User login
HRQOL deteriorates after disease progression in metastatic cancer
, results of an observational study suggest.
The findings highlight the importance of patient-relevant outcomes when evaluating novel therapies for patients with metastatic cancers, according to Norbert Marschner, MD, of Praxis für interdisziplinäre onkologie und hämatologie in Freiburg, Germany, and colleagues. The researchers reported the findings in JAMA Network Open.
They used four nationwide German registries to evaluate the association of disease progression with HRQOL in patients receiving systemic therapy for metastatic colorectal, lung, pancreatic, or breast cancer.
The analysis included 2,314 adults with documented disease progression across 203 institutions in Germany. Data collection occurred during routine follow-up visits at participating centers during 2011-2018.
Various patient-reported outcome questionnaires were used to measure HRQOL and symptom severity among participants. For the present study, the team enrolled patients at the start of any systemic palliative treatment, defined as targeted therapy, chemotherapy, or endocrine therapy.
Mixed-model analyses of more than 8,000 questionnaires showed that the first disease progression was associated with significant deterioration in 37 of 45 HRQOL scales overall, 17 of which were considered clinically meaningful.
With respect to cancer type, significant worsening after the first progression occurred in 12 of 14 colorectal cancer HRQOL scales, 11 of 14 lung cancer scales, 10 of 10 pancreatic cancer scales, and 4 of 7 breast cancer scales.
The deterioration in global HRQOL associated with the first progression was of greatest magnitude in lung cancer (6.7 points; P < .001), followed by pancreatic cancer (5.4 points; P < .001), colorectal cancer (3.5 points; P = .002), and breast cancer (2.4 points; P = .001).
The researchers also found that 38 of 45 HRQOL scales showed a greater degree of worsening after the second disease progression than after the first. They observed significant worsening after the second disease progression in 32 of 45 HRQOL scales, and all 32 were considered clinically meaningful.
The researchers acknowledged that a key limitation of this study was the observational design. As a result, the study did not include specifications related to tumor assessment, such as frequency, timing, or criteria.
“We suggest that progression-related endpoints in metastatic breast, colorectal, lung, or pancreatic cancer should be considered when evaluating the benefit of novel treatments, in addition to survival, morbidity, and HRQOL outcomes,” the researchers concluded.
The registries used in this study are funded by iOMEDICO and industry sponsors. The authors disclosed relationships with iOMEDICO and several pharmaceutical companies.
SOURCE: Marschner N et al. JAMA Netw Open. 2020 Mar 10. doi: 10.1001/jamanetworkopen.2020.0643.
, results of an observational study suggest.
The findings highlight the importance of patient-relevant outcomes when evaluating novel therapies for patients with metastatic cancers, according to Norbert Marschner, MD, of Praxis für interdisziplinäre onkologie und hämatologie in Freiburg, Germany, and colleagues. The researchers reported the findings in JAMA Network Open.
They used four nationwide German registries to evaluate the association of disease progression with HRQOL in patients receiving systemic therapy for metastatic colorectal, lung, pancreatic, or breast cancer.
The analysis included 2,314 adults with documented disease progression across 203 institutions in Germany. Data collection occurred during routine follow-up visits at participating centers during 2011-2018.
Various patient-reported outcome questionnaires were used to measure HRQOL and symptom severity among participants. For the present study, the team enrolled patients at the start of any systemic palliative treatment, defined as targeted therapy, chemotherapy, or endocrine therapy.
Mixed-model analyses of more than 8,000 questionnaires showed that the first disease progression was associated with significant deterioration in 37 of 45 HRQOL scales overall, 17 of which were considered clinically meaningful.
With respect to cancer type, significant worsening after the first progression occurred in 12 of 14 colorectal cancer HRQOL scales, 11 of 14 lung cancer scales, 10 of 10 pancreatic cancer scales, and 4 of 7 breast cancer scales.
The deterioration in global HRQOL associated with the first progression was of greatest magnitude in lung cancer (6.7 points; P < .001), followed by pancreatic cancer (5.4 points; P < .001), colorectal cancer (3.5 points; P = .002), and breast cancer (2.4 points; P = .001).
The researchers also found that 38 of 45 HRQOL scales showed a greater degree of worsening after the second disease progression than after the first. They observed significant worsening after the second disease progression in 32 of 45 HRQOL scales, and all 32 were considered clinically meaningful.
The researchers acknowledged that a key limitation of this study was the observational design. As a result, the study did not include specifications related to tumor assessment, such as frequency, timing, or criteria.
“We suggest that progression-related endpoints in metastatic breast, colorectal, lung, or pancreatic cancer should be considered when evaluating the benefit of novel treatments, in addition to survival, morbidity, and HRQOL outcomes,” the researchers concluded.
The registries used in this study are funded by iOMEDICO and industry sponsors. The authors disclosed relationships with iOMEDICO and several pharmaceutical companies.
SOURCE: Marschner N et al. JAMA Netw Open. 2020 Mar 10. doi: 10.1001/jamanetworkopen.2020.0643.
, results of an observational study suggest.
The findings highlight the importance of patient-relevant outcomes when evaluating novel therapies for patients with metastatic cancers, according to Norbert Marschner, MD, of Praxis für interdisziplinäre onkologie und hämatologie in Freiburg, Germany, and colleagues. The researchers reported the findings in JAMA Network Open.
They used four nationwide German registries to evaluate the association of disease progression with HRQOL in patients receiving systemic therapy for metastatic colorectal, lung, pancreatic, or breast cancer.
The analysis included 2,314 adults with documented disease progression across 203 institutions in Germany. Data collection occurred during routine follow-up visits at participating centers during 2011-2018.
Various patient-reported outcome questionnaires were used to measure HRQOL and symptom severity among participants. For the present study, the team enrolled patients at the start of any systemic palliative treatment, defined as targeted therapy, chemotherapy, or endocrine therapy.
Mixed-model analyses of more than 8,000 questionnaires showed that the first disease progression was associated with significant deterioration in 37 of 45 HRQOL scales overall, 17 of which were considered clinically meaningful.
With respect to cancer type, significant worsening after the first progression occurred in 12 of 14 colorectal cancer HRQOL scales, 11 of 14 lung cancer scales, 10 of 10 pancreatic cancer scales, and 4 of 7 breast cancer scales.
The deterioration in global HRQOL associated with the first progression was of greatest magnitude in lung cancer (6.7 points; P < .001), followed by pancreatic cancer (5.4 points; P < .001), colorectal cancer (3.5 points; P = .002), and breast cancer (2.4 points; P = .001).
The researchers also found that 38 of 45 HRQOL scales showed a greater degree of worsening after the second disease progression than after the first. They observed significant worsening after the second disease progression in 32 of 45 HRQOL scales, and all 32 were considered clinically meaningful.
The researchers acknowledged that a key limitation of this study was the observational design. As a result, the study did not include specifications related to tumor assessment, such as frequency, timing, or criteria.
“We suggest that progression-related endpoints in metastatic breast, colorectal, lung, or pancreatic cancer should be considered when evaluating the benefit of novel treatments, in addition to survival, morbidity, and HRQOL outcomes,” the researchers concluded.
The registries used in this study are funded by iOMEDICO and industry sponsors. The authors disclosed relationships with iOMEDICO and several pharmaceutical companies.
SOURCE: Marschner N et al. JAMA Netw Open. 2020 Mar 10. doi: 10.1001/jamanetworkopen.2020.0643.
FROM JAMA NETWORK OPEN
NMA haploidentical allo-BMT plus post-transplant cyclophosphamide deemed safe, effective for CLL
for patients with chronic lymphocytic leukemia (CLL), according to a study published in Biology of Blood and Marrow Transplantation.
The number of patients undergoing haploidentical allo-BMT has increased substantially, with the advent of new graft-versus-host disease (GVHD) prophylaxis strategies, such as posttransplantation cyclophosphamide (PTCy), that reduce the risk of GVHD complications; however there have been few studies assessing the results of this treatment regimen, according to the authors.
The study assessed 64 consecutive patients with CLL between Jan. 2005 and Aug. 2018 who underwent haploidentical allo-BMT. The median age was 59 years; 4 patients (6.2%) underwent allo-BMT after first-line treatment; 20 patients (31.2%) underwent allo-BMT after second-line treatment, and 40 patients (62.5%) underwent allo-BMT after three or more lines of treatment for relapsed and/or refractory disease.
All patients received a nonmyeloablative (NMA) conditioning regimen consisting of fludarabine, cyclophosphamide, and 200 cGy total body irradiation. Patients received PTCy (i.v. 50 mg/kg per day) on days +3 and +4, along with additional GVHD prophylaxis with mycophenolate mofetil between days +5 and +35 and tacrolimus or sirolimus between days +5 and +180.
For all 64 patients, the median duration of follow-up was 4.4 years based on the reverse Kaplan-Meier method. The 4-year overall survival (OS) was 52%, and the 4-year progression-free survival (PFS) was 37%. The 56 patients with less than 20% marrow CLL involvement before undergoing allo-BMT had a 4-year OS of 61%, a 4-year PFS of 43%, and a median OS of 4.8 years, according to the authors.
Regression analysis demonstrated that donor age, stem cell source, IGHV mutation status, or grade II-III acute GVHD did not affect risk of progression or survival.
“The majority of our patients had unfavorable risk factors, and collectively our data show that haploidentical allo-BMT with PTCy in CLL with less than 20% marrow involvement is a safe treatment option carrying a low risk of serious GVHD and other toxicities,” the researchers concluded.
The study was supported by National Institutes of Health, National Cancer Institute grants. The authors reported that they had no disclosures.
SOURCE: Suman P et al. Biol Blood Marrow Transplant. 2020 Mar 1;26:502-8. doi: 10.1016/j.bbmt.2019.11.008
for patients with chronic lymphocytic leukemia (CLL), according to a study published in Biology of Blood and Marrow Transplantation.
The number of patients undergoing haploidentical allo-BMT has increased substantially, with the advent of new graft-versus-host disease (GVHD) prophylaxis strategies, such as posttransplantation cyclophosphamide (PTCy), that reduce the risk of GVHD complications; however there have been few studies assessing the results of this treatment regimen, according to the authors.
The study assessed 64 consecutive patients with CLL between Jan. 2005 and Aug. 2018 who underwent haploidentical allo-BMT. The median age was 59 years; 4 patients (6.2%) underwent allo-BMT after first-line treatment; 20 patients (31.2%) underwent allo-BMT after second-line treatment, and 40 patients (62.5%) underwent allo-BMT after three or more lines of treatment for relapsed and/or refractory disease.
All patients received a nonmyeloablative (NMA) conditioning regimen consisting of fludarabine, cyclophosphamide, and 200 cGy total body irradiation. Patients received PTCy (i.v. 50 mg/kg per day) on days +3 and +4, along with additional GVHD prophylaxis with mycophenolate mofetil between days +5 and +35 and tacrolimus or sirolimus between days +5 and +180.
For all 64 patients, the median duration of follow-up was 4.4 years based on the reverse Kaplan-Meier method. The 4-year overall survival (OS) was 52%, and the 4-year progression-free survival (PFS) was 37%. The 56 patients with less than 20% marrow CLL involvement before undergoing allo-BMT had a 4-year OS of 61%, a 4-year PFS of 43%, and a median OS of 4.8 years, according to the authors.
Regression analysis demonstrated that donor age, stem cell source, IGHV mutation status, or grade II-III acute GVHD did not affect risk of progression or survival.
“The majority of our patients had unfavorable risk factors, and collectively our data show that haploidentical allo-BMT with PTCy in CLL with less than 20% marrow involvement is a safe treatment option carrying a low risk of serious GVHD and other toxicities,” the researchers concluded.
The study was supported by National Institutes of Health, National Cancer Institute grants. The authors reported that they had no disclosures.
SOURCE: Suman P et al. Biol Blood Marrow Transplant. 2020 Mar 1;26:502-8. doi: 10.1016/j.bbmt.2019.11.008
for patients with chronic lymphocytic leukemia (CLL), according to a study published in Biology of Blood and Marrow Transplantation.
The number of patients undergoing haploidentical allo-BMT has increased substantially, with the advent of new graft-versus-host disease (GVHD) prophylaxis strategies, such as posttransplantation cyclophosphamide (PTCy), that reduce the risk of GVHD complications; however there have been few studies assessing the results of this treatment regimen, according to the authors.
The study assessed 64 consecutive patients with CLL between Jan. 2005 and Aug. 2018 who underwent haploidentical allo-BMT. The median age was 59 years; 4 patients (6.2%) underwent allo-BMT after first-line treatment; 20 patients (31.2%) underwent allo-BMT after second-line treatment, and 40 patients (62.5%) underwent allo-BMT after three or more lines of treatment for relapsed and/or refractory disease.
All patients received a nonmyeloablative (NMA) conditioning regimen consisting of fludarabine, cyclophosphamide, and 200 cGy total body irradiation. Patients received PTCy (i.v. 50 mg/kg per day) on days +3 and +4, along with additional GVHD prophylaxis with mycophenolate mofetil between days +5 and +35 and tacrolimus or sirolimus between days +5 and +180.
For all 64 patients, the median duration of follow-up was 4.4 years based on the reverse Kaplan-Meier method. The 4-year overall survival (OS) was 52%, and the 4-year progression-free survival (PFS) was 37%. The 56 patients with less than 20% marrow CLL involvement before undergoing allo-BMT had a 4-year OS of 61%, a 4-year PFS of 43%, and a median OS of 4.8 years, according to the authors.
Regression analysis demonstrated that donor age, stem cell source, IGHV mutation status, or grade II-III acute GVHD did not affect risk of progression or survival.
“The majority of our patients had unfavorable risk factors, and collectively our data show that haploidentical allo-BMT with PTCy in CLL with less than 20% marrow involvement is a safe treatment option carrying a low risk of serious GVHD and other toxicities,” the researchers concluded.
The study was supported by National Institutes of Health, National Cancer Institute grants. The authors reported that they had no disclosures.
SOURCE: Suman P et al. Biol Blood Marrow Transplant. 2020 Mar 1;26:502-8. doi: 10.1016/j.bbmt.2019.11.008
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
As physicians, accountability is part of our innate identity
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Recently, Nicolas Badre, MD, challenged psychiatrists who care for patients involved in the legal system. He encouraged “a resurgence of personal accountability and responsibility.”
Using the chronically disenfranchised patients who are repetitiously shuttled between jails and mental hospitals as examples, he pointed out that we psychiatrists must “step up to the plate” and approach clinical problems with the attitude that “the buck stops with me.” As Dr. Badre pointed out, this is especially true when dealing with large, complex systems in which fragmented care exists without clear leadership. This, in turn, allows for a dissolution of accountability.
Accountability is a natural continuation of our training as physicians. We all remember the transition from medical student to intern, the steep learning curve as well as growth and maturation during this changeover. A dramatic transformation occurs over the course of 1 year, from medical students who tag along learning from patients to interns expected to be on their own for endless hours.
Over the course of those hours, we came to the understanding that people’s lives were in our hands. This causes a shift in our identity. This process continues throughout residency and onward in our careers. At some point, it becomes part of our innate identity as physicians or our professional sense of self – which is hard to describe to nonphysicians.
