User login
FDA issues warning to all duodenoscope manufacturers
The Food and Drug Administration on March 9 issued warning letters to all three duodenoscope manufacturers for failing to comply with the requirements of federal law under which they were ordered to conduct postmarket surveillance studies to assess the effectiveness of reprocessing the devices.
The warning is part of an ongoing effort to prevent patient infections associated with the transmission of bacteria from contaminated duodenoscopes. The three manufacturers – Olympus, Fujifilm, and Pentax – are required to conduct studies to sample and culture reprocessed duodenoscopes that are in clinical use to learn more about issues that contribute to contamination, and to study human factors to determine how hospital staff who have had training are following the reprocessing instructions. In 2015, the FDA ordered the companies to conduct a postmarket surveillance study to determine whether health care facilities were able to properly clean and disinfect the devices.
Currently, the Olympus manufacturer has failed to start data collection, while both Pentax and Fujifilm have failed to provide sufficient data required for their respective studies to sample and culture reprocessed duodenoscopes that are in clinical use. In addition, Olympus and Pentax have not complied with requirements to assess how well staff members have followed the reprocessing instructions after the human factors studies and Fujifilm has been meeting its requirements for its human factors study only.
“The FDA has taken important steps to improve the reprocessing of duodenoscopes, and we’ve seen a reduction in reports of patient infections, but we need the required postmarket studies to determine whether these measures are being properly implemented in real-world clinical settings and whether we need to take additional action to further improve the safety of these devices,” said Jeff Shuren, MD, director of the FDA’s Center for Devices and Radiological Health in a press release. “We expect these device manufacturers to meet their study obligations to ensure patient safety.”
The companies have until March 24 to submit a plan that outlines how study milestones will be achieved. If the companies fail to respond to the warning letter, the FDA states that they may take additional action, such as seizure, injunction, and civil monetary penalties.
Read the full press release on the FDA’s website.
The Food and Drug Administration on March 9 issued warning letters to all three duodenoscope manufacturers for failing to comply with the requirements of federal law under which they were ordered to conduct postmarket surveillance studies to assess the effectiveness of reprocessing the devices.
The warning is part of an ongoing effort to prevent patient infections associated with the transmission of bacteria from contaminated duodenoscopes. The three manufacturers – Olympus, Fujifilm, and Pentax – are required to conduct studies to sample and culture reprocessed duodenoscopes that are in clinical use to learn more about issues that contribute to contamination, and to study human factors to determine how hospital staff who have had training are following the reprocessing instructions. In 2015, the FDA ordered the companies to conduct a postmarket surveillance study to determine whether health care facilities were able to properly clean and disinfect the devices.
Currently, the Olympus manufacturer has failed to start data collection, while both Pentax and Fujifilm have failed to provide sufficient data required for their respective studies to sample and culture reprocessed duodenoscopes that are in clinical use. In addition, Olympus and Pentax have not complied with requirements to assess how well staff members have followed the reprocessing instructions after the human factors studies and Fujifilm has been meeting its requirements for its human factors study only.
“The FDA has taken important steps to improve the reprocessing of duodenoscopes, and we’ve seen a reduction in reports of patient infections, but we need the required postmarket studies to determine whether these measures are being properly implemented in real-world clinical settings and whether we need to take additional action to further improve the safety of these devices,” said Jeff Shuren, MD, director of the FDA’s Center for Devices and Radiological Health in a press release. “We expect these device manufacturers to meet their study obligations to ensure patient safety.”
The companies have until March 24 to submit a plan that outlines how study milestones will be achieved. If the companies fail to respond to the warning letter, the FDA states that they may take additional action, such as seizure, injunction, and civil monetary penalties.
Read the full press release on the FDA’s website.
The Food and Drug Administration on March 9 issued warning letters to all three duodenoscope manufacturers for failing to comply with the requirements of federal law under which they were ordered to conduct postmarket surveillance studies to assess the effectiveness of reprocessing the devices.
The warning is part of an ongoing effort to prevent patient infections associated with the transmission of bacteria from contaminated duodenoscopes. The three manufacturers – Olympus, Fujifilm, and Pentax – are required to conduct studies to sample and culture reprocessed duodenoscopes that are in clinical use to learn more about issues that contribute to contamination, and to study human factors to determine how hospital staff who have had training are following the reprocessing instructions. In 2015, the FDA ordered the companies to conduct a postmarket surveillance study to determine whether health care facilities were able to properly clean and disinfect the devices.
Currently, the Olympus manufacturer has failed to start data collection, while both Pentax and Fujifilm have failed to provide sufficient data required for their respective studies to sample and culture reprocessed duodenoscopes that are in clinical use. In addition, Olympus and Pentax have not complied with requirements to assess how well staff members have followed the reprocessing instructions after the human factors studies and Fujifilm has been meeting its requirements for its human factors study only.
“The FDA has taken important steps to improve the reprocessing of duodenoscopes, and we’ve seen a reduction in reports of patient infections, but we need the required postmarket studies to determine whether these measures are being properly implemented in real-world clinical settings and whether we need to take additional action to further improve the safety of these devices,” said Jeff Shuren, MD, director of the FDA’s Center for Devices and Radiological Health in a press release. “We expect these device manufacturers to meet their study obligations to ensure patient safety.”
The companies have until March 24 to submit a plan that outlines how study milestones will be achieved. If the companies fail to respond to the warning letter, the FDA states that they may take additional action, such as seizure, injunction, and civil monetary penalties.
Read the full press release on the FDA’s website.
Rare Neurological Disease Special Report
Looking to increase PrEP uptake
BOSTON – More than 1.1 million Americans are at substantial risk for HIV and would benefit from preexposure prophylaxis (PrEP), but only 90,000 prescriptions were filled by retail or mail-order pharmacies in the United States from Sept. 2015 to August 2016, according to the Centers for Disease Control and Prevention.
The CDC estimated that 500,340 blacks in the United States have indications for preexposure prophylaxis, but only about 7,000 (less than 1%) filled a prescription during that time. Among an estimated 282,260 Hispanics who might benefit, just about 7,600 (3%) filled prescriptions. Uptake was a bit higher among whites: about 42,000 prescriptions among 303,230 at-risk people (14%).
PrEP uptake might be particularly low among black and Hispanic people because, in addition to the well-known disparities in health care access and other issues: “There’s a stigma with being gay: ‘If I’m taking this drug, does that mean I’m gay?’ ” Dr. Smith said.
To address the problem, “get more serious about HIV testing. You want to find people who are positive, who need to be on treatment. The second step is to find ways to collect risk-behavior data.” That could be as simple as having the nurse ask a few extra questions before the office visit, or adding a few questions to the intake form, she said at the Conference On Retroviruses And Opportunistic Infections.
“You are trying to help patients acknowledge that they are engaging in behaviors that might have exposed them to HIV, and providers need to be able to hear the answers. One of the problems we have is providers who say ‘my patients aren’t like that,’ or ‘this person is married; I don’t need to ask them.’” Another easy way to find at-risk patients is to look at STD history. If a patient has had syphilis, or two episodes of gonorrhea in the past year, you “need to talk to them about PrEP,” she said.
For black and Hispanic patients, “it’s a higher index of suspicion. For example, you take blood pressure in all your patients, but you are also aware that hypertension is more common in African Americans. So if you’re rushed, you are still going to do a blood pressure in African American patients, but maybe not in the young white jogger; you get that next time.” Especially in high-prevalence HIV settings, “every patient should be aware of PrEP. It should be part of the conversation with everybody,” she said.
The CDC used national pharmacy data and estimates of risky behavior to draw its conclusions. Commercial pharmacies account for maybe 90% of all PrEP prescriptions, so the data slightly underestimate the true use numbers. The more than 1.1 million people included an estimated 813,970 gay and bisexual men, 258,080 heterosexuals, and 72,510 intravenous drug users. The ultimate goal of the work is target PrEP interventions where they are needed most. The agency plans to release state-by-state data soon.
CDC funded the work. Dr. Smith didn’t have any disclosures.
SOURCE: Smith DK et al. 2018 CROI, Abstract 86.
BOSTON – More than 1.1 million Americans are at substantial risk for HIV and would benefit from preexposure prophylaxis (PrEP), but only 90,000 prescriptions were filled by retail or mail-order pharmacies in the United States from Sept. 2015 to August 2016, according to the Centers for Disease Control and Prevention.
The CDC estimated that 500,340 blacks in the United States have indications for preexposure prophylaxis, but only about 7,000 (less than 1%) filled a prescription during that time. Among an estimated 282,260 Hispanics who might benefit, just about 7,600 (3%) filled prescriptions. Uptake was a bit higher among whites: about 42,000 prescriptions among 303,230 at-risk people (14%).
PrEP uptake might be particularly low among black and Hispanic people because, in addition to the well-known disparities in health care access and other issues: “There’s a stigma with being gay: ‘If I’m taking this drug, does that mean I’m gay?’ ” Dr. Smith said.
To address the problem, “get more serious about HIV testing. You want to find people who are positive, who need to be on treatment. The second step is to find ways to collect risk-behavior data.” That could be as simple as having the nurse ask a few extra questions before the office visit, or adding a few questions to the intake form, she said at the Conference On Retroviruses And Opportunistic Infections.
“You are trying to help patients acknowledge that they are engaging in behaviors that might have exposed them to HIV, and providers need to be able to hear the answers. One of the problems we have is providers who say ‘my patients aren’t like that,’ or ‘this person is married; I don’t need to ask them.’” Another easy way to find at-risk patients is to look at STD history. If a patient has had syphilis, or two episodes of gonorrhea in the past year, you “need to talk to them about PrEP,” she said.
For black and Hispanic patients, “it’s a higher index of suspicion. For example, you take blood pressure in all your patients, but you are also aware that hypertension is more common in African Americans. So if you’re rushed, you are still going to do a blood pressure in African American patients, but maybe not in the young white jogger; you get that next time.” Especially in high-prevalence HIV settings, “every patient should be aware of PrEP. It should be part of the conversation with everybody,” she said.
The CDC used national pharmacy data and estimates of risky behavior to draw its conclusions. Commercial pharmacies account for maybe 90% of all PrEP prescriptions, so the data slightly underestimate the true use numbers. The more than 1.1 million people included an estimated 813,970 gay and bisexual men, 258,080 heterosexuals, and 72,510 intravenous drug users. The ultimate goal of the work is target PrEP interventions where they are needed most. The agency plans to release state-by-state data soon.
CDC funded the work. Dr. Smith didn’t have any disclosures.
SOURCE: Smith DK et al. 2018 CROI, Abstract 86.
BOSTON – More than 1.1 million Americans are at substantial risk for HIV and would benefit from preexposure prophylaxis (PrEP), but only 90,000 prescriptions were filled by retail or mail-order pharmacies in the United States from Sept. 2015 to August 2016, according to the Centers for Disease Control and Prevention.
The CDC estimated that 500,340 blacks in the United States have indications for preexposure prophylaxis, but only about 7,000 (less than 1%) filled a prescription during that time. Among an estimated 282,260 Hispanics who might benefit, just about 7,600 (3%) filled prescriptions. Uptake was a bit higher among whites: about 42,000 prescriptions among 303,230 at-risk people (14%).
PrEP uptake might be particularly low among black and Hispanic people because, in addition to the well-known disparities in health care access and other issues: “There’s a stigma with being gay: ‘If I’m taking this drug, does that mean I’m gay?’ ” Dr. Smith said.
