User login
In Case You Missed It: COVID
HCPs and COVID-19 Risk: Safer at Home or at Work?
The Centers for Disease Control and Prevention (CDC) and Michigan Department of Health and Human Services surveyed health care personnel in 27 hospitals and 7 medical control agencies that coordinate emergency medical services in the Detroit metropolitan area. Of 16,397 participants, 6.9% had COVID-19 antibodies (although only 2.7% reported a history of a positive real-time transcription polymerase chain reaction test); however, participants had about 6 times the odds of exposure to the virus at home when compared with the workplace. Of those who reported close contact (within 6 feet) of a person with confirmed COVID-19 for ≥ 10 minutes, seroprevalence was highest among those with exposure to a household member (34.3%).
The survey revealed a pattern that suggested community acquisition was a common underlying factor of infection risk, the researchers say. Workers were only more vulnerable at home and when they were closer to the metropolitan center. Seropositivity was more common within 9 miles of Detroit’s center, regardless of occupation and health care setting. The farther away from the center, the lower the seroprevalence.
By work location, seroprevalence was highest among participants who worked in hospital wards (8.8%) and lowest among those in police departments (3.9%). In hospitals, participants working in wards and EDs had higher seropositivity (8.8% and 8.1%, respectively) than did those in ICUs and ORs (6.1% and 4.5%, respectively). Nurses and nurse assistants were more likely to be seropositive than physicians. Nurse assistants had the highest incidence, regardless of where they worked.
Reducing community spread through population-based measures may directly protect healthcare workers on 2 fronts, the researchers say: reduced occupational exposure as a result of fewer infected patients in the less controlled workplace setting such as the ED, and reduced exposure in their homes and communities.
The Centers for Disease Control and Prevention (CDC) and Michigan Department of Health and Human Services surveyed health care personnel in 27 hospitals and 7 medical control agencies that coordinate emergency medical services in the Detroit metropolitan area. Of 16,397 participants, 6.9% had COVID-19 antibodies (although only 2.7% reported a history of a positive real-time transcription polymerase chain reaction test); however, participants had about 6 times the odds of exposure to the virus at home when compared with the workplace. Of those who reported close contact (within 6 feet) of a person with confirmed COVID-19 for ≥ 10 minutes, seroprevalence was highest among those with exposure to a household member (34.3%).
The survey revealed a pattern that suggested community acquisition was a common underlying factor of infection risk, the researchers say. Workers were only more vulnerable at home and when they were closer to the metropolitan center. Seropositivity was more common within 9 miles of Detroit’s center, regardless of occupation and health care setting. The farther away from the center, the lower the seroprevalence.
By work location, seroprevalence was highest among participants who worked in hospital wards (8.8%) and lowest among those in police departments (3.9%). In hospitals, participants working in wards and EDs had higher seropositivity (8.8% and 8.1%, respectively) than did those in ICUs and ORs (6.1% and 4.5%, respectively). Nurses and nurse assistants were more likely to be seropositive than physicians. Nurse assistants had the highest incidence, regardless of where they worked.
Reducing community spread through population-based measures may directly protect healthcare workers on 2 fronts, the researchers say: reduced occupational exposure as a result of fewer infected patients in the less controlled workplace setting such as the ED, and reduced exposure in their homes and communities.
The Centers for Disease Control and Prevention (CDC) and Michigan Department of Health and Human Services surveyed health care personnel in 27 hospitals and 7 medical control agencies that coordinate emergency medical services in the Detroit metropolitan area. Of 16,397 participants, 6.9% had COVID-19 antibodies (although only 2.7% reported a history of a positive real-time transcription polymerase chain reaction test); however, participants had about 6 times the odds of exposure to the virus at home when compared with the workplace. Of those who reported close contact (within 6 feet) of a person with confirmed COVID-19 for ≥ 10 minutes, seroprevalence was highest among those with exposure to a household member (34.3%).
The survey revealed a pattern that suggested community acquisition was a common underlying factor of infection risk, the researchers say. Workers were only more vulnerable at home and when they were closer to the metropolitan center. Seropositivity was more common within 9 miles of Detroit’s center, regardless of occupation and health care setting. The farther away from the center, the lower the seroprevalence.
By work location, seroprevalence was highest among participants who worked in hospital wards (8.8%) and lowest among those in police departments (3.9%). In hospitals, participants working in wards and EDs had higher seropositivity (8.8% and 8.1%, respectively) than did those in ICUs and ORs (6.1% and 4.5%, respectively). Nurses and nurse assistants were more likely to be seropositive than physicians. Nurse assistants had the highest incidence, regardless of where they worked.
Reducing community spread through population-based measures may directly protect healthcare workers on 2 fronts, the researchers say: reduced occupational exposure as a result of fewer infected patients in the less controlled workplace setting such as the ED, and reduced exposure in their homes and communities.
Patients with lung and blood cancers most vulnerable to COVID-19
Patients with cancer are at significantly increased risk for COVID-19 and worse outcomes, a new review confirms. It also found that patients with leukemia, non-Hodgkin lymphoma, and lung cancer are at greatest risk.
Blacks with cancer are at even higher risk, and for patients with colorectal cancer and non-Hodgkin lymphoma, the risk is higher for women than for men. (This contrasts with findings in noncancer populations, where men are more at risk from COVID-19 and severe outcomes than women.)
These findings come from a huge review of electronic health records of 73.4 million patients in the United States. They “highlight the need to protect and monitor patients with cancer as part of the strategy to control the pandemic,” the authors wrote.
The review was published online Dec. 10 in JAMA Oncology.
The greater risk for COVID-19 among patients with cancer is well known, but breaking the risk down by cancer type is novel, wrote the investigators, led by Quanqiu Wang, MS, Center for Artificial Intelligence in Drug Discovery, Case Western Reserve University, Cleveland.
Cancer patients are immunocompromised and have more contact with the health care system, which increases their risk for COVID-19. But which bodily systems are affected by cancer seems to matter. In patients with blood cancer, for example, COVID-19 is probably more dangerous, because blood cancer weakens the immune system directly, the authors suggested.
The increased risk for infection and hospitalization with SARS-CoV-2 among Black patients with cancer might be because of biology, but it is more likely because of factors that weren’t captured in the database review. Such factors include social adversity, economic status, access to health care, and lifestyle, the researchers noted.
For this study, the investigators analyzed electronic health records held in the IBM Watson Health Explorys system, which captures about 15% of new cancer diagnoses in the United States.
The analysis found that, as of Aug. 14, 2020, 16,570 patients (0.02%) had been diagnosed with COVID-19; about 1,200 also had been diagnosed with cancer. Of those, 690 were diagnosed with cancer in the previous year, which counted as a recent cancer diagnosis in the analysis. The study included 13 common cancers, including endometrial, kidney, liver, lung, gastrointestinal, prostate, skin, and thyroid cancers, among others.
Patients with any cancer diagnosis (adjusted odds ratio, 1.46) as well as those with a recent cancer diagnosis (aOR, 7.14) had a significantly higher risk for COVID-19 than those without cancer, after adjusting for asthma, cardiovascular diseases, nursing home stays, and other risk factors.
The risk for COVID-19 was highest among patients recently diagnosed with leukemia (aOR, 12.16), non-Hodgkin lymphoma (aOR, 8.54), and lung cancer (aOR 7.66). The risk for COVID-19 was lower for patients with cancers associated with worse prognoses, including pancreatic (aOR, 6.26) and liver (aOR, 6.49) cancer. It was weakest for patients with thyroid cancer (aOR, 3.10; P for all < .001).
Hospitalization was more common in recent cancer patients with COVID-19 than in COVID-19 patients without cancer (47.46% vs. 24.6%), as was COVID-19–related death (14.93% vs. 5.26%). Among cancer patients who did not have COVID-19, 12.39% were hospitalized, and 4.03% died. The findings suggest a synergistic effect between the COVID-19 and cancer, the team noted.
Among patients recently diagnosed with cancer, Black patients – 10.3% of the overall study population – had a significantly higher risk for COVID-19 than White patients. The racial disparity was largest for patients with breast cancer (aOR, 5.44), followed by patients with prostate cancer (aOR, 5.10), colorectal cancer (aOR, 3.30), and lung cancer (aOR, 2.53; P for all < .001).
Hospitalizations were more common among Black patients with cancer and COVID-19 than White patients. There was also a trend toward higher mortality among Black patients (18.52% vs. 13.51%; P = .11)
However, these differences may not be related to race, oncologist Aakash Desai, MBBS, of the Mayo Clinic, Rochester, Minn., and colleagues noted in an accompanying commentary. “Interestingly, a previous study of hospitalized patients with COVID-19 without cancer demonstrated that mortality rates for Black patients were comparable to those for White patients after adjustment for both comorbidities and deprivation index, suggesting that observed differences are mainly owing to societal disparities rather than biology.”
The editorialists also noted that the finding that Black patients with cancer are at greater risk for COVID-19 (aOR, 1.58-5.44, depending on cancer) echoes the findings in the general population. The Centers for Disease Control and Prevention estimates a severalfold increased risk among Black patients. These higher rates may largely be explained by social determinants, they suggested. Such factors include increased burden of comorbidities, crowded living conditions (inner cities, multigenerational homes, etc.), dependence on public transportation or child care, and higher work-related exposures. “Until such societal disparities are accounted for, we cannot presume these findings are caused by any inherent differences among racial groups,” the editorialists wrote.
“Clearly, the haunting spotlight of COVID-19 has dramatically illuminated known U.S. health care and societal disparities,” Dr. Desai and colleagues wrote. “This situation should be a wake-up call that brings much-needed improvements in U.S. equity policies, including but not limited to better health care access. Nothing appears more critical for alleviating these disparate clinical outcomes in this time of crisis and beyond,” they declared.
