User login
Stepping Forward With Real-Time Continuous Glucose Monitoring in the Primary Care Practice
Whose responsibility is it to bring new diabetes technologies and standards of care to patients’ attention?
Read More
Whose responsibility is it to bring new diabetes technologies and standards of care to patients’ attention?
Read More
Whose responsibility is it to bring new diabetes technologies and standards of care to patients’ attention?
Read More
House passes prior authorization bill, Senate path unclear
The path through the U.S. Senate is not yet certain for a bill intended to speed the prior authorization process of insurer-run Medicare Advantage plans, despite the measure having breezed through the House.
House leaders opted to move the Improving Seniors’ Timely Access to Care Act of 2021 (H.R. 3173) without requiring a roll-call vote. The measure was passed on Sept. 14 by a voice vote, an approach used in general with only uncontroversial measures that have broad support. The bill has 191 Democratic and 135 Republican sponsors, representing about three-quarters of the members of the House.
“There is no reason that patients should be waiting for medically appropriate care, especially when we know that this can lead to worse outcomes,” Rep. Earl Blumenauer (D-Ore.) said in a Sept. 14 speech on the House floor. “The fundamental promise of Medicare Advantage is undermined when people are delaying care, getting sicker, and ultimately costing Medicare more money.”
Rep. Greg Murphy, MD (R-N.C.), spoke on the House floor that day as well, bringing up cases he has seen in his own urology practice in which prior authorization delays disrupted medical care. One patient wound up in the hospital with abscess after an insurer denied an antibiotic prescription, Rep. Murphy said.
The Senate currently appears unlikely to move the prior authorization bill as a standalone measure. Instead, the bill may become part of a larger legislative package focused on health care that the Senate Finance Committee intends to prepare later this year.
The House-passed bill would require insurer-run Medicare plans to respond to expedited requests for prior authorization of services within 24 hours and to other requests within 7 days. This bill also would establish an electronic program for prior authorizations and mandate increased transparency as to how insurers use this tool.
CBO: Cost of change would be billions
In seeking to mandate changes in prior authorization, lawmakers likely will need to contend with the issue of a $16 billion cumulative cost estimate for the bill from the Congressional Budget Office. Members of Congress often seek to offset new spending by pairing bills that add to expected costs for the federal government with ones expected to produce savings.
Unlike Rep. Blumenauer, Rep. Murphy, and other backers of the prior authorization streamlining bill, CBO staff estimates that making the mandated changes would raise federal spending, inasmuch as there would be “a greater use of services.”
On Sept. 14, CBO issued a one-page report on the costs of the bill. The CBO report concerns only the bill in question, as is common practice with the office’s estimates.
Prior authorization changes would begin in fiscal 2025 and would add $899 million in spending, or outlays, that year, CBO said. The annual costs from the streamlined prior authorization practices through fiscal 2026 to 2032 range from $1.6 billion to $2.7 billion.
Looking at the CBO estimate against a backdrop of total Medicare Advantage costs may provide important context.
The increases in spending estimated by CBO may suggest that there would be little change in federal spending as a result of streamlining prior authorization practices. These estimates of increased annual spending of $1.6 billion–$2.7 billion are only a small fraction of the current annual cost of insurer-run Medicare, and they represent an even smaller share of the projected expense.
The federal government last year spent about $350 billion on insurer-run plans, excluding Part D drug plan payments, according to the Medicare Advisory Payment Commission (MedPAC).
As of 2021, about 27 million people were enrolled in these plans, accounting for about 46% of the total Medicare population. Enrollment has doubled since 2010, MedPAC said, and it is expected to continue to grow. By 2027, insurer-run Medicare could cover 50% of the program’s population, a figure that may reach 53% by 2031.
Federal payments to these plans will accelerate in the years ahead as insurers attract more people eligible for Medicare as customers. Payments to these private health plans could rise from an expected $418 billion this year to $940.6 billion by 2031, according to the most recent Medicare trustees report.
Good intentions, poor implementation?
Insurer-run Medicare has long enjoyed deep bipartisan support in Congress. That’s due in part to its potential for reducing spending on what are considered low-value treatments, or ones considered unlikely to provide a significant medical benefit, but Rep. Blumenauer is among the members of Congress who see insurer-run Medicare as a path for preserving the giant federal health program. Traditional Medicare has far fewer restrictions on services, which sometimes opens a path for tests and treatments that offer less value for patients.
“I believe that the way traditional fee-for-service Medicare operates is not sustainable and that Medicare Advantage is one of the tools we can use to demonstrate how we can incentivize value,” Rep. Blumenauer said on the House floor. “But this is only possible when the program operates as intended. I have been deeply concerned about the reports of delays in care” caused by the clunky prior authorization processes.
He highlighted a recent report from the internal watchdog group for the Department of Health & Human Services that raises concerns about denials of appropriate care. About 18% of a set of payment denials examined by the Office of Inspector General of HHS in April actually met Medicare coverage rules and plan billing rules.
“For patients and their families, being told that you need to wait longer for care that your doctor tells you that you need is incredibly frustrating and frightening,” Rep. Blumenauer said. “There’s no comfort to be found in the fact that your insurance company needs time to decide if your doctor is right.”
Trends in prior authorization
The CBO report does not provide detail on what kind of medical spending would increase under a streamlined prior authorization process in insurer-run Medicare plans.
From trends reported in prior authorization, though, two factors could be at play in what appear to be relatively small estimated increases in Medicare spending from streamlined prior authorization.
The work already underway to create less burdensome electronic systems for these requests, such as the Fast Prior Authorization Technology Highway initiative run by the America’s Health Insurance Plans trade association.
The other factor could be the number of cases in which prior authorization merely causes delays in treatments and tests and thus simply postpones spending while adding to clinicians’ administrative work.
An analysis of prior authorization requests for dermatologic practices affiliated with the University of Utah may represent an extreme example. In a report published in JAMA Dermatology in 2020, researchers described what happened with requests made during 1 month, September 2016.
The approval rate for procedures was 99.6% – 100% (95 of 95) for Mohs surgery, and 96% (130 of 131, with 4 additional cases pending) for excisions. These findings supported calls for simplifying prior authorization procedures, “perhaps first by eliminating unnecessary PAs [prior authorizations] and appeals,” Aaron M. Secrest, MD, PhD, of the University of Utah, Salt Lake City, and coauthors wrote in the article.
Still, there is some evidence that insurer-run Medicare policies reduce the use of low-value care.
In a study published in JAMA Health Forum, Emily Boudreau, PhD, of insurer Humana Inc, and coauthors from Tufts University, Boston, and the University of Pennsylvania, Philadelphia investigated whether insurer-run Medicare could do a better job in reducing the amount of low-value care delivered than the traditional program. They analyzed a set of claims data from 2017 to 2019 for people enrolled in insurer-run and traditional Medicare.
They reported a rate of 23.07 low-value services provided per 100 people in insurer-run Medicare, compared with 25.39 for those in traditional Medicare. Some of the biggest differences reported in the article were in cancer screenings for older people.
As an example, the U.S. Preventive Services Task Force recommends that women older than 65 years not be screened for cervical cancer if they have undergone adequate screening in the past and are not at high risk for cervical cancer. There was an annual count of 1.76 screenings for cervical cancer per 100 women older than 65 in the insurer-run Medicare group versus 3.18 for those in traditional Medicare.
The Better Medicare Alliance issued a statement in favor of the House passage of the Improving Seniors’ Timely Access to Care Act.
In it, the group said the measure would “modernize prior authorization while protecting its essential function in facilitating safe, high-value, evidence-based care.” The alliance promotes use of insurer-run Medicare. The board of the Better Medicare Alliance includes executives who serve with firms that run Advantage plans as well as medical organizations and universities.
“With studies showing that up to one-quarter of all health care expenditures are wasted on services with no benefit to the patient, we need a robust, next-generation prior authorization program to deter low-value, and even harmful, care while protecting access to needed treatment and effective therapies,” said A. Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, in a statement issued by the Better Medicare Alliance. He is a member of the group’s council of scholars.
On the House floor on September 14, Rep. Ami Bera, MD (D-Calif.), said he has heard from former colleagues and his medical school classmates that they now spend as much as 40% of their time on administrative work. These distractions from patient care are helping drive physicians away from the practice of medicine.
Still, the internist defended the basic premise of prior authorization while strongly appealing for better systems of handling it.
“Yes, there is a role for prior authorization in limited cases. There is also a role to go back and retrospectively look at how care is being delivered,” Rep. Bera said. “But what is happening today is a travesty. It wasn’t the intention of prior authorization. It is a prior authorization process gone awry.”
AGA’s stance: This is a huge victory for patients! Advocating for prior authorization reform has been AGA’s top priority. Learn more about prior authorization and how it impacts gastroenterology on the AGA website.
A version of this article first appeared on Medscape.com.
The path through the U.S. Senate is not yet certain for a bill intended to speed the prior authorization process of insurer-run Medicare Advantage plans, despite the measure having breezed through the House.
House leaders opted to move the Improving Seniors’ Timely Access to Care Act of 2021 (H.R. 3173) without requiring a roll-call vote. The measure was passed on Sept. 14 by a voice vote, an approach used in general with only uncontroversial measures that have broad support. The bill has 191 Democratic and 135 Republican sponsors, representing about three-quarters of the members of the House.
“There is no reason that patients should be waiting for medically appropriate care, especially when we know that this can lead to worse outcomes,” Rep. Earl Blumenauer (D-Ore.) said in a Sept. 14 speech on the House floor. “The fundamental promise of Medicare Advantage is undermined when people are delaying care, getting sicker, and ultimately costing Medicare more money.”
Rep. Greg Murphy, MD (R-N.C.), spoke on the House floor that day as well, bringing up cases he has seen in his own urology practice in which prior authorization delays disrupted medical care. One patient wound up in the hospital with abscess after an insurer denied an antibiotic prescription, Rep. Murphy said.
The Senate currently appears unlikely to move the prior authorization bill as a standalone measure. Instead, the bill may become part of a larger legislative package focused on health care that the Senate Finance Committee intends to prepare later this year.
The House-passed bill would require insurer-run Medicare plans to respond to expedited requests for prior authorization of services within 24 hours and to other requests within 7 days. This bill also would establish an electronic program for prior authorizations and mandate increased transparency as to how insurers use this tool.
CBO: Cost of change would be billions
In seeking to mandate changes in prior authorization, lawmakers likely will need to contend with the issue of a $16 billion cumulative cost estimate for the bill from the Congressional Budget Office. Members of Congress often seek to offset new spending by pairing bills that add to expected costs for the federal government with ones expected to produce savings.
Unlike Rep. Blumenauer, Rep. Murphy, and other backers of the prior authorization streamlining bill, CBO staff estimates that making the mandated changes would raise federal spending, inasmuch as there would be “a greater use of services.”
On Sept. 14, CBO issued a one-page report on the costs of the bill. The CBO report concerns only the bill in question, as is common practice with the office’s estimates.
Prior authorization changes would begin in fiscal 2025 and would add $899 million in spending, or outlays, that year, CBO said. The annual costs from the streamlined prior authorization practices through fiscal 2026 to 2032 range from $1.6 billion to $2.7 billion.
Looking at the CBO estimate against a backdrop of total Medicare Advantage costs may provide important context.
The increases in spending estimated by CBO may suggest that there would be little change in federal spending as a result of streamlining prior authorization practices. These estimates of increased annual spending of $1.6 billion–$2.7 billion are only a small fraction of the current annual cost of insurer-run Medicare, and they represent an even smaller share of the projected expense.
The federal government last year spent about $350 billion on insurer-run plans, excluding Part D drug plan payments, according to the Medicare Advisory Payment Commission (MedPAC).
As of 2021, about 27 million people were enrolled in these plans, accounting for about 46% of the total Medicare population. Enrollment has doubled since 2010, MedPAC said, and it is expected to continue to grow. By 2027, insurer-run Medicare could cover 50% of the program’s population, a figure that may reach 53% by 2031.
Federal payments to these plans will accelerate in the years ahead as insurers attract more people eligible for Medicare as customers. Payments to these private health plans could rise from an expected $418 billion this year to $940.6 billion by 2031, according to the most recent Medicare trustees report.
Good intentions, poor implementation?
Insurer-run Medicare has long enjoyed deep bipartisan support in Congress. That’s due in part to its potential for reducing spending on what are considered low-value treatments, or ones considered unlikely to provide a significant medical benefit, but Rep. Blumenauer is among the members of Congress who see insurer-run Medicare as a path for preserving the giant federal health program. Traditional Medicare has far fewer restrictions on services, which sometimes opens a path for tests and treatments that offer less value for patients.
“I believe that the way traditional fee-for-service Medicare operates is not sustainable and that Medicare Advantage is one of the tools we can use to demonstrate how we can incentivize value,” Rep. Blumenauer said on the House floor. “But this is only possible when the program operates as intended. I have been deeply concerned about the reports of delays in care” caused by the clunky prior authorization processes.
He highlighted a recent report from the internal watchdog group for the Department of Health & Human Services that raises concerns about denials of appropriate care. About 18% of a set of payment denials examined by the Office of Inspector General of HHS in April actually met Medicare coverage rules and plan billing rules.
“For patients and their families, being told that you need to wait longer for care that your doctor tells you that you need is incredibly frustrating and frightening,” Rep. Blumenauer said. “There’s no comfort to be found in the fact that your insurance company needs time to decide if your doctor is right.”
Trends in prior authorization
The CBO report does not provide detail on what kind of medical spending would increase under a streamlined prior authorization process in insurer-run Medicare plans.
From trends reported in prior authorization, though, two factors could be at play in what appear to be relatively small estimated increases in Medicare spending from streamlined prior authorization.
The work already underway to create less burdensome electronic systems for these requests, such as the Fast Prior Authorization Technology Highway initiative run by the America’s Health Insurance Plans trade association.
