User login
Keeping Pain A Priority
Before pain was introduced as the “fifth vital sign” and the Joint Commission issued its standards, more than a decade’s worth of international research indicated that pain was largely ignored, untreated, or undertreated. The best tools available to treat pain (opioids) were reserved for patients on their deathbed. The horrific results of the SUPPORT study at the nation’s leading hospitals revealed that most patients had severe, uncontrolled pain up until their final days of life.1 Unfortunately, research suggests we are still reserving opioids for the last days or weeks of life.2
In 1992 and 1994, the Department of Health and Human Services issued clinical practice guidelines highlighting the huge gap between the availability of evidence-based pain control methods and the lack of pain assessment and treatment in practice.3 When these guidelines failed to change practice, the Joint Commission added “attending to pain” to its standards—the first effort to require that evidence-based practices be utilized. Twenty years later, the National Academy of Science issued a report stating that, despite transient improvements, the current state is inadequate since pain is the leading reason people seek health care. Patients with pain report an inability to get help, which is “viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”4 Since I started working as an NP in 1983, I have never seen as many patients with pain stigmatized, ignored, labeled, and denied access to treatment as I have in the past year.
Pain afflicts more than 100 million Americans and is the leading cause of disability worldwide.5 Acute pain that is not effectively treated progresses to chronic pain in 51% of cases.6 An estimated 23 million Americans report frequent intense pain, 25 million endure daily chronic pain, and 40 million adults have high-impact, disabling, chronic pain that degrades health and requires health care intervention.6,7 The most notable damage is to the structure and function of the central nervous system.8 Brain remodeling and loss of gray matter occurs, producing changes in the brain similar to those observed with 10 to 20 years of aging; this explains why some of the learning, memory, and emotional difficulties endured by many with ongoing pain can be partially reversed with effective treatment.9 Left untreated, pain can result in significant biopsychosocial problems, frailty, financial ruin, and premature death.10-14
Prescription drug misuse and addiction also affect millions and have been a largely ignored public health problem for decades. Trying to fix the pain problem without attending equally to the problems of nonmedical drug use, addiction, and overdose deaths has contributed to the escalation of health problems to “epidemic” and “crisis” proportions. Although most patients who are prescribed medically indicated opioids for pain do not misuse their medications or become addicted, the failure to subsequently identify and properly treat an emergent substance use disorder is a problem in our current system.15 Unfortunately, making prescription opioids inaccessible to patients forces some to abuse alcohol or seek drugs from illicit sources, which only exacerbates the situation.16 A national study performed over a five-year period revealed that only 10% of patients admitted for prescription opioid treatment were referred from their health care providers.17 So, health care providers may have been part of the problem but have not been fully engaged in the solution.
Although opioids are neither the firstline, nor only, treatment option in our current evidence-based treatment toolbox, their prudent use does not cause addiction. Only 1% of patients who receive postoperative opioids go on to develop chronic opioid use, and adolescents treated with medically necessary opioids have no greater risk for future addiction than unexposed children. It is the nonmedical use of opioids, rather than proper medical use, that predisposes people to addiction.18,19 Discharging or not treating patients suspected of “drug-seeking” exacerbates the problem. Rates of opioid prescription have declined, while overdoses of illicitly manufactured fentanyl increased by 79% in 27 states from 2013 to 2014.20 In Massachusetts, only 8% of people who fatally overdosed had a prescription, while illicit fentanyl accounted for 54% of overdose deaths in 2015 and more than 74% in the third quarter of 2016.21 We need to screen for nonmedical use, drug misuse, and addiction before, during, and after we treat with this particular tool.
Unfortunately, the prevalence of pain and addiction are both increasing, especially for women and minorities—but there are safe, effective medications and non-drug approaches available to combat this.22-24 These problems will not go away on their own, and every health care professional must choose to be part of the solution rather than perpetuate the problem. A good place to start is to become familiar with the Surgeon General’s Report and the National Pain Strategy. Educate your patients, colleagues, and policy makers about the true nature of these problems. Take a public health approach to primary, secondary, and tertiary prevention by recognizing and treating these conditions in an expedient and effective matter. When problems persist, expand the treatment team to include specialists who can develop a patient-centered, multimodal treatment plan that treats co-occurring conditions. If we continue to ignore these problems, or focus on one at the expense of the other, both problems will worsen and our patients will suffer serious consequences.
Paul Arnstein, PhD, NP-C, FAAN, FNP-C
Boston, MA
1. Lynn J, Teno JM, Phillips RS, et al; SUPPORT Investigators. Perceptions by family members of the dying experience of older and seriously ill patients. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106.
2. Ziegler L, Mulvey M, Blenkinsopp A, et al. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain. 2016;157(11):2445-2451.
3. Agency for Health Care Policy and Research [AHCPR]. Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1992.
4. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press; 2011.
5. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602.
6. Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157(10):2158-2159.
7. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769-780.
8. Pozek JP, Beausang D, Baratta JL, Viscusi ER. The acute to chronic pain transition: can chronic pain be prevented? Med Clin North Am. 2016;100(1):17-30.
9. Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011; 31(20):7540-7550.
10. Wade KF, Lee DM, McBeth J, et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing. 2016;45(2):268-274.
11. Torrance N, Elliott A, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380-386.
12. Tang NK, Beckwith P, Ashworth P. Mental defeat is associated with suicide intent in patients with chronic pain. Clin J Pain. 2016;32(5):411-419.
13. Schaefer C, Sadosky A, Mann R, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483-496.
14. Schofield D, Kelly S, Shrestha R, et al. The impact of back problems on retirement wealth. Pain. 2012;153(1):203-210.
15. Chou R, Deyo R, Devine B, et al. The effectiveness and risks of long-term opioid treatment of chronic pain. AHRQ Report No. 218. Agency for Healthcare Research and Quality; September 2014. www.effectivehealthcare.ahrq.gov/ehc/products/557/1988/chronic-pain-opioid-treat ment-executive-141022.pdf. Accessed December 2, 2016.
16. Alford DP, German JS, Samet JH, et al. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
17. St. Marie BJ, Sahker E, Arndt S. Referrals and treatment completion for prescription opioid admissions: five years of national data. J Subst Abus Treat. 2015;59:109-114.
18. Sun EC, Darnall B, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9):1286-1293.
19. McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder (SUD) symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2171-2178.
20. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
21. Massachusetts Department of Public Health. Data Brief: Opioid-related Overdose Deaths Among Massachusetts Residents. www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/data-brief-overdose-deaths-may-2016.pdf. Accessed December 2, 2016.
22. Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
23. US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Executive Summary. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/executive-summary.pdf. Accessed December 2, 2016.
24. Herndon CM, Arnstein P, Darnall B, et al. Principles of Analgesic Use. 7th ed. Chicago, IL: American Pain Society Press; 2016.
Before pain was introduced as the “fifth vital sign” and the Joint Commission issued its standards, more than a decade’s worth of international research indicated that pain was largely ignored, untreated, or undertreated. The best tools available to treat pain (opioids) were reserved for patients on their deathbed. The horrific results of the SUPPORT study at the nation’s leading hospitals revealed that most patients had severe, uncontrolled pain up until their final days of life.1 Unfortunately, research suggests we are still reserving opioids for the last days or weeks of life.2
In 1992 and 1994, the Department of Health and Human Services issued clinical practice guidelines highlighting the huge gap between the availability of evidence-based pain control methods and the lack of pain assessment and treatment in practice.3 When these guidelines failed to change practice, the Joint Commission added “attending to pain” to its standards—the first effort to require that evidence-based practices be utilized. Twenty years later, the National Academy of Science issued a report stating that, despite transient improvements, the current state is inadequate since pain is the leading reason people seek health care. Patients with pain report an inability to get help, which is “viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”4 Since I started working as an NP in 1983, I have never seen as many patients with pain stigmatized, ignored, labeled, and denied access to treatment as I have in the past year.
Pain afflicts more than 100 million Americans and is the leading cause of disability worldwide.5 Acute pain that is not effectively treated progresses to chronic pain in 51% of cases.6 An estimated 23 million Americans report frequent intense pain, 25 million endure daily chronic pain, and 40 million adults have high-impact, disabling, chronic pain that degrades health and requires health care intervention.6,7 The most notable damage is to the structure and function of the central nervous system.8 Brain remodeling and loss of gray matter occurs, producing changes in the brain similar to those observed with 10 to 20 years of aging; this explains why some of the learning, memory, and emotional difficulties endured by many with ongoing pain can be partially reversed with effective treatment.9 Left untreated, pain can result in significant biopsychosocial problems, frailty, financial ruin, and premature death.10-14
Prescription drug misuse and addiction also affect millions and have been a largely ignored public health problem for decades. Trying to fix the pain problem without attending equally to the problems of nonmedical drug use, addiction, and overdose deaths has contributed to the escalation of health problems to “epidemic” and “crisis” proportions. Although most patients who are prescribed medically indicated opioids for pain do not misuse their medications or become addicted, the failure to subsequently identify and properly treat an emergent substance use disorder is a problem in our current system.15 Unfortunately, making prescription opioids inaccessible to patients forces some to abuse alcohol or seek drugs from illicit sources, which only exacerbates the situation.16 A national study performed over a five-year period revealed that only 10% of patients admitted for prescription opioid treatment were referred from their health care providers.17 So, health care providers may have been part of the problem but have not been fully engaged in the solution.
Although opioids are neither the firstline, nor only, treatment option in our current evidence-based treatment toolbox, their prudent use does not cause addiction. Only 1% of patients who receive postoperative opioids go on to develop chronic opioid use, and adolescents treated with medically necessary opioids have no greater risk for future addiction than unexposed children. It is the nonmedical use of opioids, rather than proper medical use, that predisposes people to addiction.18,19 Discharging or not treating patients suspected of “drug-seeking” exacerbates the problem. Rates of opioid prescription have declined, while overdoses of illicitly manufactured fentanyl increased by 79% in 27 states from 2013 to 2014.20 In Massachusetts, only 8% of people who fatally overdosed had a prescription, while illicit fentanyl accounted for 54% of overdose deaths in 2015 and more than 74% in the third quarter of 2016.21 We need to screen for nonmedical use, drug misuse, and addiction before, during, and after we treat with this particular tool.
Unfortunately, the prevalence of pain and addiction are both increasing, especially for women and minorities—but there are safe, effective medications and non-drug approaches available to combat this.22-24 These problems will not go away on their own, and every health care professional must choose to be part of the solution rather than perpetuate the problem. A good place to start is to become familiar with the Surgeon General’s Report and the National Pain Strategy. Educate your patients, colleagues, and policy makers about the true nature of these problems. Take a public health approach to primary, secondary, and tertiary prevention by recognizing and treating these conditions in an expedient and effective matter. When problems persist, expand the treatment team to include specialists who can develop a patient-centered, multimodal treatment plan that treats co-occurring conditions. If we continue to ignore these problems, or focus on one at the expense of the other, both problems will worsen and our patients will suffer serious consequences.
Paul Arnstein, PhD, NP-C, FAAN, FNP-C
Boston, MA
Before pain was introduced as the “fifth vital sign” and the Joint Commission issued its standards, more than a decade’s worth of international research indicated that pain was largely ignored, untreated, or undertreated. The best tools available to treat pain (opioids) were reserved for patients on their deathbed. The horrific results of the SUPPORT study at the nation’s leading hospitals revealed that most patients had severe, uncontrolled pain up until their final days of life.1 Unfortunately, research suggests we are still reserving opioids for the last days or weeks of life.2
In 1992 and 1994, the Department of Health and Human Services issued clinical practice guidelines highlighting the huge gap between the availability of evidence-based pain control methods and the lack of pain assessment and treatment in practice.3 When these guidelines failed to change practice, the Joint Commission added “attending to pain” to its standards—the first effort to require that evidence-based practices be utilized. Twenty years later, the National Academy of Science issued a report stating that, despite transient improvements, the current state is inadequate since pain is the leading reason people seek health care. Patients with pain report an inability to get help, which is “viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”4 Since I started working as an NP in 1983, I have never seen as many patients with pain stigmatized, ignored, labeled, and denied access to treatment as I have in the past year.
Pain afflicts more than 100 million Americans and is the leading cause of disability worldwide.5 Acute pain that is not effectively treated progresses to chronic pain in 51% of cases.6 An estimated 23 million Americans report frequent intense pain, 25 million endure daily chronic pain, and 40 million adults have high-impact, disabling, chronic pain that degrades health and requires health care intervention.6,7 The most notable damage is to the structure and function of the central nervous system.8 Brain remodeling and loss of gray matter occurs, producing changes in the brain similar to those observed with 10 to 20 years of aging; this explains why some of the learning, memory, and emotional difficulties endured by many with ongoing pain can be partially reversed with effective treatment.9 Left untreated, pain can result in significant biopsychosocial problems, frailty, financial ruin, and premature death.10-14
Prescription drug misuse and addiction also affect millions and have been a largely ignored public health problem for decades. Trying to fix the pain problem without attending equally to the problems of nonmedical drug use, addiction, and overdose deaths has contributed to the escalation of health problems to “epidemic” and “crisis” proportions. Although most patients who are prescribed medically indicated opioids for pain do not misuse their medications or become addicted, the failure to subsequently identify and properly treat an emergent substance use disorder is a problem in our current system.15 Unfortunately, making prescription opioids inaccessible to patients forces some to abuse alcohol or seek drugs from illicit sources, which only exacerbates the situation.16 A national study performed over a five-year period revealed that only 10% of patients admitted for prescription opioid treatment were referred from their health care providers.17 So, health care providers may have been part of the problem but have not been fully engaged in the solution.
