User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
2019-2020 flu season ends with ‘very high’ activity in New Jersey
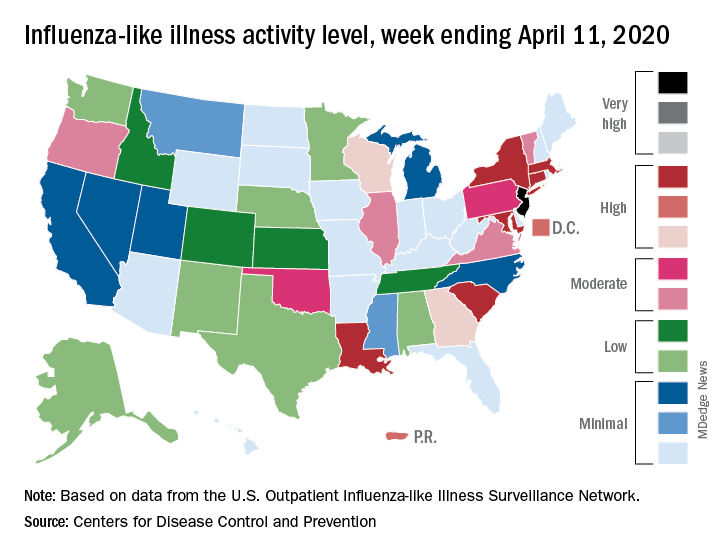
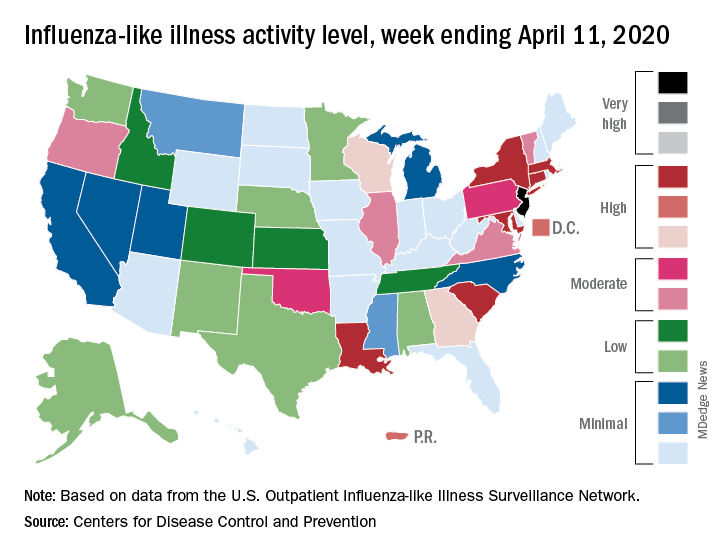
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
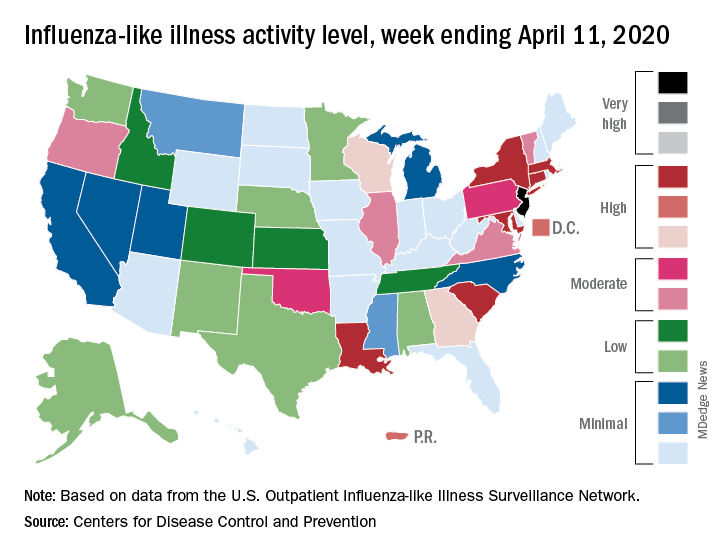
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
N.Y. universal testing: Many COVID-19+ pregnant women are asymptomatic
based on data from 215 pregnant women in New York City.
“The obstetrical population presents a unique challenge during this pandemic, since these patients have multiple interactions with the health care system and eventually most are admitted to the hospital for delivery,” wrote Desmond Sutton, MD, and colleagues at Columbia University Irving Medical Center, New York
In a letter published in the New England Journal of Medicine, the researchers reviewed their experiences with 215 pregnant women who delivered infants during March 22–April 4, 2020, at the New York–Presbyterian Allen Hospital and Columbia University Irving Medical Center. All the women were screened for symptoms of the COVID-19 infection on admission.
Overall, four women (1.9%) had fevers or other symptoms on admission, and all of these women tested positive for the virus that causes COVID-19. The other 211 women were afebrile and asymptomatic at admission, and 210 of them were tested via nasopharyngeal swabs. A total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection.
“Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote.
Three of the 29 COVID-19-positive women who were asymptomatic on admission developed fevers before they were discharged from the hospital after a median stay of 2 days. Of these, two received antibiotics for presumed endomyometritis and one patient with presumed COVID-19 infection received supportive care. In addition, one patient who was initially negative developed COVID-19 symptoms after delivery and tested positive 3 days after her initial negative test.
“Our use of universal SARS-CoV-2 testing in all pregnant patients presenting for delivery revealed that at this point in the pandemic in New York City, most of the patients who were positive for SARS-CoV-2 at delivery were asymptomatic,” Dr. Sutton and colleagues said.
Although their numbers may not be generalizable to areas with lower infection rates, they highlight the risk of COVID-19 infection in asymptomatic pregnant women, they noted.
“The potential benefits of a universal testing approach include the ability to use COVID-19 status to determine hospital isolation practices and bed assignments, inform neonatal care, and guide the use of personal protective equipment,” they concluded.
Continuing challenges
“What I have seen in our institute is the debate about rapid testing and the inherent problems with false negatives and false positives,” Catherine Cansino, MD, of the University of California, Davis, said in an interview. “I think there is definitely a role for universal testing, especially in areas with high prevalence,” and the New York clinicians have made a strong case.
However, the challenge remains of obtaining quick test results that would still be reliable, as many rapid tests have a false-negative rate of as much as 20%, noted Dr. Cansino, who was not involved in the New York study.
Her institution is using a test with a higher level of accuracy, “but it can take several hours or a day to get the results,” at which point the women may have gone through labor and delivery and been in contact with multiple health care workers who have used personal protective equipment accordingly if they don’t know a patient’s status.
To help guide policies, Dr. Cansino said that outcome data would be useful. “It’s hard to know how outcomes are different, and it would be good to know how transmission rates differ between symptomatic carriers and those who are asymptomatic.”
“As SARS-CoV-2, the virus responsible for COVID-19, continues to spread, pregnant women remain a unique population with required frequent health system contacts and ultimate need for delivery,” Iris Krishna, MD, of the Emory Healthcare Network in Atlanta, said in an interview. “This report in a high prevalence area demonstrated 1 out of 8 asymptomatic pregnant patients presenting for delivery were SARS-CoV-2 positive, illustrating a need for universal screening.
“As this pandemic evolves, we are learning more and more, and it is important to expand our understanding of asymptomatic transmission and the risk this may pose,” said Dr. Krishna, who was not part of the New York study.
“Key benefits to universal screening are the capability for labor and delivery units to implement best hospital practices in their care of mothers and babies, such as admitting positive patients to cohort units,” she noted. Such units would “allow for closer monitoring of mothers and babies, as well as ensuring proper use of personal protective equipment by health care teams” and also would help preserve supplies of personal protective equipment.
Dr. Krishna cited hospital testing capacity as an obvious barrier to universal screening of pregnant women, as well as factors including the need for additional protective equipment to be used during swab collection. Also, “If you get a negative result and there is a strong suspicion for COVID-19 infection, when do you retest?” she asked. “These are key questions or areas of assessment that should be considered before embarking on universal screening for pregnant women.” In addition, some patients may refuse testing out of fear of stigma or separation from their newborn.
“Implementing an ‘opt out’ approach to screening is encouraged, whereby a patient is informed that a test will be included in standard preventive screening, and they may decline the test,” Dr. Krishna said. “Routine, opt-out screening approaches have proven to be highly effective as it removes the stigma associated with testing, fosters earlier diagnosis and treatment, reduces risk of transmission, and has proven to be cost effective. Pregnant women should be reassured that universal screening is beneficial for their care and the care of their newborn baby,” she emphasized.
“Institutions should consider implementing universal screening on labor and delivery as several geographic areas are predicted to reach their peak time of COVID-19 transmission, and it is clear that asymptomatic individuals continue to play a role in its transmission,” Dr. Krishna concluded.
Dr. Sutton and associates had no financial conflicts to disclose. Neither Dr. Cansino nor Dr. Krishna had any financial conflicts to disclose. Dr. Cansino and Dr. Krishna are members of the Ob.Gyn. News Editorial Advisory Board.
SOURCE: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
based on data from 215 pregnant women in New York City.
“The obstetrical population presents a unique challenge during this pandemic, since these patients have multiple interactions with the health care system and eventually most are admitted to the hospital for delivery,” wrote Desmond Sutton, MD, and colleagues at Columbia University Irving Medical Center, New York
In a letter published in the New England Journal of Medicine, the researchers reviewed their experiences with 215 pregnant women who delivered infants during March 22–April 4, 2020, at the New York–Presbyterian Allen Hospital and Columbia University Irving Medical Center. All the women were screened for symptoms of the COVID-19 infection on admission.
Overall, four women (1.9%) had fevers or other symptoms on admission, and all of these women tested positive for the virus that causes COVID-19. The other 211 women were afebrile and asymptomatic at admission, and 210 of them were tested via nasopharyngeal swabs. A total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection.
“Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote.
Three of the 29 COVID-19-positive women who were asymptomatic on admission developed fevers before they were discharged from the hospital after a median stay of 2 days. Of these, two received antibiotics for presumed endomyometritis and one patient with presumed COVID-19 infection received supportive care. In addition, one patient who was initially negative developed COVID-19 symptoms after delivery and tested positive 3 days after her initial negative test.
“Our use of universal SARS-CoV-2 testing in all pregnant patients presenting for delivery revealed that at this point in the pandemic in New York City, most of the patients who were positive for SARS-CoV-2 at delivery were asymptomatic,” Dr. Sutton and colleagues said.
Although their numbers may not be generalizable to areas with lower infection rates, they highlight the risk of COVID-19 infection in asymptomatic pregnant women, they noted.
“The potential benefits of a universal testing approach include the ability to use COVID-19 status to determine hospital isolation practices and bed assignments, inform neonatal care, and guide the use of personal protective equipment,” they concluded.
Continuing challenges
“What I have seen in our institute is the debate about rapid testing and the inherent problems with false negatives and false positives,” Catherine Cansino, MD, of the University of California, Davis, said in an interview. “I think there is definitely a role for universal testing, especially in areas with high prevalence,” and the New York clinicians have made a strong case.
However, the challenge remains of obtaining quick test results that would still be reliable, as many rapid tests have a false-negative rate of as much as 20%, noted Dr. Cansino, who was not involved in the New York study.
Her institution is using a test with a higher level of accuracy, “but it can take several hours or a day to get the results,” at which point the women may have gone through labor and delivery and been in contact with multiple health care workers who have used personal protective equipment accordingly if they don’t know a patient’s status.
To help guide policies, Dr. Cansino said that outcome data would be useful. “It’s hard to know how outcomes are different, and it would be good to know how transmission rates differ between symptomatic carriers and those who are asymptomatic.”
“As SARS-CoV-2, the virus responsible for COVID-19, continues to spread, pregnant women remain a unique population with required frequent health system contacts and ultimate need for delivery,” Iris Krishna, MD, of the Emory Healthcare Network in Atlanta, said in an interview. “This report in a high prevalence area demonstrated 1 out of 8 asymptomatic pregnant patients presenting for delivery were SARS-CoV-2 positive, illustrating a need for universal screening.
“As this pandemic evolves, we are learning more and more, and it is important to expand our understanding of asymptomatic transmission and the risk this may pose,” said Dr. Krishna, who was not part of the New York study.
“Key benefits to universal screening are the capability for labor and delivery units to implement best hospital practices in their care of mothers and babies, such as admitting positive patients to cohort units,” she noted. Such units would “allow for closer monitoring of mothers and babies, as well as ensuring proper use of personal protective equipment by health care teams” and also would help preserve supplies of personal protective equipment.
Dr. Krishna cited hospital testing capacity as an obvious barrier to universal screening of pregnant women, as well as factors including the need for additional protective equipment to be used during swab collection. Also, “If you get a negative result and there is a strong suspicion for COVID-19 infection, when do you retest?” she asked. “These are key questions or areas of assessment that should be considered before embarking on universal screening for pregnant women.” In addition, some patients may refuse testing out of fear of stigma or separation from their newborn.
“Implementing an ‘opt out’ approach to screening is encouraged, whereby a patient is informed that a test will be included in standard preventive screening, and they may decline the test,” Dr. Krishna said. “Routine, opt-out screening approaches have proven to be highly effective as it removes the stigma associated with testing, fosters earlier diagnosis and treatment, reduces risk of transmission, and has proven to be cost effective. Pregnant women should be reassured that universal screening is beneficial for their care and the care of their newborn baby,” she emphasized.
“Institutions should consider implementing universal screening on labor and delivery as several geographic areas are predicted to reach their peak time of COVID-19 transmission, and it is clear that asymptomatic individuals continue to play a role in its transmission,” Dr. Krishna concluded.
Dr. Sutton and associates had no financial conflicts to disclose. Neither Dr. Cansino nor Dr. Krishna had any financial conflicts to disclose. Dr. Cansino and Dr. Krishna are members of the Ob.Gyn. News Editorial Advisory Board.
SOURCE: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
based on data from 215 pregnant women in New York City.
“The obstetrical population presents a unique challenge during this pandemic, since these patients have multiple interactions with the health care system and eventually most are admitted to the hospital for delivery,” wrote Desmond Sutton, MD, and colleagues at Columbia University Irving Medical Center, New York
In a letter published in the New England Journal of Medicine, the researchers reviewed their experiences with 215 pregnant women who delivered infants during March 22–April 4, 2020, at the New York–Presbyterian Allen Hospital and Columbia University Irving Medical Center. All the women were screened for symptoms of the COVID-19 infection on admission.
Overall, four women (1.9%) had fevers or other symptoms on admission, and all of these women tested positive for the virus that causes COVID-19. The other 211 women were afebrile and asymptomatic at admission, and 210 of them were tested via nasopharyngeal swabs. A total of 29 asymptomatic women (13.7%) tested positive for COVID-19 infection.
