User login
Dear VESS Members and Attendees: Welcome to Spring Meeting
On the advent of this year’s Society for Vascular Surgery’s (SVS) Vascular Annual Meeting (VAM), I would like to welcome you to the 2018 annual spring meeting for VESS, which convenes in conjunction with VAM on June 20 at the Hynes Convention Center in Boston. Our Wednesday program looks very diverse and outstanding, covering key topics in aortic and branch aortic, cerebrovascular, lower extremity, venous disease, hemodialysis, physician wellness/burnout, academic issues, and the medical management of vascular disease. Thank you to Matthew Smeds and the rest of the program committee for putting together such an engaging lineup for this year’s spring meeting! I would also encourage you to visit our industry sponsors for this event; exhibits will be available for perusal June 21-22 within the convention center. Finally, we will be cosponsoring an event Thursday, June 21, at 7 p.m. in the Independence West Room of the Sheraton Hotel as a Networking Reception for Women, Diversity, and Young Surgeons. All residents and students are invited to attend this networking reception hosted by SVS and VESS. Thanks also to the SVS for hosting this meeting and for the ongoing collaboration we have enjoyed between our societies!
VESS members and leadership have continued to elevate the practice of vascular surgery and the research that has defined it. The more than 40-year history of this society is well outlined by Dr. Vik Kashyap in J Vasc Surg 2014;60(4):1123-4. VESS remains focused on engaging vascular trainees and vascular surgeons within a framework of collegial academic excellence. We continue to support research through grant funding at both the trainee and young investigator levels, and our presenters at both the spring VESS/VAM and Winter Annual Meetings enjoy a very high acceptance rate for publication of their findings. For more information about VESS, just visit vesurgery.org. The leadership for this society is proud of what it stands for. We are committed to exploring relevant and educational topics in vascular surgery. We hope this year’s spring meeting enhances your understanding and practice of vascular surgery. See you June 20th!
Jon Eliason, MD
VESS President
On the advent of this year’s Society for Vascular Surgery’s (SVS) Vascular Annual Meeting (VAM), I would like to welcome you to the 2018 annual spring meeting for VESS, which convenes in conjunction with VAM on June 20 at the Hynes Convention Center in Boston. Our Wednesday program looks very diverse and outstanding, covering key topics in aortic and branch aortic, cerebrovascular, lower extremity, venous disease, hemodialysis, physician wellness/burnout, academic issues, and the medical management of vascular disease. Thank you to Matthew Smeds and the rest of the program committee for putting together such an engaging lineup for this year’s spring meeting! I would also encourage you to visit our industry sponsors for this event; exhibits will be available for perusal June 21-22 within the convention center. Finally, we will be cosponsoring an event Thursday, June 21, at 7 p.m. in the Independence West Room of the Sheraton Hotel as a Networking Reception for Women, Diversity, and Young Surgeons. All residents and students are invited to attend this networking reception hosted by SVS and VESS. Thanks also to the SVS for hosting this meeting and for the ongoing collaboration we have enjoyed between our societies!
VESS members and leadership have continued to elevate the practice of vascular surgery and the research that has defined it. The more than 40-year history of this society is well outlined by Dr. Vik Kashyap in J Vasc Surg 2014;60(4):1123-4. VESS remains focused on engaging vascular trainees and vascular surgeons within a framework of collegial academic excellence. We continue to support research through grant funding at both the trainee and young investigator levels, and our presenters at both the spring VESS/VAM and Winter Annual Meetings enjoy a very high acceptance rate for publication of their findings. For more information about VESS, just visit vesurgery.org. The leadership for this society is proud of what it stands for. We are committed to exploring relevant and educational topics in vascular surgery. We hope this year’s spring meeting enhances your understanding and practice of vascular surgery. See you June 20th!
Jon Eliason, MD
VESS President
On the advent of this year’s Society for Vascular Surgery’s (SVS) Vascular Annual Meeting (VAM), I would like to welcome you to the 2018 annual spring meeting for VESS, which convenes in conjunction with VAM on June 20 at the Hynes Convention Center in Boston. Our Wednesday program looks very diverse and outstanding, covering key topics in aortic and branch aortic, cerebrovascular, lower extremity, venous disease, hemodialysis, physician wellness/burnout, academic issues, and the medical management of vascular disease. Thank you to Matthew Smeds and the rest of the program committee for putting together such an engaging lineup for this year’s spring meeting! I would also encourage you to visit our industry sponsors for this event; exhibits will be available for perusal June 21-22 within the convention center. Finally, we will be cosponsoring an event Thursday, June 21, at 7 p.m. in the Independence West Room of the Sheraton Hotel as a Networking Reception for Women, Diversity, and Young Surgeons. All residents and students are invited to attend this networking reception hosted by SVS and VESS. Thanks also to the SVS for hosting this meeting and for the ongoing collaboration we have enjoyed between our societies!
VESS members and leadership have continued to elevate the practice of vascular surgery and the research that has defined it. The more than 40-year history of this society is well outlined by Dr. Vik Kashyap in J Vasc Surg 2014;60(4):1123-4. VESS remains focused on engaging vascular trainees and vascular surgeons within a framework of collegial academic excellence. We continue to support research through grant funding at both the trainee and young investigator levels, and our presenters at both the spring VESS/VAM and Winter Annual Meetings enjoy a very high acceptance rate for publication of their findings. For more information about VESS, just visit vesurgery.org. The leadership for this society is proud of what it stands for. We are committed to exploring relevant and educational topics in vascular surgery. We hope this year’s spring meeting enhances your understanding and practice of vascular surgery. See you June 20th!
Jon Eliason, MD
VESS President
With Collaboration the Norm, Fitting For Nurses, Surgeons to Have Meetings in Tandem
It seems fitting, said Tiffany Street, President of the Society for Vascular Nursing, that SVN and SVS have their conferences in the same location and with overlapping times.
“It parallels what we do every day in clinical practice,” she said. “Recently, we have focused our attention on the emphasis of the clinical vascular care team. Physicians and nurses collaborate daily on the care of vascular patients so collaboration in the learning environment is imperative.”
SVN’s 36th Annual Conference, SVN @SVS, will be held June 20 to 21, coinciding with the opening two days of VAM. The SVN conference registration fee permits entrance to VAM, as well.
Both organizations are emphasizing the team approach to vascular care this year, with SVN also stressing vascular education and the holistic approach to vascular patient care, Ms. Street said. An abstract session Thursday will focus on “The Vascular Team Connections,” with two abstract presentations plus a panel discussion on “How Collaboration Changes a Patient.” Speakers include surgeon and SVS President R. Clement Darling III, MD; a physician assistant, Erin Hanlon, PA-PAC; and two nurses, Marie Rossi, BS, RN, and Karen Fitzgerald, MSN, RN, NP.
The team approach is vitally important, Ms. Street said. “Vascular nursing is responsible for the care of the patient across the continuum in collaboration with the surgeon,” she said.
Undergoing a surgical procedure affects not only the patient but also the patient’s family, she pointed out. “Because the family support system is vital to good postoperative outcomes, vascular nurses support the family as well.” Nurses cover with the patient and family what they all might expect during the patient’s recovery, helping them think through the various issues and how best to manage them, she said. “It’s all part of the team approach.”
Abstract sessions at SVN @SVS will focus on CLI, AAA, carotid artery, PAD, venous and arterial compression, and vascular team connections. Concurrent sessions will target both the novice and experienced nurse, plus include other emphases, as well. Several SVS members will be presenters at SVN sessions.
The keynote address will cover the care of patients from the Boston Marathon bombing in 2013. Jonathan Gates, MD, who was Medical Director of Trauma Services at Brigham and Women’s Hospital at the time of the bombing and operated on bombing victims that day, will present the address. Other sessions at the Vascular Annual Meeting also stress the vascular team and patient benefits, including “Team Forum: Improving Metrics in Clinical Practice,” from 1:30 to 3 p.m. Friday. Nurses are sure to find topics of interest at VAM, said Dr. Darling. “I find the team approach integral to optimal patient outcomes,” he said. “I could not be happier at including all members of the team at this year’s VAM, from the special programming for physician assistants on Thursday afternoon to SVN @SVS.
“When we work together,” he said, “everyone benefits, especially the patient.”
Visit vsweb.org/SVN18conference or the VAM Planner (vsweb.org/VAMPlanner) for the complete schedule and more information.
It seems fitting, said Tiffany Street, President of the Society for Vascular Nursing, that SVN and SVS have their conferences in the same location and with overlapping times.
“It parallels what we do every day in clinical practice,” she said. “Recently, we have focused our attention on the emphasis of the clinical vascular care team. Physicians and nurses collaborate daily on the care of vascular patients so collaboration in the learning environment is imperative.”
SVN’s 36th Annual Conference, SVN @SVS, will be held June 20 to 21, coinciding with the opening two days of VAM. The SVN conference registration fee permits entrance to VAM, as well.
