User login
Virtual visits may cut no-show rate for follow-up HF appointment
PHILADELPHIA – For patients transitioning to home after a heart failure hospitalization, substituting in-person visits with virtual, video-based visits is feasible, safe, and may reduce appointment no-show rates, results of a randomized study suggest.
Connecting patients with clinicians over secure video cut no-show rates at 7 days post-discharge by about one-third, with no difference in risk of readmission, emergency department visits, or death, compared with the traditional in-person follow-up visit, investigator Eiran Z. Gorodeski, MD, MPH, reported here at the annual scientific meeting of the Heart Failure Society of America.
While the video meet-up doesn’t allow for a physical exam, it’s still possible to collect history of what happened since hospital discharge, assess breathing, and complete other aspects of the follow-up visit, according to Dr. Gorodeski, director of advanced heart failure section at the University Hospitals Cleveland Medical Center.
“The way we view use of virtual visits 7 days post-discharge is, in many ways, as a screening platform,” he said in a panel discussion. “If someone seems to be doing poorly, you can always invite them to come in, but most patients post discharge are not congested, and they’re doing quite well. Probably the more relevant issues are things like: Do they have their medications? Do they understand what their follow-up appointments are?”
During the virtual visit, patients are asked to hold their medication bottles up to the camera so the clinician can see what they are taking.
“Frequently, we are able to catch mistakes,” Dr. Gorodeski said. “Of note, most patients don’t bring their pill bottles to the clinic, so in some ways doing the virtual visit for that aspect was more valuable.”
Patients who opt for a virtual visit can do so from any smart phone, laptop, or desktop computer. Once logged in, they enter a virtual waiting room as the clinician receives a text notification to log in and begin the visit.
“It’s very efficient with time, and my questions were answered quickly,” said a patient in a short video Dr. Gorodeski played to illustrate the technology.
“I still feel the same connectivity with the patient,” a clinician in the video said.
There is currently no way to bill insurance companies for this type of visit, Dr. Gorodeski said when asked what initial barriers other institutions might have implementing a similar approach.
In the randomized, single-center clinical trial Dr. Gorodeski presented here at the HFSA meeting, called VIV-HF (Virtual Visits in Heart Failure Care Transitions), a total of 108 patients were randomized to the virtual visit (52 patients) or an in-person visit (56 patients).
The majority of patients (over 60%) had heart failure with reduced ejection fraction, according to the reported study results.
No-show rates were 50% for the in-person visit, and 34.6% for the virtual visit, for a relative risk reduction of 31%. However, this difference did not reach statistical significance, likely because the study was underpowered, according to Dr. Gorodeski.
“This strategy may reduce postdischarge appointment no-show rates, and this needs to be studied further in larger and appropriately powered clinical trials,” he said in presenting the results.
The 7-day postdischarge outpatient clinic visit is recommended in guidelines and viewed as a way to increase care engagement while reducing risk of poor outcomes, according to VIV-HF investigators.
Support for the study came from the Hunnell Fund. Dr. Gorodeski reported being a consultant and advisor to Abbott.
cardnews@mdedge
SOURCE: Gorodeski EZ, et al. HFSA 2019. Late-Breaking Clinical Trials session.
PHILADELPHIA – For patients transitioning to home after a heart failure hospitalization, substituting in-person visits with virtual, video-based visits is feasible, safe, and may reduce appointment no-show rates, results of a randomized study suggest.
Connecting patients with clinicians over secure video cut no-show rates at 7 days post-discharge by about one-third, with no difference in risk of readmission, emergency department visits, or death, compared with the traditional in-person follow-up visit, investigator Eiran Z. Gorodeski, MD, MPH, reported here at the annual scientific meeting of the Heart Failure Society of America.
While the video meet-up doesn’t allow for a physical exam, it’s still possible to collect history of what happened since hospital discharge, assess breathing, and complete other aspects of the follow-up visit, according to Dr. Gorodeski, director of advanced heart failure section at the University Hospitals Cleveland Medical Center.
“The way we view use of virtual visits 7 days post-discharge is, in many ways, as a screening platform,” he said in a panel discussion. “If someone seems to be doing poorly, you can always invite them to come in, but most patients post discharge are not congested, and they’re doing quite well. Probably the more relevant issues are things like: Do they have their medications? Do they understand what their follow-up appointments are?”
During the virtual visit, patients are asked to hold their medication bottles up to the camera so the clinician can see what they are taking.
“Frequently, we are able to catch mistakes,” Dr. Gorodeski said. “Of note, most patients don’t bring their pill bottles to the clinic, so in some ways doing the virtual visit for that aspect was more valuable.”
Patients who opt for a virtual visit can do so from any smart phone, laptop, or desktop computer. Once logged in, they enter a virtual waiting room as the clinician receives a text notification to log in and begin the visit.
“It’s very efficient with time, and my questions were answered quickly,” said a patient in a short video Dr. Gorodeski played to illustrate the technology.
“I still feel the same connectivity with the patient,” a clinician in the video said.
There is currently no way to bill insurance companies for this type of visit, Dr. Gorodeski said when asked what initial barriers other institutions might have implementing a similar approach.
In the randomized, single-center clinical trial Dr. Gorodeski presented here at the HFSA meeting, called VIV-HF (Virtual Visits in Heart Failure Care Transitions), a total of 108 patients were randomized to the virtual visit (52 patients) or an in-person visit (56 patients).
The majority of patients (over 60%) had heart failure with reduced ejection fraction, according to the reported study results.
No-show rates were 50% for the in-person visit, and 34.6% for the virtual visit, for a relative risk reduction of 31%. However, this difference did not reach statistical significance, likely because the study was underpowered, according to Dr. Gorodeski.
“This strategy may reduce postdischarge appointment no-show rates, and this needs to be studied further in larger and appropriately powered clinical trials,” he said in presenting the results.
The 7-day postdischarge outpatient clinic visit is recommended in guidelines and viewed as a way to increase care engagement while reducing risk of poor outcomes, according to VIV-HF investigators.
Support for the study came from the Hunnell Fund. Dr. Gorodeski reported being a consultant and advisor to Abbott.
cardnews@mdedge
SOURCE: Gorodeski EZ, et al. HFSA 2019. Late-Breaking Clinical Trials session.
PHILADELPHIA – For patients transitioning to home after a heart failure hospitalization, substituting in-person visits with virtual, video-based visits is feasible, safe, and may reduce appointment no-show rates, results of a randomized study suggest.
Connecting patients with clinicians over secure video cut no-show rates at 7 days post-discharge by about one-third, with no difference in risk of readmission, emergency department visits, or death, compared with the traditional in-person follow-up visit, investigator Eiran Z. Gorodeski, MD, MPH, reported here at the annual scientific meeting of the Heart Failure Society of America.
While the video meet-up doesn’t allow for a physical exam, it’s still possible to collect history of what happened since hospital discharge, assess breathing, and complete other aspects of the follow-up visit, according to Dr. Gorodeski, director of advanced heart failure section at the University Hospitals Cleveland Medical Center.
“The way we view use of virtual visits 7 days post-discharge is, in many ways, as a screening platform,” he said in a panel discussion. “If someone seems to be doing poorly, you can always invite them to come in, but most patients post discharge are not congested, and they’re doing quite well. Probably the more relevant issues are things like: Do they have their medications? Do they understand what their follow-up appointments are?”
During the virtual visit, patients are asked to hold their medication bottles up to the camera so the clinician can see what they are taking.
“Frequently, we are able to catch mistakes,” Dr. Gorodeski said. “Of note, most patients don’t bring their pill bottles to the clinic, so in some ways doing the virtual visit for that aspect was more valuable.”
Patients who opt for a virtual visit can do so from any smart phone, laptop, or desktop computer. Once logged in, they enter a virtual waiting room as the clinician receives a text notification to log in and begin the visit.
“It’s very efficient with time, and my questions were answered quickly,” said a patient in a short video Dr. Gorodeski played to illustrate the technology.
“I still feel the same connectivity with the patient,” a clinician in the video said.
There is currently no way to bill insurance companies for this type of visit, Dr. Gorodeski said when asked what initial barriers other institutions might have implementing a similar approach.
In the randomized, single-center clinical trial Dr. Gorodeski presented here at the HFSA meeting, called VIV-HF (Virtual Visits in Heart Failure Care Transitions), a total of 108 patients were randomized to the virtual visit (52 patients) or an in-person visit (56 patients).
The majority of patients (over 60%) had heart failure with reduced ejection fraction, according to the reported study results.
No-show rates were 50% for the in-person visit, and 34.6% for the virtual visit, for a relative risk reduction of 31%. However, this difference did not reach statistical significance, likely because the study was underpowered, according to Dr. Gorodeski.
“This strategy may reduce postdischarge appointment no-show rates, and this needs to be studied further in larger and appropriately powered clinical trials,” he said in presenting the results.
The 7-day postdischarge outpatient clinic visit is recommended in guidelines and viewed as a way to increase care engagement while reducing risk of poor outcomes, according to VIV-HF investigators.
