User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Doctors have failed them, say those with transgender regret
In a unique Zoom conference,
The forum was convened on what was dubbed #DetransitionAwarenessDay by Genspect, a parent-based organization that seeks to put the brakes on medical transitions for children and adolescents. The group has doubts about the gender-affirming care model supported by the World Professional Association for Transgender Health, the American Medical Association, the American Academy of Pediatrics, and other medical groups.
“Affirmative” medical care is defined as treatment with puberty blockers and cross-sex hormones for those with gender dysphoria to transition to the opposite sex and is often followed by gender reassignment surgery. However, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed for those under aged 18, in particular, with several countries pulling back on medical treatment and instead emphasizing psychotherapy first.
The purpose of the second annual Genspect meeting was to shed light on the experiences of individuals who have detransitioned – those that identified as transgender and transitioned, but then decided to end their medical transition. People logged on from all over the United States, Canada, New Zealand, Australia, the United Kingdom, Germany, Spain, Chile, and Brazil, among other countries.
“This is a minority within a minority,” said Genspect advisor Stella O’Malley, adding that the first meeting in 2021 was held because “too many people were dismissing the stories of the detransitioners.” Ms. O’Malley is a psychotherapist, a clinical advisor to the Society for Evidence-Based Gender Medicine, and a founding member of the International Association of Therapists for Desisters and Detransitioners.
“It’s become blindingly obvious over the last year that ... ‘detrans’ is a huge part of the trans phenomenon,” said Ms. O’Malley, adding that detransitioners have been “undermined and dismissed.”
Laura Edwards-Leeper, PhD (@DrLauraEL), a prominent gender therapist who has recently expressed concern regarding adequate gatekeeping when treating youth with gender dysphoria, agreed.
She tweeted: “You simply can’t call yourself a legit gender provider if you don’t believe that detransitioners exist. As part of the informed consent process for transitioning, it is unethical to not discuss this possibility with young people.” Dr. Edwards-Leeper is professor emeritus at Pacific University in Hillsboro, Ore.
Speakers in the forum largely offered experiences, not data. They pointed out that there has been little to no study of detransition, but all testified that it was less rare than it has been portrayed by the transgender community.
Struggles with going back
“There are so many reasons why people detransition,” said Sinead Watson, aged 30, a Genspect advisor who transitioned from female to male, starting in 2015, and who decided to detransition in 2019. Citing a study by Lisa Littman, MD, MPH, published in 2021, Ms. Watson said the most common reasons for detransitioning were realizing that gender dysphoria was caused by other issues; internal homophobia; and the unbearable nature of transphobia.
Ms. Watson said the hardest part of detransitioning was admitting to herself that her transition had been a mistake. “It’s embarrassing and you feel ashamed and guilty,” she said, adding that it may mean losing friends who now regard you as a “bigot, while you’re also dealing with transition regret.”
“It’s a living hell, especially when none of your therapists or counselors will listen to you,” she said. “Detransitioning isn’t fun.”
Carol (@sourpatches2077) said she knew for a year that her transition had been a mistake.
“The biggest part was I couldn’t tell my family,” said Carol, who identifies as a lesbian. “I put them through so much. It seems ridiculous to go: ‘Oops, I made this huge [expletive] mistake,’ ” she said, describing the moment she did tell them as “devastating.”
Grace (@hormonehangover) said she remembers finally hitting a moment of “undeniability” some years after transitioning. “I accept it, I’ve ruined my life, this is wrong,” she remembers thinking. “It was devastating, but I couldn’t deny it anymore.”
Don’t trust therapists
People experiencing feelings of unease “need a therapist who will listen to them,” said Ms. Watson. When she first detransitioned, her therapists treated her badly. “They just didn’t want to speak about detransition,” she said, adding that “it was like a kick in the stomach.”
Ms. Watson said she’d like to see more training about detransition, but also on “preventative techniques,” adding that many people transition who should not. “I don’t want more detransitioners – I want less.
“In order for that to happen, we need to treat people with gender dysphoria properly,” said Ms. Watson, adding that the affirmative model is “disgusting, and that’s what needs to change.”
“I would tell somebody to not go to a therapist,” said Carol. Identifying as a butch lesbian, she felt like her therapists had pushed her into transitioning to male. “The No. 1 thing not understood by the mental health professionals is that the vast majority of homosexuals were gender-nonconforming children.” She added that this is especially true of butch lesbians.
Therapists – and doctors – also need to acknowledge both the trauma of transition and detransition, she said.
Kaiser, where she had transitioned, offered her breast reconstruction. Carol said it felt demeaning. “Like you’re Mr. Potatohead: ‘Here, we can just ... put on some new parts and you’re good to go.’ ”
“Doctors are concretizing transient obsessions,” said Helena Kerschner (@lacroicsz), quoting a chatroom user.
Ms. Kerschner gave a presentation on “fandom”: becoming obsessed with a movie, book, TV show, musician, or celebrity, spending every waking hour chatting online or writing fan fiction, or attempting to interact with the celebrity online. It’s a fantasy-dominated world and “the vast majority” of participants are teenage girls who are “identifying as trans,” in part, because they are fed a community-reinforced message that it’s better to be a boy.
Therapists and physicians who help them transition “are harming them for life based on something they would have grown out of or overcome without the permanent damage,” Ms. Kerschner added.
Doctors ‘gaslighting’ people into believing that transition is the answer
A pervasive theme during the webinar was that many people are being misdiagnosed with gender dysphoria, which may not be resolved by medical transition.
Allie, a 22-year-old who stopped taking testosterone after 1½ years, said she initially started the transition to male when she gave up trying to figure out why she could not identify with, or befriend, women, and after a childhood and adolescence spent mostly in the company of boys and being more interested in traditionally male activities.
She endured sexual abuse as a teenager and her parents divorced while she was in high school. Allie also had multiple suicide attempts and many incidents of self-harm. When she decided to transition, at age 18, she went to a private clinic and received cross-sex hormones within a few months of her first and only 30-minute consultation. “There was no explorative therapy,” she said, adding that she was never given a formal diagnosis of gender dysphoria.
For the first year, she said she was “over the freaking moon” because she felt like it was the answer. But things started to unravel while she attended university, and she attempted suicide attempt at age 20. A social worker at the school identified her symptoms – which had been the same since childhood – as autism. She then decided to cease her transition.
Another detransitioner, Laura Becker, said it took 5 years after her transition to recognize that she had undiagnosed PTSD from emotional and psychiatric abuse. Despite a history of substance abuse, self-harm, suicidal ideation, and other mental health issues, she was given testosterone and had a double mastectomy at age 20. She became fixated on gay men, which devolved into a methamphetamine- and crack-fueled relationship with a man she met on the gay dating platform Grindr.
“No one around me knew any better or knew how to help, including the medical professionals who performed the mastectomy and who casually signed off and administered my medical transition,” she said.
Once she was aware of her PTSD she started to detransition, which itself was traumatic, said Laura.
Limpida, aged 24, said he felt pushed into transitioning after seeking help at a Planned Parenthood clinic. He identified as trans at age 15 and spent years attempting to be a woman socially, but every step made him feel more miserable, he said. When he went to the clinic at age 21 to get estrogen, he said he felt like the staff was dismissive of his mental health concerns – including that he was suicidal, had substance abuse, and was severely depressed. He was told he was the “perfect candidate” for transitioning.
A year later, he said he felt worse. The nurse suggested he seek out surgery. After Limpida researched what was involved, he decided to detransition. He has since received an autism diagnosis.
Robin, also aged 24, said the idea of surgery had helped push him into detransitioning, which began in 2020 after 4 years of estrogen. He said he had always been gender nonconforming and knew he was gay at an early age. He believes that gender-nonconforming people are “gaslighted” into thinking that transitioning is the answer.
Lack of evidence-based, informed consent
Michelle Alleva, who stopped identifying as transgender in 2020 but had ceased testosterone 4 years earlier because of side effects, cited what she called a lack of evidence base for the effectiveness and safety of medical transitions.
“You need to have a really, really good evidence base in place if you’re going straight to an invasive treatment that is going to cause permanent changes to your body,” she said.
Access to medical transition used to involve more “gatekeeping” through mental health evaluations and other interventions, she said, but there has been a shift from treating what was considered a psychiatric issue to essentially affirming an identity.
“This shift was activist driven, not evidence based,” she emphasized.
Most studies showing satisfaction with transition only involve a few years of follow-up, she said. She added that the longest follow-up study of transition, published in 2011 and spanning 30 years, showed that the suicide rate 10-15 years post surgery was 20 times higher than the general population.
Studies of regret were primarily conducted before the rapid increase in the number of trans-identifying individuals, she said, which makes it hard to draw conclusions about pediatric transition. Getting estimates on this population is difficult because so many who detransition do not tell their clinicians, and many studies have short follow-up times or a high loss to follow-up.
Ms. Alleva also took issue with the notion that physicians were offering true informed consent, noting that it’s not possible to know if someone is psychologically sound if they haven’t had a thorough mental health evaluation and that there are so many unknowns with medical transition, including that many of the therapies are not approved for the uses being employed.
With regret on the rise, “we need professionals that are prepared for detransitioners,” said Ms. Alleva. “Some of us have lost trust in health care professionals as a result of our experience.”
“It’s a huge feeling of institutional betrayal,” said Grace.
A version of this article first appeared on Medscape.com.
In a unique Zoom conference,
The forum was convened on what was dubbed #DetransitionAwarenessDay by Genspect, a parent-based organization that seeks to put the brakes on medical transitions for children and adolescents. The group has doubts about the gender-affirming care model supported by the World Professional Association for Transgender Health, the American Medical Association, the American Academy of Pediatrics, and other medical groups.
“Affirmative” medical care is defined as treatment with puberty blockers and cross-sex hormones for those with gender dysphoria to transition to the opposite sex and is often followed by gender reassignment surgery. However, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed for those under aged 18, in particular, with several countries pulling back on medical treatment and instead emphasizing psychotherapy first.
The purpose of the second annual Genspect meeting was to shed light on the experiences of individuals who have detransitioned – those that identified as transgender and transitioned, but then decided to end their medical transition. People logged on from all over the United States, Canada, New Zealand, Australia, the United Kingdom, Germany, Spain, Chile, and Brazil, among other countries.
“This is a minority within a minority,” said Genspect advisor Stella O’Malley, adding that the first meeting in 2021 was held because “too many people were dismissing the stories of the detransitioners.” Ms. O’Malley is a psychotherapist, a clinical advisor to the Society for Evidence-Based Gender Medicine, and a founding member of the International Association of Therapists for Desisters and Detransitioners.
“It’s become blindingly obvious over the last year that ... ‘detrans’ is a huge part of the trans phenomenon,” said Ms. O’Malley, adding that detransitioners have been “undermined and dismissed.”
Laura Edwards-Leeper, PhD (@DrLauraEL), a prominent gender therapist who has recently expressed concern regarding adequate gatekeeping when treating youth with gender dysphoria, agreed.
She tweeted: “You simply can’t call yourself a legit gender provider if you don’t believe that detransitioners exist. As part of the informed consent process for transitioning, it is unethical to not discuss this possibility with young people.” Dr. Edwards-Leeper is professor emeritus at Pacific University in Hillsboro, Ore.
Speakers in the forum largely offered experiences, not data. They pointed out that there has been little to no study of detransition, but all testified that it was less rare than it has been portrayed by the transgender community.
Struggles with going back
“There are so many reasons why people detransition,” said Sinead Watson, aged 30, a Genspect advisor who transitioned from female to male, starting in 2015, and who decided to detransition in 2019. Citing a study by Lisa Littman, MD, MPH, published in 2021, Ms. Watson said the most common reasons for detransitioning were realizing that gender dysphoria was caused by other issues; internal homophobia; and the unbearable nature of transphobia.
Ms. Watson said the hardest part of detransitioning was admitting to herself that her transition had been a mistake. “It’s embarrassing and you feel ashamed and guilty,” she said, adding that it may mean losing friends who now regard you as a “bigot, while you’re also dealing with transition regret.”
“It’s a living hell, especially when none of your therapists or counselors will listen to you,” she said. “Detransitioning isn’t fun.”
Carol (@sourpatches2077) said she knew for a year that her transition had been a mistake.
“The biggest part was I couldn’t tell my family,” said Carol, who identifies as a lesbian. “I put them through so much. It seems ridiculous to go: ‘Oops, I made this huge [expletive] mistake,’ ” she said, describing the moment she did tell them as “devastating.”
Grace (@hormonehangover) said she remembers finally hitting a moment of “undeniability” some years after transitioning. “I accept it, I’ve ruined my life, this is wrong,” she remembers thinking. “It was devastating, but I couldn’t deny it anymore.”
Don’t trust therapists
People experiencing feelings of unease “need a therapist who will listen to them,” said Ms. Watson. When she first detransitioned, her therapists treated her badly. “They just didn’t want to speak about detransition,” she said, adding that “it was like a kick in the stomach.”
Ms. Watson said she’d like to see more training about detransition, but also on “preventative techniques,” adding that many people transition who should not. “I don’t want more detransitioners – I want less.
“In order for that to happen, we need to treat people with gender dysphoria properly,” said Ms. Watson, adding that the affirmative model is “disgusting, and that’s what needs to change.”
“I would tell somebody to not go to a therapist,” said Carol. Identifying as a butch lesbian, she felt like her therapists had pushed her into transitioning to male. “The No. 1 thing not understood by the mental health professionals is that the vast majority of homosexuals were gender-nonconforming children.” She added that this is especially true of butch lesbians.
Therapists – and doctors – also need to acknowledge both the trauma of transition and detransition, she said.
Kaiser, where she had transitioned, offered her breast reconstruction. Carol said it felt demeaning. “Like you’re Mr. Potatohead: ‘Here, we can just ... put on some new parts and you’re good to go.’ ”
“Doctors are concretizing transient obsessions,” said Helena Kerschner (@lacroicsz), quoting a chatroom user.
Ms. Kerschner gave a presentation on “fandom”: becoming obsessed with a movie, book, TV show, musician, or celebrity, spending every waking hour chatting online or writing fan fiction, or attempting to interact with the celebrity online. It’s a fantasy-dominated world and “the vast majority” of participants are teenage girls who are “identifying as trans,” in part, because they are fed a community-reinforced message that it’s better to be a boy.
Therapists and physicians who help them transition “are harming them for life based on something they would have grown out of or overcome without the permanent damage,” Ms. Kerschner added.
Doctors ‘gaslighting’ people into believing that transition is the answer
A pervasive theme during the webinar was that many people are being misdiagnosed with gender dysphoria, which may not be resolved by medical transition.
Allie, a 22-year-old who stopped taking testosterone after 1½ years, said she initially started the transition to male when she gave up trying to figure out why she could not identify with, or befriend, women, and after a childhood and adolescence spent mostly in the company of boys and being more interested in traditionally male activities.
She endured sexual abuse as a teenager and her parents divorced while she was in high school. Allie also had multiple suicide attempts and many incidents of self-harm. When she decided to transition, at age 18, she went to a private clinic and received cross-sex hormones within a few months of her first and only 30-minute consultation. “There was no explorative therapy,” she said, adding that she was never given a formal diagnosis of gender dysphoria.
For the first year, she said she was “over the freaking moon” because she felt like it was the answer. But things started to unravel while she attended university, and she attempted suicide attempt at age 20. A social worker at the school identified her symptoms – which had been the same since childhood – as autism. She then decided to cease her transition.
