User login
COVID-19 in the era of loneliness
The natural state of human beings is to live together and function as organized groups. The beginnings of communities have primeval origins; evolutionarily, societies that worked together were more productive, efficient and—probably most important—safer. Thousands of years of evolution have ingrained these behaviors as part of our genetic constitution and developmental process. Social integration and acceptance thus are an integral part of basic human behavior and provide a sense of protection, pleasure, and purpose in life.
Unfortunately, the social isolation necessary to address the coronavirus disease 2019 (COVID-19) pandemic is preventing this integration, and is likely to worsen what some have called an epidemic of loneliness. As mental health clinicians, we need to use technology to strengthen our patients’ social support systems.
Loneliness: A growing problem
Changes in society over the last few decades have led to increased isolation. In the last 50 years, there has been a rise in single-person households in the United States. This is most common in large cities, where the prevalence is approximately 40%.1 The average number of confidants or the size of an American’s social network reduced by more than one-third from 1985 to 2009.2 In a study published in 2018, the health service company Cigna used the UCLA Loneliness Scale to survey >20,000 American adults.3 Nearly half of respondents reported always feeling alone (46%) or left out (47%), and individuals age 18 to 22 were the loneliest age group and claimed to be in worse health than older age groups. Furthermore, the results suggested that people who felt lonelier were more likely to have poor sleep and be less physically active. Americans who lived with others were less likely to report feeling lonely, except for single parents living only with their children. The results also showed that people who engage in meaningful interactions with others had lower loneliness scores and perceived that they were in better overall health.3
Studies have consistently demonstrated a link between loneliness and health problems such as cardiovascular disease, substance use disorders (SUDs), and mood disorders. A 2010 meta-analysis of 148 prospective studies with 308,849 participants found that the influence of social relationships on the risk of mortality is comparable to well-established risk factors for mortality such as smoking and alcohol consumption.4 These findings were confirmed in a 2015 meta-analysis that included 70 studies with 3.4 million participants followed for an average of 7 years. 5
Loneliness has been identified as a social determinant of health and is considered by many to be epidemic in proportion in developed countries. According to a 2019 Business Insider survey, almost 20% of US health care leaders planned to address social isolation in the next 12 months.6
Increased vulnerability during COVID-19 isolation
The forced quarantines and social distancing imposed by the COVID-19 crisis are likely to further exacerbate the loneliness epidemic. Hopefully, this increased isolation will not last more than several months, and its effect on chronic medical illnesses will be minor. However, for patients with mental illness, this further isolation, in conjunction with rising societal anxiety and fear of the potentially devastating financial consequences, could worsen their illness, and might even lead to suicidal ideation or behavior.
Individuals with SUDs are particularly vulnerable to the social limitations required by COVID-19. While social isolation is essential to limit the spread of COVID-19, this restriction poses unique challenges for these patients because connection and social support are important aspects of achieving and maintaining sobriety.7
Continue to: A call to action
A call to action
As mental health clinicians, we need to proactively engage with our patients to develop a plan to strengthen their social support systems. This may mean suggesting that they stay in contact with their network of people via video conferencing or by using the phone. We need to identify high-risk patients and continue to provide treatment via telepsychiatry. This is especially necessary to prevent relapse among patients with SUDs or mood disorders, and to minimize the risk of suicide.
We are ethically required to provide an atmosphere of trust, safety, and social inclusion by using resources, such as telehealth, video conferencing, and other online tools, to ameliorate the short- and long-term impact of COVID-19 isolation. Providing avenues that are easily accessible, are supportive, and maintain standards of care are essential. These resources should be implemented as early as possible to avoid negative outcomes regarding both COVID-19 and mental health.
There is also a significant risk that once circumstances improve, there will be a surge in the number of patients seeking a higher level of mental health care. Our actions and preparedness today will define the trajectory of our patients’ mental health in the future, potentially for years to come. While presently we are forced to be reactive, hopefully what is borne out of this crisis will translate into proactive measures for future crises.
Let this brief commentary serve as a call to action. As society finds ways to work from home, mental health clinicians need to lead the charge to use these same technologies to increase our patients’ social interactions. If we do not find ways to address the mental health burden of the COVID-19 pandemic, who will? We are all part of the mental health community, and we need to continue to function as an organized group, as has been the natural state of human beings for thousands of years.
Bottom Line
The social isolation required to limit the spread of the coronavirus disease 2019 pandemic is likely to increase loneliness, particularly among vulnerable patients with mood disorders and/or substance use disorders. As mental health clinicians, we need to work to strengthen our patients’ social support systems using resources such as video conferencing and other technologies.
Related Resources
- Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238-249.
- Geriatric loneliness with Dr. Steven Wengel. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/geriatricloneliness-dr-steven-wengel. Published April 1, 2020.
1. Howe N. Millennials and the loneliness epidemic. Forbes. https://www.forbes.com/sites/neilhowe/2019/05/03/millennials-and-the-loneliness-epidemic/. Published May 3, 2019. Accessed April 10, 2020.
2. The Economist. All the lonely people: loneliness is a serious public-health problem. https://www.economist.com/international/2018/09/01/loneliness-is-a-serious-public-health-problem. Published September 1, 2018. Accessed April 10, 2020.
3. Cigna. New Cigna study reveals loneliness at epidemic levels in America. https://www.cigna.com/newsroom/news-releases/2018/new-cigna-study-reveals-loneliness-at-epidemic-levels-in-america. Published May 1, 2018. Accessed April 10, 2020.
4. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
5. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-237.
6. Finley D. How increased social distancing for the coronavirus could spur a loneliness epidemic. Business Insider. https://www.businessinsider.com/coronavirus-could-spur-loneliness-epidemic-2020-3. Published March 16, 2020. Accessed April 10, 2020.
7. Roy L. Addiction treatment facilities: are they prepared for the COVID-19 coronavirus outbreak? Forbes. https://www.forbes.com/sites/lipiroy/2020/03/16/addiction-treatment-facilities-are-they-prepared-for-covid-19/#555149b544ea. Published March 16, 2020. Accessed April 10, 2020.
The natural state of human beings is to live together and function as organized groups. The beginnings of communities have primeval origins; evolutionarily, societies that worked together were more productive, efficient and—probably most important—safer. Thousands of years of evolution have ingrained these behaviors as part of our genetic constitution and developmental process. Social integration and acceptance thus are an integral part of basic human behavior and provide a sense of protection, pleasure, and purpose in life.
Unfortunately, the social isolation necessary to address the coronavirus disease 2019 (COVID-19) pandemic is preventing this integration, and is likely to worsen what some have called an epidemic of loneliness. As mental health clinicians, we need to use technology to strengthen our patients’ social support systems.
Loneliness: A growing problem
Changes in society over the last few decades have led to increased isolation. In the last 50 years, there has been a rise in single-person households in the United States. This is most common in large cities, where the prevalence is approximately 40%.1 The average number of confidants or the size of an American’s social network reduced by more than one-third from 1985 to 2009.2 In a study published in 2018, the health service company Cigna used the UCLA Loneliness Scale to survey >20,000 American adults.3 Nearly half of respondents reported always feeling alone (46%) or left out (47%), and individuals age 18 to 22 were the loneliest age group and claimed to be in worse health than older age groups. Furthermore, the results suggested that people who felt lonelier were more likely to have poor sleep and be less physically active. Americans who lived with others were less likely to report feeling lonely, except for single parents living only with their children. The results also showed that people who engage in meaningful interactions with others had lower loneliness scores and perceived that they were in better overall health.3
Studies have consistently demonstrated a link between loneliness and health problems such as cardiovascular disease, substance use disorders (SUDs), and mood disorders. A 2010 meta-analysis of 148 prospective studies with 308,849 participants found that the influence of social relationships on the risk of mortality is comparable to well-established risk factors for mortality such as smoking and alcohol consumption.4 These findings were confirmed in a 2015 meta-analysis that included 70 studies with 3.4 million participants followed for an average of 7 years. 5
Loneliness has been identified as a social determinant of health and is considered by many to be epidemic in proportion in developed countries. According to a 2019 Business Insider survey, almost 20% of US health care leaders planned to address social isolation in the next 12 months.6
Increased vulnerability during COVID-19 isolation
The forced quarantines and social distancing imposed by the COVID-19 crisis are likely to further exacerbate the loneliness epidemic. Hopefully, this increased isolation will not last more than several months, and its effect on chronic medical illnesses will be minor. However, for patients with mental illness, this further isolation, in conjunction with rising societal anxiety and fear of the potentially devastating financial consequences, could worsen their illness, and might even lead to suicidal ideation or behavior.
Individuals with SUDs are particularly vulnerable to the social limitations required by COVID-19. While social isolation is essential to limit the spread of COVID-19, this restriction poses unique challenges for these patients because connection and social support are important aspects of achieving and maintaining sobriety.7
Continue to: A call to action
A call to action
As mental health clinicians, we need to proactively engage with our patients to develop a plan to strengthen their social support systems. This may mean suggesting that they stay in contact with their network of people via video conferencing or by using the phone. We need to identify high-risk patients and continue to provide treatment via telepsychiatry. This is especially necessary to prevent relapse among patients with SUDs or mood disorders, and to minimize the risk of suicide.
We are ethically required to provide an atmosphere of trust, safety, and social inclusion by using resources, such as telehealth, video conferencing, and other online tools, to ameliorate the short- and long-term impact of COVID-19 isolation. Providing avenues that are easily accessible, are supportive, and maintain standards of care are essential. These resources should be implemented as early as possible to avoid negative outcomes regarding both COVID-19 and mental health.
There is also a significant risk that once circumstances improve, there will be a surge in the number of patients seeking a higher level of mental health care. Our actions and preparedness today will define the trajectory of our patients’ mental health in the future, potentially for years to come. While presently we are forced to be reactive, hopefully what is borne out of this crisis will translate into proactive measures for future crises.
Let this brief commentary serve as a call to action. As society finds ways to work from home, mental health clinicians need to lead the charge to use these same technologies to increase our patients’ social interactions. If we do not find ways to address the mental health burden of the COVID-19 pandemic, who will? We are all part of the mental health community, and we need to continue to function as an organized group, as has been the natural state of human beings for thousands of years.
Bottom Line
The social isolation required to limit the spread of the coronavirus disease 2019 pandemic is likely to increase loneliness, particularly among vulnerable patients with mood disorders and/or substance use disorders. As mental health clinicians, we need to work to strengthen our patients’ social support systems using resources such as video conferencing and other technologies.
Related Resources
- Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238-249.
- Geriatric loneliness with Dr. Steven Wengel. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/geriatricloneliness-dr-steven-wengel. Published April 1, 2020.
The natural state of human beings is to live together and function as organized groups. The beginnings of communities have primeval origins; evolutionarily, societies that worked together were more productive, efficient and—probably most important—safer. Thousands of years of evolution have ingrained these behaviors as part of our genetic constitution and developmental process. Social integration and acceptance thus are an integral part of basic human behavior and provide a sense of protection, pleasure, and purpose in life.
Unfortunately, the social isolation necessary to address the coronavirus disease 2019 (COVID-19) pandemic is preventing this integration, and is likely to worsen what some have called an epidemic of loneliness. As mental health clinicians, we need to use technology to strengthen our patients’ social support systems.
Loneliness: A growing problem
Changes in society over the last few decades have led to increased isolation. In the last 50 years, there has been a rise in single-person households in the United States. This is most common in large cities, where the prevalence is approximately 40%.1 The average number of confidants or the size of an American’s social network reduced by more than one-third from 1985 to 2009.2 In a study published in 2018, the health service company Cigna used the UCLA Loneliness Scale to survey >20,000 American adults.3 Nearly half of respondents reported always feeling alone (46%) or left out (47%), and individuals age 18 to 22 were the loneliest age group and claimed to be in worse health than older age groups. Furthermore, the results suggested that people who felt lonelier were more likely to have poor sleep and be less physically active. Americans who lived with others were less likely to report feeling lonely, except for single parents living only with their children. The results also showed that people who engage in meaningful interactions with others had lower loneliness scores and perceived that they were in better overall health.3
Studies have consistently demonstrated a link between loneliness and health problems such as cardiovascular disease, substance use disorders (SUDs), and mood disorders. A 2010 meta-analysis of 148 prospective studies with 308,849 participants found that the influence of social relationships on the risk of mortality is comparable to well-established risk factors for mortality such as smoking and alcohol consumption.4 These findings were confirmed in a 2015 meta-analysis that included 70 studies with 3.4 million participants followed for an average of 7 years. 5
Loneliness has been identified as a social determinant of health and is considered by many to be epidemic in proportion in developed countries. According to a 2019 Business Insider survey, almost 20% of US health care leaders planned to address social isolation in the next 12 months.6
Increased vulnerability during COVID-19 isolation
The forced quarantines and social distancing imposed by the COVID-19 crisis are likely to further exacerbate the loneliness epidemic. Hopefully, this increased isolation will not last more than several months, and its effect on chronic medical illnesses will be minor. However, for patients with mental illness, this further isolation, in conjunction with rising societal anxiety and fear of the potentially devastating financial consequences, could worsen their illness, and might even lead to suicidal ideation or behavior.
Individuals with SUDs are particularly vulnerable to the social limitations required by COVID-19. While social isolation is essential to limit the spread of COVID-19, this restriction poses unique challenges for these patients because connection and social support are important aspects of achieving and maintaining sobriety.7
Continue to: A call to action
A call to action
As mental health clinicians, we need to proactively engage with our patients to develop a plan to strengthen their social support systems. This may mean suggesting that they stay in contact with their network of people via video conferencing or by using the phone. We need to identify high-risk patients and continue to provide treatment via telepsychiatry. This is especially necessary to prevent relapse among patients with SUDs or mood disorders, and to minimize the risk of suicide.
We are ethically required to provide an atmosphere of trust, safety, and social inclusion by using resources, such as telehealth, video conferencing, and other online tools, to ameliorate the short- and long-term impact of COVID-19 isolation. Providing avenues that are easily accessible, are supportive, and maintain standards of care are essential. These resources should be implemented as early as possible to avoid negative outcomes regarding both COVID-19 and mental health.
There is also a significant risk that once circumstances improve, there will be a surge in the number of patients seeking a higher level of mental health care. Our actions and preparedness today will define the trajectory of our patients’ mental health in the future, potentially for years to come. While presently we are forced to be reactive, hopefully what is borne out of this crisis will translate into proactive measures for future crises.
Let this brief commentary serve as a call to action. As society finds ways to work from home, mental health clinicians need to lead the charge to use these same technologies to increase our patients’ social interactions. If we do not find ways to address the mental health burden of the COVID-19 pandemic, who will? We are all part of the mental health community, and we need to continue to function as an organized group, as has been the natural state of human beings for thousands of years.
Bottom Line
The social isolation required to limit the spread of the coronavirus disease 2019 pandemic is likely to increase loneliness, particularly among vulnerable patients with mood disorders and/or substance use disorders. As mental health clinicians, we need to work to strengthen our patients’ social support systems using resources such as video conferencing and other technologies.
Related Resources
- Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238-249.
- Geriatric loneliness with Dr. Steven Wengel. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/geriatricloneliness-dr-steven-wengel. Published April 1, 2020.
1. Howe N. Millennials and the loneliness epidemic. Forbes. https://www.forbes.com/sites/neilhowe/2019/05/03/millennials-and-the-loneliness-epidemic/. Published May 3, 2019. Accessed April 10, 2020.
2. The Economist. All the lonely people: loneliness is a serious public-health problem. https://www.economist.com/international/2018/09/01/loneliness-is-a-serious-public-health-problem. Published September 1, 2018. Accessed April 10, 2020.
3. Cigna. New Cigna study reveals loneliness at epidemic levels in America. https://www.cigna.com/newsroom/news-releases/2018/new-cigna-study-reveals-loneliness-at-epidemic-levels-in-america. Published May 1, 2018. Accessed April 10, 2020.
4. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
5. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-237.
6. Finley D. How increased social distancing for the coronavirus could spur a loneliness epidemic. Business Insider. https://www.businessinsider.com/coronavirus-could-spur-loneliness-epidemic-2020-3. Published March 16, 2020. Accessed April 10, 2020.
7. Roy L. Addiction treatment facilities: are they prepared for the COVID-19 coronavirus outbreak? Forbes. https://www.forbes.com/sites/lipiroy/2020/03/16/addiction-treatment-facilities-are-they-prepared-for-covid-19/#555149b544ea. Published March 16, 2020. Accessed April 10, 2020.
1. Howe N. Millennials and the loneliness epidemic. Forbes. https://www.forbes.com/sites/neilhowe/2019/05/03/millennials-and-the-loneliness-epidemic/. Published May 3, 2019. Accessed April 10, 2020.
2. The Economist. All the lonely people: loneliness is a serious public-health problem. https://www.economist.com/international/2018/09/01/loneliness-is-a-serious-public-health-problem. Published September 1, 2018. Accessed April 10, 2020.
3. Cigna. New Cigna study reveals loneliness at epidemic levels in America. https://www.cigna.com/newsroom/news-releases/2018/new-cigna-study-reveals-loneliness-at-epidemic-levels-in-america. Published May 1, 2018. Accessed April 10, 2020.
4. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
5. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-237.
6. Finley D. How increased social distancing for the coronavirus could spur a loneliness epidemic. Business Insider. https://www.businessinsider.com/coronavirus-could-spur-loneliness-epidemic-2020-3. Published March 16, 2020. Accessed April 10, 2020.
7. Roy L. Addiction treatment facilities: are they prepared for the COVID-19 coronavirus outbreak? Forbes. https://www.forbes.com/sites/lipiroy/2020/03/16/addiction-treatment-facilities-are-they-prepared-for-covid-19/#555149b544ea. Published March 16, 2020. Accessed April 10, 2020.
COVID-19: A psychiatry resident’s perspective
During these unprecedented times, venturing into the unknown of the coronavirus disease 2019 (COVID-19) pandemic, a feeling of impending doom prevails. Almost all of us have been restricted to our homes. Although the physical dimensions of what we call home may vary, the meaning of this restriction is fairly universal. No matter how our sociodemographics differ, with no guidance for this situation from anything even remotely comparable in the past, our lives have been transformed into a work in progress.
During this pandemic, I have observed a wide range of human emotions and behavior—many of them familiar and predictable, some abysmal, and some inspiring.
’Why should I care?’
On December 31, 2019, health officials in China informed the World Health Organization about a pneumonia-like presentation in a group of people in Wuhan. On January 7, 2020, a novel coronavirus was identified as the cause, and the first death was reported a few days later. In the following days and weeks the disease rapidly spread, as did the growing sense that this was not a typical virus.
While these events occurred, the rest of the world was in what I call a ”Why should I care?” mode. Most humans tend to suffer from this indifference. This has been observed repeatedly through the years, such as when the Ebola outbreak occurred in Africa in 2014-2016. It was only when cases started to develop in Europe and the United States that other countries started to pay attention. A similar phenomenon has been observed every time we’ve faced a global outbreak (avian influenza, Middle East respiratory syndrome, etc.).
When are we going to learn? It is time to realize that global borders are more porous than we think, and human interactions cannot be blocked by any wall. When a catastrophic event, outbreak, or disaster starts in any part of the world, it is naive to assume that we will not be affected. We will eventually be affected—the only question is how, when, and to what extent? We are always all in this together.
An abundance of ignorance and stupidity
Within a few weeks of the first reports from China, cases of COVID-19 were reported in South Korea, Italy, Spain, Germany, and many other countries. Slowly, COVID-19 reached the United States, which as of mid-April had the highest number of cases worldwide. When COVID-19 hit the United States, the response was that of shock and anger. How could this happen to us? Why is the government not doing anything?
Amidst this pandemonium, ignorance and stupidity of the highest degree were commonplace. This was not restricted to any particular country or region. Almost 2 months into the pandemic, the Ministry of Tourism in my home country of Nepal declared Nepal a ”coronavirus-free zone” and took measures to bring in tourists, focusing specifically on China, where COVID-19 had already killed hundreds. In India, some people were drinking cow urine in hopes of warding off the virus. In the United Sates, thousands of young people flocked to beaches for Spring Break, disregarding measures for social distancing. ”If I get corona, I get corona,” one young man said in an interview that went viral. Personally, I have encountered people who responded to this pandemic by saying the disease was ”cooties” or ”just a flu,” and dismissing it with ”If I die from this, I die.”
Continue to: Rising panic and fear
Rising panic and fear
For most people, seeing COVID-19 at their doorstep triggered a panic, and sent many into a frenzy of buying and hoarding. Once again, we proved that people everywhere are equally stupid, as toilet paper began to vanish from stores across the globe. And yet, this again was a moment when some people began to experience a false sense of immunity: ”I have enough food, money, and toilet paper to last me for 2 years. Why should I be worried?”