Support for the study came from the Hunnell Fund. Dr. Gorodeski reported being a consultant and advisor to Abbott.
cardnews@mdedge
SOURCE: Gorodeski EZ, et al. HFSA 2019. Late-Breaking Clinical Trials session.
REPORTING FROM HFSA 2019
Urban or rural, children’s gun-related injuries equally deadly
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
AT AAP 2019
Ovarian cryopreservation should no longer be experimental
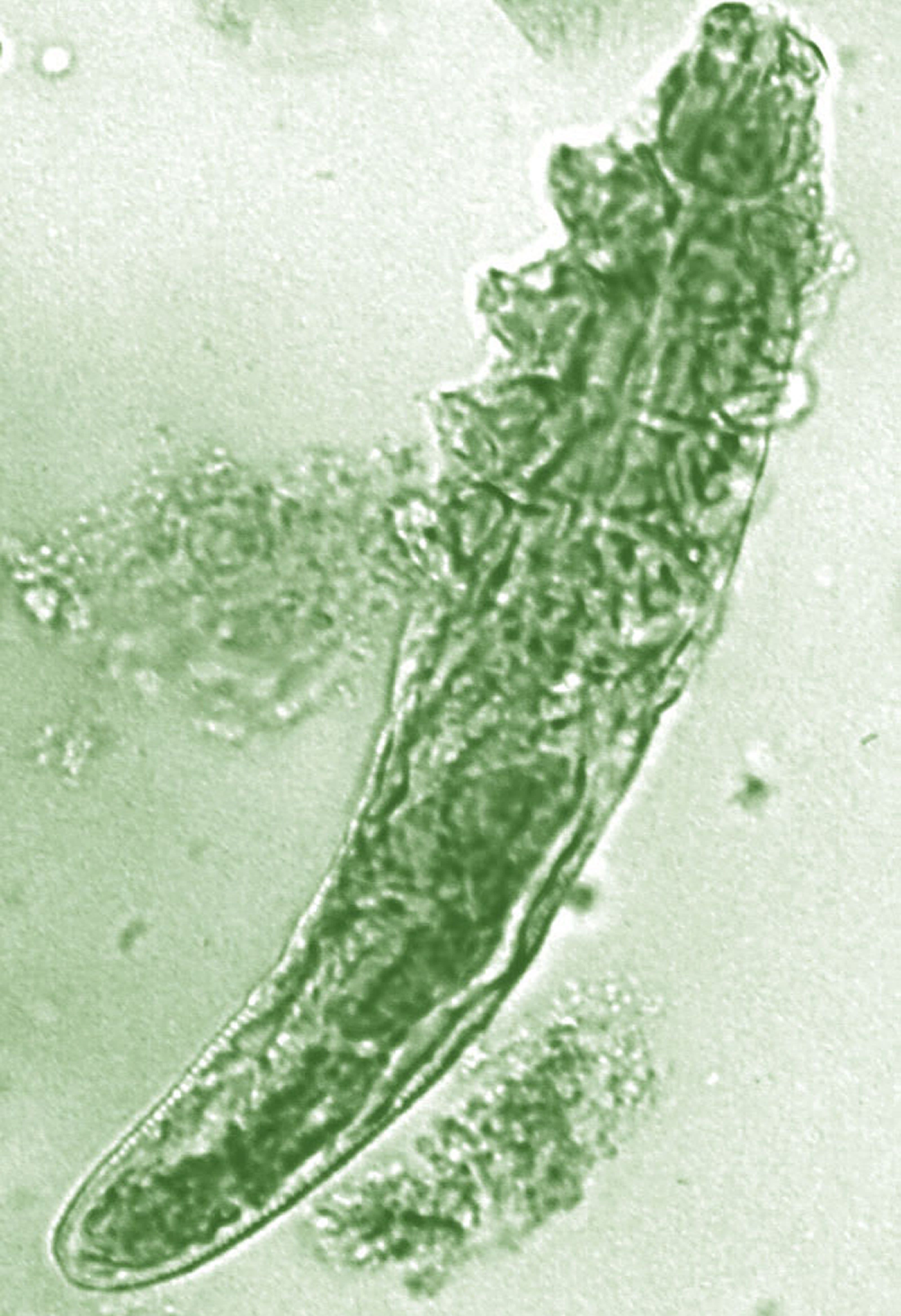
PHILADELPHIA – Ovarian tissue cryopreservation should no longer be considered experimental, Sherman J. Silber, MD, said at the annual meeting of the American Society for Reproductive Medicine.
That claim is based on more than 20 years of experience at his center performing the procedure and results he presented from patients for whom frozen ovarian tissue has been reimplanted resulting in a spontaneous pregnancy.
“For prepubertal girls with cancer and for patients who have already had a preliminary round of chemotherapy, ovarian tissue freezing is the only method available to preserve their fertility,” said Dr. Silber, of the Infertility Center of St. Louis in Chesterfield, Missouri. “It is also the only method available to preserve their fertility.”
“I have very strong feelings about this,” he added. “It has huge societal implications for insurance payments.”
Dr. Silber presented results of ovarian tissue freezing and reimplantation at his center beginning in 1997, where 115 patients between the ages of 2 and 35 years underwent the procedure using the same technique. Of these patients, 14 women came back years later to have their frozen ovary cortex reimplanted. Dr. Silber and his group followed these patients monthly for more than 2 years after reimplantation for signs of return of menses, hormonal changes, pregnancy, and live birth.
Most of the patients who chose ovarian tissue freezing had cancer. Eight patients underwent the procedure after being diagnosed with solid tissue cancer and three had leukemia, while two patients underwent ovarian tissue freezing due to premature ovarian failure, and one because of multiple sclerosis. Patients who underwent reimplantation were menopausal for at least 3 years, said Dr. Silber.
Dr. Silber also described the technique used for reimplantation. After the cortical tissue was thawed, the tissue was quilted into one piece from three to five slices using 9-0 nylon interrupted sutures. The quilted tissue was then sutured to the medulla after the surgeon completely removed the dead cortex from the other ovary. “Hemostasis was achieved with micro bipolar forceps,” said Dr. Silber. “Constant irrigation was employed with pulsed heparinized media because we wanted to avoid adhesions, and we wanted to try for spontaneous pregnancy rather than IVF.”
“Then, we put [the quilted ovarian slices] on to the medulla on the other side in such a way that the fallopian tube would be able to reach and catch any egg that’s ovulated during that time,” he added.
Dr. Silber and his group found that, over time, follicle-stimulating hormone (FSH) levels sharply decreased to normal or near-normal levels between 69 days and 133 days after the procedure while Anti-Müllerian hormone (AMH) levels dramatically rose to higher levels between 133 days and 227 days post-procedure before dropping to very low levels, “and the AMH remained at low levels despite the fact that [transplants] would last 8 to 10 years,” said Dr. Silber.
Of the 14 cases where frozen ovarian tissue was reimplanted, 11 patients (78%) achieved pregnancy, 10 patients (71%) delivered healthy babies, and 1 patient (9%) experienced a miscarriage. All patients had spontaneous pregnancies, and none used in vitro fertilization (IVF), noted Dr. Silber. There were 2 patients who had four children from transplanted ovarian tissue, and 2 of 3 patients with leukemia had a total of five children.
Additionally, Dr. Silber’s group examined the literature for other examples of ovarian tissue reimplantation after cryopreservation to determine how many live births resulted from the procedure. They found an additional 170 live births in addition to the 15 live births at their center, with a pregnancy rate ranging from 31% to 71% in different studies. Cancer was not transmitted from mother to child in any case, said Dr. Silber.
Compared with egg freezing, there is a benefit to performing ovarian tissue freezing, even after chemotherapy has begun, noted Dr. Silber. The cost of ovarian tissue freezing is also roughly one-tenth that of egg freezing, and the procedure is less burdensome than multiple cycles with the potential for ovarian hyperstimulation, and it restores the hormone function and the fertility of eggs after reimplantation.
“Because the greater primordial follicle recruitment decreases as the ovarian reserve decreases, you can put a piece of ovary tissue back every 8 years, and a woman can have endocrine function until she’s 100 years old,” said Dr. Silber.
Dr. Silber reported no relevant conflicts of interest.
SOURCE: Silber SJ. ASRM 2019. Abstract O-203.
PHILADELPHIA – Ovarian tissue cryopreservation should no longer be considered experimental, Sherman J. Silber, MD, said at the annual meeting of the American Society for Reproductive Medicine.
That claim is based on more than 20 years of experience at his center performing the procedure and results he presented from patients for whom frozen ovarian tissue has been reimplanted resulting in a spontaneous pregnancy.
“For prepubertal girls with cancer and for patients who have already had a preliminary round of chemotherapy, ovarian tissue freezing is the only method available to preserve their fertility,” said Dr. Silber, of the Infertility Center of St. Louis in Chesterfield, Missouri. “It is also the only method available to preserve their fertility.”
“I have very strong feelings about this,” he added. “It has huge societal implications for insurance payments.”
