User login
Ukraine war likely to cause infection outbreaks that will spread beyond borders
Every day we see stark images of the war in Ukraine – bombed-out buildings, explosions, and bodies lying in the streets. But there’s another, less visible war against the bacteria and viruses that are gathering their forces together. They, too, will infect parts of the population and may spread throughout Europe. Here’s what Ukrainians, and their neighbors, are facing on the infectious disease front.
Andrey Zinchuk, MD, MHS, a pulmonary/critical care physician at Yale and a native of Ukraine who immigrated to the U.S. at the age of 14 with his family, set the background for understanding this crisis. He said that TB and HIV rates in Ukraine have long been especially high, even before the current conflict: “Part of the challenge of the health care system in Ukraine is that it’s difficult to maintain a steady policy because of political instability,” he said. “We’ve had three revolutions in the last 20 years,” not counting the current Russian invasion.
The first was the breakup of the Soviet Union, which led to “an epidemic of people with HIV, hepatitis, and opioid use.” Next was the Orange Revolution in 2004 over fraud during a presidential election. In 2014 came the Maiden Revolution, after the government chose closer ties to Russia rather than Europe. Then-president Viktor Yanukovych fled to Russia.
“That’s when Russia annexed Crimea. There was essentially infiltration in Russian propaganda in the east of the country,” Dr. Zinchuk said. “This helped the Russians manufacture uprisings there to create a separatist state (the Luhansk and Donetsk People’s Republics) which were mostly Russian-speaking parts of the country,” an area known as the Donbas. This resulted in a war in eastern Ukraine that began 2014, with more than 10,000 deaths.
After the 2014 revolution, Dr. Zinchuk said, “There was a tremendous change in the way ... medical care was provided, and tremendous growth and stability in the medical supply for those chronic medical conditions.”
Nevertheless, health care expenditures in Ukraine have been quite low. Even before the current conflict, Dr. Zinchuk noted, annual health care expenditures in Ukraine were about $600 per capita. In comparison, it’s about $4,500 per person in Germany and $12,530 in the United States.
Despite those low per-capita expenditures in Ukraine, access to medicines – such as insulin for diabetes and antibiotics for tuberculosis – was stable before the war. But now, Dr. Zinchuk said, his aunt and uncle have had to flee Kyiv for the countryside and, while safe, they have “no plumbing and have to heat the house by burning firewood.” More significantly, their supply of medicine is unstable.
Asked what infections are of most immediate concern, Sten Vermund, MD, PhD, Dean of the Yale School of Public Health, told this news organization that it was “diarrheal diseases, especially in kids ... The water supply [of Mariupol] is no longer potable, but people are drinking it anyway. And sewage systems are destroyed, and raw sewage is just released into the rivers and streams. So the whole family of diarrheal diseases and war are bedfellows. So are respiratory diseases, whenever we have mass migrations and mixing of ... homeless people and transients.”
There is one notable piece of good news that may reduce the spread of infectious diseases. Unlike the aftermath of World War II or the ongoing conflicts in the Middle East, Africa, and South Asia, refugees from the war in Ukraine are being taken into individual households throughout Poland, Germany, and other countries and are not being held in large displaced-persons camps. Dr. Vermund added, “The Syrian refugee camps in Lebanon are just tent camps with a million, 2 million people in them ... In theory, what the Poles are doing is a good thing from the point of view of preventing the spread of infection.”
One way of examining infections in war zones is by considering them based on how they are spread.
Respiratory infections
Although not as high on the list of concerns as TB or HIV, COVID-19 remains a big problem for infectious disease experts. Last fall, Ukraine ranked just behind the U.S. and Russia in deaths from COVID and in the top 10 in infections. Despite these dismal numbers, only 35% of people had completed the initial vaccination series.
The same conditions that fuel TB and COVID – crowding, especially in poorly ventilated settings – could lead to another measles outbreak. One occurred in Ukraine from 2017-2020, resulting in more than 115,000 cases. Even though the immunization rate for measles has now reached about 80%, the CDC considers Ukraine at high risk for another large outbreak since measles is so highly contagious.
According to the European Centre for Disease Prevention and Control (ECDC), Ukraine reported the second-highest number of TB cases in Europe (28,539). It is also one of the top 10 countries globally with the highest burden of multidrug-resistant tuberculosis (MDR-TB) – 27%. Equally disturbing is its ranking as having the second-highest rate of HIV/TB co-infection (26%) even before the war. Experts say war is a perfect breeding ground for TB, since starvation and overcrowding in poorly ventilated spaces encourages its spread.
Before the war, COVID had already caused severe disruptions in TB diagnosis and treatment access in Ukraine, and the World Health Organization suggested that the pandemic has set back efforts to end TB by more than a decade.
Drug-resistant TB has been one of the biggest worries. In their report on TB in Ukraine, British tuberculosis experts Tom Wingfield, MBChB, PhD, from the Liverpool School of Tropical Medicine, and Jessica Potter MBBCh, PhD, from Queen Mary University of London, pointed out that “drug resistance thrives on fractured health systems and sporadic medicine supply.”
Frederick Altice, MD, a Yale epidemiologist and addiction specialist, noted, “[if] medication for tuberculosis is discontinued, that not only causes potential recurrence of disease but multidrug-resistant TB disease,” and patients could become infectious again.
Dr. Wingfield expressed concern that people will not seek care because they see it as unaffordable, although he told this news organization that he’s impressed at the Polish government’s efforts to ensure care. Especially with the triad of HIV, TB, and opioid use, Dr. Wingfield and Dr. Potter emphasized that these problems reflect the social determinants of health – “the experiences and conditions in which people live.” These medical conditions are all quite treatable with support, and once treated they pose no risk to others.
HIV and opioid use
Before the war, an estimated 260,000 people were living with HIV in Ukraine. Their rate of new HIV diagnoses in 2017 was second highest in the world – 37 out of every 100,000, exceeded only by Russia, with 71 out of 100,000.
Dr. Vermund told this news organization that “when Crimea was seized by the Russians in 2014, there was an immediate crisis among injection drug users who were in drug treatment programs, because it’s illegal in Russia to use buprenorphine or methadone ... So immediately, those programs were shut down, and all the drug users who were holding jobs, supporting their families, were withdrawing from their addictions and searching for a replacement, which was illegal heroin.”
Dr. Altice added that of 800 patients in the region who had to go cold turkey, “ten percent were dead within 6 months. Dependent on unreliable street drugs, some overdosed or committed suicide because they could not get treatment. They went through terrible withdrawal and stress.”
And as they relapsed, the HIV rate soared. “Fifty percent of the methadone patients have got HIV,” Dr. Altice said, “and if they stop taking the methadone, they’re going to stop taking their HIV medications as well. Their lives will become chaotic and very destabilized.”
This experience may soon repeat itself. There were two methadone factories in Ukraine – in Odessa and Kharkiv – that are now shut down by the war. Although there are efforts to import methadone and many other drugs, supply chain issues are “devastating,” Dr. Altice said. “If their medication for tuberculosis is discontinued, that not only causes potential recurrence of disease but multidrug-resistant TB disease,” and they could become infectious again. “[With a] lack of medication, lack of sterile syringes, people will be sharing syringes; they’ll be desperate. So as the desperation level goes up, the risk environment goes up, so that people have decreased opportunities to protect themselves,” and there will be an explosion in HIV.
Dr. Altice observed that with the immigration to Poland and the west, many Ukrainian refugees “are relying on the kindness of strangers.” They are likely to be “fearful to disclose either their HIV or their TB treatment status,” being afraid of being regarded as modern-day lepers, even though they are likely not infectious. Both Dr. Altice and Dr. Potter emphasized the need for the governments of Poland and other receiving countries to provide the refugees with “reassurance that their health information will not be shared with others.” Dr. Altice emphasized that “this is one of the things that I would say that these other countries have to get right.”
Dr. Potter echoed that, noting that extraordinary care needs to be taken so that shared information is not used for deportation.
When refugees are housed with rural hosts, transportation problems sometimes arise, creating major barriers to accessing care and treatment. In particular, refugees with TB, HIV, and addiction who are placed in small, remote locations may have difficulty securing transportation to sites where treatments for their complex illnesses are available, including specialists and medications.
Ukrainian-born microbiologist Olena Rzhepishevska, PhD, of Umeå University in Sweden, said in an interview that a network of European TB researchers have developed a database on TBNet where patients with TB can be specifically placed with understanding and helpful hosts outside of Ukraine. They can receive housing and medication through this network.
So far, 4 million Ukrainians have fled the country and millions more have been displaced internally. Dr. Altice noted that there is an “increased vulnerability beyond the vulnerability that they already [have] just by being a refugee” that we generally don’t recognize. Additionally, Poland and Hungary are not very progressive about methadone therapy nor are those nations well-equipped to provide it.
Dr. Altice explained that even within Ukraine, those who want to move to better their chance of getting their methadone are then at risk of being conscripted. He spoke of the grave calculations men must make, choosing to become internally displaced and risk conscription or losing life-saving methadone or medicines for HIV or TB.
One other unfortunate consequence of war might be a spike in rape, sexual abuse, prostitution, unwanted pregnancies, HIV, and sexually transmitted infections.
There were an estimated 80,100 female sex workers in Ukraine in 2016, with 5.2% HIV positive. In times of war, with no home or income, some women turn to prostitution to survive. Others are victims of sex trafficking, both within Ukraine and as refugees. The Russian invasion increased the risks of a surge in HIV infections, unwanted pregnancies, and abortions. Women who find themselves pregnant due to rape (a common tool of war) or sex trafficking may also struggle to access safe abortions. Poland, for example, has severe restrictions on abortion, and Ukrainian women may turn to unsafe, back-alley abortions, with their resulting high risk of infection.
Waterborne infections
Another concern involves waterborne infections. In addition to the common diarrheal diseases such as E coli, which can be expected from poor sanitation, polio is a significant concern. In the fall of 2021, Ukraine had an outbreak of vaccine-derived polio, with two cases of paralysis and 20 additional cases. As polio only paralyzes 1 person in 200 of those infected, many other cases were likely undetected. A vaccination campaign was just beginning when the war began.
Wound infections and antimicrobial resistance
The ECDC also reports high rates of antimicrobial resistance (AMR) in Ukraine, particularly involving common gram-negative bacteria, including Escherichia coli (53% resistance to third-generation cephalosporins), Klebsiella pneumoniae (54% resistance to carbapenems), and Acinetobacter spp. (77% resistance to carbapenems). Because of this, they recommend refugees requiring hospital admission be isolated on admission and screened for AMR. These AMR often complicate traumatic injuries of war.
Prevention
Many of these potential problems stemming from the war in Ukraine and the displacement of millions of its citizens can be avoided.
Attempts are being made to immunize refugees. WHO has made working with countries receiving refugees a priority, particularly by vaccinating children against measles, rubella, and COVID. The European Union has also purchased vaccines for polio and tuberculosis.
But Russia has waged an active anti-vaccine campaign against COVID in Ukraine, while at the same time advocating for vaccines in Russia. According to UNICEF, other countries with relatively low vaccination rates and high vaccine skepticism – Moldova, Romania, and Bulgaria – are at higher risk of polio and measles than those with high vaccination levels.
The continuing war in Ukraine has exacerbated the medical challenges the citizens of Ukraine face at home and as refugees fleeing to neighboring countries. Improving communication among agencies and governments and building trust with the refugees could go a long way toward limiting the spread of preventable infectious diseases as a result of the war.
Continuing to try to keep supply chains open within Ukraine and ensuring adequate supplies of medications and vaccines to refugees will also be essential. But, of course, the better solution is to end the war.
Dr. Altice, Dr. Potter, Dr. Wingfield, Dr. Vermund, and Dr. Zinchuk all report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Every day we see stark images of the war in Ukraine – bombed-out buildings, explosions, and bodies lying in the streets. But there’s another, less visible war against the bacteria and viruses that are gathering their forces together. They, too, will infect parts of the population and may spread throughout Europe. Here’s what Ukrainians, and their neighbors, are facing on the infectious disease front.
Andrey Zinchuk, MD, MHS, a pulmonary/critical care physician at Yale and a native of Ukraine who immigrated to the U.S. at the age of 14 with his family, set the background for understanding this crisis. He said that TB and HIV rates in Ukraine have long been especially high, even before the current conflict: “Part of the challenge of the health care system in Ukraine is that it’s difficult to maintain a steady policy because of political instability,” he said. “We’ve had three revolutions in the last 20 years,” not counting the current Russian invasion.
The first was the breakup of the Soviet Union, which led to “an epidemic of people with HIV, hepatitis, and opioid use.” Next was the Orange Revolution in 2004 over fraud during a presidential election. In 2014 came the Maiden Revolution, after the government chose closer ties to Russia rather than Europe. Then-president Viktor Yanukovych fled to Russia.
“That’s when Russia annexed Crimea. There was essentially infiltration in Russian propaganda in the east of the country,” Dr. Zinchuk said. “This helped the Russians manufacture uprisings there to create a separatist state (the Luhansk and Donetsk People’s Republics) which were mostly Russian-speaking parts of the country,” an area known as the Donbas. This resulted in a war in eastern Ukraine that began 2014, with more than 10,000 deaths.
After the 2014 revolution, Dr. Zinchuk said, “There was a tremendous change in the way ... medical care was provided, and tremendous growth and stability in the medical supply for those chronic medical conditions.”
Nevertheless, health care expenditures in Ukraine have been quite low. Even before the current conflict, Dr. Zinchuk noted, annual health care expenditures in Ukraine were about $600 per capita. In comparison, it’s about $4,500 per person in Germany and $12,530 in the United States.
Despite those low per-capita expenditures in Ukraine, access to medicines – such as insulin for diabetes and antibiotics for tuberculosis – was stable before the war. But now, Dr. Zinchuk said, his aunt and uncle have had to flee Kyiv for the countryside and, while safe, they have “no plumbing and have to heat the house by burning firewood.” More significantly, their supply of medicine is unstable.
Asked what infections are of most immediate concern, Sten Vermund, MD, PhD, Dean of the Yale School of Public Health, told this news organization that it was “diarrheal diseases, especially in kids ... The water supply [of Mariupol] is no longer potable, but people are drinking it anyway. And sewage systems are destroyed, and raw sewage is just released into the rivers and streams. So the whole family of diarrheal diseases and war are bedfellows. So are respiratory diseases, whenever we have mass migrations and mixing of ... homeless people and transients.”
There is one notable piece of good news that may reduce the spread of infectious diseases. Unlike the aftermath of World War II or the ongoing conflicts in the Middle East, Africa, and South Asia, refugees from the war in Ukraine are being taken into individual households throughout Poland, Germany, and other countries and are not being held in large displaced-persons camps. Dr. Vermund added, “The Syrian refugee camps in Lebanon are just tent camps with a million, 2 million people in them ... In theory, what the Poles are doing is a good thing from the point of view of preventing the spread of infection.”
One way of examining infections in war zones is by considering them based on how they are spread.
Respiratory infections
Although not as high on the list of concerns as TB or HIV, COVID-19 remains a big problem for infectious disease experts. Last fall, Ukraine ranked just behind the U.S. and Russia in deaths from COVID and in the top 10 in infections. Despite these dismal numbers, only 35% of people had completed the initial vaccination series.
The same conditions that fuel TB and COVID – crowding, especially in poorly ventilated settings – could lead to another measles outbreak. One occurred in Ukraine from 2017-2020, resulting in more than 115,000 cases. Even though the immunization rate for measles has now reached about 80%, the CDC considers Ukraine at high risk for another large outbreak since measles is so highly contagious.
According to the European Centre for Disease Prevention and Control (ECDC), Ukraine reported the second-highest number of TB cases in Europe (28,539). It is also one of the top 10 countries globally with the highest burden of multidrug-resistant tuberculosis (MDR-TB) – 27%. Equally disturbing is its ranking as having the second-highest rate of HIV/TB co-infection (26%) even before the war. Experts say war is a perfect breeding ground for TB, since starvation and overcrowding in poorly ventilated spaces encourages its spread.
Before the war, COVID had already caused severe disruptions in TB diagnosis and treatment access in Ukraine, and the World Health Organization suggested that the pandemic has set back efforts to end TB by more than a decade.
Drug-resistant TB has been one of the biggest worries. In their report on TB in Ukraine, British tuberculosis experts Tom Wingfield, MBChB, PhD, from the Liverpool School of Tropical Medicine, and Jessica Potter MBBCh, PhD, from Queen Mary University of London, pointed out that “drug resistance thrives on fractured health systems and sporadic medicine supply.”
Frederick Altice, MD, a Yale epidemiologist and addiction specialist, noted, “[if] medication for tuberculosis is discontinued, that not only causes potential recurrence of disease but multidrug-resistant TB disease,” and patients could become infectious again.
Dr. Wingfield expressed concern that people will not seek care because they see it as unaffordable, although he told this news organization that he’s impressed at the Polish government’s efforts to ensure care. Especially with the triad of HIV, TB, and opioid use, Dr. Wingfield and Dr. Potter emphasized that these problems reflect the social determinants of health – “the experiences and conditions in which people live.” These medical conditions are all quite treatable with support, and once treated they pose no risk to others.
HIV and opioid use
Before the war, an estimated 260,000 people were living with HIV in Ukraine. Their rate of new HIV diagnoses in 2017 was second highest in the world – 37 out of every 100,000, exceeded only by Russia, with 71 out of 100,000.
Dr. Vermund told this news organization that “when Crimea was seized by the Russians in 2014, there was an immediate crisis among injection drug users who were in drug treatment programs, because it’s illegal in Russia to use buprenorphine or methadone ... So immediately, those programs were shut down, and all the drug users who were holding jobs, supporting their families, were withdrawing from their addictions and searching for a replacement, which was illegal heroin.”
Dr. Altice added that of 800 patients in the region who had to go cold turkey, “ten percent were dead within 6 months. Dependent on unreliable street drugs, some overdosed or committed suicide because they could not get treatment. They went through terrible withdrawal and stress.”
And as they relapsed, the HIV rate soared. “Fifty percent of the methadone patients have got HIV,” Dr. Altice said, “and if they stop taking the methadone, they’re going to stop taking their HIV medications as well. Their lives will become chaotic and very destabilized.”
This experience may soon repeat itself. There were two methadone factories in Ukraine – in Odessa and Kharkiv – that are now shut down by the war. Although there are efforts to import methadone and many other drugs, supply chain issues are “devastating,” Dr. Altice said. “If their medication for tuberculosis is discontinued, that not only causes potential recurrence of disease but multidrug-resistant TB disease,” and they could become infectious again. “[With a] lack of medication, lack of sterile syringes, people will be sharing syringes; they’ll be desperate. So as the desperation level goes up, the risk environment goes up, so that people have decreased opportunities to protect themselves,” and there will be an explosion in HIV.
Dr. Altice observed that with the immigration to Poland and the west, many Ukrainian refugees “are relying on the kindness of strangers.” They are likely to be “fearful to disclose either their HIV or their TB treatment status,” being afraid of being regarded as modern-day lepers, even though they are likely not infectious. Both Dr. Altice and Dr. Potter emphasized the need for the governments of Poland and other receiving countries to provide the refugees with “reassurance that their health information will not be shared with others.” Dr. Altice emphasized that “this is one of the things that I would say that these other countries have to get right.”
Dr. Potter echoed that, noting that extraordinary care needs to be taken so that shared information is not used for deportation.
When refugees are housed with rural hosts, transportation problems sometimes arise, creating major barriers to accessing care and treatment. In particular, refugees with TB, HIV, and addiction who are placed in small, remote locations may have difficulty securing transportation to sites where treatments for their complex illnesses are available, including specialists and medications.
Ukrainian-born microbiologist Olena Rzhepishevska, PhD, of Umeå University in Sweden, said in an interview that a network of European TB researchers have developed a database on TBNet where patients with TB can be specifically placed with understanding and helpful hosts outside of Ukraine. They can receive housing and medication through this network.
So far, 4 million Ukrainians have fled the country and millions more have been displaced internally. Dr. Altice noted that there is an “increased vulnerability beyond the vulnerability that they already [have] just by being a refugee” that we generally don’t recognize. Additionally, Poland and Hungary are not very progressive about methadone therapy nor are those nations well-equipped to provide it.
Dr. Altice explained that even within Ukraine, those who want to move to better their chance of getting their methadone are then at risk of being conscripted. He spoke of the grave calculations men must make, choosing to become internally displaced and risk conscription or losing life-saving methadone or medicines for HIV or TB.
One other unfortunate consequence of war might be a spike in rape, sexual abuse, prostitution, unwanted pregnancies, HIV, and sexually transmitted infections.
There were an estimated 80,100 female sex workers in Ukraine in 2016, with 5.2% HIV positive. In times of war, with no home or income, some women turn to prostitution to survive. Others are victims of sex trafficking, both within Ukraine and as refugees. The Russian invasion increased the risks of a surge in HIV infections, unwanted pregnancies, and abortions. Women who find themselves pregnant due to rape (a common tool of war) or sex trafficking may also struggle to access safe abortions. Poland, for example, has severe restrictions on abortion, and Ukrainian women may turn to unsafe, back-alley abortions, with their resulting high risk of infection.
