively with change in TNF levels.
The investigators also assessed the response rates according to American College of Rheumatology criteria. At day 42, 71% of those in the methotrexate-resistant group had achieved a 20% response; 57% a 50% response; and 28.6% a 70% response. Response was not as dramatic in the group resistant to both drug classes: rates were 70%, 30%, and 0%.
By day 42, nearly 30% of patients overall achieved remission, which was defined as a DAS28 score of less than 2.6. This constituted improvement in all the score components, including tender joint count, swollen joint count, patient’s assessment of pain, patient’s global assessment, physician’s global assessment, and C-reactive protein.
Finally, the investigators noted decreased levels of most serum cytokines. Most, including serum TNF, IL-10, IL-12p70, IL-13, IL-1alpha, IL-1beta, IL-2, IL-4, IL-5, and TNF-a-beta, were below 1 pg/ml.
Adverse events were common (16 patients) but reported as mild-moderate. The included hoarseness (5), hypoesthesia (4), parasthesia (2), dyspnea (2), and bradycardia (1), among others. There were no implantation-related infections. One patient reported postimplantation pain.
SetPoint Medical, of Valencia, Calif., makes the device and conducted the study. Dr. Koopman made no financial disclosures. However, several of the other authors are employees of Set Point, and of GlaxoSmithKline, which holds equity interest in the company.
On Twitter @Alz_Gal
An implanted vagus nerve stimulator like that used for epilepsy treatment reduced inflammatory markers and significantly improved symptoms and function in a small cohort of patients with rheumatoid arthritis.
After 42 days, almost 30% of patients had achieved disease remission, Frieda A. Koopman, MD, and her colleagues reported in the July issue of the Proceedings of the National Academy of Science (doi: 10.1073/pnas.1605635113). The improvements disappeared rapidly when the devices were turned off, but were quickly reestablished after stimulation resumed.
“This first-in-class study supports a conceptual framework for further studies of electronic medical devices in diseases currently treated with drugs, an approach termed ‘bioelectronic medicine,’” wrote Dr. Koopman of the University of Amsterdam, and her coauthors.
The team built on evidence of what they termed a “reflex neural circuit” in the vagus that strongly influences the production of inflammatory cytokines. Animal studies showed that electrical stimulation of the vagus nerve encouraged choline acetyltransferase–positive T cells to secrete acetylcholine in the spleen and other tissues. Acetylcholine binds to a class of nicotinic receptors on monocytes, macrophages, and stromal cells, and inhibits their inflammatory response.
“Inflammatory reflex signaling, which is enhanced by electrically stimulating the vagus nerve, significantly reduces cytokine production and attenuates disease severity in experimental models of endotoxemia, sepsis, colitis, and other preclinical animal models of inflammatory syndromes,” the team noted.
The group reported on two human studies, totaling 25 patients. The first comprised seven patients with epilepsy who received the implanted vagus nerve stimulator for medically refractory seizures. None of these patients had a history of RA or any other inflammatory disease. The second group was all patients with active RA.
Each epilepsy patient contributed peripheral blood for study, which was collected before, during and after the implantation surgery. The team studied inflammatory markers by adding endotoxin to the samples. Those collected after the patient had been exposed to a single 30-second stimulation at 20 Hertz showed significantly inhibited production of TNF-alpha, compared with that seen in unexposed blood. Interleukin (IL)-6 and IL-1beta was also inhibited significantly by vagus nerve stimulation.
The next study involved 17 patients who had active RA, but not epilepsy. Of these, seven had failed methotrexate but were naïve to biologics; the rest had failed methotrexate and at least two biologics from different classes. Their average disease duration was 11 years.
The 86-day study gradually titrated the stimulation dose, but even at its highest, stimulation was far less than what is typically employed in epilepsy, “in which current is delivered at 60-second intervals, followed by an off interval of 5-180 minutes, repeated continuously,” the investigators wrote. “Thus, epilepsy patients may receive electrical current delivery for up to 240 minutes daily. Preclinical studies have established that stimulation of the inflammatory reflex for as little as 60 seconds confers significant inhibition of cytokine production for up to 24 hours.”
There was a 14-day post-implantation washout period with no stimulation, followed by 28 days of treatment titration. During that time, stimulation was ramped up from single 60-second stimulation with electric pulses of 250-microseconds duration at 10 Hertz and an output current between 0.25-2.0 milliamps, to the highest amperage tolerated (up to 2.0 milliamps).
That dose was the treatment target, and delivered once daily for 60 seconds in 250-microsecond pulse widths at 10 Hertz. At day 28, patients who had not had good clinical response according to EULAR response criteria, had their stimulation increased to four times daily.
In the group of seven methotrexate-resistant patients, two received electric current pulses four times daily. In the group of 10 methotrexate- and biologic-resistant patients, 6 received the four-dose stimulation.
On day 42, TNF-alpha levels in cultured peripheral blood were significantly reduced from baseline.
At that time, the vagus nerve stimulator was turned off for 14 days. By the end of the silent period, TNF-alpha levels had risen significantly from the day 42 levels. The stimulator was restarted on day 56. By day 84, after 28 more days of stimulation, TNF-alpha levels had again decreased significantly.
Symptoms and function as measured by the Disease Activity Score 28 followed a similar trajectory, improving during the initial treatment, worsening during the period of no stimulation, and improving again when stimulation was restarted. Symptom and function scores correlated positively with change in TNF levels.
The investigators also assessed the response rates according to American College of Rheumatology criteria. At day 42, 71% of those in the methotrexate-resistant group had achieved a 20% response; 57% a 50% response; and 28.6% a 70% response. Response was not as dramatic in the group resistant to both drug classes: rates were 70%, 30%, and 0%.
By day 42, nearly 30% of patients overall achieved remission, which was defined as a DAS28 score of less than 2.6. This constituted improvement in all the score components, including tender joint count, swollen joint count, patient’s assessment of pain, patient’s global assessment, physician’s global assessment, and C-reactive protein.
Finally, the investigators noted decreased levels of most serum cytokines. Most, including serum TNF, IL-10, IL-12p70, IL-13, IL-1alpha, IL-1beta, IL-2, IL-4, IL-5, and TNF-a-beta, were below 1 pg/ml.
Adverse events were common (16 patients) but reported as mild-moderate. The included hoarseness (5), hypoesthesia (4), parasthesia (2), dyspnea (2), and bradycardia (1), among others. There were no implantation-related infections. One patient reported postimplantation pain.
SetPoint Medical, of Valencia, Calif., makes the device and conducted the study. Dr. Koopman made no financial disclosures. However, several of the other authors are employees of Set Point, and of GlaxoSmithKline, which holds equity interest in the company.
On Twitter @Alz_Gal
FROM PNAS
Key clinical point: A vagus nerve stimulator reduced inflammatory markers and improved symptoms in patients with medication-refractory RA.
Major finding: About 30% of patients experienced clinical disease remission by day 42.
Data source: The open-label, prospective study comprised 17 patients with RA.
Disclosures: SetPoint Medical, of Valencia, Calif., makes the device and conducted the study. Dr. Koopman made no financial disclosures. However, several of the other authors are employees of SetPoint, and of GlaxoSmithKline, which holds equity interest in the company.
Safety of sentinel node dissection alone holds up a decade out
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
CHICAGO – Women with clinical early-stage breast cancer and a positive sentinel lymph node who receive breast-conserving therapy can safely skip an axillary lymph node dissection (ALND), and therefore avoid its associated morbidity, confirms long-term follow-up of the Z0011 trial conducted by the American College of Surgeons Oncology Group and the Alliance for Clinical Trials in Oncology.
The phase III trial enrolled 891 women with clinical T1-2,N0,M0 disease who underwent lumpectomy and were found to have sentinel node involvement. They were randomized to ALND or no further surgery, followed by whole-breast radiation therapy and, in most cases, systemic adjuvant therapy.
The trial was closed early because of low rates of accrual and events. Results at 6.3 years of follow-up showed that compared with peers who had an ALND, the women who skipped this surgery did not have inferior 5-year rates of locoregional recurrence or overall survival (JAMA. 2011;305:569-75).
“The study, however, like most breast cancer studies, contained mostly postmenopausal women with hormone receptor–positive tumors who are known to have late recurrences, and it was criticized for short follow-up,” commented first author Armando E. Giuliano, MD, executive vice chair of surgical oncology in the department of surgery, and associate director of surgical oncology in the Samuel Oschin Comprehensive Cancer Institute, Los Angeles.
In an update of the findings, now with a median follow-up of 9.3 years, the groups were statistically indistinguishable with respect to 10-year rates of the same outcomes, he reported at the annual meeting of the American Society of Clinical Oncology.
“This study... shows that sentinel node biopsy alone provides excellent 10-year locoregional control and survival comparable to completion axillary lymph node dissection for these patients, even with long-term follow-up,” he maintained. “Routine use of axillary lymph node dissection should be abandoned.”
“This was designed as a noninferiority trial, and I would suggest that based on the data we have seen, even if they had hit their target accrual, the outcomes would not be different,” said invited discussant Elizabeth A. Mittendorf, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston. “Clearly, even before today’s presentation, Z0011 has been identified as a practice-changing trial, as evidenced by the NCCN guidelines.”
In fact, a study last year showed that among patients in the general U.S. population meeting the trial’s enrollment criteria, the use of sentinel lymph node dissection alone has increased significantly since the Z0011 results were first reported (J Am Coll Surg. 2015;221:71-81).
“However, I would highlight that we have also seen an increase in omission of axillary lymph node dissection for patients who do not meet the Z0011 criteria to include those not planned for radiotherapy, those receiving APBI [accelerated partial breast irradiation], and those undergoing mastectomy,” she added. “I highlight these examples specifically because it’s been suggested that one of the reasons the patients on the trial have outstanding regional control is because of the radiation administered as part of their breast-conserving therapy.”
“We will obtain additional data on the locoregional management of these early-stage patients with clinically node-negative breast cancer,” Dr. Mittendorf predicted, pointing to the similar POSNOC trial (which is comparing systemic therapy with versus without axillary treatment) and SOUND trial (which is comparing sentinel node dissection versus no axillary surgery).
In Z0011, all women had tumor in sentinel nodes detected with hematoxylin and eosin staining. Those with sentinel node tumor detected only by immunohistochemistry were excluded, as were those who had matted nodes, three or more involved sentinel nodes, or planned third-field (nodal) irradiation.
Overall, 27.4% of the patients in the ALND group had additional positive nodes removed beyond their sentinel nodes. “There is no reason to suspect that women with sentinel node biopsy [only] had fewer involved nodes than the women treated with axillary lymph node dissection,” Dr. Giuliano commented; thus, a similar share of the former group likely had residual axillary disease that went unresected.
The updated findings showed that the women received ALND and the women who did not were statistically indistinguishable with respect to the 10-year rate of locoregional recurrence (6.2% and 5.3%). Of note, only a single regional recurrence was seen after the initial 5 years of follow-up, and it occurred in the group that did not have ALND.
The groups treated with and without ALND were also statistically indistinguishable with respect to 10-year rates of disease-free survival (78.2% and 80.2%), locoregional recurrence–free survival (81.2% and 83.0%), and overall survival (83.6% and 86.3%).
In multivariate analysis, omission of ALND did not significantly predict locoregional recurrence or overall survival, reported Dr. Giuliano. Additionally, stratified analysis showed that the lack of difference in overall survival between study groups was the same whether tumors had hormone receptors or not.
In a related analysis of radiation protocol deviations in a subset of women from the trial, 11% did not receive any radiation therapy, while 18.9% received third-field radiation, with equal distribution of the latter between study groups (J Clin Oncol. 2014;32:3600-6). Omission of radiation was associated with an increased risk of local recurrence and death, but it did not affect nodal recurrences. Receipt of third-field radiation did not influence survival.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: In women with clinical early-stage breast cancer who have a positive sentinel node and undergo breast-conserving therapy, skipping ALND does not compromise outcomes.
Major finding: Women treated with and without ALND were statistically indistinguishable with respect to 10-year rates of locoregional recurrence (6.2% and 5.3%), disease-free survival (78.2% and 80.2%), and overall survival (83.6% and 86.3%).
Data source: A randomized phase III trial among 891 women with clinical T1-2,N0,M0 breast cancer and positive sentinel nodes treated with breast-conserving therapy and usually adjuvant systemic therapy (ACOSOG Z0011).
Disclosures: Dr. Giuliano disclosed that he had no relevant conflicts of interest.
