User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Despite retraction, study using fraudulent Surgisphere data still cited
A retracted study on the safety of blood pressure medications in patients with COVID-19 continues to be cited nearly a year later, new research shows.
The study in question, published on May 1, 2020, in the New England Journal of Medicine, showed no increased risk for in-hospital death with the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) in hospitalized patients with COVID-19.
Concerns about the veracity of the Surgisphere database used for the study, however, led to a June 4 retraction and to the June 13 retraction of a second study, published in the Lancet, that focused on hydroxychloroquine as a COVID-19 treatment.
Although the Surgisphere scandal caused a global reckoning of COVID-19 scientific studies, the new analysis identified 652 citations of the NEJM article as of May 31.
More than a third of the citations occurred in the first 2 months after the retraction, 54% were at least 3 months later, and 2.8% at least 6 months later. In May, 11 months after the article was retracted, it was cited 21 times, senior author Emily G. McDonald, MD, MSc, McGill University, Montreal, and colleagues reported in a research letter in JAMA Internal Medicine.
“In early May and June there were already more than 200 citations in one of the world’s leading scientific journals, so I do believe it was a highly influential article early on and had an impact on different types of studies or research taking place,” she said in an interview.
Dr. McDonald said she’s also “certain that it impacted patient care,” observing that when there are no guidelines available on how to manage patients, physicians will turn to the most recent evidence in the most reputable journals.
“In the case of ACE [inhibitors] and ARBs, although the study was based on fraudulent data, we were lucky that the overall message was in the end probably correct, but that might not have been the case for another study or dataset,” she said.
Early in the pandemic, concerns existed that ACE inhibitors and ARBs could be harmful, increasing the expression of ACE2 receptors, which the SARS-CoV-2 virus uses to gain entry into cells. The first randomized trial to examine the issue, BRACE CORONA, showed no clinical benefit to interrupting use of the agents in hospitalized patients. An observational study suggested ACE inhibitors may even be protective.
Of two high-profile retractions, McDonald said they chose to bypass the hydroxychloroquine study, which had an eye-popping Altmetric attention score of 23,084, compared with 3,727 for the NEJM paper, because it may have been cited for “other” reasons. “We wanted to focus less on the politics and more on the problem of retracted work.”
The team found that researchers across the globe were citing the retracted ACE/ARB paper (18.7% in the United States, 8.1% in Italy, and 44% other countries). Most citations were used to support a statement in the main text of a study, but in nearly 3% of cases, the data were incorporated into new analyses.
Just 17.6% of the studies cited or noted the retraction. “For sure, that was surprising to us. We suspected it, but our study confirmed it,” Dr. McDonald said.
Although retracted articles can be identified by a watermark or line of text, in some cases that can be easily missed, she noted. What’s more, not all citation software points out when a study has been retracted, a fate shared by the copyediting process.
“There are a lot of mechanisms in place and, in general, what’s happening is rare but there isn’t a perfect automated system solution to absolutely prevent this from happening,” she said. “It’s still subject to human error.”
The findings also have to be taken in the context of a rapidly emerging pandemic and the unprecedented torrent of scientific papers released over the past year.
“That might have contributed to why this happened, but the takeaway message is that this can happen despite our best efforts, and we need to challenge ourselves to come up with a system solution to prevent this from happening in the future,” Dr. McDonald said. “Current mechanisms are probably capturing 95% of it, but we need to do better.”
Limitations of the present analysis are that it was limited to the single retracted study; used only a single search engine, Google Scholar, to identify the citing works; and that additional citations may have been missed, the authors noted.
McDonald and coauthor Todd C. Lee, MD, report being signatories on a public letter calling for the retraction of the Surgisphere papers. Dr. Lee also reported receiving research support from Fonds De Recherche du Quebec-Sante during the conduct of the study.
A version of this article first appeared on Medscape.com.
A retracted study on the safety of blood pressure medications in patients with COVID-19 continues to be cited nearly a year later, new research shows.
The study in question, published on May 1, 2020, in the New England Journal of Medicine, showed no increased risk for in-hospital death with the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) in hospitalized patients with COVID-19.
Concerns about the veracity of the Surgisphere database used for the study, however, led to a June 4 retraction and to the June 13 retraction of a second study, published in the Lancet, that focused on hydroxychloroquine as a COVID-19 treatment.
Although the Surgisphere scandal caused a global reckoning of COVID-19 scientific studies, the new analysis identified 652 citations of the NEJM article as of May 31.
More than a third of the citations occurred in the first 2 months after the retraction, 54% were at least 3 months later, and 2.8% at least 6 months later. In May, 11 months after the article was retracted, it was cited 21 times, senior author Emily G. McDonald, MD, MSc, McGill University, Montreal, and colleagues reported in a research letter in JAMA Internal Medicine.
“In early May and June there were already more than 200 citations in one of the world’s leading scientific journals, so I do believe it was a highly influential article early on and had an impact on different types of studies or research taking place,” she said in an interview.
Dr. McDonald said she’s also “certain that it impacted patient care,” observing that when there are no guidelines available on how to manage patients, physicians will turn to the most recent evidence in the most reputable journals.
“In the case of ACE [inhibitors] and ARBs, although the study was based on fraudulent data, we were lucky that the overall message was in the end probably correct, but that might not have been the case for another study or dataset,” she said.
Early in the pandemic, concerns existed that ACE inhibitors and ARBs could be harmful, increasing the expression of ACE2 receptors, which the SARS-CoV-2 virus uses to gain entry into cells. The first randomized trial to examine the issue, BRACE CORONA, showed no clinical benefit to interrupting use of the agents in hospitalized patients. An observational study suggested ACE inhibitors may even be protective.
Of two high-profile retractions, McDonald said they chose to bypass the hydroxychloroquine study, which had an eye-popping Altmetric attention score of 23,084, compared with 3,727 for the NEJM paper, because it may have been cited for “other” reasons. “We wanted to focus less on the politics and more on the problem of retracted work.”
The team found that researchers across the globe were citing the retracted ACE/ARB paper (18.7% in the United States, 8.1% in Italy, and 44% other countries). Most citations were used to support a statement in the main text of a study, but in nearly 3% of cases, the data were incorporated into new analyses.
Just 17.6% of the studies cited or noted the retraction. “For sure, that was surprising to us. We suspected it, but our study confirmed it,” Dr. McDonald said.
Although retracted articles can be identified by a watermark or line of text, in some cases that can be easily missed, she noted. What’s more, not all citation software points out when a study has been retracted, a fate shared by the copyediting process.
“There are a lot of mechanisms in place and, in general, what’s happening is rare but there isn’t a perfect automated system solution to absolutely prevent this from happening,” she said. “It’s still subject to human error.”
The findings also have to be taken in the context of a rapidly emerging pandemic and the unprecedented torrent of scientific papers released over the past year.
“That might have contributed to why this happened, but the takeaway message is that this can happen despite our best efforts, and we need to challenge ourselves to come up with a system solution to prevent this from happening in the future,” Dr. McDonald said. “Current mechanisms are probably capturing 95% of it, but we need to do better.”
Limitations of the present analysis are that it was limited to the single retracted study; used only a single search engine, Google Scholar, to identify the citing works; and that additional citations may have been missed, the authors noted.
McDonald and coauthor Todd C. Lee, MD, report being signatories on a public letter calling for the retraction of the Surgisphere papers. Dr. Lee also reported receiving research support from Fonds De Recherche du Quebec-Sante during the conduct of the study.
A version of this article first appeared on Medscape.com.
A retracted study on the safety of blood pressure medications in patients with COVID-19 continues to be cited nearly a year later, new research shows.
The study in question, published on May 1, 2020, in the New England Journal of Medicine, showed no increased risk for in-hospital death with the use of ACE inhibitors or angiotensin-receptor blockers (ARBs) in hospitalized patients with COVID-19.
Concerns about the veracity of the Surgisphere database used for the study, however, led to a June 4 retraction and to the June 13 retraction of a second study, published in the Lancet, that focused on hydroxychloroquine as a COVID-19 treatment.
Although the Surgisphere scandal caused a global reckoning of COVID-19 scientific studies, the new analysis identified 652 citations of the NEJM article as of May 31.
More than a third of the citations occurred in the first 2 months after the retraction, 54% were at least 3 months later, and 2.8% at least 6 months later. In May, 11 months after the article was retracted, it was cited 21 times, senior author Emily G. McDonald, MD, MSc, McGill University, Montreal, and colleagues reported in a research letter in JAMA Internal Medicine.
“In early May and June there were already more than 200 citations in one of the world’s leading scientific journals, so I do believe it was a highly influential article early on and had an impact on different types of studies or research taking place,” she said in an interview.
Dr. McDonald said she’s also “certain that it impacted patient care,” observing that when there are no guidelines available on how to manage patients, physicians will turn to the most recent evidence in the most reputable journals.
“In the case of ACE [inhibitors] and ARBs, although the study was based on fraudulent data, we were lucky that the overall message was in the end probably correct, but that might not have been the case for another study or dataset,” she said.
Early in the pandemic, concerns existed that ACE inhibitors and ARBs could be harmful, increasing the expression of ACE2 receptors, which the SARS-CoV-2 virus uses to gain entry into cells. The first randomized trial to examine the issue, BRACE CORONA, showed no clinical benefit to interrupting use of the agents in hospitalized patients. An observational study suggested ACE inhibitors may even be protective.
Of two high-profile retractions, McDonald said they chose to bypass the hydroxychloroquine study, which had an eye-popping Altmetric attention score of 23,084, compared with 3,727 for the NEJM paper, because it may have been cited for “other” reasons. “We wanted to focus less on the politics and more on the problem of retracted work.”
The team found that researchers across the globe were citing the retracted ACE/ARB paper (18.7% in the United States, 8.1% in Italy, and 44% other countries). Most citations were used to support a statement in the main text of a study, but in nearly 3% of cases, the data were incorporated into new analyses.
Just 17.6% of the studies cited or noted the retraction. “For sure, that was surprising to us. We suspected it, but our study confirmed it,” Dr. McDonald said.
Although retracted articles can be identified by a watermark or line of text, in some cases that can be easily missed, she noted. What’s more, not all citation software points out when a study has been retracted, a fate shared by the copyediting process.
“There are a lot of mechanisms in place and, in general, what’s happening is rare but there isn’t a perfect automated system solution to absolutely prevent this from happening,” she said. “It’s still subject to human error.”
The findings also have to be taken in the context of a rapidly emerging pandemic and the unprecedented torrent of scientific papers released over the past year.
“That might have contributed to why this happened, but the takeaway message is that this can happen despite our best efforts, and we need to challenge ourselves to come up with a system solution to prevent this from happening in the future,” Dr. McDonald said. “Current mechanisms are probably capturing 95% of it, but we need to do better.”
Limitations of the present analysis are that it was limited to the single retracted study; used only a single search engine, Google Scholar, to identify the citing works; and that additional citations may have been missed, the authors noted.
McDonald and coauthor Todd C. Lee, MD, report being signatories on a public letter calling for the retraction of the Surgisphere papers. Dr. Lee also reported receiving research support from Fonds De Recherche du Quebec-Sante during the conduct of the study.
A version of this article first appeared on Medscape.com.
Myocarditis tied to COVID-19 shots more common than reported?
While cases of pericarditis or myocarditis temporally linked to COVID-19 vaccination remain rare, they may happen more often than reported, according to a large review of electronic medical records (EMRs).
They also appear to represent two “distinct syndromes,” George Diaz, MD, Providence Regional Medical Center Everett (Washington), said in an interview.
Myocarditis typically occurs soon after vaccination in younger patients and mostly after the second dose, while pericarditis occurs later in older patients, after the first or second dose.
Dr. Diaz and colleagues reported their analysis in a research letter published online August 4 in JAMA.
They reviewed the records of 2,000,287 people who received at least one COVID-19 vaccination at 40 hospitals in Washington, Oregon, Montana, and California that are part of the Providence health care system and use the same EMRs.
The median age of the cohort was 57 years and 59% were women.
A little more than three quarters (77%) received more than one dose; most received the mRNA vaccines made by Pfizer (53%) and Moderna (44%); 3% received the Johnson & Johnson vaccine.
The records showed that 20 people had vaccine-related myocarditis (1.0 per 100,000) and 37 had pericarditis (1.8 per 100,000).
A recent report, based on data from the Centers for Disease Control and Prevention’s Vaccine Adverse Events Reporting System, suggested an incidence of myocarditis of about 4.8 cases per 1 million following receipt of mRNA COVID-19 vaccine.
The new study shows a “similar pattern, although at higher incidence, suggesting vaccine adverse event underreporting. In addition, pericarditis may be more common than myocarditis among older patients,” the study team wrote.
“Our study resulted in higher numbers of cases probably because we searched the EMR, and VAERS requires doctors to report suspected cases voluntarily,” Dr. Diaz said in an interview.
Also, in the governments’ statistics, pericarditis and myocarditis were “lumped together,” he noted.
Myocarditis cases
The 20 myocarditis cases occurred a median of 3.5 days after vaccination (11 after the Moderna vaccine and 9 after the Pfizer vaccine), 15 of the patients (75%) were men, and the median age was 36 years.
Four individuals (20%) developed myocarditis symptoms after the first vaccination and 16 (80%) after the second dose. Nineteen of the patients (95%) were admitted to the hospital and all were discharged after a median of 2 days.
None of the 20 patients were readmitted or died. Two received a second vaccination after onset of myocarditis; neither had worsening of symptoms. At last available follow-up (median, 23.5 days after symptom onset), 13 patients (65%) had a resolution of their myocarditis symptoms and seven (35%) were improving.
Pericarditis cases
The 37 pericarditis cases occurred a median of 20 days after the most recent COVID-19 vaccination: 23 (62%) with Pfizer, 12 (32%) with Moderna, and 2 (5%) with the J&J vaccine. Fifteen developed pericarditis after the first vaccine dose (41%) and 22 (59%) after the second.
Twenty-seven (73%) of the cases occurred in men; the median age was 59 years.
Thirteen patients (35%) were admitted to the hospital, none to intensive care. The median hospital stay was 1 day. Seven patients with pericarditis received a second vaccination. No patient died.
At last available follow-up (median, 28 days), 7 patients (19%) had resolved symptoms and 23 (62%) were improving.
The researchers also calculate that the average monthly number of cases of myocarditis or myopericarditis during the prevaccine period of January 2019 through January 2021 was 16.9 (95% confidence interval, 15.3-18.6) compared with 27.3 (95% CI, 22.4-32.9) during the vaccine period of February through May 2021 (P < .001).
The mean numbers of pericarditis cases during the same periods were 49.1 (95% CI, 46.4-51.9) and 78.8 (95% CI, 70.3-87.9), respectively (P < .001).
The authors say limitations of their analysis include potential missed cases outside care settings and missed diagnoses of myocarditis or pericarditis, which would underestimate the incidence, as well as inaccurate EMR vaccination information.
“Temporal association does not prove causation, although the short span between vaccination and myocarditis onset and the elevated incidence of myocarditis and pericarditis in the study hospitals lend support to a possible relationship,” they wrote.
In late June, the Food and Drug Administration added a warning to the fact sheets accompanying the Pfizer and Moderna mRNA COVID-19 vaccines, flagging the rare risk of heart inflammation after their use.
Dr. Diaz cautioned that myocarditis and pericarditis events remain “a rare occurrence” after COVID-19 vaccination.
“When discussing vaccination with patients, [health care providers] can advise them that patients generally recover in the rare event they get pericarditis or myocarditis and no deaths were found, and that the vaccines are safe and effective,” Dr. Diaz said.
The study had no specific funding. Dr. Diaz reported receipt of clinical trial research support from Gilead Sciences, Regeneron, Roche, Boehringer Ingelheim, and Edesa Biotech and scientific advisory board membership for Safeology.
A version of this article first appeared on Medscape.com.
While cases of pericarditis or myocarditis temporally linked to COVID-19 vaccination remain rare, they may happen more often than reported, according to a large review of electronic medical records (EMRs).
They also appear to represent two “distinct syndromes,” George Diaz, MD, Providence Regional Medical Center Everett (Washington), said in an interview.
Myocarditis typically occurs soon after vaccination in younger patients and mostly after the second dose, while pericarditis occurs later in older patients, after the first or second dose.
Dr. Diaz and colleagues reported their analysis in a research letter published online August 4 in JAMA.
They reviewed the records of 2,000,287 people who received at least one COVID-19 vaccination at 40 hospitals in Washington, Oregon, Montana, and California that are part of the Providence health care system and use the same EMRs.
The median age of the cohort was 57 years and 59% were women.
A little more than three quarters (77%) received more than one dose; most received the mRNA vaccines made by Pfizer (53%) and Moderna (44%); 3% received the Johnson & Johnson vaccine.
The records showed that 20 people had vaccine-related myocarditis (1.0 per 100,000) and 37 had pericarditis (1.8 per 100,000).
A recent report, based on data from the Centers for Disease Control and Prevention’s Vaccine Adverse Events Reporting System, suggested an incidence of myocarditis of about 4.8 cases per 1 million following receipt of mRNA COVID-19 vaccine.
The new study shows a “similar pattern, although at higher incidence, suggesting vaccine adverse event underreporting. In addition, pericarditis may be more common than myocarditis among older patients,” the study team wrote.
“Our study resulted in higher numbers of cases probably because we searched the EMR, and VAERS requires doctors to report suspected cases voluntarily,” Dr. Diaz said in an interview.
Also, in the governments’ statistics, pericarditis and myocarditis were “lumped together,” he noted.
Myocarditis cases
The 20 myocarditis cases occurred a median of 3.5 days after vaccination (11 after the Moderna vaccine and 9 after the Pfizer vaccine), 15 of the patients (75%) were men, and the median age was 36 years.
Four individuals (20%) developed myocarditis symptoms after the first vaccination and 16 (80%) after the second dose. Nineteen of the patients (95%) were admitted to the hospital and all were discharged after a median of 2 days.
None of the 20 patients were readmitted or died. Two received a second vaccination after onset of myocarditis; neither had worsening of symptoms. At last available follow-up (median, 23.5 days after symptom onset), 13 patients (65%) had a resolution of their myocarditis symptoms and seven (35%) were improving.
Pericarditis cases
The 37 pericarditis cases occurred a median of 20 days after the most recent COVID-19 vaccination: 23 (62%) with Pfizer, 12 (32%) with Moderna, and 2 (5%) with the J&J vaccine. Fifteen developed pericarditis after the first vaccine dose (41%) and 22 (59%) after the second.
Twenty-seven (73%) of the cases occurred in men; the median age was 59 years.
Thirteen patients (35%) were admitted to the hospital, none to intensive care. The median hospital stay was 1 day. Seven patients with pericarditis received a second vaccination. No patient died.
At last available follow-up (median, 28 days), 7 patients (19%) had resolved symptoms and 23 (62%) were improving.
The researchers also calculate that the average monthly number of cases of myocarditis or myopericarditis during the prevaccine period of January 2019 through January 2021 was 16.9 (95% confidence interval, 15.3-18.6) compared with 27.3 (95% CI, 22.4-32.9) during the vaccine period of February through May 2021 (P < .001).
The mean numbers of pericarditis cases during the same periods were 49.1 (95% CI, 46.4-51.9) and 78.8 (95% CI, 70.3-87.9), respectively (P < .001).
The authors say limitations of their analysis include potential missed cases outside care settings and missed diagnoses of myocarditis or pericarditis, which would underestimate the incidence, as well as inaccurate EMR vaccination information.
“Temporal association does not prove causation, although the short span between vaccination and myocarditis onset and the elevated incidence of myocarditis and pericarditis in the study hospitals lend support to a possible relationship,” they wrote.
In late June, the Food and Drug Administration added a warning to the fact sheets accompanying the Pfizer and Moderna mRNA COVID-19 vaccines, flagging the rare risk of heart inflammation after their use.
Dr. Diaz cautioned that myocarditis and pericarditis events remain “a rare occurrence” after COVID-19 vaccination.
“When discussing vaccination with patients, [health care providers] can advise them that patients generally recover in the rare event they get pericarditis or myocarditis and no deaths were found, and that the vaccines are safe and effective,” Dr. Diaz said.
The study had no specific funding. Dr. Diaz reported receipt of clinical trial research support from Gilead Sciences, Regeneron, Roche, Boehringer Ingelheim, and Edesa Biotech and scientific advisory board membership for Safeology.
A version of this article first appeared on Medscape.com.