Dr. Silber presented results of ovarian tissue freezing and reimplantation at his center beginning in 1997, where 115 patients between the ages of 2 and 35 years underwent the procedure using the same technique. Of these patients, 14 women came back years later to have their frozen ovary cortex reimplanted. Dr. Silber and his group followed these patients monthly for more than 2 years after reimplantation for signs of return of menses, hormonal changes, pregnancy, and live birth.
Most of the patients who chose ovarian tissue freezing had cancer. Eight patients underwent the procedure after being diagnosed with solid tissue cancer and three had leukemia, while two patients underwent ovarian tissue freezing due to premature ovarian failure, and one because of multiple sclerosis. Patients who underwent reimplantation were menopausal for at least 3 years, said Dr. Silber.
Dr. Silber also described the technique used for reimplantation. After the cortical tissue was thawed, the tissue was quilted into one piece from three to five slices using 9-0 nylon interrupted sutures. The quilted tissue was then sutured to the medulla after the surgeon completely removed the dead cortex from the other ovary. “Hemostasis was achieved with micro bipolar forceps,” said Dr. Silber. “Constant irrigation was employed with pulsed heparinized media because we wanted to avoid adhesions, and we wanted to try for spontaneous pregnancy rather than IVF.”
“Then, we put [the quilted ovarian slices] on to the medulla on the other side in such a way that the fallopian tube would be able to reach and catch any egg that’s ovulated during that time,” he added.
Dr. Silber and his group found that, over time, follicle-stimulating hormone (FSH) levels sharply decreased to normal or near-normal levels between 69 days and 133 days after the procedure while Anti-Müllerian hormone (AMH) levels dramatically rose to higher levels between 133 days and 227 days post-procedure before dropping to very low levels, “and the AMH remained at low levels despite the fact that [transplants] would last 8 to 10 years,” said Dr. Silber.
Of the 14 cases where frozen ovarian tissue was reimplanted, 11 patients (78%) achieved pregnancy, 10 patients (71%) delivered healthy babies, and 1 patient (9%) experienced a miscarriage. All patients had spontaneous pregnancies, and none used in vitro fertilization (IVF), noted Dr. Silber. There were 2 patients who had four children from transplanted ovarian tissue, and 2 of 3 patients with leukemia had a total of five children.
Additionally, Dr. Silber’s group examined the literature for other examples of ovarian tissue reimplantation after cryopreservation to determine how many live births resulted from the procedure. They found an additional 170 live births in addition to the 15 live births at their center, with a pregnancy rate ranging from 31% to 71% in different studies. Cancer was not transmitted from mother to child in any case, said Dr. Silber.
Compared with egg freezing, there is a benefit to performing ovarian tissue freezing, even after chemotherapy has begun, noted Dr. Silber. The cost of ovarian tissue freezing is also roughly one-tenth that of egg freezing, and the procedure is less burdensome than multiple cycles with the potential for ovarian hyperstimulation, and it restores the hormone function and the fertility of eggs after reimplantation.
“Because the greater primordial follicle recruitment decreases as the ovarian reserve decreases, you can put a piece of ovary tissue back every 8 years, and a woman can have endocrine function until she’s 100 years old,” said Dr. Silber.
Dr. Silber reported no relevant conflicts of interest.
SOURCE: Silber SJ. ASRM 2019. Abstract O-203.
PHILADELPHIA – Ovarian tissue cryopreservation should no longer be considered experimental, Sherman J. Silber, MD, said at the annual meeting of the American Society for Reproductive Medicine.
That claim is based on more than 20 years of experience at his center performing the procedure and results he presented from patients for whom frozen ovarian tissue has been reimplanted resulting in a spontaneous pregnancy.
“For prepubertal girls with cancer and for patients who have already had a preliminary round of chemotherapy, ovarian tissue freezing is the only method available to preserve their fertility,” said Dr. Silber, of the Infertility Center of St. Louis in Chesterfield, Missouri. “It is also the only method available to preserve their fertility.”
“I have very strong feelings about this,” he added. “It has huge societal implications for insurance payments.”
Dr. Silber presented results of ovarian tissue freezing and reimplantation at his center beginning in 1997, where 115 patients between the ages of 2 and 35 years underwent the procedure using the same technique. Of these patients, 14 women came back years later to have their frozen ovary cortex reimplanted. Dr. Silber and his group followed these patients monthly for more than 2 years after reimplantation for signs of return of menses, hormonal changes, pregnancy, and live birth.
Most of the patients who chose ovarian tissue freezing had cancer. Eight patients underwent the procedure after being diagnosed with solid tissue cancer and three had leukemia, while two patients underwent ovarian tissue freezing due to premature ovarian failure, and one because of multiple sclerosis. Patients who underwent reimplantation were menopausal for at least 3 years, said Dr. Silber.
Dr. Silber also described the technique used for reimplantation. After the cortical tissue was thawed, the tissue was quilted into one piece from three to five slices using 9-0 nylon interrupted sutures. The quilted tissue was then sutured to the medulla after the surgeon completely removed the dead cortex from the other ovary. “Hemostasis was achieved with micro bipolar forceps,” said Dr. Silber. “Constant irrigation was employed with pulsed heparinized media because we wanted to avoid adhesions, and we wanted to try for spontaneous pregnancy rather than IVF.”
“Then, we put [the quilted ovarian slices] on to the medulla on the other side in such a way that the fallopian tube would be able to reach and catch any egg that’s ovulated during that time,” he added.
Dr. Silber and his group found that, over time, follicle-stimulating hormone (FSH) levels sharply decreased to normal or near-normal levels between 69 days and 133 days after the procedure while Anti-Müllerian hormone (AMH) levels dramatically rose to higher levels between 133 days and 227 days post-procedure before dropping to very low levels, “and the AMH remained at low levels despite the fact that [transplants] would last 8 to 10 years,” said Dr. Silber.
Of the 14 cases where frozen ovarian tissue was reimplanted, 11 patients (78%) achieved pregnancy, 10 patients (71%) delivered healthy babies, and 1 patient (9%) experienced a miscarriage. All patients had spontaneous pregnancies, and none used in vitro fertilization (IVF), noted Dr. Silber. There were 2 patients who had four children from transplanted ovarian tissue, and 2 of 3 patients with leukemia had a total of five children.
Additionally, Dr. Silber’s group examined the literature for other examples of ovarian tissue reimplantation after cryopreservation to determine how many live births resulted from the procedure. They found an additional 170 live births in addition to the 15 live births at their center, with a pregnancy rate ranging from 31% to 71% in different studies. Cancer was not transmitted from mother to child in any case, said Dr. Silber.
Compared with egg freezing, there is a benefit to performing ovarian tissue freezing, even after chemotherapy has begun, noted Dr. Silber. The cost of ovarian tissue freezing is also roughly one-tenth that of egg freezing, and the procedure is less burdensome than multiple cycles with the potential for ovarian hyperstimulation, and it restores the hormone function and the fertility of eggs after reimplantation.
“Because the greater primordial follicle recruitment decreases as the ovarian reserve decreases, you can put a piece of ovary tissue back every 8 years, and a woman can have endocrine function until she’s 100 years old,” said Dr. Silber.
Dr. Silber reported no relevant conflicts of interest.
SOURCE: Silber SJ. ASRM 2019. Abstract O-203.
REPORTING FROM ASRM 2019
Patients frequently drive too soon after ICD implantation
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
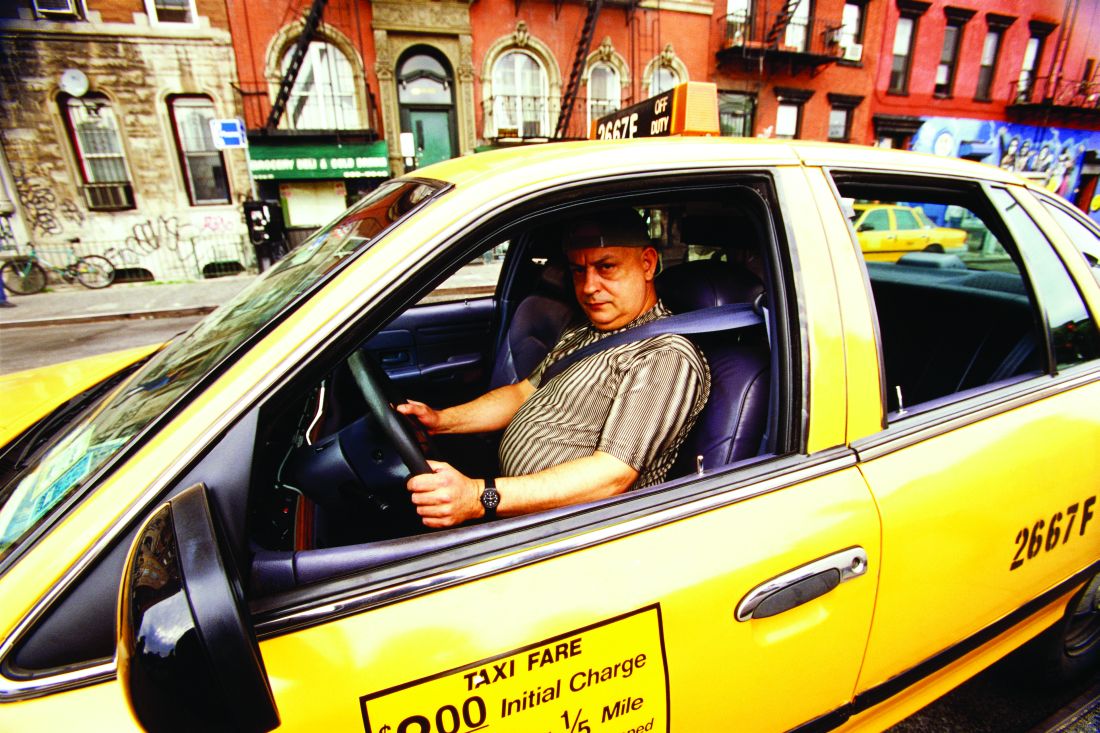
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
REPORTING FROM ESC CONGRESS 2019
Serlopitant improves psoriatic itch in phase 2 study
MADRID – Serlopitant, an investigational once-daily oral neurokinin-1 receptor antagonist, resulted in clinically meaningful improvement in psoriatic itch in a phase 2, double-blind, placebo-controlled randomized trial, David M. Pariser, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
The drug is not an effective stand alone treatment for psoriasis, though.
