User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
MD jailed for road rage, career spirals downhill
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
Bariatric surgery leads to better cardiovascular function in pregnancy
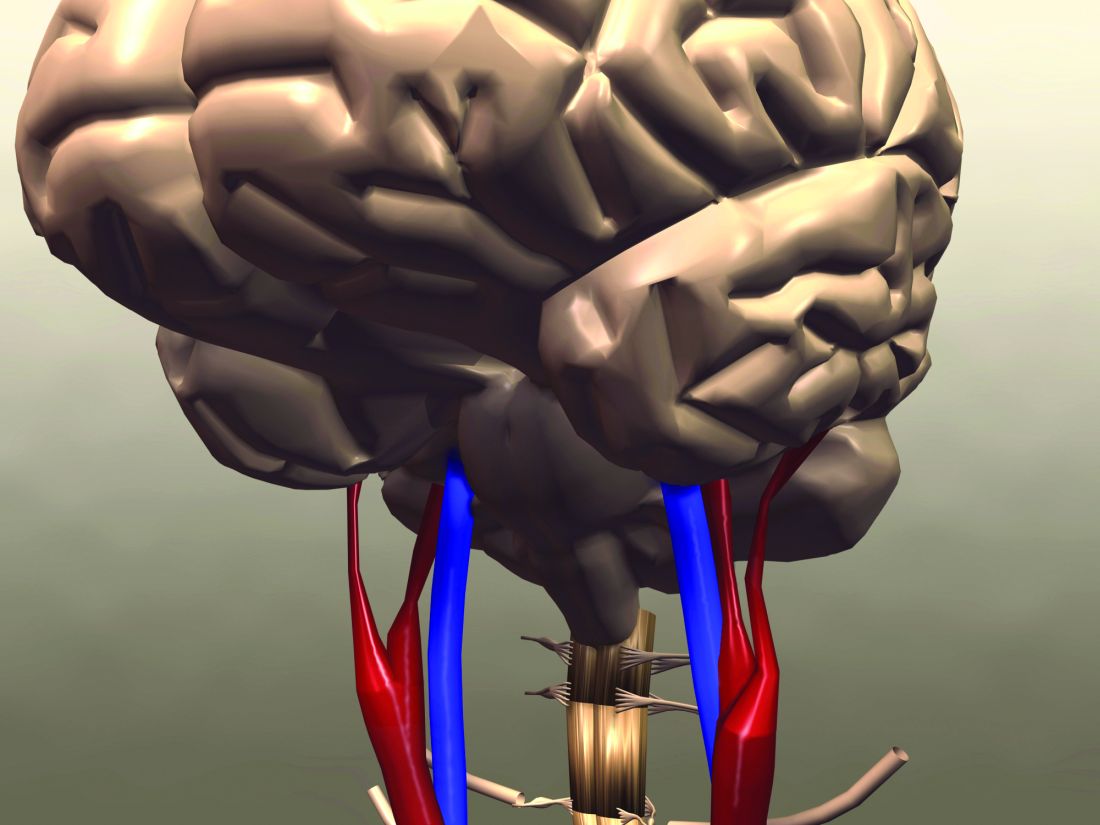
Pregnant women with a history of bariatric surgery have better cardiovascular adaptation to pregnancy compared with women who have similar early-pregnancy body mass index (BMI) but no history of weight loss surgery, new data suggest.
“Pregnant women who have had bariatric surgery demonstrate better cardiovascular adaptation through lower blood pressure, heart rate, and cardiac output, more favorable diastolic indices, and better systolic function,” reported Deesha Patel, MBBS MRCOG, specialist registrar, Chelsea and Westminster Hospital, London.
“Because the groups were matched for early pregnancy BMI, it’s unlikely that the results are due to weight loss alone but indicate that the metabolic alterations as a result of the surgery, via the enterocardiac axis, play an important role,” Dr. Patel continued.
The findings were presented at the Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress.
Although obesity is known for its inflammatory and toxic effects on the cardiovascular system, it is not clear to what extent the various treatment options for obesity modify these risks in the long term, said Hutan Ashrafian, MD, clinical lecturer in surgery, Imperial College London.
“It is even less clear how anti-obesity interventions affect the cardiovascular system in pregnancy,” Dr. Ashrafian told this news organization.
“This very novel study in pregnant mothers having undergone the most successful and consistent intervention for severe obesity – bariatric or metabolic surgery – gives new clues as to the extent that bariatric procedures can alter cardiovascular risk in pregnant mothers,” continued Dr. Ashrafian, who was not involved in the study.
The results show how bariatric surgery has favorable effects on cardiac adaptation in pregnancy and in turn “might offer protection from pregnancy-related cardiovascular pathology such as preeclampsia,” explained Dr. Ashrafian. “This adds to the known effects of cardiovascular protection of bariatric surgery through the enterocardiac axis, which may explain a wider range of effects that can be translated within pregnancy and possibly following pregnancy in the postpartum era and beyond.”
A history of bariatric surgery versus no surgery
The prospective, longitudinal study compared 41 women who had a history of bariatric surgery with 41 women who had not undergone surgery. Patients’ characteristics were closely matched for age, BMI (34.5 kg/m2 and 34.3 kg/m2 in the surgery and bariatric surgery groups, respectively) and race. Hypertensive disorders in the post-surgery group were significantly less common compared with the no-surgery group (0% vs. 9.8%).
During the study, participants underwent cardiovascular assessment at 12-14 weeks, 20-24 weeks, and 30-32 weeks of gestation. The assessment included measurement of blood pressure and heart rate, transthoracic echocardiography, and 2D speckle tracking, performed offline to assess global longitudinal and circumferential strain.
Blood pressure readings across the three trimesters were consistently lower in the women who had undergone bariatric surgery compared with those in the no-surgery group, and all differences were statistically significant. Likewise, heart rate and cardiac output across the three trimesters were lower in the post-surgery cohort. However, there was no difference in stroke volume between the two groups.
As for diastolic function, there were more favorable indices in the post-surgery group with a higher E/A ratio, a marker of left ventricle filling (P < .001), and lower left atrial volume (P < .05), Dr. Patel reported.
With respect to systolic function, there was no difference in ejection fraction, but there was lower global longitudinal strain (P < .01) and global circumferential strain in the post-bariatric group (P = .02), suggesting better systolic function.
“Strain is a measure of differences in motion and velocity between regions of the myocardium through the cardiac cycle and can detect subclinical changes when ejection fraction is normal,” she added.
“This is a fascinating piece of work. The author should be congratulated on gathering so many [pregnant] women who had had bariatric surgery. The work gives a unique glimpse into metabolic syndrome,” said Philip Toozs-Hobson, MD, who moderated the session.
“We are increasingly recognizing the impact [of bariatric surgery] on metabolic syndrome, and the fact that this study demonstrates that there is more to it than just weight is important,” continued Dr. Toosz-Hobson, who is a consultant gynecologist at Birmingham Women’s Hospital NHS Foundation Trust, United Kingdom.
Cardiovascular benefits of bariatric surgery
Bariatric surgery has been associated with loss of excess body weight of up to 55% and with approximately 40% reduction in all-cause mortality in the general population. The procedure also reduces the risk for heart disease, diabetes, and cancer.
The cardiovascular benefits of bariatric surgery include reduced hypertension, remodeling of the heart with a reduction in left ventricular mass, and an improvement in diastolic and systolic function.
“Traditionally, the cardiac changes were thought to be due to weight loss and blood pressure reduction, but it is now conceivable that the metabolic components contribute to the reverse modeling via changes to the enterocardiac axis involving changes to gut hormones,” said Dr. Patel. These hormones include secretin, glucagon, and vasoactive intestinal peptide, which are known to have inotropic effects, as well as adiponectin and leptin, which are known to have cardiac effects, she added.
“Pregnancy following bariatric surgery is associated with a reduced risk of hypertensive disorders, as well as a reduced risk of gestational diabetes, large-for-gestational-age neonates, and a small increased risk of small-for-gestational-age neonates,” said Dr. Patel.
Dr. Patel and Dr. Toosz-Hobson have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women with a history of bariatric surgery have better cardiovascular adaptation to pregnancy compared with women who have similar early-pregnancy body mass index (BMI) but no history of weight loss surgery, new data suggest.
“Pregnant women who have had bariatric surgery demonstrate better cardiovascular adaptation through lower blood pressure, heart rate, and cardiac output, more favorable diastolic indices, and better systolic function,” reported Deesha Patel, MBBS MRCOG, specialist registrar, Chelsea and Westminster Hospital, London.
“Because the groups were matched for early pregnancy BMI, it’s unlikely that the results are due to weight loss alone but indicate that the metabolic alterations as a result of the surgery, via the enterocardiac axis, play an important role,” Dr. Patel continued.
The findings were presented at the Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress.
Although obesity is known for its inflammatory and toxic effects on the cardiovascular system, it is not clear to what extent the various treatment options for obesity modify these risks in the long term, said Hutan Ashrafian, MD, clinical lecturer in surgery, Imperial College London.
“It is even less clear how anti-obesity interventions affect the cardiovascular system in pregnancy,” Dr. Ashrafian told this news organization.
“This very novel study in pregnant mothers having undergone the most successful and consistent intervention for severe obesity – bariatric or metabolic surgery – gives new clues as to the extent that bariatric procedures can alter cardiovascular risk in pregnant mothers,” continued Dr. Ashrafian, who was not involved in the study.
The results show how bariatric surgery has favorable effects on cardiac adaptation in pregnancy and in turn “might offer protection from pregnancy-related cardiovascular pathology such as preeclampsia,” explained Dr. Ashrafian. “This adds to the known effects of cardiovascular protection of bariatric surgery through the enterocardiac axis, which may explain a wider range of effects that can be translated within pregnancy and possibly following pregnancy in the postpartum era and beyond.”
A history of bariatric surgery versus no surgery
The prospective, longitudinal study compared 41 women who had a history of bariatric surgery with 41 women who had not undergone surgery. Patients’ characteristics were closely matched for age, BMI (34.5 kg/m2 and 34.3 kg/m2 in the surgery and bariatric surgery groups, respectively) and race. Hypertensive disorders in the post-surgery group were significantly less common compared with the no-surgery group (0% vs. 9.8%).
During the study, participants underwent cardiovascular assessment at 12-14 weeks, 20-24 weeks, and 30-32 weeks of gestation. The assessment included measurement of blood pressure and heart rate, transthoracic echocardiography, and 2D speckle tracking, performed offline to assess global longitudinal and circumferential strain.
Blood pressure readings across the three trimesters were consistently lower in the women who had undergone bariatric surgery compared with those in the no-surgery group, and all differences were statistically significant. Likewise, heart rate and cardiac output across the three trimesters were lower in the post-surgery cohort. However, there was no difference in stroke volume between the two groups.
As for diastolic function, there were more favorable indices in the post-surgery group with a higher E/A ratio, a marker of left ventricle filling (P < .001), and lower left atrial volume (P < .05), Dr. Patel reported.
With respect to systolic function, there was no difference in ejection fraction, but there was lower global longitudinal strain (P < .01) and global circumferential strain in the post-bariatric group (P = .02), suggesting better systolic function.
“Strain is a measure of differences in motion and velocity between regions of the myocardium through the cardiac cycle and can detect subclinical changes when ejection fraction is normal,” she added.
“This is a fascinating piece of work. The author should be congratulated on gathering so many [pregnant] women who had had bariatric surgery. The work gives a unique glimpse into metabolic syndrome,” said Philip Toozs-Hobson, MD, who moderated the session.
“We are increasingly recognizing the impact [of bariatric surgery] on metabolic syndrome, and the fact that this study demonstrates that there is more to it than just weight is important,” continued Dr. Toosz-Hobson, who is a consultant gynecologist at Birmingham Women’s Hospital NHS Foundation Trust, United Kingdom.
Cardiovascular benefits of bariatric surgery
Bariatric surgery has been associated with loss of excess body weight of up to 55% and with approximately 40% reduction in all-cause mortality in the general population. The procedure also reduces the risk for heart disease, diabetes, and cancer.
The cardiovascular benefits of bariatric surgery include reduced hypertension, remodeling of the heart with a reduction in left ventricular mass, and an improvement in diastolic and systolic function.
“Traditionally, the cardiac changes were thought to be due to weight loss and blood pressure reduction, but it is now conceivable that the metabolic components contribute to the reverse modeling via changes to the enterocardiac axis involving changes to gut hormones,” said Dr. Patel. These hormones include secretin, glucagon, and vasoactive intestinal peptide, which are known to have inotropic effects, as well as adiponectin and leptin, which are known to have cardiac effects, she added.
“Pregnancy following bariatric surgery is associated with a reduced risk of hypertensive disorders, as well as a reduced risk of gestational diabetes, large-for-gestational-age neonates, and a small increased risk of small-for-gestational-age neonates,” said Dr. Patel.
Dr. Patel and Dr. Toosz-Hobson have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women with a history of bariatric surgery have better cardiovascular adaptation to pregnancy compared with women who have similar early-pregnancy body mass index (BMI) but no history of weight loss surgery, new data suggest.
“Pregnant women who have had bariatric surgery demonstrate better cardiovascular adaptation through lower blood pressure, heart rate, and cardiac output, more favorable diastolic indices, and better systolic function,” reported Deesha Patel, MBBS MRCOG, specialist registrar, Chelsea and Westminster Hospital, London.
“Because the groups were matched for early pregnancy BMI, it’s unlikely that the results are due to weight loss alone but indicate that the metabolic alterations as a result of the surgery, via the enterocardiac axis, play an important role,” Dr. Patel continued.
The findings were presented at the Royal College of Obstetricians and Gynecologists 2021 Virtual World Congress.
Although obesity is known for its inflammatory and toxic effects on the cardiovascular system, it is not clear to what extent the various treatment options for obesity modify these risks in the long term, said Hutan Ashrafian, MD, clinical lecturer in surgery, Imperial College London.
