User login
Anastrozole-Induced Subacute Cutaneous Lupus Erythematosus
Drug-induced subacute cutaneous lupus erythematosus (DI-SCLE) was first described in 1985 in 5 patients who had been taking hydrochlorothiazide.1 The skin lesions in these patients were identical to those seen in idiopathic subacute cutaneous lupus erythematosus (SCLE) and were accompanied by the same autoantibodies (anti-Ro/Sjögren syndrome antigen A [SS-A] and anti-La/Sjögren syndrome antigen B [SS-B]) and HLA type (HLA-DR2/DR3) that are known to be associated with idiopathic SCLE. The skin lesions of SCLE in these 5 patients resolved spontaneously after discontinuing hydrochlorothiazide; however, anti-Ro/SS-A antibodies persisted in all except 1 patient.1 Over the last decade, an increasing number of drugs from different classes have been implicated to be associated with DI-SCLE. Since the concept of DI-SCLE was introduced, it has been reported to look identical to idiopathic SCLE, both clinically and histopathologically; however, one report suggested that the 2 entities can be distinguished based on clinical variations.2 In general, patients with DI-SCLE develop the same anti-Ro antibodies as seen in idiopathic SCLE. In addition, although the rash in DI-SCLE typically resolves with withdrawal of the offending drug, the antibodies tend to persist. Herein, we report a case of a patient being treated with an aromatase inhibitor who presented with clinical, serologic, and histopathologic evidence of DI-SCLE.
Case Report
A 69-year-old woman diagnosed with breast cancer 4 years prior to her presentation to dermatology initially underwent a lumpectomy and radiation treatment. She was subsequently started on anastrozole 2 years later. After 16 months of treatment with anastrozole, she developed an erythematous scaly rash on sun-exposed areas of the skin. The patient was seen by an outside dermatologist who treated her for a patient-perceived drug rash based on biopsy results that simply demonstrated interface dermatitis. She was treated with both topical and oral steroids with little improvement and therefore presented to our office approximately 6 months after starting treatment seeking a second opinion.
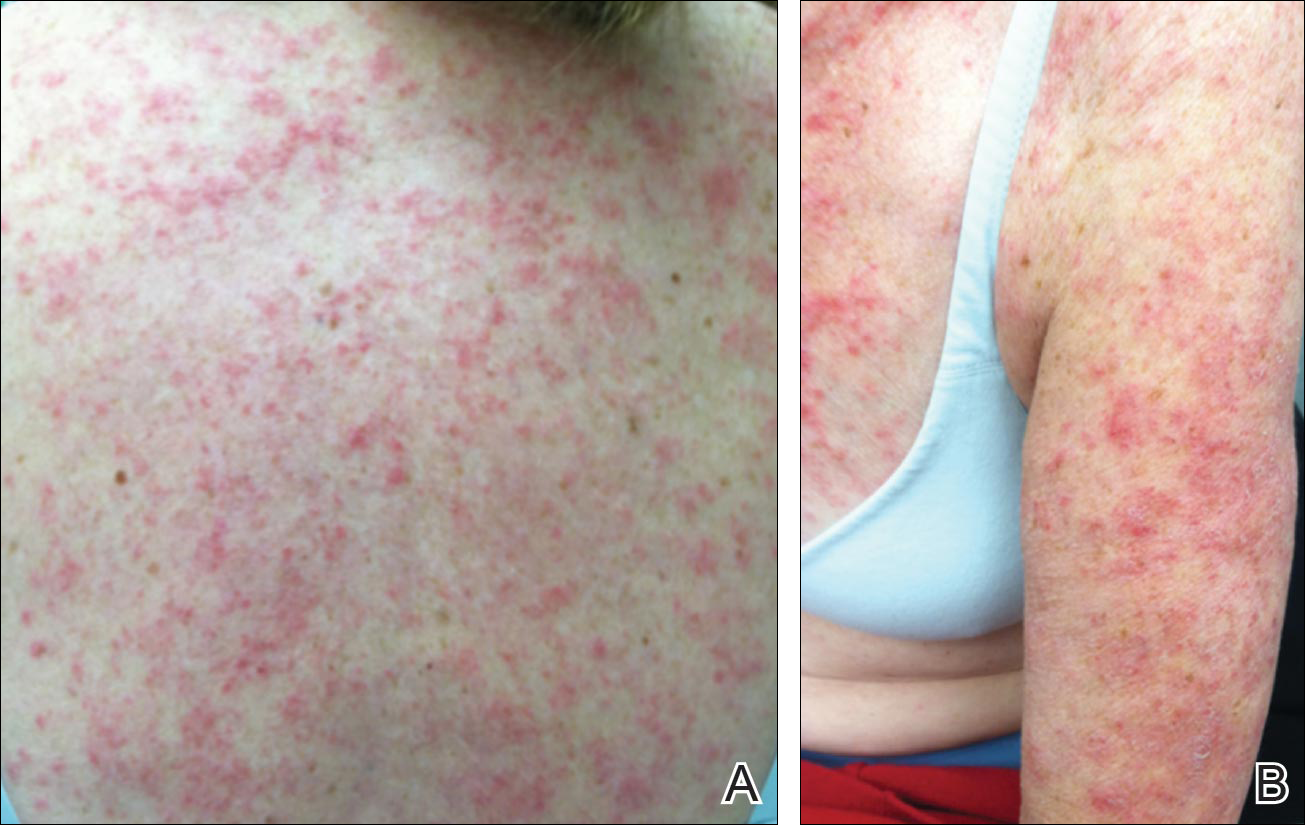
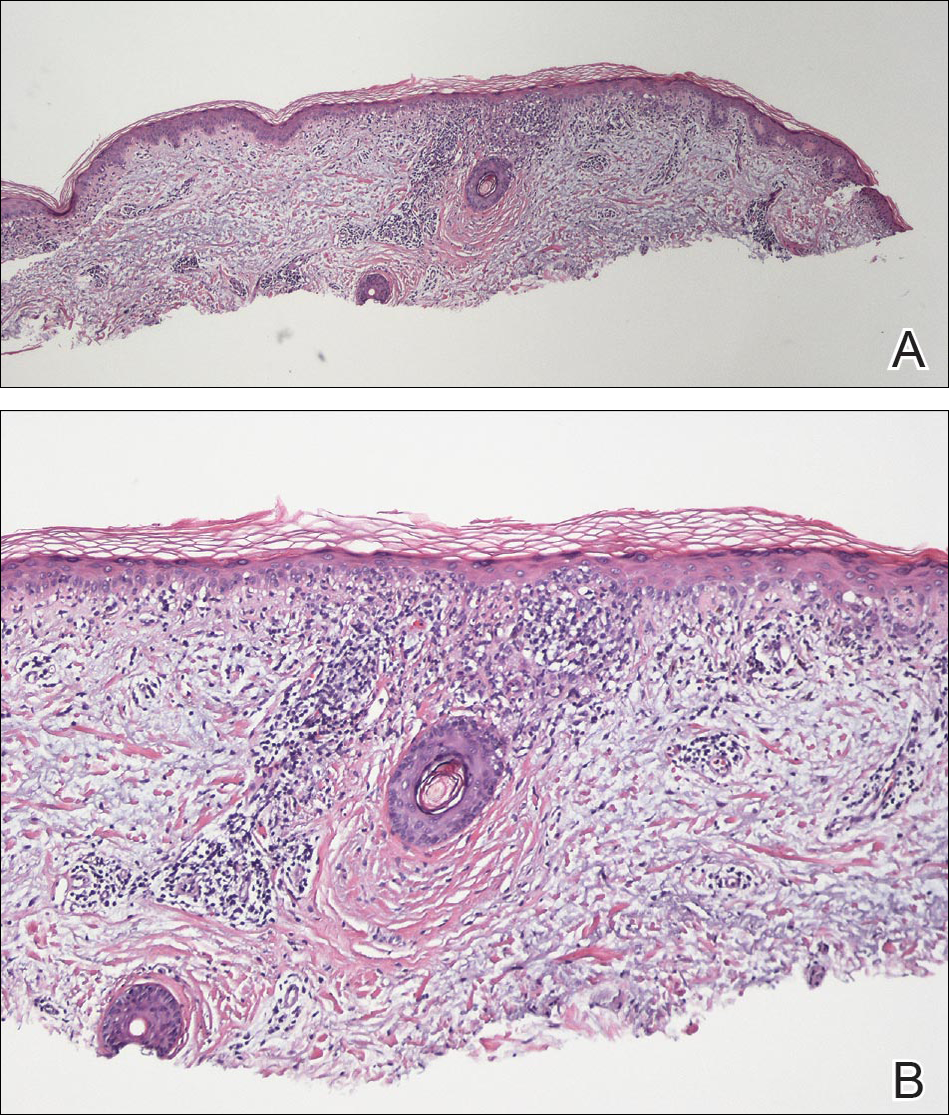
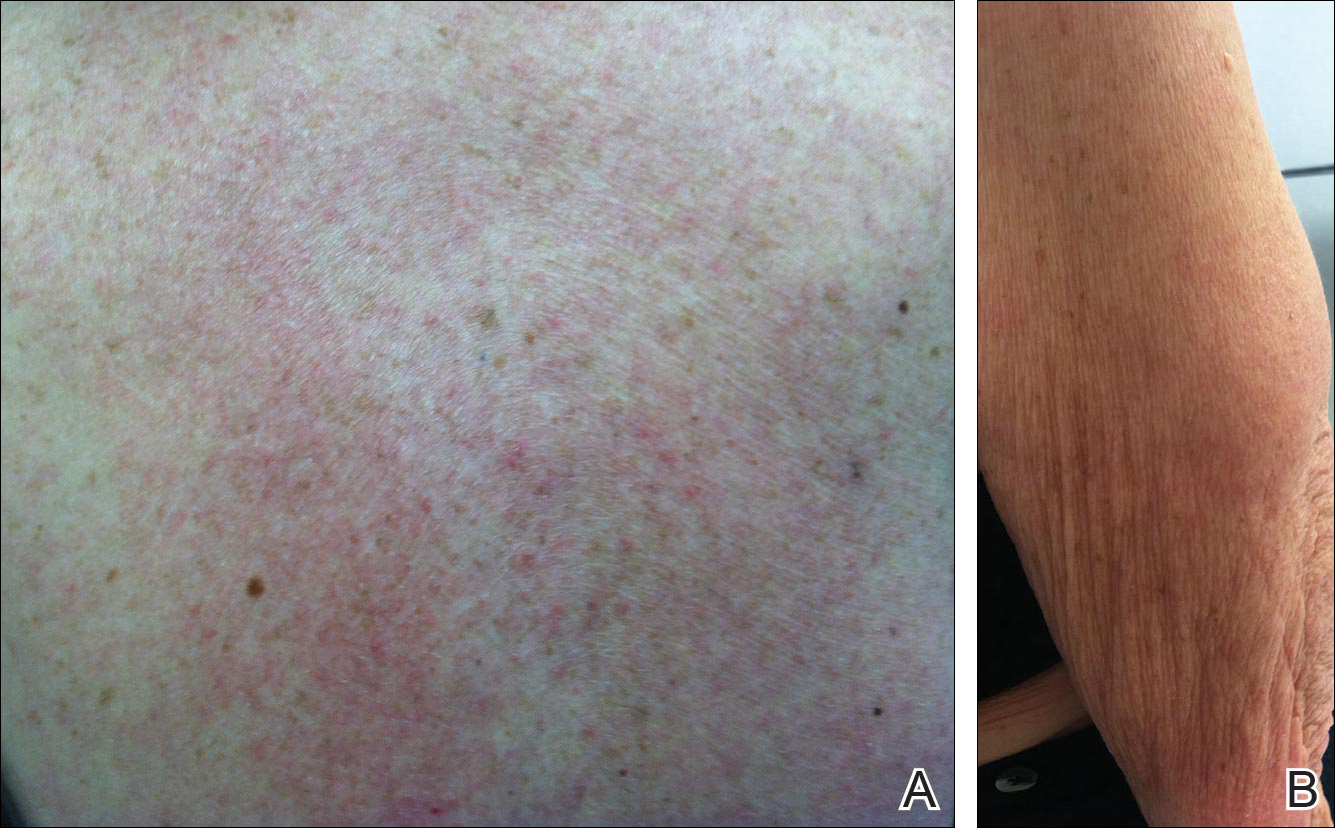
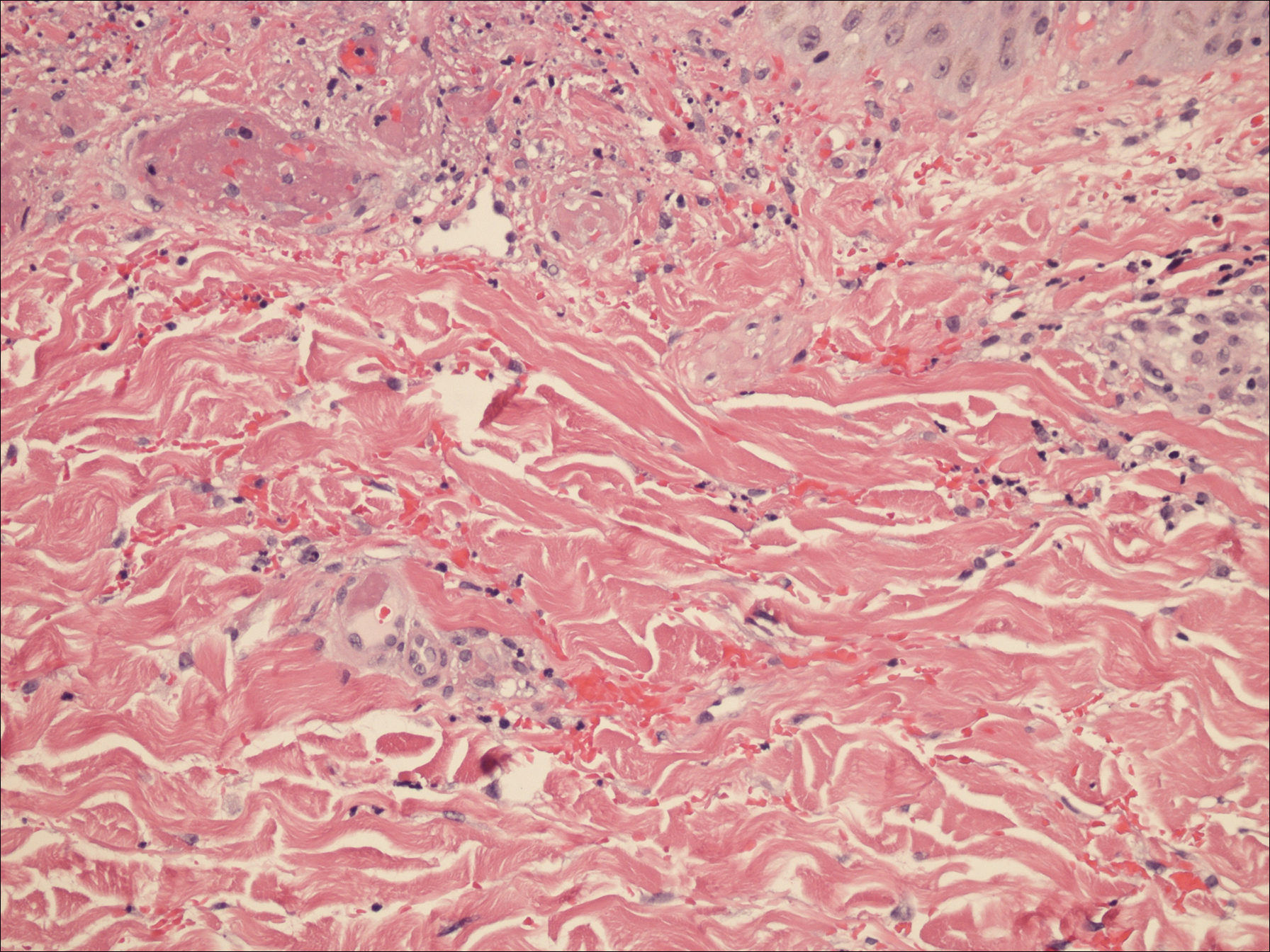
Physical examination revealed numerous erythematous scaly papules and plaques in a photodistributed pattern on the chest, back, legs, and arms (Figure 1). On further questioning, the patient noted that the rash became worse when she was at the beach or playing tennis outside as well as under indoor lights. A repeat biopsy was performed, revealing interface and perivascular dermatitis with an infiltrate composed of lymphocytes, histiocytes, and scattered pigment-laden macrophages (Figure 2). Given the appearance and distribution of the rash as well as the clinical scenario, drug-induced lupus was suspected. Anastrozole was the only medication being taken. Laboratory evaluation was performed and was negative for antinuclear antibodies, antihistone antibodies, and anti-La/SS-B antibodies but was positive for anti-Ro/SS-A antibodies (>8.0 U [reference range, <1.0 U]). Based on these findings, anastrozole-induced SCLE was the most likely explanation for this presentation. The patient was started on a sun-protective regimen (ie, wide-brimmed hat, daily sunscreen) and anastrozole was discontinued by her oncologist; the combination led to moderate improvement in symptoms. One week later, oral hydroxychloroquine 200 mg twice daily was started, which led to notable improvement (Figure 3). The patient was seen for 2 additional follow-up visits, each time with sustained resolution of the rash. The hydroxychloroquine was then stopped at her last visit 3 months after diagnosis. The patient was subsequently lost to follow-up.
Comment
Presentation of SCLE
Subacute cutaneous lupus erythematosus is a form of lupus erythematosus characterized by nonscarring, annular, scaly, erythematous plaques that occur on sun-exposed skin. The lesions are classically distributed on the upper back, chest, dorsal arms, and lateral neck but also can be found in other locations.3,4 Subacute cutaneous lupus erythematosus may be idiopathic; may occur in patients with systemic lupus erythematosus, Sjögren syndrome, or deficiency of the second component of complement (C2d); or may be drug induced.5 On histology SCLE presents as a lichenoid tissue reaction with focal vacuolization of the epidermal basal layer and perivascular lymphocytic infiltrate. On direct immunofluorescence, both idiopathic and drug-induced SCLE present with granular deposition of IgM, IgG, and C3 in a bandlike array at the dermoepidermal junction and circulating anti-Ro/SS-A antibodies. Therefore, histopathologically and immunologically, DI-SCLE is indistinguishable from idiopathic cases.6
Differential Diagnosis
It was previously thought that the clinical presentation of DI-SCLE and idiopathic SCLE were indistinguishable; however, Marzano et al2 described remarkable differences in the cutaneous manifestations of the 2 diseases. Drug-induced SCLE lesions are more widespread, occur more frequently on the legs, and may be bullous or erythema multiforme–like versus the idiopathic lesions, which tend to be more concentrated on the upper body and classically present as scaly erythematous plaques. Additionally, malar rash and vasculitic lesions, such as purpura and necrotic-ulcerative lesions, are seen more often in DI-SCLE.
Drug-induced systemic lupus erythematosus (DI-SLE) is a lupuslike syndrome that can be differentiated from DI-SCLE by virtue of its clinical and serological presentation. It differs from DI-SCLE in that DI-SLE typically does not present with skin symptoms; rather, systemic symptoms such as fever, weight loss, arthralgia, polyarthritis, pericarditis, and pleuritis are more commonly seen. Additionally, it has been associated with antihistone antibodies.4 More than 80 drugs have been reported to cause DI-SLE, including procainamide, hydralazine, and quinidine.7
To be classified as either DI-SCLE or DI-SLE, symptoms need to present after administration of the triggering drug and must resolve after the drug is discontinued.7 The drugs most commonly associated with DI-SCLE are thiazides, calcium channel blockers, tumor necrosis factor α inhibitors, angiotensin-converting enzyme inhibitors, and terbinafine, with few cases citing anastrozole as the inciting agent.4,6,8,9 The incubation period for DI-SCLE varies substantially. Thiazide diuretics and calcium channel blockers typically have the longest incubation period, ranging from 6 months to 5 years for thiazides,1,6,10,11 while calcium channel blockers have an average incubation period of 3 years.12 Drug-induced SCLE associated with antifungals, however, usually is much more rapid in onset; the incubation period on average is 5 weeks for terbinafine and 2 weeks for griseofulvin.13-15
Antiestrogen Drugs and SCLE
Anastrozole, the inciting agent in our case, is a third-generation, selective, nonsteroidal, aromatase inhibitor with no progestogenic, androgenic, or estrogenic activity. Anastrozole, when taken at its recommended dosage of 1 mg daily, will suppress estradiol. It is used as an adjuvant treatment of estrogen-sensitive breast cancer in postmenopausal women. In contrast to a prior case of DI-SCLE secondary to anastrozole in which the incubation period was approximately 1 month,8 our patient had an incubation period of approximately 16 months. Tamoxifen, another antiestrogen drug, also has been associated with DI-SCLE.9 In cases of tamoxifen-induced SCLE, the incubation period was several years, which is more similar to our patient. Although these drugs do not have the same mechanism of action, they both have antiestrogen properties.9 A systemic review of DI-SCLE reported that incubation periods between drug exposure and appearance of DI-SCLE varied greatly and were drug class dependent. It is possible that reactions associated with antiestrogen medications have a delayed presentation; however, given there are limited cases of anastrozole-induced DI-SCLE, we cannot make a clear statement on incubation periods.6
Reports of DI-SCLE caused by antiestrogen drugs are particularly interesting because sex hormones in relation to lupus disease activity have been the subject of debate for decades. Women are considerably more likely to develop autoimmune diseases than men, suggesting that steroid hormones, especially estrogen and progesterone, influence the immune system.16 Estrogen actions are proinflammatory, while the actions of progesterone, androgens, and glucocorticoids are anti-inflammatory.17 Studies in women with lupus revealed an increased rate of mild- to moderate-intensity disease flares associated with estrogen-containing hormone replace-ment therapy.18-20
Over the years, several antiestrogen therapies have been used in murine models, which showed remarkable clinical improvement in the course of SLE. The precise mechanisms involved in disease immunomodulation by these therapies have not been elucidated.21-23 It is thought that estrogen plays a role in the synthesis and expression of Ro antigens on the surface of keratinocytes, increasing the fixation of anti-Ro antibodies in keratinocytes and provoking the appearance of a cutaneous eruption in patients with a susceptible HLA profile.6
Conclusion
We report a rare case of SCLE induced by anastrozole use. Cases such as ours and others that implicate antiestrogen drugs in association with DI-SCLE are particularly noteworthy, considering many studies are looking at the potential usefulness of antiestrogen therapy in the treatment of SLE. Further research on this relationship is warranted.
- Reed B, Huff J, Jones S, et al. Subacute cutaneous lupus erythematosus associated with hydrochlorothiazide therapy. Ann Intern Med. 1985;103:49-51.
- Marzano A, Lazzari R, Polloni I, et al. Drug-induced subacute cutaneous lupus erythematosus: evidence for differences from its idiopathic counterpart. Br J Dermatol. 2011;165:335-341.
- Bonsmann G, Schiller M, Luger T, et al. Terbinafine-induced subacute cutaneous lupus erythematosus. J Am Acad Dermatol. 2001;44:925-931.
- Callen J. Review: drug induced subacute cutaneous lupus erythematosus. Lupus. 2010;19:1107-1111.
- Lin J, Callen JP. Subacute cutaneous lupus erythematosus (SCLE). Medscape website. http://emedicine.medscape.com/article/1065657-overview. Updated March 7, 2016. Accessed April 29, 2016.
- Lowe GC, Henderson CL, Grau RH, et al. A systematic review of drug-induced subacute cutaneous lupus erythematosus. Br J Dermatol. 2011;164:465-472.
- Vedove C, Giglio M, Schena D, et al. Drug-induced lupus erythematosus. Arch Dermatol Res. 2009;301:99-105.
- Trancart M, Cavailhes A, Balme B, et al. Anastrozole-induced subacute cutaneous lupus erythematosus [published online December 6, 2007]. Br J Dermatol. 2008;158:628-629.
- Fumal I, Danchin A, Cosserat F, et al. Subacute cutaneous lupus erythematosus associated with tamoxifen therapy: two cases. Dermatology. 2005;210:251-252.