The other factor could be the number of cases in which prior authorization merely causes delays in treatments and tests and thus simply postpones spending while adding to clinicians’ administrative work.
An analysis of prior authorization requests for dermatologic practices affiliated with the University of Utah may represent an extreme example. In a report published in JAMA Dermatology in 2020, researchers described what happened with requests made during 1 month, September 2016.
The approval rate for procedures was 99.6% – 100% (95 of 95) for Mohs surgery, and 96% (130 of 131, with 4 additional cases pending) for excisions. These findings supported calls for simplifying prior authorization procedures, “perhaps first by eliminating unnecessary PAs [prior authorizations] and appeals,” Aaron M. Secrest, MD, PhD, of the University of Utah, Salt Lake City, and coauthors wrote in the article.
Still, there is some evidence that insurer-run Medicare policies reduce the use of low-value care.
In a study published in JAMA Health Forum, Emily Boudreau, PhD, of insurer Humana Inc, and coauthors from Tufts University, Boston, and the University of Pennsylvania, Philadelphia investigated whether insurer-run Medicare could do a better job in reducing the amount of low-value care delivered than the traditional program. They analyzed a set of claims data from 2017 to 2019 for people enrolled in insurer-run and traditional Medicare.
They reported a rate of 23.07 low-value services provided per 100 people in insurer-run Medicare, compared with 25.39 for those in traditional Medicare. Some of the biggest differences reported in the article were in cancer screenings for older people.
As an example, the U.S. Preventive Services Task Force recommends that women older than 65 years not be screened for cervical cancer if they have undergone adequate screening in the past and are not at high risk for cervical cancer. There was an annual count of 1.76 screenings for cervical cancer per 100 women older than 65 in the insurer-run Medicare group versus 3.18 for those in traditional Medicare.
The Better Medicare Alliance issued a statement in favor of the House passage of the Improving Seniors’ Timely Access to Care Act.
In it, the group said the measure would “modernize prior authorization while protecting its essential function in facilitating safe, high-value, evidence-based care.” The alliance promotes use of insurer-run Medicare. The board of the Better Medicare Alliance includes executives who serve with firms that run Advantage plans as well as medical organizations and universities.
“With studies showing that up to one-quarter of all health care expenditures are wasted on services with no benefit to the patient, we need a robust, next-generation prior authorization program to deter low-value, and even harmful, care while protecting access to needed treatment and effective therapies,” said A. Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, in a statement issued by the Better Medicare Alliance. He is a member of the group’s council of scholars.
On the House floor on September 14, Rep. Ami Bera, MD (D-Calif.), said he has heard from former colleagues and his medical school classmates that they now spend as much as 40% of their time on administrative work. These distractions from patient care are helping drive physicians away from the practice of medicine.
Still, the internist defended the basic premise of prior authorization while strongly appealing for better systems of handling it.
“Yes, there is a role for prior authorization in limited cases. There is also a role to go back and retrospectively look at how care is being delivered,” Rep. Bera said. “But what is happening today is a travesty. It wasn’t the intention of prior authorization. It is a prior authorization process gone awry.”
AGA’s stance: This is a huge victory for patients! Advocating for prior authorization reform has been AGA’s top priority. Learn more about prior authorization and how it impacts gastroenterology on the AGA website.
A version of this article first appeared on Medscape.com.
The path through the U.S. Senate is not yet certain for a bill intended to speed the prior authorization process of insurer-run Medicare Advantage plans, despite the measure having breezed through the House.
House leaders opted to move the Improving Seniors’ Timely Access to Care Act of 2021 (H.R. 3173) without requiring a roll-call vote. The measure was passed on Sept. 14 by a voice vote, an approach used in general with only uncontroversial measures that have broad support. The bill has 191 Democratic and 135 Republican sponsors, representing about three-quarters of the members of the House.
“There is no reason that patients should be waiting for medically appropriate care, especially when we know that this can lead to worse outcomes,” Rep. Earl Blumenauer (D-Ore.) said in a Sept. 14 speech on the House floor. “The fundamental promise of Medicare Advantage is undermined when people are delaying care, getting sicker, and ultimately costing Medicare more money.”
Rep. Greg Murphy, MD (R-N.C.), spoke on the House floor that day as well, bringing up cases he has seen in his own urology practice in which prior authorization delays disrupted medical care. One patient wound up in the hospital with abscess after an insurer denied an antibiotic prescription, Rep. Murphy said.
The Senate currently appears unlikely to move the prior authorization bill as a standalone measure. Instead, the bill may become part of a larger legislative package focused on health care that the Senate Finance Committee intends to prepare later this year.
The House-passed bill would require insurer-run Medicare plans to respond to expedited requests for prior authorization of services within 24 hours and to other requests within 7 days. This bill also would establish an electronic program for prior authorizations and mandate increased transparency as to how insurers use this tool.
CBO: Cost of change would be billions
In seeking to mandate changes in prior authorization, lawmakers likely will need to contend with the issue of a $16 billion cumulative cost estimate for the bill from the Congressional Budget Office. Members of Congress often seek to offset new spending by pairing bills that add to expected costs for the federal government with ones expected to produce savings.
Unlike Rep. Blumenauer, Rep. Murphy, and other backers of the prior authorization streamlining bill, CBO staff estimates that making the mandated changes would raise federal spending, inasmuch as there would be “a greater use of services.”
On Sept. 14, CBO issued a one-page report on the costs of the bill. The CBO report concerns only the bill in question, as is common practice with the office’s estimates.
Prior authorization changes would begin in fiscal 2025 and would add $899 million in spending, or outlays, that year, CBO said. The annual costs from the streamlined prior authorization practices through fiscal 2026 to 2032 range from $1.6 billion to $2.7 billion.
Looking at the CBO estimate against a backdrop of total Medicare Advantage costs may provide important context.
The increases in spending estimated by CBO may suggest that there would be little change in federal spending as a result of streamlining prior authorization practices. These estimates of increased annual spending of $1.6 billion–$2.7 billion are only a small fraction of the current annual cost of insurer-run Medicare, and they represent an even smaller share of the projected expense.
The federal government last year spent about $350 billion on insurer-run plans, excluding Part D drug plan payments, according to the Medicare Advisory Payment Commission (MedPAC).
As of 2021, about 27 million people were enrolled in these plans, accounting for about 46% of the total Medicare population. Enrollment has doubled since 2010, MedPAC said, and it is expected to continue to grow. By 2027, insurer-run Medicare could cover 50% of the program’s population, a figure that may reach 53% by 2031.
Federal payments to these plans will accelerate in the years ahead as insurers attract more people eligible for Medicare as customers. Payments to these private health plans could rise from an expected $418 billion this year to $940.6 billion by 2031, according to the most recent Medicare trustees report.
Good intentions, poor implementation?
Insurer-run Medicare has long enjoyed deep bipartisan support in Congress. That’s due in part to its potential for reducing spending on what are considered low-value treatments, or ones considered unlikely to provide a significant medical benefit, but Rep. Blumenauer is among the members of Congress who see insurer-run Medicare as a path for preserving the giant federal health program. Traditional Medicare has far fewer restrictions on services, which sometimes opens a path for tests and treatments that offer less value for patients.
“I believe that the way traditional fee-for-service Medicare operates is not sustainable and that Medicare Advantage is one of the tools we can use to demonstrate how we can incentivize value,” Rep. Blumenauer said on the House floor. “But this is only possible when the program operates as intended. I have been deeply concerned about the reports of delays in care” caused by the clunky prior authorization processes.
He highlighted a recent report from the internal watchdog group for the Department of Health & Human Services that raises concerns about denials of appropriate care. About 18% of a set of payment denials examined by the Office of Inspector General of HHS in April actually met Medicare coverage rules and plan billing rules.
“For patients and their families, being told that you need to wait longer for care that your doctor tells you that you need is incredibly frustrating and frightening,” Rep. Blumenauer said. “There’s no comfort to be found in the fact that your insurance company needs time to decide if your doctor is right.”
Trends in prior authorization
The CBO report does not provide detail on what kind of medical spending would increase under a streamlined prior authorization process in insurer-run Medicare plans.
From trends reported in prior authorization, though, two factors could be at play in what appear to be relatively small estimated increases in Medicare spending from streamlined prior authorization.
The work already underway to create less burdensome electronic systems for these requests, such as the Fast Prior Authorization Technology Highway initiative run by the America’s Health Insurance Plans trade association.
The other factor could be the number of cases in which prior authorization merely causes delays in treatments and tests and thus simply postpones spending while adding to clinicians’ administrative work.
An analysis of prior authorization requests for dermatologic practices affiliated with the University of Utah may represent an extreme example. In a report published in JAMA Dermatology in 2020, researchers described what happened with requests made during 1 month, September 2016.
The approval rate for procedures was 99.6% – 100% (95 of 95) for Mohs surgery, and 96% (130 of 131, with 4 additional cases pending) for excisions. These findings supported calls for simplifying prior authorization procedures, “perhaps first by eliminating unnecessary PAs [prior authorizations] and appeals,” Aaron M. Secrest, MD, PhD, of the University of Utah, Salt Lake City, and coauthors wrote in the article.
Still, there is some evidence that insurer-run Medicare policies reduce the use of low-value care.
In a study published in JAMA Health Forum, Emily Boudreau, PhD, of insurer Humana Inc, and coauthors from Tufts University, Boston, and the University of Pennsylvania, Philadelphia investigated whether insurer-run Medicare could do a better job in reducing the amount of low-value care delivered than the traditional program. They analyzed a set of claims data from 2017 to 2019 for people enrolled in insurer-run and traditional Medicare.
They reported a rate of 23.07 low-value services provided per 100 people in insurer-run Medicare, compared with 25.39 for those in traditional Medicare. Some of the biggest differences reported in the article were in cancer screenings for older people.
As an example, the U.S. Preventive Services Task Force recommends that women older than 65 years not be screened for cervical cancer if they have undergone adequate screening in the past and are not at high risk for cervical cancer. There was an annual count of 1.76 screenings for cervical cancer per 100 women older than 65 in the insurer-run Medicare group versus 3.18 for those in traditional Medicare.
The Better Medicare Alliance issued a statement in favor of the House passage of the Improving Seniors’ Timely Access to Care Act.
In it, the group said the measure would “modernize prior authorization while protecting its essential function in facilitating safe, high-value, evidence-based care.” The alliance promotes use of insurer-run Medicare. The board of the Better Medicare Alliance includes executives who serve with firms that run Advantage plans as well as medical organizations and universities.
“With studies showing that up to one-quarter of all health care expenditures are wasted on services with no benefit to the patient, we need a robust, next-generation prior authorization program to deter low-value, and even harmful, care while protecting access to needed treatment and effective therapies,” said A. Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, in a statement issued by the Better Medicare Alliance. He is a member of the group’s council of scholars.
On the House floor on September 14, Rep. Ami Bera, MD (D-Calif.), said he has heard from former colleagues and his medical school classmates that they now spend as much as 40% of their time on administrative work. These distractions from patient care are helping drive physicians away from the practice of medicine.
Still, the internist defended the basic premise of prior authorization while strongly appealing for better systems of handling it.
“Yes, there is a role for prior authorization in limited cases. There is also a role to go back and retrospectively look at how care is being delivered,” Rep. Bera said. “But what is happening today is a travesty. It wasn’t the intention of prior authorization. It is a prior authorization process gone awry.”
AGA’s stance: This is a huge victory for patients! Advocating for prior authorization reform has been AGA’s top priority. Learn more about prior authorization and how it impacts gastroenterology on the AGA website.
A version of this article first appeared on Medscape.com.
Mothers’ diabetes linked to ADHD in their children
Children born to women who develop diabetes either before or during their pregnancy could be at risk for developing attention-deficit/hyperactivity disorder, data from a large multinational cohort study appear to show.
Considering more than 4.5 million mother-child pairs, it was found that children whose mothers had diabetes around the time of their pregnancy were 16% more likely to have ADHD diagnosed than were those whose mothers did not.
An increased risk was seen regardless of the type of diabetes, and regardless of whether or not the diabetes was present before or appeared during the pregnancy.
“We found a small increased risk of ADHD in children born to mothers with diabetes, including pregestational diabetes and gestational diabetes,” Carolyn Cesta, PhD, reported at the annual meeting of the European Association for the Study of Diabetes.
Dr. Cesta, a postdoctoral researcher in the Centre for Pharmacoepidemiology at the Karolinska Institutet in Stockholm noted that the effect sizes seen were lower than had been reported previously.
“This may be because we adjusted for a large number of covariates, including maternal ADHD and psychiatric disorders,” Dr. Cesta said.
ADHD and diabetes
“Previous studies have reported an increase in the risk of ADHD in children born to mothers with diabetes,” explained Dr. Cesta.
However, “these studies have been limited by the use of self-reported data, small sample sizes, lack of adjustment for important confounders, and they’re often limited to [White] populations,” she added. “There’s a lot of heterogeneity between these studies,” she said.
To try to iron out the differences seen in the prior studies, Dr. Cesta and associates looked at data from several databases based in Hong Kong (Clinical Data Analysis and Reporting System), four Nordic countries (Population Health Registers for Finland, Iceland, Norway, and Sweden), and Taiwan (National Health Insurance Database).
To create the matched mother-child pairs, the databases were searched to find women who had children born between 2001 and 2018, and who had follow-up data available up to 2020 on not only their diabetes status and child’s ADHD status, but also other parameters, such as other maternal diagnoses, maternal medications, and a host of sociodemographic factors.
More than 24 potentially confounding or covariates were considered in the analysis, which used Cox proportional hazard regression modeling and propensity score analysis to calculate hazard ratios with 95% confidence intervals.
“We looked at whether [mothers] had a diagnosis of ADHD themselves, or other psychiatric disorders, because there is high heritability for these disorders,” Dr. Cesta said, indicating that all bases had endeavored to be covered.