To address the problem, “get more serious about HIV testing. You want to find people who are positive, who need to be on treatment. The second step is to find ways to collect risk-behavior data.” That could be as simple as having the nurse ask a few extra questions before the office visit, or adding a few questions to the intake form, she said at the Conference On Retroviruses And Opportunistic Infections.
“You are trying to help patients acknowledge that they are engaging in behaviors that might have exposed them to HIV, and providers need to be able to hear the answers. One of the problems we have is providers who say ‘my patients aren’t like that,’ or ‘this person is married; I don’t need to ask them.’” Another easy way to find at-risk patients is to look at STD history. If a patient has had syphilis, or two episodes of gonorrhea in the past year, you “need to talk to them about PrEP,” she said.
For black and Hispanic patients, “it’s a higher index of suspicion. For example, you take blood pressure in all your patients, but you are also aware that hypertension is more common in African Americans. So if you’re rushed, you are still going to do a blood pressure in African American patients, but maybe not in the young white jogger; you get that next time.” Especially in high-prevalence HIV settings, “every patient should be aware of PrEP. It should be part of the conversation with everybody,” she said.
The CDC used national pharmacy data and estimates of risky behavior to draw its conclusions. Commercial pharmacies account for maybe 90% of all PrEP prescriptions, so the data slightly underestimate the true use numbers. The more than 1.1 million people included an estimated 813,970 gay and bisexual men, 258,080 heterosexuals, and 72,510 intravenous drug users. The ultimate goal of the work is target PrEP interventions where they are needed most. The agency plans to release state-by-state data soon.
CDC funded the work. Dr. Smith didn’t have any disclosures.
SOURCE: Smith DK et al. 2018 CROI, Abstract 86.
REPORTING FROM CROI
Key clinical point: To know if patients need PrEP, you first have to ask about at-risk behaviors.
Major finding: About 500,340 blacks have indications for preexposure prophylaxis (PrEP), but only about 7,000 filled a prescription from Sept. 2015-August 2016.
Study details: The findings are based on pharmacy data and estimates of risky behavior.
Disclosures: CDC funded the work. The lead investigator didn’t have any disclosures.
Source: Smith DK et al. 2018 CROI, Abstract 86.
Unassigned school epinephrine used more than assigned injectors
ORLANDO –
In the 2015-2016 and 2016-2017 school years, epinephrine was administered to students 31 times at schools in the Austin Independent School District, which began to stock unassigned epinephrine in its schools after state legislators approved a law in 2015 allowing, but not requiring, school districts to do so. In 21 of those cases, or 68% of the time, it was the unassigned stockpile that was used, Kathryn Neupert, MD, said at the joint congress of the American Academy of Allergy, Asthma, and Immunology and the World Asthma Organization.
She drew attention to the finding that 22% of the time in the study, the epinephrine use involved the unassigned stock for children with no history of anaphylaxis or allergy.
“It kind of argues that, for those people that we don’t know have anaphylaxis to anything, it’s definitely important to have it available to them,” reported Dr. Neupert, a resident at the University of Texas, Austin.
In 45% of the cases, epinephrine was administered to children who had a known history of allergic reactions but, for whatever reason, did not have an epinephrine injector assigned to them.
Food was the most common trigger for use of epinephrine, accounting for 48% of the injections, with fragrance at 16%, insect stings at 10%, and exercise and overheating at 7%.
Dr. Neupert and her associates said the frequency with which epinephrine was administered after exposure to a fragrance – seen in about the same amount for unassigned and assigned epinephrine – might signal a need for greater education.
She emphasized the importance of follow-up after the use of unassigned injectors. If children get epinephrine that was unassigned and they have known allergies, “be sure that they subsequently get back in with their pediatrician or their allergist [and] that they’re getting their up-to-date epinephrine pens renewed,” she noted.
Carla Davis, MD, a pediatrician at Baylor College of Medicine, Houston, said she hopes more school districts adopt the stock epinephrine policy, despite barriers of cost and education. “I do think that it’s important for these schools to have these, because 20% of children will have their first episode of food allergic reaction – and in some of those cases it will be anaphylaxis – in schools.”
Dr. Neupert had no relevant financial disclosures.
SOURCE: AAAAI/WAO Joint Congress Abstract 465.
ORLANDO –
In the 2015-2016 and 2016-2017 school years, epinephrine was administered to students 31 times at schools in the Austin Independent School District, which began to stock unassigned epinephrine in its schools after state legislators approved a law in 2015 allowing, but not requiring, school districts to do so. In 21 of those cases, or 68% of the time, it was the unassigned stockpile that was used, Kathryn Neupert, MD, said at the joint congress of the American Academy of Allergy, Asthma, and Immunology and the World Asthma Organization.
She drew attention to the finding that 22% of the time in the study, the epinephrine use involved the unassigned stock for children with no history of anaphylaxis or allergy.
“It kind of argues that, for those people that we don’t know have anaphylaxis to anything, it’s definitely important to have it available to them,” reported Dr. Neupert, a resident at the University of Texas, Austin.
In 45% of the cases, epinephrine was administered to children who had a known history of allergic reactions but, for whatever reason, did not have an epinephrine injector assigned to them.
Food was the most common trigger for use of epinephrine, accounting for 48% of the injections, with fragrance at 16%, insect stings at 10%, and exercise and overheating at 7%.
Dr. Neupert and her associates said the frequency with which epinephrine was administered after exposure to a fragrance – seen in about the same amount for unassigned and assigned epinephrine – might signal a need for greater education.
She emphasized the importance of follow-up after the use of unassigned injectors. If children get epinephrine that was unassigned and they have known allergies, “be sure that they subsequently get back in with their pediatrician or their allergist [and] that they’re getting their up-to-date epinephrine pens renewed,” she noted.
Carla Davis, MD, a pediatrician at Baylor College of Medicine, Houston, said she hopes more school districts adopt the stock epinephrine policy, despite barriers of cost and education. “I do think that it’s important for these schools to have these, because 20% of children will have their first episode of food allergic reaction – and in some of those cases it will be anaphylaxis – in schools.”
Dr. Neupert had no relevant financial disclosures.
SOURCE: AAAAI/WAO Joint Congress Abstract 465.
ORLANDO –
In the 2015-2016 and 2016-2017 school years, epinephrine was administered to students 31 times at schools in the Austin Independent School District, which began to stock unassigned epinephrine in its schools after state legislators approved a law in 2015 allowing, but not requiring, school districts to do so. In 21 of those cases, or 68% of the time, it was the unassigned stockpile that was used, Kathryn Neupert, MD, said at the joint congress of the American Academy of Allergy, Asthma, and Immunology and the World Asthma Organization.
She drew attention to the finding that 22% of the time in the study, the epinephrine use involved the unassigned stock for children with no history of anaphylaxis or allergy.
“It kind of argues that, for those people that we don’t know have anaphylaxis to anything, it’s definitely important to have it available to them,” reported Dr. Neupert, a resident at the University of Texas, Austin.
In 45% of the cases, epinephrine was administered to children who had a known history of allergic reactions but, for whatever reason, did not have an epinephrine injector assigned to them.
Food was the most common trigger for use of epinephrine, accounting for 48% of the injections, with fragrance at 16%, insect stings at 10%, and exercise and overheating at 7%.
Dr. Neupert and her associates said the frequency with which epinephrine was administered after exposure to a fragrance – seen in about the same amount for unassigned and assigned epinephrine – might signal a need for greater education.
She emphasized the importance of follow-up after the use of unassigned injectors. If children get epinephrine that was unassigned and they have known allergies, “be sure that they subsequently get back in with their pediatrician or their allergist [and] that they’re getting their up-to-date epinephrine pens renewed,” she noted.
Carla Davis, MD, a pediatrician at Baylor College of Medicine, Houston, said she hopes more school districts adopt the stock epinephrine policy, despite barriers of cost and education. “I do think that it’s important for these schools to have these, because 20% of children will have their first episode of food allergic reaction – and in some of those cases it will be anaphylaxis – in schools.”
Dr. Neupert had no relevant financial disclosures.
SOURCE: AAAAI/WAO Joint Congress Abstract 465.
REPORTING FROM AAAAI/WAO JOINT CONGRESS
Key clinical point: Unassigned epinephrine was used more often in a Texas school district than assigned epinephrine.
Major finding: Over 2 years, 31 epinephrine injections were administered, and in 68% of the cases, it was the unassigned stock that was used.
Study details: A review of nursing records for the Austin Independent School District.
Disclosures: Dr. Kathryn Neupert had no relevant financial disclosures.
Source: Neupert K et al. Abstract 465.
Study highlights need to investigate psoriasis treatment outcomes in skin of color patients
MIAMI – Psoriasis often presents differently in skin of color patients, but an unanswered question remains: Does response to treatment with an agent like a fixed-dose combination foam also differ by ethnicity?
Researchers at Mount Sinai St. Luke’s Hospital in New York addressed this question using phase 2 and 3 study data for 1,104 people with psoriasis, about half of whom were randomized to topical treatment with calcipotriene and betamethasone dipropionate foam 0.005%/0.064% (Enstilar); the rest received a single component or vehicle only. The data were obtained from LEO Pharma, the product’s manufacturer.
“We were very interested in knowing if there was any difference in efficacy between the specific ethnic groups – the skin of color and non–skin of color patients,” said Bridget Kaufman, MD, a dermatopharmacology fellow at Mount Sinai St. Luke’s Hospital. “So we went back to look at the data to see if there was any difference in side effects or efficacy between ethnic groups.”
Strength in numbers?
The three randomized, pooled clinical studies included many ethnic groups. However, only 6.5% of participants were black and even fewer were Asian, American Indian, or native Hawaiian, Dr. Kaufman said. “It’s hard to see meaningful differences when you don’t have a substantial skin of color population.”
As a result, no significant associations emerged from the pooled data. “That is the main take-home message of this study: We don’t have a great understanding now of the difference in efficacy between white and nonwhite ethnic groups,” Dr. Kaufman said.
The researchers defined treatment success at 4 weeks as a two-point improvement to “clear” or “almost clear” on the Investigator Global Assessment of psoriasis. Of the adult participants with chronic plaque psoriasis randomized to the combination foam product, 54% of the white patients; 30% of black patients; 69% of Asian patients; and one of the two Hawaiian/Pacific Islander patients achieved treatment success after 4 weeks of topical treatment.
“All subgroups analyzed had a good response to treatment at 4 weeks. Numerically it appears African Americans in particular did not do quite as well, but we can’t [definitively] draw that conclusion,” Dr. Kaufman said in an interview.
More data, please
The study is just the first step in investigating the efficacy of this particular product in diverse ethnic groups, Dr. Kaufman added. “That really emphasizes the importance of studying these medications in skin of color populations in particular.”
More guidance on psoriasis in skin of color patients is available in a published review article by Dr. Kaufman and Andrew F. Alexis, MD, director of the Skin of Color Center at Mount Sinai St. Luke’s and Mount Sinai West, New York (Am J Clin Dermatol. 2017 Dec 5. doi: 10.1007/s40257-017-0332-7).
Enstilar manufacturer LEO Pharma supplied the clinical data but did not fund the study. Dr. Kaufman had no relevant financial disclosures.