The study was funded by the National Institutes of Health, the American Cancer Society, and other organizations. The investigators disclosed having no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with cancer are at significantly increased risk for COVID-19 and worse outcomes, a new review confirms. It also found that patients with leukemia, non-Hodgkin lymphoma, and lung cancer are at greatest risk.
Blacks with cancer are at even higher risk, and for patients with colorectal cancer and non-Hodgkin lymphoma, the risk is higher for women than for men. (This contrasts with findings in noncancer populations, where men are more at risk from COVID-19 and severe outcomes than women.)
These findings come from a huge review of electronic health records of 73.4 million patients in the United States. They “highlight the need to protect and monitor patients with cancer as part of the strategy to control the pandemic,” the authors wrote.
The review was published online Dec. 10 in JAMA Oncology.
The greater risk for COVID-19 among patients with cancer is well known, but breaking the risk down by cancer type is novel, wrote the investigators, led by Quanqiu Wang, MS, Center for Artificial Intelligence in Drug Discovery, Case Western Reserve University, Cleveland.
Cancer patients are immunocompromised and have more contact with the health care system, which increases their risk for COVID-19. But which bodily systems are affected by cancer seems to matter. In patients with blood cancer, for example, COVID-19 is probably more dangerous, because blood cancer weakens the immune system directly, the authors suggested.
The increased risk for infection and hospitalization with SARS-CoV-2 among Black patients with cancer might be because of biology, but it is more likely because of factors that weren’t captured in the database review. Such factors include social adversity, economic status, access to health care, and lifestyle, the researchers noted.
For this study, the investigators analyzed electronic health records held in the IBM Watson Health Explorys system, which captures about 15% of new cancer diagnoses in the United States.
The analysis found that, as of Aug. 14, 2020, 16,570 patients (0.02%) had been diagnosed with COVID-19; about 1,200 also had been diagnosed with cancer. Of those, 690 were diagnosed with cancer in the previous year, which counted as a recent cancer diagnosis in the analysis. The study included 13 common cancers, including endometrial, kidney, liver, lung, gastrointestinal, prostate, skin, and thyroid cancers, among others.
Patients with any cancer diagnosis (adjusted odds ratio, 1.46) as well as those with a recent cancer diagnosis (aOR, 7.14) had a significantly higher risk for COVID-19 than those without cancer, after adjusting for asthma, cardiovascular diseases, nursing home stays, and other risk factors.
The risk for COVID-19 was highest among patients recently diagnosed with leukemia (aOR, 12.16), non-Hodgkin lymphoma (aOR, 8.54), and lung cancer (aOR 7.66). The risk for COVID-19 was lower for patients with cancers associated with worse prognoses, including pancreatic (aOR, 6.26) and liver (aOR, 6.49) cancer. It was weakest for patients with thyroid cancer (aOR, 3.10; P for all < .001).
Hospitalization was more common in recent cancer patients with COVID-19 than in COVID-19 patients without cancer (47.46% vs. 24.6%), as was COVID-19–related death (14.93% vs. 5.26%). Among cancer patients who did not have COVID-19, 12.39% were hospitalized, and 4.03% died. The findings suggest a synergistic effect between the COVID-19 and cancer, the team noted.
Among patients recently diagnosed with cancer, Black patients – 10.3% of the overall study population – had a significantly higher risk for COVID-19 than White patients. The racial disparity was largest for patients with breast cancer (aOR, 5.44), followed by patients with prostate cancer (aOR, 5.10), colorectal cancer (aOR, 3.30), and lung cancer (aOR, 2.53; P for all < .001).
Hospitalizations were more common among Black patients with cancer and COVID-19 than White patients. There was also a trend toward higher mortality among Black patients (18.52% vs. 13.51%; P = .11)
However, these differences may not be related to race, oncologist Aakash Desai, MBBS, of the Mayo Clinic, Rochester, Minn., and colleagues noted in an accompanying commentary. “Interestingly, a previous study of hospitalized patients with COVID-19 without cancer demonstrated that mortality rates for Black patients were comparable to those for White patients after adjustment for both comorbidities and deprivation index, suggesting that observed differences are mainly owing to societal disparities rather than biology.”
The editorialists also noted that the finding that Black patients with cancer are at greater risk for COVID-19 (aOR, 1.58-5.44, depending on cancer) echoes the findings in the general population. The Centers for Disease Control and Prevention estimates a severalfold increased risk among Black patients. These higher rates may largely be explained by social determinants, they suggested. Such factors include increased burden of comorbidities, crowded living conditions (inner cities, multigenerational homes, etc.), dependence on public transportation or child care, and higher work-related exposures. “Until such societal disparities are accounted for, we cannot presume these findings are caused by any inherent differences among racial groups,” the editorialists wrote.
“Clearly, the haunting spotlight of COVID-19 has dramatically illuminated known U.S. health care and societal disparities,” Dr. Desai and colleagues wrote. “This situation should be a wake-up call that brings much-needed improvements in U.S. equity policies, including but not limited to better health care access. Nothing appears more critical for alleviating these disparate clinical outcomes in this time of crisis and beyond,” they declared.
The study was funded by the National Institutes of Health, the American Cancer Society, and other organizations. The investigators disclosed having no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with cancer are at significantly increased risk for COVID-19 and worse outcomes, a new review confirms. It also found that patients with leukemia, non-Hodgkin lymphoma, and lung cancer are at greatest risk.
Blacks with cancer are at even higher risk, and for patients with colorectal cancer and non-Hodgkin lymphoma, the risk is higher for women than for men. (This contrasts with findings in noncancer populations, where men are more at risk from COVID-19 and severe outcomes than women.)
These findings come from a huge review of electronic health records of 73.4 million patients in the United States. They “highlight the need to protect and monitor patients with cancer as part of the strategy to control the pandemic,” the authors wrote.
The review was published online Dec. 10 in JAMA Oncology.
The greater risk for COVID-19 among patients with cancer is well known, but breaking the risk down by cancer type is novel, wrote the investigators, led by Quanqiu Wang, MS, Center for Artificial Intelligence in Drug Discovery, Case Western Reserve University, Cleveland.
Cancer patients are immunocompromised and have more contact with the health care system, which increases their risk for COVID-19. But which bodily systems are affected by cancer seems to matter. In patients with blood cancer, for example, COVID-19 is probably more dangerous, because blood cancer weakens the immune system directly, the authors suggested.
The increased risk for infection and hospitalization with SARS-CoV-2 among Black patients with cancer might be because of biology, but it is more likely because of factors that weren’t captured in the database review. Such factors include social adversity, economic status, access to health care, and lifestyle, the researchers noted.
For this study, the investigators analyzed electronic health records held in the IBM Watson Health Explorys system, which captures about 15% of new cancer diagnoses in the United States.
The analysis found that, as of Aug. 14, 2020, 16,570 patients (0.02%) had been diagnosed with COVID-19; about 1,200 also had been diagnosed with cancer. Of those, 690 were diagnosed with cancer in the previous year, which counted as a recent cancer diagnosis in the analysis. The study included 13 common cancers, including endometrial, kidney, liver, lung, gastrointestinal, prostate, skin, and thyroid cancers, among others.
Patients with any cancer diagnosis (adjusted odds ratio, 1.46) as well as those with a recent cancer diagnosis (aOR, 7.14) had a significantly higher risk for COVID-19 than those without cancer, after adjusting for asthma, cardiovascular diseases, nursing home stays, and other risk factors.
The risk for COVID-19 was highest among patients recently diagnosed with leukemia (aOR, 12.16), non-Hodgkin lymphoma (aOR, 8.54), and lung cancer (aOR 7.66). The risk for COVID-19 was lower for patients with cancers associated with worse prognoses, including pancreatic (aOR, 6.26) and liver (aOR, 6.49) cancer. It was weakest for patients with thyroid cancer (aOR, 3.10; P for all < .001).
Hospitalization was more common in recent cancer patients with COVID-19 than in COVID-19 patients without cancer (47.46% vs. 24.6%), as was COVID-19–related death (14.93% vs. 5.26%). Among cancer patients who did not have COVID-19, 12.39% were hospitalized, and 4.03% died. The findings suggest a synergistic effect between the COVID-19 and cancer, the team noted.
Among patients recently diagnosed with cancer, Black patients – 10.3% of the overall study population – had a significantly higher risk for COVID-19 than White patients. The racial disparity was largest for patients with breast cancer (aOR, 5.44), followed by patients with prostate cancer (aOR, 5.10), colorectal cancer (aOR, 3.30), and lung cancer (aOR, 2.53; P for all < .001).
Hospitalizations were more common among Black patients with cancer and COVID-19 than White patients. There was also a trend toward higher mortality among Black patients (18.52% vs. 13.51%; P = .11)
However, these differences may not be related to race, oncologist Aakash Desai, MBBS, of the Mayo Clinic, Rochester, Minn., and colleagues noted in an accompanying commentary. “Interestingly, a previous study of hospitalized patients with COVID-19 without cancer demonstrated that mortality rates for Black patients were comparable to those for White patients after adjustment for both comorbidities and deprivation index, suggesting that observed differences are mainly owing to societal disparities rather than biology.”
The editorialists also noted that the finding that Black patients with cancer are at greater risk for COVID-19 (aOR, 1.58-5.44, depending on cancer) echoes the findings in the general population. The Centers for Disease Control and Prevention estimates a severalfold increased risk among Black patients. These higher rates may largely be explained by social determinants, they suggested. Such factors include increased burden of comorbidities, crowded living conditions (inner cities, multigenerational homes, etc.), dependence on public transportation or child care, and higher work-related exposures. “Until such societal disparities are accounted for, we cannot presume these findings are caused by any inherent differences among racial groups,” the editorialists wrote.