When the numbers of COVID-19 deaths in Europe were first reported, the fear became palpable. In Italy and Spain, towns were locked down, and tens of thousands of people (mostly older adults) have died. It was truly heartbreaking to see people alone and at their weakest with no family members allowed to be by their side.
A glimmer of hope
Despite all of this, there were superheroes—the nurses, physicians, allied health professionals, first responders, store workers, restaurant workers, delivery personnel, and others who didn’t have the option of staying home, or who volunteered to help people in need. In moments like this, the actions of these individuals give us hope, reminding us that the human spirit is resilient, and that we will get through this.
A rotation in the emergency department during COVID-19
As a psychiatry resident, it is unlikely that my peers and I face the same risks as our colleagues in other medical specialities. But those of us who happened to be in medical rotations during this time have had the chance to experience this very closely. My personal experience, albeit a brief one, of working in an emergency department with suspected COVID-19 patients has been sobering. Watching nurses and physicians walk into a room wearing personal protective equipment, fearful inside but with a reassuring smile for a scared patient, definitely was one of the most compelling moments of my life. Living in a distant land, with my daughter, wife, parents, and extended family back home in Nepal, has made this even more challenging.
We will overcome this as we have overcome previous challenges in the past. There will be death and chaos, but we will prevail. The only thing is to ask ourselves: How do we want to continue living when this is over?
During these unprecedented times, venturing into the unknown of the coronavirus disease 2019 (COVID-19) pandemic, a feeling of impending doom prevails. Almost all of us have been restricted to our homes. Although the physical dimensions of what we call home may vary, the meaning of this restriction is fairly universal. No matter how our sociodemographics differ, with no guidance for this situation from anything even remotely comparable in the past, our lives have been transformed into a work in progress.
During this pandemic, I have observed a wide range of human emotions and behavior—many of them familiar and predictable, some abysmal, and some inspiring.
’Why should I care?’
On December 31, 2019, health officials in China informed the World Health Organization about a pneumonia-like presentation in a group of people in Wuhan. On January 7, 2020, a novel coronavirus was identified as the cause, and the first death was reported a few days later. In the following days and weeks the disease rapidly spread, as did the growing sense that this was not a typical virus.
While these events occurred, the rest of the world was in what I call a ”Why should I care?” mode. Most humans tend to suffer from this indifference. This has been observed repeatedly through the years, such as when the Ebola outbreak occurred in Africa in 2014-2016. It was only when cases started to develop in Europe and the United States that other countries started to pay attention. A similar phenomenon has been observed every time we’ve faced a global outbreak (avian influenza, Middle East respiratory syndrome, etc.).
When are we going to learn? It is time to realize that global borders are more porous than we think, and human interactions cannot be blocked by any wall. When a catastrophic event, outbreak, or disaster starts in any part of the world, it is naive to assume that we will not be affected. We will eventually be affected—the only question is how, when, and to what extent? We are always all in this together.
An abundance of ignorance and stupidity
Within a few weeks of the first reports from China, cases of COVID-19 were reported in South Korea, Italy, Spain, Germany, and many other countries. Slowly, COVID-19 reached the United States, which as of mid-April had the highest number of cases worldwide. When COVID-19 hit the United States, the response was that of shock and anger. How could this happen to us? Why is the government not doing anything?
Amidst this pandemonium, ignorance and stupidity of the highest degree were commonplace. This was not restricted to any particular country or region. Almost 2 months into the pandemic, the Ministry of Tourism in my home country of Nepal declared Nepal a ”coronavirus-free zone” and took measures to bring in tourists, focusing specifically on China, where COVID-19 had already killed hundreds. In India, some people were drinking cow urine in hopes of warding off the virus. In the United Sates, thousands of young people flocked to beaches for Spring Break, disregarding measures for social distancing. ”If I get corona, I get corona,” one young man said in an interview that went viral. Personally, I have encountered people who responded to this pandemic by saying the disease was ”cooties” or ”just a flu,” and dismissing it with ”If I die from this, I die.”
Continue to: Rising panic and fear
Rising panic and fear
For most people, seeing COVID-19 at their doorstep triggered a panic, and sent many into a frenzy of buying and hoarding. Once again, we proved that people everywhere are equally stupid, as toilet paper began to vanish from stores across the globe. And yet, this again was a moment when some people began to experience a false sense of immunity: ”I have enough food, money, and toilet paper to last me for 2 years. Why should I be worried?”
When the numbers of COVID-19 deaths in Europe were first reported, the fear became palpable. In Italy and Spain, towns were locked down, and tens of thousands of people (mostly older adults) have died. It was truly heartbreaking to see people alone and at their weakest with no family members allowed to be by their side.
A glimmer of hope
Despite all of this, there were superheroes—the nurses, physicians, allied health professionals, first responders, store workers, restaurant workers, delivery personnel, and others who didn’t have the option of staying home, or who volunteered to help people in need. In moments like this, the actions of these individuals give us hope, reminding us that the human spirit is resilient, and that we will get through this.
A rotation in the emergency department during COVID-19
As a psychiatry resident, it is unlikely that my peers and I face the same risks as our colleagues in other medical specialities. But those of us who happened to be in medical rotations during this time have had the chance to experience this very closely. My personal experience, albeit a brief one, of working in an emergency department with suspected COVID-19 patients has been sobering. Watching nurses and physicians walk into a room wearing personal protective equipment, fearful inside but with a reassuring smile for a scared patient, definitely was one of the most compelling moments of my life. Living in a distant land, with my daughter, wife, parents, and extended family back home in Nepal, has made this even more challenging.
We will overcome this as we have overcome previous challenges in the past. There will be death and chaos, but we will prevail. The only thing is to ask ourselves: How do we want to continue living when this is over?
During these unprecedented times, venturing into the unknown of the coronavirus disease 2019 (COVID-19) pandemic, a feeling of impending doom prevails. Almost all of us have been restricted to our homes. Although the physical dimensions of what we call home may vary, the meaning of this restriction is fairly universal. No matter how our sociodemographics differ, with no guidance for this situation from anything even remotely comparable in the past, our lives have been transformed into a work in progress.
During this pandemic, I have observed a wide range of human emotions and behavior—many of them familiar and predictable, some abysmal, and some inspiring.
’Why should I care?’
On December 31, 2019, health officials in China informed the World Health Organization about a pneumonia-like presentation in a group of people in Wuhan. On January 7, 2020, a novel coronavirus was identified as the cause, and the first death was reported a few days later. In the following days and weeks the disease rapidly spread, as did the growing sense that this was not a typical virus.
While these events occurred, the rest of the world was in what I call a ”Why should I care?” mode. Most humans tend to suffer from this indifference. This has been observed repeatedly through the years, such as when the Ebola outbreak occurred in Africa in 2014-2016. It was only when cases started to develop in Europe and the United States that other countries started to pay attention. A similar phenomenon has been observed every time we’ve faced a global outbreak (avian influenza, Middle East respiratory syndrome, etc.).
When are we going to learn? It is time to realize that global borders are more porous than we think, and human interactions cannot be blocked by any wall. When a catastrophic event, outbreak, or disaster starts in any part of the world, it is naive to assume that we will not be affected. We will eventually be affected—the only question is how, when, and to what extent? We are always all in this together.
An abundance of ignorance and stupidity
Within a few weeks of the first reports from China, cases of COVID-19 were reported in South Korea, Italy, Spain, Germany, and many other countries. Slowly, COVID-19 reached the United States, which as of mid-April had the highest number of cases worldwide. When COVID-19 hit the United States, the response was that of shock and anger. How could this happen to us? Why is the government not doing anything?
Amidst this pandemonium, ignorance and stupidity of the highest degree were commonplace. This was not restricted to any particular country or region. Almost 2 months into the pandemic, the Ministry of Tourism in my home country of Nepal declared Nepal a ”coronavirus-free zone” and took measures to bring in tourists, focusing specifically on China, where COVID-19 had already killed hundreds. In India, some people were drinking cow urine in hopes of warding off the virus. In the United Sates, thousands of young people flocked to beaches for Spring Break, disregarding measures for social distancing. ”If I get corona, I get corona,” one young man said in an interview that went viral. Personally, I have encountered people who responded to this pandemic by saying the disease was ”cooties” or ”just a flu,” and dismissing it with ”If I die from this, I die.”
Continue to: Rising panic and fear
Rising panic and fear
For most people, seeing COVID-19 at their doorstep triggered a panic, and sent many into a frenzy of buying and hoarding. Once again, we proved that people everywhere are equally stupid, as toilet paper began to vanish from stores across the globe. And yet, this again was a moment when some people began to experience a false sense of immunity: ”I have enough food, money, and toilet paper to last me for 2 years. Why should I be worried?”
When the numbers of COVID-19 deaths in Europe were first reported, the fear became palpable. In Italy and Spain, towns were locked down, and tens of thousands of people (mostly older adults) have died. It was truly heartbreaking to see people alone and at their weakest with no family members allowed to be by their side.
A glimmer of hope
Despite all of this, there were superheroes—the nurses, physicians, allied health professionals, first responders, store workers, restaurant workers, delivery personnel, and others who didn’t have the option of staying home, or who volunteered to help people in need. In moments like this, the actions of these individuals give us hope, reminding us that the human spirit is resilient, and that we will get through this.
A rotation in the emergency department during COVID-19
As a psychiatry resident, it is unlikely that my peers and I face the same risks as our colleagues in other medical specialities. But those of us who happened to be in medical rotations during this time have had the chance to experience this very closely. My personal experience, albeit a brief one, of working in an emergency department with suspected COVID-19 patients has been sobering. Watching nurses and physicians walk into a room wearing personal protective equipment, fearful inside but with a reassuring smile for a scared patient, definitely was one of the most compelling moments of my life. Living in a distant land, with my daughter, wife, parents, and extended family back home in Nepal, has made this even more challenging.
We will overcome this as we have overcome previous challenges in the past. There will be death and chaos, but we will prevail. The only thing is to ask ourselves: How do we want to continue living when this is over?
Screening for adolescent substance use; Changing routines during COVID-19
Screening for adolescent substance use
I want to congratulate Dr. Verma on her article “Opioid use disorder in adolescents: An overview” (Evidence-Based Reviews,
Because evidence suggests there are continued barriers, such as time constraints, in evaluating for adolescent SUD,1,2 I believe the Screen to Brief Intervention (S2BI) and Brief Screener for Tobacco, Alcohol and Drug (BSTAD) should be included.3,4 The S2BI and BSTAD are brief screeners that assess substance use, are validated for adolescent patients, can be completed online, and can assist in identifying DSM-5 criteria for SUD.
The S2BI has demonstrated high sensitivity and specificity for identifying SUD.3 The single screening assessment for “past-year use” is quick and can be administered in a variety of clinical settings. The S2BI begins by asking a patient about his/her frequency of tobacco, alcohol, and/or marijuana use in the past year. If the patient endorses past-year use of any of these substances, the S2BI prompts follow-up questions about the use of prescription medications, illicit drugs, inhalants, and herbal products. A patient’s frequency of use is strongly correlated with the likelihood of having a SUD. Adolescents who report using a substance “once or twice” in the past year are very unlikely to have a SUD. Patients who endorse “monthly” use are more likely to meet the criteria for a mild or moderate SUD, and those reporting “weekly or more” use are more likely to have a severe SUD.
The BSTAD is an electronic, validated, high-sensitivity, high-specificity instrument for identifying SUD.1 It asks a single frequency question about past-year use of tobacco, alcohol, and marijuana, which are the most commonly used substances among adolescents. Patients who report using any of these substances are then asked about additional substance use. Based on the patient’s self-report of past year use, the screen places him/her into 1 of 3 risk categories for SUD: no reported use, lower risk, and higher risk. Each risk level maps to suggested clinical actions that are summarized in the results section.
Kevin M. Simon, MD
Child & Adolescent Psychiatry Fellow
Boston Children’s Hospital
Clinical Fellow in Psychiatry
Harvard Medical School
Boston, Massachusetts
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70(5):409-412.
2. D’Souza-Li L, Harris SK. The future of screening, brief intervention and referral to treatment in adolescent primary care: research directions and dissemination challenges. Curr Opin Pediatr. 2016;28(4):434-440.
3. Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr. 2014;168(9):822-828.
4. Kelly SM, Gryczynski J, Mitchell SG, et al. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819-826.
Continue to: The author responds
The author responds
I thank Dr. Simon for his words of encouragement. I agree that both the S2BI and BSTAD have high sensitivity and specificity and are easy to use for screening for the use of multiple substances. Once substance use is established, both tools recommend administering high-risk assessment with additional scales such as the CRAFFT. During the initial evaluation, many psychiatrists take their patient’s history of substance use in detail, including age of onset, frequency, amount used, severity, and the time of his/her last use, without using a screening instrument. My article focused on instruments that can determine whether there is need for a further detailed evaluation. I agree that the S2BI and BSTAD would assist psychiatrists or physicians in other specialties (eg, pediatrics, family medicine) who might not take a complete substance use history during their initial evaluations.
Shikha Verma, MD
Rogers Behavioral Health
Kenosha, Wisconsin
Assistant Professor
Department of Psychiatry and Behavioral Health
Rosalind Franklin University of Medicine and Science
North Chicago, Illinois
Continue to: Changes as a result of COVID-19
Changes as a result of COVID-19
I thank Dr. Nasrallah for his editorial “During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19” (From the Editor,
I appreciated the editorial because it got me thinking about how the pandemic has changed me and my family:
1. We are engaging more in social media.
2. I feel uncomfortable when I go to the grocery store.
3. I feel better when I don’t access the news about COVID-19.
4. My children need physical socialization with their friends (sports, games, other activities, etc.).
5. My children function better with a schedule, but we find it difficult to keep them on a good schedule. Our teenagers stay up late at night (because all of their friends do), and they sleep in late the next morning.
Here are some positive changes:
1. Creating a weekly family calendar on a dry-erase board, so the family can see what is going on during the week.
2. Creating responsibility for our older children (eg, washing their own clothes, cleaning their bathroom).
3. Eating most meals as a family and organizing meals better, too.
4. Playing games together.
5. Cleaning the house together.
6. Getting outside to walk the dog and appreciate nature more.
7. Exercising.
8. Utilizing positive social media.
9. Getting caught up on life.
Again, I thank Dr. Nasrallah for writing this editorial because it led me to self-reflect on this situation, and helped me feel normal.
Doug Dolenc
Westfield, Indiana
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Screening for adolescent substance use
I want to congratulate Dr. Verma on her article “Opioid use disorder in adolescents: An overview” (Evidence-Based Reviews,
Because evidence suggests there are continued barriers, such as time constraints, in evaluating for adolescent SUD,1,2 I believe the Screen to Brief Intervention (S2BI) and Brief Screener for Tobacco, Alcohol and Drug (BSTAD) should be included.3,4 The S2BI and BSTAD are brief screeners that assess substance use, are validated for adolescent patients, can be completed online, and can assist in identifying DSM-5 criteria for SUD.
The S2BI has demonstrated high sensitivity and specificity for identifying SUD.3 The single screening assessment for “past-year use” is quick and can be administered in a variety of clinical settings. The S2BI begins by asking a patient about his/her frequency of tobacco, alcohol, and/or marijuana use in the past year. If the patient endorses past-year use of any of these substances, the S2BI prompts follow-up questions about the use of prescription medications, illicit drugs, inhalants, and herbal products. A patient’s frequency of use is strongly correlated with the likelihood of having a SUD. Adolescents who report using a substance “once or twice” in the past year are very unlikely to have a SUD. Patients who endorse “monthly” use are more likely to meet the criteria for a mild or moderate SUD, and those reporting “weekly or more” use are more likely to have a severe SUD.
The BSTAD is an electronic, validated, high-sensitivity, high-specificity instrument for identifying SUD.1 It asks a single frequency question about past-year use of tobacco, alcohol, and marijuana, which are the most commonly used substances among adolescents. Patients who report using any of these substances are then asked about additional substance use. Based on the patient’s self-report of past year use, the screen places him/her into 1 of 3 risk categories for SUD: no reported use, lower risk, and higher risk. Each risk level maps to suggested clinical actions that are summarized in the results section.
Kevin M. Simon, MD
Child & Adolescent Psychiatry Fellow
Boston Children’s Hospital
Clinical Fellow in Psychiatry
Harvard Medical School
Boston, Massachusetts
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70(5):409-412.
2. D’Souza-Li L, Harris SK. The future of screening, brief intervention and referral to treatment in adolescent primary care: research directions and dissemination challenges. Curr Opin Pediatr. 2016;28(4):434-440.
3. Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr. 2014;168(9):822-828.
4. Kelly SM, Gryczynski J, Mitchell SG, et al. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819-826.
Continue to: The author responds
The author responds
I thank Dr. Simon for his words of encouragement. I agree that both the S2BI and BSTAD have high sensitivity and specificity and are easy to use for screening for the use of multiple substances. Once substance use is established, both tools recommend administering high-risk assessment with additional scales such as the CRAFFT. During the initial evaluation, many psychiatrists take their patient’s history of substance use in detail, including age of onset, frequency, amount used, severity, and the time of his/her last use, without using a screening instrument. My article focused on instruments that can determine whether there is need for a further detailed evaluation. I agree that the S2BI and BSTAD would assist psychiatrists or physicians in other specialties (eg, pediatrics, family medicine) who might not take a complete substance use history during their initial evaluations.
Shikha Verma, MD
Rogers Behavioral Health
Kenosha, Wisconsin
Assistant Professor
Department of Psychiatry and Behavioral Health
Rosalind Franklin University of Medicine and Science
North Chicago, Illinois
Continue to: Changes as a result of COVID-19
Changes as a result of COVID-19
I thank Dr. Nasrallah for his editorial “During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19” (From the Editor,
I appreciated the editorial because it got me thinking about how the pandemic has changed me and my family:
1. We are engaging more in social media.
2. I feel uncomfortable when I go to the grocery store.
3. I feel better when I don’t access the news about COVID-19.
4. My children need physical socialization with their friends (sports, games, other activities, etc.).
5. My children function better with a schedule, but we find it difficult to keep them on a good schedule. Our teenagers stay up late at night (because all of their friends do), and they sleep in late the next morning.
Here are some positive changes:
1. Creating a weekly family calendar on a dry-erase board, so the family can see what is going on during the week.
2. Creating responsibility for our older children (eg, washing their own clothes, cleaning their bathroom).
3. Eating most meals as a family and organizing meals better, too.
4. Playing games together.
5. Cleaning the house together.
6. Getting outside to walk the dog and appreciate nature more.
7. Exercising.
8. Utilizing positive social media.
9. Getting caught up on life.
Again, I thank Dr. Nasrallah for writing this editorial because it led me to self-reflect on this situation, and helped me feel normal.
Doug Dolenc
Westfield, Indiana
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Screening for adolescent substance use
I want to congratulate Dr. Verma on her article “Opioid use disorder in adolescents: An overview” (Evidence-Based Reviews,
Because evidence suggests there are continued barriers, such as time constraints, in evaluating for adolescent SUD,1,2 I believe the Screen to Brief Intervention (S2BI) and Brief Screener for Tobacco, Alcohol and Drug (BSTAD) should be included.3,4 The S2BI and BSTAD are brief screeners that assess substance use, are validated for adolescent patients, can be completed online, and can assist in identifying DSM-5 criteria for SUD.
The S2BI has demonstrated high sensitivity and specificity for identifying SUD.3 The single screening assessment for “past-year use” is quick and can be administered in a variety of clinical settings. The S2BI begins by asking a patient about his/her frequency of tobacco, alcohol, and/or marijuana use in the past year. If the patient endorses past-year use of any of these substances, the S2BI prompts follow-up questions about the use of prescription medications, illicit drugs, inhalants, and herbal products. A patient’s frequency of use is strongly correlated with the likelihood of having a SUD. Adolescents who report using a substance “once or twice” in the past year are very unlikely to have a SUD. Patients who endorse “monthly” use are more likely to meet the criteria for a mild or moderate SUD, and those reporting “weekly or more” use are more likely to have a severe SUD.
The BSTAD is an electronic, validated, high-sensitivity, high-specificity instrument for identifying SUD.1 It asks a single frequency question about past-year use of tobacco, alcohol, and marijuana, which are the most commonly used substances among adolescents. Patients who report using any of these substances are then asked about additional substance use. Based on the patient’s self-report of past year use, the screen places him/her into 1 of 3 risk categories for SUD: no reported use, lower risk, and higher risk. Each risk level maps to suggested clinical actions that are summarized in the results section.