Another detransitioner, Laura Becker, said it took 5 years after her transition to recognize that she had undiagnosed PTSD from emotional and psychiatric abuse. Despite a history of substance abuse, self-harm, suicidal ideation, and other mental health issues, she was given testosterone and had a double mastectomy at age 20. She became fixated on gay men, which devolved into a methamphetamine- and crack-fueled relationship with a man she met on the gay dating platform Grindr.
“No one around me knew any better or knew how to help, including the medical professionals who performed the mastectomy and who casually signed off and administered my medical transition,” she said.
Once she was aware of her PTSD she started to detransition, which itself was traumatic, said Laura.
Limpida, aged 24, said he felt pushed into transitioning after seeking help at a Planned Parenthood clinic. He identified as trans at age 15 and spent years attempting to be a woman socially, but every step made him feel more miserable, he said. When he went to the clinic at age 21 to get estrogen, he said he felt like the staff was dismissive of his mental health concerns – including that he was suicidal, had substance abuse, and was severely depressed. He was told he was the “perfect candidate” for transitioning.
A year later, he said he felt worse. The nurse suggested he seek out surgery. After Limpida researched what was involved, he decided to detransition. He has since received an autism diagnosis.
Robin, also aged 24, said the idea of surgery had helped push him into detransitioning, which began in 2020 after 4 years of estrogen. He said he had always been gender nonconforming and knew he was gay at an early age. He believes that gender-nonconforming people are “gaslighted” into thinking that transitioning is the answer.
Lack of evidence-based, informed consent
Michelle Alleva, who stopped identifying as transgender in 2020 but had ceased testosterone 4 years earlier because of side effects, cited what she called a lack of evidence base for the effectiveness and safety of medical transitions.
“You need to have a really, really good evidence base in place if you’re going straight to an invasive treatment that is going to cause permanent changes to your body,” she said.
Access to medical transition used to involve more “gatekeeping” through mental health evaluations and other interventions, she said, but there has been a shift from treating what was considered a psychiatric issue to essentially affirming an identity.
“This shift was activist driven, not evidence based,” she emphasized.
Most studies showing satisfaction with transition only involve a few years of follow-up, she said. She added that the longest follow-up study of transition, published in 2011 and spanning 30 years, showed that the suicide rate 10-15 years post surgery was 20 times higher than the general population.
Studies of regret were primarily conducted before the rapid increase in the number of trans-identifying individuals, she said, which makes it hard to draw conclusions about pediatric transition. Getting estimates on this population is difficult because so many who detransition do not tell their clinicians, and many studies have short follow-up times or a high loss to follow-up.
Ms. Alleva also took issue with the notion that physicians were offering true informed consent, noting that it’s not possible to know if someone is psychologically sound if they haven’t had a thorough mental health evaluation and that there are so many unknowns with medical transition, including that many of the therapies are not approved for the uses being employed.
With regret on the rise, “we need professionals that are prepared for detransitioners,” said Ms. Alleva. “Some of us have lost trust in health care professionals as a result of our experience.”
“It’s a huge feeling of institutional betrayal,” said Grace.
A version of this article first appeared on Medscape.com.
In a unique Zoom conference,
The forum was convened on what was dubbed #DetransitionAwarenessDay by Genspect, a parent-based organization that seeks to put the brakes on medical transitions for children and adolescents. The group has doubts about the gender-affirming care model supported by the World Professional Association for Transgender Health, the American Medical Association, the American Academy of Pediatrics, and other medical groups.
“Affirmative” medical care is defined as treatment with puberty blockers and cross-sex hormones for those with gender dysphoria to transition to the opposite sex and is often followed by gender reassignment surgery. However, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed for those under aged 18, in particular, with several countries pulling back on medical treatment and instead emphasizing psychotherapy first.
The purpose of the second annual Genspect meeting was to shed light on the experiences of individuals who have detransitioned – those that identified as transgender and transitioned, but then decided to end their medical transition. People logged on from all over the United States, Canada, New Zealand, Australia, the United Kingdom, Germany, Spain, Chile, and Brazil, among other countries.
“This is a minority within a minority,” said Genspect advisor Stella O’Malley, adding that the first meeting in 2021 was held because “too many people were dismissing the stories of the detransitioners.” Ms. O’Malley is a psychotherapist, a clinical advisor to the Society for Evidence-Based Gender Medicine, and a founding member of the International Association of Therapists for Desisters and Detransitioners.
“It’s become blindingly obvious over the last year that ... ‘detrans’ is a huge part of the trans phenomenon,” said Ms. O’Malley, adding that detransitioners have been “undermined and dismissed.”
Laura Edwards-Leeper, PhD (@DrLauraEL), a prominent gender therapist who has recently expressed concern regarding adequate gatekeeping when treating youth with gender dysphoria, agreed.
She tweeted: “You simply can’t call yourself a legit gender provider if you don’t believe that detransitioners exist. As part of the informed consent process for transitioning, it is unethical to not discuss this possibility with young people.” Dr. Edwards-Leeper is professor emeritus at Pacific University in Hillsboro, Ore.
Speakers in the forum largely offered experiences, not data. They pointed out that there has been little to no study of detransition, but all testified that it was less rare than it has been portrayed by the transgender community.
Struggles with going back
“There are so many reasons why people detransition,” said Sinead Watson, aged 30, a Genspect advisor who transitioned from female to male, starting in 2015, and who decided to detransition in 2019. Citing a study by Lisa Littman, MD, MPH, published in 2021, Ms. Watson said the most common reasons for detransitioning were realizing that gender dysphoria was caused by other issues; internal homophobia; and the unbearable nature of transphobia.
Ms. Watson said the hardest part of detransitioning was admitting to herself that her transition had been a mistake. “It’s embarrassing and you feel ashamed and guilty,” she said, adding that it may mean losing friends who now regard you as a “bigot, while you’re also dealing with transition regret.”
“It’s a living hell, especially when none of your therapists or counselors will listen to you,” she said. “Detransitioning isn’t fun.”
Carol (@sourpatches2077) said she knew for a year that her transition had been a mistake.
“The biggest part was I couldn’t tell my family,” said Carol, who identifies as a lesbian. “I put them through so much. It seems ridiculous to go: ‘Oops, I made this huge [expletive] mistake,’ ” she said, describing the moment she did tell them as “devastating.”
Grace (@hormonehangover) said she remembers finally hitting a moment of “undeniability” some years after transitioning. “I accept it, I’ve ruined my life, this is wrong,” she remembers thinking. “It was devastating, but I couldn’t deny it anymore.”
Don’t trust therapists
People experiencing feelings of unease “need a therapist who will listen to them,” said Ms. Watson. When she first detransitioned, her therapists treated her badly. “They just didn’t want to speak about detransition,” she said, adding that “it was like a kick in the stomach.”
Ms. Watson said she’d like to see more training about detransition, but also on “preventative techniques,” adding that many people transition who should not. “I don’t want more detransitioners – I want less.
“In order for that to happen, we need to treat people with gender dysphoria properly,” said Ms. Watson, adding that the affirmative model is “disgusting, and that’s what needs to change.”
“I would tell somebody to not go to a therapist,” said Carol. Identifying as a butch lesbian, she felt like her therapists had pushed her into transitioning to male. “The No. 1 thing not understood by the mental health professionals is that the vast majority of homosexuals were gender-nonconforming children.” She added that this is especially true of butch lesbians.
Therapists – and doctors – also need to acknowledge both the trauma of transition and detransition, she said.
Kaiser, where she had transitioned, offered her breast reconstruction. Carol said it felt demeaning. “Like you’re Mr. Potatohead: ‘Here, we can just ... put on some new parts and you’re good to go.’ ”
“Doctors are concretizing transient obsessions,” said Helena Kerschner (@lacroicsz), quoting a chatroom user.
Ms. Kerschner gave a presentation on “fandom”: becoming obsessed with a movie, book, TV show, musician, or celebrity, spending every waking hour chatting online or writing fan fiction, or attempting to interact with the celebrity online. It’s a fantasy-dominated world and “the vast majority” of participants are teenage girls who are “identifying as trans,” in part, because they are fed a community-reinforced message that it’s better to be a boy.
Therapists and physicians who help them transition “are harming them for life based on something they would have grown out of or overcome without the permanent damage,” Ms. Kerschner added.
Doctors ‘gaslighting’ people into believing that transition is the answer
A pervasive theme during the webinar was that many people are being misdiagnosed with gender dysphoria, which may not be resolved by medical transition.
Allie, a 22-year-old who stopped taking testosterone after 1½ years, said she initially started the transition to male when she gave up trying to figure out why she could not identify with, or befriend, women, and after a childhood and adolescence spent mostly in the company of boys and being more interested in traditionally male activities.
She endured sexual abuse as a teenager and her parents divorced while she was in high school. Allie also had multiple suicide attempts and many incidents of self-harm. When she decided to transition, at age 18, she went to a private clinic and received cross-sex hormones within a few months of her first and only 30-minute consultation. “There was no explorative therapy,” she said, adding that she was never given a formal diagnosis of gender dysphoria.
For the first year, she said she was “over the freaking moon” because she felt like it was the answer. But things started to unravel while she attended university, and she attempted suicide attempt at age 20. A social worker at the school identified her symptoms – which had been the same since childhood – as autism. She then decided to cease her transition.
Another detransitioner, Laura Becker, said it took 5 years after her transition to recognize that she had undiagnosed PTSD from emotional and psychiatric abuse. Despite a history of substance abuse, self-harm, suicidal ideation, and other mental health issues, she was given testosterone and had a double mastectomy at age 20. She became fixated on gay men, which devolved into a methamphetamine- and crack-fueled relationship with a man she met on the gay dating platform Grindr.
“No one around me knew any better or knew how to help, including the medical professionals who performed the mastectomy and who casually signed off and administered my medical transition,” she said.
Once she was aware of her PTSD she started to detransition, which itself was traumatic, said Laura.
Limpida, aged 24, said he felt pushed into transitioning after seeking help at a Planned Parenthood clinic. He identified as trans at age 15 and spent years attempting to be a woman socially, but every step made him feel more miserable, he said. When he went to the clinic at age 21 to get estrogen, he said he felt like the staff was dismissive of his mental health concerns – including that he was suicidal, had substance abuse, and was severely depressed. He was told he was the “perfect candidate” for transitioning.
A year later, he said he felt worse. The nurse suggested he seek out surgery. After Limpida researched what was involved, he decided to detransition. He has since received an autism diagnosis.
Robin, also aged 24, said the idea of surgery had helped push him into detransitioning, which began in 2020 after 4 years of estrogen. He said he had always been gender nonconforming and knew he was gay at an early age. He believes that gender-nonconforming people are “gaslighted” into thinking that transitioning is the answer.
Lack of evidence-based, informed consent
Michelle Alleva, who stopped identifying as transgender in 2020 but had ceased testosterone 4 years earlier because of side effects, cited what she called a lack of evidence base for the effectiveness and safety of medical transitions.
“You need to have a really, really good evidence base in place if you’re going straight to an invasive treatment that is going to cause permanent changes to your body,” she said.
Access to medical transition used to involve more “gatekeeping” through mental health evaluations and other interventions, she said, but there has been a shift from treating what was considered a psychiatric issue to essentially affirming an identity.
“This shift was activist driven, not evidence based,” she emphasized.
Most studies showing satisfaction with transition only involve a few years of follow-up, she said. She added that the longest follow-up study of transition, published in 2011 and spanning 30 years, showed that the suicide rate 10-15 years post surgery was 20 times higher than the general population.
Studies of regret were primarily conducted before the rapid increase in the number of trans-identifying individuals, she said, which makes it hard to draw conclusions about pediatric transition. Getting estimates on this population is difficult because so many who detransition do not tell their clinicians, and many studies have short follow-up times or a high loss to follow-up.
Ms. Alleva also took issue with the notion that physicians were offering true informed consent, noting that it’s not possible to know if someone is psychologically sound if they haven’t had a thorough mental health evaluation and that there are so many unknowns with medical transition, including that many of the therapies are not approved for the uses being employed.
With regret on the rise, “we need professionals that are prepared for detransitioners,” said Ms. Alleva. “Some of us have lost trust in health care professionals as a result of our experience.”
“It’s a huge feeling of institutional betrayal,” said Grace.
A version of this article first appeared on Medscape.com.
Don’t drink calories: Artificial sweeteners beat sugar in new analysis
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
When I counsel patients who are trying to lose weight, there is something I always discuss: “Don’t drink calories.” The idea is that it is so easy to consume sweetened beverages (and alcoholic ones, for that matter) and we don’t really get a sense of how many calories we’re taking in.
Some patients balk at the idea, saying they can’t stand the taste of water or just can’t bring themselves to drink it. While, as a nephrologist, this pains me deeply to hear, I often suggest going for low- or zero-calorie flavored drinks instead of the sugary stuff.
And yet ... I need to admit that recently I’ve been more nervous about that advice. A very nice study in Nature, for example, found that artificial sweeteners induce glucose intolerance and weight gain – in mice.
Several observational studies have suggested that the use of nonnutritive sweeteners – sucralose, aspartame, and so on – are associated with higher body weight and type 2 diabetes. Of course,
Randomized trials, as ever, are the key to deeper understanding, but most trials in this space are relatively small. That makes a good case for this study, appearing in JAMA Network Open, which combines data from 17 randomized trials to determine what effects substituting sugary drinks with low- and zero-calorie drinks truly has.
So, what’s the bottom line? Should I ditch the Splenda in my morning coffee and drop in some sugar cubes?
It turns out that the effects of drinking low- or zero-calorie drinks instead of sugary ones is modest, but overall beneficial, depending on the outcome you’re trying to achieve.
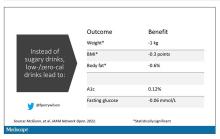
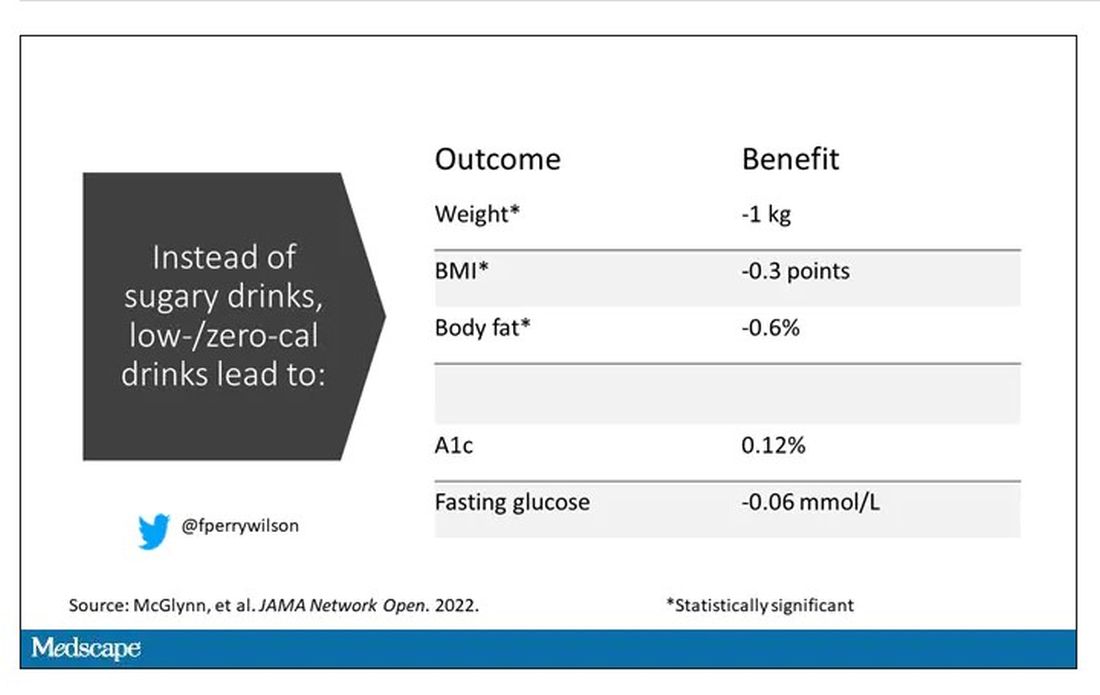
Randomized trials show that switching to low-cal drinks reduces body weight by about a kilogram, and BMI by 0.3 points. It also reduces body fat by about half a percent.
