User login
The Amygdala Know
In a recent issue of Pediatric News, the Child Psychiatry Consult column featured an excellent discussion by Dr. David Rettew of some new research into a possible association between excessive crying in infancy and emotional problems later in childhood. This longitudinal study of almost 5,000 children included an assessment at 3 months and an MRI at age 10, which found that the infants who were excessive criers also had smaller amygdala. While the orders of magnitude of the researchers’ observations is small, it is interesting that the mothers of excessive criers were slightly more likely to experience mental health problems.
Dr. Rettew wisely cautions us to take note of this study’s findings but avoid overreacting. If indeed excessive crying in infancy is a marker for future problems, at the moment we may want to increase our efforts in helping parents improve their parenting skills using a nonjudgmental approach.
Using Dr. Rettew’s sage advice as a leaping off point, I will add the reminder that we must continue to meet head on the venerable myth that “colic” is a gastrointestinal problem. We must promise to never code out a parental complaint as “colic.” If we want to label it “excessive crying of infancy,” that’s one thing, but using “colic” only serves to perpetuate the myth and all the old, and sometimes dangerous, remedies that continue to cling to it.
Whether we use the term “colicky behavior” or call it “excessive crying,” we must remember these are merely descriptive terms. We have not made a diagnosis and are obligated to keep our minds open to serious and life-threatening conditions that make infants cry excessively — aberrant coronary arteries and urinary obstructions to name just two.
I can’t leave the phenomenon of colic without adding a nickel to the two cents I have already gifted you. When I was in medical school, I am sure I was told something about the amygdala. But, I suspect that I was only expected to recall where it lived. In the 50+ years since that brief encounter, other folks have learned much more. Prompted by this study, I searched what is known about small amygdala. Turns out that sleep deprivation has been associated with smaller amygdala, as has episodic migraine headaches, both in adults.
Regular readers of Letters from Maine can already smell where this is going. For decades I have believed that both excessive crying in infancy and episodic migraine in children are associated with, and my bias would say “caused” by, sleep deprivation. We learned from this study that mothers of excessively crying infants are more likely to have mental health problems. And, I will add that at least one study has shown that mothers and fathers of excessively crying infants are more likely to suffer from migraines.
Whether you join me in my biased interpretation isn’t important. What this study tells us is that there is likely to be something going on in infancy that may be a marker for future mental health problems. Were these children born with small or vulnerable amygdala? Did poor sleep hygiene contribute to the problem by interfering with the growth of their amygdala? I can envision studies that could provide some clarity. I’m not sure many parents would agree to have their happy and well-slept 3-month-olds slid into an MRI tube to serve as controls. But, I wouldn’t be surprised that we could find a sizable number of sleep deprived and frazzled parents of colicky infants who would agree if we told them it might help find an answer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In a recent issue of Pediatric News, the Child Psychiatry Consult column featured an excellent discussion by Dr. David Rettew of some new research into a possible association between excessive crying in infancy and emotional problems later in childhood. This longitudinal study of almost 5,000 children included an assessment at 3 months and an MRI at age 10, which found that the infants who were excessive criers also had smaller amygdala. While the orders of magnitude of the researchers’ observations is small, it is interesting that the mothers of excessive criers were slightly more likely to experience mental health problems.
Dr. Rettew wisely cautions us to take note of this study’s findings but avoid overreacting. If indeed excessive crying in infancy is a marker for future problems, at the moment we may want to increase our efforts in helping parents improve their parenting skills using a nonjudgmental approach.
Using Dr. Rettew’s sage advice as a leaping off point, I will add the reminder that we must continue to meet head on the venerable myth that “colic” is a gastrointestinal problem. We must promise to never code out a parental complaint as “colic.” If we want to label it “excessive crying of infancy,” that’s one thing, but using “colic” only serves to perpetuate the myth and all the old, and sometimes dangerous, remedies that continue to cling to it.
Whether we use the term “colicky behavior” or call it “excessive crying,” we must remember these are merely descriptive terms. We have not made a diagnosis and are obligated to keep our minds open to serious and life-threatening conditions that make infants cry excessively — aberrant coronary arteries and urinary obstructions to name just two.
I can’t leave the phenomenon of colic without adding a nickel to the two cents I have already gifted you. When I was in medical school, I am sure I was told something about the amygdala. But, I suspect that I was only expected to recall where it lived. In the 50+ years since that brief encounter, other folks have learned much more. Prompted by this study, I searched what is known about small amygdala. Turns out that sleep deprivation has been associated with smaller amygdala, as has episodic migraine headaches, both in adults.
Regular readers of Letters from Maine can already smell where this is going. For decades I have believed that both excessive crying in infancy and episodic migraine in children are associated with, and my bias would say “caused” by, sleep deprivation. We learned from this study that mothers of excessively crying infants are more likely to have mental health problems. And, I will add that at least one study has shown that mothers and fathers of excessively crying infants are more likely to suffer from migraines.
Whether you join me in my biased interpretation isn’t important. What this study tells us is that there is likely to be something going on in infancy that may be a marker for future mental health problems. Were these children born with small or vulnerable amygdala? Did poor sleep hygiene contribute to the problem by interfering with the growth of their amygdala? I can envision studies that could provide some clarity. I’m not sure many parents would agree to have their happy and well-slept 3-month-olds slid into an MRI tube to serve as controls. But, I wouldn’t be surprised that we could find a sizable number of sleep deprived and frazzled parents of colicky infants who would agree if we told them it might help find an answer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In a recent issue of Pediatric News, the Child Psychiatry Consult column featured an excellent discussion by Dr. David Rettew of some new research into a possible association between excessive crying in infancy and emotional problems later in childhood. This longitudinal study of almost 5,000 children included an assessment at 3 months and an MRI at age 10, which found that the infants who were excessive criers also had smaller amygdala. While the orders of magnitude of the researchers’ observations is small, it is interesting that the mothers of excessive criers were slightly more likely to experience mental health problems.
Dr. Rettew wisely cautions us to take note of this study’s findings but avoid overreacting. If indeed excessive crying in infancy is a marker for future problems, at the moment we may want to increase our efforts in helping parents improve their parenting skills using a nonjudgmental approach.
Using Dr. Rettew’s sage advice as a leaping off point, I will add the reminder that we must continue to meet head on the venerable myth that “colic” is a gastrointestinal problem. We must promise to never code out a parental complaint as “colic.” If we want to label it “excessive crying of infancy,” that’s one thing, but using “colic” only serves to perpetuate the myth and all the old, and sometimes dangerous, remedies that continue to cling to it.
Whether we use the term “colicky behavior” or call it “excessive crying,” we must remember these are merely descriptive terms. We have not made a diagnosis and are obligated to keep our minds open to serious and life-threatening conditions that make infants cry excessively — aberrant coronary arteries and urinary obstructions to name just two.
I can’t leave the phenomenon of colic without adding a nickel to the two cents I have already gifted you. When I was in medical school, I am sure I was told something about the amygdala. But, I suspect that I was only expected to recall where it lived. In the 50+ years since that brief encounter, other folks have learned much more. Prompted by this study, I searched what is known about small amygdala. Turns out that sleep deprivation has been associated with smaller amygdala, as has episodic migraine headaches, both in adults.
Regular readers of Letters from Maine can already smell where this is going. For decades I have believed that both excessive crying in infancy and episodic migraine in children are associated with, and my bias would say “caused” by, sleep deprivation. We learned from this study that mothers of excessively crying infants are more likely to have mental health problems. And, I will add that at least one study has shown that mothers and fathers of excessively crying infants are more likely to suffer from migraines.
Whether you join me in my biased interpretation isn’t important. What this study tells us is that there is likely to be something going on in infancy that may be a marker for future mental health problems. Were these children born with small or vulnerable amygdala? Did poor sleep hygiene contribute to the problem by interfering with the growth of their amygdala? I can envision studies that could provide some clarity. I’m not sure many parents would agree to have their happy and well-slept 3-month-olds slid into an MRI tube to serve as controls. But, I wouldn’t be surprised that we could find a sizable number of sleep deprived and frazzled parents of colicky infants who would agree if we told them it might help find an answer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Adequate Transition of Epilepsy Care from Pediatric to Adult Is Often Lacking
, according to a recent survey. Many respondents received little to no information regarding the process, and many adults were still receiving care from family physicians or pediatric neurologists. The study was published online in Epilepsy & Behavior.
Room for Improvement
“We are not doing as good a job with planning for transition as we should,” said Elaine C. Wirrell, MD, who was not involved with the study. “It is not just a simple issue of sending your patient to an adult neurologist. Transition is a process that happens over time, so we need to do a better job getting our families ready for moving on to an adult provider.” Dr. Wirrell is director of pediatric epilepsy and professor of neurology at the Mayo Clinic in Rochester, Minnesota.
Clumsy Transitions
Investigators distributed a 25-question survey to patients and caregivers who attended the 2019 Epilepsy Awareness Day at Disneyland, and through online support groups in North America. Among 58 responses, 32 came from patients between ages 12 and 17 years or their caregivers.
Despite attempts to recruit a diverse cross-section of respondents, most patients had severe epilepsy and comorbidities: 43% had daily or weekly seizures; 45% were on three or more antiseizure medications; and 74% had intellectual disabilities.
Many children with early-life epilepsies suffer from developmental and epileptic encephalopathy, which has associated non-seizure symptoms including learning challenges, behavioral issues, and other medical concerns, Dr. Wirrell said. Therefore, she said, finding a neurologist who treats adults — and has the expertise and interest to care for such patients — can be difficult.
“We’re seeing many patients not making that transition, or maybe not making it appropriately, so they’re not necessarily getting to the providers who have the most expertise in managing their epilepsy.” Among adults surveyed, 27% were still being followed by pediatric neurologists, and 35% were visiting family doctors for epilepsy-related treatment.
Because the needs of children with complex epilepsy can extend well beyond neurology, Dr. Wirrell added, managing such cases often requires multidisciplinary pediatric teams. “Finding that team on the adult side is more challenging.” As a result, she said, patients may transfer their neurology care without getting additional support for comorbidities such as mood disorders and learning disabilities.
The foregoing challenges are complicated by the fact that pediatric neurologists often lack the time (and in the United States, reimbursement) to adequately address the transition process, said Dr. Wirrell. Providers in freestanding children’s hospitals may face additional challenges coordinating with adult-care providers outside their facilities, she said.
“There’s also potentially a reluctance of both families and physicians to transition the patient on, because there’s concern that maybe there isn’t anybody on the adult side who is able to do as good a job as what they have on the pediatric side.”
Well-Coordinated Transitions Should Have No Surprises
Transition should be a planned, independence-promoting process that results in smooth, well-coordinated movement of pediatric patients into adult care — one without surprises or disconnections, the authors wrote. However, 55% of respondents never heard the term “transition” from any provider, even though 69% of patients were being treated in academic specialty centers.
Among 12- to 17-year-olds, 72% had never discussed transition with their healthcare team. That figure includes no 17-year-olds. Approximately 90% of respondents said they received sufficient time during healthcare visits, but 54% reported feeling stressed when moving from pediatric to adult care.
Given resource constraints in many pediatric epilepsy programs, the study authors recommended patient-empowerment tools such as a transition toolkit to help patients and families navigate the transition process even in places without formal transition programs.
“Many of these children are coming over with boatloads of medical records,” Dr. Wirrell said. “It’s not fair to the adult provider, who then has to go through all those records.” Instead, she said, pediatric teams should provide succinct summaries of relevant test results, medication side effects, prior treatments tried, and the like. “Those summaries are critically important so that we can get information to the person who needs it.”
Although successful transition requires significant coordination, she added, much of the process can often be handled by nonphysicians. “There are some very good nurse-led transition programs. Often, we can have a nurse providing education to the family and even potentially having a joint visit with an adult epilepsy nurse for complex patients.”
Pediatric providers also must know when to begin the transition process, Dr. Wirrell said. As soon as patients are 13 or 14 years old, she suggested discussing the process with them and their families every 6 to 12 months, covering specifics ranging from how to order medications to why adult patients may need power of attorney designees.
On a broader scale, said Dr. Wirrell, a smooth handoff requires planning. Fortunately, she said, the topic is becoming a significant priority for a growing number of children’s hospitals specific not only to epilepsy, but also to other chronic illnesses.
Dr. Wirrell is co–editor-in-chief for epilepsy.com. She reports no relevant financial interests.
, according to a recent survey. Many respondents received little to no information regarding the process, and many adults were still receiving care from family physicians or pediatric neurologists. The study was published online in Epilepsy & Behavior.
Room for Improvement
“We are not doing as good a job with planning for transition as we should,” said Elaine C. Wirrell, MD, who was not involved with the study. “It is not just a simple issue of sending your patient to an adult neurologist. Transition is a process that happens over time, so we need to do a better job getting our families ready for moving on to an adult provider.” Dr. Wirrell is director of pediatric epilepsy and professor of neurology at the Mayo Clinic in Rochester, Minnesota.
Clumsy Transitions
Investigators distributed a 25-question survey to patients and caregivers who attended the 2019 Epilepsy Awareness Day at Disneyland, and through online support groups in North America. Among 58 responses, 32 came from patients between ages 12 and 17 years or their caregivers.
Despite attempts to recruit a diverse cross-section of respondents, most patients had severe epilepsy and comorbidities: 43% had daily or weekly seizures; 45% were on three or more antiseizure medications; and 74% had intellectual disabilities.
Many children with early-life epilepsies suffer from developmental and epileptic encephalopathy, which has associated non-seizure symptoms including learning challenges, behavioral issues, and other medical concerns, Dr. Wirrell said. Therefore, she said, finding a neurologist who treats adults — and has the expertise and interest to care for such patients — can be difficult.
“We’re seeing many patients not making that transition, or maybe not making it appropriately, so they’re not necessarily getting to the providers who have the most expertise in managing their epilepsy.” Among adults surveyed, 27% were still being followed by pediatric neurologists, and 35% were visiting family doctors for epilepsy-related treatment.
Because the needs of children with complex epilepsy can extend well beyond neurology, Dr. Wirrell added, managing such cases often requires multidisciplinary pediatric teams. “Finding that team on the adult side is more challenging.” As a result, she said, patients may transfer their neurology care without getting additional support for comorbidities such as mood disorders and learning disabilities.
The foregoing challenges are complicated by the fact that pediatric neurologists often lack the time (and in the United States, reimbursement) to adequately address the transition process, said Dr. Wirrell. Providers in freestanding children’s hospitals may face additional challenges coordinating with adult-care providers outside their facilities, she said.
“There’s also potentially a reluctance of both families and physicians to transition the patient on, because there’s concern that maybe there isn’t anybody on the adult side who is able to do as good a job as what they have on the pediatric side.”
Well-Coordinated Transitions Should Have No Surprises
Transition should be a planned, independence-promoting process that results in smooth, well-coordinated movement of pediatric patients into adult care — one without surprises or disconnections, the authors wrote. However, 55% of respondents never heard the term “transition” from any provider, even though 69% of patients were being treated in academic specialty centers.
Among 12- to 17-year-olds, 72% had never discussed transition with their healthcare team. That figure includes no 17-year-olds. Approximately 90% of respondents said they received sufficient time during healthcare visits, but 54% reported feeling stressed when moving from pediatric to adult care.
