User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Analysis questions tocilizumab in ventilated COVID patients
A new statistical analysis of an existing meta-analysis reaffirms a finding that hospitalized patients with COVID-19 who are on simple oxygen or noninvasive ventilation can benefit from treatment with the arthritis drug tocilizumab (Actemra) in conjunction with corticosteroids. But the report also casts doubt on the effectiveness of tocilizumab in patients who are on ventilators.
“Clinicians should prescribe steroids and tocilizumab for hospitalized patients needing simple oxygen or noninvasive ventilation,” epidemiologist and study coauthor James (Jay) Brophy, MD, PhD, of McGill University, Montreal, said in an interview. “Further research is required to answer the question of whether tocilizumab is beneficial in patients requiring invasive ventilation, and consideration of participation in further tocilizumab studies seems reasonable.”
The new analysis was published Feb. 28, 2022, in JAMA Network Open.
The initial meta-analysis, published in 2021 in JAMA, was conducted by the WHO Rapid Evidence Appraisal for COVID-19 Therapies Working Group. It analyzed the results of 27 randomized trials that explored the use of interleukin-6 antagonists, including tocilizumab, and found that “28-day all-cause mortality was lower among patients who received IL-6 antagonists, compared with those who received usual care or placebo (summary odds ratio, 0.86). The summary ORs for the association of IL-6 antagonist treatment with 28-day all-cause mortality were 0.78 with concomitant administration of corticosteroids versus 1.09 without administration of corticosteroids.”
For the new report, researchers conducted a Bayesian statistical analysis of 15 studies within the meta-analysis that specifically examined the use of the rheumatoid arthritis drug tocilizumab. “Bayesian analysis allows one to make direct probability statements regarding the exact magnitude and the certainty of any benefit,” Dr. Brophy said. “This provides clinicians with the information they require to make well-informed decisions.”
The analysis estimated that the probability of a “clinically meaningful association” (absolute mortality risk difference, >1%) because of use of tocilizumab was higher than 95% in patients receiving simple oxygen and higher than 90% in those receiving noninvasive ventilation. But the probability was only about 67% higher in those receiving invasive mechanical ventilation.
Also, the researchers estimated that about 72% of future tocilizumab studies in patients on invasive mechanical ventilation would show a benefit.
The new analysis findings don’t add much to existing knowledge, said nephrologist David E. Leaf, MD, MMSc, of Harvard Medical School, Boston, who’s studied tocilizumab in COVID-19.
“The signal seems to be consistent that there is a greater benefit of tocilizumab in less ill patients than those who are more ill – e.g., those who are receiving invasive mechanical ventilation,” Dr. Leaf said in an interview. “This is interesting because in clinical practice the opposite approach is often undertaken, with tocilizumab use only being used in the sickest patients, even though the patients most likely to benefit seem to be those who are less ill.”
Clinically, he said, “hospitalized patients with COVID-19 should receive tocilizumab unless they have a clear contraindication and assuming it can be administered relatively early in their disease course. Earlier administration, before the onset of irreversible organ injury, is likely to have greater benefit.”
Dr. Leaf also noted it’s unknown whether the drug is helpful in several groups – patients presenting later in the course of COVID-19 illness, patients with additional infections, and immunocompromised patients.
It’s also not clear if tocilizumab benefits patients with lower levels of C-reactive protein, Shruti Gupta, MD, MPH, a nephrologist at Brigham and Women’s Hospital in Boston, said in an interview. The RECOVERY trial, for example, limited subjects to those with C-reactive protein of at least 75 mg/L.
Dr. Leaf and Dr. Gupta coauthored a 2021 cohort study analyzing mortality rates in patients with COVID-19 who were treated with tocilizumab versus those who were not.
No study funding was reported. Dr. Brophy, Dr. Leaf, and Dr. Gupta disclosed no relevant financial relationships. One study author reported participating in one of the randomized clinical trials included in the analysis.
A version of this article first appeared on Medscape.com.
A new statistical analysis of an existing meta-analysis reaffirms a finding that hospitalized patients with COVID-19 who are on simple oxygen or noninvasive ventilation can benefit from treatment with the arthritis drug tocilizumab (Actemra) in conjunction with corticosteroids. But the report also casts doubt on the effectiveness of tocilizumab in patients who are on ventilators.
“Clinicians should prescribe steroids and tocilizumab for hospitalized patients needing simple oxygen or noninvasive ventilation,” epidemiologist and study coauthor James (Jay) Brophy, MD, PhD, of McGill University, Montreal, said in an interview. “Further research is required to answer the question of whether tocilizumab is beneficial in patients requiring invasive ventilation, and consideration of participation in further tocilizumab studies seems reasonable.”
The new analysis was published Feb. 28, 2022, in JAMA Network Open.
The initial meta-analysis, published in 2021 in JAMA, was conducted by the WHO Rapid Evidence Appraisal for COVID-19 Therapies Working Group. It analyzed the results of 27 randomized trials that explored the use of interleukin-6 antagonists, including tocilizumab, and found that “28-day all-cause mortality was lower among patients who received IL-6 antagonists, compared with those who received usual care or placebo (summary odds ratio, 0.86). The summary ORs for the association of IL-6 antagonist treatment with 28-day all-cause mortality were 0.78 with concomitant administration of corticosteroids versus 1.09 without administration of corticosteroids.”
For the new report, researchers conducted a Bayesian statistical analysis of 15 studies within the meta-analysis that specifically examined the use of the rheumatoid arthritis drug tocilizumab. “Bayesian analysis allows one to make direct probability statements regarding the exact magnitude and the certainty of any benefit,” Dr. Brophy said. “This provides clinicians with the information they require to make well-informed decisions.”
The analysis estimated that the probability of a “clinically meaningful association” (absolute mortality risk difference, >1%) because of use of tocilizumab was higher than 95% in patients receiving simple oxygen and higher than 90% in those receiving noninvasive ventilation. But the probability was only about 67% higher in those receiving invasive mechanical ventilation.
Also, the researchers estimated that about 72% of future tocilizumab studies in patients on invasive mechanical ventilation would show a benefit.
The new analysis findings don’t add much to existing knowledge, said nephrologist David E. Leaf, MD, MMSc, of Harvard Medical School, Boston, who’s studied tocilizumab in COVID-19.
“The signal seems to be consistent that there is a greater benefit of tocilizumab in less ill patients than those who are more ill – e.g., those who are receiving invasive mechanical ventilation,” Dr. Leaf said in an interview. “This is interesting because in clinical practice the opposite approach is often undertaken, with tocilizumab use only being used in the sickest patients, even though the patients most likely to benefit seem to be those who are less ill.”
Clinically, he said, “hospitalized patients with COVID-19 should receive tocilizumab unless they have a clear contraindication and assuming it can be administered relatively early in their disease course. Earlier administration, before the onset of irreversible organ injury, is likely to have greater benefit.”
Dr. Leaf also noted it’s unknown whether the drug is helpful in several groups – patients presenting later in the course of COVID-19 illness, patients with additional infections, and immunocompromised patients.
It’s also not clear if tocilizumab benefits patients with lower levels of C-reactive protein, Shruti Gupta, MD, MPH, a nephrologist at Brigham and Women’s Hospital in Boston, said in an interview. The RECOVERY trial, for example, limited subjects to those with C-reactive protein of at least 75 mg/L.
Dr. Leaf and Dr. Gupta coauthored a 2021 cohort study analyzing mortality rates in patients with COVID-19 who were treated with tocilizumab versus those who were not.
No study funding was reported. Dr. Brophy, Dr. Leaf, and Dr. Gupta disclosed no relevant financial relationships. One study author reported participating in one of the randomized clinical trials included in the analysis.
A version of this article first appeared on Medscape.com.
A new statistical analysis of an existing meta-analysis reaffirms a finding that hospitalized patients with COVID-19 who are on simple oxygen or noninvasive ventilation can benefit from treatment with the arthritis drug tocilizumab (Actemra) in conjunction with corticosteroids. But the report also casts doubt on the effectiveness of tocilizumab in patients who are on ventilators.
“Clinicians should prescribe steroids and tocilizumab for hospitalized patients needing simple oxygen or noninvasive ventilation,” epidemiologist and study coauthor James (Jay) Brophy, MD, PhD, of McGill University, Montreal, said in an interview. “Further research is required to answer the question of whether tocilizumab is beneficial in patients requiring invasive ventilation, and consideration of participation in further tocilizumab studies seems reasonable.”
The new analysis was published Feb. 28, 2022, in JAMA Network Open.
The initial meta-analysis, published in 2021 in JAMA, was conducted by the WHO Rapid Evidence Appraisal for COVID-19 Therapies Working Group. It analyzed the results of 27 randomized trials that explored the use of interleukin-6 antagonists, including tocilizumab, and found that “28-day all-cause mortality was lower among patients who received IL-6 antagonists, compared with those who received usual care or placebo (summary odds ratio, 0.86). The summary ORs for the association of IL-6 antagonist treatment with 28-day all-cause mortality were 0.78 with concomitant administration of corticosteroids versus 1.09 without administration of corticosteroids.”
For the new report, researchers conducted a Bayesian statistical analysis of 15 studies within the meta-analysis that specifically examined the use of the rheumatoid arthritis drug tocilizumab. “Bayesian analysis allows one to make direct probability statements regarding the exact magnitude and the certainty of any benefit,” Dr. Brophy said. “This provides clinicians with the information they require to make well-informed decisions.”
The analysis estimated that the probability of a “clinically meaningful association” (absolute mortality risk difference, >1%) because of use of tocilizumab was higher than 95% in patients receiving simple oxygen and higher than 90% in those receiving noninvasive ventilation. But the probability was only about 67% higher in those receiving invasive mechanical ventilation.
Also, the researchers estimated that about 72% of future tocilizumab studies in patients on invasive mechanical ventilation would show a benefit.
The new analysis findings don’t add much to existing knowledge, said nephrologist David E. Leaf, MD, MMSc, of Harvard Medical School, Boston, who’s studied tocilizumab in COVID-19.
“The signal seems to be consistent that there is a greater benefit of tocilizumab in less ill patients than those who are more ill – e.g., those who are receiving invasive mechanical ventilation,” Dr. Leaf said in an interview. “This is interesting because in clinical practice the opposite approach is often undertaken, with tocilizumab use only being used in the sickest patients, even though the patients most likely to benefit seem to be those who are less ill.”
Clinically, he said, “hospitalized patients with COVID-19 should receive tocilizumab unless they have a clear contraindication and assuming it can be administered relatively early in their disease course. Earlier administration, before the onset of irreversible organ injury, is likely to have greater benefit.”
Dr. Leaf also noted it’s unknown whether the drug is helpful in several groups – patients presenting later in the course of COVID-19 illness, patients with additional infections, and immunocompromised patients.
It’s also not clear if tocilizumab benefits patients with lower levels of C-reactive protein, Shruti Gupta, MD, MPH, a nephrologist at Brigham and Women’s Hospital in Boston, said in an interview. The RECOVERY trial, for example, limited subjects to those with C-reactive protein of at least 75 mg/L.
Dr. Leaf and Dr. Gupta coauthored a 2021 cohort study analyzing mortality rates in patients with COVID-19 who were treated with tocilizumab versus those who were not.
No study funding was reported. Dr. Brophy, Dr. Leaf, and Dr. Gupta disclosed no relevant financial relationships. One study author reported participating in one of the randomized clinical trials included in the analysis.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Proper steps for physicians to follow if they find themselves under investigation
Physician clients will find themselves in difficult legal situations from time to time. Sometimes it’s an investigation for Medicare fraud or other illegal conduct. Other times it’s a review related to Drug Enforcement Administration or licensure compliance. More commonly, physicians are involved in employer inquiries into workplace misconduct.
but how they choose to deal with the issue can have significant consequences.
In my opinion, physicians should have a relationship with a health care lawyer or firm in place before any investigation occurs. Whether they are being investigated for a license or medical staff issue, Medicare fraud, or contract issue, it’s important to know where to go for help quickly. Even if the physician does not retain a lawyer in advance, having the name of a qualified person who can be called for a variety of health care issues is already a step in the right direction.
More important than having a knowledgeable lawyer is actually contacting that lawyer. Some physicians will sit and chat with the Federal Bureau of Investigation or other investigators for hours, only to call me after the visitors leave. I have other clients who handle important medical staff hearings, discipline meetings, and license investigations on their own without consulting counsel first. In all of these situations, it can be too late to help a physician once their case has progressed too far down the road.
Employment issues arising in the workplace setting are the most common and troubling. Physicians will – without a second thought – attend a human resources–called or other meeting without thinking through the reason for the meeting, whether they are prepared or not, and without considering whether counsel could be helpful. Sometimes in the moment, there may be no choice, but most meetings are scheduled in advance with ample time for consultation and planning.
Many issues that arise in the workplace setting are troubling because they can be easily avoided. The No. 1 piece of advice which I offer to young physician clients as they enter the workplace is: Remember that nobody in the workplace is your friend. Every word that is said, text that is sent, gesture that is made, can put you at risk. You must assume that all conversations and messages will be shared with others. Joking around in the operating room about sexual escapades, sending texts with flirtatious comments, making comments that can be construed as racist or homophobic, or raising your voice in a moment of frustration are all real examples of situations where physicians ended up disciplined and terminated. Are these innocent comments or ones the doctor thought they could get away with among “friends?” From a human resources perspective, there is little tolerance for such conduct, regardless of the doctor’s intent.
There are also situations in the workplace that are more troubling. Many times a physician is accused of noncompliance with a contract or a policy, when in fact the accuser is retaliating or engaging in efforts to discredit a doctor. I have seen this happen where minority physicians complain about how they are treated and are suddenly investigated for a performance issue. I have had female physicians criticize a business decision at a committee meeting, only to receive a formal notice that their “negative attitude” violated a policy.
In these situations, talking with counsel before a meeting with the employer representative is recommended and can impact the trajectory of a physician’s career. Physicians cannot and should not handle such events on their own.
If a physician is forced or chooses to attend a meeting with an investigator or other party without counsel, there are some steps to consider (subject to the type of meeting and the specific circumstances).
- Listen more than you talk. Make sure you know the name of everyone who is present and their role within the organization.
- If you have previously provided any written or oral statements, or have written correspondence related to the issues at hand, review all materials in advance. If there is anything you think needs to be corrected or added, let the interviewer know that at the outset.
- Be familiar with your own employment agreement/policies and the terms that may be relevant to the discussion or meeting.
- Be calm, honest, and forthcoming in response to the questions, and don’t embellish or exaggerate.
- Avoid personal attacks on anyone. This generally serves to weaken an argument and credibility.
- Be prepared to explain your allegations or defense, and when you do so, keep in mind that the interviewer may not know the history, background, or details of any of the issues.
- If the reason for the situation relates to race or national origin, age, gender, sexual orientation, disability, or other protected category, don’t hesitate to say so.
- Answer the question you’re asked, but if you feel that the interviewer needs more information or is not understanding what you’ve said, feel free to explain. Be forthcoming, but don’t dominate the conversation.
- If they ask whether you have counsel, be honest, but decline to provide them any information about what you discussed with counsel, as those conversations are privileged.
- If the interviewer asks to record the conversation, you can agree, but ask to be provided a copy of the recording.
- Know your rights in advance. If the subject of the meeting is governed by bylaws or policies, for example, you may have the right to bring an attorney or adviser to the meeting, receive advance notice of who will be attending the meeting and the subject matter, and avail yourself of specific procedures or appeal rights of any discipline or decisions decided during the meeting.
There are many circumstances that can lead to a physician being under investigation or interrogation. In every single circumstance, it is ideal to seek legal counsel immediately. Whether the physician has actually engaged in wrongful conduct or not, without proper handling a physician’s career can be permanently, and sometimes irrevocably, affected.
Ms. Adler is a shareholder and health law practice group manager for Chicago-based law firm Roetzel, a member of the Illinois Association of Healthcare Attorneys, and a current advisory board member at DePaul College of Law Health Law Institute. She disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physician clients will find themselves in difficult legal situations from time to time. Sometimes it’s an investigation for Medicare fraud or other illegal conduct. Other times it’s a review related to Drug Enforcement Administration or licensure compliance. More commonly, physicians are involved in employer inquiries into workplace misconduct.
but how they choose to deal with the issue can have significant consequences.
In my opinion, physicians should have a relationship with a health care lawyer or firm in place before any investigation occurs. Whether they are being investigated for a license or medical staff issue, Medicare fraud, or contract issue, it’s important to know where to go for help quickly. Even if the physician does not retain a lawyer in advance, having the name of a qualified person who can be called for a variety of health care issues is already a step in the right direction.
More important than having a knowledgeable lawyer is actually contacting that lawyer. Some physicians will sit and chat with the Federal Bureau of Investigation or other investigators for hours, only to call me after the visitors leave. I have other clients who handle important medical staff hearings, discipline meetings, and license investigations on their own without consulting counsel first. In all of these situations, it can be too late to help a physician once their case has progressed too far down the road.
Employment issues arising in the workplace setting are the most common and troubling. Physicians will – without a second thought – attend a human resources–called or other meeting without thinking through the reason for the meeting, whether they are prepared or not, and without considering whether counsel could be helpful. Sometimes in the moment, there may be no choice, but most meetings are scheduled in advance with ample time for consultation and planning.