Effects on glucose homeostasis – hemoglobin A1c level and fasting glucose – were not that impressive, though.
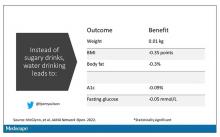
The authors also compared sugar-sweetened beverages with plain old water. I expected this analysis to show more dramatic benefits. After all, we’re all just ugly, giant bags of mostly water. Interestingly, the effects of switching to water were not as dramatic and largely nonsignificant with respect to most outcomes evaluated.
So, what do we make of this? If someone is a habitual drinker of sugar-sweetened beverages, is it preferable to switch to a zero-calorie flavored drink, compared with plain water?
One possibility is that in the trials where people are randomized to switch to water, they aren’t as adherent. Just because we ask someone to drink water doesn’t mean they do it, and so there may be a tendency to “cheat” with sugar-sweetened beverages. However, if told that low- or zero-calorie flavored drinks are okay, maybe it’s easier to stick to the plan? This is essentially the argument you get from people who say that vaping is a good way to quit smoking. It may or may not be true.
It could also be that we just don’t have enough rigorous data to make a firm conclusion. Of the 17 trials examined, only three of them used water substitution as an intervention.
All in all, these data provide some reassurance that the zero-calorie sweeteners aren’t secretly exacerbating the obesity epidemic. I’d certainly rather my patients drink Diet Coke than regular Coke. That said, these studies are necessarily short term; the longer-term effects of sugar substitutes, while perhaps not as bad as the long-term effects of sugar, must necessarily be worse than the long-term effects of drinking water. Maybe this is the nephrologist in me talking again, but I doubt that there could possibly be a fluid better for the human body than good old H2O. Except coffee, of course.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
When I counsel patients who are trying to lose weight, there is something I always discuss: “Don’t drink calories.” The idea is that it is so easy to consume sweetened beverages (and alcoholic ones, for that matter) and we don’t really get a sense of how many calories we’re taking in.
Some patients balk at the idea, saying they can’t stand the taste of water or just can’t bring themselves to drink it. While, as a nephrologist, this pains me deeply to hear, I often suggest going for low- or zero-calorie flavored drinks instead of the sugary stuff.
And yet ... I need to admit that recently I’ve been more nervous about that advice. A very nice study in Nature, for example, found that artificial sweeteners induce glucose intolerance and weight gain – in mice.
Several observational studies have suggested that the use of nonnutritive sweeteners – sucralose, aspartame, and so on – are associated with higher body weight and type 2 diabetes. Of course,
Randomized trials, as ever, are the key to deeper understanding, but most trials in this space are relatively small. That makes a good case for this study, appearing in JAMA Network Open, which combines data from 17 randomized trials to determine what effects substituting sugary drinks with low- and zero-calorie drinks truly has.
So, what’s the bottom line? Should I ditch the Splenda in my morning coffee and drop in some sugar cubes?
It turns out that the effects of drinking low- or zero-calorie drinks instead of sugary ones is modest, but overall beneficial, depending on the outcome you’re trying to achieve.
Randomized trials show that switching to low-cal drinks reduces body weight by about a kilogram, and BMI by 0.3 points. It also reduces body fat by about half a percent.
Effects on glucose homeostasis – hemoglobin A1c level and fasting glucose – were not that impressive, though.
The authors also compared sugar-sweetened beverages with plain old water. I expected this analysis to show more dramatic benefits. After all, we’re all just ugly, giant bags of mostly water. Interestingly, the effects of switching to water were not as dramatic and largely nonsignificant with respect to most outcomes evaluated.
So, what do we make of this? If someone is a habitual drinker of sugar-sweetened beverages, is it preferable to switch to a zero-calorie flavored drink, compared with plain water?
One possibility is that in the trials where people are randomized to switch to water, they aren’t as adherent. Just because we ask someone to drink water doesn’t mean they do it, and so there may be a tendency to “cheat” with sugar-sweetened beverages. However, if told that low- or zero-calorie flavored drinks are okay, maybe it’s easier to stick to the plan? This is essentially the argument you get from people who say that vaping is a good way to quit smoking. It may or may not be true.
It could also be that we just don’t have enough rigorous data to make a firm conclusion. Of the 17 trials examined, only three of them used water substitution as an intervention.
All in all, these data provide some reassurance that the zero-calorie sweeteners aren’t secretly exacerbating the obesity epidemic. I’d certainly rather my patients drink Diet Coke than regular Coke. That said, these studies are necessarily short term; the longer-term effects of sugar substitutes, while perhaps not as bad as the long-term effects of sugar, must necessarily be worse than the long-term effects of drinking water. Maybe this is the nephrologist in me talking again, but I doubt that there could possibly be a fluid better for the human body than good old H2O. Except coffee, of course.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
When I counsel patients who are trying to lose weight, there is something I always discuss: “Don’t drink calories.” The idea is that it is so easy to consume sweetened beverages (and alcoholic ones, for that matter) and we don’t really get a sense of how many calories we’re taking in.
Some patients balk at the idea, saying they can’t stand the taste of water or just can’t bring themselves to drink it. While, as a nephrologist, this pains me deeply to hear, I often suggest going for low- or zero-calorie flavored drinks instead of the sugary stuff.
And yet ... I need to admit that recently I’ve been more nervous about that advice. A very nice study in Nature, for example, found that artificial sweeteners induce glucose intolerance and weight gain – in mice.
Several observational studies have suggested that the use of nonnutritive sweeteners – sucralose, aspartame, and so on – are associated with higher body weight and type 2 diabetes. Of course,
Randomized trials, as ever, are the key to deeper understanding, but most trials in this space are relatively small. That makes a good case for this study, appearing in JAMA Network Open, which combines data from 17 randomized trials to determine what effects substituting sugary drinks with low- and zero-calorie drinks truly has.
So, what’s the bottom line? Should I ditch the Splenda in my morning coffee and drop in some sugar cubes?
It turns out that the effects of drinking low- or zero-calorie drinks instead of sugary ones is modest, but overall beneficial, depending on the outcome you’re trying to achieve.
Randomized trials show that switching to low-cal drinks reduces body weight by about a kilogram, and BMI by 0.3 points. It also reduces body fat by about half a percent.
Effects on glucose homeostasis – hemoglobin A1c level and fasting glucose – were not that impressive, though.
The authors also compared sugar-sweetened beverages with plain old water. I expected this analysis to show more dramatic benefits. After all, we’re all just ugly, giant bags of mostly water. Interestingly, the effects of switching to water were not as dramatic and largely nonsignificant with respect to most outcomes evaluated.
So, what do we make of this? If someone is a habitual drinker of sugar-sweetened beverages, is it preferable to switch to a zero-calorie flavored drink, compared with plain water?
One possibility is that in the trials where people are randomized to switch to water, they aren’t as adherent. Just because we ask someone to drink water doesn’t mean they do it, and so there may be a tendency to “cheat” with sugar-sweetened beverages. However, if told that low- or zero-calorie flavored drinks are okay, maybe it’s easier to stick to the plan? This is essentially the argument you get from people who say that vaping is a good way to quit smoking. It may or may not be true.
It could also be that we just don’t have enough rigorous data to make a firm conclusion. Of the 17 trials examined, only three of them used water substitution as an intervention.
All in all, these data provide some reassurance that the zero-calorie sweeteners aren’t secretly exacerbating the obesity epidemic. I’d certainly rather my patients drink Diet Coke than regular Coke. That said, these studies are necessarily short term; the longer-term effects of sugar substitutes, while perhaps not as bad as the long-term effects of sugar, must necessarily be worse than the long-term effects of drinking water. Maybe this is the nephrologist in me talking again, but I doubt that there could possibly be a fluid better for the human body than good old H2O. Except coffee, of course.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
French fries vs. almonds every day for a month: What changes?
Eat french fries every day for a month? Sure, as long as it’s for science.
That’s exactly what 107 people did in a scientific study, while 58 others ate a daily serving of almonds with the same number of calories.
At the end of the study, the researchers found no significant differences between the groups in people’s total amount of fat or their fasting glucose measures, according to the study, published Feb. 18 in the American Journal of Clinical Nutrition.
The french fry eaters gained a little more weight, but it was not statistically significant. The people who ate french fries gained 0.49 kilograms (just over a pound), vs. about a tenth of a kilogram (about one-fifth of a pound) in the group of people who ate almonds.
“The take-home is if you like almonds, eat some almonds. If you like potatoes, eat some potatoes, but don’t overeat either,” said study leader David B. Allison, PhD, a professor at Indiana University’s School of Public Health in Bloomington. ‘It’s probably good to have a little bit of each – each has some unique advantages in terms of nutrition.”
“This study confirms what registered dietitian nutritionists already know – all foods can fit. We can eat almonds, french fries, kale, and cookies,” said Melissa Majumdar, a registered dietitian and certified specialist in obesity and weight management at Emory University Hospital Midtown in Atlanta. ‘The consumption of one food or the avoidance of another does not make a healthy diet.”
At the same time, people should not interpret the results to mean it’s OK to eat french fries all day, every day. “We know that while potatoes are nutrient dense, the frying process reduces the nutritional value,” Ms. Majumdar said.
“Because french fries are often consumed alongside other nutrient-poor or high-fat foods, they should not be consumed daily but can fit into an overall balanced diet,” she added.
Would you like fries with that?
The researchers compared french fries to almonds because almonds are known for positive effects on energy balance, body composition, and low glycemic index. The research was partly funded by the Alliance for Potato Research and Education.
French fries are an incredibly popular food in the United States. According to an August 2021 post on the food website Mashed, Americans eat an average of 30 pounds of french fries each year.
Although consumption of almonds is increasing, Americans eat far less in volume each year than they do fries – an estimated 2.4 pounds of almonds per person, according to August 2021 figures from the Almond Board of California.
Dr. Allison and colleagues recruited 180 healthy adults for the study. Their average age was 30, and about two-thirds were women.
They randomly assigned 60 people to add about a medium serving of plain french fries (Tater Pals Ovenable Crinkle Cut Fries, Simplot Foods) to their diet. Another 60 people were assigned to the same amount of Tater Pals fries with herbs (oregano, basil, garlic, onion, and rosemary), and another 60 people ate Wonderful brand roasted and salted almonds.
Investigators told people to add either the potatoes or nuts to their diet every day for a month and gave no further instructions.
After some people dropped out of the study, results were based on 55 who ate regular french fries, 52 who ate french fries with herbs and spices, and 58 who ate the nuts.
The researchers scanned people to detect any changes in fat mass. They also measured changes in body weight, carbohydrate metabolism, and fasting blood glucose and insulin.
Key findings
Changes in total body fat mass and fat mass were not significantly different between the french fry groups and the almond group.
In terms of glycemic control, eating french fries for a month “is no better or worse than consuming a caloric equivalent of nuts,” the researchers noted.
Similarly, the change in total fat mass did not differ significantly among the three treatment groups.
Adding the herb and spice mix to the french fries did not make a significant difference on glycemic control, contrary to what the researchers thought might happen.
And fasting glucose, insulin, and HbA1c levels did not differ significantly between the combined french fry and almond groups. When comparisons were made among the three groups, the almond group had a lower insulin response, compared to the plain french fry group.
Many different things could be explored in future research, said study coauthor Rebecca Hanson, a registered dietitian nutritionist and research study coordinator at the University of Alabama at Birmingham. “People were not told to change their exercise or diet, so there are so many different variables,” she said. Repeating the research in people with diabetes is another possibility going forward.
The researchers acknowledged that 30 days may not have been long enough to show a significant difference. But they also noted that many previous studies were observational while they used a randomized controlled trial, considered a more robust study design.
Dr. Allison, the senior author, emphasized that this is just one study. “No one study has all the answers.
“I don’t want to tell you our results are the be all and end all or that we’ve now learned everything there is to learn about potatoes and almonds,” he said.
“Our study shows for the variables we looked at ... we did not see important, discernible differences,” he said. “That doesn’t mean if you ate 500 potatoes a day or 500 kilograms of almonds it would be the same. But at these modest levels, it doesn’t seem to make much difference.”
The study was funded by grants from the National Institutes of Health and from the Alliance for Potato Research and Education.
Asked if the industry support should be a concern, Ms. Majumdar said, “Funding from a specific food board does not necessarily dilute the results of a well-designed study. It’s not uncommon for a funding source to come from a food board that may benefit from the findings. Research money has to come from somewhere.
“This study has reputable researchers, some of the best in the field,” she said.
The U.S. produces the most almonds in the world, and California is the only state where almonds are grown commercially. Asked for the almond industry’s take on the findings, “We don’t have a comment,” said Rick Kushman, a spokesman for the Almond Board of California.
A version of this article first appeared on WebMD.com.
Eat french fries every day for a month? Sure, as long as it’s for science.
That’s exactly what 107 people did in a scientific study, while 58 others ate a daily serving of almonds with the same number of calories.
At the end of the study, the researchers found no significant differences between the groups in people’s total amount of fat or their fasting glucose measures, according to the study, published Feb. 18 in the American Journal of Clinical Nutrition.
The french fry eaters gained a little more weight, but it was not statistically significant. The people who ate french fries gained 0.49 kilograms (just over a pound), vs. about a tenth of a kilogram (about one-fifth of a pound) in the group of people who ate almonds.
“The take-home is if you like almonds, eat some almonds. If you like potatoes, eat some potatoes, but don’t overeat either,” said study leader David B. Allison, PhD, a professor at Indiana University’s School of Public Health in Bloomington. ‘It’s probably good to have a little bit of each – each has some unique advantages in terms of nutrition.”
“This study confirms what registered dietitian nutritionists already know – all foods can fit. We can eat almonds, french fries, kale, and cookies,” said Melissa Majumdar, a registered dietitian and certified specialist in obesity and weight management at Emory University Hospital Midtown in Atlanta. ‘The consumption of one food or the avoidance of another does not make a healthy diet.”
At the same time, people should not interpret the results to mean it’s OK to eat french fries all day, every day. “We know that while potatoes are nutrient dense, the frying process reduces the nutritional value,” Ms. Majumdar said.
“Because french fries are often consumed alongside other nutrient-poor or high-fat foods, they should not be consumed daily but can fit into an overall balanced diet,” she added.
Would you like fries with that?
The researchers compared french fries to almonds because almonds are known for positive effects on energy balance, body composition, and low glycemic index. The research was partly funded by the Alliance for Potato Research and Education.
French fries are an incredibly popular food in the United States. According to an August 2021 post on the food website Mashed, Americans eat an average of 30 pounds of french fries each year.
Although consumption of almonds is increasing, Americans eat far less in volume each year than they do fries – an estimated 2.4 pounds of almonds per person, according to August 2021 figures from the Almond Board of California.
Dr. Allison and colleagues recruited 180 healthy adults for the study. Their average age was 30, and about two-thirds were women.