Drug’s benefits outweigh risks, PRAC says

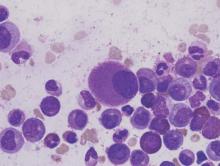
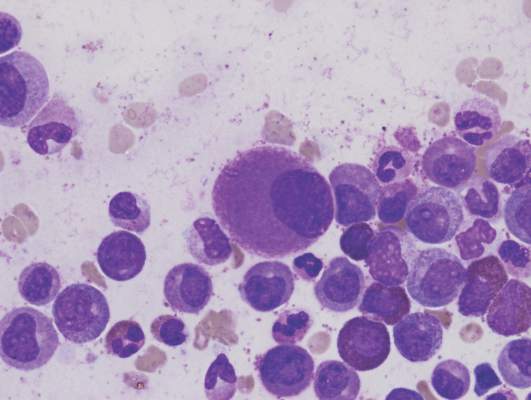
Photo courtesy of
Gilead Sciences, Inc.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) has completed its review of the PI3Kδ inhibitor idelalisib (Zyedelig) and concluded that the drug’s benefits outweigh its risks in the treatment of chronic lymphocytic leukemia (CLL) and follicular lymphoma.
However, the PRAC also confirmed that the drug increases the risk of serious infections, including Pneumocystis jirovecii pneumonia.
And the committee updated its previous recommendations to manage this risk.
The PRAC’s recommendations will now be sent to the Committee for Medicinal Products for Human Use, which will adopt the EMA’s final opinion. The final stage of the review procedure is the adoption by the European Commission of a legally binding decision applicable in all member states of the European Union (EU).
About idelalisib
In the EU, idelalisib is approved for use in combination with rituximab to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment in the presence of 17p deletion or TP53 mutation in CLL patients unsuitable for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment.
About the review
The PRAC’s review of idelalisib began after a higher rate of serious adverse events, including deaths, was seen in 3 clinical trials evaluating the addition of idelalisib to standard therapy in first-line CLL and relapsed indolent non-Hodgkin lymphoma (NHL).
Most of the deaths were related to infections such as Pneumocystis jirovecii pneumonia and cytomegalovirus infection. Other excess deaths were related mainly to respiratory events.
The NHL studies (NCT01732926 and NCT01732913) included patients with disease characteristics different from those covered by the currently approved indications for idelalisib and investigated combinations of drugs that are not currently approved in the EU—idelalisib plus rituximab for NHL and idelalisib plus bendamustine and rituximab for NHL.
The CLL trial (NCT01980888) involved patients who had not received previous treatment, some of whom had the 17p deletion or TP53 mutation. However, the trial also investigated a combination of drugs not currently approved in the EU—idelalisib plus bendamustine and rituximab.
PRAC’s recommendations
The PRAC noted that, although the aforementioned trials did not all use idelalisib as currently authorized, the risk of serious infection is considered relevant to the authorized use.
Therefore, the PRAC recommends that all patients treated with idelalisib receive antibiotics to prevent Pneumocystis jirovecii pneumonia during treatment and for up to 2 to 6 months after treatment has stopped.
Patients should also be monitored for infection and have regular blood tests for white cell counts because low counts can increase their risk of infection.
Furthermore, idelalisib should not be started in patients with a generalized infection.
At the beginning of its review, the PRAC had said idelalisib should not be started in patients with previously untreated CLL and 17p deletion or TP53 mutation.
Now, the PRAC has concluded that idelalisib can be initiated in these patients, provided they cannot take any alternative treatment and that the recommended measures to prevent infection are followed. ![]()

Photo courtesy of
Gilead Sciences, Inc.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) has completed its review of the PI3Kδ inhibitor idelalisib (Zyedelig) and concluded that the drug’s benefits outweigh its risks in the treatment of chronic lymphocytic leukemia (CLL) and follicular lymphoma.
However, the PRAC also confirmed that the drug increases the risk of serious infections, including Pneumocystis jirovecii pneumonia.
And the committee updated its previous recommendations to manage this risk.
The PRAC’s recommendations will now be sent to the Committee for Medicinal Products for Human Use, which will adopt the EMA’s final opinion. The final stage of the review procedure is the adoption by the European Commission of a legally binding decision applicable in all member states of the European Union (EU).
About idelalisib
In the EU, idelalisib is approved for use in combination with rituximab to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment in the presence of 17p deletion or TP53 mutation in CLL patients unsuitable for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment.
About the review
The PRAC’s review of idelalisib began after a higher rate of serious adverse events, including deaths, was seen in 3 clinical trials evaluating the addition of idelalisib to standard therapy in first-line CLL and relapsed indolent non-Hodgkin lymphoma (NHL).
Most of the deaths were related to infections such as Pneumocystis jirovecii pneumonia and cytomegalovirus infection. Other excess deaths were related mainly to respiratory events.
The NHL studies (NCT01732926 and NCT01732913) included patients with disease characteristics different from those covered by the currently approved indications for idelalisib and investigated combinations of drugs that are not currently approved in the EU—idelalisib plus rituximab for NHL and idelalisib plus bendamustine and rituximab for NHL.
The CLL trial (NCT01980888) involved patients who had not received previous treatment, some of whom had the 17p deletion or TP53 mutation. However, the trial also investigated a combination of drugs not currently approved in the EU—idelalisib plus bendamustine and rituximab.
PRAC’s recommendations
The PRAC noted that, although the aforementioned trials did not all use idelalisib as currently authorized, the risk of serious infection is considered relevant to the authorized use.
Therefore, the PRAC recommends that all patients treated with idelalisib receive antibiotics to prevent Pneumocystis jirovecii pneumonia during treatment and for up to 2 to 6 months after treatment has stopped.
Patients should also be monitored for infection and have regular blood tests for white cell counts because low counts can increase their risk of infection.
Furthermore, idelalisib should not be started in patients with a generalized infection.
At the beginning of its review, the PRAC had said idelalisib should not be started in patients with previously untreated CLL and 17p deletion or TP53 mutation.
Now, the PRAC has concluded that idelalisib can be initiated in these patients, provided they cannot take any alternative treatment and that the recommended measures to prevent infection are followed. ![]()

Photo courtesy of
Gilead Sciences, Inc.
The European Medicines Agency’s Pharmacovigilance Risk Assessment Committee (PRAC) has completed its review of the PI3Kδ inhibitor idelalisib (Zyedelig) and concluded that the drug’s benefits outweigh its risks in the treatment of chronic lymphocytic leukemia (CLL) and follicular lymphoma.
However, the PRAC also confirmed that the drug increases the risk of serious infections, including Pneumocystis jirovecii pneumonia.
And the committee updated its previous recommendations to manage this risk.
The PRAC’s recommendations will now be sent to the Committee for Medicinal Products for Human Use, which will adopt the EMA’s final opinion. The final stage of the review procedure is the adoption by the European Commission of a legally binding decision applicable in all member states of the European Union (EU).
About idelalisib
In the EU, idelalisib is approved for use in combination with rituximab to treat adults with CLL who have received at least 1 prior therapy or as first-line treatment in the presence of 17p deletion or TP53 mutation in CLL patients unsuitable for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for adults with follicular lymphoma that is refractory to 2 prior lines of treatment.
About the review
The PRAC’s review of idelalisib began after a higher rate of serious adverse events, including deaths, was seen in 3 clinical trials evaluating the addition of idelalisib to standard therapy in first-line CLL and relapsed indolent non-Hodgkin lymphoma (NHL).
Most of the deaths were related to infections such as Pneumocystis jirovecii pneumonia and cytomegalovirus infection. Other excess deaths were related mainly to respiratory events.
The NHL studies (NCT01732926 and NCT01732913) included patients with disease characteristics different from those covered by the currently approved indications for idelalisib and investigated combinations of drugs that are not currently approved in the EU—idelalisib plus rituximab for NHL and idelalisib plus bendamustine and rituximab for NHL.
The CLL trial (NCT01980888) involved patients who had not received previous treatment, some of whom had the 17p deletion or TP53 mutation. However, the trial also investigated a combination of drugs not currently approved in the EU—idelalisib plus bendamustine and rituximab.
PRAC’s recommendations
The PRAC noted that, although the aforementioned trials did not all use idelalisib as currently authorized, the risk of serious infection is considered relevant to the authorized use.
Therefore, the PRAC recommends that all patients treated with idelalisib receive antibiotics to prevent Pneumocystis jirovecii pneumonia during treatment and for up to 2 to 6 months after treatment has stopped.
Patients should also be monitored for infection and have regular blood tests for white cell counts because low counts can increase their risk of infection.
Furthermore, idelalisib should not be started in patients with a generalized infection.
At the beginning of its review, the PRAC had said idelalisib should not be started in patients with previously untreated CLL and 17p deletion or TP53 mutation.
Now, the PRAC has concluded that idelalisib can be initiated in these patients, provided they cannot take any alternative treatment and that the recommended measures to prevent infection are followed. ![]()
Bioabsorbable percutaneous device fully closes large femoral arteriotomies
PARIS – A new bioabsorbable sutureless device provides operators with a safe, simple, and dependable option for fully percutaneous closure of the large, 12-24 French femoral arteriotomies created for transcatheter aortic valve replacement or endovascular abdominal aortic aneurysm repair, Arne Schwindt, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He presented the 12-month follow-up results of the FRONTIER II study of the Vivasure PerQseal device. The device recently received European marketing approval on the strength of FRONTIER II but remains investigational in the United States.
The PerQseal device is deployed in less than 1 minute at the end of the primary procedure and achieves immediate hemostasis. It’s a simple three-step deployment process with essentially no learning curve, as evidenced by the fact that in FRONTIER II, the technical success rate starting from no experience was 97%, explained Dr. Schwindt of St. Franziskus Hospital in Muenster, Germany.
The large femoral arteriotomies created for TAVR or endovascular abdominal aortic aneurysm repair have typically required surgical cut down and sutured repair with a 3- to 5-cm incision. Vascular complications have been common. Indeed, the literature shows this method entails on average a 14.7% rate of major vascular complications up to 3 months post procedure, so that was the bar set in FRONTIER II: In order for the PerQseal to be deemed noninferior to surgical cut down and sutured repair, the rate of major complications directly related to the novel device at 3 months follow-up could be no greater than 14.7%. The current Valve Academic Research Consortium (VARC) 2 definition of major complications was used.
In fact, the vascular complication rate proved to be zero. Moreover, at 12 months of follow-up, no cases of groin fibrosis or scarring had been observed, Dr. Schwindt reported.
FRONTIER II was a single-arm, prospective, multicenter European study of 58 patients who received the PerQseal device for 66 closures. They were evaluated at discharge and 1, 3, and 12 months post procedure by Doppler ultrasound, with uniformly unremarkable findings.
PerQseal features a synthetic low-profile implant with over-the-wire delivery. The implant is loaded into a sheath, released by pulling back on the sheath, then pulled up against the arteriotomy from the inside. Blood pressure molds the device to the arterial wall and seals it. The device is fully absorbed in 180 days.
Session co-chair Dr. Ted E. Feldman was favorably impressed.
“This is really terrific. It’s very nice to see we’re finally making progress with large-bore closure devices,” commented Dr. Feldman, professor of medicine at Northwestern University, Chicago.
Dr. Schwindt reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study. In addition, he serves as a consultant to a half dozen medical device companies.
PARIS – A new bioabsorbable sutureless device provides operators with a safe, simple, and dependable option for fully percutaneous closure of the large, 12-24 French femoral arteriotomies created for transcatheter aortic valve replacement or endovascular abdominal aortic aneurysm repair, Arne Schwindt, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He presented the 12-month follow-up results of the FRONTIER II study of the Vivasure PerQseal device. The device recently received European marketing approval on the strength of FRONTIER II but remains investigational in the United States.
The PerQseal device is deployed in less than 1 minute at the end of the primary procedure and achieves immediate hemostasis. It’s a simple three-step deployment process with essentially no learning curve, as evidenced by the fact that in FRONTIER II, the technical success rate starting from no experience was 97%, explained Dr. Schwindt of St. Franziskus Hospital in Muenster, Germany.
The large femoral arteriotomies created for TAVR or endovascular abdominal aortic aneurysm repair have typically required surgical cut down and sutured repair with a 3- to 5-cm incision. Vascular complications have been common. Indeed, the literature shows this method entails on average a 14.7% rate of major vascular complications up to 3 months post procedure, so that was the bar set in FRONTIER II: In order for the PerQseal to be deemed noninferior to surgical cut down and sutured repair, the rate of major complications directly related to the novel device at 3 months follow-up could be no greater than 14.7%. The current Valve Academic Research Consortium (VARC) 2 definition of major complications was used.
