User login
Ixazomib/lenalidomide maintenance promising after ASCT in MM
ATLANTA—Adding ixazomib to lenalidomide as maintenance therapy for newly diagnosed multiple myeloma (MM) patients after upfront autologous stem cell transplant (ASCT) appears promising, according to an update of a phase 2 study.
The oral doublet produced an overall response rate of 90% and an estimated 2-year progression-free survival (PFS) rate of 81%.
The incidence of peripheral neuropathy was mostly limited to grade 1/2 events, and hematologic adverse events were manageable with dose reductions.
Krina K. Patel, MD, of MD Anderson Cancer Center in Houston, Texas, presented these results at the 2017 ASH Annual Meeting (abstract 437*).
Dr Patel and her colleagues conducted a single-arm, phase 2 study to evaluate the safety and efficacy of adding ixazomib to lenalidomide maintenance in MM patients after ASCT.
“[O]ur phase 2 hypothesis was that ixazomib would provide a safe, more effective, and more convenient alternative maintenance therapy, which would allow better quality of life and improve PFS when combined with lenalidomide,” Dr Patel said.
Study design
Patients had to have received ASCT within 12 months of induction therapy in order to be eligible for the study.
Maintenance therapy was initiated within 60 to 180 days after transplant. It consisted of 28-day cycles of ixazomib at 4 mg on days 1, 8, and 15 and lenalidomide at 10 mg daily on days 1 to 28.
After 3 months, patients’ lenalidomide dose could increase to 15 mg if they tolerated the drug.
Investigators amended the protocol during the first year of the study to reduce the dose of ixazomib to 3 mg.
“Based on other studies at the time,” Dr Patel explained, “they showed increased neutropenia with the higher dose of ixazomib.”
Patient characteristics
The investigators enrolled 64 evaluable patients from December 2012 to June 2015. They had a median age of 60 (range, 39 – 74).
Forty-two patients (66%) were male, and 22 were female.
Thirty-three had ISS stage I disease, 13 had stage II, and 9 had stage III. Fourteen patients (21.8%) had high-risk disease.
At the time of the presentation, 34 patients (52%) remained on therapy. As of September 2017, patients had received a median of 30 cycles of maintenance therapy (range, 1 – 55).
Safety
Forty-eight patients (75%) had neuropathy at enrollment. Most of these patients had received bortezomib-based induction therapy, Dr Patel explained.
Twenty-two patients (34%) had grade 1/2 peripheral neuropathy at last follow-up, and 6 patients (9%) had grade 3.
Baseline neuropathy worsened in 6 patients, and this necessitated dose reductions. One patient had new-onset neuropathy, also requiring dose reduction. And 8 patients had new-onset neuropathy that did not require dose reductions.
“Most of these patients had a break [in therapy] of about 2 to 8 weeks,” Dr Patel noted, “and were able to either go back on a lower dose versus stopping the therapy.”
Three patients had a secondary primary malignancy: 1 with breast ductal carcinoma in situ and 2 with squamous cell carcinoma of the skin.
Other grade 3 adverse events included: anemia (3%), neutropenia (41%), thrombocytopenia (6%), elevated liver enzymes (11%), back pain (3%), constipation (6%), elevated creatinine (1.6%), nausea/vomiting (11%), diarrhea (9%), fatigue (11%), rash (13%), peripheral neuropathy (9%), myalgia (5%), urinary tract infection (5%), and upper respiratory tract infection/pneumonia (36%).
Grade 4 adverse events included neutropenia (5%), thrombocytopenia (8%), and respiratory failure (1.6%).
Thirty patients are off study, 16 due to progressive disease, 3 at the investigator’s discretion, and 11 withdrew their consent.
Eight of the 16 patients who progressed had high-risk disease. Among the 16, the median PFS was 17 months (range, 3 – 43).
Seven patients died with an overall survival of 4 months (n=1), 16 months (n=2), 20 months (n=2), or 48 months (n=2).
Dose reductions
Sixteen patients started ixazomib at a dose of 4 mg, and 48 started at 3 mg.
Fifteen patients had their ixazomib dose reduced to 2.4 mg due to peripheral neuropathy (n=8), neutropenia (n=3), hearing loss (n=2), rash (n=1), or thrombocytopenia (n=1).
Five patients had a second dose reduction to 1.5 mg due to neuropathy (n=3), neutropenia (n=1), or thrombocytopenia (n=1).
Four patients who required a third dose reduction for neuropathy (n=2), neutropenia (n=1), and thrombocytopenia (n=1) went off study.
All patients started lenalidomide at 10 mg for 28 days.
Twenty-four patients required a lenalidomide dose reduction. Fifteen patients stayed at 10 mg but for 21 of 28 days, and 9 patients reduced to 5 mg for 28 days.
Reasons for these reductions were neutropenia (n=12), rash (n=4), thrombocytopenia (n=3), fatigue (n=2), memory impairment (n=1), infection (n=1), and pruritis (n=1).
Five patients required a second dose reduction to 5 mg for 21 of 28 days. Reasons for these reductions were neutropenia (n=2), neuropathy (n=1), thrombocytopenia (n=1), and fatigue (n=1).
“There are about 10 patients who did not have any ixazomib reductions that needed lenalidomide reductions, mostly for the pancytopenia,” Dr Patel noted.
Efficacy
Fifty-six percent of patients achieved a very good partial response, 26% a complete response (CR), 8% a stringent CR, and 10% a partial response.
Twenty-nine patients (45%) experienced an improvement in their best overall response from post-transplant baseline.
The median time to response was 10.1 months. The median duration of response has not yet been reached. Investigators estimated the 4-year duration of response to be 62%.
At a median follow-up of 38.2 months, the median PFS had not yet been reached. Investigators estimated the 2-year PFS to be 81%.
The median PFS for patients with high-risk disease is 21.85 months.
Based on these results, the investigators believe ixazomib-lenalidomide maintenance is safe, feasible, and well-tolerated and should be further explored in phase 3 studies.
Dr Patel has received research funding from and served on an advisory committee for Pfizer. She has consulted for Juno and Celgene.
The study was supported by Takeda Oncology. ![]()
* Data in the presentation differ slightly from the abstract.
ATLANTA—Adding ixazomib to lenalidomide as maintenance therapy for newly diagnosed multiple myeloma (MM) patients after upfront autologous stem cell transplant (ASCT) appears promising, according to an update of a phase 2 study.
The oral doublet produced an overall response rate of 90% and an estimated 2-year progression-free survival (PFS) rate of 81%.
The incidence of peripheral neuropathy was mostly limited to grade 1/2 events, and hematologic adverse events were manageable with dose reductions.
Krina K. Patel, MD, of MD Anderson Cancer Center in Houston, Texas, presented these results at the 2017 ASH Annual Meeting (abstract 437*).
Dr Patel and her colleagues conducted a single-arm, phase 2 study to evaluate the safety and efficacy of adding ixazomib to lenalidomide maintenance in MM patients after ASCT.
“[O]ur phase 2 hypothesis was that ixazomib would provide a safe, more effective, and more convenient alternative maintenance therapy, which would allow better quality of life and improve PFS when combined with lenalidomide,” Dr Patel said.
Study design
Patients had to have received ASCT within 12 months of induction therapy in order to be eligible for the study.
Maintenance therapy was initiated within 60 to 180 days after transplant. It consisted of 28-day cycles of ixazomib at 4 mg on days 1, 8, and 15 and lenalidomide at 10 mg daily on days 1 to 28.
After 3 months, patients’ lenalidomide dose could increase to 15 mg if they tolerated the drug.
Investigators amended the protocol during the first year of the study to reduce the dose of ixazomib to 3 mg.
“Based on other studies at the time,” Dr Patel explained, “they showed increased neutropenia with the higher dose of ixazomib.”
Patient characteristics
The investigators enrolled 64 evaluable patients from December 2012 to June 2015. They had a median age of 60 (range, 39 – 74).
Forty-two patients (66%) were male, and 22 were female.
Thirty-three had ISS stage I disease, 13 had stage II, and 9 had stage III. Fourteen patients (21.8%) had high-risk disease.
At the time of the presentation, 34 patients (52%) remained on therapy. As of September 2017, patients had received a median of 30 cycles of maintenance therapy (range, 1 – 55).
Safety
Forty-eight patients (75%) had neuropathy at enrollment. Most of these patients had received bortezomib-based induction therapy, Dr Patel explained.
Twenty-two patients (34%) had grade 1/2 peripheral neuropathy at last follow-up, and 6 patients (9%) had grade 3.
Baseline neuropathy worsened in 6 patients, and this necessitated dose reductions. One patient had new-onset neuropathy, also requiring dose reduction. And 8 patients had new-onset neuropathy that did not require dose reductions.
“Most of these patients had a break [in therapy] of about 2 to 8 weeks,” Dr Patel noted, “and were able to either go back on a lower dose versus stopping the therapy.”
Three patients had a secondary primary malignancy: 1 with breast ductal carcinoma in situ and 2 with squamous cell carcinoma of the skin.
Other grade 3 adverse events included: anemia (3%), neutropenia (41%), thrombocytopenia (6%), elevated liver enzymes (11%), back pain (3%), constipation (6%), elevated creatinine (1.6%), nausea/vomiting (11%), diarrhea (9%), fatigue (11%), rash (13%), peripheral neuropathy (9%), myalgia (5%), urinary tract infection (5%), and upper respiratory tract infection/pneumonia (36%).
Grade 4 adverse events included neutropenia (5%), thrombocytopenia (8%), and respiratory failure (1.6%).
Thirty patients are off study, 16 due to progressive disease, 3 at the investigator’s discretion, and 11 withdrew their consent.
Eight of the 16 patients who progressed had high-risk disease. Among the 16, the median PFS was 17 months (range, 3 – 43).
Seven patients died with an overall survival of 4 months (n=1), 16 months (n=2), 20 months (n=2), or 48 months (n=2).
Dose reductions
Sixteen patients started ixazomib at a dose of 4 mg, and 48 started at 3 mg.
Fifteen patients had their ixazomib dose reduced to 2.4 mg due to peripheral neuropathy (n=8), neutropenia (n=3), hearing loss (n=2), rash (n=1), or thrombocytopenia (n=1).
Five patients had a second dose reduction to 1.5 mg due to neuropathy (n=3), neutropenia (n=1), or thrombocytopenia (n=1).
Four patients who required a third dose reduction for neuropathy (n=2), neutropenia (n=1), and thrombocytopenia (n=1) went off study.
All patients started lenalidomide at 10 mg for 28 days.
Twenty-four patients required a lenalidomide dose reduction. Fifteen patients stayed at 10 mg but for 21 of 28 days, and 9 patients reduced to 5 mg for 28 days.
Reasons for these reductions were neutropenia (n=12), rash (n=4), thrombocytopenia (n=3), fatigue (n=2), memory impairment (n=1), infection (n=1), and pruritis (n=1).
Five patients required a second dose reduction to 5 mg for 21 of 28 days. Reasons for these reductions were neutropenia (n=2), neuropathy (n=1), thrombocytopenia (n=1), and fatigue (n=1).
“There are about 10 patients who did not have any ixazomib reductions that needed lenalidomide reductions, mostly for the pancytopenia,” Dr Patel noted.
Efficacy
Fifty-six percent of patients achieved a very good partial response, 26% a complete response (CR), 8% a stringent CR, and 10% a partial response.
Twenty-nine patients (45%) experienced an improvement in their best overall response from post-transplant baseline.
The median time to response was 10.1 months. The median duration of response has not yet been reached. Investigators estimated the 4-year duration of response to be 62%.
At a median follow-up of 38.2 months, the median PFS had not yet been reached. Investigators estimated the 2-year PFS to be 81%.
The median PFS for patients with high-risk disease is 21.85 months.
Based on these results, the investigators believe ixazomib-lenalidomide maintenance is safe, feasible, and well-tolerated and should be further explored in phase 3 studies.
Dr Patel has received research funding from and served on an advisory committee for Pfizer. She has consulted for Juno and Celgene.
The study was supported by Takeda Oncology. ![]()
* Data in the presentation differ slightly from the abstract.
ATLANTA—Adding ixazomib to lenalidomide as maintenance therapy for newly diagnosed multiple myeloma (MM) patients after upfront autologous stem cell transplant (ASCT) appears promising, according to an update of a phase 2 study.
The oral doublet produced an overall response rate of 90% and an estimated 2-year progression-free survival (PFS) rate of 81%.
The incidence of peripheral neuropathy was mostly limited to grade 1/2 events, and hematologic adverse events were manageable with dose reductions.
Krina K. Patel, MD, of MD Anderson Cancer Center in Houston, Texas, presented these results at the 2017 ASH Annual Meeting (abstract 437*).
Dr Patel and her colleagues conducted a single-arm, phase 2 study to evaluate the safety and efficacy of adding ixazomib to lenalidomide maintenance in MM patients after ASCT.
“[O]ur phase 2 hypothesis was that ixazomib would provide a safe, more effective, and more convenient alternative maintenance therapy, which would allow better quality of life and improve PFS when combined with lenalidomide,” Dr Patel said.
Study design
Patients had to have received ASCT within 12 months of induction therapy in order to be eligible for the study.
Maintenance therapy was initiated within 60 to 180 days after transplant. It consisted of 28-day cycles of ixazomib at 4 mg on days 1, 8, and 15 and lenalidomide at 10 mg daily on days 1 to 28.
After 3 months, patients’ lenalidomide dose could increase to 15 mg if they tolerated the drug.
Investigators amended the protocol during the first year of the study to reduce the dose of ixazomib to 3 mg.
“Based on other studies at the time,” Dr Patel explained, “they showed increased neutropenia with the higher dose of ixazomib.”
Patient characteristics
The investigators enrolled 64 evaluable patients from December 2012 to June 2015. They had a median age of 60 (range, 39 – 74).
Forty-two patients (66%) were male, and 22 were female.
Thirty-three had ISS stage I disease, 13 had stage II, and 9 had stage III. Fourteen patients (21.8%) had high-risk disease.
At the time of the presentation, 34 patients (52%) remained on therapy. As of September 2017, patients had received a median of 30 cycles of maintenance therapy (range, 1 – 55).
Safety
Forty-eight patients (75%) had neuropathy at enrollment. Most of these patients had received bortezomib-based induction therapy, Dr Patel explained.
Twenty-two patients (34%) had grade 1/2 peripheral neuropathy at last follow-up, and 6 patients (9%) had grade 3.
Baseline neuropathy worsened in 6 patients, and this necessitated dose reductions. One patient had new-onset neuropathy, also requiring dose reduction. And 8 patients had new-onset neuropathy that did not require dose reductions.
“Most of these patients had a break [in therapy] of about 2 to 8 weeks,” Dr Patel noted, “and were able to either go back on a lower dose versus stopping the therapy.”
Three patients had a secondary primary malignancy: 1 with breast ductal carcinoma in situ and 2 with squamous cell carcinoma of the skin.
Other grade 3 adverse events included: anemia (3%), neutropenia (41%), thrombocytopenia (6%), elevated liver enzymes (11%), back pain (3%), constipation (6%), elevated creatinine (1.6%), nausea/vomiting (11%), diarrhea (9%), fatigue (11%), rash (13%), peripheral neuropathy (9%), myalgia (5%), urinary tract infection (5%), and upper respiratory tract infection/pneumonia (36%).
Grade 4 adverse events included neutropenia (5%), thrombocytopenia (8%), and respiratory failure (1.6%).
Thirty patients are off study, 16 due to progressive disease, 3 at the investigator’s discretion, and 11 withdrew their consent.
Eight of the 16 patients who progressed had high-risk disease. Among the 16, the median PFS was 17 months (range, 3 – 43).
Seven patients died with an overall survival of 4 months (n=1), 16 months (n=2), 20 months (n=2), or 48 months (n=2).
Dose reductions
Sixteen patients started ixazomib at a dose of 4 mg, and 48 started at 3 mg.
Fifteen patients had their ixazomib dose reduced to 2.4 mg due to peripheral neuropathy (n=8), neutropenia (n=3), hearing loss (n=2), rash (n=1), or thrombocytopenia (n=1).
Five patients had a second dose reduction to 1.5 mg due to neuropathy (n=3), neutropenia (n=1), or thrombocytopenia (n=1).
Four patients who required a third dose reduction for neuropathy (n=2), neutropenia (n=1), and thrombocytopenia (n=1) went off study.
All patients started lenalidomide at 10 mg for 28 days.
Twenty-four patients required a lenalidomide dose reduction. Fifteen patients stayed at 10 mg but for 21 of 28 days, and 9 patients reduced to 5 mg for 28 days.
Reasons for these reductions were neutropenia (n=12), rash (n=4), thrombocytopenia (n=3), fatigue (n=2), memory impairment (n=1), infection (n=1), and pruritis (n=1).
Five patients required a second dose reduction to 5 mg for 21 of 28 days. Reasons for these reductions were neutropenia (n=2), neuropathy (n=1), thrombocytopenia (n=1), and fatigue (n=1).
“There are about 10 patients who did not have any ixazomib reductions that needed lenalidomide reductions, mostly for the pancytopenia,” Dr Patel noted.
Efficacy
Fifty-six percent of patients achieved a very good partial response, 26% a complete response (CR), 8% a stringent CR, and 10% a partial response.
Twenty-nine patients (45%) experienced an improvement in their best overall response from post-transplant baseline.
The median time to response was 10.1 months. The median duration of response has not yet been reached. Investigators estimated the 4-year duration of response to be 62%.
At a median follow-up of 38.2 months, the median PFS had not yet been reached. Investigators estimated the 2-year PFS to be 81%.
The median PFS for patients with high-risk disease is 21.85 months.
Based on these results, the investigators believe ixazomib-lenalidomide maintenance is safe, feasible, and well-tolerated and should be further explored in phase 3 studies.
Dr Patel has received research funding from and served on an advisory committee for Pfizer. She has consulted for Juno and Celgene.
The study was supported by Takeda Oncology. ![]()
* Data in the presentation differ slightly from the abstract.
Heart failure treatment: Keeping up with best practices
Heart failure (HF) affects nearly 6 million Americans and accounts for one million hospital admissions each year.1 The condition, which results from a structural or functional disorder that impairs the ventricles’ ability to fill, empty, or both,2 is a major cause of morbidity and mortality. The 5-year mortality rate ranges from 44% to 77%.3,4
Growing evidence demonstrates reduced morbidity and mortality when patients with HF with reduced ejection fraction (HFrEF) are treated with an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB); a beta-blocker; and a mineralocorticoid/aldosterone receptor antagonist (MRA) in appropriate doses.5 In addition, 2 new medications representing novel drug classes have recently entered the market and are recommended in select patients who remain symptomatic despite standard treatment.
The first is sacubitril, which is available in a combination pill with the ARB valsartan, and the second is ivabradine.6 Additionally, implanted medical devices are proving useful, particularly in the management of patients with refractory symptoms.
This article will briefly review the diagnosis and initial evaluation of the patient with suspected HF and then describe how newer treatments fit within HF management priorities and strategies. But first, a word about what causes HF.
Causes are many and diverse
HF has a variety of cardiac and non-cardiac etiologies.2,7,8 Some important cardiac causes include hypertension (HTN), coronary artery disease (CAD), valvular heart disease, arrhythmias, myocarditis, Takotsubo cardiomyopathy, and postpartum cardiomyopathy. Common and important non-cardiac causes of HF include alcoholic cardiomyopathy, pulmonary embolism, pulmonary hypertension, obstructive sleep apnea, anemia, hemochromatosis, amyloidosis, sarcoidosis, thyroid dysfunction, nephrotic syndrome, and cardiac toxins (especially stimulants and certain chemotherapy drugs).2,7,8
Diagnosing an elusive culprit
HF remains a clinical diagnosis. Common symptoms include dyspnea, cough, pedal edema, and decreased exercise tolerance, but these symptoms are not at all specific. Given the varied causes and manifestations of HF, the diagnosis can be somewhat elusive. Fortunately, there are a number of objective methods to help identify patients with HF.
Framingham criteria. One commonly used tool for making the diagnosis of HF is the Framingham criteria (see https://www.mdcalc.com/framingham-heart-failure-diagnostic-criteria),9 which diagnoses HF based on historical and physical exam findings. Another well-validated decision tool is the Heart Failure Diagnostic Rule (see http://circ.ahajournals.org/content/124/25/2865.long),10 which incorporates N-terminal pro–B-type natriuretic peptide (NT-proBNP) results, as well as exam findings.
Measurement of natriuretic peptides, either B-type natriuretic peptide (BNP) or NT-proBNP, aids in the diagnosis of HF.5 Although several factors (including age, weight, and renal function) can affect BNP levels, a normal BNP value effectively rules out HF5,7 and an elevated BNP can help to make the diagnosis in the context of a patient with corresponding symptoms.
The initial evaluation: Necessary lab work and imaging studies
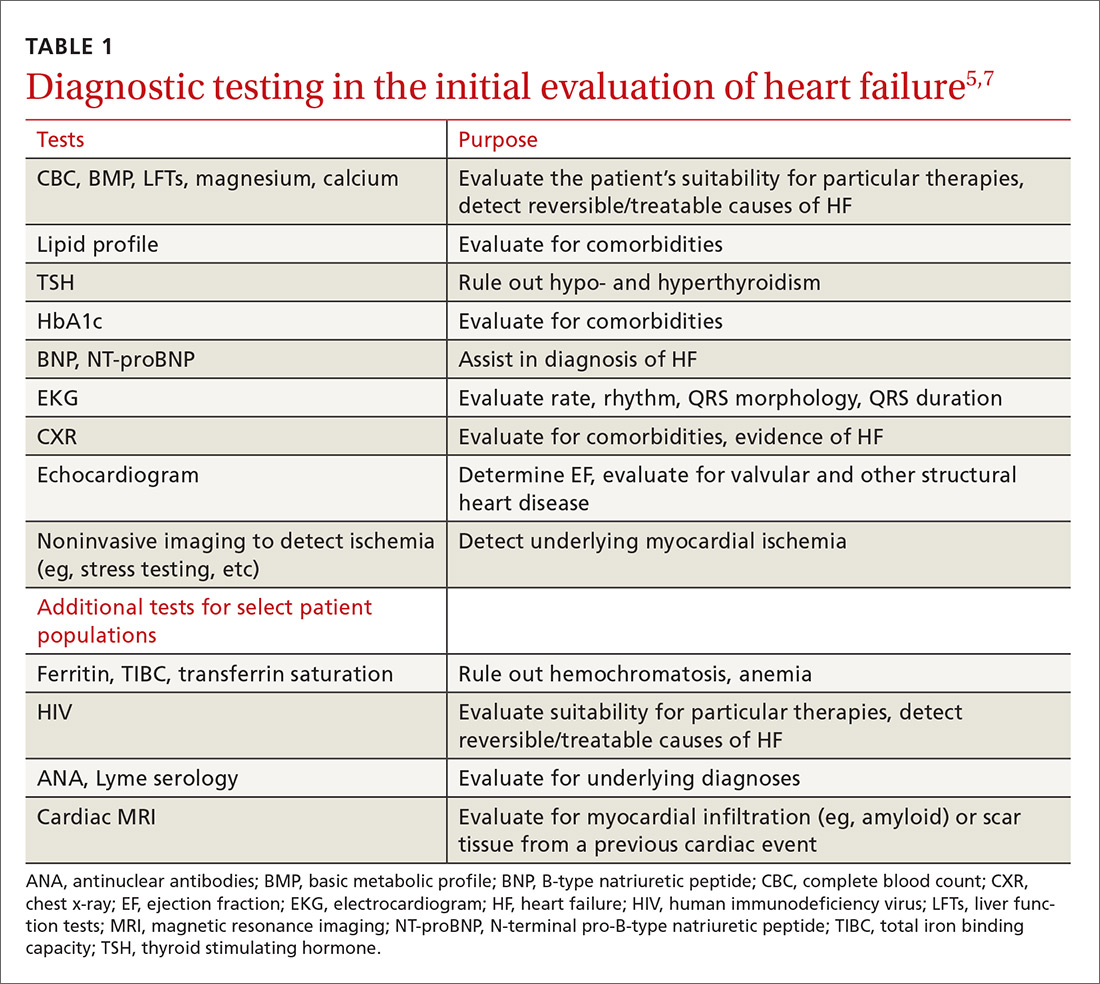
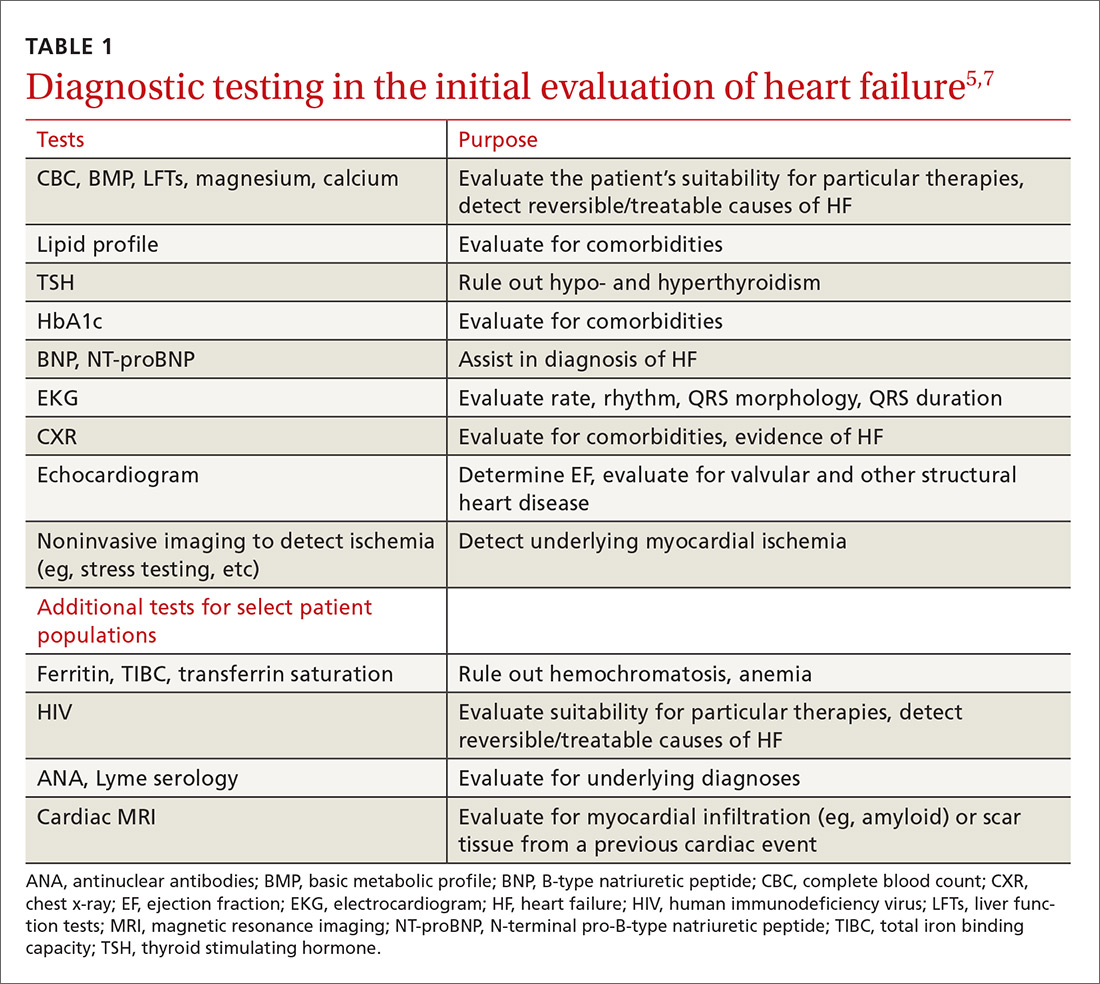
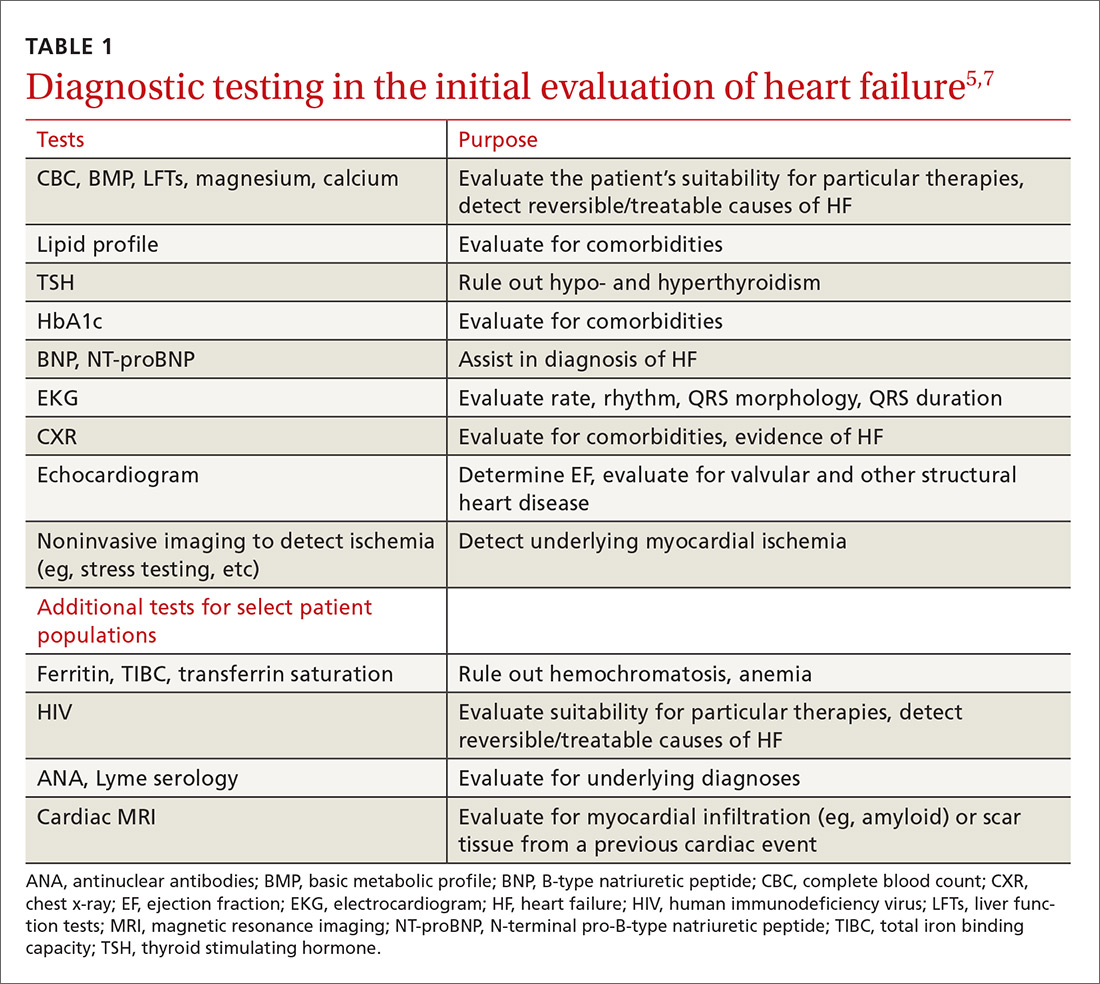
The purpose of the initial evaluation of the patient with suspected HF is to establish the diagnosis, look for underlying etiologies of HF, identify comorbidities, and establish baseline values (eg, of potassium and creatinine) for elements monitored during treatment.5,7 TABLE 15,7 lists the lab work and imaging tests that are commonly ordered in the initial evaluation of the patient with HF.
