User login
Older CLL and NHL patients are more vulnerable to toxicities
Older patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) have an increased odds of experiencing treatment-related toxicities, even when treated with novel agents, according to findings reported in the Journal of Geriatric Oncology.
An analysis of 1,199 patients showed that CLL patients aged 65 years and older had significantly higher odds than younger patients of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI, 1.39-1.55).
Investigators analyzed data obtained from the Alliance for Clinical Trials in Oncology to compare the incidence of toxicities between age groups. Of the 1,199 patients included in the analysis, 409 were 65 years of age or older, and 790 were younger than 65 years. Among these patients, 438 received only therapy with novel agents including biologic combinations, monoclonal antibodies, cell cycle inhibitors, chemoimmunotherapy, and immunomodulators, and 761 received novel agents in addition to chemotherapy.
Overall, 68% of CLL patients and 35% of NHL patients had at least one grade three or four hematologic toxicity, compared with 48% and 54% for nonhematologic toxicities, respectively.
Older CLL patients with at least one grade three or four toxicity in the first 3 months had similar overall survival (OS) and progression-free survival (PFS) as those without a toxicity. In contrast, older NHL patients with at least one grade three or four hematologic toxicity in the first 3 months had worse OS (HR, 3.14; P = .006; 95% CI, 2.25-4.39) and PFS (HR, 3.06; P = .011; 95% CI, 2.10-4.45) than patients without these toxicities. Nonhematologic toxicities were not significantly associated with survival outcomes for patients with NHL.
“The observed associations between hematologic toxicity and OS/PFS among older patients with NHL require further investigation,” the researchers wrote. “These findings could represent a direct effect of toxicity due to decreased physiologic reserve, decreased drug clearance, or an increased sensitivity of tissue to novel agents.”
The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
SOURCE: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
Older patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) have an increased odds of experiencing treatment-related toxicities, even when treated with novel agents, according to findings reported in the Journal of Geriatric Oncology.
An analysis of 1,199 patients showed that CLL patients aged 65 years and older had significantly higher odds than younger patients of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI, 1.39-1.55).
Investigators analyzed data obtained from the Alliance for Clinical Trials in Oncology to compare the incidence of toxicities between age groups. Of the 1,199 patients included in the analysis, 409 were 65 years of age or older, and 790 were younger than 65 years. Among these patients, 438 received only therapy with novel agents including biologic combinations, monoclonal antibodies, cell cycle inhibitors, chemoimmunotherapy, and immunomodulators, and 761 received novel agents in addition to chemotherapy.
Overall, 68% of CLL patients and 35% of NHL patients had at least one grade three or four hematologic toxicity, compared with 48% and 54% for nonhematologic toxicities, respectively.
Older CLL patients with at least one grade three or four toxicity in the first 3 months had similar overall survival (OS) and progression-free survival (PFS) as those without a toxicity. In contrast, older NHL patients with at least one grade three or four hematologic toxicity in the first 3 months had worse OS (HR, 3.14; P = .006; 95% CI, 2.25-4.39) and PFS (HR, 3.06; P = .011; 95% CI, 2.10-4.45) than patients without these toxicities. Nonhematologic toxicities were not significantly associated with survival outcomes for patients with NHL.
“The observed associations between hematologic toxicity and OS/PFS among older patients with NHL require further investigation,” the researchers wrote. “These findings could represent a direct effect of toxicity due to decreased physiologic reserve, decreased drug clearance, or an increased sensitivity of tissue to novel agents.”
The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
SOURCE: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
Older patients with chronic lymphocytic leukemia (CLL) and non-Hodgkin lymphoma (NHL) have an increased odds of experiencing treatment-related toxicities, even when treated with novel agents, according to findings reported in the Journal of Geriatric Oncology.
An analysis of 1,199 patients showed that CLL patients aged 65 years and older had significantly higher odds than younger patients of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI, 1.39-1.55).
Investigators analyzed data obtained from the Alliance for Clinical Trials in Oncology to compare the incidence of toxicities between age groups. Of the 1,199 patients included in the analysis, 409 were 65 years of age or older, and 790 were younger than 65 years. Among these patients, 438 received only therapy with novel agents including biologic combinations, monoclonal antibodies, cell cycle inhibitors, chemoimmunotherapy, and immunomodulators, and 761 received novel agents in addition to chemotherapy.
Overall, 68% of CLL patients and 35% of NHL patients had at least one grade three or four hematologic toxicity, compared with 48% and 54% for nonhematologic toxicities, respectively.
Older CLL patients with at least one grade three or four toxicity in the first 3 months had similar overall survival (OS) and progression-free survival (PFS) as those without a toxicity. In contrast, older NHL patients with at least one grade three or four hematologic toxicity in the first 3 months had worse OS (HR, 3.14; P = .006; 95% CI, 2.25-4.39) and PFS (HR, 3.06; P = .011; 95% CI, 2.10-4.45) than patients without these toxicities. Nonhematologic toxicities were not significantly associated with survival outcomes for patients with NHL.
“The observed associations between hematologic toxicity and OS/PFS among older patients with NHL require further investigation,” the researchers wrote. “These findings could represent a direct effect of toxicity due to decreased physiologic reserve, decreased drug clearance, or an increased sensitivity of tissue to novel agents.”
The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
SOURCE: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
Key clinical point:
Major finding: Older CLL patients had significantly higher odds of developing a grade three or four hematologic toxicity (adjusted odds ratio, 1.70; P = .009; 95% confidence interval, 1.57-1.84) or nonhematologic toxicity (OR, 1.47; P = .022; 95% CI 1.39-1.55).
Study details: An analysis of data from 1,199 CLL and NHL patients in the Alliance for Clinical Trials in Oncology.
Disclosures: The study was supported by a National Institutes of Health grant. Researchers reported relationships with Bartlett, KITE, Pfizer, Seattle Genetics, Roche-Genentech, Celgene, Pharmacyclics, and Gilead.
Source: Tallarico M et al. J Geriatr Oncol. 2018 Apr 16. pii: S1879-4068(18)30131-0.
Comorbid spondyloarthritis and fibromyalgia lower response to TNF inhibitors
LIVERPOOL, ENGLAND – Individuals with axial spondyloarthritis (axSpA) who have comorbid fibromyalgia do respond to biologic therapy but at a seemingly lower rate if they have a high symptom score during early assessments.
Data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) showed that participants with axSpA who were starting biologic therapy with a tumor necrosis factor inhibitor (TNFi) for the first time also had worse disease activity at baseline if they met fibromyalgia research criteria than if they did not.
“The issue of fibromyalgia as a comorbidity in axial SpA has been the subject of current considerable interest,” said Dr. Macfarlane, who is Clinical Chair in Epidemiology at the University of Aberdeen (Scotland), where the BSRBR-AS is run. This is for several reasons: “One is the challenge of identifying patients with axial SpA who have comorbid fibromyalgia.
“The second is the concern that comorbid fibromyalgia may have an effect on disease indices such as BASDAI [Bath Ankylosing Spondylitis Disease Activity Index],” Dr. Macfarlane observed.
This leads to the third issue: “Are patients with comorbid fibromyalgia inappropriately receiving biological therapy, and how do they respond if they do receive it?”
Previous data from the BSRBR-AS have shown that approximately one in five patients with axSpA meet research criteria for fibromyalgia (Arthritis Rheumatol. 2017;69:2144-50) and that the prevalence of the comorbidity was higher in those who met Assessment of SpondyloArthritis International Society imaging criteria and lower in those who only met clinical criteria (25% vs. 10%).
The current aims of the study presented by Dr. Macfarlane were to first quantify the extent to which meeting fibromyalgia criteria was associated with higher measures of disease activity and impact, and then to see if meeting these criteria was associated with a poorer response to first use of a TNFi.
In order to find out, Dr. Macfarlane and his associates examined data from the prospective BSRBR-AS, which has been running since 2012. The BSRBR-AS recruits patients with ASAS-confirmed axSpA who are newly starting biologics from 83 U.K. centers.
At recruitment and at 3 months, patients starting biologic treatment undergo several assessments, which since 2015 has included research criteria for fibromyalgia (J Rheumatol. 2011;38:1113–22). The latter incorporate a Widespread Pain Index rated 0-19 and a Symptom Severity Scale rated 0-12 and cover items such as fatigue and waking up unrefreshed, and the presence of lower abdominal pain or headaches.
To date, around 1,750 participants in the BSRBR-AS have completed the fibromyalgia criteria, Dr. Macfarlane said.
Across the board, baseline measures of disease activity were lower in patients who met the fibromyalgia criteria versus those who did not. This included the BASDAI and the Bath Ankylosing Spondylitis Functional Index, where scores were approximately 6.5 and 4.5 for each measure.
“Quality of life was significantly lower in those who were fibromyalgia positive,” Dr. Macfarlane said. Indeed, whatever the measure used, from the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) Scale to the general EuroQoL Quality of Life Scale, there were significant differences between those who did and did not meet fibromyalgia criteria. There were also higher scores for depression, anxiety, poorer-quality sleep, and higher levels of fatigue.
Patients treated with TNFi therapy showed improvement in both BASDAI and ASQoL scores regardless of whether they met fibromyalgia criteria, but crucially, the responses were still lower and significantly different from those without fibromyalgia.
An ASAS20 response to TNFi therapy was met by “slightly fewer” patients who met the fibromyalgia criteria than by those who did not at all follow-up points: at 3 months (about 35% vs. 45%), 6 months (about 58% vs. 61%), and 12 months (about 60% vs. 62%).
A high score on the Symptom Severity Scale but not the Widespread Pain Index of the fibromyalgia criteria was associated with a lower response to TNFi therapy at 3 months. “Such patients may benefit from the use of TNFi and nonpharmacological therapy,” Dr. Macfarlane said.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
SOURCE: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
LIVERPOOL, ENGLAND – Individuals with axial spondyloarthritis (axSpA) who have comorbid fibromyalgia do respond to biologic therapy but at a seemingly lower rate if they have a high symptom score during early assessments.
Data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) showed that participants with axSpA who were starting biologic therapy with a tumor necrosis factor inhibitor (TNFi) for the first time also had worse disease activity at baseline if they met fibromyalgia research criteria than if they did not.
“The issue of fibromyalgia as a comorbidity in axial SpA has been the subject of current considerable interest,” said Dr. Macfarlane, who is Clinical Chair in Epidemiology at the University of Aberdeen (Scotland), where the BSRBR-AS is run. This is for several reasons: “One is the challenge of identifying patients with axial SpA who have comorbid fibromyalgia.
“The second is the concern that comorbid fibromyalgia may have an effect on disease indices such as BASDAI [Bath Ankylosing Spondylitis Disease Activity Index],” Dr. Macfarlane observed.
This leads to the third issue: “Are patients with comorbid fibromyalgia inappropriately receiving biological therapy, and how do they respond if they do receive it?”
Previous data from the BSRBR-AS have shown that approximately one in five patients with axSpA meet research criteria for fibromyalgia (Arthritis Rheumatol. 2017;69:2144-50) and that the prevalence of the comorbidity was higher in those who met Assessment of SpondyloArthritis International Society imaging criteria and lower in those who only met clinical criteria (25% vs. 10%).
The current aims of the study presented by Dr. Macfarlane were to first quantify the extent to which meeting fibromyalgia criteria was associated with higher measures of disease activity and impact, and then to see if meeting these criteria was associated with a poorer response to first use of a TNFi.
In order to find out, Dr. Macfarlane and his associates examined data from the prospective BSRBR-AS, which has been running since 2012. The BSRBR-AS recruits patients with ASAS-confirmed axSpA who are newly starting biologics from 83 U.K. centers.
At recruitment and at 3 months, patients starting biologic treatment undergo several assessments, which since 2015 has included research criteria for fibromyalgia (J Rheumatol. 2011;38:1113–22). The latter incorporate a Widespread Pain Index rated 0-19 and a Symptom Severity Scale rated 0-12 and cover items such as fatigue and waking up unrefreshed, and the presence of lower abdominal pain or headaches.
To date, around 1,750 participants in the BSRBR-AS have completed the fibromyalgia criteria, Dr. Macfarlane said.
Across the board, baseline measures of disease activity were lower in patients who met the fibromyalgia criteria versus those who did not. This included the BASDAI and the Bath Ankylosing Spondylitis Functional Index, where scores were approximately 6.5 and 4.5 for each measure.
“Quality of life was significantly lower in those who were fibromyalgia positive,” Dr. Macfarlane said. Indeed, whatever the measure used, from the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) Scale to the general EuroQoL Quality of Life Scale, there were significant differences between those who did and did not meet fibromyalgia criteria. There were also higher scores for depression, anxiety, poorer-quality sleep, and higher levels of fatigue.
Patients treated with TNFi therapy showed improvement in both BASDAI and ASQoL scores regardless of whether they met fibromyalgia criteria, but crucially, the responses were still lower and significantly different from those without fibromyalgia.
An ASAS20 response to TNFi therapy was met by “slightly fewer” patients who met the fibromyalgia criteria than by those who did not at all follow-up points: at 3 months (about 35% vs. 45%), 6 months (about 58% vs. 61%), and 12 months (about 60% vs. 62%).
A high score on the Symptom Severity Scale but not the Widespread Pain Index of the fibromyalgia criteria was associated with a lower response to TNFi therapy at 3 months. “Such patients may benefit from the use of TNFi and nonpharmacological therapy,” Dr. Macfarlane said.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
SOURCE: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
LIVERPOOL, ENGLAND – Individuals with axial spondyloarthritis (axSpA) who have comorbid fibromyalgia do respond to biologic therapy but at a seemingly lower rate if they have a high symptom score during early assessments.
Data from the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS) showed that participants with axSpA who were starting biologic therapy with a tumor necrosis factor inhibitor (TNFi) for the first time also had worse disease activity at baseline if they met fibromyalgia research criteria than if they did not.
“The issue of fibromyalgia as a comorbidity in axial SpA has been the subject of current considerable interest,” said Dr. Macfarlane, who is Clinical Chair in Epidemiology at the University of Aberdeen (Scotland), where the BSRBR-AS is run. This is for several reasons: “One is the challenge of identifying patients with axial SpA who have comorbid fibromyalgia.
“The second is the concern that comorbid fibromyalgia may have an effect on disease indices such as BASDAI [Bath Ankylosing Spondylitis Disease Activity Index],” Dr. Macfarlane observed.
This leads to the third issue: “Are patients with comorbid fibromyalgia inappropriately receiving biological therapy, and how do they respond if they do receive it?”
Previous data from the BSRBR-AS have shown that approximately one in five patients with axSpA meet research criteria for fibromyalgia (Arthritis Rheumatol. 2017;69:2144-50) and that the prevalence of the comorbidity was higher in those who met Assessment of SpondyloArthritis International Society imaging criteria and lower in those who only met clinical criteria (25% vs. 10%).
The current aims of the study presented by Dr. Macfarlane were to first quantify the extent to which meeting fibromyalgia criteria was associated with higher measures of disease activity and impact, and then to see if meeting these criteria was associated with a poorer response to first use of a TNFi.
In order to find out, Dr. Macfarlane and his associates examined data from the prospective BSRBR-AS, which has been running since 2012. The BSRBR-AS recruits patients with ASAS-confirmed axSpA who are newly starting biologics from 83 U.K. centers.
At recruitment and at 3 months, patients starting biologic treatment undergo several assessments, which since 2015 has included research criteria for fibromyalgia (J Rheumatol. 2011;38:1113–22). The latter incorporate a Widespread Pain Index rated 0-19 and a Symptom Severity Scale rated 0-12 and cover items such as fatigue and waking up unrefreshed, and the presence of lower abdominal pain or headaches.
To date, around 1,750 participants in the BSRBR-AS have completed the fibromyalgia criteria, Dr. Macfarlane said.
Across the board, baseline measures of disease activity were lower in patients who met the fibromyalgia criteria versus those who did not. This included the BASDAI and the Bath Ankylosing Spondylitis Functional Index, where scores were approximately 6.5 and 4.5 for each measure.
“Quality of life was significantly lower in those who were fibromyalgia positive,” Dr. Macfarlane said. Indeed, whatever the measure used, from the disease-specific Ankylosing Spondylitis Quality of Life (ASQoL) Scale to the general EuroQoL Quality of Life Scale, there were significant differences between those who did and did not meet fibromyalgia criteria. There were also higher scores for depression, anxiety, poorer-quality sleep, and higher levels of fatigue.
Patients treated with TNFi therapy showed improvement in both BASDAI and ASQoL scores regardless of whether they met fibromyalgia criteria, but crucially, the responses were still lower and significantly different from those without fibromyalgia.
An ASAS20 response to TNFi therapy was met by “slightly fewer” patients who met the fibromyalgia criteria than by those who did not at all follow-up points: at 3 months (about 35% vs. 45%), 6 months (about 58% vs. 61%), and 12 months (about 60% vs. 62%).
A high score on the Symptom Severity Scale but not the Widespread Pain Index of the fibromyalgia criteria was associated with a lower response to TNFi therapy at 3 months. “Such patients may benefit from the use of TNFi and nonpharmacological therapy,” Dr. Macfarlane said.
The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
SOURCE: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
REPORTING FROM RHEUMATOLOGY 2018
Key clinical point: Comorbid axial spondyloarthritis and fibromyalgia are associated with a lower response to biologic therapy.
Major finding: About 35% vs. 45% of patients who did and did not meet research criteria for fibromyalgia had an ASAS20 response at 3 months.
Study details: Data on 1,750 participants of the British Society for Rheumatology Biologics Register in Ankylosing Spondylitis (BSRBR-AS).
Disclosures: The BSRBR-AS is funded by the British Society for Rheumatology, which in turn receives funding from AbbVie, Pfizer, and UCB. Dr. Macfarlane did not provide any disclosures but has previously acknowledged receiving an honorarium from Pfizer and research funding from AbbVie and Pfizer for the Scotland Registry for Ankylosing Spondylitis study.
Source: Macfarlane GJ et al. Rheumatology. 2018;57(Suppl. 3):key075.183.
Tailored hemophilia prophylaxis could cut costs
Tailored frequency-escalated prophylaxis produced good outcomes with little arthropathy among boys with hemophilia A, according to findings from a prospective study.
The potential to use smaller amounts of clotting factor concentrates (CFCs) also offers a possible cost savings, Brian M. Feldman, MD, of the Hospital for Sick Children, Toronto, and his colleagues reported in the Lancet Haematology.
Prophylactic treatment to prevent bleeding episodes and avoid long term complications using regular CFCs is very effective but also very expensive. The Canadian Hemophilia Prophylaxis Study (CHPS) began 2 decades ago with the premise that, since CFC use accounts for most of the financial burden in severe hemophilia and because primary prophylaxis is started at a very young age, the burden on both the patient and the health care system could potentially be reduced by starting prophylaxis with CFC infusions at reduced frequency intervals. The individual’s subsequent bleeding episodes would then determine how the dose and frequency could be tailored.
In the study, 56 boys between the ages of 1 and 2.5 years with severe hemophilia A from 12 Canadian centers were enrolled in the CHPS, with a median time in the study of 10.2 years. Treatment was with standard half-life recombinant factor VIII (SHL-rFVIII), beginning as once weekly prophylaxis with 50 IU/kg and then escalating in frequency with appropriate dose adjustments as needed (step 1). The primary endpoint for this analysis was joint health, as measured by the modified Colorado Child Physical Examination Scores at completion of the study.
Participants were able to stay on once a week prophylaxis, without unacceptable bleeding, until a median age of 4.5 years. At this time, boys who developed unacceptable bleeding were escalated to twice-weekly prophylaxis at 30 IU/kg (step 2). The median age for beginning alternate day prophylaxis at 25 IU/kg (step 3) was 9.9 years of age.
The median annual SHL-rFVIII use was 3,582 IU/kg at age 2 years (n = 56), 4,041 IU/kg at age 6 years (n = 53), 3,638 IU/kg at age 10 years (n = 40), and 3,663 IU/kg at 14 years of age (n = 18). Overall adherence to the tailored regimen was a median of 86%, and no treatment-related safety events were observed during the study, including central venous catheter infections.
The median use of SHL-rFVIII on the tailored frequency-escalated prophylaxis is considerably less than the 6,000 IU/kg per year used in standard prophylaxis regimens, the researchers noted.
“We have previously shown, with a formal cost-benefit analysis using the value-of-information approach, that tailored frequency escalated prophylaxis provides substantial cost-benefit in a variety of scenarios. Our results from this study lend further support to these findings,” they wrote.
The median annualized index joint bleeding rate was 0.95 per year, but 30% of the boys in the study experienced “unacceptable breakthrough bleeding” during the study.
Overall joint health was “well preserved,” according to the researchers. The median Colorado Child Physical Examination Score at the end of the CHPS was 1 (range 0-12) for the left ankle and 1 for the right ankle, with all other joints having a median score of 0.
Activities of daily living and physical function, as well as health-related quality of life were generally good, the researchers reported.
The study was initially funded by grants from the Medical Research Council of Canada/Pharmaceutical Manufacturers Association of Canada Partnership Fund and by the Bayer/Canadian Blood Services/Héma-Québec Partnership Fund. Subsequent renewals were funded by Bayer. Dr. Feldman reported grants from Bayer during the conduct of the study and grants from Baxter/Baxalta/Shire outside the submitted work. Several coauthors also report multiple relationships with industry.
SOURCE: Feldman BM et al. Lancet Haematol. 2018 May 3. doi: 10.1016/S2352-3026(18)30048-6.
Tailored frequency-escalated prophylaxis produced good outcomes with little arthropathy among boys with hemophilia A, according to findings from a prospective study.
The potential to use smaller amounts of clotting factor concentrates (CFCs) also offers a possible cost savings, Brian M. Feldman, MD, of the Hospital for Sick Children, Toronto, and his colleagues reported in the Lancet Haematology.
Prophylactic treatment to prevent bleeding episodes and avoid long term complications using regular CFCs is very effective but also very expensive. The Canadian Hemophilia Prophylaxis Study (CHPS) began 2 decades ago with the premise that, since CFC use accounts for most of the financial burden in severe hemophilia and because primary prophylaxis is started at a very young age, the burden on both the patient and the health care system could potentially be reduced by starting prophylaxis with CFC infusions at reduced frequency intervals. The individual’s subsequent bleeding episodes would then determine how the dose and frequency could be tailored.
In the study, 56 boys between the ages of 1 and 2.5 years with severe hemophilia A from 12 Canadian centers were enrolled in the CHPS, with a median time in the study of 10.2 years. Treatment was with standard half-life recombinant factor VIII (SHL-rFVIII), beginning as once weekly prophylaxis with 50 IU/kg and then escalating in frequency with appropriate dose adjustments as needed (step 1). The primary endpoint for this analysis was joint health, as measured by the modified Colorado Child Physical Examination Scores at completion of the study.
Participants were able to stay on once a week prophylaxis, without unacceptable bleeding, until a median age of 4.5 years. At this time, boys who developed unacceptable bleeding were escalated to twice-weekly prophylaxis at 30 IU/kg (step 2). The median age for beginning alternate day prophylaxis at 25 IU/kg (step 3) was 9.9 years of age.
The median annual SHL-rFVIII use was 3,582 IU/kg at age 2 years (n = 56), 4,041 IU/kg at age 6 years (n = 53), 3,638 IU/kg at age 10 years (n = 40), and 3,663 IU/kg at 14 years of age (n = 18). Overall adherence to the tailored regimen was a median of 86%, and no treatment-related safety events were observed during the study, including central venous catheter infections.
The median use of SHL-rFVIII on the tailored frequency-escalated prophylaxis is considerably less than the 6,000 IU/kg per year used in standard prophylaxis regimens, the researchers noted.
“We have previously shown, with a formal cost-benefit analysis using the value-of-information approach, that tailored frequency escalated prophylaxis provides substantial cost-benefit in a variety of scenarios. Our results from this study lend further support to these findings,” they wrote.
The median annualized index joint bleeding rate was 0.95 per year, but 30% of the boys in the study experienced “unacceptable breakthrough bleeding” during the study.
Overall joint health was “well preserved,” according to the researchers. The median Colorado Child Physical Examination Score at the end of the CHPS was 1 (range 0-12) for the left ankle and 1 for the right ankle, with all other joints having a median score of 0.
Activities of daily living and physical function, as well as health-related quality of life were generally good, the researchers reported.