In fact, the vascular complication rate proved to be zero. Moreover, at 12 months of follow-up, no cases of groin fibrosis or scarring had been observed, Dr. Schwindt reported.
FRONTIER II was a single-arm, prospective, multicenter European study of 58 patients who received the PerQseal device for 66 closures. They were evaluated at discharge and 1, 3, and 12 months post procedure by Doppler ultrasound, with uniformly unremarkable findings.
PerQseal features a synthetic low-profile implant with over-the-wire delivery. The implant is loaded into a sheath, released by pulling back on the sheath, then pulled up against the arteriotomy from the inside. Blood pressure molds the device to the arterial wall and seals it. The device is fully absorbed in 180 days.
Session co-chair Dr. Ted E. Feldman was favorably impressed.
“This is really terrific. It’s very nice to see we’re finally making progress with large-bore closure devices,” commented Dr. Feldman, professor of medicine at Northwestern University, Chicago.
Dr. Schwindt reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study. In addition, he serves as a consultant to a half dozen medical device companies.
PARIS – A new bioabsorbable sutureless device provides operators with a safe, simple, and dependable option for fully percutaneous closure of the large, 12-24 French femoral arteriotomies created for transcatheter aortic valve replacement or endovascular abdominal aortic aneurysm repair, Arne Schwindt, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
He presented the 12-month follow-up results of the FRONTIER II study of the Vivasure PerQseal device. The device recently received European marketing approval on the strength of FRONTIER II but remains investigational in the United States.
The PerQseal device is deployed in less than 1 minute at the end of the primary procedure and achieves immediate hemostasis. It’s a simple three-step deployment process with essentially no learning curve, as evidenced by the fact that in FRONTIER II, the technical success rate starting from no experience was 97%, explained Dr. Schwindt of St. Franziskus Hospital in Muenster, Germany.
The large femoral arteriotomies created for TAVR or endovascular abdominal aortic aneurysm repair have typically required surgical cut down and sutured repair with a 3- to 5-cm incision. Vascular complications have been common. Indeed, the literature shows this method entails on average a 14.7% rate of major vascular complications up to 3 months post procedure, so that was the bar set in FRONTIER II: In order for the PerQseal to be deemed noninferior to surgical cut down and sutured repair, the rate of major complications directly related to the novel device at 3 months follow-up could be no greater than 14.7%. The current Valve Academic Research Consortium (VARC) 2 definition of major complications was used.
In fact, the vascular complication rate proved to be zero. Moreover, at 12 months of follow-up, no cases of groin fibrosis or scarring had been observed, Dr. Schwindt reported.
FRONTIER II was a single-arm, prospective, multicenter European study of 58 patients who received the PerQseal device for 66 closures. They were evaluated at discharge and 1, 3, and 12 months post procedure by Doppler ultrasound, with uniformly unremarkable findings.
PerQseal features a synthetic low-profile implant with over-the-wire delivery. The implant is loaded into a sheath, released by pulling back on the sheath, then pulled up against the arteriotomy from the inside. Blood pressure molds the device to the arterial wall and seals it. The device is fully absorbed in 180 days.
Session co-chair Dr. Ted E. Feldman was favorably impressed.
“This is really terrific. It’s very nice to see we’re finally making progress with large-bore closure devices,” commented Dr. Feldman, professor of medicine at Northwestern University, Chicago.
Dr. Schwindt reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study. In addition, he serves as a consultant to a half dozen medical device companies.
AT EUROPCR 2016
Key clinical point: The PerQseal device provides a simpler alternative to existing closure methods.
Major finding: No major vascular complications were seen during structured follow-up of recipients of the novel bioabsorbable fully percutaneous PerQseal device for closure of large-bore femoral arteriotomies.
Data source: FRONTIER II was a prospective, single-arm, 12-month multicenter study including 58 patients who underwent closure of 66 large femoral arteriotomies using the PerQseal device.
Disclosures: The presenter reported receiving a research grant from Vivasure, which sponsored the FRONTIER II study.
Long-term analysis shows dwindling RT benefit for DLBCL
Long-term follow-up from two randomized trials shows that the treatment advantage initially seen by adding radiotherapy to the CHOP regimen in patients with limited-stage diffuse large B-cell lymphoma disappeared over time.
After a median follow-up of nearly 18 years, there were no significant differences in either progression-free survival (PFS) or overall survival between patients who had received standard CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone) for 8 cycles (CHOP8), or 3 cycles of CHOP with involved-field radiotherapy (CHOP3RT), reported Deborah M. Stephens, DO, of the University of Utah in Salt Lake City, and her colleagues.
The addition of rituximab to CHOP plus involved-field radiotherapy (IFRT) in a separate cohort did not appear to reduce the continued relapse risk, the investigators noted (J Clin Oncol. 2016 Jul. doi: 10.1200/JCO.2015.65.4582).
The findings suggest that long-term follow-up of patients enrolled in clinical trials may provide clinically important additional information, and that limited-stage diffuse large B-cell lymphoma (DLBCL) may have a biology that is distinctly different from that of advanced stage DLBCL, the investigators wrote.
Initial results from the SWOG (Southwest Oncology Group) Study 8736, published after a median follow-up of 4.4 years, showed that CHOP3RT was associated with significantly better 5-year PFS and OS rates, compared with patients treated with CHOP8.
A second trial, SWOG Study 0014, looked at the addition of rituximab (Rituxan) to CHOP plus IFRT in patients with high-risk DLBCL with at least one adverse feature of the stage-modified International Prognostic Index. In this trial, after a median follow-up of 5.3 years, 4-year PFS was 88%, and 4-year OS was 92%.
5 years not enough
Results of both trials were published around the 5-year follow-up mark. However, an analysis of 10-year follow-up data from the S8736 trial, published only as an abstract (Blood. 98:724a-725a, 2001; abstr 3024), showed that “the survival curves for CHOP8 and CHOP3RT, surprisingly, began to overlap,” Dr. Stephens and her colleagues wrote.
“Additionally, for both S8736 and S0014, no plateau had been reached in the PFS curves. These data contrasted the expected cure rates for advanced-stage DLBCL, leading to the hypothesis that limited-stage DLBCL may have a unique biology from its advanced-stage counterpart,” they added.
Although more than half of patients with advanced-stage diffuse large B-cell lymphoma (DLBCL) can be cured with anthracycline-based chemotherapy, cure rates are markedly lower among patients with limited-stage disease, defined as Ann Arbor stage I or II, confined to a single irradiation field. Limited-stage disease accounts for approximately one-third DLBCL cases.
To see whether the trends observed at 10 years continued, the investigators conducted a survival analysis from S8736 and compared the data from similar patients in the S0014 study.
They found that after a median follow-up of 17.7 years in S8736, median PFS was 12.0 years for patients treated with CHOP8, and 11.1 years for patients treated with CHOP3RT, a difference that was not statistically significant.
Median OS was 13.0 and 13.7 years, respectively, and was also not significant.
In S0014, after a median follow-up of 12 years, the 5-year OS rate was 82%, and 10-year rate was 67%. In this trial, the investigators observed “a persistent pattern of relapse despite the addition of rituximab.”
“The populations were not entirely identical; however, even the addition of rituximab as per S0014 to combined-modality therapy did not seem to mitigate the continued relapse risk, underscoring the value of prolonged observation of clinical trial patients and possible unique biology of limited-stage DLBCL,” Dr. Stephens and her associates wrote.
The study was sponsored by grants from the National Institutes of Health. Dr. Stephens reported having no financial disclosures. Several coauthors disclosed research funding, consulting, speakers’ bureau participation or travel expenses from various oncology drug makers.
Long-term follow-up from two randomized trials shows that the treatment advantage initially seen by adding radiotherapy to the CHOP regimen in patients with limited-stage diffuse large B-cell lymphoma disappeared over time.
After a median follow-up of nearly 18 years, there were no significant differences in either progression-free survival (PFS) or overall survival between patients who had received standard CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone) for 8 cycles (CHOP8), or 3 cycles of CHOP with involved-field radiotherapy (CHOP3RT), reported Deborah M. Stephens, DO, of the University of Utah in Salt Lake City, and her colleagues.
The addition of rituximab to CHOP plus involved-field radiotherapy (IFRT) in a separate cohort did not appear to reduce the continued relapse risk, the investigators noted (J Clin Oncol. 2016 Jul. doi: 10.1200/JCO.2015.65.4582).
The findings suggest that long-term follow-up of patients enrolled in clinical trials may provide clinically important additional information, and that limited-stage diffuse large B-cell lymphoma (DLBCL) may have a biology that is distinctly different from that of advanced stage DLBCL, the investigators wrote.
Initial results from the SWOG (Southwest Oncology Group) Study 8736, published after a median follow-up of 4.4 years, showed that CHOP3RT was associated with significantly better 5-year PFS and OS rates, compared with patients treated with CHOP8.
A second trial, SWOG Study 0014, looked at the addition of rituximab (Rituxan) to CHOP plus IFRT in patients with high-risk DLBCL with at least one adverse feature of the stage-modified International Prognostic Index. In this trial, after a median follow-up of 5.3 years, 4-year PFS was 88%, and 4-year OS was 92%.
5 years not enough
Results of both trials were published around the 5-year follow-up mark. However, an analysis of 10-year follow-up data from the S8736 trial, published only as an abstract (Blood. 98:724a-725a, 2001; abstr 3024), showed that “the survival curves for CHOP8 and CHOP3RT, surprisingly, began to overlap,” Dr. Stephens and her colleagues wrote.
“Additionally, for both S8736 and S0014, no plateau had been reached in the PFS curves. These data contrasted the expected cure rates for advanced-stage DLBCL, leading to the hypothesis that limited-stage DLBCL may have a unique biology from its advanced-stage counterpart,” they added.
Although more than half of patients with advanced-stage diffuse large B-cell lymphoma (DLBCL) can be cured with anthracycline-based chemotherapy, cure rates are markedly lower among patients with limited-stage disease, defined as Ann Arbor stage I or II, confined to a single irradiation field. Limited-stage disease accounts for approximately one-third DLBCL cases.
To see whether the trends observed at 10 years continued, the investigators conducted a survival analysis from S8736 and compared the data from similar patients in the S0014 study.
They found that after a median follow-up of 17.7 years in S8736, median PFS was 12.0 years for patients treated with CHOP8, and 11.1 years for patients treated with CHOP3RT, a difference that was not statistically significant.
Median OS was 13.0 and 13.7 years, respectively, and was also not significant.
In S0014, after a median follow-up of 12 years, the 5-year OS rate was 82%, and 10-year rate was 67%. In this trial, the investigators observed “a persistent pattern of relapse despite the addition of rituximab.”
“The populations were not entirely identical; however, even the addition of rituximab as per S0014 to combined-modality therapy did not seem to mitigate the continued relapse risk, underscoring the value of prolonged observation of clinical trial patients and possible unique biology of limited-stage DLBCL,” Dr. Stephens and her associates wrote.
The study was sponsored by grants from the National Institutes of Health. Dr. Stephens reported having no financial disclosures. Several coauthors disclosed research funding, consulting, speakers’ bureau participation or travel expenses from various oncology drug makers.
Long-term follow-up from two randomized trials shows that the treatment advantage initially seen by adding radiotherapy to the CHOP regimen in patients with limited-stage diffuse large B-cell lymphoma disappeared over time.
After a median follow-up of nearly 18 years, there were no significant differences in either progression-free survival (PFS) or overall survival between patients who had received standard CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone) for 8 cycles (CHOP8), or 3 cycles of CHOP with involved-field radiotherapy (CHOP3RT), reported Deborah M. Stephens, DO, of the University of Utah in Salt Lake City, and her colleagues.
The addition of rituximab to CHOP plus involved-field radiotherapy (IFRT) in a separate cohort did not appear to reduce the continued relapse risk, the investigators noted (J Clin Oncol. 2016 Jul. doi: 10.1200/JCO.2015.65.4582).
The findings suggest that long-term follow-up of patients enrolled in clinical trials may provide clinically important additional information, and that limited-stage diffuse large B-cell lymphoma (DLBCL) may have a biology that is distinctly different from that of advanced stage DLBCL, the investigators wrote.
Initial results from the SWOG (Southwest Oncology Group) Study 8736, published after a median follow-up of 4.4 years, showed that CHOP3RT was associated with significantly better 5-year PFS and OS rates, compared with patients treated with CHOP8.