“It is even less clear how anti-obesity interventions affect the cardiovascular system in pregnancy,” Dr. Ashrafian told this news organization.
“This very novel study in pregnant mothers having undergone the most successful and consistent intervention for severe obesity – bariatric or metabolic surgery – gives new clues as to the extent that bariatric procedures can alter cardiovascular risk in pregnant mothers,” continued Dr. Ashrafian, who was not involved in the study.
The results show how bariatric surgery has favorable effects on cardiac adaptation in pregnancy and in turn “might offer protection from pregnancy-related cardiovascular pathology such as preeclampsia,” explained Dr. Ashrafian. “This adds to the known effects of cardiovascular protection of bariatric surgery through the enterocardiac axis, which may explain a wider range of effects that can be translated within pregnancy and possibly following pregnancy in the postpartum era and beyond.”
A history of bariatric surgery versus no surgery
The prospective, longitudinal study compared 41 women who had a history of bariatric surgery with 41 women who had not undergone surgery. Patients’ characteristics were closely matched for age, BMI (34.5 kg/m2 and 34.3 kg/m2 in the surgery and bariatric surgery groups, respectively) and race. Hypertensive disorders in the post-surgery group were significantly less common compared with the no-surgery group (0% vs. 9.8%).
During the study, participants underwent cardiovascular assessment at 12-14 weeks, 20-24 weeks, and 30-32 weeks of gestation. The assessment included measurement of blood pressure and heart rate, transthoracic echocardiography, and 2D speckle tracking, performed offline to assess global longitudinal and circumferential strain.
Blood pressure readings across the three trimesters were consistently lower in the women who had undergone bariatric surgery compared with those in the no-surgery group, and all differences were statistically significant. Likewise, heart rate and cardiac output across the three trimesters were lower in the post-surgery cohort. However, there was no difference in stroke volume between the two groups.
As for diastolic function, there were more favorable indices in the post-surgery group with a higher E/A ratio, a marker of left ventricle filling (P < .001), and lower left atrial volume (P < .05), Dr. Patel reported.
With respect to systolic function, there was no difference in ejection fraction, but there was lower global longitudinal strain (P < .01) and global circumferential strain in the post-bariatric group (P = .02), suggesting better systolic function.
“Strain is a measure of differences in motion and velocity between regions of the myocardium through the cardiac cycle and can detect subclinical changes when ejection fraction is normal,” she added.
“This is a fascinating piece of work. The author should be congratulated on gathering so many [pregnant] women who had had bariatric surgery. The work gives a unique glimpse into metabolic syndrome,” said Philip Toozs-Hobson, MD, who moderated the session.
“We are increasingly recognizing the impact [of bariatric surgery] on metabolic syndrome, and the fact that this study demonstrates that there is more to it than just weight is important,” continued Dr. Toosz-Hobson, who is a consultant gynecologist at Birmingham Women’s Hospital NHS Foundation Trust, United Kingdom.
Cardiovascular benefits of bariatric surgery
Bariatric surgery has been associated with loss of excess body weight of up to 55% and with approximately 40% reduction in all-cause mortality in the general population. The procedure also reduces the risk for heart disease, diabetes, and cancer.
The cardiovascular benefits of bariatric surgery include reduced hypertension, remodeling of the heart with a reduction in left ventricular mass, and an improvement in diastolic and systolic function.
“Traditionally, the cardiac changes were thought to be due to weight loss and blood pressure reduction, but it is now conceivable that the metabolic components contribute to the reverse modeling via changes to the enterocardiac axis involving changes to gut hormones,” said Dr. Patel. These hormones include secretin, glucagon, and vasoactive intestinal peptide, which are known to have inotropic effects, as well as adiponectin and leptin, which are known to have cardiac effects, she added.
“Pregnancy following bariatric surgery is associated with a reduced risk of hypertensive disorders, as well as a reduced risk of gestational diabetes, large-for-gestational-age neonates, and a small increased risk of small-for-gestational-age neonates,” said Dr. Patel.
Dr. Patel and Dr. Toosz-Hobson have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gray hair goes away and squids go to space
Goodbye stress, goodbye gray hair
Last year was a doozy, so it wouldn’t be too surprising if we all had a few new gray strands in our hair. But what if we told you that you don’t need to start dying them or plucking them out? What if they could magically go back to the way they were? Well, it may be possible, sans magic and sans stress.
Investigators recently discovered that the age-old belief that stress will permanently turn your hair gray may not be true after all. There’s a strong possibility that it could turn back to its original color once the stressful agent is eliminated.
“Understanding the mechanisms that allow ‘old’ gray hairs to return to their ‘young’ pigmented states could yield new clues about the malleability of human aging in general and how it is influenced by stress,” said senior author Martin Picard, PhD, of Columbia University, New York.
For the study, 14 volunteers were asked to keep a stress diary and review their levels of stress throughout the week. The researchers used a new method of viewing and capturing the images of tiny parts of the hairs to see how much graying took place in each part of the strand. And what they found – some strands naturally turning back to the original color – had never been documented before.
How did it happen? Our good friend the mitochondria. We haven’t really heard that word since eighth-grade biology, but it’s actually the key link between stress hormones and hair pigmentation. Think of them as little radars picking up all different kinds of signals in your body, like mental/emotional stress. They get a big enough alert and they’re going to react, thus gray hair.
So that’s all it takes? Cut the stress and a full head of gray can go back to brown? Not exactly. The researchers said there may be a “threshold because of biological age and other factors.” They believe middle age is near that threshold and it could easily be pushed over due to stress and could potentially go back. But if you’ve been rocking the salt and pepper or silver fox for a number of years and are looking for change, you might want to just eliminate the stress and pick up a bottle of dye.
One small step for squid
Space does a number on the human body. Forget the obvious like going for a walk outside without a spacesuit, or even the well-known risks like the degradation of bone in microgravity; there are numerous smaller but still important changes to the body during spaceflight, like the disruption of the symbiotic relationship between gut bacteria and the human body. This causes the immune system to lose the ability to recognize threats, and illnesses spread more easily.
Naturally, if astronauts are going to undertake years-long journeys to Mars and beyond, a thorough understanding of this disturbance is necessary, and that’s why NASA has sent a bunch of squid to the International Space Station.
When it comes to animal studies, squid aren’t the usual culprits, but there’s a reason NASA chose calamari over the alternatives: The Hawaiian bobtail squid has a symbiotic relationship with bacteria that regulate their bioluminescence in much the same way that we have a symbiotic relationship with our gut bacteria, but the squid is a much simpler animal. If the bioluminescence-regulating bacteria are disturbed during their time in space, it will be much easier to figure out what’s going wrong.
The experiment is ongoing, but we should salute the brave squid who have taken a giant leap for squidkind. Though if NASA didn’t send them up in a giant bubble, we’re going to be very disappointed.
Less plastic, more vanilla
Have you been racked by guilt over the number of plastic water bottles you use? What about the amount of ice cream you eat? Well, this one’s for you.
Plastic isn’t the first thing you think about when you open up a pint of vanilla ice cream and catch the sweet, spicy vanilla scent, or when you smell those fresh vanilla scones coming out of the oven at the coffee shop, but a new study shows that the flavor of vanilla can come from water bottles.
Here’s the deal. A compound called vanillin is responsible for the scent of vanilla, and it can come naturally from the bean or it can be made synthetically. Believe it or not, 85% of vanillin is made synthetically from fossil fuels!
We’ve definitely grown accustomed to our favorite vanilla scents, foods, and cosmetics. In 2018, the global demand for vanillin was about 40,800 tons and is expected to grow to 65,000 tons by 2025, which far exceeds the supply of natural vanilla.
So what can we do? Well, we can use genetically engineered bacteria to turn plastic water bottles into vanillin, according to a study published in the journal Green Chemistry.
The plastic can be broken down into terephthalic acid, which is very similar, chemically speaking, to vanillin. Similar enough that a bit of bioengineering produced Escherichia coli that could convert the acid into the tasty treat, according to researchers at the University of Edinburgh.
A perfect solution? Decreasing plastic waste while producing a valued food product? The thought of consuming plastic isn’t appetizing, so just eat your ice cream and try to forget about it.
No withdrawals from this bank
Into each life, some milestones must fall: High school graduation, birth of a child, first house, 50th wedding anniversary, COVID-19. One LOTME staffer got really excited – way too excited, actually – when his Nissan Sentra reached 300,000 miles.
Well, there are milestones, and then there are milestones. “1,000 Reasons for Hope” is a report celebrating the first 1,000 brains donated to the VA-BU-CLF Brain Bank. For those of you keeping score at home, that would be the Department of Veterans Affairs, Boston University, and the Concussion Legacy Foundation.
The Brain Bank, created in 2008 to study concussions and chronic traumatic encephalopathy, is the brainchild – yes, we went there – of Chris Nowinski, PhD, a former professional wrestler, and Ann McKee, MD, an expert on neurogenerative disease. “Our discoveries have already inspired changes to sports that will prevent many future cases of CTE in the next generation of athletes,” Dr. Nowinski, the CEO of CLF, said in a written statement.
Data from the first thousand brains show that 706 men, including 305 former NFL players, had football as their primary exposure to head impacts. Women were underrepresented, making up only 2.8% of brain donations, so recruiting females is a priority. Anyone interested in pledging can go to PledgeMyBrain.org or call 617-992-0615 for the 24-hour emergency donation pager.
LOTME wanted to help, so we called the Brain Bank to find out about donating. They asked a few questions and we told them what we do for a living. “Oh, you’re with LOTME? Yeah, we’ve … um, seen that before. It’s, um … funny. Can we put you on hold?” We’re starting to get a little sick of the on-hold music by now.
Goodbye stress, goodbye gray hair
Last year was a doozy, so it wouldn’t be too surprising if we all had a few new gray strands in our hair. But what if we told you that you don’t need to start dying them or plucking them out? What if they could magically go back to the way they were? Well, it may be possible, sans magic and sans stress.
Investigators recently discovered that the age-old belief that stress will permanently turn your hair gray may not be true after all. There’s a strong possibility that it could turn back to its original color once the stressful agent is eliminated.
“Understanding the mechanisms that allow ‘old’ gray hairs to return to their ‘young’ pigmented states could yield new clues about the malleability of human aging in general and how it is influenced by stress,” said senior author Martin Picard, PhD, of Columbia University, New York.
For the study, 14 volunteers were asked to keep a stress diary and review their levels of stress throughout the week. The researchers used a new method of viewing and capturing the images of tiny parts of the hairs to see how much graying took place in each part of the strand. And what they found – some strands naturally turning back to the original color – had never been documented before.
How did it happen? Our good friend the mitochondria. We haven’t really heard that word since eighth-grade biology, but it’s actually the key link between stress hormones and hair pigmentation. Think of them as little radars picking up all different kinds of signals in your body, like mental/emotional stress. They get a big enough alert and they’re going to react, thus gray hair.
So that’s all it takes? Cut the stress and a full head of gray can go back to brown? Not exactly. The researchers said there may be a “threshold because of biological age and other factors.” They believe middle age is near that threshold and it could easily be pushed over due to stress and could potentially go back. But if you’ve been rocking the salt and pepper or silver fox for a number of years and are looking for change, you might want to just eliminate the stress and pick up a bottle of dye.
One small step for squid
Space does a number on the human body. Forget the obvious like going for a walk outside without a spacesuit, or even the well-known risks like the degradation of bone in microgravity; there are numerous smaller but still important changes to the body during spaceflight, like the disruption of the symbiotic relationship between gut bacteria and the human body. This causes the immune system to lose the ability to recognize threats, and illnesses spread more easily.
Naturally, if astronauts are going to undertake years-long journeys to Mars and beyond, a thorough understanding of this disturbance is necessary, and that’s why NASA has sent a bunch of squid to the International Space Station.
When it comes to animal studies, squid aren’t the usual culprits, but there’s a reason NASA chose calamari over the alternatives: The Hawaiian bobtail squid has a symbiotic relationship with bacteria that regulate their bioluminescence in much the same way that we have a symbiotic relationship with our gut bacteria, but the squid is a much simpler animal. If the bioluminescence-regulating bacteria are disturbed during their time in space, it will be much easier to figure out what’s going wrong.
The experiment is ongoing, but we should salute the brave squid who have taken a giant leap for squidkind. Though if NASA didn’t send them up in a giant bubble, we’re going to be very disappointed.
Less plastic, more vanilla
Have you been racked by guilt over the number of plastic water bottles you use? What about the amount of ice cream you eat? Well, this one’s for you.
Plastic isn’t the first thing you think about when you open up a pint of vanilla ice cream and catch the sweet, spicy vanilla scent, or when you smell those fresh vanilla scones coming out of the oven at the coffee shop, but a new study shows that the flavor of vanilla can come from water bottles.
Here’s the deal. A compound called vanillin is responsible for the scent of vanilla, and it can come naturally from the bean or it can be made synthetically. Believe it or not, 85% of vanillin is made synthetically from fossil fuels!
We’ve definitely grown accustomed to our favorite vanilla scents, foods, and cosmetics. In 2018, the global demand for vanillin was about 40,800 tons and is expected to grow to 65,000 tons by 2025, which far exceeds the supply of natural vanilla.
So what can we do? Well, we can use genetically engineered bacteria to turn plastic water bottles into vanillin, according to a study published in the journal Green Chemistry.
The plastic can be broken down into terephthalic acid, which is very similar, chemically speaking, to vanillin. Similar enough that a bit of bioengineering produced Escherichia coli that could convert the acid into the tasty treat, according to researchers at the University of Edinburgh.
A perfect solution? Decreasing plastic waste while producing a valued food product? The thought of consuming plastic isn’t appetizing, so just eat your ice cream and try to forget about it.
