User login
The Ads Say ‘Get Your Flu Shot Today,’ But It May Be Wiser To Wait
The pharmacy chain pitches started in August: Come in and get your flu shot.
Convenience is touted. So are incentives: CVS offers a 20-percent-off shopping pass for everyone who gets a shot, while Walgreens donates toward international vaccination efforts.
The start of flu season is still weeks — if not months — away. Yet marketing of the vaccine has become an almost year-round effort, beginning when the shots become available in August and hyped as long as the supply lasts, often into April or May.
Not that long ago, most flu-shot campaigns started as the leaves began to turn in October. But the rise of retail medical clinics inside drug stores over the past decade — and state laws allowing pharmacists to give vaccinations — has stretched the flu-shot season.
The stores have figured out how “to deliver medical services in an on-demand way” which appeals to customers, particularly millennials, said Tom Charland, founder and CEO of Merchant Medicine, which tracks the walk-in clinic industry. “It’s a way to get people into the store to buy other things.”
But some experts say the marketing may be overtaking medical wisdom since it’s unclear how long the immunity imparted by the vaccine lasts, particularly in older people.
Federal health officials say it’s better to get the shot whenever you can. An early flu shot is better than no flu shot at all. But the science is mixed when it comes to how long a flu shot promoted and given during the waning days of summer will provide optimal protection, especially because flu season generally peaks in mid-winter or beyond. Experts are divided on how patients should respond to such offers.
“If you’re over 65, don’t get the flu vaccine in September. Or August. It’s a marketing scheme,” said Laura Haynes, an immunologist at the University of Connecticut Center on Aging.
That’s because a combination of factors makes it more difficult for the immune systems of people older than age 65 to respond to the vaccination in the first place. And its protective effects may wear off faster for this age group than it does for young people.
When is the best time to vaccinate? It’s a question even doctors have.
“Should I wait until October or November to vaccinate my elderly or medically frail patients?” That’s one of the queries on the website of the board that advises the Centers for Disease Control and Prevention on immunizations. The answer is that it is safe to make the shots available to all age groups when the vaccine becomes available, although it does include a caution.
The board says antibodies created by the vaccine decline in the months following vaccination “primarily affecting persons age 65 and older,” citing a study done during the 2011-2012 flu season. Still, while “delaying vaccination might permit greater immunity later in the season,” the CDC notes that “deferral could result in missed opportunities to vaccinate.”
How long will the immunity last?
“The data are very mixed,” said. John J. Treanor, a vaccine expert at the University of Rochester medical school. Some studies suggest vaccines lose some protectiveness during the course of a single flu season. Flu activity generally starts in the fall, but peaks in January or February and can run into the spring.
“So some might worry that if [they] got vaccinated very early and flu didn’t show up until very late, it might not work as well,” he said.
But other studies “show you still have protection from the shot you got last year if it’s a year when the strains didn’t change, Treanor said.
In any given flu season, vaccine effectiveness varies. One factor is how well the vaccines match the virus that is actually prevalent. Other factors influencing effectiveness include the age and general health of the recipient. In the overall population, the CDC says studies show vaccines can reduce the risk of flu by about 50 to 60 percent when the vaccines are well matched.
Health officials say it’s especially important to vaccinate children because they often spread the disease, are better able to develop antibodies from the vaccines and, if they don’t get sick, they won’t expose grandma and grandpa. While most people who get the flu recover, it is a serious disease responsible for many deaths each year, particularly among older adults and young children. Influenza’s intensity varies annually, with the CDC saying deaths associated with the flu have ranged from about 3,300 a year to 49,000 during the past 31 seasons.
To develop vaccines, manufacturers and scientists study what’s circulating in the Southern Hemisphere during its winter, which is our summer. Then — based on that evidence — forecast what flu strains might circulate here to make vaccines that are generally delivered in late July.
For the upcoming season, the vaccines will include three or four strains, including two A strains, an H1N1 and an H3N2, as well as one or two B strains, according to the CDC. It recommends that everyone older than 6 months get vaccinated, unless they have health conditions that would prevent it.
The vaccines can’t give a person the flu because the virus is killed before it’s included in the shot. This year, the nasal vaccine is not recommended for use, as studies showed it was not effective during several of the past flu seasons.
But when to go?
“The ideal time is between Halloween and Thanksgiving,” said Haynes at UConn. “If you can’t wait and the only chance is to get it in September, then go ahead and get it. It’s best to get it early rather than not at all.”
This Kaiser Health News story also ran on NPR.
The pharmacy chain pitches started in August: Come in and get your flu shot.
Convenience is touted. So are incentives: CVS offers a 20-percent-off shopping pass for everyone who gets a shot, while Walgreens donates toward international vaccination efforts.
The start of flu season is still weeks — if not months — away. Yet marketing of the vaccine has become an almost year-round effort, beginning when the shots become available in August and hyped as long as the supply lasts, often into April or May.
Not that long ago, most flu-shot campaigns started as the leaves began to turn in October. But the rise of retail medical clinics inside drug stores over the past decade — and state laws allowing pharmacists to give vaccinations — has stretched the flu-shot season.
The stores have figured out how “to deliver medical services in an on-demand way” which appeals to customers, particularly millennials, said Tom Charland, founder and CEO of Merchant Medicine, which tracks the walk-in clinic industry. “It’s a way to get people into the store to buy other things.”
But some experts say the marketing may be overtaking medical wisdom since it’s unclear how long the immunity imparted by the vaccine lasts, particularly in older people.
Federal health officials say it’s better to get the shot whenever you can. An early flu shot is better than no flu shot at all. But the science is mixed when it comes to how long a flu shot promoted and given during the waning days of summer will provide optimal protection, especially because flu season generally peaks in mid-winter or beyond. Experts are divided on how patients should respond to such offers.
“If you’re over 65, don’t get the flu vaccine in September. Or August. It’s a marketing scheme,” said Laura Haynes, an immunologist at the University of Connecticut Center on Aging.
That’s because a combination of factors makes it more difficult for the immune systems of people older than age 65 to respond to the vaccination in the first place. And its protective effects may wear off faster for this age group than it does for young people.
When is the best time to vaccinate? It’s a question even doctors have.
“Should I wait until October or November to vaccinate my elderly or medically frail patients?” That’s one of the queries on the website of the board that advises the Centers for Disease Control and Prevention on immunizations. The answer is that it is safe to make the shots available to all age groups when the vaccine becomes available, although it does include a caution.
The board says antibodies created by the vaccine decline in the months following vaccination “primarily affecting persons age 65 and older,” citing a study done during the 2011-2012 flu season. Still, while “delaying vaccination might permit greater immunity later in the season,” the CDC notes that “deferral could result in missed opportunities to vaccinate.”
How long will the immunity last?
“The data are very mixed,” said. John J. Treanor, a vaccine expert at the University of Rochester medical school. Some studies suggest vaccines lose some protectiveness during the course of a single flu season. Flu activity generally starts in the fall, but peaks in January or February and can run into the spring.
“So some might worry that if [they] got vaccinated very early and flu didn’t show up until very late, it might not work as well,” he said.
But other studies “show you still have protection from the shot you got last year if it’s a year when the strains didn’t change, Treanor said.
In any given flu season, vaccine effectiveness varies. One factor is how well the vaccines match the virus that is actually prevalent. Other factors influencing effectiveness include the age and general health of the recipient. In the overall population, the CDC says studies show vaccines can reduce the risk of flu by about 50 to 60 percent when the vaccines are well matched.
Health officials say it’s especially important to vaccinate children because they often spread the disease, are better able to develop antibodies from the vaccines and, if they don’t get sick, they won’t expose grandma and grandpa. While most people who get the flu recover, it is a serious disease responsible for many deaths each year, particularly among older adults and young children. Influenza’s intensity varies annually, with the CDC saying deaths associated with the flu have ranged from about 3,300 a year to 49,000 during the past 31 seasons.
To develop vaccines, manufacturers and scientists study what’s circulating in the Southern Hemisphere during its winter, which is our summer. Then — based on that evidence — forecast what flu strains might circulate here to make vaccines that are generally delivered in late July.
For the upcoming season, the vaccines will include three or four strains, including two A strains, an H1N1 and an H3N2, as well as one or two B strains, according to the CDC. It recommends that everyone older than 6 months get vaccinated, unless they have health conditions that would prevent it.
The vaccines can’t give a person the flu because the virus is killed before it’s included in the shot. This year, the nasal vaccine is not recommended for use, as studies showed it was not effective during several of the past flu seasons.
But when to go?
“The ideal time is between Halloween and Thanksgiving,” said Haynes at UConn. “If you can’t wait and the only chance is to get it in September, then go ahead and get it. It’s best to get it early rather than not at all.”
This Kaiser Health News story also ran on NPR.
The pharmacy chain pitches started in August: Come in and get your flu shot.
Convenience is touted. So are incentives: CVS offers a 20-percent-off shopping pass for everyone who gets a shot, while Walgreens donates toward international vaccination efforts.
The start of flu season is still weeks — if not months — away. Yet marketing of the vaccine has become an almost year-round effort, beginning when the shots become available in August and hyped as long as the supply lasts, often into April or May.
Not that long ago, most flu-shot campaigns started as the leaves began to turn in October. But the rise of retail medical clinics inside drug stores over the past decade — and state laws allowing pharmacists to give vaccinations — has stretched the flu-shot season.
The stores have figured out how “to deliver medical services in an on-demand way” which appeals to customers, particularly millennials, said Tom Charland, founder and CEO of Merchant Medicine, which tracks the walk-in clinic industry. “It’s a way to get people into the store to buy other things.”
But some experts say the marketing may be overtaking medical wisdom since it’s unclear how long the immunity imparted by the vaccine lasts, particularly in older people.
Federal health officials say it’s better to get the shot whenever you can. An early flu shot is better than no flu shot at all. But the science is mixed when it comes to how long a flu shot promoted and given during the waning days of summer will provide optimal protection, especially because flu season generally peaks in mid-winter or beyond. Experts are divided on how patients should respond to such offers.
“If you’re over 65, don’t get the flu vaccine in September. Or August. It’s a marketing scheme,” said Laura Haynes, an immunologist at the University of Connecticut Center on Aging.
That’s because a combination of factors makes it more difficult for the immune systems of people older than age 65 to respond to the vaccination in the first place. And its protective effects may wear off faster for this age group than it does for young people.
When is the best time to vaccinate? It’s a question even doctors have.
“Should I wait until October or November to vaccinate my elderly or medically frail patients?” That’s one of the queries on the website of the board that advises the Centers for Disease Control and Prevention on immunizations. The answer is that it is safe to make the shots available to all age groups when the vaccine becomes available, although it does include a caution.
The board says antibodies created by the vaccine decline in the months following vaccination “primarily affecting persons age 65 and older,” citing a study done during the 2011-2012 flu season. Still, while “delaying vaccination might permit greater immunity later in the season,” the CDC notes that “deferral could result in missed opportunities to vaccinate.”
How long will the immunity last?
“The data are very mixed,” said. John J. Treanor, a vaccine expert at the University of Rochester medical school. Some studies suggest vaccines lose some protectiveness during the course of a single flu season. Flu activity generally starts in the fall, but peaks in January or February and can run into the spring.
“So some might worry that if [they] got vaccinated very early and flu didn’t show up until very late, it might not work as well,” he said.
But other studies “show you still have protection from the shot you got last year if it’s a year when the strains didn’t change, Treanor said.
In any given flu season, vaccine effectiveness varies. One factor is how well the vaccines match the virus that is actually prevalent. Other factors influencing effectiveness include the age and general health of the recipient. In the overall population, the CDC says studies show vaccines can reduce the risk of flu by about 50 to 60 percent when the vaccines are well matched.
Health officials say it’s especially important to vaccinate children because they often spread the disease, are better able to develop antibodies from the vaccines and, if they don’t get sick, they won’t expose grandma and grandpa. While most people who get the flu recover, it is a serious disease responsible for many deaths each year, particularly among older adults and young children. Influenza’s intensity varies annually, with the CDC saying deaths associated with the flu have ranged from about 3,300 a year to 49,000 during the past 31 seasons.
To develop vaccines, manufacturers and scientists study what’s circulating in the Southern Hemisphere during its winter, which is our summer. Then — based on that evidence — forecast what flu strains might circulate here to make vaccines that are generally delivered in late July.
For the upcoming season, the vaccines will include three or four strains, including two A strains, an H1N1 and an H3N2, as well as one or two B strains, according to the CDC. It recommends that everyone older than 6 months get vaccinated, unless they have health conditions that would prevent it.
The vaccines can’t give a person the flu because the virus is killed before it’s included in the shot. This year, the nasal vaccine is not recommended for use, as studies showed it was not effective during several of the past flu seasons.
But when to go?
“The ideal time is between Halloween and Thanksgiving,” said Haynes at UConn. “If you can’t wait and the only chance is to get it in September, then go ahead and get it. It’s best to get it early rather than not at all.”
This Kaiser Health News story also ran on NPR.
Novel De Novo Heterozygous Frameshift Mutation of the ADAR1 Gene in Heavy Dyschromatosis Symmetrica Hereditaria
To the Editor:
Dyschromatosis symmetrica hereditaria (DSH)(Online Mendelian Inheritance in Man 127400), also called reticulate acropigmentation of Dohi, is a pigmentary genodermatosis characterized by a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet. Linkage analysis has revealed that the DSH gene locus resides on chromosome 1q11-q21,1 and the adenosine deaminase RNA specific gene, ADAR1 (also called DSRAD), in this region has been identified as being responsible for the development of DSH.2 We report a sporadic case of severe DSH with the ADAR1 gene detected in a mutation analysis.
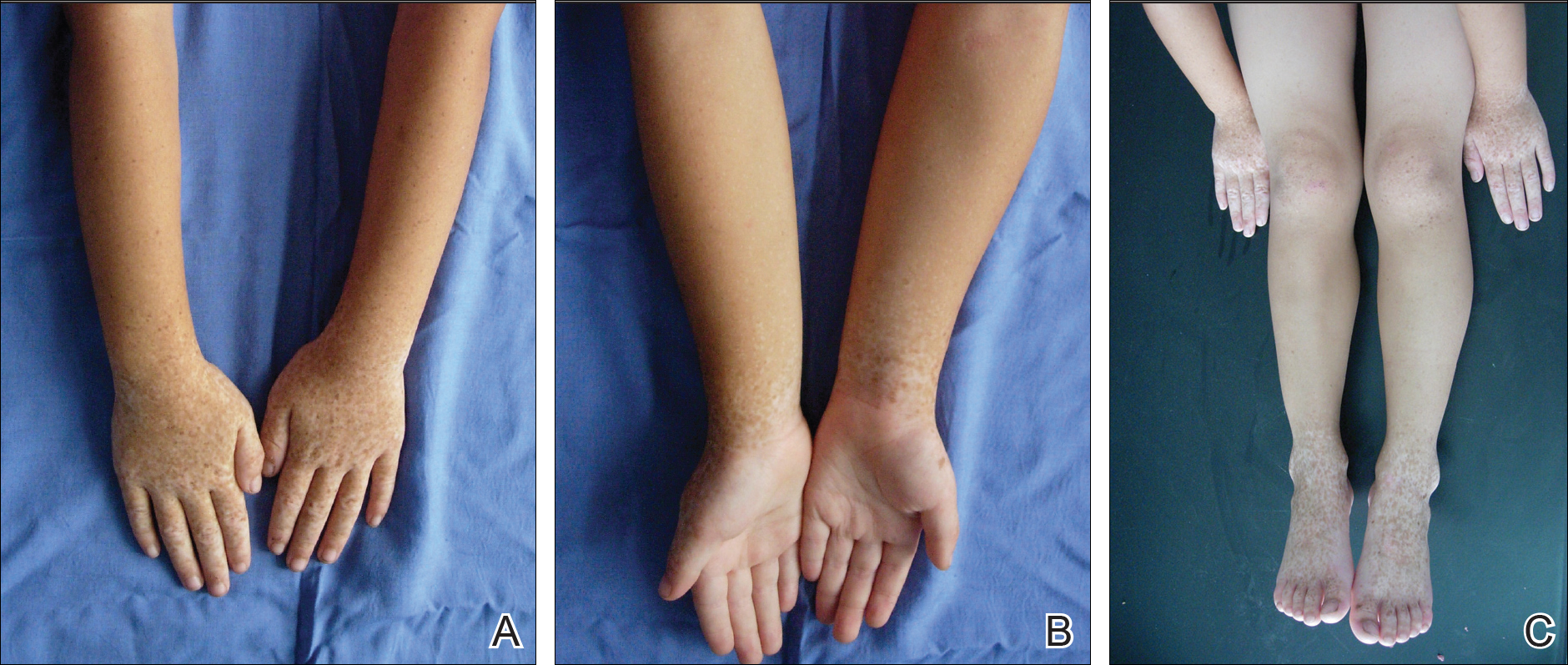
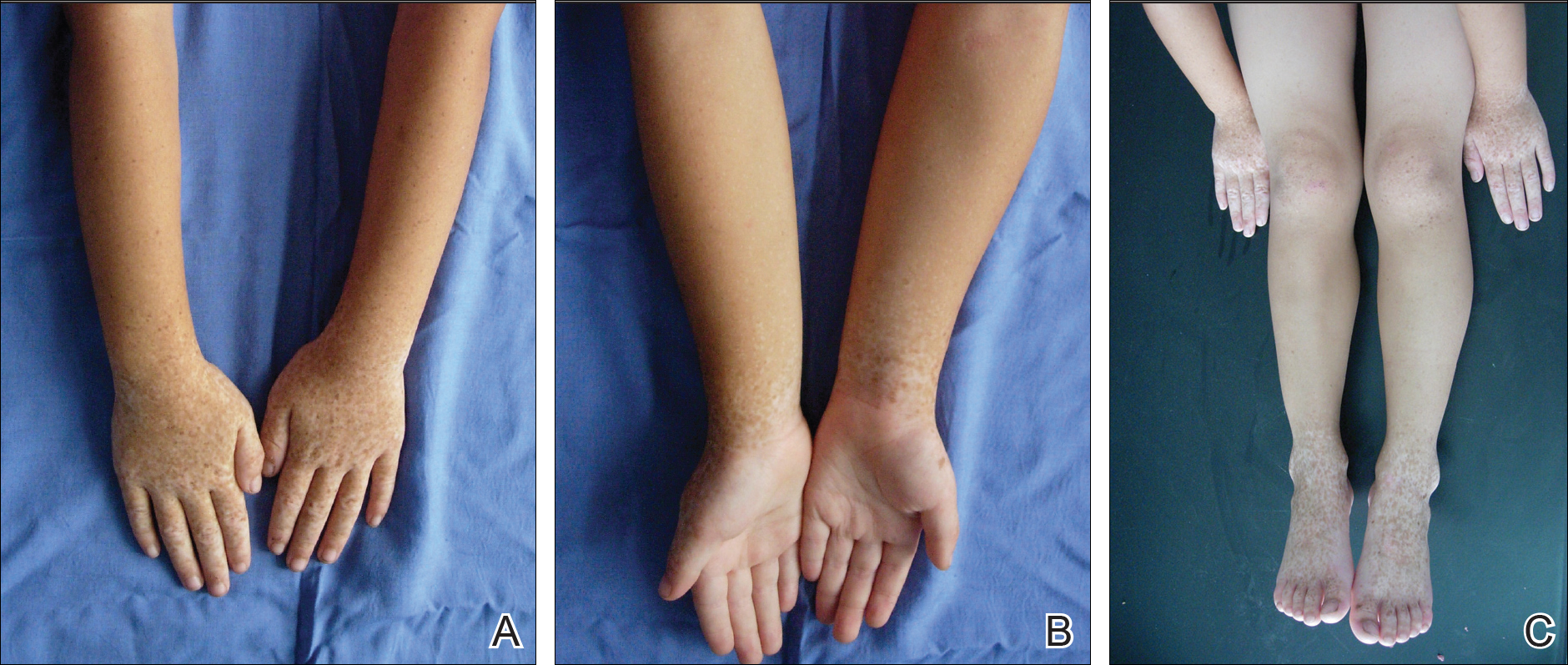
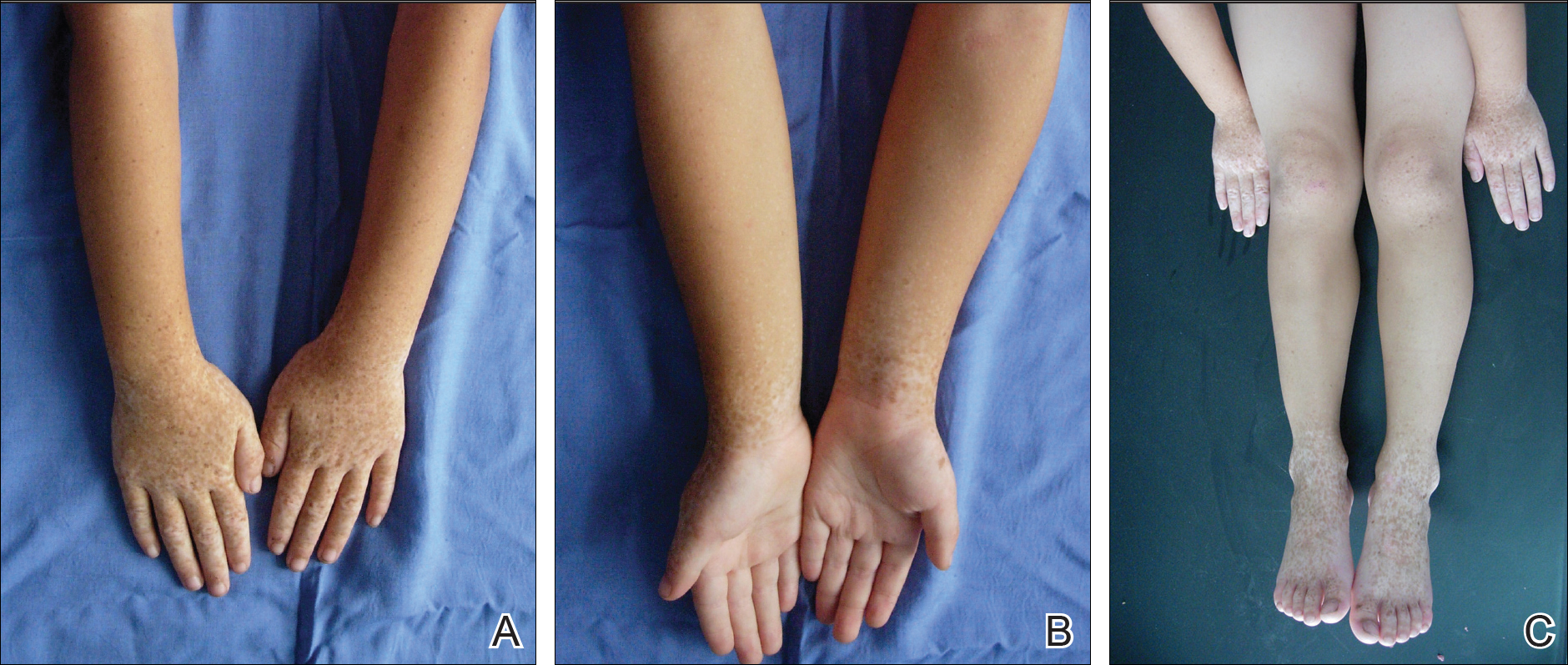
A 6-year-old girl presented with a mixture of hyperpigmented and hypopigmented macules on the dorsal aspects of the hands and feet and the curved side of the wrists, heels, and knees, as well as scattered frecklelike and depigmented spots on the face, ears, neck, arms, and upper back (Figure 1). Her parents noted that hyperpigmented and hypopigmented macules on the dorsal aspects of the hands developed at 5 months of age. Exacerbation after exposure to sunlight resulted in the eruption becoming remarkable in summer and fainter in winter. The skin lesions gradually became more progressive. Physical examination revealed that the patient generally was healthy.