A second trial, SWOG Study 0014, looked at the addition of rituximab (Rituxan) to CHOP plus IFRT in patients with high-risk DLBCL with at least one adverse feature of the stage-modified International Prognostic Index. In this trial, after a median follow-up of 5.3 years, 4-year PFS was 88%, and 4-year OS was 92%.
5 years not enough
Results of both trials were published around the 5-year follow-up mark. However, an analysis of 10-year follow-up data from the S8736 trial, published only as an abstract (Blood. 98:724a-725a, 2001; abstr 3024), showed that “the survival curves for CHOP8 and CHOP3RT, surprisingly, began to overlap,” Dr. Stephens and her colleagues wrote.
“Additionally, for both S8736 and S0014, no plateau had been reached in the PFS curves. These data contrasted the expected cure rates for advanced-stage DLBCL, leading to the hypothesis that limited-stage DLBCL may have a unique biology from its advanced-stage counterpart,” they added.
Although more than half of patients with advanced-stage diffuse large B-cell lymphoma (DLBCL) can be cured with anthracycline-based chemotherapy, cure rates are markedly lower among patients with limited-stage disease, defined as Ann Arbor stage I or II, confined to a single irradiation field. Limited-stage disease accounts for approximately one-third DLBCL cases.
To see whether the trends observed at 10 years continued, the investigators conducted a survival analysis from S8736 and compared the data from similar patients in the S0014 study.
They found that after a median follow-up of 17.7 years in S8736, median PFS was 12.0 years for patients treated with CHOP8, and 11.1 years for patients treated with CHOP3RT, a difference that was not statistically significant.
Median OS was 13.0 and 13.7 years, respectively, and was also not significant.
In S0014, after a median follow-up of 12 years, the 5-year OS rate was 82%, and 10-year rate was 67%. In this trial, the investigators observed “a persistent pattern of relapse despite the addition of rituximab.”
“The populations were not entirely identical; however, even the addition of rituximab as per S0014 to combined-modality therapy did not seem to mitigate the continued relapse risk, underscoring the value of prolonged observation of clinical trial patients and possible unique biology of limited-stage DLBCL,” Dr. Stephens and her associates wrote.
The study was sponsored by grants from the National Institutes of Health. Dr. Stephens reported having no financial disclosures. Several coauthors disclosed research funding, consulting, speakers’ bureau participation or travel expenses from various oncology drug makers.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Long-term observation of clinical trial patients revealed a dwindling of initial survival benefit from radiation added to chemotherapy in limited-stage DLBCL.
Major finding: At a median 17.7 years of follow-up, there were no significant differences in progression-free or overall survival with eight cycles of CHOP or three cycles with IFRT.
Data source: Final analysis of randomized controlled trial in 401 patients with limited-stage diffuse large B-cell lymphoma.
Disclosures: The study was sponsored by grants from the National Institutes of Health. Dr. Stephens reported having no financial disclosures. Several coauthors disclosed research funding, consulting, speakers’ bureau participation or travel expenses from various oncology drug makers.
Docs to CMS: MACRA is too complex and should be delayed
The proposed federal regulations to implement the MACRA health care reforms are too complex, too onerous on small and solo practices, lack opportunities for many to participate in alternative payment models, and should be delayed for a full year, at least.
That was the message that emerged from hundreds of comments regarding the proposed rule that were submitted by physician organizations and other stakeholders.
“The intent of [the Medicare Access and CHIP Reauthorization Act of 2015] was not to merely move the current incentive program into [the Merit-based Incentive Payment System], but to improve and simplify these programs into a single more unified approach,” the American Medical Association said in its comments, noting that “numerous changes” will be needed in the way cost and quality are measured.
AMA also called for a better, faster way for physicians to develop alternative payment models. “We strongly urge CMS to vigorously pursue this objective and establish a much more progressive and welcoming environment for the development and implementation of specialty-defined APMs than proposed in the [proposed rule].”
AMA also suggested that CMS provide more flexibility for solo and small practices, align the four components of MIPS so it operates as a single program, simplifying and lowering the financial risk for advanced APMs, and providing more timely feedback to physicians.
The organization also called for CMS to “create an initial transitional performance period from July 1, 2017, to December 31, 2017, to ensure the successful and appropriate implementation of the MACRA program. In future years, for all reporting requirements, CMS should allow physicians to select periods of less than a full calendar year to provide flexibility.”
In its comments, the American Medical Group Association questioned whether the proposed rule actually would lead to improved quality of care and reward value.
In the proposed rule, “CMS will measure and score quality and resource use or spending separately,” AMGA wrote in its comments. “CMS will not measure outcomes in relation to spending. CMS will not measure for value. If value is left unaddressed in the final rule, it will be difficult at best for the agency to meet MACRA and the [HHS] secretary’s overarching goals.”
While expressing support for MACRA conceptually, officials with the American Academy of Family Physicians wrote that they “see a strong and definite need and opportunity for CMS to step back and reconsider the approach to this proposed rule which we view as overly complex and burdensome to our members and indeed for all physicians. Given the significant complexity of the rule, we strongly encourage CMS to issue an interim final rule with comment period rather than to issue a final rule.”
Specifically, AAFP criticized the proposed rule for allowing small and solo practices to form “virtual groups” in order to earn bonuses, despite it being mandated by law.
Solo and small group practices who participate in MIPS to should “be eligible for positive payment updates if their performance yields such payments, but would be exempt from any negative payment update until such a time that the virtual group option is available,” AAFP officials wrote.
They also called for medical home delivery models to be included in APMs, in an effort to improve on the limited opportunities for family practices in particular to participate in alternative payment models.
The American College of Physicians also called for safe harbors for small and solo practices until virtual group options can be established.
ACP, like other groups, questioned that medical homes are not recognized as alternative payment models and argued that Congress intended medical homes to qualify as APMs “without bearing more than nominal financial risk.”
Despite the flexible approach to the overall quality payment program, CMS has “created a degree of complexity” and must “continue to seek ways to further streamline and simplify” the move to quality payments, according to comments from the American College of Cardiology.
The ACC also expressed concerns that the reporting requirements under MIPS and some of the APMs will limit the ability for cardiologists to report the most meaningful measures, particularly if they are part of a multi-specialty group, and suggested changes in scoring methodology or to allow more than one data file to be submitted in multi-specialty situations.
It also expressed concerns that the rule as proposed could adversely effect small practices, rural practices, and practices in health professional shortage areas, and “in the absence of other solutions such as virtual groups in 2017, CMS should monitor policies and provide effective practice assistance to these practices.”
The proposed rule provides no support for small practices, according to the American Gastroenterological Association.
“Upon release of the proposed rule, we were disappointed to see that not only will APMs be essentially closed off to small practices in the first years of implementation, but the MIPS program will significantly harm practices with less than 25 eligible clinicians,” AGA noted, citing data presented by CMS that 87% of solo practitioners will receive a negative adjustment with an aggregate negative impact of $300 million and for all practices with less than 25 eligible clinicians, the aggregate negative adjustment will total $649 million.
“Any system in which smaller practices are so heavily disadvantaged is unacceptable,” AGA said. CMS has previously stated that the regulatory impact statement would likely change and reflect a smaller impact for small and solo practices once more updated information can be modeled when the rule is final.
Additionally, AGA expressed concern over the limited engagement in APMs that will be possible under the proposed rule. “Given the importance of APM participation to both the practice and reimbursement of Medicare physicians, access to advanced APMs should be provided to all physicians.”
The association also expressed concern that the definition of APM is not broad enough and suggested that it be widened in scope so that it can capture payment models that have been created using the AGA’s Roadmap to the Future of GI Practice. It recommended a number of models be classified as APMs, including the colonoscopy bundled payment, gastroesophageal reflux disease episode payment, obesity bundled payment, Project Sonar (a chronic disease management program for IBD), and the Medical Home Neighbor.
The American College of Rheumatology called for a delay in the implementation of any final MACRA regulations, noting in its comments that with requirements set to begin in 2017, the current implementation schedule “does not provide enough time for providers to implement the required changes,” though ACR does not recommend a specific start time.
ACR also questioned how the criteria for APMs was set up, noting expressly that Physician Focused Payment Models may not meet the APM requirements. The group is seeking clarification on whether these models will qualify as an APM.
“Medical home APMs should also permit specialty physicians to participate, including small group and multispeciality groups, in keeping with the need for APMs to be flexible with their criteria and the role of specialty physicians in providing chronic care.
The American Academy of Dermatology Association echoed a number of concerns voiced across the medical profession and is calling for a delay in the implementation of MACRA’s regulations.
In particular, AADA noted that the regulations are not friendly for small and solo practices in general and little is contained within the proposal to “meaningfully engage specialist physicians in APMs.”
The association also is calling for broader mechanisms to allow for the development and recognition of APMs, including recognizing specialty-focused medical homes.
The group also is calling for pilot programs to test the validity of the measures that will form the basis of quality payment incentives and penalties.
In an effort to protect small and solo practices, AADA is calling for an exemption from MIPS or APM requirements until a virtual group option is developed, tested, and is fully operational.
The American Psychiatric Association echoed a number of broad concerns raised across the physician spectrum, including calling for a to the first year of implementation to July 1, 2017, and lasting through Dec. 31, 2017, as well as enabling the formation of virtual groups at the onset of implementation in its comments.
But APA also noted that mental health presents a variety of unique issues that need to be addressed.
For example, the association notes that psychiatrists work across a number of practice settings, including academic health centers, hospitals, clinics, nursing homes, and private practices, as well as offering services via telemedicine.
“This makes it difficult for psychiatrists to capture all the work they do, because of the combination of settings that utilize multiple, and potentially differing reporting programs and methods,” APA noted.
It added that psychiatrists generally have limited time and resources that can be devoted to Medicare quality reporting, which would make participation in MIPS and APMs more challenging, particularly because many operate in small or solo practices that do not own electronic health record systems, which would complicate reporting requirements to qualify for MIPS or APMs.
In addition to concerns with reporting in general, APA said that psychiatrists “also have limited choices in outcome quality measures.”
The proposed federal regulations to implement the MACRA health care reforms are too complex, too onerous on small and solo practices, lack opportunities for many to participate in alternative payment models, and should be delayed for a full year, at least.
That was the message that emerged from hundreds of comments regarding the proposed rule that were submitted by physician organizations and other stakeholders.
“The intent of [the Medicare Access and CHIP Reauthorization Act of 2015] was not to merely move the current incentive program into [the Merit-based Incentive Payment System], but to improve and simplify these programs into a single more unified approach,” the American Medical Association said in its comments, noting that “numerous changes” will be needed in the way cost and quality are measured.
AMA also called for a better, faster way for physicians to develop alternative payment models. “We strongly urge CMS to vigorously pursue this objective and establish a much more progressive and welcoming environment for the development and implementation of specialty-defined APMs than proposed in the [proposed rule].”
AMA also suggested that CMS provide more flexibility for solo and small practices, align the four components of MIPS so it operates as a single program, simplifying and lowering the financial risk for advanced APMs, and providing more timely feedback to physicians.
The organization also called for CMS to “create an initial transitional performance period from July 1, 2017, to December 31, 2017, to ensure the successful and appropriate implementation of the MACRA program. In future years, for all reporting requirements, CMS should allow physicians to select periods of less than a full calendar year to provide flexibility.”
In its comments, the American Medical Group Association questioned whether the proposed rule actually would lead to improved quality of care and reward value.
In the proposed rule, “CMS will measure and score quality and resource use or spending separately,” AMGA wrote in its comments. “CMS will not measure outcomes in relation to spending. CMS will not measure for value. If value is left unaddressed in the final rule, it will be difficult at best for the agency to meet MACRA and the [HHS] secretary’s overarching goals.”
While expressing support for MACRA conceptually, officials with the American Academy of Family Physicians wrote that they “see a strong and definite need and opportunity for CMS to step back and reconsider the approach to this proposed rule which we view as overly complex and burdensome to our members and indeed for all physicians. Given the significant complexity of the rule, we strongly encourage CMS to issue an interim final rule with comment period rather than to issue a final rule.”
Specifically, AAFP criticized the proposed rule for allowing small and solo practices to form “virtual groups” in order to earn bonuses, despite it being mandated by law.
Solo and small group practices who participate in MIPS to should “be eligible for positive payment updates if their performance yields such payments, but would be exempt from any negative payment update until such a time that the virtual group option is available,” AAFP officials wrote.
