User login
New study establishes IBD severity index
Experts have established a severity index for inflammatory bowel disease (IBD), according to results of an analysis published in the journal Gut (doi: 10.1136/gutjnl-2016-312648).
The index, conceived by a panel of IBD specialists from the International Organization for the Study of Inflammatory Bowel Diseases, is a step toward the standardization of disease severity definitions in ulcerative colitis and Crohn’s disease.
The panel determined 16 severity attributes for Crohn’s disease and 13 for ulcerative colitis. The analysis found that, in Crohn’s disease, mucosal lesions, fistulas, and abscesses were the greatest contributors to disease severity at 15.8%, 10.9%, and 9.7%, respectively. In ulcerative colitis, 18.1% of disease severity was attributed to mucosal lesions, 14% to impact on daily activities, and 11.2% to C-reactive protein, wrote Corey A. Siegel, MD, MS, of the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and his coauthors.
Investigators used a PubMed literature search to identify three broad elements of disease severity: impact of disease symptoms on daily activities, inflammatory burden, and disease course.
A panel of 16 experts then conducted a series of votes to determine which attributes within each domain would be used to assess disease severity. Two sets of attributes were defined as disease markers in Crohn’s disease and ulcerative colitis.
A type of conjoint analysis called adaptive choice-based conjoint was then performed to ascertain how different clinical factors influenced specialists’ decision making and impressions of disease severity.
A series of questions was asked, with each response determining subsequent questions, until “ample consistency” was found in their choices.
The exercise first had participants decide which hypothetical patient profiles met their evaluation criteria; it then showed them two final profiles and asked which was the more severe case. Survey length depended on the consistency of participants’ responses, with those lacking consistency being given more tasks to complete, Dr. Siegel and his colleagues reported.
Respondents completed the exercise three times: first independently without discussion, then after discussion in a group setting with an automated response system, and finally, independently following group discussion.
Disease severity indexes were created on a 100-point scale, and average part-worth utility scores were used to determine minimum and maximum scores for each attribute, with zero representing the absence of a symptom.
This analysis “helps redefine overall disease severity for IBD,” the authors wrote. Once validated, the indexes will offer “both further research opportunities and a practical tool by which to classify overall disease severity of patients and offer appropriate treatment without relying on present symptoms alone,” they added.
Dr. Siegel and his colleagues noted that future studies should focus on prospective validation of the disease indexes in different patient populations, as well as conducting a conjoint analysis with patients.
“We expect this work to begin to address a change in how we think about patients with IBD and how to identify those at the higher end of the risk spectrum so that appropriate intensive treatment can be initiated and optimized in an efficient, precise, and cost-effective manner,” they concluded.
The study was funded by AbbVie and Tillotts Pharma. The authors disclosed financial relationships with numerous additional pharmaceutical companies.
SOURCE: Siegel CA et al. Gut. 2018 Feb;67(2):244-54.
AGA patient education materials can help your IBD patients better understand and manage their disease. Learn more at www.gastro.org/IBD
Experts have established a severity index for inflammatory bowel disease (IBD), according to results of an analysis published in the journal Gut (doi: 10.1136/gutjnl-2016-312648).
The index, conceived by a panel of IBD specialists from the International Organization for the Study of Inflammatory Bowel Diseases, is a step toward the standardization of disease severity definitions in ulcerative colitis and Crohn’s disease.
The panel determined 16 severity attributes for Crohn’s disease and 13 for ulcerative colitis. The analysis found that, in Crohn’s disease, mucosal lesions, fistulas, and abscesses were the greatest contributors to disease severity at 15.8%, 10.9%, and 9.7%, respectively. In ulcerative colitis, 18.1% of disease severity was attributed to mucosal lesions, 14% to impact on daily activities, and 11.2% to C-reactive protein, wrote Corey A. Siegel, MD, MS, of the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and his coauthors.
Investigators used a PubMed literature search to identify three broad elements of disease severity: impact of disease symptoms on daily activities, inflammatory burden, and disease course.
A panel of 16 experts then conducted a series of votes to determine which attributes within each domain would be used to assess disease severity. Two sets of attributes were defined as disease markers in Crohn’s disease and ulcerative colitis.
A type of conjoint analysis called adaptive choice-based conjoint was then performed to ascertain how different clinical factors influenced specialists’ decision making and impressions of disease severity.
A series of questions was asked, with each response determining subsequent questions, until “ample consistency” was found in their choices.
The exercise first had participants decide which hypothetical patient profiles met their evaluation criteria; it then showed them two final profiles and asked which was the more severe case. Survey length depended on the consistency of participants’ responses, with those lacking consistency being given more tasks to complete, Dr. Siegel and his colleagues reported.
Respondents completed the exercise three times: first independently without discussion, then after discussion in a group setting with an automated response system, and finally, independently following group discussion.
Disease severity indexes were created on a 100-point scale, and average part-worth utility scores were used to determine minimum and maximum scores for each attribute, with zero representing the absence of a symptom.
This analysis “helps redefine overall disease severity for IBD,” the authors wrote. Once validated, the indexes will offer “both further research opportunities and a practical tool by which to classify overall disease severity of patients and offer appropriate treatment without relying on present symptoms alone,” they added.
Dr. Siegel and his colleagues noted that future studies should focus on prospective validation of the disease indexes in different patient populations, as well as conducting a conjoint analysis with patients.
“We expect this work to begin to address a change in how we think about patients with IBD and how to identify those at the higher end of the risk spectrum so that appropriate intensive treatment can be initiated and optimized in an efficient, precise, and cost-effective manner,” they concluded.
The study was funded by AbbVie and Tillotts Pharma. The authors disclosed financial relationships with numerous additional pharmaceutical companies.
SOURCE: Siegel CA et al. Gut. 2018 Feb;67(2):244-54.
AGA patient education materials can help your IBD patients better understand and manage their disease. Learn more at www.gastro.org/IBD
Experts have established a severity index for inflammatory bowel disease (IBD), according to results of an analysis published in the journal Gut (doi: 10.1136/gutjnl-2016-312648).
The index, conceived by a panel of IBD specialists from the International Organization for the Study of Inflammatory Bowel Diseases, is a step toward the standardization of disease severity definitions in ulcerative colitis and Crohn’s disease.
The panel determined 16 severity attributes for Crohn’s disease and 13 for ulcerative colitis. The analysis found that, in Crohn’s disease, mucosal lesions, fistulas, and abscesses were the greatest contributors to disease severity at 15.8%, 10.9%, and 9.7%, respectively. In ulcerative colitis, 18.1% of disease severity was attributed to mucosal lesions, 14% to impact on daily activities, and 11.2% to C-reactive protein, wrote Corey A. Siegel, MD, MS, of the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and his coauthors.
Investigators used a PubMed literature search to identify three broad elements of disease severity: impact of disease symptoms on daily activities, inflammatory burden, and disease course.
A panel of 16 experts then conducted a series of votes to determine which attributes within each domain would be used to assess disease severity. Two sets of attributes were defined as disease markers in Crohn’s disease and ulcerative colitis.
A type of conjoint analysis called adaptive choice-based conjoint was then performed to ascertain how different clinical factors influenced specialists’ decision making and impressions of disease severity.
A series of questions was asked, with each response determining subsequent questions, until “ample consistency” was found in their choices.
The exercise first had participants decide which hypothetical patient profiles met their evaluation criteria; it then showed them two final profiles and asked which was the more severe case. Survey length depended on the consistency of participants’ responses, with those lacking consistency being given more tasks to complete, Dr. Siegel and his colleagues reported.
Respondents completed the exercise three times: first independently without discussion, then after discussion in a group setting with an automated response system, and finally, independently following group discussion.
Disease severity indexes were created on a 100-point scale, and average part-worth utility scores were used to determine minimum and maximum scores for each attribute, with zero representing the absence of a symptom.
This analysis “helps redefine overall disease severity for IBD,” the authors wrote. Once validated, the indexes will offer “both further research opportunities and a practical tool by which to classify overall disease severity of patients and offer appropriate treatment without relying on present symptoms alone,” they added.
Dr. Siegel and his colleagues noted that future studies should focus on prospective validation of the disease indexes in different patient populations, as well as conducting a conjoint analysis with patients.
“We expect this work to begin to address a change in how we think about patients with IBD and how to identify those at the higher end of the risk spectrum so that appropriate intensive treatment can be initiated and optimized in an efficient, precise, and cost-effective manner,” they concluded.
The study was funded by AbbVie and Tillotts Pharma. The authors disclosed financial relationships with numerous additional pharmaceutical companies.
SOURCE: Siegel CA et al. Gut. 2018 Feb;67(2):244-54.
AGA patient education materials can help your IBD patients better understand and manage their disease. Learn more at www.gastro.org/IBD
FROM GUT
Does measuring episiotomy rates really benefit the quality of care our patients receive?
Like most California institutions performing deliveries, St. Joseph Hospital in Orange, California, started releasing 2016 maternal quality metrics internally at first. Data for the first 9 months of 2016 were distributed in December 2016. These metrics depend on a denominator based on the number of deliveries attributed to each obstetrician.
- I was very pleased to see that I ranked first in the vaginal birth after cesarean (VBAC) rate at 36.8%.
- I also was pleased that I ranked the fourth lowest, at 15.9%, for my cesarean delivery rate in the low-risk, nulliparous term singleton vertex (NTSV) population.
- I was neither pleased nor displeased that I ranked number 29 of 31 physicians at 59.1% (39/66) for the episiotomy rate. The denominator range was 1 to 287. I knew I would hear about this! Sure enough, a medical director asked me how 2 of my metrics could be so good, yet the third be so abysmal.
After the release of the data and the somewhat humorous chastisement by the medical director, I decided to try complying with the new American College of Obstetricians and Gynecologists (ACOG) guidelines1 again beginning in January 2017.
A little personal history
Allow me to date myself. I completed my residency in 1981 and was Board Certified in 1984. My wife refers to me as a “Dinosaur!” As an ObGyn in solo practice, I take my own call.
During my training, episiotomies were commonly performed but were not always necessary. We were taught to not perform an episiotomy if the patient could safely and easily deliver without one. However, if clinically indicated, an episiotomy should be performed. If a 3rd- or 4th-degree laceration occurred, we were taught to anatomically repair it. Nowadays in my practice, these lacerations are rare in conjunction with an episiotomy, and with a controlled delivery of the fetal head.
Our nursing staff will tell you that I resist change. However, I usually attempt and often do adapt the latest national guidelines into my practice. Although I did not agree when restrictive episiotomies became a national goal a few years ago, I tried to adhere to the new national episiotomy recommendations.1 I am meticulous: a standard episiotomy repair that does not involve excessive bleeding usually takes 20 minutes to restore normal anatomy with a simple, straightforward, layered closure.
My episiotomy performance record
In 2015, I restricted my use of episiotomies. When I did not perform one, the patient usually experienced lacerations. These were labial or periurethral as well as complex 3-dimensional “Z” or “Y” shaped vaginal/perineal lacerations, not just the 1st- and 2nd-degree perineal lacerations to which the literature refers.
The problems associated with complex, geometric vaginal lacerations are multifactorial:
- Lacerations occur at multiple locations.
- Significant bleeding often occurs. Because the lacerations are in multiple locations, the bleeding cannot be addressed easily, quickly, or at once.
- Visualization is difficult because of the bleeding, thus further prolonging the repair.
- These lacerations are often deeper than an episiotomy would have been and are very friable as all the layers have been stretched to their breaking point before tearing.
- Sometimes the lacerations include avulsion of the hymen with extensive bleeding.
- Difficult-to-repair lacerations can tear upon suturing, requiring layer upon layer of sutures at the same site. Future scarring and vaginal stricture leading to sexual dysfunction are concerns.
- At times, the friability and bleeding is so brisk that once the bleeding is controlled and the episiotomy is partially repaired, I can see that it is has not been an anatomic repair. I then have to take it down and re-do the repair with an obscured field from bleeding again!
- Some repairs are so fragile that when I express retained blood from the uterus and upper vagina after completing the repair, the tissue tears, bleeds, and requires additional restoration.
- These tears usually require an hour to repair and achieve hemostasis. At times, an assistant and a retractor are necessary.
After 2015, when I spent the year complying with the new guidelines, I returned to my original protocol: I performed an episiotomy only when I thought the patient was going to experience a significant laceration. I did not perform an episiotomy if I thought the mother could deliver easily without one. That is how I attained the 59.1% episiotomy rate in 2016.
Another try
After the 2016 hospital data were released, I decided to comply with the new guidelines1 again beginning in January 2017. Here I share the details of 3 deliveries that occurred in 2017:
- A 30-year-old woman (G2P1) planned to have a repeat cesarean delivery. At 38 3/7 weeks’ gestation, she was admitted in active labor with the cervix dilated to 5 cm. She requested a VBAC. After successful vaginal delivery without episiotomy of a 7 lb 5 oz infant, there were bilateral periurethral and right labia minora abrasions/lacerations.
- A 21-year-old woman (G1P0) at 40 4/7 weeks’ gestation was admitted in early labor. The cervix was 2-cm dilated and 70% effaced after spontaneous rupture of membranes. I exercised my clinical judgment and performed a midline episiotomy. A 9 lb 3 oz infant was delivered by vaginal delivery.
- A 16-year-old woman (G1P0) at 41 weeks’ gestation was admitted for induction of labor with an unripe cervix. I was delayed, and the laborist performed a vaginal delivery after 1 attempt at vacuum extraction and no episiotomy. The 7 lb 3 oz baby had Apgar scores of 4 and 9 at 1 and 5 minutes, respectively. There was significant bleeding from bilateral vaginal lacerations with bilateral hymeneal avulsions.
What is the benefit?
Are we really benefitting our patients by restricting the use of episiotomy? Consider these questions:
- Should we delay the mother’s bonding with her baby for an hour’s complex repair versus 20 minutes for a simple, layered episiotomy repair?
- In a busy labor and delivery unit, should resources be tied up for this extra time? With all due respect to the national experts advocating this recommendation, are they in the trenches performing deliveries and spending hours repairing complex lacerations?
- Should we not use our clinical judgment instead of allowing the mother to experience an extensive vaginal/perineal laceration after a vaginal delivery of a 9- or 10-lb baby?
- Where are the long-term data showing that it is better for a woman to stretch and attenuate her perineal and vaginal muscles to the breaking point, and then tear?
- Do all the additional sutures lead to vaginal scarring, vaginal stricture, and sexual dysfunction in later years?
- Which protocol better enables the mother to maintain pelvic organ support and avoid pelvic organ prolapse and stress urinary incontinence?
