User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Uptick in lung cancer in younger women, not related to smoking
A study of lung cancer in younger adults (less than 50 years) has found a recent trend of higher lung cancer rates in women, compared with men. The increase is driven by cases of adenocarcinoma of the lung.
The “emerging pattern of higher lung cancer incidence in young females” is not confined to geographic areas and income levels and “is not fully explained by sex-differences in smoking prevalence,” the authors comment.
Miranda M. Fidler-Benaoudia, PhD, Cancer Control Alberta, Alberta Health Services, Calgary, and colleagues examined lung cancer cases in 40 countries from 1993 to 2012.
They found that the female-to-male incidence rate ratio (IRR) had significantly crossed over from men to women in six countries, including the United States and Canada, and had nonsignificantly crossed over in a further 23 countries.
The research was published online Feb. 5 in the International Journal of Cancer.
These findings “forewarn of a higher lung cancer burden in women than men at older ages in the decades to follow, especially in higher-income settings,” write the authors. They highlight “the need for etiologic studies.”
Historically, lung cancer higher in men
Historically, lung cancer rates have been higher among men than women, owing to the fact that men start smoking in large numbers earlier and smoke at higher rates, the researchers comment.
However, there has been a convergence in lung cancer incidence between men and women. A recent study suggests that, in the United States, the incidence in young women is higher than that in their male counterparts.
To determine the degree to which this phenomenon is occurring globally, the team used national or subnational registry data from Cancer Incidence in Five Continents, volumes VIII–XI.
These included lung and bronchial cancer cases in 40 countries from 1993 to 2012, divided into 5-year periods. Individuals were categorized into 5-year age bands.
In addition, the team used the Global Health Data Exchange to extract data from the Global Burden of Disease Study 2015 and derive country- and sex-specific daily smoking prevalence rates.
The researchers found that among young men and women, there were three patterns in the occurrence of lung cancer between the periods 1993-1997 and 2008-2012:
- A significant crossover from male to female dominance, seen in six countries.
- An insignificant crossover from male to female dominance, found in 23 countries.
- A continued male dominance, observed in 11 countries.
Higher incidence in women in six countries
The six countries with significant crossover from male to female dominance were Canada, Denmark, Germany, New Zealand, the Netherlands, and the United States.
Further analysis showed that, in general, age-specific lung cancer incidence rates decreased in successive male birth cohorts in these six countries. There was more variation across female birth cohorts.
Calculating female-to-male incidence rate ratios, the team found, for example, the IRR increased in New Zealand from 1.0 in the 1953 birth cohort to 1.6 in the 1968 birth cohort for people aged 40-44 years.
In addition, among adults aged 45-49 years in the Netherlands, the IRR rose from 0.7 in those born in the circa 1948 cohort to 1.4 in those from the circa 1958 cohort.
Overall, female-to-male IRRs increased notably among the following groups:
- Individuals aged 30-34 years in Canada, Denmark, and Germany.
- Those aged 40-44 years in Germany, the Netherlands, and the United States.
- Those aged 44-50 years in the Netherlands and the United States.
- Those aged 50-54 years in Canada, Denmark, and New Zealand.
Countries with an insignificant crossover from male to female dominance of lung cancer were located across Africa, the Americas, Asia, Europe, and Oceania.
Again, incidence rates were typically characterized by falling rates of lung cancer among men in more recent birth cohorts, and lung cancer incidence trends were more variable in women.
The team writes: “Of note, the six countries demonstrating a significant crossover are among those considered to be more advanced in the tobacco epidemic.
“Many of the countries where the crossover was insignificant or when there was no crossover are considered to be late adopters of the tobacco epidemic, with the effects of the epidemic on the burden of lung cancer and other smoking-related diseases beginning to manifest more recently, or perhaps yet to come.”
They suggest that low- and middle-resource countries may not follow the tobacco epidemic pattern of high-income countries, and so “we may not see higher lung cancer incidence rates in women than men for the foreseeable future in these countries.”
No funding for the study has been disclosed. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
A study of lung cancer in younger adults (less than 50 years) has found a recent trend of higher lung cancer rates in women, compared with men. The increase is driven by cases of adenocarcinoma of the lung.
The “emerging pattern of higher lung cancer incidence in young females” is not confined to geographic areas and income levels and “is not fully explained by sex-differences in smoking prevalence,” the authors comment.
Miranda M. Fidler-Benaoudia, PhD, Cancer Control Alberta, Alberta Health Services, Calgary, and colleagues examined lung cancer cases in 40 countries from 1993 to 2012.
They found that the female-to-male incidence rate ratio (IRR) had significantly crossed over from men to women in six countries, including the United States and Canada, and had nonsignificantly crossed over in a further 23 countries.
The research was published online Feb. 5 in the International Journal of Cancer.
These findings “forewarn of a higher lung cancer burden in women than men at older ages in the decades to follow, especially in higher-income settings,” write the authors. They highlight “the need for etiologic studies.”
Historically, lung cancer higher in men
Historically, lung cancer rates have been higher among men than women, owing to the fact that men start smoking in large numbers earlier and smoke at higher rates, the researchers comment.
However, there has been a convergence in lung cancer incidence between men and women. A recent study suggests that, in the United States, the incidence in young women is higher than that in their male counterparts.
To determine the degree to which this phenomenon is occurring globally, the team used national or subnational registry data from Cancer Incidence in Five Continents, volumes VIII–XI.
These included lung and bronchial cancer cases in 40 countries from 1993 to 2012, divided into 5-year periods. Individuals were categorized into 5-year age bands.
In addition, the team used the Global Health Data Exchange to extract data from the Global Burden of Disease Study 2015 and derive country- and sex-specific daily smoking prevalence rates.
The researchers found that among young men and women, there were three patterns in the occurrence of lung cancer between the periods 1993-1997 and 2008-2012:
- A significant crossover from male to female dominance, seen in six countries.
- An insignificant crossover from male to female dominance, found in 23 countries.
- A continued male dominance, observed in 11 countries.
Higher incidence in women in six countries
The six countries with significant crossover from male to female dominance were Canada, Denmark, Germany, New Zealand, the Netherlands, and the United States.
Further analysis showed that, in general, age-specific lung cancer incidence rates decreased in successive male birth cohorts in these six countries. There was more variation across female birth cohorts.
Calculating female-to-male incidence rate ratios, the team found, for example, the IRR increased in New Zealand from 1.0 in the 1953 birth cohort to 1.6 in the 1968 birth cohort for people aged 40-44 years.
In addition, among adults aged 45-49 years in the Netherlands, the IRR rose from 0.7 in those born in the circa 1948 cohort to 1.4 in those from the circa 1958 cohort.
Overall, female-to-male IRRs increased notably among the following groups:
- Individuals aged 30-34 years in Canada, Denmark, and Germany.
- Those aged 40-44 years in Germany, the Netherlands, and the United States.
- Those aged 44-50 years in the Netherlands and the United States.
- Those aged 50-54 years in Canada, Denmark, and New Zealand.
Countries with an insignificant crossover from male to female dominance of lung cancer were located across Africa, the Americas, Asia, Europe, and Oceania.
Again, incidence rates were typically characterized by falling rates of lung cancer among men in more recent birth cohorts, and lung cancer incidence trends were more variable in women.
The team writes: “Of note, the six countries demonstrating a significant crossover are among those considered to be more advanced in the tobacco epidemic.
“Many of the countries where the crossover was insignificant or when there was no crossover are considered to be late adopters of the tobacco epidemic, with the effects of the epidemic on the burden of lung cancer and other smoking-related diseases beginning to manifest more recently, or perhaps yet to come.”
They suggest that low- and middle-resource countries may not follow the tobacco epidemic pattern of high-income countries, and so “we may not see higher lung cancer incidence rates in women than men for the foreseeable future in these countries.”
No funding for the study has been disclosed. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
A study of lung cancer in younger adults (less than 50 years) has found a recent trend of higher lung cancer rates in women, compared with men. The increase is driven by cases of adenocarcinoma of the lung.
The “emerging pattern of higher lung cancer incidence in young females” is not confined to geographic areas and income levels and “is not fully explained by sex-differences in smoking prevalence,” the authors comment.
Miranda M. Fidler-Benaoudia, PhD, Cancer Control Alberta, Alberta Health Services, Calgary, and colleagues examined lung cancer cases in 40 countries from 1993 to 2012.
They found that the female-to-male incidence rate ratio (IRR) had significantly crossed over from men to women in six countries, including the United States and Canada, and had nonsignificantly crossed over in a further 23 countries.
The research was published online Feb. 5 in the International Journal of Cancer.
These findings “forewarn of a higher lung cancer burden in women than men at older ages in the decades to follow, especially in higher-income settings,” write the authors. They highlight “the need for etiologic studies.”
Historically, lung cancer higher in men
Historically, lung cancer rates have been higher among men than women, owing to the fact that men start smoking in large numbers earlier and smoke at higher rates, the researchers comment.
However, there has been a convergence in lung cancer incidence between men and women. A recent study suggests that, in the United States, the incidence in young women is higher than that in their male counterparts.
To determine the degree to which this phenomenon is occurring globally, the team used national or subnational registry data from Cancer Incidence in Five Continents, volumes VIII–XI.
These included lung and bronchial cancer cases in 40 countries from 1993 to 2012, divided into 5-year periods. Individuals were categorized into 5-year age bands.
In addition, the team used the Global Health Data Exchange to extract data from the Global Burden of Disease Study 2015 and derive country- and sex-specific daily smoking prevalence rates.
The researchers found that among young men and women, there were three patterns in the occurrence of lung cancer between the periods 1993-1997 and 2008-2012:
- A significant crossover from male to female dominance, seen in six countries.
- An insignificant crossover from male to female dominance, found in 23 countries.
- A continued male dominance, observed in 11 countries.
Higher incidence in women in six countries
The six countries with significant crossover from male to female dominance were Canada, Denmark, Germany, New Zealand, the Netherlands, and the United States.
Further analysis showed that, in general, age-specific lung cancer incidence rates decreased in successive male birth cohorts in these six countries. There was more variation across female birth cohorts.
Calculating female-to-male incidence rate ratios, the team found, for example, the IRR increased in New Zealand from 1.0 in the 1953 birth cohort to 1.6 in the 1968 birth cohort for people aged 40-44 years.
In addition, among adults aged 45-49 years in the Netherlands, the IRR rose from 0.7 in those born in the circa 1948 cohort to 1.4 in those from the circa 1958 cohort.
Overall, female-to-male IRRs increased notably among the following groups:
- Individuals aged 30-34 years in Canada, Denmark, and Germany.
- Those aged 40-44 years in Germany, the Netherlands, and the United States.
- Those aged 44-50 years in the Netherlands and the United States.
- Those aged 50-54 years in Canada, Denmark, and New Zealand.
Countries with an insignificant crossover from male to female dominance of lung cancer were located across Africa, the Americas, Asia, Europe, and Oceania.
Again, incidence rates were typically characterized by falling rates of lung cancer among men in more recent birth cohorts, and lung cancer incidence trends were more variable in women.
The team writes: “Of note, the six countries demonstrating a significant crossover are among those considered to be more advanced in the tobacco epidemic.
“Many of the countries where the crossover was insignificant or when there was no crossover are considered to be late adopters of the tobacco epidemic, with the effects of the epidemic on the burden of lung cancer and other smoking-related diseases beginning to manifest more recently, or perhaps yet to come.”
They suggest that low- and middle-resource countries may not follow the tobacco epidemic pattern of high-income countries, and so “we may not see higher lung cancer incidence rates in women than men for the foreseeable future in these countries.”
No funding for the study has been disclosed. The authors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Vaccinating most girls could eliminate cervical cancer within a century
Cervical cancer is the second most common cancer among women in lower- and middle-income countries, but universal human papillomavirus vaccination for girls would reduce new cervical cancer cases by about 90% over the next century, according to researchers.
Adding twice-lifetime cervical screening with human papillomavirus (HPV) testing would further reduce the incidence of cervical cancer, including in countries with the highest burden, the researchers reported in The Lancet.
Marc Brisson, PhD, of Laval University, Quebec City, and colleagues conducted this study using three models identified by the World Health Organization. The models were used to project reductions in cervical cancer incidence for women in 78 low- and middle-income countries based on the following HPV vaccination and screening scenarios:
- Universal girls-only vaccination at age 9 years, assuming 90% of girls vaccinated and a vaccine that is perfectly effective
- Girls-only vaccination plus cervical screening with HPV testing at age 35 years
- Girls-only vaccination plus screening at ages 35 and 45.
All three scenarios modeled would result in the elimination of cervical cancer, Dr. Brisson and colleagues found. Elimination was defined as four or fewer new cases per 100,000 women-years.
The simplest scenario, universal girls-only vaccination, was predicted to reduce age-standardized cervical cancer incidence from 19.8 cases per 100,000 women-years to 2.1 cases per 100,000 women-years (89.4% reduction) by 2120. That amounts to about 61 million potential cases avoided, with elimination targets reached in 60% of the countries studied.
HPV vaccination plus one-time screening was predicted to reduce the incidence of cervical cancer to 1.0 case per 100,000 women-years (95.0% reduction), and HPV vaccination plus twice-lifetime screening was predicted to reduce the incidence to 0.7 cases per 100,000 women-years (96.7% reduction).
Dr. Brisson and colleagues reported that, for the countries with the highest burden of cervical cancer (more than 25 cases per 100,000 women-years), adding screening would be necessary to achieve elimination.
To meet the same targets across all 78 countries, “our models predict that scale-up of both girls-only HPV vaccination and twice-lifetime screening is necessary, with 90% HPV vaccination coverage, 90% screening uptake, and long-term protection against HPV types 16, 18, 31, 33, 45, 52, and 58,” the researchers wrote.
Dr. Brisson and colleagues claimed that a strength of this study is the modeling approach, which compared three models “that have been extensively peer reviewed and validated with postvaccination surveillance data.”
The researchers acknowledged, however, that their modeling could not account for variations in sexual behavior from country to country, and the study was not designed to anticipate behavioral or technological changes that could affect cervical cancer incidence in the decades to come.
The study was funded by the WHO, the United Nations, and the Canadian and Australian governments. The WHO contributed to the study design, data analysis and interpretation, and writing of the manuscript. Two study authors reported receiving indirect industry funding for a cervical screening trial in Australia.
SOURCE: Brisson M et al. Lancet. 2020 Jan 30. doi: 10.1016/S0140-6736(20)30068-4.
Cervical cancer is the second most common cancer among women in lower- and middle-income countries, but universal human papillomavirus vaccination for girls would reduce new cervical cancer cases by about 90% over the next century, according to researchers.
Adding twice-lifetime cervical screening with human papillomavirus (HPV) testing would further reduce the incidence of cervical cancer, including in countries with the highest burden, the researchers reported in The Lancet.
Marc Brisson, PhD, of Laval University, Quebec City, and colleagues conducted this study using three models identified by the World Health Organization. The models were used to project reductions in cervical cancer incidence for women in 78 low- and middle-income countries based on the following HPV vaccination and screening scenarios:
- Universal girls-only vaccination at age 9 years, assuming 90% of girls vaccinated and a vaccine that is perfectly effective
- Girls-only vaccination plus cervical screening with HPV testing at age 35 years
- Girls-only vaccination plus screening at ages 35 and 45.
All three scenarios modeled would result in the elimination of cervical cancer, Dr. Brisson and colleagues found. Elimination was defined as four or fewer new cases per 100,000 women-years.
The simplest scenario, universal girls-only vaccination, was predicted to reduce age-standardized cervical cancer incidence from 19.8 cases per 100,000 women-years to 2.1 cases per 100,000 women-years (89.4% reduction) by 2120. That amounts to about 61 million potential cases avoided, with elimination targets reached in 60% of the countries studied.
HPV vaccination plus one-time screening was predicted to reduce the incidence of cervical cancer to 1.0 case per 100,000 women-years (95.0% reduction), and HPV vaccination plus twice-lifetime screening was predicted to reduce the incidence to 0.7 cases per 100,000 women-years (96.7% reduction).
Dr. Brisson and colleagues reported that, for the countries with the highest burden of cervical cancer (more than 25 cases per 100,000 women-years), adding screening would be necessary to achieve elimination.