No withdrawals from this bank
Into each life, some milestones must fall: High school graduation, birth of a child, first house, 50th wedding anniversary, COVID-19. One LOTME staffer got really excited – way too excited, actually – when his Nissan Sentra reached 300,000 miles.
Well, there are milestones, and then there are milestones. “1,000 Reasons for Hope” is a report celebrating the first 1,000 brains donated to the VA-BU-CLF Brain Bank. For those of you keeping score at home, that would be the Department of Veterans Affairs, Boston University, and the Concussion Legacy Foundation.
The Brain Bank, created in 2008 to study concussions and chronic traumatic encephalopathy, is the brainchild – yes, we went there – of Chris Nowinski, PhD, a former professional wrestler, and Ann McKee, MD, an expert on neurogenerative disease. “Our discoveries have already inspired changes to sports that will prevent many future cases of CTE in the next generation of athletes,” Dr. Nowinski, the CEO of CLF, said in a written statement.
Data from the first thousand brains show that 706 men, including 305 former NFL players, had football as their primary exposure to head impacts. Women were underrepresented, making up only 2.8% of brain donations, so recruiting females is a priority. Anyone interested in pledging can go to PledgeMyBrain.org or call 617-992-0615 for the 24-hour emergency donation pager.
LOTME wanted to help, so we called the Brain Bank to find out about donating. They asked a few questions and we told them what we do for a living. “Oh, you’re with LOTME? Yeah, we’ve … um, seen that before. It’s, um … funny. Can we put you on hold?” We’re starting to get a little sick of the on-hold music by now.
Goodbye stress, goodbye gray hair
Last year was a doozy, so it wouldn’t be too surprising if we all had a few new gray strands in our hair. But what if we told you that you don’t need to start dying them or plucking them out? What if they could magically go back to the way they were? Well, it may be possible, sans magic and sans stress.
Investigators recently discovered that the age-old belief that stress will permanently turn your hair gray may not be true after all. There’s a strong possibility that it could turn back to its original color once the stressful agent is eliminated.
“Understanding the mechanisms that allow ‘old’ gray hairs to return to their ‘young’ pigmented states could yield new clues about the malleability of human aging in general and how it is influenced by stress,” said senior author Martin Picard, PhD, of Columbia University, New York.
For the study, 14 volunteers were asked to keep a stress diary and review their levels of stress throughout the week. The researchers used a new method of viewing and capturing the images of tiny parts of the hairs to see how much graying took place in each part of the strand. And what they found – some strands naturally turning back to the original color – had never been documented before.
How did it happen? Our good friend the mitochondria. We haven’t really heard that word since eighth-grade biology, but it’s actually the key link between stress hormones and hair pigmentation. Think of them as little radars picking up all different kinds of signals in your body, like mental/emotional stress. They get a big enough alert and they’re going to react, thus gray hair.
So that’s all it takes? Cut the stress and a full head of gray can go back to brown? Not exactly. The researchers said there may be a “threshold because of biological age and other factors.” They believe middle age is near that threshold and it could easily be pushed over due to stress and could potentially go back. But if you’ve been rocking the salt and pepper or silver fox for a number of years and are looking for change, you might want to just eliminate the stress and pick up a bottle of dye.
One small step for squid
Space does a number on the human body. Forget the obvious like going for a walk outside without a spacesuit, or even the well-known risks like the degradation of bone in microgravity; there are numerous smaller but still important changes to the body during spaceflight, like the disruption of the symbiotic relationship between gut bacteria and the human body. This causes the immune system to lose the ability to recognize threats, and illnesses spread more easily.
Naturally, if astronauts are going to undertake years-long journeys to Mars and beyond, a thorough understanding of this disturbance is necessary, and that’s why NASA has sent a bunch of squid to the International Space Station.
When it comes to animal studies, squid aren’t the usual culprits, but there’s a reason NASA chose calamari over the alternatives: The Hawaiian bobtail squid has a symbiotic relationship with bacteria that regulate their bioluminescence in much the same way that we have a symbiotic relationship with our gut bacteria, but the squid is a much simpler animal. If the bioluminescence-regulating bacteria are disturbed during their time in space, it will be much easier to figure out what’s going wrong.
The experiment is ongoing, but we should salute the brave squid who have taken a giant leap for squidkind. Though if NASA didn’t send them up in a giant bubble, we’re going to be very disappointed.
Less plastic, more vanilla
Have you been racked by guilt over the number of plastic water bottles you use? What about the amount of ice cream you eat? Well, this one’s for you.
Plastic isn’t the first thing you think about when you open up a pint of vanilla ice cream and catch the sweet, spicy vanilla scent, or when you smell those fresh vanilla scones coming out of the oven at the coffee shop, but a new study shows that the flavor of vanilla can come from water bottles.
Here’s the deal. A compound called vanillin is responsible for the scent of vanilla, and it can come naturally from the bean or it can be made synthetically. Believe it or not, 85% of vanillin is made synthetically from fossil fuels!
We’ve definitely grown accustomed to our favorite vanilla scents, foods, and cosmetics. In 2018, the global demand for vanillin was about 40,800 tons and is expected to grow to 65,000 tons by 2025, which far exceeds the supply of natural vanilla.
So what can we do? Well, we can use genetically engineered bacteria to turn plastic water bottles into vanillin, according to a study published in the journal Green Chemistry.
The plastic can be broken down into terephthalic acid, which is very similar, chemically speaking, to vanillin. Similar enough that a bit of bioengineering produced Escherichia coli that could convert the acid into the tasty treat, according to researchers at the University of Edinburgh.
A perfect solution? Decreasing plastic waste while producing a valued food product? The thought of consuming plastic isn’t appetizing, so just eat your ice cream and try to forget about it.
No withdrawals from this bank
Into each life, some milestones must fall: High school graduation, birth of a child, first house, 50th wedding anniversary, COVID-19. One LOTME staffer got really excited – way too excited, actually – when his Nissan Sentra reached 300,000 miles.
Well, there are milestones, and then there are milestones. “1,000 Reasons for Hope” is a report celebrating the first 1,000 brains donated to the VA-BU-CLF Brain Bank. For those of you keeping score at home, that would be the Department of Veterans Affairs, Boston University, and the Concussion Legacy Foundation.
The Brain Bank, created in 2008 to study concussions and chronic traumatic encephalopathy, is the brainchild – yes, we went there – of Chris Nowinski, PhD, a former professional wrestler, and Ann McKee, MD, an expert on neurogenerative disease. “Our discoveries have already inspired changes to sports that will prevent many future cases of CTE in the next generation of athletes,” Dr. Nowinski, the CEO of CLF, said in a written statement.
Data from the first thousand brains show that 706 men, including 305 former NFL players, had football as their primary exposure to head impacts. Women were underrepresented, making up only 2.8% of brain donations, so recruiting females is a priority. Anyone interested in pledging can go to PledgeMyBrain.org or call 617-992-0615 for the 24-hour emergency donation pager.
LOTME wanted to help, so we called the Brain Bank to find out about donating. They asked a few questions and we told them what we do for a living. “Oh, you’re with LOTME? Yeah, we’ve … um, seen that before. It’s, um … funny. Can we put you on hold?” We’re starting to get a little sick of the on-hold music by now.
Can laparoscopic lavage beat resection for acute perforated diverticulitis?
Severe complications at 5 years were no different for patients with perforated purulent diverticulitis who underwent laparoscopic peritoneal lavage or colon resection, according to data from 199 individuals treated at 21 hospitals in Norway and Sweden. But it may yet prove appropriate in the right patient.
Acute perforated diverticulitis with peritonitis remains a challenging complication with high morbidity and mortality among patients with diverticular disease, and bowel resection remains the standard of treatment, Najia Azhar, MD, of Skåne University Hospital, Malmö, Sweden, and colleagues wrote.
Short-term data suggest that laparoscopic lavage with drainage and antibiotics might be a viable alternative, but long-term data are lacking, they said.
In the Scandinavian Diverticulitis (SCANDIV) trial, published in JAMA Surgery, researchers randomized 101 patients to laparoscopic peritoneal lavage and 98 to colon resection. With 3 patients lost to follow-up, the final analysis included 73 patients who underwent laparoscopic lavage and 69 who underwent resection. The mean age of the lavage patients was 66.4 years, and 39 were men. The mean age of the resection patients was 63.5 years, and 36 were men. The primary outcome was severe complications – excluding stoma reversals and elective sigmoid resections because of recurrence – at an average of 5 years’ follow-up. Secondary outcomes included stoma prevalence, diverticulitis recurrence, and secondary sigmoid resection.
Severe complications were similar for the lavage and resection groups (36% and 35%, respectively), as were the overall mortality rates (32% and 25%, respectively).
The prevalence of stoma was significantly lower in the lavage group, compared with the resection group (8% vs. 33%, P = .002). However, secondary operations (including reversal of stoma) were similar between the lavage and resection groups, performed in 26 lavage patients (36%) versus 24 resection patients (35%).
Diverticulitis recurrence was significantly more common in the lavage, compared with the resection group (21% vs. 4%, P = .004), the researchers noted.
In the laparoscopic lavage group, 30% (n = 21) underwent a sigmoid resection; all but one of these occurred within a year of the index procedure, the researchers wrote. In addition, overall length of hospital stay was similar for both groups.
No significant differences in quality of life were noted between the groups, based on the EuroQoL-5D questionnaire or Cleveland Global Quality of Life scores.
Balance secondary pros and cons
Laparoscopic lavage is not common practice today in the United States, the researchers noted. In clinical practice guidelines issued in 2020, the American Society of Colon and Rectal Surgeons strongly recommend colectomy over laparoscopic lavage for the treatment of left-sided colonic diverticulitis. However, the European Society of Coloproctology’s guidelines state that laparoscopic lavage is feasible for patients with peritonitis at Hinchey stage III.
The findings of the current study were limited primarily by the exclusion of 50% of eligible patients because of challenges associated with conducting randomized trials in emergency settings, the researchers noted. However, the number of excluded patients and their baseline characteristics after exclusion were very similar in the two groups, and the study represents the largest randomized trial to date to examine long-term outcomes in patients with perforated diverticulitis.
“Laparoscopic lavage is faster and cost-effective but leads to a higher reoperation rate and recurrence rate, often requiring secondary sigmoid resection,” the researchers emphasized. Consequently, patients undergoing lavage should have consented for resection surgery.
The similar rates of severe complications and quality of life scores support laparoscopic lavage as an option for perforated purulent diverticulitis, but shared decision-making will be essential for better optimal patient management, the researchers concluded.
Similar outcomes, but unanswered questions
Even though the primary outcome of disease-related morbidity was similar for both groups, “the issue still remains regarding when and how, if ever, this therapeutic approach should be considered for purulent peritonitis,” Kellie E. Cunningham, MD, and Brian S. Zuckerbraun, MD, both of the University of Pittsburgh, wrote in an accompanying editorial.
Although laparoscopic lavage has the obvious advantages of avoiding a laparotomy and stoma, previous studies have shown a higher rate of early reoperations and recurrent diverticulitis, despite lower stoma prevalence and equal mortality rates, they said. In addition, “patients who are immunosuppressed or would be expected to have a higher mortality rate with failure to achieve definitive source control should likely not be offered this therapy.”
A “philosophical” argument could be made in favor of laparoscopic lavage based on the potential consequences of early treatment failure, they wrote.
“Although one may consider the need for early reoperation a complication, some would argue it affects the minority of patients, thus avoiding the more morbid procedure with creation of a stoma at the index operation in the majority of patients,” they noted. “Additionally, patients who underwent lavage that subsequently proceed to colectomy would have otherwise been offered this therapy initially at the time of the index operation.”
More research is needed to answer questions such as which, if any, operative findings are associated with failure. In addition, an analysis of long-term cost benefits between the two options should be explored, the authors wrote.
Based on current evidence, shared decision-making is necessary, with individualized care and short and long-term trade-offs taken into account, they wrote.
Gastroenterologist perspective: Study fills gap in follow-up data
In an interview, David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia School of Medicine, Norfolk, said the study is important because data have been lacking on outcomes of a laparoscopic lavage without a resection.
The findings represent “a major shift” in the growing consensus among surgeons that laparoscopic lavage is a viable option in appropriate patients, he said.
A key issue is the high rate of morbidity in patients who undergo traditional diverticulitis surgery. Complications can include wound infection and poor quality of life associated with stoma, Dr. Johnson said. Consequently, “a nonoperative approach from a patient perspective is certainly refreshing.”
Dr. Johnson said he was surprised by how well the patients fared after lavage given the severity of the diverticulitis in the patient population. However, this may be in part because of the relatively small numbers of patients at highest risk for complications, such as those with diabetes or immunocompromising conditions.
Dr. Johnson also said he was struck by the fact that the adenocarcinomas in the lavage group were diagnosed within the first year after the procedure. “The cancer diagnosis shouldn’t reflect on the lavage group,” but emphasizes the importance of having an earlier colonoscopy, he noted.
Next steps for research might include identifying a standardized endpoint for lavage, and determining how expanded use of the procedure might impact community practice, Dr. Johnson said. In addition, more research is needed to more clearly define patients most likely to benefit from laparoscopic lavage.
The study was supported in part by the department of surgery at Skåne University Hospital, Akershus University Hospital, and a fellowship to one of the study coauthors from the Southeastern Norway Regional Health Authority. Lead author Dr. Azhar disclosed grants from the department of surgery of Skåne University Hospital. Dr. Cunningham and Dr. Zuckerbraun had no financial conflicts to disclose. Dr. Johnson had no relevant financial disclosures.
Severe complications at 5 years were no different for patients with perforated purulent diverticulitis who underwent laparoscopic peritoneal lavage or colon resection, according to data from 199 individuals treated at 21 hospitals in Norway and Sweden. But it may yet prove appropriate in the right patient.