Although opioids are neither the firstline, nor only, treatment option in our current evidence-based treatment toolbox, their prudent use does not cause addiction. Only 1% of patients who receive postoperative opioids go on to develop chronic opioid use, and adolescents treated with medically necessary opioids have no greater risk for future addiction than unexposed children. It is the nonmedical use of opioids, rather than proper medical use, that predisposes people to addiction.18,19 Discharging or not treating patients suspected of “drug-seeking” exacerbates the problem. Rates of opioid prescription have declined, while overdoses of illicitly manufactured fentanyl increased by 79% in 27 states from 2013 to 2014.20 In Massachusetts, only 8% of people who fatally overdosed had a prescription, while illicit fentanyl accounted for 54% of overdose deaths in 2015 and more than 74% in the third quarter of 2016.21 We need to screen for nonmedical use, drug misuse, and addiction before, during, and after we treat with this particular tool.
Unfortunately, the prevalence of pain and addiction are both increasing, especially for women and minorities—but there are safe, effective medications and non-drug approaches available to combat this.22-24 These problems will not go away on their own, and every health care professional must choose to be part of the solution rather than perpetuate the problem. A good place to start is to become familiar with the Surgeon General’s Report and the National Pain Strategy. Educate your patients, colleagues, and policy makers about the true nature of these problems. Take a public health approach to primary, secondary, and tertiary prevention by recognizing and treating these conditions in an expedient and effective matter. When problems persist, expand the treatment team to include specialists who can develop a patient-centered, multimodal treatment plan that treats co-occurring conditions. If we continue to ignore these problems, or focus on one at the expense of the other, both problems will worsen and our patients will suffer serious consequences.
Paul Arnstein, PhD, NP-C, FAAN, FNP-C
Boston, MA
1. Lynn J, Teno JM, Phillips RS, et al; SUPPORT Investigators. Perceptions by family members of the dying experience of older and seriously ill patients. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106.
2. Ziegler L, Mulvey M, Blenkinsopp A, et al. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain. 2016;157(11):2445-2451.
3. Agency for Health Care Policy and Research [AHCPR]. Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1992.
4. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press; 2011.
5. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602.
6. Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157(10):2158-2159.
7. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769-780.
8. Pozek JP, Beausang D, Baratta JL, Viscusi ER. The acute to chronic pain transition: can chronic pain be prevented? Med Clin North Am. 2016;100(1):17-30.
9. Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011; 31(20):7540-7550.
10. Wade KF, Lee DM, McBeth J, et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing. 2016;45(2):268-274.
11. Torrance N, Elliott A, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380-386.
12. Tang NK, Beckwith P, Ashworth P. Mental defeat is associated with suicide intent in patients with chronic pain. Clin J Pain. 2016;32(5):411-419.
13. Schaefer C, Sadosky A, Mann R, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483-496.
14. Schofield D, Kelly S, Shrestha R, et al. The impact of back problems on retirement wealth. Pain. 2012;153(1):203-210.
15. Chou R, Deyo R, Devine B, et al. The effectiveness and risks of long-term opioid treatment of chronic pain. AHRQ Report No. 218. Agency for Healthcare Research and Quality; September 2014. www.effectivehealthcare.ahrq.gov/ehc/products/557/1988/chronic-pain-opioid-treat ment-executive-141022.pdf. Accessed December 2, 2016.
16. Alford DP, German JS, Samet JH, et al. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
17. St. Marie BJ, Sahker E, Arndt S. Referrals and treatment completion for prescription opioid admissions: five years of national data. J Subst Abus Treat. 2015;59:109-114.
18. Sun EC, Darnall B, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9):1286-1293.
19. McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder (SUD) symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2171-2178.
20. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
21. Massachusetts Department of Public Health. Data Brief: Opioid-related Overdose Deaths Among Massachusetts Residents. www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/data-brief-overdose-deaths-may-2016.pdf. Accessed December 2, 2016.
22. Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
23. US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Executive Summary. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/executive-summary.pdf. Accessed December 2, 2016.
24. Herndon CM, Arnstein P, Darnall B, et al. Principles of Analgesic Use. 7th ed. Chicago, IL: American Pain Society Press; 2016.
1. Lynn J, Teno JM, Phillips RS, et al; SUPPORT Investigators. Perceptions by family members of the dying experience of older and seriously ill patients. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106.
2. Ziegler L, Mulvey M, Blenkinsopp A, et al. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain. 2016;157(11):2445-2451.
3. Agency for Health Care Policy and Research [AHCPR]. Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1992.
4. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press; 2011.
5. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602.
6. Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157(10):2158-2159.
7. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769-780.
8. Pozek JP, Beausang D, Baratta JL, Viscusi ER. The acute to chronic pain transition: can chronic pain be prevented? Med Clin North Am. 2016;100(1):17-30.
9. Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011; 31(20):7540-7550.
10. Wade KF, Lee DM, McBeth J, et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing. 2016;45(2):268-274.
11. Torrance N, Elliott A, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380-386.
12. Tang NK, Beckwith P, Ashworth P. Mental defeat is associated with suicide intent in patients with chronic pain. Clin J Pain. 2016;32(5):411-419.
13. Schaefer C, Sadosky A, Mann R, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483-496.
14. Schofield D, Kelly S, Shrestha R, et al. The impact of back problems on retirement wealth. Pain. 2012;153(1):203-210.
15. Chou R, Deyo R, Devine B, et al. The effectiveness and risks of long-term opioid treatment of chronic pain. AHRQ Report No. 218. Agency for Healthcare Research and Quality; September 2014. www.effectivehealthcare.ahrq.gov/ehc/products/557/1988/chronic-pain-opioid-treat ment-executive-141022.pdf. Accessed December 2, 2016.
16. Alford DP, German JS, Samet JH, et al. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
17. St. Marie BJ, Sahker E, Arndt S. Referrals and treatment completion for prescription opioid admissions: five years of national data. J Subst Abus Treat. 2015;59:109-114.
18. Sun EC, Darnall B, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9):1286-1293.
19. McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder (SUD) symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2171-2178.
20. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
21. Massachusetts Department of Public Health. Data Brief: Opioid-related Overdose Deaths Among Massachusetts Residents. www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/data-brief-overdose-deaths-may-2016.pdf. Accessed December 2, 2016.
22. Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
23. US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Executive Summary. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/executive-summary.pdf. Accessed December 2, 2016.
24. Herndon CM, Arnstein P, Darnall B, et al. Principles of Analgesic Use. 7th ed. Chicago, IL: American Pain Society Press; 2016.
Gene, risk signatures could predict PARP inhibitor response in breast cancer
SAN ANTONIO – PARPi 7, BRCAness, and MammaPrint high1/(ultra)high2 signatures could help predict response to combination therapy with the poly ADP ribose polymerase (PARP) inhibitors veliparib and carboplatin among high-risk breast cancer patients and thereby improve patient care, according to findings from the I-SPY 2 clinical trial.
“I-SPY 2 is a phase II adaptively randomized neoadjuvant clinical trial with a shared control arm where patients receive standard neoadjuvant chemotherapy, and up to 4 simultaneous investigational arms. The primary endpoint of the trial is pathologic complete response, or pCR. The goal is to match therapies with the most responsive breast cancer subtypes,” Denise M. Wolf, PhD, of the University of California, San Francisco, explained at the San Antonio Breast Cancer Symposium.
The current analysis of I-Spy 2 data focuses on veliparib/carboplatin (VC), and the subtypes Dr. Wolf mentioned are defined by hormone receptor (HR) and HER2 expression, and by MammaPrint high1 or (ultra)high2 risk status, which, “roughly speaking, is a further stratification of the poor prognosis group into high- and extra-high-risk groups,” she said.
“This arm was open to HER2-negative patients, and graduated successfully in the triple-negative subset,” she noted, explaining that “agents or combinations graduate for efficacy if they reach 85% predicted probability of success in a subsequent phase III trial in the most responsive patient subset.”
The biomarker component of the trial aimed to evaluate biomarkers associated with the mechanisms of action of each investigational agent along with the predefined subsets.
Although the findings require verification in a larger trial, Dr. Wolf and her colleagues found that three biomarkers – the PARPi 7 gene signature, the 77-gene BRCAness signature (which both relate to DNA damage repair deficiency), and the MammaPrint high1 and (ultra)high2 risk categories – were each moderately correlated with treatment response in 72 patients receiving veliparib/carboplatin (VC), but not in 44 controls, and that the treatment-biomarker interactions retained statistical significance after adjusting for hormone receptor status.
“And so we asked the question, ‘Are these signatures identifying the same patients – and if not, might there be a way to combine them to identify a subset of patients who are especially likely to respond to VC?’” she said.
Further analysis showed that even though each of the biomarkers was a predictor of response, the biomarkers did not appear to identify exactly the same patients, therefore combining them might be of benefit.
“We did this using a simple voting scheme to combine pairs of biomarkers,” she said, adding that if the two paired biomarkers predicted resistance, the biomarker also predicted resistance. If only 1 predicted resistance, the combination predicted resistance, and only if both biomarkers predicted sensitivity did the combination predict sensitivity.
In the graduated triple-negative subset, for example, the 40% of patients who were PARPi 7–high and MammaPrint high2 (the two biomarkers most predictive of response) a dramatic separation was seen in the pCR probability curves, with an estimated pCR of 79% with VC treatment vs. 23% in the control arm.
“In contrast, triple-negative patients who were negative for one or more of the sensitivity markers had nearly overlapping probability response curves, from which we conclude that nearly all of the specific sensitivity to VC seen in the triple-negative patients is found in that subset who are positive for both sensitivity markers,” she said.
Additionally, although only 9% of HR-positive/HER2-negative patients were PARPi 7-high and MammaPrint high2, those patients also appeared to be more responsive to VC vs. the control arm (49% vs. 15%).
The results also demonstrate the value of an exploratory voting method for combining multiple biomarkers for the same treatment, Dr. Wolf noted.
However, the findings are limited by the small sample size and need to be evaluated in larger trials, and the biomarkers also need to be evaluated in carboplatin-only arms in order to “tease out whether the biomarkers are really specific to a PARP inhibitor with carboplatin or whether they might also apply to carboplatin alone.
“Our ongoing and future work is to develop predictive biomarkers for other I-Spy 2 agents,” she said.
Dr. Wolf reported having no disclosures.
SAN ANTONIO – PARPi 7, BRCAness, and MammaPrint high1/(ultra)high2 signatures could help predict response to combination therapy with the poly ADP ribose polymerase (PARP) inhibitors veliparib and carboplatin among high-risk breast cancer patients and thereby improve patient care, according to findings from the I-SPY 2 clinical trial.
“I-SPY 2 is a phase II adaptively randomized neoadjuvant clinical trial with a shared control arm where patients receive standard neoadjuvant chemotherapy, and up to 4 simultaneous investigational arms. The primary endpoint of the trial is pathologic complete response, or pCR. The goal is to match therapies with the most responsive breast cancer subtypes,” Denise M. Wolf, PhD, of the University of California, San Francisco, explained at the San Antonio Breast Cancer Symposium.
The current analysis of I-Spy 2 data focuses on veliparib/carboplatin (VC), and the subtypes Dr. Wolf mentioned are defined by hormone receptor (HR) and HER2 expression, and by MammaPrint high1 or (ultra)high2 risk status, which, “roughly speaking, is a further stratification of the poor prognosis group into high- and extra-high-risk groups,” she said.
“This arm was open to HER2-negative patients, and graduated successfully in the triple-negative subset,” she noted, explaining that “agents or combinations graduate for efficacy if they reach 85% predicted probability of success in a subsequent phase III trial in the most responsive patient subset.”
The biomarker component of the trial aimed to evaluate biomarkers associated with the mechanisms of action of each investigational agent along with the predefined subsets.
Although the findings require verification in a larger trial, Dr. Wolf and her colleagues found that three biomarkers – the PARPi 7 gene signature, the 77-gene BRCAness signature (which both relate to DNA damage repair deficiency), and the MammaPrint high1 and (ultra)high2 risk categories – were each moderately correlated with treatment response in 72 patients receiving veliparib/carboplatin (VC), but not in 44 controls, and that the treatment-biomarker interactions retained statistical significance after adjusting for hormone receptor status.
“And so we asked the question, ‘Are these signatures identifying the same patients – and if not, might there be a way to combine them to identify a subset of patients who are especially likely to respond to VC?’” she said.
Further analysis showed that even though each of the biomarkers was a predictor of response, the biomarkers did not appear to identify exactly the same patients, therefore combining them might be of benefit.
“We did this using a simple voting scheme to combine pairs of biomarkers,” she said, adding that if the two paired biomarkers predicted resistance, the biomarker also predicted resistance. If only 1 predicted resistance, the combination predicted resistance, and only if both biomarkers predicted sensitivity did the combination predict sensitivity.
In the graduated triple-negative subset, for example, the 40% of patients who were PARPi 7–high and MammaPrint high2 (the two biomarkers most predictive of response) a dramatic separation was seen in the pCR probability curves, with an estimated pCR of 79% with VC treatment vs. 23% in the control arm.
“In contrast, triple-negative patients who were negative for one or more of the sensitivity markers had nearly overlapping probability response curves, from which we conclude that nearly all of the specific sensitivity to VC seen in the triple-negative patients is found in that subset who are positive for both sensitivity markers,” she said.
Additionally, although only 9% of HR-positive/HER2-negative patients were PARPi 7-high and MammaPrint high2, those patients also appeared to be more responsive to VC vs. the control arm (49% vs. 15%).
The results also demonstrate the value of an exploratory voting method for combining multiple biomarkers for the same treatment, Dr. Wolf noted.
However, the findings are limited by the small sample size and need to be evaluated in larger trials, and the biomarkers also need to be evaluated in carboplatin-only arms in order to “tease out whether the biomarkers are really specific to a PARP inhibitor with carboplatin or whether they might also apply to carboplatin alone.
“Our ongoing and future work is to develop predictive biomarkers for other I-Spy 2 agents,” she said.
