User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Persistent asthma linked to higher carotid plaque burden
Persistent asthma is associated with increased carotid plaque burden and higher levels of inflammation, putting these patients at risk for atherosclerotic cardiovascular disease (ASCVD) events, new research suggests.
Using data from the MESA study, investigators analyzed more than 5,000 individuals, comparing carotid plaque and inflammatory markers in those with and without asthma.
They found that carotid plaque was present in half of participants without asthma and half of those with intermittent asthma but in close to 70% of participants with persistent asthma.
.
“The take-home message is that the current study, paired with prior studies, highlights that individuals with more significant forms of asthma may be at higher cardiovascular risk and makes it imperative to address modifiable risk factors among patients with asthma,” lead author Matthew Tattersall, DO, MS, assistant professor of cardiovascular medicine, University of Wisconsin School of Medicine and Public Health, Madison, told this news organization.
The study was published online in the Journal of the American Heart Association.
Limited data
Asthma and ASCVD are “highly prevalent inflammatory diseases,” the authors write. Carotid artery plaque detected by B-mode ultrasound “represents advanced, typically subclinical atherosclerosis that is a strong independent predictor of incident ASCVD events,” with inflammation playing a “key role” in precipitating these events, they note.
Serum inflammatory markers such as C-reactive protein (CRP) and IL-6 are associated with increased ASCVD events, and in asthma, CRP and other inflammatory biomarkers are elevated and tend to further increase during exacerbations.
Currently, there are limited data looking at the associations of asthma, asthma severity, and atherosclerotic plaque burden, they note, so the researchers turned to the MESA study – a multiethnic population of individuals free of prevalent ASCVD at baseline. They hypothesized that persistent asthma would be associated with higher carotid plaque presence and burden.
They also wanted to explore “whether these associations would be attenuated after adjustment for baseline inflammatory biomarkers.”
Dr. Tattersall said the current study “links our previous work studying the manifestations of asthma,” in which he and his colleagues demonstrated increased cardiovascular events among MESA participants with persistent asthma, as well as late-onset asthma participants in the Wisconsin Sleep Cohort. His group also showed that early arterial injury occurs in adolescents with asthma.
However, there are also few data looking at the association with carotid plaque, “a late manifestation of arterial injury and a strong predictor of future cardiovascular events and asthma,” Dr. Tattersall added.
He and his group therefore “wanted to explore the entire spectrum of arterial injury, from the initial increase in the carotid media thickness to plaque formation to cardiovascular events.”
To do so, they studied participants in MESA, a study of close to 7,000 adults that began in the year 2000 and continues to follow participants today. At the time of enrollment, all were free from CVD.
The current analysis looked at 5,029 MESA participants (mean age 61.6 years, 53% female, 26% Black, 23% Hispanic, 12% Asian), comparing those with persistent asthma, defined as “asthma requiring use of controller medications,” intermittent asthma, defined as “asthma without controller medications,” and no asthma.
Participants underwent B-mode carotid ultrasound to detect carotid plaques, with a total plaque score (TPS) ranging from 0-12. The researchers used multivariable regression modeling to evaluate the association of asthma subtype and carotid plaque burden.
Interpret cautiously
Participants with persistent asthma were more likely to be female, have higher body mass index (BMI), and higher high-density lipoprotein (HDL) cholesterol levels, compared with those without asthma.
Participants with persistent asthma had the highest burden of carotid plaque (P ≤ .003 for comparison of proportions and .002 for comparison of means).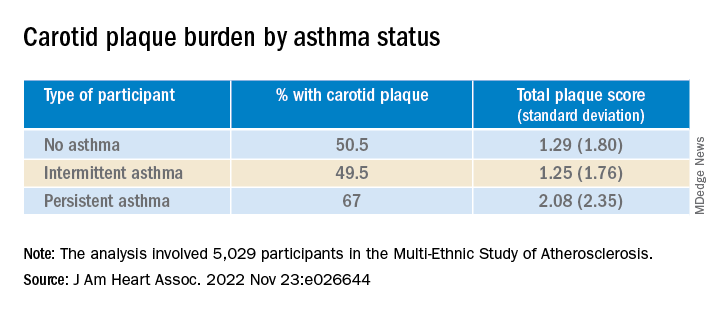
Moreover, participants with persistent asthma also had the highest systemic inflammatory marker levels – both CRP and IL-6 – compared with those without asthma. While participants with intermittent asthma also had higher average CRP, compared with those without asthma, their IL-6 levels were comparable.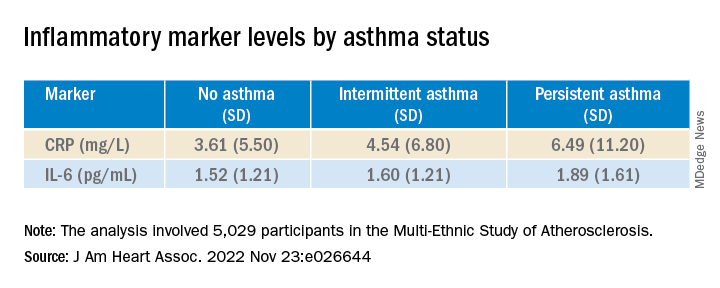
In unadjusted models, persistent asthma was associated with higher odds of carotid plaque presence (odds ratio, 1.97; 95% confidence interval, 1.32-2.95) – an association that persisted even in models that adjusted for biologic confounders (both P < .01). There also was an association between persistent asthma and higher carotid TPS (P < .001).
In further adjusted models, IL-6 was independently associated with presence of carotid plaque (P = .0001 per 1-SD increment of 1.53), as well as TPS (P < .001). CRP was “slightly associated” with carotid TPS (P = .04) but not carotid plaque presence (P = .07).
There was no attenuation after the researchers evaluated the associations of asthma subtype and carotid plaque presence or TPS and fully adjusted for baseline IL-6 or CRP (P = .02 and P = .01, respectively).
“Since this study is observational, we cannot confirm causation, but the study adds to the growing literature exploring the systemic effects of asthma,” Dr. Tattersall commented.
“Our initial hypothesis was that it was driven by inflammation, as both asthma and CVD are inflammatory conditions,” he continued. “We did adjust for inflammatory biomarkers in this analysis, but there was no change in the association.”
Nevertheless, Dr. Tattersall and colleagues are “cautious in the interpretation,” since the inflammatory biomarkers “were only collected at one point, and these measures can be dynamic, thus adjustment may not tell the whole story.”
Heightened awareness
Robert Brook, MD, professor and director of cardiovascular disease prevention, Wayne State University, Detroit, said the “main contribution of this study is the novel demonstration of a significant association between persistent (but not intermittent) asthma with carotid atherosclerosis in the MESA cohort, a large multi-ethnic population.”
These findings “support the biological plausibility of the growing epidemiological evidence that asthma independently increases the risk for cardiovascular morbidity and mortality,” added Dr. Brook, who was not involved with the study.
“The main take-home message for clinicians is that, just like in COPD (which is well-established), asthma is often a systemic condition in that the inflammation and disease process can impact the whole body,” he said.
“Health care providers should have a heightened awareness of the potentially increased cardiovascular risk of their patients with asthma and pay special attention to controlling their heart disease risk factors (for example, hyperlipidemia, hypertension),” Dr. Brook stated.
Dr. Tattersall was supported by an American Heart Association Career Development Award. The Multi-Ethnic Study of Atherosclerosis was supported by the National Heart, Lung, and Blood Institute and the National Center for Research Resources. Dr. Tattersall and co-authors and Dr. Brook declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Persistent asthma is associated with increased carotid plaque burden and higher levels of inflammation, putting these patients at risk for atherosclerotic cardiovascular disease (ASCVD) events, new research suggests.
Using data from the MESA study, investigators analyzed more than 5,000 individuals, comparing carotid plaque and inflammatory markers in those with and without asthma.
They found that carotid plaque was present in half of participants without asthma and half of those with intermittent asthma but in close to 70% of participants with persistent asthma.
.
“The take-home message is that the current study, paired with prior studies, highlights that individuals with more significant forms of asthma may be at higher cardiovascular risk and makes it imperative to address modifiable risk factors among patients with asthma,” lead author Matthew Tattersall, DO, MS, assistant professor of cardiovascular medicine, University of Wisconsin School of Medicine and Public Health, Madison, told this news organization.
The study was published online in the Journal of the American Heart Association.
Limited data
Asthma and ASCVD are “highly prevalent inflammatory diseases,” the authors write. Carotid artery plaque detected by B-mode ultrasound “represents advanced, typically subclinical atherosclerosis that is a strong independent predictor of incident ASCVD events,” with inflammation playing a “key role” in precipitating these events, they note.
Serum inflammatory markers such as C-reactive protein (CRP) and IL-6 are associated with increased ASCVD events, and in asthma, CRP and other inflammatory biomarkers are elevated and tend to further increase during exacerbations.
Currently, there are limited data looking at the associations of asthma, asthma severity, and atherosclerotic plaque burden, they note, so the researchers turned to the MESA study – a multiethnic population of individuals free of prevalent ASCVD at baseline. They hypothesized that persistent asthma would be associated with higher carotid plaque presence and burden.
They also wanted to explore “whether these associations would be attenuated after adjustment for baseline inflammatory biomarkers.”
Dr. Tattersall said the current study “links our previous work studying the manifestations of asthma,” in which he and his colleagues demonstrated increased cardiovascular events among MESA participants with persistent asthma, as well as late-onset asthma participants in the Wisconsin Sleep Cohort. His group also showed that early arterial injury occurs in adolescents with asthma.
However, there are also few data looking at the association with carotid plaque, “a late manifestation of arterial injury and a strong predictor of future cardiovascular events and asthma,” Dr. Tattersall added.
He and his group therefore “wanted to explore the entire spectrum of arterial injury, from the initial increase in the carotid media thickness to plaque formation to cardiovascular events.”
To do so, they studied participants in MESA, a study of close to 7,000 adults that began in the year 2000 and continues to follow participants today. At the time of enrollment, all were free from CVD.
The current analysis looked at 5,029 MESA participants (mean age 61.6 years, 53% female, 26% Black, 23% Hispanic, 12% Asian), comparing those with persistent asthma, defined as “asthma requiring use of controller medications,” intermittent asthma, defined as “asthma without controller medications,” and no asthma.
Participants underwent B-mode carotid ultrasound to detect carotid plaques, with a total plaque score (TPS) ranging from 0-12. The researchers used multivariable regression modeling to evaluate the association of asthma subtype and carotid plaque burden.
Interpret cautiously
Participants with persistent asthma were more likely to be female, have higher body mass index (BMI), and higher high-density lipoprotein (HDL) cholesterol levels, compared with those without asthma.
Participants with persistent asthma had the highest burden of carotid plaque (P ≤ .003 for comparison of proportions and .002 for comparison of means).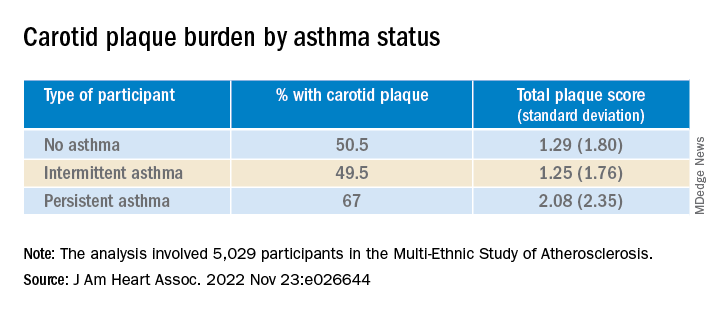
Moreover, participants with persistent asthma also had the highest systemic inflammatory marker levels – both CRP and IL-6 – compared with those without asthma. While participants with intermittent asthma also had higher average CRP, compared with those without asthma, their IL-6 levels were comparable.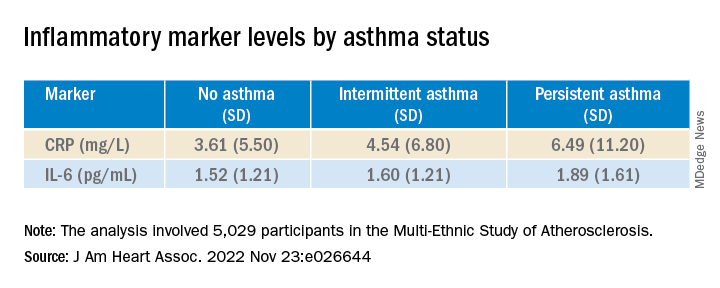
In unadjusted models, persistent asthma was associated with higher odds of carotid plaque presence (odds ratio, 1.97; 95% confidence interval, 1.32-2.95) – an association that persisted even in models that adjusted for biologic confounders (both P < .01). There also was an association between persistent asthma and higher carotid TPS (P < .001).
In further adjusted models, IL-6 was independently associated with presence of carotid plaque (P = .0001 per 1-SD increment of 1.53), as well as TPS (P < .001). CRP was “slightly associated” with carotid TPS (P = .04) but not carotid plaque presence (P = .07).
There was no attenuation after the researchers evaluated the associations of asthma subtype and carotid plaque presence or TPS and fully adjusted for baseline IL-6 or CRP (P = .02 and P = .01, respectively).
“Since this study is observational, we cannot confirm causation, but the study adds to the growing literature exploring the systemic effects of asthma,” Dr. Tattersall commented.
“Our initial hypothesis was that it was driven by inflammation, as both asthma and CVD are inflammatory conditions,” he continued. “We did adjust for inflammatory biomarkers in this analysis, but there was no change in the association.”