Given resource constraints in many pediatric epilepsy programs, the study authors recommended patient-empowerment tools such as a transition toolkit to help patients and families navigate the transition process even in places without formal transition programs.
“Many of these children are coming over with boatloads of medical records,” Dr. Wirrell said. “It’s not fair to the adult provider, who then has to go through all those records.” Instead, she said, pediatric teams should provide succinct summaries of relevant test results, medication side effects, prior treatments tried, and the like. “Those summaries are critically important so that we can get information to the person who needs it.”
Although successful transition requires significant coordination, she added, much of the process can often be handled by nonphysicians. “There are some very good nurse-led transition programs. Often, we can have a nurse providing education to the family and even potentially having a joint visit with an adult epilepsy nurse for complex patients.”
Pediatric providers also must know when to begin the transition process, Dr. Wirrell said. As soon as patients are 13 or 14 years old, she suggested discussing the process with them and their families every 6 to 12 months, covering specifics ranging from how to order medications to why adult patients may need power of attorney designees.
On a broader scale, said Dr. Wirrell, a smooth handoff requires planning. Fortunately, she said, the topic is becoming a significant priority for a growing number of children’s hospitals specific not only to epilepsy, but also to other chronic illnesses.
Dr. Wirrell is co–editor-in-chief for epilepsy.com. She reports no relevant financial interests.
, according to a recent survey. Many respondents received little to no information regarding the process, and many adults were still receiving care from family physicians or pediatric neurologists. The study was published online in Epilepsy & Behavior.
Room for Improvement
“We are not doing as good a job with planning for transition as we should,” said Elaine C. Wirrell, MD, who was not involved with the study. “It is not just a simple issue of sending your patient to an adult neurologist. Transition is a process that happens over time, so we need to do a better job getting our families ready for moving on to an adult provider.” Dr. Wirrell is director of pediatric epilepsy and professor of neurology at the Mayo Clinic in Rochester, Minnesota.
Clumsy Transitions
Investigators distributed a 25-question survey to patients and caregivers who attended the 2019 Epilepsy Awareness Day at Disneyland, and through online support groups in North America. Among 58 responses, 32 came from patients between ages 12 and 17 years or their caregivers.
Despite attempts to recruit a diverse cross-section of respondents, most patients had severe epilepsy and comorbidities: 43% had daily or weekly seizures; 45% were on three or more antiseizure medications; and 74% had intellectual disabilities.
Many children with early-life epilepsies suffer from developmental and epileptic encephalopathy, which has associated non-seizure symptoms including learning challenges, behavioral issues, and other medical concerns, Dr. Wirrell said. Therefore, she said, finding a neurologist who treats adults — and has the expertise and interest to care for such patients — can be difficult.
“We’re seeing many patients not making that transition, or maybe not making it appropriately, so they’re not necessarily getting to the providers who have the most expertise in managing their epilepsy.” Among adults surveyed, 27% were still being followed by pediatric neurologists, and 35% were visiting family doctors for epilepsy-related treatment.
Because the needs of children with complex epilepsy can extend well beyond neurology, Dr. Wirrell added, managing such cases often requires multidisciplinary pediatric teams. “Finding that team on the adult side is more challenging.” As a result, she said, patients may transfer their neurology care without getting additional support for comorbidities such as mood disorders and learning disabilities.
The foregoing challenges are complicated by the fact that pediatric neurologists often lack the time (and in the United States, reimbursement) to adequately address the transition process, said Dr. Wirrell. Providers in freestanding children’s hospitals may face additional challenges coordinating with adult-care providers outside their facilities, she said.
“There’s also potentially a reluctance of both families and physicians to transition the patient on, because there’s concern that maybe there isn’t anybody on the adult side who is able to do as good a job as what they have on the pediatric side.”
Well-Coordinated Transitions Should Have No Surprises
Transition should be a planned, independence-promoting process that results in smooth, well-coordinated movement of pediatric patients into adult care — one without surprises or disconnections, the authors wrote. However, 55% of respondents never heard the term “transition” from any provider, even though 69% of patients were being treated in academic specialty centers.
Among 12- to 17-year-olds, 72% had never discussed transition with their healthcare team. That figure includes no 17-year-olds. Approximately 90% of respondents said they received sufficient time during healthcare visits, but 54% reported feeling stressed when moving from pediatric to adult care.
Given resource constraints in many pediatric epilepsy programs, the study authors recommended patient-empowerment tools such as a transition toolkit to help patients and families navigate the transition process even in places without formal transition programs.
“Many of these children are coming over with boatloads of medical records,” Dr. Wirrell said. “It’s not fair to the adult provider, who then has to go through all those records.” Instead, she said, pediatric teams should provide succinct summaries of relevant test results, medication side effects, prior treatments tried, and the like. “Those summaries are critically important so that we can get information to the person who needs it.”
Although successful transition requires significant coordination, she added, much of the process can often be handled by nonphysicians. “There are some very good nurse-led transition programs. Often, we can have a nurse providing education to the family and even potentially having a joint visit with an adult epilepsy nurse for complex patients.”
Pediatric providers also must know when to begin the transition process, Dr. Wirrell said. As soon as patients are 13 or 14 years old, she suggested discussing the process with them and their families every 6 to 12 months, covering specifics ranging from how to order medications to why adult patients may need power of attorney designees.
On a broader scale, said Dr. Wirrell, a smooth handoff requires planning. Fortunately, she said, the topic is becoming a significant priority for a growing number of children’s hospitals specific not only to epilepsy, but also to other chronic illnesses.
Dr. Wirrell is co–editor-in-chief for epilepsy.com. She reports no relevant financial interests.
FROM EPILEPSY & BEHAVIOR
Bone Mineral Density Higher in Children Living Near Green Areas
A recently published prospective study in JAMA Network Open identified a significant association between children’s bone health and their proximity to green areas.
The literature emphasized the benefits of childhood exposure to green spaces for neurocognitive, social, behavioral, and mental development, as well as well-being. In addition, such exposure is linked to lower body mass index, increased physical activity, and reduced risks for overweight, obesity, and hypertension. However, specific data on bone mineral density implications are limited.
To address this gap, Hanne Sleurs, PhD, a researcher at the Universiteit Hasselt in Belgium, and colleagues followed the bone health of 327 participants from birth to 4-6 years and examined correlations with individuals’ exposure to green areas. Data collection occurred from October 2014 to July 2021.
Green spaces were categorized as high (vegetation height > 3 m), low (vegetation height ≤ 3 m), and mixed (combination of both). The distances of green spaces from participants’ residences ranged from a radius of 100 m to 3 km. Radial bone mineral density assessment was conducted using quantitative ultrasound during follow-up consultations.
The scientists found that participants frequently exposed to high and mixed vegetation areas within a 500-m radius of their homes had significantly higher bone mineral density than those at other distances or those frequenting spaces with different vegetation. In addition, access to larger green spaces with mixed and high vegetation within a 1-km radius was significantly associated with a lower likelihood of low bone density in children.
“These findings illustrate the positive impact on bone health of early childhood exposure to green areas near their homes during critical growth and development periods, with long-term implications,” wrote the researchers.
The results aligned with those of a prior study in which authors noted factors contributing to families’ frequent park visits, including shorter distances, safety, and park organization, as well as the natural diversity and activities offered.
One hypothesis explaining improved bone density in children visiting green areas was increased physical activity practiced in these locations. The mechanical load from exercise can activate signaling pathways favoring bone development. Literature also gathered data on the influence of green areas on young populations engaging in physical activities, showing positive outcomes.
According to the study authors, the findings are crucial for public health because they emphasize the need for urban investments in accessible green spaces as a strategy for fracture and osteoporosis prevention. In the long term, such initiatives translate to reduced public health expenses, along with physical and emotional gains in communities adopting environmental strategies, they concluded.
This article was translated from the Medscape Portuguese edition. A version of this article appeared on Medscape.com.
A recently published prospective study in JAMA Network Open identified a significant association between children’s bone health and their proximity to green areas.
The literature emphasized the benefits of childhood exposure to green spaces for neurocognitive, social, behavioral, and mental development, as well as well-being. In addition, such exposure is linked to lower body mass index, increased physical activity, and reduced risks for overweight, obesity, and hypertension. However, specific data on bone mineral density implications are limited.
To address this gap, Hanne Sleurs, PhD, a researcher at the Universiteit Hasselt in Belgium, and colleagues followed the bone health of 327 participants from birth to 4-6 years and examined correlations with individuals’ exposure to green areas. Data collection occurred from October 2014 to July 2021.
Green spaces were categorized as high (vegetation height > 3 m), low (vegetation height ≤ 3 m), and mixed (combination of both). The distances of green spaces from participants’ residences ranged from a radius of 100 m to 3 km. Radial bone mineral density assessment was conducted using quantitative ultrasound during follow-up consultations.
The scientists found that participants frequently exposed to high and mixed vegetation areas within a 500-m radius of their homes had significantly higher bone mineral density than those at other distances or those frequenting spaces with different vegetation. In addition, access to larger green spaces with mixed and high vegetation within a 1-km radius was significantly associated with a lower likelihood of low bone density in children.
“These findings illustrate the positive impact on bone health of early childhood exposure to green areas near their homes during critical growth and development periods, with long-term implications,” wrote the researchers.
The results aligned with those of a prior study in which authors noted factors contributing to families’ frequent park visits, including shorter distances, safety, and park organization, as well as the natural diversity and activities offered.
One hypothesis explaining improved bone density in children visiting green areas was increased physical activity practiced in these locations. The mechanical load from exercise can activate signaling pathways favoring bone development. Literature also gathered data on the influence of green areas on young populations engaging in physical activities, showing positive outcomes.
According to the study authors, the findings are crucial for public health because they emphasize the need for urban investments in accessible green spaces as a strategy for fracture and osteoporosis prevention. In the long term, such initiatives translate to reduced public health expenses, along with physical and emotional gains in communities adopting environmental strategies, they concluded.
This article was translated from the Medscape Portuguese edition. A version of this article appeared on Medscape.com.
A recently published prospective study in JAMA Network Open identified a significant association between children’s bone health and their proximity to green areas.
The literature emphasized the benefits of childhood exposure to green spaces for neurocognitive, social, behavioral, and mental development, as well as well-being. In addition, such exposure is linked to lower body mass index, increased physical activity, and reduced risks for overweight, obesity, and hypertension. However, specific data on bone mineral density implications are limited.
To address this gap, Hanne Sleurs, PhD, a researcher at the Universiteit Hasselt in Belgium, and colleagues followed the bone health of 327 participants from birth to 4-6 years and examined correlations with individuals’ exposure to green areas. Data collection occurred from October 2014 to July 2021.
Green spaces were categorized as high (vegetation height > 3 m), low (vegetation height ≤ 3 m), and mixed (combination of both). The distances of green spaces from participants’ residences ranged from a radius of 100 m to 3 km. Radial bone mineral density assessment was conducted using quantitative ultrasound during follow-up consultations.
The scientists found that participants frequently exposed to high and mixed vegetation areas within a 500-m radius of their homes had significantly higher bone mineral density than those at other distances or those frequenting spaces with different vegetation. In addition, access to larger green spaces with mixed and high vegetation within a 1-km radius was significantly associated with a lower likelihood of low bone density in children.
“These findings illustrate the positive impact on bone health of early childhood exposure to green areas near their homes during critical growth and development periods, with long-term implications,” wrote the researchers.
The results aligned with those of a prior study in which authors noted factors contributing to families’ frequent park visits, including shorter distances, safety, and park organization, as well as the natural diversity and activities offered.
One hypothesis explaining improved bone density in children visiting green areas was increased physical activity practiced in these locations. The mechanical load from exercise can activate signaling pathways favoring bone development. Literature also gathered data on the influence of green areas on young populations engaging in physical activities, showing positive outcomes.
According to the study authors, the findings are crucial for public health because they emphasize the need for urban investments in accessible green spaces as a strategy for fracture and osteoporosis prevention. In the long term, such initiatives translate to reduced public health expenses, along with physical and emotional gains in communities adopting environmental strategies, they concluded.
This article was translated from the Medscape Portuguese edition. A version of this article appeared on Medscape.com.
Treatment Sequence May Impact Pancreatic Cancer Survival
TOPLINE:
METHODOLOGY:
- Despite therapeutic advances, survival among patients with unresectable and/or metastatic pancreatic ductal adenocarcinoma has not markedly improved in recent years.
- In the current analysis, researchers evaluated whether treatment sequence could affect survival outcomes in this patient population.
- To this end , researchers conducted a single institution, retrospective analysis of patients who received different lines of treatment between January 2015 and December 2021.
- The most common first-line therapy was nab-paclitaxel plus S-1 (58%), followed by FOLFIRINOX (10%), nab-paclitaxel plus gemcitabine (8%), gemcitabine alone (7%), gemcitabine plus oxaliplatin (6%); second-line therapies, in order of frequency, included gemcitabine combination therapy (48%), nab-paclitaxel combination therapy (19%), FOLFIRINOX (10%), and gemcitabine alone (7%); third-line treatments consisted of FOLFIRINOX (31%), irinotecan or oxaliplatin combination therapy (23%), immunotherapy (19%), and gemcitabine combination therapy (10%).
TAKEAWAY:
- Overall, progression occurred in 90% of patients, and the median overall survival was 12.0 months, with only 48% of patients able to start a third-line therapy.
- The researchers focused on three common therapy sequences: nab-paclitaxel plus gemcitabine or nab-paclitaxel combination therapy as first-line and FOLFIRINOX as second-line (line A); nab-paclitaxel combination therapy to gemcitabine combination therapy to FOLFIRINOX (line B); and nab-paclitaxel combination therapy, to gemcitabine combination therapy, to oxaliplatin or irinotecan combination therapy (line C).
- Overall, the researchers observed a median overall survival of 14 months among patients receiving line A and C sequences and 18 months with line B.
- Patients receiving line B therapy demonstrated a 52% lower risk for death compared with those receiving line A treatment (hazard ratio [HR], 0.48; P = .018) and a 75% reduced risk for death compared with those on the line C sequence (HR, 0.25; P = .040).
IN PRACTICE:
“Our study provides real-world evidence for the effectiveness of different treatment sequences and underscores the [impact of] treatment sequences on survival outcome when considering the entire management in advanced pancreatic ductal adenocarcinoma,” the authors concluded.
SOURCE:
The study, led by Guanghai Dai, MD, from the Chinese People’s Liberation Army General Hospital, Beijing, was published in BMC Cancer on January 12, 2024.
LIMITATIONS:
The study was a single-center, retrospective analysis.
DISCLOSURES:
The paper was funded by Beijing natural science foundation. The authors did not declare any relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Despite therapeutic advances, survival among patients with unresectable and/or metastatic pancreatic ductal adenocarcinoma has not markedly improved in recent years.
- In the current analysis, researchers evaluated whether treatment sequence could affect survival outcomes in this patient population.
- To this end , researchers conducted a single institution, retrospective analysis of patients who received different lines of treatment between January 2015 and December 2021.