Echocardiography is useful in determining the ejection fraction (EF), which is essential in guiding treatment. Echocardiography can also identify important structural abnormalities including significant valvular disease. Refer patients with severe valvular disease for evaluation for valve repair/replacement, regardless of EF.8
Noninvasive testing (stress nuclear imaging or echocardiography) to evaluate for underlying CAD is reasonable in patients with unknown CAD status.8,11 Patients for whom there is a high suspicion of obstructive CAD should undergo coronary angiography if they are candidates for revascularization.5,7 Noninvasive testing may also be an acceptable option for assessing ischemia in patients presenting with HF who have known CAD and no angina.5
Classification of HF is determined by ejection fraction
Physicians have traditionally classified patients with HF as having either systolic or diastolic dysfunction. Patients with HF symptoms and a reduced EF were said to have systolic dysfunction; those with a normal EF were said to have diastolic dysfunction.
More recently, researchers have learned that patients with reduced EF and those with preserved EF can have both systolic and diastolic dysfunction simultaneously.8 Therefore, the current preferred terminology is HFpEF (heart failure with preserved ejection fraction) for those with an EF ≥50% and HFrEF (heart failure with reduced ejection fraction) for those with an EF ≤40%.5 Both the American Heart Association (AHA) and the European Society of Cardiology recognize a category of HF with moderately reduced ejection fraction defined as an EF between 40% and 50%.5,7 Practically speaking, this group is treated as per the guidelines for HFrEF.5
Treatment of HFrEF: The evidence is clear
The cornerstone of medical treatment for HFrEF is the combination of an ACE inhibitor or ARB with a beta-blocker.2,5,7,8 Several early trials showed clear benefits of these medications. For example, the Studies Of Left Ventricular Dysfunction trial (SOLVD), compared enalapril to placebo in patients receiving standard therapy (consisting chiefly of digitalis, diuretics, and nitrates). This study demonstrated a reduction in all-cause mortality or first hospitalization for HF (number needed to treat [NNT]=21) in the enalapril group vs the placebo group.12
Similarly, a subgroup analysis of the Valsartan Heart Failure Treatment (Val-HeFT) trial demonstrated morbidity (NNT=10) and all-cause mortality benefits (NNT=6) when valsartan (an ARB) was given to patients who were not receiving an ACE inhibitor.13
MERIT-HF (Metoprolol CR/XL Randomised Intervention Trial in congestive Heart Failure) compared the beta-blocker metoprolol succinate to placebo and found fewer deaths from HF and lower all-cause mortality (NNT=26) associated with the treatment group vs the placebo group.14
And a comparison of 2 beta-blockers—carvedilol and metoprolol tartrate—on clinical outcomes in patients with chronic HF in the Carvedilol Or Metoprolol European Trial (COMET) showed that carvedilol extended survival compared with metoprolol tartrate (NNT=19).15
Unlike ACE inhibitors and ARBs, which seem to show a class benefit, only 3 beta-blockers available in the United States have been proven to reduce mortality: sustained-release metoprolol succinate, carvedilol, and bisoprolol.2,7,8
Unless contraindicated, all patients with a reduced EF—even those without symptoms—should receive a beta-blocker and an ACE inhibitor or ARB.5,7,8
Cautionary notes
Remember the following caveats when treating patients with ACE inhibitors, ARBs, and beta-blockers:
- Use ACE inhibitors and ARBs with caution in patients with impaired renal function (serum creatinine >2.5 mg/dL) or elevated serum potassium (>5 mEq/L).16,17
- ARBs are associated with a much lower incidence of cough and angioedema than ACE inhibitors.18
- Although physicians frequently start patients on low doses of beta-blockers and ACE inhibitors or ARBs to minimize hypotension and other adverse effects, the goal of therapy is to titrate up to the therapeutic doses used in clinical trials.5-7 (For dosages of medications commonly used in the treatment of heart failure, see Table 3 in the American College of Cardiology/AHA/Heart Failure Society of America guidelines available at https://www.sciencedirect.com/science/article/pii/S0735109717370870?via%3Dihub#tbl3 and Table 7.2 in the European Society of Cardiology guidelines available at https://academic.oup.com/eurheartj/article/37/27/2129/1748921.)
- Because beta-blockers can exacerbate fluid retention, do not initiate them in patients with fluid overload unless such patients are being treated with diuretics.5,19
When more Tx is needed
For patients who remain symptomatic despite treatment with an ACE inhibitor or ARB and a beta-blocker, consider the following add-on therapies.
Diuretics are the only medications used in the treatment of HF that adequately reduce fluid overload.2,7 While thiazide diuretics confer greater blood pressure control, loop diuretics are generally preferred in the treatment of HF because they are more efficacious.5 Loop diuretics should be prescribed to all patients with fluid overload, as few patients can maintain their target (“dry”) weight without diuretic therapy.5,7 Common adverse effects include hypokalemia, dehydration, and azotemia.
Two MRAs are currently available in the United States: spironolactone and eplerenone. MRAs are used as add-on therapy for symptomatic patients with an EF ≤35% or an EF ≤40% following an acute myocardial infarction (MI).5 They significantly reduce all-cause mortality (NNT=26).20
Because hyperkalemia is a risk with MRAs, do not prescribe them for patients who are already taking both an ACE inhibitor and an ARB.5 Also, do not initiate MRA therapy in patients who have an elevated creatinine level (≥2.5 mg/dL in men; ≥2 mg/dL in women) or a potassium level ≥5 mEq/L.5,7,8 Discontinue MRA therapy if a patient’s potassium level rises to ≥5.5 mEq/L.5
Hydralazine combined with isosorbide dinitrate (H/ID) is an alternative in patients for whom ACE inhibitor/ARB therapy is contraindicated.5,8
H/ID is also an add-on option in African American patients. Trials have demonstrated that H/ID reduces both first hospitalization for HF (NNT=13) and all-cause mortality (NNT=25) when it is used as add-on therapy in African Americans already receiving standard therapy with an ACE inhibitor or ARB, a beta-blocker, and an MRA.21 Headache and dizziness are commonly reported adverse effects.
Digoxin does not reduce mortality, but it does improve both quality of life and exercise tolerance and reduces hospital admissions for patients with HF.5,7 Significant adverse effects of digoxin include anorexia, nausea, visual disturbances, and cardiac arrhythmias.22
Also, hypokalemia can intensify digoxin toxicity.23 Because of these concerns, digoxin is typically dosed at 0.125 mg/d (0.125 mg every other day in patients >70 years or patients with impaired renal function or low body weight) with a target therapeutic range of 0.5 to 0.9 ng/mL.5
New classes, new agents
Sacubitril, a neprilysin inhibitor, is the first drug from this class approved for use in the United States. Neprilysin is the enzyme responsible for the degradation of natriuretic peptides; as such it increases endogenous NPs, promoting diuresis and lowering blood pressure.24,25 Early trials with sacubitril alone showed limited clinical efficacy;25 however, when it was combined with the ARB, valsartan (the combination being called angiotensin receptor blocker + neprilysin inhibitor [ARNI] therapy), it was found to be of significant benefit.6,25
The PARADIGM-HF (Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure) trial compared outcomes in patients receiving ARNI therapy to those receiving enalapril.26 The authors stopped the trial early due to the overwhelming benefit seen in the ARNI arm.
After a median follow-up of 27 months, the researchers found a reduction in the primary outcomes of either cardiovascular death or first hospitalization for HF (26.5% in the enalapril-treated group vs 21.8% in the ARNI-treated group; NNT=21).26 There were slightly more cases of angioedema in the ARNI arm than in the enalapril arm (0.5% vs 0.2%), although there were no patients in the trial who required endotracheal intubation.26
Because of this increased risk, do not prescribe ARNI therapy for any patient with a history of angioedema.6 Hypotension was more common in the ARNI-treated group than in the enalapril group (14% vs 9.2%), but there were lower rates of hyperkalemia, elevated serum creatinine, and cough in the ARNI-treated group than in the enalapril group.26
Consider ARNI treatment for all patients with an EF ≤40% who remain symptomatic despite appropriate doses of an ACE inhibitor or ARB plus a beta-blocker. Do not administer ARNI therapy concomitantly with an ACE inhibitor or ARB. When switching, do not start ARNI therapy for at least 36 hours after the last dose of an ACE inhibitor or ARB.6
Ivabradine is a sinoatrial node modulator that provides additional heart rate reduction. It does not affect ventricular repolarization or myocardial contractility.27 Early trials with this medication have shown reduced cardiac mortality and an NNT to prevent one first HF hospitalization within one year of 27.28 Adverse effects include symptomatic and asymptomatic bradycardia and luminous phenomena.28
Recommend ivabradine as add-on therapy to all patients with an EF ≤35%, normal sinus rhythm, and resting heart rate ≥70 bpm who remain symptomatic despite taking the maximum-tolerated dose of a beta-blocker.6 The dose is adjusted to achieve a resting heart rate of 50 to 60 bpm.27
Nonpharmacologic options
Implantable cardioverter defibrillators (ICDs) are recommended as primary prevention in select HFrEF patients to reduce the risk of sudden cardiac death and all-cause mortality. The 2013 American College of Cardiology Foundation/AHA Guideline for the Management of Heart Failure recommends an ICD for primary prevention for: 1) patients with symptomatic HF and an LVEF ≤35% despite ≥3 months of optimal medical therapy, and 2) patients at least 40 days post-MI with an LVEF of ≤30%.5,29 ICDs are not recommended for patients who have a life expectancy of less than one year, and the devices are of unclear benefit for patients ≥75 years of age.5
Cardiac resynchronization therapy (CRT), although not new to the field of cardiology, is new to the treatment of heart failure. A number of patients with HFrEF have QRS prolongation and in particular, left bundle branch block (LBBB).5 CRT uses biventricular pacing to restore synchronous contraction of the left and right ventricles.30 It is strongly recommended for patients with an EF ≤35%, sinus rhythm, LBBB, QRS ≥150 ms, and a life expectancy of at least one year.5,7 It is weakly recommended for patients with an EF ≤35% and a QRS ≥150 ms but without LBBB. It’s also weakly recommended for patients with an EF ≤35% and LBBB with a QRS of 120 to 150 ms.5,31
Left ventricular assist devices (LVADs) and cardiac transplantation are considerations for patients with severe symptoms refractory to all other interventions.5 LVADs may be used either while awaiting cardiac transplantation (bridge therapy) or as definitive treatment (destination therapy). Appropriate patient selection for such therapies requires a team of experts that ideally includes HF and transplantation cardiologists, cardiothoracic surgeons, nurses, social workers, and palliative care clinicians.5
Treatment of HFpEF: Evidence is lacking
While HFpEF is common—affecting about half of all patients with HF—ideal treatment remains unclear.32 Some trials have shown promise, but to date no unequivocal evidence exists that any standard therapy reduces mortality in patients with HFpEF.33-37 Underlying mechanisms of action of HFpEF include cardiac rate and rhythm abnormalities, atrial dysfunction, and stiffening of the ventricles. In a sense, it represents an exaggerated expression of the pathophysiology seen with the normal aging of the heart and can be conceptualized as “presbycardia.”37 Indeed, HFpEF is more common in the elderly, but it is also more common in patients of African descent.38,39 Common contributing causes (which we’ll get to in a bit) include HTN, CAD, atrial fibrillation (AF), obesity, and obstructive sleep apnea (OSA).
Trials have failed to show clear benefit for ACE inhibitors, ARBs, or beta-blockers.7,33 The evidence for MRAs is somewhat unclear; however, they have recently been recommended as an option for patients who have been hospitalized in the last year to reduce the risk of subsequent hospitalizations.40 Digoxin is used primarily for rate control in the setting of AF, but otherwise is of unclear benefit.7 A low-sodium diet (ie, ≤2 g/d) may be useful in those patients who are prone to fluid overload.5,7 The cornerstone of treatment of HFpEF is the relief of volume overload with diuretics and the treatment of coexisting conditions.33
Common contributing causes of HFpEF
HTN is not only a common contributing cause, but also the most common comorbid condition affecting patients with HFpEF. As such, treatment of HTN represents the most important management goal.33,34 Based on recent data, the American College of Cardiology, the AHA, and the Heart Failure Society of America have recommended a systolic blood pressure goal <130 mm Hg for patients with HFpEF.40 Most patients with HFpEF and HTN will have some degree of fluid overload and, therefore, should receive a diuretic.
CAD. Patients with HFpEF should be evaluated for CAD and treated with medical management and coronary revascularization, as appropriate.
AF is poorly tolerated by patients with HFpEF.37 Patients with AF should receive anticoagulation and rate control medications, and those with persistent HF symptoms should be evaluated for rhythm control.33
Obesity is more prevalent in patients with HFpEF than in those with HFrEF.41 Although there is indirect evidence that weight loss improves cardiac function,34,42,43 and studies have shown bariatric surgery to improve diastolic function,44,45 there are no studies reporting clinical outcomes.
Treatment of OSA with continuous positive airway pressure appears to alleviate some symptoms of HF and to reduce all-cause mortality.46,47
Keeping HF patients out of the hospital
Many readmissions to the hospital for HF exacerbation are preventable. Patients often do not understand hospital discharge instructions or the nature of their chronic disease and its management.48-51 Routine follow-up in the office or clinic provides an opportunity to improve quality of life for patients and decrease admissions.7,52
A major role for the family physician is in the co-creation of, and adherence to, an individualized, comprehensive care plan. Make sure such a plan is easily understood not only by the patient with HF, but also by his or her care team. In addition, it should be evidence-based and reflect the patient’s culture, values, and goals of treatment.5,7
At each visit, the family physician or a member of the health care team should assess adherence to guideline-directed medical therapy, measure weight, evaluate fluid status, and provide ongoing patient education including information on the importance of activity, monitoring weight daily, and moderating fluid, salt, and alcohol intake.5,52
Research shows that cardiac rehabilitation improves functional capacity, exercise duration, quality of life, and mortality. Therefore, recommend it to all symptomatic patients with HF who are clinically stable.2
Consider collaboration with a subspecialist. Patients who remain symptomatic despite optimal medical management and patients with recurrent hospitalizations are best managed in conjunction with a subspecialist in HF treatment.2,5
CORRESPONDENCE
Darin Brink, MD, 420 Delaware St. SE, MMC 381, Minneapolis, MN 55455; [email protected].
1. Hall MJ, Levant S, DeFrances CJ. Hospitalization for congestive heart failure: United States, 2000-2010. NCHS Data Brief. 2012;(108):1-8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23102190. Accessed April 26, 2017.
2. Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused Update Incorporated Into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1-e90.
3. Passantino A, Guida P, Lagioia R, et al. Predictors of long-term mortality in older patients hospitalized for acutely decompensated heart failure: clinical relevance of natriuretic peptides. J Am Geriatr Soc. 2017;65:822-826.
4. Lassus JP, Siirilä-Waris K, Nieminen MS, et al. Long-term survival after hospitalization for acute heart failure—differences in prognosis of acutely decompensated chronic and new-onset acute heart failure. Int J Cardiol. 2013;168:458-462.
5. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327.
6. Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure. J Am Coll Cardiol. 2016;68:1476-1488.
7. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.
8. Pinkerman CP, Sander JE, Breeding D, et al. Institute for Clinical Systems Improvement. Heart failure in adults. Available at: https://www.scribd.com/document/310893227/HeartFailure-pdf. Accessed December 6, 2017.
9. McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham Study. N Engl J Med. 1971;285:1441-1446.
10. Kelder JC, Cramer MJ, van Wijngaarden J, et al. The diagnostic value of physical examination and additional testing in primary care patients with suspected heart failure. Circulation. 2011;124:2865-2873.
11. Heart Failure Society of America, Lindenfeld J, Albert NM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1-194.
12. Pouleur H, The SOLVD Investigators. Results of the treatment trial of the studies of left ventricular dysfunction (SOLVD). Am J Cardiol. 1992;70:135-136.
13. Maggioni AP, Anand I, Gottlieb SO, et al. Effects of valsartan on morbidity and mortality in patients with heart failure not receiving angiotensin-converting enzyme inhibitors. J Am Coll Cardiol. 2002;40:1414-1421.
14. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353:2001-2007.
15. Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet. 2003;362:7-13.
16. Gehr TW, Sica DA. Pharmacotherapy in congestive heart failure: Hyperkalemia in congestive heart failure. Congest Heart Fail. 2001;7:97-100.
17. National Institute for Health and Clinical Excellence (NICE). Chronic heart failure in adults: management. 2010. Available at: https://www.nice.org.uk/guidance/cg108. Accessed November 27, 2017.
18. Barreras A, Gurk-Turner C. Angiotensin II receptor blockers. Proc (Bayl Univ Med Cent). 2003;16:123-126.
19. Epstein SE, Braunwald E. The effect of beta adrenergic blockade on patterns of urinary sodium excretion: studies in normal subjects and in patients with heart disease. Ann Intern Med. 1966;65:20-27.
20. Berbenetz NM, Mrkobrada M. Mineralocorticoid receptor antagonists for heart failure: systematic review and meta-analysis. BMC Cardiovasc Disord. 2016;16:246.
21. Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049-2057.
22. Kelly RA, Smith TW. Recognition and management of digitalis toxicity. Am J Cardiol. 1992;69:108G-118G.
23. Sundar S, Burma DP, Vaish SK. Digoxin toxicity and electrolytes: a correlative study. Acta Cardiol. 1983;38:115-123.
24. McDowell G, Nicholls DP. The endopeptidase inhibitor, candoxatril, and its therapeutic potential in the treatment of chronic cardiac failure in man. Expert Opin Investig Drugs. 1999;8:79-84.
25. Prenner SB, Shah SJ, Yancy CW. Role of angiotensin receptor-neprilysin inhibition in heart failure. Curr Atheroscler Rep. 2016;18:48.
26. McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993-1004.
27. Corlanor package insert. Amgen Inc., Thousand Oaks, CA. Available at: http://pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/corlanor/corlanor_pi.pdf. Accessed November 28, 2017.
28. Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875-885.
29. Kusumoto FM, Calkins H, Boehmer J, et al. HRS/ACC/AHA expert consensus statement on the use of implantable cardioverter-defibrillator therapy in patients who are not included or not well represented in clinical trials. Circulation. 2014;130:94-125.
30. Leyva F, Nisam S, Auricchio A. 20 years of cardiac resynchronization therapy. J Am Coll Cardiol. 2014;64:1047-1058.
31. Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS Focused Update Incorporated Into the ACCF/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2013;127:e283-e352.
32. Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
33. Redfield MM. Heart failure with preserved ejection fraction. N Engl J Med. 2016;375:1868-1877.
34. Nanayakkara S, Kaye DM. Management of heart failure with preserved ejection fraction: a review. Clin Ther. 2015;37:2186-2198.
35. Cleland JG, Pellicori P, Dierckx R. Clinical trials in patients with heart failure and preserved left ventricular ejection fraction. Heart Fail Clin. 2014;10:511-523.
36. Ferrari R, Böhm M, Cleland JGF, et al. Heart failure with preserved ejection fraction: uncertainties and dilemmas. Eur J Heart Fail. 2015;17:665-671.
37. Borlaug BA. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2014;11:507-515.
38. Sharp A, Tapp R, Francis DP, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol. 2008;52:1015-1021.
39. Zile MR. Heart failure with a preserved ejection fraction. In: Mann DL, Zipes D, Libby P BR, eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Phila
40. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776-803.
41. Mentz RJ, Kelly JP, von Lueder TG, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2014;64:2281-2293.
42. de las Fuentes L, Waggoner AD, Mohammed BS, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009;54:2376-2381.
43. Kitzman DW, Brubaker P, Morgan T, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction. JAMA. 2016;315:36-46.
44. Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54:718-726.
45. Ristow B, Rabkin J, Haeusslein E. Improvement in dilated cardiomyopathy after bariatric surgery. J Card Fail. 2008;14:198-202.
46. Yoshihisa A, Suzuki S, Yamauchi H, et al. Beneficial effects of positive airway pressure therapy for sleep-disordered breathing in heart failure patients with preserved left ventricular ejection fraction. Clin Cardiol. 2015;38:413-421.
47. Shah RV, Abbasi SA, Heydari B, et al. Obesity and sleep apnea are independently associated with adverse left ventricular remodeling and clinical outcome in patients with atrial fibrillation and preserved ventricular function. Am Heart J. 2014;167:620-626.
48. Riegel B, Moser DK, Anker SD, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141-1163.
49. Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150:984.
50. Bernheim SM, Grady JN, Lin Z, et al. National patterns of risk-standardized mortality and readmission for acute myocardial infarction and heart failure: update on publicly reported outcomes measures based on the 2010 release. Circ Cardiovasc Qual Outcomes. 2010;3:459-467.
51. Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407-413.
52. Cowie MR, Anker SD, Cleland JG, et al. Improving care for patients with acute heart failure: before, during and after hospitalization. Available at: http://www.oxfordhealthpolicyforum.org/files/reports/ahf-report.pdf. Accessed November 27, 2017.
Heart failure (HF) affects nearly 6 million Americans and accounts for one million hospital admissions each year.1 The condition, which results from a structural or functional disorder that impairs the ventricles’ ability to fill, empty, or both,2 is a major cause of morbidity and mortality. The 5-year mortality rate ranges from 44% to 77%.3,4
Growing evidence demonstrates reduced morbidity and mortality when patients with HF with reduced ejection fraction (HFrEF) are treated with an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB); a beta-blocker; and a mineralocorticoid/aldosterone receptor antagonist (MRA) in appropriate doses.5 In addition, 2 new medications representing novel drug classes have recently entered the market and are recommended in select patients who remain symptomatic despite standard treatment.
