User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Seniors face higher risk of other medical conditions after COVID-19
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
FROM BMJ
Heavy cannabis use tied to less diabetes in women
Women who used marijuana (cannabis) at least four times in the previous month (heavy users) were less likely to have type 2 diabetes than women who were light users or nonusers, in a nationally representative U.S. observational study.
In contrast, there were no differences in the prevalence of type 2 diabetes in men who were light or heavy cannabis users versus nonusers.
These findings are based on data from the 2013-2018 National Health and Nutrition Examination Survey (NHANES), whereby participants self-reported their cannabis use.
The study by Ayobami S. Ogunsola, MD, MPH, a graduate student at Texas A&M University, College Station, and colleagues was recently published in Cannabis and Cannabinoid Research.
What do the findings mean?
Although overall findings linking cannabis use and diabetes have been inconsistent, the gender differences in the current study are consistent with animal studies and some clinical studies, senior author Ibraheem M. Karaye, MD, MPH, said in an interview.
However, these gender differences need to be confirmed, and “we strongly recommend that more biological or biochemical studies be conducted that could actually tell us the mechanisms,” said Dr. Karaye, an assistant professor in the department of population health, Hofstra University, Hempstead, N.Y.
“It’s indisputable that medical marijuana has some medical benefits,” he added. “Women [who use cannabis] have been shown to lose more weight than men, for example.”
“If women [cannabis users] are less likely to develop diabetes or more likely to express improvement of symptoms of diabetes,” he noted, “this means that hyperglycemic medications that are being prescribed should be watched scrupulously. Otherwise, there is a risk that [women] may overrespond.”
That is, Dr. Karaye continued, women “may be at risk of developing hypoglycemia because the cannabis is acting synergistically with the regular drug that is being used to treat the diabetes.”
U.S. clinicians, especially in states with legalized medical marijuana, need to be aware of the potential synergy.
“One would have to consider the patient as a whole,” he stressed. “For example, a woman that uses medical marijuana may actually respond differently to hyperglycemic medication.”
Conflicting reports explained by sex differences?
Evidence on whether cannabis use is linked with type 2 diabetes is limited and conflicting, the researchers wrote. They hypothesized that these conflicting findings might be explained by sex differences.
To “help inform current diabetes prevention and mitigation efforts,” they investigated sex differences in cannabis use and prevalence of type 2 diabetes in 15,602 men and women in the 2013-2014, 2015-2016, and 2017-2018 NHANES surveys.
Participants were classified as having type 2 diabetes if they had a physician’s diagnosis; a 2-hour plasma glucose of at least 200 mg/dL (in a glucose tolerance test); fasting blood glucose of at least 126 mg/dL; or A1c of at least 6.5%.
About half of respondents were women (52%) and close to half (44%) were age 18-39.
More than a third (38%) had a body mass index (BMI) of at least 30 kg/m2, indicating obesity.
Roughly 1 in 10 had a diagnosis of type 2 diabetes (13.5%) or A1c of at least 6.5% (9.8%).
Close to a fifth smoked cigarettes (16%). Similarly, 14.5% used cannabis at least four times a week, 3.3% used it less often, and the rest did not use it. Half of participants were not physically active (49%).
Just over half had at least a college education (55%).
Heavy cannabis users were more likely to be younger than age 40 (57% of men, 57% of women), college graduates (54% of men, 63% of women), cigarette smokers (79% of men, 83% of women), and physically inactive (39% of men, 49% of women).
Among women, heavy cannabis users were 49% less likely to have type 2 diabetes than nonusers, after adjusting for age, sex, race/ethnicity, educational level, physical activity, tobacco use, alcohol use, marital status, difficulty walking, employment status, income, and BMI (adjusted odds ratio, 0.51; 95% confidence interval, 0.31-0.84).
There were no significant differences between light cannabis users versus nonusers and diabetes prevalence in women, or between light or heavy cannabis users versus nonusers and diabetes prevalence in men.
Limitations, yet biologically plausible
The researchers acknowledged several study limitations.
They do not know how long participants had used marijuana. The men and women may have underreported their cannabis use, especially in states where medical marijuana was not legal, and the NHANES data did not specify whether the cannabis was recreational or medicinal.
The study may have been underpowered to detect a smaller difference in men who used versus did not use marijuana.
And importantly, this was an observational study (a snapshot at one point in time), so it cannot say whether the heavy cannabis use in women caused a decreased likelihood of diabetes.
Nevertheless, the inverse association between cannabis use and presence of type 2 diabetes is biologically plausible, Dr. Ogunsola and colleagues wrote.
The two major cannabis compounds, cannabidiol and delta-9-tetrahydrocannabinol, stimulate CBD1 and CBD2 receptors in the central and peripheral nervous systems, respectively. And “activation of the CBD1 receptor increases insulin secretion, glucagon, and somatostatin, and activates metabolic processes in fat and skeletal muscles – mechanisms that improve glucose disposal,” they explained.
The researchers speculated that the sex differences they found for this association may be caused by differences in sex hormones, or the endocannabinoid system, or fat deposits.
Therefore, “additional studies are needed to investigate the sex-based heterogeneity reported in this study and to elucidate potential mechanisms for the observation,” they concluded.
The study did not receive any funding and the researchers have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Women who used marijuana (cannabis) at least four times in the previous month (heavy users) were less likely to have type 2 diabetes than women who were light users or nonusers, in a nationally representative U.S. observational study.
In contrast, there were no differences in the prevalence of type 2 diabetes in men who were light or heavy cannabis users versus nonusers.
These findings are based on data from the 2013-2018 National Health and Nutrition Examination Survey (NHANES), whereby participants self-reported their cannabis use.
The study by Ayobami S. Ogunsola, MD, MPH, a graduate student at Texas A&M University, College Station, and colleagues was recently published in Cannabis and Cannabinoid Research.
What do the findings mean?
Although overall findings linking cannabis use and diabetes have been inconsistent, the gender differences in the current study are consistent with animal studies and some clinical studies, senior author Ibraheem M. Karaye, MD, MPH, said in an interview.
However, these gender differences need to be confirmed, and “we strongly recommend that more biological or biochemical studies be conducted that could actually tell us the mechanisms,” said Dr. Karaye, an assistant professor in the department of population health, Hofstra University, Hempstead, N.Y.
“It’s indisputable that medical marijuana has some medical benefits,” he added. “Women [who use cannabis] have been shown to lose more weight than men, for example.”
“If women [cannabis users] are less likely to develop diabetes or more likely to express improvement of symptoms of diabetes,” he noted, “this means that hyperglycemic medications that are being prescribed should be watched scrupulously. Otherwise, there is a risk that [women] may overrespond.”
That is, Dr. Karaye continued, women “may be at risk of developing hypoglycemia because the cannabis is acting synergistically with the regular drug that is being used to treat the diabetes.”
U.S. clinicians, especially in states with legalized medical marijuana, need to be aware of the potential synergy.
“One would have to consider the patient as a whole,” he stressed. “For example, a woman that uses medical marijuana may actually respond differently to hyperglycemic medication.”
Conflicting reports explained by sex differences?
Evidence on whether cannabis use is linked with type 2 diabetes is limited and conflicting, the researchers wrote. They hypothesized that these conflicting findings might be explained by sex differences.