“Thus, 29 of the 33 patients who were positive for SARS-CoV-2 at admission (87.9%) had no symptoms of COVID-19 at presentation,” Dr. Sutton and colleagues wrote.
Three of the 29 COVID-19-positive women who were asymptomatic on admission developed fevers before they were discharged from the hospital after a median stay of 2 days. Of these, two received antibiotics for presumed endomyometritis and one patient with presumed COVID-19 infection received supportive care. In addition, one patient who was initially negative developed COVID-19 symptoms after delivery and tested positive 3 days after her initial negative test.
“Our use of universal SARS-CoV-2 testing in all pregnant patients presenting for delivery revealed that at this point in the pandemic in New York City, most of the patients who were positive for SARS-CoV-2 at delivery were asymptomatic,” Dr. Sutton and colleagues said.
Although their numbers may not be generalizable to areas with lower infection rates, they highlight the risk of COVID-19 infection in asymptomatic pregnant women, they noted.
“The potential benefits of a universal testing approach include the ability to use COVID-19 status to determine hospital isolation practices and bed assignments, inform neonatal care, and guide the use of personal protective equipment,” they concluded.
Continuing challenges
“What I have seen in our institute is the debate about rapid testing and the inherent problems with false negatives and false positives,” Catherine Cansino, MD, of the University of California, Davis, said in an interview. “I think there is definitely a role for universal testing, especially in areas with high prevalence,” and the New York clinicians have made a strong case.
However, the challenge remains of obtaining quick test results that would still be reliable, as many rapid tests have a false-negative rate of as much as 20%, noted Dr. Cansino, who was not involved in the New York study.
Her institution is using a test with a higher level of accuracy, “but it can take several hours or a day to get the results,” at which point the women may have gone through labor and delivery and been in contact with multiple health care workers who have used personal protective equipment accordingly if they don’t know a patient’s status.
To help guide policies, Dr. Cansino said that outcome data would be useful. “It’s hard to know how outcomes are different, and it would be good to know how transmission rates differ between symptomatic carriers and those who are asymptomatic.”
“As SARS-CoV-2, the virus responsible for COVID-19, continues to spread, pregnant women remain a unique population with required frequent health system contacts and ultimate need for delivery,” Iris Krishna, MD, of the Emory Healthcare Network in Atlanta, said in an interview. “This report in a high prevalence area demonstrated 1 out of 8 asymptomatic pregnant patients presenting for delivery were SARS-CoV-2 positive, illustrating a need for universal screening.
“As this pandemic evolves, we are learning more and more, and it is important to expand our understanding of asymptomatic transmission and the risk this may pose,” said Dr. Krishna, who was not part of the New York study.
“Key benefits to universal screening are the capability for labor and delivery units to implement best hospital practices in their care of mothers and babies, such as admitting positive patients to cohort units,” she noted. Such units would “allow for closer monitoring of mothers and babies, as well as ensuring proper use of personal protective equipment by health care teams” and also would help preserve supplies of personal protective equipment.
Dr. Krishna cited hospital testing capacity as an obvious barrier to universal screening of pregnant women, as well as factors including the need for additional protective equipment to be used during swab collection. Also, “If you get a negative result and there is a strong suspicion for COVID-19 infection, when do you retest?” she asked. “These are key questions or areas of assessment that should be considered before embarking on universal screening for pregnant women.” In addition, some patients may refuse testing out of fear of stigma or separation from their newborn.
“Implementing an ‘opt out’ approach to screening is encouraged, whereby a patient is informed that a test will be included in standard preventive screening, and they may decline the test,” Dr. Krishna said. “Routine, opt-out screening approaches have proven to be highly effective as it removes the stigma associated with testing, fosters earlier diagnosis and treatment, reduces risk of transmission, and has proven to be cost effective. Pregnant women should be reassured that universal screening is beneficial for their care and the care of their newborn baby,” she emphasized.
“Institutions should consider implementing universal screening on labor and delivery as several geographic areas are predicted to reach their peak time of COVID-19 transmission, and it is clear that asymptomatic individuals continue to play a role in its transmission,” Dr. Krishna concluded.
Dr. Sutton and associates had no financial conflicts to disclose. Neither Dr. Cansino nor Dr. Krishna had any financial conflicts to disclose. Dr. Cansino and Dr. Krishna are members of the Ob.Gyn. News Editorial Advisory Board.
SOURCE: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Universal COVID-19 testing for pregnant women entering hospitals for delivery could better protect patients and staff.
Major finding: Approximately 88% of 33 pregnant women who tested positive for COVID-19 infection at hospital admission were asymptomatic; about 14% of the 215 women overall tested positive for the novel coronavirus.
Study details: The data come from a review of 215 pregnant women who delivered infants between March 22 and April 4, 2020, in New York City.
Disclosures: The authors had no financial conflicts to disclose.
Source: Sutton D et al. N Engl J Med. 2020 Apr 13. doi: 10.1056/NEJMc2009316.
Infectious disease experts say testing is key to reopening
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
How to sanitize N95 masks for reuse: NIH study
Exposing contaminated N95 respirators to vaporized hydrogen peroxide (VHP) or ultraviolet (UV) light appears to eliminate the SARS-CoV-2 virus from the material and preserve the integrity of the masks fit for up to three uses, a National Institutes of Health (NIH) study shows.
Dry heat (70° C) was also found to eliminate the virus on masks but was effective for two uses instead of three.
Robert Fischer, PhD, with the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, and colleagues posted the findings on a preprint server on April 15. The paper has not yet been peer reviewed.
Four methods tested
Fischer and colleagues compared four methods for decontaminating the masks, which are designed for one-time use: UV radiation (260-285 nm); 70° C dry heat; 70% ethanol spray; and VHP.
For each method, the researchers compared the rate at which SARS-CoV-2 is inactivated on N95 filter fabric to that on stainless steel.
All four methods eliminated detectable SARS-CoV-2 virus from the fabric test samples, though the time needed for decontamination varied. VHP was the quickest, requiring 10 minutes. Dry heat and UV light each required approximately 60 minutes. Ethanol required an intermediate amount of time.
To test durability over three uses, the researchers treated intact, clean masks with the same decontamination method and assessed function via quantitative fit testing.
Volunteers from the Rocky Mountain laboratory wore the masks for 2 hours to test fit and seal.
The researchers found that masks that had been decontaminated with ethanol spray did not function effectively after decontamination, and they did not recommend use of that method.
By contrast, masks decontaminated with UV and VHP could be used up to three times and function properly. Masks decontaminated with dry heat could be used two times before function declined.
“Our results indicate that N95 respirators can be decontaminated and reused in times of shortage for up to three times for UV and HPV, and up to two times for dry heat,” the authors write. “However, utmost care should be given to ensure the proper functioning of the N95 respirator after each decontamination using readily available qualitative fit testing tools and to ensure that treatments are carried out for sufficient time to achieve desired risk-reduction.”
Reassurance for clinicians
The results will reassure clinicians, many of whom are already using these decontamination methods, Ravina Kullar, PharmD, MPH, an infectious disease expert with the Infectious Diseases Society of America, told Medscape Medical News.
Kullar, who is also an adjunct faculty member at the David Geffen School of Medicine of the University of California, Los Angeles, said the most widely used methods have been UV light and VPH.
UV light has been used for years to decontaminate rooms, she said. She also said that so far, supplies of hydrogen peroxide are adequate.
A shortcoming of the study, Kullar said, is that it tested the masks for only 2 hours, whereas in clinical practice, they are being worn for much longer periods.
After the study is peer reviewed, the Centers for Disease Control and Prevention (CDC) may update its recommendations, she said.
So far, she noted, the CDC has not approved any method for decontaminating masks, “but it has said that it does not object to using these sterilizers, disinfectants, devices, and air purifiers for effectively killing this virus.”
Safe, multiple use of the masks is critical in the COVID-19 crisis, she said.
“We have to look at other mechanisms to keep these N95 respirators in use when there’s such a shortage,” she said.
Integrity of the fit was an important factor in the study.
“All health care workers have to go through a fitting to have that mask fitted appropriately. That’s why these N95s are only approved for health care professionals, not the lay public,” she said.
The study was supported by the National Institutes of Health; the Defense Advanced Research Projects Agency; the University of California, Los Angeles; the US National Science Foundation; and the US Department of Defense.
This article first appeared on Medscape.com.
Exposing contaminated N95 respirators to vaporized hydrogen peroxide (VHP) or ultraviolet (UV) light appears to eliminate the SARS-CoV-2 virus from the material and preserve the integrity of the masks fit for up to three uses, a National Institutes of Health (NIH) study shows.
Dry heat (70° C) was also found to eliminate the virus on masks but was effective for two uses instead of three.
Robert Fischer, PhD, with the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, and colleagues posted the findings on a preprint server on April 15. The paper has not yet been peer reviewed.
Four methods tested
Fischer and colleagues compared four methods for decontaminating the masks, which are designed for one-time use: UV radiation (260-285 nm); 70° C dry heat; 70% ethanol spray; and VHP.
For each method, the researchers compared the rate at which SARS-CoV-2 is inactivated on N95 filter fabric to that on stainless steel.
All four methods eliminated detectable SARS-CoV-2 virus from the fabric test samples, though the time needed for decontamination varied. VHP was the quickest, requiring 10 minutes. Dry heat and UV light each required approximately 60 minutes. Ethanol required an intermediate amount of time.
To test durability over three uses, the researchers treated intact, clean masks with the same decontamination method and assessed function via quantitative fit testing.
Volunteers from the Rocky Mountain laboratory wore the masks for 2 hours to test fit and seal.
The researchers found that masks that had been decontaminated with ethanol spray did not function effectively after decontamination, and they did not recommend use of that method.
By contrast, masks decontaminated with UV and VHP could be used up to three times and function properly. Masks decontaminated with dry heat could be used two times before function declined.
“Our results indicate that N95 respirators can be decontaminated and reused in times of shortage for up to three times for UV and HPV, and up to two times for dry heat,” the authors write. “However, utmost care should be given to ensure the proper functioning of the N95 respirator after each decontamination using readily available qualitative fit testing tools and to ensure that treatments are carried out for sufficient time to achieve desired risk-reduction.”
Reassurance for clinicians
The results will reassure clinicians, many of whom are already using these decontamination methods, Ravina Kullar, PharmD, MPH, an infectious disease expert with the Infectious Diseases Society of America, told Medscape Medical News.
Kullar, who is also an adjunct faculty member at the David Geffen School of Medicine of the University of California, Los Angeles, said the most widely used methods have been UV light and VPH.
UV light has been used for years to decontaminate rooms, she said. She also said that so far, supplies of hydrogen peroxide are adequate.
A shortcoming of the study, Kullar said, is that it tested the masks for only 2 hours, whereas in clinical practice, they are being worn for much longer periods.
After the study is peer reviewed, the Centers for Disease Control and Prevention (CDC) may update its recommendations, she said.
So far, she noted, the CDC has not approved any method for decontaminating masks, “but it has said that it does not object to using these sterilizers, disinfectants, devices, and air purifiers for effectively killing this virus.”
Safe, multiple use of the masks is critical in the COVID-19 crisis, she said.
“We have to look at other mechanisms to keep these N95 respirators in use when there’s such a shortage,” she said.
Integrity of the fit was an important factor in the study.
“All health care workers have to go through a fitting to have that mask fitted appropriately. That’s why these N95s are only approved for health care professionals, not the lay public,” she said.
The study was supported by the National Institutes of Health; the Defense Advanced Research Projects Agency; the University of California, Los Angeles; the US National Science Foundation; and the US Department of Defense.
This article first appeared on Medscape.com.
Exposing contaminated N95 respirators to vaporized hydrogen peroxide (VHP) or ultraviolet (UV) light appears to eliminate the SARS-CoV-2 virus from the material and preserve the integrity of the masks fit for up to three uses, a National Institutes of Health (NIH) study shows.
Dry heat (70° C) was also found to eliminate the virus on masks but was effective for two uses instead of three.
Robert Fischer, PhD, with the National Institute of Allergy and Infectious Diseases in Hamilton, Montana, and colleagues posted the findings on a preprint server on April 15. The paper has not yet been peer reviewed.
Four methods tested
Fischer and colleagues compared four methods for decontaminating the masks, which are designed for one-time use: UV radiation (260-285 nm); 70° C dry heat; 70% ethanol spray; and VHP.
For each method, the researchers compared the rate at which SARS-CoV-2 is inactivated on N95 filter fabric to that on stainless steel.
All four methods eliminated detectable SARS-CoV-2 virus from the fabric test samples, though the time needed for decontamination varied. VHP was the quickest, requiring 10 minutes. Dry heat and UV light each required approximately 60 minutes. Ethanol required an intermediate amount of time.
To test durability over three uses, the researchers treated intact, clean masks with the same decontamination method and assessed function via quantitative fit testing.
Volunteers from the Rocky Mountain laboratory wore the masks for 2 hours to test fit and seal.
The researchers found that masks that had been decontaminated with ethanol spray did not function effectively after decontamination, and they did not recommend use of that method.
By contrast, masks decontaminated with UV and VHP could be used up to three times and function properly. Masks decontaminated with dry heat could be used two times before function declined.
“Our results indicate that N95 respirators can be decontaminated and reused in times of shortage for up to three times for UV and HPV, and up to two times for dry heat,” the authors write. “However, utmost care should be given to ensure the proper functioning of the N95 respirator after each decontamination using readily available qualitative fit testing tools and to ensure that treatments are carried out for sufficient time to achieve desired risk-reduction.”
Reassurance for clinicians
The results will reassure clinicians, many of whom are already using these decontamination methods, Ravina Kullar, PharmD, MPH, an infectious disease expert with the Infectious Diseases Society of America, told Medscape Medical News.
Kullar, who is also an adjunct faculty member at the David Geffen School of Medicine of the University of California, Los Angeles, said the most widely used methods have been UV light and VPH.
UV light has been used for years to decontaminate rooms, she said. She also said that so far, supplies of hydrogen peroxide are adequate.
A shortcoming of the study, Kullar said, is that it tested the masks for only 2 hours, whereas in clinical practice, they are being worn for much longer periods.
After the study is peer reviewed, the Centers for Disease Control and Prevention (CDC) may update its recommendations, she said.
So far, she noted, the CDC has not approved any method for decontaminating masks, “but it has said that it does not object to using these sterilizers, disinfectants, devices, and air purifiers for effectively killing this virus.”
Safe, multiple use of the masks is critical in the COVID-19 crisis, she said.
“We have to look at other mechanisms to keep these N95 respirators in use when there’s such a shortage,” she said.
Integrity of the fit was an important factor in the study.
“All health care workers have to go through a fitting to have that mask fitted appropriately. That’s why these N95s are only approved for health care professionals, not the lay public,” she said.
The study was supported by the National Institutes of Health; the Defense Advanced Research Projects Agency; the University of California, Los Angeles; the US National Science Foundation; and the US Department of Defense.