Main findings
Results showed some differences in the prevalence of diabetes and ADHD between the three cohorts used in the analysis. The prevalence of any maternal diabetes ranged from 8.8% in the Hong Kong cohort to 3.3% in the Taiwan cohort, with a prevalence of 6.8% for the Nordic cohort.
Rates of pregestational diabetes were lowest in the Taiwan and Hong Kong cohorts, at 0.2% and 0.5%, respectively, and 2.2% in the Nordic cohort. Gestational diabetes rates were a respective 3.1%, 7.8%, and 4.6%.
The highest rate of ADHD in children was seen in the Taiwan cohort, at 9.6%, followed by 4.2% for the Hong Kong cohort, and 2.6% for the Nordic cohort.
The hazard ratio for having childhood ADHD was 1.16 when comparing any maternal diabetes to no maternal diabetes, 1.40 comparing mothers with and without pregestational diabetes, and a respective 1.36 and 1.37 comparing those with and without type 1 diabetes, and those with and without type 2 diabetes.
The HR for childhood ADHD comparing mothers with and without gestational diabetes was 1.13.
“Within the analysis for gestational diabetes, we had enough numbers to look at siblings that are discordant for maternal gestational diabetes,” Dr. Cesta said. Essentially “we’re comparing two siblings from the same mother, one that was exposed to gestational diabetes, one that wasn’t,” she explained.
Interestingly there was no association between ADHD and maternal gestational diabetes in the sibling analysis (HR, 1.0).
“When it comes to gestational diabetes, the evidence from our sibling analysis indicate that the association may actually be confounded by shared genetics and environmental factors,” said Dr. Cesta.
“So, future studies should explore the role of specific genetic factors in glycemic control during pregnancy and the relationship between maternal diabetes and ADHD.”
Answering long-standing questions
These data will help a lot in answering questions that clinicians have been asking themselves a long time, commented Jardena Puder, MD, who chaired the session.
“It still remains a bit puzzling that genetic and environmental factors could be responsible, if you see the same effect in type 1 [diabetes], and in type 2 [diabetes], and gestational diabetes,” said Dr. Puder, who is an endocrinologist and diabetologist at the woman-mother-child department at the Vaud University Hospital Center, Lausanne, Switzerland.
Type 1 and type 2 are “very distinct” in terms of the genetic and environmental factors involved, “so, the fact that you see [the effect] in both remains a bit puzzling,” said Dr. Puder.
“I wish we had the numbers to be able to do the sibling analysis for type 1 and type 2, just to see if we could tease anything out,” said Dr. Cesta.
“I do think this is part of the bigger question of what the relationship is between, like, metabolic disorders and psychiatric disorders, because even outside of pregnancy, we see that there’s often a comorbidity with them. So, it’s a good point.”
The next step is to look at the role of treatment and what effects glycemic control might have on the small, but still apparent, association between maternal diabetes and ADHD.
The study had multiple funders including the Hong Kong Research Grant Council, NordForsk, the Research Council of Norway, the Norwegian ADHD Research Network, the Hong Kong Innovation and Technology Commission, and European Horizon 2020.
Dr. Cesta had no conflicts of interest to disclose. Dr. Puder chaired the session in which the findings were presented and made no specific disclosures.
Children born to women who develop diabetes either before or during their pregnancy could be at risk for developing attention-deficit/hyperactivity disorder, data from a large multinational cohort study appear to show.
Considering more than 4.5 million mother-child pairs, it was found that children whose mothers had diabetes around the time of their pregnancy were 16% more likely to have ADHD diagnosed than were those whose mothers did not.
An increased risk was seen regardless of the type of diabetes, and regardless of whether or not the diabetes was present before or appeared during the pregnancy.
“We found a small increased risk of ADHD in children born to mothers with diabetes, including pregestational diabetes and gestational diabetes,” Carolyn Cesta, PhD, reported at the annual meeting of the European Association for the Study of Diabetes.
Dr. Cesta, a postdoctoral researcher in the Centre for Pharmacoepidemiology at the Karolinska Institutet in Stockholm noted that the effect sizes seen were lower than had been reported previously.
“This may be because we adjusted for a large number of covariates, including maternal ADHD and psychiatric disorders,” Dr. Cesta said.
ADHD and diabetes
“Previous studies have reported an increase in the risk of ADHD in children born to mothers with diabetes,” explained Dr. Cesta.
However, “these studies have been limited by the use of self-reported data, small sample sizes, lack of adjustment for important confounders, and they’re often limited to [White] populations,” she added. “There’s a lot of heterogeneity between these studies,” she said.
To try to iron out the differences seen in the prior studies, Dr. Cesta and associates looked at data from several databases based in Hong Kong (Clinical Data Analysis and Reporting System), four Nordic countries (Population Health Registers for Finland, Iceland, Norway, and Sweden), and Taiwan (National Health Insurance Database).
To create the matched mother-child pairs, the databases were searched to find women who had children born between 2001 and 2018, and who had follow-up data available up to 2020 on not only their diabetes status and child’s ADHD status, but also other parameters, such as other maternal diagnoses, maternal medications, and a host of sociodemographic factors.
More than 24 potentially confounding or covariates were considered in the analysis, which used Cox proportional hazard regression modeling and propensity score analysis to calculate hazard ratios with 95% confidence intervals.
“We looked at whether [mothers] had a diagnosis of ADHD themselves, or other psychiatric disorders, because there is high heritability for these disorders,” Dr. Cesta said, indicating that all bases had endeavored to be covered.
Main findings
Results showed some differences in the prevalence of diabetes and ADHD between the three cohorts used in the analysis. The prevalence of any maternal diabetes ranged from 8.8% in the Hong Kong cohort to 3.3% in the Taiwan cohort, with a prevalence of 6.8% for the Nordic cohort.
Rates of pregestational diabetes were lowest in the Taiwan and Hong Kong cohorts, at 0.2% and 0.5%, respectively, and 2.2% in the Nordic cohort. Gestational diabetes rates were a respective 3.1%, 7.8%, and 4.6%.
The highest rate of ADHD in children was seen in the Taiwan cohort, at 9.6%, followed by 4.2% for the Hong Kong cohort, and 2.6% for the Nordic cohort.
The hazard ratio for having childhood ADHD was 1.16 when comparing any maternal diabetes to no maternal diabetes, 1.40 comparing mothers with and without pregestational diabetes, and a respective 1.36 and 1.37 comparing those with and without type 1 diabetes, and those with and without type 2 diabetes.
The HR for childhood ADHD comparing mothers with and without gestational diabetes was 1.13.
“Within the analysis for gestational diabetes, we had enough numbers to look at siblings that are discordant for maternal gestational diabetes,” Dr. Cesta said. Essentially “we’re comparing two siblings from the same mother, one that was exposed to gestational diabetes, one that wasn’t,” she explained.
Interestingly there was no association between ADHD and maternal gestational diabetes in the sibling analysis (HR, 1.0).
“When it comes to gestational diabetes, the evidence from our sibling analysis indicate that the association may actually be confounded by shared genetics and environmental factors,” said Dr. Cesta.
“So, future studies should explore the role of specific genetic factors in glycemic control during pregnancy and the relationship between maternal diabetes and ADHD.”
Answering long-standing questions
These data will help a lot in answering questions that clinicians have been asking themselves a long time, commented Jardena Puder, MD, who chaired the session.
“It still remains a bit puzzling that genetic and environmental factors could be responsible, if you see the same effect in type 1 [diabetes], and in type 2 [diabetes], and gestational diabetes,” said Dr. Puder, who is an endocrinologist and diabetologist at the woman-mother-child department at the Vaud University Hospital Center, Lausanne, Switzerland.
Type 1 and type 2 are “very distinct” in terms of the genetic and environmental factors involved, “so, the fact that you see [the effect] in both remains a bit puzzling,” said Dr. Puder.
“I wish we had the numbers to be able to do the sibling analysis for type 1 and type 2, just to see if we could tease anything out,” said Dr. Cesta.
“I do think this is part of the bigger question of what the relationship is between, like, metabolic disorders and psychiatric disorders, because even outside of pregnancy, we see that there’s often a comorbidity with them. So, it’s a good point.”
The next step is to look at the role of treatment and what effects glycemic control might have on the small, but still apparent, association between maternal diabetes and ADHD.
The study had multiple funders including the Hong Kong Research Grant Council, NordForsk, the Research Council of Norway, the Norwegian ADHD Research Network, the Hong Kong Innovation and Technology Commission, and European Horizon 2020.
Dr. Cesta had no conflicts of interest to disclose. Dr. Puder chaired the session in which the findings were presented and made no specific disclosures.
Children born to women who develop diabetes either before or during their pregnancy could be at risk for developing attention-deficit/hyperactivity disorder, data from a large multinational cohort study appear to show.
Considering more than 4.5 million mother-child pairs, it was found that children whose mothers had diabetes around the time of their pregnancy were 16% more likely to have ADHD diagnosed than were those whose mothers did not.
An increased risk was seen regardless of the type of diabetes, and regardless of whether or not the diabetes was present before or appeared during the pregnancy.
“We found a small increased risk of ADHD in children born to mothers with diabetes, including pregestational diabetes and gestational diabetes,” Carolyn Cesta, PhD, reported at the annual meeting of the European Association for the Study of Diabetes.
Dr. Cesta, a postdoctoral researcher in the Centre for Pharmacoepidemiology at the Karolinska Institutet in Stockholm noted that the effect sizes seen were lower than had been reported previously.
“This may be because we adjusted for a large number of covariates, including maternal ADHD and psychiatric disorders,” Dr. Cesta said.
ADHD and diabetes
“Previous studies have reported an increase in the risk of ADHD in children born to mothers with diabetes,” explained Dr. Cesta.
However, “these studies have been limited by the use of self-reported data, small sample sizes, lack of adjustment for important confounders, and they’re often limited to [White] populations,” she added. “There’s a lot of heterogeneity between these studies,” she said.
To try to iron out the differences seen in the prior studies, Dr. Cesta and associates looked at data from several databases based in Hong Kong (Clinical Data Analysis and Reporting System), four Nordic countries (Population Health Registers for Finland, Iceland, Norway, and Sweden), and Taiwan (National Health Insurance Database).
To create the matched mother-child pairs, the databases were searched to find women who had children born between 2001 and 2018, and who had follow-up data available up to 2020 on not only their diabetes status and child’s ADHD status, but also other parameters, such as other maternal diagnoses, maternal medications, and a host of sociodemographic factors.
More than 24 potentially confounding or covariates were considered in the analysis, which used Cox proportional hazard regression modeling and propensity score analysis to calculate hazard ratios with 95% confidence intervals.
“We looked at whether [mothers] had a diagnosis of ADHD themselves, or other psychiatric disorders, because there is high heritability for these disorders,” Dr. Cesta said, indicating that all bases had endeavored to be covered.
Main findings
Results showed some differences in the prevalence of diabetes and ADHD between the three cohorts used in the analysis. The prevalence of any maternal diabetes ranged from 8.8% in the Hong Kong cohort to 3.3% in the Taiwan cohort, with a prevalence of 6.8% for the Nordic cohort.
Rates of pregestational diabetes were lowest in the Taiwan and Hong Kong cohorts, at 0.2% and 0.5%, respectively, and 2.2% in the Nordic cohort. Gestational diabetes rates were a respective 3.1%, 7.8%, and 4.6%.
The highest rate of ADHD in children was seen in the Taiwan cohort, at 9.6%, followed by 4.2% for the Hong Kong cohort, and 2.6% for the Nordic cohort.
The hazard ratio for having childhood ADHD was 1.16 when comparing any maternal diabetes to no maternal diabetes, 1.40 comparing mothers with and without pregestational diabetes, and a respective 1.36 and 1.37 comparing those with and without type 1 diabetes, and those with and without type 2 diabetes.
The HR for childhood ADHD comparing mothers with and without gestational diabetes was 1.13.
“Within the analysis for gestational diabetes, we had enough numbers to look at siblings that are discordant for maternal gestational diabetes,” Dr. Cesta said. Essentially “we’re comparing two siblings from the same mother, one that was exposed to gestational diabetes, one that wasn’t,” she explained.
Interestingly there was no association between ADHD and maternal gestational diabetes in the sibling analysis (HR, 1.0).
“When it comes to gestational diabetes, the evidence from our sibling analysis indicate that the association may actually be confounded by shared genetics and environmental factors,” said Dr. Cesta.
“So, future studies should explore the role of specific genetic factors in glycemic control during pregnancy and the relationship between maternal diabetes and ADHD.”
Answering long-standing questions
These data will help a lot in answering questions that clinicians have been asking themselves a long time, commented Jardena Puder, MD, who chaired the session.
“It still remains a bit puzzling that genetic and environmental factors could be responsible, if you see the same effect in type 1 [diabetes], and in type 2 [diabetes], and gestational diabetes,” said Dr. Puder, who is an endocrinologist and diabetologist at the woman-mother-child department at the Vaud University Hospital Center, Lausanne, Switzerland.
Type 1 and type 2 are “very distinct” in terms of the genetic and environmental factors involved, “so, the fact that you see [the effect] in both remains a bit puzzling,” said Dr. Puder.
“I wish we had the numbers to be able to do the sibling analysis for type 1 and type 2, just to see if we could tease anything out,” said Dr. Cesta.
“I do think this is part of the bigger question of what the relationship is between, like, metabolic disorders and psychiatric disorders, because even outside of pregnancy, we see that there’s often a comorbidity with them. So, it’s a good point.”
The next step is to look at the role of treatment and what effects glycemic control might have on the small, but still apparent, association between maternal diabetes and ADHD.
The study had multiple funders including the Hong Kong Research Grant Council, NordForsk, the Research Council of Norway, the Norwegian ADHD Research Network, the Hong Kong Innovation and Technology Commission, and European Horizon 2020.