While cases of pericarditis or myocarditis temporally linked to COVID-19 vaccination remain rare, they may happen more often than reported, according to a large review of electronic medical records (EMRs).
They also appear to represent two “distinct syndromes,” George Diaz, MD, Providence Regional Medical Center Everett (Washington), said in an interview.
Myocarditis typically occurs soon after vaccination in younger patients and mostly after the second dose, while pericarditis occurs later in older patients, after the first or second dose.
Dr. Diaz and colleagues reported their analysis in a research letter published online August 4 in JAMA.
They reviewed the records of 2,000,287 people who received at least one COVID-19 vaccination at 40 hospitals in Washington, Oregon, Montana, and California that are part of the Providence health care system and use the same EMRs.
The median age of the cohort was 57 years and 59% were women.
A little more than three quarters (77%) received more than one dose; most received the mRNA vaccines made by Pfizer (53%) and Moderna (44%); 3% received the Johnson & Johnson vaccine.
The records showed that 20 people had vaccine-related myocarditis (1.0 per 100,000) and 37 had pericarditis (1.8 per 100,000).
A recent report, based on data from the Centers for Disease Control and Prevention’s Vaccine Adverse Events Reporting System, suggested an incidence of myocarditis of about 4.8 cases per 1 million following receipt of mRNA COVID-19 vaccine.
The new study shows a “similar pattern, although at higher incidence, suggesting vaccine adverse event underreporting. In addition, pericarditis may be more common than myocarditis among older patients,” the study team wrote.
“Our study resulted in higher numbers of cases probably because we searched the EMR, and VAERS requires doctors to report suspected cases voluntarily,” Dr. Diaz said in an interview.
Also, in the governments’ statistics, pericarditis and myocarditis were “lumped together,” he noted.
Myocarditis cases
The 20 myocarditis cases occurred a median of 3.5 days after vaccination (11 after the Moderna vaccine and 9 after the Pfizer vaccine), 15 of the patients (75%) were men, and the median age was 36 years.
Four individuals (20%) developed myocarditis symptoms after the first vaccination and 16 (80%) after the second dose. Nineteen of the patients (95%) were admitted to the hospital and all were discharged after a median of 2 days.
None of the 20 patients were readmitted or died. Two received a second vaccination after onset of myocarditis; neither had worsening of symptoms. At last available follow-up (median, 23.5 days after symptom onset), 13 patients (65%) had a resolution of their myocarditis symptoms and seven (35%) were improving.
Pericarditis cases
The 37 pericarditis cases occurred a median of 20 days after the most recent COVID-19 vaccination: 23 (62%) with Pfizer, 12 (32%) with Moderna, and 2 (5%) with the J&J vaccine. Fifteen developed pericarditis after the first vaccine dose (41%) and 22 (59%) after the second.
Twenty-seven (73%) of the cases occurred in men; the median age was 59 years.
Thirteen patients (35%) were admitted to the hospital, none to intensive care. The median hospital stay was 1 day. Seven patients with pericarditis received a second vaccination. No patient died.
At last available follow-up (median, 28 days), 7 patients (19%) had resolved symptoms and 23 (62%) were improving.
The researchers also calculate that the average monthly number of cases of myocarditis or myopericarditis during the prevaccine period of January 2019 through January 2021 was 16.9 (95% confidence interval, 15.3-18.6) compared with 27.3 (95% CI, 22.4-32.9) during the vaccine period of February through May 2021 (P < .001).
The mean numbers of pericarditis cases during the same periods were 49.1 (95% CI, 46.4-51.9) and 78.8 (95% CI, 70.3-87.9), respectively (P < .001).
The authors say limitations of their analysis include potential missed cases outside care settings and missed diagnoses of myocarditis or pericarditis, which would underestimate the incidence, as well as inaccurate EMR vaccination information.
“Temporal association does not prove causation, although the short span between vaccination and myocarditis onset and the elevated incidence of myocarditis and pericarditis in the study hospitals lend support to a possible relationship,” they wrote.
In late June, the Food and Drug Administration added a warning to the fact sheets accompanying the Pfizer and Moderna mRNA COVID-19 vaccines, flagging the rare risk of heart inflammation after their use.
Dr. Diaz cautioned that myocarditis and pericarditis events remain “a rare occurrence” after COVID-19 vaccination.
“When discussing vaccination with patients, [health care providers] can advise them that patients generally recover in the rare event they get pericarditis or myocarditis and no deaths were found, and that the vaccines are safe and effective,” Dr. Diaz said.
The study had no specific funding. Dr. Diaz reported receipt of clinical trial research support from Gilead Sciences, Regeneron, Roche, Boehringer Ingelheim, and Edesa Biotech and scientific advisory board membership for Safeology.
A version of this article first appeared on Medscape.com.
FDA clears app for FreeStyle Libre 2 glucose monitor
The Food and Drug Administration has cleared the FreeStyle Libre 2 iOS application for use with compatible iPhones.
The new app works with the FreeStyle Libre 2 with optional glucose alarms, which was approved in the United States in June 2020 for people with diabetes aged 4 years and older.
Until now, it was only a reader device with no app compatibility. The older FreeStyle Libre 14-day, available in the United States since July 2018, has both a reader and an app, but not optional alarms.
The new app, which will soon be available for download from the App Store, enables users to view glucose readings on their iPhones and allows for caregivers or other individuals to remotely monitor the patient’s glucose levels and receive real-time alarms via the LibreLinkUp app.
Worn for 14 days before replacement is needed, the FreeStyle Libre 2 is the longest-lasting integrated continuous glucose monitoring (iCGM) sensor currently on the market. The first iCGM, the Dexcom G6, is worn for 10 days.
The Libre 2 is available at pharmacies, typically at a lower cost than other CGM systems based on a list price comparison. The actual cost for patients varies depending on insurance coverage.
Abbott has secured partial or full reimbursement for the FreeStyle Libre system in 38 countries, including Canada, France, Germany, Japan, the United Kingdom, and the United States.
The FreeStyle Libre 3 is approved for use in the European Union.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has cleared the FreeStyle Libre 2 iOS application for use with compatible iPhones.
The new app works with the FreeStyle Libre 2 with optional glucose alarms, which was approved in the United States in June 2020 for people with diabetes aged 4 years and older.
Until now, it was only a reader device with no app compatibility. The older FreeStyle Libre 14-day, available in the United States since July 2018, has both a reader and an app, but not optional alarms.
The new app, which will soon be available for download from the App Store, enables users to view glucose readings on their iPhones and allows for caregivers or other individuals to remotely monitor the patient’s glucose levels and receive real-time alarms via the LibreLinkUp app.
Worn for 14 days before replacement is needed, the FreeStyle Libre 2 is the longest-lasting integrated continuous glucose monitoring (iCGM) sensor currently on the market. The first iCGM, the Dexcom G6, is worn for 10 days.
The Libre 2 is available at pharmacies, typically at a lower cost than other CGM systems based on a list price comparison. The actual cost for patients varies depending on insurance coverage.
Abbott has secured partial or full reimbursement for the FreeStyle Libre system in 38 countries, including Canada, France, Germany, Japan, the United Kingdom, and the United States.
The FreeStyle Libre 3 is approved for use in the European Union.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has cleared the FreeStyle Libre 2 iOS application for use with compatible iPhones.
The new app works with the FreeStyle Libre 2 with optional glucose alarms, which was approved in the United States in June 2020 for people with diabetes aged 4 years and older.
Until now, it was only a reader device with no app compatibility. The older FreeStyle Libre 14-day, available in the United States since July 2018, has both a reader and an app, but not optional alarms.
The new app, which will soon be available for download from the App Store, enables users to view glucose readings on their iPhones and allows for caregivers or other individuals to remotely monitor the patient’s glucose levels and receive real-time alarms via the LibreLinkUp app.
Worn for 14 days before replacement is needed, the FreeStyle Libre 2 is the longest-lasting integrated continuous glucose monitoring (iCGM) sensor currently on the market. The first iCGM, the Dexcom G6, is worn for 10 days.
The Libre 2 is available at pharmacies, typically at a lower cost than other CGM systems based on a list price comparison. The actual cost for patients varies depending on insurance coverage.
Abbott has secured partial or full reimbursement for the FreeStyle Libre system in 38 countries, including Canada, France, Germany, Japan, the United Kingdom, and the United States.
The FreeStyle Libre 3 is approved for use in the European Union.
A version of this article first appeared on Medscape.com.
Thousands of patients were implanted with heart pumps that the FDA knew could be dangerous
John Winkler II was dying of heart failure when doctors came to his hospital bedside, offering a chance to prolong his life. The HeartWare Ventricular Assist Device, or HVAD, could be implanted in Winkler’s chest until a transplant was possible. The heart pump came with disclaimers of risk, but Winkler wanted to fight for time. He was only 46 and had a loving wife and four children, and his second grandchild was on the way.
So, in August 2014, Winkler had surgery to implant the device. A golf-ball–sized rotor was attached to his left ventricle to pump blood through a tube and into his aorta. A cable threading out of a small incision in his waist connected to a battery-powered controller strapped to his body. If something went wrong, an alarm as loud as a fire drill would sound.
Winkler returned home weeks later and, as he regained his strength, became hopeful about the future. He started making plans to visit colleges with his daughter, and was able to host his parents and new grandchild for Christmas. “He was doing so much better,” his wife, Tina Winkler, said. “We thought he was coasting until he got his transplant.”
What John Winkler didn’t know: Months before his implant, the Food and Drug Administration put HeartWare on notice for not properly monitoring or repairing HVAD defects, such as faulty batteries and short circuits caused by static electricity, that had killed patients. The agency issued a warning letter, one of its most serious citations. It demanded fixes within 15 days, but took no decisive action as problems persisted.
Ten days after Christmas of 2014, Winkler’s two teenage children heard the HVAD’s piercing alarm and ran upstairs. They found their father collapsed on his bedroom floor, completely unresponsive. Kelly, 17, dropped to his side and tried to copy how people on television did CPR. She told her brother to call 911, and over the device’s siren did her best to hear instructions from the operator.
When paramedics arrived and assessed her father, one made a passing comment that has haunted Kelly ever since: “Well, his toes are already cold.” He died 2 days later. Medtronic, the company that acquired HeartWare in 2016, settled a lawsuit by the family last year, admitting no fault. Tina Winkler believes her children blamed themselves for their father’s death. “Those two kids have never been the same,” she said. “I think they feel like they didn’t do things they needed to do.”
But it was the FDA that failed to protect Winkler and thousands of other patients whose survival depended on the HVAD, a ProPublica investigation found.
As HeartWare and Medtronic failed inspection after inspection and reports of device-related deaths piled up, the FDA relied on the device makers to fix the problems voluntarily rather than compelling them to do so.
The HVAD was implanted into more than 19,000 patients, the majority of whom got it after the FDA found in 2014 that the device didn’t meet federal standards. By the end of last year, the agency had received more than 3,000 reports of patient deaths that may have been caused or contributed to by the device.
Among them were reports of deaths the company linked to serious device problems: a patient who vomited blood as a family member struggled to restart a defective HVAD; a patient who bled out internally and died after implant surgery because a tube attached to the pump tore open; a patient whose heart tissue was left charred after an HVAD short-circuited and voltage surged through the pump.
The ineffective regulatory oversight of the HVAD is emblematic of larger, more systemic weaknesses.
For decades, the FDA and its Center for Devices and Radiological Health have been responsible for ensuring that high-risk medical devices are safe and effective. Yet they rely mostly on manufacturers to identify and correct problems. The agency says it can seize products, order injunctions against companies, or issue fines, but it rarely does so, preferring instead for companies to make fixes voluntarily.
When federal investigators found repeated manufacturing issues with the HVAD for years, the FDA didn’t penalize the company, even as the company issued 15 serious recalls of the device starting in 2014, the most of any single high-risk device in the FDA’s database. Thousands of patients with recalled models needed to have external HVAD parts replaced or take extra caution while handling their devices and monitor them for signs of malfunctions that could cause injury or death.
Meanwhile, the processes to inform the public through formal FDA notices and messages to health care providers repeatedly failed and left patients in the dark about known problems with the HVAD.
“Patients have no idea, and they rely on the FDA to ensure the safety and effectiveness of high-risk devices,” said Dr. Rita Redberg, a cardiologist at the University of California, San Francisco, who studies medical device regulation. “How can you not take action on a warning letter with these serious issues with very sick patients?”
In response to ProPublica’s findings, the FDA said it had been closely monitoring issues with the HVAD. It said that after Medtronic acquired HeartWare in 2016, it met with the company more than 100 times to ensure problems were being fixed and to review safety concerns related to the heart pump. The agency also said it initiated formal reviews of new device modifications and continually tracked whether the HVAD had a “reasonable assurance of safety and effectiveness.”
“Our decisions that we made along the way have always been patient focused,” said Dr. William Maisel, director of product evaluation and quality at the FDA’s device division. He added that more than 80% of companies fix their problems by the time the FDA reinspects.
That did not happen with the HVAD. In 2016 and 2018, inspectors found that issues detailed in the 2014 warning letter remained unresolved. Medtronic told the FDA last year that it had fixed the problems, but, before the agency could verify the claim, inspections were paused because of the coronavirus pandemic.
In June, Medtronic stopped HVAD sales and implants. The company conceded that a competing device was safer after a new study showed the HVAD had higher rates of death and neurological injury. Medtronic also cited a 12-year-old problem with its devices not restarting if they disconnect from power, leaving patients’ hearts without support.
Medtronic declined to make Geoffrey Martha, CEO, or Nnamdi Njoku, president of mechanical heart support, available for interviews. In an email, a spokesperson said, “There is nothing more important to Medtronic than the safety and well-being of patients.”
The email continued: “Medtronic takes this matter very seriously and, over the past five years, we have worked closely with FDA and engaged external experts to resolve the issues noted in the warning letter. FDA is aware of the steps Medtronic has taken to address the underlying concerns.”
The company said it will have a support system in place for the 4,000 patients worldwide and 2,000 in the United States who still rely on the HVAD. Medtronic will station 20 specialists across the globe to help with device maintenance and patient education. A centralized engineering team will provide technical support and troubleshooting for patients and medical staff. Medtronic said it will offer financial assistance if insurance doesn’t fully cover the surgery to replace a device with a competing product, but only if a doctor decides it’s medically necessary.
Patients with HVADs have little choice but to hope the devices keep working: The surgery to remove HVADs is so risky that both Medtronic and the FDA advise against it. The device is meant to be left in place until its wearer gets a heart transplant. Or dies.
Warning signs
In late 2012, HeartWare, then an independent company headquartered in Massachusetts, won FDA approval to sell a new device that could keep heart failure patients alive and mobile while awaiting a transplant.
A competing device, the HeartMate, was already gaining attention, with high-profile patients like former Vice President Dick Cheney, a heart attack survivor who eventually got a transplant after using the device for 20 months.
The HVAD offered a smaller option that could even be used in children, and it led to a string of publicized successes. A fitness model was able to return to the gym. A 13-year-old with heart defects could attend school again. Medtronic’s YouTube page features 16 interviews with grateful patients and families.
The patients who received HVADs had already been in grave peril. They had advanced heart failure, serious enough to need blood pumped out of their hearts artificially. Most patients were older than 50, but there were also younger patients with heart defects or other cardiac conditions. The device provided help but brought its own risks. Implanting it required invasive open-heart surgery, and clots could develop inside the pump, which, in the worst cases, led to deadly strokes.
The device also came with a steep price tag. Each HVAD cost about $80,000, and, even though HeartWare never made a profit as an independent company, in 2015 device sales brought in $276 million in revenue.
For many severe heart failure patients, the opportunity to survive longer and return to normal life made the device worth the risks and cost.
But patients were unaware the FDA started finding manufacturing issues at HeartWare’s Miami Lakes, Florida, plant as early as 2011, when the device was still seeking approval.
Among the findings, a federal inspector expressed concerns that engineering staff “were not completely reviewing documents before approving them” and found one employee assigned to monitoring device quality had missed several required monthly trainings. HeartWare leadership promised quick corrective action, according to FDA documents.
Then, in 2014, the FDA found more serious lapses, detailed in federal inspection reports.
For example, HeartWare knew of 119 instances in which batteries failed unexpectedly, which could leave the pump powerless, stopping support for the patient’s heart. But the company didn’t test the batteries in inventory for defects, or the batteries of current patients, even though one person’s death had already been linked to battery failure.
The company also received complaints that static electricity could short-circuit its devices. It learned of at least 27 such cases between 2010 and 2013, including four that resulted in serious injuries and two that led to death. HVAD patients would need to avoid contact with certain household objects like televisions or vacuum cleaners — anything that could create strong static electricity. HeartWare added warnings to the patient manual and redesigned its shield to protect the device controller, but the FDA found that the company didn’t replace shields for devices already being used by current patients or produced and sitting in inventory.
Continuing quality control concerns led to the FDA warning letter in June 2014. The document labeled the HVAD as “adulterated,” meaning the device did not meet federal manufacturing standards. The agency gave HeartWare 15 days to correct the problems or face regulatory action.
Still, investment analysts who followed HeartWare believed the warning posed little risk to the company’s business prospects. One described it as being “as benign as possible.”
The 15-day deadline passed, and the FDA never penalized the company.
The agency told ProPublica it had provided additional time because HeartWare was a relatively new manufacturer and the HVAD was a complicated device. It also said it avoided punitive action to make sure patients with severe heart failure had access to this treatment option. “We’re talking about the sickest of the sick patients who really have very few alternatives,” Maisel, the head of device quality, said.
But the HeartMate, the competing device, was available and already being used by the majority of patients. When Medtronic stopped HVAD sales, both companies said the HeartMate could fill the gap.
Inspectors continued to find problems at HeartWare facilities in 2015, 2016, 2017 and 2018. In the most recent report in 2018, inspectors identified seven separate violations at the HVAD plant, including three previously cited in the 2014 warning letter. The company was still mishandling newly discovered defects like pins connecting the controller to a power source that could bend and become unusable, and controllers built with incompatible parts that could chemically react and “attack” the plastic exterior.
Again, the inspection report said the company “promised to correct” the issues.
“What penalty is there for noncompliance? There isn’t one,” said Madris Kinard, a former public health analyst with the FDA and the CEO of Device Events, a software company that analyzes FDA device data. “There’s nothing the FDA is doing that penalizes, in any true sense of the matter, the manufacturer.”
By the time sales were halted last month, the HVAD had become the subject of 15 company-initiated “Class I” recalls for dangerous device problems that could cause injury or death.
One recall came with a warning sent to health care providers in December that said pumps were failing to start up properly. The pattern of malfunctions was almost as old as the device itself, the company later admitted when it halted device sales in June. But even recent patients were completely unaware of the problem.
“A no-brainer”
When children asked Latoya Johnson Keelen about the cable that came out of her side and connected to a controller on her hip, she told them she was Iron Woman.
For a while, she felt invulnerable with the HVAD on her heart.
Johnson Keelen, who lives in the Atlanta suburbs, learned she needed the device after delivering her fourth child, Isaiah, in early 2018. Doctors diagnosed her with postpartum cardiomyopathy, a rare and mysterious form of heart failure that afflicts mothers during pregnancy or after birth. Black mothers in the South have among the highest rates of the illness. Some mothers quickly regain heart function, some only partially recuperate and others never recover.
Tests showed that Johnson Keelen, then 42, was suddenly in end-stage heart failure.
Her body’s immune response at the time was too strong for her to receive a heart transplant. Doctors gave her two choices: an HVAD or end-of-life hospice care.
“It became a no-brainer,” she said. “I just had a baby. I just gave birth. I’m not ready to plan for a funeral.”
Johnson Keelen, a woman of faith, believed God would heal her, either through a medical advancement or a miracle. She thought the HVAD was the answer.
Living with a life-sustaining medical device was difficult at first for the fiercely independent mother. She had to leave her job as a public health communications specialist, ask her older sons to change her bandages and lean heavily on her new husband, only a year into their marriage.
But, for about three years, she found comfort in the soft humming of the HVAD’s spinning rotor at night. It served as a lullaby for her new baby when he lay on her chest.
She said she was never told about the manufacturing problems the FDA repeatedly found at HeartWare’s facilities or about device recalls, including one sent to patients in December 2020. The notice said the device sometimes wouldn’t restart properly, which had led to two patient deaths at that point. It warned that current patients should always keep at least one power source, a battery or an AC or DC adapter, connected at all times to avoid the need for a restart.