A profound example of a sense of accountability within the medical profession can be found in “How We Live,” a book by National Book Award winner Sherwin B. Nuland, MD. In the book, the late Dr. Nuland recounted how, as a 49-year-old seasoned surgeon working at Yale University, New Haven, Conn., and casually rounding on patients, he heard a frantic message: “Any general surgeon! Any general surgeon! Go immediately to the operating room – immediately – any general surgeon!”
The case involved a 42-year-old wife and mother who had been rushed to the ED after having been found in the community in a profound state of shock. In the ED, it was suspected that the patient was bleeding heavily from a ruptured tubal pregnancy. She was sped rapidly to the operating room with an undetectable blood pressure and a barely palpable pulse. The on-call ob.gyn. had been summoned from home, and he rushed to the operating room along with his department chairman.
Because the woman had lost much of her blood supply, there was no time for crossmatching. The anesthesiologist had placed large-bore intravenous lines and transfused her with O-negative blood (the universal donor blood type) to try maintain some level of blood pressure. Before she could be even fully anesthetized, the ob.gyn had made an incision in her lower abdomen. The bleeding he encountered was profound.
After a quick evaluation, the ob.gyn. realized that the blood was coming from above, not below, leading to the emergency page that Dr. Nuland heard. Dr. Nuland described bounding up the stairs three at a time. He recalled: “[A] very real apprehension had entered my mind. I might encounter a situation that was beyond me, something that I might make even worse, something that would cause me to regret for the rest of my life that I had answered the page’s insistent call instead of simply turning my back on its urgency and slinking off to my car before anyone noticed I was there.”
However, he could not see himself doing such a thing and he rushed up to the operating room because, “walking away from that kind of cry for help would have violated every precept taught me by my life and my training, and every bit of moral sense I had. … . I bear an obsessive preoccupation with accepting responsibility, amounting really to a compulsively neurotic sense of duty.”
And yet in the next few seconds, as he was running to the operating room, he wondered: “Am I about to botch something up? Will I, in one quick stroke of ineptness and fate, bring my career crashing down around my feet and with it my sense of what I am? Am I on my way to destroy an unknown patient and myself at the same time?”
In Dr. Nuland’s thoughts lie the conundrum of responsibility for physicians. Thankfully for Dr. Nuland, he was able to save the day and diagnose a rare case of rupture of an aneurysm of the splenic artery and keep the patient alive. This dramatic story involved a surgical colleague who had to make split-second decisions while a patient’s life hanged in the balance, but the same principles apply to us as psychiatrists.
I would note that, in the above example of the surgical patient, the “system” for saving the woman’s life was well organized and resourced to allow for a comprehensive and time-limited intervention into a life-threatening situation. There was an operating room staffed by various professionals who all had a defined role. It required the leader, Dr. Nuland, to step in, make the right diagnosis, and then issue commands to the identified professionals who all recognized his leadership and were skilled in carrying out their assigned duties. Dr. Nuland clearly was the leader once he took charge.
An outpatient psychiatrist facing a suicidal patient must deal with a different set of challenges, often involving various complex systems as well as multiple barriers. Clinical barriers include available interdisciplinary resources/personnel to assist not only with the critical encounter, but also with extended evaluation and treatment in a secure, well-resourced environment. Administrative barriers can include justifying the optimal treatment plan to payors. Our lethal patients often require both outpatient and inpatient services with sometimes-conflicting agendas. In a recent article, I pointed out some of the vexing problems that arise when communication and collaboration are poor between inpatient and outpatient psychiatrists. In such complex environments, it is less clear what is involved in the outpatient psychiatrist stepping up to the plate and asserting leadership.
An emotionally wrenching article about an emergency physician, Matthew E. Seaman, MD, who died by suicide, reminds us of the potential for suicide in a complicated patient (in this case, a medical colleague) involving complex systems. Plagued by a review of his care by the medical board (they had forced him to surrender his medical license and allowed the allegations to go public in lieu of further disciplinary proceedings), a subsequent lawsuit and an ultimate attempt by the plaintiff to obtain Dr. Seaman’s personal assets led to his worsening mental health. According to his wife, also a physician, he was getting “more depressed by the insults and assaults on his integrity and professionalism.”
Just before the investigation, he had received a 30-year pin from the American Board of Emergency Medicine for his “dedication to the specialty.” He fell into a deep depression from which he could not recover despite several psychiatric admissions and several medication trials. Along with his depression, he suffered from severe anxiety, a known risk factor for suicide. Dr. Seaman was feeling overwhelmed by the lengthy legal process targeting him as being negligent. He begged his attorney to settle the case, but his insurance carrier would not allow it. According to his wife: “All sense of human worth had been beaten out of him.”
Dr. Seaman had been known as resilient. He could handle complex ED situations, including simultaneously dealing with multiple traumas. He previously had been named in three malpractice lawsuits and had prevailed in each one. But his resilience had greatly diminished, and he became overwhelmed. He previously had, as a physician, been able to step up to the plate of accountability. But now, because of a confluence of depression and anxiety as well as the “insults and assaults on his integrity and professionalism,” he found life to be unbearable with the resulting tragic end.
So how would we as psychiatrists step up to the plate and be accountable when faced with a struggling fellow physician at risk for suicide such as Dr. Seaman?
Be aware of relevant risk factors
In addition to being aware of the usual risk factors for suicide, it would behoove us to also understand how physician suicides differ from suicides among nonphysicians.1 For example, physicians who have died by suicide were far more likely to have experienced job-related problems than nonphysicians, but less likely to have experienced the recent death of a loved one. Also noteworthy is that physicians who end their lives were more often married. In addition, Michael F. Myers, MD, a psychiatrist who has studied physician suicides, noted in the article about Dr. Seaman that struggling physicians are likely to suffer from shame and embarrassment.
Consider shame, burdensomeness, and secrecy
When suicide risk factors are taught to students and professionals, rarely is shame mentioned. Perhaps it is not a common risk factor in the general population, but shame and its cousin, disgrace, are known risk factors that likely apply more to people – such as physicians – who have built a reputation over their careers. One whole chapter is given to disgrace suicides in a book about suicide notes.2 A reputation often is one of the most important factors for professionals, which creates their sense of identity and, by extension, a sense of purpose in life.
When a doctor perceives that his or her reputation is being destroyed, it can produce a profound sense of shame, one of the most powerful of negative emotions.3 Another feature among completed suicides that applies more generally is perceived burdensomeness, according to Thomas E. Joiner Jr., PhD, one of the deep and innovative researchers in the field of suicidology.4 Once a doctor starts feeling that he has been a failure in his professional life and starts ruminating about it, the feelings of failure may generalize to other areas of his life, so that he starts feeling that he is a burden to his spouse. This, then, only increases his shame.
The issue of secrecy also is noteworthy. I was struck reading a book by Dr. Myers on physician suicide by the many spouses and family members who were caught completely unaware of problems when their spouse, a doctor, ended their lives by suicide.5 The doctors hid their problems well, perhaps not wanting to burden their family members. Also, if feelings of shame are an issue, then concealment tends to occur. This concealment of suicidality runs counter to the current narrative among some in the professional community that suicides are preventable (this despite the continuing increase in rates of suicide at the same time that there are increases in mental health services and suicide prevention programs).6
As pointed out in some of the letters quoted in Dr. Myers’s book, those who completed suicide are smart and know how to hide their symptoms well. Although Dr. Seaman’s wife, Linda Seaman, MD, was aware of her husband’s suicidality, when he eventually determined that he was going to end his life, he apparently did not reveal his more serious intention to her. Aside from spouses and family, determined suicide completers often hide their intentions from their clinicians.7
Attempt to obtain collateral information
By being aware of the usual and less-usual risk factors for suicide that our physician colleagues may present with as explained above, we can use strategies for mitigating risk. If secrecy because of shame and embarrassment prevents our physician patient from being fully candid, include the spouse or another significant family member in sessions. While the physician might hide his suicidal intent from both the clinician and spouse, it remains prudent to include the spouse in the treatment plan. Give the spouse a telephone number with which they can contact you if they notice any worrisome change in functioning or behavior. Collateral information often is helpful. (Example: Is the patient not eating, not sleeping, or giving away valued possessions?)
Assess for competency
In Dr. Seaman’s case, it was noted that, with a trial approaching, Dr. Seaman had written in a journal entry that he could not mentally endure a trial. “For me, the stress is overwhelming.” Such a patient, suffering from severe depression, often is unable to properly assist his attorney in his defense. The outpatient psychiatrist can notify the court or one of the attorneys that the competency of the physician patient is questionable (or express a definite opinion of incompetency), and offer the opinion that it would be best to postpone further legal action until the patient is in a more healthy state of mind.
Know when hospitalization is needed
Obviously, the process will go smoother if the admission is voluntary. If the patient physician resists and the psychiatrist believes that the risk for self-harm is too high for the physician patient to remain as an outpatient, try to get a spouse or family member to persuade him to be admitted. An involuntary admission opens up a whole new can of worms and may fracture the therapeutic alliance.
In the end, it might be better to take that risk rather than having a dead patient on your hands. If a hospitalization is necessary, contact the admitting psychiatrist and verbally express your concerns and the reasons why a hospitalization is needed. Ask the inpatient psychiatrist to contact you when a discharge is approaching so that you have an opportunity to ask relevant questions.
For example, during his second psychiatric admission, as the time for discharge was approaching, Dr. Seaman wrote: “I am not well enough for discharge. I am still mentally ill.” Ask the inpatient doctor whether the patient has gotten sufficiently better and he feels confident he can function as an outpatient. If there is a conflicting opinion about the readiness of the patient for discharge, notify the medical director of the service or an administrator about your concerns.
Ask for consultation
At any stage of the process consider getting consultation for a trusted colleague or senior clinician if you are failing to make progress. Sometimes it helps to get the perspective from a fresh pair of eyes or ears.
Get a reality check
Having recounted the inspiring story of Dr. Nuland’s magnificent efforts and joyous success in preserving a life that was on the verge of being lost in the battle against death at the last possible second, I would note the following: Surgeons will tell you that, despite their most heroic efforts and teamwork, there are times when luck runs out and the patient dies on the operating table. Also, small lapses, which all mortals are prone to despite their best efforts at conscientiousness, sometimes can lead to a bad outcome.
Similarly, in psychiatry, no matter how much effort we put into saving a life, sometimes it is all to no avail. Despite all we have learned about suicide and its risk factors, and no matter how much care we take to contain risk, our patients who are determined will find a way of ending their own lives. The vexing problem of suicide seems intractable. A suicide among our patients humbles us, but also hopefully inspires us to keep trying harder to step up to the plate of accountability.
In conclusion, for us physicians, accountability is not a facet, a trait, or even a pursuit, accountability is at the core of who are and how we define ourselves. Accountability is the reason we leap stairs three at time when we are urgently paged. Accountability is the reason malpractice lawsuits cut at the core of our self-image. Accountability allows us to always have hope for a positive outcome, despite overwhelming barriers, and gives our lives a sense of purpose.
For me, in preparing this article, accountability was reviewing and studying physician suicide and then applying best practices in risk assessment after reading the tragic story of Dr. Seaman. I hope I inspire you to do the same in the pursuit of helping our vulnerable patients.
Learning how to care for our complex patients is a never-ending journey.
References
1. Gold KJ. Gen Hosp Psychiatry. 2013 Jan;35(1):45-9.
2. Etkind M. ...Or Not to Be: A Collection of Suicide Notes. New York: Riverhead Books, 1997.
3. Lamia LC. Shame: A concealed, contagious, and dangerous emotion. Psychology Today. 2011 Apr 4.
4. Joiner TE. Why People Die by Suicide. Cambridge: Harvard University Press, 2005.
5. Myers MF. Why Physicians Die by Suicide. 2017.
6. National Institutes of Health. Suicide Prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml.
7. Levy AG et al. JAMA Netw Open. 2019 Aug 14. doi: 10.1001/jamanetworkopen.2019.9277.
Dr. Kausch is a clinical and forensic psychiatrist who is on the faculty at Case Western Reserve University, Cleveland, as an assistant clinical professor. He spends most of his time seeing patients through the Akron General/Cleveland Clinic health system. He has published in the area of forensic psychiatry, addictions, pathological gambling, and suicide. He has recently taken an interest in conducting marital therapy and is now publishing in that area as well.
Bariatric surgery may curtail colorectal cancer risk
Bariatric surgery was associated with a significant reduction in the risk of colorectal cancer among obese adults in a retrospective study of more than 1 million individuals.
Although some studies have suggested that bariatric surgery may reduce the risk of obesity-associated cancers, such as colorectal cancer, other studies have shown an increased colorectal cancer risk after surgery, according to Laurent Bailly, MD, of Université Côte d’Azur in Nice, France, and colleagues.
In a study published in JAMA Surgery, Dr. Bailly and colleagues compared the incidence of colorectal cancer in obese patients who underwent bariatric surgery with the incidence in obese patients who did not have surgery and the incidence in the general population.
Using the French National Health Insurance Information System database, the researchers identified 1,045,348 obese adults aged 50-75 years who had no colorectal cancer at baseline. Of these patients, 74,131 underwent bariatric surgery and 971,217 did not. The mean age was 57.3 years in the surgery group and 63.4 years in the nonsurgery group.
The mean follow-up period was 6.2 years for patients who underwent adjustable gastric banding, 5.5 years for those with sleeve gastrectomy, 5.7 years for those who underwent gastric bypass, and 5.3 years for the nonsurgery group.
Results
Overall, the colorectal cancer rate was 0.6% in the surgery group and 1.3% in the nonsurgery group (P < .001).
The researchers calculated standardized incidence ratios (SIRs) to compare the risk of colorectal cancer in the study population with the risk among the French general population; in other words, the number of observed colorectal cancer cases divided by the number of expected cases.
In the surgery group, 423 cases of colorectal cancer were observed and 428 cases were expected, which leads to an SIR of 1.0. In the nonsurgery group, 12,629 cases were observed and 9,417 cases were expected, leading to an SIR of 1.34.
These results suggest patients in the nonsurgery group had a 34% higher risk of colorectal cancer compared with the general population, whereas the risk in the surgery group was similar to that in the general population.
Patients who underwent either gastric bypass or sleeve gastrectomy had fewer new colorectal cancer diagnoses (0.5% for both) compared with patients who had adjustable gastric banding (0.7%).
The researchers noted that this study was limited by several factors, including the retrospective, observational design and potential selection bias among surgery patients. However, the results were strengthened by the large study population and long-term follow-up.
Putting results into context
The authors of an invited commentary noted that this study is supported by results from a retrospective, U.S.-based study, which indicated that bariatric surgery has a “protective effect” against colorectal cancer (Ann Surg. 2019 Jan;269[1]:95-101).
However, these results conflict with other retrospective studies. A study of Nordic patients suggested that bariatric surgery is associated with an increased risk of colon cancer but perhaps not rectal cancer (Int J Cancer. 2019. doi: 10.1002/ijc.32770).
And a study of English patients showed an increased risk of colorectal cancer in patients who underwent gastric bypass but not in those who underwent gastric banding or sleeve gastrectomy (Br J Surg. 2018;105(12):1650-7).
These conflicting results “imply that the jury is still out on whether bariatric surgery increases or decreases” the risk of colorectal cancer, the commentators wrote. They added that future studies “must account for differences in study population (i.e., race/ethnicity and national origin), mechanistic variation in bariatric surgical type, and length of follow-up, while also distinguishing between rectal and colon cancer before the case is settled.”
This study had no outside sponsorship, and the researchers and commentators had no financial conflicts to disclose.