- Brown C, Deng J. Thiazide diuretics induce cutaneous lupus-like adverse reaction. J Toxicol Clin Toxicol. 1995;33:729-733.
- Sontheimer R. Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmun Rev. 2005;4:253-263.
- Crowson A, Magro C. Subacute cutaneous lupus erythematosus arising in the setting of calcium channel blocker therapy. Hum Pathol. 1997;28:67-73.
- Lorentz K, Booken N, Goerdt S, et al. Subacute cutaneous lupus erythematosus induced by terbinafine: case report and review of literature. J Dtsch Dermatol Ges. 2008;6:823-837.
- Kasperkiewicz M, Anemüller W, Angelova-Fischer I, et al. Subacute cutaneous lupus erythematosus associated with terbinafine. Clin Exp Dermatol. 2009;34:403-404.
- Miyagawa S, Okuchi T, Shiomi Y, et al. Subacute cutaneous lupus erythematosus lesions precipitated by griseofulvin. J Am Acad Dermatol. 1989;21:343-346.
- Inman RD. Immunologic sex differences and the female predominance in systemic lupus erythematosus. Arthritis Rheum. 1978;21:849-854.
- Cutolo M, Wilder RL. Different roles of androgens and estrogens in the susceptibility to autoimmune rheumatic diseases. Rheum Dis Clin North Am. 2000;26:825-839.
- Petri M. Sex hormones and systemic lupus erythematosus. Lupus. 2008;17:412-415.
- Lateef A, Petri M. Hormone replacement and contraceptive therapy in autoimmune diseases [published online January 18, 2012]. J Autoimmun. 2012;38:J170-J176.
- Buyon JP, Petri M, Kim MY, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med. 2005;142:954-962.
- Wu W, Suen J, Lin B, et al. Tamoxifen alleviates disease severity and decreases double negative T cells in autoimmune MRL-lpr/lpr mice. Immunology. 2000;100:110-118.
- Dayan M, Zinger H, Kalush F, et al. The beneficial effects of treatment with tamoxifen and anti-oestradiol antibody on experimental systemic lupus erythematosus are associated with cytokine modulations. Immunology. 1997;90:101-108.
- Sthoeger Z, Zinger H, Mozes E. Beneficial effects of the anti-oestrogen tamoxifen on systemic lupus erythematosus of (NZBxNZW)F1 female mice are associated with specific reduction of IgG3 autoantibodies. Ann Rheum Dis. 2003;62:341-346.
Drug-induced subacute cutaneous lupus erythematosus (DI-SCLE) was first described in 1985 in 5 patients who had been taking hydrochlorothiazide.1 The skin lesions in these patients were identical to those seen in idiopathic subacute cutaneous lupus erythematosus (SCLE) and were accompanied by the same autoantibodies (anti-Ro/Sjögren syndrome antigen A [SS-A] and anti-La/Sjögren syndrome antigen B [SS-B]) and HLA type (HLA-DR2/DR3) that are known to be associated with idiopathic SCLE. The skin lesions of SCLE in these 5 patients resolved spontaneously after discontinuing hydrochlorothiazide; however, anti-Ro/SS-A antibodies persisted in all except 1 patient.1 Over the last decade, an increasing number of drugs from different classes have been implicated to be associated with DI-SCLE. Since the concept of DI-SCLE was introduced, it has been reported to look identical to idiopathic SCLE, both clinically and histopathologically; however, one report suggested that the 2 entities can be distinguished based on clinical variations.2 In general, patients with DI-SCLE develop the same anti-Ro antibodies as seen in idiopathic SCLE. In addition, although the rash in DI-SCLE typically resolves with withdrawal of the offending drug, the antibodies tend to persist. Herein, we report a case of a patient being treated with an aromatase inhibitor who presented with clinical, serologic, and histopathologic evidence of DI-SCLE.
Case Report
A 69-year-old woman diagnosed with breast cancer 4 years prior to her presentation to dermatology initially underwent a lumpectomy and radiation treatment. She was subsequently started on anastrozole 2 years later. After 16 months of treatment with anastrozole, she developed an erythematous scaly rash on sun-exposed areas of the skin. The patient was seen by an outside dermatologist who treated her for a patient-perceived drug rash based on biopsy results that simply demonstrated interface dermatitis. She was treated with both topical and oral steroids with little improvement and therefore presented to our office approximately 6 months after starting treatment seeking a second opinion.
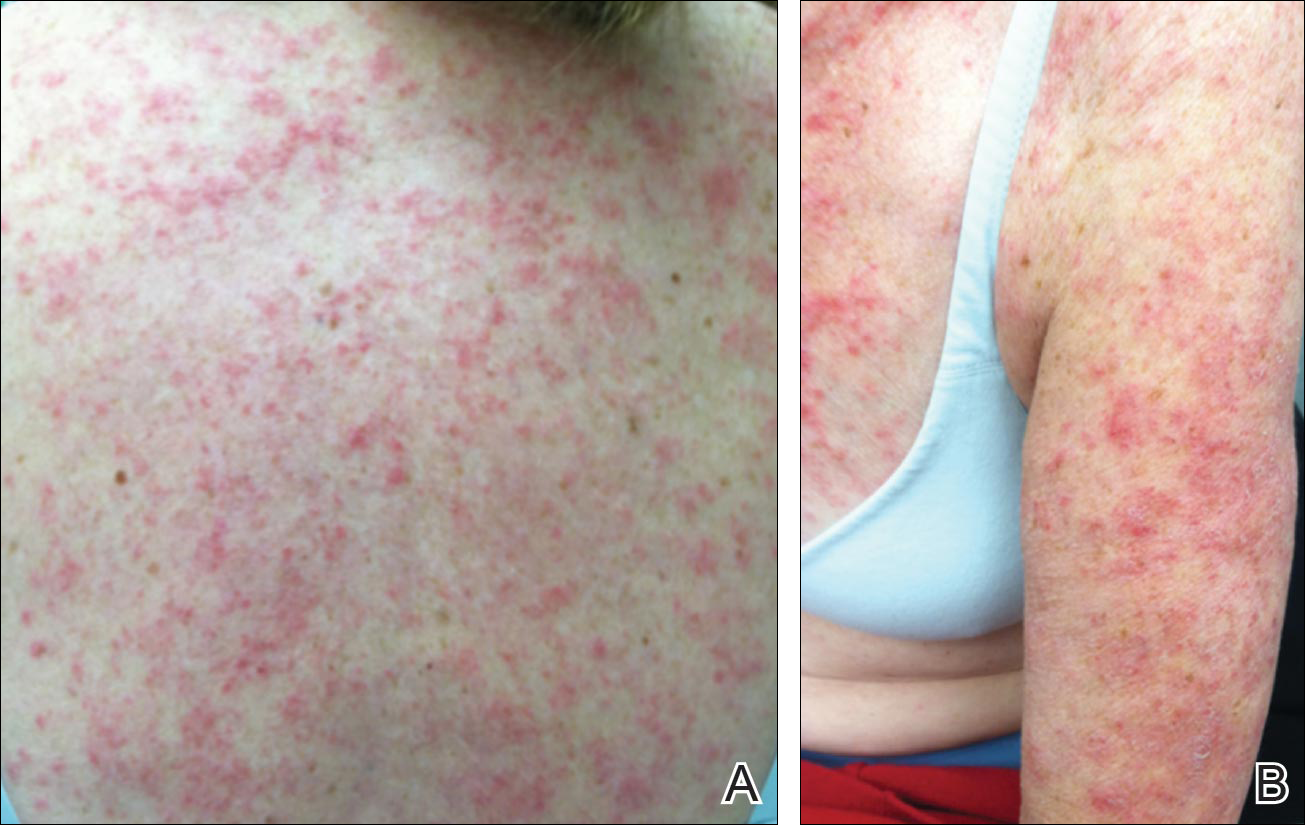
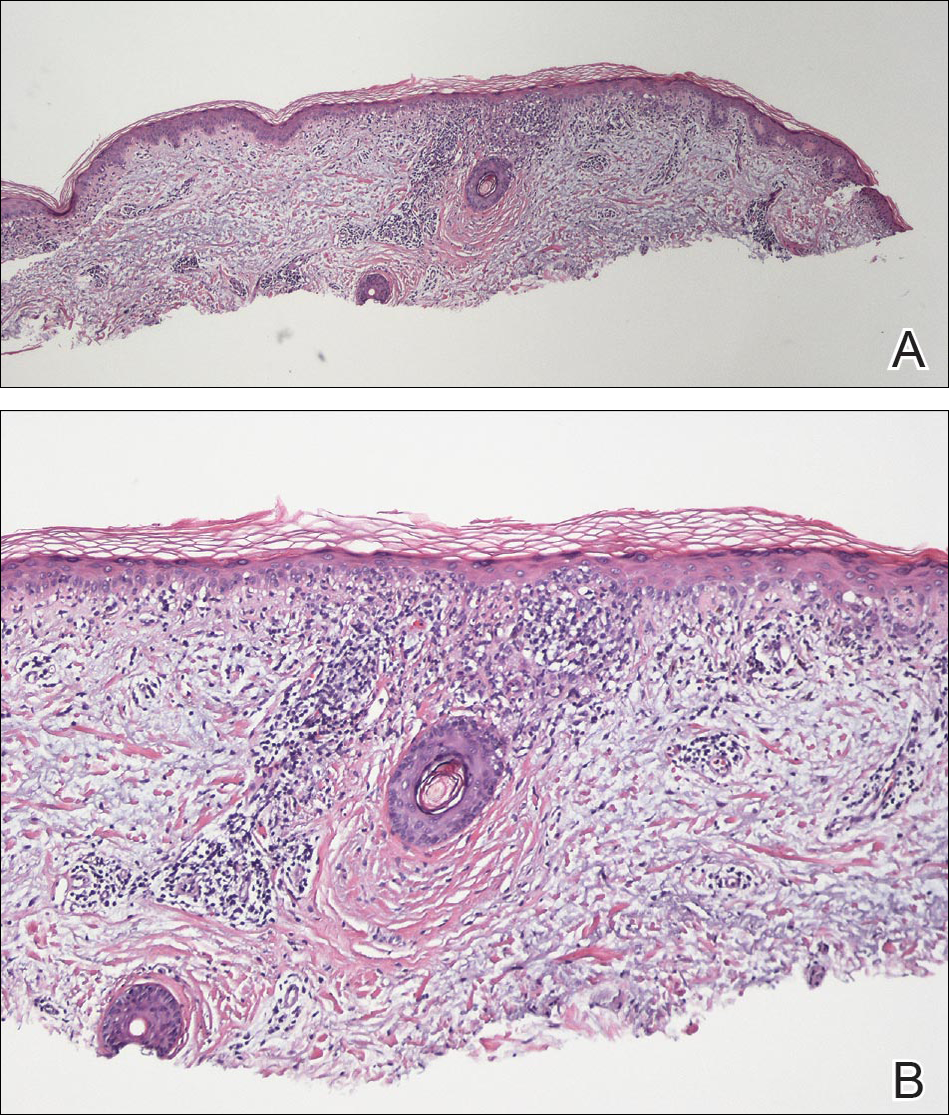
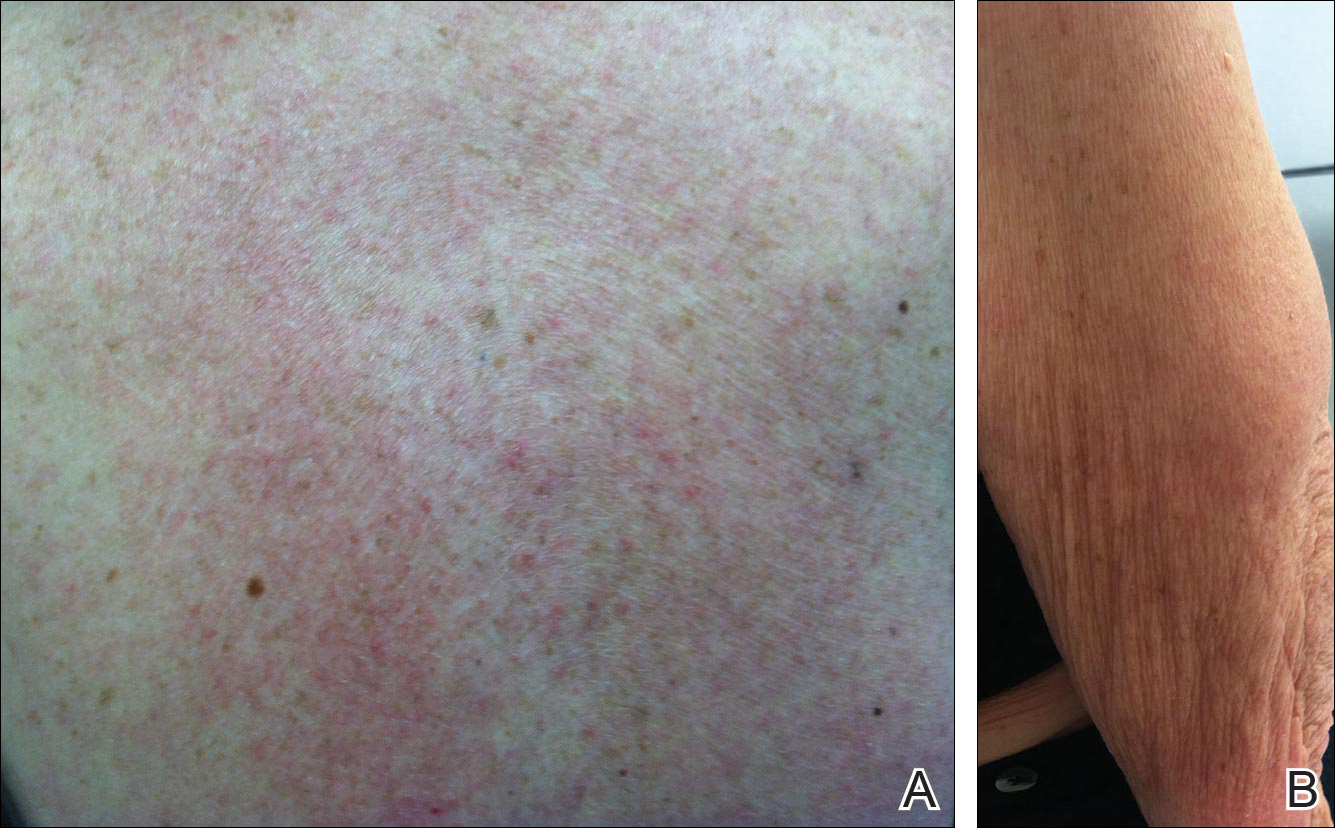
Physical examination revealed numerous erythematous scaly papules and plaques in a photodistributed pattern on the chest, back, legs, and arms (Figure 1). On further questioning, the patient noted that the rash became worse when she was at the beach or playing tennis outside as well as under indoor lights. A repeat biopsy was performed, revealing interface and perivascular dermatitis with an infiltrate composed of lymphocytes, histiocytes, and scattered pigment-laden macrophages (Figure 2). Given the appearance and distribution of the rash as well as the clinical scenario, drug-induced lupus was suspected. Anastrozole was the only medication being taken. Laboratory evaluation was performed and was negative for antinuclear antibodies, antihistone antibodies, and anti-La/SS-B antibodies but was positive for anti-Ro/SS-A antibodies (>8.0 U [reference range, <1.0 U]). Based on these findings, anastrozole-induced SCLE was the most likely explanation for this presentation. The patient was started on a sun-protective regimen (ie, wide-brimmed hat, daily sunscreen) and anastrozole was discontinued by her oncologist; the combination led to moderate improvement in symptoms. One week later, oral hydroxychloroquine 200 mg twice daily was started, which led to notable improvement (Figure 3). The patient was seen for 2 additional follow-up visits, each time with sustained resolution of the rash. The hydroxychloroquine was then stopped at her last visit 3 months after diagnosis. The patient was subsequently lost to follow-up.
Comment
Presentation of SCLE
Subacute cutaneous lupus erythematosus is a form of lupus erythematosus characterized by nonscarring, annular, scaly, erythematous plaques that occur on sun-exposed skin. The lesions are classically distributed on the upper back, chest, dorsal arms, and lateral neck but also can be found in other locations.3,4 Subacute cutaneous lupus erythematosus may be idiopathic; may occur in patients with systemic lupus erythematosus, Sjögren syndrome, or deficiency of the second component of complement (C2d); or may be drug induced.5 On histology SCLE presents as a lichenoid tissue reaction with focal vacuolization of the epidermal basal layer and perivascular lymphocytic infiltrate. On direct immunofluorescence, both idiopathic and drug-induced SCLE present with granular deposition of IgM, IgG, and C3 in a bandlike array at the dermoepidermal junction and circulating anti-Ro/SS-A antibodies. Therefore, histopathologically and immunologically, DI-SCLE is indistinguishable from idiopathic cases.6
Differential Diagnosis
It was previously thought that the clinical presentation of DI-SCLE and idiopathic SCLE were indistinguishable; however, Marzano et al2 described remarkable differences in the cutaneous manifestations of the 2 diseases. Drug-induced SCLE lesions are more widespread, occur more frequently on the legs, and may be bullous or erythema multiforme–like versus the idiopathic lesions, which tend to be more concentrated on the upper body and classically present as scaly erythematous plaques. Additionally, malar rash and vasculitic lesions, such as purpura and necrotic-ulcerative lesions, are seen more often in DI-SCLE.
Drug-induced systemic lupus erythematosus (DI-SLE) is a lupuslike syndrome that can be differentiated from DI-SCLE by virtue of its clinical and serological presentation. It differs from DI-SCLE in that DI-SLE typically does not present with skin symptoms; rather, systemic symptoms such as fever, weight loss, arthralgia, polyarthritis, pericarditis, and pleuritis are more commonly seen. Additionally, it has been associated with antihistone antibodies.4 More than 80 drugs have been reported to cause DI-SLE, including procainamide, hydralazine, and quinidine.7
To be classified as either DI-SCLE or DI-SLE, symptoms need to present after administration of the triggering drug and must resolve after the drug is discontinued.7 The drugs most commonly associated with DI-SCLE are thiazides, calcium channel blockers, tumor necrosis factor α inhibitors, angiotensin-converting enzyme inhibitors, and terbinafine, with few cases citing anastrozole as the inciting agent.4,6,8,9 The incubation period for DI-SCLE varies substantially. Thiazide diuretics and calcium channel blockers typically have the longest incubation period, ranging from 6 months to 5 years for thiazides,1,6,10,11 while calcium channel blockers have an average incubation period of 3 years.12 Drug-induced SCLE associated with antifungals, however, usually is much more rapid in onset; the incubation period on average is 5 weeks for terbinafine and 2 weeks for griseofulvin.13-15
Antiestrogen Drugs and SCLE
Anastrozole, the inciting agent in our case, is a third-generation, selective, nonsteroidal, aromatase inhibitor with no progestogenic, androgenic, or estrogenic activity. Anastrozole, when taken at its recommended dosage of 1 mg daily, will suppress estradiol. It is used as an adjuvant treatment of estrogen-sensitive breast cancer in postmenopausal women. In contrast to a prior case of DI-SCLE secondary to anastrozole in which the incubation period was approximately 1 month,8 our patient had an incubation period of approximately 16 months. Tamoxifen, another antiestrogen drug, also has been associated with DI-SCLE.9 In cases of tamoxifen-induced SCLE, the incubation period was several years, which is more similar to our patient. Although these drugs do not have the same mechanism of action, they both have antiestrogen properties.9 A systemic review of DI-SCLE reported that incubation periods between drug exposure and appearance of DI-SCLE varied greatly and were drug class dependent. It is possible that reactions associated with antiestrogen medications have a delayed presentation; however, given there are limited cases of anastrozole-induced DI-SCLE, we cannot make a clear statement on incubation periods.6
Reports of DI-SCLE caused by antiestrogen drugs are particularly interesting because sex hormones in relation to lupus disease activity have been the subject of debate for decades. Women are considerably more likely to develop autoimmune diseases than men, suggesting that steroid hormones, especially estrogen and progesterone, influence the immune system.16 Estrogen actions are proinflammatory, while the actions of progesterone, androgens, and glucocorticoids are anti-inflammatory.17 Studies in women with lupus revealed an increased rate of mild- to moderate-intensity disease flares associated with estrogen-containing hormone replace-ment therapy.18-20
Over the years, several antiestrogen therapies have been used in murine models, which showed remarkable clinical improvement in the course of SLE. The precise mechanisms involved in disease immunomodulation by these therapies have not been elucidated.21-23 It is thought that estrogen plays a role in the synthesis and expression of Ro antigens on the surface of keratinocytes, increasing the fixation of anti-Ro antibodies in keratinocytes and provoking the appearance of a cutaneous eruption in patients with a susceptible HLA profile.6
Conclusion
We report a rare case of SCLE induced by anastrozole use. Cases such as ours and others that implicate antiestrogen drugs in association with DI-SCLE are particularly noteworthy, considering many studies are looking at the potential usefulness of antiestrogen therapy in the treatment of SLE. Further research on this relationship is warranted.
Drug-induced subacute cutaneous lupus erythematosus (DI-SCLE) was first described in 1985 in 5 patients who had been taking hydrochlorothiazide.1 The skin lesions in these patients were identical to those seen in idiopathic subacute cutaneous lupus erythematosus (SCLE) and were accompanied by the same autoantibodies (anti-Ro/Sjögren syndrome antigen A [SS-A] and anti-La/Sjögren syndrome antigen B [SS-B]) and HLA type (HLA-DR2/DR3) that are known to be associated with idiopathic SCLE. The skin lesions of SCLE in these 5 patients resolved spontaneously after discontinuing hydrochlorothiazide; however, anti-Ro/SS-A antibodies persisted in all except 1 patient.1 Over the last decade, an increasing number of drugs from different classes have been implicated to be associated with DI-SCLE. Since the concept of DI-SCLE was introduced, it has been reported to look identical to idiopathic SCLE, both clinically and histopathologically; however, one report suggested that the 2 entities can be distinguished based on clinical variations.2 In general, patients with DI-SCLE develop the same anti-Ro antibodies as seen in idiopathic SCLE. In addition, although the rash in DI-SCLE typically resolves with withdrawal of the offending drug, the antibodies tend to persist. Herein, we report a case of a patient being treated with an aromatase inhibitor who presented with clinical, serologic, and histopathologic evidence of DI-SCLE.
Case Report
A 69-year-old woman diagnosed with breast cancer 4 years prior to her presentation to dermatology initially underwent a lumpectomy and radiation treatment. She was subsequently started on anastrozole 2 years later. After 16 months of treatment with anastrozole, she developed an erythematous scaly rash on sun-exposed areas of the skin. The patient was seen by an outside dermatologist who treated her for a patient-perceived drug rash based on biopsy results that simply demonstrated interface dermatitis. She was treated with both topical and oral steroids with little improvement and therefore presented to our office approximately 6 months after starting treatment seeking a second opinion.
