User login
Less vacuum may reduce post–cryolipolysis adipose hyperplasia
KAUAI, HAWAII – Gentler vacuum pressure seems to reduce the risk of paradoxical adipose hyperplasia after cryolipolysis, according to Suzanne Kilmer, MD, director of the Laser and Skin Surgery Center of Northern California, Sacramento.
She and her colleagues have noticed a reduction with the newer CoolAdvantage applicators from Zeltiq Aesthetics, the manufacturer of CoolSculpting equipment. CoolAdvantage runs colder and with less suction than earlier applicators. “It seems to work equally as well,” but with shorter treatment times, less bruising, and less discomfort. Although paradoxical adipose hyperplasia (PAH) “is incredibly rare, it is something we want to reduce, and we do see decreased incidence with these new applicators,” Dr. Kilmer said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Typically, one CoolSculpting session will get rid of about 20%-25% of the fat sucked up into the cryolipolysis cup. There can be some discomfort, for instance, when ice crystals are massaged afterward. To ensure patient satisfaction, “you really need to be realistic about what they can expect. It’s likely to be more than one session,” she said.
Another newer option from the manufacturer is the CoolMini applicator for submental fat. Dr. Kilmer generally does two overlapping applications with the CoolMini in the same session, in order to cover as much chin fat as possible. There will be what looks like a stick of butter under the chin when the applicators are removed; it goes away after a few minutes of massage. Patient satisfaction is high, but there can be unveiling of the platysmal bands, which is “something you want to talk to patients about ahead of time,” she said.
She sometimes uses the CoolMini first, followed by the other recently available option for submental fat, deoxycholic acid (Kybella). “We shrink down everything we can with CoolSculpting, and then come back with Kybella to clean up whatever’s left.” Using this approach, patients are injected with less deoxycholic acid, with less inflammation, she said.
“I think you get more fat loss out of a given CoolSculpting treatment than you do with Kybella,” said Dr. Kilmer, who noted that deoxycholic acid is also an option for PAH.
As for going off label with CoolSculpting for jowls, “we’ve done it, and I tell everybody there’s a chance of a 2-3 month palsy. All you are really doing is demyelinating the nerve, not injuring it. If you do liposuction, you actually have a little bit of risk of actually injuring it. You can use a nerve stimulator to map out the nerves beforehand,” she said.
Dr. Kilmer is a consultant for Zeltiq Aesthetics, and an investigator on many of the company’s development trials. She’s also a consultant for Allergan, manufacturer of Kybella, which recently acquired Zeltiq. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – Gentler vacuum pressure seems to reduce the risk of paradoxical adipose hyperplasia after cryolipolysis, according to Suzanne Kilmer, MD, director of the Laser and Skin Surgery Center of Northern California, Sacramento.
She and her colleagues have noticed a reduction with the newer CoolAdvantage applicators from Zeltiq Aesthetics, the manufacturer of CoolSculpting equipment. CoolAdvantage runs colder and with less suction than earlier applicators. “It seems to work equally as well,” but with shorter treatment times, less bruising, and less discomfort. Although paradoxical adipose hyperplasia (PAH) “is incredibly rare, it is something we want to reduce, and we do see decreased incidence with these new applicators,” Dr. Kilmer said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Typically, one CoolSculpting session will get rid of about 20%-25% of the fat sucked up into the cryolipolysis cup. There can be some discomfort, for instance, when ice crystals are massaged afterward. To ensure patient satisfaction, “you really need to be realistic about what they can expect. It’s likely to be more than one session,” she said.
Another newer option from the manufacturer is the CoolMini applicator for submental fat. Dr. Kilmer generally does two overlapping applications with the CoolMini in the same session, in order to cover as much chin fat as possible. There will be what looks like a stick of butter under the chin when the applicators are removed; it goes away after a few minutes of massage. Patient satisfaction is high, but there can be unveiling of the platysmal bands, which is “something you want to talk to patients about ahead of time,” she said.
She sometimes uses the CoolMini first, followed by the other recently available option for submental fat, deoxycholic acid (Kybella). “We shrink down everything we can with CoolSculpting, and then come back with Kybella to clean up whatever’s left.” Using this approach, patients are injected with less deoxycholic acid, with less inflammation, she said.
“I think you get more fat loss out of a given CoolSculpting treatment than you do with Kybella,” said Dr. Kilmer, who noted that deoxycholic acid is also an option for PAH.
As for going off label with CoolSculpting for jowls, “we’ve done it, and I tell everybody there’s a chance of a 2-3 month palsy. All you are really doing is demyelinating the nerve, not injuring it. If you do liposuction, you actually have a little bit of risk of actually injuring it. You can use a nerve stimulator to map out the nerves beforehand,” she said.
Dr. Kilmer is a consultant for Zeltiq Aesthetics, and an investigator on many of the company’s development trials. She’s also a consultant for Allergan, manufacturer of Kybella, which recently acquired Zeltiq. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – Gentler vacuum pressure seems to reduce the risk of paradoxical adipose hyperplasia after cryolipolysis, according to Suzanne Kilmer, MD, director of the Laser and Skin Surgery Center of Northern California, Sacramento.
She and her colleagues have noticed a reduction with the newer CoolAdvantage applicators from Zeltiq Aesthetics, the manufacturer of CoolSculpting equipment. CoolAdvantage runs colder and with less suction than earlier applicators. “It seems to work equally as well,” but with shorter treatment times, less bruising, and less discomfort. Although paradoxical adipose hyperplasia (PAH) “is incredibly rare, it is something we want to reduce, and we do see decreased incidence with these new applicators,” Dr. Kilmer said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
Typically, one CoolSculpting session will get rid of about 20%-25% of the fat sucked up into the cryolipolysis cup. There can be some discomfort, for instance, when ice crystals are massaged afterward. To ensure patient satisfaction, “you really need to be realistic about what they can expect. It’s likely to be more than one session,” she said.
Another newer option from the manufacturer is the CoolMini applicator for submental fat. Dr. Kilmer generally does two overlapping applications with the CoolMini in the same session, in order to cover as much chin fat as possible. There will be what looks like a stick of butter under the chin when the applicators are removed; it goes away after a few minutes of massage. Patient satisfaction is high, but there can be unveiling of the platysmal bands, which is “something you want to talk to patients about ahead of time,” she said.
She sometimes uses the CoolMini first, followed by the other recently available option for submental fat, deoxycholic acid (Kybella). “We shrink down everything we can with CoolSculpting, and then come back with Kybella to clean up whatever’s left.” Using this approach, patients are injected with less deoxycholic acid, with less inflammation, she said.
“I think you get more fat loss out of a given CoolSculpting treatment than you do with Kybella,” said Dr. Kilmer, who noted that deoxycholic acid is also an option for PAH.
As for going off label with CoolSculpting for jowls, “we’ve done it, and I tell everybody there’s a chance of a 2-3 month palsy. All you are really doing is demyelinating the nerve, not injuring it. If you do liposuction, you actually have a little bit of risk of actually injuring it. You can use a nerve stimulator to map out the nerves beforehand,” she said.
Dr. Kilmer is a consultant for Zeltiq Aesthetics, and an investigator on many of the company’s development trials. She’s also a consultant for Allergan, manufacturer of Kybella, which recently acquired Zeltiq. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Low vitamin D common in chronically anticoagulated children
SAN DIEGO – Pediatric hematologists should consider testing for vitamin D deficiency to optimize bone health in children who will be receiving chronic anticoagulation. That’s a key message from a single-center retrospective review presented during a poster session at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
“More research is needed to determine which children should be targeted for screening for low [bone mineral density], though our research suggests that children with prolonged treatment with steroids may be at the highest risk,” Kavita N. Patel, MD, one of the study’s authors, said in an interview.
“A few studies have shown reduced BMD in children taking warfarin,” she said. “Subsequently, recommendations have been published that children receiving chronic anticoagulation undergo bone density testing. This study sought to determine if children who were receiving chronic anticoagulation [not only warfarin but also low molecular weight heparins and direct oral anticoagulants] had low BMD and whether the length of anticoagulation or any other medical conditions or medications affected the probability of having low BMD. We also wanted to report on the prevalence of low vitamin D in this same group of children since low vitamin D is a known risk for low BMD.”
The study population was a retrospective cohort of children aged 10-21 years who received anticoagulation for more than 1 year at Children’s Healthcare of Atlanta between Jan. 2, 2012, and Oct. 15, 2017. The researchers evaluated a number of factors, including demographic variables, anticoagulants used, vitamin D status, previously reported comorbid conditions and medications associated with changes in BMD. They defined vitamin D deficiency as less than 20 ng/mL and insufficiency as 20-29 ng/mL.
Dr. Patel reported results from 27 males and 23 females. Of these, 15 (30%) underwent bone density testing with dual-energy X-ray absorptiometry; 5 (10%) did not undergo dual-energy X-ray absorptiometry testing because there is no age-specific standardization below the age of 5 years. Nearly half of the patients (42%) were Caucasian, 34% were African American, 16% were Hispanic, and the rest were from other ethnicities. The top four common indications for extended anticoagulation were recurrent venous thromboembolism (26%), extended treatment for deep vein thrombosis (18%), antiphospholipid syndrome (14%), and thrombophilia plus a single venous thromboembolism (14%).
The anticoagulants most often utilized were enoxaparin (59%), warfarin (29%), and rivaroxaban (7%). The most frequent risk factor for low BMD was long-term use of steroids (16%; defined as greater than 6 months of continuous use in the year prior to BMD testing).
Vitamin D deficiency was identified in 52% of subjects who were tested, while another 24% had insufficient levels of vitamin D. Overall, the median lumbar spine z score was –1.4. Five (30%) subjects who completed BMD testing had low BMD, with median z score of –2.5. None met fracture criteria for pediatric osteoporosis. On linear regression, the only factor found to be significantly associated with a BMD lumbar spine z score in chronically anticoagulated children was the long-term use of steroids (P = .04).
Dr. Patel acknowledged certain limitations of the study, including its single-center design and the fact that not all of the children receiving chronic anticoagulation could be tested.
She reported having no financial disclosures.
SOURCE: Patel KN et al. THSNA 2018, Poster 65.
SAN DIEGO – Pediatric hematologists should consider testing for vitamin D deficiency to optimize bone health in children who will be receiving chronic anticoagulation. That’s a key message from a single-center retrospective review presented during a poster session at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
“More research is needed to determine which children should be targeted for screening for low [bone mineral density], though our research suggests that children with prolonged treatment with steroids may be at the highest risk,” Kavita N. Patel, MD, one of the study’s authors, said in an interview.
“A few studies have shown reduced BMD in children taking warfarin,” she said. “Subsequently, recommendations have been published that children receiving chronic anticoagulation undergo bone density testing. This study sought to determine if children who were receiving chronic anticoagulation [not only warfarin but also low molecular weight heparins and direct oral anticoagulants] had low BMD and whether the length of anticoagulation or any other medical conditions or medications affected the probability of having low BMD. We also wanted to report on the prevalence of low vitamin D in this same group of children since low vitamin D is a known risk for low BMD.”
The study population was a retrospective cohort of children aged 10-21 years who received anticoagulation for more than 1 year at Children’s Healthcare of Atlanta between Jan. 2, 2012, and Oct. 15, 2017. The researchers evaluated a number of factors, including demographic variables, anticoagulants used, vitamin D status, previously reported comorbid conditions and medications associated with changes in BMD. They defined vitamin D deficiency as less than 20 ng/mL and insufficiency as 20-29 ng/mL.
Dr. Patel reported results from 27 males and 23 females. Of these, 15 (30%) underwent bone density testing with dual-energy X-ray absorptiometry; 5 (10%) did not undergo dual-energy X-ray absorptiometry testing because there is no age-specific standardization below the age of 5 years. Nearly half of the patients (42%) were Caucasian, 34% were African American, 16% were Hispanic, and the rest were from other ethnicities. The top four common indications for extended anticoagulation were recurrent venous thromboembolism (26%), extended treatment for deep vein thrombosis (18%), antiphospholipid syndrome (14%), and thrombophilia plus a single venous thromboembolism (14%).
The anticoagulants most often utilized were enoxaparin (59%), warfarin (29%), and rivaroxaban (7%). The most frequent risk factor for low BMD was long-term use of steroids (16%; defined as greater than 6 months of continuous use in the year prior to BMD testing).
Vitamin D deficiency was identified in 52% of subjects who were tested, while another 24% had insufficient levels of vitamin D. Overall, the median lumbar spine z score was –1.4. Five (30%) subjects who completed BMD testing had low BMD, with median z score of –2.5. None met fracture criteria for pediatric osteoporosis. On linear regression, the only factor found to be significantly associated with a BMD lumbar spine z score in chronically anticoagulated children was the long-term use of steroids (P = .04).
Dr. Patel acknowledged certain limitations of the study, including its single-center design and the fact that not all of the children receiving chronic anticoagulation could be tested.
She reported having no financial disclosures.
