User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Popularity of virtual conferences may mean a permanent shift
Fifteen days. That’s how much time the American College of Cardiology (ACC) had to convert its annual conference, scheduled for the end of March this year in Chicago, into a virtual meeting for the estimated 17,000 people who had planned to attend.
Because of the coronavirus pandemic, Illinois announced restrictions on the size of gatherings on March 13, causing the ACC to pivot to an online-only model.
“One big advantage was that we already had all of our content planned,” Janice Sibley, the ACC’s executive vice president of education, told Medscape Medical News. “We knew who the faculty would be for different sessions, and many of them had already planned their slides.”
But determining how to present those hundreds of presentations at an online conference, not to mention addressing the logistics related to registrations, tech platforms, exhibit hall sponsors, and other aspects of an annual meeting, would be no small task.
But according to a Medscape poll, many physicians think that, while the virtual experience is worthwhile and getting better, it’s never going to be the same as spending several days on site, immersed in the experience of an annual meeting.
As one respondent commented, “I miss the intellectual excitement, the electricity in the room, when there is a live presentation that announces a major breakthrough.”
Large medical societies have an advantage
As ACC rapidly prepared for its virtual conference, the society first refunded all registration and expo fees and worked with the vendor partners to resolve the cancellation of rental space, food and beverage services, and decorating. Then they organized a team of 15 people split into three groups. One group focused on the intellectual, scientific, and educational elements of the virtual conference. They chose 24 sessions to livestream and decided to prerecord the rest for on-demand access, limiting the number of presenters they needed to train for online presentation.
A second team focused on business and worked with industry partners on how to translate a large expo into digital offerings. They developed virtual pages, advertisements, promotions, and industry-sponsored education.
The third team’s focus, Ms. Sibley said, was most critical, and the hardest: addressing socio-emotional needs.
“That group was responsible for trying to create the buzz and excitement we would have had at the event,” she said, “pivoting that experience we would have had in a live event to a virtual environment. What we were worried about was, would anyone even come?”
But ACC built it, and they did indeed come. Within a half hour of the opening session, nearly 13,000 people logged on from around the world. “It worked beautifully,” Ms. Sibley said.
By the end of the 3-day event, approximately 34,000 unique visitors had logged in for live or prerecorded sessions. Although ACC worried at first about technical glitches and bandwidth needs, everything ran smoothly. By 90 days after the meeting, 63,000 unique users had logged in to access the conference content.
ACC was among the first organizations forced to switch from an in-person to all-online meeting, but dozens of other organizations have now done the same, discovering the benefits and drawbacks of a virtual environment while experimenting with different formats and offerings. Talks with a few large medical societies about the experience revealed several common themes, including the following:
- Finding new ways to attract and measure attendance.
- Ensuring the actual scientific content was as robust online as in person.
- Realizing the value of social media in enhancing the socio-emotional experience.
- Believing that virtual meetings will become a permanent fixture in a future of “hybrid” conferences.
New ways of attracting and measuring attendance
Previous ways to measure meeting attendance were straightforward: number of registrations and number of people physically walking into sessions. An online conference, however, offers dozens of ways to measure attendance. While the number of registrations remained one tool – and all the organizations interviewed reported record numbers of registrations – organizations also used other metrics to measure success, such as “participation,” “engagement,” and “viewing time.”
ACC defined “participation” as a unique user logging in, and it defined “engagement” as sticking around for a while, possibly using chat functions or discussing the content on social media. The American Society of Clinical Oncology (ASCO) annual conference in May, which attracted more than 44,000 registered attendees, also measured total content views – more than 2.5 million during the meeting – and monitored social media. More than 8,800 Twitter users posted more than 45,000 tweets with the #ASCO20 hashtag during the meeting, generating 750 million likes, shares, and comments. The European League Against Rheumatism (EULAR) annual congress registered a record 18,700 delegates – up from 14,500 in 2019 – but it also measured attendance by average viewing time and visits by congress day and by category.
Organizations shifted fee structures as well. While ACC refunded fees for its first online meeting, it has since developed tiers to match fees to anticipated value, such as charging more for livestreamed sessions that allow interactivity than for viewing recordings. ASCO offered a one-time fee waiver for members plus free registration to cancer survivors and caregivers, discounted registration for patient advocates, and reduced fees for other categories. But adjusting how to measure attendance and charge for events were the easy parts of transitioning to online.
Priority for having robust content
The biggest difficulty for most organizations was the short time they had to move online, with a host of challenges accompanying the switch, said the executive director of EULAR, Julia Rautenstrauch, DrMed. These included technical requirements, communication, training, finances, legal issues, compliance rules, and other logistics.
“The year 2020 will be remembered for being the year of unexpected transformation,” said a spokesperson from European Society for Medical Oncology (ESMO), who declined to be named. “The number of fundamental questions we had to ask ourselves is pages long. The solutions we have implemented so far have been successful, but we won’t rest on our laurels.”
ASCO had an advantage in the pivot, despite only 6 weeks to make the switch, because they already had a robust online platform to build on. “We weren’t starting from scratch, but we were sure changing the way we prepared,” ASCO CEO Clifford Hudis, MD, said.
All of the organizations made the breadth and quality of scientific and educational content a top priority, and those who have already hosted meetings this year report positive feedback.
“The rating of the scientific content was excellent, and the event did indeed fulfill the educational goals and expected learning outcomes for the vast majority of delegates,” EULAR’s Dr. Rautenstrauch said.
“Our goal, when we went into this, was that, in the future when somebody looks back at ASCO20, they should not be able to tell that it was a different year from any other in terms of the science,” Dr. Hudis said.
Missing out on networking and social interaction
Even when logistics run smoothly, virtual conferences must overcome two other challenges: the loss of in-person interactions and the potential for “Zoom burnout.”
“You do miss that human contact, the unsaid reactions in the room when you’re speaking or providing a controversial statement, even the facial expression or seeing people lean in or being distracted,” Ms. Sibley said.
Taher Modarressi, MD, an endocrinologist with Diabetes and Endocrine Associates of Hunterdon in Flemington, N.J., said all the digital conferences he has attended were missing those key social elements: “seeing old friends, sideline discussions that generate new ideas, and meeting new colleagues. However, this has been partly alleviated with the robust rise of social media and ‘MedTwitter,’ in particular, where these discussions and interactions continue.”
To attempt to meet that need for social interaction, societies came up with a variety of options. EULAR offered chatrooms, “Meet the Expert” sessions, and other virtual opportunities for live interaction. ASCO hosted discussion groups with subsets of participants, such as virtual meetings with oncology fellows, and it plans to offer networking sessions and “poster walks” during future meetings.
“The value of an in-person meeting is connecting with people, exchanging ideas over coffee, and making new contacts,” ASCO’s Dr. Hudis said. While virtual meetings lose many of those personal interactions, knowledge can also be shared with more people, he said.
The key to combating digital fatigue is focusing on opportunities for interactivity, ACC’s Ms. Sibley said. “When you are creating a virtual environment, it’s important that you offer choices.” Online learners tend to have shorter attention spans than in-person learners, so people need opportunities to flip between sessions, like flipping between TV channels. Different engagement options are also essential, such as chat functions on the video platforms, asking questions of presenters orally or in writing, and using the familiar hashtags for social media discussion.
“We set up all those different ways to interact, and you allow the user to choose,” Ms. Sibley said.
Some conferences, however, had less time or fewer resources to adjust to a virtual format and couldn’t make up for the lost social interaction. Andy Bowman, MD, a neonatologist in Lubbock, Tex., was supposed to attend the Neonatal & Pediatric Airborne Transport Conference sponsored by International Biomed in the spring, but it was canceled at the last minute. Several weeks later, the organizers released videos of scheduled speakers giving their talks, but it was less engaging and too easy to get distracted, Dr. Bowman said.
“There is a noticeable decrease in energy – you can’t look around to feed off other’s reactions when a speaker says something off the wall, or new, or contrary to expectations,” he said. He also especially missed the social interactions, such as “missing out on the chance encounters in the hallway or seeing the same face in back-to-back sessions and figuring out you have shared interest.” He was also sorry to miss the expo because neonatal transport requires a lot of specialty equipment, and he appreciates the chance to actually touch and see it in person.
Advantages of an online meeting
Despite the challenges, online meetings can overcome obstacles of in-person meetings, particularly for those in low- and middle-income countries, such as travel and registration costs, the hardships of being away from practice, and visa restrictions.
“You really have the potential to broaden your reach,” Ms. Sibley said, noting that people in 157 countries participated in ACC.20.
Another advantage is keeping the experience available to people after the livestreamed event.
“Virtual events have demonstrated the potential for a more democratic conference world, expanding the dissemination of information to a much wider community of stakeholders,” ESMO’s spokesperson said.
Not traveling can actually mean getting more out of the conference, said Atisha Patel Manhas, MD, a hematologist/oncologist in Dallas, who attended ASCO. “I have really enjoyed the access aspect – on the virtual platform there is so much more content available to you, and travel time doesn’t cut into conference time,” she said, though she also missed the interaction with colleagues.
Others found that virtual conferences provided more engagement than in-person conferences. Marwah Abdalla, MD, MPH, an assistant professor of medicine and director of education for the Cardiac Intensive Care Unit at Columbia University Medical Center, New York, felt that moderated Q&A sessions offered more interaction among participants. She attended and spoke on a panel during virtual SLEEP 2020, a joint meeting of the American Academy of Sleep Medicine (AASM) and the Sleep Research Society (SRS).
“Usually during in-person sessions, only a few questions are possible, and participants rarely have an opportunity to discuss the presentations within the session due to time limits,” Dr. Abdalla said. “Because the conference presentations can also be viewed asynchronously, participants have been able to comment on lectures and continue the discussion offline, either via social media or via email.” She acknowledged drawbacks of the virtual experience, such as an inability to socialize in person and participate in activities but appreciated the new opportunities to network and learn from international colleagues who would not have been able to attend in person.
Ritu Thamman, MD, assistant professor of medicine at the University of Pittsburgh School of Medicine, pointed out that many institutions have cut their travel budgets, and physicians would be unable to attend in-person conferences for financial or other reasons. She especially appreciated that the European Society of Cardiology had no registration fee for ESC 2020 and made their content free for all of September, which led to more than 100,000 participants.
“That meant anyone anywhere could learn,” she said. “It makes it much more diverse and more egalitarian. That feels like a good step in the right direction for all of us.”
Dr. Modarressi, who found ESC “exhilarating,” similarly noted the benefit of such an equitably accessible conference. “Decreasing barriers and improving access to top-line results and up-to-date information has always been a challenge to the global health community,” he said, noting that the map of attendance for the virtual meeting was “astonishing.”
Given these benefits, organizers said they expect a future of hybrid conferences: physical meetings for those able to attend in person and virtual ones for those who cannot.
“We also expect that the hybrid congress will cater to the needs of people on-site by allowing them additional access to more scientific content than by physical attendance alone,” Dr. Rautenstrauch said.
Everyone has been in reactive mode this year, Ms. Sibley said, but the future looks bright as they seek ways to overcome challenges such as socio-emotional needs and virtual expo spaces.
“We’ve been thrust into the virtual world much faster than we expected, but we’re finding it’s opening more opportunities than we had live,” Ms. Sibley said. “This has catapulted us, for better or worse, into a new way to deliver education and other types of information.
“I think, if we’re smart, we’ll continue to think of ways this can augment our live environment and not replace it.”
A version of this article originally appeared on Medscape.com.
Fifteen days. That’s how much time the American College of Cardiology (ACC) had to convert its annual conference, scheduled for the end of March this year in Chicago, into a virtual meeting for the estimated 17,000 people who had planned to attend.
Because of the coronavirus pandemic, Illinois announced restrictions on the size of gatherings on March 13, causing the ACC to pivot to an online-only model.
“One big advantage was that we already had all of our content planned,” Janice Sibley, the ACC’s executive vice president of education, told Medscape Medical News. “We knew who the faculty would be for different sessions, and many of them had already planned their slides.”
But determining how to present those hundreds of presentations at an online conference, not to mention addressing the logistics related to registrations, tech platforms, exhibit hall sponsors, and other aspects of an annual meeting, would be no small task.
But according to a Medscape poll, many physicians think that, while the virtual experience is worthwhile and getting better, it’s never going to be the same as spending several days on site, immersed in the experience of an annual meeting.
As one respondent commented, “I miss the intellectual excitement, the electricity in the room, when there is a live presentation that announces a major breakthrough.”
Large medical societies have an advantage
As ACC rapidly prepared for its virtual conference, the society first refunded all registration and expo fees and worked with the vendor partners to resolve the cancellation of rental space, food and beverage services, and decorating. Then they organized a team of 15 people split into three groups. One group focused on the intellectual, scientific, and educational elements of the virtual conference. They chose 24 sessions to livestream and decided to prerecord the rest for on-demand access, limiting the number of presenters they needed to train for online presentation.
A second team focused on business and worked with industry partners on how to translate a large expo into digital offerings. They developed virtual pages, advertisements, promotions, and industry-sponsored education.
The third team’s focus, Ms. Sibley said, was most critical, and the hardest: addressing socio-emotional needs.
“That group was responsible for trying to create the buzz and excitement we would have had at the event,” she said, “pivoting that experience we would have had in a live event to a virtual environment. What we were worried about was, would anyone even come?”
But ACC built it, and they did indeed come. Within a half hour of the opening session, nearly 13,000 people logged on from around the world. “It worked beautifully,” Ms. Sibley said.
By the end of the 3-day event, approximately 34,000 unique visitors had logged in for live or prerecorded sessions. Although ACC worried at first about technical glitches and bandwidth needs, everything ran smoothly. By 90 days after the meeting, 63,000 unique users had logged in to access the conference content.
ACC was among the first organizations forced to switch from an in-person to all-online meeting, but dozens of other organizations have now done the same, discovering the benefits and drawbacks of a virtual environment while experimenting with different formats and offerings. Talks with a few large medical societies about the experience revealed several common themes, including the following:
- Finding new ways to attract and measure attendance.
- Ensuring the actual scientific content was as robust online as in person.
- Realizing the value of social media in enhancing the socio-emotional experience.
- Believing that virtual meetings will become a permanent fixture in a future of “hybrid” conferences.
New ways of attracting and measuring attendance
Previous ways to measure meeting attendance were straightforward: number of registrations and number of people physically walking into sessions. An online conference, however, offers dozens of ways to measure attendance. While the number of registrations remained one tool – and all the organizations interviewed reported record numbers of registrations – organizations also used other metrics to measure success, such as “participation,” “engagement,” and “viewing time.”
ACC defined “participation” as a unique user logging in, and it defined “engagement” as sticking around for a while, possibly using chat functions or discussing the content on social media. The American Society of Clinical Oncology (ASCO) annual conference in May, which attracted more than 44,000 registered attendees, also measured total content views – more than 2.5 million during the meeting – and monitored social media. More than 8,800 Twitter users posted more than 45,000 tweets with the #ASCO20 hashtag during the meeting, generating 750 million likes, shares, and comments. The European League Against Rheumatism (EULAR) annual congress registered a record 18,700 delegates – up from 14,500 in 2019 – but it also measured attendance by average viewing time and visits by congress day and by category.
Organizations shifted fee structures as well. While ACC refunded fees for its first online meeting, it has since developed tiers to match fees to anticipated value, such as charging more for livestreamed sessions that allow interactivity than for viewing recordings. ASCO offered a one-time fee waiver for members plus free registration to cancer survivors and caregivers, discounted registration for patient advocates, and reduced fees for other categories. But adjusting how to measure attendance and charge for events were the easy parts of transitioning to online.
Priority for having robust content
The biggest difficulty for most organizations was the short time they had to move online, with a host of challenges accompanying the switch, said the executive director of EULAR, Julia Rautenstrauch, DrMed. These included technical requirements, communication, training, finances, legal issues, compliance rules, and other logistics.
“The year 2020 will be remembered for being the year of unexpected transformation,” said a spokesperson from European Society for Medical Oncology (ESMO), who declined to be named. “The number of fundamental questions we had to ask ourselves is pages long. The solutions we have implemented so far have been successful, but we won’t rest on our laurels.”
ASCO had an advantage in the pivot, despite only 6 weeks to make the switch, because they already had a robust online platform to build on. “We weren’t starting from scratch, but we were sure changing the way we prepared,” ASCO CEO Clifford Hudis, MD, said.
All of the organizations made the breadth and quality of scientific and educational content a top priority, and those who have already hosted meetings this year report positive feedback.
“The rating of the scientific content was excellent, and the event did indeed fulfill the educational goals and expected learning outcomes for the vast majority of delegates,” EULAR’s Dr. Rautenstrauch said.
“Our goal, when we went into this, was that, in the future when somebody looks back at ASCO20, they should not be able to tell that it was a different year from any other in terms of the science,” Dr. Hudis said.
Missing out on networking and social interaction
Even when logistics run smoothly, virtual conferences must overcome two other challenges: the loss of in-person interactions and the potential for “Zoom burnout.”
“You do miss that human contact, the unsaid reactions in the room when you’re speaking or providing a controversial statement, even the facial expression or seeing people lean in or being distracted,” Ms. Sibley said.
Taher Modarressi, MD, an endocrinologist with Diabetes and Endocrine Associates of Hunterdon in Flemington, N.J., said all the digital conferences he has attended were missing those key social elements: “seeing old friends, sideline discussions that generate new ideas, and meeting new colleagues. However, this has been partly alleviated with the robust rise of social media and ‘MedTwitter,’ in particular, where these discussions and interactions continue.”
To attempt to meet that need for social interaction, societies came up with a variety of options. EULAR offered chatrooms, “Meet the Expert” sessions, and other virtual opportunities for live interaction. ASCO hosted discussion groups with subsets of participants, such as virtual meetings with oncology fellows, and it plans to offer networking sessions and “poster walks” during future meetings.
“The value of an in-person meeting is connecting with people, exchanging ideas over coffee, and making new contacts,” ASCO’s Dr. Hudis said. While virtual meetings lose many of those personal interactions, knowledge can also be shared with more people, he said.
The key to combating digital fatigue is focusing on opportunities for interactivity, ACC’s Ms. Sibley said. “When you are creating a virtual environment, it’s important that you offer choices.” Online learners tend to have shorter attention spans than in-person learners, so people need opportunities to flip between sessions, like flipping between TV channels. Different engagement options are also essential, such as chat functions on the video platforms, asking questions of presenters orally or in writing, and using the familiar hashtags for social media discussion.
“We set up all those different ways to interact, and you allow the user to choose,” Ms. Sibley said.
Some conferences, however, had less time or fewer resources to adjust to a virtual format and couldn’t make up for the lost social interaction. Andy Bowman, MD, a neonatologist in Lubbock, Tex., was supposed to attend the Neonatal & Pediatric Airborne Transport Conference sponsored by International Biomed in the spring, but it was canceled at the last minute. Several weeks later, the organizers released videos of scheduled speakers giving their talks, but it was less engaging and too easy to get distracted, Dr. Bowman said.
“There is a noticeable decrease in energy – you can’t look around to feed off other’s reactions when a speaker says something off the wall, or new, or contrary to expectations,” he said. He also especially missed the social interactions, such as “missing out on the chance encounters in the hallway or seeing the same face in back-to-back sessions and figuring out you have shared interest.” He was also sorry to miss the expo because neonatal transport requires a lot of specialty equipment, and he appreciates the chance to actually touch and see it in person.