The first is sacubitril, which is available in a combination pill with the ARB valsartan, and the second is ivabradine.6 Additionally, implanted medical devices are proving useful, particularly in the management of patients with refractory symptoms.
This article will briefly review the diagnosis and initial evaluation of the patient with suspected HF and then describe how newer treatments fit within HF management priorities and strategies. But first, a word about what causes HF.
Causes are many and diverse
HF has a variety of cardiac and non-cardiac etiologies.2,7,8 Some important cardiac causes include hypertension (HTN), coronary artery disease (CAD), valvular heart disease, arrhythmias, myocarditis, Takotsubo cardiomyopathy, and postpartum cardiomyopathy. Common and important non-cardiac causes of HF include alcoholic cardiomyopathy, pulmonary embolism, pulmonary hypertension, obstructive sleep apnea, anemia, hemochromatosis, amyloidosis, sarcoidosis, thyroid dysfunction, nephrotic syndrome, and cardiac toxins (especially stimulants and certain chemotherapy drugs).2,7,8
Diagnosing an elusive culprit
HF remains a clinical diagnosis. Common symptoms include dyspnea, cough, pedal edema, and decreased exercise tolerance, but these symptoms are not at all specific. Given the varied causes and manifestations of HF, the diagnosis can be somewhat elusive. Fortunately, there are a number of objective methods to help identify patients with HF.
Framingham criteria. One commonly used tool for making the diagnosis of HF is the Framingham criteria (see https://www.mdcalc.com/framingham-heart-failure-diagnostic-criteria),9 which diagnoses HF based on historical and physical exam findings. Another well-validated decision tool is the Heart Failure Diagnostic Rule (see http://circ.ahajournals.org/content/124/25/2865.long),10 which incorporates N-terminal pro–B-type natriuretic peptide (NT-proBNP) results, as well as exam findings.
Measurement of natriuretic peptides, either B-type natriuretic peptide (BNP) or NT-proBNP, aids in the diagnosis of HF.5 Although several factors (including age, weight, and renal function) can affect BNP levels, a normal BNP value effectively rules out HF5,7 and an elevated BNP can help to make the diagnosis in the context of a patient with corresponding symptoms.
The initial evaluation: Necessary lab work and imaging studies
The purpose of the initial evaluation of the patient with suspected HF is to establish the diagnosis, look for underlying etiologies of HF, identify comorbidities, and establish baseline values (eg, of potassium and creatinine) for elements monitored during treatment.5,7 TABLE 15,7 lists the lab work and imaging tests that are commonly ordered in the initial evaluation of the patient with HF.
Echocardiography is useful in determining the ejection fraction (EF), which is essential in guiding treatment. Echocardiography can also identify important structural abnormalities including significant valvular disease. Refer patients with severe valvular disease for evaluation for valve repair/replacement, regardless of EF.8
Noninvasive testing (stress nuclear imaging or echocardiography) to evaluate for underlying CAD is reasonable in patients with unknown CAD status.8,11 Patients for whom there is a high suspicion of obstructive CAD should undergo coronary angiography if they are candidates for revascularization.5,7 Noninvasive testing may also be an acceptable option for assessing ischemia in patients presenting with HF who have known CAD and no angina.5
Classification of HF is determined by ejection fraction
Physicians have traditionally classified patients with HF as having either systolic or diastolic dysfunction. Patients with HF symptoms and a reduced EF were said to have systolic dysfunction; those with a normal EF were said to have diastolic dysfunction.
More recently, researchers have learned that patients with reduced EF and those with preserved EF can have both systolic and diastolic dysfunction simultaneously.8 Therefore, the current preferred terminology is HFpEF (heart failure with preserved ejection fraction) for those with an EF ≥50% and HFrEF (heart failure with reduced ejection fraction) for those with an EF ≤40%.5 Both the American Heart Association (AHA) and the European Society of Cardiology recognize a category of HF with moderately reduced ejection fraction defined as an EF between 40% and 50%.5,7 Practically speaking, this group is treated as per the guidelines for HFrEF.5
Treatment of HFrEF: The evidence is clear
The cornerstone of medical treatment for HFrEF is the combination of an ACE inhibitor or ARB with a beta-blocker.2,5,7,8 Several early trials showed clear benefits of these medications. For example, the Studies Of Left Ventricular Dysfunction trial (SOLVD), compared enalapril to placebo in patients receiving standard therapy (consisting chiefly of digitalis, diuretics, and nitrates). This study demonstrated a reduction in all-cause mortality or first hospitalization for HF (number needed to treat [NNT]=21) in the enalapril group vs the placebo group.12
Similarly, a subgroup analysis of the Valsartan Heart Failure Treatment (Val-HeFT) trial demonstrated morbidity (NNT=10) and all-cause mortality benefits (NNT=6) when valsartan (an ARB) was given to patients who were not receiving an ACE inhibitor.13
MERIT-HF (Metoprolol CR/XL Randomised Intervention Trial in congestive Heart Failure) compared the beta-blocker metoprolol succinate to placebo and found fewer deaths from HF and lower all-cause mortality (NNT=26) associated with the treatment group vs the placebo group.14
And a comparison of 2 beta-blockers—carvedilol and metoprolol tartrate—on clinical outcomes in patients with chronic HF in the Carvedilol Or Metoprolol European Trial (COMET) showed that carvedilol extended survival compared with metoprolol tartrate (NNT=19).15
Unlike ACE inhibitors and ARBs, which seem to show a class benefit, only 3 beta-blockers available in the United States have been proven to reduce mortality: sustained-release metoprolol succinate, carvedilol, and bisoprolol.2,7,8
Unless contraindicated, all patients with a reduced EF—even those without symptoms—should receive a beta-blocker and an ACE inhibitor or ARB.5,7,8
Cautionary notes
Remember the following caveats when treating patients with ACE inhibitors, ARBs, and beta-blockers:
- Use ACE inhibitors and ARBs with caution in patients with impaired renal function (serum creatinine >2.5 mg/dL) or elevated serum potassium (>5 mEq/L).16,17
- ARBs are associated with a much lower incidence of cough and angioedema than ACE inhibitors.18
- Although physicians frequently start patients on low doses of beta-blockers and ACE inhibitors or ARBs to minimize hypotension and other adverse effects, the goal of therapy is to titrate up to the therapeutic doses used in clinical trials.5-7 (For dosages of medications commonly used in the treatment of heart failure, see Table 3 in the American College of Cardiology/AHA/Heart Failure Society of America guidelines available at https://www.sciencedirect.com/science/article/pii/S0735109717370870?via%3Dihub#tbl3 and Table 7.2 in the European Society of Cardiology guidelines available at https://academic.oup.com/eurheartj/article/37/27/2129/1748921.)
- Because beta-blockers can exacerbate fluid retention, do not initiate them in patients with fluid overload unless such patients are being treated with diuretics.5,19
When more Tx is needed
For patients who remain symptomatic despite treatment with an ACE inhibitor or ARB and a beta-blocker, consider the following add-on therapies.
Diuretics are the only medications used in the treatment of HF that adequately reduce fluid overload.2,7 While thiazide diuretics confer greater blood pressure control, loop diuretics are generally preferred in the treatment of HF because they are more efficacious.5 Loop diuretics should be prescribed to all patients with fluid overload, as few patients can maintain their target (“dry”) weight without diuretic therapy.5,7 Common adverse effects include hypokalemia, dehydration, and azotemia.
Two MRAs are currently available in the United States: spironolactone and eplerenone. MRAs are used as add-on therapy for symptomatic patients with an EF ≤35% or an EF ≤40% following an acute myocardial infarction (MI).5 They significantly reduce all-cause mortality (NNT=26).20
Because hyperkalemia is a risk with MRAs, do not prescribe them for patients who are already taking both an ACE inhibitor and an ARB.5 Also, do not initiate MRA therapy in patients who have an elevated creatinine level (≥2.5 mg/dL in men; ≥2 mg/dL in women) or a potassium level ≥5 mEq/L.5,7,8 Discontinue MRA therapy if a patient’s potassium level rises to ≥5.5 mEq/L.5
Hydralazine combined with isosorbide dinitrate (H/ID) is an alternative in patients for whom ACE inhibitor/ARB therapy is contraindicated.5,8
H/ID is also an add-on option in African American patients. Trials have demonstrated that H/ID reduces both first hospitalization for HF (NNT=13) and all-cause mortality (NNT=25) when it is used as add-on therapy in African Americans already receiving standard therapy with an ACE inhibitor or ARB, a beta-blocker, and an MRA.21 Headache and dizziness are commonly reported adverse effects.
Digoxin does not reduce mortality, but it does improve both quality of life and exercise tolerance and reduces hospital admissions for patients with HF.5,7 Significant adverse effects of digoxin include anorexia, nausea, visual disturbances, and cardiac arrhythmias.22
Also, hypokalemia can intensify digoxin toxicity.23 Because of these concerns, digoxin is typically dosed at 0.125 mg/d (0.125 mg every other day in patients >70 years or patients with impaired renal function or low body weight) with a target therapeutic range of 0.5 to 0.9 ng/mL.5
New classes, new agents
Sacubitril, a neprilysin inhibitor, is the first drug from this class approved for use in the United States. Neprilysin is the enzyme responsible for the degradation of natriuretic peptides; as such it increases endogenous NPs, promoting diuresis and lowering blood pressure.24,25 Early trials with sacubitril alone showed limited clinical efficacy;25 however, when it was combined with the ARB, valsartan (the combination being called angiotensin receptor blocker + neprilysin inhibitor [ARNI] therapy), it was found to be of significant benefit.6,25
The PARADIGM-HF (Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure) trial compared outcomes in patients receiving ARNI therapy to those receiving enalapril.26 The authors stopped the trial early due to the overwhelming benefit seen in the ARNI arm.
After a median follow-up of 27 months, the researchers found a reduction in the primary outcomes of either cardiovascular death or first hospitalization for HF (26.5% in the enalapril-treated group vs 21.8% in the ARNI-treated group; NNT=21).26 There were slightly more cases of angioedema in the ARNI arm than in the enalapril arm (0.5% vs 0.2%), although there were no patients in the trial who required endotracheal intubation.26
Because of this increased risk, do not prescribe ARNI therapy for any patient with a history of angioedema.6 Hypotension was more common in the ARNI-treated group than in the enalapril group (14% vs 9.2%), but there were lower rates of hyperkalemia, elevated serum creatinine, and cough in the ARNI-treated group than in the enalapril group.26
Consider ARNI treatment for all patients with an EF ≤40% who remain symptomatic despite appropriate doses of an ACE inhibitor or ARB plus a beta-blocker. Do not administer ARNI therapy concomitantly with an ACE inhibitor or ARB. When switching, do not start ARNI therapy for at least 36 hours after the last dose of an ACE inhibitor or ARB.6
Ivabradine is a sinoatrial node modulator that provides additional heart rate reduction. It does not affect ventricular repolarization or myocardial contractility.27 Early trials with this medication have shown reduced cardiac mortality and an NNT to prevent one first HF hospitalization within one year of 27.28 Adverse effects include symptomatic and asymptomatic bradycardia and luminous phenomena.28
Recommend ivabradine as add-on therapy to all patients with an EF ≤35%, normal sinus rhythm, and resting heart rate ≥70 bpm who remain symptomatic despite taking the maximum-tolerated dose of a beta-blocker.6 The dose is adjusted to achieve a resting heart rate of 50 to 60 bpm.27
Nonpharmacologic options
Implantable cardioverter defibrillators (ICDs) are recommended as primary prevention in select HFrEF patients to reduce the risk of sudden cardiac death and all-cause mortality. The 2013 American College of Cardiology Foundation/AHA Guideline for the Management of Heart Failure recommends an ICD for primary prevention for: 1) patients with symptomatic HF and an LVEF ≤35% despite ≥3 months of optimal medical therapy, and 2) patients at least 40 days post-MI with an LVEF of ≤30%.5,29 ICDs are not recommended for patients who have a life expectancy of less than one year, and the devices are of unclear benefit for patients ≥75 years of age.5
Cardiac resynchronization therapy (CRT), although not new to the field of cardiology, is new to the treatment of heart failure. A number of patients with HFrEF have QRS prolongation and in particular, left bundle branch block (LBBB).5 CRT uses biventricular pacing to restore synchronous contraction of the left and right ventricles.30 It is strongly recommended for patients with an EF ≤35%, sinus rhythm, LBBB, QRS ≥150 ms, and a life expectancy of at least one year.5,7 It is weakly recommended for patients with an EF ≤35% and a QRS ≥150 ms but without LBBB. It’s also weakly recommended for patients with an EF ≤35% and LBBB with a QRS of 120 to 150 ms.5,31
Left ventricular assist devices (LVADs) and cardiac transplantation are considerations for patients with severe symptoms refractory to all other interventions.5 LVADs may be used either while awaiting cardiac transplantation (bridge therapy) or as definitive treatment (destination therapy). Appropriate patient selection for such therapies requires a team of experts that ideally includes HF and transplantation cardiologists, cardiothoracic surgeons, nurses, social workers, and palliative care clinicians.5
Treatment of HFpEF: Evidence is lacking
While HFpEF is common—affecting about half of all patients with HF—ideal treatment remains unclear.32 Some trials have shown promise, but to date no unequivocal evidence exists that any standard therapy reduces mortality in patients with HFpEF.33-37 Underlying mechanisms of action of HFpEF include cardiac rate and rhythm abnormalities, atrial dysfunction, and stiffening of the ventricles. In a sense, it represents an exaggerated expression of the pathophysiology seen with the normal aging of the heart and can be conceptualized as “presbycardia.”37 Indeed, HFpEF is more common in the elderly, but it is also more common in patients of African descent.38,39 Common contributing causes (which we’ll get to in a bit) include HTN, CAD, atrial fibrillation (AF), obesity, and obstructive sleep apnea (OSA).
Trials have failed to show clear benefit for ACE inhibitors, ARBs, or beta-blockers.7,33 The evidence for MRAs is somewhat unclear; however, they have recently been recommended as an option for patients who have been hospitalized in the last year to reduce the risk of subsequent hospitalizations.40 Digoxin is used primarily for rate control in the setting of AF, but otherwise is of unclear benefit.7 A low-sodium diet (ie, ≤2 g/d) may be useful in those patients who are prone to fluid overload.5,7 The cornerstone of treatment of HFpEF is the relief of volume overload with diuretics and the treatment of coexisting conditions.33
Common contributing causes of HFpEF
HTN is not only a common contributing cause, but also the most common comorbid condition affecting patients with HFpEF. As such, treatment of HTN represents the most important management goal.33,34 Based on recent data, the American College of Cardiology, the AHA, and the Heart Failure Society of America have recommended a systolic blood pressure goal <130 mm Hg for patients with HFpEF.40 Most patients with HFpEF and HTN will have some degree of fluid overload and, therefore, should receive a diuretic.
CAD. Patients with HFpEF should be evaluated for CAD and treated with medical management and coronary revascularization, as appropriate.
AF is poorly tolerated by patients with HFpEF.37 Patients with AF should receive anticoagulation and rate control medications, and those with persistent HF symptoms should be evaluated for rhythm control.33
Obesity is more prevalent in patients with HFpEF than in those with HFrEF.41 Although there is indirect evidence that weight loss improves cardiac function,34,42,43 and studies have shown bariatric surgery to improve diastolic function,44,45 there are no studies reporting clinical outcomes.
Treatment of OSA with continuous positive airway pressure appears to alleviate some symptoms of HF and to reduce all-cause mortality.46,47
Keeping HF patients out of the hospital
Many readmissions to the hospital for HF exacerbation are preventable. Patients often do not understand hospital discharge instructions or the nature of their chronic disease and its management.48-51 Routine follow-up in the office or clinic provides an opportunity to improve quality of life for patients and decrease admissions.7,52
A major role for the family physician is in the co-creation of, and adherence to, an individualized, comprehensive care plan. Make sure such a plan is easily understood not only by the patient with HF, but also by his or her care team. In addition, it should be evidence-based and reflect the patient’s culture, values, and goals of treatment.5,7
At each visit, the family physician or a member of the health care team should assess adherence to guideline-directed medical therapy, measure weight, evaluate fluid status, and provide ongoing patient education including information on the importance of activity, monitoring weight daily, and moderating fluid, salt, and alcohol intake.5,52
Research shows that cardiac rehabilitation improves functional capacity, exercise duration, quality of life, and mortality. Therefore, recommend it to all symptomatic patients with HF who are clinically stable.2
Consider collaboration with a subspecialist. Patients who remain symptomatic despite optimal medical management and patients with recurrent hospitalizations are best managed in conjunction with a subspecialist in HF treatment.2,5
CORRESPONDENCE
Darin Brink, MD, 420 Delaware St. SE, MMC 381, Minneapolis, MN 55455; [email protected].
Heart failure (HF) affects nearly 6 million Americans and accounts for one million hospital admissions each year.1 The condition, which results from a structural or functional disorder that impairs the ventricles’ ability to fill, empty, or both,2 is a major cause of morbidity and mortality. The 5-year mortality rate ranges from 44% to 77%.3,4
Growing evidence demonstrates reduced morbidity and mortality when patients with HF with reduced ejection fraction (HFrEF) are treated with an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB); a beta-blocker; and a mineralocorticoid/aldosterone receptor antagonist (MRA) in appropriate doses.5 In addition, 2 new medications representing novel drug classes have recently entered the market and are recommended in select patients who remain symptomatic despite standard treatment.
The first is sacubitril, which is available in a combination pill with the ARB valsartan, and the second is ivabradine.6 Additionally, implanted medical devices are proving useful, particularly in the management of patients with refractory symptoms.
This article will briefly review the diagnosis and initial evaluation of the patient with suspected HF and then describe how newer treatments fit within HF management priorities and strategies. But first, a word about what causes HF.
Causes are many and diverse
HF has a variety of cardiac and non-cardiac etiologies.2,7,8 Some important cardiac causes include hypertension (HTN), coronary artery disease (CAD), valvular heart disease, arrhythmias, myocarditis, Takotsubo cardiomyopathy, and postpartum cardiomyopathy. Common and important non-cardiac causes of HF include alcoholic cardiomyopathy, pulmonary embolism, pulmonary hypertension, obstructive sleep apnea, anemia, hemochromatosis, amyloidosis, sarcoidosis, thyroid dysfunction, nephrotic syndrome, and cardiac toxins (especially stimulants and certain chemotherapy drugs).2,7,8
Diagnosing an elusive culprit
HF remains a clinical diagnosis. Common symptoms include dyspnea, cough, pedal edema, and decreased exercise tolerance, but these symptoms are not at all specific. Given the varied causes and manifestations of HF, the diagnosis can be somewhat elusive. Fortunately, there are a number of objective methods to help identify patients with HF.
Framingham criteria. One commonly used tool for making the diagnosis of HF is the Framingham criteria (see https://www.mdcalc.com/framingham-heart-failure-diagnostic-criteria),9 which diagnoses HF based on historical and physical exam findings. Another well-validated decision tool is the Heart Failure Diagnostic Rule (see http://circ.ahajournals.org/content/124/25/2865.long),10 which incorporates N-terminal pro–B-type natriuretic peptide (NT-proBNP) results, as well as exam findings.
Measurement of natriuretic peptides, either B-type natriuretic peptide (BNP) or NT-proBNP, aids in the diagnosis of HF.5 Although several factors (including age, weight, and renal function) can affect BNP levels, a normal BNP value effectively rules out HF5,7 and an elevated BNP can help to make the diagnosis in the context of a patient with corresponding symptoms.
The initial evaluation: Necessary lab work and imaging studies
The purpose of the initial evaluation of the patient with suspected HF is to establish the diagnosis, look for underlying etiologies of HF, identify comorbidities, and establish baseline values (eg, of potassium and creatinine) for elements monitored during treatment.5,7 TABLE 15,7 lists the lab work and imaging tests that are commonly ordered in the initial evaluation of the patient with HF.
Echocardiography is useful in determining the ejection fraction (EF), which is essential in guiding treatment. Echocardiography can also identify important structural abnormalities including significant valvular disease. Refer patients with severe valvular disease for evaluation for valve repair/replacement, regardless of EF.8
Noninvasive testing (stress nuclear imaging or echocardiography) to evaluate for underlying CAD is reasonable in patients with unknown CAD status.8,11 Patients for whom there is a high suspicion of obstructive CAD should undergo coronary angiography if they are candidates for revascularization.5,7 Noninvasive testing may also be an acceptable option for assessing ischemia in patients presenting with HF who have known CAD and no angina.5
Classification of HF is determined by ejection fraction
Physicians have traditionally classified patients with HF as having either systolic or diastolic dysfunction. Patients with HF symptoms and a reduced EF were said to have systolic dysfunction; those with a normal EF were said to have diastolic dysfunction.
More recently, researchers have learned that patients with reduced EF and those with preserved EF can have both systolic and diastolic dysfunction simultaneously.8 Therefore, the current preferred terminology is HFpEF (heart failure with preserved ejection fraction) for those with an EF ≥50% and HFrEF (heart failure with reduced ejection fraction) for those with an EF ≤40%.5 Both the American Heart Association (AHA) and the European Society of Cardiology recognize a category of HF with moderately reduced ejection fraction defined as an EF between 40% and 50%.5,7 Practically speaking, this group is treated as per the guidelines for HFrEF.5
Treatment of HFrEF: The evidence is clear
The cornerstone of medical treatment for HFrEF is the combination of an ACE inhibitor or ARB with a beta-blocker.2,5,7,8 Several early trials showed clear benefits of these medications. For example, the Studies Of Left Ventricular Dysfunction trial (SOLVD), compared enalapril to placebo in patients receiving standard therapy (consisting chiefly of digitalis, diuretics, and nitrates). This study demonstrated a reduction in all-cause mortality or first hospitalization for HF (number needed to treat [NNT]=21) in the enalapril group vs the placebo group.12
Similarly, a subgroup analysis of the Valsartan Heart Failure Treatment (Val-HeFT) trial demonstrated morbidity (NNT=10) and all-cause mortality benefits (NNT=6) when valsartan (an ARB) was given to patients who were not receiving an ACE inhibitor.13
MERIT-HF (Metoprolol CR/XL Randomised Intervention Trial in congestive Heart Failure) compared the beta-blocker metoprolol succinate to placebo and found fewer deaths from HF and lower all-cause mortality (NNT=26) associated with the treatment group vs the placebo group.14
And a comparison of 2 beta-blockers—carvedilol and metoprolol tartrate—on clinical outcomes in patients with chronic HF in the Carvedilol Or Metoprolol European Trial (COMET) showed that carvedilol extended survival compared with metoprolol tartrate (NNT=19).15
Unlike ACE inhibitors and ARBs, which seem to show a class benefit, only 3 beta-blockers available in the United States have been proven to reduce mortality: sustained-release metoprolol succinate, carvedilol, and bisoprolol.2,7,8
Unless contraindicated, all patients with a reduced EF—even those without symptoms—should receive a beta-blocker and an ACE inhibitor or ARB.5,7,8
Cautionary notes
Remember the following caveats when treating patients with ACE inhibitors, ARBs, and beta-blockers:
- Use ACE inhibitors and ARBs with caution in patients with impaired renal function (serum creatinine >2.5 mg/dL) or elevated serum potassium (>5 mEq/L).16,17
- ARBs are associated with a much lower incidence of cough and angioedema than ACE inhibitors.18
- Although physicians frequently start patients on low doses of beta-blockers and ACE inhibitors or ARBs to minimize hypotension and other adverse effects, the goal of therapy is to titrate up to the therapeutic doses used in clinical trials.5-7 (For dosages of medications commonly used in the treatment of heart failure, see Table 3 in the American College of Cardiology/AHA/Heart Failure Society of America guidelines available at https://www.sciencedirect.com/science/article/pii/S0735109717370870?via%3Dihub#tbl3 and Table 7.2 in the European Society of Cardiology guidelines available at https://academic.oup.com/eurheartj/article/37/27/2129/1748921.)
- Because beta-blockers can exacerbate fluid retention, do not initiate them in patients with fluid overload unless such patients are being treated with diuretics.5,19
When more Tx is needed
For patients who remain symptomatic despite treatment with an ACE inhibitor or ARB and a beta-blocker, consider the following add-on therapies.
Diuretics are the only medications used in the treatment of HF that adequately reduce fluid overload.2,7 While thiazide diuretics confer greater blood pressure control, loop diuretics are generally preferred in the treatment of HF because they are more efficacious.5 Loop diuretics should be prescribed to all patients with fluid overload, as few patients can maintain their target (“dry”) weight without diuretic therapy.5,7 Common adverse effects include hypokalemia, dehydration, and azotemia.
Two MRAs are currently available in the United States: spironolactone and eplerenone. MRAs are used as add-on therapy for symptomatic patients with an EF ≤35% or an EF ≤40% following an acute myocardial infarction (MI).5 They significantly reduce all-cause mortality (NNT=26).20
Because hyperkalemia is a risk with MRAs, do not prescribe them for patients who are already taking both an ACE inhibitor and an ARB.5 Also, do not initiate MRA therapy in patients who have an elevated creatinine level (≥2.5 mg/dL in men; ≥2 mg/dL in women) or a potassium level ≥5 mEq/L.5,7,8 Discontinue MRA therapy if a patient’s potassium level rises to ≥5.5 mEq/L.5
Hydralazine combined with isosorbide dinitrate (H/ID) is an alternative in patients for whom ACE inhibitor/ARB therapy is contraindicated.5,8
H/ID is also an add-on option in African American patients. Trials have demonstrated that H/ID reduces both first hospitalization for HF (NNT=13) and all-cause mortality (NNT=25) when it is used as add-on therapy in African Americans already receiving standard therapy with an ACE inhibitor or ARB, a beta-blocker, and an MRA.21 Headache and dizziness are commonly reported adverse effects.
Digoxin does not reduce mortality, but it does improve both quality of life and exercise tolerance and reduces hospital admissions for patients with HF.5,7 Significant adverse effects of digoxin include anorexia, nausea, visual disturbances, and cardiac arrhythmias.22
Also, hypokalemia can intensify digoxin toxicity.23 Because of these concerns, digoxin is typically dosed at 0.125 mg/d (0.125 mg every other day in patients >70 years or patients with impaired renal function or low body weight) with a target therapeutic range of 0.5 to 0.9 ng/mL.5
New classes, new agents
Sacubitril, a neprilysin inhibitor, is the first drug from this class approved for use in the United States. Neprilysin is the enzyme responsible for the degradation of natriuretic peptides; as such it increases endogenous NPs, promoting diuresis and lowering blood pressure.24,25 Early trials with sacubitril alone showed limited clinical efficacy;25 however, when it was combined with the ARB, valsartan (the combination being called angiotensin receptor blocker + neprilysin inhibitor [ARNI] therapy), it was found to be of significant benefit.6,25
The PARADIGM-HF (Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart Failure) trial compared outcomes in patients receiving ARNI therapy to those receiving enalapril.26 The authors stopped the trial early due to the overwhelming benefit seen in the ARNI arm.