[email protected]
SOURCE: Kaufman B et al. ODAC 2018
MIAMI – Psoriasis often presents differently in skin of color patients, but an unanswered question remains: Does response to treatment with an agent like a fixed-dose combination foam also differ by ethnicity?
Researchers at Mount Sinai St. Luke’s Hospital in New York addressed this question using phase 2 and 3 study data for 1,104 people with psoriasis, about half of whom were randomized to topical treatment with calcipotriene and betamethasone dipropionate foam 0.005%/0.064% (Enstilar); the rest received a single component or vehicle only. The data were obtained from LEO Pharma, the product’s manufacturer.
“We were very interested in knowing if there was any difference in efficacy between the specific ethnic groups – the skin of color and non–skin of color patients,” said Bridget Kaufman, MD, a dermatopharmacology fellow at Mount Sinai St. Luke’s Hospital. “So we went back to look at the data to see if there was any difference in side effects or efficacy between ethnic groups.”
Strength in numbers?
The three randomized, pooled clinical studies included many ethnic groups. However, only 6.5% of participants were black and even fewer were Asian, American Indian, or native Hawaiian, Dr. Kaufman said. “It’s hard to see meaningful differences when you don’t have a substantial skin of color population.”
As a result, no significant associations emerged from the pooled data. “That is the main take-home message of this study: We don’t have a great understanding now of the difference in efficacy between white and nonwhite ethnic groups,” Dr. Kaufman said.
The researchers defined treatment success at 4 weeks as a two-point improvement to “clear” or “almost clear” on the Investigator Global Assessment of psoriasis. Of the adult participants with chronic plaque psoriasis randomized to the combination foam product, 54% of the white patients; 30% of black patients; 69% of Asian patients; and one of the two Hawaiian/Pacific Islander patients achieved treatment success after 4 weeks of topical treatment.
“All subgroups analyzed had a good response to treatment at 4 weeks. Numerically it appears African Americans in particular did not do quite as well, but we can’t [definitively] draw that conclusion,” Dr. Kaufman said in an interview.
More data, please
The study is just the first step in investigating the efficacy of this particular product in diverse ethnic groups, Dr. Kaufman added. “That really emphasizes the importance of studying these medications in skin of color populations in particular.”
More guidance on psoriasis in skin of color patients is available in a published review article by Dr. Kaufman and Andrew F. Alexis, MD, director of the Skin of Color Center at Mount Sinai St. Luke’s and Mount Sinai West, New York (Am J Clin Dermatol. 2017 Dec 5. doi: 10.1007/s40257-017-0332-7).
Enstilar manufacturer LEO Pharma supplied the clinical data but did not fund the study. Dr. Kaufman had no relevant financial disclosures.
[email protected]
SOURCE: Kaufman B et al. ODAC 2018
MIAMI – Psoriasis often presents differently in skin of color patients, but an unanswered question remains: Does response to treatment with an agent like a fixed-dose combination foam also differ by ethnicity?
Researchers at Mount Sinai St. Luke’s Hospital in New York addressed this question using phase 2 and 3 study data for 1,104 people with psoriasis, about half of whom were randomized to topical treatment with calcipotriene and betamethasone dipropionate foam 0.005%/0.064% (Enstilar); the rest received a single component or vehicle only. The data were obtained from LEO Pharma, the product’s manufacturer.
“We were very interested in knowing if there was any difference in efficacy between the specific ethnic groups – the skin of color and non–skin of color patients,” said Bridget Kaufman, MD, a dermatopharmacology fellow at Mount Sinai St. Luke’s Hospital. “So we went back to look at the data to see if there was any difference in side effects or efficacy between ethnic groups.”
Strength in numbers?
The three randomized, pooled clinical studies included many ethnic groups. However, only 6.5% of participants were black and even fewer were Asian, American Indian, or native Hawaiian, Dr. Kaufman said. “It’s hard to see meaningful differences when you don’t have a substantial skin of color population.”
As a result, no significant associations emerged from the pooled data. “That is the main take-home message of this study: We don’t have a great understanding now of the difference in efficacy between white and nonwhite ethnic groups,” Dr. Kaufman said.
The researchers defined treatment success at 4 weeks as a two-point improvement to “clear” or “almost clear” on the Investigator Global Assessment of psoriasis. Of the adult participants with chronic plaque psoriasis randomized to the combination foam product, 54% of the white patients; 30% of black patients; 69% of Asian patients; and one of the two Hawaiian/Pacific Islander patients achieved treatment success after 4 weeks of topical treatment.
“All subgroups analyzed had a good response to treatment at 4 weeks. Numerically it appears African Americans in particular did not do quite as well, but we can’t [definitively] draw that conclusion,” Dr. Kaufman said in an interview.
More data, please
The study is just the first step in investigating the efficacy of this particular product in diverse ethnic groups, Dr. Kaufman added. “That really emphasizes the importance of studying these medications in skin of color populations in particular.”
More guidance on psoriasis in skin of color patients is available in a published review article by Dr. Kaufman and Andrew F. Alexis, MD, director of the Skin of Color Center at Mount Sinai St. Luke’s and Mount Sinai West, New York (Am J Clin Dermatol. 2017 Dec 5. doi: 10.1007/s40257-017-0332-7).
Enstilar manufacturer LEO Pharma supplied the clinical data but did not fund the study. Dr. Kaufman had no relevant financial disclosures.
[email protected]
SOURCE: Kaufman B et al. ODAC 2018
REPORTING FROM ODAC 2018
Key clinical point: There were no significant differences in response to calcipotriene and betamethasone dipropionate foam in phase 2 and 3 trials, possibly because of small percentages of skin of color participants in these studies.
Major finding: Treatment success rates at 4 weeks were 30% among black patients, 54% among white patients, and 69% among Asian patients, but not enough skin of color patients were enrolled for differences to reach statistical significance.
Study details: A retrospective analysis of pooled phase 2 and phase 3 studies with 1,104 participants with psoriasis.
Disclosures: LEO Pharma supplied the clinical data but did not fund the study. Dr. Kaufman had no relevant financial disclosures.
Source: Kaufman B et al. ODAC 2018.
2017 was a big year for psoriatic arthritis
MAUI, HAWAII – 2017 was a banner year in the field of psoriatic arthritis, marked by a huge bump in the number of publications on the topic along with the approval of three additional drugs, Arthur Kavanaugh, MD, said at the 2018 Rheumatology Winter Clinical Symposium.
“There is a tremendous amount of excitement now in the field of psoriatic arthritis,” observed Dr. Kavanaugh, professor of medicine and director of the Center for Innovative Therapy at the University of California, San Diego.
Together with his colleague Eric M. Ruderman, MD, Dr. Kavanaugh highlighted the three new drug approvals for psoriatic arthritis in 2017 – abatacept(Orencia), tofacitinib(Xeljanz), and ixekizumab(Taltz) – and also discussed important recent studies of several drugs already available.
Abatacept
In the pivotal double-blind, phase 3 trial involving 424 psoriatic arthritis patients, roughly 60% with prior exposure to a tumor necrosis factor inhibitor and 60% on concomitant methotrexate, the proportion of patients with at least 20% improvement in the American College of Rheumatology criteria (ACR20) was 39.4% in patients on the selective T-cell costimulation modulator, compared with 22.3% among placebo-treated controls. The benefit on psoriasis lesions was modest, and there was no significant difference between the two study arms in terms of Health Assessment Questionnaire-Disability Index response rates (Ann Rheum Dis. 2017 Sep;76[9]:1550-8).
“I think we could say the effect is modest,” Dr. Kavanaugh said. “The challenge to us still is to identify patients who are going to have a good response, likely the patients with more joint than skin symptoms.”
An attractive feature of the drug is that its safety profile is well known as a result of its extensive track record in treating RA, he added.
Tofacitinib
On the basis of the phase 3 OPAL Beyond (N Engl J Med. 2017 Oct 19;377[16]:1525-36) and OPAL Broaden (N Engl J Med. 2017 Oct 19;377[16]:1537-50) clinical trials, the dose approved by the Food and Drug Administration for psoriatic arthritis was 5 mg b.i.d.. There was a higher ACR20 response rate with 10 mg than 5 mg b.i.d. in OPAL Broaden, but not in OPAL Beyond. And since there was a suggestion of a higher adverse event rate with the 10-mg b.i.d. dosing without unequivocal evidence of superior efficacy, the Food and Drug Administration – which always puts safety first – went with 5 mg b.i.d., Dr. Ruderman explained.
Ixekizumab
In the phase 3, double-blind SPIRIT-P1 trial, featuring 417 biologic-naive psoriatic arthritis patients, the ACR20 response rate at week 24 was 62.1% with the interleukin-17A antagonist at 80 mg given subcutaneously every 2 weeks and 57.9% when dosed every 4 weeks, compared with 57.4% with adalimumab(Humira) at 40 mg every 2 weeks and 30.2% with placebo (Ann Rheum Dis. 2017 Jan;76[1]:79-87). The FDA-approved regimen was a 160-mg loading dose of ixekizumab, followed by 80 mg every 4 weeks.
Dr. Kavanaugh noted that an international team of investigators has identified beta-defensin 2 as an easily measurable biomarker of interleukin-17A–driven skin pathology after evaluating 170 proteins expressed in blood, psoriasis lesions, and nonlesional skin. It was a small study, with eight psoriasis patients and eight healthy controls studied before and after receiving secukinumab(Cosentyx), a monoclonal antibody directed against interleukin-17A (J Allergy Clin Immunol. 2017 Mar;139[3]:923-932.e8). But it’s a study with big potential implications.
“This natural antibiotic compound we make that’s in the skin might be a marker of responsiveness to anti–interleukin-17 therapy. It could help in deciding which patients get which drugs. This needs further study, especially now that we’re using anti–interleukin-17 drugs more now,” the rheumatologist said.
The year 2017 also brought important new studies of several drugs already available for psoriatic arthritis.
Intravenous golimumab (Simponi Aria)
Dr. Kavanaugh was first author of the GO-VIBRANT study, a phase 3, double-blind clinical trial in which 480 biologic-naive psoriatic arthritis patients were randomized to a 30-minute infusion of IV golimumab at 2 mg/kg or placebo at weeks 0, 4, 12, and 20.
The primary endpoint, an ACR20 response at week 14, was achieved in 75.1% of patients on the tumor necrosis factor inhibitor versus 21.8% on placebo. An ACR50 response occurred in 43.6% of patients on IV golimumab, compared with 6.3% on placebo, and a Psoriasis and Area Severity Index 75 skin response was achieved in 59.2% on IV golimumab and 13.6% of controls. At week 24, the IV golimumab group demonstrated significantly less radiographic progression as measured by the total modified Sharp/van der Heijde score. The drug was well tolerated, with no opportunistic infections or tuberculosis, and the infusion reaction rate was below 2% (Arthritis Rheumatol. 2017 Nov;69[11]:2151-61).
Secukinumab
In a recent update of the 606-patient FUTURE 1 trial, secukinumab resulted in clinically meaningful improvement in key patient-reported outcomes at week 24, including global assessment of disease activity, which decreased by a mean of 20.6 and 20 points in patients on 150 and 75 mg, respectively, every 4 weeks, compared with a 7.4-point drop in placebo-treated controls.