To meet the same targets across all 78 countries, “our models predict that scale-up of both girls-only HPV vaccination and twice-lifetime screening is necessary, with 90% HPV vaccination coverage, 90% screening uptake, and long-term protection against HPV types 16, 18, 31, 33, 45, 52, and 58,” the researchers wrote.
Dr. Brisson and colleagues claimed that a strength of this study is the modeling approach, which compared three models “that have been extensively peer reviewed and validated with postvaccination surveillance data.”
The researchers acknowledged, however, that their modeling could not account for variations in sexual behavior from country to country, and the study was not designed to anticipate behavioral or technological changes that could affect cervical cancer incidence in the decades to come.
The study was funded by the WHO, the United Nations, and the Canadian and Australian governments. The WHO contributed to the study design, data analysis and interpretation, and writing of the manuscript. Two study authors reported receiving indirect industry funding for a cervical screening trial in Australia.
SOURCE: Brisson M et al. Lancet. 2020 Jan 30. doi: 10.1016/S0140-6736(20)30068-4.
Cervical cancer is the second most common cancer among women in lower- and middle-income countries, but universal human papillomavirus vaccination for girls would reduce new cervical cancer cases by about 90% over the next century, according to researchers.
Adding twice-lifetime cervical screening with human papillomavirus (HPV) testing would further reduce the incidence of cervical cancer, including in countries with the highest burden, the researchers reported in The Lancet.
Marc Brisson, PhD, of Laval University, Quebec City, and colleagues conducted this study using three models identified by the World Health Organization. The models were used to project reductions in cervical cancer incidence for women in 78 low- and middle-income countries based on the following HPV vaccination and screening scenarios:
- Universal girls-only vaccination at age 9 years, assuming 90% of girls vaccinated and a vaccine that is perfectly effective
- Girls-only vaccination plus cervical screening with HPV testing at age 35 years
- Girls-only vaccination plus screening at ages 35 and 45.
All three scenarios modeled would result in the elimination of cervical cancer, Dr. Brisson and colleagues found. Elimination was defined as four or fewer new cases per 100,000 women-years.
The simplest scenario, universal girls-only vaccination, was predicted to reduce age-standardized cervical cancer incidence from 19.8 cases per 100,000 women-years to 2.1 cases per 100,000 women-years (89.4% reduction) by 2120. That amounts to about 61 million potential cases avoided, with elimination targets reached in 60% of the countries studied.
HPV vaccination plus one-time screening was predicted to reduce the incidence of cervical cancer to 1.0 case per 100,000 women-years (95.0% reduction), and HPV vaccination plus twice-lifetime screening was predicted to reduce the incidence to 0.7 cases per 100,000 women-years (96.7% reduction).
Dr. Brisson and colleagues reported that, for the countries with the highest burden of cervical cancer (more than 25 cases per 100,000 women-years), adding screening would be necessary to achieve elimination.
To meet the same targets across all 78 countries, “our models predict that scale-up of both girls-only HPV vaccination and twice-lifetime screening is necessary, with 90% HPV vaccination coverage, 90% screening uptake, and long-term protection against HPV types 16, 18, 31, 33, 45, 52, and 58,” the researchers wrote.
Dr. Brisson and colleagues claimed that a strength of this study is the modeling approach, which compared three models “that have been extensively peer reviewed and validated with postvaccination surveillance data.”
The researchers acknowledged, however, that their modeling could not account for variations in sexual behavior from country to country, and the study was not designed to anticipate behavioral or technological changes that could affect cervical cancer incidence in the decades to come.
The study was funded by the WHO, the United Nations, and the Canadian and Australian governments. The WHO contributed to the study design, data analysis and interpretation, and writing of the manuscript. Two study authors reported receiving indirect industry funding for a cervical screening trial in Australia.
SOURCE: Brisson M et al. Lancet. 2020 Jan 30. doi: 10.1016/S0140-6736(20)30068-4.
FROM THE LANCET
Cardiac arrest: Targeted temperature management a game changer
SNOWMASS, COLO. – Targeted temperature management maintained at 32-36 degrees Celsius is now a strong class I recommendation for all comatose patients who experience return of spontaneous circulation after out-of-hospital cardiac arrest, including those with nonshockable rhythms, Erin A. Bohula, MD, PhD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Our practice is that ,” said Dr. Bohula, a cardiologist and critical care specialist at Brigham and Women’s Hospital and Harvard Medical School, Boston.
The current ACC/AHA guidelines declare: “There are essentially no patients for whom temperature control somewhere in the range between 32 degrees C [89.6 F) and 36 degrees C [96.8 F] is contraindicated.” The writing committee cited “recent clinical trial data enrolling patients with all rhythms, the rarity of adverse effects in trials, the high neurologic morbidity and mortality without any specific interventions, and the preponderance of data suggesting that temperature is an important variable for neurologic recovery” (Circulation. 2015 Nov 3;132[18 Suppl 2]:S465-82).
“That’s a pretty strong statement,” Dr. Bohula observed.
The current guidelines, which date back to 2015, give a class I, level of evidence B recommendation for targeted temperature management (TTM) in patients who are comatose with return of spontaneous circulation (ROSC) after out-of-hospital cardiac arrest involving ventricular fibrillation or pulseless ventricular fibrillation. The bedside definition of comatose is lack of meaningful response to verbal commands to squeeze hands, blink, or move toes.
The current recommendation for TTM in patients resuscitated from out-of-hospital cardiac arrest with a nonshockable rhythm is class I, level of evidence C, meaning it’s based on expert consensus. However, that recommendation is now out of date and due for a level-of-evidence upgrade in light of the recent results of the French HYPERION trial, an open-label randomized trial of 584 patients resuscitated from cardiac arrest with a nonshockable rhythm. Although 90-day mortality was similarly high in the TTM and targeted normothermia groups, the rate of favorable neurologic outcome as assessed by a Cerebral Performance Category scale score of 1 or 2 was 10.2% in the TTM group, significantly better than the 5.7% rate in controls (N Engl J Med. 2019 Dec 12;381[24]:2327-37).
The 2010, ACC/AHA guidelines recommended a TTM range of 32-34 degrees C, but on the basis of subsequent persuasive randomized trial data, that range was broadened to 32-36 degrees C in the 2015 guidelines, with a class IB recommendation. Maintenance of TTM for at least 24 hours has a IIa, level of evidence C recommendation in the current guidelines.
The guidelines emphasize that specific features may favor selection of one temperature for TTM over another. For example, patients with seizures or cerebral edema might be better off with TTM at a lower temperature, while a higher temperature may be best for those with bleeding or severe bradycardia. At Brigham and Women’s Hospital, the default temperature is 33 degrees C. However, TTM with a goal of 36 degrees C is seriously considered in patients with recent head trauma, major surgery within the past 2 weeks, refractory hypotension, severe sepsis, pregnancy, or high bleeding risk. Rewarming is done at a rate of 0.25 degrees C per hour, with sedation maintained until the patient has been returned to 98.6 degrees F, according to Dr. Bohula.
Based on several negative studies of TTM using rapid infusion of chilled fluids in the ambulance en route to the hospital, the guidelines rate that practice class IIIA, meaning don’t do it. Avoidance of a systolic blood pressure below 90 mm Hg and a mean arterial pressure of less than 65 mm Hg gets a class IIb level of evidence C recommendation to lessen the risk of cerebral hypoxia.
TTM a major breakthrough
Prior to the introduction of TTM, comatose patients with ROSC after out-of-hospital cardiac arrest had a dreadful prognosis, with survival rates of 1%-10% in registry studies. In contrast, the survival rate in the landmark TTM clinical trials was 50%-60%. And while that’s a dramatic improvement, ROSC after cardiac arrest remains a high-mortality condition. Dr. Bohula was first author of a report by the Critical Care Cardiology Trials Network, composed of 16 tertiary cardiac intensive care units in the United States and Canada. Cardiac arrest was the primary indication for 8.7% of 3,049 consecutive admissions, and its 38% mortality rate was the highest of all cardiac critical care indications (JAMA Cardiol. 2019 Jul 24;4[9]:928-35).
TTM was developed in response to a recognition that two-thirds of deaths in patients who make it to the hospital after out-of-hospital cardiac arrest are neurologic – the result of brain anoxia – rather than being due to the myocardial ischemia that may have initially brought them to medical attention.
“Time is brain cells, the same way we think of time as cardiac muscle,” Dr. Bohula observed.
The main idea behind therapeutic hypothermia is that it lowers the cerebral metabolic rate of oxygen to reduce the consequences of ongoing anoxia. The brain doesn’t require as much perfusion when cooled.
TTM has other beneficial neurologic effects as well: It reduces cerebral blood volume via autoregulation, decreases intracranial pressure, and blunts the inflammatory response involved in the postcardiac arrest syndrome. In addition, TTM has anticonvulsant properties, an important effect because seizures and/or myoclonus occur in up to 15% of adults who achieve ROSC after cardiac arrest – and in even more of those who are comatose after doing so. And seizures increase the brain’s metabolic rate threefold, resulting in more cerebral ischemic injury, she explained.
Seizure activity can be difficult to distinguish from shivering in a patient on TTM. For this reason Dr. Bohula recommends putting patients on continuous EEG monitoring from the time of admission, as is the routine practice at the Brigham.
She reported serving as a consultant to Daiichi Sankyo, Servier, Lexicon, Kowa, Merck, Novartis, Novo Nordisk, and the National Institutes of Health. In addition, she generates institutional research grants provided by a half-dozen pharmaceutical companies.
SNOWMASS, COLO. – Targeted temperature management maintained at 32-36 degrees Celsius is now a strong class I recommendation for all comatose patients who experience return of spontaneous circulation after out-of-hospital cardiac arrest, including those with nonshockable rhythms, Erin A. Bohula, MD, PhD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Our practice is that ,” said Dr. Bohula, a cardiologist and critical care specialist at Brigham and Women’s Hospital and Harvard Medical School, Boston.
The current ACC/AHA guidelines declare: “There are essentially no patients for whom temperature control somewhere in the range between 32 degrees C [89.6 F) and 36 degrees C [96.8 F] is contraindicated.” The writing committee cited “recent clinical trial data enrolling patients with all rhythms, the rarity of adverse effects in trials, the high neurologic morbidity and mortality without any specific interventions, and the preponderance of data suggesting that temperature is an important variable for neurologic recovery” (Circulation. 2015 Nov 3;132[18 Suppl 2]:S465-82).
“That’s a pretty strong statement,” Dr. Bohula observed.
The current guidelines, which date back to 2015, give a class I, level of evidence B recommendation for targeted temperature management (TTM) in patients who are comatose with return of spontaneous circulation (ROSC) after out-of-hospital cardiac arrest involving ventricular fibrillation or pulseless ventricular fibrillation. The bedside definition of comatose is lack of meaningful response to verbal commands to squeeze hands, blink, or move toes.
The current recommendation for TTM in patients resuscitated from out-of-hospital cardiac arrest with a nonshockable rhythm is class I, level of evidence C, meaning it’s based on expert consensus. However, that recommendation is now out of date and due for a level-of-evidence upgrade in light of the recent results of the French HYPERION trial, an open-label randomized trial of 584 patients resuscitated from cardiac arrest with a nonshockable rhythm. Although 90-day mortality was similarly high in the TTM and targeted normothermia groups, the rate of favorable neurologic outcome as assessed by a Cerebral Performance Category scale score of 1 or 2 was 10.2% in the TTM group, significantly better than the 5.7% rate in controls (N Engl J Med. 2019 Dec 12;381[24]:2327-37).
The 2010, ACC/AHA guidelines recommended a TTM range of 32-34 degrees C, but on the basis of subsequent persuasive randomized trial data, that range was broadened to 32-36 degrees C in the 2015 guidelines, with a class IB recommendation. Maintenance of TTM for at least 24 hours has a IIa, level of evidence C recommendation in the current guidelines.
The guidelines emphasize that specific features may favor selection of one temperature for TTM over another. For example, patients with seizures or cerebral edema might be better off with TTM at a lower temperature, while a higher temperature may be best for those with bleeding or severe bradycardia. At Brigham and Women’s Hospital, the default temperature is 33 degrees C. However, TTM with a goal of 36 degrees C is seriously considered in patients with recent head trauma, major surgery within the past 2 weeks, refractory hypotension, severe sepsis, pregnancy, or high bleeding risk. Rewarming is done at a rate of 0.25 degrees C per hour, with sedation maintained until the patient has been returned to 98.6 degrees F, according to Dr. Bohula.
Based on several negative studies of TTM using rapid infusion of chilled fluids in the ambulance en route to the hospital, the guidelines rate that practice class IIIA, meaning don’t do it. Avoidance of a systolic blood pressure below 90 mm Hg and a mean arterial pressure of less than 65 mm Hg gets a class IIb level of evidence C recommendation to lessen the risk of cerebral hypoxia.
TTM a major breakthrough
Prior to the introduction of TTM, comatose patients with ROSC after out-of-hospital cardiac arrest had a dreadful prognosis, with survival rates of 1%-10% in registry studies. In contrast, the survival rate in the landmark TTM clinical trials was 50%-60%. And while that’s a dramatic improvement, ROSC after cardiac arrest remains a high-mortality condition. Dr. Bohula was first author of a report by the Critical Care Cardiology Trials Network, composed of 16 tertiary cardiac intensive care units in the United States and Canada. Cardiac arrest was the primary indication for 8.7% of 3,049 consecutive admissions, and its 38% mortality rate was the highest of all cardiac critical care indications (JAMA Cardiol. 2019 Jul 24;4[9]:928-35).
TTM was developed in response to a recognition that two-thirds of deaths in patients who make it to the hospital after out-of-hospital cardiac arrest are neurologic – the result of brain anoxia – rather than being due to the myocardial ischemia that may have initially brought them to medical attention.
“Time is brain cells, the same way we think of time as cardiac muscle,” Dr. Bohula observed.
The main idea behind therapeutic hypothermia is that it lowers the cerebral metabolic rate of oxygen to reduce the consequences of ongoing anoxia. The brain doesn’t require as much perfusion when cooled.
TTM has other beneficial neurologic effects as well: It reduces cerebral blood volume via autoregulation, decreases intracranial pressure, and blunts the inflammatory response involved in the postcardiac arrest syndrome. In addition, TTM has anticonvulsant properties, an important effect because seizures and/or myoclonus occur in up to 15% of adults who achieve ROSC after cardiac arrest – and in even more of those who are comatose after doing so. And seizures increase the brain’s metabolic rate threefold, resulting in more cerebral ischemic injury, she explained.
Seizure activity can be difficult to distinguish from shivering in a patient on TTM. For this reason Dr. Bohula recommends putting patients on continuous EEG monitoring from the time of admission, as is the routine practice at the Brigham.
She reported serving as a consultant to Daiichi Sankyo, Servier, Lexicon, Kowa, Merck, Novartis, Novo Nordisk, and the National Institutes of Health. In addition, she generates institutional research grants provided by a half-dozen pharmaceutical companies.
SNOWMASS, COLO. – Targeted temperature management maintained at 32-36 degrees Celsius is now a strong class I recommendation for all comatose patients who experience return of spontaneous circulation after out-of-hospital cardiac arrest, including those with nonshockable rhythms, Erin A. Bohula, MD, PhD, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“Our practice is that ,” said Dr. Bohula, a cardiologist and critical care specialist at Brigham and Women’s Hospital and Harvard Medical School, Boston.
The current ACC/AHA guidelines declare: “There are essentially no patients for whom temperature control somewhere in the range between 32 degrees C [89.6 F) and 36 degrees C [96.8 F] is contraindicated.” The writing committee cited “recent clinical trial data enrolling patients with all rhythms, the rarity of adverse effects in trials, the high neurologic morbidity and mortality without any specific interventions, and the preponderance of data suggesting that temperature is an important variable for neurologic recovery” (Circulation. 2015 Nov 3;132[18 Suppl 2]:S465-82).
“That’s a pretty strong statement,” Dr. Bohula observed.
The current guidelines, which date back to 2015, give a class I, level of evidence B recommendation for targeted temperature management (TTM) in patients who are comatose with return of spontaneous circulation (ROSC) after out-of-hospital cardiac arrest involving ventricular fibrillation or pulseless ventricular fibrillation. The bedside definition of comatose is lack of meaningful response to verbal commands to squeeze hands, blink, or move toes.