“Clearly, the haunting spotlight of COVID-19 has dramatically illuminated known U.S. health care and societal disparities,” Dr. Desai and colleagues wrote. “This situation should be a wake-up call that brings much-needed improvements in U.S. equity policies, including but not limited to better health care access. Nothing appears more critical for alleviating these disparate clinical outcomes in this time of crisis and beyond,” they declared.
The study was funded by the National Institutes of Health, the American Cancer Society, and other organizations. The investigators disclosed having no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Pfizer can’t supply additional vaccines to U.S. until June
Pfizer won’t be able to provide more COVID-19 vaccine doses to the United States until late June or July because other countries have bought up the available supply, according to The Washington Post.
The U.S. government signed a deal with the giant pharmaceutical company earlier this year to provide 100 million doses for $1.95 billion – enough for 50 million Americans to receive the two-dose vaccine. At that time, Pfizer officials encouraged Operation Warp Speed officials to purchase an additional 100 million doses, The New York Times first reported Dec. 7, but the federal officials declined.
Since then, other countries have signed vaccine deals with Pfizer, so the U.S. may not be able to receive a second major allotment until the summer of 2021, The Washington Post reported. Without a substantial number of additional doses, the U.S. may not be able to follow its schedule of vaccinating the majority of Americans against COVID-19 by April or May.
However, Trump administration officials told the newspaper that there won’t be issues, citing other vaccine companies such as Moderna.
“I’m not concerned about our ability to buy vaccines to offer to all of the American public,” Gen. Paul Ostrowski, who oversees logistics for Operation Warp Speed, told The Washington Post.
“It’s clear that Pfizer made plans with other countries. Many have been announced. We understand those pieces,” he said.
With Pfizer’s COVID-19 vaccine on the verge of FDA approval, federal officials contacted the company last weekend to buy another 100 million doses, but the company said its current supply is already committed, the newspaper reported.
The vaccine from Pfizer and BioNTech is expected to win emergency approval within days and has been shown to be effective against COVID-19.
Pfizer added that it may be able to provide 50 million doses at the end of the second quarter and another 50 million doses during the third quarter. However, the company can’t offer anything “substantial” until next summer.
Beyond the initial 100 million doses that the U.S. has already secured, Pfizer and federal officials would need to negotiate a new, “separate and mutually acceptable agreement,” Amy Rose, a spokeswoman for Pfizer, told the newspaper.
On Dec. 8, President Donald Trump was expected to sign an executive order prioritizing vaccination for Americans first before providing doses to other countries, according to Fox News.
The order will provide guidelines to the Department of Health and Human Services, the U.S. Agency for International Development and the U.S. International Development Finance Corporation for foreign assistance with vaccines, the news outlet reported.
It’s unclear whether the executive order is related to the Pfizer issue, whether the president can prevent a private company from fulfilling contracts with other countries, and whether President-elect Joe Biden will create his own policy, according to CNBC. The order may prove to be mostly symbolic.
The FDA could issue an emergency use authorization for Pfizer’s coronavirus vaccine this week and will likely approve Moderna’s vaccine next week. The U.S. has signed a contract with Moderna for 100 million doses.
During a call with reporters on Dec. 7, a spokeswoman for the Department of Health and Human Services said, “We are confident that we will have 100 million doses of Pfizer’s vaccine as agreed to in our contract, and beyond that, we have five other vaccine candidates, including 100 million doses on the way from Moderna.”
Federal officials are counting on vaccine candidates from AstraZeneca and Johnson & Johnson to seek FDA approval in January and be ready for shipment in February.
“We could have all of them,” Moncef Slaoui, the chief science adviser for Operation Warp Speed, told The Washington Post on Dec. 7.
“And for this reason, we feel confident we could cover the needs without a specific cliff,” he said. “We have planned things in such a way as we would indeed avoid a cliff.”
This article first appeared on WebMD.com.
Pfizer won’t be able to provide more COVID-19 vaccine doses to the United States until late June or July because other countries have bought up the available supply, according to The Washington Post.
The U.S. government signed a deal with the giant pharmaceutical company earlier this year to provide 100 million doses for $1.95 billion – enough for 50 million Americans to receive the two-dose vaccine. At that time, Pfizer officials encouraged Operation Warp Speed officials to purchase an additional 100 million doses, The New York Times first reported Dec. 7, but the federal officials declined.
Since then, other countries have signed vaccine deals with Pfizer, so the U.S. may not be able to receive a second major allotment until the summer of 2021, The Washington Post reported. Without a substantial number of additional doses, the U.S. may not be able to follow its schedule of vaccinating the majority of Americans against COVID-19 by April or May.
However, Trump administration officials told the newspaper that there won’t be issues, citing other vaccine companies such as Moderna.
“I’m not concerned about our ability to buy vaccines to offer to all of the American public,” Gen. Paul Ostrowski, who oversees logistics for Operation Warp Speed, told The Washington Post.
“It’s clear that Pfizer made plans with other countries. Many have been announced. We understand those pieces,” he said.
With Pfizer’s COVID-19 vaccine on the verge of FDA approval, federal officials contacted the company last weekend to buy another 100 million doses, but the company said its current supply is already committed, the newspaper reported.
The vaccine from Pfizer and BioNTech is expected to win emergency approval within days and has been shown to be effective against COVID-19.
Pfizer added that it may be able to provide 50 million doses at the end of the second quarter and another 50 million doses during the third quarter. However, the company can’t offer anything “substantial” until next summer.
Beyond the initial 100 million doses that the U.S. has already secured, Pfizer and federal officials would need to negotiate a new, “separate and mutually acceptable agreement,” Amy Rose, a spokeswoman for Pfizer, told the newspaper.
On Dec. 8, President Donald Trump was expected to sign an executive order prioritizing vaccination for Americans first before providing doses to other countries, according to Fox News.
The order will provide guidelines to the Department of Health and Human Services, the U.S. Agency for International Development and the U.S. International Development Finance Corporation for foreign assistance with vaccines, the news outlet reported.
It’s unclear whether the executive order is related to the Pfizer issue, whether the president can prevent a private company from fulfilling contracts with other countries, and whether President-elect Joe Biden will create his own policy, according to CNBC. The order may prove to be mostly symbolic.
The FDA could issue an emergency use authorization for Pfizer’s coronavirus vaccine this week and will likely approve Moderna’s vaccine next week. The U.S. has signed a contract with Moderna for 100 million doses.
During a call with reporters on Dec. 7, a spokeswoman for the Department of Health and Human Services said, “We are confident that we will have 100 million doses of Pfizer’s vaccine as agreed to in our contract, and beyond that, we have five other vaccine candidates, including 100 million doses on the way from Moderna.”
Federal officials are counting on vaccine candidates from AstraZeneca and Johnson & Johnson to seek FDA approval in January and be ready for shipment in February.
“We could have all of them,” Moncef Slaoui, the chief science adviser for Operation Warp Speed, told The Washington Post on Dec. 7.
“And for this reason, we feel confident we could cover the needs without a specific cliff,” he said. “We have planned things in such a way as we would indeed avoid a cliff.”
This article first appeared on WebMD.com.
Pfizer won’t be able to provide more COVID-19 vaccine doses to the United States until late June or July because other countries have bought up the available supply, according to The Washington Post.
The U.S. government signed a deal with the giant pharmaceutical company earlier this year to provide 100 million doses for $1.95 billion – enough for 50 million Americans to receive the two-dose vaccine. At that time, Pfizer officials encouraged Operation Warp Speed officials to purchase an additional 100 million doses, The New York Times first reported Dec. 7, but the federal officials declined.
Since then, other countries have signed vaccine deals with Pfizer, so the U.S. may not be able to receive a second major allotment until the summer of 2021, The Washington Post reported. Without a substantial number of additional doses, the U.S. may not be able to follow its schedule of vaccinating the majority of Americans against COVID-19 by April or May.
However, Trump administration officials told the newspaper that there won’t be issues, citing other vaccine companies such as Moderna.
“I’m not concerned about our ability to buy vaccines to offer to all of the American public,” Gen. Paul Ostrowski, who oversees logistics for Operation Warp Speed, told The Washington Post.
“It’s clear that Pfizer made plans with other countries. Many have been announced. We understand those pieces,” he said.
With Pfizer’s COVID-19 vaccine on the verge of FDA approval, federal officials contacted the company last weekend to buy another 100 million doses, but the company said its current supply is already committed, the newspaper reported.
The vaccine from Pfizer and BioNTech is expected to win emergency approval within days and has been shown to be effective against COVID-19.
Pfizer added that it may be able to provide 50 million doses at the end of the second quarter and another 50 million doses during the third quarter. However, the company can’t offer anything “substantial” until next summer.
Beyond the initial 100 million doses that the U.S. has already secured, Pfizer and federal officials would need to negotiate a new, “separate and mutually acceptable agreement,” Amy Rose, a spokeswoman for Pfizer, told the newspaper.
On Dec. 8, President Donald Trump was expected to sign an executive order prioritizing vaccination for Americans first before providing doses to other countries, according to Fox News.
The order will provide guidelines to the Department of Health and Human Services, the U.S. Agency for International Development and the U.S. International Development Finance Corporation for foreign assistance with vaccines, the news outlet reported.
It’s unclear whether the executive order is related to the Pfizer issue, whether the president can prevent a private company from fulfilling contracts with other countries, and whether President-elect Joe Biden will create his own policy, according to CNBC. The order may prove to be mostly symbolic.
The FDA could issue an emergency use authorization for Pfizer’s coronavirus vaccine this week and will likely approve Moderna’s vaccine next week. The U.S. has signed a contract with Moderna for 100 million doses.
During a call with reporters on Dec. 7, a spokeswoman for the Department of Health and Human Services said, “We are confident that we will have 100 million doses of Pfizer’s vaccine as agreed to in our contract, and beyond that, we have five other vaccine candidates, including 100 million doses on the way from Moderna.”