This article first appeared on Medscape.com.
COVID-19: How intensive care cardiology can inform the response
Because of their place at the interface between critical care and cardiovascular medicine, critical care cardiologists are in a good position to come up with novel approaches to adapting critical care systems to the current crisis. Health care and clinical resources have been severely strained in some places, and increasing evidence suggests that SARS-CoV-2 can cause injury to most organ systems. More than a quarter of hospitalized patients have cardiac injury, which can be a key reason for clinical deterioration.
An international group of critical care cardiologists led by Jason Katz, MD, of Duke University, Durham, N.C., offered suggestions for scalable models for critical care delivery in the context of COVID-19 in the Journal of the American College of Cardiology.
Critical care cardiology developed in response to changes in patient populations and their clinical needs. Respiratory insufficiency, heart failure, structural heart disease, and multisystem organ dysfunction became more common than patients with complicated acute MI, leading cardiologists in critical care cardiology to become more proficient in general critical care medicine, and to become leaders in forming collaborative multidisciplinary teams. The authors argued that COVID-19 is precipitating a similar need to adapt to the changing needs of patients.
“This pandemic should serve as a clarion call to our health care systems that we should continue to develop a nimble workforce that can adapt to change quickly during a crisis. We believe critical care cardiologists are well positioned to help serve society in this capacity,” the authors wrote.
Surge staging
They proposed four surge stages based in part on an American College of Chest Physicians–endorsed model (Chest 2014 Oct;146:e61S-74S), which regards a 25% capacity surge as minor. At the other end of the spectrum, a 200% surge is defined as a “disaster.” In minor surges (less than 25% increase), the traditional cardiac ICU (CICU) model can continue to be applied. During moderate (25%-100% increases) or major (100%-200%) surges, the critical care cardiologist should collaborate or consult within multiple health care teams. Physicians not trained in critical care can assist with care of intubated and critically ill patients under the supervision of a critical care cardiologist or under the supervision of a partnership between a non–cardiac critical care medicine provider and a cardiologist. The number of patients cared for by each team should increase in step with the size of the surge.
In disaster situations (more than 200% surge), there should be adaptive and dynamic staffing reorganization. The report included an illustration of a range of steps that can be taken, including alterations to staffing, regional care systems, resource management, and triage practices. Scoring systems such as Sequential Organ Failure Assessment may be useful for triaging, but the authors also suggest employment of validated cardiac disease–specific scores, because traditional ICU measures don’t always apply well to CICU populations.
At the hospital level, deferrals should be made for elective cardiac procedures that require CICU or postanesthesia care unit recovery periods. Semielective procedures should be considered after risk-benefit considerations when delays could lead to morbidity or mortality. Even some traditional emergency procedures may need to be reevaluated in the COVID-19 context: For example, some low-risk ST-segment elevation MI (STEMI) patients don’t require ICU care but are manageable in cardiac intermediate care beds instead. Historical triage practices should be reexamined to predict which STEMI patients will require ICU care.
Resource allocation
The CICU work flow will be affected as some of its beds are opened up to COVID-19 patients. Standard philosophies of concentrating intense resources will have to give way to a utilitarian approach that evaluates operations based on efficiency, equity, and justice. Physician-patient contact should be minimized using technological links when possible, and rounds might be reorganized to first examine patients without COVID-19, in order to minimize between-patient spread.
Military medicine, which is used to ramping up operations during times of crisis, has potential lessons for the current pandemic. In the face of mass casualties, military physicians often turn to the North Atlantic Treaty Organization triage system, which separates patients into four categories: immediate, requiring lifesaving intervention; delayed, requiring intervention within hours to days; minimal, where the patient is injured but ambulatory; and expectant patients who are deceased or too injured to save. Impersonal though this system may be, it may be required in the most severe scenarios when resources are scarce or absent.
The authors reported no relevant financial disclosures.
SOURCE: Katz J et al. J Am Coll Cardiol. 2020 Apr 15. doi: 10.1016/j.annonc.2020.02.01.
Because of their place at the interface between critical care and cardiovascular medicine, critical care cardiologists are in a good position to come up with novel approaches to adapting critical care systems to the current crisis. Health care and clinical resources have been severely strained in some places, and increasing evidence suggests that SARS-CoV-2 can cause injury to most organ systems. More than a quarter of hospitalized patients have cardiac injury, which can be a key reason for clinical deterioration.
An international group of critical care cardiologists led by Jason Katz, MD, of Duke University, Durham, N.C., offered suggestions for scalable models for critical care delivery in the context of COVID-19 in the Journal of the American College of Cardiology.
Critical care cardiology developed in response to changes in patient populations and their clinical needs. Respiratory insufficiency, heart failure, structural heart disease, and multisystem organ dysfunction became more common than patients with complicated acute MI, leading cardiologists in critical care cardiology to become more proficient in general critical care medicine, and to become leaders in forming collaborative multidisciplinary teams. The authors argued that COVID-19 is precipitating a similar need to adapt to the changing needs of patients.
“This pandemic should serve as a clarion call to our health care systems that we should continue to develop a nimble workforce that can adapt to change quickly during a crisis. We believe critical care cardiologists are well positioned to help serve society in this capacity,” the authors wrote.
Surge staging
They proposed four surge stages based in part on an American College of Chest Physicians–endorsed model (Chest 2014 Oct;146:e61S-74S), which regards a 25% capacity surge as minor. At the other end of the spectrum, a 200% surge is defined as a “disaster.” In minor surges (less than 25% increase), the traditional cardiac ICU (CICU) model can continue to be applied. During moderate (25%-100% increases) or major (100%-200%) surges, the critical care cardiologist should collaborate or consult within multiple health care teams. Physicians not trained in critical care can assist with care of intubated and critically ill patients under the supervision of a critical care cardiologist or under the supervision of a partnership between a non–cardiac critical care medicine provider and a cardiologist. The number of patients cared for by each team should increase in step with the size of the surge.
In disaster situations (more than 200% surge), there should be adaptive and dynamic staffing reorganization. The report included an illustration of a range of steps that can be taken, including alterations to staffing, regional care systems, resource management, and triage practices. Scoring systems such as Sequential Organ Failure Assessment may be useful for triaging, but the authors also suggest employment of validated cardiac disease–specific scores, because traditional ICU measures don’t always apply well to CICU populations.
At the hospital level, deferrals should be made for elective cardiac procedures that require CICU or postanesthesia care unit recovery periods. Semielective procedures should be considered after risk-benefit considerations when delays could lead to morbidity or mortality. Even some traditional emergency procedures may need to be reevaluated in the COVID-19 context: For example, some low-risk ST-segment elevation MI (STEMI) patients don’t require ICU care but are manageable in cardiac intermediate care beds instead. Historical triage practices should be reexamined to predict which STEMI patients will require ICU care.
Resource allocation
The CICU work flow will be affected as some of its beds are opened up to COVID-19 patients. Standard philosophies of concentrating intense resources will have to give way to a utilitarian approach that evaluates operations based on efficiency, equity, and justice. Physician-patient contact should be minimized using technological links when possible, and rounds might be reorganized to first examine patients without COVID-19, in order to minimize between-patient spread.
Military medicine, which is used to ramping up operations during times of crisis, has potential lessons for the current pandemic. In the face of mass casualties, military physicians often turn to the North Atlantic Treaty Organization triage system, which separates patients into four categories: immediate, requiring lifesaving intervention; delayed, requiring intervention within hours to days; minimal, where the patient is injured but ambulatory; and expectant patients who are deceased or too injured to save. Impersonal though this system may be, it may be required in the most severe scenarios when resources are scarce or absent.
The authors reported no relevant financial disclosures.
SOURCE: Katz J et al. J Am Coll Cardiol. 2020 Apr 15. doi: 10.1016/j.annonc.2020.02.01.
Because of their place at the interface between critical care and cardiovascular medicine, critical care cardiologists are in a good position to come up with novel approaches to adapting critical care systems to the current crisis. Health care and clinical resources have been severely strained in some places, and increasing evidence suggests that SARS-CoV-2 can cause injury to most organ systems. More than a quarter of hospitalized patients have cardiac injury, which can be a key reason for clinical deterioration.
An international group of critical care cardiologists led by Jason Katz, MD, of Duke University, Durham, N.C., offered suggestions for scalable models for critical care delivery in the context of COVID-19 in the Journal of the American College of Cardiology.
Critical care cardiology developed in response to changes in patient populations and their clinical needs. Respiratory insufficiency, heart failure, structural heart disease, and multisystem organ dysfunction became more common than patients with complicated acute MI, leading cardiologists in critical care cardiology to become more proficient in general critical care medicine, and to become leaders in forming collaborative multidisciplinary teams. The authors argued that COVID-19 is precipitating a similar need to adapt to the changing needs of patients.
“This pandemic should serve as a clarion call to our health care systems that we should continue to develop a nimble workforce that can adapt to change quickly during a crisis. We believe critical care cardiologists are well positioned to help serve society in this capacity,” the authors wrote.
Surge staging
They proposed four surge stages based in part on an American College of Chest Physicians–endorsed model (Chest 2014 Oct;146:e61S-74S), which regards a 25% capacity surge as minor. At the other end of the spectrum, a 200% surge is defined as a “disaster.” In minor surges (less than 25% increase), the traditional cardiac ICU (CICU) model can continue to be applied. During moderate (25%-100% increases) or major (100%-200%) surges, the critical care cardiologist should collaborate or consult within multiple health care teams. Physicians not trained in critical care can assist with care of intubated and critically ill patients under the supervision of a critical care cardiologist or under the supervision of a partnership between a non–cardiac critical care medicine provider and a cardiologist. The number of patients cared for by each team should increase in step with the size of the surge.
In disaster situations (more than 200% surge), there should be adaptive and dynamic staffing reorganization. The report included an illustration of a range of steps that can be taken, including alterations to staffing, regional care systems, resource management, and triage practices. Scoring systems such as Sequential Organ Failure Assessment may be useful for triaging, but the authors also suggest employment of validated cardiac disease–specific scores, because traditional ICU measures don’t always apply well to CICU populations.
At the hospital level, deferrals should be made for elective cardiac procedures that require CICU or postanesthesia care unit recovery periods. Semielective procedures should be considered after risk-benefit considerations when delays could lead to morbidity or mortality. Even some traditional emergency procedures may need to be reevaluated in the COVID-19 context: For example, some low-risk ST-segment elevation MI (STEMI) patients don’t require ICU care but are manageable in cardiac intermediate care beds instead. Historical triage practices should be reexamined to predict which STEMI patients will require ICU care.
Resource allocation
The CICU work flow will be affected as some of its beds are opened up to COVID-19 patients. Standard philosophies of concentrating intense resources will have to give way to a utilitarian approach that evaluates operations based on efficiency, equity, and justice. Physician-patient contact should be minimized using technological links when possible, and rounds might be reorganized to first examine patients without COVID-19, in order to minimize between-patient spread.
Military medicine, which is used to ramping up operations during times of crisis, has potential lessons for the current pandemic. In the face of mass casualties, military physicians often turn to the North Atlantic Treaty Organization triage system, which separates patients into four categories: immediate, requiring lifesaving intervention; delayed, requiring intervention within hours to days; minimal, where the patient is injured but ambulatory; and expectant patients who are deceased or too injured to save. Impersonal though this system may be, it may be required in the most severe scenarios when resources are scarce or absent.
The authors reported no relevant financial disclosures.
SOURCE: Katz J et al. J Am Coll Cardiol. 2020 Apr 15. doi: 10.1016/j.annonc.2020.02.01.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Obesity link to severe COVID-19, especially in patients aged under 60
It is becoming increasingly clear that obesity is one of the biggest risk factors for severe COVID-19 disease, particularly among younger patients.
Newly published data from New York show that, among those aged under 60 years, obesity was twice as likely to result in hospitalization for COVID-19 and also significantly increased the likelihood that a person would end up in intensive care.
“Obesity [in people younger than 60] appears to be a previously unrecognized risk factor for hospital admission and need for critical care. This has important and practical implications when nearly 40% of adults in the U.S. are obese with a body mass index [BMI] of [at least] 30,” wrote Jennifer Lighter, MD, of New York University Langone Health, and colleagues in their research letter published in Clinical Infectious Diseases.
Similar findings in a preprint publication, yet to be peer reviewed, from another New York hospital show that, with the exception of older age, obesity (BMI greater than 40 kg/m2) had the strongest association with hospitalization for COVID-19, increasing the risk more than 500%.
Meanwhile, a new French study shows a high frequency of obesity among patients admitted to one ICU for COVID-19; furthermore, disease severity increased with increasing BMI. One of the authors said in an interview that many of the presenting patients were younger, with their only risk factor being obesity.
“Patients with obesity should avoid any COVID-19 contamination by enforcing all prevention measures during the current pandemic,” wrote the authors, led by Arthur Simonnet, MD, Centre Hospitalier Universitaire de Lille (France).
They also stressed that COVID-19 patients “with severe obesity should be monitored more closely.”
Those with obesity are young and become very sick, very quickly
François Pattou, MD, PhD, coauthor of the French article published in Obesity said in an interview that, when patients with COVID-19 began to arrive at their ICU in Lille, there were young patients who did not have any other comorbidities.
“They were just obese,” he observed, adding that they seemed “to have a very specific disease, something different” from that seen before, with patients becoming very sick, very quickly.
In their study, they examined 124 consecutive patients admitted to intensive care with COVID-19 between Feb. 25 and April 5, 2020, and compared them with a historical control group of 306 patients admitted to the ICU at the same hospital for non–COVID-19-related severe acute respiratory disease in 2019.
By April 6, 60 patients with COVID-19 had been discharged from intensive care, 18 had died, and 46 remained in the unit. The majority (73%) were male, and their median age was 60 years. Obesity and severe obesity were significantly more prevalent among the patients with COVID-19, at 47.6% and 28.2% versus 25.2% and 10.8% among historical controls (P < .001 for trend).
A key finding was that those with a BMI greater than 35 had a more than 600% increased risk of requiring mechanical ventilation (odds ratio, 7.36; P = .021), compared with those with a BMI less than 25, even after adjusting for age, diabetes, and hypertension.
Obesity in under 60s at least doubles risk of admission in U.S.
The studies out of New York, one of which was stratified by age, paint a similar picture.
Dr. Lighter and colleagues found that, of the 3,615 individuals who tested positive for COVID-19 in their series, 775 (21%) had a BMI of 30-34 and 595 (16%) had a BMI of at least 35. Obesity wasn’t a predictor of admission to hospital or the ICU in those over the age of 60 years, but in those younger than 60 years, it was.