They randomly assigned 60 people to add about a medium serving of plain french fries (Tater Pals Ovenable Crinkle Cut Fries, Simplot Foods) to their diet. Another 60 people were assigned to the same amount of Tater Pals fries with herbs (oregano, basil, garlic, onion, and rosemary), and another 60 people ate Wonderful brand roasted and salted almonds.
Investigators told people to add either the potatoes or nuts to their diet every day for a month and gave no further instructions.
After some people dropped out of the study, results were based on 55 who ate regular french fries, 52 who ate french fries with herbs and spices, and 58 who ate the nuts.
The researchers scanned people to detect any changes in fat mass. They also measured changes in body weight, carbohydrate metabolism, and fasting blood glucose and insulin.
Key findings
Changes in total body fat mass and fat mass were not significantly different between the french fry groups and the almond group.
In terms of glycemic control, eating french fries for a month “is no better or worse than consuming a caloric equivalent of nuts,” the researchers noted.
Similarly, the change in total fat mass did not differ significantly among the three treatment groups.
Adding the herb and spice mix to the french fries did not make a significant difference on glycemic control, contrary to what the researchers thought might happen.
And fasting glucose, insulin, and HbA1c levels did not differ significantly between the combined french fry and almond groups. When comparisons were made among the three groups, the almond group had a lower insulin response, compared to the plain french fry group.
Many different things could be explored in future research, said study coauthor Rebecca Hanson, a registered dietitian nutritionist and research study coordinator at the University of Alabama at Birmingham. “People were not told to change their exercise or diet, so there are so many different variables,” she said. Repeating the research in people with diabetes is another possibility going forward.
The researchers acknowledged that 30 days may not have been long enough to show a significant difference. But they also noted that many previous studies were observational while they used a randomized controlled trial, considered a more robust study design.
Dr. Allison, the senior author, emphasized that this is just one study. “No one study has all the answers.
“I don’t want to tell you our results are the be all and end all or that we’ve now learned everything there is to learn about potatoes and almonds,” he said.
“Our study shows for the variables we looked at ... we did not see important, discernible differences,” he said. “That doesn’t mean if you ate 500 potatoes a day or 500 kilograms of almonds it would be the same. But at these modest levels, it doesn’t seem to make much difference.”
The study was funded by grants from the National Institutes of Health and from the Alliance for Potato Research and Education.
Asked if the industry support should be a concern, Ms. Majumdar said, “Funding from a specific food board does not necessarily dilute the results of a well-designed study. It’s not uncommon for a funding source to come from a food board that may benefit from the findings. Research money has to come from somewhere.
“This study has reputable researchers, some of the best in the field,” she said.
The U.S. produces the most almonds in the world, and California is the only state where almonds are grown commercially. Asked for the almond industry’s take on the findings, “We don’t have a comment,” said Rick Kushman, a spokesman for the Almond Board of California.
A version of this article first appeared on WebMD.com.
Eat french fries every day for a month? Sure, as long as it’s for science.
That’s exactly what 107 people did in a scientific study, while 58 others ate a daily serving of almonds with the same number of calories.
At the end of the study, the researchers found no significant differences between the groups in people’s total amount of fat or their fasting glucose measures, according to the study, published Feb. 18 in the American Journal of Clinical Nutrition.
The french fry eaters gained a little more weight, but it was not statistically significant. The people who ate french fries gained 0.49 kilograms (just over a pound), vs. about a tenth of a kilogram (about one-fifth of a pound) in the group of people who ate almonds.
“The take-home is if you like almonds, eat some almonds. If you like potatoes, eat some potatoes, but don’t overeat either,” said study leader David B. Allison, PhD, a professor at Indiana University’s School of Public Health in Bloomington. ‘It’s probably good to have a little bit of each – each has some unique advantages in terms of nutrition.”
“This study confirms what registered dietitian nutritionists already know – all foods can fit. We can eat almonds, french fries, kale, and cookies,” said Melissa Majumdar, a registered dietitian and certified specialist in obesity and weight management at Emory University Hospital Midtown in Atlanta. ‘The consumption of one food or the avoidance of another does not make a healthy diet.”
At the same time, people should not interpret the results to mean it’s OK to eat french fries all day, every day. “We know that while potatoes are nutrient dense, the frying process reduces the nutritional value,” Ms. Majumdar said.
“Because french fries are often consumed alongside other nutrient-poor or high-fat foods, they should not be consumed daily but can fit into an overall balanced diet,” she added.
Would you like fries with that?
The researchers compared french fries to almonds because almonds are known for positive effects on energy balance, body composition, and low glycemic index. The research was partly funded by the Alliance for Potato Research and Education.
French fries are an incredibly popular food in the United States. According to an August 2021 post on the food website Mashed, Americans eat an average of 30 pounds of french fries each year.
Although consumption of almonds is increasing, Americans eat far less in volume each year than they do fries – an estimated 2.4 pounds of almonds per person, according to August 2021 figures from the Almond Board of California.
Dr. Allison and colleagues recruited 180 healthy adults for the study. Their average age was 30, and about two-thirds were women.
They randomly assigned 60 people to add about a medium serving of plain french fries (Tater Pals Ovenable Crinkle Cut Fries, Simplot Foods) to their diet. Another 60 people were assigned to the same amount of Tater Pals fries with herbs (oregano, basil, garlic, onion, and rosemary), and another 60 people ate Wonderful brand roasted and salted almonds.
Investigators told people to add either the potatoes or nuts to their diet every day for a month and gave no further instructions.
After some people dropped out of the study, results were based on 55 who ate regular french fries, 52 who ate french fries with herbs and spices, and 58 who ate the nuts.
The researchers scanned people to detect any changes in fat mass. They also measured changes in body weight, carbohydrate metabolism, and fasting blood glucose and insulin.
Key findings
Changes in total body fat mass and fat mass were not significantly different between the french fry groups and the almond group.
In terms of glycemic control, eating french fries for a month “is no better or worse than consuming a caloric equivalent of nuts,” the researchers noted.
Similarly, the change in total fat mass did not differ significantly among the three treatment groups.
Adding the herb and spice mix to the french fries did not make a significant difference on glycemic control, contrary to what the researchers thought might happen.
And fasting glucose, insulin, and HbA1c levels did not differ significantly between the combined french fry and almond groups. When comparisons were made among the three groups, the almond group had a lower insulin response, compared to the plain french fry group.
Many different things could be explored in future research, said study coauthor Rebecca Hanson, a registered dietitian nutritionist and research study coordinator at the University of Alabama at Birmingham. “People were not told to change their exercise or diet, so there are so many different variables,” she said. Repeating the research in people with diabetes is another possibility going forward.
The researchers acknowledged that 30 days may not have been long enough to show a significant difference. But they also noted that many previous studies were observational while they used a randomized controlled trial, considered a more robust study design.
Dr. Allison, the senior author, emphasized that this is just one study. “No one study has all the answers.
“I don’t want to tell you our results are the be all and end all or that we’ve now learned everything there is to learn about potatoes and almonds,” he said.
“Our study shows for the variables we looked at ... we did not see important, discernible differences,” he said. “That doesn’t mean if you ate 500 potatoes a day or 500 kilograms of almonds it would be the same. But at these modest levels, it doesn’t seem to make much difference.”
The study was funded by grants from the National Institutes of Health and from the Alliance for Potato Research and Education.
Asked if the industry support should be a concern, Ms. Majumdar said, “Funding from a specific food board does not necessarily dilute the results of a well-designed study. It’s not uncommon for a funding source to come from a food board that may benefit from the findings. Research money has to come from somewhere.
“This study has reputable researchers, some of the best in the field,” she said.
The U.S. produces the most almonds in the world, and California is the only state where almonds are grown commercially. Asked for the almond industry’s take on the findings, “We don’t have a comment,” said Rick Kushman, a spokesman for the Almond Board of California.
A version of this article first appeared on WebMD.com.
FROM AMERICAN JOURNAL OF CLINICAL NUTRITION
Is cancer testing going to the dogs? Nope, ants
The oncologist’s new best friend
We know that dogs have very sensitive noses. They can track criminals and missing persons and sniff out drugs and bombs. They can even detect cancer cells … after months of training.
And then there are ants.
Cancer cells produce volatile organic compounds (VOCs), which can be sniffed out by dogs and other animals with sufficiently sophisticated olfactory senses. A group of French investigators decided to find out if Formica fusca is such an animal.
First, they placed breast cancer cells and healthy cells in a petri dish. The sample of cancer cells, however, included a sugary treat. “Over successive trials, the ants got quicker and quicker at finding the treat, indicating that they had learned to recognize the VOCs produced by the cancerous cells, using these as a beacon to guide their way to the sugary delight,” according to IFL Science.
When the researchers removed the treat, the ants still went straight for the cancer cells. Then they removed the healthy cells and substituted another type of breast cancer cell, with just one type getting the treat. They went for the cancer cells with the treat, “indicating that they were capable of distinguishing between the different cancer types based on the unique pattern of VOCs emitted by each one,” IFL Science explained.
It’s just another chapter in the eternal struggle between dogs and ants. Dogs need months of training to learn to detect cancer cells; ants can do it in 30 minutes. Over the course of a dog’s training, Fido eats more food than 10,000 ants combined. (Okay, we’re guessing here, but it’s got to be a pretty big number, right?)
Then there’s the warm and fuzzy factor. Just look at that picture. Who wouldn’t want a cutie like that curling up in the bed next to you?
Console War II: Battle of the Twitter users
Video games can be a lot of fun, provided you’re not playing something like Rock Simulator. Or Surgeon Simulator. Or Surgeon Simulator 2. Yes, those are all real games. But calling yourself a video gamer invites a certain negative connotation, and nowhere can that be better exemplified than the increasingly ridiculous console war.
For those who don’t know their video game history, back in the early 90s Nintendo and Sega were the main video game console makers. Nintendo had Mario, Sega had Sonic, and everyone had an opinion on which was best. With Sega now but a shell of its former self and Nintendo viewed as too “casual” for the true gaming connoisseur, today’s battle pits Playstation against Xbox, and fans of both consoles spend their time trying to one-up each other in increasingly silly online arguments.
That brings us nicely to a Twitter user named “Shreeveera,” who is very vocal about his love of Playstation and hatred of the Xbox. Importantly, for LOTME purposes, Shreeveera identified himself as a doctor on his profile, and in the middle of an argument, Xbox enthusiasts called his credentials into question.
At this point, most people would recognize that there are very few noteworthy console-exclusive video games in today’s world and that any argument about consoles essentially comes down to which console design you like or which company you find less distasteful, and they would step away from the Twitter argument. Shreeveera is not most people, and he decided the next logical move was to post a video of himself and an anesthetized patient about to undergo a laparoscopic cholecystectomy.
This move did prove that he was indeed a doctor, but the ethics of posting such a video with a patient in the room is a bit dubious at best. Since Shreeveera also listed the hospital he worked at, numerous Twitter users review bombed the hospital with one-star reviews. Shreeveera’s fate is unknown, but he did take down the video and removed “doctor by profession” from his profile. He also made a second video asking Twitter to stop trying to ruin his life. We’re sure that’ll go well. Twitter is known for being completely fair and reasonable.
Use your words to gain power
We live in the age of the emoji. The use of emojis in texts and emails is basically the new shorthand. It’s a fun and easy way to chat with people close to us, but a new study shows that it doesn’t help in a business setting. In fact, it may do a little damage.
The use of images such as emojis in communication or logos can make a person seem less powerful than someone who opts for written words, according to Elinor Amit, PhD, of Tel Aviv University and associates.
Participants in their study were asked to imagine shopping with a person wearing a T-shirt. Half were then shown the logo of the Red Sox baseball team and half saw the words “Red Sox.” In another scenario, they were asked to imagine attending a retreat of a company called Lotus. Then half were shown an employee wearing a shirt with an image of lotus flower and half saw the verbal logo “Lotus.” In both scenarios, the individuals wearing shirts with images were seen as less powerful than the people who wore shirts with words on them.
Why is that? In a Eurekalert statement, Dr. Amit said that “visual messages are often interpreted as a signal for desire for social proximity.” In a world with COVID-19, that could give anyone pause.
That desire for more social proximity, in turn, equals a suggested loss of power because research shows that people who want to be around other people more are less powerful than people who don’t.
With the reduced social proximity we have these days, we may want to keep things cool and lighthearted, especially in work emails with people who we’ve never met. It may be, however, that using your words to say thank you in the multitude of emails you respond to on a regular basis is better than that thumbs-up emoji. Nobody will think less of you.
Should Daylight Savings Time still be a thing?
This past week, we just experienced the spring-forward portion of Daylight Savings Time, which took an hour of sleep away from us all. Some of us may still be struggling to find our footing with the time change, but at least it’s still sunny out at 7 pm. For those who don’t really see the point of changing the clocks twice a year, there are actually some good reasons to do so.
Sen. Marco Rubio, sponsor of a bill to make the time change permanent, put it simply: “If we can get this passed, we don’t have to do this stupidity anymore.” Message received, apparently, since the measure just passed unanimously in the Senate.
It’s not clear if President Biden will approve it, though, because there’s a lot that comes into play: economic needs, seasonal depression, and safety.
“I know this is not the most important issue confronting America, but it’s one of those issues where there’s a lot of agreement,” Sen. Rubio said.
Not total agreement, though. The National Association of Convenience Stores is opposed to the bill, and Reuters noted that one witness at a recent hearing said the time change “is like living in the wrong time zone for almost eight months out of the year.”
Many people, however, seem to be leaning toward the permanent spring-forward as it gives businesses a longer window to provide entertainment in the evenings and kids are able to play outside longer after school.
Honestly, we’re leaning toward whichever one can reduce seasonal depression.
The oncologist’s new best friend
We know that dogs have very sensitive noses. They can track criminals and missing persons and sniff out drugs and bombs. They can even detect cancer cells … after months of training.
And then there are ants.
Cancer cells produce volatile organic compounds (VOCs), which can be sniffed out by dogs and other animals with sufficiently sophisticated olfactory senses. A group of French investigators decided to find out if Formica fusca is such an animal.
First, they placed breast cancer cells and healthy cells in a petri dish. The sample of cancer cells, however, included a sugary treat. “Over successive trials, the ants got quicker and quicker at finding the treat, indicating that they had learned to recognize the VOCs produced by the cancerous cells, using these as a beacon to guide their way to the sugary delight,” according to IFL Science.
When the researchers removed the treat, the ants still went straight for the cancer cells. Then they removed the healthy cells and substituted another type of breast cancer cell, with just one type getting the treat. They went for the cancer cells with the treat, “indicating that they were capable of distinguishing between the different cancer types based on the unique pattern of VOCs emitted by each one,” IFL Science explained.
It’s just another chapter in the eternal struggle between dogs and ants. Dogs need months of training to learn to detect cancer cells; ants can do it in 30 minutes. Over the course of a dog’s training, Fido eats more food than 10,000 ants combined. (Okay, we’re guessing here, but it’s got to be a pretty big number, right?)
Then there’s the warm and fuzzy factor. Just look at that picture. Who wouldn’t want a cutie like that curling up in the bed next to you?
Console War II: Battle of the Twitter users
Video games can be a lot of fun, provided you’re not playing something like Rock Simulator. Or Surgeon Simulator. Or Surgeon Simulator 2. Yes, those are all real games. But calling yourself a video gamer invites a certain negative connotation, and nowhere can that be better exemplified than the increasingly ridiculous console war.
For those who don’t know their video game history, back in the early 90s Nintendo and Sega were the main video game console makers. Nintendo had Mario, Sega had Sonic, and everyone had an opinion on which was best. With Sega now but a shell of its former self and Nintendo viewed as too “casual” for the true gaming connoisseur, today’s battle pits Playstation against Xbox, and fans of both consoles spend their time trying to one-up each other in increasingly silly online arguments.