Advantages of an online meeting
Despite the challenges, online meetings can overcome obstacles of in-person meetings, particularly for those in low- and middle-income countries, such as travel and registration costs, the hardships of being away from practice, and visa restrictions.
“You really have the potential to broaden your reach,” Ms. Sibley said, noting that people in 157 countries participated in ACC.20.
Another advantage is keeping the experience available to people after the livestreamed event.
“Virtual events have demonstrated the potential for a more democratic conference world, expanding the dissemination of information to a much wider community of stakeholders,” ESMO’s spokesperson said.
Not traveling can actually mean getting more out of the conference, said Atisha Patel Manhas, MD, a hematologist/oncologist in Dallas, who attended ASCO. “I have really enjoyed the access aspect – on the virtual platform there is so much more content available to you, and travel time doesn’t cut into conference time,” she said, though she also missed the interaction with colleagues.
Others found that virtual conferences provided more engagement than in-person conferences. Marwah Abdalla, MD, MPH, an assistant professor of medicine and director of education for the Cardiac Intensive Care Unit at Columbia University Medical Center, New York, felt that moderated Q&A sessions offered more interaction among participants. She attended and spoke on a panel during virtual SLEEP 2020, a joint meeting of the American Academy of Sleep Medicine (AASM) and the Sleep Research Society (SRS).
“Usually during in-person sessions, only a few questions are possible, and participants rarely have an opportunity to discuss the presentations within the session due to time limits,” Dr. Abdalla said. “Because the conference presentations can also be viewed asynchronously, participants have been able to comment on lectures and continue the discussion offline, either via social media or via email.” She acknowledged drawbacks of the virtual experience, such as an inability to socialize in person and participate in activities but appreciated the new opportunities to network and learn from international colleagues who would not have been able to attend in person.
Ritu Thamman, MD, assistant professor of medicine at the University of Pittsburgh School of Medicine, pointed out that many institutions have cut their travel budgets, and physicians would be unable to attend in-person conferences for financial or other reasons. She especially appreciated that the European Society of Cardiology had no registration fee for ESC 2020 and made their content free for all of September, which led to more than 100,000 participants.
“That meant anyone anywhere could learn,” she said. “It makes it much more diverse and more egalitarian. That feels like a good step in the right direction for all of us.”
Dr. Modarressi, who found ESC “exhilarating,” similarly noted the benefit of such an equitably accessible conference. “Decreasing barriers and improving access to top-line results and up-to-date information has always been a challenge to the global health community,” he said, noting that the map of attendance for the virtual meeting was “astonishing.”
Given these benefits, organizers said they expect a future of hybrid conferences: physical meetings for those able to attend in person and virtual ones for those who cannot.
“We also expect that the hybrid congress will cater to the needs of people on-site by allowing them additional access to more scientific content than by physical attendance alone,” Dr. Rautenstrauch said.
Everyone has been in reactive mode this year, Ms. Sibley said, but the future looks bright as they seek ways to overcome challenges such as socio-emotional needs and virtual expo spaces.
“We’ve been thrust into the virtual world much faster than we expected, but we’re finding it’s opening more opportunities than we had live,” Ms. Sibley said. “This has catapulted us, for better or worse, into a new way to deliver education and other types of information.
“I think, if we’re smart, we’ll continue to think of ways this can augment our live environment and not replace it.”
A version of this article originally appeared on Medscape.com.
Fifteen days. That’s how much time the American College of Cardiology (ACC) had to convert its annual conference, scheduled for the end of March this year in Chicago, into a virtual meeting for the estimated 17,000 people who had planned to attend.
Because of the coronavirus pandemic, Illinois announced restrictions on the size of gatherings on March 13, causing the ACC to pivot to an online-only model.
“One big advantage was that we already had all of our content planned,” Janice Sibley, the ACC’s executive vice president of education, told Medscape Medical News. “We knew who the faculty would be for different sessions, and many of them had already planned their slides.”
But determining how to present those hundreds of presentations at an online conference, not to mention addressing the logistics related to registrations, tech platforms, exhibit hall sponsors, and other aspects of an annual meeting, would be no small task.
But according to a Medscape poll, many physicians think that, while the virtual experience is worthwhile and getting better, it’s never going to be the same as spending several days on site, immersed in the experience of an annual meeting.
As one respondent commented, “I miss the intellectual excitement, the electricity in the room, when there is a live presentation that announces a major breakthrough.”
Large medical societies have an advantage
As ACC rapidly prepared for its virtual conference, the society first refunded all registration and expo fees and worked with the vendor partners to resolve the cancellation of rental space, food and beverage services, and decorating. Then they organized a team of 15 people split into three groups. One group focused on the intellectual, scientific, and educational elements of the virtual conference. They chose 24 sessions to livestream and decided to prerecord the rest for on-demand access, limiting the number of presenters they needed to train for online presentation.
A second team focused on business and worked with industry partners on how to translate a large expo into digital offerings. They developed virtual pages, advertisements, promotions, and industry-sponsored education.
The third team’s focus, Ms. Sibley said, was most critical, and the hardest: addressing socio-emotional needs.
“That group was responsible for trying to create the buzz and excitement we would have had at the event,” she said, “pivoting that experience we would have had in a live event to a virtual environment. What we were worried about was, would anyone even come?”
But ACC built it, and they did indeed come. Within a half hour of the opening session, nearly 13,000 people logged on from around the world. “It worked beautifully,” Ms. Sibley said.
By the end of the 3-day event, approximately 34,000 unique visitors had logged in for live or prerecorded sessions. Although ACC worried at first about technical glitches and bandwidth needs, everything ran smoothly. By 90 days after the meeting, 63,000 unique users had logged in to access the conference content.
ACC was among the first organizations forced to switch from an in-person to all-online meeting, but dozens of other organizations have now done the same, discovering the benefits and drawbacks of a virtual environment while experimenting with different formats and offerings. Talks with a few large medical societies about the experience revealed several common themes, including the following:
- Finding new ways to attract and measure attendance.
- Ensuring the actual scientific content was as robust online as in person.
- Realizing the value of social media in enhancing the socio-emotional experience.
- Believing that virtual meetings will become a permanent fixture in a future of “hybrid” conferences.
New ways of attracting and measuring attendance
Previous ways to measure meeting attendance were straightforward: number of registrations and number of people physically walking into sessions. An online conference, however, offers dozens of ways to measure attendance. While the number of registrations remained one tool – and all the organizations interviewed reported record numbers of registrations – organizations also used other metrics to measure success, such as “participation,” “engagement,” and “viewing time.”
ACC defined “participation” as a unique user logging in, and it defined “engagement” as sticking around for a while, possibly using chat functions or discussing the content on social media. The American Society of Clinical Oncology (ASCO) annual conference in May, which attracted more than 44,000 registered attendees, also measured total content views – more than 2.5 million during the meeting – and monitored social media. More than 8,800 Twitter users posted more than 45,000 tweets with the #ASCO20 hashtag during the meeting, generating 750 million likes, shares, and comments. The European League Against Rheumatism (EULAR) annual congress registered a record 18,700 delegates – up from 14,500 in 2019 – but it also measured attendance by average viewing time and visits by congress day and by category.
Organizations shifted fee structures as well. While ACC refunded fees for its first online meeting, it has since developed tiers to match fees to anticipated value, such as charging more for livestreamed sessions that allow interactivity than for viewing recordings. ASCO offered a one-time fee waiver for members plus free registration to cancer survivors and caregivers, discounted registration for patient advocates, and reduced fees for other categories. But adjusting how to measure attendance and charge for events were the easy parts of transitioning to online.
Priority for having robust content
The biggest difficulty for most organizations was the short time they had to move online, with a host of challenges accompanying the switch, said the executive director of EULAR, Julia Rautenstrauch, DrMed. These included technical requirements, communication, training, finances, legal issues, compliance rules, and other logistics.
“The year 2020 will be remembered for being the year of unexpected transformation,” said a spokesperson from European Society for Medical Oncology (ESMO), who declined to be named. “The number of fundamental questions we had to ask ourselves is pages long. The solutions we have implemented so far have been successful, but we won’t rest on our laurels.”
ASCO had an advantage in the pivot, despite only 6 weeks to make the switch, because they already had a robust online platform to build on. “We weren’t starting from scratch, but we were sure changing the way we prepared,” ASCO CEO Clifford Hudis, MD, said.
All of the organizations made the breadth and quality of scientific and educational content a top priority, and those who have already hosted meetings this year report positive feedback.
“The rating of the scientific content was excellent, and the event did indeed fulfill the educational goals and expected learning outcomes for the vast majority of delegates,” EULAR’s Dr. Rautenstrauch said.
“Our goal, when we went into this, was that, in the future when somebody looks back at ASCO20, they should not be able to tell that it was a different year from any other in terms of the science,” Dr. Hudis said.
Missing out on networking and social interaction
Even when logistics run smoothly, virtual conferences must overcome two other challenges: the loss of in-person interactions and the potential for “Zoom burnout.”
“You do miss that human contact, the unsaid reactions in the room when you’re speaking or providing a controversial statement, even the facial expression or seeing people lean in or being distracted,” Ms. Sibley said.
Taher Modarressi, MD, an endocrinologist with Diabetes and Endocrine Associates of Hunterdon in Flemington, N.J., said all the digital conferences he has attended were missing those key social elements: “seeing old friends, sideline discussions that generate new ideas, and meeting new colleagues. However, this has been partly alleviated with the robust rise of social media and ‘MedTwitter,’ in particular, where these discussions and interactions continue.”
To attempt to meet that need for social interaction, societies came up with a variety of options. EULAR offered chatrooms, “Meet the Expert” sessions, and other virtual opportunities for live interaction. ASCO hosted discussion groups with subsets of participants, such as virtual meetings with oncology fellows, and it plans to offer networking sessions and “poster walks” during future meetings.
“The value of an in-person meeting is connecting with people, exchanging ideas over coffee, and making new contacts,” ASCO’s Dr. Hudis said. While virtual meetings lose many of those personal interactions, knowledge can also be shared with more people, he said.
The key to combating digital fatigue is focusing on opportunities for interactivity, ACC’s Ms. Sibley said. “When you are creating a virtual environment, it’s important that you offer choices.” Online learners tend to have shorter attention spans than in-person learners, so people need opportunities to flip between sessions, like flipping between TV channels. Different engagement options are also essential, such as chat functions on the video platforms, asking questions of presenters orally or in writing, and using the familiar hashtags for social media discussion.
“We set up all those different ways to interact, and you allow the user to choose,” Ms. Sibley said.
Some conferences, however, had less time or fewer resources to adjust to a virtual format and couldn’t make up for the lost social interaction. Andy Bowman, MD, a neonatologist in Lubbock, Tex., was supposed to attend the Neonatal & Pediatric Airborne Transport Conference sponsored by International Biomed in the spring, but it was canceled at the last minute. Several weeks later, the organizers released videos of scheduled speakers giving their talks, but it was less engaging and too easy to get distracted, Dr. Bowman said.
“There is a noticeable decrease in energy – you can’t look around to feed off other’s reactions when a speaker says something off the wall, or new, or contrary to expectations,” he said. He also especially missed the social interactions, such as “missing out on the chance encounters in the hallway or seeing the same face in back-to-back sessions and figuring out you have shared interest.” He was also sorry to miss the expo because neonatal transport requires a lot of specialty equipment, and he appreciates the chance to actually touch and see it in person.
Advantages of an online meeting
Despite the challenges, online meetings can overcome obstacles of in-person meetings, particularly for those in low- and middle-income countries, such as travel and registration costs, the hardships of being away from practice, and visa restrictions.
“You really have the potential to broaden your reach,” Ms. Sibley said, noting that people in 157 countries participated in ACC.20.
Another advantage is keeping the experience available to people after the livestreamed event.
“Virtual events have demonstrated the potential for a more democratic conference world, expanding the dissemination of information to a much wider community of stakeholders,” ESMO’s spokesperson said.
Not traveling can actually mean getting more out of the conference, said Atisha Patel Manhas, MD, a hematologist/oncologist in Dallas, who attended ASCO. “I have really enjoyed the access aspect – on the virtual platform there is so much more content available to you, and travel time doesn’t cut into conference time,” she said, though she also missed the interaction with colleagues.
Others found that virtual conferences provided more engagement than in-person conferences. Marwah Abdalla, MD, MPH, an assistant professor of medicine and director of education for the Cardiac Intensive Care Unit at Columbia University Medical Center, New York, felt that moderated Q&A sessions offered more interaction among participants. She attended and spoke on a panel during virtual SLEEP 2020, a joint meeting of the American Academy of Sleep Medicine (AASM) and the Sleep Research Society (SRS).
“Usually during in-person sessions, only a few questions are possible, and participants rarely have an opportunity to discuss the presentations within the session due to time limits,” Dr. Abdalla said. “Because the conference presentations can also be viewed asynchronously, participants have been able to comment on lectures and continue the discussion offline, either via social media or via email.” She acknowledged drawbacks of the virtual experience, such as an inability to socialize in person and participate in activities but appreciated the new opportunities to network and learn from international colleagues who would not have been able to attend in person.
Ritu Thamman, MD, assistant professor of medicine at the University of Pittsburgh School of Medicine, pointed out that many institutions have cut their travel budgets, and physicians would be unable to attend in-person conferences for financial or other reasons. She especially appreciated that the European Society of Cardiology had no registration fee for ESC 2020 and made their content free for all of September, which led to more than 100,000 participants.
“That meant anyone anywhere could learn,” she said. “It makes it much more diverse and more egalitarian. That feels like a good step in the right direction for all of us.”
Dr. Modarressi, who found ESC “exhilarating,” similarly noted the benefit of such an equitably accessible conference. “Decreasing barriers and improving access to top-line results and up-to-date information has always been a challenge to the global health community,” he said, noting that the map of attendance for the virtual meeting was “astonishing.”
Given these benefits, organizers said they expect a future of hybrid conferences: physical meetings for those able to attend in person and virtual ones for those who cannot.
“We also expect that the hybrid congress will cater to the needs of people on-site by allowing them additional access to more scientific content than by physical attendance alone,” Dr. Rautenstrauch said.
Everyone has been in reactive mode this year, Ms. Sibley said, but the future looks bright as they seek ways to overcome challenges such as socio-emotional needs and virtual expo spaces.
“We’ve been thrust into the virtual world much faster than we expected, but we’re finding it’s opening more opportunities than we had live,” Ms. Sibley said. “This has catapulted us, for better or worse, into a new way to deliver education and other types of information.
“I think, if we’re smart, we’ll continue to think of ways this can augment our live environment and not replace it.”
A version of this article originally appeared on Medscape.com.
Brazil confirms death of volunteer in COVID-19 vaccine trial
The Brazilian National Health Surveillance Agency (Anvisa) announced Oct. 21 that it is investigating data received on the death of a volunteer in a clinical trial of the COVID-19 vaccine developed by Oxford University and the pharmaceutical company AstraZeneca.
In an email sent to Medscape Medical News, the agency states that it was formally informed of the death on October 19. It has already received data regarding the investigation of the case, which is now being conducted by the Brazilian International Security Assessment Committee.
The identity of the volunteer and cause of death have not yet been confirmed by any official source linked to the study. In the email, Anvisa reiterated that “according to national and international regulations on good clinical practices, data on clinical research volunteers must be kept confidential, in accordance with the principles of confidentiality, human dignity, and protection of participants.”
A report in the Brazilian newspaper O Globo, however, states that the patient who died is a 28-year-old doctor, recently graduated, who worked on the front line of combating COVID-19 in three hospitals in Rio de Janeiro. . Due to the study design, it is impossible to know whether the volunteer received the vaccine or placebo.
It is imperative to wait for the results of the investigations, said Sergio Cimerman, MD, the scientific coordinator of the Brazilian Society of Infectious Diseases (SBI), because death is possible during any vaccine trial, even more so in cases in which the final goal is to immunize the population in record time.
“It is precisely the phase 3 study that assesses efficacy and safety so that the vaccine can be used for the entire population. We cannot let ourselves lose hope, and we must move forward, as safely as possible, in search of an ideal vaccine,” said Cimerman, who works at the Instituto de Infectologia Emílio Ribas and is also an advisor to the Portuguese edition of Medscape.
This article was translated and adapted from the Portuguese edition of Medscape.
The Brazilian National Health Surveillance Agency (Anvisa) announced Oct. 21 that it is investigating data received on the death of a volunteer in a clinical trial of the COVID-19 vaccine developed by Oxford University and the pharmaceutical company AstraZeneca.
In an email sent to Medscape Medical News, the agency states that it was formally informed of the death on October 19. It has already received data regarding the investigation of the case, which is now being conducted by the Brazilian International Security Assessment Committee.
The identity of the volunteer and cause of death have not yet been confirmed by any official source linked to the study. In the email, Anvisa reiterated that “according to national and international regulations on good clinical practices, data on clinical research volunteers must be kept confidential, in accordance with the principles of confidentiality, human dignity, and protection of participants.”
A report in the Brazilian newspaper O Globo, however, states that the patient who died is a 28-year-old doctor, recently graduated, who worked on the front line of combating COVID-19 in three hospitals in Rio de Janeiro. . Due to the study design, it is impossible to know whether the volunteer received the vaccine or placebo.
It is imperative to wait for the results of the investigations, said Sergio Cimerman, MD, the scientific coordinator of the Brazilian Society of Infectious Diseases (SBI), because death is possible during any vaccine trial, even more so in cases in which the final goal is to immunize the population in record time.
“It is precisely the phase 3 study that assesses efficacy and safety so that the vaccine can be used for the entire population. We cannot let ourselves lose hope, and we must move forward, as safely as possible, in search of an ideal vaccine,” said Cimerman, who works at the Instituto de Infectologia Emílio Ribas and is also an advisor to the Portuguese edition of Medscape.
This article was translated and adapted from the Portuguese edition of Medscape.
The Brazilian National Health Surveillance Agency (Anvisa) announced Oct. 21 that it is investigating data received on the death of a volunteer in a clinical trial of the COVID-19 vaccine developed by Oxford University and the pharmaceutical company AstraZeneca.
In an email sent to Medscape Medical News, the agency states that it was formally informed of the death on October 19. It has already received data regarding the investigation of the case, which is now being conducted by the Brazilian International Security Assessment Committee.
The identity of the volunteer and cause of death have not yet been confirmed by any official source linked to the study. In the email, Anvisa reiterated that “according to national and international regulations on good clinical practices, data on clinical research volunteers must be kept confidential, in accordance with the principles of confidentiality, human dignity, and protection of participants.”
A report in the Brazilian newspaper O Globo, however, states that the patient who died is a 28-year-old doctor, recently graduated, who worked on the front line of combating COVID-19 in three hospitals in Rio de Janeiro. . Due to the study design, it is impossible to know whether the volunteer received the vaccine or placebo.
It is imperative to wait for the results of the investigations, said Sergio Cimerman, MD, the scientific coordinator of the Brazilian Society of Infectious Diseases (SBI), because death is possible during any vaccine trial, even more so in cases in which the final goal is to immunize the population in record time.