To “help inform current diabetes prevention and mitigation efforts,” they investigated sex differences in cannabis use and prevalence of type 2 diabetes in 15,602 men and women in the 2013-2014, 2015-2016, and 2017-2018 NHANES surveys.
Participants were classified as having type 2 diabetes if they had a physician’s diagnosis; a 2-hour plasma glucose of at least 200 mg/dL (in a glucose tolerance test); fasting blood glucose of at least 126 mg/dL; or A1c of at least 6.5%.
About half of respondents were women (52%) and close to half (44%) were age 18-39.
More than a third (38%) had a body mass index (BMI) of at least 30 kg/m2, indicating obesity.
Roughly 1 in 10 had a diagnosis of type 2 diabetes (13.5%) or A1c of at least 6.5% (9.8%).
Close to a fifth smoked cigarettes (16%). Similarly, 14.5% used cannabis at least four times a week, 3.3% used it less often, and the rest did not use it. Half of participants were not physically active (49%).
Just over half had at least a college education (55%).
Heavy cannabis users were more likely to be younger than age 40 (57% of men, 57% of women), college graduates (54% of men, 63% of women), cigarette smokers (79% of men, 83% of women), and physically inactive (39% of men, 49% of women).
Among women, heavy cannabis users were 49% less likely to have type 2 diabetes than nonusers, after adjusting for age, sex, race/ethnicity, educational level, physical activity, tobacco use, alcohol use, marital status, difficulty walking, employment status, income, and BMI (adjusted odds ratio, 0.51; 95% confidence interval, 0.31-0.84).
There were no significant differences between light cannabis users versus nonusers and diabetes prevalence in women, or between light or heavy cannabis users versus nonusers and diabetes prevalence in men.
Limitations, yet biologically plausible
The researchers acknowledged several study limitations.
They do not know how long participants had used marijuana. The men and women may have underreported their cannabis use, especially in states where medical marijuana was not legal, and the NHANES data did not specify whether the cannabis was recreational or medicinal.
The study may have been underpowered to detect a smaller difference in men who used versus did not use marijuana.
And importantly, this was an observational study (a snapshot at one point in time), so it cannot say whether the heavy cannabis use in women caused a decreased likelihood of diabetes.
Nevertheless, the inverse association between cannabis use and presence of type 2 diabetes is biologically plausible, Dr. Ogunsola and colleagues wrote.
The two major cannabis compounds, cannabidiol and delta-9-tetrahydrocannabinol, stimulate CBD1 and CBD2 receptors in the central and peripheral nervous systems, respectively. And “activation of the CBD1 receptor increases insulin secretion, glucagon, and somatostatin, and activates metabolic processes in fat and skeletal muscles – mechanisms that improve glucose disposal,” they explained.
The researchers speculated that the sex differences they found for this association may be caused by differences in sex hormones, or the endocannabinoid system, or fat deposits.
Therefore, “additional studies are needed to investigate the sex-based heterogeneity reported in this study and to elucidate potential mechanisms for the observation,” they concluded.
The study did not receive any funding and the researchers have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Women who used marijuana (cannabis) at least four times in the previous month (heavy users) were less likely to have type 2 diabetes than women who were light users or nonusers, in a nationally representative U.S. observational study.
In contrast, there were no differences in the prevalence of type 2 diabetes in men who were light or heavy cannabis users versus nonusers.
These findings are based on data from the 2013-2018 National Health and Nutrition Examination Survey (NHANES), whereby participants self-reported their cannabis use.
The study by Ayobami S. Ogunsola, MD, MPH, a graduate student at Texas A&M University, College Station, and colleagues was recently published in Cannabis and Cannabinoid Research.
What do the findings mean?
Although overall findings linking cannabis use and diabetes have been inconsistent, the gender differences in the current study are consistent with animal studies and some clinical studies, senior author Ibraheem M. Karaye, MD, MPH, said in an interview.
However, these gender differences need to be confirmed, and “we strongly recommend that more biological or biochemical studies be conducted that could actually tell us the mechanisms,” said Dr. Karaye, an assistant professor in the department of population health, Hofstra University, Hempstead, N.Y.
“It’s indisputable that medical marijuana has some medical benefits,” he added. “Women [who use cannabis] have been shown to lose more weight than men, for example.”
“If women [cannabis users] are less likely to develop diabetes or more likely to express improvement of symptoms of diabetes,” he noted, “this means that hyperglycemic medications that are being prescribed should be watched scrupulously. Otherwise, there is a risk that [women] may overrespond.”
That is, Dr. Karaye continued, women “may be at risk of developing hypoglycemia because the cannabis is acting synergistically with the regular drug that is being used to treat the diabetes.”
U.S. clinicians, especially in states with legalized medical marijuana, need to be aware of the potential synergy.
“One would have to consider the patient as a whole,” he stressed. “For example, a woman that uses medical marijuana may actually respond differently to hyperglycemic medication.”
Conflicting reports explained by sex differences?
Evidence on whether cannabis use is linked with type 2 diabetes is limited and conflicting, the researchers wrote. They hypothesized that these conflicting findings might be explained by sex differences.
To “help inform current diabetes prevention and mitigation efforts,” they investigated sex differences in cannabis use and prevalence of type 2 diabetes in 15,602 men and women in the 2013-2014, 2015-2016, and 2017-2018 NHANES surveys.
Participants were classified as having type 2 diabetes if they had a physician’s diagnosis; a 2-hour plasma glucose of at least 200 mg/dL (in a glucose tolerance test); fasting blood glucose of at least 126 mg/dL; or A1c of at least 6.5%.
About half of respondents were women (52%) and close to half (44%) were age 18-39.
More than a third (38%) had a body mass index (BMI) of at least 30 kg/m2, indicating obesity.
Roughly 1 in 10 had a diagnosis of type 2 diabetes (13.5%) or A1c of at least 6.5% (9.8%).
Close to a fifth smoked cigarettes (16%). Similarly, 14.5% used cannabis at least four times a week, 3.3% used it less often, and the rest did not use it. Half of participants were not physically active (49%).
Just over half had at least a college education (55%).
Heavy cannabis users were more likely to be younger than age 40 (57% of men, 57% of women), college graduates (54% of men, 63% of women), cigarette smokers (79% of men, 83% of women), and physically inactive (39% of men, 49% of women).
Among women, heavy cannabis users were 49% less likely to have type 2 diabetes than nonusers, after adjusting for age, sex, race/ethnicity, educational level, physical activity, tobacco use, alcohol use, marital status, difficulty walking, employment status, income, and BMI (adjusted odds ratio, 0.51; 95% confidence interval, 0.31-0.84).
There were no significant differences between light cannabis users versus nonusers and diabetes prevalence in women, or between light or heavy cannabis users versus nonusers and diabetes prevalence in men.
Limitations, yet biologically plausible
The researchers acknowledged several study limitations.
They do not know how long participants had used marijuana. The men and women may have underreported their cannabis use, especially in states where medical marijuana was not legal, and the NHANES data did not specify whether the cannabis was recreational or medicinal.
The study may have been underpowered to detect a smaller difference in men who used versus did not use marijuana.