- The most common first-line therapy was nab-paclitaxel plus S-1 (58%), followed by FOLFIRINOX (10%), nab-paclitaxel plus gemcitabine (8%), gemcitabine alone (7%), gemcitabine plus oxaliplatin (6%); second-line therapies, in order of frequency, included gemcitabine combination therapy (48%), nab-paclitaxel combination therapy (19%), FOLFIRINOX (10%), and gemcitabine alone (7%); third-line treatments consisted of FOLFIRINOX (31%), irinotecan or oxaliplatin combination therapy (23%), immunotherapy (19%), and gemcitabine combination therapy (10%).
TAKEAWAY:
- Overall, progression occurred in 90% of patients, and the median overall survival was 12.0 months, with only 48% of patients able to start a third-line therapy.
- The researchers focused on three common therapy sequences: nab-paclitaxel plus gemcitabine or nab-paclitaxel combination therapy as first-line and FOLFIRINOX as second-line (line A); nab-paclitaxel combination therapy to gemcitabine combination therapy to FOLFIRINOX (line B); and nab-paclitaxel combination therapy, to gemcitabine combination therapy, to oxaliplatin or irinotecan combination therapy (line C).
- Overall, the researchers observed a median overall survival of 14 months among patients receiving line A and C sequences and 18 months with line B.
- Patients receiving line B therapy demonstrated a 52% lower risk for death compared with those receiving line A treatment (hazard ratio [HR], 0.48; P = .018) and a 75% reduced risk for death compared with those on the line C sequence (HR, 0.25; P = .040).
IN PRACTICE:
“Our study provides real-world evidence for the effectiveness of different treatment sequences and underscores the [impact of] treatment sequences on survival outcome when considering the entire management in advanced pancreatic ductal adenocarcinoma,” the authors concluded.
SOURCE:
The study, led by Guanghai Dai, MD, from the Chinese People’s Liberation Army General Hospital, Beijing, was published in BMC Cancer on January 12, 2024.
LIMITATIONS:
The study was a single-center, retrospective analysis.
DISCLOSURES:
The paper was funded by Beijing natural science foundation. The authors did not declare any relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Despite therapeutic advances, survival among patients with unresectable and/or metastatic pancreatic ductal adenocarcinoma has not markedly improved in recent years.
- In the current analysis, researchers evaluated whether treatment sequence could affect survival outcomes in this patient population.
- To this end , researchers conducted a single institution, retrospective analysis of patients who received different lines of treatment between January 2015 and December 2021.
- The most common first-line therapy was nab-paclitaxel plus S-1 (58%), followed by FOLFIRINOX (10%), nab-paclitaxel plus gemcitabine (8%), gemcitabine alone (7%), gemcitabine plus oxaliplatin (6%); second-line therapies, in order of frequency, included gemcitabine combination therapy (48%), nab-paclitaxel combination therapy (19%), FOLFIRINOX (10%), and gemcitabine alone (7%); third-line treatments consisted of FOLFIRINOX (31%), irinotecan or oxaliplatin combination therapy (23%), immunotherapy (19%), and gemcitabine combination therapy (10%).
TAKEAWAY:
- Overall, progression occurred in 90% of patients, and the median overall survival was 12.0 months, with only 48% of patients able to start a third-line therapy.
- The researchers focused on three common therapy sequences: nab-paclitaxel plus gemcitabine or nab-paclitaxel combination therapy as first-line and FOLFIRINOX as second-line (line A); nab-paclitaxel combination therapy to gemcitabine combination therapy to FOLFIRINOX (line B); and nab-paclitaxel combination therapy, to gemcitabine combination therapy, to oxaliplatin or irinotecan combination therapy (line C).
- Overall, the researchers observed a median overall survival of 14 months among patients receiving line A and C sequences and 18 months with line B.
- Patients receiving line B therapy demonstrated a 52% lower risk for death compared with those receiving line A treatment (hazard ratio [HR], 0.48; P = .018) and a 75% reduced risk for death compared with those on the line C sequence (HR, 0.25; P = .040).
IN PRACTICE:
“Our study provides real-world evidence for the effectiveness of different treatment sequences and underscores the [impact of] treatment sequences on survival outcome when considering the entire management in advanced pancreatic ductal adenocarcinoma,” the authors concluded.
SOURCE:
The study, led by Guanghai Dai, MD, from the Chinese People’s Liberation Army General Hospital, Beijing, was published in BMC Cancer on January 12, 2024.
LIMITATIONS:
The study was a single-center, retrospective analysis.
DISCLOSURES:
The paper was funded by Beijing natural science foundation. The authors did not declare any relevant financial relationships.
A version of this article appeared on Medscape.com.
Ob.Gyns. Face ‘Occupational Crisis’ Navigating Abortion Ban
A 14-year-old girl arrived at a South Carolina clinic just one day after the state’s anti-abortion law would have allowed her to terminate a pregnancy in instances of rape or incest.
Angela Dempsey-Fanning, MD, MPH, an ob.gyn. in Charleston, had to inform the teenager, a victim of incest, that she could not legally provide abortion care, so the girl and her mother decided to seek treatment in a different state.
“I couldn’t shake the sense that so many principles of medical ethics were being violated in denying care to her,” said Dr. Dempsey-Fanning, president of the Society of Family Planning, a nonprofit that advocates for abortion access. “When I interact with patients in these situations ... I carry the emotional and mental burden for weeks.”
South Carolina is one of 16 states to put in place severe abortion restrictions in the wake of the US Supreme Court ruling in June 2022 on the Dobbs v. Jackson Women’s Health Organization case that overturned Roe v. Wade.
according to a study recently published in the JAMA Network Open.
Public discourse on the Dobbs v. Jackson ruling has mostly centered on the impact to patients, according to Mara Buchbinder, PhD, professor and vice chair in the Department of Social Medicine at University of North Carolina Chapel Hill School of Medicine, and a coauthor of the study.
“We were interested in what the impacts would be for the obstetric workforce as well,” she said.
In 2022 and 2023, Dr. Buchbinder and her colleagues interviewed 54 ob.gyns. practicing in 13 states where abortion had become illegal with limited exceptions, including Texas, West Virginia, and South Dakota.
Clinicians who participated in the study described instances in which the state restrictions on abortion forced them to delay what they deemed to be medically necessary care until a patient faced severe complications or even death. More than 90% reported moral distress concerning situations where legal constraints prevented them or their colleagues from following clinical standards.
“You have somebody hemorrhaging with an intrauterine pregnancy with a heartbeat ... I [didn’t yet] have legal coverage for that, but there’s only so many times you can transfuse somebody and they’re begging for their life before you say, ‘This is unconscionable,’ ” one clinician reported to researchers.
Another clinician said, “Is a 5% risk of death enough? Does it take 20%? Does it take 50%? What is enough legally?”
The US Department of Health and Human Services has announced a new team to ensure hospitals in all states comply with the Emergency Medical Treatment and Labor Act, which, according to the Biden administration, includes emergency abortions. Still, some hospitals may not have clear policies that define pregnancy-related emergencies, making it challenging for clinicians to feel protected in clinically complex situations.
The study also highlighted aiding and abetting clauses, which prevent ob.gyns. from providing referrals for abortions or discussing the option with patients. Participants described the limitations as undermining their medical expertise.
“Some of the harm that is done to these ob.gyns. is not only from the laws themselves, but from their own institutions,” Dr. Buchbinder said. “Hospitals have to decide, ‘what does this law mean and how are we going to put it to practice here?’ ”
Angela Hawkins, MD, a hospitalist practicing in Oklahoma, encountered a patient who was experiencing an obvious miscarriage. But because the situation could not yet be established as life-threatening, Dr. Hawkins felt that she could not intervene.
“There are things I know are straightforward and I would’ve handled them completely differently in the past,” Dr. Hawkins said, adding that she needed to seek reassurance from her hospital employer that she would not face legal ramifications if she provided care.
“It’s frustrating to know that this is medicine and I can’t practice it without calling legal and ethics in the middle of the night,” said Dr. Hawkins, chair of the Oklahoma section of the American College of Obstetrics and Gynecology.
Still, more than half of Oklahoma’s 77 counties are considered maternity care deserts, meaning they have little to no obstetric services available for pregnant patients. Dr. Hawkins recently completed her own survey of practicing ob.gyns. in the state. In soon-to-be published research, almost 60% of the 63 respondents reported thinking about leaving or were planning to leave the state to practice in areas that are less restrictive.
“That’s very concerning to the ob.gyns. that are left,” she said. “I feel like, if everyone leaves, who is left to take care of the patients?”
The study in JAMA Network Open also highlighted that 11% of participants had moved their practices to less restrictive states with stronger abortion protections.
In addition to losing existing clinicians, the laws have made it difficult for medical centers to recruit new ones, according to Kavita Shah Arora, MD, MBE, MS, director for Division of General Obstetrics, Gynecology, and Midwifery at the University of North Carolina at Chapel Hill, and a coauthor of the study. North Carolina enacted a new law in July 2023 that reduced the time allowed for an abortion from 20 weeks to 12 weeks under most circumstances.
“Our department faces new challenges in recruitment and retention being in a restrictive state that we haven’t had to deal with before,” Dr. Arora said. “It’s impacting how medical students choose which residency programs to apply to.”
Ob.gyns. may not be the only clinicians who feel the effect of laws restricting abortion, according to Deborah Nucatola, MD, chief medical officer of Planned Parenthood Great Northwest, Hawai’i, Alaska, Indiana, Kentucky.
Patients who live in areas with limited access to obstetrics services often present to urgent care facilities or emergency departments for medical care that are staffed with family, internal medicine, and emergency physicians, Dr. Nucatola said.
“I don’t want anyone by any means to think this is isolated to one specialty,” said Dr. Nucatola, who was not involved with the study. “It’s going to affect everyone who cares for these patients; you lose the ability to use your medical knowledge and then have to navigate this legal restriction that doesn’t correlate with anything that happens in medicine.”
Dr. Dempsey-Fanning’s 14-year-old patient did eventually receive abortion care outside of South Carolina. Dr. Dempsey-Fanning said that she and her colleagues have spent hours coordinating for patients to receive care in a different state. Then, patients and their families must come up with the money for travel and any missed work to get to another clinician working where abortion is legal.
Despite this, she said, “You are left still feeling as though you abandoned this patient in many practical ways.
“I know I weigh the decision about my future practice almost daily, wondering how long I can stay and keep fighting for patients in an environment ripe with fear, worry, and an overriding sense of injustice,” said Dr. Dempsey-Fanning.
The study authors and experts quoted in the story report no relevant disclosures.
A version of this article appeared on Medscape.com.
A 14-year-old girl arrived at a South Carolina clinic just one day after the state’s anti-abortion law would have allowed her to terminate a pregnancy in instances of rape or incest.
Angela Dempsey-Fanning, MD, MPH, an ob.gyn. in Charleston, had to inform the teenager, a victim of incest, that she could not legally provide abortion care, so the girl and her mother decided to seek treatment in a different state.
“I couldn’t shake the sense that so many principles of medical ethics were being violated in denying care to her,” said Dr. Dempsey-Fanning, president of the Society of Family Planning, a nonprofit that advocates for abortion access. “When I interact with patients in these situations ... I carry the emotional and mental burden for weeks.”
South Carolina is one of 16 states to put in place severe abortion restrictions in the wake of the US Supreme Court ruling in June 2022 on the Dobbs v. Jackson Women’s Health Organization case that overturned Roe v. Wade.
according to a study recently published in the JAMA Network Open.
Public discourse on the Dobbs v. Jackson ruling has mostly centered on the impact to patients, according to Mara Buchbinder, PhD, professor and vice chair in the Department of Social Medicine at University of North Carolina Chapel Hill School of Medicine, and a coauthor of the study.
“We were interested in what the impacts would be for the obstetric workforce as well,” she said.
In 2022 and 2023, Dr. Buchbinder and her colleagues interviewed 54 ob.gyns. practicing in 13 states where abortion had become illegal with limited exceptions, including Texas, West Virginia, and South Dakota.
Clinicians who participated in the study described instances in which the state restrictions on abortion forced them to delay what they deemed to be medically necessary care until a patient faced severe complications or even death. More than 90% reported moral distress concerning situations where legal constraints prevented them or their colleagues from following clinical standards.
“You have somebody hemorrhaging with an intrauterine pregnancy with a heartbeat ... I [didn’t yet] have legal coverage for that, but there’s only so many times you can transfuse somebody and they’re begging for their life before you say, ‘This is unconscionable,’ ” one clinician reported to researchers.
Another clinician said, “Is a 5% risk of death enough? Does it take 20%? Does it take 50%? What is enough legally?”
The US Department of Health and Human Services has announced a new team to ensure hospitals in all states comply with the Emergency Medical Treatment and Labor Act, which, according to the Biden administration, includes emergency abortions. Still, some hospitals may not have clear policies that define pregnancy-related emergencies, making it challenging for clinicians to feel protected in clinically complex situations.
The study also highlighted aiding and abetting clauses, which prevent ob.gyns. from providing referrals for abortions or discussing the option with patients. Participants described the limitations as undermining their medical expertise.
“Some of the harm that is done to these ob.gyns. is not only from the laws themselves, but from their own institutions,” Dr. Buchbinder said. “Hospitals have to decide, ‘what does this law mean and how are we going to put it to practice here?’ ”
Angela Hawkins, MD, a hospitalist practicing in Oklahoma, encountered a patient who was experiencing an obvious miscarriage. But because the situation could not yet be established as life-threatening, Dr. Hawkins felt that she could not intervene.
“There are things I know are straightforward and I would’ve handled them completely differently in the past,” Dr. Hawkins said, adding that she needed to seek reassurance from her hospital employer that she would not face legal ramifications if she provided care.
“It’s frustrating to know that this is medicine and I can’t practice it without calling legal and ethics in the middle of the night,” said Dr. Hawkins, chair of the Oklahoma section of the American College of Obstetrics and Gynecology.
Still, more than half of Oklahoma’s 77 counties are considered maternity care deserts, meaning they have little to no obstetric services available for pregnant patients. Dr. Hawkins recently completed her own survey of practicing ob.gyns. in the state. In soon-to-be published research, almost 60% of the 63 respondents reported thinking about leaving or were planning to leave the state to practice in areas that are less restrictive.
“That’s very concerning to the ob.gyns. that are left,” she said. “I feel like, if everyone leaves, who is left to take care of the patients?”
The study in JAMA Network Open also highlighted that 11% of participants had moved their practices to less restrictive states with stronger abortion protections.
In addition to losing existing clinicians, the laws have made it difficult for medical centers to recruit new ones, according to Kavita Shah Arora, MD, MBE, MS, director for Division of General Obstetrics, Gynecology, and Midwifery at the University of North Carolina at Chapel Hill, and a coauthor of the study. North Carolina enacted a new law in July 2023 that reduced the time allowed for an abortion from 20 weeks to 12 weeks under most circumstances.
“Our department faces new challenges in recruitment and retention being in a restrictive state that we haven’t had to deal with before,” Dr. Arora said. “It’s impacting how medical students choose which residency programs to apply to.”
Ob.gyns. may not be the only clinicians who feel the effect of laws restricting abortion, according to Deborah Nucatola, MD, chief medical officer of Planned Parenthood Great Northwest, Hawai’i, Alaska, Indiana, Kentucky.
Patients who live in areas with limited access to obstetrics services often present to urgent care facilities or emergency departments for medical care that are staffed with family, internal medicine, and emergency physicians, Dr. Nucatola said.