In Williams Obstetrics, the authors state: “We are of the view that episiotomy should be applied selectively for the appropriate indications. The final rule is that there is no substitute for surgical judgment and common sense.”2
Consider other metrics
Patients might be better served by measuring quality and safety metrics other than episiotomy. These might include, for example, measuring:
- the use of prophylactic oxytocin after the anterior shoulder is delivered in order to decrease the risk of postpartum hemorrhage, as advocated by the California Maternal Quality Care Collaborative3
- the number of patients admitted before active labor and those receiving an epidural before active labor (with the aim of decreasing the primary cesarean rate in the NTSV population)
- the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, in whom no interventions have been instituted to improve the labor pattern, and who subsequently deliver by primary cesarean.
Recommendation
I recommend that performing an episiotomy should be an individual clinical decision for the individual patient by the individual obstetrician, and not a national mandate. We can provide quality care to our patients by performing selective episiotomies when clinically necessary, and not avoid them to an extreme that harms our patients. In my opinion, using the episiotomy rate as a quality metric should be abandoned.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- CambriaAmerican College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1Times New Roman MT Std–e15.
- Vaginal delivery. In: Cunnigham FG, Leveno KJ, Bloom SL, et al, eds. Williams Obstetrics. 24th ed. New York, NY: McGraw-Hill Medical; 2014:550.
- CMQCC: California Maternal Quality Care Collaborative website. https://www.cmqcc.org/. Accessed March 12, 2018.
Like most California institutions performing deliveries, St. Joseph Hospital in Orange, California, started releasing 2016 maternal quality metrics internally at first. Data for the first 9 months of 2016 were distributed in December 2016. These metrics depend on a denominator based on the number of deliveries attributed to each obstetrician.
- I was very pleased to see that I ranked first in the vaginal birth after cesarean (VBAC) rate at 36.8%.
- I also was pleased that I ranked the fourth lowest, at 15.9%, for my cesarean delivery rate in the low-risk, nulliparous term singleton vertex (NTSV) population.
- I was neither pleased nor displeased that I ranked number 29 of 31 physicians at 59.1% (39/66) for the episiotomy rate. The denominator range was 1 to 287. I knew I would hear about this! Sure enough, a medical director asked me how 2 of my metrics could be so good, yet the third be so abysmal.
After the release of the data and the somewhat humorous chastisement by the medical director, I decided to try complying with the new American College of Obstetricians and Gynecologists (ACOG) guidelines1 again beginning in January 2017.
A little personal history
Allow me to date myself. I completed my residency in 1981 and was Board Certified in 1984. My wife refers to me as a “Dinosaur!” As an ObGyn in solo practice, I take my own call.
During my training, episiotomies were commonly performed but were not always necessary. We were taught to not perform an episiotomy if the patient could safely and easily deliver without one. However, if clinically indicated, an episiotomy should be performed. If a 3rd- or 4th-degree laceration occurred, we were taught to anatomically repair it. Nowadays in my practice, these lacerations are rare in conjunction with an episiotomy, and with a controlled delivery of the fetal head.
Our nursing staff will tell you that I resist change. However, I usually attempt and often do adapt the latest national guidelines into my practice. Although I did not agree when restrictive episiotomies became a national goal a few years ago, I tried to adhere to the new national episiotomy recommendations.1 I am meticulous: a standard episiotomy repair that does not involve excessive bleeding usually takes 20 minutes to restore normal anatomy with a simple, straightforward, layered closure.
My episiotomy performance record
In 2015, I restricted my use of episiotomies. When I did not perform one, the patient usually experienced lacerations. These were labial or periurethral as well as complex 3-dimensional “Z” or “Y” shaped vaginal/perineal lacerations, not just the 1st- and 2nd-degree perineal lacerations to which the literature refers.
The problems associated with complex, geometric vaginal lacerations are multifactorial:
- Lacerations occur at multiple locations.
- Significant bleeding often occurs. Because the lacerations are in multiple locations, the bleeding cannot be addressed easily, quickly, or at once.
- Visualization is difficult because of the bleeding, thus further prolonging the repair.
- These lacerations are often deeper than an episiotomy would have been and are very friable as all the layers have been stretched to their breaking point before tearing.
- Sometimes the lacerations include avulsion of the hymen with extensive bleeding.
- Difficult-to-repair lacerations can tear upon suturing, requiring layer upon layer of sutures at the same site. Future scarring and vaginal stricture leading to sexual dysfunction are concerns.
- At times, the friability and bleeding is so brisk that once the bleeding is controlled and the episiotomy is partially repaired, I can see that it is has not been an anatomic repair. I then have to take it down and re-do the repair with an obscured field from bleeding again!
- Some repairs are so fragile that when I express retained blood from the uterus and upper vagina after completing the repair, the tissue tears, bleeds, and requires additional restoration.
- These tears usually require an hour to repair and achieve hemostasis. At times, an assistant and a retractor are necessary.
After 2015, when I spent the year complying with the new guidelines, I returned to my original protocol: I performed an episiotomy only when I thought the patient was going to experience a significant laceration. I did not perform an episiotomy if I thought the mother could deliver easily without one. That is how I attained the 59.1% episiotomy rate in 2016.
Another try
After the 2016 hospital data were released, I decided to comply with the new guidelines1 again beginning in January 2017. Here I share the details of 3 deliveries that occurred in 2017:
- A 30-year-old woman (G2P1) planned to have a repeat cesarean delivery. At 38 3/7 weeks’ gestation, she was admitted in active labor with the cervix dilated to 5 cm. She requested a VBAC. After successful vaginal delivery without episiotomy of a 7 lb 5 oz infant, there were bilateral periurethral and right labia minora abrasions/lacerations.
- A 21-year-old woman (G1P0) at 40 4/7 weeks’ gestation was admitted in early labor. The cervix was 2-cm dilated and 70% effaced after spontaneous rupture of membranes. I exercised my clinical judgment and performed a midline episiotomy. A 9 lb 3 oz infant was delivered by vaginal delivery.
- A 16-year-old woman (G1P0) at 41 weeks’ gestation was admitted for induction of labor with an unripe cervix. I was delayed, and the laborist performed a vaginal delivery after 1 attempt at vacuum extraction and no episiotomy. The 7 lb 3 oz baby had Apgar scores of 4 and 9 at 1 and 5 minutes, respectively. There was significant bleeding from bilateral vaginal lacerations with bilateral hymeneal avulsions.
What is the benefit?
Are we really benefitting our patients by restricting the use of episiotomy? Consider these questions:
- Should we delay the mother’s bonding with her baby for an hour’s complex repair versus 20 minutes for a simple, layered episiotomy repair?
- In a busy labor and delivery unit, should resources be tied up for this extra time? With all due respect to the national experts advocating this recommendation, are they in the trenches performing deliveries and spending hours repairing complex lacerations?
- Should we not use our clinical judgment instead of allowing the mother to experience an extensive vaginal/perineal laceration after a vaginal delivery of a 9- or 10-lb baby?
- Where are the long-term data showing that it is better for a woman to stretch and attenuate her perineal and vaginal muscles to the breaking point, and then tear?
- Do all the additional sutures lead to vaginal scarring, vaginal stricture, and sexual dysfunction in later years?
- Which protocol better enables the mother to maintain pelvic organ support and avoid pelvic organ prolapse and stress urinary incontinence?
In Williams Obstetrics, the authors state: “We are of the view that episiotomy should be applied selectively for the appropriate indications. The final rule is that there is no substitute for surgical judgment and common sense.”2
Consider other metrics
Patients might be better served by measuring quality and safety metrics other than episiotomy. These might include, for example, measuring:
- the use of prophylactic oxytocin after the anterior shoulder is delivered in order to decrease the risk of postpartum hemorrhage, as advocated by the California Maternal Quality Care Collaborative3
- the number of patients admitted before active labor and those receiving an epidural before active labor (with the aim of decreasing the primary cesarean rate in the NTSV population)
- the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, in whom no interventions have been instituted to improve the labor pattern, and who subsequently deliver by primary cesarean.
Recommendation
I recommend that performing an episiotomy should be an individual clinical decision for the individual patient by the individual obstetrician, and not a national mandate. We can provide quality care to our patients by performing selective episiotomies when clinically necessary, and not avoid them to an extreme that harms our patients. In my opinion, using the episiotomy rate as a quality metric should be abandoned.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Like most California institutions performing deliveries, St. Joseph Hospital in Orange, California, started releasing 2016 maternal quality metrics internally at first. Data for the first 9 months of 2016 were distributed in December 2016. These metrics depend on a denominator based on the number of deliveries attributed to each obstetrician.
- I was very pleased to see that I ranked first in the vaginal birth after cesarean (VBAC) rate at 36.8%.
- I also was pleased that I ranked the fourth lowest, at 15.9%, for my cesarean delivery rate in the low-risk, nulliparous term singleton vertex (NTSV) population.
- I was neither pleased nor displeased that I ranked number 29 of 31 physicians at 59.1% (39/66) for the episiotomy rate. The denominator range was 1 to 287. I knew I would hear about this! Sure enough, a medical director asked me how 2 of my metrics could be so good, yet the third be so abysmal.
After the release of the data and the somewhat humorous chastisement by the medical director, I decided to try complying with the new American College of Obstetricians and Gynecologists (ACOG) guidelines1 again beginning in January 2017.
A little personal history
Allow me to date myself. I completed my residency in 1981 and was Board Certified in 1984. My wife refers to me as a “Dinosaur!” As an ObGyn in solo practice, I take my own call.
During my training, episiotomies were commonly performed but were not always necessary. We were taught to not perform an episiotomy if the patient could safely and easily deliver without one. However, if clinically indicated, an episiotomy should be performed. If a 3rd- or 4th-degree laceration occurred, we were taught to anatomically repair it. Nowadays in my practice, these lacerations are rare in conjunction with an episiotomy, and with a controlled delivery of the fetal head.
Our nursing staff will tell you that I resist change. However, I usually attempt and often do adapt the latest national guidelines into my practice. Although I did not agree when restrictive episiotomies became a national goal a few years ago, I tried to adhere to the new national episiotomy recommendations.1 I am meticulous: a standard episiotomy repair that does not involve excessive bleeding usually takes 20 minutes to restore normal anatomy with a simple, straightforward, layered closure.
My episiotomy performance record
In 2015, I restricted my use of episiotomies. When I did not perform one, the patient usually experienced lacerations. These were labial or periurethral as well as complex 3-dimensional “Z” or “Y” shaped vaginal/perineal lacerations, not just the 1st- and 2nd-degree perineal lacerations to which the literature refers.
The problems associated with complex, geometric vaginal lacerations are multifactorial:
- Lacerations occur at multiple locations.
- Significant bleeding often occurs. Because the lacerations are in multiple locations, the bleeding cannot be addressed easily, quickly, or at once.
- Visualization is difficult because of the bleeding, thus further prolonging the repair.
- These lacerations are often deeper than an episiotomy would have been and are very friable as all the layers have been stretched to their breaking point before tearing.
- Sometimes the lacerations include avulsion of the hymen with extensive bleeding.
- Difficult-to-repair lacerations can tear upon suturing, requiring layer upon layer of sutures at the same site. Future scarring and vaginal stricture leading to sexual dysfunction are concerns.
- At times, the friability and bleeding is so brisk that once the bleeding is controlled and the episiotomy is partially repaired, I can see that it is has not been an anatomic repair. I then have to take it down and re-do the repair with an obscured field from bleeding again!
- Some repairs are so fragile that when I express retained blood from the uterus and upper vagina after completing the repair, the tissue tears, bleeds, and requires additional restoration.
- These tears usually require an hour to repair and achieve hemostasis. At times, an assistant and a retractor are necessary.
After 2015, when I spent the year complying with the new guidelines, I returned to my original protocol: I performed an episiotomy only when I thought the patient was going to experience a significant laceration. I did not perform an episiotomy if I thought the mother could deliver easily without one. That is how I attained the 59.1% episiotomy rate in 2016.
Another try
After the 2016 hospital data were released, I decided to comply with the new guidelines1 again beginning in January 2017. Here I share the details of 3 deliveries that occurred in 2017:
- A 30-year-old woman (G2P1) planned to have a repeat cesarean delivery. At 38 3/7 weeks’ gestation, she was admitted in active labor with the cervix dilated to 5 cm. She requested a VBAC. After successful vaginal delivery without episiotomy of a 7 lb 5 oz infant, there were bilateral periurethral and right labia minora abrasions/lacerations.
- A 21-year-old woman (G1P0) at 40 4/7 weeks’ gestation was admitted in early labor. The cervix was 2-cm dilated and 70% effaced after spontaneous rupture of membranes. I exercised my clinical judgment and performed a midline episiotomy. A 9 lb 3 oz infant was delivered by vaginal delivery.
- A 16-year-old woman (G1P0) at 41 weeks’ gestation was admitted for induction of labor with an unripe cervix. I was delayed, and the laborist performed a vaginal delivery after 1 attempt at vacuum extraction and no episiotomy. The 7 lb 3 oz baby had Apgar scores of 4 and 9 at 1 and 5 minutes, respectively. There was significant bleeding from bilateral vaginal lacerations with bilateral hymeneal avulsions.
What is the benefit?
Are we really benefitting our patients by restricting the use of episiotomy? Consider these questions:
- Should we delay the mother’s bonding with her baby for an hour’s complex repair versus 20 minutes for a simple, layered episiotomy repair?
- In a busy labor and delivery unit, should resources be tied up for this extra time? With all due respect to the national experts advocating this recommendation, are they in the trenches performing deliveries and spending hours repairing complex lacerations?
- Should we not use our clinical judgment instead of allowing the mother to experience an extensive vaginal/perineal laceration after a vaginal delivery of a 9- or 10-lb baby?
- Where are the long-term data showing that it is better for a woman to stretch and attenuate her perineal and vaginal muscles to the breaking point, and then tear?
- Do all the additional sutures lead to vaginal scarring, vaginal stricture, and sexual dysfunction in later years?
- Which protocol better enables the mother to maintain pelvic organ support and avoid pelvic organ prolapse and stress urinary incontinence?
In Williams Obstetrics, the authors state: “We are of the view that episiotomy should be applied selectively for the appropriate indications. The final rule is that there is no substitute for surgical judgment and common sense.”2
Consider other metrics
Patients might be better served by measuring quality and safety metrics other than episiotomy. These might include, for example, measuring:
- the use of prophylactic oxytocin after the anterior shoulder is delivered in order to decrease the risk of postpartum hemorrhage, as advocated by the California Maternal Quality Care Collaborative3
- the number of patients admitted before active labor and those receiving an epidural before active labor (with the aim of decreasing the primary cesarean rate in the NTSV population)
- the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, in whom no interventions have been instituted to improve the labor pattern, and who subsequently deliver by primary cesarean.