After a median follow-up of 27 months, the researchers found a reduction in the primary outcomes of either cardiovascular death or first hospitalization for HF (26.5% in the enalapril-treated group vs 21.8% in the ARNI-treated group; NNT=21).26 There were slightly more cases of angioedema in the ARNI arm than in the enalapril arm (0.5% vs 0.2%), although there were no patients in the trial who required endotracheal intubation.26
Because of this increased risk, do not prescribe ARNI therapy for any patient with a history of angioedema.6 Hypotension was more common in the ARNI-treated group than in the enalapril group (14% vs 9.2%), but there were lower rates of hyperkalemia, elevated serum creatinine, and cough in the ARNI-treated group than in the enalapril group.26
Consider ARNI treatment for all patients with an EF ≤40% who remain symptomatic despite appropriate doses of an ACE inhibitor or ARB plus a beta-blocker. Do not administer ARNI therapy concomitantly with an ACE inhibitor or ARB. When switching, do not start ARNI therapy for at least 36 hours after the last dose of an ACE inhibitor or ARB.6
Ivabradine is a sinoatrial node modulator that provides additional heart rate reduction. It does not affect ventricular repolarization or myocardial contractility.27 Early trials with this medication have shown reduced cardiac mortality and an NNT to prevent one first HF hospitalization within one year of 27.28 Adverse effects include symptomatic and asymptomatic bradycardia and luminous phenomena.28
Recommend ivabradine as add-on therapy to all patients with an EF ≤35%, normal sinus rhythm, and resting heart rate ≥70 bpm who remain symptomatic despite taking the maximum-tolerated dose of a beta-blocker.6 The dose is adjusted to achieve a resting heart rate of 50 to 60 bpm.27
Nonpharmacologic options
Implantable cardioverter defibrillators (ICDs) are recommended as primary prevention in select HFrEF patients to reduce the risk of sudden cardiac death and all-cause mortality. The 2013 American College of Cardiology Foundation/AHA Guideline for the Management of Heart Failure recommends an ICD for primary prevention for: 1) patients with symptomatic HF and an LVEF ≤35% despite ≥3 months of optimal medical therapy, and 2) patients at least 40 days post-MI with an LVEF of ≤30%.5,29 ICDs are not recommended for patients who have a life expectancy of less than one year, and the devices are of unclear benefit for patients ≥75 years of age.5
Cardiac resynchronization therapy (CRT), although not new to the field of cardiology, is new to the treatment of heart failure. A number of patients with HFrEF have QRS prolongation and in particular, left bundle branch block (LBBB).5 CRT uses biventricular pacing to restore synchronous contraction of the left and right ventricles.30 It is strongly recommended for patients with an EF ≤35%, sinus rhythm, LBBB, QRS ≥150 ms, and a life expectancy of at least one year.5,7 It is weakly recommended for patients with an EF ≤35% and a QRS ≥150 ms but without LBBB. It’s also weakly recommended for patients with an EF ≤35% and LBBB with a QRS of 120 to 150 ms.5,31
Left ventricular assist devices (LVADs) and cardiac transplantation are considerations for patients with severe symptoms refractory to all other interventions.5 LVADs may be used either while awaiting cardiac transplantation (bridge therapy) or as definitive treatment (destination therapy). Appropriate patient selection for such therapies requires a team of experts that ideally includes HF and transplantation cardiologists, cardiothoracic surgeons, nurses, social workers, and palliative care clinicians.5
Treatment of HFpEF: Evidence is lacking
While HFpEF is common—affecting about half of all patients with HF—ideal treatment remains unclear.32 Some trials have shown promise, but to date no unequivocal evidence exists that any standard therapy reduces mortality in patients with HFpEF.33-37 Underlying mechanisms of action of HFpEF include cardiac rate and rhythm abnormalities, atrial dysfunction, and stiffening of the ventricles. In a sense, it represents an exaggerated expression of the pathophysiology seen with the normal aging of the heart and can be conceptualized as “presbycardia.”37 Indeed, HFpEF is more common in the elderly, but it is also more common in patients of African descent.38,39 Common contributing causes (which we’ll get to in a bit) include HTN, CAD, atrial fibrillation (AF), obesity, and obstructive sleep apnea (OSA).
Trials have failed to show clear benefit for ACE inhibitors, ARBs, or beta-blockers.7,33 The evidence for MRAs is somewhat unclear; however, they have recently been recommended as an option for patients who have been hospitalized in the last year to reduce the risk of subsequent hospitalizations.40 Digoxin is used primarily for rate control in the setting of AF, but otherwise is of unclear benefit.7 A low-sodium diet (ie, ≤2 g/d) may be useful in those patients who are prone to fluid overload.5,7 The cornerstone of treatment of HFpEF is the relief of volume overload with diuretics and the treatment of coexisting conditions.33
Common contributing causes of HFpEF
HTN is not only a common contributing cause, but also the most common comorbid condition affecting patients with HFpEF. As such, treatment of HTN represents the most important management goal.33,34 Based on recent data, the American College of Cardiology, the AHA, and the Heart Failure Society of America have recommended a systolic blood pressure goal <130 mm Hg for patients with HFpEF.40 Most patients with HFpEF and HTN will have some degree of fluid overload and, therefore, should receive a diuretic.
CAD. Patients with HFpEF should be evaluated for CAD and treated with medical management and coronary revascularization, as appropriate.
AF is poorly tolerated by patients with HFpEF.37 Patients with AF should receive anticoagulation and rate control medications, and those with persistent HF symptoms should be evaluated for rhythm control.33
Obesity is more prevalent in patients with HFpEF than in those with HFrEF.41 Although there is indirect evidence that weight loss improves cardiac function,34,42,43 and studies have shown bariatric surgery to improve diastolic function,44,45 there are no studies reporting clinical outcomes.
Treatment of OSA with continuous positive airway pressure appears to alleviate some symptoms of HF and to reduce all-cause mortality.46,47
Keeping HF patients out of the hospital
Many readmissions to the hospital for HF exacerbation are preventable. Patients often do not understand hospital discharge instructions or the nature of their chronic disease and its management.48-51 Routine follow-up in the office or clinic provides an opportunity to improve quality of life for patients and decrease admissions.7,52
A major role for the family physician is in the co-creation of, and adherence to, an individualized, comprehensive care plan. Make sure such a plan is easily understood not only by the patient with HF, but also by his or her care team. In addition, it should be evidence-based and reflect the patient’s culture, values, and goals of treatment.5,7
At each visit, the family physician or a member of the health care team should assess adherence to guideline-directed medical therapy, measure weight, evaluate fluid status, and provide ongoing patient education including information on the importance of activity, monitoring weight daily, and moderating fluid, salt, and alcohol intake.5,52
Research shows that cardiac rehabilitation improves functional capacity, exercise duration, quality of life, and mortality. Therefore, recommend it to all symptomatic patients with HF who are clinically stable.2
Consider collaboration with a subspecialist. Patients who remain symptomatic despite optimal medical management and patients with recurrent hospitalizations are best managed in conjunction with a subspecialist in HF treatment.2,5
CORRESPONDENCE
Darin Brink, MD, 420 Delaware St. SE, MMC 381, Minneapolis, MN 55455; [email protected].
1. Hall MJ, Levant S, DeFrances CJ. Hospitalization for congestive heart failure: United States, 2000-2010. NCHS Data Brief. 2012;(108):1-8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23102190. Accessed April 26, 2017.
2. Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused Update Incorporated Into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1-e90.
3. Passantino A, Guida P, Lagioia R, et al. Predictors of long-term mortality in older patients hospitalized for acutely decompensated heart failure: clinical relevance of natriuretic peptides. J Am Geriatr Soc. 2017;65:822-826.
4. Lassus JP, Siirilä-Waris K, Nieminen MS, et al. Long-term survival after hospitalization for acute heart failure—differences in prognosis of acutely decompensated chronic and new-onset acute heart failure. Int J Cardiol. 2013;168:458-462.
5. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327.
6. Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure. J Am Coll Cardiol. 2016;68:1476-1488.
7. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.
8. Pinkerman CP, Sander JE, Breeding D, et al. Institute for Clinical Systems Improvement. Heart failure in adults. Available at: https://www.scribd.com/document/310893227/HeartFailure-pdf. Accessed December 6, 2017.
9. McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham Study. N Engl J Med. 1971;285:1441-1446.
10. Kelder JC, Cramer MJ, van Wijngaarden J, et al. The diagnostic value of physical examination and additional testing in primary care patients with suspected heart failure. Circulation. 2011;124:2865-2873.
11. Heart Failure Society of America, Lindenfeld J, Albert NM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1-194.
12. Pouleur H, The SOLVD Investigators. Results of the treatment trial of the studies of left ventricular dysfunction (SOLVD). Am J Cardiol. 1992;70:135-136.
13. Maggioni AP, Anand I, Gottlieb SO, et al. Effects of valsartan on morbidity and mortality in patients with heart failure not receiving angiotensin-converting enzyme inhibitors. J Am Coll Cardiol. 2002;40:1414-1421.
14. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353:2001-2007.
15. Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet. 2003;362:7-13.
16. Gehr TW, Sica DA. Pharmacotherapy in congestive heart failure: Hyperkalemia in congestive heart failure. Congest Heart Fail. 2001;7:97-100.
17. National Institute for Health and Clinical Excellence (NICE). Chronic heart failure in adults: management. 2010. Available at: https://www.nice.org.uk/guidance/cg108. Accessed November 27, 2017.
18. Barreras A, Gurk-Turner C. Angiotensin II receptor blockers. Proc (Bayl Univ Med Cent). 2003;16:123-126.
19. Epstein SE, Braunwald E. The effect of beta adrenergic blockade on patterns of urinary sodium excretion: studies in normal subjects and in patients with heart disease. Ann Intern Med. 1966;65:20-27.
20. Berbenetz NM, Mrkobrada M. Mineralocorticoid receptor antagonists for heart failure: systematic review and meta-analysis. BMC Cardiovasc Disord. 2016;16:246.
21. Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049-2057.
22. Kelly RA, Smith TW. Recognition and management of digitalis toxicity. Am J Cardiol. 1992;69:108G-118G.
23. Sundar S, Burma DP, Vaish SK. Digoxin toxicity and electrolytes: a correlative study. Acta Cardiol. 1983;38:115-123.
24. McDowell G, Nicholls DP. The endopeptidase inhibitor, candoxatril, and its therapeutic potential in the treatment of chronic cardiac failure in man. Expert Opin Investig Drugs. 1999;8:79-84.
25. Prenner SB, Shah SJ, Yancy CW. Role of angiotensin receptor-neprilysin inhibition in heart failure. Curr Atheroscler Rep. 2016;18:48.
26. McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993-1004.
27. Corlanor package insert. Amgen Inc., Thousand Oaks, CA. Available at: http://pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/corlanor/corlanor_pi.pdf. Accessed November 28, 2017.
28. Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875-885.
29. Kusumoto FM, Calkins H, Boehmer J, et al. HRS/ACC/AHA expert consensus statement on the use of implantable cardioverter-defibrillator therapy in patients who are not included or not well represented in clinical trials. Circulation. 2014;130:94-125.
30. Leyva F, Nisam S, Auricchio A. 20 years of cardiac resynchronization therapy. J Am Coll Cardiol. 2014;64:1047-1058.
31. Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS Focused Update Incorporated Into the ACCF/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2013;127:e283-e352.
32. Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
33. Redfield MM. Heart failure with preserved ejection fraction. N Engl J Med. 2016;375:1868-1877.
34. Nanayakkara S, Kaye DM. Management of heart failure with preserved ejection fraction: a review. Clin Ther. 2015;37:2186-2198.
35. Cleland JG, Pellicori P, Dierckx R. Clinical trials in patients with heart failure and preserved left ventricular ejection fraction. Heart Fail Clin. 2014;10:511-523.
36. Ferrari R, Böhm M, Cleland JGF, et al. Heart failure with preserved ejection fraction: uncertainties and dilemmas. Eur J Heart Fail. 2015;17:665-671.
37. Borlaug BA. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2014;11:507-515.
38. Sharp A, Tapp R, Francis DP, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol. 2008;52:1015-1021.
39. Zile MR. Heart failure with a preserved ejection fraction. In: Mann DL, Zipes D, Libby P BR, eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Phila
40. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776-803.
41. Mentz RJ, Kelly JP, von Lueder TG, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2014;64:2281-2293.
42. de las Fuentes L, Waggoner AD, Mohammed BS, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009;54:2376-2381.
43. Kitzman DW, Brubaker P, Morgan T, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction. JAMA. 2016;315:36-46.
44. Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54:718-726.
45. Ristow B, Rabkin J, Haeusslein E. Improvement in dilated cardiomyopathy after bariatric surgery. J Card Fail. 2008;14:198-202.
46. Yoshihisa A, Suzuki S, Yamauchi H, et al. Beneficial effects of positive airway pressure therapy for sleep-disordered breathing in heart failure patients with preserved left ventricular ejection fraction. Clin Cardiol. 2015;38:413-421.
47. Shah RV, Abbasi SA, Heydari B, et al. Obesity and sleep apnea are independently associated with adverse left ventricular remodeling and clinical outcome in patients with atrial fibrillation and preserved ventricular function. Am Heart J. 2014;167:620-626.
48. Riegel B, Moser DK, Anker SD, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141-1163.
49. Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150:984.
50. Bernheim SM, Grady JN, Lin Z, et al. National patterns of risk-standardized mortality and readmission for acute myocardial infarction and heart failure: update on publicly reported outcomes measures based on the 2010 release. Circ Cardiovasc Qual Outcomes. 2010;3:459-467.
51. Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407-413.
52. Cowie MR, Anker SD, Cleland JG, et al. Improving care for patients with acute heart failure: before, during and after hospitalization. Available at: http://www.oxfordhealthpolicyforum.org/files/reports/ahf-report.pdf. Accessed November 27, 2017.
1. Hall MJ, Levant S, DeFrances CJ. Hospitalization for congestive heart failure: United States, 2000-2010. NCHS Data Brief. 2012;(108):1-8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/23102190. Accessed April 26, 2017.
2. Hunt SA, Abraham WT, Chin MH, et al. 2009 Focused Update Incorporated Into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the International Society for Heart and Lung Transplantation. J Am Coll Cardiol. 2009;53:e1-e90.
3. Passantino A, Guida P, Lagioia R, et al. Predictors of long-term mortality in older patients hospitalized for acutely decompensated heart failure: clinical relevance of natriuretic peptides. J Am Geriatr Soc. 2017;65:822-826.
4. Lassus JP, Siirilä-Waris K, Nieminen MS, et al. Long-term survival after hospitalization for acute heart failure—differences in prognosis of acutely decompensated chronic and new-onset acute heart failure. Int J Cardiol. 2013;168:458-462.
5. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240-e327.
6. Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure. J Am Coll Cardiol. 2016;68:1476-1488.
7. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.
8. Pinkerman CP, Sander JE, Breeding D, et al. Institute for Clinical Systems Improvement. Heart failure in adults. Available at: https://www.scribd.com/document/310893227/HeartFailure-pdf. Accessed December 6, 2017.
9. McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham Study. N Engl J Med. 1971;285:1441-1446.
10. Kelder JC, Cramer MJ, van Wijngaarden J, et al. The diagnostic value of physical examination and additional testing in primary care patients with suspected heart failure. Circulation. 2011;124:2865-2873.
11. Heart Failure Society of America, Lindenfeld J, Albert NM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1-194.
12. Pouleur H, The SOLVD Investigators. Results of the treatment trial of the studies of left ventricular dysfunction (SOLVD). Am J Cardiol. 1992;70:135-136.
13. Maggioni AP, Anand I, Gottlieb SO, et al. Effects of valsartan on morbidity and mortality in patients with heart failure not receiving angiotensin-converting enzyme inhibitors. J Am Coll Cardiol. 2002;40:1414-1421.
14. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353:2001-2007.
15. Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet. 2003;362:7-13.
16. Gehr TW, Sica DA. Pharmacotherapy in congestive heart failure: Hyperkalemia in congestive heart failure. Congest Heart Fail. 2001;7:97-100.
17. National Institute for Health and Clinical Excellence (NICE). Chronic heart failure in adults: management. 2010. Available at: https://www.nice.org.uk/guidance/cg108. Accessed November 27, 2017.
18. Barreras A, Gurk-Turner C. Angiotensin II receptor blockers. Proc (Bayl Univ Med Cent). 2003;16:123-126.
19. Epstein SE, Braunwald E. The effect of beta adrenergic blockade on patterns of urinary sodium excretion: studies in normal subjects and in patients with heart disease. Ann Intern Med. 1966;65:20-27.
20. Berbenetz NM, Mrkobrada M. Mineralocorticoid receptor antagonists for heart failure: systematic review and meta-analysis. BMC Cardiovasc Disord. 2016;16:246.
21. Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049-2057.
22. Kelly RA, Smith TW. Recognition and management of digitalis toxicity. Am J Cardiol. 1992;69:108G-118G.
23. Sundar S, Burma DP, Vaish SK. Digoxin toxicity and electrolytes: a correlative study. Acta Cardiol. 1983;38:115-123.
24. McDowell G, Nicholls DP. The endopeptidase inhibitor, candoxatril, and its therapeutic potential in the treatment of chronic cardiac failure in man. Expert Opin Investig Drugs. 1999;8:79-84.
25. Prenner SB, Shah SJ, Yancy CW. Role of angiotensin receptor-neprilysin inhibition in heart failure. Curr Atheroscler Rep. 2016;18:48.
26. McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993-1004.
27. Corlanor package insert. Amgen Inc., Thousand Oaks, CA. Available at: http://pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/corlanor/corlanor_pi.pdf. Accessed November 28, 2017.
28. Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875-885.
29. Kusumoto FM, Calkins H, Boehmer J, et al. HRS/ACC/AHA expert consensus statement on the use of implantable cardioverter-defibrillator therapy in patients who are not included or not well represented in clinical trials. Circulation. 2014;130:94-125.
30. Leyva F, Nisam S, Auricchio A. 20 years of cardiac resynchronization therapy. J Am Coll Cardiol. 2014;64:1047-1058.
31. Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS Focused Update Incorporated Into the ACCF/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2013;127:e283-e352.
32. Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
33. Redfield MM. Heart failure with preserved ejection fraction. N Engl J Med. 2016;375:1868-1877.
34. Nanayakkara S, Kaye DM. Management of heart failure with preserved ejection fraction: a review. Clin Ther. 2015;37:2186-2198.
35. Cleland JG, Pellicori P, Dierckx R. Clinical trials in patients with heart failure and preserved left ventricular ejection fraction. Heart Fail Clin. 2014;10:511-523.
36. Ferrari R, Böhm M, Cleland JGF, et al. Heart failure with preserved ejection fraction: uncertainties and dilemmas. Eur J Heart Fail. 2015;17:665-671.
37. Borlaug BA. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2014;11:507-515.
38. Sharp A, Tapp R, Francis DP, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) substudy. J Am Coll Cardiol. 2008;52:1015-1021.
39. Zile MR. Heart failure with a preserved ejection fraction. In: Mann DL, Zipes D, Libby P BR, eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Phila
40. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776-803.
41. Mentz RJ, Kelly JP, von Lueder TG, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2014;64:2281-2293.
42. de las Fuentes L, Waggoner AD, Mohammed BS, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009;54:2376-2381.
43. Kitzman DW, Brubaker P, Morgan T, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction. JAMA. 2016;315:36-46.
44. Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54:718-726.
45. Ristow B, Rabkin J, Haeusslein E. Improvement in dilated cardiomyopathy after bariatric surgery. J Card Fail. 2008;14:198-202.
46. Yoshihisa A, Suzuki S, Yamauchi H, et al. Beneficial effects of positive airway pressure therapy for sleep-disordered breathing in heart failure patients with preserved left ventricular ejection fraction. Clin Cardiol. 2015;38:413-421.
47. Shah RV, Abbasi SA, Heydari B, et al. Obesity and sleep apnea are independently associated with adverse left ventricular remodeling and clinical outcome in patients with atrial fibrillation and preserved ventricular function. Am Heart J. 2014;167:620-626.
48. Riegel B, Moser DK, Anker SD, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141-1163.
49. Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150:984.
50. Bernheim SM, Grady JN, Lin Z, et al. National patterns of risk-standardized mortality and readmission for acute myocardial infarction and heart failure: update on publicly reported outcomes measures based on the 2010 release. Circ Cardiovasc Qual Outcomes. 2010;3:459-467.
51. Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407-413.
52. Cowie MR, Anker SD, Cleland JG, et al. Improving care for patients with acute heart failure: before, during and after hospitalization. Available at: http://www.oxfordhealthpolicyforum.org/files/reports/ahf-report.pdf. Accessed November 27, 2017.
From The Journal of Family Practice | 2018;67(1):18-26.
PRACTICE RECOMMENDATIONS
› Order a measurement of B-type natriuretic peptide or N-terminal pro-B-type natriuretic peptide in patients with dyspnea to help diagnose and manage heart failure (HF). A
› Refer patients with symptomatic HF and a left ventricular ejection fraction (LVEF) ≤35% that persists despite ≥3 months of optimal medical therapy for an implantable cardioverter defibrillator to reduce the risk of sudden death and all-cause mortality. A
› Consider cardiac resynchronization therapy for patients with an LVEF ≤35%, sinus rhythm, left bundle branch block, and a QRS duration ≥150 ms who remain symptomatic despite optimal medical therapy. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Cancer-survivor pain: What’s the PCP to do?
How do hyaluronic acid and corticosteroid injections compare for knee OA relief?
EVIDENCE SUMMARY
A 2015 network meta-analysis of 137 RCTs with 33,243 patients (ages 45-76 years) with knee OA compared the effectiveness of a variety of treatments including intra-articular CS and HA.1 At 3 months, the effect on pain was not significantly different between the CS and HA groups (12 trials; effect size [ES]=0.02; 95% confidence interval [CI], -0.12 to 0.17). However, a small but significant improvement in function was noted (scoring system not defined) at 3 months favoring HA (ES=0.24; 95% CI, 0.06-0.43; number of trials not specified).
At 3 and 6 months, HA improves pain, but not function, more than CS
Another meta-analysis published in 2015 examined the effectiveness of intra-articular CS and HA in 7 RCTs with 583 patients with knee OA.2 All 7 trials were included in the network meta-analysis and discussed separately to evaluate different time points.
Pain at one month wasn’t significantly different using a visual analog score (VAS) of one to 100 (4 trials; 245 patients; mean difference [MD]=1.66 points; 95% CI, -0.90 to 4.23). At 3 and 6 months, the HA group reported significantly reduced pain compared with the CS group (3 months: 3 trials; 320 patients; MD=12.58 points; 95% CI, -17.76 to -7.40; 6 months: 5 trials; 411 patients; MD=9.01 points; 95% CI, -12.62 to -5.40). There were no significant differences in function outcomes (Index of severity for OA of the knee by Lequesne et al; The Knee Society Clinical Rating System), maximum flexion, or adverse events.
Triamcinolone improves pain, function, but not for long
A 2016 double-blind RCT of 110 patients with knee OA compared intra-articular HA and triamcinolone, assessing pain and function at intervals between 24 hours and 6 months.3 Patients in the HA group received a single injection of 6 mL hylan G-F 20 (Synvisc); patients in the CS group received 1 mL of triamcinolone acetonide 40 mg and 5 mL of 1% lidocaine with epinephrine.
The CS group reported significantly less pain (VAS score 1 to 100) at 24 hours than the HA group (24 points vs 36 points; P=.002); relief lasted as long as one week (14 points vs 23 points; P=.018). After the first week, no difference was seen in pain between groups for as long as 6 months.
Function, assessed by a modified Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC 1 to 100; higher score indicates worse pain, stiffness, and function) showed a significant improvement with CS at 2 weeks (25 points vs 31 points; P=.03), but no difference at any other time point up to 6 months.
HA (mostly) improves pain, function more than betamethasone
A 2015 RCT of 200 patients with knee OA compared the effectiveness of intra-articular HA and betamethasone.4 Evaluators were blinded and assessments were made at 3, 6, 9, and 12 months. The HA group received 2.5 mL of 1% HA (Suprahyal); the CS group received betamethasone dipropionate 5 mg plus betamethasone sodium phosphate 2 mg in 1 mL.
The CS group had significantly less pain (VAS 1 to 10) at 3 months compared with the HA group (2.2 points vs 3.1 points; P=.004), but the HA group had less pain at all other time points (6 months: 3.9 points vs 2.4 points; P=.0001; 9 months: 5.5 points vs 3.6 points; P=.0001; 12 months: 6 points vs 4.1 points; P=.0001).
The WOMAC function subscores (0 to 68; lower indicates more function) were significantly better at all follow-up points in the HA group compared with the CS group (3 months: 19 vs 25; P=.0001; 6 months: 17 vs 29; P=.0001; 9 months: 25 vs 42; P=.0001; 12 months: 28 vs 42; P=.0001).4
RECOMMENDATIONS
The American Academy of Orthopaedic Surgeons 2013 work group couldn’t recommend for or against using intra-articular CS for patients with symptomatic knee OA based on inconclusive evidence.5 They also couldn’t recommend using HA (SOR: strong).
The National Institute for Health and Care Excellence (NICE) stated in 2008 that intra-articular CS injections should be considered as an adjunct to core treatments for the relief of moderate to severe pain in people with OA.6 In 2014, NICE recommended against offering intra-articular HA injections for managing OA.
The US Veterans Administration and Department of Defense have issued guidelines stating that clinicians may consider intra-articular CS injections for patients with symptomatic knee OA (US Preventive Services Task Force [USPSTF] Grade B).7 They report insufficient evidence to recommend for or against the use of intra-articular HA with the caveat that HA may be considered for patients who don’t respond adequately to nonpharmacologic measures and who have an inadequate response, intolerable adverse events, or contraindications to other pharmacologic therapies (USPSTF Grade I).
1. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162:46-54.
2. Wang F, He X. Intra-articular hyaluronic acid and corticosteroids in the treatment of knee osteoarthritis: a meta-analysis. Exp Ther Med. 2015;9:493-500.