SOURCE: Patel KN et al. THSNA 2018, Poster 65.
SAN DIEGO – Pediatric hematologists should consider testing for vitamin D deficiency to optimize bone health in children who will be receiving chronic anticoagulation. That’s a key message from a single-center retrospective review presented during a poster session at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
“More research is needed to determine which children should be targeted for screening for low [bone mineral density], though our research suggests that children with prolonged treatment with steroids may be at the highest risk,” Kavita N. Patel, MD, one of the study’s authors, said in an interview.
“A few studies have shown reduced BMD in children taking warfarin,” she said. “Subsequently, recommendations have been published that children receiving chronic anticoagulation undergo bone density testing. This study sought to determine if children who were receiving chronic anticoagulation [not only warfarin but also low molecular weight heparins and direct oral anticoagulants] had low BMD and whether the length of anticoagulation or any other medical conditions or medications affected the probability of having low BMD. We also wanted to report on the prevalence of low vitamin D in this same group of children since low vitamin D is a known risk for low BMD.”
The study population was a retrospective cohort of children aged 10-21 years who received anticoagulation for more than 1 year at Children’s Healthcare of Atlanta between Jan. 2, 2012, and Oct. 15, 2017. The researchers evaluated a number of factors, including demographic variables, anticoagulants used, vitamin D status, previously reported comorbid conditions and medications associated with changes in BMD. They defined vitamin D deficiency as less than 20 ng/mL and insufficiency as 20-29 ng/mL.
Dr. Patel reported results from 27 males and 23 females. Of these, 15 (30%) underwent bone density testing with dual-energy X-ray absorptiometry; 5 (10%) did not undergo dual-energy X-ray absorptiometry testing because there is no age-specific standardization below the age of 5 years. Nearly half of the patients (42%) were Caucasian, 34% were African American, 16% were Hispanic, and the rest were from other ethnicities. The top four common indications for extended anticoagulation were recurrent venous thromboembolism (26%), extended treatment for deep vein thrombosis (18%), antiphospholipid syndrome (14%), and thrombophilia plus a single venous thromboembolism (14%).
The anticoagulants most often utilized were enoxaparin (59%), warfarin (29%), and rivaroxaban (7%). The most frequent risk factor for low BMD was long-term use of steroids (16%; defined as greater than 6 months of continuous use in the year prior to BMD testing).
Vitamin D deficiency was identified in 52% of subjects who were tested, while another 24% had insufficient levels of vitamin D. Overall, the median lumbar spine z score was –1.4. Five (30%) subjects who completed BMD testing had low BMD, with median z score of –2.5. None met fracture criteria for pediatric osteoporosis. On linear regression, the only factor found to be significantly associated with a BMD lumbar spine z score in chronically anticoagulated children was the long-term use of steroids (P = .04).
Dr. Patel acknowledged certain limitations of the study, including its single-center design and the fact that not all of the children receiving chronic anticoagulation could be tested.
She reported having no financial disclosures.
SOURCE: Patel KN et al. THSNA 2018, Poster 65.
REPORTING FROM THSNA 2018
Key clinical point:
Major finding: Of chronically anticoagulated children, 52% were vitamin D deficient and another 24% had insufficient levels of the nutrient.
Study details: A retrospective, single-center cohort study of 50 chronically anticoagulated children.
Disclosures: Dr. Patel reported having no financial disclosures.
Source: Patel KN et al. THSNA 2018, Poster 65.
Colorectal cancer risk stratification enhanced by combining family history and genetic risk scores
Stratification of colorectal cancer (CRC) risk was enhanced by joint consideration of the independent family history and genetic risk score predictors, according to an ongoing population-based, case-control study of patients recruited during 2003-2010.
The research was conducted using data from DACHS (Colorectal Cancer: Chances for Prevention Through Screening), an ongoing population-based, case-control study in Germany, reported Korbinian Weigl, PhD, and his colleagues in the journal Clinical Epidemiology (doi: 10.2147/CLEP.S145636). They included 2,363 eligible CRC patients who were identified by 22 participating hospitals and frequency matched with respect to sex, age, and residential location to 2,198 randomly selected controls that had genome-wide association studies data. The population consisted of 40% women, and the median ages for cases and controls were 69 and 70 years, respectively.
Genetic risk score was calculated by genotyping 53 single-nucleotide polymorphisms reported in published literature to be associated with higher CRC risk for individuals of European descent. Seven genetic risk score groups – very low, low, low-medium, medium, medium-high, high, and very high – were established according to categories generated on the basis of weighted risk allele distribution among controls. Family history referred to CRC in first-degree and second-degree relatives. Selected potential confounders included age, sex, body mass index, education, hormone replacement therapy in women, smoking, and colonoscopy history. Odds ratios with 95% confidence intervals were estimated by multiple logistic regression models that included adjustment for potential confounders. Statistical calculations examined individual and joint family history and genetic risk score associations with risk for CRC and the effect of potential confounding factors.
At least one colonoscopy was performed on over half the individuals in the control group, while a significantly lower number (P less than .0001) were performed on case individuals (22.1%). Family history of CRC in first-degree relatives was reported by 316 case participants (13.4%) and 214 controls (9.7%; P less than .0001). The calculated genetic risk score ranged from 20 to 48, with a substantially higher proportion of cases in the higher deciles.
Investigators compared the risk for CRC in the top decile with that in the lowest and found an increased risk of 2.9-fold (OR, 2.94) based on genetic risk analysis adjusted for sex and age and an increased risk of 3.0-fold (OR, 3.0) when all other covariates except family history were included. Comparing results against analysis with the 27 single-nucleotide polymorphisms that had been used in previous studies indicated a sizable improvement in genetic risk stratification as a result of increasing the number of single-nucleotide polymorphisms (P value for increase in c statistic = .003) included in the analysis.
Risk associated with having a family history of CRC in a first-degree relative was 1.5-fold (OR, 1.47) higher in an age- and sex-adjusted analysis. Risk prediction increased to an OR of 1.86 when calculations were adjusted with covariates, especially with previous colonoscopies. Using genetic risk scoring as a calculation adjustment only slightly changed the result (OR, 1.83). A similar trend, but with lower-magnitude associations, was observed with family history of CRC in second-degree relatives.
A dose-response association between the number of risk alleles and CRC risk determined by a logistic regression model revealed a curvilinear relationship between genetic risk score and CRC risk. At higher genetic risk score levels, the increase in CRC risk was particularly strong. The dose-response association indicated an independent relationship between family history and CRC such that individuals with first-degree relatives with CRC will reach the same risk level with a lower genetic risk score as those with a higher genetic risk score but no first-degree relatives with CRC.
Joint risk stratification that combined family history and genetic risk scores was compared with risks determined by each predictor. As the genetic risk score increased there was an observed increased risk for individuals with first-degree relatives, second-degree relatives, or without family history. Considering only genetic risk score, the increase in risk from the lowest to highest decile was 2.8-fold. In contrast, the increased risk from the lowest to highest decile was 6.14-fold when stratification included both genetic risk score and considering family history in first-degree relatives, thus demonstrating the enhancing effect of combining the independent relationship of these two predictors.
The investigators concluded from their results that, by combining the genetic risk scores with family history and other easy-to-collect risk factor information,
The authors reported that they had no conflicts of interest.
SOURCE: Weigl K et al. Clin Epidemiol. 2018;10:143-52.
Stratification of colorectal cancer (CRC) risk was enhanced by joint consideration of the independent family history and genetic risk score predictors, according to an ongoing population-based, case-control study of patients recruited during 2003-2010.
The research was conducted using data from DACHS (Colorectal Cancer: Chances for Prevention Through Screening), an ongoing population-based, case-control study in Germany, reported Korbinian Weigl, PhD, and his colleagues in the journal Clinical Epidemiology (doi: 10.2147/CLEP.S145636). They included 2,363 eligible CRC patients who were identified by 22 participating hospitals and frequency matched with respect to sex, age, and residential location to 2,198 randomly selected controls that had genome-wide association studies data. The population consisted of 40% women, and the median ages for cases and controls were 69 and 70 years, respectively.
Genetic risk score was calculated by genotyping 53 single-nucleotide polymorphisms reported in published literature to be associated with higher CRC risk for individuals of European descent. Seven genetic risk score groups – very low, low, low-medium, medium, medium-high, high, and very high – were established according to categories generated on the basis of weighted risk allele distribution among controls. Family history referred to CRC in first-degree and second-degree relatives. Selected potential confounders included age, sex, body mass index, education, hormone replacement therapy in women, smoking, and colonoscopy history. Odds ratios with 95% confidence intervals were estimated by multiple logistic regression models that included adjustment for potential confounders. Statistical calculations examined individual and joint family history and genetic risk score associations with risk for CRC and the effect of potential confounding factors.
At least one colonoscopy was performed on over half the individuals in the control group, while a significantly lower number (P less than .0001) were performed on case individuals (22.1%). Family history of CRC in first-degree relatives was reported by 316 case participants (13.4%) and 214 controls (9.7%; P less than .0001). The calculated genetic risk score ranged from 20 to 48, with a substantially higher proportion of cases in the higher deciles.
Investigators compared the risk for CRC in the top decile with that in the lowest and found an increased risk of 2.9-fold (OR, 2.94) based on genetic risk analysis adjusted for sex and age and an increased risk of 3.0-fold (OR, 3.0) when all other covariates except family history were included. Comparing results against analysis with the 27 single-nucleotide polymorphisms that had been used in previous studies indicated a sizable improvement in genetic risk stratification as a result of increasing the number of single-nucleotide polymorphisms (P value for increase in c statistic = .003) included in the analysis.
Risk associated with having a family history of CRC in a first-degree relative was 1.5-fold (OR, 1.47) higher in an age- and sex-adjusted analysis. Risk prediction increased to an OR of 1.86 when calculations were adjusted with covariates, especially with previous colonoscopies. Using genetic risk scoring as a calculation adjustment only slightly changed the result (OR, 1.83). A similar trend, but with lower-magnitude associations, was observed with family history of CRC in second-degree relatives.
A dose-response association between the number of risk alleles and CRC risk determined by a logistic regression model revealed a curvilinear relationship between genetic risk score and CRC risk. At higher genetic risk score levels, the increase in CRC risk was particularly strong. The dose-response association indicated an independent relationship between family history and CRC such that individuals with first-degree relatives with CRC will reach the same risk level with a lower genetic risk score as those with a higher genetic risk score but no first-degree relatives with CRC.
Joint risk stratification that combined family history and genetic risk scores was compared with risks determined by each predictor. As the genetic risk score increased there was an observed increased risk for individuals with first-degree relatives, second-degree relatives, or without family history. Considering only genetic risk score, the increase in risk from the lowest to highest decile was 2.8-fold. In contrast, the increased risk from the lowest to highest decile was 6.14-fold when stratification included both genetic risk score and considering family history in first-degree relatives, thus demonstrating the enhancing effect of combining the independent relationship of these two predictors.
The investigators concluded from their results that, by combining the genetic risk scores with family history and other easy-to-collect risk factor information,
The authors reported that they had no conflicts of interest.
SOURCE: Weigl K et al. Clin Epidemiol. 2018;10:143-52.
Stratification of colorectal cancer (CRC) risk was enhanced by joint consideration of the independent family history and genetic risk score predictors, according to an ongoing population-based, case-control study of patients recruited during 2003-2010.
The research was conducted using data from DACHS (Colorectal Cancer: Chances for Prevention Through Screening), an ongoing population-based, case-control study in Germany, reported Korbinian Weigl, PhD, and his colleagues in the journal Clinical Epidemiology (doi: 10.2147/CLEP.S145636). They included 2,363 eligible CRC patients who were identified by 22 participating hospitals and frequency matched with respect to sex, age, and residential location to 2,198 randomly selected controls that had genome-wide association studies data. The population consisted of 40% women, and the median ages for cases and controls were 69 and 70 years, respectively.
Genetic risk score was calculated by genotyping 53 single-nucleotide polymorphisms reported in published literature to be associated with higher CRC risk for individuals of European descent. Seven genetic risk score groups – very low, low, low-medium, medium, medium-high, high, and very high – were established according to categories generated on the basis of weighted risk allele distribution among controls. Family history referred to CRC in first-degree and second-degree relatives. Selected potential confounders included age, sex, body mass index, education, hormone replacement therapy in women, smoking, and colonoscopy history. Odds ratios with 95% confidence intervals were estimated by multiple logistic regression models that included adjustment for potential confounders. Statistical calculations examined individual and joint family history and genetic risk score associations with risk for CRC and the effect of potential confounding factors.
At least one colonoscopy was performed on over half the individuals in the control group, while a significantly lower number (P less than .0001) were performed on case individuals (22.1%). Family history of CRC in first-degree relatives was reported by 316 case participants (13.4%) and 214 controls (9.7%; P less than .0001). The calculated genetic risk score ranged from 20 to 48, with a substantially higher proportion of cases in the higher deciles.