SOURCE: Bailly L et al. JAMA Surg. 2020 Mar 11. doi:10.1001/jamasurg.2020.0089; Davidson LE et al. JAMA Surg. 2020 Mar. 11. doi:10.1001/jamasurg.2020.0090.
Bariatric surgery was associated with a significant reduction in the risk of colorectal cancer among obese adults in a retrospective study of more than 1 million individuals.
Although some studies have suggested that bariatric surgery may reduce the risk of obesity-associated cancers, such as colorectal cancer, other studies have shown an increased colorectal cancer risk after surgery, according to Laurent Bailly, MD, of Université Côte d’Azur in Nice, France, and colleagues.
In a study published in JAMA Surgery, Dr. Bailly and colleagues compared the incidence of colorectal cancer in obese patients who underwent bariatric surgery with the incidence in obese patients who did not have surgery and the incidence in the general population.
Using the French National Health Insurance Information System database, the researchers identified 1,045,348 obese adults aged 50-75 years who had no colorectal cancer at baseline. Of these patients, 74,131 underwent bariatric surgery and 971,217 did not. The mean age was 57.3 years in the surgery group and 63.4 years in the nonsurgery group.
The mean follow-up period was 6.2 years for patients who underwent adjustable gastric banding, 5.5 years for those with sleeve gastrectomy, 5.7 years for those who underwent gastric bypass, and 5.3 years for the nonsurgery group.
Results
Overall, the colorectal cancer rate was 0.6% in the surgery group and 1.3% in the nonsurgery group (P < .001).
The researchers calculated standardized incidence ratios (SIRs) to compare the risk of colorectal cancer in the study population with the risk among the French general population; in other words, the number of observed colorectal cancer cases divided by the number of expected cases.
In the surgery group, 423 cases of colorectal cancer were observed and 428 cases were expected, which leads to an SIR of 1.0. In the nonsurgery group, 12,629 cases were observed and 9,417 cases were expected, leading to an SIR of 1.34.
These results suggest patients in the nonsurgery group had a 34% higher risk of colorectal cancer compared with the general population, whereas the risk in the surgery group was similar to that in the general population.
Patients who underwent either gastric bypass or sleeve gastrectomy had fewer new colorectal cancer diagnoses (0.5% for both) compared with patients who had adjustable gastric banding (0.7%).
The researchers noted that this study was limited by several factors, including the retrospective, observational design and potential selection bias among surgery patients. However, the results were strengthened by the large study population and long-term follow-up.
Putting results into context
The authors of an invited commentary noted that this study is supported by results from a retrospective, U.S.-based study, which indicated that bariatric surgery has a “protective effect” against colorectal cancer (Ann Surg. 2019 Jan;269[1]:95-101).
However, these results conflict with other retrospective studies. A study of Nordic patients suggested that bariatric surgery is associated with an increased risk of colon cancer but perhaps not rectal cancer (Int J Cancer. 2019. doi: 10.1002/ijc.32770).
And a study of English patients showed an increased risk of colorectal cancer in patients who underwent gastric bypass but not in those who underwent gastric banding or sleeve gastrectomy (Br J Surg. 2018;105(12):1650-7).
These conflicting results “imply that the jury is still out on whether bariatric surgery increases or decreases” the risk of colorectal cancer, the commentators wrote. They added that future studies “must account for differences in study population (i.e., race/ethnicity and national origin), mechanistic variation in bariatric surgical type, and length of follow-up, while also distinguishing between rectal and colon cancer before the case is settled.”
This study had no outside sponsorship, and the researchers and commentators had no financial conflicts to disclose.
SOURCE: Bailly L et al. JAMA Surg. 2020 Mar 11. doi:10.1001/jamasurg.2020.0089; Davidson LE et al. JAMA Surg. 2020 Mar. 11. doi:10.1001/jamasurg.2020.0090.
Bariatric surgery was associated with a significant reduction in the risk of colorectal cancer among obese adults in a retrospective study of more than 1 million individuals.
Although some studies have suggested that bariatric surgery may reduce the risk of obesity-associated cancers, such as colorectal cancer, other studies have shown an increased colorectal cancer risk after surgery, according to Laurent Bailly, MD, of Université Côte d’Azur in Nice, France, and colleagues.
In a study published in JAMA Surgery, Dr. Bailly and colleagues compared the incidence of colorectal cancer in obese patients who underwent bariatric surgery with the incidence in obese patients who did not have surgery and the incidence in the general population.
Using the French National Health Insurance Information System database, the researchers identified 1,045,348 obese adults aged 50-75 years who had no colorectal cancer at baseline. Of these patients, 74,131 underwent bariatric surgery and 971,217 did not. The mean age was 57.3 years in the surgery group and 63.4 years in the nonsurgery group.
The mean follow-up period was 6.2 years for patients who underwent adjustable gastric banding, 5.5 years for those with sleeve gastrectomy, 5.7 years for those who underwent gastric bypass, and 5.3 years for the nonsurgery group.
Results
Overall, the colorectal cancer rate was 0.6% in the surgery group and 1.3% in the nonsurgery group (P < .001).
The researchers calculated standardized incidence ratios (SIRs) to compare the risk of colorectal cancer in the study population with the risk among the French general population; in other words, the number of observed colorectal cancer cases divided by the number of expected cases.
In the surgery group, 423 cases of colorectal cancer were observed and 428 cases were expected, which leads to an SIR of 1.0. In the nonsurgery group, 12,629 cases were observed and 9,417 cases were expected, leading to an SIR of 1.34.
These results suggest patients in the nonsurgery group had a 34% higher risk of colorectal cancer compared with the general population, whereas the risk in the surgery group was similar to that in the general population.
Patients who underwent either gastric bypass or sleeve gastrectomy had fewer new colorectal cancer diagnoses (0.5% for both) compared with patients who had adjustable gastric banding (0.7%).
The researchers noted that this study was limited by several factors, including the retrospective, observational design and potential selection bias among surgery patients. However, the results were strengthened by the large study population and long-term follow-up.
Putting results into context
The authors of an invited commentary noted that this study is supported by results from a retrospective, U.S.-based study, which indicated that bariatric surgery has a “protective effect” against colorectal cancer (Ann Surg. 2019 Jan;269[1]:95-101).
However, these results conflict with other retrospective studies. A study of Nordic patients suggested that bariatric surgery is associated with an increased risk of colon cancer but perhaps not rectal cancer (Int J Cancer. 2019. doi: 10.1002/ijc.32770).
And a study of English patients showed an increased risk of colorectal cancer in patients who underwent gastric bypass but not in those who underwent gastric banding or sleeve gastrectomy (Br J Surg. 2018;105(12):1650-7).
These conflicting results “imply that the jury is still out on whether bariatric surgery increases or decreases” the risk of colorectal cancer, the commentators wrote. They added that future studies “must account for differences in study population (i.e., race/ethnicity and national origin), mechanistic variation in bariatric surgical type, and length of follow-up, while also distinguishing between rectal and colon cancer before the case is settled.”
This study had no outside sponsorship, and the researchers and commentators had no financial conflicts to disclose.
SOURCE: Bailly L et al. JAMA Surg. 2020 Mar 11. doi:10.1001/jamasurg.2020.0089; Davidson LE et al. JAMA Surg. 2020 Mar. 11. doi:10.1001/jamasurg.2020.0090.
FROM JAMA SURGERY
Rare Neurological Disease Special Report
Our sixth annual Rare Neurological Disease Special Report is our biggest issue yet. It is very gratifying to know we are part of the rare disease community and witness to some of the exciting developments that are transforming this field. There are many newly approved therapies highlighted in the articles in this issue, as well as brief profiles of a number of research groups within the NIH’s Rare Diseases Clinical Research Network and an intriguing profile of how the Netflix show Diagnosis used crowdsourcing to solve medical mysteries, many of which involved rare neurologic conditions. That’s just a sampling of what this issue has to offer. There are too many articles to mention each one, but I hope you take the time to read the entire issue.
—Glenn S. Williams, vice president, group editor, Neurology Reviews
Our sixth annual Rare Neurological Disease Special Report is our biggest issue yet. It is very gratifying to know we are part of the rare disease community and witness to some of the exciting developments that are transforming this field. There are many newly approved therapies highlighted in the articles in this issue, as well as brief profiles of a number of research groups within the NIH’s Rare Diseases Clinical Research Network and an intriguing profile of how the Netflix show Diagnosis used crowdsourcing to solve medical mysteries, many of which involved rare neurologic conditions. That’s just a sampling of what this issue has to offer. There are too many articles to mention each one, but I hope you take the time to read the entire issue.
—Glenn S. Williams, vice president, group editor, Neurology Reviews
Our sixth annual Rare Neurological Disease Special Report is our biggest issue yet. It is very gratifying to know we are part of the rare disease community and witness to some of the exciting developments that are transforming this field. There are many newly approved therapies highlighted in the articles in this issue, as well as brief profiles of a number of research groups within the NIH’s Rare Diseases Clinical Research Network and an intriguing profile of how the Netflix show Diagnosis used crowdsourcing to solve medical mysteries, many of which involved rare neurologic conditions. That’s just a sampling of what this issue has to offer. There are too many articles to mention each one, but I hope you take the time to read the entire issue.
—Glenn S. Williams, vice president, group editor, Neurology Reviews
Microbiome profiling ready to take personalized medicine to next level
Standards and technology are now available for microbiome profiling to take personalized medicine to the next level, but prospective trials are needed to realize this possibility, according to a leading expert.
The need for prospective microbiomics trials is increasing with the incidence of immune disorders, many of which have been linked with disturbances in the gut, reported Jöel Doré, PhD, at the annual Gut Microbiota for Health World Summit.
“In spite of considerable progress in medicine, together with hygiene, antibiotics, and vaccination developments, we are still seeing an increasing incidence – uncontrolled, that started over 60 years ago – of immune-mediated conditions,” said Dr. Doré, research director at the French National Research Institute for Agriculture, Food, and the Environment.
According to the World Health Organization, one out of four people will be affected by such a disorder in their lifetime, and the incidence rate of some conditions is accelerating faster than others, with geographical distributions that suggest environmental risk factors.
“The rate of incidence of autism in the U.S.A. is a quite scary exponential curve, where less than 1 birth per 5,000 was [affected] in the 1970s, where today it is 1 birth out of 50,” Dr. Doré said at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility. “Prevention is an urgent need, and possibly if we do not manage to understand what’s going on, human longevity might be at stake.”
Multiple studies have shown that transferring microbiota from humans with immune disorders to healthy mice can induce clinical signs of immune disorders, he said. And between humans, fecal transplants from healthy donors have reduced symptoms in patients with conditions such as inflammatory bowel disease.
While these studies support the link between microbe-host relationships and immune function, most of the underlying mechanisms remain unknown, Dr. Doré said. He highlighted the fact that the complex network of interactions involved separates microbiomics research from conventional approaches to disease.
“I want to stress the fact that clinical trials [in the past] have been designed in the situation where infection was the problem, [but] infection is essentially a linear thing; one agent, one risk, one disease,” Dr. Doré said. “What we are dealing with – with the increasing incidence of immune disorders – is host-microbe interaction at the center of everything, and alteration of host-microbe leading to risk, which may lead to disease. But host-microbe interaction is under the control of a vast number of environmental aspects ... so tools to deal with innovation and translation in a totally different or systemic configuration have yet to be invented.”
According to Dr. Doré, to develop clinical applications, research procedures must first be standardized.
“To be of use for the clinician and general practitioner, microbiome profiling will have to rely on pipelines of standardized preanalytical and analytical procedures,” he said. “This starts from sample collection and shipment.”
For the past 5 years, Dr. Doré and colleagues have been working to standardize procedures with a number of organizations around the world, and progress has been made.
“Today we have very good standards for shotgun sequencing,” he said.
With standards solidifying, microbiomics may lead to new clinical strategies for a range of conditions, even beyond immune disorders, Dr. Doré said. He noted that, as a relatively simple measure, gene richness in the microbiome may be used as a health stratifier. Studies have shown that low gene count has been associated with more severe metabolic and inflammatory traits among overweight patients, a lack of response to low-calorie diets among overweight and obese patients, severity of related conditions and risk of mortality among patients with liver cirrhosis, and poorer responses to immunotherapy among patients with cancer.
Certain patterns of flora may be prognostic, Dr. Doré said, citing a study by Gopalakrishnan et al. that involved 112 melanoma patients, in which those with a high abundance of Faecalibacterium had significantly longer progression-free survival than patients with a low abundance of the same bacteria. Further, a multivariate model showed that a high abundance of Faecalibacterium was the strongest predictor of response to immunotherapy, (hazard ratio, 2.95; P = .03), followed closely by prior immunotherapy (HR, 2.87; P = .03). In contrast, patients with a high abundance of Bacteroidales had shorter progression-free survival than patients with a low abundance of the same bacteria.
Dr. Doré also referred to one of the first interventional microbiomics studies in oncology. Mohty et al. conducted the ODYSSEE phase 1b/2a trial involving 25 patients with acute myeloid leukemia, in which patients were given autologous fecal microbiota transplants after induction chemotherapy and antibiotics. The treatment recovered 90% of original microbiota, and the estimated 1-year overall survival rate was 84%, compared with a historical rate of 70%.
The ODYSSEE study serves as proof of concept that microbiomics may eventually offer the next level of personalized medicine, Dr. Doré said. And now, with standards and technology available, researchers can move forward.
Dr. Doré disclosed relationships with BioFortis, Janssen, Sanofi, and other pharmaceutical companies.
Standards and technology are now available for microbiome profiling to take personalized medicine to the next level, but prospective trials are needed to realize this possibility, according to a leading expert.
The need for prospective microbiomics trials is increasing with the incidence of immune disorders, many of which have been linked with disturbances in the gut, reported Jöel Doré, PhD, at the annual Gut Microbiota for Health World Summit.
“In spite of considerable progress in medicine, together with hygiene, antibiotics, and vaccination developments, we are still seeing an increasing incidence – uncontrolled, that started over 60 years ago – of immune-mediated conditions,” said Dr. Doré, research director at the French National Research Institute for Agriculture, Food, and the Environment.
According to the World Health Organization, one out of four people will be affected by such a disorder in their lifetime, and the incidence rate of some conditions is accelerating faster than others, with geographical distributions that suggest environmental risk factors.
“The rate of incidence of autism in the U.S.A. is a quite scary exponential curve, where less than 1 birth per 5,000 was [affected] in the 1970s, where today it is 1 birth out of 50,” Dr. Doré said at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility. “Prevention is an urgent need, and possibly if we do not manage to understand what’s going on, human longevity might be at stake.”
Multiple studies have shown that transferring microbiota from humans with immune disorders to healthy mice can induce clinical signs of immune disorders, he said. And between humans, fecal transplants from healthy donors have reduced symptoms in patients with conditions such as inflammatory bowel disease.
While these studies support the link between microbe-host relationships and immune function, most of the underlying mechanisms remain unknown, Dr. Doré said. He highlighted the fact that the complex network of interactions involved separates microbiomics research from conventional approaches to disease.
“I want to stress the fact that clinical trials [in the past] have been designed in the situation where infection was the problem, [but] infection is essentially a linear thing; one agent, one risk, one disease,” Dr. Doré said. “What we are dealing with – with the increasing incidence of immune disorders – is host-microbe interaction at the center of everything, and alteration of host-microbe leading to risk, which may lead to disease. But host-microbe interaction is under the control of a vast number of environmental aspects ... so tools to deal with innovation and translation in a totally different or systemic configuration have yet to be invented.”