The study was initially funded by grants from the Medical Research Council of Canada/Pharmaceutical Manufacturers Association of Canada Partnership Fund and by the Bayer/Canadian Blood Services/Héma-Québec Partnership Fund. Subsequent renewals were funded by Bayer. Dr. Feldman reported grants from Bayer during the conduct of the study and grants from Baxter/Baxalta/Shire outside the submitted work. Several coauthors also report multiple relationships with industry.
SOURCE: Feldman BM et al. Lancet Haematol. 2018 May 3. doi: 10.1016/S2352-3026(18)30048-6.
Tailored frequency-escalated prophylaxis produced good outcomes with little arthropathy among boys with hemophilia A, according to findings from a prospective study.
The potential to use smaller amounts of clotting factor concentrates (CFCs) also offers a possible cost savings, Brian M. Feldman, MD, of the Hospital for Sick Children, Toronto, and his colleagues reported in the Lancet Haematology.
Prophylactic treatment to prevent bleeding episodes and avoid long term complications using regular CFCs is very effective but also very expensive. The Canadian Hemophilia Prophylaxis Study (CHPS) began 2 decades ago with the premise that, since CFC use accounts for most of the financial burden in severe hemophilia and because primary prophylaxis is started at a very young age, the burden on both the patient and the health care system could potentially be reduced by starting prophylaxis with CFC infusions at reduced frequency intervals. The individual’s subsequent bleeding episodes would then determine how the dose and frequency could be tailored.
In the study, 56 boys between the ages of 1 and 2.5 years with severe hemophilia A from 12 Canadian centers were enrolled in the CHPS, with a median time in the study of 10.2 years. Treatment was with standard half-life recombinant factor VIII (SHL-rFVIII), beginning as once weekly prophylaxis with 50 IU/kg and then escalating in frequency with appropriate dose adjustments as needed (step 1). The primary endpoint for this analysis was joint health, as measured by the modified Colorado Child Physical Examination Scores at completion of the study.
Participants were able to stay on once a week prophylaxis, without unacceptable bleeding, until a median age of 4.5 years. At this time, boys who developed unacceptable bleeding were escalated to twice-weekly prophylaxis at 30 IU/kg (step 2). The median age for beginning alternate day prophylaxis at 25 IU/kg (step 3) was 9.9 years of age.
The median annual SHL-rFVIII use was 3,582 IU/kg at age 2 years (n = 56), 4,041 IU/kg at age 6 years (n = 53), 3,638 IU/kg at age 10 years (n = 40), and 3,663 IU/kg at 14 years of age (n = 18). Overall adherence to the tailored regimen was a median of 86%, and no treatment-related safety events were observed during the study, including central venous catheter infections.
The median use of SHL-rFVIII on the tailored frequency-escalated prophylaxis is considerably less than the 6,000 IU/kg per year used in standard prophylaxis regimens, the researchers noted.
“We have previously shown, with a formal cost-benefit analysis using the value-of-information approach, that tailored frequency escalated prophylaxis provides substantial cost-benefit in a variety of scenarios. Our results from this study lend further support to these findings,” they wrote.
The median annualized index joint bleeding rate was 0.95 per year, but 30% of the boys in the study experienced “unacceptable breakthrough bleeding” during the study.
Overall joint health was “well preserved,” according to the researchers. The median Colorado Child Physical Examination Score at the end of the CHPS was 1 (range 0-12) for the left ankle and 1 for the right ankle, with all other joints having a median score of 0.
Activities of daily living and physical function, as well as health-related quality of life were generally good, the researchers reported.
The study was initially funded by grants from the Medical Research Council of Canada/Pharmaceutical Manufacturers Association of Canada Partnership Fund and by the Bayer/Canadian Blood Services/Héma-Québec Partnership Fund. Subsequent renewals were funded by Bayer. Dr. Feldman reported grants from Bayer during the conduct of the study and grants from Baxter/Baxalta/Shire outside the submitted work. Several coauthors also report multiple relationships with industry.
SOURCE: Feldman BM et al. Lancet Haematol. 2018 May 3. doi: 10.1016/S2352-3026(18)30048-6.
LANCET HAEMATOLOGY
Key clinical point:
Major finding: The median CPPES score at the end of the study was 1 (range 0-12) for the left ankle and 1 for the right ankle, with all other joints having a median score of 0.
Study details: Longitudinal design comprising 56 boys with severe hemophilia A who were followed for up to 16.1 years.
Disclosures: The study was initially funded by grants from the Medical Research Council of Canada/Pharmaceutical Manufacturers Association of Canada Partnership Fund and by the Bayer/Canadian Blood Services/Héma-Québec Partnership Fund. Subsequent renewals were funded by Bayer. Dr. Feldman reported grants from Bayer during the conduct of the study and grants from Baxter/Baxalta/Shire outside the submitted work. Several coauthors also report multiple relationships with industry.
Source: Feldman BM et al. Lancet Haematol. 2018 May 3. doi: 10.1016/S2352-3026(18)30048-6.
Congress passes ‘right to try’ legislation
Both houses of Congress have now approved a bill to provide terminally ill patients with access to experimental treatments, despite opposition from many Democrats and more than 100 patient and physician groups. President Trump is expected to sign the legislation.
By a vote of 250-169, the House passed S. 204, the Trickett Wendler, Frank Mongiello, Jordan McLinn, and Matthew Bellina Right to Try Act of 2017 on May 22. All Republication House members voted for the bill, as did 22 Democrats. The Senate had passed the bill by unanimous consent in August 2017.
“This is dangerous legislation that threatens FDA’s [Food and Drug Administration’s] authority over insuring that medical treatments are effective,” Rep. Frank Pallone (D-N.J.), ranking member of the House Energy and Commerce Committee, said during the debate on the bill. “This bill needlessly exposes vulnerable patients to the risk of unproven medications.”
He noted the language will apply broadly to anyone who has been diagnosed with a disease but may not be terminal.
“The term ‘life-threatening disease or condition’ could include chronic and often manageable diseases, such as diabetes or chronic heart failure,” he said. “If all patients with diabetes and other chronic but manageable illnesses were eligible, you have greatly expanded the scope of the legislation well beyond the scope of most state laws and FDA’s expanded access program. This exposes an even greater number of patients to risk and undermines our clinical trial program by diverting patients from trials that could support full approval to the alternate pathway.”
The law notes that the experimental drug must have cleared phase 1 testing and experimentation, and development and testing must be ongoing. Treating physicians will not be compensated for certifying a patient as eligible to gain access to an investigational drug.
Patient and physician groups, including the American Society of Clinical Oncology, Friends of Cancer Research, American Lung Association, Cystic Fibrosis Foundation, and National Organization for Rare Disorders, voiced their opposition in a May 21 letter to House Republican and Democratic leaders.
“The Senate version of the legislation is less safe than the pathway proposed in the House version and is dangerous compared to the current [FDA] expanded access program,” according to the groups. “Both House and Senate versions would also remove FDA’s consultation on dosing, route of administration, dosing schedule, and other important safety measures available under FDA’s current expanded access program.”
The organizations noted that, while they did not support the House version, it “includes improved patient safeguards compared to the Senate version. The Senate version would negatively impact patient safety substantially, and our collective organizations are strongly opposed.”
President Trump has signaled he will sign the bill.
Both houses of Congress have now approved a bill to provide terminally ill patients with access to experimental treatments, despite opposition from many Democrats and more than 100 patient and physician groups. President Trump is expected to sign the legislation.
By a vote of 250-169, the House passed S. 204, the Trickett Wendler, Frank Mongiello, Jordan McLinn, and Matthew Bellina Right to Try Act of 2017 on May 22. All Republication House members voted for the bill, as did 22 Democrats. The Senate had passed the bill by unanimous consent in August 2017.
“This is dangerous legislation that threatens FDA’s [Food and Drug Administration’s] authority over insuring that medical treatments are effective,” Rep. Frank Pallone (D-N.J.), ranking member of the House Energy and Commerce Committee, said during the debate on the bill. “This bill needlessly exposes vulnerable patients to the risk of unproven medications.”
He noted the language will apply broadly to anyone who has been diagnosed with a disease but may not be terminal.
“The term ‘life-threatening disease or condition’ could include chronic and often manageable diseases, such as diabetes or chronic heart failure,” he said. “If all patients with diabetes and other chronic but manageable illnesses were eligible, you have greatly expanded the scope of the legislation well beyond the scope of most state laws and FDA’s expanded access program. This exposes an even greater number of patients to risk and undermines our clinical trial program by diverting patients from trials that could support full approval to the alternate pathway.”
The law notes that the experimental drug must have cleared phase 1 testing and experimentation, and development and testing must be ongoing. Treating physicians will not be compensated for certifying a patient as eligible to gain access to an investigational drug.
Patient and physician groups, including the American Society of Clinical Oncology, Friends of Cancer Research, American Lung Association, Cystic Fibrosis Foundation, and National Organization for Rare Disorders, voiced their opposition in a May 21 letter to House Republican and Democratic leaders.
“The Senate version of the legislation is less safe than the pathway proposed in the House version and is dangerous compared to the current [FDA] expanded access program,” according to the groups. “Both House and Senate versions would also remove FDA’s consultation on dosing, route of administration, dosing schedule, and other important safety measures available under FDA’s current expanded access program.”
The organizations noted that, while they did not support the House version, it “includes improved patient safeguards compared to the Senate version. The Senate version would negatively impact patient safety substantially, and our collective organizations are strongly opposed.”
President Trump has signaled he will sign the bill.
Both houses of Congress have now approved a bill to provide terminally ill patients with access to experimental treatments, despite opposition from many Democrats and more than 100 patient and physician groups. President Trump is expected to sign the legislation.
By a vote of 250-169, the House passed S. 204, the Trickett Wendler, Frank Mongiello, Jordan McLinn, and Matthew Bellina Right to Try Act of 2017 on May 22. All Republication House members voted for the bill, as did 22 Democrats. The Senate had passed the bill by unanimous consent in August 2017.
“This is dangerous legislation that threatens FDA’s [Food and Drug Administration’s] authority over insuring that medical treatments are effective,” Rep. Frank Pallone (D-N.J.), ranking member of the House Energy and Commerce Committee, said during the debate on the bill. “This bill needlessly exposes vulnerable patients to the risk of unproven medications.”
He noted the language will apply broadly to anyone who has been diagnosed with a disease but may not be terminal.
“The term ‘life-threatening disease or condition’ could include chronic and often manageable diseases, such as diabetes or chronic heart failure,” he said. “If all patients with diabetes and other chronic but manageable illnesses were eligible, you have greatly expanded the scope of the legislation well beyond the scope of most state laws and FDA’s expanded access program. This exposes an even greater number of patients to risk and undermines our clinical trial program by diverting patients from trials that could support full approval to the alternate pathway.”
The law notes that the experimental drug must have cleared phase 1 testing and experimentation, and development and testing must be ongoing. Treating physicians will not be compensated for certifying a patient as eligible to gain access to an investigational drug.
Patient and physician groups, including the American Society of Clinical Oncology, Friends of Cancer Research, American Lung Association, Cystic Fibrosis Foundation, and National Organization for Rare Disorders, voiced their opposition in a May 21 letter to House Republican and Democratic leaders.
“The Senate version of the legislation is less safe than the pathway proposed in the House version and is dangerous compared to the current [FDA] expanded access program,” according to the groups. “Both House and Senate versions would also remove FDA’s consultation on dosing, route of administration, dosing schedule, and other important safety measures available under FDA’s current expanded access program.”
The organizations noted that, while they did not support the House version, it “includes improved patient safeguards compared to the Senate version. The Senate version would negatively impact patient safety substantially, and our collective organizations are strongly opposed.”
President Trump has signaled he will sign the bill.
Breakthrough in noninvasive assessment of multivessel CAD
PARIS – A completely noninvasive method of identifying functionally significant lesions in patients with triple-vessel coronary artery disease yielded results comparable to conventional invasive angiographic assessment accompanied by an intracoronary pressure wire, in a prespecified secondary analysis of the SYNTAX II study.
That noninvasive method uses fractional flow reserve calculated from computed tomographic angiography, Carlos Collet, MD, said at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
The results were hailed as a harbinger of a coming era in which interventional decision making will be based entirely upon noninvasively acquired anatomic and physiologic data. Conventional diagnostic angiography is predicted to fall by the wayside, with resultant savings in time and cost as well as avoidance of the risks of percutaneous diagnostic angiography, which entails considerably more radiation exposure than does noninvasive CT angiography (CTA).
“We are on the verge of a major change,” said Patrick W. Serruys, MD, PhD, professor of cardiology at Imperial College London, who was the senior coinvestigator in the study. “I think that the next disruptive moment in cardiology will be the introduction of the new generation of multislice CT scans replacing conventional cineangiography in the next 5-10 years. For the interventional cardiologist, to have the results of a multislice CT scan the day before a procedure is a wonderful bonus. You know in advance what you’re going to see, you can develop your treatment strategy, and you can spare contrast.”
Compared with conventional invasive angiographic assessment with the use of an intracoronary pressure wire to measure iFR, the noninvasively calculated SYNTAX II score had 95% sensitivity and 61% specificity for detection of functionally significant stenosis, with a positive predictive value of 81% and a negative predictive value of 87%. And this was achieved using older scanners and software considerably less accurate than today’s rapidly evolving state of the art, Dr. Collet noted.
Background
The original landmark SYNTAX trial led to development of an anatomically based SYNTAX score for use in stratifying risk and guiding treatment planning – coronary artery bypass grafting versus PCI – in patients with multivessel CAD. Both the U.S. and European guidelines recommend the use of this score, based on invasive angiography, giving it a Class IIa and I recommendation, respectively. Patients with a low-risk SYNTAX score of 22 or less were shown to have similar outcomes with PCI and coronary artery bypass grafting, while those with a score of 23 or more had better outcomes at 5-year follow-up with CABG.
Subsequently, incorporation of clinical characteristics formed the basis of the updated SYNTAX II score, with enhanced predictive accuracy allowing for projections of 4-year all-cause mortality with CABG versus PCI in a given patient (www.syntaxscore.com). The new SYNTAX II substudy takes things a giant step further by rendering the coronary imaging and physiology assessment noninvasive.
Simultaneous with Dr. Collet’s presentation at EuroPCR 2018, the study results were published in the Journal of the American College of Cardiology.
In an accompanying editorial, Bjarne L. Norgaard, MD, PhD, of Aarhus (Denmark) University and coauthors enthused, “These data suggest that we may be entering a new era in the management of CAD. The days of having patients entering the catheterization laboratory with nothing more than symptoms and a positive stress test result may be coming to an end. This study may be signaling a shifting paradigm in which CAD is diagnosed and thoroughly characterized noninvasively, and revascularization planning made in a collaborative fashion integrating the heart team, and a wealth of noninvasive data that will hopefully lead to more effective and cost-efficient revascularization strategies.”
What’s next
Elsewhere at EuroPCR 2018, Dr. Serruys presented the results of the SYNTAX III Revolution Trial, which randomized six pairs of heart teams – each comprising an interventional cardiologist, surgeon, and radiologist – to collectively assess and plan revascularization strategies for 223 patients with left main or triple-vessel CAD. One heart team in each pair was provided with a patient’s noninvasive CTA and FFR results, while the other team was given only the results of conventional angiography.
“There was almost perfect agreement between the heart teams on their decisions,” according to Dr. Serruys. “We were impressed that the surgeons were enthusiastic about the prospect of operating based on multislice CT alone.
On the basis of this evidence that heart teams found, the noninvasive assessment to be acceptable, he and his coinvestigators are organizing a multicenter trial to assess the feasibility and safety of the fully noninvasive stratification, compared with conventional angiography and invasive physiologic assessment of lesions. The primary safety endpoint will be the 1-month patency of bypass grafts.
The multislice scanner used in the SYNTAX III Revolution trial was the General Electric Revolution CT scanner, which enables imaging of the heart during a single heart beat. But Dr. Serruys said most of the big medical imaging companies with an eye to the near future are now developing multislice scanners specifically for the heart.
“They cost half the price and take only half the space of conventional scanners. I think these small units – which are not used for the brain, the abdomen, and all the rest – are going to play a big role in cardiology,” he predicted.
William Wijns, MD, codirector of EuroPCR, called the results of the SYNTAX II and SYNTAX III Revolution studies “transformative.” He and the other meeting organizers highlighted the studies in a special “deep-dive” session, which he urged younger interventionalists in particular to attend because he believes it’s likely they will be relying on these noninvasive assessments in the near future.
The SYNTAX III Revolution trial was sponsored by the European Cardiovascular Research Institute with support from GE Healthcare and HeartFlow. Dr. Serruys reported having no financial relationship with either company.
SOURCE: Collet C. EuroPCR 2018, Simultaneous publication (J Am Coll Cardiol 2018;71:40-53).
PARIS – A completely noninvasive method of identifying functionally significant lesions in patients with triple-vessel coronary artery disease yielded results comparable to conventional invasive angiographic assessment accompanied by an intracoronary pressure wire, in a prespecified secondary analysis of the SYNTAX II study.
That noninvasive method uses fractional flow reserve calculated from computed tomographic angiography, Carlos Collet, MD, said at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
The results were hailed as a harbinger of a coming era in which interventional decision making will be based entirely upon noninvasively acquired anatomic and physiologic data. Conventional diagnostic angiography is predicted to fall by the wayside, with resultant savings in time and cost as well as avoidance of the risks of percutaneous diagnostic angiography, which entails considerably more radiation exposure than does noninvasive CT angiography (CTA).
“We are on the verge of a major change,” said Patrick W. Serruys, MD, PhD, professor of cardiology at Imperial College London, who was the senior coinvestigator in the study. “I think that the next disruptive moment in cardiology will be the introduction of the new generation of multislice CT scans replacing conventional cineangiography in the next 5-10 years. For the interventional cardiologist, to have the results of a multislice CT scan the day before a procedure is a wonderful bonus. You know in advance what you’re going to see, you can develop your treatment strategy, and you can spare contrast.”
Compared with conventional invasive angiographic assessment with the use of an intracoronary pressure wire to measure iFR, the noninvasively calculated SYNTAX II score had 95% sensitivity and 61% specificity for detection of functionally significant stenosis, with a positive predictive value of 81% and a negative predictive value of 87%. And this was achieved using older scanners and software considerably less accurate than today’s rapidly evolving state of the art, Dr. Collet noted.
Background
The original landmark SYNTAX trial led to development of an anatomically based SYNTAX score for use in stratifying risk and guiding treatment planning – coronary artery bypass grafting versus PCI – in patients with multivessel CAD. Both the U.S. and European guidelines recommend the use of this score, based on invasive angiography, giving it a Class IIa and I recommendation, respectively. Patients with a low-risk SYNTAX score of 22 or less were shown to have similar outcomes with PCI and coronary artery bypass grafting, while those with a score of 23 or more had better outcomes at 5-year follow-up with CABG.
Subsequently, incorporation of clinical characteristics formed the basis of the updated SYNTAX II score, with enhanced predictive accuracy allowing for projections of 4-year all-cause mortality with CABG versus PCI in a given patient (www.syntaxscore.com). The new SYNTAX II substudy takes things a giant step further by rendering the coronary imaging and physiology assessment noninvasive.
Simultaneous with Dr. Collet’s presentation at EuroPCR 2018, the study results were published in the Journal of the American College of Cardiology.
In an accompanying editorial, Bjarne L. Norgaard, MD, PhD, of Aarhus (Denmark) University and coauthors enthused, “These data suggest that we may be entering a new era in the management of CAD. The days of having patients entering the catheterization laboratory with nothing more than symptoms and a positive stress test result may be coming to an end. This study may be signaling a shifting paradigm in which CAD is diagnosed and thoroughly characterized noninvasively, and revascularization planning made in a collaborative fashion integrating the heart team, and a wealth of noninvasive data that will hopefully lead to more effective and cost-efficient revascularization strategies.”
What’s next
Elsewhere at EuroPCR 2018, Dr. Serruys presented the results of the SYNTAX III Revolution Trial, which randomized six pairs of heart teams – each comprising an interventional cardiologist, surgeon, and radiologist – to collectively assess and plan revascularization strategies for 223 patients with left main or triple-vessel CAD. One heart team in each pair was provided with a patient’s noninvasive CTA and FFR results, while the other team was given only the results of conventional angiography.
“There was almost perfect agreement between the heart teams on their decisions,” according to Dr. Serruys. “We were impressed that the surgeons were enthusiastic about the prospect of operating based on multislice CT alone.
On the basis of this evidence that heart teams found, the noninvasive assessment to be acceptable, he and his coinvestigators are organizing a multicenter trial to assess the feasibility and safety of the fully noninvasive stratification, compared with conventional angiography and invasive physiologic assessment of lesions. The primary safety endpoint will be the 1-month patency of bypass grafts.
The multislice scanner used in the SYNTAX III Revolution trial was the General Electric Revolution CT scanner, which enables imaging of the heart during a single heart beat. But Dr. Serruys said most of the big medical imaging companies with an eye to the near future are now developing multislice scanners specifically for the heart.
“They cost half the price and take only half the space of conventional scanners. I think these small units – which are not used for the brain, the abdomen, and all the rest – are going to play a big role in cardiology,” he predicted.
William Wijns, MD, codirector of EuroPCR, called the results of the SYNTAX II and SYNTAX III Revolution studies “transformative.” He and the other meeting organizers highlighted the studies in a special “deep-dive” session, which he urged younger interventionalists in particular to attend because he believes it’s likely they will be relying on these noninvasive assessments in the near future.
The SYNTAX III Revolution trial was sponsored by the European Cardiovascular Research Institute with support from GE Healthcare and HeartFlow. Dr. Serruys reported having no financial relationship with either company.
SOURCE: Collet C. EuroPCR 2018, Simultaneous publication (J Am Coll Cardiol 2018;71:40-53).
PARIS – A completely noninvasive method of identifying functionally significant lesions in patients with triple-vessel coronary artery disease yielded results comparable to conventional invasive angiographic assessment accompanied by an intracoronary pressure wire, in a prespecified secondary analysis of the SYNTAX II study.
That noninvasive method uses fractional flow reserve calculated from computed tomographic angiography, Carlos Collet, MD, said at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
The results were hailed as a harbinger of a coming era in which interventional decision making will be based entirely upon noninvasively acquired anatomic and physiologic data. Conventional diagnostic angiography is predicted to fall by the wayside, with resultant savings in time and cost as well as avoidance of the risks of percutaneous diagnostic angiography, which entails considerably more radiation exposure than does noninvasive CT angiography (CTA).
“We are on the verge of a major change,” said Patrick W. Serruys, MD, PhD, professor of cardiology at Imperial College London, who was the senior coinvestigator in the study. “I think that the next disruptive moment in cardiology will be the introduction of the new generation of multislice CT scans replacing conventional cineangiography in the next 5-10 years. For the interventional cardiologist, to have the results of a multislice CT scan the day before a procedure is a wonderful bonus. You know in advance what you’re going to see, you can develop your treatment strategy, and you can spare contrast.”
Compared with conventional invasive angiographic assessment with the use of an intracoronary pressure wire to measure iFR, the noninvasively calculated SYNTAX II score had 95% sensitivity and 61% specificity for detection of functionally significant stenosis, with a positive predictive value of 81% and a negative predictive value of 87%. And this was achieved using older scanners and software considerably less accurate than today’s rapidly evolving state of the art, Dr. Collet noted.
Background
The original landmark SYNTAX trial led to development of an anatomically based SYNTAX score for use in stratifying risk and guiding treatment planning – coronary artery bypass grafting versus PCI – in patients with multivessel CAD. Both the U.S. and European guidelines recommend the use of this score, based on invasive angiography, giving it a Class IIa and I recommendation, respectively. Patients with a low-risk SYNTAX score of 22 or less were shown to have similar outcomes with PCI and coronary artery bypass grafting, while those with a score of 23 or more had better outcomes at 5-year follow-up with CABG.
Subsequently, incorporation of clinical characteristics formed the basis of the updated SYNTAX II score, with enhanced predictive accuracy allowing for projections of 4-year all-cause mortality with CABG versus PCI in a given patient (www.syntaxscore.com). The new SYNTAX II substudy takes things a giant step further by rendering the coronary imaging and physiology assessment noninvasive.
Simultaneous with Dr. Collet’s presentation at EuroPCR 2018, the study results were published in the Journal of the American College of Cardiology.