Psoriatic arthritis quality of life scores improved by 3.5 and 3.2 points in the two secukinumab arms, compared with 0.4 points in controls. Dermatology Life Quality Index scores improved by 8.8 and 7.9 points, versus 0.7 in controls. Patients on the interleukin-17A inhibitor also showed significantly greater improvement in self-assessments measuring pain and fatigue (Ann Rheum Dis. 2017 Jan;76[1]:203-7).
Apremilast (Otezla)
At the 2018 meeting of the American Academy of Dermatology, Dr. Kavanaugh presented 5-year outcomes of the open-label extension of the 504-patient, phase 3 PALACE-1 trial. In an as-observed analysis, patients on apremilast 30 mg b.i.d. up to week 260 had a 71.7% ACR20 response rate, a 48.6% ACR50 response rate, and a 28.4% ACR70 response. Eighty percent of patients on the oral phosphodiesterase-4 (PDE-4) inhibitor had a dactylitis count of 0, and 54.5% had a Maastricht Ankylosing Spondylitis Enthesitis Score of 0.
In a report from the 219-patient, phase 3B ACTIVE trial, investigators showed that biologic-naive patients randomized to apremilast at 30 mg b.i.d. had a significantly greater ACR20 response as early as week 2, which was the first assessment. At that point, the ACR20 rate was 16.4% with apremilast, compared with 6.4% in placebo-treated controls. The apremilast group also demonstrated significant early improvements in patient-reported outcomes, including the Health Assessment Questionnaire-Disability Index, morning stiffness, and enthesitis severity.
The primary outcome, the ACR20 rate at week 16, was 38.2% with active treatment versus 20.2% in controls (Ann Rheum Dis. 2018 Jan 17. doi: 10.1136/annrheumdis-2017-211568).
“The main advantage of apremilast is safety – and that’s a big advantage,” Dr. Kavanaugh commented.
Military physicians tell him they are prescribing a lot of apremilast for armed forces deploying overseas because it’s not immunosuppressive and doesn’t entail laboratory testing.
The research agenda for PDE-4 inhibition in psoriatic disease is extensive, he noted. There is a need for formal studies of PDE-4 inhibition in combination with conventional disease-modifying antirheumatic drugs or biologics. Topical formulations, once-daily dosing, and the possibility that PDE-4 inhibition might be the preferred therapy in patients with certain comorbid conditions, such as chronic obstructive pulmonary disease or a history of recurrent infections, are all topics worthy of study. A biomarker to identify in advance which patients with psoriatic arthritis or psoriasis will attain maximum clinical benefit from apremilast, and in which domains, would be of enormous help to clinicians.
Dr. Kavanaugh and Dr. Ruderman reported serving as consultants to and receiving research grants from numerous pharmaceutical companies.
MAUI, HAWAII – 2017 was a banner year in the field of psoriatic arthritis, marked by a huge bump in the number of publications on the topic along with the approval of three additional drugs, Arthur Kavanaugh, MD, said at the 2018 Rheumatology Winter Clinical Symposium.
“There is a tremendous amount of excitement now in the field of psoriatic arthritis,” observed Dr. Kavanaugh, professor of medicine and director of the Center for Innovative Therapy at the University of California, San Diego.
Together with his colleague Eric M. Ruderman, MD, Dr. Kavanaugh highlighted the three new drug approvals for psoriatic arthritis in 2017 – abatacept(Orencia), tofacitinib(Xeljanz), and ixekizumab(Taltz) – and also discussed important recent studies of several drugs already available.
Abatacept
In the pivotal double-blind, phase 3 trial involving 424 psoriatic arthritis patients, roughly 60% with prior exposure to a tumor necrosis factor inhibitor and 60% on concomitant methotrexate, the proportion of patients with at least 20% improvement in the American College of Rheumatology criteria (ACR20) was 39.4% in patients on the selective T-cell costimulation modulator, compared with 22.3% among placebo-treated controls. The benefit on psoriasis lesions was modest, and there was no significant difference between the two study arms in terms of Health Assessment Questionnaire-Disability Index response rates (Ann Rheum Dis. 2017 Sep;76[9]:1550-8).
“I think we could say the effect is modest,” Dr. Kavanaugh said. “The challenge to us still is to identify patients who are going to have a good response, likely the patients with more joint than skin symptoms.”
An attractive feature of the drug is that its safety profile is well known as a result of its extensive track record in treating RA, he added.
Tofacitinib
On the basis of the phase 3 OPAL Beyond (N Engl J Med. 2017 Oct 19;377[16]:1525-36) and OPAL Broaden (N Engl J Med. 2017 Oct 19;377[16]:1537-50) clinical trials, the dose approved by the Food and Drug Administration for psoriatic arthritis was 5 mg b.i.d.. There was a higher ACR20 response rate with 10 mg than 5 mg b.i.d. in OPAL Broaden, but not in OPAL Beyond. And since there was a suggestion of a higher adverse event rate with the 10-mg b.i.d. dosing without unequivocal evidence of superior efficacy, the Food and Drug Administration – which always puts safety first – went with 5 mg b.i.d., Dr. Ruderman explained.
Ixekizumab
In the phase 3, double-blind SPIRIT-P1 trial, featuring 417 biologic-naive psoriatic arthritis patients, the ACR20 response rate at week 24 was 62.1% with the interleukin-17A antagonist at 80 mg given subcutaneously every 2 weeks and 57.9% when dosed every 4 weeks, compared with 57.4% with adalimumab(Humira) at 40 mg every 2 weeks and 30.2% with placebo (Ann Rheum Dis. 2017 Jan;76[1]:79-87). The FDA-approved regimen was a 160-mg loading dose of ixekizumab, followed by 80 mg every 4 weeks.
Dr. Kavanaugh noted that an international team of investigators has identified beta-defensin 2 as an easily measurable biomarker of interleukin-17A–driven skin pathology after evaluating 170 proteins expressed in blood, psoriasis lesions, and nonlesional skin. It was a small study, with eight psoriasis patients and eight healthy controls studied before and after receiving secukinumab(Cosentyx), a monoclonal antibody directed against interleukin-17A (J Allergy Clin Immunol. 2017 Mar;139[3]:923-932.e8). But it’s a study with big potential implications.
“This natural antibiotic compound we make that’s in the skin might be a marker of responsiveness to anti–interleukin-17 therapy. It could help in deciding which patients get which drugs. This needs further study, especially now that we’re using anti–interleukin-17 drugs more now,” the rheumatologist said.
The year 2017 also brought important new studies of several drugs already available for psoriatic arthritis.
Intravenous golimumab (Simponi Aria)
Dr. Kavanaugh was first author of the GO-VIBRANT study, a phase 3, double-blind clinical trial in which 480 biologic-naive psoriatic arthritis patients were randomized to a 30-minute infusion of IV golimumab at 2 mg/kg or placebo at weeks 0, 4, 12, and 20.
The primary endpoint, an ACR20 response at week 14, was achieved in 75.1% of patients on the tumor necrosis factor inhibitor versus 21.8% on placebo. An ACR50 response occurred in 43.6% of patients on IV golimumab, compared with 6.3% on placebo, and a Psoriasis and Area Severity Index 75 skin response was achieved in 59.2% on IV golimumab and 13.6% of controls. At week 24, the IV golimumab group demonstrated significantly less radiographic progression as measured by the total modified Sharp/van der Heijde score. The drug was well tolerated, with no opportunistic infections or tuberculosis, and the infusion reaction rate was below 2% (Arthritis Rheumatol. 2017 Nov;69[11]:2151-61).
Secukinumab
In a recent update of the 606-patient FUTURE 1 trial, secukinumab resulted in clinically meaningful improvement in key patient-reported outcomes at week 24, including global assessment of disease activity, which decreased by a mean of 20.6 and 20 points in patients on 150 and 75 mg, respectively, every 4 weeks, compared with a 7.4-point drop in placebo-treated controls.
Psoriatic arthritis quality of life scores improved by 3.5 and 3.2 points in the two secukinumab arms, compared with 0.4 points in controls. Dermatology Life Quality Index scores improved by 8.8 and 7.9 points, versus 0.7 in controls. Patients on the interleukin-17A inhibitor also showed significantly greater improvement in self-assessments measuring pain and fatigue (Ann Rheum Dis. 2017 Jan;76[1]:203-7).
Apremilast (Otezla)
At the 2018 meeting of the American Academy of Dermatology, Dr. Kavanaugh presented 5-year outcomes of the open-label extension of the 504-patient, phase 3 PALACE-1 trial. In an as-observed analysis, patients on apremilast 30 mg b.i.d. up to week 260 had a 71.7% ACR20 response rate, a 48.6% ACR50 response rate, and a 28.4% ACR70 response. Eighty percent of patients on the oral phosphodiesterase-4 (PDE-4) inhibitor had a dactylitis count of 0, and 54.5% had a Maastricht Ankylosing Spondylitis Enthesitis Score of 0.
In a report from the 219-patient, phase 3B ACTIVE trial, investigators showed that biologic-naive patients randomized to apremilast at 30 mg b.i.d. had a significantly greater ACR20 response as early as week 2, which was the first assessment. At that point, the ACR20 rate was 16.4% with apremilast, compared with 6.4% in placebo-treated controls. The apremilast group also demonstrated significant early improvements in patient-reported outcomes, including the Health Assessment Questionnaire-Disability Index, morning stiffness, and enthesitis severity.
The primary outcome, the ACR20 rate at week 16, was 38.2% with active treatment versus 20.2% in controls (Ann Rheum Dis. 2018 Jan 17. doi: 10.1136/annrheumdis-2017-211568).
“The main advantage of apremilast is safety – and that’s a big advantage,” Dr. Kavanaugh commented.
Military physicians tell him they are prescribing a lot of apremilast for armed forces deploying overseas because it’s not immunosuppressive and doesn’t entail laboratory testing.
The research agenda for PDE-4 inhibition in psoriatic disease is extensive, he noted. There is a need for formal studies of PDE-4 inhibition in combination with conventional disease-modifying antirheumatic drugs or biologics. Topical formulations, once-daily dosing, and the possibility that PDE-4 inhibition might be the preferred therapy in patients with certain comorbid conditions, such as chronic obstructive pulmonary disease or a history of recurrent infections, are all topics worthy of study. A biomarker to identify in advance which patients with psoriatic arthritis or psoriasis will attain maximum clinical benefit from apremilast, and in which domains, would be of enormous help to clinicians.
Dr. Kavanaugh and Dr. Ruderman reported serving as consultants to and receiving research grants from numerous pharmaceutical companies.
MAUI, HAWAII – 2017 was a banner year in the field of psoriatic arthritis, marked by a huge bump in the number of publications on the topic along with the approval of three additional drugs, Arthur Kavanaugh, MD, said at the 2018 Rheumatology Winter Clinical Symposium.
“There is a tremendous amount of excitement now in the field of psoriatic arthritis,” observed Dr. Kavanaugh, professor of medicine and director of the Center for Innovative Therapy at the University of California, San Diego.
Together with his colleague Eric M. Ruderman, MD, Dr. Kavanaugh highlighted the three new drug approvals for psoriatic arthritis in 2017 – abatacept(Orencia), tofacitinib(Xeljanz), and ixekizumab(Taltz) – and also discussed important recent studies of several drugs already available.