Dr. Wolf reported having no disclosures.
SAN ANTONIO – PARPi 7, BRCAness, and MammaPrint high1/(ultra)high2 signatures could help predict response to combination therapy with the poly ADP ribose polymerase (PARP) inhibitors veliparib and carboplatin among high-risk breast cancer patients and thereby improve patient care, according to findings from the I-SPY 2 clinical trial.
“I-SPY 2 is a phase II adaptively randomized neoadjuvant clinical trial with a shared control arm where patients receive standard neoadjuvant chemotherapy, and up to 4 simultaneous investigational arms. The primary endpoint of the trial is pathologic complete response, or pCR. The goal is to match therapies with the most responsive breast cancer subtypes,” Denise M. Wolf, PhD, of the University of California, San Francisco, explained at the San Antonio Breast Cancer Symposium.
The current analysis of I-Spy 2 data focuses on veliparib/carboplatin (VC), and the subtypes Dr. Wolf mentioned are defined by hormone receptor (HR) and HER2 expression, and by MammaPrint high1 or (ultra)high2 risk status, which, “roughly speaking, is a further stratification of the poor prognosis group into high- and extra-high-risk groups,” she said.
“This arm was open to HER2-negative patients, and graduated successfully in the triple-negative subset,” she noted, explaining that “agents or combinations graduate for efficacy if they reach 85% predicted probability of success in a subsequent phase III trial in the most responsive patient subset.”
The biomarker component of the trial aimed to evaluate biomarkers associated with the mechanisms of action of each investigational agent along with the predefined subsets.
Although the findings require verification in a larger trial, Dr. Wolf and her colleagues found that three biomarkers – the PARPi 7 gene signature, the 77-gene BRCAness signature (which both relate to DNA damage repair deficiency), and the MammaPrint high1 and (ultra)high2 risk categories – were each moderately correlated with treatment response in 72 patients receiving veliparib/carboplatin (VC), but not in 44 controls, and that the treatment-biomarker interactions retained statistical significance after adjusting for hormone receptor status.
“And so we asked the question, ‘Are these signatures identifying the same patients – and if not, might there be a way to combine them to identify a subset of patients who are especially likely to respond to VC?’” she said.
Further analysis showed that even though each of the biomarkers was a predictor of response, the biomarkers did not appear to identify exactly the same patients, therefore combining them might be of benefit.
“We did this using a simple voting scheme to combine pairs of biomarkers,” she said, adding that if the two paired biomarkers predicted resistance, the biomarker also predicted resistance. If only 1 predicted resistance, the combination predicted resistance, and only if both biomarkers predicted sensitivity did the combination predict sensitivity.
In the graduated triple-negative subset, for example, the 40% of patients who were PARPi 7–high and MammaPrint high2 (the two biomarkers most predictive of response) a dramatic separation was seen in the pCR probability curves, with an estimated pCR of 79% with VC treatment vs. 23% in the control arm.
“In contrast, triple-negative patients who were negative for one or more of the sensitivity markers had nearly overlapping probability response curves, from which we conclude that nearly all of the specific sensitivity to VC seen in the triple-negative patients is found in that subset who are positive for both sensitivity markers,” she said.
Additionally, although only 9% of HR-positive/HER2-negative patients were PARPi 7-high and MammaPrint high2, those patients also appeared to be more responsive to VC vs. the control arm (49% vs. 15%).
The results also demonstrate the value of an exploratory voting method for combining multiple biomarkers for the same treatment, Dr. Wolf noted.
However, the findings are limited by the small sample size and need to be evaluated in larger trials, and the biomarkers also need to be evaluated in carboplatin-only arms in order to “tease out whether the biomarkers are really specific to a PARP inhibitor with carboplatin or whether they might also apply to carboplatin alone.
“Our ongoing and future work is to develop predictive biomarkers for other I-Spy 2 agents,” she said.
Dr. Wolf reported having no disclosures.
AT SABCS 2016
Key clinical point:
Major finding: Estimated pCR in PARPi 7–high and MammaPrint 2 triple-negative patients was 79% vs. 23% for the VC arm vs. control arm.
Data source: The phase II adaptively randomized I-Spy 2 clinical trial of 116 subjects.
Disclosures: Dr. Wolf reported having no disclosures.
Study eyes fracture risk in pediatric patients taking antiepileptic drugs
HOUSTON – The incidence of fractures in pediatric patients taking antiepileptic medication stands at an estimated 1.1%, according to results from a 4-year period at a children’s hospital.
“Understanding the prevalence of fractures in pediatric patients on an AED [antiepileptic drug] will allow clinicians to weigh the risk versus benefit of therapy,” researchers led by Shannon DiCarlo, MD, wrote in an abstract presented during a poster session at the annual meeting of the American Epilepsy Society. “Recognizing a risk of fractures with AEDs will permit clinicians to provide appropriate supportive care and monitoring from the initiation of therapy.”
Dr. DiCarlo of Texas Children’s Hospital, Houston, and her associates went on to note that adults with epilepsy have a twofold to sixfold greater risk of experiencing fractures, compared with the general population, and that fractures secondary to seizures “are a major concern in pediatrics.” In fact, one survey of 404 pediatric neurologists found that only 41% of respondents were aware of the association between AEDs and reduced bone mass (Arch Neurol. 2001;58[9]:1369-74).
In an effort to evaluate the prevalence of fractures in pediatric patients on an antiepileptic drug, the researchers conducted a cohort study of 10,153 patients younger than 18 years of age who received an AED at Texas Children’s Hospital from 2011 to 2014. Half of the study population were female, and the most common concomitant disease was epilepsy (52.6%), followed by cerebral palsy (8.3%), epilepsy plus cerebral palsy (6.9%), osteoporosis (0.2%), and osteopenia (0.3%). In all, 113 patients (1.1%) experienced a fracture while on an antiepileptic drug, and the mean time from initiation of an AED to time of fracture was 1.6 years. Patients on enzyme-inducing AEDs were two times more likely to experience a fracture, while those with cerebral palsy and epilepsy were three times more likely to experience a fracture. Proton pump inhibitors and corticosteroids were the most common concomitant drugs. The researchers also found that less than 10% of patients were on calcium or vitamin D supplementation.
“Vigilant monitoring should be employed for at-risk patients,” the researchers concluded. “Regular monitoring of calcium and vitamin D levels may be warranted; further studies are needed to evaluate the roll of prophylactic calcium and vitamin D supplements.”
The researchers reported having no relevant financial disclosures.
HOUSTON – The incidence of fractures in pediatric patients taking antiepileptic medication stands at an estimated 1.1%, according to results from a 4-year period at a children’s hospital.
“Understanding the prevalence of fractures in pediatric patients on an AED [antiepileptic drug] will allow clinicians to weigh the risk versus benefit of therapy,” researchers led by Shannon DiCarlo, MD, wrote in an abstract presented during a poster session at the annual meeting of the American Epilepsy Society. “Recognizing a risk of fractures with AEDs will permit clinicians to provide appropriate supportive care and monitoring from the initiation of therapy.”
Dr. DiCarlo of Texas Children’s Hospital, Houston, and her associates went on to note that adults with epilepsy have a twofold to sixfold greater risk of experiencing fractures, compared with the general population, and that fractures secondary to seizures “are a major concern in pediatrics.” In fact, one survey of 404 pediatric neurologists found that only 41% of respondents were aware of the association between AEDs and reduced bone mass (Arch Neurol. 2001;58[9]:1369-74).
In an effort to evaluate the prevalence of fractures in pediatric patients on an antiepileptic drug, the researchers conducted a cohort study of 10,153 patients younger than 18 years of age who received an AED at Texas Children’s Hospital from 2011 to 2014. Half of the study population were female, and the most common concomitant disease was epilepsy (52.6%), followed by cerebral palsy (8.3%), epilepsy plus cerebral palsy (6.9%), osteoporosis (0.2%), and osteopenia (0.3%). In all, 113 patients (1.1%) experienced a fracture while on an antiepileptic drug, and the mean time from initiation of an AED to time of fracture was 1.6 years. Patients on enzyme-inducing AEDs were two times more likely to experience a fracture, while those with cerebral palsy and epilepsy were three times more likely to experience a fracture. Proton pump inhibitors and corticosteroids were the most common concomitant drugs. The researchers also found that less than 10% of patients were on calcium or vitamin D supplementation.
“Vigilant monitoring should be employed for at-risk patients,” the researchers concluded. “Regular monitoring of calcium and vitamin D levels may be warranted; further studies are needed to evaluate the roll of prophylactic calcium and vitamin D supplements.”
The researchers reported having no relevant financial disclosures.
HOUSTON – The incidence of fractures in pediatric patients taking antiepileptic medication stands at an estimated 1.1%, according to results from a 4-year period at a children’s hospital.
“Understanding the prevalence of fractures in pediatric patients on an AED [antiepileptic drug] will allow clinicians to weigh the risk versus benefit of therapy,” researchers led by Shannon DiCarlo, MD, wrote in an abstract presented during a poster session at the annual meeting of the American Epilepsy Society. “Recognizing a risk of fractures with AEDs will permit clinicians to provide appropriate supportive care and monitoring from the initiation of therapy.”
Dr. DiCarlo of Texas Children’s Hospital, Houston, and her associates went on to note that adults with epilepsy have a twofold to sixfold greater risk of experiencing fractures, compared with the general population, and that fractures secondary to seizures “are a major concern in pediatrics.” In fact, one survey of 404 pediatric neurologists found that only 41% of respondents were aware of the association between AEDs and reduced bone mass (Arch Neurol. 2001;58[9]:1369-74).
In an effort to evaluate the prevalence of fractures in pediatric patients on an antiepileptic drug, the researchers conducted a cohort study of 10,153 patients younger than 18 years of age who received an AED at Texas Children’s Hospital from 2011 to 2014. Half of the study population were female, and the most common concomitant disease was epilepsy (52.6%), followed by cerebral palsy (8.3%), epilepsy plus cerebral palsy (6.9%), osteoporosis (0.2%), and osteopenia (0.3%). In all, 113 patients (1.1%) experienced a fracture while on an antiepileptic drug, and the mean time from initiation of an AED to time of fracture was 1.6 years. Patients on enzyme-inducing AEDs were two times more likely to experience a fracture, while those with cerebral palsy and epilepsy were three times more likely to experience a fracture. Proton pump inhibitors and corticosteroids were the most common concomitant drugs. The researchers also found that less than 10% of patients were on calcium or vitamin D supplementation.
“Vigilant monitoring should be employed for at-risk patients,” the researchers concluded. “Regular monitoring of calcium and vitamin D levels may be warranted; further studies are needed to evaluate the roll of prophylactic calcium and vitamin D supplements.”
The researchers reported having no relevant financial disclosures.
Key clinical point:
Major finding: In all, 113 patients (1.1%) experienced a fracture while on an antiepileptic drug, and the mean time from initiation of AED to time of fracture was 1.6 years.
Data source: A cohort study of 10,153 patients younger than 18 years of age who received an AED at Texas Children’s Hospital from 2011 to 2014.
Disclosures: The researchers reported having no relevant financial disclosures.
Which maternal beta-blockers boost SGA risk?
NEW ORLEANS – The use of labetalol or atenolol in pregnancy is associated with significantly increased risk of having a small-for-gestational-age (SGA) baby; metoprolol and propranolol are not.
And none of these four beta-blockers are associated with increased risk of congenital cardiac anomalies, Angie Ng, MD, reported at the American Heart Association scientific sessions.
Overall, the average birth weight for babies whose mothers were on a beta-blocker was 2,996 g, significantly less than the 3,353 g in 374,391 controls who weren’t exposed to beta-blockers during pregnancy. But beta-blockers are not a monolithic class of drugs; their pharmacokinetics and physical properties differ. And so did their associated incidence of SGA, according to Dr. Ng of Kaiser Permanente Los Angeles.
The rate of SGA below the 10th percentile was 17.6% in the 3,357 women on labetalol during pregnancy and the same in the 638 women on atenolol. In contrast, the SGA rates in women on metoprolol or propranolol – 10.8% and 10.3%, respectively – weren’t significantly different from the 8.7% incidence in controls.
To deal with the possibility of confounding by indication, Dr. Ng and her coinvestigators performed a multivariate analysis adjusted for maternal age, white race, body mass index, gestational age, diabetes, hypertension, arrhythmias, dyslipidemia, and renal insufficiency. The resultant adjusted risk of having an SGA baby was 2.9-fold greater in women on labetalol and 2.4-fold greater in those on atenolol than in controls. Women on the other two beta-blockers faced no increased risk.
The incidence of congenital cardiac anomalies was 5.1% in women exposed to beta-blockers in pregnancy and 1.9% in controls who weren’t. The most commonly diagnosed anomalies – patent ductus arteriosus, atrial septal defect, and ventricular septal defect – were two- to threefold more frequent in the setting of maternal beta-blocker exposure. However, in a multivariate analysis the use of any beta-blocker was no longer associated with significantly elevated risk of congenital cardiac anomalies.
“This suggests that the initial association we see in the unadjusted analysis is likely due to confounders and not due to the beta-blocker exposure,” Dr. Ng said.
Labetalol and atenolol were prescribed during pregnancy most often for hypertension, while metoprolol and propranolol were typically prescribed to control arrhythmias.
Previous reports by other investigators have yielded conflicting results as to whether maternal beta-blocker therapy is associated with increased risk of SGA. A major limitation of those studies was that they examined beta-blockers as a class rather than assessing the impact of specific agents, according to Dr. Ng.
She reported having no financial conflicts of interest regarding her study, which was conducted free of commercial support.
NEW ORLEANS – The use of labetalol or atenolol in pregnancy is associated with significantly increased risk of having a small-for-gestational-age (SGA) baby; metoprolol and propranolol are not.