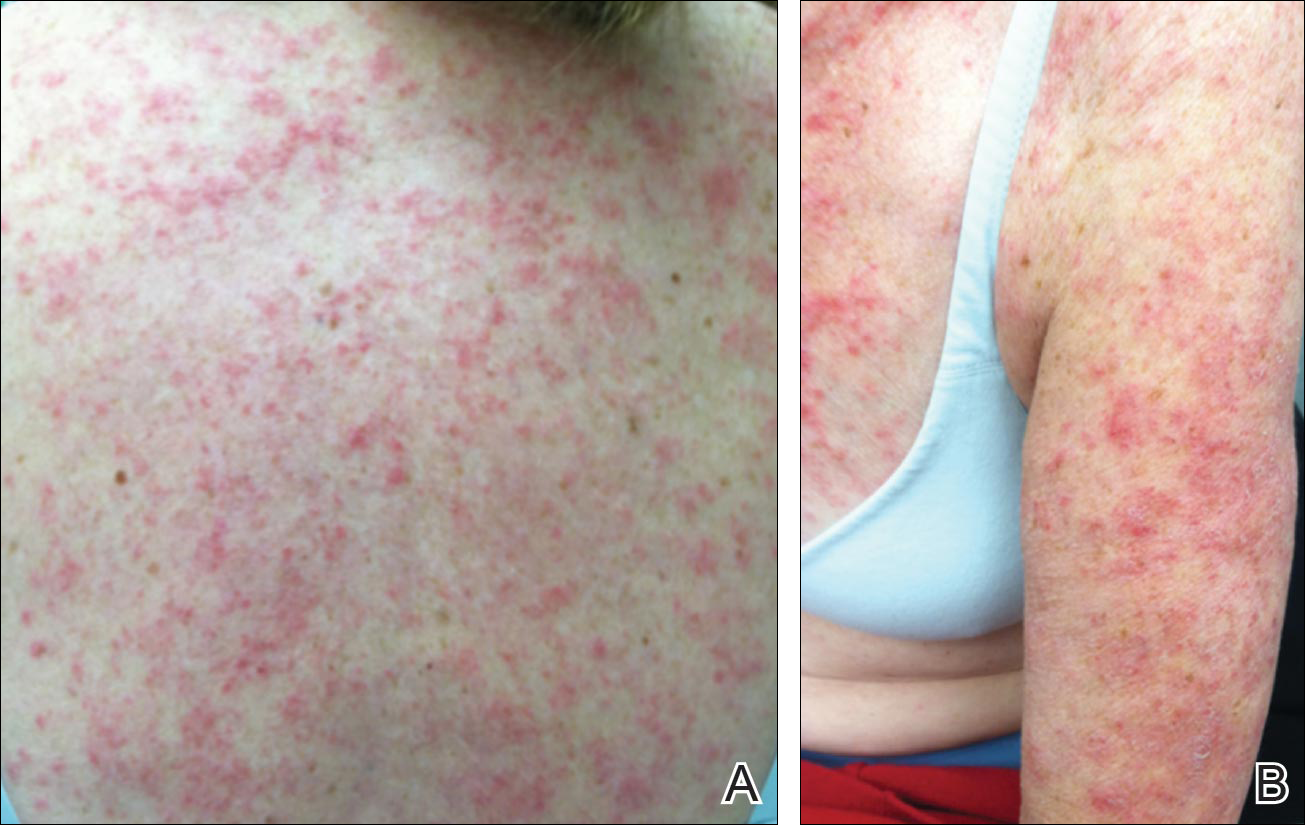
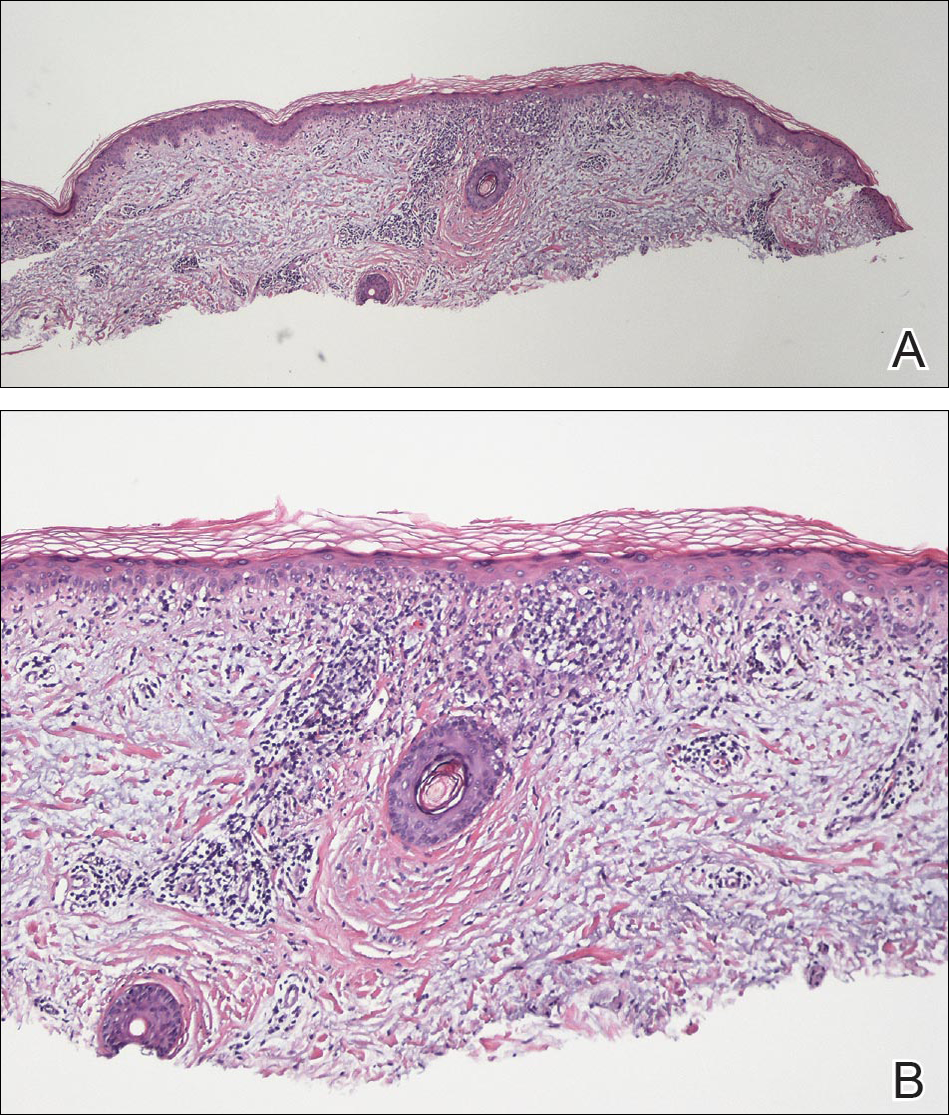
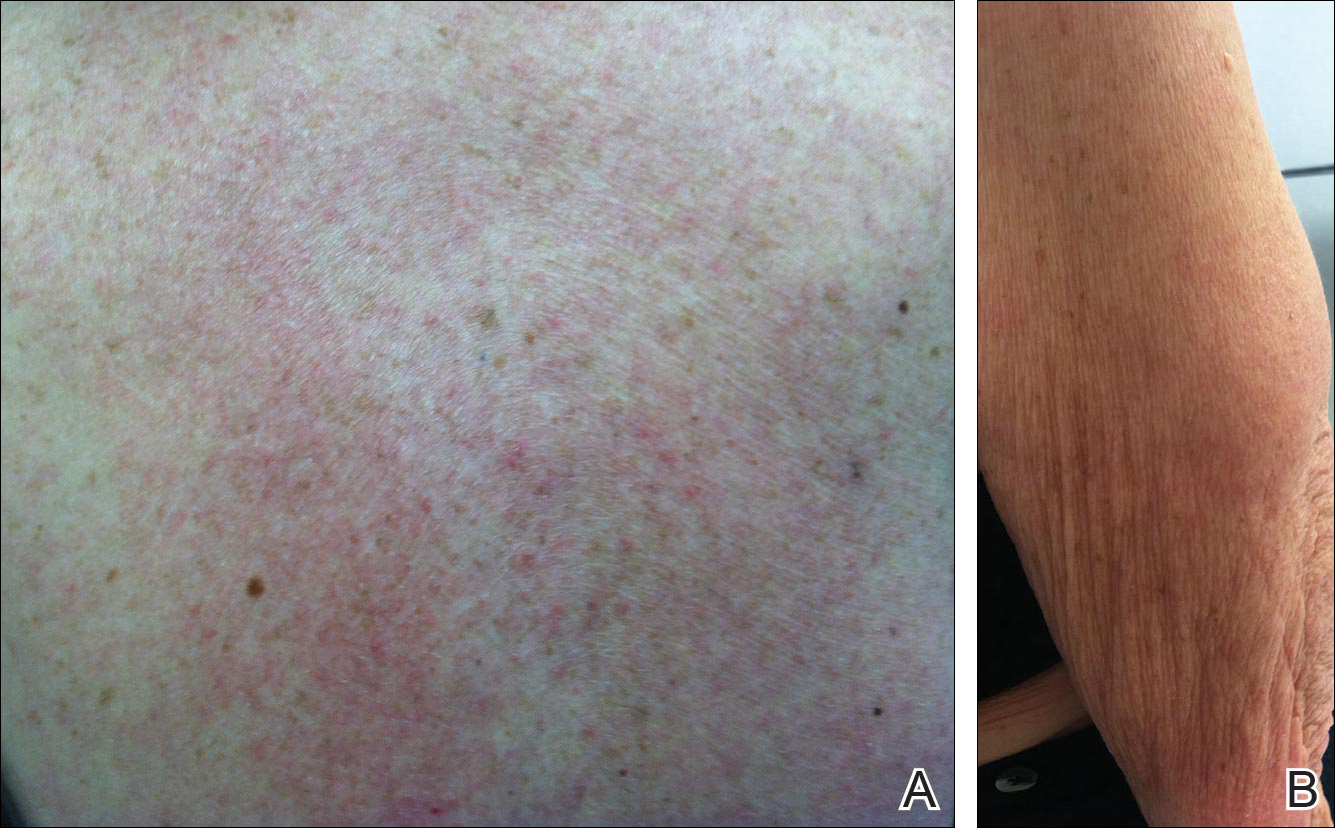
Physical examination revealed numerous erythematous scaly papules and plaques in a photodistributed pattern on the chest, back, legs, and arms (Figure 1). On further questioning, the patient noted that the rash became worse when she was at the beach or playing tennis outside as well as under indoor lights. A repeat biopsy was performed, revealing interface and perivascular dermatitis with an infiltrate composed of lymphocytes, histiocytes, and scattered pigment-laden macrophages (Figure 2). Given the appearance and distribution of the rash as well as the clinical scenario, drug-induced lupus was suspected. Anastrozole was the only medication being taken. Laboratory evaluation was performed and was negative for antinuclear antibodies, antihistone antibodies, and anti-La/SS-B antibodies but was positive for anti-Ro/SS-A antibodies (>8.0 U [reference range, <1.0 U]). Based on these findings, anastrozole-induced SCLE was the most likely explanation for this presentation. The patient was started on a sun-protective regimen (ie, wide-brimmed hat, daily sunscreen) and anastrozole was discontinued by her oncologist; the combination led to moderate improvement in symptoms. One week later, oral hydroxychloroquine 200 mg twice daily was started, which led to notable improvement (Figure 3). The patient was seen for 2 additional follow-up visits, each time with sustained resolution of the rash. The hydroxychloroquine was then stopped at her last visit 3 months after diagnosis. The patient was subsequently lost to follow-up.
Comment
Presentation of SCLE
Subacute cutaneous lupus erythematosus is a form of lupus erythematosus characterized by nonscarring, annular, scaly, erythematous plaques that occur on sun-exposed skin. The lesions are classically distributed on the upper back, chest, dorsal arms, and lateral neck but also can be found in other locations.3,4 Subacute cutaneous lupus erythematosus may be idiopathic; may occur in patients with systemic lupus erythematosus, Sjögren syndrome, or deficiency of the second component of complement (C2d); or may be drug induced.5 On histology SCLE presents as a lichenoid tissue reaction with focal vacuolization of the epidermal basal layer and perivascular lymphocytic infiltrate. On direct immunofluorescence, both idiopathic and drug-induced SCLE present with granular deposition of IgM, IgG, and C3 in a bandlike array at the dermoepidermal junction and circulating anti-Ro/SS-A antibodies. Therefore, histopathologically and immunologically, DI-SCLE is indistinguishable from idiopathic cases.6
Differential Diagnosis
It was previously thought that the clinical presentation of DI-SCLE and idiopathic SCLE were indistinguishable; however, Marzano et al2 described remarkable differences in the cutaneous manifestations of the 2 diseases. Drug-induced SCLE lesions are more widespread, occur more frequently on the legs, and may be bullous or erythema multiforme–like versus the idiopathic lesions, which tend to be more concentrated on the upper body and classically present as scaly erythematous plaques. Additionally, malar rash and vasculitic lesions, such as purpura and necrotic-ulcerative lesions, are seen more often in DI-SCLE.
Drug-induced systemic lupus erythematosus (DI-SLE) is a lupuslike syndrome that can be differentiated from DI-SCLE by virtue of its clinical and serological presentation. It differs from DI-SCLE in that DI-SLE typically does not present with skin symptoms; rather, systemic symptoms such as fever, weight loss, arthralgia, polyarthritis, pericarditis, and pleuritis are more commonly seen. Additionally, it has been associated with antihistone antibodies.4 More than 80 drugs have been reported to cause DI-SLE, including procainamide, hydralazine, and quinidine.7
To be classified as either DI-SCLE or DI-SLE, symptoms need to present after administration of the triggering drug and must resolve after the drug is discontinued.7 The drugs most commonly associated with DI-SCLE are thiazides, calcium channel blockers, tumor necrosis factor α inhibitors, angiotensin-converting enzyme inhibitors, and terbinafine, with few cases citing anastrozole as the inciting agent.4,6,8,9 The incubation period for DI-SCLE varies substantially. Thiazide diuretics and calcium channel blockers typically have the longest incubation period, ranging from 6 months to 5 years for thiazides,1,6,10,11 while calcium channel blockers have an average incubation period of 3 years.12 Drug-induced SCLE associated with antifungals, however, usually is much more rapid in onset; the incubation period on average is 5 weeks for terbinafine and 2 weeks for griseofulvin.13-15
Antiestrogen Drugs and SCLE
Anastrozole, the inciting agent in our case, is a third-generation, selective, nonsteroidal, aromatase inhibitor with no progestogenic, androgenic, or estrogenic activity. Anastrozole, when taken at its recommended dosage of 1 mg daily, will suppress estradiol. It is used as an adjuvant treatment of estrogen-sensitive breast cancer in postmenopausal women. In contrast to a prior case of DI-SCLE secondary to anastrozole in which the incubation period was approximately 1 month,8 our patient had an incubation period of approximately 16 months. Tamoxifen, another antiestrogen drug, also has been associated with DI-SCLE.9 In cases of tamoxifen-induced SCLE, the incubation period was several years, which is more similar to our patient. Although these drugs do not have the same mechanism of action, they both have antiestrogen properties.9 A systemic review of DI-SCLE reported that incubation periods between drug exposure and appearance of DI-SCLE varied greatly and were drug class dependent. It is possible that reactions associated with antiestrogen medications have a delayed presentation; however, given there are limited cases of anastrozole-induced DI-SCLE, we cannot make a clear statement on incubation periods.6
Reports of DI-SCLE caused by antiestrogen drugs are particularly interesting because sex hormones in relation to lupus disease activity have been the subject of debate for decades. Women are considerably more likely to develop autoimmune diseases than men, suggesting that steroid hormones, especially estrogen and progesterone, influence the immune system.16 Estrogen actions are proinflammatory, while the actions of progesterone, androgens, and glucocorticoids are anti-inflammatory.17 Studies in women with lupus revealed an increased rate of mild- to moderate-intensity disease flares associated with estrogen-containing hormone replace-ment therapy.18-20
Over the years, several antiestrogen therapies have been used in murine models, which showed remarkable clinical improvement in the course of SLE. The precise mechanisms involved in disease immunomodulation by these therapies have not been elucidated.21-23 It is thought that estrogen plays a role in the synthesis and expression of Ro antigens on the surface of keratinocytes, increasing the fixation of anti-Ro antibodies in keratinocytes and provoking the appearance of a cutaneous eruption in patients with a susceptible HLA profile.6
Conclusion
We report a rare case of SCLE induced by anastrozole use. Cases such as ours and others that implicate antiestrogen drugs in association with DI-SCLE are particularly noteworthy, considering many studies are looking at the potential usefulness of antiestrogen therapy in the treatment of SLE. Further research on this relationship is warranted.
- Reed B, Huff J, Jones S, et al. Subacute cutaneous lupus erythematosus associated with hydrochlorothiazide therapy. Ann Intern Med. 1985;103:49-51.
- Marzano A, Lazzari R, Polloni I, et al. Drug-induced subacute cutaneous lupus erythematosus: evidence for differences from its idiopathic counterpart. Br J Dermatol. 2011;165:335-341.
- Bonsmann G, Schiller M, Luger T, et al. Terbinafine-induced subacute cutaneous lupus erythematosus. J Am Acad Dermatol. 2001;44:925-931.
- Callen J. Review: drug induced subacute cutaneous lupus erythematosus. Lupus. 2010;19:1107-1111.
- Lin J, Callen JP. Subacute cutaneous lupus erythematosus (SCLE). Medscape website. http://emedicine.medscape.com/article/1065657-overview. Updated March 7, 2016. Accessed April 29, 2016.
- Lowe GC, Henderson CL, Grau RH, et al. A systematic review of drug-induced subacute cutaneous lupus erythematosus. Br J Dermatol. 2011;164:465-472.
- Vedove C, Giglio M, Schena D, et al. Drug-induced lupus erythematosus. Arch Dermatol Res. 2009;301:99-105.
- Trancart M, Cavailhes A, Balme B, et al. Anastrozole-induced subacute cutaneous lupus erythematosus [published online December 6, 2007]. Br J Dermatol. 2008;158:628-629.
- Fumal I, Danchin A, Cosserat F, et al. Subacute cutaneous lupus erythematosus associated with tamoxifen therapy: two cases. Dermatology. 2005;210:251-252.
- Brown C, Deng J. Thiazide diuretics induce cutaneous lupus-like adverse reaction. J Toxicol Clin Toxicol. 1995;33:729-733.
- Sontheimer R. Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmun Rev. 2005;4:253-263.
- Crowson A, Magro C. Subacute cutaneous lupus erythematosus arising in the setting of calcium channel blocker therapy. Hum Pathol. 1997;28:67-73.
- Lorentz K, Booken N, Goerdt S, et al. Subacute cutaneous lupus erythematosus induced by terbinafine: case report and review of literature. J Dtsch Dermatol Ges. 2008;6:823-837.
- Kasperkiewicz M, Anemüller W, Angelova-Fischer I, et al. Subacute cutaneous lupus erythematosus associated with terbinafine. Clin Exp Dermatol. 2009;34:403-404.
- Miyagawa S, Okuchi T, Shiomi Y, et al. Subacute cutaneous lupus erythematosus lesions precipitated by griseofulvin. J Am Acad Dermatol. 1989;21:343-346.
- Inman RD. Immunologic sex differences and the female predominance in systemic lupus erythematosus. Arthritis Rheum. 1978;21:849-854.
- Cutolo M, Wilder RL. Different roles of androgens and estrogens in the susceptibility to autoimmune rheumatic diseases. Rheum Dis Clin North Am. 2000;26:825-839.
- Petri M. Sex hormones and systemic lupus erythematosus. Lupus. 2008;17:412-415.
- Lateef A, Petri M. Hormone replacement and contraceptive therapy in autoimmune diseases [published online January 18, 2012]. J Autoimmun. 2012;38:J170-J176.
- Buyon JP, Petri M, Kim MY, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med. 2005;142:954-962.
- Wu W, Suen J, Lin B, et al. Tamoxifen alleviates disease severity and decreases double negative T cells in autoimmune MRL-lpr/lpr mice. Immunology. 2000;100:110-118.
- Dayan M, Zinger H, Kalush F, et al. The beneficial effects of treatment with tamoxifen and anti-oestradiol antibody on experimental systemic lupus erythematosus are associated with cytokine modulations. Immunology. 1997;90:101-108.
- Sthoeger Z, Zinger H, Mozes E. Beneficial effects of the anti-oestrogen tamoxifen on systemic lupus erythematosus of (NZBxNZW)F1 female mice are associated with specific reduction of IgG3 autoantibodies. Ann Rheum Dis. 2003;62:341-346.
- Reed B, Huff J, Jones S, et al. Subacute cutaneous lupus erythematosus associated with hydrochlorothiazide therapy. Ann Intern Med. 1985;103:49-51.
- Marzano A, Lazzari R, Polloni I, et al. Drug-induced subacute cutaneous lupus erythematosus: evidence for differences from its idiopathic counterpart. Br J Dermatol. 2011;165:335-341.
- Bonsmann G, Schiller M, Luger T, et al. Terbinafine-induced subacute cutaneous lupus erythematosus. J Am Acad Dermatol. 2001;44:925-931.
- Callen J. Review: drug induced subacute cutaneous lupus erythematosus. Lupus. 2010;19:1107-1111.
- Lin J, Callen JP. Subacute cutaneous lupus erythematosus (SCLE). Medscape website. http://emedicine.medscape.com/article/1065657-overview. Updated March 7, 2016. Accessed April 29, 2016.
- Lowe GC, Henderson CL, Grau RH, et al. A systematic review of drug-induced subacute cutaneous lupus erythematosus. Br J Dermatol. 2011;164:465-472.
- Vedove C, Giglio M, Schena D, et al. Drug-induced lupus erythematosus. Arch Dermatol Res. 2009;301:99-105.
- Trancart M, Cavailhes A, Balme B, et al. Anastrozole-induced subacute cutaneous lupus erythematosus [published online December 6, 2007]. Br J Dermatol. 2008;158:628-629.
- Fumal I, Danchin A, Cosserat F, et al. Subacute cutaneous lupus erythematosus associated with tamoxifen therapy: two cases. Dermatology. 2005;210:251-252.
- Brown C, Deng J. Thiazide diuretics induce cutaneous lupus-like adverse reaction. J Toxicol Clin Toxicol. 1995;33:729-733.
- Sontheimer R. Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmun Rev. 2005;4:253-263.
- Crowson A, Magro C. Subacute cutaneous lupus erythematosus arising in the setting of calcium channel blocker therapy. Hum Pathol. 1997;28:67-73.
- Lorentz K, Booken N, Goerdt S, et al. Subacute cutaneous lupus erythematosus induced by terbinafine: case report and review of literature. J Dtsch Dermatol Ges. 2008;6:823-837.
- Kasperkiewicz M, Anemüller W, Angelova-Fischer I, et al. Subacute cutaneous lupus erythematosus associated with terbinafine. Clin Exp Dermatol. 2009;34:403-404.
- Miyagawa S, Okuchi T, Shiomi Y, et al. Subacute cutaneous lupus erythematosus lesions precipitated by griseofulvin. J Am Acad Dermatol. 1989;21:343-346.
- Inman RD. Immunologic sex differences and the female predominance in systemic lupus erythematosus. Arthritis Rheum. 1978;21:849-854.
- Cutolo M, Wilder RL. Different roles of androgens and estrogens in the susceptibility to autoimmune rheumatic diseases. Rheum Dis Clin North Am. 2000;26:825-839.
- Petri M. Sex hormones and systemic lupus erythematosus. Lupus. 2008;17:412-415.
- Lateef A, Petri M. Hormone replacement and contraceptive therapy in autoimmune diseases [published online January 18, 2012]. J Autoimmun. 2012;38:J170-J176.
- Buyon JP, Petri M, Kim MY, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med. 2005;142:954-962.
- Wu W, Suen J, Lin B, et al. Tamoxifen alleviates disease severity and decreases double negative T cells in autoimmune MRL-lpr/lpr mice. Immunology. 2000;100:110-118.
- Dayan M, Zinger H, Kalush F, et al. The beneficial effects of treatment with tamoxifen and anti-oestradiol antibody on experimental systemic lupus erythematosus are associated with cytokine modulations. Immunology. 1997;90:101-108.
- Sthoeger Z, Zinger H, Mozes E. Beneficial effects of the anti-oestrogen tamoxifen on systemic lupus erythematosus of (NZBxNZW)F1 female mice are associated with specific reduction of IgG3 autoantibodies. Ann Rheum Dis. 2003;62:341-346.
Practice Points
- There are numerous cases of drug-induced subacute cutaneous lupus erythematosus (DI-SCLE) published in the literature; however, there are limited reports with anastrozole implicated as the causative agent.
- Cases of DI-SCLE are clinically and histologically indistinguishable from idiopathic cases. It is important to recognize and withdraw the offending agent.
Studies suggest moving SNAP outside of Alzheimer’s framework
Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology – a brain biomarker construct suspected by some to be an Alzheimer’s disease precursor – truly belongs on the Alzheimer’s spectrum.
A team from Washington University in St. Louis concluded that neurodegeneration in isolation without beta-amyloid deposition – the definition of suspected non-Alzheimer’s pathophysiology (SNAP) – “often represents comorbid influences rather than emerging” Alzheimer’s disease (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2642).