In an accompanying editorial, Bjarne L. Norgaard, MD, PhD, of Aarhus (Denmark) University and coauthors enthused, “These data suggest that we may be entering a new era in the management of CAD. The days of having patients entering the catheterization laboratory with nothing more than symptoms and a positive stress test result may be coming to an end. This study may be signaling a shifting paradigm in which CAD is diagnosed and thoroughly characterized noninvasively, and revascularization planning made in a collaborative fashion integrating the heart team, and a wealth of noninvasive data that will hopefully lead to more effective and cost-efficient revascularization strategies.”
What’s next
Elsewhere at EuroPCR 2018, Dr. Serruys presented the results of the SYNTAX III Revolution Trial, which randomized six pairs of heart teams – each comprising an interventional cardiologist, surgeon, and radiologist – to collectively assess and plan revascularization strategies for 223 patients with left main or triple-vessel CAD. One heart team in each pair was provided with a patient’s noninvasive CTA and FFR results, while the other team was given only the results of conventional angiography.
“There was almost perfect agreement between the heart teams on their decisions,” according to Dr. Serruys. “We were impressed that the surgeons were enthusiastic about the prospect of operating based on multislice CT alone.
On the basis of this evidence that heart teams found, the noninvasive assessment to be acceptable, he and his coinvestigators are organizing a multicenter trial to assess the feasibility and safety of the fully noninvasive stratification, compared with conventional angiography and invasive physiologic assessment of lesions. The primary safety endpoint will be the 1-month patency of bypass grafts.
The multislice scanner used in the SYNTAX III Revolution trial was the General Electric Revolution CT scanner, which enables imaging of the heart during a single heart beat. But Dr. Serruys said most of the big medical imaging companies with an eye to the near future are now developing multislice scanners specifically for the heart.
“They cost half the price and take only half the space of conventional scanners. I think these small units – which are not used for the brain, the abdomen, and all the rest – are going to play a big role in cardiology,” he predicted.
William Wijns, MD, codirector of EuroPCR, called the results of the SYNTAX II and SYNTAX III Revolution studies “transformative.” He and the other meeting organizers highlighted the studies in a special “deep-dive” session, which he urged younger interventionalists in particular to attend because he believes it’s likely they will be relying on these noninvasive assessments in the near future.
The SYNTAX III Revolution trial was sponsored by the European Cardiovascular Research Institute with support from GE Healthcare and HeartFlow. Dr. Serruys reported having no financial relationship with either company.
SOURCE: Collet C. EuroPCR 2018, Simultaneous publication (J Am Coll Cardiol 2018;71:40-53).
REPORTING FROM EUROPCR 2018
Key clinical point:
Major finding: A completely noninvasive method of identifying functionally significant lesions in patients with triple-vessel CAD by means of fractional flow reserve calculated from CT angiography yielded results comparable to conventional pressure-wire-based invasive angiographic assessment.
Study details: This prespecified secondary analysis of the SYNTAX II trial compared the results of noninvasive assessment of patients with triple-vessel CAD using FFR calculated from CT angiography with conventional angiography plus an invasive pressure wire.
Disclosures: The study was sponsored by the European Cardiovascular Research Institute with research grant support from Volcano and Boston Scientific. The presenter reported financial relationships with half a dozen medical device companies, but neither of those two.
Source: Collet C. EuroPCR 2018, simultaneous publication (J Am Coll Cardiol 2018;71:40-53).
A fib ablation in HFrEF patients gains momentum
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Results from two recent trials suggest that cardiologists may have a new way to improve outcomes in patients with heart failure with reduced ejection fraction if they also have atrial fibrillation: Cut the patient’s atrial fibrillation burden with catheter ablation.
This seemingly off-target approach to improving survival, avoiding heart failure hospitalizations, and possibly reducing other adverse events first gained attention with results from the CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) randomized trial, first reported in 2017. The study showed in 363 patients that atrial fibrillation (AF) ablation in patients with heart failure with reduced ejection fraction (HFrEF) led to a statistically significant 38% relative reduction in the primary endpoint of mortality or heart failure hospitalization during a median 38 months of follow-up (N Engl J Med. 2018 Feb 1;378[5]:417-27).
This groundbreaking finding then received some degree of confirmation when Douglas L. Packer, MD, reported primary results from CABANA (Catheter Ablation vs Anti-arrhythmic Drug Therapy for Atrial Fibrillation Trial) at the annual scientific sessions of the Heart Rhythm Society. CABANA compared upfront ablation against first-line medical management of AF in 2,203 patients. While the primary endpoint of the cumulative rate of all-cause death, disabling stroke, serious bleeding, or cardiac arrest over a median follow-up of just over 4 years was neutral, with no statistically significant difference between the two treatment arms, a subgroup analysis showed a tantalizing suggestion of benefit in the 337 enrolled patients with a history of congestive heart failure (15% of the total study group).
In this subgroup, treatment with ablation cut the primary endpoint by 39% relative to those treated upfront with medical management, an effect that came close to statistical significance. In addition, Dr. Packer took special note of the per-protocol analysis, which censored out the crossover patients who constituted roughly a fifth of all enrolled patients. In the subgroup analysis using the per-protocol data, ablation was linked with a statistically significant 49% relative reduction in the primary endpoint among patients with a history of heart failure.
The patients for whom there may be the quickest shift to upfront ablation to treat AF based on the CABANA results will be those with heart failure and others with high underlying risk, Dr. Packer predicted at the meeting.
“The CASTLE-AF results were interesting, but in fewer than 400 patients. Now we’ve basically seen the same thing” in CABANA, said Dr. Packer, professor and a cardiac electrophysiologist at the Mayo Clinic in Rochester, Minn.
Notably however, the results Dr. Packer reported on the heart failure subgroup did not include any information on how many of these were patients who had HFrEF or heart failure with preserved ejection fraction and how the apparent benefit from AF ablation affected each of these two heart failure types. In addition, the reported CABANA results did not have an endpoint result that completely matched the mortality and heart failure hospitalization composite endpoint used in CASTLE-AF. The closest endpoint that Dr. Packer reported from CABANA was a composite of mortality and cardiovascular hospitalization that showed, for the entire CABANA cohort, a statistically significant 17% relative reduction with ablation in the intention-to-treat analysis. Dr. Packer gave no data on how this outcome shook out in the subgroup of heart failure patients.
Despite these limitations, in trying to synthesize the CABANA and CASTLE-AF results, several electrophysiologists who heard the results agreed with Dr. Packer that the CABANA results confirmed the CASTLE-AF findings and helped strengthen the case for strongly considering AF ablation as first-line treatment in patients with heart failure.
“It’s clear that sinus rhythm is important in patients with heart failure. CASTLE-AF and now these results; that’s very strong to me,” said Eric N. Prystowsky, MD, a cardiac electrophysiologist with the St. Vincent Medical Group in Indianapolis and designated discussant for CABANA at the meeting.
“It’s confirmatory,” said Nassir F. Marrouche, MD, lead investigator for CASTLE-AF, and professor and director of the electrophysiology laboratory at the University of Utah in Salt Lake City.
The “signal” of benefit from AF ablation in heart failure patients in CABANA “replicates what was seen in CASTLE-AF. The results are highly consistent and very important regarding how to treat patients with AF and heart failure,” said Jeremy N. Ruskin, MD, professor of medicine at Harvard Medical School and director of the cardiac arrhythmia service at Massachusetts General Hospital, both in Boston. “The data strongly suggest that catheter ablation is helpful for restoring and preserving [heart] muscle function,” Dr. Ruskin said in a video interview. He noted that AF occurs in at least about a quarter of heart failure patients.
Other cardiologists at the meeting noted that, on the basis of the CASTLE-AF results alone, they have already become more aggressive about treating AF with ablation in patients with heart failure in routine practice.
“It adds to the armamentarium for treatment of patients with heart failure,” said Johannes Brachmann, MD, professor and chief of cardiology at the Coburg (Germany) Clinic and a senior coinvestigator for CASTLE-AF.
William T. Abraham, MD, a heart failure specialist at The Ohio State University in Columbus, offered a broader perspective on where AF diagnosis, treatment, and ablation currently stand in U.S. heart failure practice.
“There is a very tight link between AF burden and worse outcomes in heart failure, so there is something intuitively appealing about restoring sinus rhythm in heart failure patients. I think most heart failure clinicians believe, like me, that heart failure patients with AF benefit from restoration of normal sinus rhythm. But I don’t believe that the CASTLE-AF results have so far had much impact on practice, in part because it was a relatively small study. The heart failure community is looking for some confirmation,” said Dr. Abraham, professor and director of cardiovascular medicine at Ohio State.
“I think the CABANA results are encouraging, but they came from only 15% of the enrolled patients who also had heart failure. CABANA adds to our knowledge, but I’m not sure it’s definitive for the heart failure population. I’m not sure it tells us if you treat patients with heart failure with anti-arrhythmia drugs and successfully maintain sinus rhythm do those patients do just as well as those who get ablated,” he said in an interview. “I’d love to see a study of heart failure patients maintained in sinus rhythm with drugs compared with those treated with ablation.”
For most patients with heart failure, the coexistence of AF is identified because of AF symptoms, or when asymptomatic AF is found in recordings made by an implanted cardiac device. “I’m more aggressive about addressing asymptomatic AF in my heart failure patients, and I believe the heart failure community is moving rapidly in that direction because of the association between higher AF burden and worse heart failure outcomes,” Dr. Abraham said.
A more cautious view came from another heart failure specialist, Clyde Yancy, MD, professor and chief of cardiology at Northwestern University in Chicago. “It’s pretty evident that in certain patients with heart failure AF ablation might be the right treatment, but is it every HFrEF patient with AF?” he wondered. “It’s nice to have more evidence so we can be more comfortable sending heart failure patients for ablation, but I want to see more information about the risk” from ablation in heart failure patients, “the sustainability of the effect, and the consequences of ablation.”
But the reservations expressed by cardiologists like Dr. Yancy contrasted with the views of colleagues who consider the current evidence much more convincing.
“It seems logical to look harder for AF” in heart failure patients, based on the accumulated evidence from CASTLE-AF and CABANA, said Dr. Ruskin. “I don’t think we can offer advice to heart failure physicians to screen their heart failure patients for AF, but if it’s seen I think we have some useful information on how to address it.”
CASTLE-AF was funded by Biotronik. CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and has received research funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude, and also from several other companies. Dr. Prystowsky as been a consultant to CardioNet and Medtronic, he has an equity interest in Stereotaxis, and he receives fellowship support from Medtronic and St. Jude. Dr. Marrouche has been a consultant to Biosense Webster, Biotronik, Boston Scientific, and St. Jude. He has received research support from Medtronic, and he has had financial relationships with several other companies. Dr. Ruskin has been a consultant to Biosense Webster and Medtronic and several other companies, has an ownership interest in Amgen, Cameron Health, InfoBionic, Newpace, Portola, and Regeneron, and has a fiduciary role in Pharmaco-Kinesis. Dr. Russo and Dr. Yancy had no disclosures. Dr. Brachmann has been a consultant to and has received research funding from Biotronik, Boston Scientific, St. Jude, and several other companies. Dr. Abraham has been a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Results from two recent trials suggest that cardiologists may have a new way to improve outcomes in patients with heart failure with reduced ejection fraction if they also have atrial fibrillation: Cut the patient’s atrial fibrillation burden with catheter ablation.
This seemingly off-target approach to improving survival, avoiding heart failure hospitalizations, and possibly reducing other adverse events first gained attention with results from the CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) randomized trial, first reported in 2017. The study showed in 363 patients that atrial fibrillation (AF) ablation in patients with heart failure with reduced ejection fraction (HFrEF) led to a statistically significant 38% relative reduction in the primary endpoint of mortality or heart failure hospitalization during a median 38 months of follow-up (N Engl J Med. 2018 Feb 1;378[5]:417-27).
This groundbreaking finding then received some degree of confirmation when Douglas L. Packer, MD, reported primary results from CABANA (Catheter Ablation vs Anti-arrhythmic Drug Therapy for Atrial Fibrillation Trial) at the annual scientific sessions of the Heart Rhythm Society. CABANA compared upfront ablation against first-line medical management of AF in 2,203 patients. While the primary endpoint of the cumulative rate of all-cause death, disabling stroke, serious bleeding, or cardiac arrest over a median follow-up of just over 4 years was neutral, with no statistically significant difference between the two treatment arms, a subgroup analysis showed a tantalizing suggestion of benefit in the 337 enrolled patients with a history of congestive heart failure (15% of the total study group).
In this subgroup, treatment with ablation cut the primary endpoint by 39% relative to those treated upfront with medical management, an effect that came close to statistical significance. In addition, Dr. Packer took special note of the per-protocol analysis, which censored out the crossover patients who constituted roughly a fifth of all enrolled patients. In the subgroup analysis using the per-protocol data, ablation was linked with a statistically significant 49% relative reduction in the primary endpoint among patients with a history of heart failure.
The patients for whom there may be the quickest shift to upfront ablation to treat AF based on the CABANA results will be those with heart failure and others with high underlying risk, Dr. Packer predicted at the meeting.
“The CASTLE-AF results were interesting, but in fewer than 400 patients. Now we’ve basically seen the same thing” in CABANA, said Dr. Packer, professor and a cardiac electrophysiologist at the Mayo Clinic in Rochester, Minn.
Notably however, the results Dr. Packer reported on the heart failure subgroup did not include any information on how many of these were patients who had HFrEF or heart failure with preserved ejection fraction and how the apparent benefit from AF ablation affected each of these two heart failure types. In addition, the reported CABANA results did not have an endpoint result that completely matched the mortality and heart failure hospitalization composite endpoint used in CASTLE-AF. The closest endpoint that Dr. Packer reported from CABANA was a composite of mortality and cardiovascular hospitalization that showed, for the entire CABANA cohort, a statistically significant 17% relative reduction with ablation in the intention-to-treat analysis. Dr. Packer gave no data on how this outcome shook out in the subgroup of heart failure patients.
Despite these limitations, in trying to synthesize the CABANA and CASTLE-AF results, several electrophysiologists who heard the results agreed with Dr. Packer that the CABANA results confirmed the CASTLE-AF findings and helped strengthen the case for strongly considering AF ablation as first-line treatment in patients with heart failure.
“It’s clear that sinus rhythm is important in patients with heart failure. CASTLE-AF and now these results; that’s very strong to me,” said Eric N. Prystowsky, MD, a cardiac electrophysiologist with the St. Vincent Medical Group in Indianapolis and designated discussant for CABANA at the meeting.
“It’s confirmatory,” said Nassir F. Marrouche, MD, lead investigator for CASTLE-AF, and professor and director of the electrophysiology laboratory at the University of Utah in Salt Lake City.
The “signal” of benefit from AF ablation in heart failure patients in CABANA “replicates what was seen in CASTLE-AF. The results are highly consistent and very important regarding how to treat patients with AF and heart failure,” said Jeremy N. Ruskin, MD, professor of medicine at Harvard Medical School and director of the cardiac arrhythmia service at Massachusetts General Hospital, both in Boston. “The data strongly suggest that catheter ablation is helpful for restoring and preserving [heart] muscle function,” Dr. Ruskin said in a video interview. He noted that AF occurs in at least about a quarter of heart failure patients.
Other cardiologists at the meeting noted that, on the basis of the CASTLE-AF results alone, they have already become more aggressive about treating AF with ablation in patients with heart failure in routine practice.
“It adds to the armamentarium for treatment of patients with heart failure,” said Johannes Brachmann, MD, professor and chief of cardiology at the Coburg (Germany) Clinic and a senior coinvestigator for CASTLE-AF.
William T. Abraham, MD, a heart failure specialist at The Ohio State University in Columbus, offered a broader perspective on where AF diagnosis, treatment, and ablation currently stand in U.S. heart failure practice.
“There is a very tight link between AF burden and worse outcomes in heart failure, so there is something intuitively appealing about restoring sinus rhythm in heart failure patients. I think most heart failure clinicians believe, like me, that heart failure patients with AF benefit from restoration of normal sinus rhythm. But I don’t believe that the CASTLE-AF results have so far had much impact on practice, in part because it was a relatively small study. The heart failure community is looking for some confirmation,” said Dr. Abraham, professor and director of cardiovascular medicine at Ohio State.
“I think the CABANA results are encouraging, but they came from only 15% of the enrolled patients who also had heart failure. CABANA adds to our knowledge, but I’m not sure it’s definitive for the heart failure population. I’m not sure it tells us if you treat patients with heart failure with anti-arrhythmia drugs and successfully maintain sinus rhythm do those patients do just as well as those who get ablated,” he said in an interview. “I’d love to see a study of heart failure patients maintained in sinus rhythm with drugs compared with those treated with ablation.”
For most patients with heart failure, the coexistence of AF is identified because of AF symptoms, or when asymptomatic AF is found in recordings made by an implanted cardiac device. “I’m more aggressive about addressing asymptomatic AF in my heart failure patients, and I believe the heart failure community is moving rapidly in that direction because of the association between higher AF burden and worse heart failure outcomes,” Dr. Abraham said.
A more cautious view came from another heart failure specialist, Clyde Yancy, MD, professor and chief of cardiology at Northwestern University in Chicago. “It’s pretty evident that in certain patients with heart failure AF ablation might be the right treatment, but is it every HFrEF patient with AF?” he wondered. “It’s nice to have more evidence so we can be more comfortable sending heart failure patients for ablation, but I want to see more information about the risk” from ablation in heart failure patients, “the sustainability of the effect, and the consequences of ablation.”
But the reservations expressed by cardiologists like Dr. Yancy contrasted with the views of colleagues who consider the current evidence much more convincing.
“It seems logical to look harder for AF” in heart failure patients, based on the accumulated evidence from CASTLE-AF and CABANA, said Dr. Ruskin. “I don’t think we can offer advice to heart failure physicians to screen their heart failure patients for AF, but if it’s seen I think we have some useful information on how to address it.”
CASTLE-AF was funded by Biotronik. CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and has received research funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude, and also from several other companies. Dr. Prystowsky as been a consultant to CardioNet and Medtronic, he has an equity interest in Stereotaxis, and he receives fellowship support from Medtronic and St. Jude. Dr. Marrouche has been a consultant to Biosense Webster, Biotronik, Boston Scientific, and St. Jude. He has received research support from Medtronic, and he has had financial relationships with several other companies. Dr. Ruskin has been a consultant to Biosense Webster and Medtronic and several other companies, has an ownership interest in Amgen, Cameron Health, InfoBionic, Newpace, Portola, and Regeneron, and has a fiduciary role in Pharmaco-Kinesis. Dr. Russo and Dr. Yancy had no disclosures. Dr. Brachmann has been a consultant to and has received research funding from Biotronik, Boston Scientific, St. Jude, and several other companies. Dr. Abraham has been a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Results from two recent trials suggest that cardiologists may have a new way to improve outcomes in patients with heart failure with reduced ejection fraction if they also have atrial fibrillation: Cut the patient’s atrial fibrillation burden with catheter ablation.
This seemingly off-target approach to improving survival, avoiding heart failure hospitalizations, and possibly reducing other adverse events first gained attention with results from the CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) randomized trial, first reported in 2017. The study showed in 363 patients that atrial fibrillation (AF) ablation in patients with heart failure with reduced ejection fraction (HFrEF) led to a statistically significant 38% relative reduction in the primary endpoint of mortality or heart failure hospitalization during a median 38 months of follow-up (N Engl J Med. 2018 Feb 1;378[5]:417-27).
This groundbreaking finding then received some degree of confirmation when Douglas L. Packer, MD, reported primary results from CABANA (Catheter Ablation vs Anti-arrhythmic Drug Therapy for Atrial Fibrillation Trial) at the annual scientific sessions of the Heart Rhythm Society. CABANA compared upfront ablation against first-line medical management of AF in 2,203 patients. While the primary endpoint of the cumulative rate of all-cause death, disabling stroke, serious bleeding, or cardiac arrest over a median follow-up of just over 4 years was neutral, with no statistically significant difference between the two treatment arms, a subgroup analysis showed a tantalizing suggestion of benefit in the 337 enrolled patients with a history of congestive heart failure (15% of the total study group).
In this subgroup, treatment with ablation cut the primary endpoint by 39% relative to those treated upfront with medical management, an effect that came close to statistical significance. In addition, Dr. Packer took special note of the per-protocol analysis, which censored out the crossover patients who constituted roughly a fifth of all enrolled patients. In the subgroup analysis using the per-protocol data, ablation was linked with a statistically significant 49% relative reduction in the primary endpoint among patients with a history of heart failure.
The patients for whom there may be the quickest shift to upfront ablation to treat AF based on the CABANA results will be those with heart failure and others with high underlying risk, Dr. Packer predicted at the meeting.
“The CASTLE-AF results were interesting, but in fewer than 400 patients. Now we’ve basically seen the same thing” in CABANA, said Dr. Packer, professor and a cardiac electrophysiologist at the Mayo Clinic in Rochester, Minn.
Notably however, the results Dr. Packer reported on the heart failure subgroup did not include any information on how many of these were patients who had HFrEF or heart failure with preserved ejection fraction and how the apparent benefit from AF ablation affected each of these two heart failure types. In addition, the reported CABANA results did not have an endpoint result that completely matched the mortality and heart failure hospitalization composite endpoint used in CASTLE-AF. The closest endpoint that Dr. Packer reported from CABANA was a composite of mortality and cardiovascular hospitalization that showed, for the entire CABANA cohort, a statistically significant 17% relative reduction with ablation in the intention-to-treat analysis. Dr. Packer gave no data on how this outcome shook out in the subgroup of heart failure patients.
Despite these limitations, in trying to synthesize the CABANA and CASTLE-AF results, several electrophysiologists who heard the results agreed with Dr. Packer that the CABANA results confirmed the CASTLE-AF findings and helped strengthen the case for strongly considering AF ablation as first-line treatment in patients with heart failure.
“It’s clear that sinus rhythm is important in patients with heart failure. CASTLE-AF and now these results; that’s very strong to me,” said Eric N. Prystowsky, MD, a cardiac electrophysiologist with the St. Vincent Medical Group in Indianapolis and designated discussant for CABANA at the meeting.
“It’s confirmatory,” said Nassir F. Marrouche, MD, lead investigator for CASTLE-AF, and professor and director of the electrophysiology laboratory at the University of Utah in Salt Lake City.
The “signal” of benefit from AF ablation in heart failure patients in CABANA “replicates what was seen in CASTLE-AF. The results are highly consistent and very important regarding how to treat patients with AF and heart failure,” said Jeremy N. Ruskin, MD, professor of medicine at Harvard Medical School and director of the cardiac arrhythmia service at Massachusetts General Hospital, both in Boston. “The data strongly suggest that catheter ablation is helpful for restoring and preserving [heart] muscle function,” Dr. Ruskin said in a video interview. He noted that AF occurs in at least about a quarter of heart failure patients.
Other cardiologists at the meeting noted that, on the basis of the CASTLE-AF results alone, they have already become more aggressive about treating AF with ablation in patients with heart failure in routine practice.
“It adds to the armamentarium for treatment of patients with heart failure,” said Johannes Brachmann, MD, professor and chief of cardiology at the Coburg (Germany) Clinic and a senior coinvestigator for CASTLE-AF.
William T. Abraham, MD, a heart failure specialist at The Ohio State University in Columbus, offered a broader perspective on where AF diagnosis, treatment, and ablation currently stand in U.S. heart failure practice.
“There is a very tight link between AF burden and worse outcomes in heart failure, so there is something intuitively appealing about restoring sinus rhythm in heart failure patients. I think most heart failure clinicians believe, like me, that heart failure patients with AF benefit from restoration of normal sinus rhythm. But I don’t believe that the CASTLE-AF results have so far had much impact on practice, in part because it was a relatively small study. The heart failure community is looking for some confirmation,” said Dr. Abraham, professor and director of cardiovascular medicine at Ohio State.
“I think the CABANA results are encouraging, but they came from only 15% of the enrolled patients who also had heart failure. CABANA adds to our knowledge, but I’m not sure it’s definitive for the heart failure population. I’m not sure it tells us if you treat patients with heart failure with anti-arrhythmia drugs and successfully maintain sinus rhythm do those patients do just as well as those who get ablated,” he said in an interview. “I’d love to see a study of heart failure patients maintained in sinus rhythm with drugs compared with those treated with ablation.”