The current recommendation for TTM in patients resuscitated from out-of-hospital cardiac arrest with a nonshockable rhythm is class I, level of evidence C, meaning it’s based on expert consensus. However, that recommendation is now out of date and due for a level-of-evidence upgrade in light of the recent results of the French HYPERION trial, an open-label randomized trial of 584 patients resuscitated from cardiac arrest with a nonshockable rhythm. Although 90-day mortality was similarly high in the TTM and targeted normothermia groups, the rate of favorable neurologic outcome as assessed by a Cerebral Performance Category scale score of 1 or 2 was 10.2% in the TTM group, significantly better than the 5.7% rate in controls (N Engl J Med. 2019 Dec 12;381[24]:2327-37).
The 2010, ACC/AHA guidelines recommended a TTM range of 32-34 degrees C, but on the basis of subsequent persuasive randomized trial data, that range was broadened to 32-36 degrees C in the 2015 guidelines, with a class IB recommendation. Maintenance of TTM for at least 24 hours has a IIa, level of evidence C recommendation in the current guidelines.
The guidelines emphasize that specific features may favor selection of one temperature for TTM over another. For example, patients with seizures or cerebral edema might be better off with TTM at a lower temperature, while a higher temperature may be best for those with bleeding or severe bradycardia. At Brigham and Women’s Hospital, the default temperature is 33 degrees C. However, TTM with a goal of 36 degrees C is seriously considered in patients with recent head trauma, major surgery within the past 2 weeks, refractory hypotension, severe sepsis, pregnancy, or high bleeding risk. Rewarming is done at a rate of 0.25 degrees C per hour, with sedation maintained until the patient has been returned to 98.6 degrees F, according to Dr. Bohula.
Based on several negative studies of TTM using rapid infusion of chilled fluids in the ambulance en route to the hospital, the guidelines rate that practice class IIIA, meaning don’t do it. Avoidance of a systolic blood pressure below 90 mm Hg and a mean arterial pressure of less than 65 mm Hg gets a class IIb level of evidence C recommendation to lessen the risk of cerebral hypoxia.
TTM a major breakthrough
Prior to the introduction of TTM, comatose patients with ROSC after out-of-hospital cardiac arrest had a dreadful prognosis, with survival rates of 1%-10% in registry studies. In contrast, the survival rate in the landmark TTM clinical trials was 50%-60%. And while that’s a dramatic improvement, ROSC after cardiac arrest remains a high-mortality condition. Dr. Bohula was first author of a report by the Critical Care Cardiology Trials Network, composed of 16 tertiary cardiac intensive care units in the United States and Canada. Cardiac arrest was the primary indication for 8.7% of 3,049 consecutive admissions, and its 38% mortality rate was the highest of all cardiac critical care indications (JAMA Cardiol. 2019 Jul 24;4[9]:928-35).
TTM was developed in response to a recognition that two-thirds of deaths in patients who make it to the hospital after out-of-hospital cardiac arrest are neurologic – the result of brain anoxia – rather than being due to the myocardial ischemia that may have initially brought them to medical attention.
“Time is brain cells, the same way we think of time as cardiac muscle,” Dr. Bohula observed.
The main idea behind therapeutic hypothermia is that it lowers the cerebral metabolic rate of oxygen to reduce the consequences of ongoing anoxia. The brain doesn’t require as much perfusion when cooled.
TTM has other beneficial neurologic effects as well: It reduces cerebral blood volume via autoregulation, decreases intracranial pressure, and blunts the inflammatory response involved in the postcardiac arrest syndrome. In addition, TTM has anticonvulsant properties, an important effect because seizures and/or myoclonus occur in up to 15% of adults who achieve ROSC after cardiac arrest – and in even more of those who are comatose after doing so. And seizures increase the brain’s metabolic rate threefold, resulting in more cerebral ischemic injury, she explained.
Seizure activity can be difficult to distinguish from shivering in a patient on TTM. For this reason Dr. Bohula recommends putting patients on continuous EEG monitoring from the time of admission, as is the routine practice at the Brigham.
She reported serving as a consultant to Daiichi Sankyo, Servier, Lexicon, Kowa, Merck, Novartis, Novo Nordisk, and the National Institutes of Health. In addition, she generates institutional research grants provided by a half-dozen pharmaceutical companies.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
CDC begins coronavirus diagnostic test kit distribution; new case confirmed in Wisconsin
The Centers for Disease Control and Prevention and the Wisconsin Department of Health Services confirmed a new case of the 2019 Novel Coronavirus (2019-nCoV) on Feb. 5, 2020, bringing the total number of cases in the United States to 12.*
Earlier in the day, Nancy Messonnier, MD, director of the CDC National Center for Immunization and Respiratory Diseases, told reporters that 206 individuals under investigation had tested negative for infection with the novel virus and that tests were pending on another 76 individuals.
The agency also announced during a press briefing call that diagnostic test kits will begin shipping on Feb. 5, less than 24 hours after receiving an emergency use authorization from the Food and Drug Administration. Full information is available in an article published in the Morbidity and Mortality Weekly Report.
The emergency use authorization will allow for broader use of the CDC’s 2019-nCoV Real Time RT-PCR Diagnostic Panel, which to date has been limited for use at CDC laboratories. Under the emergency use authorization, the diagnostic kit is authorized for patients who meed the CDC criteria for 2019-nCoV testing. The diagnostic test is a reverse transcriptase polymerase chain reaction test that provides presumptive detection of 2019-nCoV from respiratory secretions, such as nasal or oral swabs. A positive test indicates likely infection, although a negative test does not preclude infection and should not be the sole determination for patient management decisions.
“Today, the test kits will start shipping to over 100 U.S. public health labs,” she said. “Each of these labs is required to perform international verification for [Clinical Laboratory Improvement Amendments] compliance prior to reporting out. This process is expected to take a few days.”
Dr. Messonnier said that 200 test kits will be distributed to domestic labs and another 200 test kits will go to select international labs. Each kit can perform diagnostics on 700-800 patient samples.
“What that means is that, by the start of next week, we expect there to be much enhanced capacity for laboratory testing closer to our patients,” she said, adding that additional test kits are being produced and will be available for ordering in the future. Each laboratory that places an order will receive one test kit.
“Distribution of these tests will improve the global capacity to detect and respond to this new virus,” Dr. Messonnier said. “Availability of this test is a starting place for greater commercial availability of diagnostic testing for nCoV.”
The CDC also said that the next batch of passengers arriving from Wuhan, China, will be arriving in one of four locations: Travis Air Force Base, Fairfield, Calif.; Marine Corps Air Station Miramar, San Diego; Lackland Air Force Base, San Antonio; and Eppley Airfield, Omaha, Neb. Passengers will be quarantined for up to 14 days from the day the flight left Wuhan and medical care will be provided if needed.
“We do not believe these people pose a threat to the communities where they are being housed as we are taking measures to minimize any contact,” she said, adding that confirmed infections are expected among these and other returning travelers.
Dr. Messonnier warned that the quarantine measures “may not catch every single returning traveler returning with novel coronavirus, given the nature of this virus and how it is spreading. But if we can catch the majority of them, that will slow the entry of this virus into the United States.”
*This story was updated on 02/05/2020.
The Centers for Disease Control and Prevention and the Wisconsin Department of Health Services confirmed a new case of the 2019 Novel Coronavirus (2019-nCoV) on Feb. 5, 2020, bringing the total number of cases in the United States to 12.*
Earlier in the day, Nancy Messonnier, MD, director of the CDC National Center for Immunization and Respiratory Diseases, told reporters that 206 individuals under investigation had tested negative for infection with the novel virus and that tests were pending on another 76 individuals.
The agency also announced during a press briefing call that diagnostic test kits will begin shipping on Feb. 5, less than 24 hours after receiving an emergency use authorization from the Food and Drug Administration. Full information is available in an article published in the Morbidity and Mortality Weekly Report.
The emergency use authorization will allow for broader use of the CDC’s 2019-nCoV Real Time RT-PCR Diagnostic Panel, which to date has been limited for use at CDC laboratories. Under the emergency use authorization, the diagnostic kit is authorized for patients who meed the CDC criteria for 2019-nCoV testing. The diagnostic test is a reverse transcriptase polymerase chain reaction test that provides presumptive detection of 2019-nCoV from respiratory secretions, such as nasal or oral swabs. A positive test indicates likely infection, although a negative test does not preclude infection and should not be the sole determination for patient management decisions.
“Today, the test kits will start shipping to over 100 U.S. public health labs,” she said. “Each of these labs is required to perform international verification for [Clinical Laboratory Improvement Amendments] compliance prior to reporting out. This process is expected to take a few days.”
Dr. Messonnier said that 200 test kits will be distributed to domestic labs and another 200 test kits will go to select international labs. Each kit can perform diagnostics on 700-800 patient samples.
“What that means is that, by the start of next week, we expect there to be much enhanced capacity for laboratory testing closer to our patients,” she said, adding that additional test kits are being produced and will be available for ordering in the future. Each laboratory that places an order will receive one test kit.
“Distribution of these tests will improve the global capacity to detect and respond to this new virus,” Dr. Messonnier said. “Availability of this test is a starting place for greater commercial availability of diagnostic testing for nCoV.”
The CDC also said that the next batch of passengers arriving from Wuhan, China, will be arriving in one of four locations: Travis Air Force Base, Fairfield, Calif.; Marine Corps Air Station Miramar, San Diego; Lackland Air Force Base, San Antonio; and Eppley Airfield, Omaha, Neb. Passengers will be quarantined for up to 14 days from the day the flight left Wuhan and medical care will be provided if needed.
“We do not believe these people pose a threat to the communities where they are being housed as we are taking measures to minimize any contact,” she said, adding that confirmed infections are expected among these and other returning travelers.
Dr. Messonnier warned that the quarantine measures “may not catch every single returning traveler returning with novel coronavirus, given the nature of this virus and how it is spreading. But if we can catch the majority of them, that will slow the entry of this virus into the United States.”
*This story was updated on 02/05/2020.
The Centers for Disease Control and Prevention and the Wisconsin Department of Health Services confirmed a new case of the 2019 Novel Coronavirus (2019-nCoV) on Feb. 5, 2020, bringing the total number of cases in the United States to 12.*
Earlier in the day, Nancy Messonnier, MD, director of the CDC National Center for Immunization and Respiratory Diseases, told reporters that 206 individuals under investigation had tested negative for infection with the novel virus and that tests were pending on another 76 individuals.
The agency also announced during a press briefing call that diagnostic test kits will begin shipping on Feb. 5, less than 24 hours after receiving an emergency use authorization from the Food and Drug Administration. Full information is available in an article published in the Morbidity and Mortality Weekly Report.
The emergency use authorization will allow for broader use of the CDC’s 2019-nCoV Real Time RT-PCR Diagnostic Panel, which to date has been limited for use at CDC laboratories. Under the emergency use authorization, the diagnostic kit is authorized for patients who meed the CDC criteria for 2019-nCoV testing. The diagnostic test is a reverse transcriptase polymerase chain reaction test that provides presumptive detection of 2019-nCoV from respiratory secretions, such as nasal or oral swabs. A positive test indicates likely infection, although a negative test does not preclude infection and should not be the sole determination for patient management decisions.
“Today, the test kits will start shipping to over 100 U.S. public health labs,” she said. “Each of these labs is required to perform international verification for [Clinical Laboratory Improvement Amendments] compliance prior to reporting out. This process is expected to take a few days.”
Dr. Messonnier said that 200 test kits will be distributed to domestic labs and another 200 test kits will go to select international labs. Each kit can perform diagnostics on 700-800 patient samples.
“What that means is that, by the start of next week, we expect there to be much enhanced capacity for laboratory testing closer to our patients,” she said, adding that additional test kits are being produced and will be available for ordering in the future. Each laboratory that places an order will receive one test kit.
“Distribution of these tests will improve the global capacity to detect and respond to this new virus,” Dr. Messonnier said. “Availability of this test is a starting place for greater commercial availability of diagnostic testing for nCoV.”
The CDC also said that the next batch of passengers arriving from Wuhan, China, will be arriving in one of four locations: Travis Air Force Base, Fairfield, Calif.; Marine Corps Air Station Miramar, San Diego; Lackland Air Force Base, San Antonio; and Eppley Airfield, Omaha, Neb. Passengers will be quarantined for up to 14 days from the day the flight left Wuhan and medical care will be provided if needed.
“We do not believe these people pose a threat to the communities where they are being housed as we are taking measures to minimize any contact,” she said, adding that confirmed infections are expected among these and other returning travelers.
Dr. Messonnier warned that the quarantine measures “may not catch every single returning traveler returning with novel coronavirus, given the nature of this virus and how it is spreading. But if we can catch the majority of them, that will slow the entry of this virus into the United States.”
*This story was updated on 02/05/2020.
Global project reveals cancer’s genomic playbook
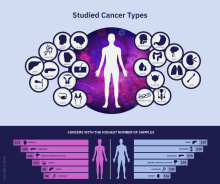
A massive collaborative project spanning four continents and 744 research centers has revealed driver mutations in both protein-coding and noncoding regions of 38 cancer types.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) is an integrative analysis of the whole-genome sequences from 2,658 donors across 38 common tumor types. The findings are expected to add exponentially to what’s currently known about the complex genetics of cancer, and they point to possible strategies for improving cancer prevention, diagnosis, and care.
Six articles summarizing the findings are presented in a series of papers in Nature, and 16 more appear in affiliated publications.
“It’s humbling that it was only 14 years ago that the genomics community sequenced its very first cancer exome, and it was able to identify mutations within the roughly 20,000 protein-coding genes in the human cell,” investigator Lincoln Stein, MD, PhD, of the Ontario Institute for Cancer Research in Toronto, said in a telephone briefing.
Exome sequencing, however, covers only protein-coding genomic regions, which constitute only about 1% of the entire genome, “so assembling an accurate portrait of the cancer genome using just the exome data is like trying to put together a 100,000-piece jigsaw puzzle when you’re missing 99% of the pieces and there’s no puzzle box with a completed picture to guide you,” Dr. Stein said.
Members of the PCAWG from centers in North America, Europe, Asia, and Australia screened 2,658 whole-cancer genomes and matched samples of noncancerous tissues from the same individuals, along with 1,188 transcriptomes cataloging the sequences and expression of RNA transcripts in a given tumor. The 6-year project netted more than 800 terabytes of genomic data, roughly equivalent to the digital holdings of the U.S. Library of Congress multiplied by 11.
The findings are summarized in papers focusing on cancer drivers, noncoding changes, mutational signatures, structural variants, cancer evolution over time, and RNA alterations.
Driver mutations
Investigators found that the average cancer genome contains four or five driver mutations located in both coding and noncoding regions. They also found, however, that in approximately 5% of cases no driver mutations could be identified.
A substantial proportion of tumors displayed “hallmarks of genomic catastrophes.” About 22% of tumors exhibited chromothripsis, a mutational process marked by hundreds or even thousands of clustered chromosomal rearrangements. About 18% showed chromoplexy, which is characterized by scattering and rearrangement of multiple strands of DNA from one or more chromosomes.
Analyzing driver point mutations and structural variants in noncoding regions, the investigators found the usual suspects – previously reported culprits – as well as novel candidates.
For example, they identified point mutations in the five prime region of the tumor suppressor gene TP53 and the three prime untranslated regions of NFKBIZ (a nuclear factor kappa B inhibitor) and TOB1 (an antiproliferative protein), focal deletion in BRD4 (a transcriptional and epigenetic regulator), and rearrangements in chromosomal loci in members of the AKR1C family of enzymes thought to play a role in disease progression.
In addition, investigators identified mutations in noncoding regions of TERT, a telomerase gene. These mutations result in ramped-up expression of telomerase, which in turn promotes uncontrollable division of tumor cells.
Mutational signatures
In a related line of research, PCAWG investigators identified new DNA mutational signatures ranging from single nucleotide polymorphisms to insertions and deletions, as well as to structural variants – rearrangements of large sections of the genome.
“The substantial size of our dataset, compared with previous analyses, enabled the discovery of new signatures, the separation of overlapping signatures, and the decomposition of signatures into components that may represent associated – but distinct – DNA damage, repair, and/or replication mechanisms. By estimating the contribution of each signature to the mutational catalogs of individual cancer genomes, we revealed associations of signatures to exogenous or endogenous exposures, as well as to defective DNA maintenance processes,” the investigators wrote.