A team from Harvard Medical School in Boston came to a similar conclusion, finding that patterns of neurodegeneration in brain regions vulnerable to Alzheimer’s disease (AD) “are not specific to AD processes among [clinically normal] individuals. Instead, multiple causes likely contribute to the biomarker construct of SNAP” (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2237).
The relationship between SNAP and AD is, for now, mostly of concern to researchers. SNAP was originally linked to cerebral vascular disease and other age-related problems, but since it was proposed a few years ago as an addition to the National Institute on Aging (NIA)–Alzheimer’s Association’s research criteria for preclinical AD, it’s been unclear how – or if – it really fits. The two research groups tackled the issue.
Patients in stage 1 of the NIA scheme have biomarker evidence of amyloid deposition without neurodegeneration (ND); stage 2 patients have both. Stage 3 adds cognitive decline to the amyloid and ND signs. SNAP captures cognitively normal patients with ND but no evidence of amyloid deposition.
Over a period of 9 years, the St. Louis team split 174 cognitively normal adults – about equal numbers of men and women with an average age of 66 – into the four groups at baseline, plus a fifth: no evidence of ND or amyloid. Amyloid deposition was assessed by positron emission tomography, and ND was assessed by both hippocampal volume loss on MRI and cerebrospinal fluid levels of the AD-linked tau protein.
Amyloid accumulation and hippocampal loss were greater in the later NIA stages than in either SNAP or biomarker-free subjects. Among the 34 SNAP patients (20%), only about 5 went on to deposit amyloid.
“The rates of [amyloid] accumulation and loss of hippocampal volume in individuals with SNAP were indistinguishable from those without any pathologic features at baseline. … SNAP appears most likely to capture inherent individual variability in brain structure or to represent comorbid pathologic features rather than early emerging AD. Low hippocampal volumes or elevated levels of [tau protein] in isolation may not accurately represent ongoing neurodegenerative processes,” said investigators led by Brian Gordon, PhD.
Meanwhile, in the Harvard study, only “a small subset” of the 64 SNAP patients went on to rapid cognitive decline. SNAP seems to be “heterogeneous, and further biomarker refinement will be necessary to characterize this group,” said investigators led by Elizabeth Mormino, PhD.
The Harvard team split 247 clinically normal individuals – a bit more women than men this time, with an average age of 74 years – into NIA categories, SNAP, and patients with no ND or amyloid biomarkers. Hippocampal volume was again assessed by MRI; positron emission tomography scans were used to assess amyloid deposition, but also regional brain tau protein levels and other pathologies, and there was serial cognitive testing. The study started in 2010 and is ongoing, with subjects evaluated yearly.
SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories, and had levels of amyloid deposition no greater than biomarker-free subjects. Tau protein “levels in the medial and inferior temporal lobes were indistinguishable between” the two groups.
SNAP patients did slightly worse on serial cognitive tests, but these findings were driven mostly by two SNAP patients who declined faster than the others. (The study by Dr. Gordon and his associates did not report cognitive outcomes.)
Overall, “clinically normal adults with SNAP,” the Harvard group said, “did not exhibit evidence of elevated tau levels, which suggests that this biomarker construct does not represent amyloid-independent tauopathy,” one of the bridges proposed from SNAP to AD.
“SNAP is likely heterogeneous,” with only a subset of patients at risk “for short-term decline. Future refinement of biomarkers will be necessary to subclassify this group and determine the biologic correlates of ND markers.” SNAP does not “appear to be specific to AD,” and is likely influenced by “age-related pathologic processes, the normal aging process, and [individual] differences,” the investigators said.
When asked to comment on the studies, Richard J. Caselli, MD, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., noted that the Mormino study’s findings of a flattened test-retest effect on the serial cognitive tests seemed to be a sensitive cognitive correlate of SNAP, and consistent with the previously reported increased rate of decline in MCI [mild cognitive impairment] patients with SNAP relative to both preclinical stage 0 and preclinical stage 1 (Neurology. 2015 Feb 13;84[5]:508-15).
Overall, the two studies support SNAP as a “generally non-AD heterogeneous diagnosis that does in fact exhibit greater cognitive decline with age, even if subtle in the Mormino study, with an increased risk of MCI and dementia. If we look at the neuropathology of AD cases, we find similar additional pathologies, so maybe SNAP is that minus the AD piece,” said Dr. Caselli, who was not involved in either study.
The heterogeneity explains “our difficulties understanding” the nature of SNAP, Sylvia Villeneuve, PhD, said in an editorial to the Harvard study (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2842).
“Given that the cognitive and brain profile of most SNAP individuals are stable over time, some authors have suggested that neurodegeneration should not be a defining feature of SNAP. … Part of what we capture as SNAP represents a tail of the normal aging distribution,” said Dr. Villeneuve of McGill University in Montreal. “A better comprehension of the biomarkers used to characterize SNAP will be important, with an awareness of the limitations of bimodal markers” – the yes/no answers used for NIA and SNAP classification – “especially those with cutoffs that do not have a biological basis.”
Both studies were funded at least in part by the National Institutes of Health. Dr. Gordon reported research work with Avid Radiopharmaceuticals; Dr. Mormino had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer. Dr. Villeneuve had no disclosures.
The authors have provided a valuable contribution to an area that is receiving increasing attention. While they seem to ascribe small hippocampal volumes to variability in anatomic brain development, it may be that in older individuals, this is more appropriately ascribed to variability in non-Alzheimer’s disease pathologies, resistance to age-related neurodegeneration, or both – all of which should have slow rates of atrophy.
The authors recommended that the field shift from using hippocampal volume as a neurodegenerative measure to using a summary volumetric signature selective for Alzheimer’s disease. This seems justified, although not because hippocampal volume loss with increasing age represents individual variation in brain development. We recommend an Alzheimer’s disease signature (cortical) thickness measure because cortical thickness, unlike volume, is not dependent on head size. Thus, thickness does not need to be adjusted for variation in head size, which imparts a sex effect to all volume adjustments.
Clifford Jack, MD, is a professor of radiology at the Mayo Clinic in Rochester, Minn. He is an originator of the concept of suspected non-Alzheimer’s pathophysiology (SNAP) and also the National Institute on Aging–Alzheimer’s Association’s research criteria for preclinical Alzheimer’s disease. He is a consultant for Eli Lilly and owns stock in Johnson and Johnson. His commentary is adapted from his editorial accompanying the report from Dr. Gordon and his associates (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2843).
The authors have provided a valuable contribution to an area that is receiving increasing attention. While they seem to ascribe small hippocampal volumes to variability in anatomic brain development, it may be that in older individuals, this is more appropriately ascribed to variability in non-Alzheimer’s disease pathologies, resistance to age-related neurodegeneration, or both – all of which should have slow rates of atrophy.
The authors recommended that the field shift from using hippocampal volume as a neurodegenerative measure to using a summary volumetric signature selective for Alzheimer’s disease. This seems justified, although not because hippocampal volume loss with increasing age represents individual variation in brain development. We recommend an Alzheimer’s disease signature (cortical) thickness measure because cortical thickness, unlike volume, is not dependent on head size. Thus, thickness does not need to be adjusted for variation in head size, which imparts a sex effect to all volume adjustments.
Clifford Jack, MD, is a professor of radiology at the Mayo Clinic in Rochester, Minn. He is an originator of the concept of suspected non-Alzheimer’s pathophysiology (SNAP) and also the National Institute on Aging–Alzheimer’s Association’s research criteria for preclinical Alzheimer’s disease. He is a consultant for Eli Lilly and owns stock in Johnson and Johnson. His commentary is adapted from his editorial accompanying the report from Dr. Gordon and his associates (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2843).
The authors have provided a valuable contribution to an area that is receiving increasing attention. While they seem to ascribe small hippocampal volumes to variability in anatomic brain development, it may be that in older individuals, this is more appropriately ascribed to variability in non-Alzheimer’s disease pathologies, resistance to age-related neurodegeneration, or both – all of which should have slow rates of atrophy.
The authors recommended that the field shift from using hippocampal volume as a neurodegenerative measure to using a summary volumetric signature selective for Alzheimer’s disease. This seems justified, although not because hippocampal volume loss with increasing age represents individual variation in brain development. We recommend an Alzheimer’s disease signature (cortical) thickness measure because cortical thickness, unlike volume, is not dependent on head size. Thus, thickness does not need to be adjusted for variation in head size, which imparts a sex effect to all volume adjustments.
Clifford Jack, MD, is a professor of radiology at the Mayo Clinic in Rochester, Minn. He is an originator of the concept of suspected non-Alzheimer’s pathophysiology (SNAP) and also the National Institute on Aging–Alzheimer’s Association’s research criteria for preclinical Alzheimer’s disease. He is a consultant for Eli Lilly and owns stock in Johnson and Johnson. His commentary is adapted from his editorial accompanying the report from Dr. Gordon and his associates (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2843).
Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology – a brain biomarker construct suspected by some to be an Alzheimer’s disease precursor – truly belongs on the Alzheimer’s spectrum.
A team from Washington University in St. Louis concluded that neurodegeneration in isolation without beta-amyloid deposition – the definition of suspected non-Alzheimer’s pathophysiology (SNAP) – “often represents comorbid influences rather than emerging” Alzheimer’s disease (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2642).
A team from Harvard Medical School in Boston came to a similar conclusion, finding that patterns of neurodegeneration in brain regions vulnerable to Alzheimer’s disease (AD) “are not specific to AD processes among [clinically normal] individuals. Instead, multiple causes likely contribute to the biomarker construct of SNAP” (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2237).
The relationship between SNAP and AD is, for now, mostly of concern to researchers. SNAP was originally linked to cerebral vascular disease and other age-related problems, but since it was proposed a few years ago as an addition to the National Institute on Aging (NIA)–Alzheimer’s Association’s research criteria for preclinical AD, it’s been unclear how – or if – it really fits. The two research groups tackled the issue.
Patients in stage 1 of the NIA scheme have biomarker evidence of amyloid deposition without neurodegeneration (ND); stage 2 patients have both. Stage 3 adds cognitive decline to the amyloid and ND signs. SNAP captures cognitively normal patients with ND but no evidence of amyloid deposition.
Over a period of 9 years, the St. Louis team split 174 cognitively normal adults – about equal numbers of men and women with an average age of 66 – into the four groups at baseline, plus a fifth: no evidence of ND or amyloid. Amyloid deposition was assessed by positron emission tomography, and ND was assessed by both hippocampal volume loss on MRI and cerebrospinal fluid levels of the AD-linked tau protein.
Amyloid accumulation and hippocampal loss were greater in the later NIA stages than in either SNAP or biomarker-free subjects. Among the 34 SNAP patients (20%), only about 5 went on to deposit amyloid.
“The rates of [amyloid] accumulation and loss of hippocampal volume in individuals with SNAP were indistinguishable from those without any pathologic features at baseline. … SNAP appears most likely to capture inherent individual variability in brain structure or to represent comorbid pathologic features rather than early emerging AD. Low hippocampal volumes or elevated levels of [tau protein] in isolation may not accurately represent ongoing neurodegenerative processes,” said investigators led by Brian Gordon, PhD.
Meanwhile, in the Harvard study, only “a small subset” of the 64 SNAP patients went on to rapid cognitive decline. SNAP seems to be “heterogeneous, and further biomarker refinement will be necessary to characterize this group,” said investigators led by Elizabeth Mormino, PhD.
The Harvard team split 247 clinically normal individuals – a bit more women than men this time, with an average age of 74 years – into NIA categories, SNAP, and patients with no ND or amyloid biomarkers. Hippocampal volume was again assessed by MRI; positron emission tomography scans were used to assess amyloid deposition, but also regional brain tau protein levels and other pathologies, and there was serial cognitive testing. The study started in 2010 and is ongoing, with subjects evaluated yearly.
SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories, and had levels of amyloid deposition no greater than biomarker-free subjects. Tau protein “levels in the medial and inferior temporal lobes were indistinguishable between” the two groups.
SNAP patients did slightly worse on serial cognitive tests, but these findings were driven mostly by two SNAP patients who declined faster than the others. (The study by Dr. Gordon and his associates did not report cognitive outcomes.)
Overall, “clinically normal adults with SNAP,” the Harvard group said, “did not exhibit evidence of elevated tau levels, which suggests that this biomarker construct does not represent amyloid-independent tauopathy,” one of the bridges proposed from SNAP to AD.
“SNAP is likely heterogeneous,” with only a subset of patients at risk “for short-term decline. Future refinement of biomarkers will be necessary to subclassify this group and determine the biologic correlates of ND markers.” SNAP does not “appear to be specific to AD,” and is likely influenced by “age-related pathologic processes, the normal aging process, and [individual] differences,” the investigators said.
When asked to comment on the studies, Richard J. Caselli, MD, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., noted that the Mormino study’s findings of a flattened test-retest effect on the serial cognitive tests seemed to be a sensitive cognitive correlate of SNAP, and consistent with the previously reported increased rate of decline in MCI [mild cognitive impairment] patients with SNAP relative to both preclinical stage 0 and preclinical stage 1 (Neurology. 2015 Feb 13;84[5]:508-15).
Overall, the two studies support SNAP as a “generally non-AD heterogeneous diagnosis that does in fact exhibit greater cognitive decline with age, even if subtle in the Mormino study, with an increased risk of MCI and dementia. If we look at the neuropathology of AD cases, we find similar additional pathologies, so maybe SNAP is that minus the AD piece,” said Dr. Caselli, who was not involved in either study.
The heterogeneity explains “our difficulties understanding” the nature of SNAP, Sylvia Villeneuve, PhD, said in an editorial to the Harvard study (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2842).
“Given that the cognitive and brain profile of most SNAP individuals are stable over time, some authors have suggested that neurodegeneration should not be a defining feature of SNAP. … Part of what we capture as SNAP represents a tail of the normal aging distribution,” said Dr. Villeneuve of McGill University in Montreal. “A better comprehension of the biomarkers used to characterize SNAP will be important, with an awareness of the limitations of bimodal markers” – the yes/no answers used for NIA and SNAP classification – “especially those with cutoffs that do not have a biological basis.”
Both studies were funded at least in part by the National Institutes of Health. Dr. Gordon reported research work with Avid Radiopharmaceuticals; Dr. Mormino had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer. Dr. Villeneuve had no disclosures.
Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology – a brain biomarker construct suspected by some to be an Alzheimer’s disease precursor – truly belongs on the Alzheimer’s spectrum.
A team from Washington University in St. Louis concluded that neurodegeneration in isolation without beta-amyloid deposition – the definition of suspected non-Alzheimer’s pathophysiology (SNAP) – “often represents comorbid influences rather than emerging” Alzheimer’s disease (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2642).
A team from Harvard Medical School in Boston came to a similar conclusion, finding that patterns of neurodegeneration in brain regions vulnerable to Alzheimer’s disease (AD) “are not specific to AD processes among [clinically normal] individuals. Instead, multiple causes likely contribute to the biomarker construct of SNAP” (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2237).
The relationship between SNAP and AD is, for now, mostly of concern to researchers. SNAP was originally linked to cerebral vascular disease and other age-related problems, but since it was proposed a few years ago as an addition to the National Institute on Aging (NIA)–Alzheimer’s Association’s research criteria for preclinical AD, it’s been unclear how – or if – it really fits. The two research groups tackled the issue.
Patients in stage 1 of the NIA scheme have biomarker evidence of amyloid deposition without neurodegeneration (ND); stage 2 patients have both. Stage 3 adds cognitive decline to the amyloid and ND signs. SNAP captures cognitively normal patients with ND but no evidence of amyloid deposition.
Over a period of 9 years, the St. Louis team split 174 cognitively normal adults – about equal numbers of men and women with an average age of 66 – into the four groups at baseline, plus a fifth: no evidence of ND or amyloid. Amyloid deposition was assessed by positron emission tomography, and ND was assessed by both hippocampal volume loss on MRI and cerebrospinal fluid levels of the AD-linked tau protein.
Amyloid accumulation and hippocampal loss were greater in the later NIA stages than in either SNAP or biomarker-free subjects. Among the 34 SNAP patients (20%), only about 5 went on to deposit amyloid.
“The rates of [amyloid] accumulation and loss of hippocampal volume in individuals with SNAP were indistinguishable from those without any pathologic features at baseline. … SNAP appears most likely to capture inherent individual variability in brain structure or to represent comorbid pathologic features rather than early emerging AD. Low hippocampal volumes or elevated levels of [tau protein] in isolation may not accurately represent ongoing neurodegenerative processes,” said investigators led by Brian Gordon, PhD.
Meanwhile, in the Harvard study, only “a small subset” of the 64 SNAP patients went on to rapid cognitive decline. SNAP seems to be “heterogeneous, and further biomarker refinement will be necessary to characterize this group,” said investigators led by Elizabeth Mormino, PhD.
The Harvard team split 247 clinically normal individuals – a bit more women than men this time, with an average age of 74 years – into NIA categories, SNAP, and patients with no ND or amyloid biomarkers. Hippocampal volume was again assessed by MRI; positron emission tomography scans were used to assess amyloid deposition, but also regional brain tau protein levels and other pathologies, and there was serial cognitive testing. The study started in 2010 and is ongoing, with subjects evaluated yearly.
SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories, and had levels of amyloid deposition no greater than biomarker-free subjects. Tau protein “levels in the medial and inferior temporal lobes were indistinguishable between” the two groups.
SNAP patients did slightly worse on serial cognitive tests, but these findings were driven mostly by two SNAP patients who declined faster than the others. (The study by Dr. Gordon and his associates did not report cognitive outcomes.)
Overall, “clinically normal adults with SNAP,” the Harvard group said, “did not exhibit evidence of elevated tau levels, which suggests that this biomarker construct does not represent amyloid-independent tauopathy,” one of the bridges proposed from SNAP to AD.
“SNAP is likely heterogeneous,” with only a subset of patients at risk “for short-term decline. Future refinement of biomarkers will be necessary to subclassify this group and determine the biologic correlates of ND markers.” SNAP does not “appear to be specific to AD,” and is likely influenced by “age-related pathologic processes, the normal aging process, and [individual] differences,” the investigators said.
When asked to comment on the studies, Richard J. Caselli, MD, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., noted that the Mormino study’s findings of a flattened test-retest effect on the serial cognitive tests seemed to be a sensitive cognitive correlate of SNAP, and consistent with the previously reported increased rate of decline in MCI [mild cognitive impairment] patients with SNAP relative to both preclinical stage 0 and preclinical stage 1 (Neurology. 2015 Feb 13;84[5]:508-15).
Overall, the two studies support SNAP as a “generally non-AD heterogeneous diagnosis that does in fact exhibit greater cognitive decline with age, even if subtle in the Mormino study, with an increased risk of MCI and dementia. If we look at the neuropathology of AD cases, we find similar additional pathologies, so maybe SNAP is that minus the AD piece,” said Dr. Caselli, who was not involved in either study.
The heterogeneity explains “our difficulties understanding” the nature of SNAP, Sylvia Villeneuve, PhD, said in an editorial to the Harvard study (JAMA Neurol. 2016 Aug 22. doi:10.1001/jamaneurol.2016.2842).
“Given that the cognitive and brain profile of most SNAP individuals are stable over time, some authors have suggested that neurodegeneration should not be a defining feature of SNAP. … Part of what we capture as SNAP represents a tail of the normal aging distribution,” said Dr. Villeneuve of McGill University in Montreal. “A better comprehension of the biomarkers used to characterize SNAP will be important, with an awareness of the limitations of bimodal markers” – the yes/no answers used for NIA and SNAP classification – “especially those with cutoffs that do not have a biological basis.”
Both studies were funded at least in part by the National Institutes of Health. Dr. Gordon reported research work with Avid Radiopharmaceuticals; Dr. Mormino had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer. Dr. Villeneuve had no disclosures.
FROM JAMA NEUROLOGY
Key clinical point: Two studies from JAMA Neurology raise doubts about whether suspected non-Alzheimer’s pathophysiology truly belongs on the Alzheimer’s spectrum.
Major finding: SNAP patients had less pathology and better ongoing cognitive function than peers in the accepted NIA categories and had levels of amyloid deposition no greater than biomarker-free subjects.
Data source: One longitudinal study from Harvard Medical School, Boston, and one from Washington University, St. Louis.
Disclosures: Both studies were funded at least in part by the National Institutes of Health. One lead investigator reported research work with Avid Radiopharmaceuticals; the other had no industry disclosures. Other investigators in both projects reported ties to several companies, including Eli Lilly, Janssen, AbbVie, Roche, and Pfizer.
Prednisone and Vardenafil Hydrochloride for Refractory Levamisole-Induced Vasculitis
Levamisole is an immunomodulatory drug that had been used to treat various medical conditions, including parasitic infections, nephrotic syndrome, and colorectal cancer,1 before being withdrawn from the US market in 2000. The most common reasons for levamisole discontinuation were leukopenia and rashes (1%–2%),1 many of which included leg ulcers and necrotizing purpura of the ears.1,2 The drug is currently available only as a deworming agent in veterinary medicine.
Since 2007, increasing amounts of levamisole have been used as an adulterant in cocaine. In 2007, less than 10% of cocaine was contaminated with levamisole, with an increase to 77% by 2010.3 In addition, 78% of 249 urine toxicology screens that were positive for cocaine in an inner city hospital also tested positive for levamisole.4 Levamisole-cut cocaine has become a concern because it is associated with a life-threatening syndrome involving a necrotizing purpuric rash, autoantibody production, and leukopenia.5
Levamisole-induced vasculitis is an independent entity from cocaine-induced vasculitis, which is associated with skin findings ranging from palpable purpura and chronic ulcers to digital infarction secondary to its vasospastic activity.6-8 Cocaine-induced vasculopathy has been related to cytoplasmic antineutrophil cytoplasmic antibody positivity and often resembles Wegener granulomatosis.6 Although both cocaine and levamisole have reportedly caused acrally distributed purpura and vasculopathy, levamisole is specifically associated with retiform purpura, ear involvement, and leukopenia.6,9 In addition, levamisole-induced skin reactions have been linked to specific antibodies, including antinuclear, antiphospholipid, and perinuclear antineutrophil cytoplasmic antibody (p-ANCA).2,5-7,9-14
We present a case of refractory levamisole-induced vasculitis and review its clinical presentation, diagnostic approach, laboratory findings, histology, and management. Furthermore, we discuss the possibility of a new treatment option for levamisole-induced vasculitis for patients with refractory disease or for patients who continue to use levamisole.
Case Report
A 49-year-old man with a history of polysubstance abuse presented with intermittent fevers and painful swollen ears as well as joint pain of 3 weeks’ duration. One week after the lesions developed on the ears, similar lesions were seen on the legs, arms, and trunk. He admitted to cocaine use 3 weeks prior to presentation when the symptoms began.
On physical examination, violaceous patches with necrotic bleeding edges and overlying black eschars were noted on the helices, antihelices, and ear lobules bilaterally (Figure 1). Retiform, purpuric to dark brown patches, some with signs of epidermal necrosis, were scattered on the arms, legs, and chest (Figure 2).