“The psoriasis itself did not improve during the trial. It’s the itch that improved. This drug is not designed for psoriasis; it’s going to be used for itching. If this does materialize as a treatment for psoriasis, it would be as an adjunct,” according to Dr. Pariser, a dermatologist at the Eastern Virginia School of Medicine, Norfolk.
Still, serlopitant addresses an unmet need for better treatment options for psoriatic itch. Up to 90% of psoriasis patients report experiencing pruritus, regardless of their disease severity.
“Although patients consider pruritus one of the most important, severe, and troublesome symptoms of psoriasis, clinicians have not historically recognized itch as a significant symptom, and treatments for psoriasis often don’t alleviate the associated pruritus,” he said.
Serlopitant has already shown efficacy and good tolerability in phase 2 studies in patients with prurigo nodularis and chronic pruritus.
The 8-week psoriatic itch trial included 204 adults with plaque psoriasis randomized to 5 mg of serlopitant once daily or placebo. Patients averaged 4.3% involved body surface area, and nearly two-thirds of them had moderate psoriasis by physician global assessment. The majority of patients rated their itch as severe; The average baseline score on the 0-10 Worst Itch Numeric Rating Scale was 8.2.
The primary study endpoint was achievement of at least a 4-point improvement on the Worst Itch Numeric Rating Scale. This was achieved in 33.9% of the serlopitant group and 21.1% of placebo-treated controls. The therapeutic benefit was consistent regardless of baseline body weight, gender, age, or extent of psoriasis-involved body surface area.
The safety data were consistent with what was seen in prior phase 2 studies for other dermatologic disorders. There were no serious adverse events, and the type and frequency of adverse events deemed related to treatment was similar in the two study arms.
“These results support the ongoing development of serlopitant across the spectrum of psoriatic disease,” Dr. Pariser declared.
The study was funded by Menlo Therapeutics. Dr. Pariser reported receiving research funding from and/or serving as a consultant to or advisory board member for roughly two dozen pharmaceutical companies.
MADRID – Serlopitant, an investigational once-daily oral neurokinin-1 receptor antagonist, resulted in clinically meaningful improvement in psoriatic itch in a phase 2, double-blind, placebo-controlled randomized trial, David M. Pariser, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
The drug is not an effective stand alone treatment for psoriasis, though.
“The psoriasis itself did not improve during the trial. It’s the itch that improved. This drug is not designed for psoriasis; it’s going to be used for itching. If this does materialize as a treatment for psoriasis, it would be as an adjunct,” according to Dr. Pariser, a dermatologist at the Eastern Virginia School of Medicine, Norfolk.
Still, serlopitant addresses an unmet need for better treatment options for psoriatic itch. Up to 90% of psoriasis patients report experiencing pruritus, regardless of their disease severity.
“Although patients consider pruritus one of the most important, severe, and troublesome symptoms of psoriasis, clinicians have not historically recognized itch as a significant symptom, and treatments for psoriasis often don’t alleviate the associated pruritus,” he said.
Serlopitant has already shown efficacy and good tolerability in phase 2 studies in patients with prurigo nodularis and chronic pruritus.
The 8-week psoriatic itch trial included 204 adults with plaque psoriasis randomized to 5 mg of serlopitant once daily or placebo. Patients averaged 4.3% involved body surface area, and nearly two-thirds of them had moderate psoriasis by physician global assessment. The majority of patients rated their itch as severe; The average baseline score on the 0-10 Worst Itch Numeric Rating Scale was 8.2.
The primary study endpoint was achievement of at least a 4-point improvement on the Worst Itch Numeric Rating Scale. This was achieved in 33.9% of the serlopitant group and 21.1% of placebo-treated controls. The therapeutic benefit was consistent regardless of baseline body weight, gender, age, or extent of psoriasis-involved body surface area.
The safety data were consistent with what was seen in prior phase 2 studies for other dermatologic disorders. There were no serious adverse events, and the type and frequency of adverse events deemed related to treatment was similar in the two study arms.
“These results support the ongoing development of serlopitant across the spectrum of psoriatic disease,” Dr. Pariser declared.
The study was funded by Menlo Therapeutics. Dr. Pariser reported receiving research funding from and/or serving as a consultant to or advisory board member for roughly two dozen pharmaceutical companies.
MADRID – Serlopitant, an investigational once-daily oral neurokinin-1 receptor antagonist, resulted in clinically meaningful improvement in psoriatic itch in a phase 2, double-blind, placebo-controlled randomized trial, David M. Pariser, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
The drug is not an effective stand alone treatment for psoriasis, though.
“The psoriasis itself did not improve during the trial. It’s the itch that improved. This drug is not designed for psoriasis; it’s going to be used for itching. If this does materialize as a treatment for psoriasis, it would be as an adjunct,” according to Dr. Pariser, a dermatologist at the Eastern Virginia School of Medicine, Norfolk.
Still, serlopitant addresses an unmet need for better treatment options for psoriatic itch. Up to 90% of psoriasis patients report experiencing pruritus, regardless of their disease severity.
“Although patients consider pruritus one of the most important, severe, and troublesome symptoms of psoriasis, clinicians have not historically recognized itch as a significant symptom, and treatments for psoriasis often don’t alleviate the associated pruritus,” he said.
Serlopitant has already shown efficacy and good tolerability in phase 2 studies in patients with prurigo nodularis and chronic pruritus.
The 8-week psoriatic itch trial included 204 adults with plaque psoriasis randomized to 5 mg of serlopitant once daily or placebo. Patients averaged 4.3% involved body surface area, and nearly two-thirds of them had moderate psoriasis by physician global assessment. The majority of patients rated their itch as severe; The average baseline score on the 0-10 Worst Itch Numeric Rating Scale was 8.2.
The primary study endpoint was achievement of at least a 4-point improvement on the Worst Itch Numeric Rating Scale. This was achieved in 33.9% of the serlopitant group and 21.1% of placebo-treated controls. The therapeutic benefit was consistent regardless of baseline body weight, gender, age, or extent of psoriasis-involved body surface area.
The safety data were consistent with what was seen in prior phase 2 studies for other dermatologic disorders. There were no serious adverse events, and the type and frequency of adverse events deemed related to treatment was similar in the two study arms.
“These results support the ongoing development of serlopitant across the spectrum of psoriatic disease,” Dr. Pariser declared.
The study was funded by Menlo Therapeutics. Dr. Pariser reported receiving research funding from and/or serving as a consultant to or advisory board member for roughly two dozen pharmaceutical companies.
REPORTING FROM EADV 2019
Cancer overtakes CVD as cause of death in high-income countries
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
REPORTING FROM ESC CONGRESS 2019
Patients have good recall on lung cancer screening scan benefits, not risks
NEW ORLEANS – in a recent survey, underscoring the need for ongoing patient education beyond the initial shared decision-making encounter, a researcher said.
While about 9 in 10 patients recalled key information on the benefits, only about 4 in 10 recalled information on risks, according to Erin Hirsch, MSPH, of the Colorado School of Public Health in Aurora.
“This may mean we need ongoing clinician involvement or continued education about this important information, especially if the patients aren’t screening annually,” Ms. Hirsch said in a podium presentation at the annual meeting of the American College of Chest Physicians.
Even fewer patients could correctly recall eligibility criteria for lung cancer screening, which suggests “ongoing clinician involvement” is needed to identify appropriate patients, Hirsch added in her presentation.
Shared decision making about lung cancer screening, which is supposed to entail a balanced patient-provider conversation about eligibility, risks, and benefits, is required by the Centers for Medicare & Medicaid Services to cover the cost of lung cancer screening as a preventative service, Hirsch noted in her presentation.