Kevin M. Simon, MD
Child & Adolescent Psychiatry Fellow
Boston Children’s Hospital
Clinical Fellow in Psychiatry
Harvard Medical School
Boston, Massachusetts
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70(5):409-412.
2. D’Souza-Li L, Harris SK. The future of screening, brief intervention and referral to treatment in adolescent primary care: research directions and dissemination challenges. Curr Opin Pediatr. 2016;28(4):434-440.
3. Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr. 2014;168(9):822-828.
4. Kelly SM, Gryczynski J, Mitchell SG, et al. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819-826.
Continue to: The author responds
The author responds
I thank Dr. Simon for his words of encouragement. I agree that both the S2BI and BSTAD have high sensitivity and specificity and are easy to use for screening for the use of multiple substances. Once substance use is established, both tools recommend administering high-risk assessment with additional scales such as the CRAFFT. During the initial evaluation, many psychiatrists take their patient’s history of substance use in detail, including age of onset, frequency, amount used, severity, and the time of his/her last use, without using a screening instrument. My article focused on instruments that can determine whether there is need for a further detailed evaluation. I agree that the S2BI and BSTAD would assist psychiatrists or physicians in other specialties (eg, pediatrics, family medicine) who might not take a complete substance use history during their initial evaluations.
Shikha Verma, MD
Rogers Behavioral Health
Kenosha, Wisconsin
Assistant Professor
Department of Psychiatry and Behavioral Health
Rosalind Franklin University of Medicine and Science
North Chicago, Illinois
Continue to: Changes as a result of COVID-19
Changes as a result of COVID-19
I thank Dr. Nasrallah for his editorial “During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19” (From the Editor,
I appreciated the editorial because it got me thinking about how the pandemic has changed me and my family:
1. We are engaging more in social media.
2. I feel uncomfortable when I go to the grocery store.
3. I feel better when I don’t access the news about COVID-19.
4. My children need physical socialization with their friends (sports, games, other activities, etc.).
5. My children function better with a schedule, but we find it difficult to keep them on a good schedule. Our teenagers stay up late at night (because all of their friends do), and they sleep in late the next morning.
Here are some positive changes:
1. Creating a weekly family calendar on a dry-erase board, so the family can see what is going on during the week.
2. Creating responsibility for our older children (eg, washing their own clothes, cleaning their bathroom).
3. Eating most meals as a family and organizing meals better, too.
4. Playing games together.
5. Cleaning the house together.
6. Getting outside to walk the dog and appreciate nature more.
7. Exercising.
8. Utilizing positive social media.
9. Getting caught up on life.
Again, I thank Dr. Nasrallah for writing this editorial because it led me to self-reflect on this situation, and helped me feel normal.
Doug Dolenc
Westfield, Indiana
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Love in the time of coronavirus
Several months ago, I sat with a woman just a few days after the emergent Cesarean section delivery of her first child. She cried as she told me about her entire life—childhood trauma, a pattern of difficult relationships, several miscarriages, and now, finally, a baby—delivered under circumstances so scary, all she remembered was overwhelming fear. Now, she had returned to the hospital with severe postpartum depression, layered with struggles that are common during the first days with a newborn—little sleep, loss of autonomy, guilt, and loneliness. It was hard to listen to it all, but I encouraged her to express her pain, believing that burdens are lighter when shared.
Words often fail us in times of desperation. Much of my education has involved borrowing words, phrases, or ideas from my experienced attendings and mentors, applying them like a salve when I don’t know what else to say. Sitting with another person in silence is often powerful enough, but when something needs to be said, I fall back on these inherited ideas. One of the mantras I often use, and what I said to my patient that day, is about hope: “When you’re down in this depression, you feel hopeless, and you can’t see the hope. It doesn’t mean there isn’t hope; just that you can’t see it.” I’ve watched that idea take root in patients who—despite their own beliefs in the moment—do get better, thus proving the point. Another favorite phrase: “With any luck at all, tomorrow will be better than today.” When you talk to someone on the worst day of their life, what else is there to say?
Today, my conversation with that woman seems like an eternity ago. Public discourse has been overtaken by coronavirus disease 2019 (COVID-19)—the journalism, reflections on the journalism, medical advice, debate about the medical advice, and the innumerable ways in which this worldwide strife has created pain: celebrations and long-awaited plans cancelled, weddings and funerals put on hold, isolation, loneliness, death, and, of course, the fear of death. Those feelings and any other permutations are valid; another phrase, “It’s OK to feel what you are feeling,” carries weight for me these days. I work in a hospital, so I add to the list the breathless fears about what’s going to happen in our local environment. The chronic uncertainty was wearing us thin even before we had begun to do here in Ohio what was already being done elsewhere: working extra shifts, intubating new patients, praying we don’t get sick ourselves.
Our work during COVID-19
Amidst this, my colleagues and I continue our work as psychiatrists, sitting with humans experiencing complex grief (a man whose wife died alone in a nursing home, because of visitor restrictions), confusion (delirium resulting from respiratory failure), and even psychosis (inability to access stabilizing medications coupled with crippling paranoia). These remain just as real and debilitating in a pandemic as they do in other times. In addition to pre-existing mental illnesses, for some individuals, the shared anxiety will progress to clinically significant disorders that may last even longer than the effects of the virus. The resulting complex symptoms could affect everything from home lives to interpersonal relationships to our local and global economies. These are not minor issues. Although often triaged aside in a disaster, our collective mental health remains in some ways more central than ever.
Modern psychiatry would not often use the word “love,” but that’s what I am trying to do—show love to the people who need it the most right now (which is all of us, really). This love takes strange shapes, and sometimes new forms, but it’s just about all I have to give. Like everyone else, I don’t have concrete answers for the grief and fear and panic. But I’m content to share the burden of pain, believing that burdens are lighter when shared. And I have a few words that, however little comfort they offer in the moment, are eventually proven true: Just because you can’t see the hope doesn’t mean it isn’t there. It’s OK to feel what you are feeling. With any luck at all, tomorrow will be better than today.
Several months ago, I sat with a woman just a few days after the emergent Cesarean section delivery of her first child. She cried as she told me about her entire life—childhood trauma, a pattern of difficult relationships, several miscarriages, and now, finally, a baby—delivered under circumstances so scary, all she remembered was overwhelming fear. Now, she had returned to the hospital with severe postpartum depression, layered with struggles that are common during the first days with a newborn—little sleep, loss of autonomy, guilt, and loneliness. It was hard to listen to it all, but I encouraged her to express her pain, believing that burdens are lighter when shared.
Words often fail us in times of desperation. Much of my education has involved borrowing words, phrases, or ideas from my experienced attendings and mentors, applying them like a salve when I don’t know what else to say. Sitting with another person in silence is often powerful enough, but when something needs to be said, I fall back on these inherited ideas. One of the mantras I often use, and what I said to my patient that day, is about hope: “When you’re down in this depression, you feel hopeless, and you can’t see the hope. It doesn’t mean there isn’t hope; just that you can’t see it.” I’ve watched that idea take root in patients who—despite their own beliefs in the moment—do get better, thus proving the point. Another favorite phrase: “With any luck at all, tomorrow will be better than today.” When you talk to someone on the worst day of their life, what else is there to say?
Today, my conversation with that woman seems like an eternity ago. Public discourse has been overtaken by coronavirus disease 2019 (COVID-19)—the journalism, reflections on the journalism, medical advice, debate about the medical advice, and the innumerable ways in which this worldwide strife has created pain: celebrations and long-awaited plans cancelled, weddings and funerals put on hold, isolation, loneliness, death, and, of course, the fear of death. Those feelings and any other permutations are valid; another phrase, “It’s OK to feel what you are feeling,” carries weight for me these days. I work in a hospital, so I add to the list the breathless fears about what’s going to happen in our local environment. The chronic uncertainty was wearing us thin even before we had begun to do here in Ohio what was already being done elsewhere: working extra shifts, intubating new patients, praying we don’t get sick ourselves.
Our work during COVID-19
Amidst this, my colleagues and I continue our work as psychiatrists, sitting with humans experiencing complex grief (a man whose wife died alone in a nursing home, because of visitor restrictions), confusion (delirium resulting from respiratory failure), and even psychosis (inability to access stabilizing medications coupled with crippling paranoia). These remain just as real and debilitating in a pandemic as they do in other times. In addition to pre-existing mental illnesses, for some individuals, the shared anxiety will progress to clinically significant disorders that may last even longer than the effects of the virus. The resulting complex symptoms could affect everything from home lives to interpersonal relationships to our local and global economies. These are not minor issues. Although often triaged aside in a disaster, our collective mental health remains in some ways more central than ever.
Modern psychiatry would not often use the word “love,” but that’s what I am trying to do—show love to the people who need it the most right now (which is all of us, really). This love takes strange shapes, and sometimes new forms, but it’s just about all I have to give. Like everyone else, I don’t have concrete answers for the grief and fear and panic. But I’m content to share the burden of pain, believing that burdens are lighter when shared. And I have a few words that, however little comfort they offer in the moment, are eventually proven true: Just because you can’t see the hope doesn’t mean it isn’t there. It’s OK to feel what you are feeling. With any luck at all, tomorrow will be better than today.
Several months ago, I sat with a woman just a few days after the emergent Cesarean section delivery of her first child. She cried as she told me about her entire life—childhood trauma, a pattern of difficult relationships, several miscarriages, and now, finally, a baby—delivered under circumstances so scary, all she remembered was overwhelming fear. Now, she had returned to the hospital with severe postpartum depression, layered with struggles that are common during the first days with a newborn—little sleep, loss of autonomy, guilt, and loneliness. It was hard to listen to it all, but I encouraged her to express her pain, believing that burdens are lighter when shared.
Words often fail us in times of desperation. Much of my education has involved borrowing words, phrases, or ideas from my experienced attendings and mentors, applying them like a salve when I don’t know what else to say. Sitting with another person in silence is often powerful enough, but when something needs to be said, I fall back on these inherited ideas. One of the mantras I often use, and what I said to my patient that day, is about hope: “When you’re down in this depression, you feel hopeless, and you can’t see the hope. It doesn’t mean there isn’t hope; just that you can’t see it.” I’ve watched that idea take root in patients who—despite their own beliefs in the moment—do get better, thus proving the point. Another favorite phrase: “With any luck at all, tomorrow will be better than today.” When you talk to someone on the worst day of their life, what else is there to say?
Today, my conversation with that woman seems like an eternity ago. Public discourse has been overtaken by coronavirus disease 2019 (COVID-19)—the journalism, reflections on the journalism, medical advice, debate about the medical advice, and the innumerable ways in which this worldwide strife has created pain: celebrations and long-awaited plans cancelled, weddings and funerals put on hold, isolation, loneliness, death, and, of course, the fear of death. Those feelings and any other permutations are valid; another phrase, “It’s OK to feel what you are feeling,” carries weight for me these days. I work in a hospital, so I add to the list the breathless fears about what’s going to happen in our local environment. The chronic uncertainty was wearing us thin even before we had begun to do here in Ohio what was already being done elsewhere: working extra shifts, intubating new patients, praying we don’t get sick ourselves.
Our work during COVID-19
Amidst this, my colleagues and I continue our work as psychiatrists, sitting with humans experiencing complex grief (a man whose wife died alone in a nursing home, because of visitor restrictions), confusion (delirium resulting from respiratory failure), and even psychosis (inability to access stabilizing medications coupled with crippling paranoia). These remain just as real and debilitating in a pandemic as they do in other times. In addition to pre-existing mental illnesses, for some individuals, the shared anxiety will progress to clinically significant disorders that may last even longer than the effects of the virus. The resulting complex symptoms could affect everything from home lives to interpersonal relationships to our local and global economies. These are not minor issues. Although often triaged aside in a disaster, our collective mental health remains in some ways more central than ever.
Modern psychiatry would not often use the word “love,” but that’s what I am trying to do—show love to the people who need it the most right now (which is all of us, really). This love takes strange shapes, and sometimes new forms, but it’s just about all I have to give. Like everyone else, I don’t have concrete answers for the grief and fear and panic. But I’m content to share the burden of pain, believing that burdens are lighter when shared. And I have a few words that, however little comfort they offer in the moment, are eventually proven true: Just because you can’t see the hope doesn’t mean it isn’t there. It’s OK to feel what you are feeling. With any luck at all, tomorrow will be better than today.
Posttraumatic stress disorder: From pathophysiology to pharmacology
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
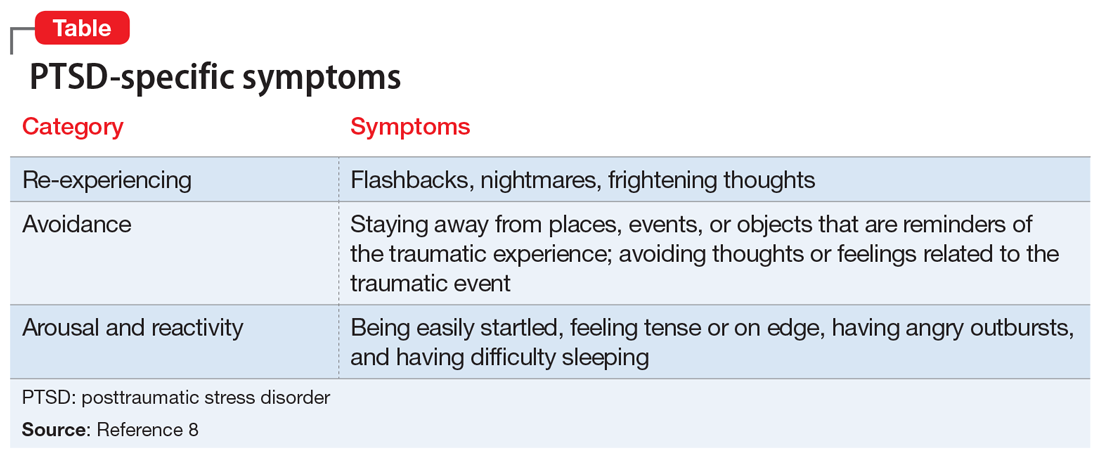
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
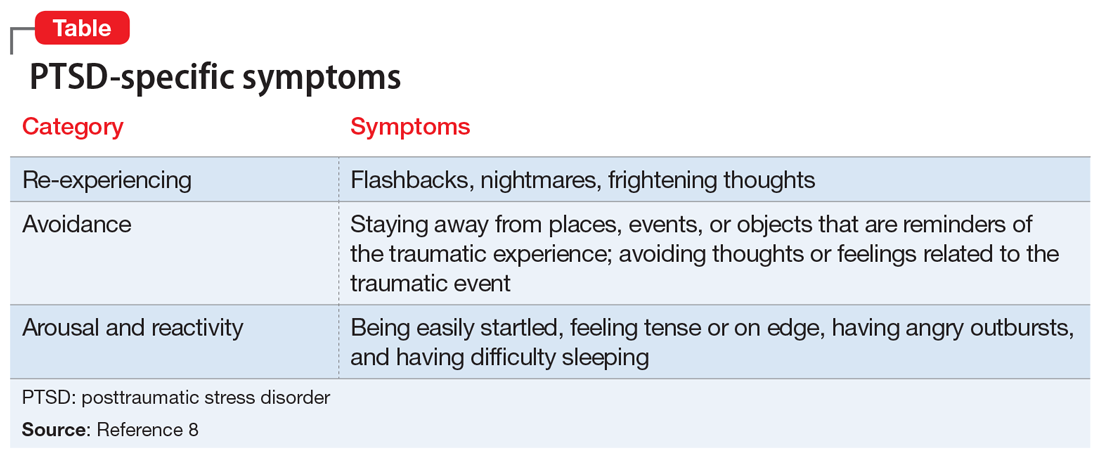
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
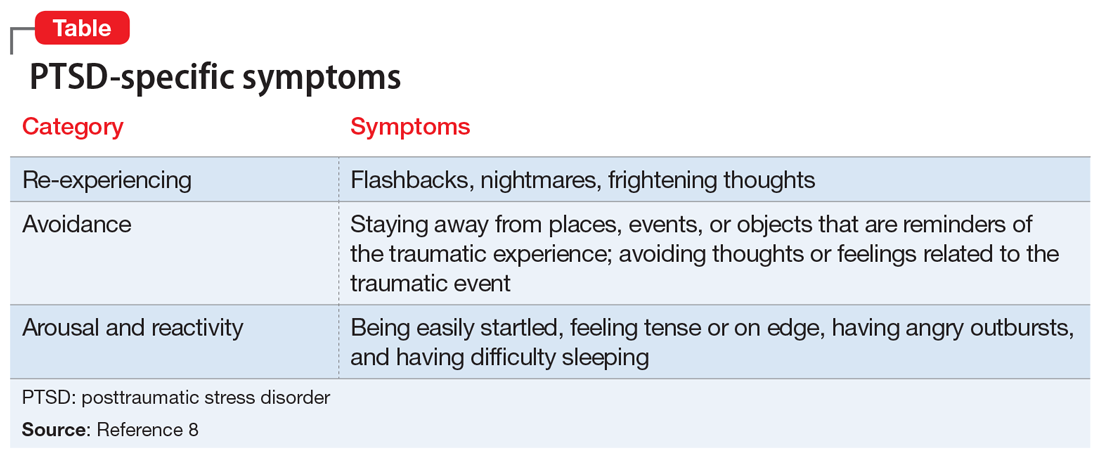
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
When mania isn’t what it seems
CASE Aggressive, impulsive, and not sleeping
Mr. S, age 22, is brought by his family to his outpatient psychiatrist because he has begun to
Mr. S has significant language impairment and is unreliable as a narrator. His family reports that Mr. S’s behavior has resulted in declining academic performance, and they have curtailed his social activities due to behavioral issues. Both his family and teachers report that it is increasingly difficult to redirect Mr. S’s behavior. Although not physically aggressive, Mr. S becomes verbally agitated when rituals are incomplete. He has gone from sleeping 8 hours each night to only 3 to 4 hours, but he does not appear tired during the day.
HISTORY Multiple hospitalizations
As a child, Mr. S had been diagnosed with autism and intellectual disability. When he was 13, he began exhibiting marked stereotypy, restlessness, impulsivity, frenzy, agitation, combativeness, and purposeless motor activity. At that time, he was not receiving any medications. Mr. S had not slept for 2 days and had been walking in circles nonstop. He became aggressive whenever anyone attempted to redirect his behavior. The family took Mr. S to the emergency department (ED), where clinicians ruled out organic causes for his behavioral disturbances, including infections, drug intoxication, and use of illicit substances. Mr. S was transferred from the ED to a child and adolescent psychiatry ward at a nearby university hospital for inpatient treatment.
On the inpatient unit, the treatment team diagnosed Mr. S with bipolar disorder and believed that he was experiencing a manic episode. He was prescribed quetiapine, 25 mg by mouth during the day and 75 mg by mouth at night, to stabilize his agitation, and was discharged with a plan to follow up with his outpatient psychiatrist. However, within 1 week, his symptoms returned, with markedly increased aggression and agitation, so he was readmitted, tapered off quetiapine, and prescribed valproic acid, 125 mg by mouth during the day and 375 mg by mouth at bedtime. With this regimen, Mr. S became calmer, but when he was discharged home, he was subdued and withdrawn, overly adherent to rules and routines, constantly irritable, and often unable to focus.
Two years later, Mr. S developed hyperammonemia. Valproic acid was discontinued, and many of his behavioral issues resolved. He flourished both academically and socially. He experienced no exacerbation of symptoms until his current presentation.
[polldaddy:10544547]
EVALUATION Pinpointing the cause
Mr. S’s physical examination reveals that his vital signs are within normal limits. Mr. S is mildly tachycardic (heart rate, 105 bpm), with regular rate and rhythm. No murmurs, gallops, or rubs are auscultated. The remainder of the physical exam, including a detailed neurologic exam, is normal.
On mental status examination, Mr. S makes limited eye contact. He has difficulty sitting in the chair, with increased rocking, finger flicking, and hand flapping from baseline. Some compulsive behaviors are noted, such as tapping his neck. He has increased tics (eye blinking and mouth opening) and increased verbigeration and repetitive verbal statements. He loudly and repeatedly demands to go home, and uses short sentences with incorrect pronouns. His affect is difficult to assess, but he is agitated. His thought process is concrete. There is no evidence of suicidal ideation, homicidal ideation, or psychosis. Mr. S denies auditory hallucinations. His insight and judgment are limited.
Continue to: The psychiatrist rules out...