According to Dr. Doré, to develop clinical applications, research procedures must first be standardized.
“To be of use for the clinician and general practitioner, microbiome profiling will have to rely on pipelines of standardized preanalytical and analytical procedures,” he said. “This starts from sample collection and shipment.”
For the past 5 years, Dr. Doré and colleagues have been working to standardize procedures with a number of organizations around the world, and progress has been made.
“Today we have very good standards for shotgun sequencing,” he said.
With standards solidifying, microbiomics may lead to new clinical strategies for a range of conditions, even beyond immune disorders, Dr. Doré said. He noted that, as a relatively simple measure, gene richness in the microbiome may be used as a health stratifier. Studies have shown that low gene count has been associated with more severe metabolic and inflammatory traits among overweight patients, a lack of response to low-calorie diets among overweight and obese patients, severity of related conditions and risk of mortality among patients with liver cirrhosis, and poorer responses to immunotherapy among patients with cancer.
Certain patterns of flora may be prognostic, Dr. Doré said, citing a study by Gopalakrishnan et al. that involved 112 melanoma patients, in which those with a high abundance of Faecalibacterium had significantly longer progression-free survival than patients with a low abundance of the same bacteria. Further, a multivariate model showed that a high abundance of Faecalibacterium was the strongest predictor of response to immunotherapy, (hazard ratio, 2.95; P = .03), followed closely by prior immunotherapy (HR, 2.87; P = .03). In contrast, patients with a high abundance of Bacteroidales had shorter progression-free survival than patients with a low abundance of the same bacteria.
Dr. Doré also referred to one of the first interventional microbiomics studies in oncology. Mohty et al. conducted the ODYSSEE phase 1b/2a trial involving 25 patients with acute myeloid leukemia, in which patients were given autologous fecal microbiota transplants after induction chemotherapy and antibiotics. The treatment recovered 90% of original microbiota, and the estimated 1-year overall survival rate was 84%, compared with a historical rate of 70%.
The ODYSSEE study serves as proof of concept that microbiomics may eventually offer the next level of personalized medicine, Dr. Doré said. And now, with standards and technology available, researchers can move forward.
Dr. Doré disclosed relationships with BioFortis, Janssen, Sanofi, and other pharmaceutical companies.
Standards and technology are now available for microbiome profiling to take personalized medicine to the next level, but prospective trials are needed to realize this possibility, according to a leading expert.
The need for prospective microbiomics trials is increasing with the incidence of immune disorders, many of which have been linked with disturbances in the gut, reported Jöel Doré, PhD, at the annual Gut Microbiota for Health World Summit.
“In spite of considerable progress in medicine, together with hygiene, antibiotics, and vaccination developments, we are still seeing an increasing incidence – uncontrolled, that started over 60 years ago – of immune-mediated conditions,” said Dr. Doré, research director at the French National Research Institute for Agriculture, Food, and the Environment.
According to the World Health Organization, one out of four people will be affected by such a disorder in their lifetime, and the incidence rate of some conditions is accelerating faster than others, with geographical distributions that suggest environmental risk factors.
“The rate of incidence of autism in the U.S.A. is a quite scary exponential curve, where less than 1 birth per 5,000 was [affected] in the 1970s, where today it is 1 birth out of 50,” Dr. Doré said at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility. “Prevention is an urgent need, and possibly if we do not manage to understand what’s going on, human longevity might be at stake.”
Multiple studies have shown that transferring microbiota from humans with immune disorders to healthy mice can induce clinical signs of immune disorders, he said. And between humans, fecal transplants from healthy donors have reduced symptoms in patients with conditions such as inflammatory bowel disease.
While these studies support the link between microbe-host relationships and immune function, most of the underlying mechanisms remain unknown, Dr. Doré said. He highlighted the fact that the complex network of interactions involved separates microbiomics research from conventional approaches to disease.
“I want to stress the fact that clinical trials [in the past] have been designed in the situation where infection was the problem, [but] infection is essentially a linear thing; one agent, one risk, one disease,” Dr. Doré said. “What we are dealing with – with the increasing incidence of immune disorders – is host-microbe interaction at the center of everything, and alteration of host-microbe leading to risk, which may lead to disease. But host-microbe interaction is under the control of a vast number of environmental aspects ... so tools to deal with innovation and translation in a totally different or systemic configuration have yet to be invented.”
According to Dr. Doré, to develop clinical applications, research procedures must first be standardized.
“To be of use for the clinician and general practitioner, microbiome profiling will have to rely on pipelines of standardized preanalytical and analytical procedures,” he said. “This starts from sample collection and shipment.”
For the past 5 years, Dr. Doré and colleagues have been working to standardize procedures with a number of organizations around the world, and progress has been made.
“Today we have very good standards for shotgun sequencing,” he said.
With standards solidifying, microbiomics may lead to new clinical strategies for a range of conditions, even beyond immune disorders, Dr. Doré said. He noted that, as a relatively simple measure, gene richness in the microbiome may be used as a health stratifier. Studies have shown that low gene count has been associated with more severe metabolic and inflammatory traits among overweight patients, a lack of response to low-calorie diets among overweight and obese patients, severity of related conditions and risk of mortality among patients with liver cirrhosis, and poorer responses to immunotherapy among patients with cancer.
Certain patterns of flora may be prognostic, Dr. Doré said, citing a study by Gopalakrishnan et al. that involved 112 melanoma patients, in which those with a high abundance of Faecalibacterium had significantly longer progression-free survival than patients with a low abundance of the same bacteria. Further, a multivariate model showed that a high abundance of Faecalibacterium was the strongest predictor of response to immunotherapy, (hazard ratio, 2.95; P = .03), followed closely by prior immunotherapy (HR, 2.87; P = .03). In contrast, patients with a high abundance of Bacteroidales had shorter progression-free survival than patients with a low abundance of the same bacteria.
Dr. Doré also referred to one of the first interventional microbiomics studies in oncology. Mohty et al. conducted the ODYSSEE phase 1b/2a trial involving 25 patients with acute myeloid leukemia, in which patients were given autologous fecal microbiota transplants after induction chemotherapy and antibiotics. The treatment recovered 90% of original microbiota, and the estimated 1-year overall survival rate was 84%, compared with a historical rate of 70%.
The ODYSSEE study serves as proof of concept that microbiomics may eventually offer the next level of personalized medicine, Dr. Doré said. And now, with standards and technology available, researchers can move forward.
Dr. Doré disclosed relationships with BioFortis, Janssen, Sanofi, and other pharmaceutical companies.
EXPERT ANALYSIS FROM GMFH 2020
Rapid Development of Perifolliculitis Following Mesotherapy
To the Editor:
Mesotherapy, also known as intradermotherapy, is a cosmetic procedure in which multiple intradermal or subcutaneous injections of homeopathic substances, vitamins, chemicals, and plant extracts are administered.1 First conceived in Europe, mesotherapy is not approved by the US Food and Drug Administration but is gaining popularity in the United States as an alternative cosmetic procedure for various purposes, including lipolysis, body contouring, stretch marks, acne scars, actinic damage, and skin rejuvenation.1,2 We report a case of a healthy woman who developed perifolliculitis, transaminitis, and neutropenia 2 weeks after mesotherapy administration to the face, neck, and chest. We also review other potential side effects of this procedure.
A 36-year-old woman with no notable medical history presented to the emergency department with a worsening pruritic and painful rash on the face, chest, and neck of 2 weeks’ duration. The rash had developed 3 days after the patient received mesotherapy with an unknown substance for cosmetic rejuvenation; the rash was localized only to the injection sites. She did not note any fever, chills, nausea, vomiting, diarrhea, headache, arthralgia, or upper respiratory tract symptoms. She further denied starting any new medications, herbal products, or topical therapies apart from the procedure she had received 2 weeks prior.
The patient was found to be in no acute distress and vital signs were stable. Laboratory testing was remarkable for elevations in alanine aminotransferase (62 U/L [reference range, 10–40 U/L]) and aspartate aminotransferase (72 U/L [reference range 10–30 U/L]). Moreover, she had an absolute neutrophil count of 0.5×103 cells/µL (reference range 1.8–8.0×103 cells/µL). An electrolyte panel, creatinine level, and urinalysis were normal. Physical examination revealed numerous 4- to 5-mm erythematous papules in a gridlike distribution across the face, neck, and chest (Figure 1). No pustules or nodules were present. There was no discharge, crust, excoriations, or secondary lesions. Additionally, there was no lymphadenopathy and no mucous membrane or ocular involvement.

A 4-mm punch biopsy from a representative papule on the right lateral aspect of the neck demonstrated a perifollicular and perivascular lymphohistiocytic infiltrate with some focal granulomatous changes. No polarizable foreign body material was found (Figure 2). Bacterial, fungal, mycobacterial, and skin cultures were obtained, and results were all negative after several weeks.
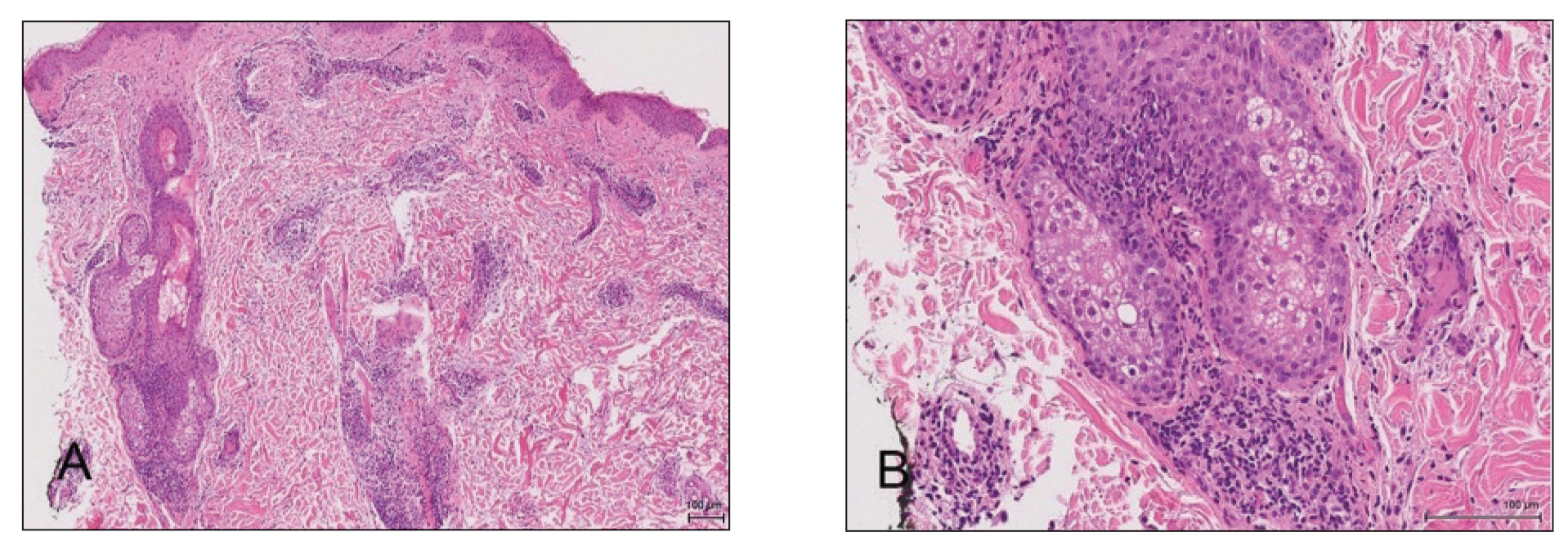
A diagnosis of perifolliculitis from the mesotherapy procedure was on the top of the differential vs a fast-growing mycobacterial or granulomatous reaction. The patient was started on a prednisone taper at 40 mg once daily tapered down completely over 3 weeks in addition to triamcinolone cream 0.1% applied 2 to 4 times daily as needed. Although she did not return to our outpatient clinic for follow-up, she informed us that her rash had improved 1 month after starting the prednisone taper. She was later lost to follow-up. It is unclear if the transaminitis and neutropenia were related to the materials injected during the mesotherapy procedure or from long-standing health issues.
Mesotherapy promises aesthetic benefits through a minimally invasive procedure and therefore is rapidly gaining popularity in aesthetic spas and treatment centers. Due to the lack of regulation in treatment protocols and substances used, there have been numerous reported cases of adverse side effects following mesotherapy, such as pain, allergic reactions, urticaria, panniculitis, ulceration, hair loss, necrosis, paraffinoma, cutaneous tuberculosis, and rapidly growing nontuberculous mycobacterial infections.1-5 More serious side effects also have been reported, such as permanent scarring, deformities, delirium, and massive subcutaneous emphysema (Table).2,4-18
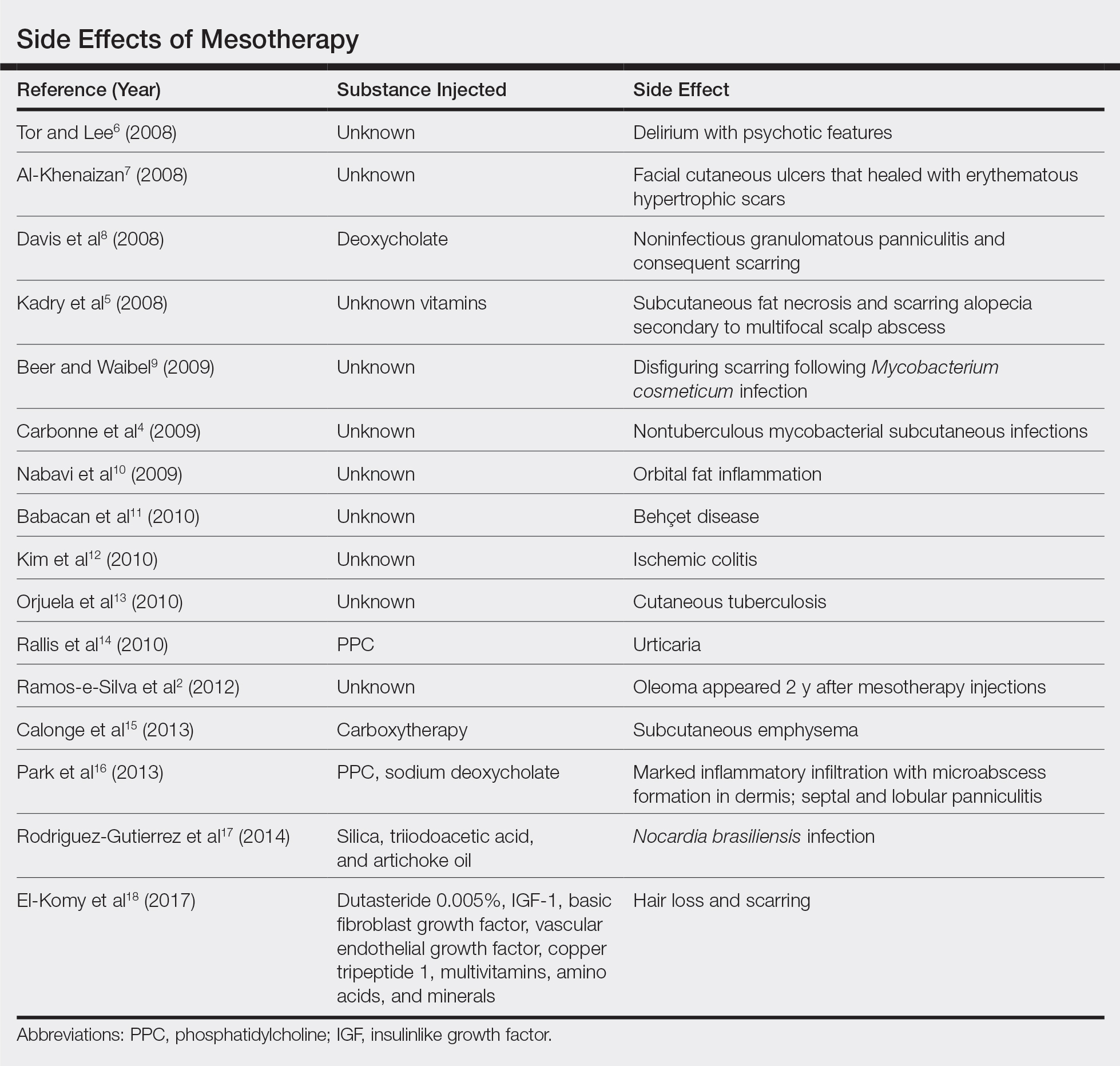
Given the potential complications of mesotherapy documented in the literature, we believe clinical investigations and trials must be performed to appropriately assess the safety and efficacy of this potentially hazardous procedure. Because there currently is insufficient research showing why certain patients are developing these adverse side effects, aesthetic spas and treatment centers should inform patients of all potential side effects associated with mesotherapy for the patient to make an informed decision about the procedure. Mesotherapy should be a point of focus for both the US Food and Drug Administration and researchers to determine its efficacy, safety, and standardization of the procedure.