“It is precisely the phase 3 study that assesses efficacy and safety so that the vaccine can be used for the entire population. We cannot let ourselves lose hope, and we must move forward, as safely as possible, in search of an ideal vaccine,” said Cimerman, who works at the Instituto de Infectologia Emílio Ribas and is also an advisor to the Portuguese edition of Medscape.
This article was translated and adapted from the Portuguese edition of Medscape.
Outpatient visits rebound for most specialties to pre-COVID-19 levels
, according to new data.
Overall visits plunged by almost 60% at the low point in late March and did not start recovering until late June, when visits were still off by 10%. Visits began to rise again – by 2% over the March 1 baseline – around Labor Day.
As of Oct. 4, visits had returned to that March 1 baseline, which was slightly higher than in late February, according to data analyzed by Harvard University, the Commonwealth Fund, and the healthcare technology company Phreesia, which helps medical practices with patient registration, insurance verification, and payments, and has data on 50,000 providers in all 50 states.
The study was published online by the Commonwealth Fund.
In-person visits are still down 6% from the March 1 baseline. Telemedicine visits – which surged in mid-April to account for some 13%-14% of visits – have subsided to 6% of visits.
Many states reopened businesses and lifted travel restrictions in early September, benefiting medical practices in some areas. But clinicians in some regions are still facing rising COVID-19 cases, as well as “the challenges of keeping patients and clinicians safe while also maintaining revenue,” wrote the report authors.
Some specialties are still hard hit. For the week starting Oct. 4, visits to pulmonologists were off 20% from March 1. Otolaryngology visits were down 17%, and behavioral health visits were down 14%. Cardiology, allergy/immunology, neurology, gastroenterology, and endocrinology also saw drops of 5%-10% from March.
Patients were flocking to dermatologists, however. Visits were up 17% over baseline. Primary care also was popular, with a 13% increase over March 1.
At the height of the pandemic shutdown in late March, Medicare beneficiaries stayed away from doctors the most. Visits dipped 63%, compared with 56% for the commercially insured, and 52% for those on Medicaid. Now, Medicare visits are up 3% over baseline, while Medicaid visits are down 1% and commercially insured visits have risen 1% from March.
The over-65 age group did not have the steepest drop in visits when analyzed by age. Children aged 3-17 years saw the biggest decline at the height of the shutdown. Infants to 5-year-olds have still not returned to prepandemic visit levels. Those visits are off by 10%-18%. The 65-and-older group is up 4% from March.
Larger practices – with more than six clinicians – have seen the biggest rebound, after having had the largest dip in visits, from a decline of 53% in late March to a 14% rise over that baseline. Practices with fewer than five clinicians are still 6% down from the March baseline.
Wide variation in telemedicine use
The researchers reported a massive gap in the percentage of various specialties that are using telemedicine. At the top end are behavioral health specialists, where 41% of visits are by telemedicine.
The next-closest specialty is endocrinology, which has 14% of visits via telemedicine, on par with rheumatology, neurology, and gastroenterology. At the low end: ophthalmology, with zero virtual visits; otolaryngology (1%), orthopedics (1%), surgery (2%), and dermatology and ob.gyn., both at 3%.
Smaller practices – with fewer than five clinicians – never adopted telemedicine at the rate of the larger practices. During the mid-April peak, about 10% of the smaller practices were using telemedicine in adult primary care practices, compared with 19% of those primary care practices with more than six clinicians.
The gap persists. Currently, 9% of the larger practices are using telemedicine, compared with 4% of small practices.
One-third of all provider organizations analyzed never-adopted telemedicine. And while use continues, it is now mostly minimal. At the April peak, 35% of the practices with telemedicine reported heavy use – that is, in more than 20% of visits. In September, 9% said they had such heavy use.
A version of this article originally appeared on Medscape.com.
, according to new data.
Overall visits plunged by almost 60% at the low point in late March and did not start recovering until late June, when visits were still off by 10%. Visits began to rise again – by 2% over the March 1 baseline – around Labor Day.
As of Oct. 4, visits had returned to that March 1 baseline, which was slightly higher than in late February, according to data analyzed by Harvard University, the Commonwealth Fund, and the healthcare technology company Phreesia, which helps medical practices with patient registration, insurance verification, and payments, and has data on 50,000 providers in all 50 states.
The study was published online by the Commonwealth Fund.
In-person visits are still down 6% from the March 1 baseline. Telemedicine visits – which surged in mid-April to account for some 13%-14% of visits – have subsided to 6% of visits.
Many states reopened businesses and lifted travel restrictions in early September, benefiting medical practices in some areas. But clinicians in some regions are still facing rising COVID-19 cases, as well as “the challenges of keeping patients and clinicians safe while also maintaining revenue,” wrote the report authors.
Some specialties are still hard hit. For the week starting Oct. 4, visits to pulmonologists were off 20% from March 1. Otolaryngology visits were down 17%, and behavioral health visits were down 14%. Cardiology, allergy/immunology, neurology, gastroenterology, and endocrinology also saw drops of 5%-10% from March.
Patients were flocking to dermatologists, however. Visits were up 17% over baseline. Primary care also was popular, with a 13% increase over March 1.
At the height of the pandemic shutdown in late March, Medicare beneficiaries stayed away from doctors the most. Visits dipped 63%, compared with 56% for the commercially insured, and 52% for those on Medicaid. Now, Medicare visits are up 3% over baseline, while Medicaid visits are down 1% and commercially insured visits have risen 1% from March.
The over-65 age group did not have the steepest drop in visits when analyzed by age. Children aged 3-17 years saw the biggest decline at the height of the shutdown. Infants to 5-year-olds have still not returned to prepandemic visit levels. Those visits are off by 10%-18%. The 65-and-older group is up 4% from March.
Larger practices – with more than six clinicians – have seen the biggest rebound, after having had the largest dip in visits, from a decline of 53% in late March to a 14% rise over that baseline. Practices with fewer than five clinicians are still 6% down from the March baseline.
Wide variation in telemedicine use
The researchers reported a massive gap in the percentage of various specialties that are using telemedicine. At the top end are behavioral health specialists, where 41% of visits are by telemedicine.
The next-closest specialty is endocrinology, which has 14% of visits via telemedicine, on par with rheumatology, neurology, and gastroenterology. At the low end: ophthalmology, with zero virtual visits; otolaryngology (1%), orthopedics (1%), surgery (2%), and dermatology and ob.gyn., both at 3%.
Smaller practices – with fewer than five clinicians – never adopted telemedicine at the rate of the larger practices. During the mid-April peak, about 10% of the smaller practices were using telemedicine in adult primary care practices, compared with 19% of those primary care practices with more than six clinicians.
The gap persists. Currently, 9% of the larger practices are using telemedicine, compared with 4% of small practices.
One-third of all provider organizations analyzed never-adopted telemedicine. And while use continues, it is now mostly minimal. At the April peak, 35% of the practices with telemedicine reported heavy use – that is, in more than 20% of visits. In September, 9% said they had such heavy use.
A version of this article originally appeared on Medscape.com.
, according to new data.
Overall visits plunged by almost 60% at the low point in late March and did not start recovering until late June, when visits were still off by 10%. Visits began to rise again – by 2% over the March 1 baseline – around Labor Day.
As of Oct. 4, visits had returned to that March 1 baseline, which was slightly higher than in late February, according to data analyzed by Harvard University, the Commonwealth Fund, and the healthcare technology company Phreesia, which helps medical practices with patient registration, insurance verification, and payments, and has data on 50,000 providers in all 50 states.
The study was published online by the Commonwealth Fund.
In-person visits are still down 6% from the March 1 baseline. Telemedicine visits – which surged in mid-April to account for some 13%-14% of visits – have subsided to 6% of visits.
Many states reopened businesses and lifted travel restrictions in early September, benefiting medical practices in some areas. But clinicians in some regions are still facing rising COVID-19 cases, as well as “the challenges of keeping patients and clinicians safe while also maintaining revenue,” wrote the report authors.
Some specialties are still hard hit. For the week starting Oct. 4, visits to pulmonologists were off 20% from March 1. Otolaryngology visits were down 17%, and behavioral health visits were down 14%. Cardiology, allergy/immunology, neurology, gastroenterology, and endocrinology also saw drops of 5%-10% from March.
Patients were flocking to dermatologists, however. Visits were up 17% over baseline. Primary care also was popular, with a 13% increase over March 1.
At the height of the pandemic shutdown in late March, Medicare beneficiaries stayed away from doctors the most. Visits dipped 63%, compared with 56% for the commercially insured, and 52% for those on Medicaid. Now, Medicare visits are up 3% over baseline, while Medicaid visits are down 1% and commercially insured visits have risen 1% from March.
The over-65 age group did not have the steepest drop in visits when analyzed by age. Children aged 3-17 years saw the biggest decline at the height of the shutdown. Infants to 5-year-olds have still not returned to prepandemic visit levels. Those visits are off by 10%-18%. The 65-and-older group is up 4% from March.
Larger practices – with more than six clinicians – have seen the biggest rebound, after having had the largest dip in visits, from a decline of 53% in late March to a 14% rise over that baseline. Practices with fewer than five clinicians are still 6% down from the March baseline.
Wide variation in telemedicine use
The researchers reported a massive gap in the percentage of various specialties that are using telemedicine. At the top end are behavioral health specialists, where 41% of visits are by telemedicine.
The next-closest specialty is endocrinology, which has 14% of visits via telemedicine, on par with rheumatology, neurology, and gastroenterology. At the low end: ophthalmology, with zero virtual visits; otolaryngology (1%), orthopedics (1%), surgery (2%), and dermatology and ob.gyn., both at 3%.
Smaller practices – with fewer than five clinicians – never adopted telemedicine at the rate of the larger practices. During the mid-April peak, about 10% of the smaller practices were using telemedicine in adult primary care practices, compared with 19% of those primary care practices with more than six clinicians.
The gap persists. Currently, 9% of the larger practices are using telemedicine, compared with 4% of small practices.
One-third of all provider organizations analyzed never-adopted telemedicine. And while use continues, it is now mostly minimal. At the April peak, 35% of the practices with telemedicine reported heavy use – that is, in more than 20% of visits. In September, 9% said they had such heavy use.
A version of this article originally appeared on Medscape.com.
Scrubs ad that insulted women and DOs pulled after outcry
A video that advertised scrubs but denigrated women and DOs has been removed from the company’s website after fierce backlash.
On Tuesday Kevin Klauer, DO, EJD, directed this tweet to the medical uniform company Figs: “@wearfigs REMOVE YOUR DO offensive web ad immediately or the @AOAforDOs will proceed promptly with a defamation lawsuit on behalf of our members and profession.”
Also on Tuesday, the American Association of Colleges of Osteopathic Medicine demanded a public apology.
The video ad featured a woman carrying a “Medical Terminology for Dummies” book upside down while modeling the pink scrubs from all angles and dancing. At one point in the ad, the camera zooms in on the badge clipped to her waistband that read “DO.”
Agnieszka Solberg, MD, a vascular and interventional radiologist and assistant clinical professor at the University of North Dakota in Grand Forks, was among those voicing pointed criticism on social media.
“This was another hit for our DO colleagues,” she said in an interview, emphasizing that MDs and DOs provide the same level of care.
AACOM tweeted: “We are outraged women physicians & doctors of osteopathic medicine are still attacked in ignorant marketing campaigns. A company like @wearfigs should be ashamed for promoting these stereotypes. We demand the respect we’ve earned AND a public apology.”
Dr. Solberg says this is not the first offense by the company. She said she had stopped buying the company’s scrubs a year ago because the ads “have been portraying female providers as dumb and silly. This was the final straw.”
She said the timing of the ad is suspect as DOs had been swept into a storm of negativity earlier this month, as Medscape Medical News reported, when some questioned the qualifications of President Donald Trump’s physician, Sean Conley, who is a DO.
The scrubs ad ignited criticism across specialties, provider levels, and genders.
Jessica K. Willett, MD, tweeted: “As women physicians in 2020, we still struggle to be taken seriously compared to our male counterparts, as we battle stereotypes like THIS EXACT ONE. We expect the brands we support to reflect the badasses we are.”
The company responded to her tweet: “Thank you so much for the feedback! Totally not our intent – we’re taking down both the men’s and women’s versions of this ASAP! I really appreciate you taking the time to share this.”
The company did not respond to a request for comment but issued an apology on social media: “A lot of you guys have pointed out an insensitive video we had on our site – we are incredibly sorry for any hurt this has caused you, especially our female DOs (who are amazing!) FIGS is a female founded company whose only mission is to make you guys feel awesome.”
The Los Angeles–based company, which Forbes estimated will make $250 million in sales this year, was founded by co-CEOs Heather Hasson and Trina Spear.
A med student wrote on Twitter: “As a female and a DO student, how would I ever “feel awesome” about myself knowing that this is how you view me??? And how you want others to view me??? Women and DO’s have fought stereotypes way too long for you to go ahead and put this out there. Do better.”
Even the company’s apology was tinged with disrespect, some noted, with the use of “you guys” and for what it didn’t include.
As Liesl Young, MD, tweeted: “We are not “guys”, we are women. MD = DO. We stand together.”
Dr. Solberg said the apology came across as an apology that feelings were hurt. It should have detailed the changes the company would make to prevent another incident and address the processes that led to the video.
Dr. Solberg said she is seeing something positive come from the whole incident in that, “women are taking up the torch of feminism in such a volatile and divisive time.”
Dr. Solberg reported no relevant financial relationships.
This article first appeared on Medscape.com.
A video that advertised scrubs but denigrated women and DOs has been removed from the company’s website after fierce backlash.
On Tuesday Kevin Klauer, DO, EJD, directed this tweet to the medical uniform company Figs: “@wearfigs REMOVE YOUR DO offensive web ad immediately or the @AOAforDOs will proceed promptly with a defamation lawsuit on behalf of our members and profession.”
Also on Tuesday, the American Association of Colleges of Osteopathic Medicine demanded a public apology.
The video ad featured a woman carrying a “Medical Terminology for Dummies” book upside down while modeling the pink scrubs from all angles and dancing. At one point in the ad, the camera zooms in on the badge clipped to her waistband that read “DO.”
Agnieszka Solberg, MD, a vascular and interventional radiologist and assistant clinical professor at the University of North Dakota in Grand Forks, was among those voicing pointed criticism on social media.
“This was another hit for our DO colleagues,” she said in an interview, emphasizing that MDs and DOs provide the same level of care.
AACOM tweeted: “We are outraged women physicians & doctors of osteopathic medicine are still attacked in ignorant marketing campaigns. A company like @wearfigs should be ashamed for promoting these stereotypes. We demand the respect we’ve earned AND a public apology.”
Dr. Solberg says this is not the first offense by the company. She said she had stopped buying the company’s scrubs a year ago because the ads “have been portraying female providers as dumb and silly. This was the final straw.”
She said the timing of the ad is suspect as DOs had been swept into a storm of negativity earlier this month, as Medscape Medical News reported, when some questioned the qualifications of President Donald Trump’s physician, Sean Conley, who is a DO.
The scrubs ad ignited criticism across specialties, provider levels, and genders.
Jessica K. Willett, MD, tweeted: “As women physicians in 2020, we still struggle to be taken seriously compared to our male counterparts, as we battle stereotypes like THIS EXACT ONE. We expect the brands we support to reflect the badasses we are.”
The company responded to her tweet: “Thank you so much for the feedback! Totally not our intent – we’re taking down both the men’s and women’s versions of this ASAP! I really appreciate you taking the time to share this.”
The company did not respond to a request for comment but issued an apology on social media: “A lot of you guys have pointed out an insensitive video we had on our site – we are incredibly sorry for any hurt this has caused you, especially our female DOs (who are amazing!) FIGS is a female founded company whose only mission is to make you guys feel awesome.”
The Los Angeles–based company, which Forbes estimated will make $250 million in sales this year, was founded by co-CEOs Heather Hasson and Trina Spear.
A med student wrote on Twitter: “As a female and a DO student, how would I ever “feel awesome” about myself knowing that this is how you view me??? And how you want others to view me??? Women and DO’s have fought stereotypes way too long for you to go ahead and put this out there. Do better.”
Even the company’s apology was tinged with disrespect, some noted, with the use of “you guys” and for what it didn’t include.
As Liesl Young, MD, tweeted: “We are not “guys”, we are women. MD = DO. We stand together.”
Dr. Solberg said the apology came across as an apology that feelings were hurt. It should have detailed the changes the company would make to prevent another incident and address the processes that led to the video.
Dr. Solberg said she is seeing something positive come from the whole incident in that, “women are taking up the torch of feminism in such a volatile and divisive time.”
Dr. Solberg reported no relevant financial relationships.
This article first appeared on Medscape.com.
A video that advertised scrubs but denigrated women and DOs has been removed from the company’s website after fierce backlash.
On Tuesday Kevin Klauer, DO, EJD, directed this tweet to the medical uniform company Figs: “@wearfigs REMOVE YOUR DO offensive web ad immediately or the @AOAforDOs will proceed promptly with a defamation lawsuit on behalf of our members and profession.”
Also on Tuesday, the American Association of Colleges of Osteopathic Medicine demanded a public apology.
The video ad featured a woman carrying a “Medical Terminology for Dummies” book upside down while modeling the pink scrubs from all angles and dancing. At one point in the ad, the camera zooms in on the badge clipped to her waistband that read “DO.”
Agnieszka Solberg, MD, a vascular and interventional radiologist and assistant clinical professor at the University of North Dakota in Grand Forks, was among those voicing pointed criticism on social media.
“This was another hit for our DO colleagues,” she said in an interview, emphasizing that MDs and DOs provide the same level of care.
AACOM tweeted: “We are outraged women physicians & doctors of osteopathic medicine are still attacked in ignorant marketing campaigns. A company like @wearfigs should be ashamed for promoting these stereotypes. We demand the respect we’ve earned AND a public apology.”
Dr. Solberg says this is not the first offense by the company. She said she had stopped buying the company’s scrubs a year ago because the ads “have been portraying female providers as dumb and silly. This was the final straw.”
She said the timing of the ad is suspect as DOs had been swept into a storm of negativity earlier this month, as Medscape Medical News reported, when some questioned the qualifications of President Donald Trump’s physician, Sean Conley, who is a DO.
The scrubs ad ignited criticism across specialties, provider levels, and genders.
Jessica K. Willett, MD, tweeted: “As women physicians in 2020, we still struggle to be taken seriously compared to our male counterparts, as we battle stereotypes like THIS EXACT ONE. We expect the brands we support to reflect the badasses we are.”
The company responded to her tweet: “Thank you so much for the feedback! Totally not our intent – we’re taking down both the men’s and women’s versions of this ASAP! I really appreciate you taking the time to share this.”
The company did not respond to a request for comment but issued an apology on social media: “A lot of you guys have pointed out an insensitive video we had on our site – we are incredibly sorry for any hurt this has caused you, especially our female DOs (who are amazing!) FIGS is a female founded company whose only mission is to make you guys feel awesome.”
The Los Angeles–based company, which Forbes estimated will make $250 million in sales this year, was founded by co-CEOs Heather Hasson and Trina Spear.
A med student wrote on Twitter: “As a female and a DO student, how would I ever “feel awesome” about myself knowing that this is how you view me??? And how you want others to view me??? Women and DO’s have fought stereotypes way too long for you to go ahead and put this out there. Do better.”