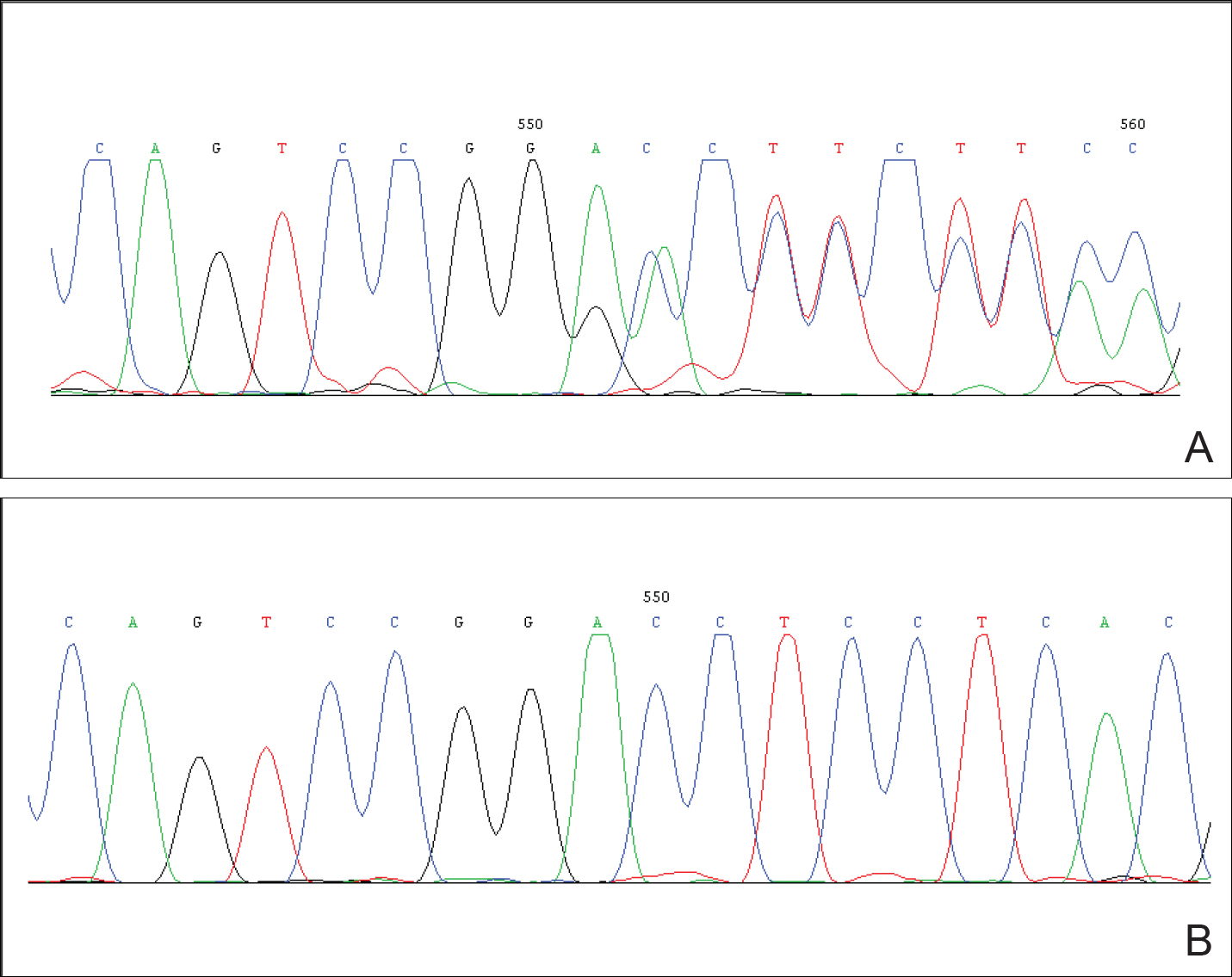
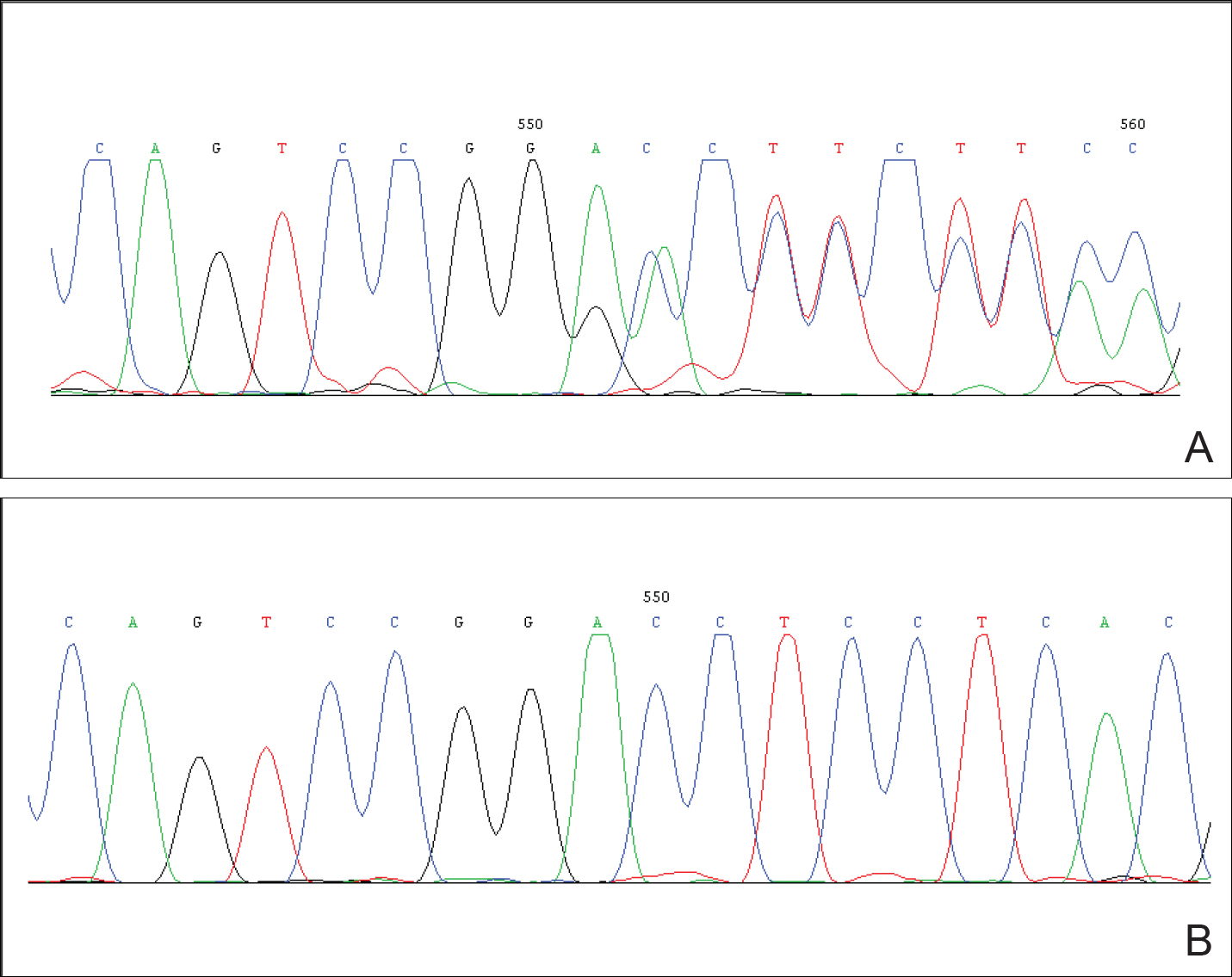
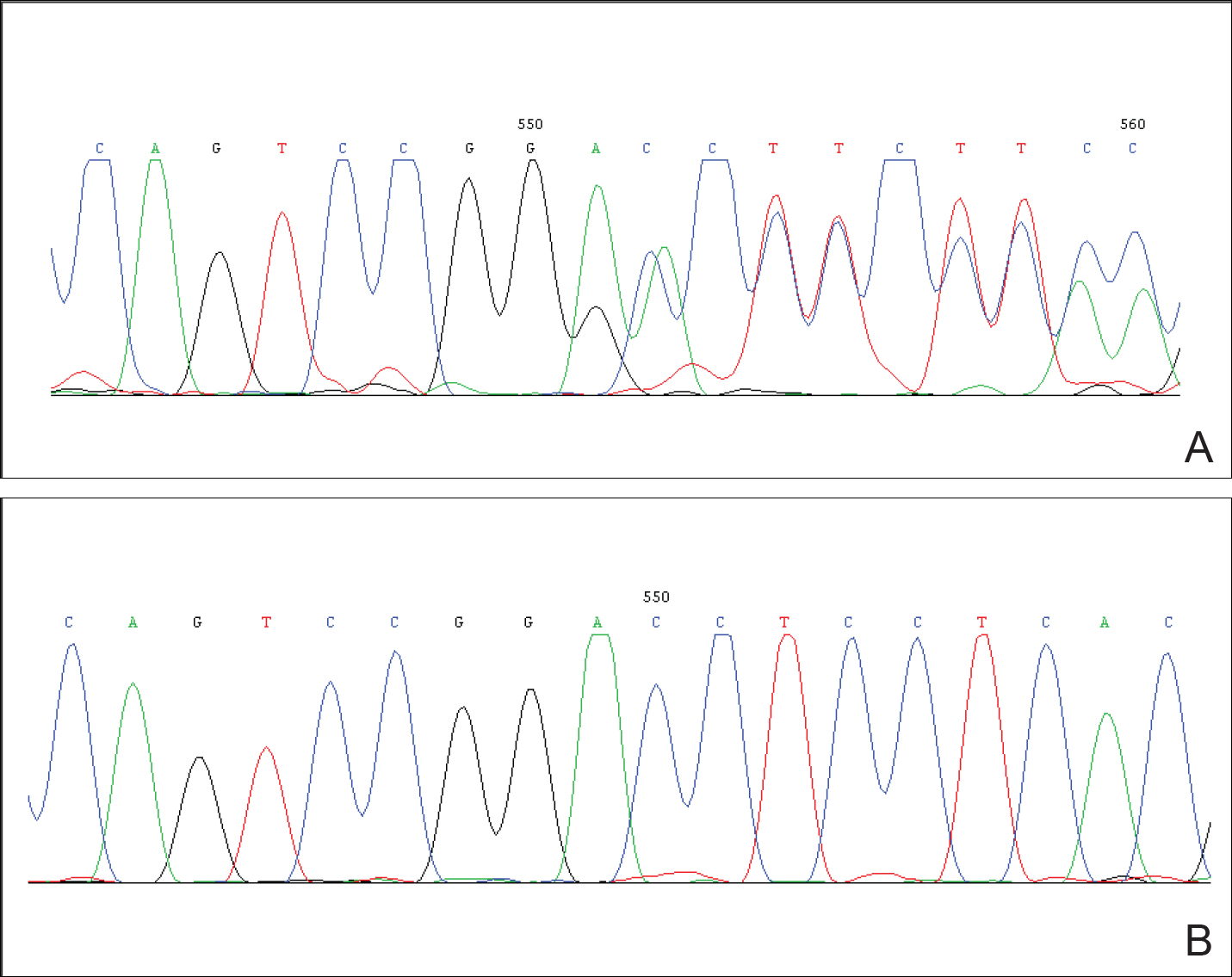
After obtaining informed consent, we performed a mutation analysis of the ADAR1 gene in our patient and her parents. We used a kit to extract genomic DNA from peripheral blood, which was then used to amplify the exons of the ADAR1 gene with intronic flanking sequences by polymerase chain reaction with the primer.3 After amplification, polymerase chain reaction products were purified. We sequenced the ADAR1 gene. Sequence comparisons and analysis found that the patient (proband) carried a heterozygous insertional mutation c.2253insG in exon 6 of the ADAR1 gene. This mutation was not detected in the proband’s healthy parents and 100 normal individuals (Figure 2).
Dyschromatosis symmetrica hereditaria is acquired by autosomal-dominant inheritance and is mainly reported in Asians, especially in Japan and China. Oyama et al4 reviewed 185 cases of DSH in Japan and found the onset of this disease usually was during infancy or childhood; 73% of patients developed the skin lesions before 6 years of age. Suzuki et al5 reported 10 unrelated Japanese patients and found the onset of disease ranged from 1 year of age to childhood. Zhang et al1,6 investigated 78 Chinese patients with DSH including 8 multigenerational families and 2 sporadic patients and found the age of disease onset ranged from 6 months to 15 years of age. The age of onset in our patient (5 months) was younger than these prior reports.
Patients with DSH have a characteristic appearance including a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet. Few patients have similar lesions on the knees and elbows. Many patients have frecklelike macules on the face and arms.1-6 One patient has been described with scattered depigmented spots on the face and chest.1 Our patient had a characteristic appearance as well as some special manifestations including skin lesions on the curved side of the wrist, ears, neck, and upper back.
The human ADAR1 gene spans 30 kilobase and contains 15 exons. It encodes RNA-specific adenosine deaminase composed of 1226 amino acid residues. This enzyme is important for various functions such as site-specific RNA editing and nuclear translation. This enzyme has 2 Z-alpha domains, 3 double-stranded RNA–binding domains, and the putative deaminase domain corresponding to exon 2, exons 2 to 7, and exons 9 to 14 of ADAR1, respectively.6
Mutation analysis of the ADAR1 gene in this case showed heterozygous insertion mutation c.2253insG in exon 6 of the ADAR1 gene, which changed the reading frame, and 475 amino acid residues in C-terminus are replaced by 90 amino acid residues (TSSRAQVRLPSKSWGSLVPSRLRTQQEA RQAGSSRCGSPCLDWGEREGRTHGFHRG NPSDRGQSQKNYAPPLKVPRSTAKT DTPSHWQHLP). This mutation was not detected in the proband’s healthy parents and the 100 control individuals, which indicated that it was a de novo mutation and the pathogenic mutation of DSH rather than a common polymorphism.
In conclusion, we report a novel mutation of the ADAR1 gene with a heavy clinical phenotype in DSH. This study expands the spectrum of clinical manifestations and demonstrates the ADAR1 mutation in DSH.
Acknowledgments
We are most grateful to the patient and her family for taking part in our study.
- Zhang XJ, Gao M, Li M, et al. Identification of a locus for dyschromatosis symmetrica hereditaria at chromosome 1q11-1q21. J Invest Dermatol. 2003;120:776-780.
- Miyamura Y, Suzuki T, Kono M, et al. Mutations of the RNA-specific adenosine deaminase gene (DSRAD) are involved in dyschromatosis symmetrica hereditaria [published online August 11, 2003]. Am J Hum Genet. 2003;73:693-699.
- Li M, Li C, Hua H, et al. Identification of two novel mutations in Chinese patients with dyschromatosis symmetrica hereditaria [published online October 8, 2005]. Arch Dermatol Res. 2005;297:196-200.
- Oyama M, Shimizu H, Ohata Y, et al. Dyschromatosis symmetrica hereditaria (reticulate acropigmentation of Dohi): report of a Japanese family with the condition and a literature review of 185 cases. Br J Dermatol. 1999;140:491-496.
- Suzuki N, Suzuki T, Inagaki K, et al. Ten novel mutations of the ADAR1 gene in Japanese patients with dyschromatosis symmetrica hereditaria [published online August 17, 2006]. J Invest Dermatol. 2007;127:309-311.
- Zhang XJ, He PP, Li M, et al. Seven novel mutations of the ADAR gene in Chinese families and sporadic patients with dyschromatosis symmetrica hereditaria (DSH). Hum Mutat. 2004;23:629-630.
To the Editor:
Dyschromatosis symmetrica hereditaria (DSH)(Online Mendelian Inheritance in Man 127400), also called reticulate acropigmentation of Dohi, is a pigmentary genodermatosis characterized by a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet. Linkage analysis has revealed that the DSH gene locus resides on chromosome 1q11-q21,1 and the adenosine deaminase RNA specific gene, ADAR1 (also called DSRAD), in this region has been identified as being responsible for the development of DSH.2 We report a sporadic case of severe DSH with the ADAR1 gene detected in a mutation analysis.