They also acknowledged, however, that “many signatures are of unknown cause.”
Cancer evolution
One of the six main studies focused on the evolution of cancer over time. Instead of providing a “snapshot” of the genome as captured by sequencing tissue from a single biopsy, consortium investigators created full-length features of the “life history and evolution of mutational processes and driver mutation sequences.”
They found that early cancer development was marked by relatively few mutations in driver genes and by identifiable copy-number gains, including trisomy 7 in glioblastoma, and an abnormal mirroring of the arms (isochromosome) of chromosome 17 in medulloblastoma.
In 40% of the samples, however, there were significant changes in the mutational spectrum as the cancers grew, leading to a near quadrupling of driver genes and increased genomic instability in later-stage tumors.
“Copy-number alterations often occur in mitotic crises and lead to simultaneous gains of chromosomal segments,” the investigators wrote. “Timing analyses suggest that driver mutations often precede diagnosis by many years, if not decades. Together, these results determine the evolutionary trajectories of cancer and highlight opportunities for early cancer detection.”
Implications for cancer care
“When I used to treat patients with cancer, I was always completely amazed and puzzled by how two patients could have what looked like the same tumor. It would look the same under the microscope, have the same size, and the two patients would receive exactly the same treatment, but the two patients would have completely opposite outcomes; one would survive, and one would die. What this analysis … has done is really laid bare the reasons for that unpredictability in clinical outcomes,” Peter Campbell, MD, PhD, of the Wellcome Sanger Institute in Hinxton, England, said during the telebriefing.
“The most striking finding out of all of the suite of papers is just how different one person’s cancer genome is from another person’s. We see thousands of different combinations of mutations that can cause the cancer, and more than 80 different underlying processes generating the mutations in a cancer, and that leads to very different shapes and patterns in the genome that result,” he added.
On a positive note, the research shows that one or more driver mutations can be identified in about 95% of all cancer patients, and it elucidates the sequence of events leading to oncogenesis and tumor evolution, providing opportunities for earlier identification and potential interventions to prevent cancer, Dr. Campbell said.
The PCAWG was a collaborative multinational effort with multiple funding sources and many investigators.
SOURCE: Nature. 2020 Feb 5. https://www.nature.com/collections/pcawg/
A massive collaborative project spanning four continents and 744 research centers has revealed driver mutations in both protein-coding and noncoding regions of 38 cancer types.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) is an integrative analysis of the whole-genome sequences from 2,658 donors across 38 common tumor types. The findings are expected to add exponentially to what’s currently known about the complex genetics of cancer, and they point to possible strategies for improving cancer prevention, diagnosis, and care.
Six articles summarizing the findings are presented in a series of papers in Nature, and 16 more appear in affiliated publications.
“It’s humbling that it was only 14 years ago that the genomics community sequenced its very first cancer exome, and it was able to identify mutations within the roughly 20,000 protein-coding genes in the human cell,” investigator Lincoln Stein, MD, PhD, of the Ontario Institute for Cancer Research in Toronto, said in a telephone briefing.
Exome sequencing, however, covers only protein-coding genomic regions, which constitute only about 1% of the entire genome, “so assembling an accurate portrait of the cancer genome using just the exome data is like trying to put together a 100,000-piece jigsaw puzzle when you’re missing 99% of the pieces and there’s no puzzle box with a completed picture to guide you,” Dr. Stein said.
Members of the PCAWG from centers in North America, Europe, Asia, and Australia screened 2,658 whole-cancer genomes and matched samples of noncancerous tissues from the same individuals, along with 1,188 transcriptomes cataloging the sequences and expression of RNA transcripts in a given tumor. The 6-year project netted more than 800 terabytes of genomic data, roughly equivalent to the digital holdings of the U.S. Library of Congress multiplied by 11.
The findings are summarized in papers focusing on cancer drivers, noncoding changes, mutational signatures, structural variants, cancer evolution over time, and RNA alterations.
Driver mutations
Investigators found that the average cancer genome contains four or five driver mutations located in both coding and noncoding regions. They also found, however, that in approximately 5% of cases no driver mutations could be identified.
A substantial proportion of tumors displayed “hallmarks of genomic catastrophes.” About 22% of tumors exhibited chromothripsis, a mutational process marked by hundreds or even thousands of clustered chromosomal rearrangements. About 18% showed chromoplexy, which is characterized by scattering and rearrangement of multiple strands of DNA from one or more chromosomes.
Analyzing driver point mutations and structural variants in noncoding regions, the investigators found the usual suspects – previously reported culprits – as well as novel candidates.
For example, they identified point mutations in the five prime region of the tumor suppressor gene TP53 and the three prime untranslated regions of NFKBIZ (a nuclear factor kappa B inhibitor) and TOB1 (an antiproliferative protein), focal deletion in BRD4 (a transcriptional and epigenetic regulator), and rearrangements in chromosomal loci in members of the AKR1C family of enzymes thought to play a role in disease progression.
In addition, investigators identified mutations in noncoding regions of TERT, a telomerase gene. These mutations result in ramped-up expression of telomerase, which in turn promotes uncontrollable division of tumor cells.
Mutational signatures
In a related line of research, PCAWG investigators identified new DNA mutational signatures ranging from single nucleotide polymorphisms to insertions and deletions, as well as to structural variants – rearrangements of large sections of the genome.
“The substantial size of our dataset, compared with previous analyses, enabled the discovery of new signatures, the separation of overlapping signatures, and the decomposition of signatures into components that may represent associated – but distinct – DNA damage, repair, and/or replication mechanisms. By estimating the contribution of each signature to the mutational catalogs of individual cancer genomes, we revealed associations of signatures to exogenous or endogenous exposures, as well as to defective DNA maintenance processes,” the investigators wrote.
They also acknowledged, however, that “many signatures are of unknown cause.”
Cancer evolution
One of the six main studies focused on the evolution of cancer over time. Instead of providing a “snapshot” of the genome as captured by sequencing tissue from a single biopsy, consortium investigators created full-length features of the “life history and evolution of mutational processes and driver mutation sequences.”
They found that early cancer development was marked by relatively few mutations in driver genes and by identifiable copy-number gains, including trisomy 7 in glioblastoma, and an abnormal mirroring of the arms (isochromosome) of chromosome 17 in medulloblastoma.
In 40% of the samples, however, there were significant changes in the mutational spectrum as the cancers grew, leading to a near quadrupling of driver genes and increased genomic instability in later-stage tumors.
“Copy-number alterations often occur in mitotic crises and lead to simultaneous gains of chromosomal segments,” the investigators wrote. “Timing analyses suggest that driver mutations often precede diagnosis by many years, if not decades. Together, these results determine the evolutionary trajectories of cancer and highlight opportunities for early cancer detection.”
Implications for cancer care
“When I used to treat patients with cancer, I was always completely amazed and puzzled by how two patients could have what looked like the same tumor. It would look the same under the microscope, have the same size, and the two patients would receive exactly the same treatment, but the two patients would have completely opposite outcomes; one would survive, and one would die. What this analysis … has done is really laid bare the reasons for that unpredictability in clinical outcomes,” Peter Campbell, MD, PhD, of the Wellcome Sanger Institute in Hinxton, England, said during the telebriefing.
“The most striking finding out of all of the suite of papers is just how different one person’s cancer genome is from another person’s. We see thousands of different combinations of mutations that can cause the cancer, and more than 80 different underlying processes generating the mutations in a cancer, and that leads to very different shapes and patterns in the genome that result,” he added.
On a positive note, the research shows that one or more driver mutations can be identified in about 95% of all cancer patients, and it elucidates the sequence of events leading to oncogenesis and tumor evolution, providing opportunities for earlier identification and potential interventions to prevent cancer, Dr. Campbell said.
The PCAWG was a collaborative multinational effort with multiple funding sources and many investigators.
SOURCE: Nature. 2020 Feb 5. https://www.nature.com/collections/pcawg/
A massive collaborative project spanning four continents and 744 research centers has revealed driver mutations in both protein-coding and noncoding regions of 38 cancer types.
The Pan-Cancer Analysis of Whole Genomes (PCAWG) is an integrative analysis of the whole-genome sequences from 2,658 donors across 38 common tumor types. The findings are expected to add exponentially to what’s currently known about the complex genetics of cancer, and they point to possible strategies for improving cancer prevention, diagnosis, and care.
Six articles summarizing the findings are presented in a series of papers in Nature, and 16 more appear in affiliated publications.
“It’s humbling that it was only 14 years ago that the genomics community sequenced its very first cancer exome, and it was able to identify mutations within the roughly 20,000 protein-coding genes in the human cell,” investigator Lincoln Stein, MD, PhD, of the Ontario Institute for Cancer Research in Toronto, said in a telephone briefing.
Exome sequencing, however, covers only protein-coding genomic regions, which constitute only about 1% of the entire genome, “so assembling an accurate portrait of the cancer genome using just the exome data is like trying to put together a 100,000-piece jigsaw puzzle when you’re missing 99% of the pieces and there’s no puzzle box with a completed picture to guide you,” Dr. Stein said.
Members of the PCAWG from centers in North America, Europe, Asia, and Australia screened 2,658 whole-cancer genomes and matched samples of noncancerous tissues from the same individuals, along with 1,188 transcriptomes cataloging the sequences and expression of RNA transcripts in a given tumor. The 6-year project netted more than 800 terabytes of genomic data, roughly equivalent to the digital holdings of the U.S. Library of Congress multiplied by 11.
The findings are summarized in papers focusing on cancer drivers, noncoding changes, mutational signatures, structural variants, cancer evolution over time, and RNA alterations.
Driver mutations
Investigators found that the average cancer genome contains four or five driver mutations located in both coding and noncoding regions. They also found, however, that in approximately 5% of cases no driver mutations could be identified.
A substantial proportion of tumors displayed “hallmarks of genomic catastrophes.” About 22% of tumors exhibited chromothripsis, a mutational process marked by hundreds or even thousands of clustered chromosomal rearrangements. About 18% showed chromoplexy, which is characterized by scattering and rearrangement of multiple strands of DNA from one or more chromosomes.
Analyzing driver point mutations and structural variants in noncoding regions, the investigators found the usual suspects – previously reported culprits – as well as novel candidates.
For example, they identified point mutations in the five prime region of the tumor suppressor gene TP53 and the three prime untranslated regions of NFKBIZ (a nuclear factor kappa B inhibitor) and TOB1 (an antiproliferative protein), focal deletion in BRD4 (a transcriptional and epigenetic regulator), and rearrangements in chromosomal loci in members of the AKR1C family of enzymes thought to play a role in disease progression.
In addition, investigators identified mutations in noncoding regions of TERT, a telomerase gene. These mutations result in ramped-up expression of telomerase, which in turn promotes uncontrollable division of tumor cells.
Mutational signatures
In a related line of research, PCAWG investigators identified new DNA mutational signatures ranging from single nucleotide polymorphisms to insertions and deletions, as well as to structural variants – rearrangements of large sections of the genome.
“The substantial size of our dataset, compared with previous analyses, enabled the discovery of new signatures, the separation of overlapping signatures, and the decomposition of signatures into components that may represent associated – but distinct – DNA damage, repair, and/or replication mechanisms. By estimating the contribution of each signature to the mutational catalogs of individual cancer genomes, we revealed associations of signatures to exogenous or endogenous exposures, as well as to defective DNA maintenance processes,” the investigators wrote.
They also acknowledged, however, that “many signatures are of unknown cause.”
Cancer evolution
One of the six main studies focused on the evolution of cancer over time. Instead of providing a “snapshot” of the genome as captured by sequencing tissue from a single biopsy, consortium investigators created full-length features of the “life history and evolution of mutational processes and driver mutation sequences.”
They found that early cancer development was marked by relatively few mutations in driver genes and by identifiable copy-number gains, including trisomy 7 in glioblastoma, and an abnormal mirroring of the arms (isochromosome) of chromosome 17 in medulloblastoma.
In 40% of the samples, however, there were significant changes in the mutational spectrum as the cancers grew, leading to a near quadrupling of driver genes and increased genomic instability in later-stage tumors.
“Copy-number alterations often occur in mitotic crises and lead to simultaneous gains of chromosomal segments,” the investigators wrote. “Timing analyses suggest that driver mutations often precede diagnosis by many years, if not decades. Together, these results determine the evolutionary trajectories of cancer and highlight opportunities for early cancer detection.”
Implications for cancer care
“When I used to treat patients with cancer, I was always completely amazed and puzzled by how two patients could have what looked like the same tumor. It would look the same under the microscope, have the same size, and the two patients would receive exactly the same treatment, but the two patients would have completely opposite outcomes; one would survive, and one would die. What this analysis … has done is really laid bare the reasons for that unpredictability in clinical outcomes,” Peter Campbell, MD, PhD, of the Wellcome Sanger Institute in Hinxton, England, said during the telebriefing.
“The most striking finding out of all of the suite of papers is just how different one person’s cancer genome is from another person’s. We see thousands of different combinations of mutations that can cause the cancer, and more than 80 different underlying processes generating the mutations in a cancer, and that leads to very different shapes and patterns in the genome that result,” he added.
On a positive note, the research shows that one or more driver mutations can be identified in about 95% of all cancer patients, and it elucidates the sequence of events leading to oncogenesis and tumor evolution, providing opportunities for earlier identification and potential interventions to prevent cancer, Dr. Campbell said.
The PCAWG was a collaborative multinational effort with multiple funding sources and many investigators.
SOURCE: Nature. 2020 Feb 5. https://www.nature.com/collections/pcawg/
FROM NATURE
Measles, scarlet fever among infectious diseases to watch for in 2020
ORLANDO – – leading into 2020, Justin Finch, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
While group A streptococcus has declined over the past century, there has been “an unprecedented” resurgence in severe, invasive group A streptococcal infections and severe epidemics of scarlet fever worldwide, including in industrialized regions like the United Kingdom. Shedding some light on why this may be occurring, Dr. Finch referred to a recently published population-based molecular epidemiologic study identified a new dominant emm1UK lineage of Streptococcus pyogenes associated with such cases in England (Lancet Infect Dis. 2019 Nov;19(11):1209-18). This new lineage of S. pyogenes was genotypically distinct from other emm1 isolates and had greatly increased expression of the streptococcal pyrogenic exotoxin A, one of the exotoxins responsible for the clinical features of scarlet fever.
“We have not, to my knowledge, seen the strain yet in the United States,” said Dr. Finch, of Central Connecticut Dermatology in Cromwell. “Have it on your radar. With all of the worldwide travel patterns, I expect that you will see this in the United States at some point in the not-too-distant future.”
Also in 2019, promising data on the safety and effectiveness of the recombinant herpes zoster vaccine in immunocompromised patients became available for the first time. A randomized clinical trial published in JAMA of 1,846 patients who were immunosuppressed after autologous hematopoietic stem cell transplantation and received two doses of a recombinant zoster vaccine found that the patients had a reduced incidence of herpes zoster after a median follow-up of 21 months (JAMA. 2019 Jul 9;322[2]:123-33). The study found that the recombinant vaccine was both safe and effective in these immunocompromised patients, “so we can easily generalize this to our dermatology population as well,” Dr. Finch said. In comparing the live attenuated and recombinant vaccines, he noted the recombinant vaccine requires two doses but appears to be slightly more effective. “The number needed to treat to prevent [one case] of zoster is about half as high as that for the live vaccine, and most importantly for us is, it’s safe in immunocompromised patients.”
2019 also saw a record high in the number of measles cases in the United States, the highest since 1993, Dr. Finch pointed out. Most cases were seen in the area in and around New York City, but the percentage of people across the United States who are vaccinated against measles is below the threshold for herd immunity to protect immunocompromised patients. Measles requires a population vaccination rate of 94%, and less than half of U.S. counties in 2014 and 2015 reached that vaccination rate.
“Furthermore, if we look at that over the last 20 years, comparing the domestic measles cases to imported measles cases, we are increasingly breeding these measles epidemics right here at home, whereas they used to be imported from throughout the world,” said Dr. Finch. Patients with measles can be treated with vitamin A, he added, referring to a Cochrane review showing that 200,000 units of vitamin A given daily for 2 days decreased the mortality rate of measles by about 80%. Measles is on the Centers for Disease Control and Prevention’s list of reportable diseases, so should be reported to local health authorities, and will be followed up with confirmatory testing.