Many issues that arise in the workplace setting are troubling because they can be easily avoided. The No. 1 piece of advice which I offer to young physician clients as they enter the workplace is: Remember that nobody in the workplace is your friend. Every word that is said, text that is sent, gesture that is made, can put you at risk. You must assume that all conversations and messages will be shared with others. Joking around in the operating room about sexual escapades, sending texts with flirtatious comments, making comments that can be construed as racist or homophobic, or raising your voice in a moment of frustration are all real examples of situations where physicians ended up disciplined and terminated. Are these innocent comments or ones the doctor thought they could get away with among “friends?” From a human resources perspective, there is little tolerance for such conduct, regardless of the doctor’s intent.
There are also situations in the workplace that are more troubling. Many times a physician is accused of noncompliance with a contract or a policy, when in fact the accuser is retaliating or engaging in efforts to discredit a doctor. I have seen this happen where minority physicians complain about how they are treated and are suddenly investigated for a performance issue. I have had female physicians criticize a business decision at a committee meeting, only to receive a formal notice that their “negative attitude” violated a policy.
In these situations, talking with counsel before a meeting with the employer representative is recommended and can impact the trajectory of a physician’s career. Physicians cannot and should not handle such events on their own.
If a physician is forced or chooses to attend a meeting with an investigator or other party without counsel, there are some steps to consider (subject to the type of meeting and the specific circumstances).
- Listen more than you talk. Make sure you know the name of everyone who is present and their role within the organization.
- If you have previously provided any written or oral statements, or have written correspondence related to the issues at hand, review all materials in advance. If there is anything you think needs to be corrected or added, let the interviewer know that at the outset.
- Be familiar with your own employment agreement/policies and the terms that may be relevant to the discussion or meeting.
- Be calm, honest, and forthcoming in response to the questions, and don’t embellish or exaggerate.
- Avoid personal attacks on anyone. This generally serves to weaken an argument and credibility.
- Be prepared to explain your allegations or defense, and when you do so, keep in mind that the interviewer may not know the history, background, or details of any of the issues.
- If the reason for the situation relates to race or national origin, age, gender, sexual orientation, disability, or other protected category, don’t hesitate to say so.
- Answer the question you’re asked, but if you feel that the interviewer needs more information or is not understanding what you’ve said, feel free to explain. Be forthcoming, but don’t dominate the conversation.
- If they ask whether you have counsel, be honest, but decline to provide them any information about what you discussed with counsel, as those conversations are privileged.
- If the interviewer asks to record the conversation, you can agree, but ask to be provided a copy of the recording.
- Know your rights in advance. If the subject of the meeting is governed by bylaws or policies, for example, you may have the right to bring an attorney or adviser to the meeting, receive advance notice of who will be attending the meeting and the subject matter, and avail yourself of specific procedures or appeal rights of any discipline or decisions decided during the meeting.
There are many circumstances that can lead to a physician being under investigation or interrogation. In every single circumstance, it is ideal to seek legal counsel immediately. Whether the physician has actually engaged in wrongful conduct or not, without proper handling a physician’s career can be permanently, and sometimes irrevocably, affected.
Ms. Adler is a shareholder and health law practice group manager for Chicago-based law firm Roetzel, a member of the Illinois Association of Healthcare Attorneys, and a current advisory board member at DePaul College of Law Health Law Institute. She disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physician clients will find themselves in difficult legal situations from time to time. Sometimes it’s an investigation for Medicare fraud or other illegal conduct. Other times it’s a review related to Drug Enforcement Administration or licensure compliance. More commonly, physicians are involved in employer inquiries into workplace misconduct.
but how they choose to deal with the issue can have significant consequences.
In my opinion, physicians should have a relationship with a health care lawyer or firm in place before any investigation occurs. Whether they are being investigated for a license or medical staff issue, Medicare fraud, or contract issue, it’s important to know where to go for help quickly. Even if the physician does not retain a lawyer in advance, having the name of a qualified person who can be called for a variety of health care issues is already a step in the right direction.
More important than having a knowledgeable lawyer is actually contacting that lawyer. Some physicians will sit and chat with the Federal Bureau of Investigation or other investigators for hours, only to call me after the visitors leave. I have other clients who handle important medical staff hearings, discipline meetings, and license investigations on their own without consulting counsel first. In all of these situations, it can be too late to help a physician once their case has progressed too far down the road.
Employment issues arising in the workplace setting are the most common and troubling. Physicians will – without a second thought – attend a human resources–called or other meeting without thinking through the reason for the meeting, whether they are prepared or not, and without considering whether counsel could be helpful. Sometimes in the moment, there may be no choice, but most meetings are scheduled in advance with ample time for consultation and planning.
Many issues that arise in the workplace setting are troubling because they can be easily avoided. The No. 1 piece of advice which I offer to young physician clients as they enter the workplace is: Remember that nobody in the workplace is your friend. Every word that is said, text that is sent, gesture that is made, can put you at risk. You must assume that all conversations and messages will be shared with others. Joking around in the operating room about sexual escapades, sending texts with flirtatious comments, making comments that can be construed as racist or homophobic, or raising your voice in a moment of frustration are all real examples of situations where physicians ended up disciplined and terminated. Are these innocent comments or ones the doctor thought they could get away with among “friends?” From a human resources perspective, there is little tolerance for such conduct, regardless of the doctor’s intent.
There are also situations in the workplace that are more troubling. Many times a physician is accused of noncompliance with a contract or a policy, when in fact the accuser is retaliating or engaging in efforts to discredit a doctor. I have seen this happen where minority physicians complain about how they are treated and are suddenly investigated for a performance issue. I have had female physicians criticize a business decision at a committee meeting, only to receive a formal notice that their “negative attitude” violated a policy.
In these situations, talking with counsel before a meeting with the employer representative is recommended and can impact the trajectory of a physician’s career. Physicians cannot and should not handle such events on their own.
If a physician is forced or chooses to attend a meeting with an investigator or other party without counsel, there are some steps to consider (subject to the type of meeting and the specific circumstances).
- Listen more than you talk. Make sure you know the name of everyone who is present and their role within the organization.
- If you have previously provided any written or oral statements, or have written correspondence related to the issues at hand, review all materials in advance. If there is anything you think needs to be corrected or added, let the interviewer know that at the outset.
- Be familiar with your own employment agreement/policies and the terms that may be relevant to the discussion or meeting.
- Be calm, honest, and forthcoming in response to the questions, and don’t embellish or exaggerate.
- Avoid personal attacks on anyone. This generally serves to weaken an argument and credibility.
- Be prepared to explain your allegations or defense, and when you do so, keep in mind that the interviewer may not know the history, background, or details of any of the issues.
- If the reason for the situation relates to race or national origin, age, gender, sexual orientation, disability, or other protected category, don’t hesitate to say so.
- Answer the question you’re asked, but if you feel that the interviewer needs more information or is not understanding what you’ve said, feel free to explain. Be forthcoming, but don’t dominate the conversation.
- If they ask whether you have counsel, be honest, but decline to provide them any information about what you discussed with counsel, as those conversations are privileged.
- If the interviewer asks to record the conversation, you can agree, but ask to be provided a copy of the recording.
- Know your rights in advance. If the subject of the meeting is governed by bylaws or policies, for example, you may have the right to bring an attorney or adviser to the meeting, receive advance notice of who will be attending the meeting and the subject matter, and avail yourself of specific procedures or appeal rights of any discipline or decisions decided during the meeting.
There are many circumstances that can lead to a physician being under investigation or interrogation. In every single circumstance, it is ideal to seek legal counsel immediately. Whether the physician has actually engaged in wrongful conduct or not, without proper handling a physician’s career can be permanently, and sometimes irrevocably, affected.
Ms. Adler is a shareholder and health law practice group manager for Chicago-based law firm Roetzel, a member of the Illinois Association of Healthcare Attorneys, and a current advisory board member at DePaul College of Law Health Law Institute. She disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Self-care tips for clinicians as COVID-19 lingers
LAS VEGAS – according to Jon A. Levenson, MD.
“There are those who will need mental health treatment, so creating an easy way to reach out for help and facilitate linkage with care is critically important,” Dr. Levenson, associate professor of psychiatry at Columbia University Irving Medical Center, New York, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “The vast majority of our workforce will thrive with proper support. But what can each of us do to take care of ourselves?”
Step one is to recognize common stress reactions as well as signs of distress. He offered the oxygen mask metaphor, the idea that before we can take care of and support anyone else, we must first take care of ourselves. “When people are stressed, they don’t always think about the oxygen mask metaphor,” Dr. Levenson said. Step two is to practice and model self-care by adopting principles often discussed in acceptance and commitment therapy: to focus on what you can control, not on what you can’t control.
“We can’t control the amount of toilet paper at the grocery store, how long the pandemic will last, or how others have reacted,” Dr. Levenson said. “We also can’t control other people’s motives, predict what will happen, or the actions of others, including whether they will follow social distancing guidelines or not.”
How about what we can control? One is a positive attitude, “which can sustain people during times of intense stress,” he said. “Other things that we can do include turn off the news and find fun and enriching activities to do at home, whether it be playing a game with family or reaching out to friends through an iPad or a smartphone. You can also follow [Centers for Disease Control and Prevention] recommendations, control your own social distancing, and limit social media activity, which can be stressful. We can also control our kindness and grace.” He added that resilience does not mean “snapping back” to how you were before the pandemic, but rather “learning to integrate the adverse experiences into who you are and growing with them, which is sometimes known as posttraumatic growth.”
Dr. Levenson encouraged health care workers to use their coping resources, connect to others, and cultivate their values and purpose in life as they navigate these challenging times. “You also want to promote realistic optimism; find a way to stay positive,” he said. “We emphasize to our staff that while you won’t forget this time, focus on what you can control – your positive relationships – and remind yourself of your values and sources of gratitude. Figure out, and reflect on, what you care about, and then care about it. Remind yourself in a deliberate, purposeful way what anchors you to your job, which in the health care setting tends to be a desire to care for others, to assist those in need, and to work in teams. We also encourage staff to refrain from judgment. Guilt is a normal and near-universal response to this stressor, but there are many ways to contribute without a judgmental or guilty tone.”
Other tips for self-support are to remind yourself that it is not selfish to take breaks. “The needs of your patients are not more important than your own needs,” Dr. Levenson said. “Working nonstop can put you at higher risk for stress, exhaustion, and illness. You may need to give yourself more time to step back and recover from workplace challenges or extended coverage for peers; this is important. We remind our staff that your work may feel more emotionally draining than usual because everything is more intense overall during the COVID-19 pandemic. This reminder helps staff normalize what they already may be experiencing, and in turn, to further support each other.”
Soothing activities to relieve stress include meditation, prayer, deep and slow breathing, relaxation exercises, yoga, mindfulness, stretching, staying hydrated, eating healthfully, exercise, and getting sufficient sleep. Other stress management tips include avoiding excessive alcohol intake, reaching out to others, asking for assistance, and delegating when possible. “We want to promote psychological flexibility: the ability to stay in contact with the present moment,” he said. “We encourage our peers to be aware of unpleasant thoughts and feelings, and to try to redirect negative thought patterns to a proactive problem-solving approach; this includes choosing one’s behaviors based on the situation and personal values.”
Dr. Levenson reported having no disclosures related to his presentation.
LAS VEGAS – according to Jon A. Levenson, MD.
“There are those who will need mental health treatment, so creating an easy way to reach out for help and facilitate linkage with care is critically important,” Dr. Levenson, associate professor of psychiatry at Columbia University Irving Medical Center, New York, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “The vast majority of our workforce will thrive with proper support. But what can each of us do to take care of ourselves?”
Step one is to recognize common stress reactions as well as signs of distress. He offered the oxygen mask metaphor, the idea that before we can take care of and support anyone else, we must first take care of ourselves. “When people are stressed, they don’t always think about the oxygen mask metaphor,” Dr. Levenson said. Step two is to practice and model self-care by adopting principles often discussed in acceptance and commitment therapy: to focus on what you can control, not on what you can’t control.
“We can’t control the amount of toilet paper at the grocery store, how long the pandemic will last, or how others have reacted,” Dr. Levenson said. “We also can’t control other people’s motives, predict what will happen, or the actions of others, including whether they will follow social distancing guidelines or not.”
How about what we can control? One is a positive attitude, “which can sustain people during times of intense stress,” he said. “Other things that we can do include turn off the news and find fun and enriching activities to do at home, whether it be playing a game with family or reaching out to friends through an iPad or a smartphone. You can also follow [Centers for Disease Control and Prevention] recommendations, control your own social distancing, and limit social media activity, which can be stressful. We can also control our kindness and grace.” He added that resilience does not mean “snapping back” to how you were before the pandemic, but rather “learning to integrate the adverse experiences into who you are and growing with them, which is sometimes known as posttraumatic growth.”
Dr. Levenson encouraged health care workers to use their coping resources, connect to others, and cultivate their values and purpose in life as they navigate these challenging times. “You also want to promote realistic optimism; find a way to stay positive,” he said. “We emphasize to our staff that while you won’t forget this time, focus on what you can control – your positive relationships – and remind yourself of your values and sources of gratitude. Figure out, and reflect on, what you care about, and then care about it. Remind yourself in a deliberate, purposeful way what anchors you to your job, which in the health care setting tends to be a desire to care for others, to assist those in need, and to work in teams. We also encourage staff to refrain from judgment. Guilt is a normal and near-universal response to this stressor, but there are many ways to contribute without a judgmental or guilty tone.”
Other tips for self-support are to remind yourself that it is not selfish to take breaks. “The needs of your patients are not more important than your own needs,” Dr. Levenson said. “Working nonstop can put you at higher risk for stress, exhaustion, and illness. You may need to give yourself more time to step back and recover from workplace challenges or extended coverage for peers; this is important. We remind our staff that your work may feel more emotionally draining than usual because everything is more intense overall during the COVID-19 pandemic. This reminder helps staff normalize what they already may be experiencing, and in turn, to further support each other.”
Soothing activities to relieve stress include meditation, prayer, deep and slow breathing, relaxation exercises, yoga, mindfulness, stretching, staying hydrated, eating healthfully, exercise, and getting sufficient sleep. Other stress management tips include avoiding excessive alcohol intake, reaching out to others, asking for assistance, and delegating when possible. “We want to promote psychological flexibility: the ability to stay in contact with the present moment,” he said. “We encourage our peers to be aware of unpleasant thoughts and feelings, and to try to redirect negative thought patterns to a proactive problem-solving approach; this includes choosing one’s behaviors based on the situation and personal values.”
Dr. Levenson reported having no disclosures related to his presentation.
LAS VEGAS – according to Jon A. Levenson, MD.
“There are those who will need mental health treatment, so creating an easy way to reach out for help and facilitate linkage with care is critically important,” Dr. Levenson, associate professor of psychiatry at Columbia University Irving Medical Center, New York, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “The vast majority of our workforce will thrive with proper support. But what can each of us do to take care of ourselves?”
Step one is to recognize common stress reactions as well as signs of distress. He offered the oxygen mask metaphor, the idea that before we can take care of and support anyone else, we must first take care of ourselves. “When people are stressed, they don’t always think about the oxygen mask metaphor,” Dr. Levenson said. Step two is to practice and model self-care by adopting principles often discussed in acceptance and commitment therapy: to focus on what you can control, not on what you can’t control.
“We can’t control the amount of toilet paper at the grocery store, how long the pandemic will last, or how others have reacted,” Dr. Levenson said. “We also can’t control other people’s motives, predict what will happen, or the actions of others, including whether they will follow social distancing guidelines or not.”
How about what we can control? One is a positive attitude, “which can sustain people during times of intense stress,” he said. “Other things that we can do include turn off the news and find fun and enriching activities to do at home, whether it be playing a game with family or reaching out to friends through an iPad or a smartphone. You can also follow [Centers for Disease Control and Prevention] recommendations, control your own social distancing, and limit social media activity, which can be stressful. We can also control our kindness and grace.” He added that resilience does not mean “snapping back” to how you were before the pandemic, but rather “learning to integrate the adverse experiences into who you are and growing with them, which is sometimes known as posttraumatic growth.”
Dr. Levenson encouraged health care workers to use their coping resources, connect to others, and cultivate their values and purpose in life as they navigate these challenging times. “You also want to promote realistic optimism; find a way to stay positive,” he said. “We emphasize to our staff that while you won’t forget this time, focus on what you can control – your positive relationships – and remind yourself of your values and sources of gratitude. Figure out, and reflect on, what you care about, and then care about it. Remind yourself in a deliberate, purposeful way what anchors you to your job, which in the health care setting tends to be a desire to care for others, to assist those in need, and to work in teams. We also encourage staff to refrain from judgment. Guilt is a normal and near-universal response to this stressor, but there are many ways to contribute without a judgmental or guilty tone.”
Other tips for self-support are to remind yourself that it is not selfish to take breaks. “The needs of your patients are not more important than your own needs,” Dr. Levenson said. “Working nonstop can put you at higher risk for stress, exhaustion, and illness. You may need to give yourself more time to step back and recover from workplace challenges or extended coverage for peers; this is important. We remind our staff that your work may feel more emotionally draining than usual because everything is more intense overall during the COVID-19 pandemic. This reminder helps staff normalize what they already may be experiencing, and in turn, to further support each other.”