However, it’s largely unknown to what extent patients due for an annual screening recall information that should have been imparted in that initial discussion.
“The gap in knowledge centers around the fact that shared decision making is only required for baseline scan, but screening is recommended on an annual basis,” she said.
To test patient recall, Hirsch and colleagues developed a knowledge survey including 34 questions about lung cancer screening eligibility, risks, and benefits. The surveys went out by mail or email to 228 patients who had a baseline screening CT scan 6-12 months earlier; a total of 53 complete responses were included in the analysis, which focused on seven key questions about benefit, risk, and eligibility.
Recall was “excellent” for the benefit questions, Ms. Hirsch said, with 91% of patients able to recall that a computed tomography (CT) scan is better at detecting a possible lung cancer than a chest x-ray, while 87% recalled that without screening lung cancer is often found at a later stage when cure is less likely.
By contrast, a “moderate” amount (40%) remembered that a CT scan can suggest the patient has lung cancer when in fact they do not, she said, and only 38% recalled that radiation exposure was one of the harms of lung cancer screening, she added.
Eligibility recall was “poor,” she added, with only 21% affirming that not all current and former smokers need to be screened for lung cancer. Just 8% recalled that 55 years is the age at which beginning lung cancer screening is recommended, and 4% knew that 30 is the minimum number of pack-years required to be eligible for screening.
While these results may have clinical implications, Ms. Hirsch acknowledged a number of limitations to this pilot study. Among those was the fact that the content of the initial shared decision-making conversation could not be assessed: “We assumed that the patients were exposed to the information asked about in the survey ahead of time, but we can’t say for sure if that was true,” she explained.
Ms. Hirsch and coauthors disclosed no relationships relevant to their study.
SOURCE: Hirsch E et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.107.
NEW ORLEANS – in a recent survey, underscoring the need for ongoing patient education beyond the initial shared decision-making encounter, a researcher said.
While about 9 in 10 patients recalled key information on the benefits, only about 4 in 10 recalled information on risks, according to Erin Hirsch, MSPH, of the Colorado School of Public Health in Aurora.
“This may mean we need ongoing clinician involvement or continued education about this important information, especially if the patients aren’t screening annually,” Ms. Hirsch said in a podium presentation at the annual meeting of the American College of Chest Physicians.
Even fewer patients could correctly recall eligibility criteria for lung cancer screening, which suggests “ongoing clinician involvement” is needed to identify appropriate patients, Hirsch added in her presentation.
Shared decision making about lung cancer screening, which is supposed to entail a balanced patient-provider conversation about eligibility, risks, and benefits, is required by the Centers for Medicare & Medicaid Services to cover the cost of lung cancer screening as a preventative service, Hirsch noted in her presentation.
However, it’s largely unknown to what extent patients due for an annual screening recall information that should have been imparted in that initial discussion.
“The gap in knowledge centers around the fact that shared decision making is only required for baseline scan, but screening is recommended on an annual basis,” she said.
To test patient recall, Hirsch and colleagues developed a knowledge survey including 34 questions about lung cancer screening eligibility, risks, and benefits. The surveys went out by mail or email to 228 patients who had a baseline screening CT scan 6-12 months earlier; a total of 53 complete responses were included in the analysis, which focused on seven key questions about benefit, risk, and eligibility.
Recall was “excellent” for the benefit questions, Ms. Hirsch said, with 91% of patients able to recall that a computed tomography (CT) scan is better at detecting a possible lung cancer than a chest x-ray, while 87% recalled that without screening lung cancer is often found at a later stage when cure is less likely.
By contrast, a “moderate” amount (40%) remembered that a CT scan can suggest the patient has lung cancer when in fact they do not, she said, and only 38% recalled that radiation exposure was one of the harms of lung cancer screening, she added.
Eligibility recall was “poor,” she added, with only 21% affirming that not all current and former smokers need to be screened for lung cancer. Just 8% recalled that 55 years is the age at which beginning lung cancer screening is recommended, and 4% knew that 30 is the minimum number of pack-years required to be eligible for screening.
While these results may have clinical implications, Ms. Hirsch acknowledged a number of limitations to this pilot study. Among those was the fact that the content of the initial shared decision-making conversation could not be assessed: “We assumed that the patients were exposed to the information asked about in the survey ahead of time, but we can’t say for sure if that was true,” she explained.
Ms. Hirsch and coauthors disclosed no relationships relevant to their study.
SOURCE: Hirsch E et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.107.
NEW ORLEANS – in a recent survey, underscoring the need for ongoing patient education beyond the initial shared decision-making encounter, a researcher said.
While about 9 in 10 patients recalled key information on the benefits, only about 4 in 10 recalled information on risks, according to Erin Hirsch, MSPH, of the Colorado School of Public Health in Aurora.
“This may mean we need ongoing clinician involvement or continued education about this important information, especially if the patients aren’t screening annually,” Ms. Hirsch said in a podium presentation at the annual meeting of the American College of Chest Physicians.
Even fewer patients could correctly recall eligibility criteria for lung cancer screening, which suggests “ongoing clinician involvement” is needed to identify appropriate patients, Hirsch added in her presentation.
Shared decision making about lung cancer screening, which is supposed to entail a balanced patient-provider conversation about eligibility, risks, and benefits, is required by the Centers for Medicare & Medicaid Services to cover the cost of lung cancer screening as a preventative service, Hirsch noted in her presentation.
However, it’s largely unknown to what extent patients due for an annual screening recall information that should have been imparted in that initial discussion.
“The gap in knowledge centers around the fact that shared decision making is only required for baseline scan, but screening is recommended on an annual basis,” she said.
To test patient recall, Hirsch and colleagues developed a knowledge survey including 34 questions about lung cancer screening eligibility, risks, and benefits. The surveys went out by mail or email to 228 patients who had a baseline screening CT scan 6-12 months earlier; a total of 53 complete responses were included in the analysis, which focused on seven key questions about benefit, risk, and eligibility.
Recall was “excellent” for the benefit questions, Ms. Hirsch said, with 91% of patients able to recall that a computed tomography (CT) scan is better at detecting a possible lung cancer than a chest x-ray, while 87% recalled that without screening lung cancer is often found at a later stage when cure is less likely.
By contrast, a “moderate” amount (40%) remembered that a CT scan can suggest the patient has lung cancer when in fact they do not, she said, and only 38% recalled that radiation exposure was one of the harms of lung cancer screening, she added.
Eligibility recall was “poor,” she added, with only 21% affirming that not all current and former smokers need to be screened for lung cancer. Just 8% recalled that 55 years is the age at which beginning lung cancer screening is recommended, and 4% knew that 30 is the minimum number of pack-years required to be eligible for screening.
While these results may have clinical implications, Ms. Hirsch acknowledged a number of limitations to this pilot study. Among those was the fact that the content of the initial shared decision-making conversation could not be assessed: “We assumed that the patients were exposed to the information asked about in the survey ahead of time, but we can’t say for sure if that was true,” she explained.
Ms. Hirsch and coauthors disclosed no relationships relevant to their study.
SOURCE: Hirsch E et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.107.
REPORTING FROM CHEST 2019
NIH seeks gene-based cures for HIV, sickle cell disease
The National Institutes of Health and the Bill & Melinda Gates Foundation have announced that they plan to invest $100 million each over the next 4 years to develop affordable, gene-based cures for sickle cell disease (SCD) and HIV.
The initiative follows an announcement from President Trump that set a goal of ending the HIV epidemic in the United States in the next 10 years, seeking to reduce the number of diagnoses by 90% by 2030. The Trump administration has also identified SCD as an “intractable health challenge with the potential for dramatic advances in the coming years,” the NIH said in a statement.
Gene-based therapy has become a reality in recent years thanks to dramatic advances, but the cost is prohibitive in many parts of the world. “The collaboration between the NIH and the Gates Foundation sets out a bold goal of advancing safe, effective, and durable gene-based cures to clinical trials in the United States and relevant countries in sub-Saharan Africa within the next 7-10 years. The ultimate goal is to scale and implement these treatments globally in areas hardest hit by these diseases,” the NIH said.
Both diseases are a significant burden on low- and middle-income countries, as 95% of the 38 million people living with HIV globally are in the developing world, with 67% living in sub-Saharan Africa; about half of the HIV-infected population receives no treatment for the disease. An estimated 15 million children will be born with SCD over the next 30 years, with three-quarters of those births occurring in sub-Saharan Africa. About 50%-90% of children born with SCD will die before age 5 years.
The collaboration will focus on coordination in two areas: identifying potential candidate cures for SCD and HIV for preclinical and clinical evaluation, and defining long-term opportunities to work together and with African partners on advancing promising candidates to late-phase clinical trials, with funding to be determined as candidates progress.