3. Tammachote N, Kanitnate S, Yakumpor T, et al. Intra-articular, single-shot Hylan G-F 20 hyaluronic acid injection compared with corticosteroid in knee osteoarthritis: a double-blind, randomized controlled trial. J Bone Joint Surg Am. 2016;98:885-892.
4. Trueba Davalillo CA, Trueba Vasavilbaso C, Navarrete Alvarez JM, et al. Clinical efficacy of intra-articular injections in knee osteoarthritis: a prospective randomized study comparing hyaluronic acid and betamethasone. Open Access Rheumatol Res Rev. 2015;7:9-18.
5. American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee: Evidence-Based Guideline. 2nd ed. Available at: http://www.aaos.org/cc_files/aaosorg/research/guidelines/treatmentofosteoarthritisofthekneeguideline.pdf. Accessed May 15, 2016.
6. National Institute for Health and Care Excellence. Osteoarthritis: Care and Management. Available at: https://www.nice.org.uk/guidance/cg177/chapter/1-recommendations. Accessed May 15, 2016.
7. United States Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Non-Surgical Management of Hip and Knee Osteoarthritis. Available at: http://www.healthquality.va.gov/guidelines/CD/OA/VADoDOACPGFINAL090214.pdf. Accessed May 15, 2016.
EVIDENCE SUMMARY
A 2015 network meta-analysis of 137 RCTs with 33,243 patients (ages 45-76 years) with knee OA compared the effectiveness of a variety of treatments including intra-articular CS and HA.1 At 3 months, the effect on pain was not significantly different between the CS and HA groups (12 trials; effect size [ES]=0.02; 95% confidence interval [CI], -0.12 to 0.17). However, a small but significant improvement in function was noted (scoring system not defined) at 3 months favoring HA (ES=0.24; 95% CI, 0.06-0.43; number of trials not specified).
At 3 and 6 months, HA improves pain, but not function, more than CS
Another meta-analysis published in 2015 examined the effectiveness of intra-articular CS and HA in 7 RCTs with 583 patients with knee OA.2 All 7 trials were included in the network meta-analysis and discussed separately to evaluate different time points.
Pain at one month wasn’t significantly different using a visual analog score (VAS) of one to 100 (4 trials; 245 patients; mean difference [MD]=1.66 points; 95% CI, -0.90 to 4.23). At 3 and 6 months, the HA group reported significantly reduced pain compared with the CS group (3 months: 3 trials; 320 patients; MD=12.58 points; 95% CI, -17.76 to -7.40; 6 months: 5 trials; 411 patients; MD=9.01 points; 95% CI, -12.62 to -5.40). There were no significant differences in function outcomes (Index of severity for OA of the knee by Lequesne et al; The Knee Society Clinical Rating System), maximum flexion, or adverse events.
Triamcinolone improves pain, function, but not for long
A 2016 double-blind RCT of 110 patients with knee OA compared intra-articular HA and triamcinolone, assessing pain and function at intervals between 24 hours and 6 months.3 Patients in the HA group received a single injection of 6 mL hylan G-F 20 (Synvisc); patients in the CS group received 1 mL of triamcinolone acetonide 40 mg and 5 mL of 1% lidocaine with epinephrine.
The CS group reported significantly less pain (VAS score 1 to 100) at 24 hours than the HA group (24 points vs 36 points; P=.002); relief lasted as long as one week (14 points vs 23 points; P=.018). After the first week, no difference was seen in pain between groups for as long as 6 months.
Function, assessed by a modified Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC 1 to 100; higher score indicates worse pain, stiffness, and function) showed a significant improvement with CS at 2 weeks (25 points vs 31 points; P=.03), but no difference at any other time point up to 6 months.
HA (mostly) improves pain, function more than betamethasone
A 2015 RCT of 200 patients with knee OA compared the effectiveness of intra-articular HA and betamethasone.4 Evaluators were blinded and assessments were made at 3, 6, 9, and 12 months. The HA group received 2.5 mL of 1% HA (Suprahyal); the CS group received betamethasone dipropionate 5 mg plus betamethasone sodium phosphate 2 mg in 1 mL.
The CS group had significantly less pain (VAS 1 to 10) at 3 months compared with the HA group (2.2 points vs 3.1 points; P=.004), but the HA group had less pain at all other time points (6 months: 3.9 points vs 2.4 points; P=.0001; 9 months: 5.5 points vs 3.6 points; P=.0001; 12 months: 6 points vs 4.1 points; P=.0001).
The WOMAC function subscores (0 to 68; lower indicates more function) were significantly better at all follow-up points in the HA group compared with the CS group (3 months: 19 vs 25; P=.0001; 6 months: 17 vs 29; P=.0001; 9 months: 25 vs 42; P=.0001; 12 months: 28 vs 42; P=.0001).4
RECOMMENDATIONS
The American Academy of Orthopaedic Surgeons 2013 work group couldn’t recommend for or against using intra-articular CS for patients with symptomatic knee OA based on inconclusive evidence.5 They also couldn’t recommend using HA (SOR: strong).
The National Institute for Health and Care Excellence (NICE) stated in 2008 that intra-articular CS injections should be considered as an adjunct to core treatments for the relief of moderate to severe pain in people with OA.6 In 2014, NICE recommended against offering intra-articular HA injections for managing OA.
The US Veterans Administration and Department of Defense have issued guidelines stating that clinicians may consider intra-articular CS injections for patients with symptomatic knee OA (US Preventive Services Task Force [USPSTF] Grade B).7 They report insufficient evidence to recommend for or against the use of intra-articular HA with the caveat that HA may be considered for patients who don’t respond adequately to nonpharmacologic measures and who have an inadequate response, intolerable adverse events, or contraindications to other pharmacologic therapies (USPSTF Grade I).
EVIDENCE SUMMARY
A 2015 network meta-analysis of 137 RCTs with 33,243 patients (ages 45-76 years) with knee OA compared the effectiveness of a variety of treatments including intra-articular CS and HA.1 At 3 months, the effect on pain was not significantly different between the CS and HA groups (12 trials; effect size [ES]=0.02; 95% confidence interval [CI], -0.12 to 0.17). However, a small but significant improvement in function was noted (scoring system not defined) at 3 months favoring HA (ES=0.24; 95% CI, 0.06-0.43; number of trials not specified).
At 3 and 6 months, HA improves pain, but not function, more than CS
Another meta-analysis published in 2015 examined the effectiveness of intra-articular CS and HA in 7 RCTs with 583 patients with knee OA.2 All 7 trials were included in the network meta-analysis and discussed separately to evaluate different time points.
Pain at one month wasn’t significantly different using a visual analog score (VAS) of one to 100 (4 trials; 245 patients; mean difference [MD]=1.66 points; 95% CI, -0.90 to 4.23). At 3 and 6 months, the HA group reported significantly reduced pain compared with the CS group (3 months: 3 trials; 320 patients; MD=12.58 points; 95% CI, -17.76 to -7.40; 6 months: 5 trials; 411 patients; MD=9.01 points; 95% CI, -12.62 to -5.40). There were no significant differences in function outcomes (Index of severity for OA of the knee by Lequesne et al; The Knee Society Clinical Rating System), maximum flexion, or adverse events.
Triamcinolone improves pain, function, but not for long
A 2016 double-blind RCT of 110 patients with knee OA compared intra-articular HA and triamcinolone, assessing pain and function at intervals between 24 hours and 6 months.3 Patients in the HA group received a single injection of 6 mL hylan G-F 20 (Synvisc); patients in the CS group received 1 mL of triamcinolone acetonide 40 mg and 5 mL of 1% lidocaine with epinephrine.
The CS group reported significantly less pain (VAS score 1 to 100) at 24 hours than the HA group (24 points vs 36 points; P=.002); relief lasted as long as one week (14 points vs 23 points; P=.018). After the first week, no difference was seen in pain between groups for as long as 6 months.
Function, assessed by a modified Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC 1 to 100; higher score indicates worse pain, stiffness, and function) showed a significant improvement with CS at 2 weeks (25 points vs 31 points; P=.03), but no difference at any other time point up to 6 months.
HA (mostly) improves pain, function more than betamethasone
A 2015 RCT of 200 patients with knee OA compared the effectiveness of intra-articular HA and betamethasone.4 Evaluators were blinded and assessments were made at 3, 6, 9, and 12 months. The HA group received 2.5 mL of 1% HA (Suprahyal); the CS group received betamethasone dipropionate 5 mg plus betamethasone sodium phosphate 2 mg in 1 mL.
The CS group had significantly less pain (VAS 1 to 10) at 3 months compared with the HA group (2.2 points vs 3.1 points; P=.004), but the HA group had less pain at all other time points (6 months: 3.9 points vs 2.4 points; P=.0001; 9 months: 5.5 points vs 3.6 points; P=.0001; 12 months: 6 points vs 4.1 points; P=.0001).
The WOMAC function subscores (0 to 68; lower indicates more function) were significantly better at all follow-up points in the HA group compared with the CS group (3 months: 19 vs 25; P=.0001; 6 months: 17 vs 29; P=.0001; 9 months: 25 vs 42; P=.0001; 12 months: 28 vs 42; P=.0001).4
RECOMMENDATIONS
The American Academy of Orthopaedic Surgeons 2013 work group couldn’t recommend for or against using intra-articular CS for patients with symptomatic knee OA based on inconclusive evidence.5 They also couldn’t recommend using HA (SOR: strong).
The National Institute for Health and Care Excellence (NICE) stated in 2008 that intra-articular CS injections should be considered as an adjunct to core treatments for the relief of moderate to severe pain in people with OA.6 In 2014, NICE recommended against offering intra-articular HA injections for managing OA.
The US Veterans Administration and Department of Defense have issued guidelines stating that clinicians may consider intra-articular CS injections for patients with symptomatic knee OA (US Preventive Services Task Force [USPSTF] Grade B).7 They report insufficient evidence to recommend for or against the use of intra-articular HA with the caveat that HA may be considered for patients who don’t respond adequately to nonpharmacologic measures and who have an inadequate response, intolerable adverse events, or contraindications to other pharmacologic therapies (USPSTF Grade I).
1. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162:46-54.
2. Wang F, He X. Intra-articular hyaluronic acid and corticosteroids in the treatment of knee osteoarthritis: a meta-analysis. Exp Ther Med. 2015;9:493-500.
3. Tammachote N, Kanitnate S, Yakumpor T, et al. Intra-articular, single-shot Hylan G-F 20 hyaluronic acid injection compared with corticosteroid in knee osteoarthritis: a double-blind, randomized controlled trial. J Bone Joint Surg Am. 2016;98:885-892.
4. Trueba Davalillo CA, Trueba Vasavilbaso C, Navarrete Alvarez JM, et al. Clinical efficacy of intra-articular injections in knee osteoarthritis: a prospective randomized study comparing hyaluronic acid and betamethasone. Open Access Rheumatol Res Rev. 2015;7:9-18.
5. American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee: Evidence-Based Guideline. 2nd ed. Available at: http://www.aaos.org/cc_files/aaosorg/research/guidelines/treatmentofosteoarthritisofthekneeguideline.pdf. Accessed May 15, 2016.
6. National Institute for Health and Care Excellence. Osteoarthritis: Care and Management. Available at: https://www.nice.org.uk/guidance/cg177/chapter/1-recommendations. Accessed May 15, 2016.
7. United States Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Non-Surgical Management of Hip and Knee Osteoarthritis. Available at: http://www.healthquality.va.gov/guidelines/CD/OA/VADoDOACPGFINAL090214.pdf. Accessed May 15, 2016.
1. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162:46-54.
2. Wang F, He X. Intra-articular hyaluronic acid and corticosteroids in the treatment of knee osteoarthritis: a meta-analysis. Exp Ther Med. 2015;9:493-500.
3. Tammachote N, Kanitnate S, Yakumpor T, et al. Intra-articular, single-shot Hylan G-F 20 hyaluronic acid injection compared with corticosteroid in knee osteoarthritis: a double-blind, randomized controlled trial. J Bone Joint Surg Am. 2016;98:885-892.
4. Trueba Davalillo CA, Trueba Vasavilbaso C, Navarrete Alvarez JM, et al. Clinical efficacy of intra-articular injections in knee osteoarthritis: a prospective randomized study comparing hyaluronic acid and betamethasone. Open Access Rheumatol Res Rev. 2015;7:9-18.
5. American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee: Evidence-Based Guideline. 2nd ed. Available at: http://www.aaos.org/cc_files/aaosorg/research/guidelines/treatmentofosteoarthritisofthekneeguideline.pdf. Accessed May 15, 2016.
6. National Institute for Health and Care Excellence. Osteoarthritis: Care and Management. Available at: https://www.nice.org.uk/guidance/cg177/chapter/1-recommendations. Accessed May 15, 2016.
7. United States Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Non-Surgical Management of Hip and Knee Osteoarthritis. Available at: http://www.healthquality.va.gov/guidelines/CD/OA/VADoDOACPGFINAL090214.pdf. Accessed May 15, 2016.
Evidence-based answers from the Family Physicians Inquiries Network
EVIDENCE-BASED ANSWER:
Inconsistent evidence shows a small amount of pain relief early (one week to 3 months) with corticosteroid (CS) injections and an equally small improvement in pain relief and function later (3 to 12 months) with hyaluronic acid (HA) injections (strength of recommendation [SOR]: B, meta-analysis of a randomized controlled trial [RCT] and inconsistent RCTs).
Guidelines state that CS injections can be considered for symptomatic knee osteoarthritis (OA), but that insufficient evidence exists to recommend HA injections (SOR: B, evidence-based guidelines).
Time for another cup of coffee … or two
Nutrition enthusiasts have been saying for years that “we are what we eat.” In this issue of JFP, Drs. Malone and Tsai review the evidence regarding the medicinal properties of certain herbal and botanical supplements. (See here.) Although there are many unfounded claims about the health effects of a wide variety of supplements, increasing evidence from well-conducted randomized trials and large epidemiologic studies demonstrates that certain items we ingest have therapeutic value for a variety of conditions.
However, as Dr. Malone points out, herbal supplements and botanicals are not regulated by the US Food and Drug Administration, so manufacturers are not required to provide proof of effectiveness or safety to market their products. Some of these products have adverse effects. For example, butterbur can cause liver toxicity.1
Because about 38% of Americans use supplements, all primary care clinicians should know which products do—and do not—have evidence of efficacy.2 I suggest you read Dr. Malone’s 2-part article (part 2 is available here), but I can’t resist highlighting several of my favorites:
Coffee. Coffee used to be maligned because of its caffeine content, but more recent evidence suggests it protects against liver disease and has positive effects on cardiovascular disease and even mortality. (See Dr. Malone’s article for references.) There are no randomized trials, however, so we can’t be entirely sure if these associations are causal, but at least I can feel better about the 4 cups of coffee I drink every day!
Tea, especially green tea, appears to have many positive effects on health, including potential roles in reducing the risk of cancer, cardiovascular disease, type 2 diabetes, and even dementia. As with coffee, these associations are based on large observational studies and not randomized trials.
Chamomile. If your coffee gives you too much of a buzz and causes you to feel anxious, calm down with chamomile tea or oil. Evidence from randomized trials indicates it has positive effects on insomnia and anxiety.
Peppermint oil. The data for calming irritable bowel syndrome is fairly strong, and it may be effective in aborting migraines when applied to the forehead. It’s certainly worth a try for these difficult-to-treat conditions.
When patients ask you about botanicals and herbals, a great resource is
Now I will finish my fourth cup of coffee . . .
1. Daniel O, Mauskop A. Nutraceuticals in acute and prophylactic treatment of migraine. Curr Treat Options Neurol. 2016;18:14.
2. National Center for Complementary and Integrative Health. The use of complementary and alternative medicine in the United States. Available at: https://nccih.nih.gov/research/statistics/2007/camsurvey_fs1.htm. Accessed December 14, 2017.
Nutrition enthusiasts have been saying for years that “we are what we eat.” In this issue of JFP, Drs. Malone and Tsai review the evidence regarding the medicinal properties of certain herbal and botanical supplements. (See here.) Although there are many unfounded claims about the health effects of a wide variety of supplements, increasing evidence from well-conducted randomized trials and large epidemiologic studies demonstrates that certain items we ingest have therapeutic value for a variety of conditions.
However, as Dr. Malone points out, herbal supplements and botanicals are not regulated by the US Food and Drug Administration, so manufacturers are not required to provide proof of effectiveness or safety to market their products. Some of these products have adverse effects. For example, butterbur can cause liver toxicity.1
Because about 38% of Americans use supplements, all primary care clinicians should know which products do—and do not—have evidence of efficacy.2 I suggest you read Dr. Malone’s 2-part article (part 2 is available here), but I can’t resist highlighting several of my favorites:
Coffee. Coffee used to be maligned because of its caffeine content, but more recent evidence suggests it protects against liver disease and has positive effects on cardiovascular disease and even mortality. (See Dr. Malone’s article for references.) There are no randomized trials, however, so we can’t be entirely sure if these associations are causal, but at least I can feel better about the 4 cups of coffee I drink every day!
Tea, especially green tea, appears to have many positive effects on health, including potential roles in reducing the risk of cancer, cardiovascular disease, type 2 diabetes, and even dementia. As with coffee, these associations are based on large observational studies and not randomized trials.
Chamomile. If your coffee gives you too much of a buzz and causes you to feel anxious, calm down with chamomile tea or oil. Evidence from randomized trials indicates it has positive effects on insomnia and anxiety.
Peppermint oil. The data for calming irritable bowel syndrome is fairly strong, and it may be effective in aborting migraines when applied to the forehead. It’s certainly worth a try for these difficult-to-treat conditions.
When patients ask you about botanicals and herbals, a great resource is
Now I will finish my fourth cup of coffee . . .
Nutrition enthusiasts have been saying for years that “we are what we eat.” In this issue of JFP, Drs. Malone and Tsai review the evidence regarding the medicinal properties of certain herbal and botanical supplements. (See here.) Although there are many unfounded claims about the health effects of a wide variety of supplements, increasing evidence from well-conducted randomized trials and large epidemiologic studies demonstrates that certain items we ingest have therapeutic value for a variety of conditions.
However, as Dr. Malone points out, herbal supplements and botanicals are not regulated by the US Food and Drug Administration, so manufacturers are not required to provide proof of effectiveness or safety to market their products. Some of these products have adverse effects. For example, butterbur can cause liver toxicity.1
Because about 38% of Americans use supplements, all primary care clinicians should know which products do—and do not—have evidence of efficacy.2 I suggest you read Dr. Malone’s 2-part article (part 2 is available here), but I can’t resist highlighting several of my favorites:
Coffee. Coffee used to be maligned because of its caffeine content, but more recent evidence suggests it protects against liver disease and has positive effects on cardiovascular disease and even mortality. (See Dr. Malone’s article for references.) There are no randomized trials, however, so we can’t be entirely sure if these associations are causal, but at least I can feel better about the 4 cups of coffee I drink every day!
Tea, especially green tea, appears to have many positive effects on health, including potential roles in reducing the risk of cancer, cardiovascular disease, type 2 diabetes, and even dementia. As with coffee, these associations are based on large observational studies and not randomized trials.
Chamomile. If your coffee gives you too much of a buzz and causes you to feel anxious, calm down with chamomile tea or oil. Evidence from randomized trials indicates it has positive effects on insomnia and anxiety.
Peppermint oil. The data for calming irritable bowel syndrome is fairly strong, and it may be effective in aborting migraines when applied to the forehead. It’s certainly worth a try for these difficult-to-treat conditions.
When patients ask you about botanicals and herbals, a great resource is
Now I will finish my fourth cup of coffee . . .
1. Daniel O, Mauskop A. Nutraceuticals in acute and prophylactic treatment of migraine. Curr Treat Options Neurol. 2016;18:14.
2. National Center for Complementary and Integrative Health. The use of complementary and alternative medicine in the United States. Available at: https://nccih.nih.gov/research/statistics/2007/camsurvey_fs1.htm. Accessed December 14, 2017.
1. Daniel O, Mauskop A. Nutraceuticals in acute and prophylactic treatment of migraine. Curr Treat Options Neurol. 2016;18:14.
2. National Center for Complementary and Integrative Health. The use of complementary and alternative medicine in the United States. Available at: https://nccih.nih.gov/research/statistics/2007/camsurvey_fs1.htm. Accessed December 14, 2017.
Is this hypertension treatment strategy based on SOR “A” evidence?
In the article, “Hypertension treatment strategies for older adults” (J Fam Pract. 2017;66:546-554), Hansell et al gave an “A” Strength of Recommendation (SOR) rating to the Practice Recommendation that read: “Target a systolic blood pressure (SBP) <120 mm Hg in community-dwelling, nondiabetic patients ≥75 years of age if it is achievable without undue burden.”
As justification for this SBP target, the authors cited a subgroup analysis from the Systolic Blood Pressure Intervention Trial (SPRINT),1 which consisted of patients ≥75 years of age.2 I posit that the inconsistencies of the data cited by Hansell et al contradict an “A” rating, and that the methodology used in SPRINT greatly mitigates the generalizability of the results.
First, Hansell et al admit that no consensus exists on an optimal BP target for older patients. SOR taxonomy requires that the evidence behind an SOR of “A” be based on consistent and good-quality patient-oriented evidence.3 One source cited by the authors states that evidence supporting lower targets is inconsistent,4 while a recent Cochrane review does not support low BP targets.5 Given that the evidence is inconsistent, the SOR should be a “B”, at best.
Second, the evidence to target a systolic BP <120 mm Hg primarily comes from SPRINT.1,2,4 In a Letter to the Editor that appeared in The New England Journal of Medicine, Dr. Marc A. Pfeffer addressed a key methodology issue of that trial: SPRINT protocol called for the withdrawal of antihypertensive therapy in the standard treatment group if a single systolic BP reading was <130 mm Hg, or if readings at 2 or more consecutive visits were <135 mm Hg, regardless of patient symptoms.6
The letter also questioned how frequently this withdrawal occurred, to which the SPRINT authors replied that 87% of participants required at least one reduction in the dose of medication to maintain the treatment target in the standard group, and complete withdrawal of medication was required in <7.5% of participants.7 While this dose adjustment may have been necessary to adequately test the SPRINT hypothesis that lower systolic BP targets are better, routine dose reduction in an asymptomatic patient is not standard practice.
Given the small benefit in absolute risk reduction in SPRINT’s aggressive hypertensive treatment arm of 0.54% per year for the primary composite outcome and 0.37% per year for all-cause mortality,2 the frequent medication dose reductions in the standard treatment arm likely contributed significantly to the statistical benefit seen in the aggressive treatment group in SPRINT.
If an SOR of “A” for BP targets is to be made, the print publication of Hansell et al’s article should communicate the degree of benefit, preferably in terms of absolute risk reduction. Only the online publication of TABLE W1 stated the degree of benefit in the SPRINT subgroup study, but it was stated in terms of relative risk.
Given the current suboptimal rates of hypertension control, primary care physicians would do well to impact morbidity and mortality in older adults by working to achieve standard targets, such as an SBP of <140 mm Hg or <150 mm Hg. Once standard targets are achieved, a conversation could then ensue about the potential benefits and harms of lower BP targets.
Chris Fallert, MD
St. Paul, Minn
1. Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
2. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2106.
3. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556.
4. Weiss J, Freeman M, Low A, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: a systematic review and meta-analysis. Ann Intern Med. 2017;166:419-429.
5. Garrison SR, Kolber MR, Korownyk CS, et al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev. 2017;8:CD011575.
6. Pfeffer MA. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2290.
7. Wright JT Jr, Whelton PK, Reboussin DM. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2294.
Authors’ response:
An SOR of “A” is based on consistent and good-quality patient-oriented evidence, which is further defined for treatment, prevention, and screening studies as (a) systematic reviews/meta-analyses of randomized controlled trials (RCTs) with consistent findings or (b) a high-quality individual RCT.1 The recommendation to “target a systolic blood pressure (BP) <120 mm Hg in community-dwelling, nondiabetic patients ≥75 years of age if it is achievable without undue burden” meets level 1 evidence based on both (a) and (b).
While a Cochrane review of hypertension did not support a systolic BP target <120 mm Hg, the populations evaluated included a variety of ages; the studies did not specifically focus on those ≥75 years of age with inherently high cardiovascular risk while excluding patients with diabetes.2 The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial results,3 which are often viewed as inconsistent with SPRINT,4 included patients with diabetes and patients of a younger average age than SPRINT. Although no overall mortality benefit of intensive BP control was found in the ACCORD trial, there was significant reduction in stroke, as well as additional benefit in the ACCORD standard glycemia group.3,5
The American College of Cardiology/American Heart Association 2017 BP guidelines summarize several meta-analyses that consistently support tighter BP control with recommendations for a lower BP target of <130 mm Hg systolic.5,6 They selected a target of <130 mm Hg, rather than <120 mm Hg, assuming that general health care providers cannot be as efficacious at lowering BP as researchers in efficacy trials.5
With regard to medication withdrawal as a flaw in the SPRINT design,4 an accepted geriatric principle is reduction in polypharmacy whenever possible. Medication reduction or withdrawal when a patient is too far below target is prudent. The 2 different target groups in an RCT have to be statistically different to draw conclusions about the differences. This strategy has been employed in other BP trials. Medication withdrawal is an appropriate means to achieve targets, which the SPRINT investigators did successfully with a least-square mean systolic BP for patients ≥75 years of age in the control group of 134.8 mm Hg and 123.4 mm Hg in the intensive group.4 Even with reduction in polypharmacy in the standard group, SPRINT demonstrated cardiovascular and mortality benefit with tighter control.4
With regard to Dr. Fallert’s comments about a small absolute risk reduction for the entire SPRINT study population, our article in JFP specifically pertains to adults ≥75 years of age. The numbers needed to treat for composite cardiovascular outcomes and all-cause mortality in the ≥75 SPRINT group are 27 (95% confidence interval [CI], 19-61) and 41 (95% CI, 27-145), respectively.4
We agree that there is suboptimal hypertension control at present. However, physicians should not only focus on this modifiable risk factor to reduce CVD risk and mortality in appropriate patients, but they should focus on doing it to the evidence-based goal.
Maggie W. Hansell, MD; Emily M. Mann, MD; Julienne K. Kirk, PharmD
Winston-Salem, NC
1. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556.
2. Garrison SR, Kolber MR, Korownyk CS, et al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev. 2017;8:CD011575.
3. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive blood-pressure control in type 2 diabetes. N Engl J Med. 2010;362:1575-1585.