That brings us nicely to a Twitter user named “Shreeveera,” who is very vocal about his love of Playstation and hatred of the Xbox. Importantly, for LOTME purposes, Shreeveera identified himself as a doctor on his profile, and in the middle of an argument, Xbox enthusiasts called his credentials into question.
At this point, most people would recognize that there are very few noteworthy console-exclusive video games in today’s world and that any argument about consoles essentially comes down to which console design you like or which company you find less distasteful, and they would step away from the Twitter argument. Shreeveera is not most people, and he decided the next logical move was to post a video of himself and an anesthetized patient about to undergo a laparoscopic cholecystectomy.
This move did prove that he was indeed a doctor, but the ethics of posting such a video with a patient in the room is a bit dubious at best. Since Shreeveera also listed the hospital he worked at, numerous Twitter users review bombed the hospital with one-star reviews. Shreeveera’s fate is unknown, but he did take down the video and removed “doctor by profession” from his profile. He also made a second video asking Twitter to stop trying to ruin his life. We’re sure that’ll go well. Twitter is known for being completely fair and reasonable.
Use your words to gain power
We live in the age of the emoji. The use of emojis in texts and emails is basically the new shorthand. It’s a fun and easy way to chat with people close to us, but a new study shows that it doesn’t help in a business setting. In fact, it may do a little damage.
The use of images such as emojis in communication or logos can make a person seem less powerful than someone who opts for written words, according to Elinor Amit, PhD, of Tel Aviv University and associates.
Participants in their study were asked to imagine shopping with a person wearing a T-shirt. Half were then shown the logo of the Red Sox baseball team and half saw the words “Red Sox.” In another scenario, they were asked to imagine attending a retreat of a company called Lotus. Then half were shown an employee wearing a shirt with an image of lotus flower and half saw the verbal logo “Lotus.” In both scenarios, the individuals wearing shirts with images were seen as less powerful than the people who wore shirts with words on them.
Why is that? In a Eurekalert statement, Dr. Amit said that “visual messages are often interpreted as a signal for desire for social proximity.” In a world with COVID-19, that could give anyone pause.
That desire for more social proximity, in turn, equals a suggested loss of power because research shows that people who want to be around other people more are less powerful than people who don’t.
With the reduced social proximity we have these days, we may want to keep things cool and lighthearted, especially in work emails with people who we’ve never met. It may be, however, that using your words to say thank you in the multitude of emails you respond to on a regular basis is better than that thumbs-up emoji. Nobody will think less of you.
Should Daylight Savings Time still be a thing?
This past week, we just experienced the spring-forward portion of Daylight Savings Time, which took an hour of sleep away from us all. Some of us may still be struggling to find our footing with the time change, but at least it’s still sunny out at 7 pm. For those who don’t really see the point of changing the clocks twice a year, there are actually some good reasons to do so.
Sen. Marco Rubio, sponsor of a bill to make the time change permanent, put it simply: “If we can get this passed, we don’t have to do this stupidity anymore.” Message received, apparently, since the measure just passed unanimously in the Senate.
It’s not clear if President Biden will approve it, though, because there’s a lot that comes into play: economic needs, seasonal depression, and safety.
“I know this is not the most important issue confronting America, but it’s one of those issues where there’s a lot of agreement,” Sen. Rubio said.
Not total agreement, though. The National Association of Convenience Stores is opposed to the bill, and Reuters noted that one witness at a recent hearing said the time change “is like living in the wrong time zone for almost eight months out of the year.”
Many people, however, seem to be leaning toward the permanent spring-forward as it gives businesses a longer window to provide entertainment in the evenings and kids are able to play outside longer after school.
Honestly, we’re leaning toward whichever one can reduce seasonal depression.
The oncologist’s new best friend
We know that dogs have very sensitive noses. They can track criminals and missing persons and sniff out drugs and bombs. They can even detect cancer cells … after months of training.
And then there are ants.
Cancer cells produce volatile organic compounds (VOCs), which can be sniffed out by dogs and other animals with sufficiently sophisticated olfactory senses. A group of French investigators decided to find out if Formica fusca is such an animal.
First, they placed breast cancer cells and healthy cells in a petri dish. The sample of cancer cells, however, included a sugary treat. “Over successive trials, the ants got quicker and quicker at finding the treat, indicating that they had learned to recognize the VOCs produced by the cancerous cells, using these as a beacon to guide their way to the sugary delight,” according to IFL Science.
When the researchers removed the treat, the ants still went straight for the cancer cells. Then they removed the healthy cells and substituted another type of breast cancer cell, with just one type getting the treat. They went for the cancer cells with the treat, “indicating that they were capable of distinguishing between the different cancer types based on the unique pattern of VOCs emitted by each one,” IFL Science explained.
It’s just another chapter in the eternal struggle between dogs and ants. Dogs need months of training to learn to detect cancer cells; ants can do it in 30 minutes. Over the course of a dog’s training, Fido eats more food than 10,000 ants combined. (Okay, we’re guessing here, but it’s got to be a pretty big number, right?)
Then there’s the warm and fuzzy factor. Just look at that picture. Who wouldn’t want a cutie like that curling up in the bed next to you?
Console War II: Battle of the Twitter users
Video games can be a lot of fun, provided you’re not playing something like Rock Simulator. Or Surgeon Simulator. Or Surgeon Simulator 2. Yes, those are all real games. But calling yourself a video gamer invites a certain negative connotation, and nowhere can that be better exemplified than the increasingly ridiculous console war.
For those who don’t know their video game history, back in the early 90s Nintendo and Sega were the main video game console makers. Nintendo had Mario, Sega had Sonic, and everyone had an opinion on which was best. With Sega now but a shell of its former self and Nintendo viewed as too “casual” for the true gaming connoisseur, today’s battle pits Playstation against Xbox, and fans of both consoles spend their time trying to one-up each other in increasingly silly online arguments.
That brings us nicely to a Twitter user named “Shreeveera,” who is very vocal about his love of Playstation and hatred of the Xbox. Importantly, for LOTME purposes, Shreeveera identified himself as a doctor on his profile, and in the middle of an argument, Xbox enthusiasts called his credentials into question.
At this point, most people would recognize that there are very few noteworthy console-exclusive video games in today’s world and that any argument about consoles essentially comes down to which console design you like or which company you find less distasteful, and they would step away from the Twitter argument. Shreeveera is not most people, and he decided the next logical move was to post a video of himself and an anesthetized patient about to undergo a laparoscopic cholecystectomy.
This move did prove that he was indeed a doctor, but the ethics of posting such a video with a patient in the room is a bit dubious at best. Since Shreeveera also listed the hospital he worked at, numerous Twitter users review bombed the hospital with one-star reviews. Shreeveera’s fate is unknown, but he did take down the video and removed “doctor by profession” from his profile. He also made a second video asking Twitter to stop trying to ruin his life. We’re sure that’ll go well. Twitter is known for being completely fair and reasonable.
Use your words to gain power
We live in the age of the emoji. The use of emojis in texts and emails is basically the new shorthand. It’s a fun and easy way to chat with people close to us, but a new study shows that it doesn’t help in a business setting. In fact, it may do a little damage.
The use of images such as emojis in communication or logos can make a person seem less powerful than someone who opts for written words, according to Elinor Amit, PhD, of Tel Aviv University and associates.
Participants in their study were asked to imagine shopping with a person wearing a T-shirt. Half were then shown the logo of the Red Sox baseball team and half saw the words “Red Sox.” In another scenario, they were asked to imagine attending a retreat of a company called Lotus. Then half were shown an employee wearing a shirt with an image of lotus flower and half saw the verbal logo “Lotus.” In both scenarios, the individuals wearing shirts with images were seen as less powerful than the people who wore shirts with words on them.
Why is that? In a Eurekalert statement, Dr. Amit said that “visual messages are often interpreted as a signal for desire for social proximity.” In a world with COVID-19, that could give anyone pause.
That desire for more social proximity, in turn, equals a suggested loss of power because research shows that people who want to be around other people more are less powerful than people who don’t.
With the reduced social proximity we have these days, we may want to keep things cool and lighthearted, especially in work emails with people who we’ve never met. It may be, however, that using your words to say thank you in the multitude of emails you respond to on a regular basis is better than that thumbs-up emoji. Nobody will think less of you.
Should Daylight Savings Time still be a thing?
This past week, we just experienced the spring-forward portion of Daylight Savings Time, which took an hour of sleep away from us all. Some of us may still be struggling to find our footing with the time change, but at least it’s still sunny out at 7 pm. For those who don’t really see the point of changing the clocks twice a year, there are actually some good reasons to do so.
Sen. Marco Rubio, sponsor of a bill to make the time change permanent, put it simply: “If we can get this passed, we don’t have to do this stupidity anymore.” Message received, apparently, since the measure just passed unanimously in the Senate.
It’s not clear if President Biden will approve it, though, because there’s a lot that comes into play: economic needs, seasonal depression, and safety.
“I know this is not the most important issue confronting America, but it’s one of those issues where there’s a lot of agreement,” Sen. Rubio said.
Not total agreement, though. The National Association of Convenience Stores is opposed to the bill, and Reuters noted that one witness at a recent hearing said the time change “is like living in the wrong time zone for almost eight months out of the year.”
Many people, however, seem to be leaning toward the permanent spring-forward as it gives businesses a longer window to provide entertainment in the evenings and kids are able to play outside longer after school.
Honestly, we’re leaning toward whichever one can reduce seasonal depression.
High-intensity exercise vs. omega-3s for heart failure risk reduction
A year of high-intensity interval training seemed to benefit obese middle-aged adults at a high risk of heart failure, but omega-3 fatty acid supplementation didn’t have any effect on cardiac biomarkers measured in a small, single-center, prospective study.
“One year of HIIT training reduces adiposity but had no consistent effect on myocardial triglyceride content or visceral adiposity,” wrote lead author Christopher M. Hearon Jr., PhD, and colleagues in JACC: Heart Failure. “However, long-duration HIIT improves fitness and induces favorable cardiac remodeling.” Omega-3 supplementation, however, had “no independent or additive effect.” Dr. Hearon is an instructor of applied clinical research at University of Texas Southwestern Medical Center in Dallas.
Investigators there and at the Institute for Exercise and Environmental Medicine at Texas Health Presbyterian Hospital Dallas studied 80 patients aged 40-55 years classified as high risk for HF and obese, randomizing them to a year of high-intensity interval training (HIIT) with supplementation of either 1.6 g omega-3 FA or placebo daily; or to a control group split between supplementation or placebo. Fifty-six patients completed the 1-year study, with a compliance rate of 90% in the HIIT group and 92% in those assigned omega-3 FA supplementation.
Carl J. “Chip” Lavie, MD, of the John Ochsner Heart and Vascular Institute in New Orleans, commented that, although the study was “extremely well done from an excellent research group,” it was limited by its small population and relatively short follow-up. Future research should evaluate HIIT and moderate exercise on clinical events over a longer term as well as different doses of omega-3 “There is tremendous potential for omega-3 in heart failure prevention and treatment.”
HIIT boosts exercise capacity, more
In the study, the HIIT group showed improvement in a number of cardiac markers: around a 22% improvement in exercise capacity as measured by absolute peak and relative peak oxygen uptake (VO2), even without significant weight loss. They improved an average of 0.43 L/min (0.32-0.53; P < .0001) and 4.46 mL/kg per minute (3.18-5.56; P < .0001), respectively.
The researchers attributed the increase in peak VO2 to an increase in peak cardiac output averaging 2.15 L/min (95% confidence interval, 0.90-3.39; P = .001) and stroke volume averaging 9.46 mL (95% CI, 0.65-18.27; P = .04). A year of exercise training also resulted in changes in cardiac remodeling, including increases in left ventricle mass and LV end diastolic volume, averaging 9.4 g (95% CI, 4.36-14.44; P < .001) and 12.33 mL (95% CI, 5.61-19.05; P < .001), respectively.
The study also found that neither intervention had any appreciable impact on body weight, body mass index, body surface area or lean mass, or markers of arterial or local carotid stiffness. The exercise group had a modest decrease in fat mass, averaging 2.63 kg (95% CI,–4.81 to –0.46; P = .02), but without any effect from omega-3 supplementation.
The study acknowledged that high-dose omega-3 supplements have been found to lower triglyceride levels in people with severe hypertriglyceridemia, and hypothesized that HIIT alone or with omega-3 supplementation would improve fitness and biomarkers in people with stage A HF. “Contrary to our hypothesis, we found that one year of n-3FA [omega-3 FA] supplementation had no detectable effect on any parameter related to cardiopulmonary fitness, cardiovascular remodeling/stiffness, visceral adiposity, or myocardial triglyceride content,” Dr. Hearon and colleagues wrote.
The study “shows that obese middle-aged patients with heart failure with preserved ejection fraction [HFpEF] can markedly improve their fitness with HIIT and, generally, fitness is one of the strongest if not the strongest predictor of prognosis and survival,” said Dr. Lavie.
“Studies are needed on exercise that improves fitness in both HF with reduced ejection fraction and HFpEF, but especially HFpEF,” he said.
The study received funding from the American Heart Association Strategically Focused Research Network. Dr. Hearon and coauthors have no relevant disclosures. Dr. Lavie is a speaker and consultant for PAI Health, the Global Organization for EPA and DHA Omega-3s and DSM Nutritional Products.
A year of high-intensity interval training seemed to benefit obese middle-aged adults at a high risk of heart failure, but omega-3 fatty acid supplementation didn’t have any effect on cardiac biomarkers measured in a small, single-center, prospective study.
“One year of HIIT training reduces adiposity but had no consistent effect on myocardial triglyceride content or visceral adiposity,” wrote lead author Christopher M. Hearon Jr., PhD, and colleagues in JACC: Heart Failure. “However, long-duration HIIT improves fitness and induces favorable cardiac remodeling.” Omega-3 supplementation, however, had “no independent or additive effect.” Dr. Hearon is an instructor of applied clinical research at University of Texas Southwestern Medical Center in Dallas.
Investigators there and at the Institute for Exercise and Environmental Medicine at Texas Health Presbyterian Hospital Dallas studied 80 patients aged 40-55 years classified as high risk for HF and obese, randomizing them to a year of high-intensity interval training (HIIT) with supplementation of either 1.6 g omega-3 FA or placebo daily; or to a control group split between supplementation or placebo. Fifty-six patients completed the 1-year study, with a compliance rate of 90% in the HIIT group and 92% in those assigned omega-3 FA supplementation.
Carl J. “Chip” Lavie, MD, of the John Ochsner Heart and Vascular Institute in New Orleans, commented that, although the study was “extremely well done from an excellent research group,” it was limited by its small population and relatively short follow-up. Future research should evaluate HIIT and moderate exercise on clinical events over a longer term as well as different doses of omega-3 “There is tremendous potential for omega-3 in heart failure prevention and treatment.”
HIIT boosts exercise capacity, more
In the study, the HIIT group showed improvement in a number of cardiac markers: around a 22% improvement in exercise capacity as measured by absolute peak and relative peak oxygen uptake (VO2), even without significant weight loss. They improved an average of 0.43 L/min (0.32-0.53; P < .0001) and 4.46 mL/kg per minute (3.18-5.56; P < .0001), respectively.