Dr. Cesta had no conflicts of interest to disclose. Dr. Puder chaired the session in which the findings were presented and made no specific disclosures.
FROM EASD 2022
FDA warns against cooking chicken in NyQuil
Called the “sleepy chicken challenge,” the trend tells people to cook chicken in NyQuil or similar over-the-counter cough and cold medications, which include ingredients such as acetaminophen, dextromethorphan, and doxylamine.
“The challenge sounds silly and unappetizing – and it is. But it could also be very unsafe,” the FDA said. “Boiling a medication can make it much more concentrated and change its properties in other ways.”
Even if someone doesn’t plan to eat the chicken, inhaling the vapors of the medication while it cooks could cause high levels of the drug to enter the body.
“It could also hurt your lungs,” the FDA said. “Put simply: Someone could take a dangerously high amount of the cough and cold medicine without even realizing it.”
This isn’t the first time that social media challenges involving medicine have gone viral. In a 2020 TikTok challenge, people were encouraged to take large doses of the allergy medicine diphenhydramine, called the “Benadryl challenge,” to cause hallucinations. The FDA received several reports of teens who were hospitalized or died, and it issued a warning about taking high doses of the drug.
“These video challenges, which often target youths, can harm people – and even cause death,” the FDA said. “Nonprescription (also called over-the-counter or OTC) drugs are readily available in many homes, making these challenges even more risky.”
In the latest warning, the FDA provided several ways for parents to make it less likely for children to do the social media challenges, such as locking up prescription and over-the-counter medications to prevent accidental overdoses. The FDA also encouraged parents and guardians to have open conversations with their children.
“Sit down with your children and discuss the dangers of misusing drugs and how social media trends can lead to real, sometimes irreversible, damage,” the FDA said. “Remind your children that overdoses can occur with OTC drugs as well as with prescription drugs.”
Following the FDA warning, the American Academy of Pediatrics also issued an advisory about social media trends. Some challenges, such as the ALS ice bucket challenge or the mannequin challenge, can be fun and positive activities. But medication-related challenges, such as the sleepy chicken and Benadryl challenges, can cause serious heart problems, seizures, coma, and even death.
“Teens’ brains are still developing. The part of the brain that handles rational thought, the prefrontal cortex, is not fully developed until the mid-20s,” the American Academy of Pediatrics said. “This means teens are naturally more impulsive and likely to act before thinking through all of the ramifications.”
Social media rewards outrageous behavior, it wrote, and the more outrageous the behavior, the more likely someone will get more engagement online.
“It’s a quick moving, impulsive environment, and the fear of losing out is real for teens,” the academy said. “What they will focus on is that a popular kid in class did this and got hundreds of likes and comments.”
The academy suggested that parents and guardians talk with teens about which challenges are trending on social media and at school.
“Sometimes kids are more willing to talk about their peers than themselves,” it said. “Asking questions about school trends, friends and fads may yield more answers than direct questions about their own activities.”
A version of this article first appeared on WebMD.com.
Called the “sleepy chicken challenge,” the trend tells people to cook chicken in NyQuil or similar over-the-counter cough and cold medications, which include ingredients such as acetaminophen, dextromethorphan, and doxylamine.
“The challenge sounds silly and unappetizing – and it is. But it could also be very unsafe,” the FDA said. “Boiling a medication can make it much more concentrated and change its properties in other ways.”
Even if someone doesn’t plan to eat the chicken, inhaling the vapors of the medication while it cooks could cause high levels of the drug to enter the body.
“It could also hurt your lungs,” the FDA said. “Put simply: Someone could take a dangerously high amount of the cough and cold medicine without even realizing it.”
This isn’t the first time that social media challenges involving medicine have gone viral. In a 2020 TikTok challenge, people were encouraged to take large doses of the allergy medicine diphenhydramine, called the “Benadryl challenge,” to cause hallucinations. The FDA received several reports of teens who were hospitalized or died, and it issued a warning about taking high doses of the drug.
“These video challenges, which often target youths, can harm people – and even cause death,” the FDA said. “Nonprescription (also called over-the-counter or OTC) drugs are readily available in many homes, making these challenges even more risky.”
In the latest warning, the FDA provided several ways for parents to make it less likely for children to do the social media challenges, such as locking up prescription and over-the-counter medications to prevent accidental overdoses. The FDA also encouraged parents and guardians to have open conversations with their children.
“Sit down with your children and discuss the dangers of misusing drugs and how social media trends can lead to real, sometimes irreversible, damage,” the FDA said. “Remind your children that overdoses can occur with OTC drugs as well as with prescription drugs.”
Following the FDA warning, the American Academy of Pediatrics also issued an advisory about social media trends. Some challenges, such as the ALS ice bucket challenge or the mannequin challenge, can be fun and positive activities. But medication-related challenges, such as the sleepy chicken and Benadryl challenges, can cause serious heart problems, seizures, coma, and even death.
“Teens’ brains are still developing. The part of the brain that handles rational thought, the prefrontal cortex, is not fully developed until the mid-20s,” the American Academy of Pediatrics said. “This means teens are naturally more impulsive and likely to act before thinking through all of the ramifications.”
Social media rewards outrageous behavior, it wrote, and the more outrageous the behavior, the more likely someone will get more engagement online.
“It’s a quick moving, impulsive environment, and the fear of losing out is real for teens,” the academy said. “What they will focus on is that a popular kid in class did this and got hundreds of likes and comments.”
The academy suggested that parents and guardians talk with teens about which challenges are trending on social media and at school.
“Sometimes kids are more willing to talk about their peers than themselves,” it said. “Asking questions about school trends, friends and fads may yield more answers than direct questions about their own activities.”
A version of this article first appeared on WebMD.com.
Called the “sleepy chicken challenge,” the trend tells people to cook chicken in NyQuil or similar over-the-counter cough and cold medications, which include ingredients such as acetaminophen, dextromethorphan, and doxylamine.
“The challenge sounds silly and unappetizing – and it is. But it could also be very unsafe,” the FDA said. “Boiling a medication can make it much more concentrated and change its properties in other ways.”
Even if someone doesn’t plan to eat the chicken, inhaling the vapors of the medication while it cooks could cause high levels of the drug to enter the body.
“It could also hurt your lungs,” the FDA said. “Put simply: Someone could take a dangerously high amount of the cough and cold medicine without even realizing it.”
This isn’t the first time that social media challenges involving medicine have gone viral. In a 2020 TikTok challenge, people were encouraged to take large doses of the allergy medicine diphenhydramine, called the “Benadryl challenge,” to cause hallucinations. The FDA received several reports of teens who were hospitalized or died, and it issued a warning about taking high doses of the drug.
“These video challenges, which often target youths, can harm people – and even cause death,” the FDA said. “Nonprescription (also called over-the-counter or OTC) drugs are readily available in many homes, making these challenges even more risky.”
In the latest warning, the FDA provided several ways for parents to make it less likely for children to do the social media challenges, such as locking up prescription and over-the-counter medications to prevent accidental overdoses. The FDA also encouraged parents and guardians to have open conversations with their children.
“Sit down with your children and discuss the dangers of misusing drugs and how social media trends can lead to real, sometimes irreversible, damage,” the FDA said. “Remind your children that overdoses can occur with OTC drugs as well as with prescription drugs.”
Following the FDA warning, the American Academy of Pediatrics also issued an advisory about social media trends. Some challenges, such as the ALS ice bucket challenge or the mannequin challenge, can be fun and positive activities. But medication-related challenges, such as the sleepy chicken and Benadryl challenges, can cause serious heart problems, seizures, coma, and even death.
“Teens’ brains are still developing. The part of the brain that handles rational thought, the prefrontal cortex, is not fully developed until the mid-20s,” the American Academy of Pediatrics said. “This means teens are naturally more impulsive and likely to act before thinking through all of the ramifications.”
Social media rewards outrageous behavior, it wrote, and the more outrageous the behavior, the more likely someone will get more engagement online.
“It’s a quick moving, impulsive environment, and the fear of losing out is real for teens,” the academy said. “What they will focus on is that a popular kid in class did this and got hundreds of likes and comments.”
The academy suggested that parents and guardians talk with teens about which challenges are trending on social media and at school.
“Sometimes kids are more willing to talk about their peers than themselves,” it said. “Asking questions about school trends, friends and fads may yield more answers than direct questions about their own activities.”
A version of this article first appeared on WebMD.com.
Telehealth effective in managing patients with movement disorders
Researchers presented their findings at the International Congress of Parkinson’s Disease and Movement Disorders.
Serving the underserved
One of the studies – from Kenya, Africa – documented a 2-year experience with telemedicine in a rural patient population.
Kenya suffers from a dearth of neurologists and movement disorder specialists. Most are based in the capital city of Nairobi, “leaving regions with a population of more than 30 million without access to their care,” wrote the study’s investigators. Internists with an interest in neurology usually manage the bulk of these patients.
Telemedicine has helped to bridge gaps between providers in this part of Africa.
Investigators in their study reviewed all cases of movement disorders at Meru Teaching and Referral Hospital and an affiliated clinic, Oregon Health Services, Meru, Kenya, during 2020 and 2021.
They also reviewed WhatsApp messaging, video calls via WhatsApp, patient videos, and phone calls to see how final diagnoses were arrived at using these platforms.
“For instance, a relative would send a video of a patient experiencing a tremor,” explained lead study author Bundi Karau, MD, a consultant physician. “We also shared the diagnostic challenges with experienced neurologists in Kenya and abroad by forwarding WhatsApp and recorded videos of the patients,” he added.
Telemedicine bridged the gap between rural doctors and patients in several ways. It enabled physicians to discuss cases with neurologists in and out of Kenya. “We were able to advise on medical management or further investigations in a more structured pattern and without spending months to make a diagnosis,” said Dr. Karau.
Patients no longer had to travel to Nairobi for care. “Where a direct link could be expensive or out of reach, we bridged this and consequently brought care closer to the patient,” he added.
More than 100 patients were diagnosed with a movement disorder and enrolled in care and follow-up during this 2-year time. Patients averaged about 62 years of age and more than 60% were male. Parkinson’s disease was the most common diagnosed condition (38.9%) followed by drug-induced movement disorders (30.6%), dystonia (11.1%), and functional movement disorders (11.1%).
Investigators found 3 cases of diabetic striatopathy, 8 cases of myoclonus, and 2 cases of Sydenham’s chorea.
Looking ahead, Dr. Karau and colleagues plan to do a cost benefit analysis vis-a-vis traditional physician visits and a trial model for follow-up visits for other neurological diseases.
Wearable devices and apps improve care
Moving from Africa to Greece, investigators in another study assessed the feasibility of using wearable devices to monitor symptoms in patients with Parkinson’s disease.
Such devices may enhance physical exams during virtual visits. Studies have shown that patients can commit to using such devices or mobile apps. What’s lacking is real-world data from everyday device usage, noted lead author George Rigas, PhD, and colleagues.
Fifty-two private physicians instructed a total of 133 patients to wear a device for Parkinson’s disease motor symptom telemonitoring for 1 week per month during waking hours.
Patients used a mobile app to report symptoms, medication, and nutrition adherence and to message their doctor.
The study team noticed that adherence rates stayed above 70% over a 12-month period. Medication and nutrition were among the most popular app features, an encouraging finding given that patients averaged 67 years of age.
“The high adherence percentage is significant, considering the target population and the early stage of telemedicine in Greece,” they concluded. Additional real-world data could help better inform longer-term adherence.
“These studies from all over the world demonstrate that we are only scratching the surface of the telehealth’s potential to improve care and the lives of individuals with Parkinson’s disease,” said Ray Dorsey, MD, a professor of neurology with the Center for Health + Technology at the University of Rochester (N.Y.).
Dr. Dorsey was not involved with the studies but has written and researched extensively on this topic.
Dr. Dorsey is a consultant for and has equity interests in Mediflix and Included Health, two digital health companies.
Researchers presented their findings at the International Congress of Parkinson’s Disease and Movement Disorders.
Serving the underserved
One of the studies – from Kenya, Africa – documented a 2-year experience with telemedicine in a rural patient population.
Kenya suffers from a dearth of neurologists and movement disorder specialists. Most are based in the capital city of Nairobi, “leaving regions with a population of more than 30 million without access to their care,” wrote the study’s investigators. Internists with an interest in neurology usually manage the bulk of these patients.
Telemedicine has helped to bridge gaps between providers in this part of Africa.
Investigators in their study reviewed all cases of movement disorders at Meru Teaching and Referral Hospital and an affiliated clinic, Oregon Health Services, Meru, Kenya, during 2020 and 2021.
They also reviewed WhatsApp messaging, video calls via WhatsApp, patient videos, and phone calls to see how final diagnoses were arrived at using these platforms.
“For instance, a relative would send a video of a patient experiencing a tremor,” explained lead study author Bundi Karau, MD, a consultant physician. “We also shared the diagnostic challenges with experienced neurologists in Kenya and abroad by forwarding WhatsApp and recorded videos of the patients,” he added.
Telemedicine bridged the gap between rural doctors and patients in several ways. It enabled physicians to discuss cases with neurologists in and out of Kenya. “We were able to advise on medical management or further investigations in a more structured pattern and without spending months to make a diagnosis,” said Dr. Karau.
Patients no longer had to travel to Nairobi for care. “Where a direct link could be expensive or out of reach, we bridged this and consequently brought care closer to the patient,” he added.
More than 100 patients were diagnosed with a movement disorder and enrolled in care and follow-up during this 2-year time. Patients averaged about 62 years of age and more than 60% were male. Parkinson’s disease was the most common diagnosed condition (38.9%) followed by drug-induced movement disorders (30.6%), dystonia (11.1%), and functional movement disorders (11.1%).