Acute perforated diverticulitis with peritonitis remains a challenging complication with high morbidity and mortality among patients with diverticular disease, and bowel resection remains the standard of treatment, Najia Azhar, MD, of Skåne University Hospital, Malmö, Sweden, and colleagues wrote.
Short-term data suggest that laparoscopic lavage with drainage and antibiotics might be a viable alternative, but long-term data are lacking, they said.
In the Scandinavian Diverticulitis (SCANDIV) trial, published in JAMA Surgery, researchers randomized 101 patients to laparoscopic peritoneal lavage and 98 to colon resection. With 3 patients lost to follow-up, the final analysis included 73 patients who underwent laparoscopic lavage and 69 who underwent resection. The mean age of the lavage patients was 66.4 years, and 39 were men. The mean age of the resection patients was 63.5 years, and 36 were men. The primary outcome was severe complications – excluding stoma reversals and elective sigmoid resections because of recurrence – at an average of 5 years’ follow-up. Secondary outcomes included stoma prevalence, diverticulitis recurrence, and secondary sigmoid resection.
Severe complications were similar for the lavage and resection groups (36% and 35%, respectively), as were the overall mortality rates (32% and 25%, respectively).
The prevalence of stoma was significantly lower in the lavage group, compared with the resection group (8% vs. 33%, P = .002). However, secondary operations (including reversal of stoma) were similar between the lavage and resection groups, performed in 26 lavage patients (36%) versus 24 resection patients (35%).
Diverticulitis recurrence was significantly more common in the lavage, compared with the resection group (21% vs. 4%, P = .004), the researchers noted.
In the laparoscopic lavage group, 30% (n = 21) underwent a sigmoid resection; all but one of these occurred within a year of the index procedure, the researchers wrote. In addition, overall length of hospital stay was similar for both groups.
No significant differences in quality of life were noted between the groups, based on the EuroQoL-5D questionnaire or Cleveland Global Quality of Life scores.
Balance secondary pros and cons
Laparoscopic lavage is not common practice today in the United States, the researchers noted. In clinical practice guidelines issued in 2020, the American Society of Colon and Rectal Surgeons strongly recommend colectomy over laparoscopic lavage for the treatment of left-sided colonic diverticulitis. However, the European Society of Coloproctology’s guidelines state that laparoscopic lavage is feasible for patients with peritonitis at Hinchey stage III.
The findings of the current study were limited primarily by the exclusion of 50% of eligible patients because of challenges associated with conducting randomized trials in emergency settings, the researchers noted. However, the number of excluded patients and their baseline characteristics after exclusion were very similar in the two groups, and the study represents the largest randomized trial to date to examine long-term outcomes in patients with perforated diverticulitis.
“Laparoscopic lavage is faster and cost-effective but leads to a higher reoperation rate and recurrence rate, often requiring secondary sigmoid resection,” the researchers emphasized. Consequently, patients undergoing lavage should have consented for resection surgery.
The similar rates of severe complications and quality of life scores support laparoscopic lavage as an option for perforated purulent diverticulitis, but shared decision-making will be essential for better optimal patient management, the researchers concluded.
Similar outcomes, but unanswered questions
Even though the primary outcome of disease-related morbidity was similar for both groups, “the issue still remains regarding when and how, if ever, this therapeutic approach should be considered for purulent peritonitis,” Kellie E. Cunningham, MD, and Brian S. Zuckerbraun, MD, both of the University of Pittsburgh, wrote in an accompanying editorial.
Although laparoscopic lavage has the obvious advantages of avoiding a laparotomy and stoma, previous studies have shown a higher rate of early reoperations and recurrent diverticulitis, despite lower stoma prevalence and equal mortality rates, they said. In addition, “patients who are immunosuppressed or would be expected to have a higher mortality rate with failure to achieve definitive source control should likely not be offered this therapy.”
A “philosophical” argument could be made in favor of laparoscopic lavage based on the potential consequences of early treatment failure, they wrote.
“Although one may consider the need for early reoperation a complication, some would argue it affects the minority of patients, thus avoiding the more morbid procedure with creation of a stoma at the index operation in the majority of patients,” they noted. “Additionally, patients who underwent lavage that subsequently proceed to colectomy would have otherwise been offered this therapy initially at the time of the index operation.”
More research is needed to answer questions such as which, if any, operative findings are associated with failure. In addition, an analysis of long-term cost benefits between the two options should be explored, the authors wrote.
Based on current evidence, shared decision-making is necessary, with individualized care and short and long-term trade-offs taken into account, they wrote.
Gastroenterologist perspective: Study fills gap in follow-up data
In an interview, David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia School of Medicine, Norfolk, said the study is important because data have been lacking on outcomes of a laparoscopic lavage without a resection.
The findings represent “a major shift” in the growing consensus among surgeons that laparoscopic lavage is a viable option in appropriate patients, he said.
A key issue is the high rate of morbidity in patients who undergo traditional diverticulitis surgery. Complications can include wound infection and poor quality of life associated with stoma, Dr. Johnson said. Consequently, “a nonoperative approach from a patient perspective is certainly refreshing.”
Dr. Johnson said he was surprised by how well the patients fared after lavage given the severity of the diverticulitis in the patient population. However, this may be in part because of the relatively small numbers of patients at highest risk for complications, such as those with diabetes or immunocompromising conditions.
Dr. Johnson also said he was struck by the fact that the adenocarcinomas in the lavage group were diagnosed within the first year after the procedure. “The cancer diagnosis shouldn’t reflect on the lavage group,” but emphasizes the importance of having an earlier colonoscopy, he noted.
Next steps for research might include identifying a standardized endpoint for lavage, and determining how expanded use of the procedure might impact community practice, Dr. Johnson said. In addition, more research is needed to more clearly define patients most likely to benefit from laparoscopic lavage.
The study was supported in part by the department of surgery at Skåne University Hospital, Akershus University Hospital, and a fellowship to one of the study coauthors from the Southeastern Norway Regional Health Authority. Lead author Dr. Azhar disclosed grants from the department of surgery of Skåne University Hospital. Dr. Cunningham and Dr. Zuckerbraun had no financial conflicts to disclose. Dr. Johnson had no relevant financial disclosures.
Severe complications at 5 years were no different for patients with perforated purulent diverticulitis who underwent laparoscopic peritoneal lavage or colon resection, according to data from 199 individuals treated at 21 hospitals in Norway and Sweden. But it may yet prove appropriate in the right patient.
Acute perforated diverticulitis with peritonitis remains a challenging complication with high morbidity and mortality among patients with diverticular disease, and bowel resection remains the standard of treatment, Najia Azhar, MD, of Skåne University Hospital, Malmö, Sweden, and colleagues wrote.
Short-term data suggest that laparoscopic lavage with drainage and antibiotics might be a viable alternative, but long-term data are lacking, they said.
In the Scandinavian Diverticulitis (SCANDIV) trial, published in JAMA Surgery, researchers randomized 101 patients to laparoscopic peritoneal lavage and 98 to colon resection. With 3 patients lost to follow-up, the final analysis included 73 patients who underwent laparoscopic lavage and 69 who underwent resection. The mean age of the lavage patients was 66.4 years, and 39 were men. The mean age of the resection patients was 63.5 years, and 36 were men. The primary outcome was severe complications – excluding stoma reversals and elective sigmoid resections because of recurrence – at an average of 5 years’ follow-up. Secondary outcomes included stoma prevalence, diverticulitis recurrence, and secondary sigmoid resection.
Severe complications were similar for the lavage and resection groups (36% and 35%, respectively), as were the overall mortality rates (32% and 25%, respectively).
The prevalence of stoma was significantly lower in the lavage group, compared with the resection group (8% vs. 33%, P = .002). However, secondary operations (including reversal of stoma) were similar between the lavage and resection groups, performed in 26 lavage patients (36%) versus 24 resection patients (35%).
Diverticulitis recurrence was significantly more common in the lavage, compared with the resection group (21% vs. 4%, P = .004), the researchers noted.
In the laparoscopic lavage group, 30% (n = 21) underwent a sigmoid resection; all but one of these occurred within a year of the index procedure, the researchers wrote. In addition, overall length of hospital stay was similar for both groups.
No significant differences in quality of life were noted between the groups, based on the EuroQoL-5D questionnaire or Cleveland Global Quality of Life scores.
Balance secondary pros and cons
Laparoscopic lavage is not common practice today in the United States, the researchers noted. In clinical practice guidelines issued in 2020, the American Society of Colon and Rectal Surgeons strongly recommend colectomy over laparoscopic lavage for the treatment of left-sided colonic diverticulitis. However, the European Society of Coloproctology’s guidelines state that laparoscopic lavage is feasible for patients with peritonitis at Hinchey stage III.
The findings of the current study were limited primarily by the exclusion of 50% of eligible patients because of challenges associated with conducting randomized trials in emergency settings, the researchers noted. However, the number of excluded patients and their baseline characteristics after exclusion were very similar in the two groups, and the study represents the largest randomized trial to date to examine long-term outcomes in patients with perforated diverticulitis.
“Laparoscopic lavage is faster and cost-effective but leads to a higher reoperation rate and recurrence rate, often requiring secondary sigmoid resection,” the researchers emphasized. Consequently, patients undergoing lavage should have consented for resection surgery.
The similar rates of severe complications and quality of life scores support laparoscopic lavage as an option for perforated purulent diverticulitis, but shared decision-making will be essential for better optimal patient management, the researchers concluded.
Similar outcomes, but unanswered questions
Even though the primary outcome of disease-related morbidity was similar for both groups, “the issue still remains regarding when and how, if ever, this therapeutic approach should be considered for purulent peritonitis,” Kellie E. Cunningham, MD, and Brian S. Zuckerbraun, MD, both of the University of Pittsburgh, wrote in an accompanying editorial.
Although laparoscopic lavage has the obvious advantages of avoiding a laparotomy and stoma, previous studies have shown a higher rate of early reoperations and recurrent diverticulitis, despite lower stoma prevalence and equal mortality rates, they said. In addition, “patients who are immunosuppressed or would be expected to have a higher mortality rate with failure to achieve definitive source control should likely not be offered this therapy.”
A “philosophical” argument could be made in favor of laparoscopic lavage based on the potential consequences of early treatment failure, they wrote.
“Although one may consider the need for early reoperation a complication, some would argue it affects the minority of patients, thus avoiding the more morbid procedure with creation of a stoma at the index operation in the majority of patients,” they noted. “Additionally, patients who underwent lavage that subsequently proceed to colectomy would have otherwise been offered this therapy initially at the time of the index operation.”
More research is needed to answer questions such as which, if any, operative findings are associated with failure. In addition, an analysis of long-term cost benefits between the two options should be explored, the authors wrote.
Based on current evidence, shared decision-making is necessary, with individualized care and short and long-term trade-offs taken into account, they wrote.
Gastroenterologist perspective: Study fills gap in follow-up data
In an interview, David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia School of Medicine, Norfolk, said the study is important because data have been lacking on outcomes of a laparoscopic lavage without a resection.
The findings represent “a major shift” in the growing consensus among surgeons that laparoscopic lavage is a viable option in appropriate patients, he said.
A key issue is the high rate of morbidity in patients who undergo traditional diverticulitis surgery. Complications can include wound infection and poor quality of life associated with stoma, Dr. Johnson said. Consequently, “a nonoperative approach from a patient perspective is certainly refreshing.”
Dr. Johnson said he was surprised by how well the patients fared after lavage given the severity of the diverticulitis in the patient population. However, this may be in part because of the relatively small numbers of patients at highest risk for complications, such as those with diabetes or immunocompromising conditions.
Dr. Johnson also said he was struck by the fact that the adenocarcinomas in the lavage group were diagnosed within the first year after the procedure. “The cancer diagnosis shouldn’t reflect on the lavage group,” but emphasizes the importance of having an earlier colonoscopy, he noted.
Next steps for research might include identifying a standardized endpoint for lavage, and determining how expanded use of the procedure might impact community practice, Dr. Johnson said. In addition, more research is needed to more clearly define patients most likely to benefit from laparoscopic lavage.
The study was supported in part by the department of surgery at Skåne University Hospital, Akershus University Hospital, and a fellowship to one of the study coauthors from the Southeastern Norway Regional Health Authority. Lead author Dr. Azhar disclosed grants from the department of surgery of Skåne University Hospital. Dr. Cunningham and Dr. Zuckerbraun had no financial conflicts to disclose. Dr. Johnson had no relevant financial disclosures.
FROM JAMA SURGERY
Bariatric surgery tied to 22% lower 5-year stroke risk
Patients with obesity who underwent bariatric surgery had 46% lower odds of stroke 1 year later, similar odds of stroke 3 years later, and 22% lower odds of stroke 5 years later, compared with matched control patients, in new research.
Michael D. Williams, MD, presented the study findings (abstract A002) at the annual meeting of the American Society for Metabolic & Bariatric Surgery.
The findings are “very good news,” even though the protection against stroke declined further out from the surgery, John D. Scott, MD, scientific program chair of the ASMBS meeting, told this news organization.
The investigators matched more than 56,000 patients with obesity who had bariatric surgery with an equal number of similar patients who did not have this surgery, from a large national insurance database, in what they believe is the largest study of this to date.
“Any intervention that decreases your risk of [cardiovascular] events is good news,” said Dr. Scott, a clinical professor of surgery at the University of South Carolina, Greenville, and metabolic and bariatric surgery director at Prisma Health in Greenville, S.C. “And having a 22%-45% chance of reduction in stroke risk is a very worthwhile intervention.”
Asked how this would change the way clinicians inform patients of what to expect from bariatric surgery, he said: “I would advise patients that studies like this show that surgery would not increase your risk of having a stroke.
“This is consistent with many studies that show that the risks of all macrovascular events decrease after the comorbidity reductions seen after surgery.”