Abatacept
In the pivotal double-blind, phase 3 trial involving 424 psoriatic arthritis patients, roughly 60% with prior exposure to a tumor necrosis factor inhibitor and 60% on concomitant methotrexate, the proportion of patients with at least 20% improvement in the American College of Rheumatology criteria (ACR20) was 39.4% in patients on the selective T-cell costimulation modulator, compared with 22.3% among placebo-treated controls. The benefit on psoriasis lesions was modest, and there was no significant difference between the two study arms in terms of Health Assessment Questionnaire-Disability Index response rates (Ann Rheum Dis. 2017 Sep;76[9]:1550-8).
“I think we could say the effect is modest,” Dr. Kavanaugh said. “The challenge to us still is to identify patients who are going to have a good response, likely the patients with more joint than skin symptoms.”
An attractive feature of the drug is that its safety profile is well known as a result of its extensive track record in treating RA, he added.
Tofacitinib
On the basis of the phase 3 OPAL Beyond (N Engl J Med. 2017 Oct 19;377[16]:1525-36) and OPAL Broaden (N Engl J Med. 2017 Oct 19;377[16]:1537-50) clinical trials, the dose approved by the Food and Drug Administration for psoriatic arthritis was 5 mg b.i.d.. There was a higher ACR20 response rate with 10 mg than 5 mg b.i.d. in OPAL Broaden, but not in OPAL Beyond. And since there was a suggestion of a higher adverse event rate with the 10-mg b.i.d. dosing without unequivocal evidence of superior efficacy, the Food and Drug Administration – which always puts safety first – went with 5 mg b.i.d., Dr. Ruderman explained.
Ixekizumab
In the phase 3, double-blind SPIRIT-P1 trial, featuring 417 biologic-naive psoriatic arthritis patients, the ACR20 response rate at week 24 was 62.1% with the interleukin-17A antagonist at 80 mg given subcutaneously every 2 weeks and 57.9% when dosed every 4 weeks, compared with 57.4% with adalimumab(Humira) at 40 mg every 2 weeks and 30.2% with placebo (Ann Rheum Dis. 2017 Jan;76[1]:79-87). The FDA-approved regimen was a 160-mg loading dose of ixekizumab, followed by 80 mg every 4 weeks.
Dr. Kavanaugh noted that an international team of investigators has identified beta-defensin 2 as an easily measurable biomarker of interleukin-17A–driven skin pathology after evaluating 170 proteins expressed in blood, psoriasis lesions, and nonlesional skin. It was a small study, with eight psoriasis patients and eight healthy controls studied before and after receiving secukinumab(Cosentyx), a monoclonal antibody directed against interleukin-17A (J Allergy Clin Immunol. 2017 Mar;139[3]:923-932.e8). But it’s a study with big potential implications.
“This natural antibiotic compound we make that’s in the skin might be a marker of responsiveness to anti–interleukin-17 therapy. It could help in deciding which patients get which drugs. This needs further study, especially now that we’re using anti–interleukin-17 drugs more now,” the rheumatologist said.
The year 2017 also brought important new studies of several drugs already available for psoriatic arthritis.
Intravenous golimumab (Simponi Aria)
Dr. Kavanaugh was first author of the GO-VIBRANT study, a phase 3, double-blind clinical trial in which 480 biologic-naive psoriatic arthritis patients were randomized to a 30-minute infusion of IV golimumab at 2 mg/kg or placebo at weeks 0, 4, 12, and 20.
The primary endpoint, an ACR20 response at week 14, was achieved in 75.1% of patients on the tumor necrosis factor inhibitor versus 21.8% on placebo. An ACR50 response occurred in 43.6% of patients on IV golimumab, compared with 6.3% on placebo, and a Psoriasis and Area Severity Index 75 skin response was achieved in 59.2% on IV golimumab and 13.6% of controls. At week 24, the IV golimumab group demonstrated significantly less radiographic progression as measured by the total modified Sharp/van der Heijde score. The drug was well tolerated, with no opportunistic infections or tuberculosis, and the infusion reaction rate was below 2% (Arthritis Rheumatol. 2017 Nov;69[11]:2151-61).
Secukinumab
In a recent update of the 606-patient FUTURE 1 trial, secukinumab resulted in clinically meaningful improvement in key patient-reported outcomes at week 24, including global assessment of disease activity, which decreased by a mean of 20.6 and 20 points in patients on 150 and 75 mg, respectively, every 4 weeks, compared with a 7.4-point drop in placebo-treated controls.
Psoriatic arthritis quality of life scores improved by 3.5 and 3.2 points in the two secukinumab arms, compared with 0.4 points in controls. Dermatology Life Quality Index scores improved by 8.8 and 7.9 points, versus 0.7 in controls. Patients on the interleukin-17A inhibitor also showed significantly greater improvement in self-assessments measuring pain and fatigue (Ann Rheum Dis. 2017 Jan;76[1]:203-7).
Apremilast (Otezla)
At the 2018 meeting of the American Academy of Dermatology, Dr. Kavanaugh presented 5-year outcomes of the open-label extension of the 504-patient, phase 3 PALACE-1 trial. In an as-observed analysis, patients on apremilast 30 mg b.i.d. up to week 260 had a 71.7% ACR20 response rate, a 48.6% ACR50 response rate, and a 28.4% ACR70 response. Eighty percent of patients on the oral phosphodiesterase-4 (PDE-4) inhibitor had a dactylitis count of 0, and 54.5% had a Maastricht Ankylosing Spondylitis Enthesitis Score of 0.
In a report from the 219-patient, phase 3B ACTIVE trial, investigators showed that biologic-naive patients randomized to apremilast at 30 mg b.i.d. had a significantly greater ACR20 response as early as week 2, which was the first assessment. At that point, the ACR20 rate was 16.4% with apremilast, compared with 6.4% in placebo-treated controls. The apremilast group also demonstrated significant early improvements in patient-reported outcomes, including the Health Assessment Questionnaire-Disability Index, morning stiffness, and enthesitis severity.
The primary outcome, the ACR20 rate at week 16, was 38.2% with active treatment versus 20.2% in controls (Ann Rheum Dis. 2018 Jan 17. doi: 10.1136/annrheumdis-2017-211568).
“The main advantage of apremilast is safety – and that’s a big advantage,” Dr. Kavanaugh commented.
Military physicians tell him they are prescribing a lot of apremilast for armed forces deploying overseas because it’s not immunosuppressive and doesn’t entail laboratory testing.
The research agenda for PDE-4 inhibition in psoriatic disease is extensive, he noted. There is a need for formal studies of PDE-4 inhibition in combination with conventional disease-modifying antirheumatic drugs or biologics. Topical formulations, once-daily dosing, and the possibility that PDE-4 inhibition might be the preferred therapy in patients with certain comorbid conditions, such as chronic obstructive pulmonary disease or a history of recurrent infections, are all topics worthy of study. A biomarker to identify in advance which patients with psoriatic arthritis or psoriasis will attain maximum clinical benefit from apremilast, and in which domains, would be of enormous help to clinicians.
Dr. Kavanaugh and Dr. Ruderman reported serving as consultants to and receiving research grants from numerous pharmaceutical companies.
EXPERT ANALYSIS FROM RWCS 2018
Toxicology reveals worse maternal and fetal outcomes with teen marijuana use
DALLAS – . Also, hypertensive disorders of pregnancy were higher in marijuana users, according to a study that incorporated universal urine toxicology testing of adolescents.
The study compared maternal and fetal/neonatal outcomes in 211 marijuana-exposed with 995 unexposed pregnancies. Christina Rodriguez, MD, and her coinvestigators found that the risk of a composite adverse pregnancy outcome was higher in marijuana users, occurring in 97/211 marijuana users (46%), and in 337/995 (33.9%) of the non–marijuana users (P less than .001).
Dr. Rodriguez said that since it used biological samples to confirm marijuana exposure, the study helps fill a gap in the literature. She presented the retrospective cohort study at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Previous work, she said, had established that up to 70% of pregnant women who had positive tests for tetrahydrocannabinol also denied marijuana use. “If marijuana use is determined by self-report, some women are misclassified as nonusers,” making it difficult to ascertain the true association between marijuana use during pregnancy and pregnancy outcomes, said Dr. Rodriguez of the University of Colorado, Denver.
Whether marijuana is associated with adverse pregnancy outcomes is an increasingly pressing question given rapidly shifting legislation, said Dr. Rodriguez. “In a state with legal access to marijuana, use is common in adolescent pregnancies,” she said.
Participants who were enrolled in prenatal care through the University of Colorado’s adolescent maternity program, where Dr. Rodriguez is a fellow, and who delivered at the University of Colorado Hospital, Aurora, were eligible to participate; adolescents were excluded for multiple gestation and for known major fetal anomalies or aneuploidy.
In addition to urine toxicology testing, participants also completed a uniformly administered substance use questionnaire. Marijuana exposure was defined as either having a positive urine toxicology result or self-reported marijuana use on the questionnaire (or both). Of the marijuana-exposed pregnancies, 133 (63%) of the adolescents tested positive on urine toxicology, 18 (9%) were positive by self-report, and 60 (28%) had both positive marijuana urine toxicology and positive self-report. Toxicology was available for 91% of participants.
Participants were negative for marijuana exposure if they had a negative toxicology screen, regardless of their response on the substance-use questionnaire.
The study’s primary outcome was a composite of adverse pregnancy outcomes, including stillbirth, defined as Apgar score of 0; any hypertensive disorder of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count); preterm birth, defined as spontaneous delivery before 37 weeks gestation; and infants born small for gestational age, defined as a birth weight below the 10th percentile after adjustment for gestational age and sex.
Secondary outcomes included pregnancy outcomes including placental abruption, mode of delivery, and gestational age at delivery. Neonatal outcomes included weight, length, and head circumference at birth, and neonatal intensive care unit admission. An Apgar score less than 7 at 5 minutes was considered an adverse neonatal outcome.
The sample size was determined by an estimate drawn from previous chart abstraction that the composite outcome would be seen in 16% of the clinic’s non–marijuana exposed patients, and 24% of the marijuana-exposed patients. The investigators also factored in that 18% of adolescents in the clinic database were marijuana users.
Dr. Rodriguez and her collaborators used a variety of models for statistical analysis, some of which included self-report alone or in conjunction with urine toxicology. In the end, they found that significant associations between their composite endpoint and marijuana use were seen when patients were dichotomized into those who had at least one positive urine toxicology test, versus those who had no positive toxicology results.
One of the study limitations was that the study didn’t permit investigators to get accurate information about the quantity, timing, or route of marijuana dosing. Also, this methodology may primarily identify heavier marijuana users, said Dr. Rodriguez.
Tobacco use was determined only by self-report, and outcomes were followed over a relatively short period of time.
Still, said Dr. Rodriguez, the study had many strengths, including the use of biological sampling to determine exposure and the near-universal participant urine toxicology testing. The investigators were able to capture and account for many important factors that could confound the results, she said. “Uncertainty regarding the impact of [marijuana] on pregnancy outcomes in the literature may result from incomplete ascertainment of exposure,” she and her coinvestigators wrote in the abstract accompanying the presentation.
SOURCE: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
DALLAS – . Also, hypertensive disorders of pregnancy were higher in marijuana users, according to a study that incorporated universal urine toxicology testing of adolescents.
The study compared maternal and fetal/neonatal outcomes in 211 marijuana-exposed with 995 unexposed pregnancies. Christina Rodriguez, MD, and her coinvestigators found that the risk of a composite adverse pregnancy outcome was higher in marijuana users, occurring in 97/211 marijuana users (46%), and in 337/995 (33.9%) of the non–marijuana users (P less than .001).