In 2019, a study examining herd protection of oral human papillomavirus infection in men and women compared the prevalence of oral HPV infection based on the 4 HPV types present in the quadrivalent HPV vaccine with 33 nonvaccine types from 2009 to 2016. There was no change in the prevalence of nonvaccine type oral HPV infections among men who were unvaccinated, but the prevalence of oral HPV infections because of the four strains in the quadrivalent HPV vaccine declined from 2.7% in 2009-2010 to 1.6% in 2015-2016 (JAMA. 2019 Sep 10;322[10]:977-9). Among unvaccinated women, the prevalence of nonvaccine- and vaccine-type oral HPV infections did not change between the two time periods.
“Notably, this only occurred in men,” Dr. Finch said. Herd immunity is being achieved in men “because we’re vaccinating all women, [but] we’re not seeing that herd immunity in women. Which begs the question: Why are we still vaccinating only half of our population?”
One study published in 2019 (Br J Dermatol. 2019 Nov;181[5]:1093-5) described a patient with CARD9 mutations, which predispose individuals to deep invasive infections – a disseminated Microsporum infection in this case, Dr. Finch said. “You shouldn’t see that,” he added, noting that these mutations are known to predispose individuals to severe Trichophyton infections and familial candidiasis.
“What I think is interesting about this is that, as we look forward to 2020, we’re going to increasingly see studies like this that are identifying specific mutations in our community that underlie a lot of these weird infections,” he added. “I wouldn’t be surprised if within the span of our careers, we find that a lot of those severe treatment-refractory reports that so commonly plague your everyday clinic have some underlying, specific immunity.”
Dr. Finch reported no relevant conflicts of interest.
ORLANDO – – leading into 2020, Justin Finch, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
While group A streptococcus has declined over the past century, there has been “an unprecedented” resurgence in severe, invasive group A streptococcal infections and severe epidemics of scarlet fever worldwide, including in industrialized regions like the United Kingdom. Shedding some light on why this may be occurring, Dr. Finch referred to a recently published population-based molecular epidemiologic study identified a new dominant emm1UK lineage of Streptococcus pyogenes associated with such cases in England (Lancet Infect Dis. 2019 Nov;19(11):1209-18). This new lineage of S. pyogenes was genotypically distinct from other emm1 isolates and had greatly increased expression of the streptococcal pyrogenic exotoxin A, one of the exotoxins responsible for the clinical features of scarlet fever.
“We have not, to my knowledge, seen the strain yet in the United States,” said Dr. Finch, of Central Connecticut Dermatology in Cromwell. “Have it on your radar. With all of the worldwide travel patterns, I expect that you will see this in the United States at some point in the not-too-distant future.”
Also in 2019, promising data on the safety and effectiveness of the recombinant herpes zoster vaccine in immunocompromised patients became available for the first time. A randomized clinical trial published in JAMA of 1,846 patients who were immunosuppressed after autologous hematopoietic stem cell transplantation and received two doses of a recombinant zoster vaccine found that the patients had a reduced incidence of herpes zoster after a median follow-up of 21 months (JAMA. 2019 Jul 9;322[2]:123-33). The study found that the recombinant vaccine was both safe and effective in these immunocompromised patients, “so we can easily generalize this to our dermatology population as well,” Dr. Finch said. In comparing the live attenuated and recombinant vaccines, he noted the recombinant vaccine requires two doses but appears to be slightly more effective. “The number needed to treat to prevent [one case] of zoster is about half as high as that for the live vaccine, and most importantly for us is, it’s safe in immunocompromised patients.”
2019 also saw a record high in the number of measles cases in the United States, the highest since 1993, Dr. Finch pointed out. Most cases were seen in the area in and around New York City, but the percentage of people across the United States who are vaccinated against measles is below the threshold for herd immunity to protect immunocompromised patients. Measles requires a population vaccination rate of 94%, and less than half of U.S. counties in 2014 and 2015 reached that vaccination rate.
“Furthermore, if we look at that over the last 20 years, comparing the domestic measles cases to imported measles cases, we are increasingly breeding these measles epidemics right here at home, whereas they used to be imported from throughout the world,” said Dr. Finch. Patients with measles can be treated with vitamin A, he added, referring to a Cochrane review showing that 200,000 units of vitamin A given daily for 2 days decreased the mortality rate of measles by about 80%. Measles is on the Centers for Disease Control and Prevention’s list of reportable diseases, so should be reported to local health authorities, and will be followed up with confirmatory testing.
In 2019, a study examining herd protection of oral human papillomavirus infection in men and women compared the prevalence of oral HPV infection based on the 4 HPV types present in the quadrivalent HPV vaccine with 33 nonvaccine types from 2009 to 2016. There was no change in the prevalence of nonvaccine type oral HPV infections among men who were unvaccinated, but the prevalence of oral HPV infections because of the four strains in the quadrivalent HPV vaccine declined from 2.7% in 2009-2010 to 1.6% in 2015-2016 (JAMA. 2019 Sep 10;322[10]:977-9). Among unvaccinated women, the prevalence of nonvaccine- and vaccine-type oral HPV infections did not change between the two time periods.
“Notably, this only occurred in men,” Dr. Finch said. Herd immunity is being achieved in men “because we’re vaccinating all women, [but] we’re not seeing that herd immunity in women. Which begs the question: Why are we still vaccinating only half of our population?”
One study published in 2019 (Br J Dermatol. 2019 Nov;181[5]:1093-5) described a patient with CARD9 mutations, which predispose individuals to deep invasive infections – a disseminated Microsporum infection in this case, Dr. Finch said. “You shouldn’t see that,” he added, noting that these mutations are known to predispose individuals to severe Trichophyton infections and familial candidiasis.
“What I think is interesting about this is that, as we look forward to 2020, we’re going to increasingly see studies like this that are identifying specific mutations in our community that underlie a lot of these weird infections,” he added. “I wouldn’t be surprised if within the span of our careers, we find that a lot of those severe treatment-refractory reports that so commonly plague your everyday clinic have some underlying, specific immunity.”
Dr. Finch reported no relevant conflicts of interest.
ORLANDO – – leading into 2020, Justin Finch, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
While group A streptococcus has declined over the past century, there has been “an unprecedented” resurgence in severe, invasive group A streptococcal infections and severe epidemics of scarlet fever worldwide, including in industrialized regions like the United Kingdom. Shedding some light on why this may be occurring, Dr. Finch referred to a recently published population-based molecular epidemiologic study identified a new dominant emm1UK lineage of Streptococcus pyogenes associated with such cases in England (Lancet Infect Dis. 2019 Nov;19(11):1209-18). This new lineage of S. pyogenes was genotypically distinct from other emm1 isolates and had greatly increased expression of the streptococcal pyrogenic exotoxin A, one of the exotoxins responsible for the clinical features of scarlet fever.
“We have not, to my knowledge, seen the strain yet in the United States,” said Dr. Finch, of Central Connecticut Dermatology in Cromwell. “Have it on your radar. With all of the worldwide travel patterns, I expect that you will see this in the United States at some point in the not-too-distant future.”
Also in 2019, promising data on the safety and effectiveness of the recombinant herpes zoster vaccine in immunocompromised patients became available for the first time. A randomized clinical trial published in JAMA of 1,846 patients who were immunosuppressed after autologous hematopoietic stem cell transplantation and received two doses of a recombinant zoster vaccine found that the patients had a reduced incidence of herpes zoster after a median follow-up of 21 months (JAMA. 2019 Jul 9;322[2]:123-33). The study found that the recombinant vaccine was both safe and effective in these immunocompromised patients, “so we can easily generalize this to our dermatology population as well,” Dr. Finch said. In comparing the live attenuated and recombinant vaccines, he noted the recombinant vaccine requires two doses but appears to be slightly more effective. “The number needed to treat to prevent [one case] of zoster is about half as high as that for the live vaccine, and most importantly for us is, it’s safe in immunocompromised patients.”
2019 also saw a record high in the number of measles cases in the United States, the highest since 1993, Dr. Finch pointed out. Most cases were seen in the area in and around New York City, but the percentage of people across the United States who are vaccinated against measles is below the threshold for herd immunity to protect immunocompromised patients. Measles requires a population vaccination rate of 94%, and less than half of U.S. counties in 2014 and 2015 reached that vaccination rate.
“Furthermore, if we look at that over the last 20 years, comparing the domestic measles cases to imported measles cases, we are increasingly breeding these measles epidemics right here at home, whereas they used to be imported from throughout the world,” said Dr. Finch. Patients with measles can be treated with vitamin A, he added, referring to a Cochrane review showing that 200,000 units of vitamin A given daily for 2 days decreased the mortality rate of measles by about 80%. Measles is on the Centers for Disease Control and Prevention’s list of reportable diseases, so should be reported to local health authorities, and will be followed up with confirmatory testing.
In 2019, a study examining herd protection of oral human papillomavirus infection in men and women compared the prevalence of oral HPV infection based on the 4 HPV types present in the quadrivalent HPV vaccine with 33 nonvaccine types from 2009 to 2016. There was no change in the prevalence of nonvaccine type oral HPV infections among men who were unvaccinated, but the prevalence of oral HPV infections because of the four strains in the quadrivalent HPV vaccine declined from 2.7% in 2009-2010 to 1.6% in 2015-2016 (JAMA. 2019 Sep 10;322[10]:977-9). Among unvaccinated women, the prevalence of nonvaccine- and vaccine-type oral HPV infections did not change between the two time periods.
“Notably, this only occurred in men,” Dr. Finch said. Herd immunity is being achieved in men “because we’re vaccinating all women, [but] we’re not seeing that herd immunity in women. Which begs the question: Why are we still vaccinating only half of our population?”
One study published in 2019 (Br J Dermatol. 2019 Nov;181[5]:1093-5) described a patient with CARD9 mutations, which predispose individuals to deep invasive infections – a disseminated Microsporum infection in this case, Dr. Finch said. “You shouldn’t see that,” he added, noting that these mutations are known to predispose individuals to severe Trichophyton infections and familial candidiasis.
“What I think is interesting about this is that, as we look forward to 2020, we’re going to increasingly see studies like this that are identifying specific mutations in our community that underlie a lot of these weird infections,” he added. “I wouldn’t be surprised if within the span of our careers, we find that a lot of those severe treatment-refractory reports that so commonly plague your everyday clinic have some underlying, specific immunity.”
Dr. Finch reported no relevant conflicts of interest.
REPORTING FROM ODAC 2020
Home BP now a class Ia recommendation, with good reason
SNOWMASS, COLO. – The redefinition of hypertension as 130/80 mm Hg or higher introduced in the current American College of Cardiology/American Heart Association hypertension management guidelines has generated considerable controversy. Often overlooked, however, has been another major innovation included in the 2017 guidelines: the rise in the status of out-of-office 24-hour ambulatory blood pressure monitoring and home blood pressure self-measurement to a class I, level of evidence A recommendation, Andrew M. Kates, MD, observed at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
It’s a guideline he strongly endorses.
“We do a lot of this. It can be a challenge to get 24-hour ambulatory blood pressure monitoring covered by payers, so said Dr. Kates, professor of medicine and director of the cardiology fellowship program at Washington University, St. Louis.
He explained that one of the four key questions the guideline committee was tasked with answering at the outset of deliberations was this: What’s the evidence base for self-directed out-of-office blood pressure monitoring? Based on the panel’s systematic review of the literature, this practice wound up receiving the strongest possible class Ia recommendation, specifically for confirming the diagnosis of hypertension and for titration of antihypertensive medications. Moreover, the guidelines also endorsed home blood pressure monitoring for the detection of white-coat hypertension, this time as a Class IIa recommendation, as well as for identification of patients with masked hypertension, with class IIb status (Circulation. 2018 Oct 23;138[17]:e484-594).
The 2017 ACC/AHA guidelines include a detailed checklist for obtaining accurate measurements of office blood pressure. The suggestions include having the patient sit relaxed in a chair with both feet on the floor for at least 5 minutes before taking the measurement, no coffee or exercise for 30 minutes beforehand, empty the bladder, no talking, no clothing over the arm, and other recommendations. Many busy clinicians roll their eyes at the impracticality of doing all this on a routine basis.
“I don’t want to take an audience survey, but I’ll say that even in our office we are not successful in doing this. Patients run up the stairs to the office after dealing with traffic and the parking garage, they’re late for their appointment, in winter they’re wearing a sweater and don’t want to take it off. These are things we don’t do well, and they’re low-hanging fruit where we could do better,” Dr. Kates commented.
The challenges inherent in performing by-the-book office blood pressure measurement reinforce the importance of home self-monitoring of blood pressure in what is hopefully a more stress-free environment.
“We can give patients specific guidance about checking their blood pressure an hour after taking their medications, sitting for 5 minutes, and checking the pressures on a bare arm and not with the sleeve rolled up,” he noted.
The guidelines recommend using home blood pressure monitoring or ambulatory monitoring to detect white-coat hypertension in patients with an office blood pressure of 130/80 mm Hg or more, but less than 160/100 mm Hg, after a 3-month trial of lifestyle modification. If the home blood pressure is less than 130/80 mm Hg, that’s evidence of white-coat hypertension, for which the recommended treatment consists of continued lifestyle modification plus periodic monitoring of out-of-office blood pressures in order to promptly detect progression to hypertension. If, however, the out-of-office blood pressure is not less than 130/80 mm Hg, that’s hypertension, and the guidelines recommend starting dual-agent antihypertensive drug therapy while continuing lifestyle modification.
A confusing array of definitions of hypertension are now in use by various medical societies. While the 2017 ACC/AHA hypertension guidelines define hypertension as office blood pressure of 130/80 mm Hg or more, the 2018 European Society of Cardiology/European Society of Hypertension guidelines use a threshold of 140/90 mm Hg or more. Joint American Academy of Family Physicians/American College of Physicians guidelines recommend a treatment target of less than 150 mm Hg in hypertensive patients aged 60 years or older. And at the other end of the spectrum, the SPRINT trial showed a significant cardiovascular benefit for intensive treatment of hypertension to a target systolic blood pressure below 120 mm Hg, rather than less than 140 mm Hg (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
Dr. Kates believes the debate over the “right” treatment target misses the central point, which is that hypertension is staggeringly undertreated. Indeed, the Centers for Disease Control and Prevention estimates only one in four adults with hypertension have their disease under control. That’s a disconcerting statistic given that hypertension accounts for more cardiovascular deaths than any other modifiable cardiovascular risk factor.
“There’s been some concern raised that maybe too much weight has been put on the SPRINT trial in making the ACC/AHA recommendations, but I think it’s helpful to understand that we vastly undertreat patients with hypertension. So I think that, rather than being so concerned that we’re going to be treating people to too low a target or we’re being overly aggressive, it should give us some pause to think about the fact that we’re ordinarily not being aggressive enough with many of our patients as it is,” the cardiologist said.
Dr. Kates reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – The redefinition of hypertension as 130/80 mm Hg or higher introduced in the current American College of Cardiology/American Heart Association hypertension management guidelines has generated considerable controversy. Often overlooked, however, has been another major innovation included in the 2017 guidelines: the rise in the status of out-of-office 24-hour ambulatory blood pressure monitoring and home blood pressure self-measurement to a class I, level of evidence A recommendation, Andrew M. Kates, MD, observed at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
It’s a guideline he strongly endorses.
“We do a lot of this. It can be a challenge to get 24-hour ambulatory blood pressure monitoring covered by payers, so said Dr. Kates, professor of medicine and director of the cardiology fellowship program at Washington University, St. Louis.
He explained that one of the four key questions the guideline committee was tasked with answering at the outset of deliberations was this: What’s the evidence base for self-directed out-of-office blood pressure monitoring? Based on the panel’s systematic review of the literature, this practice wound up receiving the strongest possible class Ia recommendation, specifically for confirming the diagnosis of hypertension and for titration of antihypertensive medications. Moreover, the guidelines also endorsed home blood pressure monitoring for the detection of white-coat hypertension, this time as a Class IIa recommendation, as well as for identification of patients with masked hypertension, with class IIb status (Circulation. 2018 Oct 23;138[17]:e484-594).