According to Dr. Scott, “the next steps might include a prospective randomized trial of medical treatment versus surgery alone for [cardiovascular]/stroke outcomes, but this is unlikely.”
Similarly, Dr. Williams told this news organization that “I would tell [patients] that surgery is an effective and durable method for weight loss. It also can improve comorbid conditions, particularly diabetes and hypertension.”
Even with this study, “I’m not sure it’s appropriate to say that bariatric surgery will reduce the risk of stroke,” he cautioned.
“However, as we continue to investigate the effects of bariatric surgery, this study contributes to the greater body of knowledge that suggests that reduction in ischemic stroke risk is yet another benefit of bariatric surgery.”
The assigned discussant, Corrigan L. McBride, MD, MBA wanted to know if the lower odds ratio at 1 year might be because preoperative patient selection might eliminate patients at high risk of poor cardiovascular outcomes.
Dr. Williams, a resident at Rush Medical College, Chicago, replied that it is difficult to eliminate potential selection bias, despite best efforts, but this study shows that he can tell patients: “Having surgery is not going to increases your risk of stroke.”
“This is an important study,” Dr. McBride, professor and chief of minimally invasive surgery and bariatric surgery, University of Nebraska Medical Center, Omaha, told this news organization.
“It is the first large study to show a decreased [or no increased] risk of stroke 1, 3, and 5 years after bariatric surgery compared to matched patients, and it had enough data to look at stroke as a standalone endpoint,” Dr. McBride said. “It is important too, for patients and their physicians to understand that there is a lower chance of them having a stroke if they have surgery than if they do not.”
‘Important,’ ‘good news’ for stroke risk after bariatric surgery
The impact of bariatric surgery on remission of type 2 diabetes is well known, Dr. Williams noted, and other studies have reported how bariatric surgery affects the risk of major adverse cardiovascular events – a composite of stroke, myocardial infarction, coronary artery disease, and all-cause death – including a study presented in the same meeting session.
However, a very large sample size is needed to be able to demonstrate the effect of bariatric surgery on stroke, since stroke is a rare event.
The researchers analyzed data from the Mariner (PearlDiver.) all-payer insurance national claims database of patients in the United States.
They matched 56,514 patients with a body mass index over 35 kg/m2 and comorbidities or a BMI of more than 40 who underwent sleeve gastrectomy or Roux-en-Y gastric bypass during 2010-2019 with 56,514 control patients who did not undergo bariatric surgery.
A year after bariatric surgery, patients in that group had a lower stroke rate than patients in the control group (0.6% vs. 1.2%), and they had close to 50% lower odds of having a stroke (odds ratio, 0.54; 95% CI, 0.47-0.61).
Three years after bariatric surgery, there were 44,948 patients in each group; the rate of stroke was 2.1% in the surgery group and 2.2% in the control group, and there was no significant difference in the odds of having a stroke (OR, 0.96; 95% CI, 0.91-1.00).
Five years after bariatric surgery, there were 27,619 patients in each group; the stroke rate was lower in the bariatric surgery group than in the control group (2.8% vs 3.6%), but reduced odds of stroke was not as great as after 1 year (OR, 0.78; 95% CI, 0.65-0.90).
Dr. Williams has no relevant financial disclosures. Dr. McBride and Dr. Scott disclosed that they are speakers/trainers/faculty advisers for Gore. Dr. Scott is also a consultant for C-SATS (part of Johnson & Johnson).
Patients with obesity who underwent bariatric surgery had 46% lower odds of stroke 1 year later, similar odds of stroke 3 years later, and 22% lower odds of stroke 5 years later, compared with matched control patients, in new research.
Michael D. Williams, MD, presented the study findings (abstract A002) at the annual meeting of the American Society for Metabolic & Bariatric Surgery.
The findings are “very good news,” even though the protection against stroke declined further out from the surgery, John D. Scott, MD, scientific program chair of the ASMBS meeting, told this news organization.
The investigators matched more than 56,000 patients with obesity who had bariatric surgery with an equal number of similar patients who did not have this surgery, from a large national insurance database, in what they believe is the largest study of this to date.
“Any intervention that decreases your risk of [cardiovascular] events is good news,” said Dr. Scott, a clinical professor of surgery at the University of South Carolina, Greenville, and metabolic and bariatric surgery director at Prisma Health in Greenville, S.C. “And having a 22%-45% chance of reduction in stroke risk is a very worthwhile intervention.”
Asked how this would change the way clinicians inform patients of what to expect from bariatric surgery, he said: “I would advise patients that studies like this show that surgery would not increase your risk of having a stroke.
“This is consistent with many studies that show that the risks of all macrovascular events decrease after the comorbidity reductions seen after surgery.”
According to Dr. Scott, “the next steps might include a prospective randomized trial of medical treatment versus surgery alone for [cardiovascular]/stroke outcomes, but this is unlikely.”
Similarly, Dr. Williams told this news organization that “I would tell [patients] that surgery is an effective and durable method for weight loss. It also can improve comorbid conditions, particularly diabetes and hypertension.”
Even with this study, “I’m not sure it’s appropriate to say that bariatric surgery will reduce the risk of stroke,” he cautioned.
“However, as we continue to investigate the effects of bariatric surgery, this study contributes to the greater body of knowledge that suggests that reduction in ischemic stroke risk is yet another benefit of bariatric surgery.”
The assigned discussant, Corrigan L. McBride, MD, MBA wanted to know if the lower odds ratio at 1 year might be because preoperative patient selection might eliminate patients at high risk of poor cardiovascular outcomes.
Dr. Williams, a resident at Rush Medical College, Chicago, replied that it is difficult to eliminate potential selection bias, despite best efforts, but this study shows that he can tell patients: “Having surgery is not going to increases your risk of stroke.”
“This is an important study,” Dr. McBride, professor and chief of minimally invasive surgery and bariatric surgery, University of Nebraska Medical Center, Omaha, told this news organization.
“It is the first large study to show a decreased [or no increased] risk of stroke 1, 3, and 5 years after bariatric surgery compared to matched patients, and it had enough data to look at stroke as a standalone endpoint,” Dr. McBride said. “It is important too, for patients and their physicians to understand that there is a lower chance of them having a stroke if they have surgery than if they do not.”
‘Important,’ ‘good news’ for stroke risk after bariatric surgery
The impact of bariatric surgery on remission of type 2 diabetes is well known, Dr. Williams noted, and other studies have reported how bariatric surgery affects the risk of major adverse cardiovascular events – a composite of stroke, myocardial infarction, coronary artery disease, and all-cause death – including a study presented in the same meeting session.
However, a very large sample size is needed to be able to demonstrate the effect of bariatric surgery on stroke, since stroke is a rare event.
The researchers analyzed data from the Mariner (PearlDiver.) all-payer insurance national claims database of patients in the United States.
They matched 56,514 patients with a body mass index over 35 kg/m2 and comorbidities or a BMI of more than 40 who underwent sleeve gastrectomy or Roux-en-Y gastric bypass during 2010-2019 with 56,514 control patients who did not undergo bariatric surgery.
A year after bariatric surgery, patients in that group had a lower stroke rate than patients in the control group (0.6% vs. 1.2%), and they had close to 50% lower odds of having a stroke (odds ratio, 0.54; 95% CI, 0.47-0.61).
Three years after bariatric surgery, there were 44,948 patients in each group; the rate of stroke was 2.1% in the surgery group and 2.2% in the control group, and there was no significant difference in the odds of having a stroke (OR, 0.96; 95% CI, 0.91-1.00).
Five years after bariatric surgery, there were 27,619 patients in each group; the stroke rate was lower in the bariatric surgery group than in the control group (2.8% vs 3.6%), but reduced odds of stroke was not as great as after 1 year (OR, 0.78; 95% CI, 0.65-0.90).
Dr. Williams has no relevant financial disclosures. Dr. McBride and Dr. Scott disclosed that they are speakers/trainers/faculty advisers for Gore. Dr. Scott is also a consultant for C-SATS (part of Johnson & Johnson).
Patients with obesity who underwent bariatric surgery had 46% lower odds of stroke 1 year later, similar odds of stroke 3 years later, and 22% lower odds of stroke 5 years later, compared with matched control patients, in new research.
Michael D. Williams, MD, presented the study findings (abstract A002) at the annual meeting of the American Society for Metabolic & Bariatric Surgery.
The findings are “very good news,” even though the protection against stroke declined further out from the surgery, John D. Scott, MD, scientific program chair of the ASMBS meeting, told this news organization.
The investigators matched more than 56,000 patients with obesity who had bariatric surgery with an equal number of similar patients who did not have this surgery, from a large national insurance database, in what they believe is the largest study of this to date.
“Any intervention that decreases your risk of [cardiovascular] events is good news,” said Dr. Scott, a clinical professor of surgery at the University of South Carolina, Greenville, and metabolic and bariatric surgery director at Prisma Health in Greenville, S.C. “And having a 22%-45% chance of reduction in stroke risk is a very worthwhile intervention.”
Asked how this would change the way clinicians inform patients of what to expect from bariatric surgery, he said: “I would advise patients that studies like this show that surgery would not increase your risk of having a stroke.
“This is consistent with many studies that show that the risks of all macrovascular events decrease after the comorbidity reductions seen after surgery.”
According to Dr. Scott, “the next steps might include a prospective randomized trial of medical treatment versus surgery alone for [cardiovascular]/stroke outcomes, but this is unlikely.”
Similarly, Dr. Williams told this news organization that “I would tell [patients] that surgery is an effective and durable method for weight loss. It also can improve comorbid conditions, particularly diabetes and hypertension.”
Even with this study, “I’m not sure it’s appropriate to say that bariatric surgery will reduce the risk of stroke,” he cautioned.
“However, as we continue to investigate the effects of bariatric surgery, this study contributes to the greater body of knowledge that suggests that reduction in ischemic stroke risk is yet another benefit of bariatric surgery.”
The assigned discussant, Corrigan L. McBride, MD, MBA wanted to know if the lower odds ratio at 1 year might be because preoperative patient selection might eliminate patients at high risk of poor cardiovascular outcomes.
Dr. Williams, a resident at Rush Medical College, Chicago, replied that it is difficult to eliminate potential selection bias, despite best efforts, but this study shows that he can tell patients: “Having surgery is not going to increases your risk of stroke.”
“This is an important study,” Dr. McBride, professor and chief of minimally invasive surgery and bariatric surgery, University of Nebraska Medical Center, Omaha, told this news organization.
“It is the first large study to show a decreased [or no increased] risk of stroke 1, 3, and 5 years after bariatric surgery compared to matched patients, and it had enough data to look at stroke as a standalone endpoint,” Dr. McBride said. “It is important too, for patients and their physicians to understand that there is a lower chance of them having a stroke if they have surgery than if they do not.”
‘Important,’ ‘good news’ for stroke risk after bariatric surgery
The impact of bariatric surgery on remission of type 2 diabetes is well known, Dr. Williams noted, and other studies have reported how bariatric surgery affects the risk of major adverse cardiovascular events – a composite of stroke, myocardial infarction, coronary artery disease, and all-cause death – including a study presented in the same meeting session.
However, a very large sample size is needed to be able to demonstrate the effect of bariatric surgery on stroke, since stroke is a rare event.
The researchers analyzed data from the Mariner (PearlDiver.) all-payer insurance national claims database of patients in the United States.
They matched 56,514 patients with a body mass index over 35 kg/m2 and comorbidities or a BMI of more than 40 who underwent sleeve gastrectomy or Roux-en-Y gastric bypass during 2010-2019 with 56,514 control patients who did not undergo bariatric surgery.
A year after bariatric surgery, patients in that group had a lower stroke rate than patients in the control group (0.6% vs. 1.2%), and they had close to 50% lower odds of having a stroke (odds ratio, 0.54; 95% CI, 0.47-0.61).
Three years after bariatric surgery, there were 44,948 patients in each group; the rate of stroke was 2.1% in the surgery group and 2.2% in the control group, and there was no significant difference in the odds of having a stroke (OR, 0.96; 95% CI, 0.91-1.00).
Five years after bariatric surgery, there were 27,619 patients in each group; the stroke rate was lower in the bariatric surgery group than in the control group (2.8% vs 3.6%), but reduced odds of stroke was not as great as after 1 year (OR, 0.78; 95% CI, 0.65-0.90).
Dr. Williams has no relevant financial disclosures. Dr. McBride and Dr. Scott disclosed that they are speakers/trainers/faculty advisers for Gore. Dr. Scott is also a consultant for C-SATS (part of Johnson & Johnson).
FROM ASMBS 2021
Medically suspect criterion can determine bariatric surgery coverage
A delaying tactic used by some U.S. health insurers to limit coverage of bariatric surgery does not jibe with the clinical experience at one U.S. center with 461 patients who underwent primary or revisional bariatric surgery.
The tactic applies to patients with a baseline body mass index (BMI) of 35-39 kg/m2 who usually also need at least one comorbidity to qualify for insurance coverage for bariatric surgery, and specifically to the subgroup for whom hypertension is the qualifying comorbidity.
Some insurers limit surgery coverage to patients with hypertension who fail to reach their goal blood pressure on agents from three different drug classes, a policy that is “extremely frustrating and dangerous,” said Yannis Raftopoulos, MD, PhD, in his presentation at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
Using number of antihypertensive drugs ‘is not correct’
“Using the number of antihypertensive medications to justify surgery is not correct because blood pressure control is not [always] better when patients take two or three medications, compared with when they are taking one. This harms patients because the more severe their hypertension, the worse their control,” said Dr. Raftopoulos, director of the weight management program at Holyoke (Mass.) Medical Center.