Those under age 60 with a BMI of 30-34 were twice as likely to be admitted to hospital (hazard ratio, 2.0; P < .0001) and critical care (HR, 1.8; P = .006), compared with those under age 60 with a BMI less than 30. Likewise, those under age 60 with a BMI of at least 35 were 2.2 (P < .0001) and 3.6 (P < .0001) times more likely to be admitted to acute and critical care.
“Unfortunately, obesity in people [less than] 60 years is a newly identified epidemiologic risk factor which may contribute to increased morbidity rates [with COVID-19] experienced in the U.S.,” they concluded.
And in the other U.S. study, Christopher M. Petrilli, MD, of New York University, and colleagues looked at 4,103 patients with COVID-19 treated between March 1 and April 2, 2020, and followed to April 7.
Just under half of patients (48.7%) were hospitalized, of whom 22.3% required mechanical ventilation and 14.6% died or were discharged to hospice. The research was published on medRxiv, showing that, apart from age, the strongest predictors of hospitalization were BMI greater than 40 (OR, 6.2) and heart failure (OR, 4.3).
“It is notable that the chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” they noted.
Inflammation is a possible culprit
Dr. Pattou believes that the culprit behind the increased risk of disease severity seen with obesity in COVID-19 is inflammation, mediated by fibrin deposits in the circulation, which his colleagues have seen on autopsy, and which “block oxygen passage through the blood.”
This may help explain why mechanical ventilation can be less successful in these patients. “The answer is to get rid of this inflammation,” Dr. Pattou observed.
Dr. Petrilli and colleagues also observed that obesity “is well-recognized to be a proinflammatory condition.”
And their findings showed “the importance of inflammatory markers in distinguishing future critical from noncritical illness,” they said, noting that, among these markers, early elevations in C-reactive protein and D-dimer “had the strongest association with mechanical ventilation or mortality.”
Livio Luzi, MD, of IRCCS MultiMedica, Milan, Italy, has previously written on the relationship between influenza and obesity, and discussed in an interview the potential lessons for the COVID-19 pandemic.
“Obesity is characterized by an impairment of immune response and by a low-grade chronic inflammation. Furthermore, obese subjects have an altered dynamic of pulmonary ventilation, with reduced diaphragmatic excursion,” Dr. Luzi said. These factors, alongside others, “may help to explain” the current results, and stress the importance of close monitoring of those with obesity and COVID-19.
No relevant financial relationships were declared.
This article first appeared on Medscape.com.
It is becoming increasingly clear that obesity is one of the biggest risk factors for severe COVID-19 disease, particularly among younger patients.
Newly published data from New York show that, among those aged under 60 years, obesity was twice as likely to result in hospitalization for COVID-19 and also significantly increased the likelihood that a person would end up in intensive care.
“Obesity [in people younger than 60] appears to be a previously unrecognized risk factor for hospital admission and need for critical care. This has important and practical implications when nearly 40% of adults in the U.S. are obese with a body mass index [BMI] of [at least] 30,” wrote Jennifer Lighter, MD, of New York University Langone Health, and colleagues in their research letter published in Clinical Infectious Diseases.
Similar findings in a preprint publication, yet to be peer reviewed, from another New York hospital show that, with the exception of older age, obesity (BMI greater than 40 kg/m2) had the strongest association with hospitalization for COVID-19, increasing the risk more than 500%.
Meanwhile, a new French study shows a high frequency of obesity among patients admitted to one ICU for COVID-19; furthermore, disease severity increased with increasing BMI. One of the authors said in an interview that many of the presenting patients were younger, with their only risk factor being obesity.
“Patients with obesity should avoid any COVID-19 contamination by enforcing all prevention measures during the current pandemic,” wrote the authors, led by Arthur Simonnet, MD, Centre Hospitalier Universitaire de Lille (France).
They also stressed that COVID-19 patients “with severe obesity should be monitored more closely.”
Those with obesity are young and become very sick, very quickly
François Pattou, MD, PhD, coauthor of the French article published in Obesity said in an interview that, when patients with COVID-19 began to arrive at their ICU in Lille, there were young patients who did not have any other comorbidities.
“They were just obese,” he observed, adding that they seemed “to have a very specific disease, something different” from that seen before, with patients becoming very sick, very quickly.
In their study, they examined 124 consecutive patients admitted to intensive care with COVID-19 between Feb. 25 and April 5, 2020, and compared them with a historical control group of 306 patients admitted to the ICU at the same hospital for non–COVID-19-related severe acute respiratory disease in 2019.
By April 6, 60 patients with COVID-19 had been discharged from intensive care, 18 had died, and 46 remained in the unit. The majority (73%) were male, and their median age was 60 years. Obesity and severe obesity were significantly more prevalent among the patients with COVID-19, at 47.6% and 28.2% versus 25.2% and 10.8% among historical controls (P < .001 for trend).
A key finding was that those with a BMI greater than 35 had a more than 600% increased risk of requiring mechanical ventilation (odds ratio, 7.36; P = .021), compared with those with a BMI less than 25, even after adjusting for age, diabetes, and hypertension.
Obesity in under 60s at least doubles risk of admission in U.S.
The studies out of New York, one of which was stratified by age, paint a similar picture.
Dr. Lighter and colleagues found that, of the 3,615 individuals who tested positive for COVID-19 in their series, 775 (21%) had a BMI of 30-34 and 595 (16%) had a BMI of at least 35. Obesity wasn’t a predictor of admission to hospital or the ICU in those over the age of 60 years, but in those younger than 60 years, it was.
Those under age 60 with a BMI of 30-34 were twice as likely to be admitted to hospital (hazard ratio, 2.0; P < .0001) and critical care (HR, 1.8; P = .006), compared with those under age 60 with a BMI less than 30. Likewise, those under age 60 with a BMI of at least 35 were 2.2 (P < .0001) and 3.6 (P < .0001) times more likely to be admitted to acute and critical care.
“Unfortunately, obesity in people [less than] 60 years is a newly identified epidemiologic risk factor which may contribute to increased morbidity rates [with COVID-19] experienced in the U.S.,” they concluded.
And in the other U.S. study, Christopher M. Petrilli, MD, of New York University, and colleagues looked at 4,103 patients with COVID-19 treated between March 1 and April 2, 2020, and followed to April 7.
Just under half of patients (48.7%) were hospitalized, of whom 22.3% required mechanical ventilation and 14.6% died or were discharged to hospice. The research was published on medRxiv, showing that, apart from age, the strongest predictors of hospitalization were BMI greater than 40 (OR, 6.2) and heart failure (OR, 4.3).
“It is notable that the chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” they noted.
Inflammation is a possible culprit
Dr. Pattou believes that the culprit behind the increased risk of disease severity seen with obesity in COVID-19 is inflammation, mediated by fibrin deposits in the circulation, which his colleagues have seen on autopsy, and which “block oxygen passage through the blood.”
This may help explain why mechanical ventilation can be less successful in these patients. “The answer is to get rid of this inflammation,” Dr. Pattou observed.
Dr. Petrilli and colleagues also observed that obesity “is well-recognized to be a proinflammatory condition.”
And their findings showed “the importance of inflammatory markers in distinguishing future critical from noncritical illness,” they said, noting that, among these markers, early elevations in C-reactive protein and D-dimer “had the strongest association with mechanical ventilation or mortality.”
Livio Luzi, MD, of IRCCS MultiMedica, Milan, Italy, has previously written on the relationship between influenza and obesity, and discussed in an interview the potential lessons for the COVID-19 pandemic.
“Obesity is characterized by an impairment of immune response and by a low-grade chronic inflammation. Furthermore, obese subjects have an altered dynamic of pulmonary ventilation, with reduced diaphragmatic excursion,” Dr. Luzi said. These factors, alongside others, “may help to explain” the current results, and stress the importance of close monitoring of those with obesity and COVID-19.
No relevant financial relationships were declared.
This article first appeared on Medscape.com.
It is becoming increasingly clear that obesity is one of the biggest risk factors for severe COVID-19 disease, particularly among younger patients.
Newly published data from New York show that, among those aged under 60 years, obesity was twice as likely to result in hospitalization for COVID-19 and also significantly increased the likelihood that a person would end up in intensive care.
“Obesity [in people younger than 60] appears to be a previously unrecognized risk factor for hospital admission and need for critical care. This has important and practical implications when nearly 40% of adults in the U.S. are obese with a body mass index [BMI] of [at least] 30,” wrote Jennifer Lighter, MD, of New York University Langone Health, and colleagues in their research letter published in Clinical Infectious Diseases.
Similar findings in a preprint publication, yet to be peer reviewed, from another New York hospital show that, with the exception of older age, obesity (BMI greater than 40 kg/m2) had the strongest association with hospitalization for COVID-19, increasing the risk more than 500%.
Meanwhile, a new French study shows a high frequency of obesity among patients admitted to one ICU for COVID-19; furthermore, disease severity increased with increasing BMI. One of the authors said in an interview that many of the presenting patients were younger, with their only risk factor being obesity.
“Patients with obesity should avoid any COVID-19 contamination by enforcing all prevention measures during the current pandemic,” wrote the authors, led by Arthur Simonnet, MD, Centre Hospitalier Universitaire de Lille (France).
They also stressed that COVID-19 patients “with severe obesity should be monitored more closely.”
Those with obesity are young and become very sick, very quickly
François Pattou, MD, PhD, coauthor of the French article published in Obesity said in an interview that, when patients with COVID-19 began to arrive at their ICU in Lille, there were young patients who did not have any other comorbidities.
“They were just obese,” he observed, adding that they seemed “to have a very specific disease, something different” from that seen before, with patients becoming very sick, very quickly.
In their study, they examined 124 consecutive patients admitted to intensive care with COVID-19 between Feb. 25 and April 5, 2020, and compared them with a historical control group of 306 patients admitted to the ICU at the same hospital for non–COVID-19-related severe acute respiratory disease in 2019.
By April 6, 60 patients with COVID-19 had been discharged from intensive care, 18 had died, and 46 remained in the unit. The majority (73%) were male, and their median age was 60 years. Obesity and severe obesity were significantly more prevalent among the patients with COVID-19, at 47.6% and 28.2% versus 25.2% and 10.8% among historical controls (P < .001 for trend).
A key finding was that those with a BMI greater than 35 had a more than 600% increased risk of requiring mechanical ventilation (odds ratio, 7.36; P = .021), compared with those with a BMI less than 25, even after adjusting for age, diabetes, and hypertension.
Obesity in under 60s at least doubles risk of admission in U.S.
The studies out of New York, one of which was stratified by age, paint a similar picture.
Dr. Lighter and colleagues found that, of the 3,615 individuals who tested positive for COVID-19 in their series, 775 (21%) had a BMI of 30-34 and 595 (16%) had a BMI of at least 35. Obesity wasn’t a predictor of admission to hospital or the ICU in those over the age of 60 years, but in those younger than 60 years, it was.
Those under age 60 with a BMI of 30-34 were twice as likely to be admitted to hospital (hazard ratio, 2.0; P < .0001) and critical care (HR, 1.8; P = .006), compared with those under age 60 with a BMI less than 30. Likewise, those under age 60 with a BMI of at least 35 were 2.2 (P < .0001) and 3.6 (P < .0001) times more likely to be admitted to acute and critical care.
“Unfortunately, obesity in people [less than] 60 years is a newly identified epidemiologic risk factor which may contribute to increased morbidity rates [with COVID-19] experienced in the U.S.,” they concluded.
And in the other U.S. study, Christopher M. Petrilli, MD, of New York University, and colleagues looked at 4,103 patients with COVID-19 treated between March 1 and April 2, 2020, and followed to April 7.
Just under half of patients (48.7%) were hospitalized, of whom 22.3% required mechanical ventilation and 14.6% died or were discharged to hospice. The research was published on medRxiv, showing that, apart from age, the strongest predictors of hospitalization were BMI greater than 40 (OR, 6.2) and heart failure (OR, 4.3).
“It is notable that the chronic condition with the strongest association with critical illness was obesity, with a substantially higher odds ratio than any cardiovascular or pulmonary disease,” they noted.
Inflammation is a possible culprit
Dr. Pattou believes that the culprit behind the increased risk of disease severity seen with obesity in COVID-19 is inflammation, mediated by fibrin deposits in the circulation, which his colleagues have seen on autopsy, and which “block oxygen passage through the blood.”
This may help explain why mechanical ventilation can be less successful in these patients. “The answer is to get rid of this inflammation,” Dr. Pattou observed.
Dr. Petrilli and colleagues also observed that obesity “is well-recognized to be a proinflammatory condition.”
And their findings showed “the importance of inflammatory markers in distinguishing future critical from noncritical illness,” they said, noting that, among these markers, early elevations in C-reactive protein and D-dimer “had the strongest association with mechanical ventilation or mortality.”
Livio Luzi, MD, of IRCCS MultiMedica, Milan, Italy, has previously written on the relationship between influenza and obesity, and discussed in an interview the potential lessons for the COVID-19 pandemic.
“Obesity is characterized by an impairment of immune response and by a low-grade chronic inflammation. Furthermore, obese subjects have an altered dynamic of pulmonary ventilation, with reduced diaphragmatic excursion,” Dr. Luzi said. These factors, alongside others, “may help to explain” the current results, and stress the importance of close monitoring of those with obesity and COVID-19.
No relevant financial relationships were declared.
This article first appeared on Medscape.com.
Can convalescent plasma treat COVID-19 patients?
As an Episcopal priest, Father Robert Pace of Fort Worth, TX, is used to putting others first and reaching out to help. So when the pulmonologist who helped him through his ordeal with COVID-19 asked if he would like to donate blood to help other patients, he did not hesitate.
“I said, ‘Absolutely,’” Pace, 53, recalls. He says the idea was ‘very appealing.’ ” During his ordeal with COVID-19 in March, he had spent 3 days in the hospital, isolated and on IV fluids and oxygen. He was short of breath, with a heartbeat more rapid than usual.
Now, fully recovered, his blood was a precious commodity, antibody-rich and potentially life-saving.
As researchers scramble to test drugs to fight COVID-19, others are turning to an age-old treatment. They’re collecting the blood of survivors and giving it to patients in the throes of a severe infection, a treatment known as convalescent plasma therapy.
Doctors say the treatment will probably serve as a bridge until other drugs and a vaccine become available.
Although the FDA considers the treatment investigational, in late March, it eased access to it. Patients can get it as part of a clinical trial or through an expanded access program overseen by hospitals or universities. A doctor can also request permission to use the treatment for a single patient.
“It is considered an emergent, compassionate need,” says John Burk, MD, a pulmonologist at Texas Health Harris Methodist Hospital, Fort Worth, who treated Pace. “It is a way to bring it to the bedside.” And the approval can happen quickly. Burk says he got one from the FDA just 20 minutes after requesting it for a severely ill patient.