Investigators found 3 cases of diabetic striatopathy, 8 cases of myoclonus, and 2 cases of Sydenham’s chorea.
Looking ahead, Dr. Karau and colleagues plan to do a cost benefit analysis vis-a-vis traditional physician visits and a trial model for follow-up visits for other neurological diseases.
Wearable devices and apps improve care
Moving from Africa to Greece, investigators in another study assessed the feasibility of using wearable devices to monitor symptoms in patients with Parkinson’s disease.
Such devices may enhance physical exams during virtual visits. Studies have shown that patients can commit to using such devices or mobile apps. What’s lacking is real-world data from everyday device usage, noted lead author George Rigas, PhD, and colleagues.
Fifty-two private physicians instructed a total of 133 patients to wear a device for Parkinson’s disease motor symptom telemonitoring for 1 week per month during waking hours.
Patients used a mobile app to report symptoms, medication, and nutrition adherence and to message their doctor.
The study team noticed that adherence rates stayed above 70% over a 12-month period. Medication and nutrition were among the most popular app features, an encouraging finding given that patients averaged 67 years of age.
“The high adherence percentage is significant, considering the target population and the early stage of telemedicine in Greece,” they concluded. Additional real-world data could help better inform longer-term adherence.
“These studies from all over the world demonstrate that we are only scratching the surface of the telehealth’s potential to improve care and the lives of individuals with Parkinson’s disease,” said Ray Dorsey, MD, a professor of neurology with the Center for Health + Technology at the University of Rochester (N.Y.).
Dr. Dorsey was not involved with the studies but has written and researched extensively on this topic.
Dr. Dorsey is a consultant for and has equity interests in Mediflix and Included Health, two digital health companies.
Researchers presented their findings at the International Congress of Parkinson’s Disease and Movement Disorders.
Serving the underserved
One of the studies – from Kenya, Africa – documented a 2-year experience with telemedicine in a rural patient population.
Kenya suffers from a dearth of neurologists and movement disorder specialists. Most are based in the capital city of Nairobi, “leaving regions with a population of more than 30 million without access to their care,” wrote the study’s investigators. Internists with an interest in neurology usually manage the bulk of these patients.
Telemedicine has helped to bridge gaps between providers in this part of Africa.
Investigators in their study reviewed all cases of movement disorders at Meru Teaching and Referral Hospital and an affiliated clinic, Oregon Health Services, Meru, Kenya, during 2020 and 2021.
They also reviewed WhatsApp messaging, video calls via WhatsApp, patient videos, and phone calls to see how final diagnoses were arrived at using these platforms.
“For instance, a relative would send a video of a patient experiencing a tremor,” explained lead study author Bundi Karau, MD, a consultant physician. “We also shared the diagnostic challenges with experienced neurologists in Kenya and abroad by forwarding WhatsApp and recorded videos of the patients,” he added.
Telemedicine bridged the gap between rural doctors and patients in several ways. It enabled physicians to discuss cases with neurologists in and out of Kenya. “We were able to advise on medical management or further investigations in a more structured pattern and without spending months to make a diagnosis,” said Dr. Karau.
Patients no longer had to travel to Nairobi for care. “Where a direct link could be expensive or out of reach, we bridged this and consequently brought care closer to the patient,” he added.
More than 100 patients were diagnosed with a movement disorder and enrolled in care and follow-up during this 2-year time. Patients averaged about 62 years of age and more than 60% were male. Parkinson’s disease was the most common diagnosed condition (38.9%) followed by drug-induced movement disorders (30.6%), dystonia (11.1%), and functional movement disorders (11.1%).
Investigators found 3 cases of diabetic striatopathy, 8 cases of myoclonus, and 2 cases of Sydenham’s chorea.
Looking ahead, Dr. Karau and colleagues plan to do a cost benefit analysis vis-a-vis traditional physician visits and a trial model for follow-up visits for other neurological diseases.
Wearable devices and apps improve care
Moving from Africa to Greece, investigators in another study assessed the feasibility of using wearable devices to monitor symptoms in patients with Parkinson’s disease.
Such devices may enhance physical exams during virtual visits. Studies have shown that patients can commit to using such devices or mobile apps. What’s lacking is real-world data from everyday device usage, noted lead author George Rigas, PhD, and colleagues.
Fifty-two private physicians instructed a total of 133 patients to wear a device for Parkinson’s disease motor symptom telemonitoring for 1 week per month during waking hours.
Patients used a mobile app to report symptoms, medication, and nutrition adherence and to message their doctor.
The study team noticed that adherence rates stayed above 70% over a 12-month period. Medication and nutrition were among the most popular app features, an encouraging finding given that patients averaged 67 years of age.
“The high adherence percentage is significant, considering the target population and the early stage of telemedicine in Greece,” they concluded. Additional real-world data could help better inform longer-term adherence.
“These studies from all over the world demonstrate that we are only scratching the surface of the telehealth’s potential to improve care and the lives of individuals with Parkinson’s disease,” said Ray Dorsey, MD, a professor of neurology with the Center for Health + Technology at the University of Rochester (N.Y.).
Dr. Dorsey was not involved with the studies but has written and researched extensively on this topic.
Dr. Dorsey is a consultant for and has equity interests in Mediflix and Included Health, two digital health companies.
From MDS 2022
Triple threat: Novel agent shows potent T2D weight loss in phase 1
STOCKHOLM – First came the GLP-1 receptor agonists as treatments for patients with type 2 diabetes, then came tirzepatide (Mounjaro) which added a second incretin agonism for the receptor to the glucose-dependent insulinotropic polypeptide (GIP). Now coming onto the clinical scene is a molecule with triple agonism to the GLP-1 receptor, the GIP receptor, and to the glucagon receptor.
That molecule, LY3437943, showed reasonable safety and tolerability and an apparent incremental uptick in weight loss compared with the approved incretin-based agents for people with type 2 diabetes in a 12-week, dose-ranging study involving a 52 patients with type 2 diabetes who received the new agent.
The 12 people who uptitrated for a total of 12 weeks and reached the highest tested dose of LY3437943, 12 mg, injected once weekly during the final 4 weeks, showed an average weight loss of 8.65 kg, while the 11 patients who maxed out at a weekly dose of 6 mg of LY3437943 had an average 12-week weight loss of 7.52 kg, Zvonko Milicevic, MD, reported at the annual meeting of the European Association for the Study of Diabetes.
Fifteen more participants received placebo and five received a comparator GLP-1 receptor agonist. All 72 patients in the study were also already on treatment with metformin when they entered, and they were maintained on metformin throughout the study period.
The new agent showed “greater weight loss efficacy than currently approved medications,” said Dr. Milicevic, a staff researcher who works in Vienna for Eli Lilly, the company developing LY3437943.
‘Really impressive’ weight loss
Martin Haluzik, MD, who chaired the session where Dr. Milicevic spoke, agreed. “The data, especially for weight reduction, were really impressive,” Dr. Haluzik said in an interview. “It looks stronger than the best we have at the moment,” the dual incretin agonist tirzepatide, he added.
Cross-study comparisons are very unreliable, but to put the weight loss seen with LY3437943 in perspective, the 12-week weight reduction that occurred with the highest dose of tirzepatide tested (15 mg/weekly) in the pivotal SURPASS-2 trial with 1,879 randomized patients with type 2 diabetes was an average of roughly 5 kg, while the comparator of 1 mg weekly of semaglutide (Ozempic) tested in the same study produced an average weight loss of about 4 kg.
Other notable efficacy results for LY3437943 after 12 weeks on treatment included an average reduction in hemoglobin A1c from baseline of 1.90%, achieved in the group that received 6 mg weekly as their maximum dose for 8 weeks after a 4-week run-in at a lower dose; a reduction in systolic blood pressure of 7.99 mm Hg on the 6-mg maximum weekly dose and of 12.06 mm Hg on the maximum 12-mg weekly dose; and “robust” reductions in lipids including cuts from baseline of about 40% for both triglycerides and very-LDL cholesterol, Dr. Milicevic reported.
Adverse effects resemble approved incretin-based agents
The study, which ran at four U.S. sites, had a primary objective of safety assessment, and Dr. Milicevic said the results showed acceptable safety and tolerability consistent with the glucagon-like peptide-1 (GLP-1) receptor agonists and tirzepatide. Like those agents, LY3437943 caused primarily mild gastrointestinal adverse effects such as nausea and diarrhea. Of the 52 patients in the study who received the triple agonist, 4 discontinued treatment because of a treatment-emergent adverse effect, including 1 patient in the subgroup who received the maximum dose.
The only concerning adverse effect noted by Dr. Haluzik was the average increase in heart rate from baseline of 10.26 beats/min in the subgroup that received the maximum dose, roughly twice the increase seen with tirzepatide and semaglutide in SURPASS-2. The average heart rate increase was about half that, 5.30 beats/min compared with baseline, in the subgroup that received a maximum weekly dose of 6 mg.
Overall, the results showed “no major adverse effects that might hamper use,” said Dr. Haluzik, an endocrinologist and professor at Charles University in Prague.
Two phase 2 studies of LY3437943 are underway and are scheduled to finish before the end of 2022. They include a study of about 300 people with type 2 diabetes that’s running at 43 U.S. sites, and a second study of about 500 people with overweight or obesity running at 28 U.S. sites.
The study was sponsored by Eli Lilly, the company developing LY3437943. Dr. Milicevic is an employee of and stockholder of Eli Lilly. Dr. Haluzik has been an adviser to, consultant to, and received honoraria and research support from Eli Lilly. He has had similar relationships with Amgen, AstraZeneca, Boehringer Ingelheim, BristolMyersSquibb, Janssen, Johnson & Johnson, Mundipharma, Novo Nordisk, and Sanofi.
STOCKHOLM – First came the GLP-1 receptor agonists as treatments for patients with type 2 diabetes, then came tirzepatide (Mounjaro) which added a second incretin agonism for the receptor to the glucose-dependent insulinotropic polypeptide (GIP). Now coming onto the clinical scene is a molecule with triple agonism to the GLP-1 receptor, the GIP receptor, and to the glucagon receptor.
That molecule, LY3437943, showed reasonable safety and tolerability and an apparent incremental uptick in weight loss compared with the approved incretin-based agents for people with type 2 diabetes in a 12-week, dose-ranging study involving a 52 patients with type 2 diabetes who received the new agent.
The 12 people who uptitrated for a total of 12 weeks and reached the highest tested dose of LY3437943, 12 mg, injected once weekly during the final 4 weeks, showed an average weight loss of 8.65 kg, while the 11 patients who maxed out at a weekly dose of 6 mg of LY3437943 had an average 12-week weight loss of 7.52 kg, Zvonko Milicevic, MD, reported at the annual meeting of the European Association for the Study of Diabetes.
Fifteen more participants received placebo and five received a comparator GLP-1 receptor agonist. All 72 patients in the study were also already on treatment with metformin when they entered, and they were maintained on metformin throughout the study period.
The new agent showed “greater weight loss efficacy than currently approved medications,” said Dr. Milicevic, a staff researcher who works in Vienna for Eli Lilly, the company developing LY3437943.
‘Really impressive’ weight loss
Martin Haluzik, MD, who chaired the session where Dr. Milicevic spoke, agreed. “The data, especially for weight reduction, were really impressive,” Dr. Haluzik said in an interview. “It looks stronger than the best we have at the moment,” the dual incretin agonist tirzepatide, he added.
Cross-study comparisons are very unreliable, but to put the weight loss seen with LY3437943 in perspective, the 12-week weight reduction that occurred with the highest dose of tirzepatide tested (15 mg/weekly) in the pivotal SURPASS-2 trial with 1,879 randomized patients with type 2 diabetes was an average of roughly 5 kg, while the comparator of 1 mg weekly of semaglutide (Ozempic) tested in the same study produced an average weight loss of about 4 kg.
Other notable efficacy results for LY3437943 after 12 weeks on treatment included an average reduction in hemoglobin A1c from baseline of 1.90%, achieved in the group that received 6 mg weekly as their maximum dose for 8 weeks after a 4-week run-in at a lower dose; a reduction in systolic blood pressure of 7.99 mm Hg on the 6-mg maximum weekly dose and of 12.06 mm Hg on the maximum 12-mg weekly dose; and “robust” reductions in lipids including cuts from baseline of about 40% for both triglycerides and very-LDL cholesterol, Dr. Milicevic reported.
Adverse effects resemble approved incretin-based agents
The study, which ran at four U.S. sites, had a primary objective of safety assessment, and Dr. Milicevic said the results showed acceptable safety and tolerability consistent with the glucagon-like peptide-1 (GLP-1) receptor agonists and tirzepatide. Like those agents, LY3437943 caused primarily mild gastrointestinal adverse effects such as nausea and diarrhea. Of the 52 patients in the study who received the triple agonist, 4 discontinued treatment because of a treatment-emergent adverse effect, including 1 patient in the subgroup who received the maximum dose.
The only concerning adverse effect noted by Dr. Haluzik was the average increase in heart rate from baseline of 10.26 beats/min in the subgroup that received the maximum dose, roughly twice the increase seen with tirzepatide and semaglutide in SURPASS-2. The average heart rate increase was about half that, 5.30 beats/min compared with baseline, in the subgroup that received a maximum weekly dose of 6 mg.
Overall, the results showed “no major adverse effects that might hamper use,” said Dr. Haluzik, an endocrinologist and professor at Charles University in Prague.
Two phase 2 studies of LY3437943 are underway and are scheduled to finish before the end of 2022. They include a study of about 300 people with type 2 diabetes that’s running at 43 U.S. sites, and a second study of about 500 people with overweight or obesity running at 28 U.S. sites.
The study was sponsored by Eli Lilly, the company developing LY3437943. Dr. Milicevic is an employee of and stockholder of Eli Lilly. Dr. Haluzik has been an adviser to, consultant to, and received honoraria and research support from Eli Lilly. He has had similar relationships with Amgen, AstraZeneca, Boehringer Ingelheim, BristolMyersSquibb, Janssen, Johnson & Johnson, Mundipharma, Novo Nordisk, and Sanofi.