Waterborne infections
Another concern involves waterborne infections. In addition to the common diarrheal diseases such as E coli, which can be expected from poor sanitation, polio is a significant concern. In the fall of 2021, Ukraine had an outbreak of vaccine-derived polio, with two cases of paralysis and 20 additional cases. As polio only paralyzes 1 person in 200 of those infected, many other cases were likely undetected. A vaccination campaign was just beginning when the war began.
Wound infections and antimicrobial resistance
The ECDC also reports high rates of antimicrobial resistance (AMR) in Ukraine, particularly involving common gram-negative bacteria, including Escherichia coli (53% resistance to third-generation cephalosporins), Klebsiella pneumoniae (54% resistance to carbapenems), and Acinetobacter spp. (77% resistance to carbapenems). Because of this, they recommend refugees requiring hospital admission be isolated on admission and screened for AMR. These AMR often complicate traumatic injuries of war.
Prevention
Many of these potential problems stemming from the war in Ukraine and the displacement of millions of its citizens can be avoided.
Attempts are being made to immunize refugees. WHO has made working with countries receiving refugees a priority, particularly by vaccinating children against measles, rubella, and COVID. The European Union has also purchased vaccines for polio and tuberculosis.
But Russia has waged an active anti-vaccine campaign against COVID in Ukraine, while at the same time advocating for vaccines in Russia. According to UNICEF, other countries with relatively low vaccination rates and high vaccine skepticism – Moldova, Romania, and Bulgaria – are at higher risk of polio and measles than those with high vaccination levels.
The continuing war in Ukraine has exacerbated the medical challenges the citizens of Ukraine face at home and as refugees fleeing to neighboring countries. Improving communication among agencies and governments and building trust with the refugees could go a long way toward limiting the spread of preventable infectious diseases as a result of the war.
Continuing to try to keep supply chains open within Ukraine and ensuring adequate supplies of medications and vaccines to refugees will also be essential. But, of course, the better solution is to end the war.
Dr. Altice, Dr. Potter, Dr. Wingfield, Dr. Vermund, and Dr. Zinchuk all report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Every day we see stark images of the war in Ukraine – bombed-out buildings, explosions, and bodies lying in the streets. But there’s another, less visible war against the bacteria and viruses that are gathering their forces together. They, too, will infect parts of the population and may spread throughout Europe. Here’s what Ukrainians, and their neighbors, are facing on the infectious disease front.
Andrey Zinchuk, MD, MHS, a pulmonary/critical care physician at Yale and a native of Ukraine who immigrated to the U.S. at the age of 14 with his family, set the background for understanding this crisis. He said that TB and HIV rates in Ukraine have long been especially high, even before the current conflict: “Part of the challenge of the health care system in Ukraine is that it’s difficult to maintain a steady policy because of political instability,” he said. “We’ve had three revolutions in the last 20 years,” not counting the current Russian invasion.
The first was the breakup of the Soviet Union, which led to “an epidemic of people with HIV, hepatitis, and opioid use.” Next was the Orange Revolution in 2004 over fraud during a presidential election. In 2014 came the Maiden Revolution, after the government chose closer ties to Russia rather than Europe. Then-president Viktor Yanukovych fled to Russia.
“That’s when Russia annexed Crimea. There was essentially infiltration in Russian propaganda in the east of the country,” Dr. Zinchuk said. “This helped the Russians manufacture uprisings there to create a separatist state (the Luhansk and Donetsk People’s Republics) which were mostly Russian-speaking parts of the country,” an area known as the Donbas. This resulted in a war in eastern Ukraine that began 2014, with more than 10,000 deaths.
After the 2014 revolution, Dr. Zinchuk said, “There was a tremendous change in the way ... medical care was provided, and tremendous growth and stability in the medical supply for those chronic medical conditions.”
Nevertheless, health care expenditures in Ukraine have been quite low. Even before the current conflict, Dr. Zinchuk noted, annual health care expenditures in Ukraine were about $600 per capita. In comparison, it’s about $4,500 per person in Germany and $12,530 in the United States.
Despite those low per-capita expenditures in Ukraine, access to medicines – such as insulin for diabetes and antibiotics for tuberculosis – was stable before the war. But now, Dr. Zinchuk said, his aunt and uncle have had to flee Kyiv for the countryside and, while safe, they have “no plumbing and have to heat the house by burning firewood.” More significantly, their supply of medicine is unstable.
Asked what infections are of most immediate concern, Sten Vermund, MD, PhD, Dean of the Yale School of Public Health, told this news organization that it was “diarrheal diseases, especially in kids ... The water supply [of Mariupol] is no longer potable, but people are drinking it anyway. And sewage systems are destroyed, and raw sewage is just released into the rivers and streams. So the whole family of diarrheal diseases and war are bedfellows. So are respiratory diseases, whenever we have mass migrations and mixing of ... homeless people and transients.”
There is one notable piece of good news that may reduce the spread of infectious diseases. Unlike the aftermath of World War II or the ongoing conflicts in the Middle East, Africa, and South Asia, refugees from the war in Ukraine are being taken into individual households throughout Poland, Germany, and other countries and are not being held in large displaced-persons camps. Dr. Vermund added, “The Syrian refugee camps in Lebanon are just tent camps with a million, 2 million people in them ... In theory, what the Poles are doing is a good thing from the point of view of preventing the spread of infection.”
One way of examining infections in war zones is by considering them based on how they are spread.
Respiratory infections
Although not as high on the list of concerns as TB or HIV, COVID-19 remains a big problem for infectious disease experts. Last fall, Ukraine ranked just behind the U.S. and Russia in deaths from COVID and in the top 10 in infections. Despite these dismal numbers, only 35% of people had completed the initial vaccination series.
The same conditions that fuel TB and COVID – crowding, especially in poorly ventilated settings – could lead to another measles outbreak. One occurred in Ukraine from 2017-2020, resulting in more than 115,000 cases. Even though the immunization rate for measles has now reached about 80%, the CDC considers Ukraine at high risk for another large outbreak since measles is so highly contagious.
According to the European Centre for Disease Prevention and Control (ECDC), Ukraine reported the second-highest number of TB cases in Europe (28,539). It is also one of the top 10 countries globally with the highest burden of multidrug-resistant tuberculosis (MDR-TB) – 27%. Equally disturbing is its ranking as having the second-highest rate of HIV/TB co-infection (26%) even before the war. Experts say war is a perfect breeding ground for TB, since starvation and overcrowding in poorly ventilated spaces encourages its spread.
Before the war, COVID had already caused severe disruptions in TB diagnosis and treatment access in Ukraine, and the World Health Organization suggested that the pandemic has set back efforts to end TB by more than a decade.
Drug-resistant TB has been one of the biggest worries. In their report on TB in Ukraine, British tuberculosis experts Tom Wingfield, MBChB, PhD, from the Liverpool School of Tropical Medicine, and Jessica Potter MBBCh, PhD, from Queen Mary University of London, pointed out that “drug resistance thrives on fractured health systems and sporadic medicine supply.”
Frederick Altice, MD, a Yale epidemiologist and addiction specialist, noted, “[if] medication for tuberculosis is discontinued, that not only causes potential recurrence of disease but multidrug-resistant TB disease,” and patients could become infectious again.
Dr. Wingfield expressed concern that people will not seek care because they see it as unaffordable, although he told this news organization that he’s impressed at the Polish government’s efforts to ensure care. Especially with the triad of HIV, TB, and opioid use, Dr. Wingfield and Dr. Potter emphasized that these problems reflect the social determinants of health – “the experiences and conditions in which people live.” These medical conditions are all quite treatable with support, and once treated they pose no risk to others.
HIV and opioid use
Before the war, an estimated 260,000 people were living with HIV in Ukraine. Their rate of new HIV diagnoses in 2017 was second highest in the world – 37 out of every 100,000, exceeded only by Russia, with 71 out of 100,000.
Dr. Vermund told this news organization that “when Crimea was seized by the Russians in 2014, there was an immediate crisis among injection drug users who were in drug treatment programs, because it’s illegal in Russia to use buprenorphine or methadone ... So immediately, those programs were shut down, and all the drug users who were holding jobs, supporting their families, were withdrawing from their addictions and searching for a replacement, which was illegal heroin.”
Dr. Altice added that of 800 patients in the region who had to go cold turkey, “ten percent were dead within 6 months. Dependent on unreliable street drugs, some overdosed or committed suicide because they could not get treatment. They went through terrible withdrawal and stress.”
And as they relapsed, the HIV rate soared. “Fifty percent of the methadone patients have got HIV,” Dr. Altice said, “and if they stop taking the methadone, they’re going to stop taking their HIV medications as well. Their lives will become chaotic and very destabilized.”
This experience may soon repeat itself. There were two methadone factories in Ukraine – in Odessa and Kharkiv – that are now shut down by the war. Although there are efforts to import methadone and many other drugs, supply chain issues are “devastating,” Dr. Altice said. “If their medication for tuberculosis is discontinued, that not only causes potential recurrence of disease but multidrug-resistant TB disease,” and they could become infectious again. “[With a] lack of medication, lack of sterile syringes, people will be sharing syringes; they’ll be desperate. So as the desperation level goes up, the risk environment goes up, so that people have decreased opportunities to protect themselves,” and there will be an explosion in HIV.
Dr. Altice observed that with the immigration to Poland and the west, many Ukrainian refugees “are relying on the kindness of strangers.” They are likely to be “fearful to disclose either their HIV or their TB treatment status,” being afraid of being regarded as modern-day lepers, even though they are likely not infectious. Both Dr. Altice and Dr. Potter emphasized the need for the governments of Poland and other receiving countries to provide the refugees with “reassurance that their health information will not be shared with others.” Dr. Altice emphasized that “this is one of the things that I would say that these other countries have to get right.”
Dr. Potter echoed that, noting that extraordinary care needs to be taken so that shared information is not used for deportation.
When refugees are housed with rural hosts, transportation problems sometimes arise, creating major barriers to accessing care and treatment. In particular, refugees with TB, HIV, and addiction who are placed in small, remote locations may have difficulty securing transportation to sites where treatments for their complex illnesses are available, including specialists and medications.
Ukrainian-born microbiologist Olena Rzhepishevska, PhD, of Umeå University in Sweden, said in an interview that a network of European TB researchers have developed a database on TBNet where patients with TB can be specifically placed with understanding and helpful hosts outside of Ukraine. They can receive housing and medication through this network.
So far, 4 million Ukrainians have fled the country and millions more have been displaced internally. Dr. Altice noted that there is an “increased vulnerability beyond the vulnerability that they already [have] just by being a refugee” that we generally don’t recognize. Additionally, Poland and Hungary are not very progressive about methadone therapy nor are those nations well-equipped to provide it.
Dr. Altice explained that even within Ukraine, those who want to move to better their chance of getting their methadone are then at risk of being conscripted. He spoke of the grave calculations men must make, choosing to become internally displaced and risk conscription or losing life-saving methadone or medicines for HIV or TB.
One other unfortunate consequence of war might be a spike in rape, sexual abuse, prostitution, unwanted pregnancies, HIV, and sexually transmitted infections.
There were an estimated 80,100 female sex workers in Ukraine in 2016, with 5.2% HIV positive. In times of war, with no home or income, some women turn to prostitution to survive. Others are victims of sex trafficking, both within Ukraine and as refugees. The Russian invasion increased the risks of a surge in HIV infections, unwanted pregnancies, and abortions. Women who find themselves pregnant due to rape (a common tool of war) or sex trafficking may also struggle to access safe abortions. Poland, for example, has severe restrictions on abortion, and Ukrainian women may turn to unsafe, back-alley abortions, with their resulting high risk of infection.
Waterborne infections
Another concern involves waterborne infections. In addition to the common diarrheal diseases such as E coli, which can be expected from poor sanitation, polio is a significant concern. In the fall of 2021, Ukraine had an outbreak of vaccine-derived polio, with two cases of paralysis and 20 additional cases. As polio only paralyzes 1 person in 200 of those infected, many other cases were likely undetected. A vaccination campaign was just beginning when the war began.
Wound infections and antimicrobial resistance
The ECDC also reports high rates of antimicrobial resistance (AMR) in Ukraine, particularly involving common gram-negative bacteria, including Escherichia coli (53% resistance to third-generation cephalosporins), Klebsiella pneumoniae (54% resistance to carbapenems), and Acinetobacter spp. (77% resistance to carbapenems). Because of this, they recommend refugees requiring hospital admission be isolated on admission and screened for AMR. These AMR often complicate traumatic injuries of war.
Prevention
Many of these potential problems stemming from the war in Ukraine and the displacement of millions of its citizens can be avoided.
Attempts are being made to immunize refugees. WHO has made working with countries receiving refugees a priority, particularly by vaccinating children against measles, rubella, and COVID. The European Union has also purchased vaccines for polio and tuberculosis.
But Russia has waged an active anti-vaccine campaign against COVID in Ukraine, while at the same time advocating for vaccines in Russia. According to UNICEF, other countries with relatively low vaccination rates and high vaccine skepticism – Moldova, Romania, and Bulgaria – are at higher risk of polio and measles than those with high vaccination levels.
The continuing war in Ukraine has exacerbated the medical challenges the citizens of Ukraine face at home and as refugees fleeing to neighboring countries. Improving communication among agencies and governments and building trust with the refugees could go a long way toward limiting the spread of preventable infectious diseases as a result of the war.
Continuing to try to keep supply chains open within Ukraine and ensuring adequate supplies of medications and vaccines to refugees will also be essential. But, of course, the better solution is to end the war.
Dr. Altice, Dr. Potter, Dr. Wingfield, Dr. Vermund, and Dr. Zinchuk all report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The importance of treating insomnia in psychiatric illness
Data suggests this symptom, defined as chronic sleep onset and/or sleep continuity problems associated with impaired daytime functioning, is common in psychiatric illnesses, and can worsen their course.2
The incidence of psychiatric illness in patients with insomnia is estimated at near 50%, with the highest rates found in mood disorders such as depression and bipolar disorder, as well as anxiety disorders.3 In patients with diagnosed major depressive disorder, insomnia rates can approach 90%.4-6
Insomnia has been identified as a risk factor for development of mental illness, including doubling the risk of major depressive disorder and tripling the risk of any depressive or anxiety disorder.7,8 It can also significantly increase the risk of alcohol abuse and psychosis.8
Sleep disturbances can worsen symptoms of diagnosed mental illness, including substance abuse, mood and psychotic disorders.9-10 In one study, nearly 75% of patients with a diagnosis of schizophrenia or bipolar spectrum disorder had at least one type of sleep disturbance (insomnia, hypersomnia, or delayed sleep phase).10 This was almost twice the rate in healthy controls. Importantly, compared with well-rested subjects with mental illness in this study, sleep-disordered participants had higher rates of negative and depressive symptoms on the Positive and Negative Syndrome Scale, as well as significantly lower function via the global assessment of functioning.11,12
Additional data suggests simply being awake during the night (00:00-05:59) elevates risk of suicide. The mean incident rate of completed suicide in one study was a striking four times the rate noted during daytime hours (06:00-23:59 ) (P < .001).13
Although insomnia symptoms can resolve after relief from a particular life stressor, as many as half of patients with more severe symptoms develop a chronic course.14 This then leads to an extended use of many types of sedative-hypnotics designed and studied primarily for short-term use.15 In a survey reviewing national use of prescription drugs for insomnia, as many as 20% of individuals use a medication to target insomnia in a given month.16
Fortunately, despite the many challenges posed by COVID-19, particularly for those with psychiatric illness and limited access to care, telehealth has become more readily available. Additionally, digital versions of evidence-based treatments specifically for sleep problems, such as cognitive-behavioral therapy for insomnia (CBT-I), are regularly being developed.
The benefits of CBT-I have been demonstrated repeatedly and it is recommended as the first line treatment for insomnia by the Clinical Guidelines of the American Academy of Sleep Medicine, the Centers for Disease Control and Prevention, and the National Institutes of Health.17-21 Studies suggest benefits persist long-term, even after completing the therapy sessions, which differ in durability from medication choices.18
One group that may be particularly suited for treatment with CBT-I is women with insomnia during pregnancy or the postpartum period. In these women, options for treatment may be limited by risk of medication during breastfeeding, as well as difficulty traveling to a physician’s or therapist’s office to receive psychotherapy. However, two recent studies evaluated the use of digital CBT-I to treat insomnia during pregnancy and in the postpartum period, respectively.22-23
In both studies,the same group of women with insomnia diagnosed during pregnancy were given six weekly 20-minute sessions of digital CBT-I or standard treatment for insomnia, including medication and psychotherapy per their usual provider.
By study end, the pregnant women receiving the CBT-I intervention not only had significantly improved severity of insomnia, they also experienced improved depression and anxiety symptoms, and a decrease in the use of prescription or over-the-counter sleep aides, compared with the standard treatment group, lowering the fetal exposure to medication during pregnancy.22
In the more recent study, the same group was followed for 6 months post partum.23 Results were again notable, with the women who received CBT-I reporting significantly less insomnia, as well as significantly lower rates of probable major depression at 3 and 6 months (18% vs. 4%, 10% vs. 0%, respectively.) They also exhibited lower rates of moderate to severe anxiety (17% vs. 4%) at 3 months, compared with those receiving standard care. With as many as one in seven women suffering from postpartum depression, these findings represent a substantial public health benefit.
In summary, insomnia is a critical area of focus for any provider diagnosing and treating psychiatric illness. Attempts to optimize sleep, whether through CBT-I or other psychotherapy approaches, or evidence-based medications dosed for appropriate lengths and at safe doses, should be a part of most, if not all, clinical encounters.
Dr. Reid is a board-certified psychiatrist and award-winning medical educator with a private practice in Philadelphia, as well as a clinical faculty role at the University of Pennsylvania, also in Philadelphia. She attended medical school at Columbia University, New York, and completed her psychiatry residency at the University of California, Los Angeles. Dr. Reid is a regular contributor to Psychology Today with her blog, “Think Like a Shrink,” and writes and podcasts as The Reflective Doc.
References
1. Voitsidis P et al. Psychiatry Res. 2020 Jul;289:113076. doi: 10.1016/j.psychres.2020.113076.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, Va.: American Psychiatric Publishing, 2013.
3. Ford DE and Kamerow DB. JAMA. 1989;262(11):1479-84. doi: 10.1001/jama.1989.03430110069030.
4. Ohayon MM and Roth T. J Psychiatr Res. Jan-Feb 2003;37(1):9-15. doi: 10.1016/s0022-3956(02)00052-3.
5. Seow LSE et al. J Ment Health. 2016 Dec;25(6):492-9. doi: 10.3109/09638237.2015.1124390.
6. Thase ME. J Clin Psychiatry. 1999;60 Suppl 17:28-31; discussion 46-8.
7. Baglioni C et al. J Affect Disord. 2011 Dec;135(1-3):10-9. doi: 10.1016/j.jad.2011.01.011.
8. Hertenstein E et al. Sleep Med Rev. 2019 Feb;43:96-105. doi: 10.1016/j.smrv.2018.10.006.
9. Brower KJ et al. Medical Hypotheses. 2010;74(5):928-33. doi: 10.1016/j.mehy.2009.10.020.
10. Laskemoen JF et al. Compr Psychiatry. 2019 May;91:6-12. doi: 10.1016/j.comppsych.2019.02.006.
11. Kay SR et al. Schizophr Bull. 1987;13(2):261-76. doi: 10.1093/schbul/13.2.261.
12. Hall R. Psychosomatics. May-Jun 1995;36(3):267-75. doi: 10.1016/S0033-3182(95)71666-8.
13. Perlis ML et al. J Clin Psychiatry. 2016 Jun;77(6):e726-33. doi: 10.4088/JCP.15m10131.
14. Morin CM et al. Arch Intern Med. 2009 Mar 9. doi: 10.1001/archinternmed.2008.610.
15. Cheung J et al. Sleep Med Clin. 2019 Jun;14(2):253-65. doi: 10.1016/j.jsmc.2019.01.006.
16. Bertisch SM et al. Sleep. 2014 Feb 1. doi: 10.5665/sleep.3410.
17. Okajima I et al. Sleep Biol Rhythms. 2010 Nov 28. doi: 10.1111/j.1479-8425.2010.00481.x.
18. Trauer JM et al. Ann Intern Med. 2015 Aug 4. doi: 10.7326/M14-2841.
19. Edinger J et al. J Clin Sleep Med. 2021 Feb 1. doi: 10.5664/jcsm.8986.
20. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/for-clinicians.html.
21. National Institutes of Health. Sleep Health. https://www.nhlbi.nih.gov/health-topics/education-and-awareness/sleep-health.