Investigators compared the risk for CRC in the top decile with that in the lowest and found an increased risk of 2.9-fold (OR, 2.94) based on genetic risk analysis adjusted for sex and age and an increased risk of 3.0-fold (OR, 3.0) when all other covariates except family history were included. Comparing results against analysis with the 27 single-nucleotide polymorphisms that had been used in previous studies indicated a sizable improvement in genetic risk stratification as a result of increasing the number of single-nucleotide polymorphisms (P value for increase in c statistic = .003) included in the analysis.
Risk associated with having a family history of CRC in a first-degree relative was 1.5-fold (OR, 1.47) higher in an age- and sex-adjusted analysis. Risk prediction increased to an OR of 1.86 when calculations were adjusted with covariates, especially with previous colonoscopies. Using genetic risk scoring as a calculation adjustment only slightly changed the result (OR, 1.83). A similar trend, but with lower-magnitude associations, was observed with family history of CRC in second-degree relatives.
A dose-response association between the number of risk alleles and CRC risk determined by a logistic regression model revealed a curvilinear relationship between genetic risk score and CRC risk. At higher genetic risk score levels, the increase in CRC risk was particularly strong. The dose-response association indicated an independent relationship between family history and CRC such that individuals with first-degree relatives with CRC will reach the same risk level with a lower genetic risk score as those with a higher genetic risk score but no first-degree relatives with CRC.
Joint risk stratification that combined family history and genetic risk scores was compared with risks determined by each predictor. As the genetic risk score increased there was an observed increased risk for individuals with first-degree relatives, second-degree relatives, or without family history. Considering only genetic risk score, the increase in risk from the lowest to highest decile was 2.8-fold. In contrast, the increased risk from the lowest to highest decile was 6.14-fold when stratification included both genetic risk score and considering family history in first-degree relatives, thus demonstrating the enhancing effect of combining the independent relationship of these two predictors.
The investigators concluded from their results that, by combining the genetic risk scores with family history and other easy-to-collect risk factor information,
The authors reported that they had no conflicts of interest.
SOURCE: Weigl K et al. Clin Epidemiol. 2018;10:143-52.
FROM CLINICAL EPIDEMIOLOGY
Key clinical point: Jointly using family history and genetic risk scores enhances their independent considerations for CRC risk stratifications.
Major finding: CRC in the highest decile compared with lowest decile was associated with 3.0-fold and 6.1-fold increased risks when considering genetic risk scores independently and jointly with family history, respectively.
Study details: Ongoing population-based study involving 22 hospitals in Germany with 2,363 CRC cases compared to 2,198 controls.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Weigl K et al. Clin Epidemiol. 2018;10:143-52.
Excessive daytime sleepiness linked to increase in Alzheimer’s biomarker
, results of a prospective, longitudinal cohort study suggest.
In the study, excessive daytime sleepiness (EDS) was associated with increased accumulation of beta-amyloid, an important biomarker of AD that manifests in early preclinical stages, wrote first author Diego Z. Carvalho, MD, and his colleagues at the Mayo Clinic, Rochester, Minn. The report was published online March 12 in JAMA Neurology.
“It remains unclear whether EDS is a result of greater sleep instability, synaptic or network overload, or neurodegeneration of wakefulness-promoting centers,” Dr. Carvalho and colleagues wrote in their report. “However, participants with EDS were more vulnerable to AD pathologic processes.”
The prospective, longitudinal cohort analysis from Dr. Carvalho and his colleagues included 283 participants age 70 or older without a diagnosis of dementia who filled out a sleepiness assessment survey and underwent baseline and follow-up imaging studies as part of the Mayo Clinic Study of Aging.
All participants included in the analysis underwent at least two consecutive carbon 11–labeled Pittsburgh compound B PET (PiB-PET) scans. EDS, defined as a score of at least 10 on the Epworth Sleepiness Scale, was seen in 63 participants (22.3%), the researchers found.
At baseline, EDS was significantly associated with increased beta-amyloid accumulation in the anterior cingulate (P = .04), posterior cingulate-precuneus (P = .02), and parietal (P = .04) regions. The association between EDS and longitudinal beta-amyloid accumulation was most pronounced in participants who had global PiB positivity at baseline in anterior cingulate and cingulate-precuneus regions (P = .02 for both), they reported.
Findings of the study are consistent with a previous investigation of middle-aged participants without dementia, Dr. Carvalho and coauthors said in a discussion of the results. In that study, increased daytime somnolence was associated with increased beta-amyloid burden in regions including the precuneus and anterior cingulate. Daytime sleepiness in that study was measured using a different measure, the Sleep Scale, which was originally developed as part of the Medical Outcomes Study.
Further investigation of the link between EDS and beta-amyloid accumulation is needed. In particular, the researchers suggested that future studies might evaluate whether amyloid accumulation can be avoided through early recognition of EDS and subsequent treatment of the underlying sleep disorder.
The study was funded by grants from the National Institutes of Health and several foundations. Dr. Carvalho reported no disclosures related to the study. Many of his coauthors reported relationships with a variety of pharmaceutical companies developing therapies for Alzheimer’s.
SOURCE: Carvalho D et al., JAMA Neurol. 2018 Mar 12. doi: 10.1001/jamaneurol.2018.0049
The study by Dr. Carvalho and his colleagues advances the understanding of sleep disturbance as a risk factor for Alzheimer’s disease.
Findings of the study suggest that poor sleep quality may be an early warning sign of AD-related processes, but we advise caution in interpreting the results of this prospective cohort study given that daytime sleepiness was assessed subjectively using the Epworth Sleepiness Scale (ESS), which may reflect declining sleep quality, but is not necessarily a warning sign for impending amyloidosis because of the low specificity of subjective sleepiness and the many underlying causes that could contribute to ESS scores.
Nevertheless, the results hint at a time in the future when sleep dysfunction might be managed with sleep-based interventions that are deployed at the most optimal time to intervene in the beta-amyloid cascade.
Future studies would ideally include other markers of AD progression, such as cortical atrophy, tau deposition, or cardiovascular changes, and better explain a physiologic link between subjective daytime sleepiness and longitudinal change in beta-amyloid.
Joseph R. Winer is with the department of psychology at the University of California, Berkeley, and Bryce A. Mander, PhD, is with the University of California, Irvine. The text above is derived from their editorial appearing in JAMA Neurology (2018 Mar 12. doi: 10.1001/jamaneurol.2018.0005). The authors reported no conflict of interest disclosures related to their editorial contribution.
The study by Dr. Carvalho and his colleagues advances the understanding of sleep disturbance as a risk factor for Alzheimer’s disease.
Findings of the study suggest that poor sleep quality may be an early warning sign of AD-related processes, but we advise caution in interpreting the results of this prospective cohort study given that daytime sleepiness was assessed subjectively using the Epworth Sleepiness Scale (ESS), which may reflect declining sleep quality, but is not necessarily a warning sign for impending amyloidosis because of the low specificity of subjective sleepiness and the many underlying causes that could contribute to ESS scores.
Nevertheless, the results hint at a time in the future when sleep dysfunction might be managed with sleep-based interventions that are deployed at the most optimal time to intervene in the beta-amyloid cascade.
Future studies would ideally include other markers of AD progression, such as cortical atrophy, tau deposition, or cardiovascular changes, and better explain a physiologic link between subjective daytime sleepiness and longitudinal change in beta-amyloid.
Joseph R. Winer is with the department of psychology at the University of California, Berkeley, and Bryce A. Mander, PhD, is with the University of California, Irvine. The text above is derived from their editorial appearing in JAMA Neurology (2018 Mar 12. doi: 10.1001/jamaneurol.2018.0005). The authors reported no conflict of interest disclosures related to their editorial contribution.
The study by Dr. Carvalho and his colleagues advances the understanding of sleep disturbance as a risk factor for Alzheimer’s disease.
Findings of the study suggest that poor sleep quality may be an early warning sign of AD-related processes, but we advise caution in interpreting the results of this prospective cohort study given that daytime sleepiness was assessed subjectively using the Epworth Sleepiness Scale (ESS), which may reflect declining sleep quality, but is not necessarily a warning sign for impending amyloidosis because of the low specificity of subjective sleepiness and the many underlying causes that could contribute to ESS scores.
Nevertheless, the results hint at a time in the future when sleep dysfunction might be managed with sleep-based interventions that are deployed at the most optimal time to intervene in the beta-amyloid cascade.
Future studies would ideally include other markers of AD progression, such as cortical atrophy, tau deposition, or cardiovascular changes, and better explain a physiologic link between subjective daytime sleepiness and longitudinal change in beta-amyloid.
Joseph R. Winer is with the department of psychology at the University of California, Berkeley, and Bryce A. Mander, PhD, is with the University of California, Irvine. The text above is derived from their editorial appearing in JAMA Neurology (2018 Mar 12. doi: 10.1001/jamaneurol.2018.0005). The authors reported no conflict of interest disclosures related to their editorial contribution.
, results of a prospective, longitudinal cohort study suggest.
In the study, excessive daytime sleepiness (EDS) was associated with increased accumulation of beta-amyloid, an important biomarker of AD that manifests in early preclinical stages, wrote first author Diego Z. Carvalho, MD, and his colleagues at the Mayo Clinic, Rochester, Minn. The report was published online March 12 in JAMA Neurology.
“It remains unclear whether EDS is a result of greater sleep instability, synaptic or network overload, or neurodegeneration of wakefulness-promoting centers,” Dr. Carvalho and colleagues wrote in their report. “However, participants with EDS were more vulnerable to AD pathologic processes.”
The prospective, longitudinal cohort analysis from Dr. Carvalho and his colleagues included 283 participants age 70 or older without a diagnosis of dementia who filled out a sleepiness assessment survey and underwent baseline and follow-up imaging studies as part of the Mayo Clinic Study of Aging.
All participants included in the analysis underwent at least two consecutive carbon 11–labeled Pittsburgh compound B PET (PiB-PET) scans. EDS, defined as a score of at least 10 on the Epworth Sleepiness Scale, was seen in 63 participants (22.3%), the researchers found.
At baseline, EDS was significantly associated with increased beta-amyloid accumulation in the anterior cingulate (P = .04), posterior cingulate-precuneus (P = .02), and parietal (P = .04) regions. The association between EDS and longitudinal beta-amyloid accumulation was most pronounced in participants who had global PiB positivity at baseline in anterior cingulate and cingulate-precuneus regions (P = .02 for both), they reported.
Findings of the study are consistent with a previous investigation of middle-aged participants without dementia, Dr. Carvalho and coauthors said in a discussion of the results. In that study, increased daytime somnolence was associated with increased beta-amyloid burden in regions including the precuneus and anterior cingulate. Daytime sleepiness in that study was measured using a different measure, the Sleep Scale, which was originally developed as part of the Medical Outcomes Study.
Further investigation of the link between EDS and beta-amyloid accumulation is needed. In particular, the researchers suggested that future studies might evaluate whether amyloid accumulation can be avoided through early recognition of EDS and subsequent treatment of the underlying sleep disorder.
The study was funded by grants from the National Institutes of Health and several foundations. Dr. Carvalho reported no disclosures related to the study. Many of his coauthors reported relationships with a variety of pharmaceutical companies developing therapies for Alzheimer’s.
SOURCE: Carvalho D et al., JAMA Neurol. 2018 Mar 12. doi: 10.1001/jamaneurol.2018.0049
, results of a prospective, longitudinal cohort study suggest.
In the study, excessive daytime sleepiness (EDS) was associated with increased accumulation of beta-amyloid, an important biomarker of AD that manifests in early preclinical stages, wrote first author Diego Z. Carvalho, MD, and his colleagues at the Mayo Clinic, Rochester, Minn. The report was published online March 12 in JAMA Neurology.
“It remains unclear whether EDS is a result of greater sleep instability, synaptic or network overload, or neurodegeneration of wakefulness-promoting centers,” Dr. Carvalho and colleagues wrote in their report. “However, participants with EDS were more vulnerable to AD pathologic processes.”
The prospective, longitudinal cohort analysis from Dr. Carvalho and his colleagues included 283 participants age 70 or older without a diagnosis of dementia who filled out a sleepiness assessment survey and underwent baseline and follow-up imaging studies as part of the Mayo Clinic Study of Aging.
All participants included in the analysis underwent at least two consecutive carbon 11–labeled Pittsburgh compound B PET (PiB-PET) scans. EDS, defined as a score of at least 10 on the Epworth Sleepiness Scale, was seen in 63 participants (22.3%), the researchers found.
At baseline, EDS was significantly associated with increased beta-amyloid accumulation in the anterior cingulate (P = .04), posterior cingulate-precuneus (P = .02), and parietal (P = .04) regions. The association between EDS and longitudinal beta-amyloid accumulation was most pronounced in participants who had global PiB positivity at baseline in anterior cingulate and cingulate-precuneus regions (P = .02 for both), they reported.