STOCKHOLM – First came the GLP-1 receptor agonists as treatments for patients with type 2 diabetes, then came tirzepatide (Mounjaro) which added a second incretin agonism for the receptor to the glucose-dependent insulinotropic polypeptide (GIP). Now coming onto the clinical scene is a molecule with triple agonism to the GLP-1 receptor, the GIP receptor, and to the glucagon receptor.
That molecule, LY3437943, showed reasonable safety and tolerability and an apparent incremental uptick in weight loss compared with the approved incretin-based agents for people with type 2 diabetes in a 12-week, dose-ranging study involving a 52 patients with type 2 diabetes who received the new agent.
The 12 people who uptitrated for a total of 12 weeks and reached the highest tested dose of LY3437943, 12 mg, injected once weekly during the final 4 weeks, showed an average weight loss of 8.65 kg, while the 11 patients who maxed out at a weekly dose of 6 mg of LY3437943 had an average 12-week weight loss of 7.52 kg, Zvonko Milicevic, MD, reported at the annual meeting of the European Association for the Study of Diabetes.
Fifteen more participants received placebo and five received a comparator GLP-1 receptor agonist. All 72 patients in the study were also already on treatment with metformin when they entered, and they were maintained on metformin throughout the study period.
The new agent showed “greater weight loss efficacy than currently approved medications,” said Dr. Milicevic, a staff researcher who works in Vienna for Eli Lilly, the company developing LY3437943.
‘Really impressive’ weight loss
Martin Haluzik, MD, who chaired the session where Dr. Milicevic spoke, agreed. “The data, especially for weight reduction, were really impressive,” Dr. Haluzik said in an interview. “It looks stronger than the best we have at the moment,” the dual incretin agonist tirzepatide, he added.
Cross-study comparisons are very unreliable, but to put the weight loss seen with LY3437943 in perspective, the 12-week weight reduction that occurred with the highest dose of tirzepatide tested (15 mg/weekly) in the pivotal SURPASS-2 trial with 1,879 randomized patients with type 2 diabetes was an average of roughly 5 kg, while the comparator of 1 mg weekly of semaglutide (Ozempic) tested in the same study produced an average weight loss of about 4 kg.
Other notable efficacy results for LY3437943 after 12 weeks on treatment included an average reduction in hemoglobin A1c from baseline of 1.90%, achieved in the group that received 6 mg weekly as their maximum dose for 8 weeks after a 4-week run-in at a lower dose; a reduction in systolic blood pressure of 7.99 mm Hg on the 6-mg maximum weekly dose and of 12.06 mm Hg on the maximum 12-mg weekly dose; and “robust” reductions in lipids including cuts from baseline of about 40% for both triglycerides and very-LDL cholesterol, Dr. Milicevic reported.
Adverse effects resemble approved incretin-based agents
The study, which ran at four U.S. sites, had a primary objective of safety assessment, and Dr. Milicevic said the results showed acceptable safety and tolerability consistent with the glucagon-like peptide-1 (GLP-1) receptor agonists and tirzepatide. Like those agents, LY3437943 caused primarily mild gastrointestinal adverse effects such as nausea and diarrhea. Of the 52 patients in the study who received the triple agonist, 4 discontinued treatment because of a treatment-emergent adverse effect, including 1 patient in the subgroup who received the maximum dose.
The only concerning adverse effect noted by Dr. Haluzik was the average increase in heart rate from baseline of 10.26 beats/min in the subgroup that received the maximum dose, roughly twice the increase seen with tirzepatide and semaglutide in SURPASS-2. The average heart rate increase was about half that, 5.30 beats/min compared with baseline, in the subgroup that received a maximum weekly dose of 6 mg.
Overall, the results showed “no major adverse effects that might hamper use,” said Dr. Haluzik, an endocrinologist and professor at Charles University in Prague.
Two phase 2 studies of LY3437943 are underway and are scheduled to finish before the end of 2022. They include a study of about 300 people with type 2 diabetes that’s running at 43 U.S. sites, and a second study of about 500 people with overweight or obesity running at 28 U.S. sites.
The study was sponsored by Eli Lilly, the company developing LY3437943. Dr. Milicevic is an employee of and stockholder of Eli Lilly. Dr. Haluzik has been an adviser to, consultant to, and received honoraria and research support from Eli Lilly. He has had similar relationships with Amgen, AstraZeneca, Boehringer Ingelheim, BristolMyersSquibb, Janssen, Johnson & Johnson, Mundipharma, Novo Nordisk, and Sanofi.
AT EASD 2022
Hep C, HIV coinfection tied to higher MI risk with age
, a new analysis suggests.
By contrast, the risk increases by 30% every 10 years among PWH without HCV infection.
“There is other evidence that suggests people with HIV and HCV have a greater burden of negative health outcomes,” senior author Keri N. Althoff, PhD, MPH, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, said in an interview. “But the magnitude of ‘greater’ was bigger than I expected.”
“Understanding the difference HCV can make in the risk of MI with increasing age among those with – compared to without – HCV is an important step for understanding additional potential benefits of HCV treatment (among PWH),” she said.
The amplified risk with age occurred even though, overall, the association between HCV coinfection and increased risk of type 1 myocardial infarction (T1MI) was not significant, the analysis showed.
The study was published online in the Journal of the American Heart Association.
How age counts
Dr. Althoff and colleagues analyzed data from 23,361 PWH aged 40-79 who had initiated antiretroviral therapy between 2000 and 2017. The primary outcome was T1MI.
A total of 4,677 participants (20%) had HCV. Eighty-nine T1MIs occurred among PWH with HCV (1.9%) vs. 314 among PWH without HCV (1.7%). In adjusted analyses, HCV was not associated with increased T1MI risk (adjusted hazard ratio, 0.98).
However, the risk of T1MI increased with age and was augmented in those with HCV (aHR per 10-year increase in age, 1.85) vs. those without HCV (aHR, 1.30).
Specifically, compared with those without HCV, the estimated T1MI risk was 17% higher among 50- to 59-year-olds with HCV and 77% higher among those 60 and older; neither association was statistically significant, although the authors suggest this probably was because of the smaller number of participants in the older age categories.
Even without HCV, the risk of T1MI increased in participants who had traditional risk factors. The risk was significantly higher among PWH aged 40-49 with diabetes, hypertension, chronic kidney disease, protease inhibitor (PI) use, and smoking, whereas among PWH aged 50-59, the T1MI risk was significantly greater among those with hypertension, PI use, and smoking.
Among those aged 60 or older, hypertension and low CD4 counts were associated with a significantly increased T1MI risk.
“Clinicians providing health care to people with HIV should know their patients’ HCV status,” Dr. Althoff said, “and provide support regarding HCV treatment and ways to reduce their cardiovascular risk, including smoking cessation, reaching and maintaining a healthy BMI, and substance use treatment.”
Truly additive?
American Heart Association expert volunteer Nieca Goldberg, MD, a clinical associate professor of medicine at New York University and medical director of Atria NY, said the increased T1MI risk with coinfection “makes sense” because both HIV and HCV are linked to inflammation.
However, she said in an interview, “the fact that the authors didn’t control for other, more traditional heart attack risk factors is a limitation. I would like to see a study that takes other risk factors into consideration to see if HCV is truly additive.”
Meanwhile, like Dr. Althoff, she said, “Clinicians should be taking a careful history that includes chronic infections as well as traditional heart risk factors.”
Additional studies are needed, Dr. Althoff agreed. “There are two paths we are keenly interested in pursuing. The first is understanding how metabolic risk factors for MI change after HCV treatment. We are working on this.”
“Ultimately,” she said, “we want to compare MI risk in people with HIV who had successful HCV treatment to those who have not had successful HCV treatment.”
In their current study, they had nearly 2 decades of follow-up, she noted. “Although we don’t need to wait that long, we would like to have close to a decade of potential follow-up time (since 2016, when sofosbuvir/velpatasvir became available) so that we have a large enough sample size to observe a sufficient number of MIs within the first 5 years after successful HCV treatment.”
No commercial funding or relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
, a new analysis suggests.
By contrast, the risk increases by 30% every 10 years among PWH without HCV infection.
“There is other evidence that suggests people with HIV and HCV have a greater burden of negative health outcomes,” senior author Keri N. Althoff, PhD, MPH, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, said in an interview. “But the magnitude of ‘greater’ was bigger than I expected.”
“Understanding the difference HCV can make in the risk of MI with increasing age among those with – compared to without – HCV is an important step for understanding additional potential benefits of HCV treatment (among PWH),” she said.
The amplified risk with age occurred even though, overall, the association between HCV coinfection and increased risk of type 1 myocardial infarction (T1MI) was not significant, the analysis showed.
The study was published online in the Journal of the American Heart Association.
How age counts
Dr. Althoff and colleagues analyzed data from 23,361 PWH aged 40-79 who had initiated antiretroviral therapy between 2000 and 2017. The primary outcome was T1MI.
A total of 4,677 participants (20%) had HCV. Eighty-nine T1MIs occurred among PWH with HCV (1.9%) vs. 314 among PWH without HCV (1.7%). In adjusted analyses, HCV was not associated with increased T1MI risk (adjusted hazard ratio, 0.98).
However, the risk of T1MI increased with age and was augmented in those with HCV (aHR per 10-year increase in age, 1.85) vs. those without HCV (aHR, 1.30).
Specifically, compared with those without HCV, the estimated T1MI risk was 17% higher among 50- to 59-year-olds with HCV and 77% higher among those 60 and older; neither association was statistically significant, although the authors suggest this probably was because of the smaller number of participants in the older age categories.
Even without HCV, the risk of T1MI increased in participants who had traditional risk factors. The risk was significantly higher among PWH aged 40-49 with diabetes, hypertension, chronic kidney disease, protease inhibitor (PI) use, and smoking, whereas among PWH aged 50-59, the T1MI risk was significantly greater among those with hypertension, PI use, and smoking.
Among those aged 60 or older, hypertension and low CD4 counts were associated with a significantly increased T1MI risk.
“Clinicians providing health care to people with HIV should know their patients’ HCV status,” Dr. Althoff said, “and provide support regarding HCV treatment and ways to reduce their cardiovascular risk, including smoking cessation, reaching and maintaining a healthy BMI, and substance use treatment.”
Truly additive?
American Heart Association expert volunteer Nieca Goldberg, MD, a clinical associate professor of medicine at New York University and medical director of Atria NY, said the increased T1MI risk with coinfection “makes sense” because both HIV and HCV are linked to inflammation.
However, she said in an interview, “the fact that the authors didn’t control for other, more traditional heart attack risk factors is a limitation. I would like to see a study that takes other risk factors into consideration to see if HCV is truly additive.”
Meanwhile, like Dr. Althoff, she said, “Clinicians should be taking a careful history that includes chronic infections as well as traditional heart risk factors.”
Additional studies are needed, Dr. Althoff agreed. “There are two paths we are keenly interested in pursuing. The first is understanding how metabolic risk factors for MI change after HCV treatment. We are working on this.”
“Ultimately,” she said, “we want to compare MI risk in people with HIV who had successful HCV treatment to those who have not had successful HCV treatment.”
In their current study, they had nearly 2 decades of follow-up, she noted. “Although we don’t need to wait that long, we would like to have close to a decade of potential follow-up time (since 2016, when sofosbuvir/velpatasvir became available) so that we have a large enough sample size to observe a sufficient number of MIs within the first 5 years after successful HCV treatment.”
No commercial funding or relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
, a new analysis suggests.
By contrast, the risk increases by 30% every 10 years among PWH without HCV infection.
“There is other evidence that suggests people with HIV and HCV have a greater burden of negative health outcomes,” senior author Keri N. Althoff, PhD, MPH, of the Johns Hopkins Bloomberg School of Public Health in Baltimore, said in an interview. “But the magnitude of ‘greater’ was bigger than I expected.”
“Understanding the difference HCV can make in the risk of MI with increasing age among those with – compared to without – HCV is an important step for understanding additional potential benefits of HCV treatment (among PWH),” she said.
The amplified risk with age occurred even though, overall, the association between HCV coinfection and increased risk of type 1 myocardial infarction (T1MI) was not significant, the analysis showed.
The study was published online in the Journal of the American Heart Association.
How age counts
Dr. Althoff and colleagues analyzed data from 23,361 PWH aged 40-79 who had initiated antiretroviral therapy between 2000 and 2017. The primary outcome was T1MI.
A total of 4,677 participants (20%) had HCV. Eighty-nine T1MIs occurred among PWH with HCV (1.9%) vs. 314 among PWH without HCV (1.7%). In adjusted analyses, HCV was not associated with increased T1MI risk (adjusted hazard ratio, 0.98).
However, the risk of T1MI increased with age and was augmented in those with HCV (aHR per 10-year increase in age, 1.85) vs. those without HCV (aHR, 1.30).
Specifically, compared with those without HCV, the estimated T1MI risk was 17% higher among 50- to 59-year-olds with HCV and 77% higher among those 60 and older; neither association was statistically significant, although the authors suggest this probably was because of the smaller number of participants in the older age categories.
Even without HCV, the risk of T1MI increased in participants who had traditional risk factors. The risk was significantly higher among PWH aged 40-49 with diabetes, hypertension, chronic kidney disease, protease inhibitor (PI) use, and smoking, whereas among PWH aged 50-59, the T1MI risk was significantly greater among those with hypertension, PI use, and smoking.
Among those aged 60 or older, hypertension and low CD4 counts were associated with a significantly increased T1MI risk.