And none of these four beta-blockers are associated with increased risk of congenital cardiac anomalies, Angie Ng, MD, reported at the American Heart Association scientific sessions.
Overall, the average birth weight for babies whose mothers were on a beta-blocker was 2,996 g, significantly less than the 3,353 g in 374,391 controls who weren’t exposed to beta-blockers during pregnancy. But beta-blockers are not a monolithic class of drugs; their pharmacokinetics and physical properties differ. And so did their associated incidence of SGA, according to Dr. Ng of Kaiser Permanente Los Angeles.
The rate of SGA below the 10th percentile was 17.6% in the 3,357 women on labetalol during pregnancy and the same in the 638 women on atenolol. In contrast, the SGA rates in women on metoprolol or propranolol – 10.8% and 10.3%, respectively – weren’t significantly different from the 8.7% incidence in controls.
To deal with the possibility of confounding by indication, Dr. Ng and her coinvestigators performed a multivariate analysis adjusted for maternal age, white race, body mass index, gestational age, diabetes, hypertension, arrhythmias, dyslipidemia, and renal insufficiency. The resultant adjusted risk of having an SGA baby was 2.9-fold greater in women on labetalol and 2.4-fold greater in those on atenolol than in controls. Women on the other two beta-blockers faced no increased risk.
The incidence of congenital cardiac anomalies was 5.1% in women exposed to beta-blockers in pregnancy and 1.9% in controls who weren’t. The most commonly diagnosed anomalies – patent ductus arteriosus, atrial septal defect, and ventricular septal defect – were two- to threefold more frequent in the setting of maternal beta-blocker exposure. However, in a multivariate analysis the use of any beta-blocker was no longer associated with significantly elevated risk of congenital cardiac anomalies.
“This suggests that the initial association we see in the unadjusted analysis is likely due to confounders and not due to the beta-blocker exposure,” Dr. Ng said.
Labetalol and atenolol were prescribed during pregnancy most often for hypertension, while metoprolol and propranolol were typically prescribed to control arrhythmias.
Previous reports by other investigators have yielded conflicting results as to whether maternal beta-blocker therapy is associated with increased risk of SGA. A major limitation of those studies was that they examined beta-blockers as a class rather than assessing the impact of specific agents, according to Dr. Ng.
She reported having no financial conflicts of interest regarding her study, which was conducted free of commercial support.
NEW ORLEANS – The use of labetalol or atenolol in pregnancy is associated with significantly increased risk of having a small-for-gestational-age (SGA) baby; metoprolol and propranolol are not.
And none of these four beta-blockers are associated with increased risk of congenital cardiac anomalies, Angie Ng, MD, reported at the American Heart Association scientific sessions.
Overall, the average birth weight for babies whose mothers were on a beta-blocker was 2,996 g, significantly less than the 3,353 g in 374,391 controls who weren’t exposed to beta-blockers during pregnancy. But beta-blockers are not a monolithic class of drugs; their pharmacokinetics and physical properties differ. And so did their associated incidence of SGA, according to Dr. Ng of Kaiser Permanente Los Angeles.
The rate of SGA below the 10th percentile was 17.6% in the 3,357 women on labetalol during pregnancy and the same in the 638 women on atenolol. In contrast, the SGA rates in women on metoprolol or propranolol – 10.8% and 10.3%, respectively – weren’t significantly different from the 8.7% incidence in controls.
To deal with the possibility of confounding by indication, Dr. Ng and her coinvestigators performed a multivariate analysis adjusted for maternal age, white race, body mass index, gestational age, diabetes, hypertension, arrhythmias, dyslipidemia, and renal insufficiency. The resultant adjusted risk of having an SGA baby was 2.9-fold greater in women on labetalol and 2.4-fold greater in those on atenolol than in controls. Women on the other two beta-blockers faced no increased risk.
The incidence of congenital cardiac anomalies was 5.1% in women exposed to beta-blockers in pregnancy and 1.9% in controls who weren’t. The most commonly diagnosed anomalies – patent ductus arteriosus, atrial septal defect, and ventricular septal defect – were two- to threefold more frequent in the setting of maternal beta-blocker exposure. However, in a multivariate analysis the use of any beta-blocker was no longer associated with significantly elevated risk of congenital cardiac anomalies.
“This suggests that the initial association we see in the unadjusted analysis is likely due to confounders and not due to the beta-blocker exposure,” Dr. Ng said.
Labetalol and atenolol were prescribed during pregnancy most often for hypertension, while metoprolol and propranolol were typically prescribed to control arrhythmias.
Previous reports by other investigators have yielded conflicting results as to whether maternal beta-blocker therapy is associated with increased risk of SGA. A major limitation of those studies was that they examined beta-blockers as a class rather than assessing the impact of specific agents, according to Dr. Ng.
She reported having no financial conflicts of interest regarding her study, which was conducted free of commercial support.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Women on labetalol or atenolol during pregnancy had a 17.6% incidence of small-for-gestational-age babies, a rate more than twice that in women not exposed to a beta-blocker during pregnancy.
Data source: This was a retrospective study of fetal outcomes in nearly 380,000 pregnant women, 4,847 of whom were on beta-blocker therapy during their pregnancy.
Disclosures: The presenter reported having no financial conflicts of interest regarding her study, which was conducted free of commercial support.
Infantile spasms diagnosis, treatment too often delayed
HOUSTON – The appropriate evaluation and treatment of infantile spasms often comes after significant delays that are largely attributable to lack of recognition of the condition, according to recent survey results.
“Parental suspicions that ‘something was wrong’ were often discounted by health care providers, and survey respondents frequently reported that health care providers (including neurologists) were unfamiliar with infantile spasms [IS],” wrote Johnson Lay and his collaborators, in presenting results of the recently-completed Assessment of Symptoms and Specialists in Infantile Spasms (ASSIST) study at the annual meeting of the American Epilepsy Society. It’s critically important not to discount parental concerns, senior author Shaun Hussain, MD, said in an interview about the study, which surveyed parents of children with IS: “Sometimes we get in the habit of reassuring patients too much.”
On average, a pediatrician will see two cases of infantile spasms in a career of caring for children, Dr. Hussain said. These characteristically brief episodes last just a second or so, and frequently come in clusters, during or after which crying is common. Though the classic presentation of IS is a brief drop of the head with accompanying elevation of the shoulders – and perhaps a lifting of the arms – there’s wide variation in presentation. “Infantile spasms can present in a lot of different ways; babies haven’t read the neurology textbooks,” Dr. Hussain said. A curated collection of videos showing the variety of infantile spasms is available on the Infantile Spasms Project website.
Mr. Lay and his collaborators surveyed the parents of 100 children with IS in order to understand and describe their experiences in having their child receive the correct diagnosis and treatment. Also, they sought to determine whether socioeconomic factors affected prompt access to care. Dr. Lay completed the study with Dr. Hussain and other coauthors after graduating from UCLA in 2015.
The study, presented during a poster session at the meeting, measured the time between the parents’ first identification of IS and their contact with an “effective provider.” A provider was deemed effective if he or she correctly diagnosed IS and prescribed a first-line therapy: adrenocorticotropin-releasing hormone (ACTH), corticosteroids, or vigabatrin (Sabril).
Of the 100 children whose families were surveyed, 29% were seen by an effective provider within a week of the onset of IS. The median time from the onset of IS to the patient’s being seen by an effective provider was 24.5 days, with a wide range seen in the population surveyed (interquartile range, 0-110.5 days). This exceeds the 7 days that has been identified as the goal cumulative latency to treatment, Mr. Lay and his coauthors said.
The median age of onset of IS was 6.6 months in the study population, 45% of whom were female.
A total of 64 patients were first seen for IS concerns by a provider who was not a neurologist. Of those, the cumulative latency to seeing the first effective provider was over 100 days, with some patients’ wait time stretching to over 200 days.
The survey asked about socioeconomic factors, including income, health insurance status, proximity to specialty care, ethnicity, and parental language preference. Of these, only a non-English parental language preference was associated with increased time to seeing an effective provider (hazard ratio, 0.37; 95% confidence interval, 0.20-0.68; P = .002).
“These results suggest that a simple lack of awareness of infantile spasms among health care providers may be responsible for potentially catastrophic delays in IS care,” wrote Mr. Lay and his coauthors. Dr. Hussain concurred: “The clear driver of treatment delay is the failure of health care providers to recognize the appearance, importance, and urgency of infantile spasms. Delay in diagnosis and treatment of infantile spasms is common, costly – to both patients and the health care system – and almost entirely preventable.”
The Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute funded the study. Dr. Hussain has received research support from and been on the advisory boards of several pharmaceutical companies. Mr. Lay reported no disclosures.
[email protected]
On Twitter @karioakes
HOUSTON – The appropriate evaluation and treatment of infantile spasms often comes after significant delays that are largely attributable to lack of recognition of the condition, according to recent survey results.
“Parental suspicions that ‘something was wrong’ were often discounted by health care providers, and survey respondents frequently reported that health care providers (including neurologists) were unfamiliar with infantile spasms [IS],” wrote Johnson Lay and his collaborators, in presenting results of the recently-completed Assessment of Symptoms and Specialists in Infantile Spasms (ASSIST) study at the annual meeting of the American Epilepsy Society. It’s critically important not to discount parental concerns, senior author Shaun Hussain, MD, said in an interview about the study, which surveyed parents of children with IS: “Sometimes we get in the habit of reassuring patients too much.”
On average, a pediatrician will see two cases of infantile spasms in a career of caring for children, Dr. Hussain said. These characteristically brief episodes last just a second or so, and frequently come in clusters, during or after which crying is common. Though the classic presentation of IS is a brief drop of the head with accompanying elevation of the shoulders – and perhaps a lifting of the arms – there’s wide variation in presentation. “Infantile spasms can present in a lot of different ways; babies haven’t read the neurology textbooks,” Dr. Hussain said. A curated collection of videos showing the variety of infantile spasms is available on the Infantile Spasms Project website.
Mr. Lay and his collaborators surveyed the parents of 100 children with IS in order to understand and describe their experiences in having their child receive the correct diagnosis and treatment. Also, they sought to determine whether socioeconomic factors affected prompt access to care. Dr. Lay completed the study with Dr. Hussain and other coauthors after graduating from UCLA in 2015.
The study, presented during a poster session at the meeting, measured the time between the parents’ first identification of IS and their contact with an “effective provider.” A provider was deemed effective if he or she correctly diagnosed IS and prescribed a first-line therapy: adrenocorticotropin-releasing hormone (ACTH), corticosteroids, or vigabatrin (Sabril).
Of the 100 children whose families were surveyed, 29% were seen by an effective provider within a week of the onset of IS. The median time from the onset of IS to the patient’s being seen by an effective provider was 24.5 days, with a wide range seen in the population surveyed (interquartile range, 0-110.5 days). This exceeds the 7 days that has been identified as the goal cumulative latency to treatment, Mr. Lay and his coauthors said.
The median age of onset of IS was 6.6 months in the study population, 45% of whom were female.
A total of 64 patients were first seen for IS concerns by a provider who was not a neurologist. Of those, the cumulative latency to seeing the first effective provider was over 100 days, with some patients’ wait time stretching to over 200 days.
The survey asked about socioeconomic factors, including income, health insurance status, proximity to specialty care, ethnicity, and parental language preference. Of these, only a non-English parental language preference was associated with increased time to seeing an effective provider (hazard ratio, 0.37; 95% confidence interval, 0.20-0.68; P = .002).
“These results suggest that a simple lack of awareness of infantile spasms among health care providers may be responsible for potentially catastrophic delays in IS care,” wrote Mr. Lay and his coauthors. Dr. Hussain concurred: “The clear driver of treatment delay is the failure of health care providers to recognize the appearance, importance, and urgency of infantile spasms. Delay in diagnosis and treatment of infantile spasms is common, costly – to both patients and the health care system – and almost entirely preventable.”
The Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute funded the study. Dr. Hussain has received research support from and been on the advisory boards of several pharmaceutical companies. Mr. Lay reported no disclosures.
[email protected]
On Twitter @karioakes
HOUSTON – The appropriate evaluation and treatment of infantile spasms often comes after significant delays that are largely attributable to lack of recognition of the condition, according to recent survey results.
“Parental suspicions that ‘something was wrong’ were often discounted by health care providers, and survey respondents frequently reported that health care providers (including neurologists) were unfamiliar with infantile spasms [IS],” wrote Johnson Lay and his collaborators, in presenting results of the recently-completed Assessment of Symptoms and Specialists in Infantile Spasms (ASSIST) study at the annual meeting of the American Epilepsy Society. It’s critically important not to discount parental concerns, senior author Shaun Hussain, MD, said in an interview about the study, which surveyed parents of children with IS: “Sometimes we get in the habit of reassuring patients too much.”
On average, a pediatrician will see two cases of infantile spasms in a career of caring for children, Dr. Hussain said. These characteristically brief episodes last just a second or so, and frequently come in clusters, during or after which crying is common. Though the classic presentation of IS is a brief drop of the head with accompanying elevation of the shoulders – and perhaps a lifting of the arms – there’s wide variation in presentation. “Infantile spasms can present in a lot of different ways; babies haven’t read the neurology textbooks,” Dr. Hussain said. A curated collection of videos showing the variety of infantile spasms is available on the Infantile Spasms Project website.
Mr. Lay and his collaborators surveyed the parents of 100 children with IS in order to understand and describe their experiences in having their child receive the correct diagnosis and treatment. Also, they sought to determine whether socioeconomic factors affected prompt access to care. Dr. Lay completed the study with Dr. Hussain and other coauthors after graduating from UCLA in 2015.
The study, presented during a poster session at the meeting, measured the time between the parents’ first identification of IS and their contact with an “effective provider.” A provider was deemed effective if he or she correctly diagnosed IS and prescribed a first-line therapy: adrenocorticotropin-releasing hormone (ACTH), corticosteroids, or vigabatrin (Sabril).