Findings of the study are consistent with a previous investigation of middle-aged participants without dementia, Dr. Carvalho and coauthors said in a discussion of the results. In that study, increased daytime somnolence was associated with increased beta-amyloid burden in regions including the precuneus and anterior cingulate. Daytime sleepiness in that study was measured using a different measure, the Sleep Scale, which was originally developed as part of the Medical Outcomes Study.
Further investigation of the link between EDS and beta-amyloid accumulation is needed. In particular, the researchers suggested that future studies might evaluate whether amyloid accumulation can be avoided through early recognition of EDS and subsequent treatment of the underlying sleep disorder.
The study was funded by grants from the National Institutes of Health and several foundations. Dr. Carvalho reported no disclosures related to the study. Many of his coauthors reported relationships with a variety of pharmaceutical companies developing therapies for Alzheimer’s.
SOURCE: Carvalho D et al., JAMA Neurol. 2018 Mar 12. doi: 10.1001/jamaneurol.2018.0049
FROM JAMA NEUROLOGY
Key clinical point: Elderly individuals who have excessive daytime sleepiness might be more susceptible to accumulation of beta-amyloid, an important biomarker of Alzheimer’s disease that manifests in early preclinical stages.
Major finding: Excessive daytime sleepiness was significantly associated with increased accumulation of beta-amyloid in the cingulate gyrus and precuneus regions (P = .02 for both brain regions).
Study details: A prospective, longitudinal, population-based study including 283 elderly participants without a diagnosis of dementia who filled out a sleepiness assessment survey and underwent imaging studies.
Disclosures: The study was funded by grants from the National Institutes of Health and several foundations. Many authors reported relationships with a variety of pharmaceutical companies developing therapies for Alzheimer’s.
Source: Carvalho D et al., JAMA Neurol. 2018 Mar 12. doi: 10.1001/jamaneurol.2018.0049.
Epilepsy in the Elderly: Could it Be a Seizure?
The fastest growing segment of the American population is the elderly. Moreover, they are also the fastest growing segment of the population with new-onset epilepsy and recurrent seizures. Many medical conditions that are common among the elderly population—including stroke, intracranial hemorrhage, brain tumor, and dementia—have a higher risk for resultant epilepsy, hence the higher incidence of epilepsy in this age group. This special subgroup of epilepsy patients presents unique challenges, including diagnosis, management, risk factors, and medication choice. Many of these challenges are interrelated.
The first and possibly the most difficult challenge is diagnosis. Seizures can begin at any age, not necessarily childhood. There does not have to be a genetic family history of epilepsy. Seizures in the elderly can present in a subtle fashion and are often not recognized as such. In addition, these symptoms are often attributed to other common medical conditions or lumped together with other generic symptoms that are frequently seen in the elderly.
For example, seizures can present with one or more of the following: slow speech, pauses in speech, confusion, memory loss, loss of track of time, trembling of the extremities, blinking, staring, slow responsiveness, chewing movements, and grabbing movements. As such, seizures may be misidentified as dementia, tremor, a movement disorder, delirium, overall slowness, or “aging.”
The potential implication has a compounding effect. Individuals with these symptoms can be diagnosed with a condition that they do not have, prescribed medication that they do not need, and be subject to the side effects of this incorrect medication. In addition, the patient could have unnecessary diagnostic testing, which can be a hardship in this population.
The correct diagnosis, in this case seizures/epilepsy, may be delayed, which could lead to potential consequences such as recurrent seizures, falls, injury, memory loss, and possible sudden death. This contributes to a decreased quality of life.
What are the central issues that lead to the delayed diagnosis? First, as mentioned above, the presentation can be quite subtle. Unlike what is most often portrayed in the media, not all seizures involve a loss of consciousness, body stiffening, and/or body shaking. Second, the patient is not necessarily aware that the above symptoms have occurred. It is often a friend or family member that reports them, and the patient may deny the occurrence. Third, even after the diagnosis is confirmed the patient may still be skeptical because he/she is still “functioning.” Often the question becomes how long have these signs/symptoms actually been present?
Epilepsy in the elderly is real and increasing. Unfortunately, it is frequently this subgroup of the population that has the least education about the disease. Increasing awareness of epilepsy is an ongoing goal by epilepsy advocacy organizations. Along with these organizations, physicians and other health care provides need to play an active role in increasing awareness for this special subpopulation with epilepsy.
The fastest growing segment of the American population is the elderly. Moreover, they are also the fastest growing segment of the population with new-onset epilepsy and recurrent seizures. Many medical conditions that are common among the elderly population—including stroke, intracranial hemorrhage, brain tumor, and dementia—have a higher risk for resultant epilepsy, hence the higher incidence of epilepsy in this age group. This special subgroup of epilepsy patients presents unique challenges, including diagnosis, management, risk factors, and medication choice. Many of these challenges are interrelated.
The first and possibly the most difficult challenge is diagnosis. Seizures can begin at any age, not necessarily childhood. There does not have to be a genetic family history of epilepsy. Seizures in the elderly can present in a subtle fashion and are often not recognized as such. In addition, these symptoms are often attributed to other common medical conditions or lumped together with other generic symptoms that are frequently seen in the elderly.
For example, seizures can present with one or more of the following: slow speech, pauses in speech, confusion, memory loss, loss of track of time, trembling of the extremities, blinking, staring, slow responsiveness, chewing movements, and grabbing movements. As such, seizures may be misidentified as dementia, tremor, a movement disorder, delirium, overall slowness, or “aging.”
The potential implication has a compounding effect. Individuals with these symptoms can be diagnosed with a condition that they do not have, prescribed medication that they do not need, and be subject to the side effects of this incorrect medication. In addition, the patient could have unnecessary diagnostic testing, which can be a hardship in this population.
The correct diagnosis, in this case seizures/epilepsy, may be delayed, which could lead to potential consequences such as recurrent seizures, falls, injury, memory loss, and possible sudden death. This contributes to a decreased quality of life.
What are the central issues that lead to the delayed diagnosis? First, as mentioned above, the presentation can be quite subtle. Unlike what is most often portrayed in the media, not all seizures involve a loss of consciousness, body stiffening, and/or body shaking. Second, the patient is not necessarily aware that the above symptoms have occurred. It is often a friend or family member that reports them, and the patient may deny the occurrence. Third, even after the diagnosis is confirmed the patient may still be skeptical because he/she is still “functioning.” Often the question becomes how long have these signs/symptoms actually been present?
Epilepsy in the elderly is real and increasing. Unfortunately, it is frequently this subgroup of the population that has the least education about the disease. Increasing awareness of epilepsy is an ongoing goal by epilepsy advocacy organizations. Along with these organizations, physicians and other health care provides need to play an active role in increasing awareness for this special subpopulation with epilepsy.
The fastest growing segment of the American population is the elderly. Moreover, they are also the fastest growing segment of the population with new-onset epilepsy and recurrent seizures. Many medical conditions that are common among the elderly population—including stroke, intracranial hemorrhage, brain tumor, and dementia—have a higher risk for resultant epilepsy, hence the higher incidence of epilepsy in this age group. This special subgroup of epilepsy patients presents unique challenges, including diagnosis, management, risk factors, and medication choice. Many of these challenges are interrelated.
The first and possibly the most difficult challenge is diagnosis. Seizures can begin at any age, not necessarily childhood. There does not have to be a genetic family history of epilepsy. Seizures in the elderly can present in a subtle fashion and are often not recognized as such. In addition, these symptoms are often attributed to other common medical conditions or lumped together with other generic symptoms that are frequently seen in the elderly.
For example, seizures can present with one or more of the following: slow speech, pauses in speech, confusion, memory loss, loss of track of time, trembling of the extremities, blinking, staring, slow responsiveness, chewing movements, and grabbing movements. As such, seizures may be misidentified as dementia, tremor, a movement disorder, delirium, overall slowness, or “aging.”
The potential implication has a compounding effect. Individuals with these symptoms can be diagnosed with a condition that they do not have, prescribed medication that they do not need, and be subject to the side effects of this incorrect medication. In addition, the patient could have unnecessary diagnostic testing, which can be a hardship in this population.
The correct diagnosis, in this case seizures/epilepsy, may be delayed, which could lead to potential consequences such as recurrent seizures, falls, injury, memory loss, and possible sudden death. This contributes to a decreased quality of life.
What are the central issues that lead to the delayed diagnosis? First, as mentioned above, the presentation can be quite subtle. Unlike what is most often portrayed in the media, not all seizures involve a loss of consciousness, body stiffening, and/or body shaking. Second, the patient is not necessarily aware that the above symptoms have occurred. It is often a friend or family member that reports them, and the patient may deny the occurrence. Third, even after the diagnosis is confirmed the patient may still be skeptical because he/she is still “functioning.” Often the question becomes how long have these signs/symptoms actually been present?
Epilepsy in the elderly is real and increasing. Unfortunately, it is frequently this subgroup of the population that has the least education about the disease. Increasing awareness of epilepsy is an ongoing goal by epilepsy advocacy organizations. Along with these organizations, physicians and other health care provides need to play an active role in increasing awareness for this special subpopulation with epilepsy.
Gut bacteria could drive autoimmune response in genetically predisposed
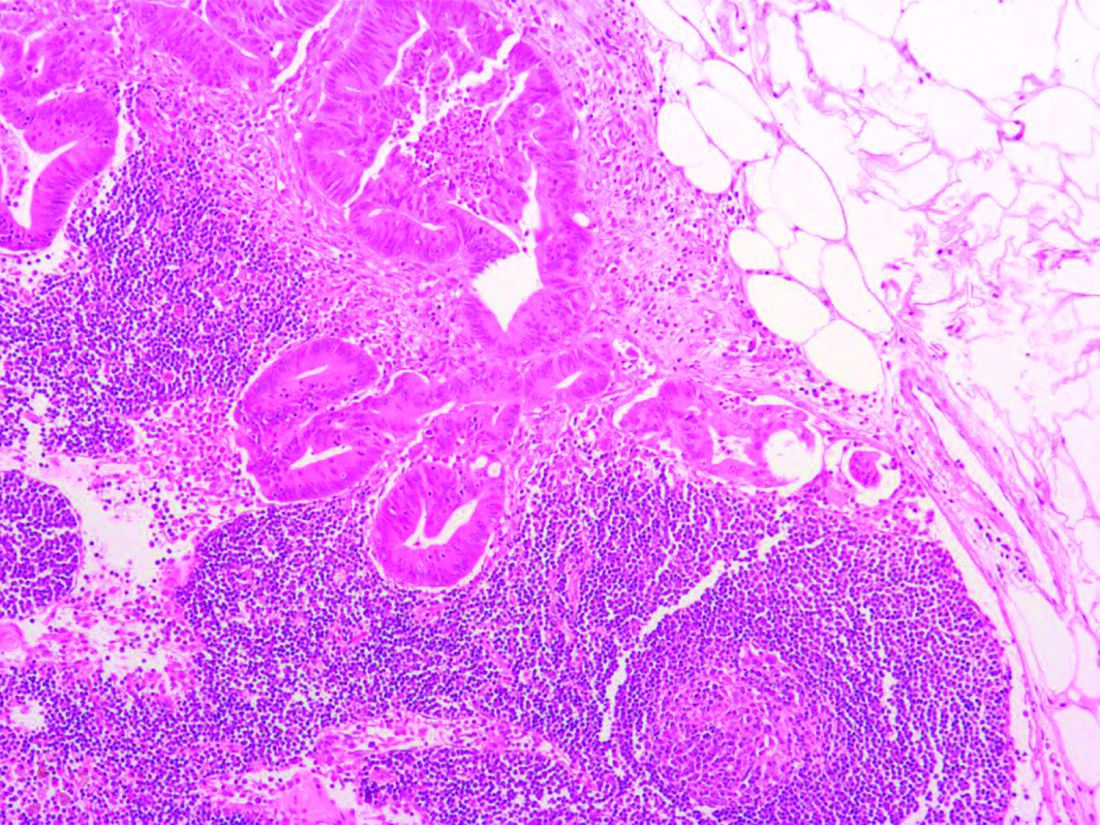
Gut bacteria found in the small intestines could play a role in triggering an autoimmune response in genetically predisposed individuals, such as those with lupus, a research report suggests.
Recent studies have shown that gut commensals can reside within gastrointestinal-associated lymph tissues of healthy hosts, but it has been unclear whether pathobiont translocation was involved in systemic autoimmunity. Silvio Manfredo Vieira, PhD, and his colleagues at Yale University, New Haven, Conn., addressed this knowledge gap by studying the Gram-positive gut commensal Enterococcus gallinarum, which was identified in mesenteric lymph nodes, liver, and spleen cultures from genetically susceptible mouse models.
The researchers found that they could suppress the autoimmunity with antibiotics or an intramuscular vaccine targeted at E. gallinarum. The vaccine reduced levels of serum autoantibodies, prolonged survival in the mice, and also prevented translocation, as no growth of E. gallinarum was observed in internal organs.
“Pathobiont-specific treatment can abrogate host autoimmune processes without needing to suppress the immune system, which can lead to systemic adverse events in current clinical practice,” they wrote.