A 6-year-old girl presented with a mixture of hyperpigmented and hypopigmented macules on the dorsal aspects of the hands and feet and the curved side of the wrists, heels, and knees, as well as scattered frecklelike and depigmented spots on the face, ears, neck, arms, and upper back (Figure 1). Her parents noted that hyperpigmented and hypopigmented macules on the dorsal aspects of the hands developed at 5 months of age. Exacerbation after exposure to sunlight resulted in the eruption becoming remarkable in summer and fainter in winter. The skin lesions gradually became more progressive. Physical examination revealed that the patient generally was healthy.
After obtaining informed consent, we performed a mutation analysis of the ADAR1 gene in our patient and her parents. We used a kit to extract genomic DNA from peripheral blood, which was then used to amplify the exons of the ADAR1 gene with intronic flanking sequences by polymerase chain reaction with the primer.3 After amplification, polymerase chain reaction products were purified. We sequenced the ADAR1 gene. Sequence comparisons and analysis found that the patient (proband) carried a heterozygous insertional mutation c.2253insG in exon 6 of the ADAR1 gene. This mutation was not detected in the proband’s healthy parents and 100 normal individuals (Figure 2).
Dyschromatosis symmetrica hereditaria is acquired by autosomal-dominant inheritance and is mainly reported in Asians, especially in Japan and China. Oyama et al4 reviewed 185 cases of DSH in Japan and found the onset of this disease usually was during infancy or childhood; 73% of patients developed the skin lesions before 6 years of age. Suzuki et al5 reported 10 unrelated Japanese patients and found the onset of disease ranged from 1 year of age to childhood. Zhang et al1,6 investigated 78 Chinese patients with DSH including 8 multigenerational families and 2 sporadic patients and found the age of disease onset ranged from 6 months to 15 years of age. The age of onset in our patient (5 months) was younger than these prior reports.
Patients with DSH have a characteristic appearance including a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet. Few patients have similar lesions on the knees and elbows. Many patients have frecklelike macules on the face and arms.1-6 One patient has been described with scattered depigmented spots on the face and chest.1 Our patient had a characteristic appearance as well as some special manifestations including skin lesions on the curved side of the wrist, ears, neck, and upper back.
The human ADAR1 gene spans 30 kilobase and contains 15 exons. It encodes RNA-specific adenosine deaminase composed of 1226 amino acid residues. This enzyme is important for various functions such as site-specific RNA editing and nuclear translation. This enzyme has 2 Z-alpha domains, 3 double-stranded RNA–binding domains, and the putative deaminase domain corresponding to exon 2, exons 2 to 7, and exons 9 to 14 of ADAR1, respectively.6
Mutation analysis of the ADAR1 gene in this case showed heterozygous insertion mutation c.2253insG in exon 6 of the ADAR1 gene, which changed the reading frame, and 475 amino acid residues in C-terminus are replaced by 90 amino acid residues (TSSRAQVRLPSKSWGSLVPSRLRTQQEA RQAGSSRCGSPCLDWGEREGRTHGFHRG NPSDRGQSQKNYAPPLKVPRSTAKT DTPSHWQHLP). This mutation was not detected in the proband’s healthy parents and the 100 control individuals, which indicated that it was a de novo mutation and the pathogenic mutation of DSH rather than a common polymorphism.
In conclusion, we report a novel mutation of the ADAR1 gene with a heavy clinical phenotype in DSH. This study expands the spectrum of clinical manifestations and demonstrates the ADAR1 mutation in DSH.
Acknowledgments
We are most grateful to the patient and her family for taking part in our study.
To the Editor:
Dyschromatosis symmetrica hereditaria (DSH)(Online Mendelian Inheritance in Man 127400), also called reticulate acropigmentation of Dohi, is a pigmentary genodermatosis characterized by a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet. Linkage analysis has revealed that the DSH gene locus resides on chromosome 1q11-q21,1 and the adenosine deaminase RNA specific gene, ADAR1 (also called DSRAD), in this region has been identified as being responsible for the development of DSH.2 We report a sporadic case of severe DSH with the ADAR1 gene detected in a mutation analysis.
A 6-year-old girl presented with a mixture of hyperpigmented and hypopigmented macules on the dorsal aspects of the hands and feet and the curved side of the wrists, heels, and knees, as well as scattered frecklelike and depigmented spots on the face, ears, neck, arms, and upper back (Figure 1). Her parents noted that hyperpigmented and hypopigmented macules on the dorsal aspects of the hands developed at 5 months of age. Exacerbation after exposure to sunlight resulted in the eruption becoming remarkable in summer and fainter in winter. The skin lesions gradually became more progressive. Physical examination revealed that the patient generally was healthy.
After obtaining informed consent, we performed a mutation analysis of the ADAR1 gene in our patient and her parents. We used a kit to extract genomic DNA from peripheral blood, which was then used to amplify the exons of the ADAR1 gene with intronic flanking sequences by polymerase chain reaction with the primer.3 After amplification, polymerase chain reaction products were purified. We sequenced the ADAR1 gene. Sequence comparisons and analysis found that the patient (proband) carried a heterozygous insertional mutation c.2253insG in exon 6 of the ADAR1 gene. This mutation was not detected in the proband’s healthy parents and 100 normal individuals (Figure 2).
Dyschromatosis symmetrica hereditaria is acquired by autosomal-dominant inheritance and is mainly reported in Asians, especially in Japan and China. Oyama et al4 reviewed 185 cases of DSH in Japan and found the onset of this disease usually was during infancy or childhood; 73% of patients developed the skin lesions before 6 years of age. Suzuki et al5 reported 10 unrelated Japanese patients and found the onset of disease ranged from 1 year of age to childhood. Zhang et al1,6 investigated 78 Chinese patients with DSH including 8 multigenerational families and 2 sporadic patients and found the age of disease onset ranged from 6 months to 15 years of age. The age of onset in our patient (5 months) was younger than these prior reports.
Patients with DSH have a characteristic appearance including a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet. Few patients have similar lesions on the knees and elbows. Many patients have frecklelike macules on the face and arms.1-6 One patient has been described with scattered depigmented spots on the face and chest.1 Our patient had a characteristic appearance as well as some special manifestations including skin lesions on the curved side of the wrist, ears, neck, and upper back.
The human ADAR1 gene spans 30 kilobase and contains 15 exons. It encodes RNA-specific adenosine deaminase composed of 1226 amino acid residues. This enzyme is important for various functions such as site-specific RNA editing and nuclear translation. This enzyme has 2 Z-alpha domains, 3 double-stranded RNA–binding domains, and the putative deaminase domain corresponding to exon 2, exons 2 to 7, and exons 9 to 14 of ADAR1, respectively.6
Mutation analysis of the ADAR1 gene in this case showed heterozygous insertion mutation c.2253insG in exon 6 of the ADAR1 gene, which changed the reading frame, and 475 amino acid residues in C-terminus are replaced by 90 amino acid residues (TSSRAQVRLPSKSWGSLVPSRLRTQQEA RQAGSSRCGSPCLDWGEREGRTHGFHRG NPSDRGQSQKNYAPPLKVPRSTAKT DTPSHWQHLP). This mutation was not detected in the proband’s healthy parents and the 100 control individuals, which indicated that it was a de novo mutation and the pathogenic mutation of DSH rather than a common polymorphism.
In conclusion, we report a novel mutation of the ADAR1 gene with a heavy clinical phenotype in DSH. This study expands the spectrum of clinical manifestations and demonstrates the ADAR1 mutation in DSH.
Acknowledgments
We are most grateful to the patient and her family for taking part in our study.
- Zhang XJ, Gao M, Li M, et al. Identification of a locus for dyschromatosis symmetrica hereditaria at chromosome 1q11-1q21. J Invest Dermatol. 2003;120:776-780.
- Miyamura Y, Suzuki T, Kono M, et al. Mutations of the RNA-specific adenosine deaminase gene (DSRAD) are involved in dyschromatosis symmetrica hereditaria [published online August 11, 2003]. Am J Hum Genet. 2003;73:693-699.
- Li M, Li C, Hua H, et al. Identification of two novel mutations in Chinese patients with dyschromatosis symmetrica hereditaria [published online October 8, 2005]. Arch Dermatol Res. 2005;297:196-200.
- Oyama M, Shimizu H, Ohata Y, et al. Dyschromatosis symmetrica hereditaria (reticulate acropigmentation of Dohi): report of a Japanese family with the condition and a literature review of 185 cases. Br J Dermatol. 1999;140:491-496.
- Suzuki N, Suzuki T, Inagaki K, et al. Ten novel mutations of the ADAR1 gene in Japanese patients with dyschromatosis symmetrica hereditaria [published online August 17, 2006]. J Invest Dermatol. 2007;127:309-311.
- Zhang XJ, He PP, Li M, et al. Seven novel mutations of the ADAR gene in Chinese families and sporadic patients with dyschromatosis symmetrica hereditaria (DSH). Hum Mutat. 2004;23:629-630.
- Zhang XJ, Gao M, Li M, et al. Identification of a locus for dyschromatosis symmetrica hereditaria at chromosome 1q11-1q21. J Invest Dermatol. 2003;120:776-780.
- Miyamura Y, Suzuki T, Kono M, et al. Mutations of the RNA-specific adenosine deaminase gene (DSRAD) are involved in dyschromatosis symmetrica hereditaria [published online August 11, 2003]. Am J Hum Genet. 2003;73:693-699.
- Li M, Li C, Hua H, et al. Identification of two novel mutations in Chinese patients with dyschromatosis symmetrica hereditaria [published online October 8, 2005]. Arch Dermatol Res. 2005;297:196-200.
- Oyama M, Shimizu H, Ohata Y, et al. Dyschromatosis symmetrica hereditaria (reticulate acropigmentation of Dohi): report of a Japanese family with the condition and a literature review of 185 cases. Br J Dermatol. 1999;140:491-496.
- Suzuki N, Suzuki T, Inagaki K, et al. Ten novel mutations of the ADAR1 gene in Japanese patients with dyschromatosis symmetrica hereditaria [published online August 17, 2006]. J Invest Dermatol. 2007;127:309-311.
- Zhang XJ, He PP, Li M, et al. Seven novel mutations of the ADAR gene in Chinese families and sporadic patients with dyschromatosis symmetrica hereditaria (DSH). Hum Mutat. 2004;23:629-630.
Practice Points
- The adenosine deaminase RNA specific gene, ADAR1, has been identified as being responsible for the development of dyschromatosis symmetrica hereditaria (DSH).
- The characteristic appearance of DSH is a mixture of hyperpigmented and hypopigmented macules of various sizes on the dorsal aspects of the hands and feet.
Should I throw out my expired medications?
A 55-year-old patient requests new prescriptions at a routine appointment. She will be traveling internationally next month and wants to replace her emergency medication kit, as the medications in it (ciprofloxacin, loperamide, and oxycodone) have all expired.
What do you do?
A) Replace the prescription for ciprofloxacin.
B) Replace all three medications.
C) Tell the patient that all the meds should still be fine.
This is a common concern brought up by patients. Many patients discard medications when they pass the expiration date on the package. Is this necessary? Is there a health risk to taking expired medications, and is it okay from a therapeutic standpoint to use medications past their expiration date?
The expiration date is not a date that the drug stops being effective or potentially becomes toxic. It is a date, required by law, that the manufacturer can guarantee greater than 90% original potency of the medication. There really isn’t incentive for pharmaceutical companies to extend the expiration dates, as it is profitable for patients to throw away expired medications and replace them with new prescriptions.
The U.S. military purchases a large stockpile of drugs and has the potential for having a great deal of expired medications. To help reduce this problem, the Food and Drug Administration administers the shelf-life extension program (SLEP) for the U.S. military as a testing and evaluation program designed to justify an extension of the shelf life of stockpiled drug products.1
Robbe Lyon, MD, and colleagues reported data from the SLEP.2 A total of 122 drugs were studied representing 3,005 lots, with 88% of these extended at least 1 year past the expiration date, with an average extension of more than 5 years. Several antibiotics were studied, including ciprofloxacin (mean extension, 55 months), amoxicillin (mean extension, 23 months), and doxycycline (mean extension, 50 months).
Lee Cantrell, PharmD, and coinvestigators looked at sealed drugs from a retail pharmacy that were 28-40 years past their expiration date.3 Amazingly, 12 of the 14 compounds tested were in concentrations that were at least 90% of the labeled amount. Among the drugs that were tested that maintained greater than 90% of the labeled amount were acetaminophen, codeine, hydrocodone, and barbiturates. Aspirin and amphetamine were the two drugs that did not have greater than 90% of the labeled amount. The aspirin amounts were very low, about 1% of the listed amount on the package.
The major myth surrounding expired medications is that taking an expired medication could be toxic.
There is one case report of toxicity from the use of expired tetracycline.4 This was a case series of three patients who developed reversible Fanconi syndrome linked to using an expired tetracycline preparation. That preparation of tetracycline is no longer available.
There are no other reports of toxicity due to use of expired medications.5,6 There appears to be no direct risk of toxicity to the patient by using medication past the expiration date.
The risk that isn’t answered is the risk of using medications that may not be effective if potency isn’t guaranteed beyond the expiration date. It appears that most drugs are effective for years past the expiration date.
This isn’t an issue for medications for treatment of chronic conditions, as patients take the medications every day, and the medications will be used up long before they expire. For medications that are used infrequently – analgesics, antihistamines, and medications for traveler’s diarrhea – they appear to be stable for years past expiration, and there is little risk to the patient if the medications are not fully effective.
I think aspirin should not be used past expiration, given the data showing that it breaks down more so than other medications. For the case at the start of this article, I think having the patient use the expired medications should be fine.
References
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 55-year-old patient requests new prescriptions at a routine appointment. She will be traveling internationally next month and wants to replace her emergency medication kit, as the medications in it (ciprofloxacin, loperamide, and oxycodone) have all expired.
What do you do?
A) Replace the prescription for ciprofloxacin.
B) Replace all three medications.
C) Tell the patient that all the meds should still be fine.
This is a common concern brought up by patients. Many patients discard medications when they pass the expiration date on the package. Is this necessary? Is there a health risk to taking expired medications, and is it okay from a therapeutic standpoint to use medications past their expiration date?
The expiration date is not a date that the drug stops being effective or potentially becomes toxic. It is a date, required by law, that the manufacturer can guarantee greater than 90% original potency of the medication. There really isn’t incentive for pharmaceutical companies to extend the expiration dates, as it is profitable for patients to throw away expired medications and replace them with new prescriptions.
The U.S. military purchases a large stockpile of drugs and has the potential for having a great deal of expired medications. To help reduce this problem, the Food and Drug Administration administers the shelf-life extension program (SLEP) for the U.S. military as a testing and evaluation program designed to justify an extension of the shelf life of stockpiled drug products.1
Robbe Lyon, MD, and colleagues reported data from the SLEP.2 A total of 122 drugs were studied representing 3,005 lots, with 88% of these extended at least 1 year past the expiration date, with an average extension of more than 5 years. Several antibiotics were studied, including ciprofloxacin (mean extension, 55 months), amoxicillin (mean extension, 23 months), and doxycycline (mean extension, 50 months).
Lee Cantrell, PharmD, and coinvestigators looked at sealed drugs from a retail pharmacy that were 28-40 years past their expiration date.3 Amazingly, 12 of the 14 compounds tested were in concentrations that were at least 90% of the labeled amount. Among the drugs that were tested that maintained greater than 90% of the labeled amount were acetaminophen, codeine, hydrocodone, and barbiturates. Aspirin and amphetamine were the two drugs that did not have greater than 90% of the labeled amount. The aspirin amounts were very low, about 1% of the listed amount on the package.
The major myth surrounding expired medications is that taking an expired medication could be toxic.
There is one case report of toxicity from the use of expired tetracycline.4 This was a case series of three patients who developed reversible Fanconi syndrome linked to using an expired tetracycline preparation. That preparation of tetracycline is no longer available.
There are no other reports of toxicity due to use of expired medications.5,6 There appears to be no direct risk of toxicity to the patient by using medication past the expiration date.
The risk that isn’t answered is the risk of using medications that may not be effective if potency isn’t guaranteed beyond the expiration date. It appears that most drugs are effective for years past the expiration date.
This isn’t an issue for medications for treatment of chronic conditions, as patients take the medications every day, and the medications will be used up long before they expire. For medications that are used infrequently – analgesics, antihistamines, and medications for traveler’s diarrhea – they appear to be stable for years past expiration, and there is little risk to the patient if the medications are not fully effective.
I think aspirin should not be used past expiration, given the data showing that it breaks down more so than other medications. For the case at the start of this article, I think having the patient use the expired medications should be fine.
References
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
A 55-year-old patient requests new prescriptions at a routine appointment. She will be traveling internationally next month and wants to replace her emergency medication kit, as the medications in it (ciprofloxacin, loperamide, and oxycodone) have all expired.
What do you do?
A) Replace the prescription for ciprofloxacin.
B) Replace all three medications.
C) Tell the patient that all the meds should still be fine.
This is a common concern brought up by patients. Many patients discard medications when they pass the expiration date on the package. Is this necessary? Is there a health risk to taking expired medications, and is it okay from a therapeutic standpoint to use medications past their expiration date?
The expiration date is not a date that the drug stops being effective or potentially becomes toxic. It is a date, required by law, that the manufacturer can guarantee greater than 90% original potency of the medication. There really isn’t incentive for pharmaceutical companies to extend the expiration dates, as it is profitable for patients to throw away expired medications and replace them with new prescriptions.
The U.S. military purchases a large stockpile of drugs and has the potential for having a great deal of expired medications. To help reduce this problem, the Food and Drug Administration administers the shelf-life extension program (SLEP) for the U.S. military as a testing and evaluation program designed to justify an extension of the shelf life of stockpiled drug products.1
Robbe Lyon, MD, and colleagues reported data from the SLEP.2 A total of 122 drugs were studied representing 3,005 lots, with 88% of these extended at least 1 year past the expiration date, with an average extension of more than 5 years. Several antibiotics were studied, including ciprofloxacin (mean extension, 55 months), amoxicillin (mean extension, 23 months), and doxycycline (mean extension, 50 months).
Lee Cantrell, PharmD, and coinvestigators looked at sealed drugs from a retail pharmacy that were 28-40 years past their expiration date.3 Amazingly, 12 of the 14 compounds tested were in concentrations that were at least 90% of the labeled amount. Among the drugs that were tested that maintained greater than 90% of the labeled amount were acetaminophen, codeine, hydrocodone, and barbiturates. Aspirin and amphetamine were the two drugs that did not have greater than 90% of the labeled amount. The aspirin amounts were very low, about 1% of the listed amount on the package.
The major myth surrounding expired medications is that taking an expired medication could be toxic.
There is one case report of toxicity from the use of expired tetracycline.4 This was a case series of three patients who developed reversible Fanconi syndrome linked to using an expired tetracycline preparation. That preparation of tetracycline is no longer available.
There are no other reports of toxicity due to use of expired medications.5,6 There appears to be no direct risk of toxicity to the patient by using medication past the expiration date.
The risk that isn’t answered is the risk of using medications that may not be effective if potency isn’t guaranteed beyond the expiration date. It appears that most drugs are effective for years past the expiration date.
This isn’t an issue for medications for treatment of chronic conditions, as patients take the medications every day, and the medications will be used up long before they expire. For medications that are used infrequently – analgesics, antihistamines, and medications for traveler’s diarrhea – they appear to be stable for years past expiration, and there is little risk to the patient if the medications are not fully effective.
I think aspirin should not be used past expiration, given the data showing that it breaks down more so than other medications. For the case at the start of this article, I think having the patient use the expired medications should be fine.
References
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Metastatic Crohn Disease Clinically Reminiscent of Erythema Nodosum on the Right Leg
Metastatic Crohn disease (MCD) is defined by the presence of cutaneous noncaseating granulomatous lesions that are noncontiguous with the gastrointestinal (GI) tract or fistulae.1 The clinical presentation of MCD is so variable that its diagnosis requires a high index of suspicion.1,2 In particular, the presence of erythematous tender nodules on the legs is easily mistaken for erythema nodosum (EN). Skin biopsy has an important role in confirming the diagnosis, as histopathological examination would reveal a noncaseating granuloma similar to those in the involved GI tract.2 Herein, we report a case of MCD on the right leg that was clinically reminiscent of unilateral EN.