22. Felder JN et al. JAMA Psychiatry. 2020;77(5):484-92. doi:10.1001/jamapsychiatry.2019.4491.
23. Felder JN et al. Sleep. 2022 Feb 14. doi: 10.1093/sleep/zsab280.
Data suggests this symptom, defined as chronic sleep onset and/or sleep continuity problems associated with impaired daytime functioning, is common in psychiatric illnesses, and can worsen their course.2
The incidence of psychiatric illness in patients with insomnia is estimated at near 50%, with the highest rates found in mood disorders such as depression and bipolar disorder, as well as anxiety disorders.3 In patients with diagnosed major depressive disorder, insomnia rates can approach 90%.4-6
Insomnia has been identified as a risk factor for development of mental illness, including doubling the risk of major depressive disorder and tripling the risk of any depressive or anxiety disorder.7,8 It can also significantly increase the risk of alcohol abuse and psychosis.8
Sleep disturbances can worsen symptoms of diagnosed mental illness, including substance abuse, mood and psychotic disorders.9-10 In one study, nearly 75% of patients with a diagnosis of schizophrenia or bipolar spectrum disorder had at least one type of sleep disturbance (insomnia, hypersomnia, or delayed sleep phase).10 This was almost twice the rate in healthy controls. Importantly, compared with well-rested subjects with mental illness in this study, sleep-disordered participants had higher rates of negative and depressive symptoms on the Positive and Negative Syndrome Scale, as well as significantly lower function via the global assessment of functioning.11,12
Additional data suggests simply being awake during the night (00:00-05:59) elevates risk of suicide. The mean incident rate of completed suicide in one study was a striking four times the rate noted during daytime hours (06:00-23:59 ) (P < .001).13
Although insomnia symptoms can resolve after relief from a particular life stressor, as many as half of patients with more severe symptoms develop a chronic course.14 This then leads to an extended use of many types of sedative-hypnotics designed and studied primarily for short-term use.15 In a survey reviewing national use of prescription drugs for insomnia, as many as 20% of individuals use a medication to target insomnia in a given month.16
Fortunately, despite the many challenges posed by COVID-19, particularly for those with psychiatric illness and limited access to care, telehealth has become more readily available. Additionally, digital versions of evidence-based treatments specifically for sleep problems, such as cognitive-behavioral therapy for insomnia (CBT-I), are regularly being developed.
The benefits of CBT-I have been demonstrated repeatedly and it is recommended as the first line treatment for insomnia by the Clinical Guidelines of the American Academy of Sleep Medicine, the Centers for Disease Control and Prevention, and the National Institutes of Health.17-21 Studies suggest benefits persist long-term, even after completing the therapy sessions, which differ in durability from medication choices.18
One group that may be particularly suited for treatment with CBT-I is women with insomnia during pregnancy or the postpartum period. In these women, options for treatment may be limited by risk of medication during breastfeeding, as well as difficulty traveling to a physician’s or therapist’s office to receive psychotherapy. However, two recent studies evaluated the use of digital CBT-I to treat insomnia during pregnancy and in the postpartum period, respectively.22-23
In both studies,the same group of women with insomnia diagnosed during pregnancy were given six weekly 20-minute sessions of digital CBT-I or standard treatment for insomnia, including medication and psychotherapy per their usual provider.
By study end, the pregnant women receiving the CBT-I intervention not only had significantly improved severity of insomnia, they also experienced improved depression and anxiety symptoms, and a decrease in the use of prescription or over-the-counter sleep aides, compared with the standard treatment group, lowering the fetal exposure to medication during pregnancy.22
In the more recent study, the same group was followed for 6 months post partum.23 Results were again notable, with the women who received CBT-I reporting significantly less insomnia, as well as significantly lower rates of probable major depression at 3 and 6 months (18% vs. 4%, 10% vs. 0%, respectively.) They also exhibited lower rates of moderate to severe anxiety (17% vs. 4%) at 3 months, compared with those receiving standard care. With as many as one in seven women suffering from postpartum depression, these findings represent a substantial public health benefit.
In summary, insomnia is a critical area of focus for any provider diagnosing and treating psychiatric illness. Attempts to optimize sleep, whether through CBT-I or other psychotherapy approaches, or evidence-based medications dosed for appropriate lengths and at safe doses, should be a part of most, if not all, clinical encounters.
Dr. Reid is a board-certified psychiatrist and award-winning medical educator with a private practice in Philadelphia, as well as a clinical faculty role at the University of Pennsylvania, also in Philadelphia. She attended medical school at Columbia University, New York, and completed her psychiatry residency at the University of California, Los Angeles. Dr. Reid is a regular contributor to Psychology Today with her blog, “Think Like a Shrink,” and writes and podcasts as The Reflective Doc.
References
1. Voitsidis P et al. Psychiatry Res. 2020 Jul;289:113076. doi: 10.1016/j.psychres.2020.113076.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, Va.: American Psychiatric Publishing, 2013.
3. Ford DE and Kamerow DB. JAMA. 1989;262(11):1479-84. doi: 10.1001/jama.1989.03430110069030.
4. Ohayon MM and Roth T. J Psychiatr Res. Jan-Feb 2003;37(1):9-15. doi: 10.1016/s0022-3956(02)00052-3.
5. Seow LSE et al. J Ment Health. 2016 Dec;25(6):492-9. doi: 10.3109/09638237.2015.1124390.
6. Thase ME. J Clin Psychiatry. 1999;60 Suppl 17:28-31; discussion 46-8.
7. Baglioni C et al. J Affect Disord. 2011 Dec;135(1-3):10-9. doi: 10.1016/j.jad.2011.01.011.
8. Hertenstein E et al. Sleep Med Rev. 2019 Feb;43:96-105. doi: 10.1016/j.smrv.2018.10.006.
9. Brower KJ et al. Medical Hypotheses. 2010;74(5):928-33. doi: 10.1016/j.mehy.2009.10.020.
10. Laskemoen JF et al. Compr Psychiatry. 2019 May;91:6-12. doi: 10.1016/j.comppsych.2019.02.006.
11. Kay SR et al. Schizophr Bull. 1987;13(2):261-76. doi: 10.1093/schbul/13.2.261.
12. Hall R. Psychosomatics. May-Jun 1995;36(3):267-75. doi: 10.1016/S0033-3182(95)71666-8.
13. Perlis ML et al. J Clin Psychiatry. 2016 Jun;77(6):e726-33. doi: 10.4088/JCP.15m10131.
14. Morin CM et al. Arch Intern Med. 2009 Mar 9. doi: 10.1001/archinternmed.2008.610.
15. Cheung J et al. Sleep Med Clin. 2019 Jun;14(2):253-65. doi: 10.1016/j.jsmc.2019.01.006.
16. Bertisch SM et al. Sleep. 2014 Feb 1. doi: 10.5665/sleep.3410.
17. Okajima I et al. Sleep Biol Rhythms. 2010 Nov 28. doi: 10.1111/j.1479-8425.2010.00481.x.
18. Trauer JM et al. Ann Intern Med. 2015 Aug 4. doi: 10.7326/M14-2841.
19. Edinger J et al. J Clin Sleep Med. 2021 Feb 1. doi: 10.5664/jcsm.8986.
20. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/for-clinicians.html.
21. National Institutes of Health. Sleep Health. https://www.nhlbi.nih.gov/health-topics/education-and-awareness/sleep-health.
22. Felder JN et al. JAMA Psychiatry. 2020;77(5):484-92. doi:10.1001/jamapsychiatry.2019.4491.
23. Felder JN et al. Sleep. 2022 Feb 14. doi: 10.1093/sleep/zsab280.
Data suggests this symptom, defined as chronic sleep onset and/or sleep continuity problems associated with impaired daytime functioning, is common in psychiatric illnesses, and can worsen their course.2
The incidence of psychiatric illness in patients with insomnia is estimated at near 50%, with the highest rates found in mood disorders such as depression and bipolar disorder, as well as anxiety disorders.3 In patients with diagnosed major depressive disorder, insomnia rates can approach 90%.4-6
Insomnia has been identified as a risk factor for development of mental illness, including doubling the risk of major depressive disorder and tripling the risk of any depressive or anxiety disorder.7,8 It can also significantly increase the risk of alcohol abuse and psychosis.8
Sleep disturbances can worsen symptoms of diagnosed mental illness, including substance abuse, mood and psychotic disorders.9-10 In one study, nearly 75% of patients with a diagnosis of schizophrenia or bipolar spectrum disorder had at least one type of sleep disturbance (insomnia, hypersomnia, or delayed sleep phase).10 This was almost twice the rate in healthy controls. Importantly, compared with well-rested subjects with mental illness in this study, sleep-disordered participants had higher rates of negative and depressive symptoms on the Positive and Negative Syndrome Scale, as well as significantly lower function via the global assessment of functioning.11,12
Additional data suggests simply being awake during the night (00:00-05:59) elevates risk of suicide. The mean incident rate of completed suicide in one study was a striking four times the rate noted during daytime hours (06:00-23:59 ) (P < .001).13
Although insomnia symptoms can resolve after relief from a particular life stressor, as many as half of patients with more severe symptoms develop a chronic course.14 This then leads to an extended use of many types of sedative-hypnotics designed and studied primarily for short-term use.15 In a survey reviewing national use of prescription drugs for insomnia, as many as 20% of individuals use a medication to target insomnia in a given month.16
Fortunately, despite the many challenges posed by COVID-19, particularly for those with psychiatric illness and limited access to care, telehealth has become more readily available. Additionally, digital versions of evidence-based treatments specifically for sleep problems, such as cognitive-behavioral therapy for insomnia (CBT-I), are regularly being developed.
The benefits of CBT-I have been demonstrated repeatedly and it is recommended as the first line treatment for insomnia by the Clinical Guidelines of the American Academy of Sleep Medicine, the Centers for Disease Control and Prevention, and the National Institutes of Health.17-21 Studies suggest benefits persist long-term, even after completing the therapy sessions, which differ in durability from medication choices.18
One group that may be particularly suited for treatment with CBT-I is women with insomnia during pregnancy or the postpartum period. In these women, options for treatment may be limited by risk of medication during breastfeeding, as well as difficulty traveling to a physician’s or therapist’s office to receive psychotherapy. However, two recent studies evaluated the use of digital CBT-I to treat insomnia during pregnancy and in the postpartum period, respectively.22-23
In both studies,the same group of women with insomnia diagnosed during pregnancy were given six weekly 20-minute sessions of digital CBT-I or standard treatment for insomnia, including medication and psychotherapy per their usual provider.
By study end, the pregnant women receiving the CBT-I intervention not only had significantly improved severity of insomnia, they also experienced improved depression and anxiety symptoms, and a decrease in the use of prescription or over-the-counter sleep aides, compared with the standard treatment group, lowering the fetal exposure to medication during pregnancy.22
In the more recent study, the same group was followed for 6 months post partum.23 Results were again notable, with the women who received CBT-I reporting significantly less insomnia, as well as significantly lower rates of probable major depression at 3 and 6 months (18% vs. 4%, 10% vs. 0%, respectively.) They also exhibited lower rates of moderate to severe anxiety (17% vs. 4%) at 3 months, compared with those receiving standard care. With as many as one in seven women suffering from postpartum depression, these findings represent a substantial public health benefit.
In summary, insomnia is a critical area of focus for any provider diagnosing and treating psychiatric illness. Attempts to optimize sleep, whether through CBT-I or other psychotherapy approaches, or evidence-based medications dosed for appropriate lengths and at safe doses, should be a part of most, if not all, clinical encounters.
Dr. Reid is a board-certified psychiatrist and award-winning medical educator with a private practice in Philadelphia, as well as a clinical faculty role at the University of Pennsylvania, also in Philadelphia. She attended medical school at Columbia University, New York, and completed her psychiatry residency at the University of California, Los Angeles. Dr. Reid is a regular contributor to Psychology Today with her blog, “Think Like a Shrink,” and writes and podcasts as The Reflective Doc.
References
1. Voitsidis P et al. Psychiatry Res. 2020 Jul;289:113076. doi: 10.1016/j.psychres.2020.113076.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, Va.: American Psychiatric Publishing, 2013.
3. Ford DE and Kamerow DB. JAMA. 1989;262(11):1479-84. doi: 10.1001/jama.1989.03430110069030.
4. Ohayon MM and Roth T. J Psychiatr Res. Jan-Feb 2003;37(1):9-15. doi: 10.1016/s0022-3956(02)00052-3.
5. Seow LSE et al. J Ment Health. 2016 Dec;25(6):492-9. doi: 10.3109/09638237.2015.1124390.
6. Thase ME. J Clin Psychiatry. 1999;60 Suppl 17:28-31; discussion 46-8.
7. Baglioni C et al. J Affect Disord. 2011 Dec;135(1-3):10-9. doi: 10.1016/j.jad.2011.01.011.
8. Hertenstein E et al. Sleep Med Rev. 2019 Feb;43:96-105. doi: 10.1016/j.smrv.2018.10.006.
9. Brower KJ et al. Medical Hypotheses. 2010;74(5):928-33. doi: 10.1016/j.mehy.2009.10.020.
10. Laskemoen JF et al. Compr Psychiatry. 2019 May;91:6-12. doi: 10.1016/j.comppsych.2019.02.006.
11. Kay SR et al. Schizophr Bull. 1987;13(2):261-76. doi: 10.1093/schbul/13.2.261.
12. Hall R. Psychosomatics. May-Jun 1995;36(3):267-75. doi: 10.1016/S0033-3182(95)71666-8.
13. Perlis ML et al. J Clin Psychiatry. 2016 Jun;77(6):e726-33. doi: 10.4088/JCP.15m10131.
14. Morin CM et al. Arch Intern Med. 2009 Mar 9. doi: 10.1001/archinternmed.2008.610.
15. Cheung J et al. Sleep Med Clin. 2019 Jun;14(2):253-65. doi: 10.1016/j.jsmc.2019.01.006.
16. Bertisch SM et al. Sleep. 2014 Feb 1. doi: 10.5665/sleep.3410.
17. Okajima I et al. Sleep Biol Rhythms. 2010 Nov 28. doi: 10.1111/j.1479-8425.2010.00481.x.
18. Trauer JM et al. Ann Intern Med. 2015 Aug 4. doi: 10.7326/M14-2841.
19. Edinger J et al. J Clin Sleep Med. 2021 Feb 1. doi: 10.5664/jcsm.8986.
20. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/for-clinicians.html.
21. National Institutes of Health. Sleep Health. https://www.nhlbi.nih.gov/health-topics/education-and-awareness/sleep-health.
22. Felder JN et al. JAMA Psychiatry. 2020;77(5):484-92. doi:10.1001/jamapsychiatry.2019.4491.
23. Felder JN et al. Sleep. 2022 Feb 14. doi: 10.1093/sleep/zsab280.
IBD: Patients struggle with presenteeism, mental health
Anxiety and depression are common among individuals with inflammatory bowel disease (IBD) who are in remission, and the conditions are linked to unemployment and presenteeism, according to a prospective study.
Previous studies have found a heightened risk of anxiety and depression in IBD, as well as an association with poor treatment compliance and greater morbidity. Presenteeism, defined as reduced productivity due to a physical or mental condition, is increasingly recognized as an indirect economic cost of chronic conditions that may exact a higher cost than absenteeism.
More than one-third of patients with IBD experienced presenteeism in one study. Other studies have examined exercise in chronic diseases, and most find an association between more exercise and lower rates of anxiety and depression. To date, few studies have examined a combination of physical activity, mental health, and presenteeism in the context of IBD.
The new study, published in the Journal of Crohn’s and Colitis, “is very important, as presenteeism is not commonly discussed in any formal, measurable way in the IBD space,” said Laurie Keefer, PhD, professor of medicine and a gastropsychologist at Icahn School of Medicine, who was asked to comment on the research. “While conducted in Europe and Israel, the study also has relevance in the U.S. since, here, employers typically pay for health care – so absenteeism, presenteeism, and health care cost are all intertwined.”
“The study confirmed high rates of depression and anxiety after a diagnosis of IBD. One high-quality aspect of this study was that the diagnosis of depression and anxiety was confirmed by a medical practitioner,” said Dr. Keefer.
The results suggest that current efforts to screen IBD patients for depression and anxiety may not be enough, according to Stephen Lupe, PsyD, who was also asked to comment on the study. He noted that almost half of the patients had symptoms of anxiety or depression as measured by the Hospital Anxiety and Depression Score (HADS). “We’re missing all kinds of people,” said Dr. Lupe, who is director of behavioral medicine for the department of gastroenterology, hepatology, and nutrition at the Cleveland Clinic. He cited other data that show that, if someone develops depression, they are more likely to have a surgical outcome, and they are more likely to have problems with medication adherence. They likely will have more flares and less time in remission. “We need to be screening for it as part of care,” he said.
The researchers prospectively studied 585 IBD patients who were in clinical remission at 8 centers in Europe and Israel between September 2020 and March 2021. Participants filled out the HADS and The Stanford Presenteeism scale (SPS-6). A total of 62.2% of the participants had CD; 53.0% were male. Participants’ mean age was 39 years. Among the group, 10.8% had a pre existing diagnosis of anxiety or depression at the time of IBD diagnosis, and an additional 14.2% were later diagnosed with anxiety or depression.
Less than half, 46.1%, of IBD patients had a score 8 or higher in the HADS-anxiety (HADS-A) or HADS-depression (HADS-D) subscale, a cutoff that suggests evidence of clinical depression or anxiety. A total of 27.4% had a score of 11 or higher, indicating a mood disorder. High HADS-A score was associated with female gender (odds ratio, 1.91; P < 0.05), long duration of disease (OR, 1.04; P < 0.01), and perianal disease (P < 0.023). The authors speculate that the latter result may be due to a higher burden of symptoms. Three-quarters, 74.5%, of patients were employed; 34.0% experienced presenteeism as defined by SPS-6 score less than or equal to 18.
The researchers found that 23.0% of the patients were sedentary, and this was more common among individuals with HADS-A or HADS-D scores greater than or equal to 8. Among those experiencing presenteeism, 50% were sedentary, 29.4% were active, and 20.6% were moderately active (P < 0.01). Individuals with higher HADS-A or HADS-D scores had a greater likelihood of being sedentary (P < 0.05).
One limitation of the study was that the questionnaires were translated into the respective languages and scores were taken at only one time point.
“Rather than relying on the patient to come forward and seek help,” physicians should familiarize themselves with these validated screening tools “in order to increase the diagnostic rate of such pathologies and enable a better holistic care for the IBD patients,” the authors concluded. “Active involvement of a psychologist and/or a psychiatrist, as part of the IBD team, should be pursued to further improve the patients’ quality of life, which has emerged as one of the top priority outcomes in IBD.”
Dr. Lupe said that the findings regarding presenteeism are consistent with his experience. He pointed out that IBD patients must be more aware of their body and vigilant in managing symptoms, and he speculated that that could detract from concentration at work. He said that the study shows the need for a holistic approach to treatment. “When someone is coping with a chronic disease, like ulcerative colitis or Crohn’s disease, it affects the whole person,” including psychologically, professionally, and personally. “These are bidirectional relationships, so that if someone’s social life starts falling down, it’s more contributory to the development of something like depression and anxiety, and maybe that’s contributory to complications that come up in a disease state like Crohn’s disease or ulcerative colitis.”
The study did not receive funding, but two authors disclosed relations with AbbVie, Janssen, Pfizer, and other companies. Dr. Keefer is a cofounder and has equity ownership In Trellus Health. Dr. Lupe has no relevant financial disclosures.
Anxiety and depression are common among individuals with inflammatory bowel disease (IBD) who are in remission, and the conditions are linked to unemployment and presenteeism, according to a prospective study.
Previous studies have found a heightened risk of anxiety and depression in IBD, as well as an association with poor treatment compliance and greater morbidity. Presenteeism, defined as reduced productivity due to a physical or mental condition, is increasingly recognized as an indirect economic cost of chronic conditions that may exact a higher cost than absenteeism.
More than one-third of patients with IBD experienced presenteeism in one study. Other studies have examined exercise in chronic diseases, and most find an association between more exercise and lower rates of anxiety and depression. To date, few studies have examined a combination of physical activity, mental health, and presenteeism in the context of IBD.
The new study, published in the Journal of Crohn’s and Colitis, “is very important, as presenteeism is not commonly discussed in any formal, measurable way in the IBD space,” said Laurie Keefer, PhD, professor of medicine and a gastropsychologist at Icahn School of Medicine, who was asked to comment on the research. “While conducted in Europe and Israel, the study also has relevance in the U.S. since, here, employers typically pay for health care – so absenteeism, presenteeism, and health care cost are all intertwined.”
“The study confirmed high rates of depression and anxiety after a diagnosis of IBD. One high-quality aspect of this study was that the diagnosis of depression and anxiety was confirmed by a medical practitioner,” said Dr. Keefer.
The results suggest that current efforts to screen IBD patients for depression and anxiety may not be enough, according to Stephen Lupe, PsyD, who was also asked to comment on the study. He noted that almost half of the patients had symptoms of anxiety or depression as measured by the Hospital Anxiety and Depression Score (HADS). “We’re missing all kinds of people,” said Dr. Lupe, who is director of behavioral medicine for the department of gastroenterology, hepatology, and nutrition at the Cleveland Clinic. He cited other data that show that, if someone develops depression, they are more likely to have a surgical outcome, and they are more likely to have problems with medication adherence. They likely will have more flares and less time in remission. “We need to be screening for it as part of care,” he said.
The researchers prospectively studied 585 IBD patients who were in clinical remission at 8 centers in Europe and Israel between September 2020 and March 2021. Participants filled out the HADS and The Stanford Presenteeism scale (SPS-6). A total of 62.2% of the participants had CD; 53.0% were male. Participants’ mean age was 39 years. Among the group, 10.8% had a pre existing diagnosis of anxiety or depression at the time of IBD diagnosis, and an additional 14.2% were later diagnosed with anxiety or depression.