“Clinicians providing health care to people with HIV should know their patients’ HCV status,” Dr. Althoff said, “and provide support regarding HCV treatment and ways to reduce their cardiovascular risk, including smoking cessation, reaching and maintaining a healthy BMI, and substance use treatment.”
Truly additive?
American Heart Association expert volunteer Nieca Goldberg, MD, a clinical associate professor of medicine at New York University and medical director of Atria NY, said the increased T1MI risk with coinfection “makes sense” because both HIV and HCV are linked to inflammation.
However, she said in an interview, “the fact that the authors didn’t control for other, more traditional heart attack risk factors is a limitation. I would like to see a study that takes other risk factors into consideration to see if HCV is truly additive.”
Meanwhile, like Dr. Althoff, she said, “Clinicians should be taking a careful history that includes chronic infections as well as traditional heart risk factors.”
Additional studies are needed, Dr. Althoff agreed. “There are two paths we are keenly interested in pursuing. The first is understanding how metabolic risk factors for MI change after HCV treatment. We are working on this.”
“Ultimately,” she said, “we want to compare MI risk in people with HIV who had successful HCV treatment to those who have not had successful HCV treatment.”
In their current study, they had nearly 2 decades of follow-up, she noted. “Although we don’t need to wait that long, we would like to have close to a decade of potential follow-up time (since 2016, when sofosbuvir/velpatasvir became available) so that we have a large enough sample size to observe a sufficient number of MIs within the first 5 years after successful HCV treatment.”
No commercial funding or relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
High BMI linked to better survival for cancer patients treated with ICI, but for men only
That is the conclusion of a new retrospective analysis presented during a poster session given at the annual meeting of the European Society for Medical Oncology. The study sought to better understand ICI outcomes. “These are complex new treatments and, because they harness the immune system, no two patients are likely to respond in the same way. BMI has previously been associated with improved survival in patients with advanced lung cancer treated with immunotherapy. However, the reasons behind this observation, and the implications for treatment are unknown, as is whether this observation is specific for patients with only certain types of cancers,” study author Dwight Owen, MD, said in an email.
He pointed out that the retrospective nature of the findings means that they have no immediate clinical implications. “The reason for the discrepancy in males remains unclear. Although our study included a relatively large number of patients, it is a heterogenous cohort and there may be confounding factors that we haven’t recognized, so these findings need to be replicated in larger cohorts,” said Dr. Owen, a medical oncologist with The Ohio State University Comprehensive Cancer Center, Columbus.
Asked if there is a potential biological explanation for a difference between males and females, Dr. Owen said that this is an area of intense research. One recent study examined whether androgen could help explain why men are more likely than women to both develop and have more aggressive nonreproductive cancers. They concluded that androgen receptor signaling may be leading to loss of effector and proliferative potential of CD8+ T cells in the tumor microenvironment. Once exhausted, these cells do not respond well to stimulation that can occur after ICI treatment.
On the opposite end of the spectrum, cancer cachexia is also a key subject of study. It is characterized by weight loss and is associated with worse clinical outcomes. A cachexia mouse model found that weight loss can lead to more clearance of immune checkpoint antibodies.
Still, much more work needs to be done. “For now, how BMI, obesity, and cachexia relate to other factors, for instance the microbiome and tumor immunogenicity, are still not fully understood,” Dr. Owen said.
The study data
The researchers analyzed data from 688 patients with metastatic cancer treated at their center between 2011 and 2017. 94% were White and 5% were Black. 41% were female and the mean age was 61.9 years. The mean BMI was 28.8 kg/m2; 40% of patients had melanoma, 23% had non–small cell lung cancer, 10% had renal cancer, and 27% had another form of cancer.
For every unit decrease in BMI, the researchers observed a 1.8% decrease in mortality (hazard ratio, 0.982; P = .007). Patients with a BMI of 40 or above had better survival than all other patients grouped by 5 BMI increments (that is, 35-40, 30-35, etc.). When separated by sex, males had a significant decrease in mortality for every increase in BMI unit (HR, 0.964; P = .004), but there was no significant difference among women (HR, 1.003; P = .706). The relationship in men held up after adjustment for Eastern Cooperative Oncology Group score, line of therapy, and cancer type (HR, 0.979; P = .0308). The researchers also looked at a separate cohort of 185 normal weight and 15 obese (BMI ≥ 40) NSCLC patients. Median survival was 27.5 months in the obese group and 9.1 months in the normal weight group (HR, 0.474; 95% CI, 0.232-0.969).
Dr. Owen has received research funding through his institution from Bristol-Myers Squibb, Genentech, Pfizer, Palobiofarma, and Onc.AI.
That is the conclusion of a new retrospective analysis presented during a poster session given at the annual meeting of the European Society for Medical Oncology. The study sought to better understand ICI outcomes. “These are complex new treatments and, because they harness the immune system, no two patients are likely to respond in the same way. BMI has previously been associated with improved survival in patients with advanced lung cancer treated with immunotherapy. However, the reasons behind this observation, and the implications for treatment are unknown, as is whether this observation is specific for patients with only certain types of cancers,” study author Dwight Owen, MD, said in an email.
He pointed out that the retrospective nature of the findings means that they have no immediate clinical implications. “The reason for the discrepancy in males remains unclear. Although our study included a relatively large number of patients, it is a heterogenous cohort and there may be confounding factors that we haven’t recognized, so these findings need to be replicated in larger cohorts,” said Dr. Owen, a medical oncologist with The Ohio State University Comprehensive Cancer Center, Columbus.
Asked if there is a potential biological explanation for a difference between males and females, Dr. Owen said that this is an area of intense research. One recent study examined whether androgen could help explain why men are more likely than women to both develop and have more aggressive nonreproductive cancers. They concluded that androgen receptor signaling may be leading to loss of effector and proliferative potential of CD8+ T cells in the tumor microenvironment. Once exhausted, these cells do not respond well to stimulation that can occur after ICI treatment.
On the opposite end of the spectrum, cancer cachexia is also a key subject of study. It is characterized by weight loss and is associated with worse clinical outcomes. A cachexia mouse model found that weight loss can lead to more clearance of immune checkpoint antibodies.
Still, much more work needs to be done. “For now, how BMI, obesity, and cachexia relate to other factors, for instance the microbiome and tumor immunogenicity, are still not fully understood,” Dr. Owen said.
The study data
The researchers analyzed data from 688 patients with metastatic cancer treated at their center between 2011 and 2017. 94% were White and 5% were Black. 41% were female and the mean age was 61.9 years. The mean BMI was 28.8 kg/m2; 40% of patients had melanoma, 23% had non–small cell lung cancer, 10% had renal cancer, and 27% had another form of cancer.
For every unit decrease in BMI, the researchers observed a 1.8% decrease in mortality (hazard ratio, 0.982; P = .007). Patients with a BMI of 40 or above had better survival than all other patients grouped by 5 BMI increments (that is, 35-40, 30-35, etc.). When separated by sex, males had a significant decrease in mortality for every increase in BMI unit (HR, 0.964; P = .004), but there was no significant difference among women (HR, 1.003; P = .706). The relationship in men held up after adjustment for Eastern Cooperative Oncology Group score, line of therapy, and cancer type (HR, 0.979; P = .0308). The researchers also looked at a separate cohort of 185 normal weight and 15 obese (BMI ≥ 40) NSCLC patients. Median survival was 27.5 months in the obese group and 9.1 months in the normal weight group (HR, 0.474; 95% CI, 0.232-0.969).
Dr. Owen has received research funding through his institution from Bristol-Myers Squibb, Genentech, Pfizer, Palobiofarma, and Onc.AI.
That is the conclusion of a new retrospective analysis presented during a poster session given at the annual meeting of the European Society for Medical Oncology. The study sought to better understand ICI outcomes. “These are complex new treatments and, because they harness the immune system, no two patients are likely to respond in the same way. BMI has previously been associated with improved survival in patients with advanced lung cancer treated with immunotherapy. However, the reasons behind this observation, and the implications for treatment are unknown, as is whether this observation is specific for patients with only certain types of cancers,” study author Dwight Owen, MD, said in an email.
He pointed out that the retrospective nature of the findings means that they have no immediate clinical implications. “The reason for the discrepancy in males remains unclear. Although our study included a relatively large number of patients, it is a heterogenous cohort and there may be confounding factors that we haven’t recognized, so these findings need to be replicated in larger cohorts,” said Dr. Owen, a medical oncologist with The Ohio State University Comprehensive Cancer Center, Columbus.
Asked if there is a potential biological explanation for a difference between males and females, Dr. Owen said that this is an area of intense research. One recent study examined whether androgen could help explain why men are more likely than women to both develop and have more aggressive nonreproductive cancers. They concluded that androgen receptor signaling may be leading to loss of effector and proliferative potential of CD8+ T cells in the tumor microenvironment. Once exhausted, these cells do not respond well to stimulation that can occur after ICI treatment.
On the opposite end of the spectrum, cancer cachexia is also a key subject of study. It is characterized by weight loss and is associated with worse clinical outcomes. A cachexia mouse model found that weight loss can lead to more clearance of immune checkpoint antibodies.
Still, much more work needs to be done. “For now, how BMI, obesity, and cachexia relate to other factors, for instance the microbiome and tumor immunogenicity, are still not fully understood,” Dr. Owen said.
The study data
The researchers analyzed data from 688 patients with metastatic cancer treated at their center between 2011 and 2017. 94% were White and 5% were Black. 41% were female and the mean age was 61.9 years. The mean BMI was 28.8 kg/m2; 40% of patients had melanoma, 23% had non–small cell lung cancer, 10% had renal cancer, and 27% had another form of cancer.
For every unit decrease in BMI, the researchers observed a 1.8% decrease in mortality (hazard ratio, 0.982; P = .007). Patients with a BMI of 40 or above had better survival than all other patients grouped by 5 BMI increments (that is, 35-40, 30-35, etc.). When separated by sex, males had a significant decrease in mortality for every increase in BMI unit (HR, 0.964; P = .004), but there was no significant difference among women (HR, 1.003; P = .706). The relationship in men held up after adjustment for Eastern Cooperative Oncology Group score, line of therapy, and cancer type (HR, 0.979; P = .0308). The researchers also looked at a separate cohort of 185 normal weight and 15 obese (BMI ≥ 40) NSCLC patients. Median survival was 27.5 months in the obese group and 9.1 months in the normal weight group (HR, 0.474; 95% CI, 0.232-0.969).
Dr. Owen has received research funding through his institution from Bristol-Myers Squibb, Genentech, Pfizer, Palobiofarma, and Onc.AI.
FROM ESMO CONGRESS 2022
Scalp plaque
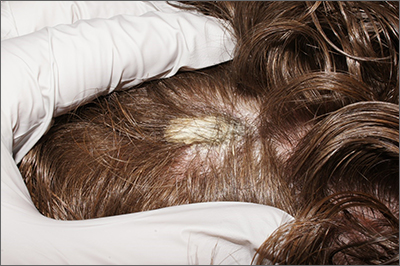
A punch biopsy was performed, and the results were consistent with pityriasis amiantacea arising from psoriasis. In an older patient, a keratinaceous horn would be worrisome for a squamous cell carcinoma. In a younger patient, like this one, it is more likely an atypical manifestation of a more common dermatosis.
Pityriasis amiantacea is an unusual disorder in which thick adherent scales form on the scalp; it is most common in children, adolescents, and young adults. There is no racial predilection. With this condition, patients complain of a fixed plaque that may shed scale but not as quickly as it accumulates. It can be an isolated finding, but more often it is a secondary manifestation of an underlying case of psoriasis, seborrheic dermatitis, tinea capitis, or atopic dermatitis.1
A punch biopsy performed on the scalp should include the skin underlying the compact keratin scale. However, to avoid excessive bleeding, use lidocaine with epinephrine. Allow 15 minutes for the anesthesia to take effect before beginning the procedure.
Treatment depends on the underlying cause but includes debridement of the aggregated scale with a topical keratolytic (such as salicylic acid or topical fluocinolone oil 0.01% applied) at night and washed out 7 to 10 hours later.
The patient was advised to use over-the-counter 2% salicylic acid shampoo daily and to apply topical clobetasol 0.05% solution nightly for 4 weeks and once weekly after clearance for another 3 months. At the 3-month follow-up, the patient’s scalp was clear.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Ettler J, Wetter DA, Pittelkow MR. Pityriasis amiantacea: a distinctive presentation of psoriasis associated with tumour necrosis factor-α inhibitor therapy. Clin Exp Dermatol. 2012;37:639-641. doi: 10.1111/j.1365-2230.2011.04286.x
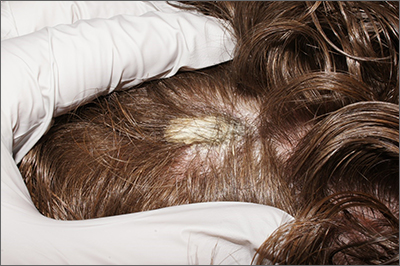
A punch biopsy was performed, and the results were consistent with pityriasis amiantacea arising from psoriasis. In an older patient, a keratinaceous horn would be worrisome for a squamous cell carcinoma. In a younger patient, like this one, it is more likely an atypical manifestation of a more common dermatosis.
Pityriasis amiantacea is an unusual disorder in which thick adherent scales form on the scalp; it is most common in children, adolescents, and young adults. There is no racial predilection. With this condition, patients complain of a fixed plaque that may shed scale but not as quickly as it accumulates. It can be an isolated finding, but more often it is a secondary manifestation of an underlying case of psoriasis, seborrheic dermatitis, tinea capitis, or atopic dermatitis.1
A punch biopsy performed on the scalp should include the skin underlying the compact keratin scale. However, to avoid excessive bleeding, use lidocaine with epinephrine. Allow 15 minutes for the anesthesia to take effect before beginning the procedure.
Treatment depends on the underlying cause but includes debridement of the aggregated scale with a topical keratolytic (such as salicylic acid or topical fluocinolone oil 0.01% applied) at night and washed out 7 to 10 hours later.