Nevertheless, Dr. Tattersall and colleagues are “cautious in the interpretation,” since the inflammatory biomarkers “were only collected at one point, and these measures can be dynamic, thus adjustment may not tell the whole story.”
Heightened awareness
Robert Brook, MD, professor and director of cardiovascular disease prevention, Wayne State University, Detroit, said the “main contribution of this study is the novel demonstration of a significant association between persistent (but not intermittent) asthma with carotid atherosclerosis in the MESA cohort, a large multi-ethnic population.”
These findings “support the biological plausibility of the growing epidemiological evidence that asthma independently increases the risk for cardiovascular morbidity and mortality,” added Dr. Brook, who was not involved with the study.
“The main take-home message for clinicians is that, just like in COPD (which is well-established), asthma is often a systemic condition in that the inflammation and disease process can impact the whole body,” he said.
“Health care providers should have a heightened awareness of the potentially increased cardiovascular risk of their patients with asthma and pay special attention to controlling their heart disease risk factors (for example, hyperlipidemia, hypertension),” Dr. Brook stated.
Dr. Tattersall was supported by an American Heart Association Career Development Award. The Multi-Ethnic Study of Atherosclerosis was supported by the National Heart, Lung, and Blood Institute and the National Center for Research Resources. Dr. Tattersall and co-authors and Dr. Brook declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Persistent asthma is associated with increased carotid plaque burden and higher levels of inflammation, putting these patients at risk for atherosclerotic cardiovascular disease (ASCVD) events, new research suggests.
Using data from the MESA study, investigators analyzed more than 5,000 individuals, comparing carotid plaque and inflammatory markers in those with and without asthma.
They found that carotid plaque was present in half of participants without asthma and half of those with intermittent asthma but in close to 70% of participants with persistent asthma.
.
“The take-home message is that the current study, paired with prior studies, highlights that individuals with more significant forms of asthma may be at higher cardiovascular risk and makes it imperative to address modifiable risk factors among patients with asthma,” lead author Matthew Tattersall, DO, MS, assistant professor of cardiovascular medicine, University of Wisconsin School of Medicine and Public Health, Madison, told this news organization.
The study was published online in the Journal of the American Heart Association.
Limited data
Asthma and ASCVD are “highly prevalent inflammatory diseases,” the authors write. Carotid artery plaque detected by B-mode ultrasound “represents advanced, typically subclinical atherosclerosis that is a strong independent predictor of incident ASCVD events,” with inflammation playing a “key role” in precipitating these events, they note.
Serum inflammatory markers such as C-reactive protein (CRP) and IL-6 are associated with increased ASCVD events, and in asthma, CRP and other inflammatory biomarkers are elevated and tend to further increase during exacerbations.
Currently, there are limited data looking at the associations of asthma, asthma severity, and atherosclerotic plaque burden, they note, so the researchers turned to the MESA study – a multiethnic population of individuals free of prevalent ASCVD at baseline. They hypothesized that persistent asthma would be associated with higher carotid plaque presence and burden.
They also wanted to explore “whether these associations would be attenuated after adjustment for baseline inflammatory biomarkers.”
Dr. Tattersall said the current study “links our previous work studying the manifestations of asthma,” in which he and his colleagues demonstrated increased cardiovascular events among MESA participants with persistent asthma, as well as late-onset asthma participants in the Wisconsin Sleep Cohort. His group also showed that early arterial injury occurs in adolescents with asthma.
However, there are also few data looking at the association with carotid plaque, “a late manifestation of arterial injury and a strong predictor of future cardiovascular events and asthma,” Dr. Tattersall added.
He and his group therefore “wanted to explore the entire spectrum of arterial injury, from the initial increase in the carotid media thickness to plaque formation to cardiovascular events.”
To do so, they studied participants in MESA, a study of close to 7,000 adults that began in the year 2000 and continues to follow participants today. At the time of enrollment, all were free from CVD.
The current analysis looked at 5,029 MESA participants (mean age 61.6 years, 53% female, 26% Black, 23% Hispanic, 12% Asian), comparing those with persistent asthma, defined as “asthma requiring use of controller medications,” intermittent asthma, defined as “asthma without controller medications,” and no asthma.
Participants underwent B-mode carotid ultrasound to detect carotid plaques, with a total plaque score (TPS) ranging from 0-12. The researchers used multivariable regression modeling to evaluate the association of asthma subtype and carotid plaque burden.
Interpret cautiously
Participants with persistent asthma were more likely to be female, have higher body mass index (BMI), and higher high-density lipoprotein (HDL) cholesterol levels, compared with those without asthma.
Participants with persistent asthma had the highest burden of carotid plaque (P ≤ .003 for comparison of proportions and .002 for comparison of means).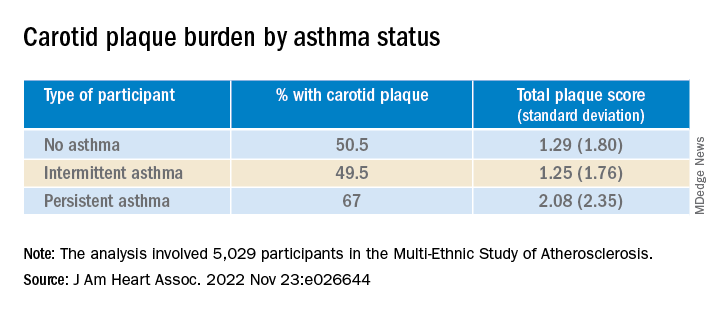
Moreover, participants with persistent asthma also had the highest systemic inflammatory marker levels – both CRP and IL-6 – compared with those without asthma. While participants with intermittent asthma also had higher average CRP, compared with those without asthma, their IL-6 levels were comparable.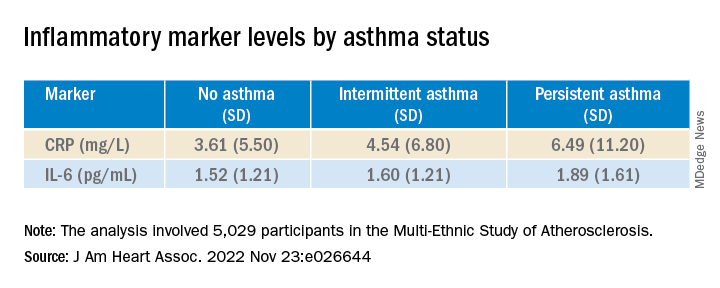
In unadjusted models, persistent asthma was associated with higher odds of carotid plaque presence (odds ratio, 1.97; 95% confidence interval, 1.32-2.95) – an association that persisted even in models that adjusted for biologic confounders (both P < .01). There also was an association between persistent asthma and higher carotid TPS (P < .001).
In further adjusted models, IL-6 was independently associated with presence of carotid plaque (P = .0001 per 1-SD increment of 1.53), as well as TPS (P < .001). CRP was “slightly associated” with carotid TPS (P = .04) but not carotid plaque presence (P = .07).
There was no attenuation after the researchers evaluated the associations of asthma subtype and carotid plaque presence or TPS and fully adjusted for baseline IL-6 or CRP (P = .02 and P = .01, respectively).
“Since this study is observational, we cannot confirm causation, but the study adds to the growing literature exploring the systemic effects of asthma,” Dr. Tattersall commented.
“Our initial hypothesis was that it was driven by inflammation, as both asthma and CVD are inflammatory conditions,” he continued. “We did adjust for inflammatory biomarkers in this analysis, but there was no change in the association.”
Nevertheless, Dr. Tattersall and colleagues are “cautious in the interpretation,” since the inflammatory biomarkers “were only collected at one point, and these measures can be dynamic, thus adjustment may not tell the whole story.”
Heightened awareness
Robert Brook, MD, professor and director of cardiovascular disease prevention, Wayne State University, Detroit, said the “main contribution of this study is the novel demonstration of a significant association between persistent (but not intermittent) asthma with carotid atherosclerosis in the MESA cohort, a large multi-ethnic population.”
These findings “support the biological plausibility of the growing epidemiological evidence that asthma independently increases the risk for cardiovascular morbidity and mortality,” added Dr. Brook, who was not involved with the study.
“The main take-home message for clinicians is that, just like in COPD (which is well-established), asthma is often a systemic condition in that the inflammation and disease process can impact the whole body,” he said.
“Health care providers should have a heightened awareness of the potentially increased cardiovascular risk of their patients with asthma and pay special attention to controlling their heart disease risk factors (for example, hyperlipidemia, hypertension),” Dr. Brook stated.
Dr. Tattersall was supported by an American Heart Association Career Development Award. The Multi-Ethnic Study of Atherosclerosis was supported by the National Heart, Lung, and Blood Institute and the National Center for Research Resources. Dr. Tattersall and co-authors and Dr. Brook declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Just 8 minutes of exercise a day is all you need
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
FROM EUROPEAN HEART JOURNAL
Vitamin D fails to stave off statin-related muscle symptoms
Vitamin D supplements do not prevent muscle symptoms in new statin users or affect the likelihood of discontinuing a statin due to muscle pain and discomfort, a substudy of the VITAL trial indicates.
Among more than 2,000 randomized participants, statin-associated muscle symptoms (SAMS) were reported by 31% assigned to vitamin D and 31% assigned to placebo.
The two groups were equally likely to stop taking a statin due to muscle symptoms, at 13%.
No significant difference was observed in SAMS (odds ratio [OR], 0.97; 95% confidence interval [CI], 0.80-1.18) or statin discontinuations (OR, 1.04; 95% CI, 0.80-1.35) after adjustment for baseline variables and other characteristics, namely age, sex, and African-American race, previously found to be associated with SAMS in VITAL.
“We actually thought when we started out that maybe we were going to show something, that maybe it was going to be that the people who got the vitamin D were least likely to have a problem with a statin than all those who didn’t get vitamin D, but that is not what we showed,” senior author Neil J. Stone, MD, Northwestern University, Chicago, told this news organization.
He noted that patients in the clinic with low levels of vitamin D often have muscle pain and discomfort and that previous unblinded studies suggested vitamin D might benefit patients with SAMS and reduce statin intolerance.
As previously reported, the double-blind VITAL trial showed no difference in the primary prevention of cardiovascular disease or cancer at 5 years among 25,871 middle-aged adults randomized to vitamin D3 at 2000 IU/d or placebo, regardless of their baseline vitamin D level.
Unlike previous studies showing a benefit with vitamin D on SAMS, importantly, VITAL participants were unaware of whether they were taking vitamin D or placebo and were not expecting any help with their muscle symptoms, first author Mark A. Hlatky, MD, Stanford (Calif.) University, pointed out in an interview.
As to how many statin users turn to the popular supplement for SAMS, he said that number couldn’t be pinned down, despite a lengthy search. “But I think it’s very common, because up to half of people stop taking their statins within a year and many of these do so because of statin-associated muscle symptoms, and we found it in about 30% of people who have them. I have them myself and was motivated to study it because I thought this was an interesting question.”
The results were published online in JAMA Cardiology.
SAMS by baseline 25-OHD
The substudy included 2,083 patients who initiated statin therapy after randomization and were surveyed in early 2016 about their statin use and muscle symptoms.
Two-thirds, or 1,397 patients, had 25-hydroxy vitamin D (25-OHD) measured at baseline, with 47% having levels < 30 ng/mL and 13% levels < 20 ng/mL.
Serum 25-OHD levels were virtually identical in the two treatment groups (mean, 30.4 ng/mL; median, 30.0 ng/mL). The frequency of SAMS did not differ between those assigned to vitamin D or placebo (28% vs. 31%).
The odds ratios for the association with vitamin D on SAMS were:
- 0.86 in all respondents with 25-OHD measured (95% CI, 0.69-1.09).
- 0.87 in those with levels ≥ 30 ng/mL (95% CI, 0.64-1.19).
- 0.85 with levels of 20-30 ng/mL (95% CI, 0.56-1.28).
- 0.93 with levels < 20 ng/mL (95% CI, 0.50-1.74).
The test for treatment effect modification by baseline serum 25-OHD level was not significant (P for interaction = .83).
In addition, the rate of muscle symptoms was similar between participants randomized to vitamin D and placebo when researchers used a cutpoint to define low 25-OHD of < 30 ng/mL (27% vs. 30%) or < 20 ng/mL (33% vs. 35%).
“We didn’t find any evidence at all that the people who came into the study with low levels of vitamin D did better with the supplement in this case,” Dr. Hlatky said. “So that wasn’t the reason we didn’t see anything.”
Critics may suggest the trial didn’t use a high enough dose of vitamin D, but both Dr. Hlatky and Dr. Stone say that’s unlikely to be a factor in the results because 2,000 IU/d is a substantial dose and well above the recommended adult daily dose of 600-800 IU.
They caution that the substudy wasn’t prespecified, was smaller than the parent trial, and did not have a protocol in place to detail SAMS. They also can’t rule out the possibility that vitamin D may have an effect in patients who have confirmed intolerance to multiple statins, especially after adjustment for the statin type and dose.
“If you’re taking vitamin D to keep from having statin-associated muscle symptoms, this very carefully done substudy with the various caveats doesn’t support that and that’s not something I would give my patients,” Dr. Stone said.
“The most important thing from a negative study is that it allows you to focus your attention on things that may be much more productive rather than assuming that just giving everybody vitamin D will take care of the statin issue,” he added. “Maybe the answer is going to be somewhere else, and there’ll be a lot of people I’m sure who will offer their advice as what the answer is but, I would argue, we want to see more studies to pin it down. So people can get some science behind what they do to try to reduce statin-associated muscle symptoms.”