How it works
The premise of how it works is “quite straightforward,” says Michael Joyner, MD, a professor of anesthesiology at the Mayo Clinic, Rochester, MN. “When someone is recovered and no longer symptomatic, you can harvest those antibodies from their blood and give them to someone else, and hopefully alter the course of their disease.” Joyner is the principal investigator for the FDA’s national Expanded Access to Convalescent Plasma for the Treatment of Patients with COVID-19, with 1,000 sites already signed on.
Convalescent therapy has been used to fight many other viruses, including Ebola, severe acute respiratory syndrome (SARS), the “bird” flu, H1N1 flu, and during the 1918 flu pandemic. Joyner says the strongest evidence for it comes from the 1950s, when it was used to treat a rodent-borne illness called Argentine hemorrhagic fever. Using convalescent plasma therapy for this infection reduced the death rate from nearly 43% before the treatment became common in the late 1950s to about 3% after it was widely used, one report found.
Data about convalescent therapy specifically for COVID-19 is limited. Chinese researchers reported on five critically ill patients, all on mechanical ventilation, treated with convalescent plasma after they had received antiviral and anti-inflammatory medicines. Three could leave the hospital after 51-55 days, and two were in stable condition in the hospital 37 days after the transfusion.
In another study of 10 severely ill patients, symptoms went away or improved in all 10 within 1 to 3 days after the transfusion. Two of the three on ventilators were weaned off and put on oxygen instead. None died.
Chinese researchers also reported three cases of patients with COVID-19 given the convalescent therapy who had a satisfactory recovery.
Researchers who reviewed the track record of convalescent therapy for other conditions recently concluded that the treatment doesn’t appear to cause severe side effects and it should be studied for COVID-19.
Although information on side effects specific to this treatment is evolving, Joyner says they are “very, very low.”
According to the FDA, allergic reactions can occur with plasma therapies. Because the treatment for COVID-19 is new, it is not known if patients might have other types of reactions.
Who can donate?
Blood bank officials and researchers running the convalescent plasma programs say the desire to help is widespread, and they’ve been deluged with offers to donate. But requirements are strict.
Donors must have evidence of COVID-19 infection, documented in a variety of ways, such as a diagnostic test by nasal swab or a blood test showing antibodies. And they must be symptom-free for 14 days, with test results, or 28 days without.
The treatment involves collecting plasma, not whole blood. Plasma, the liquid part of the blood, helps with clotting and supports immunity. During the collection, a donor’s blood is put through a machine that collects the plasma only and sends the red blood cells and platelets back to the donor.
Clinical trials
Requirements may be more stringent for donors joining a formal clinical trial rather than an expanded access program. For instance, potential donors in a randomized clinical trial underway at Stony Brook University must have higher antibody levels than required by the FDA, says study leader Elliott Bennett-Guerrero, MD, medical director of perioperative quality and patient safety and professor at the Renaissance School of Medicine.
He hopes to enroll up to 500 patients from the Long Island, NY, area. While clinical trials typically have a 50-50 split, with half of subjects getting a treatment and half a placebo, Bennett-Guerrero’s study will give 80% of patients the convalescent plasma and 20% standard plasma.
Julia Sabia Motley, 57, of Merrick, NY, is hoping to become a donor for the Stony Brook study. She and her husband, Sean Motley, 59, tested positive in late March. She has to pass one more test to join the trial. Her husband is also planning to try to donate. “I can finally do something,” Sabia Motley says. Her son is in the MD-PhD program at Stony Brook and told her about the study.
Many questions remain
The treatment for COVID-19 is in its infancy. Burk has given the convalescent plasma to two patients. One is now recovering at home, and the other is on a ventilator but improving, he says.
About 200 nationwide have received the therapy, Joyner says. He expects blood supplies to increase as more people are eligible to donate.
Questions remain about how effective the convalescent therapy will be. While experts know that the COVID-19 antibodies “can be helpful in fighting the virus, we don’t know how long the antibodies in the plasma would stay in place,” Bennett-Guerrero says.
Nor do doctors know who the therapy might work best for, beyond people with a severe or life-threatening illness. When it’s been used for other infections, it’s generally given in early stages once someone has symptoms, Joyner says.
Joyner says he sees the treatment as a stopgap ‘’until concentrated antibodies are available.” Several drug companies are working to retrieve antibodies from donors and make concentrated antibody drugs.
“Typically we would think convalescent plasma might be a helpful bridge until therapies that are safe and effective and can be mass-produced are available, such as a vaccine or a drug,” Bennett-Guerrero says.
Even so, he says that he doesn’t think he will have a problem attracting donors, and that he will have repeat donors eager to help.
More information for potential donors
Blood banks, the American Red Cross, and others involved in convalescent plasma therapy have posted information online for potential donors. People who don’t meet the qualifications for COVID-19 plasma donations are welcomed as regular blood donors if they meet those criteria
According to the FDA, a donation could potentially help save the lives of up to four COVID-19 patients.
Father Pace is already planning another visit to the blood bank. To pass the time last time, he says, he prayed for the person who would eventually get his blood.
This article first appeared on WebMD.com.
As an Episcopal priest, Father Robert Pace of Fort Worth, TX, is used to putting others first and reaching out to help. So when the pulmonologist who helped him through his ordeal with COVID-19 asked if he would like to donate blood to help other patients, he did not hesitate.
“I said, ‘Absolutely,’” Pace, 53, recalls. He says the idea was ‘very appealing.’ ” During his ordeal with COVID-19 in March, he had spent 3 days in the hospital, isolated and on IV fluids and oxygen. He was short of breath, with a heartbeat more rapid than usual.
Now, fully recovered, his blood was a precious commodity, antibody-rich and potentially life-saving.
As researchers scramble to test drugs to fight COVID-19, others are turning to an age-old treatment. They’re collecting the blood of survivors and giving it to patients in the throes of a severe infection, a treatment known as convalescent plasma therapy.
Doctors say the treatment will probably serve as a bridge until other drugs and a vaccine become available.
Although the FDA considers the treatment investigational, in late March, it eased access to it. Patients can get it as part of a clinical trial or through an expanded access program overseen by hospitals or universities. A doctor can also request permission to use the treatment for a single patient.
“It is considered an emergent, compassionate need,” says John Burk, MD, a pulmonologist at Texas Health Harris Methodist Hospital, Fort Worth, who treated Pace. “It is a way to bring it to the bedside.” And the approval can happen quickly. Burk says he got one from the FDA just 20 minutes after requesting it for a severely ill patient.
How it works
The premise of how it works is “quite straightforward,” says Michael Joyner, MD, a professor of anesthesiology at the Mayo Clinic, Rochester, MN. “When someone is recovered and no longer symptomatic, you can harvest those antibodies from their blood and give them to someone else, and hopefully alter the course of their disease.” Joyner is the principal investigator for the FDA’s national Expanded Access to Convalescent Plasma for the Treatment of Patients with COVID-19, with 1,000 sites already signed on.
Convalescent therapy has been used to fight many other viruses, including Ebola, severe acute respiratory syndrome (SARS), the “bird” flu, H1N1 flu, and during the 1918 flu pandemic. Joyner says the strongest evidence for it comes from the 1950s, when it was used to treat a rodent-borne illness called Argentine hemorrhagic fever. Using convalescent plasma therapy for this infection reduced the death rate from nearly 43% before the treatment became common in the late 1950s to about 3% after it was widely used, one report found.
Data about convalescent therapy specifically for COVID-19 is limited. Chinese researchers reported on five critically ill patients, all on mechanical ventilation, treated with convalescent plasma after they had received antiviral and anti-inflammatory medicines. Three could leave the hospital after 51-55 days, and two were in stable condition in the hospital 37 days after the transfusion.
In another study of 10 severely ill patients, symptoms went away or improved in all 10 within 1 to 3 days after the transfusion. Two of the three on ventilators were weaned off and put on oxygen instead. None died.
Chinese researchers also reported three cases of patients with COVID-19 given the convalescent therapy who had a satisfactory recovery.
Researchers who reviewed the track record of convalescent therapy for other conditions recently concluded that the treatment doesn’t appear to cause severe side effects and it should be studied for COVID-19.
Although information on side effects specific to this treatment is evolving, Joyner says they are “very, very low.”
According to the FDA, allergic reactions can occur with plasma therapies. Because the treatment for COVID-19 is new, it is not known if patients might have other types of reactions.
Who can donate?
Blood bank officials and researchers running the convalescent plasma programs say the desire to help is widespread, and they’ve been deluged with offers to donate. But requirements are strict.
Donors must have evidence of COVID-19 infection, documented in a variety of ways, such as a diagnostic test by nasal swab or a blood test showing antibodies. And they must be symptom-free for 14 days, with test results, or 28 days without.
The treatment involves collecting plasma, not whole blood. Plasma, the liquid part of the blood, helps with clotting and supports immunity. During the collection, a donor’s blood is put through a machine that collects the plasma only and sends the red blood cells and platelets back to the donor.
Clinical trials
Requirements may be more stringent for donors joining a formal clinical trial rather than an expanded access program. For instance, potential donors in a randomized clinical trial underway at Stony Brook University must have higher antibody levels than required by the FDA, says study leader Elliott Bennett-Guerrero, MD, medical director of perioperative quality and patient safety and professor at the Renaissance School of Medicine.
He hopes to enroll up to 500 patients from the Long Island, NY, area. While clinical trials typically have a 50-50 split, with half of subjects getting a treatment and half a placebo, Bennett-Guerrero’s study will give 80% of patients the convalescent plasma and 20% standard plasma.
Julia Sabia Motley, 57, of Merrick, NY, is hoping to become a donor for the Stony Brook study. She and her husband, Sean Motley, 59, tested positive in late March. She has to pass one more test to join the trial. Her husband is also planning to try to donate. “I can finally do something,” Sabia Motley says. Her son is in the MD-PhD program at Stony Brook and told her about the study.
Many questions remain
The treatment for COVID-19 is in its infancy. Burk has given the convalescent plasma to two patients. One is now recovering at home, and the other is on a ventilator but improving, he says.
About 200 nationwide have received the therapy, Joyner says. He expects blood supplies to increase as more people are eligible to donate.
Questions remain about how effective the convalescent therapy will be. While experts know that the COVID-19 antibodies “can be helpful in fighting the virus, we don’t know how long the antibodies in the plasma would stay in place,” Bennett-Guerrero says.
Nor do doctors know who the therapy might work best for, beyond people with a severe or life-threatening illness. When it’s been used for other infections, it’s generally given in early stages once someone has symptoms, Joyner says.
Joyner says he sees the treatment as a stopgap ‘’until concentrated antibodies are available.” Several drug companies are working to retrieve antibodies from donors and make concentrated antibody drugs.
“Typically we would think convalescent plasma might be a helpful bridge until therapies that are safe and effective and can be mass-produced are available, such as a vaccine or a drug,” Bennett-Guerrero says.
Even so, he says that he doesn’t think he will have a problem attracting donors, and that he will have repeat donors eager to help.
More information for potential donors
Blood banks, the American Red Cross, and others involved in convalescent plasma therapy have posted information online for potential donors. People who don’t meet the qualifications for COVID-19 plasma donations are welcomed as regular blood donors if they meet those criteria
According to the FDA, a donation could potentially help save the lives of up to four COVID-19 patients.
Father Pace is already planning another visit to the blood bank. To pass the time last time, he says, he prayed for the person who would eventually get his blood.
This article first appeared on WebMD.com.
As an Episcopal priest, Father Robert Pace of Fort Worth, TX, is used to putting others first and reaching out to help. So when the pulmonologist who helped him through his ordeal with COVID-19 asked if he would like to donate blood to help other patients, he did not hesitate.
“I said, ‘Absolutely,’” Pace, 53, recalls. He says the idea was ‘very appealing.’ ” During his ordeal with COVID-19 in March, he had spent 3 days in the hospital, isolated and on IV fluids and oxygen. He was short of breath, with a heartbeat more rapid than usual.
Now, fully recovered, his blood was a precious commodity, antibody-rich and potentially life-saving.
As researchers scramble to test drugs to fight COVID-19, others are turning to an age-old treatment. They’re collecting the blood of survivors and giving it to patients in the throes of a severe infection, a treatment known as convalescent plasma therapy.
Doctors say the treatment will probably serve as a bridge until other drugs and a vaccine become available.
Although the FDA considers the treatment investigational, in late March, it eased access to it. Patients can get it as part of a clinical trial or through an expanded access program overseen by hospitals or universities. A doctor can also request permission to use the treatment for a single patient.
“It is considered an emergent, compassionate need,” says John Burk, MD, a pulmonologist at Texas Health Harris Methodist Hospital, Fort Worth, who treated Pace. “It is a way to bring it to the bedside.” And the approval can happen quickly. Burk says he got one from the FDA just 20 minutes after requesting it for a severely ill patient.
How it works
The premise of how it works is “quite straightforward,” says Michael Joyner, MD, a professor of anesthesiology at the Mayo Clinic, Rochester, MN. “When someone is recovered and no longer symptomatic, you can harvest those antibodies from their blood and give them to someone else, and hopefully alter the course of their disease.” Joyner is the principal investigator for the FDA’s national Expanded Access to Convalescent Plasma for the Treatment of Patients with COVID-19, with 1,000 sites already signed on.
Convalescent therapy has been used to fight many other viruses, including Ebola, severe acute respiratory syndrome (SARS), the “bird” flu, H1N1 flu, and during the 1918 flu pandemic. Joyner says the strongest evidence for it comes from the 1950s, when it was used to treat a rodent-borne illness called Argentine hemorrhagic fever. Using convalescent plasma therapy for this infection reduced the death rate from nearly 43% before the treatment became common in the late 1950s to about 3% after it was widely used, one report found.
Data about convalescent therapy specifically for COVID-19 is limited. Chinese researchers reported on five critically ill patients, all on mechanical ventilation, treated with convalescent plasma after they had received antiviral and anti-inflammatory medicines. Three could leave the hospital after 51-55 days, and two were in stable condition in the hospital 37 days after the transfusion.
In another study of 10 severely ill patients, symptoms went away or improved in all 10 within 1 to 3 days after the transfusion. Two of the three on ventilators were weaned off and put on oxygen instead. None died.
Chinese researchers also reported three cases of patients with COVID-19 given the convalescent therapy who had a satisfactory recovery.
Researchers who reviewed the track record of convalescent therapy for other conditions recently concluded that the treatment doesn’t appear to cause severe side effects and it should be studied for COVID-19.
Although information on side effects specific to this treatment is evolving, Joyner says they are “very, very low.”
According to the FDA, allergic reactions can occur with plasma therapies. Because the treatment for COVID-19 is new, it is not known if patients might have other types of reactions.
Who can donate?
Blood bank officials and researchers running the convalescent plasma programs say the desire to help is widespread, and they’ve been deluged with offers to donate. But requirements are strict.