Soothing activities to relieve stress include meditation, prayer, deep and slow breathing, relaxation exercises, yoga, mindfulness, stretching, staying hydrated, eating healthfully, exercise, and getting sufficient sleep. Other stress management tips include avoiding excessive alcohol intake, reaching out to others, asking for assistance, and delegating when possible. “We want to promote psychological flexibility: the ability to stay in contact with the present moment,” he said. “We encourage our peers to be aware of unpleasant thoughts and feelings, and to try to redirect negative thought patterns to a proactive problem-solving approach; this includes choosing one’s behaviors based on the situation and personal values.”
Dr. Levenson reported having no disclosures related to his presentation.
AT NPA 2022
Tastier chocolate may be healthier chocolate
Chocolate: Now part of a well-balanced diet
Asking if someone loves chocolate is like asking if they love breathing. It’s really not a question that needs to be asked. The thing with chocolate, however, is that most people who love chocolate actually love sugar, since your typical milk chocolate contains only about 30% cacao. The rest, of course, is sugar.
Now, dark chocolate is actually kind of good for you since it contains beneficial flavonoids and less sugar. But that healthiness comes at a cost: Dark chocolate is quite bitter, and gets more so as the cacao content rises, to the point where 100% cacao chocolate is very nearly inedible. That’s the chocolate conundrum, the healthier it is, the worse it tastes. But what if there’s another way? What if you can have tasty chocolate that’s good for you?
That’s the question a group of researchers from Penn State University dared to ask. The secret, they discovered, is to subject the cacao beans to extra-intense roasting. We’re not sure how screaming insults at a bunch of beans will help, but if science says so ... YOU USELESS LUMP OF BARELY EDIBLE FOOD! HOW DARE YOU EXIST!
Oh, not that kind of roasting. Oops.
For their study, the researchers made 27 unsweetened chocolates, prepared using various cacao bean roasting times and temperatures, and served them to volunteers. Those volunteers reported that chocolates made with cacao beans roasted more intensely (such as 20 minutes at 340° F, 80 min at 275° F, and 54 min at 304° F) were far more acceptable than were chocolates prepared with raw or lightly roasted cacao beans.
The implications of healthy yet tasty chocolate are obvious: Master the chocolate and you’ll make millions. Imagine a future where parents say to their kids: “Don’t forget to eat your chocolate.” So, we’re off to do some cooking. Don’t want Hershey to make all the money off of this revelation.
The villain hiding in dairy for some MS patients
For some of us, lactose can be a real heartbreaker when it comes to dairy consumption, but for people with multiple sclerosis (MS) there’s another villain they may also have to face that can make their symptoms worse.
Physicians at the Institute of Anatomy at University Hospital Bonn (Germany) were getting so many complaints from patients with MS about how much worse they felt about after having cheese, yogurt, and milk that they decided to get to the bottom of it. The culprit, it seems, is casein, a protein specifically found in cow’s milk.
The researchers injected mice with various proteins found in cow’s milk and found perforated myelin sheaths in those given casein. In MS, the patient’s own immune system destroys that sheath, which leads to paresthesia, vision problems, and movement disorders.
“The body’s defenses actually attack the casein, but in the process they also destroy proteins involved in the formation of myelin, “ said Rittika Chunder, a postdoctoral fellow at the University of Bonn. How? Apparently it’s all a big misunderstanding.
While looking at molecules needed for myelin production, the researchers came across MAG, which is very similar to casein, which is a problem when patients with MS are allergic to casein. After they have dairy products, the B-cell squad gets called in to clean up the evil twin, casein, but can’t differentiate it from the good twin, MAG, so it all gets a wash and the myelin sheath suffers.
Since this happens only to patients with MS who have a casein allergy, the researchers advise them to stay away from milk, yogurt, or cottage cheese while they work on a self-test to check if patients carry the antibodies.
A small price to pay, perhaps, to stop a villainous evil twin.
You would even say it glows
If you’re anything like us – and we think you are since you’re reading this – you’ve been asking yourself: Are there any common medications in my house that will make good radiation sensors?
Not that anyone needs to worry about excess radiation or anything. Far from it. We were just wondering.
It just so happens that Anna Mrozik and Paweł Bilski, both of the Institute of Nuclear Physics Polish Academy of Sciences (IFJ PAN) in Kraków, Poland, were wondering the same thing: “During an uncontrolled release of radiation, it is highly unlikely that members of the public will be equipped with personal radiation dose monitors.”
People would need to use something they had lying around the house. A smartphone would work, the investigators explained in a statement from the IFJ PAN, but the process of converting one to radiation-sensor duty, which involves dismantling it and breaking the display glass, “is laborious and time-consuming [and] the destruction of a valuable and useful device does not seem to be the optimal solution.”
Naturally, they turned to drugs. The key, in this case, is optically stimulated luminescence. They needed to find materials that would glow with greater intensity as the radiation dose increased. Turns out that ibuprofen- and paracetamol-based painkillers fit the bill quite nicely, although aspirin also works.
It’s not known exactly which substance is causing the luminescence, but rest assured, the “physicists from the IFJ PAN intend to identify it.”
This is why you don’t interrupt someone using headphones
There’s nothing like taking a nice relaxing walk with your headphones. Whether you’re listening to a podcast or a song or talking on the phone, it’s an escape from reality that makes you feel like you’re completely in tune with what you’re listening to.
According to a new study, headphones, as opposed to speakers, make people feel more connected to what they are listening to. Data collected from more than 4,000 people showed that listening with headphones makes more of an impact than listening to speakers.
“Headphones produce a phenomenon called in-head localization, which makes the speaker sound as if they’re inside your head,” study coauthor On Amir of the University of California, San Diego, said in a statement. Because of this, people feel like the speakers are close to them and there’s more of a sense of empathy for the speakers and the listener is more likely to be swayed toward the ideas of the speaker.
These findings could lead to more efficient training programs, online work, and advertising, the investigators suggested.
We now finally understand why people get so mad when they have to take out their headphones to answer or talk to us. We ruined a satisfying moment going on in their brains.
Chocolate: Now part of a well-balanced diet
Asking if someone loves chocolate is like asking if they love breathing. It’s really not a question that needs to be asked. The thing with chocolate, however, is that most people who love chocolate actually love sugar, since your typical milk chocolate contains only about 30% cacao. The rest, of course, is sugar.
Now, dark chocolate is actually kind of good for you since it contains beneficial flavonoids and less sugar. But that healthiness comes at a cost: Dark chocolate is quite bitter, and gets more so as the cacao content rises, to the point where 100% cacao chocolate is very nearly inedible. That’s the chocolate conundrum, the healthier it is, the worse it tastes. But what if there’s another way? What if you can have tasty chocolate that’s good for you?
That’s the question a group of researchers from Penn State University dared to ask. The secret, they discovered, is to subject the cacao beans to extra-intense roasting. We’re not sure how screaming insults at a bunch of beans will help, but if science says so ... YOU USELESS LUMP OF BARELY EDIBLE FOOD! HOW DARE YOU EXIST!
Oh, not that kind of roasting. Oops.
For their study, the researchers made 27 unsweetened chocolates, prepared using various cacao bean roasting times and temperatures, and served them to volunteers. Those volunteers reported that chocolates made with cacao beans roasted more intensely (such as 20 minutes at 340° F, 80 min at 275° F, and 54 min at 304° F) were far more acceptable than were chocolates prepared with raw or lightly roasted cacao beans.
The implications of healthy yet tasty chocolate are obvious: Master the chocolate and you’ll make millions. Imagine a future where parents say to their kids: “Don’t forget to eat your chocolate.” So, we’re off to do some cooking. Don’t want Hershey to make all the money off of this revelation.
The villain hiding in dairy for some MS patients
For some of us, lactose can be a real heartbreaker when it comes to dairy consumption, but for people with multiple sclerosis (MS) there’s another villain they may also have to face that can make their symptoms worse.
Physicians at the Institute of Anatomy at University Hospital Bonn (Germany) were getting so many complaints from patients with MS about how much worse they felt about after having cheese, yogurt, and milk that they decided to get to the bottom of it. The culprit, it seems, is casein, a protein specifically found in cow’s milk.
The researchers injected mice with various proteins found in cow’s milk and found perforated myelin sheaths in those given casein. In MS, the patient’s own immune system destroys that sheath, which leads to paresthesia, vision problems, and movement disorders.
“The body’s defenses actually attack the casein, but in the process they also destroy proteins involved in the formation of myelin, “ said Rittika Chunder, a postdoctoral fellow at the University of Bonn. How? Apparently it’s all a big misunderstanding.
While looking at molecules needed for myelin production, the researchers came across MAG, which is very similar to casein, which is a problem when patients with MS are allergic to casein. After they have dairy products, the B-cell squad gets called in to clean up the evil twin, casein, but can’t differentiate it from the good twin, MAG, so it all gets a wash and the myelin sheath suffers.
Since this happens only to patients with MS who have a casein allergy, the researchers advise them to stay away from milk, yogurt, or cottage cheese while they work on a self-test to check if patients carry the antibodies.
A small price to pay, perhaps, to stop a villainous evil twin.
You would even say it glows
If you’re anything like us – and we think you are since you’re reading this – you’ve been asking yourself: Are there any common medications in my house that will make good radiation sensors?
Not that anyone needs to worry about excess radiation or anything. Far from it. We were just wondering.
It just so happens that Anna Mrozik and Paweł Bilski, both of the Institute of Nuclear Physics Polish Academy of Sciences (IFJ PAN) in Kraków, Poland, were wondering the same thing: “During an uncontrolled release of radiation, it is highly unlikely that members of the public will be equipped with personal radiation dose monitors.”
People would need to use something they had lying around the house. A smartphone would work, the investigators explained in a statement from the IFJ PAN, but the process of converting one to radiation-sensor duty, which involves dismantling it and breaking the display glass, “is laborious and time-consuming [and] the destruction of a valuable and useful device does not seem to be the optimal solution.”
Naturally, they turned to drugs. The key, in this case, is optically stimulated luminescence. They needed to find materials that would glow with greater intensity as the radiation dose increased. Turns out that ibuprofen- and paracetamol-based painkillers fit the bill quite nicely, although aspirin also works.
It’s not known exactly which substance is causing the luminescence, but rest assured, the “physicists from the IFJ PAN intend to identify it.”
This is why you don’t interrupt someone using headphones
There’s nothing like taking a nice relaxing walk with your headphones. Whether you’re listening to a podcast or a song or talking on the phone, it’s an escape from reality that makes you feel like you’re completely in tune with what you’re listening to.
According to a new study, headphones, as opposed to speakers, make people feel more connected to what they are listening to. Data collected from more than 4,000 people showed that listening with headphones makes more of an impact than listening to speakers.
“Headphones produce a phenomenon called in-head localization, which makes the speaker sound as if they’re inside your head,” study coauthor On Amir of the University of California, San Diego, said in a statement. Because of this, people feel like the speakers are close to them and there’s more of a sense of empathy for the speakers and the listener is more likely to be swayed toward the ideas of the speaker.
These findings could lead to more efficient training programs, online work, and advertising, the investigators suggested.
We now finally understand why people get so mad when they have to take out their headphones to answer or talk to us. We ruined a satisfying moment going on in their brains.
Chocolate: Now part of a well-balanced diet
Asking if someone loves chocolate is like asking if they love breathing. It’s really not a question that needs to be asked. The thing with chocolate, however, is that most people who love chocolate actually love sugar, since your typical milk chocolate contains only about 30% cacao. The rest, of course, is sugar.
Now, dark chocolate is actually kind of good for you since it contains beneficial flavonoids and less sugar. But that healthiness comes at a cost: Dark chocolate is quite bitter, and gets more so as the cacao content rises, to the point where 100% cacao chocolate is very nearly inedible. That’s the chocolate conundrum, the healthier it is, the worse it tastes. But what if there’s another way? What if you can have tasty chocolate that’s good for you?
That’s the question a group of researchers from Penn State University dared to ask. The secret, they discovered, is to subject the cacao beans to extra-intense roasting. We’re not sure how screaming insults at a bunch of beans will help, but if science says so ... YOU USELESS LUMP OF BARELY EDIBLE FOOD! HOW DARE YOU EXIST!
Oh, not that kind of roasting. Oops.
For their study, the researchers made 27 unsweetened chocolates, prepared using various cacao bean roasting times and temperatures, and served them to volunteers. Those volunteers reported that chocolates made with cacao beans roasted more intensely (such as 20 minutes at 340° F, 80 min at 275° F, and 54 min at 304° F) were far more acceptable than were chocolates prepared with raw or lightly roasted cacao beans.
The implications of healthy yet tasty chocolate are obvious: Master the chocolate and you’ll make millions. Imagine a future where parents say to their kids: “Don’t forget to eat your chocolate.” So, we’re off to do some cooking. Don’t want Hershey to make all the money off of this revelation.
The villain hiding in dairy for some MS patients
For some of us, lactose can be a real heartbreaker when it comes to dairy consumption, but for people with multiple sclerosis (MS) there’s another villain they may also have to face that can make their symptoms worse.
Physicians at the Institute of Anatomy at University Hospital Bonn (Germany) were getting so many complaints from patients with MS about how much worse they felt about after having cheese, yogurt, and milk that they decided to get to the bottom of it. The culprit, it seems, is casein, a protein specifically found in cow’s milk.
The researchers injected mice with various proteins found in cow’s milk and found perforated myelin sheaths in those given casein. In MS, the patient’s own immune system destroys that sheath, which leads to paresthesia, vision problems, and movement disorders.
“The body’s defenses actually attack the casein, but in the process they also destroy proteins involved in the formation of myelin, “ said Rittika Chunder, a postdoctoral fellow at the University of Bonn. How? Apparently it’s all a big misunderstanding.
While looking at molecules needed for myelin production, the researchers came across MAG, which is very similar to casein, which is a problem when patients with MS are allergic to casein. After they have dairy products, the B-cell squad gets called in to clean up the evil twin, casein, but can’t differentiate it from the good twin, MAG, so it all gets a wash and the myelin sheath suffers.
Since this happens only to patients with MS who have a casein allergy, the researchers advise them to stay away from milk, yogurt, or cottage cheese while they work on a self-test to check if patients carry the antibodies.
A small price to pay, perhaps, to stop a villainous evil twin.
You would even say it glows
If you’re anything like us – and we think you are since you’re reading this – you’ve been asking yourself: Are there any common medications in my house that will make good radiation sensors?
Not that anyone needs to worry about excess radiation or anything. Far from it. We were just wondering.
It just so happens that Anna Mrozik and Paweł Bilski, both of the Institute of Nuclear Physics Polish Academy of Sciences (IFJ PAN) in Kraków, Poland, were wondering the same thing: “During an uncontrolled release of radiation, it is highly unlikely that members of the public will be equipped with personal radiation dose monitors.”
People would need to use something they had lying around the house. A smartphone would work, the investigators explained in a statement from the IFJ PAN, but the process of converting one to radiation-sensor duty, which involves dismantling it and breaking the display glass, “is laborious and time-consuming [and] the destruction of a valuable and useful device does not seem to be the optimal solution.”
Naturally, they turned to drugs. The key, in this case, is optically stimulated luminescence. They needed to find materials that would glow with greater intensity as the radiation dose increased. Turns out that ibuprofen- and paracetamol-based painkillers fit the bill quite nicely, although aspirin also works.
It’s not known exactly which substance is causing the luminescence, but rest assured, the “physicists from the IFJ PAN intend to identify it.”
This is why you don’t interrupt someone using headphones
There’s nothing like taking a nice relaxing walk with your headphones. Whether you’re listening to a podcast or a song or talking on the phone, it’s an escape from reality that makes you feel like you’re completely in tune with what you’re listening to.
According to a new study, headphones, as opposed to speakers, make people feel more connected to what they are listening to. Data collected from more than 4,000 people showed that listening with headphones makes more of an impact than listening to speakers.
“Headphones produce a phenomenon called in-head localization, which makes the speaker sound as if they’re inside your head,” study coauthor On Amir of the University of California, San Diego, said in a statement. Because of this, people feel like the speakers are close to them and there’s more of a sense of empathy for the speakers and the listener is more likely to be swayed toward the ideas of the speaker.
These findings could lead to more efficient training programs, online work, and advertising, the investigators suggested.
We now finally understand why people get so mad when they have to take out their headphones to answer or talk to us. We ruined a satisfying moment going on in their brains.
‘Striking’ differences in BP when wrong cuff size is used
Strong new evidence on the need to use an appropriately sized cuff in blood pressure measurement has come from the cross-sectional randomized trial Cuff(SZ).
The study found that in people in whom a small adult cuff was appropriate, systolic BP readings were on average 3.6 mm Hg lower when a regular adult size cuff was used.
However, systolic readings were on average 4.8 mm Hg higher when a regular cuff was used in people who required a large adult cuff and 19.5 mm Hg higher in those needing an extra-large cuff based on their mid-arm circumference.