The psychiatrist rules out a behavioral exacerbation of autism based on an interview with Mr. S’s family and established rapport from treating him for several years. Mr. S’s family reports that many of his behaviors are not new but that the increased drive and intensity is worrisome. Further, his family cannot identify any stressors or precipitants for the behaviors and reports that offering preferred reinforcers did not help. An anxiety disorder is ruled out because according to the family, Mr. S’s drive to constantly move and complete rituals is fueling his anxiety. Schizoaffective disorder is ruled out because Mr. S denies auditory hallucinations and has not been observed responding to internal stimuli.
His Bush-Francis Catatonia Rating Scale (BFCRS) score is 26, which suggests a high likelihood of catatonia. Based on the BFCRS score, Mr. S’s psychiatrist makes the diagnosis of hyperkinetic catatonia.
The authors’ observations
The psychiatrist determined that Mr. S had been misdiagnosed with bipolar disorder at age 13. At that time, he had experienced his first episode of hyperkinetic catatonia and his symptoms decreased after he received lorazepam in the ED. However, the treatment team did not correctly identify this, most likely due to limited knowledge of catatonia among emergency medicine clinicians.
This case exemplifies a cognitive error of premature closure. Rather than considering catatonia as a complication of autism when Mr. S was 13, the clinicians added a second psychiatric diagnosis of bipolar disorder.Although premature closure errors generally occur when the physician assumes the patient is having a common complication of a known illness,1 in Mr. S’s case, the opposite occurred.
Conceptualizing catatonia
One helpful model for conceptualizing catatonia is to think of it as a basal ganglia disorder, with lesions in the basal ganglia thalamocortical tracts and the anterior cingulate/medial orbitofrontal circuit. Disrupting these pathways can result in symptoms such as mutism or repetitive and imitative behaviors. This is likely due to decreased disinhibition by gamma-aminobutyric acid (GABA), resulting in a hypodopaminergic state. This explains why benzodiazepines, which act to increase GABA, are effective for treating catatonia, and antipsychotics that act to decrease dopamine can exacerbate symptoms. Fricchione et al2 developed a model to visually represent the neurobiologic pathophysiology of catatonia (Figure2).
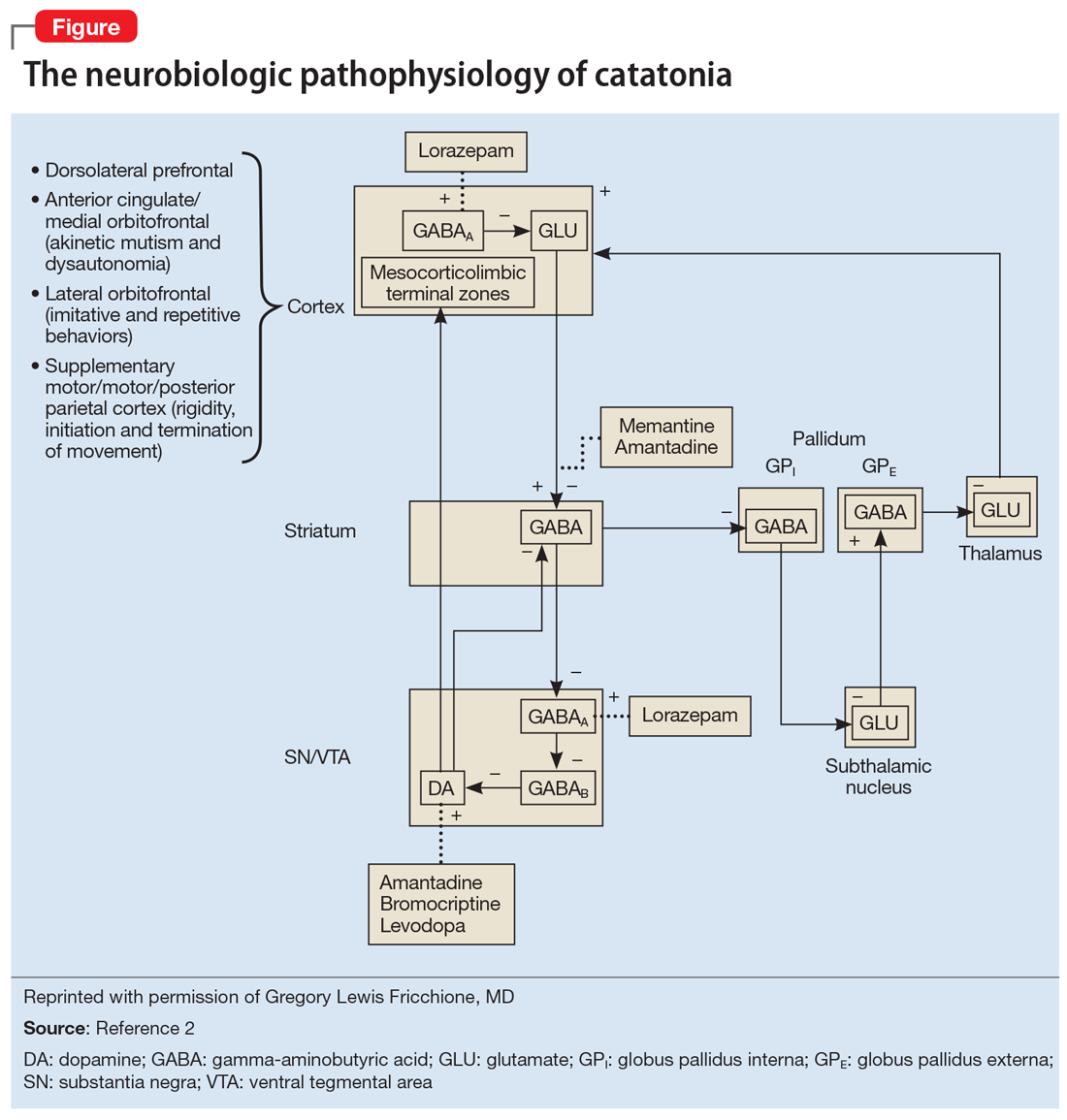
Continue to: Underlying causes of catatonia
Underlying causes of catatonia
Catatonia is most often seen in individuals with an underlying psychiatric condition such as schizophrenia, mood disorders, or autism. However, catatonia also occurs in the context of general neurologic and medical disorders, including (but not limited to) infections, metabolic disorders, endocrinopathies, epilepsy, neurodegenerative diseases, delirium, hypertensive encephalopathy, autoimmune encephalitis, and liver and kidney transplantation.3
Subtypes of catatonia include4:
- hypokinetic catatonia, which presents as stupor, mutism, and negativism
- hyperkinetic catatonia, which presents as hyperactivity, agitation, and stereotypy (as observed in Mr. S)
- malignant catatonia, which is a potentially lethal form of catatonia that occurs when hypo- or hyperkinetic catatonia is accompanied by autonomic instability such as tachycardia, tachypnea, hypertension, fever, and muscle rigidity
- periodic catatonia, which is characterized by brief episodes of stupor or excitatory catatonia lasting 4 to 10 days. These episodes recur over weeks to years, with patients remaining asymptomatic between episodes, or showing mild symptoms, such as facial grimacing or negativisms. Periodic catatonia often is autosomal dominant, involves linkage for the long arm of chromosome 15, and has a better prognosis than the other forms.
Autism and catatonia
Most individuals with autism who experience a catatonic episode first do so between age 10 and 19, and many episodes are precipitated by sudden changes in routine resulting in stress.5 An estimated 12% to 18% of patients with autism are diagnosed with catatonia in their lifetime, but the actual prevalence is likely higher.4
One of the reasons for this might be that although catatonia is well known in the psychiatric community, it is relatively unknown in the general medical community. Children and adolescents with psychiatric illness are likely to have symptoms of catatonia overlooked because catatonia often is not included in the differential diagnosis.6
In Mr. S’s case, it became clear that he did not have a mood disorder, but was prone to episodes of hyperkinetic catatonia due to his autism.
Continue to: Better recognition of catatonia
Better recognition of catatonia
As catatonia becomes better elucidated and more clearly described in the literature, there is increasing awareness that symptoms do not always involve stupor, mutism, and slowed motor activity, but can include increased motor activity, agitation, and stereotypies. The BFCRS is extremely useful for quantifying symptoms of catatonia. The best way to confirm the diagnosis is to use a lorazepam challenge in an inpatient setting, or a trial of lorazepam in an outpatient setting.5
[polldaddy:10544548]
The authors’ observations
Lorazepam is often considered the first-line treatment for catatonia because it is one of the most widely studied medications. Other benzodiazepines, such as oxazepam and clonazepam, and the sedative/hypnotic zolpidem have also been shown to be effective. Antipsychotics with dopamine-blocking mechanisms can exacerbate symptoms of catatonia and should be avoided in these patients. Furthermore, in cases of refractory catatonia, bilateral electroconvulsive therapy is an important and necessary treatment.7
TREATMENT Pharmacologic agents decrease BFCRS score
Mr. S is prescribed a regimen of lorazepam, 2 mg by mouth daily, and the supplement N-acetylcysteine, 600 mg by mouth daily. Within 2 weeks of starting this regimen, Mr. S’s BFCRS score decreases from 26 to 14. After 6 months of treatment with lorazepam, Mr. S shows considerable improvement. The stereotypic behaviors and impulsivity decrease significantly, leading to improved sleep and performance in school. After 6 months Mr. S is successfully tapered off the lorazepam, with a complete return to baseline.
Bottom Line
Hyperkinetic catatonia is easily overlooked, especially in the emergency setting. Catatonia should always be ruled out, particularly in patients with underlying conditions associated with it. Hyperkinetic catatonia is an underrecognized comorbidity in patients with autism.
Related Resources
- Dhossche DM, Wing L, Ohta M, et al. International Review of Neurobiology: Catatonia in autism spectrum disorders, vol 72. New York, NY: Academic Press/Elsevier; 2006.
- Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
Drug Brand Names
Amantadine • Symmetrel
Bromocriptine • Parlodel
Clonazepam • Klonopin
Lorazepam • Ativan
Memantine • Namenda
Oxazepam • Serax
Quetiapine • Seroquel
Valproic acid • Depakene, Depakote
Zolpidem • Ambien
1. McGee DL. Cognitive errors in clinical decision making. Merck Manual. https://www.merckmanuals.com/professional/special-subjects/clinical-decision-making/cognitive-errors-in-clinical-decision-making. Published November 2018. Accessed February 10, 2020.
2. Fricchione GL, Gross AF, Stern TA. Catatonia, neuroleptic malignant syndrome, and serotonin syndrome. Fricchione GL, Huffman JC, Stern TA, Bush G, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 6th ed. Philadelphia, PA: Saunders Elsevier; 2004:513-530.
3. Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37(6):554-559.
4. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2014;86(8):825-832.
5. Dhossche DM, Shah A, Wing L. Blueprints for the assessment, treatment, and future study of catatonia in autism spectrum disorders. Int Rev Neurobiol. 2006:72;267-284.
6. Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry. 2000:176(4):357-362.
7. Seinaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
CASE Aggressive, impulsive, and not sleeping
Mr. S, age 22, is brought by his family to his outpatient psychiatrist because he has begun to
Mr. S has significant language impairment and is unreliable as a narrator. His family reports that Mr. S’s behavior has resulted in declining academic performance, and they have curtailed his social activities due to behavioral issues. Both his family and teachers report that it is increasingly difficult to redirect Mr. S’s behavior. Although not physically aggressive, Mr. S becomes verbally agitated when rituals are incomplete. He has gone from sleeping 8 hours each night to only 3 to 4 hours, but he does not appear tired during the day.
HISTORY Multiple hospitalizations
As a child, Mr. S had been diagnosed with autism and intellectual disability. When he was 13, he began exhibiting marked stereotypy, restlessness, impulsivity, frenzy, agitation, combativeness, and purposeless motor activity. At that time, he was not receiving any medications. Mr. S had not slept for 2 days and had been walking in circles nonstop. He became aggressive whenever anyone attempted to redirect his behavior. The family took Mr. S to the emergency department (ED), where clinicians ruled out organic causes for his behavioral disturbances, including infections, drug intoxication, and use of illicit substances. Mr. S was transferred from the ED to a child and adolescent psychiatry ward at a nearby university hospital for inpatient treatment.
On the inpatient unit, the treatment team diagnosed Mr. S with bipolar disorder and believed that he was experiencing a manic episode. He was prescribed quetiapine, 25 mg by mouth during the day and 75 mg by mouth at night, to stabilize his agitation, and was discharged with a plan to follow up with his outpatient psychiatrist. However, within 1 week, his symptoms returned, with markedly increased aggression and agitation, so he was readmitted, tapered off quetiapine, and prescribed valproic acid, 125 mg by mouth during the day and 375 mg by mouth at bedtime. With this regimen, Mr. S became calmer, but when he was discharged home, he was subdued and withdrawn, overly adherent to rules and routines, constantly irritable, and often unable to focus.
Two years later, Mr. S developed hyperammonemia. Valproic acid was discontinued, and many of his behavioral issues resolved. He flourished both academically and socially. He experienced no exacerbation of symptoms until his current presentation.
[polldaddy:10544547]
EVALUATION Pinpointing the cause
Mr. S’s physical examination reveals that his vital signs are within normal limits. Mr. S is mildly tachycardic (heart rate, 105 bpm), with regular rate and rhythm. No murmurs, gallops, or rubs are auscultated. The remainder of the physical exam, including a detailed neurologic exam, is normal.
On mental status examination, Mr. S makes limited eye contact. He has difficulty sitting in the chair, with increased rocking, finger flicking, and hand flapping from baseline. Some compulsive behaviors are noted, such as tapping his neck. He has increased tics (eye blinking and mouth opening) and increased verbigeration and repetitive verbal statements. He loudly and repeatedly demands to go home, and uses short sentences with incorrect pronouns. His affect is difficult to assess, but he is agitated. His thought process is concrete. There is no evidence of suicidal ideation, homicidal ideation, or psychosis. Mr. S denies auditory hallucinations. His insight and judgment are limited.
Continue to: The psychiatrist rules out...
The psychiatrist rules out a behavioral exacerbation of autism based on an interview with Mr. S’s family and established rapport from treating him for several years. Mr. S’s family reports that many of his behaviors are not new but that the increased drive and intensity is worrisome. Further, his family cannot identify any stressors or precipitants for the behaviors and reports that offering preferred reinforcers did not help. An anxiety disorder is ruled out because according to the family, Mr. S’s drive to constantly move and complete rituals is fueling his anxiety. Schizoaffective disorder is ruled out because Mr. S denies auditory hallucinations and has not been observed responding to internal stimuli.
His Bush-Francis Catatonia Rating Scale (BFCRS) score is 26, which suggests a high likelihood of catatonia. Based on the BFCRS score, Mr. S’s psychiatrist makes the diagnosis of hyperkinetic catatonia.
The authors’ observations
The psychiatrist determined that Mr. S had been misdiagnosed with bipolar disorder at age 13. At that time, he had experienced his first episode of hyperkinetic catatonia and his symptoms decreased after he received lorazepam in the ED. However, the treatment team did not correctly identify this, most likely due to limited knowledge of catatonia among emergency medicine clinicians.
This case exemplifies a cognitive error of premature closure. Rather than considering catatonia as a complication of autism when Mr. S was 13, the clinicians added a second psychiatric diagnosis of bipolar disorder.Although premature closure errors generally occur when the physician assumes the patient is having a common complication of a known illness,1 in Mr. S’s case, the opposite occurred.
Conceptualizing catatonia
One helpful model for conceptualizing catatonia is to think of it as a basal ganglia disorder, with lesions in the basal ganglia thalamocortical tracts and the anterior cingulate/medial orbitofrontal circuit. Disrupting these pathways can result in symptoms such as mutism or repetitive and imitative behaviors. This is likely due to decreased disinhibition by gamma-aminobutyric acid (GABA), resulting in a hypodopaminergic state. This explains why benzodiazepines, which act to increase GABA, are effective for treating catatonia, and antipsychotics that act to decrease dopamine can exacerbate symptoms. Fricchione et al2 developed a model to visually represent the neurobiologic pathophysiology of catatonia (Figure2).
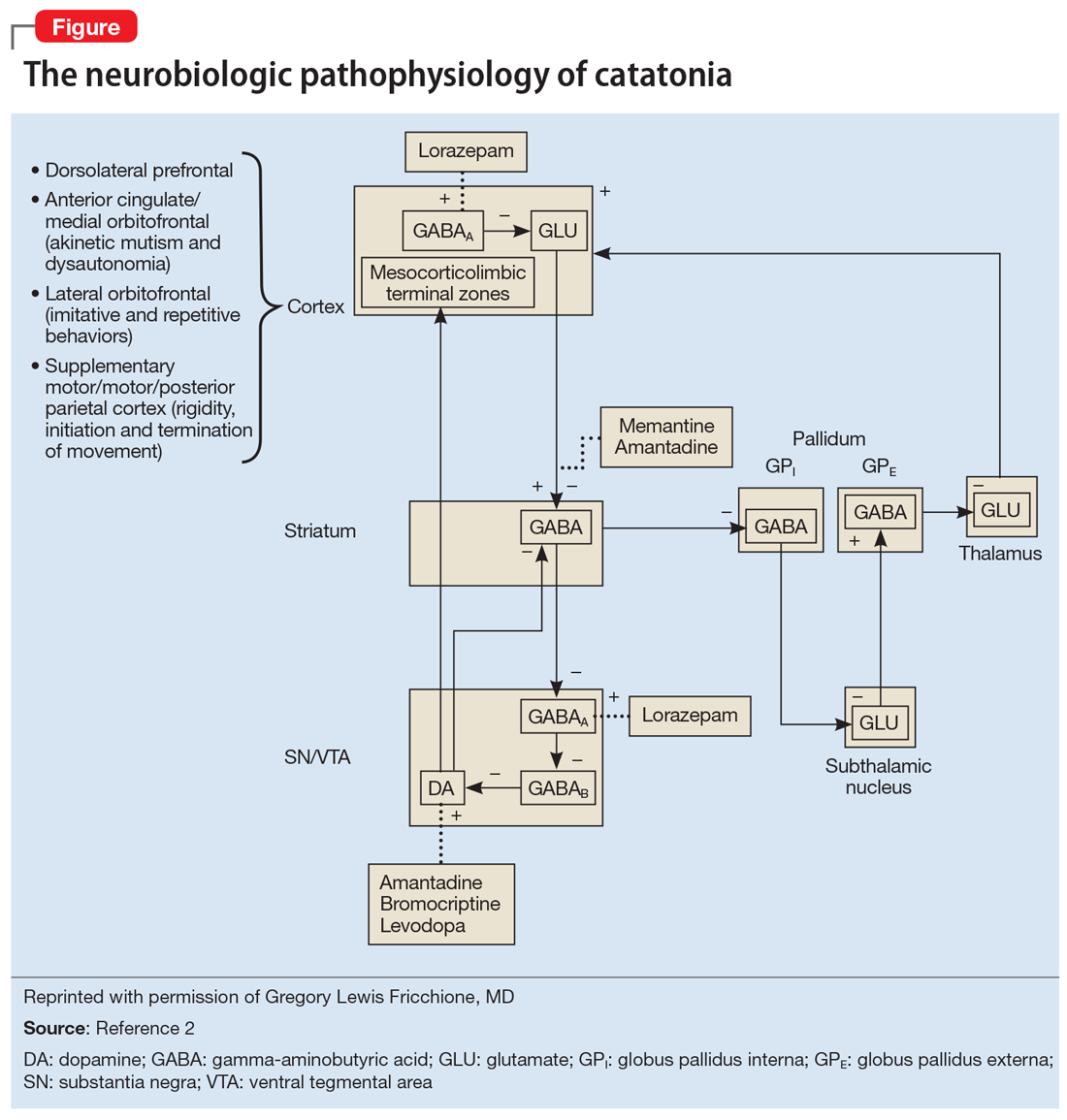
Continue to: Underlying causes of catatonia
Underlying causes of catatonia
Catatonia is most often seen in individuals with an underlying psychiatric condition such as schizophrenia, mood disorders, or autism. However, catatonia also occurs in the context of general neurologic and medical disorders, including (but not limited to) infections, metabolic disorders, endocrinopathies, epilepsy, neurodegenerative diseases, delirium, hypertensive encephalopathy, autoimmune encephalitis, and liver and kidney transplantation.3
Subtypes of catatonia include4:
- hypokinetic catatonia, which presents as stupor, mutism, and negativism
- hyperkinetic catatonia, which presents as hyperactivity, agitation, and stereotypy (as observed in Mr. S)
- malignant catatonia, which is a potentially lethal form of catatonia that occurs when hypo- or hyperkinetic catatonia is accompanied by autonomic instability such as tachycardia, tachypnea, hypertension, fever, and muscle rigidity
- periodic catatonia, which is characterized by brief episodes of stupor or excitatory catatonia lasting 4 to 10 days. These episodes recur over weeks to years, with patients remaining asymptomatic between episodes, or showing mild symptoms, such as facial grimacing or negativisms. Periodic catatonia often is autosomal dominant, involves linkage for the long arm of chromosome 15, and has a better prognosis than the other forms.