Paul D. Thompson, MD, chief of cardiology emeritus at Hartford (Conn.) Hospital, and a SAMS expert who was not involved with the research, said, “This is a useful publication, and it’s smart in that it took advantage of a study that was already done.”
He acknowledged being skeptical of a beneficial effect of vitamin D supplementation on SAMS, because some previous data have been retracted, but said that potential treatments are best tested in patients with confirmed statin myalgia, as was the case in his team’s negative trial of CoQ10 supplementation.
That said, the present “study was able to at least give some of the best evidence so far that vitamin D doesn’t do anything to improve symptoms,” Dr. Thompson said. “So maybe it will cut down on so many vitamin D levels [being measured] and use of vitamin D when you don’t really need it.”
The study was sponsored by the Hyperlipidemia Research Fund at Northwestern University. The VITAL trial was supported by grants from the National Institutes of Health, and Quest Diagnostics performed the laboratory measurements at no additional costs. Dr. Hlatky reports no relevant financial relationships. Dr. Stone reports a grant from the Hyperlipidemia Research Fund at Northwestern and honorarium for educational activity for Knowledge to Practice. Dr. Thompson is on the executive committee for a study examining bempedoic acid in patients with statin-associated muscle symptoms.
A version of this article first appeared on Medscape.com.
Vitamin D supplements do not prevent muscle symptoms in new statin users or affect the likelihood of discontinuing a statin due to muscle pain and discomfort, a substudy of the VITAL trial indicates.
Among more than 2,000 randomized participants, statin-associated muscle symptoms (SAMS) were reported by 31% assigned to vitamin D and 31% assigned to placebo.
The two groups were equally likely to stop taking a statin due to muscle symptoms, at 13%.
No significant difference was observed in SAMS (odds ratio [OR], 0.97; 95% confidence interval [CI], 0.80-1.18) or statin discontinuations (OR, 1.04; 95% CI, 0.80-1.35) after adjustment for baseline variables and other characteristics, namely age, sex, and African-American race, previously found to be associated with SAMS in VITAL.
“We actually thought when we started out that maybe we were going to show something, that maybe it was going to be that the people who got the vitamin D were least likely to have a problem with a statin than all those who didn’t get vitamin D, but that is not what we showed,” senior author Neil J. Stone, MD, Northwestern University, Chicago, told this news organization.
He noted that patients in the clinic with low levels of vitamin D often have muscle pain and discomfort and that previous unblinded studies suggested vitamin D might benefit patients with SAMS and reduce statin intolerance.
As previously reported, the double-blind VITAL trial showed no difference in the primary prevention of cardiovascular disease or cancer at 5 years among 25,871 middle-aged adults randomized to vitamin D3 at 2000 IU/d or placebo, regardless of their baseline vitamin D level.
Unlike previous studies showing a benefit with vitamin D on SAMS, importantly, VITAL participants were unaware of whether they were taking vitamin D or placebo and were not expecting any help with their muscle symptoms, first author Mark A. Hlatky, MD, Stanford (Calif.) University, pointed out in an interview.
As to how many statin users turn to the popular supplement for SAMS, he said that number couldn’t be pinned down, despite a lengthy search. “But I think it’s very common, because up to half of people stop taking their statins within a year and many of these do so because of statin-associated muscle symptoms, and we found it in about 30% of people who have them. I have them myself and was motivated to study it because I thought this was an interesting question.”
The results were published online in JAMA Cardiology.
SAMS by baseline 25-OHD
The substudy included 2,083 patients who initiated statin therapy after randomization and were surveyed in early 2016 about their statin use and muscle symptoms.
Two-thirds, or 1,397 patients, had 25-hydroxy vitamin D (25-OHD) measured at baseline, with 47% having levels < 30 ng/mL and 13% levels < 20 ng/mL.
Serum 25-OHD levels were virtually identical in the two treatment groups (mean, 30.4 ng/mL; median, 30.0 ng/mL). The frequency of SAMS did not differ between those assigned to vitamin D or placebo (28% vs. 31%).
The odds ratios for the association with vitamin D on SAMS were:
- 0.86 in all respondents with 25-OHD measured (95% CI, 0.69-1.09).
- 0.87 in those with levels ≥ 30 ng/mL (95% CI, 0.64-1.19).
- 0.85 with levels of 20-30 ng/mL (95% CI, 0.56-1.28).
- 0.93 with levels < 20 ng/mL (95% CI, 0.50-1.74).
The test for treatment effect modification by baseline serum 25-OHD level was not significant (P for interaction = .83).
In addition, the rate of muscle symptoms was similar between participants randomized to vitamin D and placebo when researchers used a cutpoint to define low 25-OHD of < 30 ng/mL (27% vs. 30%) or < 20 ng/mL (33% vs. 35%).
“We didn’t find any evidence at all that the people who came into the study with low levels of vitamin D did better with the supplement in this case,” Dr. Hlatky said. “So that wasn’t the reason we didn’t see anything.”
Critics may suggest the trial didn’t use a high enough dose of vitamin D, but both Dr. Hlatky and Dr. Stone say that’s unlikely to be a factor in the results because 2,000 IU/d is a substantial dose and well above the recommended adult daily dose of 600-800 IU.
They caution that the substudy wasn’t prespecified, was smaller than the parent trial, and did not have a protocol in place to detail SAMS. They also can’t rule out the possibility that vitamin D may have an effect in patients who have confirmed intolerance to multiple statins, especially after adjustment for the statin type and dose.
“If you’re taking vitamin D to keep from having statin-associated muscle symptoms, this very carefully done substudy with the various caveats doesn’t support that and that’s not something I would give my patients,” Dr. Stone said.
“The most important thing from a negative study is that it allows you to focus your attention on things that may be much more productive rather than assuming that just giving everybody vitamin D will take care of the statin issue,” he added. “Maybe the answer is going to be somewhere else, and there’ll be a lot of people I’m sure who will offer their advice as what the answer is but, I would argue, we want to see more studies to pin it down. So people can get some science behind what they do to try to reduce statin-associated muscle symptoms.”
Paul D. Thompson, MD, chief of cardiology emeritus at Hartford (Conn.) Hospital, and a SAMS expert who was not involved with the research, said, “This is a useful publication, and it’s smart in that it took advantage of a study that was already done.”
He acknowledged being skeptical of a beneficial effect of vitamin D supplementation on SAMS, because some previous data have been retracted, but said that potential treatments are best tested in patients with confirmed statin myalgia, as was the case in his team’s negative trial of CoQ10 supplementation.
That said, the present “study was able to at least give some of the best evidence so far that vitamin D doesn’t do anything to improve symptoms,” Dr. Thompson said. “So maybe it will cut down on so many vitamin D levels [being measured] and use of vitamin D when you don’t really need it.”
The study was sponsored by the Hyperlipidemia Research Fund at Northwestern University. The VITAL trial was supported by grants from the National Institutes of Health, and Quest Diagnostics performed the laboratory measurements at no additional costs. Dr. Hlatky reports no relevant financial relationships. Dr. Stone reports a grant from the Hyperlipidemia Research Fund at Northwestern and honorarium for educational activity for Knowledge to Practice. Dr. Thompson is on the executive committee for a study examining bempedoic acid in patients with statin-associated muscle symptoms.
A version of this article first appeared on Medscape.com.
Vitamin D supplements do not prevent muscle symptoms in new statin users or affect the likelihood of discontinuing a statin due to muscle pain and discomfort, a substudy of the VITAL trial indicates.
Among more than 2,000 randomized participants, statin-associated muscle symptoms (SAMS) were reported by 31% assigned to vitamin D and 31% assigned to placebo.
The two groups were equally likely to stop taking a statin due to muscle symptoms, at 13%.
No significant difference was observed in SAMS (odds ratio [OR], 0.97; 95% confidence interval [CI], 0.80-1.18) or statin discontinuations (OR, 1.04; 95% CI, 0.80-1.35) after adjustment for baseline variables and other characteristics, namely age, sex, and African-American race, previously found to be associated with SAMS in VITAL.
“We actually thought when we started out that maybe we were going to show something, that maybe it was going to be that the people who got the vitamin D were least likely to have a problem with a statin than all those who didn’t get vitamin D, but that is not what we showed,” senior author Neil J. Stone, MD, Northwestern University, Chicago, told this news organization.
He noted that patients in the clinic with low levels of vitamin D often have muscle pain and discomfort and that previous unblinded studies suggested vitamin D might benefit patients with SAMS and reduce statin intolerance.
As previously reported, the double-blind VITAL trial showed no difference in the primary prevention of cardiovascular disease or cancer at 5 years among 25,871 middle-aged adults randomized to vitamin D3 at 2000 IU/d or placebo, regardless of their baseline vitamin D level.
Unlike previous studies showing a benefit with vitamin D on SAMS, importantly, VITAL participants were unaware of whether they were taking vitamin D or placebo and were not expecting any help with their muscle symptoms, first author Mark A. Hlatky, MD, Stanford (Calif.) University, pointed out in an interview.
As to how many statin users turn to the popular supplement for SAMS, he said that number couldn’t be pinned down, despite a lengthy search. “But I think it’s very common, because up to half of people stop taking their statins within a year and many of these do so because of statin-associated muscle symptoms, and we found it in about 30% of people who have them. I have them myself and was motivated to study it because I thought this was an interesting question.”
The results were published online in JAMA Cardiology.
SAMS by baseline 25-OHD
The substudy included 2,083 patients who initiated statin therapy after randomization and were surveyed in early 2016 about their statin use and muscle symptoms.
Two-thirds, or 1,397 patients, had 25-hydroxy vitamin D (25-OHD) measured at baseline, with 47% having levels < 30 ng/mL and 13% levels < 20 ng/mL.
Serum 25-OHD levels were virtually identical in the two treatment groups (mean, 30.4 ng/mL; median, 30.0 ng/mL). The frequency of SAMS did not differ between those assigned to vitamin D or placebo (28% vs. 31%).
The odds ratios for the association with vitamin D on SAMS were:
- 0.86 in all respondents with 25-OHD measured (95% CI, 0.69-1.09).
- 0.87 in those with levels ≥ 30 ng/mL (95% CI, 0.64-1.19).
- 0.85 with levels of 20-30 ng/mL (95% CI, 0.56-1.28).
- 0.93 with levels < 20 ng/mL (95% CI, 0.50-1.74).
The test for treatment effect modification by baseline serum 25-OHD level was not significant (P for interaction = .83).
In addition, the rate of muscle symptoms was similar between participants randomized to vitamin D and placebo when researchers used a cutpoint to define low 25-OHD of < 30 ng/mL (27% vs. 30%) or < 20 ng/mL (33% vs. 35%).
“We didn’t find any evidence at all that the people who came into the study with low levels of vitamin D did better with the supplement in this case,” Dr. Hlatky said. “So that wasn’t the reason we didn’t see anything.”
Critics may suggest the trial didn’t use a high enough dose of vitamin D, but both Dr. Hlatky and Dr. Stone say that’s unlikely to be a factor in the results because 2,000 IU/d is a substantial dose and well above the recommended adult daily dose of 600-800 IU.
They caution that the substudy wasn’t prespecified, was smaller than the parent trial, and did not have a protocol in place to detail SAMS. They also can’t rule out the possibility that vitamin D may have an effect in patients who have confirmed intolerance to multiple statins, especially after adjustment for the statin type and dose.
“If you’re taking vitamin D to keep from having statin-associated muscle symptoms, this very carefully done substudy with the various caveats doesn’t support that and that’s not something I would give my patients,” Dr. Stone said.
“The most important thing from a negative study is that it allows you to focus your attention on things that may be much more productive rather than assuming that just giving everybody vitamin D will take care of the statin issue,” he added. “Maybe the answer is going to be somewhere else, and there’ll be a lot of people I’m sure who will offer their advice as what the answer is but, I would argue, we want to see more studies to pin it down. So people can get some science behind what they do to try to reduce statin-associated muscle symptoms.”
Paul D. Thompson, MD, chief of cardiology emeritus at Hartford (Conn.) Hospital, and a SAMS expert who was not involved with the research, said, “This is a useful publication, and it’s smart in that it took advantage of a study that was already done.”
He acknowledged being skeptical of a beneficial effect of vitamin D supplementation on SAMS, because some previous data have been retracted, but said that potential treatments are best tested in patients with confirmed statin myalgia, as was the case in his team’s negative trial of CoQ10 supplementation.
That said, the present “study was able to at least give some of the best evidence so far that vitamin D doesn’t do anything to improve symptoms,” Dr. Thompson said. “So maybe it will cut down on so many vitamin D levels [being measured] and use of vitamin D when you don’t really need it.”
The study was sponsored by the Hyperlipidemia Research Fund at Northwestern University. The VITAL trial was supported by grants from the National Institutes of Health, and Quest Diagnostics performed the laboratory measurements at no additional costs. Dr. Hlatky reports no relevant financial relationships. Dr. Stone reports a grant from the Hyperlipidemia Research Fund at Northwestern and honorarium for educational activity for Knowledge to Practice. Dr. Thompson is on the executive committee for a study examining bempedoic acid in patients with statin-associated muscle symptoms.
A version of this article first appeared on Medscape.com.