4. Williamson JD, Suplano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
5. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Available at: http://hyper.ahajournals.org/content/hypertensionaha/early/2017/11/10/HYP.0000000000000066.full.pdf. Accessed December 12, 2017.
6. Reboussin DM, Allen NB, Griswold ME, et al. Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Available at: http://hyper.ahajournals.org/content/early/2017/11/10/HYP.0000000000000067. Accessed December 12, 2017.
In the article, “Hypertension treatment strategies for older adults” (J Fam Pract. 2017;66:546-554), Hansell et al gave an “A” Strength of Recommendation (SOR) rating to the Practice Recommendation that read: “Target a systolic blood pressure (SBP) <120 mm Hg in community-dwelling, nondiabetic patients ≥75 years of age if it is achievable without undue burden.”
As justification for this SBP target, the authors cited a subgroup analysis from the Systolic Blood Pressure Intervention Trial (SPRINT),1 which consisted of patients ≥75 years of age.2 I posit that the inconsistencies of the data cited by Hansell et al contradict an “A” rating, and that the methodology used in SPRINT greatly mitigates the generalizability of the results.
First, Hansell et al admit that no consensus exists on an optimal BP target for older patients. SOR taxonomy requires that the evidence behind an SOR of “A” be based on consistent and good-quality patient-oriented evidence.3 One source cited by the authors states that evidence supporting lower targets is inconsistent,4 while a recent Cochrane review does not support low BP targets.5 Given that the evidence is inconsistent, the SOR should be a “B”, at best.
Second, the evidence to target a systolic BP <120 mm Hg primarily comes from SPRINT.1,2,4 In a Letter to the Editor that appeared in The New England Journal of Medicine, Dr. Marc A. Pfeffer addressed a key methodology issue of that trial: SPRINT protocol called for the withdrawal of antihypertensive therapy in the standard treatment group if a single systolic BP reading was <130 mm Hg, or if readings at 2 or more consecutive visits were <135 mm Hg, regardless of patient symptoms.6
The letter also questioned how frequently this withdrawal occurred, to which the SPRINT authors replied that 87% of participants required at least one reduction in the dose of medication to maintain the treatment target in the standard group, and complete withdrawal of medication was required in <7.5% of participants.7 While this dose adjustment may have been necessary to adequately test the SPRINT hypothesis that lower systolic BP targets are better, routine dose reduction in an asymptomatic patient is not standard practice.
Given the small benefit in absolute risk reduction in SPRINT’s aggressive hypertensive treatment arm of 0.54% per year for the primary composite outcome and 0.37% per year for all-cause mortality,2 the frequent medication dose reductions in the standard treatment arm likely contributed significantly to the statistical benefit seen in the aggressive treatment group in SPRINT.
If an SOR of “A” for BP targets is to be made, the print publication of Hansell et al’s article should communicate the degree of benefit, preferably in terms of absolute risk reduction. Only the online publication of TABLE W1 stated the degree of benefit in the SPRINT subgroup study, but it was stated in terms of relative risk.
Given the current suboptimal rates of hypertension control, primary care physicians would do well to impact morbidity and mortality in older adults by working to achieve standard targets, such as an SBP of <140 mm Hg or <150 mm Hg. Once standard targets are achieved, a conversation could then ensue about the potential benefits and harms of lower BP targets.
Chris Fallert, MD
St. Paul, Minn
1. Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
2. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2106.
3. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556.
4. Weiss J, Freeman M, Low A, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: a systematic review and meta-analysis. Ann Intern Med. 2017;166:419-429.
5. Garrison SR, Kolber MR, Korownyk CS, et al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev. 2017;8:CD011575.
6. Pfeffer MA. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2290.
7. Wright JT Jr, Whelton PK, Reboussin DM. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2294.
Authors’ response:
An SOR of “A” is based on consistent and good-quality patient-oriented evidence, which is further defined for treatment, prevention, and screening studies as (a) systematic reviews/meta-analyses of randomized controlled trials (RCTs) with consistent findings or (b) a high-quality individual RCT.1 The recommendation to “target a systolic blood pressure (BP) <120 mm Hg in community-dwelling, nondiabetic patients ≥75 years of age if it is achievable without undue burden” meets level 1 evidence based on both (a) and (b).
While a Cochrane review of hypertension did not support a systolic BP target <120 mm Hg, the populations evaluated included a variety of ages; the studies did not specifically focus on those ≥75 years of age with inherently high cardiovascular risk while excluding patients with diabetes.2 The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial results,3 which are often viewed as inconsistent with SPRINT,4 included patients with diabetes and patients of a younger average age than SPRINT. Although no overall mortality benefit of intensive BP control was found in the ACCORD trial, there was significant reduction in stroke, as well as additional benefit in the ACCORD standard glycemia group.3,5
The American College of Cardiology/American Heart Association 2017 BP guidelines summarize several meta-analyses that consistently support tighter BP control with recommendations for a lower BP target of <130 mm Hg systolic.5,6 They selected a target of <130 mm Hg, rather than <120 mm Hg, assuming that general health care providers cannot be as efficacious at lowering BP as researchers in efficacy trials.5
With regard to medication withdrawal as a flaw in the SPRINT design,4 an accepted geriatric principle is reduction in polypharmacy whenever possible. Medication reduction or withdrawal when a patient is too far below target is prudent. The 2 different target groups in an RCT have to be statistically different to draw conclusions about the differences. This strategy has been employed in other BP trials. Medication withdrawal is an appropriate means to achieve targets, which the SPRINT investigators did successfully with a least-square mean systolic BP for patients ≥75 years of age in the control group of 134.8 mm Hg and 123.4 mm Hg in the intensive group.4 Even with reduction in polypharmacy in the standard group, SPRINT demonstrated cardiovascular and mortality benefit with tighter control.4
With regard to Dr. Fallert’s comments about a small absolute risk reduction for the entire SPRINT study population, our article in JFP specifically pertains to adults ≥75 years of age. The numbers needed to treat for composite cardiovascular outcomes and all-cause mortality in the ≥75 SPRINT group are 27 (95% confidence interval [CI], 19-61) and 41 (95% CI, 27-145), respectively.4
We agree that there is suboptimal hypertension control at present. However, physicians should not only focus on this modifiable risk factor to reduce CVD risk and mortality in appropriate patients, but they should focus on doing it to the evidence-based goal.
Maggie W. Hansell, MD; Emily M. Mann, MD; Julienne K. Kirk, PharmD
Winston-Salem, NC
1. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556.
2. Garrison SR, Kolber MR, Korownyk CS, et al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev. 2017;8:CD011575.
3. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive blood-pressure control in type 2 diabetes. N Engl J Med. 2010;362:1575-1585.
4. Williamson JD, Suplano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
5. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Available at: http://hyper.ahajournals.org/content/hypertensionaha/early/2017/11/10/HYP.0000000000000066.full.pdf. Accessed December 12, 2017.
6. Reboussin DM, Allen NB, Griswold ME, et al. Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Available at: http://hyper.ahajournals.org/content/early/2017/11/10/HYP.0000000000000067. Accessed December 12, 2017.
In the article, “Hypertension treatment strategies for older adults” (J Fam Pract. 2017;66:546-554), Hansell et al gave an “A” Strength of Recommendation (SOR) rating to the Practice Recommendation that read: “Target a systolic blood pressure (SBP) <120 mm Hg in community-dwelling, nondiabetic patients ≥75 years of age if it is achievable without undue burden.”
As justification for this SBP target, the authors cited a subgroup analysis from the Systolic Blood Pressure Intervention Trial (SPRINT),1 which consisted of patients ≥75 years of age.2 I posit that the inconsistencies of the data cited by Hansell et al contradict an “A” rating, and that the methodology used in SPRINT greatly mitigates the generalizability of the results.
First, Hansell et al admit that no consensus exists on an optimal BP target for older patients. SOR taxonomy requires that the evidence behind an SOR of “A” be based on consistent and good-quality patient-oriented evidence.3 One source cited by the authors states that evidence supporting lower targets is inconsistent,4 while a recent Cochrane review does not support low BP targets.5 Given that the evidence is inconsistent, the SOR should be a “B”, at best.
Second, the evidence to target a systolic BP <120 mm Hg primarily comes from SPRINT.1,2,4 In a Letter to the Editor that appeared in The New England Journal of Medicine, Dr. Marc A. Pfeffer addressed a key methodology issue of that trial: SPRINT protocol called for the withdrawal of antihypertensive therapy in the standard treatment group if a single systolic BP reading was <130 mm Hg, or if readings at 2 or more consecutive visits were <135 mm Hg, regardless of patient symptoms.6
The letter also questioned how frequently this withdrawal occurred, to which the SPRINT authors replied that 87% of participants required at least one reduction in the dose of medication to maintain the treatment target in the standard group, and complete withdrawal of medication was required in <7.5% of participants.7 While this dose adjustment may have been necessary to adequately test the SPRINT hypothesis that lower systolic BP targets are better, routine dose reduction in an asymptomatic patient is not standard practice.
Given the small benefit in absolute risk reduction in SPRINT’s aggressive hypertensive treatment arm of 0.54% per year for the primary composite outcome and 0.37% per year for all-cause mortality,2 the frequent medication dose reductions in the standard treatment arm likely contributed significantly to the statistical benefit seen in the aggressive treatment group in SPRINT.
If an SOR of “A” for BP targets is to be made, the print publication of Hansell et al’s article should communicate the degree of benefit, preferably in terms of absolute risk reduction. Only the online publication of TABLE W1 stated the degree of benefit in the SPRINT subgroup study, but it was stated in terms of relative risk.
Given the current suboptimal rates of hypertension control, primary care physicians would do well to impact morbidity and mortality in older adults by working to achieve standard targets, such as an SBP of <140 mm Hg or <150 mm Hg. Once standard targets are achieved, a conversation could then ensue about the potential benefits and harms of lower BP targets.
Chris Fallert, MD
St. Paul, Minn
1. Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
2. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2106.
3. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556.
4. Weiss J, Freeman M, Low A, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: a systematic review and meta-analysis. Ann Intern Med. 2017;166:419-429.
5. Garrison SR, Kolber MR, Korownyk CS, et al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev. 2017;8:CD011575.
6. Pfeffer MA. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2290.
7. Wright JT Jr, Whelton PK, Reboussin DM. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2016;374:2294.
Authors’ response:
An SOR of “A” is based on consistent and good-quality patient-oriented evidence, which is further defined for treatment, prevention, and screening studies as (a) systematic reviews/meta-analyses of randomized controlled trials (RCTs) with consistent findings or (b) a high-quality individual RCT.1 The recommendation to “target a systolic blood pressure (BP) <120 mm Hg in community-dwelling, nondiabetic patients ≥75 years of age if it is achievable without undue burden” meets level 1 evidence based on both (a) and (b).
While a Cochrane review of hypertension did not support a systolic BP target <120 mm Hg, the populations evaluated included a variety of ages; the studies did not specifically focus on those ≥75 years of age with inherently high cardiovascular risk while excluding patients with diabetes.2 The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial results,3 which are often viewed as inconsistent with SPRINT,4 included patients with diabetes and patients of a younger average age than SPRINT. Although no overall mortality benefit of intensive BP control was found in the ACCORD trial, there was significant reduction in stroke, as well as additional benefit in the ACCORD standard glycemia group.3,5
The American College of Cardiology/American Heart Association 2017 BP guidelines summarize several meta-analyses that consistently support tighter BP control with recommendations for a lower BP target of <130 mm Hg systolic.5,6 They selected a target of <130 mm Hg, rather than <120 mm Hg, assuming that general health care providers cannot be as efficacious at lowering BP as researchers in efficacy trials.5
With regard to medication withdrawal as a flaw in the SPRINT design,4 an accepted geriatric principle is reduction in polypharmacy whenever possible. Medication reduction or withdrawal when a patient is too far below target is prudent. The 2 different target groups in an RCT have to be statistically different to draw conclusions about the differences. This strategy has been employed in other BP trials. Medication withdrawal is an appropriate means to achieve targets, which the SPRINT investigators did successfully with a least-square mean systolic BP for patients ≥75 years of age in the control group of 134.8 mm Hg and 123.4 mm Hg in the intensive group.4 Even with reduction in polypharmacy in the standard group, SPRINT demonstrated cardiovascular and mortality benefit with tighter control.4
With regard to Dr. Fallert’s comments about a small absolute risk reduction for the entire SPRINT study population, our article in JFP specifically pertains to adults ≥75 years of age. The numbers needed to treat for composite cardiovascular outcomes and all-cause mortality in the ≥75 SPRINT group are 27 (95% confidence interval [CI], 19-61) and 41 (95% CI, 27-145), respectively.4
We agree that there is suboptimal hypertension control at present. However, physicians should not only focus on this modifiable risk factor to reduce CVD risk and mortality in appropriate patients, but they should focus on doing it to the evidence-based goal.
Maggie W. Hansell, MD; Emily M. Mann, MD; Julienne K. Kirk, PharmD
Winston-Salem, NC
1. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69:548-556.
2. Garrison SR, Kolber MR, Korownyk CS, et al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev. 2017;8:CD011575.
3. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive blood-pressure control in type 2 diabetes. N Engl J Med. 2010;362:1575-1585.
4. Williamson JD, Suplano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
5. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Available at: http://hyper.ahajournals.org/content/hypertensionaha/early/2017/11/10/HYP.0000000000000066.full.pdf. Accessed December 12, 2017.
6. Reboussin DM, Allen NB, Griswold ME, et al. Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Available at: http://hyper.ahajournals.org/content/early/2017/11/10/HYP.0000000000000067. Accessed December 12, 2017.
Let’s recognize Dr. John Geyman, too
Thank you for your tribute to David Warfield Stires, The Journal of Family Practice’s founding publisher (J Fam Pract. 2017;66:654-655). The real hero of the story, however, is Dr. John Geyman, who had the vision to found a research journal at the birth of our specialty. This was no easy task, as John faced a challenging chicken-and-egg problem: how to establish a research journal when academic family medicine was just getting underway and had no track record of generating a steady stream of quality research. The latter problem was due, in part, to the lack of a research journal devoted to promoting and publishing research in the field.
Yet, John did it, putting family medicine research on the publishing map. His groundbreaking work set the stage for future journals, including the Journal of the American Board of Family Medicine, the American Medical Association’s now-defunct Archives of Family Medicine, and the American Academy of Family Physicians’ Annals of Family Medicine.
As a family medicine resident in the 1970s, I remember coveting JFP so much that I managed to collect every issue from Volume 1, Issue 1, through the turn of the century. And as a young faculty member at Georgetown University Medical Center in the 1980s, I painstakingly created an annotated bibliography of the then-published content of JFP to use for teaching, research, and administration.
When I became editor of American Family Physician in 1988, I made a pilgrimage to the University of Washington School of Medicine in Seattle, where John was chairman of the Department of Family Medicine. I wanted to seek his advice, learn from his vast experience, and pay tribute to all that he’d done for our specialty. Over the past 30 years, John has continued to leave his mark. (See http://www.johngeymanmd.org/bio.html.)
A tribute to David Warfield Stires is incomplete without a corresponding acknowledgement and celebration of John’s decades-long visionary leadership in family medicine.
Jay Siwek, MD
Washington, DC
Thank you for your tribute to David Warfield Stires, The Journal of Family Practice’s founding publisher (J Fam Pract. 2017;66:654-655). The real hero of the story, however, is Dr. John Geyman, who had the vision to found a research journal at the birth of our specialty. This was no easy task, as John faced a challenging chicken-and-egg problem: how to establish a research journal when academic family medicine was just getting underway and had no track record of generating a steady stream of quality research. The latter problem was due, in part, to the lack of a research journal devoted to promoting and publishing research in the field.
Yet, John did it, putting family medicine research on the publishing map. His groundbreaking work set the stage for future journals, including the Journal of the American Board of Family Medicine, the American Medical Association’s now-defunct Archives of Family Medicine, and the American Academy of Family Physicians’ Annals of Family Medicine.
As a family medicine resident in the 1970s, I remember coveting JFP so much that I managed to collect every issue from Volume 1, Issue 1, through the turn of the century. And as a young faculty member at Georgetown University Medical Center in the 1980s, I painstakingly created an annotated bibliography of the then-published content of JFP to use for teaching, research, and administration.
When I became editor of American Family Physician in 1988, I made a pilgrimage to the University of Washington School of Medicine in Seattle, where John was chairman of the Department of Family Medicine. I wanted to seek his advice, learn from his vast experience, and pay tribute to all that he’d done for our specialty. Over the past 30 years, John has continued to leave his mark. (See http://www.johngeymanmd.org/bio.html.)
A tribute to David Warfield Stires is incomplete without a corresponding acknowledgement and celebration of John’s decades-long visionary leadership in family medicine.
Jay Siwek, MD
Washington, DC
Thank you for your tribute to David Warfield Stires, The Journal of Family Practice’s founding publisher (J Fam Pract. 2017;66:654-655). The real hero of the story, however, is Dr. John Geyman, who had the vision to found a research journal at the birth of our specialty. This was no easy task, as John faced a challenging chicken-and-egg problem: how to establish a research journal when academic family medicine was just getting underway and had no track record of generating a steady stream of quality research. The latter problem was due, in part, to the lack of a research journal devoted to promoting and publishing research in the field.
Yet, John did it, putting family medicine research on the publishing map. His groundbreaking work set the stage for future journals, including the Journal of the American Board of Family Medicine, the American Medical Association’s now-defunct Archives of Family Medicine, and the American Academy of Family Physicians’ Annals of Family Medicine.
As a family medicine resident in the 1970s, I remember coveting JFP so much that I managed to collect every issue from Volume 1, Issue 1, through the turn of the century. And as a young faculty member at Georgetown University Medical Center in the 1980s, I painstakingly created an annotated bibliography of the then-published content of JFP to use for teaching, research, and administration.
When I became editor of American Family Physician in 1988, I made a pilgrimage to the University of Washington School of Medicine in Seattle, where John was chairman of the Department of Family Medicine. I wanted to seek his advice, learn from his vast experience, and pay tribute to all that he’d done for our specialty. Over the past 30 years, John has continued to leave his mark. (See http://www.johngeymanmd.org/bio.html.)
A tribute to David Warfield Stires is incomplete without a corresponding acknowledgement and celebration of John’s decades-long visionary leadership in family medicine.
Jay Siwek, MD
Washington, DC
Utilize guidelines, but customize BP treatment in older patients
In the article, “Hypertension treatment strategies for older adults” (J Fam Pract. 2017;66:546-554), Hansell et al recommend a systolic blood pressure (SBP) treatment target of <120 mm Hg for community-dwelling, nondiabetic patients ≥75 years of age. This recommendation is not supported by the authors’ cited guidelines, and we have serious concerns about the risk of harm from such overly stringent BP control in this population.
While Hansell et al acknowledge that no consensus exists regarding an optimal BP target for older patients, the authors cite the Eighth Joint National Committee (JNC 8), the American College of Physicians (ACP), the Systolic Blood Pressure Intervention Trial (SPRINT) subgroup analysis, and the BP arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial to justify their recommendation. But as the authors mention, JNC 8 conducted a comprehensive review of the available evidence and determined that a BP target of <150/90 mm Hg for hypertensive patients ≥60 years of age is appropriate.1
The authors also state that ACP recommends an SBP target of <140 mm Hg, while, in fact, the recommendations from ACP (which are joint guidelines published with the American Academy of Family Physicians) say that high-quality evidence strongly supports an SBP target of <150 mm Hg to reduce the risk for mortality, stroke, and cardiac events in adults ≥60 years of age.2
SPRINT does support Hansell et al’s recommended SBP target of <120 mm Hg, but this trial provided only composite data of adults ≥75 years of age and did not differentiate between the outcomes in otherwise healthy adults ≥75 years of age vs those with cardiovascular conditions.3 As Hansell et al point out, the SPRINT trial was halted prematurely, which compromises the validity of their findings.
Lastly, the ACCORD trial did not find benefit to treating SBP <120 mm Hg compared with <140 mm Hg in adults with diabetes, but it did find substantial harms in the <120 mm Hg group, including an increased risk of renal impairment and hypokalemia.4
Hansel et al’s overreliance on the SPRINT subgroup analysis represents a significant flaw in the assertion that an SBP target <120 mm Hg is reasonable for all community-dwelling, non-diabetic adults ≥75 years of age. While the authors made the allowance that a higher target (<140 mm Hg) is acceptable if a target of <120 mm Hg places undue burden on the patient, the guidelines they cited, when considered together, suggest that starting at a higher target is not only sufficient to prevent complications, but also reduces overtreatment.
Adults ≥75 years of age are a diverse group regarding disease conditions, life expectancy, and personal priorities. While it is tempting to make generalizations about BP treatment targets, we owe it to our patients to understand the nuances of applicable guidelines so that we can tailor BP treatment targets to each patient’s unique clinical situation and personal priorities. Applying a blanket recommendation to this heterogeneous population may result in significant harms from overtreatment.
Jennifer L. Middleton, MD, MPH, FAAFP; Miriam Chan, PharmD, CDE
Columbus, Ohio
1. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
2. Qaseem A, Wilt TJ, Rich R, et al. Pharmacological treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.
3. Williamson JD, Suplano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
4. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575-1585.
Authors’ response:
We agree with the title of this letter, “Utilize guidelines, but customize BP treatment in older patients.” Our recommendations are not limited to targeting a systolic BP <120 mm Hg for community-dwelling, nondiabetic adults ≥75 years of age, but include consideration for “undue burden.” Our third practice recommendation, which recommends that one consider cognitive function, polypharmacy, multimorbidity, and frailty, is an equally—if not more—important recommendation.
With regard to the specific concerns about the current guidelines:
- The American College of Physicians and American Academy of Family Physicians’ “Recommendation 1” advocates a systolic BP goal <150 mm Hg for adults ≥60 years of age. However, “Recommendation 3” endorses intensifying treatment in adults ≥60 years of age at high cardiovascular (CV) risk. Based on Framingham criteria, all adults ≥75 years of age are considered at high risk for CV disease, as stated in our article. Therefore, “Recommendation 3” for a target of <140 mm Hg is applicable for the population addressed in our article.1
- The Eighth Joint National Committee (JNC 8) does recommend a BP target <150 mm Hg for adults ≥60 years of age, but does not take into account recent data, which is why we wanted to highlight that data for physicians.2
- Since submission of our article, The American College of Cardiology/American Heart Association (ACC/AHA) has published its first set of guidelines since 2003, which lowered BP target to <130 mm Hg in patients with high CV risk. Those guidelines outline the validity of SPRINT and the consistency of the existing evidence, including the linear relationship of BP and mortality.3
- SPRINT was halted early specifically because of the mortality benefit in the intensive treatment group, which is ethically appropriate.4 It is unclear to us how this compromises the validity of the trial. There is often concern for bias from early cessation in small trials, but this was a large, well-powered trial.
- The ACC/AHA guidelines also address some of the nuances of ACCORD, which is specific to patients with diabetes (whom we excluded from our first Practice Recommendation). Although no overall mortality benefit was found, there was stroke reduction in this group and additional benefit in the standard glycemia group.3,5 A meta-analysis of SPRINT and ACCORD showed CV disease reduction with a BP target <120 mm Hg.6
Although we do believe that SPRINT is a landmark trial contributing a great deal to our recommendations, we strongly emphasized that comorbidities, frailty, and dementia greatly impact treatment decisions. We stressed that prescribers use caution and slow titration because of adverse effects. Geriatric medicine is a complex art, and one of the goals of our article was to highlight this complexity and emphasize the importance of considering goals of care, comorbidity, frailty, and cognitive function when choosing optimal BP targets.
Maggie W. Hansell, MD; Emily M. Mann, MD; Julienne K. Kirk, PharmD
Winston-Salem, NC
1. Qaseem A, Wilt TJ, Rich R, et al. Pharmacological treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.
2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
3. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Available at: http://hyper.ahajournals.org/content/hypertensionaha/early/2017/11/10/HYP.0000000000000066.full.pdf. Accessed December 12, 2017.
4. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2106.
5. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive blood-pressure control in type 2 diabetes. N Engl J Med. 2010;362:1575-1585.
6. Perkovic V, Rodgers A. Redefining blood-pressure targets—SPRINT starts the marathon. N Engl Med. 2015;373:2175-2178.
In the article, “Hypertension treatment strategies for older adults” (J Fam Pract. 2017;66:546-554), Hansell et al recommend a systolic blood pressure (SBP) treatment target of <120 mm Hg for community-dwelling, nondiabetic patients ≥75 years of age. This recommendation is not supported by the authors’ cited guidelines, and we have serious concerns about the risk of harm from such overly stringent BP control in this population.
While Hansell et al acknowledge that no consensus exists regarding an optimal BP target for older patients, the authors cite the Eighth Joint National Committee (JNC 8), the American College of Physicians (ACP), the Systolic Blood Pressure Intervention Trial (SPRINT) subgroup analysis, and the BP arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial to justify their recommendation. But as the authors mention, JNC 8 conducted a comprehensive review of the available evidence and determined that a BP target of <150/90 mm Hg for hypertensive patients ≥60 years of age is appropriate.1
The authors also state that ACP recommends an SBP target of <140 mm Hg, while, in fact, the recommendations from ACP (which are joint guidelines published with the American Academy of Family Physicians) say that high-quality evidence strongly supports an SBP target of <150 mm Hg to reduce the risk for mortality, stroke, and cardiac events in adults ≥60 years of age.2
SPRINT does support Hansell et al’s recommended SBP target of <120 mm Hg, but this trial provided only composite data of adults ≥75 years of age and did not differentiate between the outcomes in otherwise healthy adults ≥75 years of age vs those with cardiovascular conditions.3 As Hansell et al point out, the SPRINT trial was halted prematurely, which compromises the validity of their findings.
Lastly, the ACCORD trial did not find benefit to treating SBP <120 mm Hg compared with <140 mm Hg in adults with diabetes, but it did find substantial harms in the <120 mm Hg group, including an increased risk of renal impairment and hypokalemia.4
Hansel et al’s overreliance on the SPRINT subgroup analysis represents a significant flaw in the assertion that an SBP target <120 mm Hg is reasonable for all community-dwelling, non-diabetic adults ≥75 years of age. While the authors made the allowance that a higher target (<140 mm Hg) is acceptable if a target of <120 mm Hg places undue burden on the patient, the guidelines they cited, when considered together, suggest that starting at a higher target is not only sufficient to prevent complications, but also reduces overtreatment.