Autism and catatonia
Most individuals with autism who experience a catatonic episode first do so between age 10 and 19, and many episodes are precipitated by sudden changes in routine resulting in stress.5 An estimated 12% to 18% of patients with autism are diagnosed with catatonia in their lifetime, but the actual prevalence is likely higher.4
One of the reasons for this might be that although catatonia is well known in the psychiatric community, it is relatively unknown in the general medical community. Children and adolescents with psychiatric illness are likely to have symptoms of catatonia overlooked because catatonia often is not included in the differential diagnosis.6
In Mr. S’s case, it became clear that he did not have a mood disorder, but was prone to episodes of hyperkinetic catatonia due to his autism.
Continue to: Better recognition of catatonia
Better recognition of catatonia
As catatonia becomes better elucidated and more clearly described in the literature, there is increasing awareness that symptoms do not always involve stupor, mutism, and slowed motor activity, but can include increased motor activity, agitation, and stereotypies. The BFCRS is extremely useful for quantifying symptoms of catatonia. The best way to confirm the diagnosis is to use a lorazepam challenge in an inpatient setting, or a trial of lorazepam in an outpatient setting.5
[polldaddy:10544548]
The authors’ observations
Lorazepam is often considered the first-line treatment for catatonia because it is one of the most widely studied medications. Other benzodiazepines, such as oxazepam and clonazepam, and the sedative/hypnotic zolpidem have also been shown to be effective. Antipsychotics with dopamine-blocking mechanisms can exacerbate symptoms of catatonia and should be avoided in these patients. Furthermore, in cases of refractory catatonia, bilateral electroconvulsive therapy is an important and necessary treatment.7
TREATMENT Pharmacologic agents decrease BFCRS score
Mr. S is prescribed a regimen of lorazepam, 2 mg by mouth daily, and the supplement N-acetylcysteine, 600 mg by mouth daily. Within 2 weeks of starting this regimen, Mr. S’s BFCRS score decreases from 26 to 14. After 6 months of treatment with lorazepam, Mr. S shows considerable improvement. The stereotypic behaviors and impulsivity decrease significantly, leading to improved sleep and performance in school. After 6 months Mr. S is successfully tapered off the lorazepam, with a complete return to baseline.
Bottom Line
Hyperkinetic catatonia is easily overlooked, especially in the emergency setting. Catatonia should always be ruled out, particularly in patients with underlying conditions associated with it. Hyperkinetic catatonia is an underrecognized comorbidity in patients with autism.
Related Resources
- Dhossche DM, Wing L, Ohta M, et al. International Review of Neurobiology: Catatonia in autism spectrum disorders, vol 72. New York, NY: Academic Press/Elsevier; 2006.
- Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
Drug Brand Names
Amantadine • Symmetrel
Bromocriptine • Parlodel
Clonazepam • Klonopin
Lorazepam • Ativan
Memantine • Namenda
Oxazepam • Serax
Quetiapine • Seroquel
Valproic acid • Depakene, Depakote
Zolpidem • Ambien
CASE Aggressive, impulsive, and not sleeping
Mr. S, age 22, is brought by his family to his outpatient psychiatrist because he has begun to
Mr. S has significant language impairment and is unreliable as a narrator. His family reports that Mr. S’s behavior has resulted in declining academic performance, and they have curtailed his social activities due to behavioral issues. Both his family and teachers report that it is increasingly difficult to redirect Mr. S’s behavior. Although not physically aggressive, Mr. S becomes verbally agitated when rituals are incomplete. He has gone from sleeping 8 hours each night to only 3 to 4 hours, but he does not appear tired during the day.
HISTORY Multiple hospitalizations
As a child, Mr. S had been diagnosed with autism and intellectual disability. When he was 13, he began exhibiting marked stereotypy, restlessness, impulsivity, frenzy, agitation, combativeness, and purposeless motor activity. At that time, he was not receiving any medications. Mr. S had not slept for 2 days and had been walking in circles nonstop. He became aggressive whenever anyone attempted to redirect his behavior. The family took Mr. S to the emergency department (ED), where clinicians ruled out organic causes for his behavioral disturbances, including infections, drug intoxication, and use of illicit substances. Mr. S was transferred from the ED to a child and adolescent psychiatry ward at a nearby university hospital for inpatient treatment.
On the inpatient unit, the treatment team diagnosed Mr. S with bipolar disorder and believed that he was experiencing a manic episode. He was prescribed quetiapine, 25 mg by mouth during the day and 75 mg by mouth at night, to stabilize his agitation, and was discharged with a plan to follow up with his outpatient psychiatrist. However, within 1 week, his symptoms returned, with markedly increased aggression and agitation, so he was readmitted, tapered off quetiapine, and prescribed valproic acid, 125 mg by mouth during the day and 375 mg by mouth at bedtime. With this regimen, Mr. S became calmer, but when he was discharged home, he was subdued and withdrawn, overly adherent to rules and routines, constantly irritable, and often unable to focus.
Two years later, Mr. S developed hyperammonemia. Valproic acid was discontinued, and many of his behavioral issues resolved. He flourished both academically and socially. He experienced no exacerbation of symptoms until his current presentation.
[polldaddy:10544547]
EVALUATION Pinpointing the cause
Mr. S’s physical examination reveals that his vital signs are within normal limits. Mr. S is mildly tachycardic (heart rate, 105 bpm), with regular rate and rhythm. No murmurs, gallops, or rubs are auscultated. The remainder of the physical exam, including a detailed neurologic exam, is normal.
On mental status examination, Mr. S makes limited eye contact. He has difficulty sitting in the chair, with increased rocking, finger flicking, and hand flapping from baseline. Some compulsive behaviors are noted, such as tapping his neck. He has increased tics (eye blinking and mouth opening) and increased verbigeration and repetitive verbal statements. He loudly and repeatedly demands to go home, and uses short sentences with incorrect pronouns. His affect is difficult to assess, but he is agitated. His thought process is concrete. There is no evidence of suicidal ideation, homicidal ideation, or psychosis. Mr. S denies auditory hallucinations. His insight and judgment are limited.
Continue to: The psychiatrist rules out...
The psychiatrist rules out a behavioral exacerbation of autism based on an interview with Mr. S’s family and established rapport from treating him for several years. Mr. S’s family reports that many of his behaviors are not new but that the increased drive and intensity is worrisome. Further, his family cannot identify any stressors or precipitants for the behaviors and reports that offering preferred reinforcers did not help. An anxiety disorder is ruled out because according to the family, Mr. S’s drive to constantly move and complete rituals is fueling his anxiety. Schizoaffective disorder is ruled out because Mr. S denies auditory hallucinations and has not been observed responding to internal stimuli.
His Bush-Francis Catatonia Rating Scale (BFCRS) score is 26, which suggests a high likelihood of catatonia. Based on the BFCRS score, Mr. S’s psychiatrist makes the diagnosis of hyperkinetic catatonia.
The authors’ observations
The psychiatrist determined that Mr. S had been misdiagnosed with bipolar disorder at age 13. At that time, he had experienced his first episode of hyperkinetic catatonia and his symptoms decreased after he received lorazepam in the ED. However, the treatment team did not correctly identify this, most likely due to limited knowledge of catatonia among emergency medicine clinicians.
This case exemplifies a cognitive error of premature closure. Rather than considering catatonia as a complication of autism when Mr. S was 13, the clinicians added a second psychiatric diagnosis of bipolar disorder.Although premature closure errors generally occur when the physician assumes the patient is having a common complication of a known illness,1 in Mr. S’s case, the opposite occurred.
Conceptualizing catatonia
One helpful model for conceptualizing catatonia is to think of it as a basal ganglia disorder, with lesions in the basal ganglia thalamocortical tracts and the anterior cingulate/medial orbitofrontal circuit. Disrupting these pathways can result in symptoms such as mutism or repetitive and imitative behaviors. This is likely due to decreased disinhibition by gamma-aminobutyric acid (GABA), resulting in a hypodopaminergic state. This explains why benzodiazepines, which act to increase GABA, are effective for treating catatonia, and antipsychotics that act to decrease dopamine can exacerbate symptoms. Fricchione et al2 developed a model to visually represent the neurobiologic pathophysiology of catatonia (Figure2).
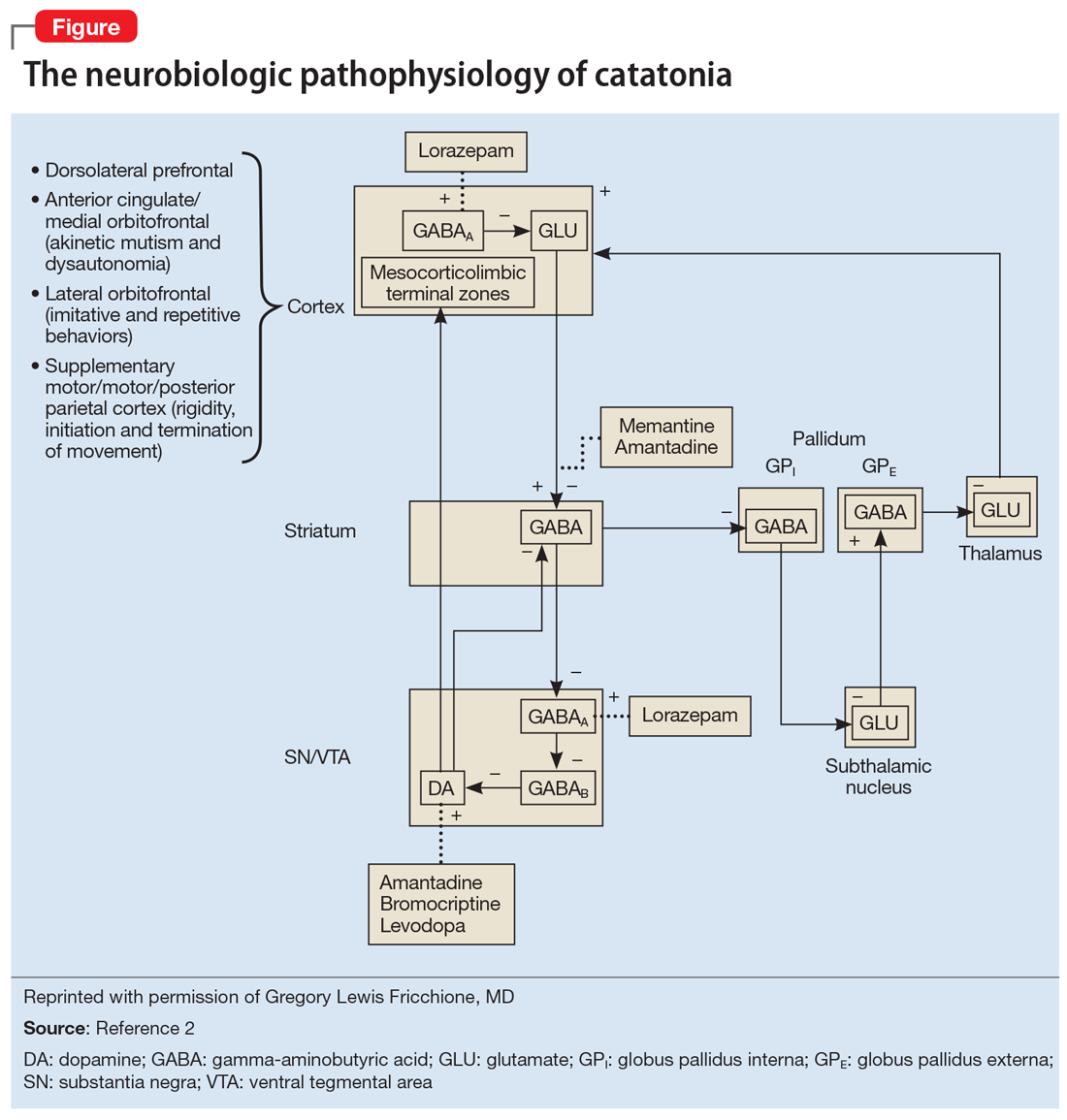
Continue to: Underlying causes of catatonia
Underlying causes of catatonia
Catatonia is most often seen in individuals with an underlying psychiatric condition such as schizophrenia, mood disorders, or autism. However, catatonia also occurs in the context of general neurologic and medical disorders, including (but not limited to) infections, metabolic disorders, endocrinopathies, epilepsy, neurodegenerative diseases, delirium, hypertensive encephalopathy, autoimmune encephalitis, and liver and kidney transplantation.3
Subtypes of catatonia include4:
- hypokinetic catatonia, which presents as stupor, mutism, and negativism
- hyperkinetic catatonia, which presents as hyperactivity, agitation, and stereotypy (as observed in Mr. S)
- malignant catatonia, which is a potentially lethal form of catatonia that occurs when hypo- or hyperkinetic catatonia is accompanied by autonomic instability such as tachycardia, tachypnea, hypertension, fever, and muscle rigidity
- periodic catatonia, which is characterized by brief episodes of stupor or excitatory catatonia lasting 4 to 10 days. These episodes recur over weeks to years, with patients remaining asymptomatic between episodes, or showing mild symptoms, such as facial grimacing or negativisms. Periodic catatonia often is autosomal dominant, involves linkage for the long arm of chromosome 15, and has a better prognosis than the other forms.
Autism and catatonia
Most individuals with autism who experience a catatonic episode first do so between age 10 and 19, and many episodes are precipitated by sudden changes in routine resulting in stress.5 An estimated 12% to 18% of patients with autism are diagnosed with catatonia in their lifetime, but the actual prevalence is likely higher.4
One of the reasons for this might be that although catatonia is well known in the psychiatric community, it is relatively unknown in the general medical community. Children and adolescents with psychiatric illness are likely to have symptoms of catatonia overlooked because catatonia often is not included in the differential diagnosis.6
In Mr. S’s case, it became clear that he did not have a mood disorder, but was prone to episodes of hyperkinetic catatonia due to his autism.
Continue to: Better recognition of catatonia
Better recognition of catatonia
As catatonia becomes better elucidated and more clearly described in the literature, there is increasing awareness that symptoms do not always involve stupor, mutism, and slowed motor activity, but can include increased motor activity, agitation, and stereotypies. The BFCRS is extremely useful for quantifying symptoms of catatonia. The best way to confirm the diagnosis is to use a lorazepam challenge in an inpatient setting, or a trial of lorazepam in an outpatient setting.5
[polldaddy:10544548]
The authors’ observations
Lorazepam is often considered the first-line treatment for catatonia because it is one of the most widely studied medications. Other benzodiazepines, such as oxazepam and clonazepam, and the sedative/hypnotic zolpidem have also been shown to be effective. Antipsychotics with dopamine-blocking mechanisms can exacerbate symptoms of catatonia and should be avoided in these patients. Furthermore, in cases of refractory catatonia, bilateral electroconvulsive therapy is an important and necessary treatment.7
TREATMENT Pharmacologic agents decrease BFCRS score
Mr. S is prescribed a regimen of lorazepam, 2 mg by mouth daily, and the supplement N-acetylcysteine, 600 mg by mouth daily. Within 2 weeks of starting this regimen, Mr. S’s BFCRS score decreases from 26 to 14. After 6 months of treatment with lorazepam, Mr. S shows considerable improvement. The stereotypic behaviors and impulsivity decrease significantly, leading to improved sleep and performance in school. After 6 months Mr. S is successfully tapered off the lorazepam, with a complete return to baseline.
Bottom Line
Hyperkinetic catatonia is easily overlooked, especially in the emergency setting. Catatonia should always be ruled out, particularly in patients with underlying conditions associated with it. Hyperkinetic catatonia is an underrecognized comorbidity in patients with autism.
Related Resources
- Dhossche DM, Wing L, Ohta M, et al. International Review of Neurobiology: Catatonia in autism spectrum disorders, vol 72. New York, NY: Academic Press/Elsevier; 2006.
- Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
Drug Brand Names
Amantadine • Symmetrel
Bromocriptine • Parlodel
Clonazepam • Klonopin
Lorazepam • Ativan
Memantine • Namenda
Oxazepam • Serax
Quetiapine • Seroquel
Valproic acid • Depakene, Depakote
Zolpidem • Ambien
1. McGee DL. Cognitive errors in clinical decision making. Merck Manual. https://www.merckmanuals.com/professional/special-subjects/clinical-decision-making/cognitive-errors-in-clinical-decision-making. Published November 2018. Accessed February 10, 2020.
2. Fricchione GL, Gross AF, Stern TA. Catatonia, neuroleptic malignant syndrome, and serotonin syndrome. Fricchione GL, Huffman JC, Stern TA, Bush G, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 6th ed. Philadelphia, PA: Saunders Elsevier; 2004:513-530.
3. Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37(6):554-559.
4. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2014;86(8):825-832.
5. Dhossche DM, Shah A, Wing L. Blueprints for the assessment, treatment, and future study of catatonia in autism spectrum disorders. Int Rev Neurobiol. 2006:72;267-284.
6. Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry. 2000:176(4):357-362.
7. Seinaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
1. McGee DL. Cognitive errors in clinical decision making. Merck Manual. https://www.merckmanuals.com/professional/special-subjects/clinical-decision-making/cognitive-errors-in-clinical-decision-making. Published November 2018. Accessed February 10, 2020.
2. Fricchione GL, Gross AF, Stern TA. Catatonia, neuroleptic malignant syndrome, and serotonin syndrome. Fricchione GL, Huffman JC, Stern TA, Bush G, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 6th ed. Philadelphia, PA: Saunders Elsevier; 2004:513-530.
3. Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37(6):554-559.
4. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2014;86(8):825-832.
5. Dhossche DM, Shah A, Wing L. Blueprints for the assessment, treatment, and future study of catatonia in autism spectrum disorders. Int Rev Neurobiol. 2006:72;267-284.
6. Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry. 2000:176(4):357-362.
7. Seinaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
Multigene panel testing for colorectal cancer
Dear colleagues and friends,
I write to introduce to you the new Perspectives section of GI & Hepatology News.
A more appropriate description is perhaps old-new, because Perspectives is the continuation and legacy of AGA Perspectives, the content of which has been consolidated into GI & Hepatology News. Perspectives will continue to feature the point/counterpoint expert debates about an important GI topic, which has historically been immensely popular with readers. In this edition, experts from Mayo Clinic and Cleveland Clinic discuss the pros and cons of universal multigene panel testing for colorectal cancer. These debates never end with the publication itself, and I hope they will continue to stimulate further thought and discussion. As always, I welcome your comments and suggestions for future topics.
–Charles I. Kahi, MD, MS, AGAF, is professor of medicine at Indiana University School of Medicine, Indianapolis. He is also an Associate Editor for GI & Hepatology News.
For everyone
By N. Jewel Samadder, MD, MSC
Traditionally, health care structure has been directed predominantly toward treatment rather than prevention. Advances in genomic medicine offer the opportunity to deliver a more personalized, predictive, and preventive strategy toward colorectal cancer. Approximately 150,000 men and women are diagnosed with colorectal cancer (CRC) every year in the United States.1 An estimated 10%-15% of these cancers are likely attributable to hereditary (germline) causes.2 Several genes are associated with an increased risk of developing CRC, and those of key interest include those for Lynch syndrome, MLH1, MSH2, MSH6, PMS2, EPCAM; adenomatous polyposis conditions (APC), MUTYH, POLE, POLD1, NTHL1; hamartomatous polyposis syndromes PTEN, SMAD4, STK11, and other rare cancer predisposition states where colorectal cancer is part of the phenotype, CHEK2 and TP532.
A universal strategy for multigene panel testing in all patients with CRC is an option versus the current strategy of guideline-based testing using family history and tumor features. In addition, the identification of germline alterations has substantial clinical implications including targeted therapies and future cancer prevention in the patient and relatives. This article will focus on the benefits of universal strategy for germline genetic evaluation in all patients with colorectal cancer.
The role and utility of current guideline-based testing
Given the therapeutic and prevention implications, the National Comprehensive Cancer Network (along with other professional organizations) has guidance on when patients with CRC should undergo genetic evaluation.3 Currently, these guidelines advocate an approach based heavily on family cancer history or utilizing colorectal phenotype based on the number and histology of polyps or tumor-based molecular features. Although family history is important for the diagnosis of hereditary CRC, the ability to accurately capture extended family cancer history in routine practice, from multiple generations and for different cancer types can be a challenge. The largest drawback of all such approaches is the focus on Lynch syndrome or only a few of the cancer predisposition syndromes. Recent studies have reported a substantial number (7%-10%) of CRC patients will have mutations in non–Lynch syndrome–associated genes and over half of these would be missed by using standard criteria for genetic evaluation.