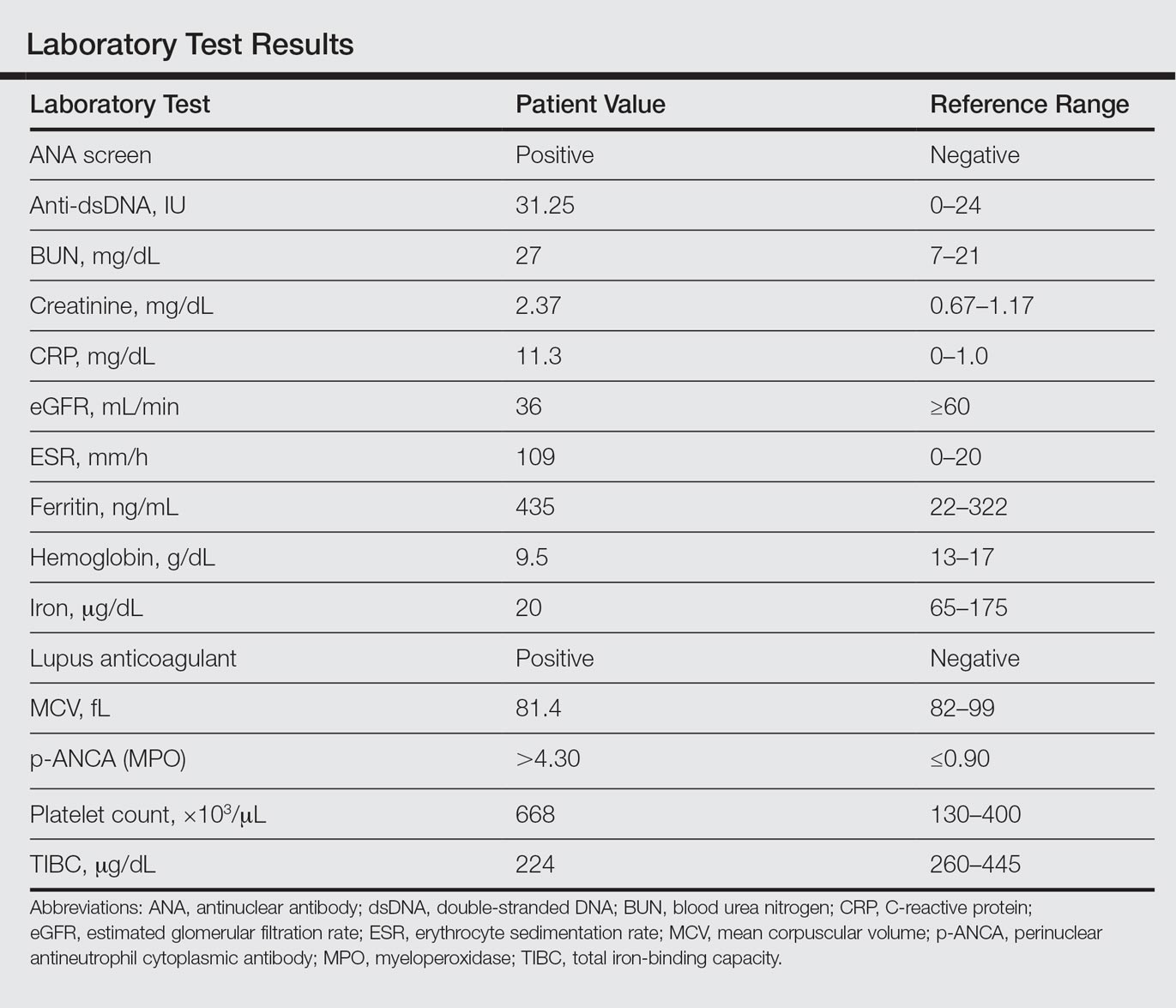
Laboratory examination revealed renal failure, anemia of chronic disease, and thrombocytosis (Table). The patient also screened positive for lupus anticoagulant and antinuclear antibodies and had elevated p-ANCA and anti–double-stranded DNA (Table). He also had an elevated sedimentation rate (109 mm/h [reference range, 0–20 mm/h]) and C-reactive protein level (11.3 mg/dL [reference range, 0–1.0 mg/dL])(Table). Urine toxicology was positive for cocaine.
A punch biopsy of the left thigh was performed on the edge of a retiform purpuric patch. Histopathologic examination revealed epidermal necrosis with subjacent intraluminal vascular thrombi along with extravasated red blood cells and neutrophilic debris (leukocytoclasis) and fibrin in and around vessel walls, consistent with vasculitis (Figure 3).
The patient was admitted to the hospital for pain management and wound care. Despite cocaine cessation and oral prednisone taper, the lesions on the legs worsened over the next several weeks. His condition was further complicated by wound infections, nonhealing ulcers, and subjective fevers and chills requiring frequent hospitalization. The patient was managed by the dermatology department as an outpatient and in clinic between hospital visits. He was treated with antibiotics, ulcer debridement, compression wraps, and aspirin (81 mg once daily) with moderate improvement.
Ten weeks after the first visit, the patient returned with worsening and recurrent leg and ear lesions. He denied any cocaine use since the initial hospital admission; however, a toxicology screen was never obtained. It was decided that the patient would need additional treatment along with traditional trigger (cocaine) avoidance and wound care. Combined treatment with aspirin (81 mg once daily), oral prednisone (40 mg once daily), and vardenafil hydrochloride (20 mg twice weekly) was initiated. At the end of week 1, the patient began to exhibit signs of improvement, which continued over the next 4 weeks. He was then lost to follow-up.
Comment
Our patient presented with severe necrotizing cutaneous vasculitis, likely secondary to levamisole exposure. Some of our patient’s cutaneous findings may be explained exclusively on the basis of cocaine exposure, but the characteristic lesion distribution and histopathologic findings along with the evidence of autoantibody positivity and concurrent arthralgias make the combination of levamisole and cocaine a more likely cause. Similar skin lesions were first described in children treated with levamisole for nephrotic syndrome.2 The most common site of clinical involvement in these children was the ears, as seen in our patient. Our patient tested positive for p-ANCA, which is the most commonly reported autoantibody associated with this patient population. Sixty-one percent (20/33) of patients with levamisole-induced vasculitis from 2 separate reviews showed p-ANCA positivity.7,10
On histopathology, our patient’s skin biopsy findings were consistent with those of prior reports of levamisole-induced vasculitis, which describe patterns of thrombotic vasculitis, leukocytoclasis, and fibrin deposition or occlusive disease.2,6,7,9-14 Mixed histologic findings of vasculitis and thrombosis, usually with varying ages of thrombi, are characteristic of levamisole-induced purpura. In addition, the disease can present nonspecifically with pure microvascular thrombosis without vasculitis, especially later in the course.9
The recommended management of levamisole-induced vasculitis currently involves the withdrawal of the culprit adulterated cocaine along with supportive treatment. Spontaneous and complete clinical resolution of lesions has been reported within 2 to 3 weeks and serology normalization within 2 to 14 months of levamisole cessation.2,6 A 2011 review of patients with levamisole-induced vasculitis reported 66% (19/29) of cases with either full cutaneous resolution after levamisole withdrawal or recurrence with resumed use, supporting a causal relationship.7 Walsh et al9 described 2 patients with recurrent and exacerbated retiform purpura following cocaine binges. Both of these patients had urine samples that tested positive for levamisole.9 In more severe cases, medications shown to be effective include colchicine, polidocanol, antibiotics, methotrexate, anticoagulants, and most commonly systemic corticosteroids.7,10,11,15 Nonsteroidal anti-inflammatory drugs were successful in treating lesions in 2 patients with concurrent arthralgia.7 Rarely, patients have required surgical debridement or skin grafting due to advanced disease at initial presentation.9,12-14 One of the most severe cases of levamisole-induced vasculitis reported in the literature involved 52% of the patient’s total body surface area with skin, soft tissue, and bony necrosis requiring nasal amputation, upper lip excision, skin grafting, and extremity amputation.14 Another severe case with widespread skin involvement was recently reported.16
For unclear reasons, our patient continued to develop cutaneous lesions despite self-reported cocaine cessation. Complete resolution required the combination of vardenafil, prednisone, and aspirin, along with debridement and wound care. Vardenafil, a selective phosphodiesterase 5 inhibitor, enhances the effect of nitrous oxide by increasing levels of cyclic guanosine monophosphate,17 which results in smooth muscle relaxation and vasodilatation. The primary indication for vardenafil is the treatment of erectile dysfunction, but it often is used off label in diseases that may benefit from vasodilatation. Because of its mechanism of action, it is understandable that a vasodilator such as vardenafil could be therapeutic in a condition associated with thrombosis. Moreover, the autoinflammatory nature of levamisole-induced vasculitis makes corticosteroid treatment effective. Given the 10-week delay in improvement, we suspect that it was the combination of treatment or an individual agent that led to our patient’s eventual recovery.
There are few reports in the literature focusing on optimal treatment of levamisole-induced vasculitis and none that mention alternative management for patients who continue to develop new lesions despite cocaine avoidance. Although the discontinuation of levamisole seems to be imperative for resolution of cutaneous lesions, it may not always be enough. It is possible that there is a subpopulation of patients that may not respond to the simple withdrawal of cocaine. It also should be mentioned that there was no urine toxicology screen obtained to support our patient’s reported cocaine cessation. Therefore, it is possible that his worsening condition was secondary to continued cocaine use. However, the patient successfully responded to the combination of vardenafil and prednisone, regardless of whether his condition persisted due to continued use of cocaine or not. This case suggests the possibility of a new treatment option for levamisole-induced vasculitis for patients who continue to use levamisole despite instruction for cessation or for patients with refractory disease.
Conclusion
A trial of prednisone and vardenafil should be considered for patients with refractory levamisole-induced vasculitis. Further studies and discussions of disease course are needed to identify the best treatment of this skin condition, especially for patients with refractory lesions.
- Scheinfeld N, Rosenberg JD, Weinberg JM. Levamisole in dermatology: a review. Am J Clin Dermatol. 2004;5:97-104.
- Rongioletti F, Ghio L, Ginevri F, et al. Purpura of the ears: a distinctive vasculopathy with circulating autoantibodies complicating long-term treatment with levamisole in children. Br J Dermatol. 1999;140:948-951.
- National Drug Threat Assessment 2011. US Department of Justice National Drug Intelligence Center website. https://www.justice.gov/archive/ndic/pubs44/44849/44849p.pdf. Published August 2011. Accessed August 7, 2016.
- Buchanan JA, Heard K, Burbach C, et al. Prevalence of levamisole in urine toxicology screens positive for cocaine in an inner-city hospital. JAMA. 2011;305:1657-1658.
- Gross RL, Brucker J, Bahce-Altuntas A, et al. A novel cutaneous vasculitis syndrome induced by levamisole-contaminated cocaine. Clin Rheumatol. 2011;30:1385-1392.
- Waller JM, Feramisco JD, Alberta-Wszolek L, et al. Cocaine-associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol. 2010;63:530-535.
- Poon SH, Baliog CR, Sams RN, et al. Syndrome of cocaine-levamisole-induced cutaneous vasculitis and immune-mediated leukopenia. Semin Arthritis Rheum. 2011;41:434-444.
- Brewer JD, Meves A, Bostwick JM, et al. Cocaine abuse: dermatologic manifestations and therapeutic approaches. J Am Acad Dermatol. 2008;59:483-487.
- Walsh NMG, Green PJ, Burlingame RW, et al. Cocaine-related retiform purpura: evidence to incriminate the adulterant, levamisole. J Cutan Pathol. 2010;37:1212-1219.
- Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia—a potential public health epidemic associated with levamisole adultered cocaine. J Am Acad Dermatol. 2011;65:722-725.
- Kahn TA, Cuchacovich R, Espinoza LR, et al. Vasculopathy, hematological, and immune abnormalities associated with levamisole-contaminated cocaine use. Semin Arthritis Rheum. 2011;41:445-454.
- Graf J, Lynch K, Yeh CL, et al. Purpura, cutaneous necrosis, and antineutrophil cytoplasmic antibodies associated with levamisole-adulterated cocaine. Arthritis Rheum. 2011;63:3998-4001.
- Farmer RW, Malhotra PS, Mays MP, et al. Necrotizing peripheral vasculitis/vasculopathy following the use of cocaine laced with levamisole. J Burn Care Res. 2012;33:e6-e11.
- Ching JA, Smith DJ Jr. Levamisole-induced skin necrosis of skin, soft tissue, and bone: case report and review of literature. J Burn Care Res. 2012;33:e1-e5.
- Buchanan JA, Vogel JA, Eberhardt AM. Levamisole-induced occlusive necrotizing vasculitis of the ears after use of cocaine contaminated with levamisole. J Med Toxicol. 2011;7:83-84.
- Graff N, Whitworth K, Trigger C. Purpuric skin eruption in an illicit drug user: levamisole-induced vasculitis. Am J Emer Med. 2016;34:1321.
- Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
Levamisole is an immunomodulatory drug that had been used to treat various medical conditions, including parasitic infections, nephrotic syndrome, and colorectal cancer,1 before being withdrawn from the US market in 2000. The most common reasons for levamisole discontinuation were leukopenia and rashes (1%–2%),1 many of which included leg ulcers and necrotizing purpura of the ears.1,2 The drug is currently available only as a deworming agent in veterinary medicine.
Since 2007, increasing amounts of levamisole have been used as an adulterant in cocaine. In 2007, less than 10% of cocaine was contaminated with levamisole, with an increase to 77% by 2010.3 In addition, 78% of 249 urine toxicology screens that were positive for cocaine in an inner city hospital also tested positive for levamisole.4 Levamisole-cut cocaine has become a concern because it is associated with a life-threatening syndrome involving a necrotizing purpuric rash, autoantibody production, and leukopenia.5
Levamisole-induced vasculitis is an independent entity from cocaine-induced vasculitis, which is associated with skin findings ranging from palpable purpura and chronic ulcers to digital infarction secondary to its vasospastic activity.6-8 Cocaine-induced vasculopathy has been related to cytoplasmic antineutrophil cytoplasmic antibody positivity and often resembles Wegener granulomatosis.6 Although both cocaine and levamisole have reportedly caused acrally distributed purpura and vasculopathy, levamisole is specifically associated with retiform purpura, ear involvement, and leukopenia.6,9 In addition, levamisole-induced skin reactions have been linked to specific antibodies, including antinuclear, antiphospholipid, and perinuclear antineutrophil cytoplasmic antibody (p-ANCA).2,5-7,9-14
We present a case of refractory levamisole-induced vasculitis and review its clinical presentation, diagnostic approach, laboratory findings, histology, and management. Furthermore, we discuss the possibility of a new treatment option for levamisole-induced vasculitis for patients with refractory disease or for patients who continue to use levamisole.
Case Report
A 49-year-old man with a history of polysubstance abuse presented with intermittent fevers and painful swollen ears as well as joint pain of 3 weeks’ duration. One week after the lesions developed on the ears, similar lesions were seen on the legs, arms, and trunk. He admitted to cocaine use 3 weeks prior to presentation when the symptoms began.
On physical examination, violaceous patches with necrotic bleeding edges and overlying black eschars were noted on the helices, antihelices, and ear lobules bilaterally (Figure 1). Retiform, purpuric to dark brown patches, some with signs of epidermal necrosis, were scattered on the arms, legs, and chest (Figure 2).


Laboratory examination revealed renal failure, anemia of chronic disease, and thrombocytosis (Table). The patient also screened positive for lupus anticoagulant and antinuclear antibodies and had elevated p-ANCA and anti–double-stranded DNA (Table). He also had an elevated sedimentation rate (109 mm/h [reference range, 0–20 mm/h]) and C-reactive protein level (11.3 mg/dL [reference range, 0–1.0 mg/dL])(Table). Urine toxicology was positive for cocaine.
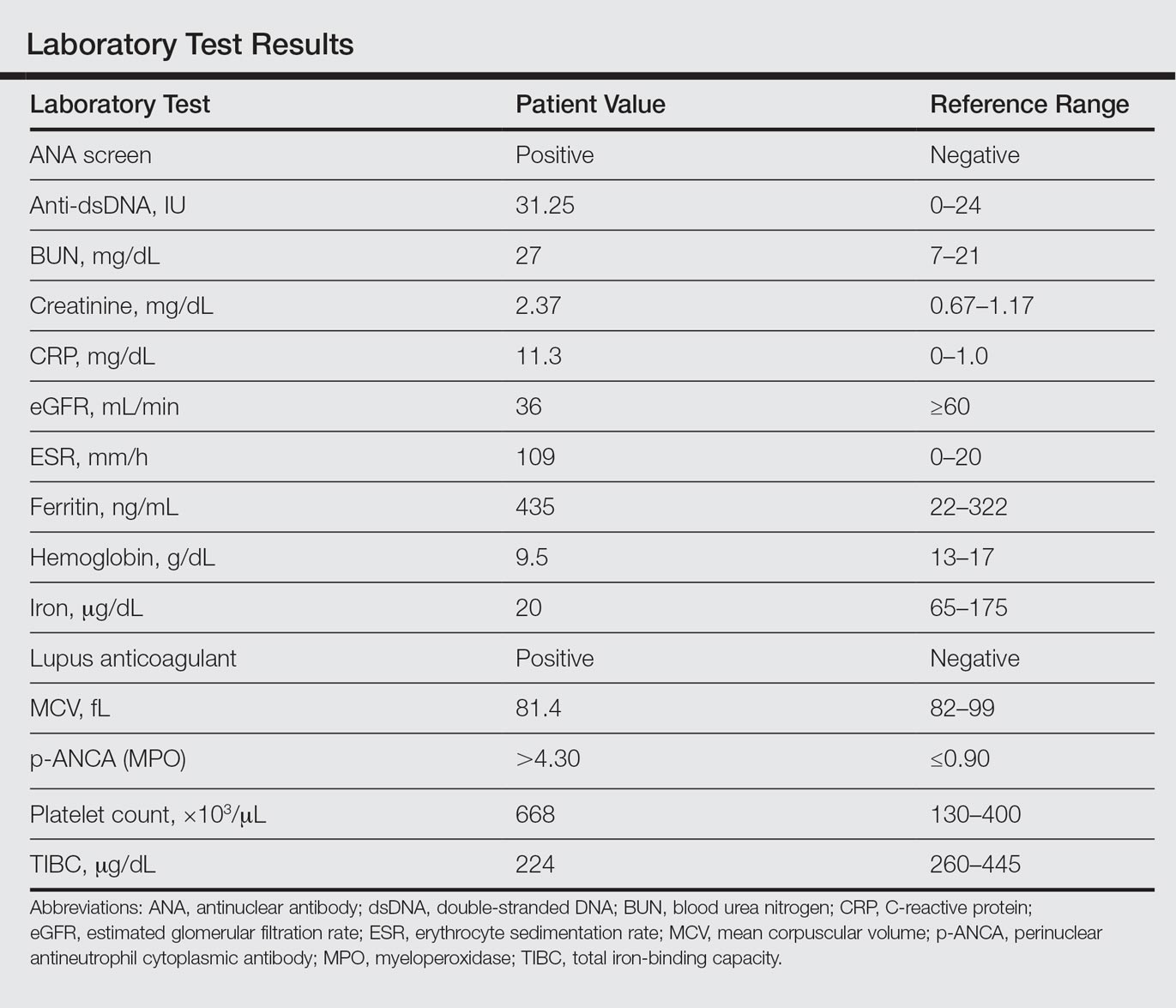
A punch biopsy of the left thigh was performed on the edge of a retiform purpuric patch. Histopathologic examination revealed epidermal necrosis with subjacent intraluminal vascular thrombi along with extravasated red blood cells and neutrophilic debris (leukocytoclasis) and fibrin in and around vessel walls, consistent with vasculitis (Figure 3).
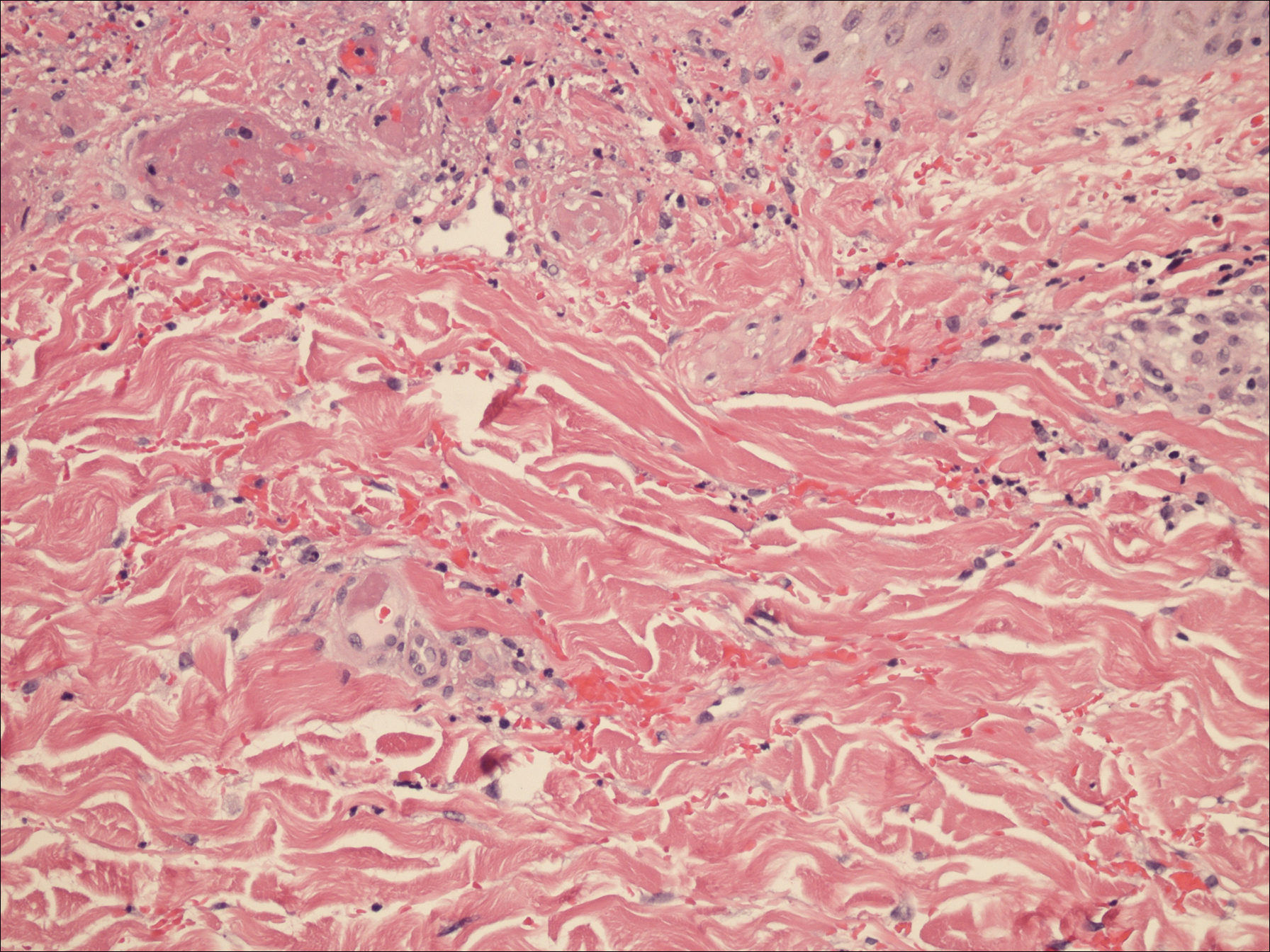
The patient was admitted to the hospital for pain management and wound care. Despite cocaine cessation and oral prednisone taper, the lesions on the legs worsened over the next several weeks. His condition was further complicated by wound infections, nonhealing ulcers, and subjective fevers and chills requiring frequent hospitalization. The patient was managed by the dermatology department as an outpatient and in clinic between hospital visits. He was treated with antibiotics, ulcer debridement, compression wraps, and aspirin (81 mg once daily) with moderate improvement.
Ten weeks after the first visit, the patient returned with worsening and recurrent leg and ear lesions. He denied any cocaine use since the initial hospital admission; however, a toxicology screen was never obtained. It was decided that the patient would need additional treatment along with traditional trigger (cocaine) avoidance and wound care. Combined treatment with aspirin (81 mg once daily), oral prednisone (40 mg once daily), and vardenafil hydrochloride (20 mg twice weekly) was initiated. At the end of week 1, the patient began to exhibit signs of improvement, which continued over the next 4 weeks. He was then lost to follow-up.