And importantly, this was an observational study (a snapshot at one point in time), so it cannot say whether the heavy cannabis use in women caused a decreased likelihood of diabetes.
Nevertheless, the inverse association between cannabis use and presence of type 2 diabetes is biologically plausible, Dr. Ogunsola and colleagues wrote.
The two major cannabis compounds, cannabidiol and delta-9-tetrahydrocannabinol, stimulate CBD1 and CBD2 receptors in the central and peripheral nervous systems, respectively. And “activation of the CBD1 receptor increases insulin secretion, glucagon, and somatostatin, and activates metabolic processes in fat and skeletal muscles – mechanisms that improve glucose disposal,” they explained.
The researchers speculated that the sex differences they found for this association may be caused by differences in sex hormones, or the endocannabinoid system, or fat deposits.
Therefore, “additional studies are needed to investigate the sex-based heterogeneity reported in this study and to elucidate potential mechanisms for the observation,” they concluded.
The study did not receive any funding and the researchers have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM CANNABIS AND CANNABINOID RESEARCH
If you’ve got 3 seconds, then you’ve got time to work out
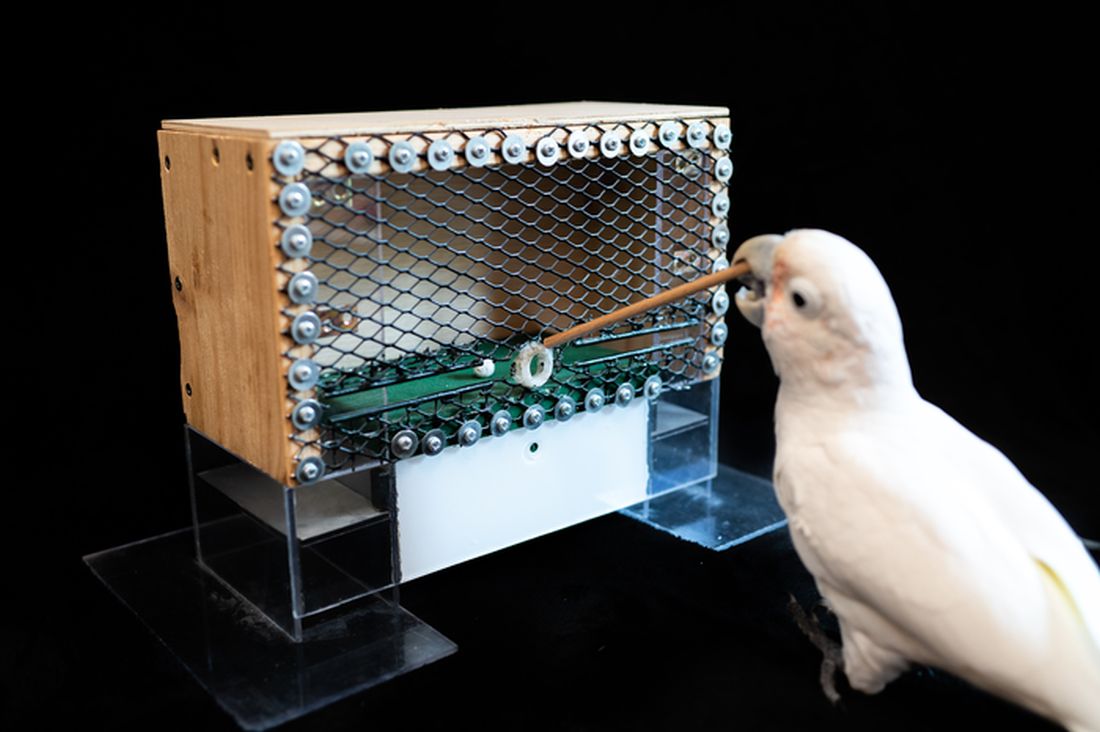
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Chronic marijuana use linked to recurrent stroke
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ISC 2022
Switching to a healthy diet can add 10 years to life
Just a few changes to your diet could add years to your life, but the sooner you start the better.
Maintaining a healthy diet is important, but most people find this difficult to do daily. In a new study, researchers examined the effects of individual healthful and nonhealthful types of foods and estimated the impact by age and sex of swapping some for others.
say the Norwegian scientists who conducted the study, published in PLOS Medicine on Feb. 8.
They developed an online tool that anyone can use to get an idea of how individual food choices can affect life expectancy.
The biggest overall impact comes from eating more plant-based foods (legumes), whole grains and nuts, and less red and processed meat. Fruits and vegetables also have a positive health impact, but on average people who eat a typical Western diet are already consuming those in relatively high amounts. Fish is included on the healthful list, whereas sugar-sweetened beverages (sodas) and foods based on refined [white] grains, such as white bread, are among those to be avoided.
The study found that although it’s never too late to start, young adults can expect to see more years gained by adopting healthful eating than would older adults.
“Our results indicate that for individuals with a typical Western diet, sustained dietary changes at any age may give substantial health benefits, although the gains are the largest if changes start early in life,” said the researchers.
Depending on how many healthy dietary “switches” are made and maintained and the amounts consumed, a 20-year-old man in the United States could extend his life up to 13 years, and a 20-year old woman by 11 years.
That number drops with age but changing from a typical diet to the optimized diet at age 60 years could still increase life expectancy by 8 years for women and 9 years for men, and even an 80-year-old female could gain more than 3 years with healthier food choices.
Until now, research in this area has shown health benefits associated with separate food groups or specific diet patterns, while focusing less on the health impact of other dietary changes. The statistical ‘modeling’ approach used in this study bridges that gap, the researchers said.
“Understanding the relative health potential of different food groups could enable people to make feasible and significant health gains,” they concluded.
A version of this article was first published on WebMD.com.
Just a few changes to your diet could add years to your life, but the sooner you start the better.
Maintaining a healthy diet is important, but most people find this difficult to do daily. In a new study, researchers examined the effects of individual healthful and nonhealthful types of foods and estimated the impact by age and sex of swapping some for others.
say the Norwegian scientists who conducted the study, published in PLOS Medicine on Feb. 8.
They developed an online tool that anyone can use to get an idea of how individual food choices can affect life expectancy.
The biggest overall impact comes from eating more plant-based foods (legumes), whole grains and nuts, and less red and processed meat. Fruits and vegetables also have a positive health impact, but on average people who eat a typical Western diet are already consuming those in relatively high amounts. Fish is included on the healthful list, whereas sugar-sweetened beverages (sodas) and foods based on refined [white] grains, such as white bread, are among those to be avoided.
The study found that although it’s never too late to start, young adults can expect to see more years gained by adopting healthful eating than would older adults.
“Our results indicate that for individuals with a typical Western diet, sustained dietary changes at any age may give substantial health benefits, although the gains are the largest if changes start early in life,” said the researchers.
Depending on how many healthy dietary “switches” are made and maintained and the amounts consumed, a 20-year-old man in the United States could extend his life up to 13 years, and a 20-year old woman by 11 years.
That number drops with age but changing from a typical diet to the optimized diet at age 60 years could still increase life expectancy by 8 years for women and 9 years for men, and even an 80-year-old female could gain more than 3 years with healthier food choices.