Two months after that notice, Johnson Keelen was getting her kids ready for school when the HVAD’s low-battery alarm blared. She had unplugged the battery to replace it without realizing her wall adapter was disconnected.
Once before, Johnson Keelen had simply plugged the charger back into the outlet and her device restarted. But this time it wouldn’t.
As an emergency alarm sounded, she called the ventricular-assist team assigned to her case, and a specialist directed her to switch out the device controller.
Nothing changed, and panic crept into the voice on the phone.
An ambulance took Johnson Keelen to a hospital where medical staff used several backup controllers to try to start the pump.
Still nothing.
Doctors and nurses tried to keep calm, but Johnson Keelen could see fear and shock on their faces. Without the HVAD, her only options were a transplant or a completely new pump.
Doctors scurried to locate a donor heart and airlifted her for an emergency transplant. But while running tests, the medical team was stunned to find that Johnson Keelen’s miracle had occurred: Her heart was once again pumping blood on its own.
She had a new choice. She could avoid the risks of transplant rejection and open heart surgery during the pandemic by leaving the device on her functioning heart, while cutting the wires, removing the external components and sealing the pump.
She chose to trust her newly functioning heart, and leave the decommissioned HVAD inside her.
Three months later, when Medtronic said it was stopping HeartWare sales and implants, its announcement cited the problem with pumps not restarting among the reasons.
Company-led oversight
If evidence suggests a medical device may be linked to a serious patient injury or death, hospitals and other health care facilities must submit a report to the manufacturer and the FDA. Device companies must also submit reports if they learn independently of any incidents.
By the end of 2020, roughly 3,000 death reports and 20,000 injury reports related to the HVAD had been filed with the FDA.
Any details that could identify patients, like their age or gender, are removed from the publicly available reports. Most only have limited details about circumstances surrounding deaths or injuries. But it’s clear from the reports on the HVAD that some of these outcomes could be linked to problems previously identified by FDA inspectors.
Doctors attempted CPR for two hours after an electrostatic shock short-circuited one patient’s device in 2014, a few months after the FDA inspection that year. An autopsy revealed voltage had caused “deep charring” of the tissue inside the patient’s chest.
Friends found another patient dead in the kitchen, with groceries still on the counter, in 2018 after their device, which did not have the recommended static shield, short-circuited.
Last year, paramedics found a patient with the device disconnected from power. They struggled to restart the device, but it wouldn’t plug back into the power source because the connector pins were bent. The patient would die at the hospital.
In most cases, the FDA turned to the company to investigate whether a malfunction caused or contributed to the incidents.
But the FDA has long known HeartWare and Medtronic could not be relied on to properly submit HVAD incident reports.
In 2014, the FDA cited HeartWare because in at least 10 cases, there were no documents showing the company attempted to investigate.
In 2016, the agency wrote another citation when the company was late in reporting more than 200 cases, some more than a year past their 30-day reporting deadlines, and failed to report malfunctions that occurred during clinical trials.
The FDA told ProPublica the agency increased its monitoring of HVAD reports, and Medtronic hired new employees to submit timely reports. But by 2018, its backlog had only grown, with 677 late case filings. Again, the FDA did nothing beyond telling the company to fix the problem and further increasing its monitoring.
In an email, Medtronic said it “has robust systems in place to monitor the safety of all of our products, including the HVAD device.”
The email said, “When any potential safety issues are identified, those issues are thoroughly investigated and relevant information is shared with regulators and healthcare providers.” The company didn’t respond to the pattern of late reports and incomplete investigations identified in FDA inspections.
Maisel, the director of FDA device evaluation and quality, once criticized asking companies to investigate their own devices. In 2008, as a practicing cardiologist, he testified to the U.S. House oversight committee about his concerns.
“In the majority of cases, FDA relies on industry to identify, correct and report the problems,” he said. “But there is obviously an inherent financial conflict of interest for the manufacturers, sometimes measured in billions of dollars.”
Maisel has since had a change of heart. When asked about his 2008 testimony, he told ProPublica that he now believes the regulatory system “generally serves patients well” and “most companies are well intentioned.”
HeartWare’s track record of questionable investigations was glaring in John Winkler II’s case.
A report submitted by HeartWare that matches the dates and details of Winkler’s case shows the company decided there was “no indication of any device malfunctions.” It told the FDA that the device couldn’t be removed from the body because the hospital said his family declined an autopsy. HeartWare added that the evidence of the device’s role in Winkler’s death was inconclusive.
Yet little of this appears to be true. Documents reviewed by ProPublica show an autopsy of the heart and lungs was performed a day after the death. Tina Winkler said she was told the pump was removed from her husband’s body and was available for inspection.
A year after John Winkler’s death, HeartWare recalled 18,000 potentially faulty batteries produced between 2013 and 2015. Tina Winkler came across the notice online and found her husband’s battery serial numbers on the list. The company never contacted her about it or any further investigation, she said.
Rewards, not penalties
As deaths and recalls mounted, HeartWare and Medtronic touted additional FDA approval to treat more patients and their attempts to develop new cutting-edge devices.
With the company on notice under the 2014 warning letter, HeartWare geared up to begin human trials on a smaller heart pump, called the MVAD or Miniaturized Ventricular Assist Device. It would be powered by a new algorithm to more efficiently pump blood. Industry analysts predicted robust sales.
In July 2015, implantations were set to begin on a select group of 60 patients in Europe and Australia. But they were abruptly stopped less than two months later after only 11 implants. Patients experienced numerous adverse events, including major bleeding, infection and device malfunction, according to published data.
HeartWare’s stock price plummeted from about $85 to $35 by October 2015. The next year, Medtronic bought HeartWare for $1.1 billion, replacing much of the company’s leadership shortly after.
Some former HeartWare investors filed a class action lawsuit in January 2016 alleging deception in the development of the MVAD.
According to the accounts of six anonymous former employees in the lawsuit, the details mirror the scandal surrounding Theranos, the former blood test company charged with fraud for raising more than $700 million by allegedly lying about its technology.
Where Theranos made empty promises of a test that only needed a few drops of blood, the suit alleges HeartWare promoted a life-sustaining medical device that former employees said had many problems and actually worsened blood flow, increasing clotting risks.
“Nothing really worked right,” one former HeartWare manager said in the lawsuit, citing “improper alarms, improper touch screen performance, gibberish on display screens — just so many alerts and problems.”
Leadership proceeded with human testing anyway, the suit alleges.
Months later, at an investor conference, HeartWare leadership acknowledged the pump and algorithm led to multiple adverse events. For two patients in particular, the algorithm would direct the pump to speed up so fast that it would try to suck up more blood than was available inside the heart for prolonged periods of time.
HeartWare and Medtronic settled the investor suit for $54.5 million in 2018, admitting no fault.
None of the allegations slowed the FDA as it gave Medtronic additional approval and support for its heart pump technologies.
In September 2017, the agency approved the HVAD as “destination therapy” for patients who were not heart transplant candidates and would rely on the device for the rest of their lives.
“We’re really excited about our HVAD destination therapy approval,” a Medtronic executive said on an investor earnings call. “That’s a real game changer for us in that market.”
Two years later, Medtronic announced it was developing a fully implantable version of the HVAD that would no longer need a cable coming through the waist to connect to power.
Even though issues with the HeartWare device had been unresolved for five years at that point, the FDA accepted the pitch into its new fast-track approval process for high-risk devices.
“Slipped Through The Cracks”
After Johnson Keelen’s pump failed in February, she found a news story about the recall notice sent to medical providers two months prior.
It said the company had identified a problem with pump restarts that could cause heart attacks or serious patient harm. Nineteen patients had been seriously injured so far, and two people had died. The recall warned that patients should be careful to avoid disconnecting the device’s power sources.
“I kept seeing Medtronic on record saying they notified patients,” Johnson Keelen said. “Who did they contact? No one told me.”
Her doctor later told her she must have “slipped through the cracks,” she said.
The current system for informing patients of new safety concerns with high-risk devices relies on a communication chain that can easily break. The device company contacts the FDA and health care providers that work with device patients. The FDA typically issues a public notice, while health professionals contact their patients.
But the agency admits most patients don’t know to look for formal FDA postings. And, experts say, the medical system can lose track of who needs to be notified, especially if a patient moves or switches primary care physicians.
Tina Winkler still wonders why she was never told about FDA-known safety issues with the HVAD. She said her husband’s medical team “had to teach me how to clean his wound, how to change his batteries and what to do if alarms go off. And they never mentioned any of this.”
She said, “If we had all the facts, there’s no way he would have gotten that device implanted in his heart.”
When FDA inspectors find serious safety issues with a medical device, inspection reports are not posted online or sent to patients. The public can obtain reports through a Freedom of Information Act request, but the agency’s records department has said new requests can be stuck behind a year-long backlog.
Patients can find warning letters online in a searchable database of thousands of letters from different FDA divisions, including the center for devices. But HeartWare’s 2014 letter is no longer available for public review because the website purges letters older than five years.
There are also few documents available in state courts about faulty products, because of restrictions on lawsuits related to medical devices. The restrictions date back to a 2008 Supreme Court decision in a case against Medtronic. The court found that U.S. law bars patients and their survivors from suing device makers in state court, essentially because their products go through such a rigorous FDA approval process.
Two recent patient lawsuits against HeartWare and Medtronic, including one filed by Tina Winkler, were moved from state court to federal court. In both cases, Medtronic filed to dismiss the cases because of the U.S. law that protects device companies. Medtronic and the families reached private settlements soon after.
Winkler and an attorney for the other family said they could not comment on their settlements.
Johnson Keelen, with a decommissioned HVAD still attached to her heart, wonders what that means for her and other patients’ chances of recourse.
“Why isn’t anyone now stepping up for the patient?” she asked. “They are now liable for taking care of us because we relied on them.”
“Run its course”
Deserae Cain, 33, is one of the 4,000 patients still relying on a HeartWare device.
She was implanted with the heart pump in late 2017, after suddenly being diagnosed with heart failure. Scans showed her heart was three times normal size. It took time for her to come to terms with needing a life-sustaining device — not long before her diagnosis, she had been going on five-mile runs. In the four years since, though, Cain has built a life around the HVAD with her fiance in their Dayton, Ohio, home.
They know the device can malfunction. In 2019, the pump failed for almost an hour as doctors at a nearby hospital struggled to restart it. Cain just tried to stay calm, knowing anxiety could threaten her unsupported weak heart. Months later, she needed an emergency experimental procedure to clear out blood clots developed within her HVAD.
Then, in 2020, Cain developed a widespread infection. Doctors told her she needed surgery to clean out and replace the pump.
Cain asked her medical team if she could switch to the alternative HeartMate device, which other patients told her presented fewer problems, she said. Doctors said the HVAD was better suited for her smaller frame.
But her new pump had problems soon after the surgery.
The device’s suction alarms, which alert when the pump is trying to pull in more blood than is available within the heart, sounded multiple times a day, for hours at a time, she said. Baffled by the issue for months, her medical team eventually turned off that specific alarm.
Soon after, her ventricular-assist specialist called her about a patient’s death linked to the belt that holds the device controller, she said. The belt had ripped and the equipment had fallen, yanking on the cable that connected the controller to the pump. Cain replaced her belt but it quickly frayed and had to be replaced again within six weeks.
Then, in June, she found out about Medtronic’s decision to stop sales and implants. Cain received a letter from her hospital mentioning a Medtronic support program, but it provided few specifics.
Cain wondered if things would be any different than before. Anxious about her future, she asked: “Are they just going to let it run its course until there is none of us left?”
This article first appeared on Propublica.
John Winkler II was dying of heart failure when doctors came to his hospital bedside, offering a chance to prolong his life. The HeartWare Ventricular Assist Device, or HVAD, could be implanted in Winkler’s chest until a transplant was possible. The heart pump came with disclaimers of risk, but Winkler wanted to fight for time. He was only 46 and had a loving wife and four children, and his second grandchild was on the way.
So, in August 2014, Winkler had surgery to implant the device. A golf-ball–sized rotor was attached to his left ventricle to pump blood through a tube and into his aorta. A cable threading out of a small incision in his waist connected to a battery-powered controller strapped to his body. If something went wrong, an alarm as loud as a fire drill would sound.
Winkler returned home weeks later and, as he regained his strength, became hopeful about the future. He started making plans to visit colleges with his daughter, and was able to host his parents and new grandchild for Christmas. “He was doing so much better,” his wife, Tina Winkler, said. “We thought he was coasting until he got his transplant.”
What John Winkler didn’t know: Months before his implant, the Food and Drug Administration put HeartWare on notice for not properly monitoring or repairing HVAD defects, such as faulty batteries and short circuits caused by static electricity, that had killed patients. The agency issued a warning letter, one of its most serious citations. It demanded fixes within 15 days, but took no decisive action as problems persisted.
Ten days after Christmas of 2014, Winkler’s two teenage children heard the HVAD’s piercing alarm and ran upstairs. They found their father collapsed on his bedroom floor, completely unresponsive. Kelly, 17, dropped to his side and tried to copy how people on television did CPR. She told her brother to call 911, and over the device’s siren did her best to hear instructions from the operator.
When paramedics arrived and assessed her father, one made a passing comment that has haunted Kelly ever since: “Well, his toes are already cold.” He died 2 days later. Medtronic, the company that acquired HeartWare in 2016, settled a lawsuit by the family last year, admitting no fault. Tina Winkler believes her children blamed themselves for their father’s death. “Those two kids have never been the same,” she said. “I think they feel like they didn’t do things they needed to do.”
But it was the FDA that failed to protect Winkler and thousands of other patients whose survival depended on the HVAD, a ProPublica investigation found.
As HeartWare and Medtronic failed inspection after inspection and reports of device-related deaths piled up, the FDA relied on the device makers to fix the problems voluntarily rather than compelling them to do so.
The HVAD was implanted into more than 19,000 patients, the majority of whom got it after the FDA found in 2014 that the device didn’t meet federal standards. By the end of last year, the agency had received more than 3,000 reports of patient deaths that may have been caused or contributed to by the device.
Among them were reports of deaths the company linked to serious device problems: a patient who vomited blood as a family member struggled to restart a defective HVAD; a patient who bled out internally and died after implant surgery because a tube attached to the pump tore open; a patient whose heart tissue was left charred after an HVAD short-circuited and voltage surged through the pump.
The ineffective regulatory oversight of the HVAD is emblematic of larger, more systemic weaknesses.
For decades, the FDA and its Center for Devices and Radiological Health have been responsible for ensuring that high-risk medical devices are safe and effective. Yet they rely mostly on manufacturers to identify and correct problems. The agency says it can seize products, order injunctions against companies, or issue fines, but it rarely does so, preferring instead for companies to make fixes voluntarily.
When federal investigators found repeated manufacturing issues with the HVAD for years, the FDA didn’t penalize the company, even as the company issued 15 serious recalls of the device starting in 2014, the most of any single high-risk device in the FDA’s database. Thousands of patients with recalled models needed to have external HVAD parts replaced or take extra caution while handling their devices and monitor them for signs of malfunctions that could cause injury or death.
Meanwhile, the processes to inform the public through formal FDA notices and messages to health care providers repeatedly failed and left patients in the dark about known problems with the HVAD.
“Patients have no idea, and they rely on the FDA to ensure the safety and effectiveness of high-risk devices,” said Dr. Rita Redberg, a cardiologist at the University of California, San Francisco, who studies medical device regulation. “How can you not take action on a warning letter with these serious issues with very sick patients?”
In response to ProPublica’s findings, the FDA said it had been closely monitoring issues with the HVAD. It said that after Medtronic acquired HeartWare in 2016, it met with the company more than 100 times to ensure problems were being fixed and to review safety concerns related to the heart pump. The agency also said it initiated formal reviews of new device modifications and continually tracked whether the HVAD had a “reasonable assurance of safety and effectiveness.”
“Our decisions that we made along the way have always been patient focused,” said Dr. William Maisel, director of product evaluation and quality at the FDA’s device division. He added that more than 80% of companies fix their problems by the time the FDA reinspects.
That did not happen with the HVAD. In 2016 and 2018, inspectors found that issues detailed in the 2014 warning letter remained unresolved. Medtronic told the FDA last year that it had fixed the problems, but, before the agency could verify the claim, inspections were paused because of the coronavirus pandemic.
In June, Medtronic stopped HVAD sales and implants. The company conceded that a competing device was safer after a new study showed the HVAD had higher rates of death and neurological injury. Medtronic also cited a 12-year-old problem with its devices not restarting if they disconnect from power, leaving patients’ hearts without support.
Medtronic declined to make Geoffrey Martha, CEO, or Nnamdi Njoku, president of mechanical heart support, available for interviews. In an email, a spokesperson said, “There is nothing more important to Medtronic than the safety and well-being of patients.”
The email continued: “Medtronic takes this matter very seriously and, over the past five years, we have worked closely with FDA and engaged external experts to resolve the issues noted in the warning letter. FDA is aware of the steps Medtronic has taken to address the underlying concerns.”
The company said it will have a support system in place for the 4,000 patients worldwide and 2,000 in the United States who still rely on the HVAD. Medtronic will station 20 specialists across the globe to help with device maintenance and patient education. A centralized engineering team will provide technical support and troubleshooting for patients and medical staff. Medtronic said it will offer financial assistance if insurance doesn’t fully cover the surgery to replace a device with a competing product, but only if a doctor decides it’s medically necessary.
Patients with HVADs have little choice but to hope the devices keep working: The surgery to remove HVADs is so risky that both Medtronic and the FDA advise against it. The device is meant to be left in place until its wearer gets a heart transplant. Or dies.
Warning signs
In late 2012, HeartWare, then an independent company headquartered in Massachusetts, won FDA approval to sell a new device that could keep heart failure patients alive and mobile while awaiting a transplant.
A competing device, the HeartMate, was already gaining attention, with high-profile patients like former Vice President Dick Cheney, a heart attack survivor who eventually got a transplant after using the device for 20 months.
The HVAD offered a smaller option that could even be used in children, and it led to a string of publicized successes. A fitness model was able to return to the gym. A 13-year-old with heart defects could attend school again. Medtronic’s YouTube page features 16 interviews with grateful patients and families.
The patients who received HVADs had already been in grave peril. They had advanced heart failure, serious enough to need blood pumped out of their hearts artificially. Most patients were older than 50, but there were also younger patients with heart defects or other cardiac conditions. The device provided help but brought its own risks. Implanting it required invasive open-heart surgery, and clots could develop inside the pump, which, in the worst cases, led to deadly strokes.
The device also came with a steep price tag. Each HVAD cost about $80,000, and, even though HeartWare never made a profit as an independent company, in 2015 device sales brought in $276 million in revenue.
For many severe heart failure patients, the opportunity to survive longer and return to normal life made the device worth the risks and cost.
But patients were unaware the FDA started finding manufacturing issues at HeartWare’s Miami Lakes, Florida, plant as early as 2011, when the device was still seeking approval.
Among the findings, a federal inspector expressed concerns that engineering staff “were not completely reviewing documents before approving them” and found one employee assigned to monitoring device quality had missed several required monthly trainings. HeartWare leadership promised quick corrective action, according to FDA documents.
Then, in 2014, the FDA found more serious lapses, detailed in federal inspection reports.
For example, HeartWare knew of 119 instances in which batteries failed unexpectedly, which could leave the pump powerless, stopping support for the patient’s heart. But the company didn’t test the batteries in inventory for defects, or the batteries of current patients, even though one person’s death had already been linked to battery failure.
The company also received complaints that static electricity could short-circuit its devices. It learned of at least 27 such cases between 2010 and 2013, including four that resulted in serious injuries and two that led to death. HVAD patients would need to avoid contact with certain household objects like televisions or vacuum cleaners — anything that could create strong static electricity. HeartWare added warnings to the patient manual and redesigned its shield to protect the device controller, but the FDA found that the company didn’t replace shields for devices already being used by current patients or produced and sitting in inventory.
Continuing quality control concerns led to the FDA warning letter in June 2014. The document labeled the HVAD as “adulterated,” meaning the device did not meet federal manufacturing standards. The agency gave HeartWare 15 days to correct the problems or face regulatory action.
Still, investment analysts who followed HeartWare believed the warning posed little risk to the company’s business prospects. One described it as being “as benign as possible.”
The 15-day deadline passed, and the FDA never penalized the company.