Role of tumor-based screening approaches
More recently, health care institutions have begun to widely adopt “universal” tumor screening using microsatellite instability and/or immunohistochemistry (IHC) showing deficient expression of the mismatch repair proteins (MLH1, MSH2, MSH6, PMS2) to identify patients with colorectal or endometrial cancers that are likely to have Lynch syndrome. However, the sensitivity and specificity of IHC for Lynch syndrome ranges between 60% and 75% and there is considerable interobserver variation by pathologists in their interpretation.
Thus, both clinical guidelines (largely focused around family history and patient phenotype) and tumor molecular features will fail to identify a significant number of patients with inherited cancer predisposition.
Cost and availability of genetic testing
In the past, cost and availability of genetic testing were an impediment to such care. This has rapidly changed in the last few years. With modern next-generation sequencing technology and an ever increasing number of testing laboratories, the cost of genetic testing has dropped to below $500 and multigene panels can now test for dozens of genes in parallel offering comprehensive testing of genetic predisposition across multiple cancer types. The popularity of direct-to-consumer health-related genetic testing (with the inclusion of certain BRCA variants on these panels) has also fueled the public interest in cancer genetic testing.
Cancer prevention for family members
In individuals with CRC and hereditary cancer predisposition, implications for family members are clinically meaningful and include increased colorectal and extracolonic surveillance, consideration of risk-reducing hysterectomy, salpingo-oophorectomy, and bilateral mastectomy for colorectal, uterine, ovarian, breast, and other cancer prevention depending on the germline mutation.2 The goal of these intensive surveillance strategies is to either prevent the occurrence of cancer altogether or detect cancer at an earlier stage when cure is likely. Identifying these high-risk groups can thus play a significant role in our goal to reduce the burden of cancer in society.
Precision targeted treatment and chemoprevention
The treatment implications for patients with CRC and pathogenic mutations in the Lynch syndrome MMR genes are the best characterized and include response to immune checkpoint inhibitor therapy.4 Mismatch repair deficiency is highly predictive of response to immunotherapy in metastatic CRCs and led to expedited approval of both pembrolizumab and nivolumab monotherapies with disease control rates of 69%-77% with durable response and combination therapy with nivolumab and ipilimumab with likely even greater benefit. Multiple clinical trials are examining the role of immune checkpoint inhibitor therapy for first-line palliative treatment of MSI-high CRC (ClinicalTrials.gov ID NCT02563002; NCT02997228), adjuvant therapy (ClinicalTrials.gov ID NCT02912559), and even as potential chemoprevention in those with Lynch syndrome (ClinicalTrials.gov ID NCT03631641).
Long-term cancer prevention using a chemopreventive approach has long been a desire in the hereditary cancer community.5 The most well-studied group to date has been Lynch syndrome, where a large randomized clinical trial showed the effect of high-dose aspirin in decreasing the incidence of colorectal and other Lynch-associated cancers by nearly 60%.6 Similar smaller (earlier-phase) studies in familial adenomatous polyposis have suggested targeted chemoprevention options for the regression of colorectal or duodenal polyposis with COX inhibitors, EGFR inhibitors, DFMO (NCT01483144), and IL-23 blockade (ClinicalTrials.gov ID NCT03649971) may all be possible.
Cancer programs have already started to introduce genomic profiling (germline and tumor somatic) into the frontline care of their patients to help guide precision therapy approaches that optimize disease control, minimize side effects, and reduce risk of long-term recurrence.
The future
The approach to genomic profiling of cancer patients is rapidly changing because of the lack of sensitivity for the identification of these hereditary cancer predisposition syndromes utilizing current approaches focused on family history, clinical phenotype, and tumor features. The wide availability of low-cost/affordable multigene panel testing has implications for cancer therapy selection and cancer prevention. This supports establishing a universal approach to multigene panel testing of all patients with CRC.
It will be important for physicians of many different specialties – including gastroenterology and oncology – to become more adept in this changing landscape of genomic medicine and to work closely with the genetic counseling resources available in their communities to provide the best care for these high-risk cancer patients.
References
1. Siegel RL et al. CA Cancer J Clin. 2017;67:177-93.
2. Kanth P et al. Am J Gastroenterol. 2017;112:1509-25.
3. Gupta S et al. J Natl Compr Canc Netw. 2019;17:1032-41.
4. Ribas A, Wolchok JD. Science. 2018;359:1350-5.
5. Ramamurthy C et al. Surg Oncol Clin N Am. 2017;26:729-50.
6. Burn J et al. Lancet 2011;378:2081-7.
Dr. Samadder is a gastroenterologist in the division of gastroenterology and hepatology, Mayo Clinic, Phoenix. He is a consultant for Janssen Research & Development and Cancer Prevention Pharmaceuticals.
Not for everyone
By Carol A. Burke, MD, AGAF, and Brandie Heald Leach, MS
Multigene panel testing (MGPT) takes advantage of next-generation sequencing (NGS) a non-Sanger-based DNA sequencing technology which has revolutionized genomic research and clinical care because it can be run quickly, is lower cost than Sanger sequencing, can sequence an entire genome or exome, or specific genes of interest. Currently, cancer gene panels (disease specific or pan-cancer) are commonly utilized.
Approximately 10% of colorectal cancers (CRCs) are heritable because of a germline pathogenic variant (PV), most commonly in Lynch syndrome genes. Identification of patients with hereditary CRC is important because they are at greatest CRC and extracolonic cancer risk, benefit from aggressive cancer surveillance. and when indicated may need prophylactic surgery of at-risk organs, require multidisciplinary care, and may have at-risk family members who need testing.
Red flags regarding family cancer history may allow clinical inference as to the cause of CRC and direct who is offered germline testing. These include young age of cancer (age less than 50), synchronous or metachronous cancers, multiple relatives with CRC or extracolonic cancers, and cumulative lifetime numbers of adenomas or hamartomas. While overt clinical manifestations can be specific for predicting the causative gene defect, such as Amsterdam criteria for Lynch syndrome or numerous adenomas at a young age in familial adenomatous polyposis, overlap can occur between syndromes and single gene testing has its limitations. While family pedigrees with a phenotype that meets clinical criteria, such as Amsterdam II, can be very specific (although less sensitive) for predicting Lynch syndrome, or overt clinical manifestations such as 100 adenomatous polyps in an individual by the age of 40 is highly suggestive of familial adenomatous polyposis, overlap can occur between syndromes and single gene testing has its limitations.
The current standard of care for patients with CRC is germline testing after assessment of tumor mismatch repair (MMR) proficiency by microsatellite instability (MSI) testing and/or immunohistochemistry (IHC). Broadly, tumors that show high levels of MSI and or loss of expression of MMR proteins (not attributed to MLH1 promoter hypermethylation or double somatic mutations/loss of heterozygosity) are considered MMR deficient (MMRd) and suggestive of Lynch syndrome. MMRd directs treatment (immune check point inhibitors) and is a hallmark of Lynch syndrome as 95% of Lynch syndrome–related CRCs are MMRd.
The utility of MGPT in individuals with CRC can be inferred from two studies. In both, a 25-gene pan-cancer panel test was performed. In the first, 1,058 unselected individuals with CRC at a mean age of 56 were assessed regardless of MMR status; 9.9% were diagnosed with moderately (4.7%) or highly penetrant (5.2%) PV.1 In these individuals with CRC, 31% were diagnosed with Lynch syndrome and nearly all Lynch syndrome patients had MMRd tumors and met criteria for germline testing for Lynch syndrome; 22% of patients had other high-penetrance PV found, the majority lacking clinical features consistent with the PV. The second study,2 tested 450 patients with CRC diagnosed under the age of 50. Germline PV were detected in 16%. The majority of patients with an MMRd tumor were diagnosed with Lynch syndrome. Eight percent of patients with an MMR-proficient tumor had a PV detected. Nearly one-third did not meet clinical criteria for testing. Germline variants of uncertain significance (VUS) were noted in approximately 32% of patients in both studies. These data support the current standard of tumor assessment for MMRd, followed by Lynch syndrome germline testing as directed by IHC.
While MGPT for patients with CRC is feasible, the high rates of VUS, detection of moderate and low penetrance PV for which no clinical guidance exists, and dearth of evidence on penetrance and cancer risk attributable to incidentally found PV, need consideration. Prior to germline testing, patients and providers must understand potential testing outcomes, possible detection of incidental findings and VUS, and how each influence patient cancer risks and management. The commercial genetic testing companies accumulate information on VUS over time and reclassify the significance of the finding, but this process could take months to years. Providers ordering genetic testing must have a system to inform the patient when a VUS is reclassified.
Pre- and post-test genetic counseling, ideally by an individual with understanding of medical genetics, should be offered, including caveats, risks, benefits, and alternatives to germline testing, a plan for results disclosure, including to family members, and a plan for follow-up care. Patients with uninformative findings and VUS need to be followed as technology and research evolve. Patient preferences regarding genetic testing need to be considered. There still remains stigma and fear associated with genetic testing. Despite protections from the Genetic Information Non-Discrimination Act, many patients remain fearful of genetic discrimination. A genetic diagnosis comes with the burden that it reveals not only information about the patient’s risks, but potentially also his/her family members’ risks. These are valid patient concerns that need to be vetted and addressed.
Selection of correct testing strategy is important. A patient with a known PV in the family might benefit most from single-site analysis for the family mutation. For a patient with an affected relative who had negative genetic testing, additional genetic testing for that patients is unlikely to be beneficial. For a patient with no known PV in the family who meet genetic testing criteria, a cancer gene panel should be considered. However, guidance on which MGPT to order is lacking in professional guidelines and often left to the discretion of the provider and patient. Utilization of a “disease specific panel” (i.e., a panel of genes related to CRC risk) is useful for understanding the cause of the patient’s disease and guiding treatment, screening, and cascade testing while minimizing the number of VUS identified. Pan-cancer gene panels increase diagnostic yield, but include identification of PV in genes unrelated to phenotype or more poorly described risk and management recommendations and have a higher rate of VUS.
Finally, the cost of MGPT to the health care system needs to be considered. Despite dropping costs, the process of genetic counseling and testing remains expensive and will rise if and when testing is expanded to all patients with CRC.
MGPT is not for everyone.
References
1. Yurgelun MB et al. J Clin Oncol. 2017;35:1086-95.
2. Pearlman R et al. JAMA Oncol. 2017 Apr 01;3(4):464-71.
Dr. Burke is with the department of gastroenterology, hepatology, and nutrition, Sanford R. Weiss Center for Hereditary Colorectal Neoplasia, Digestive Disease and Surgical Institute, Cleveland Clinic; Ms. Leach is with the Center for Personalized Genetic Healthcare, Sanford R. Weiss Center for Hereditary Colorectal Neoplasia, Digestive Disease and Surgical Institute, Cleveland Clinic. Dr. Burke has no conflicts of interest, Ms. Leach serves on the advisory board of Invitae.
Dear colleagues and friends,
I write to introduce to you the new Perspectives section of GI & Hepatology News.
A more appropriate description is perhaps old-new, because Perspectives is the continuation and legacy of AGA Perspectives, the content of which has been consolidated into GI & Hepatology News. Perspectives will continue to feature the point/counterpoint expert debates about an important GI topic, which has historically been immensely popular with readers. In this edition, experts from Mayo Clinic and Cleveland Clinic discuss the pros and cons of universal multigene panel testing for colorectal cancer. These debates never end with the publication itself, and I hope they will continue to stimulate further thought and discussion. As always, I welcome your comments and suggestions for future topics.
–Charles I. Kahi, MD, MS, AGAF, is professor of medicine at Indiana University School of Medicine, Indianapolis. He is also an Associate Editor for GI & Hepatology News.
For everyone
By N. Jewel Samadder, MD, MSC
Traditionally, health care structure has been directed predominantly toward treatment rather than prevention. Advances in genomic medicine offer the opportunity to deliver a more personalized, predictive, and preventive strategy toward colorectal cancer. Approximately 150,000 men and women are diagnosed with colorectal cancer (CRC) every year in the United States.1 An estimated 10%-15% of these cancers are likely attributable to hereditary (germline) causes.2 Several genes are associated with an increased risk of developing CRC, and those of key interest include those for Lynch syndrome, MLH1, MSH2, MSH6, PMS2, EPCAM; adenomatous polyposis conditions (APC), MUTYH, POLE, POLD1, NTHL1; hamartomatous polyposis syndromes PTEN, SMAD4, STK11, and other rare cancer predisposition states where colorectal cancer is part of the phenotype, CHEK2 and TP532.
A universal strategy for multigene panel testing in all patients with CRC is an option versus the current strategy of guideline-based testing using family history and tumor features. In addition, the identification of germline alterations has substantial clinical implications including targeted therapies and future cancer prevention in the patient and relatives. This article will focus on the benefits of universal strategy for germline genetic evaluation in all patients with colorectal cancer.
The role and utility of current guideline-based testing
Given the therapeutic and prevention implications, the National Comprehensive Cancer Network (along with other professional organizations) has guidance on when patients with CRC should undergo genetic evaluation.3 Currently, these guidelines advocate an approach based heavily on family cancer history or utilizing colorectal phenotype based on the number and histology of polyps or tumor-based molecular features. Although family history is important for the diagnosis of hereditary CRC, the ability to accurately capture extended family cancer history in routine practice, from multiple generations and for different cancer types can be a challenge. The largest drawback of all such approaches is the focus on Lynch syndrome or only a few of the cancer predisposition syndromes. Recent studies have reported a substantial number (7%-10%) of CRC patients will have mutations in non–Lynch syndrome–associated genes and over half of these would be missed by using standard criteria for genetic evaluation.
Role of tumor-based screening approaches
More recently, health care institutions have begun to widely adopt “universal” tumor screening using microsatellite instability and/or immunohistochemistry (IHC) showing deficient expression of the mismatch repair proteins (MLH1, MSH2, MSH6, PMS2) to identify patients with colorectal or endometrial cancers that are likely to have Lynch syndrome. However, the sensitivity and specificity of IHC for Lynch syndrome ranges between 60% and 75% and there is considerable interobserver variation by pathologists in their interpretation.
Thus, both clinical guidelines (largely focused around family history and patient phenotype) and tumor molecular features will fail to identify a significant number of patients with inherited cancer predisposition.
Cost and availability of genetic testing
In the past, cost and availability of genetic testing were an impediment to such care. This has rapidly changed in the last few years. With modern next-generation sequencing technology and an ever increasing number of testing laboratories, the cost of genetic testing has dropped to below $500 and multigene panels can now test for dozens of genes in parallel offering comprehensive testing of genetic predisposition across multiple cancer types. The popularity of direct-to-consumer health-related genetic testing (with the inclusion of certain BRCA variants on these panels) has also fueled the public interest in cancer genetic testing.
Cancer prevention for family members
In individuals with CRC and hereditary cancer predisposition, implications for family members are clinically meaningful and include increased colorectal and extracolonic surveillance, consideration of risk-reducing hysterectomy, salpingo-oophorectomy, and bilateral mastectomy for colorectal, uterine, ovarian, breast, and other cancer prevention depending on the germline mutation.2 The goal of these intensive surveillance strategies is to either prevent the occurrence of cancer altogether or detect cancer at an earlier stage when cure is likely. Identifying these high-risk groups can thus play a significant role in our goal to reduce the burden of cancer in society.
Precision targeted treatment and chemoprevention
The treatment implications for patients with CRC and pathogenic mutations in the Lynch syndrome MMR genes are the best characterized and include response to immune checkpoint inhibitor therapy.4 Mismatch repair deficiency is highly predictive of response to immunotherapy in metastatic CRCs and led to expedited approval of both pembrolizumab and nivolumab monotherapies with disease control rates of 69%-77% with durable response and combination therapy with nivolumab and ipilimumab with likely even greater benefit. Multiple clinical trials are examining the role of immune checkpoint inhibitor therapy for first-line palliative treatment of MSI-high CRC (ClinicalTrials.gov ID NCT02563002; NCT02997228), adjuvant therapy (ClinicalTrials.gov ID NCT02912559), and even as potential chemoprevention in those with Lynch syndrome (ClinicalTrials.gov ID NCT03631641).
Long-term cancer prevention using a chemopreventive approach has long been a desire in the hereditary cancer community.5 The most well-studied group to date has been Lynch syndrome, where a large randomized clinical trial showed the effect of high-dose aspirin in decreasing the incidence of colorectal and other Lynch-associated cancers by nearly 60%.6 Similar smaller (earlier-phase) studies in familial adenomatous polyposis have suggested targeted chemoprevention options for the regression of colorectal or duodenal polyposis with COX inhibitors, EGFR inhibitors, DFMO (NCT01483144), and IL-23 blockade (ClinicalTrials.gov ID NCT03649971) may all be possible.
Cancer programs have already started to introduce genomic profiling (germline and tumor somatic) into the frontline care of their patients to help guide precision therapy approaches that optimize disease control, minimize side effects, and reduce risk of long-term recurrence.
The future
The approach to genomic profiling of cancer patients is rapidly changing because of the lack of sensitivity for the identification of these hereditary cancer predisposition syndromes utilizing current approaches focused on family history, clinical phenotype, and tumor features. The wide availability of low-cost/affordable multigene panel testing has implications for cancer therapy selection and cancer prevention. This supports establishing a universal approach to multigene panel testing of all patients with CRC.
It will be important for physicians of many different specialties – including gastroenterology and oncology – to become more adept in this changing landscape of genomic medicine and to work closely with the genetic counseling resources available in their communities to provide the best care for these high-risk cancer patients.
References
1. Siegel RL et al. CA Cancer J Clin. 2017;67:177-93.
2. Kanth P et al. Am J Gastroenterol. 2017;112:1509-25.
3. Gupta S et al. J Natl Compr Canc Netw. 2019;17:1032-41.
4. Ribas A, Wolchok JD. Science. 2018;359:1350-5.
5. Ramamurthy C et al. Surg Oncol Clin N Am. 2017;26:729-50.
6. Burn J et al. Lancet 2011;378:2081-7.
Dr. Samadder is a gastroenterologist in the division of gastroenterology and hepatology, Mayo Clinic, Phoenix. He is a consultant for Janssen Research & Development and Cancer Prevention Pharmaceuticals.
Not for everyone
By Carol A. Burke, MD, AGAF, and Brandie Heald Leach, MS
Multigene panel testing (MGPT) takes advantage of next-generation sequencing (NGS) a non-Sanger-based DNA sequencing technology which has revolutionized genomic research and clinical care because it can be run quickly, is lower cost than Sanger sequencing, can sequence an entire genome or exome, or specific genes of interest. Currently, cancer gene panels (disease specific or pan-cancer) are commonly utilized.
Approximately 10% of colorectal cancers (CRCs) are heritable because of a germline pathogenic variant (PV), most commonly in Lynch syndrome genes. Identification of patients with hereditary CRC is important because they are at greatest CRC and extracolonic cancer risk, benefit from aggressive cancer surveillance. and when indicated may need prophylactic surgery of at-risk organs, require multidisciplinary care, and may have at-risk family members who need testing.
Red flags regarding family cancer history may allow clinical inference as to the cause of CRC and direct who is offered germline testing. These include young age of cancer (age less than 50), synchronous or metachronous cancers, multiple relatives with CRC or extracolonic cancers, and cumulative lifetime numbers of adenomas or hamartomas. While overt clinical manifestations can be specific for predicting the causative gene defect, such as Amsterdam criteria for Lynch syndrome or numerous adenomas at a young age in familial adenomatous polyposis, overlap can occur between syndromes and single gene testing has its limitations. While family pedigrees with a phenotype that meets clinical criteria, such as Amsterdam II, can be very specific (although less sensitive) for predicting Lynch syndrome, or overt clinical manifestations such as 100 adenomatous polyps in an individual by the age of 40 is highly suggestive of familial adenomatous polyposis, overlap can occur between syndromes and single gene testing has its limitations.
The current standard of care for patients with CRC is germline testing after assessment of tumor mismatch repair (MMR) proficiency by microsatellite instability (MSI) testing and/or immunohistochemistry (IHC). Broadly, tumors that show high levels of MSI and or loss of expression of MMR proteins (not attributed to MLH1 promoter hypermethylation or double somatic mutations/loss of heterozygosity) are considered MMR deficient (MMRd) and suggestive of Lynch syndrome. MMRd directs treatment (immune check point inhibitors) and is a hallmark of Lynch syndrome as 95% of Lynch syndrome–related CRCs are MMRd.