Until now, research in this area has shown health benefits associated with separate food groups or specific diet patterns, while focusing less on the health impact of other dietary changes. The statistical ‘modeling’ approach used in this study bridges that gap, the researchers said.
“Understanding the relative health potential of different food groups could enable people to make feasible and significant health gains,” they concluded.
A version of this article was first published on WebMD.com.
Just a few changes to your diet could add years to your life, but the sooner you start the better.
Maintaining a healthy diet is important, but most people find this difficult to do daily. In a new study, researchers examined the effects of individual healthful and nonhealthful types of foods and estimated the impact by age and sex of swapping some for others.
say the Norwegian scientists who conducted the study, published in PLOS Medicine on Feb. 8.
They developed an online tool that anyone can use to get an idea of how individual food choices can affect life expectancy.
The biggest overall impact comes from eating more plant-based foods (legumes), whole grains and nuts, and less red and processed meat. Fruits and vegetables also have a positive health impact, but on average people who eat a typical Western diet are already consuming those in relatively high amounts. Fish is included on the healthful list, whereas sugar-sweetened beverages (sodas) and foods based on refined [white] grains, such as white bread, are among those to be avoided.
The study found that although it’s never too late to start, young adults can expect to see more years gained by adopting healthful eating than would older adults.
“Our results indicate that for individuals with a typical Western diet, sustained dietary changes at any age may give substantial health benefits, although the gains are the largest if changes start early in life,” said the researchers.
Depending on how many healthy dietary “switches” are made and maintained and the amounts consumed, a 20-year-old man in the United States could extend his life up to 13 years, and a 20-year old woman by 11 years.
That number drops with age but changing from a typical diet to the optimized diet at age 60 years could still increase life expectancy by 8 years for women and 9 years for men, and even an 80-year-old female could gain more than 3 years with healthier food choices.
Until now, research in this area has shown health benefits associated with separate food groups or specific diet patterns, while focusing less on the health impact of other dietary changes. The statistical ‘modeling’ approach used in this study bridges that gap, the researchers said.
“Understanding the relative health potential of different food groups could enable people to make feasible and significant health gains,” they concluded.
A version of this article was first published on WebMD.com.
FROM PLOS MEDICINE
Promising leads to crack long COVID discovered
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
Endocrine Society and others to FDA: Restrict BPA
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
PAH care turns corner with new therapies, intensified monitoring
Aggressive up-front combination therapy, more lofty treatment goals, and earlier and more frequent reassessments to guide treatment are improving care of patients with pulmonary arterial hypertension (PAH) while at the same time making it more complex.
A larger number of oral and generic treatment options have in some respects ushered in more management ease. But overall, “I don’t know if management of these patients has ever been more complicated, given the treatment options and strategies,” said Murali M. Chakinala, MD, professor of medicine at Washington University, St. Louis. “We’re always thinking through approaches.”
Diagnosis continues to be challenging given the rarity of PAH and its nonspecific presentation – and in some cases it’s now harder. Experts such as Dr. Chakinala are seeing increasing number of aging patients with left heart disease, chronic kidney disease, and other comorbidities who have significant precapillary pulmonary hypertension and who exhibit hemodynamics consistent with PAH, or group 1 PH.
The question experts face is, do such patients have “true PAH,” as do a reported 25-50 people per million, or do they have another type of PH in the classification schema – or a mixture?
Deciding which patients “really fit into group 1 and should be managed like group 1,” Dr. Chakinala said, requires clinical acumen and has important implications, as patients with PAH are the main beneficiaries of vasodilator therapy. Most other patients with PH will not respond to or tolerate such treatment.
“These older patients may be getting PAH through different mechanisms than our younger patients, but because we define PAH through hemodynamic criteria and by ruling out other obvious explanations, they all get lumped together,” said Dr. Chakinala. “We need to parse these patients out better in the future, much like our oncology colleagues are doing.”
Personalized medicine hopefully is the next horizon for this condition, characterized by severe remodeling of the distal pulmonary arteries. Researchers are pushing to achieve deep phenotyping, identify biomarkers and improve risk assessment tools.
And with 80 or so centers now accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Care Centers, referred patients are accessing clinical trials of new nonvasodilatory drugs. Currently available therapies improve hemodynamics and symptoms, and can slow disease progression, but are not truly disease modifying, sources say.
“The endothelin, nitric oxide, and prostacyclin pathways have been exhaustively studied and we now have great drugs for those pathways,” said Dr. Chakinala, who leads the PHA’s scientific leadership council. But “we’re not going to put a greater dent into this disease until we have new drugs that work on different biologic pathways.”
Diagnostic challenges
The diagnosis of PAH – a remarkably heterogeneous condition that encompasses heritable forms and idiopathic forms, and that comprises a broad mix of predisposing conditions and exposures, from scleroderma to methamphetamine use – is still too often missed or delayed. Delayed diagnoses and misdiagnoses of PAH and other types of PH have been reported in up to 85% of at-risk patients, according to a 2016 literature review.
Being able to pivot from thinking about common pulmonary ailments or heart failure to considering PAH is a key part of earlier diagnosis and better treatment outcomes. “If someone has unexplained dyspnea or if they’re treated for other lung diseases and are not improving, think about a screening echocardiogram,” said Timothy L. Williamson, MD, vice president of quality and safety and a pulmonary and critical care physician at the University of Kansas Health Center, Kansas City.
One of the most common reasons Dr. Chakinala sees for missed diagnoses are right heart catheterizations that are incomplete or misinterpreted. (Right heart catheterizations are required to confirm the diagnosis.) “One can’t simply measure pressures and stop,” he said. “We need the full hemodynamic profile to know that it’s truly precapillary PAH ... and we need proper interpretation of [elements like] the waveforms.”
The 2019 World Symposium on Pulmonary Hypertension shifted the definition of PH from an arbitrarily defined mean pulmonary arterial pressure of at least 25 mm Hg at rest (as measured by right heart catheterization) to a more scientifically determined mPAP of at least 20 mm Hg.
The classification document also requires pulmonary vascular resistance (PVR) of at least 3 Wood units in the definition of all forms of precapillary PH. PAH specifically is defined as the presence of mPAP of at least 20 mm Hg, PVR of at least 3 Wood units, and pulmonary arterial wedge pressure 15 mm Hg or less.
Trends in treatment
The value of initial combination therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 (PDE5) inhibitor in treatment-naive PAH was cemented in 2015 by the AMBITION trial. The primary endpoint (death, PAH hospitalization, or unsatisfactory clinical response) occurred in 18%, 34%, and 28% of patients who were randomized, respectively, to combination therapy, monotherapy with the ERA ambrisentan, or monotherapy with the PDE-5 inhibitor tadalafil – and in 31% of the two monotherapy groups combined.
The trial reported a 50% reduction in the primary endpoint in the combination-therapy group versus the pooled monotherapy group, as well as greater reductions in N-terminal of the prohormone brain natriuretic peptide levels, more satisfactory clinical response and greater improvement in 6-minute walking distance.
In practice, a minority of patients – typically older patients with multiple comorbidities – still receive initial monotherapy with sequential add-on therapies based on tolerance, but “for the most part PAH patients will start on combination therapy, most commonly with a ERA and PDE5 inhibitor,” Dr. Chakinala said.