Recommendation
I recommend that performing an episiotomy should be an individual clinical decision for the individual patient by the individual obstetrician, and not a national mandate. We can provide quality care to our patients by performing selective episiotomies when clinically necessary, and not avoid them to an extreme that harms our patients. In my opinion, using the episiotomy rate as a quality metric should be abandoned.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- CambriaAmerican College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1Times New Roman MT Std–e15.
- Vaginal delivery. In: Cunnigham FG, Leveno KJ, Bloom SL, et al, eds. Williams Obstetrics. 24th ed. New York, NY: McGraw-Hill Medical; 2014:550.
- CMQCC: California Maternal Quality Care Collaborative website. https://www.cmqcc.org/. Accessed March 12, 2018.
- CambriaAmerican College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1Times New Roman MT Std–e15.
- Vaginal delivery. In: Cunnigham FG, Leveno KJ, Bloom SL, et al, eds. Williams Obstetrics. 24th ed. New York, NY: McGraw-Hill Medical; 2014:550.
- CMQCC: California Maternal Quality Care Collaborative website. https://www.cmqcc.org/. Accessed March 12, 2018.
VIDEO: Interventions target opioid overprescribing after gynecologic surgery
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – U.S. clinicians prescribe opioid tablets to postsurgical patients too often and at too high a pill count, according to results from two independent studies that examined prescribing patterns and opioid use in patients following gynecologic surgery.
In addition, “setting preoperative expectations about pain management led to increased compliance at discharge,” said Dr. Mark, a gynecologic oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
Findings from the second study, of 122 women who underwent gynecologic surgery at Women and Infants Hospital in Providence, R.I., showed that 32% did not use any opioids for pain following hospital discharge, and that opioid use during hospitalization was a significant predictor of postdischarge opioid needs. This finding provided a way to devise a new prescribing guide for postsurgical patients based on their opioid use while hospitalized, said Erica Weston, MD, a gynecologic oncologist at Johns Hopkins University, Baltimore.

“No question, we are overprescribing,” Dr. Dowdy said, and described a program he and his colleagues at Mayo recently put in place that capped routine opioid pill prescriptions following various surgeries based on historic patient needs. For example, most laparotomy patients receive a prescription for 10 opioid doses on discharge. Based on the first 6 months of this program, it’s on track to cut the annual number of opioid tablets prescribed to postsurgical patients at Mayo by 35,000 for all gynecologic surgeries and by 1.5 million tablets for all Mayo surgical subspecialties, he said.
The study reported by Dr. Mark ran after the Roswell Park gynecologic oncology department implemented new guidelines for dispensing pain control medications following surgery. The guidelines called for comprehensive teaching for patients about pain expectations and pain management both before and after surgery and also established four dispensing categories:
- Patients undergoing minimally invasive or outpatient surgery and with no history of chronic pain and low opioid need while hospitalized received the default dispense of 600 mg ibuprofen every 6 hours as needed for 7 days and 500 mg acetaminophen every 6 hours as needed for 7 days.
- Patients who underwent this surgery but required 5 or more opioid tablets while hospitalized or those with a history of chronic pain and opioid use received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply with 1 tablet taken every 6 hours as needed.
- Patients who underwent laparotomy and had no chronic pain and opioid history and low opioid use while hospitalized received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply.
- Patients who underwent laparotomy and showed a higher opioid need based on their use during the 24 hours before discharge received the ibuprofen and acetaminophen regimen plus 24 opioid tablets for 3 days so they could take 2 tablets every 6 hours as needed.
Dr. Mark and his associates collected data from 337 patients managed with these guidelines during June 2017–January 2018 and compared them with 626 patients who underwent gynecologic surgery at Roswell Park during July 2016–June 2017. The data showed the average number of opioid tablets dispensed per patient for all discharges fell from 31.7 before the new guideline to 3.5, an 89% reduction. For the subgroup of patients who had undergone a laparotomy, the average pill number fell from 43.6 to 11.6, a 72% drop. Among patients treated with minimally invasive or outpatient surgery, average tablets dispensed fell from 28.1 before to 0.9 after, a 97% reduction. The reduction among opioid-naive patients was 90%, and it was 83% among patients who used opioids prior to their surgery.
Under the new program, patients requested an opioid refill 14% of the time after laparotomy and 8% of the time after minimally invasive surgery, rates that did not significantly differ from the prior era. Average postoperative pain scores were identical among patients treated under the new dispensing guidelines and those treated during the prior years, and 96% of patients said they were satisfied with the care they received during the new, restricted dispensing period, Dr. Mark reported.
The single-center experience reviewed by Dr. Weston tracked opioid use by 122 women who underwent a minimally invasive hysterectomy at Women and Infants both as inpatients and out to both 1-2 weeks and 4-6 weeks following discharge. The patients were an average age of 61 years, and included 16% who reported chronic pain and 5% with a history of chronic opioid use.
During the inpatient phase, median opioid use was three doses, with 25% of the patients using no opioids. During the first 1-2 weeks following discharge, median opioid use was nine tablets, with 37% of the patients using no opioids. By the 4- to 6-week follow-up (which collected data from 114 of the patients), median opioid use was a cumulative 11 tablets with 67% of the patients reporting no opioid use during the time between their first and second follow-up visit. During the total postdischarge period, 90% of the patients used 30 or fewer opioid tablets.
A multivariate analysis of the findings showed that opioid use while in hospital was the only significant predictor of opioid use after discharge. Age of 65 years or older showed a nonsignificant trend toward less postdischarge opioid use.
Based on these data Dr. Weston and her associates proposed a formula for estimating a patient’s opioid needs at discharge: Gynecologic surgery patients who needed no opioid medication as inpatients could receive 1-5 opioid tablets at discharge, patients who used opioids at or below the median level should receive 10-15 tablets at discharge, and those who used more than the median number of opioid tablets as inpatients should receive 25-30 tablets at discharge. For patients who undergo surgery as outpatients and have no record of pain medication needs, Dr. Weston recommended discharging them with a prescription for 25-30 tablets, possibly reducing this to 10-15 tablets for patients aged 65 years or older.
Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
SOURCE: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
The important and thought provoking reports by Dr. Mark and by Dr. Weston and their associates present innovative ways for clinicians to address the opioid crisis by prescribing fewer narcotics to postsurgical patients when they leave the hospital. Their work suggests that doing this can have little or no negative impact on patient satisfaction with their care. Their findings give us important documentation for prescribing fewer opioid tablets, while still giving patients adequate pain relief.

Their findings also provide clear documentation that, in current practice, without guidance like this opioids are often overprescribed, not out of negligence but because clinicians are simply not sure what a patient will need once they go home following gynecologic surgery. By reviewing the pain medication a patient needed in hospital we can better estimate what patients will need when they go home, and we can better avoid giving patients more opioid tablets than they will really need.
Brent Smith, MD , is a gynecologic oncologist at Ohio State University, Columbus. He had no disclosures. Dr. Smith made these comments in a video interview.
The important and thought provoking reports by Dr. Mark and by Dr. Weston and their associates present innovative ways for clinicians to address the opioid crisis by prescribing fewer narcotics to postsurgical patients when they leave the hospital. Their work suggests that doing this can have little or no negative impact on patient satisfaction with their care. Their findings give us important documentation for prescribing fewer opioid tablets, while still giving patients adequate pain relief.

Their findings also provide clear documentation that, in current practice, without guidance like this opioids are often overprescribed, not out of negligence but because clinicians are simply not sure what a patient will need once they go home following gynecologic surgery. By reviewing the pain medication a patient needed in hospital we can better estimate what patients will need when they go home, and we can better avoid giving patients more opioid tablets than they will really need.
Brent Smith, MD , is a gynecologic oncologist at Ohio State University, Columbus. He had no disclosures. Dr. Smith made these comments in a video interview.
The important and thought provoking reports by Dr. Mark and by Dr. Weston and their associates present innovative ways for clinicians to address the opioid crisis by prescribing fewer narcotics to postsurgical patients when they leave the hospital. Their work suggests that doing this can have little or no negative impact on patient satisfaction with their care. Their findings give us important documentation for prescribing fewer opioid tablets, while still giving patients adequate pain relief.

Their findings also provide clear documentation that, in current practice, without guidance like this opioids are often overprescribed, not out of negligence but because clinicians are simply not sure what a patient will need once they go home following gynecologic surgery. By reviewing the pain medication a patient needed in hospital we can better estimate what patients will need when they go home, and we can better avoid giving patients more opioid tablets than they will really need.
Brent Smith, MD , is a gynecologic oncologist at Ohio State University, Columbus. He had no disclosures. Dr. Smith made these comments in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – U.S. clinicians prescribe opioid tablets to postsurgical patients too often and at too high a pill count, according to results from two independent studies that examined prescribing patterns and opioid use in patients following gynecologic surgery.
In addition, “setting preoperative expectations about pain management led to increased compliance at discharge,” said Dr. Mark, a gynecologic oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
Findings from the second study, of 122 women who underwent gynecologic surgery at Women and Infants Hospital in Providence, R.I., showed that 32% did not use any opioids for pain following hospital discharge, and that opioid use during hospitalization was a significant predictor of postdischarge opioid needs. This finding provided a way to devise a new prescribing guide for postsurgical patients based on their opioid use while hospitalized, said Erica Weston, MD, a gynecologic oncologist at Johns Hopkins University, Baltimore.

“No question, we are overprescribing,” Dr. Dowdy said, and described a program he and his colleagues at Mayo recently put in place that capped routine opioid pill prescriptions following various surgeries based on historic patient needs. For example, most laparotomy patients receive a prescription for 10 opioid doses on discharge. Based on the first 6 months of this program, it’s on track to cut the annual number of opioid tablets prescribed to postsurgical patients at Mayo by 35,000 for all gynecologic surgeries and by 1.5 million tablets for all Mayo surgical subspecialties, he said.
The study reported by Dr. Mark ran after the Roswell Park gynecologic oncology department implemented new guidelines for dispensing pain control medications following surgery. The guidelines called for comprehensive teaching for patients about pain expectations and pain management both before and after surgery and also established four dispensing categories:
- Patients undergoing minimally invasive or outpatient surgery and with no history of chronic pain and low opioid need while hospitalized received the default dispense of 600 mg ibuprofen every 6 hours as needed for 7 days and 500 mg acetaminophen every 6 hours as needed for 7 days.
- Patients who underwent this surgery but required 5 or more opioid tablets while hospitalized or those with a history of chronic pain and opioid use received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply with 1 tablet taken every 6 hours as needed.
- Patients who underwent laparotomy and had no chronic pain and opioid history and low opioid use while hospitalized received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply.
- Patients who underwent laparotomy and showed a higher opioid need based on their use during the 24 hours before discharge received the ibuprofen and acetaminophen regimen plus 24 opioid tablets for 3 days so they could take 2 tablets every 6 hours as needed.
Dr. Mark and his associates collected data from 337 patients managed with these guidelines during June 2017–January 2018 and compared them with 626 patients who underwent gynecologic surgery at Roswell Park during July 2016–June 2017. The data showed the average number of opioid tablets dispensed per patient for all discharges fell from 31.7 before the new guideline to 3.5, an 89% reduction. For the subgroup of patients who had undergone a laparotomy, the average pill number fell from 43.6 to 11.6, a 72% drop. Among patients treated with minimally invasive or outpatient surgery, average tablets dispensed fell from 28.1 before to 0.9 after, a 97% reduction. The reduction among opioid-naive patients was 90%, and it was 83% among patients who used opioids prior to their surgery.
Under the new program, patients requested an opioid refill 14% of the time after laparotomy and 8% of the time after minimally invasive surgery, rates that did not significantly differ from the prior era. Average postoperative pain scores were identical among patients treated under the new dispensing guidelines and those treated during the prior years, and 96% of patients said they were satisfied with the care they received during the new, restricted dispensing period, Dr. Mark reported.
The single-center experience reviewed by Dr. Weston tracked opioid use by 122 women who underwent a minimally invasive hysterectomy at Women and Infants both as inpatients and out to both 1-2 weeks and 4-6 weeks following discharge. The patients were an average age of 61 years, and included 16% who reported chronic pain and 5% with a history of chronic opioid use.
During the inpatient phase, median opioid use was three doses, with 25% of the patients using no opioids. During the first 1-2 weeks following discharge, median opioid use was nine tablets, with 37% of the patients using no opioids. By the 4- to 6-week follow-up (which collected data from 114 of the patients), median opioid use was a cumulative 11 tablets with 67% of the patients reporting no opioid use during the time between their first and second follow-up visit. During the total postdischarge period, 90% of the patients used 30 or fewer opioid tablets.
A multivariate analysis of the findings showed that opioid use while in hospital was the only significant predictor of opioid use after discharge. Age of 65 years or older showed a nonsignificant trend toward less postdischarge opioid use.
Based on these data Dr. Weston and her associates proposed a formula for estimating a patient’s opioid needs at discharge: Gynecologic surgery patients who needed no opioid medication as inpatients could receive 1-5 opioid tablets at discharge, patients who used opioids at or below the median level should receive 10-15 tablets at discharge, and those who used more than the median number of opioid tablets as inpatients should receive 25-30 tablets at discharge. For patients who undergo surgery as outpatients and have no record of pain medication needs, Dr. Weston recommended discharging them with a prescription for 25-30 tablets, possibly reducing this to 10-15 tablets for patients aged 65 years or older.
Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
SOURCE: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – U.S. clinicians prescribe opioid tablets to postsurgical patients too often and at too high a pill count, according to results from two independent studies that examined prescribing patterns and opioid use in patients following gynecologic surgery.
In addition, “setting preoperative expectations about pain management led to increased compliance at discharge,” said Dr. Mark, a gynecologic oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y.
Findings from the second study, of 122 women who underwent gynecologic surgery at Women and Infants Hospital in Providence, R.I., showed that 32% did not use any opioids for pain following hospital discharge, and that opioid use during hospitalization was a significant predictor of postdischarge opioid needs. This finding provided a way to devise a new prescribing guide for postsurgical patients based on their opioid use while hospitalized, said Erica Weston, MD, a gynecologic oncologist at Johns Hopkins University, Baltimore.

“No question, we are overprescribing,” Dr. Dowdy said, and described a program he and his colleagues at Mayo recently put in place that capped routine opioid pill prescriptions following various surgeries based on historic patient needs. For example, most laparotomy patients receive a prescription for 10 opioid doses on discharge. Based on the first 6 months of this program, it’s on track to cut the annual number of opioid tablets prescribed to postsurgical patients at Mayo by 35,000 for all gynecologic surgeries and by 1.5 million tablets for all Mayo surgical subspecialties, he said.