Federal officials are counting on vaccine candidates from AstraZeneca and Johnson & Johnson to seek FDA approval in January and be ready for shipment in February.
“We could have all of them,” Moncef Slaoui, the chief science adviser for Operation Warp Speed, told The Washington Post on Dec. 7.
“And for this reason, we feel confident we could cover the needs without a specific cliff,” he said. “We have planned things in such a way as we would indeed avoid a cliff.”
This article first appeared on WebMD.com.
Can a health care worker refuse the COVID-19 vaccine?
As hospitals across the country develop their plans to vaccinate their health care employees against COVID-19, a key question has come to the fore: What if an employee – whether nurse, physician, or other health care worker – refuses to receive the vaccine? Can hospitals require their employees to be vaccinated against COVID-19? And what consequences could an employee face for refusing the vaccine?
My answer needs to be based, in part, on the law related to previous vaccines – influenza, for example – because at the time of this writing (early December 2020), no vaccine for COVID-19 has been approved, although approval of at least one vaccine is expected within a week. So there have been no offers of vaccine and refusals yet, nor are there any cases to date involving an employee who refused a COVID-19 vaccine. As of December 2020, there are no state or federal laws that either require an employee to be vaccinated against COVID-19 or that protect an employee who refuses vaccination against COVID-19. It will take a while after the vaccine is approved and distributed before refusals, reactions, policies, cases, and laws begin to emerge.
If we look at the law related to health care workers refusing to be vaccinated against the closest relative to COVID-19 – influenza – then the answer would be yes, employers can require employees to be vaccinated.
An employer can fire an employee who refuses influenza vaccination. If an employee who refused and was fired sues the employer for wrongful termination, the employee has more or less chance of success depending on the reason for refusal. Some courts and the Equal Employment Opportunity Commission have held that a refusal on religious grounds is protected by the U.S. Constitution, as in this recent case. The Constitution protects freedom to practice one’s religion. Specific religions may have a range of tenets that support refusal to be vaccinated.
A refusal on medical grounds has been successful if the medical grounds fall under the protections of the Americans with Disabilities Act but may fail when the medical grounds for the claim are not covered by the ADA.
Refusal for secular, nonmedical reasons, such as a health care worker’s policy of treating their body as their temple, has not gone over well with employers or courts. However, in at least one case, a nurse who refused vaccination on secular, nonmedical grounds won her case against her employer, on appeal. The appeals court found that the hospital violated her First Amendment rights.
Employees who refuse vaccination for religious or medical reasons still will need to take measures to protect patients and other employees from infection. An employer such as a hospital can, rather than fire the employee, offer the employee an accommodation, such as requiring that the employee wear a mask or quarantine. There are no cases that have upheld an employee’s right to refuse to wear a mask or quarantine.
The situation with the COVID-19 vaccine is different from the situation surrounding influenza vaccines. There are plenty of data on effectiveness and side effects of influenza vaccines, but there is very little evidence of short- or long-term effects of the COVID-19 vaccines currently being tested and/or considered for approval. One could argue that the process of vaccine development is the same for all virus vaccines. However, public confidence in the vaccine vetting process is not what it once was. It has been widely publicized that the COVID-19 vaccine trials have been rushed. As of December 2020, only 60% of the general population say they would take the vaccine, although researchers say confidence is increasing.
The Centers for Disease Control and Prevention has designated health care workers as first in line to get the vaccine, but some health care workers may not want to be the first to try it. A CDC survey found that 63% of health care workers polled in recent months said they would get a COVID-19 vaccine.
Unions have entered the conversation. A coalition of unions that represent health care workers said, “we need a transparent, evidence-based federal vaccine strategy based on principles of equity, safety, and priority, as well as robust efforts to address a high degree of skepticism about safety of an authorized vaccine.” The organization declined to promote a vaccine until more is known.
As of publication date, the EEOC guidance for employers responding to COVID-19 does not address vaccines.
The CDC’s Interim Guidance for Businesses and Employers Responding to Coronavirus Disease 2019, May 2020, updated Dec. 4, 2020, does not address vaccines. The CDC’s page on COVID-19 vaccination for health care workers does not address a health care worker’s refusal. The site does assure health care workers that the vaccine development process is sound: “The current vaccine safety system is strong and robust, with the capacity to effectively monitor COVID-19 vaccine safety. Existing data systems have validated analytic methods that can rapidly detect statistical signals for possible vaccine safety problems. These systems are being scaled up to fully meet the needs of the nation. Additional systems and data sources are also being developed to further enhance safety monitoring capabilities. CDC is committed to ensuring that COVID-19 vaccines are safe.”
In the coming months, government officials and vaccine manufacturers will be working to reassure the public of the safety of the vaccine and the rigor of the vaccine development process. In November 2020, National Institute of Allergy and Infectious Diseases Director Anthony Fauci, MD, told Kaiser Health News: “The company looks at the data. I look at the data. Then the company puts the data to the FDA. The FDA will make the decision to do an emergency-use authorization or a license application approval. And they have career scientists who are really independent. They’re not beholden to anybody. Then there’s another independent group, the Vaccines and Related Biological Products Advisory Committee. The FDA commissioner has vowed publicly that he will go according to the opinion of the career scientists and the advisory board.” President-elect Joe Biden said he would get a vaccine when Dr. Fauci thinks it is safe.
An employee who, after researching the vaccine and the process, still wants to refuse when offered the vaccine is not likely to be fired for that reason right away, as long as the employee takes other precautions, such as wearing a mask. If the employer does fire the employee and the employee sues the employer, it is impossible to predict how a court would decide the case.
Related legal questions may arise in the coming months. For example:
- Is an employer exempt from paying workers’ compensation to an employee who refuses to be vaccinated and then contracts the virus while on the job?
- Can a prospective employer require COVID-19 vaccination as a precondition of employment?
- Is it within a patient’s rights to receive an answer to the question: Has my health care worker been vaccinated against COVID-19?
- If a hospital allows employees to refuse vaccination and keep working, and an outbreak occurs, and it is suggested through contact tracing that unvaccinated workers infected patients, will a court hold the hospital liable for patients’ damages?
Answers to these questions are yet to be determined.
Carolyn Buppert (www.buppert.com) is an attorney and former nurse practitioner who focuses on the legal issues affecting nurse practitioners.
A version of this article originally appeared on Medscape.com.
As hospitals across the country develop their plans to vaccinate their health care employees against COVID-19, a key question has come to the fore: What if an employee – whether nurse, physician, or other health care worker – refuses to receive the vaccine? Can hospitals require their employees to be vaccinated against COVID-19? And what consequences could an employee face for refusing the vaccine?
My answer needs to be based, in part, on the law related to previous vaccines – influenza, for example – because at the time of this writing (early December 2020), no vaccine for COVID-19 has been approved, although approval of at least one vaccine is expected within a week. So there have been no offers of vaccine and refusals yet, nor are there any cases to date involving an employee who refused a COVID-19 vaccine. As of December 2020, there are no state or federal laws that either require an employee to be vaccinated against COVID-19 or that protect an employee who refuses vaccination against COVID-19. It will take a while after the vaccine is approved and distributed before refusals, reactions, policies, cases, and laws begin to emerge.
If we look at the law related to health care workers refusing to be vaccinated against the closest relative to COVID-19 – influenza – then the answer would be yes, employers can require employees to be vaccinated.
An employer can fire an employee who refuses influenza vaccination. If an employee who refused and was fired sues the employer for wrongful termination, the employee has more or less chance of success depending on the reason for refusal. Some courts and the Equal Employment Opportunity Commission have held that a refusal on religious grounds is protected by the U.S. Constitution, as in this recent case. The Constitution protects freedom to practice one’s religion. Specific religions may have a range of tenets that support refusal to be vaccinated.
A refusal on medical grounds has been successful if the medical grounds fall under the protections of the Americans with Disabilities Act but may fail when the medical grounds for the claim are not covered by the ADA.
Refusal for secular, nonmedical reasons, such as a health care worker’s policy of treating their body as their temple, has not gone over well with employers or courts. However, in at least one case, a nurse who refused vaccination on secular, nonmedical grounds won her case against her employer, on appeal. The appeals court found that the hospital violated her First Amendment rights.
Employees who refuse vaccination for religious or medical reasons still will need to take measures to protect patients and other employees from infection. An employer such as a hospital can, rather than fire the employee, offer the employee an accommodation, such as requiring that the employee wear a mask or quarantine. There are no cases that have upheld an employee’s right to refuse to wear a mask or quarantine.
The situation with the COVID-19 vaccine is different from the situation surrounding influenza vaccines. There are plenty of data on effectiveness and side effects of influenza vaccines, but there is very little evidence of short- or long-term effects of the COVID-19 vaccines currently being tested and/or considered for approval. One could argue that the process of vaccine development is the same for all virus vaccines. However, public confidence in the vaccine vetting process is not what it once was. It has been widely publicized that the COVID-19 vaccine trials have been rushed. As of December 2020, only 60% of the general population say they would take the vaccine, although researchers say confidence is increasing.
The Centers for Disease Control and Prevention has designated health care workers as first in line to get the vaccine, but some health care workers may not want to be the first to try it. A CDC survey found that 63% of health care workers polled in recent months said they would get a COVID-19 vaccine.
Unions have entered the conversation. A coalition of unions that represent health care workers said, “we need a transparent, evidence-based federal vaccine strategy based on principles of equity, safety, and priority, as well as robust efforts to address a high degree of skepticism about safety of an authorized vaccine.” The organization declined to promote a vaccine until more is known.
As of publication date, the EEOC guidance for employers responding to COVID-19 does not address vaccines.