They also called for medical home delivery models to be included in APMs, in an effort to improve on the limited opportunities for family practices in particular to participate in alternative payment models.
The American College of Physicians also called for safe harbors for small and solo practices until virtual group options can be established.
ACP, like other groups, questioned that medical homes are not recognized as alternative payment models and argued that Congress intended medical homes to qualify as APMs “without bearing more than nominal financial risk.”
Despite the flexible approach to the overall quality payment program, CMS has “created a degree of complexity” and must “continue to seek ways to further streamline and simplify” the move to quality payments, according to comments from the American College of Cardiology.
The ACC also expressed concerns that the reporting requirements under MIPS and some of the APMs will limit the ability for cardiologists to report the most meaningful measures, particularly if they are part of a multi-specialty group, and suggested changes in scoring methodology or to allow more than one data file to be submitted in multi-specialty situations.
It also expressed concerns that the rule as proposed could adversely effect small practices, rural practices, and practices in health professional shortage areas, and “in the absence of other solutions such as virtual groups in 2017, CMS should monitor policies and provide effective practice assistance to these practices.”
The proposed rule provides no support for small practices, according to the American Gastroenterological Association.
“Upon release of the proposed rule, we were disappointed to see that not only will APMs be essentially closed off to small practices in the first years of implementation, but the MIPS program will significantly harm practices with less than 25 eligible clinicians,” AGA noted, citing data presented by CMS that 87% of solo practitioners will receive a negative adjustment with an aggregate negative impact of $300 million and for all practices with less than 25 eligible clinicians, the aggregate negative adjustment will total $649 million.
“Any system in which smaller practices are so heavily disadvantaged is unacceptable,” AGA said. CMS has previously stated that the regulatory impact statement would likely change and reflect a smaller impact for small and solo practices once more updated information can be modeled when the rule is final.
Additionally, AGA expressed concern over the limited engagement in APMs that will be possible under the proposed rule. “Given the importance of APM participation to both the practice and reimbursement of Medicare physicians, access to advanced APMs should be provided to all physicians.”
The association also expressed concern that the definition of APM is not broad enough and suggested that it be widened in scope so that it can capture payment models that have been created using the AGA’s Roadmap to the Future of GI Practice. It recommended a number of models be classified as APMs, including the colonoscopy bundled payment, gastroesophageal reflux disease episode payment, obesity bundled payment, Project Sonar (a chronic disease management program for IBD), and the Medical Home Neighbor.
The American College of Rheumatology called for a delay in the implementation of any final MACRA regulations, noting in its comments that with requirements set to begin in 2017, the current implementation schedule “does not provide enough time for providers to implement the required changes,” though ACR does not recommend a specific start time.
ACR also questioned how the criteria for APMs was set up, noting expressly that Physician Focused Payment Models may not meet the APM requirements. The group is seeking clarification on whether these models will qualify as an APM.
“Medical home APMs should also permit specialty physicians to participate, including small group and multispeciality groups, in keeping with the need for APMs to be flexible with their criteria and the role of specialty physicians in providing chronic care.
The American Academy of Dermatology Association echoed a number of concerns voiced across the medical profession and is calling for a delay in the implementation of MACRA’s regulations.
In particular, AADA noted that the regulations are not friendly for small and solo practices in general and little is contained within the proposal to “meaningfully engage specialist physicians in APMs.”
The association also is calling for broader mechanisms to allow for the development and recognition of APMs, including recognizing specialty-focused medical homes.
The group also is calling for pilot programs to test the validity of the measures that will form the basis of quality payment incentives and penalties.
In an effort to protect small and solo practices, AADA is calling for an exemption from MIPS or APM requirements until a virtual group option is developed, tested, and is fully operational.
The American Psychiatric Association echoed a number of broad concerns raised across the physician spectrum, including calling for a to the first year of implementation to July 1, 2017, and lasting through Dec. 31, 2017, as well as enabling the formation of virtual groups at the onset of implementation in its comments.
But APA also noted that mental health presents a variety of unique issues that need to be addressed.
For example, the association notes that psychiatrists work across a number of practice settings, including academic health centers, hospitals, clinics, nursing homes, and private practices, as well as offering services via telemedicine.
“This makes it difficult for psychiatrists to capture all the work they do, because of the combination of settings that utilize multiple, and potentially differing reporting programs and methods,” APA noted.
It added that psychiatrists generally have limited time and resources that can be devoted to Medicare quality reporting, which would make participation in MIPS and APMs more challenging, particularly because many operate in small or solo practices that do not own electronic health record systems, which would complicate reporting requirements to qualify for MIPS or APMs.
In addition to concerns with reporting in general, APA said that psychiatrists “also have limited choices in outcome quality measures.”
The proposed federal regulations to implement the MACRA health care reforms are too complex, too onerous on small and solo practices, lack opportunities for many to participate in alternative payment models, and should be delayed for a full year, at least.
That was the message that emerged from hundreds of comments regarding the proposed rule that were submitted by physician organizations and other stakeholders.
“The intent of [the Medicare Access and CHIP Reauthorization Act of 2015] was not to merely move the current incentive program into [the Merit-based Incentive Payment System], but to improve and simplify these programs into a single more unified approach,” the American Medical Association said in its comments, noting that “numerous changes” will be needed in the way cost and quality are measured.
AMA also called for a better, faster way for physicians to develop alternative payment models. “We strongly urge CMS to vigorously pursue this objective and establish a much more progressive and welcoming environment for the development and implementation of specialty-defined APMs than proposed in the [proposed rule].”
AMA also suggested that CMS provide more flexibility for solo and small practices, align the four components of MIPS so it operates as a single program, simplifying and lowering the financial risk for advanced APMs, and providing more timely feedback to physicians.
The organization also called for CMS to “create an initial transitional performance period from July 1, 2017, to December 31, 2017, to ensure the successful and appropriate implementation of the MACRA program. In future years, for all reporting requirements, CMS should allow physicians to select periods of less than a full calendar year to provide flexibility.”
In its comments, the American Medical Group Association questioned whether the proposed rule actually would lead to improved quality of care and reward value.
In the proposed rule, “CMS will measure and score quality and resource use or spending separately,” AMGA wrote in its comments. “CMS will not measure outcomes in relation to spending. CMS will not measure for value. If value is left unaddressed in the final rule, it will be difficult at best for the agency to meet MACRA and the [HHS] secretary’s overarching goals.”
While expressing support for MACRA conceptually, officials with the American Academy of Family Physicians wrote that they “see a strong and definite need and opportunity for CMS to step back and reconsider the approach to this proposed rule which we view as overly complex and burdensome to our members and indeed for all physicians. Given the significant complexity of the rule, we strongly encourage CMS to issue an interim final rule with comment period rather than to issue a final rule.”
Specifically, AAFP criticized the proposed rule for allowing small and solo practices to form “virtual groups” in order to earn bonuses, despite it being mandated by law.
Solo and small group practices who participate in MIPS to should “be eligible for positive payment updates if their performance yields such payments, but would be exempt from any negative payment update until such a time that the virtual group option is available,” AAFP officials wrote.
They also called for medical home delivery models to be included in APMs, in an effort to improve on the limited opportunities for family practices in particular to participate in alternative payment models.
The American College of Physicians also called for safe harbors for small and solo practices until virtual group options can be established.
ACP, like other groups, questioned that medical homes are not recognized as alternative payment models and argued that Congress intended medical homes to qualify as APMs “without bearing more than nominal financial risk.”
Despite the flexible approach to the overall quality payment program, CMS has “created a degree of complexity” and must “continue to seek ways to further streamline and simplify” the move to quality payments, according to comments from the American College of Cardiology.
The ACC also expressed concerns that the reporting requirements under MIPS and some of the APMs will limit the ability for cardiologists to report the most meaningful measures, particularly if they are part of a multi-specialty group, and suggested changes in scoring methodology or to allow more than one data file to be submitted in multi-specialty situations.
It also expressed concerns that the rule as proposed could adversely effect small practices, rural practices, and practices in health professional shortage areas, and “in the absence of other solutions such as virtual groups in 2017, CMS should monitor policies and provide effective practice assistance to these practices.”
The proposed rule provides no support for small practices, according to the American Gastroenterological Association.
“Upon release of the proposed rule, we were disappointed to see that not only will APMs be essentially closed off to small practices in the first years of implementation, but the MIPS program will significantly harm practices with less than 25 eligible clinicians,” AGA noted, citing data presented by CMS that 87% of solo practitioners will receive a negative adjustment with an aggregate negative impact of $300 million and for all practices with less than 25 eligible clinicians, the aggregate negative adjustment will total $649 million.
“Any system in which smaller practices are so heavily disadvantaged is unacceptable,” AGA said. CMS has previously stated that the regulatory impact statement would likely change and reflect a smaller impact for small and solo practices once more updated information can be modeled when the rule is final.
Additionally, AGA expressed concern over the limited engagement in APMs that will be possible under the proposed rule. “Given the importance of APM participation to both the practice and reimbursement of Medicare physicians, access to advanced APMs should be provided to all physicians.”
The association also expressed concern that the definition of APM is not broad enough and suggested that it be widened in scope so that it can capture payment models that have been created using the AGA’s Roadmap to the Future of GI Practice. It recommended a number of models be classified as APMs, including the colonoscopy bundled payment, gastroesophageal reflux disease episode payment, obesity bundled payment, Project Sonar (a chronic disease management program for IBD), and the Medical Home Neighbor.
The American College of Rheumatology called for a delay in the implementation of any final MACRA regulations, noting in its comments that with requirements set to begin in 2017, the current implementation schedule “does not provide enough time for providers to implement the required changes,” though ACR does not recommend a specific start time.
ACR also questioned how the criteria for APMs was set up, noting expressly that Physician Focused Payment Models may not meet the APM requirements. The group is seeking clarification on whether these models will qualify as an APM.
“Medical home APMs should also permit specialty physicians to participate, including small group and multispeciality groups, in keeping with the need for APMs to be flexible with their criteria and the role of specialty physicians in providing chronic care.
The American Academy of Dermatology Association echoed a number of concerns voiced across the medical profession and is calling for a delay in the implementation of MACRA’s regulations.
In particular, AADA noted that the regulations are not friendly for small and solo practices in general and little is contained within the proposal to “meaningfully engage specialist physicians in APMs.”
The association also is calling for broader mechanisms to allow for the development and recognition of APMs, including recognizing specialty-focused medical homes.
The group also is calling for pilot programs to test the validity of the measures that will form the basis of quality payment incentives and penalties.
In an effort to protect small and solo practices, AADA is calling for an exemption from MIPS or APM requirements until a virtual group option is developed, tested, and is fully operational.
The American Psychiatric Association echoed a number of broad concerns raised across the physician spectrum, including calling for a to the first year of implementation to July 1, 2017, and lasting through Dec. 31, 2017, as well as enabling the formation of virtual groups at the onset of implementation in its comments.
But APA also noted that mental health presents a variety of unique issues that need to be addressed.
For example, the association notes that psychiatrists work across a number of practice settings, including academic health centers, hospitals, clinics, nursing homes, and private practices, as well as offering services via telemedicine.
“This makes it difficult for psychiatrists to capture all the work they do, because of the combination of settings that utilize multiple, and potentially differing reporting programs and methods,” APA noted.
It added that psychiatrists generally have limited time and resources that can be devoted to Medicare quality reporting, which would make participation in MIPS and APMs more challenging, particularly because many operate in small or solo practices that do not own electronic health record systems, which would complicate reporting requirements to qualify for MIPS or APMs.
In addition to concerns with reporting in general, APA said that psychiatrists “also have limited choices in outcome quality measures.”
Deaths prompt clinical hold for JCAR015 trial

Image from UNSW
Update: The hold on this trial has been lifted. Click here for additional details.
A trial of the chimeric antigen receptor (CAR) T-cell therapy JCAR015 has been placed on clinical hold following 3 patient deaths.
The trial, known as ROCKET, is a phase 2 study of adults with relapsed or refractory B-cell acute lymphoblastic leukemia.
The US Food and Drug Administration (FDA) placed a hold on the trial after 3 patients died of cerebral edema.
All 3 patients had received conditioning with fludarabine, and Juno Therapeutics, the company developing JCAR015, believes this may have caused the patients’ deaths.
Patients enrolled on the ROCKET trial previously received conditioning with cyclophosphamide alone, but investigators decided to add fludarabine in hopes of increasing efficacy.
The addition of fludarabine to conditioning had been shown to increase the efficacy of 2 of Juno’s other CAR T-cell therapies, JCAR014 and JCAR017, in phase 1/2 trials.