Of the 100 children whose families were surveyed, 29% were seen by an effective provider within a week of the onset of IS. The median time from the onset of IS to the patient’s being seen by an effective provider was 24.5 days, with a wide range seen in the population surveyed (interquartile range, 0-110.5 days). This exceeds the 7 days that has been identified as the goal cumulative latency to treatment, Mr. Lay and his coauthors said.
The median age of onset of IS was 6.6 months in the study population, 45% of whom were female.
A total of 64 patients were first seen for IS concerns by a provider who was not a neurologist. Of those, the cumulative latency to seeing the first effective provider was over 100 days, with some patients’ wait time stretching to over 200 days.
The survey asked about socioeconomic factors, including income, health insurance status, proximity to specialty care, ethnicity, and parental language preference. Of these, only a non-English parental language preference was associated with increased time to seeing an effective provider (hazard ratio, 0.37; 95% confidence interval, 0.20-0.68; P = .002).
“These results suggest that a simple lack of awareness of infantile spasms among health care providers may be responsible for potentially catastrophic delays in IS care,” wrote Mr. Lay and his coauthors. Dr. Hussain concurred: “The clear driver of treatment delay is the failure of health care providers to recognize the appearance, importance, and urgency of infantile spasms. Delay in diagnosis and treatment of infantile spasms is common, costly – to both patients and the health care system – and almost entirely preventable.”
The Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute funded the study. Dr. Hussain has received research support from and been on the advisory boards of several pharmaceutical companies. Mr. Lay reported no disclosures.
[email protected]
On Twitter @karioakes
AT AES 2016
Key clinical point:
Major finding: The cumulative latency to seeing an effective provider was over 100 days for IS patients initially seen by a nonneurologist.
Data source: Survey of parent(s) of 100 children with infantile spasms.
Disclosures: The Elsie and Isaac Fogelman Endowment, the Hughes Family Foundation, and the UCLA Children’s Discovery and Innovation Institute funded the study. Dr. Hussain has received research support from and been on the advisory boards of several pharmaceutical companies. Mr. Lay reported no disclosures.
Intermittent energy restriction
My patients find it extremely difficult to determine the number of calories they consume on a daily basis. This activity can be laborious and time consuming, even when you have the right “app.”
So, when I tell my overweight and obese patients to restrict their caloric consumption to lose weight, the discussion usually begins with, “I know this might be difficult, but …” And it usually ends with me feeling a little less than anemic optimism.
But is it effective for weight loss?
C.S. Davis of Monash University, Melbourne, and colleagues conducted a systematic review of IER for weight loss (Eur J Clin Nutr. 2016 Mar;70[3]:292-9). The authors searched for articles evaluating the IER for weight loss among overweight and obese adults aged 18 years or older. IER was defined as periods of low energy intake (fast) alternating with periods of normal food intake (feed).
Eight studies were included in this review. Included studies defined low energy intake as 25%-50% of daily energy, or 400-1,400 kcal/day. The feed period was defined as either eating ad libitum or no less than 1,400 kcal/day. Studies varied in their approach and ranged from 2-4 consecutive fast days per week, followed by consecutive feed days, to three cycles of 5 weeks of fasting, followed by 5 weeks of ad lib eating.
IER was associated with 0.2-0.8 kg of weight loss per week. IER was associated with weight loss comparable to daily energy restriction (DER; that is, a typical diet). IER was comparable to typical daily energy restriction diets for fat mass, free-fat mass, and waist circumference.
The authors state that the amount of weight loss achieved with IER for a 100-kg individual would be associated with a 5% reduction in weight over a 5-week to 6-month time period. A 5% reduction is associated with a clinically significant reduction in health risk.
However, the authors found that fewer study participants planned to stick with IER beyond 6 months, compared with DER. Perhaps despite the difficulty that may exist in counting calories every day, the habit of doing the counting every day may be easier than doing it on an intermittent basis.
Regardless, IER is an option that may be beneficial to some patients. If other things haven’t worked for your patients, it is definitely worth a try.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
My patients find it extremely difficult to determine the number of calories they consume on a daily basis. This activity can be laborious and time consuming, even when you have the right “app.”
So, when I tell my overweight and obese patients to restrict their caloric consumption to lose weight, the discussion usually begins with, “I know this might be difficult, but …” And it usually ends with me feeling a little less than anemic optimism.
But is it effective for weight loss?
C.S. Davis of Monash University, Melbourne, and colleagues conducted a systematic review of IER for weight loss (Eur J Clin Nutr. 2016 Mar;70[3]:292-9). The authors searched for articles evaluating the IER for weight loss among overweight and obese adults aged 18 years or older. IER was defined as periods of low energy intake (fast) alternating with periods of normal food intake (feed).
Eight studies were included in this review. Included studies defined low energy intake as 25%-50% of daily energy, or 400-1,400 kcal/day. The feed period was defined as either eating ad libitum or no less than 1,400 kcal/day. Studies varied in their approach and ranged from 2-4 consecutive fast days per week, followed by consecutive feed days, to three cycles of 5 weeks of fasting, followed by 5 weeks of ad lib eating.
IER was associated with 0.2-0.8 kg of weight loss per week. IER was associated with weight loss comparable to daily energy restriction (DER; that is, a typical diet). IER was comparable to typical daily energy restriction diets for fat mass, free-fat mass, and waist circumference.
The authors state that the amount of weight loss achieved with IER for a 100-kg individual would be associated with a 5% reduction in weight over a 5-week to 6-month time period. A 5% reduction is associated with a clinically significant reduction in health risk.
However, the authors found that fewer study participants planned to stick with IER beyond 6 months, compared with DER. Perhaps despite the difficulty that may exist in counting calories every day, the habit of doing the counting every day may be easier than doing it on an intermittent basis.
Regardless, IER is an option that may be beneficial to some patients. If other things haven’t worked for your patients, it is definitely worth a try.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
My patients find it extremely difficult to determine the number of calories they consume on a daily basis. This activity can be laborious and time consuming, even when you have the right “app.”
So, when I tell my overweight and obese patients to restrict their caloric consumption to lose weight, the discussion usually begins with, “I know this might be difficult, but …” And it usually ends with me feeling a little less than anemic optimism.
But is it effective for weight loss?
C.S. Davis of Monash University, Melbourne, and colleagues conducted a systematic review of IER for weight loss (Eur J Clin Nutr. 2016 Mar;70[3]:292-9). The authors searched for articles evaluating the IER for weight loss among overweight and obese adults aged 18 years or older. IER was defined as periods of low energy intake (fast) alternating with periods of normal food intake (feed).
Eight studies were included in this review. Included studies defined low energy intake as 25%-50% of daily energy, or 400-1,400 kcal/day. The feed period was defined as either eating ad libitum or no less than 1,400 kcal/day. Studies varied in their approach and ranged from 2-4 consecutive fast days per week, followed by consecutive feed days, to three cycles of 5 weeks of fasting, followed by 5 weeks of ad lib eating.
IER was associated with 0.2-0.8 kg of weight loss per week. IER was associated with weight loss comparable to daily energy restriction (DER; that is, a typical diet). IER was comparable to typical daily energy restriction diets for fat mass, free-fat mass, and waist circumference.
The authors state that the amount of weight loss achieved with IER for a 100-kg individual would be associated with a 5% reduction in weight over a 5-week to 6-month time period. A 5% reduction is associated with a clinically significant reduction in health risk.
However, the authors found that fewer study participants planned to stick with IER beyond 6 months, compared with DER. Perhaps despite the difficulty that may exist in counting calories every day, the habit of doing the counting every day may be easier than doing it on an intermittent basis.
Regardless, IER is an option that may be beneficial to some patients. If other things haven’t worked for your patients, it is definitely worth a try.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition, nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician. Dr. Ebbert has no relevant financial disclosures about this article.
ILAE Approves New Seizure Classification
HOUSTON—The International League Against Epilepsy (ILAE) has approved a new seizure classification. Robert S. Fisher, MD, PhD, Director of the Epilepsy Center at Stanford University in California and Chair of the ILAE’s Seizure Classification Task Force, described the classification at the 70th Annual Meeting of the American Epilepsy Society.
The existing classification, published in 1981, worked well, but its limitations became apparent over time, Dr. Fisher said. For example, certain seizure types (eg, tonic) only existed in the generalized seizure category, even though they can occur focally. In addition, it was impossible to classify a seizure without knowing its onset, and some common seizures could not be classified at all.
The 2017 ILAE Seizure Classification addresses those limitations and updates certain terms to make them clearer to patients and people who do not specialize in seizure classification. “Some patients construe the word ‘simple’ to mean easy, and they feel that their seizures are not simple at all,” Dr. Fisher said. “So, a simple partial seizure is now going to be called a focal aware seizure. A complex partial seizure is a focal impaired awareness seizure.”
Impairment of consciousness has always played a key role in classifying seizures. The 2017 classification uses awareness as a surrogate marker of consciousness. Awareness can be used to classify focal, but not generalized onset, seizures in the new classification.
Focal seizures optionally may be further classified as motor or nonmotor. Nonmotor seizure types include behavior arrest, autonomic, cognitive, emotional, and sensory. Motor seizure types include atonic seizures, automatisms, clonic seizures, epileptic spasms, hyperkinetic seizures, myoclonic seizures, and tonic seizures.New generalized seizures include absence with eyelid myoclonia, epileptic spasms, myoclonic–atonic (as in Doose syndrome), and myoclonic–tonic–clonic (as in juvenile myoclonic epilepsy). A combined seizure type—focal to bilateral tonic–clonic—previously was known as secondarily generalized tonic–clonic.
Rules for Classifying Seizures
When classifying seizures, physicians should decide whether seizure onset is focal or generalized, using an 80% confidence level. Neurologists may classify focal seizures by degree of awareness or omit awareness as a classifier. If awareness is impaired at any point during a focal seizure, it is a focal impaired awareness seizure.
The first prominent sign or symptom of a focal seizure should be used for classification, not counting transient behavior arrest. A focal seizure is only considered a behavior arrest seizure if behavior arrest is the prominent feature of the entire seizure.
Clinicians are encouraged to add descriptions of other signs and symptoms, but these additions do not alter the seizure type (eg, focal emotional seizure with tonic right arm activity and hyperventilation). Seizures may be unclassified due to inadequate information or inability to place them in other categories, Dr. Fisher said.
Implications of Seizure Type
Seizure type may suggest a particular treatment, prognosis, restriction of an activity like driving, or an underlying disease process. The ILAE task force initially was interested in developing an entirely new seizure classification based anatomy, brain networks, or pathophysiology. “But we quickly realized that we just did not know enough about the underlying science,” Dr. Fisher said. Instead, they updated the existing, primarily observational classification.
The ILAE plans to publish the classification in an upcoming isssue of Epilepsia. A mapping table will allow neurologists to match old and new seizure terms.
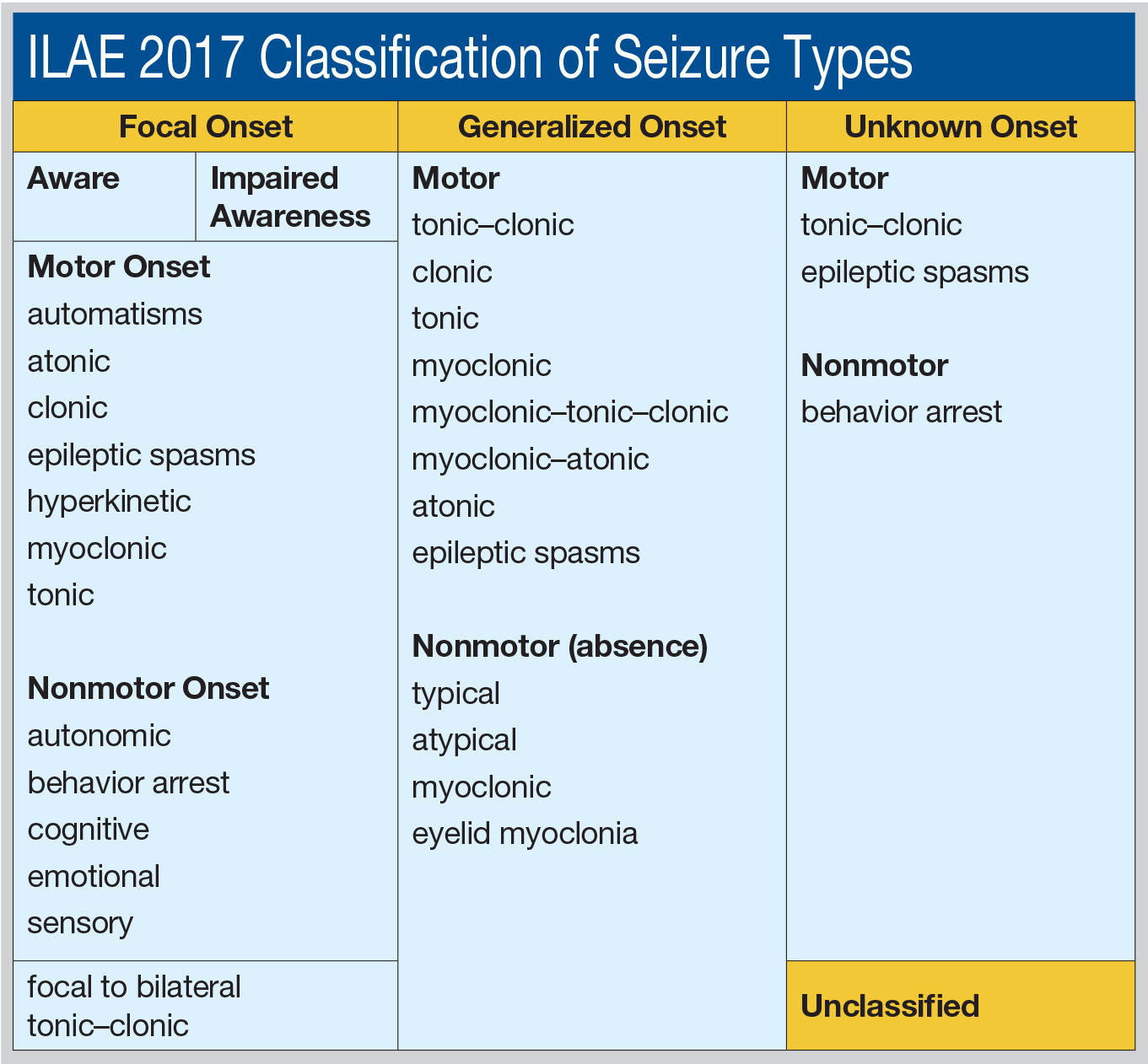
—Jake Remaly
HOUSTON—The International League Against Epilepsy (ILAE) has approved a new seizure classification. Robert S. Fisher, MD, PhD, Director of the Epilepsy Center at Stanford University in California and Chair of the ILAE’s Seizure Classification Task Force, described the classification at the 70th Annual Meeting of the American Epilepsy Society.