For patients who are not improving on the ERA-PDE5 inhibitor approach – typically those who remain in the intermediate-risk category for intermediate-term mortality – substitution of the PDE5 inhibitor with the soluble guanylate cyclase stimulator riociguat may be considered, he and Dr. Williamson said. Clinical improvement with this substitution was demonstrated in the REPLACE trial.
Experts at PH care centers are also utilizing triple therapy for patients who do not improve to low-risk status after 2-4 months of dual combination therapy. The availability of oral prostacyclin analogues (selexipag and treprostinil) makes it easier to consider adding these agents early on, Dr. Chakinala and Dr. Richardson said.
Patients who fall into the high-risk category, at any point, are still best managed with parenteral prostacyclin analogues, Dr. Chakinala said.
In general, said Dr. Williamson, who also directs the University of Kansas Pulmonary Hypertension Comprehensive Care Center, “the PH community tends to be fairly aggressive up front, and with a low threshold for using prostacyclin analogues.”
The agents are “always part of the picture for someone who is really ill, in functional class IV, or has really impaired right ventricular function,” he said. “And we’re finding increased roles in patients who are not as ill but still have decompensated right ventricular dysfunction. It’s something we now consider.”
Recently published research on up-front oral triple therapy suggests possible benefit for some patients – but it’s far from conclusive, said Dr. Chakinala. The TRITON study randomized treatment-naive patients to the traditional ERA-PDE5 combination and either oral selexipag (a selective prostacyclin receptor agonist) or placebo as a third agent. It found no significant difference in reduction in PVR, the primary outcome, at week 26. However, the authors reported a “possible signal” for improved long-term outcomes with triple therapy.
“Based on this best evidence from a randomized clinical trial, I think it’s unfair to say that all patients should be on triple combination therapy right out of the gate,” he said. “Having said that, more recent [European] data showed that two drugs fell short of the mark in some patients, with high rates of clinical progression. And even in AMBITION, there were a number of patients in the combination arm who didn’t have a robust response.”
A 2021 retrospective analysis from the French Pulmonary Hypertension Registry – one of the European studies – assessed survival with monotherapy, dual therapy, or triple-combination therapy (two orals with a parenteral prostacyclin), and found no difference between monotherapy and dual therapy in high-risk patients.
Experts have been upping the ante, therefore, on early assessment and frequent reassessment of treatment response. Not long ago, patients were typically reassessed 6-12 months after the initiation of treatment. Now, experts at the PH care centers want to assess patients at 3-4 months and adjust or intensify treatment regimens for those who don’t yet qualify as low risk using a multidimensional risk score calculator.
The REVEAL (Registry to Evaluate Early and Long-Term PAH Management) risk score calculator, for instance, predicts the probability of 1-year survival and assigns patients to a strata of risk level based on either 12 or 6 variables (for the full or “lite” versions).]
Even better monitoring and risk assessment is needed, however, to “help sift out which patients are not improving enough on initial therapy or who are starting to fall off after being on a regimen for a period of time,” Dr. Chakinala said.
Today, with a network of accredited centers of expertise and a desire and need for many patients to remain close to home, Dr. Chakinala encourages finding a balance. Well-resourced clinicians can strive for early diagnosis and management – potentially initiating ERA–PDE-5 inhibitor combination therapy – but still should collaborate with PH experts.
“It’s a good idea to comanage these patients and let the experts see them periodically to help you determine when your patient may be declining,” he said. “The timetable for reassessment, the complexity of the reassessment, and the need to escalate to more advanced therapies has never been more important.”
Research highlights
Therapies that target inflammation and altered metabolism – including metformin – are among those being investigated for PAH. So are therapies targeting dysfunctional bone morphogenetic protein pathway signaling, which has been shown to be associated with hereditary, idiopathic, and likely other forms of PAH; one such drug, called sotatercept, is currently at the phase 3 trial stage.
Most promising for PAH may be the research efforts involving deep phenotyping, said Andrew J. Sweatt, MD, of Stanford (Calif.) University and the Vera Moulton Wall Center for Pulmonary Vascular Disease.
“It’s where a lot of research is headed – deep phenotyping to deconstruct the molecular and clinical heterogeneity that exists within PAH ... to detect distinct subphenotypes of patients who would respond to particular therapies,” said Dr. Sweatt, who led a review of PH clinical research presented at the 2020 American Thoracic Society International Conference
“Right now, we largely treat all patients the same ... [while] we know that patients have a wide response to therapies and there’s a lot of clinical heterogeneity in how their disease evolves over time,” he said.
Data from a large National Institutes of Health–funded multicenter phenotyping study of PH is being analyzed and should yield findings and publications starting this year, said Anna R. Hemnes, MD, associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., and an investigator with the initiative, coined “Redefining Pulmonary Hypertension through Pulmonary Disease Phenomics (PVDOMICS).”
Patients have undergone advanced imaging (for example, echocardiography, cardiac MRI, chest CT, ventilation/perfusion scans), advanced testing through right heart catheterization, body composition testing, quality of life questionnaires, and blood draws that have been analyzed for DNA and RNA expression, proteomics, and metabolomics, said Dr. Hemnes, assistant director of Vanderbilt’s Pulmonary Vascular Center.
The initiative aims to refine the classification of all kinds of PH and “to bring precision medicine to the field so we’re no longer characterizing somebody [based on imaging] and right heart catheterization, but we also incorporating molecular pieces and biomarkers into the diagnostic evaluation,” she said.
In the short term, the results of deep phenotyping should “allow us to be more effective with our therapy recommendations,” Dr. Hemnes said. “Then hopefully in the longer term, [identified biomarkers] will help us to develop new, more effective therapies.”
Dr. Sweatt and Dr. Williamson reported that they have no relevant financial disclosures. Dr. Hemnes reported that she holds stock in Tenax (which is studying a tyrosine kinase inhibitor for PAH) and serves as a consultant for Acceleron, Bayer, GossamerBio, United Therapeutics, and Janssen. She also receives research funding from Imara. Dr. Chakinala reported that he is an investigator on clinical trials for a number of pharmaceutical companies. He also serves on advisory boards for Phase Bio, Liquidia/Rare Gen, Bayer, Janssen, Trio Health Analytics, and Aerovate.
Aggressive up-front combination therapy, more lofty treatment goals, and earlier and more frequent reassessments to guide treatment are improving care of patients with pulmonary arterial hypertension (PAH) while at the same time making it more complex.
A larger number of oral and generic treatment options have in some respects ushered in more management ease. But overall, “I don’t know if management of these patients has ever been more complicated, given the treatment options and strategies,” said Murali M. Chakinala, MD, professor of medicine at Washington University, St. Louis. “We’re always thinking through approaches.”
Diagnosis continues to be challenging given the rarity of PAH and its nonspecific presentation – and in some cases it’s now harder. Experts such as Dr. Chakinala are seeing increasing number of aging patients with left heart disease, chronic kidney disease, and other comorbidities who have significant precapillary pulmonary hypertension and who exhibit hemodynamics consistent with PAH, or group 1 PH.
The question experts face is, do such patients have “true PAH,” as do a reported 25-50 people per million, or do they have another type of PH in the classification schema – or a mixture?