For most patients with heart failure, the coexistence of AF is identified because of AF symptoms, or when asymptomatic AF is found in recordings made by an implanted cardiac device. “I’m more aggressive about addressing asymptomatic AF in my heart failure patients, and I believe the heart failure community is moving rapidly in that direction because of the association between higher AF burden and worse heart failure outcomes,” Dr. Abraham said.
A more cautious view came from another heart failure specialist, Clyde Yancy, MD, professor and chief of cardiology at Northwestern University in Chicago. “It’s pretty evident that in certain patients with heart failure AF ablation might be the right treatment, but is it every HFrEF patient with AF?” he wondered. “It’s nice to have more evidence so we can be more comfortable sending heart failure patients for ablation, but I want to see more information about the risk” from ablation in heart failure patients, “the sustainability of the effect, and the consequences of ablation.”
But the reservations expressed by cardiologists like Dr. Yancy contrasted with the views of colleagues who consider the current evidence much more convincing.
“It seems logical to look harder for AF” in heart failure patients, based on the accumulated evidence from CASTLE-AF and CABANA, said Dr. Ruskin. “I don’t think we can offer advice to heart failure physicians to screen their heart failure patients for AF, but if it’s seen I think we have some useful information on how to address it.”
CASTLE-AF was funded by Biotronik. CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and has received research funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude, and also from several other companies. Dr. Prystowsky as been a consultant to CardioNet and Medtronic, he has an equity interest in Stereotaxis, and he receives fellowship support from Medtronic and St. Jude. Dr. Marrouche has been a consultant to Biosense Webster, Biotronik, Boston Scientific, and St. Jude. He has received research support from Medtronic, and he has had financial relationships with several other companies. Dr. Ruskin has been a consultant to Biosense Webster and Medtronic and several other companies, has an ownership interest in Amgen, Cameron Health, InfoBionic, Newpace, Portola, and Regeneron, and has a fiduciary role in Pharmaco-Kinesis. Dr. Russo and Dr. Yancy had no disclosures. Dr. Brachmann has been a consultant to and has received research funding from Biotronik, Boston Scientific, St. Jude, and several other companies. Dr. Abraham has been a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude.
EXPERT ANALYSIS FROM HEART RHYTHM 2018
Establishing Financial Literacy: What Every Resident Needs to Know
The average debt of graduating medical students today is $190,000, which has increased from $32,000 since 1986 (or the equivalent of $70,000 in 2017 dollars when adjusted for inflation).1 This fact is especially disconcerting given that medical trainees and professionals are not known for being financially sophisticated, and rising levels of high-interest educational debt, increasing years of training, and stagnant or decreasing physician salaries make this status quo untenable.2 Building foundational financial literacy and establishing good financial practices should start during medical school and residency; these basics are a crucial component of long-term job satisfaction and professional resilience.
One prominent physician finance writer advocates that residents should consider the following 5 big-ticket financial steps: acquire life and disability insurance, open a Roth IRA, engage yearly in some type of financial education, and learn about billing and coding in your specialty.3 These exercises, except life insurance for a resident without dependents, are all nonnegotiable, yet alone are insufficient actions to build a solid financial foundation. The purpose of this article is to address additional steps every resident should take, including establishing a workable budget, learning how and why to calculate net worth yearly, determining what percentage of income to save for retirement and basic investing strategies, and managing student loans.
Establish a Workable Budget
Living on a budget is a form of reality acceptance. It may feel impossible to save or budget on a resident salary, but residents earn approximately the median US household income of $59,039, according to the US Census Bureau from September 2017.4,5 There are many tools that can be used to create a budget and to track monthly expenses. However, the simplest way to budget is to pay yourself first with automatic deductions to retirement and savings accounts as well as automated bill payments. Making a habit of reviewing all expenses at the end of every month allows you to see if expenditures remain aligned to your personal values and to reallocate funds for the upcoming month if they are not.
Calculate Net Worth Yearly
Calculating personal net worth may appear to be a discouraging activity to advocate for residents, as many will have a negative 6-figure net worth. The purpose is two-fold: Firstly, to compel you to become well acquainted with your varying types of debt and their respective interest rates. Secondly, similar to taking serial photographs of vitiligo patients to monitor for improvement, it may be the only thing in a long slow slog that indicates beneficial change is occurring because small daily efforts over time yield surprisingly impressive results and the calculation factors in both debt repayment and contributions to all savings vehicles. An example of a simplified method to calculate net worth is demonstrated in the Table.
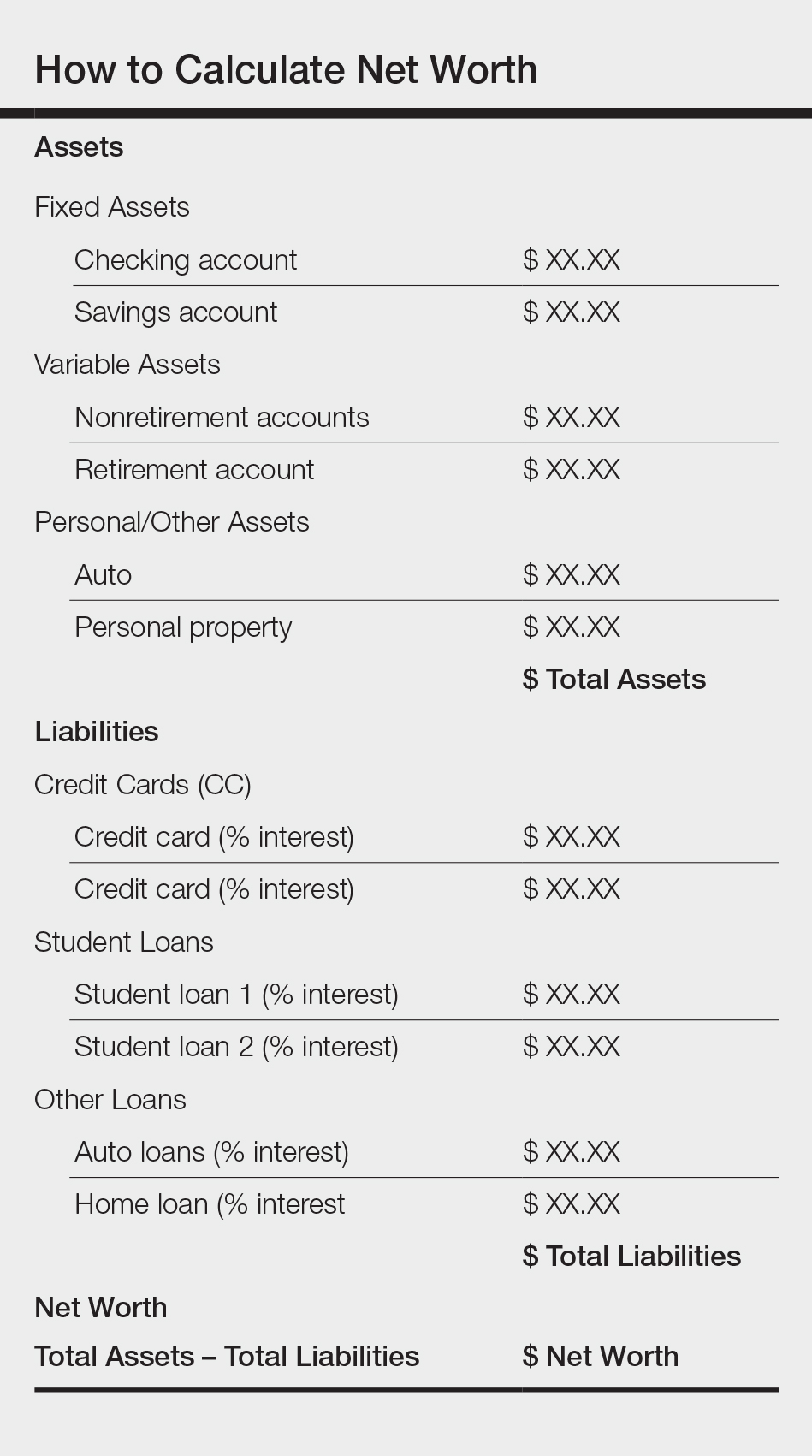
Understand Your Retirement Account and Asset Distribution
Contributing to a retirement account should start day 1 of intern year. A simple rule of thumb to estimate how much money you need to save for retirement is to divide how much you expect to spend on a yearly basis by 4%. For example, if you anticipate spending $80,000 per year during retirement, you will need $2 million in savings (0.04×$2,000,000=$80,000). The amount saved depends on the aggressiveness of your financial goals, but it should be a minimum of 10% to 15% of income during residency and at least 20% afterwards. This strategy allows even a resident to save $25,000 to $50,000 over a 4-year period (depending on employer match), which can accrue additional value in the stock market. One advantage of contributing to an employer-based retirement account, which usually is a 403(b) plan for residents, is that it lowers your tax burden for the year because the savings are tax deferred, in contrast to a Roth IRA, which is funded with posttax dollars. Roth accounts often are recommended for residents because contributions are made during a period in which the physician is presumably in the lowest tax bracket, as account earnings and withdrawals from a Roth IRA after 59.5 years of age, when most physicians expect to be in a higher tax bracket, are tax free. Another advantage of contributing to a 403(b) account is that many residency programs offer a match, which provides for an immediate and substantial return on invested money. Because most residents do not have the cash flow to fully fund both a Roth IRA and 403(b) account (2018 contribution limits are $5500 and $18,500, respectively),6,7 one strategy to utilize both is to save enough to the 403(b) to capture the employer match and place whatever additional savings you can afford into the Roth IRA.
Many different investment strategies exist, and a thorough discussion of them is beyond the scope of this article. Simply speaking, there are 4 major asset classes in which to invest: US stocks, foreign stocks, real estate, and bonds. The variation of recommended contributions to each asset is limitless, and every resident should spend time considering the best strategy for his/her goals. One example of a simple effective investing strategy is to utilize index funds, which track the market and therefore rise with the market, as they tend to go up (at least historically, though temporary setbacks occur).8 If you are investing in funds available through your employer-sponsored retirement account, examine the funds you are automatically assigned and their associated fee and expense ratio (ER) disclosures, which are typically available through the online portal. A general rule of thumb is that good funds have ERs of less than 0.5% and bad funds have ERs greater than 1% and additional associated fees. The funds available to you also can be researched on the Morningstar, Inc, website (www.morningstar.com). My institution (University of Texas Dell Medical School, Austin) offers a variety of options with ERs varying from 0.02% to 1.02%. The difference in the costs associated with these funds over decades is notable, and it pays (literally) to understand the nuances. Reallocation of funds usually can be done easily online and are effective within 24 hours.
Student Loans
Although many residents agonize most over management of student loans, the simple solution is do not defer them. Refinancing federal loans with a private company versus enrolling in an income-based repayment program depends on many factors, including whether you have a high-earning spouse, how many dependents you have, and whether you expect to stay in academia and will be eligible for Public Service Loan Forgiveness, among others. Look critically at your situation and likely future employment to decide what is most appropriate for you; doing so can save you thousands of dollars in interest over the course of your residency.
Final Thoughts
To the detriment of residents and the attending physicians they will become, discussing financial matters in medicine remains rare, perhaps because it seems to shift what should be the singular focus of our profession, namely to help the sick, to thoughts of personal gain, which is a false dichotomy. Unquestionably, the physician’s role that supersedes all others is to care for the patient and to honor the oath we all took: “Into whatsoever houses I enter, I will enter to help the sick.” But this commitment should not preclude the mastery of financial concepts that promote personal and professional health and well-being. After all, the joy in work is maximized when you are not enslaved to it.
Your reading assignment, paper revision, or presentation can wait. Making time to understand your current financial health, to build your own financial literacy, and to plan for your future is an important component of a long satisfying career. Start now.
- Grischkan J, George BP, Chaiyachati K, et al. Distribution of medical education debt by specialty, 2010-2016. JAMA Intern Med. 2017;177:1532-1535.
- Ahmad FA, White AJ, Hiller KM, et al. An assessment of residents’ and fellows’ personal finance literacy: an unmet medical education need. Int J Med Educ. 2017;8:192-204.
- The five big money items you should do as a resident. The White Coat Investor website. https://www.whitecoatinvestor.com/the-five-big-money-items-you-should-do-as-a-resident. Published July 7, 2011. Accessed May 14, 2018.
- Income, poverty and health insurance coverage in the United States: 2016. United States Census Bureau website. https://www.census.gov/newsroom/press-releases/2017/income-povery.html. Published September 12, 2017. Accessed May 14, 2018.
- Levy S. Residents salary and debt report 2017. Medscape website. https://www.medscape.com/slideshow/residents-salary-and-debt-report-2017-6008931. Published July 26, 2017. Accessed May 22, 2018.
- Retirement topics - IRA contribution limits. Internal Revenue Service website. https://www.irs.gov/retirement-plans/plan-participant-employee/retirement-topics-ira-contribution-limits. Updated October 20, 2017. Accessed May 22, 2018.
- Retirement plan FAQs regarding 403(b) tax-sheltered annuity plans. Internal Revenue Service website. https://www.irs.gov/retirement-plans/retirement-plans-faqs-regarding-403b-tax-sheltered-annuity-plans#conts. Updated November 14, 2017. Accessed May 22, 2018.
- Collins JL. Stock series. JLCollins website. http://jlcollinsnh.com/stock-series/. Accessed May 14, 2018.
The average debt of graduating medical students today is $190,000, which has increased from $32,000 since 1986 (or the equivalent of $70,000 in 2017 dollars when adjusted for inflation).1 This fact is especially disconcerting given that medical trainees and professionals are not known for being financially sophisticated, and rising levels of high-interest educational debt, increasing years of training, and stagnant or decreasing physician salaries make this status quo untenable.2 Building foundational financial literacy and establishing good financial practices should start during medical school and residency; these basics are a crucial component of long-term job satisfaction and professional resilience.
One prominent physician finance writer advocates that residents should consider the following 5 big-ticket financial steps: acquire life and disability insurance, open a Roth IRA, engage yearly in some type of financial education, and learn about billing and coding in your specialty.3 These exercises, except life insurance for a resident without dependents, are all nonnegotiable, yet alone are insufficient actions to build a solid financial foundation. The purpose of this article is to address additional steps every resident should take, including establishing a workable budget, learning how and why to calculate net worth yearly, determining what percentage of income to save for retirement and basic investing strategies, and managing student loans.
Establish a Workable Budget
Living on a budget is a form of reality acceptance. It may feel impossible to save or budget on a resident salary, but residents earn approximately the median US household income of $59,039, according to the US Census Bureau from September 2017.4,5 There are many tools that can be used to create a budget and to track monthly expenses. However, the simplest way to budget is to pay yourself first with automatic deductions to retirement and savings accounts as well as automated bill payments. Making a habit of reviewing all expenses at the end of every month allows you to see if expenditures remain aligned to your personal values and to reallocate funds for the upcoming month if they are not.
Calculate Net Worth Yearly
Calculating personal net worth may appear to be a discouraging activity to advocate for residents, as many will have a negative 6-figure net worth. The purpose is two-fold: Firstly, to compel you to become well acquainted with your varying types of debt and their respective interest rates. Secondly, similar to taking serial photographs of vitiligo patients to monitor for improvement, it may be the only thing in a long slow slog that indicates beneficial change is occurring because small daily efforts over time yield surprisingly impressive results and the calculation factors in both debt repayment and contributions to all savings vehicles. An example of a simplified method to calculate net worth is demonstrated in the Table.
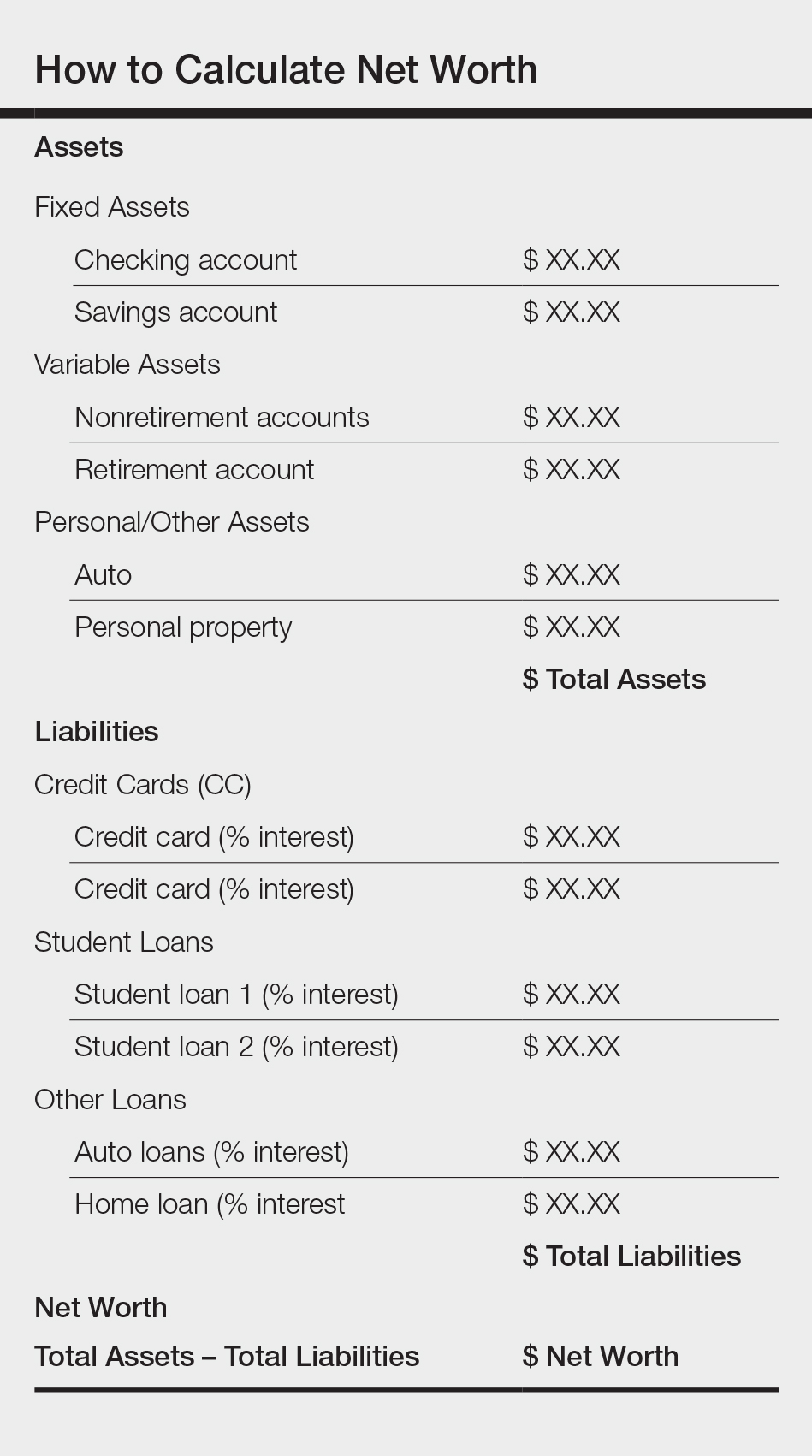
Understand Your Retirement Account and Asset Distribution
Contributing to a retirement account should start day 1 of intern year. A simple rule of thumb to estimate how much money you need to save for retirement is to divide how much you expect to spend on a yearly basis by 4%. For example, if you anticipate spending $80,000 per year during retirement, you will need $2 million in savings (0.04×$2,000,000=$80,000). The amount saved depends on the aggressiveness of your financial goals, but it should be a minimum of 10% to 15% of income during residency and at least 20% afterwards. This strategy allows even a resident to save $25,000 to $50,000 over a 4-year period (depending on employer match), which can accrue additional value in the stock market. One advantage of contributing to an employer-based retirement account, which usually is a 403(b) plan for residents, is that it lowers your tax burden for the year because the savings are tax deferred, in contrast to a Roth IRA, which is funded with posttax dollars. Roth accounts often are recommended for residents because contributions are made during a period in which the physician is presumably in the lowest tax bracket, as account earnings and withdrawals from a Roth IRA after 59.5 years of age, when most physicians expect to be in a higher tax bracket, are tax free. Another advantage of contributing to a 403(b) account is that many residency programs offer a match, which provides for an immediate and substantial return on invested money. Because most residents do not have the cash flow to fully fund both a Roth IRA and 403(b) account (2018 contribution limits are $5500 and $18,500, respectively),6,7 one strategy to utilize both is to save enough to the 403(b) to capture the employer match and place whatever additional savings you can afford into the Roth IRA.
Many different investment strategies exist, and a thorough discussion of them is beyond the scope of this article. Simply speaking, there are 4 major asset classes in which to invest: US stocks, foreign stocks, real estate, and bonds. The variation of recommended contributions to each asset is limitless, and every resident should spend time considering the best strategy for his/her goals. One example of a simple effective investing strategy is to utilize index funds, which track the market and therefore rise with the market, as they tend to go up (at least historically, though temporary setbacks occur).8 If you are investing in funds available through your employer-sponsored retirement account, examine the funds you are automatically assigned and their associated fee and expense ratio (ER) disclosures, which are typically available through the online portal. A general rule of thumb is that good funds have ERs of less than 0.5% and bad funds have ERs greater than 1% and additional associated fees. The funds available to you also can be researched on the Morningstar, Inc, website (www.morningstar.com). My institution (University of Texas Dell Medical School, Austin) offers a variety of options with ERs varying from 0.02% to 1.02%. The difference in the costs associated with these funds over decades is notable, and it pays (literally) to understand the nuances. Reallocation of funds usually can be done easily online and are effective within 24 hours.
Student Loans
Although many residents agonize most over management of student loans, the simple solution is do not defer them. Refinancing federal loans with a private company versus enrolling in an income-based repayment program depends on many factors, including whether you have a high-earning spouse, how many dependents you have, and whether you expect to stay in academia and will be eligible for Public Service Loan Forgiveness, among others. Look critically at your situation and likely future employment to decide what is most appropriate for you; doing so can save you thousands of dollars in interest over the course of your residency.
Final Thoughts
To the detriment of residents and the attending physicians they will become, discussing financial matters in medicine remains rare, perhaps because it seems to shift what should be the singular focus of our profession, namely to help the sick, to thoughts of personal gain, which is a false dichotomy. Unquestionably, the physician’s role that supersedes all others is to care for the patient and to honor the oath we all took: “Into whatsoever houses I enter, I will enter to help the sick.” But this commitment should not preclude the mastery of financial concepts that promote personal and professional health and well-being. After all, the joy in work is maximized when you are not enslaved to it.
Your reading assignment, paper revision, or presentation can wait. Making time to understand your current financial health, to build your own financial literacy, and to plan for your future is an important component of a long satisfying career. Start now.
The average debt of graduating medical students today is $190,000, which has increased from $32,000 since 1986 (or the equivalent of $70,000 in 2017 dollars when adjusted for inflation).1 This fact is especially disconcerting given that medical trainees and professionals are not known for being financially sophisticated, and rising levels of high-interest educational debt, increasing years of training, and stagnant or decreasing physician salaries make this status quo untenable.2 Building foundational financial literacy and establishing good financial practices should start during medical school and residency; these basics are a crucial component of long-term job satisfaction and professional resilience.
One prominent physician finance writer advocates that residents should consider the following 5 big-ticket financial steps: acquire life and disability insurance, open a Roth IRA, engage yearly in some type of financial education, and learn about billing and coding in your specialty.3 These exercises, except life insurance for a resident without dependents, are all nonnegotiable, yet alone are insufficient actions to build a solid financial foundation. The purpose of this article is to address additional steps every resident should take, including establishing a workable budget, learning how and why to calculate net worth yearly, determining what percentage of income to save for retirement and basic investing strategies, and managing student loans.
Establish a Workable Budget
Living on a budget is a form of reality acceptance. It may feel impossible to save or budget on a resident salary, but residents earn approximately the median US household income of $59,039, according to the US Census Bureau from September 2017.4,5 There are many tools that can be used to create a budget and to track monthly expenses. However, the simplest way to budget is to pay yourself first with automatic deductions to retirement and savings accounts as well as automated bill payments. Making a habit of reviewing all expenses at the end of every month allows you to see if expenditures remain aligned to your personal values and to reallocate funds for the upcoming month if they are not.