- Bishara AS, Ibrahim AE, Dibo SA. Cosmetic mesotherapy: between scientific evidence, science fiction, and lucrative business. Aesth Plast Surg. 2008;32:842-849.
- Ramos-e-Silva M, Pereira AL, Ramos-e-Silva S, et al. Oleoma: a rare complication of mesotherapy for cellulite. Int J Dermatol. 2012;51:162-167.
- Rotunda AM, Kolodney MS. Mesotherapy and phosphatidylcholine injections: historical clarification and review. Dermatol Surg. 2006;32:465-480.
- Carbonne A, Brossier F, Arnaud I, et al. Outbreak of nontuberculous mycobacterial subcutaneous infections related to multiple mesotherapy injections. J Clin Microbiol. 2009;47:1961-1964.
- Kadry R, Hamadah I, Al-Issa A, et al. Multifocal scalp abscess with subcutaneous fat necrosis and scarring alopecia as a complication of scalp mesotherapy. J Drugs Dermatol. 2008;7:72-73.
- Tor PC, Lee TS. Delirium with psychotic features possibly associated with mesotherapy. Psychosomatics. 2008;49:273-274.
- Al-Khenaizan S. Facial cutaneous ulcers following mesotherapy. Dermatol Surg. 2008;34:832-834.
- Davis MD, Wright TI, Shehan JM. A complication of mesotherapy: noninfectious granulomatous panniculitis. Arch Dermatol. 2008;144:808-809.
- Beer K, Waibel J. Disfiguring scarring following mesotherapy-associated Mycobacterium cosmeticum infection. J Drugs Dermatol. 2009;8:391-393.
- Nabavi CB, Minckler DS, Tao JP. Histologic features of mesotherapy-induced orbital fat inflammation. Opthalmic Plast Reconstr Surg. 2009;25:69-70.
- Babacan T, Onat AM, Pehlivan Y, et al. A case of Behçet’s disease diagnosed by the panniculitis after mesotherapy. Rheumatol Int. 2010;30:1657-1659.
- Kim JB, Moon W, Park SJ, et al. Ischemic colitis after mesotherapy combined with anti-obesity medications. World J Gastroenterol. 2010;16:1537-1540.
- Orjuela D, Puerto G, Mejia G, et al. Cutaneous tuberculosis after mesotherapy: report of six cases. Biomedica. 2010;30:321-326.
- Rallis E, Kintzoglou S, Moussatou V, et al. Mesotherapy-induced urticaria. Dermatol Surg. 2010;36:1355-1356.
- Calonge WM, Lesbros-Pantoflickova D, Hodina M, et al. Massive subcutaneous emphysema after carbon dioxide mesotherapy. Aesthetic Plast Surg. 2013;37:194-197.
- Park EJ, Kim HS, Kim M, et al. Histological changes after treatment for localized fat deposits with phosphatidylcholine and sodium deoxycholate. J Cosmet Dermatol. 2013;3:240-243.
- Rodriguez-Gutierrez G, Toussaint S, Hernandez-Castro R, et al. Norcardia brasiliensis infection: an emergent suppurative granuloma after mesotherapy. Int J Dermatol. 2014;53:888-890.
- El-Komy M, Hassan A, Tawdy A, et al. Hair loss at injection sites of mesotherapy for alopecia [published online February 3, 2017]. J Cosmet Dermatol. 2017;16:E28-E30.
To the Editor:
Mesotherapy, also known as intradermotherapy, is a cosmetic procedure in which multiple intradermal or subcutaneous injections of homeopathic substances, vitamins, chemicals, and plant extracts are administered.1 First conceived in Europe, mesotherapy is not approved by the US Food and Drug Administration but is gaining popularity in the United States as an alternative cosmetic procedure for various purposes, including lipolysis, body contouring, stretch marks, acne scars, actinic damage, and skin rejuvenation.1,2 We report a case of a healthy woman who developed perifolliculitis, transaminitis, and neutropenia 2 weeks after mesotherapy administration to the face, neck, and chest. We also review other potential side effects of this procedure.
A 36-year-old woman with no notable medical history presented to the emergency department with a worsening pruritic and painful rash on the face, chest, and neck of 2 weeks’ duration. The rash had developed 3 days after the patient received mesotherapy with an unknown substance for cosmetic rejuvenation; the rash was localized only to the injection sites. She did not note any fever, chills, nausea, vomiting, diarrhea, headache, arthralgia, or upper respiratory tract symptoms. She further denied starting any new medications, herbal products, or topical therapies apart from the procedure she had received 2 weeks prior.
The patient was found to be in no acute distress and vital signs were stable. Laboratory testing was remarkable for elevations in alanine aminotransferase (62 U/L [reference range, 10–40 U/L]) and aspartate aminotransferase (72 U/L [reference range 10–30 U/L]). Moreover, she had an absolute neutrophil count of 0.5×103 cells/µL (reference range 1.8–8.0×103 cells/µL). An electrolyte panel, creatinine level, and urinalysis were normal. Physical examination revealed numerous 4- to 5-mm erythematous papules in a gridlike distribution across the face, neck, and chest (Figure 1). No pustules or nodules were present. There was no discharge, crust, excoriations, or secondary lesions. Additionally, there was no lymphadenopathy and no mucous membrane or ocular involvement.

A 4-mm punch biopsy from a representative papule on the right lateral aspect of the neck demonstrated a perifollicular and perivascular lymphohistiocytic infiltrate with some focal granulomatous changes. No polarizable foreign body material was found (Figure 2). Bacterial, fungal, mycobacterial, and skin cultures were obtained, and results were all negative after several weeks.
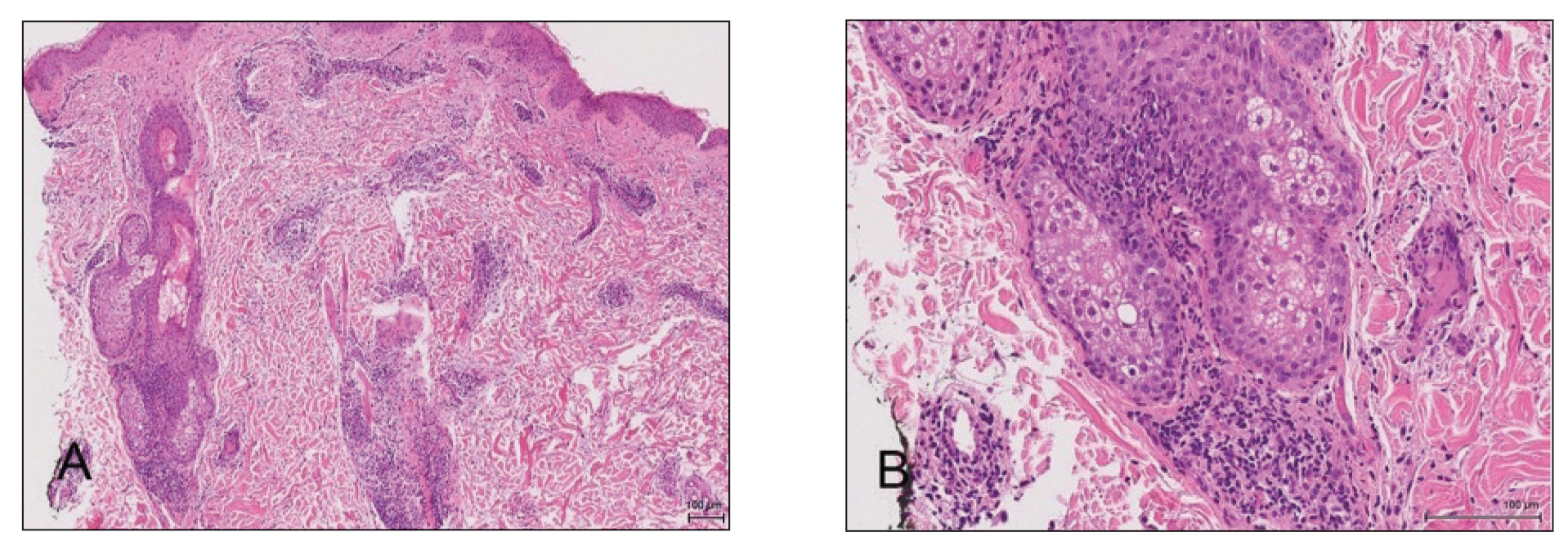
A diagnosis of perifolliculitis from the mesotherapy procedure was on the top of the differential vs a fast-growing mycobacterial or granulomatous reaction. The patient was started on a prednisone taper at 40 mg once daily tapered down completely over 3 weeks in addition to triamcinolone cream 0.1% applied 2 to 4 times daily as needed. Although she did not return to our outpatient clinic for follow-up, she informed us that her rash had improved 1 month after starting the prednisone taper. She was later lost to follow-up. It is unclear if the transaminitis and neutropenia were related to the materials injected during the mesotherapy procedure or from long-standing health issues.
Mesotherapy promises aesthetic benefits through a minimally invasive procedure and therefore is rapidly gaining popularity in aesthetic spas and treatment centers. Due to the lack of regulation in treatment protocols and substances used, there have been numerous reported cases of adverse side effects following mesotherapy, such as pain, allergic reactions, urticaria, panniculitis, ulceration, hair loss, necrosis, paraffinoma, cutaneous tuberculosis, and rapidly growing nontuberculous mycobacterial infections.1-5 More serious side effects also have been reported, such as permanent scarring, deformities, delirium, and massive subcutaneous emphysema (Table).2,4-18
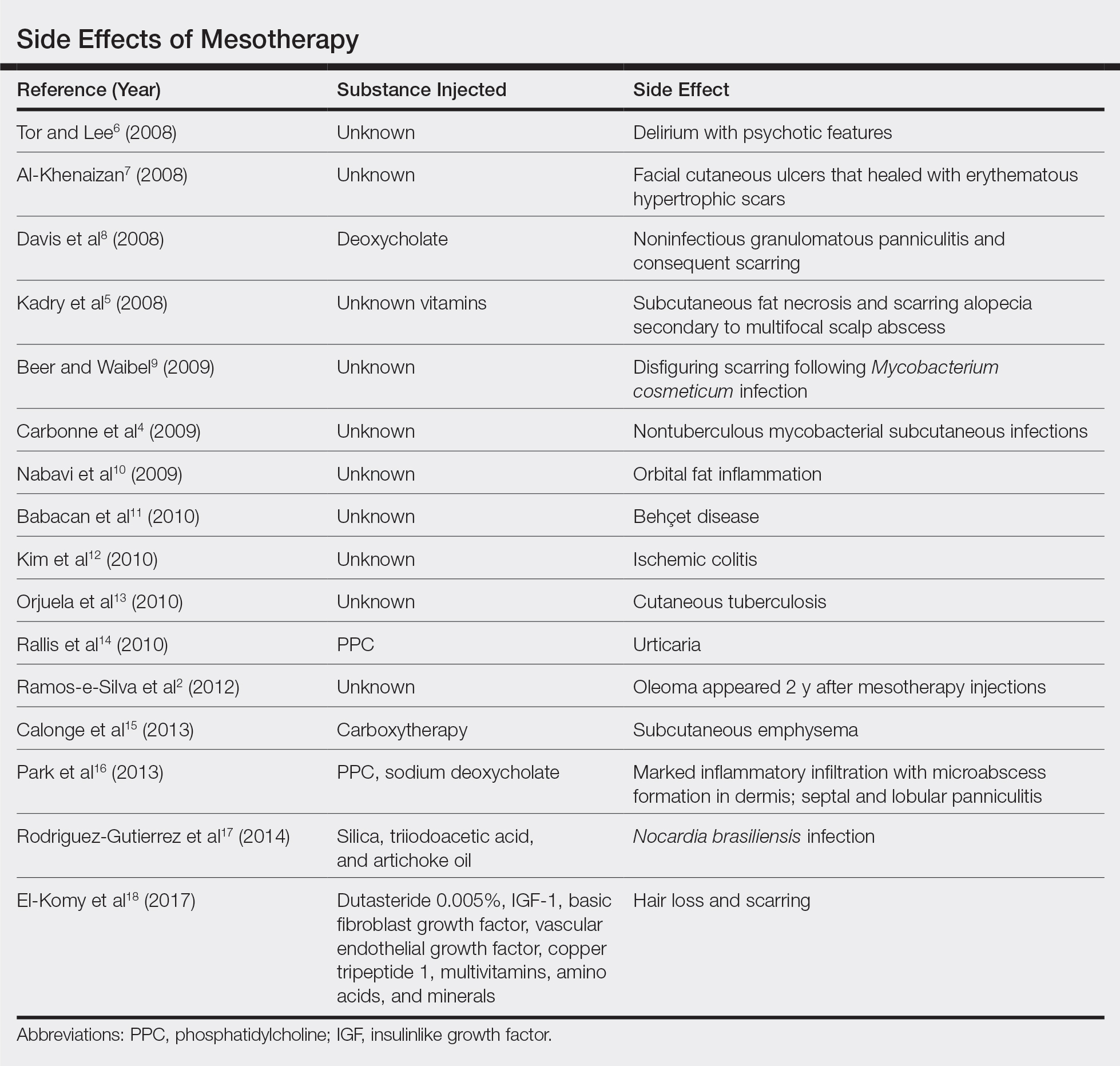
Given the potential complications of mesotherapy documented in the literature, we believe clinical investigations and trials must be performed to appropriately assess the safety and efficacy of this potentially hazardous procedure. Because there currently is insufficient research showing why certain patients are developing these adverse side effects, aesthetic spas and treatment centers should inform patients of all potential side effects associated with mesotherapy for the patient to make an informed decision about the procedure. Mesotherapy should be a point of focus for both the US Food and Drug Administration and researchers to determine its efficacy, safety, and standardization of the procedure.