The researchers then tested for E. gallinarum translocation to human livers in patients with systemic lupus erythematosus (SLE) and autoimmune hepatitis (AIH) with serologic features of lupus, including antinuclear antibodies and anti-dsDNA immunoglobulin G antibodies.
Liver biopsies from three SLE patients were positive for E. gallinarum, whereas samples from four of six healthy liver transplant donors with normal liver histology tested positive for the presence of other Enterococcus species but not E. gallinarum.
“Consistent with enhanced adaptive immune responses to E. gallinarum, the majority of SLE and AIH patients also showed increased serum antibody titers against E. gallinarum and particularly its RNA,” they said.
The authors said their findings showed that E. gallinarum translocates into systemic organs as a result of the breakdown of the gut barrier in autoimmune-prone hosts to drive autoimmune pathogenesis. They suggested that the translocating bacteria skewed T helper cell differentiation but also acted directly on colonized tissues such as the liver to induce autoantigens, endogenous retrovirus proteins, cytokines, and other autoimmune-promoting factors.
“If the complexity of host-tissue microbiota interactions is considered in chronic autoimmunity, it may offer new therapeutic avenues for these debilitating and potentially lethal diseases,” they concluded.
The study was supported by grants from various institutes and initiatives within the National Institutes of Health as well as from the Arthritis National Research Foundation, the Arthritis Foundation, and the Lupus Research Institute. Dr. Vieira and the senior author, Martin A. Kriegel, MD, PhD, are inventors on a patent application filed by Yale University related to the use of antibiotics and commensal vaccination to treat autoimmunity.
SOURCE: Vieira S et al. Science. 2018;359(6380):1156-61.
Gut bacteria found in the small intestines could play a role in triggering an autoimmune response in genetically predisposed individuals, such as those with lupus, a research report suggests.
Recent studies have shown that gut commensals can reside within gastrointestinal-associated lymph tissues of healthy hosts, but it has been unclear whether pathobiont translocation was involved in systemic autoimmunity. Silvio Manfredo Vieira, PhD, and his colleagues at Yale University, New Haven, Conn., addressed this knowledge gap by studying the Gram-positive gut commensal Enterococcus gallinarum, which was identified in mesenteric lymph nodes, liver, and spleen cultures from genetically susceptible mouse models.
The researchers found that they could suppress the autoimmunity with antibiotics or an intramuscular vaccine targeted at E. gallinarum. The vaccine reduced levels of serum autoantibodies, prolonged survival in the mice, and also prevented translocation, as no growth of E. gallinarum was observed in internal organs.
“Pathobiont-specific treatment can abrogate host autoimmune processes without needing to suppress the immune system, which can lead to systemic adverse events in current clinical practice,” they wrote.
The researchers then tested for E. gallinarum translocation to human livers in patients with systemic lupus erythematosus (SLE) and autoimmune hepatitis (AIH) with serologic features of lupus, including antinuclear antibodies and anti-dsDNA immunoglobulin G antibodies.
Liver biopsies from three SLE patients were positive for E. gallinarum, whereas samples from four of six healthy liver transplant donors with normal liver histology tested positive for the presence of other Enterococcus species but not E. gallinarum.
“Consistent with enhanced adaptive immune responses to E. gallinarum, the majority of SLE and AIH patients also showed increased serum antibody titers against E. gallinarum and particularly its RNA,” they said.
The authors said their findings showed that E. gallinarum translocates into systemic organs as a result of the breakdown of the gut barrier in autoimmune-prone hosts to drive autoimmune pathogenesis. They suggested that the translocating bacteria skewed T helper cell differentiation but also acted directly on colonized tissues such as the liver to induce autoantigens, endogenous retrovirus proteins, cytokines, and other autoimmune-promoting factors.
“If the complexity of host-tissue microbiota interactions is considered in chronic autoimmunity, it may offer new therapeutic avenues for these debilitating and potentially lethal diseases,” they concluded.
The study was supported by grants from various institutes and initiatives within the National Institutes of Health as well as from the Arthritis National Research Foundation, the Arthritis Foundation, and the Lupus Research Institute. Dr. Vieira and the senior author, Martin A. Kriegel, MD, PhD, are inventors on a patent application filed by Yale University related to the use of antibiotics and commensal vaccination to treat autoimmunity.
SOURCE: Vieira S et al. Science. 2018;359(6380):1156-61.
Gut bacteria found in the small intestines could play a role in triggering an autoimmune response in genetically predisposed individuals, such as those with lupus, a research report suggests.
Recent studies have shown that gut commensals can reside within gastrointestinal-associated lymph tissues of healthy hosts, but it has been unclear whether pathobiont translocation was involved in systemic autoimmunity. Silvio Manfredo Vieira, PhD, and his colleagues at Yale University, New Haven, Conn., addressed this knowledge gap by studying the Gram-positive gut commensal Enterococcus gallinarum, which was identified in mesenteric lymph nodes, liver, and spleen cultures from genetically susceptible mouse models.
The researchers found that they could suppress the autoimmunity with antibiotics or an intramuscular vaccine targeted at E. gallinarum. The vaccine reduced levels of serum autoantibodies, prolonged survival in the mice, and also prevented translocation, as no growth of E. gallinarum was observed in internal organs.
“Pathobiont-specific treatment can abrogate host autoimmune processes without needing to suppress the immune system, which can lead to systemic adverse events in current clinical practice,” they wrote.
The researchers then tested for E. gallinarum translocation to human livers in patients with systemic lupus erythematosus (SLE) and autoimmune hepatitis (AIH) with serologic features of lupus, including antinuclear antibodies and anti-dsDNA immunoglobulin G antibodies.
Liver biopsies from three SLE patients were positive for E. gallinarum, whereas samples from four of six healthy liver transplant donors with normal liver histology tested positive for the presence of other Enterococcus species but not E. gallinarum.
“Consistent with enhanced adaptive immune responses to E. gallinarum, the majority of SLE and AIH patients also showed increased serum antibody titers against E. gallinarum and particularly its RNA,” they said.
The authors said their findings showed that E. gallinarum translocates into systemic organs as a result of the breakdown of the gut barrier in autoimmune-prone hosts to drive autoimmune pathogenesis. They suggested that the translocating bacteria skewed T helper cell differentiation but also acted directly on colonized tissues such as the liver to induce autoantigens, endogenous retrovirus proteins, cytokines, and other autoimmune-promoting factors.
“If the complexity of host-tissue microbiota interactions is considered in chronic autoimmunity, it may offer new therapeutic avenues for these debilitating and potentially lethal diseases,” they concluded.
The study was supported by grants from various institutes and initiatives within the National Institutes of Health as well as from the Arthritis National Research Foundation, the Arthritis Foundation, and the Lupus Research Institute. Dr. Vieira and the senior author, Martin A. Kriegel, MD, PhD, are inventors on a patent application filed by Yale University related to the use of antibiotics and commensal vaccination to treat autoimmunity.
SOURCE: Vieira S et al. Science. 2018;359(6380):1156-61.
FROM SCIENCE
Key clinical point: The discovery that gut bacteria found in the small intestines can trigger autoimmune responses in predisposed individuals could lead to new therapeutic avenues for autoimmune diseases.
Major finding: In mice and humans, the Gram-positive gut bacteria pathobiont E. gallinarum translocated into systemic organs in autoimmune-prone hosts to drive autoimmune pathogenesis.
Study details: A mouse model that was replicated in cultured liver cells of healthy controls and patients with autoimmune disease.
Disclosures: The study was supported by grants from various institutes and initiatives within the National Institutes of Health as well as from the Arthritis National Research Foundation, the Arthritis Foundation, and the Lupus Research Institute. The first author and senior author are inventors on a patent application filed by Yale University related to the use of antibiotics and commensal vaccination to treat autoimmunity.
Source: Vieira S et al. Science. 2018;359(6380):1156-61.
Endocrine Society Preview: The 2018 meeting will be ‘a journey to innovation’
Attendees at the upcoming Endocrine Society annual meeting in Chicago can expect many of the scheduled sessions to be practice changing, according to Ann Danoff, MD, clinical chair of this year’s meeting program.
Endocrine Society President Lynnette K. Nieman, MD, will lead off the plenary sessions on March 17, by presenting awards to six visionary investigators. Noteworthy among these will be the work of Diana Lynn Blithe, PhD, National Institutes of Health, for her research on male contraception. Dr. Blithe will speak about what’s in the clinical pipeline and what direction future research will take.
The second plenary session has an intriguing title – Rhythm and Blues. This session will cover circadian rhythmicity, which is, coincidentally, the research area of the three joint winners of the 2017 Nobel Prize in Physiology or Medicine.
In a plenary sessions scheduled for March 17, at 3:00 p.m., the topic under discussion will be the issue of circadian rhythm and metabolic health. Dysregulation of light and dark exposure puts people at risk for a variety of metabolic disease, said Dr. Danoff, who is chief of the medical service at the Philadelphia Veterans Affairs Medical Center. Specifically, two of the presentations – one on Circadian Rhythms, Blue Light, and Setting Your Internal Clock and the other on Improving Health by Time-Restricted Eating – are likely to be enlightening.
The Endocrine Society has revamped this year’s approach to sessions on guidelines to take the format of a discussion of how the guidelines affect patients on case-by-case basis. The moderator of each session will not be a member of the guideline-writing committee, but the panelists will be committee members.
New guidelines to be discussed are those dealing with gender incongruence and testosterone therapy. The session on transgender issues in endocrinology will take place on March 19, and is entitled Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. The session on testosterone therapy is entitled: Testosterone Therapy in Men with Hypogonadism: An Endocrine Society Clinical Practice Guideline, also on March 19.
Another change to the approach taken to guidelines are sessions that go beyond the guidelines to discuss patients who fall between the cracks. Topics of these sessions are osteoporosis, indeterminate thyroid nodules, and challenging hyperprolactinemia and prolactinoma cases The panels involved in these discussions may include a surgeon, and two-thirds of them will include a fellow. “I am committed to the bringing along of young trainees,” said Dr. Danoff.
And what is an annual meeting without a few debates? On March 18, there will be a debate on Debate: This House Believes that Adrenal Vein Sampling Has a Major Role to Play in the Management of Patients with Primary Aldosteronism. Speaking in favor will be William F. Young Jr., MD, of the Mayo Clinic in Rochester, Minn., and against will be Paul Michael Stewart, MD, of the University of Leeds (England). Another debate topic, scheduled for March 17, will be The LDL Limbo: How Low Should You Go? Taking up the side that Benefits of LDL Reduction Are Continuous and Extend to Extremely Low Levels will be Steven Nissen, MD, of the Cleveland Clinic. There to discuss Lower LDL Is Better but What About Very-Low LDL? will be Henry N. Ginsberg, MD, Columbia University College of Physicians and Surgeons, New York.
Attendees at the upcoming Endocrine Society annual meeting in Chicago can expect many of the scheduled sessions to be practice changing, according to Ann Danoff, MD, clinical chair of this year’s meeting program.
Endocrine Society President Lynnette K. Nieman, MD, will lead off the plenary sessions on March 17, by presenting awards to six visionary investigators. Noteworthy among these will be the work of Diana Lynn Blithe, PhD, National Institutes of Health, for her research on male contraception. Dr. Blithe will speak about what’s in the clinical pipeline and what direction future research will take.
The second plenary session has an intriguing title – Rhythm and Blues. This session will cover circadian rhythmicity, which is, coincidentally, the research area of the three joint winners of the 2017 Nobel Prize in Physiology or Medicine.
In a plenary sessions scheduled for March 17, at 3:00 p.m., the topic under discussion will be the issue of circadian rhythm and metabolic health. Dysregulation of light and dark exposure puts people at risk for a variety of metabolic disease, said Dr. Danoff, who is chief of the medical service at the Philadelphia Veterans Affairs Medical Center. Specifically, two of the presentations – one on Circadian Rhythms, Blue Light, and Setting Your Internal Clock and the other on Improving Health by Time-Restricted Eating – are likely to be enlightening.
The Endocrine Society has revamped this year’s approach to sessions on guidelines to take the format of a discussion of how the guidelines affect patients on case-by-case basis. The moderator of each session will not be a member of the guideline-writing committee, but the panelists will be committee members.
New guidelines to be discussed are those dealing with gender incongruence and testosterone therapy. The session on transgender issues in endocrinology will take place on March 19, and is entitled Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. The session on testosterone therapy is entitled: Testosterone Therapy in Men with Hypogonadism: An Endocrine Society Clinical Practice Guideline, also on March 19.
Another change to the approach taken to guidelines are sessions that go beyond the guidelines to discuss patients who fall between the cracks. Topics of these sessions are osteoporosis, indeterminate thyroid nodules, and challenging hyperprolactinemia and prolactinoma cases The panels involved in these discussions may include a surgeon, and two-thirds of them will include a fellow. “I am committed to the bringing along of young trainees,” said Dr. Danoff.