Even the company’s apology was tinged with disrespect, some noted, with the use of “you guys” and for what it didn’t include.
As Liesl Young, MD, tweeted: “We are not “guys”, we are women. MD = DO. We stand together.”
Dr. Solberg said the apology came across as an apology that feelings were hurt. It should have detailed the changes the company would make to prevent another incident and address the processes that led to the video.
Dr. Solberg said she is seeing something positive come from the whole incident in that, “women are taking up the torch of feminism in such a volatile and divisive time.”
Dr. Solberg reported no relevant financial relationships.
This article first appeared on Medscape.com.
Bariatric surgery tied to lower aortic dissection risk
The finding is the latest in a series of benefits researchers have linked to the surgery, not all of which appear to directly result from weight loss.
“It has an incredible impact on hyperlipidemia and hypertension,” said Luis Felipe Okida, MD, from Cleveland Clinic Florida, Weston. “Those are the main risk factors for aortic dissection.”
He presented the finding at the virtual American Congress of Surgeons Clinical Congress 2020. The study was also published online in the Journal of the American College of Surgeons.
Although uncommon, acute aortic dissection proves fatal to half the people it strikes if patients do not receive treatment within 72 hours, Dr. Okida said in an interview.
To learn whether there is an association between bariatric surgery and risk for aortic dissection, Dr. Okida and colleagues analyzed data from the National Inpatient Sample (NIS) database from 2010 to 2015. The NIS comprises about 20% of hospital inpatient admissions in the United States.
Among the patients in the sample, 296,041 adults had undergone bariatric surgery, and 2,004,804 adults had obesity (body mass index ≥35 kg/m2) but had never undergone bariatric surgery. This latter group represented the control group.
Among the control group, 1,411 patients (.070%) experienced aortic dissection; among the bariatric surgery group, 94 patients (0.032%) experienced aortic dissection. This was a statistically significant difference (P < .0001).
The groups differed significantly in many ways. The mean age of the patients in the control group was 54.4 years, which was a mean of 2.5 years older than the bariatric surgery group. Additionally, the control group included a higher percentage of women and a lower percentage of White persons.
Those in the control group were also more likely to have a history of tobacco use, hypertension (64.2% vs. 48.9% in the surgery group), hyperlipidemia (32.7% vs. 18.3%), diabetes, aortic aneurysm (20.6% vs. 12.0%), and bicuspid aortic valves but were less likely to have Marfan/Ehlers-Danlos syndrome.
A multivariate analysis showed that gender, age, history of tobacco use, hypertension, hyperlipidemia, and Marfan/Ehlers-Danlos syndrome were associated with an increased risk for aortic dissection. Diabetes was associated with a lower risk. All of these findings had previously been reported in the literature, Dr. Okida said, but the reasons for the negative association with diabetes is not well understood.
The association between the surgery and aortic dissection applied to younger patients as well as older ones.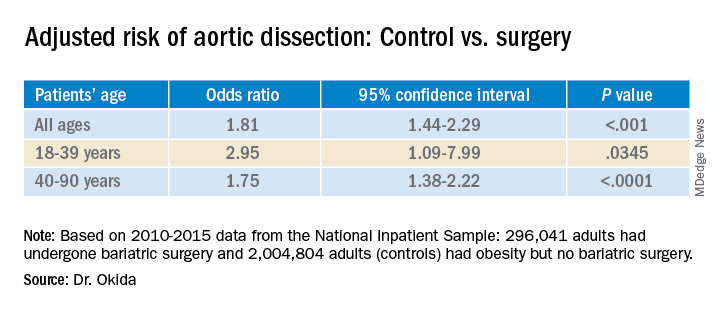
“In elderly patients, the main risk factor for aortic dissection is hypertension, and in younger patients, below 40 years old, the main risk factors are diseases of the collagen and diseases of the aorta,” said Dr. Okida during his presentation. “But these younger patients still have a high prevalence of hypertension, and that’s why bariatric surgery is beneficial.”
Although the finding regarding risk for aortic dissection supports the value of bariatric surgery, it does not in itself provide justification for undergoing the procedure. “It’s not even one of the comorbidities that insurance companies would recognize as key in approving this procedure,” said senior author Emanuele Lo Menzo, MD, PhD, also from the Cleveland Clinic Florida.
“I don’t think a physician would ever recommend this procedure specifically to avoid aortic dissection,” he said in an interview. “It’s sort of an extended benefit.”
The study raises interesting questions about the effects of the surgery, said Shanu Kothari, MD, president-elect of the American Society for Metabolic and Bariatric Surgery.
“We’ve known for a long time that patients with chronic obesity who undergo weight-loss surgery live longer than those who don’t,” he said in an interview. “They have less cardiovascular disease and cancer. Is this one more reason that they live longer?”
Bariatric surgery produces benefits for people with diabetes the day after the surgery, long before patients lose weight as a result of the procedure, Dr. Kothari said.
The effects on metabolism are complex, he added. Besides caloric restriction, they include changes in bile salt absorption and the gut microbiome, which in turn can affect hormones and inflammation.
A key question is how long after the surgery the risk for aortic dissection starts to decline, said Dr. Kothari.
The study could not answer such questions, and Dr. Okida could not find any previous studies that explored the association. He also couldn’t find any study that examined whether weight loss by other means might also reduce the risk for aortic dissection.
Dr. Okida, Dr. Lo Menzo, and Dr. Kothari disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The finding is the latest in a series of benefits researchers have linked to the surgery, not all of which appear to directly result from weight loss.
“It has an incredible impact on hyperlipidemia and hypertension,” said Luis Felipe Okida, MD, from Cleveland Clinic Florida, Weston. “Those are the main risk factors for aortic dissection.”
He presented the finding at the virtual American Congress of Surgeons Clinical Congress 2020. The study was also published online in the Journal of the American College of Surgeons.
Although uncommon, acute aortic dissection proves fatal to half the people it strikes if patients do not receive treatment within 72 hours, Dr. Okida said in an interview.
To learn whether there is an association between bariatric surgery and risk for aortic dissection, Dr. Okida and colleagues analyzed data from the National Inpatient Sample (NIS) database from 2010 to 2015. The NIS comprises about 20% of hospital inpatient admissions in the United States.
Among the patients in the sample, 296,041 adults had undergone bariatric surgery, and 2,004,804 adults had obesity (body mass index ≥35 kg/m2) but had never undergone bariatric surgery. This latter group represented the control group.
Among the control group, 1,411 patients (.070%) experienced aortic dissection; among the bariatric surgery group, 94 patients (0.032%) experienced aortic dissection. This was a statistically significant difference (P < .0001).
The groups differed significantly in many ways. The mean age of the patients in the control group was 54.4 years, which was a mean of 2.5 years older than the bariatric surgery group. Additionally, the control group included a higher percentage of women and a lower percentage of White persons.
Those in the control group were also more likely to have a history of tobacco use, hypertension (64.2% vs. 48.9% in the surgery group), hyperlipidemia (32.7% vs. 18.3%), diabetes, aortic aneurysm (20.6% vs. 12.0%), and bicuspid aortic valves but were less likely to have Marfan/Ehlers-Danlos syndrome.
A multivariate analysis showed that gender, age, history of tobacco use, hypertension, hyperlipidemia, and Marfan/Ehlers-Danlos syndrome were associated with an increased risk for aortic dissection. Diabetes was associated with a lower risk. All of these findings had previously been reported in the literature, Dr. Okida said, but the reasons for the negative association with diabetes is not well understood.
The association between the surgery and aortic dissection applied to younger patients as well as older ones.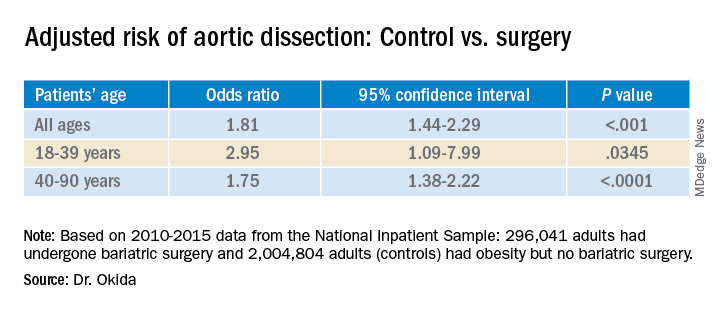
“In elderly patients, the main risk factor for aortic dissection is hypertension, and in younger patients, below 40 years old, the main risk factors are diseases of the collagen and diseases of the aorta,” said Dr. Okida during his presentation. “But these younger patients still have a high prevalence of hypertension, and that’s why bariatric surgery is beneficial.”
Although the finding regarding risk for aortic dissection supports the value of bariatric surgery, it does not in itself provide justification for undergoing the procedure. “It’s not even one of the comorbidities that insurance companies would recognize as key in approving this procedure,” said senior author Emanuele Lo Menzo, MD, PhD, also from the Cleveland Clinic Florida.
“I don’t think a physician would ever recommend this procedure specifically to avoid aortic dissection,” he said in an interview. “It’s sort of an extended benefit.”
The study raises interesting questions about the effects of the surgery, said Shanu Kothari, MD, president-elect of the American Society for Metabolic and Bariatric Surgery.
“We’ve known for a long time that patients with chronic obesity who undergo weight-loss surgery live longer than those who don’t,” he said in an interview. “They have less cardiovascular disease and cancer. Is this one more reason that they live longer?”
Bariatric surgery produces benefits for people with diabetes the day after the surgery, long before patients lose weight as a result of the procedure, Dr. Kothari said.
The effects on metabolism are complex, he added. Besides caloric restriction, they include changes in bile salt absorption and the gut microbiome, which in turn can affect hormones and inflammation.
A key question is how long after the surgery the risk for aortic dissection starts to decline, said Dr. Kothari.
The study could not answer such questions, and Dr. Okida could not find any previous studies that explored the association. He also couldn’t find any study that examined whether weight loss by other means might also reduce the risk for aortic dissection.
Dr. Okida, Dr. Lo Menzo, and Dr. Kothari disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The finding is the latest in a series of benefits researchers have linked to the surgery, not all of which appear to directly result from weight loss.
“It has an incredible impact on hyperlipidemia and hypertension,” said Luis Felipe Okida, MD, from Cleveland Clinic Florida, Weston. “Those are the main risk factors for aortic dissection.”
He presented the finding at the virtual American Congress of Surgeons Clinical Congress 2020. The study was also published online in the Journal of the American College of Surgeons.
Although uncommon, acute aortic dissection proves fatal to half the people it strikes if patients do not receive treatment within 72 hours, Dr. Okida said in an interview.
To learn whether there is an association between bariatric surgery and risk for aortic dissection, Dr. Okida and colleagues analyzed data from the National Inpatient Sample (NIS) database from 2010 to 2015. The NIS comprises about 20% of hospital inpatient admissions in the United States.
Among the patients in the sample, 296,041 adults had undergone bariatric surgery, and 2,004,804 adults had obesity (body mass index ≥35 kg/m2) but had never undergone bariatric surgery. This latter group represented the control group.
Among the control group, 1,411 patients (.070%) experienced aortic dissection; among the bariatric surgery group, 94 patients (0.032%) experienced aortic dissection. This was a statistically significant difference (P < .0001).
The groups differed significantly in many ways. The mean age of the patients in the control group was 54.4 years, which was a mean of 2.5 years older than the bariatric surgery group. Additionally, the control group included a higher percentage of women and a lower percentage of White persons.
Those in the control group were also more likely to have a history of tobacco use, hypertension (64.2% vs. 48.9% in the surgery group), hyperlipidemia (32.7% vs. 18.3%), diabetes, aortic aneurysm (20.6% vs. 12.0%), and bicuspid aortic valves but were less likely to have Marfan/Ehlers-Danlos syndrome.
A multivariate analysis showed that gender, age, history of tobacco use, hypertension, hyperlipidemia, and Marfan/Ehlers-Danlos syndrome were associated with an increased risk for aortic dissection. Diabetes was associated with a lower risk. All of these findings had previously been reported in the literature, Dr. Okida said, but the reasons for the negative association with diabetes is not well understood.
The association between the surgery and aortic dissection applied to younger patients as well as older ones.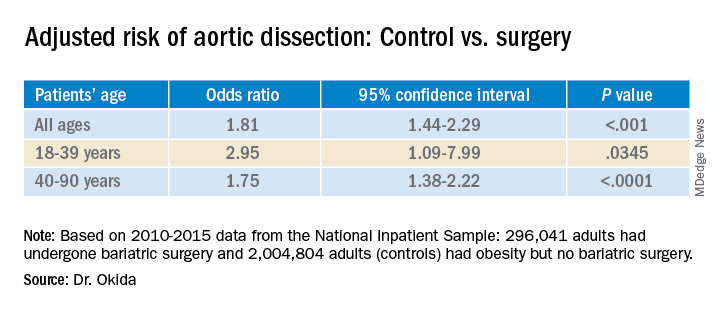
“In elderly patients, the main risk factor for aortic dissection is hypertension, and in younger patients, below 40 years old, the main risk factors are diseases of the collagen and diseases of the aorta,” said Dr. Okida during his presentation. “But these younger patients still have a high prevalence of hypertension, and that’s why bariatric surgery is beneficial.”
Although the finding regarding risk for aortic dissection supports the value of bariatric surgery, it does not in itself provide justification for undergoing the procedure. “It’s not even one of the comorbidities that insurance companies would recognize as key in approving this procedure,” said senior author Emanuele Lo Menzo, MD, PhD, also from the Cleveland Clinic Florida.
“I don’t think a physician would ever recommend this procedure specifically to avoid aortic dissection,” he said in an interview. “It’s sort of an extended benefit.”
The study raises interesting questions about the effects of the surgery, said Shanu Kothari, MD, president-elect of the American Society for Metabolic and Bariatric Surgery.
“We’ve known for a long time that patients with chronic obesity who undergo weight-loss surgery live longer than those who don’t,” he said in an interview. “They have less cardiovascular disease and cancer. Is this one more reason that they live longer?”
Bariatric surgery produces benefits for people with diabetes the day after the surgery, long before patients lose weight as a result of the procedure, Dr. Kothari said.
The effects on metabolism are complex, he added. Besides caloric restriction, they include changes in bile salt absorption and the gut microbiome, which in turn can affect hormones and inflammation.
A key question is how long after the surgery the risk for aortic dissection starts to decline, said Dr. Kothari.
The study could not answer such questions, and Dr. Okida could not find any previous studies that explored the association. He also couldn’t find any study that examined whether weight loss by other means might also reduce the risk for aortic dissection.
Dr. Okida, Dr. Lo Menzo, and Dr. Kothari disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Sleepless nights, hair loss, and cracked teeth: Pandemic stress takes its toll
In late March, shortly after New York state closed nonessential businesses and asked people to stay home, Ashley Laderer began waking each morning with a throbbing headache.
“The pressure was so intense it felt like my head was going to explode,” recalled the 27-year-old freelance writer from Long Island.
She tried spending less time on the computer and taking over-the-counter pain medication, but the pounding kept breaking through – a constant drumbeat to accompany her equally incessant worries about COVID-19.
“Every day I lived in fear that I was going to get it and I was going to infect my whole family,” she said.
After a month and a half, Ms. Laderer decided to visit a neurologist, who ordered an MRI. But the doctor found no physical cause. The scan was clear.
Then he asked: “Are you under a lot of stress?”
excruciating headaches, episodes of hair loss, upset stomach for weeks on end, sudden outbreaks of shingles, and flare-ups of autoimmune disorders. The disparate symptoms, often in otherwise-healthy individuals, have puzzled doctors and patients alike, sometimes resulting in a series of visits to specialists with few answers. But it turns out there’s a common thread among many of these conditions, one that has been months in the making: chronic stress.
Although people often underestimate the influence of the mind on the body, a growing catalog of research shows that high levels of stress over an extended time can drastically alter physical function and affect nearly every organ system.
Now, at least 8 months into the pandemic, alongside a divisive election cycle and racial unrest, those effects are showing up in a variety of symptoms.
“The mental health component of COVID is starting to come like a tsunami,” said Jennifer Love, MD, a California-based psychiatrist and coauthor of an upcoming book on how to heal from chronic stress.
Nationwide, surveys have found increasing rates of depression, anxiety and suicidal thoughts during the pandemic. But many medical experts said it’s too soon to measure the related physical symptoms, since they generally appear months after the stress begins.
Still, some early research, such as a small Chinese study and an online survey of more than 500 people in Turkey, points to an uptick.
In the United States, data from FAIR Health, a nonprofit database that provides cost information to the health industry and consumers, showed slight to moderate increases in the percentage of medical claims related to conditions triggered or exacerbated by stress, like multiple sclerosis and shingles. The portion of claims for the autoimmune disease lupus, for example, showed one of the biggest increases – 12% this year – compared with the same period last year (January to August).
Express Scripts, a major pharmacy benefit manager, reported that prescriptions for anti-insomnia medications increased 15% early in the pandemic.
Perhaps the strongest indicator comes from doctors reporting a growing number of patients with physical symptoms for which they can’t determine a cause.
Shilpi Khetarpal, MD, a dermatologist at the Cleveland Clinic, used to see about five patients a week with stress-related hair loss. Since mid-June, that number has jumped to 20 or 25. Mostly women, ages 20-80, are reporting hair coming out in fistfuls, Dr. Khetarpal said.
In Houston, at least a dozen patients have told fertility specialist Rashmi Kudesia, MD, they’re having irregular menstrual cycles, changes in cervical discharge and breast tenderness, despite normal hormone levels.
Stress is also the culprit dentists are pointing to for the rapid increase in patients with teeth grinding, teeth fractures, and temporomandibular joint dysfunction.
“We, as humans, like to have the idea that we are in control of our minds and that stress isn’t a big deal,” Dr. Love said. “But it’s simply not true.”
How mental stress becomes physical
Stress causes physical changes in the body that can affect nearly every organ system.
Although symptoms of chronic stress are often dismissed as being in one’s head, the pain is very real, said Kate Harkness, PhD, a professor of psychology and psychiatry at Queen’s University, Kingston, Ont.
When the body feels unsafe – whether it’s a physical threat of attack or a psychological fear of losing a job or catching a disease – the brain signals adrenal glands to pump stress hormones. Adrenaline and cortisol flood the body, activating the fight-or-flight response. They also disrupt bodily functions that aren’t necessary for immediate survival, like digestion and reproduction.
When the danger is over, the hormones return to normal levels. But during times of chronic stress, like a pandemic, the body keeps pumping out stress hormones until it tires itself out. This leads to increased inflammation throughout the body and brain, and a poorly functioning immune system.
Studies link chronic stress to heart disease, muscle tension, gastrointestinal issues and even physical shrinking of the hippocampus, an area of the brain associated with memory and learning. As the immune system acts up, some people can even develop new allergic reactions, Dr. Harkness said.
The good news is that many of these symptoms are reversible. But it’s important to recognize them early, especially when it comes to the brain, said Barbara Sahakian, FBA, FMedSci, a professor of clinical neuropsychology at the University of Cambridge (England).
“The brain is plastic, so we can to some extent modify it,” Dr. Sahakian said. “But we don’t know if there’s a cliff beyond which you can’t reverse a change. So the sooner you catch something, the better.”