Less than half, 46.1%, of IBD patients had a score 8 or higher in the HADS-anxiety (HADS-A) or HADS-depression (HADS-D) subscale, a cutoff that suggests evidence of clinical depression or anxiety. A total of 27.4% had a score of 11 or higher, indicating a mood disorder. High HADS-A score was associated with female gender (odds ratio, 1.91; P < 0.05), long duration of disease (OR, 1.04; P < 0.01), and perianal disease (P < 0.023). The authors speculate that the latter result may be due to a higher burden of symptoms. Three-quarters, 74.5%, of patients were employed; 34.0% experienced presenteeism as defined by SPS-6 score less than or equal to 18.
The researchers found that 23.0% of the patients were sedentary, and this was more common among individuals with HADS-A or HADS-D scores greater than or equal to 8. Among those experiencing presenteeism, 50% were sedentary, 29.4% were active, and 20.6% were moderately active (P < 0.01). Individuals with higher HADS-A or HADS-D scores had a greater likelihood of being sedentary (P < 0.05).
One limitation of the study was that the questionnaires were translated into the respective languages and scores were taken at only one time point.
“Rather than relying on the patient to come forward and seek help,” physicians should familiarize themselves with these validated screening tools “in order to increase the diagnostic rate of such pathologies and enable a better holistic care for the IBD patients,” the authors concluded. “Active involvement of a psychologist and/or a psychiatrist, as part of the IBD team, should be pursued to further improve the patients’ quality of life, which has emerged as one of the top priority outcomes in IBD.”
Dr. Lupe said that the findings regarding presenteeism are consistent with his experience. He pointed out that IBD patients must be more aware of their body and vigilant in managing symptoms, and he speculated that that could detract from concentration at work. He said that the study shows the need for a holistic approach to treatment. “When someone is coping with a chronic disease, like ulcerative colitis or Crohn’s disease, it affects the whole person,” including psychologically, professionally, and personally. “These are bidirectional relationships, so that if someone’s social life starts falling down, it’s more contributory to the development of something like depression and anxiety, and maybe that’s contributory to complications that come up in a disease state like Crohn’s disease or ulcerative colitis.”
The study did not receive funding, but two authors disclosed relations with AbbVie, Janssen, Pfizer, and other companies. Dr. Keefer is a cofounder and has equity ownership In Trellus Health. Dr. Lupe has no relevant financial disclosures.
Anxiety and depression are common among individuals with inflammatory bowel disease (IBD) who are in remission, and the conditions are linked to unemployment and presenteeism, according to a prospective study.
Previous studies have found a heightened risk of anxiety and depression in IBD, as well as an association with poor treatment compliance and greater morbidity. Presenteeism, defined as reduced productivity due to a physical or mental condition, is increasingly recognized as an indirect economic cost of chronic conditions that may exact a higher cost than absenteeism.
More than one-third of patients with IBD experienced presenteeism in one study. Other studies have examined exercise in chronic diseases, and most find an association between more exercise and lower rates of anxiety and depression. To date, few studies have examined a combination of physical activity, mental health, and presenteeism in the context of IBD.
The new study, published in the Journal of Crohn’s and Colitis, “is very important, as presenteeism is not commonly discussed in any formal, measurable way in the IBD space,” said Laurie Keefer, PhD, professor of medicine and a gastropsychologist at Icahn School of Medicine, who was asked to comment on the research. “While conducted in Europe and Israel, the study also has relevance in the U.S. since, here, employers typically pay for health care – so absenteeism, presenteeism, and health care cost are all intertwined.”
“The study confirmed high rates of depression and anxiety after a diagnosis of IBD. One high-quality aspect of this study was that the diagnosis of depression and anxiety was confirmed by a medical practitioner,” said Dr. Keefer.
The results suggest that current efforts to screen IBD patients for depression and anxiety may not be enough, according to Stephen Lupe, PsyD, who was also asked to comment on the study. He noted that almost half of the patients had symptoms of anxiety or depression as measured by the Hospital Anxiety and Depression Score (HADS). “We’re missing all kinds of people,” said Dr. Lupe, who is director of behavioral medicine for the department of gastroenterology, hepatology, and nutrition at the Cleveland Clinic. He cited other data that show that, if someone develops depression, they are more likely to have a surgical outcome, and they are more likely to have problems with medication adherence. They likely will have more flares and less time in remission. “We need to be screening for it as part of care,” he said.
The researchers prospectively studied 585 IBD patients who were in clinical remission at 8 centers in Europe and Israel between September 2020 and March 2021. Participants filled out the HADS and The Stanford Presenteeism scale (SPS-6). A total of 62.2% of the participants had CD; 53.0% were male. Participants’ mean age was 39 years. Among the group, 10.8% had a pre existing diagnosis of anxiety or depression at the time of IBD diagnosis, and an additional 14.2% were later diagnosed with anxiety or depression.
Less than half, 46.1%, of IBD patients had a score 8 or higher in the HADS-anxiety (HADS-A) or HADS-depression (HADS-D) subscale, a cutoff that suggests evidence of clinical depression or anxiety. A total of 27.4% had a score of 11 or higher, indicating a mood disorder. High HADS-A score was associated with female gender (odds ratio, 1.91; P < 0.05), long duration of disease (OR, 1.04; P < 0.01), and perianal disease (P < 0.023). The authors speculate that the latter result may be due to a higher burden of symptoms. Three-quarters, 74.5%, of patients were employed; 34.0% experienced presenteeism as defined by SPS-6 score less than or equal to 18.
The researchers found that 23.0% of the patients were sedentary, and this was more common among individuals with HADS-A or HADS-D scores greater than or equal to 8. Among those experiencing presenteeism, 50% were sedentary, 29.4% were active, and 20.6% were moderately active (P < 0.01). Individuals with higher HADS-A or HADS-D scores had a greater likelihood of being sedentary (P < 0.05).
One limitation of the study was that the questionnaires were translated into the respective languages and scores were taken at only one time point.
“Rather than relying on the patient to come forward and seek help,” physicians should familiarize themselves with these validated screening tools “in order to increase the diagnostic rate of such pathologies and enable a better holistic care for the IBD patients,” the authors concluded. “Active involvement of a psychologist and/or a psychiatrist, as part of the IBD team, should be pursued to further improve the patients’ quality of life, which has emerged as one of the top priority outcomes in IBD.”
Dr. Lupe said that the findings regarding presenteeism are consistent with his experience. He pointed out that IBD patients must be more aware of their body and vigilant in managing symptoms, and he speculated that that could detract from concentration at work. He said that the study shows the need for a holistic approach to treatment. “When someone is coping with a chronic disease, like ulcerative colitis or Crohn’s disease, it affects the whole person,” including psychologically, professionally, and personally. “These are bidirectional relationships, so that if someone’s social life starts falling down, it’s more contributory to the development of something like depression and anxiety, and maybe that’s contributory to complications that come up in a disease state like Crohn’s disease or ulcerative colitis.”
The study did not receive funding, but two authors disclosed relations with AbbVie, Janssen, Pfizer, and other companies. Dr. Keefer is a cofounder and has equity ownership In Trellus Health. Dr. Lupe has no relevant financial disclosures.
REPORTING FROM JOURNAL OF CROHN'S AND COLITIS
Locoregional therapy lowers waitlist dropout in HCC
The use of bridging locoregional therapy (LRT) before liver transplantation in patients with hepatocellular carcinoma (HCC) has significantly increased in the United States within the past 15 years, a recent analysis suggests. Data show that liver transplant candidates with HCC who have elevated tumor burden and patients with more compensated liver disease have received a greater number of treatments while awaiting transplant.
According to the researchers, led by Allison Kwong, MD, of Stanford (Calif.) University, liver transplant remains a curative option for individuals with unresectable HCC who meet prespecified size criteria. In the United States, a mandated waiting period of 6 months prior “to gaining exception points has been implemented” in an effort “to allow for consideration of tumor biology and reduce the disparities in waitlist dropout between HCC and non-HCC patients,” the researchers wrote.
Several forms of LRT are now available for HCC, including chemoembolization, external beam radiation, radioembolization, and radiofrequency or microwave ablation. In the liver transplant setting, these LRT options enable management of intrahepatic disease in patients who are waiting for liver transplant, Dr. Kwong and colleagues explained.
The researchers, who published their study findings online August 3 in Clinical Gastroenterology and Hepatology, sought to examine the national temporal trends and waitlist outcomes of LRT in 31,609 patients eligible for liver transplant with greater than or equal to 1 approved HCC exception application in the United States.
Patient data were obtained from the Organ Procurement and Transplantation Network database and comprised primary adult LT candidates who were listed from the years 2003 to 2018. The investigators assessed explant histology and performed multivariable competing risk analysis to examine the relationship between the type of first LRT and time to waitlist dropout.
The waitlist dropout variable was defined by list removal due to death or excessive illness. The researchers noted that list removal likely represents disease progression “beyond transplantable criteria and beyond which patients were unlikely to benefit from or be eligible for further LRT.”
In the study population, the median age was 59 years, and approximately 77% of patients were male. More than half (53.1%) of the cohort had hepatitis C as the predominant liver disease etiology. Patients had a median follow-up period of 214 days on the waitlist.
Most patients (79%) received deceased or living-donor transplants, and 18.6% of patients were removed from the waitlist. Between the 2003 and 2006 period, the median waitlist time was 123 days, but this median waitlist duration increased to 257 days for patients listed between 2015 and 2018.
A total of 34,610 LRTs were performed among 24,145 liver transplant candidates during the study period. From 2003 to 2018, the proportion of patients with greater than or equal to 1 LRT recorded in the database rose from 42.3% to 92.4%, respectively. Most patients (67.8%) who received liver-directed therapy had a single LRT, while 23.8% of patients had 2 LRTs, 6.2% had 3 LRTs, and 2.2% had greater than or equal to 4 LRTs.
The most frequent type of LRT performed was chemoembolization, followed by thermal ablation. Radioembolization increased from less than 5% in 2013 to 19% in 2018. Moreover, in 2018, chemoembolization accounted for 50% of LRTs, while thermal ablation accounted for 22% of LRTs.
The incidence rates of LRT per 100 waitlist days was above average in patients who had an initial tumor burden beyond the Milan criteria (0.188), an alpha-fetoprotein level of 21-40 (0.171) or 41-500 ng/mL (0.179), Child-Pugh class A (0.160), patients in short (0.151) and medium (0.154) wait-time regions, as well as patients who were listed following implementation of cap-and-delay in October 2015 (0.192).
In the multivariable competing-risk analysis for waitlist dropout, adjusting for initial tumor burden and AFP, Child-Pugh class, wait region, and listing era, no locoregional therapy was associated with an increased risk of waitlist dropout versus chemoembolization as the first LRT in a multivariable competing-risk analysis (subhazard ratio [sHR], 1.37; 95% CI, 1.28-1.47). The inverse probability of treatment weighting–adjusted analysis found an association between radioembolization, when compared with chemoembolization, and a reduced risk of waitlist dropout (sHR, 0.85; 95% CI, 0.81-0.89). Thermal ablation was also associated with a reduced risk of waitlist dropout, compared with chemoembolization (sHR, 0.95; 95% CI, 0.91-0.99). “Radioembolization and thermal ablation may be superior to chemoembolization and prove to be more cost-effective options, depending on the clinical context,” the researchers wrote.
The researchers noted that they were unable to distinguish patients who were removed from the waitlist between those with disease progression versus liver failure.
The researchers reported no conflicts of interest with the pharmaceutical industry. The study received no industry funding.
The use of bridging locoregional therapy (LRT) before liver transplantation in patients with hepatocellular carcinoma (HCC) has significantly increased in the United States within the past 15 years, a recent analysis suggests. Data show that liver transplant candidates with HCC who have elevated tumor burden and patients with more compensated liver disease have received a greater number of treatments while awaiting transplant.
According to the researchers, led by Allison Kwong, MD, of Stanford (Calif.) University, liver transplant remains a curative option for individuals with unresectable HCC who meet prespecified size criteria. In the United States, a mandated waiting period of 6 months prior “to gaining exception points has been implemented” in an effort “to allow for consideration of tumor biology and reduce the disparities in waitlist dropout between HCC and non-HCC patients,” the researchers wrote.
Several forms of LRT are now available for HCC, including chemoembolization, external beam radiation, radioembolization, and radiofrequency or microwave ablation. In the liver transplant setting, these LRT options enable management of intrahepatic disease in patients who are waiting for liver transplant, Dr. Kwong and colleagues explained.
The researchers, who published their study findings online August 3 in Clinical Gastroenterology and Hepatology, sought to examine the national temporal trends and waitlist outcomes of LRT in 31,609 patients eligible for liver transplant with greater than or equal to 1 approved HCC exception application in the United States.
Patient data were obtained from the Organ Procurement and Transplantation Network database and comprised primary adult LT candidates who were listed from the years 2003 to 2018. The investigators assessed explant histology and performed multivariable competing risk analysis to examine the relationship between the type of first LRT and time to waitlist dropout.
The waitlist dropout variable was defined by list removal due to death or excessive illness. The researchers noted that list removal likely represents disease progression “beyond transplantable criteria and beyond which patients were unlikely to benefit from or be eligible for further LRT.”
In the study population, the median age was 59 years, and approximately 77% of patients were male. More than half (53.1%) of the cohort had hepatitis C as the predominant liver disease etiology. Patients had a median follow-up period of 214 days on the waitlist.
Most patients (79%) received deceased or living-donor transplants, and 18.6% of patients were removed from the waitlist. Between the 2003 and 2006 period, the median waitlist time was 123 days, but this median waitlist duration increased to 257 days for patients listed between 2015 and 2018.
A total of 34,610 LRTs were performed among 24,145 liver transplant candidates during the study period. From 2003 to 2018, the proportion of patients with greater than or equal to 1 LRT recorded in the database rose from 42.3% to 92.4%, respectively. Most patients (67.8%) who received liver-directed therapy had a single LRT, while 23.8% of patients had 2 LRTs, 6.2% had 3 LRTs, and 2.2% had greater than or equal to 4 LRTs.
The most frequent type of LRT performed was chemoembolization, followed by thermal ablation. Radioembolization increased from less than 5% in 2013 to 19% in 2018. Moreover, in 2018, chemoembolization accounted for 50% of LRTs, while thermal ablation accounted for 22% of LRTs.
The incidence rates of LRT per 100 waitlist days was above average in patients who had an initial tumor burden beyond the Milan criteria (0.188), an alpha-fetoprotein level of 21-40 (0.171) or 41-500 ng/mL (0.179), Child-Pugh class A (0.160), patients in short (0.151) and medium (0.154) wait-time regions, as well as patients who were listed following implementation of cap-and-delay in October 2015 (0.192).
In the multivariable competing-risk analysis for waitlist dropout, adjusting for initial tumor burden and AFP, Child-Pugh class, wait region, and listing era, no locoregional therapy was associated with an increased risk of waitlist dropout versus chemoembolization as the first LRT in a multivariable competing-risk analysis (subhazard ratio [sHR], 1.37; 95% CI, 1.28-1.47). The inverse probability of treatment weighting–adjusted analysis found an association between radioembolization, when compared with chemoembolization, and a reduced risk of waitlist dropout (sHR, 0.85; 95% CI, 0.81-0.89). Thermal ablation was also associated with a reduced risk of waitlist dropout, compared with chemoembolization (sHR, 0.95; 95% CI, 0.91-0.99). “Radioembolization and thermal ablation may be superior to chemoembolization and prove to be more cost-effective options, depending on the clinical context,” the researchers wrote.
The researchers noted that they were unable to distinguish patients who were removed from the waitlist between those with disease progression versus liver failure.
The researchers reported no conflicts of interest with the pharmaceutical industry. The study received no industry funding.
The use of bridging locoregional therapy (LRT) before liver transplantation in patients with hepatocellular carcinoma (HCC) has significantly increased in the United States within the past 15 years, a recent analysis suggests. Data show that liver transplant candidates with HCC who have elevated tumor burden and patients with more compensated liver disease have received a greater number of treatments while awaiting transplant.
According to the researchers, led by Allison Kwong, MD, of Stanford (Calif.) University, liver transplant remains a curative option for individuals with unresectable HCC who meet prespecified size criteria. In the United States, a mandated waiting period of 6 months prior “to gaining exception points has been implemented” in an effort “to allow for consideration of tumor biology and reduce the disparities in waitlist dropout between HCC and non-HCC patients,” the researchers wrote.
Several forms of LRT are now available for HCC, including chemoembolization, external beam radiation, radioembolization, and radiofrequency or microwave ablation. In the liver transplant setting, these LRT options enable management of intrahepatic disease in patients who are waiting for liver transplant, Dr. Kwong and colleagues explained.
The researchers, who published their study findings online August 3 in Clinical Gastroenterology and Hepatology, sought to examine the national temporal trends and waitlist outcomes of LRT in 31,609 patients eligible for liver transplant with greater than or equal to 1 approved HCC exception application in the United States.
Patient data were obtained from the Organ Procurement and Transplantation Network database and comprised primary adult LT candidates who were listed from the years 2003 to 2018. The investigators assessed explant histology and performed multivariable competing risk analysis to examine the relationship between the type of first LRT and time to waitlist dropout.
The waitlist dropout variable was defined by list removal due to death or excessive illness. The researchers noted that list removal likely represents disease progression “beyond transplantable criteria and beyond which patients were unlikely to benefit from or be eligible for further LRT.”
In the study population, the median age was 59 years, and approximately 77% of patients were male. More than half (53.1%) of the cohort had hepatitis C as the predominant liver disease etiology. Patients had a median follow-up period of 214 days on the waitlist.
Most patients (79%) received deceased or living-donor transplants, and 18.6% of patients were removed from the waitlist. Between the 2003 and 2006 period, the median waitlist time was 123 days, but this median waitlist duration increased to 257 days for patients listed between 2015 and 2018.
A total of 34,610 LRTs were performed among 24,145 liver transplant candidates during the study period. From 2003 to 2018, the proportion of patients with greater than or equal to 1 LRT recorded in the database rose from 42.3% to 92.4%, respectively. Most patients (67.8%) who received liver-directed therapy had a single LRT, while 23.8% of patients had 2 LRTs, 6.2% had 3 LRTs, and 2.2% had greater than or equal to 4 LRTs.
The most frequent type of LRT performed was chemoembolization, followed by thermal ablation. Radioembolization increased from less than 5% in 2013 to 19% in 2018. Moreover, in 2018, chemoembolization accounted for 50% of LRTs, while thermal ablation accounted for 22% of LRTs.
The incidence rates of LRT per 100 waitlist days was above average in patients who had an initial tumor burden beyond the Milan criteria (0.188), an alpha-fetoprotein level of 21-40 (0.171) or 41-500 ng/mL (0.179), Child-Pugh class A (0.160), patients in short (0.151) and medium (0.154) wait-time regions, as well as patients who were listed following implementation of cap-and-delay in October 2015 (0.192).
In the multivariable competing-risk analysis for waitlist dropout, adjusting for initial tumor burden and AFP, Child-Pugh class, wait region, and listing era, no locoregional therapy was associated with an increased risk of waitlist dropout versus chemoembolization as the first LRT in a multivariable competing-risk analysis (subhazard ratio [sHR], 1.37; 95% CI, 1.28-1.47). The inverse probability of treatment weighting–adjusted analysis found an association between radioembolization, when compared with chemoembolization, and a reduced risk of waitlist dropout (sHR, 0.85; 95% CI, 0.81-0.89). Thermal ablation was also associated with a reduced risk of waitlist dropout, compared with chemoembolization (sHR, 0.95; 95% CI, 0.91-0.99). “Radioembolization and thermal ablation may be superior to chemoembolization and prove to be more cost-effective options, depending on the clinical context,” the researchers wrote.
The researchers noted that they were unable to distinguish patients who were removed from the waitlist between those with disease progression versus liver failure.
The researchers reported no conflicts of interest with the pharmaceutical industry. The study received no industry funding.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Tech Glitches at One VA Site Raise Concerns About a Nationwide Rollout
Spokane, Washington, was supposed to be the center of the Department of Veterans Affairs’ tech reinvention, the first site in the agency’s decade-long project to change its medical records software. But one morning in early March, the latest system malfunction made some clinicians snap.
At Spokane’s Mann-Grandstaff VA Medical Center, the records system — developed by Cerner Corp., based in North Kansas City, Missouri — went down. Staffers, inside the hospital and its outpatient facilities, were back to relying on pen and paper. Computerized schedules were inaccessible. Physicians couldn’t enter new orders or change patients’ medications.
By the next day, the electronic health records were only partially available. Dozens of records remained “sequestered,” meaning that doctors and nurses struggled to update patient charts.
The snafu, the latest in a series at Mann-Grandstaff, heightened Spokane medical staff members’ frustration with a system that has been problematic since it was installed a year and a half ago. The VA said no patients had been harmed because of the problems.
But physicians on the ground there said it’s only a matter of time before serious safety problems — those causing injury or death — emerge, pointing to the program’s ongoing weaknesses amid VA leadership’s full-bore push toward implementation nationwide. One provider said she was glad she didn’t have a relative in Mann-Grandstaff.
The one-two punch of a dangerous outage and staff grievances is the latest setback in the VA’s more than $16 billion effort to upgrade its record-keeping technology. The issues have at times forced clinicians to see fewer patients and file tens of thousands of requests for help to Cerner with patient-safety problems, congressional and agency watchdog reviews show.
If those issues multiply over the vast VA system — which employs more than a quarter-million workers and serves 6.3 million active patients — it could create rampant patient-safety and productivity problems. Despite the VA’s goals of using the technology upgrade to provide seamless records for patients from enlistment in the military until discharge, the doctors and clinicians who spoke to KHN are convinced that the problems experienced in Spokane will be repeated again and again.