Cardiovascular societies less apt to recognize women, minorities
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
New genetic variant linked to maturity-onset diabetes of the young
A newly discovered genetic variant that is associated with type 2 diabetes (T2D) is responsible for almost 7% of all diabetes cases in Greenland, according to a whole-genome sequencing analysis of 448 Greenlandic Inuit individuals.
The variant, identified as c.1108G>T, “has the largest population impact of any previously reported variant” within the HNF1A gene – a gene that can cause maturity-onset diabetes of the young (MODY), reported senior author Torben Hansen, MD, PhD, of the University of Copenhagen, and colleagues in The Lancet Regional Health–Europe. The c.1108G>T variant does not cause MODY, but other variants within the HNF1A gene do. However, carriers of this variant, which is present in 1.9% of the Greenlandic Inuit population and has not been found elsewhere, have normal insulin sensitivity, but decreased beta-cell function and a more than fourfold risk of developing type 2 diabetes. “This adds to a previous discovery that about 11% of all diabetes in Greenlandic Inuit is explained by a mutation in the TBC1D4 variant,” Dr. Hansen told this publication. “Thus 1 in 5 patients diagnosed with type 2 diabetes in Greenland have a specific mutation explaining their diabetes. In European populations only about 1%-2% of patients diagnosed with type 2 diabetes have a known genetic etiology.”
The finding “provides new avenues to subgroup patients, detect diabetes in family members, and pursue precision treatment trials,” noted the authors, although they acknowledged that treatment choices for individuals with this variant still need to be explored. “We know from HNF1A-mutation carriers with European ancestry that they benefit from sulfonylurea treatment,” said Dr. Hansen. “However, we have not yet done treatment studies in Inuit.” The investigators noted that “it is not always the case that variants in HNF1A result in an increased insulin secretory response to sulfonylurea. ... Whether carriers of the c.1108G>T variant could benefit from treatment with sulfonylurea should be pursued within the context of a randomized clinical trial establishing both short- and long-term efficacy of sulfonylurea in these patients.”
A total of 4,497 study participants were randomly sampled from two cross-sectional cohorts in an adult Greenlandic population health survey. Among 448 participants who had whole genome sequencing, 14 known MODY genes were screened for both previously identified as well as novel variants. This identified the c.1108G>T variant, which was then genotyped in the full cohort in order to estimate an allele frequency of 1.3% in the general Greenlandic population, and 1.9% in the Inuit component. The variant was not found in genome sequences of other populations.
The researchers then tested the association of the variant with T2D and showed strong association with T2D (odds ratio, 4.35) and higher hemoglobin A1c levels.
“This is very well-conducted and exciting research that highlights the importance of studying the genetics of diverse populations,” said Miriam Udler, MD, PhD, director of the Massachusetts General Diabetes Genetics Clinic, and assistant professor at Harvard University, both in Boston. “This manuscript builds on prior work from the researchers identifying another genetic variant specific to the Greenlandic Inuit population in the gene TBC1D4,” she added. “About 3.8% of people in this population carry two copies of the TBC1D4 variant and have about a 10-fold increased risk of diabetes. Together the two variants affect 18% of Greenlanders with diabetes.”
With its fourfold increased risk of diabetes, the new variant falls into “an ever-growing category” of “intermediate risk” genetic variants, explained Dr. Udler – “meaning that they have a large impact on diabetes risk, but cannot fully predict whether someone will get diabetes. The contribution of additional risk factors is particularly important for ‘intermediate risk’ genetic variants,” she added. “Thus, clinically, we can tell patients who have variants such as HNF1A c.1108>T that they are at substantial increased risk of diabetes, but that many will not develop diabetes. And for those who do develop diabetes, we are not yet able to advise on particular therapeutic strategies.”
Still, she emphasized, the importance of studying diverse populations with specific genetic risk factors is the end-goal of precision medicine. “An active area of research is determining whether and how to return such information about ‘intermediate risk’ variants to patients who get clinical genetic testing for diabetes, since typically only variants that are very high risk ... are returned in clinical testing reports.” Dr. Udler added that “many more such “intermediate risk’ variants likely exist in all populations, but have yet to be characterized because they are less common than HNF1A c.1108>T; however, ongoing worldwide efforts to increase the sample sizes of human genetic studies will facilitate such discovery.”
The study was funded by Novo Nordisk Foundation, Independent Research Fund Denmark, and Karen Elise Jensen’s Foundation. Dr. Hansen and Dr. Udler had no disclosures.
A newly discovered genetic variant that is associated with type 2 diabetes (T2D) is responsible for almost 7% of all diabetes cases in Greenland, according to a whole-genome sequencing analysis of 448 Greenlandic Inuit individuals.
The variant, identified as c.1108G>T, “has the largest population impact of any previously reported variant” within the HNF1A gene – a gene that can cause maturity-onset diabetes of the young (MODY), reported senior author Torben Hansen, MD, PhD, of the University of Copenhagen, and colleagues in The Lancet Regional Health–Europe. The c.1108G>T variant does not cause MODY, but other variants within the HNF1A gene do. However, carriers of this variant, which is present in 1.9% of the Greenlandic Inuit population and has not been found elsewhere, have normal insulin sensitivity, but decreased beta-cell function and a more than fourfold risk of developing type 2 diabetes. “This adds to a previous discovery that about 11% of all diabetes in Greenlandic Inuit is explained by a mutation in the TBC1D4 variant,” Dr. Hansen told this publication. “Thus 1 in 5 patients diagnosed with type 2 diabetes in Greenland have a specific mutation explaining their diabetes. In European populations only about 1%-2% of patients diagnosed with type 2 diabetes have a known genetic etiology.”
The finding “provides new avenues to subgroup patients, detect diabetes in family members, and pursue precision treatment trials,” noted the authors, although they acknowledged that treatment choices for individuals with this variant still need to be explored. “We know from HNF1A-mutation carriers with European ancestry that they benefit from sulfonylurea treatment,” said Dr. Hansen. “However, we have not yet done treatment studies in Inuit.” The investigators noted that “it is not always the case that variants in HNF1A result in an increased insulin secretory response to sulfonylurea. ... Whether carriers of the c.1108G>T variant could benefit from treatment with sulfonylurea should be pursued within the context of a randomized clinical trial establishing both short- and long-term efficacy of sulfonylurea in these patients.”
A total of 4,497 study participants were randomly sampled from two cross-sectional cohorts in an adult Greenlandic population health survey. Among 448 participants who had whole genome sequencing, 14 known MODY genes were screened for both previously identified as well as novel variants. This identified the c.1108G>T variant, which was then genotyped in the full cohort in order to estimate an allele frequency of 1.3% in the general Greenlandic population, and 1.9% in the Inuit component. The variant was not found in genome sequences of other populations.
The researchers then tested the association of the variant with T2D and showed strong association with T2D (odds ratio, 4.35) and higher hemoglobin A1c levels.
“This is very well-conducted and exciting research that highlights the importance of studying the genetics of diverse populations,” said Miriam Udler, MD, PhD, director of the Massachusetts General Diabetes Genetics Clinic, and assistant professor at Harvard University, both in Boston. “This manuscript builds on prior work from the researchers identifying another genetic variant specific to the Greenlandic Inuit population in the gene TBC1D4,” she added. “About 3.8% of people in this population carry two copies of the TBC1D4 variant and have about a 10-fold increased risk of diabetes. Together the two variants affect 18% of Greenlanders with diabetes.”
With its fourfold increased risk of diabetes, the new variant falls into “an ever-growing category” of “intermediate risk” genetic variants, explained Dr. Udler – “meaning that they have a large impact on diabetes risk, but cannot fully predict whether someone will get diabetes. The contribution of additional risk factors is particularly important for ‘intermediate risk’ genetic variants,” she added. “Thus, clinically, we can tell patients who have variants such as HNF1A c.1108>T that they are at substantial increased risk of diabetes, but that many will not develop diabetes. And for those who do develop diabetes, we are not yet able to advise on particular therapeutic strategies.”
Still, she emphasized, the importance of studying diverse populations with specific genetic risk factors is the end-goal of precision medicine. “An active area of research is determining whether and how to return such information about ‘intermediate risk’ variants to patients who get clinical genetic testing for diabetes, since typically only variants that are very high risk ... are returned in clinical testing reports.” Dr. Udler added that “many more such “intermediate risk’ variants likely exist in all populations, but have yet to be characterized because they are less common than HNF1A c.1108>T; however, ongoing worldwide efforts to increase the sample sizes of human genetic studies will facilitate such discovery.”
The study was funded by Novo Nordisk Foundation, Independent Research Fund Denmark, and Karen Elise Jensen’s Foundation. Dr. Hansen and Dr. Udler had no disclosures.
A newly discovered genetic variant that is associated with type 2 diabetes (T2D) is responsible for almost 7% of all diabetes cases in Greenland, according to a whole-genome sequencing analysis of 448 Greenlandic Inuit individuals.
The variant, identified as c.1108G>T, “has the largest population impact of any previously reported variant” within the HNF1A gene – a gene that can cause maturity-onset diabetes of the young (MODY), reported senior author Torben Hansen, MD, PhD, of the University of Copenhagen, and colleagues in The Lancet Regional Health–Europe. The c.1108G>T variant does not cause MODY, but other variants within the HNF1A gene do. However, carriers of this variant, which is present in 1.9% of the Greenlandic Inuit population and has not been found elsewhere, have normal insulin sensitivity, but decreased beta-cell function and a more than fourfold risk of developing type 2 diabetes. “This adds to a previous discovery that about 11% of all diabetes in Greenlandic Inuit is explained by a mutation in the TBC1D4 variant,” Dr. Hansen told this publication. “Thus 1 in 5 patients diagnosed with type 2 diabetes in Greenland have a specific mutation explaining their diabetes. In European populations only about 1%-2% of patients diagnosed with type 2 diabetes have a known genetic etiology.”
The finding “provides new avenues to subgroup patients, detect diabetes in family members, and pursue precision treatment trials,” noted the authors, although they acknowledged that treatment choices for individuals with this variant still need to be explored. “We know from HNF1A-mutation carriers with European ancestry that they benefit from sulfonylurea treatment,” said Dr. Hansen. “However, we have not yet done treatment studies in Inuit.” The investigators noted that “it is not always the case that variants in HNF1A result in an increased insulin secretory response to sulfonylurea. ... Whether carriers of the c.1108G>T variant could benefit from treatment with sulfonylurea should be pursued within the context of a randomized clinical trial establishing both short- and long-term efficacy of sulfonylurea in these patients.”
A total of 4,497 study participants were randomly sampled from two cross-sectional cohorts in an adult Greenlandic population health survey. Among 448 participants who had whole genome sequencing, 14 known MODY genes were screened for both previously identified as well as novel variants. This identified the c.1108G>T variant, which was then genotyped in the full cohort in order to estimate an allele frequency of 1.3% in the general Greenlandic population, and 1.9% in the Inuit component. The variant was not found in genome sequences of other populations.
The researchers then tested the association of the variant with T2D and showed strong association with T2D (odds ratio, 4.35) and higher hemoglobin A1c levels.
“This is very well-conducted and exciting research that highlights the importance of studying the genetics of diverse populations,” said Miriam Udler, MD, PhD, director of the Massachusetts General Diabetes Genetics Clinic, and assistant professor at Harvard University, both in Boston. “This manuscript builds on prior work from the researchers identifying another genetic variant specific to the Greenlandic Inuit population in the gene TBC1D4,” she added. “About 3.8% of people in this population carry two copies of the TBC1D4 variant and have about a 10-fold increased risk of diabetes. Together the two variants affect 18% of Greenlanders with diabetes.”
With its fourfold increased risk of diabetes, the new variant falls into “an ever-growing category” of “intermediate risk” genetic variants, explained Dr. Udler – “meaning that they have a large impact on diabetes risk, but cannot fully predict whether someone will get diabetes. The contribution of additional risk factors is particularly important for ‘intermediate risk’ genetic variants,” she added. “Thus, clinically, we can tell patients who have variants such as HNF1A c.1108>T that they are at substantial increased risk of diabetes, but that many will not develop diabetes. And for those who do develop diabetes, we are not yet able to advise on particular therapeutic strategies.”
Still, she emphasized, the importance of studying diverse populations with specific genetic risk factors is the end-goal of precision medicine. “An active area of research is determining whether and how to return such information about ‘intermediate risk’ variants to patients who get clinical genetic testing for diabetes, since typically only variants that are very high risk ... are returned in clinical testing reports.” Dr. Udler added that “many more such “intermediate risk’ variants likely exist in all populations, but have yet to be characterized because they are less common than HNF1A c.1108>T; however, ongoing worldwide efforts to increase the sample sizes of human genetic studies will facilitate such discovery.”
The study was funded by Novo Nordisk Foundation, Independent Research Fund Denmark, and Karen Elise Jensen’s Foundation. Dr. Hansen and Dr. Udler had no disclosures.
FROM THE LANCET REGIONAL HEALTH–EUROPE
Don’t call me ‘Dr.,’ say some physicians – but most prefer the title
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
The right indoor relative humidity could ward off COVID
The “sweet spot” associated with reduced COVID-19 cases and deaths is 40%-60% indoor relative humidity, an MIT news release said. People who maintained indoor relative humidity outside those parameters had higher rates of catching COVID-19.
Most people are comfortable with 30%-50% relative humidity, researchers said. An airplane cabin has about 20% relative humidity.
Relative humidity is the amount of moisture in the air, compared with the total moisture the air can hold at a given temperature before saturating and forming condensation.
The study was published in The Journal of the Royal Society Interface. Researchers examined COVID-19 data and meteorological measurements from 121 countries from January 2020 through August 2020, before vaccines became available to the public.