Case Report
A 21-year-old woman presented to the dermatology department with 2 painful erythematous nodules on the lower right leg of 2 weeks’ duration. She also reported abdominal pain, diarrhea, and bloody stool. She had been diagnosed with Crohn disease (CD) 6 years prior that had been well controlled with systemic low-dose steroids (5–15 mg/d), metronidazole (750 mg/d), and intermittent mesalamine and antidiarrheal drugs. However, she had not taken her medication for several weeks on her own authority. Subsequently, the patient developed skin lesions, which were characterized by ill-defined erythematous nodules with tenderness on the right lower leg along with GI symptoms (Figure 1). Laboratory studies revealed anemia (hemoglobin, 9.9 g/dL [reference range, 12.0–16.0 g/dL]) and an elevated C-reactive protein level (4.3 mg/dL [reference range, 0–0.3 mg/dL]). Other routine laboratory findings were normal.

Histopathologically, a skin biopsy from the right ankle showed vague, ill-defined, noncaseating granulomas scattered in the deep dermis and lobules of the subcutis (Figure 2). The granulomas were composed of epithelioid cells and Langerhans-type giant cells. Lymphocytes and neutrophils also were present, but eosinophils were absent. Immunohistochemical staining revealed that the infiltrating cells were mostly CD4+ helper/inducer T cells intermixed with CD8+ suppressor/cytotoxic T cells. The CD4:CD8 ratio was approximately 2:1. Counts of CD20+ B cells were low. Epithelioid cells and giant cells were positive for CD68.
×20). The skin biopsy showed granulomas composed of epithelioid cells and multinucleated giant cells in the deep dermis and in the lobules of the subcutis (B)(H&E, original magnification ×200). Histopathologic features such as small vessel vasculitis characterized by a fibrin deposit in the small blood vessels and swelling of the endothelial cells as well as granulomatous perivasculitis with perivascular infiltration of the epithelioid cells were present (C)(H&E, original magnification ×200).
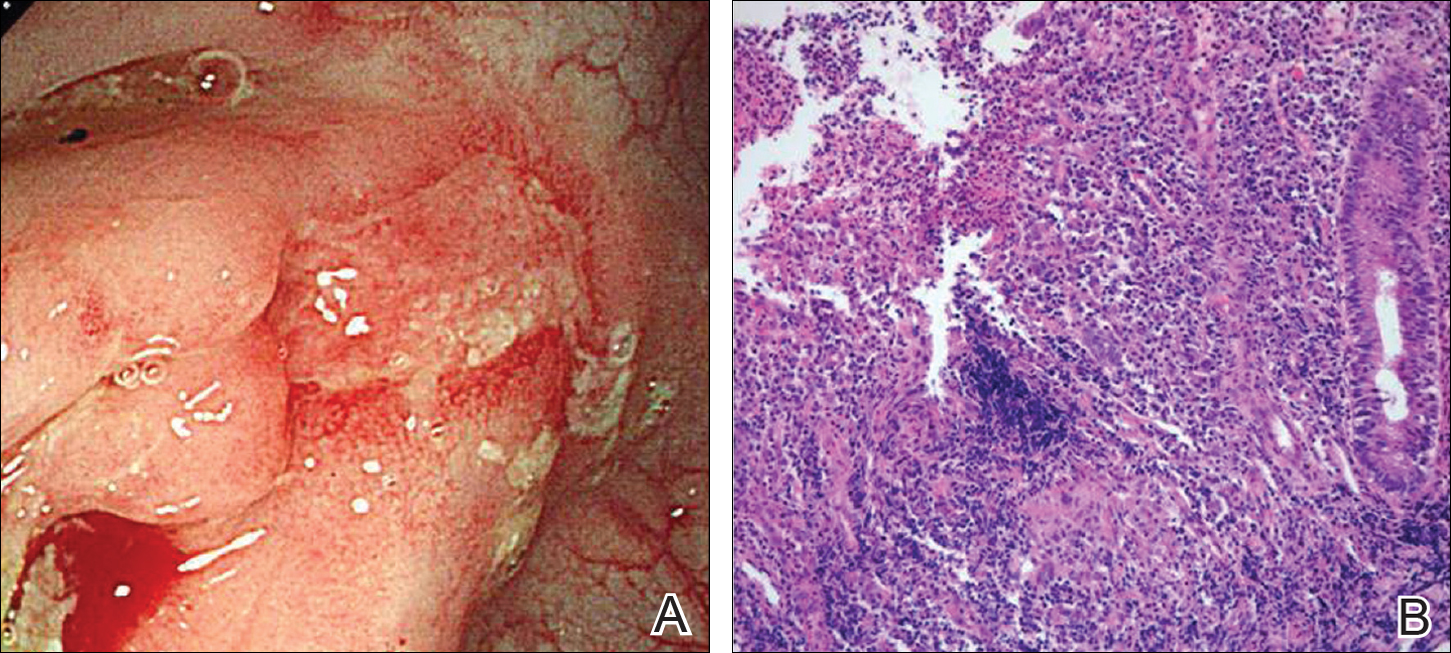
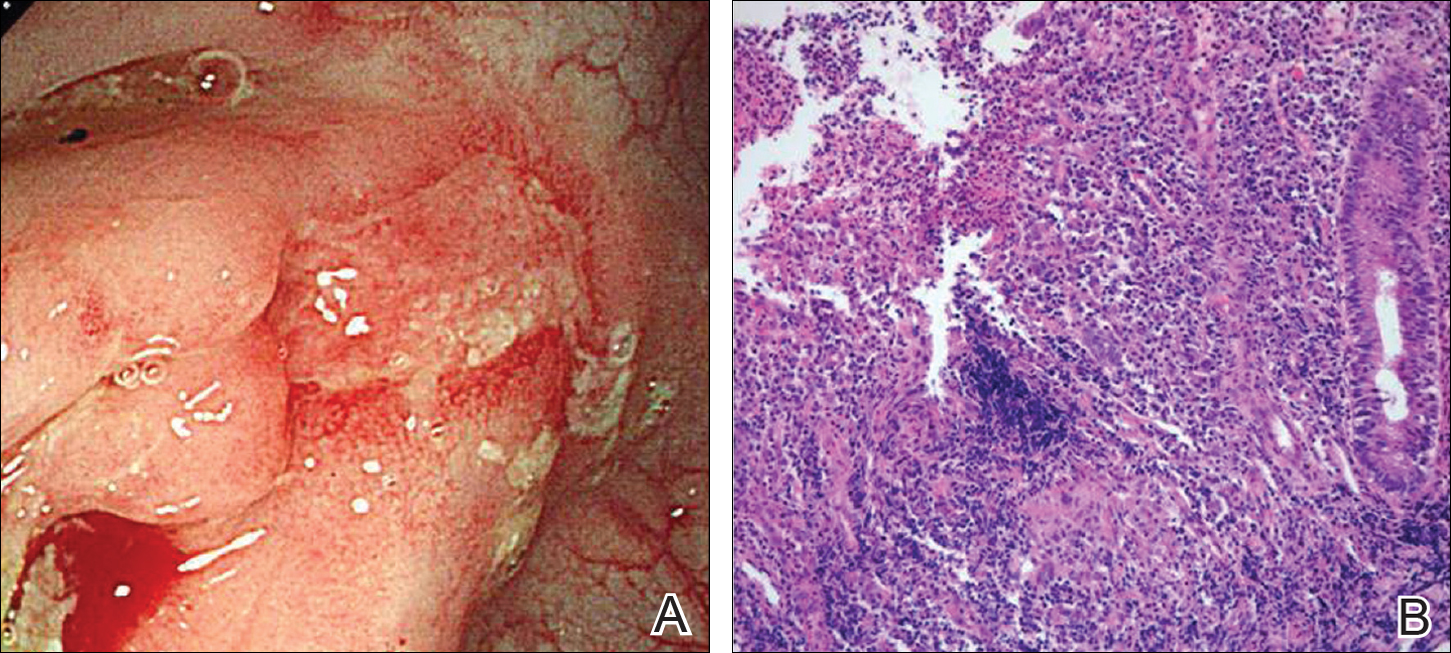
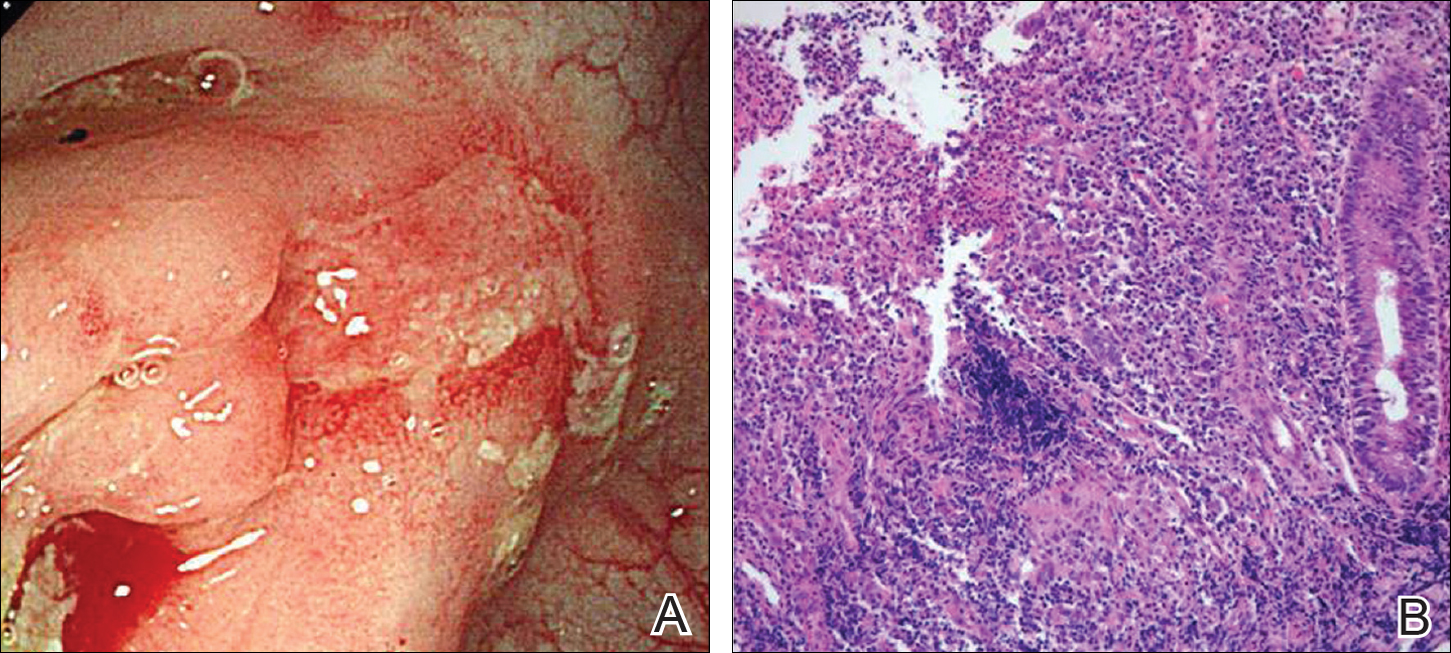
A colonoscopy was performed to evaluate the aggravation of CD. Multiple longitudinal ulcers were observed in the ileocecal valve area and from the transverse colon to the sigmoid colon (Figure 3A). Histopathologic findings from the colon showed mucosal ulceration and noncaseating granulomas with heavy infiltration of lymphocytes and plasma cells (Figure 3B). Staining for infectious microorganisms (eg, Ziehl-Neelsen, periodic acid–Schiff, Gram) was negative. A polymerase chain reaction performed on sections cut from the paraffin block of the skin biopsy was negative for Mycobacterium tuberculosis DNA.
Based on the clinical and histopathologic findings, the patient was diagnosed with MCD that was clinically reminiscent of unilateral EN. Four weeks after the initiation of therapy with systemic corticosteroids (25 mg/d), oral metronidazole (750 mg/d), and mesalamine (1200 mg/d) for CD, the skin lesions were completely resolved and the patient’s GI symptoms improved simultaneously.
Comment
Crohn disease is a chronic inflammatory granulomatous disease of the GI tract that often is associated with reactive cutaneous lesions including EN, pyoderma gangrenosum, necrotizing vasculitis, and epidermolysis bullosa acquisita. Of these, EN is the most common to appear in CD patients and has been reported to occur in 1% to 15% of patients.3-5 In particular, skin lesions on the leg presenting as tender erythematous nodules and patches are often diagnosed as EN, which is relatively common. In our case, we initially suspected EN due to the rare presentation of MCD and lack of specific clinical features; however, the skin biopsy revealed noncaseating granulomas in the mid to deep dermis and subcutis consistent with MCD.
Metastatic Crohn disease is a rare disease entity and is characterized by the presence of noncaseating granulomas of the skin at sites separated from the GI tract by normal tissue.1 Although its pathogenesis is unclear, it has been suggested that immune complexes deposited in the skin could be responsible for the granulomatous reactions.4 A T lymphocyte–mediated type IV hypersensitivity reaction also could be responsible.6,7 Because antimicrobial therapy can be curative for infection-related MCD, special histologic stains and/or tissue cultures can help to exclude an infectious etiology.8
Clinical presentations of MCD vary greatly, with observations such as single or multiple erythematous swellings, papules, plaques, nodules, abscesses, and ulcers.1,2 The relationship between these clinical presentations and the intestinal activity of CD still is unknown; in some cases, however, the metastatic granulomatous lesions and the bowel disease show comparable severity.2,9,10 In a review of the literature, MCD was generally reported to present in the genital area in children. In adults, lesions most frequently present in the genital area, followed by ulcers on the arms and legs.1,2 These variations in clinical features and location resemble benign or infectious disease and can lead to delays in diagnosis.
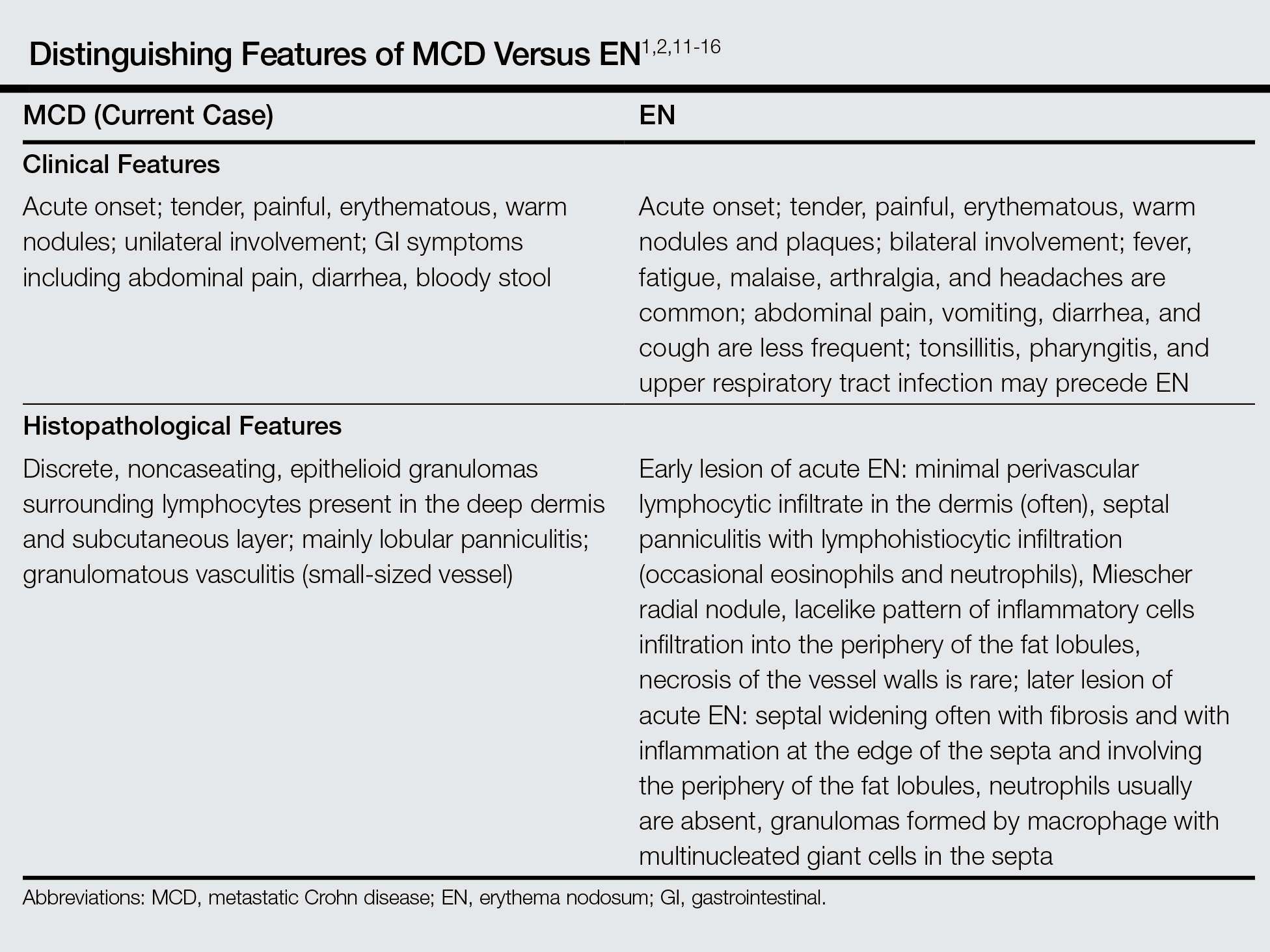
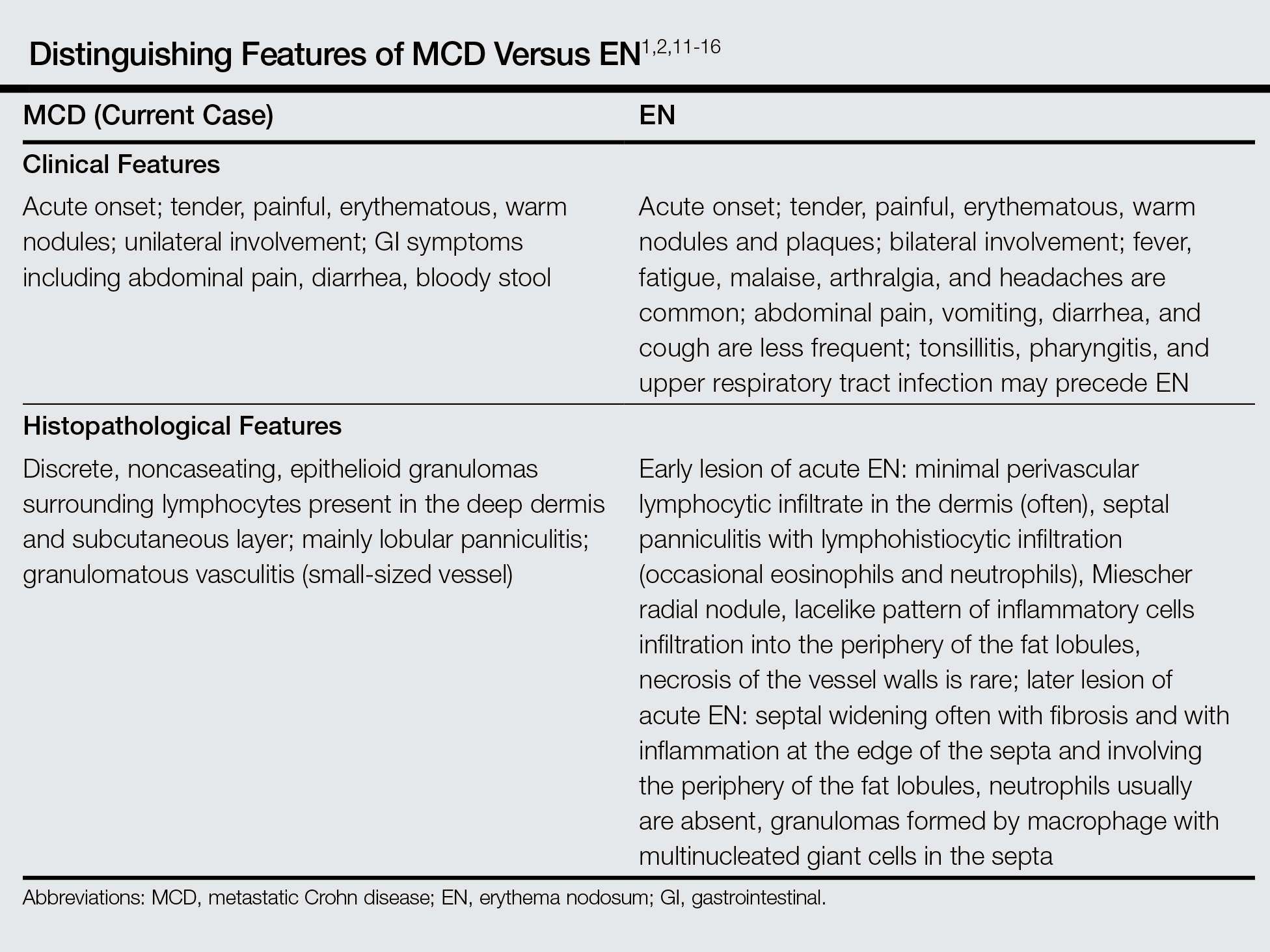
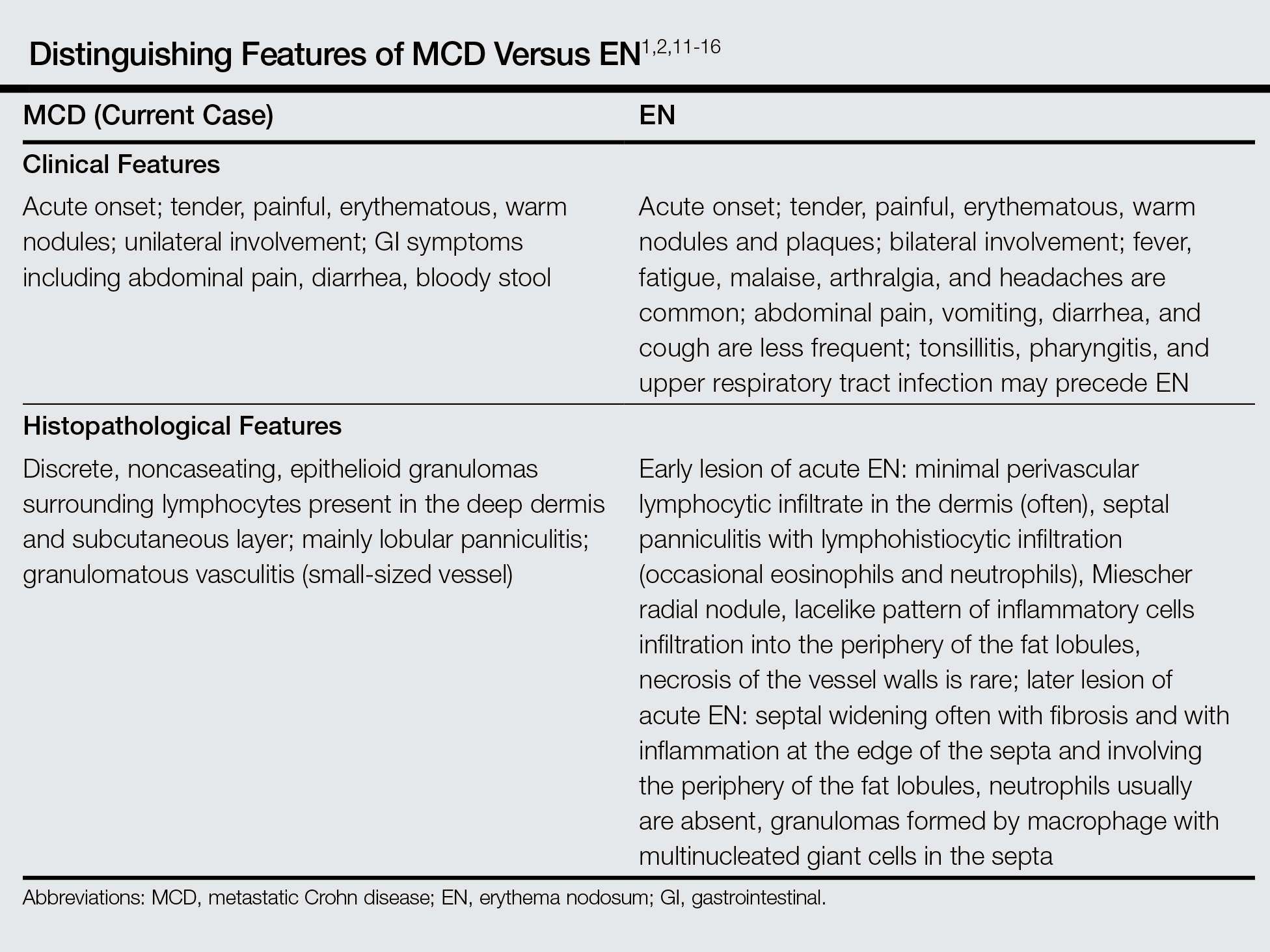
Histopathologically, MCD lesions usually are ill-defined noncaseating granulomas with numerous multinucleated giant cells and lymphomononuclear cells located mostly in the dermis and occasionally extending into the subcutis. The cutaneous granulomata are similar to those present in the affected GI tract. Lymphocytes and plasma cells also are commonly present and eosinophils can be prominent.1,2,11 In some cases of MCD, granulomatous vasculitis of small- to medium-sized vessels can be found and is associated with dermal and subcutaneous granulomatous inflammation.8,11,12 Misago and Narisawa13 suggested that granulomatous vasculitis and panniculitis associated with CD is considered to be a rare subtype of MCD. Few cases of MCD presenting as granulomatous panniculitis have been described in the literature.14-16 Our patient presented with lesions that clinically resembled EN; however, the biopsy was more consistent with MCD. The Table summarizes the distinguishing clinical and histopathological features of MCD in our case and classic EN.
Although some authors believe that MCD is not related to CD activity, others assert that MCD lesions may parallel GI activity.1,2 Our patient was treated with systemic corticosteroids, oral metronidazole, and mesalamine to control the GI symptoms associated with CD. Four weeks after treatment, the GI symptoms and skin lesions improved simultaneously without any additional dermatologic treatment. We believe that MCD has the potential to serve as an early marker of the recurrence of CD and can help with the early diagnosis of CD aggravation, though an association between MCD and CD activity has not been confirmed.
Conclusion
We reported a case of MCD that was clinically reminiscent of unilateral EN and associated with GI disease activity. Physicians should be aware of the possibility of skin manifestations in CD, especially when erythematous nodular lesions are present on the leg.
- Calonje E, Brenn T, Lazar AJ, et al. Mckee’s Pathology of the Skin: With Clinical Correlations. 4th ed. Philadelphia, PA: Saunders Elsevier; 2012.
- Palamaras I, El-Jabbour J, Pietropaolo N, et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol. 2008;22:1033-1043.
- Sonia F, Richard SB. Inflammatory bowel disease. In: Kasper DL, Braunwald E, Fauci AS, et al, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:1776-1789.
- Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5:689-695.
- Crowson AN, Nuovo GJ, Mihm MC Jr, et al. Cutaneous manifestations of Crohn’s disease, its spectrum, and its pathogenesis: intracellular consensus bacterial 16S rRNA is associated with the gastrointestinal but not the cutaneous manifestations of Crohn’s disease. Hum Pathol. 2003;34:1185-1192.
- Tatnall FM, Dodd HJ, Sarkany I. Crohn’s disease with metastatic cutaneous involvement and granulomatous cheilitis. J R Soc Med. 1987;80:49-51.
- Shum DT, Guenther L. Metastatic Crohn’s disease. case report and review of the literature. Arch Dermatol. 1990;126:645-648.
- Emanuel PO, Phelps RG. Metastatic Crohn’s disease: a histopathologic study of 12 cases. J Cutan Pathol. 2008;35:457-461.
- Chalvardjian A, Nethercott JR. Cutaneous granulomatous vasculitis associated with Crohn’s disease. Cutis. 1982;30:645-655.