The day-to-day impact
In some ways, mental health awareness has increased during the pandemic. TV shows are flush with ads for therapy and meditation apps, like Talkspace and Calm, and companies are announcing mental health days off for staff. But those spurts of attention fail to reveal the full impact of poor mental health on people’s daily lives.
For Alex Kostka, pandemic-related stress has brought on mood swings, nightmares, and jaw pain.
He’d been working at a Whole Foods coffee bar in New York City for only about a month before the pandemic hit, suddenly anointing him an essential worker. As deaths in the city soared, Mr. Kostka continued riding the subway to work, interacting with coworkers in the store and working longer hours for just a $2-per-hour wage increase. (Months later, he’d get a $500 bonus.) It left the 28-year-old feeling constantly unsafe and helpless.
“It was hard not to break down on the subway the minute I got on it,” Mr. Kostka said.
Soon he began waking in the middle of the night with pain from clenching his jaw so tightly. Often his teeth grinding and chomping were loud enough to wake his girlfriend.
Mr. Kostka tried Talkspace, but found texting about his troubles felt impersonal. By the end of the summer, he decided to start using the seven free counseling sessions offered by his employer. That’s helped, he said. But as the sessions run out, he worries the symptoms might return if he’s unable to find a new therapist covered by his insurance.
“Eventually, I will be able to leave this behind me, but it will take time,” Mr. Kostka said. “I’m still very much a work in progress.”
How to mitigate chronic stress
When it comes to chronic stress, seeing a doctor for stomach pain, headaches, or skin rashes may address those physical symptoms. But the root cause is mental, medical experts said.
That means the solution will often involve stress-management techniques. And there’s plenty we can do to feel better:
- Exercise. Even low- to moderate-intensity physical activity can help counteract stress-induced inflammation in the body. It can also increase neuronal connections in the brain.
- Meditation and mindfulness. Research shows this can lead to positive, structural, and functional changes in the brain.
- Fostering social connections. Talking to family and friends, even virtually, or staring into a pet’s eyes can release a hormone that may counteract inflammation.
- Learning something new. Whether it’s a formal class or taking up a casual hobby, learning supports brain plasticity, the ability to change and adapt as a result of experience, which can be protective against depression and other mental illness.
“We shouldn’t think of this stressful situation as a negative sentence for the brain,” said Dr. Harkness. “Because stress changes the brain, that means positive stuff can change the brain, too. And there is plenty we can do to help ourselves feel better in the face of adversity.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In late March, shortly after New York state closed nonessential businesses and asked people to stay home, Ashley Laderer began waking each morning with a throbbing headache.
“The pressure was so intense it felt like my head was going to explode,” recalled the 27-year-old freelance writer from Long Island.
She tried spending less time on the computer and taking over-the-counter pain medication, but the pounding kept breaking through – a constant drumbeat to accompany her equally incessant worries about COVID-19.
“Every day I lived in fear that I was going to get it and I was going to infect my whole family,” she said.
After a month and a half, Ms. Laderer decided to visit a neurologist, who ordered an MRI. But the doctor found no physical cause. The scan was clear.
Then he asked: “Are you under a lot of stress?”
excruciating headaches, episodes of hair loss, upset stomach for weeks on end, sudden outbreaks of shingles, and flare-ups of autoimmune disorders. The disparate symptoms, often in otherwise-healthy individuals, have puzzled doctors and patients alike, sometimes resulting in a series of visits to specialists with few answers. But it turns out there’s a common thread among many of these conditions, one that has been months in the making: chronic stress.
Although people often underestimate the influence of the mind on the body, a growing catalog of research shows that high levels of stress over an extended time can drastically alter physical function and affect nearly every organ system.
Now, at least 8 months into the pandemic, alongside a divisive election cycle and racial unrest, those effects are showing up in a variety of symptoms.
“The mental health component of COVID is starting to come like a tsunami,” said Jennifer Love, MD, a California-based psychiatrist and coauthor of an upcoming book on how to heal from chronic stress.
Nationwide, surveys have found increasing rates of depression, anxiety and suicidal thoughts during the pandemic. But many medical experts said it’s too soon to measure the related physical symptoms, since they generally appear months after the stress begins.
Still, some early research, such as a small Chinese study and an online survey of more than 500 people in Turkey, points to an uptick.
In the United States, data from FAIR Health, a nonprofit database that provides cost information to the health industry and consumers, showed slight to moderate increases in the percentage of medical claims related to conditions triggered or exacerbated by stress, like multiple sclerosis and shingles. The portion of claims for the autoimmune disease lupus, for example, showed one of the biggest increases – 12% this year – compared with the same period last year (January to August).
Express Scripts, a major pharmacy benefit manager, reported that prescriptions for anti-insomnia medications increased 15% early in the pandemic.
Perhaps the strongest indicator comes from doctors reporting a growing number of patients with physical symptoms for which they can’t determine a cause.
Shilpi Khetarpal, MD, a dermatologist at the Cleveland Clinic, used to see about five patients a week with stress-related hair loss. Since mid-June, that number has jumped to 20 or 25. Mostly women, ages 20-80, are reporting hair coming out in fistfuls, Dr. Khetarpal said.
In Houston, at least a dozen patients have told fertility specialist Rashmi Kudesia, MD, they’re having irregular menstrual cycles, changes in cervical discharge and breast tenderness, despite normal hormone levels.
Stress is also the culprit dentists are pointing to for the rapid increase in patients with teeth grinding, teeth fractures, and temporomandibular joint dysfunction.
“We, as humans, like to have the idea that we are in control of our minds and that stress isn’t a big deal,” Dr. Love said. “But it’s simply not true.”
How mental stress becomes physical
Stress causes physical changes in the body that can affect nearly every organ system.
Although symptoms of chronic stress are often dismissed as being in one’s head, the pain is very real, said Kate Harkness, PhD, a professor of psychology and psychiatry at Queen’s University, Kingston, Ont.
When the body feels unsafe – whether it’s a physical threat of attack or a psychological fear of losing a job or catching a disease – the brain signals adrenal glands to pump stress hormones. Adrenaline and cortisol flood the body, activating the fight-or-flight response. They also disrupt bodily functions that aren’t necessary for immediate survival, like digestion and reproduction.
When the danger is over, the hormones return to normal levels. But during times of chronic stress, like a pandemic, the body keeps pumping out stress hormones until it tires itself out. This leads to increased inflammation throughout the body and brain, and a poorly functioning immune system.
Studies link chronic stress to heart disease, muscle tension, gastrointestinal issues and even physical shrinking of the hippocampus, an area of the brain associated with memory and learning. As the immune system acts up, some people can even develop new allergic reactions, Dr. Harkness said.
The good news is that many of these symptoms are reversible. But it’s important to recognize them early, especially when it comes to the brain, said Barbara Sahakian, FBA, FMedSci, a professor of clinical neuropsychology at the University of Cambridge (England).
“The brain is plastic, so we can to some extent modify it,” Dr. Sahakian said. “But we don’t know if there’s a cliff beyond which you can’t reverse a change. So the sooner you catch something, the better.”
The day-to-day impact
In some ways, mental health awareness has increased during the pandemic. TV shows are flush with ads for therapy and meditation apps, like Talkspace and Calm, and companies are announcing mental health days off for staff. But those spurts of attention fail to reveal the full impact of poor mental health on people’s daily lives.
For Alex Kostka, pandemic-related stress has brought on mood swings, nightmares, and jaw pain.
He’d been working at a Whole Foods coffee bar in New York City for only about a month before the pandemic hit, suddenly anointing him an essential worker. As deaths in the city soared, Mr. Kostka continued riding the subway to work, interacting with coworkers in the store and working longer hours for just a $2-per-hour wage increase. (Months later, he’d get a $500 bonus.) It left the 28-year-old feeling constantly unsafe and helpless.
“It was hard not to break down on the subway the minute I got on it,” Mr. Kostka said.
Soon he began waking in the middle of the night with pain from clenching his jaw so tightly. Often his teeth grinding and chomping were loud enough to wake his girlfriend.
Mr. Kostka tried Talkspace, but found texting about his troubles felt impersonal. By the end of the summer, he decided to start using the seven free counseling sessions offered by his employer. That’s helped, he said. But as the sessions run out, he worries the symptoms might return if he’s unable to find a new therapist covered by his insurance.
“Eventually, I will be able to leave this behind me, but it will take time,” Mr. Kostka said. “I’m still very much a work in progress.”
How to mitigate chronic stress
When it comes to chronic stress, seeing a doctor for stomach pain, headaches, or skin rashes may address those physical symptoms. But the root cause is mental, medical experts said.
That means the solution will often involve stress-management techniques. And there’s plenty we can do to feel better:
- Exercise. Even low- to moderate-intensity physical activity can help counteract stress-induced inflammation in the body. It can also increase neuronal connections in the brain.
- Meditation and mindfulness. Research shows this can lead to positive, structural, and functional changes in the brain.
- Fostering social connections. Talking to family and friends, even virtually, or staring into a pet’s eyes can release a hormone that may counteract inflammation.
- Learning something new. Whether it’s a formal class or taking up a casual hobby, learning supports brain plasticity, the ability to change and adapt as a result of experience, which can be protective against depression and other mental illness.
“We shouldn’t think of this stressful situation as a negative sentence for the brain,” said Dr. Harkness. “Because stress changes the brain, that means positive stuff can change the brain, too. And there is plenty we can do to help ourselves feel better in the face of adversity.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In late March, shortly after New York state closed nonessential businesses and asked people to stay home, Ashley Laderer began waking each morning with a throbbing headache.
“The pressure was so intense it felt like my head was going to explode,” recalled the 27-year-old freelance writer from Long Island.
She tried spending less time on the computer and taking over-the-counter pain medication, but the pounding kept breaking through – a constant drumbeat to accompany her equally incessant worries about COVID-19.
“Every day I lived in fear that I was going to get it and I was going to infect my whole family,” she said.
After a month and a half, Ms. Laderer decided to visit a neurologist, who ordered an MRI. But the doctor found no physical cause. The scan was clear.
Then he asked: “Are you under a lot of stress?”
excruciating headaches, episodes of hair loss, upset stomach for weeks on end, sudden outbreaks of shingles, and flare-ups of autoimmune disorders. The disparate symptoms, often in otherwise-healthy individuals, have puzzled doctors and patients alike, sometimes resulting in a series of visits to specialists with few answers. But it turns out there’s a common thread among many of these conditions, one that has been months in the making: chronic stress.
Although people often underestimate the influence of the mind on the body, a growing catalog of research shows that high levels of stress over an extended time can drastically alter physical function and affect nearly every organ system.
Now, at least 8 months into the pandemic, alongside a divisive election cycle and racial unrest, those effects are showing up in a variety of symptoms.
“The mental health component of COVID is starting to come like a tsunami,” said Jennifer Love, MD, a California-based psychiatrist and coauthor of an upcoming book on how to heal from chronic stress.
Nationwide, surveys have found increasing rates of depression, anxiety and suicidal thoughts during the pandemic. But many medical experts said it’s too soon to measure the related physical symptoms, since they generally appear months after the stress begins.
Still, some early research, such as a small Chinese study and an online survey of more than 500 people in Turkey, points to an uptick.
In the United States, data from FAIR Health, a nonprofit database that provides cost information to the health industry and consumers, showed slight to moderate increases in the percentage of medical claims related to conditions triggered or exacerbated by stress, like multiple sclerosis and shingles. The portion of claims for the autoimmune disease lupus, for example, showed one of the biggest increases – 12% this year – compared with the same period last year (January to August).
Express Scripts, a major pharmacy benefit manager, reported that prescriptions for anti-insomnia medications increased 15% early in the pandemic.
Perhaps the strongest indicator comes from doctors reporting a growing number of patients with physical symptoms for which they can’t determine a cause.
Shilpi Khetarpal, MD, a dermatologist at the Cleveland Clinic, used to see about five patients a week with stress-related hair loss. Since mid-June, that number has jumped to 20 or 25. Mostly women, ages 20-80, are reporting hair coming out in fistfuls, Dr. Khetarpal said.
In Houston, at least a dozen patients have told fertility specialist Rashmi Kudesia, MD, they’re having irregular menstrual cycles, changes in cervical discharge and breast tenderness, despite normal hormone levels.
Stress is also the culprit dentists are pointing to for the rapid increase in patients with teeth grinding, teeth fractures, and temporomandibular joint dysfunction.
“We, as humans, like to have the idea that we are in control of our minds and that stress isn’t a big deal,” Dr. Love said. “But it’s simply not true.”
How mental stress becomes physical
Stress causes physical changes in the body that can affect nearly every organ system.
Although symptoms of chronic stress are often dismissed as being in one’s head, the pain is very real, said Kate Harkness, PhD, a professor of psychology and psychiatry at Queen’s University, Kingston, Ont.
When the body feels unsafe – whether it’s a physical threat of attack or a psychological fear of losing a job or catching a disease – the brain signals adrenal glands to pump stress hormones. Adrenaline and cortisol flood the body, activating the fight-or-flight response. They also disrupt bodily functions that aren’t necessary for immediate survival, like digestion and reproduction.
When the danger is over, the hormones return to normal levels. But during times of chronic stress, like a pandemic, the body keeps pumping out stress hormones until it tires itself out. This leads to increased inflammation throughout the body and brain, and a poorly functioning immune system.
Studies link chronic stress to heart disease, muscle tension, gastrointestinal issues and even physical shrinking of the hippocampus, an area of the brain associated with memory and learning. As the immune system acts up, some people can even develop new allergic reactions, Dr. Harkness said.
The good news is that many of these symptoms are reversible. But it’s important to recognize them early, especially when it comes to the brain, said Barbara Sahakian, FBA, FMedSci, a professor of clinical neuropsychology at the University of Cambridge (England).
“The brain is plastic, so we can to some extent modify it,” Dr. Sahakian said. “But we don’t know if there’s a cliff beyond which you can’t reverse a change. So the sooner you catch something, the better.”
The day-to-day impact
In some ways, mental health awareness has increased during the pandemic. TV shows are flush with ads for therapy and meditation apps, like Talkspace and Calm, and companies are announcing mental health days off for staff. But those spurts of attention fail to reveal the full impact of poor mental health on people’s daily lives.
For Alex Kostka, pandemic-related stress has brought on mood swings, nightmares, and jaw pain.
He’d been working at a Whole Foods coffee bar in New York City for only about a month before the pandemic hit, suddenly anointing him an essential worker. As deaths in the city soared, Mr. Kostka continued riding the subway to work, interacting with coworkers in the store and working longer hours for just a $2-per-hour wage increase. (Months later, he’d get a $500 bonus.) It left the 28-year-old feeling constantly unsafe and helpless.
“It was hard not to break down on the subway the minute I got on it,” Mr. Kostka said.
Soon he began waking in the middle of the night with pain from clenching his jaw so tightly. Often his teeth grinding and chomping were loud enough to wake his girlfriend.
Mr. Kostka tried Talkspace, but found texting about his troubles felt impersonal. By the end of the summer, he decided to start using the seven free counseling sessions offered by his employer. That’s helped, he said. But as the sessions run out, he worries the symptoms might return if he’s unable to find a new therapist covered by his insurance.
“Eventually, I will be able to leave this behind me, but it will take time,” Mr. Kostka said. “I’m still very much a work in progress.”
How to mitigate chronic stress
When it comes to chronic stress, seeing a doctor for stomach pain, headaches, or skin rashes may address those physical symptoms. But the root cause is mental, medical experts said.
That means the solution will often involve stress-management techniques. And there’s plenty we can do to feel better:
- Exercise. Even low- to moderate-intensity physical activity can help counteract stress-induced inflammation in the body. It can also increase neuronal connections in the brain.
- Meditation and mindfulness. Research shows this can lead to positive, structural, and functional changes in the brain.
- Fostering social connections. Talking to family and friends, even virtually, or staring into a pet’s eyes can release a hormone that may counteract inflammation.
- Learning something new. Whether it’s a formal class or taking up a casual hobby, learning supports brain plasticity, the ability to change and adapt as a result of experience, which can be protective against depression and other mental illness.
“We shouldn’t think of this stressful situation as a negative sentence for the brain,” said Dr. Harkness. “Because stress changes the brain, that means positive stuff can change the brain, too. And there is plenty we can do to help ourselves feel better in the face of adversity.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Survey: Doctors lonely, burned out in COVID-19
Patrick Ross, MD, a critical care physician at Children’s Hospital of Los Angeles, was plagued with increasing worry about his health and that of his family, patients, and colleagues. While distancing from his wife and daughter, he became terrified of falling ill and dying alone.
As he grew more anxious, Ross withdrew from family, colleagues, and friends, although his clinical and academic responsibilities were unaffected. He barely ate; his weight plummeted, and he began to have suicidal thoughts.
Rebecca Margolis, DO, a pediatric anesthesiologist whom Ross was mentoring, noticed something was amiss and suggested that he go to a therapist. That suggestion may have saved him.
“Once I started therapy, I no longer had suicidal ideations, but I still remained anxious on a day-to-day basis,” said Ross, who is an associate professor of clinical anesthesiology and pediatrics at the University of Southern California, Los Angeles. “As soon as I learned to manage or mitigate the anxiety, I was no longer consumed to the degree I had been by the sense of day-to-day threat.”
Ross openly shares his story because “many other physicians may be going through versions of what I experienced, and I want to encourage them to get help if they’re feeling stressed, anxious, lonely, depressed, or burned out, and to recognize that they are not alone.”
Physicians feel a sense of betrayal
Ross’ experience, although extreme, is not unique. According to a Medscape survey of almost 7,500 physicians, about two-thirds (64%) of U.S. physicians reported experiencing more intense burnout, and close to half (46%) reported feeling more lonely and isolated during the pandemic.
“We know that stress, which was already significant in physicians, has increased dramatically for many physicians during the pandemic. That’s understandable, given the circumstances they’ve been working under,” said Christine A. Sinsky, MD, vice president of professional satisfaction at the American Medical Association.
Physicians are stressed about potentially contracting the virus or infecting family members; being overworked and fatigued; witnessing wrenching scenes of patients dying alone; grieving the loss of patients, colleagues, or family members; and sometimes lacking adequate personal protective equipment (PPE), she said.
Lack of PPE has been identified as one of the most significant contributors to burnout and stress among physicians and other health care professionals. In all eight countries surveyed by Medscape, a significant number of respondents reported lacking appropriate PPE “sometimes,” “often,” or “always” when treating COVID-19 patients. Only 54% of U.S. respondents said they were always adequately protected.
The PPE shortage not only jeopardizes physical health but also has a negative effect on mental health and morale. A U.S.-based rheumatologist said, “The fact that we were sent to take care of infectious patients without proper PPE makes me feel we were betrayed in this fight.”
Not what they signed up for
Many physicians expressed fear regarding their personal safety, but that was often superseded by concern for family – especially elderly relatives or young children. (Medscape’s survey found that 9% of US respondents had immediate family members who had been diagnosed with COVID-19.)
Larissa Thomas, MD, MPH, University of California, San Francisco, said her greatest fear was bringing the virus home to her new baby and other vulnerable family members. Thomas is associate clinical professor of medicine and is a faculty hospitalist at Zuckerberg San Francisco General Hospital.