“When outdoor temperatures were below the typical human comfort range, they assumed indoor spaces were heated to reach that comfort range. Based on the added heating, they calculated the associated drop in indoor relative humidity,” the MIT news release said.
The research teams found that when a region reported a rise in COVID-19 cases and deaths, the region’s estimated indoor relative humidity was either lower than 40% or higher than 60%, the release said.
“There’s potentially a protective effect of this intermediate indoor relative humidity,” said Connor Verheyen, the lead author and a PhD student in medical engineering and medical physics in the Harvard-MIT Program in Health Sciences and Technology.
Widespread use of the 40%-60% indoor humidity range could reduce the need for lockdowns and other widespread restrictions, the study concluded.
“Unlike measures that depend on individual compliance (for example, masking or hand-washing), indoor RH optimization would achieve high compliance because all occupants of a common indoor space would be exposed to similar ambient conditions,” the study said. “Compared to the long timelines and high costs of vaccine production and distribution, humidity control systems could potentially be implemented more quickly and cheaply in certain indoor settings.”
A version of this article first appeared on WebMD.com.
The “sweet spot” associated with reduced COVID-19 cases and deaths is 40%-60% indoor relative humidity, an MIT news release said. People who maintained indoor relative humidity outside those parameters had higher rates of catching COVID-19.
Most people are comfortable with 30%-50% relative humidity, researchers said. An airplane cabin has about 20% relative humidity.
Relative humidity is the amount of moisture in the air, compared with the total moisture the air can hold at a given temperature before saturating and forming condensation.
The study was published in The Journal of the Royal Society Interface. Researchers examined COVID-19 data and meteorological measurements from 121 countries from January 2020 through August 2020, before vaccines became available to the public.
“When outdoor temperatures were below the typical human comfort range, they assumed indoor spaces were heated to reach that comfort range. Based on the added heating, they calculated the associated drop in indoor relative humidity,” the MIT news release said.
The research teams found that when a region reported a rise in COVID-19 cases and deaths, the region’s estimated indoor relative humidity was either lower than 40% or higher than 60%, the release said.
“There’s potentially a protective effect of this intermediate indoor relative humidity,” said Connor Verheyen, the lead author and a PhD student in medical engineering and medical physics in the Harvard-MIT Program in Health Sciences and Technology.
Widespread use of the 40%-60% indoor humidity range could reduce the need for lockdowns and other widespread restrictions, the study concluded.
“Unlike measures that depend on individual compliance (for example, masking or hand-washing), indoor RH optimization would achieve high compliance because all occupants of a common indoor space would be exposed to similar ambient conditions,” the study said. “Compared to the long timelines and high costs of vaccine production and distribution, humidity control systems could potentially be implemented more quickly and cheaply in certain indoor settings.”
A version of this article first appeared on WebMD.com.
The “sweet spot” associated with reduced COVID-19 cases and deaths is 40%-60% indoor relative humidity, an MIT news release said. People who maintained indoor relative humidity outside those parameters had higher rates of catching COVID-19.
Most people are comfortable with 30%-50% relative humidity, researchers said. An airplane cabin has about 20% relative humidity.
Relative humidity is the amount of moisture in the air, compared with the total moisture the air can hold at a given temperature before saturating and forming condensation.
The study was published in The Journal of the Royal Society Interface. Researchers examined COVID-19 data and meteorological measurements from 121 countries from January 2020 through August 2020, before vaccines became available to the public.
“When outdoor temperatures were below the typical human comfort range, they assumed indoor spaces were heated to reach that comfort range. Based on the added heating, they calculated the associated drop in indoor relative humidity,” the MIT news release said.
The research teams found that when a region reported a rise in COVID-19 cases and deaths, the region’s estimated indoor relative humidity was either lower than 40% or higher than 60%, the release said.
“There’s potentially a protective effect of this intermediate indoor relative humidity,” said Connor Verheyen, the lead author and a PhD student in medical engineering and medical physics in the Harvard-MIT Program in Health Sciences and Technology.
Widespread use of the 40%-60% indoor humidity range could reduce the need for lockdowns and other widespread restrictions, the study concluded.
“Unlike measures that depend on individual compliance (for example, masking or hand-washing), indoor RH optimization would achieve high compliance because all occupants of a common indoor space would be exposed to similar ambient conditions,” the study said. “Compared to the long timelines and high costs of vaccine production and distribution, humidity control systems could potentially be implemented more quickly and cheaply in certain indoor settings.”
A version of this article first appeared on WebMD.com.
FROM THE JOURNAL OF THE ROYAL SOCIETY INTERFACE
HDL cholesterol not linked to CHD risk in Blacks: REGARDS
High-density lipoprotein cholesterol may not be as effective a biomarker of cardiovascular disease risk as once thought, particularly in Black adults, according to results from a large biracial cohort study that also raised questions about the validity of high HDL cholesterol as a potentially protective factor in White and Black adults alike.
“I think this opens the door to suggest that every biomarker we use might have a race-specific association with disease outcome,” Nathalie Pamir, PhD, an associate professor at Oregon Health & Science University in Portland, said in an interview. “So, something as basic as HDL cholesterol – we’ve known about it since 1970 – has a race signature.”
Dr. Pamir and colleagues reported their findings from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) cohort study that recruited 30,239 Black and White individuals aged 45 years and older from the contiguous United States from 2003 to 2007.
The study found that LDL cholesterol “modestly” predicted coronary heart disease (CHD) risk in Black and White adults. However, low HDL cholesterol, while associated with an increased risk in White patients (hazard ratio, 1.22; 95% confidence interval, 1.05-1.43), did not have a similar association in Blacks (HR, 0.94; 95% CI: 0.78-1.14). And high HDL cholesterol wasn’t found to be predictive in either group (HR, 0.96; 95% CI, 0.79-1.16 for White participants: HR, 0.91; 95% CI, 0.74-1.12 for Black participants).
Among 23,901 study participants who were CHD-risk free over a 10-year follow-up, 664 and 951 CHD events occurred in Black and White participants, respectively. The study cohort was 57.8% White and 58.4% women, with a mean age of 65 years.
The study noted that LDL cholesterol and triglycerides conferred similar risks for CHD in both White and Black participants.
Acknowledging that this study focused on Blacks, Dr. Pamir added that “we need to know about Asian Americans; we need to know about Hispanic Americans.”
Change of approach to lipid management called for
Dr. Pamir noted that the current understanding about HDL cholesterol and CHD risk comes from the Framingham heart study in the 1970s, whose population was 100% White.
Care algorithms derived from the Framingham study as well as the Multi-Ethnic Study of Atherosclerosis incorporate that association between HDL cholesterol and CHD risk, she noted, but these findings from REGARDS should change how cardiologists approach lipid management in Black and White patients.
“The conversation would go something like: High HDL cholesterol levels put you in a higher risk [bracket] but HDL cholesterol levels are not something we treat; we have no drugs for that,” Dr. Pamir said.
“The conversation would continue along the lines that: ‘You need to do more exercise, you need to change your diet, incorporate healthy fats, walnuts, and omega 3s.’
“But what might the conversation be for Black patients? ‘We don’t see the association that we see for White patients. Do adopt the good habits to exercise and dietary changes, but don’t get too worried about it.’ ”
The study report raises “caution” about using the Framingham, MESA, and other algorithms for evaluating CHD risk. Dr. Pamir explained what that means. “We might be underestimating risk, because what our study showed was that, when we looked at clinically high HDL cholesterol, about 60 mg/dL, it has no benefit for White and Black patients.”
She added, “So that pat on the back we get for patients that have high HDL-C levels? Maybe that pat on the back shouldn’t be there.”
In an invited commentary, Keith C. Ferdinand, MD, of Tulane University in New Orleans, wrote that using HDL cholesterol in risk calculations could inaccurately assess atherosclerotic cardiovascular risk in Black adults “and become a barrier to optimal care.”
In an interview, he said the REGARDS findings call for consideration of other biomarkers for evaluating CHD risk and point to the importance of socioeconomic factors in health outcomes.
“Physicians and other clinicians need to recognize the powerful impact of the social determinants of health and to also recognize the limits of HDL itself as either protective if it’s high or a definitive predictor of risk if it’s low, and focus on some more modern approaches, including coronary artery calcium scoring.”
He also said risk evaluation should include lipoprotein(a), which, he noted in the editorial, the European Atherosclerosis Society recommends measuring. “One of the reasons it’s underutilized is that we really don’t have a specific treatment for it,” he said of Lp(a) in the United States.
In his editorial comment, Dr. Ferdinand called for future research aimed at eliminating health disparities. “Regardless of the development of better tools for the assessment of risk, newer drugs to treat CVD, the use of coronary artery calcium, if we don’t apply evidence-based medicine equally across the population based on race, ethnicity, sex, gender, socioeconomic status, or geography, then the disparities are going to persist,” he said.
The National Institute of Neurological Disorders and Stroke and the National Institute on Aging provided funding for the study. Dr. Pamir has no relevant relationships to disclose. Dr. Ferdinand disclosed relationships with Boehringer Ingelheim, Novartis, Janssen, and Lilly.
High-density lipoprotein cholesterol may not be as effective a biomarker of cardiovascular disease risk as once thought, particularly in Black adults, according to results from a large biracial cohort study that also raised questions about the validity of high HDL cholesterol as a potentially protective factor in White and Black adults alike.
“I think this opens the door to suggest that every biomarker we use might have a race-specific association with disease outcome,” Nathalie Pamir, PhD, an associate professor at Oregon Health & Science University in Portland, said in an interview. “So, something as basic as HDL cholesterol – we’ve known about it since 1970 – has a race signature.”
Dr. Pamir and colleagues reported their findings from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) cohort study that recruited 30,239 Black and White individuals aged 45 years and older from the contiguous United States from 2003 to 2007.
The study found that LDL cholesterol “modestly” predicted coronary heart disease (CHD) risk in Black and White adults. However, low HDL cholesterol, while associated with an increased risk in White patients (hazard ratio, 1.22; 95% confidence interval, 1.05-1.43), did not have a similar association in Blacks (HR, 0.94; 95% CI: 0.78-1.14). And high HDL cholesterol wasn’t found to be predictive in either group (HR, 0.96; 95% CI, 0.79-1.16 for White participants: HR, 0.91; 95% CI, 0.74-1.12 for Black participants).
Among 23,901 study participants who were CHD-risk free over a 10-year follow-up, 664 and 951 CHD events occurred in Black and White participants, respectively. The study cohort was 57.8% White and 58.4% women, with a mean age of 65 years.
The study noted that LDL cholesterol and triglycerides conferred similar risks for CHD in both White and Black participants.
Acknowledging that this study focused on Blacks, Dr. Pamir added that “we need to know about Asian Americans; we need to know about Hispanic Americans.”
Change of approach to lipid management called for
Dr. Pamir noted that the current understanding about HDL cholesterol and CHD risk comes from the Framingham heart study in the 1970s, whose population was 100% White.
Care algorithms derived from the Framingham study as well as the Multi-Ethnic Study of Atherosclerosis incorporate that association between HDL cholesterol and CHD risk, she noted, but these findings from REGARDS should change how cardiologists approach lipid management in Black and White patients.
“The conversation would go something like: High HDL cholesterol levels put you in a higher risk [bracket] but HDL cholesterol levels are not something we treat; we have no drugs for that,” Dr. Pamir said.
“The conversation would continue along the lines that: ‘You need to do more exercise, you need to change your diet, incorporate healthy fats, walnuts, and omega 3s.’
“But what might the conversation be for Black patients? ‘We don’t see the association that we see for White patients. Do adopt the good habits to exercise and dietary changes, but don’t get too worried about it.’ ”
The study report raises “caution” about using the Framingham, MESA, and other algorithms for evaluating CHD risk. Dr. Pamir explained what that means. “We might be underestimating risk, because what our study showed was that, when we looked at clinically high HDL cholesterol, about 60 mg/dL, it has no benefit for White and Black patients.”
She added, “So that pat on the back we get for patients that have high HDL-C levels? Maybe that pat on the back shouldn’t be there.”
In an invited commentary, Keith C. Ferdinand, MD, of Tulane University in New Orleans, wrote that using HDL cholesterol in risk calculations could inaccurately assess atherosclerotic cardiovascular risk in Black adults “and become a barrier to optimal care.”
In an interview, he said the REGARDS findings call for consideration of other biomarkers for evaluating CHD risk and point to the importance of socioeconomic factors in health outcomes.
“Physicians and other clinicians need to recognize the powerful impact of the social determinants of health and to also recognize the limits of HDL itself as either protective if it’s high or a definitive predictor of risk if it’s low, and focus on some more modern approaches, including coronary artery calcium scoring.”
He also said risk evaluation should include lipoprotein(a), which, he noted in the editorial, the European Atherosclerosis Society recommends measuring. “One of the reasons it’s underutilized is that we really don’t have a specific treatment for it,” he said of Lp(a) in the United States.
In his editorial comment, Dr. Ferdinand called for future research aimed at eliminating health disparities. “Regardless of the development of better tools for the assessment of risk, newer drugs to treat CVD, the use of coronary artery calcium, if we don’t apply evidence-based medicine equally across the population based on race, ethnicity, sex, gender, socioeconomic status, or geography, then the disparities are going to persist,” he said.
The National Institute of Neurological Disorders and Stroke and the National Institute on Aging provided funding for the study. Dr. Pamir has no relevant relationships to disclose. Dr. Ferdinand disclosed relationships with Boehringer Ingelheim, Novartis, Janssen, and Lilly.