Calculate Net Worth Yearly
Calculating personal net worth may appear to be a discouraging activity to advocate for residents, as many will have a negative 6-figure net worth. The purpose is two-fold: Firstly, to compel you to become well acquainted with your varying types of debt and their respective interest rates. Secondly, similar to taking serial photographs of vitiligo patients to monitor for improvement, it may be the only thing in a long slow slog that indicates beneficial change is occurring because small daily efforts over time yield surprisingly impressive results and the calculation factors in both debt repayment and contributions to all savings vehicles. An example of a simplified method to calculate net worth is demonstrated in the Table.
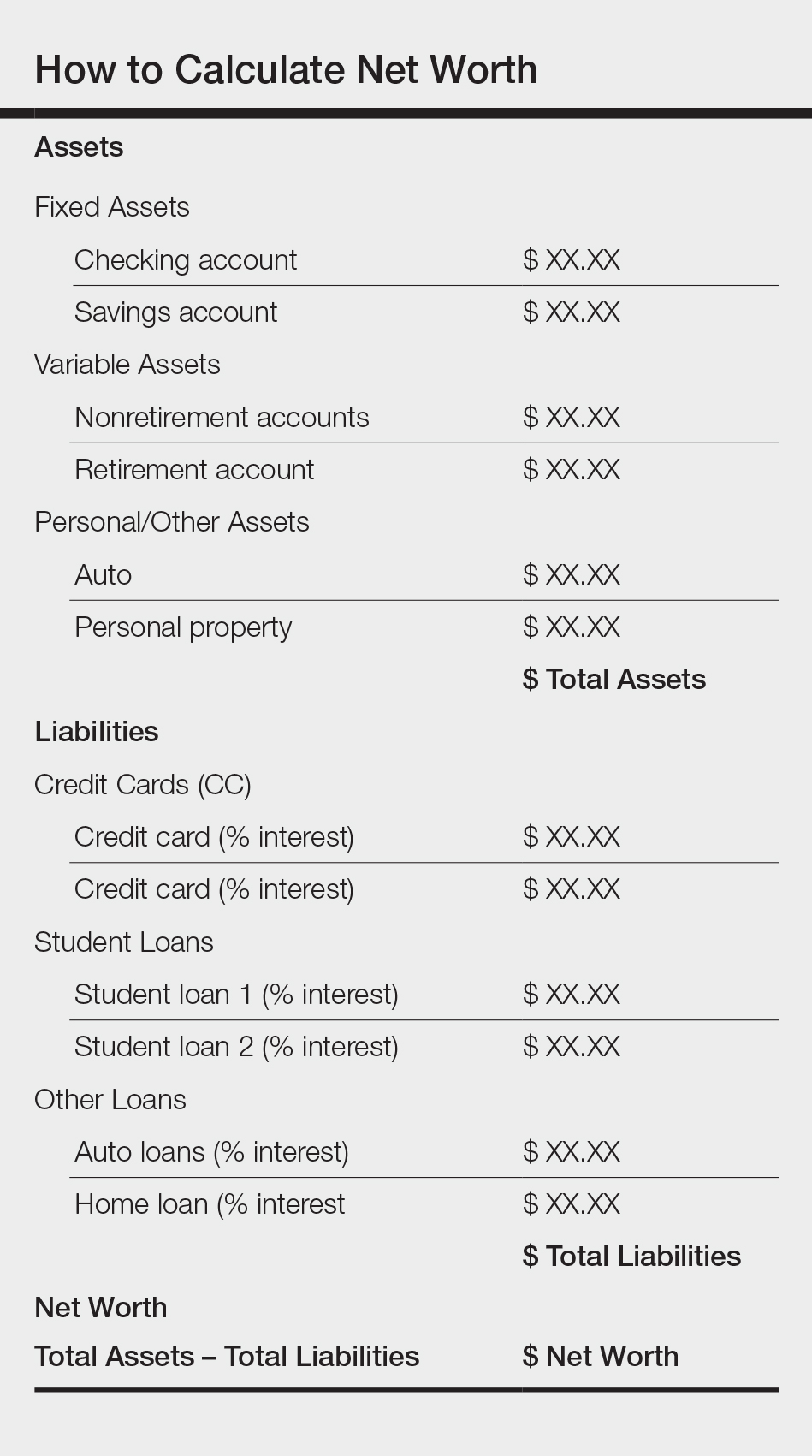
Understand Your Retirement Account and Asset Distribution
Contributing to a retirement account should start day 1 of intern year. A simple rule of thumb to estimate how much money you need to save for retirement is to divide how much you expect to spend on a yearly basis by 4%. For example, if you anticipate spending $80,000 per year during retirement, you will need $2 million in savings (0.04×$2,000,000=$80,000). The amount saved depends on the aggressiveness of your financial goals, but it should be a minimum of 10% to 15% of income during residency and at least 20% afterwards. This strategy allows even a resident to save $25,000 to $50,000 over a 4-year period (depending on employer match), which can accrue additional value in the stock market. One advantage of contributing to an employer-based retirement account, which usually is a 403(b) plan for residents, is that it lowers your tax burden for the year because the savings are tax deferred, in contrast to a Roth IRA, which is funded with posttax dollars. Roth accounts often are recommended for residents because contributions are made during a period in which the physician is presumably in the lowest tax bracket, as account earnings and withdrawals from a Roth IRA after 59.5 years of age, when most physicians expect to be in a higher tax bracket, are tax free. Another advantage of contributing to a 403(b) account is that many residency programs offer a match, which provides for an immediate and substantial return on invested money. Because most residents do not have the cash flow to fully fund both a Roth IRA and 403(b) account (2018 contribution limits are $5500 and $18,500, respectively),6,7 one strategy to utilize both is to save enough to the 403(b) to capture the employer match and place whatever additional savings you can afford into the Roth IRA.
Many different investment strategies exist, and a thorough discussion of them is beyond the scope of this article. Simply speaking, there are 4 major asset classes in which to invest: US stocks, foreign stocks, real estate, and bonds. The variation of recommended contributions to each asset is limitless, and every resident should spend time considering the best strategy for his/her goals. One example of a simple effective investing strategy is to utilize index funds, which track the market and therefore rise with the market, as they tend to go up (at least historically, though temporary setbacks occur).8 If you are investing in funds available through your employer-sponsored retirement account, examine the funds you are automatically assigned and their associated fee and expense ratio (ER) disclosures, which are typically available through the online portal. A general rule of thumb is that good funds have ERs of less than 0.5% and bad funds have ERs greater than 1% and additional associated fees. The funds available to you also can be researched on the Morningstar, Inc, website (www.morningstar.com). My institution (University of Texas Dell Medical School, Austin) offers a variety of options with ERs varying from 0.02% to 1.02%. The difference in the costs associated with these funds over decades is notable, and it pays (literally) to understand the nuances. Reallocation of funds usually can be done easily online and are effective within 24 hours.
Student Loans
Although many residents agonize most over management of student loans, the simple solution is do not defer them. Refinancing federal loans with a private company versus enrolling in an income-based repayment program depends on many factors, including whether you have a high-earning spouse, how many dependents you have, and whether you expect to stay in academia and will be eligible for Public Service Loan Forgiveness, among others. Look critically at your situation and likely future employment to decide what is most appropriate for you; doing so can save you thousands of dollars in interest over the course of your residency.
Final Thoughts
To the detriment of residents and the attending physicians they will become, discussing financial matters in medicine remains rare, perhaps because it seems to shift what should be the singular focus of our profession, namely to help the sick, to thoughts of personal gain, which is a false dichotomy. Unquestionably, the physician’s role that supersedes all others is to care for the patient and to honor the oath we all took: “Into whatsoever houses I enter, I will enter to help the sick.” But this commitment should not preclude the mastery of financial concepts that promote personal and professional health and well-being. After all, the joy in work is maximized when you are not enslaved to it.
Your reading assignment, paper revision, or presentation can wait. Making time to understand your current financial health, to build your own financial literacy, and to plan for your future is an important component of a long satisfying career. Start now.
- Grischkan J, George BP, Chaiyachati K, et al. Distribution of medical education debt by specialty, 2010-2016. JAMA Intern Med. 2017;177:1532-1535.
- Ahmad FA, White AJ, Hiller KM, et al. An assessment of residents’ and fellows’ personal finance literacy: an unmet medical education need. Int J Med Educ. 2017;8:192-204.
- The five big money items you should do as a resident. The White Coat Investor website. https://www.whitecoatinvestor.com/the-five-big-money-items-you-should-do-as-a-resident. Published July 7, 2011. Accessed May 14, 2018.
- Income, poverty and health insurance coverage in the United States: 2016. United States Census Bureau website. https://www.census.gov/newsroom/press-releases/2017/income-povery.html. Published September 12, 2017. Accessed May 14, 2018.
- Levy S. Residents salary and debt report 2017. Medscape website. https://www.medscape.com/slideshow/residents-salary-and-debt-report-2017-6008931. Published July 26, 2017. Accessed May 22, 2018.
- Retirement topics - IRA contribution limits. Internal Revenue Service website. https://www.irs.gov/retirement-plans/plan-participant-employee/retirement-topics-ira-contribution-limits. Updated October 20, 2017. Accessed May 22, 2018.
- Retirement plan FAQs regarding 403(b) tax-sheltered annuity plans. Internal Revenue Service website. https://www.irs.gov/retirement-plans/retirement-plans-faqs-regarding-403b-tax-sheltered-annuity-plans#conts. Updated November 14, 2017. Accessed May 22, 2018.
- Collins JL. Stock series. JLCollins website. http://jlcollinsnh.com/stock-series/. Accessed May 14, 2018.
- Grischkan J, George BP, Chaiyachati K, et al. Distribution of medical education debt by specialty, 2010-2016. JAMA Intern Med. 2017;177:1532-1535.
- Ahmad FA, White AJ, Hiller KM, et al. An assessment of residents’ and fellows’ personal finance literacy: an unmet medical education need. Int J Med Educ. 2017;8:192-204.
- The five big money items you should do as a resident. The White Coat Investor website. https://www.whitecoatinvestor.com/the-five-big-money-items-you-should-do-as-a-resident. Published July 7, 2011. Accessed May 14, 2018.
- Income, poverty and health insurance coverage in the United States: 2016. United States Census Bureau website. https://www.census.gov/newsroom/press-releases/2017/income-povery.html. Published September 12, 2017. Accessed May 14, 2018.
- Levy S. Residents salary and debt report 2017. Medscape website. https://www.medscape.com/slideshow/residents-salary-and-debt-report-2017-6008931. Published July 26, 2017. Accessed May 22, 2018.
- Retirement topics - IRA contribution limits. Internal Revenue Service website. https://www.irs.gov/retirement-plans/plan-participant-employee/retirement-topics-ira-contribution-limits. Updated October 20, 2017. Accessed May 22, 2018.
- Retirement plan FAQs regarding 403(b) tax-sheltered annuity plans. Internal Revenue Service website. https://www.irs.gov/retirement-plans/retirement-plans-faqs-regarding-403b-tax-sheltered-annuity-plans#conts. Updated November 14, 2017. Accessed May 22, 2018.
- Collins JL. Stock series. JLCollins website. http://jlcollinsnh.com/stock-series/. Accessed May 14, 2018.
Participation in Work and Sport Following Reverse and Total Shoulder Arthroplasty
ABSTRACT
Both anatomical total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA) are routinely performed for patients who desire to continuously work or participate in sports. This study analyzes and compares the ability of patients to work and partake in sports following shoulder arthroplasty based on responses to clinical outcome surveys.
A retrospective review of the shoulder surgery repository was performed for all patients treated with TSA and RSA and who completed questions 9 and 10 on the activity patient self-evaluation portion of the American Shoulder and Elbow Surgeons (ASES) Assessment Form. Patients with a minimum of 1-year follow-up were included if a sport or work was identified. The analysis included 162 patients with TSA and 114 patients with RSA. Comparisons were made between TSA and RSA in terms of the specific ASES scores (rated 0-3) reported for ability to work and participate in sports and total ASES scores, and scores based on specific sports or line of work reported. Comparisons were also made between sports predominantly using shoulder function and those that do not.
TSA patients had a 27% higher ability to participate in sports (average specific ASES score: 2.5 vs 1.9, P < .001) than RSA patients and presented significantly higher scores for swimming and golf. Compared with RSA patients, TSA patients demonstrated more ability to participate in sports requiring shoulder function without difficulty, as 63% reported maximal scores (P = .003). Total shoulder arthroplasty patients also demonstrated a 21% higher ability to work than RSA patients (average specific ASES scores: 2.6 vs 2.1, P < .001), yielding significantly higher scores for housework and gardening.
Both TSA and RSA allow for participation in work and sports, with TSA patients reporting better overall ability to participate. For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
End-stage shoulder arthritis has been successfully treated with anatomical total shoulder arthroplasty (TSA) with high rates of functional recovery.1 With the introduction of reverse shoulder arthroplasty (RSA), indications for TSA have expanded.2-6 With continuing expansion of surgical indications, a more diverse and potentially active patient population is now being treated. As patients exhibit increased awareness of health and wellness, they demonstrate significant interest in understanding their ability to work or participate in sports after surgery.7 Patients no longer focus on pain relief as the only goal of surgery. A recent study of patients aged 65 years and undergoing shoulder arthroplasty revealed that 64% of the patients listed the ability to return to sports as the main reason for undergoing surgery,8 highlighting the significance of sports play in a patient’s life. Prior to surgery, shoulder pathologies lead to impairment in function, range of motion, and pain,9 hindering a patient to participate in both work and sports. With the intervention yielding improvement to these areas6,9-13 with increased patient satisfaction,10,13 accurately tailoring patient expectations for participation in sports and work postoperatively becomes increasingly important.
Continue to: Although several studies...
Although several studies have demonstrated the ability of patients to return to sports following TSA,8,14-18 a limited number of studies discuss the return to sports following RSA.19-21 Despite known postoperative improvements, no clear consensus is reached as to which specific sports patients can return to and at what level of participation is to be expected. Surveyed members of the American Shoulder and Elbow Surgeons (ASES) universally favored full return to sports, except for contact sports for TSA patients, whereas other surgeons are more conservative to allow RSA patients to return to activities.22 To our knowledge, no other study has investigated the ability to work following RSA. Furthermore, no other study has used patient-reported outcomes to compare the quality of participation in sports or work between TSA and RSA patients following surgery. This study reports the ability of patients treated with TSA and RSA to work and participate in sports based on clinical outcome surveys. We hypothesize that TSA patients will be allowed to work and participate in sports with less difficulty than RSA patients.
MATERIALS AND METHODS
Following Institutional Review Board approval, a retrospective review was performed on all patients treated with TSA or RSA and who completed questions 9 and/or 10 (by score and named usual sport and/or work) on the activity patient self-evaluation portion of the ASES23 Assessment Form between 2007 to 2014; queries were made via the Shoulder Outcomes Repository. A minimum of 12-month follow-up was required, as functional recovery has been shown to plateau or nearly plateau by 12 months.11 Patients were excluded if <12 months of follow-up was available, if they failed to provide a written answer for questions 9 or 10 on the activity patient self-evaluation portion of the ASES Assessment Form, or if they required a revision shoulder arthroplasty. A single fellowship-trained shoulder and elbow surgeon performed all procedures via the same deltopectoral approach and prescribed identical postoperative rehabilitation for both TSA and RSA patients. The database query yielded 162 TSA and 114 RSA patients, for a total of 276 patients eligible for the study.
For all patients, the most recent follow-up ASES score was used. Comparisons were made between TSA and RSA for total ASES scores and response groups for usual sport (ASES question 9) and usual work (ASES question 10). The ASES questionnaire provides patients with 4 choices for each question based on the ability to perform each activity: 0, unable to do; 1, very difficult; 2, somewhat difficult; and 3, not difficult. The questionnaire also allows the patients to identify their usual work and sports. If patients noted >1 sport or work activity, they were included within multiple subgroups. Patients were further compared by age and gender.
Work was subdivided to include retired, housework, desk jobs, prolonged standing, gardening/yard work, jobs requiring lifting, carpenter/construction, cook/food preparation, and creative jobs (Table 1).
Statistical analysis was performed with SPSS Version 21 (IBM). Unpaired t tests were used to determine differences between groups. A P-value of <.05 was deemed significant.
Continue to: A total of 276 patients...
RESULTS
A total of 276 patients that met the inclusion criteria were eligible for the study, with 162 having undergone TSA and 114 with RSA. Overall average follow-up totaled 29 months (range, 12-91 months). RSA patients (average age, 75 years old; range, 46-88 years) were significantly older than TSA patients (average age, 69 years old; range, 32-89 years; P = .001). Significantly more women were treated with TSA (52% TSA; 48% RSA; P = .012), whereas significantly more men were treated with TSA (67% TSA; 33% RSA, P = .012). Total ASES scores were significantly higher for TSA patients than RSA patients in work (P = .012) (Table 4) but not in sports (P = .063) (Table 5) categories.
SPORTS
A total of 186 patients, comprising of 71 RSA and 115 TSA individuals, responded to question 9 of the ASES questionnaire (Table 5). Among usually reported sports, golf (25%), swimming (17%), and walking (18%) were the most commonly cited. RSA patients indicating a sport were significantly older than TSA patients (74 years vs 69 years, P < .001). TSA patients reported a 27% higher difference in overall ability to participate in sports, with an average ASES sport-specific score of 2.5 compared with the 1.9 for RSA patients (P < .001).
Among specific sports, TSA patients reported significantly higher scores for swimming (2.6 vs 1.8, P = .007) and golf (2.5 vs 1.8, P = .050). However, no significant differences were observed for walking, gym exercises, and racquet sports (Table 5). Among sport subsets, RSA patients were significantly older for golf (77 years vs 70 years, P = .006) and bowling (80 years vs 68 years, P = .005). Five TSA patients reported biking as their sport, whereas no RSA patient reported such activity. Within each subset of sports, no significant differences were noted in average ASES total scores.
TSA patients demonstrated a more significant ability to perform usual sports that involve shoulder function without difficulty (score of 3). In shoulder dominant sports, a total of 63% of TSA patients reported a score of 3 compared with the 39% of RSA patients (P = .003). RSA patients more often reported an inability to perform shoulder specific sports, as proven by 20% of RSA patients reporting a score of 0 compared with 4% of TSA patients (P < .001) (Table 6).
WORK
A total of 265 patients, including 106 RSA and 159 TSA patients, responded to question 10 of the ASES questionnaire. Among usually reported work, retirement (43%), housework (27%), and desk jobs (18%) were the most commonly cited. RSA patients denoting a work were significantly older than TSA patients (75 years vs 69 years, P < .001). Patients with TSA presented a 21% higher difference in the overall ability to work, featuring an average ASES work-specific score of 2.6 compared with the 2.1 for RSA patients (P < .001) (Table 4).
Continue to: Among specific work activities...
Among specific work activities, TSA patients reported significantly higher scores for housework (2.7 vs 2; 34% difference; P = .001) and gardening (2.8 vs 1.7; 65% difference; P = .009) in comparison with RSA patients. However, no significant differences were observed for other work activities, including retirement, desk job, prolonged standing, creative jobs, lifting jobs, or construction (Table 4). Among the work subgroups, RSA patients were older than TSA patients for the retired group (77 years vs 72 years; P < .001) and gardening (81 years vs 68 years; P = .002).
DISCUSSION
The ability to participate in sports and work is a common goal for shoulder arthroplasty patients. However, the ability at which participation occurs has not been examined. This study illustrates not only the ability to engage in usual work or sport, but provides some insights into patient-reported quality of participation. Overall, TSA patients featured 27% higher sport-specific ASES scores and 21% higher work-specific ASES scores than RSA patients, confirming our hypothesis that TSA patients can participate in work or sports with less difficulty in general. This study is the first to stratify the difficulty of participating in sports in general and in specific sports identified by patients. Although statistical analysis was performed for individual sports and work reported, the use of small cohorts possibly affected the ability to detect significant differences. The data presented in this study can thus be used as descriptive evidence of what a patient may expect to be able to do following surgery, helping to define patient expectations prior to electing to undergo shoulder arthroplasty.
Among specific sports identified by patients, a few significant differences were observed between RSA and TSA patients. However, ASES-specific scores almost universally favored TSA. Of the sport subgroups, swimming and golf showed significant differences. For swimming, this difference was fairly significant, as TSA patients demonstrated a 49% higher score than their RSA counterparts, but without differences in age or total ASES score (Table 5). Alteration in shoulder mechanics after RSA may be used to explain the difficulty in returning to swimming, as additional time may be needed to adapt to new mechanics.24 McCarty and colleagues8 demonstrated that 90% of patients following TSA fully resumed participation in swimming within 6 months of surgery, and further stated that repetitive motions of swimming caused no effects on short-term outcomes. No similar analysis of swimming has been reported for RSA patients. Based upon our findings, the average RSA patient can experience some difficulties when returning to swimming after surgery (average specific ASES score, 1.8).
Jensen and Rockwood16 were among the first to demonstrate successful return to golf of 24 patients who had undergone either TSA or hemiarthroplasty (HA), showing a 5-stroke improvement in their game. A recent study investigating patient-reported activity in patients aged 75 years and undergoing RSA showed that 23% of patients returned to high-level activity sports, such as golf, motorcycle riding, or free weights.19 All patients who participated in golf before surgery resumed playing following surgery; however, golf was listed among the top activities that patients wanted to participate in but could not for any reason.19 Our data suggest that golfers with TSA will face less difficulty returning to sports compared with their RSA counterparts (average specific ASES score, 2.5 vs 1.8, who might find golf somewhat difficult.
Although no study has provided a clear consensus as to which activities are safe to perform following shoulder arthroplasty, experts have suggested that activities that impart high loads on the glenohumeral joint should be avoided.15 Among TSA patients, McCarty and colleagues8 reported high rates of return for swimmers, golfers, and tennis players; however, relatively low rates were reported for weight lifting, bowling, and softball (20%). Within our study group, golf, swimming, and walking were listed among the most popular sports performed. Although weight lifting, bowling, and softball were less commonly identified as usual sports within our study, patients treated with TSA demonstrated more ease to participate than RSA patients. This result was observed with ASES-specific scores noted for weight lifting and gym exercises (TSA, 2.5; RSA, 2.3) and team sports, such as softball (TSA, 2; RSA, 1.3). However, for bowling, RSA patients showed a trend toward more ability (RSA, 2.7; TSA, 1.7).
Continue to: Among specific work activities...
Successful return to sports that involve shoulder function, such as golf and swimming, has been demonstrated for TSA.8,14,16,17 However, studies have reported that return to these sports can be difficult for RSA patients.20 Fink and colleagues19 reported that following RSA, 48.7% of patients returned to moderate-intensity sports, such as swimming and golf. Consistent with these findings, in our study, TSA patients demonstrated a significantly higher ability to participate in their usual sports without difficulty (ASES-specific score of 3). This observation may relate to lower ultimate achievements in range of motion and strength in patients treated with RSA, when compared with TSA patients,24,25 and the generalized practice of utilizing RSA for lower-demand patients (RSA patients in this study were older).
Overall, participation in work was 21% easier for TSA patients than RSA patients. Although the majority of our patients cited retirement as their primary work, which is consistent with what one would expect with the mean age of this study’s cohorts (RSA, 75 years; TSA, 69 years), housework and gardening were the only specifically identified forms of work that demonstrated significant differences between RSA and TSA patients. A few reports in the literature documented the ability to return to work after shoulder arthroplasty. In a recent report on 13 workers’ compensation patients treated with TSA, only 1 patient returned to the same job, and 54% did not return to work.26 In a study comparing 14 workers’ compensation to a matched group of controls with all members treated with RSA, the workers’ compensation group yielded a lower return-to-work rate (14.2%) than the controls (41.7%).27 In a large study of 154 TSA patients, 14% returned to work, but specific jobs were not described in this analysis.14
The results of this study suggest that more TSA patients successfully participate in low-demand activities, such as gardening or housework. Zarkadas and colleagues18 reported that 65% of TSA and 47% of HA patients successfully returned to gardening compared with 42% of RSA patients observed in a continuation study.20 This study showed that TSA patients yielded a 65% difference in ability to work in gardening and 34% difference in ability to perform housework compared with RSA patients. Based on these findings, TSA patients can expect to experience no difficulty in performing housework or gardening, whereas RSA patients may find these tasks difficult to a certain degree.