He presented findings from a retrospective study of 461 patients who underwent either sleeve gastrectomy or laparoscopic Roux-en-Y gastric bypass at his center, including 213 (46%) diagnosed with hypertension at the time of their surgery. Within this group were 68 patients with a BMI of 35-39, which meant that they could get insurance coverage for bariatric surgery only if they also had a relevant comorbidity such as hypertension, diabetes, or severe sleep apnea.
Among these patients, 36 (17% of those with hypertension) had only hypertension as their relevant comorbidity and would not have qualified for bariatric surgery under the strictest criteria applied by some insurers that require patients to remain hypertensive despite treatment with at least three different antihypertensive medications. (These 36 patients underwent bariatric surgery because their insurance coverage did not have this restriction.)
The analyses Dr. Raftopoulos presented also documented the rate of hypertension resolution among patients in the series who had hypertension at baseline and 1-year follow-up results. Among 65 patients on one antihypertensive drug at baseline, 43 (66%) had complete resolution of their hypertension after 1 year, defined as blood pressure of less than 130/90 mm Hg while completely off antihypertensive treatment. In contrast, among 55 patients on two antihypertensive medications at baseline, 28 (51%) had complete resolution after 1 year, and among 24 patients on three or more antihypertensive medications at baseline, 3 (13%) had complete resolution 1 year after bariatric surgery, he reported.
“Patients who were treated with one oral antihypertensive medication preoperatively had a higher likelihood of postoperative hypertension resolution,” concluded Dr. Raftopoulos.
Restricting access to bariatric surgery to patients with a BMI of less than 40 based on the preoperative intensity of their antihypertensive treatment “is not supported by our data, and can be potentially harmful,” he declared.
“This study was the result of discussions about this problem with multiple insurers in my area,” he added. “This affects a good number of patients.”
Waiting for hypertension to become less treatable
The results Dr. Raftopoulos presented “are not surprising, because they confirm the hypothesis that earlier intervention in the course of a disease like hypertension is more likely to be successful,” commented Bruce D. Schirmer, MD, a professor of surgery at the University of Virginia, Charlottesville, and designated discussant for the report.
The policy followed by some health insurers to delay coverage for bariatric surgery until patients fail three medications “forces patients with more treatable hypertension to wait until their disease worsens and becomes less treatable before they can receive appropriate treatment,” he said.
Dr. Schirmer attributed the motivation for this approach to a “despicable” and “reprehensible” reason: “Actuarial calculations that show paying for curative therapy is not cost effective in the short term. The duration of a patient’s policy may not be long enough to yield a positive financial outcome, so it becomes more appropriate to deny optimal care and have patients become sicker from their disease.”
“I applaud the authors for accumulating the data that point out this unfortunate rule of some insurance companies,” Dr. Schirmer added.
The practice is comparable with an insurer requiring that a patient’s cancer must be metastatic before allowing coverage for treatment, commented Ann M. Rogers, MD, professor and director of the Penn State University surgical weight loss program in Hershey, Penn., and a moderator of the session.
Dr. Raftopoulos, Dr. Schirmer, and Dr. Rogers had no disclosures.
A delaying tactic used by some U.S. health insurers to limit coverage of bariatric surgery does not jibe with the clinical experience at one U.S. center with 461 patients who underwent primary or revisional bariatric surgery.
The tactic applies to patients with a baseline body mass index (BMI) of 35-39 kg/m2 who usually also need at least one comorbidity to qualify for insurance coverage for bariatric surgery, and specifically to the subgroup for whom hypertension is the qualifying comorbidity.
Some insurers limit surgery coverage to patients with hypertension who fail to reach their goal blood pressure on agents from three different drug classes, a policy that is “extremely frustrating and dangerous,” said Yannis Raftopoulos, MD, PhD, in his presentation at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
Using number of antihypertensive drugs ‘is not correct’
“Using the number of antihypertensive medications to justify surgery is not correct because blood pressure control is not [always] better when patients take two or three medications, compared with when they are taking one. This harms patients because the more severe their hypertension, the worse their control,” said Dr. Raftopoulos, director of the weight management program at Holyoke (Mass.) Medical Center.
He presented findings from a retrospective study of 461 patients who underwent either sleeve gastrectomy or laparoscopic Roux-en-Y gastric bypass at his center, including 213 (46%) diagnosed with hypertension at the time of their surgery. Within this group were 68 patients with a BMI of 35-39, which meant that they could get insurance coverage for bariatric surgery only if they also had a relevant comorbidity such as hypertension, diabetes, or severe sleep apnea.
Among these patients, 36 (17% of those with hypertension) had only hypertension as their relevant comorbidity and would not have qualified for bariatric surgery under the strictest criteria applied by some insurers that require patients to remain hypertensive despite treatment with at least three different antihypertensive medications. (These 36 patients underwent bariatric surgery because their insurance coverage did not have this restriction.)
The analyses Dr. Raftopoulos presented also documented the rate of hypertension resolution among patients in the series who had hypertension at baseline and 1-year follow-up results. Among 65 patients on one antihypertensive drug at baseline, 43 (66%) had complete resolution of their hypertension after 1 year, defined as blood pressure of less than 130/90 mm Hg while completely off antihypertensive treatment. In contrast, among 55 patients on two antihypertensive medications at baseline, 28 (51%) had complete resolution after 1 year, and among 24 patients on three or more antihypertensive medications at baseline, 3 (13%) had complete resolution 1 year after bariatric surgery, he reported.
“Patients who were treated with one oral antihypertensive medication preoperatively had a higher likelihood of postoperative hypertension resolution,” concluded Dr. Raftopoulos.
Restricting access to bariatric surgery to patients with a BMI of less than 40 based on the preoperative intensity of their antihypertensive treatment “is not supported by our data, and can be potentially harmful,” he declared.
“This study was the result of discussions about this problem with multiple insurers in my area,” he added. “This affects a good number of patients.”
Waiting for hypertension to become less treatable
The results Dr. Raftopoulos presented “are not surprising, because they confirm the hypothesis that earlier intervention in the course of a disease like hypertension is more likely to be successful,” commented Bruce D. Schirmer, MD, a professor of surgery at the University of Virginia, Charlottesville, and designated discussant for the report.
The policy followed by some health insurers to delay coverage for bariatric surgery until patients fail three medications “forces patients with more treatable hypertension to wait until their disease worsens and becomes less treatable before they can receive appropriate treatment,” he said.
Dr. Schirmer attributed the motivation for this approach to a “despicable” and “reprehensible” reason: “Actuarial calculations that show paying for curative therapy is not cost effective in the short term. The duration of a patient’s policy may not be long enough to yield a positive financial outcome, so it becomes more appropriate to deny optimal care and have patients become sicker from their disease.”
“I applaud the authors for accumulating the data that point out this unfortunate rule of some insurance companies,” Dr. Schirmer added.
The practice is comparable with an insurer requiring that a patient’s cancer must be metastatic before allowing coverage for treatment, commented Ann M. Rogers, MD, professor and director of the Penn State University surgical weight loss program in Hershey, Penn., and a moderator of the session.
Dr. Raftopoulos, Dr. Schirmer, and Dr. Rogers had no disclosures.
A delaying tactic used by some U.S. health insurers to limit coverage of bariatric surgery does not jibe with the clinical experience at one U.S. center with 461 patients who underwent primary or revisional bariatric surgery.
The tactic applies to patients with a baseline body mass index (BMI) of 35-39 kg/m2 who usually also need at least one comorbidity to qualify for insurance coverage for bariatric surgery, and specifically to the subgroup for whom hypertension is the qualifying comorbidity.
Some insurers limit surgery coverage to patients with hypertension who fail to reach their goal blood pressure on agents from three different drug classes, a policy that is “extremely frustrating and dangerous,” said Yannis Raftopoulos, MD, PhD, in his presentation at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
Using number of antihypertensive drugs ‘is not correct’
“Using the number of antihypertensive medications to justify surgery is not correct because blood pressure control is not [always] better when patients take two or three medications, compared with when they are taking one. This harms patients because the more severe their hypertension, the worse their control,” said Dr. Raftopoulos, director of the weight management program at Holyoke (Mass.) Medical Center.
He presented findings from a retrospective study of 461 patients who underwent either sleeve gastrectomy or laparoscopic Roux-en-Y gastric bypass at his center, including 213 (46%) diagnosed with hypertension at the time of their surgery. Within this group were 68 patients with a BMI of 35-39, which meant that they could get insurance coverage for bariatric surgery only if they also had a relevant comorbidity such as hypertension, diabetes, or severe sleep apnea.
Among these patients, 36 (17% of those with hypertension) had only hypertension as their relevant comorbidity and would not have qualified for bariatric surgery under the strictest criteria applied by some insurers that require patients to remain hypertensive despite treatment with at least three different antihypertensive medications. (These 36 patients underwent bariatric surgery because their insurance coverage did not have this restriction.)
The analyses Dr. Raftopoulos presented also documented the rate of hypertension resolution among patients in the series who had hypertension at baseline and 1-year follow-up results. Among 65 patients on one antihypertensive drug at baseline, 43 (66%) had complete resolution of their hypertension after 1 year, defined as blood pressure of less than 130/90 mm Hg while completely off antihypertensive treatment. In contrast, among 55 patients on two antihypertensive medications at baseline, 28 (51%) had complete resolution after 1 year, and among 24 patients on three or more antihypertensive medications at baseline, 3 (13%) had complete resolution 1 year after bariatric surgery, he reported.
“Patients who were treated with one oral antihypertensive medication preoperatively had a higher likelihood of postoperative hypertension resolution,” concluded Dr. Raftopoulos.
Restricting access to bariatric surgery to patients with a BMI of less than 40 based on the preoperative intensity of their antihypertensive treatment “is not supported by our data, and can be potentially harmful,” he declared.
“This study was the result of discussions about this problem with multiple insurers in my area,” he added. “This affects a good number of patients.”
Waiting for hypertension to become less treatable
The results Dr. Raftopoulos presented “are not surprising, because they confirm the hypothesis that earlier intervention in the course of a disease like hypertension is more likely to be successful,” commented Bruce D. Schirmer, MD, a professor of surgery at the University of Virginia, Charlottesville, and designated discussant for the report.
The policy followed by some health insurers to delay coverage for bariatric surgery until patients fail three medications “forces patients with more treatable hypertension to wait until their disease worsens and becomes less treatable before they can receive appropriate treatment,” he said.
Dr. Schirmer attributed the motivation for this approach to a “despicable” and “reprehensible” reason: “Actuarial calculations that show paying for curative therapy is not cost effective in the short term. The duration of a patient’s policy may not be long enough to yield a positive financial outcome, so it becomes more appropriate to deny optimal care and have patients become sicker from their disease.”
“I applaud the authors for accumulating the data that point out this unfortunate rule of some insurance companies,” Dr. Schirmer added.
The practice is comparable with an insurer requiring that a patient’s cancer must be metastatic before allowing coverage for treatment, commented Ann M. Rogers, MD, professor and director of the Penn State University surgical weight loss program in Hershey, Penn., and a moderator of the session.
Dr. Raftopoulos, Dr. Schirmer, and Dr. Rogers had no disclosures.
FROM ASMBS 2021
Supreme Court upholds Affordable Care Act
The challengers were comprised of 18 GOP-dominated states, led by Texas, that took issue with the ACA’s individual mandate – which required most Americans to have health insurance or pay a tax penalty.
But Congress reduced the penalty to zero in 2017. Challengers argued that without the mandate, the rest of the law should be scrapped, too. The court ruled that eliminated the harm the states were claiming.
“To have standing, a plaintiff must ‘allege personal injury fairly traceable to the defendant’s allegedly unlawful conduct and likely to be redressed by the requested relief,’” the majority wrote. “No plaintiff has shown such an injury ‘fairly traceable’ to the ‘allegedly unlawful conduct’ challenged here.”
Justice Stephen Breyer authored the opinion. Justices Samuel Alito and Neil Gorsuch dissented.
The decision said that the mandate in question did not require the 18 states that brought the complaint to pay anything, and therefore they had no standing.
President Joe Biden has said he plans to build on the ACA – which was enacted while he was vice president – to offer coverage to more Americans.
This marks the third time the Supreme Court spared the Obama-era law from GOP attacks. The mandate was also upheld in 2012 in a 5 to 4 ruling.
American Medical Association president Gerald Harmon, MD, also called for building on the ruling to expand the law.
“With yet another court decision upholding the ACA now behind us, we remain committed to strengthening the current law and look forward to policymakers advancing solutions to improve the ACA,” Dr. Harmon said in a statement. “The AMA will continue working to expand access to health care and ensure that all Americans have meaningful, comprehensive, and affordable health coverage to improve the health of the nation.”
House Speaker Nancy Pelosi (D-Calif.), a longtime advocate for the ACA, called the decision a “landmark victory for Democrats.”
“Thanks to the tireless advocacy of Americans across the country and Democrats in Congress, the Affordable Care Act endures as a pillar of American health and economic security alongside Medicare, Medicaid and Social Security,” she said in a statement.
Senate Majority Leader Chuck Schumer (D-N.Y.) also celebrated the ruling.
“The Affordable Care Act has won. The Supreme Court has just ruled: the ACA is here to stay and now we’re going to try to make it bigger and better,” he said, according to CNN. “For more than a decade, the assault on our health care law was relentless from Republicans in Congress, from the executive branch itself and from Republican attorneys general in the courts. Each time in each arena, the ACA has prevailed.”
This article was updated June 17, 2021.
A version of this article first appeared on WebMD.com.
The challengers were comprised of 18 GOP-dominated states, led by Texas, that took issue with the ACA’s individual mandate – which required most Americans to have health insurance or pay a tax penalty.
But Congress reduced the penalty to zero in 2017. Challengers argued that without the mandate, the rest of the law should be scrapped, too. The court ruled that eliminated the harm the states were claiming.