“I don’t want anyone by any means to think this is isolated to one specialty,” said Dr. Nucatola, who was not involved with the study. “It’s going to affect everyone who cares for these patients; you lose the ability to use your medical knowledge and then have to navigate this legal restriction that doesn’t correlate with anything that happens in medicine.”
Dr. Dempsey-Fanning’s 14-year-old patient did eventually receive abortion care outside of South Carolina. Dr. Dempsey-Fanning said that she and her colleagues have spent hours coordinating for patients to receive care in a different state. Then, patients and their families must come up with the money for travel and any missed work to get to another clinician working where abortion is legal.
Despite this, she said, “You are left still feeling as though you abandoned this patient in many practical ways.
“I know I weigh the decision about my future practice almost daily, wondering how long I can stay and keep fighting for patients in an environment ripe with fear, worry, and an overriding sense of injustice,” said Dr. Dempsey-Fanning.
The study authors and experts quoted in the story report no relevant disclosures.
A version of this article appeared on Medscape.com.
A 14-year-old girl arrived at a South Carolina clinic just one day after the state’s anti-abortion law would have allowed her to terminate a pregnancy in instances of rape or incest.
Angela Dempsey-Fanning, MD, MPH, an ob.gyn. in Charleston, had to inform the teenager, a victim of incest, that she could not legally provide abortion care, so the girl and her mother decided to seek treatment in a different state.
“I couldn’t shake the sense that so many principles of medical ethics were being violated in denying care to her,” said Dr. Dempsey-Fanning, president of the Society of Family Planning, a nonprofit that advocates for abortion access. “When I interact with patients in these situations ... I carry the emotional and mental burden for weeks.”
South Carolina is one of 16 states to put in place severe abortion restrictions in the wake of the US Supreme Court ruling in June 2022 on the Dobbs v. Jackson Women’s Health Organization case that overturned Roe v. Wade.
according to a study recently published in the JAMA Network Open.
Public discourse on the Dobbs v. Jackson ruling has mostly centered on the impact to patients, according to Mara Buchbinder, PhD, professor and vice chair in the Department of Social Medicine at University of North Carolina Chapel Hill School of Medicine, and a coauthor of the study.
“We were interested in what the impacts would be for the obstetric workforce as well,” she said.
In 2022 and 2023, Dr. Buchbinder and her colleagues interviewed 54 ob.gyns. practicing in 13 states where abortion had become illegal with limited exceptions, including Texas, West Virginia, and South Dakota.
Clinicians who participated in the study described instances in which the state restrictions on abortion forced them to delay what they deemed to be medically necessary care until a patient faced severe complications or even death. More than 90% reported moral distress concerning situations where legal constraints prevented them or their colleagues from following clinical standards.
“You have somebody hemorrhaging with an intrauterine pregnancy with a heartbeat ... I [didn’t yet] have legal coverage for that, but there’s only so many times you can transfuse somebody and they’re begging for their life before you say, ‘This is unconscionable,’ ” one clinician reported to researchers.
Another clinician said, “Is a 5% risk of death enough? Does it take 20%? Does it take 50%? What is enough legally?”
The US Department of Health and Human Services has announced a new team to ensure hospitals in all states comply with the Emergency Medical Treatment and Labor Act, which, according to the Biden administration, includes emergency abortions. Still, some hospitals may not have clear policies that define pregnancy-related emergencies, making it challenging for clinicians to feel protected in clinically complex situations.
The study also highlighted aiding and abetting clauses, which prevent ob.gyns. from providing referrals for abortions or discussing the option with patients. Participants described the limitations as undermining their medical expertise.
“Some of the harm that is done to these ob.gyns. is not only from the laws themselves, but from their own institutions,” Dr. Buchbinder said. “Hospitals have to decide, ‘what does this law mean and how are we going to put it to practice here?’ ”
Angela Hawkins, MD, a hospitalist practicing in Oklahoma, encountered a patient who was experiencing an obvious miscarriage. But because the situation could not yet be established as life-threatening, Dr. Hawkins felt that she could not intervene.
“There are things I know are straightforward and I would’ve handled them completely differently in the past,” Dr. Hawkins said, adding that she needed to seek reassurance from her hospital employer that she would not face legal ramifications if she provided care.
“It’s frustrating to know that this is medicine and I can’t practice it without calling legal and ethics in the middle of the night,” said Dr. Hawkins, chair of the Oklahoma section of the American College of Obstetrics and Gynecology.
Still, more than half of Oklahoma’s 77 counties are considered maternity care deserts, meaning they have little to no obstetric services available for pregnant patients. Dr. Hawkins recently completed her own survey of practicing ob.gyns. in the state. In soon-to-be published research, almost 60% of the 63 respondents reported thinking about leaving or were planning to leave the state to practice in areas that are less restrictive.
“That’s very concerning to the ob.gyns. that are left,” she said. “I feel like, if everyone leaves, who is left to take care of the patients?”
The study in JAMA Network Open also highlighted that 11% of participants had moved their practices to less restrictive states with stronger abortion protections.
In addition to losing existing clinicians, the laws have made it difficult for medical centers to recruit new ones, according to Kavita Shah Arora, MD, MBE, MS, director for Division of General Obstetrics, Gynecology, and Midwifery at the University of North Carolina at Chapel Hill, and a coauthor of the study. North Carolina enacted a new law in July 2023 that reduced the time allowed for an abortion from 20 weeks to 12 weeks under most circumstances.
“Our department faces new challenges in recruitment and retention being in a restrictive state that we haven’t had to deal with before,” Dr. Arora said. “It’s impacting how medical students choose which residency programs to apply to.”
Ob.gyns. may not be the only clinicians who feel the effect of laws restricting abortion, according to Deborah Nucatola, MD, chief medical officer of Planned Parenthood Great Northwest, Hawai’i, Alaska, Indiana, Kentucky.
Patients who live in areas with limited access to obstetrics services often present to urgent care facilities or emergency departments for medical care that are staffed with family, internal medicine, and emergency physicians, Dr. Nucatola said.
“I don’t want anyone by any means to think this is isolated to one specialty,” said Dr. Nucatola, who was not involved with the study. “It’s going to affect everyone who cares for these patients; you lose the ability to use your medical knowledge and then have to navigate this legal restriction that doesn’t correlate with anything that happens in medicine.”
Dr. Dempsey-Fanning’s 14-year-old patient did eventually receive abortion care outside of South Carolina. Dr. Dempsey-Fanning said that she and her colleagues have spent hours coordinating for patients to receive care in a different state. Then, patients and their families must come up with the money for travel and any missed work to get to another clinician working where abortion is legal.
Despite this, she said, “You are left still feeling as though you abandoned this patient in many practical ways.
“I know I weigh the decision about my future practice almost daily, wondering how long I can stay and keep fighting for patients in an environment ripe with fear, worry, and an overriding sense of injustice,” said Dr. Dempsey-Fanning.
The study authors and experts quoted in the story report no relevant disclosures.
A version of this article appeared on Medscape.com.
Wearable Device Tracks IBD from Sweat
LAS VEGAS —
The device, in development by EnLiSense, can rapidly detect calprotectin, C-reactive protein (CRP), and interleukin-6 (IL-6), using miniaturized versions of biochemical lab tests.
Patient monitoring relies on identifying trends, whether biomarker levels are increasing or decreasing, according to Shalini Prasad, PhD, who presented the study during a poster session at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “In a blood test you don’t get that unless you’re willing to sample every month. That’s the benefit [of the device],” said Dr. Prasad, professor of bioengineering at University of Texas at Dallas and a cofounder of EnLiSense.
The project grew out of the involvement of EnLiSense with the Biomedical Advanced Research Development Authority (BARDA). “We were tracking infections, and we were looking at inflammatory markers associated with infections: Cytokines and chemokines. We thought it was a natural pivot for us because the disease of inflammation is IBD,” said Dr. Prasad.
The device need only be worn when the physician determines the disease is in a variable state. The patient “will wear it for the duration of time as determined by the clinician,” said Dr. Prasad.
The watch face–sized device, typically worn on the forearm, absorbs sweat and performs automated biochemical analysis independently, then beams its findings to the cloud. “What you get back is concentration [of inflammatory biomarkers]. It is essentially trend line reporting of how the concentration is fluctuating over time for markers,” said Dr. Prasad.
The Crohn’s and Colitis Foundation is supporting the company through its IBD Ventures program. EnLiSense is currently conducting a study tracking patients over 4 weeks to correlate biomarker concentrations in sweat with concentrations in stool.
A key remaining question is how long the device should be worn and during what clinical periods. The technology has the potential to provide too much information. “Just figuring the balance. We’re trying to find the right spot where it makes sense for both the clinician and the patient. This is something that is a work in progress. We don’t want this to be just like any other consumer wearable which gives you something but you’re not sure what it means,” said Dr. Prasad.
The study included 33 patients with IBD who were monitored between 40 and 130 minutes. The device measured levels of CRP, IL-6, and calprotectin. Serum samples were also measured the same day.
The researchers found higher levels of calprotectin among patients with active disease in perspiration (P = .0260), serum (P = .022), and in fecal samples (P = .0411). There were no significant differences between patients who are active and those in remission with respect to CRP levels in perspiration or serum, or IL-6 in perspiration. Serum Il-6 levels were higher in those with active disease.
There was no significant difference between serum and sweat calprotectin levels among patients who were active or in remission, but the median expression of IL-6 in perspiration was higher in the active group (P = .0016). In the active group, calprotectin was elevated in sweat, serum, and stool.
Levels of calprotectin measured in perspiration correlated with levels in the serum (R2 = 0.7195), as did CRP (R2 = 0.615) and IL-6 (R2 = 0.5411).
Treating to Target
The poster caught the interest of Jeremiah Faith, PhD, who attended the session and was asked to comment. “I think patients want to know what’s happening [with their disease], and we could probably give better care if we know day to day the status of someone, especially because every time we test them we get a point in time, but the reality is probably that people are kind of wavy, and knowing the wave is much better,” he said.
He noted that there was not a strong separation between mean perspiration calprotectin values, but he said the ability to take frequent measurements could overcome that weakness. “The difference between active and remission is not as drastic as what you’d see from blood, for example. But it’s the same thing with your watch. Your watch is a really poor sensor of what your heartbeat is doing, but if you measure it every few seconds, and you average over a long period of time, it can actually more be more [accurate]. So there’s a lot of potential for this,” said Dr. Faith, associate professor of genetics and genomic sciences at the Icahn School of Medicine at Mount Sinai in New York.
If perfected, the device could help efforts at treating to target, in which therapies are adjusted to achieve minimal disease. Currently, physicians are forced to adjust doses or change therapies based on infrequent testing. “If this is accurate ... maybe at some point we will have the tools to be smarter about it,” said Dr. Faith.
Dr. Prasad is a cofounder of EnLiSense. Dr. Faith has no relevant financial disclosures.
LAS VEGAS —
The device, in development by EnLiSense, can rapidly detect calprotectin, C-reactive protein (CRP), and interleukin-6 (IL-6), using miniaturized versions of biochemical lab tests.
Patient monitoring relies on identifying trends, whether biomarker levels are increasing or decreasing, according to Shalini Prasad, PhD, who presented the study during a poster session at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “In a blood test you don’t get that unless you’re willing to sample every month. That’s the benefit [of the device],” said Dr. Prasad, professor of bioengineering at University of Texas at Dallas and a cofounder of EnLiSense.
The project grew out of the involvement of EnLiSense with the Biomedical Advanced Research Development Authority (BARDA). “We were tracking infections, and we were looking at inflammatory markers associated with infections: Cytokines and chemokines. We thought it was a natural pivot for us because the disease of inflammation is IBD,” said Dr. Prasad.
The device need only be worn when the physician determines the disease is in a variable state. The patient “will wear it for the duration of time as determined by the clinician,” said Dr. Prasad.
The watch face–sized device, typically worn on the forearm, absorbs sweat and performs automated biochemical analysis independently, then beams its findings to the cloud. “What you get back is concentration [of inflammatory biomarkers]. It is essentially trend line reporting of how the concentration is fluctuating over time for markers,” said Dr. Prasad.
The Crohn’s and Colitis Foundation is supporting the company through its IBD Ventures program. EnLiSense is currently conducting a study tracking patients over 4 weeks to correlate biomarker concentrations in sweat with concentrations in stool.
A key remaining question is how long the device should be worn and during what clinical periods. The technology has the potential to provide too much information. “Just figuring the balance. We’re trying to find the right spot where it makes sense for both the clinician and the patient. This is something that is a work in progress. We don’t want this to be just like any other consumer wearable which gives you something but you’re not sure what it means,” said Dr. Prasad.
The study included 33 patients with IBD who were monitored between 40 and 130 minutes. The device measured levels of CRP, IL-6, and calprotectin. Serum samples were also measured the same day.
The researchers found higher levels of calprotectin among patients with active disease in perspiration (P = .0260), serum (P = .022), and in fecal samples (P = .0411). There were no significant differences between patients who are active and those in remission with respect to CRP levels in perspiration or serum, or IL-6 in perspiration. Serum Il-6 levels were higher in those with active disease.
There was no significant difference between serum and sweat calprotectin levels among patients who were active or in remission, but the median expression of IL-6 in perspiration was higher in the active group (P = .0016). In the active group, calprotectin was elevated in sweat, serum, and stool.
Levels of calprotectin measured in perspiration correlated with levels in the serum (R2 = 0.7195), as did CRP (R2 = 0.615) and IL-6 (R2 = 0.5411).
Treating to Target
The poster caught the interest of Jeremiah Faith, PhD, who attended the session and was asked to comment. “I think patients want to know what’s happening [with their disease], and we could probably give better care if we know day to day the status of someone, especially because every time we test them we get a point in time, but the reality is probably that people are kind of wavy, and knowing the wave is much better,” he said.
He noted that there was not a strong separation between mean perspiration calprotectin values, but he said the ability to take frequent measurements could overcome that weakness. “The difference between active and remission is not as drastic as what you’d see from blood, for example. But it’s the same thing with your watch. Your watch is a really poor sensor of what your heartbeat is doing, but if you measure it every few seconds, and you average over a long period of time, it can actually more be more [accurate]. So there’s a lot of potential for this,” said Dr. Faith, associate professor of genetics and genomic sciences at the Icahn School of Medicine at Mount Sinai in New York.
If perfected, the device could help efforts at treating to target, in which therapies are adjusted to achieve minimal disease. Currently, physicians are forced to adjust doses or change therapies based on infrequent testing. “If this is accurate ... maybe at some point we will have the tools to be smarter about it,” said Dr. Faith.
Dr. Prasad is a cofounder of EnLiSense. Dr. Faith has no relevant financial disclosures.
LAS VEGAS —
The device, in development by EnLiSense, can rapidly detect calprotectin, C-reactive protein (CRP), and interleukin-6 (IL-6), using miniaturized versions of biochemical lab tests.
Patient monitoring relies on identifying trends, whether biomarker levels are increasing or decreasing, according to Shalini Prasad, PhD, who presented the study during a poster session at the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association. “In a blood test you don’t get that unless you’re willing to sample every month. That’s the benefit [of the device],” said Dr. Prasad, professor of bioengineering at University of Texas at Dallas and a cofounder of EnLiSense.