The main limitation of this study is the reporting bias that results from survey-based studies. Possibly, more people engage in specific sports or work than what were reported. This type of study also features an inherent selection bias, as patients with highly and physically demanding jobs or usual sports were less likely to have been offered either TSA or RSA. An additional important limitation is the relatively small cohorts within sport and work subgroups; the small cohorts probably underpowered the statistical results of this study and made these findings valuable mostly as descriptive observations. Larger studies focusing on each subgroup will further clarify the ability of shoulder arthroplasty to perform individual sports or work. Further studies evaluating preoperative to postoperative sports- and work-specific ASES scores would provide notable insights into the functional improvements observed within each sport or work following surgery. The relatively large study population of 276 patients strengthened the findings, which relate to the overall ability to participate in sports and work for TSA and RSA patients. Finally, the evaluated TSA and RSA patients possibly represent different groups (significant difference in age and gender) with different underlying pathologies and potentially different demands and expectations. However, comparisons among these groups of patients bear importance in defining patient expectations related to surgery. Still, the ability to participate in sport or work possibly relates more to the limitations of the implant used than patient pathology. This possibility warrants further investigation.
CONCLUSION
Both TSA and RSA allow for participation in work and sports, with TSA patients reporting easier overall ability to participate. For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
1. Fehringer EV, Kopjar B, Boorman RS, Churchill RS, Smith KL, Matsen FA 3rd. Characterizing the functional improvement after total shoulder arthroplasty for osteoarthritis. J Bone Joint Surg Am. 2002;84-A(8):1349-1353.
2. Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013;95(22):2050-2055. doi:10.2106/JBJS.L.01637.
3. Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742-1747.
4. Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89(2):189-195.
5. Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(11):1478-1483. doi:10.1016/j.jse.2011.11.004.
6. Sebastia-Forcada E, Cebrian-Gomez R, Lizaur-Utrilla A, Gil-Guillen V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23(10):1419-1426. doi:10.1016/j.jse.2014.06.035.
7. Henn RF 3rd, Ghomrawi H, Rutledge JR, Mazumdar M, Mancuso CA, Marx RG. Preoperative patient expectations of total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93(22):2110-2115. doi:10.2106/JBJS.J.01114.
8. McCarty EC, Marx RG, Maerz D, Altchek D, Warren RF. Sports participation after shoulder replacement surgery. Am J Sports Med. 2008;36(8):1577-1581. doi:10.1177/0363546508317126.
9. Puskas B, Harreld K, Clark R, Downes K, Virani NA, Frankle M. Isometric strength, range of motion, and impairment before and after total and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(7):869-876. doi:10.1016/j.jse.2012.09.004.
10. Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471-479.
11. Levy JC, Everding NG, Gil CC Jr., Stephens S, Giveans MR. Speed of recovery after shoulder arthroplasty: a comparison of reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(12):1872-1881. doi:10.1016/j.jse.2014.04.014.
12. Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011;469(9):2476-2482. doi:10.1007/s11999-010-1683-z.
13. Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11(2):130-135.
14. Bulhoff M, Sattler P, Bruckner T, Loew M, Zeifang F, Raiss P. Do patients return to sports and work after total shoulder replacement surgery? Am J Sports Med. 2015;43(2):423-427. doi:10.1177/0363546514557940.
15. Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377-388.
16. Jensen KL, Rockwood CA Jr. Shoulder arthroplasty in recreational golfers. J Shoulder Elbow Surg. 1998;7(4):362-367.
17. Schumann K, Flury MP, Schwyzer HK, Simmen BR, Drerup S, Goldhahn J. Sports activity after anatomical total shoulder arthroplasty. Am J Sports Med. 2010;38(10):2097-2105. doi:10.1177/0363546510371368.
18. Zarkadas PC, Throckmorton TQ, Dahm DL, Sperling J, Schleck CD, Cofield R. Patient reported activities after shoulder replacement: total and hemiarthroplasty. J Shoulder Elbow Surg. 2011;20(2):273-280. doi:10.1016/j.jse.2010.06.007.
19. Fink Barnes LA, Grantham WJ, Meadows MC, Bigliani LU, Levine WN, Ahmad CS. Sports activity after reverse total shoulder arthroplasty with minimum 2-year follow-up. Am J Orthop. 2015;44(2):68-72.
20. Lawrence TM, Ahmadi S, Sanchez-Sotelo J, Sperling JW, Cofield RH. Patient reported activities after reverse shoulder arthroplasty: part II. J Shoulder Elbow Surg. 2012;21(11):1464-1469. doi:10.1016/j.jse.2011.11.012.
21. Simovitch RW, Gerard BK, Brees JA, Fullick R, Kearse JC. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. J Shoulder Elbow Surg. 2015;24(9):1481-1485. doi:10.1016/j.jse.2015.03.011.
22. Golant A, Christoforou D, Zuckerman JD, Kwon YW. Return to sports after shoulder arthroplasty: a survey of surgeons' preferences. J Shoulder Elbow Surg. 2012;21(4):554-560. doi:10.1016/j.jse.2010.11.021.
23. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594.
24. Alta TD, de Toledo JM, Veeger HE, Janssen TW, Willems WJ. The active and passive kinematic difference between primary reverse and total shoulder prostheses. J Shoulder Elbow Surg. 2014;23(9):1395-1402. doi:10.1016/j.jse.2014.01.040.
25. Alta TD, Veeger DH, de Toledo JM, Janssen TW, Willems WJ. Isokinetic strength differences between patients with primary reverse and total shoulder prostheses: muscle strength quantified with a dynamometer. Clin Biomech (Bristol, Avon). 2014;29(9):965-970. doi:10.1016/j.clinbiomech.2014.08.018.
26. Jawa A, Dasti UR, Fasulo SM, Vaickus MH, Curtis AS, Miller SL. Anatomic total shoulder arthroplasty for patients receiving workers' compensation. J Shoulder Elbow Surg. 2015;24(11):1694-1697. doi:10.1016/j.jse.2015.04.017.
27. Morris BJ, Haigler RE, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB. Workers' compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(3):453-459. doi:10.1016/j.jse.2014.07.009.
ABSTRACT
Both anatomical total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA) are routinely performed for patients who desire to continuously work or participate in sports. This study analyzes and compares the ability of patients to work and partake in sports following shoulder arthroplasty based on responses to clinical outcome surveys.
A retrospective review of the shoulder surgery repository was performed for all patients treated with TSA and RSA and who completed questions 9 and 10 on the activity patient self-evaluation portion of the American Shoulder and Elbow Surgeons (ASES) Assessment Form. Patients with a minimum of 1-year follow-up were included if a sport or work was identified. The analysis included 162 patients with TSA and 114 patients with RSA. Comparisons were made between TSA and RSA in terms of the specific ASES scores (rated 0-3) reported for ability to work and participate in sports and total ASES scores, and scores based on specific sports or line of work reported. Comparisons were also made between sports predominantly using shoulder function and those that do not.
TSA patients had a 27% higher ability to participate in sports (average specific ASES score: 2.5 vs 1.9, P < .001) than RSA patients and presented significantly higher scores for swimming and golf. Compared with RSA patients, TSA patients demonstrated more ability to participate in sports requiring shoulder function without difficulty, as 63% reported maximal scores (P = .003). Total shoulder arthroplasty patients also demonstrated a 21% higher ability to work than RSA patients (average specific ASES scores: 2.6 vs 2.1, P < .001), yielding significantly higher scores for housework and gardening.
Both TSA and RSA allow for participation in work and sports, with TSA patients reporting better overall ability to participate. For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
End-stage shoulder arthritis has been successfully treated with anatomical total shoulder arthroplasty (TSA) with high rates of functional recovery.1 With the introduction of reverse shoulder arthroplasty (RSA), indications for TSA have expanded.2-6 With continuing expansion of surgical indications, a more diverse and potentially active patient population is now being treated. As patients exhibit increased awareness of health and wellness, they demonstrate significant interest in understanding their ability to work or participate in sports after surgery.7 Patients no longer focus on pain relief as the only goal of surgery. A recent study of patients aged 65 years and undergoing shoulder arthroplasty revealed that 64% of the patients listed the ability to return to sports as the main reason for undergoing surgery,8 highlighting the significance of sports play in a patient’s life. Prior to surgery, shoulder pathologies lead to impairment in function, range of motion, and pain,9 hindering a patient to participate in both work and sports. With the intervention yielding improvement to these areas6,9-13 with increased patient satisfaction,10,13 accurately tailoring patient expectations for participation in sports and work postoperatively becomes increasingly important.
Continue to: Although several studies...
Although several studies have demonstrated the ability of patients to return to sports following TSA,8,14-18 a limited number of studies discuss the return to sports following RSA.19-21 Despite known postoperative improvements, no clear consensus is reached as to which specific sports patients can return to and at what level of participation is to be expected. Surveyed members of the American Shoulder and Elbow Surgeons (ASES) universally favored full return to sports, except for contact sports for TSA patients, whereas other surgeons are more conservative to allow RSA patients to return to activities.22 To our knowledge, no other study has investigated the ability to work following RSA. Furthermore, no other study has used patient-reported outcomes to compare the quality of participation in sports or work between TSA and RSA patients following surgery. This study reports the ability of patients treated with TSA and RSA to work and participate in sports based on clinical outcome surveys. We hypothesize that TSA patients will be allowed to work and participate in sports with less difficulty than RSA patients.
MATERIALS AND METHODS
Following Institutional Review Board approval, a retrospective review was performed on all patients treated with TSA or RSA and who completed questions 9 and/or 10 (by score and named usual sport and/or work) on the activity patient self-evaluation portion of the ASES23 Assessment Form between 2007 to 2014; queries were made via the Shoulder Outcomes Repository. A minimum of 12-month follow-up was required, as functional recovery has been shown to plateau or nearly plateau by 12 months.11 Patients were excluded if <12 months of follow-up was available, if they failed to provide a written answer for questions 9 or 10 on the activity patient self-evaluation portion of the ASES Assessment Form, or if they required a revision shoulder arthroplasty. A single fellowship-trained shoulder and elbow surgeon performed all procedures via the same deltopectoral approach and prescribed identical postoperative rehabilitation for both TSA and RSA patients. The database query yielded 162 TSA and 114 RSA patients, for a total of 276 patients eligible for the study.
For all patients, the most recent follow-up ASES score was used. Comparisons were made between TSA and RSA for total ASES scores and response groups for usual sport (ASES question 9) and usual work (ASES question 10). The ASES questionnaire provides patients with 4 choices for each question based on the ability to perform each activity: 0, unable to do; 1, very difficult; 2, somewhat difficult; and 3, not difficult. The questionnaire also allows the patients to identify their usual work and sports. If patients noted >1 sport or work activity, they were included within multiple subgroups. Patients were further compared by age and gender.
Work was subdivided to include retired, housework, desk jobs, prolonged standing, gardening/yard work, jobs requiring lifting, carpenter/construction, cook/food preparation, and creative jobs (Table 1).
Statistical analysis was performed with SPSS Version 21 (IBM). Unpaired t tests were used to determine differences between groups. A P-value of <.05 was deemed significant.
Continue to: A total of 276 patients...
RESULTS
A total of 276 patients that met the inclusion criteria were eligible for the study, with 162 having undergone TSA and 114 with RSA. Overall average follow-up totaled 29 months (range, 12-91 months). RSA patients (average age, 75 years old; range, 46-88 years) were significantly older than TSA patients (average age, 69 years old; range, 32-89 years; P = .001). Significantly more women were treated with TSA (52% TSA; 48% RSA; P = .012), whereas significantly more men were treated with TSA (67% TSA; 33% RSA, P = .012). Total ASES scores were significantly higher for TSA patients than RSA patients in work (P = .012) (Table 4) but not in sports (P = .063) (Table 5) categories.
SPORTS
A total of 186 patients, comprising of 71 RSA and 115 TSA individuals, responded to question 9 of the ASES questionnaire (Table 5). Among usually reported sports, golf (25%), swimming (17%), and walking (18%) were the most commonly cited. RSA patients indicating a sport were significantly older than TSA patients (74 years vs 69 years, P < .001). TSA patients reported a 27% higher difference in overall ability to participate in sports, with an average ASES sport-specific score of 2.5 compared with the 1.9 for RSA patients (P < .001).
Among specific sports, TSA patients reported significantly higher scores for swimming (2.6 vs 1.8, P = .007) and golf (2.5 vs 1.8, P = .050). However, no significant differences were observed for walking, gym exercises, and racquet sports (Table 5). Among sport subsets, RSA patients were significantly older for golf (77 years vs 70 years, P = .006) and bowling (80 years vs 68 years, P = .005). Five TSA patients reported biking as their sport, whereas no RSA patient reported such activity. Within each subset of sports, no significant differences were noted in average ASES total scores.
TSA patients demonstrated a more significant ability to perform usual sports that involve shoulder function without difficulty (score of 3). In shoulder dominant sports, a total of 63% of TSA patients reported a score of 3 compared with the 39% of RSA patients (P = .003). RSA patients more often reported an inability to perform shoulder specific sports, as proven by 20% of RSA patients reporting a score of 0 compared with 4% of TSA patients (P < .001) (Table 6).
WORK
A total of 265 patients, including 106 RSA and 159 TSA patients, responded to question 10 of the ASES questionnaire. Among usually reported work, retirement (43%), housework (27%), and desk jobs (18%) were the most commonly cited. RSA patients denoting a work were significantly older than TSA patients (75 years vs 69 years, P < .001). Patients with TSA presented a 21% higher difference in the overall ability to work, featuring an average ASES work-specific score of 2.6 compared with the 2.1 for RSA patients (P < .001) (Table 4).
Continue to: Among specific work activities...
Among specific work activities, TSA patients reported significantly higher scores for housework (2.7 vs 2; 34% difference; P = .001) and gardening (2.8 vs 1.7; 65% difference; P = .009) in comparison with RSA patients. However, no significant differences were observed for other work activities, including retirement, desk job, prolonged standing, creative jobs, lifting jobs, or construction (Table 4). Among the work subgroups, RSA patients were older than TSA patients for the retired group (77 years vs 72 years; P < .001) and gardening (81 years vs 68 years; P = .002).
DISCUSSION
The ability to participate in sports and work is a common goal for shoulder arthroplasty patients. However, the ability at which participation occurs has not been examined. This study illustrates not only the ability to engage in usual work or sport, but provides some insights into patient-reported quality of participation. Overall, TSA patients featured 27% higher sport-specific ASES scores and 21% higher work-specific ASES scores than RSA patients, confirming our hypothesis that TSA patients can participate in work or sports with less difficulty in general. This study is the first to stratify the difficulty of participating in sports in general and in specific sports identified by patients. Although statistical analysis was performed for individual sports and work reported, the use of small cohorts possibly affected the ability to detect significant differences. The data presented in this study can thus be used as descriptive evidence of what a patient may expect to be able to do following surgery, helping to define patient expectations prior to electing to undergo shoulder arthroplasty.
Among specific sports identified by patients, a few significant differences were observed between RSA and TSA patients. However, ASES-specific scores almost universally favored TSA. Of the sport subgroups, swimming and golf showed significant differences. For swimming, this difference was fairly significant, as TSA patients demonstrated a 49% higher score than their RSA counterparts, but without differences in age or total ASES score (Table 5). Alteration in shoulder mechanics after RSA may be used to explain the difficulty in returning to swimming, as additional time may be needed to adapt to new mechanics.24 McCarty and colleagues8 demonstrated that 90% of patients following TSA fully resumed participation in swimming within 6 months of surgery, and further stated that repetitive motions of swimming caused no effects on short-term outcomes. No similar analysis of swimming has been reported for RSA patients. Based upon our findings, the average RSA patient can experience some difficulties when returning to swimming after surgery (average specific ASES score, 1.8).
Jensen and Rockwood16 were among the first to demonstrate successful return to golf of 24 patients who had undergone either TSA or hemiarthroplasty (HA), showing a 5-stroke improvement in their game. A recent study investigating patient-reported activity in patients aged 75 years and undergoing RSA showed that 23% of patients returned to high-level activity sports, such as golf, motorcycle riding, or free weights.19 All patients who participated in golf before surgery resumed playing following surgery; however, golf was listed among the top activities that patients wanted to participate in but could not for any reason.19 Our data suggest that golfers with TSA will face less difficulty returning to sports compared with their RSA counterparts (average specific ASES score, 2.5 vs 1.8, who might find golf somewhat difficult.
Although no study has provided a clear consensus as to which activities are safe to perform following shoulder arthroplasty, experts have suggested that activities that impart high loads on the glenohumeral joint should be avoided.15 Among TSA patients, McCarty and colleagues8 reported high rates of return for swimmers, golfers, and tennis players; however, relatively low rates were reported for weight lifting, bowling, and softball (20%). Within our study group, golf, swimming, and walking were listed among the most popular sports performed. Although weight lifting, bowling, and softball were less commonly identified as usual sports within our study, patients treated with TSA demonstrated more ease to participate than RSA patients. This result was observed with ASES-specific scores noted for weight lifting and gym exercises (TSA, 2.5; RSA, 2.3) and team sports, such as softball (TSA, 2; RSA, 1.3). However, for bowling, RSA patients showed a trend toward more ability (RSA, 2.7; TSA, 1.7).
Continue to: Among specific work activities...
Successful return to sports that involve shoulder function, such as golf and swimming, has been demonstrated for TSA.8,14,16,17 However, studies have reported that return to these sports can be difficult for RSA patients.20 Fink and colleagues19 reported that following RSA, 48.7% of patients returned to moderate-intensity sports, such as swimming and golf. Consistent with these findings, in our study, TSA patients demonstrated a significantly higher ability to participate in their usual sports without difficulty (ASES-specific score of 3). This observation may relate to lower ultimate achievements in range of motion and strength in patients treated with RSA, when compared with TSA patients,24,25 and the generalized practice of utilizing RSA for lower-demand patients (RSA patients in this study were older).
Overall, participation in work was 21% easier for TSA patients than RSA patients. Although the majority of our patients cited retirement as their primary work, which is consistent with what one would expect with the mean age of this study’s cohorts (RSA, 75 years; TSA, 69 years), housework and gardening were the only specifically identified forms of work that demonstrated significant differences between RSA and TSA patients. A few reports in the literature documented the ability to return to work after shoulder arthroplasty. In a recent report on 13 workers’ compensation patients treated with TSA, only 1 patient returned to the same job, and 54% did not return to work.26 In a study comparing 14 workers’ compensation to a matched group of controls with all members treated with RSA, the workers’ compensation group yielded a lower return-to-work rate (14.2%) than the controls (41.7%).27 In a large study of 154 TSA patients, 14% returned to work, but specific jobs were not described in this analysis.14
The results of this study suggest that more TSA patients successfully participate in low-demand activities, such as gardening or housework. Zarkadas and colleagues18 reported that 65% of TSA and 47% of HA patients successfully returned to gardening compared with 42% of RSA patients observed in a continuation study.20 This study showed that TSA patients yielded a 65% difference in ability to work in gardening and 34% difference in ability to perform housework compared with RSA patients. Based on these findings, TSA patients can expect to experience no difficulty in performing housework or gardening, whereas RSA patients may find these tasks difficult to a certain degree.
The main limitation of this study is the reporting bias that results from survey-based studies. Possibly, more people engage in specific sports or work than what were reported. This type of study also features an inherent selection bias, as patients with highly and physically demanding jobs or usual sports were less likely to have been offered either TSA or RSA. An additional important limitation is the relatively small cohorts within sport and work subgroups; the small cohorts probably underpowered the statistical results of this study and made these findings valuable mostly as descriptive observations. Larger studies focusing on each subgroup will further clarify the ability of shoulder arthroplasty to perform individual sports or work. Further studies evaluating preoperative to postoperative sports- and work-specific ASES scores would provide notable insights into the functional improvements observed within each sport or work following surgery. The relatively large study population of 276 patients strengthened the findings, which relate to the overall ability to participate in sports and work for TSA and RSA patients. Finally, the evaluated TSA and RSA patients possibly represent different groups (significant difference in age and gender) with different underlying pathologies and potentially different demands and expectations. However, comparisons among these groups of patients bear importance in defining patient expectations related to surgery. Still, the ability to participate in sport or work possibly relates more to the limitations of the implant used than patient pathology. This possibility warrants further investigation.
CONCLUSION
Both TSA and RSA allow for participation in work and sports, with TSA patients reporting easier overall ability to participate. For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
ABSTRACT
Both anatomical total shoulder arthroplasty (TSA) and reverse shoulder arthroplasty (RSA) are routinely performed for patients who desire to continuously work or participate in sports. This study analyzes and compares the ability of patients to work and partake in sports following shoulder arthroplasty based on responses to clinical outcome surveys.
A retrospective review of the shoulder surgery repository was performed for all patients treated with TSA and RSA and who completed questions 9 and 10 on the activity patient self-evaluation portion of the American Shoulder and Elbow Surgeons (ASES) Assessment Form. Patients with a minimum of 1-year follow-up were included if a sport or work was identified. The analysis included 162 patients with TSA and 114 patients with RSA. Comparisons were made between TSA and RSA in terms of the specific ASES scores (rated 0-3) reported for ability to work and participate in sports and total ASES scores, and scores based on specific sports or line of work reported. Comparisons were also made between sports predominantly using shoulder function and those that do not.
TSA patients had a 27% higher ability to participate in sports (average specific ASES score: 2.5 vs 1.9, P < .001) than RSA patients and presented significantly higher scores for swimming and golf. Compared with RSA patients, TSA patients demonstrated more ability to participate in sports requiring shoulder function without difficulty, as 63% reported maximal scores (P = .003). Total shoulder arthroplasty patients also demonstrated a 21% higher ability to work than RSA patients (average specific ASES scores: 2.6 vs 2.1, P < .001), yielding significantly higher scores for housework and gardening.
Both TSA and RSA allow for participation in work and sports, with TSA patients reporting better overall ability to participate. For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
End-stage shoulder arthritis has been successfully treated with anatomical total shoulder arthroplasty (TSA) with high rates of functional recovery.1 With the introduction of reverse shoulder arthroplasty (RSA), indications for TSA have expanded.2-6 With continuing expansion of surgical indications, a more diverse and potentially active patient population is now being treated. As patients exhibit increased awareness of health and wellness, they demonstrate significant interest in understanding their ability to work or participate in sports after surgery.7 Patients no longer focus on pain relief as the only goal of surgery. A recent study of patients aged 65 years and undergoing shoulder arthroplasty revealed that 64% of the patients listed the ability to return to sports as the main reason for undergoing surgery,8 highlighting the significance of sports play in a patient’s life. Prior to surgery, shoulder pathologies lead to impairment in function, range of motion, and pain,9 hindering a patient to participate in both work and sports. With the intervention yielding improvement to these areas6,9-13 with increased patient satisfaction,10,13 accurately tailoring patient expectations for participation in sports and work postoperatively becomes increasingly important.
Continue to: Although several studies...
Although several studies have demonstrated the ability of patients to return to sports following TSA,8,14-18 a limited number of studies discuss the return to sports following RSA.19-21 Despite known postoperative improvements, no clear consensus is reached as to which specific sports patients can return to and at what level of participation is to be expected. Surveyed members of the American Shoulder and Elbow Surgeons (ASES) universally favored full return to sports, except for contact sports for TSA patients, whereas other surgeons are more conservative to allow RSA patients to return to activities.22 To our knowledge, no other study has investigated the ability to work following RSA. Furthermore, no other study has used patient-reported outcomes to compare the quality of participation in sports or work between TSA and RSA patients following surgery. This study reports the ability of patients treated with TSA and RSA to work and participate in sports based on clinical outcome surveys. We hypothesize that TSA patients will be allowed to work and participate in sports with less difficulty than RSA patients.
MATERIALS AND METHODS
Following Institutional Review Board approval, a retrospective review was performed on all patients treated with TSA or RSA and who completed questions 9 and/or 10 (by score and named usual sport and/or work) on the activity patient self-evaluation portion of the ASES23 Assessment Form between 2007 to 2014; queries were made via the Shoulder Outcomes Repository. A minimum of 12-month follow-up was required, as functional recovery has been shown to plateau or nearly plateau by 12 months.11 Patients were excluded if <12 months of follow-up was available, if they failed to provide a written answer for questions 9 or 10 on the activity patient self-evaluation portion of the ASES Assessment Form, or if they required a revision shoulder arthroplasty. A single fellowship-trained shoulder and elbow surgeon performed all procedures via the same deltopectoral approach and prescribed identical postoperative rehabilitation for both TSA and RSA patients. The database query yielded 162 TSA and 114 RSA patients, for a total of 276 patients eligible for the study.