The CDC’s Interim Guidance for Businesses and Employers Responding to Coronavirus Disease 2019, May 2020, updated Dec. 4, 2020, does not address vaccines. The CDC’s page on COVID-19 vaccination for health care workers does not address a health care worker’s refusal. The site does assure health care workers that the vaccine development process is sound: “The current vaccine safety system is strong and robust, with the capacity to effectively monitor COVID-19 vaccine safety. Existing data systems have validated analytic methods that can rapidly detect statistical signals for possible vaccine safety problems. These systems are being scaled up to fully meet the needs of the nation. Additional systems and data sources are also being developed to further enhance safety monitoring capabilities. CDC is committed to ensuring that COVID-19 vaccines are safe.”
In the coming months, government officials and vaccine manufacturers will be working to reassure the public of the safety of the vaccine and the rigor of the vaccine development process. In November 2020, National Institute of Allergy and Infectious Diseases Director Anthony Fauci, MD, told Kaiser Health News: “The company looks at the data. I look at the data. Then the company puts the data to the FDA. The FDA will make the decision to do an emergency-use authorization or a license application approval. And they have career scientists who are really independent. They’re not beholden to anybody. Then there’s another independent group, the Vaccines and Related Biological Products Advisory Committee. The FDA commissioner has vowed publicly that he will go according to the opinion of the career scientists and the advisory board.” President-elect Joe Biden said he would get a vaccine when Dr. Fauci thinks it is safe.
An employee who, after researching the vaccine and the process, still wants to refuse when offered the vaccine is not likely to be fired for that reason right away, as long as the employee takes other precautions, such as wearing a mask. If the employer does fire the employee and the employee sues the employer, it is impossible to predict how a court would decide the case.
Related legal questions may arise in the coming months. For example:
- Is an employer exempt from paying workers’ compensation to an employee who refuses to be vaccinated and then contracts the virus while on the job?
- Can a prospective employer require COVID-19 vaccination as a precondition of employment?
- Is it within a patient’s rights to receive an answer to the question: Has my health care worker been vaccinated against COVID-19?
- If a hospital allows employees to refuse vaccination and keep working, and an outbreak occurs, and it is suggested through contact tracing that unvaccinated workers infected patients, will a court hold the hospital liable for patients’ damages?
Answers to these questions are yet to be determined.
Carolyn Buppert (www.buppert.com) is an attorney and former nurse practitioner who focuses on the legal issues affecting nurse practitioners.
A version of this article originally appeared on Medscape.com.
As hospitals across the country develop their plans to vaccinate their health care employees against COVID-19, a key question has come to the fore: What if an employee – whether nurse, physician, or other health care worker – refuses to receive the vaccine? Can hospitals require their employees to be vaccinated against COVID-19? And what consequences could an employee face for refusing the vaccine?
My answer needs to be based, in part, on the law related to previous vaccines – influenza, for example – because at the time of this writing (early December 2020), no vaccine for COVID-19 has been approved, although approval of at least one vaccine is expected within a week. So there have been no offers of vaccine and refusals yet, nor are there any cases to date involving an employee who refused a COVID-19 vaccine. As of December 2020, there are no state or federal laws that either require an employee to be vaccinated against COVID-19 or that protect an employee who refuses vaccination against COVID-19. It will take a while after the vaccine is approved and distributed before refusals, reactions, policies, cases, and laws begin to emerge.
If we look at the law related to health care workers refusing to be vaccinated against the closest relative to COVID-19 – influenza – then the answer would be yes, employers can require employees to be vaccinated.
An employer can fire an employee who refuses influenza vaccination. If an employee who refused and was fired sues the employer for wrongful termination, the employee has more or less chance of success depending on the reason for refusal. Some courts and the Equal Employment Opportunity Commission have held that a refusal on religious grounds is protected by the U.S. Constitution, as in this recent case. The Constitution protects freedom to practice one’s religion. Specific religions may have a range of tenets that support refusal to be vaccinated.
A refusal on medical grounds has been successful if the medical grounds fall under the protections of the Americans with Disabilities Act but may fail when the medical grounds for the claim are not covered by the ADA.
Refusal for secular, nonmedical reasons, such as a health care worker’s policy of treating their body as their temple, has not gone over well with employers or courts. However, in at least one case, a nurse who refused vaccination on secular, nonmedical grounds won her case against her employer, on appeal. The appeals court found that the hospital violated her First Amendment rights.
Employees who refuse vaccination for religious or medical reasons still will need to take measures to protect patients and other employees from infection. An employer such as a hospital can, rather than fire the employee, offer the employee an accommodation, such as requiring that the employee wear a mask or quarantine. There are no cases that have upheld an employee’s right to refuse to wear a mask or quarantine.
The situation with the COVID-19 vaccine is different from the situation surrounding influenza vaccines. There are plenty of data on effectiveness and side effects of influenza vaccines, but there is very little evidence of short- or long-term effects of the COVID-19 vaccines currently being tested and/or considered for approval. One could argue that the process of vaccine development is the same for all virus vaccines. However, public confidence in the vaccine vetting process is not what it once was. It has been widely publicized that the COVID-19 vaccine trials have been rushed. As of December 2020, only 60% of the general population say they would take the vaccine, although researchers say confidence is increasing.
The Centers for Disease Control and Prevention has designated health care workers as first in line to get the vaccine, but some health care workers may not want to be the first to try it. A CDC survey found that 63% of health care workers polled in recent months said they would get a COVID-19 vaccine.
Unions have entered the conversation. A coalition of unions that represent health care workers said, “we need a transparent, evidence-based federal vaccine strategy based on principles of equity, safety, and priority, as well as robust efforts to address a high degree of skepticism about safety of an authorized vaccine.” The organization declined to promote a vaccine until more is known.
As of publication date, the EEOC guidance for employers responding to COVID-19 does not address vaccines.
The CDC’s Interim Guidance for Businesses and Employers Responding to Coronavirus Disease 2019, May 2020, updated Dec. 4, 2020, does not address vaccines. The CDC’s page on COVID-19 vaccination for health care workers does not address a health care worker’s refusal. The site does assure health care workers that the vaccine development process is sound: “The current vaccine safety system is strong and robust, with the capacity to effectively monitor COVID-19 vaccine safety. Existing data systems have validated analytic methods that can rapidly detect statistical signals for possible vaccine safety problems. These systems are being scaled up to fully meet the needs of the nation. Additional systems and data sources are also being developed to further enhance safety monitoring capabilities. CDC is committed to ensuring that COVID-19 vaccines are safe.”
In the coming months, government officials and vaccine manufacturers will be working to reassure the public of the safety of the vaccine and the rigor of the vaccine development process. In November 2020, National Institute of Allergy and Infectious Diseases Director Anthony Fauci, MD, told Kaiser Health News: “The company looks at the data. I look at the data. Then the company puts the data to the FDA. The FDA will make the decision to do an emergency-use authorization or a license application approval. And they have career scientists who are really independent. They’re not beholden to anybody. Then there’s another independent group, the Vaccines and Related Biological Products Advisory Committee. The FDA commissioner has vowed publicly that he will go according to the opinion of the career scientists and the advisory board.” President-elect Joe Biden said he would get a vaccine when Dr. Fauci thinks it is safe.
An employee who, after researching the vaccine and the process, still wants to refuse when offered the vaccine is not likely to be fired for that reason right away, as long as the employee takes other precautions, such as wearing a mask. If the employer does fire the employee and the employee sues the employer, it is impossible to predict how a court would decide the case.
Related legal questions may arise in the coming months. For example:
- Is an employer exempt from paying workers’ compensation to an employee who refuses to be vaccinated and then contracts the virus while on the job?
- Can a prospective employer require COVID-19 vaccination as a precondition of employment?
- Is it within a patient’s rights to receive an answer to the question: Has my health care worker been vaccinated against COVID-19?
- If a hospital allows employees to refuse vaccination and keep working, and an outbreak occurs, and it is suggested through contact tracing that unvaccinated workers infected patients, will a court hold the hospital liable for patients’ damages?
Answers to these questions are yet to be determined.
Carolyn Buppert (www.buppert.com) is an attorney and former nurse practitioner who focuses on the legal issues affecting nurse practitioners.
A version of this article originally appeared on Medscape.com.
Extended virus shedding after COVID-19 in some patients with cancer
Live-virus shedding was detected in 18 patients who had undergone hematopoietic stem cell transplants or chimeric antigen receptor (CAR) T-cell therapy and in 2 patients with lymphoma.
The finding was reported Dec. 1 in a research letter in the New England Journal of Medicine.
Individuals who are otherwise healthy when they get COVID-19 are “no longer infectious after the first week of illness,” said lead author Mini Kamboj, MD, chief medical epidemiologist, Memorial Sloan Kettering Cancer Center, New York.
“We need to keep an open mind about how [much] longer immunocompromised patients could pose an infection risk to others,” she added.
Dr. Kamboj said in an interview that her team’s previous experience with stem cell transplant recipients had suggested that severely immunocompromised patients shed other viruses (such as respiratory syncytial virus, parainfluenza, and influenza) for longer periods of time than do healthy controls.
Based on their latest findings, the investigators suggest that current guidelines for COVID-19 isolation precautions may need to be revised for immunocompromised patients. Even if only a small proportion of patients with cancer who have COVID-19 remain contagious for prolonged periods of time, “it’s a residual risk that we need to address,” Dr. Kamboj said.
Dr. Kamboj also suggested that physicians follow test-based criteria to determine when a patient undergoing transplant can be released from isolation.
Shedding of viable virus
For this study, the investigators used cell cultures to detect viable virus in serially collected nasopharyngeal and sputum samples from 20 immunocompromised patients who had COVID-19 (diagnosed with COVID-19 between March 10 and April 20).
Patients had lymphoma (n = 8), multiple myeloma (n= 7), acute leukemia/myelodysplastic syndrome (n = 4), and chronic leukemia (n = 1). There were 16 patients who had undergone transplant, 2 who had received CAR T-cell therapy, and 2 who had received other therapy.