The project grew out of the involvement of EnLiSense with the Biomedical Advanced Research Development Authority (BARDA). “We were tracking infections, and we were looking at inflammatory markers associated with infections: Cytokines and chemokines. We thought it was a natural pivot for us because the disease of inflammation is IBD,” said Dr. Prasad.
The device need only be worn when the physician determines the disease is in a variable state. The patient “will wear it for the duration of time as determined by the clinician,” said Dr. Prasad.
The watch face–sized device, typically worn on the forearm, absorbs sweat and performs automated biochemical analysis independently, then beams its findings to the cloud. “What you get back is concentration [of inflammatory biomarkers]. It is essentially trend line reporting of how the concentration is fluctuating over time for markers,” said Dr. Prasad.
The Crohn’s and Colitis Foundation is supporting the company through its IBD Ventures program. EnLiSense is currently conducting a study tracking patients over 4 weeks to correlate biomarker concentrations in sweat with concentrations in stool.
A key remaining question is how long the device should be worn and during what clinical periods. The technology has the potential to provide too much information. “Just figuring the balance. We’re trying to find the right spot where it makes sense for both the clinician and the patient. This is something that is a work in progress. We don’t want this to be just like any other consumer wearable which gives you something but you’re not sure what it means,” said Dr. Prasad.
The study included 33 patients with IBD who were monitored between 40 and 130 minutes. The device measured levels of CRP, IL-6, and calprotectin. Serum samples were also measured the same day.
The researchers found higher levels of calprotectin among patients with active disease in perspiration (P = .0260), serum (P = .022), and in fecal samples (P = .0411). There were no significant differences between patients who are active and those in remission with respect to CRP levels in perspiration or serum, or IL-6 in perspiration. Serum Il-6 levels were higher in those with active disease.
There was no significant difference between serum and sweat calprotectin levels among patients who were active or in remission, but the median expression of IL-6 in perspiration was higher in the active group (P = .0016). In the active group, calprotectin was elevated in sweat, serum, and stool.
Levels of calprotectin measured in perspiration correlated with levels in the serum (R2 = 0.7195), as did CRP (R2 = 0.615) and IL-6 (R2 = 0.5411).
Treating to Target
The poster caught the interest of Jeremiah Faith, PhD, who attended the session and was asked to comment. “I think patients want to know what’s happening [with their disease], and we could probably give better care if we know day to day the status of someone, especially because every time we test them we get a point in time, but the reality is probably that people are kind of wavy, and knowing the wave is much better,” he said.
He noted that there was not a strong separation between mean perspiration calprotectin values, but he said the ability to take frequent measurements could overcome that weakness. “The difference between active and remission is not as drastic as what you’d see from blood, for example. But it’s the same thing with your watch. Your watch is a really poor sensor of what your heartbeat is doing, but if you measure it every few seconds, and you average over a long period of time, it can actually more be more [accurate]. So there’s a lot of potential for this,” said Dr. Faith, associate professor of genetics and genomic sciences at the Icahn School of Medicine at Mount Sinai in New York.
If perfected, the device could help efforts at treating to target, in which therapies are adjusted to achieve minimal disease. Currently, physicians are forced to adjust doses or change therapies based on infrequent testing. “If this is accurate ... maybe at some point we will have the tools to be smarter about it,” said Dr. Faith.
Dr. Prasad is a cofounder of EnLiSense. Dr. Faith has no relevant financial disclosures.
FROM CROHN’S & COLITIS CONGRESS
Diffusely Scattered Macules Following Radiation Therapy
The Diagnosis: Cutaneous Mastocytosis
A shave skin biopsy from the right lateral breast and a punch skin biopsy from the right thigh showed similar histopathology. There were dermal predominantly perivascular aggregates of cells demonstrating basophilic granular cytoplasm and round to oval nuclei (Figure, A and B). These cells were highlighted by CD117 immunohistochemical stain (Figure, C), consistent with mastocytes. Additionally, occasional lymphocytes and rare eosinophils were noted. These histopathologic findings confirmed the diagnosis of cutaneous mastocytosis (CM). The patient’s complete blood cell count was within reference range, but serum tryptase was elevated at 15.7 μg/L (reference range, <11.0 μg/L), which prompted a bone marrow biopsy to rule out systemic mastocytosis (SM). The result showed normocellular bone marrow with no evidence of dysplasia or increased blasts, granuloma, lymphoproliferative disorder, or malignancy. Fluorescence in situ hybridization for PDGFRA (platelet-derived growth factor receptor alpha) and KIT mutation was negative. Because CM developed predominantly on the right breast where the patient previously had received radiation therapy, we concluded that this reaction was triggered by exposure to ionizing radiation.
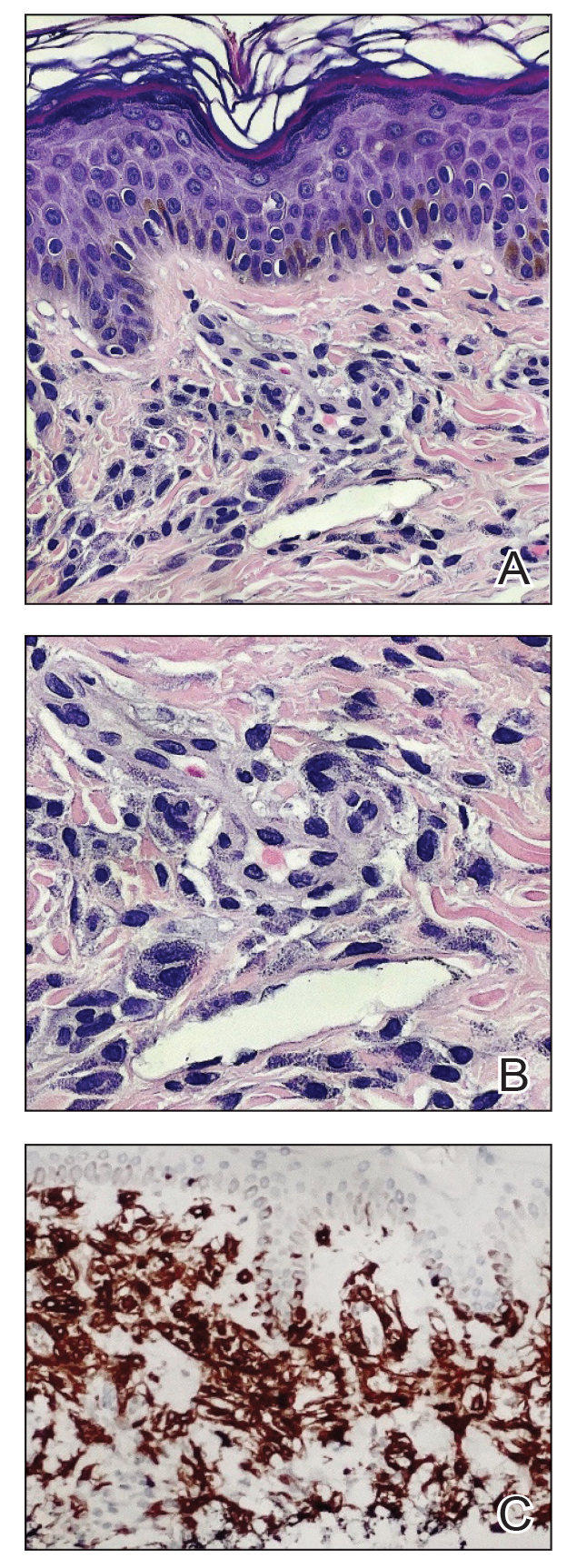
Mastocytosis can be divided into 2 groups: CM and SM.1 The histologic differential diagnosis of CM includes solitary mastocytoma, urticaria pigmentosa, telangiectasia macularis eruptiva perstans, and diffuse mastocytosis.2 Clinicopathologic correlation is of crucial importance to render the final diagnosis in these disorders. Immunohistochemically, mast cells express CD177, CD5, CD68, tryptase, and chymase. Unlike normal mast cells, neoplastic cells express CD2 and/or CD25; CD25 is commonly expressed in cutaneous involvement by SM.2
Macdonald and Feiwel3 reported the first case of CM following ionizing radiation. Cutaneous mastocytosis is most common in female patients and presents with redbrown macules originating at the site of radiation therapy. Prior literature suggests that radiation-associated CM has a predilection for White patients4; however, our patient was Hispanic. It also is important to note that the presentation of this rash may differ in individuals with skin of color. In one case it spread beyond the radiation site.2 Systemic mast call–mediated symptoms can occur in both CM and SM. The macules manifest as blanching with pressure.5 Typically these macules also are asymptomatic, though a positive Darier sign has been reported.6,7 The interval between radiotherapy and CM has ranged from 3 to 24 months.2
Patients with CM should have a serum tryptase evaluation along with a complete blood cell count, serum biochemistry, and liver function tests. Elevated serum tryptase has a high positive predictive value for SM and should prompt a bone marrow biopsy. Our patient’s bone marrow biopsy results failed to establish SM; however, her serum tryptase levels will be carefully monitored going forward. At the time of publication, the skin macules were still persistent but not worsening or symptomatic.
Treatment is focused on symptomatic relief of cutaneous symptoms, if present; avoiding triggers of mast cell degranulation; and implementing the use of oral antihistamines and leukotriene antagonists as needed. Because our patient was completely asymptomatic, we did not recommend any topical or oral treatment. However, we do counsel patients on avoiding triggers of mast cell degranulation including nonsteroidal anti-inflammatory drugs, morphine and codeine derivatives, alcohol, certain anesthetics, and anticholinergic medications.8
Additional diagnoses were ruled out for the following reasons: Although lichen planus pigmentosus presents with ill-defined, oval, gray-brown macules, histopathology shows a bandlike lymphocytic infiltrate at the dermoepidermal junction. Solar lentiginosis is characterized by grouped tan macules in a sun-exposed distribution. A fixed drug eruption is a delayed hypersensitivity reaction, usually to an ingested medication, characterized by violaceous or hyperpigmented patches, with histopathology showing interface dermatitis with a lymphoeosinophilic infiltrate. Eruptive seborrheic keratoses can result from sunburn or dermatitis but does not show mastocytes on histopathology.8
In conclusion, dermatologists should be reminded of the rare possibility of CM when evaluating an atypical eruption in a prior radiation field.
- Landy RE, Stross WC, May JM, et al. Idiopathic mast cell activation syndrome and radiation therapy: a case study, literature review, and discussion of mast cell disorders and radiotherapy [published online December 9, 2019]. Radiat Oncol. 2019;14:222. doi:10.1186 /s13014-019-1434-6
- Easwaralingam N, Wu Y, Cheung D, et al. Radiotherapy for breast cancer associated with a cutaneous presentation of systemic mastocytosis—a case report and literature review. J Surg Case Rep. 2018;2018:1-3. doi:10.1093/jscr/rjy317
- Macdonald A, Feiwel M. Cutaneous mastocytosis: an unusual radiation dermatitis. Proc R Soc Med. 1971;64:29-30.
- Kirshenbaum AS, Abuhay H, Bolan H, et al. Maculopapular cutaneous mastocytosis in a diverse population. J Allergy Clin Immunol Pract. 2019;7:2845-2847. doi:10.1016/j.jaip.2019.04.003
- Soilleux EJ, Brown VL, Bowling J. Cutaneous mastocytosis localized to a radiotherapy field. Clin Exp Dermatol. 2008;34:111-112. doi:10.1111 /j.1365-2230.2008.02931.x
- Comte C, Bessis D, Dereure O, et al. Urticaria pigmentosa localized on radiation field. Eur J Dermatol. 2003;13:408-409.
- Davidson SJ, Coates D. Cutaneous mastocytosis extending beyond a radiotherapy site: a form of radiodermatitis or a neoplastic phenomenon? Australas J Dermatol. 2012;54:E85-E87. doi:10.1111 /j.1440-0960.2012.00961.x
- Bolognia J, Schaffer JV, Duncan KO, et al, eds. Dermatology Essentials. 2nd ed. Elsevier; 2022.
The Diagnosis: Cutaneous Mastocytosis
A shave skin biopsy from the right lateral breast and a punch skin biopsy from the right thigh showed similar histopathology. There were dermal predominantly perivascular aggregates of cells demonstrating basophilic granular cytoplasm and round to oval nuclei (Figure, A and B). These cells were highlighted by CD117 immunohistochemical stain (Figure, C), consistent with mastocytes. Additionally, occasional lymphocytes and rare eosinophils were noted. These histopathologic findings confirmed the diagnosis of cutaneous mastocytosis (CM). The patient’s complete blood cell count was within reference range, but serum tryptase was elevated at 15.7 μg/L (reference range, <11.0 μg/L), which prompted a bone marrow biopsy to rule out systemic mastocytosis (SM). The result showed normocellular bone marrow with no evidence of dysplasia or increased blasts, granuloma, lymphoproliferative disorder, or malignancy. Fluorescence in situ hybridization for PDGFRA (platelet-derived growth factor receptor alpha) and KIT mutation was negative. Because CM developed predominantly on the right breast where the patient previously had received radiation therapy, we concluded that this reaction was triggered by exposure to ionizing radiation.