Deciding which patients “really fit into group 1 and should be managed like group 1,” Dr. Chakinala said, requires clinical acumen and has important implications, as patients with PAH are the main beneficiaries of vasodilator therapy. Most other patients with PH will not respond to or tolerate such treatment.
“These older patients may be getting PAH through different mechanisms than our younger patients, but because we define PAH through hemodynamic criteria and by ruling out other obvious explanations, they all get lumped together,” said Dr. Chakinala. “We need to parse these patients out better in the future, much like our oncology colleagues are doing.”
Personalized medicine hopefully is the next horizon for this condition, characterized by severe remodeling of the distal pulmonary arteries. Researchers are pushing to achieve deep phenotyping, identify biomarkers and improve risk assessment tools.
And with 80 or so centers now accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Care Centers, referred patients are accessing clinical trials of new nonvasodilatory drugs. Currently available therapies improve hemodynamics and symptoms, and can slow disease progression, but are not truly disease modifying, sources say.
“The endothelin, nitric oxide, and prostacyclin pathways have been exhaustively studied and we now have great drugs for those pathways,” said Dr. Chakinala, who leads the PHA’s scientific leadership council. But “we’re not going to put a greater dent into this disease until we have new drugs that work on different biologic pathways.”
Diagnostic challenges
The diagnosis of PAH – a remarkably heterogeneous condition that encompasses heritable forms and idiopathic forms, and that comprises a broad mix of predisposing conditions and exposures, from scleroderma to methamphetamine use – is still too often missed or delayed. Delayed diagnoses and misdiagnoses of PAH and other types of PH have been reported in up to 85% of at-risk patients, according to a 2016 literature review.
Being able to pivot from thinking about common pulmonary ailments or heart failure to considering PAH is a key part of earlier diagnosis and better treatment outcomes. “If someone has unexplained dyspnea or if they’re treated for other lung diseases and are not improving, think about a screening echocardiogram,” said Timothy L. Williamson, MD, vice president of quality and safety and a pulmonary and critical care physician at the University of Kansas Health Center, Kansas City.
One of the most common reasons Dr. Chakinala sees for missed diagnoses are right heart catheterizations that are incomplete or misinterpreted. (Right heart catheterizations are required to confirm the diagnosis.) “One can’t simply measure pressures and stop,” he said. “We need the full hemodynamic profile to know that it’s truly precapillary PAH ... and we need proper interpretation of [elements like] the waveforms.”
The 2019 World Symposium on Pulmonary Hypertension shifted the definition of PH from an arbitrarily defined mean pulmonary arterial pressure of at least 25 mm Hg at rest (as measured by right heart catheterization) to a more scientifically determined mPAP of at least 20 mm Hg.
The classification document also requires pulmonary vascular resistance (PVR) of at least 3 Wood units in the definition of all forms of precapillary PH. PAH specifically is defined as the presence of mPAP of at least 20 mm Hg, PVR of at least 3 Wood units, and pulmonary arterial wedge pressure 15 mm Hg or less.
Trends in treatment
The value of initial combination therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 (PDE5) inhibitor in treatment-naive PAH was cemented in 2015 by the AMBITION trial. The primary endpoint (death, PAH hospitalization, or unsatisfactory clinical response) occurred in 18%, 34%, and 28% of patients who were randomized, respectively, to combination therapy, monotherapy with the ERA ambrisentan, or monotherapy with the PDE-5 inhibitor tadalafil – and in 31% of the two monotherapy groups combined.
The trial reported a 50% reduction in the primary endpoint in the combination-therapy group versus the pooled monotherapy group, as well as greater reductions in N-terminal of the prohormone brain natriuretic peptide levels, more satisfactory clinical response and greater improvement in 6-minute walking distance.
In practice, a minority of patients – typically older patients with multiple comorbidities – still receive initial monotherapy with sequential add-on therapies based on tolerance, but “for the most part PAH patients will start on combination therapy, most commonly with a ERA and PDE5 inhibitor,” Dr. Chakinala said.
For patients who are not improving on the ERA-PDE5 inhibitor approach – typically those who remain in the intermediate-risk category for intermediate-term mortality – substitution of the PDE5 inhibitor with the soluble guanylate cyclase stimulator riociguat may be considered, he and Dr. Williamson said. Clinical improvement with this substitution was demonstrated in the REPLACE trial.
Experts at PH care centers are also utilizing triple therapy for patients who do not improve to low-risk status after 2-4 months of dual combination therapy. The availability of oral prostacyclin analogues (selexipag and treprostinil) makes it easier to consider adding these agents early on, Dr. Chakinala and Dr. Richardson said.
Patients who fall into the high-risk category, at any point, are still best managed with parenteral prostacyclin analogues, Dr. Chakinala said.
In general, said Dr. Williamson, who also directs the University of Kansas Pulmonary Hypertension Comprehensive Care Center, “the PH community tends to be fairly aggressive up front, and with a low threshold for using prostacyclin analogues.”
The agents are “always part of the picture for someone who is really ill, in functional class IV, or has really impaired right ventricular function,” he said. “And we’re finding increased roles in patients who are not as ill but still have decompensated right ventricular dysfunction. It’s something we now consider.”
Recently published research on up-front oral triple therapy suggests possible benefit for some patients – but it’s far from conclusive, said Dr. Chakinala. The TRITON study randomized treatment-naive patients to the traditional ERA-PDE5 combination and either oral selexipag (a selective prostacyclin receptor agonist) or placebo as a third agent. It found no significant difference in reduction in PVR, the primary outcome, at week 26. However, the authors reported a “possible signal” for improved long-term outcomes with triple therapy.
“Based on this best evidence from a randomized clinical trial, I think it’s unfair to say that all patients should be on triple combination therapy right out of the gate,” he said. “Having said that, more recent [European] data showed that two drugs fell short of the mark in some patients, with high rates of clinical progression. And even in AMBITION, there were a number of patients in the combination arm who didn’t have a robust response.”
A 2021 retrospective analysis from the French Pulmonary Hypertension Registry – one of the European studies – assessed survival with monotherapy, dual therapy, or triple-combination therapy (two orals with a parenteral prostacyclin), and found no difference between monotherapy and dual therapy in high-risk patients.
Experts have been upping the ante, therefore, on early assessment and frequent reassessment of treatment response. Not long ago, patients were typically reassessed 6-12 months after the initiation of treatment. Now, experts at the PH care centers want to assess patients at 3-4 months and adjust or intensify treatment regimens for those who don’t yet qualify as low risk using a multidimensional risk score calculator.
The REVEAL (Registry to Evaluate Early and Long-Term PAH Management) risk score calculator, for instance, predicts the probability of 1-year survival and assigns patients to a strata of risk level based on either 12 or 6 variables (for the full or “lite” versions).]
Even better monitoring and risk assessment is needed, however, to “help sift out which patients are not improving enough on initial therapy or who are starting to fall off after being on a regimen for a period of time,” Dr. Chakinala said.
Today, with a network of accredited centers of expertise and a desire and need for many patients to remain close to home, Dr. Chakinala encourages finding a balance. Well-resourced clinicians can strive for early diagnosis and management – potentially initiating ERA–PDE-5 inhibitor combination therapy – but still should collaborate with PH experts.