The 2017 ACC/AHA guidelines include a detailed checklist for obtaining accurate measurements of office blood pressure. The suggestions include having the patient sit relaxed in a chair with both feet on the floor for at least 5 minutes before taking the measurement, no coffee or exercise for 30 minutes beforehand, empty the bladder, no talking, no clothing over the arm, and other recommendations. Many busy clinicians roll their eyes at the impracticality of doing all this on a routine basis.
“I don’t want to take an audience survey, but I’ll say that even in our office we are not successful in doing this. Patients run up the stairs to the office after dealing with traffic and the parking garage, they’re late for their appointment, in winter they’re wearing a sweater and don’t want to take it off. These are things we don’t do well, and they’re low-hanging fruit where we could do better,” Dr. Kates commented.
The challenges inherent in performing by-the-book office blood pressure measurement reinforce the importance of home self-monitoring of blood pressure in what is hopefully a more stress-free environment.
“We can give patients specific guidance about checking their blood pressure an hour after taking their medications, sitting for 5 minutes, and checking the pressures on a bare arm and not with the sleeve rolled up,” he noted.
The guidelines recommend using home blood pressure monitoring or ambulatory monitoring to detect white-coat hypertension in patients with an office blood pressure of 130/80 mm Hg or more, but less than 160/100 mm Hg, after a 3-month trial of lifestyle modification. If the home blood pressure is less than 130/80 mm Hg, that’s evidence of white-coat hypertension, for which the recommended treatment consists of continued lifestyle modification plus periodic monitoring of out-of-office blood pressures in order to promptly detect progression to hypertension. If, however, the out-of-office blood pressure is not less than 130/80 mm Hg, that’s hypertension, and the guidelines recommend starting dual-agent antihypertensive drug therapy while continuing lifestyle modification.
A confusing array of definitions of hypertension are now in use by various medical societies. While the 2017 ACC/AHA hypertension guidelines define hypertension as office blood pressure of 130/80 mm Hg or more, the 2018 European Society of Cardiology/European Society of Hypertension guidelines use a threshold of 140/90 mm Hg or more. Joint American Academy of Family Physicians/American College of Physicians guidelines recommend a treatment target of less than 150 mm Hg in hypertensive patients aged 60 years or older. And at the other end of the spectrum, the SPRINT trial showed a significant cardiovascular benefit for intensive treatment of hypertension to a target systolic blood pressure below 120 mm Hg, rather than less than 140 mm Hg (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
Dr. Kates believes the debate over the “right” treatment target misses the central point, which is that hypertension is staggeringly undertreated. Indeed, the Centers for Disease Control and Prevention estimates only one in four adults with hypertension have their disease under control. That’s a disconcerting statistic given that hypertension accounts for more cardiovascular deaths than any other modifiable cardiovascular risk factor.
“There’s been some concern raised that maybe too much weight has been put on the SPRINT trial in making the ACC/AHA recommendations, but I think it’s helpful to understand that we vastly undertreat patients with hypertension. So I think that, rather than being so concerned that we’re going to be treating people to too low a target or we’re being overly aggressive, it should give us some pause to think about the fact that we’re ordinarily not being aggressive enough with many of our patients as it is,” the cardiologist said.
Dr. Kates reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – The redefinition of hypertension as 130/80 mm Hg or higher introduced in the current American College of Cardiology/American Heart Association hypertension management guidelines has generated considerable controversy. Often overlooked, however, has been another major innovation included in the 2017 guidelines: the rise in the status of out-of-office 24-hour ambulatory blood pressure monitoring and home blood pressure self-measurement to a class I, level of evidence A recommendation, Andrew M. Kates, MD, observed at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
It’s a guideline he strongly endorses.
“We do a lot of this. It can be a challenge to get 24-hour ambulatory blood pressure monitoring covered by payers, so said Dr. Kates, professor of medicine and director of the cardiology fellowship program at Washington University, St. Louis.
He explained that one of the four key questions the guideline committee was tasked with answering at the outset of deliberations was this: What’s the evidence base for self-directed out-of-office blood pressure monitoring? Based on the panel’s systematic review of the literature, this practice wound up receiving the strongest possible class Ia recommendation, specifically for confirming the diagnosis of hypertension and for titration of antihypertensive medications. Moreover, the guidelines also endorsed home blood pressure monitoring for the detection of white-coat hypertension, this time as a Class IIa recommendation, as well as for identification of patients with masked hypertension, with class IIb status (Circulation. 2018 Oct 23;138[17]:e484-594).
The 2017 ACC/AHA guidelines include a detailed checklist for obtaining accurate measurements of office blood pressure. The suggestions include having the patient sit relaxed in a chair with both feet on the floor for at least 5 minutes before taking the measurement, no coffee or exercise for 30 minutes beforehand, empty the bladder, no talking, no clothing over the arm, and other recommendations. Many busy clinicians roll their eyes at the impracticality of doing all this on a routine basis.
“I don’t want to take an audience survey, but I’ll say that even in our office we are not successful in doing this. Patients run up the stairs to the office after dealing with traffic and the parking garage, they’re late for their appointment, in winter they’re wearing a sweater and don’t want to take it off. These are things we don’t do well, and they’re low-hanging fruit where we could do better,” Dr. Kates commented.
The challenges inherent in performing by-the-book office blood pressure measurement reinforce the importance of home self-monitoring of blood pressure in what is hopefully a more stress-free environment.
“We can give patients specific guidance about checking their blood pressure an hour after taking their medications, sitting for 5 minutes, and checking the pressures on a bare arm and not with the sleeve rolled up,” he noted.
The guidelines recommend using home blood pressure monitoring or ambulatory monitoring to detect white-coat hypertension in patients with an office blood pressure of 130/80 mm Hg or more, but less than 160/100 mm Hg, after a 3-month trial of lifestyle modification. If the home blood pressure is less than 130/80 mm Hg, that’s evidence of white-coat hypertension, for which the recommended treatment consists of continued lifestyle modification plus periodic monitoring of out-of-office blood pressures in order to promptly detect progression to hypertension. If, however, the out-of-office blood pressure is not less than 130/80 mm Hg, that’s hypertension, and the guidelines recommend starting dual-agent antihypertensive drug therapy while continuing lifestyle modification.
A confusing array of definitions of hypertension are now in use by various medical societies. While the 2017 ACC/AHA hypertension guidelines define hypertension as office blood pressure of 130/80 mm Hg or more, the 2018 European Society of Cardiology/European Society of Hypertension guidelines use a threshold of 140/90 mm Hg or more. Joint American Academy of Family Physicians/American College of Physicians guidelines recommend a treatment target of less than 150 mm Hg in hypertensive patients aged 60 years or older. And at the other end of the spectrum, the SPRINT trial showed a significant cardiovascular benefit for intensive treatment of hypertension to a target systolic blood pressure below 120 mm Hg, rather than less than 140 mm Hg (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
Dr. Kates believes the debate over the “right” treatment target misses the central point, which is that hypertension is staggeringly undertreated. Indeed, the Centers for Disease Control and Prevention estimates only one in four adults with hypertension have their disease under control. That’s a disconcerting statistic given that hypertension accounts for more cardiovascular deaths than any other modifiable cardiovascular risk factor.
“There’s been some concern raised that maybe too much weight has been put on the SPRINT trial in making the ACC/AHA recommendations, but I think it’s helpful to understand that we vastly undertreat patients with hypertension. So I think that, rather than being so concerned that we’re going to be treating people to too low a target or we’re being overly aggressive, it should give us some pause to think about the fact that we’re ordinarily not being aggressive enough with many of our patients as it is,” the cardiologist said.
Dr. Kates reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM ACC SNOWMASS 2020
Statin, antihypertensive treatment don’t guarantee healthier lifestyles
When people learn they have enough cardiovascular disease risk to start treatment with a statin or antihypertensive drug, the impact on their healthy-lifestyle choices seems to often be a wash, based on findings from more than 40,000 Finland residents followed for at least 4 years after starting their primary-prevention regimen.
“Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” wrote Maarit J. Korhonen, PhD, and associates in a report published in the Journal of the American Heart Association.
“Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative,” wrote Dr. Korhonen, a pharmacoepidemiologist at the University of Turku (Finland), and associates. This was the first reported study to assess a large-scale and prospectively followed cohort to look for associations between the use of medicines that prevent cardiovascular disease (CVD) and lifestyle changes. Most previous studies of these associations “have been cross sectional and provide no information on potential lifestyle changes during the time window around the initiation of medication use,” they added.
The new study specifically found that, on average, people who began treatment with at least one CVD-prevention medication for the first time were more likely to gain weight and more likely to become less active during the years following their treatment onset. But at the same time, these patients were also more likely to either quit or cut down on their smoking and alcohol consumption, the researchers found.
Their analysis used data from 41,225 people enrolled in the Finnish Public Sector Study, which prospectively began collecting data on a large number of Finland residents in the 1990s. They specifically focused on 81,772 completed questionnaires – collected at 4-year intervals – from people who completed at least two consecutive rounds of the survey during 2000-2013, and who were also at least 40 years old and free of prevalent CVD at the time of their first survey. The participants averaged nearly 53 years of age at their first survey, and 84% were women.
The researchers subdivided the survey responses into 8,837 (11%) people who began a statin, antihypertensive drug, or both during their participation; 26,914 (33%) already on a statin or antihypertensive drug when they completed their first questionnaire; and 46,021 response sets (56%) from people who never began treatment with either drug class. People who initiated a relevant drug began a median of 1.7 years following completion of their first survey, and a median of 2.4 years before their next survey. During follow-up, about 2% of all participants became newly diagnosed with some form of CVD.
The results showed that, after full adjustment for possible confounders, the mean increase in body mass index was larger among those who initiated a CVD-prevention drug, compared with those who did not. Among participants who were obese at entry, those who started a CVD drug had a statistically significant 37% increased rate of remaining obese, compared with those not starting these drugs. Among those who were not obese at baseline, those who began a CVD prevention drug had a statistically significant 82%% higher rate of becoming obese, compared with those not on a CVD-prevention drug. In addition, average daily energy expenditure, a measure of physical activity, showed a statistically significant decline among those who started a CVD drug, compared with those who did not. In contrast, CVD drug initiators had an average 1.85 gram/week decline in alcohol intake, compared with noninitiators, and those who were current smokers at the first survey and then started a CVD drug had a 26% relative drop in their smoking prevalence, compared with those who did not start a CVD drug, both statistically significant differences.
The findings suggest that “patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” the authors concluded. “This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level.”
The study received no commercial funding. Dr. Korhonen had no disclosures.
SOURCE: Korhonen MJ et al. J Am Heart Assoc. 2020 Feb 5. doi: 10.1161/JAHA.119.014.168.
When people learn they have enough cardiovascular disease risk to start treatment with a statin or antihypertensive drug, the impact on their healthy-lifestyle choices seems to often be a wash, based on findings from more than 40,000 Finland residents followed for at least 4 years after starting their primary-prevention regimen.
“Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” wrote Maarit J. Korhonen, PhD, and associates in a report published in the Journal of the American Heart Association.
“Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative,” wrote Dr. Korhonen, a pharmacoepidemiologist at the University of Turku (Finland), and associates. This was the first reported study to assess a large-scale and prospectively followed cohort to look for associations between the use of medicines that prevent cardiovascular disease (CVD) and lifestyle changes. Most previous studies of these associations “have been cross sectional and provide no information on potential lifestyle changes during the time window around the initiation of medication use,” they added.
The new study specifically found that, on average, people who began treatment with at least one CVD-prevention medication for the first time were more likely to gain weight and more likely to become less active during the years following their treatment onset. But at the same time, these patients were also more likely to either quit or cut down on their smoking and alcohol consumption, the researchers found.
Their analysis used data from 41,225 people enrolled in the Finnish Public Sector Study, which prospectively began collecting data on a large number of Finland residents in the 1990s. They specifically focused on 81,772 completed questionnaires – collected at 4-year intervals – from people who completed at least two consecutive rounds of the survey during 2000-2013, and who were also at least 40 years old and free of prevalent CVD at the time of their first survey. The participants averaged nearly 53 years of age at their first survey, and 84% were women.
The researchers subdivided the survey responses into 8,837 (11%) people who began a statin, antihypertensive drug, or both during their participation; 26,914 (33%) already on a statin or antihypertensive drug when they completed their first questionnaire; and 46,021 response sets (56%) from people who never began treatment with either drug class. People who initiated a relevant drug began a median of 1.7 years following completion of their first survey, and a median of 2.4 years before their next survey. During follow-up, about 2% of all participants became newly diagnosed with some form of CVD.
The results showed that, after full adjustment for possible confounders, the mean increase in body mass index was larger among those who initiated a CVD-prevention drug, compared with those who did not. Among participants who were obese at entry, those who started a CVD drug had a statistically significant 37% increased rate of remaining obese, compared with those not starting these drugs. Among those who were not obese at baseline, those who began a CVD prevention drug had a statistically significant 82%% higher rate of becoming obese, compared with those not on a CVD-prevention drug. In addition, average daily energy expenditure, a measure of physical activity, showed a statistically significant decline among those who started a CVD drug, compared with those who did not. In contrast, CVD drug initiators had an average 1.85 gram/week decline in alcohol intake, compared with noninitiators, and those who were current smokers at the first survey and then started a CVD drug had a 26% relative drop in their smoking prevalence, compared with those who did not start a CVD drug, both statistically significant differences.
The findings suggest that “patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” the authors concluded. “This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level.”
The study received no commercial funding. Dr. Korhonen had no disclosures.
SOURCE: Korhonen MJ et al. J Am Heart Assoc. 2020 Feb 5. doi: 10.1161/JAHA.119.014.168.
When people learn they have enough cardiovascular disease risk to start treatment with a statin or antihypertensive drug, the impact on their healthy-lifestyle choices seems to often be a wash, based on findings from more than 40,000 Finland residents followed for at least 4 years after starting their primary-prevention regimen.
“Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” wrote Maarit J. Korhonen, PhD, and associates in a report published in the Journal of the American Heart Association.
“Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative,” wrote Dr. Korhonen, a pharmacoepidemiologist at the University of Turku (Finland), and associates. This was the first reported study to assess a large-scale and prospectively followed cohort to look for associations between the use of medicines that prevent cardiovascular disease (CVD) and lifestyle changes. Most previous studies of these associations “have been cross sectional and provide no information on potential lifestyle changes during the time window around the initiation of medication use,” they added.
The new study specifically found that, on average, people who began treatment with at least one CVD-prevention medication for the first time were more likely to gain weight and more likely to become less active during the years following their treatment onset. But at the same time, these patients were also more likely to either quit or cut down on their smoking and alcohol consumption, the researchers found.
Their analysis used data from 41,225 people enrolled in the Finnish Public Sector Study, which prospectively began collecting data on a large number of Finland residents in the 1990s. They specifically focused on 81,772 completed questionnaires – collected at 4-year intervals – from people who completed at least two consecutive rounds of the survey during 2000-2013, and who were also at least 40 years old and free of prevalent CVD at the time of their first survey. The participants averaged nearly 53 years of age at their first survey, and 84% were women.
The researchers subdivided the survey responses into 8,837 (11%) people who began a statin, antihypertensive drug, or both during their participation; 26,914 (33%) already on a statin or antihypertensive drug when they completed their first questionnaire; and 46,021 response sets (56%) from people who never began treatment with either drug class. People who initiated a relevant drug began a median of 1.7 years following completion of their first survey, and a median of 2.4 years before their next survey. During follow-up, about 2% of all participants became newly diagnosed with some form of CVD.
The results showed that, after full adjustment for possible confounders, the mean increase in body mass index was larger among those who initiated a CVD-prevention drug, compared with those who did not. Among participants who were obese at entry, those who started a CVD drug had a statistically significant 37% increased rate of remaining obese, compared with those not starting these drugs. Among those who were not obese at baseline, those who began a CVD prevention drug had a statistically significant 82%% higher rate of becoming obese, compared with those not on a CVD-prevention drug. In addition, average daily energy expenditure, a measure of physical activity, showed a statistically significant decline among those who started a CVD drug, compared with those who did not. In contrast, CVD drug initiators had an average 1.85 gram/week decline in alcohol intake, compared with noninitiators, and those who were current smokers at the first survey and then started a CVD drug had a 26% relative drop in their smoking prevalence, compared with those who did not start a CVD drug, both statistically significant differences.