- Lebwohl M, Fleischmajer R, Janowitz H, et al. Metastatic Crohn’s disease. J Am Acad Dermatol. 1984;10:33-38.
- Sabat M, Leulmo J, Saez A. Cutaneous granulomatous vasculitis in metastatic Crohn’s disease. J Eur Acad Dermatol Venereol. 2005;19:652-653.
- Burns AM, Walsh N, Green PJ. Granulomatous vasculitis in Crohn’s disease: a clinicopathologic correlate of two unusual cases. J Cutan Pathol. 2010;37:1077-1083.
- Misago N, Narisawa Y. Erythema induratum (nodular vasculitis) associated with Crohn’s disease: a rare type of metastatic Crohn’s disease. Am J Dermatopathol. 2012;34:325-329.
- Liebermann TR, Greene JF Jr. Transient subcutaneous granulomatosis of the upper extremities in Crohn’s disease. Am J Gastroenterol. 1979;72:89-91.
- Levine N, Bangert J. Cutaneous granulomatosis in Crohn’s disease. Arch Dermatol. 1982;118:1006-1009.
- Hackzell-Bradley M, Hedblad MA, Stephansson EA. Metastatic Crohn’s disease. report of 3 cases with special reference to histopathologic findings. Arch Dermatol. 1996;132:928-932.
Metastatic Crohn disease (MCD) is defined by the presence of cutaneous noncaseating granulomatous lesions that are noncontiguous with the gastrointestinal (GI) tract or fistulae.1 The clinical presentation of MCD is so variable that its diagnosis requires a high index of suspicion.1,2 In particular, the presence of erythematous tender nodules on the legs is easily mistaken for erythema nodosum (EN). Skin biopsy has an important role in confirming the diagnosis, as histopathological examination would reveal a noncaseating granuloma similar to those in the involved GI tract.2 Herein, we report a case of MCD on the right leg that was clinically reminiscent of unilateral EN.
Case Report
A 21-year-old woman presented to the dermatology department with 2 painful erythematous nodules on the lower right leg of 2 weeks’ duration. She also reported abdominal pain, diarrhea, and bloody stool. She had been diagnosed with Crohn disease (CD) 6 years prior that had been well controlled with systemic low-dose steroids (5–15 mg/d), metronidazole (750 mg/d), and intermittent mesalamine and antidiarrheal drugs. However, she had not taken her medication for several weeks on her own authority. Subsequently, the patient developed skin lesions, which were characterized by ill-defined erythematous nodules with tenderness on the right lower leg along with GI symptoms (Figure 1). Laboratory studies revealed anemia (hemoglobin, 9.9 g/dL [reference range, 12.0–16.0 g/dL]) and an elevated C-reactive protein level (4.3 mg/dL [reference range, 0–0.3 mg/dL]). Other routine laboratory findings were normal.

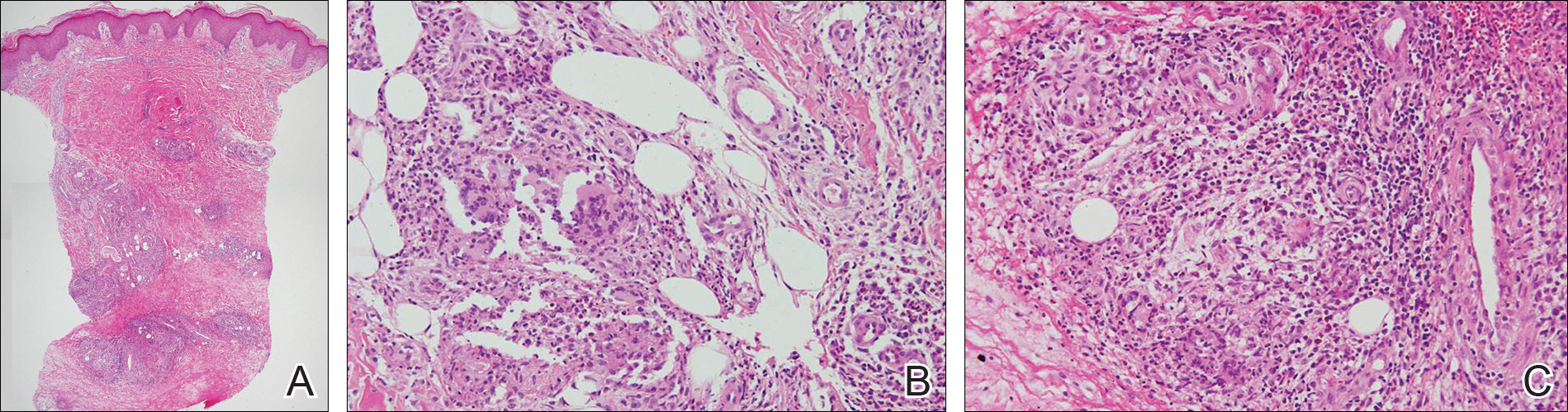
Histopathologically, a skin biopsy from the right ankle showed vague, ill-defined, noncaseating granulomas scattered in the deep dermis and lobules of the subcutis (Figure 2). The granulomas were composed of epithelioid cells and Langerhans-type giant cells. Lymphocytes and neutrophils also were present, but eosinophils were absent. Immunohistochemical staining revealed that the infiltrating cells were mostly CD4+ helper/inducer T cells intermixed with CD8+ suppressor/cytotoxic T cells. The CD4:CD8 ratio was approximately 2:1. Counts of CD20+ B cells were low. Epithelioid cells and giant cells were positive for CD68.
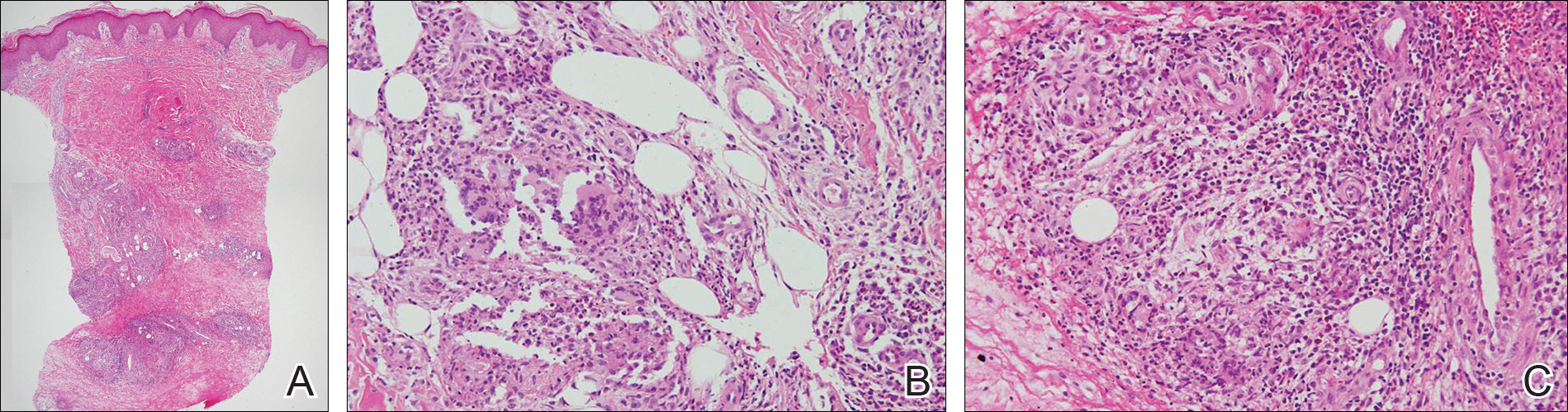
×20). The skin biopsy showed granulomas composed of epithelioid cells and multinucleated giant cells in the deep dermis and in the lobules of the subcutis (B)(H&E, original magnification ×200). Histopathologic features such as small vessel vasculitis characterized by a fibrin deposit in the small blood vessels and swelling of the endothelial cells as well as granulomatous perivasculitis with perivascular infiltration of the epithelioid cells were present (C)(H&E, original magnification ×200).
A colonoscopy was performed to evaluate the aggravation of CD. Multiple longitudinal ulcers were observed in the ileocecal valve area and from the transverse colon to the sigmoid colon (Figure 3A). Histopathologic findings from the colon showed mucosal ulceration and noncaseating granulomas with heavy infiltration of lymphocytes and plasma cells (Figure 3B). Staining for infectious microorganisms (eg, Ziehl-Neelsen, periodic acid–Schiff, Gram) was negative. A polymerase chain reaction performed on sections cut from the paraffin block of the skin biopsy was negative for Mycobacterium tuberculosis DNA.
Based on the clinical and histopathologic findings, the patient was diagnosed with MCD that was clinically reminiscent of unilateral EN. Four weeks after the initiation of therapy with systemic corticosteroids (25 mg/d), oral metronidazole (750 mg/d), and mesalamine (1200 mg/d) for CD, the skin lesions were completely resolved and the patient’s GI symptoms improved simultaneously.
Comment
Crohn disease is a chronic inflammatory granulomatous disease of the GI tract that often is associated with reactive cutaneous lesions including EN, pyoderma gangrenosum, necrotizing vasculitis, and epidermolysis bullosa acquisita. Of these, EN is the most common to appear in CD patients and has been reported to occur in 1% to 15% of patients.3-5 In particular, skin lesions on the leg presenting as tender erythematous nodules and patches are often diagnosed as EN, which is relatively common. In our case, we initially suspected EN due to the rare presentation of MCD and lack of specific clinical features; however, the skin biopsy revealed noncaseating granulomas in the mid to deep dermis and subcutis consistent with MCD.
Metastatic Crohn disease is a rare disease entity and is characterized by the presence of noncaseating granulomas of the skin at sites separated from the GI tract by normal tissue.1 Although its pathogenesis is unclear, it has been suggested that immune complexes deposited in the skin could be responsible for the granulomatous reactions.4 A T lymphocyte–mediated type IV hypersensitivity reaction also could be responsible.6,7 Because antimicrobial therapy can be curative for infection-related MCD, special histologic stains and/or tissue cultures can help to exclude an infectious etiology.8
Clinical presentations of MCD vary greatly, with observations such as single or multiple erythematous swellings, papules, plaques, nodules, abscesses, and ulcers.1,2 The relationship between these clinical presentations and the intestinal activity of CD still is unknown; in some cases, however, the metastatic granulomatous lesions and the bowel disease show comparable severity.2,9,10 In a review of the literature, MCD was generally reported to present in the genital area in children. In adults, lesions most frequently present in the genital area, followed by ulcers on the arms and legs.1,2 These variations in clinical features and location resemble benign or infectious disease and can lead to delays in diagnosis.
Histopathologically, MCD lesions usually are ill-defined noncaseating granulomas with numerous multinucleated giant cells and lymphomononuclear cells located mostly in the dermis and occasionally extending into the subcutis. The cutaneous granulomata are similar to those present in the affected GI tract. Lymphocytes and plasma cells also are commonly present and eosinophils can be prominent.1,2,11 In some cases of MCD, granulomatous vasculitis of small- to medium-sized vessels can be found and is associated with dermal and subcutaneous granulomatous inflammation.8,11,12 Misago and Narisawa13 suggested that granulomatous vasculitis and panniculitis associated with CD is considered to be a rare subtype of MCD. Few cases of MCD presenting as granulomatous panniculitis have been described in the literature.14-16 Our patient presented with lesions that clinically resembled EN; however, the biopsy was more consistent with MCD. The Table summarizes the distinguishing clinical and histopathological features of MCD in our case and classic EN.
Although some authors believe that MCD is not related to CD activity, others assert that MCD lesions may parallel GI activity.1,2 Our patient was treated with systemic corticosteroids, oral metronidazole, and mesalamine to control the GI symptoms associated with CD. Four weeks after treatment, the GI symptoms and skin lesions improved simultaneously without any additional dermatologic treatment. We believe that MCD has the potential to serve as an early marker of the recurrence of CD and can help with the early diagnosis of CD aggravation, though an association between MCD and CD activity has not been confirmed.