Dr. Rodriguez said that since it used biological samples to confirm marijuana exposure, the study helps fill a gap in the literature. She presented the retrospective cohort study at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Previous work, she said, had established that up to 70% of pregnant women who had positive tests for tetrahydrocannabinol also denied marijuana use. “If marijuana use is determined by self-report, some women are misclassified as nonusers,” making it difficult to ascertain the true association between marijuana use during pregnancy and pregnancy outcomes, said Dr. Rodriguez of the University of Colorado, Denver.
Whether marijuana is associated with adverse pregnancy outcomes is an increasingly pressing question given rapidly shifting legislation, said Dr. Rodriguez. “In a state with legal access to marijuana, use is common in adolescent pregnancies,” she said.
Participants who were enrolled in prenatal care through the University of Colorado’s adolescent maternity program, where Dr. Rodriguez is a fellow, and who delivered at the University of Colorado Hospital, Aurora, were eligible to participate; adolescents were excluded for multiple gestation and for known major fetal anomalies or aneuploidy.
In addition to urine toxicology testing, participants also completed a uniformly administered substance use questionnaire. Marijuana exposure was defined as either having a positive urine toxicology result or self-reported marijuana use on the questionnaire (or both). Of the marijuana-exposed pregnancies, 133 (63%) of the adolescents tested positive on urine toxicology, 18 (9%) were positive by self-report, and 60 (28%) had both positive marijuana urine toxicology and positive self-report. Toxicology was available for 91% of participants.
Participants were negative for marijuana exposure if they had a negative toxicology screen, regardless of their response on the substance-use questionnaire.
The study’s primary outcome was a composite of adverse pregnancy outcomes, including stillbirth, defined as Apgar score of 0; any hypertensive disorder of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count); preterm birth, defined as spontaneous delivery before 37 weeks gestation; and infants born small for gestational age, defined as a birth weight below the 10th percentile after adjustment for gestational age and sex.
Secondary outcomes included pregnancy outcomes including placental abruption, mode of delivery, and gestational age at delivery. Neonatal outcomes included weight, length, and head circumference at birth, and neonatal intensive care unit admission. An Apgar score less than 7 at 5 minutes was considered an adverse neonatal outcome.
The sample size was determined by an estimate drawn from previous chart abstraction that the composite outcome would be seen in 16% of the clinic’s non–marijuana exposed patients, and 24% of the marijuana-exposed patients. The investigators also factored in that 18% of adolescents in the clinic database were marijuana users.
Dr. Rodriguez and her collaborators used a variety of models for statistical analysis, some of which included self-report alone or in conjunction with urine toxicology. In the end, they found that significant associations between their composite endpoint and marijuana use were seen when patients were dichotomized into those who had at least one positive urine toxicology test, versus those who had no positive toxicology results.
One of the study limitations was that the study didn’t permit investigators to get accurate information about the quantity, timing, or route of marijuana dosing. Also, this methodology may primarily identify heavier marijuana users, said Dr. Rodriguez.
Tobacco use was determined only by self-report, and outcomes were followed over a relatively short period of time.
Still, said Dr. Rodriguez, the study had many strengths, including the use of biological sampling to determine exposure and the near-universal participant urine toxicology testing. The investigators were able to capture and account for many important factors that could confound the results, she said. “Uncertainty regarding the impact of [marijuana] on pregnancy outcomes in the literature may result from incomplete ascertainment of exposure,” she and her coinvestigators wrote in the abstract accompanying the presentation.
SOURCE: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
DALLAS – . Also, hypertensive disorders of pregnancy were higher in marijuana users, according to a study that incorporated universal urine toxicology testing of adolescents.
The study compared maternal and fetal/neonatal outcomes in 211 marijuana-exposed with 995 unexposed pregnancies. Christina Rodriguez, MD, and her coinvestigators found that the risk of a composite adverse pregnancy outcome was higher in marijuana users, occurring in 97/211 marijuana users (46%), and in 337/995 (33.9%) of the non–marijuana users (P less than .001).
Dr. Rodriguez said that since it used biological samples to confirm marijuana exposure, the study helps fill a gap in the literature. She presented the retrospective cohort study at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Previous work, she said, had established that up to 70% of pregnant women who had positive tests for tetrahydrocannabinol also denied marijuana use. “If marijuana use is determined by self-report, some women are misclassified as nonusers,” making it difficult to ascertain the true association between marijuana use during pregnancy and pregnancy outcomes, said Dr. Rodriguez of the University of Colorado, Denver.
Whether marijuana is associated with adverse pregnancy outcomes is an increasingly pressing question given rapidly shifting legislation, said Dr. Rodriguez. “In a state with legal access to marijuana, use is common in adolescent pregnancies,” she said.
Participants who were enrolled in prenatal care through the University of Colorado’s adolescent maternity program, where Dr. Rodriguez is a fellow, and who delivered at the University of Colorado Hospital, Aurora, were eligible to participate; adolescents were excluded for multiple gestation and for known major fetal anomalies or aneuploidy.
In addition to urine toxicology testing, participants also completed a uniformly administered substance use questionnaire. Marijuana exposure was defined as either having a positive urine toxicology result or self-reported marijuana use on the questionnaire (or both). Of the marijuana-exposed pregnancies, 133 (63%) of the adolescents tested positive on urine toxicology, 18 (9%) were positive by self-report, and 60 (28%) had both positive marijuana urine toxicology and positive self-report. Toxicology was available for 91% of participants.
Participants were negative for marijuana exposure if they had a negative toxicology screen, regardless of their response on the substance-use questionnaire.
The study’s primary outcome was a composite of adverse pregnancy outcomes, including stillbirth, defined as Apgar score of 0; any hypertensive disorder of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count); preterm birth, defined as spontaneous delivery before 37 weeks gestation; and infants born small for gestational age, defined as a birth weight below the 10th percentile after adjustment for gestational age and sex.
Secondary outcomes included pregnancy outcomes including placental abruption, mode of delivery, and gestational age at delivery. Neonatal outcomes included weight, length, and head circumference at birth, and neonatal intensive care unit admission. An Apgar score less than 7 at 5 minutes was considered an adverse neonatal outcome.
The sample size was determined by an estimate drawn from previous chart abstraction that the composite outcome would be seen in 16% of the clinic’s non–marijuana exposed patients, and 24% of the marijuana-exposed patients. The investigators also factored in that 18% of adolescents in the clinic database were marijuana users.
Dr. Rodriguez and her collaborators used a variety of models for statistical analysis, some of which included self-report alone or in conjunction with urine toxicology. In the end, they found that significant associations between their composite endpoint and marijuana use were seen when patients were dichotomized into those who had at least one positive urine toxicology test, versus those who had no positive toxicology results.
One of the study limitations was that the study didn’t permit investigators to get accurate information about the quantity, timing, or route of marijuana dosing. Also, this methodology may primarily identify heavier marijuana users, said Dr. Rodriguez.
Tobacco use was determined only by self-report, and outcomes were followed over a relatively short period of time.
Still, said Dr. Rodriguez, the study had many strengths, including the use of biological sampling to determine exposure and the near-universal participant urine toxicology testing. The investigators were able to capture and account for many important factors that could confound the results, she said. “Uncertainty regarding the impact of [marijuana] on pregnancy outcomes in the literature may result from incomplete ascertainment of exposure,” she and her coinvestigators wrote in the abstract accompanying the presentation.
SOURCE: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Maternal and fetal outcomes were worse when marijuana use was detected by urine toxicology.
Major finding: A composite adverse outcome occurred in 46% of adolescent marijuana users, compared with 34% of non–marijuana users (P less than .001).
Study details: Retrospective cohort study of participants in an adolescent maternity clinic.
Disclosures: The authors reported no conflicts of interest.
Source: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
Cancer groups offer guidance on immune-related adverse events
The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have released new guidelines designed to help clinicians manage the unique and sometimes severe side effects associated with cancer immunotherapy agents.
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“The mechanism of action of these anticancer therapies is so much different from anything that we’re used to,” Dr. Schneider said in an interview.
Critical need for guidance
The ASCO and NCCN guidelines are “critically important” to ensure uniform management of common immune-related adverse events, according to Stephen M. Ansell, MD, PhD, professor of medicine and chair of the Lymphoma Group at Mayo Clinic, Rochester, Minn.
“I think it also specifically highlights a few side effects that many people may not necessarily think about, from eye toxicities to thyroid effects, or the type of things that the average oncologist who is now using this in their practice quite regularly may not necessarily think about,” Dr. Ansell said. “Those kind of effects are now clearly outlined with clear guidance about what should be done, and I think that allows oncologists a resource to go and look at this carefully so that they do the right thing.”
The spectrum of adverse effects associated with checkpoint inhibitors is markedly different from what is seen with cytotoxic chemotherapy, the guidelines note. Most often, the side effects are seen in the skin, GI tract, and lungs, as well as the endocrine, adrenal, nervous, thyroid, pituitary, musculoskeletal, cardiovascular, ocular, and hematologic systems.
Stepwise approach
Side effects of checkpoint inhibitors are typically mild, but they can be severe and sometimes life-threatening, according to ASCO and NCCN.
If immune-related adverse events are mild (i.e., grade 1), treatment can continue with close monitoring, according to the guidelines. By contrast, moderate to severe immune-related adverse events can lead to severe declines in organ function and quality of life, or even fatal outcomes, so early detection and proper management are needed.
Grade 2 toxicities warrant suspending immune checkpoint inhibitor treatment, and resuming it once symptoms subside to grade 1 or less, according to the guidelines. Grade 3 toxicities should also prompt suspension of treatment, plus initiation of high-dose corticosteroids tapered over at least 4-6 weeks.
For most toxicities that reach grade 4, permanent discontinuation of checkpoint inhibitors is recommended.
A thoughtful discussion of potential risks and benefits is needed before using immune checkpoint inhibitors in patients who have autoimmune disease or prior organ transplant, according to the guidelines.
Vigilance required
Checkpoint inhibitors have been approved by the Food and Drug Administration to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because immune-related adverse event symptoms can be subtle, according to Julie Brahmer, MD, of The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focuses specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T-cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have released new guidelines designed to help clinicians manage the unique and sometimes severe side effects associated with cancer immunotherapy agents.
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“The mechanism of action of these anticancer therapies is so much different from anything that we’re used to,” Dr. Schneider said in an interview.
Critical need for guidance
The ASCO and NCCN guidelines are “critically important” to ensure uniform management of common immune-related adverse events, according to Stephen M. Ansell, MD, PhD, professor of medicine and chair of the Lymphoma Group at Mayo Clinic, Rochester, Minn.
“I think it also specifically highlights a few side effects that many people may not necessarily think about, from eye toxicities to thyroid effects, or the type of things that the average oncologist who is now using this in their practice quite regularly may not necessarily think about,” Dr. Ansell said. “Those kind of effects are now clearly outlined with clear guidance about what should be done, and I think that allows oncologists a resource to go and look at this carefully so that they do the right thing.”
The spectrum of adverse effects associated with checkpoint inhibitors is markedly different from what is seen with cytotoxic chemotherapy, the guidelines note. Most often, the side effects are seen in the skin, GI tract, and lungs, as well as the endocrine, adrenal, nervous, thyroid, pituitary, musculoskeletal, cardiovascular, ocular, and hematologic systems.