The patient was advised to use over-the-counter 2% salicylic acid shampoo daily and to apply topical clobetasol 0.05% solution nightly for 4 weeks and once weekly after clearance for another 3 months. At the 3-month follow-up, the patient’s scalp was clear.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
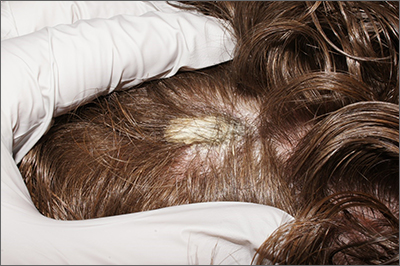
A punch biopsy was performed, and the results were consistent with pityriasis amiantacea arising from psoriasis. In an older patient, a keratinaceous horn would be worrisome for a squamous cell carcinoma. In a younger patient, like this one, it is more likely an atypical manifestation of a more common dermatosis.
Pityriasis amiantacea is an unusual disorder in which thick adherent scales form on the scalp; it is most common in children, adolescents, and young adults. There is no racial predilection. With this condition, patients complain of a fixed plaque that may shed scale but not as quickly as it accumulates. It can be an isolated finding, but more often it is a secondary manifestation of an underlying case of psoriasis, seborrheic dermatitis, tinea capitis, or atopic dermatitis.1
A punch biopsy performed on the scalp should include the skin underlying the compact keratin scale. However, to avoid excessive bleeding, use lidocaine with epinephrine. Allow 15 minutes for the anesthesia to take effect before beginning the procedure.
Treatment depends on the underlying cause but includes debridement of the aggregated scale with a topical keratolytic (such as salicylic acid or topical fluocinolone oil 0.01% applied) at night and washed out 7 to 10 hours later.
The patient was advised to use over-the-counter 2% salicylic acid shampoo daily and to apply topical clobetasol 0.05% solution nightly for 4 weeks and once weekly after clearance for another 3 months. At the 3-month follow-up, the patient’s scalp was clear.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Ettler J, Wetter DA, Pittelkow MR. Pityriasis amiantacea: a distinctive presentation of psoriasis associated with tumour necrosis factor-α inhibitor therapy. Clin Exp Dermatol. 2012;37:639-641. doi: 10.1111/j.1365-2230.2011.04286.x
1. Ettler J, Wetter DA, Pittelkow MR. Pityriasis amiantacea: a distinctive presentation of psoriasis associated with tumour necrosis factor-α inhibitor therapy. Clin Exp Dermatol. 2012;37:639-641. doi: 10.1111/j.1365-2230.2011.04286.x
New liver stiffness thresholds refine NASH risk stratification
New liver stiffness (LS) thresholds offer accurate prediction of disease progression and clinical outcomes in patients with nonalcoholic steatohepatitis (NASH) and advanced fibrosis, according to investigators.
These new LS thresholds are more reliable because they are based on high-quality prospective data drawn from four randomized controlled trials, reported lead author Rohit Loomba, MD, of the University of California, San Diego, and colleagues.
“Retrospective studies report that increasing baseline LS by VCTE [vibration-controlled transient elastography] is associated with the risk of disease progression in patients with NAFLD [non-alcoholic fatty liver disease], but prospective data in well-characterized NASH cohorts with biopsy-confirmed advanced fibrosis are limited,” the investigators wrote in Gut. “The optimal LS thresholds for prognostication of fibrosis progression and decompensation are unknown.”
Seeking clarity, Dr. Loomba and colleagues leveraged data from two phase 3 placebo-controlled trials for selonsertib and two phase 2b placebo-controlled trials for simtuzumab.
“While the studies were discontinued prematurely due to lack of efficacy, the prospectively collected data in these well-characterized participants with serial liver biopsies provides a unique opportunity to study the association between baseline LS by VCTE and disease progression,” the investigators wrote.
Across all four studies, bridging fibrosis (F3) was present in 664 participants, while 734 individuals had cirrhosis (F4). In the selonsertib studies, fibrosis was staged at baseline and week 48. The simtuzumab studies measured liver fibrosis at baseline and week 96. Out of the 664 participants with bridging fibrosis, 103 (16%) progressed to cirrhosis. Among the 734 patients with cirrhosis, 27 (4%) experienced liver-related events. Comparing these outcomes with LS data at baseline and throughout the study revealed optimal LS thresholds.
The best threshold for predicting progression from bridging fibrosis to cirrhosis was 16.6 kPa. According to the authors, the sensitivity, specificity, positive predictive value, and negative predictive value of this threshold for progression to cirrhosis were 58%, 76%, 31%, and 91%, respectively. Among patients at or above 16.6 kPa, 31% progressed to cirrhosis, compared with 9.1% of those under that threshold. Furthermore, individuals with a baseline LS at or above 16.6 kPa had nearly four times greater risk of developing cirrhosis (adjusted hazard ratio, 3.99; 95% CI, 2.66-5.98; P < .0001).
For patients with cirrhosis at baseline, the optimal threshold for predicting liver-related events, such as ascites, hepatic encephalopathy, and portal hypertension–related GI bleeding, liver transplantation, or mortality, was 30.7 kPa. The sensitivity, specificity, PPV, and NPV of this threshold for liver-related events were 62%, 87%, 10%, and 99%, respectively, according to the authors. Patients with an LS above this mark were 10 times as likely to experience liver-related events (aHR, 10.13; 95% CI, 4.38-23.41; P < .0001).
Scott L. Friedman, MD, chief of the division of liver diseases and dean for Therapeutic Discovery at the Icahn School of Medicine at Mount Sinai, New York, called the study “an important effort” that offers valuable insights for both researchers and practitioners.
“For clinical trials, [these thresholds] really allow for greater refinement or enrichment of patients who are suitable for enrollment in the trial because they’re at a higher risk of clinical problems that might be mitigated if the drug is effective,” Dr. Friedman said in an interview. “For clinical practice, it might indicate that the patient should either be fast tracked for a clinical trial or, more importantly, maybe needs to be referred for evaluation for a liver transplant. It may also indicate – although they didn’t look at it in this study – that there’s a need to begin or accelerate screening for liver cancer, which becomes an encroaching risk as the fibrosis advances to later stages.”
The study was funded by Gilead Sciences. The investigators disclosed additional relationships with Amgen, Eli Lilly, CohBar, and others. Dr. Friedman reported no relevant conflicts of interest.
New liver stiffness (LS) thresholds offer accurate prediction of disease progression and clinical outcomes in patients with nonalcoholic steatohepatitis (NASH) and advanced fibrosis, according to investigators.
These new LS thresholds are more reliable because they are based on high-quality prospective data drawn from four randomized controlled trials, reported lead author Rohit Loomba, MD, of the University of California, San Diego, and colleagues.
“Retrospective studies report that increasing baseline LS by VCTE [vibration-controlled transient elastography] is associated with the risk of disease progression in patients with NAFLD [non-alcoholic fatty liver disease], but prospective data in well-characterized NASH cohorts with biopsy-confirmed advanced fibrosis are limited,” the investigators wrote in Gut. “The optimal LS thresholds for prognostication of fibrosis progression and decompensation are unknown.”
Seeking clarity, Dr. Loomba and colleagues leveraged data from two phase 3 placebo-controlled trials for selonsertib and two phase 2b placebo-controlled trials for simtuzumab.
“While the studies were discontinued prematurely due to lack of efficacy, the prospectively collected data in these well-characterized participants with serial liver biopsies provides a unique opportunity to study the association between baseline LS by VCTE and disease progression,” the investigators wrote.
Across all four studies, bridging fibrosis (F3) was present in 664 participants, while 734 individuals had cirrhosis (F4). In the selonsertib studies, fibrosis was staged at baseline and week 48. The simtuzumab studies measured liver fibrosis at baseline and week 96. Out of the 664 participants with bridging fibrosis, 103 (16%) progressed to cirrhosis. Among the 734 patients with cirrhosis, 27 (4%) experienced liver-related events. Comparing these outcomes with LS data at baseline and throughout the study revealed optimal LS thresholds.
The best threshold for predicting progression from bridging fibrosis to cirrhosis was 16.6 kPa. According to the authors, the sensitivity, specificity, positive predictive value, and negative predictive value of this threshold for progression to cirrhosis were 58%, 76%, 31%, and 91%, respectively. Among patients at or above 16.6 kPa, 31% progressed to cirrhosis, compared with 9.1% of those under that threshold. Furthermore, individuals with a baseline LS at or above 16.6 kPa had nearly four times greater risk of developing cirrhosis (adjusted hazard ratio, 3.99; 95% CI, 2.66-5.98; P < .0001).
For patients with cirrhosis at baseline, the optimal threshold for predicting liver-related events, such as ascites, hepatic encephalopathy, and portal hypertension–related GI bleeding, liver transplantation, or mortality, was 30.7 kPa. The sensitivity, specificity, PPV, and NPV of this threshold for liver-related events were 62%, 87%, 10%, and 99%, respectively, according to the authors. Patients with an LS above this mark were 10 times as likely to experience liver-related events (aHR, 10.13; 95% CI, 4.38-23.41; P < .0001).
Scott L. Friedman, MD, chief of the division of liver diseases and dean for Therapeutic Discovery at the Icahn School of Medicine at Mount Sinai, New York, called the study “an important effort” that offers valuable insights for both researchers and practitioners.
“For clinical trials, [these thresholds] really allow for greater refinement or enrichment of patients who are suitable for enrollment in the trial because they’re at a higher risk of clinical problems that might be mitigated if the drug is effective,” Dr. Friedman said in an interview. “For clinical practice, it might indicate that the patient should either be fast tracked for a clinical trial or, more importantly, maybe needs to be referred for evaluation for a liver transplant. It may also indicate – although they didn’t look at it in this study – that there’s a need to begin or accelerate screening for liver cancer, which becomes an encroaching risk as the fibrosis advances to later stages.”
The study was funded by Gilead Sciences. The investigators disclosed additional relationships with Amgen, Eli Lilly, CohBar, and others. Dr. Friedman reported no relevant conflicts of interest.
New liver stiffness (LS) thresholds offer accurate prediction of disease progression and clinical outcomes in patients with nonalcoholic steatohepatitis (NASH) and advanced fibrosis, according to investigators.
These new LS thresholds are more reliable because they are based on high-quality prospective data drawn from four randomized controlled trials, reported lead author Rohit Loomba, MD, of the University of California, San Diego, and colleagues.
“Retrospective studies report that increasing baseline LS by VCTE [vibration-controlled transient elastography] is associated with the risk of disease progression in patients with NAFLD [non-alcoholic fatty liver disease], but prospective data in well-characterized NASH cohorts with biopsy-confirmed advanced fibrosis are limited,” the investigators wrote in Gut. “The optimal LS thresholds for prognostication of fibrosis progression and decompensation are unknown.”
Seeking clarity, Dr. Loomba and colleagues leveraged data from two phase 3 placebo-controlled trials for selonsertib and two phase 2b placebo-controlled trials for simtuzumab.
“While the studies were discontinued prematurely due to lack of efficacy, the prospectively collected data in these well-characterized participants with serial liver biopsies provides a unique opportunity to study the association between baseline LS by VCTE and disease progression,” the investigators wrote.
Across all four studies, bridging fibrosis (F3) was present in 664 participants, while 734 individuals had cirrhosis (F4). In the selonsertib studies, fibrosis was staged at baseline and week 48. The simtuzumab studies measured liver fibrosis at baseline and week 96. Out of the 664 participants with bridging fibrosis, 103 (16%) progressed to cirrhosis. Among the 734 patients with cirrhosis, 27 (4%) experienced liver-related events. Comparing these outcomes with LS data at baseline and throughout the study revealed optimal LS thresholds.
The best threshold for predicting progression from bridging fibrosis to cirrhosis was 16.6 kPa. According to the authors, the sensitivity, specificity, positive predictive value, and negative predictive value of this threshold for progression to cirrhosis were 58%, 76%, 31%, and 91%, respectively. Among patients at or above 16.6 kPa, 31% progressed to cirrhosis, compared with 9.1% of those under that threshold. Furthermore, individuals with a baseline LS at or above 16.6 kPa had nearly four times greater risk of developing cirrhosis (adjusted hazard ratio, 3.99; 95% CI, 2.66-5.98; P < .0001).
For patients with cirrhosis at baseline, the optimal threshold for predicting liver-related events, such as ascites, hepatic encephalopathy, and portal hypertension–related GI bleeding, liver transplantation, or mortality, was 30.7 kPa. The sensitivity, specificity, PPV, and NPV of this threshold for liver-related events were 62%, 87%, 10%, and 99%, respectively, according to the authors. Patients with an LS above this mark were 10 times as likely to experience liver-related events (aHR, 10.13; 95% CI, 4.38-23.41; P < .0001).
Scott L. Friedman, MD, chief of the division of liver diseases and dean for Therapeutic Discovery at the Icahn School of Medicine at Mount Sinai, New York, called the study “an important effort” that offers valuable insights for both researchers and practitioners.
“For clinical trials, [these thresholds] really allow for greater refinement or enrichment of patients who are suitable for enrollment in the trial because they’re at a higher risk of clinical problems that might be mitigated if the drug is effective,” Dr. Friedman said in an interview. “For clinical practice, it might indicate that the patient should either be fast tracked for a clinical trial or, more importantly, maybe needs to be referred for evaluation for a liver transplant. It may also indicate – although they didn’t look at it in this study – that there’s a need to begin or accelerate screening for liver cancer, which becomes an encroaching risk as the fibrosis advances to later stages.”
The study was funded by Gilead Sciences. The investigators disclosed additional relationships with Amgen, Eli Lilly, CohBar, and others. Dr. Friedman reported no relevant conflicts of interest.
FROM GUT