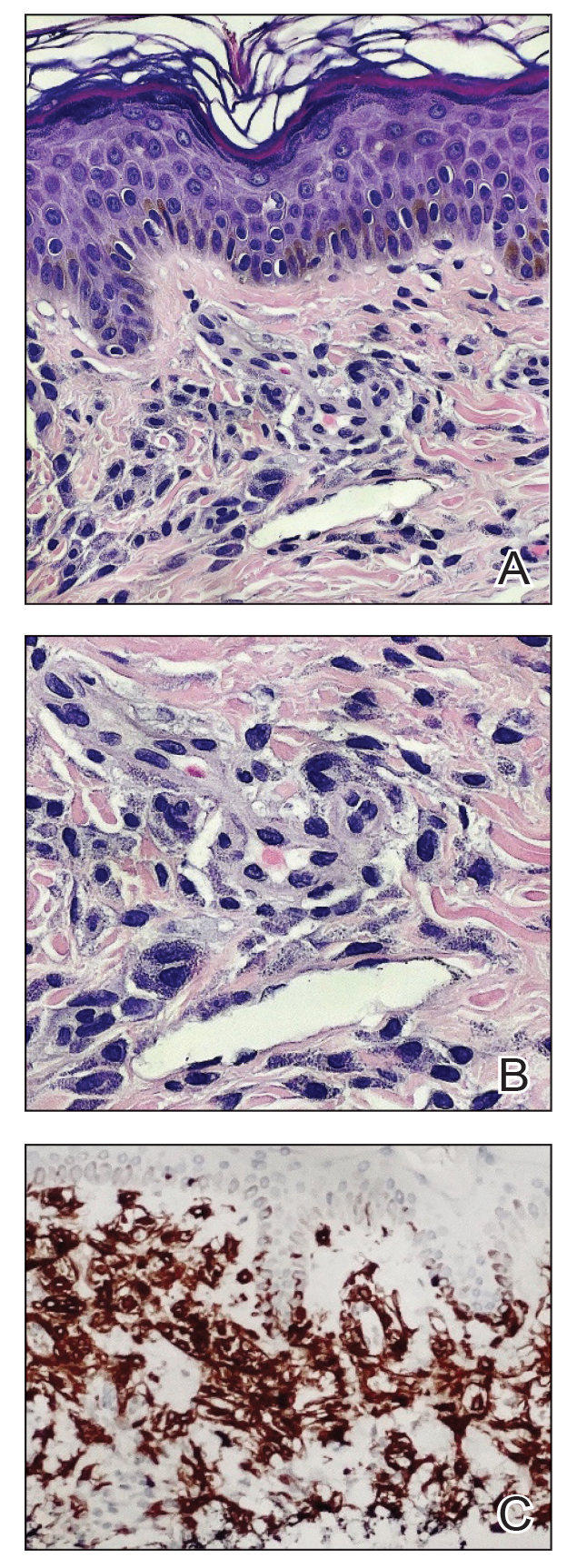
Mastocytosis can be divided into 2 groups: CM and SM.1 The histologic differential diagnosis of CM includes solitary mastocytoma, urticaria pigmentosa, telangiectasia macularis eruptiva perstans, and diffuse mastocytosis.2 Clinicopathologic correlation is of crucial importance to render the final diagnosis in these disorders. Immunohistochemically, mast cells express CD177, CD5, CD68, tryptase, and chymase. Unlike normal mast cells, neoplastic cells express CD2 and/or CD25; CD25 is commonly expressed in cutaneous involvement by SM.2
Macdonald and Feiwel3 reported the first case of CM following ionizing radiation. Cutaneous mastocytosis is most common in female patients and presents with redbrown macules originating at the site of radiation therapy. Prior literature suggests that radiation-associated CM has a predilection for White patients4; however, our patient was Hispanic. It also is important to note that the presentation of this rash may differ in individuals with skin of color. In one case it spread beyond the radiation site.2 Systemic mast call–mediated symptoms can occur in both CM and SM. The macules manifest as blanching with pressure.5 Typically these macules also are asymptomatic, though a positive Darier sign has been reported.6,7 The interval between radiotherapy and CM has ranged from 3 to 24 months.2
Patients with CM should have a serum tryptase evaluation along with a complete blood cell count, serum biochemistry, and liver function tests. Elevated serum tryptase has a high positive predictive value for SM and should prompt a bone marrow biopsy. Our patient’s bone marrow biopsy results failed to establish SM; however, her serum tryptase levels will be carefully monitored going forward. At the time of publication, the skin macules were still persistent but not worsening or symptomatic.
Treatment is focused on symptomatic relief of cutaneous symptoms, if present; avoiding triggers of mast cell degranulation; and implementing the use of oral antihistamines and leukotriene antagonists as needed. Because our patient was completely asymptomatic, we did not recommend any topical or oral treatment. However, we do counsel patients on avoiding triggers of mast cell degranulation including nonsteroidal anti-inflammatory drugs, morphine and codeine derivatives, alcohol, certain anesthetics, and anticholinergic medications.8
Additional diagnoses were ruled out for the following reasons: Although lichen planus pigmentosus presents with ill-defined, oval, gray-brown macules, histopathology shows a bandlike lymphocytic infiltrate at the dermoepidermal junction. Solar lentiginosis is characterized by grouped tan macules in a sun-exposed distribution. A fixed drug eruption is a delayed hypersensitivity reaction, usually to an ingested medication, characterized by violaceous or hyperpigmented patches, with histopathology showing interface dermatitis with a lymphoeosinophilic infiltrate. Eruptive seborrheic keratoses can result from sunburn or dermatitis but does not show mastocytes on histopathology.8
In conclusion, dermatologists should be reminded of the rare possibility of CM when evaluating an atypical eruption in a prior radiation field.
The Diagnosis: Cutaneous Mastocytosis
A shave skin biopsy from the right lateral breast and a punch skin biopsy from the right thigh showed similar histopathology. There were dermal predominantly perivascular aggregates of cells demonstrating basophilic granular cytoplasm and round to oval nuclei (Figure, A and B). These cells were highlighted by CD117 immunohistochemical stain (Figure, C), consistent with mastocytes. Additionally, occasional lymphocytes and rare eosinophils were noted. These histopathologic findings confirmed the diagnosis of cutaneous mastocytosis (CM). The patient’s complete blood cell count was within reference range, but serum tryptase was elevated at 15.7 μg/L (reference range, <11.0 μg/L), which prompted a bone marrow biopsy to rule out systemic mastocytosis (SM). The result showed normocellular bone marrow with no evidence of dysplasia or increased blasts, granuloma, lymphoproliferative disorder, or malignancy. Fluorescence in situ hybridization for PDGFRA (platelet-derived growth factor receptor alpha) and KIT mutation was negative. Because CM developed predominantly on the right breast where the patient previously had received radiation therapy, we concluded that this reaction was triggered by exposure to ionizing radiation.
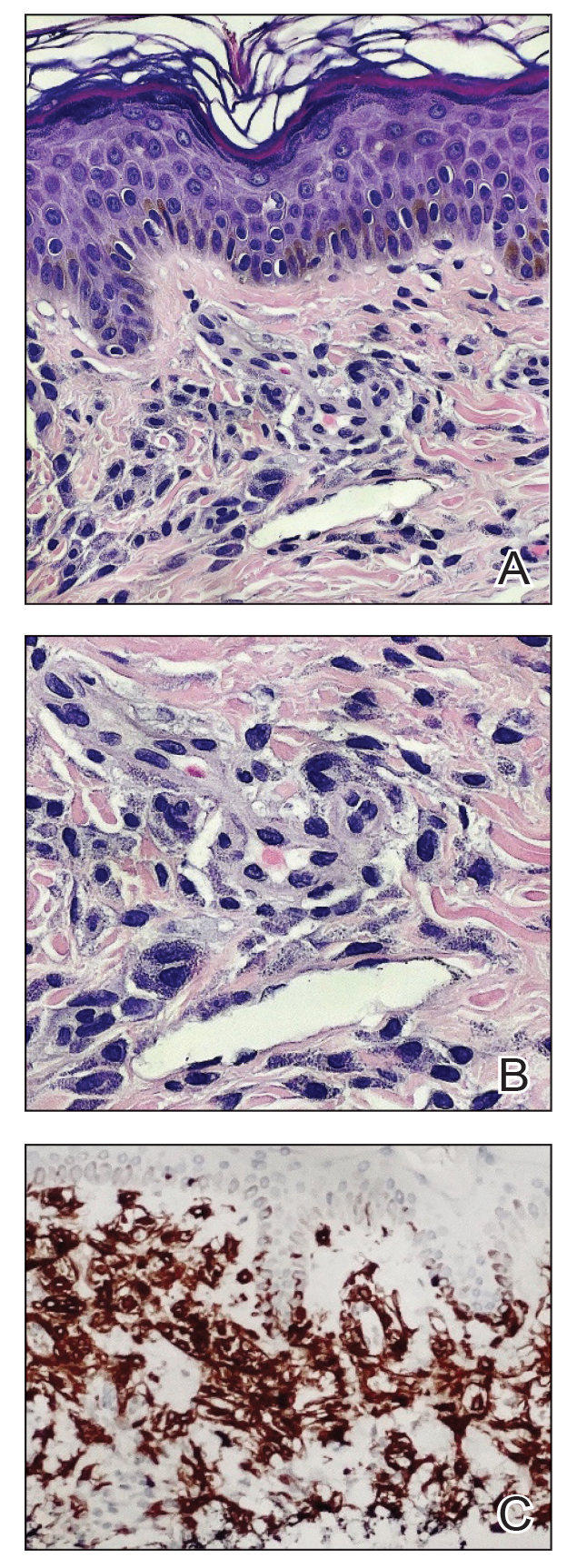
Mastocytosis can be divided into 2 groups: CM and SM.1 The histologic differential diagnosis of CM includes solitary mastocytoma, urticaria pigmentosa, telangiectasia macularis eruptiva perstans, and diffuse mastocytosis.2 Clinicopathologic correlation is of crucial importance to render the final diagnosis in these disorders. Immunohistochemically, mast cells express CD177, CD5, CD68, tryptase, and chymase. Unlike normal mast cells, neoplastic cells express CD2 and/or CD25; CD25 is commonly expressed in cutaneous involvement by SM.2
Macdonald and Feiwel3 reported the first case of CM following ionizing radiation. Cutaneous mastocytosis is most common in female patients and presents with redbrown macules originating at the site of radiation therapy. Prior literature suggests that radiation-associated CM has a predilection for White patients4; however, our patient was Hispanic. It also is important to note that the presentation of this rash may differ in individuals with skin of color. In one case it spread beyond the radiation site.2 Systemic mast call–mediated symptoms can occur in both CM and SM. The macules manifest as blanching with pressure.5 Typically these macules also are asymptomatic, though a positive Darier sign has been reported.6,7 The interval between radiotherapy and CM has ranged from 3 to 24 months.2
Patients with CM should have a serum tryptase evaluation along with a complete blood cell count, serum biochemistry, and liver function tests. Elevated serum tryptase has a high positive predictive value for SM and should prompt a bone marrow biopsy. Our patient’s bone marrow biopsy results failed to establish SM; however, her serum tryptase levels will be carefully monitored going forward. At the time of publication, the skin macules were still persistent but not worsening or symptomatic.
Treatment is focused on symptomatic relief of cutaneous symptoms, if present; avoiding triggers of mast cell degranulation; and implementing the use of oral antihistamines and leukotriene antagonists as needed. Because our patient was completely asymptomatic, we did not recommend any topical or oral treatment. However, we do counsel patients on avoiding triggers of mast cell degranulation including nonsteroidal anti-inflammatory drugs, morphine and codeine derivatives, alcohol, certain anesthetics, and anticholinergic medications.8
Additional diagnoses were ruled out for the following reasons: Although lichen planus pigmentosus presents with ill-defined, oval, gray-brown macules, histopathology shows a bandlike lymphocytic infiltrate at the dermoepidermal junction. Solar lentiginosis is characterized by grouped tan macules in a sun-exposed distribution. A fixed drug eruption is a delayed hypersensitivity reaction, usually to an ingested medication, characterized by violaceous or hyperpigmented patches, with histopathology showing interface dermatitis with a lymphoeosinophilic infiltrate. Eruptive seborrheic keratoses can result from sunburn or dermatitis but does not show mastocytes on histopathology.8
In conclusion, dermatologists should be reminded of the rare possibility of CM when evaluating an atypical eruption in a prior radiation field.
- Landy RE, Stross WC, May JM, et al. Idiopathic mast cell activation syndrome and radiation therapy: a case study, literature review, and discussion of mast cell disorders and radiotherapy [published online December 9, 2019]. Radiat Oncol. 2019;14:222. doi:10.1186 /s13014-019-1434-6
- Easwaralingam N, Wu Y, Cheung D, et al. Radiotherapy for breast cancer associated with a cutaneous presentation of systemic mastocytosis—a case report and literature review. J Surg Case Rep. 2018;2018:1-3. doi:10.1093/jscr/rjy317
- Macdonald A, Feiwel M. Cutaneous mastocytosis: an unusual radiation dermatitis. Proc R Soc Med. 1971;64:29-30.
- Kirshenbaum AS, Abuhay H, Bolan H, et al. Maculopapular cutaneous mastocytosis in a diverse population. J Allergy Clin Immunol Pract. 2019;7:2845-2847. doi:10.1016/j.jaip.2019.04.003
- Soilleux EJ, Brown VL, Bowling J. Cutaneous mastocytosis localized to a radiotherapy field. Clin Exp Dermatol. 2008;34:111-112. doi:10.1111 /j.1365-2230.2008.02931.x
- Comte C, Bessis D, Dereure O, et al. Urticaria pigmentosa localized on radiation field. Eur J Dermatol. 2003;13:408-409.
- Davidson SJ, Coates D. Cutaneous mastocytosis extending beyond a radiotherapy site: a form of radiodermatitis or a neoplastic phenomenon? Australas J Dermatol. 2012;54:E85-E87. doi:10.1111 /j.1440-0960.2012.00961.x
- Bolognia J, Schaffer JV, Duncan KO, et al, eds. Dermatology Essentials. 2nd ed. Elsevier; 2022.
- Landy RE, Stross WC, May JM, et al. Idiopathic mast cell activation syndrome and radiation therapy: a case study, literature review, and discussion of mast cell disorders and radiotherapy [published online December 9, 2019]. Radiat Oncol. 2019;14:222. doi:10.1186 /s13014-019-1434-6
- Easwaralingam N, Wu Y, Cheung D, et al. Radiotherapy for breast cancer associated with a cutaneous presentation of systemic mastocytosis—a case report and literature review. J Surg Case Rep. 2018;2018:1-3. doi:10.1093/jscr/rjy317
- Macdonald A, Feiwel M. Cutaneous mastocytosis: an unusual radiation dermatitis. Proc R Soc Med. 1971;64:29-30.
- Kirshenbaum AS, Abuhay H, Bolan H, et al. Maculopapular cutaneous mastocytosis in a diverse population. J Allergy Clin Immunol Pract. 2019;7:2845-2847. doi:10.1016/j.jaip.2019.04.003
- Soilleux EJ, Brown VL, Bowling J. Cutaneous mastocytosis localized to a radiotherapy field. Clin Exp Dermatol. 2008;34:111-112. doi:10.1111 /j.1365-2230.2008.02931.x
- Comte C, Bessis D, Dereure O, et al. Urticaria pigmentosa localized on radiation field. Eur J Dermatol. 2003;13:408-409.
- Davidson SJ, Coates D. Cutaneous mastocytosis extending beyond a radiotherapy site: a form of radiodermatitis or a neoplastic phenomenon? Australas J Dermatol. 2012;54:E85-E87. doi:10.1111 /j.1440-0960.2012.00961.x
- Bolognia J, Schaffer JV, Duncan KO, et al, eds. Dermatology Essentials. 2nd ed. Elsevier; 2022.
A 41-year-old woman was referred to dermatology by her radiation oncologist for evaluation of a rash on the right breast at the site of prior radiation therapy of 4 to 6 weeks’ duration. Approximately 2 years prior, the patient was diagnosed with triple-negative invasive ductal carcinoma of the right breast. She was treated with neoadjuvant chemotherapy, bilateral simple mastectomies, and 28 doses of adjuvant radiation therapy. Thirteen months after completing radiation therapy, the patient noted the onset of asymptomatic freckles on the right breast that had appeared over weeks and seemed to be multiplying. Physical examination at the time of dermatology consultation revealed multiple diffusely scattered, brownishred, 3- to 5-mm macules concentrated on the right breast but also involving the right supraclavicular and right axillary areas, abdomen, and thighs.