The diastolic readings followed a similar pattern (-1.3 mm Hg, 1.8 mm Hg, and 7.4 mm Hg, respectively).
“We found that using the regular adult cuff in all individuals had striking differences in blood pressure,” lead author Tammy M. Brady, MD, PhD, Johns Hopkins University School of Medicine, Baltimore, told this news organization. “And that has a lot of clinical implications.”
She noted, for example, that people who required an extra-large cuff and were measured with a regular cuff had an average BP of 144/86.7 mm Hg, which is in the stage 2 hypertension range. But when the correct size cuff was used, the average BP was 124.5/79.3 mm Hg, or in the prehypertensive range.
Overall, the overestimation of BP due to using too small a cuff misclassified 39% of people as being hypertensive, while the underestimation of BP due to using a cuff that was too large missed 22% of people with hypertension.
“So, I think clinicians really need to have a renewed emphasis on cuff size, especially in populations where obesity is highly prevalent and many of their patients require extra-large cuffs, because those are the populations that are most impacted by mis-cuffing,” Dr. Brady said.
The findings were presented in an E-poster at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health (EPI/Lifestyle) 2022 conference sponsored by the American Heart Association.
Willie Lawrence, MD, chair of the AHA’s National Hypertension Control Initiative Advisory Committee, said in an interview that the magnitude of inaccuracy observed by the researchers “makes this a very, very important study.”
“Is it the first of its kind, no, but it’s incredibly important because it was so well done, and it comes at a time when people are once again dealing with issues around equity, and this study can have a significant impact on the state of hypertension in diverse communities,” said Dr. Lawrence, a cardiologist with Spectrum Health Lakeland, Benton Harbor, Michigan.
Previous studies examining the issue were older, had few participants, and used mercury sphygmomanometers instead of automated devices, which are typically recommended by professional societies for screening hypertension in adults, Dr. Brady explained.
For the Cuff Size Blood Pressure Measurement trial, 195 adults recruited from the community underwent 2 to 3 sets of 3 BP readings, 30 seconds apart, with an automated and validated device (Welch Allyn ProB 2000) using a BP cuff that was appropriated sized, one size lower, and one size higher. The order of cuff sizes was randomized. Before each set, patients walked for 2 minutes, followed by 5 minutes of rest to eliminate the potential effect of longer resting periods between tests on the results. The room was also kept quiet and participants were asked not to speak or use a smart phone.
Participants had a mean age of 54 years, 34% were male, 68% were Black, and 36% had a body mass index of at least 30 kg/m2, meeting the criteria for obesity.
Roughly one-half had a self-reported hypertension diagnosis, 31% had a systolic BP of 130 mm Hg or greater, and 26% had a diastolic BP of 80 mm Hg or greater.
Based on arm circumference (mean, 34 cm), the appropriate adult cuff size was small (20-25 cm) in 18%, regular (25.1-32 cm) in 28%, large (32.1-40 cm) in 34%, and extra-large (40.1-55 cm) in 21%.
Dr. Brady pointed out that the most recent hypertension guidelines detail sources of inaccuracy in BP measurement and say that if too small a cuff size is used, the blood pressure could be different by 2 to 11 mm Hg. “And what we show, is it can be anywhere from 5 to 20 mm Hg. So, I think that’s a significant difference from what studies have shown so far and is going to be very surprising to clinicians.”
A 2019 AHA scientific statement on the measurement of blood pressure stresses the importance of cuff size, and last year, the American Medical Association launched a new initiative to standardize training in BP measurement for future physicians and health care professionals.
Previous work also showed that children as young as 3 to 5 years of age often require an adult cuff size, and those in the 12- to 15-year age group may need an extra-large cuff, or what is often referred to as a thigh cuff, said Dr. Brady, who is also the medical director of the pediatric hypertension program at Johns Hopkins Children’s Center.
“Part of the problem is that many physicians aren’t often the one doing the measurement and that others may not be as in tune with some of these data and initiatives,” she said.
Other barriers are cost and availability. Offices and clinics don’t routinely stock multiple cuff sizes in exam rooms, and devices sold over the counter typically come with a regular adult cuff, Dr. Brady said. An extra cuff could add $25 to $50 on top of the $25 to $50 for the device for the growing number of patients measuring BP remotely.
“During the pandemic, I was trying to do telemedicine with my hypertensive patients, but the children who had significant obesity couldn’t afford or find blood pressure devices that had a cuff that was big enough for them,” she said. “It just wasn’t something that they could get. So I think people just don’t recognize how important this is.”
A version of this article first appeared on Medscape.com.
Strong new evidence on the need to use an appropriately sized cuff in blood pressure measurement has come from the cross-sectional randomized trial Cuff(SZ).
The study found that in people in whom a small adult cuff was appropriate, systolic BP readings were on average 3.6 mm Hg lower when a regular adult size cuff was used.
However, systolic readings were on average 4.8 mm Hg higher when a regular cuff was used in people who required a large adult cuff and 19.5 mm Hg higher in those needing an extra-large cuff based on their mid-arm circumference.
The diastolic readings followed a similar pattern (-1.3 mm Hg, 1.8 mm Hg, and 7.4 mm Hg, respectively).
“We found that using the regular adult cuff in all individuals had striking differences in blood pressure,” lead author Tammy M. Brady, MD, PhD, Johns Hopkins University School of Medicine, Baltimore, told this news organization. “And that has a lot of clinical implications.”
She noted, for example, that people who required an extra-large cuff and were measured with a regular cuff had an average BP of 144/86.7 mm Hg, which is in the stage 2 hypertension range. But when the correct size cuff was used, the average BP was 124.5/79.3 mm Hg, or in the prehypertensive range.
Overall, the overestimation of BP due to using too small a cuff misclassified 39% of people as being hypertensive, while the underestimation of BP due to using a cuff that was too large missed 22% of people with hypertension.
“So, I think clinicians really need to have a renewed emphasis on cuff size, especially in populations where obesity is highly prevalent and many of their patients require extra-large cuffs, because those are the populations that are most impacted by mis-cuffing,” Dr. Brady said.
The findings were presented in an E-poster at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health (EPI/Lifestyle) 2022 conference sponsored by the American Heart Association.
Willie Lawrence, MD, chair of the AHA’s National Hypertension Control Initiative Advisory Committee, said in an interview that the magnitude of inaccuracy observed by the researchers “makes this a very, very important study.”
“Is it the first of its kind, no, but it’s incredibly important because it was so well done, and it comes at a time when people are once again dealing with issues around equity, and this study can have a significant impact on the state of hypertension in diverse communities,” said Dr. Lawrence, a cardiologist with Spectrum Health Lakeland, Benton Harbor, Michigan.
Previous studies examining the issue were older, had few participants, and used mercury sphygmomanometers instead of automated devices, which are typically recommended by professional societies for screening hypertension in adults, Dr. Brady explained.
For the Cuff Size Blood Pressure Measurement trial, 195 adults recruited from the community underwent 2 to 3 sets of 3 BP readings, 30 seconds apart, with an automated and validated device (Welch Allyn ProB 2000) using a BP cuff that was appropriated sized, one size lower, and one size higher. The order of cuff sizes was randomized. Before each set, patients walked for 2 minutes, followed by 5 minutes of rest to eliminate the potential effect of longer resting periods between tests on the results. The room was also kept quiet and participants were asked not to speak or use a smart phone.
Participants had a mean age of 54 years, 34% were male, 68% were Black, and 36% had a body mass index of at least 30 kg/m2, meeting the criteria for obesity.
Roughly one-half had a self-reported hypertension diagnosis, 31% had a systolic BP of 130 mm Hg or greater, and 26% had a diastolic BP of 80 mm Hg or greater.
Based on arm circumference (mean, 34 cm), the appropriate adult cuff size was small (20-25 cm) in 18%, regular (25.1-32 cm) in 28%, large (32.1-40 cm) in 34%, and extra-large (40.1-55 cm) in 21%.
Dr. Brady pointed out that the most recent hypertension guidelines detail sources of inaccuracy in BP measurement and say that if too small a cuff size is used, the blood pressure could be different by 2 to 11 mm Hg. “And what we show, is it can be anywhere from 5 to 20 mm Hg. So, I think that’s a significant difference from what studies have shown so far and is going to be very surprising to clinicians.”
A 2019 AHA scientific statement on the measurement of blood pressure stresses the importance of cuff size, and last year, the American Medical Association launched a new initiative to standardize training in BP measurement for future physicians and health care professionals.
Previous work also showed that children as young as 3 to 5 years of age often require an adult cuff size, and those in the 12- to 15-year age group may need an extra-large cuff, or what is often referred to as a thigh cuff, said Dr. Brady, who is also the medical director of the pediatric hypertension program at Johns Hopkins Children’s Center.
“Part of the problem is that many physicians aren’t often the one doing the measurement and that others may not be as in tune with some of these data and initiatives,” she said.
Other barriers are cost and availability. Offices and clinics don’t routinely stock multiple cuff sizes in exam rooms, and devices sold over the counter typically come with a regular adult cuff, Dr. Brady said. An extra cuff could add $25 to $50 on top of the $25 to $50 for the device for the growing number of patients measuring BP remotely.
“During the pandemic, I was trying to do telemedicine with my hypertensive patients, but the children who had significant obesity couldn’t afford or find blood pressure devices that had a cuff that was big enough for them,” she said. “It just wasn’t something that they could get. So I think people just don’t recognize how important this is.”
A version of this article first appeared on Medscape.com.
Strong new evidence on the need to use an appropriately sized cuff in blood pressure measurement has come from the cross-sectional randomized trial Cuff(SZ).
The study found that in people in whom a small adult cuff was appropriate, systolic BP readings were on average 3.6 mm Hg lower when a regular adult size cuff was used.
However, systolic readings were on average 4.8 mm Hg higher when a regular cuff was used in people who required a large adult cuff and 19.5 mm Hg higher in those needing an extra-large cuff based on their mid-arm circumference.
The diastolic readings followed a similar pattern (-1.3 mm Hg, 1.8 mm Hg, and 7.4 mm Hg, respectively).
“We found that using the regular adult cuff in all individuals had striking differences in blood pressure,” lead author Tammy M. Brady, MD, PhD, Johns Hopkins University School of Medicine, Baltimore, told this news organization. “And that has a lot of clinical implications.”
She noted, for example, that people who required an extra-large cuff and were measured with a regular cuff had an average BP of 144/86.7 mm Hg, which is in the stage 2 hypertension range. But when the correct size cuff was used, the average BP was 124.5/79.3 mm Hg, or in the prehypertensive range.
Overall, the overestimation of BP due to using too small a cuff misclassified 39% of people as being hypertensive, while the underestimation of BP due to using a cuff that was too large missed 22% of people with hypertension.
“So, I think clinicians really need to have a renewed emphasis on cuff size, especially in populations where obesity is highly prevalent and many of their patients require extra-large cuffs, because those are the populations that are most impacted by mis-cuffing,” Dr. Brady said.
The findings were presented in an E-poster at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health (EPI/Lifestyle) 2022 conference sponsored by the American Heart Association.
Willie Lawrence, MD, chair of the AHA’s National Hypertension Control Initiative Advisory Committee, said in an interview that the magnitude of inaccuracy observed by the researchers “makes this a very, very important study.”
“Is it the first of its kind, no, but it’s incredibly important because it was so well done, and it comes at a time when people are once again dealing with issues around equity, and this study can have a significant impact on the state of hypertension in diverse communities,” said Dr. Lawrence, a cardiologist with Spectrum Health Lakeland, Benton Harbor, Michigan.
Previous studies examining the issue were older, had few participants, and used mercury sphygmomanometers instead of automated devices, which are typically recommended by professional societies for screening hypertension in adults, Dr. Brady explained.
For the Cuff Size Blood Pressure Measurement trial, 195 adults recruited from the community underwent 2 to 3 sets of 3 BP readings, 30 seconds apart, with an automated and validated device (Welch Allyn ProB 2000) using a BP cuff that was appropriated sized, one size lower, and one size higher. The order of cuff sizes was randomized. Before each set, patients walked for 2 minutes, followed by 5 minutes of rest to eliminate the potential effect of longer resting periods between tests on the results. The room was also kept quiet and participants were asked not to speak or use a smart phone.
Participants had a mean age of 54 years, 34% were male, 68% were Black, and 36% had a body mass index of at least 30 kg/m2, meeting the criteria for obesity.
Roughly one-half had a self-reported hypertension diagnosis, 31% had a systolic BP of 130 mm Hg or greater, and 26% had a diastolic BP of 80 mm Hg or greater.
Based on arm circumference (mean, 34 cm), the appropriate adult cuff size was small (20-25 cm) in 18%, regular (25.1-32 cm) in 28%, large (32.1-40 cm) in 34%, and extra-large (40.1-55 cm) in 21%.
Dr. Brady pointed out that the most recent hypertension guidelines detail sources of inaccuracy in BP measurement and say that if too small a cuff size is used, the blood pressure could be different by 2 to 11 mm Hg. “And what we show, is it can be anywhere from 5 to 20 mm Hg. So, I think that’s a significant difference from what studies have shown so far and is going to be very surprising to clinicians.”
A 2019 AHA scientific statement on the measurement of blood pressure stresses the importance of cuff size, and last year, the American Medical Association launched a new initiative to standardize training in BP measurement for future physicians and health care professionals.
Previous work also showed that children as young as 3 to 5 years of age often require an adult cuff size, and those in the 12- to 15-year age group may need an extra-large cuff, or what is often referred to as a thigh cuff, said Dr. Brady, who is also the medical director of the pediatric hypertension program at Johns Hopkins Children’s Center.
“Part of the problem is that many physicians aren’t often the one doing the measurement and that others may not be as in tune with some of these data and initiatives,” she said.
Other barriers are cost and availability. Offices and clinics don’t routinely stock multiple cuff sizes in exam rooms, and devices sold over the counter typically come with a regular adult cuff, Dr. Brady said. An extra cuff could add $25 to $50 on top of the $25 to $50 for the device for the growing number of patients measuring BP remotely.
“During the pandemic, I was trying to do telemedicine with my hypertensive patients, but the children who had significant obesity couldn’t afford or find blood pressure devices that had a cuff that was big enough for them,” she said. “It just wasn’t something that they could get. So I think people just don’t recognize how important this is.”
A version of this article first appeared on Medscape.com.
First possible case of deer-to-human COVID transmission identified
according a new preprint study that hasn’t yet been peer-reviewed.
Typically, humans spread the virus to deer, and then deer spread it to other deer. But new evidence suggests that the virus could spill over from deer into humans. The researchers identified a COVID-19 case in someone from Ontario who had recently been in contact with deer.
“This particular case, while raising a red flag, doesn’t seem to be hugely alarming,” Finlay Maguire, PhD, one of the study authors and an epidemiologist at Dalhousie University, told CBC News.
“While we haven’t seen [transmission from deer to humans] happen directly, we sampled from the human case around the same time we sampled from the deer, and we sampled from around the same location,” he said. “There is also a plausible link by which it could have happened, in that the individual involved is known to have had considerable contact with deer.”
Dr. Maguire and colleagues have been monitoring the spread of the coronavirus among animals. They analyzed nasal swabs and lymph node samples taken from hundreds of deer that were killed by hunters in fall 2021 in southwestern and eastern Ontario. Among 298 sampled deer, 17 tested positive -- all from southwestern Ontario.
During the analysis, they found a “highly divergent” coronavirus lineage, which means a cluster of samples with many mutations. Around the same time, they found a genetically similar version in a person from the same region.
The study points to the need for better surveillance of the coronavirus, Dr. Maguire told CBC News, including in humans, animals, plants, and the broader environment. Researchers aren’t quite sure how deer contract the virus from humans, but it could happen through contaminated water, direct contact, food, farming, or other animals such as mink.
The coronavirus lineage identified in the study is different from what’s circulating among humans now, and it’s not related to the Delta or Omicron variants. The closest genetic relative came from samples taken from humans and mink in Michigan in 2020, which means the divergent lineage mutated and evolved over time.
“It’s reassuring that we found no evidence of further transmission, during a time when we were doing a lot of sampling and a lot of sequencing,” Samira Mubareka, MD, one of the study authors and a virologist at Sunnybrook Health Sciences Centre, told CBC News.
“If we continue to do this surveillance, we’ll get a much better sense of what the actual risk is,” she said.
So far, the coronavirus has been found in wild white-tailed deer in the northeastern United States and central Canadian provinces.
Other known cases of transmission from animals to humans have been identified in farmed mink and potentially hamsters, the news outlet reported. But for the most part, humans transmit the virus to animals and are most likely to catch the virus from other people.
At the same time, the Public Health Agency of Canada has issued guidance for hunters, trappers, and those who handle wild deer. People should wear gloves, goggles, and a mask when they could be exposed to respiratory tissues and fluids, especially indoors.
Coronaviruses are killed by normal cooking temperatures, the agency said, and there has been no evidence that cooked venison can spread the virus.
A version of this article first appeared on WebMD.com.
according a new preprint study that hasn’t yet been peer-reviewed.
Typically, humans spread the virus to deer, and then deer spread it to other deer. But new evidence suggests that the virus could spill over from deer into humans. The researchers identified a COVID-19 case in someone from Ontario who had recently been in contact with deer.