Conclusion
We reported a case of MCD that was clinically reminiscent of unilateral EN and associated with GI disease activity. Physicians should be aware of the possibility of skin manifestations in CD, especially when erythematous nodular lesions are present on the leg.
Metastatic Crohn disease (MCD) is defined by the presence of cutaneous noncaseating granulomatous lesions that are noncontiguous with the gastrointestinal (GI) tract or fistulae.1 The clinical presentation of MCD is so variable that its diagnosis requires a high index of suspicion.1,2 In particular, the presence of erythematous tender nodules on the legs is easily mistaken for erythema nodosum (EN). Skin biopsy has an important role in confirming the diagnosis, as histopathological examination would reveal a noncaseating granuloma similar to those in the involved GI tract.2 Herein, we report a case of MCD on the right leg that was clinically reminiscent of unilateral EN.
Case Report
A 21-year-old woman presented to the dermatology department with 2 painful erythematous nodules on the lower right leg of 2 weeks’ duration. She also reported abdominal pain, diarrhea, and bloody stool. She had been diagnosed with Crohn disease (CD) 6 years prior that had been well controlled with systemic low-dose steroids (5–15 mg/d), metronidazole (750 mg/d), and intermittent mesalamine and antidiarrheal drugs. However, she had not taken her medication for several weeks on her own authority. Subsequently, the patient developed skin lesions, which were characterized by ill-defined erythematous nodules with tenderness on the right lower leg along with GI symptoms (Figure 1). Laboratory studies revealed anemia (hemoglobin, 9.9 g/dL [reference range, 12.0–16.0 g/dL]) and an elevated C-reactive protein level (4.3 mg/dL [reference range, 0–0.3 mg/dL]). Other routine laboratory findings were normal.

Histopathologically, a skin biopsy from the right ankle showed vague, ill-defined, noncaseating granulomas scattered in the deep dermis and lobules of the subcutis (Figure 2). The granulomas were composed of epithelioid cells and Langerhans-type giant cells. Lymphocytes and neutrophils also were present, but eosinophils were absent. Immunohistochemical staining revealed that the infiltrating cells were mostly CD4+ helper/inducer T cells intermixed with CD8+ suppressor/cytotoxic T cells. The CD4:CD8 ratio was approximately 2:1. Counts of CD20+ B cells were low. Epithelioid cells and giant cells were positive for CD68.
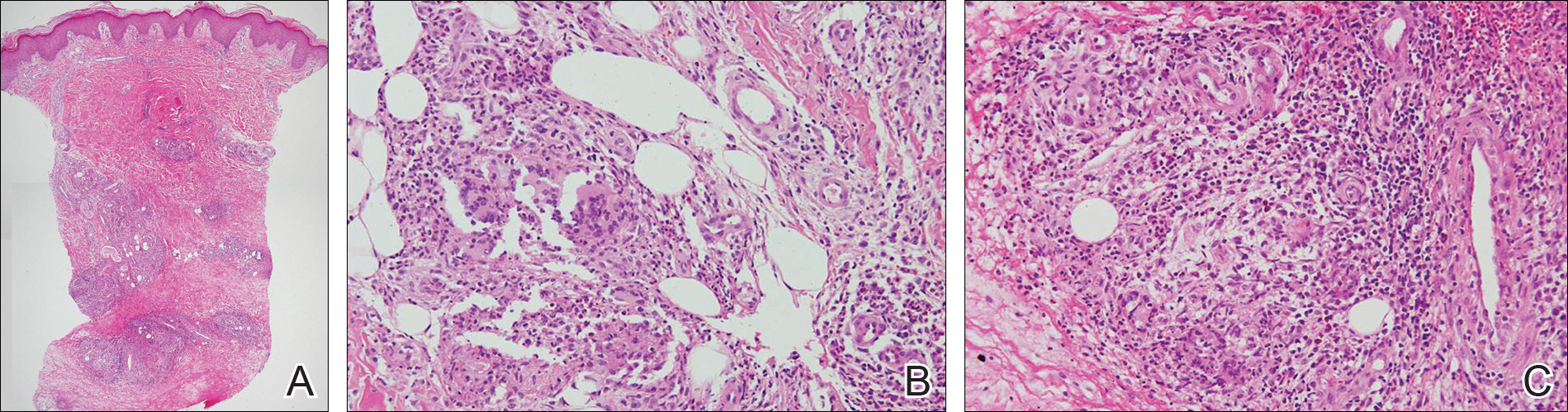
×20). The skin biopsy showed granulomas composed of epithelioid cells and multinucleated giant cells in the deep dermis and in the lobules of the subcutis (B)(H&E, original magnification ×200). Histopathologic features such as small vessel vasculitis characterized by a fibrin deposit in the small blood vessels and swelling of the endothelial cells as well as granulomatous perivasculitis with perivascular infiltration of the epithelioid cells were present (C)(H&E, original magnification ×200).
A colonoscopy was performed to evaluate the aggravation of CD. Multiple longitudinal ulcers were observed in the ileocecal valve area and from the transverse colon to the sigmoid colon (Figure 3A). Histopathologic findings from the colon showed mucosal ulceration and noncaseating granulomas with heavy infiltration of lymphocytes and plasma cells (Figure 3B). Staining for infectious microorganisms (eg, Ziehl-Neelsen, periodic acid–Schiff, Gram) was negative. A polymerase chain reaction performed on sections cut from the paraffin block of the skin biopsy was negative for Mycobacterium tuberculosis DNA.
Based on the clinical and histopathologic findings, the patient was diagnosed with MCD that was clinically reminiscent of unilateral EN. Four weeks after the initiation of therapy with systemic corticosteroids (25 mg/d), oral metronidazole (750 mg/d), and mesalamine (1200 mg/d) for CD, the skin lesions were completely resolved and the patient’s GI symptoms improved simultaneously.
Comment
Crohn disease is a chronic inflammatory granulomatous disease of the GI tract that often is associated with reactive cutaneous lesions including EN, pyoderma gangrenosum, necrotizing vasculitis, and epidermolysis bullosa acquisita. Of these, EN is the most common to appear in CD patients and has been reported to occur in 1% to 15% of patients.3-5 In particular, skin lesions on the leg presenting as tender erythematous nodules and patches are often diagnosed as EN, which is relatively common. In our case, we initially suspected EN due to the rare presentation of MCD and lack of specific clinical features; however, the skin biopsy revealed noncaseating granulomas in the mid to deep dermis and subcutis consistent with MCD.
Metastatic Crohn disease is a rare disease entity and is characterized by the presence of noncaseating granulomas of the skin at sites separated from the GI tract by normal tissue.1 Although its pathogenesis is unclear, it has been suggested that immune complexes deposited in the skin could be responsible for the granulomatous reactions.4 A T lymphocyte–mediated type IV hypersensitivity reaction also could be responsible.6,7 Because antimicrobial therapy can be curative for infection-related MCD, special histologic stains and/or tissue cultures can help to exclude an infectious etiology.8
Clinical presentations of MCD vary greatly, with observations such as single or multiple erythematous swellings, papules, plaques, nodules, abscesses, and ulcers.1,2 The relationship between these clinical presentations and the intestinal activity of CD still is unknown; in some cases, however, the metastatic granulomatous lesions and the bowel disease show comparable severity.2,9,10 In a review of the literature, MCD was generally reported to present in the genital area in children. In adults, lesions most frequently present in the genital area, followed by ulcers on the arms and legs.1,2 These variations in clinical features and location resemble benign or infectious disease and can lead to delays in diagnosis.
Histopathologically, MCD lesions usually are ill-defined noncaseating granulomas with numerous multinucleated giant cells and lymphomononuclear cells located mostly in the dermis and occasionally extending into the subcutis. The cutaneous granulomata are similar to those present in the affected GI tract. Lymphocytes and plasma cells also are commonly present and eosinophils can be prominent.1,2,11 In some cases of MCD, granulomatous vasculitis of small- to medium-sized vessels can be found and is associated with dermal and subcutaneous granulomatous inflammation.8,11,12 Misago and Narisawa13 suggested that granulomatous vasculitis and panniculitis associated with CD is considered to be a rare subtype of MCD. Few cases of MCD presenting as granulomatous panniculitis have been described in the literature.14-16 Our patient presented with lesions that clinically resembled EN; however, the biopsy was more consistent with MCD. The Table summarizes the distinguishing clinical and histopathological features of MCD in our case and classic EN.
Although some authors believe that MCD is not related to CD activity, others assert that MCD lesions may parallel GI activity.1,2 Our patient was treated with systemic corticosteroids, oral metronidazole, and mesalamine to control the GI symptoms associated with CD. Four weeks after treatment, the GI symptoms and skin lesions improved simultaneously without any additional dermatologic treatment. We believe that MCD has the potential to serve as an early marker of the recurrence of CD and can help with the early diagnosis of CD aggravation, though an association between MCD and CD activity has not been confirmed.
Conclusion
We reported a case of MCD that was clinically reminiscent of unilateral EN and associated with GI disease activity. Physicians should be aware of the possibility of skin manifestations in CD, especially when erythematous nodular lesions are present on the leg.
- Calonje E, Brenn T, Lazar AJ, et al. Mckee’s Pathology of the Skin: With Clinical Correlations. 4th ed. Philadelphia, PA: Saunders Elsevier; 2012.
- Palamaras I, El-Jabbour J, Pietropaolo N, et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol. 2008;22:1033-1043.
- Sonia F, Richard SB. Inflammatory bowel disease. In: Kasper DL, Braunwald E, Fauci AS, et al, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:1776-1789.
- Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5:689-695.
- Crowson AN, Nuovo GJ, Mihm MC Jr, et al. Cutaneous manifestations of Crohn’s disease, its spectrum, and its pathogenesis: intracellular consensus bacterial 16S rRNA is associated with the gastrointestinal but not the cutaneous manifestations of Crohn’s disease. Hum Pathol. 2003;34:1185-1192.
- Tatnall FM, Dodd HJ, Sarkany I. Crohn’s disease with metastatic cutaneous involvement and granulomatous cheilitis. J R Soc Med. 1987;80:49-51.
- Shum DT, Guenther L. Metastatic Crohn’s disease. case report and review of the literature. Arch Dermatol. 1990;126:645-648.
- Emanuel PO, Phelps RG. Metastatic Crohn’s disease: a histopathologic study of 12 cases. J Cutan Pathol. 2008;35:457-461.
- Chalvardjian A, Nethercott JR. Cutaneous granulomatous vasculitis associated with Crohn’s disease. Cutis. 1982;30:645-655.
- Lebwohl M, Fleischmajer R, Janowitz H, et al. Metastatic Crohn’s disease. J Am Acad Dermatol. 1984;10:33-38.
- Sabat M, Leulmo J, Saez A. Cutaneous granulomatous vasculitis in metastatic Crohn’s disease. J Eur Acad Dermatol Venereol. 2005;19:652-653.
- Burns AM, Walsh N, Green PJ. Granulomatous vasculitis in Crohn’s disease: a clinicopathologic correlate of two unusual cases. J Cutan Pathol. 2010;37:1077-1083.
- Misago N, Narisawa Y. Erythema induratum (nodular vasculitis) associated with Crohn’s disease: a rare type of metastatic Crohn’s disease. Am J Dermatopathol. 2012;34:325-329.
- Liebermann TR, Greene JF Jr. Transient subcutaneous granulomatosis of the upper extremities in Crohn’s disease. Am J Gastroenterol. 1979;72:89-91.
- Levine N, Bangert J. Cutaneous granulomatosis in Crohn’s disease. Arch Dermatol. 1982;118:1006-1009.
- Hackzell-Bradley M, Hedblad MA, Stephansson EA. Metastatic Crohn’s disease. report of 3 cases with special reference to histopathologic findings. Arch Dermatol. 1996;132:928-932.
- Calonje E, Brenn T, Lazar AJ, et al. Mckee’s Pathology of the Skin: With Clinical Correlations. 4th ed. Philadelphia, PA: Saunders Elsevier; 2012.
- Palamaras I, El-Jabbour J, Pietropaolo N, et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol. 2008;22:1033-1043.
- Sonia F, Richard SB. Inflammatory bowel disease. In: Kasper DL, Braunwald E, Fauci AS, et al, eds. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:1776-1789.
- Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5:689-695.
- Crowson AN, Nuovo GJ, Mihm MC Jr, et al. Cutaneous manifestations of Crohn’s disease, its spectrum, and its pathogenesis: intracellular consensus bacterial 16S rRNA is associated with the gastrointestinal but not the cutaneous manifestations of Crohn’s disease. Hum Pathol. 2003;34:1185-1192.
- Tatnall FM, Dodd HJ, Sarkany I. Crohn’s disease with metastatic cutaneous involvement and granulomatous cheilitis. J R Soc Med. 1987;80:49-51.
- Shum DT, Guenther L. Metastatic Crohn’s disease. case report and review of the literature. Arch Dermatol. 1990;126:645-648.
- Emanuel PO, Phelps RG. Metastatic Crohn’s disease: a histopathologic study of 12 cases. J Cutan Pathol. 2008;35:457-461.
- Chalvardjian A, Nethercott JR. Cutaneous granulomatous vasculitis associated with Crohn’s disease. Cutis. 1982;30:645-655.
- Lebwohl M, Fleischmajer R, Janowitz H, et al. Metastatic Crohn’s disease. J Am Acad Dermatol. 1984;10:33-38.
- Sabat M, Leulmo J, Saez A. Cutaneous granulomatous vasculitis in metastatic Crohn’s disease. J Eur Acad Dermatol Venereol. 2005;19:652-653.
- Burns AM, Walsh N, Green PJ. Granulomatous vasculitis in Crohn’s disease: a clinicopathologic correlate of two unusual cases. J Cutan Pathol. 2010;37:1077-1083.
- Misago N, Narisawa Y. Erythema induratum (nodular vasculitis) associated with Crohn’s disease: a rare type of metastatic Crohn’s disease. Am J Dermatopathol. 2012;34:325-329.
- Liebermann TR, Greene JF Jr. Transient subcutaneous granulomatosis of the upper extremities in Crohn’s disease. Am J Gastroenterol. 1979;72:89-91.
- Levine N, Bangert J. Cutaneous granulomatosis in Crohn’s disease. Arch Dermatol. 1982;118:1006-1009.
- Hackzell-Bradley M, Hedblad MA, Stephansson EA. Metastatic Crohn’s disease. report of 3 cases with special reference to histopathologic findings. Arch Dermatol. 1996;132:928-932.
Practice Points
- Metastatic Crohn disease (MCD) may be an initial sign indicating the aggravation of intestinal Crohn disease (CD).
- Metastatic Crohn disease on the legs could be clinically reminiscent of erythema nodosum (EN).
- Physicians should be aware of the possibility of MCD when encountering EN-like lesions on the legs in a CD patient.
Should we pursue board certification in Mohs micrographic surgery?
The medical director was direct and blunt: “You’ve got a problem with two very different levels of training in Mohs surgery. This is a big problem for your specialty.”
The remarks came at a medical director summit that I was attending to speak on the value of dermatology. I was explaining to medical directors how including small dermatology practices in their plans would realize cost savings when treating skin cancer in the office setting. An awkward silence followed the medical director’s remarks. Then I uttered a lame “we may have a board certification someday.”
My interview with the New York Times reporter before the meeting quickly became adversarial. “What about these guys who do Mohs after a 3-day course?” I explained that there is more involved than just the 3-day course, that there is a preceptorship and case reviews. Plus, some of “those guys” wrote some of the best Mohs textbooks. The reporter wasn’t buying it, and the rest of the interview went downhill.
And the training issues surrounding Mohs surgery are playing out in practice. One dermatologist wrote me complaining that an insurer will no longer let him bill for Mohs because “he can’t document his residency training in Mohs and did not do a fellowship.” Another wrote me saying he can no longer teach Mohs surgery at the VA or the medical school “because he didn’t do a formal Mohs fellowship.”
The issue of who is qualified to perform Mohs surgery is coming to a head. There are more than 2,500 dermatologists billing Medicare for Mohs, and insurers are groaning at the expense. They are looking for any possible reason to exclude dermatologists from billing for Mohs surgery.
A possible solution is a board certification in Mohs surgery. Osteopathic dermatologists have had this option for 20 years. Unfortunately, allopathic dermatologists cannot sit for the osteopathic exam. A new certification exam for allopathic dermatologists who have successfully completed a dermatology residency accredited by the Accreditation Council for Graduate Medical Education (ACGME) seems worthy of a discussion.
Downsides of certification include the likely $1,000 or more cost of a test, the costs of preparing for the test, and the risk of failing a test. A new certification would give the Maintenance of Certification (MOC) haters another reason to complain, since about 600 lifetime certified, board-exempt dermatologists would be dragged back into MOC to maintain a Mohs surgery subspecialty certification. Some of the current fellowship-trained Mohs surgeons will not like being grouped with the nonfellowship-trained surgeons, whom they consider their inferiors and who will now have the opportunity to be board certified.
The name of the fellowship, which is “micrographic surgery and dermatologic oncology,” also has some paranoid types fearing that they will lose the right to treat skin cancer if such a subspecialty is created. That shouldn’t be an issue, since all dermatologists are trained in residency to treat skin cancer. The formal fellowships already exist. There are already 1,600 fellowship-trained Mohs surgeons out there, and they have not cornered the market on skin cancer. The situation should not change since general dermatologists remain the gatekeepers – and entry point – for most skin cancer patients. Certification exams in dermatopathology and pediatric dermatology have not had a negative impact on general dermatologists, who still read their own slides and see kids for skin disease. In fact, having dermatopathology as a certified part of dermatology has been a huge benefit in our struggle to maintain the right to read our own slides.
Developing a certification exam would take at least 2 years if the American Board of Dermatology decided to do it. There would be no “grandfathering” automatic certification. Everyone would have to take the same exam – young, old, formally trained, or not.
Members of the American Board of Dermatology explained the qualifiers to sit for an exam (if there was an exam) at a summit I held in Cincinnati in 2015. They are interested in including all ABD dermatologists who currently practice Mohs surgery, fellowship trained or not. Suggested parameters included any ABD fellow whose practice is 20% Mohs and reconstructive surgery (by volume or income), or anyone who performs Mohs once a week. Fellowship-trained micrographic surgeons could be eligible, and this would be a self-attestation! There would be no case log reviews, no visits by inspectors, no secret questions or passwords. This pathway would remain open for 5 years as were the exams for dermatopathology and pediatric dermatology. After that point, only ACGME fellowship–trained Mohs surgeons would be eligible to take the exam.
Upsides to this approach include decreasing divisiveness in the specialty, creating a better brand, and elevating the specialty. A board certification will help in obtaining a Medicare specialty designation, which will help stop the delisting of Mohs surgeons from insurance networks based on their average charges compared with general dermatologists. This action would particularly help small practices.
The American Academy of Dermatology board of directors sent this issue to the education committee to inform and poll the membership. You should expect to hear more about the proposed process. As an AAD member, you will get to express your opinion so make sure you are well informed. The AAD membership opinion will be important in whether or not the American Board of Dermatology decides to pursue this. Remember, this is an American Board of Dermatology decision, not an AAD decision.
More reasons for a board certification include that the ACGME expects its fellowships to develop a board exam at some point (although not all have). The 1,000 ACGME fellowship–trained micrographic surgeons deserve a chance to be board certified, which is the medical profession’s way to demonstrate competence to the public.
Having all Mohs surgeons board certified would heal a huge rift in the house of dermatology, and give us a united, consistent face to present to other specialties, the Congress, and the media. Physicians are judged by their training and credentials. Love them or hate them, the ACGME is the gold standard. Perhaps the greatest beneficiaries would be those practicing Mohs who did not complete a formal fellowship. I think a board exam is overdue, and will be a boon to all of dermatology.
Dr. Coldiron is a past president of the American Academy of Dermatology. He is currently in private practice, but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics.
The medical director was direct and blunt: “You’ve got a problem with two very different levels of training in Mohs surgery. This is a big problem for your specialty.”
The remarks came at a medical director summit that I was attending to speak on the value of dermatology. I was explaining to medical directors how including small dermatology practices in their plans would realize cost savings when treating skin cancer in the office setting. An awkward silence followed the medical director’s remarks. Then I uttered a lame “we may have a board certification someday.”