The agency told ProPublica it had provided additional time because HeartWare was a relatively new manufacturer and the HVAD was a complicated device. It also said it avoided punitive action to make sure patients with severe heart failure had access to this treatment option. “We’re talking about the sickest of the sick patients who really have very few alternatives,” Maisel, the head of device quality, said.
But the HeartMate, the competing device, was available and already being used by the majority of patients. When Medtronic stopped HVAD sales, both companies said the HeartMate could fill the gap.
Inspectors continued to find problems at HeartWare facilities in 2015, 2016, 2017 and 2018. In the most recent report in 2018, inspectors identified seven separate violations at the HVAD plant, including three previously cited in the 2014 warning letter. The company was still mishandling newly discovered defects like pins connecting the controller to a power source that could bend and become unusable, and controllers built with incompatible parts that could chemically react and “attack” the plastic exterior.
Again, the inspection report said the company “promised to correct” the issues.
“What penalty is there for noncompliance? There isn’t one,” said Madris Kinard, a former public health analyst with the FDA and the CEO of Device Events, a software company that analyzes FDA device data. “There’s nothing the FDA is doing that penalizes, in any true sense of the matter, the manufacturer.”
By the time sales were halted last month, the HVAD had become the subject of 15 company-initiated “Class I” recalls for dangerous device problems that could cause injury or death.
One recall came with a warning sent to health care providers in December that said pumps were failing to start up properly. The pattern of malfunctions was almost as old as the device itself, the company later admitted when it halted device sales in June. But even recent patients were completely unaware of the problem.
“A no-brainer”
When children asked Latoya Johnson Keelen about the cable that came out of her side and connected to a controller on her hip, she told them she was Iron Woman.
For a while, she felt invulnerable with the HVAD on her heart.
Johnson Keelen, who lives in the Atlanta suburbs, learned she needed the device after delivering her fourth child, Isaiah, in early 2018. Doctors diagnosed her with postpartum cardiomyopathy, a rare and mysterious form of heart failure that afflicts mothers during pregnancy or after birth. Black mothers in the South have among the highest rates of the illness. Some mothers quickly regain heart function, some only partially recuperate and others never recover.
Tests showed that Johnson Keelen, then 42, was suddenly in end-stage heart failure.
Her body’s immune response at the time was too strong for her to receive a heart transplant. Doctors gave her two choices: an HVAD or end-of-life hospice care.
“It became a no-brainer,” she said. “I just had a baby. I just gave birth. I’m not ready to plan for a funeral.”
Johnson Keelen, a woman of faith, believed God would heal her, either through a medical advancement or a miracle. She thought the HVAD was the answer.
Living with a life-sustaining medical device was difficult at first for the fiercely independent mother. She had to leave her job as a public health communications specialist, ask her older sons to change her bandages and lean heavily on her new husband, only a year into their marriage.
But, for about three years, she found comfort in the soft humming of the HVAD’s spinning rotor at night. It served as a lullaby for her new baby when he lay on her chest.
She said she was never told about the manufacturing problems the FDA repeatedly found at HeartWare’s facilities or about device recalls, including one sent to patients in December 2020. The notice said the device sometimes wouldn’t restart properly, which had led to two patient deaths at that point. It warned that current patients should always keep at least one power source, a battery or an AC or DC adapter, connected at all times to avoid the need for a restart.
Two months after that notice, Johnson Keelen was getting her kids ready for school when the HVAD’s low-battery alarm blared. She had unplugged the battery to replace it without realizing her wall adapter was disconnected.
Once before, Johnson Keelen had simply plugged the charger back into the outlet and her device restarted. But this time it wouldn’t.
As an emergency alarm sounded, she called the ventricular-assist team assigned to her case, and a specialist directed her to switch out the device controller.
Nothing changed, and panic crept into the voice on the phone.
An ambulance took Johnson Keelen to a hospital where medical staff used several backup controllers to try to start the pump.
Still nothing.
Doctors and nurses tried to keep calm, but Johnson Keelen could see fear and shock on their faces. Without the HVAD, her only options were a transplant or a completely new pump.
Doctors scurried to locate a donor heart and airlifted her for an emergency transplant. But while running tests, the medical team was stunned to find that Johnson Keelen’s miracle had occurred: Her heart was once again pumping blood on its own.
She had a new choice. She could avoid the risks of transplant rejection and open heart surgery during the pandemic by leaving the device on her functioning heart, while cutting the wires, removing the external components and sealing the pump.
She chose to trust her newly functioning heart, and leave the decommissioned HVAD inside her.
Three months later, when Medtronic said it was stopping HeartWare sales and implants, its announcement cited the problem with pumps not restarting among the reasons.
Company-led oversight
If evidence suggests a medical device may be linked to a serious patient injury or death, hospitals and other health care facilities must submit a report to the manufacturer and the FDA. Device companies must also submit reports if they learn independently of any incidents.
By the end of 2020, roughly 3,000 death reports and 20,000 injury reports related to the HVAD had been filed with the FDA.
Any details that could identify patients, like their age or gender, are removed from the publicly available reports. Most only have limited details about circumstances surrounding deaths or injuries. But it’s clear from the reports on the HVAD that some of these outcomes could be linked to problems previously identified by FDA inspectors.
Doctors attempted CPR for two hours after an electrostatic shock short-circuited one patient’s device in 2014, a few months after the FDA inspection that year. An autopsy revealed voltage had caused “deep charring” of the tissue inside the patient’s chest.
Friends found another patient dead in the kitchen, with groceries still on the counter, in 2018 after their device, which did not have the recommended static shield, short-circuited.
Last year, paramedics found a patient with the device disconnected from power. They struggled to restart the device, but it wouldn’t plug back into the power source because the connector pins were bent. The patient would die at the hospital.
In most cases, the FDA turned to the company to investigate whether a malfunction caused or contributed to the incidents.
But the FDA has long known HeartWare and Medtronic could not be relied on to properly submit HVAD incident reports.
In 2014, the FDA cited HeartWare because in at least 10 cases, there were no documents showing the company attempted to investigate.
In 2016, the agency wrote another citation when the company was late in reporting more than 200 cases, some more than a year past their 30-day reporting deadlines, and failed to report malfunctions that occurred during clinical trials.
The FDA told ProPublica the agency increased its monitoring of HVAD reports, and Medtronic hired new employees to submit timely reports. But by 2018, its backlog had only grown, with 677 late case filings. Again, the FDA did nothing beyond telling the company to fix the problem and further increasing its monitoring.
In an email, Medtronic said it “has robust systems in place to monitor the safety of all of our products, including the HVAD device.”
The email said, “When any potential safety issues are identified, those issues are thoroughly investigated and relevant information is shared with regulators and healthcare providers.” The company didn’t respond to the pattern of late reports and incomplete investigations identified in FDA inspections.
Maisel, the director of FDA device evaluation and quality, once criticized asking companies to investigate their own devices. In 2008, as a practicing cardiologist, he testified to the U.S. House oversight committee about his concerns.
“In the majority of cases, FDA relies on industry to identify, correct and report the problems,” he said. “But there is obviously an inherent financial conflict of interest for the manufacturers, sometimes measured in billions of dollars.”
Maisel has since had a change of heart. When asked about his 2008 testimony, he told ProPublica that he now believes the regulatory system “generally serves patients well” and “most companies are well intentioned.”
HeartWare’s track record of questionable investigations was glaring in John Winkler II’s case.
A report submitted by HeartWare that matches the dates and details of Winkler’s case shows the company decided there was “no indication of any device malfunctions.” It told the FDA that the device couldn’t be removed from the body because the hospital said his family declined an autopsy. HeartWare added that the evidence of the device’s role in Winkler’s death was inconclusive.
Yet little of this appears to be true. Documents reviewed by ProPublica show an autopsy of the heart and lungs was performed a day after the death. Tina Winkler said she was told the pump was removed from her husband’s body and was available for inspection.
A year after John Winkler’s death, HeartWare recalled 18,000 potentially faulty batteries produced between 2013 and 2015. Tina Winkler came across the notice online and found her husband’s battery serial numbers on the list. The company never contacted her about it or any further investigation, she said.
Rewards, not penalties
As deaths and recalls mounted, HeartWare and Medtronic touted additional FDA approval to treat more patients and their attempts to develop new cutting-edge devices.
With the company on notice under the 2014 warning letter, HeartWare geared up to begin human trials on a smaller heart pump, called the MVAD or Miniaturized Ventricular Assist Device. It would be powered by a new algorithm to more efficiently pump blood. Industry analysts predicted robust sales.
In July 2015, implantations were set to begin on a select group of 60 patients in Europe and Australia. But they were abruptly stopped less than two months later after only 11 implants. Patients experienced numerous adverse events, including major bleeding, infection and device malfunction, according to published data.
HeartWare’s stock price plummeted from about $85 to $35 by October 2015. The next year, Medtronic bought HeartWare for $1.1 billion, replacing much of the company’s leadership shortly after.
Some former HeartWare investors filed a class action lawsuit in January 2016 alleging deception in the development of the MVAD.
According to the accounts of six anonymous former employees in the lawsuit, the details mirror the scandal surrounding Theranos, the former blood test company charged with fraud for raising more than $700 million by allegedly lying about its technology.
Where Theranos made empty promises of a test that only needed a few drops of blood, the suit alleges HeartWare promoted a life-sustaining medical device that former employees said had many problems and actually worsened blood flow, increasing clotting risks.
“Nothing really worked right,” one former HeartWare manager said in the lawsuit, citing “improper alarms, improper touch screen performance, gibberish on display screens — just so many alerts and problems.”
Leadership proceeded with human testing anyway, the suit alleges.
Months later, at an investor conference, HeartWare leadership acknowledged the pump and algorithm led to multiple adverse events. For two patients in particular, the algorithm would direct the pump to speed up so fast that it would try to suck up more blood than was available inside the heart for prolonged periods of time.
HeartWare and Medtronic settled the investor suit for $54.5 million in 2018, admitting no fault.
None of the allegations slowed the FDA as it gave Medtronic additional approval and support for its heart pump technologies.
In September 2017, the agency approved the HVAD as “destination therapy” for patients who were not heart transplant candidates and would rely on the device for the rest of their lives.
“We’re really excited about our HVAD destination therapy approval,” a Medtronic executive said on an investor earnings call. “That’s a real game changer for us in that market.”
Two years later, Medtronic announced it was developing a fully implantable version of the HVAD that would no longer need a cable coming through the waist to connect to power.
Even though issues with the HeartWare device had been unresolved for five years at that point, the FDA accepted the pitch into its new fast-track approval process for high-risk devices.
“Slipped Through The Cracks”
After Johnson Keelen’s pump failed in February, she found a news story about the recall notice sent to medical providers two months prior.
It said the company had identified a problem with pump restarts that could cause heart attacks or serious patient harm. Nineteen patients had been seriously injured so far, and two people had died. The recall warned that patients should be careful to avoid disconnecting the device’s power sources.
“I kept seeing Medtronic on record saying they notified patients,” Johnson Keelen said. “Who did they contact? No one told me.”
Her doctor later told her she must have “slipped through the cracks,” she said.
The current system for informing patients of new safety concerns with high-risk devices relies on a communication chain that can easily break. The device company contacts the FDA and health care providers that work with device patients. The FDA typically issues a public notice, while health professionals contact their patients.
But the agency admits most patients don’t know to look for formal FDA postings. And, experts say, the medical system can lose track of who needs to be notified, especially if a patient moves or switches primary care physicians.
Tina Winkler still wonders why she was never told about FDA-known safety issues with the HVAD. She said her husband’s medical team “had to teach me how to clean his wound, how to change his batteries and what to do if alarms go off. And they never mentioned any of this.”
She said, “If we had all the facts, there’s no way he would have gotten that device implanted in his heart.”
When FDA inspectors find serious safety issues with a medical device, inspection reports are not posted online or sent to patients. The public can obtain reports through a Freedom of Information Act request, but the agency’s records department has said new requests can be stuck behind a year-long backlog.
Patients can find warning letters online in a searchable database of thousands of letters from different FDA divisions, including the center for devices. But HeartWare’s 2014 letter is no longer available for public review because the website purges letters older than five years.
There are also few documents available in state courts about faulty products, because of restrictions on lawsuits related to medical devices. The restrictions date back to a 2008 Supreme Court decision in a case against Medtronic. The court found that U.S. law bars patients and their survivors from suing device makers in state court, essentially because their products go through such a rigorous FDA approval process.
Two recent patient lawsuits against HeartWare and Medtronic, including one filed by Tina Winkler, were moved from state court to federal court. In both cases, Medtronic filed to dismiss the cases because of the U.S. law that protects device companies. Medtronic and the families reached private settlements soon after.
Winkler and an attorney for the other family said they could not comment on their settlements.
Johnson Keelen, with a decommissioned HVAD still attached to her heart, wonders what that means for her and other patients’ chances of recourse.
“Why isn’t anyone now stepping up for the patient?” she asked. “They are now liable for taking care of us because we relied on them.”
“Run its course”
Deserae Cain, 33, is one of the 4,000 patients still relying on a HeartWare device.
She was implanted with the heart pump in late 2017, after suddenly being diagnosed with heart failure. Scans showed her heart was three times normal size. It took time for her to come to terms with needing a life-sustaining device — not long before her diagnosis, she had been going on five-mile runs. In the four years since, though, Cain has built a life around the HVAD with her fiance in their Dayton, Ohio, home.
They know the device can malfunction. In 2019, the pump failed for almost an hour as doctors at a nearby hospital struggled to restart it. Cain just tried to stay calm, knowing anxiety could threaten her unsupported weak heart. Months later, she needed an emergency experimental procedure to clear out blood clots developed within her HVAD.
Then, in 2020, Cain developed a widespread infection. Doctors told her she needed surgery to clean out and replace the pump.
Cain asked her medical team if she could switch to the alternative HeartMate device, which other patients told her presented fewer problems, she said. Doctors said the HVAD was better suited for her smaller frame.
But her new pump had problems soon after the surgery.
The device’s suction alarms, which alert when the pump is trying to pull in more blood than is available within the heart, sounded multiple times a day, for hours at a time, she said. Baffled by the issue for months, her medical team eventually turned off that specific alarm.
Soon after, her ventricular-assist specialist called her about a patient’s death linked to the belt that holds the device controller, she said. The belt had ripped and the equipment had fallen, yanking on the cable that connected the controller to the pump. Cain replaced her belt but it quickly frayed and had to be replaced again within six weeks.
Then, in June, she found out about Medtronic’s decision to stop sales and implants. Cain received a letter from her hospital mentioning a Medtronic support program, but it provided few specifics.
Cain wondered if things would be any different than before. Anxious about her future, she asked: “Are they just going to let it run its course until there is none of us left?”
This article first appeared on Propublica.
John Winkler II was dying of heart failure when doctors came to his hospital bedside, offering a chance to prolong his life. The HeartWare Ventricular Assist Device, or HVAD, could be implanted in Winkler’s chest until a transplant was possible. The heart pump came with disclaimers of risk, but Winkler wanted to fight for time. He was only 46 and had a loving wife and four children, and his second grandchild was on the way.
So, in August 2014, Winkler had surgery to implant the device. A golf-ball–sized rotor was attached to his left ventricle to pump blood through a tube and into his aorta. A cable threading out of a small incision in his waist connected to a battery-powered controller strapped to his body. If something went wrong, an alarm as loud as a fire drill would sound.
Winkler returned home weeks later and, as he regained his strength, became hopeful about the future. He started making plans to visit colleges with his daughter, and was able to host his parents and new grandchild for Christmas. “He was doing so much better,” his wife, Tina Winkler, said. “We thought he was coasting until he got his transplant.”
What John Winkler didn’t know: Months before his implant, the Food and Drug Administration put HeartWare on notice for not properly monitoring or repairing HVAD defects, such as faulty batteries and short circuits caused by static electricity, that had killed patients. The agency issued a warning letter, one of its most serious citations. It demanded fixes within 15 days, but took no decisive action as problems persisted.
Ten days after Christmas of 2014, Winkler’s two teenage children heard the HVAD’s piercing alarm and ran upstairs. They found their father collapsed on his bedroom floor, completely unresponsive. Kelly, 17, dropped to his side and tried to copy how people on television did CPR. She told her brother to call 911, and over the device’s siren did her best to hear instructions from the operator.
When paramedics arrived and assessed her father, one made a passing comment that has haunted Kelly ever since: “Well, his toes are already cold.” He died 2 days later. Medtronic, the company that acquired HeartWare in 2016, settled a lawsuit by the family last year, admitting no fault. Tina Winkler believes her children blamed themselves for their father’s death. “Those two kids have never been the same,” she said. “I think they feel like they didn’t do things they needed to do.”
But it was the FDA that failed to protect Winkler and thousands of other patients whose survival depended on the HVAD, a ProPublica investigation found.
As HeartWare and Medtronic failed inspection after inspection and reports of device-related deaths piled up, the FDA relied on the device makers to fix the problems voluntarily rather than compelling them to do so.
The HVAD was implanted into more than 19,000 patients, the majority of whom got it after the FDA found in 2014 that the device didn’t meet federal standards. By the end of last year, the agency had received more than 3,000 reports of patient deaths that may have been caused or contributed to by the device.
Among them were reports of deaths the company linked to serious device problems: a patient who vomited blood as a family member struggled to restart a defective HVAD; a patient who bled out internally and died after implant surgery because a tube attached to the pump tore open; a patient whose heart tissue was left charred after an HVAD short-circuited and voltage surged through the pump.
The ineffective regulatory oversight of the HVAD is emblematic of larger, more systemic weaknesses.
For decades, the FDA and its Center for Devices and Radiological Health have been responsible for ensuring that high-risk medical devices are safe and effective. Yet they rely mostly on manufacturers to identify and correct problems. The agency says it can seize products, order injunctions against companies, or issue fines, but it rarely does so, preferring instead for companies to make fixes voluntarily.
When federal investigators found repeated manufacturing issues with the HVAD for years, the FDA didn’t penalize the company, even as the company issued 15 serious recalls of the device starting in 2014, the most of any single high-risk device in the FDA’s database. Thousands of patients with recalled models needed to have external HVAD parts replaced or take extra caution while handling their devices and monitor them for signs of malfunctions that could cause injury or death.
Meanwhile, the processes to inform the public through formal FDA notices and messages to health care providers repeatedly failed and left patients in the dark about known problems with the HVAD.
“Patients have no idea, and they rely on the FDA to ensure the safety and effectiveness of high-risk devices,” said Dr. Rita Redberg, a cardiologist at the University of California, San Francisco, who studies medical device regulation. “How can you not take action on a warning letter with these serious issues with very sick patients?”
In response to ProPublica’s findings, the FDA said it had been closely monitoring issues with the HVAD. It said that after Medtronic acquired HeartWare in 2016, it met with the company more than 100 times to ensure problems were being fixed and to review safety concerns related to the heart pump. The agency also said it initiated formal reviews of new device modifications and continually tracked whether the HVAD had a “reasonable assurance of safety and effectiveness.”
“Our decisions that we made along the way have always been patient focused,” said Dr. William Maisel, director of product evaluation and quality at the FDA’s device division. He added that more than 80% of companies fix their problems by the time the FDA reinspects.
That did not happen with the HVAD. In 2016 and 2018, inspectors found that issues detailed in the 2014 warning letter remained unresolved. Medtronic told the FDA last year that it had fixed the problems, but, before the agency could verify the claim, inspections were paused because of the coronavirus pandemic.
In June, Medtronic stopped HVAD sales and implants. The company conceded that a competing device was safer after a new study showed the HVAD had higher rates of death and neurological injury. Medtronic also cited a 12-year-old problem with its devices not restarting if they disconnect from power, leaving patients’ hearts without support.
Medtronic declined to make Geoffrey Martha, CEO, or Nnamdi Njoku, president of mechanical heart support, available for interviews. In an email, a spokesperson said, “There is nothing more important to Medtronic than the safety and well-being of patients.”
The email continued: “Medtronic takes this matter very seriously and, over the past five years, we have worked closely with FDA and engaged external experts to resolve the issues noted in the warning letter. FDA is aware of the steps Medtronic has taken to address the underlying concerns.”
The company said it will have a support system in place for the 4,000 patients worldwide and 2,000 in the United States who still rely on the HVAD. Medtronic will station 20 specialists across the globe to help with device maintenance and patient education. A centralized engineering team will provide technical support and troubleshooting for patients and medical staff. Medtronic said it will offer financial assistance if insurance doesn’t fully cover the surgery to replace a device with a competing product, but only if a doctor decides it’s medically necessary.