Both organizations are emphasizing the team approach to vascular care this year, with SVN also stressing vascular education and the holistic approach to vascular patient care, Ms. Street said. An abstract session Thursday will focus on “The Vascular Team Connections,” with two abstract presentations plus a panel discussion on “How Collaboration Changes a Patient.” Speakers include surgeon and SVS President R. Clement Darling III, MD; a physician assistant, Erin Hanlon, PA-PAC; and two nurses, Marie Rossi, BS, RN, and Karen Fitzgerald, MSN, RN, NP.
The team approach is vitally important, Ms. Street said. “Vascular nursing is responsible for the care of the patient across the continuum in collaboration with the surgeon,” she said.
Undergoing a surgical procedure affects not only the patient but also the patient’s family, she pointed out. “Because the family support system is vital to good postoperative outcomes, vascular nurses support the family as well.” Nurses cover with the patient and family what they all might expect during the patient’s recovery, helping them think through the various issues and how best to manage them, she said. “It’s all part of the team approach.”
Abstract sessions at SVN @SVS will focus on CLI, AAA, carotid artery, PAD, venous and arterial compression, and vascular team connections. Concurrent sessions will target both the novice and experienced nurse, plus include other emphases, as well. Several SVS members will be presenters at SVN sessions.
The keynote address will cover the care of patients from the Boston Marathon bombing in 2013. Jonathan Gates, MD, who was Medical Director of Trauma Services at Brigham and Women’s Hospital at the time of the bombing and operated on bombing victims that day, will present the address. Other sessions at the Vascular Annual Meeting also stress the vascular team and patient benefits, including “Team Forum: Improving Metrics in Clinical Practice,” from 1:30 to 3 p.m. Friday. Nurses are sure to find topics of interest at VAM, said Dr. Darling. “I find the team approach integral to optimal patient outcomes,” he said. “I could not be happier at including all members of the team at this year’s VAM, from the special programming for physician assistants on Thursday afternoon to SVN @SVS.
“When we work together,” he said, “everyone benefits, especially the patient.”
Visit vsweb.org/SVN18conference or the VAM Planner (vsweb.org/VAMPlanner) for the complete schedule and more information.
It seems fitting, said Tiffany Street, President of the Society for Vascular Nursing, that SVN and SVS have their conferences in the same location and with overlapping times.
“It parallels what we do every day in clinical practice,” she said. “Recently, we have focused our attention on the emphasis of the clinical vascular care team. Physicians and nurses collaborate daily on the care of vascular patients so collaboration in the learning environment is imperative.”
SVN’s 36th Annual Conference, SVN @SVS, will be held June 20 to 21, coinciding with the opening two days of VAM. The SVN conference registration fee permits entrance to VAM, as well.
Both organizations are emphasizing the team approach to vascular care this year, with SVN also stressing vascular education and the holistic approach to vascular patient care, Ms. Street said. An abstract session Thursday will focus on “The Vascular Team Connections,” with two abstract presentations plus a panel discussion on “How Collaboration Changes a Patient.” Speakers include surgeon and SVS President R. Clement Darling III, MD; a physician assistant, Erin Hanlon, PA-PAC; and two nurses, Marie Rossi, BS, RN, and Karen Fitzgerald, MSN, RN, NP.
The team approach is vitally important, Ms. Street said. “Vascular nursing is responsible for the care of the patient across the continuum in collaboration with the surgeon,” she said.
Undergoing a surgical procedure affects not only the patient but also the patient’s family, she pointed out. “Because the family support system is vital to good postoperative outcomes, vascular nurses support the family as well.” Nurses cover with the patient and family what they all might expect during the patient’s recovery, helping them think through the various issues and how best to manage them, she said. “It’s all part of the team approach.”
Abstract sessions at SVN @SVS will focus on CLI, AAA, carotid artery, PAD, venous and arterial compression, and vascular team connections. Concurrent sessions will target both the novice and experienced nurse, plus include other emphases, as well. Several SVS members will be presenters at SVN sessions.
The keynote address will cover the care of patients from the Boston Marathon bombing in 2013. Jonathan Gates, MD, who was Medical Director of Trauma Services at Brigham and Women’s Hospital at the time of the bombing and operated on bombing victims that day, will present the address. Other sessions at the Vascular Annual Meeting also stress the vascular team and patient benefits, including “Team Forum: Improving Metrics in Clinical Practice,” from 1:30 to 3 p.m. Friday. Nurses are sure to find topics of interest at VAM, said Dr. Darling. “I find the team approach integral to optimal patient outcomes,” he said. “I could not be happier at including all members of the team at this year’s VAM, from the special programming for physician assistants on Thursday afternoon to SVN @SVS.
“When we work together,” he said, “everyone benefits, especially the patient.”
Visit vsweb.org/SVN18conference or the VAM Planner (vsweb.org/VAMPlanner) for the complete schedule and more information.
Call for Serious Mental Illness and Substance Use Disorder Manuscripts
Federal Practitioner is inviting VA, DoD, and PHS health care providers and researchers to contribute to a special issue that will be published in October 2018 and will examine series mental health and substance use disorders. Articles that address serious mental illnesses, including schizophrenia, bipolar disorder, major depressive disorder, and alcohol or opioid misuse are especially desired. Articles may include new research, review articles, case studies, quality improvement/quality assurance programs, and patient-centered care best practices.
The full text of all accepted Federal Practitioner articles are now included in the PubMed Central database and are part of any PubMed search result.
Interested authors can submit articles at http://www.editorialmanager.com/fedprac or submit a brief 2 to 3 sentence abstract to [email protected] by July 15, 2018. The updated and complete submission guidelines, including details about the style and format, can be found here:
http://www.mdedge.com/fedprac/page/submission-guidelines
Federal Practitioner uses Editorial Manager, a web-based manuscript submission and review system. All manuscripts must be submitted through this system.
All manuscripts submitted to Federal Practitioner for both special and regular issues will be subject to peer review. Peer reviews are conducted in a double-blind fashion, and the reviewers are asked to comment on the manuscript’s importance, accuracy, relevance, clarity, timeliness, balance, and reference citation. Final decisions on all submitted manuscripts are made by the Editor-in-Chief (or, in the event of a potential conflict of interest, a designated surrogate from the journal’s Editorial Advisory Association).
Federal Practitioner is inviting VA, DoD, and PHS health care providers and researchers to contribute to a special issue that will be published in October 2018 and will examine series mental health and substance use disorders. Articles that address serious mental illnesses, including schizophrenia, bipolar disorder, major depressive disorder, and alcohol or opioid misuse are especially desired. Articles may include new research, review articles, case studies, quality improvement/quality assurance programs, and patient-centered care best practices.
The full text of all accepted Federal Practitioner articles are now included in the PubMed Central database and are part of any PubMed search result.
Interested authors can submit articles at http://www.editorialmanager.com/fedprac or submit a brief 2 to 3 sentence abstract to [email protected] by July 15, 2018. The updated and complete submission guidelines, including details about the style and format, can be found here:
http://www.mdedge.com/fedprac/page/submission-guidelines
Federal Practitioner uses Editorial Manager, a web-based manuscript submission and review system. All manuscripts must be submitted through this system.
All manuscripts submitted to Federal Practitioner for both special and regular issues will be subject to peer review. Peer reviews are conducted in a double-blind fashion, and the reviewers are asked to comment on the manuscript’s importance, accuracy, relevance, clarity, timeliness, balance, and reference citation. Final decisions on all submitted manuscripts are made by the Editor-in-Chief (or, in the event of a potential conflict of interest, a designated surrogate from the journal’s Editorial Advisory Association).
Federal Practitioner is inviting VA, DoD, and PHS health care providers and researchers to contribute to a special issue that will be published in October 2018 and will examine series mental health and substance use disorders. Articles that address serious mental illnesses, including schizophrenia, bipolar disorder, major depressive disorder, and alcohol or opioid misuse are especially desired. Articles may include new research, review articles, case studies, quality improvement/quality assurance programs, and patient-centered care best practices.
The full text of all accepted Federal Practitioner articles are now included in the PubMed Central database and are part of any PubMed search result.
Interested authors can submit articles at http://www.editorialmanager.com/fedprac or submit a brief 2 to 3 sentence abstract to [email protected] by July 15, 2018. The updated and complete submission guidelines, including details about the style and format, can be found here:
http://www.mdedge.com/fedprac/page/submission-guidelines
Federal Practitioner uses Editorial Manager, a web-based manuscript submission and review system. All manuscripts must be submitted through this system.
All manuscripts submitted to Federal Practitioner for both special and regular issues will be subject to peer review. Peer reviews are conducted in a double-blind fashion, and the reviewers are asked to comment on the manuscript’s importance, accuracy, relevance, clarity, timeliness, balance, and reference citation. Final decisions on all submitted manuscripts are made by the Editor-in-Chief (or, in the event of a potential conflict of interest, a designated surrogate from the journal’s Editorial Advisory Association).
Crawford Forum Celebrates 25 Years
The E. Stanley Crawford Critical Issues Forum – marking 25 years under that name this year – is a mainstay of the Vascular Annual Meeting.
But who was E. Stanley Crawford?