My interview with the New York Times reporter before the meeting quickly became adversarial. “What about these guys who do Mohs after a 3-day course?” I explained that there is more involved than just the 3-day course, that there is a preceptorship and case reviews. Plus, some of “those guys” wrote some of the best Mohs textbooks. The reporter wasn’t buying it, and the rest of the interview went downhill.
And the training issues surrounding Mohs surgery are playing out in practice. One dermatologist wrote me complaining that an insurer will no longer let him bill for Mohs because “he can’t document his residency training in Mohs and did not do a fellowship.” Another wrote me saying he can no longer teach Mohs surgery at the VA or the medical school “because he didn’t do a formal Mohs fellowship.”
The issue of who is qualified to perform Mohs surgery is coming to a head. There are more than 2,500 dermatologists billing Medicare for Mohs, and insurers are groaning at the expense. They are looking for any possible reason to exclude dermatologists from billing for Mohs surgery.
A possible solution is a board certification in Mohs surgery. Osteopathic dermatologists have had this option for 20 years. Unfortunately, allopathic dermatologists cannot sit for the osteopathic exam. A new certification exam for allopathic dermatologists who have successfully completed a dermatology residency accredited by the Accreditation Council for Graduate Medical Education (ACGME) seems worthy of a discussion.
Downsides of certification include the likely $1,000 or more cost of a test, the costs of preparing for the test, and the risk of failing a test. A new certification would give the Maintenance of Certification (MOC) haters another reason to complain, since about 600 lifetime certified, board-exempt dermatologists would be dragged back into MOC to maintain a Mohs surgery subspecialty certification. Some of the current fellowship-trained Mohs surgeons will not like being grouped with the nonfellowship-trained surgeons, whom they consider their inferiors and who will now have the opportunity to be board certified.
The name of the fellowship, which is “micrographic surgery and dermatologic oncology,” also has some paranoid types fearing that they will lose the right to treat skin cancer if such a subspecialty is created. That shouldn’t be an issue, since all dermatologists are trained in residency to treat skin cancer. The formal fellowships already exist. There are already 1,600 fellowship-trained Mohs surgeons out there, and they have not cornered the market on skin cancer. The situation should not change since general dermatologists remain the gatekeepers – and entry point – for most skin cancer patients. Certification exams in dermatopathology and pediatric dermatology have not had a negative impact on general dermatologists, who still read their own slides and see kids for skin disease. In fact, having dermatopathology as a certified part of dermatology has been a huge benefit in our struggle to maintain the right to read our own slides.
Developing a certification exam would take at least 2 years if the American Board of Dermatology decided to do it. There would be no “grandfathering” automatic certification. Everyone would have to take the same exam – young, old, formally trained, or not.
Members of the American Board of Dermatology explained the qualifiers to sit for an exam (if there was an exam) at a summit I held in Cincinnati in 2015. They are interested in including all ABD dermatologists who currently practice Mohs surgery, fellowship trained or not. Suggested parameters included any ABD fellow whose practice is 20% Mohs and reconstructive surgery (by volume or income), or anyone who performs Mohs once a week. Fellowship-trained micrographic surgeons could be eligible, and this would be a self-attestation! There would be no case log reviews, no visits by inspectors, no secret questions or passwords. This pathway would remain open for 5 years as were the exams for dermatopathology and pediatric dermatology. After that point, only ACGME fellowship–trained Mohs surgeons would be eligible to take the exam.
Upsides to this approach include decreasing divisiveness in the specialty, creating a better brand, and elevating the specialty. A board certification will help in obtaining a Medicare specialty designation, which will help stop the delisting of Mohs surgeons from insurance networks based on their average charges compared with general dermatologists. This action would particularly help small practices.
The American Academy of Dermatology board of directors sent this issue to the education committee to inform and poll the membership. You should expect to hear more about the proposed process. As an AAD member, you will get to express your opinion so make sure you are well informed. The AAD membership opinion will be important in whether or not the American Board of Dermatology decides to pursue this. Remember, this is an American Board of Dermatology decision, not an AAD decision.
More reasons for a board certification include that the ACGME expects its fellowships to develop a board exam at some point (although not all have). The 1,000 ACGME fellowship–trained micrographic surgeons deserve a chance to be board certified, which is the medical profession’s way to demonstrate competence to the public.
Having all Mohs surgeons board certified would heal a huge rift in the house of dermatology, and give us a united, consistent face to present to other specialties, the Congress, and the media. Physicians are judged by their training and credentials. Love them or hate them, the ACGME is the gold standard. Perhaps the greatest beneficiaries would be those practicing Mohs who did not complete a formal fellowship. I think a board exam is overdue, and will be a boon to all of dermatology.
Dr. Coldiron is a past president of the American Academy of Dermatology. He is currently in private practice, but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics.
The medical director was direct and blunt: “You’ve got a problem with two very different levels of training in Mohs surgery. This is a big problem for your specialty.”
The remarks came at a medical director summit that I was attending to speak on the value of dermatology. I was explaining to medical directors how including small dermatology practices in their plans would realize cost savings when treating skin cancer in the office setting. An awkward silence followed the medical director’s remarks. Then I uttered a lame “we may have a board certification someday.”
My interview with the New York Times reporter before the meeting quickly became adversarial. “What about these guys who do Mohs after a 3-day course?” I explained that there is more involved than just the 3-day course, that there is a preceptorship and case reviews. Plus, some of “those guys” wrote some of the best Mohs textbooks. The reporter wasn’t buying it, and the rest of the interview went downhill.
And the training issues surrounding Mohs surgery are playing out in practice. One dermatologist wrote me complaining that an insurer will no longer let him bill for Mohs because “he can’t document his residency training in Mohs and did not do a fellowship.” Another wrote me saying he can no longer teach Mohs surgery at the VA or the medical school “because he didn’t do a formal Mohs fellowship.”
The issue of who is qualified to perform Mohs surgery is coming to a head. There are more than 2,500 dermatologists billing Medicare for Mohs, and insurers are groaning at the expense. They are looking for any possible reason to exclude dermatologists from billing for Mohs surgery.
A possible solution is a board certification in Mohs surgery. Osteopathic dermatologists have had this option for 20 years. Unfortunately, allopathic dermatologists cannot sit for the osteopathic exam. A new certification exam for allopathic dermatologists who have successfully completed a dermatology residency accredited by the Accreditation Council for Graduate Medical Education (ACGME) seems worthy of a discussion.
Downsides of certification include the likely $1,000 or more cost of a test, the costs of preparing for the test, and the risk of failing a test. A new certification would give the Maintenance of Certification (MOC) haters another reason to complain, since about 600 lifetime certified, board-exempt dermatologists would be dragged back into MOC to maintain a Mohs surgery subspecialty certification. Some of the current fellowship-trained Mohs surgeons will not like being grouped with the nonfellowship-trained surgeons, whom they consider their inferiors and who will now have the opportunity to be board certified.
The name of the fellowship, which is “micrographic surgery and dermatologic oncology,” also has some paranoid types fearing that they will lose the right to treat skin cancer if such a subspecialty is created. That shouldn’t be an issue, since all dermatologists are trained in residency to treat skin cancer. The formal fellowships already exist. There are already 1,600 fellowship-trained Mohs surgeons out there, and they have not cornered the market on skin cancer. The situation should not change since general dermatologists remain the gatekeepers – and entry point – for most skin cancer patients. Certification exams in dermatopathology and pediatric dermatology have not had a negative impact on general dermatologists, who still read their own slides and see kids for skin disease. In fact, having dermatopathology as a certified part of dermatology has been a huge benefit in our struggle to maintain the right to read our own slides.
Developing a certification exam would take at least 2 years if the American Board of Dermatology decided to do it. There would be no “grandfathering” automatic certification. Everyone would have to take the same exam – young, old, formally trained, or not.
Members of the American Board of Dermatology explained the qualifiers to sit for an exam (if there was an exam) at a summit I held in Cincinnati in 2015. They are interested in including all ABD dermatologists who currently practice Mohs surgery, fellowship trained or not. Suggested parameters included any ABD fellow whose practice is 20% Mohs and reconstructive surgery (by volume or income), or anyone who performs Mohs once a week. Fellowship-trained micrographic surgeons could be eligible, and this would be a self-attestation! There would be no case log reviews, no visits by inspectors, no secret questions or passwords. This pathway would remain open for 5 years as were the exams for dermatopathology and pediatric dermatology. After that point, only ACGME fellowship–trained Mohs surgeons would be eligible to take the exam.
Upsides to this approach include decreasing divisiveness in the specialty, creating a better brand, and elevating the specialty. A board certification will help in obtaining a Medicare specialty designation, which will help stop the delisting of Mohs surgeons from insurance networks based on their average charges compared with general dermatologists. This action would particularly help small practices.
The American Academy of Dermatology board of directors sent this issue to the education committee to inform and poll the membership. You should expect to hear more about the proposed process. As an AAD member, you will get to express your opinion so make sure you are well informed. The AAD membership opinion will be important in whether or not the American Board of Dermatology decides to pursue this. Remember, this is an American Board of Dermatology decision, not an AAD decision.
More reasons for a board certification include that the ACGME expects its fellowships to develop a board exam at some point (although not all have). The 1,000 ACGME fellowship–trained micrographic surgeons deserve a chance to be board certified, which is the medical profession’s way to demonstrate competence to the public.
Having all Mohs surgeons board certified would heal a huge rift in the house of dermatology, and give us a united, consistent face to present to other specialties, the Congress, and the media. Physicians are judged by their training and credentials. Love them or hate them, the ACGME is the gold standard. Perhaps the greatest beneficiaries would be those practicing Mohs who did not complete a formal fellowship. I think a board exam is overdue, and will be a boon to all of dermatology.
Dr. Coldiron is a past president of the American Academy of Dermatology. He is currently in private practice, but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics.
VIDEO: MOC + Me: Maintenance of Certification in Hospital Medicine
Dr. Marianne Green and Dr. Jeffrey Wiese, two members of the ABIM Council, talk about ABIM's Maintenance of Certification process, and the importance of professional assessment. Dr. Green works on Internal Medicine MOC, Dr. Wiese was part of the team that developed the Focused Practice in Hospital Medicine MOC.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Marianne Green and Dr. Jeffrey Wiese, two members of the ABIM Council, talk about ABIM's Maintenance of Certification process, and the importance of professional assessment. Dr. Green works on Internal Medicine MOC, Dr. Wiese was part of the team that developed the Focused Practice in Hospital Medicine MOC.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Marianne Green and Dr. Jeffrey Wiese, two members of the ABIM Council, talk about ABIM's Maintenance of Certification process, and the importance of professional assessment. Dr. Green works on Internal Medicine MOC, Dr. Wiese was part of the team that developed the Focused Practice in Hospital Medicine MOC.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Spending on Complementary Health Care
Americans spend billions of dollars out-of-pocket on complementary health care, according to an analysis of data from the 2012 National Health Interview Survey conducted by the National Center for Complementary and Integrative Health (NCCIH) and the CDC.
Of the more than $30 billion spent by consumers, nearly $15 billion went to visits to chiropractors, acupuncturists, massage therapists, and other complementary practitioners—almost 30% of what Americans spent on out-of-pocket services by conventional physicians. The mean annual out-of-pocket expenditure for practitioner visits was $433. This analysis also included the first-ever data on spending for children: almost $2 billion.
Related: Complementary Therapp-y
Americans also spent billions on natural product supplements for an annual mean of $368 or about one-fourth of what they spent on prescription drugs.
Income level made little difference in expenditure. People with family incomes of < $25,000 averaged $314 for visits to complementary practitioners, vs $518 for those with incomes of more than $100,000.
The fact that so many people spent money on complementary approaches is “an indication that users believe enough in the value of these approaches to pay for them,” said Richard Nahin, PhD, lead author of the analysis and lead epidemiologist for National Center for Complementary and Integrative Health, which conducted the analysis.
Related: Complementary and Alternative Medicine for Chronic Musculoskeletal Pain
It’s also the reason that it’s “extremely important for us to provide the public with evidence-based information to help inform decisions,” said Josephine Briggs, MD, director of NCCIH. “This underscores the importance of conducting rigorous research to know whether the products and practices being used are safe and effective.”
Americans spend billions of dollars out-of-pocket on complementary health care, according to an analysis of data from the 2012 National Health Interview Survey conducted by the National Center for Complementary and Integrative Health (NCCIH) and the CDC.
Of the more than $30 billion spent by consumers, nearly $15 billion went to visits to chiropractors, acupuncturists, massage therapists, and other complementary practitioners—almost 30% of what Americans spent on out-of-pocket services by conventional physicians. The mean annual out-of-pocket expenditure for practitioner visits was $433. This analysis also included the first-ever data on spending for children: almost $2 billion.
Related: Complementary Therapp-y
Americans also spent billions on natural product supplements for an annual mean of $368 or about one-fourth of what they spent on prescription drugs.
Income level made little difference in expenditure. People with family incomes of < $25,000 averaged $314 for visits to complementary practitioners, vs $518 for those with incomes of more than $100,000.
The fact that so many people spent money on complementary approaches is “an indication that users believe enough in the value of these approaches to pay for them,” said Richard Nahin, PhD, lead author of the analysis and lead epidemiologist for National Center for Complementary and Integrative Health, which conducted the analysis.
Related: Complementary and Alternative Medicine for Chronic Musculoskeletal Pain
It’s also the reason that it’s “extremely important for us to provide the public with evidence-based information to help inform decisions,” said Josephine Briggs, MD, director of NCCIH. “This underscores the importance of conducting rigorous research to know whether the products and practices being used are safe and effective.”
Americans spend billions of dollars out-of-pocket on complementary health care, according to an analysis of data from the 2012 National Health Interview Survey conducted by the National Center for Complementary and Integrative Health (NCCIH) and the CDC.
Of the more than $30 billion spent by consumers, nearly $15 billion went to visits to chiropractors, acupuncturists, massage therapists, and other complementary practitioners—almost 30% of what Americans spent on out-of-pocket services by conventional physicians. The mean annual out-of-pocket expenditure for practitioner visits was $433. This analysis also included the first-ever data on spending for children: almost $2 billion.
Related: Complementary Therapp-y
Americans also spent billions on natural product supplements for an annual mean of $368 or about one-fourth of what they spent on prescription drugs.
Income level made little difference in expenditure. People with family incomes of < $25,000 averaged $314 for visits to complementary practitioners, vs $518 for those with incomes of more than $100,000.
The fact that so many people spent money on complementary approaches is “an indication that users believe enough in the value of these approaches to pay for them,” said Richard Nahin, PhD, lead author of the analysis and lead epidemiologist for National Center for Complementary and Integrative Health, which conducted the analysis.
Related: Complementary and Alternative Medicine for Chronic Musculoskeletal Pain
It’s also the reason that it’s “extremely important for us to provide the public with evidence-based information to help inform decisions,” said Josephine Briggs, MD, director of NCCIH. “This underscores the importance of conducting rigorous research to know whether the products and practices being used are safe and effective.”
MRD status should be endpoint in MM trials, team says

Photo courtesy of the
Dana-Farber Cancer Institute
Patients with newly diagnosed multiple myeloma (MM) have better survival outcomes if they are minimal residual disease (MRD)-negative after treatment, according to research published in JAMA Oncology.
MRD negativity was significantly associated with better progression-free survival (PFS) and overall survival (OS).
Researchers therefore concluded that MRD status after treatment should be considered as an endpoint in clinical trials of MM.
Nikhil C. Munshi, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues conducted this study.
The team evaluated the prognostic value of MRD in patients with MM by performing a meta-analysis of 21 studies published between January 1990 and January 2016.
The impact of MRD on PFS was assessed in 14 of the studies (n=1273), and the impact of MRD on OS was assessed in 12 studies (n=1100).
Five of the PFS studies (n=574) had results reported specifically in patients with a complete response (CR), as did 6 of the OS studies (n=616).
Dr Munchi and his colleagues found that MRD negativity was associated with significantly better PFS—both overall and in studies looking specifically at patients with CRs. The hazard ratios were 0.41 (95% CI, 0.36-0.48) and 0.44 (95% CI, 0.34-0.56), respectively (P<0.001 for both).
Likewise, MRD negativity was associated with significantly better OS—both overall and in studies looking at patients with CRs. The hazard ratios were 0.57 (95% CI, 0.46-0.71) and 0.47 (95% CI, 0.33-0.67), respectively (P<0.001 for both).
The researchers said there were no significant differences among the studies for PFS and OS.
The team therefore concluded that this study provides quantitative evidence to support the integration of MRD assessment as an endpoint in trials of MM patients. ![]()

Photo courtesy of the
Dana-Farber Cancer Institute
Patients with newly diagnosed multiple myeloma (MM) have better survival outcomes if they are minimal residual disease (MRD)-negative after treatment, according to research published in JAMA Oncology.
MRD negativity was significantly associated with better progression-free survival (PFS) and overall survival (OS).
Researchers therefore concluded that MRD status after treatment should be considered as an endpoint in clinical trials of MM.
Nikhil C. Munshi, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues conducted this study.
The team evaluated the prognostic value of MRD in patients with MM by performing a meta-analysis of 21 studies published between January 1990 and January 2016.
The impact of MRD on PFS was assessed in 14 of the studies (n=1273), and the impact of MRD on OS was assessed in 12 studies (n=1100).
Five of the PFS studies (n=574) had results reported specifically in patients with a complete response (CR), as did 6 of the OS studies (n=616).
Dr Munchi and his colleagues found that MRD negativity was associated with significantly better PFS—both overall and in studies looking specifically at patients with CRs. The hazard ratios were 0.41 (95% CI, 0.36-0.48) and 0.44 (95% CI, 0.34-0.56), respectively (P<0.001 for both).
Likewise, MRD negativity was associated with significantly better OS—both overall and in studies looking at patients with CRs. The hazard ratios were 0.57 (95% CI, 0.46-0.71) and 0.47 (95% CI, 0.33-0.67), respectively (P<0.001 for both).
The researchers said there were no significant differences among the studies for PFS and OS.
The team therefore concluded that this study provides quantitative evidence to support the integration of MRD assessment as an endpoint in trials of MM patients. ![]()

Photo courtesy of the
Dana-Farber Cancer Institute
Patients with newly diagnosed multiple myeloma (MM) have better survival outcomes if they are minimal residual disease (MRD)-negative after treatment, according to research published in JAMA Oncology.
MRD negativity was significantly associated with better progression-free survival (PFS) and overall survival (OS).
Researchers therefore concluded that MRD status after treatment should be considered as an endpoint in clinical trials of MM.
Nikhil C. Munshi, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues conducted this study.
The team evaluated the prognostic value of MRD in patients with MM by performing a meta-analysis of 21 studies published between January 1990 and January 2016.
The impact of MRD on PFS was assessed in 14 of the studies (n=1273), and the impact of MRD on OS was assessed in 12 studies (n=1100).
Five of the PFS studies (n=574) had results reported specifically in patients with a complete response (CR), as did 6 of the OS studies (n=616).
Dr Munchi and his colleagues found that MRD negativity was associated with significantly better PFS—both overall and in studies looking specifically at patients with CRs. The hazard ratios were 0.41 (95% CI, 0.36-0.48) and 0.44 (95% CI, 0.34-0.56), respectively (P<0.001 for both).
Likewise, MRD negativity was associated with significantly better OS—both overall and in studies looking at patients with CRs. The hazard ratios were 0.57 (95% CI, 0.46-0.71) and 0.47 (95% CI, 0.33-0.67), respectively (P<0.001 for both).
The researchers said there were no significant differences among the studies for PFS and OS.
The team therefore concluded that this study provides quantitative evidence to support the integration of MRD assessment as an endpoint in trials of MM patients. ![]()
EZH2 inhibitors could improve treatment of CML, studies suggest

Image by Difu Wu
Two preclinical studies published in Cancer Discovery suggest that EZH2 inhibitors might enhance the efficacy of treatment with tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML).
One study showed that CML leukemic stem cells (LSCs) are dependent upon EZH2.