“This particular case, while raising a red flag, doesn’t seem to be hugely alarming,” Finlay Maguire, PhD, one of the study authors and an epidemiologist at Dalhousie University, told CBC News.
“While we haven’t seen [transmission from deer to humans] happen directly, we sampled from the human case around the same time we sampled from the deer, and we sampled from around the same location,” he said. “There is also a plausible link by which it could have happened, in that the individual involved is known to have had considerable contact with deer.”
Dr. Maguire and colleagues have been monitoring the spread of the coronavirus among animals. They analyzed nasal swabs and lymph node samples taken from hundreds of deer that were killed by hunters in fall 2021 in southwestern and eastern Ontario. Among 298 sampled deer, 17 tested positive -- all from southwestern Ontario.
During the analysis, they found a “highly divergent” coronavirus lineage, which means a cluster of samples with many mutations. Around the same time, they found a genetically similar version in a person from the same region.
The study points to the need for better surveillance of the coronavirus, Dr. Maguire told CBC News, including in humans, animals, plants, and the broader environment. Researchers aren’t quite sure how deer contract the virus from humans, but it could happen through contaminated water, direct contact, food, farming, or other animals such as mink.
The coronavirus lineage identified in the study is different from what’s circulating among humans now, and it’s not related to the Delta or Omicron variants. The closest genetic relative came from samples taken from humans and mink in Michigan in 2020, which means the divergent lineage mutated and evolved over time.
“It’s reassuring that we found no evidence of further transmission, during a time when we were doing a lot of sampling and a lot of sequencing,” Samira Mubareka, MD, one of the study authors and a virologist at Sunnybrook Health Sciences Centre, told CBC News.
“If we continue to do this surveillance, we’ll get a much better sense of what the actual risk is,” she said.
So far, the coronavirus has been found in wild white-tailed deer in the northeastern United States and central Canadian provinces.
Other known cases of transmission from animals to humans have been identified in farmed mink and potentially hamsters, the news outlet reported. But for the most part, humans transmit the virus to animals and are most likely to catch the virus from other people.
At the same time, the Public Health Agency of Canada has issued guidance for hunters, trappers, and those who handle wild deer. People should wear gloves, goggles, and a mask when they could be exposed to respiratory tissues and fluids, especially indoors.
Coronaviruses are killed by normal cooking temperatures, the agency said, and there has been no evidence that cooked venison can spread the virus.
A version of this article first appeared on WebMD.com.
according a new preprint study that hasn’t yet been peer-reviewed.
Typically, humans spread the virus to deer, and then deer spread it to other deer. But new evidence suggests that the virus could spill over from deer into humans. The researchers identified a COVID-19 case in someone from Ontario who had recently been in contact with deer.
“This particular case, while raising a red flag, doesn’t seem to be hugely alarming,” Finlay Maguire, PhD, one of the study authors and an epidemiologist at Dalhousie University, told CBC News.
“While we haven’t seen [transmission from deer to humans] happen directly, we sampled from the human case around the same time we sampled from the deer, and we sampled from around the same location,” he said. “There is also a plausible link by which it could have happened, in that the individual involved is known to have had considerable contact with deer.”
Dr. Maguire and colleagues have been monitoring the spread of the coronavirus among animals. They analyzed nasal swabs and lymph node samples taken from hundreds of deer that were killed by hunters in fall 2021 in southwestern and eastern Ontario. Among 298 sampled deer, 17 tested positive -- all from southwestern Ontario.
During the analysis, they found a “highly divergent” coronavirus lineage, which means a cluster of samples with many mutations. Around the same time, they found a genetically similar version in a person from the same region.
The study points to the need for better surveillance of the coronavirus, Dr. Maguire told CBC News, including in humans, animals, plants, and the broader environment. Researchers aren’t quite sure how deer contract the virus from humans, but it could happen through contaminated water, direct contact, food, farming, or other animals such as mink.
The coronavirus lineage identified in the study is different from what’s circulating among humans now, and it’s not related to the Delta or Omicron variants. The closest genetic relative came from samples taken from humans and mink in Michigan in 2020, which means the divergent lineage mutated and evolved over time.
“It’s reassuring that we found no evidence of further transmission, during a time when we were doing a lot of sampling and a lot of sequencing,” Samira Mubareka, MD, one of the study authors and a virologist at Sunnybrook Health Sciences Centre, told CBC News.
“If we continue to do this surveillance, we’ll get a much better sense of what the actual risk is,” she said.
So far, the coronavirus has been found in wild white-tailed deer in the northeastern United States and central Canadian provinces.
Other known cases of transmission from animals to humans have been identified in farmed mink and potentially hamsters, the news outlet reported. But for the most part, humans transmit the virus to animals and are most likely to catch the virus from other people.
At the same time, the Public Health Agency of Canada has issued guidance for hunters, trappers, and those who handle wild deer. People should wear gloves, goggles, and a mask when they could be exposed to respiratory tissues and fluids, especially indoors.
Coronaviruses are killed by normal cooking temperatures, the agency said, and there has been no evidence that cooked venison can spread the virus.
A version of this article first appeared on WebMD.com.
IBD-VTE score serves as reminder to assess postdischarge risk
The chances of developing a blood clot after hospital admission for inflammatory bowel disease (IBD) may persist for several months after being discharged, but a new simple score might help clinicians identify patients who are at greatest risk.
The score – which takes eight, easily captured factors into consideration – had a reasonable ability to distinguish between people who did and did not develop venous thromboembolism (VTE), with an area under the curve of 0.71 (95% confidence interval, 0.69-0.72).
“There is clearly an excess of risk for VTE in patients admitted for IBD in the 90 days following their hospital discharge,” said Philip Harvey, MD, a consultant gastroenterologist with the Royal Wolverhampton (England) NHS Trust at the 17th congress of the European Crohn’s and Colitis Organisation.
“Advancing age, male gender, emergency admission, longer admissions, and ulcerative colitis are particularly important risk factors,” he noted.
“We have proposed a risk-scoring system that will be generalizable to patients under the age of 60 using readily identifiable clinical data so that clinicians can identify patients who are at the greatest risk,” Dr. Harvey added when presenting the work.
“This research provides much needed evidence to guide posthospitalization anticoagulation in patients hospitalized for IBD flares,” Bharati Kochar, MD, MS, independently commented.
“Surgeons are already discharging select patients on anticoagulation for DVT [deep vein thrombosis] prophylaxis [but] we need to consider this more systematically after medical IBD admissions,” suggested Dr. Kochar, who is a gastroenterologist and IBD specialist at Massachusetts General Hospital in Boston.
“This research should spur prospective investigation into type of anticoagulation upon discharge, dose, duration and whether the intervention makes a difference in postdischarge clotting events in patients hospitalized for a flare of IBD,” she added.
VTE risk in IBD patients
The risk and prevention of VTE and arterial thrombosis in IBD patients was the focus of a recent international consensus project in which 14 international IBD experts and three thrombosis experts from 12 countries came together to develop evidence-based guidance. Nineteen statements and 10 core recommendations were made, notably that “patients with IBD should be screened for VTE risk factors” and that “thromboprophylaxis should be given to patients with IBD during hospitalization of any cause and maintained during the inpatient period.”
Although met with a high level of agreement among the expert panel, these recommendations were supported by a low (grade C/D) level of evidence.
The expert panel observed in their conclusions that “development of specific risk-assessment tools for thrombotic complications in patients with IBD are needed, as they might influence management in some clinical scenarios (such as thromboprophylaxis during ambulatory flares).”
Large hospitalized IBD population considered
Dr. Harvey and fellow investigators’ IBD-VTE risk score was created using data from almost 102,000 patients (49,385 of whom were men) with just greater than 201,000 hospital admissions between 2006 and 2019. These data were taken from the Hospital Episode Statistics (HES), a “data warehouse” that collects details of all emergency, routine, and outpatient hospital attendances at NHS hospitals in England.
“The HES database is advantageous due to its size because VTE events are relatively uncommon in this group, and therefore it’s important to capture as many patients as possible,” Dr. Harvey explained.
All admissions, from emergencies without surgery to those involving surgery, and those for more routine cases of elective surgery were considered, with the most common (79.3%) admission type being nonsurgical emergencies.
A multilevel logistic regression model was used to identify patient and admission factors that might influence the risk for VTE.
With regard to the number of VTE events seen, Dr. Harvey noted: “There was an enormous excess of events and risk in that 0-90 day period, compared to 180-270 days later. This was true across all admission types.”
Indeed, VTE rates per 100,000 people in the 0-90 day postoperative period were 36.9 for emergency surgical admissions, and 15.6 for both nonsurgical emergencies and elective surgeries. Rates in the later period were a respective 0.84, 1.59, and 1.70.
Key risk factors for VTE were male gender, older age, emergency admission with or without surgery, longer hospital stays, and having ulcerative colitis which were included in the scoring system together with number of prior IBD hospital admissions in the past 3 months, ethnicity, and number of comorbidities.
Ideal thromboprophylaxis duration under investigation
“A higher risk of DVT is known in these patients and all should be considered for postoperative VTE prevention,” said Robert Neil Goldstone, MD, who is assistant professor of surgery at Massachusetts General Hospital.
“Many scores can be used, including the Caprini score, which also adds a point for patient history of IBD,” he observed.
The flip-side of VTE is of course the risk for postsurgical bleeding. While this is something clinicians need to be cognizant of there is “not generally increased risk” with some of the more commonly used anticoagulants, Dr. Goldstone noted. In his practice, “high-risk” IBD patients who have undergone bowel surgery will commonly be discharged on a low-molecular-weight heparin treatment for at least 3-4 weeks.
“The bigger question that remains is whether prolonged postoperative thromboprophylaxis is required,” Dr. Goldstone said. This is something that needs examining in a large randomized controlled trial.
Dr. Harvey and coinvestigators had no conflicts of interest to disclose. Dr. Kochar is on the Board of Editors for GI & Hepatology News but had no other conflicts of interest. Dr. Goldstone was also not involved in the study and had nothing to disclose.
The chances of developing a blood clot after hospital admission for inflammatory bowel disease (IBD) may persist for several months after being discharged, but a new simple score might help clinicians identify patients who are at greatest risk.
The score – which takes eight, easily captured factors into consideration – had a reasonable ability to distinguish between people who did and did not develop venous thromboembolism (VTE), with an area under the curve of 0.71 (95% confidence interval, 0.69-0.72).
“There is clearly an excess of risk for VTE in patients admitted for IBD in the 90 days following their hospital discharge,” said Philip Harvey, MD, a consultant gastroenterologist with the Royal Wolverhampton (England) NHS Trust at the 17th congress of the European Crohn’s and Colitis Organisation.
“Advancing age, male gender, emergency admission, longer admissions, and ulcerative colitis are particularly important risk factors,” he noted.
“We have proposed a risk-scoring system that will be generalizable to patients under the age of 60 using readily identifiable clinical data so that clinicians can identify patients who are at the greatest risk,” Dr. Harvey added when presenting the work.
“This research provides much needed evidence to guide posthospitalization anticoagulation in patients hospitalized for IBD flares,” Bharati Kochar, MD, MS, independently commented.
“Surgeons are already discharging select patients on anticoagulation for DVT [deep vein thrombosis] prophylaxis [but] we need to consider this more systematically after medical IBD admissions,” suggested Dr. Kochar, who is a gastroenterologist and IBD specialist at Massachusetts General Hospital in Boston.
“This research should spur prospective investigation into type of anticoagulation upon discharge, dose, duration and whether the intervention makes a difference in postdischarge clotting events in patients hospitalized for a flare of IBD,” she added.
VTE risk in IBD patients
The risk and prevention of VTE and arterial thrombosis in IBD patients was the focus of a recent international consensus project in which 14 international IBD experts and three thrombosis experts from 12 countries came together to develop evidence-based guidance. Nineteen statements and 10 core recommendations were made, notably that “patients with IBD should be screened for VTE risk factors” and that “thromboprophylaxis should be given to patients with IBD during hospitalization of any cause and maintained during the inpatient period.”
Although met with a high level of agreement among the expert panel, these recommendations were supported by a low (grade C/D) level of evidence.
The expert panel observed in their conclusions that “development of specific risk-assessment tools for thrombotic complications in patients with IBD are needed, as they might influence management in some clinical scenarios (such as thromboprophylaxis during ambulatory flares).”
Large hospitalized IBD population considered
Dr. Harvey and fellow investigators’ IBD-VTE risk score was created using data from almost 102,000 patients (49,385 of whom were men) with just greater than 201,000 hospital admissions between 2006 and 2019. These data were taken from the Hospital Episode Statistics (HES), a “data warehouse” that collects details of all emergency, routine, and outpatient hospital attendances at NHS hospitals in England.
“The HES database is advantageous due to its size because VTE events are relatively uncommon in this group, and therefore it’s important to capture as many patients as possible,” Dr. Harvey explained.
All admissions, from emergencies without surgery to those involving surgery, and those for more routine cases of elective surgery were considered, with the most common (79.3%) admission type being nonsurgical emergencies.
A multilevel logistic regression model was used to identify patient and admission factors that might influence the risk for VTE.
With regard to the number of VTE events seen, Dr. Harvey noted: “There was an enormous excess of events and risk in that 0-90 day period, compared to 180-270 days later. This was true across all admission types.”
Indeed, VTE rates per 100,000 people in the 0-90 day postoperative period were 36.9 for emergency surgical admissions, and 15.6 for both nonsurgical emergencies and elective surgeries. Rates in the later period were a respective 0.84, 1.59, and 1.70.
Key risk factors for VTE were male gender, older age, emergency admission with or without surgery, longer hospital stays, and having ulcerative colitis which were included in the scoring system together with number of prior IBD hospital admissions in the past 3 months, ethnicity, and number of comorbidities.
Ideal thromboprophylaxis duration under investigation
“A higher risk of DVT is known in these patients and all should be considered for postoperative VTE prevention,” said Robert Neil Goldstone, MD, who is assistant professor of surgery at Massachusetts General Hospital.
“Many scores can be used, including the Caprini score, which also adds a point for patient history of IBD,” he observed.
The flip-side of VTE is of course the risk for postsurgical bleeding. While this is something clinicians need to be cognizant of there is “not generally increased risk” with some of the more commonly used anticoagulants, Dr. Goldstone noted. In his practice, “high-risk” IBD patients who have undergone bowel surgery will commonly be discharged on a low-molecular-weight heparin treatment for at least 3-4 weeks.
“The bigger question that remains is whether prolonged postoperative thromboprophylaxis is required,” Dr. Goldstone said. This is something that needs examining in a large randomized controlled trial.
Dr. Harvey and coinvestigators had no conflicts of interest to disclose. Dr. Kochar is on the Board of Editors for GI & Hepatology News but had no other conflicts of interest. Dr. Goldstone was also not involved in the study and had nothing to disclose.
The chances of developing a blood clot after hospital admission for inflammatory bowel disease (IBD) may persist for several months after being discharged, but a new simple score might help clinicians identify patients who are at greatest risk.
The score – which takes eight, easily captured factors into consideration – had a reasonable ability to distinguish between people who did and did not develop venous thromboembolism (VTE), with an area under the curve of 0.71 (95% confidence interval, 0.69-0.72).
“There is clearly an excess of risk for VTE in patients admitted for IBD in the 90 days following their hospital discharge,” said Philip Harvey, MD, a consultant gastroenterologist with the Royal Wolverhampton (England) NHS Trust at the 17th congress of the European Crohn’s and Colitis Organisation.
“Advancing age, male gender, emergency admission, longer admissions, and ulcerative colitis are particularly important risk factors,” he noted.
“We have proposed a risk-scoring system that will be generalizable to patients under the age of 60 using readily identifiable clinical data so that clinicians can identify patients who are at the greatest risk,” Dr. Harvey added when presenting the work.
“This research provides much needed evidence to guide posthospitalization anticoagulation in patients hospitalized for IBD flares,” Bharati Kochar, MD, MS, independently commented.
“Surgeons are already discharging select patients on anticoagulation for DVT [deep vein thrombosis] prophylaxis [but] we need to consider this more systematically after medical IBD admissions,” suggested Dr. Kochar, who is a gastroenterologist and IBD specialist at Massachusetts General Hospital in Boston.
“This research should spur prospective investigation into type of anticoagulation upon discharge, dose, duration and whether the intervention makes a difference in postdischarge clotting events in patients hospitalized for a flare of IBD,” she added.
VTE risk in IBD patients
The risk and prevention of VTE and arterial thrombosis in IBD patients was the focus of a recent international consensus project in which 14 international IBD experts and three thrombosis experts from 12 countries came together to develop evidence-based guidance. Nineteen statements and 10 core recommendations were made, notably that “patients with IBD should be screened for VTE risk factors” and that “thromboprophylaxis should be given to patients with IBD during hospitalization of any cause and maintained during the inpatient period.”
Although met with a high level of agreement among the expert panel, these recommendations were supported by a low (grade C/D) level of evidence.
The expert panel observed in their conclusions that “development of specific risk-assessment tools for thrombotic complications in patients with IBD are needed, as they might influence management in some clinical scenarios (such as thromboprophylaxis during ambulatory flares).”