He was a “cardiovascular surgeon extraordinare,” according to the late Calvin Ernst, MD, writing after Dr. Crawford’s death in late 1992. Dr. Crawford developed new techniques for treating AAA; was a coinventor of the Baylor (College of Medicine, where he worked from 1956 until his death) Rapid Autologus Transfusion System, a machine that recycles a patient’s red blood cells during surgery; and wrote more than 300 peer-reviewed publications and book chapters. With his son, Dr. John Lloyd Crawford II, he wrote the “Diseases of the Aorta” textbook, which Dr. Ernst called “a standard reference text on aortic surgery.”
Dr. Crawford also helped develop the SVS Forum on Critical Issues, convening the first session during the 1988 VAM. It was decided the forum should address socioeconomic and research issues, as they impact vascular surgery, and be led by that year’s president-elect.
Dr. Ernst said Dr. Crawford believed the vascular surgery specialty had become “increasingly vague, its mission ill-defined, and its future membership uncertain. The big question: 'Who would want to go into vascular surgery today with the uncertainties of tomorrow and how can those already committed remain dominant?’ ” Dr. Ernst wrote.
Dr. Crawford felt the SVS needed to take a leadership role in this and other questions; he believed the SVS and its members were eminently qualified to do so successfully.
After his death, the SVS Executive Council unanimously agreed to rename the Critical Issues Forum for Dr. Crawford. The first such named forum was held 25 years ago, at the 1993 VAM.
This year’s Crawford Forum will focus on the vascular surgery workforce, addressing challenges and solutions. President-Elect Michel S. Makaroun, MD, who spearheaded a survey of SVS members on workforce data in late December 2017, will moderate.
The E. Stanley Crawford Critical Issues Forum – marking 25 years under that name this year – is a mainstay of the Vascular Annual Meeting.
But who was E. Stanley Crawford?
He was a “cardiovascular surgeon extraordinare,” according to the late Calvin Ernst, MD, writing after Dr. Crawford’s death in late 1992. Dr. Crawford developed new techniques for treating AAA; was a coinventor of the Baylor (College of Medicine, where he worked from 1956 until his death) Rapid Autologus Transfusion System, a machine that recycles a patient’s red blood cells during surgery; and wrote more than 300 peer-reviewed publications and book chapters. With his son, Dr. John Lloyd Crawford II, he wrote the “Diseases of the Aorta” textbook, which Dr. Ernst called “a standard reference text on aortic surgery.”
Dr. Crawford also helped develop the SVS Forum on Critical Issues, convening the first session during the 1988 VAM. It was decided the forum should address socioeconomic and research issues, as they impact vascular surgery, and be led by that year’s president-elect.
Dr. Ernst said Dr. Crawford believed the vascular surgery specialty had become “increasingly vague, its mission ill-defined, and its future membership uncertain. The big question: 'Who would want to go into vascular surgery today with the uncertainties of tomorrow and how can those already committed remain dominant?’ ” Dr. Ernst wrote.
Dr. Crawford felt the SVS needed to take a leadership role in this and other questions; he believed the SVS and its members were eminently qualified to do so successfully.
After his death, the SVS Executive Council unanimously agreed to rename the Critical Issues Forum for Dr. Crawford. The first such named forum was held 25 years ago, at the 1993 VAM.
This year’s Crawford Forum will focus on the vascular surgery workforce, addressing challenges and solutions. President-Elect Michel S. Makaroun, MD, who spearheaded a survey of SVS members on workforce data in late December 2017, will moderate.
The E. Stanley Crawford Critical Issues Forum – marking 25 years under that name this year – is a mainstay of the Vascular Annual Meeting.
But who was E. Stanley Crawford?
He was a “cardiovascular surgeon extraordinare,” according to the late Calvin Ernst, MD, writing after Dr. Crawford’s death in late 1992. Dr. Crawford developed new techniques for treating AAA; was a coinventor of the Baylor (College of Medicine, where he worked from 1956 until his death) Rapid Autologus Transfusion System, a machine that recycles a patient’s red blood cells during surgery; and wrote more than 300 peer-reviewed publications and book chapters. With his son, Dr. John Lloyd Crawford II, he wrote the “Diseases of the Aorta” textbook, which Dr. Ernst called “a standard reference text on aortic surgery.”
Dr. Crawford also helped develop the SVS Forum on Critical Issues, convening the first session during the 1988 VAM. It was decided the forum should address socioeconomic and research issues, as they impact vascular surgery, and be led by that year’s president-elect.
Dr. Ernst said Dr. Crawford believed the vascular surgery specialty had become “increasingly vague, its mission ill-defined, and its future membership uncertain. The big question: 'Who would want to go into vascular surgery today with the uncertainties of tomorrow and how can those already committed remain dominant?’ ” Dr. Ernst wrote.
Dr. Crawford felt the SVS needed to take a leadership role in this and other questions; he believed the SVS and its members were eminently qualified to do so successfully.
After his death, the SVS Executive Council unanimously agreed to rename the Critical Issues Forum for Dr. Crawford. The first such named forum was held 25 years ago, at the 1993 VAM.
This year’s Crawford Forum will focus on the vascular surgery workforce, addressing challenges and solutions. President-Elect Michel S. Makaroun, MD, who spearheaded a survey of SVS members on workforce data in late December 2017, will moderate.
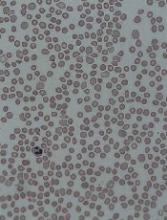
Early infection could prevent ALL, doc says
Childhood acute lymphoblastic leukemia (ALL) may be preventable, according to a researcher.
Mel Greaves, PhD, of The Institute of Cancer Research in London, UK, reviewed more than 30 years of research and concluded that ALL develops in 2 steps—genetic mutation before birth and further genetic change after birth triggered by infection.
The evidence suggests that infection early in life is beneficial to prime the immune system, but later infection without earlier priming can trigger ALL.
So priming the immune system in the first year of life could potentially prevent childhood ALL, according to Dr Greaves.
He outlined this theory in Nature Reviews Cancer.
Dr Greaves compiled more than 30 years of research into genetics, cell biology, immunology, epidemiology, and animal modelling of ALL.
The evidence led him to conclude that ALL begins with a genetic mutation that occurs before birth and predisposes a child to leukemia.
The disease is triggered later, in childhood, by exposure to one or more common infections. This primarily occurs in children who experienced “clean” childhoods in their first year of life, without much interaction with other infants or older children.
Dr Greaves challenged previous reports of possible environmental causes for ALL, such as ionizing radiation, electromagnetic waves, or man-made chemicals. He argued that none of these reports are supported by robust evidence.
Instead, he believes there is strong evidence suggesting that infection later in childhood, in the absence of earlier priming, can trigger ALL.
Dr Greaves’ studies of identical twins with ALL showed that 2 mutations were required for ALL development. The first arises in one twin in the womb but produces a population of pre-malignant cells that spread to the other twin via their shared blood supply. The second mutation arises after birth and is different in the twins.
Population studies and animal experiments suggest this second genetic hit can be triggered by infection, probably by a range of common viruses and bacteria. In one unique cluster of cases investigated by Dr Greaves and his colleagues, all cases were infected with flu virus.
In other work, researchers engineered mice with an active leukemia-initiating gene. When the team moved the mice from an ultra-clean, germ-free environment to one that had common microbes, the mice developed ALL.
Population studies have indicated that early exposure to infection in infancy, such as via day care attendance and breast feeding, can protect against ALL, probably by priming the immune system. This suggests childhood ALL may be preventable.
Dr Greaves is now investigating whether earlier exposure to harmless microbes could prevent leukemia in mice.
“I have spent more than 40 years researching childhood leukemia, and, over that time, there has been huge progress in our understanding of its biology and its treatment . . . ,” Dr Greaves said. “But it has always struck me that something big was missing, a gap in our knowledge [that failed to explain] why or how otherwise healthy children develop leukemia and whether this cancer is preventable.”
“This body of research is a culmination of decades of work and at last provides a credible explanation for how the major type of childhood leukemia develops. The research strongly suggests that ALL has a clear biological cause and is triggered by a variety of infections in predisposed children whose immune systems have not been properly primed. It also busts some persistent myths about the causes of leukemia, such as the damaging but unsubstantiated claims that the disease is commonly caused by exposure to electro-magnetic waves or pollution.”
“I hope this research will have a real impact on the lives of children. The most important implication is that most cases of childhood leukemia are likely to be preventable. It might be done in the same way that is currently under consideration for autoimmune disease or allergies, perhaps with simple and safe interventions to expose infants to a variety of common and harmless ‘bugs.’”
Childhood acute lymphoblastic leukemia (ALL) may be preventable, according to a researcher.
Mel Greaves, PhD, of The Institute of Cancer Research in London, UK, reviewed more than 30 years of research and concluded that ALL develops in 2 steps—genetic mutation before birth and further genetic change after birth triggered by infection.
The evidence suggests that infection early in life is beneficial to prime the immune system, but later infection without earlier priming can trigger ALL.
So priming the immune system in the first year of life could potentially prevent childhood ALL, according to Dr Greaves.
He outlined this theory in Nature Reviews Cancer.
Dr Greaves compiled more than 30 years of research into genetics, cell biology, immunology, epidemiology, and animal modelling of ALL.