The other study revealed that epigenetic reprogramming sensitizes CML LSCs to combined treatment with an EZH2 inhibitor and a TKI.
EZH2 dependence
In the first study, in vitro experiments revealed that LSCs have an overabundance of EZH2. In fact, the researchers found that EZH2 helps LSCs survive and give rise to full-fledged CML cells.
Experiments in mice showed that inactivating EZH2 through gene-editing techniques caused LSCs to die, halting CML at its source.
“The stem cells’ dependence on EZH2 suggests they will be especially vulnerable to drugs that target the protein,” said study author Stuart Orkin, MD, of Boston Children’s Hospital in Massachusetts.
“Our findings suggest inhibition of EZH2 should be considered as a way to eradicate CML when used in combination with current targeted therapies. It offers a promising approach to shortening the duration of therapy in order to achieve a cure. If successful, the cost savings of such an approach could also be significant.”
Combination treatment
The second study supports the idea that combining EZH2 inhibitors and TKIs could benefit patients with CML.
Mary T. Scott, of the University of Glasgow in the UK, and her colleagues found that EZH2 and H3K27me3 reprogramming is important for LSC survival and renders the cells sensitive to combined treatment with an EZH2 inhibitor and a TKI.
The researchers treated CML CD34+ cells, normal CD34+ cells, and LSCs with the EZH2 inhibitor GSK343 and the TKI dasatinib, both alone and in combination. The team said that GSK343 selectively targeted the loss of H3K27me3 in the presence of dasatinib.
In addition, combination treatment led to a significant reduction in cell viability (even in “TKI-persistent” cells), an increase in apoptosis, and a reduction in colony-forming cell and granulocyte/erythroid/macrophage/megakaryocyte outputs, when compared to dasatinib alone.
The researchers also evaluated a TKI and an EZH2 inhibitor in a mouse model of CML. The mice received nilotinib and EPZ-6438, both alone and in combination, for either 14 days or 25 days.
After 14 days of treatment, mice that received the combination had significant reductions in levels of leukemic (Ph+) human CD45+ cells, CD45+CD34+ progenitor cells, and primitive CD45+CD34+CD38− stem cells in the bone marrow, when compared to mice that received nilotinib alone.
After 25 days of treatment, mice that received the combination had near-complete elimination of CD45+CD34+ progenitor cells and a greater than 70% reduction of CD45+CD34+CD38− cells, when compared to mice that received nilotinib alone.
The researchers said these results demonstrate a clear rationale for combining TKI treatment with an EZH2 inhibitor, as an EZH2 inhibitor can target primitive CML cells not eradicated by a TKI alone. ![]()

Image by Difu Wu
Two preclinical studies published in Cancer Discovery suggest that EZH2 inhibitors might enhance the efficacy of treatment with tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML).
One study showed that CML leukemic stem cells (LSCs) are dependent upon EZH2.
The other study revealed that epigenetic reprogramming sensitizes CML LSCs to combined treatment with an EZH2 inhibitor and a TKI.
EZH2 dependence
In the first study, in vitro experiments revealed that LSCs have an overabundance of EZH2. In fact, the researchers found that EZH2 helps LSCs survive and give rise to full-fledged CML cells.
Experiments in mice showed that inactivating EZH2 through gene-editing techniques caused LSCs to die, halting CML at its source.
“The stem cells’ dependence on EZH2 suggests they will be especially vulnerable to drugs that target the protein,” said study author Stuart Orkin, MD, of Boston Children’s Hospital in Massachusetts.
“Our findings suggest inhibition of EZH2 should be considered as a way to eradicate CML when used in combination with current targeted therapies. It offers a promising approach to shortening the duration of therapy in order to achieve a cure. If successful, the cost savings of such an approach could also be significant.”
Combination treatment
The second study supports the idea that combining EZH2 inhibitors and TKIs could benefit patients with CML.
Mary T. Scott, of the University of Glasgow in the UK, and her colleagues found that EZH2 and H3K27me3 reprogramming is important for LSC survival and renders the cells sensitive to combined treatment with an EZH2 inhibitor and a TKI.
The researchers treated CML CD34+ cells, normal CD34+ cells, and LSCs with the EZH2 inhibitor GSK343 and the TKI dasatinib, both alone and in combination. The team said that GSK343 selectively targeted the loss of H3K27me3 in the presence of dasatinib.
In addition, combination treatment led to a significant reduction in cell viability (even in “TKI-persistent” cells), an increase in apoptosis, and a reduction in colony-forming cell and granulocyte/erythroid/macrophage/megakaryocyte outputs, when compared to dasatinib alone.
The researchers also evaluated a TKI and an EZH2 inhibitor in a mouse model of CML. The mice received nilotinib and EPZ-6438, both alone and in combination, for either 14 days or 25 days.
After 14 days of treatment, mice that received the combination had significant reductions in levels of leukemic (Ph+) human CD45+ cells, CD45+CD34+ progenitor cells, and primitive CD45+CD34+CD38− stem cells in the bone marrow, when compared to mice that received nilotinib alone.
After 25 days of treatment, mice that received the combination had near-complete elimination of CD45+CD34+ progenitor cells and a greater than 70% reduction of CD45+CD34+CD38− cells, when compared to mice that received nilotinib alone.
The researchers said these results demonstrate a clear rationale for combining TKI treatment with an EZH2 inhibitor, as an EZH2 inhibitor can target primitive CML cells not eradicated by a TKI alone. ![]()

Image by Difu Wu
Two preclinical studies published in Cancer Discovery suggest that EZH2 inhibitors might enhance the efficacy of treatment with tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML).
One study showed that CML leukemic stem cells (LSCs) are dependent upon EZH2.
The other study revealed that epigenetic reprogramming sensitizes CML LSCs to combined treatment with an EZH2 inhibitor and a TKI.
EZH2 dependence
In the first study, in vitro experiments revealed that LSCs have an overabundance of EZH2. In fact, the researchers found that EZH2 helps LSCs survive and give rise to full-fledged CML cells.
Experiments in mice showed that inactivating EZH2 through gene-editing techniques caused LSCs to die, halting CML at its source.
“The stem cells’ dependence on EZH2 suggests they will be especially vulnerable to drugs that target the protein,” said study author Stuart Orkin, MD, of Boston Children’s Hospital in Massachusetts.
“Our findings suggest inhibition of EZH2 should be considered as a way to eradicate CML when used in combination with current targeted therapies. It offers a promising approach to shortening the duration of therapy in order to achieve a cure. If successful, the cost savings of such an approach could also be significant.”
Combination treatment
The second study supports the idea that combining EZH2 inhibitors and TKIs could benefit patients with CML.
Mary T. Scott, of the University of Glasgow in the UK, and her colleagues found that EZH2 and H3K27me3 reprogramming is important for LSC survival and renders the cells sensitive to combined treatment with an EZH2 inhibitor and a TKI.
The researchers treated CML CD34+ cells, normal CD34+ cells, and LSCs with the EZH2 inhibitor GSK343 and the TKI dasatinib, both alone and in combination. The team said that GSK343 selectively targeted the loss of H3K27me3 in the presence of dasatinib.
In addition, combination treatment led to a significant reduction in cell viability (even in “TKI-persistent” cells), an increase in apoptosis, and a reduction in colony-forming cell and granulocyte/erythroid/macrophage/megakaryocyte outputs, when compared to dasatinib alone.
The researchers also evaluated a TKI and an EZH2 inhibitor in a mouse model of CML. The mice received nilotinib and EPZ-6438, both alone and in combination, for either 14 days or 25 days.
After 14 days of treatment, mice that received the combination had significant reductions in levels of leukemic (Ph+) human CD45+ cells, CD45+CD34+ progenitor cells, and primitive CD45+CD34+CD38− stem cells in the bone marrow, when compared to mice that received nilotinib alone.
After 25 days of treatment, mice that received the combination had near-complete elimination of CD45+CD34+ progenitor cells and a greater than 70% reduction of CD45+CD34+CD38− cells, when compared to mice that received nilotinib alone.
The researchers said these results demonstrate a clear rationale for combining TKI treatment with an EZH2 inhibitor, as an EZH2 inhibitor can target primitive CML cells not eradicated by a TKI alone. ![]()
Smartphone app measures hemoglobin

Photo by Daniel Sone
HEIDELBERG, GERMANY—Scientists have developed a smartphone application called HemaApp that can be used to measure hemoglobin levels and screen for anemia non-invasively.
HemaApp uses illumination sources from a smartphone, in combination with other light sources, and algorithms that analyze the color of a patient’s blood to estimate hemoglobin levels.
In a trial of 31 patients, HemaApp’s results compared favorably to an approved medical device that measures hemoglobin non-invasively.
Researchers described HemaApp in a paper presented at the Association for Computing Machinery’s 2016 International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp 2016).
“In developing countries, community health workers have so much specialized equipment to monitor different conditions that they literally have whole bags full of devices,” said study author Edward Wang, a doctoral student at the University of Washington in Seattle.
“We are trying to make these screening tools work on one ubiquitous platform—a smartphone.”
How the app works
By shining light from the phone’s camera flash through the patient’s finger, HemaApp analyzes the color of the patient’s blood to estimate hemoglobin concentrations.
HemaApp bombards the finger with different wavelengths of light and infrared energy and creates a series of videos. By analyzing how colors are absorbed and reflected across those wavelengths, it can detect concentrations of hemoglobin and other blood components like plasma.
To ensure that the app works on different skin tones and body masses, the researchers developed processing algorithms that use the patient’s pulse to distinguish between the properties of the patient’s blood and the physical characteristics of his or her finger.
Testing
The researchers tested HemaApp on 31 subjects, including healthy students and staff at the University of Washington, inpatients at a children’s cancer and transfusion clinic, and inpatients at an adult cancer and bone marrow transplant clinic.
The subjects ranged in age from 6 to 77. Their hemoglobin levels ranged from 8 to 16 g/dL, and they had skin tones ranging from pale to dark.
The researchers compared results with HemaApp to results obtained via a complete blood count (CBC) and via the Masimo Pronto 7, a device that non-invasively measures hemoglobin by clipping a sensor onto a person’s finger.
The team tested HemaApp under 3 different scenarios—using the smartphone camera’s flash alone, in combination with a common incandescent lightbulb, and with a low-cost LED lighting attachment.
The additional illumination sources tap into other parts of the electromagnetic spectrum that have useful absorption properties but that aren’t currently found on all smartphone cameras.
“New phones are beginning to have more advanced infrared and multi-color LED capabilities,” said study author Shwetak Patel, PhD, of the University of Washington.
“But what we found is that even if your phone doesn’t have all that, you can put your finger near an external light source like a common lightbulb and boost the accuracy rates.”
Results
HemaApp’s hemoglobin measurements using a smartphone camera alone had a 69% correlation to results with the CBC. The app had a 74% correlation with the CBC when used with an incandescent light bulb and an 82% correlation when used with the LED lights.
In comparison, the Masimo Pronto 7’s measurements had an 81% correlation to the CBC.
When used to screen for anemia, HemaApp had higher sensitivity than the Masimo Pronto but lower specificity.
The app’s sensitivity was 79% using just the phone camera and 86% when used with the incandescent light bulb or LED lights, whereas Masimo Pronto’s sensitivity was 69%.
The app’s specificity was 71% when using just the phone or the incandescent light bulb and 77% with the LED lights, whereas Masimo Pronto’s specificity was 88%.
Next steps
The researchers said HemaApp is not intended to replace blood tests, which remain the most accurate way to measure hemoglobin. But the early test results suggest HemaApp can be an effective and affordable initial screening tool to determine whether further blood testing is warranted.
“Anemia is one of the most common problems affecting adults and children worldwide,” said study author Doug Hawkins, MD, of Seattle Children’s Hospital.
“The ability to screen quickly with a smartphone-based test could be a huge improvement to delivering care in limited-resource environments.”
Next research steps include wider national and international testing of HemaApp, collecting more data to improve accuracy rates, and using smartphones to try to detect abnormal hemoglobin properties that could help screen for sickle cell disease and other blood disorders.
“We’re just starting to scratch the surface here,” Dr Patel said. “There’s a lot that we want to tackle in using phones for non-invasively screening disease.” ![]()

Photo by Daniel Sone
HEIDELBERG, GERMANY—Scientists have developed a smartphone application called HemaApp that can be used to measure hemoglobin levels and screen for anemia non-invasively.
HemaApp uses illumination sources from a smartphone, in combination with other light sources, and algorithms that analyze the color of a patient’s blood to estimate hemoglobin levels.
In a trial of 31 patients, HemaApp’s results compared favorably to an approved medical device that measures hemoglobin non-invasively.
Researchers described HemaApp in a paper presented at the Association for Computing Machinery’s 2016 International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp 2016).
“In developing countries, community health workers have so much specialized equipment to monitor different conditions that they literally have whole bags full of devices,” said study author Edward Wang, a doctoral student at the University of Washington in Seattle.
“We are trying to make these screening tools work on one ubiquitous platform—a smartphone.”
How the app works
By shining light from the phone’s camera flash through the patient’s finger, HemaApp analyzes the color of the patient’s blood to estimate hemoglobin concentrations.
HemaApp bombards the finger with different wavelengths of light and infrared energy and creates a series of videos. By analyzing how colors are absorbed and reflected across those wavelengths, it can detect concentrations of hemoglobin and other blood components like plasma.
To ensure that the app works on different skin tones and body masses, the researchers developed processing algorithms that use the patient’s pulse to distinguish between the properties of the patient’s blood and the physical characteristics of his or her finger.
Testing
The researchers tested HemaApp on 31 subjects, including healthy students and staff at the University of Washington, inpatients at a children’s cancer and transfusion clinic, and inpatients at an adult cancer and bone marrow transplant clinic.
The subjects ranged in age from 6 to 77. Their hemoglobin levels ranged from 8 to 16 g/dL, and they had skin tones ranging from pale to dark.
The researchers compared results with HemaApp to results obtained via a complete blood count (CBC) and via the Masimo Pronto 7, a device that non-invasively measures hemoglobin by clipping a sensor onto a person’s finger.
The team tested HemaApp under 3 different scenarios—using the smartphone camera’s flash alone, in combination with a common incandescent lightbulb, and with a low-cost LED lighting attachment.
The additional illumination sources tap into other parts of the electromagnetic spectrum that have useful absorption properties but that aren’t currently found on all smartphone cameras.
“New phones are beginning to have more advanced infrared and multi-color LED capabilities,” said study author Shwetak Patel, PhD, of the University of Washington.
“But what we found is that even if your phone doesn’t have all that, you can put your finger near an external light source like a common lightbulb and boost the accuracy rates.”
Results
HemaApp’s hemoglobin measurements using a smartphone camera alone had a 69% correlation to results with the CBC. The app had a 74% correlation with the CBC when used with an incandescent light bulb and an 82% correlation when used with the LED lights.
In comparison, the Masimo Pronto 7’s measurements had an 81% correlation to the CBC.
When used to screen for anemia, HemaApp had higher sensitivity than the Masimo Pronto but lower specificity.
The app’s sensitivity was 79% using just the phone camera and 86% when used with the incandescent light bulb or LED lights, whereas Masimo Pronto’s sensitivity was 69%.
The app’s specificity was 71% when using just the phone or the incandescent light bulb and 77% with the LED lights, whereas Masimo Pronto’s specificity was 88%.
Next steps
The researchers said HemaApp is not intended to replace blood tests, which remain the most accurate way to measure hemoglobin. But the early test results suggest HemaApp can be an effective and affordable initial screening tool to determine whether further blood testing is warranted.
“Anemia is one of the most common problems affecting adults and children worldwide,” said study author Doug Hawkins, MD, of Seattle Children’s Hospital.
“The ability to screen quickly with a smartphone-based test could be a huge improvement to delivering care in limited-resource environments.”
Next research steps include wider national and international testing of HemaApp, collecting more data to improve accuracy rates, and using smartphones to try to detect abnormal hemoglobin properties that could help screen for sickle cell disease and other blood disorders.
“We’re just starting to scratch the surface here,” Dr Patel said. “There’s a lot that we want to tackle in using phones for non-invasively screening disease.” ![]()

Photo by Daniel Sone
HEIDELBERG, GERMANY—Scientists have developed a smartphone application called HemaApp that can be used to measure hemoglobin levels and screen for anemia non-invasively.
HemaApp uses illumination sources from a smartphone, in combination with other light sources, and algorithms that analyze the color of a patient’s blood to estimate hemoglobin levels.
In a trial of 31 patients, HemaApp’s results compared favorably to an approved medical device that measures hemoglobin non-invasively.
Researchers described HemaApp in a paper presented at the Association for Computing Machinery’s 2016 International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp 2016).
“In developing countries, community health workers have so much specialized equipment to monitor different conditions that they literally have whole bags full of devices,” said study author Edward Wang, a doctoral student at the University of Washington in Seattle.
“We are trying to make these screening tools work on one ubiquitous platform—a smartphone.”
How the app works
By shining light from the phone’s camera flash through the patient’s finger, HemaApp analyzes the color of the patient’s blood to estimate hemoglobin concentrations.
HemaApp bombards the finger with different wavelengths of light and infrared energy and creates a series of videos. By analyzing how colors are absorbed and reflected across those wavelengths, it can detect concentrations of hemoglobin and other blood components like plasma.
To ensure that the app works on different skin tones and body masses, the researchers developed processing algorithms that use the patient’s pulse to distinguish between the properties of the patient’s blood and the physical characteristics of his or her finger.
Testing
The researchers tested HemaApp on 31 subjects, including healthy students and staff at the University of Washington, inpatients at a children’s cancer and transfusion clinic, and inpatients at an adult cancer and bone marrow transplant clinic.
The subjects ranged in age from 6 to 77. Their hemoglobin levels ranged from 8 to 16 g/dL, and they had skin tones ranging from pale to dark.
The researchers compared results with HemaApp to results obtained via a complete blood count (CBC) and via the Masimo Pronto 7, a device that non-invasively measures hemoglobin by clipping a sensor onto a person’s finger.
The team tested HemaApp under 3 different scenarios—using the smartphone camera’s flash alone, in combination with a common incandescent lightbulb, and with a low-cost LED lighting attachment.
The additional illumination sources tap into other parts of the electromagnetic spectrum that have useful absorption properties but that aren’t currently found on all smartphone cameras.
“New phones are beginning to have more advanced infrared and multi-color LED capabilities,” said study author Shwetak Patel, PhD, of the University of Washington.
“But what we found is that even if your phone doesn’t have all that, you can put your finger near an external light source like a common lightbulb and boost the accuracy rates.”
Results
HemaApp’s hemoglobin measurements using a smartphone camera alone had a 69% correlation to results with the CBC. The app had a 74% correlation with the CBC when used with an incandescent light bulb and an 82% correlation when used with the LED lights.
In comparison, the Masimo Pronto 7’s measurements had an 81% correlation to the CBC.
When used to screen for anemia, HemaApp had higher sensitivity than the Masimo Pronto but lower specificity.
The app’s sensitivity was 79% using just the phone camera and 86% when used with the incandescent light bulb or LED lights, whereas Masimo Pronto’s sensitivity was 69%.
The app’s specificity was 71% when using just the phone or the incandescent light bulb and 77% with the LED lights, whereas Masimo Pronto’s specificity was 88%.
Next steps
The researchers said HemaApp is not intended to replace blood tests, which remain the most accurate way to measure hemoglobin. But the early test results suggest HemaApp can be an effective and affordable initial screening tool to determine whether further blood testing is warranted.
“Anemia is one of the most common problems affecting adults and children worldwide,” said study author Doug Hawkins, MD, of Seattle Children’s Hospital.
“The ability to screen quickly with a smartphone-based test could be a huge improvement to delivering care in limited-resource environments.”
Next research steps include wider national and international testing of HemaApp, collecting more data to improve accuracy rates, and using smartphones to try to detect abnormal hemoglobin properties that could help screen for sickle cell disease and other blood disorders.
“We’re just starting to scratch the surface here,” Dr Patel said. “There’s a lot that we want to tackle in using phones for non-invasively screening disease.” ![]()