Patients with HVADs have little choice but to hope the devices keep working: The surgery to remove HVADs is so risky that both Medtronic and the FDA advise against it. The device is meant to be left in place until its wearer gets a heart transplant. Or dies.
Warning signs
In late 2012, HeartWare, then an independent company headquartered in Massachusetts, won FDA approval to sell a new device that could keep heart failure patients alive and mobile while awaiting a transplant.
A competing device, the HeartMate, was already gaining attention, with high-profile patients like former Vice President Dick Cheney, a heart attack survivor who eventually got a transplant after using the device for 20 months.
The HVAD offered a smaller option that could even be used in children, and it led to a string of publicized successes. A fitness model was able to return to the gym. A 13-year-old with heart defects could attend school again. Medtronic’s YouTube page features 16 interviews with grateful patients and families.
The patients who received HVADs had already been in grave peril. They had advanced heart failure, serious enough to need blood pumped out of their hearts artificially. Most patients were older than 50, but there were also younger patients with heart defects or other cardiac conditions. The device provided help but brought its own risks. Implanting it required invasive open-heart surgery, and clots could develop inside the pump, which, in the worst cases, led to deadly strokes.
The device also came with a steep price tag. Each HVAD cost about $80,000, and, even though HeartWare never made a profit as an independent company, in 2015 device sales brought in $276 million in revenue.
For many severe heart failure patients, the opportunity to survive longer and return to normal life made the device worth the risks and cost.
But patients were unaware the FDA started finding manufacturing issues at HeartWare’s Miami Lakes, Florida, plant as early as 2011, when the device was still seeking approval.
Among the findings, a federal inspector expressed concerns that engineering staff “were not completely reviewing documents before approving them” and found one employee assigned to monitoring device quality had missed several required monthly trainings. HeartWare leadership promised quick corrective action, according to FDA documents.
Then, in 2014, the FDA found more serious lapses, detailed in federal inspection reports.
For example, HeartWare knew of 119 instances in which batteries failed unexpectedly, which could leave the pump powerless, stopping support for the patient’s heart. But the company didn’t test the batteries in inventory for defects, or the batteries of current patients, even though one person’s death had already been linked to battery failure.
The company also received complaints that static electricity could short-circuit its devices. It learned of at least 27 such cases between 2010 and 2013, including four that resulted in serious injuries and two that led to death. HVAD patients would need to avoid contact with certain household objects like televisions or vacuum cleaners — anything that could create strong static electricity. HeartWare added warnings to the patient manual and redesigned its shield to protect the device controller, but the FDA found that the company didn’t replace shields for devices already being used by current patients or produced and sitting in inventory.
Continuing quality control concerns led to the FDA warning letter in June 2014. The document labeled the HVAD as “adulterated,” meaning the device did not meet federal manufacturing standards. The agency gave HeartWare 15 days to correct the problems or face regulatory action.
Still, investment analysts who followed HeartWare believed the warning posed little risk to the company’s business prospects. One described it as being “as benign as possible.”
The 15-day deadline passed, and the FDA never penalized the company.
The agency told ProPublica it had provided additional time because HeartWare was a relatively new manufacturer and the HVAD was a complicated device. It also said it avoided punitive action to make sure patients with severe heart failure had access to this treatment option. “We’re talking about the sickest of the sick patients who really have very few alternatives,” Maisel, the head of device quality, said.
But the HeartMate, the competing device, was available and already being used by the majority of patients. When Medtronic stopped HVAD sales, both companies said the HeartMate could fill the gap.
Inspectors continued to find problems at HeartWare facilities in 2015, 2016, 2017 and 2018. In the most recent report in 2018, inspectors identified seven separate violations at the HVAD plant, including three previously cited in the 2014 warning letter. The company was still mishandling newly discovered defects like pins connecting the controller to a power source that could bend and become unusable, and controllers built with incompatible parts that could chemically react and “attack” the plastic exterior.
Again, the inspection report said the company “promised to correct” the issues.
“What penalty is there for noncompliance? There isn’t one,” said Madris Kinard, a former public health analyst with the FDA and the CEO of Device Events, a software company that analyzes FDA device data. “There’s nothing the FDA is doing that penalizes, in any true sense of the matter, the manufacturer.”
By the time sales were halted last month, the HVAD had become the subject of 15 company-initiated “Class I” recalls for dangerous device problems that could cause injury or death.
One recall came with a warning sent to health care providers in December that said pumps were failing to start up properly. The pattern of malfunctions was almost as old as the device itself, the company later admitted when it halted device sales in June. But even recent patients were completely unaware of the problem.
“A no-brainer”
When children asked Latoya Johnson Keelen about the cable that came out of her side and connected to a controller on her hip, she told them she was Iron Woman.
For a while, she felt invulnerable with the HVAD on her heart.
Johnson Keelen, who lives in the Atlanta suburbs, learned she needed the device after delivering her fourth child, Isaiah, in early 2018. Doctors diagnosed her with postpartum cardiomyopathy, a rare and mysterious form of heart failure that afflicts mothers during pregnancy or after birth. Black mothers in the South have among the highest rates of the illness. Some mothers quickly regain heart function, some only partially recuperate and others never recover.
Tests showed that Johnson Keelen, then 42, was suddenly in end-stage heart failure.
Her body’s immune response at the time was too strong for her to receive a heart transplant. Doctors gave her two choices: an HVAD or end-of-life hospice care.
“It became a no-brainer,” she said. “I just had a baby. I just gave birth. I’m not ready to plan for a funeral.”
Johnson Keelen, a woman of faith, believed God would heal her, either through a medical advancement or a miracle. She thought the HVAD was the answer.
Living with a life-sustaining medical device was difficult at first for the fiercely independent mother. She had to leave her job as a public health communications specialist, ask her older sons to change her bandages and lean heavily on her new husband, only a year into their marriage.
But, for about three years, she found comfort in the soft humming of the HVAD’s spinning rotor at night. It served as a lullaby for her new baby when he lay on her chest.
She said she was never told about the manufacturing problems the FDA repeatedly found at HeartWare’s facilities or about device recalls, including one sent to patients in December 2020. The notice said the device sometimes wouldn’t restart properly, which had led to two patient deaths at that point. It warned that current patients should always keep at least one power source, a battery or an AC or DC adapter, connected at all times to avoid the need for a restart.
Two months after that notice, Johnson Keelen was getting her kids ready for school when the HVAD’s low-battery alarm blared. She had unplugged the battery to replace it without realizing her wall adapter was disconnected.
Once before, Johnson Keelen had simply plugged the charger back into the outlet and her device restarted. But this time it wouldn’t.
As an emergency alarm sounded, she called the ventricular-assist team assigned to her case, and a specialist directed her to switch out the device controller.
Nothing changed, and panic crept into the voice on the phone.
An ambulance took Johnson Keelen to a hospital where medical staff used several backup controllers to try to start the pump.
Still nothing.
Doctors and nurses tried to keep calm, but Johnson Keelen could see fear and shock on their faces. Without the HVAD, her only options were a transplant or a completely new pump.
Doctors scurried to locate a donor heart and airlifted her for an emergency transplant. But while running tests, the medical team was stunned to find that Johnson Keelen’s miracle had occurred: Her heart was once again pumping blood on its own.
She had a new choice. She could avoid the risks of transplant rejection and open heart surgery during the pandemic by leaving the device on her functioning heart, while cutting the wires, removing the external components and sealing the pump.
She chose to trust her newly functioning heart, and leave the decommissioned HVAD inside her.
Three months later, when Medtronic said it was stopping HeartWare sales and implants, its announcement cited the problem with pumps not restarting among the reasons.
Company-led oversight
If evidence suggests a medical device may be linked to a serious patient injury or death, hospitals and other health care facilities must submit a report to the manufacturer and the FDA. Device companies must also submit reports if they learn independently of any incidents.
By the end of 2020, roughly 3,000 death reports and 20,000 injury reports related to the HVAD had been filed with the FDA.
Any details that could identify patients, like their age or gender, are removed from the publicly available reports. Most only have limited details about circumstances surrounding deaths or injuries. But it’s clear from the reports on the HVAD that some of these outcomes could be linked to problems previously identified by FDA inspectors.
Doctors attempted CPR for two hours after an electrostatic shock short-circuited one patient’s device in 2014, a few months after the FDA inspection that year. An autopsy revealed voltage had caused “deep charring” of the tissue inside the patient’s chest.
Friends found another patient dead in the kitchen, with groceries still on the counter, in 2018 after their device, which did not have the recommended static shield, short-circuited.
Last year, paramedics found a patient with the device disconnected from power. They struggled to restart the device, but it wouldn’t plug back into the power source because the connector pins were bent. The patient would die at the hospital.
In most cases, the FDA turned to the company to investigate whether a malfunction caused or contributed to the incidents.
But the FDA has long known HeartWare and Medtronic could not be relied on to properly submit HVAD incident reports.
In 2014, the FDA cited HeartWare because in at least 10 cases, there were no documents showing the company attempted to investigate.
In 2016, the agency wrote another citation when the company was late in reporting more than 200 cases, some more than a year past their 30-day reporting deadlines, and failed to report malfunctions that occurred during clinical trials.
The FDA told ProPublica the agency increased its monitoring of HVAD reports, and Medtronic hired new employees to submit timely reports. But by 2018, its backlog had only grown, with 677 late case filings. Again, the FDA did nothing beyond telling the company to fix the problem and further increasing its monitoring.
In an email, Medtronic said it “has robust systems in place to monitor the safety of all of our products, including the HVAD device.”
The email said, “When any potential safety issues are identified, those issues are thoroughly investigated and relevant information is shared with regulators and healthcare providers.” The company didn’t respond to the pattern of late reports and incomplete investigations identified in FDA inspections.
Maisel, the director of FDA device evaluation and quality, once criticized asking companies to investigate their own devices. In 2008, as a practicing cardiologist, he testified to the U.S. House oversight committee about his concerns.
“In the majority of cases, FDA relies on industry to identify, correct and report the problems,” he said. “But there is obviously an inherent financial conflict of interest for the manufacturers, sometimes measured in billions of dollars.”
Maisel has since had a change of heart. When asked about his 2008 testimony, he told ProPublica that he now believes the regulatory system “generally serves patients well” and “most companies are well intentioned.”
HeartWare’s track record of questionable investigations was glaring in John Winkler II’s case.
A report submitted by HeartWare that matches the dates and details of Winkler’s case shows the company decided there was “no indication of any device malfunctions.” It told the FDA that the device couldn’t be removed from the body because the hospital said his family declined an autopsy. HeartWare added that the evidence of the device’s role in Winkler’s death was inconclusive.
Yet little of this appears to be true. Documents reviewed by ProPublica show an autopsy of the heart and lungs was performed a day after the death. Tina Winkler said she was told the pump was removed from her husband’s body and was available for inspection.
A year after John Winkler’s death, HeartWare recalled 18,000 potentially faulty batteries produced between 2013 and 2015. Tina Winkler came across the notice online and found her husband’s battery serial numbers on the list. The company never contacted her about it or any further investigation, she said.
Rewards, not penalties
As deaths and recalls mounted, HeartWare and Medtronic touted additional FDA approval to treat more patients and their attempts to develop new cutting-edge devices.
With the company on notice under the 2014 warning letter, HeartWare geared up to begin human trials on a smaller heart pump, called the MVAD or Miniaturized Ventricular Assist Device. It would be powered by a new algorithm to more efficiently pump blood. Industry analysts predicted robust sales.
In July 2015, implantations were set to begin on a select group of 60 patients in Europe and Australia. But they were abruptly stopped less than two months later after only 11 implants. Patients experienced numerous adverse events, including major bleeding, infection and device malfunction, according to published data.
HeartWare’s stock price plummeted from about $85 to $35 by October 2015. The next year, Medtronic bought HeartWare for $1.1 billion, replacing much of the company’s leadership shortly after.
Some former HeartWare investors filed a class action lawsuit in January 2016 alleging deception in the development of the MVAD.
According to the accounts of six anonymous former employees in the lawsuit, the details mirror the scandal surrounding Theranos, the former blood test company charged with fraud for raising more than $700 million by allegedly lying about its technology.
Where Theranos made empty promises of a test that only needed a few drops of blood, the suit alleges HeartWare promoted a life-sustaining medical device that former employees said had many problems and actually worsened blood flow, increasing clotting risks.
“Nothing really worked right,” one former HeartWare manager said in the lawsuit, citing “improper alarms, improper touch screen performance, gibberish on display screens — just so many alerts and problems.”
Leadership proceeded with human testing anyway, the suit alleges.
Months later, at an investor conference, HeartWare leadership acknowledged the pump and algorithm led to multiple adverse events. For two patients in particular, the algorithm would direct the pump to speed up so fast that it would try to suck up more blood than was available inside the heart for prolonged periods of time.
HeartWare and Medtronic settled the investor suit for $54.5 million in 2018, admitting no fault.
None of the allegations slowed the FDA as it gave Medtronic additional approval and support for its heart pump technologies.
In September 2017, the agency approved the HVAD as “destination therapy” for patients who were not heart transplant candidates and would rely on the device for the rest of their lives.
“We’re really excited about our HVAD destination therapy approval,” a Medtronic executive said on an investor earnings call. “That’s a real game changer for us in that market.”
Two years later, Medtronic announced it was developing a fully implantable version of the HVAD that would no longer need a cable coming through the waist to connect to power.
Even though issues with the HeartWare device had been unresolved for five years at that point, the FDA accepted the pitch into its new fast-track approval process for high-risk devices.
“Slipped Through The Cracks”
After Johnson Keelen’s pump failed in February, she found a news story about the recall notice sent to medical providers two months prior.
It said the company had identified a problem with pump restarts that could cause heart attacks or serious patient harm. Nineteen patients had been seriously injured so far, and two people had died. The recall warned that patients should be careful to avoid disconnecting the device’s power sources.
“I kept seeing Medtronic on record saying they notified patients,” Johnson Keelen said. “Who did they contact? No one told me.”
Her doctor later told her she must have “slipped through the cracks,” she said.
The current system for informing patients of new safety concerns with high-risk devices relies on a communication chain that can easily break. The device company contacts the FDA and health care providers that work with device patients. The FDA typically issues a public notice, while health professionals contact their patients.
But the agency admits most patients don’t know to look for formal FDA postings. And, experts say, the medical system can lose track of who needs to be notified, especially if a patient moves or switches primary care physicians.
Tina Winkler still wonders why she was never told about FDA-known safety issues with the HVAD. She said her husband’s medical team “had to teach me how to clean his wound, how to change his batteries and what to do if alarms go off. And they never mentioned any of this.”
She said, “If we had all the facts, there’s no way he would have gotten that device implanted in his heart.”
When FDA inspectors find serious safety issues with a medical device, inspection reports are not posted online or sent to patients. The public can obtain reports through a Freedom of Information Act request, but the agency’s records department has said new requests can be stuck behind a year-long backlog.
Patients can find warning letters online in a searchable database of thousands of letters from different FDA divisions, including the center for devices. But HeartWare’s 2014 letter is no longer available for public review because the website purges letters older than five years.
There are also few documents available in state courts about faulty products, because of restrictions on lawsuits related to medical devices. The restrictions date back to a 2008 Supreme Court decision in a case against Medtronic. The court found that U.S. law bars patients and their survivors from suing device makers in state court, essentially because their products go through such a rigorous FDA approval process.
Two recent patient lawsuits against HeartWare and Medtronic, including one filed by Tina Winkler, were moved from state court to federal court. In both cases, Medtronic filed to dismiss the cases because of the U.S. law that protects device companies. Medtronic and the families reached private settlements soon after.
Winkler and an attorney for the other family said they could not comment on their settlements.
Johnson Keelen, with a decommissioned HVAD still attached to her heart, wonders what that means for her and other patients’ chances of recourse.
“Why isn’t anyone now stepping up for the patient?” she asked. “They are now liable for taking care of us because we relied on them.”
“Run its course”
Deserae Cain, 33, is one of the 4,000 patients still relying on a HeartWare device.
She was implanted with the heart pump in late 2017, after suddenly being diagnosed with heart failure. Scans showed her heart was three times normal size. It took time for her to come to terms with needing a life-sustaining device — not long before her diagnosis, she had been going on five-mile runs. In the four years since, though, Cain has built a life around the HVAD with her fiance in their Dayton, Ohio, home.
They know the device can malfunction. In 2019, the pump failed for almost an hour as doctors at a nearby hospital struggled to restart it. Cain just tried to stay calm, knowing anxiety could threaten her unsupported weak heart. Months later, she needed an emergency experimental procedure to clear out blood clots developed within her HVAD.
Then, in 2020, Cain developed a widespread infection. Doctors told her she needed surgery to clean out and replace the pump.
Cain asked her medical team if she could switch to the alternative HeartMate device, which other patients told her presented fewer problems, she said. Doctors said the HVAD was better suited for her smaller frame.
But her new pump had problems soon after the surgery.
The device’s suction alarms, which alert when the pump is trying to pull in more blood than is available within the heart, sounded multiple times a day, for hours at a time, she said. Baffled by the issue for months, her medical team eventually turned off that specific alarm.
Soon after, her ventricular-assist specialist called her about a patient’s death linked to the belt that holds the device controller, she said. The belt had ripped and the equipment had fallen, yanking on the cable that connected the controller to the pump. Cain replaced her belt but it quickly frayed and had to be replaced again within six weeks.
Then, in June, she found out about Medtronic’s decision to stop sales and implants. Cain received a letter from her hospital mentioning a Medtronic support program, but it provided few specifics.
Cain wondered if things would be any different than before. Anxious about her future, she asked: “Are they just going to let it run its course until there is none of us left?”
This article first appeared on Propublica.
Please interrupt me, but don't heat your fish
Bother me, I’m working
Although some of us have been comfortably functioning in a virtual work environment, others are now trickling back into the office. And you know what that means? People come to your desk to show you pictures of their cat or tell you about their kid’s birthday party. You may sneer at the interruption, but a study shows you actually like it.
A team of researchers at the University of Cincinnati surveyed 111 full-time employees twice a day for 3 weeks about their work experience. They asked about mental exhaustion, workplace interruptions, sense of belonging, and overall job satisfaction. They found that employees had a higher sense of belonging and job satisfaction when interrupted with a social versus work interruption.
“Interruptions can actually benefit individuals from an interpersonal perspective – people feel like they belong when others come and talk to them or ask them questions, even while being distracted from their tasks,” said Heather C. Vough, senior investigator and a former university faculty member.
Chitchatting at work is often seen as a distraction, but this study suggests that it’s not like heating up fish in the breakroom microwave.
So the next time someone hits you with the “Hey, do you have a sec?,” do yourself a favor and enjoy the interruption.
A smorgasbord of science
It’s probably difficult to recruit patients for some medical trials. Try this new drug and potentially get all sorts of interesting and unpleasant side effects. Pass. We suggest the approach a group of researchers from the University of Kansas took for a recent study into weight gain: Invite a bunch of 20-something adults to an all-you-can-eat buffet. They’ll be beating down your door in no time.
Their study, published in Appetite, focused on hyperpalatable food – the sort of food you can keep eating – and compared it with high-energy-dense food and ultra processed food. The test patients had their body composition measured, were let loose on the buffet, and were measured again a year later.
The patients who favored salty/carbohydrate-filled hyperpalatable food (such as pretzels or popcorn) were much more likely to gain weight, compared with those who focused on salty/fat-filled food of any variety. As a matter of fact, those who stuck to fatty food during the buffet had no change in weight over the 1-year study period. The researchers noted that those who ate the carb-filled food tended more toward hedonic eating, or the act of eating simply for pleasure.
The study is no doubt helpful in the long battle against obesity and overeating, but it’s also a very helpful guide to getting the most bang for your buck at the buffet. Stay away from the cheap salty snack food. Go for the steak and seafood. Get your money’s worth. In the long run you won’t even gain any weight. No promises about tomorrow though.
There’s a cheat code for that
For a large percentage of kids and young adults, and maybe even older adults (we don’t judge), a storm warning means a cozy night in playing video games. Staying inside is probably the safest bet when there’s a storm, and the weatherman never says to avoid playing video games when there’s lightning.
Maybe he should, though, since a man from Tennessee reportedly got struck by lightning through his game controller. Emergency crews determined that lightning either hit the man’s house or struck near it and went through the controller. The type of console was not revealed, even though some people may want to know the specifics before playing during the next storm.