Comment
Our patient presented with severe necrotizing cutaneous vasculitis, likely secondary to levamisole exposure. Some of our patient’s cutaneous findings may be explained exclusively on the basis of cocaine exposure, but the characteristic lesion distribution and histopathologic findings along with the evidence of autoantibody positivity and concurrent arthralgias make the combination of levamisole and cocaine a more likely cause. Similar skin lesions were first described in children treated with levamisole for nephrotic syndrome.2 The most common site of clinical involvement in these children was the ears, as seen in our patient. Our patient tested positive for p-ANCA, which is the most commonly reported autoantibody associated with this patient population. Sixty-one percent (20/33) of patients with levamisole-induced vasculitis from 2 separate reviews showed p-ANCA positivity.7,10
On histopathology, our patient’s skin biopsy findings were consistent with those of prior reports of levamisole-induced vasculitis, which describe patterns of thrombotic vasculitis, leukocytoclasis, and fibrin deposition or occlusive disease.2,6,7,9-14 Mixed histologic findings of vasculitis and thrombosis, usually with varying ages of thrombi, are characteristic of levamisole-induced purpura. In addition, the disease can present nonspecifically with pure microvascular thrombosis without vasculitis, especially later in the course.9
The recommended management of levamisole-induced vasculitis currently involves the withdrawal of the culprit adulterated cocaine along with supportive treatment. Spontaneous and complete clinical resolution of lesions has been reported within 2 to 3 weeks and serology normalization within 2 to 14 months of levamisole cessation.2,6 A 2011 review of patients with levamisole-induced vasculitis reported 66% (19/29) of cases with either full cutaneous resolution after levamisole withdrawal or recurrence with resumed use, supporting a causal relationship.7 Walsh et al9 described 2 patients with recurrent and exacerbated retiform purpura following cocaine binges. Both of these patients had urine samples that tested positive for levamisole.9 In more severe cases, medications shown to be effective include colchicine, polidocanol, antibiotics, methotrexate, anticoagulants, and most commonly systemic corticosteroids.7,10,11,15 Nonsteroidal anti-inflammatory drugs were successful in treating lesions in 2 patients with concurrent arthralgia.7 Rarely, patients have required surgical debridement or skin grafting due to advanced disease at initial presentation.9,12-14 One of the most severe cases of levamisole-induced vasculitis reported in the literature involved 52% of the patient’s total body surface area with skin, soft tissue, and bony necrosis requiring nasal amputation, upper lip excision, skin grafting, and extremity amputation.14 Another severe case with widespread skin involvement was recently reported.16
For unclear reasons, our patient continued to develop cutaneous lesions despite self-reported cocaine cessation. Complete resolution required the combination of vardenafil, prednisone, and aspirin, along with debridement and wound care. Vardenafil, a selective phosphodiesterase 5 inhibitor, enhances the effect of nitrous oxide by increasing levels of cyclic guanosine monophosphate,17 which results in smooth muscle relaxation and vasodilatation. The primary indication for vardenafil is the treatment of erectile dysfunction, but it often is used off label in diseases that may benefit from vasodilatation. Because of its mechanism of action, it is understandable that a vasodilator such as vardenafil could be therapeutic in a condition associated with thrombosis. Moreover, the autoinflammatory nature of levamisole-induced vasculitis makes corticosteroid treatment effective. Given the 10-week delay in improvement, we suspect that it was the combination of treatment or an individual agent that led to our patient’s eventual recovery.
There are few reports in the literature focusing on optimal treatment of levamisole-induced vasculitis and none that mention alternative management for patients who continue to develop new lesions despite cocaine avoidance. Although the discontinuation of levamisole seems to be imperative for resolution of cutaneous lesions, it may not always be enough. It is possible that there is a subpopulation of patients that may not respond to the simple withdrawal of cocaine. It also should be mentioned that there was no urine toxicology screen obtained to support our patient’s reported cocaine cessation. Therefore, it is possible that his worsening condition was secondary to continued cocaine use. However, the patient successfully responded to the combination of vardenafil and prednisone, regardless of whether his condition persisted due to continued use of cocaine or not. This case suggests the possibility of a new treatment option for levamisole-induced vasculitis for patients who continue to use levamisole despite instruction for cessation or for patients with refractory disease.
Conclusion
A trial of prednisone and vardenafil should be considered for patients with refractory levamisole-induced vasculitis. Further studies and discussions of disease course are needed to identify the best treatment of this skin condition, especially for patients with refractory lesions.
Levamisole is an immunomodulatory drug that had been used to treat various medical conditions, including parasitic infections, nephrotic syndrome, and colorectal cancer,1 before being withdrawn from the US market in 2000. The most common reasons for levamisole discontinuation were leukopenia and rashes (1%–2%),1 many of which included leg ulcers and necrotizing purpura of the ears.1,2 The drug is currently available only as a deworming agent in veterinary medicine.
Since 2007, increasing amounts of levamisole have been used as an adulterant in cocaine. In 2007, less than 10% of cocaine was contaminated with levamisole, with an increase to 77% by 2010.3 In addition, 78% of 249 urine toxicology screens that were positive for cocaine in an inner city hospital also tested positive for levamisole.4 Levamisole-cut cocaine has become a concern because it is associated with a life-threatening syndrome involving a necrotizing purpuric rash, autoantibody production, and leukopenia.5
Levamisole-induced vasculitis is an independent entity from cocaine-induced vasculitis, which is associated with skin findings ranging from palpable purpura and chronic ulcers to digital infarction secondary to its vasospastic activity.6-8 Cocaine-induced vasculopathy has been related to cytoplasmic antineutrophil cytoplasmic antibody positivity and often resembles Wegener granulomatosis.6 Although both cocaine and levamisole have reportedly caused acrally distributed purpura and vasculopathy, levamisole is specifically associated with retiform purpura, ear involvement, and leukopenia.6,9 In addition, levamisole-induced skin reactions have been linked to specific antibodies, including antinuclear, antiphospholipid, and perinuclear antineutrophil cytoplasmic antibody (p-ANCA).2,5-7,9-14
We present a case of refractory levamisole-induced vasculitis and review its clinical presentation, diagnostic approach, laboratory findings, histology, and management. Furthermore, we discuss the possibility of a new treatment option for levamisole-induced vasculitis for patients with refractory disease or for patients who continue to use levamisole.
Case Report
A 49-year-old man with a history of polysubstance abuse presented with intermittent fevers and painful swollen ears as well as joint pain of 3 weeks’ duration. One week after the lesions developed on the ears, similar lesions were seen on the legs, arms, and trunk. He admitted to cocaine use 3 weeks prior to presentation when the symptoms began.
On physical examination, violaceous patches with necrotic bleeding edges and overlying black eschars were noted on the helices, antihelices, and ear lobules bilaterally (Figure 1). Retiform, purpuric to dark brown patches, some with signs of epidermal necrosis, were scattered on the arms, legs, and chest (Figure 2).


Laboratory examination revealed renal failure, anemia of chronic disease, and thrombocytosis (Table). The patient also screened positive for lupus anticoagulant and antinuclear antibodies and had elevated p-ANCA and anti–double-stranded DNA (Table). He also had an elevated sedimentation rate (109 mm/h [reference range, 0–20 mm/h]) and C-reactive protein level (11.3 mg/dL [reference range, 0–1.0 mg/dL])(Table). Urine toxicology was positive for cocaine.
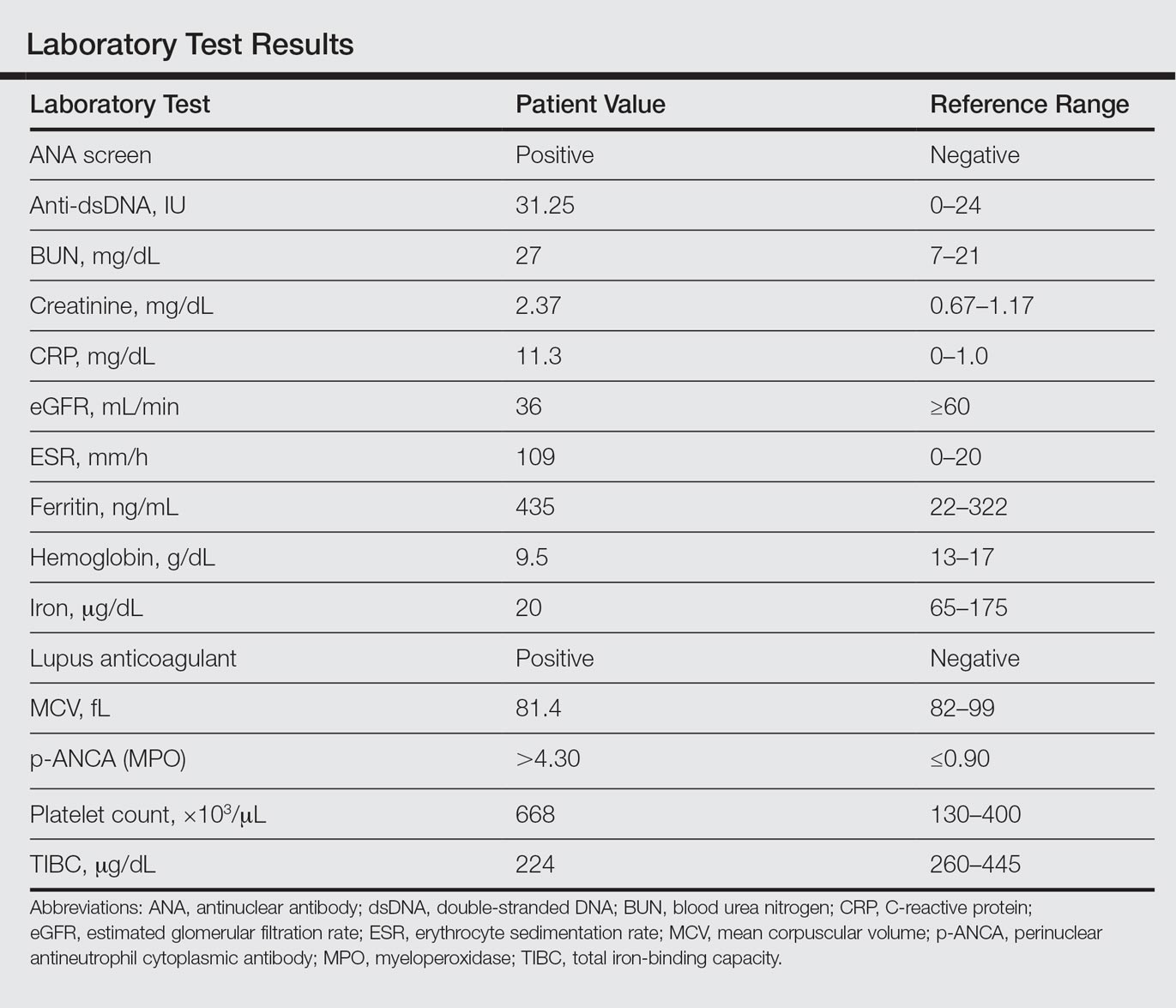
A punch biopsy of the left thigh was performed on the edge of a retiform purpuric patch. Histopathologic examination revealed epidermal necrosis with subjacent intraluminal vascular thrombi along with extravasated red blood cells and neutrophilic debris (leukocytoclasis) and fibrin in and around vessel walls, consistent with vasculitis (Figure 3).
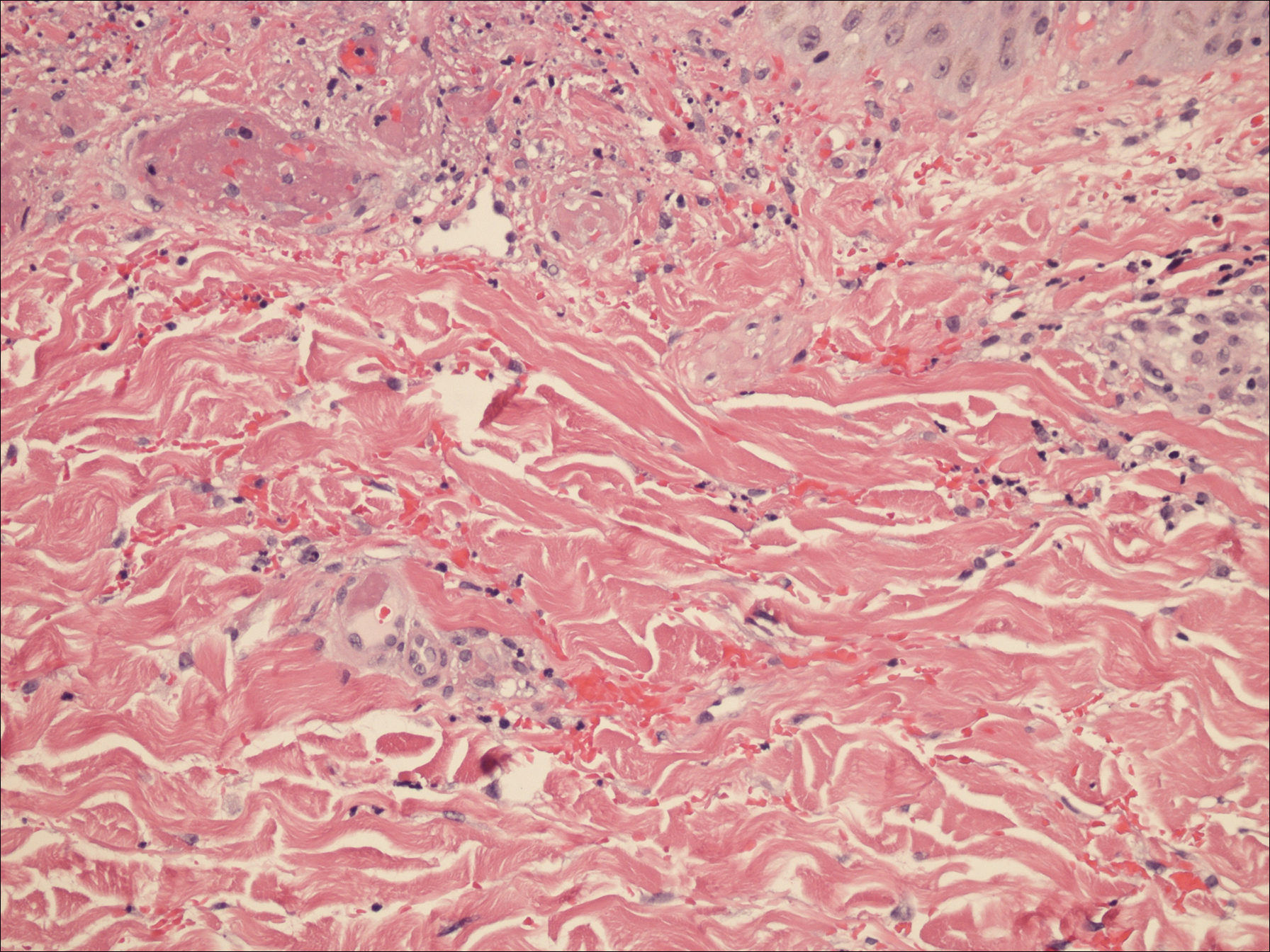
The patient was admitted to the hospital for pain management and wound care. Despite cocaine cessation and oral prednisone taper, the lesions on the legs worsened over the next several weeks. His condition was further complicated by wound infections, nonhealing ulcers, and subjective fevers and chills requiring frequent hospitalization. The patient was managed by the dermatology department as an outpatient and in clinic between hospital visits. He was treated with antibiotics, ulcer debridement, compression wraps, and aspirin (81 mg once daily) with moderate improvement.
Ten weeks after the first visit, the patient returned with worsening and recurrent leg and ear lesions. He denied any cocaine use since the initial hospital admission; however, a toxicology screen was never obtained. It was decided that the patient would need additional treatment along with traditional trigger (cocaine) avoidance and wound care. Combined treatment with aspirin (81 mg once daily), oral prednisone (40 mg once daily), and vardenafil hydrochloride (20 mg twice weekly) was initiated. At the end of week 1, the patient began to exhibit signs of improvement, which continued over the next 4 weeks. He was then lost to follow-up.
Comment
Our patient presented with severe necrotizing cutaneous vasculitis, likely secondary to levamisole exposure. Some of our patient’s cutaneous findings may be explained exclusively on the basis of cocaine exposure, but the characteristic lesion distribution and histopathologic findings along with the evidence of autoantibody positivity and concurrent arthralgias make the combination of levamisole and cocaine a more likely cause. Similar skin lesions were first described in children treated with levamisole for nephrotic syndrome.2 The most common site of clinical involvement in these children was the ears, as seen in our patient. Our patient tested positive for p-ANCA, which is the most commonly reported autoantibody associated with this patient population. Sixty-one percent (20/33) of patients with levamisole-induced vasculitis from 2 separate reviews showed p-ANCA positivity.7,10
On histopathology, our patient’s skin biopsy findings were consistent with those of prior reports of levamisole-induced vasculitis, which describe patterns of thrombotic vasculitis, leukocytoclasis, and fibrin deposition or occlusive disease.2,6,7,9-14 Mixed histologic findings of vasculitis and thrombosis, usually with varying ages of thrombi, are characteristic of levamisole-induced purpura. In addition, the disease can present nonspecifically with pure microvascular thrombosis without vasculitis, especially later in the course.9
The recommended management of levamisole-induced vasculitis currently involves the withdrawal of the culprit adulterated cocaine along with supportive treatment. Spontaneous and complete clinical resolution of lesions has been reported within 2 to 3 weeks and serology normalization within 2 to 14 months of levamisole cessation.2,6 A 2011 review of patients with levamisole-induced vasculitis reported 66% (19/29) of cases with either full cutaneous resolution after levamisole withdrawal or recurrence with resumed use, supporting a causal relationship.7 Walsh et al9 described 2 patients with recurrent and exacerbated retiform purpura following cocaine binges. Both of these patients had urine samples that tested positive for levamisole.9 In more severe cases, medications shown to be effective include colchicine, polidocanol, antibiotics, methotrexate, anticoagulants, and most commonly systemic corticosteroids.7,10,11,15 Nonsteroidal anti-inflammatory drugs were successful in treating lesions in 2 patients with concurrent arthralgia.7 Rarely, patients have required surgical debridement or skin grafting due to advanced disease at initial presentation.9,12-14 One of the most severe cases of levamisole-induced vasculitis reported in the literature involved 52% of the patient’s total body surface area with skin, soft tissue, and bony necrosis requiring nasal amputation, upper lip excision, skin grafting, and extremity amputation.14 Another severe case with widespread skin involvement was recently reported.16
For unclear reasons, our patient continued to develop cutaneous lesions despite self-reported cocaine cessation. Complete resolution required the combination of vardenafil, prednisone, and aspirin, along with debridement and wound care. Vardenafil, a selective phosphodiesterase 5 inhibitor, enhances the effect of nitrous oxide by increasing levels of cyclic guanosine monophosphate,17 which results in smooth muscle relaxation and vasodilatation. The primary indication for vardenafil is the treatment of erectile dysfunction, but it often is used off label in diseases that may benefit from vasodilatation. Because of its mechanism of action, it is understandable that a vasodilator such as vardenafil could be therapeutic in a condition associated with thrombosis. Moreover, the autoinflammatory nature of levamisole-induced vasculitis makes corticosteroid treatment effective. Given the 10-week delay in improvement, we suspect that it was the combination of treatment or an individual agent that led to our patient’s eventual recovery.
There are few reports in the literature focusing on optimal treatment of levamisole-induced vasculitis and none that mention alternative management for patients who continue to develop new lesions despite cocaine avoidance. Although the discontinuation of levamisole seems to be imperative for resolution of cutaneous lesions, it may not always be enough. It is possible that there is a subpopulation of patients that may not respond to the simple withdrawal of cocaine. It also should be mentioned that there was no urine toxicology screen obtained to support our patient’s reported cocaine cessation. Therefore, it is possible that his worsening condition was secondary to continued cocaine use. However, the patient successfully responded to the combination of vardenafil and prednisone, regardless of whether his condition persisted due to continued use of cocaine or not. This case suggests the possibility of a new treatment option for levamisole-induced vasculitis for patients who continue to use levamisole despite instruction for cessation or for patients with refractory disease.
Conclusion
A trial of prednisone and vardenafil should be considered for patients with refractory levamisole-induced vasculitis. Further studies and discussions of disease course are needed to identify the best treatment of this skin condition, especially for patients with refractory lesions.
- Scheinfeld N, Rosenberg JD, Weinberg JM. Levamisole in dermatology: a review. Am J Clin Dermatol. 2004;5:97-104.
- Rongioletti F, Ghio L, Ginevri F, et al. Purpura of the ears: a distinctive vasculopathy with circulating autoantibodies complicating long-term treatment with levamisole in children. Br J Dermatol. 1999;140:948-951.
- National Drug Threat Assessment 2011. US Department of Justice National Drug Intelligence Center website. https://www.justice.gov/archive/ndic/pubs44/44849/44849p.pdf. Published August 2011. Accessed August 7, 2016.
- Buchanan JA, Heard K, Burbach C, et al. Prevalence of levamisole in urine toxicology screens positive for cocaine in an inner-city hospital. JAMA. 2011;305:1657-1658.
- Gross RL, Brucker J, Bahce-Altuntas A, et al. A novel cutaneous vasculitis syndrome induced by levamisole-contaminated cocaine. Clin Rheumatol. 2011;30:1385-1392.
- Waller JM, Feramisco JD, Alberta-Wszolek L, et al. Cocaine-associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol. 2010;63:530-535.
- Poon SH, Baliog CR, Sams RN, et al. Syndrome of cocaine-levamisole-induced cutaneous vasculitis and immune-mediated leukopenia. Semin Arthritis Rheum. 2011;41:434-444.
- Brewer JD, Meves A, Bostwick JM, et al. Cocaine abuse: dermatologic manifestations and therapeutic approaches. J Am Acad Dermatol. 2008;59:483-487.
- Walsh NMG, Green PJ, Burlingame RW, et al. Cocaine-related retiform purpura: evidence to incriminate the adulterant, levamisole. J Cutan Pathol. 2010;37:1212-1219.
- Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia—a potential public health epidemic associated with levamisole adultered cocaine. J Am Acad Dermatol. 2011;65:722-725.
- Kahn TA, Cuchacovich R, Espinoza LR, et al. Vasculopathy, hematological, and immune abnormalities associated with levamisole-contaminated cocaine use. Semin Arthritis Rheum. 2011;41:445-454.
- Graf J, Lynch K, Yeh CL, et al. Purpura, cutaneous necrosis, and antineutrophil cytoplasmic antibodies associated with levamisole-adulterated cocaine. Arthritis Rheum. 2011;63:3998-4001.
- Farmer RW, Malhotra PS, Mays MP, et al. Necrotizing peripheral vasculitis/vasculopathy following the use of cocaine laced with levamisole. J Burn Care Res. 2012;33:e6-e11.
- Ching JA, Smith DJ Jr. Levamisole-induced skin necrosis of skin, soft tissue, and bone: case report and review of literature. J Burn Care Res. 2012;33:e1-e5.
- Buchanan JA, Vogel JA, Eberhardt AM. Levamisole-induced occlusive necrotizing vasculitis of the ears after use of cocaine contaminated with levamisole. J Med Toxicol. 2011;7:83-84.
- Graff N, Whitworth K, Trigger C. Purpuric skin eruption in an illicit drug user: levamisole-induced vasculitis. Am J Emer Med. 2016;34:1321.
- Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
- Scheinfeld N, Rosenberg JD, Weinberg JM. Levamisole in dermatology: a review. Am J Clin Dermatol. 2004;5:97-104.
- Rongioletti F, Ghio L, Ginevri F, et al. Purpura of the ears: a distinctive vasculopathy with circulating autoantibodies complicating long-term treatment with levamisole in children. Br J Dermatol. 1999;140:948-951.
- National Drug Threat Assessment 2011. US Department of Justice National Drug Intelligence Center website. https://www.justice.gov/archive/ndic/pubs44/44849/44849p.pdf. Published August 2011. Accessed August 7, 2016.
- Buchanan JA, Heard K, Burbach C, et al. Prevalence of levamisole in urine toxicology screens positive for cocaine in an inner-city hospital. JAMA. 2011;305:1657-1658.
- Gross RL, Brucker J, Bahce-Altuntas A, et al. A novel cutaneous vasculitis syndrome induced by levamisole-contaminated cocaine. Clin Rheumatol. 2011;30:1385-1392.
- Waller JM, Feramisco JD, Alberta-Wszolek L, et al. Cocaine-associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol. 2010;63:530-535.
- Poon SH, Baliog CR, Sams RN, et al. Syndrome of cocaine-levamisole-induced cutaneous vasculitis and immune-mediated leukopenia. Semin Arthritis Rheum. 2011;41:434-444.