For all patients, the most recent follow-up ASES score was used. Comparisons were made between TSA and RSA for total ASES scores and response groups for usual sport (ASES question 9) and usual work (ASES question 10). The ASES questionnaire provides patients with 4 choices for each question based on the ability to perform each activity: 0, unable to do; 1, very difficult; 2, somewhat difficult; and 3, not difficult. The questionnaire also allows the patients to identify their usual work and sports. If patients noted >1 sport or work activity, they were included within multiple subgroups. Patients were further compared by age and gender.
Work was subdivided to include retired, housework, desk jobs, prolonged standing, gardening/yard work, jobs requiring lifting, carpenter/construction, cook/food preparation, and creative jobs (Table 1).
Statistical analysis was performed with SPSS Version 21 (IBM). Unpaired t tests were used to determine differences between groups. A P-value of <.05 was deemed significant.
Continue to: A total of 276 patients...
RESULTS
A total of 276 patients that met the inclusion criteria were eligible for the study, with 162 having undergone TSA and 114 with RSA. Overall average follow-up totaled 29 months (range, 12-91 months). RSA patients (average age, 75 years old; range, 46-88 years) were significantly older than TSA patients (average age, 69 years old; range, 32-89 years; P = .001). Significantly more women were treated with TSA (52% TSA; 48% RSA; P = .012), whereas significantly more men were treated with TSA (67% TSA; 33% RSA, P = .012). Total ASES scores were significantly higher for TSA patients than RSA patients in work (P = .012) (Table 4) but not in sports (P = .063) (Table 5) categories.
SPORTS
A total of 186 patients, comprising of 71 RSA and 115 TSA individuals, responded to question 9 of the ASES questionnaire (Table 5). Among usually reported sports, golf (25%), swimming (17%), and walking (18%) were the most commonly cited. RSA patients indicating a sport were significantly older than TSA patients (74 years vs 69 years, P < .001). TSA patients reported a 27% higher difference in overall ability to participate in sports, with an average ASES sport-specific score of 2.5 compared with the 1.9 for RSA patients (P < .001).
Among specific sports, TSA patients reported significantly higher scores for swimming (2.6 vs 1.8, P = .007) and golf (2.5 vs 1.8, P = .050). However, no significant differences were observed for walking, gym exercises, and racquet sports (Table 5). Among sport subsets, RSA patients were significantly older for golf (77 years vs 70 years, P = .006) and bowling (80 years vs 68 years, P = .005). Five TSA patients reported biking as their sport, whereas no RSA patient reported such activity. Within each subset of sports, no significant differences were noted in average ASES total scores.
TSA patients demonstrated a more significant ability to perform usual sports that involve shoulder function without difficulty (score of 3). In shoulder dominant sports, a total of 63% of TSA patients reported a score of 3 compared with the 39% of RSA patients (P = .003). RSA patients more often reported an inability to perform shoulder specific sports, as proven by 20% of RSA patients reporting a score of 0 compared with 4% of TSA patients (P < .001) (Table 6).
WORK
A total of 265 patients, including 106 RSA and 159 TSA patients, responded to question 10 of the ASES questionnaire. Among usually reported work, retirement (43%), housework (27%), and desk jobs (18%) were the most commonly cited. RSA patients denoting a work were significantly older than TSA patients (75 years vs 69 years, P < .001). Patients with TSA presented a 21% higher difference in the overall ability to work, featuring an average ASES work-specific score of 2.6 compared with the 2.1 for RSA patients (P < .001) (Table 4).
Continue to: Among specific work activities...
Among specific work activities, TSA patients reported significantly higher scores for housework (2.7 vs 2; 34% difference; P = .001) and gardening (2.8 vs 1.7; 65% difference; P = .009) in comparison with RSA patients. However, no significant differences were observed for other work activities, including retirement, desk job, prolonged standing, creative jobs, lifting jobs, or construction (Table 4). Among the work subgroups, RSA patients were older than TSA patients for the retired group (77 years vs 72 years; P < .001) and gardening (81 years vs 68 years; P = .002).
DISCUSSION
The ability to participate in sports and work is a common goal for shoulder arthroplasty patients. However, the ability at which participation occurs has not been examined. This study illustrates not only the ability to engage in usual work or sport, but provides some insights into patient-reported quality of participation. Overall, TSA patients featured 27% higher sport-specific ASES scores and 21% higher work-specific ASES scores than RSA patients, confirming our hypothesis that TSA patients can participate in work or sports with less difficulty in general. This study is the first to stratify the difficulty of participating in sports in general and in specific sports identified by patients. Although statistical analysis was performed for individual sports and work reported, the use of small cohorts possibly affected the ability to detect significant differences. The data presented in this study can thus be used as descriptive evidence of what a patient may expect to be able to do following surgery, helping to define patient expectations prior to electing to undergo shoulder arthroplasty.
Among specific sports identified by patients, a few significant differences were observed between RSA and TSA patients. However, ASES-specific scores almost universally favored TSA. Of the sport subgroups, swimming and golf showed significant differences. For swimming, this difference was fairly significant, as TSA patients demonstrated a 49% higher score than their RSA counterparts, but without differences in age or total ASES score (Table 5). Alteration in shoulder mechanics after RSA may be used to explain the difficulty in returning to swimming, as additional time may be needed to adapt to new mechanics.24 McCarty and colleagues8 demonstrated that 90% of patients following TSA fully resumed participation in swimming within 6 months of surgery, and further stated that repetitive motions of swimming caused no effects on short-term outcomes. No similar analysis of swimming has been reported for RSA patients. Based upon our findings, the average RSA patient can experience some difficulties when returning to swimming after surgery (average specific ASES score, 1.8).
Jensen and Rockwood16 were among the first to demonstrate successful return to golf of 24 patients who had undergone either TSA or hemiarthroplasty (HA), showing a 5-stroke improvement in their game. A recent study investigating patient-reported activity in patients aged 75 years and undergoing RSA showed that 23% of patients returned to high-level activity sports, such as golf, motorcycle riding, or free weights.19 All patients who participated in golf before surgery resumed playing following surgery; however, golf was listed among the top activities that patients wanted to participate in but could not for any reason.19 Our data suggest that golfers with TSA will face less difficulty returning to sports compared with their RSA counterparts (average specific ASES score, 2.5 vs 1.8, who might find golf somewhat difficult.
Although no study has provided a clear consensus as to which activities are safe to perform following shoulder arthroplasty, experts have suggested that activities that impart high loads on the glenohumeral joint should be avoided.15 Among TSA patients, McCarty and colleagues8 reported high rates of return for swimmers, golfers, and tennis players; however, relatively low rates were reported for weight lifting, bowling, and softball (20%). Within our study group, golf, swimming, and walking were listed among the most popular sports performed. Although weight lifting, bowling, and softball were less commonly identified as usual sports within our study, patients treated with TSA demonstrated more ease to participate than RSA patients. This result was observed with ASES-specific scores noted for weight lifting and gym exercises (TSA, 2.5; RSA, 2.3) and team sports, such as softball (TSA, 2; RSA, 1.3). However, for bowling, RSA patients showed a trend toward more ability (RSA, 2.7; TSA, 1.7).
Continue to: Among specific work activities...
Successful return to sports that involve shoulder function, such as golf and swimming, has been demonstrated for TSA.8,14,16,17 However, studies have reported that return to these sports can be difficult for RSA patients.20 Fink and colleagues19 reported that following RSA, 48.7% of patients returned to moderate-intensity sports, such as swimming and golf. Consistent with these findings, in our study, TSA patients demonstrated a significantly higher ability to participate in their usual sports without difficulty (ASES-specific score of 3). This observation may relate to lower ultimate achievements in range of motion and strength in patients treated with RSA, when compared with TSA patients,24,25 and the generalized practice of utilizing RSA for lower-demand patients (RSA patients in this study were older).
Overall, participation in work was 21% easier for TSA patients than RSA patients. Although the majority of our patients cited retirement as their primary work, which is consistent with what one would expect with the mean age of this study’s cohorts (RSA, 75 years; TSA, 69 years), housework and gardening were the only specifically identified forms of work that demonstrated significant differences between RSA and TSA patients. A few reports in the literature documented the ability to return to work after shoulder arthroplasty. In a recent report on 13 workers’ compensation patients treated with TSA, only 1 patient returned to the same job, and 54% did not return to work.26 In a study comparing 14 workers’ compensation to a matched group of controls with all members treated with RSA, the workers’ compensation group yielded a lower return-to-work rate (14.2%) than the controls (41.7%).27 In a large study of 154 TSA patients, 14% returned to work, but specific jobs were not described in this analysis.14
The results of this study suggest that more TSA patients successfully participate in low-demand activities, such as gardening or housework. Zarkadas and colleagues18 reported that 65% of TSA and 47% of HA patients successfully returned to gardening compared with 42% of RSA patients observed in a continuation study.20 This study showed that TSA patients yielded a 65% difference in ability to work in gardening and 34% difference in ability to perform housework compared with RSA patients. Based on these findings, TSA patients can expect to experience no difficulty in performing housework or gardening, whereas RSA patients may find these tasks difficult to a certain degree.
The main limitation of this study is the reporting bias that results from survey-based studies. Possibly, more people engage in specific sports or work than what were reported. This type of study also features an inherent selection bias, as patients with highly and physically demanding jobs or usual sports were less likely to have been offered either TSA or RSA. An additional important limitation is the relatively small cohorts within sport and work subgroups; the small cohorts probably underpowered the statistical results of this study and made these findings valuable mostly as descriptive observations. Larger studies focusing on each subgroup will further clarify the ability of shoulder arthroplasty to perform individual sports or work. Further studies evaluating preoperative to postoperative sports- and work-specific ASES scores would provide notable insights into the functional improvements observed within each sport or work following surgery. The relatively large study population of 276 patients strengthened the findings, which relate to the overall ability to participate in sports and work for TSA and RSA patients. Finally, the evaluated TSA and RSA patients possibly represent different groups (significant difference in age and gender) with different underlying pathologies and potentially different demands and expectations. However, comparisons among these groups of patients bear importance in defining patient expectations related to surgery. Still, the ability to participate in sport or work possibly relates more to the limitations of the implant used than patient pathology. This possibility warrants further investigation.
CONCLUSION
Both TSA and RSA allow for participation in work and sports, with TSA patients reporting easier overall ability to participate. For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
1. Fehringer EV, Kopjar B, Boorman RS, Churchill RS, Smith KL, Matsen FA 3rd. Characterizing the functional improvement after total shoulder arthroplasty for osteoarthritis. J Bone Joint Surg Am. 2002;84-A(8):1349-1353.
2. Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013;95(22):2050-2055. doi:10.2106/JBJS.L.01637.
3. Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742-1747.
4. Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89(2):189-195.
5. Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(11):1478-1483. doi:10.1016/j.jse.2011.11.004.
6. Sebastia-Forcada E, Cebrian-Gomez R, Lizaur-Utrilla A, Gil-Guillen V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23(10):1419-1426. doi:10.1016/j.jse.2014.06.035.
7. Henn RF 3rd, Ghomrawi H, Rutledge JR, Mazumdar M, Mancuso CA, Marx RG. Preoperative patient expectations of total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93(22):2110-2115. doi:10.2106/JBJS.J.01114.
8. McCarty EC, Marx RG, Maerz D, Altchek D, Warren RF. Sports participation after shoulder replacement surgery. Am J Sports Med. 2008;36(8):1577-1581. doi:10.1177/0363546508317126.
9. Puskas B, Harreld K, Clark R, Downes K, Virani NA, Frankle M. Isometric strength, range of motion, and impairment before and after total and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(7):869-876. doi:10.1016/j.jse.2012.09.004.
10. Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471-479.
11. Levy JC, Everding NG, Gil CC Jr., Stephens S, Giveans MR. Speed of recovery after shoulder arthroplasty: a comparison of reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(12):1872-1881. doi:10.1016/j.jse.2014.04.014.
12. Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011;469(9):2476-2482. doi:10.1007/s11999-010-1683-z.
13. Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11(2):130-135.
14. Bulhoff M, Sattler P, Bruckner T, Loew M, Zeifang F, Raiss P. Do patients return to sports and work after total shoulder replacement surgery? Am J Sports Med. 2015;43(2):423-427. doi:10.1177/0363546514557940.
15. Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377-388.
16. Jensen KL, Rockwood CA Jr. Shoulder arthroplasty in recreational golfers. J Shoulder Elbow Surg. 1998;7(4):362-367.
17. Schumann K, Flury MP, Schwyzer HK, Simmen BR, Drerup S, Goldhahn J. Sports activity after anatomical total shoulder arthroplasty. Am J Sports Med. 2010;38(10):2097-2105. doi:10.1177/0363546510371368.
18. Zarkadas PC, Throckmorton TQ, Dahm DL, Sperling J, Schleck CD, Cofield R. Patient reported activities after shoulder replacement: total and hemiarthroplasty. J Shoulder Elbow Surg. 2011;20(2):273-280. doi:10.1016/j.jse.2010.06.007.
19. Fink Barnes LA, Grantham WJ, Meadows MC, Bigliani LU, Levine WN, Ahmad CS. Sports activity after reverse total shoulder arthroplasty with minimum 2-year follow-up. Am J Orthop. 2015;44(2):68-72.
20. Lawrence TM, Ahmadi S, Sanchez-Sotelo J, Sperling JW, Cofield RH. Patient reported activities after reverse shoulder arthroplasty: part II. J Shoulder Elbow Surg. 2012;21(11):1464-1469. doi:10.1016/j.jse.2011.11.012.
21. Simovitch RW, Gerard BK, Brees JA, Fullick R, Kearse JC. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. J Shoulder Elbow Surg. 2015;24(9):1481-1485. doi:10.1016/j.jse.2015.03.011.
22. Golant A, Christoforou D, Zuckerman JD, Kwon YW. Return to sports after shoulder arthroplasty: a survey of surgeons' preferences. J Shoulder Elbow Surg. 2012;21(4):554-560. doi:10.1016/j.jse.2010.11.021.
23. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594.
24. Alta TD, de Toledo JM, Veeger HE, Janssen TW, Willems WJ. The active and passive kinematic difference between primary reverse and total shoulder prostheses. J Shoulder Elbow Surg. 2014;23(9):1395-1402. doi:10.1016/j.jse.2014.01.040.
25. Alta TD, Veeger DH, de Toledo JM, Janssen TW, Willems WJ. Isokinetic strength differences between patients with primary reverse and total shoulder prostheses: muscle strength quantified with a dynamometer. Clin Biomech (Bristol, Avon). 2014;29(9):965-970. doi:10.1016/j.clinbiomech.2014.08.018.
26. Jawa A, Dasti UR, Fasulo SM, Vaickus MH, Curtis AS, Miller SL. Anatomic total shoulder arthroplasty for patients receiving workers' compensation. J Shoulder Elbow Surg. 2015;24(11):1694-1697. doi:10.1016/j.jse.2015.04.017.
27. Morris BJ, Haigler RE, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB. Workers' compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(3):453-459. doi:10.1016/j.jse.2014.07.009.
1. Fehringer EV, Kopjar B, Boorman RS, Churchill RS, Smith KL, Matsen FA 3rd. Characterizing the functional improvement after total shoulder arthroplasty for osteoarthritis. J Bone Joint Surg Am. 2002;84-A(8):1349-1353.
2. Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013;95(22):2050-2055. doi:10.2106/JBJS.L.01637.
3. Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742-1747.
4. Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89(2):189-195.
5. Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(11):1478-1483. doi:10.1016/j.jse.2011.11.004.
6. Sebastia-Forcada E, Cebrian-Gomez R, Lizaur-Utrilla A, Gil-Guillen V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg. 2014;23(10):1419-1426. doi:10.1016/j.jse.2014.06.035.
7. Henn RF 3rd, Ghomrawi H, Rutledge JR, Mazumdar M, Mancuso CA, Marx RG. Preoperative patient expectations of total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93(22):2110-2115. doi:10.2106/JBJS.J.01114.
8. McCarty EC, Marx RG, Maerz D, Altchek D, Warren RF. Sports participation after shoulder replacement surgery. Am J Sports Med. 2008;36(8):1577-1581. doi:10.1177/0363546508317126.
9. Puskas B, Harreld K, Clark R, Downes K, Virani NA, Frankle M. Isometric strength, range of motion, and impairment before and after total and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(7):869-876. doi:10.1016/j.jse.2012.09.004.
10. Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471-479.
11. Levy JC, Everding NG, Gil CC Jr., Stephens S, Giveans MR. Speed of recovery after shoulder arthroplasty: a comparison of reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(12):1872-1881. doi:10.1016/j.jse.2014.04.014.
12. Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011;469(9):2476-2482. doi:10.1007/s11999-010-1683-z.
13. Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11(2):130-135.
14. Bulhoff M, Sattler P, Bruckner T, Loew M, Zeifang F, Raiss P. Do patients return to sports and work after total shoulder replacement surgery? Am J Sports Med. 2015;43(2):423-427. doi:10.1177/0363546514557940.
15. Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377-388.
16. Jensen KL, Rockwood CA Jr. Shoulder arthroplasty in recreational golfers. J Shoulder Elbow Surg. 1998;7(4):362-367.
17. Schumann K, Flury MP, Schwyzer HK, Simmen BR, Drerup S, Goldhahn J. Sports activity after anatomical total shoulder arthroplasty. Am J Sports Med. 2010;38(10):2097-2105. doi:10.1177/0363546510371368.
18. Zarkadas PC, Throckmorton TQ, Dahm DL, Sperling J, Schleck CD, Cofield R. Patient reported activities after shoulder replacement: total and hemiarthroplasty. J Shoulder Elbow Surg. 2011;20(2):273-280. doi:10.1016/j.jse.2010.06.007.
19. Fink Barnes LA, Grantham WJ, Meadows MC, Bigliani LU, Levine WN, Ahmad CS. Sports activity after reverse total shoulder arthroplasty with minimum 2-year follow-up. Am J Orthop. 2015;44(2):68-72.
20. Lawrence TM, Ahmadi S, Sanchez-Sotelo J, Sperling JW, Cofield RH. Patient reported activities after reverse shoulder arthroplasty: part II. J Shoulder Elbow Surg. 2012;21(11):1464-1469. doi:10.1016/j.jse.2011.11.012.
21. Simovitch RW, Gerard BK, Brees JA, Fullick R, Kearse JC. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. J Shoulder Elbow Surg. 2015;24(9):1481-1485. doi:10.1016/j.jse.2015.03.011.
22. Golant A, Christoforou D, Zuckerman JD, Kwon YW. Return to sports after shoulder arthroplasty: a survey of surgeons' preferences. J Shoulder Elbow Surg. 2012;21(4):554-560. doi:10.1016/j.jse.2010.11.021.
23. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594.
24. Alta TD, de Toledo JM, Veeger HE, Janssen TW, Willems WJ. The active and passive kinematic difference between primary reverse and total shoulder prostheses. J Shoulder Elbow Surg. 2014;23(9):1395-1402. doi:10.1016/j.jse.2014.01.040.
25. Alta TD, Veeger DH, de Toledo JM, Janssen TW, Willems WJ. Isokinetic strength differences between patients with primary reverse and total shoulder prostheses: muscle strength quantified with a dynamometer. Clin Biomech (Bristol, Avon). 2014;29(9):965-970. doi:10.1016/j.clinbiomech.2014.08.018.
26. Jawa A, Dasti UR, Fasulo SM, Vaickus MH, Curtis AS, Miller SL. Anatomic total shoulder arthroplasty for patients receiving workers' compensation. J Shoulder Elbow Surg. 2015;24(11):1694-1697. doi:10.1016/j.jse.2015.04.017.
27. Morris BJ, Haigler RE, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB. Workers' compensation claims and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(3):453-459. doi:10.1016/j.jse.2014.07.009.
TAKE-HOME POINTS
- Both anatomic (TSA) and reverse shoulder arthroplasty (RSA) allow for the participation in work and sports.
- TSA patients report easier overall ability to participate in sports, specifically golf and swimming.
- For sports involving shoulder function, TSA patients more commonly report maximal ability to participate than RSA patients.
- TSA patients report easier overall ability to return to work-related activities, specifically housework and gardening.
- TSA patients featured 27% higher sport-specific ASES scores and 21% higher work-specific ASES scores than RSA patients.
CBT-I bests acupuncture for treating insomnia among cancer survivors
Cancer survivors who have trouble sleeping saw improvements with both cognitive-behavioral therapy designed specifically for insomnia (CBT-I) and acupuncture, according to results from the randomized, controlled CHOICE trial. But the former is more efficacious.
“Insomnia can have deleterious effects on quality of life and function, and occurs in up to 60% of cancer survivors,” lead study author Jun J. Mao, MD, chief of integrative medicine service at Memorial Sloan Kettering Cancer Center, New York, said in a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“CBT-I is a highly effective therapy and can be considered the gold standard of treatment,” he noted. However, this modality may be limited by poor adherence and nonresponse. Moreover, it is highly specialized and not currently available in many cancer centers or communities.
Functional imaging studies have shown that acupuncture can regulate brain regions involving cognition and emotion that are essential to sleep regulation, and clinical research has shown that it can improve pain- and hot flash–related sleep disturbances, according to Dr. Mao. About 73% of U.S. comprehensive cancer centers offer acupuncture for symptom management.
Main results of the CHOICE (Choosing Options for Insomnia in Cancer Effectively) trial showed that patients in both the CBT-I and acupuncture groups reduced their Insomnia Severity Index scores by more than one-half at the end of the 8-weeks treatment period, but the reduction was a statistically significant 2.6 points greater with CBT-I. Benefit of each treatment was still evident after 12 weeks.
Response rate was higher with CBT-I than with acupuncture only among patients having mild insomnia at baseline, and the two treatments yielded similar improvements in mental and physical quality of life.
“Among cancer patients with insomnia, we found that both acupuncture and CBT-I produced clinically meaningful and durable benefit, but overall, CBT-I is more effective in reducing insomnia severity,” Dr. Mao concluded. “Our hope is that by doing this type of research, we can help patients and clinicians pick the right kind of treatment and help them to manage their sleep. Our next step is to really examine for what type of patient treatment would be beneficial, and how to deliver this type of effective treatment to the broader community of cancer patients.”
Insomnia among cancer survivors is both prevalent and problematic, agreed ASCO President Bruce E. Johnson, MD, FASCO.
“The most common way we treat this is pharmacologically, with sleeping pills,” he noted. “This trial shows that two different methods using something other than medications can help people with sleep, and not only do they help people with sleep, but they improve their quality of life.
“We think this information will be helpful for clinicians who end up having to decide, and also, we would use this information to help decide about how the severity of the insomnia is going to influence the treatment,” maintained Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute in Boston, and a leader of the center’s lung cancer program.
Study details
The CHOICE trial did not have any restrictions on cancer type or stage; more than a half-dozen types were represented among the 160 patients enrolled, with breast cancer (31%) and prostate cancer (23%) accounting for the largest shares. The majority of patients were white (70%) and had moderate to severe insomnia (79%).
Patients were randomized to receive either acupuncture sessions (10 sessions, with points selected to treat insomnia plus comorbid symptoms such as fatigue and anxiety) or CBT-I (7 sessions), each over the course of 8 weeks.
Main results showed that at the end of treatment, the reduction in Insomnia Severity Index was 8.3 points with acupuncture and 10.9 points with CBT-I (P = .0007), Dr. Mao reported. Benefit of each treatment was sustained after 12 weeks.
In stratified analysis, the rate of response (defined as a greater than 8-point reduction) was higher with CBT-I than with acupuncture among patients with mild insomnia (Insomnia Severity Index of 8-14) (85% vs. 18%; P less than .0001), but not among patients with moderate or severe insomnia (Insomnia Severity Index of 15 or higher) (75% vs. 66%; P = .26).
The two treatments were similarly efficacious with respect to quality of life, assessed with the Patient-Reported Outcomes Measurement Information System over the entire course of the trial, for both the physical health component (P = .4) and the mental health component (P = .36).
Dr. Mao disclosed no relevant conflicts of interest. The study received funding from the Patient-Centered Outcomes Research Institute.