Adults ≥75 years of age are a diverse group regarding disease conditions, life expectancy, and personal priorities. While it is tempting to make generalizations about BP treatment targets, we owe it to our patients to understand the nuances of applicable guidelines so that we can tailor BP treatment targets to each patient’s unique clinical situation and personal priorities. Applying a blanket recommendation to this heterogeneous population may result in significant harms from overtreatment.
Jennifer L. Middleton, MD, MPH, FAAFP; Miriam Chan, PharmD, CDE
Columbus, Ohio
1. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
2. Qaseem A, Wilt TJ, Rich R, et al. Pharmacological treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.
3. Williamson JD, Suplano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
4. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575-1585.
Authors’ response:
We agree with the title of this letter, “Utilize guidelines, but customize BP treatment in older patients.” Our recommendations are not limited to targeting a systolic BP <120 mm Hg for community-dwelling, nondiabetic adults ≥75 years of age, but include consideration for “undue burden.” Our third practice recommendation, which recommends that one consider cognitive function, polypharmacy, multimorbidity, and frailty, is an equally—if not more—important recommendation.
With regard to the specific concerns about the current guidelines:
- The American College of Physicians and American Academy of Family Physicians’ “Recommendation 1” advocates a systolic BP goal <150 mm Hg for adults ≥60 years of age. However, “Recommendation 3” endorses intensifying treatment in adults ≥60 years of age at high cardiovascular (CV) risk. Based on Framingham criteria, all adults ≥75 years of age are considered at high risk for CV disease, as stated in our article. Therefore, “Recommendation 3” for a target of <140 mm Hg is applicable for the population addressed in our article.1
- The Eighth Joint National Committee (JNC 8) does recommend a BP target <150 mm Hg for adults ≥60 years of age, but does not take into account recent data, which is why we wanted to highlight that data for physicians.2
- Since submission of our article, The American College of Cardiology/American Heart Association (ACC/AHA) has published its first set of guidelines since 2003, which lowered BP target to <130 mm Hg in patients with high CV risk. Those guidelines outline the validity of SPRINT and the consistency of the existing evidence, including the linear relationship of BP and mortality.3
- SPRINT was halted early specifically because of the mortality benefit in the intensive treatment group, which is ethically appropriate.4 It is unclear to us how this compromises the validity of the trial. There is often concern for bias from early cessation in small trials, but this was a large, well-powered trial.
- The ACC/AHA guidelines also address some of the nuances of ACCORD, which is specific to patients with diabetes (whom we excluded from our first Practice Recommendation). Although no overall mortality benefit was found, there was stroke reduction in this group and additional benefit in the standard glycemia group.3,5 A meta-analysis of SPRINT and ACCORD showed CV disease reduction with a BP target <120 mm Hg.6
Although we do believe that SPRINT is a landmark trial contributing a great deal to our recommendations, we strongly emphasized that comorbidities, frailty, and dementia greatly impact treatment decisions. We stressed that prescribers use caution and slow titration because of adverse effects. Geriatric medicine is a complex art, and one of the goals of our article was to highlight this complexity and emphasize the importance of considering goals of care, comorbidity, frailty, and cognitive function when choosing optimal BP targets.
Maggie W. Hansell, MD; Emily M. Mann, MD; Julienne K. Kirk, PharmD
Winston-Salem, NC
1. Qaseem A, Wilt TJ, Rich R, et al. Pharmacological treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.
2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
3. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Available at: http://hyper.ahajournals.org/content/hypertensionaha/early/2017/11/10/HYP.0000000000000066.full.pdf. Accessed December 12, 2017.
4. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2106.
5. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive blood-pressure control in type 2 diabetes. N Engl J Med. 2010;362:1575-1585.
6. Perkovic V, Rodgers A. Redefining blood-pressure targets—SPRINT starts the marathon. N Engl Med. 2015;373:2175-2178.
In the article, “Hypertension treatment strategies for older adults” (J Fam Pract. 2017;66:546-554), Hansell et al recommend a systolic blood pressure (SBP) treatment target of <120 mm Hg for community-dwelling, nondiabetic patients ≥75 years of age. This recommendation is not supported by the authors’ cited guidelines, and we have serious concerns about the risk of harm from such overly stringent BP control in this population.
While Hansell et al acknowledge that no consensus exists regarding an optimal BP target for older patients, the authors cite the Eighth Joint National Committee (JNC 8), the American College of Physicians (ACP), the Systolic Blood Pressure Intervention Trial (SPRINT) subgroup analysis, and the BP arm of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial to justify their recommendation. But as the authors mention, JNC 8 conducted a comprehensive review of the available evidence and determined that a BP target of <150/90 mm Hg for hypertensive patients ≥60 years of age is appropriate.1
The authors also state that ACP recommends an SBP target of <140 mm Hg, while, in fact, the recommendations from ACP (which are joint guidelines published with the American Academy of Family Physicians) say that high-quality evidence strongly supports an SBP target of <150 mm Hg to reduce the risk for mortality, stroke, and cardiac events in adults ≥60 years of age.2
SPRINT does support Hansell et al’s recommended SBP target of <120 mm Hg, but this trial provided only composite data of adults ≥75 years of age and did not differentiate between the outcomes in otherwise healthy adults ≥75 years of age vs those with cardiovascular conditions.3 As Hansell et al point out, the SPRINT trial was halted prematurely, which compromises the validity of their findings.
Lastly, the ACCORD trial did not find benefit to treating SBP <120 mm Hg compared with <140 mm Hg in adults with diabetes, but it did find substantial harms in the <120 mm Hg group, including an increased risk of renal impairment and hypokalemia.4
Hansel et al’s overreliance on the SPRINT subgroup analysis represents a significant flaw in the assertion that an SBP target <120 mm Hg is reasonable for all community-dwelling, non-diabetic adults ≥75 years of age. While the authors made the allowance that a higher target (<140 mm Hg) is acceptable if a target of <120 mm Hg places undue burden on the patient, the guidelines they cited, when considered together, suggest that starting at a higher target is not only sufficient to prevent complications, but also reduces overtreatment.
Adults ≥75 years of age are a diverse group regarding disease conditions, life expectancy, and personal priorities. While it is tempting to make generalizations about BP treatment targets, we owe it to our patients to understand the nuances of applicable guidelines so that we can tailor BP treatment targets to each patient’s unique clinical situation and personal priorities. Applying a blanket recommendation to this heterogeneous population may result in significant harms from overtreatment.
Jennifer L. Middleton, MD, MPH, FAAFP; Miriam Chan, PharmD, CDE
Columbus, Ohio
1. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
2. Qaseem A, Wilt TJ, Rich R, et al. Pharmacological treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.
3. Williamson JD, Suplano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673-2682.
4. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575-1585.
Authors’ response:
We agree with the title of this letter, “Utilize guidelines, but customize BP treatment in older patients.” Our recommendations are not limited to targeting a systolic BP <120 mm Hg for community-dwelling, nondiabetic adults ≥75 years of age, but include consideration for “undue burden.” Our third practice recommendation, which recommends that one consider cognitive function, polypharmacy, multimorbidity, and frailty, is an equally—if not more—important recommendation.
With regard to the specific concerns about the current guidelines:
- The American College of Physicians and American Academy of Family Physicians’ “Recommendation 1” advocates a systolic BP goal <150 mm Hg for adults ≥60 years of age. However, “Recommendation 3” endorses intensifying treatment in adults ≥60 years of age at high cardiovascular (CV) risk. Based on Framingham criteria, all adults ≥75 years of age are considered at high risk for CV disease, as stated in our article. Therefore, “Recommendation 3” for a target of <140 mm Hg is applicable for the population addressed in our article.1
- The Eighth Joint National Committee (JNC 8) does recommend a BP target <150 mm Hg for adults ≥60 years of age, but does not take into account recent data, which is why we wanted to highlight that data for physicians.2
- Since submission of our article, The American College of Cardiology/American Heart Association (ACC/AHA) has published its first set of guidelines since 2003, which lowered BP target to <130 mm Hg in patients with high CV risk. Those guidelines outline the validity of SPRINT and the consistency of the existing evidence, including the linear relationship of BP and mortality.3
- SPRINT was halted early specifically because of the mortality benefit in the intensive treatment group, which is ethically appropriate.4 It is unclear to us how this compromises the validity of the trial. There is often concern for bias from early cessation in small trials, but this was a large, well-powered trial.
- The ACC/AHA guidelines also address some of the nuances of ACCORD, which is specific to patients with diabetes (whom we excluded from our first Practice Recommendation). Although no overall mortality benefit was found, there was stroke reduction in this group and additional benefit in the standard glycemia group.3,5 A meta-analysis of SPRINT and ACCORD showed CV disease reduction with a BP target <120 mm Hg.6
Although we do believe that SPRINT is a landmark trial contributing a great deal to our recommendations, we strongly emphasized that comorbidities, frailty, and dementia greatly impact treatment decisions. We stressed that prescribers use caution and slow titration because of adverse effects. Geriatric medicine is a complex art, and one of the goals of our article was to highlight this complexity and emphasize the importance of considering goals of care, comorbidity, frailty, and cognitive function when choosing optimal BP targets.
Maggie W. Hansell, MD; Emily M. Mann, MD; Julienne K. Kirk, PharmD
Winston-Salem, NC
1. Qaseem A, Wilt TJ, Rich R, et al. Pharmacological treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430-437.
2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520.
3. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Available at: http://hyper.ahajournals.org/content/hypertensionaha/early/2017/11/10/HYP.0000000000000066.full.pdf. Accessed December 12, 2017.
4. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103-2106.
5. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive blood-pressure control in type 2 diabetes. N Engl J Med. 2010;362:1575-1585.
6. Perkovic V, Rodgers A. Redefining blood-pressure targets—SPRINT starts the marathon. N Engl Med. 2015;373:2175-2178.
Weakness with left elbow flexion • left anterior shoulder pain • Dx?
THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
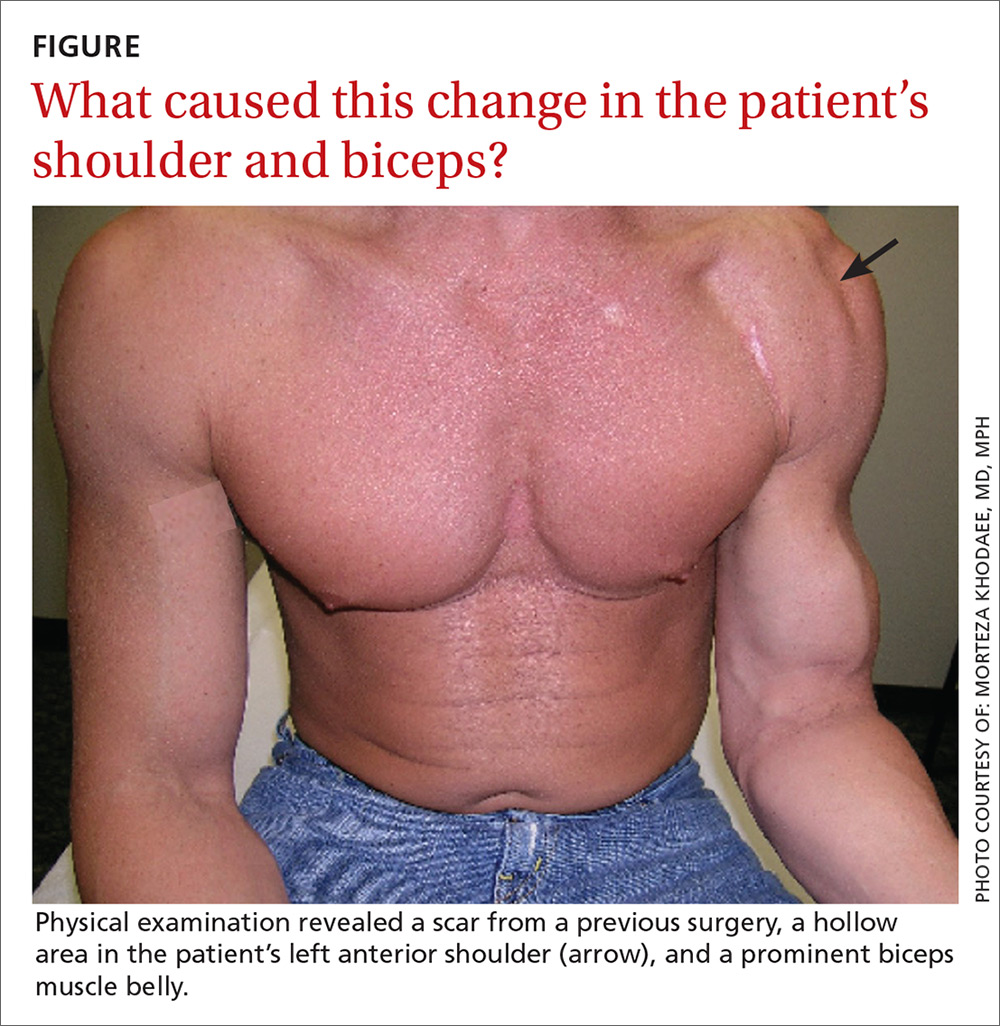
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12
Surgery is suitable for some, but not all
Surgical repair is recommended for acute ruptures in patients with high physical demands and for whom a slight loss of flexion and supination strength would not be well tolerated.13 Tenotomy and tenodesis are the main techniques used to surgically repair a rupture of the long head of the biceps brachii tendon. Although there is no consensus on which technique is superior, it seems that there is less cosmetic deformity and better post-surgery biomechanical strength with tenodesis compared with tenotomy.14 However, tenodesis is associated with a higher likelihood of bicipital pain,14 and recent case reports have suggested it is associated with an increased risk of humeral fracture.15 Therefore, each patient should be treated on an individual case basis, taking into account age, activity level, and physical demand.14
For most patients, treatment remains conservative with typically excellent outcomes. Nonoperative management includes gentle range-of-motion exercises for the prevention of contractures of the elbow and shoulder. Such exercises can be started almost immediately after injury. In one study, nonoperative management was recommended for patients with sedentary work, injury in the non-dominant arm, and acceptable cosmetic deformity. Researchers noted that patients who opt for a nonsurgical treatment generally do well with a home exercise program and rarely have stiffness.1
If the patient is a young athlete, if cosmetic deformity is unacceptable, or if the injury is in the dominant arm of a laborer, then the patient may want to consider tenodesis.1 Tangari et al found that in high-demand athletes, biceps tenodesis resulted in excellent functional and cosmetic results with no clinically significant decrease in strength after an average follow-up of 7.6 years.13 In a case s
Our patient elected to proceed with a tenodesis procedure. Two months after the surgery, he had fully recovered.
THE TAKEAWAY
Rupture of the biceps brachii tendon is relatively uncommon. In the vast majority of cases, it happens in the long head of the dominant arm of middle-aged men. Diagnosis is mainly clinical; however, ultrasound and MRI can confirm the diagnosis when there is doubt. Nonoperative management is appropriate for the majority of patients. Young athletes, patients who are concerned with cosmetic appearance, and labor workers with injury to their dominant arm should be referred to an orthopedic surgeon for possible surgery.
1. Geaney LE, Mazzocca AD. Biceps brachii tendon ruptures: a review of diagnosis and treatment of proximal and distal biceps tendon ruptures. Phys Sportsmed. 2010;38:117-125.
2. Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801-808.
3. Jayamoorthy T, Field JR, Costi JJ, et al. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160-164.
4. Mazzocca AD, Spang JT, Arciero RA. Distal biceps rupture. Orthop Clin North Am. 2008;39:237-249, vii.
5. Carter AN, Erickson SM. Proximal biceps tendon rupture: primarily an injury of middle age. Phys Sportsmed. 1999;27:95-101.
6. Elser F, Braun S, Dewing CB, et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581-592.
7. Kelly MP, Perkinson SG, Ablove RH, et al. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012-2017.
8. Schneider A, Bennett JM, O’Connor DP, et al. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18:804-807.
9. Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644-654.
10. The Physician and Sportsmedicine. Complete rupture of large tendons. Risk factors, signs, and definitive treatment. Available at: https://orthony.com/directory/uploads/flik_complete-rupture-of-large-tendons.pdf. Accessed December 8, 2017.
11. Pearl ML, Bessos K, Wong K. Strength deficits related to distal biceps tendon rupture and repair. A case report. Am J Sports Med. 1998;26:295-296.
12. Deutch SR, Gelineck J, Johannsen HV, et al. Permanent disabilities in the displaced muscle from rupture of the long head tendon of the biceps. Scand J Med Sci Sports. 2005;15:159-162.
13. Tangari M, Carbone S, Gallo M, et al. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409-413.
14. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332.
15. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7-e11.
THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
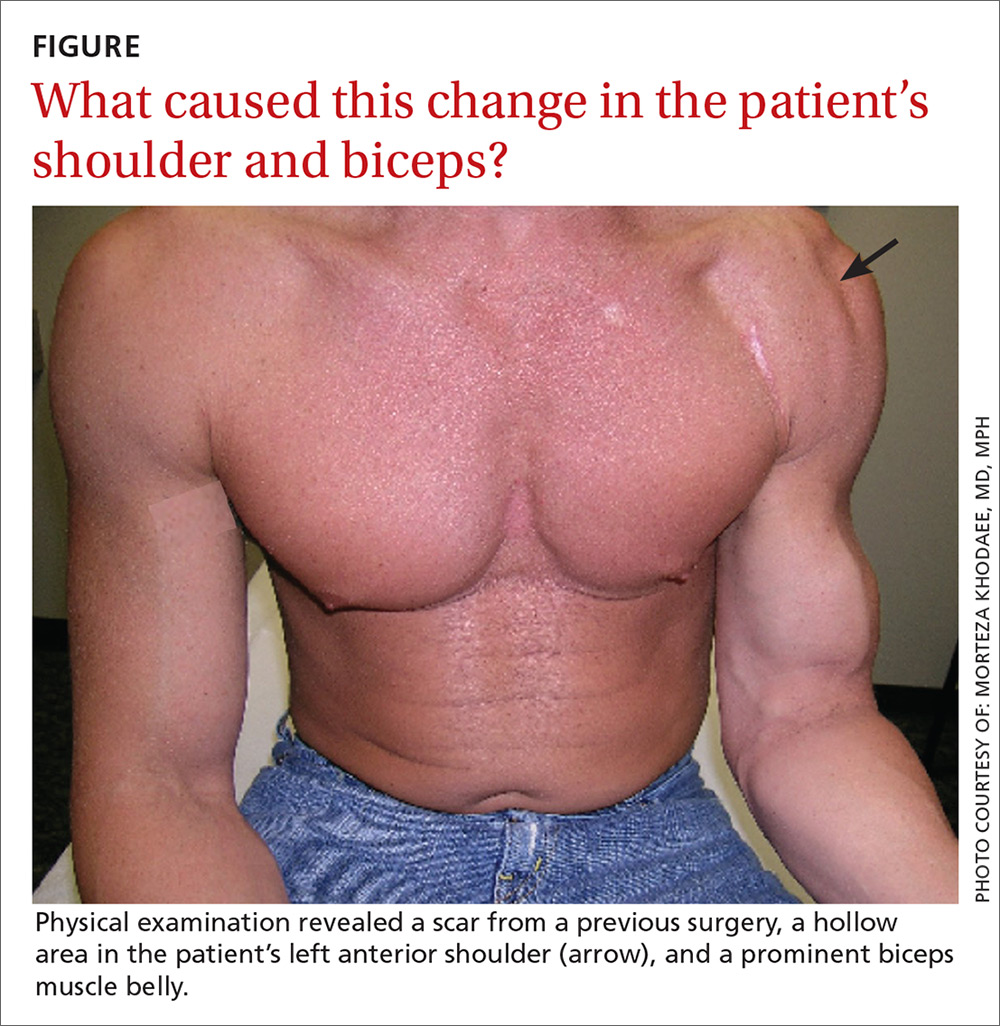
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12
Surgery is suitable for some, but not all
Surgical repair is recommended for acute ruptures in patients with high physical demands and for whom a slight loss of flexion and supination strength would not be well tolerated.13 Tenotomy and tenodesis are the main techniques used to surgically repair a rupture of the long head of the biceps brachii tendon. Although there is no consensus on which technique is superior, it seems that there is less cosmetic deformity and better post-surgery biomechanical strength with tenodesis compared with tenotomy.14 However, tenodesis is associated with a higher likelihood of bicipital pain,14 and recent case reports have suggested it is associated with an increased risk of humeral fracture.15 Therefore, each patient should be treated on an individual case basis, taking into account age, activity level, and physical demand.14
For most patients, treatment remains conservative with typically excellent outcomes. Nonoperative management includes gentle range-of-motion exercises for the prevention of contractures of the elbow and shoulder. Such exercises can be started almost immediately after injury. In one study, nonoperative management was recommended for patients with sedentary work, injury in the non-dominant arm, and acceptable cosmetic deformity. Researchers noted that patients who opt for a nonsurgical treatment generally do well with a home exercise program and rarely have stiffness.1
If the patient is a young athlete, if cosmetic deformity is unacceptable, or if the injury is in the dominant arm of a laborer, then the patient may want to consider tenodesis.1 Tangari et al found that in high-demand athletes, biceps tenodesis resulted in excellent functional and cosmetic results with no clinically significant decrease in strength after an average follow-up of 7.6 years.13 In a case s
Our patient elected to proceed with a tenodesis procedure. Two months after the surgery, he had fully recovered.
THE TAKEAWAY
Rupture of the biceps brachii tendon is relatively uncommon. In the vast majority of cases, it happens in the long head of the dominant arm of middle-aged men. Diagnosis is mainly clinical; however, ultrasound and MRI can confirm the diagnosis when there is doubt. Nonoperative management is appropriate for the majority of patients. Young athletes, patients who are concerned with cosmetic appearance, and labor workers with injury to their dominant arm should be referred to an orthopedic surgeon for possible surgery.
THE CASE
A 41-year-old, right-hand dominant man sought care at our facility one day after trying to pull his boat out of the water. He’d tried to lift the boat with his hands while his forearms were fully supinated and his elbows were flexed to about 90°. He then felt a sharp burning sensation in his left anterior shoulder and was unable to lift the boat. The patient denied feeling a popping sensation at the time of the injury. He had mild pain at night, but was able to sleep. He said that he had mild diminished strength with elbow flexion, but denied having any numbness, tingling, or discoloration of his skin.
The patient said he did weightlifting and strength training of his upper and lower extremities 4 times/week. He was in good general health, was not taking any medications or supplements, and denied smoking or using illicit drugs. His surgical history was significant for a Bankart repair 8 years ago.
On physical examination, the patient had a scar from the previous surgery, a hollow area in his left anterior shoulder, and a prominent biceps muscle belly (FIGURE). His shoulder range of motion was normal. Left shoulder Neer, Hawkins-Kennedy, drop-arm, cross-arm, empty can, and apprehension tests were negative. A left Speed’s test (resisted elbow flexion when elbow is flexed 20° to 30° with the forearm in supination and the arm in about 60° of flexion) was positive for mild anterior shoulder pain. So, too, was a Yergason’s test (resisted forearm supination and elbow flexion when forearm is pronated and elbow is flexed to 90°). The patient’s elbow flexion strength was 4 out of 5, and his supination strength was 5 out of 5. Neurovascular and sensory examinations of his upper extremities, including radial and ulnar pulses, were normal.
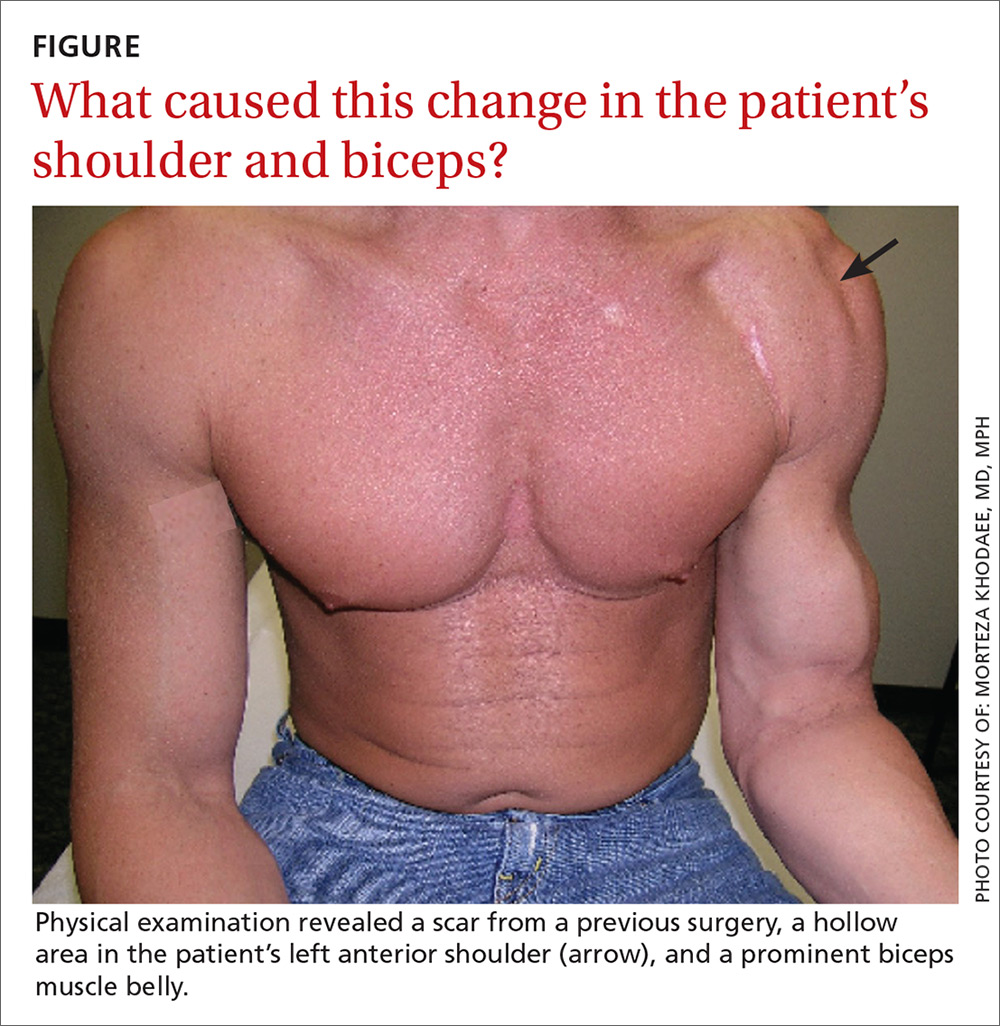
THE DIAGNOSIS
A diagnostic musculoskeletal ultrasound revealed an empty tendon sheath of the long head of the biceps in the bicipital groove and a retracted echogenic stump with associated hematoma at the proximal musculotendinous junction. Based on the patient’s history, physical examination, and ultrasound, a diagnosis of an acute rupture of the left long head of the biceps brachii tendon was made.