Large hospitalized IBD population considered
Dr. Harvey and fellow investigators’ IBD-VTE risk score was created using data from almost 102,000 patients (49,385 of whom were men) with just greater than 201,000 hospital admissions between 2006 and 2019. These data were taken from the Hospital Episode Statistics (HES), a “data warehouse” that collects details of all emergency, routine, and outpatient hospital attendances at NHS hospitals in England.
“The HES database is advantageous due to its size because VTE events are relatively uncommon in this group, and therefore it’s important to capture as many patients as possible,” Dr. Harvey explained.
All admissions, from emergencies without surgery to those involving surgery, and those for more routine cases of elective surgery were considered, with the most common (79.3%) admission type being nonsurgical emergencies.
A multilevel logistic regression model was used to identify patient and admission factors that might influence the risk for VTE.
With regard to the number of VTE events seen, Dr. Harvey noted: “There was an enormous excess of events and risk in that 0-90 day period, compared to 180-270 days later. This was true across all admission types.”
Indeed, VTE rates per 100,000 people in the 0-90 day postoperative period were 36.9 for emergency surgical admissions, and 15.6 for both nonsurgical emergencies and elective surgeries. Rates in the later period were a respective 0.84, 1.59, and 1.70.
Key risk factors for VTE were male gender, older age, emergency admission with or without surgery, longer hospital stays, and having ulcerative colitis which were included in the scoring system together with number of prior IBD hospital admissions in the past 3 months, ethnicity, and number of comorbidities.
Ideal thromboprophylaxis duration under investigation
“A higher risk of DVT is known in these patients and all should be considered for postoperative VTE prevention,” said Robert Neil Goldstone, MD, who is assistant professor of surgery at Massachusetts General Hospital.
“Many scores can be used, including the Caprini score, which also adds a point for patient history of IBD,” he observed.
The flip-side of VTE is of course the risk for postsurgical bleeding. While this is something clinicians need to be cognizant of there is “not generally increased risk” with some of the more commonly used anticoagulants, Dr. Goldstone noted. In his practice, “high-risk” IBD patients who have undergone bowel surgery will commonly be discharged on a low-molecular-weight heparin treatment for at least 3-4 weeks.
“The bigger question that remains is whether prolonged postoperative thromboprophylaxis is required,” Dr. Goldstone said. This is something that needs examining in a large randomized controlled trial.
Dr. Harvey and coinvestigators had no conflicts of interest to disclose. Dr. Kochar is on the Board of Editors for GI & Hepatology News but had no other conflicts of interest. Dr. Goldstone was also not involved in the study and had nothing to disclose.
FROM ECCO 2022
Needle-free epinephrine products could be available in 2023
Longstanding anxiety around use of epinephrine autoinjectors has prompted research into alternative delivery routes for this life-saving medication. Several companies presented posters on their needle-free epinephrine products at the American Academy of Allergy, Asthma & Immunology (AAAAI) Annual Meeting.
Intranasal formulations are under development at ARS Pharmaceuticals (San Diego) and Bryn Pharma (Raleigh, N.C.). And Aquestive Therapeutics (Warren, N.J.) is working on a sublingual film that delivers epinephrine prodrug when applied under the tongue.
Epinephrine is essential for stopping life-threatening allergic reactions, yet patients often don’t carry their autoinjectors and many hesitate to use them. “It’s needle phobia,” said ARS Pharmaceuticals CEO Richard Lowenthal in an interview with this news organization. “They’re afraid to use it. They don’t like to inject their children, so they hesitate.”
Both nasal sprays reached maximal plasma concentration in 20-30 minutes. ARS Pharmaceuticals compared its intranasal product (Neffy 1 mg) against manual intramuscular injection (0.3 mg) and two autoinjectors (EpiPen 0.3 mg and Symjepi 0.3 mg) by analyzing data from multiple randomized crossover Phase 1 studies examining pharmacokinetics and pharmacodynamics in 175 healthy adults. In this integrated analysis, EpiPen was fastest (20 minutes) at reaching maximal concentration (Tmax), followed by Symjepi and Neffy (both 30 minutes) and epinephrine 0.3 mg IM (45 minutes). In a human factors analysis, ARS Pharmaceuticals reported that untrained participants were able to administer the Neffy spray to themselves or another participant safely and effectively during a simulated emergency scenario.
Bryn Pharma compared pharmacokinetics of its nasal spray product (BRYN-NDS1C 6.6 mg) when self-administered or administered by trained professionals and found comparable profiles for each. Tmax values were also similar: 21.63 minutes (trained professional) and 19.82 minutes (self-administered).
Aquestive Therapeutics is developing a postage stamp-sized product (AQST-109) that delivers epinephrine and begins dissolving when placed under the tongue. No water or swallowing is required for administration, and its packaging is thinner and smaller than a credit card, according to CEO Keith Kendall.
Its analysis showed that the epinephrine reaches maximum plasma concentration in about 15 minutes, with a Tmax range narrower than that of the EpiPen. “The results showed dosing with AQST-109 resulted in PK concentration and Tmax values comparable to published data from autoinjectors,” said John Oppenheimer, MD, of Rutgers University School of Medicine, in a prerecorded poster summary.
Aquestive aims to move forward to the manufacture of registration batches and a pivotal pharmacokinetic study in the second half of 2022. Mr. Lowenthal said ARS Pharmaceuticals is hoping for approval and launch of its nasal spray by summer 2023.
“Having a non-needle delivery device would help many people overcome that fear and hopefully increase use in anaphylaxis,” said David Stukus, MD, an allergist-immunologist and professor of clinical pediatrics at Nationwide Children’s Hospital, Columbus, who was not involved with any of the studies on EpiPen alternatives. And “it’s not just food allergy – anaphylaxis can occur from venom stings, medications, or idiopathic causes.”
Mr. Lowenthal is the CEO of ARS Pharmaceuticals. Mr. Kendall is CEO of Aquestive Therapeutics. Dr. Oppenheimer is a consultant for Aquestive, GSK, Amgen, Sanofi, and Aimmune and sits on Aquestive’s advisory board. Dr. Stukus is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Longstanding anxiety around use of epinephrine autoinjectors has prompted research into alternative delivery routes for this life-saving medication. Several companies presented posters on their needle-free epinephrine products at the American Academy of Allergy, Asthma & Immunology (AAAAI) Annual Meeting.
Intranasal formulations are under development at ARS Pharmaceuticals (San Diego) and Bryn Pharma (Raleigh, N.C.). And Aquestive Therapeutics (Warren, N.J.) is working on a sublingual film that delivers epinephrine prodrug when applied under the tongue.
Epinephrine is essential for stopping life-threatening allergic reactions, yet patients often don’t carry their autoinjectors and many hesitate to use them. “It’s needle phobia,” said ARS Pharmaceuticals CEO Richard Lowenthal in an interview with this news organization. “They’re afraid to use it. They don’t like to inject their children, so they hesitate.”
Both nasal sprays reached maximal plasma concentration in 20-30 minutes. ARS Pharmaceuticals compared its intranasal product (Neffy 1 mg) against manual intramuscular injection (0.3 mg) and two autoinjectors (EpiPen 0.3 mg and Symjepi 0.3 mg) by analyzing data from multiple randomized crossover Phase 1 studies examining pharmacokinetics and pharmacodynamics in 175 healthy adults. In this integrated analysis, EpiPen was fastest (20 minutes) at reaching maximal concentration (Tmax), followed by Symjepi and Neffy (both 30 minutes) and epinephrine 0.3 mg IM (45 minutes). In a human factors analysis, ARS Pharmaceuticals reported that untrained participants were able to administer the Neffy spray to themselves or another participant safely and effectively during a simulated emergency scenario.
Bryn Pharma compared pharmacokinetics of its nasal spray product (BRYN-NDS1C 6.6 mg) when self-administered or administered by trained professionals and found comparable profiles for each. Tmax values were also similar: 21.63 minutes (trained professional) and 19.82 minutes (self-administered).
Aquestive Therapeutics is developing a postage stamp-sized product (AQST-109) that delivers epinephrine and begins dissolving when placed under the tongue. No water or swallowing is required for administration, and its packaging is thinner and smaller than a credit card, according to CEO Keith Kendall.
Its analysis showed that the epinephrine reaches maximum plasma concentration in about 15 minutes, with a Tmax range narrower than that of the EpiPen. “The results showed dosing with AQST-109 resulted in PK concentration and Tmax values comparable to published data from autoinjectors,” said John Oppenheimer, MD, of Rutgers University School of Medicine, in a prerecorded poster summary.
Aquestive aims to move forward to the manufacture of registration batches and a pivotal pharmacokinetic study in the second half of 2022. Mr. Lowenthal said ARS Pharmaceuticals is hoping for approval and launch of its nasal spray by summer 2023.
“Having a non-needle delivery device would help many people overcome that fear and hopefully increase use in anaphylaxis,” said David Stukus, MD, an allergist-immunologist and professor of clinical pediatrics at Nationwide Children’s Hospital, Columbus, who was not involved with any of the studies on EpiPen alternatives. And “it’s not just food allergy – anaphylaxis can occur from venom stings, medications, or idiopathic causes.”
Mr. Lowenthal is the CEO of ARS Pharmaceuticals. Mr. Kendall is CEO of Aquestive Therapeutics. Dr. Oppenheimer is a consultant for Aquestive, GSK, Amgen, Sanofi, and Aimmune and sits on Aquestive’s advisory board. Dr. Stukus is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
Longstanding anxiety around use of epinephrine autoinjectors has prompted research into alternative delivery routes for this life-saving medication. Several companies presented posters on their needle-free epinephrine products at the American Academy of Allergy, Asthma & Immunology (AAAAI) Annual Meeting.
Intranasal formulations are under development at ARS Pharmaceuticals (San Diego) and Bryn Pharma (Raleigh, N.C.). And Aquestive Therapeutics (Warren, N.J.) is working on a sublingual film that delivers epinephrine prodrug when applied under the tongue.
Epinephrine is essential for stopping life-threatening allergic reactions, yet patients often don’t carry their autoinjectors and many hesitate to use them. “It’s needle phobia,” said ARS Pharmaceuticals CEO Richard Lowenthal in an interview with this news organization. “They’re afraid to use it. They don’t like to inject their children, so they hesitate.”
Both nasal sprays reached maximal plasma concentration in 20-30 minutes. ARS Pharmaceuticals compared its intranasal product (Neffy 1 mg) against manual intramuscular injection (0.3 mg) and two autoinjectors (EpiPen 0.3 mg and Symjepi 0.3 mg) by analyzing data from multiple randomized crossover Phase 1 studies examining pharmacokinetics and pharmacodynamics in 175 healthy adults. In this integrated analysis, EpiPen was fastest (20 minutes) at reaching maximal concentration (Tmax), followed by Symjepi and Neffy (both 30 minutes) and epinephrine 0.3 mg IM (45 minutes). In a human factors analysis, ARS Pharmaceuticals reported that untrained participants were able to administer the Neffy spray to themselves or another participant safely and effectively during a simulated emergency scenario.
Bryn Pharma compared pharmacokinetics of its nasal spray product (BRYN-NDS1C 6.6 mg) when self-administered or administered by trained professionals and found comparable profiles for each. Tmax values were also similar: 21.63 minutes (trained professional) and 19.82 minutes (self-administered).
Aquestive Therapeutics is developing a postage stamp-sized product (AQST-109) that delivers epinephrine and begins dissolving when placed under the tongue. No water or swallowing is required for administration, and its packaging is thinner and smaller than a credit card, according to CEO Keith Kendall.
Its analysis showed that the epinephrine reaches maximum plasma concentration in about 15 minutes, with a Tmax range narrower than that of the EpiPen. “The results showed dosing with AQST-109 resulted in PK concentration and Tmax values comparable to published data from autoinjectors,” said John Oppenheimer, MD, of Rutgers University School of Medicine, in a prerecorded poster summary.
Aquestive aims to move forward to the manufacture of registration batches and a pivotal pharmacokinetic study in the second half of 2022. Mr. Lowenthal said ARS Pharmaceuticals is hoping for approval and launch of its nasal spray by summer 2023.
“Having a non-needle delivery device would help many people overcome that fear and hopefully increase use in anaphylaxis,” said David Stukus, MD, an allergist-immunologist and professor of clinical pediatrics at Nationwide Children’s Hospital, Columbus, who was not involved with any of the studies on EpiPen alternatives. And “it’s not just food allergy – anaphylaxis can occur from venom stings, medications, or idiopathic causes.”
Mr. Lowenthal is the CEO of ARS Pharmaceuticals. Mr. Kendall is CEO of Aquestive Therapeutics. Dr. Oppenheimer is a consultant for Aquestive, GSK, Amgen, Sanofi, and Aimmune and sits on Aquestive’s advisory board. Dr. Stukus is a consultant for Novartis.
A version of this article first appeared on Medscape.com.
FROM AAAAI
GI involvement may signal risk for MIS-C after COVID
While evaluating an adolescent who had endured a several-day history of vomiting and diarrhea, I mentioned the likelihood of a viral causation, including SARS-CoV-2 infection. His well-informed mother responded, “He has no respiratory symptoms. Does COVID cause GI disease?”
Indeed, not only is the gastrointestinal tract a potential portal of entry of the virus but it may well be the site of mediation of both local and remote injury and thus a harbinger of more severe clinical phenotypes.
As we learn more about the clinical spectrum of COVID, it is becoming increasingly clear that certain features of GI tract involvement may allow us to establish a timeline of the clinical course and perhaps predict the outcome.
The GI tract’s involvement isn’t surprising
The ways in which the GI tract serves as a target organ of SARS-CoV-2 have been postulated in the literature. In part, this is related to the presence of abundant receptors for SARS-CoV-2 cell binding and internalization. The virus uses angiotensin-converting enzyme 2 receptors to enter various cells. These receptors are highly expressed on not only lung cells but also enterocytes. Binding of SARS-CoV-2 to ACE2 receptors allows GI involvement, leading to microscopic mucosal inflammation, increased permeability, and altered intestinal absorption.
The clinical GI manifestations of this include anorexia, nausea, vomiting, diarrhea, and abdominal pain, which may be the earliest, or sole, symptoms of COVID-19, often noted before the onset of fever or respiratory symptoms. In fact, John Ong, MBBS, and colleagues, in a discussion about patients with primary GI SARS-CoV-2 infection and symptoms, use the term “GI-COVID.”
Clinical course of GI manifestations
After SARS-CoV-2 exposure, adults most commonly present with respiratory symptoms, with GI symptoms reported in 10%-15% of cases. However, the overall incidence of GI involvement during SARS-CoV-2 infection varies according to age, with children more likely than adults to manifest intestinal symptoms.
There are also differences in incidence reported when comparing hospitalized with nonhospitalized individuals. In early reports from the onset of the COVID-19 pandemic, 11%-43% of hospitalized adult patients manifested GI symptoms. Of note, the presence of GI symptoms was associated with more severe disease and thus predictive of outcomes in those admitted to hospitals.
In a multicenter study that assessed pediatric inpatients with COVID-19, GI manifestations were present in 57% of patients and were the first manifestation in 14%. Adjusted by confounding factors, those with GI symptoms had a higher risk for pediatric intensive care unit admission. Patients admitted to the PICU also had higher serum C-reactive protein and aspartate aminotransferase values.
Emerging data on MIS-C
In previously healthy children and adolescents, the severe, life-threatening complication of multisystem inflammatory syndrome in children (MIS-C) may present 2-6 weeks after acute infection with SARS-CoV-2. MIS-C appears to be an immune activation syndrome and is presumed to be the delayed immunologic sequelae of mild/asymptomatic SARS-CoV-2 infection. This response manifests as hyperinflammation in conjunction with a peak in antibody production a few weeks later.
One report of 186 children with MIS-C in the United States noted that the involved organ system included the GI tract in 92%, followed by cardiovascular in 80%, hematologic in 76%, mucocutaneous in 74%, and respiratory in 70%. Affected children were hospitalized for a median of 7 days, with 80% requiring intensive care, 20% receiving mechanical ventilation, and 48% receiving vasoactive support; 2% died. In a similar study of patients hospitalized in New York, 88% had GI symptoms (abdominal pain, vomiting, and/or diarrhea). A retrospective chart review of patients with MIS-C found that the majority had GI symptoms with any portion of the GI tract potentially involved, but ileal and colonic inflammation predominated.
Elizabeth Whittaker, MD, and colleagues described the clinical characteristics of children in eight hospitals in England who met criteria for MIS-C that were temporally associated with SARS-CoV-2. At presentation, all of the patients manifested fever and nonspecific GI symptoms, including vomiting (45%), abdominal pain (53%), and diarrhea (52%). During hospitalization, 50% developed shock with evidence of myocardial dysfunction.
Ermias D. Belay, MD, and colleagues described the clinical characteristics of a large cohort of patients with MIS-C that were reported to the U.S. Centers for Disease Control and Prevention. Of 1,733 patients identified, GI symptoms were reported in 53%-67%. Over half developed hypotension or shock and were admitted for intensive care. Younger children more frequently presented with abdominal pain in contrast with adolescents, who more frequently manifest respiratory symptoms.