The records system, scheduled for deployment at multiple VA facilities in the Pacific Northwest in the coming weeks and months, most recently rolled out at Jonathan M. Wainwright Memorial VA Medical Center in Walla Walla, Washington.
Both Cerner and Mann-Grandstaff officials declined to comment and referred KHN to officials at VA headquarters in Washington, D.C.
“If it’s a total meltdown” in Walla Walla, said Katie Purswell, the American Legion’s director of veterans affairs and rehabilitation, it’s a problem for the department and its decade-long initiative. Initial impressions from staffers are positive, but the issues in Spokane appeared over the course of weeks after the system was turned on.
The distress was particularly acute in early March. On March 2, Cerner turned on a software update to a database containing patient identification information. Problems emerged the next morning. In the record of a patient who was checking in for surgery, staff members discovered incorrect data, including gender information for a different patient. About an hour later, a staffer from the national VA’s medical records office told some clinicians at Mann-Grandstaff to “log out.”
Robert Fischer, Mann-Grandstaff’s medical center director, sent a dire warning later that morning. “Assume all electronic data is corrupted/inaccurate,” Fischer said in an email. He urged clinicians to limit orders for lab work, imaging studies, and medications. The facility shifted to “downtime procedures,” meaning a reliance on paper.
Some staffers didn’t absorb the late-morning message and continued entering information in the mixed-up records, adding to the stew of erroneous data.
According to information provided to Congress later by the VA, Cerner had informed Mann-Grandstaff of a “complete degradation” the night before — leading to questions from staffers about why it took until late morning the next day to shut down the system. Agency spokesperson Erin Crowe told KHN there wasn’t any delay in notifying staff.
Problems stretched into the following week. Some records — 70 as of March 10, according to a briefing provided to Congress — remained unusable while auditors tried to ascertain what information had been mixed in from other charts. This left clinicians in some instances unable to keep track of patients’ care. Doctors said it became a confusing and chaotic environment. They couldn’t, for example, help patients refill prescriptions.
Members of Congress are concerned — not only about the outage but also VA’s explanations about it. In a letter to agency leadership, the leading Republicans on the House Veterans’ Affairs Committee and the subcommittee overseeing technology, Rep. Mike Bost of Illinois and Rep. Matt Rosendale of Montana, expressed worries the agency was “soft-pedal[ing]” its communications and argued that veterans were misled by assurances that records had been corrected.
The full committee plans to do a deeper examination soon. It has scheduled a closed-door roundtable with VA staffers from Spokane and Walla Walla on April 5.
The outage deepened unhappiness at Mann-Grandstaff. Clinicians there were already frazzled by a deeply buggy system. Downtime was common, a congressional aide told KHN.
A March 17 VA inspector general report documented nearly 39,000 requests for technical help or improvement since the October 2020 deployment of the new records system. Cerner employees often closed requests without resolving the underlying problems, the report said. Mann-Grandstaff staffers became disengaged or devised shortcuts to bypass the malfunctioning software, the inspector general wrote — each a potential root of patient-safety incidents.
The department said the shortcuts — or workarounds — aren’t its policy. “Workarounds are not authorized nor encouraged,” Crowe said.
The Biden administration tried to overhaul the software initiative, putting the program on hiatus before installing new leadership in the medical records office at the end of 2021. But by then, low morale had sunk in. “People in Spokane VA are … demoralized and unhappy,” Rep. Frank Mrvan (D-Ind.), chair of the House subcommittee focused on the VA’s technology modernization programs, told agency leaders during a November congressional hearing. He said staffers told him they felt as though they were beating their heads against a wall to make things function.
Other observers shared Mrvan’s concerns.
Purswell of the American Legion questioned whether appropriate steps are being taken to prepare the Walla Walla facility and its staff for the technology rollout. She asked whether staffers feel as if the Cerner system has been thrust upon them or are excited about the change.
Whether the VA has been persuasive about the benefits of the program is unclear. “I think it’s incumbent on us to demonstrate it’s not a loss,” said Dr. Terry Adirim, the leader of the VA office in charge of implementing the new records technology. “We might have dropped the ball on explaining what a benefit this is.”
Indeed, Adirim conducted a virtual town hall meeting March 21 for veterans in the Walla Walla area — where she was pressed about the problems in Spokane. “If Spokane has been a year figuring this out, why is this moving forward?” one questioner asked, expressing a point made frequently during the call. Adirim said the VA had made “thousands of changes” since the initial rollout.
Medical staffers at the Spokane and Walla Walla VA facilities are part of informal networks sharing their often-negative experiences about the program despite a perception among staff members that dissent will hurt their careers.
Adirim thinks negative feelings can be addressed by stepping up technical support. She also said training programs have been overhauled since the deployment in Spokane. Bottom line: The VA is proceeding.
“People want to revert back to what they did before,” Adirim said, but that’s not going to happen.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Subscribe to KHN's free Morning Briefing.
Spokane, Washington, was supposed to be the center of the Department of Veterans Affairs’ tech reinvention, the first site in the agency’s decade-long project to change its medical records software. But one morning in early March, the latest system malfunction made some clinicians snap.
At Spokane’s Mann-Grandstaff VA Medical Center, the records system — developed by Cerner Corp., based in North Kansas City, Missouri — went down. Staffers, inside the hospital and its outpatient facilities, were back to relying on pen and paper. Computerized schedules were inaccessible. Physicians couldn’t enter new orders or change patients’ medications.
By the next day, the electronic health records were only partially available. Dozens of records remained “sequestered,” meaning that doctors and nurses struggled to update patient charts.
The snafu, the latest in a series at Mann-Grandstaff, heightened Spokane medical staff members’ frustration with a system that has been problematic since it was installed a year and a half ago. The VA said no patients had been harmed because of the problems.
But physicians on the ground there said it’s only a matter of time before serious safety problems — those causing injury or death — emerge, pointing to the program’s ongoing weaknesses amid VA leadership’s full-bore push toward implementation nationwide. One provider said she was glad she didn’t have a relative in Mann-Grandstaff.
The one-two punch of a dangerous outage and staff grievances is the latest setback in the VA’s more than $16 billion effort to upgrade its record-keeping technology. The issues have at times forced clinicians to see fewer patients and file tens of thousands of requests for help to Cerner with patient-safety problems, congressional and agency watchdog reviews show.
If those issues multiply over the vast VA system — which employs more than a quarter-million workers and serves 6.3 million active patients — it could create rampant patient-safety and productivity problems. Despite the VA’s goals of using the technology upgrade to provide seamless records for patients from enlistment in the military until discharge, the doctors and clinicians who spoke to KHN are convinced that the problems experienced in Spokane will be repeated again and again.
The records system, scheduled for deployment at multiple VA facilities in the Pacific Northwest in the coming weeks and months, most recently rolled out at Jonathan M. Wainwright Memorial VA Medical Center in Walla Walla, Washington.
Both Cerner and Mann-Grandstaff officials declined to comment and referred KHN to officials at VA headquarters in Washington, D.C.
“If it’s a total meltdown” in Walla Walla, said Katie Purswell, the American Legion’s director of veterans affairs and rehabilitation, it’s a problem for the department and its decade-long initiative. Initial impressions from staffers are positive, but the issues in Spokane appeared over the course of weeks after the system was turned on.
The distress was particularly acute in early March. On March 2, Cerner turned on a software update to a database containing patient identification information. Problems emerged the next morning. In the record of a patient who was checking in for surgery, staff members discovered incorrect data, including gender information for a different patient. About an hour later, a staffer from the national VA’s medical records office told some clinicians at Mann-Grandstaff to “log out.”
Robert Fischer, Mann-Grandstaff’s medical center director, sent a dire warning later that morning. “Assume all electronic data is corrupted/inaccurate,” Fischer said in an email. He urged clinicians to limit orders for lab work, imaging studies, and medications. The facility shifted to “downtime procedures,” meaning a reliance on paper.
Some staffers didn’t absorb the late-morning message and continued entering information in the mixed-up records, adding to the stew of erroneous data.
According to information provided to Congress later by the VA, Cerner had informed Mann-Grandstaff of a “complete degradation” the night before — leading to questions from staffers about why it took until late morning the next day to shut down the system. Agency spokesperson Erin Crowe told KHN there wasn’t any delay in notifying staff.
Problems stretched into the following week. Some records — 70 as of March 10, according to a briefing provided to Congress — remained unusable while auditors tried to ascertain what information had been mixed in from other charts. This left clinicians in some instances unable to keep track of patients’ care. Doctors said it became a confusing and chaotic environment. They couldn’t, for example, help patients refill prescriptions.
Members of Congress are concerned — not only about the outage but also VA’s explanations about it. In a letter to agency leadership, the leading Republicans on the House Veterans’ Affairs Committee and the subcommittee overseeing technology, Rep. Mike Bost of Illinois and Rep. Matt Rosendale of Montana, expressed worries the agency was “soft-pedal[ing]” its communications and argued that veterans were misled by assurances that records had been corrected.
The full committee plans to do a deeper examination soon. It has scheduled a closed-door roundtable with VA staffers from Spokane and Walla Walla on April 5.
The outage deepened unhappiness at Mann-Grandstaff. Clinicians there were already frazzled by a deeply buggy system. Downtime was common, a congressional aide told KHN.
A March 17 VA inspector general report documented nearly 39,000 requests for technical help or improvement since the October 2020 deployment of the new records system. Cerner employees often closed requests without resolving the underlying problems, the report said. Mann-Grandstaff staffers became disengaged or devised shortcuts to bypass the malfunctioning software, the inspector general wrote — each a potential root of patient-safety incidents.
The department said the shortcuts — or workarounds — aren’t its policy. “Workarounds are not authorized nor encouraged,” Crowe said.
The Biden administration tried to overhaul the software initiative, putting the program on hiatus before installing new leadership in the medical records office at the end of 2021. But by then, low morale had sunk in. “People in Spokane VA are … demoralized and unhappy,” Rep. Frank Mrvan (D-Ind.), chair of the House subcommittee focused on the VA’s technology modernization programs, told agency leaders during a November congressional hearing. He said staffers told him they felt as though they were beating their heads against a wall to make things function.
Other observers shared Mrvan’s concerns.
Purswell of the American Legion questioned whether appropriate steps are being taken to prepare the Walla Walla facility and its staff for the technology rollout. She asked whether staffers feel as if the Cerner system has been thrust upon them or are excited about the change.
Whether the VA has been persuasive about the benefits of the program is unclear. “I think it’s incumbent on us to demonstrate it’s not a loss,” said Dr. Terry Adirim, the leader of the VA office in charge of implementing the new records technology. “We might have dropped the ball on explaining what a benefit this is.”
Indeed, Adirim conducted a virtual town hall meeting March 21 for veterans in the Walla Walla area — where she was pressed about the problems in Spokane. “If Spokane has been a year figuring this out, why is this moving forward?” one questioner asked, expressing a point made frequently during the call. Adirim said the VA had made “thousands of changes” since the initial rollout.
Medical staffers at the Spokane and Walla Walla VA facilities are part of informal networks sharing their often-negative experiences about the program despite a perception among staff members that dissent will hurt their careers.
Adirim thinks negative feelings can be addressed by stepping up technical support. She also said training programs have been overhauled since the deployment in Spokane. Bottom line: The VA is proceeding.
“People want to revert back to what they did before,” Adirim said, but that’s not going to happen.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Subscribe to KHN's free Morning Briefing.
Spokane, Washington, was supposed to be the center of the Department of Veterans Affairs’ tech reinvention, the first site in the agency’s decade-long project to change its medical records software. But one morning in early March, the latest system malfunction made some clinicians snap.
At Spokane’s Mann-Grandstaff VA Medical Center, the records system — developed by Cerner Corp., based in North Kansas City, Missouri — went down. Staffers, inside the hospital and its outpatient facilities, were back to relying on pen and paper. Computerized schedules were inaccessible. Physicians couldn’t enter new orders or change patients’ medications.
By the next day, the electronic health records were only partially available. Dozens of records remained “sequestered,” meaning that doctors and nurses struggled to update patient charts.
The snafu, the latest in a series at Mann-Grandstaff, heightened Spokane medical staff members’ frustration with a system that has been problematic since it was installed a year and a half ago. The VA said no patients had been harmed because of the problems.
But physicians on the ground there said it’s only a matter of time before serious safety problems — those causing injury or death — emerge, pointing to the program’s ongoing weaknesses amid VA leadership’s full-bore push toward implementation nationwide. One provider said she was glad she didn’t have a relative in Mann-Grandstaff.
The one-two punch of a dangerous outage and staff grievances is the latest setback in the VA’s more than $16 billion effort to upgrade its record-keeping technology. The issues have at times forced clinicians to see fewer patients and file tens of thousands of requests for help to Cerner with patient-safety problems, congressional and agency watchdog reviews show.
If those issues multiply over the vast VA system — which employs more than a quarter-million workers and serves 6.3 million active patients — it could create rampant patient-safety and productivity problems. Despite the VA’s goals of using the technology upgrade to provide seamless records for patients from enlistment in the military until discharge, the doctors and clinicians who spoke to KHN are convinced that the problems experienced in Spokane will be repeated again and again.
The records system, scheduled for deployment at multiple VA facilities in the Pacific Northwest in the coming weeks and months, most recently rolled out at Jonathan M. Wainwright Memorial VA Medical Center in Walla Walla, Washington.
Both Cerner and Mann-Grandstaff officials declined to comment and referred KHN to officials at VA headquarters in Washington, D.C.
“If it’s a total meltdown” in Walla Walla, said Katie Purswell, the American Legion’s director of veterans affairs and rehabilitation, it’s a problem for the department and its decade-long initiative. Initial impressions from staffers are positive, but the issues in Spokane appeared over the course of weeks after the system was turned on.
The distress was particularly acute in early March. On March 2, Cerner turned on a software update to a database containing patient identification information. Problems emerged the next morning. In the record of a patient who was checking in for surgery, staff members discovered incorrect data, including gender information for a different patient. About an hour later, a staffer from the national VA’s medical records office told some clinicians at Mann-Grandstaff to “log out.”
Robert Fischer, Mann-Grandstaff’s medical center director, sent a dire warning later that morning. “Assume all electronic data is corrupted/inaccurate,” Fischer said in an email. He urged clinicians to limit orders for lab work, imaging studies, and medications. The facility shifted to “downtime procedures,” meaning a reliance on paper.
Some staffers didn’t absorb the late-morning message and continued entering information in the mixed-up records, adding to the stew of erroneous data.
According to information provided to Congress later by the VA, Cerner had informed Mann-Grandstaff of a “complete degradation” the night before — leading to questions from staffers about why it took until late morning the next day to shut down the system. Agency spokesperson Erin Crowe told KHN there wasn’t any delay in notifying staff.
Problems stretched into the following week. Some records — 70 as of March 10, according to a briefing provided to Congress — remained unusable while auditors tried to ascertain what information had been mixed in from other charts. This left clinicians in some instances unable to keep track of patients’ care. Doctors said it became a confusing and chaotic environment. They couldn’t, for example, help patients refill prescriptions.
Members of Congress are concerned — not only about the outage but also VA’s explanations about it. In a letter to agency leadership, the leading Republicans on the House Veterans’ Affairs Committee and the subcommittee overseeing technology, Rep. Mike Bost of Illinois and Rep. Matt Rosendale of Montana, expressed worries the agency was “soft-pedal[ing]” its communications and argued that veterans were misled by assurances that records had been corrected.
The full committee plans to do a deeper examination soon. It has scheduled a closed-door roundtable with VA staffers from Spokane and Walla Walla on April 5.
The outage deepened unhappiness at Mann-Grandstaff. Clinicians there were already frazzled by a deeply buggy system. Downtime was common, a congressional aide told KHN.
A March 17 VA inspector general report documented nearly 39,000 requests for technical help or improvement since the October 2020 deployment of the new records system. Cerner employees often closed requests without resolving the underlying problems, the report said. Mann-Grandstaff staffers became disengaged or devised shortcuts to bypass the malfunctioning software, the inspector general wrote — each a potential root of patient-safety incidents.
The department said the shortcuts — or workarounds — aren’t its policy. “Workarounds are not authorized nor encouraged,” Crowe said.
The Biden administration tried to overhaul the software initiative, putting the program on hiatus before installing new leadership in the medical records office at the end of 2021. But by then, low morale had sunk in. “People in Spokane VA are … demoralized and unhappy,” Rep. Frank Mrvan (D-Ind.), chair of the House subcommittee focused on the VA’s technology modernization programs, told agency leaders during a November congressional hearing. He said staffers told him they felt as though they were beating their heads against a wall to make things function.
Other observers shared Mrvan’s concerns.
Purswell of the American Legion questioned whether appropriate steps are being taken to prepare the Walla Walla facility and its staff for the technology rollout. She asked whether staffers feel as if the Cerner system has been thrust upon them or are excited about the change.
Whether the VA has been persuasive about the benefits of the program is unclear. “I think it’s incumbent on us to demonstrate it’s not a loss,” said Dr. Terry Adirim, the leader of the VA office in charge of implementing the new records technology. “We might have dropped the ball on explaining what a benefit this is.”
Indeed, Adirim conducted a virtual town hall meeting March 21 for veterans in the Walla Walla area — where she was pressed about the problems in Spokane. “If Spokane has been a year figuring this out, why is this moving forward?” one questioner asked, expressing a point made frequently during the call. Adirim said the VA had made “thousands of changes” since the initial rollout.
Medical staffers at the Spokane and Walla Walla VA facilities are part of informal networks sharing their often-negative experiences about the program despite a perception among staff members that dissent will hurt their careers.
Adirim thinks negative feelings can be addressed by stepping up technical support. She also said training programs have been overhauled since the deployment in Spokane. Bottom line: The VA is proceeding.
“People want to revert back to what they did before,” Adirim said, but that’s not going to happen.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Subscribe to KHN's free Morning Briefing.
Excoriated Papules and Plaques on the Arms and Legs
The Diagnosis: Reactive Perforating Collagenosis
Reactive perforating collagenosis (RPC) may be either acquired or inherited. It is 1 of 4 classical forms of transepithelial elimination, which also includes elastosis perforans serpiginosa (EPS) as well as perforating folliculitis and Kyrle disease. These 4 forms of transepithelial elimination share characteristics of the elimination of altered dermal components through the epidermis.1 The acquired subtype of RPC frequently occurs in patients with diabetes mellitus and end-stage renal disease,2 both present in our patient.
Clinical presentation typically shows pruritic hyperkeratotic papules with a central crater filled with crust that frequently are distributed on the extensor surfaces of the extremities, often in a linear pattern.3 The perforating papules and nodules occasionally may involve the trunk and face.4 Histopathologic examination is characterized by the elimination of altered collagen through the epidermis. Established lesions may show a cup-shaped depression of the epidermis filled with a keratin plug. The underlying dermis will show vertically oriented basophilic collagen fibers with focal extrusion through the epidermis, and elastic fibers will be absent.5 The exact pathophysiology of this disease is unknown, but it may represent a cutaneous response to superficial trauma caused by intense scratching.6
Standard treatment protocols are not well established for this condition, but some evidence shows that a combination of treatments can help ameliorate symptoms, even if they are not curative.7 Treatments without strong evidence have included a wide range of topical, systemic, and other therapies. Case series and anecdotal reports have used retinoids, corticosteroids, menthol, antibiotics, allopurinol antihistamines, cryotherapy, and lasers.8 One case was treated with a combination of narrowband UVB phototherapy and doxycycline with resolution in approximately 6 weeks.9 Other cases have been cured using triple therapy with antihistamines, topical or injected steroids, and emollients or oral antibiotics.7 Evidence shows that there may be benefit to combining multiple different treatment types that target pruritus, inflammation, and collagen damage.7,9 This disease usually cannot be cured, but it may be improved by the available treatments.
The differential diagnosis includes delusional parasitosis, EPS, perforating folliculitis, and prurigo nodularis. Delusional parasitosis also can be characterized by excoriated plaques and a sensation of parasites infesting the skin, as our patient described.10 However, it can be differentiated from RPC by the fact that it is a diagnosis of exclusion, which would not have the histopathologic findings of the elimination of collagen from the epidermis, as was demonstrated in our patient.11 Elastosis perforans serpiginosa is in the same family of perforating diseases as RPC; however, EPS typically appears in children or young adults and often is associated with other genetic disorders. Physical examination in a patient with EPS would reveal keratotic papules in a serpiginous pattern, whereas our patient had discrete lesions without any serpiginous pattern. The histopathologic appearance of EPS would reveal plugs of elastic fibers rather than collagen fibers, as was demonstrated in our patient.8 Perforating folliculitis, while also demonstrating transepithelial elimination similar to RPC, would appear as erythematous follicular papules with small central keratotic plugs and histopathologic findings of a widely dilated follicle with a mass of keratotic debris.12 Prurigo nodularis would appear as dome-shaped papulonodules with varying degrees of scale, crust, and erosion, with a histopathologic appearance of hyperplasia and thick hyperkeratosis.11
Overall, the histopathology is paramount in differentiating RPC from the alternative diagnoses, with the extrusion of collagen from the epidermis not being seen in these other conditions. The coupling of the medical history (type 2 diabetes mellitus and end-stage renal disease) with the clinical presentation and skin biopsy findings confirmed the diagnosis of RPC.