There were 15 patients receiving active treatment or chemotherapy, and 11 developed severe COVID-19 infection.
In total, 78 respiratory samples were collected.
“Viral RNA was detected for up to 78 days after the onset of symptoms,” the researchers reported, “[and] viable virus was detected in 10 of 14 nasopharyngeal samples (71%) that were available from the first day of laboratory testing.”
Five patients were followed up, and from these patients, the team grew virus in culture for up to 61 days after symptom onset. Two among this small group of five patients had received allogenic hematopoietic stem cell transplantation and one patient had been treated with CAR T-cell therapy within the previous 6 months. This patient remained seronegative for antibodies to the coronavirus.
For 11 patients, the team obtained serial sample genomes and found that “each patient was infected by a distinct virus and there were no major changes in the consensus sequences of the original serial specimens or cultured isolates.” These findings were consistent with persistent infection, they noted.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Live-virus shedding was detected in 18 patients who had undergone hematopoietic stem cell transplants or chimeric antigen receptor (CAR) T-cell therapy and in 2 patients with lymphoma.
The finding was reported Dec. 1 in a research letter in the New England Journal of Medicine.
Individuals who are otherwise healthy when they get COVID-19 are “no longer infectious after the first week of illness,” said lead author Mini Kamboj, MD, chief medical epidemiologist, Memorial Sloan Kettering Cancer Center, New York.
“We need to keep an open mind about how [much] longer immunocompromised patients could pose an infection risk to others,” she added.
Dr. Kamboj said in an interview that her team’s previous experience with stem cell transplant recipients had suggested that severely immunocompromised patients shed other viruses (such as respiratory syncytial virus, parainfluenza, and influenza) for longer periods of time than do healthy controls.
Based on their latest findings, the investigators suggest that current guidelines for COVID-19 isolation precautions may need to be revised for immunocompromised patients. Even if only a small proportion of patients with cancer who have COVID-19 remain contagious for prolonged periods of time, “it’s a residual risk that we need to address,” Dr. Kamboj said.
Dr. Kamboj also suggested that physicians follow test-based criteria to determine when a patient undergoing transplant can be released from isolation.
Shedding of viable virus
For this study, the investigators used cell cultures to detect viable virus in serially collected nasopharyngeal and sputum samples from 20 immunocompromised patients who had COVID-19 (diagnosed with COVID-19 between March 10 and April 20).
Patients had lymphoma (n = 8), multiple myeloma (n= 7), acute leukemia/myelodysplastic syndrome (n = 4), and chronic leukemia (n = 1). There were 16 patients who had undergone transplant, 2 who had received CAR T-cell therapy, and 2 who had received other therapy.
There were 15 patients receiving active treatment or chemotherapy, and 11 developed severe COVID-19 infection.
In total, 78 respiratory samples were collected.
“Viral RNA was detected for up to 78 days after the onset of symptoms,” the researchers reported, “[and] viable virus was detected in 10 of 14 nasopharyngeal samples (71%) that were available from the first day of laboratory testing.”
Five patients were followed up, and from these patients, the team grew virus in culture for up to 61 days after symptom onset. Two among this small group of five patients had received allogenic hematopoietic stem cell transplantation and one patient had been treated with CAR T-cell therapy within the previous 6 months. This patient remained seronegative for antibodies to the coronavirus.
For 11 patients, the team obtained serial sample genomes and found that “each patient was infected by a distinct virus and there were no major changes in the consensus sequences of the original serial specimens or cultured isolates.” These findings were consistent with persistent infection, they noted.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Live-virus shedding was detected in 18 patients who had undergone hematopoietic stem cell transplants or chimeric antigen receptor (CAR) T-cell therapy and in 2 patients with lymphoma.
The finding was reported Dec. 1 in a research letter in the New England Journal of Medicine.
Individuals who are otherwise healthy when they get COVID-19 are “no longer infectious after the first week of illness,” said lead author Mini Kamboj, MD, chief medical epidemiologist, Memorial Sloan Kettering Cancer Center, New York.
“We need to keep an open mind about how [much] longer immunocompromised patients could pose an infection risk to others,” she added.
Dr. Kamboj said in an interview that her team’s previous experience with stem cell transplant recipients had suggested that severely immunocompromised patients shed other viruses (such as respiratory syncytial virus, parainfluenza, and influenza) for longer periods of time than do healthy controls.
Based on their latest findings, the investigators suggest that current guidelines for COVID-19 isolation precautions may need to be revised for immunocompromised patients. Even if only a small proportion of patients with cancer who have COVID-19 remain contagious for prolonged periods of time, “it’s a residual risk that we need to address,” Dr. Kamboj said.
Dr. Kamboj also suggested that physicians follow test-based criteria to determine when a patient undergoing transplant can be released from isolation.
Shedding of viable virus
For this study, the investigators used cell cultures to detect viable virus in serially collected nasopharyngeal and sputum samples from 20 immunocompromised patients who had COVID-19 (diagnosed with COVID-19 between March 10 and April 20).
Patients had lymphoma (n = 8), multiple myeloma (n= 7), acute leukemia/myelodysplastic syndrome (n = 4), and chronic leukemia (n = 1). There were 16 patients who had undergone transplant, 2 who had received CAR T-cell therapy, and 2 who had received other therapy.
There were 15 patients receiving active treatment or chemotherapy, and 11 developed severe COVID-19 infection.
In total, 78 respiratory samples were collected.
“Viral RNA was detected for up to 78 days after the onset of symptoms,” the researchers reported, “[and] viable virus was detected in 10 of 14 nasopharyngeal samples (71%) that were available from the first day of laboratory testing.”
Five patients were followed up, and from these patients, the team grew virus in culture for up to 61 days after symptom onset. Two among this small group of five patients had received allogenic hematopoietic stem cell transplantation and one patient had been treated with CAR T-cell therapy within the previous 6 months. This patient remained seronegative for antibodies to the coronavirus.
For 11 patients, the team obtained serial sample genomes and found that “each patient was infected by a distinct virus and there were no major changes in the consensus sequences of the original serial specimens or cultured isolates.” These findings were consistent with persistent infection, they noted.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Upper GI bleeds in COVID-19 not related to increased mortality
A Spanish survey of COVID-19 patients suggests that upper gastrointestinal bleeding (UGB) does not affect in-hospital mortality. It also found that fewer COVID-19–positive patients underwent endoscopies, but there was no statistically significant difference in in-hospital mortality outcome as a result of delays.
“In-hospital mortality in COVID-19 patients with upper-GI bleeding seemed to be more influenced by COVID-19 than by upper-GI bleeding, and that’s something I think is important for us to know,” Gyanprakash Ketwaroo, MD, associate professor at Baylor College of Medicine, Houston, said in an interview. Dr. Ketwaroo was not involved in the study.
The results weren’t a surprise, but they do provide some reassurance. “It’s probably what I expected. Initially, we thought there might be some COVID-19 related (GI) lesions, but that didn’t seem to be borne out. So we thought the bleeding was related to (the patient) being in a hospital or the typical reasons for bleeding. It’s also what I expected that less endoscopies would be performed in these patients, and even though fewer endoscopies were performed, the outcomes were still similar. I think it’s what most people expected,” said Dr. Ketwaroo.
The study was published online Nov. 25 in the Journal of Clinical Gastroenterology, and led by Rebeca González González, MD, of Severo Ochoa University Hospital in Leganés, Madrid, and Pascual Piñera-Salmerón, MD, of Reina Sofia University General Hospital in Murcia, Spain. The researchers retrospectively analyzed data on 71,904 COVID-19 patients at 62 emergency departments in Spain, and compared 83 patients who had COVID-19 and UGB to two control groups: 249 randomly selected COVID-19 patients without UGB, and 249 randomly selected non-COVID-19 patients with UGB.
They found that 1.11% of COVID-19 patients presented with UGB, compared with 1.78% of non-COVID-19 patients at emergency departments. In patients with COVID-19, risk of UGB was associated with hemoglobin values < 10 g/L (odds ratio [OR], 34.255, 95% confidence interval [CI], 12.752-92.021), abdominal pain (OR, 11.4; 95% CI, 5.092-25.944), and systolic blood pressure < 90 mm Hg (OR, 11.096; 95% CI, 2.975-41.390).
Compared with non-COVID-19 patients with UGB, those COVID-19 patients with UGB were more likely to have interstitial lung infiltrates (OR, 66.42; 95% CI, 15.364-287.223) and ground-glass opacities (OR, 21.27; 95% CI, 9.720-46.567) in chest radiograph, as well as fever (OR, 34.67; 95% CI, 11.719-102.572) and cough (OR, 26.4; 95% CI, 8.845-78.806).
Gastroscopy and endoscopic procedures were lower in patients with COVID-19 than in the general population (gastroscopy OR, 0.269; 95% CI, 0.160-0.453: endoscopy OR, 0.26; 95% CI, 0.165-0.623). There was no difference between the two groups with respect to endoscopic findings. After adjustment for age and sex, the only significant difference between COVID-19 patients with UGB and COVID-19 patients without UGB was a higher rate of intensive care unit admission (OR, 2.98; 95% CI, 1.16-7.65). Differences between COVID-19 patients with UGB and non–COVID-19 patients with UGB included higher rates of ICU admission (OR, 3.29; 95% CI, 1.28-8.47), prolonged hospitalizations (OR, 2.02; 95% CI, 1.15-3.55), and in-hospital mortality (OR, 2.05; 95% CI, 1.09-3.86).
UGB development was not associated with increased in-hospital mortality in COVID-19 patients (OR, 1.14; 95% CI, 0.59-2.19).
A limitation to the study it was that it was performed in Spain, where endoscopies are performed in the emergency department, and where there are different thresholds for admission to the intensive care unit than in the United States.
The authors did not report a funding source. Dr. Ketwaroo has no relevant financial disclosures.