In a multicenter retrospective study of Italian children with COVID-19 that was conducted from the onset of the pandemic to early 2021, GI symptoms were noted in 38%. These manifestations were mild and self-limiting, comparable to other viral intestinal infections. However, a subset of children (9.5%) had severe GI manifestations of MIS-C, defined as a medical and/or radiologic diagnosis of acute abdomen, appendicitis, intussusception, pancreatitis, abdominal fluid collection, or diffuse adenomesenteritis requiring surgical consultation. Overall, 42% of this group underwent surgery. The authors noted that the clinical presentation of abdominal pain, lymphopenia, and increased C-reactive protein and ferritin levels were associated with a 9- to 30-fold increased probability of these severe sequelae. In addition, the severity of the GI manifestations was correlated with age (5-10 years: overall response, 8.33; >10 years: OR, 6.37). Again, the presence of GI symptoms was a harbinger of hospitalization and PICU admission.
Given that GI symptoms are a common presentation of MIS-C, its diagnosis may be delayed as clinicians first consider other GI/viral infections, inflammatory bowel disease, or Kawasaki disease. Prompt identification of GI involvement and awareness of the potential outcomes may guide the management and improve the outcome.
These studies provide a clear picture of the differential presenting features of COVID-19 and MIS-C. Although there may be other environmental/genetic factors that govern the incidence, impact, and manifestations, COVID’s status as an ongoing pandemic gives these observations worldwide relevance. This is evident in a recent report documenting pronounced GI symptoms in African children with COVID-19.
It should be noted, however, that the published data cited here reflect the impact of the initial variants of SARS-CoV-2. The GI binding, effects, and aftermath of infection with the Delta and Omicron variants is not yet known.
Cause and effect, or simply coincidental?
Some insight into MIS-C pathogenesis was provided by Lael M. Yonker, MD, and colleagues in their analysis of biospecimens from 100 children: 19 with MIS-C, 26 with acute COVID-19, and 55 controls. They demonstrated that in children with MIS-C the prolonged presence of SARS-CoV-2 in the GI tract led to the release of zonulin, a biomarker of intestinal permeability, with subsequent trafficking of SARS-CoV-2 antigens into the bloodstream, leading to hyperinflammation. They were then able to decrease plasma SARS-CoV-2 spike antigen levels and inflammatory markers, with resulting clinical improvement after administration of larazotide, a zonulin antagonist.
These observations regarding the potential mechanism and triggers of MIS-C may offer biomarkers for early detection and/or strategies for prevention and treatment of MIS-C.
Bottom line
The GI tract is the target of an immune-mediated inflammatory response that is triggered by SARS-CoV-2, with MIS-C being the major manifestation of the resultant high degree of inflammation. These observations will allow an increased awareness of nonrespiratory symptoms of SARS-CoV-2 infection by clinicians working in emergency departments and primary care settings.
Clues that may enhance the ability of pediatric clinicians to recognize the potential for severe GI involvement include the occurrence of abdominal pain, leukopenia, and elevated inflammatory markers. Their presence should raise suspicion of MIS-C and lead to early evaluation.
Of note, COVID-19 mRNA vaccination is associated with a lower incidence of MIS-C in adolescents. This underscores the importance of COVID vaccination for all eligible children. Yet, we clearly have our work cut out for us. Of 107 children with MIS-C who were hospitalized in France, 31% were adolescents eligible for vaccination; however, none had been fully vaccinated. At the end of 2021, CDC data noted that less than 1% of vaccine-eligible children (12-17 years) were fully vaccinated.
The Pfizer-BioNTech vaccine is now authorized for receipt by children aged 5-11 years, the age group that is at highest risk for MIS-C. However, despite the approval of vaccines for these younger children, there is limited access in some parts of the United States at a time of rising incidence.
We look forward to broad availability of pediatric vaccination strategies. In addition, with the intense focus on safe and effective therapeutics for SARS-CoV-2 infection, we hope to soon have strategies to prevent and/or treat the life-threatening manifestations and long-term consequences of MIS-C. For example, the recently reported central role of the gut microbiota in immunity against SARS-CoV-2 infection offer the possibility that “microbiota modulation” may both reduce GI injury and enhance vaccine efficacy.
Dr. Balistreri has disclosed no relevant financial relationships.
William F. Balistreri, MD, is the Dorothy M.M. Kersten Professor of Pediatrics; director emeritus, Pediatric Liver Care Center; medical director emeritus, liver transplantation; and professor, University of Cincinnati College of Medicine, department of pediatrics, Cincinnati Children’s Hospital Medical Center. He has served as director of the division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s for 25 years and frequently covers gastroenterology, liver, and nutrition-related topics for this news organization. Dr Balistreri is currently editor-in-chief of the Journal of Pediatrics, having previously served as editor-in-chief of several journals and textbooks. He also became the first pediatrician to act as president of the American Association for the Study of Liver Diseases. In his spare time, he coaches youth lacrosse.
A version of this article first appeared on Medscape.com.
While evaluating an adolescent who had endured a several-day history of vomiting and diarrhea, I mentioned the likelihood of a viral causation, including SARS-CoV-2 infection. His well-informed mother responded, “He has no respiratory symptoms. Does COVID cause GI disease?”
Indeed, not only is the gastrointestinal tract a potential portal of entry of the virus but it may well be the site of mediation of both local and remote injury and thus a harbinger of more severe clinical phenotypes.
As we learn more about the clinical spectrum of COVID, it is becoming increasingly clear that certain features of GI tract involvement may allow us to establish a timeline of the clinical course and perhaps predict the outcome.
The GI tract’s involvement isn’t surprising
The ways in which the GI tract serves as a target organ of SARS-CoV-2 have been postulated in the literature. In part, this is related to the presence of abundant receptors for SARS-CoV-2 cell binding and internalization. The virus uses angiotensin-converting enzyme 2 receptors to enter various cells. These receptors are highly expressed on not only lung cells but also enterocytes. Binding of SARS-CoV-2 to ACE2 receptors allows GI involvement, leading to microscopic mucosal inflammation, increased permeability, and altered intestinal absorption.
The clinical GI manifestations of this include anorexia, nausea, vomiting, diarrhea, and abdominal pain, which may be the earliest, or sole, symptoms of COVID-19, often noted before the onset of fever or respiratory symptoms. In fact, John Ong, MBBS, and colleagues, in a discussion about patients with primary GI SARS-CoV-2 infection and symptoms, use the term “GI-COVID.”
Clinical course of GI manifestations
After SARS-CoV-2 exposure, adults most commonly present with respiratory symptoms, with GI symptoms reported in 10%-15% of cases. However, the overall incidence of GI involvement during SARS-CoV-2 infection varies according to age, with children more likely than adults to manifest intestinal symptoms.
There are also differences in incidence reported when comparing hospitalized with nonhospitalized individuals. In early reports from the onset of the COVID-19 pandemic, 11%-43% of hospitalized adult patients manifested GI symptoms. Of note, the presence of GI symptoms was associated with more severe disease and thus predictive of outcomes in those admitted to hospitals.
In a multicenter study that assessed pediatric inpatients with COVID-19, GI manifestations were present in 57% of patients and were the first manifestation in 14%. Adjusted by confounding factors, those with GI symptoms had a higher risk for pediatric intensive care unit admission. Patients admitted to the PICU also had higher serum C-reactive protein and aspartate aminotransferase values.
Emerging data on MIS-C
In previously healthy children and adolescents, the severe, life-threatening complication of multisystem inflammatory syndrome in children (MIS-C) may present 2-6 weeks after acute infection with SARS-CoV-2. MIS-C appears to be an immune activation syndrome and is presumed to be the delayed immunologic sequelae of mild/asymptomatic SARS-CoV-2 infection. This response manifests as hyperinflammation in conjunction with a peak in antibody production a few weeks later.
One report of 186 children with MIS-C in the United States noted that the involved organ system included the GI tract in 92%, followed by cardiovascular in 80%, hematologic in 76%, mucocutaneous in 74%, and respiratory in 70%. Affected children were hospitalized for a median of 7 days, with 80% requiring intensive care, 20% receiving mechanical ventilation, and 48% receiving vasoactive support; 2% died. In a similar study of patients hospitalized in New York, 88% had GI symptoms (abdominal pain, vomiting, and/or diarrhea). A retrospective chart review of patients with MIS-C found that the majority had GI symptoms with any portion of the GI tract potentially involved, but ileal and colonic inflammation predominated.
Elizabeth Whittaker, MD, and colleagues described the clinical characteristics of children in eight hospitals in England who met criteria for MIS-C that were temporally associated with SARS-CoV-2. At presentation, all of the patients manifested fever and nonspecific GI symptoms, including vomiting (45%), abdominal pain (53%), and diarrhea (52%). During hospitalization, 50% developed shock with evidence of myocardial dysfunction.
Ermias D. Belay, MD, and colleagues described the clinical characteristics of a large cohort of patients with MIS-C that were reported to the U.S. Centers for Disease Control and Prevention. Of 1,733 patients identified, GI symptoms were reported in 53%-67%. Over half developed hypotension or shock and were admitted for intensive care. Younger children more frequently presented with abdominal pain in contrast with adolescents, who more frequently manifest respiratory symptoms.
In a multicenter retrospective study of Italian children with COVID-19 that was conducted from the onset of the pandemic to early 2021, GI symptoms were noted in 38%. These manifestations were mild and self-limiting, comparable to other viral intestinal infections. However, a subset of children (9.5%) had severe GI manifestations of MIS-C, defined as a medical and/or radiologic diagnosis of acute abdomen, appendicitis, intussusception, pancreatitis, abdominal fluid collection, or diffuse adenomesenteritis requiring surgical consultation. Overall, 42% of this group underwent surgery. The authors noted that the clinical presentation of abdominal pain, lymphopenia, and increased C-reactive protein and ferritin levels were associated with a 9- to 30-fold increased probability of these severe sequelae. In addition, the severity of the GI manifestations was correlated with age (5-10 years: overall response, 8.33; >10 years: OR, 6.37). Again, the presence of GI symptoms was a harbinger of hospitalization and PICU admission.
Given that GI symptoms are a common presentation of MIS-C, its diagnosis may be delayed as clinicians first consider other GI/viral infections, inflammatory bowel disease, or Kawasaki disease. Prompt identification of GI involvement and awareness of the potential outcomes may guide the management and improve the outcome.
These studies provide a clear picture of the differential presenting features of COVID-19 and MIS-C. Although there may be other environmental/genetic factors that govern the incidence, impact, and manifestations, COVID’s status as an ongoing pandemic gives these observations worldwide relevance. This is evident in a recent report documenting pronounced GI symptoms in African children with COVID-19.
It should be noted, however, that the published data cited here reflect the impact of the initial variants of SARS-CoV-2. The GI binding, effects, and aftermath of infection with the Delta and Omicron variants is not yet known.
Cause and effect, or simply coincidental?
Some insight into MIS-C pathogenesis was provided by Lael M. Yonker, MD, and colleagues in their analysis of biospecimens from 100 children: 19 with MIS-C, 26 with acute COVID-19, and 55 controls. They demonstrated that in children with MIS-C the prolonged presence of SARS-CoV-2 in the GI tract led to the release of zonulin, a biomarker of intestinal permeability, with subsequent trafficking of SARS-CoV-2 antigens into the bloodstream, leading to hyperinflammation. They were then able to decrease plasma SARS-CoV-2 spike antigen levels and inflammatory markers, with resulting clinical improvement after administration of larazotide, a zonulin antagonist.
These observations regarding the potential mechanism and triggers of MIS-C may offer biomarkers for early detection and/or strategies for prevention and treatment of MIS-C.
Bottom line
The GI tract is the target of an immune-mediated inflammatory response that is triggered by SARS-CoV-2, with MIS-C being the major manifestation of the resultant high degree of inflammation. These observations will allow an increased awareness of nonrespiratory symptoms of SARS-CoV-2 infection by clinicians working in emergency departments and primary care settings.
Clues that may enhance the ability of pediatric clinicians to recognize the potential for severe GI involvement include the occurrence of abdominal pain, leukopenia, and elevated inflammatory markers. Their presence should raise suspicion of MIS-C and lead to early evaluation.
Of note, COVID-19 mRNA vaccination is associated with a lower incidence of MIS-C in adolescents. This underscores the importance of COVID vaccination for all eligible children. Yet, we clearly have our work cut out for us. Of 107 children with MIS-C who were hospitalized in France, 31% were adolescents eligible for vaccination; however, none had been fully vaccinated. At the end of 2021, CDC data noted that less than 1% of vaccine-eligible children (12-17 years) were fully vaccinated.
The Pfizer-BioNTech vaccine is now authorized for receipt by children aged 5-11 years, the age group that is at highest risk for MIS-C. However, despite the approval of vaccines for these younger children, there is limited access in some parts of the United States at a time of rising incidence.
We look forward to broad availability of pediatric vaccination strategies. In addition, with the intense focus on safe and effective therapeutics for SARS-CoV-2 infection, we hope to soon have strategies to prevent and/or treat the life-threatening manifestations and long-term consequences of MIS-C. For example, the recently reported central role of the gut microbiota in immunity against SARS-CoV-2 infection offer the possibility that “microbiota modulation” may both reduce GI injury and enhance vaccine efficacy.
Dr. Balistreri has disclosed no relevant financial relationships.
William F. Balistreri, MD, is the Dorothy M.M. Kersten Professor of Pediatrics; director emeritus, Pediatric Liver Care Center; medical director emeritus, liver transplantation; and professor, University of Cincinnati College of Medicine, department of pediatrics, Cincinnati Children’s Hospital Medical Center. He has served as director of the division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s for 25 years and frequently covers gastroenterology, liver, and nutrition-related topics for this news organization. Dr Balistreri is currently editor-in-chief of the Journal of Pediatrics, having previously served as editor-in-chief of several journals and textbooks. He also became the first pediatrician to act as president of the American Association for the Study of Liver Diseases. In his spare time, he coaches youth lacrosse.
A version of this article first appeared on Medscape.com.
While evaluating an adolescent who had endured a several-day history of vomiting and diarrhea, I mentioned the likelihood of a viral causation, including SARS-CoV-2 infection. His well-informed mother responded, “He has no respiratory symptoms. Does COVID cause GI disease?”
Indeed, not only is the gastrointestinal tract a potential portal of entry of the virus but it may well be the site of mediation of both local and remote injury and thus a harbinger of more severe clinical phenotypes.
As we learn more about the clinical spectrum of COVID, it is becoming increasingly clear that certain features of GI tract involvement may allow us to establish a timeline of the clinical course and perhaps predict the outcome.
The GI tract’s involvement isn’t surprising
The ways in which the GI tract serves as a target organ of SARS-CoV-2 have been postulated in the literature. In part, this is related to the presence of abundant receptors for SARS-CoV-2 cell binding and internalization. The virus uses angiotensin-converting enzyme 2 receptors to enter various cells. These receptors are highly expressed on not only lung cells but also enterocytes. Binding of SARS-CoV-2 to ACE2 receptors allows GI involvement, leading to microscopic mucosal inflammation, increased permeability, and altered intestinal absorption.
The clinical GI manifestations of this include anorexia, nausea, vomiting, diarrhea, and abdominal pain, which may be the earliest, or sole, symptoms of COVID-19, often noted before the onset of fever or respiratory symptoms. In fact, John Ong, MBBS, and colleagues, in a discussion about patients with primary GI SARS-CoV-2 infection and symptoms, use the term “GI-COVID.”
Clinical course of GI manifestations
After SARS-CoV-2 exposure, adults most commonly present with respiratory symptoms, with GI symptoms reported in 10%-15% of cases. However, the overall incidence of GI involvement during SARS-CoV-2 infection varies according to age, with children more likely than adults to manifest intestinal symptoms.
There are also differences in incidence reported when comparing hospitalized with nonhospitalized individuals. In early reports from the onset of the COVID-19 pandemic, 11%-43% of hospitalized adult patients manifested GI symptoms. Of note, the presence of GI symptoms was associated with more severe disease and thus predictive of outcomes in those admitted to hospitals.
In a multicenter study that assessed pediatric inpatients with COVID-19, GI manifestations were present in 57% of patients and were the first manifestation in 14%. Adjusted by confounding factors, those with GI symptoms had a higher risk for pediatric intensive care unit admission. Patients admitted to the PICU also had higher serum C-reactive protein and aspartate aminotransferase values.
Emerging data on MIS-C
In previously healthy children and adolescents, the severe, life-threatening complication of multisystem inflammatory syndrome in children (MIS-C) may present 2-6 weeks after acute infection with SARS-CoV-2. MIS-C appears to be an immune activation syndrome and is presumed to be the delayed immunologic sequelae of mild/asymptomatic SARS-CoV-2 infection. This response manifests as hyperinflammation in conjunction with a peak in antibody production a few weeks later.
One report of 186 children with MIS-C in the United States noted that the involved organ system included the GI tract in 92%, followed by cardiovascular in 80%, hematologic in 76%, mucocutaneous in 74%, and respiratory in 70%. Affected children were hospitalized for a median of 7 days, with 80% requiring intensive care, 20% receiving mechanical ventilation, and 48% receiving vasoactive support; 2% died. In a similar study of patients hospitalized in New York, 88% had GI symptoms (abdominal pain, vomiting, and/or diarrhea). A retrospective chart review of patients with MIS-C found that the majority had GI symptoms with any portion of the GI tract potentially involved, but ileal and colonic inflammation predominated.