“Although physicians assume risk in our work, we didn’t sign up to care for patients without adequate protection, and our families certainly didn’t sign up for that risk, so the concern was acutely stressful,” said Thomas, who is also associate program director for the UCSF Internal Medicine Residency Program and is director of well-being for UCSF Graduate Medical Education.
The impact of stay-at-home restrictions on family members’ mental health also affected many physicians.
David Marcus, MD, residency director of the Combined Program in Emergency/Internal/Critical Care Medicine and chair of the GME Physician Wellbeing Committee at Northwell Health, Long Island, New York, said that a large stressor during the pandemic was having an elderly father with multiple comorbidities who lived alone and was unable to go out because of stay-at-home restrictions.
“I was worried not only for his physical health but also that his cognition might slip due to lack of socialization,” said Marcus.
Marcus was also worried about his preschool-age daughter, who seemed to be regressing and becoming desocialized from no longer being at school. “Fortunately, school has reopened, but it was a constant weight on my wife and me to see the impact of the lockdown on her development,” he said.
New situations create more anxiety
Being redeployed to new clinical roles in settings such as the emergency department or intensive care, which were not in their area of specialty, created much stress for physicians, Thomas said.
Physicians in private practice also had to adjust to new ways of practicing. In Medscape’s survey, 39% of U.S. physicians reported that their medical practice never closed during the pandemic. Keeping a practice open often meant learning to see patients virtually or becoming extremely vigilant about reducing the risk for contagion when seeing patients in person.
Relationships became more challenging
Social distancing during the pandemic had a negative effect on personal relationships for 44% of respondents, both in the United States and abroad.
One physician described her relationship with her partner as “more stressful” and argumentative. A rheumatologist reported experiencing frustration at having college-aged children living at home. Another respondent said that being with young children 24/7 left her “short-tempered,” and an emergency medicine physician respondent said she and her family were “driving each other crazy.”
Social distancing was not the only challenge to relationships. An orthopedist identified long, taxing work hours as contributing to a “decline in spousal harmony.”
On the other hand, some physicians said their relationships improved by developing shared insight. An emergency medicine physician wrote that he and his wife were “having more quarrels” but were “trying very hard and succeeding at understanding that much of this is due to the changes in our living situation.”
As a volunteer with New York City’s Medical Reserve Corps, Wilfrid Noel Raby, PhD, MD, adjunct clinical professor of psychiatry, Albert Einstein College of Medicine, New York City, chose to keep his Teaneck, New Jersey–based office open and was taking overnight shifts at Lincoln Hospital in New York City during the acute physician shortage. “After my regular hospital job treating psychiatric patients and seeing patients in my private practice, I sometimes pulled 12-hour nights caring for very ill patients. It was grueling, and I came home drained and exhausted,” he recalled.
Raby’s wife, a surgical nurse, had been redeployed to care for COVID-19 patients in the ICU – a situation she found grueling as well. Adding to the stress were the “rigorous distancing and sanitation precautions we needed to practice at home.” Fear of contagion, together with exhaustion, resulted in “occasional moments of friction,” Raby acknowledged.
Still, some physicians managed to find a bit of a silver lining. “We tried to relax, get as much sleep as possible, and keep things simple, not taking on extra tasks that could be postponed,” Raby said. “It helped that we both recognized how difficult it was to reassure each other when we were stressed and scared, so we faced the crisis together, and I think it ultimately brought us closer.”
Thomas said that the pandemic has helped her to recognize what she can and cannot control and how to take things one day at a time.
“When my husband and I can both work from home, we are grateful to have that ability and grateful for the things that we do have. These small moments of gratitude have sustained us day to day,” Thomas said.
Socializing outside the box
Several physicians expressed a sense of loneliness because stay-at-home guidelines and social distancing prevented them from socializing with friends. In all countries, physician respondents to the Medscape survey reported feeling “more lonely” than prior to the pandemic. Over half (51%) of Portuguese physicians reported feeling lonelier; 48% of physicians in Brazil felt that way. The United States came in third, at 46%.
Many physicians feel cut off, even from other physicians, and are reluctant to share feelings of distress.
“Talking to colleagues about distress is an important human connection,” Margolis emphasized. “We need to rely on each other to commiserate and receive validation and comfort.”
Some institutions have formalized this process by instituting a “battle buddy” model – a term borrowed from the military – which involves pairing clinicians of similar specialty, career stage, and life circumstances to provide mutual peer support, Margolis said. A partner who notices concerning signs in the other partner can refer the person to resources for help.
Sinsky said that an organization called PeerRxMed offers physicians a chance to sign up for a “buddy,” even outside their own institution.
The importance of ‘fixing’ the workplace
Close to half (43%) of U.S. respondents to Medscape’s survey reported that their workplace offers activities to help physicians deal with grief and stress, but 39% said that their workplace does not offer this type of support, and 18% were not sure whether these services were offered.
At times of crisis, organizations need to offer “stress first aid,” Sinsky said. This includes providing for basic needs, such as child care, transportation, and healthy food, and having “open, transparent, and honest communication” from leadership regarding what is known and not known about the pandemic, clinician responsibilities, and stress reduction measures.
Marcus notes that, at his institution, psychiatric residents and other members of the psychiatry department have “stepped up and crafted process groups and peer support contexts to debrief, engage, explore productive outlets for feelings, and facilitate communication.” In particular, residents have found cognitive-behavioral therapy to be useful.
Despite the difficult situation, seeking help can be challenging for some physicians. One reason, Marcus says, is that doctors tend to think of themselves as being at the giving rather than the receiving end of help – especially during a crisis. “We do what we need to do, and we often don’t see the toll it takes on us,” he noted. Moreover, the pressure to be at the “giving” end can lead to stigma in acknowledging vulnerability.
Ross said he hopes his story will help to destigmatize reaching out for help. “It is possible that a silver lining of this terrible crisis is to normalize physicians receiving help for mental health issues.”
Marcus likewise openly shares his own experiences about struggles with burnout and depressive symptoms. “As a physician educator, I think it’s important for me to be public about these things, which validates help-seeking for residents and colleagues.”
For physicians seeking help not offered in their workplace, the Physician Support Line is a useful resource, added Margolis. She noted that its services are free and confidential.
This article first appeared on Medscape.com.
Patrick Ross, MD, a critical care physician at Children’s Hospital of Los Angeles, was plagued with increasing worry about his health and that of his family, patients, and colleagues. While distancing from his wife and daughter, he became terrified of falling ill and dying alone.
As he grew more anxious, Ross withdrew from family, colleagues, and friends, although his clinical and academic responsibilities were unaffected. He barely ate; his weight plummeted, and he began to have suicidal thoughts.
Rebecca Margolis, DO, a pediatric anesthesiologist whom Ross was mentoring, noticed something was amiss and suggested that he go to a therapist. That suggestion may have saved him.
“Once I started therapy, I no longer had suicidal ideations, but I still remained anxious on a day-to-day basis,” said Ross, who is an associate professor of clinical anesthesiology and pediatrics at the University of Southern California, Los Angeles. “As soon as I learned to manage or mitigate the anxiety, I was no longer consumed to the degree I had been by the sense of day-to-day threat.”
Ross openly shares his story because “many other physicians may be going through versions of what I experienced, and I want to encourage them to get help if they’re feeling stressed, anxious, lonely, depressed, or burned out, and to recognize that they are not alone.”
Physicians feel a sense of betrayal
Ross’ experience, although extreme, is not unique. According to a Medscape survey of almost 7,500 physicians, about two-thirds (64%) of U.S. physicians reported experiencing more intense burnout, and close to half (46%) reported feeling more lonely and isolated during the pandemic.
“We know that stress, which was already significant in physicians, has increased dramatically for many physicians during the pandemic. That’s understandable, given the circumstances they’ve been working under,” said Christine A. Sinsky, MD, vice president of professional satisfaction at the American Medical Association.
Physicians are stressed about potentially contracting the virus or infecting family members; being overworked and fatigued; witnessing wrenching scenes of patients dying alone; grieving the loss of patients, colleagues, or family members; and sometimes lacking adequate personal protective equipment (PPE), she said.
Lack of PPE has been identified as one of the most significant contributors to burnout and stress among physicians and other health care professionals. In all eight countries surveyed by Medscape, a significant number of respondents reported lacking appropriate PPE “sometimes,” “often,” or “always” when treating COVID-19 patients. Only 54% of U.S. respondents said they were always adequately protected.
The PPE shortage not only jeopardizes physical health but also has a negative effect on mental health and morale. A U.S.-based rheumatologist said, “The fact that we were sent to take care of infectious patients without proper PPE makes me feel we were betrayed in this fight.”
Not what they signed up for
Many physicians expressed fear regarding their personal safety, but that was often superseded by concern for family – especially elderly relatives or young children. (Medscape’s survey found that 9% of US respondents had immediate family members who had been diagnosed with COVID-19.)
Larissa Thomas, MD, MPH, University of California, San Francisco, said her greatest fear was bringing the virus home to her new baby and other vulnerable family members. Thomas is associate clinical professor of medicine and is a faculty hospitalist at Zuckerberg San Francisco General Hospital.
“Although physicians assume risk in our work, we didn’t sign up to care for patients without adequate protection, and our families certainly didn’t sign up for that risk, so the concern was acutely stressful,” said Thomas, who is also associate program director for the UCSF Internal Medicine Residency Program and is director of well-being for UCSF Graduate Medical Education.
The impact of stay-at-home restrictions on family members’ mental health also affected many physicians.
David Marcus, MD, residency director of the Combined Program in Emergency/Internal/Critical Care Medicine and chair of the GME Physician Wellbeing Committee at Northwell Health, Long Island, New York, said that a large stressor during the pandemic was having an elderly father with multiple comorbidities who lived alone and was unable to go out because of stay-at-home restrictions.
“I was worried not only for his physical health but also that his cognition might slip due to lack of socialization,” said Marcus.
Marcus was also worried about his preschool-age daughter, who seemed to be regressing and becoming desocialized from no longer being at school. “Fortunately, school has reopened, but it was a constant weight on my wife and me to see the impact of the lockdown on her development,” he said.
New situations create more anxiety
Being redeployed to new clinical roles in settings such as the emergency department or intensive care, which were not in their area of specialty, created much stress for physicians, Thomas said.
Physicians in private practice also had to adjust to new ways of practicing. In Medscape’s survey, 39% of U.S. physicians reported that their medical practice never closed during the pandemic. Keeping a practice open often meant learning to see patients virtually or becoming extremely vigilant about reducing the risk for contagion when seeing patients in person.
Relationships became more challenging
Social distancing during the pandemic had a negative effect on personal relationships for 44% of respondents, both in the United States and abroad.
One physician described her relationship with her partner as “more stressful” and argumentative. A rheumatologist reported experiencing frustration at having college-aged children living at home. Another respondent said that being with young children 24/7 left her “short-tempered,” and an emergency medicine physician respondent said she and her family were “driving each other crazy.”
Social distancing was not the only challenge to relationships. An orthopedist identified long, taxing work hours as contributing to a “decline in spousal harmony.”
On the other hand, some physicians said their relationships improved by developing shared insight. An emergency medicine physician wrote that he and his wife were “having more quarrels” but were “trying very hard and succeeding at understanding that much of this is due to the changes in our living situation.”
As a volunteer with New York City’s Medical Reserve Corps, Wilfrid Noel Raby, PhD, MD, adjunct clinical professor of psychiatry, Albert Einstein College of Medicine, New York City, chose to keep his Teaneck, New Jersey–based office open and was taking overnight shifts at Lincoln Hospital in New York City during the acute physician shortage. “After my regular hospital job treating psychiatric patients and seeing patients in my private practice, I sometimes pulled 12-hour nights caring for very ill patients. It was grueling, and I came home drained and exhausted,” he recalled.
Raby’s wife, a surgical nurse, had been redeployed to care for COVID-19 patients in the ICU – a situation she found grueling as well. Adding to the stress were the “rigorous distancing and sanitation precautions we needed to practice at home.” Fear of contagion, together with exhaustion, resulted in “occasional moments of friction,” Raby acknowledged.
Still, some physicians managed to find a bit of a silver lining. “We tried to relax, get as much sleep as possible, and keep things simple, not taking on extra tasks that could be postponed,” Raby said. “It helped that we both recognized how difficult it was to reassure each other when we were stressed and scared, so we faced the crisis together, and I think it ultimately brought us closer.”
Thomas said that the pandemic has helped her to recognize what she can and cannot control and how to take things one day at a time.
“When my husband and I can both work from home, we are grateful to have that ability and grateful for the things that we do have. These small moments of gratitude have sustained us day to day,” Thomas said.
Socializing outside the box
Several physicians expressed a sense of loneliness because stay-at-home guidelines and social distancing prevented them from socializing with friends. In all countries, physician respondents to the Medscape survey reported feeling “more lonely” than prior to the pandemic. Over half (51%) of Portuguese physicians reported feeling lonelier; 48% of physicians in Brazil felt that way. The United States came in third, at 46%.
Many physicians feel cut off, even from other physicians, and are reluctant to share feelings of distress.
“Talking to colleagues about distress is an important human connection,” Margolis emphasized. “We need to rely on each other to commiserate and receive validation and comfort.”
Some institutions have formalized this process by instituting a “battle buddy” model – a term borrowed from the military – which involves pairing clinicians of similar specialty, career stage, and life circumstances to provide mutual peer support, Margolis said. A partner who notices concerning signs in the other partner can refer the person to resources for help.
Sinsky said that an organization called PeerRxMed offers physicians a chance to sign up for a “buddy,” even outside their own institution.
The importance of ‘fixing’ the workplace
Close to half (43%) of U.S. respondents to Medscape’s survey reported that their workplace offers activities to help physicians deal with grief and stress, but 39% said that their workplace does not offer this type of support, and 18% were not sure whether these services were offered.
At times of crisis, organizations need to offer “stress first aid,” Sinsky said. This includes providing for basic needs, such as child care, transportation, and healthy food, and having “open, transparent, and honest communication” from leadership regarding what is known and not known about the pandemic, clinician responsibilities, and stress reduction measures.
Marcus notes that, at his institution, psychiatric residents and other members of the psychiatry department have “stepped up and crafted process groups and peer support contexts to debrief, engage, explore productive outlets for feelings, and facilitate communication.” In particular, residents have found cognitive-behavioral therapy to be useful.
Despite the difficult situation, seeking help can be challenging for some physicians. One reason, Marcus says, is that doctors tend to think of themselves as being at the giving rather than the receiving end of help – especially during a crisis. “We do what we need to do, and we often don’t see the toll it takes on us,” he noted. Moreover, the pressure to be at the “giving” end can lead to stigma in acknowledging vulnerability.
Ross said he hopes his story will help to destigmatize reaching out for help. “It is possible that a silver lining of this terrible crisis is to normalize physicians receiving help for mental health issues.”
Marcus likewise openly shares his own experiences about struggles with burnout and depressive symptoms. “As a physician educator, I think it’s important for me to be public about these things, which validates help-seeking for residents and colleagues.”
For physicians seeking help not offered in their workplace, the Physician Support Line is a useful resource, added Margolis. She noted that its services are free and confidential.
This article first appeared on Medscape.com.
Patrick Ross, MD, a critical care physician at Children’s Hospital of Los Angeles, was plagued with increasing worry about his health and that of his family, patients, and colleagues. While distancing from his wife and daughter, he became terrified of falling ill and dying alone.
As he grew more anxious, Ross withdrew from family, colleagues, and friends, although his clinical and academic responsibilities were unaffected. He barely ate; his weight plummeted, and he began to have suicidal thoughts.
Rebecca Margolis, DO, a pediatric anesthesiologist whom Ross was mentoring, noticed something was amiss and suggested that he go to a therapist. That suggestion may have saved him.
“Once I started therapy, I no longer had suicidal ideations, but I still remained anxious on a day-to-day basis,” said Ross, who is an associate professor of clinical anesthesiology and pediatrics at the University of Southern California, Los Angeles. “As soon as I learned to manage or mitigate the anxiety, I was no longer consumed to the degree I had been by the sense of day-to-day threat.”
Ross openly shares his story because “many other physicians may be going through versions of what I experienced, and I want to encourage them to get help if they’re feeling stressed, anxious, lonely, depressed, or burned out, and to recognize that they are not alone.”
Physicians feel a sense of betrayal
Ross’ experience, although extreme, is not unique. According to a Medscape survey of almost 7,500 physicians, about two-thirds (64%) of U.S. physicians reported experiencing more intense burnout, and close to half (46%) reported feeling more lonely and isolated during the pandemic.
“We know that stress, which was already significant in physicians, has increased dramatically for many physicians during the pandemic. That’s understandable, given the circumstances they’ve been working under,” said Christine A. Sinsky, MD, vice president of professional satisfaction at the American Medical Association.
Physicians are stressed about potentially contracting the virus or infecting family members; being overworked and fatigued; witnessing wrenching scenes of patients dying alone; grieving the loss of patients, colleagues, or family members; and sometimes lacking adequate personal protective equipment (PPE), she said.
Lack of PPE has been identified as one of the most significant contributors to burnout and stress among physicians and other health care professionals. In all eight countries surveyed by Medscape, a significant number of respondents reported lacking appropriate PPE “sometimes,” “often,” or “always” when treating COVID-19 patients. Only 54% of U.S. respondents said they were always adequately protected.
The PPE shortage not only jeopardizes physical health but also has a negative effect on mental health and morale. A U.S.-based rheumatologist said, “The fact that we were sent to take care of infectious patients without proper PPE makes me feel we were betrayed in this fight.”
Not what they signed up for
Many physicians expressed fear regarding their personal safety, but that was often superseded by concern for family – especially elderly relatives or young children. (Medscape’s survey found that 9% of US respondents had immediate family members who had been diagnosed with COVID-19.)
Larissa Thomas, MD, MPH, University of California, San Francisco, said her greatest fear was bringing the virus home to her new baby and other vulnerable family members. Thomas is associate clinical professor of medicine and is a faculty hospitalist at Zuckerberg San Francisco General Hospital.
“Although physicians assume risk in our work, we didn’t sign up to care for patients without adequate protection, and our families certainly didn’t sign up for that risk, so the concern was acutely stressful,” said Thomas, who is also associate program director for the UCSF Internal Medicine Residency Program and is director of well-being for UCSF Graduate Medical Education.
The impact of stay-at-home restrictions on family members’ mental health also affected many physicians.
David Marcus, MD, residency director of the Combined Program in Emergency/Internal/Critical Care Medicine and chair of the GME Physician Wellbeing Committee at Northwell Health, Long Island, New York, said that a large stressor during the pandemic was having an elderly father with multiple comorbidities who lived alone and was unable to go out because of stay-at-home restrictions.
“I was worried not only for his physical health but also that his cognition might slip due to lack of socialization,” said Marcus.
Marcus was also worried about his preschool-age daughter, who seemed to be regressing and becoming desocialized from no longer being at school. “Fortunately, school has reopened, but it was a constant weight on my wife and me to see the impact of the lockdown on her development,” he said.
New situations create more anxiety
Being redeployed to new clinical roles in settings such as the emergency department or intensive care, which were not in their area of specialty, created much stress for physicians, Thomas said.