The evidence led him to conclude that ALL begins with a genetic mutation that occurs before birth and predisposes a child to leukemia.
The disease is triggered later, in childhood, by exposure to one or more common infections. This primarily occurs in children who experienced “clean” childhoods in their first year of life, without much interaction with other infants or older children.
Dr Greaves challenged previous reports of possible environmental causes for ALL, such as ionizing radiation, electromagnetic waves, or man-made chemicals. He argued that none of these reports are supported by robust evidence.
Instead, he believes there is strong evidence suggesting that infection later in childhood, in the absence of earlier priming, can trigger ALL.
Dr Greaves’ studies of identical twins with ALL showed that 2 mutations were required for ALL development. The first arises in one twin in the womb but produces a population of pre-malignant cells that spread to the other twin via their shared blood supply. The second mutation arises after birth and is different in the twins.
Population studies and animal experiments suggest this second genetic hit can be triggered by infection, probably by a range of common viruses and bacteria. In one unique cluster of cases investigated by Dr Greaves and his colleagues, all cases were infected with flu virus.
In other work, researchers engineered mice with an active leukemia-initiating gene. When the team moved the mice from an ultra-clean, germ-free environment to one that had common microbes, the mice developed ALL.
Population studies have indicated that early exposure to infection in infancy, such as via day care attendance and breast feeding, can protect against ALL, probably by priming the immune system. This suggests childhood ALL may be preventable.
Dr Greaves is now investigating whether earlier exposure to harmless microbes could prevent leukemia in mice.
“I have spent more than 40 years researching childhood leukemia, and, over that time, there has been huge progress in our understanding of its biology and its treatment . . . ,” Dr Greaves said. “But it has always struck me that something big was missing, a gap in our knowledge [that failed to explain] why or how otherwise healthy children develop leukemia and whether this cancer is preventable.”
“This body of research is a culmination of decades of work and at last provides a credible explanation for how the major type of childhood leukemia develops. The research strongly suggests that ALL has a clear biological cause and is triggered by a variety of infections in predisposed children whose immune systems have not been properly primed. It also busts some persistent myths about the causes of leukemia, such as the damaging but unsubstantiated claims that the disease is commonly caused by exposure to electro-magnetic waves or pollution.”
“I hope this research will have a real impact on the lives of children. The most important implication is that most cases of childhood leukemia are likely to be preventable. It might be done in the same way that is currently under consideration for autoimmune disease or allergies, perhaps with simple and safe interventions to expose infants to a variety of common and harmless ‘bugs.’”
Childhood acute lymphoblastic leukemia (ALL) may be preventable, according to a researcher.
Mel Greaves, PhD, of The Institute of Cancer Research in London, UK, reviewed more than 30 years of research and concluded that ALL develops in 2 steps—genetic mutation before birth and further genetic change after birth triggered by infection.
The evidence suggests that infection early in life is beneficial to prime the immune system, but later infection without earlier priming can trigger ALL.
So priming the immune system in the first year of life could potentially prevent childhood ALL, according to Dr Greaves.
He outlined this theory in Nature Reviews Cancer.
Dr Greaves compiled more than 30 years of research into genetics, cell biology, immunology, epidemiology, and animal modelling of ALL.
The evidence led him to conclude that ALL begins with a genetic mutation that occurs before birth and predisposes a child to leukemia.
The disease is triggered later, in childhood, by exposure to one or more common infections. This primarily occurs in children who experienced “clean” childhoods in their first year of life, without much interaction with other infants or older children.
Dr Greaves challenged previous reports of possible environmental causes for ALL, such as ionizing radiation, electromagnetic waves, or man-made chemicals. He argued that none of these reports are supported by robust evidence.
Instead, he believes there is strong evidence suggesting that infection later in childhood, in the absence of earlier priming, can trigger ALL.
Dr Greaves’ studies of identical twins with ALL showed that 2 mutations were required for ALL development. The first arises in one twin in the womb but produces a population of pre-malignant cells that spread to the other twin via their shared blood supply. The second mutation arises after birth and is different in the twins.
Population studies and animal experiments suggest this second genetic hit can be triggered by infection, probably by a range of common viruses and bacteria. In one unique cluster of cases investigated by Dr Greaves and his colleagues, all cases were infected with flu virus.
In other work, researchers engineered mice with an active leukemia-initiating gene. When the team moved the mice from an ultra-clean, germ-free environment to one that had common microbes, the mice developed ALL.
Population studies have indicated that early exposure to infection in infancy, such as via day care attendance and breast feeding, can protect against ALL, probably by priming the immune system. This suggests childhood ALL may be preventable.
Dr Greaves is now investigating whether earlier exposure to harmless microbes could prevent leukemia in mice.
“I have spent more than 40 years researching childhood leukemia, and, over that time, there has been huge progress in our understanding of its biology and its treatment . . . ,” Dr Greaves said. “But it has always struck me that something big was missing, a gap in our knowledge [that failed to explain] why or how otherwise healthy children develop leukemia and whether this cancer is preventable.”
“This body of research is a culmination of decades of work and at last provides a credible explanation for how the major type of childhood leukemia develops. The research strongly suggests that ALL has a clear biological cause and is triggered by a variety of infections in predisposed children whose immune systems have not been properly primed. It also busts some persistent myths about the causes of leukemia, such as the damaging but unsubstantiated claims that the disease is commonly caused by exposure to electro-magnetic waves or pollution.”
“I hope this research will have a real impact on the lives of children. The most important implication is that most cases of childhood leukemia are likely to be preventable. It might be done in the same way that is currently under consideration for autoimmune disease or allergies, perhaps with simple and safe interventions to expose infants to a variety of common and harmless ‘bugs.’”
Emicizumab reduces bleeding in hemophilia A
GLASGOW—Final results from the HAVEN 3 study suggest emicizumab prophylaxis can reduce bleeding in hemophilia A patients without factor VIII inhibitors.
Compared to patients who did not receive prophylaxis, those who received emicizumab prophylaxis had a 96% to 97% reduction in treated bleeds and a 94% to 95% reduction in all bleeds.
An intra-patient comparison showed a 68% reduction in treated bleeds with once-weekly emicizumab, compared to prior factor VIII prophylaxis.
“[Emicizumab] is the first medicine to show superior efficacy to prior factor VIII prophylaxis, the current standard of care therapy, as demonstrated by a statistically significant reduction in treated bleeds in the HAVEN 3 study intra-patient comparison,” said Johnny Mahlangu, MB BCh, of the University of the Witwatersrand in Johannesburg, South Africa.
Dr Mahlangu presented these results at the World Federation of Hemophilia (WFH) 2018 World Congress during the late-breaking abstract session on Monday. HAVEN 3 was sponsored by Hoffmann-La Roche.
Patients and treatment
In this phase 3 trial, researchers evaluated emicizumab in patients with hemophilia A without factor VIII inhibitors. The study included 152 patients who were 12 years of age or older and were previously treated with factor VIII therapy on-demand or as prophylaxis.
Patients previously treated with on-demand factor VIII were randomized in a 2:2:1 fashion to receive:
- Emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 1.5 mg/kg/wk until the end of study (arm A, n=36)
- Emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 3 mg/kg/2wks for at least 24 weeks (arm B, n=35)
- No prophylaxis, only episodic/on-demand factor VIII treatment (arm C, n=18).
Patients previously treated with factor VIII prophylaxis received emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 1.5 mg/kg/wk until the end of study (arm D, n=63).
Episodic treatment of breakthrough bleeds with factor VIII therapy was allowed per protocol.
Emicizumab vs no prophylaxis
The model-based (negative binomial regression model) annualized bleeding rate (ABR) for treated bleeds was 1.5 in arm A, 1.3 in arm B, and 38.2 in arm C. The median ABR for treated bleeds was 0 in arms A and B and 40.4 in arm C.
Compared to patients in arm C, those in arm A had a 96% (P<0.0001) reduction in treated bleeds, and those in arm B had a 97% (P<0.0001) reduction in treated bleeds.
None of the patients in arm C had 0 treated bleeds, compared to 55.6% of patients in arm A and 60% of patients in arm B.
The model-based ABR for all bleeds was 2.5 in arm A, 2.6 in arm B, and 47.6 in arm C.
Patients in arm A had a 95% reduction in all bleeds (P<0.0001), and patients in arm B had a 94% reduction in all bleeds (P<0.0001), compared to patients in arm C.
Fifty percent of patients in arm A had 0 total bleeds, as did 40% of patients in arm B and 0% of patients in arm C.
Intra-patient comparison
The researchers compared previous prophylaxis to once-weekly emicizumab prophylaxis in 48 patients from arm D.
The model-based ABR for treated bleeds was 4.8 with prior prophylaxis and 1.5 with emicizumab. The median ABR for treated bleeds was 1.8 and 0.0, respectively.
Patients had a 68% reduction in treated bleeds with emicizumab (P<0.0001).
With prior prophylaxis, 39.6% of patients had 0 treated bleeds. With emicizumab, 54.2% of patients had 0 treated bleeds.