Luckily, the man was not seriously hurt and did not need to go to the hospital. This is apparently not unheard of, as a professional gamer was shocked through a wired controller last year, causing burns on her hands and a broken controller.
This might be our cue to do less electrical types of activities during thunderstorms, like knitting or reading by candlelight.
Freeze, squeeze, and enjoy … cramping
As you were ingesting last week’s installment of the never-ending buffet that is LOTME, you probably wondered: What’s going on? Where’s the latest bodily insult being perpetuated by the gang over at TikTok?
Have no fear, good readers. We would never make you go 2 straight weeks without serving up some hyperpalatable TikTok tidbits.
Our bodily insult du jour is frozen honey, and it’s exploding all over TikTok … and a few other places. “The hashtag ‘#FrozenHoney’ has been viewed nearly 600 million times, and the hashtag ‘#FrozenHoneyChallenge’ has been viewed more than 80 million times,” NBC News recently reported.
After a few hours in the freezer, honey can be squeezed out of a plastic bottle as a semisolid, toothpastelike goo – it’s stiff enough to rise out of a container that’s pointed straight up – and bitten off in large chunks. And therein lies the problem.
Some people are overdoing it. “Honey is great, but having it in small amounts to sweeten is really a healthy relationship with food, and using it to get a lot of followers and a lot of attention and having it in excess amounts is crazy,” Kristin Kirkpatrick, a registered dietitian at the Cleveland Clinic, told NBC.
Besides the possible weight gain from eating massive amounts of sugar, experts warned that “gobbling up bottles of frozen honey” could lead to stomach cramping, bloating, and diarrhea. Some TikTokers, NBC noted, said that they “were running for the bathroom.”
As we said, it’s a trend that is exploding.
Be sure to tune in next week, when we learn how TikTokers use ground meat as a skin moisturizer.
Bother me, I’m working
Although some of us have been comfortably functioning in a virtual work environment, others are now trickling back into the office. And you know what that means? People come to your desk to show you pictures of their cat or tell you about their kid’s birthday party. You may sneer at the interruption, but a study shows you actually like it.
A team of researchers at the University of Cincinnati surveyed 111 full-time employees twice a day for 3 weeks about their work experience. They asked about mental exhaustion, workplace interruptions, sense of belonging, and overall job satisfaction. They found that employees had a higher sense of belonging and job satisfaction when interrupted with a social versus work interruption.
“Interruptions can actually benefit individuals from an interpersonal perspective – people feel like they belong when others come and talk to them or ask them questions, even while being distracted from their tasks,” said Heather C. Vough, senior investigator and a former university faculty member.
Chitchatting at work is often seen as a distraction, but this study suggests that it’s not like heating up fish in the breakroom microwave.
So the next time someone hits you with the “Hey, do you have a sec?,” do yourself a favor and enjoy the interruption.
A smorgasbord of science
It’s probably difficult to recruit patients for some medical trials. Try this new drug and potentially get all sorts of interesting and unpleasant side effects. Pass. We suggest the approach a group of researchers from the University of Kansas took for a recent study into weight gain: Invite a bunch of 20-something adults to an all-you-can-eat buffet. They’ll be beating down your door in no time.
Their study, published in Appetite, focused on hyperpalatable food – the sort of food you can keep eating – and compared it with high-energy-dense food and ultra processed food. The test patients had their body composition measured, were let loose on the buffet, and were measured again a year later.
The patients who favored salty/carbohydrate-filled hyperpalatable food (such as pretzels or popcorn) were much more likely to gain weight, compared with those who focused on salty/fat-filled food of any variety. As a matter of fact, those who stuck to fatty food during the buffet had no change in weight over the 1-year study period. The researchers noted that those who ate the carb-filled food tended more toward hedonic eating, or the act of eating simply for pleasure.
The study is no doubt helpful in the long battle against obesity and overeating, but it’s also a very helpful guide to getting the most bang for your buck at the buffet. Stay away from the cheap salty snack food. Go for the steak and seafood. Get your money’s worth. In the long run you won’t even gain any weight. No promises about tomorrow though.
There’s a cheat code for that
For a large percentage of kids and young adults, and maybe even older adults (we don’t judge), a storm warning means a cozy night in playing video games. Staying inside is probably the safest bet when there’s a storm, and the weatherman never says to avoid playing video games when there’s lightning.
Maybe he should, though, since a man from Tennessee reportedly got struck by lightning through his game controller. Emergency crews determined that lightning either hit the man’s house or struck near it and went through the controller. The type of console was not revealed, even though some people may want to know the specifics before playing during the next storm.
Luckily, the man was not seriously hurt and did not need to go to the hospital. This is apparently not unheard of, as a professional gamer was shocked through a wired controller last year, causing burns on her hands and a broken controller.
This might be our cue to do less electrical types of activities during thunderstorms, like knitting or reading by candlelight.
Freeze, squeeze, and enjoy … cramping
As you were ingesting last week’s installment of the never-ending buffet that is LOTME, you probably wondered: What’s going on? Where’s the latest bodily insult being perpetuated by the gang over at TikTok?
Have no fear, good readers. We would never make you go 2 straight weeks without serving up some hyperpalatable TikTok tidbits.
Our bodily insult du jour is frozen honey, and it’s exploding all over TikTok … and a few other places. “The hashtag ‘#FrozenHoney’ has been viewed nearly 600 million times, and the hashtag ‘#FrozenHoneyChallenge’ has been viewed more than 80 million times,” NBC News recently reported.
After a few hours in the freezer, honey can be squeezed out of a plastic bottle as a semisolid, toothpastelike goo – it’s stiff enough to rise out of a container that’s pointed straight up – and bitten off in large chunks. And therein lies the problem.
Some people are overdoing it. “Honey is great, but having it in small amounts to sweeten is really a healthy relationship with food, and using it to get a lot of followers and a lot of attention and having it in excess amounts is crazy,” Kristin Kirkpatrick, a registered dietitian at the Cleveland Clinic, told NBC.
Besides the possible weight gain from eating massive amounts of sugar, experts warned that “gobbling up bottles of frozen honey” could lead to stomach cramping, bloating, and diarrhea. Some TikTokers, NBC noted, said that they “were running for the bathroom.”
As we said, it’s a trend that is exploding.
Be sure to tune in next week, when we learn how TikTokers use ground meat as a skin moisturizer.
Bother me, I’m working
Although some of us have been comfortably functioning in a virtual work environment, others are now trickling back into the office. And you know what that means? People come to your desk to show you pictures of their cat or tell you about their kid’s birthday party. You may sneer at the interruption, but a study shows you actually like it.
A team of researchers at the University of Cincinnati surveyed 111 full-time employees twice a day for 3 weeks about their work experience. They asked about mental exhaustion, workplace interruptions, sense of belonging, and overall job satisfaction. They found that employees had a higher sense of belonging and job satisfaction when interrupted with a social versus work interruption.
“Interruptions can actually benefit individuals from an interpersonal perspective – people feel like they belong when others come and talk to them or ask them questions, even while being distracted from their tasks,” said Heather C. Vough, senior investigator and a former university faculty member.
Chitchatting at work is often seen as a distraction, but this study suggests that it’s not like heating up fish in the breakroom microwave.
So the next time someone hits you with the “Hey, do you have a sec?,” do yourself a favor and enjoy the interruption.
A smorgasbord of science
It’s probably difficult to recruit patients for some medical trials. Try this new drug and potentially get all sorts of interesting and unpleasant side effects. Pass. We suggest the approach a group of researchers from the University of Kansas took for a recent study into weight gain: Invite a bunch of 20-something adults to an all-you-can-eat buffet. They’ll be beating down your door in no time.
Their study, published in Appetite, focused on hyperpalatable food – the sort of food you can keep eating – and compared it with high-energy-dense food and ultra processed food. The test patients had their body composition measured, were let loose on the buffet, and were measured again a year later.
The patients who favored salty/carbohydrate-filled hyperpalatable food (such as pretzels or popcorn) were much more likely to gain weight, compared with those who focused on salty/fat-filled food of any variety. As a matter of fact, those who stuck to fatty food during the buffet had no change in weight over the 1-year study period. The researchers noted that those who ate the carb-filled food tended more toward hedonic eating, or the act of eating simply for pleasure.
The study is no doubt helpful in the long battle against obesity and overeating, but it’s also a very helpful guide to getting the most bang for your buck at the buffet. Stay away from the cheap salty snack food. Go for the steak and seafood. Get your money’s worth. In the long run you won’t even gain any weight. No promises about tomorrow though.
There’s a cheat code for that
For a large percentage of kids and young adults, and maybe even older adults (we don’t judge), a storm warning means a cozy night in playing video games. Staying inside is probably the safest bet when there’s a storm, and the weatherman never says to avoid playing video games when there’s lightning.
Maybe he should, though, since a man from Tennessee reportedly got struck by lightning through his game controller. Emergency crews determined that lightning either hit the man’s house or struck near it and went through the controller. The type of console was not revealed, even though some people may want to know the specifics before playing during the next storm.
Luckily, the man was not seriously hurt and did not need to go to the hospital. This is apparently not unheard of, as a professional gamer was shocked through a wired controller last year, causing burns on her hands and a broken controller.
This might be our cue to do less electrical types of activities during thunderstorms, like knitting or reading by candlelight.
Freeze, squeeze, and enjoy … cramping
As you were ingesting last week’s installment of the never-ending buffet that is LOTME, you probably wondered: What’s going on? Where’s the latest bodily insult being perpetuated by the gang over at TikTok?
Have no fear, good readers. We would never make you go 2 straight weeks without serving up some hyperpalatable TikTok tidbits.
Our bodily insult du jour is frozen honey, and it’s exploding all over TikTok … and a few other places. “The hashtag ‘#FrozenHoney’ has been viewed nearly 600 million times, and the hashtag ‘#FrozenHoneyChallenge’ has been viewed more than 80 million times,” NBC News recently reported.
After a few hours in the freezer, honey can be squeezed out of a plastic bottle as a semisolid, toothpastelike goo – it’s stiff enough to rise out of a container that’s pointed straight up – and bitten off in large chunks. And therein lies the problem.
Some people are overdoing it. “Honey is great, but having it in small amounts to sweeten is really a healthy relationship with food, and using it to get a lot of followers and a lot of attention and having it in excess amounts is crazy,” Kristin Kirkpatrick, a registered dietitian at the Cleveland Clinic, told NBC.
Besides the possible weight gain from eating massive amounts of sugar, experts warned that “gobbling up bottles of frozen honey” could lead to stomach cramping, bloating, and diarrhea. Some TikTokers, NBC noted, said that they “were running for the bathroom.”
As we said, it’s a trend that is exploding.
Be sure to tune in next week, when we learn how TikTokers use ground meat as a skin moisturizer.
How heat kills: Deadly weather ‘cooking’ people from within
Millions of Americans have been languishing for weeks in the oppressive heat and humidity of a merciless summer. Deadly heat has already taken the lives of hundreds in the Pacific Northwest alone, with numbers likely to grow as the full impact of heat-related deaths eventually comes to light.
In the final week of July, the National Weather Service issued excessive heat warnings for 17 states, stretching from the West Coast, across the Midwest, down south into Louisiana and Georgia. Temperatures 10° to 15° F above average threaten the lives and livelihoods of people all across the country.
After a scorching heat wave in late June, residents of the Pacific Northwest are once again likely to see triple-digit temperatures in the coming days. With the heat, hospitals may face another surge of people with heat-related illnesses.
Erika Moseson, MD, a lung and intensive care specialist, witnessed firsthand the life-threatening impacts of soaring temperatures. She happened to be running her 10-bed intensive care unit in a suburban hospital in Gresham, Ore., about 15 miles east of Portland, the weekend of June 26. Within 12 hours, almost half her ICU beds were filled with people found unconscious on the street, in the bushes, or in their own beds, all because their body’s defenses had become overwhelmed by heat.
“It was unidentified person after unidentified person, coming in, same story, temperatures through the roof, comatose,” Dr. Moseson recalled. Young people in their 20s with muscle breakdown markers through the roof, a sign of rhabdomyolysis; people with no other medical problems that would have put them in a high-risk category.
As a lifelong Oregonian, she’d never seen anything like this before. “We’re all trained for it. I know what happens to you if you have heatstroke, I know how to treat it,” she trailed off, still finding it hard to believe. Still reeling from the number of cases in just a few hours. Still shocked that this happened on what’s supposed to be the cooler, rainforest side of Oregon.
Among those she treated and resuscitated, the memory of a patient that she lost continues to gnaw at her.
“I’ve gone back to it day after day since it happened,” she reflected.
Adults, in their 50s, living at home with their children. Just 1 hour prior, they’d all said goodnight. Then 1 hour later, when a child came to check in, both parents were unconscious.
Dr. Moseson shared how her team tried everything in their power for 18 hours to save the parent that was brought to her ICU. But like hundreds of others who went through the heat wave that weekend, her patient didn’t survive.
It was too late. From Dr. Moseson’s experience, it’s what happens “if you’re cooking a human.”
How heat kills
Regardless of where we live on the planet, humans maintain a consistent internal temperature around 98° F for our systems to function properly.
Our bodies have an entire temperature-regulating system to balance heat gain with heat loss so we don’t stray too far from our ideal range. The hypothalamus functions as the thermostat, communicating with heat sensors in our skin, muscles, and spinal cord. Based on signals about our core body temperature, our nervous system makes many decisions for us – opening up blood vessels in the peripheral parts of our body, pushing more blood toward the skin, and activating sweat glands to produce more sweat.
Sweat is one of the most powerful tools we have to maintain a safe internal temperature. Of course, there are some things under our control, such as removing clothing, drinking more water, and finding shade (or preferably air conditioning). But beyond that, it’s our ability to sweat that keeps us cool. When sweat evaporates into the air, heat from our skin goes with it, cooling us off.
Over time, our sweat response can work better as we get used to warmer environments, a process that’s known as acclimatization. Over the period of a few days to weeks, the sweat glands of acclimated people can start making sweat at lower temperatures, produce more sweat, and absorb more salt back into our system, all to make us more efficient “sweaters.”
While someone who’s not used to the heat may only produce 1 liter of sweat per hour, people who have become acclimated can produce 2-3 liters every hour, allowing evaporation to eliminate more than two times the amount of heat.
Because the process of acclimatization can take some time, typically it’s the first throes of summer, or heat waves in places where people don’t typically see high temperatures, that are the most deadly. And of course, the right infrastructure, like access to air conditioning, also plays a large role in limiting heat-related death and hospitalization.
A 2019 study showed that heat-related hospitalizations peak at different temperatures in different places. For example, hospitalizations typically peak in Texas when the temperature hits 105° F. But they might be highest in the Pacific Northwest at just 81° F.
Even with acclimatization, there are limits to how much our bodies can adapt to heat. When the humidity goes up past 75%, there’s already so much moisture in the air that heat loss through evaporation no longer occurs.
It’s this connection between heat and humidity that can be deadly. This is why the heat index (a measure that takes into account temperature and relative humidity) and wet bulb globe temperature (a measure commonly used by the military and competitive athletes that takes into account temperature, humidity, wind speed, sun angle, and cloud cover) are both better at showing how dangerous the heat may be for our health, compared to temperature alone.
Kristie L. Ebi, PhD, a professor in the Center for Health and the Global Environment at the University of Washington, Seattle, has been studying the effects of heat and other climate-sensitive conditions on health for over 20 years. She stresses that it’s not just the recorded temperatures, but the prolonged exposure that kills.
If you never get a chance to bring down that core body temperature, if your internal temperatures stay above the range where your cells and your organs can work well for a long time, that’s when you can have the most dangerous effects of heat.
“It depends then on your age, your fitness, your individual physiology, underlying medical conditions, to how quickly that could affect the functioning of those organs. There’s lots of variability in there,” Dr. Ebi said.
Our hearts take on the brunt of the early response, working harder to pump blood toward the skin. Water and salt loss through our skin can start to cause electrolyte changes that can cause heat cramps and heat exhaustion. We feel tired, nauseated, dizzy. With enough water loss, we may become dehydrated, limiting the blood flow to our brains, causing us to pass out.
These early signs are like a car’s check engine light – systems are already being damaged, but resting, refueling, and, most importantly, turning off the heat are critical steps to prevent fatal injury.
If hazardous heat exposure continues and our internal temperatures continue to rise, nerves stop talking to each other, the proteins in our body unfold and lose their shape, and the cells of our organs disintegrate. This in turn sets off a fire alarm in our blood vessels, where a variety of chemical messengers, including “heat-shock proteins,” are released. The release of these inflammatory proteins, coupled with the loss of blood flow, eventually leads to the death of cells throughout the body, from the brain, to the heart, the muscles, and the kidneys.
This process is referred to as heatstroke. In essence, we melt from the inside.
At a certain point, this cascade can’t be reversed. Just like when you cool a melting block of ice, the parts that have melted will not go back to their original shape. It’s a similar process in our bodies, so delays in cooling and treatment can lead to death rates as high as 80%.
On the outside, we see people who look confused and disoriented, with hot skin and rapid breathing, and they may eventually become unconscious. Core body temperatures over 105° F clinch the diagnosis, but at the first sign of feeling unwell, cooling should be started.
There is no fancier or more effective treatment than that: Cool right away. In emergency rooms in Washington State, doctors used body bags filled with ice and water to cool victims of the heat wave in late June.
“It was all from heat ... that’s the thing, you feel so idiotic ... you’re like, ‘I’ve given you ice’ ... you bring their temperature down. But it’s already set off this cascade that you can’t stop,” Dr. Moseson said.
By the time Dr. Moseson’s patient made it to her, cooling with ice was just the beginning of the attempts to resuscitate and revive. The patient was already showing evidence of a process causing widespread bleeding and clotting, known as disseminated intravascular coagulation, along with damage to the heart and failing kidneys. Over 18 hours, her team cooled the patient, flooded the blood vessels with fluids and blood products, attempted to start dialysis, and inserted a breathing tube – all of the technology that is used to save people from serious cardiovascular collapse from other conditions. But nothing could reverse the melting that had already occurred.
Deaths from heat are 100% preventable. Until they’re not.
No respite
As Dr. Ebi says, the key to preventing heat-related death is to cool down enough to stabilize our internal cells and proteins before the irreversible cascade begins.
But for close to 80% of Americans who live in urban areas, temperatures can be even higher and more intolerable compared to surrounding areas because of the way we’ve designed our cities. In effect, we have unintentionally created hot zones called “urban heat islands.”
Jeremy Hoffman, PhD, chief scientist for the Science Museum of Virginia, explains that things like bricks, asphalt, and parking lots absorb more of the sun’s energy throughout the day and then emit that back into the air as heat throughout the afternoon and into the evening. This raises the air and surface temperatures in cities, relative to rural areas. When temperatures don’t cool enough at night, there’s no way to recover from the day’s heat. You start the next day still depleted, with less reserve to face the heat of a new day.
When you dig even deeper, it turns out that even within the same city, there are huge “thermal inequities,” as Dr. Hoffman calls them. In a 2019 study, he found that wealthier parts of cities had more natural spaces such as parks and tree-lined streets, compared to areas that had been intentionally “redlined,” or systematically deprived of investment. This pattern repeats itself in over 100 urban areas across the country and translates to huge temperature differences on the order of 10-20 degrees Fahrenheit within the same city, at the exact same time during a heat wave.
“In some ways, the way that we’ve decided to plan and build our cities physically turns up the thermostat by several tens of degrees during heat waves in particular neighborhoods,” Dr. Hoffman said.
Dr. Hoffman’s work showed that the city of Portland (where the death toll from the heat wave in late June was the highest) had some of the most intense differences between formerly redlined vs. tree-lined areas out of the more than 100 cities that he studied.
“Watching it play out, I was really concerned, not only as a climate scientist, but as a human. Understanding the urban heat island effect and the extreme nature of the inequity in our cities, thermally and otherwise, once you start to really recognize it, you can’t forget it.”
The most vulnerable
When it comes to identifying and protecting the people most vulnerable to heat stress and heat-related death, there is an ever-growing list of those most at risk. Unfortunately, very few recognize when they themselves are at risk, often until it’s too late.
According to Linda McCauley, PhD, dean of the Emory University School of Nursing in Atlanta, “the scope of who is vulnerable is quickly increasing.”
For example, we’re used to recognizing that pregnant women and young children are at risk. Public health campaigns have long advised us not to leave young children and pets in hot cars. We know that adolescents who play sports during hot summer months are at high risk for heat-related events and even death.