“To have standing, a plaintiff must ‘allege personal injury fairly traceable to the defendant’s allegedly unlawful conduct and likely to be redressed by the requested relief,’” the majority wrote. “No plaintiff has shown such an injury ‘fairly traceable’ to the ‘allegedly unlawful conduct’ challenged here.”
Justice Stephen Breyer authored the opinion. Justices Samuel Alito and Neil Gorsuch dissented.
The decision said that the mandate in question did not require the 18 states that brought the complaint to pay anything, and therefore they had no standing.
President Joe Biden has said he plans to build on the ACA – which was enacted while he was vice president – to offer coverage to more Americans.
This marks the third time the Supreme Court spared the Obama-era law from GOP attacks. The mandate was also upheld in 2012 in a 5 to 4 ruling.
American Medical Association president Gerald Harmon, MD, also called for building on the ruling to expand the law.
“With yet another court decision upholding the ACA now behind us, we remain committed to strengthening the current law and look forward to policymakers advancing solutions to improve the ACA,” Dr. Harmon said in a statement. “The AMA will continue working to expand access to health care and ensure that all Americans have meaningful, comprehensive, and affordable health coverage to improve the health of the nation.”
House Speaker Nancy Pelosi (D-Calif.), a longtime advocate for the ACA, called the decision a “landmark victory for Democrats.”
“Thanks to the tireless advocacy of Americans across the country and Democrats in Congress, the Affordable Care Act endures as a pillar of American health and economic security alongside Medicare, Medicaid and Social Security,” she said in a statement.
Senate Majority Leader Chuck Schumer (D-N.Y.) also celebrated the ruling.
“The Affordable Care Act has won. The Supreme Court has just ruled: the ACA is here to stay and now we’re going to try to make it bigger and better,” he said, according to CNN. “For more than a decade, the assault on our health care law was relentless from Republicans in Congress, from the executive branch itself and from Republican attorneys general in the courts. Each time in each arena, the ACA has prevailed.”
This article was updated June 17, 2021.
A version of this article first appeared on WebMD.com.
The challengers were comprised of 18 GOP-dominated states, led by Texas, that took issue with the ACA’s individual mandate – which required most Americans to have health insurance or pay a tax penalty.
But Congress reduced the penalty to zero in 2017. Challengers argued that without the mandate, the rest of the law should be scrapped, too. The court ruled that eliminated the harm the states were claiming.
“To have standing, a plaintiff must ‘allege personal injury fairly traceable to the defendant’s allegedly unlawful conduct and likely to be redressed by the requested relief,’” the majority wrote. “No plaintiff has shown such an injury ‘fairly traceable’ to the ‘allegedly unlawful conduct’ challenged here.”
Justice Stephen Breyer authored the opinion. Justices Samuel Alito and Neil Gorsuch dissented.
The decision said that the mandate in question did not require the 18 states that brought the complaint to pay anything, and therefore they had no standing.
President Joe Biden has said he plans to build on the ACA – which was enacted while he was vice president – to offer coverage to more Americans.
This marks the third time the Supreme Court spared the Obama-era law from GOP attacks. The mandate was also upheld in 2012 in a 5 to 4 ruling.
American Medical Association president Gerald Harmon, MD, also called for building on the ruling to expand the law.
“With yet another court decision upholding the ACA now behind us, we remain committed to strengthening the current law and look forward to policymakers advancing solutions to improve the ACA,” Dr. Harmon said in a statement. “The AMA will continue working to expand access to health care and ensure that all Americans have meaningful, comprehensive, and affordable health coverage to improve the health of the nation.”
House Speaker Nancy Pelosi (D-Calif.), a longtime advocate for the ACA, called the decision a “landmark victory for Democrats.”
“Thanks to the tireless advocacy of Americans across the country and Democrats in Congress, the Affordable Care Act endures as a pillar of American health and economic security alongside Medicare, Medicaid and Social Security,” she said in a statement.
Senate Majority Leader Chuck Schumer (D-N.Y.) also celebrated the ruling.
“The Affordable Care Act has won. The Supreme Court has just ruled: the ACA is here to stay and now we’re going to try to make it bigger and better,” he said, according to CNN. “For more than a decade, the assault on our health care law was relentless from Republicans in Congress, from the executive branch itself and from Republican attorneys general in the courts. Each time in each arena, the ACA has prevailed.”
This article was updated June 17, 2021.
A version of this article first appeared on WebMD.com.
The most important meal of the day, with extra zinc
Busting the myth of skipping breakfast
Your mother told you that breakfast was the most important meal of the day. Cereal marketing teams banked on that, selling breakfast to millions of people based on a common turn of phrase like “an apple a day keeps the doctor away.” Well, what if the notion of breakfast’s importance isn’t just marketing BS?
A new study suggests that adults who don’t eat breakfast are setting themselves up for a nutritional gap. Common breakfast foods pack a ton of calcium, fiber, and vitamin C from milk, cereals, and fruit. Christopher Taylor, PhD, senior author of the study and professor of dietetics at the Ohio State University, Columbus, said that if you’re not getting those nutrients from foods at breakfast, there’s a tendency to skip them throughout the rest of your day.
Data from a sample of the National Health and Nutrition Examination Survey – 30,889 adults aged 19 and older who participated between 2005 and 2016 – showed that 15.2% of participants reported skipping breakfast.
The research team then estimated nutrient consumption using federal dietary studies and guidelines and compared it to Food and Nutrition Board of National Academies nutrient recommendations. The breakfast skippers, they determined, were missing out on pronounced levels of fiber, magnesium, iron, calcium, and vitamins A, B1, B2, B3, C, and D and were more likely to fall prey to lower-quality snacking. Cue those Oreos at 3 pm.
You may get more total calories within the day by eating breakfast, but your lunch, dinner, and snacks are much larger when you skip it. So the case of breakfast being the most important meal of the day checks out. Who knew that Tony the Tiger – and Mom – were actually on to something?
The bitter taste of a healthy liver
Alcohol and liver disease. They go together like, well, alcohol and liver disease. But alcohol isn’t the only reason people get liver disease, and now there’s a potential new treatment for people with hepatic steatosis on the way to becoming nonalcoholic fatty liver disease: beer.
Okay, not literally beer, but a pair of compounds derived from hops, the plant that gives beer its color and bitter flavor. In a study published in eLife, researchers from Oregon State University fed mice either a low-fat diet or a high-fat diet to induce hepatic steatosis, with some on the high-fat diet receiving either xanthohumol, a prenylated flavonoid from the hop plant, or tetrahydroxanthohumol, a hydrogenated derivative of xanthohumol.
Mice that received tetrahydroxanthohumol not only gained weight at a far slower rate than that of mice on the normal high-fat diet, their blood sugar remained stable; xanthohumol was similarly effective if the dosage was higher. The researchers noted that the two chemicals were effective because they acted as antagonists for the PPAR-gamma protein, which controls glucose metabolism and fatty cell activation. The chemicals bind to the protein but don’t activate it, meaning fat is unable to build up in the cells. No fat means no hepatic steatosis, which means no liver disease.
The researchers caution that more research is needed to determine the chemicals’ effectiveness in humans, but the classic line from a great animated philosopher still holds true: Alcohol may really be the source of, and solution to, all of life’s problems.
Life’s great mysteries, from A to zinc
Thanks to science, we now have answers to what were once unanswerable questions: Is Jello a solid or a liquid? If someone leads but no one follows, are they just out for a walk? Does zinc inhibit or promote the growth of kidney stones? How many licks does it take to get to the center of a Tootsie Pop? (Turns out science really did answer this one.)
If you’re anything like us, then you’ve been following the big debate on the two competing theories involving the role of zinc in kidney stone formation for years. One theory says that zinc stops the growth of calcium oxalate crystals that make up stones. The other says that zinc alters the surfaces of crystals, which encourages growth.
We can’t stand the suspense any longer, so here goes: The answer to “does zinc inhibit or promote the growth of kidney stones?” is … yes.
“What we see with zinc is something we haven’t seen before. It does slow down calcium oxalate crystal growth and at the same time it changes the surface of the crystals, causing defects in the form of intergrowths. These abnormalities create centers for new crystals to nucleate and grow,” said senior author Jeffrey Rimer, PhD, of the University of Houston.
In vitro experimentation, computational modeling, and atomic force microscopy don’t lie: Zinc ions have a unique ability “to alter the termination of crystal surfaces.” They tried alternative ions found in urine, including magnesium, and there was no effect on crystal formation.
With this one great mystery now solved, we contacted Dr. Rimer to ask him about the whole “sound of one hand clapping” business. He hasn’t cracked that one yet, but he did want to speak to our supervisor. So many of life’s unanswered questions, so little time. Oh well.
Babies’ ‘gut instinct’ to cry
At some point or another, you’ve probably been told not to “be such a baby” when you were scared of something. If you’ve been called a crybaby, it may be an indicator that you had a different gut microbiome as an infant.
Investigators from Michigan State University and the University of North Carolina say that babies who react more strongly to scary situations have different gut microbiomes compared with babies who don’t have such a strong reaction. The way babies react to scary situations can say a lot about their future, and there is even some evidence that gut microbiomes may have something to do with mental health.
Physicians who support neurologic development may one day be able to use this research on gut microbiomes to help monitor people’s neurological health. “This early developmental period is a time of tremendous opportunity for promoting healthy brain development. The microbiome is an exciting new target that can be potentially used for that,” said Rebecca Knickmeyer of MSU, leader of the study, which was published in Nature Communications. And loyal LOTME followers already know about the OpenBiome Microbiome Library, aka the “Amazon of bacteria.”
So the next time someone tells you not to be such a baby when you’re scared of something, tell them it’s not your fault. Blame it on your gut microbiome!
Busting the myth of skipping breakfast
Your mother told you that breakfast was the most important meal of the day. Cereal marketing teams banked on that, selling breakfast to millions of people based on a common turn of phrase like “an apple a day keeps the doctor away.” Well, what if the notion of breakfast’s importance isn’t just marketing BS?
A new study suggests that adults who don’t eat breakfast are setting themselves up for a nutritional gap. Common breakfast foods pack a ton of calcium, fiber, and vitamin C from milk, cereals, and fruit. Christopher Taylor, PhD, senior author of the study and professor of dietetics at the Ohio State University, Columbus, said that if you’re not getting those nutrients from foods at breakfast, there’s a tendency to skip them throughout the rest of your day.
Data from a sample of the National Health and Nutrition Examination Survey – 30,889 adults aged 19 and older who participated between 2005 and 2016 – showed that 15.2% of participants reported skipping breakfast.
The research team then estimated nutrient consumption using federal dietary studies and guidelines and compared it to Food and Nutrition Board of National Academies nutrient recommendations. The breakfast skippers, they determined, were missing out on pronounced levels of fiber, magnesium, iron, calcium, and vitamins A, B1, B2, B3, C, and D and were more likely to fall prey to lower-quality snacking. Cue those Oreos at 3 pm.
You may get more total calories within the day by eating breakfast, but your lunch, dinner, and snacks are much larger when you skip it. So the case of breakfast being the most important meal of the day checks out. Who knew that Tony the Tiger – and Mom – were actually on to something?
The bitter taste of a healthy liver
Alcohol and liver disease. They go together like, well, alcohol and liver disease. But alcohol isn’t the only reason people get liver disease, and now there’s a potential new treatment for people with hepatic steatosis on the way to becoming nonalcoholic fatty liver disease: beer.
Okay, not literally beer, but a pair of compounds derived from hops, the plant that gives beer its color and bitter flavor. In a study published in eLife, researchers from Oregon State University fed mice either a low-fat diet or a high-fat diet to induce hepatic steatosis, with some on the high-fat diet receiving either xanthohumol, a prenylated flavonoid from the hop plant, or tetrahydroxanthohumol, a hydrogenated derivative of xanthohumol.
Mice that received tetrahydroxanthohumol not only gained weight at a far slower rate than that of mice on the normal high-fat diet, their blood sugar remained stable; xanthohumol was similarly effective if the dosage was higher. The researchers noted that the two chemicals were effective because they acted as antagonists for the PPAR-gamma protein, which controls glucose metabolism and fatty cell activation. The chemicals bind to the protein but don’t activate it, meaning fat is unable to build up in the cells. No fat means no hepatic steatosis, which means no liver disease.
The researchers caution that more research is needed to determine the chemicals’ effectiveness in humans, but the classic line from a great animated philosopher still holds true: Alcohol may really be the source of, and solution to, all of life’s problems.
Life’s great mysteries, from A to zinc
Thanks to science, we now have answers to what were once unanswerable questions: Is Jello a solid or a liquid? If someone leads but no one follows, are they just out for a walk? Does zinc inhibit or promote the growth of kidney stones? How many licks does it take to get to the center of a Tootsie Pop? (Turns out science really did answer this one.)
If you’re anything like us, then you’ve been following the big debate on the two competing theories involving the role of zinc in kidney stone formation for years. One theory says that zinc stops the growth of calcium oxalate crystals that make up stones. The other says that zinc alters the surfaces of crystals, which encourages growth.
We can’t stand the suspense any longer, so here goes: The answer to “does zinc inhibit or promote the growth of kidney stones?” is … yes.
“What we see with zinc is something we haven’t seen before. It does slow down calcium oxalate crystal growth and at the same time it changes the surface of the crystals, causing defects in the form of intergrowths. These abnormalities create centers for new crystals to nucleate and grow,” said senior author Jeffrey Rimer, PhD, of the University of Houston.
In vitro experimentation, computational modeling, and atomic force microscopy don’t lie: Zinc ions have a unique ability “to alter the termination of crystal surfaces.” They tried alternative ions found in urine, including magnesium, and there was no effect on crystal formation.
With this one great mystery now solved, we contacted Dr. Rimer to ask him about the whole “sound of one hand clapping” business. He hasn’t cracked that one yet, but he did want to speak to our supervisor. So many of life’s unanswered questions, so little time. Oh well.