Stepwise approach
Side effects of checkpoint inhibitors are typically mild, but they can be severe and sometimes life-threatening, according to ASCO and NCCN.
If immune-related adverse events are mild (i.e., grade 1), treatment can continue with close monitoring, according to the guidelines. By contrast, moderate to severe immune-related adverse events can lead to severe declines in organ function and quality of life, or even fatal outcomes, so early detection and proper management are needed.
Grade 2 toxicities warrant suspending immune checkpoint inhibitor treatment, and resuming it once symptoms subside to grade 1 or less, according to the guidelines. Grade 3 toxicities should also prompt suspension of treatment, plus initiation of high-dose corticosteroids tapered over at least 4-6 weeks.
For most toxicities that reach grade 4, permanent discontinuation of checkpoint inhibitors is recommended.
A thoughtful discussion of potential risks and benefits is needed before using immune checkpoint inhibitors in patients who have autoimmune disease or prior organ transplant, according to the guidelines.
Vigilance required
Checkpoint inhibitors have been approved by the Food and Drug Administration to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because immune-related adverse event symptoms can be subtle, according to Julie Brahmer, MD, of The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focuses specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T-cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) have released new guidelines designed to help clinicians manage the unique and sometimes severe side effects associated with cancer immunotherapy agents.
These guidelines meet a growing need to help practicing clinicians identify and best manage immune-related adverse events, according to Bryan J. Schneider, MD, of the University of Michigan Comprehensive Cancer Center, and vice chair of the NCCN Panel on Management of Immunotherapy-Related Toxicities.
“The mechanism of action of these anticancer therapies is so much different from anything that we’re used to,” Dr. Schneider said in an interview.
Critical need for guidance
The ASCO and NCCN guidelines are “critically important” to ensure uniform management of common immune-related adverse events, according to Stephen M. Ansell, MD, PhD, professor of medicine and chair of the Lymphoma Group at Mayo Clinic, Rochester, Minn.
“I think it also specifically highlights a few side effects that many people may not necessarily think about, from eye toxicities to thyroid effects, or the type of things that the average oncologist who is now using this in their practice quite regularly may not necessarily think about,” Dr. Ansell said. “Those kind of effects are now clearly outlined with clear guidance about what should be done, and I think that allows oncologists a resource to go and look at this carefully so that they do the right thing.”
The spectrum of adverse effects associated with checkpoint inhibitors is markedly different from what is seen with cytotoxic chemotherapy, the guidelines note. Most often, the side effects are seen in the skin, GI tract, and lungs, as well as the endocrine, adrenal, nervous, thyroid, pituitary, musculoskeletal, cardiovascular, ocular, and hematologic systems.
Stepwise approach
Side effects of checkpoint inhibitors are typically mild, but they can be severe and sometimes life-threatening, according to ASCO and NCCN.
If immune-related adverse events are mild (i.e., grade 1), treatment can continue with close monitoring, according to the guidelines. By contrast, moderate to severe immune-related adverse events can lead to severe declines in organ function and quality of life, or even fatal outcomes, so early detection and proper management are needed.
Grade 2 toxicities warrant suspending immune checkpoint inhibitor treatment, and resuming it once symptoms subside to grade 1 or less, according to the guidelines. Grade 3 toxicities should also prompt suspension of treatment, plus initiation of high-dose corticosteroids tapered over at least 4-6 weeks.
For most toxicities that reach grade 4, permanent discontinuation of checkpoint inhibitors is recommended.
A thoughtful discussion of potential risks and benefits is needed before using immune checkpoint inhibitors in patients who have autoimmune disease or prior organ transplant, according to the guidelines.
Vigilance required
Checkpoint inhibitors have been approved by the Food and Drug Administration to treat a variety of cancers, including melanoma, lung cancer, and Hodgkin lymphoma, as well as lung, liver, kidney, and bladder cancers.
Clinicians managing patients on checkpoint inhibitors should always be vigilant because immune-related adverse event symptoms can be subtle, according to Julie Brahmer, MD, of The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins in Baltimore.
“Everyone has to work as a team, which includes being educated on possible side effects to immunotherapy prior to prescribing it,” said Dr. Brahmer, chair of the ASCO panel and vice chair of the NCCN panel that developed the guidelines.
The guidelines were published Feb. 14 in two documents that are similar in content, but different in format. The ASCO guideline was published in the Journal of Clinical Oncology (doi: 10.1200/JCO.2017.77.6385) and the NCCN Clinical Practice Guidelines in Oncology were posted on the NCCN website.
While the first edition of the guidelines focuses specifically on immune checkpoint inhibitors, an update anticipated for 2019 will include guidance on chimeric antigen receptor (CAR) T-cell therapy, which is associated with several important side effects, notably cytokine release syndrome.
Flu activity continues to decline
The 2017-2018 flu season continued to loosen its grip on the country as both outpatient activity and pediatric deaths dropped during the week ending March 3, according to the Centers for Disease Control and Prevention.
After five consecutive weeks of double-digit pediatric deaths related to influenza-like illness (ILI), five deaths were reported for the week ending March 3, four of which occurred in previous weeks. The total for the 2017-2018 season is now 119, the CDC said in its weekly surveillance report.
The proportion of outpatient visits for ILI was 3.7% for the week, which is down from 4.9% the week before and less than half of the seasonal high of 7.5% that was recorded for the week of Feb. 3, CDC data show. The national baseline level of outpatient activity is 2.2%.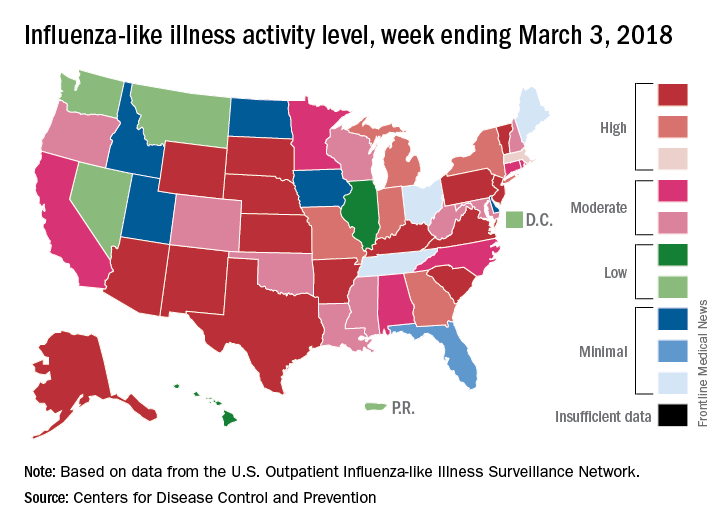
The cumulative hospitalization rate for the 2017-2018 flu season climbed from 84.2 the previous week to 86.3 per 100,000 population – well above the rate of 57.2 per 100,000 that was recorded for the corresponding week of the hospitalization-record-setting 2014-2015 season, FluView data show.
The 2017-2018 flu season continued to loosen its grip on the country as both outpatient activity and pediatric deaths dropped during the week ending March 3, according to the Centers for Disease Control and Prevention.
After five consecutive weeks of double-digit pediatric deaths related to influenza-like illness (ILI), five deaths were reported for the week ending March 3, four of which occurred in previous weeks. The total for the 2017-2018 season is now 119, the CDC said in its weekly surveillance report.
The proportion of outpatient visits for ILI was 3.7% for the week, which is down from 4.9% the week before and less than half of the seasonal high of 7.5% that was recorded for the week of Feb. 3, CDC data show. The national baseline level of outpatient activity is 2.2%.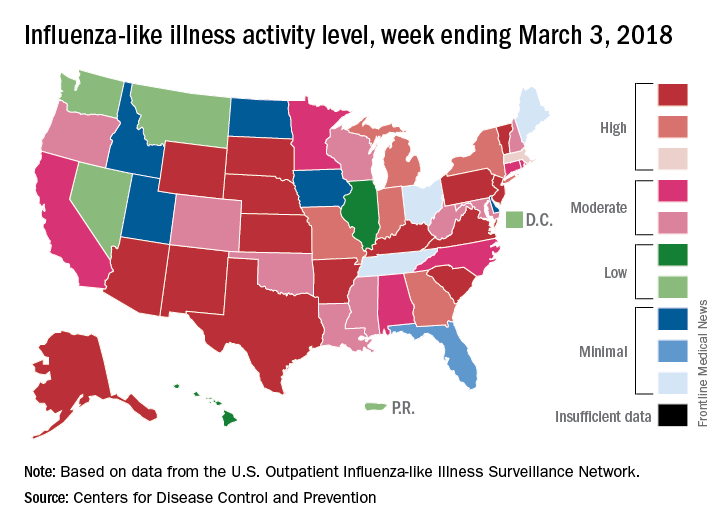
The cumulative hospitalization rate for the 2017-2018 flu season climbed from 84.2 the previous week to 86.3 per 100,000 population – well above the rate of 57.2 per 100,000 that was recorded for the corresponding week of the hospitalization-record-setting 2014-2015 season, FluView data show.
The 2017-2018 flu season continued to loosen its grip on the country as both outpatient activity and pediatric deaths dropped during the week ending March 3, according to the Centers for Disease Control and Prevention.
After five consecutive weeks of double-digit pediatric deaths related to influenza-like illness (ILI), five deaths were reported for the week ending March 3, four of which occurred in previous weeks. The total for the 2017-2018 season is now 119, the CDC said in its weekly surveillance report.
The proportion of outpatient visits for ILI was 3.7% for the week, which is down from 4.9% the week before and less than half of the seasonal high of 7.5% that was recorded for the week of Feb. 3, CDC data show. The national baseline level of outpatient activity is 2.2%.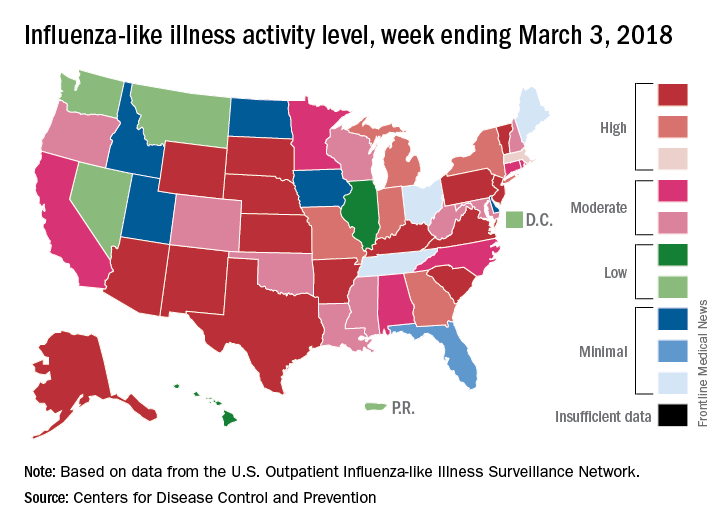
The cumulative hospitalization rate for the 2017-2018 flu season climbed from 84.2 the previous week to 86.3 per 100,000 population – well above the rate of 57.2 per 100,000 that was recorded for the corresponding week of the hospitalization-record-setting 2014-2015 season, FluView data show.
IBD: When to operate and when to punt
LAS VEGAS – Patients with inflammatory bowel disease who are in need of a surgical intervention can pose a special challenge to surgeons who encounter these patients only occasionally.