High-density lipoprotein cholesterol may not be as effective a biomarker of cardiovascular disease risk as once thought, particularly in Black adults, according to results from a large biracial cohort study that also raised questions about the validity of high HDL cholesterol as a potentially protective factor in White and Black adults alike.
“I think this opens the door to suggest that every biomarker we use might have a race-specific association with disease outcome,” Nathalie Pamir, PhD, an associate professor at Oregon Health & Science University in Portland, said in an interview. “So, something as basic as HDL cholesterol – we’ve known about it since 1970 – has a race signature.”
Dr. Pamir and colleagues reported their findings from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) cohort study that recruited 30,239 Black and White individuals aged 45 years and older from the contiguous United States from 2003 to 2007.
The study found that LDL cholesterol “modestly” predicted coronary heart disease (CHD) risk in Black and White adults. However, low HDL cholesterol, while associated with an increased risk in White patients (hazard ratio, 1.22; 95% confidence interval, 1.05-1.43), did not have a similar association in Blacks (HR, 0.94; 95% CI: 0.78-1.14). And high HDL cholesterol wasn’t found to be predictive in either group (HR, 0.96; 95% CI, 0.79-1.16 for White participants: HR, 0.91; 95% CI, 0.74-1.12 for Black participants).
Among 23,901 study participants who were CHD-risk free over a 10-year follow-up, 664 and 951 CHD events occurred in Black and White participants, respectively. The study cohort was 57.8% White and 58.4% women, with a mean age of 65 years.
The study noted that LDL cholesterol and triglycerides conferred similar risks for CHD in both White and Black participants.
Acknowledging that this study focused on Blacks, Dr. Pamir added that “we need to know about Asian Americans; we need to know about Hispanic Americans.”
Change of approach to lipid management called for
Dr. Pamir noted that the current understanding about HDL cholesterol and CHD risk comes from the Framingham heart study in the 1970s, whose population was 100% White.
Care algorithms derived from the Framingham study as well as the Multi-Ethnic Study of Atherosclerosis incorporate that association between HDL cholesterol and CHD risk, she noted, but these findings from REGARDS should change how cardiologists approach lipid management in Black and White patients.
“The conversation would go something like: High HDL cholesterol levels put you in a higher risk [bracket] but HDL cholesterol levels are not something we treat; we have no drugs for that,” Dr. Pamir said.
“The conversation would continue along the lines that: ‘You need to do more exercise, you need to change your diet, incorporate healthy fats, walnuts, and omega 3s.’
“But what might the conversation be for Black patients? ‘We don’t see the association that we see for White patients. Do adopt the good habits to exercise and dietary changes, but don’t get too worried about it.’ ”
The study report raises “caution” about using the Framingham, MESA, and other algorithms for evaluating CHD risk. Dr. Pamir explained what that means. “We might be underestimating risk, because what our study showed was that, when we looked at clinically high HDL cholesterol, about 60 mg/dL, it has no benefit for White and Black patients.”
She added, “So that pat on the back we get for patients that have high HDL-C levels? Maybe that pat on the back shouldn’t be there.”
In an invited commentary, Keith C. Ferdinand, MD, of Tulane University in New Orleans, wrote that using HDL cholesterol in risk calculations could inaccurately assess atherosclerotic cardiovascular risk in Black adults “and become a barrier to optimal care.”
In an interview, he said the REGARDS findings call for consideration of other biomarkers for evaluating CHD risk and point to the importance of socioeconomic factors in health outcomes.
“Physicians and other clinicians need to recognize the powerful impact of the social determinants of health and to also recognize the limits of HDL itself as either protective if it’s high or a definitive predictor of risk if it’s low, and focus on some more modern approaches, including coronary artery calcium scoring.”
He also said risk evaluation should include lipoprotein(a), which, he noted in the editorial, the European Atherosclerosis Society recommends measuring. “One of the reasons it’s underutilized is that we really don’t have a specific treatment for it,” he said of Lp(a) in the United States.
In his editorial comment, Dr. Ferdinand called for future research aimed at eliminating health disparities. “Regardless of the development of better tools for the assessment of risk, newer drugs to treat CVD, the use of coronary artery calcium, if we don’t apply evidence-based medicine equally across the population based on race, ethnicity, sex, gender, socioeconomic status, or geography, then the disparities are going to persist,” he said.
The National Institute of Neurological Disorders and Stroke and the National Institute on Aging provided funding for the study. Dr. Pamir has no relevant relationships to disclose. Dr. Ferdinand disclosed relationships with Boehringer Ingelheim, Novartis, Janssen, and Lilly.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Will ICER review aid bid for Medicare to pay for obesity drugs?
A report from a well-respected nonprofit group may bolster efforts to have Medicare, the largest U.S. purchaser of prescription drugs, cover obesity medicines, for which there has been accumulating evidence of significant benefit.
The Institute for Clinical and Economic Review (ICER) released a report last month on obesity medicines, based on extensive review of research done to date and input from clinicians, drug-makers, and members of the public.
Of the treatments reviewed, the ICER report gave the best ratings to two Novo Nordisk products, a B+ for semaglutide (Wegovy) and a B for liraglutide (Saxenda), while also making the case for price cuts. At an annual U.S. net price estimated at $13,618, semaglutide exceeds what ICER considers typical cost-effectiveness thresholds. ICER suggested a benchmark annual price range for semaglutide of between $7,500 and $9,800.
The ICER report also directs insurers in general to provide more generous coverage of obesity medicines, with a specific recommendation for the U.S. Congress to pass a pending bill known as the Treat and Reduce Obesity Act of 2021. The bill would undo a restriction on weight-loss drugs in the Medicare Part D plans, which covered about 49 million people last year. Sen. Tom Carper (D-Del.) and Sen. Bill Cassidy, MD, (R-La.) have repeatedly introduced versions of the bill since 2013.
“In both chambers of Congress and with bipartisan support, we’ve pushed to expand Medicare coverage of additional therapies and medications to treat obesity,” Sen. Cassidy said in an email. “This report confirms what we’ve worked on for nearly a decade – our legislation will help improve lives.”
The current House version of the bill has the backing of more than a third of the members of that chamber, with 113 Democratic and 40 Republican cosponsors. The Senate version has 22 sponsors.
Changing views
The ICER report comes amid a broader change in how clinicians view obesity.
The American Academy of Pediatrics is readying a new Clinical Practice Guideline for the Evaluation and Treatment of Pediatric Obesity that will mark a major shift in approach. Aaron S. Kelly, PhD, a professor of pediatrics at the University of Minnesota, Minneapolis, described it as a “sea change,” with obesity now seen as “a chronic, refractory, relapsing disease,” for which watchful waiting is no longer appropriate.
But the field of obesity treatment looked quite different in the early 2000s when Congress worked on a plan to add a pharmacy benefit to Medicare.
The deliberate omission of obesity medicine in the Medicare Part D benefit reflected both the state of science at the time and U.S. experience with a dangerous weight-loss drug combo in the late 1990s.
Initial expectations for weight-loss pills were high after the Food and Drug Administration cleared dexfenfluramine HCl (Redux) in 1996, which was part of the popular fen-phen combination. “Newly Approved Diet Drug Promises to Help Millions of Obese Americans – But Is No Magic Bullet,” read a headline about the Redux approval in The Washington Post
When work began in the 2000s to create a Medicare pharmacy benefit, lawmakers and congressional staff had a pool of about $400 billion available to establish what became the Part D program, Joel White, a former House staffer who helped draft the law, told this news organization in an email exchange.
Given the state of obesity research at the time, it seemed to make sense to exclude weight-loss medications, wrote Mr. White. Mr. White is now chief executive of the consulting firm Horizon, which has clients in the drug industry including the Pharmaceutical Research and Manufacturers of America.
“Now we know that obesity is a chronic disease of epidemic proportions. Decades of research have produced a series of advances in the way we understand and treat obesity. While scientists and many who work directly with those impacted by this epidemic understand how treatments have advanced, the law lags behind,” Mr. White said.
XXXCurrent payment policies for obesity treatments are based on “outdated information and ongoing misperception,” he noted. “While Part D has been a resounding success, our Medicare approach to obesity is not.”
“In addition, it makes no sense that Medicare covers the most drastic procedure (bariatric surgery) but not less-invasive, effective treatments,” he added. “We should have long ago lifted restrictions based on advances in science and medicine.”
Overcoming the stigma
Scott Kahan, MD, MPH, agreed and hopes that the new ICER report will help more patients secure needed medications, raising a “call to arms” about the need for better coverage of obesity drugs.
Dr. Kahan is director of the National Center for Weight and Wellness, a private clinic in Washington, and chair of the clinical committee for The Obesity Society. He also served as a member of a policy roundtable that ICER convened as part of research on the report on obesity drugs. Dr. Kahan, who also serves on the faculty at the Johns Hopkins Bloomberg School of Public Health, Baltimore, has received fees from drug makers such as Eli Lilly.
The ICER report may help what Dr. Kahan described as well-founded caution about obesity treatments in general.
“When it comes to weight loss, there are all of these magical treatments that are sold on social media and traditional media. There are a lot of bad actors in terms of people calling themselves experts and gurus and promising all kinds of crazy stuff,” said Dr. Kahan.
And there are long-standing stigmas about obesity, he stressed.
“That underlies a lot of the backward policies, including poor coverage for medications and the noncoverage by Medicare,” Dr. Kahan said. “There’s a societal ingrained set of beliefs and misperceptions and biases. That takes time to unwind, and I think we’re on the way, but we’re not quite there yet.”
Lifestyle changes not enough to tackle obesity
AHIP (formerly America’s Health Insurance Plans) told this news organization its members consider ICER reports when making decisions about which products to cover. “And health plans already cover obesity treatments that they consider medically necessary,” said David Allen, an AHIP spokesperson.
“It is important to note that every treatment does not work for every patient, and many patients experience adverse events and may discontinue treatment,” he added in an email. “Health insurance providers play an important role in helping [health care] providers and patients identify the treatment options that are most likely to be effective as well as affordable.”
Separately, the nonprofit watchdog group Public Citizen cautioned against liraglutide on its Worst Pills, Best Pills website. In its view, the drug is minimally effective and has many dangerous adverse effects, which are even more frequent with the higher-dose weight-loss version (a lower-dose version is approved for type 2 diabetes).
“There is currently no medication that can be used safely to achieve weight loss effortlessly and without dangerous adverse effects,” the group said. “Rather than focus on losing weight by turning to risky drugs, overweight and obese adults seeking to achieve better health should make reasonable and sustainable changes to their lifestyle, such as eating a healthy diet and getting regular exercise.”
Yet, many people find there is little help available for making lifestyle changes, and some patients and physicians say these modifications by themselves are not enough.
“The vast majority of people with obesity cannot achieve sustained weight loss through diet and exercise alone,” said David Rind, MD, chief medical officer of ICER, in an Oct. 20 statement. “As such, obesity, and its resulting physical health, mental health, and social burdens, is not a choice or failing, but a medical condition.”
The focus should now be on assuring that effective medications “are priced in alignment with their benefits so that they are accessible and affordable across U.S. society,” Dr. Rind urges.
‘My own demise with a fork and knife’
ICER sought public feedback on a draft version of the report before finalizing it.
In their comments on ICER’s work, several pharmaceutical researchers and Novo Nordisk questioned the calculations used in making judgments about the value of obesity drugs. In a statement, Novo Nordisk told this news organization that the company’s view is that ICER’s modeling “does not adequately address the real-world complexities of obesity, and consequently underestimates the health and societal impact medical treatments can have.”
Commenters also dug into aspects of ICER’s calculations, including ones that consider quality-adjusted life-years (QALYs). ICER describes QALY as an academic standard for measuring how well all different types of medical treatments can extend or improve patients’ lives. In an explainer on its website, ICER says this metric has served as a fundamental component of cost-effectiveness analyses in the United States and around the world for more than 30 years.
ICER and drug makers have been at odds for some time, with PhRMA having criticized the nonprofit group. A 2020 Reuters article detailed public relations strategies used by firms paid by drug makers to raise questions about ICER’s work. Critics accuse it of allying with insurers.
ICER’s list of its recent financial supporters includes Blue Cross Blue Shield of Massachusetts and the Kaiser Foundation Health Plan, but also many other groups, such as the U.S. Department of Veterans Affairs, the American Academy of Neurology, and the American College of Rheumatology.
The public comments on the ICER report also include one from an unidentified woman who wrote of her past struggles to lose weight.
She said her health plan wouldn’t cover behavioral programs or semaglutide as a weight-loss drug but did cover it eventually because of signs that she had developed insulin resistance. The patient said the drug worked for her, whereas other approaches to control weight had failed.
“To put it simply, I now experience hunger and satiety in a way that I can only assume people with normal metabolism do. I am 49 years old and approaching the age where serious comorbidities associated with obesity begin to manifest,” the patient wrote.
“I no longer worry about bringing about my own demise with a fork and knife because of misfiring hunger cues.”
A version of this article first appeared on Medscape.com.
A report from a well-respected nonprofit group may bolster efforts to have Medicare, the largest U.S. purchaser of prescription drugs, cover obesity medicines, for which there has been accumulating evidence of significant benefit.
The Institute for Clinical and Economic Review (ICER) released a report last month on obesity medicines, based on extensive review of research done to date and input from clinicians, drug-makers, and members of the public.