- Fei C, Wang Y, Gong Y, et al. Acquired reactive perforating collagenosis: a report of a typical case. Medicine (Baltimore). 2016;95:E4305.
- Matsui A, Nakano H, Aizu T, et al. Treatment of acquired reactive perforating collagenosis with 308‐nm excimer laser. Clin Exp Dermatol. 2016;41:820-821.
- Dey AK. Reactive perforating collagenosis: an important differential diagnosis in hemodialysis patients. Saudi J Kidney Dis Transpl. 2018;29:422-425.
- Kang S, Amagai M, Bruckner AL, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 9th ed. McGraw-Hill Education LLC; 2012.
- Plaza JA, Prieto VG. Inflammatory Skin Disorders. Demos Medical Publishing LLC; 2012.
- Kreuter A, Gambichler T. Acquired reactive perforating collagenosis. CMAJ. 2010;182:E184.
- Zhang X, Yang Y, Shao S. Acquired reactive perforating collagenosis: a case report and review of the literature. Medicine (Baltimore). 2020;99:E20391.
- Rapini RP. Perforating diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1690-1696.
- Gao L, Gu L, Chen Z, et al. Doxycycline combined with NB-UVB phototherapy for acquired reactive perforating collagenosis. Ther Clin Risk Manag. 2020;16:917-921.
- Bolognia JL, Schaffer JV, Duncan KO, et al. Psychocutaneous disorders. Dermatology Essentials. Elsevier; 2014:50-55. 11. Bolognia JL, Schaffer JV, Duncan KO, et al. Pruritus and dysesthesia. Dermatology Essentials. Elsevier; 2014:39-49. 12. Rubio FA, Herranz P, Robayna G, et al. Perforating folliculitis: report of a case in an HIV-infected man. J Am Acad Dermatol. 1999;40:300-302.
The Diagnosis: Reactive Perforating Collagenosis
Reactive perforating collagenosis (RPC) may be either acquired or inherited. It is 1 of 4 classical forms of transepithelial elimination, which also includes elastosis perforans serpiginosa (EPS) as well as perforating folliculitis and Kyrle disease. These 4 forms of transepithelial elimination share characteristics of the elimination of altered dermal components through the epidermis.1 The acquired subtype of RPC frequently occurs in patients with diabetes mellitus and end-stage renal disease,2 both present in our patient.
Clinical presentation typically shows pruritic hyperkeratotic papules with a central crater filled with crust that frequently are distributed on the extensor surfaces of the extremities, often in a linear pattern.3 The perforating papules and nodules occasionally may involve the trunk and face.4 Histopathologic examination is characterized by the elimination of altered collagen through the epidermis. Established lesions may show a cup-shaped depression of the epidermis filled with a keratin plug. The underlying dermis will show vertically oriented basophilic collagen fibers with focal extrusion through the epidermis, and elastic fibers will be absent.5 The exact pathophysiology of this disease is unknown, but it may represent a cutaneous response to superficial trauma caused by intense scratching.6
Standard treatment protocols are not well established for this condition, but some evidence shows that a combination of treatments can help ameliorate symptoms, even if they are not curative.7 Treatments without strong evidence have included a wide range of topical, systemic, and other therapies. Case series and anecdotal reports have used retinoids, corticosteroids, menthol, antibiotics, allopurinol antihistamines, cryotherapy, and lasers.8 One case was treated with a combination of narrowband UVB phototherapy and doxycycline with resolution in approximately 6 weeks.9 Other cases have been cured using triple therapy with antihistamines, topical or injected steroids, and emollients or oral antibiotics.7 Evidence shows that there may be benefit to combining multiple different treatment types that target pruritus, inflammation, and collagen damage.7,9 This disease usually cannot be cured, but it may be improved by the available treatments.
The differential diagnosis includes delusional parasitosis, EPS, perforating folliculitis, and prurigo nodularis. Delusional parasitosis also can be characterized by excoriated plaques and a sensation of parasites infesting the skin, as our patient described.10 However, it can be differentiated from RPC by the fact that it is a diagnosis of exclusion, which would not have the histopathologic findings of the elimination of collagen from the epidermis, as was demonstrated in our patient.11 Elastosis perforans serpiginosa is in the same family of perforating diseases as RPC; however, EPS typically appears in children or young adults and often is associated with other genetic disorders. Physical examination in a patient with EPS would reveal keratotic papules in a serpiginous pattern, whereas our patient had discrete lesions without any serpiginous pattern. The histopathologic appearance of EPS would reveal plugs of elastic fibers rather than collagen fibers, as was demonstrated in our patient.8 Perforating folliculitis, while also demonstrating transepithelial elimination similar to RPC, would appear as erythematous follicular papules with small central keratotic plugs and histopathologic findings of a widely dilated follicle with a mass of keratotic debris.12 Prurigo nodularis would appear as dome-shaped papulonodules with varying degrees of scale, crust, and erosion, with a histopathologic appearance of hyperplasia and thick hyperkeratosis.11
Overall, the histopathology is paramount in differentiating RPC from the alternative diagnoses, with the extrusion of collagen from the epidermis not being seen in these other conditions. The coupling of the medical history (type 2 diabetes mellitus and end-stage renal disease) with the clinical presentation and skin biopsy findings confirmed the diagnosis of RPC.
The Diagnosis: Reactive Perforating Collagenosis
Reactive perforating collagenosis (RPC) may be either acquired or inherited. It is 1 of 4 classical forms of transepithelial elimination, which also includes elastosis perforans serpiginosa (EPS) as well as perforating folliculitis and Kyrle disease. These 4 forms of transepithelial elimination share characteristics of the elimination of altered dermal components through the epidermis.1 The acquired subtype of RPC frequently occurs in patients with diabetes mellitus and end-stage renal disease,2 both present in our patient.
Clinical presentation typically shows pruritic hyperkeratotic papules with a central crater filled with crust that frequently are distributed on the extensor surfaces of the extremities, often in a linear pattern.3 The perforating papules and nodules occasionally may involve the trunk and face.4 Histopathologic examination is characterized by the elimination of altered collagen through the epidermis. Established lesions may show a cup-shaped depression of the epidermis filled with a keratin plug. The underlying dermis will show vertically oriented basophilic collagen fibers with focal extrusion through the epidermis, and elastic fibers will be absent.5 The exact pathophysiology of this disease is unknown, but it may represent a cutaneous response to superficial trauma caused by intense scratching.6
Standard treatment protocols are not well established for this condition, but some evidence shows that a combination of treatments can help ameliorate symptoms, even if they are not curative.7 Treatments without strong evidence have included a wide range of topical, systemic, and other therapies. Case series and anecdotal reports have used retinoids, corticosteroids, menthol, antibiotics, allopurinol antihistamines, cryotherapy, and lasers.8 One case was treated with a combination of narrowband UVB phototherapy and doxycycline with resolution in approximately 6 weeks.9 Other cases have been cured using triple therapy with antihistamines, topical or injected steroids, and emollients or oral antibiotics.7 Evidence shows that there may be benefit to combining multiple different treatment types that target pruritus, inflammation, and collagen damage.7,9 This disease usually cannot be cured, but it may be improved by the available treatments.
The differential diagnosis includes delusional parasitosis, EPS, perforating folliculitis, and prurigo nodularis. Delusional parasitosis also can be characterized by excoriated plaques and a sensation of parasites infesting the skin, as our patient described.10 However, it can be differentiated from RPC by the fact that it is a diagnosis of exclusion, which would not have the histopathologic findings of the elimination of collagen from the epidermis, as was demonstrated in our patient.11 Elastosis perforans serpiginosa is in the same family of perforating diseases as RPC; however, EPS typically appears in children or young adults and often is associated with other genetic disorders. Physical examination in a patient with EPS would reveal keratotic papules in a serpiginous pattern, whereas our patient had discrete lesions without any serpiginous pattern. The histopathologic appearance of EPS would reveal plugs of elastic fibers rather than collagen fibers, as was demonstrated in our patient.8 Perforating folliculitis, while also demonstrating transepithelial elimination similar to RPC, would appear as erythematous follicular papules with small central keratotic plugs and histopathologic findings of a widely dilated follicle with a mass of keratotic debris.12 Prurigo nodularis would appear as dome-shaped papulonodules with varying degrees of scale, crust, and erosion, with a histopathologic appearance of hyperplasia and thick hyperkeratosis.11
Overall, the histopathology is paramount in differentiating RPC from the alternative diagnoses, with the extrusion of collagen from the epidermis not being seen in these other conditions. The coupling of the medical history (type 2 diabetes mellitus and end-stage renal disease) with the clinical presentation and skin biopsy findings confirmed the diagnosis of RPC.
- Fei C, Wang Y, Gong Y, et al. Acquired reactive perforating collagenosis: a report of a typical case. Medicine (Baltimore). 2016;95:E4305.
- Matsui A, Nakano H, Aizu T, et al. Treatment of acquired reactive perforating collagenosis with 308‐nm excimer laser. Clin Exp Dermatol. 2016;41:820-821.
- Dey AK. Reactive perforating collagenosis: an important differential diagnosis in hemodialysis patients. Saudi J Kidney Dis Transpl. 2018;29:422-425.
- Kang S, Amagai M, Bruckner AL, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 9th ed. McGraw-Hill Education LLC; 2012.
- Plaza JA, Prieto VG. Inflammatory Skin Disorders. Demos Medical Publishing LLC; 2012.
- Kreuter A, Gambichler T. Acquired reactive perforating collagenosis. CMAJ. 2010;182:E184.
- Zhang X, Yang Y, Shao S. Acquired reactive perforating collagenosis: a case report and review of the literature. Medicine (Baltimore). 2020;99:E20391.
- Rapini RP. Perforating diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1690-1696.
- Gao L, Gu L, Chen Z, et al. Doxycycline combined with NB-UVB phototherapy for acquired reactive perforating collagenosis. Ther Clin Risk Manag. 2020;16:917-921.
- Bolognia JL, Schaffer JV, Duncan KO, et al. Psychocutaneous disorders. Dermatology Essentials. Elsevier; 2014:50-55. 11. Bolognia JL, Schaffer JV, Duncan KO, et al. Pruritus and dysesthesia. Dermatology Essentials. Elsevier; 2014:39-49. 12. Rubio FA, Herranz P, Robayna G, et al. Perforating folliculitis: report of a case in an HIV-infected man. J Am Acad Dermatol. 1999;40:300-302.
- Fei C, Wang Y, Gong Y, et al. Acquired reactive perforating collagenosis: a report of a typical case. Medicine (Baltimore). 2016;95:E4305.
- Matsui A, Nakano H, Aizu T, et al. Treatment of acquired reactive perforating collagenosis with 308‐nm excimer laser. Clin Exp Dermatol. 2016;41:820-821.
- Dey AK. Reactive perforating collagenosis: an important differential diagnosis in hemodialysis patients. Saudi J Kidney Dis Transpl. 2018;29:422-425.
- Kang S, Amagai M, Bruckner AL, et al, eds. Fitzpatrick’s Dermatology in General Medicine. 9th ed. McGraw-Hill Education LLC; 2012.
- Plaza JA, Prieto VG. Inflammatory Skin Disorders. Demos Medical Publishing LLC; 2012.
- Kreuter A, Gambichler T. Acquired reactive perforating collagenosis. CMAJ. 2010;182:E184.
- Zhang X, Yang Y, Shao S. Acquired reactive perforating collagenosis: a case report and review of the literature. Medicine (Baltimore). 2020;99:E20391.
- Rapini RP. Perforating diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:1690-1696.
- Gao L, Gu L, Chen Z, et al. Doxycycline combined with NB-UVB phototherapy for acquired reactive perforating collagenosis. Ther Clin Risk Manag. 2020;16:917-921.
- Bolognia JL, Schaffer JV, Duncan KO, et al. Psychocutaneous disorders. Dermatology Essentials. Elsevier; 2014:50-55. 11. Bolognia JL, Schaffer JV, Duncan KO, et al. Pruritus and dysesthesia. Dermatology Essentials. Elsevier; 2014:39-49. 12. Rubio FA, Herranz P, Robayna G, et al. Perforating folliculitis: report of a case in an HIV-infected man. J Am Acad Dermatol. 1999;40:300-302.
A 73-year-old woman presented for evaluation of a rash on the arms and legs of 3 months’ duration. The rash had developed abruptly, and she believed it was caused by bugs in the skin; her husband noted that she constantly picked at her arms and legs. She had a medical history of hypertension, type 2 diabetes mellitus, and endstage renal disease on dialysis. Physical examination revealed multiple pigmented papules and plaques, some with keratotic scale, on the lower legs (left) and arms, with greater involvement on the left arm (right). The lesions were of various sizes and shapes, some with a central keratotic core, and several lesions demonstrated erosion, excoriation, or ulceration. Histopathologic examination revealed slight attenuation of the epidermis with loss of normal rete peg architecture, alternating areas of hypergranulosis and hypogranulosis, central ulceration with inflammatory cells, and a basophilic hue to the ulcer base with sweeping up of the collagen fibers.
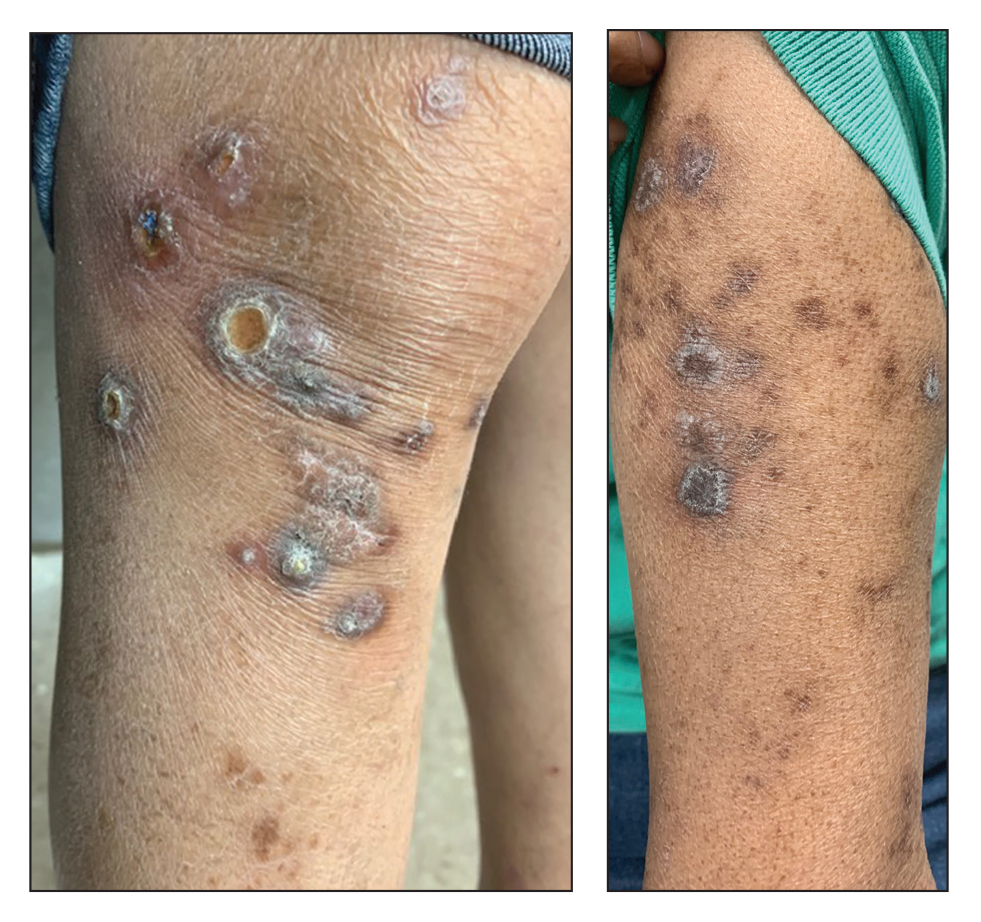
Adding immunotherapy to chemo in lung cancer improves patient outcomes, new data show
according to an analysis presented at the annual European Lung Cancer Congress (ELCC) on March 30.
“Overall, it is very clear that chemotherapy plus immunotherapy prolongs the time to symptom deterioration and actually improves symptoms” in this patient population, said study discussant Luis Paz-Ares, MD, PhD, chair of medical oncology at the Hospital Universitario 12 de Octubre, Madrid, who was not involved in the research.
Last September, investigators reported efficacy outcomes from the phase 3 POSEIDON trial, which randomized 1,013 patients with EGFR/ALK wild-type mNSCLC to one of three first-line options: chemotherapy alone, chemotherapy plus the checkpoint inhibitor durvalumab, or chemotherapy plus two check-point inhibitors, durvalumab and tremelimumab. The analysis showed improved progression-free survival in both immunotherapy arms as well as a significant 2.3-month overall survival advantage with dual immunotherapy and a nonsignificant 1.6-month advantage with single agent durvalumab.
At the ELCC meeting, study presenter and lead investigator Edward Garon, MD, reported the latest data on the trial’s secondary endpoints: patient-reported outcomes. Global health status, functioning, and symptom scores were assessed using two questionnaires, the EORTC QLQ-C30 and EORTC QLQ-LC13.
Overall, Dr. Garon and colleagues reported a longer time to deterioration in all three areas – global health status, functioning, and symptoms – for patients who received immunotherapy versus chemotherapy alone, with similar results in both immunotherapy arms.
Time to deterioration in global health status, for instance, was a median of about 8 months on both immunotherapy regimens versus 5.6 months with chemotherapy alone. The positive findings held for many patient-reported treatment side effects, including dyspnea, hemoptysis, nausea/vomiting, and insomnia, but the benefits of adding immunotherapy weren’t always statistically significant.
Adding one or both checkpoint inhibitors to chemotherapy “improved efficacy while delaying deterioration in symptoms, functioning, and [health-related quality of life] versus chemotherapy alone in patients with mNSCLC,” concluded Dr. Garon, a thoracic medical oncologist at the University of California, Los Angeles. Plus, he added, “the pattern was observed across nearly all prespecified symptoms and domains of interest.”
According to study discussant Dr. Paz-Ares, “the data seem to be very consistent with all the trials asking similar questions.” The important thing here is figuring out the ideal candidates for dual inhibitor therapy, he said.
With positive efficacy and patient-reported outcomes for single and dual immunotherapy in this trial, it’s a “relatively straightforward” decision to add immunotherapy to chemotherapy for patients with mNSCLC, Massimo Di Maio, a medical oncologist at the University of Turin, Italy, said in an editorial on the ELCC’s news site.
However, that’s not always the case for every cancer type, which makes patient-reported outcomes “crucial” for determining the right treatment for each patient. Some might opt for a modest survival benefit regardless of the side effects, while others might favor a less toxic approach, even it means not living quite as long, he said.
The problem, he stressed, is that trials often release efficacy data well before patient-reported outcomes, which makes weighing the benefits and risks of a treat-ment option more difficult. The delay between efficacy and patient-reported outcome data was about 6 months in the POSEIDON trial.
“Timing is key when it comes to using [patient reported outcomes] for decision-making in oncology,” Dr. Di Maio said. “In fact, to enable a full assessment of a treatment, results should be published concurrently with the efficacy and safety data. Unfortunately, this is generally not the case.”
POSEIDON was funded by AstraZeneca, which markets durvalumab and is developing tremelimumab. Dr. Garon reported grants from the company. Dr. Paz-Ares reported honoraria and institutional research grants from AstraZeneca. Dr. Di Maio is a consultant for AstraZeneca and reported receiving honoraria and personal fees from the company.
according to an analysis presented at the annual European Lung Cancer Congress (ELCC) on March 30.
“Overall, it is very clear that chemotherapy plus immunotherapy prolongs the time to symptom deterioration and actually improves symptoms” in this patient population, said study discussant Luis Paz-Ares, MD, PhD, chair of medical oncology at the Hospital Universitario 12 de Octubre, Madrid, who was not involved in the research.
Last September, investigators reported efficacy outcomes from the phase 3 POSEIDON trial, which randomized 1,013 patients with EGFR/ALK wild-type mNSCLC to one of three first-line options: chemotherapy alone, chemotherapy plus the checkpoint inhibitor durvalumab, or chemotherapy plus two check-point inhibitors, durvalumab and tremelimumab. The analysis showed improved progression-free survival in both immunotherapy arms as well as a significant 2.3-month overall survival advantage with dual immunotherapy and a nonsignificant 1.6-month advantage with single agent durvalumab.
At the ELCC meeting, study presenter and lead investigator Edward Garon, MD, reported the latest data on the trial’s secondary endpoints: patient-reported outcomes. Global health status, functioning, and symptom scores were assessed using two questionnaires, the EORTC QLQ-C30 and EORTC QLQ-LC13.
Overall, Dr. Garon and colleagues reported a longer time to deterioration in all three areas – global health status, functioning, and symptoms – for patients who received immunotherapy versus chemotherapy alone, with similar results in both immunotherapy arms.
Time to deterioration in global health status, for instance, was a median of about 8 months on both immunotherapy regimens versus 5.6 months with chemotherapy alone. The positive findings held for many patient-reported treatment side effects, including dyspnea, hemoptysis, nausea/vomiting, and insomnia, but the benefits of adding immunotherapy weren’t always statistically significant.