Elizabeth Whittaker, MD, and colleagues described the clinical characteristics of children in eight hospitals in England who met criteria for MIS-C that were temporally associated with SARS-CoV-2. At presentation, all of the patients manifested fever and nonspecific GI symptoms, including vomiting (45%), abdominal pain (53%), and diarrhea (52%). During hospitalization, 50% developed shock with evidence of myocardial dysfunction.
Ermias D. Belay, MD, and colleagues described the clinical characteristics of a large cohort of patients with MIS-C that were reported to the U.S. Centers for Disease Control and Prevention. Of 1,733 patients identified, GI symptoms were reported in 53%-67%. Over half developed hypotension or shock and were admitted for intensive care. Younger children more frequently presented with abdominal pain in contrast with adolescents, who more frequently manifest respiratory symptoms.
In a multicenter retrospective study of Italian children with COVID-19 that was conducted from the onset of the pandemic to early 2021, GI symptoms were noted in 38%. These manifestations were mild and self-limiting, comparable to other viral intestinal infections. However, a subset of children (9.5%) had severe GI manifestations of MIS-C, defined as a medical and/or radiologic diagnosis of acute abdomen, appendicitis, intussusception, pancreatitis, abdominal fluid collection, or diffuse adenomesenteritis requiring surgical consultation. Overall, 42% of this group underwent surgery. The authors noted that the clinical presentation of abdominal pain, lymphopenia, and increased C-reactive protein and ferritin levels were associated with a 9- to 30-fold increased probability of these severe sequelae. In addition, the severity of the GI manifestations was correlated with age (5-10 years: overall response, 8.33; >10 years: OR, 6.37). Again, the presence of GI symptoms was a harbinger of hospitalization and PICU admission.
Given that GI symptoms are a common presentation of MIS-C, its diagnosis may be delayed as clinicians first consider other GI/viral infections, inflammatory bowel disease, or Kawasaki disease. Prompt identification of GI involvement and awareness of the potential outcomes may guide the management and improve the outcome.
These studies provide a clear picture of the differential presenting features of COVID-19 and MIS-C. Although there may be other environmental/genetic factors that govern the incidence, impact, and manifestations, COVID’s status as an ongoing pandemic gives these observations worldwide relevance. This is evident in a recent report documenting pronounced GI symptoms in African children with COVID-19.
It should be noted, however, that the published data cited here reflect the impact of the initial variants of SARS-CoV-2. The GI binding, effects, and aftermath of infection with the Delta and Omicron variants is not yet known.
Cause and effect, or simply coincidental?
Some insight into MIS-C pathogenesis was provided by Lael M. Yonker, MD, and colleagues in their analysis of biospecimens from 100 children: 19 with MIS-C, 26 with acute COVID-19, and 55 controls. They demonstrated that in children with MIS-C the prolonged presence of SARS-CoV-2 in the GI tract led to the release of zonulin, a biomarker of intestinal permeability, with subsequent trafficking of SARS-CoV-2 antigens into the bloodstream, leading to hyperinflammation. They were then able to decrease plasma SARS-CoV-2 spike antigen levels and inflammatory markers, with resulting clinical improvement after administration of larazotide, a zonulin antagonist.
These observations regarding the potential mechanism and triggers of MIS-C may offer biomarkers for early detection and/or strategies for prevention and treatment of MIS-C.
Bottom line
The GI tract is the target of an immune-mediated inflammatory response that is triggered by SARS-CoV-2, with MIS-C being the major manifestation of the resultant high degree of inflammation. These observations will allow an increased awareness of nonrespiratory symptoms of SARS-CoV-2 infection by clinicians working in emergency departments and primary care settings.
Clues that may enhance the ability of pediatric clinicians to recognize the potential for severe GI involvement include the occurrence of abdominal pain, leukopenia, and elevated inflammatory markers. Their presence should raise suspicion of MIS-C and lead to early evaluation.
Of note, COVID-19 mRNA vaccination is associated with a lower incidence of MIS-C in adolescents. This underscores the importance of COVID vaccination for all eligible children. Yet, we clearly have our work cut out for us. Of 107 children with MIS-C who were hospitalized in France, 31% were adolescents eligible for vaccination; however, none had been fully vaccinated. At the end of 2021, CDC data noted that less than 1% of vaccine-eligible children (12-17 years) were fully vaccinated.
The Pfizer-BioNTech vaccine is now authorized for receipt by children aged 5-11 years, the age group that is at highest risk for MIS-C. However, despite the approval of vaccines for these younger children, there is limited access in some parts of the United States at a time of rising incidence.
We look forward to broad availability of pediatric vaccination strategies. In addition, with the intense focus on safe and effective therapeutics for SARS-CoV-2 infection, we hope to soon have strategies to prevent and/or treat the life-threatening manifestations and long-term consequences of MIS-C. For example, the recently reported central role of the gut microbiota in immunity against SARS-CoV-2 infection offer the possibility that “microbiota modulation” may both reduce GI injury and enhance vaccine efficacy.
Dr. Balistreri has disclosed no relevant financial relationships.
William F. Balistreri, MD, is the Dorothy M.M. Kersten Professor of Pediatrics; director emeritus, Pediatric Liver Care Center; medical director emeritus, liver transplantation; and professor, University of Cincinnati College of Medicine, department of pediatrics, Cincinnati Children’s Hospital Medical Center. He has served as director of the division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s for 25 years and frequently covers gastroenterology, liver, and nutrition-related topics for this news organization. Dr Balistreri is currently editor-in-chief of the Journal of Pediatrics, having previously served as editor-in-chief of several journals and textbooks. He also became the first pediatrician to act as president of the American Association for the Study of Liver Diseases. In his spare time, he coaches youth lacrosse.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases down to pre-Omicron level
New cases of COVID-19 in U.S. children dropped for the fifth consecutive week, but the rate of decline slowed considerably, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The national count of new cases has now fallen for five straight weeks since peaking Jan. 14-20, and this week’s figure is the lowest since the pre-Omicron days of mid-November, based on data collected by the AAP and CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.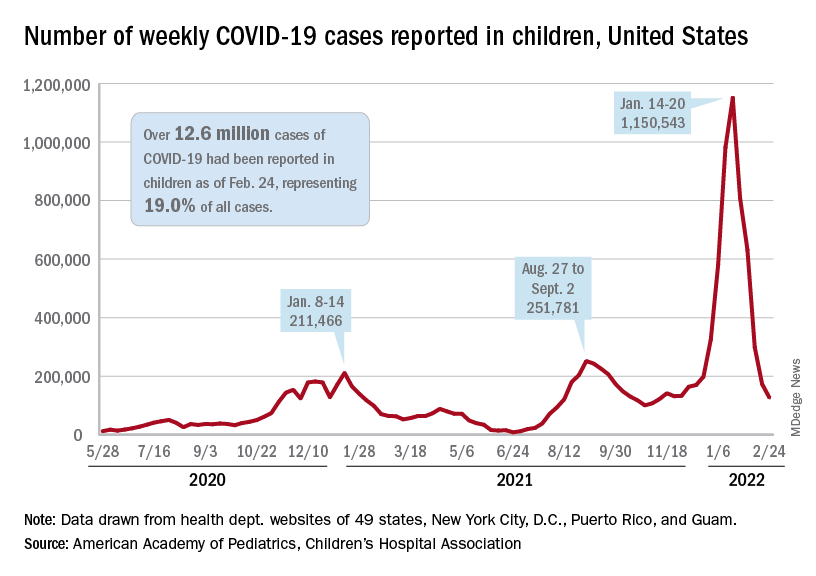
Over 12.6 million pediatric cases have been reported by those jurisdictions since the start of the pandemic, representing 19.0% of all cases in the United States, the AAP and CHA said in their weekly COVID report.
The highest cumulative rate among the states, 27.5%, can be found in Vermont, followed by New Hampshire (26.7%) and Alaska (26.6%). Alabama’s 12.1% is lower than any other jurisdiction, but the state stopped reporting during the summer of 2021, just as the Delta surge was beginning. The next two lowest states, Florida (12.8%) and Utah (13.9%), both define children as those aged 0-14 years, so the state with the lowest rate and no qualifiers is Idaho at 14.3%, the AAP/CHA data show.
The downward trend in new cases is reflected in other national measures. The daily rate of new hospital admissions for children aged 0-17 years was 0.32 per 100,000 population on Feb. 26, which is a drop of 75% since admissions peaked at 1.25 per 100,000 on Jan. 15, according to the Centers for Disease Control and Prevention.
The most recent 7-day average (Feb. 20-26) for child admissions with confirmed COVID-19 was 237 per day, compared with 914 per day during the peak week of Jan. 10-16. Emergency department visits with diagnosed COVID, measured as a percentage of all ED visits by age group, are down even more. The 7-day average was 1.2% on Feb. 25 for children aged 0-11 years, compared with a peak of 13.9% in mid-January, the CDC said on its COVID Data Tracker. The current rates for older children are even lower.
The decline of the Omicron surge over the last few weeks is allowing states to end mask mandates in schools around the country. The governors of California, Oregon, and Washington just announced that their states will be lifting their mask requirements on March 11, and New York State will end its mandate on March 2, while New York City is scheduled to go mask-free as of March 7, according to District Administration.
Those types of government moves, however, do not seem to be entirely supported by the public. In a survey conducted Feb. 9-21 by the Kaiser Family Foundation, 43% of the 1,502 respondents said that all students and staff should be required to wear masks in schools, while 40% said that there should be no mask requirements at all.
New cases of COVID-19 in U.S. children dropped for the fifth consecutive week, but the rate of decline slowed considerably, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The national count of new cases has now fallen for five straight weeks since peaking Jan. 14-20, and this week’s figure is the lowest since the pre-Omicron days of mid-November, based on data collected by the AAP and CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.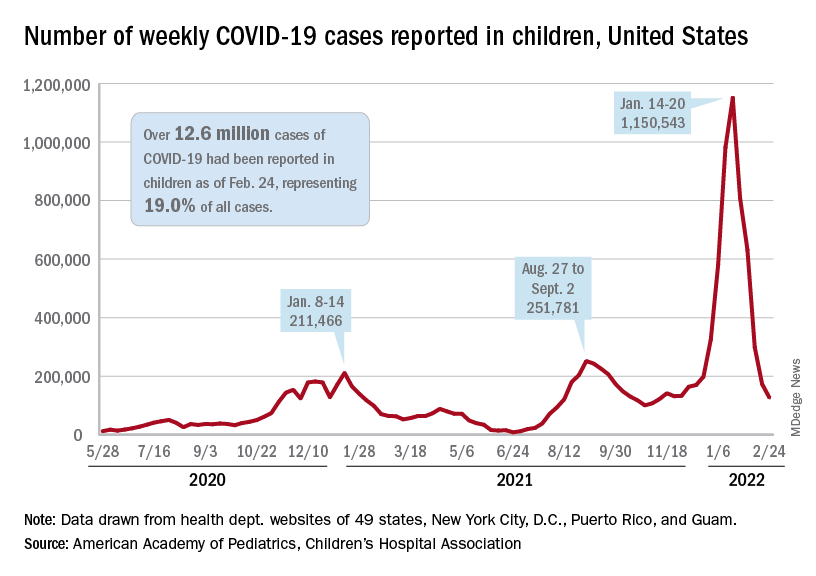
Over 12.6 million pediatric cases have been reported by those jurisdictions since the start of the pandemic, representing 19.0% of all cases in the United States, the AAP and CHA said in their weekly COVID report.
The highest cumulative rate among the states, 27.5%, can be found in Vermont, followed by New Hampshire (26.7%) and Alaska (26.6%). Alabama’s 12.1% is lower than any other jurisdiction, but the state stopped reporting during the summer of 2021, just as the Delta surge was beginning. The next two lowest states, Florida (12.8%) and Utah (13.9%), both define children as those aged 0-14 years, so the state with the lowest rate and no qualifiers is Idaho at 14.3%, the AAP/CHA data show.
The downward trend in new cases is reflected in other national measures. The daily rate of new hospital admissions for children aged 0-17 years was 0.32 per 100,000 population on Feb. 26, which is a drop of 75% since admissions peaked at 1.25 per 100,000 on Jan. 15, according to the Centers for Disease Control and Prevention.
The most recent 7-day average (Feb. 20-26) for child admissions with confirmed COVID-19 was 237 per day, compared with 914 per day during the peak week of Jan. 10-16. Emergency department visits with diagnosed COVID, measured as a percentage of all ED visits by age group, are down even more. The 7-day average was 1.2% on Feb. 25 for children aged 0-11 years, compared with a peak of 13.9% in mid-January, the CDC said on its COVID Data Tracker. The current rates for older children are even lower.
The decline of the Omicron surge over the last few weeks is allowing states to end mask mandates in schools around the country. The governors of California, Oregon, and Washington just announced that their states will be lifting their mask requirements on March 11, and New York State will end its mandate on March 2, while New York City is scheduled to go mask-free as of March 7, according to District Administration.
Those types of government moves, however, do not seem to be entirely supported by the public. In a survey conducted Feb. 9-21 by the Kaiser Family Foundation, 43% of the 1,502 respondents said that all students and staff should be required to wear masks in schools, while 40% said that there should be no mask requirements at all.
New cases of COVID-19 in U.S. children dropped for the fifth consecutive week, but the rate of decline slowed considerably, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The national count of new cases has now fallen for five straight weeks since peaking Jan. 14-20, and this week’s figure is the lowest since the pre-Omicron days of mid-November, based on data collected by the AAP and CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.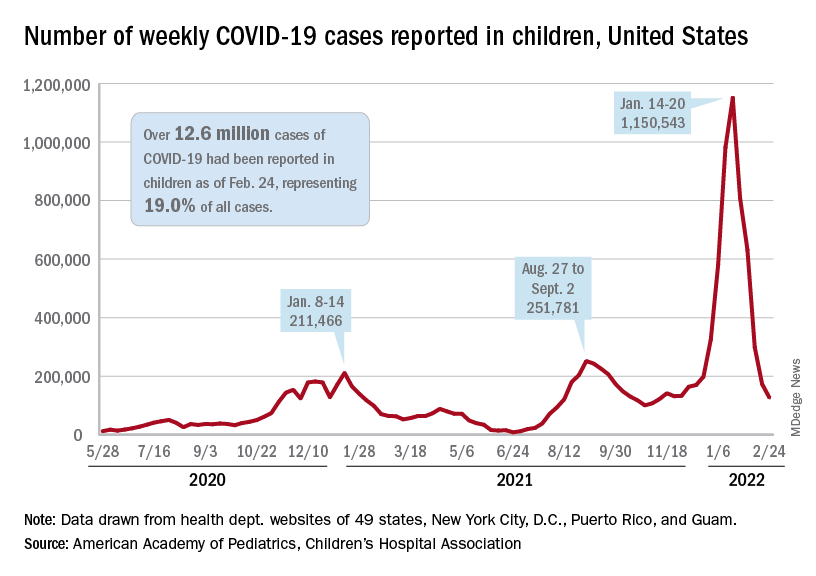
Over 12.6 million pediatric cases have been reported by those jurisdictions since the start of the pandemic, representing 19.0% of all cases in the United States, the AAP and CHA said in their weekly COVID report.
The highest cumulative rate among the states, 27.5%, can be found in Vermont, followed by New Hampshire (26.7%) and Alaska (26.6%). Alabama’s 12.1% is lower than any other jurisdiction, but the state stopped reporting during the summer of 2021, just as the Delta surge was beginning. The next two lowest states, Florida (12.8%) and Utah (13.9%), both define children as those aged 0-14 years, so the state with the lowest rate and no qualifiers is Idaho at 14.3%, the AAP/CHA data show.
The downward trend in new cases is reflected in other national measures. The daily rate of new hospital admissions for children aged 0-17 years was 0.32 per 100,000 population on Feb. 26, which is a drop of 75% since admissions peaked at 1.25 per 100,000 on Jan. 15, according to the Centers for Disease Control and Prevention.
The most recent 7-day average (Feb. 20-26) for child admissions with confirmed COVID-19 was 237 per day, compared with 914 per day during the peak week of Jan. 10-16. Emergency department visits with diagnosed COVID, measured as a percentage of all ED visits by age group, are down even more. The 7-day average was 1.2% on Feb. 25 for children aged 0-11 years, compared with a peak of 13.9% in mid-January, the CDC said on its COVID Data Tracker. The current rates for older children are even lower.
The decline of the Omicron surge over the last few weeks is allowing states to end mask mandates in schools around the country. The governors of California, Oregon, and Washington just announced that their states will be lifting their mask requirements on March 11, and New York State will end its mandate on March 2, while New York City is scheduled to go mask-free as of March 7, according to District Administration.
Those types of government moves, however, do not seem to be entirely supported by the public. In a survey conducted Feb. 9-21 by the Kaiser Family Foundation, 43% of the 1,502 respondents said that all students and staff should be required to wear masks in schools, while 40% said that there should be no mask requirements at all.