“In recent years, gene-based treatments have been groundbreaking for rare genetic disorders and infectious diseases. While these treatments are exciting, people in low- and middle-income countries do not have access to these breakthroughs. By working with the NIH and scientists across Africa, we aim to ensure these approaches will improve the lives of those most in need and bring the incredible promise of gene-based treatments to the world of public health,” said Trevor Mundel, MD, PhD, president of the global health program at the Bill & Melinda Gates Foundation.
The National Institutes of Health and the Bill & Melinda Gates Foundation have announced that they plan to invest $100 million each over the next 4 years to develop affordable, gene-based cures for sickle cell disease (SCD) and HIV.
The initiative follows an announcement from President Trump that set a goal of ending the HIV epidemic in the United States in the next 10 years, seeking to reduce the number of diagnoses by 90% by 2030. The Trump administration has also identified SCD as an “intractable health challenge with the potential for dramatic advances in the coming years,” the NIH said in a statement.
Gene-based therapy has become a reality in recent years thanks to dramatic advances, but the cost is prohibitive in many parts of the world. “The collaboration between the NIH and the Gates Foundation sets out a bold goal of advancing safe, effective, and durable gene-based cures to clinical trials in the United States and relevant countries in sub-Saharan Africa within the next 7-10 years. The ultimate goal is to scale and implement these treatments globally in areas hardest hit by these diseases,” the NIH said.
Both diseases are a significant burden on low- and middle-income countries, as 95% of the 38 million people living with HIV globally are in the developing world, with 67% living in sub-Saharan Africa; about half of the HIV-infected population receives no treatment for the disease. An estimated 15 million children will be born with SCD over the next 30 years, with three-quarters of those births occurring in sub-Saharan Africa. About 50%-90% of children born with SCD will die before age 5 years.
The collaboration will focus on coordination in two areas: identifying potential candidate cures for SCD and HIV for preclinical and clinical evaluation, and defining long-term opportunities to work together and with African partners on advancing promising candidates to late-phase clinical trials, with funding to be determined as candidates progress.
“In recent years, gene-based treatments have been groundbreaking for rare genetic disorders and infectious diseases. While these treatments are exciting, people in low- and middle-income countries do not have access to these breakthroughs. By working with the NIH and scientists across Africa, we aim to ensure these approaches will improve the lives of those most in need and bring the incredible promise of gene-based treatments to the world of public health,” said Trevor Mundel, MD, PhD, president of the global health program at the Bill & Melinda Gates Foundation.
The National Institutes of Health and the Bill & Melinda Gates Foundation have announced that they plan to invest $100 million each over the next 4 years to develop affordable, gene-based cures for sickle cell disease (SCD) and HIV.
The initiative follows an announcement from President Trump that set a goal of ending the HIV epidemic in the United States in the next 10 years, seeking to reduce the number of diagnoses by 90% by 2030. The Trump administration has also identified SCD as an “intractable health challenge with the potential for dramatic advances in the coming years,” the NIH said in a statement.
Gene-based therapy has become a reality in recent years thanks to dramatic advances, but the cost is prohibitive in many parts of the world. “The collaboration between the NIH and the Gates Foundation sets out a bold goal of advancing safe, effective, and durable gene-based cures to clinical trials in the United States and relevant countries in sub-Saharan Africa within the next 7-10 years. The ultimate goal is to scale and implement these treatments globally in areas hardest hit by these diseases,” the NIH said.
Both diseases are a significant burden on low- and middle-income countries, as 95% of the 38 million people living with HIV globally are in the developing world, with 67% living in sub-Saharan Africa; about half of the HIV-infected population receives no treatment for the disease. An estimated 15 million children will be born with SCD over the next 30 years, with three-quarters of those births occurring in sub-Saharan Africa. About 50%-90% of children born with SCD will die before age 5 years.
The collaboration will focus on coordination in two areas: identifying potential candidate cures for SCD and HIV for preclinical and clinical evaluation, and defining long-term opportunities to work together and with African partners on advancing promising candidates to late-phase clinical trials, with funding to be determined as candidates progress.
“In recent years, gene-based treatments have been groundbreaking for rare genetic disorders and infectious diseases. While these treatments are exciting, people in low- and middle-income countries do not have access to these breakthroughs. By working with the NIH and scientists across Africa, we aim to ensure these approaches will improve the lives of those most in need and bring the incredible promise of gene-based treatments to the world of public health,” said Trevor Mundel, MD, PhD, president of the global health program at the Bill & Melinda Gates Foundation.
Fibrinogen concentrate effective, safe for postop bleeding
SAN ANTONIO – Fibrinogen concentrate was noninferior to cryoprecipitate for controlling bleeding following cardiac surgery in the randomized FIBRES trial, Canadian investigators reported.
Among 827 patients undergoing cardiopulmonary bypass, there were no significant differences in the use of allogenenic transfusion products within 24 hours of surgery for patients assigned to receive fibrinogen concentrate for control of bleeding, compared with patients who received cryoprecipitate, reported Jeannie Callum, MD, from Sunnybrook Health Sciences Centre in Toronto, on behalf of coinvestigators in the FIBRES trial.
Fibrinogen concentrate, commonly used to control postoperative bleeding in Europe, was associated with numerically, but not statistically, lower incidence of both adverse events and serious adverse events than cryoprecipitate, the current standard of care in North America.
“Given its safety and logistical advantages, fibrinogen concentrate may be considered in bleeding patients with acquired hypofibrinogenemia,” Dr. Callum said at the annual meeting of the AABB, the group formerly known as the American Association of Blood Banks.
Results of the FIBRES trial were published simultaneously in JAMA (2019 Oct 21. doi: 10.1001/jama.2019.17312).
Acquired hypofibrinogenemia, defined as a fibrinogen level below the range of 1.5-2.0 g/L, is a major cause of excess bleeding after cardiac surgery. European guidelines on the management of bleeding following trauma or cardiac surgery recommend the use of either cryoprecipitate or fibrinogen concentrate to control excessive bleeding in patients with acquired hypofibrinogenemia, Dr. Callum noted.
Cryoprecipitate is a pooled plasma–derived product that contains fibrinogen, but also fibronectin, platelet microparticles, coagulation factors VIII and XIII, and von Willebrand factor.
Additionally, fibrinogen levels in cryoprecipitate can range from as low as 3 g/L to as high as 30 g/L, and the product is normally kept and shipped frozen, and is then thawed for use and pooled prior to administration, with a shelf life of just 4-6 hours.
In contrast, fibrinogen concentrates “are pathogen-reduced and purified; have standardized fibrinogen content (20 g/L); are lyophilized, allowing for easy storage, reconstitution, and administration; and have longer shelf life after reconstitution (up to 24 hours),” Dr. Callum and her colleagues reported.
Despite the North American preference for cryoprecipitate and the European preference for fibrinogen concentrate, there have been few studies directly comparing the two products, which prompted the FIBRES investigators to design a head-to-head trial.
The randomized trial was conducted in 11 Canadian hospitals with adults undergoing cardiac surgery with cardiopulmonary bypass for whom fibrinogen supplementation was ordered in accordance with accepted clinical standards.
Patients were randomly assigned to received either 4 g of fibrinogen concentrate or 10 units of cryoprecipitate for 24 hours, with all patients receiving additional cryoprecipitate as needed after the first day.
Of 15,412 cardiac patients treated at the participating sites, 827 patients met the trial criteria and were randomized. Because the trial met the prespecified stopping criterion for noninferiority of fibrinogen at the interim analysis, the trial was halted, leaving the 827 patients as the final analysis population.
The mean number of allogeneic blood component units administered – the primary outcome – was 16.3 units in the fibrinogen concentrate group and 17.0 units in the cryoprecipitate group (mean ratio, 0.96; P for noninferiority less than .001; P for superiority = .50).
Fibrinogen was also noninferior for the secondary outcomes of individual 24-hour and cumulative 7-day blood component transfusions, and in a post-hoc analysis of cumulative transfusions measured from product administration to 24 hours after termination of cardiopulmonary bypass. These endpoints should be interpreted with caution, however, because they were not corrected for type 1 error, the investigators noted.
Fibrinogen concentrate also appeared to be noninferior for all defined subgroups, except for patients who underwent nonelective procedures, which included all patients in critical state before surgery.
Adverse events (AEs) of any kind occurred in 66.7% of patients with fibrinogen concentrate vs. 72.7% of those on cryoprecipitate. Serious AEs occurred in 31.5% vs. 34.7%, respectively.
Thromboembolic events – stroke or transient ischemic attack, amaurosis fugax (temporary vision loss), myocardial infarction, deep-vein thrombosis, pulmonary embolism, other-vessel thrombosis, disseminated intravascular coagulation, or thrombophlebitis – occurred in 7% vs. 9.6%, respectively.
The investigators acknowledged that the study was limited by the inability to blind the clinical team to the product used, by the adult-only population, and by the likelihood of variable dosing in the cryoprecipitate group.
Advantages of fibrinogen concentrate over cryoprecipitate are that the former is pathogen reduced and is easier to deliver, the investigators said.
“One important consideration is the cost differential that currently favors cryoprecipitate, but this varies across regions, and the most recent economic analysis failed to include the costs of future emerging pathogens and did not include comprehensive activity-based costing,” the investigators wrote in JAMA.