Safety
There were no serious adverse events (AEs) related to emicizumab, no anti-drug antibodies detected, and none of the patients on emicizumab developed de novo factor VIII inhibitors.
Injection-site reactions occurred in 25.3% of all patients (38/150), 25% of patients in arm A (9/36), 20% in arm B (7/35), 12.5% in arm C (2/16), and 31.7% in arm D (20/63).
An additional patient in arm D (who was included in the total) reported an “injection-site erythema,” not an “injection-site reaction.”
Upper respiratory tract infections occurred in 10.7% of all patients (n=16), 11.1% (n=4) of those in arm A, 11.4% (n=4) of those in arm B, 0% of those in arm C, and 12.7% (n=8) of those in arm D.
Other AEs occurring in at least 5% of patients were arthralgia (19%), nasopharyngitis (12%), headache (11%), and influenza (6%).
One patient in arm B discontinued emicizumab due to multiple mild AEs—insomnia, hair loss, nightmare, lethargy, depressed mood, headache, and pruritus.
Two patients were lost to follow-up—1 in arm A and 1 in arm C.
GLASGOW—Final results from the HAVEN 3 study suggest emicizumab prophylaxis can reduce bleeding in hemophilia A patients without factor VIII inhibitors.
Compared to patients who did not receive prophylaxis, those who received emicizumab prophylaxis had a 96% to 97% reduction in treated bleeds and a 94% to 95% reduction in all bleeds.
An intra-patient comparison showed a 68% reduction in treated bleeds with once-weekly emicizumab, compared to prior factor VIII prophylaxis.
“[Emicizumab] is the first medicine to show superior efficacy to prior factor VIII prophylaxis, the current standard of care therapy, as demonstrated by a statistically significant reduction in treated bleeds in the HAVEN 3 study intra-patient comparison,” said Johnny Mahlangu, MB BCh, of the University of the Witwatersrand in Johannesburg, South Africa.
Dr Mahlangu presented these results at the World Federation of Hemophilia (WFH) 2018 World Congress during the late-breaking abstract session on Monday. HAVEN 3 was sponsored by Hoffmann-La Roche.
Patients and treatment
In this phase 3 trial, researchers evaluated emicizumab in patients with hemophilia A without factor VIII inhibitors. The study included 152 patients who were 12 years of age or older and were previously treated with factor VIII therapy on-demand or as prophylaxis.
Patients previously treated with on-demand factor VIII were randomized in a 2:2:1 fashion to receive:
- Emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 1.5 mg/kg/wk until the end of study (arm A, n=36)
- Emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 3 mg/kg/2wks for at least 24 weeks (arm B, n=35)
- No prophylaxis, only episodic/on-demand factor VIII treatment (arm C, n=18).
Patients previously treated with factor VIII prophylaxis received emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 1.5 mg/kg/wk until the end of study (arm D, n=63).
Episodic treatment of breakthrough bleeds with factor VIII therapy was allowed per protocol.
Emicizumab vs no prophylaxis
The model-based (negative binomial regression model) annualized bleeding rate (ABR) for treated bleeds was 1.5 in arm A, 1.3 in arm B, and 38.2 in arm C. The median ABR for treated bleeds was 0 in arms A and B and 40.4 in arm C.
Compared to patients in arm C, those in arm A had a 96% (P<0.0001) reduction in treated bleeds, and those in arm B had a 97% (P<0.0001) reduction in treated bleeds.
None of the patients in arm C had 0 treated bleeds, compared to 55.6% of patients in arm A and 60% of patients in arm B.
The model-based ABR for all bleeds was 2.5 in arm A, 2.6 in arm B, and 47.6 in arm C.
Patients in arm A had a 95% reduction in all bleeds (P<0.0001), and patients in arm B had a 94% reduction in all bleeds (P<0.0001), compared to patients in arm C.
Fifty percent of patients in arm A had 0 total bleeds, as did 40% of patients in arm B and 0% of patients in arm C.
Intra-patient comparison
The researchers compared previous prophylaxis to once-weekly emicizumab prophylaxis in 48 patients from arm D.
The model-based ABR for treated bleeds was 4.8 with prior prophylaxis and 1.5 with emicizumab. The median ABR for treated bleeds was 1.8 and 0.0, respectively.
Patients had a 68% reduction in treated bleeds with emicizumab (P<0.0001).
With prior prophylaxis, 39.6% of patients had 0 treated bleeds. With emicizumab, 54.2% of patients had 0 treated bleeds.
Safety
There were no serious adverse events (AEs) related to emicizumab, no anti-drug antibodies detected, and none of the patients on emicizumab developed de novo factor VIII inhibitors.
Injection-site reactions occurred in 25.3% of all patients (38/150), 25% of patients in arm A (9/36), 20% in arm B (7/35), 12.5% in arm C (2/16), and 31.7% in arm D (20/63).
An additional patient in arm D (who was included in the total) reported an “injection-site erythema,” not an “injection-site reaction.”
Upper respiratory tract infections occurred in 10.7% of all patients (n=16), 11.1% (n=4) of those in arm A, 11.4% (n=4) of those in arm B, 0% of those in arm C, and 12.7% (n=8) of those in arm D.
Other AEs occurring in at least 5% of patients were arthralgia (19%), nasopharyngitis (12%), headache (11%), and influenza (6%).
One patient in arm B discontinued emicizumab due to multiple mild AEs—insomnia, hair loss, nightmare, lethargy, depressed mood, headache, and pruritus.
Two patients were lost to follow-up—1 in arm A and 1 in arm C.
GLASGOW—Final results from the HAVEN 3 study suggest emicizumab prophylaxis can reduce bleeding in hemophilia A patients without factor VIII inhibitors.
Compared to patients who did not receive prophylaxis, those who received emicizumab prophylaxis had a 96% to 97% reduction in treated bleeds and a 94% to 95% reduction in all bleeds.
An intra-patient comparison showed a 68% reduction in treated bleeds with once-weekly emicizumab, compared to prior factor VIII prophylaxis.
“[Emicizumab] is the first medicine to show superior efficacy to prior factor VIII prophylaxis, the current standard of care therapy, as demonstrated by a statistically significant reduction in treated bleeds in the HAVEN 3 study intra-patient comparison,” said Johnny Mahlangu, MB BCh, of the University of the Witwatersrand in Johannesburg, South Africa.
Dr Mahlangu presented these results at the World Federation of Hemophilia (WFH) 2018 World Congress during the late-breaking abstract session on Monday. HAVEN 3 was sponsored by Hoffmann-La Roche.
Patients and treatment
In this phase 3 trial, researchers evaluated emicizumab in patients with hemophilia A without factor VIII inhibitors. The study included 152 patients who were 12 years of age or older and were previously treated with factor VIII therapy on-demand or as prophylaxis.
Patients previously treated with on-demand factor VIII were randomized in a 2:2:1 fashion to receive:
- Emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 1.5 mg/kg/wk until the end of study (arm A, n=36)
- Emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 3 mg/kg/2wks for at least 24 weeks (arm B, n=35)
- No prophylaxis, only episodic/on-demand factor VIII treatment (arm C, n=18).
Patients previously treated with factor VIII prophylaxis received emicizumab prophylaxis at 3 mg/kg/wk for 4 weeks, followed by 1.5 mg/kg/wk until the end of study (arm D, n=63).
Episodic treatment of breakthrough bleeds with factor VIII therapy was allowed per protocol.
Emicizumab vs no prophylaxis
The model-based (negative binomial regression model) annualized bleeding rate (ABR) for treated bleeds was 1.5 in arm A, 1.3 in arm B, and 38.2 in arm C. The median ABR for treated bleeds was 0 in arms A and B and 40.4 in arm C.
Compared to patients in arm C, those in arm A had a 96% (P<0.0001) reduction in treated bleeds, and those in arm B had a 97% (P<0.0001) reduction in treated bleeds.
None of the patients in arm C had 0 treated bleeds, compared to 55.6% of patients in arm A and 60% of patients in arm B.
The model-based ABR for all bleeds was 2.5 in arm A, 2.6 in arm B, and 47.6 in arm C.
Patients in arm A had a 95% reduction in all bleeds (P<0.0001), and patients in arm B had a 94% reduction in all bleeds (P<0.0001), compared to patients in arm C.
Fifty percent of patients in arm A had 0 total bleeds, as did 40% of patients in arm B and 0% of patients in arm C.
Intra-patient comparison
The researchers compared previous prophylaxis to once-weekly emicizumab prophylaxis in 48 patients from arm D.
The model-based ABR for treated bleeds was 4.8 with prior prophylaxis and 1.5 with emicizumab. The median ABR for treated bleeds was 1.8 and 0.0, respectively.
Patients had a 68% reduction in treated bleeds with emicizumab (P<0.0001).
With prior prophylaxis, 39.6% of patients had 0 treated bleeds. With emicizumab, 54.2% of patients had 0 treated bleeds.
Safety
There were no serious adverse events (AEs) related to emicizumab, no anti-drug antibodies detected, and none of the patients on emicizumab developed de novo factor VIII inhibitors.