Of the treatments reviewed, the ICER report gave the best ratings to two Novo Nordisk products, a B+ for semaglutide (Wegovy) and a B for liraglutide (Saxenda), while also making the case for price cuts. At an annual U.S. net price estimated at $13,618, semaglutide exceeds what ICER considers typical cost-effectiveness thresholds. ICER suggested a benchmark annual price range for semaglutide of between $7,500 and $9,800.
The ICER report also directs insurers in general to provide more generous coverage of obesity medicines, with a specific recommendation for the U.S. Congress to pass a pending bill known as the Treat and Reduce Obesity Act of 2021. The bill would undo a restriction on weight-loss drugs in the Medicare Part D plans, which covered about 49 million people last year. Sen. Tom Carper (D-Del.) and Sen. Bill Cassidy, MD, (R-La.) have repeatedly introduced versions of the bill since 2013.
“In both chambers of Congress and with bipartisan support, we’ve pushed to expand Medicare coverage of additional therapies and medications to treat obesity,” Sen. Cassidy said in an email. “This report confirms what we’ve worked on for nearly a decade – our legislation will help improve lives.”
The current House version of the bill has the backing of more than a third of the members of that chamber, with 113 Democratic and 40 Republican cosponsors. The Senate version has 22 sponsors.
Changing views
The ICER report comes amid a broader change in how clinicians view obesity.
The American Academy of Pediatrics is readying a new Clinical Practice Guideline for the Evaluation and Treatment of Pediatric Obesity that will mark a major shift in approach. Aaron S. Kelly, PhD, a professor of pediatrics at the University of Minnesota, Minneapolis, described it as a “sea change,” with obesity now seen as “a chronic, refractory, relapsing disease,” for which watchful waiting is no longer appropriate.
But the field of obesity treatment looked quite different in the early 2000s when Congress worked on a plan to add a pharmacy benefit to Medicare.
The deliberate omission of obesity medicine in the Medicare Part D benefit reflected both the state of science at the time and U.S. experience with a dangerous weight-loss drug combo in the late 1990s.
Initial expectations for weight-loss pills were high after the Food and Drug Administration cleared dexfenfluramine HCl (Redux) in 1996, which was part of the popular fen-phen combination. “Newly Approved Diet Drug Promises to Help Millions of Obese Americans – But Is No Magic Bullet,” read a headline about the Redux approval in The Washington Post
When work began in the 2000s to create a Medicare pharmacy benefit, lawmakers and congressional staff had a pool of about $400 billion available to establish what became the Part D program, Joel White, a former House staffer who helped draft the law, told this news organization in an email exchange.
Given the state of obesity research at the time, it seemed to make sense to exclude weight-loss medications, wrote Mr. White. Mr. White is now chief executive of the consulting firm Horizon, which has clients in the drug industry including the Pharmaceutical Research and Manufacturers of America.
“Now we know that obesity is a chronic disease of epidemic proportions. Decades of research have produced a series of advances in the way we understand and treat obesity. While scientists and many who work directly with those impacted by this epidemic understand how treatments have advanced, the law lags behind,” Mr. White said.
XXXCurrent payment policies for obesity treatments are based on “outdated information and ongoing misperception,” he noted. “While Part D has been a resounding success, our Medicare approach to obesity is not.”
“In addition, it makes no sense that Medicare covers the most drastic procedure (bariatric surgery) but not less-invasive, effective treatments,” he added. “We should have long ago lifted restrictions based on advances in science and medicine.”
Overcoming the stigma
Scott Kahan, MD, MPH, agreed and hopes that the new ICER report will help more patients secure needed medications, raising a “call to arms” about the need for better coverage of obesity drugs.
Dr. Kahan is director of the National Center for Weight and Wellness, a private clinic in Washington, and chair of the clinical committee for The Obesity Society. He also served as a member of a policy roundtable that ICER convened as part of research on the report on obesity drugs. Dr. Kahan, who also serves on the faculty at the Johns Hopkins Bloomberg School of Public Health, Baltimore, has received fees from drug makers such as Eli Lilly.
The ICER report may help what Dr. Kahan described as well-founded caution about obesity treatments in general.
“When it comes to weight loss, there are all of these magical treatments that are sold on social media and traditional media. There are a lot of bad actors in terms of people calling themselves experts and gurus and promising all kinds of crazy stuff,” said Dr. Kahan.
And there are long-standing stigmas about obesity, he stressed.
“That underlies a lot of the backward policies, including poor coverage for medications and the noncoverage by Medicare,” Dr. Kahan said. “There’s a societal ingrained set of beliefs and misperceptions and biases. That takes time to unwind, and I think we’re on the way, but we’re not quite there yet.”
Lifestyle changes not enough to tackle obesity
AHIP (formerly America’s Health Insurance Plans) told this news organization its members consider ICER reports when making decisions about which products to cover. “And health plans already cover obesity treatments that they consider medically necessary,” said David Allen, an AHIP spokesperson.
“It is important to note that every treatment does not work for every patient, and many patients experience adverse events and may discontinue treatment,” he added in an email. “Health insurance providers play an important role in helping [health care] providers and patients identify the treatment options that are most likely to be effective as well as affordable.”
Separately, the nonprofit watchdog group Public Citizen cautioned against liraglutide on its Worst Pills, Best Pills website. In its view, the drug is minimally effective and has many dangerous adverse effects, which are even more frequent with the higher-dose weight-loss version (a lower-dose version is approved for type 2 diabetes).
“There is currently no medication that can be used safely to achieve weight loss effortlessly and without dangerous adverse effects,” the group said. “Rather than focus on losing weight by turning to risky drugs, overweight and obese adults seeking to achieve better health should make reasonable and sustainable changes to their lifestyle, such as eating a healthy diet and getting regular exercise.”
Yet, many people find there is little help available for making lifestyle changes, and some patients and physicians say these modifications by themselves are not enough.
“The vast majority of people with obesity cannot achieve sustained weight loss through diet and exercise alone,” said David Rind, MD, chief medical officer of ICER, in an Oct. 20 statement. “As such, obesity, and its resulting physical health, mental health, and social burdens, is not a choice or failing, but a medical condition.”
The focus should now be on assuring that effective medications “are priced in alignment with their benefits so that they are accessible and affordable across U.S. society,” Dr. Rind urges.
‘My own demise with a fork and knife’
ICER sought public feedback on a draft version of the report before finalizing it.
In their comments on ICER’s work, several pharmaceutical researchers and Novo Nordisk questioned the calculations used in making judgments about the value of obesity drugs. In a statement, Novo Nordisk told this news organization that the company’s view is that ICER’s modeling “does not adequately address the real-world complexities of obesity, and consequently underestimates the health and societal impact medical treatments can have.”
Commenters also dug into aspects of ICER’s calculations, including ones that consider quality-adjusted life-years (QALYs). ICER describes QALY as an academic standard for measuring how well all different types of medical treatments can extend or improve patients’ lives. In an explainer on its website, ICER says this metric has served as a fundamental component of cost-effectiveness analyses in the United States and around the world for more than 30 years.
ICER and drug makers have been at odds for some time, with PhRMA having criticized the nonprofit group. A 2020 Reuters article detailed public relations strategies used by firms paid by drug makers to raise questions about ICER’s work. Critics accuse it of allying with insurers.
ICER’s list of its recent financial supporters includes Blue Cross Blue Shield of Massachusetts and the Kaiser Foundation Health Plan, but also many other groups, such as the U.S. Department of Veterans Affairs, the American Academy of Neurology, and the American College of Rheumatology.
The public comments on the ICER report also include one from an unidentified woman who wrote of her past struggles to lose weight.
She said her health plan wouldn’t cover behavioral programs or semaglutide as a weight-loss drug but did cover it eventually because of signs that she had developed insulin resistance. The patient said the drug worked for her, whereas other approaches to control weight had failed.
“To put it simply, I now experience hunger and satiety in a way that I can only assume people with normal metabolism do. I am 49 years old and approaching the age where serious comorbidities associated with obesity begin to manifest,” the patient wrote.
“I no longer worry about bringing about my own demise with a fork and knife because of misfiring hunger cues.”
A version of this article first appeared on Medscape.com.
A report from a well-respected nonprofit group may bolster efforts to have Medicare, the largest U.S. purchaser of prescription drugs, cover obesity medicines, for which there has been accumulating evidence of significant benefit.
The Institute for Clinical and Economic Review (ICER) released a report last month on obesity medicines, based on extensive review of research done to date and input from clinicians, drug-makers, and members of the public.
Of the treatments reviewed, the ICER report gave the best ratings to two Novo Nordisk products, a B+ for semaglutide (Wegovy) and a B for liraglutide (Saxenda), while also making the case for price cuts. At an annual U.S. net price estimated at $13,618, semaglutide exceeds what ICER considers typical cost-effectiveness thresholds. ICER suggested a benchmark annual price range for semaglutide of between $7,500 and $9,800.
The ICER report also directs insurers in general to provide more generous coverage of obesity medicines, with a specific recommendation for the U.S. Congress to pass a pending bill known as the Treat and Reduce Obesity Act of 2021. The bill would undo a restriction on weight-loss drugs in the Medicare Part D plans, which covered about 49 million people last year. Sen. Tom Carper (D-Del.) and Sen. Bill Cassidy, MD, (R-La.) have repeatedly introduced versions of the bill since 2013.
“In both chambers of Congress and with bipartisan support, we’ve pushed to expand Medicare coverage of additional therapies and medications to treat obesity,” Sen. Cassidy said in an email. “This report confirms what we’ve worked on for nearly a decade – our legislation will help improve lives.”
The current House version of the bill has the backing of more than a third of the members of that chamber, with 113 Democratic and 40 Republican cosponsors. The Senate version has 22 sponsors.
Changing views
The ICER report comes amid a broader change in how clinicians view obesity.
The American Academy of Pediatrics is readying a new Clinical Practice Guideline for the Evaluation and Treatment of Pediatric Obesity that will mark a major shift in approach. Aaron S. Kelly, PhD, a professor of pediatrics at the University of Minnesota, Minneapolis, described it as a “sea change,” with obesity now seen as “a chronic, refractory, relapsing disease,” for which watchful waiting is no longer appropriate.
But the field of obesity treatment looked quite different in the early 2000s when Congress worked on a plan to add a pharmacy benefit to Medicare.
The deliberate omission of obesity medicine in the Medicare Part D benefit reflected both the state of science at the time and U.S. experience with a dangerous weight-loss drug combo in the late 1990s.
Initial expectations for weight-loss pills were high after the Food and Drug Administration cleared dexfenfluramine HCl (Redux) in 1996, which was part of the popular fen-phen combination. “Newly Approved Diet Drug Promises to Help Millions of Obese Americans – But Is No Magic Bullet,” read a headline about the Redux approval in The Washington Post
When work began in the 2000s to create a Medicare pharmacy benefit, lawmakers and congressional staff had a pool of about $400 billion available to establish what became the Part D program, Joel White, a former House staffer who helped draft the law, told this news organization in an email exchange.
Given the state of obesity research at the time, it seemed to make sense to exclude weight-loss medications, wrote Mr. White. Mr. White is now chief executive of the consulting firm Horizon, which has clients in the drug industry including the Pharmaceutical Research and Manufacturers of America.
“Now we know that obesity is a chronic disease of epidemic proportions. Decades of research have produced a series of advances in the way we understand and treat obesity. While scientists and many who work directly with those impacted by this epidemic understand how treatments have advanced, the law lags behind,” Mr. White said.
XXXCurrent payment policies for obesity treatments are based on “outdated information and ongoing misperception,” he noted. “While Part D has been a resounding success, our Medicare approach to obesity is not.”
“In addition, it makes no sense that Medicare covers the most drastic procedure (bariatric surgery) but not less-invasive, effective treatments,” he added. “We should have long ago lifted restrictions based on advances in science and medicine.”
Overcoming the stigma
Scott Kahan, MD, MPH, agreed and hopes that the new ICER report will help more patients secure needed medications, raising a “call to arms” about the need for better coverage of obesity drugs.
Dr. Kahan is director of the National Center for Weight and Wellness, a private clinic in Washington, and chair of the clinical committee for The Obesity Society. He also served as a member of a policy roundtable that ICER convened as part of research on the report on obesity drugs. Dr. Kahan, who also serves on the faculty at the Johns Hopkins Bloomberg School of Public Health, Baltimore, has received fees from drug makers such as Eli Lilly.
The ICER report may help what Dr. Kahan described as well-founded caution about obesity treatments in general.
“When it comes to weight loss, there are all of these magical treatments that are sold on social media and traditional media. There are a lot of bad actors in terms of people calling themselves experts and gurus and promising all kinds of crazy stuff,” said Dr. Kahan.
And there are long-standing stigmas about obesity, he stressed.
“That underlies a lot of the backward policies, including poor coverage for medications and the noncoverage by Medicare,” Dr. Kahan said. “There’s a societal ingrained set of beliefs and misperceptions and biases. That takes time to unwind, and I think we’re on the way, but we’re not quite there yet.”
Lifestyle changes not enough to tackle obesity
AHIP (formerly America’s Health Insurance Plans) told this news organization its members consider ICER reports when making decisions about which products to cover. “And health plans already cover obesity treatments that they consider medically necessary,” said David Allen, an AHIP spokesperson.
“It is important to note that every treatment does not work for every patient, and many patients experience adverse events and may discontinue treatment,” he added in an email. “Health insurance providers play an important role in helping [health care] providers and patients identify the treatment options that are most likely to be effective as well as affordable.”