The trial was sponsored by Octapharma AG, which also provided fibrinogen concentrate. Cryoprecipitate was provided by the Canadian Blood Services and Héma-Québec. Dr. Callum reported receiving grants from Canadian Blood Services, Octapharma, and CSL Behring during the conduct of the study. Multiple coauthors had similar disclosures.
SOURCE: Callum J et al. JAMA. 2019 Oct 21. doi:10.1001/jama.2019.17312.
SAN ANTONIO – Fibrinogen concentrate was noninferior to cryoprecipitate for controlling bleeding following cardiac surgery in the randomized FIBRES trial, Canadian investigators reported.
Among 827 patients undergoing cardiopulmonary bypass, there were no significant differences in the use of allogenenic transfusion products within 24 hours of surgery for patients assigned to receive fibrinogen concentrate for control of bleeding, compared with patients who received cryoprecipitate, reported Jeannie Callum, MD, from Sunnybrook Health Sciences Centre in Toronto, on behalf of coinvestigators in the FIBRES trial.
Fibrinogen concentrate, commonly used to control postoperative bleeding in Europe, was associated with numerically, but not statistically, lower incidence of both adverse events and serious adverse events than cryoprecipitate, the current standard of care in North America.
“Given its safety and logistical advantages, fibrinogen concentrate may be considered in bleeding patients with acquired hypofibrinogenemia,” Dr. Callum said at the annual meeting of the AABB, the group formerly known as the American Association of Blood Banks.
Results of the FIBRES trial were published simultaneously in JAMA (2019 Oct 21. doi: 10.1001/jama.2019.17312).
Acquired hypofibrinogenemia, defined as a fibrinogen level below the range of 1.5-2.0 g/L, is a major cause of excess bleeding after cardiac surgery. European guidelines on the management of bleeding following trauma or cardiac surgery recommend the use of either cryoprecipitate or fibrinogen concentrate to control excessive bleeding in patients with acquired hypofibrinogenemia, Dr. Callum noted.
Cryoprecipitate is a pooled plasma–derived product that contains fibrinogen, but also fibronectin, platelet microparticles, coagulation factors VIII and XIII, and von Willebrand factor.
Additionally, fibrinogen levels in cryoprecipitate can range from as low as 3 g/L to as high as 30 g/L, and the product is normally kept and shipped frozen, and is then thawed for use and pooled prior to administration, with a shelf life of just 4-6 hours.
In contrast, fibrinogen concentrates “are pathogen-reduced and purified; have standardized fibrinogen content (20 g/L); are lyophilized, allowing for easy storage, reconstitution, and administration; and have longer shelf life after reconstitution (up to 24 hours),” Dr. Callum and her colleagues reported.
Despite the North American preference for cryoprecipitate and the European preference for fibrinogen concentrate, there have been few studies directly comparing the two products, which prompted the FIBRES investigators to design a head-to-head trial.
The randomized trial was conducted in 11 Canadian hospitals with adults undergoing cardiac surgery with cardiopulmonary bypass for whom fibrinogen supplementation was ordered in accordance with accepted clinical standards.
Patients were randomly assigned to received either 4 g of fibrinogen concentrate or 10 units of cryoprecipitate for 24 hours, with all patients receiving additional cryoprecipitate as needed after the first day.
Of 15,412 cardiac patients treated at the participating sites, 827 patients met the trial criteria and were randomized. Because the trial met the prespecified stopping criterion for noninferiority of fibrinogen at the interim analysis, the trial was halted, leaving the 827 patients as the final analysis population.
The mean number of allogeneic blood component units administered – the primary outcome – was 16.3 units in the fibrinogen concentrate group and 17.0 units in the cryoprecipitate group (mean ratio, 0.96; P for noninferiority less than .001; P for superiority = .50).
Fibrinogen was also noninferior for the secondary outcomes of individual 24-hour and cumulative 7-day blood component transfusions, and in a post-hoc analysis of cumulative transfusions measured from product administration to 24 hours after termination of cardiopulmonary bypass. These endpoints should be interpreted with caution, however, because they were not corrected for type 1 error, the investigators noted.
Fibrinogen concentrate also appeared to be noninferior for all defined subgroups, except for patients who underwent nonelective procedures, which included all patients in critical state before surgery.
Adverse events (AEs) of any kind occurred in 66.7% of patients with fibrinogen concentrate vs. 72.7% of those on cryoprecipitate. Serious AEs occurred in 31.5% vs. 34.7%, respectively.
Thromboembolic events – stroke or transient ischemic attack, amaurosis fugax (temporary vision loss), myocardial infarction, deep-vein thrombosis, pulmonary embolism, other-vessel thrombosis, disseminated intravascular coagulation, or thrombophlebitis – occurred in 7% vs. 9.6%, respectively.
The investigators acknowledged that the study was limited by the inability to blind the clinical team to the product used, by the adult-only population, and by the likelihood of variable dosing in the cryoprecipitate group.
Advantages of fibrinogen concentrate over cryoprecipitate are that the former is pathogen reduced and is easier to deliver, the investigators said.
“One important consideration is the cost differential that currently favors cryoprecipitate, but this varies across regions, and the most recent economic analysis failed to include the costs of future emerging pathogens and did not include comprehensive activity-based costing,” the investigators wrote in JAMA.
The trial was sponsored by Octapharma AG, which also provided fibrinogen concentrate. Cryoprecipitate was provided by the Canadian Blood Services and Héma-Québec. Dr. Callum reported receiving grants from Canadian Blood Services, Octapharma, and CSL Behring during the conduct of the study. Multiple coauthors had similar disclosures.
SOURCE: Callum J et al. JAMA. 2019 Oct 21. doi:10.1001/jama.2019.17312.
SAN ANTONIO – Fibrinogen concentrate was noninferior to cryoprecipitate for controlling bleeding following cardiac surgery in the randomized FIBRES trial, Canadian investigators reported.
Among 827 patients undergoing cardiopulmonary bypass, there were no significant differences in the use of allogenenic transfusion products within 24 hours of surgery for patients assigned to receive fibrinogen concentrate for control of bleeding, compared with patients who received cryoprecipitate, reported Jeannie Callum, MD, from Sunnybrook Health Sciences Centre in Toronto, on behalf of coinvestigators in the FIBRES trial.
Fibrinogen concentrate, commonly used to control postoperative bleeding in Europe, was associated with numerically, but not statistically, lower incidence of both adverse events and serious adverse events than cryoprecipitate, the current standard of care in North America.
“Given its safety and logistical advantages, fibrinogen concentrate may be considered in bleeding patients with acquired hypofibrinogenemia,” Dr. Callum said at the annual meeting of the AABB, the group formerly known as the American Association of Blood Banks.
Results of the FIBRES trial were published simultaneously in JAMA (2019 Oct 21. doi: 10.1001/jama.2019.17312).
Acquired hypofibrinogenemia, defined as a fibrinogen level below the range of 1.5-2.0 g/L, is a major cause of excess bleeding after cardiac surgery. European guidelines on the management of bleeding following trauma or cardiac surgery recommend the use of either cryoprecipitate or fibrinogen concentrate to control excessive bleeding in patients with acquired hypofibrinogenemia, Dr. Callum noted.
Cryoprecipitate is a pooled plasma–derived product that contains fibrinogen, but also fibronectin, platelet microparticles, coagulation factors VIII and XIII, and von Willebrand factor.
Additionally, fibrinogen levels in cryoprecipitate can range from as low as 3 g/L to as high as 30 g/L, and the product is normally kept and shipped frozen, and is then thawed for use and pooled prior to administration, with a shelf life of just 4-6 hours.
In contrast, fibrinogen concentrates “are pathogen-reduced and purified; have standardized fibrinogen content (20 g/L); are lyophilized, allowing for easy storage, reconstitution, and administration; and have longer shelf life after reconstitution (up to 24 hours),” Dr. Callum and her colleagues reported.
Despite the North American preference for cryoprecipitate and the European preference for fibrinogen concentrate, there have been few studies directly comparing the two products, which prompted the FIBRES investigators to design a head-to-head trial.
The randomized trial was conducted in 11 Canadian hospitals with adults undergoing cardiac surgery with cardiopulmonary bypass for whom fibrinogen supplementation was ordered in accordance with accepted clinical standards.
Patients were randomly assigned to received either 4 g of fibrinogen concentrate or 10 units of cryoprecipitate for 24 hours, with all patients receiving additional cryoprecipitate as needed after the first day.
Of 15,412 cardiac patients treated at the participating sites, 827 patients met the trial criteria and were randomized. Because the trial met the prespecified stopping criterion for noninferiority of fibrinogen at the interim analysis, the trial was halted, leaving the 827 patients as the final analysis population.
The mean number of allogeneic blood component units administered – the primary outcome – was 16.3 units in the fibrinogen concentrate group and 17.0 units in the cryoprecipitate group (mean ratio, 0.96; P for noninferiority less than .001; P for superiority = .50).