The study reported by Dr. Mark ran after the Roswell Park gynecologic oncology department implemented new guidelines for dispensing pain control medications following surgery. The guidelines called for comprehensive teaching for patients about pain expectations and pain management both before and after surgery and also established four dispensing categories:
- Patients undergoing minimally invasive or outpatient surgery and with no history of chronic pain and low opioid need while hospitalized received the default dispense of 600 mg ibuprofen every 6 hours as needed for 7 days and 500 mg acetaminophen every 6 hours as needed for 7 days.
- Patients who underwent this surgery but required 5 or more opioid tablets while hospitalized or those with a history of chronic pain and opioid use received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply with 1 tablet taken every 6 hours as needed.
- Patients who underwent laparotomy and had no chronic pain and opioid history and low opioid use while hospitalized received the ibuprofen and acetaminophen regimen plus 12 opioid tablets, a 3-day supply.
- Patients who underwent laparotomy and showed a higher opioid need based on their use during the 24 hours before discharge received the ibuprofen and acetaminophen regimen plus 24 opioid tablets for 3 days so they could take 2 tablets every 6 hours as needed.
Dr. Mark and his associates collected data from 337 patients managed with these guidelines during June 2017–January 2018 and compared them with 626 patients who underwent gynecologic surgery at Roswell Park during July 2016–June 2017. The data showed the average number of opioid tablets dispensed per patient for all discharges fell from 31.7 before the new guideline to 3.5, an 89% reduction. For the subgroup of patients who had undergone a laparotomy, the average pill number fell from 43.6 to 11.6, a 72% drop. Among patients treated with minimally invasive or outpatient surgery, average tablets dispensed fell from 28.1 before to 0.9 after, a 97% reduction. The reduction among opioid-naive patients was 90%, and it was 83% among patients who used opioids prior to their surgery.
Under the new program, patients requested an opioid refill 14% of the time after laparotomy and 8% of the time after minimally invasive surgery, rates that did not significantly differ from the prior era. Average postoperative pain scores were identical among patients treated under the new dispensing guidelines and those treated during the prior years, and 96% of patients said they were satisfied with the care they received during the new, restricted dispensing period, Dr. Mark reported.
The single-center experience reviewed by Dr. Weston tracked opioid use by 122 women who underwent a minimally invasive hysterectomy at Women and Infants both as inpatients and out to both 1-2 weeks and 4-6 weeks following discharge. The patients were an average age of 61 years, and included 16% who reported chronic pain and 5% with a history of chronic opioid use.
During the inpatient phase, median opioid use was three doses, with 25% of the patients using no opioids. During the first 1-2 weeks following discharge, median opioid use was nine tablets, with 37% of the patients using no opioids. By the 4- to 6-week follow-up (which collected data from 114 of the patients), median opioid use was a cumulative 11 tablets with 67% of the patients reporting no opioid use during the time between their first and second follow-up visit. During the total postdischarge period, 90% of the patients used 30 or fewer opioid tablets.
A multivariate analysis of the findings showed that opioid use while in hospital was the only significant predictor of opioid use after discharge. Age of 65 years or older showed a nonsignificant trend toward less postdischarge opioid use.
Based on these data Dr. Weston and her associates proposed a formula for estimating a patient’s opioid needs at discharge: Gynecologic surgery patients who needed no opioid medication as inpatients could receive 1-5 opioid tablets at discharge, patients who used opioids at or below the median level should receive 10-15 tablets at discharge, and those who used more than the median number of opioid tablets as inpatients should receive 25-30 tablets at discharge. For patients who undergo surgery as outpatients and have no record of pain medication needs, Dr. Weston recommended discharging them with a prescription for 25-30 tablets, possibly reducing this to 10-15 tablets for patients aged 65 years or older.
Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
SOURCE: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
REPORTING FROM SGO 2018
Key clinical point: Patients who underwent gynecologic surgery received adequate pain relief when receiving fewer opioid tablets.
Major finding: A protocol that restricted opioid dispensing successfully cut the discharge allotment of opioid tablets by 89%.
Study details: A single-center review of 337 patients, and a second single-center experience with 122 patients.
Disclosures: Dr. Mark, Dr. Weston, and Dr. Dowdy had no disclosures.
Source: Mark J et al. SGO 2018, Abstract 7. Weston E et al. SGO 2018, Abstract 8.
Longer poly-JIA inactivity not necessarily better before stopping anti-TNF therapy
Recent data suggest the longer a patient with polyarticular forms of juvenile idiopathic arthritis stays on anti–tumor necrosis factor therapy to maintain a clinical inactive disease state, the higher the likelihood of experiencing disease flare after discontinuing anti-TNF therapy.
Daniel J. Lovell, MD, MPH, of the Cincinnati Children’s Hospital Medical Center, and his coauthors prospectively evaluated 137 patients with clinical inactive PF-JIA who were receiving anti-TNF therapy at 16 academic pediatric centers. Of these, 7 patients dropped from the study and 24 patients did not maintain clinical inactive disease (CID) for 6 months.
Among the 106 patients who continued anti-TNF therapy for 6 months and maintained CID, the investigators then stopped anti-TNF therapy and examined patients for disease flare at 1-month, 2-month, 3-month, 4-month, 6-month, and 8-month follow-up. A total of 42% of these patients were also taking background medication such as methotrexate. Investigators found 39 patients (37%) who showed signs of disease flare within 8 months of discontinuing anti-TNF therapy. A number of factors proved to be significantly associated with disease flare, including age at disease onset (hazard ratio, 0.92; 95% confidence interval, 0.85-0.99; P = .03), age at disease diagnosis (HR, 0.91; 95% CI, 0.84-0.99; P = .02), disease duration at enrollment (HR, 1.12; 95% CI, 1.04-1.21; P less than .01) and time from onset until first CID (HR, 1.10; 95% CI, 1.01-1.20; P = .04). Flare occurred at a mean 7.01 months (standard error of the mean, 0.32) and median 8.26 months (95% CI, 7.80-8.66).
“These data certainly do not support the existence of a protective effect of longer duration of CID before considering stopping anti-TNF therapy,” the authors wrote in their study. “In fact, the data suggest that CID, even in those who did demonstrate CID consistently for the first 6 months of the study, continued to be an unstable clinical state and prolonged observation of CID resulted in a significantly greater risk for flare.”
Dr. Lovell and his colleagues noted their results suggest a “window of opportunity” where treating JIA early with “aggressive therapy” to reach CID sooner will help improve outcomes and long-term control of the disease.
The study was sponsored by a grant from the National Institutes of Health.
SOURCE: Lovell D et al. Arthritis Rheumatol. 2018 Mar 31. doi: 10.1002/art.40509.
Recent data suggest the longer a patient with polyarticular forms of juvenile idiopathic arthritis stays on anti–tumor necrosis factor therapy to maintain a clinical inactive disease state, the higher the likelihood of experiencing disease flare after discontinuing anti-TNF therapy.
Daniel J. Lovell, MD, MPH, of the Cincinnati Children’s Hospital Medical Center, and his coauthors prospectively evaluated 137 patients with clinical inactive PF-JIA who were receiving anti-TNF therapy at 16 academic pediatric centers. Of these, 7 patients dropped from the study and 24 patients did not maintain clinical inactive disease (CID) for 6 months.
Among the 106 patients who continued anti-TNF therapy for 6 months and maintained CID, the investigators then stopped anti-TNF therapy and examined patients for disease flare at 1-month, 2-month, 3-month, 4-month, 6-month, and 8-month follow-up. A total of 42% of these patients were also taking background medication such as methotrexate. Investigators found 39 patients (37%) who showed signs of disease flare within 8 months of discontinuing anti-TNF therapy. A number of factors proved to be significantly associated with disease flare, including age at disease onset (hazard ratio, 0.92; 95% confidence interval, 0.85-0.99; P = .03), age at disease diagnosis (HR, 0.91; 95% CI, 0.84-0.99; P = .02), disease duration at enrollment (HR, 1.12; 95% CI, 1.04-1.21; P less than .01) and time from onset until first CID (HR, 1.10; 95% CI, 1.01-1.20; P = .04). Flare occurred at a mean 7.01 months (standard error of the mean, 0.32) and median 8.26 months (95% CI, 7.80-8.66).
“These data certainly do not support the existence of a protective effect of longer duration of CID before considering stopping anti-TNF therapy,” the authors wrote in their study. “In fact, the data suggest that CID, even in those who did demonstrate CID consistently for the first 6 months of the study, continued to be an unstable clinical state and prolonged observation of CID resulted in a significantly greater risk for flare.”
Dr. Lovell and his colleagues noted their results suggest a “window of opportunity” where treating JIA early with “aggressive therapy” to reach CID sooner will help improve outcomes and long-term control of the disease.
The study was sponsored by a grant from the National Institutes of Health.
SOURCE: Lovell D et al. Arthritis Rheumatol. 2018 Mar 31. doi: 10.1002/art.40509.
Recent data suggest the longer a patient with polyarticular forms of juvenile idiopathic arthritis stays on anti–tumor necrosis factor therapy to maintain a clinical inactive disease state, the higher the likelihood of experiencing disease flare after discontinuing anti-TNF therapy.
Daniel J. Lovell, MD, MPH, of the Cincinnati Children’s Hospital Medical Center, and his coauthors prospectively evaluated 137 patients with clinical inactive PF-JIA who were receiving anti-TNF therapy at 16 academic pediatric centers. Of these, 7 patients dropped from the study and 24 patients did not maintain clinical inactive disease (CID) for 6 months.
Among the 106 patients who continued anti-TNF therapy for 6 months and maintained CID, the investigators then stopped anti-TNF therapy and examined patients for disease flare at 1-month, 2-month, 3-month, 4-month, 6-month, and 8-month follow-up. A total of 42% of these patients were also taking background medication such as methotrexate. Investigators found 39 patients (37%) who showed signs of disease flare within 8 months of discontinuing anti-TNF therapy. A number of factors proved to be significantly associated with disease flare, including age at disease onset (hazard ratio, 0.92; 95% confidence interval, 0.85-0.99; P = .03), age at disease diagnosis (HR, 0.91; 95% CI, 0.84-0.99; P = .02), disease duration at enrollment (HR, 1.12; 95% CI, 1.04-1.21; P less than .01) and time from onset until first CID (HR, 1.10; 95% CI, 1.01-1.20; P = .04). Flare occurred at a mean 7.01 months (standard error of the mean, 0.32) and median 8.26 months (95% CI, 7.80-8.66).
“These data certainly do not support the existence of a protective effect of longer duration of CID before considering stopping anti-TNF therapy,” the authors wrote in their study. “In fact, the data suggest that CID, even in those who did demonstrate CID consistently for the first 6 months of the study, continued to be an unstable clinical state and prolonged observation of CID resulted in a significantly greater risk for flare.”
Dr. Lovell and his colleagues noted their results suggest a “window of opportunity” where treating JIA early with “aggressive therapy” to reach CID sooner will help improve outcomes and long-term control of the disease.
The study was sponsored by a grant from the National Institutes of Health.
SOURCE: Lovell D et al. Arthritis Rheumatol. 2018 Mar 31. doi: 10.1002/art.40509.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Discontinuing anti–tumor necrosis factor therapy caused disease flare within 8 months in over one-third of children with clinically inactive polyarticular forms of juvenile idiopathic arthritis.
Major finding:
Story details: A two-phase prospective study of 137 patients with PF-JIA in CID across 16 centers over a 16-month period.
Disclosures: This study was sponsored by a grant from the National Institutes of Health.
Source: Lovell D et al. Arthritis Rheumatol. 2018 Mar 31. doi: 10.1002/art.40509.
Patients presenting with saddle pulmonary emboli (PE) versus nonsaddle PE have no mortality difference but have an increased risk for decompensation
Background: Patients with saddle PEs can differ in terms of their clinical presentation and may present as hemodynamically stable or unstable. There have been few studies to quantify the presentation, management, and outcome of patients who present with saddle PEs.
Study design: Retrospective cohort study.
Setting: Quaternary care hospital in Minnesota.
Synopsis: Using a localized database, 187 consecutive patients with saddle PEs were matched with 187 nonsaddle PEs using age and the simplified Pulmonary Embolism Severity Index (sPESI). Saddle PE patients had no significant in-hospital mortality differences versus nonsaddle PEs. However, they were more likely to present with massive and submassive hemodynamics (80% vs. 52%; P less than .05), RV dilatation (84% vs. 67%; P less than .001), and troponin elevation (71% vs. 40%; P less than .001). Patients with saddle PEs were more likely to receive thrombolytics, inferior vena cava filter placement, and require mechanical ventilation. They also had increased risk of decompensation after 6 hours (12 patients vs. 6 patients). Limitations of this study include some selection bias and use of a single-center study. Regardless, hospitalists should consider close monitoring for patients with saddle PEs upon admission, independent of hemodynamics given risk of decompensation regardless of presenting vitals.
Bottom line: Saddle PEs have an increased risk of late decompensation, clot burden, and presentation with massive and submassive hemodynamics but not an increased risk of mortality when compared with nonsaddle PEs.
Citation: Alkinj B et al. Saddle vs. nonsaddle pulmonary embolism: Clinical presentation, hemodynamics, management, and outcomes. Mayo Clin Proc. 2017 Oct;92(10):1511-8.
Dr. O’Donnell is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Background: Patients with saddle PEs can differ in terms of their clinical presentation and may present as hemodynamically stable or unstable. There have been few studies to quantify the presentation, management, and outcome of patients who present with saddle PEs.
Study design: Retrospective cohort study.
Setting: Quaternary care hospital in Minnesota.
Synopsis: Using a localized database, 187 consecutive patients with saddle PEs were matched with 187 nonsaddle PEs using age and the simplified Pulmonary Embolism Severity Index (sPESI). Saddle PE patients had no significant in-hospital mortality differences versus nonsaddle PEs. However, they were more likely to present with massive and submassive hemodynamics (80% vs. 52%; P less than .05), RV dilatation (84% vs. 67%; P less than .001), and troponin elevation (71% vs. 40%; P less than .001). Patients with saddle PEs were more likely to receive thrombolytics, inferior vena cava filter placement, and require mechanical ventilation. They also had increased risk of decompensation after 6 hours (12 patients vs. 6 patients). Limitations of this study include some selection bias and use of a single-center study. Regardless, hospitalists should consider close monitoring for patients with saddle PEs upon admission, independent of hemodynamics given risk of decompensation regardless of presenting vitals.