Injection-site reactions occurred in 25.3% of all patients (38/150), 25% of patients in arm A (9/36), 20% in arm B (7/35), 12.5% in arm C (2/16), and 31.7% in arm D (20/63).
An additional patient in arm D (who was included in the total) reported an “injection-site erythema,” not an “injection-site reaction.”
Upper respiratory tract infections occurred in 10.7% of all patients (n=16), 11.1% (n=4) of those in arm A, 11.4% (n=4) of those in arm B, 0% of those in arm C, and 12.7% (n=8) of those in arm D.
Other AEs occurring in at least 5% of patients were arthralgia (19%), nasopharyngitis (12%), headache (11%), and influenza (6%).
One patient in arm B discontinued emicizumab due to multiple mild AEs—insomnia, hair loss, nightmare, lethargy, depressed mood, headache, and pruritus.
Two patients were lost to follow-up—1 in arm A and 1 in arm C.
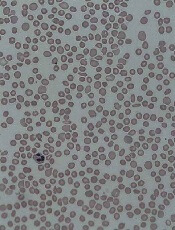
FDA approves drug for thrombocytopenia in CLD
The US Food and Drug Administration (FDA) has approved avatrombopag (DOPTELET®), a second-generation thrombopoietin receptor agonist.
Avatrombopag is now approved to treat thrombocytopenia in adults with chronic liver disease (CLD) who are scheduled to undergo a procedure.
Dova Pharmaceuticals, Inc., plans to launch the drug in June.
The FDA approved avatrombopag based on data from 2 randomized, double-blind, placebo-controlled phase 3 trials—ADAPT-1 (n=231) and ADAPT-2 (n=204).
The trials enrolled adults with thrombocytopenia (platelet count less than 50,000/µL) and CLD.
Patients received 40 mg or 60 mg of avatrombopag daily for 5 days based on their baseline platelet counts (40 to <50,000/mL or <40,000/mL, respectively), or they received placebo.
In both trials, avatrombopag reduced the need for platelet transfusions or rescue procedures for bleeding up to 7 days following a scheduled procedure.
In ADAPT-1, platelet transfusions/rescue procedures were not required for:
- 66% of patients in the 60 mg avatrombopag arm and 23% of matching placebo recipients (P<0.0001)
- 88% of the 40 mg avatrombopag arm and 38% of matching placebo recipients (P<0.0001).
In ADAPT-2, platelet transfusions/rescue procedures were not required for:
- 69% of patients in the 60 mg avatrombopag arm and 35% of matching placebo recipients (P=0.0006)
- 88% of the 40 mg avatrombopag arm and 33% of placebo recipients (P<0.0001).
The most common adverse events (AEs) in both trials (in the avatrombopag and placebo groups, respectively) were pyrexia (10% and 9%), abdominal pain (7% and 6%), nausea (7% for both), headache (6% for both), fatigue (4% and 3%), and peripheral edema (3% and 2%).
The incidence of serious AEs was 7% in the 60 mg avatrombopag group and 13% in the matching placebo group. The incidence was 8% in the 40 mg avatrombopag group and 3% in the matching placebo group.
The most common serious AE reported with avatrombopag was hyponatremia, occurring in 2 patients (0.7%).
AEs resulting in discontinuation of avatrombopag were anemia, pyrexia, and myalgia. Each of these events was reported in a single (0.4%) patient in the avatrombopag 60 mg group.
Additional data from ADAPT-1 and ADAPT-2 are available in the prescribing information for avatrombopag, which can be found at www.doptelet.com.
The US Food and Drug Administration (FDA) has approved avatrombopag (DOPTELET®), a second-generation thrombopoietin receptor agonist.
Avatrombopag is now approved to treat thrombocytopenia in adults with chronic liver disease (CLD) who are scheduled to undergo a procedure.
Dova Pharmaceuticals, Inc., plans to launch the drug in June.
The FDA approved avatrombopag based on data from 2 randomized, double-blind, placebo-controlled phase 3 trials—ADAPT-1 (n=231) and ADAPT-2 (n=204).
The trials enrolled adults with thrombocytopenia (platelet count less than 50,000/µL) and CLD.
Patients received 40 mg or 60 mg of avatrombopag daily for 5 days based on their baseline platelet counts (40 to <50,000/mL or <40,000/mL, respectively), or they received placebo.
In both trials, avatrombopag reduced the need for platelet transfusions or rescue procedures for bleeding up to 7 days following a scheduled procedure.
In ADAPT-1, platelet transfusions/rescue procedures were not required for:
- 66% of patients in the 60 mg avatrombopag arm and 23% of matching placebo recipients (P<0.0001)
- 88% of the 40 mg avatrombopag arm and 38% of matching placebo recipients (P<0.0001).
In ADAPT-2, platelet transfusions/rescue procedures were not required for:
- 69% of patients in the 60 mg avatrombopag arm and 35% of matching placebo recipients (P=0.0006)
- 88% of the 40 mg avatrombopag arm and 33% of placebo recipients (P<0.0001).
The most common adverse events (AEs) in both trials (in the avatrombopag and placebo groups, respectively) were pyrexia (10% and 9%), abdominal pain (7% and 6%), nausea (7% for both), headache (6% for both), fatigue (4% and 3%), and peripheral edema (3% and 2%).
The incidence of serious AEs was 7% in the 60 mg avatrombopag group and 13% in the matching placebo group. The incidence was 8% in the 40 mg avatrombopag group and 3% in the matching placebo group.
The most common serious AE reported with avatrombopag was hyponatremia, occurring in 2 patients (0.7%).
AEs resulting in discontinuation of avatrombopag were anemia, pyrexia, and myalgia. Each of these events was reported in a single (0.4%) patient in the avatrombopag 60 mg group.
Additional data from ADAPT-1 and ADAPT-2 are available in the prescribing information for avatrombopag, which can be found at www.doptelet.com.
The US Food and Drug Administration (FDA) has approved avatrombopag (DOPTELET®), a second-generation thrombopoietin receptor agonist.
Avatrombopag is now approved to treat thrombocytopenia in adults with chronic liver disease (CLD) who are scheduled to undergo a procedure.
Dova Pharmaceuticals, Inc., plans to launch the drug in June.
The FDA approved avatrombopag based on data from 2 randomized, double-blind, placebo-controlled phase 3 trials—ADAPT-1 (n=231) and ADAPT-2 (n=204).
The trials enrolled adults with thrombocytopenia (platelet count less than 50,000/µL) and CLD.
Patients received 40 mg or 60 mg of avatrombopag daily for 5 days based on their baseline platelet counts (40 to <50,000/mL or <40,000/mL, respectively), or they received placebo.
In both trials, avatrombopag reduced the need for platelet transfusions or rescue procedures for bleeding up to 7 days following a scheduled procedure.
In ADAPT-1, platelet transfusions/rescue procedures were not required for:
- 66% of patients in the 60 mg avatrombopag arm and 23% of matching placebo recipients (P<0.0001)
- 88% of the 40 mg avatrombopag arm and 38% of matching placebo recipients (P<0.0001).
In ADAPT-2, platelet transfusions/rescue procedures were not required for:
- 69% of patients in the 60 mg avatrombopag arm and 35% of matching placebo recipients (P=0.0006)
- 88% of the 40 mg avatrombopag arm and 33% of placebo recipients (P<0.0001).
The most common adverse events (AEs) in both trials (in the avatrombopag and placebo groups, respectively) were pyrexia (10% and 9%), abdominal pain (7% and 6%), nausea (7% for both), headache (6% for both), fatigue (4% and 3%), and peripheral edema (3% and 2%).
The incidence of serious AEs was 7% in the 60 mg avatrombopag group and 13% in the matching placebo group. The incidence was 8% in the 40 mg avatrombopag group and 3% in the matching placebo group.
The most common serious AE reported with avatrombopag was hyponatremia, occurring in 2 patients (0.7%).
AEs resulting in discontinuation of avatrombopag were anemia, pyrexia, and myalgia. Each of these events was reported in a single (0.4%) patient in the avatrombopag 60 mg group.
Additional data from ADAPT-1 and ADAPT-2 are available in the prescribing information for avatrombopag, which can be found at www.doptelet.com.
See You in Beantown!
Boston is my hometown and I can’t wait to show it off at our Vascular Annual Meeting.
Come join me there June 20-23 for the preeminent educational and social networking event of the year in vascular surgery. Scientific sessions will be June 21-23 and the Exhibit Hall will be open June 21-22.
All scientific meetings, educational sessions, and exhibits will be at the Hynes Convention Center. Committee meetings, the SVS Board of Directors meeting, and alumni and committee receptions will be held at the Sheraton Boston Hotel, the VAM headquarters hotel. Other hotel options are available. (See vsweb.org/hotels18.) Special room rates were to end May 22, so it’s possible you may need to make your own housing arrangements.
This year’s VAM is all about the vascular team. In fact, that’s the theme: “Home of the Vascular Team – Partners in Patient Care.” There are sessions for the whole team – surgeons, nurses, nurse practitioners, technologists, and physician assistants. We have special programming for PAs on Thursday afternoon, and the Vascular Quality Initiative and the Society for Vascular Nursing are holding their annual sessions in tandem with VAM.