Physicians in private practice also had to adjust to new ways of practicing. In Medscape’s survey, 39% of U.S. physicians reported that their medical practice never closed during the pandemic. Keeping a practice open often meant learning to see patients virtually or becoming extremely vigilant about reducing the risk for contagion when seeing patients in person.
Relationships became more challenging
Social distancing during the pandemic had a negative effect on personal relationships for 44% of respondents, both in the United States and abroad.
One physician described her relationship with her partner as “more stressful” and argumentative. A rheumatologist reported experiencing frustration at having college-aged children living at home. Another respondent said that being with young children 24/7 left her “short-tempered,” and an emergency medicine physician respondent said she and her family were “driving each other crazy.”
Social distancing was not the only challenge to relationships. An orthopedist identified long, taxing work hours as contributing to a “decline in spousal harmony.”
On the other hand, some physicians said their relationships improved by developing shared insight. An emergency medicine physician wrote that he and his wife were “having more quarrels” but were “trying very hard and succeeding at understanding that much of this is due to the changes in our living situation.”
As a volunteer with New York City’s Medical Reserve Corps, Wilfrid Noel Raby, PhD, MD, adjunct clinical professor of psychiatry, Albert Einstein College of Medicine, New York City, chose to keep his Teaneck, New Jersey–based office open and was taking overnight shifts at Lincoln Hospital in New York City during the acute physician shortage. “After my regular hospital job treating psychiatric patients and seeing patients in my private practice, I sometimes pulled 12-hour nights caring for very ill patients. It was grueling, and I came home drained and exhausted,” he recalled.
Raby’s wife, a surgical nurse, had been redeployed to care for COVID-19 patients in the ICU – a situation she found grueling as well. Adding to the stress were the “rigorous distancing and sanitation precautions we needed to practice at home.” Fear of contagion, together with exhaustion, resulted in “occasional moments of friction,” Raby acknowledged.
Still, some physicians managed to find a bit of a silver lining. “We tried to relax, get as much sleep as possible, and keep things simple, not taking on extra tasks that could be postponed,” Raby said. “It helped that we both recognized how difficult it was to reassure each other when we were stressed and scared, so we faced the crisis together, and I think it ultimately brought us closer.”
Thomas said that the pandemic has helped her to recognize what she can and cannot control and how to take things one day at a time.
“When my husband and I can both work from home, we are grateful to have that ability and grateful for the things that we do have. These small moments of gratitude have sustained us day to day,” Thomas said.
Socializing outside the box
Several physicians expressed a sense of loneliness because stay-at-home guidelines and social distancing prevented them from socializing with friends. In all countries, physician respondents to the Medscape survey reported feeling “more lonely” than prior to the pandemic. Over half (51%) of Portuguese physicians reported feeling lonelier; 48% of physicians in Brazil felt that way. The United States came in third, at 46%.
Many physicians feel cut off, even from other physicians, and are reluctant to share feelings of distress.
“Talking to colleagues about distress is an important human connection,” Margolis emphasized. “We need to rely on each other to commiserate and receive validation and comfort.”
Some institutions have formalized this process by instituting a “battle buddy” model – a term borrowed from the military – which involves pairing clinicians of similar specialty, career stage, and life circumstances to provide mutual peer support, Margolis said. A partner who notices concerning signs in the other partner can refer the person to resources for help.
Sinsky said that an organization called PeerRxMed offers physicians a chance to sign up for a “buddy,” even outside their own institution.
The importance of ‘fixing’ the workplace
Close to half (43%) of U.S. respondents to Medscape’s survey reported that their workplace offers activities to help physicians deal with grief and stress, but 39% said that their workplace does not offer this type of support, and 18% were not sure whether these services were offered.
At times of crisis, organizations need to offer “stress first aid,” Sinsky said. This includes providing for basic needs, such as child care, transportation, and healthy food, and having “open, transparent, and honest communication” from leadership regarding what is known and not known about the pandemic, clinician responsibilities, and stress reduction measures.
Marcus notes that, at his institution, psychiatric residents and other members of the psychiatry department have “stepped up and crafted process groups and peer support contexts to debrief, engage, explore productive outlets for feelings, and facilitate communication.” In particular, residents have found cognitive-behavioral therapy to be useful.
Despite the difficult situation, seeking help can be challenging for some physicians. One reason, Marcus says, is that doctors tend to think of themselves as being at the giving rather than the receiving end of help – especially during a crisis. “We do what we need to do, and we often don’t see the toll it takes on us,” he noted. Moreover, the pressure to be at the “giving” end can lead to stigma in acknowledging vulnerability.
Ross said he hopes his story will help to destigmatize reaching out for help. “It is possible that a silver lining of this terrible crisis is to normalize physicians receiving help for mental health issues.”
Marcus likewise openly shares his own experiences about struggles with burnout and depressive symptoms. “As a physician educator, I think it’s important for me to be public about these things, which validates help-seeking for residents and colleagues.”
For physicians seeking help not offered in their workplace, the Physician Support Line is a useful resource, added Margolis. She noted that its services are free and confidential.
This article first appeared on Medscape.com.
Fauci: Cautious optimism for COVID-19 vaccine by end of 2020
with distribution of first doses possible before the end of the year, according to Anthony S. Fauci, MD, director, National Institute of Allergy and Infectious Diseases, Bethesda, Md.
“Given the rate of infection that’s going on in this country, and the distribution of the clinical trial sites involving tens of thousands of volunteers, we project that we will have an answer as to whether or not we have a safe and effective vaccine by November or December,” Dr. Fauci said today in his virtual keynote address during the annual meeting of the American College of Chest Physicians.
“It may come earlier -- this month, in October,” he added in his remarks. “That is unlikely – it is more likely that we’ll have an answer in November and December.”
If that timing does come to pass, Dr. Fauci said, it’s possible that distribution of doses could start at the end of the year, continuing throughout the beginning and middle of 2021.
Although there are no guarantees, Dr. Fauci said he is “cautiously optimistic” regarding the timeline.
He said that his optimism is based in part on animal studies and phase 1 data that demonstrate robust neutralizing antibody responses to a vaccine that are equivalent to, if not greater than, natural infection with the SARS-CoV-2 virus that causes COVID-19.
Rapid development gives reason for hope
Ryan C. Maves, MD, FCCP, a critical care and infectious disease specialist at Naval Medical Center San Diego, said there is reason to be hopeful that a vaccine will be available by the end of the calendar year. He cautioned, however, that this timing is based on the assumption that one of the vaccines will be proven safe and effective very soon.
“We’re lucky to have multiple phase 3 trials using multiple vaccine technologies in different platforms,” Dr. Maves said in a panel discussion following Dr. Fauci’s remarks. “I think the odds are very high that one of them will be effective.”
“I’m hoping that multiple vaccines will be effective,” Dr. Maves added. “Then we’ll be in a good position of determining which is the best of several good options, as a society and as a world.”
COVID-19 vaccine development over the past year has been remarkably fast, especially given the previous record set by the mumps vaccine, which took about four years to go from initial steps to rollout, Dr. Maves noted.
Dr. Fauci said the federal government has taken a “strategic approach” to the COVID-19 vaccine that includes direct involvement in the research and development of six different vaccine candidates, five of which are now in phase 3 trials.
As part of that strategic approach, the study protocols are harmonized to have a common data and safety monitoring board, common primary and secondary endpoints, and an independent statistical group to determine correlates of protection, Dr. Fauci said.
Prioritizing COVID-19 vaccine distribution
Who gets COVID-19 vaccine first will be a challenge for governmental organizations as well as bioethicists, who have proposed different strategies for fairly prioritizing different groups for access.
Reaching communities of color will be an important consideration for prioritization, according to Dr. Maves, given the disproportionate burden of disease on Black and Hispanic individuals, among other such populations.
COVID-19–related hospitalization rates have been substantially higher in communities of color, Dr. Fauci said in his keynote address. Age-adjusted hospitalization rates for Hispanic/Latinx and Black populations are 375 to 368 per 100,000, respectively, compared with just 82 per 100,000 for White non-Hispanics, according to data from the Centers for Disease Control and Prevention.
Outreach to those communities should include building trust in those populations that they will benefit from a safe and effective vaccine, and making sure that the vaccine is available to those communities as quickly as possible, Dr. Maves said.
Dr. Fauci and Dr. Maves provided no disclosures related to their presentations.
with distribution of first doses possible before the end of the year, according to Anthony S. Fauci, MD, director, National Institute of Allergy and Infectious Diseases, Bethesda, Md.
“Given the rate of infection that’s going on in this country, and the distribution of the clinical trial sites involving tens of thousands of volunteers, we project that we will have an answer as to whether or not we have a safe and effective vaccine by November or December,” Dr. Fauci said today in his virtual keynote address during the annual meeting of the American College of Chest Physicians.
“It may come earlier -- this month, in October,” he added in his remarks. “That is unlikely – it is more likely that we’ll have an answer in November and December.”
If that timing does come to pass, Dr. Fauci said, it’s possible that distribution of doses could start at the end of the year, continuing throughout the beginning and middle of 2021.
Although there are no guarantees, Dr. Fauci said he is “cautiously optimistic” regarding the timeline.
He said that his optimism is based in part on animal studies and phase 1 data that demonstrate robust neutralizing antibody responses to a vaccine that are equivalent to, if not greater than, natural infection with the SARS-CoV-2 virus that causes COVID-19.
Rapid development gives reason for hope
Ryan C. Maves, MD, FCCP, a critical care and infectious disease specialist at Naval Medical Center San Diego, said there is reason to be hopeful that a vaccine will be available by the end of the calendar year. He cautioned, however, that this timing is based on the assumption that one of the vaccines will be proven safe and effective very soon.
“We’re lucky to have multiple phase 3 trials using multiple vaccine technologies in different platforms,” Dr. Maves said in a panel discussion following Dr. Fauci’s remarks. “I think the odds are very high that one of them will be effective.”
“I’m hoping that multiple vaccines will be effective,” Dr. Maves added. “Then we’ll be in a good position of determining which is the best of several good options, as a society and as a world.”
COVID-19 vaccine development over the past year has been remarkably fast, especially given the previous record set by the mumps vaccine, which took about four years to go from initial steps to rollout, Dr. Maves noted.
Dr. Fauci said the federal government has taken a “strategic approach” to the COVID-19 vaccine that includes direct involvement in the research and development of six different vaccine candidates, five of which are now in phase 3 trials.
As part of that strategic approach, the study protocols are harmonized to have a common data and safety monitoring board, common primary and secondary endpoints, and an independent statistical group to determine correlates of protection, Dr. Fauci said.
Prioritizing COVID-19 vaccine distribution
Who gets COVID-19 vaccine first will be a challenge for governmental organizations as well as bioethicists, who have proposed different strategies for fairly prioritizing different groups for access.
Reaching communities of color will be an important consideration for prioritization, according to Dr. Maves, given the disproportionate burden of disease on Black and Hispanic individuals, among other such populations.
COVID-19–related hospitalization rates have been substantially higher in communities of color, Dr. Fauci said in his keynote address. Age-adjusted hospitalization rates for Hispanic/Latinx and Black populations are 375 to 368 per 100,000, respectively, compared with just 82 per 100,000 for White non-Hispanics, according to data from the Centers for Disease Control and Prevention.
Outreach to those communities should include building trust in those populations that they will benefit from a safe and effective vaccine, and making sure that the vaccine is available to those communities as quickly as possible, Dr. Maves said.
Dr. Fauci and Dr. Maves provided no disclosures related to their presentations.
with distribution of first doses possible before the end of the year, according to Anthony S. Fauci, MD, director, National Institute of Allergy and Infectious Diseases, Bethesda, Md.
“Given the rate of infection that’s going on in this country, and the distribution of the clinical trial sites involving tens of thousands of volunteers, we project that we will have an answer as to whether or not we have a safe and effective vaccine by November or December,” Dr. Fauci said today in his virtual keynote address during the annual meeting of the American College of Chest Physicians.
“It may come earlier -- this month, in October,” he added in his remarks. “That is unlikely – it is more likely that we’ll have an answer in November and December.”
If that timing does come to pass, Dr. Fauci said, it’s possible that distribution of doses could start at the end of the year, continuing throughout the beginning and middle of 2021.
Although there are no guarantees, Dr. Fauci said he is “cautiously optimistic” regarding the timeline.
He said that his optimism is based in part on animal studies and phase 1 data that demonstrate robust neutralizing antibody responses to a vaccine that are equivalent to, if not greater than, natural infection with the SARS-CoV-2 virus that causes COVID-19.
Rapid development gives reason for hope
Ryan C. Maves, MD, FCCP, a critical care and infectious disease specialist at Naval Medical Center San Diego, said there is reason to be hopeful that a vaccine will be available by the end of the calendar year. He cautioned, however, that this timing is based on the assumption that one of the vaccines will be proven safe and effective very soon.
“We’re lucky to have multiple phase 3 trials using multiple vaccine technologies in different platforms,” Dr. Maves said in a panel discussion following Dr. Fauci’s remarks. “I think the odds are very high that one of them will be effective.”
“I’m hoping that multiple vaccines will be effective,” Dr. Maves added. “Then we’ll be in a good position of determining which is the best of several good options, as a society and as a world.”
COVID-19 vaccine development over the past year has been remarkably fast, especially given the previous record set by the mumps vaccine, which took about four years to go from initial steps to rollout, Dr. Maves noted.
Dr. Fauci said the federal government has taken a “strategic approach” to the COVID-19 vaccine that includes direct involvement in the research and development of six different vaccine candidates, five of which are now in phase 3 trials.
As part of that strategic approach, the study protocols are harmonized to have a common data and safety monitoring board, common primary and secondary endpoints, and an independent statistical group to determine correlates of protection, Dr. Fauci said.
Prioritizing COVID-19 vaccine distribution
Who gets COVID-19 vaccine first will be a challenge for governmental organizations as well as bioethicists, who have proposed different strategies for fairly prioritizing different groups for access.
Reaching communities of color will be an important consideration for prioritization, according to Dr. Maves, given the disproportionate burden of disease on Black and Hispanic individuals, among other such populations.
COVID-19–related hospitalization rates have been substantially higher in communities of color, Dr. Fauci said in his keynote address. Age-adjusted hospitalization rates for Hispanic/Latinx and Black populations are 375 to 368 per 100,000, respectively, compared with just 82 per 100,000 for White non-Hispanics, according to data from the Centers for Disease Control and Prevention.
Outreach to those communities should include building trust in those populations that they will benefit from a safe and effective vaccine, and making sure that the vaccine is available to those communities as quickly as possible, Dr. Maves said.
Dr. Fauci and Dr. Maves provided no disclosures related to their presentations.
FROM CHEST 2020
Survey of Mohs surgeons highlights its use in invasive melanoma
of members of the American College of Mohs Surgery.
Of 513 survey participants, 40.9% reported using MMS to treat any subtype of melanoma. Most of these surgeons reported treating both lentigo maligna (97.5%) and other melanoma in situ (MIS) subtypes (91.4%). A slight majority – 58.6% – reported treating invasive T1 melanoma, and 20.5% reported treating invasive T2 and/or higher-stage melanoma with MMS.
The analysis, published in Dermatologic Surgery, was done by Spyros M. Siscos, MD, and a team of residents and faculty in the division of dermatology at the University of Kansas Medical Center, Kansas City.
It comes on the heels of an analysis of claims data for Mohs surgery, published last year in JAMA Dermatology, which showed a more than threefold increase in the use of Mohs surgery for melanoma from 2.6% of all surgical cases in 2001 to 7.9% in 2016.
With the increased use of MMS for treatment of melanoma, “Mohs surgeons who previously treated MIS with MMS may be increasingly doing so and/or expanding their scope of treatment to include invasive melanoma,” the University of Kansas investigators wrote.
That a slight majority now report treating invasive melanoma with MMS “may be due, in part, to upstaging during the MMS procedure and the increasing evidence demonstrating improved survival of early-invasive melanoma treated with MMS compared with [wide local excision],” as well as the advent of melanocytic immunohistochemical (IHC) stains, particularly melanoma antigen recognized by T-cells 1 (MART-1), they said. However, 29% of surveyed Mohs surgeons treating melanoma with MMS do not use IHC stains “despite growing evidence supporting” their use, the authors wrote.
The advent of IHC stains, particularly MART-1, has improved the accuracy of interpreting frozen sections of melanoma, they reported, noting that MMS without IHC has been associated with a recurrence rate as high as 33%. Of the 71% who reported using IHC stains, MART-1 was the primary IHC stain for virtually all of them (97.3%).
There was also variation in the number of surgeons who reported debulking MIS. Eighty-two percent take this approach, excising the clinically visible tumor before excising the initial Mohs stage – almost all with a scalpel. More than half of these surgeons – 58.5% – submit the entire debulked MIS specimen for permanent vertical sectioning (breadloafing) to evaluate for deeper tumor invasion.
The others reported submitting the entire debulked specimen for frozen vertical sectioning, or portions of the specimen for both permanent and frozen vertical sectioning. “It is unclear why a minority of surveyed Mohs surgeons reported not debulking MIS,” wrote Dr. Siscos and his colleagues.
The average margin size of the first Mohs stage for MIS was 4.96 ± 1.74 mm, which is at the lower end of the 0.5-1.0 cm range for wide local excision (WLE) recommended by the National Comprehensive Cancer Network (NCCN) and the American Academy of Dermatology (AAD), according to a clinical practice guideline. (The survey did not investigate initial margins for invasive melanoma treated with MMS.)
Jeremy R. Etzhorn, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and an author of a 2019 claims data analysis of excisional surgery practices for melanoma, said that the new survey findings – like the prior analysis – highlight the variability in approaches to using MMS for melanoma.
“Mohs for melanoma [seems] like a one-liner ... but really, there are [a lot] of different techniques that fall under that umbrella, if you parse out all the variations,” he said in an interview.
Per the 2016 claims analysis, he noted, IHC was used in less than 40% of Mohs surgery cases for melanoma, and there were wide geographic variations. “The biggest critique of Mohs surgery for melanoma over the last two decades has been that it’s hard to see the tumor,” he said. “But with the advent of IHC, that challenge was overcome.”
Surgical excision practices are evolving without the development of best practice guidelines, said Dr. Etzkorn, who is director of clinical research for the University of Pennsylvania dermatologic oncology center. Multisociety guidelines published in 2012 on appropriate use criteria for Mohs surgery do not offer specific recommendations on the use of MMS for invasive melanoma. Nor do guidelines from the AAD and the NCCN, he said.
“What this [new] study highlights and what’s being discussed amongst Moh’s surgeons” is that Mohs for melanoma “has be to be standardized” to some extent and then clinical trials conducted comparing Mohs to conventional excision. The studies that have been published in recent years comparing MMS with WLE for MIS and invasive melanoma are “not gold standard studies,” he said.
Practice guidelines then can be informed by high-quality evidence on its safety and efficacy, he said.
The 513 participants in the newly published survey represent a 31.5% response rate. Invasive T2 and/or higher stage melanoma was more likely to be treated with MMS in academic hospitals, compared with other practice settings (30.2% v. 18.1%), Dr. Siscos and his coauthors reported.