The findings suggest that “patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors,” the authors concluded. “This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level.”
The study received no commercial funding. Dr. Korhonen had no disclosures.
SOURCE: Korhonen MJ et al. J Am Heart Assoc. 2020 Feb 5. doi: 10.1161/JAHA.119.014.168.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
U.S. cancer centers embroiled in Chinese research thefts
Academic cancer centers around the United States continue to get caught up in an ever-evolving investigation into researchers – American and Chinese – who did not disclose payments from or the work they did for Chinese institutions while simultaneously accepting taxpayer money through U.S. government grants.
The U.S. Federal Bureau of Investigation has been ferreting out researchers it says have acted illegally.
On Jan. 28, the agency arrested Charles Lieber, a chemist from Harvard University, Cambridge, Mass., and also unveiled charges against Zheng Zaosong, a cancer researcher who is in the United States on a Harvard-sponsored visa.
The FBI said Mr. Zheng, who worked at the Harvard-affiliated Beth Israel Deaconess Medical Center, Boston, tried to smuggle 21 vials of biological material and research to China. Mr. Zheng was arrested in December at Boston’s Logan Airport. He admitted he planned to conduct and publish research in China using the stolen samples, said the FBI.
“All of the individuals charged today were either directly or indirectly working for the Chinese government, at our country’s expense,” said the agent in charge of the FBI’s Boston office, Joseph R. Bonavolonta.
Sen. Charles Grassley (R-IA), who has been pushing for more government action against foreign theft of U.S. research, said in a statement, “I’m glad the FBI appears to be taking foreign threats to taxpayer-funded research seriously, but I fear that this case is only the tip of the iceberg.”
The FBI said it is investigating China-related cases in all 50 states.
Ross McKinney, MD, the chief scientific officer at the Association of American Medical Colleges (AAMC), said he is aware of some 200 investigations, not all of which are cancer related, at 70-75 institutions.
“It’s a very ubiquitous problem,” Dr. McKinney said in an interview.
He also pointed out that some 6,000 National Institutes of Health–funded principal investigators are of Asian background. “So that 200 is a pretty small proportion,” said Dr. McKinney.
The NIH warned some 10,000 institutions in August 2018 that it had uncovered Chinese manipulation of peer review and a lack of disclosure of work for Chinese institutions. It urged the institutions to report irregularities.
For universities, “the trouble is sorting out who is the violator from who is not,” said Dr. McKinney. He noted that they are not set up to investigate whether someone has a laboratory in China.
“The fact that the Chinese government exploited the fact that universities are typically fairly trusting is extremely disappointing,” he said.
Moffitt story still unfolding
The most serious allegations have been leveled against six former employees of the Moffitt Cancer Center and Research Institute in Tampa, Florida.
In December 2019, Moffitt announced that the six – including President and CEO Alan List, MD, and the center director, Thomas Sellers, PhD – had left Moffitt as a result of “violations of conflict of interest rules through their work in China.”
New details have emerged, thanks to a new investigative report from a committee of the Florida House of Representatives.
The report said that Sheng Wei, a naturalized U.S. citizen who had worked at Moffitt since 2008 – when Moffitt began its affiliation with the Tianjin Medical University Cancer Institute and Hospital – was instrumental in recruiting top executives into the Thousand Talents program, which Wei had joined in 2010, according to the report. These executives included Dr. List, Dr. Sellers, and also Daniel Sullivan, head of Moffitt’s clinical science program, and cancer biologist Pearlie Epling-Burnette, it noted.
Begun in 2008, China’s Thousand Talents Plan gave salaries, funding, laboratory space, and other incentives to researchers who promised to bring U.S.-gained knowledge and research to China.
All information about this program has been removed from the Internet, but the program may still be active, Dr. McKinney commented.
According to the report, Dr. List pledged to work for the Tianjin cancer center 9 months a year for $71,000 annually. He was appointed head of the hematology department ($85,300 a year) in 2016. He opened a bank account in China to receive that salary and other Thousand Talents payments, the report found. The report notes that the exact amount Dr. List was paid is still not known.
Initially, Dr. Sellers, who was the principal investigator for Moffitt’s National Cancer Institute core grant, said he had not been involved in the Thousand Talents program. He later admitted that he had pledged to work in China 2 months a year for the program and that he’d opened a Chinese bank account and had deposited at least $35,000 into the account, the report notes.
The others pledged to work for the Thousand Talents program and also opened bank accounts in China and received money in those accounts.
Another Moffitt employee, Howard McLeod, MD, had worked for Thousand Talents before he joined Moffitt but did not disclose his China work. Dr. McLeod also supervised and had a close relationship with another researcher, Yijing (Bob) He, MD, who was employed by Moffitt but who lived in China, unbeknownst to Moffitt. “Dr. He appears to have functioned as an agent of Dr. McLeod in China,” said the report.
The report concluded that “none of the Moffitt faculty who were Talents program participants properly or timely disclosed their Talents program involvement to Moffitt, and none disclosed the full extent of their Talents program activities prior to Moffitt’s internal investigation.”
No charges have been filed against any of the former Moffitt employees.
However, the Cancer Letter has reported that Dr. Sellers is claiming he was not involved in the program and that he is preparing to sue Moffitt.
AAMC’s Dr. McKinney notes that it is illegal for researchers to take U.S. government grant money and pledge a certain amount of time but not deliver on that commitment because they are working for someone else – in this case, China. They also lied about not having any other research support, which is also illegal, he said.
The researchers received Chinese money and deposited it in Chinese accounts, which was never reported to the U.S. Internal Revenue Service.
“One of the hallmarks of the Chinese recruitment program was that people were instructed to not tell their normal U.S. host institution and not tell any U.S. government agency about their relationship with China,” Dr. McKinney said. “It was creating a culture where dishonesty in this situation was norm,” he added.
The lack of honesty brings up bigger questions for the field, he said. “Once you start lying about one thing, do you lie about your science, too?”
Lack of oversight?
Dr. McKinney said the NIH, as well as universities and hospitals, had a long and trusting relationship with China and should not be blamed for falling prey to the Chinese government’s concerted effort to steal intellectual property.
But some government watchdog groups have chided the NIH for lax oversight. In February 2019, the federal Health & Human Services’ Office of Inspector General found that “NIH has not assessed the risks to national security when permitting data access to foreign [principal investigators].”
Federal investigators have said that Thousand Talents has been one of the biggest threats.
The U.S. Senate Permanent Subcommittee on Investigations reported in November 2019 that “the federal government’s grant-making agencies did little to prevent this from happening, nor did the FBI and other federal agencies develop a coordinated response to mitigate the threat.”
The NIH invests $31 billion a year in medical research through 50,000 competitive grants to more than 300,000 researchers, according to that report. Even after uncovering grant fraud and peer-review manipulation that benefited China, “significant gaps in NIH’s grant integrity process remain,” the report states. Site visits by the NIH’s Division of Grants Compliance and Oversight dropped from 28 in 2012 to just 3 in 2018, the report noted.
Widening dragnet
In April 2019, Science reported that the NIH identified five researchers at MD Anderson Cancer Center in Houston who had failed to disclose their ties to Chinese enterprises and who had failed to keep peer review confidential.
Two resigned before they could be fired, one was fired, another eventually left the institution, and the fifth was found to have not willfully engaged in subterfuge.
Just a month later, Emory University in Atlanta announced that it had fired a husband and wife research team. The neuroscientists were known for their studies of Huntington disease. Both were U.S. citizens and had worked at Emory for more than 2 decades, according to the Science report.
The Moffitt situation led to the Florida legislature’s investigation, and also prompted some soul searching. The Tampa Bay Times reported that U.S. Senator Rick Scott (R-FL) asked state universities to provide information on what they are doing to stop foreign influence. The University of Florida then acknowledged that four faculty members resigned or were terminated because of ties to a foreign recruitment program.
This article first appeared on Medscape.com.
Academic cancer centers around the United States continue to get caught up in an ever-evolving investigation into researchers – American and Chinese – who did not disclose payments from or the work they did for Chinese institutions while simultaneously accepting taxpayer money through U.S. government grants.
The U.S. Federal Bureau of Investigation has been ferreting out researchers it says have acted illegally.
On Jan. 28, the agency arrested Charles Lieber, a chemist from Harvard University, Cambridge, Mass., and also unveiled charges against Zheng Zaosong, a cancer researcher who is in the United States on a Harvard-sponsored visa.
The FBI said Mr. Zheng, who worked at the Harvard-affiliated Beth Israel Deaconess Medical Center, Boston, tried to smuggle 21 vials of biological material and research to China. Mr. Zheng was arrested in December at Boston’s Logan Airport. He admitted he planned to conduct and publish research in China using the stolen samples, said the FBI.
“All of the individuals charged today were either directly or indirectly working for the Chinese government, at our country’s expense,” said the agent in charge of the FBI’s Boston office, Joseph R. Bonavolonta.
Sen. Charles Grassley (R-IA), who has been pushing for more government action against foreign theft of U.S. research, said in a statement, “I’m glad the FBI appears to be taking foreign threats to taxpayer-funded research seriously, but I fear that this case is only the tip of the iceberg.”
The FBI said it is investigating China-related cases in all 50 states.
Ross McKinney, MD, the chief scientific officer at the Association of American Medical Colleges (AAMC), said he is aware of some 200 investigations, not all of which are cancer related, at 70-75 institutions.
“It’s a very ubiquitous problem,” Dr. McKinney said in an interview.
He also pointed out that some 6,000 National Institutes of Health–funded principal investigators are of Asian background. “So that 200 is a pretty small proportion,” said Dr. McKinney.
The NIH warned some 10,000 institutions in August 2018 that it had uncovered Chinese manipulation of peer review and a lack of disclosure of work for Chinese institutions. It urged the institutions to report irregularities.
For universities, “the trouble is sorting out who is the violator from who is not,” said Dr. McKinney. He noted that they are not set up to investigate whether someone has a laboratory in China.
“The fact that the Chinese government exploited the fact that universities are typically fairly trusting is extremely disappointing,” he said.
Moffitt story still unfolding
The most serious allegations have been leveled against six former employees of the Moffitt Cancer Center and Research Institute in Tampa, Florida.
In December 2019, Moffitt announced that the six – including President and CEO Alan List, MD, and the center director, Thomas Sellers, PhD – had left Moffitt as a result of “violations of conflict of interest rules through their work in China.”
New details have emerged, thanks to a new investigative report from a committee of the Florida House of Representatives.
The report said that Sheng Wei, a naturalized U.S. citizen who had worked at Moffitt since 2008 – when Moffitt began its affiliation with the Tianjin Medical University Cancer Institute and Hospital – was instrumental in recruiting top executives into the Thousand Talents program, which Wei had joined in 2010, according to the report. These executives included Dr. List, Dr. Sellers, and also Daniel Sullivan, head of Moffitt’s clinical science program, and cancer biologist Pearlie Epling-Burnette, it noted.
Begun in 2008, China’s Thousand Talents Plan gave salaries, funding, laboratory space, and other incentives to researchers who promised to bring U.S.-gained knowledge and research to China.
All information about this program has been removed from the Internet, but the program may still be active, Dr. McKinney commented.
According to the report, Dr. List pledged to work for the Tianjin cancer center 9 months a year for $71,000 annually. He was appointed head of the hematology department ($85,300 a year) in 2016. He opened a bank account in China to receive that salary and other Thousand Talents payments, the report found. The report notes that the exact amount Dr. List was paid is still not known.
Initially, Dr. Sellers, who was the principal investigator for Moffitt’s National Cancer Institute core grant, said he had not been involved in the Thousand Talents program. He later admitted that he had pledged to work in China 2 months a year for the program and that he’d opened a Chinese bank account and had deposited at least $35,000 into the account, the report notes.
The others pledged to work for the Thousand Talents program and also opened bank accounts in China and received money in those accounts.
Another Moffitt employee, Howard McLeod, MD, had worked for Thousand Talents before he joined Moffitt but did not disclose his China work. Dr. McLeod also supervised and had a close relationship with another researcher, Yijing (Bob) He, MD, who was employed by Moffitt but who lived in China, unbeknownst to Moffitt. “Dr. He appears to have functioned as an agent of Dr. McLeod in China,” said the report.
The report concluded that “none of the Moffitt faculty who were Talents program participants properly or timely disclosed their Talents program involvement to Moffitt, and none disclosed the full extent of their Talents program activities prior to Moffitt’s internal investigation.”
No charges have been filed against any of the former Moffitt employees.
However, the Cancer Letter has reported that Dr. Sellers is claiming he was not involved in the program and that he is preparing to sue Moffitt.
AAMC’s Dr. McKinney notes that it is illegal for researchers to take U.S. government grant money and pledge a certain amount of time but not deliver on that commitment because they are working for someone else – in this case, China. They also lied about not having any other research support, which is also illegal, he said.
The researchers received Chinese money and deposited it in Chinese accounts, which was never reported to the U.S. Internal Revenue Service.
“One of the hallmarks of the Chinese recruitment program was that people were instructed to not tell their normal U.S. host institution and not tell any U.S. government agency about their relationship with China,” Dr. McKinney said. “It was creating a culture where dishonesty in this situation was norm,” he added.
The lack of honesty brings up bigger questions for the field, he said. “Once you start lying about one thing, do you lie about your science, too?”
Lack of oversight?
Dr. McKinney said the NIH, as well as universities and hospitals, had a long and trusting relationship with China and should not be blamed for falling prey to the Chinese government’s concerted effort to steal intellectual property.
But some government watchdog groups have chided the NIH for lax oversight. In February 2019, the federal Health & Human Services’ Office of Inspector General found that “NIH has not assessed the risks to national security when permitting data access to foreign [principal investigators].”
Federal investigators have said that Thousand Talents has been one of the biggest threats.
The U.S. Senate Permanent Subcommittee on Investigations reported in November 2019 that “the federal government’s grant-making agencies did little to prevent this from happening, nor did the FBI and other federal agencies develop a coordinated response to mitigate the threat.”
The NIH invests $31 billion a year in medical research through 50,000 competitive grants to more than 300,000 researchers, according to that report. Even after uncovering grant fraud and peer-review manipulation that benefited China, “significant gaps in NIH’s grant integrity process remain,” the report states. Site visits by the NIH’s Division of Grants Compliance and Oversight dropped from 28 in 2012 to just 3 in 2018, the report noted.
Widening dragnet
In April 2019, Science reported that the NIH identified five researchers at MD Anderson Cancer Center in Houston who had failed to disclose their ties to Chinese enterprises and who had failed to keep peer review confidential.
Two resigned before they could be fired, one was fired, another eventually left the institution, and the fifth was found to have not willfully engaged in subterfuge.
Just a month later, Emory University in Atlanta announced that it had fired a husband and wife research team. The neuroscientists were known for their studies of Huntington disease. Both were U.S. citizens and had worked at Emory for more than 2 decades, according to the Science report.
The Moffitt situation led to the Florida legislature’s investigation, and also prompted some soul searching. The Tampa Bay Times reported that U.S. Senator Rick Scott (R-FL) asked state universities to provide information on what they are doing to stop foreign influence. The University of Florida then acknowledged that four faculty members resigned or were terminated because of ties to a foreign recruitment program.
This article first appeared on Medscape.com.
Academic cancer centers around the United States continue to get caught up in an ever-evolving investigation into researchers – American and Chinese – who did not disclose payments from or the work they did for Chinese institutions while simultaneously accepting taxpayer money through U.S. government grants.
The U.S. Federal Bureau of Investigation has been ferreting out researchers it says have acted illegally.
On Jan. 28, the agency arrested Charles Lieber, a chemist from Harvard University, Cambridge, Mass., and also unveiled charges against Zheng Zaosong, a cancer researcher who is in the United States on a Harvard-sponsored visa.
The FBI said Mr. Zheng, who worked at the Harvard-affiliated Beth Israel Deaconess Medical Center, Boston, tried to smuggle 21 vials of biological material and research to China. Mr. Zheng was arrested in December at Boston’s Logan Airport. He admitted he planned to conduct and publish research in China using the stolen samples, said the FBI.
“All of the individuals charged today were either directly or indirectly working for the Chinese government, at our country’s expense,” said the agent in charge of the FBI’s Boston office, Joseph R. Bonavolonta.