The utility of MGPT in individuals with CRC can be inferred from two studies. In both, a 25-gene pan-cancer panel test was performed. In the first, 1,058 unselected individuals with CRC at a mean age of 56 were assessed regardless of MMR status; 9.9% were diagnosed with moderately (4.7%) or highly penetrant (5.2%) PV.1 In these individuals with CRC, 31% were diagnosed with Lynch syndrome and nearly all Lynch syndrome patients had MMRd tumors and met criteria for germline testing for Lynch syndrome; 22% of patients had other high-penetrance PV found, the majority lacking clinical features consistent with the PV. The second study,2 tested 450 patients with CRC diagnosed under the age of 50. Germline PV were detected in 16%. The majority of patients with an MMRd tumor were diagnosed with Lynch syndrome. Eight percent of patients with an MMR-proficient tumor had a PV detected. Nearly one-third did not meet clinical criteria for testing. Germline variants of uncertain significance (VUS) were noted in approximately 32% of patients in both studies. These data support the current standard of tumor assessment for MMRd, followed by Lynch syndrome germline testing as directed by IHC.
While MGPT for patients with CRC is feasible, the high rates of VUS, detection of moderate and low penetrance PV for which no clinical guidance exists, and dearth of evidence on penetrance and cancer risk attributable to incidentally found PV, need consideration. Prior to germline testing, patients and providers must understand potential testing outcomes, possible detection of incidental findings and VUS, and how each influence patient cancer risks and management. The commercial genetic testing companies accumulate information on VUS over time and reclassify the significance of the finding, but this process could take months to years. Providers ordering genetic testing must have a system to inform the patient when a VUS is reclassified.
Pre- and post-test genetic counseling, ideally by an individual with understanding of medical genetics, should be offered, including caveats, risks, benefits, and alternatives to germline testing, a plan for results disclosure, including to family members, and a plan for follow-up care. Patients with uninformative findings and VUS need to be followed as technology and research evolve. Patient preferences regarding genetic testing need to be considered. There still remains stigma and fear associated with genetic testing. Despite protections from the Genetic Information Non-Discrimination Act, many patients remain fearful of genetic discrimination. A genetic diagnosis comes with the burden that it reveals not only information about the patient’s risks, but potentially also his/her family members’ risks. These are valid patient concerns that need to be vetted and addressed.
Selection of correct testing strategy is important. A patient with a known PV in the family might benefit most from single-site analysis for the family mutation. For a patient with an affected relative who had negative genetic testing, additional genetic testing for that patients is unlikely to be beneficial. For a patient with no known PV in the family who meet genetic testing criteria, a cancer gene panel should be considered. However, guidance on which MGPT to order is lacking in professional guidelines and often left to the discretion of the provider and patient. Utilization of a “disease specific panel” (i.e., a panel of genes related to CRC risk) is useful for understanding the cause of the patient’s disease and guiding treatment, screening, and cascade testing while minimizing the number of VUS identified. Pan-cancer gene panels increase diagnostic yield, but include identification of PV in genes unrelated to phenotype or more poorly described risk and management recommendations and have a higher rate of VUS.
Finally, the cost of MGPT to the health care system needs to be considered. Despite dropping costs, the process of genetic counseling and testing remains expensive and will rise if and when testing is expanded to all patients with CRC.
MGPT is not for everyone.
References
1. Yurgelun MB et al. J Clin Oncol. 2017;35:1086-95.
2. Pearlman R et al. JAMA Oncol. 2017 Apr 01;3(4):464-71.
Dr. Burke is with the department of gastroenterology, hepatology, and nutrition, Sanford R. Weiss Center for Hereditary Colorectal Neoplasia, Digestive Disease and Surgical Institute, Cleveland Clinic; Ms. Leach is with the Center for Personalized Genetic Healthcare, Sanford R. Weiss Center for Hereditary Colorectal Neoplasia, Digestive Disease and Surgical Institute, Cleveland Clinic. Dr. Burke has no conflicts of interest, Ms. Leach serves on the advisory board of Invitae.
Dear colleagues and friends,
I write to introduce to you the new Perspectives section of GI & Hepatology News.
A more appropriate description is perhaps old-new, because Perspectives is the continuation and legacy of AGA Perspectives, the content of which has been consolidated into GI & Hepatology News. Perspectives will continue to feature the point/counterpoint expert debates about an important GI topic, which has historically been immensely popular with readers. In this edition, experts from Mayo Clinic and Cleveland Clinic discuss the pros and cons of universal multigene panel testing for colorectal cancer. These debates never end with the publication itself, and I hope they will continue to stimulate further thought and discussion. As always, I welcome your comments and suggestions for future topics.
–Charles I. Kahi, MD, MS, AGAF, is professor of medicine at Indiana University School of Medicine, Indianapolis. He is also an Associate Editor for GI & Hepatology News.
For everyone
By N. Jewel Samadder, MD, MSC
Traditionally, health care structure has been directed predominantly toward treatment rather than prevention. Advances in genomic medicine offer the opportunity to deliver a more personalized, predictive, and preventive strategy toward colorectal cancer. Approximately 150,000 men and women are diagnosed with colorectal cancer (CRC) every year in the United States.1 An estimated 10%-15% of these cancers are likely attributable to hereditary (germline) causes.2 Several genes are associated with an increased risk of developing CRC, and those of key interest include those for Lynch syndrome, MLH1, MSH2, MSH6, PMS2, EPCAM; adenomatous polyposis conditions (APC), MUTYH, POLE, POLD1, NTHL1; hamartomatous polyposis syndromes PTEN, SMAD4, STK11, and other rare cancer predisposition states where colorectal cancer is part of the phenotype, CHEK2 and TP532.
A universal strategy for multigene panel testing in all patients with CRC is an option versus the current strategy of guideline-based testing using family history and tumor features. In addition, the identification of germline alterations has substantial clinical implications including targeted therapies and future cancer prevention in the patient and relatives. This article will focus on the benefits of universal strategy for germline genetic evaluation in all patients with colorectal cancer.
The role and utility of current guideline-based testing
Given the therapeutic and prevention implications, the National Comprehensive Cancer Network (along with other professional organizations) has guidance on when patients with CRC should undergo genetic evaluation.3 Currently, these guidelines advocate an approach based heavily on family cancer history or utilizing colorectal phenotype based on the number and histology of polyps or tumor-based molecular features. Although family history is important for the diagnosis of hereditary CRC, the ability to accurately capture extended family cancer history in routine practice, from multiple generations and for different cancer types can be a challenge. The largest drawback of all such approaches is the focus on Lynch syndrome or only a few of the cancer predisposition syndromes. Recent studies have reported a substantial number (7%-10%) of CRC patients will have mutations in non–Lynch syndrome–associated genes and over half of these would be missed by using standard criteria for genetic evaluation.
Role of tumor-based screening approaches
More recently, health care institutions have begun to widely adopt “universal” tumor screening using microsatellite instability and/or immunohistochemistry (IHC) showing deficient expression of the mismatch repair proteins (MLH1, MSH2, MSH6, PMS2) to identify patients with colorectal or endometrial cancers that are likely to have Lynch syndrome. However, the sensitivity and specificity of IHC for Lynch syndrome ranges between 60% and 75% and there is considerable interobserver variation by pathologists in their interpretation.
Thus, both clinical guidelines (largely focused around family history and patient phenotype) and tumor molecular features will fail to identify a significant number of patients with inherited cancer predisposition.
Cost and availability of genetic testing
In the past, cost and availability of genetic testing were an impediment to such care. This has rapidly changed in the last few years. With modern next-generation sequencing technology and an ever increasing number of testing laboratories, the cost of genetic testing has dropped to below $500 and multigene panels can now test for dozens of genes in parallel offering comprehensive testing of genetic predisposition across multiple cancer types. The popularity of direct-to-consumer health-related genetic testing (with the inclusion of certain BRCA variants on these panels) has also fueled the public interest in cancer genetic testing.
Cancer prevention for family members
In individuals with CRC and hereditary cancer predisposition, implications for family members are clinically meaningful and include increased colorectal and extracolonic surveillance, consideration of risk-reducing hysterectomy, salpingo-oophorectomy, and bilateral mastectomy for colorectal, uterine, ovarian, breast, and other cancer prevention depending on the germline mutation.2 The goal of these intensive surveillance strategies is to either prevent the occurrence of cancer altogether or detect cancer at an earlier stage when cure is likely. Identifying these high-risk groups can thus play a significant role in our goal to reduce the burden of cancer in society.
Precision targeted treatment and chemoprevention
The treatment implications for patients with CRC and pathogenic mutations in the Lynch syndrome MMR genes are the best characterized and include response to immune checkpoint inhibitor therapy.4 Mismatch repair deficiency is highly predictive of response to immunotherapy in metastatic CRCs and led to expedited approval of both pembrolizumab and nivolumab monotherapies with disease control rates of 69%-77% with durable response and combination therapy with nivolumab and ipilimumab with likely even greater benefit. Multiple clinical trials are examining the role of immune checkpoint inhibitor therapy for first-line palliative treatment of MSI-high CRC (ClinicalTrials.gov ID NCT02563002; NCT02997228), adjuvant therapy (ClinicalTrials.gov ID NCT02912559), and even as potential chemoprevention in those with Lynch syndrome (ClinicalTrials.gov ID NCT03631641).
Long-term cancer prevention using a chemopreventive approach has long been a desire in the hereditary cancer community.5 The most well-studied group to date has been Lynch syndrome, where a large randomized clinical trial showed the effect of high-dose aspirin in decreasing the incidence of colorectal and other Lynch-associated cancers by nearly 60%.6 Similar smaller (earlier-phase) studies in familial adenomatous polyposis have suggested targeted chemoprevention options for the regression of colorectal or duodenal polyposis with COX inhibitors, EGFR inhibitors, DFMO (NCT01483144), and IL-23 blockade (ClinicalTrials.gov ID NCT03649971) may all be possible.
Cancer programs have already started to introduce genomic profiling (germline and tumor somatic) into the frontline care of their patients to help guide precision therapy approaches that optimize disease control, minimize side effects, and reduce risk of long-term recurrence.
The future
The approach to genomic profiling of cancer patients is rapidly changing because of the lack of sensitivity for the identification of these hereditary cancer predisposition syndromes utilizing current approaches focused on family history, clinical phenotype, and tumor features. The wide availability of low-cost/affordable multigene panel testing has implications for cancer therapy selection and cancer prevention. This supports establishing a universal approach to multigene panel testing of all patients with CRC.
It will be important for physicians of many different specialties – including gastroenterology and oncology – to become more adept in this changing landscape of genomic medicine and to work closely with the genetic counseling resources available in their communities to provide the best care for these high-risk cancer patients.
References
1. Siegel RL et al. CA Cancer J Clin. 2017;67:177-93.
2. Kanth P et al. Am J Gastroenterol. 2017;112:1509-25.
3. Gupta S et al. J Natl Compr Canc Netw. 2019;17:1032-41.
4. Ribas A, Wolchok JD. Science. 2018;359:1350-5.
5. Ramamurthy C et al. Surg Oncol Clin N Am. 2017;26:729-50.
6. Burn J et al. Lancet 2011;378:2081-7.
Dr. Samadder is a gastroenterologist in the division of gastroenterology and hepatology, Mayo Clinic, Phoenix. He is a consultant for Janssen Research & Development and Cancer Prevention Pharmaceuticals.
Not for everyone
By Carol A. Burke, MD, AGAF, and Brandie Heald Leach, MS
Multigene panel testing (MGPT) takes advantage of next-generation sequencing (NGS) a non-Sanger-based DNA sequencing technology which has revolutionized genomic research and clinical care because it can be run quickly, is lower cost than Sanger sequencing, can sequence an entire genome or exome, or specific genes of interest. Currently, cancer gene panels (disease specific or pan-cancer) are commonly utilized.
Approximately 10% of colorectal cancers (CRCs) are heritable because of a germline pathogenic variant (PV), most commonly in Lynch syndrome genes. Identification of patients with hereditary CRC is important because they are at greatest CRC and extracolonic cancer risk, benefit from aggressive cancer surveillance. and when indicated may need prophylactic surgery of at-risk organs, require multidisciplinary care, and may have at-risk family members who need testing.
Red flags regarding family cancer history may allow clinical inference as to the cause of CRC and direct who is offered germline testing. These include young age of cancer (age less than 50), synchronous or metachronous cancers, multiple relatives with CRC or extracolonic cancers, and cumulative lifetime numbers of adenomas or hamartomas. While overt clinical manifestations can be specific for predicting the causative gene defect, such as Amsterdam criteria for Lynch syndrome or numerous adenomas at a young age in familial adenomatous polyposis, overlap can occur between syndromes and single gene testing has its limitations. While family pedigrees with a phenotype that meets clinical criteria, such as Amsterdam II, can be very specific (although less sensitive) for predicting Lynch syndrome, or overt clinical manifestations such as 100 adenomatous polyps in an individual by the age of 40 is highly suggestive of familial adenomatous polyposis, overlap can occur between syndromes and single gene testing has its limitations.
The current standard of care for patients with CRC is germline testing after assessment of tumor mismatch repair (MMR) proficiency by microsatellite instability (MSI) testing and/or immunohistochemistry (IHC). Broadly, tumors that show high levels of MSI and or loss of expression of MMR proteins (not attributed to MLH1 promoter hypermethylation or double somatic mutations/loss of heterozygosity) are considered MMR deficient (MMRd) and suggestive of Lynch syndrome. MMRd directs treatment (immune check point inhibitors) and is a hallmark of Lynch syndrome as 95% of Lynch syndrome–related CRCs are MMRd.
The utility of MGPT in individuals with CRC can be inferred from two studies. In both, a 25-gene pan-cancer panel test was performed. In the first, 1,058 unselected individuals with CRC at a mean age of 56 were assessed regardless of MMR status; 9.9% were diagnosed with moderately (4.7%) or highly penetrant (5.2%) PV.1 In these individuals with CRC, 31% were diagnosed with Lynch syndrome and nearly all Lynch syndrome patients had MMRd tumors and met criteria for germline testing for Lynch syndrome; 22% of patients had other high-penetrance PV found, the majority lacking clinical features consistent with the PV. The second study,2 tested 450 patients with CRC diagnosed under the age of 50. Germline PV were detected in 16%. The majority of patients with an MMRd tumor were diagnosed with Lynch syndrome. Eight percent of patients with an MMR-proficient tumor had a PV detected. Nearly one-third did not meet clinical criteria for testing. Germline variants of uncertain significance (VUS) were noted in approximately 32% of patients in both studies. These data support the current standard of tumor assessment for MMRd, followed by Lynch syndrome germline testing as directed by IHC.
While MGPT for patients with CRC is feasible, the high rates of VUS, detection of moderate and low penetrance PV for which no clinical guidance exists, and dearth of evidence on penetrance and cancer risk attributable to incidentally found PV, need consideration. Prior to germline testing, patients and providers must understand potential testing outcomes, possible detection of incidental findings and VUS, and how each influence patient cancer risks and management. The commercial genetic testing companies accumulate information on VUS over time and reclassify the significance of the finding, but this process could take months to years. Providers ordering genetic testing must have a system to inform the patient when a VUS is reclassified.
Pre- and post-test genetic counseling, ideally by an individual with understanding of medical genetics, should be offered, including caveats, risks, benefits, and alternatives to germline testing, a plan for results disclosure, including to family members, and a plan for follow-up care. Patients with uninformative findings and VUS need to be followed as technology and research evolve. Patient preferences regarding genetic testing need to be considered. There still remains stigma and fear associated with genetic testing. Despite protections from the Genetic Information Non-Discrimination Act, many patients remain fearful of genetic discrimination. A genetic diagnosis comes with the burden that it reveals not only information about the patient’s risks, but potentially also his/her family members’ risks. These are valid patient concerns that need to be vetted and addressed.
Selection of correct testing strategy is important. A patient with a known PV in the family might benefit most from single-site analysis for the family mutation. For a patient with an affected relative who had negative genetic testing, additional genetic testing for that patients is unlikely to be beneficial. For a patient with no known PV in the family who meet genetic testing criteria, a cancer gene panel should be considered. However, guidance on which MGPT to order is lacking in professional guidelines and often left to the discretion of the provider and patient. Utilization of a “disease specific panel” (i.e., a panel of genes related to CRC risk) is useful for understanding the cause of the patient’s disease and guiding treatment, screening, and cascade testing while minimizing the number of VUS identified. Pan-cancer gene panels increase diagnostic yield, but include identification of PV in genes unrelated to phenotype or more poorly described risk and management recommendations and have a higher rate of VUS.
Finally, the cost of MGPT to the health care system needs to be considered. Despite dropping costs, the process of genetic counseling and testing remains expensive and will rise if and when testing is expanded to all patients with CRC.
MGPT is not for everyone.
References
1. Yurgelun MB et al. J Clin Oncol. 2017;35:1086-95.
2. Pearlman R et al. JAMA Oncol. 2017 Apr 01;3(4):464-71.
Dr. Burke is with the department of gastroenterology, hepatology, and nutrition, Sanford R. Weiss Center for Hereditary Colorectal Neoplasia, Digestive Disease and Surgical Institute, Cleveland Clinic; Ms. Leach is with the Center for Personalized Genetic Healthcare, Sanford R. Weiss Center for Hereditary Colorectal Neoplasia, Digestive Disease and Surgical Institute, Cleveland Clinic. Dr. Burke has no conflicts of interest, Ms. Leach serves on the advisory board of Invitae.
Let’s learn from our experience
COVID-19 has revealed the worst and best of our country. Some have used it to validate their racism (my Korean-born son keeps me apprised of the Asian prejudice he has experienced) and a few leaders have made policy decisions based on ideology and not science, with disastrous consequences. That said, no world threat since those 13 days in October 1962 has demonstrated so decisively our interconnectedness. The best of our country has been demonstrated by our frontline health care workers, grocery clerks, people who deliver our packages, and volunteers who help feed our fellow citizens.
We are witnessing consequences of long-term health disparities that America continues to condone. Current hotspots are clustered in cities with high population density where people (usually minorities) lack ready access to health care and live with barriers to preventive care (poor nutritional options and a lack of sufficient primary care). We have underfunded our public health system and allowed politicians to ignore science. When testing was not prioritized initially, we lost the ability to isolate and trace index cases. If we want to honor those people who have died, let’s learn from our experience and change our priorities.
Private practices and health systems alike are being financially devastated. We are seeing massive numbers of people furloughed or laid off, as practices see drastic revenue loss. The transition to virtual health (video visits, remote patient monitoring) has been breath-taking with real implications about future needs for bricks and mortar. These changes in care delivery will be sustained in the future. Practice acquisitions have stopped, planned private equity exits are on hold, and the job market for graduating fellows will be challenging for the next 2 years. Now is a time for our GI societies to come together and find solutions for these problems so that our specialty can remain viable.
John I. Allen, MD, MBA, AGAF
Editor in Chief
COVID-19 has revealed the worst and best of our country. Some have used it to validate their racism (my Korean-born son keeps me apprised of the Asian prejudice he has experienced) and a few leaders have made policy decisions based on ideology and not science, with disastrous consequences. That said, no world threat since those 13 days in October 1962 has demonstrated so decisively our interconnectedness. The best of our country has been demonstrated by our frontline health care workers, grocery clerks, people who deliver our packages, and volunteers who help feed our fellow citizens.
We are witnessing consequences of long-term health disparities that America continues to condone. Current hotspots are clustered in cities with high population density where people (usually minorities) lack ready access to health care and live with barriers to preventive care (poor nutritional options and a lack of sufficient primary care). We have underfunded our public health system and allowed politicians to ignore science. When testing was not prioritized initially, we lost the ability to isolate and trace index cases. If we want to honor those people who have died, let’s learn from our experience and change our priorities.
Private practices and health systems alike are being financially devastated. We are seeing massive numbers of people furloughed or laid off, as practices see drastic revenue loss. The transition to virtual health (video visits, remote patient monitoring) has been breath-taking with real implications about future needs for bricks and mortar. These changes in care delivery will be sustained in the future. Practice acquisitions have stopped, planned private equity exits are on hold, and the job market for graduating fellows will be challenging for the next 2 years. Now is a time for our GI societies to come together and find solutions for these problems so that our specialty can remain viable.
John I. Allen, MD, MBA, AGAF
Editor in Chief
COVID-19 has revealed the worst and best of our country. Some have used it to validate their racism (my Korean-born son keeps me apprised of the Asian prejudice he has experienced) and a few leaders have made policy decisions based on ideology and not science, with disastrous consequences. That said, no world threat since those 13 days in October 1962 has demonstrated so decisively our interconnectedness. The best of our country has been demonstrated by our frontline health care workers, grocery clerks, people who deliver our packages, and volunteers who help feed our fellow citizens.