Adding one or both checkpoint inhibitors to chemotherapy “improved efficacy while delaying deterioration in symptoms, functioning, and [health-related quality of life] versus chemotherapy alone in patients with mNSCLC,” concluded Dr. Garon, a thoracic medical oncologist at the University of California, Los Angeles. Plus, he added, “the pattern was observed across nearly all prespecified symptoms and domains of interest.”
According to study discussant Dr. Paz-Ares, “the data seem to be very consistent with all the trials asking similar questions.” The important thing here is figuring out the ideal candidates for dual inhibitor therapy, he said.
With positive efficacy and patient-reported outcomes for single and dual immunotherapy in this trial, it’s a “relatively straightforward” decision to add immunotherapy to chemotherapy for patients with mNSCLC, Massimo Di Maio, a medical oncologist at the University of Turin, Italy, said in an editorial on the ELCC’s news site.
However, that’s not always the case for every cancer type, which makes patient-reported outcomes “crucial” for determining the right treatment for each patient. Some might opt for a modest survival benefit regardless of the side effects, while others might favor a less toxic approach, even it means not living quite as long, he said.
The problem, he stressed, is that trials often release efficacy data well before patient-reported outcomes, which makes weighing the benefits and risks of a treat-ment option more difficult. The delay between efficacy and patient-reported outcome data was about 6 months in the POSEIDON trial.
“Timing is key when it comes to using [patient reported outcomes] for decision-making in oncology,” Dr. Di Maio said. “In fact, to enable a full assessment of a treatment, results should be published concurrently with the efficacy and safety data. Unfortunately, this is generally not the case.”
POSEIDON was funded by AstraZeneca, which markets durvalumab and is developing tremelimumab. Dr. Garon reported grants from the company. Dr. Paz-Ares reported honoraria and institutional research grants from AstraZeneca. Dr. Di Maio is a consultant for AstraZeneca and reported receiving honoraria and personal fees from the company.
according to an analysis presented at the annual European Lung Cancer Congress (ELCC) on March 30.
“Overall, it is very clear that chemotherapy plus immunotherapy prolongs the time to symptom deterioration and actually improves symptoms” in this patient population, said study discussant Luis Paz-Ares, MD, PhD, chair of medical oncology at the Hospital Universitario 12 de Octubre, Madrid, who was not involved in the research.
Last September, investigators reported efficacy outcomes from the phase 3 POSEIDON trial, which randomized 1,013 patients with EGFR/ALK wild-type mNSCLC to one of three first-line options: chemotherapy alone, chemotherapy plus the checkpoint inhibitor durvalumab, or chemotherapy plus two check-point inhibitors, durvalumab and tremelimumab. The analysis showed improved progression-free survival in both immunotherapy arms as well as a significant 2.3-month overall survival advantage with dual immunotherapy and a nonsignificant 1.6-month advantage with single agent durvalumab.
At the ELCC meeting, study presenter and lead investigator Edward Garon, MD, reported the latest data on the trial’s secondary endpoints: patient-reported outcomes. Global health status, functioning, and symptom scores were assessed using two questionnaires, the EORTC QLQ-C30 and EORTC QLQ-LC13.
Overall, Dr. Garon and colleagues reported a longer time to deterioration in all three areas – global health status, functioning, and symptoms – for patients who received immunotherapy versus chemotherapy alone, with similar results in both immunotherapy arms.
Time to deterioration in global health status, for instance, was a median of about 8 months on both immunotherapy regimens versus 5.6 months with chemotherapy alone. The positive findings held for many patient-reported treatment side effects, including dyspnea, hemoptysis, nausea/vomiting, and insomnia, but the benefits of adding immunotherapy weren’t always statistically significant.
Adding one or both checkpoint inhibitors to chemotherapy “improved efficacy while delaying deterioration in symptoms, functioning, and [health-related quality of life] versus chemotherapy alone in patients with mNSCLC,” concluded Dr. Garon, a thoracic medical oncologist at the University of California, Los Angeles. Plus, he added, “the pattern was observed across nearly all prespecified symptoms and domains of interest.”
According to study discussant Dr. Paz-Ares, “the data seem to be very consistent with all the trials asking similar questions.” The important thing here is figuring out the ideal candidates for dual inhibitor therapy, he said.
With positive efficacy and patient-reported outcomes for single and dual immunotherapy in this trial, it’s a “relatively straightforward” decision to add immunotherapy to chemotherapy for patients with mNSCLC, Massimo Di Maio, a medical oncologist at the University of Turin, Italy, said in an editorial on the ELCC’s news site.
However, that’s not always the case for every cancer type, which makes patient-reported outcomes “crucial” for determining the right treatment for each patient. Some might opt for a modest survival benefit regardless of the side effects, while others might favor a less toxic approach, even it means not living quite as long, he said.
The problem, he stressed, is that trials often release efficacy data well before patient-reported outcomes, which makes weighing the benefits and risks of a treat-ment option more difficult. The delay between efficacy and patient-reported outcome data was about 6 months in the POSEIDON trial.
“Timing is key when it comes to using [patient reported outcomes] for decision-making in oncology,” Dr. Di Maio said. “In fact, to enable a full assessment of a treatment, results should be published concurrently with the efficacy and safety data. Unfortunately, this is generally not the case.”
POSEIDON was funded by AstraZeneca, which markets durvalumab and is developing tremelimumab. Dr. Garon reported grants from the company. Dr. Paz-Ares reported honoraria and institutional research grants from AstraZeneca. Dr. Di Maio is a consultant for AstraZeneca and reported receiving honoraria and personal fees from the company.
FROM ELCC 2022
Experimental drug may boost executive function in patients with Alzheimer’s disease
Patients performed better in cognitive testing after just 2 weeks, especially in areas of executive functioning. Clinicians involved in the study also reported improvements in patients’ ability to complete daily activities, especially in complex tasks such as using a computer, carrying out household chores, and managing their medications.
“It’s pretty incredible to see improvement over the course of a week to a week and a half,” said study investigator Aaron Koenig, MD, vice president of Early Clinical Development at Sage Therapeutics in Cambridge, Mass. “Not only are we seeing objective improvement, we’re also seeing a subjective benefit.”
The drug, SAGE-718, is also under study for MCI in patients with Huntington’s disease, the drug’s primary indication, and Parkinson’s disease.
The findings will be presented at the 2022 annual meeting of the American Academy of Neurology.
Improved executive function
SAGE-718 is in a new class of drugs called positive allosteric modulator of N-methyl-D-aspartate (NMDA) receptors, which are thought to improve neuroplasticity.
For the phase 2a open-label LUMINARY trial, researchers enrolled 26 patients ages 50-80 years with Alzheimer’s disease who had MCI. Patients completed a battery of cognitive tests at the study outset, again at the end of treatment, and again after 28 days.
Participants received SAGE-718 daily for 2 weeks and were followed for another 2 weeks.
The study’s primary outcome was safety. Seven patients (26.9%) reported mild or moderate treatment-emergent adverse events (AEs), and there were no serious AEs or deaths.
However, after 14 days, researchers also noted improvements from baseline on multiple tests of executive functioning, learning, and memory. And at 28 days, participants demonstrated significantly better Montreal Cognitive Assessment scores, compared with baseline (+2.3 points; P < .05), suggesting improvement in global cognition.
“We know that in Alzheimer’s and other neurodegenerative conditions there is a change in cognition, the ability to think, the ability to do things,” Dr. Koenig said. “What we’ve seen with SAGE-718 to date, all the way back to our phase 1 studies, is a cognitively beneficial effect, but more specifically an improvement in executive functioning.”
Intentional small study design
Commenting on the findings, Percy Griffin, PhD, MSc, director of scientific engagement for the Alzheimer’s Association, said that because of the small study size, short follow-up, and limited data available in the conference abstract, “we cannot speculate about the efficacy of this investigational therapy.”
“Bigger picture, the real-world clinical meaningfulness of research results that are generated in highly controlled circumstances is an important question that is being discussed right now throughout the Alzheimer’s field,” he added.
However, Dr. Koenig countered that the small study design was intentional. “Over the course of a year, we can get to the answer in different patient populations rather than running these rather large and arduous trials that may pan out to not be positive,” he said.
“The purpose here is to say, directionally, are we seeing improvement that warrants further investigation? If you don’t see an effect in a small number of patients, if you don’t see that effect rather quickly, and if you don’t see an effect that should translate into something meaningful, we at SAGE believe that you may not have a drug there,” he added.
Sage Therapeutics plans to launch a phase 2b placebo-controlled trial later this year to study SAGE-718 in more Alzheimer’s patients over a longer period of time.
The study was funded by SAGE Therapeutics. Dr. Koenig is an employee of SAGE and reports no other conflicts. Dr. Griffin has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients performed better in cognitive testing after just 2 weeks, especially in areas of executive functioning. Clinicians involved in the study also reported improvements in patients’ ability to complete daily activities, especially in complex tasks such as using a computer, carrying out household chores, and managing their medications.
“It’s pretty incredible to see improvement over the course of a week to a week and a half,” said study investigator Aaron Koenig, MD, vice president of Early Clinical Development at Sage Therapeutics in Cambridge, Mass. “Not only are we seeing objective improvement, we’re also seeing a subjective benefit.”
The drug, SAGE-718, is also under study for MCI in patients with Huntington’s disease, the drug’s primary indication, and Parkinson’s disease.
The findings will be presented at the 2022 annual meeting of the American Academy of Neurology.
Improved executive function
SAGE-718 is in a new class of drugs called positive allosteric modulator of N-methyl-D-aspartate (NMDA) receptors, which are thought to improve neuroplasticity.
For the phase 2a open-label LUMINARY trial, researchers enrolled 26 patients ages 50-80 years with Alzheimer’s disease who had MCI. Patients completed a battery of cognitive tests at the study outset, again at the end of treatment, and again after 28 days.
Participants received SAGE-718 daily for 2 weeks and were followed for another 2 weeks.
The study’s primary outcome was safety. Seven patients (26.9%) reported mild or moderate treatment-emergent adverse events (AEs), and there were no serious AEs or deaths.
However, after 14 days, researchers also noted improvements from baseline on multiple tests of executive functioning, learning, and memory. And at 28 days, participants demonstrated significantly better Montreal Cognitive Assessment scores, compared with baseline (+2.3 points; P < .05), suggesting improvement in global cognition.
“We know that in Alzheimer’s and other neurodegenerative conditions there is a change in cognition, the ability to think, the ability to do things,” Dr. Koenig said. “What we’ve seen with SAGE-718 to date, all the way back to our phase 1 studies, is a cognitively beneficial effect, but more specifically an improvement in executive functioning.”
Intentional small study design
Commenting on the findings, Percy Griffin, PhD, MSc, director of scientific engagement for the Alzheimer’s Association, said that because of the small study size, short follow-up, and limited data available in the conference abstract, “we cannot speculate about the efficacy of this investigational therapy.”
“Bigger picture, the real-world clinical meaningfulness of research results that are generated in highly controlled circumstances is an important question that is being discussed right now throughout the Alzheimer’s field,” he added.
However, Dr. Koenig countered that the small study design was intentional. “Over the course of a year, we can get to the answer in different patient populations rather than running these rather large and arduous trials that may pan out to not be positive,” he said.
“The purpose here is to say, directionally, are we seeing improvement that warrants further investigation? If you don’t see an effect in a small number of patients, if you don’t see that effect rather quickly, and if you don’t see an effect that should translate into something meaningful, we at SAGE believe that you may not have a drug there,” he added.
Sage Therapeutics plans to launch a phase 2b placebo-controlled trial later this year to study SAGE-718 in more Alzheimer’s patients over a longer period of time.
The study was funded by SAGE Therapeutics. Dr. Koenig is an employee of SAGE and reports no other conflicts. Dr. Griffin has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients performed better in cognitive testing after just 2 weeks, especially in areas of executive functioning. Clinicians involved in the study also reported improvements in patients’ ability to complete daily activities, especially in complex tasks such as using a computer, carrying out household chores, and managing their medications.
“It’s pretty incredible to see improvement over the course of a week to a week and a half,” said study investigator Aaron Koenig, MD, vice president of Early Clinical Development at Sage Therapeutics in Cambridge, Mass. “Not only are we seeing objective improvement, we’re also seeing a subjective benefit.”
The drug, SAGE-718, is also under study for MCI in patients with Huntington’s disease, the drug’s primary indication, and Parkinson’s disease.
The findings will be presented at the 2022 annual meeting of the American Academy of Neurology.
Improved executive function
SAGE-718 is in a new class of drugs called positive allosteric modulator of N-methyl-D-aspartate (NMDA) receptors, which are thought to improve neuroplasticity.
For the phase 2a open-label LUMINARY trial, researchers enrolled 26 patients ages 50-80 years with Alzheimer’s disease who had MCI. Patients completed a battery of cognitive tests at the study outset, again at the end of treatment, and again after 28 days.
Participants received SAGE-718 daily for 2 weeks and were followed for another 2 weeks.
The study’s primary outcome was safety. Seven patients (26.9%) reported mild or moderate treatment-emergent adverse events (AEs), and there were no serious AEs or deaths.
However, after 14 days, researchers also noted improvements from baseline on multiple tests of executive functioning, learning, and memory. And at 28 days, participants demonstrated significantly better Montreal Cognitive Assessment scores, compared with baseline (+2.3 points; P < .05), suggesting improvement in global cognition.
“We know that in Alzheimer’s and other neurodegenerative conditions there is a change in cognition, the ability to think, the ability to do things,” Dr. Koenig said. “What we’ve seen with SAGE-718 to date, all the way back to our phase 1 studies, is a cognitively beneficial effect, but more specifically an improvement in executive functioning.”
Intentional small study design
Commenting on the findings, Percy Griffin, PhD, MSc, director of scientific engagement for the Alzheimer’s Association, said that because of the small study size, short follow-up, and limited data available in the conference abstract, “we cannot speculate about the efficacy of this investigational therapy.”
“Bigger picture, the real-world clinical meaningfulness of research results that are generated in highly controlled circumstances is an important question that is being discussed right now throughout the Alzheimer’s field,” he added.
However, Dr. Koenig countered that the small study design was intentional. “Over the course of a year, we can get to the answer in different patient populations rather than running these rather large and arduous trials that may pan out to not be positive,” he said.
“The purpose here is to say, directionally, are we seeing improvement that warrants further investigation? If you don’t see an effect in a small number of patients, if you don’t see that effect rather quickly, and if you don’t see an effect that should translate into something meaningful, we at SAGE believe that you may not have a drug there,” he added.
Sage Therapeutics plans to launch a phase 2b placebo-controlled trial later this year to study SAGE-718 in more Alzheimer’s patients over a longer period of time.
The study was funded by SAGE Therapeutics. Dr. Koenig is an employee of SAGE and reports no other conflicts. Dr. Griffin has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2022
Novel drug significantly reduces tics in Tourette syndrome – without side effects
, a new study shows.
Importantly, unlike current medications for the disorder, ecocipam does not lead to weight gain, anxiety, depression, or tardive dyskinesia, compared with placebo – a factor that may lead to better adherence.
For clinicians treating children with Tourette syndrome, the results suggest “help is on the way,” said study investigator Donald Gilbert, MD, professor of pediatrics and neurology, University of Cincinnati Children’s Hospital Medical Center.
“There may be a drug available with a new mechanism of action that is effective to suppress tics without causing weight gain or unwanted neuropsychiatric side effects,” Dr. Gilbert said.
The findings will be presented at the 2022 annual meeting of the American Academy of Neurology.
First-in-class agent
Tourette syndrome is a neurologic condition that causes sudden repetitive involuntary muscle movements and sounds known as tics. These movements typically develop in childhood and worsen during adolescence.
“There’s a risk of injury, such as to the neck, with tics in childhood, so it’s good to have something that makes tics less severe and less socially impairing in junior high,” said Dr. Gilbert.
While tics generally diminish by adulthood, “about 10% of the patients we see as kids persist into adulthood enough to need medical interventions,” said Dr. Gilbert.
Ecopipam is a first-in-class selective D1 receptor antagonist in clinical development for pediatric patients with Tourette syndrome. The compound was previously tested without success in schizophrenia and in obesity, the idea being that because dopamine is linked to pleasure or reward, blocking it might result in weight loss, said Dr. Gilbert.
However, earlier studies in Tourette syndrome suggested that ecopipam reduces tics in children and adults and had low metabolic and movement-related adverse effects.
Drugs currently used to treat tics include haloperidol, pimocide, and aripiprazole. All of these agents block the dopamine-2 (D2) receptor and can cause weight gain and tardive dyskinesia, said Dr. Gilbert.
Placebo-controlled trial
The new study included 149 patients with Tourette syndrome who had a score of at least 20 on the Yale Global Tic Severity Total Tic Score (YGTSS-TTS). The scale measures five aspects of motor and vocal tics: the number, frequency, intensity, complexity, and interference.
With that scale, intensity assesses whether tics cause injury, complexity evaluates the number of muscle group, and interference assesses whether tics interrupt functions, such as speaking or walking.
For each of the five areas, scores range from 0-5, with higher scores indicating greater severity. The motor and vocal parts have a maximum of 25 points each, for a maximum total of 50.
Participants were randomly assigned to receive once-daily oral ecopipam or placebo. A 4-week titration period was followed by an 8-week maintenance period and then a 1-week tapering period.
The primary endpoint was mean change from baseline to week 12 in scores on the YGTSS-TTS.
Results on the YGTSS-TTS showed a significant improvement in the ecopipam group, compared with placebo groups (least square [LS] mean difference: -3.44; 95% confidence interval: -6.09 to -0.79; P = .011).
The analysis indicated a 30% reduction, with an effect size of 0.48, which is “pretty good,” said Dr. Gilbert. “The amount of change is comparable to other drugs that are marketed” to treat tics.
The drug was effective for younger as well as older children. Among those aged 6-11 years, the LS mean difference was -4.95 (95% CI: -9.99 to 0.10; P = .054), and for those aged 12 to 17 years, the LS mean difference was -3.37 (95% CI: -6.51 to -0.24; P = .035).
A key secondary endpoint was the score on the Clinical Global Impression of Tourette Syndrome Severity, which Dr. Gilbert said is a more subjective measure of whether a patient’s life has improved. Here, the mean change at week 12 was significant (P = .001) for the treated group (improvement of 0.91 points), compared with the placebo group (improvement of 0.5 points).
Researchers also assessed safety and tolerability. Treatment-related adverse events (AEs) occurred in 34% of patients taking ecopipam and in 21% of those taking placebo. The most common AEs were headache (9.2%), fatigue (6.6%), somnolence (6.6%), and restlessness (5.3%).
There were no metabolic or movement-related AEs or treatment-related serious AEs.
“This drug doesn’t cause weight gain at all,” said Dr. Gilbert. He noted that there was also no difference in the groups in terms of rates of depression, anxiety, or tardive dyskinesia.
Significant tic reduction
Commenting on the findings, Jessica Frey, MD, a movement disorders fellow at the University of Florida, said the new double-blind, placebo-controlled study “is promising” in that it demonstrates significant tic reduction, compared with placebo without significant side effects.
“Ecopipam could potentially expand pharmacologic treatment options for children and adolescents with Tourette syndrome in the near future,” she said.
Dr. Frey will also be presenting results at the meeting of a study showing a significant correlation between tic severity and social media use among adolescents with Tourette syndrome during the COVID pandemic.
She noted that dopamine is an important neurotransmitter in the underlying pathophysiology of Tourette syndrome. In addition, although D2 receptor blockade can provide significant tic reduction, the “intolerable” side effects often linked to medications with this mechanism “can lead to discontinuation,” said Dr. Frey.
She also noted that ecopipam has previously been evaluated in an open-label study and a follow-up placebo-controlled study that demonstrated safety as well as significant tic reduction.
The study was supported by Emalex Biosciences. Dr. Gilbert and Dr. Frey report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new study shows.
Importantly, unlike current medications for the disorder, ecocipam does not lead to weight gain, anxiety, depression, or tardive dyskinesia, compared with placebo – a factor that may lead to better adherence.
For clinicians treating children with Tourette syndrome, the results suggest “help is on the way,” said study investigator Donald Gilbert, MD, professor of pediatrics and neurology, University of Cincinnati Children’s Hospital Medical Center.
“There may be a drug available with a new mechanism of action that is effective to suppress tics without causing weight gain or unwanted neuropsychiatric side effects,” Dr. Gilbert said.
The findings will be presented at the 2022 annual meeting of the American Academy of Neurology.
First-in-class agent
Tourette syndrome is a neurologic condition that causes sudden repetitive involuntary muscle movements and sounds known as tics. These movements typically develop in childhood and worsen during adolescence.
“There’s a risk of injury, such as to the neck, with tics in childhood, so it’s good to have something that makes tics less severe and less socially impairing in junior high,” said Dr. Gilbert.
While tics generally diminish by adulthood, “about 10% of the patients we see as kids persist into adulthood enough to need medical interventions,” said Dr. Gilbert.
Ecopipam is a first-in-class selective D1 receptor antagonist in clinical development for pediatric patients with Tourette syndrome. The compound was previously tested without success in schizophrenia and in obesity, the idea being that because dopamine is linked to pleasure or reward, blocking it might result in weight loss, said Dr. Gilbert.
However, earlier studies in Tourette syndrome suggested that ecopipam reduces tics in children and adults and had low metabolic and movement-related adverse effects.