Separately, the nonprofit watchdog group Public Citizen cautioned against liraglutide on its Worst Pills, Best Pills website. In its view, the drug is minimally effective and has many dangerous adverse effects, which are even more frequent with the higher-dose weight-loss version (a lower-dose version is approved for type 2 diabetes).
“There is currently no medication that can be used safely to achieve weight loss effortlessly and without dangerous adverse effects,” the group said. “Rather than focus on losing weight by turning to risky drugs, overweight and obese adults seeking to achieve better health should make reasonable and sustainable changes to their lifestyle, such as eating a healthy diet and getting regular exercise.”
Yet, many people find there is little help available for making lifestyle changes, and some patients and physicians say these modifications by themselves are not enough.
“The vast majority of people with obesity cannot achieve sustained weight loss through diet and exercise alone,” said David Rind, MD, chief medical officer of ICER, in an Oct. 20 statement. “As such, obesity, and its resulting physical health, mental health, and social burdens, is not a choice or failing, but a medical condition.”
The focus should now be on assuring that effective medications “are priced in alignment with their benefits so that they are accessible and affordable across U.S. society,” Dr. Rind urges.
‘My own demise with a fork and knife’
ICER sought public feedback on a draft version of the report before finalizing it.
In their comments on ICER’s work, several pharmaceutical researchers and Novo Nordisk questioned the calculations used in making judgments about the value of obesity drugs. In a statement, Novo Nordisk told this news organization that the company’s view is that ICER’s modeling “does not adequately address the real-world complexities of obesity, and consequently underestimates the health and societal impact medical treatments can have.”
Commenters also dug into aspects of ICER’s calculations, including ones that consider quality-adjusted life-years (QALYs). ICER describes QALY as an academic standard for measuring how well all different types of medical treatments can extend or improve patients’ lives. In an explainer on its website, ICER says this metric has served as a fundamental component of cost-effectiveness analyses in the United States and around the world for more than 30 years.
ICER and drug makers have been at odds for some time, with PhRMA having criticized the nonprofit group. A 2020 Reuters article detailed public relations strategies used by firms paid by drug makers to raise questions about ICER’s work. Critics accuse it of allying with insurers.
ICER’s list of its recent financial supporters includes Blue Cross Blue Shield of Massachusetts and the Kaiser Foundation Health Plan, but also many other groups, such as the U.S. Department of Veterans Affairs, the American Academy of Neurology, and the American College of Rheumatology.
The public comments on the ICER report also include one from an unidentified woman who wrote of her past struggles to lose weight.
She said her health plan wouldn’t cover behavioral programs or semaglutide as a weight-loss drug but did cover it eventually because of signs that she had developed insulin resistance. The patient said the drug worked for her, whereas other approaches to control weight had failed.
“To put it simply, I now experience hunger and satiety in a way that I can only assume people with normal metabolism do. I am 49 years old and approaching the age where serious comorbidities associated with obesity begin to manifest,” the patient wrote.
“I no longer worry about bringing about my own demise with a fork and knife because of misfiring hunger cues.”
A version of this article first appeared on Medscape.com.
Nurse practitioner fined $20k for advertising herself as ‘Doctor Sarah’
Last month, the San Luis Obispo County, California, District Attorney Dan Dow filed a complaint against Sarah Erny, RN, NP, citing unfair business practices and unprofessional conduct.
According to court documents, California’s Medical Practice Act does not permit individuals to refer to themselves as “doctor, physician, or any other terms or letters indicating or implying that he or she is a physician and surgeon ... without having ... a certificate as a physician and surgeon.”
Individuals who misrepresent themselves are subject to misdemeanor charges and civil penalties.
In addition to the fine, Ms. Erny agreed to refrain from referring to herself as a doctor in her practice and on social media. She has already deleted her Twitter account.
The case underscores tensions between physicians fighting to preserve their scope of practice and the allied professionals that U.S. lawmakers increasingly see as a less expensive way to improve access to health care.
The American Medical Association and specialty groups strongly oppose a new bill, the Improving Care and Access to Nurses Act, that would expand the scope of practice for nurse practitioners and physician assistants.
Court records show that Ms. Erny earned a doctor of nursing practice (DNP) degree from Vanderbilt University, Nashville, Tenn., and that she met the state requirements to obtain licensure as a registered nurse and nurse practitioner. In 2018, she opened a practice in Arroyo Grande, California, called Holistic Women’s Healing, where she provided medical services and drug supplements to patients.
She also entered a collaborative agreement with ob.gyn. Anika Moore, MD, for approximately 3 years. Dr. Moore’s medical practice was in another county and state, and the physician returned every 2 to 3 months to review a portion of Ms. Erny’s patient files.
Ms. Erny and Dr. Moore terminated the collaborative agreement in March, according to court documents.
However, Mr. Dow alleged that Ms. Erny regularly referred to herself as “Dr. Sarah” or “Dr. Sarah Erny” in her online advertising and social media accounts. Her patients “were so proud of her” that they called her doctor, and her supervising physician instructed staff to do the same.
Mr. Dow said Ms. Erny did not clearly advise the public that she was not a medical doctor and failed to identify her supervising physician. “Simply put, there is a great need for health care providers to state their level of training and licensing clearly and honestly in all of their advertising and marketing materials,” he said in a press release.
In California, nurse practitioners who have been certified by the Board of Registered Nursing may use the following titles: Advanced Practice Registered Nurse; Certified Nurse Practitioner; APRN-CNP; RN and NP; or a combination of other letters or words to identify specialization, such as adult nurse practitioner, pediatric nurse practitioner, obstetrical-gynecological nurse practitioner, and family nurse practitioner.
As educational requirements shift for advanced practice clinicians, similar cases will likely emerge, said Grant Martsolf, PhD, MPH, RN, FAAN, professor at the University of Pittsburgh School of Nursing.
“Scope of practice is governed by states, [so they] will have to figure [it] out as more professional disciplines move to clinical doctorates as the entry to practice. Pharma, [physical therapy], and [occupational therapy] have already done this, and advanced practice nursing is on its way. [Certified registered nurse anesthetists] are already required to get a DNP to sit for certification,” he said.
More guidance is needed, especially when considering other professions like dentists, clinical psychologists, and individuals with clinical or research doctorates who often call themselves doctors, Dr. Martsolf said.
“It seems that the honorific of ‘Dr.’ emerges from the degree, not from being a physician or surgeon,” he said.
Beyond the false advertising, Mr. Dow alleged that Ms. Erny did not file a fictitious business name statement for 2020 and 2021 – a requirement under the California Business and Professions Code to identify who is operating the business.
A version of this article first appeared on Medscape.com.
Last month, the San Luis Obispo County, California, District Attorney Dan Dow filed a complaint against Sarah Erny, RN, NP, citing unfair business practices and unprofessional conduct.
According to court documents, California’s Medical Practice Act does not permit individuals to refer to themselves as “doctor, physician, or any other terms or letters indicating or implying that he or she is a physician and surgeon ... without having ... a certificate as a physician and surgeon.”
Individuals who misrepresent themselves are subject to misdemeanor charges and civil penalties.
In addition to the fine, Ms. Erny agreed to refrain from referring to herself as a doctor in her practice and on social media. She has already deleted her Twitter account.
The case underscores tensions between physicians fighting to preserve their scope of practice and the allied professionals that U.S. lawmakers increasingly see as a less expensive way to improve access to health care.
The American Medical Association and specialty groups strongly oppose a new bill, the Improving Care and Access to Nurses Act, that would expand the scope of practice for nurse practitioners and physician assistants.
Court records show that Ms. Erny earned a doctor of nursing practice (DNP) degree from Vanderbilt University, Nashville, Tenn., and that she met the state requirements to obtain licensure as a registered nurse and nurse practitioner. In 2018, she opened a practice in Arroyo Grande, California, called Holistic Women’s Healing, where she provided medical services and drug supplements to patients.
She also entered a collaborative agreement with ob.gyn. Anika Moore, MD, for approximately 3 years. Dr. Moore’s medical practice was in another county and state, and the physician returned every 2 to 3 months to review a portion of Ms. Erny’s patient files.
Ms. Erny and Dr. Moore terminated the collaborative agreement in March, according to court documents.
However, Mr. Dow alleged that Ms. Erny regularly referred to herself as “Dr. Sarah” or “Dr. Sarah Erny” in her online advertising and social media accounts. Her patients “were so proud of her” that they called her doctor, and her supervising physician instructed staff to do the same.
Mr. Dow said Ms. Erny did not clearly advise the public that she was not a medical doctor and failed to identify her supervising physician. “Simply put, there is a great need for health care providers to state their level of training and licensing clearly and honestly in all of their advertising and marketing materials,” he said in a press release.
In California, nurse practitioners who have been certified by the Board of Registered Nursing may use the following titles: Advanced Practice Registered Nurse; Certified Nurse Practitioner; APRN-CNP; RN and NP; or a combination of other letters or words to identify specialization, such as adult nurse practitioner, pediatric nurse practitioner, obstetrical-gynecological nurse practitioner, and family nurse practitioner.
As educational requirements shift for advanced practice clinicians, similar cases will likely emerge, said Grant Martsolf, PhD, MPH, RN, FAAN, professor at the University of Pittsburgh School of Nursing.
“Scope of practice is governed by states, [so they] will have to figure [it] out as more professional disciplines move to clinical doctorates as the entry to practice. Pharma, [physical therapy], and [occupational therapy] have already done this, and advanced practice nursing is on its way. [Certified registered nurse anesthetists] are already required to get a DNP to sit for certification,” he said.
More guidance is needed, especially when considering other professions like dentists, clinical psychologists, and individuals with clinical or research doctorates who often call themselves doctors, Dr. Martsolf said.
“It seems that the honorific of ‘Dr.’ emerges from the degree, not from being a physician or surgeon,” he said.
Beyond the false advertising, Mr. Dow alleged that Ms. Erny did not file a fictitious business name statement for 2020 and 2021 – a requirement under the California Business and Professions Code to identify who is operating the business.
A version of this article first appeared on Medscape.com.
Last month, the San Luis Obispo County, California, District Attorney Dan Dow filed a complaint against Sarah Erny, RN, NP, citing unfair business practices and unprofessional conduct.
According to court documents, California’s Medical Practice Act does not permit individuals to refer to themselves as “doctor, physician, or any other terms or letters indicating or implying that he or she is a physician and surgeon ... without having ... a certificate as a physician and surgeon.”
Individuals who misrepresent themselves are subject to misdemeanor charges and civil penalties.
In addition to the fine, Ms. Erny agreed to refrain from referring to herself as a doctor in her practice and on social media. She has already deleted her Twitter account.
The case underscores tensions between physicians fighting to preserve their scope of practice and the allied professionals that U.S. lawmakers increasingly see as a less expensive way to improve access to health care.
The American Medical Association and specialty groups strongly oppose a new bill, the Improving Care and Access to Nurses Act, that would expand the scope of practice for nurse practitioners and physician assistants.
Court records show that Ms. Erny earned a doctor of nursing practice (DNP) degree from Vanderbilt University, Nashville, Tenn., and that she met the state requirements to obtain licensure as a registered nurse and nurse practitioner. In 2018, she opened a practice in Arroyo Grande, California, called Holistic Women’s Healing, where she provided medical services and drug supplements to patients.
She also entered a collaborative agreement with ob.gyn. Anika Moore, MD, for approximately 3 years. Dr. Moore’s medical practice was in another county and state, and the physician returned every 2 to 3 months to review a portion of Ms. Erny’s patient files.
Ms. Erny and Dr. Moore terminated the collaborative agreement in March, according to court documents.
However, Mr. Dow alleged that Ms. Erny regularly referred to herself as “Dr. Sarah” or “Dr. Sarah Erny” in her online advertising and social media accounts. Her patients “were so proud of her” that they called her doctor, and her supervising physician instructed staff to do the same.
Mr. Dow said Ms. Erny did not clearly advise the public that she was not a medical doctor and failed to identify her supervising physician. “Simply put, there is a great need for health care providers to state their level of training and licensing clearly and honestly in all of their advertising and marketing materials,” he said in a press release.
In California, nurse practitioners who have been certified by the Board of Registered Nursing may use the following titles: Advanced Practice Registered Nurse; Certified Nurse Practitioner; APRN-CNP; RN and NP; or a combination of other letters or words to identify specialization, such as adult nurse practitioner, pediatric nurse practitioner, obstetrical-gynecological nurse practitioner, and family nurse practitioner.
As educational requirements shift for advanced practice clinicians, similar cases will likely emerge, said Grant Martsolf, PhD, MPH, RN, FAAN, professor at the University of Pittsburgh School of Nursing.
“Scope of practice is governed by states, [so they] will have to figure [it] out as more professional disciplines move to clinical doctorates as the entry to practice. Pharma, [physical therapy], and [occupational therapy] have already done this, and advanced practice nursing is on its way. [Certified registered nurse anesthetists] are already required to get a DNP to sit for certification,” he said.
More guidance is needed, especially when considering other professions like dentists, clinical psychologists, and individuals with clinical or research doctorates who often call themselves doctors, Dr. Martsolf said.
“It seems that the honorific of ‘Dr.’ emerges from the degree, not from being a physician or surgeon,” he said.
Beyond the false advertising, Mr. Dow alleged that Ms. Erny did not file a fictitious business name statement for 2020 and 2021 – a requirement under the California Business and Professions Code to identify who is operating the business.
A version of this article first appeared on Medscape.com.