- Brewer JD, Meves A, Bostwick JM, et al. Cocaine abuse: dermatologic manifestations and therapeutic approaches. J Am Acad Dermatol. 2008;59:483-487.
- Walsh NMG, Green PJ, Burlingame RW, et al. Cocaine-related retiform purpura: evidence to incriminate the adulterant, levamisole. J Cutan Pathol. 2010;37:1212-1219.
- Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia—a potential public health epidemic associated with levamisole adultered cocaine. J Am Acad Dermatol. 2011;65:722-725.
- Kahn TA, Cuchacovich R, Espinoza LR, et al. Vasculopathy, hematological, and immune abnormalities associated with levamisole-contaminated cocaine use. Semin Arthritis Rheum. 2011;41:445-454.
- Graf J, Lynch K, Yeh CL, et al. Purpura, cutaneous necrosis, and antineutrophil cytoplasmic antibodies associated with levamisole-adulterated cocaine. Arthritis Rheum. 2011;63:3998-4001.
- Farmer RW, Malhotra PS, Mays MP, et al. Necrotizing peripheral vasculitis/vasculopathy following the use of cocaine laced with levamisole. J Burn Care Res. 2012;33:e6-e11.
- Ching JA, Smith DJ Jr. Levamisole-induced skin necrosis of skin, soft tissue, and bone: case report and review of literature. J Burn Care Res. 2012;33:e1-e5.
- Buchanan JA, Vogel JA, Eberhardt AM. Levamisole-induced occlusive necrotizing vasculitis of the ears after use of cocaine contaminated with levamisole. J Med Toxicol. 2011;7:83-84.
- Graff N, Whitworth K, Trigger C. Purpuric skin eruption in an illicit drug user: levamisole-induced vasculitis. Am J Emer Med. 2016;34:1321.
- Schwartz BG, Kloner RA. Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation. 2010;122:88-95.
Practice Points
- Levamisole is an immunomodulatory drug that, before being withdrawn from the US market in 2000, was previously used to treat various medical conditions.
- A majority of the cocaine in the United States is contaminated with levamisole, which is added as an adulterant or bulking agent.
- Levamisole-cut cocaine is a concern because it is associated with a life-threatening syndrome involving a necrotizing purpuric rash, autoantibody production, and leukopenia.
- Although treatment of levamisole toxicity is primarily supportive and includes cessation of levamisole-cut cocaine, a trial of prednisone and vardenafil hydrochloride can be considered for refractory levamisole-induced vasculopathy or for patients who continue to use the drug.
Food allergy testing only rarely needed for AD patients
BOSTON – Between 15% and 30% of children with moderate to severe atopic dermatitis also have food allergies, but the allergies are a trigger for AD in only a small subset of patients, according to Mercedes E. Gonzalez, MD.
In most cases, allergy testing is not indicated, she said at the American Academy of Dermatology summer meeting.
She described a scenario involving a parent who is concerned that a food allergy is causing her child’s AD. The child has had no hives, no lip swelling, and no other signs of immediate hypersensitivity. In such a case, the best approach is to treat with topical therapies and follow the patient clinically.
“Allergy testing independent of history is not recommended,” she said.
However, in cases involving a significant concern about food allergy, such as the presence of hives or urticaria, or when the child has severe dermatitis that is not improving with optimized topical therapies, an assessment can be undertaken, said Dr. Gonzalez of the University of Miami.
She recommended limited food allergy testing – for common culprits such as cow’s milk, eggs, wheat, soy, and peanuts – in children younger than age 5 years with moderate to severe AD, if the AD persists despite optimized topical treatment and/or a history of immediate and reproducible reaction after ingestion of a specific food.
Food elimination diets based solely on the findings of food allergy test results are not recommended for managing AD, she noted.
If a patient has true immunoglobulin E–mediated allergy they should practice avoidance to prevent potential serious health sequelae, Dr. Gonzalez said.
When testing is done, keep in mind that skin prick tests and serum-specific IgE levels have high negative predictive values above 95%, but low specificity and positive predictive values of 40%-60%, she pointed out. Positive tests should be verified with a food elimination diet or oral food challenge.
Also, most children develop tolerance to the foods over time and should be retested, Dr. Gonzalez said.
Early peanut introduction advised in infants with AD
There is no need to delay the introduction of peanuts into the diet of an infant at high risk for atopic dermatitis, Dr. Gonzalez said.
A 2015 consensus communication from the American Academy of Pediatrics and numerous other organizations, including the American Academy of Allergy, Asthma & Immunology and the Society of Pediatric Dermatology, offering interim guidance on the topic calls for introduction of peanut products into the diets of high-risk infants in countries where peanut allergy is present, she said.
High-risk infants were defined in the study as those with egg allergy and/or severe eczema.
The guidance, which the AAP “endorses and accepts as its policy” pending more formal guidelines currently in development, was based largely on findings from the LEAP (Learn Early About Peanut Allergy) trial – a 5-year randomized, controlled trial of 640 high-risk infants aged 4-11 months. The trial showed that 17.2% of infants who avoided peanuts had peanut allergy at 5 years, compared with 3.2% of those with peanut consumption three times weekly, a relative risk reduction of 81% (N Engl J Med. 2015; 372:803-13).
In infants with egg allergy or severe eczema, an evaluation by an allergist or dermatologist familiar with the guidance may be warranted to assist in implementing the suggestions, Dr. Gonzalez said.
Dr. Gonzalez reported receiving honoraria for serving as a speaker and/or advisory board member for Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Between 15% and 30% of children with moderate to severe atopic dermatitis also have food allergies, but the allergies are a trigger for AD in only a small subset of patients, according to Mercedes E. Gonzalez, MD.
In most cases, allergy testing is not indicated, she said at the American Academy of Dermatology summer meeting.
She described a scenario involving a parent who is concerned that a food allergy is causing her child’s AD. The child has had no hives, no lip swelling, and no other signs of immediate hypersensitivity. In such a case, the best approach is to treat with topical therapies and follow the patient clinically.
“Allergy testing independent of history is not recommended,” she said.
However, in cases involving a significant concern about food allergy, such as the presence of hives or urticaria, or when the child has severe dermatitis that is not improving with optimized topical therapies, an assessment can be undertaken, said Dr. Gonzalez of the University of Miami.
She recommended limited food allergy testing – for common culprits such as cow’s milk, eggs, wheat, soy, and peanuts – in children younger than age 5 years with moderate to severe AD, if the AD persists despite optimized topical treatment and/or a history of immediate and reproducible reaction after ingestion of a specific food.
Food elimination diets based solely on the findings of food allergy test results are not recommended for managing AD, she noted.
If a patient has true immunoglobulin E–mediated allergy they should practice avoidance to prevent potential serious health sequelae, Dr. Gonzalez said.
When testing is done, keep in mind that skin prick tests and serum-specific IgE levels have high negative predictive values above 95%, but low specificity and positive predictive values of 40%-60%, she pointed out. Positive tests should be verified with a food elimination diet or oral food challenge.
Also, most children develop tolerance to the foods over time and should be retested, Dr. Gonzalez said.
Early peanut introduction advised in infants with AD
There is no need to delay the introduction of peanuts into the diet of an infant at high risk for atopic dermatitis, Dr. Gonzalez said.
A 2015 consensus communication from the American Academy of Pediatrics and numerous other organizations, including the American Academy of Allergy, Asthma & Immunology and the Society of Pediatric Dermatology, offering interim guidance on the topic calls for introduction of peanut products into the diets of high-risk infants in countries where peanut allergy is present, she said.
High-risk infants were defined in the study as those with egg allergy and/or severe eczema.
The guidance, which the AAP “endorses and accepts as its policy” pending more formal guidelines currently in development, was based largely on findings from the LEAP (Learn Early About Peanut Allergy) trial – a 5-year randomized, controlled trial of 640 high-risk infants aged 4-11 months. The trial showed that 17.2% of infants who avoided peanuts had peanut allergy at 5 years, compared with 3.2% of those with peanut consumption three times weekly, a relative risk reduction of 81% (N Engl J Med. 2015; 372:803-13).
In infants with egg allergy or severe eczema, an evaluation by an allergist or dermatologist familiar with the guidance may be warranted to assist in implementing the suggestions, Dr. Gonzalez said.
Dr. Gonzalez reported receiving honoraria for serving as a speaker and/or advisory board member for Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Between 15% and 30% of children with moderate to severe atopic dermatitis also have food allergies, but the allergies are a trigger for AD in only a small subset of patients, according to Mercedes E. Gonzalez, MD.
In most cases, allergy testing is not indicated, she said at the American Academy of Dermatology summer meeting.
She described a scenario involving a parent who is concerned that a food allergy is causing her child’s AD. The child has had no hives, no lip swelling, and no other signs of immediate hypersensitivity. In such a case, the best approach is to treat with topical therapies and follow the patient clinically.
“Allergy testing independent of history is not recommended,” she said.
However, in cases involving a significant concern about food allergy, such as the presence of hives or urticaria, or when the child has severe dermatitis that is not improving with optimized topical therapies, an assessment can be undertaken, said Dr. Gonzalez of the University of Miami.
She recommended limited food allergy testing – for common culprits such as cow’s milk, eggs, wheat, soy, and peanuts – in children younger than age 5 years with moderate to severe AD, if the AD persists despite optimized topical treatment and/or a history of immediate and reproducible reaction after ingestion of a specific food.
Food elimination diets based solely on the findings of food allergy test results are not recommended for managing AD, she noted.
If a patient has true immunoglobulin E–mediated allergy they should practice avoidance to prevent potential serious health sequelae, Dr. Gonzalez said.
When testing is done, keep in mind that skin prick tests and serum-specific IgE levels have high negative predictive values above 95%, but low specificity and positive predictive values of 40%-60%, she pointed out. Positive tests should be verified with a food elimination diet or oral food challenge.
Also, most children develop tolerance to the foods over time and should be retested, Dr. Gonzalez said.
Early peanut introduction advised in infants with AD
There is no need to delay the introduction of peanuts into the diet of an infant at high risk for atopic dermatitis, Dr. Gonzalez said.
A 2015 consensus communication from the American Academy of Pediatrics and numerous other organizations, including the American Academy of Allergy, Asthma & Immunology and the Society of Pediatric Dermatology, offering interim guidance on the topic calls for introduction of peanut products into the diets of high-risk infants in countries where peanut allergy is present, she said.
High-risk infants were defined in the study as those with egg allergy and/or severe eczema.
The guidance, which the AAP “endorses and accepts as its policy” pending more formal guidelines currently in development, was based largely on findings from the LEAP (Learn Early About Peanut Allergy) trial – a 5-year randomized, controlled trial of 640 high-risk infants aged 4-11 months. The trial showed that 17.2% of infants who avoided peanuts had peanut allergy at 5 years, compared with 3.2% of those with peanut consumption three times weekly, a relative risk reduction of 81% (N Engl J Med. 2015; 372:803-13).
In infants with egg allergy or severe eczema, an evaluation by an allergist or dermatologist familiar with the guidance may be warranted to assist in implementing the suggestions, Dr. Gonzalez said.
Dr. Gonzalez reported receiving honoraria for serving as a speaker and/or advisory board member for Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
EXPERT ANALYSIS FROM AAD SUMMER ACADEMY 2016
Ninlaro receives approval for use in Canada
Health Canada has approved ixazomib (Ninlaro) for use in combination with lenalidomide and dexamethasone for the treatment of adults with relapsed/refractory multiple myeloma.
The U.S. Food and Drug Administration approved ixazomib in November 2015 for patients with relapsed/refractory multiple myeloma, based on data from TOURMALINE-MM1 that showed extended progression-free survival with a manageable safety profile.
“The approval of Ninlaro offers a much-needed new option for Canadian patients with multiple myeloma who have received at least one prior therapy. Its oral delivery may help multiple myeloma patients overcome some of the logistical burdens they may face with current therapies, which are typically administered in-clinic or in-hospital requiring significant travel and time constraints,” said Donna Reece, M.D., professor and director of the program for multiple myeloma and related diseases in the department of medical oncology and haematology at Princess Margaret Hospital/University of Toronto.
Ninlaro is marketed by Takeda. Click here to read the press release.
Health Canada has approved ixazomib (Ninlaro) for use in combination with lenalidomide and dexamethasone for the treatment of adults with relapsed/refractory multiple myeloma.
The U.S. Food and Drug Administration approved ixazomib in November 2015 for patients with relapsed/refractory multiple myeloma, based on data from TOURMALINE-MM1 that showed extended progression-free survival with a manageable safety profile.
“The approval of Ninlaro offers a much-needed new option for Canadian patients with multiple myeloma who have received at least one prior therapy. Its oral delivery may help multiple myeloma patients overcome some of the logistical burdens they may face with current therapies, which are typically administered in-clinic or in-hospital requiring significant travel and time constraints,” said Donna Reece, M.D., professor and director of the program for multiple myeloma and related diseases in the department of medical oncology and haematology at Princess Margaret Hospital/University of Toronto.
Ninlaro is marketed by Takeda. Click here to read the press release.
Health Canada has approved ixazomib (Ninlaro) for use in combination with lenalidomide and dexamethasone for the treatment of adults with relapsed/refractory multiple myeloma.
The U.S. Food and Drug Administration approved ixazomib in November 2015 for patients with relapsed/refractory multiple myeloma, based on data from TOURMALINE-MM1 that showed extended progression-free survival with a manageable safety profile.
“The approval of Ninlaro offers a much-needed new option for Canadian patients with multiple myeloma who have received at least one prior therapy. Its oral delivery may help multiple myeloma patients overcome some of the logistical burdens they may face with current therapies, which are typically administered in-clinic or in-hospital requiring significant travel and time constraints,” said Donna Reece, M.D., professor and director of the program for multiple myeloma and related diseases in the department of medical oncology and haematology at Princess Margaret Hospital/University of Toronto.
Ninlaro is marketed by Takeda. Click here to read the press release.
Eradication strategies for chronic hepatitis B infection
Current treatment strategies for chronic hepatitis B virus (HBV) infection seek to suppress viral replication by blocking HBV reverse transcription. When circulating HBV viremia is suppressed, clinical outcomes improve, with slowing of fibrosis and reduced rates of hepatocellular carcinoma. However, when treatment is discontinued, viral replication typically rebounds. This is because nucleos(t)ide (NUC) therapy has no effect on existing HBV cccDNA (covalently closed circular DNA) reservoirs.
A functional cure is defined as the absence of HBV DNA and hepatitis B surface antigen (HBsAg), in the absence of antiviral therapy, with or without the development of protective hepatitis B surface antibody (HBsAb). However, rates of viral clearance are extremely low after therapy with IFN and NUC analogs. Strategies to control HBV replication, purge covalently closed circular DNA (cccDNA) reservoirs, and develop long-lasting protective immunity in patients with chronic HBV infection are desperately needed to achieve a functional cure.
Current investigational approaches to curing HBV fall into two different strategies: targeting the virus directly or manipulating the host immune response to aid in clearance.
Targeting the virus
One of the challenges of treating HBV is the stability of HBV DNA inside infected hepatocytes; supercoiled and sequestered in the host cell nucleus, HBV cccDNA is protected from cellular DNA-sensing machinery. Hepatocytes infected with HBV have a long half-life, serving as a reservoir for HBV reactivation. In addition to preventing, inactivating, or disrupting cccDNA, investigational approaches to target the virus also focus on blocking specific steps in viral replication, including viral transcription, entry into uninfected hepatocytes, capsid assembly, and antigen secretion.
Gene therapy approaches, including zinc finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs), clustered regularly interspaced palindromic repeat (CRISP-R) applications, and RNA interference (RNAi) technology may be able to inactivate target cccDNA, silencing or disrupting this viral reservoir.
Various investigational drugs are being studied for their ability to interfere with viral entry, encapsidation, or antigen release. Specific interactions between viral membrane proteins and cellular receptors are attractive targets for blocking HBV entry into host cells. Agents that interfere with assembly of the virus particle may prevent the production of infectious virus. Some innovative therapeutic strategies also seek to block the secretion of HBsAg; chronic exposure to HBsAg can lead to T-cell exhaustion, so this strategy may allow the host to develop a more effective anti-HBV adaptive immune response.
Manipulating host response
The second major strategy of novel HBV therapies involves mediating the host response, reversing immune exhaustion, selectively activating innate and/or adaptive immunity through therapeutic vaccination or passive transfer in order to produce a more effective response that results in viral clearance.
The innate immune response, the first line of defense against viral infections, is activated when toll-like receptors (TLRs) on the surface of innate immune cells are engaged, but TLR signaling is downregulated in chronic HBV infection. Stimulating innate immune cells by activating TLRs may accelerate HBV-specific immune reconstitution and help clear HBV in chronically infected individuals. Likewise, blocking the interaction of PD-1 with its ligands (PD-L1/2) may improve the antiviral function of exhausted T cells.
Reversing immune exhaustion will not work if there are no HBV-specific T cells present. Studies have pointed to the clonal deletion of HBV-specific CD8+ T cells as a mechanism of HBV persistence. T-cell responses may be “trained” to recognize infected cells by expressing HBV-specific chimeric antigen receptors (CARs), which are synthetic engineered receptors that can engage cell-surface molecules.
Therapeutic vaccination additionally presents a promising strategy to address HBV-specific T-cell exhaustion by inducing a potent CD4 T-cell response and counteracting immune tolerance against HBV antigens. Yeast-based vaccines, adenovirus vector and engineered vesicular stomatitis virus vectors have shown to be promising platforms that may be capable of eliciting a functional adaptive immune response in patients with chronic HBV, but their use is often limited by preexisting host immunity.
In summary, current therapies for HBV rarely clear or cure infection. A two-pronged approach of targeting viral and host factors may offer the best chance to reverse the immune tolerance, T-cell exhaustion, and persistent viral reservoir associated with chronic HBV infection.
Rebecca Lee is a second-year medical student at the University of Maryland School of Medicine. Eleanor Wilson, MD, is assistant professor in the Institute of Human Virology at the University of Maryland School of Medicine. Shyam Kottilil, MBBS, PhD, is professor of medicine in the Institute of Human Virology at the University of Maryland School of Medicine.
Current treatment strategies for chronic hepatitis B virus (HBV) infection seek to suppress viral replication by blocking HBV reverse transcription. When circulating HBV viremia is suppressed, clinical outcomes improve, with slowing of fibrosis and reduced rates of hepatocellular carcinoma. However, when treatment is discontinued, viral replication typically rebounds. This is because nucleos(t)ide (NUC) therapy has no effect on existing HBV cccDNA (covalently closed circular DNA) reservoirs.
A functional cure is defined as the absence of HBV DNA and hepatitis B surface antigen (HBsAg), in the absence of antiviral therapy, with or without the development of protective hepatitis B surface antibody (HBsAb). However, rates of viral clearance are extremely low after therapy with IFN and NUC analogs. Strategies to control HBV replication, purge covalently closed circular DNA (cccDNA) reservoirs, and develop long-lasting protective immunity in patients with chronic HBV infection are desperately needed to achieve a functional cure.
Current investigational approaches to curing HBV fall into two different strategies: targeting the virus directly or manipulating the host immune response to aid in clearance.
Targeting the virus
One of the challenges of treating HBV is the stability of HBV DNA inside infected hepatocytes; supercoiled and sequestered in the host cell nucleus, HBV cccDNA is protected from cellular DNA-sensing machinery. Hepatocytes infected with HBV have a long half-life, serving as a reservoir for HBV reactivation. In addition to preventing, inactivating, or disrupting cccDNA, investigational approaches to target the virus also focus on blocking specific steps in viral replication, including viral transcription, entry into uninfected hepatocytes, capsid assembly, and antigen secretion.
Gene therapy approaches, including zinc finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs), clustered regularly interspaced palindromic repeat (CRISP-R) applications, and RNA interference (RNAi) technology may be able to inactivate target cccDNA, silencing or disrupting this viral reservoir.
Various investigational drugs are being studied for their ability to interfere with viral entry, encapsidation, or antigen release. Specific interactions between viral membrane proteins and cellular receptors are attractive targets for blocking HBV entry into host cells. Agents that interfere with assembly of the virus particle may prevent the production of infectious virus. Some innovative therapeutic strategies also seek to block the secretion of HBsAg; chronic exposure to HBsAg can lead to T-cell exhaustion, so this strategy may allow the host to develop a more effective anti-HBV adaptive immune response.
Manipulating host response
The second major strategy of novel HBV therapies involves mediating the host response, reversing immune exhaustion, selectively activating innate and/or adaptive immunity through therapeutic vaccination or passive transfer in order to produce a more effective response that results in viral clearance.
The innate immune response, the first line of defense against viral infections, is activated when toll-like receptors (TLRs) on the surface of innate immune cells are engaged, but TLR signaling is downregulated in chronic HBV infection. Stimulating innate immune cells by activating TLRs may accelerate HBV-specific immune reconstitution and help clear HBV in chronically infected individuals. Likewise, blocking the interaction of PD-1 with its ligands (PD-L1/2) may improve the antiviral function of exhausted T cells.
Reversing immune exhaustion will not work if there are no HBV-specific T cells present. Studies have pointed to the clonal deletion of HBV-specific CD8+ T cells as a mechanism of HBV persistence. T-cell responses may be “trained” to recognize infected cells by expressing HBV-specific chimeric antigen receptors (CARs), which are synthetic engineered receptors that can engage cell-surface molecules.
Therapeutic vaccination additionally presents a promising strategy to address HBV-specific T-cell exhaustion by inducing a potent CD4 T-cell response and counteracting immune tolerance against HBV antigens. Yeast-based vaccines, adenovirus vector and engineered vesicular stomatitis virus vectors have shown to be promising platforms that may be capable of eliciting a functional adaptive immune response in patients with chronic HBV, but their use is often limited by preexisting host immunity.
In summary, current therapies for HBV rarely clear or cure infection. A two-pronged approach of targeting viral and host factors may offer the best chance to reverse the immune tolerance, T-cell exhaustion, and persistent viral reservoir associated with chronic HBV infection.
Rebecca Lee is a second-year medical student at the University of Maryland School of Medicine. Eleanor Wilson, MD, is assistant professor in the Institute of Human Virology at the University of Maryland School of Medicine. Shyam Kottilil, MBBS, PhD, is professor of medicine in the Institute of Human Virology at the University of Maryland School of Medicine.
Current treatment strategies for chronic hepatitis B virus (HBV) infection seek to suppress viral replication by blocking HBV reverse transcription. When circulating HBV viremia is suppressed, clinical outcomes improve, with slowing of fibrosis and reduced rates of hepatocellular carcinoma. However, when treatment is discontinued, viral replication typically rebounds. This is because nucleos(t)ide (NUC) therapy has no effect on existing HBV cccDNA (covalently closed circular DNA) reservoirs.
A functional cure is defined as the absence of HBV DNA and hepatitis B surface antigen (HBsAg), in the absence of antiviral therapy, with or without the development of protective hepatitis B surface antibody (HBsAb). However, rates of viral clearance are extremely low after therapy with IFN and NUC analogs. Strategies to control HBV replication, purge covalently closed circular DNA (cccDNA) reservoirs, and develop long-lasting protective immunity in patients with chronic HBV infection are desperately needed to achieve a functional cure.
Current investigational approaches to curing HBV fall into two different strategies: targeting the virus directly or manipulating the host immune response to aid in clearance.
Targeting the virus
One of the challenges of treating HBV is the stability of HBV DNA inside infected hepatocytes; supercoiled and sequestered in the host cell nucleus, HBV cccDNA is protected from cellular DNA-sensing machinery. Hepatocytes infected with HBV have a long half-life, serving as a reservoir for HBV reactivation. In addition to preventing, inactivating, or disrupting cccDNA, investigational approaches to target the virus also focus on blocking specific steps in viral replication, including viral transcription, entry into uninfected hepatocytes, capsid assembly, and antigen secretion.
Gene therapy approaches, including zinc finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs), clustered regularly interspaced palindromic repeat (CRISP-R) applications, and RNA interference (RNAi) technology may be able to inactivate target cccDNA, silencing or disrupting this viral reservoir.