SOURCE: Mao JJ et al. ASCO 2018. Abstract 10001.
Cancer survivors who have trouble sleeping saw improvements with both cognitive-behavioral therapy designed specifically for insomnia (CBT-I) and acupuncture, according to results from the randomized, controlled CHOICE trial. But the former is more efficacious.
“Insomnia can have deleterious effects on quality of life and function, and occurs in up to 60% of cancer survivors,” lead study author Jun J. Mao, MD, chief of integrative medicine service at Memorial Sloan Kettering Cancer Center, New York, said in a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“CBT-I is a highly effective therapy and can be considered the gold standard of treatment,” he noted. However, this modality may be limited by poor adherence and nonresponse. Moreover, it is highly specialized and not currently available in many cancer centers or communities.
Functional imaging studies have shown that acupuncture can regulate brain regions involving cognition and emotion that are essential to sleep regulation, and clinical research has shown that it can improve pain- and hot flash–related sleep disturbances, according to Dr. Mao. About 73% of U.S. comprehensive cancer centers offer acupuncture for symptom management.
Main results of the CHOICE (Choosing Options for Insomnia in Cancer Effectively) trial showed that patients in both the CBT-I and acupuncture groups reduced their Insomnia Severity Index scores by more than one-half at the end of the 8-weeks treatment period, but the reduction was a statistically significant 2.6 points greater with CBT-I. Benefit of each treatment was still evident after 12 weeks.
Response rate was higher with CBT-I than with acupuncture only among patients having mild insomnia at baseline, and the two treatments yielded similar improvements in mental and physical quality of life.
“Among cancer patients with insomnia, we found that both acupuncture and CBT-I produced clinically meaningful and durable benefit, but overall, CBT-I is more effective in reducing insomnia severity,” Dr. Mao concluded. “Our hope is that by doing this type of research, we can help patients and clinicians pick the right kind of treatment and help them to manage their sleep. Our next step is to really examine for what type of patient treatment would be beneficial, and how to deliver this type of effective treatment to the broader community of cancer patients.”
Insomnia among cancer survivors is both prevalent and problematic, agreed ASCO President Bruce E. Johnson, MD, FASCO.
“The most common way we treat this is pharmacologically, with sleeping pills,” he noted. “This trial shows that two different methods using something other than medications can help people with sleep, and not only do they help people with sleep, but they improve their quality of life.
“We think this information will be helpful for clinicians who end up having to decide, and also, we would use this information to help decide about how the severity of the insomnia is going to influence the treatment,” maintained Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute in Boston, and a leader of the center’s lung cancer program.
Study details
The CHOICE trial did not have any restrictions on cancer type or stage; more than a half-dozen types were represented among the 160 patients enrolled, with breast cancer (31%) and prostate cancer (23%) accounting for the largest shares. The majority of patients were white (70%) and had moderate to severe insomnia (79%).
Patients were randomized to receive either acupuncture sessions (10 sessions, with points selected to treat insomnia plus comorbid symptoms such as fatigue and anxiety) or CBT-I (7 sessions), each over the course of 8 weeks.
Main results showed that at the end of treatment, the reduction in Insomnia Severity Index was 8.3 points with acupuncture and 10.9 points with CBT-I (P = .0007), Dr. Mao reported. Benefit of each treatment was sustained after 12 weeks.
In stratified analysis, the rate of response (defined as a greater than 8-point reduction) was higher with CBT-I than with acupuncture among patients with mild insomnia (Insomnia Severity Index of 8-14) (85% vs. 18%; P less than .0001), but not among patients with moderate or severe insomnia (Insomnia Severity Index of 15 or higher) (75% vs. 66%; P = .26).
The two treatments were similarly efficacious with respect to quality of life, assessed with the Patient-Reported Outcomes Measurement Information System over the entire course of the trial, for both the physical health component (P = .4) and the mental health component (P = .36).
Dr. Mao disclosed no relevant conflicts of interest. The study received funding from the Patient-Centered Outcomes Research Institute.
SOURCE: Mao JJ et al. ASCO 2018. Abstract 10001.
Cancer survivors who have trouble sleeping saw improvements with both cognitive-behavioral therapy designed specifically for insomnia (CBT-I) and acupuncture, according to results from the randomized, controlled CHOICE trial. But the former is more efficacious.
“Insomnia can have deleterious effects on quality of life and function, and occurs in up to 60% of cancer survivors,” lead study author Jun J. Mao, MD, chief of integrative medicine service at Memorial Sloan Kettering Cancer Center, New York, said in a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“CBT-I is a highly effective therapy and can be considered the gold standard of treatment,” he noted. However, this modality may be limited by poor adherence and nonresponse. Moreover, it is highly specialized and not currently available in many cancer centers or communities.
Functional imaging studies have shown that acupuncture can regulate brain regions involving cognition and emotion that are essential to sleep regulation, and clinical research has shown that it can improve pain- and hot flash–related sleep disturbances, according to Dr. Mao. About 73% of U.S. comprehensive cancer centers offer acupuncture for symptom management.
Main results of the CHOICE (Choosing Options for Insomnia in Cancer Effectively) trial showed that patients in both the CBT-I and acupuncture groups reduced their Insomnia Severity Index scores by more than one-half at the end of the 8-weeks treatment period, but the reduction was a statistically significant 2.6 points greater with CBT-I. Benefit of each treatment was still evident after 12 weeks.
Response rate was higher with CBT-I than with acupuncture only among patients having mild insomnia at baseline, and the two treatments yielded similar improvements in mental and physical quality of life.
“Among cancer patients with insomnia, we found that both acupuncture and CBT-I produced clinically meaningful and durable benefit, but overall, CBT-I is more effective in reducing insomnia severity,” Dr. Mao concluded. “Our hope is that by doing this type of research, we can help patients and clinicians pick the right kind of treatment and help them to manage their sleep. Our next step is to really examine for what type of patient treatment would be beneficial, and how to deliver this type of effective treatment to the broader community of cancer patients.”
Insomnia among cancer survivors is both prevalent and problematic, agreed ASCO President Bruce E. Johnson, MD, FASCO.
“The most common way we treat this is pharmacologically, with sleeping pills,” he noted. “This trial shows that two different methods using something other than medications can help people with sleep, and not only do they help people with sleep, but they improve their quality of life.
“We think this information will be helpful for clinicians who end up having to decide, and also, we would use this information to help decide about how the severity of the insomnia is going to influence the treatment,” maintained Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute in Boston, and a leader of the center’s lung cancer program.
Study details
The CHOICE trial did not have any restrictions on cancer type or stage; more than a half-dozen types were represented among the 160 patients enrolled, with breast cancer (31%) and prostate cancer (23%) accounting for the largest shares. The majority of patients were white (70%) and had moderate to severe insomnia (79%).
Patients were randomized to receive either acupuncture sessions (10 sessions, with points selected to treat insomnia plus comorbid symptoms such as fatigue and anxiety) or CBT-I (7 sessions), each over the course of 8 weeks.
Main results showed that at the end of treatment, the reduction in Insomnia Severity Index was 8.3 points with acupuncture and 10.9 points with CBT-I (P = .0007), Dr. Mao reported. Benefit of each treatment was sustained after 12 weeks.
In stratified analysis, the rate of response (defined as a greater than 8-point reduction) was higher with CBT-I than with acupuncture among patients with mild insomnia (Insomnia Severity Index of 8-14) (85% vs. 18%; P less than .0001), but not among patients with moderate or severe insomnia (Insomnia Severity Index of 15 or higher) (75% vs. 66%; P = .26).
The two treatments were similarly efficacious with respect to quality of life, assessed with the Patient-Reported Outcomes Measurement Information System over the entire course of the trial, for both the physical health component (P = .4) and the mental health component (P = .36).
Dr. Mao disclosed no relevant conflicts of interest. The study received funding from the Patient-Centered Outcomes Research Institute.
SOURCE: Mao JJ et al. ASCO 2018. Abstract 10001.
REPORTING FROM ASCO 2018
Key clinical point:
Major finding: After 8 weeks of treatment, the reduction in Insomnia Severity Index was 8.3 points with acupuncture and 10.9 points with CBT-I (P = .0007).
Study details: A randomized, controlled trial among 160 survivors of diverse cancers having any degree of insomnia.
Disclosures: Dr. Mao disclosed no relevant conflicts of interest. The study received funding from the Patient-Centered Outcomes Research Institute.
Source: Mao JJ et al. ASCO 2018. Abstract 10001.
Uptake of lung cancer screening is exceedingly low
Most heavy smokers in the United States who are eligible for low-dose CT screening for lung cancer do not receive it, according to a cross-sectional study reported in a press briefing held before the annual meeting of the American Society of Clinical Oncology.
Results of the National Lung Screening Trial reported in 2011 showed a 20% reduction in lung cancer mortality with targeted low-dose CT (LDCT) screening, noted lead study author Danh C. Pham, MD, of the James Graham Brown Cancer Center at the University of Louisville (Ky.).
Since 2013, the U.S. Preventive Services Task Force has recommended this screening for people aged 55-80 years who are current or former heavy smokers, defined as having smoked at least 30 pack-years, he added. “More importantly, in 2015, the Centers for Medicare and Medicaid Services expanded Medicare coverage for LDCT for lung cancer screening,” he said.
However, results of the new study showed that nationally, only 1.9% of more than 7.6 million eligible current and former smokers underwent LDCT screening in 2016. By region, the South had one of the lowest rates, despite having the most accredited screening sites and the greatest number of eligible patients.
The findings are stark when juxtaposed with rates of screening for some other cancers, Dr. Pham maintained. For example, 65% of women aged 40 years or older underwent mammography for breast cancer screening in 2015.
“This ultimately begs the question as to the root of the disparity,” he said. “Are physicians not referring enough? Or perhaps, are eligible patients not wanting screening, even if they know a test is available? Unfortunately, controversy still exists among providers about costs and benefits of screening, while patients at risk for lung cancer also perhaps lack adequate awareness of the benefits of screening.”
It is also possible that the stigma attached to smoking, a modifiable risk factor, and thus to lung cancer screening may be a deterrent, Dr. Pham speculated. Specifically, patients may perceive screening-detected lung cancer as confirmation of a poor lifestyle choice.
“Regardless of the reason, this ultimately is a call to action on everyone’s part to increase this much-needed screening, whether that’s through creating awareness or conducting additional research, to urgently increase screening for the No. 1 cancer killer in America, as it has been now documented that effective screening can prevent nearly 12,000 premature lung cancer deaths per year,” he concluded.
Oncologists in the lung cancer field “would certainly like to be put out of business by an effective screening program,” commented ASCO President Bruce E. Johnson, MD, FASCO.
These new findings should be considered in light of the fact that the study period came only about a year after the change in reimbursement for LDCT, he noted. “So this is not a measure of the steady-state situation, but rather when this was first implemented.”
Nonetheless, it is “very disappointing” how little LDCT screening is being used, added Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute in Boston, and a leader of the center’s lung cancer program. “It should be saving 12,000 lives a year, and with this number, it’s about 250 lives. As correctly stated, there is a certain stigma whereby people who smoke feel as if they deserve it or that it’s sort of a self-punishment.”
He agreed that the findings represent a call to action. “We hope that the message will get out there, that people who fall into this risk pattern, folks who have smoked a pack of cigarettes daily for 30 years or longer, will get in and get themselves screened for lung cancer.”
What will it take?
Policy change would likely help increase uptake of LDCT lung cancer screening, according to Dr. Pham. “I think the most radical thing we could suggest based on our study so far would potentially be making lung cancer screening a national quality health measure, just the way that CMS made [mammograms for] breast cancer and colonoscopies [for colorectal cancer] national areas of improvement in 2008,” he elaborated.
“I agree that that could be an effective strategy, particularly since physicians are increasingly being required [to follow] our quality measures to optimize the reimbursement,” commented Richard L. Schilsky, MD, FACP, FASCO, chief medical officer of ASCO and press briefing moderator.
“Keep in mind that, generally speaking, screening of healthy or high-risk individuals for cancer is typically performed by primary care physicians, not by oncologists,” he further noted. “So one of the things that we also need to do is to be sure that primary care physicians are well aware of the screening data and the importance of referring the appropriate patients for screening, and are aware of screening centers available in their communities.”
Dr. Johnson said that the society has been active in that area. “ASCO is working with the American College of Physicians and some of the other primary care groups to try to get the message out about the screening,” as well as to educate them about the large potential impact of screening and treatment. “There are 15 million cancer survivors in the United States, and for the people who fit those criteria for smoking, [we need] to make certain they are getting screened.”
Study details
For the study, Dr. Pham and his colleagues used data from the American College of Radiology’s Lung Cancer Screening Registry, collecting total number of LDCTs performed in 2016 from all 1,796 accredited radiographic screening sites. They also used data from the 2015 National Health Interview Survey to estimate eligible smokers who could be screened based on the USPSTF recommendations.
Overall, 1.9% of 7,612,975 eligible current and former heavy smokers underwent LDCT, he reported. By census region, the rate was highest in the Northeast (3.5%) and lowest in the West (1.0%).
Notably, only 1.6% of eligible heavy smokers in the South underwent LDCT, even though that region had, by far, the most accredited screening sites (663) and the most eligible patients (3,072,095). The rate was highest in the Northeast, at 3.5%, even though that region had the second-lowest number of accredited screening sites (404) and the fewest eligible patients (1,152,141).
Dr. Pham disclosed no relevant conflicts of interest. The study received grant funding from the Bristol-Myers Squibb Foundation.
SOURCE: Pham DC et al. ASCO 2018. Abstract 6504.
Most heavy smokers in the United States who are eligible for low-dose CT screening for lung cancer do not receive it, according to a cross-sectional study reported in a press briefing held before the annual meeting of the American Society of Clinical Oncology.
Results of the National Lung Screening Trial reported in 2011 showed a 20% reduction in lung cancer mortality with targeted low-dose CT (LDCT) screening, noted lead study author Danh C. Pham, MD, of the James Graham Brown Cancer Center at the University of Louisville (Ky.).
Since 2013, the U.S. Preventive Services Task Force has recommended this screening for people aged 55-80 years who are current or former heavy smokers, defined as having smoked at least 30 pack-years, he added. “More importantly, in 2015, the Centers for Medicare and Medicaid Services expanded Medicare coverage for LDCT for lung cancer screening,” he said.
However, results of the new study showed that nationally, only 1.9% of more than 7.6 million eligible current and former smokers underwent LDCT screening in 2016. By region, the South had one of the lowest rates, despite having the most accredited screening sites and the greatest number of eligible patients.
The findings are stark when juxtaposed with rates of screening for some other cancers, Dr. Pham maintained. For example, 65% of women aged 40 years or older underwent mammography for breast cancer screening in 2015.
“This ultimately begs the question as to the root of the disparity,” he said. “Are physicians not referring enough? Or perhaps, are eligible patients not wanting screening, even if they know a test is available? Unfortunately, controversy still exists among providers about costs and benefits of screening, while patients at risk for lung cancer also perhaps lack adequate awareness of the benefits of screening.”
It is also possible that the stigma attached to smoking, a modifiable risk factor, and thus to lung cancer screening may be a deterrent, Dr. Pham speculated. Specifically, patients may perceive screening-detected lung cancer as confirmation of a poor lifestyle choice.
“Regardless of the reason, this ultimately is a call to action on everyone’s part to increase this much-needed screening, whether that’s through creating awareness or conducting additional research, to urgently increase screening for the No. 1 cancer killer in America, as it has been now documented that effective screening can prevent nearly 12,000 premature lung cancer deaths per year,” he concluded.
Oncologists in the lung cancer field “would certainly like to be put out of business by an effective screening program,” commented ASCO President Bruce E. Johnson, MD, FASCO.
These new findings should be considered in light of the fact that the study period came only about a year after the change in reimbursement for LDCT, he noted. “So this is not a measure of the steady-state situation, but rather when this was first implemented.”
Nonetheless, it is “very disappointing” how little LDCT screening is being used, added Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute in Boston, and a leader of the center’s lung cancer program. “It should be saving 12,000 lives a year, and with this number, it’s about 250 lives. As correctly stated, there is a certain stigma whereby people who smoke feel as if they deserve it or that it’s sort of a self-punishment.”
He agreed that the findings represent a call to action. “We hope that the message will get out there, that people who fall into this risk pattern, folks who have smoked a pack of cigarettes daily for 30 years or longer, will get in and get themselves screened for lung cancer.”
What will it take?
Policy change would likely help increase uptake of LDCT lung cancer screening, according to Dr. Pham. “I think the most radical thing we could suggest based on our study so far would potentially be making lung cancer screening a national quality health measure, just the way that CMS made [mammograms for] breast cancer and colonoscopies [for colorectal cancer] national areas of improvement in 2008,” he elaborated.
“I agree that that could be an effective strategy, particularly since physicians are increasingly being required [to follow] our quality measures to optimize the reimbursement,” commented Richard L. Schilsky, MD, FACP, FASCO, chief medical officer of ASCO and press briefing moderator.
“Keep in mind that, generally speaking, screening of healthy or high-risk individuals for cancer is typically performed by primary care physicians, not by oncologists,” he further noted. “So one of the things that we also need to do is to be sure that primary care physicians are well aware of the screening data and the importance of referring the appropriate patients for screening, and are aware of screening centers available in their communities.”
Dr. Johnson said that the society has been active in that area. “ASCO is working with the American College of Physicians and some of the other primary care groups to try to get the message out about the screening,” as well as to educate them about the large potential impact of screening and treatment. “There are 15 million cancer survivors in the United States, and for the people who fit those criteria for smoking, [we need] to make certain they are getting screened.”
Study details
For the study, Dr. Pham and his colleagues used data from the American College of Radiology’s Lung Cancer Screening Registry, collecting total number of LDCTs performed in 2016 from all 1,796 accredited radiographic screening sites. They also used data from the 2015 National Health Interview Survey to estimate eligible smokers who could be screened based on the USPSTF recommendations.
Overall, 1.9% of 7,612,975 eligible current and former heavy smokers underwent LDCT, he reported. By census region, the rate was highest in the Northeast (3.5%) and lowest in the West (1.0%).
Notably, only 1.6% of eligible heavy smokers in the South underwent LDCT, even though that region had, by far, the most accredited screening sites (663) and the most eligible patients (3,072,095). The rate was highest in the Northeast, at 3.5%, even though that region had the second-lowest number of accredited screening sites (404) and the fewest eligible patients (1,152,141).
Dr. Pham disclosed no relevant conflicts of interest. The study received grant funding from the Bristol-Myers Squibb Foundation.
SOURCE: Pham DC et al. ASCO 2018. Abstract 6504.
Most heavy smokers in the United States who are eligible for low-dose CT screening for lung cancer do not receive it, according to a cross-sectional study reported in a press briefing held before the annual meeting of the American Society of Clinical Oncology.
Results of the National Lung Screening Trial reported in 2011 showed a 20% reduction in lung cancer mortality with targeted low-dose CT (LDCT) screening, noted lead study author Danh C. Pham, MD, of the James Graham Brown Cancer Center at the University of Louisville (Ky.).
Since 2013, the U.S. Preventive Services Task Force has recommended this screening for people aged 55-80 years who are current or former heavy smokers, defined as having smoked at least 30 pack-years, he added. “More importantly, in 2015, the Centers for Medicare and Medicaid Services expanded Medicare coverage for LDCT for lung cancer screening,” he said.
However, results of the new study showed that nationally, only 1.9% of more than 7.6 million eligible current and former smokers underwent LDCT screening in 2016. By region, the South had one of the lowest rates, despite having the most accredited screening sites and the greatest number of eligible patients.
The findings are stark when juxtaposed with rates of screening for some other cancers, Dr. Pham maintained. For example, 65% of women aged 40 years or older underwent mammography for breast cancer screening in 2015.
“This ultimately begs the question as to the root of the disparity,” he said. “Are physicians not referring enough? Or perhaps, are eligible patients not wanting screening, even if they know a test is available? Unfortunately, controversy still exists among providers about costs and benefits of screening, while patients at risk for lung cancer also perhaps lack adequate awareness of the benefits of screening.”
It is also possible that the stigma attached to smoking, a modifiable risk factor, and thus to lung cancer screening may be a deterrent, Dr. Pham speculated. Specifically, patients may perceive screening-detected lung cancer as confirmation of a poor lifestyle choice.
“Regardless of the reason, this ultimately is a call to action on everyone’s part to increase this much-needed screening, whether that’s through creating awareness or conducting additional research, to urgently increase screening for the No. 1 cancer killer in America, as it has been now documented that effective screening can prevent nearly 12,000 premature lung cancer deaths per year,” he concluded.
Oncologists in the lung cancer field “would certainly like to be put out of business by an effective screening program,” commented ASCO President Bruce E. Johnson, MD, FASCO.
These new findings should be considered in light of the fact that the study period came only about a year after the change in reimbursement for LDCT, he noted. “So this is not a measure of the steady-state situation, but rather when this was first implemented.”
Nonetheless, it is “very disappointing” how little LDCT screening is being used, added Dr. Johnson, who is also a professor of medicine at the Dana-Farber Cancer Institute in Boston, and a leader of the center’s lung cancer program. “It should be saving 12,000 lives a year, and with this number, it’s about 250 lives. As correctly stated, there is a certain stigma whereby people who smoke feel as if they deserve it or that it’s sort of a self-punishment.”
He agreed that the findings represent a call to action. “We hope that the message will get out there, that people who fall into this risk pattern, folks who have smoked a pack of cigarettes daily for 30 years or longer, will get in and get themselves screened for lung cancer.”
What will it take?
Policy change would likely help increase uptake of LDCT lung cancer screening, according to Dr. Pham. “I think the most radical thing we could suggest based on our study so far would potentially be making lung cancer screening a national quality health measure, just the way that CMS made [mammograms for] breast cancer and colonoscopies [for colorectal cancer] national areas of improvement in 2008,” he elaborated.
“I agree that that could be an effective strategy, particularly since physicians are increasingly being required [to follow] our quality measures to optimize the reimbursement,” commented Richard L. Schilsky, MD, FACP, FASCO, chief medical officer of ASCO and press briefing moderator.
“Keep in mind that, generally speaking, screening of healthy or high-risk individuals for cancer is typically performed by primary care physicians, not by oncologists,” he further noted. “So one of the things that we also need to do is to be sure that primary care physicians are well aware of the screening data and the importance of referring the appropriate patients for screening, and are aware of screening centers available in their communities.”
Dr. Johnson said that the society has been active in that area. “ASCO is working with the American College of Physicians and some of the other primary care groups to try to get the message out about the screening,” as well as to educate them about the large potential impact of screening and treatment. “There are 15 million cancer survivors in the United States, and for the people who fit those criteria for smoking, [we need] to make certain they are getting screened.”
Study details
For the study, Dr. Pham and his colleagues used data from the American College of Radiology’s Lung Cancer Screening Registry, collecting total number of LDCTs performed in 2016 from all 1,796 accredited radiographic screening sites. They also used data from the 2015 National Health Interview Survey to estimate eligible smokers who could be screened based on the USPSTF recommendations.
Overall, 1.9% of 7,612,975 eligible current and former heavy smokers underwent LDCT, he reported. By census region, the rate was highest in the Northeast (3.5%) and lowest in the West (1.0%).
Notably, only 1.6% of eligible heavy smokers in the South underwent LDCT, even though that region had, by far, the most accredited screening sites (663) and the most eligible patients (3,072,095). The rate was highest in the Northeast, at 3.5%, even though that region had the second-lowest number of accredited screening sites (404) and the fewest eligible patients (1,152,141).
Dr. Pham disclosed no relevant conflicts of interest. The study received grant funding from the Bristol-Myers Squibb Foundation.
SOURCE: Pham DC et al. ASCO 2018. Abstract 6504.
REPORTING FROM ASCO 2018
Key clinical point: The rate of lung cancer screening among eligible patients is overall very low.
Major finding: Just 1.9% of estimated, eligible current and former heavy smokers in the United States underwent low-dose CT screening for lung cancer in 2016.
Study details: Nationwide, cross-sectional cohort study of screening among an estimated 7,612,975 eligible smokers.
Disclosures: Dr. Pham disclosed no relevant conflicts of interest. The study received grant funding from the Bristol-Myers Squibb Foundation.
Source: Pham DC et al. ASCO 2018. Abstract 6504.