Donors must have evidence of COVID-19 infection, documented in a variety of ways, such as a diagnostic test by nasal swab or a blood test showing antibodies. And they must be symptom-free for 14 days, with test results, or 28 days without.
The treatment involves collecting plasma, not whole blood. Plasma, the liquid part of the blood, helps with clotting and supports immunity. During the collection, a donor’s blood is put through a machine that collects the plasma only and sends the red blood cells and platelets back to the donor.
Clinical trials
Requirements may be more stringent for donors joining a formal clinical trial rather than an expanded access program. For instance, potential donors in a randomized clinical trial underway at Stony Brook University must have higher antibody levels than required by the FDA, says study leader Elliott Bennett-Guerrero, MD, medical director of perioperative quality and patient safety and professor at the Renaissance School of Medicine.
He hopes to enroll up to 500 patients from the Long Island, NY, area. While clinical trials typically have a 50-50 split, with half of subjects getting a treatment and half a placebo, Bennett-Guerrero’s study will give 80% of patients the convalescent plasma and 20% standard plasma.
Julia Sabia Motley, 57, of Merrick, NY, is hoping to become a donor for the Stony Brook study. She and her husband, Sean Motley, 59, tested positive in late March. She has to pass one more test to join the trial. Her husband is also planning to try to donate. “I can finally do something,” Sabia Motley says. Her son is in the MD-PhD program at Stony Brook and told her about the study.
Many questions remain
The treatment for COVID-19 is in its infancy. Burk has given the convalescent plasma to two patients. One is now recovering at home, and the other is on a ventilator but improving, he says.
About 200 nationwide have received the therapy, Joyner says. He expects blood supplies to increase as more people are eligible to donate.
Questions remain about how effective the convalescent therapy will be. While experts know that the COVID-19 antibodies “can be helpful in fighting the virus, we don’t know how long the antibodies in the plasma would stay in place,” Bennett-Guerrero says.
Nor do doctors know who the therapy might work best for, beyond people with a severe or life-threatening illness. When it’s been used for other infections, it’s generally given in early stages once someone has symptoms, Joyner says.
Joyner says he sees the treatment as a stopgap ‘’until concentrated antibodies are available.” Several drug companies are working to retrieve antibodies from donors and make concentrated antibody drugs.
“Typically we would think convalescent plasma might be a helpful bridge until therapies that are safe and effective and can be mass-produced are available, such as a vaccine or a drug,” Bennett-Guerrero says.
Even so, he says that he doesn’t think he will have a problem attracting donors, and that he will have repeat donors eager to help.
More information for potential donors
Blood banks, the American Red Cross, and others involved in convalescent plasma therapy have posted information online for potential donors. People who don’t meet the qualifications for COVID-19 plasma donations are welcomed as regular blood donors if they meet those criteria
According to the FDA, a donation could potentially help save the lives of up to four COVID-19 patients.
Father Pace is already planning another visit to the blood bank. To pass the time last time, he says, he prayed for the person who would eventually get his blood.
This article first appeared on WebMD.com.
COVID-19: Press pause on assisted reproduction?
The SARS-CoV-2 novel coronavirus has dramatically altered specialty practice across the board, including the practice of infertility treatment. Reproductive medicine societies recommend suspending new infertility treatment cycles during this time. Women and couples who have already invested time and money in their treatment may be understandably frustrated and worried about the impact of this enforced – and indefinite – delay on their chances of conceiving. This puts the physician, who can’t even guarantee when treatment can resume, in the difficult position of trying to balance the patient’s needs with expert recommendations and government mandates.
Infertility Care During COVID-19
European and American reproductive medicine societies have both offered guidelines regarding infertility care during the pandemic. Both recommend shifting to the use of telehealth rather than in-person visits when possible for initial consultations and follow-up discussions.
With respect to infertility treatments during the COVID-19 pandemic, the American Society for Reproductive Medicine (ASRM) advises the following:
- Suspend initiation of new treatment cycles, including ovulation induction; intrauterine insemination; and in vitro fertilization, including retrievals and frozen embryo transfers, and suspend nonurgent gamete cryopreservation.
- Strongly consider cancellation of all embryo transfers, whether fresh or frozen.
- Continue to care for patients who are currently “in cycle” or who require urgent stimulation and cryopreservation.
- Suspend elective surgeries and nonurgent diagnostic procedures.
In most countries, including the United States, all healthcare providers have been asked to put elective and nonurgent medical interventions on hold to ensure that personal protective equipment and other resources are available for the management of patients with COVID-19.
Infertility is a disease and, as such, not all infertility care should be considered elective. Still, for most patients, the overall chances of conceiving will not be compromised by a short delay (1-3 months) in treatment. A longer wait could have more impact on older patients or those who already have reduced ovarian reserve, but these are not indications for urgent fertility treatment.
There are clearly some cases in which infertility treatment cannot be delayed: for example, fertility preservation (oocyte or embryo vitrification) for patients who need to undergo immediate gonadotoxic oncology treatment. These patients need to be able to freeze oocytes/embryos so that later on, they have the option of having a family.
Another situation that could require new infertility treatment is a woman who needs urgent surgery for a condition such as severe symptomatic endometriosis causing ureteral or bowel stenosis/obstruction. Because the surgery itself can compromise fertility, the patient may elect to undergo oocyte embryo cryopreservation or ovarian tissue cryopreservation before the surgical procedure.
Pregnancy and COVID-19
As a precautionary measure during the COVID-19 pandemic, it is recommended that planned pregnancy be avoided. The available data on the risks presented by planning a pregnancy during the COVID pandemic are reassuring but limited.
Pregnancy itself has not been shown to alter the course of COVID-19, and most affected pregnant women will experience only mild or moderate flulike symptoms. Patients with cardiovascular or metabolic comorbidities or those requiring immunosuppressants are expected to be at increased risk for more severe forms of the infection. Currently, no strong evidence suggests a higher risk for miscarriage, stillbirth, or adverse neonatal outcomes with maternal COVID-19 infection.
A report based on 38 cases found no evidence for vertical transmission from mother to fetus, and all neonatal specimens (placental tissue) tested negative for the virus. Moreover, no maternal deaths were reported among these 38 infected women. Another study of 11 infected pregnant women likewise found no increased risk for perinatal morbidity or mortality.
On the other hand, a recent article on the perinatal outcomes of 33 neonates born to mothers with confirmed COVID-19 reported three cases of neonatal COVID-19 as a result of possible vertical transmission. In two cases, symptoms were mild and initial positive coronavirus test results turned negative within a few days. The third case – a pregnancy delivered by emergency cesarean section at 31 weeks for fetal distress – was complicated by bacterial sepsis, thrombocytopenia, and coagulopathy, but once again, the initially positive coronavirus test was negative by day 7.
No neonatal deaths were reported in these 33 cases. The authors could not rule out the possibility of vertical transmission in the three COVID-positive newborns because strict infection control measures were implemented during the care of the patients.
Counseling Patients About Suspending Infertility Treatments
Counseling women is the key to acceptance of the need to suspend or postpone infertility treatments during the pandemic. In addition to the economic hardships that some patients may face as a consequence of the pandemic, an obvious source of frustration stems from not knowing how long delays in treatment might be necessary. A discussion with patients or couples may reassure them that delaying conception is the safest route. For some women, other treatment options might be offered, such as the use of a donor gamete.
Some patients, even when counseled appropriately, may elect to accept the unknown risks. These patients should be counseled about the benefits of cryopreservation with delayed transfer. This could be a compromise, because their overall chances of pregnancy will not be affected but they will have to wait to become pregnant.
Counseling patients about the true impact of delaying treatment in their individual circumstances, providing them with emotional and (if needed) psychological support is important while they wait for their treatment to start. For now, the vast majority of the patients understand the need for delay, appreciate the opportunity to consult the physician over the phone, and are demonstrating patience as they wait for their treatment to start or resume.
Resuming Infertility Care
Recommendations could change as the pandemic continues and more information becomes available about the impact of coronavirus infection during pregnancy and the overall capacity of the healthcare system improves. ASRM acknowledges that “reproductive care professionals, in consultation with their patients, will have to consider reassessing the criteria of what represents urgent and non-urgent care.” If the data remain reassuring and social distancing measures are able to slow down the spread of the disease, the infertility care of those couples who would be most affected by a delay in their treatment could gradually be resumed. On April 14, ASRM updated its recommendations about resuming infertility treatment: “ While it is not yet prudent to resume nonemergency infertility procedures, the Task Force recognizes it is also time to begin to consider strategies and best practices for resuming time-sensitive fertility treatments in the face of COVID-19.”
It is likely that the return to “normal” daily practice will be done in a stepwise fashion. I expect the practices first to open for diagnostic infertility testing, then for the less invasive procedures (frozen embryo transfer, intrauterine insemination) and finally for the more invasive lengthy procedures (stimulation with retrieval and embryo transfer). During the reopening of practice, strict infection control measures will need to be observed.
Dr. Kovacs is the medical director of Kaali Institute IVF Center in Budapest, Hungary. He has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The SARS-CoV-2 novel coronavirus has dramatically altered specialty practice across the board, including the practice of infertility treatment. Reproductive medicine societies recommend suspending new infertility treatment cycles during this time. Women and couples who have already invested time and money in their treatment may be understandably frustrated and worried about the impact of this enforced – and indefinite – delay on their chances of conceiving. This puts the physician, who can’t even guarantee when treatment can resume, in the difficult position of trying to balance the patient’s needs with expert recommendations and government mandates.
Infertility Care During COVID-19
European and American reproductive medicine societies have both offered guidelines regarding infertility care during the pandemic. Both recommend shifting to the use of telehealth rather than in-person visits when possible for initial consultations and follow-up discussions.
With respect to infertility treatments during the COVID-19 pandemic, the American Society for Reproductive Medicine (ASRM) advises the following:
- Suspend initiation of new treatment cycles, including ovulation induction; intrauterine insemination; and in vitro fertilization, including retrievals and frozen embryo transfers, and suspend nonurgent gamete cryopreservation.
- Strongly consider cancellation of all embryo transfers, whether fresh or frozen.
- Continue to care for patients who are currently “in cycle” or who require urgent stimulation and cryopreservation.
- Suspend elective surgeries and nonurgent diagnostic procedures.
In most countries, including the United States, all healthcare providers have been asked to put elective and nonurgent medical interventions on hold to ensure that personal protective equipment and other resources are available for the management of patients with COVID-19.
Infertility is a disease and, as such, not all infertility care should be considered elective. Still, for most patients, the overall chances of conceiving will not be compromised by a short delay (1-3 months) in treatment. A longer wait could have more impact on older patients or those who already have reduced ovarian reserve, but these are not indications for urgent fertility treatment.
There are clearly some cases in which infertility treatment cannot be delayed: for example, fertility preservation (oocyte or embryo vitrification) for patients who need to undergo immediate gonadotoxic oncology treatment. These patients need to be able to freeze oocytes/embryos so that later on, they have the option of having a family.
Another situation that could require new infertility treatment is a woman who needs urgent surgery for a condition such as severe symptomatic endometriosis causing ureteral or bowel stenosis/obstruction. Because the surgery itself can compromise fertility, the patient may elect to undergo oocyte embryo cryopreservation or ovarian tissue cryopreservation before the surgical procedure.
Pregnancy and COVID-19
As a precautionary measure during the COVID-19 pandemic, it is recommended that planned pregnancy be avoided. The available data on the risks presented by planning a pregnancy during the COVID pandemic are reassuring but limited.
Pregnancy itself has not been shown to alter the course of COVID-19, and most affected pregnant women will experience only mild or moderate flulike symptoms. Patients with cardiovascular or metabolic comorbidities or those requiring immunosuppressants are expected to be at increased risk for more severe forms of the infection. Currently, no strong evidence suggests a higher risk for miscarriage, stillbirth, or adverse neonatal outcomes with maternal COVID-19 infection.
A report based on 38 cases found no evidence for vertical transmission from mother to fetus, and all neonatal specimens (placental tissue) tested negative for the virus. Moreover, no maternal deaths were reported among these 38 infected women. Another study of 11 infected pregnant women likewise found no increased risk for perinatal morbidity or mortality.
On the other hand, a recent article on the perinatal outcomes of 33 neonates born to mothers with confirmed COVID-19 reported three cases of neonatal COVID-19 as a result of possible vertical transmission. In two cases, symptoms were mild and initial positive coronavirus test results turned negative within a few days. The third case – a pregnancy delivered by emergency cesarean section at 31 weeks for fetal distress – was complicated by bacterial sepsis, thrombocytopenia, and coagulopathy, but once again, the initially positive coronavirus test was negative by day 7.
No neonatal deaths were reported in these 33 cases. The authors could not rule out the possibility of vertical transmission in the three COVID-positive newborns because strict infection control measures were implemented during the care of the patients.
Counseling Patients About Suspending Infertility Treatments
Counseling women is the key to acceptance of the need to suspend or postpone infertility treatments during the pandemic. In addition to the economic hardships that some patients may face as a consequence of the pandemic, an obvious source of frustration stems from not knowing how long delays in treatment might be necessary. A discussion with patients or couples may reassure them that delaying conception is the safest route. For some women, other treatment options might be offered, such as the use of a donor gamete.
Some patients, even when counseled appropriately, may elect to accept the unknown risks. These patients should be counseled about the benefits of cryopreservation with delayed transfer. This could be a compromise, because their overall chances of pregnancy will not be affected but they will have to wait to become pregnant.
Counseling patients about the true impact of delaying treatment in their individual circumstances, providing them with emotional and (if needed) psychological support is important while they wait for their treatment to start. For now, the vast majority of the patients understand the need for delay, appreciate the opportunity to consult the physician over the phone, and are demonstrating patience as they wait for their treatment to start or resume.
Resuming Infertility Care
Recommendations could change as the pandemic continues and more information becomes available about the impact of coronavirus infection during pregnancy and the overall capacity of the healthcare system improves. ASRM acknowledges that “reproductive care professionals, in consultation with their patients, will have to consider reassessing the criteria of what represents urgent and non-urgent care.” If the data remain reassuring and social distancing measures are able to slow down the spread of the disease, the infertility care of those couples who would be most affected by a delay in their treatment could gradually be resumed. On April 14, ASRM updated its recommendations about resuming infertility treatment: “ While it is not yet prudent to resume nonemergency infertility procedures, the Task Force recognizes it is also time to begin to consider strategies and best practices for resuming time-sensitive fertility treatments in the face of COVID-19.”
It is likely that the return to “normal” daily practice will be done in a stepwise fashion. I expect the practices first to open for diagnostic infertility testing, then for the less invasive procedures (frozen embryo transfer, intrauterine insemination) and finally for the more invasive lengthy procedures (stimulation with retrieval and embryo transfer). During the reopening of practice, strict infection control measures will need to be observed.