We are witnessing consequences of long-term health disparities that America continues to condone. Current hotspots are clustered in cities with high population density where people (usually minorities) lack ready access to health care and live with barriers to preventive care (poor nutritional options and a lack of sufficient primary care). We have underfunded our public health system and allowed politicians to ignore science. When testing was not prioritized initially, we lost the ability to isolate and trace index cases. If we want to honor those people who have died, let’s learn from our experience and change our priorities.
Private practices and health systems alike are being financially devastated. We are seeing massive numbers of people furloughed or laid off, as practices see drastic revenue loss. The transition to virtual health (video visits, remote patient monitoring) has been breath-taking with real implications about future needs for bricks and mortar. These changes in care delivery will be sustained in the future. Practice acquisitions have stopped, planned private equity exits are on hold, and the job market for graduating fellows will be challenging for the next 2 years. Now is a time for our GI societies to come together and find solutions for these problems so that our specialty can remain viable.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Leadership & Professional Development: Make a Friend Before You Need One
“Takers believe in a zero-sum world, and they end up creating one where bosses, colleagues and clients don’t trust them. Givers build deeper and broader relationships—people are rooting for them instead of gunning for them.”
—Adam Grant
To succeed in a hospital, leaders need a generous supply of social and political capital. House officers learn this very quickly, especially when they are relying on other members of the healthcare team to obtain tests and studies for their patients and calling for specialty consultations. To be successful and efficient, building relationships and trust is key. Such capital, unfortunately, takes time to develop. Therefore, healthcare leaders and clinicians at all levels of training need to make an everyday investment of goodwill and friendliness with those they encounter. The dividends may be slow in coming, but they are substantial and sustained. Friends give you the benefit of the doubt—and help you when you are most in need.
Having friends (or friendly colleagues) at work is beneficial both professionally and personally. The benefits of social interactions have been studied for years and even more so in recent times with the dramatic increase in the use of handheld devices. Eye contact between casual acquaintances passing each other in the hallway is replaced with eyes focused downward on smartphones. The result? We are becoming more socially isolated. Our personal solution? When we see professional colleagues (or patients and families in the hallways of our hospital), we nod in acknowledgement with appropriate eye contact and say “Good morning” or “Hello” even if we don’t know them—even if their eyes are focused on their devices as they walk past you in the hallway. You get a gold star if you remember the names of the professional colleagues you see frequently in the hallways or around the hospital.
This isn’t soft science; it’s backed by hard data. When we conduct site visits of different hospitals around the country to help them improve their care quality and performance, we informally divide hospitals into two groups: The “How ya doin’?” hospitals vs the “Rec-Ignore” hospitals (in which employees recognize a colleague in the hallway but choose to not acknowledge them). Most prefer to work at a “How ya doin’?” hospital. Being friendly has been linked to increased team spirit and morale, knowledge sharing, trust, prevention of burnout, and sense of a positive working environment. It also makes you feel better about yourself—and makes other people feel similarly as well.
We’ll share an example from a search for a new department chair. The dean went on reverse site visits to meet the two finalists in their home institutions and asked them for tours of their hospitals. Candidate A walked around and it seemed like everyone knew her. She smiled and said hello to the people she came in contact with during the tour. Not so for candidate B—just the opposite. Guess which candidate the dean hired?
Put away your phone, interact with your colleagues, and learn to make small talk, and not just with your supervisors or peers. Chitchat is an important “social lubricant,” fostering a sense of community and teamwork. It helps bring down the divides that come from organizational hierarchies. It helps endear you to your staff.
Developing a reputation as a nice person who is quick with a smile and even quicker with a “How ya doin’?” pays off in the end. This reputation also makes it easier to give bad news, something that all leaders must do at some point. So make a friend before you need one—it usually will pay dividends.
“Takers believe in a zero-sum world, and they end up creating one where bosses, colleagues and clients don’t trust them. Givers build deeper and broader relationships—people are rooting for them instead of gunning for them.”
—Adam Grant
To succeed in a hospital, leaders need a generous supply of social and political capital. House officers learn this very quickly, especially when they are relying on other members of the healthcare team to obtain tests and studies for their patients and calling for specialty consultations. To be successful and efficient, building relationships and trust is key. Such capital, unfortunately, takes time to develop. Therefore, healthcare leaders and clinicians at all levels of training need to make an everyday investment of goodwill and friendliness with those they encounter. The dividends may be slow in coming, but they are substantial and sustained. Friends give you the benefit of the doubt—and help you when you are most in need.
Having friends (or friendly colleagues) at work is beneficial both professionally and personally. The benefits of social interactions have been studied for years and even more so in recent times with the dramatic increase in the use of handheld devices. Eye contact between casual acquaintances passing each other in the hallway is replaced with eyes focused downward on smartphones. The result? We are becoming more socially isolated. Our personal solution? When we see professional colleagues (or patients and families in the hallways of our hospital), we nod in acknowledgement with appropriate eye contact and say “Good morning” or “Hello” even if we don’t know them—even if their eyes are focused on their devices as they walk past you in the hallway. You get a gold star if you remember the names of the professional colleagues you see frequently in the hallways or around the hospital.
This isn’t soft science; it’s backed by hard data. When we conduct site visits of different hospitals around the country to help them improve their care quality and performance, we informally divide hospitals into two groups: The “How ya doin’?” hospitals vs the “Rec-Ignore” hospitals (in which employees recognize a colleague in the hallway but choose to not acknowledge them). Most prefer to work at a “How ya doin’?” hospital. Being friendly has been linked to increased team spirit and morale, knowledge sharing, trust, prevention of burnout, and sense of a positive working environment. It also makes you feel better about yourself—and makes other people feel similarly as well.
We’ll share an example from a search for a new department chair. The dean went on reverse site visits to meet the two finalists in their home institutions and asked them for tours of their hospitals. Candidate A walked around and it seemed like everyone knew her. She smiled and said hello to the people she came in contact with during the tour. Not so for candidate B—just the opposite. Guess which candidate the dean hired?
Put away your phone, interact with your colleagues, and learn to make small talk, and not just with your supervisors or peers. Chitchat is an important “social lubricant,” fostering a sense of community and teamwork. It helps bring down the divides that come from organizational hierarchies. It helps endear you to your staff.
Developing a reputation as a nice person who is quick with a smile and even quicker with a “How ya doin’?” pays off in the end. This reputation also makes it easier to give bad news, something that all leaders must do at some point. So make a friend before you need one—it usually will pay dividends.
“Takers believe in a zero-sum world, and they end up creating one where bosses, colleagues and clients don’t trust them. Givers build deeper and broader relationships—people are rooting for them instead of gunning for them.”
—Adam Grant
To succeed in a hospital, leaders need a generous supply of social and political capital. House officers learn this very quickly, especially when they are relying on other members of the healthcare team to obtain tests and studies for their patients and calling for specialty consultations. To be successful and efficient, building relationships and trust is key. Such capital, unfortunately, takes time to develop. Therefore, healthcare leaders and clinicians at all levels of training need to make an everyday investment of goodwill and friendliness with those they encounter. The dividends may be slow in coming, but they are substantial and sustained. Friends give you the benefit of the doubt—and help you when you are most in need.
Having friends (or friendly colleagues) at work is beneficial both professionally and personally. The benefits of social interactions have been studied for years and even more so in recent times with the dramatic increase in the use of handheld devices. Eye contact between casual acquaintances passing each other in the hallway is replaced with eyes focused downward on smartphones. The result? We are becoming more socially isolated. Our personal solution? When we see professional colleagues (or patients and families in the hallways of our hospital), we nod in acknowledgement with appropriate eye contact and say “Good morning” or “Hello” even if we don’t know them—even if their eyes are focused on their devices as they walk past you in the hallway. You get a gold star if you remember the names of the professional colleagues you see frequently in the hallways or around the hospital.
This isn’t soft science; it’s backed by hard data. When we conduct site visits of different hospitals around the country to help them improve their care quality and performance, we informally divide hospitals into two groups: The “How ya doin’?” hospitals vs the “Rec-Ignore” hospitals (in which employees recognize a colleague in the hallway but choose to not acknowledge them). Most prefer to work at a “How ya doin’?” hospital. Being friendly has been linked to increased team spirit and morale, knowledge sharing, trust, prevention of burnout, and sense of a positive working environment. It also makes you feel better about yourself—and makes other people feel similarly as well.
We’ll share an example from a search for a new department chair. The dean went on reverse site visits to meet the two finalists in their home institutions and asked them for tours of their hospitals. Candidate A walked around and it seemed like everyone knew her. She smiled and said hello to the people she came in contact with during the tour. Not so for candidate B—just the opposite. Guess which candidate the dean hired?
Put away your phone, interact with your colleagues, and learn to make small talk, and not just with your supervisors or peers. Chitchat is an important “social lubricant,” fostering a sense of community and teamwork. It helps bring down the divides that come from organizational hierarchies. It helps endear you to your staff.
Developing a reputation as a nice person who is quick with a smile and even quicker with a “How ya doin’?” pays off in the end. This reputation also makes it easier to give bad news, something that all leaders must do at some point. So make a friend before you need one—it usually will pay dividends.
Yale’s COVID-19 inpatient protocol: Hydroxychloroquine plus/minus tocilizumab
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
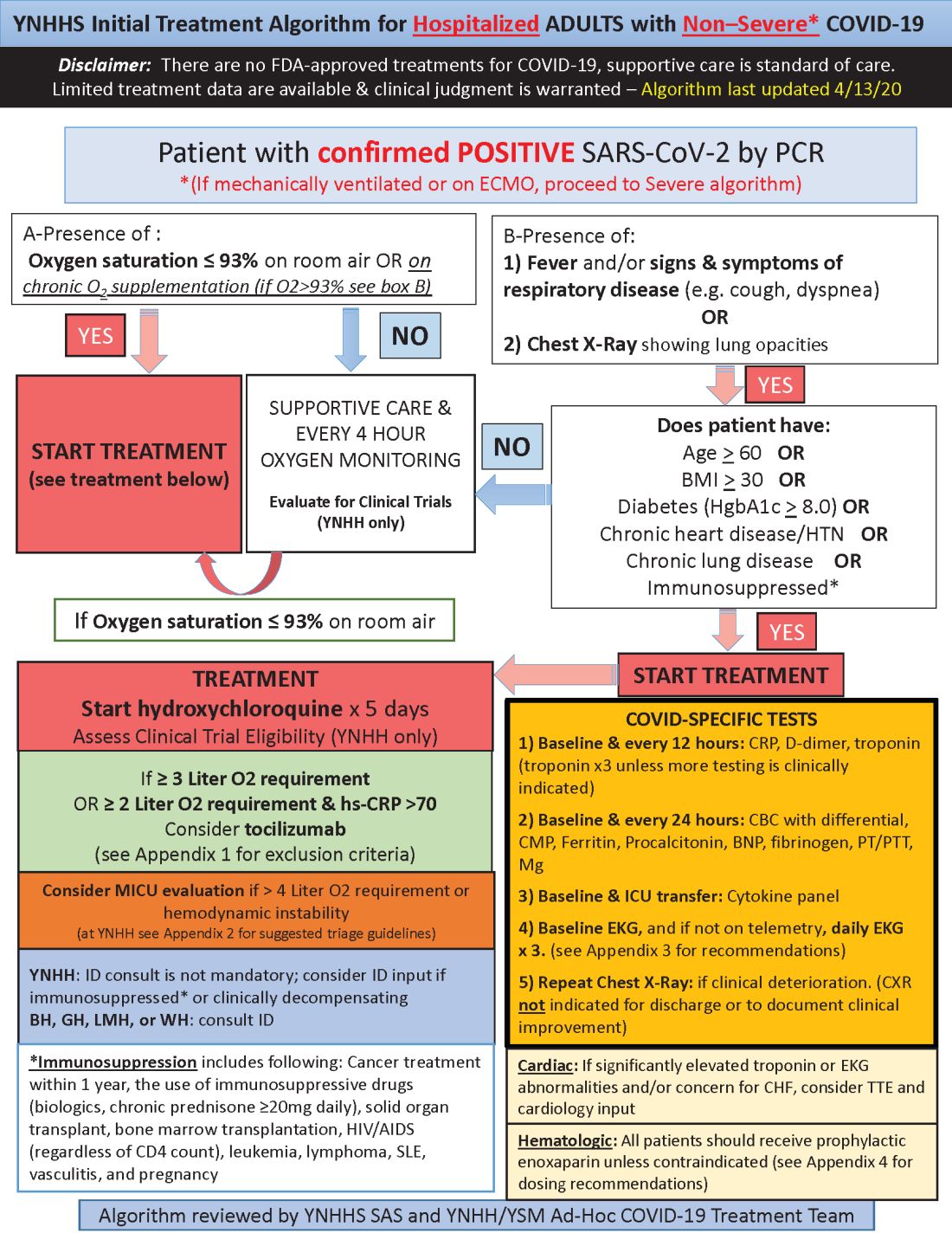
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
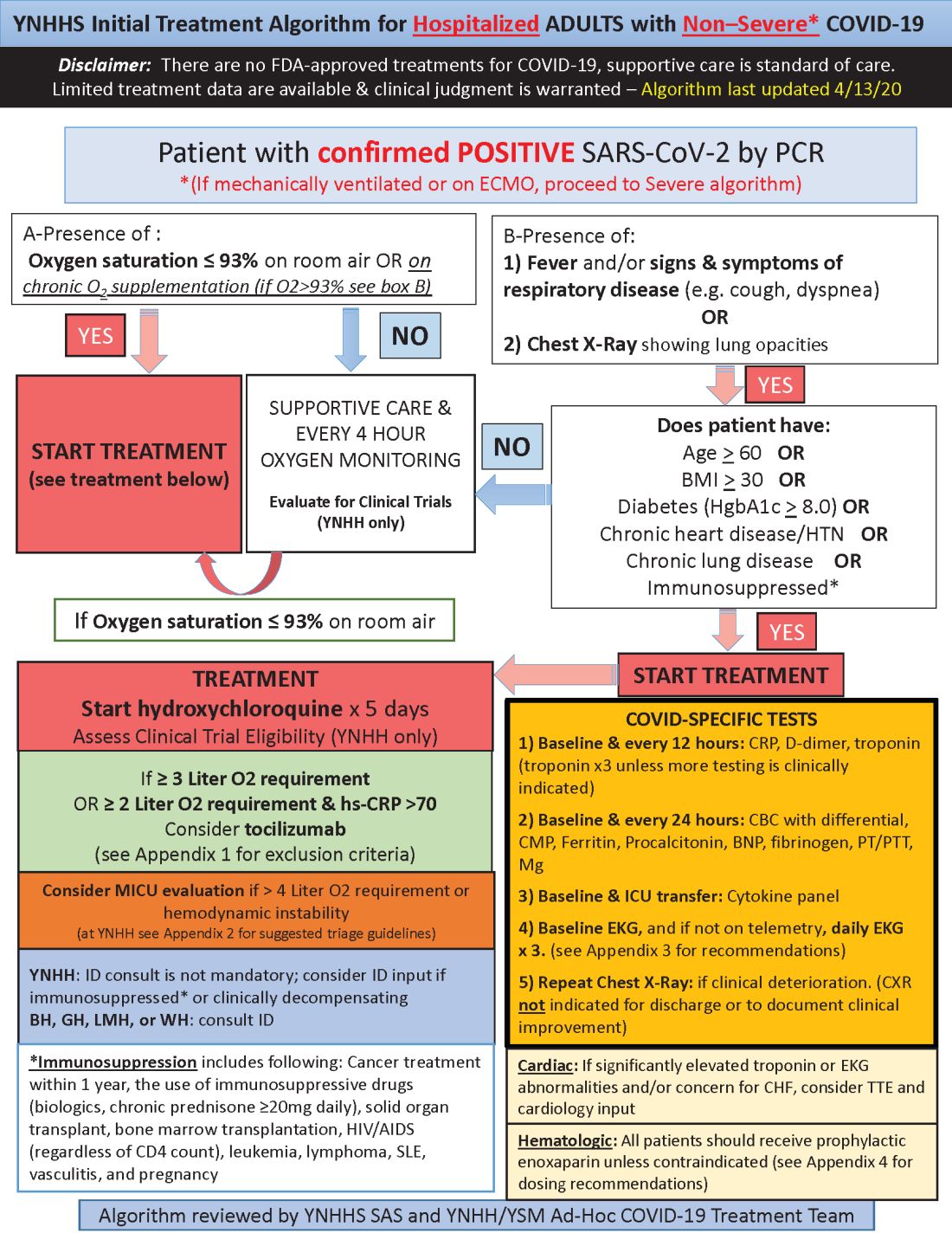
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
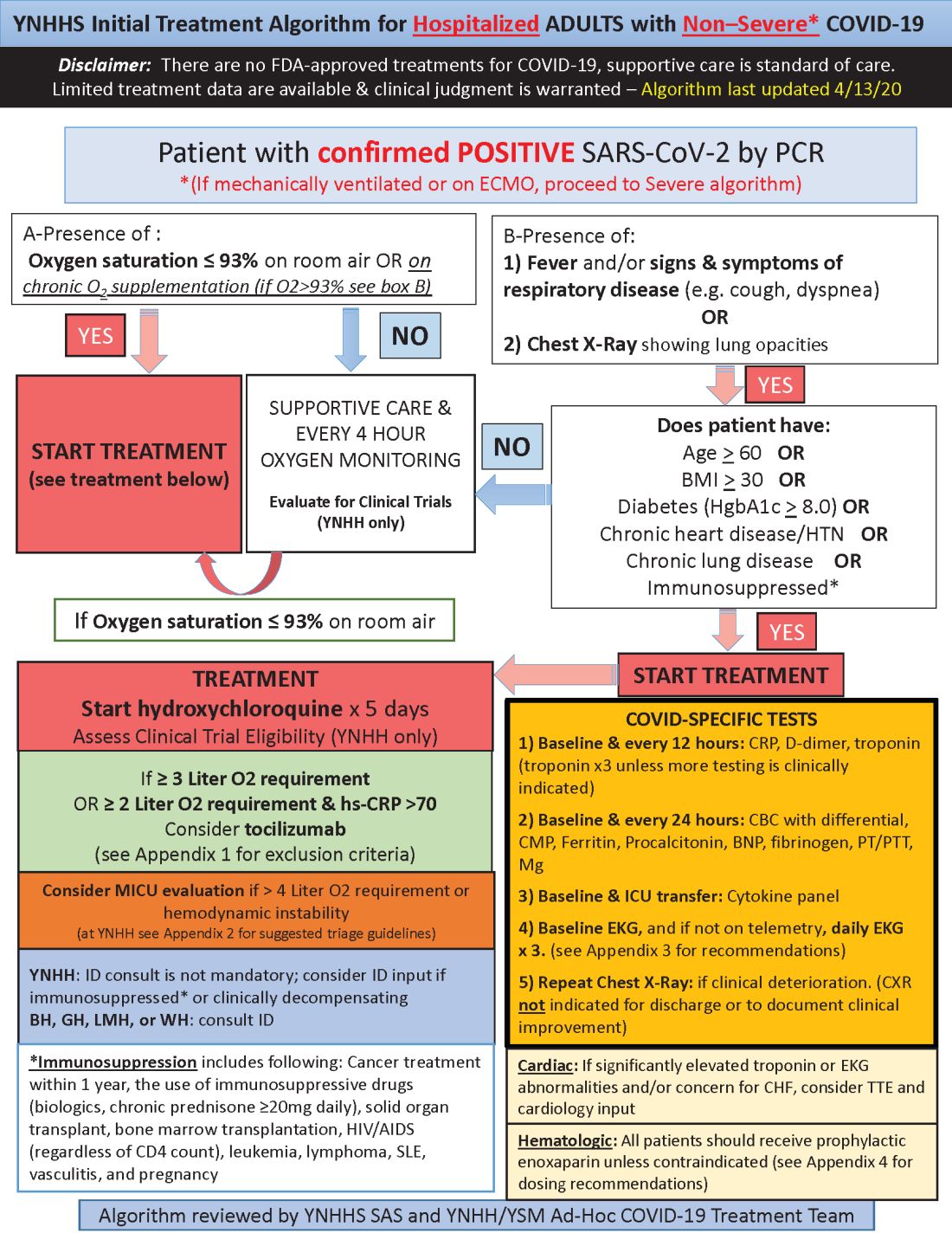
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.