SOURCE: González González R et al. J Clin Gastroenterol. 10.1097/MCG.0000000000001465.
A Spanish survey of COVID-19 patients suggests that upper gastrointestinal bleeding (UGB) does not affect in-hospital mortality. It also found that fewer COVID-19–positive patients underwent endoscopies, but there was no statistically significant difference in in-hospital mortality outcome as a result of delays.
“In-hospital mortality in COVID-19 patients with upper-GI bleeding seemed to be more influenced by COVID-19 than by upper-GI bleeding, and that’s something I think is important for us to know,” Gyanprakash Ketwaroo, MD, associate professor at Baylor College of Medicine, Houston, said in an interview. Dr. Ketwaroo was not involved in the study.
The results weren’t a surprise, but they do provide some reassurance. “It’s probably what I expected. Initially, we thought there might be some COVID-19 related (GI) lesions, but that didn’t seem to be borne out. So we thought the bleeding was related to (the patient) being in a hospital or the typical reasons for bleeding. It’s also what I expected that less endoscopies would be performed in these patients, and even though fewer endoscopies were performed, the outcomes were still similar. I think it’s what most people expected,” said Dr. Ketwaroo.
The study was published online Nov. 25 in the Journal of Clinical Gastroenterology, and led by Rebeca González González, MD, of Severo Ochoa University Hospital in Leganés, Madrid, and Pascual Piñera-Salmerón, MD, of Reina Sofia University General Hospital in Murcia, Spain. The researchers retrospectively analyzed data on 71,904 COVID-19 patients at 62 emergency departments in Spain, and compared 83 patients who had COVID-19 and UGB to two control groups: 249 randomly selected COVID-19 patients without UGB, and 249 randomly selected non-COVID-19 patients with UGB.
They found that 1.11% of COVID-19 patients presented with UGB, compared with 1.78% of non-COVID-19 patients at emergency departments. In patients with COVID-19, risk of UGB was associated with hemoglobin values < 10 g/L (odds ratio [OR], 34.255, 95% confidence interval [CI], 12.752-92.021), abdominal pain (OR, 11.4; 95% CI, 5.092-25.944), and systolic blood pressure < 90 mm Hg (OR, 11.096; 95% CI, 2.975-41.390).
Compared with non-COVID-19 patients with UGB, those COVID-19 patients with UGB were more likely to have interstitial lung infiltrates (OR, 66.42; 95% CI, 15.364-287.223) and ground-glass opacities (OR, 21.27; 95% CI, 9.720-46.567) in chest radiograph, as well as fever (OR, 34.67; 95% CI, 11.719-102.572) and cough (OR, 26.4; 95% CI, 8.845-78.806).
Gastroscopy and endoscopic procedures were lower in patients with COVID-19 than in the general population (gastroscopy OR, 0.269; 95% CI, 0.160-0.453: endoscopy OR, 0.26; 95% CI, 0.165-0.623). There was no difference between the two groups with respect to endoscopic findings. After adjustment for age and sex, the only significant difference between COVID-19 patients with UGB and COVID-19 patients without UGB was a higher rate of intensive care unit admission (OR, 2.98; 95% CI, 1.16-7.65). Differences between COVID-19 patients with UGB and non–COVID-19 patients with UGB included higher rates of ICU admission (OR, 3.29; 95% CI, 1.28-8.47), prolonged hospitalizations (OR, 2.02; 95% CI, 1.15-3.55), and in-hospital mortality (OR, 2.05; 95% CI, 1.09-3.86).
UGB development was not associated with increased in-hospital mortality in COVID-19 patients (OR, 1.14; 95% CI, 0.59-2.19).
A limitation to the study it was that it was performed in Spain, where endoscopies are performed in the emergency department, and where there are different thresholds for admission to the intensive care unit than in the United States.
The authors did not report a funding source. Dr. Ketwaroo has no relevant financial disclosures.
SOURCE: González González R et al. J Clin Gastroenterol. 10.1097/MCG.0000000000001465.
A Spanish survey of COVID-19 patients suggests that upper gastrointestinal bleeding (UGB) does not affect in-hospital mortality. It also found that fewer COVID-19–positive patients underwent endoscopies, but there was no statistically significant difference in in-hospital mortality outcome as a result of delays.
“In-hospital mortality in COVID-19 patients with upper-GI bleeding seemed to be more influenced by COVID-19 than by upper-GI bleeding, and that’s something I think is important for us to know,” Gyanprakash Ketwaroo, MD, associate professor at Baylor College of Medicine, Houston, said in an interview. Dr. Ketwaroo was not involved in the study.
The results weren’t a surprise, but they do provide some reassurance. “It’s probably what I expected. Initially, we thought there might be some COVID-19 related (GI) lesions, but that didn’t seem to be borne out. So we thought the bleeding was related to (the patient) being in a hospital or the typical reasons for bleeding. It’s also what I expected that less endoscopies would be performed in these patients, and even though fewer endoscopies were performed, the outcomes were still similar. I think it’s what most people expected,” said Dr. Ketwaroo.
The study was published online Nov. 25 in the Journal of Clinical Gastroenterology, and led by Rebeca González González, MD, of Severo Ochoa University Hospital in Leganés, Madrid, and Pascual Piñera-Salmerón, MD, of Reina Sofia University General Hospital in Murcia, Spain. The researchers retrospectively analyzed data on 71,904 COVID-19 patients at 62 emergency departments in Spain, and compared 83 patients who had COVID-19 and UGB to two control groups: 249 randomly selected COVID-19 patients without UGB, and 249 randomly selected non-COVID-19 patients with UGB.
They found that 1.11% of COVID-19 patients presented with UGB, compared with 1.78% of non-COVID-19 patients at emergency departments. In patients with COVID-19, risk of UGB was associated with hemoglobin values < 10 g/L (odds ratio [OR], 34.255, 95% confidence interval [CI], 12.752-92.021), abdominal pain (OR, 11.4; 95% CI, 5.092-25.944), and systolic blood pressure < 90 mm Hg (OR, 11.096; 95% CI, 2.975-41.390).
Compared with non-COVID-19 patients with UGB, those COVID-19 patients with UGB were more likely to have interstitial lung infiltrates (OR, 66.42; 95% CI, 15.364-287.223) and ground-glass opacities (OR, 21.27; 95% CI, 9.720-46.567) in chest radiograph, as well as fever (OR, 34.67; 95% CI, 11.719-102.572) and cough (OR, 26.4; 95% CI, 8.845-78.806).
Gastroscopy and endoscopic procedures were lower in patients with COVID-19 than in the general population (gastroscopy OR, 0.269; 95% CI, 0.160-0.453: endoscopy OR, 0.26; 95% CI, 0.165-0.623). There was no difference between the two groups with respect to endoscopic findings. After adjustment for age and sex, the only significant difference between COVID-19 patients with UGB and COVID-19 patients without UGB was a higher rate of intensive care unit admission (OR, 2.98; 95% CI, 1.16-7.65). Differences between COVID-19 patients with UGB and non–COVID-19 patients with UGB included higher rates of ICU admission (OR, 3.29; 95% CI, 1.28-8.47), prolonged hospitalizations (OR, 2.02; 95% CI, 1.15-3.55), and in-hospital mortality (OR, 2.05; 95% CI, 1.09-3.86).
UGB development was not associated with increased in-hospital mortality in COVID-19 patients (OR, 1.14; 95% CI, 0.59-2.19).
A limitation to the study it was that it was performed in Spain, where endoscopies are performed in the emergency department, and where there are different thresholds for admission to the intensive care unit than in the United States.
The authors did not report a funding source. Dr. Ketwaroo has no relevant financial disclosures.
SOURCE: González González R et al. J Clin Gastroenterol. 10.1097/MCG.0000000000001465.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Medical societies waive fees, weigh other options during pandemic
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
Are pregnant women with COVID-19 at greater risk for severe illness?