The existing classification, published in 1981, worked well, but its limitations became apparent over time, Dr. Fisher said. For example, certain seizure types (eg, tonic) only existed in the generalized seizure category, even though they can occur focally. In addition, it was impossible to classify a seizure without knowing its onset, and some common seizures could not be classified at all.
The 2017 ILAE Seizure Classification addresses those limitations and updates certain terms to make them clearer to patients and people who do not specialize in seizure classification. “Some patients construe the word ‘simple’ to mean easy, and they feel that their seizures are not simple at all,” Dr. Fisher said. “So, a simple partial seizure is now going to be called a focal aware seizure. A complex partial seizure is a focal impaired awareness seizure.”
Impairment of consciousness has always played a key role in classifying seizures. The 2017 classification uses awareness as a surrogate marker of consciousness. Awareness can be used to classify focal, but not generalized onset, seizures in the new classification.
Focal seizures optionally may be further classified as motor or nonmotor. Nonmotor seizure types include behavior arrest, autonomic, cognitive, emotional, and sensory. Motor seizure types include atonic seizures, automatisms, clonic seizures, epileptic spasms, hyperkinetic seizures, myoclonic seizures, and tonic seizures.New generalized seizures include absence with eyelid myoclonia, epileptic spasms, myoclonic–atonic (as in Doose syndrome), and myoclonic–tonic–clonic (as in juvenile myoclonic epilepsy). A combined seizure type—focal to bilateral tonic–clonic—previously was known as secondarily generalized tonic–clonic.
Rules for Classifying Seizures
When classifying seizures, physicians should decide whether seizure onset is focal or generalized, using an 80% confidence level. Neurologists may classify focal seizures by degree of awareness or omit awareness as a classifier. If awareness is impaired at any point during a focal seizure, it is a focal impaired awareness seizure.
The first prominent sign or symptom of a focal seizure should be used for classification, not counting transient behavior arrest. A focal seizure is only considered a behavior arrest seizure if behavior arrest is the prominent feature of the entire seizure.
Clinicians are encouraged to add descriptions of other signs and symptoms, but these additions do not alter the seizure type (eg, focal emotional seizure with tonic right arm activity and hyperventilation). Seizures may be unclassified due to inadequate information or inability to place them in other categories, Dr. Fisher said.
Implications of Seizure Type
Seizure type may suggest a particular treatment, prognosis, restriction of an activity like driving, or an underlying disease process. The ILAE task force initially was interested in developing an entirely new seizure classification based anatomy, brain networks, or pathophysiology. “But we quickly realized that we just did not know enough about the underlying science,” Dr. Fisher said. Instead, they updated the existing, primarily observational classification.
The ILAE plans to publish the classification in an upcoming isssue of Epilepsia. A mapping table will allow neurologists to match old and new seizure terms.
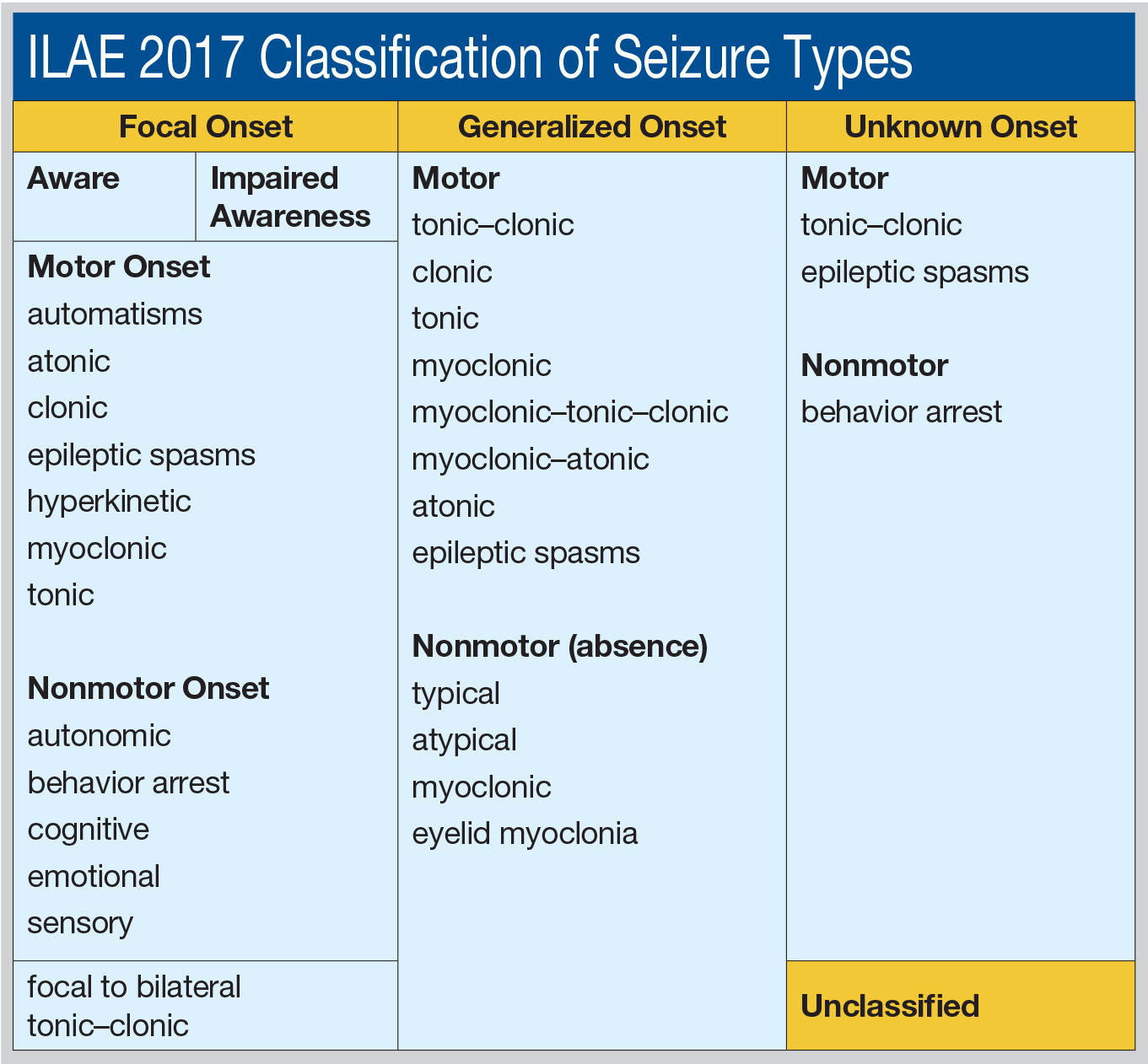
—Jake Remaly
HOUSTON—The International League Against Epilepsy (ILAE) has approved a new seizure classification. Robert S. Fisher, MD, PhD, Director of the Epilepsy Center at Stanford University in California and Chair of the ILAE’s Seizure Classification Task Force, described the classification at the 70th Annual Meeting of the American Epilepsy Society.
The existing classification, published in 1981, worked well, but its limitations became apparent over time, Dr. Fisher said. For example, certain seizure types (eg, tonic) only existed in the generalized seizure category, even though they can occur focally. In addition, it was impossible to classify a seizure without knowing its onset, and some common seizures could not be classified at all.
The 2017 ILAE Seizure Classification addresses those limitations and updates certain terms to make them clearer to patients and people who do not specialize in seizure classification. “Some patients construe the word ‘simple’ to mean easy, and they feel that their seizures are not simple at all,” Dr. Fisher said. “So, a simple partial seizure is now going to be called a focal aware seizure. A complex partial seizure is a focal impaired awareness seizure.”
Impairment of consciousness has always played a key role in classifying seizures. The 2017 classification uses awareness as a surrogate marker of consciousness. Awareness can be used to classify focal, but not generalized onset, seizures in the new classification.
Focal seizures optionally may be further classified as motor or nonmotor. Nonmotor seizure types include behavior arrest, autonomic, cognitive, emotional, and sensory. Motor seizure types include atonic seizures, automatisms, clonic seizures, epileptic spasms, hyperkinetic seizures, myoclonic seizures, and tonic seizures.New generalized seizures include absence with eyelid myoclonia, epileptic spasms, myoclonic–atonic (as in Doose syndrome), and myoclonic–tonic–clonic (as in juvenile myoclonic epilepsy). A combined seizure type—focal to bilateral tonic–clonic—previously was known as secondarily generalized tonic–clonic.
Rules for Classifying Seizures
When classifying seizures, physicians should decide whether seizure onset is focal or generalized, using an 80% confidence level. Neurologists may classify focal seizures by degree of awareness or omit awareness as a classifier. If awareness is impaired at any point during a focal seizure, it is a focal impaired awareness seizure.
The first prominent sign or symptom of a focal seizure should be used for classification, not counting transient behavior arrest. A focal seizure is only considered a behavior arrest seizure if behavior arrest is the prominent feature of the entire seizure.
Clinicians are encouraged to add descriptions of other signs and symptoms, but these additions do not alter the seizure type (eg, focal emotional seizure with tonic right arm activity and hyperventilation). Seizures may be unclassified due to inadequate information or inability to place them in other categories, Dr. Fisher said.
Implications of Seizure Type
Seizure type may suggest a particular treatment, prognosis, restriction of an activity like driving, or an underlying disease process. The ILAE task force initially was interested in developing an entirely new seizure classification based anatomy, brain networks, or pathophysiology. “But we quickly realized that we just did not know enough about the underlying science,” Dr. Fisher said. Instead, they updated the existing, primarily observational classification.
The ILAE plans to publish the classification in an upcoming isssue of Epilepsia. A mapping table will allow neurologists to match old and new seizure terms.
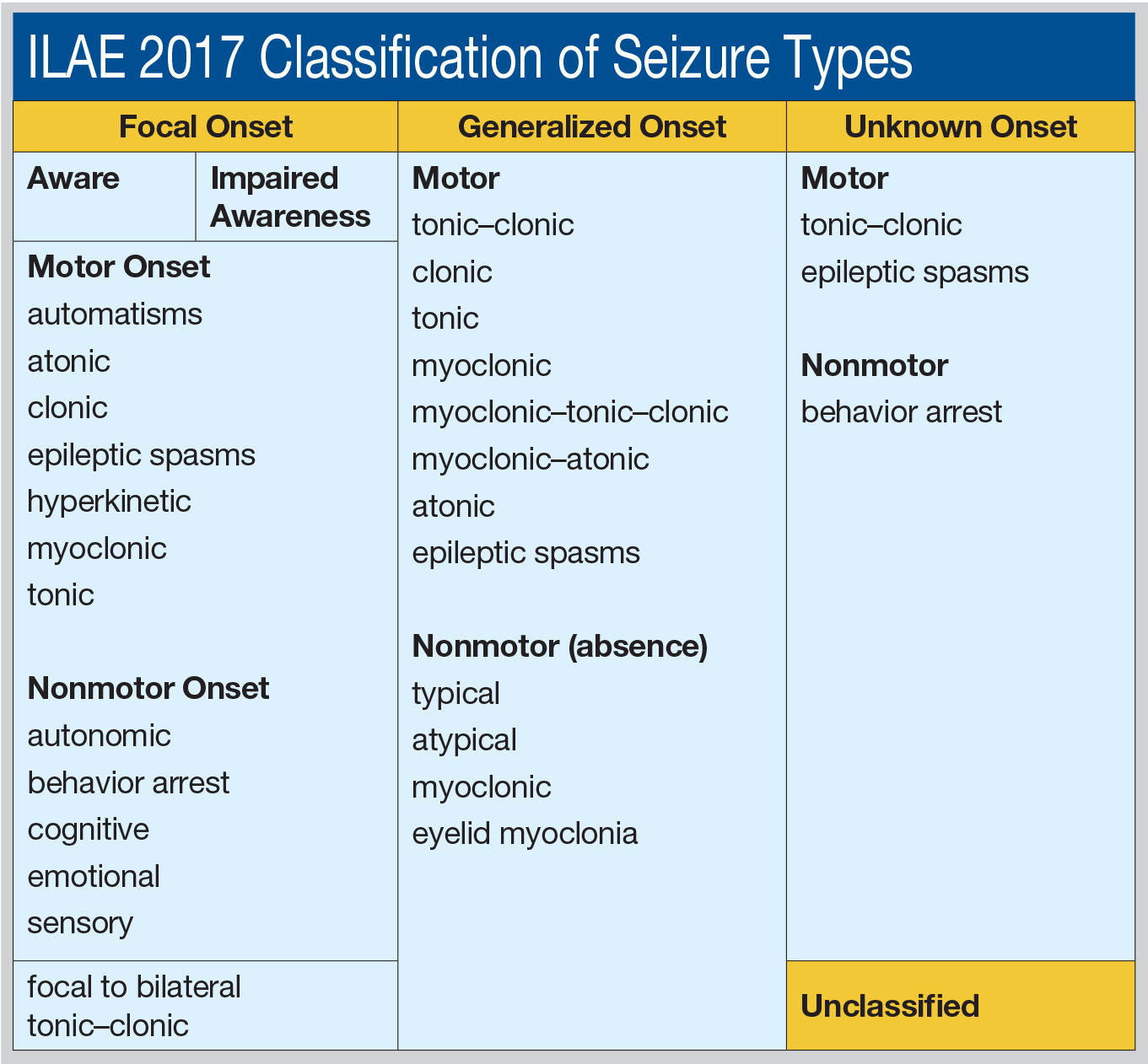
—Jake Remaly
Hypothermia does not provide neuroprotection during convulsive status epilepticus
Adding hypothermia therapy to standard care for convulsive status epilepticus is not neuroprotective, according to a report published online Dec. 22 in the New England Journal of Medicine.