“It’s a good idea to comanage these patients and let the experts see them periodically to help you determine when your patient may be declining,” he said. “The timetable for reassessment, the complexity of the reassessment, and the need to escalate to more advanced therapies has never been more important.”
Research highlights
Therapies that target inflammation and altered metabolism – including metformin – are among those being investigated for PAH. So are therapies targeting dysfunctional bone morphogenetic protein pathway signaling, which has been shown to be associated with hereditary, idiopathic, and likely other forms of PAH; one such drug, called sotatercept, is currently at the phase 3 trial stage.
Most promising for PAH may be the research efforts involving deep phenotyping, said Andrew J. Sweatt, MD, of Stanford (Calif.) University and the Vera Moulton Wall Center for Pulmonary Vascular Disease.
“It’s where a lot of research is headed – deep phenotyping to deconstruct the molecular and clinical heterogeneity that exists within PAH ... to detect distinct subphenotypes of patients who would respond to particular therapies,” said Dr. Sweatt, who led a review of PH clinical research presented at the 2020 American Thoracic Society International Conference
“Right now, we largely treat all patients the same ... [while] we know that patients have a wide response to therapies and there’s a lot of clinical heterogeneity in how their disease evolves over time,” he said.
Data from a large National Institutes of Health–funded multicenter phenotyping study of PH is being analyzed and should yield findings and publications starting this year, said Anna R. Hemnes, MD, associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., and an investigator with the initiative, coined “Redefining Pulmonary Hypertension through Pulmonary Disease Phenomics (PVDOMICS).”
Patients have undergone advanced imaging (for example, echocardiography, cardiac MRI, chest CT, ventilation/perfusion scans), advanced testing through right heart catheterization, body composition testing, quality of life questionnaires, and blood draws that have been analyzed for DNA and RNA expression, proteomics, and metabolomics, said Dr. Hemnes, assistant director of Vanderbilt’s Pulmonary Vascular Center.
The initiative aims to refine the classification of all kinds of PH and “to bring precision medicine to the field so we’re no longer characterizing somebody [based on imaging] and right heart catheterization, but we also incorporating molecular pieces and biomarkers into the diagnostic evaluation,” she said.
In the short term, the results of deep phenotyping should “allow us to be more effective with our therapy recommendations,” Dr. Hemnes said. “Then hopefully in the longer term, [identified biomarkers] will help us to develop new, more effective therapies.”
Dr. Sweatt and Dr. Williamson reported that they have no relevant financial disclosures. Dr. Hemnes reported that she holds stock in Tenax (which is studying a tyrosine kinase inhibitor for PAH) and serves as a consultant for Acceleron, Bayer, GossamerBio, United Therapeutics, and Janssen. She also receives research funding from Imara. Dr. Chakinala reported that he is an investigator on clinical trials for a number of pharmaceutical companies. He also serves on advisory boards for Phase Bio, Liquidia/Rare Gen, Bayer, Janssen, Trio Health Analytics, and Aerovate.
Aggressive up-front combination therapy, more lofty treatment goals, and earlier and more frequent reassessments to guide treatment are improving care of patients with pulmonary arterial hypertension (PAH) while at the same time making it more complex.
A larger number of oral and generic treatment options have in some respects ushered in more management ease. But overall, “I don’t know if management of these patients has ever been more complicated, given the treatment options and strategies,” said Murali M. Chakinala, MD, professor of medicine at Washington University, St. Louis. “We’re always thinking through approaches.”
Diagnosis continues to be challenging given the rarity of PAH and its nonspecific presentation – and in some cases it’s now harder. Experts such as Dr. Chakinala are seeing increasing number of aging patients with left heart disease, chronic kidney disease, and other comorbidities who have significant precapillary pulmonary hypertension and who exhibit hemodynamics consistent with PAH, or group 1 PH.
The question experts face is, do such patients have “true PAH,” as do a reported 25-50 people per million, or do they have another type of PH in the classification schema – or a mixture?
Deciding which patients “really fit into group 1 and should be managed like group 1,” Dr. Chakinala said, requires clinical acumen and has important implications, as patients with PAH are the main beneficiaries of vasodilator therapy. Most other patients with PH will not respond to or tolerate such treatment.
“These older patients may be getting PAH through different mechanisms than our younger patients, but because we define PAH through hemodynamic criteria and by ruling out other obvious explanations, they all get lumped together,” said Dr. Chakinala. “We need to parse these patients out better in the future, much like our oncology colleagues are doing.”
Personalized medicine hopefully is the next horizon for this condition, characterized by severe remodeling of the distal pulmonary arteries. Researchers are pushing to achieve deep phenotyping, identify biomarkers and improve risk assessment tools.
And with 80 or so centers now accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Care Centers, referred patients are accessing clinical trials of new nonvasodilatory drugs. Currently available therapies improve hemodynamics and symptoms, and can slow disease progression, but are not truly disease modifying, sources say.
“The endothelin, nitric oxide, and prostacyclin pathways have been exhaustively studied and we now have great drugs for those pathways,” said Dr. Chakinala, who leads the PHA’s scientific leadership council. But “we’re not going to put a greater dent into this disease until we have new drugs that work on different biologic pathways.”
Diagnostic challenges
The diagnosis of PAH – a remarkably heterogeneous condition that encompasses heritable forms and idiopathic forms, and that comprises a broad mix of predisposing conditions and exposures, from scleroderma to methamphetamine use – is still too often missed or delayed. Delayed diagnoses and misdiagnoses of PAH and other types of PH have been reported in up to 85% of at-risk patients, according to a 2016 literature review.
Being able to pivot from thinking about common pulmonary ailments or heart failure to considering PAH is a key part of earlier diagnosis and better treatment outcomes. “If someone has unexplained dyspnea or if they’re treated for other lung diseases and are not improving, think about a screening echocardiogram,” said Timothy L. Williamson, MD, vice president of quality and safety and a pulmonary and critical care physician at the University of Kansas Health Center, Kansas City.
One of the most common reasons Dr. Chakinala sees for missed diagnoses are right heart catheterizations that are incomplete or misinterpreted. (Right heart catheterizations are required to confirm the diagnosis.) “One can’t simply measure pressures and stop,” he said. “We need the full hemodynamic profile to know that it’s truly precapillary PAH ... and we need proper interpretation of [elements like] the waveforms.”
The 2019 World Symposium on Pulmonary Hypertension shifted the definition of PH from an arbitrarily defined mean pulmonary arterial pressure of at least 25 mm Hg at rest (as measured by right heart catheterization) to a more scientifically determined mPAP of at least 20 mm Hg.
The classification document also requires pulmonary vascular resistance (PVR) of at least 3 Wood units in the definition of all forms of precapillary PH. PAH specifically is defined as the presence of mPAP of at least 20 mm Hg, PVR of at least 3 Wood units, and pulmonary arterial wedge pressure 15 mm Hg or less.
Trends in treatment
The value of initial combination therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 (PDE5) inhibitor in treatment-naive PAH was cemented in 2015 by the AMBITION trial. The primary endpoint (death, PAH hospitalization, or unsatisfactory clinical response) occurred in 18%, 34%, and 28% of patients who were randomized, respectively, to combination therapy, monotherapy with the ERA ambrisentan, or monotherapy with the PDE-5 inhibitor tadalafil – and in 31% of the two monotherapy groups combined.