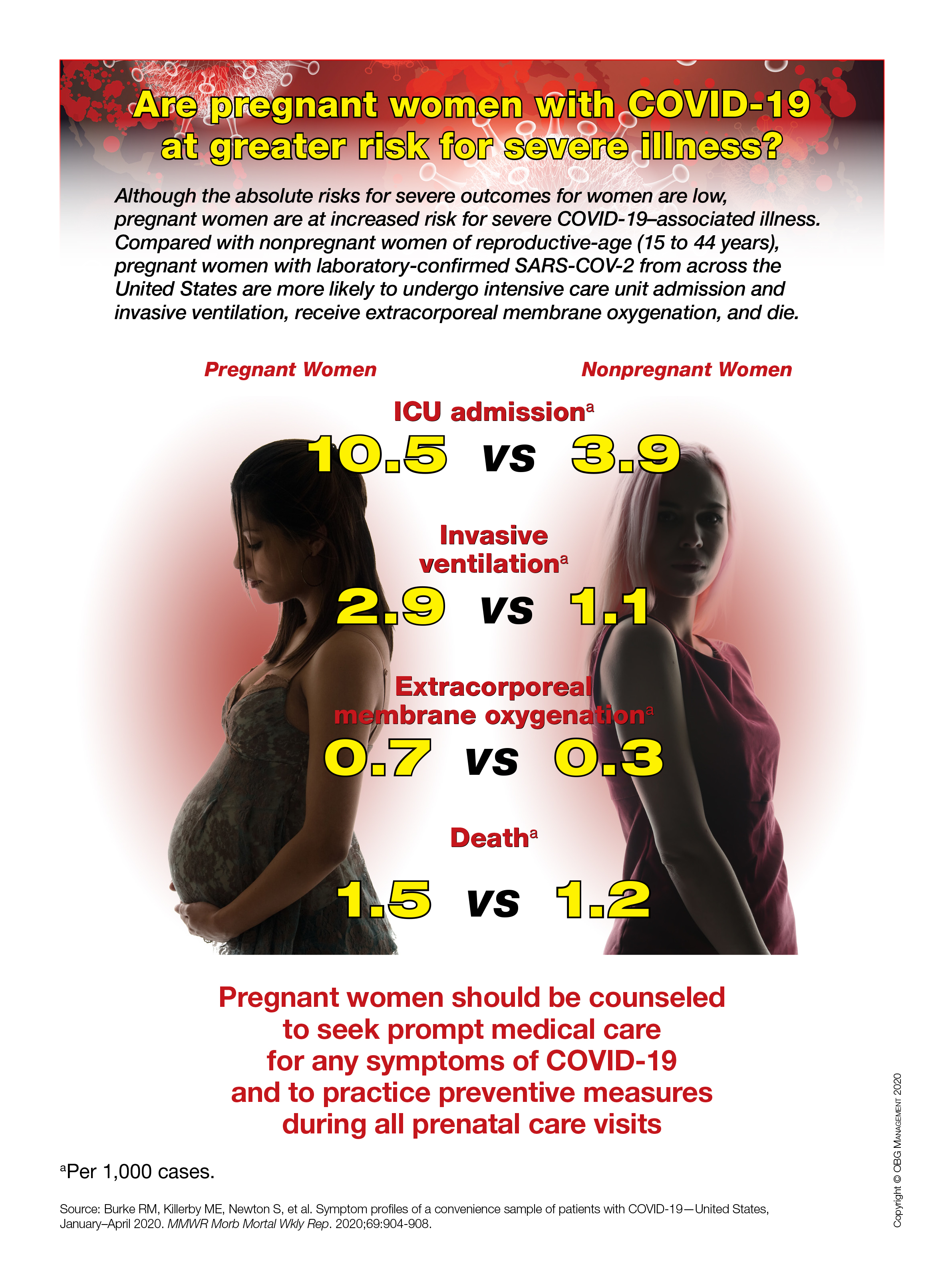
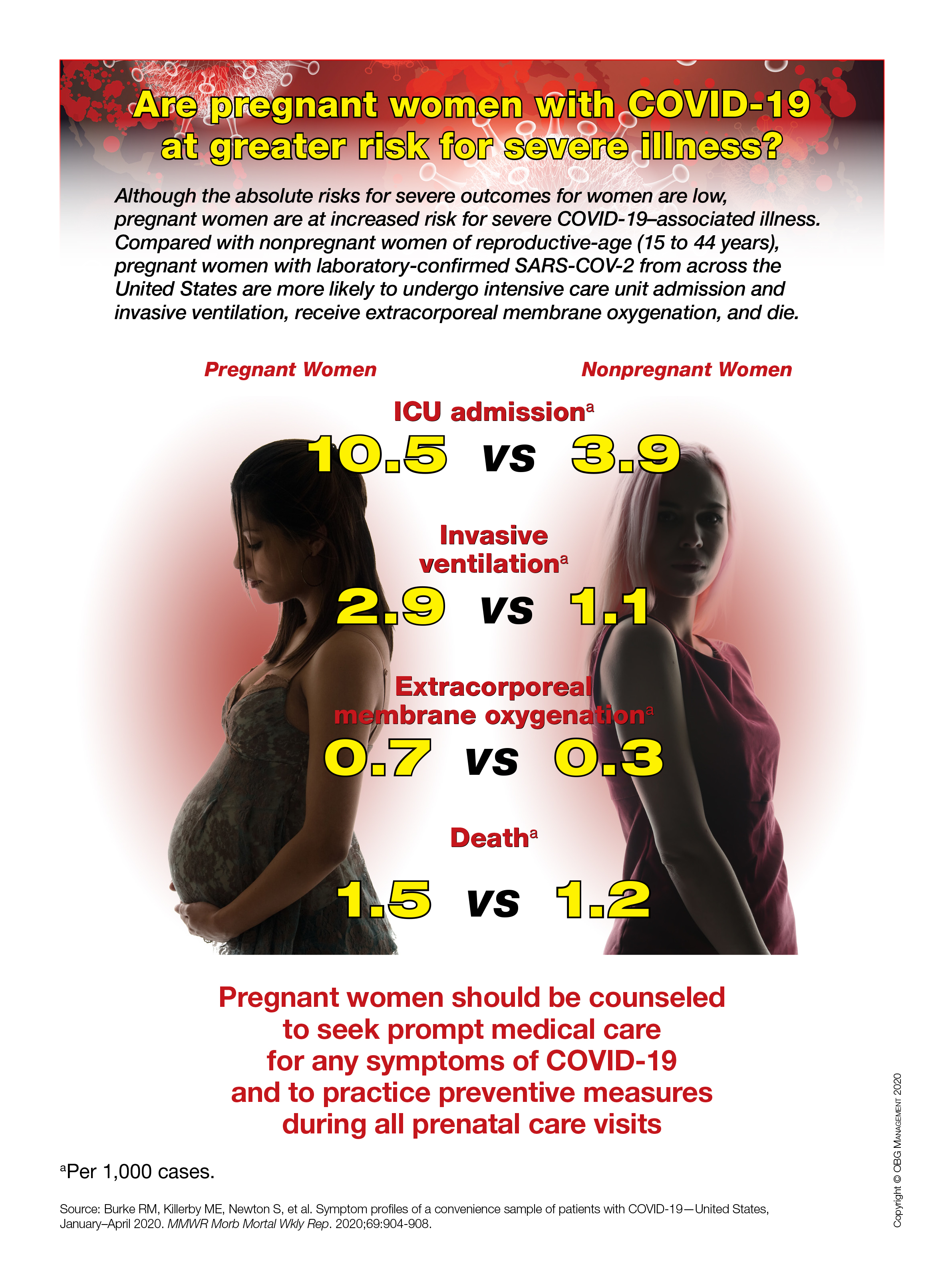
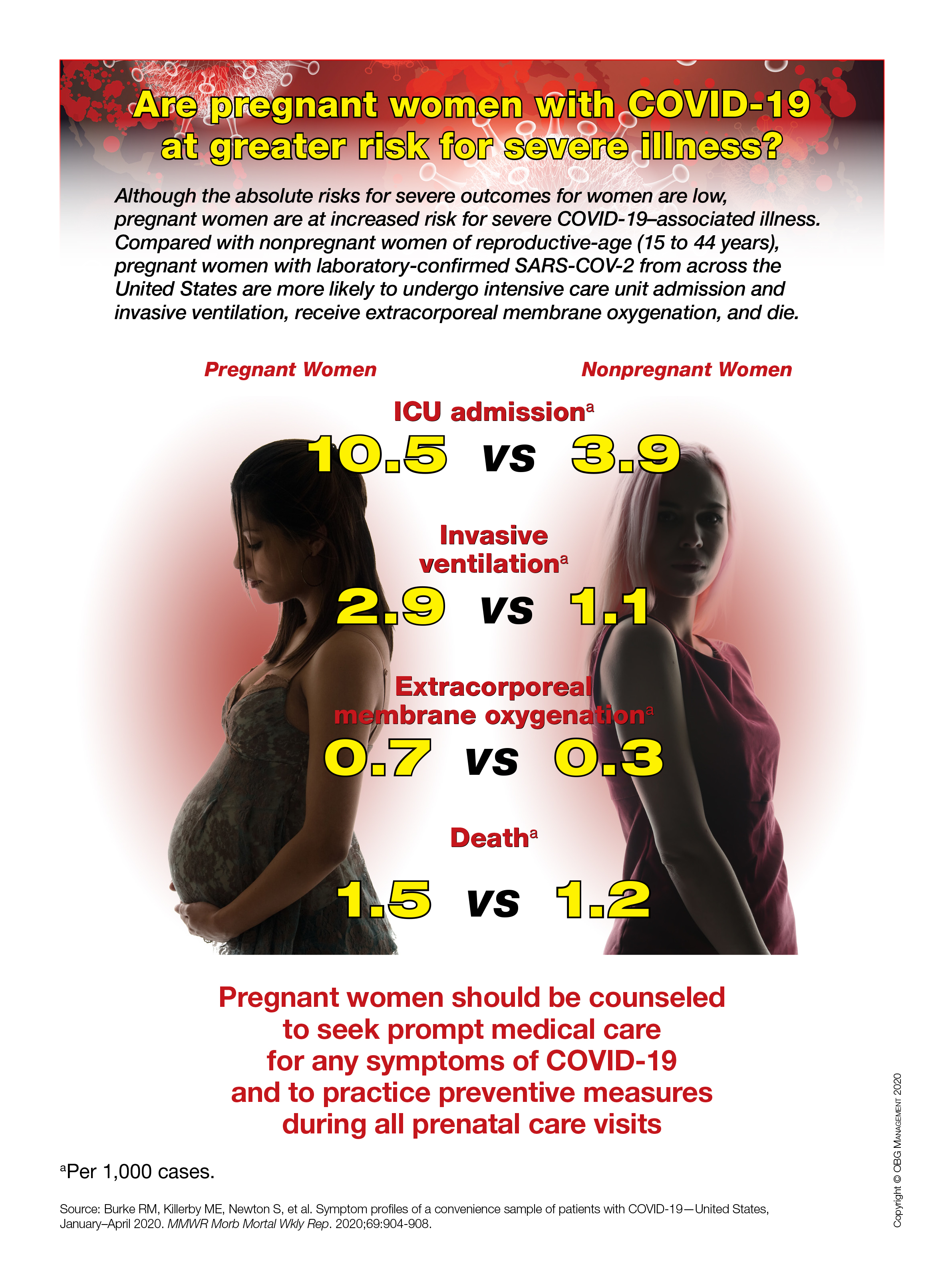
Children and school during the pandemic: What’s the answer?
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
FROM ESPID 2020
Prioritize COVID-19 vaccination in both types of diabetes, say docs
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.