And what is an annual meeting without a few debates? On March 18, there will be a debate on Debate: This House Believes that Adrenal Vein Sampling Has a Major Role to Play in the Management of Patients with Primary Aldosteronism. Speaking in favor will be William F. Young Jr., MD, of the Mayo Clinic in Rochester, Minn., and against will be Paul Michael Stewart, MD, of the University of Leeds (England). Another debate topic, scheduled for March 17, will be The LDL Limbo: How Low Should You Go? Taking up the side that Benefits of LDL Reduction Are Continuous and Extend to Extremely Low Levels will be Steven Nissen, MD, of the Cleveland Clinic. There to discuss Lower LDL Is Better but What About Very-Low LDL? will be Henry N. Ginsberg, MD, Columbia University College of Physicians and Surgeons, New York.
Attendees at the upcoming Endocrine Society annual meeting in Chicago can expect many of the scheduled sessions to be practice changing, according to Ann Danoff, MD, clinical chair of this year’s meeting program.
Endocrine Society President Lynnette K. Nieman, MD, will lead off the plenary sessions on March 17, by presenting awards to six visionary investigators. Noteworthy among these will be the work of Diana Lynn Blithe, PhD, National Institutes of Health, for her research on male contraception. Dr. Blithe will speak about what’s in the clinical pipeline and what direction future research will take.
The second plenary session has an intriguing title – Rhythm and Blues. This session will cover circadian rhythmicity, which is, coincidentally, the research area of the three joint winners of the 2017 Nobel Prize in Physiology or Medicine.
In a plenary sessions scheduled for March 17, at 3:00 p.m., the topic under discussion will be the issue of circadian rhythm and metabolic health. Dysregulation of light and dark exposure puts people at risk for a variety of metabolic disease, said Dr. Danoff, who is chief of the medical service at the Philadelphia Veterans Affairs Medical Center. Specifically, two of the presentations – one on Circadian Rhythms, Blue Light, and Setting Your Internal Clock and the other on Improving Health by Time-Restricted Eating – are likely to be enlightening.
The Endocrine Society has revamped this year’s approach to sessions on guidelines to take the format of a discussion of how the guidelines affect patients on case-by-case basis. The moderator of each session will not be a member of the guideline-writing committee, but the panelists will be committee members.
New guidelines to be discussed are those dealing with gender incongruence and testosterone therapy. The session on transgender issues in endocrinology will take place on March 19, and is entitled Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. The session on testosterone therapy is entitled: Testosterone Therapy in Men with Hypogonadism: An Endocrine Society Clinical Practice Guideline, also on March 19.
Another change to the approach taken to guidelines are sessions that go beyond the guidelines to discuss patients who fall between the cracks. Topics of these sessions are osteoporosis, indeterminate thyroid nodules, and challenging hyperprolactinemia and prolactinoma cases The panels involved in these discussions may include a surgeon, and two-thirds of them will include a fellow. “I am committed to the bringing along of young trainees,” said Dr. Danoff.
And what is an annual meeting without a few debates? On March 18, there will be a debate on Debate: This House Believes that Adrenal Vein Sampling Has a Major Role to Play in the Management of Patients with Primary Aldosteronism. Speaking in favor will be William F. Young Jr., MD, of the Mayo Clinic in Rochester, Minn., and against will be Paul Michael Stewart, MD, of the University of Leeds (England). Another debate topic, scheduled for March 17, will be The LDL Limbo: How Low Should You Go? Taking up the side that Benefits of LDL Reduction Are Continuous and Extend to Extremely Low Levels will be Steven Nissen, MD, of the Cleveland Clinic. There to discuss Lower LDL Is Better but What About Very-Low LDL? will be Henry N. Ginsberg, MD, Columbia University College of Physicians and Surgeons, New York.
MOMENTUM 3 HeartMate 3 LVAD ‘practice changing’
ORLANDO – of follow-up in patients with advanced heart failure in the large multicenter MOMENTUM 3 trial, Mandeep R. Mehra, MD, reported at the annual meeting of the American College of Cardiology.
HeartMate 3 recipients had a 90% lower risk of undergoing reoperation to replace or remove their device because of malfunction, and a stroke rate half that in the HeartMate II group.
“This was the lowest rate of stroke ever seen in any LVAD trial,” according to Dr. Mehra, medical director of the Brigham and Women’s Hospital Heart and Vascular Center, Boston, and professor of medicine at Harvard Medical School.
“We believe this is a practice-changing result in the field, and that the real implication of our findings is to reassure those who refer or treat patients with advanced heart failure that it is perhaps going to be ignorant not to refer patients for consideration for destination therapy,” he said at a press conference highlighting the MOMENTUM 3 results, also presented in a late-breaking clinical trials session.
The HeartMate 3 is a miniaturized centrifugal-flow device that fits entirely within the chest, whereas the HeartMate II requires creation of a pocket in the abdomen. The HeartMate 3 was designed to prevent pump thrombosis – a common limiting problem with the HeartMate II and other LVADs – by employing three innovations: use of wide blood-flow passages to reduce shear stress and minimize disruption of red blood cells as they pass through the pump; reliance on magnetic levitation technology to create a frictionless pump with no mechanical bearings, which are subject to wear and tear; and incorporation of an artificial fixed pulse that speeds up and slows every 2 seconds in order to minimize blood stasis, which promotes thrombosis, the cardiologist explained in a video interview.
MOMENTUM 3 is the largest-ever randomized trial of LVAD therapy, involving 1,028 advanced heart failure patients at 69 U.S. centers. The study population is a mix of bridge-to-transplant patients and others who weren’t eligible for heart transplantation and are using their device as lifelong destination therapy. In an earlier report on the first 294 patients to reach 6 months of follow-up post implantation, Dr. Mehra and his coinvestigators showed that the HeartMate 3 group had a significantly lower incidence of the composite endpoint of disabling stroke or reoperation to replace or remove the device (N Engl J Med. 2017 Feb 2;376[5]:440-50).
At ACC 2018, he presented the prespecified 2-year analysis of results in the first 366 patients to reach that benchmark. The rate of survival free of disabling stroke or reoperation for device malfunction was 79.5% in the HeartMate 3 group and 60.2% with the HeartMate II, for a highly significant 54% reduction in the risk of bad outcome. Reoperation for device malfunction occurred in 1.6% of HeartMate 3 patients versus 17% of those with a HeartMate II, for a 92% reduction in risk. Two-year survival was 82.8% in the HeartMate 3 group and 76.2% in HeartMate II recipients.
The overall stroke rate was 10% with the HeartMate 3, compared with 19% with the older, axial-flow LVAD. The incidence of disabling stroke was 3% in the HeartMate 3 group and similar at 2% with the HeartMate II; however, nondisabling stroke occurred in only 3% of HeartMate 3 recipients, compared with 14% of patients with the HeartMate II.
“There has always been this notion that, ‘There are so many complications with this device, so let’s suffer with the disease rather than suffer with the pump.’ Now we’re showing that you don’t suffer with the pump as with the earlier-generation devices. I think this is going to open the gates for more referrals and more opportunities for destination therapy in patients who are deemed ineligible for transplant,” Dr. Mehra predicted.
Discussant James L. Janzuzzi Jr., called the MOMENTUM 3 results “a very-much-needed step forward.”
“Perhaps the most dramatic observation in this study is the dramatic reduction in thrombosis events requiring reoperation. In essence, this problem was entirely prevented by the use of this magnetically levitated centrifugal-flow device. Reoperation for thrombosis accounted for two-thirds of the reoperations in the HeartMate II group and the rate was zero in the HeartMate 3 population. Essentially, with this technology we’ve addressed a very important unmet need by reducing the onset of pump thrombosis, which is the precursor to either pump dysfunction or embolic stroke,” commented Dr. Januzzi, professor of medicine at Harvard Medical School, Boston.
Given the 83% survival rate at 2 years in the HeartMate 3 group in the MOMENTUM 3 trial, the on-average 50% survival at 10 years for heart transplant recipients, and the perpetual enormous shortage of donor organs, it’s time to consider a randomized trial of an advanced LVAD such as the HeartMate 3 versus heart transplantation, with quality-of-life outcomes front and center, he asserted.
Dr. Mehra was all for the idea. He noted that within the community of physicians and surgeons who provide care for advanced heart failure patients there is a growing move to replace problematic axial-flow LVADs requiring reoperation with a HeartMate 3 upgrade.
The MOMENTUM 3 trial is funded by Abbott. Dr. Mehra reported receiving research funds from and serving as a consultant to the company.
Simultaneous with his presentation at ACC 2018, the 2-year results of MOMENTUM 3 were published online at NEJM.org (doi: 10.1056/NEJMoa1800866).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mehra M et al. ACC 18.
ORLANDO – of follow-up in patients with advanced heart failure in the large multicenter MOMENTUM 3 trial, Mandeep R. Mehra, MD, reported at the annual meeting of the American College of Cardiology.
HeartMate 3 recipients had a 90% lower risk of undergoing reoperation to replace or remove their device because of malfunction, and a stroke rate half that in the HeartMate II group.
“This was the lowest rate of stroke ever seen in any LVAD trial,” according to Dr. Mehra, medical director of the Brigham and Women’s Hospital Heart and Vascular Center, Boston, and professor of medicine at Harvard Medical School.
“We believe this is a practice-changing result in the field, and that the real implication of our findings is to reassure those who refer or treat patients with advanced heart failure that it is perhaps going to be ignorant not to refer patients for consideration for destination therapy,” he said at a press conference highlighting the MOMENTUM 3 results, also presented in a late-breaking clinical trials session.
The HeartMate 3 is a miniaturized centrifugal-flow device that fits entirely within the chest, whereas the HeartMate II requires creation of a pocket in the abdomen. The HeartMate 3 was designed to prevent pump thrombosis – a common limiting problem with the HeartMate II and other LVADs – by employing three innovations: use of wide blood-flow passages to reduce shear stress and minimize disruption of red blood cells as they pass through the pump; reliance on magnetic levitation technology to create a frictionless pump with no mechanical bearings, which are subject to wear and tear; and incorporation of an artificial fixed pulse that speeds up and slows every 2 seconds in order to minimize blood stasis, which promotes thrombosis, the cardiologist explained in a video interview.
MOMENTUM 3 is the largest-ever randomized trial of LVAD therapy, involving 1,028 advanced heart failure patients at 69 U.S. centers. The study population is a mix of bridge-to-transplant patients and others who weren’t eligible for heart transplantation and are using their device as lifelong destination therapy. In an earlier report on the first 294 patients to reach 6 months of follow-up post implantation, Dr. Mehra and his coinvestigators showed that the HeartMate 3 group had a significantly lower incidence of the composite endpoint of disabling stroke or reoperation to replace or remove the device (N Engl J Med. 2017 Feb 2;376[5]:440-50).
At ACC 2018, he presented the prespecified 2-year analysis of results in the first 366 patients to reach that benchmark. The rate of survival free of disabling stroke or reoperation for device malfunction was 79.5% in the HeartMate 3 group and 60.2% with the HeartMate II, for a highly significant 54% reduction in the risk of bad outcome. Reoperation for device malfunction occurred in 1.6% of HeartMate 3 patients versus 17% of those with a HeartMate II, for a 92% reduction in risk. Two-year survival was 82.8% in the HeartMate 3 group and 76.2% in HeartMate II recipients.
The overall stroke rate was 10% with the HeartMate 3, compared with 19% with the older, axial-flow LVAD. The incidence of disabling stroke was 3% in the HeartMate 3 group and similar at 2% with the HeartMate II; however, nondisabling stroke occurred in only 3% of HeartMate 3 recipients, compared with 14% of patients with the HeartMate II.
“There has always been this notion that, ‘There are so many complications with this device, so let’s suffer with the disease rather than suffer with the pump.’ Now we’re showing that you don’t suffer with the pump as with the earlier-generation devices. I think this is going to open the gates for more referrals and more opportunities for destination therapy in patients who are deemed ineligible for transplant,” Dr. Mehra predicted.
Discussant James L. Janzuzzi Jr., called the MOMENTUM 3 results “a very-much-needed step forward.”
“Perhaps the most dramatic observation in this study is the dramatic reduction in thrombosis events requiring reoperation. In essence, this problem was entirely prevented by the use of this magnetically levitated centrifugal-flow device. Reoperation for thrombosis accounted for two-thirds of the reoperations in the HeartMate II group and the rate was zero in the HeartMate 3 population. Essentially, with this technology we’ve addressed a very important unmet need by reducing the onset of pump thrombosis, which is the precursor to either pump dysfunction or embolic stroke,” commented Dr. Januzzi, professor of medicine at Harvard Medical School, Boston.
Given the 83% survival rate at 2 years in the HeartMate 3 group in the MOMENTUM 3 trial, the on-average 50% survival at 10 years for heart transplant recipients, and the perpetual enormous shortage of donor organs, it’s time to consider a randomized trial of an advanced LVAD such as the HeartMate 3 versus heart transplantation, with quality-of-life outcomes front and center, he asserted.