To the Editor:
Mesotherapy, also known as intradermotherapy, is a cosmetic procedure in which multiple intradermal or subcutaneous injections of homeopathic substances, vitamins, chemicals, and plant extracts are administered.1 First conceived in Europe, mesotherapy is not approved by the US Food and Drug Administration but is gaining popularity in the United States as an alternative cosmetic procedure for various purposes, including lipolysis, body contouring, stretch marks, acne scars, actinic damage, and skin rejuvenation.1,2 We report a case of a healthy woman who developed perifolliculitis, transaminitis, and neutropenia 2 weeks after mesotherapy administration to the face, neck, and chest. We also review other potential side effects of this procedure.
A 36-year-old woman with no notable medical history presented to the emergency department with a worsening pruritic and painful rash on the face, chest, and neck of 2 weeks’ duration. The rash had developed 3 days after the patient received mesotherapy with an unknown substance for cosmetic rejuvenation; the rash was localized only to the injection sites. She did not note any fever, chills, nausea, vomiting, diarrhea, headache, arthralgia, or upper respiratory tract symptoms. She further denied starting any new medications, herbal products, or topical therapies apart from the procedure she had received 2 weeks prior.
The patient was found to be in no acute distress and vital signs were stable. Laboratory testing was remarkable for elevations in alanine aminotransferase (62 U/L [reference range, 10–40 U/L]) and aspartate aminotransferase (72 U/L [reference range 10–30 U/L]). Moreover, she had an absolute neutrophil count of 0.5×103 cells/µL (reference range 1.8–8.0×103 cells/µL). An electrolyte panel, creatinine level, and urinalysis were normal. Physical examination revealed numerous 4- to 5-mm erythematous papules in a gridlike distribution across the face, neck, and chest (Figure 1). No pustules or nodules were present. There was no discharge, crust, excoriations, or secondary lesions. Additionally, there was no lymphadenopathy and no mucous membrane or ocular involvement.

A 4-mm punch biopsy from a representative papule on the right lateral aspect of the neck demonstrated a perifollicular and perivascular lymphohistiocytic infiltrate with some focal granulomatous changes. No polarizable foreign body material was found (Figure 2). Bacterial, fungal, mycobacterial, and skin cultures were obtained, and results were all negative after several weeks.
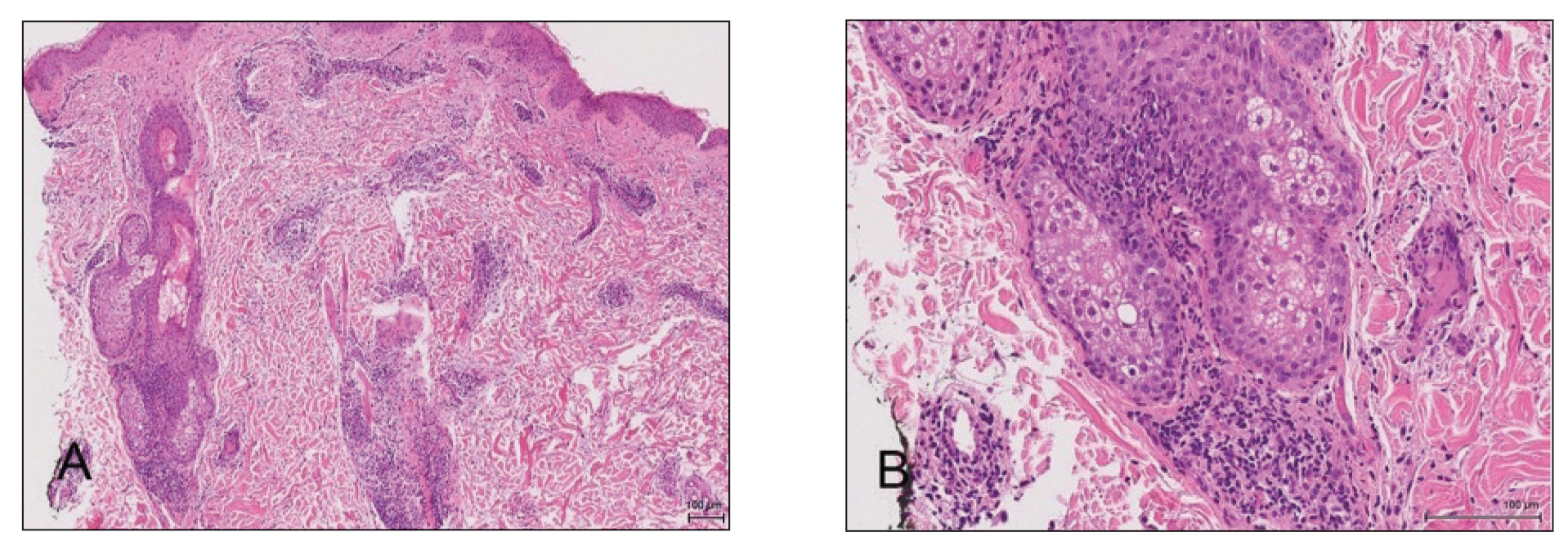
A diagnosis of perifolliculitis from the mesotherapy procedure was on the top of the differential vs a fast-growing mycobacterial or granulomatous reaction. The patient was started on a prednisone taper at 40 mg once daily tapered down completely over 3 weeks in addition to triamcinolone cream 0.1% applied 2 to 4 times daily as needed. Although she did not return to our outpatient clinic for follow-up, she informed us that her rash had improved 1 month after starting the prednisone taper. She was later lost to follow-up. It is unclear if the transaminitis and neutropenia were related to the materials injected during the mesotherapy procedure or from long-standing health issues.
Mesotherapy promises aesthetic benefits through a minimally invasive procedure and therefore is rapidly gaining popularity in aesthetic spas and treatment centers. Due to the lack of regulation in treatment protocols and substances used, there have been numerous reported cases of adverse side effects following mesotherapy, such as pain, allergic reactions, urticaria, panniculitis, ulceration, hair loss, necrosis, paraffinoma, cutaneous tuberculosis, and rapidly growing nontuberculous mycobacterial infections.1-5 More serious side effects also have been reported, such as permanent scarring, deformities, delirium, and massive subcutaneous emphysema (Table).2,4-18
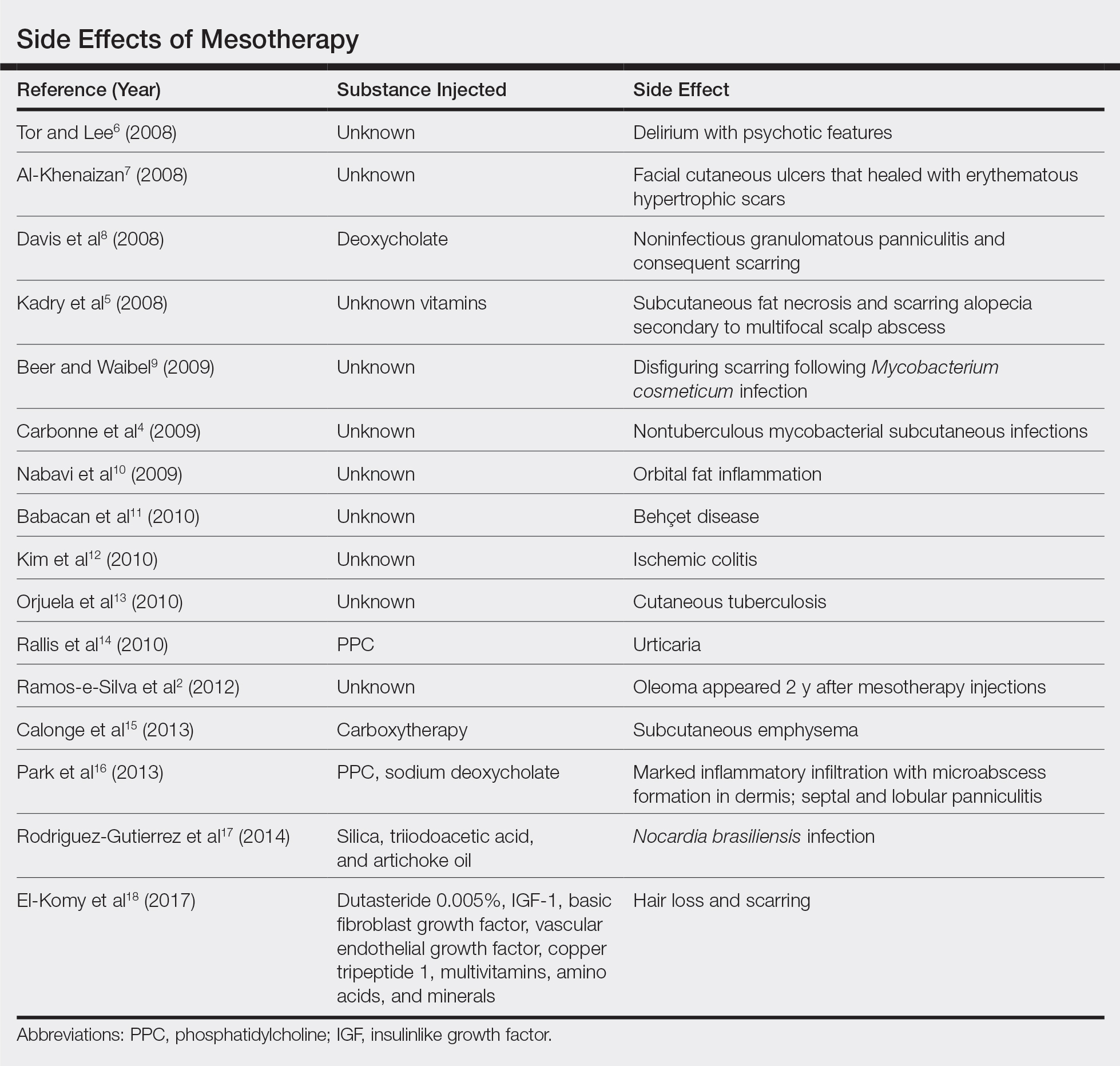
Given the potential complications of mesotherapy documented in the literature, we believe clinical investigations and trials must be performed to appropriately assess the safety and efficacy of this potentially hazardous procedure. Because there currently is insufficient research showing why certain patients are developing these adverse side effects, aesthetic spas and treatment centers should inform patients of all potential side effects associated with mesotherapy for the patient to make an informed decision about the procedure. Mesotherapy should be a point of focus for both the US Food and Drug Administration and researchers to determine its efficacy, safety, and standardization of the procedure.
- Bishara AS, Ibrahim AE, Dibo SA. Cosmetic mesotherapy: between scientific evidence, science fiction, and lucrative business. Aesth Plast Surg. 2008;32:842-849.
- Ramos-e-Silva M, Pereira AL, Ramos-e-Silva S, et al. Oleoma: a rare complication of mesotherapy for cellulite. Int J Dermatol. 2012;51:162-167.
- Rotunda AM, Kolodney MS. Mesotherapy and phosphatidylcholine injections: historical clarification and review. Dermatol Surg. 2006;32:465-480.
- Carbonne A, Brossier F, Arnaud I, et al. Outbreak of nontuberculous mycobacterial subcutaneous infections related to multiple mesotherapy injections. J Clin Microbiol. 2009;47:1961-1964.
- Kadry R, Hamadah I, Al-Issa A, et al. Multifocal scalp abscess with subcutaneous fat necrosis and scarring alopecia as a complication of scalp mesotherapy. J Drugs Dermatol. 2008;7:72-73.
- Tor PC, Lee TS. Delirium with psychotic features possibly associated with mesotherapy. Psychosomatics. 2008;49:273-274.
- Al-Khenaizan S. Facial cutaneous ulcers following mesotherapy. Dermatol Surg. 2008;34:832-834.
- Davis MD, Wright TI, Shehan JM. A complication of mesotherapy: noninfectious granulomatous panniculitis. Arch Dermatol. 2008;144:808-809.
- Beer K, Waibel J. Disfiguring scarring following mesotherapy-associated Mycobacterium cosmeticum infection. J Drugs Dermatol. 2009;8:391-393.
- Nabavi CB, Minckler DS, Tao JP. Histologic features of mesotherapy-induced orbital fat inflammation. Opthalmic Plast Reconstr Surg. 2009;25:69-70.
- Babacan T, Onat AM, Pehlivan Y, et al. A case of Behçet’s disease diagnosed by the panniculitis after mesotherapy. Rheumatol Int. 2010;30:1657-1659.
- Kim JB, Moon W, Park SJ, et al. Ischemic colitis after mesotherapy combined with anti-obesity medications. World J Gastroenterol. 2010;16:1537-1540.
- Orjuela D, Puerto G, Mejia G, et al. Cutaneous tuberculosis after mesotherapy: report of six cases. Biomedica. 2010;30:321-326.
- Rallis E, Kintzoglou S, Moussatou V, et al. Mesotherapy-induced urticaria. Dermatol Surg. 2010;36:1355-1356.
- Calonge WM, Lesbros-Pantoflickova D, Hodina M, et al. Massive subcutaneous emphysema after carbon dioxide mesotherapy. Aesthetic Plast Surg. 2013;37:194-197.
- Park EJ, Kim HS, Kim M, et al. Histological changes after treatment for localized fat deposits with phosphatidylcholine and sodium deoxycholate. J Cosmet Dermatol. 2013;3:240-243.
- Rodriguez-Gutierrez G, Toussaint S, Hernandez-Castro R, et al. Norcardia brasiliensis infection: an emergent suppurative granuloma after mesotherapy. Int J Dermatol. 2014;53:888-890.
- El-Komy M, Hassan A, Tawdy A, et al. Hair loss at injection sites of mesotherapy for alopecia [published online February 3, 2017]. J Cosmet Dermatol. 2017;16:E28-E30.
- Bishara AS, Ibrahim AE, Dibo SA. Cosmetic mesotherapy: between scientific evidence, science fiction, and lucrative business. Aesth Plast Surg. 2008;32:842-849.
- Ramos-e-Silva M, Pereira AL, Ramos-e-Silva S, et al. Oleoma: a rare complication of mesotherapy for cellulite. Int J Dermatol. 2012;51:162-167.
- Rotunda AM, Kolodney MS. Mesotherapy and phosphatidylcholine injections: historical clarification and review. Dermatol Surg. 2006;32:465-480.
- Carbonne A, Brossier F, Arnaud I, et al. Outbreak of nontuberculous mycobacterial subcutaneous infections related to multiple mesotherapy injections. J Clin Microbiol. 2009;47:1961-1964.
- Kadry R, Hamadah I, Al-Issa A, et al. Multifocal scalp abscess with subcutaneous fat necrosis and scarring alopecia as a complication of scalp mesotherapy. J Drugs Dermatol. 2008;7:72-73.
- Tor PC, Lee TS. Delirium with psychotic features possibly associated with mesotherapy. Psychosomatics. 2008;49:273-274.
- Al-Khenaizan S. Facial cutaneous ulcers following mesotherapy. Dermatol Surg. 2008;34:832-834.
- Davis MD, Wright TI, Shehan JM. A complication of mesotherapy: noninfectious granulomatous panniculitis. Arch Dermatol. 2008;144:808-809.