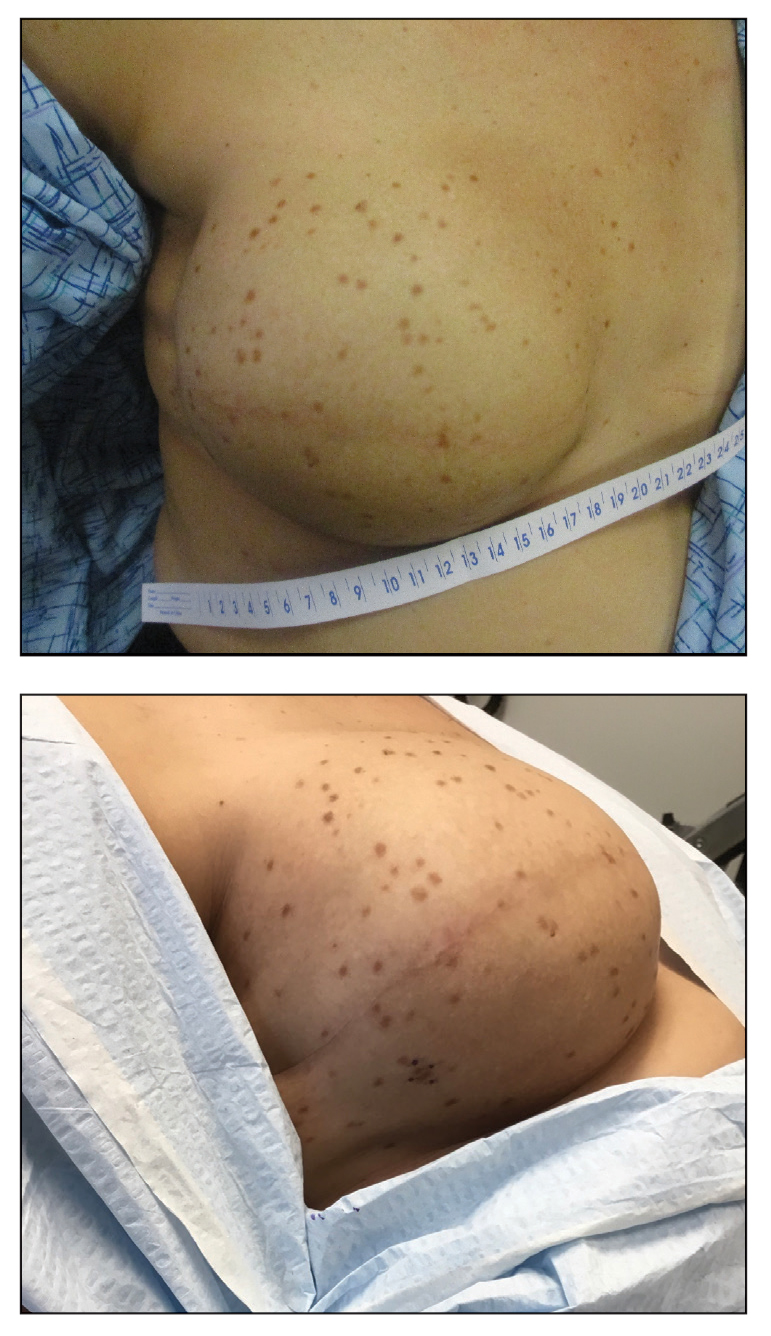
Robitussin Cough Syrup Recalled Nationwide Due to Fungus Concerns
The company that makes Robitussin syrups did not specify which microorganisms may be in the products. The recall announcement from the global consumer health products company Haleon stated that the contamination could lead to fungal infections or the presence of fungi or yeasts in a person’s blood. So far, the company has not received any reports of people being sickened by the recalled products.
The recall applies to bottles of Robitussin Honey CF Max Day and Robitussin Honey CF Max Nighttime. Both varieties are for adults. Affected products were sold nationwide and have specific lot numbers printed at the bottom of the back of the bottles. Consumers can view the lot numbers on the FDA’s recall webpage.
People with weakened immune systems have a higher risk of life-threatening health problems due to the cough syrup, the company warned.
“In non-immunocompromised consumers, the population most likely to use the product, life-threatening infections are not likely to occur,” the recall notice from Haleon stated. “However, the occurrence of an infection that may necessitate medical intervention cannot be completely ruled out.”
People who have affected products should stop using them immediately. The company asked that anyone with the products email Haleon at [email protected], or call the company at 800-245-1040 Monday through Friday from 8 a.m. to 6 p.m. Eastern time.
A version of this article appeared on WebMD.com.
The company that makes Robitussin syrups did not specify which microorganisms may be in the products. The recall announcement from the global consumer health products company Haleon stated that the contamination could lead to fungal infections or the presence of fungi or yeasts in a person’s blood. So far, the company has not received any reports of people being sickened by the recalled products.
The recall applies to bottles of Robitussin Honey CF Max Day and Robitussin Honey CF Max Nighttime. Both varieties are for adults. Affected products were sold nationwide and have specific lot numbers printed at the bottom of the back of the bottles. Consumers can view the lot numbers on the FDA’s recall webpage.
People with weakened immune systems have a higher risk of life-threatening health problems due to the cough syrup, the company warned.
“In non-immunocompromised consumers, the population most likely to use the product, life-threatening infections are not likely to occur,” the recall notice from Haleon stated. “However, the occurrence of an infection that may necessitate medical intervention cannot be completely ruled out.”
People who have affected products should stop using them immediately. The company asked that anyone with the products email Haleon at [email protected], or call the company at 800-245-1040 Monday through Friday from 8 a.m. to 6 p.m. Eastern time.
A version of this article appeared on WebMD.com.
The company that makes Robitussin syrups did not specify which microorganisms may be in the products. The recall announcement from the global consumer health products company Haleon stated that the contamination could lead to fungal infections or the presence of fungi or yeasts in a person’s blood. So far, the company has not received any reports of people being sickened by the recalled products.
The recall applies to bottles of Robitussin Honey CF Max Day and Robitussin Honey CF Max Nighttime. Both varieties are for adults. Affected products were sold nationwide and have specific lot numbers printed at the bottom of the back of the bottles. Consumers can view the lot numbers on the FDA’s recall webpage.
People with weakened immune systems have a higher risk of life-threatening health problems due to the cough syrup, the company warned.
“In non-immunocompromised consumers, the population most likely to use the product, life-threatening infections are not likely to occur,” the recall notice from Haleon stated. “However, the occurrence of an infection that may necessitate medical intervention cannot be completely ruled out.”
People who have affected products should stop using them immediately. The company asked that anyone with the products email Haleon at [email protected], or call the company at 800-245-1040 Monday through Friday from 8 a.m. to 6 p.m. Eastern time.
A version of this article appeared on WebMD.com.
Lp(a) Packs a More Powerful Atherogenic Punch Than LDL
TOPLINE:
While low-density lipoprotein (LDL) particles are much more abundant than lipoprotein(a) [Lp(a)] particles and carry the greatest overall risk for coronary heart disease (CHD), .
METHODOLOGY:
- To compare the atherogenicity of Lp(a) relative to LDL on a per-particle basis, researchers used a genetic analysis because Lp(a) and LDL both contain one apolipoprotein B (apoB) per particle.
- In a genome-wide association study of 502,413 UK Biobank participants, they identified genetic variants uniquely affecting plasma levels of either Lp(a) or LDL particles.
- For these two genetic clusters, they related the change in apoB to the respective change in CHD risk, which allowed them to directly compare the atherogenicity of LDL and Lp(a), particle to particle.
TAKEAWAY:
- The odds ratio for CHD for a 50 nmol/L higher Lp(a)-apoB was 1.28 (95% CI, 1.24-1.33) compared with 1.04 (95% CI, 1.03-1.05) for the same increment in LDL-apoB.
- Additional supporting evidence was provided by using polygenic scores to rank participants according to the difference in Lp(a)-apoB vs LDL-apoB, which revealed a greater risk for CHD per 50 nmol/L apoB for the Lp(a) cluster (hazard ratio [HR], 1.47; 95% CI, 1.36-1.58) than the LDL cluster (HR, 1.04; 95% CI, 1.02-1.05).
- Based on the data, the researchers estimate that the atherogenicity of Lp(a) is roughly sixfold greater (point estimate of 6.6; 95% CI, 5.1-8.8) than that of LDL on a per-particle basis.
IN PRACTICE:
“There are two clinical implications. First, to completely characterize atherosclerotic cardiovascular disease risk, it is imperative to measure Lp(a) in all adult patients at least once. Second, these studies provide a rationale that targeting Lp(a) with potent and specific drugs may lead to clinically meaningful benefit,” wrote the authors of an accompanying commentary on the study.
SOURCE:
The study, with first author Elias Björnson, PhD, University of Gothenburg, Gothenburg, Sweden, and an editorial by Sotirios Tsimikas, MD, University of California, San Diego, and Vera Bittner, MD, University of Alabama at Birmingham, was published in the Journal of the American College of Cardiology.
LIMITATIONS:
The UK Biobank consists primarily of a Caucasian population, and confirmatory studies in more diverse samples are needed. The working range for the Lp(a) assay used in the study did not cover the full range of Lp(a) values seen in the population. Variations in Lp(a)-apoB and LDL-apoB were estimated from genetic analysis and not measured specifically in biochemical assays.
DISCLOSURES:
The study had no commercial funding. Some authors received honoraria from the pharmaceutical industry. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
While low-density lipoprotein (LDL) particles are much more abundant than lipoprotein(a) [Lp(a)] particles and carry the greatest overall risk for coronary heart disease (CHD), .
METHODOLOGY:
- To compare the atherogenicity of Lp(a) relative to LDL on a per-particle basis, researchers used a genetic analysis because Lp(a) and LDL both contain one apolipoprotein B (apoB) per particle.
- In a genome-wide association study of 502,413 UK Biobank participants, they identified genetic variants uniquely affecting plasma levels of either Lp(a) or LDL particles.
- For these two genetic clusters, they related the change in apoB to the respective change in CHD risk, which allowed them to directly compare the atherogenicity of LDL and Lp(a), particle to particle.
TAKEAWAY:
- The odds ratio for CHD for a 50 nmol/L higher Lp(a)-apoB was 1.28 (95% CI, 1.24-1.33) compared with 1.04 (95% CI, 1.03-1.05) for the same increment in LDL-apoB.
- Additional supporting evidence was provided by using polygenic scores to rank participants according to the difference in Lp(a)-apoB vs LDL-apoB, which revealed a greater risk for CHD per 50 nmol/L apoB for the Lp(a) cluster (hazard ratio [HR], 1.47; 95% CI, 1.36-1.58) than the LDL cluster (HR, 1.04; 95% CI, 1.02-1.05).
- Based on the data, the researchers estimate that the atherogenicity of Lp(a) is roughly sixfold greater (point estimate of 6.6; 95% CI, 5.1-8.8) than that of LDL on a per-particle basis.
IN PRACTICE:
“There are two clinical implications. First, to completely characterize atherosclerotic cardiovascular disease risk, it is imperative to measure Lp(a) in all adult patients at least once. Second, these studies provide a rationale that targeting Lp(a) with potent and specific drugs may lead to clinically meaningful benefit,” wrote the authors of an accompanying commentary on the study.
SOURCE:
The study, with first author Elias Björnson, PhD, University of Gothenburg, Gothenburg, Sweden, and an editorial by Sotirios Tsimikas, MD, University of California, San Diego, and Vera Bittner, MD, University of Alabama at Birmingham, was published in the Journal of the American College of Cardiology.
LIMITATIONS:
The UK Biobank consists primarily of a Caucasian population, and confirmatory studies in more diverse samples are needed. The working range for the Lp(a) assay used in the study did not cover the full range of Lp(a) values seen in the population. Variations in Lp(a)-apoB and LDL-apoB were estimated from genetic analysis and not measured specifically in biochemical assays.
DISCLOSURES:
The study had no commercial funding. Some authors received honoraria from the pharmaceutical industry. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
TOPLINE:
While low-density lipoprotein (LDL) particles are much more abundant than lipoprotein(a) [Lp(a)] particles and carry the greatest overall risk for coronary heart disease (CHD), .
METHODOLOGY:
- To compare the atherogenicity of Lp(a) relative to LDL on a per-particle basis, researchers used a genetic analysis because Lp(a) and LDL both contain one apolipoprotein B (apoB) per particle.
- In a genome-wide association study of 502,413 UK Biobank participants, they identified genetic variants uniquely affecting plasma levels of either Lp(a) or LDL particles.
- For these two genetic clusters, they related the change in apoB to the respective change in CHD risk, which allowed them to directly compare the atherogenicity of LDL and Lp(a), particle to particle.
TAKEAWAY:
- The odds ratio for CHD for a 50 nmol/L higher Lp(a)-apoB was 1.28 (95% CI, 1.24-1.33) compared with 1.04 (95% CI, 1.03-1.05) for the same increment in LDL-apoB.
- Additional supporting evidence was provided by using polygenic scores to rank participants according to the difference in Lp(a)-apoB vs LDL-apoB, which revealed a greater risk for CHD per 50 nmol/L apoB for the Lp(a) cluster (hazard ratio [HR], 1.47; 95% CI, 1.36-1.58) than the LDL cluster (HR, 1.04; 95% CI, 1.02-1.05).
- Based on the data, the researchers estimate that the atherogenicity of Lp(a) is roughly sixfold greater (point estimate of 6.6; 95% CI, 5.1-8.8) than that of LDL on a per-particle basis.
IN PRACTICE:
“There are two clinical implications. First, to completely characterize atherosclerotic cardiovascular disease risk, it is imperative to measure Lp(a) in all adult patients at least once. Second, these studies provide a rationale that targeting Lp(a) with potent and specific drugs may lead to clinically meaningful benefit,” wrote the authors of an accompanying commentary on the study.
SOURCE:
The study, with first author Elias Björnson, PhD, University of Gothenburg, Gothenburg, Sweden, and an editorial by Sotirios Tsimikas, MD, University of California, San Diego, and Vera Bittner, MD, University of Alabama at Birmingham, was published in the Journal of the American College of Cardiology.
LIMITATIONS:
The UK Biobank consists primarily of a Caucasian population, and confirmatory studies in more diverse samples are needed. The working range for the Lp(a) assay used in the study did not cover the full range of Lp(a) values seen in the population. Variations in Lp(a)-apoB and LDL-apoB were estimated from genetic analysis and not measured specifically in biochemical assays.
DISCLOSURES:
The study had no commercial funding. Some authors received honoraria from the pharmaceutical industry. A complete list of author disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
ALL: When Should MRD Trigger Stem Cell Transplants?
Allogeneic hematopoietic stem cell transplants (HSCT) are still part of the hematology armamentarium for relapsed/refractory (R/R) patients with Ph-negative ALL who are MRD positive. However, when asked about the best treatment strategy for patients who are MRD-negative, hematologist Mark R. Litzow, MD, of the Mayo Clinic in Rochester, Minnesota, said in an interview, “There is no firm consensus about that.”
Discussing how medicine has evolved over the past 20 to 30 years, Dr. Litzow recalled that HSCT used to be standard treatment for adult patients with ALL. “We felt that in most instances, chemotherapy alone was not going to be effective in curing them. A vast majority would relapse,” he said. Nowadays, however, specialists differ on the use of HSCT in patients with Ph-negative, MRD-negative ALL.
A pair of commentaries in the January issue of The Lancet Hematology tackle this topic from different perspectives. On one hand, hematologist Patrice Chevallier, MD, of the University of Nantes in France, argues that for such patients, HSCT “remains a valid option,”and MRD status shouldn’t be the sole factor used for a decision.
However, hematologist Nicolas Boissel, MD, PhD, of Paris Cité University, contends that detectable early MRD is the “only robust predictor” of HSCT benefit in patients under 60 with Ph-negative ALL, and it has “unproven” benefit in older patients.
As Dr. Chevallier notes, “allogeneic HSCT is indicated in patients defined as having a high risk of relapse. Currently, a high level of residual leukemic cells after treatment is recognized as the strongest, and sometimes sole, criterion defining high-risk patients.”