“However, since adding fludarabine to the preconditioning on the ROCKET trial, we have seen an increase in the incidence of severe neurotoxicity, which has, unfortunately, included 2 patient deaths that occurred last week from cerebral edema that appeared to be treatment-related,” Hans Bishop, Juno’s president and chief executive officer, said in a conference call.
“After the first of these 2 deaths, we immediately paused the trial for an internal review and review with our Data Safety Monitoring Board [DSMB] and the FDA. There was also 1 previous death from cerebral edema on the trial in May. After a review of that event, we, along with the FDA and our DSMB, concluded there were confounding factors, and a change in our plans at the time was not warranted.”
After the more recent deaths, Juno investigated several factors that could have contributed, including the conditioning regimen, patient characteristics, toxicity management, product characteristics, and cell dose.
“Although more than 1 factor may have contributed, based on our review of the data available . . . , we believe the addition of fludarabine, when combined with JCAR015, is the most likely and the most appropriately modifiable factor,” Bishop said.
“Indeed, with cy[clophosphamide] alone, which we have used in the greatest number of patients treated in the ROCKET trial to date, there have not been any treatment-related deaths, and the incidence of severe neurotoxicity is within the range of what we expected in light of the Memorial Sloan-Kettering experience [phase 1 trial of JCAR015].”
Therefore, Juno has proposed continuing the ROCKET trial using conditioning with cyclophosphamide alone.
In response to this request, the FDA has requested that Juno submit:
- A revised patient informed consent form
- A revised investigator brochure
- A revised trial protocol
- A copy of a presentation the company made to the FDA.
The FDA said it will expedite the review of these documents and expects to complete the review within 30 days of receiving them.
If the clinical hold on the ROCKET trial is lifted, Juno plans to continue the trial. However, the hold will likely impact the company’s goal of gaining FDA approval for JCAR015 in 2017.
Juno’s trials and plans for its other CD19-directed CAR-T cell product candidates are not affected by the clinical hold placed on ROCKET.
ROCKET is not the first trial of JCAR015 to be placed on hold. The phase 1 trial of the therapy was placed on clinical hold in 2014, after 2 patients died of cytokine release syndrome.
That hold was lifted following changes to enrollment criteria and dosing. Results from this trial were presented at ASCO 2015 and ASCO 2016. ![]()

Image from UNSW
Update: The hold on this trial has been lifted. Click here for additional details.
A trial of the chimeric antigen receptor (CAR) T-cell therapy JCAR015 has been placed on clinical hold following 3 patient deaths.
The trial, known as ROCKET, is a phase 2 study of adults with relapsed or refractory B-cell acute lymphoblastic leukemia.
The US Food and Drug Administration (FDA) placed a hold on the trial after 3 patients died of cerebral edema.
All 3 patients had received conditioning with fludarabine, and Juno Therapeutics, the company developing JCAR015, believes this may have caused the patients’ deaths.
Patients enrolled on the ROCKET trial previously received conditioning with cyclophosphamide alone, but investigators decided to add fludarabine in hopes of increasing efficacy.
The addition of fludarabine to conditioning had been shown to increase the efficacy of 2 of Juno’s other CAR T-cell therapies, JCAR014 and JCAR017, in phase 1/2 trials.
“However, since adding fludarabine to the preconditioning on the ROCKET trial, we have seen an increase in the incidence of severe neurotoxicity, which has, unfortunately, included 2 patient deaths that occurred last week from cerebral edema that appeared to be treatment-related,” Hans Bishop, Juno’s president and chief executive officer, said in a conference call.
“After the first of these 2 deaths, we immediately paused the trial for an internal review and review with our Data Safety Monitoring Board [DSMB] and the FDA. There was also 1 previous death from cerebral edema on the trial in May. After a review of that event, we, along with the FDA and our DSMB, concluded there were confounding factors, and a change in our plans at the time was not warranted.”
After the more recent deaths, Juno investigated several factors that could have contributed, including the conditioning regimen, patient characteristics, toxicity management, product characteristics, and cell dose.
“Although more than 1 factor may have contributed, based on our review of the data available . . . , we believe the addition of fludarabine, when combined with JCAR015, is the most likely and the most appropriately modifiable factor,” Bishop said.
“Indeed, with cy[clophosphamide] alone, which we have used in the greatest number of patients treated in the ROCKET trial to date, there have not been any treatment-related deaths, and the incidence of severe neurotoxicity is within the range of what we expected in light of the Memorial Sloan-Kettering experience [phase 1 trial of JCAR015].”
Therefore, Juno has proposed continuing the ROCKET trial using conditioning with cyclophosphamide alone.
In response to this request, the FDA has requested that Juno submit:
- A revised patient informed consent form
- A revised investigator brochure
- A revised trial protocol
- A copy of a presentation the company made to the FDA.
The FDA said it will expedite the review of these documents and expects to complete the review within 30 days of receiving them.
If the clinical hold on the ROCKET trial is lifted, Juno plans to continue the trial. However, the hold will likely impact the company’s goal of gaining FDA approval for JCAR015 in 2017.
Juno’s trials and plans for its other CD19-directed CAR-T cell product candidates are not affected by the clinical hold placed on ROCKET.
ROCKET is not the first trial of JCAR015 to be placed on hold. The phase 1 trial of the therapy was placed on clinical hold in 2014, after 2 patients died of cytokine release syndrome.
That hold was lifted following changes to enrollment criteria and dosing. Results from this trial were presented at ASCO 2015 and ASCO 2016. ![]()

Image from UNSW
Update: The hold on this trial has been lifted. Click here for additional details.
A trial of the chimeric antigen receptor (CAR) T-cell therapy JCAR015 has been placed on clinical hold following 3 patient deaths.
The trial, known as ROCKET, is a phase 2 study of adults with relapsed or refractory B-cell acute lymphoblastic leukemia.
The US Food and Drug Administration (FDA) placed a hold on the trial after 3 patients died of cerebral edema.
All 3 patients had received conditioning with fludarabine, and Juno Therapeutics, the company developing JCAR015, believes this may have caused the patients’ deaths.
Patients enrolled on the ROCKET trial previously received conditioning with cyclophosphamide alone, but investigators decided to add fludarabine in hopes of increasing efficacy.
The addition of fludarabine to conditioning had been shown to increase the efficacy of 2 of Juno’s other CAR T-cell therapies, JCAR014 and JCAR017, in phase 1/2 trials.
“However, since adding fludarabine to the preconditioning on the ROCKET trial, we have seen an increase in the incidence of severe neurotoxicity, which has, unfortunately, included 2 patient deaths that occurred last week from cerebral edema that appeared to be treatment-related,” Hans Bishop, Juno’s president and chief executive officer, said in a conference call.
“After the first of these 2 deaths, we immediately paused the trial for an internal review and review with our Data Safety Monitoring Board [DSMB] and the FDA. There was also 1 previous death from cerebral edema on the trial in May. After a review of that event, we, along with the FDA and our DSMB, concluded there were confounding factors, and a change in our plans at the time was not warranted.”
After the more recent deaths, Juno investigated several factors that could have contributed, including the conditioning regimen, patient characteristics, toxicity management, product characteristics, and cell dose.
“Although more than 1 factor may have contributed, based on our review of the data available . . . , we believe the addition of fludarabine, when combined with JCAR015, is the most likely and the most appropriately modifiable factor,” Bishop said.
“Indeed, with cy[clophosphamide] alone, which we have used in the greatest number of patients treated in the ROCKET trial to date, there have not been any treatment-related deaths, and the incidence of severe neurotoxicity is within the range of what we expected in light of the Memorial Sloan-Kettering experience [phase 1 trial of JCAR015].”
Therefore, Juno has proposed continuing the ROCKET trial using conditioning with cyclophosphamide alone.
In response to this request, the FDA has requested that Juno submit:
- A revised patient informed consent form
- A revised investigator brochure
- A revised trial protocol
- A copy of a presentation the company made to the FDA.
The FDA said it will expedite the review of these documents and expects to complete the review within 30 days of receiving them.
If the clinical hold on the ROCKET trial is lifted, Juno plans to continue the trial. However, the hold will likely impact the company’s goal of gaining FDA approval for JCAR015 in 2017.
Juno’s trials and plans for its other CD19-directed CAR-T cell product candidates are not affected by the clinical hold placed on ROCKET.
ROCKET is not the first trial of JCAR015 to be placed on hold. The phase 1 trial of the therapy was placed on clinical hold in 2014, after 2 patients died of cytokine release syndrome.
That hold was lifted following changes to enrollment criteria and dosing. Results from this trial were presented at ASCO 2015 and ASCO 2016. ![]()
DNA repair mutations crop up often in mPC
The prevalence of inherited mutations in DNA repair genes such as BRCA2 in men with metastatic prostate cancer may be as high as 12%, investigators in a multicenter study report.
The prevalence of presumably harmful mutations in men with metastatic disease was more than twice that of men with localized prostate cancer, and men with metastatic prostate cancer had a 3- to 19-fold higher risk for having mutations in individual DNA repair genes, compared with men without prostate cancer in a population-wide genetic sample, reported Colin C. Pritchard, MD, PhD, of the University of Washington in Seattle and colleagues.
“Because the high frequency of DNA repair gene mutations is not exclusive to an early-onset phenotype and is associated with clinically and histologically aggressive disease, with compelling evidence for therapeutic relevance, it may be of interest to routinely examine all men with metastatic prostate cancer for the presence of germline mutations in DNA repair genes,” the investigators suggest (N Engl J Med. 2016 July. doi: 10.1056/NEJMoa1603144).
The findings point to possible therapeutic interventions for men with advanced prostate cancer with identified germline mutations in DNA repair genes, such as poly (ADP-ribose) polymerase (PARP) inhibitors or platinum compound–based chemotherapy,
To date, the only genetic factors known to be associated with aggressive prostate cancer and prostate cancer–specific mortality are mutations in DNA repair genes such as BRCA1 and BRCA2, CHEK2, and PALB2. The frequency of mutations in these genes among men with localized prostate cancer in general is relatively low, accounting for just a few percentage points of familial prostate cancer cases in a sample unselected for family predisposition, the authors noted.
To determine the frequency of mutations in advanced disease, the investigators reviewed genetic data on 692 men with metastatic prostate cancer who were enrolled in one of seven cases series and were unselected for family history of cancer or age at diagnosis.
They used multiplex genetic sequencing assays to look for mutation in 20 DNA repair genes that are associated with autosomal dominant cancer predisposition syndromes.
They found 84 presumably harmful mutations in 82 men, for an overall prevalence of 11.8%. In contrast, the frequency of germline DNA repair mutations among 499 men in the Cancer Genome Atlas prostate cancer study, including men with high-risk disease, was 4.6%, the authors noted.
The mutations occurred in 16 different genes, including, in order of prevalence, BRCA2, ATM, CHEL2, BRCA1, RAD51D and PALB2. There were no significant differences in mutation frequencies by either family history of prostate cancer or age at diagnosis.
The authors also estimated the prevalence of DNA repair gene mutations among the general population by looking at a sample of 53,105 persons without a known diagnosis of cancer who were included in the Exome Aggregation Consortium. Men with metastatic prostate cancer had a fivefold risk for having any deleterious DNA repair mutation, compared with the general population (P less than .001).
The relative risk of mutations in individual genes for men with metastatic disease, compared with men in the control sample, ranged from 3.1 for CHEK2 (P = .002) to 18.6 for BRCA2 (P less than .001).
The study was supported by a Stand Up To Cancer–Prostate Cancer Foundation (SU2C-PCF) International Prostate Cancer Dream Team Translational Cancer Research Grant and awards from the National Institutes of Health, Department of Defense, and prostate cancer foundation. Several authors reported receiving research fees, grants, honoraria, and/or travel expenses from various pharmaceutical companies.
The prevalence of inherited mutations in DNA repair genes such as BRCA2 in men with metastatic prostate cancer may be as high as 12%, investigators in a multicenter study report.
The prevalence of presumably harmful mutations in men with metastatic disease was more than twice that of men with localized prostate cancer, and men with metastatic prostate cancer had a 3- to 19-fold higher risk for having mutations in individual DNA repair genes, compared with men without prostate cancer in a population-wide genetic sample, reported Colin C. Pritchard, MD, PhD, of the University of Washington in Seattle and colleagues.