Dr. Kovacs is the medical director of Kaali Institute IVF Center in Budapest, Hungary. He has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The SARS-CoV-2 novel coronavirus has dramatically altered specialty practice across the board, including the practice of infertility treatment. Reproductive medicine societies recommend suspending new infertility treatment cycles during this time. Women and couples who have already invested time and money in their treatment may be understandably frustrated and worried about the impact of this enforced – and indefinite – delay on their chances of conceiving. This puts the physician, who can’t even guarantee when treatment can resume, in the difficult position of trying to balance the patient’s needs with expert recommendations and government mandates.
Infertility Care During COVID-19
European and American reproductive medicine societies have both offered guidelines regarding infertility care during the pandemic. Both recommend shifting to the use of telehealth rather than in-person visits when possible for initial consultations and follow-up discussions.
With respect to infertility treatments during the COVID-19 pandemic, the American Society for Reproductive Medicine (ASRM) advises the following:
- Suspend initiation of new treatment cycles, including ovulation induction; intrauterine insemination; and in vitro fertilization, including retrievals and frozen embryo transfers, and suspend nonurgent gamete cryopreservation.
- Strongly consider cancellation of all embryo transfers, whether fresh or frozen.
- Continue to care for patients who are currently “in cycle” or who require urgent stimulation and cryopreservation.
- Suspend elective surgeries and nonurgent diagnostic procedures.
In most countries, including the United States, all healthcare providers have been asked to put elective and nonurgent medical interventions on hold to ensure that personal protective equipment and other resources are available for the management of patients with COVID-19.
Infertility is a disease and, as such, not all infertility care should be considered elective. Still, for most patients, the overall chances of conceiving will not be compromised by a short delay (1-3 months) in treatment. A longer wait could have more impact on older patients or those who already have reduced ovarian reserve, but these are not indications for urgent fertility treatment.
There are clearly some cases in which infertility treatment cannot be delayed: for example, fertility preservation (oocyte or embryo vitrification) for patients who need to undergo immediate gonadotoxic oncology treatment. These patients need to be able to freeze oocytes/embryos so that later on, they have the option of having a family.
Another situation that could require new infertility treatment is a woman who needs urgent surgery for a condition such as severe symptomatic endometriosis causing ureteral or bowel stenosis/obstruction. Because the surgery itself can compromise fertility, the patient may elect to undergo oocyte embryo cryopreservation or ovarian tissue cryopreservation before the surgical procedure.
Pregnancy and COVID-19
As a precautionary measure during the COVID-19 pandemic, it is recommended that planned pregnancy be avoided. The available data on the risks presented by planning a pregnancy during the COVID pandemic are reassuring but limited.
Pregnancy itself has not been shown to alter the course of COVID-19, and most affected pregnant women will experience only mild or moderate flulike symptoms. Patients with cardiovascular or metabolic comorbidities or those requiring immunosuppressants are expected to be at increased risk for more severe forms of the infection. Currently, no strong evidence suggests a higher risk for miscarriage, stillbirth, or adverse neonatal outcomes with maternal COVID-19 infection.
A report based on 38 cases found no evidence for vertical transmission from mother to fetus, and all neonatal specimens (placental tissue) tested negative for the virus. Moreover, no maternal deaths were reported among these 38 infected women. Another study of 11 infected pregnant women likewise found no increased risk for perinatal morbidity or mortality.
On the other hand, a recent article on the perinatal outcomes of 33 neonates born to mothers with confirmed COVID-19 reported three cases of neonatal COVID-19 as a result of possible vertical transmission. In two cases, symptoms were mild and initial positive coronavirus test results turned negative within a few days. The third case – a pregnancy delivered by emergency cesarean section at 31 weeks for fetal distress – was complicated by bacterial sepsis, thrombocytopenia, and coagulopathy, but once again, the initially positive coronavirus test was negative by day 7.
No neonatal deaths were reported in these 33 cases. The authors could not rule out the possibility of vertical transmission in the three COVID-positive newborns because strict infection control measures were implemented during the care of the patients.
Counseling Patients About Suspending Infertility Treatments
Counseling women is the key to acceptance of the need to suspend or postpone infertility treatments during the pandemic. In addition to the economic hardships that some patients may face as a consequence of the pandemic, an obvious source of frustration stems from not knowing how long delays in treatment might be necessary. A discussion with patients or couples may reassure them that delaying conception is the safest route. For some women, other treatment options might be offered, such as the use of a donor gamete.
Some patients, even when counseled appropriately, may elect to accept the unknown risks. These patients should be counseled about the benefits of cryopreservation with delayed transfer. This could be a compromise, because their overall chances of pregnancy will not be affected but they will have to wait to become pregnant.
Counseling patients about the true impact of delaying treatment in their individual circumstances, providing them with emotional and (if needed) psychological support is important while they wait for their treatment to start. For now, the vast majority of the patients understand the need for delay, appreciate the opportunity to consult the physician over the phone, and are demonstrating patience as they wait for their treatment to start or resume.
Resuming Infertility Care
Recommendations could change as the pandemic continues and more information becomes available about the impact of coronavirus infection during pregnancy and the overall capacity of the healthcare system improves. ASRM acknowledges that “reproductive care professionals, in consultation with their patients, will have to consider reassessing the criteria of what represents urgent and non-urgent care.” If the data remain reassuring and social distancing measures are able to slow down the spread of the disease, the infertility care of those couples who would be most affected by a delay in their treatment could gradually be resumed. On April 14, ASRM updated its recommendations about resuming infertility treatment: “ While it is not yet prudent to resume nonemergency infertility procedures, the Task Force recognizes it is also time to begin to consider strategies and best practices for resuming time-sensitive fertility treatments in the face of COVID-19.”
It is likely that the return to “normal” daily practice will be done in a stepwise fashion. I expect the practices first to open for diagnostic infertility testing, then for the less invasive procedures (frozen embryo transfer, intrauterine insemination) and finally for the more invasive lengthy procedures (stimulation with retrieval and embryo transfer). During the reopening of practice, strict infection control measures will need to be observed.
Dr. Kovacs is the medical director of Kaali Institute IVF Center in Budapest, Hungary. He has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Cancer care ‘transformed in space of a month’ because of pandemic
, the most “revolutionary” being a deep dive into telehealth, predicts Deborah Schrag, MD, MPH, a medical oncologist specializing in gastrointestinal cancers at the Dana Farber Cancer Institute in Boston, Massachusetts.
“In the space of a month, approaches and accepted norms of cancer care delivery have been transformed of necessity,” Schrag and colleagues write in an article published in JAMA on April 13.
“Most of these changes would not have occurred without the pandemic,” they add. They predict that some changes will last after the crisis is over.
“None of us want to be thrown in the deep end.... On the other hand, sometimes it works,” Schrag told Medscape Medical News.
“The in-person visit between patient and physician has been upended,” she said.
“I don’t think there’s any going back to the way it was before because cancer patients won’t stand for it,” she said. “They’re not going to drive in to get the results of a blood test.
“I think that on balance, of course, there are situations where you need eye-to-eye contact. No one wants to have an initial oncology meeting by telehealth – doctors or patients – that’s ridiculous,” she said. “But for follow-up visits, patients are now going to be more demanding, and doctors will be more willing.”
The “essential empathy” of oncologists can still “transcend the new physical barriers presented by masks and telehealth,” Schrag and colleagues comment.
“Doctors are figuring out how to deliver empathy by Zoom,” she told Medscape Medical News. “It’s not the same, but we all convey empathy to our elderly relatives over the phone.”
Pandemic impact on oncology
While the crisis has affected all of medicine – dismantling how care is delivered and forcing clinicians to make difficult decisions regarding triage – the fact that some cancers present an immediate threat to survival means that oncology “provides a lens into the major shifts currently underway in clinical care,” Schrag and colleagues write.
They illustrate the point by highlighting systemic chemotherapy, which is provided to a large proportion of patients with advanced cancer. The pandemic has tipped the risk-benefit ratio away from treatments that have a marginal effect on quality or quantity of life, they note. It has forced an “elimination of low-value treatments that were identified by the Choosing Wisely campaign,” the authors write. Up to now, the uptake of recommendations to eliminate these treatments has been slow.
“For example, for most metastatic solid tumors, chemotherapy beyond the third regimen does not improve survival for more than a few weeks; therefore, oncologists are advising supportive care instead. For patients receiving adjuvant therapy for curable cancers, delaying initiation or abbreviating the number of cycles is appropriate. Oncologists are postponing initiation of adjuvant chemotherapy for some estrogen receptor–negative stage II breast cancers by 8 weeks and administering 6 rather than 12 cycles of adjuvant chemotherapy for stage III colorectal cancers,” Schrag and colleagues write.
On the other hand, even in the epicenters of the pandemic, thus far, oncologists are still delivering cancer treatments that have the potential to cure and cannot safely be delayed, they point out. “This includes most patients with new diagnoses of acute leukemia, high-grade lymphoma, and those with chemotherapy-responsive tumors such as testicular, ovarian, and small cell lung cancer. Despite the risks, oncologists are not modifying such treatments because these cancers are likely more lethal than COVID-19.”
It’s the cancer patients who fall in between these two extremes who pose the biggest treatment challenge during this crisis – the patients for whom a delay would have “moderate clinically important adverse influence on quality of life or survival.” In these cases, oncologists are “prescribing marginally less effective regimens that have lower risk of precipitating hospitalization,” the authors note.
These treatments include the use of “white cell growth factor, more stringent neutrophil counts for proceeding with a next cycle of therapy, and omitting use of steroids to manage nausea.” In addition, where possible, oncologists are substituting oral agents for intravenous agents and “myriad other modifications to minimize visits and hospitalizations.”
Most hospitals and outpatient infusion centers now prohibit visitors from accompanying patients, and oncologists are prioritizing conversations with patients about advance directives, healthcare proxies, and end-of-life care preferences. Yet, even here, telehealth offers a new, enhanced layer to those conversations by enabling families to gather with their loved one and the doctor, she said.
This article first appeared on Medscape.com.
, the most “revolutionary” being a deep dive into telehealth, predicts Deborah Schrag, MD, MPH, a medical oncologist specializing in gastrointestinal cancers at the Dana Farber Cancer Institute in Boston, Massachusetts.
“In the space of a month, approaches and accepted norms of cancer care delivery have been transformed of necessity,” Schrag and colleagues write in an article published in JAMA on April 13.
“Most of these changes would not have occurred without the pandemic,” they add. They predict that some changes will last after the crisis is over.
“None of us want to be thrown in the deep end.... On the other hand, sometimes it works,” Schrag told Medscape Medical News.
“The in-person visit between patient and physician has been upended,” she said.
“I don’t think there’s any going back to the way it was before because cancer patients won’t stand for it,” she said. “They’re not going to drive in to get the results of a blood test.
“I think that on balance, of course, there are situations where you need eye-to-eye contact. No one wants to have an initial oncology meeting by telehealth – doctors or patients – that’s ridiculous,” she said. “But for follow-up visits, patients are now going to be more demanding, and doctors will be more willing.”
The “essential empathy” of oncologists can still “transcend the new physical barriers presented by masks and telehealth,” Schrag and colleagues comment.
“Doctors are figuring out how to deliver empathy by Zoom,” she told Medscape Medical News. “It’s not the same, but we all convey empathy to our elderly relatives over the phone.”
Pandemic impact on oncology
While the crisis has affected all of medicine – dismantling how care is delivered and forcing clinicians to make difficult decisions regarding triage – the fact that some cancers present an immediate threat to survival means that oncology “provides a lens into the major shifts currently underway in clinical care,” Schrag and colleagues write.
They illustrate the point by highlighting systemic chemotherapy, which is provided to a large proportion of patients with advanced cancer. The pandemic has tipped the risk-benefit ratio away from treatments that have a marginal effect on quality or quantity of life, they note. It has forced an “elimination of low-value treatments that were identified by the Choosing Wisely campaign,” the authors write. Up to now, the uptake of recommendations to eliminate these treatments has been slow.
“For example, for most metastatic solid tumors, chemotherapy beyond the third regimen does not improve survival for more than a few weeks; therefore, oncologists are advising supportive care instead. For patients receiving adjuvant therapy for curable cancers, delaying initiation or abbreviating the number of cycles is appropriate. Oncologists are postponing initiation of adjuvant chemotherapy for some estrogen receptor–negative stage II breast cancers by 8 weeks and administering 6 rather than 12 cycles of adjuvant chemotherapy for stage III colorectal cancers,” Schrag and colleagues write.
On the other hand, even in the epicenters of the pandemic, thus far, oncologists are still delivering cancer treatments that have the potential to cure and cannot safely be delayed, they point out. “This includes most patients with new diagnoses of acute leukemia, high-grade lymphoma, and those with chemotherapy-responsive tumors such as testicular, ovarian, and small cell lung cancer. Despite the risks, oncologists are not modifying such treatments because these cancers are likely more lethal than COVID-19.”
It’s the cancer patients who fall in between these two extremes who pose the biggest treatment challenge during this crisis – the patients for whom a delay would have “moderate clinically important adverse influence on quality of life or survival.” In these cases, oncologists are “prescribing marginally less effective regimens that have lower risk of precipitating hospitalization,” the authors note.
These treatments include the use of “white cell growth factor, more stringent neutrophil counts for proceeding with a next cycle of therapy, and omitting use of steroids to manage nausea.” In addition, where possible, oncologists are substituting oral agents for intravenous agents and “myriad other modifications to minimize visits and hospitalizations.”
Most hospitals and outpatient infusion centers now prohibit visitors from accompanying patients, and oncologists are prioritizing conversations with patients about advance directives, healthcare proxies, and end-of-life care preferences. Yet, even here, telehealth offers a new, enhanced layer to those conversations by enabling families to gather with their loved one and the doctor, she said.
This article first appeared on Medscape.com.
, the most “revolutionary” being a deep dive into telehealth, predicts Deborah Schrag, MD, MPH, a medical oncologist specializing in gastrointestinal cancers at the Dana Farber Cancer Institute in Boston, Massachusetts.
“In the space of a month, approaches and accepted norms of cancer care delivery have been transformed of necessity,” Schrag and colleagues write in an article published in JAMA on April 13.
“Most of these changes would not have occurred without the pandemic,” they add. They predict that some changes will last after the crisis is over.
“None of us want to be thrown in the deep end.... On the other hand, sometimes it works,” Schrag told Medscape Medical News.
“The in-person visit between patient and physician has been upended,” she said.
“I don’t think there’s any going back to the way it was before because cancer patients won’t stand for it,” she said. “They’re not going to drive in to get the results of a blood test.
“I think that on balance, of course, there are situations where you need eye-to-eye contact. No one wants to have an initial oncology meeting by telehealth – doctors or patients – that’s ridiculous,” she said. “But for follow-up visits, patients are now going to be more demanding, and doctors will be more willing.”