Babies’ ‘gut instinct’ to cry
At some point or another, you’ve probably been told not to “be such a baby” when you were scared of something. If you’ve been called a crybaby, it may be an indicator that you had a different gut microbiome as an infant.
Investigators from Michigan State University and the University of North Carolina say that babies who react more strongly to scary situations have different gut microbiomes compared with babies who don’t have such a strong reaction. The way babies react to scary situations can say a lot about their future, and there is even some evidence that gut microbiomes may have something to do with mental health.
Physicians who support neurologic development may one day be able to use this research on gut microbiomes to help monitor people’s neurological health. “This early developmental period is a time of tremendous opportunity for promoting healthy brain development. The microbiome is an exciting new target that can be potentially used for that,” said Rebecca Knickmeyer of MSU, leader of the study, which was published in Nature Communications. And loyal LOTME followers already know about the OpenBiome Microbiome Library, aka the “Amazon of bacteria.”
So the next time someone tells you not to be such a baby when you’re scared of something, tell them it’s not your fault. Blame it on your gut microbiome!
Busting the myth of skipping breakfast
Your mother told you that breakfast was the most important meal of the day. Cereal marketing teams banked on that, selling breakfast to millions of people based on a common turn of phrase like “an apple a day keeps the doctor away.” Well, what if the notion of breakfast’s importance isn’t just marketing BS?
A new study suggests that adults who don’t eat breakfast are setting themselves up for a nutritional gap. Common breakfast foods pack a ton of calcium, fiber, and vitamin C from milk, cereals, and fruit. Christopher Taylor, PhD, senior author of the study and professor of dietetics at the Ohio State University, Columbus, said that if you’re not getting those nutrients from foods at breakfast, there’s a tendency to skip them throughout the rest of your day.
Data from a sample of the National Health and Nutrition Examination Survey – 30,889 adults aged 19 and older who participated between 2005 and 2016 – showed that 15.2% of participants reported skipping breakfast.
The research team then estimated nutrient consumption using federal dietary studies and guidelines and compared it to Food and Nutrition Board of National Academies nutrient recommendations. The breakfast skippers, they determined, were missing out on pronounced levels of fiber, magnesium, iron, calcium, and vitamins A, B1, B2, B3, C, and D and were more likely to fall prey to lower-quality snacking. Cue those Oreos at 3 pm.
You may get more total calories within the day by eating breakfast, but your lunch, dinner, and snacks are much larger when you skip it. So the case of breakfast being the most important meal of the day checks out. Who knew that Tony the Tiger – and Mom – were actually on to something?
The bitter taste of a healthy liver
Alcohol and liver disease. They go together like, well, alcohol and liver disease. But alcohol isn’t the only reason people get liver disease, and now there’s a potential new treatment for people with hepatic steatosis on the way to becoming nonalcoholic fatty liver disease: beer.
Okay, not literally beer, but a pair of compounds derived from hops, the plant that gives beer its color and bitter flavor. In a study published in eLife, researchers from Oregon State University fed mice either a low-fat diet or a high-fat diet to induce hepatic steatosis, with some on the high-fat diet receiving either xanthohumol, a prenylated flavonoid from the hop plant, or tetrahydroxanthohumol, a hydrogenated derivative of xanthohumol.
Mice that received tetrahydroxanthohumol not only gained weight at a far slower rate than that of mice on the normal high-fat diet, their blood sugar remained stable; xanthohumol was similarly effective if the dosage was higher. The researchers noted that the two chemicals were effective because they acted as antagonists for the PPAR-gamma protein, which controls glucose metabolism and fatty cell activation. The chemicals bind to the protein but don’t activate it, meaning fat is unable to build up in the cells. No fat means no hepatic steatosis, which means no liver disease.
The researchers caution that more research is needed to determine the chemicals’ effectiveness in humans, but the classic line from a great animated philosopher still holds true: Alcohol may really be the source of, and solution to, all of life’s problems.
Life’s great mysteries, from A to zinc
Thanks to science, we now have answers to what were once unanswerable questions: Is Jello a solid or a liquid? If someone leads but no one follows, are they just out for a walk? Does zinc inhibit or promote the growth of kidney stones? How many licks does it take to get to the center of a Tootsie Pop? (Turns out science really did answer this one.)
If you’re anything like us, then you’ve been following the big debate on the two competing theories involving the role of zinc in kidney stone formation for years. One theory says that zinc stops the growth of calcium oxalate crystals that make up stones. The other says that zinc alters the surfaces of crystals, which encourages growth.
We can’t stand the suspense any longer, so here goes: The answer to “does zinc inhibit or promote the growth of kidney stones?” is … yes.
“What we see with zinc is something we haven’t seen before. It does slow down calcium oxalate crystal growth and at the same time it changes the surface of the crystals, causing defects in the form of intergrowths. These abnormalities create centers for new crystals to nucleate and grow,” said senior author Jeffrey Rimer, PhD, of the University of Houston.
In vitro experimentation, computational modeling, and atomic force microscopy don’t lie: Zinc ions have a unique ability “to alter the termination of crystal surfaces.” They tried alternative ions found in urine, including magnesium, and there was no effect on crystal formation.
With this one great mystery now solved, we contacted Dr. Rimer to ask him about the whole “sound of one hand clapping” business. He hasn’t cracked that one yet, but he did want to speak to our supervisor. So many of life’s unanswered questions, so little time. Oh well.
Babies’ ‘gut instinct’ to cry
At some point or another, you’ve probably been told not to “be such a baby” when you were scared of something. If you’ve been called a crybaby, it may be an indicator that you had a different gut microbiome as an infant.
Investigators from Michigan State University and the University of North Carolina say that babies who react more strongly to scary situations have different gut microbiomes compared with babies who don’t have such a strong reaction. The way babies react to scary situations can say a lot about their future, and there is even some evidence that gut microbiomes may have something to do with mental health.
Physicians who support neurologic development may one day be able to use this research on gut microbiomes to help monitor people’s neurological health. “This early developmental period is a time of tremendous opportunity for promoting healthy brain development. The microbiome is an exciting new target that can be potentially used for that,” said Rebecca Knickmeyer of MSU, leader of the study, which was published in Nature Communications. And loyal LOTME followers already know about the OpenBiome Microbiome Library, aka the “Amazon of bacteria.”
So the next time someone tells you not to be such a baby when you’re scared of something, tell them it’s not your fault. Blame it on your gut microbiome!
AMA acknowledges medical education racism of past, vows better future
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
Inpatient care for HS higher for Black and Hispanic patients
National Inpatient Sample.
The differences occurred despite Black and Hispanic patients being younger at the time of admission than White patients, and may reflect increased disease severity and management challenges in these patients with skin of color, Nishadh Sutaria, BS, a medical student at Tufts University, Boston, said at the annual Skin of Color Society symposium. “They may also reflect social inequities in access to dermatologists, with racial and ethnic minorities using inpatient services in lieu of outpatient care.”
Mr. Sutaria and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified 8,040 HS admissions for White patients, 16,490 Black patients, and 2,405 for Hispanic patients during the 5-year period.
Black and Hispanic patients were significantly younger than White patients, with a mean age of 38.1 years and 35 years, respectively, compared with 42 years for White patients (P < .001 in each case). Compared with White patients, Black patients had more procedures (2.03 vs. 1.84, P = .006), a longer length of stay (5.82 days vs. 4.97 days, P = .001), and higher cost of care ($46,119 vs. $39,862, P = .010). Compared with White patients, Hispanic patients had higher cost of care ($52,334 vs. $39,862, P = .004).
“In these models, Black patients stayed almost a full day longer and accrued a charge of $8,000 more than White patients, and Hispanic patients stayed about a half-day longer and accrued a charge of almost $15,000 more than White patients,” Mr. Sutaria said.
In a multilinear regression analysis adjusting for age, sex, and insurance type, Black race correlated with more procedures, higher length of stay, and higher cost of care, and Hispanic ethnicity with more procedures and higher cost of care.
Prior research has shown that Black patients may be disproportionately affected by HS. A 2017 analysis of electronic health record data for tens of millions of patients nationally, for instance, showed an incidence of HS that was over 2.5 times greater in Blacks than Whites. And a recent analysis of electronic data in Wisconsin for patients with an HS diagnosis and 3 or more encounters for the disease showed that Blacks are more likely to have HS that is Hurley Stage 3, the most severe type.
Increased severity “has not been explicitly shown in Hispanic patients,” Dr. Kwatra said in an interview, “[but] there is a strong relationship between obesity/metabolic syndrome with HS. Because Hispanic patients have higher rates of obesity and metabolic syndrome, it’s [thought] that they may have more severe HS.”
HS patients with skin of color are underrepresented in clinical trials, he said. “Severe HS can be difficult to treat because there are few effective treatments,” he said, noting that adalimumab is the only Food and Drug Administration–approved therapy.
The National Inpatient Sample is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Sutaria is a dermatology research fellow working under the guidance of Dr. Kwatra.
National Inpatient Sample.
The differences occurred despite Black and Hispanic patients being younger at the time of admission than White patients, and may reflect increased disease severity and management challenges in these patients with skin of color, Nishadh Sutaria, BS, a medical student at Tufts University, Boston, said at the annual Skin of Color Society symposium. “They may also reflect social inequities in access to dermatologists, with racial and ethnic minorities using inpatient services in lieu of outpatient care.”
Mr. Sutaria and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified 8,040 HS admissions for White patients, 16,490 Black patients, and 2,405 for Hispanic patients during the 5-year period.
Black and Hispanic patients were significantly younger than White patients, with a mean age of 38.1 years and 35 years, respectively, compared with 42 years for White patients (P < .001 in each case). Compared with White patients, Black patients had more procedures (2.03 vs. 1.84, P = .006), a longer length of stay (5.82 days vs. 4.97 days, P = .001), and higher cost of care ($46,119 vs. $39,862, P = .010). Compared with White patients, Hispanic patients had higher cost of care ($52,334 vs. $39,862, P = .004).
“In these models, Black patients stayed almost a full day longer and accrued a charge of $8,000 more than White patients, and Hispanic patients stayed about a half-day longer and accrued a charge of almost $15,000 more than White patients,” Mr. Sutaria said.
In a multilinear regression analysis adjusting for age, sex, and insurance type, Black race correlated with more procedures, higher length of stay, and higher cost of care, and Hispanic ethnicity with more procedures and higher cost of care.
Prior research has shown that Black patients may be disproportionately affected by HS. A 2017 analysis of electronic health record data for tens of millions of patients nationally, for instance, showed an incidence of HS that was over 2.5 times greater in Blacks than Whites. And a recent analysis of electronic data in Wisconsin for patients with an HS diagnosis and 3 or more encounters for the disease showed that Blacks are more likely to have HS that is Hurley Stage 3, the most severe type.
Increased severity “has not been explicitly shown in Hispanic patients,” Dr. Kwatra said in an interview, “[but] there is a strong relationship between obesity/metabolic syndrome with HS. Because Hispanic patients have higher rates of obesity and metabolic syndrome, it’s [thought] that they may have more severe HS.”
HS patients with skin of color are underrepresented in clinical trials, he said. “Severe HS can be difficult to treat because there are few effective treatments,” he said, noting that adalimumab is the only Food and Drug Administration–approved therapy.
The National Inpatient Sample is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Sutaria is a dermatology research fellow working under the guidance of Dr. Kwatra.
National Inpatient Sample.
The differences occurred despite Black and Hispanic patients being younger at the time of admission than White patients, and may reflect increased disease severity and management challenges in these patients with skin of color, Nishadh Sutaria, BS, a medical student at Tufts University, Boston, said at the annual Skin of Color Society symposium. “They may also reflect social inequities in access to dermatologists, with racial and ethnic minorities using inpatient services in lieu of outpatient care.”
Mr. Sutaria and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified 8,040 HS admissions for White patients, 16,490 Black patients, and 2,405 for Hispanic patients during the 5-year period.
Black and Hispanic patients were significantly younger than White patients, with a mean age of 38.1 years and 35 years, respectively, compared with 42 years for White patients (P < .001 in each case). Compared with White patients, Black patients had more procedures (2.03 vs. 1.84, P = .006), a longer length of stay (5.82 days vs. 4.97 days, P = .001), and higher cost of care ($46,119 vs. $39,862, P = .010). Compared with White patients, Hispanic patients had higher cost of care ($52,334 vs. $39,862, P = .004).
“In these models, Black patients stayed almost a full day longer and accrued a charge of $8,000 more than White patients, and Hispanic patients stayed about a half-day longer and accrued a charge of almost $15,000 more than White patients,” Mr. Sutaria said.
In a multilinear regression analysis adjusting for age, sex, and insurance type, Black race correlated with more procedures, higher length of stay, and higher cost of care, and Hispanic ethnicity with more procedures and higher cost of care.
Prior research has shown that Black patients may be disproportionately affected by HS. A 2017 analysis of electronic health record data for tens of millions of patients nationally, for instance, showed an incidence of HS that was over 2.5 times greater in Blacks than Whites. And a recent analysis of electronic data in Wisconsin for patients with an HS diagnosis and 3 or more encounters for the disease showed that Blacks are more likely to have HS that is Hurley Stage 3, the most severe type.
Increased severity “has not been explicitly shown in Hispanic patients,” Dr. Kwatra said in an interview, “[but] there is a strong relationship between obesity/metabolic syndrome with HS. Because Hispanic patients have higher rates of obesity and metabolic syndrome, it’s [thought] that they may have more severe HS.”
HS patients with skin of color are underrepresented in clinical trials, he said. “Severe HS can be difficult to treat because there are few effective treatments,” he said, noting that adalimumab is the only Food and Drug Administration–approved therapy.
The National Inpatient Sample is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Sutaria is a dermatology research fellow working under the guidance of Dr. Kwatra.
FROM SOC SOCIETY 2021