“Because the high frequency of DNA repair gene mutations is not exclusive to an early-onset phenotype and is associated with clinically and histologically aggressive disease, with compelling evidence for therapeutic relevance, it may be of interest to routinely examine all men with metastatic prostate cancer for the presence of germline mutations in DNA repair genes,” the investigators suggest (N Engl J Med. 2016 July. doi: 10.1056/NEJMoa1603144).
The findings point to possible therapeutic interventions for men with advanced prostate cancer with identified germline mutations in DNA repair genes, such as poly (ADP-ribose) polymerase (PARP) inhibitors or platinum compound–based chemotherapy,
To date, the only genetic factors known to be associated with aggressive prostate cancer and prostate cancer–specific mortality are mutations in DNA repair genes such as BRCA1 and BRCA2, CHEK2, and PALB2. The frequency of mutations in these genes among men with localized prostate cancer in general is relatively low, accounting for just a few percentage points of familial prostate cancer cases in a sample unselected for family predisposition, the authors noted.
To determine the frequency of mutations in advanced disease, the investigators reviewed genetic data on 692 men with metastatic prostate cancer who were enrolled in one of seven cases series and were unselected for family history of cancer or age at diagnosis.
They used multiplex genetic sequencing assays to look for mutation in 20 DNA repair genes that are associated with autosomal dominant cancer predisposition syndromes.
They found 84 presumably harmful mutations in 82 men, for an overall prevalence of 11.8%. In contrast, the frequency of germline DNA repair mutations among 499 men in the Cancer Genome Atlas prostate cancer study, including men with high-risk disease, was 4.6%, the authors noted.
The mutations occurred in 16 different genes, including, in order of prevalence, BRCA2, ATM, CHEL2, BRCA1, RAD51D and PALB2. There were no significant differences in mutation frequencies by either family history of prostate cancer or age at diagnosis.
The authors also estimated the prevalence of DNA repair gene mutations among the general population by looking at a sample of 53,105 persons without a known diagnosis of cancer who were included in the Exome Aggregation Consortium. Men with metastatic prostate cancer had a fivefold risk for having any deleterious DNA repair mutation, compared with the general population (P less than .001).
The relative risk of mutations in individual genes for men with metastatic disease, compared with men in the control sample, ranged from 3.1 for CHEK2 (P = .002) to 18.6 for BRCA2 (P less than .001).
The study was supported by a Stand Up To Cancer–Prostate Cancer Foundation (SU2C-PCF) International Prostate Cancer Dream Team Translational Cancer Research Grant and awards from the National Institutes of Health, Department of Defense, and prostate cancer foundation. Several authors reported receiving research fees, grants, honoraria, and/or travel expenses from various pharmaceutical companies.
The prevalence of inherited mutations in DNA repair genes such as BRCA2 in men with metastatic prostate cancer may be as high as 12%, investigators in a multicenter study report.
The prevalence of presumably harmful mutations in men with metastatic disease was more than twice that of men with localized prostate cancer, and men with metastatic prostate cancer had a 3- to 19-fold higher risk for having mutations in individual DNA repair genes, compared with men without prostate cancer in a population-wide genetic sample, reported Colin C. Pritchard, MD, PhD, of the University of Washington in Seattle and colleagues.
“Because the high frequency of DNA repair gene mutations is not exclusive to an early-onset phenotype and is associated with clinically and histologically aggressive disease, with compelling evidence for therapeutic relevance, it may be of interest to routinely examine all men with metastatic prostate cancer for the presence of germline mutations in DNA repair genes,” the investigators suggest (N Engl J Med. 2016 July. doi: 10.1056/NEJMoa1603144).
The findings point to possible therapeutic interventions for men with advanced prostate cancer with identified germline mutations in DNA repair genes, such as poly (ADP-ribose) polymerase (PARP) inhibitors or platinum compound–based chemotherapy,
To date, the only genetic factors known to be associated with aggressive prostate cancer and prostate cancer–specific mortality are mutations in DNA repair genes such as BRCA1 and BRCA2, CHEK2, and PALB2. The frequency of mutations in these genes among men with localized prostate cancer in general is relatively low, accounting for just a few percentage points of familial prostate cancer cases in a sample unselected for family predisposition, the authors noted.
To determine the frequency of mutations in advanced disease, the investigators reviewed genetic data on 692 men with metastatic prostate cancer who were enrolled in one of seven cases series and were unselected for family history of cancer or age at diagnosis.
They used multiplex genetic sequencing assays to look for mutation in 20 DNA repair genes that are associated with autosomal dominant cancer predisposition syndromes.
They found 84 presumably harmful mutations in 82 men, for an overall prevalence of 11.8%. In contrast, the frequency of germline DNA repair mutations among 499 men in the Cancer Genome Atlas prostate cancer study, including men with high-risk disease, was 4.6%, the authors noted.
The mutations occurred in 16 different genes, including, in order of prevalence, BRCA2, ATM, CHEL2, BRCA1, RAD51D and PALB2. There were no significant differences in mutation frequencies by either family history of prostate cancer or age at diagnosis.
The authors also estimated the prevalence of DNA repair gene mutations among the general population by looking at a sample of 53,105 persons without a known diagnosis of cancer who were included in the Exome Aggregation Consortium. Men with metastatic prostate cancer had a fivefold risk for having any deleterious DNA repair mutation, compared with the general population (P less than .001).
The relative risk of mutations in individual genes for men with metastatic disease, compared with men in the control sample, ranged from 3.1 for CHEK2 (P = .002) to 18.6 for BRCA2 (P less than .001).
The study was supported by a Stand Up To Cancer–Prostate Cancer Foundation (SU2C-PCF) International Prostate Cancer Dream Team Translational Cancer Research Grant and awards from the National Institutes of Health, Department of Defense, and prostate cancer foundation. Several authors reported receiving research fees, grants, honoraria, and/or travel expenses from various pharmaceutical companies.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Germline mutations in DNA repair genes are potential targets for therapy in men with metastatic prostate cancer.
Major finding: There were 84 presumably deleterious mutations in 82 men with metastatic prostate cancer, for an overall prevalence of 11.8%.
Data source: Study of mutational frequencies in 692 men with metastatic prostate cancer in seven case series.
Disclosures: The study was supported by a Stand Up To Cancer–Prostate Cancer Foundation (SU2C-PCF) International Prostate Cancer Dream Team Translational Cancer Research Grant and awards from the National Institutes of Health, Department of Defense, and prostate cancer foundation. Several authors reported receiving research fees, grants, honoraria, and/or travel expenses from various pharmaceutical companies.
Fee schedule includes expansion of Diabetes Prevention Program
An expansion of the Diabetes Prevention Program (DPP), announced July 7 in the proposed Medicare Physician Fee Schedule for 2017, would allow recognized suppliers to submit claims to the Centers for Medicare & Medicaid Services for payment beginning Jan. 1, 2018.
The proposed expansion would allow patients across the United States to access community-based intervention that curbs diabetes and keeps families healthy, according to Patrick Conway, MD, CMS chief medical officer.
“This is part of our efforts for better care, smarter spending, and healthier people,” Dr. Conway said in a statement. The “proposal is an exciting milestone for prevention and population health.”
The Diabetes Prevention Program started in 2011 as an Affordable Care Act pilot program awarded to the National Council of YMCAs of the United States of America (Y-USA). Medicare patients at high risk for diabetes attended 16 intensive educational sessions in a group-based, classroom-style setting and practical training in long-term dietary change, increased physical activity, and behavior change strategies for weight control.
The pilot resulted in savings of $2,650 per enrollee over 15 months, according to CMS, compared with costs associated with nonprogram beneficiaries – enough to cover the cost of the program. Program participants also were shown to lose an average of about 5% of their body weight.
In March 2016, the U.S. Health and Human Services Department announced that the CMS Office of the Actuary had certified the pilot Diabetes Prevention Program model as a cost savings program that reduced net Medicare spending. HHS determined that the program demonstrated the ability to improve the quality of patient care without limiting coverage or benefits.
In the fee schedule proposal, CMS is suggesting that each health care provider who offers services as part of a CDC-recognized organization delivering DPP services obtain a National Provider Identification number to provide Medicare DPP services, allowing supplier enrollment beginning as early as Jan. 1, 2017. In addition, CMS envisions a payment structure tying payment for Medicare DPP services to the number of sessions attended by patients and the achievement and maintenance of minimum weight loss. Claims for payment under the Medicare DPP would be submitted following the achievement of core session attendance and minimum weight loss, and following maintenance session attendance and maintenance of minimum weight loss, according to the proposal.
CMS has not decided whether the Medicare DPP should be expanded nationally in the first year of the program or whether it should be phased in.
The American College of Physicians expressed support for DPP expansion and said that organization leaders plan to provide comments on the basic framework.
“As a practicing primary care internist myself, I am greatly encouraged that CMS is proposing substantial improvements to help me and my colleagues provide coordinated, patient-centered, high-value, and team-based care to our patients,” ACP President Nitin S. Damle, MD, said in a statement. “We look forward to providing CMS with detailed comments to support these improvements while recommending other changes to strengthen primary care.”
Robert E. Ratner, MD, chief scientific and medical officer for the American Diabetes Association agreed.
“Providing people with prediabetes with effective tools to prevent diabetes is a win for all of us,” Dr. Ratner said in a statement. “We appreciate HHS’s continued commitment to improving the nation’s health and helping us reduce the incidence and burden of diabetes across the country.”
Wanda Filer, MD, president of the American Academy of Family Physicians, said her organization was still analyzing the proposal, but that the expansion sounds positive for health care.
“We think the expansion is a great idea for patients,” she said in an interview, adding that it’s essential that doctors are reimbursed for preventive services. “Frankly, if you do the work, you need to get paid.”
CMS will accept comments on the proposed rule until Sept. 6. The proposed rule will appear in the July 15 Federal Register.
On Twitter @legal_med
An expansion of the Diabetes Prevention Program (DPP), announced July 7 in the proposed Medicare Physician Fee Schedule for 2017, would allow recognized suppliers to submit claims to the Centers for Medicare & Medicaid Services for payment beginning Jan. 1, 2018.
The proposed expansion would allow patients across the United States to access community-based intervention that curbs diabetes and keeps families healthy, according to Patrick Conway, MD, CMS chief medical officer.
“This is part of our efforts for better care, smarter spending, and healthier people,” Dr. Conway said in a statement. The “proposal is an exciting milestone for prevention and population health.”
The Diabetes Prevention Program started in 2011 as an Affordable Care Act pilot program awarded to the National Council of YMCAs of the United States of America (Y-USA). Medicare patients at high risk for diabetes attended 16 intensive educational sessions in a group-based, classroom-style setting and practical training in long-term dietary change, increased physical activity, and behavior change strategies for weight control.
The pilot resulted in savings of $2,650 per enrollee over 15 months, according to CMS, compared with costs associated with nonprogram beneficiaries – enough to cover the cost of the program. Program participants also were shown to lose an average of about 5% of their body weight.
In March 2016, the U.S. Health and Human Services Department announced that the CMS Office of the Actuary had certified the pilot Diabetes Prevention Program model as a cost savings program that reduced net Medicare spending. HHS determined that the program demonstrated the ability to improve the quality of patient care without limiting coverage or benefits.
In the fee schedule proposal, CMS is suggesting that each health care provider who offers services as part of a CDC-recognized organization delivering DPP services obtain a National Provider Identification number to provide Medicare DPP services, allowing supplier enrollment beginning as early as Jan. 1, 2017. In addition, CMS envisions a payment structure tying payment for Medicare DPP services to the number of sessions attended by patients and the achievement and maintenance of minimum weight loss. Claims for payment under the Medicare DPP would be submitted following the achievement of core session attendance and minimum weight loss, and following maintenance session attendance and maintenance of minimum weight loss, according to the proposal.
CMS has not decided whether the Medicare DPP should be expanded nationally in the first year of the program or whether it should be phased in.
The American College of Physicians expressed support for DPP expansion and said that organization leaders plan to provide comments on the basic framework.
“As a practicing primary care internist myself, I am greatly encouraged that CMS is proposing substantial improvements to help me and my colleagues provide coordinated, patient-centered, high-value, and team-based care to our patients,” ACP President Nitin S. Damle, MD, said in a statement. “We look forward to providing CMS with detailed comments to support these improvements while recommending other changes to strengthen primary care.”
Robert E. Ratner, MD, chief scientific and medical officer for the American Diabetes Association agreed.
“Providing people with prediabetes with effective tools to prevent diabetes is a win for all of us,” Dr. Ratner said in a statement. “We appreciate HHS’s continued commitment to improving the nation’s health and helping us reduce the incidence and burden of diabetes across the country.”