- Beer K, Waibel J. Disfiguring scarring following mesotherapy-associated Mycobacterium cosmeticum infection. J Drugs Dermatol. 2009;8:391-393.
- Nabavi CB, Minckler DS, Tao JP. Histologic features of mesotherapy-induced orbital fat inflammation. Opthalmic Plast Reconstr Surg. 2009;25:69-70.
- Babacan T, Onat AM, Pehlivan Y, et al. A case of Behçet’s disease diagnosed by the panniculitis after mesotherapy. Rheumatol Int. 2010;30:1657-1659.
- Kim JB, Moon W, Park SJ, et al. Ischemic colitis after mesotherapy combined with anti-obesity medications. World J Gastroenterol. 2010;16:1537-1540.
- Orjuela D, Puerto G, Mejia G, et al. Cutaneous tuberculosis after mesotherapy: report of six cases. Biomedica. 2010;30:321-326.
- Rallis E, Kintzoglou S, Moussatou V, et al. Mesotherapy-induced urticaria. Dermatol Surg. 2010;36:1355-1356.
- Calonge WM, Lesbros-Pantoflickova D, Hodina M, et al. Massive subcutaneous emphysema after carbon dioxide mesotherapy. Aesthetic Plast Surg. 2013;37:194-197.
- Park EJ, Kim HS, Kim M, et al. Histological changes after treatment for localized fat deposits with phosphatidylcholine and sodium deoxycholate. J Cosmet Dermatol. 2013;3:240-243.
- Rodriguez-Gutierrez G, Toussaint S, Hernandez-Castro R, et al. Norcardia brasiliensis infection: an emergent suppurative granuloma after mesotherapy. Int J Dermatol. 2014;53:888-890.
- El-Komy M, Hassan A, Tawdy A, et al. Hair loss at injection sites of mesotherapy for alopecia [published online February 3, 2017]. J Cosmet Dermatol. 2017;16:E28-E30.
Practice Points
- Mesotherapy—the delivery of vitamins, chemicals, and plant extracts directly into the dermis via injections—is a common procedure performed in both medical and nonmedical settings for cosmetic rejuvenation.
- Complications can occur from mesotherapy treatment.
- Patients should be advised to seek medical care with US Food and Drug Administration–approved cosmetic techniques and substances only
Human Immunodeficiency Virus Infection in a Hepatitis B Virus–Positive Psoriasis Patient Treated With Ustekinumab
To the Editor:
The incidence of psoriasis in human immunodeficiency virus (HIV)–infected patients is similar to the general population, but it usually becomes more severe as immunosuppression increases. Additionally, it tends to be more resistant to conventional therapies, and the incidence and severity of psoriatic arthropathy is increased. Psoriasis often worsens at the time of HIV primary infection.1 We describe a case of a patient with hepatitis B virus (HBV) whose severe plaque psoriasis was controlled on ustekinumab; he was later diagnosed with HIV infection.
A 42-year-old man with HBV treated with entecavir (HBV DNA viral load, <20 copies/mL [inactive carrier, <2000 copies/mL]) presented to our dermatology unit with severe plaque psoriasis (psoriasis area and severity index 23) that caused notable psychologic difficulties such as anxiety and depression. Treatment was attempted with cyclosporine; acitretin; psoralen plus UVA; infliximab; adalimumab; and eventually ustekinumab (45 mg every 3 months), which controlled the condition well (psoriasis area and severity index 0) in an almost completely sustained manner.
Serologic tests requested at one of his analytical control appointments 2 years after initiating treatment with ustekinumab revealed he was HIV positive. The patient reported unprotected sexual intercourse 4 months prior. He was referred to the infectious disease unit and was classified in subtype A1 of HIV infection (CD4 count, 583 cells/µL [reference range, 500-1200 cells/µL]; viral load, 159,268 copies/mL [rapid progression to AIDS, >100,000 copies/mL]). Treatment was initiated with raltegravir, ritonavir, darunavir, and abacavir; tolerance was suitable. Because of the patient’s history of severe psoriasis, treatment with ustekinumab was maintained. Normally, treatment with this drug would be contraindicated in patients with HIV, as it can lead to viral reactivation. Four years after his HIV diagnosis, neither the patient’s cutaneous nor HIV-associated condition had worsened.
For patients with HIV and mild or moderate psoriasis, topical therapies (eg, corticosteroids, vitamin D analogues, tazarotene) are recommended, similar to patients who are HIV negative. Human immunodeficiency virus–positive patients with severe psoriasis who do not respond to topical treatment should receive phototherapy (UVB or psoralen plus UVA) or acitretin along with their antiretroviral drugs.2 In refractory cases, immunosuppressants, including cyclosporine, methotrexate, or tumor necrosis factor α inhibitors, might be used, though experience with them is limited.3,4 Maintaining antiretroviral therapy and prophylaxis against opportunist disease is important in patients who receive such immunosuppressants, as is close monitoring of the viral load.
Ustekinumab is an IL-12/IL-23 monoclonal antibody indicated for the treatment of moderate to severe plaque psoriasis, active psoriatic arthritis, and inflammatory bowel disease. It is contraindicated in patients with clinically important active infections, such as HBV and hepatitis C virus infections.5 However, it was shown to be safe in a group of 18 patients with HBV who had received antiviral prophylaxis6; a degree of reactivation was observed in similar patients who received no such prophylaxis and in others with hepatitis C virus infection.7 The simultaneous use of methotrexate with ustekinumab in the treatment of psoriatic arthritis does not appear to affect the safety of the latter drug.8 Paparizos et al9 described a patient with HIV controlled with antiretroviral drugs who was treated with ustekinumab for psoriasis; no adverse effects were observed.
We report the case of a patient with HBV and psoriasis who was treated with ustekinumab and later became infected with HIV. His ustekinumab treatment was maintained without subsequent cutaneous or systemic complications.
- Menon K, Van Voorhees V, Bebo B, et al. Psoriasis in patients with HIV infection: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291-299.
- Chiricozzi A, Saraceno R, Cannizzaro MV. Complete resolution of erythrodermic psoriasis in an HIV and HCV patient unresponsive to antipsoriatic treatments after highly active antiretroviral therapy. Dermatology. 2012;225:333-337.
- Barco D, Puig L, Alomar A. Treatment of moderate-severe psoriasis with etanercept in patients with chronic human immunodeficiency virus infection. Actas Dermosifiliogr. 2010;101(suppl 1):77-81.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV positive patient. J Drugs Dermatol. 2014;13:869-871.
- Rustin MH. Long-term safety of biologics in the treatment of moderate to severe plaque psoriasis: review of the current data. Br J Dermatol. 2012;167(suppl 3):3-11.
- Navarro R, Vilarrasa E, Herranz P, et al. Safety and effectiveness of ustekinumab and antitumour necrosis factor therapy in patients with psoriasis and chronic viral hepatitis B or C: a retrospective, multicentre study in a clinical setting. Br J Dermatol. 2013;168:609-616.
- Chiu HY, Chen CH, Wu MS, et al. The safety profile of ustekinumab in the treatment of patients with psoriasis and concurrent hepatitis B or C. Br J Dermatol. 2013;169:1295-1303.
- Weitz JE, Ritchlin CT. Ustekinumab: targeting the IL-17 pathway to improve outcomes in psoriatic arthritis. Expert Opin Biol Ther. 2014;14:515-526.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatol Treat. 2012;23:398-399.
To the Editor:
The incidence of psoriasis in human immunodeficiency virus (HIV)–infected patients is similar to the general population, but it usually becomes more severe as immunosuppression increases. Additionally, it tends to be more resistant to conventional therapies, and the incidence and severity of psoriatic arthropathy is increased. Psoriasis often worsens at the time of HIV primary infection.1 We describe a case of a patient with hepatitis B virus (HBV) whose severe plaque psoriasis was controlled on ustekinumab; he was later diagnosed with HIV infection.
A 42-year-old man with HBV treated with entecavir (HBV DNA viral load, <20 copies/mL [inactive carrier, <2000 copies/mL]) presented to our dermatology unit with severe plaque psoriasis (psoriasis area and severity index 23) that caused notable psychologic difficulties such as anxiety and depression. Treatment was attempted with cyclosporine; acitretin; psoralen plus UVA; infliximab; adalimumab; and eventually ustekinumab (45 mg every 3 months), which controlled the condition well (psoriasis area and severity index 0) in an almost completely sustained manner.
Serologic tests requested at one of his analytical control appointments 2 years after initiating treatment with ustekinumab revealed he was HIV positive. The patient reported unprotected sexual intercourse 4 months prior. He was referred to the infectious disease unit and was classified in subtype A1 of HIV infection (CD4 count, 583 cells/µL [reference range, 500-1200 cells/µL]; viral load, 159,268 copies/mL [rapid progression to AIDS, >100,000 copies/mL]). Treatment was initiated with raltegravir, ritonavir, darunavir, and abacavir; tolerance was suitable. Because of the patient’s history of severe psoriasis, treatment with ustekinumab was maintained. Normally, treatment with this drug would be contraindicated in patients with HIV, as it can lead to viral reactivation. Four years after his HIV diagnosis, neither the patient’s cutaneous nor HIV-associated condition had worsened.
For patients with HIV and mild or moderate psoriasis, topical therapies (eg, corticosteroids, vitamin D analogues, tazarotene) are recommended, similar to patients who are HIV negative. Human immunodeficiency virus–positive patients with severe psoriasis who do not respond to topical treatment should receive phototherapy (UVB or psoralen plus UVA) or acitretin along with their antiretroviral drugs.2 In refractory cases, immunosuppressants, including cyclosporine, methotrexate, or tumor necrosis factor α inhibitors, might be used, though experience with them is limited.3,4 Maintaining antiretroviral therapy and prophylaxis against opportunist disease is important in patients who receive such immunosuppressants, as is close monitoring of the viral load.
Ustekinumab is an IL-12/IL-23 monoclonal antibody indicated for the treatment of moderate to severe plaque psoriasis, active psoriatic arthritis, and inflammatory bowel disease. It is contraindicated in patients with clinically important active infections, such as HBV and hepatitis C virus infections.5 However, it was shown to be safe in a group of 18 patients with HBV who had received antiviral prophylaxis6; a degree of reactivation was observed in similar patients who received no such prophylaxis and in others with hepatitis C virus infection.7 The simultaneous use of methotrexate with ustekinumab in the treatment of psoriatic arthritis does not appear to affect the safety of the latter drug.8 Paparizos et al9 described a patient with HIV controlled with antiretroviral drugs who was treated with ustekinumab for psoriasis; no adverse effects were observed.
We report the case of a patient with HBV and psoriasis who was treated with ustekinumab and later became infected with HIV. His ustekinumab treatment was maintained without subsequent cutaneous or systemic complications.
To the Editor:
The incidence of psoriasis in human immunodeficiency virus (HIV)–infected patients is similar to the general population, but it usually becomes more severe as immunosuppression increases. Additionally, it tends to be more resistant to conventional therapies, and the incidence and severity of psoriatic arthropathy is increased. Psoriasis often worsens at the time of HIV primary infection.1 We describe a case of a patient with hepatitis B virus (HBV) whose severe plaque psoriasis was controlled on ustekinumab; he was later diagnosed with HIV infection.
A 42-year-old man with HBV treated with entecavir (HBV DNA viral load, <20 copies/mL [inactive carrier, <2000 copies/mL]) presented to our dermatology unit with severe plaque psoriasis (psoriasis area and severity index 23) that caused notable psychologic difficulties such as anxiety and depression. Treatment was attempted with cyclosporine; acitretin; psoralen plus UVA; infliximab; adalimumab; and eventually ustekinumab (45 mg every 3 months), which controlled the condition well (psoriasis area and severity index 0) in an almost completely sustained manner.
Serologic tests requested at one of his analytical control appointments 2 years after initiating treatment with ustekinumab revealed he was HIV positive. The patient reported unprotected sexual intercourse 4 months prior. He was referred to the infectious disease unit and was classified in subtype A1 of HIV infection (CD4 count, 583 cells/µL [reference range, 500-1200 cells/µL]; viral load, 159,268 copies/mL [rapid progression to AIDS, >100,000 copies/mL]). Treatment was initiated with raltegravir, ritonavir, darunavir, and abacavir; tolerance was suitable. Because of the patient’s history of severe psoriasis, treatment with ustekinumab was maintained. Normally, treatment with this drug would be contraindicated in patients with HIV, as it can lead to viral reactivation. Four years after his HIV diagnosis, neither the patient’s cutaneous nor HIV-associated condition had worsened.
For patients with HIV and mild or moderate psoriasis, topical therapies (eg, corticosteroids, vitamin D analogues, tazarotene) are recommended, similar to patients who are HIV negative. Human immunodeficiency virus–positive patients with severe psoriasis who do not respond to topical treatment should receive phototherapy (UVB or psoralen plus UVA) or acitretin along with their antiretroviral drugs.2 In refractory cases, immunosuppressants, including cyclosporine, methotrexate, or tumor necrosis factor α inhibitors, might be used, though experience with them is limited.3,4 Maintaining antiretroviral therapy and prophylaxis against opportunist disease is important in patients who receive such immunosuppressants, as is close monitoring of the viral load.
Ustekinumab is an IL-12/IL-23 monoclonal antibody indicated for the treatment of moderate to severe plaque psoriasis, active psoriatic arthritis, and inflammatory bowel disease. It is contraindicated in patients with clinically important active infections, such as HBV and hepatitis C virus infections.5 However, it was shown to be safe in a group of 18 patients with HBV who had received antiviral prophylaxis6; a degree of reactivation was observed in similar patients who received no such prophylaxis and in others with hepatitis C virus infection.7 The simultaneous use of methotrexate with ustekinumab in the treatment of psoriatic arthritis does not appear to affect the safety of the latter drug.8 Paparizos et al9 described a patient with HIV controlled with antiretroviral drugs who was treated with ustekinumab for psoriasis; no adverse effects were observed.
We report the case of a patient with HBV and psoriasis who was treated with ustekinumab and later became infected with HIV. His ustekinumab treatment was maintained without subsequent cutaneous or systemic complications.
- Menon K, Van Voorhees V, Bebo B, et al. Psoriasis in patients with HIV infection: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291-299.
- Chiricozzi A, Saraceno R, Cannizzaro MV. Complete resolution of erythrodermic psoriasis in an HIV and HCV patient unresponsive to antipsoriatic treatments after highly active antiretroviral therapy. Dermatology. 2012;225:333-337.
- Barco D, Puig L, Alomar A. Treatment of moderate-severe psoriasis with etanercept in patients with chronic human immunodeficiency virus infection. Actas Dermosifiliogr. 2010;101(suppl 1):77-81.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV positive patient. J Drugs Dermatol. 2014;13:869-871.
- Rustin MH. Long-term safety of biologics in the treatment of moderate to severe plaque psoriasis: review of the current data. Br J Dermatol. 2012;167(suppl 3):3-11.
- Navarro R, Vilarrasa E, Herranz P, et al. Safety and effectiveness of ustekinumab and antitumour necrosis factor therapy in patients with psoriasis and chronic viral hepatitis B or C: a retrospective, multicentre study in a clinical setting. Br J Dermatol. 2013;168:609-616.
- Chiu HY, Chen CH, Wu MS, et al. The safety profile of ustekinumab in the treatment of patients with psoriasis and concurrent hepatitis B or C. Br J Dermatol. 2013;169:1295-1303.