Creating the program followed extensive surveying after the 2017 meeting. In response to member feedback, this year we are highlighting:
- Topics and practical sessions for community practitioners and young surgeons, including on clinical practice guidelines, practice management, even physician burnout.
- More opportunities to interact with presenters, particularly with the “Tips & Tricks” and “Ask the Experts” daily sessions.
- Ideas and translational research that participants can take home to their practices.
- VAM on Demand, letting you catch up on missed sessions afterwards, plus the VAM Planner and a new mobile app to help everyone design their own meetings and navigate VAM easily.
The familiar favorites will be there: workshops, concurrent and scientific sessions, postgraduate courses – free to SVS members, a $300 value – events for international members, collaborative sessions with other societies, plenty of opportunities to network and connect with friends and colleagues, and educational credits, not to mention the chance to explore the fascinating city I’ve always loved.
We have a great mix of old activities and some new initiatives. And we’re excited for you to experience it all at VAM 2018. See you in Beantown.
Boston is my hometown and I can’t wait to show it off at our Vascular Annual Meeting.
Come join me there June 20-23 for the preeminent educational and social networking event of the year in vascular surgery. Scientific sessions will be June 21-23 and the Exhibit Hall will be open June 21-22.
All scientific meetings, educational sessions, and exhibits will be at the Hynes Convention Center. Committee meetings, the SVS Board of Directors meeting, and alumni and committee receptions will be held at the Sheraton Boston Hotel, the VAM headquarters hotel. Other hotel options are available. (See vsweb.org/hotels18.) Special room rates were to end May 22, so it’s possible you may need to make your own housing arrangements.
This year’s VAM is all about the vascular team. In fact, that’s the theme: “Home of the Vascular Team – Partners in Patient Care.” There are sessions for the whole team – surgeons, nurses, nurse practitioners, technologists, and physician assistants. We have special programming for PAs on Thursday afternoon, and the Vascular Quality Initiative and the Society for Vascular Nursing are holding their annual sessions in tandem with VAM.
Creating the program followed extensive surveying after the 2017 meeting. In response to member feedback, this year we are highlighting:
- Topics and practical sessions for community practitioners and young surgeons, including on clinical practice guidelines, practice management, even physician burnout.
- More opportunities to interact with presenters, particularly with the “Tips & Tricks” and “Ask the Experts” daily sessions.
- Ideas and translational research that participants can take home to their practices.
- VAM on Demand, letting you catch up on missed sessions afterwards, plus the VAM Planner and a new mobile app to help everyone design their own meetings and navigate VAM easily.
The familiar favorites will be there: workshops, concurrent and scientific sessions, postgraduate courses – free to SVS members, a $300 value – events for international members, collaborative sessions with other societies, plenty of opportunities to network and connect with friends and colleagues, and educational credits, not to mention the chance to explore the fascinating city I’ve always loved.
We have a great mix of old activities and some new initiatives. And we’re excited for you to experience it all at VAM 2018. See you in Beantown.
Boston is my hometown and I can’t wait to show it off at our Vascular Annual Meeting.
Come join me there June 20-23 for the preeminent educational and social networking event of the year in vascular surgery. Scientific sessions will be June 21-23 and the Exhibit Hall will be open June 21-22.
All scientific meetings, educational sessions, and exhibits will be at the Hynes Convention Center. Committee meetings, the SVS Board of Directors meeting, and alumni and committee receptions will be held at the Sheraton Boston Hotel, the VAM headquarters hotel. Other hotel options are available. (See vsweb.org/hotels18.) Special room rates were to end May 22, so it’s possible you may need to make your own housing arrangements.
This year’s VAM is all about the vascular team. In fact, that’s the theme: “Home of the Vascular Team – Partners in Patient Care.” There are sessions for the whole team – surgeons, nurses, nurse practitioners, technologists, and physician assistants. We have special programming for PAs on Thursday afternoon, and the Vascular Quality Initiative and the Society for Vascular Nursing are holding their annual sessions in tandem with VAM.
Creating the program followed extensive surveying after the 2017 meeting. In response to member feedback, this year we are highlighting:
- Topics and practical sessions for community practitioners and young surgeons, including on clinical practice guidelines, practice management, even physician burnout.
- More opportunities to interact with presenters, particularly with the “Tips & Tricks” and “Ask the Experts” daily sessions.
- Ideas and translational research that participants can take home to their practices.
- VAM on Demand, letting you catch up on missed sessions afterwards, plus the VAM Planner and a new mobile app to help everyone design their own meetings and navigate VAM easily.
The familiar favorites will be there: workshops, concurrent and scientific sessions, postgraduate courses – free to SVS members, a $300 value – events for international members, collaborative sessions with other societies, plenty of opportunities to network and connect with friends and colleagues, and educational credits, not to mention the chance to explore the fascinating city I’ve always loved.
We have a great mix of old activities and some new initiatives. And we’re excited for you to experience it all at VAM 2018. See you in Beantown.
Short Takes
Association between hospitalist years of experience with mortality in hospitalized patients
Cohort study showed that Medicare patients cared for by hospitalists in their first year of practice experienced higher in-hospital and 30-day mortality, compared with patients cared for by hospitalists in their second year of practice. New hospitalists may need additional monitoring and support to ensure optimal patient outcomes.
Standardized handoff improves preparedness in the ICU
Cluster randomized stepped-wedge trial in eight ICUs in an academic center showed that a standardized handoff intervention was associated with a statistically significant reduction in the odds of clinician self-reported unpreparedness from a poor-quality handoff (odds ratio, 0.19; 95% confidence interval, 0.03-0.74; P = .03).
Citation: Parent B et al. Effect of standardized handoff curriculum on improved clinician preparedness in the intensive care: A stepped-wedge cluster randomized clinical trial. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5440.
Association between hospitalist years of experience with mortality in hospitalized patients
Cohort study showed that Medicare patients cared for by hospitalists in their first year of practice experienced higher in-hospital and 30-day mortality, compared with patients cared for by hospitalists in their second year of practice. New hospitalists may need additional monitoring and support to ensure optimal patient outcomes.
Standardized handoff improves preparedness in the ICU
Cluster randomized stepped-wedge trial in eight ICUs in an academic center showed that a standardized handoff intervention was associated with a statistically significant reduction in the odds of clinician self-reported unpreparedness from a poor-quality handoff (odds ratio, 0.19; 95% confidence interval, 0.03-0.74; P = .03).
Citation: Parent B et al. Effect of standardized handoff curriculum on improved clinician preparedness in the intensive care: A stepped-wedge cluster randomized clinical trial. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5440.
Association between hospitalist years of experience with mortality in hospitalized patients
Cohort study showed that Medicare patients cared for by hospitalists in their first year of practice experienced higher in-hospital and 30-day mortality, compared with patients cared for by hospitalists in their second year of practice. New hospitalists may need additional monitoring and support to ensure optimal patient outcomes.
Standardized handoff improves preparedness in the ICU
Cluster randomized stepped-wedge trial in eight ICUs in an academic center showed that a standardized handoff intervention was associated with a statistically significant reduction in the odds of clinician self-reported unpreparedness from a poor-quality handoff (odds ratio, 0.19; 95% confidence interval, 0.03-0.74; P = .03).
Citation: Parent B et al. Effect of standardized handoff curriculum on improved clinician preparedness in the intensive care: A stepped-wedge cluster randomized clinical trial. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5440.
FDA approval expected for CCM in heart failure patients
BOSTON – Positive results from a confirmatory trial appear to put the Optimizer by Impulse Dynamics, a cardiac contractility modulation (CCM) device for patients with function-limiting heart failure, on track for imminent U.S. marketing approval by the Food and Drug Administration. If that happens, several hundreds of thousands of U.S. heart failure patients would immediately become candidates for this treatment based on the enrolled study populations, the benefits shown, and current treatment options for advanced heart failure, experts predicted.

CCM “promises to meet a very large unmet need in heart failure,” William T. Abraham, MD, said as he presented the confirmatory study’s results at the annual scientific sessions of the Heart Rhythm Society. ”These patients aren’t doing well, but don’t qualify” for a heart transplant, left ventricular assist device, implantable cardioverter defibrillator, or cardiac resynchronization therapy (CRT), noted Dr. Abraham, professor and director of cardiovascular medicine at the Ohio State University in Columbus. In the months following the anticipated FDA approval, Dr. Abraham said he expects the device will be implanted in tens of thousands of U.S. heart failure patients who match the criteria of those who got the biggest benefit from CCM.
“There are few if any evidence-based treatments for patients with an ejection fraction of 35%-45%. This is an underserved population, so the potential of CCM is appropriately high,” Dr. Abraham said.