Dr. Mehra was all for the idea. He noted that within the community of physicians and surgeons who provide care for advanced heart failure patients there is a growing move to replace problematic axial-flow LVADs requiring reoperation with a HeartMate 3 upgrade.
The MOMENTUM 3 trial is funded by Abbott. Dr. Mehra reported receiving research funds from and serving as a consultant to the company.
Simultaneous with his presentation at ACC 2018, the 2-year results of MOMENTUM 3 were published online at NEJM.org (doi: 10.1056/NEJMoa1800866).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mehra M et al. ACC 18.
ORLANDO – of follow-up in patients with advanced heart failure in the large multicenter MOMENTUM 3 trial, Mandeep R. Mehra, MD, reported at the annual meeting of the American College of Cardiology.
HeartMate 3 recipients had a 90% lower risk of undergoing reoperation to replace or remove their device because of malfunction, and a stroke rate half that in the HeartMate II group.
“This was the lowest rate of stroke ever seen in any LVAD trial,” according to Dr. Mehra, medical director of the Brigham and Women’s Hospital Heart and Vascular Center, Boston, and professor of medicine at Harvard Medical School.
“We believe this is a practice-changing result in the field, and that the real implication of our findings is to reassure those who refer or treat patients with advanced heart failure that it is perhaps going to be ignorant not to refer patients for consideration for destination therapy,” he said at a press conference highlighting the MOMENTUM 3 results, also presented in a late-breaking clinical trials session.
The HeartMate 3 is a miniaturized centrifugal-flow device that fits entirely within the chest, whereas the HeartMate II requires creation of a pocket in the abdomen. The HeartMate 3 was designed to prevent pump thrombosis – a common limiting problem with the HeartMate II and other LVADs – by employing three innovations: use of wide blood-flow passages to reduce shear stress and minimize disruption of red blood cells as they pass through the pump; reliance on magnetic levitation technology to create a frictionless pump with no mechanical bearings, which are subject to wear and tear; and incorporation of an artificial fixed pulse that speeds up and slows every 2 seconds in order to minimize blood stasis, which promotes thrombosis, the cardiologist explained in a video interview.
MOMENTUM 3 is the largest-ever randomized trial of LVAD therapy, involving 1,028 advanced heart failure patients at 69 U.S. centers. The study population is a mix of bridge-to-transplant patients and others who weren’t eligible for heart transplantation and are using their device as lifelong destination therapy. In an earlier report on the first 294 patients to reach 6 months of follow-up post implantation, Dr. Mehra and his coinvestigators showed that the HeartMate 3 group had a significantly lower incidence of the composite endpoint of disabling stroke or reoperation to replace or remove the device (N Engl J Med. 2017 Feb 2;376[5]:440-50).
At ACC 2018, he presented the prespecified 2-year analysis of results in the first 366 patients to reach that benchmark. The rate of survival free of disabling stroke or reoperation for device malfunction was 79.5% in the HeartMate 3 group and 60.2% with the HeartMate II, for a highly significant 54% reduction in the risk of bad outcome. Reoperation for device malfunction occurred in 1.6% of HeartMate 3 patients versus 17% of those with a HeartMate II, for a 92% reduction in risk. Two-year survival was 82.8% in the HeartMate 3 group and 76.2% in HeartMate II recipients.
The overall stroke rate was 10% with the HeartMate 3, compared with 19% with the older, axial-flow LVAD. The incidence of disabling stroke was 3% in the HeartMate 3 group and similar at 2% with the HeartMate II; however, nondisabling stroke occurred in only 3% of HeartMate 3 recipients, compared with 14% of patients with the HeartMate II.
“There has always been this notion that, ‘There are so many complications with this device, so let’s suffer with the disease rather than suffer with the pump.’ Now we’re showing that you don’t suffer with the pump as with the earlier-generation devices. I think this is going to open the gates for more referrals and more opportunities for destination therapy in patients who are deemed ineligible for transplant,” Dr. Mehra predicted.
Discussant James L. Janzuzzi Jr., called the MOMENTUM 3 results “a very-much-needed step forward.”
“Perhaps the most dramatic observation in this study is the dramatic reduction in thrombosis events requiring reoperation. In essence, this problem was entirely prevented by the use of this magnetically levitated centrifugal-flow device. Reoperation for thrombosis accounted for two-thirds of the reoperations in the HeartMate II group and the rate was zero in the HeartMate 3 population. Essentially, with this technology we’ve addressed a very important unmet need by reducing the onset of pump thrombosis, which is the precursor to either pump dysfunction or embolic stroke,” commented Dr. Januzzi, professor of medicine at Harvard Medical School, Boston.
Given the 83% survival rate at 2 years in the HeartMate 3 group in the MOMENTUM 3 trial, the on-average 50% survival at 10 years for heart transplant recipients, and the perpetual enormous shortage of donor organs, it’s time to consider a randomized trial of an advanced LVAD such as the HeartMate 3 versus heart transplantation, with quality-of-life outcomes front and center, he asserted.
Dr. Mehra was all for the idea. He noted that within the community of physicians and surgeons who provide care for advanced heart failure patients there is a growing move to replace problematic axial-flow LVADs requiring reoperation with a HeartMate 3 upgrade.
The MOMENTUM 3 trial is funded by Abbott. Dr. Mehra reported receiving research funds from and serving as a consultant to the company.
Simultaneous with his presentation at ACC 2018, the 2-year results of MOMENTUM 3 were published online at NEJM.org (doi: 10.1056/NEJMoa1800866).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mehra M et al. ACC 18.
REPORTING FROM ACC 18
Key clinical point: Landmark trial paves way to much wider use of LVADs as destination therapy.
Major finding: The 2-year rate of survival free of disabling stroke or reoperation to replace or remove a malfunctioning LVAD was 79.5% with the novel HeartMate 3 LVAD, compared with 60.2% with the commonly used HeartMate II axial-flow device.
Study details: This was a randomized, unblinded, multicenter study of more than 1,000 patients with advanced heart failure.
Disclosures: The MOMENTUM 3 trial was funded by Abbott. The presenter reported receiving research grants from and serving as a consultant to the company.
Source: Mehra MR et al. ACC 18.
ABS announces new certification exam
.
The new test, required every other year, consists of a 40-question, open-book assessment that surgeons can take on their own computers within the assessment time frame, according to a March 5 announcement. The previous 10-year exam consisted of nearly 250 questions and had to be completed at a highly secure testing center.
The assessment shift was made to address diplomates’ concerns that the prior exam was burdensome, stressful, and challenging to complete because of its rigid design and location requirements, ABS Chair Mary E. Klingensmith, MD, FACS, said in an interview.
“This new method, which allows a take-from-home or office format, is much less stressful, as both the setting, and the ability to choose the content area, give diplomates much more control,” Dr. Klingensmith said. “Additionally, the testing concepts and references will be provided in advance, should a diplomate desire to know these aspects.”
On March 11, the American College of Surgeons released a statement regarding the new assessment and suggested that, while the new approach is welcomed by the ACS, some details of the process are of concern to surgeons. “The American College of Surgeons (ACS) leadership has heard your concerns both through personal conversations with many of you and through your posts on ACS Communities. In fact, many in leadership share these concerns. We have been in discussions with ABS leadership and can tell you that they are also listening. They want to get this right.”
Of the 40 questions on the new exam, 20 questions will cover core surgical principles, while the other 20 will cover a practice-related area of the diplomate’s choosing. For 2018, diplomates can select from four practice-related areas: general surgery, abdomen, alimentary tract, or breast. More areas are planned based on future feedback from diplomates and surgical societies. Other aspects of the new exam include:
- Topics and references for the various areas will be published in advance on the ABS website.
- Diplomates will be provided with immediate feedback, and will have two opportunities to answer a question correctly.
- A final score of 80% correct will be required to pass.
- Once the assessment is started, diplomates will have 2 weeks to complete the test, with the ability to save and continue when convenient.
The purpose of the new assessment is to provide practicing surgeons with a timely, relevant, and accessible method to stay current with surgical practice knowledge,” Dr. Klingensmith said.
“By selecting a practice-specific area of their own choosing, surgeons will no longer have to study for and be tested upon the entire breadth of general surgery; instead they can focus on those areas that most reflect their practice,” she said. “By submitting to a learning exercise every 2 years, which is focused in the areas of an individual surgeon’s practice, I expect important aspects of knowledge will be transmitted and integrated into a surgeon’s practice. This new program will provide practicing surgeons with an accessible method for keeping up with the constantly changing landscape of surgical practice.”
The new exam is part of an ongoing effort by ABS to revamp its maintenance of certification requirements after widespread criticism that its past provisions were burdensome and irrelevant. In July, ABS announced that it was extending its continuing medical education reporting cycle from 3 to 5 years and reducing the number of required self-assessment by a third. Surgeons now have to report 150 credits over 5 years, 50 from self-assessment CMEs. Under the old system, it was 90 credits over 3 years, 60 of which had to include self-assessment.
After the July announcement, ABS sent surveys to all diplomates to gather feedback about alternatives to the 10-year exam. Nearly 10,000 surgeons responded, according to an ABS summary. The majority of respondents said they wanted more frequent, lower-stakes, open-book assessments that would be required no frequently than every 2 years. Most surgeons were also in favor of being tested on both surgery concepts and practice-specific content.
For 2019 and beyond, the ABS’ Component Boards – Vascular, Pediatric Surgery, Surgical, and Critical Care – will develop their continuous certification processes, Dr. Klingensmith said. Additional areas for the surgery exam also will be developed in collaboration with specialty societies.
In the meantime, registration for the new general surgery assessment opens Aug. 1. The assessment will be available from Sept. 7 to Nov. 5, during which time diplomates can take the assessment at their convenience.
For more information, go to the continuous certification section on the ABS website.
.
The new test, required every other year, consists of a 40-question, open-book assessment that surgeons can take on their own computers within the assessment time frame, according to a March 5 announcement. The previous 10-year exam consisted of nearly 250 questions and had to be completed at a highly secure testing center.
The assessment shift was made to address diplomates’ concerns that the prior exam was burdensome, stressful, and challenging to complete because of its rigid design and location requirements, ABS Chair Mary E. Klingensmith, MD, FACS, said in an interview.
“This new method, which allows a take-from-home or office format, is much less stressful, as both the setting, and the ability to choose the content area, give diplomates much more control,” Dr. Klingensmith said. “Additionally, the testing concepts and references will be provided in advance, should a diplomate desire to know these aspects.”
On March 11, the American College of Surgeons released a statement regarding the new assessment and suggested that, while the new approach is welcomed by the ACS, some details of the process are of concern to surgeons. “The American College of Surgeons (ACS) leadership has heard your concerns both through personal conversations with many of you and through your posts on ACS Communities. In fact, many in leadership share these concerns. We have been in discussions with ABS leadership and can tell you that they are also listening. They want to get this right.”
Of the 40 questions on the new exam, 20 questions will cover core surgical principles, while the other 20 will cover a practice-related area of the diplomate’s choosing. For 2018, diplomates can select from four practice-related areas: general surgery, abdomen, alimentary tract, or breast. More areas are planned based on future feedback from diplomates and surgical societies. Other aspects of the new exam include:
- Topics and references for the various areas will be published in advance on the ABS website.
- Diplomates will be provided with immediate feedback, and will have two opportunities to answer a question correctly.
- A final score of 80% correct will be required to pass.
- Once the assessment is started, diplomates will have 2 weeks to complete the test, with the ability to save and continue when convenient.
The purpose of the new assessment is to provide practicing surgeons with a timely, relevant, and accessible method to stay current with surgical practice knowledge,” Dr. Klingensmith said.
“By selecting a practice-specific area of their own choosing, surgeons will no longer have to study for and be tested upon the entire breadth of general surgery; instead they can focus on those areas that most reflect their practice,” she said. “By submitting to a learning exercise every 2 years, which is focused in the areas of an individual surgeon’s practice, I expect important aspects of knowledge will be transmitted and integrated into a surgeon’s practice. This new program will provide practicing surgeons with an accessible method for keeping up with the constantly changing landscape of surgical practice.”
The new exam is part of an ongoing effort by ABS to revamp its maintenance of certification requirements after widespread criticism that its past provisions were burdensome and irrelevant. In July, ABS announced that it was extending its continuing medical education reporting cycle from 3 to 5 years and reducing the number of required self-assessment by a third. Surgeons now have to report 150 credits over 5 years, 50 from self-assessment CMEs. Under the old system, it was 90 credits over 3 years, 60 of which had to include self-assessment.
After the July announcement, ABS sent surveys to all diplomates to gather feedback about alternatives to the 10-year exam. Nearly 10,000 surgeons responded, according to an ABS summary. The majority of respondents said they wanted more frequent, lower-stakes, open-book assessments that would be required no frequently than every 2 years. Most surgeons were also in favor of being tested on both surgery concepts and practice-specific content.