- Weitz JE, Ritchlin CT. Ustekinumab: targeting the IL-17 pathway to improve outcomes in psoriatic arthritis. Expert Opin Biol Ther. 2014;14:515-526.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatol Treat. 2012;23:398-399.
- Menon K, Van Voorhees V, Bebo B, et al. Psoriasis in patients with HIV infection: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:291-299.
- Chiricozzi A, Saraceno R, Cannizzaro MV. Complete resolution of erythrodermic psoriasis in an HIV and HCV patient unresponsive to antipsoriatic treatments after highly active antiretroviral therapy. Dermatology. 2012;225:333-337.
- Barco D, Puig L, Alomar A. Treatment of moderate-severe psoriasis with etanercept in patients with chronic human immunodeficiency virus infection. Actas Dermosifiliogr. 2010;101(suppl 1):77-81.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV positive patient. J Drugs Dermatol. 2014;13:869-871.
- Rustin MH. Long-term safety of biologics in the treatment of moderate to severe plaque psoriasis: review of the current data. Br J Dermatol. 2012;167(suppl 3):3-11.
- Navarro R, Vilarrasa E, Herranz P, et al. Safety and effectiveness of ustekinumab and antitumour necrosis factor therapy in patients with psoriasis and chronic viral hepatitis B or C: a retrospective, multicentre study in a clinical setting. Br J Dermatol. 2013;168:609-616.
- Chiu HY, Chen CH, Wu MS, et al. The safety profile of ustekinumab in the treatment of patients with psoriasis and concurrent hepatitis B or C. Br J Dermatol. 2013;169:1295-1303.
- Weitz JE, Ritchlin CT. Ustekinumab: targeting the IL-17 pathway to improve outcomes in psoriatic arthritis. Expert Opin Biol Ther. 2014;14:515-526.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatol Treat. 2012;23:398-399.
Practice Points
- Psoriasis in patients with human immunodeficiency virus (HIV) tends to be more resistant to conventional therapies.
- Experience is limited in the use of immunosuppressants and biologics to treat psoriasis in HIV patients.
- Maintaining antiretroviral therapy and prophylaxis against opportunist disease is important in HIV patients who receive biologics, as is close monitoring of the viral load.
COVID-19 update: Transmission 5% or less among close contacts
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
The transmission rate of coronavirus disease 2019 (COVID-19) was 1%-5% among 38,000 Chinese people in close contact with infected patients, according to the chief epidemiologist of the Chinese Centers for Disease Control and Prevention, Beijing, Zunyou Wu, MD, PhD, who gave an update on the epidemic at the Conference on Retroviruses & Opportunistic Infections.
The rate of spread to family members – the driver of the infection in China – was 10% early in the outbreak, but fell to 3% with quicker recognition and isolation. The overall numbers are lower than might have been expected, and an important insight for clinicians trying to contain the outbreak in the United States.
, but their ability to spread the infection dropped after that, Dr. Wu and others said at a special COVID-19 session at the meeting, which was scheduled to be in Boston, but was held online instead because of concerns about spreading the virus. The session has been posted.
Transmission from presymptomatic people is rare. Shedding persists to some degree for 7-12 days in mild/moderate cases, but 2 weeks or more in severe cases.
Dr. Wu said the numbers in China are moving in the right direction, which means that containment efforts there have worked.
The virus emerged in Wuhan, the capital of Hubei province in central China, in connection with a wildlife food market in December 2019. Bats are thought to be the reservoir, with perhaps an intermediate step between civet cats and raccoon dogs. Officials shut down the market.
Essentially, the entire population of China, more than a billion people, was told to stay home for 10 days to interrupt the transmission cycle after the virus spread throughout the country in a few weeks, and almost 60 million people in Hubei were put behind a cordon sanitaire, where they have been for 50 days and will remain “for a while,” Dr. Wu said.
It’s led to a steep drop in new cases and deaths in China since mid-February; both are now more common outside China than inside, and international numbers are lower than they were at the peak in China.
Meanwhile, there’s been no evidence of perinatal transmission; the virus has not been detected in amniotic fluid, cord blood, neonatal throat swabs, or breast milk. Maternal morbidity appears to be similar to uninfected women. “The data around pregnancy are reassuring,” said John Brooks, MD, chief medical officers for HIV/AIDS prevention at the Centers for Disease Control and Prevention, Atlanta, who has been involved with CDC’s containment efforts.
There’s no data yet for immunocompromised people, but for people with HIV, he said, “we think the risk of severe illness would be greater” with lower CD4 counts and unsuppressed viral loads. “People living with HIV should take precautions against this new virus,” including having at least a 30-day supply of HIV medications; keeping up flu and pneumonia vaccinations; and having a care plan if quarantined. Setting up telemedicine might be a good idea.
The usual incubation period for COVID-19 is 4-6 days but can be longer. Recovery time is about 2 weeks in mild cases and 3-6 weeks in more severe cases. People who die do so within 2 months of symptom onset.
The most common symptoms among hospitalized patients in China are fever, dry cough, fatigue, and headache. Truly asymptomatic cases are not common; most go on to develop symptoms. There have been reports of diarrhea before other symptoms by a day or two, but it’s probably a red herring. The virus has been isolated from stool, but there is no evidence of fecal-oral transmission, Dr. Wu said.
Eighty percent of COVID-19 cases are mild or moderate and most patients recover spontaneously, especially middle aged and younger people. There is no meaningful difference in distribution between the sexes.
There are limited pediatric data perhaps due to underreporting, “but we know [children] experience milder illness than adults,” the CDC’s Dr. Brooks said.
He pegged the latest case fatality estimate at 0.5% to 3.5%, which is considerably higher than seasonal flu, but might well drop as more mild cases are detected and added to the denominator, he said.
For now, death rates top 5% in adults over 60 years old and climb further with increasing age, approaching 16% in people 80 years or older. Patients with hypertension, diabetes, cardiovascular disease, and chronic respiratory illness are at increased risk. The ultimate cause of death is acute respiratory distress syndrome, said Ralph Baric, PhD, a coronavirus expert and epidemiology professor at the University of North Carolina, Chapel Hill, who also presented at the meeting.
Several drug and vaccine candidates are under study for the infection. An intriguing possibility is that angiotensin converting enzyme (ACE) inhibitors might help. Hypertension is a known risk factor for severe infection; the virus makes use of ACE receptor pathways to infect airway epithelial cells; and there have been reports of ACE inhibitors having effect against the virus that caused severe acute respiratory syndrome (SARS), another coronavirus outbreak in 2003.
“I think it’s a very good idea to go back and re-explore use of these drugs,” Dr. Baric said.
The presenters didn’t have any relevant disclosures.
FROM CROI 2020
Serum GFAP may indicate disease severity in NMOSD
WEST PALM BEACH, FLA. – (NMOSD), according to research presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Treatment with inebilizumab decreases serum GFAP concentrations and reduces the risk of an NMOSD attack, the investigators said.
In NMOSD, autoantibodies often target aquaporin-4, a protein expressed on astrocytes. This immune response destroys astrocytes and increases levels of GFAP in cerebrospinal fluid and serum. In the N-MOmentum trial, inebilizumab reduced the risk of attacks by 73%, compared with placebo, in patients with NMOSD. Bruce Cree, MD, PhD, professor of neurology at the University of California, San Francisco, Weill Institute for Neurosciences and colleagues analyzed the data from this trial to examine the relationship between serum GFAP concentrations and disease activity.
In the study, the investigators prospectively collected 1,260 serum samples from 215 participants, 25 healthy donors, and 23 patients with relapsing-remitting multiple sclerosis (MS). Serum GFAP concentration was measured using a single-molecule array assay. The researchers and an independent adjudication committee evaluated attacks during the 28-week randomized controlled study period using predefined criteria.
The median serum GFAP concentration was higher in patients with NMOSD (128.3 pg/mL) than in patients with relapsing-remitting MS (97.5 pg/mL) and healthy controls (73.3 pg/mL). At baseline, 29% of patients with NMOSD and 9% of patients with MS had a serum GFAP concentration that was three or more standard deviations above the mean level in healthy donors.
During the study, patients with a high baseline concentration of serum GFAP were three times more likely to have an adjudicated NMOSD attack than patients with lower serum GFAP concentrations. Concentrations of serum GFAP increased within 1 week of an adjudicated attack during the randomized controlled period. Furthermore, serum GFAP concentration was significantly higher in patients with major adjudicated attacks, compared with those who had minor adjudicated attacks. This finding was true for all organ domains, including for attacks that affected only the optic nerve.
Compared with placebo, inebilizumab reduced the risk of an adjudicated attack by 79% in patients with a normal baseline serum GFAP concentration and by 61% in patients with an elevated baseline serum GFAP concentration. The increase in serum GFAP concentration following an adjudicated attack was significant in patients receiving placebo, but not in patients receiving inebilizumab. Seven samples taken during an adjudicated attack from patients receiving inebilizumab had serum GFAP concentrations within the normal range. One sample taken during an attack from a patient receiving placebo had a serum GFAP concentration within the normal range. In addition, serum GFAP concentrations decreased from baseline among patients receiving inebilizumab who did not have an adjudicated attack.
“These observations suggest that serum GFAP could be a clinically useful biomarker of disease activity and increased attack risk in NMOSD,” said Dr. Cree and colleagues.
Viela Bio, which is developing inebilizumab, and MedImmune sponsored the study. Dr. Cree has received compensation for consulting services that he provided to Alexion, Atara, Biogen, EMD Serono, Novartis, and TG Therapeutics.
SOURCE: Hartung H et al. ACTRIMS 2020, Abstract P205.
WEST PALM BEACH, FLA. – (NMOSD), according to research presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Treatment with inebilizumab decreases serum GFAP concentrations and reduces the risk of an NMOSD attack, the investigators said.
In NMOSD, autoantibodies often target aquaporin-4, a protein expressed on astrocytes. This immune response destroys astrocytes and increases levels of GFAP in cerebrospinal fluid and serum. In the N-MOmentum trial, inebilizumab reduced the risk of attacks by 73%, compared with placebo, in patients with NMOSD. Bruce Cree, MD, PhD, professor of neurology at the University of California, San Francisco, Weill Institute for Neurosciences and colleagues analyzed the data from this trial to examine the relationship between serum GFAP concentrations and disease activity.
In the study, the investigators prospectively collected 1,260 serum samples from 215 participants, 25 healthy donors, and 23 patients with relapsing-remitting multiple sclerosis (MS). Serum GFAP concentration was measured using a single-molecule array assay. The researchers and an independent adjudication committee evaluated attacks during the 28-week randomized controlled study period using predefined criteria.
The median serum GFAP concentration was higher in patients with NMOSD (128.3 pg/mL) than in patients with relapsing-remitting MS (97.5 pg/mL) and healthy controls (73.3 pg/mL). At baseline, 29% of patients with NMOSD and 9% of patients with MS had a serum GFAP concentration that was three or more standard deviations above the mean level in healthy donors.
During the study, patients with a high baseline concentration of serum GFAP were three times more likely to have an adjudicated NMOSD attack than patients with lower serum GFAP concentrations. Concentrations of serum GFAP increased within 1 week of an adjudicated attack during the randomized controlled period. Furthermore, serum GFAP concentration was significantly higher in patients with major adjudicated attacks, compared with those who had minor adjudicated attacks. This finding was true for all organ domains, including for attacks that affected only the optic nerve.
Compared with placebo, inebilizumab reduced the risk of an adjudicated attack by 79% in patients with a normal baseline serum GFAP concentration and by 61% in patients with an elevated baseline serum GFAP concentration. The increase in serum GFAP concentration following an adjudicated attack was significant in patients receiving placebo, but not in patients receiving inebilizumab. Seven samples taken during an adjudicated attack from patients receiving inebilizumab had serum GFAP concentrations within the normal range. One sample taken during an attack from a patient receiving placebo had a serum GFAP concentration within the normal range. In addition, serum GFAP concentrations decreased from baseline among patients receiving inebilizumab who did not have an adjudicated attack.
“These observations suggest that serum GFAP could be a clinically useful biomarker of disease activity and increased attack risk in NMOSD,” said Dr. Cree and colleagues.
Viela Bio, which is developing inebilizumab, and MedImmune sponsored the study. Dr. Cree has received compensation for consulting services that he provided to Alexion, Atara, Biogen, EMD Serono, Novartis, and TG Therapeutics.
SOURCE: Hartung H et al. ACTRIMS 2020, Abstract P205.
WEST PALM BEACH, FLA. – (NMOSD), according to research presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Treatment with inebilizumab decreases serum GFAP concentrations and reduces the risk of an NMOSD attack, the investigators said.
In NMOSD, autoantibodies often target aquaporin-4, a protein expressed on astrocytes. This immune response destroys astrocytes and increases levels of GFAP in cerebrospinal fluid and serum. In the N-MOmentum trial, inebilizumab reduced the risk of attacks by 73%, compared with placebo, in patients with NMOSD. Bruce Cree, MD, PhD, professor of neurology at the University of California, San Francisco, Weill Institute for Neurosciences and colleagues analyzed the data from this trial to examine the relationship between serum GFAP concentrations and disease activity.
In the study, the investigators prospectively collected 1,260 serum samples from 215 participants, 25 healthy donors, and 23 patients with relapsing-remitting multiple sclerosis (MS). Serum GFAP concentration was measured using a single-molecule array assay. The researchers and an independent adjudication committee evaluated attacks during the 28-week randomized controlled study period using predefined criteria.
The median serum GFAP concentration was higher in patients with NMOSD (128.3 pg/mL) than in patients with relapsing-remitting MS (97.5 pg/mL) and healthy controls (73.3 pg/mL). At baseline, 29% of patients with NMOSD and 9% of patients with MS had a serum GFAP concentration that was three or more standard deviations above the mean level in healthy donors.
During the study, patients with a high baseline concentration of serum GFAP were three times more likely to have an adjudicated NMOSD attack than patients with lower serum GFAP concentrations. Concentrations of serum GFAP increased within 1 week of an adjudicated attack during the randomized controlled period. Furthermore, serum GFAP concentration was significantly higher in patients with major adjudicated attacks, compared with those who had minor adjudicated attacks. This finding was true for all organ domains, including for attacks that affected only the optic nerve.
Compared with placebo, inebilizumab reduced the risk of an adjudicated attack by 79% in patients with a normal baseline serum GFAP concentration and by 61% in patients with an elevated baseline serum GFAP concentration. The increase in serum GFAP concentration following an adjudicated attack was significant in patients receiving placebo, but not in patients receiving inebilizumab. Seven samples taken during an adjudicated attack from patients receiving inebilizumab had serum GFAP concentrations within the normal range. One sample taken during an attack from a patient receiving placebo had a serum GFAP concentration within the normal range. In addition, serum GFAP concentrations decreased from baseline among patients receiving inebilizumab who did not have an adjudicated attack.
“These observations suggest that serum GFAP could be a clinically useful biomarker of disease activity and increased attack risk in NMOSD,” said Dr. Cree and colleagues.
Viela Bio, which is developing inebilizumab, and MedImmune sponsored the study. Dr. Cree has received compensation for consulting services that he provided to Alexion, Atara, Biogen, EMD Serono, Novartis, and TG Therapeutics.
SOURCE: Hartung H et al. ACTRIMS 2020, Abstract P205.
REPORTING FROM ACTRIMS FORUM 2020