Participants who reported treating melanoma with MMS were more likely to report fellowship exposure and more likely to have received fellowship training on melanocytic IHC stains. The study “highlights the importance of fellowship exposure to MMS and IHC staining for melanoma,” the authors wrote, adding that postfellowship training opportunities in MMS and IHC staining for melanoma may help broaden its use among Mohs surgeons who received inadequate fellowship exposure.
Dr. Siscos and his colleagues reported no significant interest with commercial supporters. Dr. Etzkorn had no disclosures.
SOURCE: Siscos S et al. Dermatol Surg. 2020 Oct;46(10):1267-71.
of members of the American College of Mohs Surgery.
Of 513 survey participants, 40.9% reported using MMS to treat any subtype of melanoma. Most of these surgeons reported treating both lentigo maligna (97.5%) and other melanoma in situ (MIS) subtypes (91.4%). A slight majority – 58.6% – reported treating invasive T1 melanoma, and 20.5% reported treating invasive T2 and/or higher-stage melanoma with MMS.
The analysis, published in Dermatologic Surgery, was done by Spyros M. Siscos, MD, and a team of residents and faculty in the division of dermatology at the University of Kansas Medical Center, Kansas City.
It comes on the heels of an analysis of claims data for Mohs surgery, published last year in JAMA Dermatology, which showed a more than threefold increase in the use of Mohs surgery for melanoma from 2.6% of all surgical cases in 2001 to 7.9% in 2016.
With the increased use of MMS for treatment of melanoma, “Mohs surgeons who previously treated MIS with MMS may be increasingly doing so and/or expanding their scope of treatment to include invasive melanoma,” the University of Kansas investigators wrote.
That a slight majority now report treating invasive melanoma with MMS “may be due, in part, to upstaging during the MMS procedure and the increasing evidence demonstrating improved survival of early-invasive melanoma treated with MMS compared with [wide local excision],” as well as the advent of melanocytic immunohistochemical (IHC) stains, particularly melanoma antigen recognized by T-cells 1 (MART-1), they said. However, 29% of surveyed Mohs surgeons treating melanoma with MMS do not use IHC stains “despite growing evidence supporting” their use, the authors wrote.
The advent of IHC stains, particularly MART-1, has improved the accuracy of interpreting frozen sections of melanoma, they reported, noting that MMS without IHC has been associated with a recurrence rate as high as 33%. Of the 71% who reported using IHC stains, MART-1 was the primary IHC stain for virtually all of them (97.3%).
There was also variation in the number of surgeons who reported debulking MIS. Eighty-two percent take this approach, excising the clinically visible tumor before excising the initial Mohs stage – almost all with a scalpel. More than half of these surgeons – 58.5% – submit the entire debulked MIS specimen for permanent vertical sectioning (breadloafing) to evaluate for deeper tumor invasion.
The others reported submitting the entire debulked specimen for frozen vertical sectioning, or portions of the specimen for both permanent and frozen vertical sectioning. “It is unclear why a minority of surveyed Mohs surgeons reported not debulking MIS,” wrote Dr. Siscos and his colleagues.
The average margin size of the first Mohs stage for MIS was 4.96 ± 1.74 mm, which is at the lower end of the 0.5-1.0 cm range for wide local excision (WLE) recommended by the National Comprehensive Cancer Network (NCCN) and the American Academy of Dermatology (AAD), according to a clinical practice guideline. (The survey did not investigate initial margins for invasive melanoma treated with MMS.)
Jeremy R. Etzhorn, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and an author of a 2019 claims data analysis of excisional surgery practices for melanoma, said that the new survey findings – like the prior analysis – highlight the variability in approaches to using MMS for melanoma.
“Mohs for melanoma [seems] like a one-liner ... but really, there are [a lot] of different techniques that fall under that umbrella, if you parse out all the variations,” he said in an interview.
Per the 2016 claims analysis, he noted, IHC was used in less than 40% of Mohs surgery cases for melanoma, and there were wide geographic variations. “The biggest critique of Mohs surgery for melanoma over the last two decades has been that it’s hard to see the tumor,” he said. “But with the advent of IHC, that challenge was overcome.”
Surgical excision practices are evolving without the development of best practice guidelines, said Dr. Etzkorn, who is director of clinical research for the University of Pennsylvania dermatologic oncology center. Multisociety guidelines published in 2012 on appropriate use criteria for Mohs surgery do not offer specific recommendations on the use of MMS for invasive melanoma. Nor do guidelines from the AAD and the NCCN, he said.
“What this [new] study highlights and what’s being discussed amongst Moh’s surgeons” is that Mohs for melanoma “has be to be standardized” to some extent and then clinical trials conducted comparing Mohs to conventional excision. The studies that have been published in recent years comparing MMS with WLE for MIS and invasive melanoma are “not gold standard studies,” he said.
Practice guidelines then can be informed by high-quality evidence on its safety and efficacy, he said.
The 513 participants in the newly published survey represent a 31.5% response rate. Invasive T2 and/or higher stage melanoma was more likely to be treated with MMS in academic hospitals, compared with other practice settings (30.2% v. 18.1%), Dr. Siscos and his coauthors reported.
Participants who reported treating melanoma with MMS were more likely to report fellowship exposure and more likely to have received fellowship training on melanocytic IHC stains. The study “highlights the importance of fellowship exposure to MMS and IHC staining for melanoma,” the authors wrote, adding that postfellowship training opportunities in MMS and IHC staining for melanoma may help broaden its use among Mohs surgeons who received inadequate fellowship exposure.
Dr. Siscos and his colleagues reported no significant interest with commercial supporters. Dr. Etzkorn had no disclosures.
SOURCE: Siscos S et al. Dermatol Surg. 2020 Oct;46(10):1267-71.
of members of the American College of Mohs Surgery.
Of 513 survey participants, 40.9% reported using MMS to treat any subtype of melanoma. Most of these surgeons reported treating both lentigo maligna (97.5%) and other melanoma in situ (MIS) subtypes (91.4%). A slight majority – 58.6% – reported treating invasive T1 melanoma, and 20.5% reported treating invasive T2 and/or higher-stage melanoma with MMS.
The analysis, published in Dermatologic Surgery, was done by Spyros M. Siscos, MD, and a team of residents and faculty in the division of dermatology at the University of Kansas Medical Center, Kansas City.
It comes on the heels of an analysis of claims data for Mohs surgery, published last year in JAMA Dermatology, which showed a more than threefold increase in the use of Mohs surgery for melanoma from 2.6% of all surgical cases in 2001 to 7.9% in 2016.
With the increased use of MMS for treatment of melanoma, “Mohs surgeons who previously treated MIS with MMS may be increasingly doing so and/or expanding their scope of treatment to include invasive melanoma,” the University of Kansas investigators wrote.
That a slight majority now report treating invasive melanoma with MMS “may be due, in part, to upstaging during the MMS procedure and the increasing evidence demonstrating improved survival of early-invasive melanoma treated with MMS compared with [wide local excision],” as well as the advent of melanocytic immunohistochemical (IHC) stains, particularly melanoma antigen recognized by T-cells 1 (MART-1), they said. However, 29% of surveyed Mohs surgeons treating melanoma with MMS do not use IHC stains “despite growing evidence supporting” their use, the authors wrote.
The advent of IHC stains, particularly MART-1, has improved the accuracy of interpreting frozen sections of melanoma, they reported, noting that MMS without IHC has been associated with a recurrence rate as high as 33%. Of the 71% who reported using IHC stains, MART-1 was the primary IHC stain for virtually all of them (97.3%).
There was also variation in the number of surgeons who reported debulking MIS. Eighty-two percent take this approach, excising the clinically visible tumor before excising the initial Mohs stage – almost all with a scalpel. More than half of these surgeons – 58.5% – submit the entire debulked MIS specimen for permanent vertical sectioning (breadloafing) to evaluate for deeper tumor invasion.
The others reported submitting the entire debulked specimen for frozen vertical sectioning, or portions of the specimen for both permanent and frozen vertical sectioning. “It is unclear why a minority of surveyed Mohs surgeons reported not debulking MIS,” wrote Dr. Siscos and his colleagues.
The average margin size of the first Mohs stage for MIS was 4.96 ± 1.74 mm, which is at the lower end of the 0.5-1.0 cm range for wide local excision (WLE) recommended by the National Comprehensive Cancer Network (NCCN) and the American Academy of Dermatology (AAD), according to a clinical practice guideline. (The survey did not investigate initial margins for invasive melanoma treated with MMS.)
Jeremy R. Etzhorn, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and an author of a 2019 claims data analysis of excisional surgery practices for melanoma, said that the new survey findings – like the prior analysis – highlight the variability in approaches to using MMS for melanoma.
“Mohs for melanoma [seems] like a one-liner ... but really, there are [a lot] of different techniques that fall under that umbrella, if you parse out all the variations,” he said in an interview.
Per the 2016 claims analysis, he noted, IHC was used in less than 40% of Mohs surgery cases for melanoma, and there were wide geographic variations. “The biggest critique of Mohs surgery for melanoma over the last two decades has been that it’s hard to see the tumor,” he said. “But with the advent of IHC, that challenge was overcome.”
Surgical excision practices are evolving without the development of best practice guidelines, said Dr. Etzkorn, who is director of clinical research for the University of Pennsylvania dermatologic oncology center. Multisociety guidelines published in 2012 on appropriate use criteria for Mohs surgery do not offer specific recommendations on the use of MMS for invasive melanoma. Nor do guidelines from the AAD and the NCCN, he said.
“What this [new] study highlights and what’s being discussed amongst Moh’s surgeons” is that Mohs for melanoma “has be to be standardized” to some extent and then clinical trials conducted comparing Mohs to conventional excision. The studies that have been published in recent years comparing MMS with WLE for MIS and invasive melanoma are “not gold standard studies,” he said.
Practice guidelines then can be informed by high-quality evidence on its safety and efficacy, he said.
The 513 participants in the newly published survey represent a 31.5% response rate. Invasive T2 and/or higher stage melanoma was more likely to be treated with MMS in academic hospitals, compared with other practice settings (30.2% v. 18.1%), Dr. Siscos and his coauthors reported.
Participants who reported treating melanoma with MMS were more likely to report fellowship exposure and more likely to have received fellowship training on melanocytic IHC stains. The study “highlights the importance of fellowship exposure to MMS and IHC staining for melanoma,” the authors wrote, adding that postfellowship training opportunities in MMS and IHC staining for melanoma may help broaden its use among Mohs surgeons who received inadequate fellowship exposure.
Dr. Siscos and his colleagues reported no significant interest with commercial supporters. Dr. Etzkorn had no disclosures.
SOURCE: Siscos S et al. Dermatol Surg. 2020 Oct;46(10):1267-71.
FROM DERMATOLOGIC SURGERY
The unsteady state
As the COVID-19 pandemic continues to chug along, some communities feel it slowing to a pace at which they might feel comfortable about a return to, if not quite “business as usual,” at least “business as sort of normal-ish.” They are ready to accept a level of disease that signals they have reached a steady state. However, in other communities, the virus has picked up speed and is threatening to overwhelm the medical infrastructure. If you are in one of those fortunate and skillfully managed states in which folks are beginning to talk seriously, but with little evidence, that it is time to return to normal, it is probably far too early.
Eons ago in pandemic terms, the World Health Organization in Thailand published a list of criteria to aid in determining when a community could consider lifting the limits that seemed to have been effective in halting transmission of the virus (“Transitioning to and maintaining a steady state of low-level or no transmission,” WHO, Thailand, 2020 Apr 18). While much more has been learned about the behavior of the virus since the spring of 2020, the criteria from the WHO in Thailand are worth considering.
Here is my summary of their criteria for returning to normalcy. First, virus transmission is controlled to the point that only sporadic cases and small clusters exist, and that all of these are traceable in origin. Second, health care and public health systems are in place with sufficient capacities to manage a shift from detection to treatment should the case load increase dramatically; this capacity should include detection, testing, isolation, and quarantine. Third, outbreaks in high-risk populations such as nursing homes have been minimized. Fourth, workplace prevention strategies are in place and have been demonstrated to be effective. Fifth, risk of imported cases is at manageable levels. Finally, communities are engaged.
It is hard to argue with the rationale behind each of these criteria. However, the United States is not Thailand, and just thinking about how this country would go about meeting those criteria provides a window into some of the reasons why we have done so poorly and will continue to be challenged in dealing with the pandemic.
First, notice that the criteria make no mention of a vaccine. One gets the sense that from the top down our country is banking too heavily on the effectiveness and widespread delivery of a vaccine. Even if and when a vaccine is developed and delivered, all of these criteria still must be met and kept in mind for a future pandemic.
Second, the criteria call for an effective health care system, but it is abundantly clear that the United States does not have a cohesive health care system and probably won’t for the foreseeable future. The best we can hope for is individual states cobbling together their own systems, which may in turn serve as examples for those states who haven’t had the foresight. We have had a public health system of sorts, but its credibility and effectiveness has been neutered to the point that again we must rely on each state’s ability to see through the haze and create it’s own systems for detection, testing, tracking, isolating, and quarantining – often with little help in materiel support from the federal government. The sliver of good news is that, after a bit of a stumbling start, detecting and limiting the importation of cases from abroad is being addressed.
We continue to hear and see evidence that there are segments of the population who are not engaged in the activities that we have learned are necessary to stabilize the pandemic. My sense is that those people represent a very small minority. But, it is probably large enough to make the route to a steady state on a national level long and painful. This unfortunately is to be expected in a country that was built on a framework of personal freedoms. The best you can hope for in achieving a steady state is to live in one of the states that seems to be achieving the fine balance between personal freedoms and the common good.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As the COVID-19 pandemic continues to chug along, some communities feel it slowing to a pace at which they might feel comfortable about a return to, if not quite “business as usual,” at least “business as sort of normal-ish.” They are ready to accept a level of disease that signals they have reached a steady state. However, in other communities, the virus has picked up speed and is threatening to overwhelm the medical infrastructure. If you are in one of those fortunate and skillfully managed states in which folks are beginning to talk seriously, but with little evidence, that it is time to return to normal, it is probably far too early.
Eons ago in pandemic terms, the World Health Organization in Thailand published a list of criteria to aid in determining when a community could consider lifting the limits that seemed to have been effective in halting transmission of the virus (“Transitioning to and maintaining a steady state of low-level or no transmission,” WHO, Thailand, 2020 Apr 18). While much more has been learned about the behavior of the virus since the spring of 2020, the criteria from the WHO in Thailand are worth considering.
Here is my summary of their criteria for returning to normalcy. First, virus transmission is controlled to the point that only sporadic cases and small clusters exist, and that all of these are traceable in origin. Second, health care and public health systems are in place with sufficient capacities to manage a shift from detection to treatment should the case load increase dramatically; this capacity should include detection, testing, isolation, and quarantine. Third, outbreaks in high-risk populations such as nursing homes have been minimized. Fourth, workplace prevention strategies are in place and have been demonstrated to be effective. Fifth, risk of imported cases is at manageable levels. Finally, communities are engaged.
It is hard to argue with the rationale behind each of these criteria. However, the United States is not Thailand, and just thinking about how this country would go about meeting those criteria provides a window into some of the reasons why we have done so poorly and will continue to be challenged in dealing with the pandemic.
First, notice that the criteria make no mention of a vaccine. One gets the sense that from the top down our country is banking too heavily on the effectiveness and widespread delivery of a vaccine. Even if and when a vaccine is developed and delivered, all of these criteria still must be met and kept in mind for a future pandemic.
Second, the criteria call for an effective health care system, but it is abundantly clear that the United States does not have a cohesive health care system and probably won’t for the foreseeable future. The best we can hope for is individual states cobbling together their own systems, which may in turn serve as examples for those states who haven’t had the foresight. We have had a public health system of sorts, but its credibility and effectiveness has been neutered to the point that again we must rely on each state’s ability to see through the haze and create it’s own systems for detection, testing, tracking, isolating, and quarantining – often with little help in materiel support from the federal government. The sliver of good news is that, after a bit of a stumbling start, detecting and limiting the importation of cases from abroad is being addressed.
We continue to hear and see evidence that there are segments of the population who are not engaged in the activities that we have learned are necessary to stabilize the pandemic. My sense is that those people represent a very small minority. But, it is probably large enough to make the route to a steady state on a national level long and painful. This unfortunately is to be expected in a country that was built on a framework of personal freedoms. The best you can hope for in achieving a steady state is to live in one of the states that seems to be achieving the fine balance between personal freedoms and the common good.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As the COVID-19 pandemic continues to chug along, some communities feel it slowing to a pace at which they might feel comfortable about a return to, if not quite “business as usual,” at least “business as sort of normal-ish.” They are ready to accept a level of disease that signals they have reached a steady state. However, in other communities, the virus has picked up speed and is threatening to overwhelm the medical infrastructure. If you are in one of those fortunate and skillfully managed states in which folks are beginning to talk seriously, but with little evidence, that it is time to return to normal, it is probably far too early.
Eons ago in pandemic terms, the World Health Organization in Thailand published a list of criteria to aid in determining when a community could consider lifting the limits that seemed to have been effective in halting transmission of the virus (“Transitioning to and maintaining a steady state of low-level or no transmission,” WHO, Thailand, 2020 Apr 18). While much more has been learned about the behavior of the virus since the spring of 2020, the criteria from the WHO in Thailand are worth considering.
Here is my summary of their criteria for returning to normalcy. First, virus transmission is controlled to the point that only sporadic cases and small clusters exist, and that all of these are traceable in origin. Second, health care and public health systems are in place with sufficient capacities to manage a shift from detection to treatment should the case load increase dramatically; this capacity should include detection, testing, isolation, and quarantine. Third, outbreaks in high-risk populations such as nursing homes have been minimized. Fourth, workplace prevention strategies are in place and have been demonstrated to be effective. Fifth, risk of imported cases is at manageable levels. Finally, communities are engaged.
It is hard to argue with the rationale behind each of these criteria. However, the United States is not Thailand, and just thinking about how this country would go about meeting those criteria provides a window into some of the reasons why we have done so poorly and will continue to be challenged in dealing with the pandemic.
First, notice that the criteria make no mention of a vaccine. One gets the sense that from the top down our country is banking too heavily on the effectiveness and widespread delivery of a vaccine. Even if and when a vaccine is developed and delivered, all of these criteria still must be met and kept in mind for a future pandemic.
Second, the criteria call for an effective health care system, but it is abundantly clear that the United States does not have a cohesive health care system and probably won’t for the foreseeable future. The best we can hope for is individual states cobbling together their own systems, which may in turn serve as examples for those states who haven’t had the foresight. We have had a public health system of sorts, but its credibility and effectiveness has been neutered to the point that again we must rely on each state’s ability to see through the haze and create it’s own systems for detection, testing, tracking, isolating, and quarantining – often with little help in materiel support from the federal government. The sliver of good news is that, after a bit of a stumbling start, detecting and limiting the importation of cases from abroad is being addressed.
We continue to hear and see evidence that there are segments of the population who are not engaged in the activities that we have learned are necessary to stabilize the pandemic. My sense is that those people represent a very small minority. But, it is probably large enough to make the route to a steady state on a national level long and painful. This unfortunately is to be expected in a country that was built on a framework of personal freedoms. The best you can hope for in achieving a steady state is to live in one of the states that seems to be achieving the fine balance between personal freedoms and the common good.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].