For 2019 and beyond, the ABS’ Component Boards – Vascular, Pediatric Surgery, Surgical, and Critical Care – will develop their continuous certification processes, Dr. Klingensmith said. Additional areas for the surgery exam also will be developed in collaboration with specialty societies.
In the meantime, registration for the new general surgery assessment opens Aug. 1. The assessment will be available from Sept. 7 to Nov. 5, during which time diplomates can take the assessment at their convenience.
For more information, go to the continuous certification section on the ABS website.
.
The new test, required every other year, consists of a 40-question, open-book assessment that surgeons can take on their own computers within the assessment time frame, according to a March 5 announcement. The previous 10-year exam consisted of nearly 250 questions and had to be completed at a highly secure testing center.
The assessment shift was made to address diplomates’ concerns that the prior exam was burdensome, stressful, and challenging to complete because of its rigid design and location requirements, ABS Chair Mary E. Klingensmith, MD, FACS, said in an interview.
“This new method, which allows a take-from-home or office format, is much less stressful, as both the setting, and the ability to choose the content area, give diplomates much more control,” Dr. Klingensmith said. “Additionally, the testing concepts and references will be provided in advance, should a diplomate desire to know these aspects.”
On March 11, the American College of Surgeons released a statement regarding the new assessment and suggested that, while the new approach is welcomed by the ACS, some details of the process are of concern to surgeons. “The American College of Surgeons (ACS) leadership has heard your concerns both through personal conversations with many of you and through your posts on ACS Communities. In fact, many in leadership share these concerns. We have been in discussions with ABS leadership and can tell you that they are also listening. They want to get this right.”
Of the 40 questions on the new exam, 20 questions will cover core surgical principles, while the other 20 will cover a practice-related area of the diplomate’s choosing. For 2018, diplomates can select from four practice-related areas: general surgery, abdomen, alimentary tract, or breast. More areas are planned based on future feedback from diplomates and surgical societies. Other aspects of the new exam include:
- Topics and references for the various areas will be published in advance on the ABS website.
- Diplomates will be provided with immediate feedback, and will have two opportunities to answer a question correctly.
- A final score of 80% correct will be required to pass.
- Once the assessment is started, diplomates will have 2 weeks to complete the test, with the ability to save and continue when convenient.
The purpose of the new assessment is to provide practicing surgeons with a timely, relevant, and accessible method to stay current with surgical practice knowledge,” Dr. Klingensmith said.
“By selecting a practice-specific area of their own choosing, surgeons will no longer have to study for and be tested upon the entire breadth of general surgery; instead they can focus on those areas that most reflect their practice,” she said. “By submitting to a learning exercise every 2 years, which is focused in the areas of an individual surgeon’s practice, I expect important aspects of knowledge will be transmitted and integrated into a surgeon’s practice. This new program will provide practicing surgeons with an accessible method for keeping up with the constantly changing landscape of surgical practice.”
The new exam is part of an ongoing effort by ABS to revamp its maintenance of certification requirements after widespread criticism that its past provisions were burdensome and irrelevant. In July, ABS announced that it was extending its continuing medical education reporting cycle from 3 to 5 years and reducing the number of required self-assessment by a third. Surgeons now have to report 150 credits over 5 years, 50 from self-assessment CMEs. Under the old system, it was 90 credits over 3 years, 60 of which had to include self-assessment.
After the July announcement, ABS sent surveys to all diplomates to gather feedback about alternatives to the 10-year exam. Nearly 10,000 surgeons responded, according to an ABS summary. The majority of respondents said they wanted more frequent, lower-stakes, open-book assessments that would be required no frequently than every 2 years. Most surgeons were also in favor of being tested on both surgery concepts and practice-specific content.
For 2019 and beyond, the ABS’ Component Boards – Vascular, Pediatric Surgery, Surgical, and Critical Care – will develop their continuous certification processes, Dr. Klingensmith said. Additional areas for the surgery exam also will be developed in collaboration with specialty societies.
In the meantime, registration for the new general surgery assessment opens Aug. 1. The assessment will be available from Sept. 7 to Nov. 5, during which time diplomates can take the assessment at their convenience.
For more information, go to the continuous certification section on the ABS website.
Migraine Often Results in Emergency Department Revisits
More than one-quarter of initial emergency department (ED) visits for migraine are followed by headache revisits in fewer than six months, according to a retrospective study of New York City hospitals. Reporting in the March issue of Headache, Mia T. Minen, MD, MPH, and colleagues found that among patients discharged from the ED with a diagnosis of migraine, 12.5% revisit the same ED for headache more than once within six months. “Targeted interventions might … decrease the frequency of headache revisits,” said Dr. Minen and colleagues. Dr. Minen is Director of Headache Services at NYU Langone Headache Center in New York City.
Migraine causes more than 1.2 million visits to US EDs annually. Many of these visits are revisits among patients who have already been treated in an ED for migraine. Dr. Minen and colleagues sought to determine t
A Study of New York City EDs
Using the New York City Department of Health and Mental Hygiene Syndromic Surveillance database, Dr. Minen and colleagues conducted a retrospective nested cohort study. They analyzed visits from 18 New York City EDs with discharge diagnoses in the first six months of 2015. They then conducted descriptive analyses to determine the frequency of headache revisits within six months of an index ED visit for migraine and the elapsed time to revisit. Using multivariable logistic regression, the researchers assessed associations between age, sex, poverty, and revisit.
Of 1,052 ED visits with a discharge diagnosis of migraine during the first six months of 2015, 277 (26.3%) had a headache revisit within six months of their initial migraine visit, and 131 (12.5%) had two or more revisits at the same hospital. Of the revisits for headache, 9% occurred within 72 hours, and 46% occurred within 90 days of the initial migraine visit. Sex, age, and poverty were not associated with an ED revisit.
Noting that the revisit rate in New York City EDs was similar to the 30.3% revisit rate in a prior study in Maine EDs, the researchers said that frequent revisits for headache are not surprising. “Migraine is a recurrent headache disorder, and 80% of headache patients in the ED do not visit a clinic, primary care physician, or specialist before visiting the ED. In one urban ED, nearly 60% of ED patients were not instructed to follow-up with a physician, and approximately 40% were not prescribed medications.”
Potentially Preventable
Several approaches could decrease headache revisits, the researchers said. “Within the ED, the use of evidence-based algorithms can aid in the standardization of headache diagnosis and treatment. These should include the use of dexamethasone, an evidence-based intervention to decrease the frequency of moderate or severe headache within 48 hours of ED discharge.” On discharge from the ED, patients should be advised about local headache treatment facilities. “Because ED patients with migraine and psychiatric comorbidities have higher health care utilization rates than migraine patients without psychiatric comorbidities, migraine patients with comorbid psychiatric disorders could be referred to an ED case manager to ensure further intervention.” Finally, “ED revisits for headache could be mitigated by increasing the availability and access to urgent care appointments or walk-in outpatient appointments, especially during off-hour nights and weekends,” they said.
—Glenn S. Williams
Suggested Reading
Minen MT, Boubour A, Wahnich A, et al. A retrospective nested cohort study of emergency department revisits for migraine in New York City. Headache. 2018;58(3):399-406.
More than one-quarter of initial emergency department (ED) visits for migraine are followed by headache revisits in fewer than six months, according to a retrospective study of New York City hospitals. Reporting in the March issue of Headache, Mia T. Minen, MD, MPH, and colleagues found that among patients discharged from the ED with a diagnosis of migraine, 12.5% revisit the same ED for headache more than once within six months. “Targeted interventions might … decrease the frequency of headache revisits,” said Dr. Minen and colleagues. Dr. Minen is Director of Headache Services at NYU Langone Headache Center in New York City.
Migraine causes more than 1.2 million visits to US EDs annually. Many of these visits are revisits among patients who have already been treated in an ED for migraine. Dr. Minen and colleagues sought to determine t
A Study of New York City EDs
Using the New York City Department of Health and Mental Hygiene Syndromic Surveillance database, Dr. Minen and colleagues conducted a retrospective nested cohort study. They analyzed visits from 18 New York City EDs with discharge diagnoses in the first six months of 2015. They then conducted descriptive analyses to determine the frequency of headache revisits within six months of an index ED visit for migraine and the elapsed time to revisit. Using multivariable logistic regression, the researchers assessed associations between age, sex, poverty, and revisit.
Of 1,052 ED visits with a discharge diagnosis of migraine during the first six months of 2015, 277 (26.3%) had a headache revisit within six months of their initial migraine visit, and 131 (12.5%) had two or more revisits at the same hospital. Of the revisits for headache, 9% occurred within 72 hours, and 46% occurred within 90 days of the initial migraine visit. Sex, age, and poverty were not associated with an ED revisit.
Noting that the revisit rate in New York City EDs was similar to the 30.3% revisit rate in a prior study in Maine EDs, the researchers said that frequent revisits for headache are not surprising. “Migraine is a recurrent headache disorder, and 80% of headache patients in the ED do not visit a clinic, primary care physician, or specialist before visiting the ED. In one urban ED, nearly 60% of ED patients were not instructed to follow-up with a physician, and approximately 40% were not prescribed medications.”
Potentially Preventable
Several approaches could decrease headache revisits, the researchers said. “Within the ED, the use of evidence-based algorithms can aid in the standardization of headache diagnosis and treatment. These should include the use of dexamethasone, an evidence-based intervention to decrease the frequency of moderate or severe headache within 48 hours of ED discharge.” On discharge from the ED, patients should be advised about local headache treatment facilities. “Because ED patients with migraine and psychiatric comorbidities have higher health care utilization rates than migraine patients without psychiatric comorbidities, migraine patients with comorbid psychiatric disorders could be referred to an ED case manager to ensure further intervention.” Finally, “ED revisits for headache could be mitigated by increasing the availability and access to urgent care appointments or walk-in outpatient appointments, especially during off-hour nights and weekends,” they said.
—Glenn S. Williams
Suggested Reading
Minen MT, Boubour A, Wahnich A, et al. A retrospective nested cohort study of emergency department revisits for migraine in New York City. Headache. 2018;58(3):399-406.
More than one-quarter of initial emergency department (ED) visits for migraine are followed by headache revisits in fewer than six months, according to a retrospective study of New York City hospitals. Reporting in the March issue of Headache, Mia T. Minen, MD, MPH, and colleagues found that among patients discharged from the ED with a diagnosis of migraine, 12.5% revisit the same ED for headache more than once within six months. “Targeted interventions might … decrease the frequency of headache revisits,” said Dr. Minen and colleagues. Dr. Minen is Director of Headache Services at NYU Langone Headache Center in New York City.
Migraine causes more than 1.2 million visits to US EDs annually. Many of these visits are revisits among patients who have already been treated in an ED for migraine. Dr. Minen and colleagues sought to determine t
A Study of New York City EDs
Using the New York City Department of Health and Mental Hygiene Syndromic Surveillance database, Dr. Minen and colleagues conducted a retrospective nested cohort study. They analyzed visits from 18 New York City EDs with discharge diagnoses in the first six months of 2015. They then conducted descriptive analyses to determine the frequency of headache revisits within six months of an index ED visit for migraine and the elapsed time to revisit. Using multivariable logistic regression, the researchers assessed associations between age, sex, poverty, and revisit.
Of 1,052 ED visits with a discharge diagnosis of migraine during the first six months of 2015, 277 (26.3%) had a headache revisit within six months of their initial migraine visit, and 131 (12.5%) had two or more revisits at the same hospital. Of the revisits for headache, 9% occurred within 72 hours, and 46% occurred within 90 days of the initial migraine visit. Sex, age, and poverty were not associated with an ED revisit.
Noting that the revisit rate in New York City EDs was similar to the 30.3% revisit rate in a prior study in Maine EDs, the researchers said that frequent revisits for headache are not surprising. “Migraine is a recurrent headache disorder, and 80% of headache patients in the ED do not visit a clinic, primary care physician, or specialist before visiting the ED. In one urban ED, nearly 60% of ED patients were not instructed to follow-up with a physician, and approximately 40% were not prescribed medications.”
Potentially Preventable
Several approaches could decrease headache revisits, the researchers said. “Within the ED, the use of evidence-based algorithms can aid in the standardization of headache diagnosis and treatment. These should include the use of dexamethasone, an evidence-based intervention to decrease the frequency of moderate or severe headache within 48 hours of ED discharge.” On discharge from the ED, patients should be advised about local headache treatment facilities. “Because ED patients with migraine and psychiatric comorbidities have higher health care utilization rates than migraine patients without psychiatric comorbidities, migraine patients with comorbid psychiatric disorders could be referred to an ED case manager to ensure further intervention.” Finally, “ED revisits for headache could be mitigated by increasing the availability and access to urgent care appointments or walk-in outpatient appointments, especially during off-hour nights and weekends,” they said.
—Glenn S. Williams
Suggested Reading
Minen MT, Boubour A, Wahnich A, et al. A retrospective nested cohort study of emergency department revisits for migraine in New York City. Headache. 2018;58(3):399-406.