Bottom line: Saddle PEs have an increased risk of late decompensation, clot burden, and presentation with massive and submassive hemodynamics but not an increased risk of mortality when compared with nonsaddle PEs.
Citation: Alkinj B et al. Saddle vs. nonsaddle pulmonary embolism: Clinical presentation, hemodynamics, management, and outcomes. Mayo Clin Proc. 2017 Oct;92(10):1511-8.
Dr. O’Donnell is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Background: Patients with saddle PEs can differ in terms of their clinical presentation and may present as hemodynamically stable or unstable. There have been few studies to quantify the presentation, management, and outcome of patients who present with saddle PEs.
Study design: Retrospective cohort study.
Setting: Quaternary care hospital in Minnesota.
Synopsis: Using a localized database, 187 consecutive patients with saddle PEs were matched with 187 nonsaddle PEs using age and the simplified Pulmonary Embolism Severity Index (sPESI). Saddle PE patients had no significant in-hospital mortality differences versus nonsaddle PEs. However, they were more likely to present with massive and submassive hemodynamics (80% vs. 52%; P less than .05), RV dilatation (84% vs. 67%; P less than .001), and troponin elevation (71% vs. 40%; P less than .001). Patients with saddle PEs were more likely to receive thrombolytics, inferior vena cava filter placement, and require mechanical ventilation. They also had increased risk of decompensation after 6 hours (12 patients vs. 6 patients). Limitations of this study include some selection bias and use of a single-center study. Regardless, hospitalists should consider close monitoring for patients with saddle PEs upon admission, independent of hemodynamics given risk of decompensation regardless of presenting vitals.
Bottom line: Saddle PEs have an increased risk of late decompensation, clot burden, and presentation with massive and submassive hemodynamics but not an increased risk of mortality when compared with nonsaddle PEs.
Citation: Alkinj B et al. Saddle vs. nonsaddle pulmonary embolism: Clinical presentation, hemodynamics, management, and outcomes. Mayo Clin Proc. 2017 Oct;92(10):1511-8.
Dr. O’Donnell is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
FDA grants priority review of follicular lymphoma drug
by the Food and Drug Administration.
The biopharmaceutical company Verastem is seeking full approval for duvelisib for the treatment of relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval for the treatment of relapsed/refractory follicular lymphoma. The FDA has set Oct. 5, 2018, as the target action date, according to Verastem.
by the Food and Drug Administration.
The biopharmaceutical company Verastem is seeking full approval for duvelisib for the treatment of relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval for the treatment of relapsed/refractory follicular lymphoma. The FDA has set Oct. 5, 2018, as the target action date, according to Verastem.
by the Food and Drug Administration.
The biopharmaceutical company Verastem is seeking full approval for duvelisib for the treatment of relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval for the treatment of relapsed/refractory follicular lymphoma. The FDA has set Oct. 5, 2018, as the target action date, according to Verastem.
Product News: 04 2018
Avène Mineral Light Mattifying Sunscreen Lotion
Pierre Fabre Dermo-Cosmetique introduces the Avène Mineral Light Mattifying Sunscreen Lotion with SPF 50+. This sunscreen offers broad-spectrum sun protection without irritation while delivering oil control and providing a natural mattifying finish for oily and acne-prone skin. This product absorbs quickly into the skin and can be worn under makeup. Avène Mineral Light Mattifying Sunscreen Lotion should be applied to the face 15 minutes prior to sun exposure and reapplied after 80 minutes of swimming or sweating, immediately after towel drying, or every 2 hours. For more information, visit www.aveneusa.com.
Ducray Anacaps Activ+ Dietary Supplement
Pierre Fabre Dermo-Cosmetique introduces Ducray Anacaps Activ+ Dietary Supplement, a once-daily capsule that contains zinc, molybdenum, iron, and selenium. This supplement targets factors that trigger sudden hair loss, including seasonal changes, stress, and diet. It also targets chronic hair loss with genetic, hormonal, and vascular causes. This formula provides essential nutrients needed to promote healthy hair growth from within, preserve hair density, and maintain the strength and vitality of hair. This supplement also is used for weak, devitalized nails and has a vegan formula with good digestive tolerance. For more information, visit www.ducray.com/en-us/.
Luzu
Ortho Dermatologics receives US Food and Drug Administration approval of the Supplemental New Drug Application to expand the use of Luzu (luliconazole) Cream 1% to pediatric patients. This new indication is for the topical treatment of interdigital tinea pedis and tinea cruris in patients 12 years of age and older and for tinea corporis in patients 2 years of age and older. Luzu is a topical azole antifungal agent with a 1-week, once-daily treatment regimen with results available 3 weeks post-treatment. Luzu previously was approved for use in adult patients. For more information, visit www.luzurx.com/HCP.
Xeljanz and Xeljanz XR
Pfizer Inc announces US Food and Drug Administration approval of twice-daily Xeljanz 5 mg and once-daily Xeljanz XR extended release 11 mg (tofacitinib) for the treatment of adult patients with active psoriatic arthritis who have had an inadequate response or intolerance to methotrexate or other disease-modifying antirheumatic drugs. Xeljanz and Xeljanz XR are Janus kinase inhibitors that previously were approved for the treatment of rheumatoid arthritis. For more information, visit www.xeljanz.com.
If you would like your product included in Product News, please email a press release to the Editorial Office at [email protected].
Avène Mineral Light Mattifying Sunscreen Lotion
Pierre Fabre Dermo-Cosmetique introduces the Avène Mineral Light Mattifying Sunscreen Lotion with SPF 50+. This sunscreen offers broad-spectrum sun protection without irritation while delivering oil control and providing a natural mattifying finish for oily and acne-prone skin. This product absorbs quickly into the skin and can be worn under makeup. Avène Mineral Light Mattifying Sunscreen Lotion should be applied to the face 15 minutes prior to sun exposure and reapplied after 80 minutes of swimming or sweating, immediately after towel drying, or every 2 hours. For more information, visit www.aveneusa.com.
Ducray Anacaps Activ+ Dietary Supplement
Pierre Fabre Dermo-Cosmetique introduces Ducray Anacaps Activ+ Dietary Supplement, a once-daily capsule that contains zinc, molybdenum, iron, and selenium. This supplement targets factors that trigger sudden hair loss, including seasonal changes, stress, and diet. It also targets chronic hair loss with genetic, hormonal, and vascular causes. This formula provides essential nutrients needed to promote healthy hair growth from within, preserve hair density, and maintain the strength and vitality of hair. This supplement also is used for weak, devitalized nails and has a vegan formula with good digestive tolerance. For more information, visit www.ducray.com/en-us/.
Luzu
Ortho Dermatologics receives US Food and Drug Administration approval of the Supplemental New Drug Application to expand the use of Luzu (luliconazole) Cream 1% to pediatric patients. This new indication is for the topical treatment of interdigital tinea pedis and tinea cruris in patients 12 years of age and older and for tinea corporis in patients 2 years of age and older. Luzu is a topical azole antifungal agent with a 1-week, once-daily treatment regimen with results available 3 weeks post-treatment. Luzu previously was approved for use in adult patients. For more information, visit www.luzurx.com/HCP.
Xeljanz and Xeljanz XR
Pfizer Inc announces US Food and Drug Administration approval of twice-daily Xeljanz 5 mg and once-daily Xeljanz XR extended release 11 mg (tofacitinib) for the treatment of adult patients with active psoriatic arthritis who have had an inadequate response or intolerance to methotrexate or other disease-modifying antirheumatic drugs. Xeljanz and Xeljanz XR are Janus kinase inhibitors that previously were approved for the treatment of rheumatoid arthritis. For more information, visit www.xeljanz.com.
If you would like your product included in Product News, please email a press release to the Editorial Office at [email protected].
Avène Mineral Light Mattifying Sunscreen Lotion
Pierre Fabre Dermo-Cosmetique introduces the Avène Mineral Light Mattifying Sunscreen Lotion with SPF 50+. This sunscreen offers broad-spectrum sun protection without irritation while delivering oil control and providing a natural mattifying finish for oily and acne-prone skin. This product absorbs quickly into the skin and can be worn under makeup. Avène Mineral Light Mattifying Sunscreen Lotion should be applied to the face 15 minutes prior to sun exposure and reapplied after 80 minutes of swimming or sweating, immediately after towel drying, or every 2 hours. For more information, visit www.aveneusa.com.
Ducray Anacaps Activ+ Dietary Supplement
Pierre Fabre Dermo-Cosmetique introduces Ducray Anacaps Activ+ Dietary Supplement, a once-daily capsule that contains zinc, molybdenum, iron, and selenium. This supplement targets factors that trigger sudden hair loss, including seasonal changes, stress, and diet. It also targets chronic hair loss with genetic, hormonal, and vascular causes. This formula provides essential nutrients needed to promote healthy hair growth from within, preserve hair density, and maintain the strength and vitality of hair. This supplement also is used for weak, devitalized nails and has a vegan formula with good digestive tolerance. For more information, visit www.ducray.com/en-us/.
Luzu
Ortho Dermatologics receives US Food and Drug Administration approval of the Supplemental New Drug Application to expand the use of Luzu (luliconazole) Cream 1% to pediatric patients. This new indication is for the topical treatment of interdigital tinea pedis and tinea cruris in patients 12 years of age and older and for tinea corporis in patients 2 years of age and older. Luzu is a topical azole antifungal agent with a 1-week, once-daily treatment regimen with results available 3 weeks post-treatment. Luzu previously was approved for use in adult patients. For more information, visit www.luzurx.com/HCP.
Xeljanz and Xeljanz XR
Pfizer Inc announces US Food and Drug Administration approval of twice-daily Xeljanz 5 mg and once-daily Xeljanz XR extended release 11 mg (tofacitinib) for the treatment of adult patients with active psoriatic arthritis who have had an inadequate response or intolerance to methotrexate or other disease-modifying antirheumatic drugs. Xeljanz and Xeljanz XR are Janus kinase inhibitors that previously were approved for the treatment of rheumatoid arthritis. For more information, visit www.xeljanz.com.
If you would like your product included in Product News, please email a press release to the Editorial Office at [email protected].
Genetic Screening May Reduce Carbamazepine-Induced Cutaneous Adverse Reactions
Preemptive HLA-A*31:01 genetic screening may significantly decrease the incidence of carbamazepine-induced cutaneous adverse reactions in Japanese patients, according to a report published online ahead of print April 2 in JAMA Neurology. According to the researchers, their finding suggests that such screening may be warranted in routine clinical practice.
Carbamazepine, which is widely used to treat seizures, neuropathic pain, and other disorders, is a common cause of cutaneous adverse drug reactions worldwide. The allele HLA-A*31:01 has been associated with
Genetic Screening Informed Treatment
To assess the use of HLA-A*31:01 genetic screening to identify individuals at risk of carbamazepine-induced cutaneous drug reactions, researchers from the Genotype-Based Carbamazepine Therapy Study Group conducted a cohort study in 36 hospitals in Japan from January 2012 to November 2014. The investigators enrolled 1,202 patients who were eligible to receive carbamazepine during the study period. Preemptive HLA-A*31:01 screening was performed for 1,187 study participants. Patients who did not start treatment with carbamazepine or alternative drugs were excluded. Participants were interviewed once weekly for eight weeks to monitor the development of
Neuropsychiatrists were asked to prescribe carbamazepine for patients who tested negative for HLA-A*31:01 and alternative drugs for those who tested positive for the allele. The study’s main outcome was the incidence of carbamazepine-induced cutaneous adverse drug reactions.
Of the 1,130 patients who were prescribed carbamazepine or alternative drugs, the mean age was 37.4; 614 (54.3%) were men, and 198 (17.5%) were positive for HLA-A*31:01. Dermatologists identified 23 patients (2.0%) who had carbamazepine-induced cutaneous adverse drug reactions, of whom four patients required hospitalization. Drug-induced hypersensitivity syndrome was observed for three patients, maculopapular eruption for nine patients, erythema multiforme for five patients, and an undetermined type of cutaneous adverse drug reaction for six patients. No patient developed Stevens-Johnson syndrome or toxic epidermal necrolysis.
Comparison with a historical control indicated that the preemptive use of HLA-A*31:01 screening was associated with a 40% reduction in the incidence of carbamazepine-induced cutaneous adverse drug reactions.
Two Alleles
The researchers noted that the clinical utility of the HLA-B*15:02 genetic test for reducing carbamazepine-induced cutaneous drug reactions has already been established by preemptive screening. However, the frequency of the HLA-B*15:02 allele is low in Korean, Japanese, African, and European populations.
In contrast, the frequency of the HLA-A*31:01 allele is 7% to 9% in Japanese, 5% in Korean, 2% in Chinese, 2% to 3% in European, and 1% in African populations. Moreover, HLA-A*31:01 has been associated with a full spectrum of carbamazepine-induced
A First Step in Precision Neurology?
The present study “provides initial data that preemptive strategies may allow for a more consistent approach to safely administer this commonly used medication,” said Yijing He, MD, PhD; Lucia Seminario-Vidal, MD, PhD; and Howard L. McLeod, PharmD, in an accompanying editorial. A substantial decrease in the incidence and severity of carbamazepine-associated
“However, 23 patients experienced a carbamazepine-associated cutaneous adverse drug reaction,” and four patients required hospitalization, the editorialists noted. “Therefore, the use of HLA-A*31:01 testing will not eliminate the risk of carbamazepine-associated events, nor will it decrease the need for neurologists to provide skin-focused monitoring as part of their management of cases involving carbamazepine-treated patients.”
This research, the editorialists said, indicates that there is still more to discover. “To date, a small number of heroes has relentlessly pursued mechanistic and preventive research on drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis. However, the field needs to build on these efforts with a more systematic approach that will aid more rapid progress and provide more consistent influence across the globe.” Much still needs to be learned about the basic mechanisms, clinical confounders, biomarkers, and epidemiologic aspects of the various drug reactions that become Stevens-Johnson syndrome and toxic epidermal necrolysis. Attributing this clinical, immunologic, and therapeutic problem to various idiosyncratic reactions does not serve patients well, said the editorialists.
A key first step, the editorialists said, is to “apply existing preemptive strategies, including genomic analysis. Whether this is initially implemented broadly or in regions with higher probability of the risk alleles is less important than learning how to change a culture that tolerates adverse drug events and inventing informatics tools to make proactive approaches less of a burden. Although we will not get it completely right the first time, we need to start the iterative process to eradicate severe cutaneous adverse drug reactions.”