Drugs currently used to treat tics include haloperidol, pimocide, and aripiprazole. All of these agents block the dopamine-2 (D2) receptor and can cause weight gain and tardive dyskinesia, said Dr. Gilbert.
Placebo-controlled trial
The new study included 149 patients with Tourette syndrome who had a score of at least 20 on the Yale Global Tic Severity Total Tic Score (YGTSS-TTS). The scale measures five aspects of motor and vocal tics: the number, frequency, intensity, complexity, and interference.
With that scale, intensity assesses whether tics cause injury, complexity evaluates the number of muscle group, and interference assesses whether tics interrupt functions, such as speaking or walking.
For each of the five areas, scores range from 0-5, with higher scores indicating greater severity. The motor and vocal parts have a maximum of 25 points each, for a maximum total of 50.
Participants were randomly assigned to receive once-daily oral ecopipam or placebo. A 4-week titration period was followed by an 8-week maintenance period and then a 1-week tapering period.
The primary endpoint was mean change from baseline to week 12 in scores on the YGTSS-TTS.
Results on the YGTSS-TTS showed a significant improvement in the ecopipam group, compared with placebo groups (least square [LS] mean difference: -3.44; 95% confidence interval: -6.09 to -0.79; P = .011).
The analysis indicated a 30% reduction, with an effect size of 0.48, which is “pretty good,” said Dr. Gilbert. “The amount of change is comparable to other drugs that are marketed” to treat tics.
The drug was effective for younger as well as older children. Among those aged 6-11 years, the LS mean difference was -4.95 (95% CI: -9.99 to 0.10; P = .054), and for those aged 12 to 17 years, the LS mean difference was -3.37 (95% CI: -6.51 to -0.24; P = .035).
A key secondary endpoint was the score on the Clinical Global Impression of Tourette Syndrome Severity, which Dr. Gilbert said is a more subjective measure of whether a patient’s life has improved. Here, the mean change at week 12 was significant (P = .001) for the treated group (improvement of 0.91 points), compared with the placebo group (improvement of 0.5 points).
Researchers also assessed safety and tolerability. Treatment-related adverse events (AEs) occurred in 34% of patients taking ecopipam and in 21% of those taking placebo. The most common AEs were headache (9.2%), fatigue (6.6%), somnolence (6.6%), and restlessness (5.3%).
There were no metabolic or movement-related AEs or treatment-related serious AEs.
“This drug doesn’t cause weight gain at all,” said Dr. Gilbert. He noted that there was also no difference in the groups in terms of rates of depression, anxiety, or tardive dyskinesia.
Significant tic reduction
Commenting on the findings, Jessica Frey, MD, a movement disorders fellow at the University of Florida, said the new double-blind, placebo-controlled study “is promising” in that it demonstrates significant tic reduction, compared with placebo without significant side effects.
“Ecopipam could potentially expand pharmacologic treatment options for children and adolescents with Tourette syndrome in the near future,” she said.
Dr. Frey will also be presenting results at the meeting of a study showing a significant correlation between tic severity and social media use among adolescents with Tourette syndrome during the COVID pandemic.
She noted that dopamine is an important neurotransmitter in the underlying pathophysiology of Tourette syndrome. In addition, although D2 receptor blockade can provide significant tic reduction, the “intolerable” side effects often linked to medications with this mechanism “can lead to discontinuation,” said Dr. Frey.
She also noted that ecopipam has previously been evaluated in an open-label study and a follow-up placebo-controlled study that demonstrated safety as well as significant tic reduction.
The study was supported by Emalex Biosciences. Dr. Gilbert and Dr. Frey report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new study shows.
Importantly, unlike current medications for the disorder, ecocipam does not lead to weight gain, anxiety, depression, or tardive dyskinesia, compared with placebo – a factor that may lead to better adherence.
For clinicians treating children with Tourette syndrome, the results suggest “help is on the way,” said study investigator Donald Gilbert, MD, professor of pediatrics and neurology, University of Cincinnati Children’s Hospital Medical Center.
“There may be a drug available with a new mechanism of action that is effective to suppress tics without causing weight gain or unwanted neuropsychiatric side effects,” Dr. Gilbert said.
The findings will be presented at the 2022 annual meeting of the American Academy of Neurology.
First-in-class agent
Tourette syndrome is a neurologic condition that causes sudden repetitive involuntary muscle movements and sounds known as tics. These movements typically develop in childhood and worsen during adolescence.
“There’s a risk of injury, such as to the neck, with tics in childhood, so it’s good to have something that makes tics less severe and less socially impairing in junior high,” said Dr. Gilbert.
While tics generally diminish by adulthood, “about 10% of the patients we see as kids persist into adulthood enough to need medical interventions,” said Dr. Gilbert.
Ecopipam is a first-in-class selective D1 receptor antagonist in clinical development for pediatric patients with Tourette syndrome. The compound was previously tested without success in schizophrenia and in obesity, the idea being that because dopamine is linked to pleasure or reward, blocking it might result in weight loss, said Dr. Gilbert.
However, earlier studies in Tourette syndrome suggested that ecopipam reduces tics in children and adults and had low metabolic and movement-related adverse effects.
Drugs currently used to treat tics include haloperidol, pimocide, and aripiprazole. All of these agents block the dopamine-2 (D2) receptor and can cause weight gain and tardive dyskinesia, said Dr. Gilbert.
Placebo-controlled trial
The new study included 149 patients with Tourette syndrome who had a score of at least 20 on the Yale Global Tic Severity Total Tic Score (YGTSS-TTS). The scale measures five aspects of motor and vocal tics: the number, frequency, intensity, complexity, and interference.
With that scale, intensity assesses whether tics cause injury, complexity evaluates the number of muscle group, and interference assesses whether tics interrupt functions, such as speaking or walking.
For each of the five areas, scores range from 0-5, with higher scores indicating greater severity. The motor and vocal parts have a maximum of 25 points each, for a maximum total of 50.
Participants were randomly assigned to receive once-daily oral ecopipam or placebo. A 4-week titration period was followed by an 8-week maintenance period and then a 1-week tapering period.
The primary endpoint was mean change from baseline to week 12 in scores on the YGTSS-TTS.
Results on the YGTSS-TTS showed a significant improvement in the ecopipam group, compared with placebo groups (least square [LS] mean difference: -3.44; 95% confidence interval: -6.09 to -0.79; P = .011).
The analysis indicated a 30% reduction, with an effect size of 0.48, which is “pretty good,” said Dr. Gilbert. “The amount of change is comparable to other drugs that are marketed” to treat tics.
The drug was effective for younger as well as older children. Among those aged 6-11 years, the LS mean difference was -4.95 (95% CI: -9.99 to 0.10; P = .054), and for those aged 12 to 17 years, the LS mean difference was -3.37 (95% CI: -6.51 to -0.24; P = .035).
A key secondary endpoint was the score on the Clinical Global Impression of Tourette Syndrome Severity, which Dr. Gilbert said is a more subjective measure of whether a patient’s life has improved. Here, the mean change at week 12 was significant (P = .001) for the treated group (improvement of 0.91 points), compared with the placebo group (improvement of 0.5 points).
Researchers also assessed safety and tolerability. Treatment-related adverse events (AEs) occurred in 34% of patients taking ecopipam and in 21% of those taking placebo. The most common AEs were headache (9.2%), fatigue (6.6%), somnolence (6.6%), and restlessness (5.3%).
There were no metabolic or movement-related AEs or treatment-related serious AEs.
“This drug doesn’t cause weight gain at all,” said Dr. Gilbert. He noted that there was also no difference in the groups in terms of rates of depression, anxiety, or tardive dyskinesia.
Significant tic reduction
Commenting on the findings, Jessica Frey, MD, a movement disorders fellow at the University of Florida, said the new double-blind, placebo-controlled study “is promising” in that it demonstrates significant tic reduction, compared with placebo without significant side effects.
“Ecopipam could potentially expand pharmacologic treatment options for children and adolescents with Tourette syndrome in the near future,” she said.
Dr. Frey will also be presenting results at the meeting of a study showing a significant correlation between tic severity and social media use among adolescents with Tourette syndrome during the COVID pandemic.
She noted that dopamine is an important neurotransmitter in the underlying pathophysiology of Tourette syndrome. In addition, although D2 receptor blockade can provide significant tic reduction, the “intolerable” side effects often linked to medications with this mechanism “can lead to discontinuation,” said Dr. Frey.
She also noted that ecopipam has previously been evaluated in an open-label study and a follow-up placebo-controlled study that demonstrated safety as well as significant tic reduction.
The study was supported by Emalex Biosciences. Dr. Gilbert and Dr. Frey report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2022
Anticoagulation not routinely needed after TAVR: ADAPT-TAVR
In patients undergoing transcatheter aortic valve replacement (TAVR), the incidence of leaflet thrombosis was numerically lower in those treated with the anticoagulant edoxaban for 6 months after the procedure than in those who received dual antiplatelet therapy, although the difference was not statistically significant, in the ADAPT-TAVR study.
There was no difference in new cerebral thromboembolism or neurologic/neurocognitive function between the two groups in the study.
Also, there was no significant relation between subclinical leaflet thrombosis and increased risk for cerebral thromboembolism and neurologic dysfunction.
The ADAPT-TAVR trial was presented April 4 at the American College of Cardiology (ACC) 2022 Scientific Session by Duk-Woo Park, MD, Asan Medical Center, Seoul, South Korea. It was simultaneously published online in Circulation.
“The key messages from this study are that subclinical leaflet thrombosis has not been proven to affect clinical outcomes for patients undergoing valve replacement and that in patients in whom leaflet thrombosis causes no symptoms or complications, its presence should not dictate the type of antithrombotic therapy that patients receive following the implantation of an artificial heart valve,” Dr. Park said.
“These findings do not support the routine use of computed tomography scans to detect subclinical leaflet thrombosis,” he added.
Commenting on the study at an ACC press conference, Megan Coylewright, MD, director of the Structural Heart Program at Erlanger Health System, Chattanooga, Tennessee, said: “Oftentimes when studies are negative, we’re disappointed. In this case, I think we are pleased that the study is negative because it suggests we do not have to expose our TAVR patients to anticoagulation for benefit.”
Dr. Coylewright explained that the ADAPT-TAVR study was asking whether clots form on the valve, as defined by CT.
“We are worried about that for two reasons: could that clot cause a stroke, and could that clot cause the valve to break down over time. This study looked at the first issue. And it found that there was some clot build up on the valve, but that it wasn’t significantly different between the anticoagulant and dual antiplatelet groups. And there was no correlation with embolic events, she noted.
“It shows how fast our field moves. In the U.S. now, we are using aspirin alone at 81 mg for patients who do not have an indication for oral anticoagulation after TAVR. We are moving away from dual antiplatelet therapy because the bleeding risk is so bad,” Dr. Coylewright said.
In his presentation, Dr. Park explained that it is believed that oral anticoagulants are more effective than antiplatelet therapy at reducing subclinical leaflet thrombosis, but it is not known whether there is a causal association between subclinical leaflet thrombosis and cerebral embolism, or whether oral anticoagulation can reduce cerebral embolism related to subclinical leaflet thrombosis.
The ADAPT-TAVR was conducted to look at these issues. The open-label randomized trial was conducted in five centers in Hong Kong, South Korea, and Taiwan.
For the study, 229 patients who had undergone successful TAVR and did not have an indication for anticoagulation were randomized to edoxaban 60 mg once daily, edoxaban 30 mg once daily for patients needing a reduced dose, or dual antiplatelet therapy for 6 months.
The primary endpoint was an incidence of leaflet thrombosis on four-dimensional CT at 6 months.
Results showed a strong trend toward a lower incidence of leaflet thrombosis in the edoxaban groups than in the dual antiplatelet group (9.8% vs. 18.4%; P = .076).
There was a nonsignificant difference in the percentage of patients with new cerebral lesions identified on brain MRI between the edoxaban and dual antiplatelet groups (25.0% vs. 20.2%).
The percentage of patients with worsening of neurologic and neurocognitive function was not different among the groups.
The incidence of any or major bleeding events was not different between two therapies.
There was also no significant association of the presence or extent of leaflet thrombosis with new cerebral lesions or change of neurologic or neurocognitive function.
Dr. Park noted that the trial had several limitations, including an open-label design, use of surrogate imaging outcomes for the primary outcome, and the relatively short follow-up period, so the study was underpowered to detect any meaningful differences in clinical efficacy and safety outcomes. The results should thus be considered hypothesis-generating, highlighting the need for further research, he added.
The long-term effect of leaflet thrombosis or different antithrombotic strategies on bioprosthetic valve durability is still unknown, Dr. Park said.
He also pointed out that the findings cannot be directly extrapolated to patients with an established indication for oral anticoagulant therapy.
The ADAPT-TAVR trial was an investigator-initiated trial and was funded by the CardioVascular Research Foundation (Seoul, Korea) and Daiichi Sankyo Korea.
A version of this article first appeared on Medscape.com.
In patients undergoing transcatheter aortic valve replacement (TAVR), the incidence of leaflet thrombosis was numerically lower in those treated with the anticoagulant edoxaban for 6 months after the procedure than in those who received dual antiplatelet therapy, although the difference was not statistically significant, in the ADAPT-TAVR study.
There was no difference in new cerebral thromboembolism or neurologic/neurocognitive function between the two groups in the study.
Also, there was no significant relation between subclinical leaflet thrombosis and increased risk for cerebral thromboembolism and neurologic dysfunction.
The ADAPT-TAVR trial was presented April 4 at the American College of Cardiology (ACC) 2022 Scientific Session by Duk-Woo Park, MD, Asan Medical Center, Seoul, South Korea. It was simultaneously published online in Circulation.
“The key messages from this study are that subclinical leaflet thrombosis has not been proven to affect clinical outcomes for patients undergoing valve replacement and that in patients in whom leaflet thrombosis causes no symptoms or complications, its presence should not dictate the type of antithrombotic therapy that patients receive following the implantation of an artificial heart valve,” Dr. Park said.
“These findings do not support the routine use of computed tomography scans to detect subclinical leaflet thrombosis,” he added.
Commenting on the study at an ACC press conference, Megan Coylewright, MD, director of the Structural Heart Program at Erlanger Health System, Chattanooga, Tennessee, said: “Oftentimes when studies are negative, we’re disappointed. In this case, I think we are pleased that the study is negative because it suggests we do not have to expose our TAVR patients to anticoagulation for benefit.”
Dr. Coylewright explained that the ADAPT-TAVR study was asking whether clots form on the valve, as defined by CT.
“We are worried about that for two reasons: could that clot cause a stroke, and could that clot cause the valve to break down over time. This study looked at the first issue. And it found that there was some clot build up on the valve, but that it wasn’t significantly different between the anticoagulant and dual antiplatelet groups. And there was no correlation with embolic events, she noted.
“It shows how fast our field moves. In the U.S. now, we are using aspirin alone at 81 mg for patients who do not have an indication for oral anticoagulation after TAVR. We are moving away from dual antiplatelet therapy because the bleeding risk is so bad,” Dr. Coylewright said.
In his presentation, Dr. Park explained that it is believed that oral anticoagulants are more effective than antiplatelet therapy at reducing subclinical leaflet thrombosis, but it is not known whether there is a causal association between subclinical leaflet thrombosis and cerebral embolism, or whether oral anticoagulation can reduce cerebral embolism related to subclinical leaflet thrombosis.
The ADAPT-TAVR was conducted to look at these issues. The open-label randomized trial was conducted in five centers in Hong Kong, South Korea, and Taiwan.
For the study, 229 patients who had undergone successful TAVR and did not have an indication for anticoagulation were randomized to edoxaban 60 mg once daily, edoxaban 30 mg once daily for patients needing a reduced dose, or dual antiplatelet therapy for 6 months.
The primary endpoint was an incidence of leaflet thrombosis on four-dimensional CT at 6 months.
Results showed a strong trend toward a lower incidence of leaflet thrombosis in the edoxaban groups than in the dual antiplatelet group (9.8% vs. 18.4%; P = .076).
There was a nonsignificant difference in the percentage of patients with new cerebral lesions identified on brain MRI between the edoxaban and dual antiplatelet groups (25.0% vs. 20.2%).
The percentage of patients with worsening of neurologic and neurocognitive function was not different among the groups.
The incidence of any or major bleeding events was not different between two therapies.
There was also no significant association of the presence or extent of leaflet thrombosis with new cerebral lesions or change of neurologic or neurocognitive function.
Dr. Park noted that the trial had several limitations, including an open-label design, use of surrogate imaging outcomes for the primary outcome, and the relatively short follow-up period, so the study was underpowered to detect any meaningful differences in clinical efficacy and safety outcomes. The results should thus be considered hypothesis-generating, highlighting the need for further research, he added.
The long-term effect of leaflet thrombosis or different antithrombotic strategies on bioprosthetic valve durability is still unknown, Dr. Park said.
He also pointed out that the findings cannot be directly extrapolated to patients with an established indication for oral anticoagulant therapy.
The ADAPT-TAVR trial was an investigator-initiated trial and was funded by the CardioVascular Research Foundation (Seoul, Korea) and Daiichi Sankyo Korea.
A version of this article first appeared on Medscape.com.
In patients undergoing transcatheter aortic valve replacement (TAVR), the incidence of leaflet thrombosis was numerically lower in those treated with the anticoagulant edoxaban for 6 months after the procedure than in those who received dual antiplatelet therapy, although the difference was not statistically significant, in the ADAPT-TAVR study.
There was no difference in new cerebral thromboembolism or neurologic/neurocognitive function between the two groups in the study.
Also, there was no significant relation between subclinical leaflet thrombosis and increased risk for cerebral thromboembolism and neurologic dysfunction.
The ADAPT-TAVR trial was presented April 4 at the American College of Cardiology (ACC) 2022 Scientific Session by Duk-Woo Park, MD, Asan Medical Center, Seoul, South Korea. It was simultaneously published online in Circulation.
“The key messages from this study are that subclinical leaflet thrombosis has not been proven to affect clinical outcomes for patients undergoing valve replacement and that in patients in whom leaflet thrombosis causes no symptoms or complications, its presence should not dictate the type of antithrombotic therapy that patients receive following the implantation of an artificial heart valve,” Dr. Park said.
“These findings do not support the routine use of computed tomography scans to detect subclinical leaflet thrombosis,” he added.
Commenting on the study at an ACC press conference, Megan Coylewright, MD, director of the Structural Heart Program at Erlanger Health System, Chattanooga, Tennessee, said: “Oftentimes when studies are negative, we’re disappointed. In this case, I think we are pleased that the study is negative because it suggests we do not have to expose our TAVR patients to anticoagulation for benefit.”
Dr. Coylewright explained that the ADAPT-TAVR study was asking whether clots form on the valve, as defined by CT.
“We are worried about that for two reasons: could that clot cause a stroke, and could that clot cause the valve to break down over time. This study looked at the first issue. And it found that there was some clot build up on the valve, but that it wasn’t significantly different between the anticoagulant and dual antiplatelet groups. And there was no correlation with embolic events, she noted.
“It shows how fast our field moves. In the U.S. now, we are using aspirin alone at 81 mg for patients who do not have an indication for oral anticoagulation after TAVR. We are moving away from dual antiplatelet therapy because the bleeding risk is so bad,” Dr. Coylewright said.
In his presentation, Dr. Park explained that it is believed that oral anticoagulants are more effective than antiplatelet therapy at reducing subclinical leaflet thrombosis, but it is not known whether there is a causal association between subclinical leaflet thrombosis and cerebral embolism, or whether oral anticoagulation can reduce cerebral embolism related to subclinical leaflet thrombosis.
The ADAPT-TAVR was conducted to look at these issues. The open-label randomized trial was conducted in five centers in Hong Kong, South Korea, and Taiwan.
For the study, 229 patients who had undergone successful TAVR and did not have an indication for anticoagulation were randomized to edoxaban 60 mg once daily, edoxaban 30 mg once daily for patients needing a reduced dose, or dual antiplatelet therapy for 6 months.
The primary endpoint was an incidence of leaflet thrombosis on four-dimensional CT at 6 months.
Results showed a strong trend toward a lower incidence of leaflet thrombosis in the edoxaban groups than in the dual antiplatelet group (9.8% vs. 18.4%; P = .076).
There was a nonsignificant difference in the percentage of patients with new cerebral lesions identified on brain MRI between the edoxaban and dual antiplatelet groups (25.0% vs. 20.2%).
The percentage of patients with worsening of neurologic and neurocognitive function was not different among the groups.
The incidence of any or major bleeding events was not different between two therapies.
There was also no significant association of the presence or extent of leaflet thrombosis with new cerebral lesions or change of neurologic or neurocognitive function.
Dr. Park noted that the trial had several limitations, including an open-label design, use of surrogate imaging outcomes for the primary outcome, and the relatively short follow-up period, so the study was underpowered to detect any meaningful differences in clinical efficacy and safety outcomes. The results should thus be considered hypothesis-generating, highlighting the need for further research, he added.
The long-term effect of leaflet thrombosis or different antithrombotic strategies on bioprosthetic valve durability is still unknown, Dr. Park said.
He also pointed out that the findings cannot be directly extrapolated to patients with an established indication for oral anticoagulant therapy.
The ADAPT-TAVR trial was an investigator-initiated trial and was funded by the CardioVascular Research Foundation (Seoul, Korea) and Daiichi Sankyo Korea.
A version of this article first appeared on Medscape.com.