Fibrinogen was also noninferior for the secondary outcomes of individual 24-hour and cumulative 7-day blood component transfusions, and in a post-hoc analysis of cumulative transfusions measured from product administration to 24 hours after termination of cardiopulmonary bypass. These endpoints should be interpreted with caution, however, because they were not corrected for type 1 error, the investigators noted.
Fibrinogen concentrate also appeared to be noninferior for all defined subgroups, except for patients who underwent nonelective procedures, which included all patients in critical state before surgery.
Adverse events (AEs) of any kind occurred in 66.7% of patients with fibrinogen concentrate vs. 72.7% of those on cryoprecipitate. Serious AEs occurred in 31.5% vs. 34.7%, respectively.
Thromboembolic events – stroke or transient ischemic attack, amaurosis fugax (temporary vision loss), myocardial infarction, deep-vein thrombosis, pulmonary embolism, other-vessel thrombosis, disseminated intravascular coagulation, or thrombophlebitis – occurred in 7% vs. 9.6%, respectively.
The investigators acknowledged that the study was limited by the inability to blind the clinical team to the product used, by the adult-only population, and by the likelihood of variable dosing in the cryoprecipitate group.
Advantages of fibrinogen concentrate over cryoprecipitate are that the former is pathogen reduced and is easier to deliver, the investigators said.
“One important consideration is the cost differential that currently favors cryoprecipitate, but this varies across regions, and the most recent economic analysis failed to include the costs of future emerging pathogens and did not include comprehensive activity-based costing,” the investigators wrote in JAMA.
The trial was sponsored by Octapharma AG, which also provided fibrinogen concentrate. Cryoprecipitate was provided by the Canadian Blood Services and Héma-Québec. Dr. Callum reported receiving grants from Canadian Blood Services, Octapharma, and CSL Behring during the conduct of the study. Multiple coauthors had similar disclosures.
SOURCE: Callum J et al. JAMA. 2019 Oct 21. doi:10.1001/jama.2019.17312.
REPORTING FROM AABB 2019
Topical benzyl benzoate–based treatment reduced Demodex in patients with rosacea
Daily treatment with benzyl benzoate (BB) cream reduced Demodex densities in patients with and without rosacea, and was associated with improvement in clinical signs, according to F.M.N. Forton, MD, of the Dermatology Clinic, Brussels, and his coauthor in the Journal of the European Academy of Dermatology and Venereology.
The retrospective study comprised 394 patients treated between 2002 and 2010; 117 of them had rosacea with papulopustules and the remainder only demodicosis. Their mean age was 49 years; most (278) were women. They had been treated with one of three doses of BB cream with crotamiton 10% cream: crotamiton applied in the morning, and BB 12% plus crotamiton in the evening; BB 12% plus crotamiton applied twice daily; and BB 20%-24% plus crotamiton applied once in the evening. Demodex densities (Dds) were measured with two consecutive standardized skin surface biopsies and deep biopsies at baseline and follow-up. Symptoms were measured with an investigator global assessment (IGA).
The authors said they had previously found that BB had acaricidal effects on Demodex, as did crotamiton “to a lesser extent,” but that the two treatments have not been well studied. They also referred to the increasing evidence that Demodex has a role in papulopustular rosacea, and that ivermectin, which is acaricidal, is recommended for topical treatment of papulopustular rosacea.
In the study, a mean of 2.7 months after starting treatment, mean Dds were significantly lower for the entire cohort, decreasing by 72.4% (plus or minus 2.6%) from baseline. Dds had normalized in 35% of patients, and in 31% of patients, symptoms had cleared.
Treatment was considered effective in 46% of patients and curative in 20%. Men responded slightly better, with clearance in 34% vs. 20% of women. The two regimens using the higher dose of BB were more effective than those using the lower dose and were associated with better compliance. Compliance overall was 77%.
After a mean of nearly 3 months of treatment, “topical application of BB (with crotamiton) was effective at reducing Dds and clearing clinical symptoms, not only in demodicosis but also in rosacea with papulopustules, indirectly supporting a key role of the mite in the pathophysiology of rosacea,” the authors concluded.
Neither of these products are approved in the United States for treating rosacea.
Dr. Forton disclosed that he occasionally works as a consultant for Galderma; the second author had no disclosures. The study had no funding source.
Source: Forton FMN et al. J Eur Acad Dermatol Venereol. 2019 Sep 7. doi: 10.1111/jdv.15938.
Daily treatment with benzyl benzoate (BB) cream reduced Demodex densities in patients with and without rosacea, and was associated with improvement in clinical signs, according to F.M.N. Forton, MD, of the Dermatology Clinic, Brussels, and his coauthor in the Journal of the European Academy of Dermatology and Venereology.
The retrospective study comprised 394 patients treated between 2002 and 2010; 117 of them had rosacea with papulopustules and the remainder only demodicosis. Their mean age was 49 years; most (278) were women. They had been treated with one of three doses of BB cream with crotamiton 10% cream: crotamiton applied in the morning, and BB 12% plus crotamiton in the evening; BB 12% plus crotamiton applied twice daily; and BB 20%-24% plus crotamiton applied once in the evening. Demodex densities (Dds) were measured with two consecutive standardized skin surface biopsies and deep biopsies at baseline and follow-up. Symptoms were measured with an investigator global assessment (IGA).
The authors said they had previously found that BB had acaricidal effects on Demodex, as did crotamiton “to a lesser extent,” but that the two treatments have not been well studied. They also referred to the increasing evidence that Demodex has a role in papulopustular rosacea, and that ivermectin, which is acaricidal, is recommended for topical treatment of papulopustular rosacea.
In the study, a mean of 2.7 months after starting treatment, mean Dds were significantly lower for the entire cohort, decreasing by 72.4% (plus or minus 2.6%) from baseline. Dds had normalized in 35% of patients, and in 31% of patients, symptoms had cleared.
Treatment was considered effective in 46% of patients and curative in 20%. Men responded slightly better, with clearance in 34% vs. 20% of women. The two regimens using the higher dose of BB were more effective than those using the lower dose and were associated with better compliance. Compliance overall was 77%.
After a mean of nearly 3 months of treatment, “topical application of BB (with crotamiton) was effective at reducing Dds and clearing clinical symptoms, not only in demodicosis but also in rosacea with papulopustules, indirectly supporting a key role of the mite in the pathophysiology of rosacea,” the authors concluded.
Neither of these products are approved in the United States for treating rosacea.
Dr. Forton disclosed that he occasionally works as a consultant for Galderma; the second author had no disclosures. The study had no funding source.
Source: Forton FMN et al. J Eur Acad Dermatol Venereol. 2019 Sep 7. doi: 10.1111/jdv.15938.
Daily treatment with benzyl benzoate (BB) cream reduced Demodex densities in patients with and without rosacea, and was associated with improvement in clinical signs, according to F.M.N. Forton, MD, of the Dermatology Clinic, Brussels, and his coauthor in the Journal of the European Academy of Dermatology and Venereology.
The retrospective study comprised 394 patients treated between 2002 and 2010; 117 of them had rosacea with papulopustules and the remainder only demodicosis. Their mean age was 49 years; most (278) were women. They had been treated with one of three doses of BB cream with crotamiton 10% cream: crotamiton applied in the morning, and BB 12% plus crotamiton in the evening; BB 12% plus crotamiton applied twice daily; and BB 20%-24% plus crotamiton applied once in the evening. Demodex densities (Dds) were measured with two consecutive standardized skin surface biopsies and deep biopsies at baseline and follow-up. Symptoms were measured with an investigator global assessment (IGA).
The authors said they had previously found that BB had acaricidal effects on Demodex, as did crotamiton “to a lesser extent,” but that the two treatments have not been well studied. They also referred to the increasing evidence that Demodex has a role in papulopustular rosacea, and that ivermectin, which is acaricidal, is recommended for topical treatment of papulopustular rosacea.
In the study, a mean of 2.7 months after starting treatment, mean Dds were significantly lower for the entire cohort, decreasing by 72.4% (plus or minus 2.6%) from baseline. Dds had normalized in 35% of patients, and in 31% of patients, symptoms had cleared.
Treatment was considered effective in 46% of patients and curative in 20%. Men responded slightly better, with clearance in 34% vs. 20% of women. The two regimens using the higher dose of BB were more effective than those using the lower dose and were associated with better compliance. Compliance overall was 77%.
After a mean of nearly 3 months of treatment, “topical application of BB (with crotamiton) was effective at reducing Dds and clearing clinical symptoms, not only in demodicosis but also in rosacea with papulopustules, indirectly supporting a key role of the mite in the pathophysiology of rosacea,” the authors concluded.
Neither of these products are approved in the United States for treating rosacea.
Dr. Forton disclosed that he occasionally works as a consultant for Galderma; the second author had no disclosures. The study had no funding source.
Source: Forton FMN et al. J Eur Acad Dermatol Venereol. 2019 Sep 7. doi: 10.1111/jdv.15938.
FROM JEADV