DISCUSSION
Diagnosis of acute rupture is often made clinically based on a visually apparent defect proximally and a bulbous mass distally (“Popeye deformity”).1 Ultrasound and magnetic resonance imaging (MRI) may aid in the diagnosis by demonstrating an absence of the long head in the bicipital groove or at its insertion.
The biceps brachii tendon functions in flexion and supination of the forearm. The long head of the biceps also plays a stabilizing role in the glenohumeral joint during elbow flexion and supination.2 Injury to the biceps most often occurs in middle-aged men following a traumatic sudden eccentric bicipital contraction event, during which most patients describe a snapping or popping sensation.3,4
Rupture of the proximal biceps tendon represents about 90% of all biceps ruptures, which almost exclusively involve the long head of the biceps.3,5,6 Risk factors for tendon rupture include obesity, smoking, steroid injection in or around the tendon, and previous tendinopathy.7-10
Functional limitations. It is generally thought that functional limitations following a proximal biceps rupture are relatively minimal, due to the work of other flexors and supinators, including the brachialis and brachioradialis. However, because strength and endurance of the muscle can decrease by about 25%, physical laborers and high-demand athletes may notice a degree of residual weakness with supination and elbow flexion.11,12
Surgery is suitable for some, but not all
Surgical repair is recommended for acute ruptures in patients with high physical demands and for whom a slight loss of flexion and supination strength would not be well tolerated.13 Tenotomy and tenodesis are the main techniques used to surgically repair a rupture of the long head of the biceps brachii tendon. Although there is no consensus on which technique is superior, it seems that there is less cosmetic deformity and better post-surgery biomechanical strength with tenodesis compared with tenotomy.14 However, tenodesis is associated with a higher likelihood of bicipital pain,14 and recent case reports have suggested it is associated with an increased risk of humeral fracture.15 Therefore, each patient should be treated on an individual case basis, taking into account age, activity level, and physical demand.14
For most patients, treatment remains conservative with typically excellent outcomes. Nonoperative management includes gentle range-of-motion exercises for the prevention of contractures of the elbow and shoulder. Such exercises can be started almost immediately after injury. In one study, nonoperative management was recommended for patients with sedentary work, injury in the non-dominant arm, and acceptable cosmetic deformity. Researchers noted that patients who opt for a nonsurgical treatment generally do well with a home exercise program and rarely have stiffness.1
If the patient is a young athlete, if cosmetic deformity is unacceptable, or if the injury is in the dominant arm of a laborer, then the patient may want to consider tenodesis.1 Tangari et al found that in high-demand athletes, biceps tenodesis resulted in excellent functional and cosmetic results with no clinically significant decrease in strength after an average follow-up of 7.6 years.13 In a case s
Our patient elected to proceed with a tenodesis procedure. Two months after the surgery, he had fully recovered.
THE TAKEAWAY
Rupture of the biceps brachii tendon is relatively uncommon. In the vast majority of cases, it happens in the long head of the dominant arm of middle-aged men. Diagnosis is mainly clinical; however, ultrasound and MRI can confirm the diagnosis when there is doubt. Nonoperative management is appropriate for the majority of patients. Young athletes, patients who are concerned with cosmetic appearance, and labor workers with injury to their dominant arm should be referred to an orthopedic surgeon for possible surgery.
1. Geaney LE, Mazzocca AD. Biceps brachii tendon ruptures: a review of diagnosis and treatment of proximal and distal biceps tendon ruptures. Phys Sportsmed. 2010;38:117-125.
2. Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801-808.
3. Jayamoorthy T, Field JR, Costi JJ, et al. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160-164.
4. Mazzocca AD, Spang JT, Arciero RA. Distal biceps rupture. Orthop Clin North Am. 2008;39:237-249, vii.
5. Carter AN, Erickson SM. Proximal biceps tendon rupture: primarily an injury of middle age. Phys Sportsmed. 1999;27:95-101.
6. Elser F, Braun S, Dewing CB, et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581-592.
7. Kelly MP, Perkinson SG, Ablove RH, et al. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012-2017.
8. Schneider A, Bennett JM, O’Connor DP, et al. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18:804-807.
9. Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644-654.
10. The Physician and Sportsmedicine. Complete rupture of large tendons. Risk factors, signs, and definitive treatment. Available at: https://orthony.com/directory/uploads/flik_complete-rupture-of-large-tendons.pdf. Accessed December 8, 2017.
11. Pearl ML, Bessos K, Wong K. Strength deficits related to distal biceps tendon rupture and repair. A case report. Am J Sports Med. 1998;26:295-296.
12. Deutch SR, Gelineck J, Johannsen HV, et al. Permanent disabilities in the displaced muscle from rupture of the long head tendon of the biceps. Scand J Med Sci Sports. 2005;15:159-162.
13. Tangari M, Carbone S, Gallo M, et al. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409-413.
14. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332.
15. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7-e11.
1. Geaney LE, Mazzocca AD. Biceps brachii tendon ruptures: a review of diagnosis and treatment of proximal and distal biceps tendon ruptures. Phys Sportsmed. 2010;38:117-125.
2. Payne LZ, Deng XH, Craig EV, et al. The combined dynamic and static contributions to subacromial impingement. A biomechanical analysis. Am J Sports Med. 1997;25:801-808.
3. Jayamoorthy T, Field JR, Costi JJ, et al. Biceps tenodesis: a biomechanical study of fixation methods. J Shoulder Elbow Surg. 2004;13:160-164.
4. Mazzocca AD, Spang JT, Arciero RA. Distal biceps rupture. Orthop Clin North Am. 2008;39:237-249, vii.
5. Carter AN, Erickson SM. Proximal biceps tendon rupture: primarily an injury of middle age. Phys Sportsmed. 1999;27:95-101.
6. Elser F, Braun S, Dewing CB, et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581-592.
7. Kelly MP, Perkinson SG, Ablove RH, et al. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012-2017.
8. Schneider A, Bennett JM, O’Connor DP, et al. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18:804-807.
9. Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644-654.
10. The Physician and Sportsmedicine. Complete rupture of large tendons. Risk factors, signs, and definitive treatment. Available at: https://orthony.com/directory/uploads/flik_complete-rupture-of-large-tendons.pdf. Accessed December 8, 2017.
11. Pearl ML, Bessos K, Wong K. Strength deficits related to distal biceps tendon rupture and repair. A case report. Am J Sports Med. 1998;26:295-296.
12. Deutch SR, Gelineck J, Johannsen HV, et al. Permanent disabilities in the displaced muscle from rupture of the long head tendon of the biceps. Scand J Med Sci Sports. 2005;15:159-162.
13. Tangari M, Carbone S, Gallo M, et al. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20:409-413.
14. Hsu AR, Ghodadra NS, Provencher MT, et al. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326-332.
15. Sears BW, Spencer EE, Getz CL. Humeral fracture following subpectoral biceps tenodesis in 2 active, healthy patients. J Shoulder Elbow Surg. 2011;20:e7-e11.
Painful jaw lesion
A 48-year-old Chinese woman was referred to our center with a 7-month history of a painful lesion on her left jaw that had been gradually increasing in size. The patient noted occasional purulent and bloody discharge from the lesion. She denied having a toothache.
An examination revealed an erythematous nodule with perilesional puckering superior to the left body of the mandible, measuring 7 × 8 mm, with no discharge or surrounding inflammation (FIGURE 1). There was no cervical lymphadenopathy.
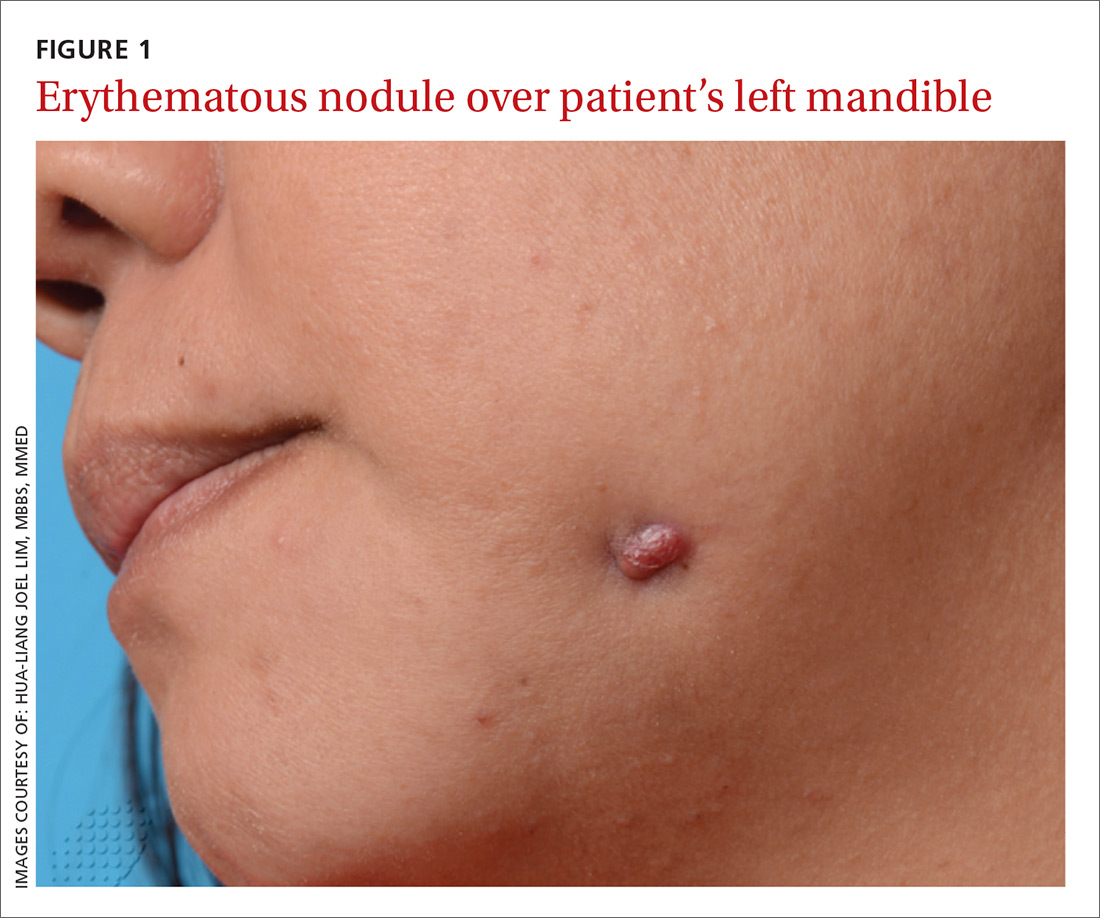
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Odontogenic sinus tract
Further examination on the inside of the patient’s mouth revealed root stumps of the left inferior molars (FIGURE 2). Based on the appearance of the lesion and molar involvement, we diagnosed odontogenic sinus tract (OST). OST, also known as odontogenic fistula or dental sinus, is a clinical diagnosis.

Symptoms such as odontalgia may be present in only 50% of patients with OST; thus, patients often initially consult their physician, rather than their dentist.1 If OST is suspected, evaluation should begin with a thorough history focusing on any recent facial trauma or past dental diseases. Dental panoramic or periapical radiography can be performed to confirm the extent of dental disease, and pulp vitality testing can determine if a diseased tooth is restorable.
A biopsy of the sinus tract is not required, as it would only reveal granulation tissue. Bimanual palpation of the oral cavity may reveal a cord-like structure from the cutaneous sinus to the underlying alveolar bone. (This structure was palpated in our patient.)
The pathogenesis of OST begins with dental caries, which progress to degeneration of the pulp and formation of periapical abscesses and root stumps. Progressive suppuration causes local destruction and subsequent tract formation through the alveolar bone and mandible. The build-up in pressure within this tract results in an eruption through the skin, manifesting as a sinus with extrusion of pus. The most common site of OST is at the angle of the mandible.2
The differential Dx is limited
There are a small number of other cutaneous conditions that may arise in the region of the mandible, but they have clinical features that distinguish them from OST.
Pyogenic granuloma presents as an erythematous papule that bleeds on contact. It usually develops rapidly following antecedent trauma.
Actinomycosis usually appears as an indolent plaque, with draining sinuses that extrude yellow grains on pressure. It may result from an underlying dental infection.
Squamous cell carcinoma of the skin often presents as a scaly plaque or non-healing ulcer with irregular margins and everted edges.
A furuncle is a tender, erythematous papule or nodule centered on a hair follicle. It is commonly associated with Staphylococcus aureus infection.
Treating OST
Treatment requires endodontic referral for root canal therapy, after which most cases resolve within a few weeks. OST can heal with post-inflammatory hyper- or hypopigmentation as a result of melanocyte damage. Systemic antibiotic administration is not necessary.3
We referred our patient to a dentist, who removed the root stumps and provided root canal treatment. The OST healed within several weeks. The patient had residual hypopigmentation after the OST healed, but was satisfied with the outcome.
CORRESPONDENCE
Hua-Liang Joel Lim, MBBS, MMed, National Skin Centre, 1 Mandalay Rd, Singapore 308205; [email protected].
1. Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
2. Brown RS, Jones R, Feimster T, et al. Cutaneous sinus tracts (or emerging sinus tracts) of odontogenic origin: a report of 3 cases. Clin Cosmet Investig Dent. 2010;2:63-67.
3. Susic M, Krakar N, Borcic J, et al. Odontogenic sinus tract to the neck skin: a case report. J Dermatol. 2004;31:920-922.
A 48-year-old Chinese woman was referred to our center with a 7-month history of a painful lesion on her left jaw that had been gradually increasing in size. The patient noted occasional purulent and bloody discharge from the lesion. She denied having a toothache.
An examination revealed an erythematous nodule with perilesional puckering superior to the left body of the mandible, measuring 7 × 8 mm, with no discharge or surrounding inflammation (FIGURE 1). There was no cervical lymphadenopathy.
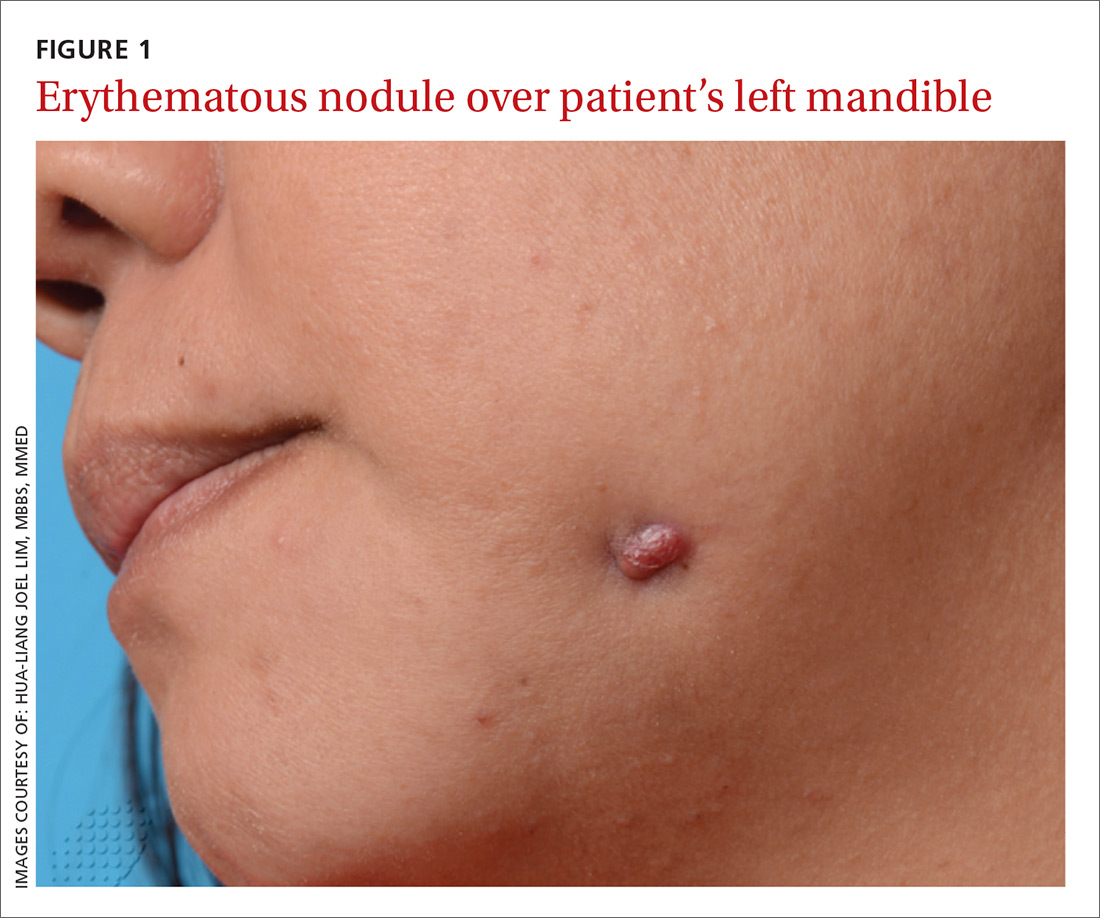
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Odontogenic sinus tract
Further examination on the inside of the patient’s mouth revealed root stumps of the left inferior molars (FIGURE 2). Based on the appearance of the lesion and molar involvement, we diagnosed odontogenic sinus tract (OST). OST, also known as odontogenic fistula or dental sinus, is a clinical diagnosis.

Symptoms such as odontalgia may be present in only 50% of patients with OST; thus, patients often initially consult their physician, rather than their dentist.1 If OST is suspected, evaluation should begin with a thorough history focusing on any recent facial trauma or past dental diseases. Dental panoramic or periapical radiography can be performed to confirm the extent of dental disease, and pulp vitality testing can determine if a diseased tooth is restorable.
A biopsy of the sinus tract is not required, as it would only reveal granulation tissue. Bimanual palpation of the oral cavity may reveal a cord-like structure from the cutaneous sinus to the underlying alveolar bone. (This structure was palpated in our patient.)
The pathogenesis of OST begins with dental caries, which progress to degeneration of the pulp and formation of periapical abscesses and root stumps. Progressive suppuration causes local destruction and subsequent tract formation through the alveolar bone and mandible. The build-up in pressure within this tract results in an eruption through the skin, manifesting as a sinus with extrusion of pus. The most common site of OST is at the angle of the mandible.2
The differential Dx is limited
There are a small number of other cutaneous conditions that may arise in the region of the mandible, but they have clinical features that distinguish them from OST.
Pyogenic granuloma presents as an erythematous papule that bleeds on contact. It usually develops rapidly following antecedent trauma.
Actinomycosis usually appears as an indolent plaque, with draining sinuses that extrude yellow grains on pressure. It may result from an underlying dental infection.
Squamous cell carcinoma of the skin often presents as a scaly plaque or non-healing ulcer with irregular margins and everted edges.
A furuncle is a tender, erythematous papule or nodule centered on a hair follicle. It is commonly associated with Staphylococcus aureus infection.
Treating OST
Treatment requires endodontic referral for root canal therapy, after which most cases resolve within a few weeks. OST can heal with post-inflammatory hyper- or hypopigmentation as a result of melanocyte damage. Systemic antibiotic administration is not necessary.3
We referred our patient to a dentist, who removed the root stumps and provided root canal treatment. The OST healed within several weeks. The patient had residual hypopigmentation after the OST healed, but was satisfied with the outcome.
CORRESPONDENCE
Hua-Liang Joel Lim, MBBS, MMed, National Skin Centre, 1 Mandalay Rd, Singapore 308205; [email protected].
A 48-year-old Chinese woman was referred to our center with a 7-month history of a painful lesion on her left jaw that had been gradually increasing in size. The patient noted occasional purulent and bloody discharge from the lesion. She denied having a toothache.
An examination revealed an erythematous nodule with perilesional puckering superior to the left body of the mandible, measuring 7 × 8 mm, with no discharge or surrounding inflammation (FIGURE 1). There was no cervical lymphadenopathy.
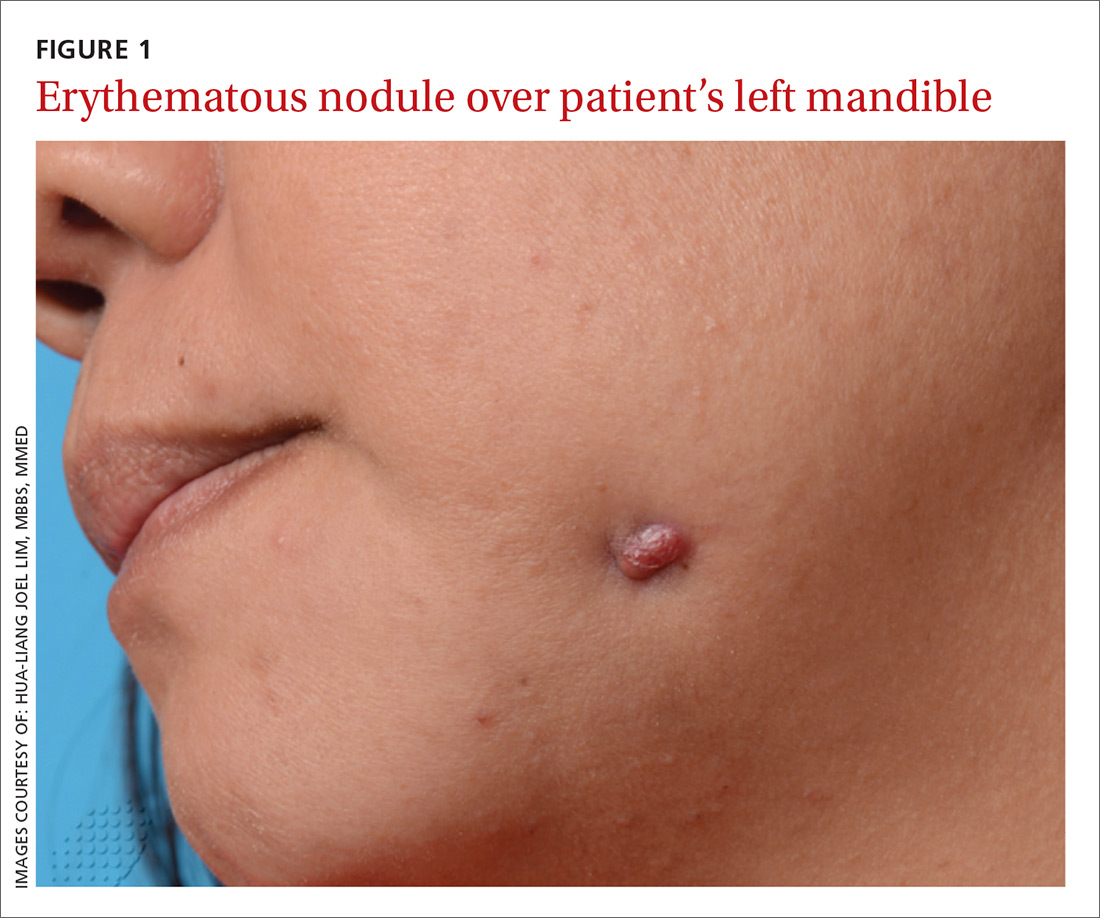
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Odontogenic sinus tract
Further examination on the inside of the patient’s mouth revealed root stumps of the left inferior molars (FIGURE 2). Based on the appearance of the lesion and molar involvement, we diagnosed odontogenic sinus tract (OST). OST, also known as odontogenic fistula or dental sinus, is a clinical diagnosis.

Symptoms such as odontalgia may be present in only 50% of patients with OST; thus, patients often initially consult their physician, rather than their dentist.1 If OST is suspected, evaluation should begin with a thorough history focusing on any recent facial trauma or past dental diseases. Dental panoramic or periapical radiography can be performed to confirm the extent of dental disease, and pulp vitality testing can determine if a diseased tooth is restorable.
A biopsy of the sinus tract is not required, as it would only reveal granulation tissue. Bimanual palpation of the oral cavity may reveal a cord-like structure from the cutaneous sinus to the underlying alveolar bone. (This structure was palpated in our patient.)
The pathogenesis of OST begins with dental caries, which progress to degeneration of the pulp and formation of periapical abscesses and root stumps. Progressive suppuration causes local destruction and subsequent tract formation through the alveolar bone and mandible. The build-up in pressure within this tract results in an eruption through the skin, manifesting as a sinus with extrusion of pus. The most common site of OST is at the angle of the mandible.2
The differential Dx is limited
There are a small number of other cutaneous conditions that may arise in the region of the mandible, but they have clinical features that distinguish them from OST.
Pyogenic granuloma presents as an erythematous papule that bleeds on contact. It usually develops rapidly following antecedent trauma.
Actinomycosis usually appears as an indolent plaque, with draining sinuses that extrude yellow grains on pressure. It may result from an underlying dental infection.
Squamous cell carcinoma of the skin often presents as a scaly plaque or non-healing ulcer with irregular margins and everted edges.
A furuncle is a tender, erythematous papule or nodule centered on a hair follicle. It is commonly associated with Staphylococcus aureus infection.
Treating OST
Treatment requires endodontic referral for root canal therapy, after which most cases resolve within a few weeks. OST can heal with post-inflammatory hyper- or hypopigmentation as a result of melanocyte damage. Systemic antibiotic administration is not necessary.3
We referred our patient to a dentist, who removed the root stumps and provided root canal treatment. The OST healed within several weeks. The patient had residual hypopigmentation after the OST healed, but was satisfied with the outcome.
CORRESPONDENCE
Hua-Liang Joel Lim, MBBS, MMed, National Skin Centre, 1 Mandalay Rd, Singapore 308205; [email protected].
1. Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
2. Brown RS, Jones R, Feimster T, et al. Cutaneous sinus tracts (or emerging sinus tracts) of odontogenic origin: a report of 3 cases. Clin Cosmet Investig Dent. 2010;2:63-67.
3. Susic M, Krakar N, Borcic J, et al. Odontogenic sinus tract to the neck skin: a case report. J Dermatol. 2004;31:920-922.
1. Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
2. Brown RS, Jones R, Feimster T, et al. Cutaneous sinus tracts (or emerging sinus tracts) of odontogenic origin: a report of 3 cases. Clin Cosmet Investig Dent. 2010;2:63-67.
3. Susic M, Krakar N, Borcic J, et al. Odontogenic sinus tract to the neck skin: a case report. J Dermatol. 2004;31:920-922.