Sen. Charles Grassley (R-IA), who has been pushing for more government action against foreign theft of U.S. research, said in a statement, “I’m glad the FBI appears to be taking foreign threats to taxpayer-funded research seriously, but I fear that this case is only the tip of the iceberg.”
The FBI said it is investigating China-related cases in all 50 states.
Ross McKinney, MD, the chief scientific officer at the Association of American Medical Colleges (AAMC), said he is aware of some 200 investigations, not all of which are cancer related, at 70-75 institutions.
“It’s a very ubiquitous problem,” Dr. McKinney said in an interview.
He also pointed out that some 6,000 National Institutes of Health–funded principal investigators are of Asian background. “So that 200 is a pretty small proportion,” said Dr. McKinney.
The NIH warned some 10,000 institutions in August 2018 that it had uncovered Chinese manipulation of peer review and a lack of disclosure of work for Chinese institutions. It urged the institutions to report irregularities.
For universities, “the trouble is sorting out who is the violator from who is not,” said Dr. McKinney. He noted that they are not set up to investigate whether someone has a laboratory in China.
“The fact that the Chinese government exploited the fact that universities are typically fairly trusting is extremely disappointing,” he said.
Moffitt story still unfolding
The most serious allegations have been leveled against six former employees of the Moffitt Cancer Center and Research Institute in Tampa, Florida.
In December 2019, Moffitt announced that the six – including President and CEO Alan List, MD, and the center director, Thomas Sellers, PhD – had left Moffitt as a result of “violations of conflict of interest rules through their work in China.”
New details have emerged, thanks to a new investigative report from a committee of the Florida House of Representatives.
The report said that Sheng Wei, a naturalized U.S. citizen who had worked at Moffitt since 2008 – when Moffitt began its affiliation with the Tianjin Medical University Cancer Institute and Hospital – was instrumental in recruiting top executives into the Thousand Talents program, which Wei had joined in 2010, according to the report. These executives included Dr. List, Dr. Sellers, and also Daniel Sullivan, head of Moffitt’s clinical science program, and cancer biologist Pearlie Epling-Burnette, it noted.
Begun in 2008, China’s Thousand Talents Plan gave salaries, funding, laboratory space, and other incentives to researchers who promised to bring U.S.-gained knowledge and research to China.
All information about this program has been removed from the Internet, but the program may still be active, Dr. McKinney commented.
According to the report, Dr. List pledged to work for the Tianjin cancer center 9 months a year for $71,000 annually. He was appointed head of the hematology department ($85,300 a year) in 2016. He opened a bank account in China to receive that salary and other Thousand Talents payments, the report found. The report notes that the exact amount Dr. List was paid is still not known.
Initially, Dr. Sellers, who was the principal investigator for Moffitt’s National Cancer Institute core grant, said he had not been involved in the Thousand Talents program. He later admitted that he had pledged to work in China 2 months a year for the program and that he’d opened a Chinese bank account and had deposited at least $35,000 into the account, the report notes.
The others pledged to work for the Thousand Talents program and also opened bank accounts in China and received money in those accounts.
Another Moffitt employee, Howard McLeod, MD, had worked for Thousand Talents before he joined Moffitt but did not disclose his China work. Dr. McLeod also supervised and had a close relationship with another researcher, Yijing (Bob) He, MD, who was employed by Moffitt but who lived in China, unbeknownst to Moffitt. “Dr. He appears to have functioned as an agent of Dr. McLeod in China,” said the report.
The report concluded that “none of the Moffitt faculty who were Talents program participants properly or timely disclosed their Talents program involvement to Moffitt, and none disclosed the full extent of their Talents program activities prior to Moffitt’s internal investigation.”
No charges have been filed against any of the former Moffitt employees.
However, the Cancer Letter has reported that Dr. Sellers is claiming he was not involved in the program and that he is preparing to sue Moffitt.
AAMC’s Dr. McKinney notes that it is illegal for researchers to take U.S. government grant money and pledge a certain amount of time but not deliver on that commitment because they are working for someone else – in this case, China. They also lied about not having any other research support, which is also illegal, he said.
The researchers received Chinese money and deposited it in Chinese accounts, which was never reported to the U.S. Internal Revenue Service.
“One of the hallmarks of the Chinese recruitment program was that people were instructed to not tell their normal U.S. host institution and not tell any U.S. government agency about their relationship with China,” Dr. McKinney said. “It was creating a culture where dishonesty in this situation was norm,” he added.
The lack of honesty brings up bigger questions for the field, he said. “Once you start lying about one thing, do you lie about your science, too?”
Lack of oversight?
Dr. McKinney said the NIH, as well as universities and hospitals, had a long and trusting relationship with China and should not be blamed for falling prey to the Chinese government’s concerted effort to steal intellectual property.
But some government watchdog groups have chided the NIH for lax oversight. In February 2019, the federal Health & Human Services’ Office of Inspector General found that “NIH has not assessed the risks to national security when permitting data access to foreign [principal investigators].”
Federal investigators have said that Thousand Talents has been one of the biggest threats.
The U.S. Senate Permanent Subcommittee on Investigations reported in November 2019 that “the federal government’s grant-making agencies did little to prevent this from happening, nor did the FBI and other federal agencies develop a coordinated response to mitigate the threat.”
The NIH invests $31 billion a year in medical research through 50,000 competitive grants to more than 300,000 researchers, according to that report. Even after uncovering grant fraud and peer-review manipulation that benefited China, “significant gaps in NIH’s grant integrity process remain,” the report states. Site visits by the NIH’s Division of Grants Compliance and Oversight dropped from 28 in 2012 to just 3 in 2018, the report noted.
Widening dragnet
In April 2019, Science reported that the NIH identified five researchers at MD Anderson Cancer Center in Houston who had failed to disclose their ties to Chinese enterprises and who had failed to keep peer review confidential.
Two resigned before they could be fired, one was fired, another eventually left the institution, and the fifth was found to have not willfully engaged in subterfuge.
Just a month later, Emory University in Atlanta announced that it had fired a husband and wife research team. The neuroscientists were known for their studies of Huntington disease. Both were U.S. citizens and had worked at Emory for more than 2 decades, according to the Science report.
The Moffitt situation led to the Florida legislature’s investigation, and also prompted some soul searching. The Tampa Bay Times reported that U.S. Senator Rick Scott (R-FL) asked state universities to provide information on what they are doing to stop foreign influence. The University of Florida then acknowledged that four faculty members resigned or were terminated because of ties to a foreign recruitment program.
This article first appeared on Medscape.com.
Chronic cough in COPD linked to more severe disease
, according to research published in CHEST.
The results indicate “that chronic cough in individuals with COPD is associated with a more severe disease phenotype, which could be helpful for stratifying management of COPD in the future,” wrote Eskild Landt, PhD, a research assistant at Zealand University Hospital in Køge, Denmark, and colleagues.
A study by published in the Journal of Allergy and Clinical Immunology: In Practice (2019;7[6]:1783-92.e8) indicated that in patients with asthma, chronic cough was associated with worse respiratory symptoms, more health care utilization, decreased lung function, and increased inflammatory markers in blood. Dr. Landt and colleagues hypothesized that patients with COPD and chronic cough had a similar pattern of disease severity.
To test their hypothesis, they identified individuals with COPD and chronic cough among 43,271 participants in the Copenhagen General Population Study, a population-based cohort study. The researchers defined COPD as a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 in individuals without asthma. Consecutive individuals answered questions about chronic cough, which was defined as a cough lasting more than 8 weeks, and responded to the Leicester Cough Questionnaire. They also underwent a physical health examination, including prebronchodilatory spirometry, and gave blood for biochemical analyses. The blood was analyzed for high-sensitive C-reactive protein, fibrinogen, leukocytes, eosinophils, neutrophils, and immunoglobulin E (i.e., inflammatory biomarkers).
Dr. Landt and colleagues identified 8,181 patients (19% of the population) with COPD, 796 (10%) of whom had chronic cough. Of the 33,364 participants without COPD, 1,585 (5%) had chronic cough. For patients with COPD and chronic cough, median total Leicester Cough Questionnaire score was 17.7, corresponding to 5.9 for the physical domain, 5.6 for the psychological domain, and 6.3 for the social domain.
Among participants with COPD, those with chronic cough had higher rates of sputum production (60% versus 8%), wheezing (46% versus 14%), dyspnea (66% versus 38%), chest pain or tightness (9% versus 4%), nighttime dyspnea (8% versus 3%), episodes of acute bronchitis or pneumonias in the past 10 years (45% versus 25%), and general practitioner visits in the past 12 months (53% versus 37%). In addition, these participants had lower FEV1% of predicted (81% versus 89%), lower ratio of FEV1 to FVC (0.64 versus 0.66), and higher levels of high-sensitive C-reactive protein, fibrinogen, leukocytes, neutrophils, eosinophils, and immunoglobulin E in blood.
“To our knowledge, this is the first study reporting Leicester Cough Questionnaire score for randomly selected individuals with COPD from a general population setting,” wrote Dr. Landt and colleagues. The study’s strengths include its randomly chosen population-based sample and investigator blinding to disease status and clinical outcome, they added. Some patients with the most severe types of COPD and chronic cough may not have attended the physical examination and participated in the study, however, and this factor could have biased the results. Furthermore, nearly the entire sample was white, so the results may not be generalizable to other ethnicities. “That said, we are not aware of results to suggest that our findings should not be relevant to individuals of all races,” wrote the investigators.
The study was funded by the private Lundbeck Foundation, as well as by the Danish Lung Association and the Danish Cancer Society. Several authors reported receiving grants and fees from AstraZeneca, GlaxoSmithKline, and Novartis that were unrelated to the study.
SOURCE: Landt E et al. CHEST. 2020 Jan 24. doi: 10.1016/j.chest.2019.12.038.
, according to research published in CHEST.
The results indicate “that chronic cough in individuals with COPD is associated with a more severe disease phenotype, which could be helpful for stratifying management of COPD in the future,” wrote Eskild Landt, PhD, a research assistant at Zealand University Hospital in Køge, Denmark, and colleagues.
A study by published in the Journal of Allergy and Clinical Immunology: In Practice (2019;7[6]:1783-92.e8) indicated that in patients with asthma, chronic cough was associated with worse respiratory symptoms, more health care utilization, decreased lung function, and increased inflammatory markers in blood. Dr. Landt and colleagues hypothesized that patients with COPD and chronic cough had a similar pattern of disease severity.
To test their hypothesis, they identified individuals with COPD and chronic cough among 43,271 participants in the Copenhagen General Population Study, a population-based cohort study. The researchers defined COPD as a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 in individuals without asthma. Consecutive individuals answered questions about chronic cough, which was defined as a cough lasting more than 8 weeks, and responded to the Leicester Cough Questionnaire. They also underwent a physical health examination, including prebronchodilatory spirometry, and gave blood for biochemical analyses. The blood was analyzed for high-sensitive C-reactive protein, fibrinogen, leukocytes, eosinophils, neutrophils, and immunoglobulin E (i.e., inflammatory biomarkers).
Dr. Landt and colleagues identified 8,181 patients (19% of the population) with COPD, 796 (10%) of whom had chronic cough. Of the 33,364 participants without COPD, 1,585 (5%) had chronic cough. For patients with COPD and chronic cough, median total Leicester Cough Questionnaire score was 17.7, corresponding to 5.9 for the physical domain, 5.6 for the psychological domain, and 6.3 for the social domain.
Among participants with COPD, those with chronic cough had higher rates of sputum production (60% versus 8%), wheezing (46% versus 14%), dyspnea (66% versus 38%), chest pain or tightness (9% versus 4%), nighttime dyspnea (8% versus 3%), episodes of acute bronchitis or pneumonias in the past 10 years (45% versus 25%), and general practitioner visits in the past 12 months (53% versus 37%). In addition, these participants had lower FEV1% of predicted (81% versus 89%), lower ratio of FEV1 to FVC (0.64 versus 0.66), and higher levels of high-sensitive C-reactive protein, fibrinogen, leukocytes, neutrophils, eosinophils, and immunoglobulin E in blood.
“To our knowledge, this is the first study reporting Leicester Cough Questionnaire score for randomly selected individuals with COPD from a general population setting,” wrote Dr. Landt and colleagues. The study’s strengths include its randomly chosen population-based sample and investigator blinding to disease status and clinical outcome, they added. Some patients with the most severe types of COPD and chronic cough may not have attended the physical examination and participated in the study, however, and this factor could have biased the results. Furthermore, nearly the entire sample was white, so the results may not be generalizable to other ethnicities. “That said, we are not aware of results to suggest that our findings should not be relevant to individuals of all races,” wrote the investigators.
The study was funded by the private Lundbeck Foundation, as well as by the Danish Lung Association and the Danish Cancer Society. Several authors reported receiving grants and fees from AstraZeneca, GlaxoSmithKline, and Novartis that were unrelated to the study.
SOURCE: Landt E et al. CHEST. 2020 Jan 24. doi: 10.1016/j.chest.2019.12.038.
, according to research published in CHEST.
The results indicate “that chronic cough in individuals with COPD is associated with a more severe disease phenotype, which could be helpful for stratifying management of COPD in the future,” wrote Eskild Landt, PhD, a research assistant at Zealand University Hospital in Køge, Denmark, and colleagues.
A study by published in the Journal of Allergy and Clinical Immunology: In Practice (2019;7[6]:1783-92.e8) indicated that in patients with asthma, chronic cough was associated with worse respiratory symptoms, more health care utilization, decreased lung function, and increased inflammatory markers in blood. Dr. Landt and colleagues hypothesized that patients with COPD and chronic cough had a similar pattern of disease severity.
To test their hypothesis, they identified individuals with COPD and chronic cough among 43,271 participants in the Copenhagen General Population Study, a population-based cohort study. The researchers defined COPD as a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 in individuals without asthma. Consecutive individuals answered questions about chronic cough, which was defined as a cough lasting more than 8 weeks, and responded to the Leicester Cough Questionnaire. They also underwent a physical health examination, including prebronchodilatory spirometry, and gave blood for biochemical analyses. The blood was analyzed for high-sensitive C-reactive protein, fibrinogen, leukocytes, eosinophils, neutrophils, and immunoglobulin E (i.e., inflammatory biomarkers).
Dr. Landt and colleagues identified 8,181 patients (19% of the population) with COPD, 796 (10%) of whom had chronic cough. Of the 33,364 participants without COPD, 1,585 (5%) had chronic cough. For patients with COPD and chronic cough, median total Leicester Cough Questionnaire score was 17.7, corresponding to 5.9 for the physical domain, 5.6 for the psychological domain, and 6.3 for the social domain.
Among participants with COPD, those with chronic cough had higher rates of sputum production (60% versus 8%), wheezing (46% versus 14%), dyspnea (66% versus 38%), chest pain or tightness (9% versus 4%), nighttime dyspnea (8% versus 3%), episodes of acute bronchitis or pneumonias in the past 10 years (45% versus 25%), and general practitioner visits in the past 12 months (53% versus 37%). In addition, these participants had lower FEV1% of predicted (81% versus 89%), lower ratio of FEV1 to FVC (0.64 versus 0.66), and higher levels of high-sensitive C-reactive protein, fibrinogen, leukocytes, neutrophils, eosinophils, and immunoglobulin E in blood.
“To our knowledge, this is the first study reporting Leicester Cough Questionnaire score for randomly selected individuals with COPD from a general population setting,” wrote Dr. Landt and colleagues. The study’s strengths include its randomly chosen population-based sample and investigator blinding to disease status and clinical outcome, they added. Some patients with the most severe types of COPD and chronic cough may not have attended the physical examination and participated in the study, however, and this factor could have biased the results. Furthermore, nearly the entire sample was white, so the results may not be generalizable to other ethnicities. “That said, we are not aware of results to suggest that our findings should not be relevant to individuals of all races,” wrote the investigators.
The study was funded by the private Lundbeck Foundation, as well as by the Danish Lung Association and the Danish Cancer Society. Several authors reported receiving grants and fees from AstraZeneca, GlaxoSmithKline, and Novartis that were unrelated to the study.
SOURCE: Landt E et al. CHEST. 2020 Jan 24. doi: 10.1016/j.chest.2019.12.038.
FROM CHEST