In Georgia, a 15-year-old boy collapsed and died after his first day back at football practice when the heat index was 105° F on July 26, even as it appears that all protocols for heat safety were being followed.
We recognize that outdoor workers face devastating consequences from prolonged exertion in the heat and must have safer working conditions.
The elderly and those with long-term medical and mental health conditions are also more vulnerable to heat. The elderly may not have the same warning signs and may not recognize that they are dehydrated until it is too late. In addition, their sweating mechanism weakens, and they may be taking medicines that interfere with their ability to regulate their temperature.
Poverty and inadequate housing are risk factors, especially for those in urban heat islands. For many people, their housing does not have enough cooling to protect them, and they can’t safely get themselves to cooling shelters.
These patterns for the most vulnerable fit for the majority of deaths in Oregon during the late June heat wave. Most victims were older, lived alone, and didn’t have air conditioning. But with climate change, the predictions are that temperatures will go higher and heat waves will last longer.
“There’s probably very few people today that are ‘immune’ to the effects of heat-related stress with climate change. All of us can be put in situations where we are susceptible,” Dr. McCauley said.
Dr. Moseson agreed. Many of her patients fit none of these risk categories – she treated people with no health problems in their 20s in her ICU, and the patient she lost would not traditionally have been thought of as high risk. That 50-something patient had no long-standing medical problems, and lived with family in a newly renovated suburban home that had air conditioning. The only problem was that the air conditioner had broken and there had been no rush to fix it based on past experience with Oregon summers.
Preventing heat deaths
Protecting ourselves and our families means monitoring the “simple things.” The first three rules are to make sure we’re drinking plenty of water – this means drinking whether we feel thirsty or not. If we’re not in an air-conditioned place, we’ve got to look for shade. And we need to take regular rest breaks.
Inside a home without air conditioning, placing ice in front of a fan to cool the air can work, but realistically, if you are in a place without air conditioning and the temperatures are approaching 90° F, it’s safest to find another place to stay, if possible.
For those playing sports, there are usually 1-week to 2-week protocols that allow for acclimatization when the season begins – this means starting slowly, without gear, and ramping up activity. Still, parents and coaches should watch advanced weather reports to make sure it’s safe to practice outside.
How we dress can also help us, so light clothing is key. And if we’re able to schedule activities for times when it is cooler, that can also protect us from overheating.
If anyone shows early signs of heat stress, removing clothing, cooling their bodies with cold water, and getting them out of the heat is critical. Any evidence of heatstroke is an emergency, and 911 should be called without delay. The faster the core temperature can be dropped, the better the chances for recovery.
On the level of communities, access to natural air conditioning in the form of healthy tree canopies, and trees at bus stops to provide shade can help a lot. According to Dr. Hoffman, these investments help almost right away. Reimagining our cities to remove the “hot zones” that we have created is another key to protecting ourselves as our climate changes.
Reaching our limits in a changing climate
Already, we are seeing more intense, more frequent, and longer-lasting heat waves throughout the country and across the globe.
Dr. Ebi, a coauthor of a recently released scientific analysis that found that the late June Pacific Northwest heat wave would have been virtually impossible without climate change, herself lived through the scorching temperatures in Seattle. Her work shows that the changing climate is killing us right now.
We are approaching a time where extreme temperatures and humidity will make it almost impossible for people to be outside in many parts of the world. Researchers have found that periods of extreme humid heat have more than doubled since 1979, and some places have already had wet-bulb temperatures at the limits of what scientists think humans can tolerate under ideal conditions, meaning for people in perfect health, completely unclothed, in gale-force winds, performing no activity. Obviously that’s less than ideal for most of us and helps explain why thousands of people die at temperatures much lower than our upper limit.
Dr. Ebi pointed out that the good news is that many local communities with a long history of managing high temperatures have a lot of knowledge to share with regions that are newly dealing with these conditions. This includes how local areas develop early warning and response systems with specific action plans.
But, she cautions, it’s going to take a lot of coordination and a lot of behavior change to stabilize the earth’s climate, understand our weak points, and protect our health.
For Dr. Moseson, this reality has hit home.
“I already spent the year being terrified that I as an ICU doctor was going to be the one who gave my mom COVID. Finally I’m vaccinated, she’s vaccinated. Now I’ve watched someone die because they don’t have AC. And my parents, they’re old-school Oregonians, they don’t have AC.”
A version of this article originally appeared on WebMD.com.
Millions of Americans have been languishing for weeks in the oppressive heat and humidity of a merciless summer. Deadly heat has already taken the lives of hundreds in the Pacific Northwest alone, with numbers likely to grow as the full impact of heat-related deaths eventually comes to light.
In the final week of July, the National Weather Service issued excessive heat warnings for 17 states, stretching from the West Coast, across the Midwest, down south into Louisiana and Georgia. Temperatures 10° to 15° F above average threaten the lives and livelihoods of people all across the country.
After a scorching heat wave in late June, residents of the Pacific Northwest are once again likely to see triple-digit temperatures in the coming days. With the heat, hospitals may face another surge of people with heat-related illnesses.
Erika Moseson, MD, a lung and intensive care specialist, witnessed firsthand the life-threatening impacts of soaring temperatures. She happened to be running her 10-bed intensive care unit in a suburban hospital in Gresham, Ore., about 15 miles east of Portland, the weekend of June 26. Within 12 hours, almost half her ICU beds were filled with people found unconscious on the street, in the bushes, or in their own beds, all because their body’s defenses had become overwhelmed by heat.
“It was unidentified person after unidentified person, coming in, same story, temperatures through the roof, comatose,” Dr. Moseson recalled. Young people in their 20s with muscle breakdown markers through the roof, a sign of rhabdomyolysis; people with no other medical problems that would have put them in a high-risk category.
As a lifelong Oregonian, she’d never seen anything like this before. “We’re all trained for it. I know what happens to you if you have heatstroke, I know how to treat it,” she trailed off, still finding it hard to believe. Still reeling from the number of cases in just a few hours. Still shocked that this happened on what’s supposed to be the cooler, rainforest side of Oregon.
Among those she treated and resuscitated, the memory of a patient that she lost continues to gnaw at her.
“I’ve gone back to it day after day since it happened,” she reflected.
Adults, in their 50s, living at home with their children. Just 1 hour prior, they’d all said goodnight. Then 1 hour later, when a child came to check in, both parents were unconscious.
Dr. Moseson shared how her team tried everything in their power for 18 hours to save the parent that was brought to her ICU. But like hundreds of others who went through the heat wave that weekend, her patient didn’t survive.
It was too late. From Dr. Moseson’s experience, it’s what happens “if you’re cooking a human.”
How heat kills
Regardless of where we live on the planet, humans maintain a consistent internal temperature around 98° F for our systems to function properly.
Our bodies have an entire temperature-regulating system to balance heat gain with heat loss so we don’t stray too far from our ideal range. The hypothalamus functions as the thermostat, communicating with heat sensors in our skin, muscles, and spinal cord. Based on signals about our core body temperature, our nervous system makes many decisions for us – opening up blood vessels in the peripheral parts of our body, pushing more blood toward the skin, and activating sweat glands to produce more sweat.
Sweat is one of the most powerful tools we have to maintain a safe internal temperature. Of course, there are some things under our control, such as removing clothing, drinking more water, and finding shade (or preferably air conditioning). But beyond that, it’s our ability to sweat that keeps us cool. When sweat evaporates into the air, heat from our skin goes with it, cooling us off.
Over time, our sweat response can work better as we get used to warmer environments, a process that’s known as acclimatization. Over the period of a few days to weeks, the sweat glands of acclimated people can start making sweat at lower temperatures, produce more sweat, and absorb more salt back into our system, all to make us more efficient “sweaters.”
While someone who’s not used to the heat may only produce 1 liter of sweat per hour, people who have become acclimated can produce 2-3 liters every hour, allowing evaporation to eliminate more than two times the amount of heat.
Because the process of acclimatization can take some time, typically it’s the first throes of summer, or heat waves in places where people don’t typically see high temperatures, that are the most deadly. And of course, the right infrastructure, like access to air conditioning, also plays a large role in limiting heat-related death and hospitalization.
A 2019 study showed that heat-related hospitalizations peak at different temperatures in different places. For example, hospitalizations typically peak in Texas when the temperature hits 105° F. But they might be highest in the Pacific Northwest at just 81° F.
Even with acclimatization, there are limits to how much our bodies can adapt to heat. When the humidity goes up past 75%, there’s already so much moisture in the air that heat loss through evaporation no longer occurs.
It’s this connection between heat and humidity that can be deadly. This is why the heat index (a measure that takes into account temperature and relative humidity) and wet bulb globe temperature (a measure commonly used by the military and competitive athletes that takes into account temperature, humidity, wind speed, sun angle, and cloud cover) are both better at showing how dangerous the heat may be for our health, compared to temperature alone.
Kristie L. Ebi, PhD, a professor in the Center for Health and the Global Environment at the University of Washington, Seattle, has been studying the effects of heat and other climate-sensitive conditions on health for over 20 years. She stresses that it’s not just the recorded temperatures, but the prolonged exposure that kills.
If you never get a chance to bring down that core body temperature, if your internal temperatures stay above the range where your cells and your organs can work well for a long time, that’s when you can have the most dangerous effects of heat.
“It depends then on your age, your fitness, your individual physiology, underlying medical conditions, to how quickly that could affect the functioning of those organs. There’s lots of variability in there,” Dr. Ebi said.
Our hearts take on the brunt of the early response, working harder to pump blood toward the skin. Water and salt loss through our skin can start to cause electrolyte changes that can cause heat cramps and heat exhaustion. We feel tired, nauseated, dizzy. With enough water loss, we may become dehydrated, limiting the blood flow to our brains, causing us to pass out.
These early signs are like a car’s check engine light – systems are already being damaged, but resting, refueling, and, most importantly, turning off the heat are critical steps to prevent fatal injury.
If hazardous heat exposure continues and our internal temperatures continue to rise, nerves stop talking to each other, the proteins in our body unfold and lose their shape, and the cells of our organs disintegrate. This in turn sets off a fire alarm in our blood vessels, where a variety of chemical messengers, including “heat-shock proteins,” are released. The release of these inflammatory proteins, coupled with the loss of blood flow, eventually leads to the death of cells throughout the body, from the brain, to the heart, the muscles, and the kidneys.
This process is referred to as heatstroke. In essence, we melt from the inside.
At a certain point, this cascade can’t be reversed. Just like when you cool a melting block of ice, the parts that have melted will not go back to their original shape. It’s a similar process in our bodies, so delays in cooling and treatment can lead to death rates as high as 80%.
On the outside, we see people who look confused and disoriented, with hot skin and rapid breathing, and they may eventually become unconscious. Core body temperatures over 105° F clinch the diagnosis, but at the first sign of feeling unwell, cooling should be started.
There is no fancier or more effective treatment than that: Cool right away. In emergency rooms in Washington State, doctors used body bags filled with ice and water to cool victims of the heat wave in late June.
“It was all from heat ... that’s the thing, you feel so idiotic ... you’re like, ‘I’ve given you ice’ ... you bring their temperature down. But it’s already set off this cascade that you can’t stop,” Dr. Moseson said.
By the time Dr. Moseson’s patient made it to her, cooling with ice was just the beginning of the attempts to resuscitate and revive. The patient was already showing evidence of a process causing widespread bleeding and clotting, known as disseminated intravascular coagulation, along with damage to the heart and failing kidneys. Over 18 hours, her team cooled the patient, flooded the blood vessels with fluids and blood products, attempted to start dialysis, and inserted a breathing tube – all of the technology that is used to save people from serious cardiovascular collapse from other conditions. But nothing could reverse the melting that had already occurred.
Deaths from heat are 100% preventable. Until they’re not.
No respite
As Dr. Ebi says, the key to preventing heat-related death is to cool down enough to stabilize our internal cells and proteins before the irreversible cascade begins.
But for close to 80% of Americans who live in urban areas, temperatures can be even higher and more intolerable compared to surrounding areas because of the way we’ve designed our cities. In effect, we have unintentionally created hot zones called “urban heat islands.”
Jeremy Hoffman, PhD, chief scientist for the Science Museum of Virginia, explains that things like bricks, asphalt, and parking lots absorb more of the sun’s energy throughout the day and then emit that back into the air as heat throughout the afternoon and into the evening. This raises the air and surface temperatures in cities, relative to rural areas. When temperatures don’t cool enough at night, there’s no way to recover from the day’s heat. You start the next day still depleted, with less reserve to face the heat of a new day.
When you dig even deeper, it turns out that even within the same city, there are huge “thermal inequities,” as Dr. Hoffman calls them. In a 2019 study, he found that wealthier parts of cities had more natural spaces such as parks and tree-lined streets, compared to areas that had been intentionally “redlined,” or systematically deprived of investment. This pattern repeats itself in over 100 urban areas across the country and translates to huge temperature differences on the order of 10-20 degrees Fahrenheit within the same city, at the exact same time during a heat wave.
“In some ways, the way that we’ve decided to plan and build our cities physically turns up the thermostat by several tens of degrees during heat waves in particular neighborhoods,” Dr. Hoffman said.
Dr. Hoffman’s work showed that the city of Portland (where the death toll from the heat wave in late June was the highest) had some of the most intense differences between formerly redlined vs. tree-lined areas out of the more than 100 cities that he studied.
“Watching it play out, I was really concerned, not only as a climate scientist, but as a human. Understanding the urban heat island effect and the extreme nature of the inequity in our cities, thermally and otherwise, once you start to really recognize it, you can’t forget it.”
The most vulnerable
When it comes to identifying and protecting the people most vulnerable to heat stress and heat-related death, there is an ever-growing list of those most at risk. Unfortunately, very few recognize when they themselves are at risk, often until it’s too late.
According to Linda McCauley, PhD, dean of the Emory University School of Nursing in Atlanta, “the scope of who is vulnerable is quickly increasing.”
For example, we’re used to recognizing that pregnant women and young children are at risk. Public health campaigns have long advised us not to leave young children and pets in hot cars. We know that adolescents who play sports during hot summer months are at high risk for heat-related events and even death.
In Georgia, a 15-year-old boy collapsed and died after his first day back at football practice when the heat index was 105° F on July 26, even as it appears that all protocols for heat safety were being followed.
We recognize that outdoor workers face devastating consequences from prolonged exertion in the heat and must have safer working conditions.
The elderly and those with long-term medical and mental health conditions are also more vulnerable to heat. The elderly may not have the same warning signs and may not recognize that they are dehydrated until it is too late. In addition, their sweating mechanism weakens, and they may be taking medicines that interfere with their ability to regulate their temperature.
Poverty and inadequate housing are risk factors, especially for those in urban heat islands. For many people, their housing does not have enough cooling to protect them, and they can’t safely get themselves to cooling shelters.
These patterns for the most vulnerable fit for the majority of deaths in Oregon during the late June heat wave. Most victims were older, lived alone, and didn’t have air conditioning. But with climate change, the predictions are that temperatures will go higher and heat waves will last longer.
“There’s probably very few people today that are ‘immune’ to the effects of heat-related stress with climate change. All of us can be put in situations where we are susceptible,” Dr. McCauley said.
Dr. Moseson agreed. Many of her patients fit none of these risk categories – she treated people with no health problems in their 20s in her ICU, and the patient she lost would not traditionally have been thought of as high risk. That 50-something patient had no long-standing medical problems, and lived with family in a newly renovated suburban home that had air conditioning. The only problem was that the air conditioner had broken and there had been no rush to fix it based on past experience with Oregon summers.
Preventing heat deaths
Protecting ourselves and our families means monitoring the “simple things.” The first three rules are to make sure we’re drinking plenty of water – this means drinking whether we feel thirsty or not. If we’re not in an air-conditioned place, we’ve got to look for shade. And we need to take regular rest breaks.
Inside a home without air conditioning, placing ice in front of a fan to cool the air can work, but realistically, if you are in a place without air conditioning and the temperatures are approaching 90° F, it’s safest to find another place to stay, if possible.
For those playing sports, there are usually 1-week to 2-week protocols that allow for acclimatization when the season begins – this means starting slowly, without gear, and ramping up activity. Still, parents and coaches should watch advanced weather reports to make sure it’s safe to practice outside.
How we dress can also help us, so light clothing is key. And if we’re able to schedule activities for times when it is cooler, that can also protect us from overheating.
If anyone shows early signs of heat stress, removing clothing, cooling their bodies with cold water, and getting them out of the heat is critical. Any evidence of heatstroke is an emergency, and 911 should be called without delay. The faster the core temperature can be dropped, the better the chances for recovery.
On the level of communities, access to natural air conditioning in the form of healthy tree canopies, and trees at bus stops to provide shade can help a lot. According to Dr. Hoffman, these investments help almost right away. Reimagining our cities to remove the “hot zones” that we have created is another key to protecting ourselves as our climate changes.
Reaching our limits in a changing climate
Already, we are seeing more intense, more frequent, and longer-lasting heat waves throughout the country and across the globe.
Dr. Ebi, a coauthor of a recently released scientific analysis that found that the late June Pacific Northwest heat wave would have been virtually impossible without climate change, herself lived through the scorching temperatures in Seattle. Her work shows that the changing climate is killing us right now.
We are approaching a time where extreme temperatures and humidity will make it almost impossible for people to be outside in many parts of the world. Researchers have found that periods of extreme humid heat have more than doubled since 1979, and some places have already had wet-bulb temperatures at the limits of what scientists think humans can tolerate under ideal conditions, meaning for people in perfect health, completely unclothed, in gale-force winds, performing no activity. Obviously that’s less than ideal for most of us and helps explain why thousands of people die at temperatures much lower than our upper limit.
Dr. Ebi pointed out that the good news is that many local communities with a long history of managing high temperatures have a lot of knowledge to share with regions that are newly dealing with these conditions. This includes how local areas develop early warning and response systems with specific action plans.
But, she cautions, it’s going to take a lot of coordination and a lot of behavior change to stabilize the earth’s climate, understand our weak points, and protect our health.
For Dr. Moseson, this reality has hit home.
“I already spent the year being terrified that I as an ICU doctor was going to be the one who gave my mom COVID. Finally I’m vaccinated, she’s vaccinated. Now I’ve watched someone die because they don’t have AC. And my parents, they’re old-school Oregonians, they don’t have AC.”
A version of this article originally appeared on WebMD.com.
Millions of Americans have been languishing for weeks in the oppressive heat and humidity of a merciless summer. Deadly heat has already taken the lives of hundreds in the Pacific Northwest alone, with numbers likely to grow as the full impact of heat-related deaths eventually comes to light.
In the final week of July, the National Weather Service issued excessive heat warnings for 17 states, stretching from the West Coast, across the Midwest, down south into Louisiana and Georgia. Temperatures 10° to 15° F above average threaten the lives and livelihoods of people all across the country.
After a scorching heat wave in late June, residents of the Pacific Northwest are once again likely to see triple-digit temperatures in the coming days. With the heat, hospitals may face another surge of people with heat-related illnesses.
Erika Moseson, MD, a lung and intensive care specialist, witnessed firsthand the life-threatening impacts of soaring temperatures. She happened to be running her 10-bed intensive care unit in a suburban hospital in Gresham, Ore., about 15 miles east of Portland, the weekend of June 26. Within 12 hours, almost half her ICU beds were filled with people found unconscious on the street, in the bushes, or in their own beds, all because their body’s defenses had become overwhelmed by heat.
“It was unidentified person after unidentified person, coming in, same story, temperatures through the roof, comatose,” Dr. Moseson recalled. Young people in their 20s with muscle breakdown markers through the roof, a sign of rhabdomyolysis; people with no other medical problems that would have put them in a high-risk category.
As a lifelong Oregonian, she’d never seen anything like this before. “We’re all trained for it. I know what happens to you if you have heatstroke, I know how to treat it,” she trailed off, still finding it hard to believe. Still reeling from the number of cases in just a few hours. Still shocked that this happened on what’s supposed to be the cooler, rainforest side of Oregon.
Among those she treated and resuscitated, the memory of a patient that she lost continues to gnaw at her.
“I’ve gone back to it day after day since it happened,” she reflected.
Adults, in their 50s, living at home with their children. Just 1 hour prior, they’d all said goodnight. Then 1 hour later, when a child came to check in, both parents were unconscious.
Dr. Moseson shared how her team tried everything in their power for 18 hours to save the parent that was brought to her ICU. But like hundreds of others who went through the heat wave that weekend, her patient didn’t survive.