The researchers attributed the increase in peak VO2 to an increase in peak cardiac output averaging 2.15 L/min (95% confidence interval, 0.90-3.39; P = .001) and stroke volume averaging 9.46 mL (95% CI, 0.65-18.27; P = .04). A year of exercise training also resulted in changes in cardiac remodeling, including increases in left ventricle mass and LV end diastolic volume, averaging 9.4 g (95% CI, 4.36-14.44; P < .001) and 12.33 mL (95% CI, 5.61-19.05; P < .001), respectively.
The study also found that neither intervention had any appreciable impact on body weight, body mass index, body surface area or lean mass, or markers of arterial or local carotid stiffness. The exercise group had a modest decrease in fat mass, averaging 2.63 kg (95% CI,–4.81 to –0.46; P = .02), but without any effect from omega-3 supplementation.
The study acknowledged that high-dose omega-3 supplements have been found to lower triglyceride levels in people with severe hypertriglyceridemia, and hypothesized that HIIT alone or with omega-3 supplementation would improve fitness and biomarkers in people with stage A HF. “Contrary to our hypothesis, we found that one year of n-3FA [omega-3 FA] supplementation had no detectable effect on any parameter related to cardiopulmonary fitness, cardiovascular remodeling/stiffness, visceral adiposity, or myocardial triglyceride content,” Dr. Hearon and colleagues wrote.
The study “shows that obese middle-aged patients with heart failure with preserved ejection fraction [HFpEF] can markedly improve their fitness with HIIT and, generally, fitness is one of the strongest if not the strongest predictor of prognosis and survival,” said Dr. Lavie.
“Studies are needed on exercise that improves fitness in both HF with reduced ejection fraction and HFpEF, but especially HFpEF,” he said.
The study received funding from the American Heart Association Strategically Focused Research Network. Dr. Hearon and coauthors have no relevant disclosures. Dr. Lavie is a speaker and consultant for PAI Health, the Global Organization for EPA and DHA Omega-3s and DSM Nutritional Products.
A year of high-intensity interval training seemed to benefit obese middle-aged adults at a high risk of heart failure, but omega-3 fatty acid supplementation didn’t have any effect on cardiac biomarkers measured in a small, single-center, prospective study.
“One year of HIIT training reduces adiposity but had no consistent effect on myocardial triglyceride content or visceral adiposity,” wrote lead author Christopher M. Hearon Jr., PhD, and colleagues in JACC: Heart Failure. “However, long-duration HIIT improves fitness and induces favorable cardiac remodeling.” Omega-3 supplementation, however, had “no independent or additive effect.” Dr. Hearon is an instructor of applied clinical research at University of Texas Southwestern Medical Center in Dallas.
Investigators there and at the Institute for Exercise and Environmental Medicine at Texas Health Presbyterian Hospital Dallas studied 80 patients aged 40-55 years classified as high risk for HF and obese, randomizing them to a year of high-intensity interval training (HIIT) with supplementation of either 1.6 g omega-3 FA or placebo daily; or to a control group split between supplementation or placebo. Fifty-six patients completed the 1-year study, with a compliance rate of 90% in the HIIT group and 92% in those assigned omega-3 FA supplementation.
Carl J. “Chip” Lavie, MD, of the John Ochsner Heart and Vascular Institute in New Orleans, commented that, although the study was “extremely well done from an excellent research group,” it was limited by its small population and relatively short follow-up. Future research should evaluate HIIT and moderate exercise on clinical events over a longer term as well as different doses of omega-3 “There is tremendous potential for omega-3 in heart failure prevention and treatment.”
HIIT boosts exercise capacity, more
In the study, the HIIT group showed improvement in a number of cardiac markers: around a 22% improvement in exercise capacity as measured by absolute peak and relative peak oxygen uptake (VO2), even without significant weight loss. They improved an average of 0.43 L/min (0.32-0.53; P < .0001) and 4.46 mL/kg per minute (3.18-5.56; P < .0001), respectively.
The researchers attributed the increase in peak VO2 to an increase in peak cardiac output averaging 2.15 L/min (95% confidence interval, 0.90-3.39; P = .001) and stroke volume averaging 9.46 mL (95% CI, 0.65-18.27; P = .04). A year of exercise training also resulted in changes in cardiac remodeling, including increases in left ventricle mass and LV end diastolic volume, averaging 9.4 g (95% CI, 4.36-14.44; P < .001) and 12.33 mL (95% CI, 5.61-19.05; P < .001), respectively.
The study also found that neither intervention had any appreciable impact on body weight, body mass index, body surface area or lean mass, or markers of arterial or local carotid stiffness. The exercise group had a modest decrease in fat mass, averaging 2.63 kg (95% CI,–4.81 to –0.46; P = .02), but without any effect from omega-3 supplementation.
The study acknowledged that high-dose omega-3 supplements have been found to lower triglyceride levels in people with severe hypertriglyceridemia, and hypothesized that HIIT alone or with omega-3 supplementation would improve fitness and biomarkers in people with stage A HF. “Contrary to our hypothesis, we found that one year of n-3FA [omega-3 FA] supplementation had no detectable effect on any parameter related to cardiopulmonary fitness, cardiovascular remodeling/stiffness, visceral adiposity, or myocardial triglyceride content,” Dr. Hearon and colleagues wrote.
The study “shows that obese middle-aged patients with heart failure with preserved ejection fraction [HFpEF] can markedly improve their fitness with HIIT and, generally, fitness is one of the strongest if not the strongest predictor of prognosis and survival,” said Dr. Lavie.
“Studies are needed on exercise that improves fitness in both HF with reduced ejection fraction and HFpEF, but especially HFpEF,” he said.
The study received funding from the American Heart Association Strategically Focused Research Network. Dr. Hearon and coauthors have no relevant disclosures. Dr. Lavie is a speaker and consultant for PAI Health, the Global Organization for EPA and DHA Omega-3s and DSM Nutritional Products.
FROM JACC: HEART FAILURE
Pollution levels linked to physical and mental health problems
Other analyses of data have found environmental air pollution from sources such as car exhaust and factory output can trigger an inflammatory response in the body. What’s new about a study published in RMD Open is that it explored an association between long-term exposure to pollution and risk of autoimmune diseases, wrote Giovanni Adami, MD, of the University of Verona (Italy) and colleagues.
“Environmental air pollution, according to the World Health Organization, is a major risk to health and 99% of the population worldwide is living in places where recommendations for air quality are not met,” said Dr. Adami in an interview. The limited data on the precise role of air pollution on rheumatic diseases in particular prompted the study, he said.
To explore the potential link between air pollution exposure and autoimmune disease, the researchers reviewed medical information from 81,363 adults via a national medical database in Italy; the data were submitted between June 2016 and November 2020.
The average age of the study population was 65 years, and 92% were women; 22% had at least one coexisting health condition. Each study participant was linked to local environmental monitoring via their residential postcode.
The researchers obtained details about concentrations of particulate matter in the environment from the Italian Institute of Environmental Protection that included 617 monitoring stations in 110 Italian provinces. They focused on concentrations of 10 and 2.5 (PM10 and PM2.5).
Exposure thresholds of 30 mcg/m3 for PM10 and 20 mcg/m3 for PM2.5 are generally considered harmful to health, they noted. On average, the long-term exposure was 16 mcg/m3 for PM2.5 and 25 mcg/m3 for PM10 between 2013 and 2019.
Overall, 9,723 individuals (12%) were diagnosed with an autoimmune disease between 2016 and 2020.
Exposure to PM10 was associated with a 7% higher risk of diagnosis with any autoimmune disease for every 10 mcg/m3 increase in concentration, but no association appeared between PM2.5 exposure and increased risk of autoimmune diseases.
However, in an adjusted model, chronic exposure to PM10 above 30 mcg/m3 and to PM2.5 above 20 mcg/m3 were associated with a 12% and 13% higher risk, respectively, of any autoimmune disease.
Chronic exposure to high levels of PM10 was specifically associated with a higher risk of rheumatoid arthritis, but no other autoimmune diseases. Chronic exposure to high levels of PM2.5 was associated with a higher risk of rheumatoid arthritis, connective tissue diseases, and inflammatory bowel diseases.
In their discussion, the researchers noted that the smaller diameter of PM2.5 molecules fluctuate less in response to rain and other weather, compared with PM10 molecules, which might make them a more accurate predictor of exposure to chronic air pollution.
The study findings were limited by several factors including the observational design, which prohibits the establishment of cause, and a lack of data on the start of symptoms and dates of diagnoses for autoimmune diseases, the researchers noted. Other limitations include the high percentage of older women in the study, which may limit generalizability, and the inability to account for additional personal exposure to pollutants outside of the environmental exposure, they said.
However, the results were strengthened by the large sample size and wide geographic distribution with variable pollution exposure, they said.
“Unfortunately, we were not surprised at all,” by the findings, Dr. Adami said in an interview.
“The biological rationale underpinning our findings is strong. Nevertheless, the magnitude of the effect was overwhelming. In addition, we saw an effect even at threshold of exposure that is widely considered as safe,” Dr. Adami noted.
Clinicians have been taught to consider cigarette smoking or other lifestyle behaviors as major risk factors for the development of several autoimmune diseases, said Dr. Adami. “In the future, we probably should include air pollution exposure as a risk factor as well. Interestingly, there is also accumulating evidence linking acute exposure to environmental air pollution with flares of chronic arthritis,” he said.
“Our study could have direct societal and political consequences,” and might help direct policy makers’ decisions on addressing strategies aimed to reduce fossil emissions, he said. As for additional research, “we certainly need multination studies to confirm our results on a larger scale,” Dr. Adami emphasized. “In addition, it is time to take action and start designing interventions aimed to reduce acute and chronic exposure to air pollution in patients suffering from RMDs.”
Consider the big picture of air quality
The Italian study is especially timely “given our evolving and emerging understanding of environmental risk factors for acute and chronic diseases, which we must first understand before we can address,” said Eileen Barrett, MD, of the University of New Mexico, Albuquerque, in an interview.
“I am largely surprised about the findings, as most physicians aren’t studying ambient air quality and risk for autoimmune disease,” said Dr. Barrett. “More often we think of air quality when we think of risk for respiratory diseases than autoimmune diseases, per se,” she said.
“There are several take-home messages from this study,” said Dr. Barrett. “The first is that we need more research to understand the consequences of air pollutants on health. Second, this study reminds us to think broadly about how air quality and our environment can affect health. And third, all clinicians should be committed to promoting science that can improve public health and reduce death and disability,” she emphasized.
The findings do not specifically reflect associations between pollution and other conditions such as chronic obstructive pulmonary disease and asthma although previous studies have shown an association between asthma and COPD exacerbations and air pollution, Dr. Barrett said.
“Further research will be needed to confirm the associations reported in this study,” Dr. Barrett said.
More research in other countries, including research related to other autoimmune diseases, and with other datasets on population and community level risks from poor air quality, would be helpful, and that information could be used to advise smart public policy, Dr. Barrett added.
Air pollution’s mental health impact
Air pollution’s effects extend beyond physical to the psychological, a new study of depression in teenagers showed. This study was published in Developmental Psychology.
Previous research on the environmental factors associated with depressive symptoms in teens has focused mainly on individual and family level contributors; the impact of the physical environment has not been well studied, the investigators, Erika M. Manczak, PhD, of the University of Denver and colleagues, wrote.
In their paper, the authors found a significant impact of neighborhood ozone exposure on the trajectory of depressive symptoms in teens over a 4-year period.
“Given that inhaling pollution activates biological pathways implicated in the development of depression, including immune, cardiovascular, and neurodevelopmental processes, exposure to ambient air pollution may influence the development and/or trajectory of depressive symptoms in youth,” they said.
The researchers recruited 213 adolescents in the San Francisco Bay area through local advertisements. The participants were aged 9-13 years at baseline, with an average age of 11 years. A total of 121 were female, 47% were white, 8.5% were African American, 12.3% were Asian, 10.4% were nonwhite Latin, and 21.7% were biracial or another ethnicity. The participants self-reported depressive symptoms and other psychopathology symptoms up to three times during the study period. Ozone exposure was calculated based on home addresses.
After controlling for other personal, family, and neighborhood variables, the researchers found that higher levels of ozone exposure were significantly associated with increased depressive symptoms over time, and the slope of trajectory of depressive symptoms became steeper as the ozone levels increased (P less than .001). Ozone did not significantly predict the trajectory of any other psychopathology symptoms.
“The results of this study provide preliminary support for the possibility that ozone is an overlooked contributor to the development or course of youth depressive symptoms,” the researchers wrote in their discussion.
“Interestingly, the association between ozone and symptom trajectories as measured by Anxious/Depressed subscale of the [Youth Self-Report] was not as strong as it was for the [Children’s Depression Inventory-Short Version] or Withdrawn/Depressed scales, suggesting that associations are more robust for behavioral withdrawal symptoms of depression than for other types of symptoms,” they noted.
The study findings were limited by the use of self-reports and by the inability of the study design to show causality, the researchers said. Other limitations include the use of average assessments of ozone that are less precise, lack of assessment of biological pathways for risk, lack of formal psychiatric diagnoses, and the small geographic region included in the study, they said.
However, the results provide preliminary evidence that ozone exposure is a potential contributing factor to depressive symptoms in youth, and serve as a jumping-off point for future research, they noted. Future studies should address changes in systemic inflammation, neurodevelopment, or stress reactivity, as well as concurrent psychosocial or biological factors, and temporal associations between air pollution and mental health symptoms, they concluded.
Environmental factors drive inflammatory responses
Peter L. Loper Jr., MD, considers the findings of the Developmental Psychology study to be unsurprising but important – because air pollution is simply getting worse.
“As the study authors cite, there is sufficient data correlating ozone to negative physical health outcomes in youth, but a paucity of data exploring the impact of poor air quality on mental health outcomes in this demographic,” noted Dr. Loper, of the University of South Carolina, Columbia, in an interview.
“As discussed by the study researchers, any environmental exposure that increases immune-mediated inflammation can result in negative health outcomes. In fact, there is already data to suggest that similar cytokines, or immune cell signalers, that get released by our immune system due to environmental exposures and that contribute to asthma, may also be implicated in depression and other mental health problems,” he noted.
“Just like downstream symptom indicators of physical illnesses such as asthma are secondary to immune-mediated pulmonary inflammation, downstream symptom indicators of mental illness, such as depression, are secondary to immune-mediated neuroinflammation,” Dr. Loper emphasized. “The most well-characterized upstream phenomenon perpetuating the downstream symptom indicators of depression involve neuroinflammatory states due to psychosocial and relational factors such as chronic stress, poor relationships, or substance use. However, any environmental factor that triggers an immune response and inflammation can promote neuroinflammation that manifests as symptoms of mental illness.”
The message for teens with depression and their families is that “we are a product of our environment,” Dr. Loper said. “When our environments are proinflammatory, or cause our immune system to become overactive, then we will develop illness; however, the most potent mediator of inflammation in the brain, and the downstream symptoms of depression, is our relationships with those we love most,” he said.
Dr. Loper suggested research aimed at identifying other sources of immune-mediated inflammation caused by physical environments and better understanding how environmental phenomenon like ozone may compound previously established risk factors for mental illness could be useful.
The RMD Open study received no outside funding, and its authors had no financial conflicts.
The Developmental Psychology study was supported by the National Institute of Mental Health and the Stanford University Precision Health and Integrated Diagnostics Center. The researchers for that report, and Dr. Loper and Dr. Barrett had no conflicts to disclose.
Other analyses of data have found environmental air pollution from sources such as car exhaust and factory output can trigger an inflammatory response in the body. What’s new about a study published in RMD Open is that it explored an association between long-term exposure to pollution and risk of autoimmune diseases, wrote Giovanni Adami, MD, of the University of Verona (Italy) and colleagues.