—Glenn S. Williams
Suggested Reading
Mushiroda T, Takahashi Y, Onuma T, et al. Association of HLA-A*31:01 screening with the incidence of carbamazepine-induced cutaneous adverse reactions in a Japanese population. JAMA Neurol. 2018 Apr 2 [Epub ahead of print].
He Y, Seminario-Vidal S, McLeod HL. Avoidance of severe cutaneous adverse drug events as a first step in precision neurology. JAMA Neurol. Apr 2 [Epub ahead of print].
Preemptive HLA-A*31:01 genetic screening may significantly decrease the incidence of carbamazepine-induced cutaneous adverse reactions in Japanese patients, according to a report published online ahead of print April 2 in JAMA Neurology. According to the researchers, their finding suggests that such screening may be warranted in routine clinical practice.
Carbamazepine, which is widely used to treat seizures, neuropathic pain, and other disorders, is a common cause of cutaneous adverse drug reactions worldwide. The allele HLA-A*31:01 has been associated with
Genetic Screening Informed Treatment
To assess the use of HLA-A*31:01 genetic screening to identify individuals at risk of carbamazepine-induced cutaneous drug reactions, researchers from the Genotype-Based Carbamazepine Therapy Study Group conducted a cohort study in 36 hospitals in Japan from January 2012 to November 2014. The investigators enrolled 1,202 patients who were eligible to receive carbamazepine during the study period. Preemptive HLA-A*31:01 screening was performed for 1,187 study participants. Patients who did not start treatment with carbamazepine or alternative drugs were excluded. Participants were interviewed once weekly for eight weeks to monitor the development of
Neuropsychiatrists were asked to prescribe carbamazepine for patients who tested negative for HLA-A*31:01 and alternative drugs for those who tested positive for the allele. The study’s main outcome was the incidence of carbamazepine-induced cutaneous adverse drug reactions.
Of the 1,130 patients who were prescribed carbamazepine or alternative drugs, the mean age was 37.4; 614 (54.3%) were men, and 198 (17.5%) were positive for HLA-A*31:01. Dermatologists identified 23 patients (2.0%) who had carbamazepine-induced cutaneous adverse drug reactions, of whom four patients required hospitalization. Drug-induced hypersensitivity syndrome was observed for three patients, maculopapular eruption for nine patients, erythema multiforme for five patients, and an undetermined type of cutaneous adverse drug reaction for six patients. No patient developed Stevens-Johnson syndrome or toxic epidermal necrolysis.
Comparison with a historical control indicated that the preemptive use of HLA-A*31:01 screening was associated with a 40% reduction in the incidence of carbamazepine-induced cutaneous adverse drug reactions.
Two Alleles
The researchers noted that the clinical utility of the HLA-B*15:02 genetic test for reducing carbamazepine-induced cutaneous drug reactions has already been established by preemptive screening. However, the frequency of the HLA-B*15:02 allele is low in Korean, Japanese, African, and European populations.
In contrast, the frequency of the HLA-A*31:01 allele is 7% to 9% in Japanese, 5% in Korean, 2% in Chinese, 2% to 3% in European, and 1% in African populations. Moreover, HLA-A*31:01 has been associated with a full spectrum of carbamazepine-induced
A First Step in Precision Neurology?
The present study “provides initial data that preemptive strategies may allow for a more consistent approach to safely administer this commonly used medication,” said Yijing He, MD, PhD; Lucia Seminario-Vidal, MD, PhD; and Howard L. McLeod, PharmD, in an accompanying editorial. A substantial decrease in the incidence and severity of carbamazepine-associated
“However, 23 patients experienced a carbamazepine-associated cutaneous adverse drug reaction,” and four patients required hospitalization, the editorialists noted. “Therefore, the use of HLA-A*31:01 testing will not eliminate the risk of carbamazepine-associated events, nor will it decrease the need for neurologists to provide skin-focused monitoring as part of their management of cases involving carbamazepine-treated patients.”
This research, the editorialists said, indicates that there is still more to discover. “To date, a small number of heroes has relentlessly pursued mechanistic and preventive research on drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis. However, the field needs to build on these efforts with a more systematic approach that will aid more rapid progress and provide more consistent influence across the globe.” Much still needs to be learned about the basic mechanisms, clinical confounders, biomarkers, and epidemiologic aspects of the various drug reactions that become Stevens-Johnson syndrome and toxic epidermal necrolysis. Attributing this clinical, immunologic, and therapeutic problem to various idiosyncratic reactions does not serve patients well, said the editorialists.
A key first step, the editorialists said, is to “apply existing preemptive strategies, including genomic analysis. Whether this is initially implemented broadly or in regions with higher probability of the risk alleles is less important than learning how to change a culture that tolerates adverse drug events and inventing informatics tools to make proactive approaches less of a burden. Although we will not get it completely right the first time, we need to start the iterative process to eradicate severe cutaneous adverse drug reactions.”
—Glenn S. Williams
Suggested Reading
Mushiroda T, Takahashi Y, Onuma T, et al. Association of HLA-A*31:01 screening with the incidence of carbamazepine-induced cutaneous adverse reactions in a Japanese population. JAMA Neurol. 2018 Apr 2 [Epub ahead of print].
He Y, Seminario-Vidal S, McLeod HL. Avoidance of severe cutaneous adverse drug events as a first step in precision neurology. JAMA Neurol. Apr 2 [Epub ahead of print].
Preemptive HLA-A*31:01 genetic screening may significantly decrease the incidence of carbamazepine-induced cutaneous adverse reactions in Japanese patients, according to a report published online ahead of print April 2 in JAMA Neurology. According to the researchers, their finding suggests that such screening may be warranted in routine clinical practice.
Carbamazepine, which is widely used to treat seizures, neuropathic pain, and other disorders, is a common cause of cutaneous adverse drug reactions worldwide. The allele HLA-A*31:01 has been associated with
Genetic Screening Informed Treatment
To assess the use of HLA-A*31:01 genetic screening to identify individuals at risk of carbamazepine-induced cutaneous drug reactions, researchers from the Genotype-Based Carbamazepine Therapy Study Group conducted a cohort study in 36 hospitals in Japan from January 2012 to November 2014. The investigators enrolled 1,202 patients who were eligible to receive carbamazepine during the study period. Preemptive HLA-A*31:01 screening was performed for 1,187 study participants. Patients who did not start treatment with carbamazepine or alternative drugs were excluded. Participants were interviewed once weekly for eight weeks to monitor the development of
Neuropsychiatrists were asked to prescribe carbamazepine for patients who tested negative for HLA-A*31:01 and alternative drugs for those who tested positive for the allele. The study’s main outcome was the incidence of carbamazepine-induced cutaneous adverse drug reactions.
Of the 1,130 patients who were prescribed carbamazepine or alternative drugs, the mean age was 37.4; 614 (54.3%) were men, and 198 (17.5%) were positive for HLA-A*31:01. Dermatologists identified 23 patients (2.0%) who had carbamazepine-induced cutaneous adverse drug reactions, of whom four patients required hospitalization. Drug-induced hypersensitivity syndrome was observed for three patients, maculopapular eruption for nine patients, erythema multiforme for five patients, and an undetermined type of cutaneous adverse drug reaction for six patients. No patient developed Stevens-Johnson syndrome or toxic epidermal necrolysis.
Comparison with a historical control indicated that the preemptive use of HLA-A*31:01 screening was associated with a 40% reduction in the incidence of carbamazepine-induced cutaneous adverse drug reactions.
Two Alleles
The researchers noted that the clinical utility of the HLA-B*15:02 genetic test for reducing carbamazepine-induced cutaneous drug reactions has already been established by preemptive screening. However, the frequency of the HLA-B*15:02 allele is low in Korean, Japanese, African, and European populations.
In contrast, the frequency of the HLA-A*31:01 allele is 7% to 9% in Japanese, 5% in Korean, 2% in Chinese, 2% to 3% in European, and 1% in African populations. Moreover, HLA-A*31:01 has been associated with a full spectrum of carbamazepine-induced
A First Step in Precision Neurology?
The present study “provides initial data that preemptive strategies may allow for a more consistent approach to safely administer this commonly used medication,” said Yijing He, MD, PhD; Lucia Seminario-Vidal, MD, PhD; and Howard L. McLeod, PharmD, in an accompanying editorial. A substantial decrease in the incidence and severity of carbamazepine-associated
“However, 23 patients experienced a carbamazepine-associated cutaneous adverse drug reaction,” and four patients required hospitalization, the editorialists noted. “Therefore, the use of HLA-A*31:01 testing will not eliminate the risk of carbamazepine-associated events, nor will it decrease the need for neurologists to provide skin-focused monitoring as part of their management of cases involving carbamazepine-treated patients.”
This research, the editorialists said, indicates that there is still more to discover. “To date, a small number of heroes has relentlessly pursued mechanistic and preventive research on drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis. However, the field needs to build on these efforts with a more systematic approach that will aid more rapid progress and provide more consistent influence across the globe.” Much still needs to be learned about the basic mechanisms, clinical confounders, biomarkers, and epidemiologic aspects of the various drug reactions that become Stevens-Johnson syndrome and toxic epidermal necrolysis. Attributing this clinical, immunologic, and therapeutic problem to various idiosyncratic reactions does not serve patients well, said the editorialists.
A key first step, the editorialists said, is to “apply existing preemptive strategies, including genomic analysis. Whether this is initially implemented broadly or in regions with higher probability of the risk alleles is less important than learning how to change a culture that tolerates adverse drug events and inventing informatics tools to make proactive approaches less of a burden. Although we will not get it completely right the first time, we need to start the iterative process to eradicate severe cutaneous adverse drug reactions.”
—Glenn S. Williams
Suggested Reading
Mushiroda T, Takahashi Y, Onuma T, et al. Association of HLA-A*31:01 screening with the incidence of carbamazepine-induced cutaneous adverse reactions in a Japanese population. JAMA Neurol. 2018 Apr 2 [Epub ahead of print].
He Y, Seminario-Vidal S, McLeod HL. Avoidance of severe cutaneous adverse drug events as a first step in precision neurology. JAMA Neurol. Apr 2 [Epub ahead of print].
Life and health are not even across the U.S.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.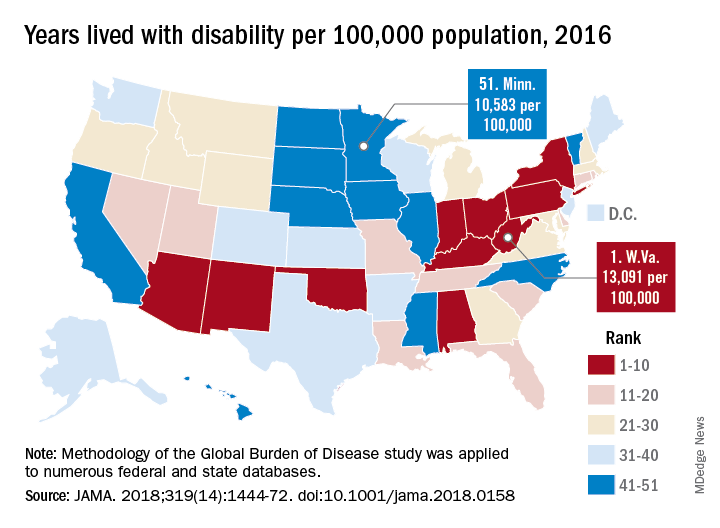
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
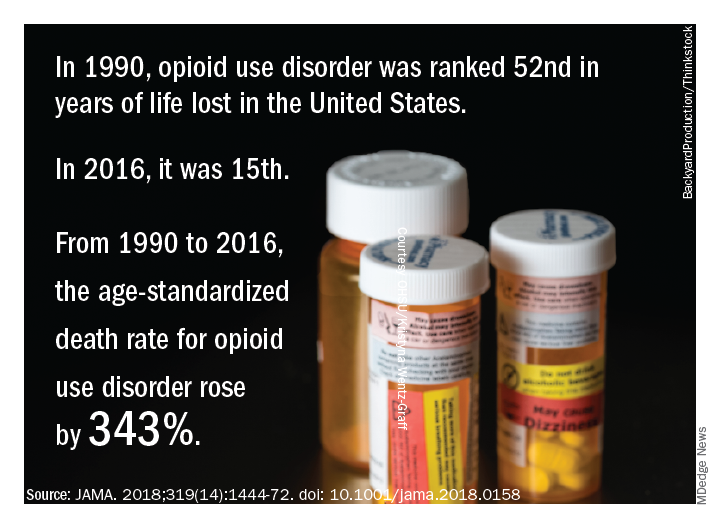
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
This report on Global Burden of Disease (GBD) study data profoundly and powerfully illuminates U.S. health trends over time and by geography. There is much unfinished business for us, nationally and at the state level.
Clinicians and policy makers can use the rankings to evaluate why many individuals are still experiencing injury, disease, and deaths that are preventable; in doing so, the entire nation could move closely resemble a United States of health.
Clinicians could use the results to help guide patients through evidence-based disease prevention and early intervention, a strategy that has led to decreases in death due to cancer and cardiovascular disease over the past few decades.
At the same time, policy makers could use GBD 2016 results to reevaluate current national attitudes toward disease prevention.
Howard K. Koh, MD, MPH, is with the Harvard T.H. Chan School of Public Health, Boston. Anand K. Parekh, MD, MPH, is with the Bipartisan Policy Center in Washington. The comments above are derived from an editorial accompanying the report from the US Burden of Disease Collaborators ( JAMA. 2018;319[14]:1438-40 ). Dr. Koh and Dr. Parekh reported no conflicts of interest related to the editorial.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.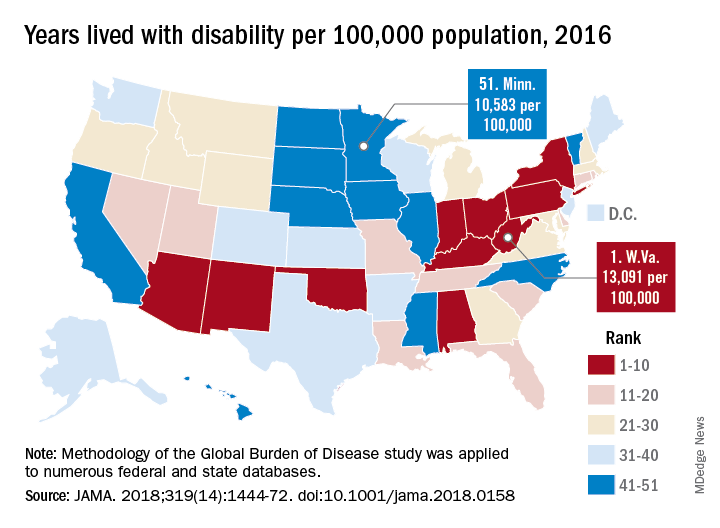
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
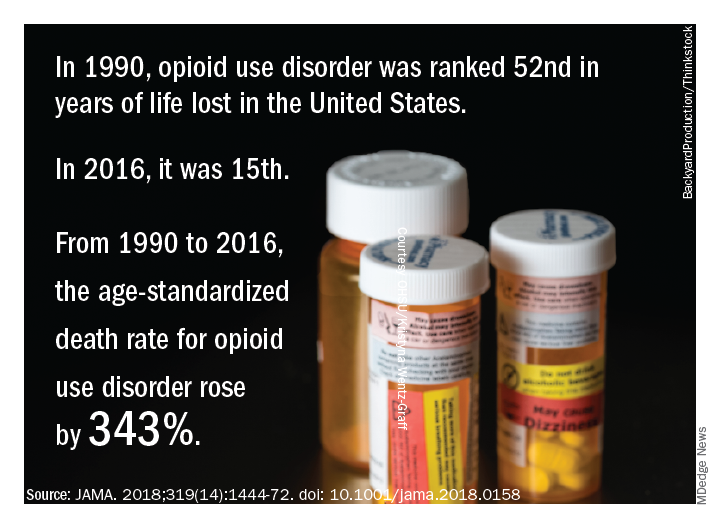
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors, according to a comprehensive analysis.