Small-animal studies recently reported that therapeutic hypothermia had antiepileptic and neuroprotective properties. Researchers performed an open-label, randomized controlled trial to examine whether the treatment would improve neurologic outcomes in 268 consecutive adults treated at 11 ICUs in France for convulsive status epilepticus during a 4-year period. The average patient age was 57 years, and approximately half the study participants had a history of epilepsy. All required mechanical ventilation.
A total of 130 patients were assigned to receive standard care, and 138 were assigned to hypothermia in which their core body temperature was rapidly lowered to 32-34 degrees C and maintained at that level for 24 hours. Hypothermia was induced using ice-cold IV fluids and was maintained by applying ice packs to the groin and neck and surrounding the patient in a cold-air tunnel, said Stephane Legriel, MD, of the Medical-Surgical ICU, Centre Hospitalier de Versailles-Site André Mignot, France, and his associates.
The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group, indicating that the addition of hypothermia was not neuroprotective. In addition, ICU mortality, in-hospital mortality, and 90-day mortality were not significantly different between the two study groups. More patients in the hypothermia group (51%) than in the standard-care group (45%) developed pneumonia that was attributed to aspiration, the investigators reported (N Engl J Med. 2016;375:2457-67).
“The results of this trial do not support a beneficial effect of therapeutic hypothermia as compared with standard care alone in patients with convulsive status epilepticus receiving mechanical ventilation,” Dr. Legriel and his associates wrote.
This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
Adding hypothermia therapy to standard care for convulsive status epilepticus is not neuroprotective, according to a report published online Dec. 22 in the New England Journal of Medicine.
Small-animal studies recently reported that therapeutic hypothermia had antiepileptic and neuroprotective properties. Researchers performed an open-label, randomized controlled trial to examine whether the treatment would improve neurologic outcomes in 268 consecutive adults treated at 11 ICUs in France for convulsive status epilepticus during a 4-year period. The average patient age was 57 years, and approximately half the study participants had a history of epilepsy. All required mechanical ventilation.
A total of 130 patients were assigned to receive standard care, and 138 were assigned to hypothermia in which their core body temperature was rapidly lowered to 32-34 degrees C and maintained at that level for 24 hours. Hypothermia was induced using ice-cold IV fluids and was maintained by applying ice packs to the groin and neck and surrounding the patient in a cold-air tunnel, said Stephane Legriel, MD, of the Medical-Surgical ICU, Centre Hospitalier de Versailles-Site André Mignot, France, and his associates.
The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group, indicating that the addition of hypothermia was not neuroprotective. In addition, ICU mortality, in-hospital mortality, and 90-day mortality were not significantly different between the two study groups. More patients in the hypothermia group (51%) than in the standard-care group (45%) developed pneumonia that was attributed to aspiration, the investigators reported (N Engl J Med. 2016;375:2457-67).
“The results of this trial do not support a beneficial effect of therapeutic hypothermia as compared with standard care alone in patients with convulsive status epilepticus receiving mechanical ventilation,” Dr. Legriel and his associates wrote.
This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
Adding hypothermia therapy to standard care for convulsive status epilepticus is not neuroprotective, according to a report published online Dec. 22 in the New England Journal of Medicine.
Small-animal studies recently reported that therapeutic hypothermia had antiepileptic and neuroprotective properties. Researchers performed an open-label, randomized controlled trial to examine whether the treatment would improve neurologic outcomes in 268 consecutive adults treated at 11 ICUs in France for convulsive status epilepticus during a 4-year period. The average patient age was 57 years, and approximately half the study participants had a history of epilepsy. All required mechanical ventilation.
A total of 130 patients were assigned to receive standard care, and 138 were assigned to hypothermia in which their core body temperature was rapidly lowered to 32-34 degrees C and maintained at that level for 24 hours. Hypothermia was induced using ice-cold IV fluids and was maintained by applying ice packs to the groin and neck and surrounding the patient in a cold-air tunnel, said Stephane Legriel, MD, of the Medical-Surgical ICU, Centre Hospitalier de Versailles-Site André Mignot, France, and his associates.
The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group, indicating that the addition of hypothermia was not neuroprotective. In addition, ICU mortality, in-hospital mortality, and 90-day mortality were not significantly different between the two study groups. More patients in the hypothermia group (51%) than in the standard-care group (45%) developed pneumonia that was attributed to aspiration, the investigators reported (N Engl J Med. 2016;375:2457-67).
“The results of this trial do not support a beneficial effect of therapeutic hypothermia as compared with standard care alone in patients with convulsive status epilepticus receiving mechanical ventilation,” Dr. Legriel and his associates wrote.
This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: The primary outcome measure – the absence of functional impairment 90 days after admission, defined as a score of 5 on the Glasgow Outcome Scale – occurred in 49% of the hypothermia group and 43% of the control group.
Data source: An open-label, multicenter, randomized controlled trial involving 268 consecutive adults treated at 11 ICUs in France during a 4-year period.
Disclosures: This study was supported by the French Ministry of Health and received no industry support or involvement. Dr. Legriel reported having no relevant financial disclosures; two of his associates reported ties to Alexion, Astellas, Bard, and Gilead.
Enterovirus D68 – An emerging threat to child health
In August 2014, we first heard of increased pediatric cases of severe respiratory tract disease, many requiring management in the ICU, and of acute flaccid myelitis/paralysis (AFM) of unknown etiology from many states across the United States. Concurrently with this outbreak in the United States, similar clinical cases were reported in Canada and Europe. Subsequently, enterovirus D68 was confirmed in some, but not all, of the paralyzed children. Although new to many of us, enterovirus D68 was already known as an atypical enterovirus sharing many of its structural and chemical properties with rhinovirus. For example, it most often was reported from respiratory samples and less common from stool samples. It also had been associated with clusters of respiratory disease since 2000 and a 2008 case of fatal AFM.
There were 120 cases of AFM, coinciding with the nationwide outbreak of enteroviral D68 disease, reported in 2014. The Centers for Disease Control and Prevention has evaluated the cerebrospinal fluid in many of these cases, and no pathogen has consistently been detected. The children were mostly school age, aged 7-11 years, presented with acute, febrile respiratory illness followed by acute onset of cranial nerve dysfunction or flaccid paralysis of one or more limbs. The CSF revealed mild pleocytosis, most often with mild elevation of protein and a normal glucose. However, the MRI was distinctly abnormal with focal lesion in the cranial nerve nuclei (in those with bulbar dysfunction) and/or in the anterior horn or spinal cord gray matter. Long-term prognosis is unknown, although most patients have persistent weakness, despite some improvement, to date.
In 2016, the CDC has reported an increase in cases after a decline in 2015 despite the absence of epidemic respiratory tract disease in the United States from enterovirus D68. In the Netherlands, an increase in respiratory disease from enterovirus D68 in children and adults also has been reported since June 2016. Respiratory disease has been observed in children as young as 3 months of age, and most of the children have underlying comorbidity, many with asthma or other pulmonary conditions. Thirteen of 17 (77%) cases in children have required ICU admission, while most of the adult cases were mild and influenzalike. One child developed bulbar dysfunction and limb weakness.
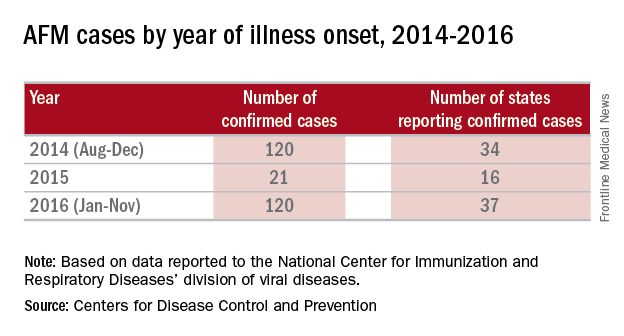
Enterovirus D68 infection should be suspected in children with moderate to severe respiratory tract infection or acute onset bulbar or flaccid paralysis of unknown etiology, especially in summer and fall. In such cases, respiratory specimens (nasopharyngeal or oral swabs or wash, tracheal secretions or bronchoalveolar lavage) should be obtained. Increasingly, hospitals and laboratories can perform multiplex polymerase chain reaction testing for enterovirus/rhinovirus. However, most do not determine the specific enterovirus. CDC and some state health departments use real-time reverse transcription polymerase chain reaction (rRT-PCR), which enables reporting of specific enterovirus species within days. CDC recommends that clinicians consider enterovirus D68 testing for children with unknown, severe respiratory illness or AFM. Details for sending specimens should be available from your state’s Department of Public Health website or the CDC.
Prevention strategies may be critical for limiting the spread of enterovirus D68 in the community. The CDC recommends:
- Wash your hands often with soap and water for 20 seconds.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Avoid close contact such as kissing, hugging, and sharing cups with people who are ill.
- Cover your coughs and sneezes with a tissue or shirt sleeve, not your hands.
- Clean and disinfect frequently touched surfaces, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are ill.
In 2014, it was speculated that the epidemic might have been a one-time event. It now appears more likely that enterovirus D68 activity has been increasing since 2000, and that children and immunocompromised hosts will be at greatest risk because of a lack of neutralizing antibody. Ongoing enterovirus surveillance will be critical to understand the potential for severe respiratory disease as will the development of new and effective antivirals. A vaccine for enterovirus 71 recently demonstrated efficacy against hand, foot, and mouth disease in children and may provide insights into the development of vaccines against enterovirus D68.
References
Lancet Infect Dis. 2016 May;16(5):e64-75
Emerg Infect Dis. 2017 Jan;23(1):140-3.
J Med Virol. 2016 May;88(5):739-45
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
In August 2014, we first heard of increased pediatric cases of severe respiratory tract disease, many requiring management in the ICU, and of acute flaccid myelitis/paralysis (AFM) of unknown etiology from many states across the United States. Concurrently with this outbreak in the United States, similar clinical cases were reported in Canada and Europe. Subsequently, enterovirus D68 was confirmed in some, but not all, of the paralyzed children. Although new to many of us, enterovirus D68 was already known as an atypical enterovirus sharing many of its structural and chemical properties with rhinovirus. For example, it most often was reported from respiratory samples and less common from stool samples. It also had been associated with clusters of respiratory disease since 2000 and a 2008 case of fatal AFM.
There were 120 cases of AFM, coinciding with the nationwide outbreak of enteroviral D68 disease, reported in 2014. The Centers for Disease Control and Prevention has evaluated the cerebrospinal fluid in many of these cases, and no pathogen has consistently been detected. The children were mostly school age, aged 7-11 years, presented with acute, febrile respiratory illness followed by acute onset of cranial nerve dysfunction or flaccid paralysis of one or more limbs. The CSF revealed mild pleocytosis, most often with mild elevation of protein and a normal glucose. However, the MRI was distinctly abnormal with focal lesion in the cranial nerve nuclei (in those with bulbar dysfunction) and/or in the anterior horn or spinal cord gray matter. Long-term prognosis is unknown, although most patients have persistent weakness, despite some improvement, to date.
In 2016, the CDC has reported an increase in cases after a decline in 2015 despite the absence of epidemic respiratory tract disease in the United States from enterovirus D68. In the Netherlands, an increase in respiratory disease from enterovirus D68 in children and adults also has been reported since June 2016. Respiratory disease has been observed in children as young as 3 months of age, and most of the children have underlying comorbidity, many with asthma or other pulmonary conditions. Thirteen of 17 (77%) cases in children have required ICU admission, while most of the adult cases were mild and influenzalike. One child developed bulbar dysfunction and limb weakness.
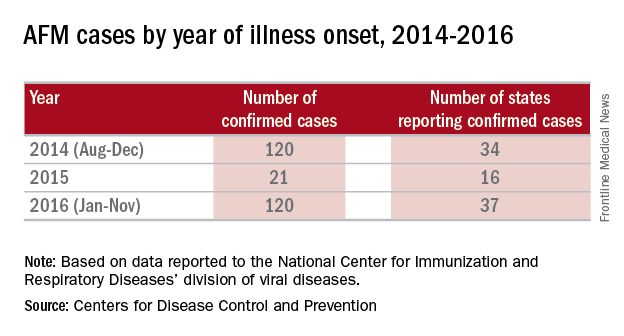
Enterovirus D68 infection should be suspected in children with moderate to severe respiratory tract infection or acute onset bulbar or flaccid paralysis of unknown etiology, especially in summer and fall. In such cases, respiratory specimens (nasopharyngeal or oral swabs or wash, tracheal secretions or bronchoalveolar lavage) should be obtained. Increasingly, hospitals and laboratories can perform multiplex polymerase chain reaction testing for enterovirus/rhinovirus. However, most do not determine the specific enterovirus. CDC and some state health departments use real-time reverse transcription polymerase chain reaction (rRT-PCR), which enables reporting of specific enterovirus species within days. CDC recommends that clinicians consider enterovirus D68 testing for children with unknown, severe respiratory illness or AFM. Details for sending specimens should be available from your state’s Department of Public Health website or the CDC.