“Environmental air pollution, according to the World Health Organization, is a major risk to health and 99% of the population worldwide is living in places where recommendations for air quality are not met,” said Dr. Adami in an interview. The limited data on the precise role of air pollution on rheumatic diseases in particular prompted the study, he said.
To explore the potential link between air pollution exposure and autoimmune disease, the researchers reviewed medical information from 81,363 adults via a national medical database in Italy; the data were submitted between June 2016 and November 2020.
The average age of the study population was 65 years, and 92% were women; 22% had at least one coexisting health condition. Each study participant was linked to local environmental monitoring via their residential postcode.
The researchers obtained details about concentrations of particulate matter in the environment from the Italian Institute of Environmental Protection that included 617 monitoring stations in 110 Italian provinces. They focused on concentrations of 10 and 2.5 (PM10 and PM2.5).
Exposure thresholds of 30 mcg/m3 for PM10 and 20 mcg/m3 for PM2.5 are generally considered harmful to health, they noted. On average, the long-term exposure was 16 mcg/m3 for PM2.5 and 25 mcg/m3 for PM10 between 2013 and 2019.
Overall, 9,723 individuals (12%) were diagnosed with an autoimmune disease between 2016 and 2020.
Exposure to PM10 was associated with a 7% higher risk of diagnosis with any autoimmune disease for every 10 mcg/m3 increase in concentration, but no association appeared between PM2.5 exposure and increased risk of autoimmune diseases.
However, in an adjusted model, chronic exposure to PM10 above 30 mcg/m3 and to PM2.5 above 20 mcg/m3 were associated with a 12% and 13% higher risk, respectively, of any autoimmune disease.
Chronic exposure to high levels of PM10 was specifically associated with a higher risk of rheumatoid arthritis, but no other autoimmune diseases. Chronic exposure to high levels of PM2.5 was associated with a higher risk of rheumatoid arthritis, connective tissue diseases, and inflammatory bowel diseases.
In their discussion, the researchers noted that the smaller diameter of PM2.5 molecules fluctuate less in response to rain and other weather, compared with PM10 molecules, which might make them a more accurate predictor of exposure to chronic air pollution.
The study findings were limited by several factors including the observational design, which prohibits the establishment of cause, and a lack of data on the start of symptoms and dates of diagnoses for autoimmune diseases, the researchers noted. Other limitations include the high percentage of older women in the study, which may limit generalizability, and the inability to account for additional personal exposure to pollutants outside of the environmental exposure, they said.
However, the results were strengthened by the large sample size and wide geographic distribution with variable pollution exposure, they said.
“Unfortunately, we were not surprised at all,” by the findings, Dr. Adami said in an interview.
“The biological rationale underpinning our findings is strong. Nevertheless, the magnitude of the effect was overwhelming. In addition, we saw an effect even at threshold of exposure that is widely considered as safe,” Dr. Adami noted.
Clinicians have been taught to consider cigarette smoking or other lifestyle behaviors as major risk factors for the development of several autoimmune diseases, said Dr. Adami. “In the future, we probably should include air pollution exposure as a risk factor as well. Interestingly, there is also accumulating evidence linking acute exposure to environmental air pollution with flares of chronic arthritis,” he said.
“Our study could have direct societal and political consequences,” and might help direct policy makers’ decisions on addressing strategies aimed to reduce fossil emissions, he said. As for additional research, “we certainly need multination studies to confirm our results on a larger scale,” Dr. Adami emphasized. “In addition, it is time to take action and start designing interventions aimed to reduce acute and chronic exposure to air pollution in patients suffering from RMDs.”
Consider the big picture of air quality
The Italian study is especially timely “given our evolving and emerging understanding of environmental risk factors for acute and chronic diseases, which we must first understand before we can address,” said Eileen Barrett, MD, of the University of New Mexico, Albuquerque, in an interview.
“I am largely surprised about the findings, as most physicians aren’t studying ambient air quality and risk for autoimmune disease,” said Dr. Barrett. “More often we think of air quality when we think of risk for respiratory diseases than autoimmune diseases, per se,” she said.
“There are several take-home messages from this study,” said Dr. Barrett. “The first is that we need more research to understand the consequences of air pollutants on health. Second, this study reminds us to think broadly about how air quality and our environment can affect health. And third, all clinicians should be committed to promoting science that can improve public health and reduce death and disability,” she emphasized.
The findings do not specifically reflect associations between pollution and other conditions such as chronic obstructive pulmonary disease and asthma although previous studies have shown an association between asthma and COPD exacerbations and air pollution, Dr. Barrett said.
“Further research will be needed to confirm the associations reported in this study,” Dr. Barrett said.
More research in other countries, including research related to other autoimmune diseases, and with other datasets on population and community level risks from poor air quality, would be helpful, and that information could be used to advise smart public policy, Dr. Barrett added.
Air pollution’s mental health impact
Air pollution’s effects extend beyond physical to the psychological, a new study of depression in teenagers showed. This study was published in Developmental Psychology.
Previous research on the environmental factors associated with depressive symptoms in teens has focused mainly on individual and family level contributors; the impact of the physical environment has not been well studied, the investigators, Erika M. Manczak, PhD, of the University of Denver and colleagues, wrote.
In their paper, the authors found a significant impact of neighborhood ozone exposure on the trajectory of depressive symptoms in teens over a 4-year period.
“Given that inhaling pollution activates biological pathways implicated in the development of depression, including immune, cardiovascular, and neurodevelopmental processes, exposure to ambient air pollution may influence the development and/or trajectory of depressive symptoms in youth,” they said.
The researchers recruited 213 adolescents in the San Francisco Bay area through local advertisements. The participants were aged 9-13 years at baseline, with an average age of 11 years. A total of 121 were female, 47% were white, 8.5% were African American, 12.3% were Asian, 10.4% were nonwhite Latin, and 21.7% were biracial or another ethnicity. The participants self-reported depressive symptoms and other psychopathology symptoms up to three times during the study period. Ozone exposure was calculated based on home addresses.
After controlling for other personal, family, and neighborhood variables, the researchers found that higher levels of ozone exposure were significantly associated with increased depressive symptoms over time, and the slope of trajectory of depressive symptoms became steeper as the ozone levels increased (P less than .001). Ozone did not significantly predict the trajectory of any other psychopathology symptoms.
“The results of this study provide preliminary support for the possibility that ozone is an overlooked contributor to the development or course of youth depressive symptoms,” the researchers wrote in their discussion.
“Interestingly, the association between ozone and symptom trajectories as measured by Anxious/Depressed subscale of the [Youth Self-Report] was not as strong as it was for the [Children’s Depression Inventory-Short Version] or Withdrawn/Depressed scales, suggesting that associations are more robust for behavioral withdrawal symptoms of depression than for other types of symptoms,” they noted.
The study findings were limited by the use of self-reports and by the inability of the study design to show causality, the researchers said. Other limitations include the use of average assessments of ozone that are less precise, lack of assessment of biological pathways for risk, lack of formal psychiatric diagnoses, and the small geographic region included in the study, they said.
However, the results provide preliminary evidence that ozone exposure is a potential contributing factor to depressive symptoms in youth, and serve as a jumping-off point for future research, they noted. Future studies should address changes in systemic inflammation, neurodevelopment, or stress reactivity, as well as concurrent psychosocial or biological factors, and temporal associations between air pollution and mental health symptoms, they concluded.
Environmental factors drive inflammatory responses
Peter L. Loper Jr., MD, considers the findings of the Developmental Psychology study to be unsurprising but important – because air pollution is simply getting worse.
“As the study authors cite, there is sufficient data correlating ozone to negative physical health outcomes in youth, but a paucity of data exploring the impact of poor air quality on mental health outcomes in this demographic,” noted Dr. Loper, of the University of South Carolina, Columbia, in an interview.
“As discussed by the study researchers, any environmental exposure that increases immune-mediated inflammation can result in negative health outcomes. In fact, there is already data to suggest that similar cytokines, or immune cell signalers, that get released by our immune system due to environmental exposures and that contribute to asthma, may also be implicated in depression and other mental health problems,” he noted.
“Just like downstream symptom indicators of physical illnesses such as asthma are secondary to immune-mediated pulmonary inflammation, downstream symptom indicators of mental illness, such as depression, are secondary to immune-mediated neuroinflammation,” Dr. Loper emphasized. “The most well-characterized upstream phenomenon perpetuating the downstream symptom indicators of depression involve neuroinflammatory states due to psychosocial and relational factors such as chronic stress, poor relationships, or substance use. However, any environmental factor that triggers an immune response and inflammation can promote neuroinflammation that manifests as symptoms of mental illness.”
The message for teens with depression and their families is that “we are a product of our environment,” Dr. Loper said. “When our environments are proinflammatory, or cause our immune system to become overactive, then we will develop illness; however, the most potent mediator of inflammation in the brain, and the downstream symptoms of depression, is our relationships with those we love most,” he said.
Dr. Loper suggested research aimed at identifying other sources of immune-mediated inflammation caused by physical environments and better understanding how environmental phenomenon like ozone may compound previously established risk factors for mental illness could be useful.
The RMD Open study received no outside funding, and its authors had no financial conflicts.
The Developmental Psychology study was supported by the National Institute of Mental Health and the Stanford University Precision Health and Integrated Diagnostics Center. The researchers for that report, and Dr. Loper and Dr. Barrett had no conflicts to disclose.
Other analyses of data have found environmental air pollution from sources such as car exhaust and factory output can trigger an inflammatory response in the body. What’s new about a study published in RMD Open is that it explored an association between long-term exposure to pollution and risk of autoimmune diseases, wrote Giovanni Adami, MD, of the University of Verona (Italy) and colleagues.
“Environmental air pollution, according to the World Health Organization, is a major risk to health and 99% of the population worldwide is living in places where recommendations for air quality are not met,” said Dr. Adami in an interview. The limited data on the precise role of air pollution on rheumatic diseases in particular prompted the study, he said.
To explore the potential link between air pollution exposure and autoimmune disease, the researchers reviewed medical information from 81,363 adults via a national medical database in Italy; the data were submitted between June 2016 and November 2020.
The average age of the study population was 65 years, and 92% were women; 22% had at least one coexisting health condition. Each study participant was linked to local environmental monitoring via their residential postcode.
The researchers obtained details about concentrations of particulate matter in the environment from the Italian Institute of Environmental Protection that included 617 monitoring stations in 110 Italian provinces. They focused on concentrations of 10 and 2.5 (PM10 and PM2.5).
Exposure thresholds of 30 mcg/m3 for PM10 and 20 mcg/m3 for PM2.5 are generally considered harmful to health, they noted. On average, the long-term exposure was 16 mcg/m3 for PM2.5 and 25 mcg/m3 for PM10 between 2013 and 2019.
Overall, 9,723 individuals (12%) were diagnosed with an autoimmune disease between 2016 and 2020.
Exposure to PM10 was associated with a 7% higher risk of diagnosis with any autoimmune disease for every 10 mcg/m3 increase in concentration, but no association appeared between PM2.5 exposure and increased risk of autoimmune diseases.
However, in an adjusted model, chronic exposure to PM10 above 30 mcg/m3 and to PM2.5 above 20 mcg/m3 were associated with a 12% and 13% higher risk, respectively, of any autoimmune disease.
Chronic exposure to high levels of PM10 was specifically associated with a higher risk of rheumatoid arthritis, but no other autoimmune diseases. Chronic exposure to high levels of PM2.5 was associated with a higher risk of rheumatoid arthritis, connective tissue diseases, and inflammatory bowel diseases.
In their discussion, the researchers noted that the smaller diameter of PM2.5 molecules fluctuate less in response to rain and other weather, compared with PM10 molecules, which might make them a more accurate predictor of exposure to chronic air pollution.
The study findings were limited by several factors including the observational design, which prohibits the establishment of cause, and a lack of data on the start of symptoms and dates of diagnoses for autoimmune diseases, the researchers noted. Other limitations include the high percentage of older women in the study, which may limit generalizability, and the inability to account for additional personal exposure to pollutants outside of the environmental exposure, they said.
However, the results were strengthened by the large sample size and wide geographic distribution with variable pollution exposure, they said.
“Unfortunately, we were not surprised at all,” by the findings, Dr. Adami said in an interview.
“The biological rationale underpinning our findings is strong. Nevertheless, the magnitude of the effect was overwhelming. In addition, we saw an effect even at threshold of exposure that is widely considered as safe,” Dr. Adami noted.
Clinicians have been taught to consider cigarette smoking or other lifestyle behaviors as major risk factors for the development of several autoimmune diseases, said Dr. Adami. “In the future, we probably should include air pollution exposure as a risk factor as well. Interestingly, there is also accumulating evidence linking acute exposure to environmental air pollution with flares of chronic arthritis,” he said.
“Our study could have direct societal and political consequences,” and might help direct policy makers’ decisions on addressing strategies aimed to reduce fossil emissions, he said. As for additional research, “we certainly need multination studies to confirm our results on a larger scale,” Dr. Adami emphasized. “In addition, it is time to take action and start designing interventions aimed to reduce acute and chronic exposure to air pollution in patients suffering from RMDs.”
Consider the big picture of air quality
The Italian study is especially timely “given our evolving and emerging understanding of environmental risk factors for acute and chronic diseases, which we must first understand before we can address,” said Eileen Barrett, MD, of the University of New Mexico, Albuquerque, in an interview.
“I am largely surprised about the findings, as most physicians aren’t studying ambient air quality and risk for autoimmune disease,” said Dr. Barrett. “More often we think of air quality when we think of risk for respiratory diseases than autoimmune diseases, per se,” she said.
“There are several take-home messages from this study,” said Dr. Barrett. “The first is that we need more research to understand the consequences of air pollutants on health. Second, this study reminds us to think broadly about how air quality and our environment can affect health. And third, all clinicians should be committed to promoting science that can improve public health and reduce death and disability,” she emphasized.
The findings do not specifically reflect associations between pollution and other conditions such as chronic obstructive pulmonary disease and asthma although previous studies have shown an association between asthma and COPD exacerbations and air pollution, Dr. Barrett said.
“Further research will be needed to confirm the associations reported in this study,” Dr. Barrett said.
More research in other countries, including research related to other autoimmune diseases, and with other datasets on population and community level risks from poor air quality, would be helpful, and that information could be used to advise smart public policy, Dr. Barrett added.
Air pollution’s mental health impact
Air pollution’s effects extend beyond physical to the psychological, a new study of depression in teenagers showed. This study was published in Developmental Psychology.
Previous research on the environmental factors associated with depressive symptoms in teens has focused mainly on individual and family level contributors; the impact of the physical environment has not been well studied, the investigators, Erika M. Manczak, PhD, of the University of Denver and colleagues, wrote.
In their paper, the authors found a significant impact of neighborhood ozone exposure on the trajectory of depressive symptoms in teens over a 4-year period.
“Given that inhaling pollution activates biological pathways implicated in the development of depression, including immune, cardiovascular, and neurodevelopmental processes, exposure to ambient air pollution may influence the development and/or trajectory of depressive symptoms in youth,” they said.
The researchers recruited 213 adolescents in the San Francisco Bay area through local advertisements. The participants were aged 9-13 years at baseline, with an average age of 11 years. A total of 121 were female, 47% were white, 8.5% were African American, 12.3% were Asian, 10.4% were nonwhite Latin, and 21.7% were biracial or another ethnicity. The participants self-reported depressive symptoms and other psychopathology symptoms up to three times during the study period. Ozone exposure was calculated based on home addresses.