The question of whether to perform surgery or refer a patient to a higher-volume specialty center can depend on proximity. In some cases, a specialty center isn’t close, or the patient can’t tolerate the required travel. In fact, a recent study showed that 85.8% of IBD patients are treated surgically in hospitals that treat fewer than 50 patients per year (Am J Gastroenterol. 2008;103:2789-98).
In a presentation at the Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education, Larry Whelan, MD, FACS, discussed some of the challenges these patients pose and offered guidance on which cases are best referred to high-volume centers, and the best way to proceed in emergencies.
IBD patients at high-volume centers have lower mortality than do those in low-volume centers, but patients treated at lower-volume centers tend to be sicker, and studies have shown no significant difference in complication rate. This suggests that surgeons shouldn’t be afraid to tackle these cases, according to Dr. Whelan, chief of colorectal surgery at Mount Sinai West, New York.
"If you get an IBD case and you don’t see a lot of those, how do you decide what to do about it, and should you just refer it to a high-volume center?” said Dr. Whelan.
These patients are often under complex medical management, frequently spanning years, and this is an important factor in surgical decisions. They are often on multiple medications, including steroids, and most patients these days are taking monoclonal antibodies, said Dr. Whelan. The latter in particular can lead patients to be susceptible to infections. “These things can all affect decision making,” said Dr. Whelan.
Sometimes the nutritional status of IBD patients is poor, and most of the time, surgery is elective in these patients. So surgery can often be delayed for a month or more to allow time for nutritional status to improve, and this gives time for a patient to go off monoclonal antibodies, and for the physician to arrange for a referral to a high-volume center, if that seems the wisest course.
Surgery should not be considered without a gastrointestinal specialist who is comfortable in managing these patients. “Having someone who knows when to operate and not to operate, and how to handle medication, is really important,” said Dr. Whelan.
Certain cases should definitely be referred out. Ileal pouches are one. Another is a Crohn’s disease patient with multiple points of obstruction. “That may be one that you’re better off to punt,” said Dr. Whelan. Other cases include patients under complex medical management, when there is no experienced GI specialist available to help.
Emergencies require quicker decisions. In ulcerative colitis, emergency cases may include toxic megacolon, perforated colon, or obstruction from either a stricture or cancer, as well as bleeding in rare cases. Scenarios in Crohn’s disease include perforation with sepsis, inaccessible abscess, and, most commonly, obstruction resulting from fibrous stricture or acute inflammation.
When surgery is required, what’s the best choice? Dr. Whelan emphasized keeping it simple. Redo ileal pouches and ileal pouch excisions should generally be avoided. “Even if you do [pouches] often. It’s not the smartest way to go. These patients are almost all on immunosuppressive medications … to make an operation that’s already big even bigger often doesn’t work out well,” he said.
In emergency chronic ulcerative colitis cases, the safest choice is total abdominal colectomy plus end ileostomy. Dr. Whelan discourages surgeons from considering proctectomy and ileal pouch in emergency cases. A number of studies have shown that delaying pouch surgery is associated with fewer minor and major adverse events, and lower reoperation rates, he said. “If you do these operations on an immunosuppressed population, they don’t do as well,” said Dr. Whelan.
Crohn’s disease emergencies can often be managed nonsurgically. Most patients have phlegmon, fistulae, or a partial obstruction. Intravenous antibiotics, percutaneous drainage, hydration, and boosting nutritional status are good options. In cases where an obstruction requires surgery, and the surgeon isn’t comfortable performing stricturoplasty, “you want to limit the resection as best you can,” he said.
Dr. Whelan disclosed financial relationships with Ethicon Endosurgery and Olympus Corporation. Global Academy for Medical Education and this news organization are owned by the same parent company.”
LAS VEGAS – Patients with inflammatory bowel disease who are in need of a surgical intervention can pose a special challenge to surgeons who encounter these patients only occasionally.
The question of whether to perform surgery or refer a patient to a higher-volume specialty center can depend on proximity. In some cases, a specialty center isn’t close, or the patient can’t tolerate the required travel. In fact, a recent study showed that 85.8% of IBD patients are treated surgically in hospitals that treat fewer than 50 patients per year (Am J Gastroenterol. 2008;103:2789-98).
In a presentation at the Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education, Larry Whelan, MD, FACS, discussed some of the challenges these patients pose and offered guidance on which cases are best referred to high-volume centers, and the best way to proceed in emergencies.
IBD patients at high-volume centers have lower mortality than do those in low-volume centers, but patients treated at lower-volume centers tend to be sicker, and studies have shown no significant difference in complication rate. This suggests that surgeons shouldn’t be afraid to tackle these cases, according to Dr. Whelan, chief of colorectal surgery at Mount Sinai West, New York.
"If you get an IBD case and you don’t see a lot of those, how do you decide what to do about it, and should you just refer it to a high-volume center?” said Dr. Whelan.
These patients are often under complex medical management, frequently spanning years, and this is an important factor in surgical decisions. They are often on multiple medications, including steroids, and most patients these days are taking monoclonal antibodies, said Dr. Whelan. The latter in particular can lead patients to be susceptible to infections. “These things can all affect decision making,” said Dr. Whelan.
Sometimes the nutritional status of IBD patients is poor, and most of the time, surgery is elective in these patients. So surgery can often be delayed for a month or more to allow time for nutritional status to improve, and this gives time for a patient to go off monoclonal antibodies, and for the physician to arrange for a referral to a high-volume center, if that seems the wisest course.
Surgery should not be considered without a gastrointestinal specialist who is comfortable in managing these patients. “Having someone who knows when to operate and not to operate, and how to handle medication, is really important,” said Dr. Whelan.
Certain cases should definitely be referred out. Ileal pouches are one. Another is a Crohn’s disease patient with multiple points of obstruction. “That may be one that you’re better off to punt,” said Dr. Whelan. Other cases include patients under complex medical management, when there is no experienced GI specialist available to help.
Emergencies require quicker decisions. In ulcerative colitis, emergency cases may include toxic megacolon, perforated colon, or obstruction from either a stricture or cancer, as well as bleeding in rare cases. Scenarios in Crohn’s disease include perforation with sepsis, inaccessible abscess, and, most commonly, obstruction resulting from fibrous stricture or acute inflammation.
When surgery is required, what’s the best choice? Dr. Whelan emphasized keeping it simple. Redo ileal pouches and ileal pouch excisions should generally be avoided. “Even if you do [pouches] often. It’s not the smartest way to go. These patients are almost all on immunosuppressive medications … to make an operation that’s already big even bigger often doesn’t work out well,” he said.
In emergency chronic ulcerative colitis cases, the safest choice is total abdominal colectomy plus end ileostomy. Dr. Whelan discourages surgeons from considering proctectomy and ileal pouch in emergency cases. A number of studies have shown that delaying pouch surgery is associated with fewer minor and major adverse events, and lower reoperation rates, he said. “If you do these operations on an immunosuppressed population, they don’t do as well,” said Dr. Whelan.
Crohn’s disease emergencies can often be managed nonsurgically. Most patients have phlegmon, fistulae, or a partial obstruction. Intravenous antibiotics, percutaneous drainage, hydration, and boosting nutritional status are good options. In cases where an obstruction requires surgery, and the surgeon isn’t comfortable performing stricturoplasty, “you want to limit the resection as best you can,” he said.
Dr. Whelan disclosed financial relationships with Ethicon Endosurgery and Olympus Corporation. Global Academy for Medical Education and this news organization are owned by the same parent company.”
LAS VEGAS – Patients with inflammatory bowel disease who are in need of a surgical intervention can pose a special challenge to surgeons who encounter these patients only occasionally.
The question of whether to perform surgery or refer a patient to a higher-volume specialty center can depend on proximity. In some cases, a specialty center isn’t close, or the patient can’t tolerate the required travel. In fact, a recent study showed that 85.8% of IBD patients are treated surgically in hospitals that treat fewer than 50 patients per year (Am J Gastroenterol. 2008;103:2789-98).
In a presentation at the Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education, Larry Whelan, MD, FACS, discussed some of the challenges these patients pose and offered guidance on which cases are best referred to high-volume centers, and the best way to proceed in emergencies.
IBD patients at high-volume centers have lower mortality than do those in low-volume centers, but patients treated at lower-volume centers tend to be sicker, and studies have shown no significant difference in complication rate. This suggests that surgeons shouldn’t be afraid to tackle these cases, according to Dr. Whelan, chief of colorectal surgery at Mount Sinai West, New York.
"If you get an IBD case and you don’t see a lot of those, how do you decide what to do about it, and should you just refer it to a high-volume center?” said Dr. Whelan.
These patients are often under complex medical management, frequently spanning years, and this is an important factor in surgical decisions. They are often on multiple medications, including steroids, and most patients these days are taking monoclonal antibodies, said Dr. Whelan. The latter in particular can lead patients to be susceptible to infections. “These things can all affect decision making,” said Dr. Whelan.
Sometimes the nutritional status of IBD patients is poor, and most of the time, surgery is elective in these patients. So surgery can often be delayed for a month or more to allow time for nutritional status to improve, and this gives time for a patient to go off monoclonal antibodies, and for the physician to arrange for a referral to a high-volume center, if that seems the wisest course.
Surgery should not be considered without a gastrointestinal specialist who is comfortable in managing these patients. “Having someone who knows when to operate and not to operate, and how to handle medication, is really important,” said Dr. Whelan.
Certain cases should definitely be referred out. Ileal pouches are one. Another is a Crohn’s disease patient with multiple points of obstruction. “That may be one that you’re better off to punt,” said Dr. Whelan. Other cases include patients under complex medical management, when there is no experienced GI specialist available to help.
Emergencies require quicker decisions. In ulcerative colitis, emergency cases may include toxic megacolon, perforated colon, or obstruction from either a stricture or cancer, as well as bleeding in rare cases. Scenarios in Crohn’s disease include perforation with sepsis, inaccessible abscess, and, most commonly, obstruction resulting from fibrous stricture or acute inflammation.
When surgery is required, what’s the best choice? Dr. Whelan emphasized keeping it simple. Redo ileal pouches and ileal pouch excisions should generally be avoided. “Even if you do [pouches] often. It’s not the smartest way to go. These patients are almost all on immunosuppressive medications … to make an operation that’s already big even bigger often doesn’t work out well,” he said.
In emergency chronic ulcerative colitis cases, the safest choice is total abdominal colectomy plus end ileostomy. Dr. Whelan discourages surgeons from considering proctectomy and ileal pouch in emergency cases. A number of studies have shown that delaying pouch surgery is associated with fewer minor and major adverse events, and lower reoperation rates, he said. “If you do these operations on an immunosuppressed population, they don’t do as well,” said Dr. Whelan.
Crohn’s disease emergencies can often be managed nonsurgically. Most patients have phlegmon, fistulae, or a partial obstruction. Intravenous antibiotics, percutaneous drainage, hydration, and boosting nutritional status are good options. In cases where an obstruction requires surgery, and the surgeon isn’t comfortable performing stricturoplasty, “you want to limit the resection as best you can,” he said.
Dr. Whelan disclosed financial relationships with Ethicon Endosurgery and Olympus Corporation. Global Academy for Medical Education and this news organization are owned by the same parent company.”
EXPERT ANALYSIS FROM MISS