Life expectancy varies substantially, for example, ranging from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, according to results from the analysis of data from the Global Burden of Disease (GBD) study (JAMA. 2018;319[14]:1444-72).
Previously decreasing death rates for adults have reversed in 19 states, according to the analysis, which covers the years 1990 to 2016.
Hardest hit were Kentucky, New Mexico, Oklahoma, West Virginia, and Wyoming, which had mortality increases of more than 10% among adults aged 20-55 years. Those increases were largely due to causes such as substance use disorders, self-harm, and cirrhosis, according to the US Burden of Disease Collaborators, who authored the report.
“These findings should be used to examine the causes of health variations and to plan, develop, and implement programs and policies to improve health overall and eliminate disparities in the United States,” the authors wrote.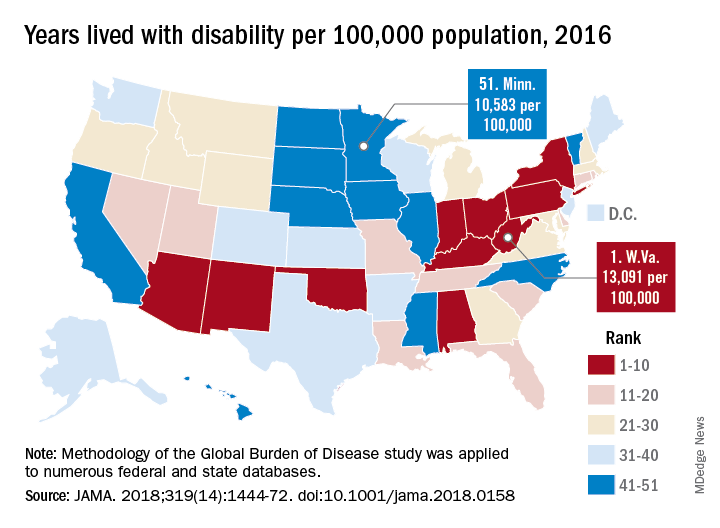
Overall, U.S. death rates have declined from 745.2 per 100,000 persons in 1990 to 578.0 per 100,000 persons in 2016, according to the report.
Likewise, health outcomes throughout the United States have improved over time for some conditions, such as ischemic heart disease, lung cancer, and neonatal preterm complications, the report says.
However, those gains are offset by rising death rates due to drug-use disorders, chronic kidney disease, cirrhosis, chronic obstructive pulmonary disease, hypertension, and self-harm.
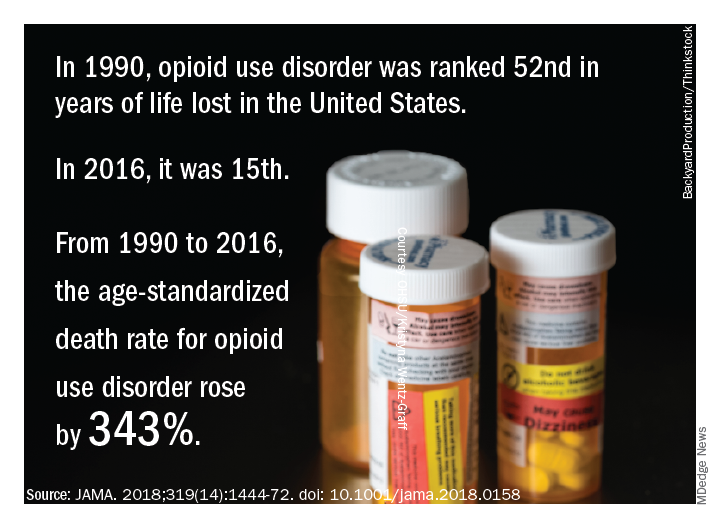
The three most important risk factors in the United States are high body mass index, smoking, and high fasting plasma glucose, the analysis showed. Of those risk factors, only smoking is decreasing, authors noted.
Many risk factors contributing to disparities in burden among states are amenable to medical treatment that emphasizes supportive behavioral and lifestyle changes, according to the authors.
“Expanding health coverage for certain conditions and medications should be considered and adopted to reduce burden,” they said.
Substance abuse disorders, cirrhosis, and self-harm, the causes of the mortality reversal in Kentucky, New Mexico, and other states, could be addressed via a wide range of interventions, according to the investigators.
Prevention programs could address the root causes of substance use and causes of relapse, while physicians can play a “major role” in addiction control through counseling of patients on pain control medication, they said.
Interventions to treat hepatitis C and decrease excessive alcohol consumption could help address cirrhosis, while for self-harm, the most promising approaches focus on restricting access to lethal means, they said, noting that a large proportion of U.S. suicides are due to firearms.
“While multiple strategies are available for dealing with these problems, they have not until very recently garnered attention,” investigators wrote.
The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Some individual study collaborators reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
SOURCE: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-72.
FROM JAMA
Key clinical point: While U.S. death rates have declined overall, marked geographic disparities exist at the state level in burden of disease, injuries, and risk factors.
Major finding: Life expectancy ranged from a high of 81.3 years in Hawaii to a low of 74.7 years in Mississippi, and previously decreasing death rates for adults have reversed in 19 states.
Study details: A U.S. state-level analysis of results from the Global Burden of Disease (GBD) study illustrating trends in diseases, injuries, risk factors, and deaths from 1990 to 2016.
Disclosures: The study was supported in part by the National Institute of Environmental Health Sciences and the Bill and Melinda Gates Foundation. Study authors reported disclosures related to Savient, Takeda, Crealta/Horizon, Regeneron, Allergan, and others.
Source: The US Burden of Disease Collaborators. JAMA 2018;319(14):1444-1472.
Multidisciplinary teams improve diagnoses in ILD
New research provides strong statistical support for the use of dynamic multidisciplinary discussion in the diagnosis of patients who may have interstitial lung diseases (ILD).
and it changed the diagnosis in 41% of the other cases.
The American Thoracic Society, European Respiratory Society, Japanese Respiratory Society, and Latin American Thoracic Association adopted joint guidelines for the treatment of idiopathic pulmonary fibrosis in 2015, and the ATS and ERS updated guidelines for the classification and terminology for idiopathic interstitial pneumonias in 2013. The Lancet Respiratory Medicine published what some consider to be a landmark evaluation of multidisciplinary team agreement on diagnosis of interstitial lung disease following the adoption of these guidelines (Walsh SLF et al. 2016;4[7]:557-65). This study showed that in idiopathic pulmonary fibrosis, multidisciplinary team meetings “have a higher level of agreement on diagnoses, assign diagnoses with higher confidence more frequently, and provide diagnoses that have nonsignificant greater prognostic separation than do clinicians or radiologists in most cases,” the researchers wrote.
In the new study, MDD failed to produce a diagnosis or suggestions about a way forward in only 3.5% of patients, according to the study, which appeared March 30 in CHEST®.
According to Dr. Antin-Ozerkis, accurate diagnosis of ILD is crucial to treatment, but it can be challenging to achieve. The MDD approach has been recommended since 2002 by the ATS and ERS, she said.
The study authors, led by Laurens J. De Sadeleer, MD, of Belgium’s University Hospitals Leuven, define the MDD approach as one “in which expert ILD clinicians, radiologists, and pathologists integrate all available clinical data, laboratory results, high-resolution computed tomography [HRCT] findings, and lung biopsy [when performed].”
For the study, the researchers tracked pre-MDD and MDD diagnoses of 938 consecutive patients with possible ILD who were discussed during 2005-2015. Of these patients, referring physicians made preliminary diagnoses in 49% of cases; in the rest, physicians either failed to develop a diagnosis or offered multiple possible diagnoses.
MDD teams produced a change in diagnosis in 191 – 42% – of patients with a pre-MDD diagnosis. Another condition was diagnosed in 118 of these patients, and the MDD teams declined to classify the other 73 patients pending further investigation.
The MDD teams also were able to produce diagnoses in 80% of cases when referring physicians could not come up with diagnoses.
“Discrepancy between pre-MDD diagnosis before work-up and discussion was remarkable,” the study authors wrote, estimating that MDD added value for 70% of referred patients.
“We believe MDD should be a common practice in the diagnosis of every patient with suspected ILD,” the researchers said.
The study doesn’t examine the challenges of putting MDD into practice, but Dr. Antin-Ozerkis provided some perspective. “It may be difficult for physicians to take the time from a busy practice to meet with a multidisciplinary team. It can require resources to gather the data necessary to comprehensively assess each patient case. Additionally, maintaining staff with experienced pulmonologists, radiologists and pathologists may be costly.”
She added that “there are various ways in which MDD may occur,” and that the pros and cons of different methods have not been well studied. “This practice will likely evolve with the development of new biomarkers and other diagnostic strategies in IPF [idiopathic pulmonary fibrosis].”
Still, she said, “this joint undertaking is clearly vital in helping to guide clinical practice, including therapeutic decisions and discussion of prognosis. For now, any discussion between clinician, radiologist, and pathologist is of benefit.”
Research Foundation-Flanders and University Hospitals Leuven funded the study. Some study authors reported various disclosures. Dr. Antin-Ozerkis disclosed serving as an investigator on several clinical trials for IPF and other ILDs by Boehringer, Promedior, Fibrogen and Roche. She noted that payments go directly to the university with no direct payments to the investigator.
SOURCE: De Sadeleer LJ et al. Chest. 2018 Mar 30. doi: 10.1016/j.chest.2018.03.026.
MDD strategy is crucial for accurate ILD diagnoses
The field of interstitial lung diseases (ILD) is challenging, with more than 200 disorders as possible diagnoses for patients who present to clinicians with similar symptoms and chest x-ray findings. The multidisciplinary discussion (MDD) strategy is very important for attaining an accurate ILD diagnosis.
We have had routine, formal, multidisciplinary discussions at our center since 2008. My guesstimate is that at least a third of patients referred as having idiopathic pulmonary fibrosis or another form of ILD by pulmonologists had been given the wrong diagnosis. Frequently, this was because of incorrect impressions provided by local radiologists and/or pathologists along with the clinician’s own limited knowledge of ILD.
In my experience, some patients described their pulmonologists as becoming irate with them when they asked for a second opinion, and I have had to try to avoid confrontations with referring physicians when trying to explain why the referral diagnosis was inaccurate.
Challenges to instituting the multidisciplinary discussion approach include coverage by health plans for a second-opinion evaluation, the willingness of physicians (for example, pulmonologists) outside of academic referral centers to refer patients to a center capable of adequately conducting an MDD, and patients’ desire to undergo an evaluation at centers of excellence where an MDD can be performed.
One must have also adequate resources to perform a proper MDD. But even in centers that refer patients, pulmonologists should confer with their colleague radiologists – and pathologists when appropriate – to try to make the most accurate diagnosis. And they should continue to question their diagnosis at follow-up appointments, as new symptoms and findings may arise or additional crucial information can become available over time that can point to an alternative diagnosis.
Kenneth C. Meyer, MD, MS, served as medical director of the lung transplant program and head of ILD at the University of Wisconsin–Madison. He reported no relevant disclosures.
Second MDD may be helpful for CTD-related ILD
Accumulating evidence suggests that multidisciplinary committees play a central role in improving the diagnostic accuracy of complex medical conditions. Interstitial lung disease (ILD) encompasses a number of clinical entities and no single diagnostic test alone can discriminate among the various causes of ILD. Instead, these diagnoses are based on a constellation of signs and symptoms, and radiographic, pathologic, and laboratory studies.
However, unanswered questions remain. First, it is unclear whether a single MDD is sufficient. The present study found that 20% of cases were unclassifiable after the MDD. A second MDD may be helpful, especially in patients with ILDs related to connective tissue disease (CTD). The rheumatic diseases most commonly associated with ILD (for example, systemic sclerosis, rheumatoid arthritis, myositis) often evolve at different rates, and not all of the signs and symptoms of these conditions may be present or apparent at the time of the ILD presentation. A second MDD discussion may be particularly helpful in patients presenting with a specific CTD-related autoantibody in the absence of clinical signs and symptoms of a CTD. Another unanswered question is whether MDDs actually improve clinically meaningful outcomes for patients, such as survival and quality of life. At our CTD-ILD Program at the University of California, Los Angeles, we have found that our MDD has augmented patient satisfaction with their care, and it has also improved our ability to identify patients who are eligible for specific clinical studies. Future research is needed to determine to assess the impact of MDD on a variety of patient-centered and practice/research-focused outcomes.
Elizabeth Volkmann, MD, is founder and codirector of the CTD-ILD Program at the University of California, Los Angeles. She disclosed serving as a consultant or as a member of an advisory board for Boehringer Ingelheim and Astellas Pharma. She has received grants from Boehringer Ingelheim, Merck Serono, and the Rheumatology Research Foundation.
MDD strategy is crucial for accurate ILD diagnoses
The field of interstitial lung diseases (ILD) is challenging, with more than 200 disorders as possible diagnoses for patients who present to clinicians with similar symptoms and chest x-ray findings. The multidisciplinary discussion (MDD) strategy is very important for attaining an accurate ILD diagnosis.
We have had routine, formal, multidisciplinary discussions at our center since 2008. My guesstimate is that at least a third of patients referred as having idiopathic pulmonary fibrosis or another form of ILD by pulmonologists had been given the wrong diagnosis. Frequently, this was because of incorrect impressions provided by local radiologists and/or pathologists along with the clinician’s own limited knowledge of ILD.