Prevention strategies may be critical for limiting the spread of enterovirus D68 in the community. The CDC recommends:
- Wash your hands often with soap and water for 20 seconds.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Avoid close contact such as kissing, hugging, and sharing cups with people who are ill.
- Cover your coughs and sneezes with a tissue or shirt sleeve, not your hands.
- Clean and disinfect frequently touched surfaces, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are ill.
In 2014, it was speculated that the epidemic might have been a one-time event. It now appears more likely that enterovirus D68 activity has been increasing since 2000, and that children and immunocompromised hosts will be at greatest risk because of a lack of neutralizing antibody. Ongoing enterovirus surveillance will be critical to understand the potential for severe respiratory disease as will the development of new and effective antivirals. A vaccine for enterovirus 71 recently demonstrated efficacy against hand, foot, and mouth disease in children and may provide insights into the development of vaccines against enterovirus D68.
References
Lancet Infect Dis. 2016 May;16(5):e64-75
Emerg Infect Dis. 2017 Jan;23(1):140-3.
J Med Virol. 2016 May;88(5):739-45
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
In August 2014, we first heard of increased pediatric cases of severe respiratory tract disease, many requiring management in the ICU, and of acute flaccid myelitis/paralysis (AFM) of unknown etiology from many states across the United States. Concurrently with this outbreak in the United States, similar clinical cases were reported in Canada and Europe. Subsequently, enterovirus D68 was confirmed in some, but not all, of the paralyzed children. Although new to many of us, enterovirus D68 was already known as an atypical enterovirus sharing many of its structural and chemical properties with rhinovirus. For example, it most often was reported from respiratory samples and less common from stool samples. It also had been associated with clusters of respiratory disease since 2000 and a 2008 case of fatal AFM.
There were 120 cases of AFM, coinciding with the nationwide outbreak of enteroviral D68 disease, reported in 2014. The Centers for Disease Control and Prevention has evaluated the cerebrospinal fluid in many of these cases, and no pathogen has consistently been detected. The children were mostly school age, aged 7-11 years, presented with acute, febrile respiratory illness followed by acute onset of cranial nerve dysfunction or flaccid paralysis of one or more limbs. The CSF revealed mild pleocytosis, most often with mild elevation of protein and a normal glucose. However, the MRI was distinctly abnormal with focal lesion in the cranial nerve nuclei (in those with bulbar dysfunction) and/or in the anterior horn or spinal cord gray matter. Long-term prognosis is unknown, although most patients have persistent weakness, despite some improvement, to date.
In 2016, the CDC has reported an increase in cases after a decline in 2015 despite the absence of epidemic respiratory tract disease in the United States from enterovirus D68. In the Netherlands, an increase in respiratory disease from enterovirus D68 in children and adults also has been reported since June 2016. Respiratory disease has been observed in children as young as 3 months of age, and most of the children have underlying comorbidity, many with asthma or other pulmonary conditions. Thirteen of 17 (77%) cases in children have required ICU admission, while most of the adult cases were mild and influenzalike. One child developed bulbar dysfunction and limb weakness.
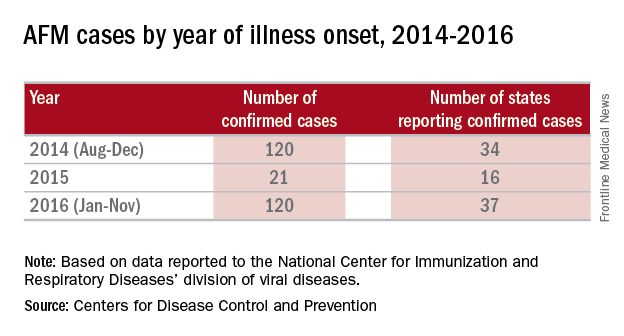
Enterovirus D68 infection should be suspected in children with moderate to severe respiratory tract infection or acute onset bulbar or flaccid paralysis of unknown etiology, especially in summer and fall. In such cases, respiratory specimens (nasopharyngeal or oral swabs or wash, tracheal secretions or bronchoalveolar lavage) should be obtained. Increasingly, hospitals and laboratories can perform multiplex polymerase chain reaction testing for enterovirus/rhinovirus. However, most do not determine the specific enterovirus. CDC and some state health departments use real-time reverse transcription polymerase chain reaction (rRT-PCR), which enables reporting of specific enterovirus species within days. CDC recommends that clinicians consider enterovirus D68 testing for children with unknown, severe respiratory illness or AFM. Details for sending specimens should be available from your state’s Department of Public Health website or the CDC.
Prevention strategies may be critical for limiting the spread of enterovirus D68 in the community. The CDC recommends:
- Wash your hands often with soap and water for 20 seconds.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Avoid close contact such as kissing, hugging, and sharing cups with people who are ill.
- Cover your coughs and sneezes with a tissue or shirt sleeve, not your hands.
- Clean and disinfect frequently touched surfaces, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are ill.
In 2014, it was speculated that the epidemic might have been a one-time event. It now appears more likely that enterovirus D68 activity has been increasing since 2000, and that children and immunocompromised hosts will be at greatest risk because of a lack of neutralizing antibody. Ongoing enterovirus surveillance will be critical to understand the potential for severe respiratory disease as will the development of new and effective antivirals. A vaccine for enterovirus 71 recently demonstrated efficacy against hand, foot, and mouth disease in children and may provide insights into the development of vaccines against enterovirus D68.
References
Lancet Infect Dis. 2016 May;16(5):e64-75
Emerg Infect Dis. 2017 Jan;23(1):140-3.
J Med Virol. 2016 May;88(5):739-45
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
Meta-analysis compares infliximab with tacrolimus in ulcerative colitis
ORLANDO – Infliximab and tacrolimus each demonstrate efficacy for treatment of moderate to severe active ulcerative colitis in published studies. However, it remains unknown if one agent offers greater efficacy than the other in this patient population, so researchers in Japan conducted a meta-analysis to find out more.
Lead investigator Shinichi Kawano, MD, at Kyushu University, Fukuoka, Japan, and his colleagues searched PubMed for relevant studies up until August 2016. They conducted a systematic review and identified 79 potential studies of tumor necrosis factor blocker infliximab (Remicade, Janssen) and the calcineurin inhibitor tacrolimus (various brands) in this patient population. They ruled out the vast majority, 75 studies, for not directly comparing therapeutic efficacy. They also excluded one additional study for insufficient data on their five outcomes of interest: rates of clinical remission, clinical response, freedom from colectomy, adverse events, and serious adverse events. They focused on three 2016 retrospective studies with a total of 244 patients, and added 13 of their own patients, 5 taking infliximab and 8 taking tacrolimus, to their dataset.
Similarly, the short-term clinical response rate favored infliximab (overall RR, 1.55), but again the difference was not statistically significant.
The investigators found the rate of colectomy was comparable between patients taking infliximab and tacrolimus (overall RR, 1.01). They reported their findings in a poster presentation at the Advances in Inflammatory Bowel Diseases meeting, sponsored by the Crohn’s & Colitis Foundation of America.
The adverse event rate favored tacrolimus over infliximab, but it was not significant (overall RR, 0.23). The serious adverse event rate slightly favored tacrolimus as well (overall RR, 0.88). The incidences of adverse events and serious adverse events were comparable between the two groups, the study authors wrote.
The trials included in the meta-analysis looked at either adults only or adults and pediatric patients with active ulcerative colitis. In one study, there were 40 patients taking infliximab and 50 taking tacrolimus (Aliment Pharmacol Ther. 2016;43:705-16); in another 48 patients took infliximab and 47 took tacrolimus (Gastroenterol Res Pract. 2016;2016:3162595); and in the third study 30 were treated with infliximab and 29 with tacrolimus (Scand J Gastroenterol. 2016;51:700-5).
“This meta-analysis demonstrates equivalent therapeutic efficacy and safety between infliximab and tacrolimus,” the authors continued. Dr. Kawano said he was not surprised by the findings. “Because there are only three retrospective studies, it is reasonable that there is no significant difference in efficacy between infliximab and tacrolimus.”
However, he added, “We think that further prospective, comparative trials are needed.”
Dr. Kawano had no relevant financial disclosures.
ORLANDO – Infliximab and tacrolimus each demonstrate efficacy for treatment of moderate to severe active ulcerative colitis in published studies. However, it remains unknown if one agent offers greater efficacy than the other in this patient population, so researchers in Japan conducted a meta-analysis to find out more.
Lead investigator Shinichi Kawano, MD, at Kyushu University, Fukuoka, Japan, and his colleagues searched PubMed for relevant studies up until August 2016. They conducted a systematic review and identified 79 potential studies of tumor necrosis factor blocker infliximab (Remicade, Janssen) and the calcineurin inhibitor tacrolimus (various brands) in this patient population. They ruled out the vast majority, 75 studies, for not directly comparing therapeutic efficacy. They also excluded one additional study for insufficient data on their five outcomes of interest: rates of clinical remission, clinical response, freedom from colectomy, adverse events, and serious adverse events. They focused on three 2016 retrospective studies with a total of 244 patients, and added 13 of their own patients, 5 taking infliximab and 8 taking tacrolimus, to their dataset.
Similarly, the short-term clinical response rate favored infliximab (overall RR, 1.55), but again the difference was not statistically significant.
The investigators found the rate of colectomy was comparable between patients taking infliximab and tacrolimus (overall RR, 1.01). They reported their findings in a poster presentation at the Advances in Inflammatory Bowel Diseases meeting, sponsored by the Crohn’s & Colitis Foundation of America.
The adverse event rate favored tacrolimus over infliximab, but it was not significant (overall RR, 0.23). The serious adverse event rate slightly favored tacrolimus as well (overall RR, 0.88). The incidences of adverse events and serious adverse events were comparable between the two groups, the study authors wrote.
The trials included in the meta-analysis looked at either adults only or adults and pediatric patients with active ulcerative colitis. In one study, there were 40 patients taking infliximab and 50 taking tacrolimus (Aliment Pharmacol Ther. 2016;43:705-16); in another 48 patients took infliximab and 47 took tacrolimus (Gastroenterol Res Pract. 2016;2016:3162595); and in the third study 30 were treated with infliximab and 29 with tacrolimus (Scand J Gastroenterol. 2016;51:700-5).
“This meta-analysis demonstrates equivalent therapeutic efficacy and safety between infliximab and tacrolimus,” the authors continued. Dr. Kawano said he was not surprised by the findings. “Because there are only three retrospective studies, it is reasonable that there is no significant difference in efficacy between infliximab and tacrolimus.”
However, he added, “We think that further prospective, comparative trials are needed.”
Dr. Kawano had no relevant financial disclosures.
ORLANDO – Infliximab and tacrolimus each demonstrate efficacy for treatment of moderate to severe active ulcerative colitis in published studies. However, it remains unknown if one agent offers greater efficacy than the other in this patient population, so researchers in Japan conducted a meta-analysis to find out more.
Lead investigator Shinichi Kawano, MD, at Kyushu University, Fukuoka, Japan, and his colleagues searched PubMed for relevant studies up until August 2016. They conducted a systematic review and identified 79 potential studies of tumor necrosis factor blocker infliximab (Remicade, Janssen) and the calcineurin inhibitor tacrolimus (various brands) in this patient population. They ruled out the vast majority, 75 studies, for not directly comparing therapeutic efficacy. They also excluded one additional study for insufficient data on their five outcomes of interest: rates of clinical remission, clinical response, freedom from colectomy, adverse events, and serious adverse events. They focused on three 2016 retrospective studies with a total of 244 patients, and added 13 of their own patients, 5 taking infliximab and 8 taking tacrolimus, to their dataset.
Similarly, the short-term clinical response rate favored infliximab (overall RR, 1.55), but again the difference was not statistically significant.
The investigators found the rate of colectomy was comparable between patients taking infliximab and tacrolimus (overall RR, 1.01). They reported their findings in a poster presentation at the Advances in Inflammatory Bowel Diseases meeting, sponsored by the Crohn’s & Colitis Foundation of America.
The adverse event rate favored tacrolimus over infliximab, but it was not significant (overall RR, 0.23). The serious adverse event rate slightly favored tacrolimus as well (overall RR, 0.88). The incidences of adverse events and serious adverse events were comparable between the two groups, the study authors wrote.
The trials included in the meta-analysis looked at either adults only or adults and pediatric patients with active ulcerative colitis. In one study, there were 40 patients taking infliximab and 50 taking tacrolimus (Aliment Pharmacol Ther. 2016;43:705-16); in another 48 patients took infliximab and 47 took tacrolimus (Gastroenterol Res Pract. 2016;2016:3162595); and in the third study 30 were treated with infliximab and 29 with tacrolimus (Scand J Gastroenterol. 2016;51:700-5).
“This meta-analysis demonstrates equivalent therapeutic efficacy and safety between infliximab and tacrolimus,” the authors continued. Dr. Kawano said he was not surprised by the findings. “Because there are only three retrospective studies, it is reasonable that there is no significant difference in efficacy between infliximab and tacrolimus.”
However, he added, “We think that further prospective, comparative trials are needed.”
Dr. Kawano had no relevant financial disclosures.
AT AIBD 2016
Key clinical point: Infliximab and tacrolimus both demonstrate efficacy for active ulcerative colitis in published studies, but few direct comparisons exist.
Major finding: The reported rate of clinical remission with infliximab was higher than with tacrolimus (risk ratio, 1.17), but the difference was not statistically significant.
Data source: Meta-analysis of relevant articles identified in a PubMed search through August 2016.
Disclosures: Dr. Kawano had no relevant financial disclosures.