Researchers designed the study in consultation with the FDA to resolve lingering regulatory concerns following completion of three prior randomized trials with a total of nearly 650 patients. Dr. Abraham simultaneously reported the results at the meeting and published them in a report (JACC Heart Failure. 2018 May 10. doi: 10.1016/j.jchf.2018.04.010); these results from 160 patients – 74 of whom received the device and 86 of whom continued medical therapy – showed the superiority of the device for the primary endpoint of change in exercise capacity (as measured by peak oxygen uptake) and for the secondary endpoints of quality of life (as measured with the Minnesota Living With Heart Failure Questionnaire) and functional status (as measured by New York Heart Association class). The boost in exercise capacity, an average increase of 0.84 ml/kg per min in peak oxygen uptake after 24 weeks, “was similar to the improvement seen with CRT in patients with a wide QRS interval” who thereby qualified for CRT placement, Dr. Abraham said.
The CCM device also met the study’s prespecified safety endpoint of a complication rate of less than 30% – with an actual rate of 10%. “The complications were those we expect from implanted leads and pulse generators and were comparable to what happens with other implanted rhythm devices. In the context of the benefits patients received and their having no other treatment options, I see the complication rate as acceptable,” Dr. Abraham said during his report.

In summing up the trial’s results, Dr. Stevenson noted that “the safety endpoint was met, the primary endpoint and other functional endpoints were met, and functional endpoints are of vital importance to patients. The CCM story is not yet the CRT story,” with CRT having produced even larger effects in its pivotal trial, also led by Dr. Abraham (New Engl J Med. 2002 June 13;346[24]:1845-53), cautioned Dr. Stevenson. But in general she put a positive spin on the CCM device, saying that it “has ingenuity and innovation, and we look forward to a better understanding of which patients benefit from CCM and what we can tell them about the magnitude and duration of the benefit.”

The FIX-HF-5C trial was sponsored by Impulse Dynamics, the company developing the CCM Optimizer device. Dr. Abraham has been a consultant to Impulse Dynamics, as well as to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical. Dr. Singh has been a consultant to Biotronik, Boston Scientific, Liva Nova, Medtronic, and St. Jude. Dr. Stevenson has received research funding from Abbott and Novartis. Dr. Yancy had no disclosures.
SOURCE: Abraham W et al. Heart Rhythm 2018, Abstract B-LBCT01-02.
BOSTON – Positive results from a confirmatory trial appear to put the Optimizer by Impulse Dynamics, a cardiac contractility modulation (CCM) device for patients with function-limiting heart failure, on track for imminent U.S. marketing approval by the Food and Drug Administration. If that happens, several hundreds of thousands of U.S. heart failure patients would immediately become candidates for this treatment based on the enrolled study populations, the benefits shown, and current treatment options for advanced heart failure, experts predicted.

CCM “promises to meet a very large unmet need in heart failure,” William T. Abraham, MD, said as he presented the confirmatory study’s results at the annual scientific sessions of the Heart Rhythm Society. ”These patients aren’t doing well, but don’t qualify” for a heart transplant, left ventricular assist device, implantable cardioverter defibrillator, or cardiac resynchronization therapy (CRT), noted Dr. Abraham, professor and director of cardiovascular medicine at the Ohio State University in Columbus. In the months following the anticipated FDA approval, Dr. Abraham said he expects the device will be implanted in tens of thousands of U.S. heart failure patients who match the criteria of those who got the biggest benefit from CCM.
“There are few if any evidence-based treatments for patients with an ejection fraction of 35%-45%. This is an underserved population, so the potential of CCM is appropriately high,” Dr. Abraham said.

Researchers designed the study in consultation with the FDA to resolve lingering regulatory concerns following completion of three prior randomized trials with a total of nearly 650 patients. Dr. Abraham simultaneously reported the results at the meeting and published them in a report (JACC Heart Failure. 2018 May 10. doi: 10.1016/j.jchf.2018.04.010); these results from 160 patients – 74 of whom received the device and 86 of whom continued medical therapy – showed the superiority of the device for the primary endpoint of change in exercise capacity (as measured by peak oxygen uptake) and for the secondary endpoints of quality of life (as measured with the Minnesota Living With Heart Failure Questionnaire) and functional status (as measured by New York Heart Association class). The boost in exercise capacity, an average increase of 0.84 ml/kg per min in peak oxygen uptake after 24 weeks, “was similar to the improvement seen with CRT in patients with a wide QRS interval” who thereby qualified for CRT placement, Dr. Abraham said.
The CCM device also met the study’s prespecified safety endpoint of a complication rate of less than 30% – with an actual rate of 10%. “The complications were those we expect from implanted leads and pulse generators and were comparable to what happens with other implanted rhythm devices. In the context of the benefits patients received and their having no other treatment options, I see the complication rate as acceptable,” Dr. Abraham said during his report.

In summing up the trial’s results, Dr. Stevenson noted that “the safety endpoint was met, the primary endpoint and other functional endpoints were met, and functional endpoints are of vital importance to patients. The CCM story is not yet the CRT story,” with CRT having produced even larger effects in its pivotal trial, also led by Dr. Abraham (New Engl J Med. 2002 June 13;346[24]:1845-53), cautioned Dr. Stevenson. But in general she put a positive spin on the CCM device, saying that it “has ingenuity and innovation, and we look forward to a better understanding of which patients benefit from CCM and what we can tell them about the magnitude and duration of the benefit.”

The FIX-HF-5C trial was sponsored by Impulse Dynamics, the company developing the CCM Optimizer device. Dr. Abraham has been a consultant to Impulse Dynamics, as well as to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical. Dr. Singh has been a consultant to Biotronik, Boston Scientific, Liva Nova, Medtronic, and St. Jude. Dr. Stevenson has received research funding from Abbott and Novartis. Dr. Yancy had no disclosures.
SOURCE: Abraham W et al. Heart Rhythm 2018, Abstract B-LBCT01-02.
BOSTON – Positive results from a confirmatory trial appear to put the Optimizer by Impulse Dynamics, a cardiac contractility modulation (CCM) device for patients with function-limiting heart failure, on track for imminent U.S. marketing approval by the Food and Drug Administration. If that happens, several hundreds of thousands of U.S. heart failure patients would immediately become candidates for this treatment based on the enrolled study populations, the benefits shown, and current treatment options for advanced heart failure, experts predicted.

CCM “promises to meet a very large unmet need in heart failure,” William T. Abraham, MD, said as he presented the confirmatory study’s results at the annual scientific sessions of the Heart Rhythm Society. ”These patients aren’t doing well, but don’t qualify” for a heart transplant, left ventricular assist device, implantable cardioverter defibrillator, or cardiac resynchronization therapy (CRT), noted Dr. Abraham, professor and director of cardiovascular medicine at the Ohio State University in Columbus. In the months following the anticipated FDA approval, Dr. Abraham said he expects the device will be implanted in tens of thousands of U.S. heart failure patients who match the criteria of those who got the biggest benefit from CCM.
“There are few if any evidence-based treatments for patients with an ejection fraction of 35%-45%. This is an underserved population, so the potential of CCM is appropriately high,” Dr. Abraham said.

Researchers designed the study in consultation with the FDA to resolve lingering regulatory concerns following completion of three prior randomized trials with a total of nearly 650 patients. Dr. Abraham simultaneously reported the results at the meeting and published them in a report (JACC Heart Failure. 2018 May 10. doi: 10.1016/j.jchf.2018.04.010); these results from 160 patients – 74 of whom received the device and 86 of whom continued medical therapy – showed the superiority of the device for the primary endpoint of change in exercise capacity (as measured by peak oxygen uptake) and for the secondary endpoints of quality of life (as measured with the Minnesota Living With Heart Failure Questionnaire) and functional status (as measured by New York Heart Association class). The boost in exercise capacity, an average increase of 0.84 ml/kg per min in peak oxygen uptake after 24 weeks, “was similar to the improvement seen with CRT in patients with a wide QRS interval” who thereby qualified for CRT placement, Dr. Abraham said.
The CCM device also met the study’s prespecified safety endpoint of a complication rate of less than 30% – with an actual rate of 10%. “The complications were those we expect from implanted leads and pulse generators and were comparable to what happens with other implanted rhythm devices. In the context of the benefits patients received and their having no other treatment options, I see the complication rate as acceptable,” Dr. Abraham said during his report.

In summing up the trial’s results, Dr. Stevenson noted that “the safety endpoint was met, the primary endpoint and other functional endpoints were met, and functional endpoints are of vital importance to patients. The CCM story is not yet the CRT story,” with CRT having produced even larger effects in its pivotal trial, also led by Dr. Abraham (New Engl J Med. 2002 June 13;346[24]:1845-53), cautioned Dr. Stevenson. But in general she put a positive spin on the CCM device, saying that it “has ingenuity and innovation, and we look forward to a better understanding of which patients benefit from CCM and what we can tell them about the magnitude and duration of the benefit.”

The FIX-HF-5C trial was sponsored by Impulse Dynamics, the company developing the CCM Optimizer device. Dr. Abraham has been a consultant to Impulse Dynamics, as well as to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical. Dr. Singh has been a consultant to Biotronik, Boston Scientific, Liva Nova, Medtronic, and St. Jude. Dr. Stevenson has received research funding from Abbott and Novartis. Dr. Yancy had no disclosures.
SOURCE: Abraham W et al. Heart Rhythm 2018, Abstract B-LBCT01-02.
REPORTING FROM HEART RHYTHM 2018