The trial reported a 50% reduction in the primary endpoint in the combination-therapy group versus the pooled monotherapy group, as well as greater reductions in N-terminal of the prohormone brain natriuretic peptide levels, more satisfactory clinical response and greater improvement in 6-minute walking distance.
In practice, a minority of patients – typically older patients with multiple comorbidities – still receive initial monotherapy with sequential add-on therapies based on tolerance, but “for the most part PAH patients will start on combination therapy, most commonly with a ERA and PDE5 inhibitor,” Dr. Chakinala said.
For patients who are not improving on the ERA-PDE5 inhibitor approach – typically those who remain in the intermediate-risk category for intermediate-term mortality – substitution of the PDE5 inhibitor with the soluble guanylate cyclase stimulator riociguat may be considered, he and Dr. Williamson said. Clinical improvement with this substitution was demonstrated in the REPLACE trial.
Experts at PH care centers are also utilizing triple therapy for patients who do not improve to low-risk status after 2-4 months of dual combination therapy. The availability of oral prostacyclin analogues (selexipag and treprostinil) makes it easier to consider adding these agents early on, Dr. Chakinala and Dr. Richardson said.
Patients who fall into the high-risk category, at any point, are still best managed with parenteral prostacyclin analogues, Dr. Chakinala said.
In general, said Dr. Williamson, who also directs the University of Kansas Pulmonary Hypertension Comprehensive Care Center, “the PH community tends to be fairly aggressive up front, and with a low threshold for using prostacyclin analogues.”
The agents are “always part of the picture for someone who is really ill, in functional class IV, or has really impaired right ventricular function,” he said. “And we’re finding increased roles in patients who are not as ill but still have decompensated right ventricular dysfunction. It’s something we now consider.”
Recently published research on up-front oral triple therapy suggests possible benefit for some patients – but it’s far from conclusive, said Dr. Chakinala. The TRITON study randomized treatment-naive patients to the traditional ERA-PDE5 combination and either oral selexipag (a selective prostacyclin receptor agonist) or placebo as a third agent. It found no significant difference in reduction in PVR, the primary outcome, at week 26. However, the authors reported a “possible signal” for improved long-term outcomes with triple therapy.
“Based on this best evidence from a randomized clinical trial, I think it’s unfair to say that all patients should be on triple combination therapy right out of the gate,” he said. “Having said that, more recent [European] data showed that two drugs fell short of the mark in some patients, with high rates of clinical progression. And even in AMBITION, there were a number of patients in the combination arm who didn’t have a robust response.”
A 2021 retrospective analysis from the French Pulmonary Hypertension Registry – one of the European studies – assessed survival with monotherapy, dual therapy, or triple-combination therapy (two orals with a parenteral prostacyclin), and found no difference between monotherapy and dual therapy in high-risk patients.
Experts have been upping the ante, therefore, on early assessment and frequent reassessment of treatment response. Not long ago, patients were typically reassessed 6-12 months after the initiation of treatment. Now, experts at the PH care centers want to assess patients at 3-4 months and adjust or intensify treatment regimens for those who don’t yet qualify as low risk using a multidimensional risk score calculator.
The REVEAL (Registry to Evaluate Early and Long-Term PAH Management) risk score calculator, for instance, predicts the probability of 1-year survival and assigns patients to a strata of risk level based on either 12 or 6 variables (for the full or “lite” versions).]
Even better monitoring and risk assessment is needed, however, to “help sift out which patients are not improving enough on initial therapy or who are starting to fall off after being on a regimen for a period of time,” Dr. Chakinala said.
Today, with a network of accredited centers of expertise and a desire and need for many patients to remain close to home, Dr. Chakinala encourages finding a balance. Well-resourced clinicians can strive for early diagnosis and management – potentially initiating ERA–PDE-5 inhibitor combination therapy – but still should collaborate with PH experts.
“It’s a good idea to comanage these patients and let the experts see them periodically to help you determine when your patient may be declining,” he said. “The timetable for reassessment, the complexity of the reassessment, and the need to escalate to more advanced therapies has never been more important.”
Research highlights
Therapies that target inflammation and altered metabolism – including metformin – are among those being investigated for PAH. So are therapies targeting dysfunctional bone morphogenetic protein pathway signaling, which has been shown to be associated with hereditary, idiopathic, and likely other forms of PAH; one such drug, called sotatercept, is currently at the phase 3 trial stage.
Most promising for PAH may be the research efforts involving deep phenotyping, said Andrew J. Sweatt, MD, of Stanford (Calif.) University and the Vera Moulton Wall Center for Pulmonary Vascular Disease.
“It’s where a lot of research is headed – deep phenotyping to deconstruct the molecular and clinical heterogeneity that exists within PAH ... to detect distinct subphenotypes of patients who would respond to particular therapies,” said Dr. Sweatt, who led a review of PH clinical research presented at the 2020 American Thoracic Society International Conference
“Right now, we largely treat all patients the same ... [while] we know that patients have a wide response to therapies and there’s a lot of clinical heterogeneity in how their disease evolves over time,” he said.
Data from a large National Institutes of Health–funded multicenter phenotyping study of PH is being analyzed and should yield findings and publications starting this year, said Anna R. Hemnes, MD, associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., and an investigator with the initiative, coined “Redefining Pulmonary Hypertension through Pulmonary Disease Phenomics (PVDOMICS).”
Patients have undergone advanced imaging (for example, echocardiography, cardiac MRI, chest CT, ventilation/perfusion scans), advanced testing through right heart catheterization, body composition testing, quality of life questionnaires, and blood draws that have been analyzed for DNA and RNA expression, proteomics, and metabolomics, said Dr. Hemnes, assistant director of Vanderbilt’s Pulmonary Vascular Center.
The initiative aims to refine the classification of all kinds of PH and “to bring precision medicine to the field so we’re no longer characterizing somebody [based on imaging] and right heart catheterization, but we also incorporating molecular pieces and biomarkers into the diagnostic evaluation,” she said.
In the short term, the results of deep phenotyping should “allow us to be more effective with our therapy recommendations,” Dr. Hemnes said. “Then hopefully in the longer term, [identified biomarkers] will help us to develop new, more effective therapies.”
Dr. Sweatt and Dr. Williamson reported that they have no relevant financial disclosures. Dr. Hemnes reported that she holds stock in Tenax (which is studying a tyrosine kinase inhibitor for PAH) and serves as a consultant for Acceleron, Bayer, GossamerBio, United Therapeutics, and Janssen. She also receives research funding from Imara. Dr. Chakinala reported that he is an investigator on clinical trials for a number of pharmaceutical companies. He also serves on advisory boards for Phase Bio, Liquidia/Rare Gen, Bayer, Janssen, Trio Health Analytics, and Aerovate.
Absolute increase in Kawasaki CV risk remains small in long-term follow-up
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
FROM THE ANNUAL MEETING OF THE CANADIAN RHEUMATOLOGY ASSOCIATION
Q&A: Long COVID symptoms, management, and where we’re headed
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.