It was too late. From Dr. Moseson’s experience, it’s what happens “if you’re cooking a human.”
How heat kills
Regardless of where we live on the planet, humans maintain a consistent internal temperature around 98° F for our systems to function properly.
Our bodies have an entire temperature-regulating system to balance heat gain with heat loss so we don’t stray too far from our ideal range. The hypothalamus functions as the thermostat, communicating with heat sensors in our skin, muscles, and spinal cord. Based on signals about our core body temperature, our nervous system makes many decisions for us – opening up blood vessels in the peripheral parts of our body, pushing more blood toward the skin, and activating sweat glands to produce more sweat.
Sweat is one of the most powerful tools we have to maintain a safe internal temperature. Of course, there are some things under our control, such as removing clothing, drinking more water, and finding shade (or preferably air conditioning). But beyond that, it’s our ability to sweat that keeps us cool. When sweat evaporates into the air, heat from our skin goes with it, cooling us off.
Over time, our sweat response can work better as we get used to warmer environments, a process that’s known as acclimatization. Over the period of a few days to weeks, the sweat glands of acclimated people can start making sweat at lower temperatures, produce more sweat, and absorb more salt back into our system, all to make us more efficient “sweaters.”
While someone who’s not used to the heat may only produce 1 liter of sweat per hour, people who have become acclimated can produce 2-3 liters every hour, allowing evaporation to eliminate more than two times the amount of heat.
Because the process of acclimatization can take some time, typically it’s the first throes of summer, or heat waves in places where people don’t typically see high temperatures, that are the most deadly. And of course, the right infrastructure, like access to air conditioning, also plays a large role in limiting heat-related death and hospitalization.
A 2019 study showed that heat-related hospitalizations peak at different temperatures in different places. For example, hospitalizations typically peak in Texas when the temperature hits 105° F. But they might be highest in the Pacific Northwest at just 81° F.
Even with acclimatization, there are limits to how much our bodies can adapt to heat. When the humidity goes up past 75%, there’s already so much moisture in the air that heat loss through evaporation no longer occurs.
It’s this connection between heat and humidity that can be deadly. This is why the heat index (a measure that takes into account temperature and relative humidity) and wet bulb globe temperature (a measure commonly used by the military and competitive athletes that takes into account temperature, humidity, wind speed, sun angle, and cloud cover) are both better at showing how dangerous the heat may be for our health, compared to temperature alone.
Kristie L. Ebi, PhD, a professor in the Center for Health and the Global Environment at the University of Washington, Seattle, has been studying the effects of heat and other climate-sensitive conditions on health for over 20 years. She stresses that it’s not just the recorded temperatures, but the prolonged exposure that kills.
If you never get a chance to bring down that core body temperature, if your internal temperatures stay above the range where your cells and your organs can work well for a long time, that’s when you can have the most dangerous effects of heat.
“It depends then on your age, your fitness, your individual physiology, underlying medical conditions, to how quickly that could affect the functioning of those organs. There’s lots of variability in there,” Dr. Ebi said.
Our hearts take on the brunt of the early response, working harder to pump blood toward the skin. Water and salt loss through our skin can start to cause electrolyte changes that can cause heat cramps and heat exhaustion. We feel tired, nauseated, dizzy. With enough water loss, we may become dehydrated, limiting the blood flow to our brains, causing us to pass out.
These early signs are like a car’s check engine light – systems are already being damaged, but resting, refueling, and, most importantly, turning off the heat are critical steps to prevent fatal injury.
If hazardous heat exposure continues and our internal temperatures continue to rise, nerves stop talking to each other, the proteins in our body unfold and lose their shape, and the cells of our organs disintegrate. This in turn sets off a fire alarm in our blood vessels, where a variety of chemical messengers, including “heat-shock proteins,” are released. The release of these inflammatory proteins, coupled with the loss of blood flow, eventually leads to the death of cells throughout the body, from the brain, to the heart, the muscles, and the kidneys.
This process is referred to as heatstroke. In essence, we melt from the inside.
At a certain point, this cascade can’t be reversed. Just like when you cool a melting block of ice, the parts that have melted will not go back to their original shape. It’s a similar process in our bodies, so delays in cooling and treatment can lead to death rates as high as 80%.
On the outside, we see people who look confused and disoriented, with hot skin and rapid breathing, and they may eventually become unconscious. Core body temperatures over 105° F clinch the diagnosis, but at the first sign of feeling unwell, cooling should be started.
There is no fancier or more effective treatment than that: Cool right away. In emergency rooms in Washington State, doctors used body bags filled with ice and water to cool victims of the heat wave in late June.
“It was all from heat ... that’s the thing, you feel so idiotic ... you’re like, ‘I’ve given you ice’ ... you bring their temperature down. But it’s already set off this cascade that you can’t stop,” Dr. Moseson said.
By the time Dr. Moseson’s patient made it to her, cooling with ice was just the beginning of the attempts to resuscitate and revive. The patient was already showing evidence of a process causing widespread bleeding and clotting, known as disseminated intravascular coagulation, along with damage to the heart and failing kidneys. Over 18 hours, her team cooled the patient, flooded the blood vessels with fluids and blood products, attempted to start dialysis, and inserted a breathing tube – all of the technology that is used to save people from serious cardiovascular collapse from other conditions. But nothing could reverse the melting that had already occurred.
Deaths from heat are 100% preventable. Until they’re not.
No respite
As Dr. Ebi says, the key to preventing heat-related death is to cool down enough to stabilize our internal cells and proteins before the irreversible cascade begins.
But for close to 80% of Americans who live in urban areas, temperatures can be even higher and more intolerable compared to surrounding areas because of the way we’ve designed our cities. In effect, we have unintentionally created hot zones called “urban heat islands.”
Jeremy Hoffman, PhD, chief scientist for the Science Museum of Virginia, explains that things like bricks, asphalt, and parking lots absorb more of the sun’s energy throughout the day and then emit that back into the air as heat throughout the afternoon and into the evening. This raises the air and surface temperatures in cities, relative to rural areas. When temperatures don’t cool enough at night, there’s no way to recover from the day’s heat. You start the next day still depleted, with less reserve to face the heat of a new day.
When you dig even deeper, it turns out that even within the same city, there are huge “thermal inequities,” as Dr. Hoffman calls them. In a 2019 study, he found that wealthier parts of cities had more natural spaces such as parks and tree-lined streets, compared to areas that had been intentionally “redlined,” or systematically deprived of investment. This pattern repeats itself in over 100 urban areas across the country and translates to huge temperature differences on the order of 10-20 degrees Fahrenheit within the same city, at the exact same time during a heat wave.
“In some ways, the way that we’ve decided to plan and build our cities physically turns up the thermostat by several tens of degrees during heat waves in particular neighborhoods,” Dr. Hoffman said.
Dr. Hoffman’s work showed that the city of Portland (where the death toll from the heat wave in late June was the highest) had some of the most intense differences between formerly redlined vs. tree-lined areas out of the more than 100 cities that he studied.
“Watching it play out, I was really concerned, not only as a climate scientist, but as a human. Understanding the urban heat island effect and the extreme nature of the inequity in our cities, thermally and otherwise, once you start to really recognize it, you can’t forget it.”
The most vulnerable
When it comes to identifying and protecting the people most vulnerable to heat stress and heat-related death, there is an ever-growing list of those most at risk. Unfortunately, very few recognize when they themselves are at risk, often until it’s too late.
According to Linda McCauley, PhD, dean of the Emory University School of Nursing in Atlanta, “the scope of who is vulnerable is quickly increasing.”
For example, we’re used to recognizing that pregnant women and young children are at risk. Public health campaigns have long advised us not to leave young children and pets in hot cars. We know that adolescents who play sports during hot summer months are at high risk for heat-related events and even death.
In Georgia, a 15-year-old boy collapsed and died after his first day back at football practice when the heat index was 105° F on July 26, even as it appears that all protocols for heat safety were being followed.
We recognize that outdoor workers face devastating consequences from prolonged exertion in the heat and must have safer working conditions.
The elderly and those with long-term medical and mental health conditions are also more vulnerable to heat. The elderly may not have the same warning signs and may not recognize that they are dehydrated until it is too late. In addition, their sweating mechanism weakens, and they may be taking medicines that interfere with their ability to regulate their temperature.
Poverty and inadequate housing are risk factors, especially for those in urban heat islands. For many people, their housing does not have enough cooling to protect them, and they can’t safely get themselves to cooling shelters.
These patterns for the most vulnerable fit for the majority of deaths in Oregon during the late June heat wave. Most victims were older, lived alone, and didn’t have air conditioning. But with climate change, the predictions are that temperatures will go higher and heat waves will last longer.
“There’s probably very few people today that are ‘immune’ to the effects of heat-related stress with climate change. All of us can be put in situations where we are susceptible,” Dr. McCauley said.
Dr. Moseson agreed. Many of her patients fit none of these risk categories – she treated people with no health problems in their 20s in her ICU, and the patient she lost would not traditionally have been thought of as high risk. That 50-something patient had no long-standing medical problems, and lived with family in a newly renovated suburban home that had air conditioning. The only problem was that the air conditioner had broken and there had been no rush to fix it based on past experience with Oregon summers.
Preventing heat deaths
Protecting ourselves and our families means monitoring the “simple things.” The first three rules are to make sure we’re drinking plenty of water – this means drinking whether we feel thirsty or not. If we’re not in an air-conditioned place, we’ve got to look for shade. And we need to take regular rest breaks.
Inside a home without air conditioning, placing ice in front of a fan to cool the air can work, but realistically, if you are in a place without air conditioning and the temperatures are approaching 90° F, it’s safest to find another place to stay, if possible.
For those playing sports, there are usually 1-week to 2-week protocols that allow for acclimatization when the season begins – this means starting slowly, without gear, and ramping up activity. Still, parents and coaches should watch advanced weather reports to make sure it’s safe to practice outside.
How we dress can also help us, so light clothing is key. And if we’re able to schedule activities for times when it is cooler, that can also protect us from overheating.
If anyone shows early signs of heat stress, removing clothing, cooling their bodies with cold water, and getting them out of the heat is critical. Any evidence of heatstroke is an emergency, and 911 should be called without delay. The faster the core temperature can be dropped, the better the chances for recovery.
On the level of communities, access to natural air conditioning in the form of healthy tree canopies, and trees at bus stops to provide shade can help a lot. According to Dr. Hoffman, these investments help almost right away. Reimagining our cities to remove the “hot zones” that we have created is another key to protecting ourselves as our climate changes.
Reaching our limits in a changing climate
Already, we are seeing more intense, more frequent, and longer-lasting heat waves throughout the country and across the globe.
Dr. Ebi, a coauthor of a recently released scientific analysis that found that the late June Pacific Northwest heat wave would have been virtually impossible without climate change, herself lived through the scorching temperatures in Seattle. Her work shows that the changing climate is killing us right now.
We are approaching a time where extreme temperatures and humidity will make it almost impossible for people to be outside in many parts of the world. Researchers have found that periods of extreme humid heat have more than doubled since 1979, and some places have already had wet-bulb temperatures at the limits of what scientists think humans can tolerate under ideal conditions, meaning for people in perfect health, completely unclothed, in gale-force winds, performing no activity. Obviously that’s less than ideal for most of us and helps explain why thousands of people die at temperatures much lower than our upper limit.
Dr. Ebi pointed out that the good news is that many local communities with a long history of managing high temperatures have a lot of knowledge to share with regions that are newly dealing with these conditions. This includes how local areas develop early warning and response systems with specific action plans.
But, she cautions, it’s going to take a lot of coordination and a lot of behavior change to stabilize the earth’s climate, understand our weak points, and protect our health.
For Dr. Moseson, this reality has hit home.
“I already spent the year being terrified that I as an ICU doctor was going to be the one who gave my mom COVID. Finally I’m vaccinated, she’s vaccinated. Now I’ve watched someone die because they don’t have AC. And my parents, they’re old-school Oregonians, they don’t have AC.”
A version of this article originally appeared on WebMD.com.
Delta variant could drive herd immunity threshold over 80%
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Increases in new COVID cases among children far outpace vaccinations
New COVID-19 cases in children soared by almost 86% over the course of just 1 week, while the number of 12- to 17-year-old children who have received at least one dose of vaccine rose by 5.4%, according to two separate sources.
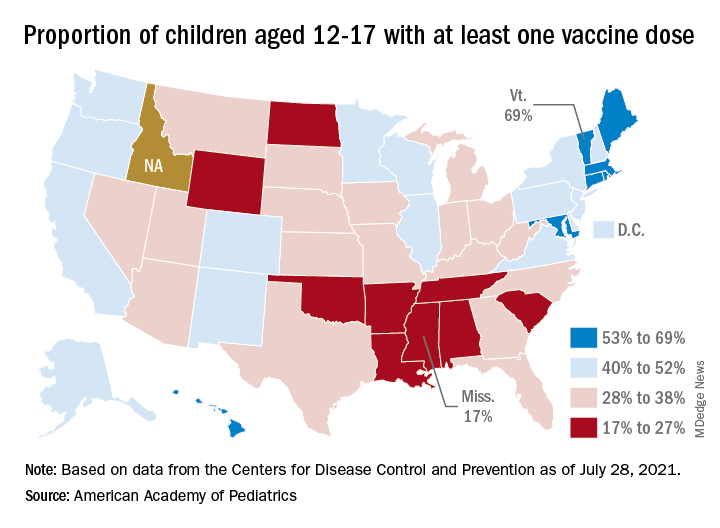
Meanwhile, the increase over the past 2 weeks – from 23,551 new cases for July 16-22 to almost 72,000 – works out to almost 205%, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Children represented 19.0% of the cases reported during the week of July 23-29, and they have made up 14.3% of all cases since the pandemic began, with the total number of cases in children now approaching 4.2 million, the AAP and CHA said in their weekly COVID report. About 22% of the U.S. population is under the age of 18 years.
As of Aug. 2, just over 9.8 million children aged 12-17 years had received at least one dose of the COVID vaccine, which was up by about 500,000, or 5.4%, from a week earlier, based on data from the Centers for Disease Control and Prevention.
Children aged 16-17 have reached a notable milestone on the journey that started with vaccine approval in December: 50.2% have gotten at least one dose and 40.3% are fully vaccinated. Among children aged 12-15 years, the proportion with at least one dose of vaccine is up to 39.5%, compared with 37.1% the previous week, while 29.0% are fully vaccinated (27.8% the week before), the CDC said on its COVID Data Tracker.
The national rates for child vaccination, however, tend to hide the disparities between states. There is a gap between Mississippi (lowest), where just 17% of children aged 12-17 years have gotten at least one dose, and Vermont (highest), which is up to 69%. Vermont also has the highest rate of vaccine completion (60%), while Alabama and Mississippi have the lowest (10%), according to a solo report from the AAP.
New COVID-19 cases in children soared by almost 86% over the course of just 1 week, while the number of 12- to 17-year-old children who have received at least one dose of vaccine rose by 5.4%, according to two separate sources.
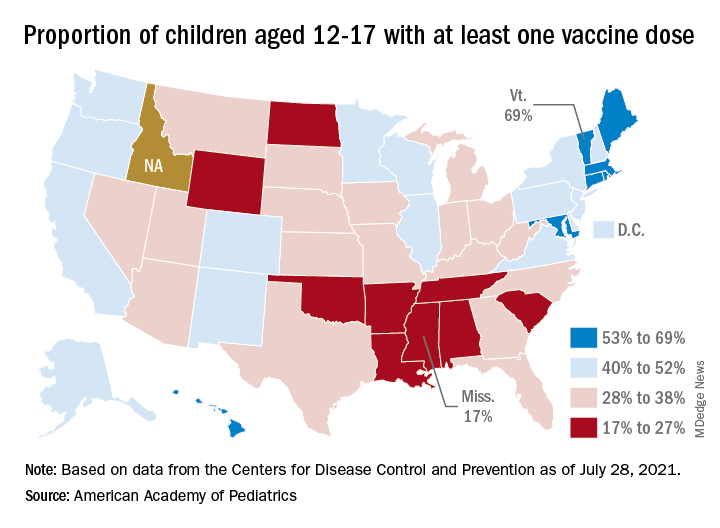
Meanwhile, the increase over the past 2 weeks – from 23,551 new cases for July 16-22 to almost 72,000 – works out to almost 205%, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Children represented 19.0% of the cases reported during the week of July 23-29, and they have made up 14.3% of all cases since the pandemic began, with the total number of cases in children now approaching 4.2 million, the AAP and CHA said in their weekly COVID report. About 22% of the U.S. population is under the age of 18 years.
As of Aug. 2, just over 9.8 million children aged 12-17 years had received at least one dose of the COVID vaccine, which was up by about 500,000, or 5.4%, from a week earlier, based on data from the Centers for Disease Control and Prevention.
Children aged 16-17 have reached a notable milestone on the journey that started with vaccine approval in December: 50.2% have gotten at least one dose and 40.3% are fully vaccinated. Among children aged 12-15 years, the proportion with at least one dose of vaccine is up to 39.5%, compared with 37.1% the previous week, while 29.0% are fully vaccinated (27.8% the week before), the CDC said on its COVID Data Tracker.
The national rates for child vaccination, however, tend to hide the disparities between states. There is a gap between Mississippi (lowest), where just 17% of children aged 12-17 years have gotten at least one dose, and Vermont (highest), which is up to 69%. Vermont also has the highest rate of vaccine completion (60%), while Alabama and Mississippi have the lowest (10%), according to a solo report from the AAP.
New COVID-19 cases in children soared by almost 86% over the course of just 1 week, while the number of 12- to 17-year-old children who have received at least one dose of vaccine rose by 5.4%, according to two separate sources.
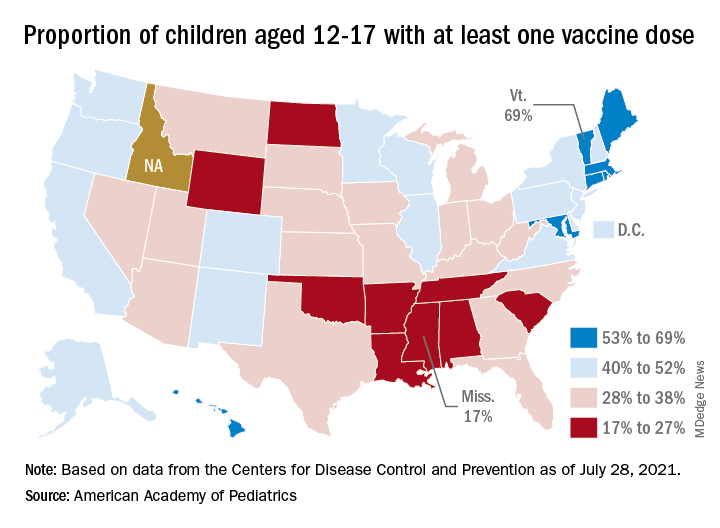
Meanwhile, the increase over the past 2 weeks – from 23,551 new cases for July 16-22 to almost 72,000 – works out to almost 205%, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Children represented 19.0% of the cases reported during the week of July 23-29, and they have made up 14.3% of all cases since the pandemic began, with the total number of cases in children now approaching 4.2 million, the AAP and CHA said in their weekly COVID report. About 22% of the U.S. population is under the age of 18 years.
As of Aug. 2, just over 9.8 million children aged 12-17 years had received at least one dose of the COVID vaccine, which was up by about 500,000, or 5.4%, from a week earlier, based on data from the Centers for Disease Control and Prevention.
Children aged 16-17 have reached a notable milestone on the journey that started with vaccine approval in December: 50.2% have gotten at least one dose and 40.3% are fully vaccinated. Among children aged 12-15 years, the proportion with at least one dose of vaccine is up to 39.5%, compared with 37.1% the previous week, while 29.0% are fully vaccinated (27.8% the week before), the CDC said on its COVID Data Tracker.
The national rates for child vaccination, however, tend to hide the disparities between states. There is a gap between Mississippi (lowest), where just 17% of children aged 12-17 years have gotten at least one dose, and Vermont (highest), which is up to 69%. Vermont also has the highest rate of vaccine completion (60%), while Alabama and Mississippi have the lowest (10%), according to a solo report from the AAP.
ACOG, SMFM urge all pregnant women to get COVID-19 vaccine
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
COVID-19: Delta variant is raising the stakes
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Empathetic conversations with unvaccinated people desperately needed
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.