The “essential empathy” of oncologists can still “transcend the new physical barriers presented by masks and telehealth,” Schrag and colleagues comment.
“Doctors are figuring out how to deliver empathy by Zoom,” she told Medscape Medical News. “It’s not the same, but we all convey empathy to our elderly relatives over the phone.”
Pandemic impact on oncology
While the crisis has affected all of medicine – dismantling how care is delivered and forcing clinicians to make difficult decisions regarding triage – the fact that some cancers present an immediate threat to survival means that oncology “provides a lens into the major shifts currently underway in clinical care,” Schrag and colleagues write.
They illustrate the point by highlighting systemic chemotherapy, which is provided to a large proportion of patients with advanced cancer. The pandemic has tipped the risk-benefit ratio away from treatments that have a marginal effect on quality or quantity of life, they note. It has forced an “elimination of low-value treatments that were identified by the Choosing Wisely campaign,” the authors write. Up to now, the uptake of recommendations to eliminate these treatments has been slow.
“For example, for most metastatic solid tumors, chemotherapy beyond the third regimen does not improve survival for more than a few weeks; therefore, oncologists are advising supportive care instead. For patients receiving adjuvant therapy for curable cancers, delaying initiation or abbreviating the number of cycles is appropriate. Oncologists are postponing initiation of adjuvant chemotherapy for some estrogen receptor–negative stage II breast cancers by 8 weeks and administering 6 rather than 12 cycles of adjuvant chemotherapy for stage III colorectal cancers,” Schrag and colleagues write.
On the other hand, even in the epicenters of the pandemic, thus far, oncologists are still delivering cancer treatments that have the potential to cure and cannot safely be delayed, they point out. “This includes most patients with new diagnoses of acute leukemia, high-grade lymphoma, and those with chemotherapy-responsive tumors such as testicular, ovarian, and small cell lung cancer. Despite the risks, oncologists are not modifying such treatments because these cancers are likely more lethal than COVID-19.”
It’s the cancer patients who fall in between these two extremes who pose the biggest treatment challenge during this crisis – the patients for whom a delay would have “moderate clinically important adverse influence on quality of life or survival.” In these cases, oncologists are “prescribing marginally less effective regimens that have lower risk of precipitating hospitalization,” the authors note.
These treatments include the use of “white cell growth factor, more stringent neutrophil counts for proceeding with a next cycle of therapy, and omitting use of steroids to manage nausea.” In addition, where possible, oncologists are substituting oral agents for intravenous agents and “myriad other modifications to minimize visits and hospitalizations.”
Most hospitals and outpatient infusion centers now prohibit visitors from accompanying patients, and oncologists are prioritizing conversations with patients about advance directives, healthcare proxies, and end-of-life care preferences. Yet, even here, telehealth offers a new, enhanced layer to those conversations by enabling families to gather with their loved one and the doctor, she said.
This article first appeared on Medscape.com.
COVID-19 pandemic spells trouble for children’s health
Although priority number one lies in controlling the spread of COVID-19, public health researchers are calling attention to the long-term repercussions of the pandemic on children’s health.
School closures could noticeably worsen the epidemic of childhood obesity that already threatens many children in the United States, say Paul Rundle, DrPH, and colleagues from Columbia University Mailman School of Public Health, New York City, in a perspective published online March 30 in Obesity.
“In part, we wrote the perspective to remind people that summer unhealthy weight gain seems to accumulate year to year,” he told Medscape Medical News in an email.
Rundle and colleagues estimate that time spent out of school will double this year because of school closures due to COVID-19. That, along with shelter-in-place orders, will pose challenges both for physical activity and healthy eating among children.
In addition, playgrounds have closed in many areas, and even where parks remain open, social distancing decreases opportunities for exercise. Team sports are on hold, and without physical education taught in schools, many children will not be getting as much active outdoor play as needed.
That’s especially true for children in urban areas, who may find it even more difficult to exercise inside cramped apartments, they add.
As a result, more and more children may turn to sedentary activities, and increased screen time goes hand in hand with childhood overweight and obesity, not just because of the lack of exercise but also because of snacking on unhealthy, empty-calorie foods while glued to the screen.
“We were hoping to get the word out on this issue, do some education or reminding, and at least let people know that this should be something to keep an eye on, among so many other things,” Rundle added.
Excess Eating Because of Stress and Boredom
Jessica Sparks Lilley, MD, director of the Pediatric Diabetes and Lipid Program at the Mississippi Center for Advanced Medicine in Madison, agrees that it is crucial to address these issues.
“Just like adults, children eat in response to emotions, including stress and boredom, and stress levels are high during these uncertain times,” she told Medscape Medical News.
Although both Rundle and Sparks Lilley acknowledged the challenges of finding good solutions at this time, they do offer some tips.
Schools should make physical education and at-home exercise a priority alongside other remote teaching. Physical education teachers could even stream exercise classes to children at home.
Even just walking in the park while maintaining social distancing could be better than nothing, and a brisk walk is probably even better.
Depending on the age of the child, online yoga may also be useful. Even though yoga burns relatively few calories, it incorporates mindfulness training that may be helpful.
“I think focusing on promoting mindful eating as compared to mindless or distracted eating is important. Even in the best of circumstances, it is hard to exercise enough to burn off high energy snacks,” Rundle said.
Additional Stressors From Poverty: Schools Can Help With Meals
Children living in poverty, already the most vulnerable to obesity and related health problems, have additional stressors, add the two experts.
“As more Americans are losing jobs, poverty is a real threat to many of the children I care for. Families living in poverty often rely on processed, high-calorie, low-nutrient foods for survival, because they are inexpensive and shelf-stable,” Sparks Lilley said.
Rundle and colleagues agree: “Our own experiences in supermarkets show...shelves that held...crackers, chips, ramen noodles, soda, sugary cereals, and processed ready-to-eat meals are quite empty. We anticipate that many children will experience higher calorie diets during the pandemic response.”
Similar to how they address food insecurity during summer holidays, school districts have responded by offering grab-and-go meals, Rundle and colleagues note.
To maintain social distancing for people with vulnerable family members, some school districts have also started delivering food using school buses that run along regularly scheduled routes.
Rundle also stresses that farmers’ markets, which often provide foods that appeal to immigrant and ethnic communities, should be considered part of essential food services.
As such, social distancing protocols should be established for them and they should be allowed to stay open, he argues.
“The safety of American children is at stake in many ways. The threat to themselves or their caregivers being infected with COVID-19 is rightly foremost in our concerns,” Sparks Lilley stressed.
“However, there is other fallout to consider. We’ve seen very clearly the need for public health and preventive medicine and can’t let vulnerable children fall through the cracks.”
Rundle agrees. Although it is a “priority” to mitigate the immediate impact of COVID-19, “it is important to consider ways to prevent its long-term effects, including new risks for childhood obesity.”
Rundle and coauthors, as well as Sparks Lilley, have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Although priority number one lies in controlling the spread of COVID-19, public health researchers are calling attention to the long-term repercussions of the pandemic on children’s health.
School closures could noticeably worsen the epidemic of childhood obesity that already threatens many children in the United States, say Paul Rundle, DrPH, and colleagues from Columbia University Mailman School of Public Health, New York City, in a perspective published online March 30 in Obesity.
“In part, we wrote the perspective to remind people that summer unhealthy weight gain seems to accumulate year to year,” he told Medscape Medical News in an email.
Rundle and colleagues estimate that time spent out of school will double this year because of school closures due to COVID-19. That, along with shelter-in-place orders, will pose challenges both for physical activity and healthy eating among children.
In addition, playgrounds have closed in many areas, and even where parks remain open, social distancing decreases opportunities for exercise. Team sports are on hold, and without physical education taught in schools, many children will not be getting as much active outdoor play as needed.
That’s especially true for children in urban areas, who may find it even more difficult to exercise inside cramped apartments, they add.
As a result, more and more children may turn to sedentary activities, and increased screen time goes hand in hand with childhood overweight and obesity, not just because of the lack of exercise but also because of snacking on unhealthy, empty-calorie foods while glued to the screen.
“We were hoping to get the word out on this issue, do some education or reminding, and at least let people know that this should be something to keep an eye on, among so many other things,” Rundle added.
Excess Eating Because of Stress and Boredom
Jessica Sparks Lilley, MD, director of the Pediatric Diabetes and Lipid Program at the Mississippi Center for Advanced Medicine in Madison, agrees that it is crucial to address these issues.
“Just like adults, children eat in response to emotions, including stress and boredom, and stress levels are high during these uncertain times,” she told Medscape Medical News.
Although both Rundle and Sparks Lilley acknowledged the challenges of finding good solutions at this time, they do offer some tips.
Schools should make physical education and at-home exercise a priority alongside other remote teaching. Physical education teachers could even stream exercise classes to children at home.
Even just walking in the park while maintaining social distancing could be better than nothing, and a brisk walk is probably even better.
Depending on the age of the child, online yoga may also be useful. Even though yoga burns relatively few calories, it incorporates mindfulness training that may be helpful.
“I think focusing on promoting mindful eating as compared to mindless or distracted eating is important. Even in the best of circumstances, it is hard to exercise enough to burn off high energy snacks,” Rundle said.
Additional Stressors From Poverty: Schools Can Help With Meals
Children living in poverty, already the most vulnerable to obesity and related health problems, have additional stressors, add the two experts.
“As more Americans are losing jobs, poverty is a real threat to many of the children I care for. Families living in poverty often rely on processed, high-calorie, low-nutrient foods for survival, because they are inexpensive and shelf-stable,” Sparks Lilley said.
Rundle and colleagues agree: “Our own experiences in supermarkets show...shelves that held...crackers, chips, ramen noodles, soda, sugary cereals, and processed ready-to-eat meals are quite empty. We anticipate that many children will experience higher calorie diets during the pandemic response.”
Similar to how they address food insecurity during summer holidays, school districts have responded by offering grab-and-go meals, Rundle and colleagues note.
To maintain social distancing for people with vulnerable family members, some school districts have also started delivering food using school buses that run along regularly scheduled routes.
Rundle also stresses that farmers’ markets, which often provide foods that appeal to immigrant and ethnic communities, should be considered part of essential food services.
As such, social distancing protocols should be established for them and they should be allowed to stay open, he argues.
“The safety of American children is at stake in many ways. The threat to themselves or their caregivers being infected with COVID-19 is rightly foremost in our concerns,” Sparks Lilley stressed.
“However, there is other fallout to consider. We’ve seen very clearly the need for public health and preventive medicine and can’t let vulnerable children fall through the cracks.”
Rundle agrees. Although it is a “priority” to mitigate the immediate impact of COVID-19, “it is important to consider ways to prevent its long-term effects, including new risks for childhood obesity.”
Rundle and coauthors, as well as Sparks Lilley, have reported no relevant financial relationships.
This article first appeared on Medscape.com.
Although priority number one lies in controlling the spread of COVID-19, public health researchers are calling attention to the long-term repercussions of the pandemic on children’s health.
School closures could noticeably worsen the epidemic of childhood obesity that already threatens many children in the United States, say Paul Rundle, DrPH, and colleagues from Columbia University Mailman School of Public Health, New York City, in a perspective published online March 30 in Obesity.
“In part, we wrote the perspective to remind people that summer unhealthy weight gain seems to accumulate year to year,” he told Medscape Medical News in an email.
Rundle and colleagues estimate that time spent out of school will double this year because of school closures due to COVID-19. That, along with shelter-in-place orders, will pose challenges both for physical activity and healthy eating among children.
In addition, playgrounds have closed in many areas, and even where parks remain open, social distancing decreases opportunities for exercise. Team sports are on hold, and without physical education taught in schools, many children will not be getting as much active outdoor play as needed.
That’s especially true for children in urban areas, who may find it even more difficult to exercise inside cramped apartments, they add.
As a result, more and more children may turn to sedentary activities, and increased screen time goes hand in hand with childhood overweight and obesity, not just because of the lack of exercise but also because of snacking on unhealthy, empty-calorie foods while glued to the screen.
“We were hoping to get the word out on this issue, do some education or reminding, and at least let people know that this should be something to keep an eye on, among so many other things,” Rundle added.
Excess Eating Because of Stress and Boredom
Jessica Sparks Lilley, MD, director of the Pediatric Diabetes and Lipid Program at the Mississippi Center for Advanced Medicine in Madison, agrees that it is crucial to address these issues.
“Just like adults, children eat in response to emotions, including stress and boredom, and stress levels are high during these uncertain times,” she told Medscape Medical News.
Although both Rundle and Sparks Lilley acknowledged the challenges of finding good solutions at this time, they do offer some tips.
Schools should make physical education and at-home exercise a priority alongside other remote teaching. Physical education teachers could even stream exercise classes to children at home.
Even just walking in the park while maintaining social distancing could be better than nothing, and a brisk walk is probably even better.
Depending on the age of the child, online yoga may also be useful. Even though yoga burns relatively few calories, it incorporates mindfulness training that may be helpful.
“I think focusing on promoting mindful eating as compared to mindless or distracted eating is important. Even in the best of circumstances, it is hard to exercise enough to burn off high energy snacks,” Rundle said.
Additional Stressors From Poverty: Schools Can Help With Meals
Children living in poverty, already the most vulnerable to obesity and related health problems, have additional stressors, add the two experts.
“As more Americans are losing jobs, poverty is a real threat to many of the children I care for. Families living in poverty often rely on processed, high-calorie, low-nutrient foods for survival, because they are inexpensive and shelf-stable,” Sparks Lilley said.
Rundle and colleagues agree: “Our own experiences in supermarkets show...shelves that held...crackers, chips, ramen noodles, soda, sugary cereals, and processed ready-to-eat meals are quite empty. We anticipate that many children will experience higher calorie diets during the pandemic response.”
Similar to how they address food insecurity during summer holidays, school districts have responded by offering grab-and-go meals, Rundle and colleagues note.
To maintain social distancing for people with vulnerable family members, some school districts have also started delivering food using school buses that run along regularly scheduled routes.
Rundle also stresses that farmers’ markets, which often provide foods that appeal to immigrant and ethnic communities, should be considered part of essential food services.
As such, social distancing protocols should be established for them and they should be allowed to stay open, he argues.
“The safety of American children is at stake in many ways. The threat to themselves or their caregivers being infected with COVID-19 is rightly foremost in our concerns,” Sparks Lilley stressed.
“However, there is other fallout to consider. We’ve seen very clearly the need for public health and preventive medicine and can’t let vulnerable children fall through the cracks.”
Rundle agrees. Although it is a “priority” to mitigate the immediate impact of COVID-19, “it is important to consider ways to prevent its long-term effects, including new risks for childhood obesity.”
Rundle and coauthors, as well as Sparks Lilley, have reported no relevant financial relationships.
This article first appeared on Medscape.com.