As first- and second-line therapy in pediatric patients and as first-line therapy in adults, the “rule” is to offer HSCT to MRD-positive patients but not MRD-negative ones, he writes. “In older patients and those who are relapsed or refractory, the recent demonstration of efficient immunotherapies and cell therapies has launched the debate on the role of MRD status and the question of whether or not to transplant patients who are MRD-negative in both settings.”
Dr. Chevallier notes that “there is no standard definition of an MRD-negative status,” and the best timing for evaluation is unknown. Further, he adds, a “variable proportion of MRD-negative patients still relapse after treatment — up to 25% of patients who respond early and more than 50% of patients who respond late.”
He also points out that there’s an 80% chance that patients will convert from MRD negative to MRD positive after blinatumomab therapy, and he highlights the low long-term survival rate (20%) after brexucabtagene autoleucel (Tecartus), a CAR T-cell therapy.
As for older patients, Dr. Chevallier observes that improved chemo-immunotherapy and conditioning regimens could spark a rethinking of the feasibility of HSCT. However, for now, in those patients, “MRD is not decisional, and allogeneic HSCT is not a routine practice,” he writes.
In his commentary, Dr. Boissel points out that there have been no controlled studies of HSCT in the first-remission setting, although he writes that some data suggests that HSCT may be helpful for patients in high-risk genetic subgroups, regardless of MRD status. On the other hand, “converging observations suggest no benefit of HSCT in MRD-positive patients treated with blinatumomab in the front-line setting.”
If MRD monitoring is unavailable, Dr. Boissel adds, “it seems reasonable to use early blast clearance or other baseline high-risk features to indicate HSCT.”
How can hematologists make the best decision about HSCT?
In an interview, City of Hope Medical Center (Duarte, California) hematologist-oncologist Ibrahim T. Aldoss, MD, said that chemotherapy — with or without immunotherapy — can often be enough to treat younger patients without high-risk genetic factors. “Potentially, these patients can be spared from transplants,” he said, although patients with resistant MRD “clearly need transplants.”
The risks of transplants are significant, he noted. While they can reduce the risk of relapse, the risk of dying during remission is higher vs chemotherapy. “So you have to balance the risks that you’re willing to take,” he said, keeping in mind that some patients can be cured with chemotherapy.
In addition, Dr. Aldoss said, acute graft-versus-host disease in the first few months after transplant can become chronic. “Many years later, patients can be struggling to where it actually impacts their daily activity. And unfortunately, patients can die from it.”
In the big picture, “you cannot have a generalized statement about whether you shouldn’t do transplants in every MRD-negative patient,” he said. However, “if you do achieve MRD negativity, most patients likely don’t need transplants.”
The Mayo Clinic’s Dr. Litzow urged colleagues to consider several factors when making decisions. Do patients have a high level of comorbidities that would raise the risk of death from HSCT? He noted that there’s nearly a 20% risk of death from HSCT, and comorbidities can boost the risk to 40%-50%.
Also, does the patient have a suitable donor? While advances have boosted the number of eligible donors, he said, “not everybody has an ideal donor.”
If a patient is MRD-negative but not a good candidate for a transplant, Dr. Litzow said consolidation therapy followed by maintenance therapy may be indicated. “Continue to check their bone marrow and their blood periodically as they’re going through treatment and reassess their MRD status to make sure they’re staying negative. If they turn MRD-positive during the course of their therapy, then we have to step back and rethink the role of transplant.”
As for cost, Dr. Litzow points out that HSCT is very expensive, although ALL is an accepted indication for HSCT. However, “if someone doesn’t have medical insurance, then it can be difficult to consider them having a transplant.”
What’s next? In his commentary, Dr. Boissel writes that his team aims to study whether HSCT is helpful in patients with high-risk B-cell ALL “who reach MRD negativity after a consolidation phase including blinatumomab.”
Dr. Aldoss discloses relationships with Amgen, Kite, Pfizer, Jazz, AbbVie, Sobi, Agios, Autolus, and MacroGenics. Dr. Litzow reports ties with Amgen. Dr. Boissel declares relationships with Amgen, Pfizer, Novartis, and Servier. Dr. Chevallier has no disclosures.
Allogeneic hematopoietic stem cell transplants (HSCT) are still part of the hematology armamentarium for relapsed/refractory (R/R) patients with Ph-negative ALL who are MRD positive. However, when asked about the best treatment strategy for patients who are MRD-negative, hematologist Mark R. Litzow, MD, of the Mayo Clinic in Rochester, Minnesota, said in an interview, “There is no firm consensus about that.”
Discussing how medicine has evolved over the past 20 to 30 years, Dr. Litzow recalled that HSCT used to be standard treatment for adult patients with ALL. “We felt that in most instances, chemotherapy alone was not going to be effective in curing them. A vast majority would relapse,” he said. Nowadays, however, specialists differ on the use of HSCT in patients with Ph-negative, MRD-negative ALL.
A pair of commentaries in the January issue of The Lancet Hematology tackle this topic from different perspectives. On one hand, hematologist Patrice Chevallier, MD, of the University of Nantes in France, argues that for such patients, HSCT “remains a valid option,”and MRD status shouldn’t be the sole factor used for a decision.
However, hematologist Nicolas Boissel, MD, PhD, of Paris Cité University, contends that detectable early MRD is the “only robust predictor” of HSCT benefit in patients under 60 with Ph-negative ALL, and it has “unproven” benefit in older patients.
As Dr. Chevallier notes, “allogeneic HSCT is indicated in patients defined as having a high risk of relapse. Currently, a high level of residual leukemic cells after treatment is recognized as the strongest, and sometimes sole, criterion defining high-risk patients.”
As first- and second-line therapy in pediatric patients and as first-line therapy in adults, the “rule” is to offer HSCT to MRD-positive patients but not MRD-negative ones, he writes. “In older patients and those who are relapsed or refractory, the recent demonstration of efficient immunotherapies and cell therapies has launched the debate on the role of MRD status and the question of whether or not to transplant patients who are MRD-negative in both settings.”
Dr. Chevallier notes that “there is no standard definition of an MRD-negative status,” and the best timing for evaluation is unknown. Further, he adds, a “variable proportion of MRD-negative patients still relapse after treatment — up to 25% of patients who respond early and more than 50% of patients who respond late.”
He also points out that there’s an 80% chance that patients will convert from MRD negative to MRD positive after blinatumomab therapy, and he highlights the low long-term survival rate (20%) after brexucabtagene autoleucel (Tecartus), a CAR T-cell therapy.
As for older patients, Dr. Chevallier observes that improved chemo-immunotherapy and conditioning regimens could spark a rethinking of the feasibility of HSCT. However, for now, in those patients, “MRD is not decisional, and allogeneic HSCT is not a routine practice,” he writes.
In his commentary, Dr. Boissel points out that there have been no controlled studies of HSCT in the first-remission setting, although he writes that some data suggests that HSCT may be helpful for patients in high-risk genetic subgroups, regardless of MRD status. On the other hand, “converging observations suggest no benefit of HSCT in MRD-positive patients treated with blinatumomab in the front-line setting.”
If MRD monitoring is unavailable, Dr. Boissel adds, “it seems reasonable to use early blast clearance or other baseline high-risk features to indicate HSCT.”
How can hematologists make the best decision about HSCT?
In an interview, City of Hope Medical Center (Duarte, California) hematologist-oncologist Ibrahim T. Aldoss, MD, said that chemotherapy — with or without immunotherapy — can often be enough to treat younger patients without high-risk genetic factors. “Potentially, these patients can be spared from transplants,” he said, although patients with resistant MRD “clearly need transplants.”
The risks of transplants are significant, he noted. While they can reduce the risk of relapse, the risk of dying during remission is higher vs chemotherapy. “So you have to balance the risks that you’re willing to take,” he said, keeping in mind that some patients can be cured with chemotherapy.
In addition, Dr. Aldoss said, acute graft-versus-host disease in the first few months after transplant can become chronic. “Many years later, patients can be struggling to where it actually impacts their daily activity. And unfortunately, patients can die from it.”
In the big picture, “you cannot have a generalized statement about whether you shouldn’t do transplants in every MRD-negative patient,” he said. However, “if you do achieve MRD negativity, most patients likely don’t need transplants.”
The Mayo Clinic’s Dr. Litzow urged colleagues to consider several factors when making decisions. Do patients have a high level of comorbidities that would raise the risk of death from HSCT? He noted that there’s nearly a 20% risk of death from HSCT, and comorbidities can boost the risk to 40%-50%.
Also, does the patient have a suitable donor? While advances have boosted the number of eligible donors, he said, “not everybody has an ideal donor.”
If a patient is MRD-negative but not a good candidate for a transplant, Dr. Litzow said consolidation therapy followed by maintenance therapy may be indicated. “Continue to check their bone marrow and their blood periodically as they’re going through treatment and reassess their MRD status to make sure they’re staying negative. If they turn MRD-positive during the course of their therapy, then we have to step back and rethink the role of transplant.”
As for cost, Dr. Litzow points out that HSCT is very expensive, although ALL is an accepted indication for HSCT. However, “if someone doesn’t have medical insurance, then it can be difficult to consider them having a transplant.”
What’s next? In his commentary, Dr. Boissel writes that his team aims to study whether HSCT is helpful in patients with high-risk B-cell ALL “who reach MRD negativity after a consolidation phase including blinatumomab.”
Dr. Aldoss discloses relationships with Amgen, Kite, Pfizer, Jazz, AbbVie, Sobi, Agios, Autolus, and MacroGenics. Dr. Litzow reports ties with Amgen. Dr. Boissel declares relationships with Amgen, Pfizer, Novartis, and Servier. Dr. Chevallier has no disclosures.
Allogeneic hematopoietic stem cell transplants (HSCT) are still part of the hematology armamentarium for relapsed/refractory (R/R) patients with Ph-negative ALL who are MRD positive. However, when asked about the best treatment strategy for patients who are MRD-negative, hematologist Mark R. Litzow, MD, of the Mayo Clinic in Rochester, Minnesota, said in an interview, “There is no firm consensus about that.”
Discussing how medicine has evolved over the past 20 to 30 years, Dr. Litzow recalled that HSCT used to be standard treatment for adult patients with ALL. “We felt that in most instances, chemotherapy alone was not going to be effective in curing them. A vast majority would relapse,” he said. Nowadays, however, specialists differ on the use of HSCT in patients with Ph-negative, MRD-negative ALL.
A pair of commentaries in the January issue of The Lancet Hematology tackle this topic from different perspectives. On one hand, hematologist Patrice Chevallier, MD, of the University of Nantes in France, argues that for such patients, HSCT “remains a valid option,”and MRD status shouldn’t be the sole factor used for a decision.
However, hematologist Nicolas Boissel, MD, PhD, of Paris Cité University, contends that detectable early MRD is the “only robust predictor” of HSCT benefit in patients under 60 with Ph-negative ALL, and it has “unproven” benefit in older patients.
As Dr. Chevallier notes, “allogeneic HSCT is indicated in patients defined as having a high risk of relapse. Currently, a high level of residual leukemic cells after treatment is recognized as the strongest, and sometimes sole, criterion defining high-risk patients.”
As first- and second-line therapy in pediatric patients and as first-line therapy in adults, the “rule” is to offer HSCT to MRD-positive patients but not MRD-negative ones, he writes. “In older patients and those who are relapsed or refractory, the recent demonstration of efficient immunotherapies and cell therapies has launched the debate on the role of MRD status and the question of whether or not to transplant patients who are MRD-negative in both settings.”
Dr. Chevallier notes that “there is no standard definition of an MRD-negative status,” and the best timing for evaluation is unknown. Further, he adds, a “variable proportion of MRD-negative patients still relapse after treatment — up to 25% of patients who respond early and more than 50% of patients who respond late.”
He also points out that there’s an 80% chance that patients will convert from MRD negative to MRD positive after blinatumomab therapy, and he highlights the low long-term survival rate (20%) after brexucabtagene autoleucel (Tecartus), a CAR T-cell therapy.
As for older patients, Dr. Chevallier observes that improved chemo-immunotherapy and conditioning regimens could spark a rethinking of the feasibility of HSCT. However, for now, in those patients, “MRD is not decisional, and allogeneic HSCT is not a routine practice,” he writes.
In his commentary, Dr. Boissel points out that there have been no controlled studies of HSCT in the first-remission setting, although he writes that some data suggests that HSCT may be helpful for patients in high-risk genetic subgroups, regardless of MRD status. On the other hand, “converging observations suggest no benefit of HSCT in MRD-positive patients treated with blinatumomab in the front-line setting.”
If MRD monitoring is unavailable, Dr. Boissel adds, “it seems reasonable to use early blast clearance or other baseline high-risk features to indicate HSCT.”
How can hematologists make the best decision about HSCT?
In an interview, City of Hope Medical Center (Duarte, California) hematologist-oncologist Ibrahim T. Aldoss, MD, said that chemotherapy — with or without immunotherapy — can often be enough to treat younger patients without high-risk genetic factors. “Potentially, these patients can be spared from transplants,” he said, although patients with resistant MRD “clearly need transplants.”
The risks of transplants are significant, he noted. While they can reduce the risk of relapse, the risk of dying during remission is higher vs chemotherapy. “So you have to balance the risks that you’re willing to take,” he said, keeping in mind that some patients can be cured with chemotherapy.
In addition, Dr. Aldoss said, acute graft-versus-host disease in the first few months after transplant can become chronic. “Many years later, patients can be struggling to where it actually impacts their daily activity. And unfortunately, patients can die from it.”
In the big picture, “you cannot have a generalized statement about whether you shouldn’t do transplants in every MRD-negative patient,” he said. However, “if you do achieve MRD negativity, most patients likely don’t need transplants.”
The Mayo Clinic’s Dr. Litzow urged colleagues to consider several factors when making decisions. Do patients have a high level of comorbidities that would raise the risk of death from HSCT? He noted that there’s nearly a 20% risk of death from HSCT, and comorbidities can boost the risk to 40%-50%.
Also, does the patient have a suitable donor? While advances have boosted the number of eligible donors, he said, “not everybody has an ideal donor.”
If a patient is MRD-negative but not a good candidate for a transplant, Dr. Litzow said consolidation therapy followed by maintenance therapy may be indicated. “Continue to check their bone marrow and their blood periodically as they’re going through treatment and reassess their MRD status to make sure they’re staying negative. If they turn MRD-positive during the course of their therapy, then we have to step back and rethink the role of transplant.”
As for cost, Dr. Litzow points out that HSCT is very expensive, although ALL is an accepted indication for HSCT. However, “if someone doesn’t have medical insurance, then it can be difficult to consider them having a transplant.”
What’s next? In his commentary, Dr. Boissel writes that his team aims to study whether HSCT is helpful in patients with high-risk B-cell ALL “who reach MRD negativity after a consolidation phase including blinatumomab.”
Dr. Aldoss discloses relationships with Amgen, Kite, Pfizer, Jazz, AbbVie, Sobi, Agios, Autolus, and MacroGenics. Dr. Litzow reports ties with Amgen. Dr. Boissel declares relationships with Amgen, Pfizer, Novartis, and Servier. Dr. Chevallier has no disclosures.