Various investigational drugs are being studied for their ability to interfere with viral entry, encapsidation, or antigen release. Specific interactions between viral membrane proteins and cellular receptors are attractive targets for blocking HBV entry into host cells. Agents that interfere with assembly of the virus particle may prevent the production of infectious virus. Some innovative therapeutic strategies also seek to block the secretion of HBsAg; chronic exposure to HBsAg can lead to T-cell exhaustion, so this strategy may allow the host to develop a more effective anti-HBV adaptive immune response.
Manipulating host response
The second major strategy of novel HBV therapies involves mediating the host response, reversing immune exhaustion, selectively activating innate and/or adaptive immunity through therapeutic vaccination or passive transfer in order to produce a more effective response that results in viral clearance.
The innate immune response, the first line of defense against viral infections, is activated when toll-like receptors (TLRs) on the surface of innate immune cells are engaged, but TLR signaling is downregulated in chronic HBV infection. Stimulating innate immune cells by activating TLRs may accelerate HBV-specific immune reconstitution and help clear HBV in chronically infected individuals. Likewise, blocking the interaction of PD-1 with its ligands (PD-L1/2) may improve the antiviral function of exhausted T cells.
Reversing immune exhaustion will not work if there are no HBV-specific T cells present. Studies have pointed to the clonal deletion of HBV-specific CD8+ T cells as a mechanism of HBV persistence. T-cell responses may be “trained” to recognize infected cells by expressing HBV-specific chimeric antigen receptors (CARs), which are synthetic engineered receptors that can engage cell-surface molecules.
Therapeutic vaccination additionally presents a promising strategy to address HBV-specific T-cell exhaustion by inducing a potent CD4 T-cell response and counteracting immune tolerance against HBV antigens. Yeast-based vaccines, adenovirus vector and engineered vesicular stomatitis virus vectors have shown to be promising platforms that may be capable of eliciting a functional adaptive immune response in patients with chronic HBV, but their use is often limited by preexisting host immunity.
In summary, current therapies for HBV rarely clear or cure infection. A two-pronged approach of targeting viral and host factors may offer the best chance to reverse the immune tolerance, T-cell exhaustion, and persistent viral reservoir associated with chronic HBV infection.
Rebecca Lee is a second-year medical student at the University of Maryland School of Medicine. Eleanor Wilson, MD, is assistant professor in the Institute of Human Virology at the University of Maryland School of Medicine. Shyam Kottilil, MBBS, PhD, is professor of medicine in the Institute of Human Virology at the University of Maryland School of Medicine.
Nanoparticles speed blood clotting in multiple models
form clots in injured liver
Image courtesy of Erin Lavik
PHILADELPHIA—Researchers say they have developed nanoparticles that can congregate at sites of injury and speed blood clotting in vitro and in vivo.
The nanoparticles are designed to bind with activated platelets and help them join together to form clots faster.
The nanoparticles have helped stop bleeding and improved animals’ survival in different models of injury, without producing off-target clotting.
“When you have uncontrolled internal bleeding, that’s when these particles could really make a difference,” said Erin B. Lavik, ScD, of the University of Maryland, Baltimore County (UMBC) in Baltimore, Maryland.
“Compared to injuries that aren’t treated with the nanoparticles, we can cut bleeding time in half and reduce total blood loss.”
Dr Lavik discussed this work at the 252nd National Meeting & Exposition of the American Chemical Society.
She and her colleagues have been testing different versions of these nanoparticles for years. They previously reported results with the particles in 2012 and 2014.
The current nanoparticles are made from polylactic acid or polylactic co-glycolic acid. Dr Lavik said that by using the 2 different materials, the researchers can change the temperature at which the nanoparticles melt. Thus far, the team has developed nanoparticles that are stable up to 50° C (122° F).
The nanoparticles have an outer coating of polyethylene glycol and an attached peptide—RGD—that enables them to bind to natural platelets. Dr Lavik said the researchers chose RGD because platelets have receptors for that peptide, it’s ubiquitous in the body, and it wouldn’t alter the chemistry of the nanoparticles.
The researchers have tested the nanoparticles in a femoral injury model, a liver injury model, and blast injury model. The team has also started testing in models of brain and spinal cord injury, but the results are “very preliminary,” according to Dr Lavik.
In the femoral injury model, the nanoparticles halved bleeding time when compared to no treatment. In both the liver injury model and the blast injury model, the nanoparticles stopped bleeding and improved survival.
Dr Lavik said these experiments have shown that the nanoparticles successfully speed clotting, and the clots formed are mechanically robust.
The nanoparticles also clear the body easily. When the particles are bound into a clot, they stay as long as the clot remains. They begin to degrade once the clot does and clear out of the bloodstream quickly.
Dr Lavik said the researchers haven’t seen non-specific clotting with the nanoparticles yet. However, this side effect remains a possibility because the particles are designed to bind to activated platelets, which may not be confined to the site of injury.
One unfortunate side effect occurred with an earlier version of the nanoparticles. They triggered an immune response, activating complement in pig’s blood. However, the researchers were able to modify the particles to reduce complement activation and the accompanying complications.
In future studies, Dr Lavik and her colleagues plan to test whether the new nanoparticles activate complement in human blood. The team also aims to verify that the nanoparticles don’t cause non-specific clotting. ![]()
form clots in injured liver
Image courtesy of Erin Lavik
PHILADELPHIA—Researchers say they have developed nanoparticles that can congregate at sites of injury and speed blood clotting in vitro and in vivo.
The nanoparticles are designed to bind with activated platelets and help them join together to form clots faster.
The nanoparticles have helped stop bleeding and improved animals’ survival in different models of injury, without producing off-target clotting.
“When you have uncontrolled internal bleeding, that’s when these particles could really make a difference,” said Erin B. Lavik, ScD, of the University of Maryland, Baltimore County (UMBC) in Baltimore, Maryland.
“Compared to injuries that aren’t treated with the nanoparticles, we can cut bleeding time in half and reduce total blood loss.”
Dr Lavik discussed this work at the 252nd National Meeting & Exposition of the American Chemical Society.
She and her colleagues have been testing different versions of these nanoparticles for years. They previously reported results with the particles in 2012 and 2014.
The current nanoparticles are made from polylactic acid or polylactic co-glycolic acid. Dr Lavik said that by using the 2 different materials, the researchers can change the temperature at which the nanoparticles melt. Thus far, the team has developed nanoparticles that are stable up to 50° C (122° F).
The nanoparticles have an outer coating of polyethylene glycol and an attached peptide—RGD—that enables them to bind to natural platelets. Dr Lavik said the researchers chose RGD because platelets have receptors for that peptide, it’s ubiquitous in the body, and it wouldn’t alter the chemistry of the nanoparticles.
The researchers have tested the nanoparticles in a femoral injury model, a liver injury model, and blast injury model. The team has also started testing in models of brain and spinal cord injury, but the results are “very preliminary,” according to Dr Lavik.
In the femoral injury model, the nanoparticles halved bleeding time when compared to no treatment. In both the liver injury model and the blast injury model, the nanoparticles stopped bleeding and improved survival.
Dr Lavik said these experiments have shown that the nanoparticles successfully speed clotting, and the clots formed are mechanically robust.
The nanoparticles also clear the body easily. When the particles are bound into a clot, they stay as long as the clot remains. They begin to degrade once the clot does and clear out of the bloodstream quickly.
Dr Lavik said the researchers haven’t seen non-specific clotting with the nanoparticles yet. However, this side effect remains a possibility because the particles are designed to bind to activated platelets, which may not be confined to the site of injury.
One unfortunate side effect occurred with an earlier version of the nanoparticles. They triggered an immune response, activating complement in pig’s blood. However, the researchers were able to modify the particles to reduce complement activation and the accompanying complications.
In future studies, Dr Lavik and her colleagues plan to test whether the new nanoparticles activate complement in human blood. The team also aims to verify that the nanoparticles don’t cause non-specific clotting. ![]()
form clots in injured liver
Image courtesy of Erin Lavik
PHILADELPHIA—Researchers say they have developed nanoparticles that can congregate at sites of injury and speed blood clotting in vitro and in vivo.
The nanoparticles are designed to bind with activated platelets and help them join together to form clots faster.
The nanoparticles have helped stop bleeding and improved animals’ survival in different models of injury, without producing off-target clotting.
“When you have uncontrolled internal bleeding, that’s when these particles could really make a difference,” said Erin B. Lavik, ScD, of the University of Maryland, Baltimore County (UMBC) in Baltimore, Maryland.
“Compared to injuries that aren’t treated with the nanoparticles, we can cut bleeding time in half and reduce total blood loss.”
Dr Lavik discussed this work at the 252nd National Meeting & Exposition of the American Chemical Society.
She and her colleagues have been testing different versions of these nanoparticles for years. They previously reported results with the particles in 2012 and 2014.
The current nanoparticles are made from polylactic acid or polylactic co-glycolic acid. Dr Lavik said that by using the 2 different materials, the researchers can change the temperature at which the nanoparticles melt. Thus far, the team has developed nanoparticles that are stable up to 50° C (122° F).
The nanoparticles have an outer coating of polyethylene glycol and an attached peptide—RGD—that enables them to bind to natural platelets. Dr Lavik said the researchers chose RGD because platelets have receptors for that peptide, it’s ubiquitous in the body, and it wouldn’t alter the chemistry of the nanoparticles.
The researchers have tested the nanoparticles in a femoral injury model, a liver injury model, and blast injury model. The team has also started testing in models of brain and spinal cord injury, but the results are “very preliminary,” according to Dr Lavik.
In the femoral injury model, the nanoparticles halved bleeding time when compared to no treatment. In both the liver injury model and the blast injury model, the nanoparticles stopped bleeding and improved survival.
Dr Lavik said these experiments have shown that the nanoparticles successfully speed clotting, and the clots formed are mechanically robust.
The nanoparticles also clear the body easily. When the particles are bound into a clot, they stay as long as the clot remains. They begin to degrade once the clot does and clear out of the bloodstream quickly.
Dr Lavik said the researchers haven’t seen non-specific clotting with the nanoparticles yet. However, this side effect remains a possibility because the particles are designed to bind to activated platelets, which may not be confined to the site of injury.
One unfortunate side effect occurred with an earlier version of the nanoparticles. They triggered an immune response, activating complement in pig’s blood. However, the researchers were able to modify the particles to reduce complement activation and the accompanying complications.
In future studies, Dr Lavik and her colleagues plan to test whether the new nanoparticles activate complement in human blood. The team also aims to verify that the nanoparticles don’t cause non-specific clotting. ![]()
LETTER: 6 Tips When Practicing Telemedicine
In early 2014, I decided to use the six state licenses I had obtained as a locum tenens physician to start practicing telemedicine. Since then, I have worked with several telemedicine platforms. I have found that telemedicine companies differ dramatically in their overall ease of use for the provider. Here are my top tips for deciding which telemedicine company to work with.
- Technology support: Telemedicine is dependent on technology. If it is difficult to get help from tech support, do not credential with the company. Tech support is your lifeline to your patients. Make sure you can get help right away if you are having problems finishing or starting a consult. Companies that send automatic emails saying they will get back to you within 24 hours are the most difficult to work with.
- Nursing support: All of the telemedicine companies that I have worked with have amazing nurses, but some are overwhelmed with work. Telemedicine nurses are able to connect to your patients via direct callback numbers in a way that you cannot connect. They are able to call in prescriptions to pharmacies if the platform is down or if the patient put in the wrong pharmacy information. Make sure that the company has a nurse that is able to call you back right away. A few telemedicine companies are understaffed with nurses, and it can take hours for a callback. If the key to telemedicine is volume, this is frustrating to deal with.
- Chief complaints: Many telemedicine companies are moving away from making the “chief complaint” visible to providers before choosing to take the consult. For me, this is a big red flag. It can be as simple as, “I have a cold.” I like this because if I see a patient who says, “I have abdominal pain,” I know to triage them first.
- Volume: Telemedicine is great for staying connected to outpatient medicine. If you are looking to work on a telemedicine platform for your main source of income, then volume is key. A lot of telemedicine companies will tell you how many calls they get per day; the key question is how many calls they get for the states that you are licensed in and how many providers they have licensed in those states. If you want higher volume, then ask if they will pay for your license in states with higher needs (some will). If you are willing to pay to be licensed in additional states, make sure the volume is high enough to make that extra out-of-pocket cost worth it.
- Malpractice coverage: Many companies provide malpractice coverage as part of their credentialing package. If they do not, make sure your malpractice coverage covers you for telemedicine.
- Documentation: Documentation during your telemedicine consult is arguably even more important than in an outpatient visit. Everything is on the phone or by video, so make sure, in the subjective area, that you are quoting what the patient is telling you. You are not able to do a physical exam, so your recommendations will be based on what the patient is saying.
Have fun! Telemedicine has been really enjoyable for me. I like being able to have the time to educate my patients about things like antibiotics. I enjoy the technological aspects and understanding all of the different platforms. Telemedicine gives you a unique opportunity to practice your skills from the comfort of your own home. TH
In early 2014, I decided to use the six state licenses I had obtained as a locum tenens physician to start practicing telemedicine. Since then, I have worked with several telemedicine platforms. I have found that telemedicine companies differ dramatically in their overall ease of use for the provider. Here are my top tips for deciding which telemedicine company to work with.
- Technology support: Telemedicine is dependent on technology. If it is difficult to get help from tech support, do not credential with the company. Tech support is your lifeline to your patients. Make sure you can get help right away if you are having problems finishing or starting a consult. Companies that send automatic emails saying they will get back to you within 24 hours are the most difficult to work with.
- Nursing support: All of the telemedicine companies that I have worked with have amazing nurses, but some are overwhelmed with work. Telemedicine nurses are able to connect to your patients via direct callback numbers in a way that you cannot connect. They are able to call in prescriptions to pharmacies if the platform is down or if the patient put in the wrong pharmacy information. Make sure that the company has a nurse that is able to call you back right away. A few telemedicine companies are understaffed with nurses, and it can take hours for a callback. If the key to telemedicine is volume, this is frustrating to deal with.
- Chief complaints: Many telemedicine companies are moving away from making the “chief complaint” visible to providers before choosing to take the consult. For me, this is a big red flag. It can be as simple as, “I have a cold.” I like this because if I see a patient who says, “I have abdominal pain,” I know to triage them first.
- Volume: Telemedicine is great for staying connected to outpatient medicine. If you are looking to work on a telemedicine platform for your main source of income, then volume is key. A lot of telemedicine companies will tell you how many calls they get per day; the key question is how many calls they get for the states that you are licensed in and how many providers they have licensed in those states. If you want higher volume, then ask if they will pay for your license in states with higher needs (some will). If you are willing to pay to be licensed in additional states, make sure the volume is high enough to make that extra out-of-pocket cost worth it.
- Malpractice coverage: Many companies provide malpractice coverage as part of their credentialing package. If they do not, make sure your malpractice coverage covers you for telemedicine.
- Documentation: Documentation during your telemedicine consult is arguably even more important than in an outpatient visit. Everything is on the phone or by video, so make sure, in the subjective area, that you are quoting what the patient is telling you. You are not able to do a physical exam, so your recommendations will be based on what the patient is saying.
Have fun! Telemedicine has been really enjoyable for me. I like being able to have the time to educate my patients about things like antibiotics. I enjoy the technological aspects and understanding all of the different platforms. Telemedicine gives you a unique opportunity to practice your skills from the comfort of your own home. TH
In early 2014, I decided to use the six state licenses I had obtained as a locum tenens physician to start practicing telemedicine. Since then, I have worked with several telemedicine platforms. I have found that telemedicine companies differ dramatically in their overall ease of use for the provider. Here are my top tips for deciding which telemedicine company to work with.
- Technology support: Telemedicine is dependent on technology. If it is difficult to get help from tech support, do not credential with the company. Tech support is your lifeline to your patients. Make sure you can get help right away if you are having problems finishing or starting a consult. Companies that send automatic emails saying they will get back to you within 24 hours are the most difficult to work with.
- Nursing support: All of the telemedicine companies that I have worked with have amazing nurses, but some are overwhelmed with work. Telemedicine nurses are able to connect to your patients via direct callback numbers in a way that you cannot connect. They are able to call in prescriptions to pharmacies if the platform is down or if the patient put in the wrong pharmacy information. Make sure that the company has a nurse that is able to call you back right away. A few telemedicine companies are understaffed with nurses, and it can take hours for a callback. If the key to telemedicine is volume, this is frustrating to deal with.
- Chief complaints: Many telemedicine companies are moving away from making the “chief complaint” visible to providers before choosing to take the consult. For me, this is a big red flag. It can be as simple as, “I have a cold.” I like this because if I see a patient who says, “I have abdominal pain,” I know to triage them first.
- Volume: Telemedicine is great for staying connected to outpatient medicine. If you are looking to work on a telemedicine platform for your main source of income, then volume is key. A lot of telemedicine companies will tell you how many calls they get per day; the key question is how many calls they get for the states that you are licensed in and how many providers they have licensed in those states. If you want higher volume, then ask if they will pay for your license in states with higher needs (some will). If you are willing to pay to be licensed in additional states, make sure the volume is high enough to make that extra out-of-pocket cost worth it.
- Malpractice coverage: Many companies provide malpractice coverage as part of their credentialing package. If they do not, make sure your malpractice coverage covers you for telemedicine.
- Documentation: Documentation during your telemedicine consult is arguably even more important than in an outpatient visit. Everything is on the phone or by video, so make sure, in the subjective area, that you are quoting what the patient is telling you. You are not able to do a physical exam, so your recommendations will be based on what the patient is saying.
Have fun! Telemedicine has been really enjoyable for me. I like being able to have the time to educate my patients about things like antibiotics. I enjoy the technological aspects and understanding all of the different platforms. Telemedicine gives you a unique opportunity to practice your skills from the comfort of your own home. TH
Massage therapy seems to benefit cancer patients

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()
Drug granted breakthrough designation for BPDCN

The US Food and Drug Administration (FDA) has granted breakthrough therapy designation for SL-401 in the treatment of blastic plasmacytoid dendritic cell neoplasm (BPDCN).
SL-401 is a targeted therapy directed to the interleukin-3 receptor (IL-3R), which is present in BPDCN and other hematologic malignancies.
SL-401 is composed of human IL-3 coupled to a truncated diphtheria toxin payload that inhibits protein synthesis.
The drug is under development by Stemline Therapeutics, Inc.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new therapies for serious or life-threatening conditions.
To earn the designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Phase 2 trial of SL-401
The breakthrough designation for SL-401 was supported by data from a phase 2 trial of patients with BPDCN or acute myeloid leukemia. Results observed in the BPDCN patients were presented at the 2016 EHA Congress (abstract S812).
The study consists of a lead-in dose-escalation stage (stage 1) and subsequent expansion stage (stage 2). In stage 1, patients received SL-401 as a daily intravenous infusion for up to 5 days (7, 9, 12, or 16 μg/kg/day) every 21 days. In stage 2, patients received SL-401 at the optimal stage 1 dose—12 μg/kg.
At the data cut-off, 18 BPDCN patients had received SL-401 at 7 μg/kg (n=3, stage 1) or 12 μg/kg (n=15, 6 in stage 1, 9 in stage 2).
Fifteen of these patients were evaluable for response. The overall response rate was 87% (13/15). All 10 previously untreated BPDCN patients achieved a response, including 7 complete responses (CRs).
All 8 previously untreated BPDCN patients treated at the optimal dose (12 μg/kg) achieved a response, including 6 CRs. Four of these patients were still on SL-401 and in CR at the data cutoff, and 2 had gone on to stem cell transplant.
The most common treatment-related adverse events in the BPDCN patients were transient transaminase elevation (57%), hypoalbuminemia (40%), and transient thrombocytopenia (15%).
In stage 1, two patients had capillary leak syndrome (CLS)—one grade 5 (7 μg/kg) and one grade 4 (12 μg/kg). After this, safety precautions were implemented to minimize the risk of severe CLS. There have been no cases of severe CLS since then. ![]()

The US Food and Drug Administration (FDA) has granted breakthrough therapy designation for SL-401 in the treatment of blastic plasmacytoid dendritic cell neoplasm (BPDCN).
SL-401 is a targeted therapy directed to the interleukin-3 receptor (IL-3R), which is present in BPDCN and other hematologic malignancies.
SL-401 is composed of human IL-3 coupled to a truncated diphtheria toxin payload that inhibits protein synthesis.
The drug is under development by Stemline Therapeutics, Inc.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new therapies for serious or life-threatening conditions.
To earn the designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Phase 2 trial of SL-401
The breakthrough designation for SL-401 was supported by data from a phase 2 trial of patients with BPDCN or acute myeloid leukemia. Results observed in the BPDCN patients were presented at the 2016 EHA Congress (abstract S812).
The study consists of a lead-in dose-escalation stage (stage 1) and subsequent expansion stage (stage 2). In stage 1, patients received SL-401 as a daily intravenous infusion for up to 5 days (7, 9, 12, or 16 μg/kg/day) every 21 days. In stage 2, patients received SL-401 at the optimal stage 1 dose—12 μg/kg.
At the data cut-off, 18 BPDCN patients had received SL-401 at 7 μg/kg (n=3, stage 1) or 12 μg/kg (n=15, 6 in stage 1, 9 in stage 2).
Fifteen of these patients were evaluable for response. The overall response rate was 87% (13/15). All 10 previously untreated BPDCN patients achieved a response, including 7 complete responses (CRs).
All 8 previously untreated BPDCN patients treated at the optimal dose (12 μg/kg) achieved a response, including 6 CRs. Four of these patients were still on SL-401 and in CR at the data cutoff, and 2 had gone on to stem cell transplant.
The most common treatment-related adverse events in the BPDCN patients were transient transaminase elevation (57%), hypoalbuminemia (40%), and transient thrombocytopenia (15%).
In stage 1, two patients had capillary leak syndrome (CLS)—one grade 5 (7 μg/kg) and one grade 4 (12 μg/kg). After this, safety precautions were implemented to minimize the risk of severe CLS. There have been no cases of severe CLS since then. ![]()

The US Food and Drug Administration (FDA) has granted breakthrough therapy designation for SL-401 in the treatment of blastic plasmacytoid dendritic cell neoplasm (BPDCN).
SL-401 is a targeted therapy directed to the interleukin-3 receptor (IL-3R), which is present in BPDCN and other hematologic malignancies.
SL-401 is composed of human IL-3 coupled to a truncated diphtheria toxin payload that inhibits protein synthesis.
The drug is under development by Stemline Therapeutics, Inc.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new therapies for serious or life-threatening conditions.
To earn the designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Phase 2 trial of SL-401
The breakthrough designation for SL-401 was supported by data from a phase 2 trial of patients with BPDCN or acute myeloid leukemia. Results observed in the BPDCN patients were presented at the 2016 EHA Congress (abstract S812).
The study consists of a lead-in dose-escalation stage (stage 1) and subsequent expansion stage (stage 2). In stage 1, patients received SL-401 as a daily intravenous infusion for up to 5 days (7, 9, 12, or 16 μg/kg/day) every 21 days. In stage 2, patients received SL-401 at the optimal stage 1 dose—12 μg/kg.
At the data cut-off, 18 BPDCN patients had received SL-401 at 7 μg/kg (n=3, stage 1) or 12 μg/kg (n=15, 6 in stage 1, 9 in stage 2).
Fifteen of these patients were evaluable for response. The overall response rate was 87% (13/15). All 10 previously untreated BPDCN patients achieved a response, including 7 complete responses (CRs).
All 8 previously untreated BPDCN patients treated at the optimal dose (12 μg/kg) achieved a response, including 6 CRs. Four of these patients were still on SL-401 and in CR at the data cutoff, and 2 had gone on to stem cell transplant.
The most common treatment-related adverse events in the BPDCN patients were transient transaminase elevation (57%), hypoalbuminemia (40%), and transient thrombocytopenia (15%).
In stage 1, two patients had capillary leak syndrome (CLS)—one grade 5 (7 μg/kg) and one grade 4 (12 μg/kg). After this, safety precautions were implemented to minimize the risk of severe CLS. There have been no cases of severe CLS since then. ![]()