Wanda Filer, MD, president of the American Academy of Family Physicians, said her organization was still analyzing the proposal, but that the expansion sounds positive for health care.
“We think the expansion is a great idea for patients,” she said in an interview, adding that it’s essential that doctors are reimbursed for preventive services. “Frankly, if you do the work, you need to get paid.”
CMS will accept comments on the proposed rule until Sept. 6. The proposed rule will appear in the July 15 Federal Register.
On Twitter @legal_med
An expansion of the Diabetes Prevention Program (DPP), announced July 7 in the proposed Medicare Physician Fee Schedule for 2017, would allow recognized suppliers to submit claims to the Centers for Medicare & Medicaid Services for payment beginning Jan. 1, 2018.
The proposed expansion would allow patients across the United States to access community-based intervention that curbs diabetes and keeps families healthy, according to Patrick Conway, MD, CMS chief medical officer.
“This is part of our efforts for better care, smarter spending, and healthier people,” Dr. Conway said in a statement. The “proposal is an exciting milestone for prevention and population health.”
The Diabetes Prevention Program started in 2011 as an Affordable Care Act pilot program awarded to the National Council of YMCAs of the United States of America (Y-USA). Medicare patients at high risk for diabetes attended 16 intensive educational sessions in a group-based, classroom-style setting and practical training in long-term dietary change, increased physical activity, and behavior change strategies for weight control.
The pilot resulted in savings of $2,650 per enrollee over 15 months, according to CMS, compared with costs associated with nonprogram beneficiaries – enough to cover the cost of the program. Program participants also were shown to lose an average of about 5% of their body weight.
In March 2016, the U.S. Health and Human Services Department announced that the CMS Office of the Actuary had certified the pilot Diabetes Prevention Program model as a cost savings program that reduced net Medicare spending. HHS determined that the program demonstrated the ability to improve the quality of patient care without limiting coverage or benefits.
In the fee schedule proposal, CMS is suggesting that each health care provider who offers services as part of a CDC-recognized organization delivering DPP services obtain a National Provider Identification number to provide Medicare DPP services, allowing supplier enrollment beginning as early as Jan. 1, 2017. In addition, CMS envisions a payment structure tying payment for Medicare DPP services to the number of sessions attended by patients and the achievement and maintenance of minimum weight loss. Claims for payment under the Medicare DPP would be submitted following the achievement of core session attendance and minimum weight loss, and following maintenance session attendance and maintenance of minimum weight loss, according to the proposal.
CMS has not decided whether the Medicare DPP should be expanded nationally in the first year of the program or whether it should be phased in.
The American College of Physicians expressed support for DPP expansion and said that organization leaders plan to provide comments on the basic framework.
“As a practicing primary care internist myself, I am greatly encouraged that CMS is proposing substantial improvements to help me and my colleagues provide coordinated, patient-centered, high-value, and team-based care to our patients,” ACP President Nitin S. Damle, MD, said in a statement. “We look forward to providing CMS with detailed comments to support these improvements while recommending other changes to strengthen primary care.”
Robert E. Ratner, MD, chief scientific and medical officer for the American Diabetes Association agreed.
“Providing people with prediabetes with effective tools to prevent diabetes is a win for all of us,” Dr. Ratner said in a statement. “We appreciate HHS’s continued commitment to improving the nation’s health and helping us reduce the incidence and burden of diabetes across the country.”
Wanda Filer, MD, president of the American Academy of Family Physicians, said her organization was still analyzing the proposal, but that the expansion sounds positive for health care.
“We think the expansion is a great idea for patients,” she said in an interview, adding that it’s essential that doctors are reimbursed for preventive services. “Frankly, if you do the work, you need to get paid.”
CMS will accept comments on the proposed rule until Sept. 6. The proposed rule will appear in the July 15 Federal Register.
On Twitter @legal_med
Treatment-free remissions achieved in patients with chronic myeloid leukemia
Treatment-free remission attempts are safe and are achievable in most patients with chronic myeloid leukemia (CML) in chronic phase, Timothy P. Hughes, MD, and his colleagues in the international ENESTop trial reported at the annual meeting of the American Society of Clinical Oncology.
The conclusion is based on follow-up data on 126 patients who achieved a sustained deep molecular response (MR4.5) after switching from imatinib (Gleevec) to nilotinib (Tasigna) and discontinued nilotinib. So far, these are the largest prospective treatment-free remission data set in a population of patients who achieved a sustained deep molecular response after switching from imatinib to nilotinib, Dr. Hughes, head of hematology at the University of Adelaide and his colleagues wrote in a poster presentation.
The ENESTop study is a single-arm, phase II study. Patients eligible for the study started treatment with imatinib when they were first diagnosed with CML, then switched to nilotinib for at least 2 years with the combined time on the drugs of at least 3 years and small amounts of leukemia cells remaining after the nilotinib treatment.
For the consolidation phase of the study, patients continued their nilotinib therapy for 1 year. Patients without confirmed loss of MR4.5 after 1 year were eligible to stop nilotinib. RQ-PCR (reverse transcriptase–polymerase chain reaction) was monitored every 12 weeks in the consolidation phase of the study and every 4 weeks during first 48 weeks of treatment-free remission. Nilotinib was restarted if patients had confirmed loss of deep molecular response (MR4 [consecutive BCR-ABL1IS greater than 0.01%]) or loss of major molecular response ([MMR] BCR-ABL1IS greater than 0.1%).
Of the 163 patients in the consolidation phase of the study, 126 entered treatment-free remission. Their median duration of tyrosine kinase inhibitor use prior to treatment-free remission was nearly 88 months, with a 53-month median duration of nilotinib therapy. At data cut-off, with median follow up of 50 weeks, 58% of the 126 patients were still in treatment-free remission at 48 weeks.
During treatment-free remission, 18 patients had confirmed loss of MR4 and 34 lost MMR. One patient had atypical transcript and came off the study. All but one of the 52 patients reinitiated nilotinib; 50 (98%) regained at least MMR by data cut-off, 48 (94%) regained MR4, and 47 (92%) regained MR4.5. One patient switched to another tyrosine kinase inhibitor at 22 weeks after restarting therapy.
Of those who restarted therapy, the median time was 12 weeks to regain MR4 and was 13 weeks to regain MR4.5. No new safety findings were observed on treatment.
The study is sponsored by Novartis, the maker of nilotinib (Tasigna). Dr. Hughes receives research support and honoraria from, and is a consultant or advisor to Novartis as well as Ariad and Bristol-Myers Squibb.
On Twitter @maryjodales
Treatment-free remission attempts are safe and are achievable in most patients with chronic myeloid leukemia (CML) in chronic phase, Timothy P. Hughes, MD, and his colleagues in the international ENESTop trial reported at the annual meeting of the American Society of Clinical Oncology.
The conclusion is based on follow-up data on 126 patients who achieved a sustained deep molecular response (MR4.5) after switching from imatinib (Gleevec) to nilotinib (Tasigna) and discontinued nilotinib. So far, these are the largest prospective treatment-free remission data set in a population of patients who achieved a sustained deep molecular response after switching from imatinib to nilotinib, Dr. Hughes, head of hematology at the University of Adelaide and his colleagues wrote in a poster presentation.
The ENESTop study is a single-arm, phase II study. Patients eligible for the study started treatment with imatinib when they were first diagnosed with CML, then switched to nilotinib for at least 2 years with the combined time on the drugs of at least 3 years and small amounts of leukemia cells remaining after the nilotinib treatment.
For the consolidation phase of the study, patients continued their nilotinib therapy for 1 year. Patients without confirmed loss of MR4.5 after 1 year were eligible to stop nilotinib. RQ-PCR (reverse transcriptase–polymerase chain reaction) was monitored every 12 weeks in the consolidation phase of the study and every 4 weeks during first 48 weeks of treatment-free remission. Nilotinib was restarted if patients had confirmed loss of deep molecular response (MR4 [consecutive BCR-ABL1IS greater than 0.01%]) or loss of major molecular response ([MMR] BCR-ABL1IS greater than 0.1%).
Of the 163 patients in the consolidation phase of the study, 126 entered treatment-free remission. Their median duration of tyrosine kinase inhibitor use prior to treatment-free remission was nearly 88 months, with a 53-month median duration of nilotinib therapy. At data cut-off, with median follow up of 50 weeks, 58% of the 126 patients were still in treatment-free remission at 48 weeks.
During treatment-free remission, 18 patients had confirmed loss of MR4 and 34 lost MMR. One patient had atypical transcript and came off the study. All but one of the 52 patients reinitiated nilotinib; 50 (98%) regained at least MMR by data cut-off, 48 (94%) regained MR4, and 47 (92%) regained MR4.5. One patient switched to another tyrosine kinase inhibitor at 22 weeks after restarting therapy.
Of those who restarted therapy, the median time was 12 weeks to regain MR4 and was 13 weeks to regain MR4.5. No new safety findings were observed on treatment.
The study is sponsored by Novartis, the maker of nilotinib (Tasigna). Dr. Hughes receives research support and honoraria from, and is a consultant or advisor to Novartis as well as Ariad and Bristol-Myers Squibb.
On Twitter @maryjodales
Treatment-free remission attempts are safe and are achievable in most patients with chronic myeloid leukemia (CML) in chronic phase, Timothy P. Hughes, MD, and his colleagues in the international ENESTop trial reported at the annual meeting of the American Society of Clinical Oncology.
The conclusion is based on follow-up data on 126 patients who achieved a sustained deep molecular response (MR4.5) after switching from imatinib (Gleevec) to nilotinib (Tasigna) and discontinued nilotinib. So far, these are the largest prospective treatment-free remission data set in a population of patients who achieved a sustained deep molecular response after switching from imatinib to nilotinib, Dr. Hughes, head of hematology at the University of Adelaide and his colleagues wrote in a poster presentation.
The ENESTop study is a single-arm, phase II study. Patients eligible for the study started treatment with imatinib when they were first diagnosed with CML, then switched to nilotinib for at least 2 years with the combined time on the drugs of at least 3 years and small amounts of leukemia cells remaining after the nilotinib treatment.
For the consolidation phase of the study, patients continued their nilotinib therapy for 1 year. Patients without confirmed loss of MR4.5 after 1 year were eligible to stop nilotinib. RQ-PCR (reverse transcriptase–polymerase chain reaction) was monitored every 12 weeks in the consolidation phase of the study and every 4 weeks during first 48 weeks of treatment-free remission. Nilotinib was restarted if patients had confirmed loss of deep molecular response (MR4 [consecutive BCR-ABL1IS greater than 0.01%]) or loss of major molecular response ([MMR] BCR-ABL1IS greater than 0.1%).
Of the 163 patients in the consolidation phase of the study, 126 entered treatment-free remission. Their median duration of tyrosine kinase inhibitor use prior to treatment-free remission was nearly 88 months, with a 53-month median duration of nilotinib therapy. At data cut-off, with median follow up of 50 weeks, 58% of the 126 patients were still in treatment-free remission at 48 weeks.
During treatment-free remission, 18 patients had confirmed loss of MR4 and 34 lost MMR. One patient had atypical transcript and came off the study. All but one of the 52 patients reinitiated nilotinib; 50 (98%) regained at least MMR by data cut-off, 48 (94%) regained MR4, and 47 (92%) regained MR4.5. One patient switched to another tyrosine kinase inhibitor at 22 weeks after restarting therapy.
Of those who restarted therapy, the median time was 12 weeks to regain MR4 and was 13 weeks to regain MR4.5. No new safety findings were observed on treatment.
The study is sponsored by Novartis, the maker of nilotinib (Tasigna). Dr. Hughes receives research support and honoraria from, and is a consultant or advisor to Novartis as well as Ariad and Bristol-Myers Squibb.
On Twitter @maryjodales
FROM 2016 ASCO ANNUAL MEETING
Key clinical point: Treatment-free remission attempts are safe and are achievable in most patients with chronic myeloid leukemia in chronic phase.
Major finding: At data cut-off, with median follow-up of 50 weeks, 58% of the 126 patients who entered the treatment-free stage of the study were still in treatment-free remission at 48 weeks.
Data source: The ENESTop study is a single-arm, phase II study that included 163 patients.
Disclosures: The study is sponsored by Novartis, the maker of nilotinib (Tasigna). Dr. Hughes receives research support and honoraria from, and is a consultant or advisor to Novartis as well as Ariad and Bristol-Myers Squibb.