In my experience, some patients described their pulmonologists as becoming irate with them when they asked for a second opinion, and I have had to try to avoid confrontations with referring physicians when trying to explain why the referral diagnosis was inaccurate.
Challenges to instituting the multidisciplinary discussion approach include coverage by health plans for a second-opinion evaluation, the willingness of physicians (for example, pulmonologists) outside of academic referral centers to refer patients to a center capable of adequately conducting an MDD, and patients’ desire to undergo an evaluation at centers of excellence where an MDD can be performed.
One must have also adequate resources to perform a proper MDD. But even in centers that refer patients, pulmonologists should confer with their colleague radiologists – and pathologists when appropriate – to try to make the most accurate diagnosis. And they should continue to question their diagnosis at follow-up appointments, as new symptoms and findings may arise or additional crucial information can become available over time that can point to an alternative diagnosis.
Kenneth C. Meyer, MD, MS, served as medical director of the lung transplant program and head of ILD at the University of Wisconsin–Madison. He reported no relevant disclosures.
Second MDD may be helpful for CTD-related ILD
Accumulating evidence suggests that multidisciplinary committees play a central role in improving the diagnostic accuracy of complex medical conditions. Interstitial lung disease (ILD) encompasses a number of clinical entities and no single diagnostic test alone can discriminate among the various causes of ILD. Instead, these diagnoses are based on a constellation of signs and symptoms, and radiographic, pathologic, and laboratory studies.
However, unanswered questions remain. First, it is unclear whether a single MDD is sufficient. The present study found that 20% of cases were unclassifiable after the MDD. A second MDD may be helpful, especially in patients with ILDs related to connective tissue disease (CTD). The rheumatic diseases most commonly associated with ILD (for example, systemic sclerosis, rheumatoid arthritis, myositis) often evolve at different rates, and not all of the signs and symptoms of these conditions may be present or apparent at the time of the ILD presentation. A second MDD discussion may be particularly helpful in patients presenting with a specific CTD-related autoantibody in the absence of clinical signs and symptoms of a CTD. Another unanswered question is whether MDDs actually improve clinically meaningful outcomes for patients, such as survival and quality of life. At our CTD-ILD Program at the University of California, Los Angeles, we have found that our MDD has augmented patient satisfaction with their care, and it has also improved our ability to identify patients who are eligible for specific clinical studies. Future research is needed to determine to assess the impact of MDD on a variety of patient-centered and practice/research-focused outcomes.
Elizabeth Volkmann, MD, is founder and codirector of the CTD-ILD Program at the University of California, Los Angeles. She disclosed serving as a consultant or as a member of an advisory board for Boehringer Ingelheim and Astellas Pharma. She has received grants from Boehringer Ingelheim, Merck Serono, and the Rheumatology Research Foundation.
MDD strategy is crucial for accurate ILD diagnoses
The field of interstitial lung diseases (ILD) is challenging, with more than 200 disorders as possible diagnoses for patients who present to clinicians with similar symptoms and chest x-ray findings. The multidisciplinary discussion (MDD) strategy is very important for attaining an accurate ILD diagnosis.
We have had routine, formal, multidisciplinary discussions at our center since 2008. My guesstimate is that at least a third of patients referred as having idiopathic pulmonary fibrosis or another form of ILD by pulmonologists had been given the wrong diagnosis. Frequently, this was because of incorrect impressions provided by local radiologists and/or pathologists along with the clinician’s own limited knowledge of ILD.
In my experience, some patients described their pulmonologists as becoming irate with them when they asked for a second opinion, and I have had to try to avoid confrontations with referring physicians when trying to explain why the referral diagnosis was inaccurate.
Challenges to instituting the multidisciplinary discussion approach include coverage by health plans for a second-opinion evaluation, the willingness of physicians (for example, pulmonologists) outside of academic referral centers to refer patients to a center capable of adequately conducting an MDD, and patients’ desire to undergo an evaluation at centers of excellence where an MDD can be performed.
One must have also adequate resources to perform a proper MDD. But even in centers that refer patients, pulmonologists should confer with their colleague radiologists – and pathologists when appropriate – to try to make the most accurate diagnosis. And they should continue to question their diagnosis at follow-up appointments, as new symptoms and findings may arise or additional crucial information can become available over time that can point to an alternative diagnosis.
Kenneth C. Meyer, MD, MS, served as medical director of the lung transplant program and head of ILD at the University of Wisconsin–Madison. He reported no relevant disclosures.
Second MDD may be helpful for CTD-related ILD
Accumulating evidence suggests that multidisciplinary committees play a central role in improving the diagnostic accuracy of complex medical conditions. Interstitial lung disease (ILD) encompasses a number of clinical entities and no single diagnostic test alone can discriminate among the various causes of ILD. Instead, these diagnoses are based on a constellation of signs and symptoms, and radiographic, pathologic, and laboratory studies.
However, unanswered questions remain. First, it is unclear whether a single MDD is sufficient. The present study found that 20% of cases were unclassifiable after the MDD. A second MDD may be helpful, especially in patients with ILDs related to connective tissue disease (CTD). The rheumatic diseases most commonly associated with ILD (for example, systemic sclerosis, rheumatoid arthritis, myositis) often evolve at different rates, and not all of the signs and symptoms of these conditions may be present or apparent at the time of the ILD presentation. A second MDD discussion may be particularly helpful in patients presenting with a specific CTD-related autoantibody in the absence of clinical signs and symptoms of a CTD. Another unanswered question is whether MDDs actually improve clinically meaningful outcomes for patients, such as survival and quality of life. At our CTD-ILD Program at the University of California, Los Angeles, we have found that our MDD has augmented patient satisfaction with their care, and it has also improved our ability to identify patients who are eligible for specific clinical studies. Future research is needed to determine to assess the impact of MDD on a variety of patient-centered and practice/research-focused outcomes.
Elizabeth Volkmann, MD, is founder and codirector of the CTD-ILD Program at the University of California, Los Angeles. She disclosed serving as a consultant or as a member of an advisory board for Boehringer Ingelheim and Astellas Pharma. She has received grants from Boehringer Ingelheim, Merck Serono, and the Rheumatology Research Foundation.
New research provides strong statistical support for the use of dynamic multidisciplinary discussion in the diagnosis of patients who may have interstitial lung diseases (ILD).
and it changed the diagnosis in 41% of the other cases.
The American Thoracic Society, European Respiratory Society, Japanese Respiratory Society, and Latin American Thoracic Association adopted joint guidelines for the treatment of idiopathic pulmonary fibrosis in 2015, and the ATS and ERS updated guidelines for the classification and terminology for idiopathic interstitial pneumonias in 2013. The Lancet Respiratory Medicine published what some consider to be a landmark evaluation of multidisciplinary team agreement on diagnosis of interstitial lung disease following the adoption of these guidelines (Walsh SLF et al. 2016;4[7]:557-65). This study showed that in idiopathic pulmonary fibrosis, multidisciplinary team meetings “have a higher level of agreement on diagnoses, assign diagnoses with higher confidence more frequently, and provide diagnoses that have nonsignificant greater prognostic separation than do clinicians or radiologists in most cases,” the researchers wrote.
In the new study, MDD failed to produce a diagnosis or suggestions about a way forward in only 3.5% of patients, according to the study, which appeared March 30 in CHEST®.
According to Dr. Antin-Ozerkis, accurate diagnosis of ILD is crucial to treatment, but it can be challenging to achieve. The MDD approach has been recommended since 2002 by the ATS and ERS, she said.
The study authors, led by Laurens J. De Sadeleer, MD, of Belgium’s University Hospitals Leuven, define the MDD approach as one “in which expert ILD clinicians, radiologists, and pathologists integrate all available clinical data, laboratory results, high-resolution computed tomography [HRCT] findings, and lung biopsy [when performed].”
For the study, the researchers tracked pre-MDD and MDD diagnoses of 938 consecutive patients with possible ILD who were discussed during 2005-2015. Of these patients, referring physicians made preliminary diagnoses in 49% of cases; in the rest, physicians either failed to develop a diagnosis or offered multiple possible diagnoses.
MDD teams produced a change in diagnosis in 191 – 42% – of patients with a pre-MDD diagnosis. Another condition was diagnosed in 118 of these patients, and the MDD teams declined to classify the other 73 patients pending further investigation.
The MDD teams also were able to produce diagnoses in 80% of cases when referring physicians could not come up with diagnoses.
“Discrepancy between pre-MDD diagnosis before work-up and discussion was remarkable,” the study authors wrote, estimating that MDD added value for 70% of referred patients.
“We believe MDD should be a common practice in the diagnosis of every patient with suspected ILD,” the researchers said.
The study doesn’t examine the challenges of putting MDD into practice, but Dr. Antin-Ozerkis provided some perspective. “It may be difficult for physicians to take the time from a busy practice to meet with a multidisciplinary team. It can require resources to gather the data necessary to comprehensively assess each patient case. Additionally, maintaining staff with experienced pulmonologists, radiologists and pathologists may be costly.”
She added that “there are various ways in which MDD may occur,” and that the pros and cons of different methods have not been well studied. “This practice will likely evolve with the development of new biomarkers and other diagnostic strategies in IPF [idiopathic pulmonary fibrosis].”
Still, she said, “this joint undertaking is clearly vital in helping to guide clinical practice, including therapeutic decisions and discussion of prognosis. For now, any discussion between clinician, radiologist, and pathologist is of benefit.”
Research Foundation-Flanders and University Hospitals Leuven funded the study. Some study authors reported various disclosures. Dr. Antin-Ozerkis disclosed serving as an investigator on several clinical trials for IPF and other ILDs by Boehringer, Promedior, Fibrogen and Roche. She noted that payments go directly to the university with no direct payments to the investigator.
SOURCE: De Sadeleer LJ et al. Chest. 2018 Mar 30. doi: 10.1016/j.chest.2018.03.026.
New research provides strong statistical support for the use of dynamic multidisciplinary discussion in the diagnosis of patients who may have interstitial lung diseases (ILD).
and it changed the diagnosis in 41% of the other cases.
The American Thoracic Society, European Respiratory Society, Japanese Respiratory Society, and Latin American Thoracic Association adopted joint guidelines for the treatment of idiopathic pulmonary fibrosis in 2015, and the ATS and ERS updated guidelines for the classification and terminology for idiopathic interstitial pneumonias in 2013. The Lancet Respiratory Medicine published what some consider to be a landmark evaluation of multidisciplinary team agreement on diagnosis of interstitial lung disease following the adoption of these guidelines (Walsh SLF et al. 2016;4[7]:557-65). This study showed that in idiopathic pulmonary fibrosis, multidisciplinary team meetings “have a higher level of agreement on diagnoses, assign diagnoses with higher confidence more frequently, and provide diagnoses that have nonsignificant greater prognostic separation than do clinicians or radiologists in most cases,” the researchers wrote.
In the new study, MDD failed to produce a diagnosis or suggestions about a way forward in only 3.5% of patients, according to the study, which appeared March 30 in CHEST®.
According to Dr. Antin-Ozerkis, accurate diagnosis of ILD is crucial to treatment, but it can be challenging to achieve. The MDD approach has been recommended since 2002 by the ATS and ERS, she said.
The study authors, led by Laurens J. De Sadeleer, MD, of Belgium’s University Hospitals Leuven, define the MDD approach as one “in which expert ILD clinicians, radiologists, and pathologists integrate all available clinical data, laboratory results, high-resolution computed tomography [HRCT] findings, and lung biopsy [when performed].”
For the study, the researchers tracked pre-MDD and MDD diagnoses of 938 consecutive patients with possible ILD who were discussed during 2005-2015. Of these patients, referring physicians made preliminary diagnoses in 49% of cases; in the rest, physicians either failed to develop a diagnosis or offered multiple possible diagnoses.
MDD teams produced a change in diagnosis in 191 – 42% – of patients with a pre-MDD diagnosis. Another condition was diagnosed in 118 of these patients, and the MDD teams declined to classify the other 73 patients pending further investigation.
The MDD teams also were able to produce diagnoses in 80% of cases when referring physicians could not come up with diagnoses.
“Discrepancy between pre-MDD diagnosis before work-up and discussion was remarkable,” the study authors wrote, estimating that MDD added value for 70% of referred patients.
“We believe MDD should be a common practice in the diagnosis of every patient with suspected ILD,” the researchers said.
The study doesn’t examine the challenges of putting MDD into practice, but Dr. Antin-Ozerkis provided some perspective. “It may be difficult for physicians to take the time from a busy practice to meet with a multidisciplinary team. It can require resources to gather the data necessary to comprehensively assess each patient case. Additionally, maintaining staff with experienced pulmonologists, radiologists and pathologists may be costly.”
She added that “there are various ways in which MDD may occur,” and that the pros and cons of different methods have not been well studied. “This practice will likely evolve with the development of new biomarkers and other diagnostic strategies in IPF [idiopathic pulmonary fibrosis].”
Still, she said, “this joint undertaking is clearly vital in helping to guide clinical practice, including therapeutic decisions and discussion of prognosis. For now, any discussion between clinician, radiologist, and pathologist is of benefit.”
Research Foundation-Flanders and University Hospitals Leuven funded the study. Some study authors reported various disclosures. Dr. Antin-Ozerkis disclosed serving as an investigator on several clinical trials for IPF and other ILDs by Boehringer, Promedior, Fibrogen and Roche. She noted that payments go directly to the university with no direct payments to the investigator.
SOURCE: De Sadeleer LJ et al. Chest. 2018 Mar 30. doi: 10.1016/j.chest.2018.03.026.
FROM CHEST
Key clinical point: Multidisciplinary discussion (MDD) in cases of suspected interstitial lung disease frequently produces adjustments of previous diagnoses and new diagnoses when none existed previously.
Major finding: MDD teams produced a change in diagnosis in 42% of patients with a pre-MDD diagnosis and in 80% of those without one.
Study details: 938 consecutive patients at University Hospitals Leuven, Belgium, with possible ILD who underwent MDD diagnostics during 2005-2015.
Disclosures: Research Foundation–Flanders and University Hospitals Leuven funded the study. Some study authors reported various disclosures. Dr. Antin-Ozerkis disclosed serving as an investigator on several clinical trials for idiopathic pulmonary fibrosis and other ILDs by Boehringer, Promedior, FibroGen, and Roche. She noted that payments go directly to the university, with no direct payments to the investigator.
Source: De Sadeleer LJ et al. Chest 2018. 2018 Mar 30. doi: 10.1016/j.chest.2018.03.026.