After controlling for other personal, family, and neighborhood variables, the researchers found that higher levels of ozone exposure were significantly associated with increased depressive symptoms over time, and the slope of trajectory of depressive symptoms became steeper as the ozone levels increased (P less than .001). Ozone did not significantly predict the trajectory of any other psychopathology symptoms.
“The results of this study provide preliminary support for the possibility that ozone is an overlooked contributor to the development or course of youth depressive symptoms,” the researchers wrote in their discussion.
“Interestingly, the association between ozone and symptom trajectories as measured by Anxious/Depressed subscale of the [Youth Self-Report] was not as strong as it was for the [Children’s Depression Inventory-Short Version] or Withdrawn/Depressed scales, suggesting that associations are more robust for behavioral withdrawal symptoms of depression than for other types of symptoms,” they noted.
The study findings were limited by the use of self-reports and by the inability of the study design to show causality, the researchers said. Other limitations include the use of average assessments of ozone that are less precise, lack of assessment of biological pathways for risk, lack of formal psychiatric diagnoses, and the small geographic region included in the study, they said.
However, the results provide preliminary evidence that ozone exposure is a potential contributing factor to depressive symptoms in youth, and serve as a jumping-off point for future research, they noted. Future studies should address changes in systemic inflammation, neurodevelopment, or stress reactivity, as well as concurrent psychosocial or biological factors, and temporal associations between air pollution and mental health symptoms, they concluded.
Environmental factors drive inflammatory responses
Peter L. Loper Jr., MD, considers the findings of the Developmental Psychology study to be unsurprising but important – because air pollution is simply getting worse.
“As the study authors cite, there is sufficient data correlating ozone to negative physical health outcomes in youth, but a paucity of data exploring the impact of poor air quality on mental health outcomes in this demographic,” noted Dr. Loper, of the University of South Carolina, Columbia, in an interview.
“As discussed by the study researchers, any environmental exposure that increases immune-mediated inflammation can result in negative health outcomes. In fact, there is already data to suggest that similar cytokines, or immune cell signalers, that get released by our immune system due to environmental exposures and that contribute to asthma, may also be implicated in depression and other mental health problems,” he noted.
“Just like downstream symptom indicators of physical illnesses such as asthma are secondary to immune-mediated pulmonary inflammation, downstream symptom indicators of mental illness, such as depression, are secondary to immune-mediated neuroinflammation,” Dr. Loper emphasized. “The most well-characterized upstream phenomenon perpetuating the downstream symptom indicators of depression involve neuroinflammatory states due to psychosocial and relational factors such as chronic stress, poor relationships, or substance use. However, any environmental factor that triggers an immune response and inflammation can promote neuroinflammation that manifests as symptoms of mental illness.”
The message for teens with depression and their families is that “we are a product of our environment,” Dr. Loper said. “When our environments are proinflammatory, or cause our immune system to become overactive, then we will develop illness; however, the most potent mediator of inflammation in the brain, and the downstream symptoms of depression, is our relationships with those we love most,” he said.
Dr. Loper suggested research aimed at identifying other sources of immune-mediated inflammation caused by physical environments and better understanding how environmental phenomenon like ozone may compound previously established risk factors for mental illness could be useful.
The RMD Open study received no outside funding, and its authors had no financial conflicts.
The Developmental Psychology study was supported by the National Institute of Mental Health and the Stanford University Precision Health and Integrated Diagnostics Center. The researchers for that report, and Dr. Loper and Dr. Barrett had no conflicts to disclose.
FROM RMD OPEN
Cardiologists say rights to maternity leave violated
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Burden of thyroid cancer: Substantial and increasing
in many developed countries, including the Unites States, concluded a new analysis based on 30 years of observational data.
“We report overall increases in the burden of thyroid cancer across the majority of EU15+ countries between 1990 and 2019, evidenced by plateaus in incidence rates and reductions in mortality and DALY [disability-adjusted life-years] rates,” the authors reported.
“However, in a number of countries, including the U.S., there are unfavorable increasing mortality and DALY trends over this time period ... [and] a better understanding of the trends in the disease burden of thyroid cancer may help to inform future health system planning,” they added.
The study was published online March 10, 2022, in JAMA Otolaryngology–Head & Neck Surgery.
Trends in thyroid cancer
For the analysis, James Schuster-Bruce, MBChB, from St. George’s University Hospital NHS Foundation Trust, London, and colleagues compared trends in thyroid cancer across 30 years of follow-up among 15 countries of the (pre-2004) European Union as well as those in the United States, Australia, Canada, and Norway (EU15+).
Data from the Global Burden of Disease study database were used to track these trends. “We extracted age-standardized incidence rates (ASIRs), age-standardized mortality rates (ASMRs), and DALYs for thyroid cancer from EU15+ countries between 1990 and 2019 using the dedicated GBD study results tool,” the investigators explained.
In 2019, ASIRs were highest in Italy at 6.36 per 100,000 population, followed by the United States at a rate of 5.59 per 100,000 population – although incidence rates of thyroid cancer have actually recently decreased in U.S. women, they noted.
“Thirteen of 19 countries showed an average annual percentage increase in ASIR across the study period,” the investigators added. Out of all the EU15+ countries, the average annual percentage change (AAPC) was the highest in Australia at 2.5 per 100,000 population and the United States at 1.2 per 100,000.
On the other hand, a largely plateauing trend in incidence rates across the majority of EU15+ nations has been observed since 1990, as reflected by incidence rates ranging from –0.8 to 0.8 per 100,000 in the most recent period, the researchers added. ASMRs ranged from a 0.40 per 100,000 in Greece to 0.57 per 100,000 in Luxembourg.
In the United States, the ASMR in 2019 was 0.43 per 100,000 population while the ASMR was the lowest in the United Kingdom in the same year at 0.38 per 100,000 population.
Australia, Denmark, and the United States were the only countries showing positive AAPC changes, the team observed. For example, in the most recent period to 2019, Denmark and Australia had reductions in ASMR trends, whereas in the United States, the trend was toward increasing ASMRs
In 2019, the DALYs of the EU15+ nations ranged from 9.63 per 100,000 in the United Kingdom to 14.46 per 100,000 in Luxembourg. In the most recent period, a downward trend in DALYs was observed in Australia and Denmark while it plateaued in the United States.
“Overall, we identified improvements in thyroid cancer mortality and DALYs, but overall increases in thyroid cancer incidence in EU15+ countries over the past 3 decades,” the investigators commented.
It has been widely suggested that improvements in diagnostic techniques have contributed significantly to increasing incidence rates of thyroid cancer, but there is concern about overdiagnosis. Newer diagnostic techniques detect significant numbers of slow-growing, subclinical papillary thyroid cancers that make up at least one quarter of all thyroid cancer subtypes, the authors pointed out.
“It has therefore been suggested that an increase in subclinical disease has inflated the data to look more substantial than the clinical reality,” the authors wrote. However, they insisted that overdiagnosis alone is unlikely to account entirely for increasing incidence trends in the current analysis.
Rather, their concern for countries with high incidence rates of thyroid cancer is the surveillance burden of disease that does not affect mortality. “Close observation of future time trends in thyroid cancer disease burden should be performed in the context of recent changes in international clinical practice guidelines, which have suggested more conservative diagnostic and management strategies,” the authors suggested.
“In the context of the more conservative treatment guidelines and reported increase in true disease, it is important to closely observe mortality and DALYs over the coming years to ensure optimum thyroid cancer management in these nations,” they added.
The study had no specific funding. Dr. Schuster-Bruce disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in many developed countries, including the Unites States, concluded a new analysis based on 30 years of observational data.
“We report overall increases in the burden of thyroid cancer across the majority of EU15+ countries between 1990 and 2019, evidenced by plateaus in incidence rates and reductions in mortality and DALY [disability-adjusted life-years] rates,” the authors reported.
“However, in a number of countries, including the U.S., there are unfavorable increasing mortality and DALY trends over this time period ... [and] a better understanding of the trends in the disease burden of thyroid cancer may help to inform future health system planning,” they added.
The study was published online March 10, 2022, in JAMA Otolaryngology–Head & Neck Surgery.
Trends in thyroid cancer
For the analysis, James Schuster-Bruce, MBChB, from St. George’s University Hospital NHS Foundation Trust, London, and colleagues compared trends in thyroid cancer across 30 years of follow-up among 15 countries of the (pre-2004) European Union as well as those in the United States, Australia, Canada, and Norway (EU15+).
Data from the Global Burden of Disease study database were used to track these trends. “We extracted age-standardized incidence rates (ASIRs), age-standardized mortality rates (ASMRs), and DALYs for thyroid cancer from EU15+ countries between 1990 and 2019 using the dedicated GBD study results tool,” the investigators explained.
In 2019, ASIRs were highest in Italy at 6.36 per 100,000 population, followed by the United States at a rate of 5.59 per 100,000 population – although incidence rates of thyroid cancer have actually recently decreased in U.S. women, they noted.
“Thirteen of 19 countries showed an average annual percentage increase in ASIR across the study period,” the investigators added. Out of all the EU15+ countries, the average annual percentage change (AAPC) was the highest in Australia at 2.5 per 100,000 population and the United States at 1.2 per 100,000.
On the other hand, a largely plateauing trend in incidence rates across the majority of EU15+ nations has been observed since 1990, as reflected by incidence rates ranging from –0.8 to 0.8 per 100,000 in the most recent period, the researchers added. ASMRs ranged from a 0.40 per 100,000 in Greece to 0.57 per 100,000 in Luxembourg.
In the United States, the ASMR in 2019 was 0.43 per 100,000 population while the ASMR was the lowest in the United Kingdom in the same year at 0.38 per 100,000 population.
Australia, Denmark, and the United States were the only countries showing positive AAPC changes, the team observed. For example, in the most recent period to 2019, Denmark and Australia had reductions in ASMR trends, whereas in the United States, the trend was toward increasing ASMRs
In 2019, the DALYs of the EU15+ nations ranged from 9.63 per 100,000 in the United Kingdom to 14.46 per 100,000 in Luxembourg. In the most recent period, a downward trend in DALYs was observed in Australia and Denmark while it plateaued in the United States.
“Overall, we identified improvements in thyroid cancer mortality and DALYs, but overall increases in thyroid cancer incidence in EU15+ countries over the past 3 decades,” the investigators commented.
It has been widely suggested that improvements in diagnostic techniques have contributed significantly to increasing incidence rates of thyroid cancer, but there is concern about overdiagnosis. Newer diagnostic techniques detect significant numbers of slow-growing, subclinical papillary thyroid cancers that make up at least one quarter of all thyroid cancer subtypes, the authors pointed out.
“It has therefore been suggested that an increase in subclinical disease has inflated the data to look more substantial than the clinical reality,” the authors wrote. However, they insisted that overdiagnosis alone is unlikely to account entirely for increasing incidence trends in the current analysis.
Rather, their concern for countries with high incidence rates of thyroid cancer is the surveillance burden of disease that does not affect mortality. “Close observation of future time trends in thyroid cancer disease burden should be performed in the context of recent changes in international clinical practice guidelines, which have suggested more conservative diagnostic and management strategies,” the authors suggested.
“In the context of the more conservative treatment guidelines and reported increase in true disease, it is important to closely observe mortality and DALYs over the coming years to ensure optimum thyroid cancer management in these nations,” they added.
The study had no specific funding. Dr. Schuster-Bruce disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in many developed countries, including the Unites States, concluded a new analysis based on 30 years of observational data.
“We report overall increases in the burden of thyroid cancer across the majority of EU15+ countries between 1990 and 2019, evidenced by plateaus in incidence rates and reductions in mortality and DALY [disability-adjusted life-years] rates,” the authors reported.
“However, in a number of countries, including the U.S., there are unfavorable increasing mortality and DALY trends over this time period ... [and] a better understanding of the trends in the disease burden of thyroid cancer may help to inform future health system planning,” they added.
The study was published online March 10, 2022, in JAMA Otolaryngology–Head & Neck Surgery.
Trends in thyroid cancer
For the analysis, James Schuster-Bruce, MBChB, from St. George’s University Hospital NHS Foundation Trust, London, and colleagues compared trends in thyroid cancer across 30 years of follow-up among 15 countries of the (pre-2004) European Union as well as those in the United States, Australia, Canada, and Norway (EU15+).
Data from the Global Burden of Disease study database were used to track these trends. “We extracted age-standardized incidence rates (ASIRs), age-standardized mortality rates (ASMRs), and DALYs for thyroid cancer from EU15+ countries between 1990 and 2019 using the dedicated GBD study results tool,” the investigators explained.
In 2019, ASIRs were highest in Italy at 6.36 per 100,000 population, followed by the United States at a rate of 5.59 per 100,000 population – although incidence rates of thyroid cancer have actually recently decreased in U.S. women, they noted.
“Thirteen of 19 countries showed an average annual percentage increase in ASIR across the study period,” the investigators added. Out of all the EU15+ countries, the average annual percentage change (AAPC) was the highest in Australia at 2.5 per 100,000 population and the United States at 1.2 per 100,000.
On the other hand, a largely plateauing trend in incidence rates across the majority of EU15+ nations has been observed since 1990, as reflected by incidence rates ranging from –0.8 to 0.8 per 100,000 in the most recent period, the researchers added. ASMRs ranged from a 0.40 per 100,000 in Greece to 0.57 per 100,000 in Luxembourg.
In the United States, the ASMR in 2019 was 0.43 per 100,000 population while the ASMR was the lowest in the United Kingdom in the same year at 0.38 per 100,000 population.
Australia, Denmark, and the United States were the only countries showing positive AAPC changes, the team observed. For example, in the most recent period to 2019, Denmark and Australia had reductions in ASMR trends, whereas in the United States, the trend was toward increasing ASMRs
In 2019, the DALYs of the EU15+ nations ranged from 9.63 per 100,000 in the United Kingdom to 14.46 per 100,000 in Luxembourg. In the most recent period, a downward trend in DALYs was observed in Australia and Denmark while it plateaued in the United States.
“Overall, we identified improvements in thyroid cancer mortality and DALYs, but overall increases in thyroid cancer incidence in EU15+ countries over the past 3 decades,” the investigators commented.
It has been widely suggested that improvements in diagnostic techniques have contributed significantly to increasing incidence rates of thyroid cancer, but there is concern about overdiagnosis. Newer diagnostic techniques detect significant numbers of slow-growing, subclinical papillary thyroid cancers that make up at least one quarter of all thyroid cancer subtypes, the authors pointed out.
“It has therefore been suggested that an increase in subclinical disease has inflated the data to look more substantial than the clinical reality,” the authors wrote. However, they insisted that overdiagnosis alone is unlikely to account entirely for increasing incidence trends in the current analysis.
Rather, their concern for countries with high incidence rates of thyroid cancer is the surveillance burden of disease that does not affect mortality. “Close observation of future time trends in thyroid cancer disease burden should be performed in the context of recent changes in international clinical practice guidelines, which have suggested more conservative diagnostic and management strategies,” the authors suggested.
“In the context of the more conservative treatment guidelines and reported increase in true disease, it is important to closely observe mortality and DALYs over the coming years to ensure optimum thyroid cancer management in these nations,” they added.
The study had no specific funding. Dr. Schuster-Bruce disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA OTOLARYNGOLOGY–HEAD & NECK SURGERY.
Study: Majority of research on homeopathic remedies unpublished or unregistered
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
FROM BMJ EVIDENCE BASED MEDICINE
Food insecurity linked to metabolic syndrome in Hispanic/Latino youth
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
FROM PEDIATRICS