User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Patients trying to lose weight overestimate their diet quality
Only 28% of the participants had good agreement – defined as a difference of 6 points or less – between their perceived diet quality and its actual quality based on Healthy Eating Index–2015 (HEI) scores at the end of the 12-month intervention.
Even fewer – only 13% – had good agreement with their perceived and actual improvement in diet quality.
Jessica Cheng, PhD, Harvard School of Public Health, Boston, presented the findings in an oral session at the American Heart Association scientific sessions.
The study suggests that “patients can benefit from concrete advice on aspects of their diet that could most benefit by being changed,” Dr. Cheng said in an interview.
“But once they know what to change, they may need additional advice on how to make and sustain those changes. Providers may direct their patients to resources such as dietitians, medically tailored meals, MyPlate, healthy recipes, etc.,” she advised.
“The findings are not surprising given that dietary recalls are subject to recall bias and depend on the person’s baseline nutrition knowledge or literacy,” Deepika Laddu, PhD, who was not involved with this research, said in an interview.
Misperception of diet intake is common in individuals with overweight or obesity, and one 90-minute session with a dietitian is not enough, according to Dr. Laddu, assistant professor at the University of Illinois at Chicago.
“The Dietary Guidelines for Americans does a really nice job at presenting all of the options,” she said. However, “understanding what a healthy diet pattern is, or how to adopt it, is confusing, due to a lot of ‘noise’, that is, the mixed messaging and unproven health claims, which add to inadequacies in health or nutrition literacy.”
“It is important to recognize that changing dietary practices is behaviorally challenging and complex,” she emphasized.
People who are interested in making dietary changes need to have ongoing conversations with a qualified health care professional, which most often starts with their primary care clinician.
“Given the well-known time constraints during a typical clinical visit, beyond that initial conversation, it is absolutely critical that patients be referred to qualified healthcare professionals such as a registered dietitian, nurse practitioner, health coach/educator or diabetes educator, etc, for ongoing support.”
These providers can assess the patient’s initial diet, perceptions of a healthy diet, and diet goals, and address any gaps in health literacy, to enable the patient to develop long-lasting, realistic, and healthy eating behaviors.
Perceived vs. actual diet quality
Healthy eating is essential for heart and general health and longevity, but it is unclear if people who make lifestyle (diet and physical activity) changes to lose weight have an accurate perception of diet quality.
The researchers analyzed data from the SMARTER trial of 502 adults aged 35-58 living in the greater Pittsburgh area who were trying to lose weight.
Participants received a 90-minute weight loss counseling session addressing behavioral strategies and establishing dietary and physical activity goals. They all received instructions on how to monitor their diet, physical activity, and weight daily, using a smartphone app, a wristband tracker (Fitbit Charge 2), and a smart wireless scale. Half of the participants also received real-time personalized feedback on those behaviors, up to three times a day, via the study app.
The participants replied to two 24-hour dietary recall questionnaires at study entry and two questionnaires at 12 months.
Researchers analyzed data from the 116 participants who provided information about diet quality. At 1 year, they were asked to rate their diet quality, but also rate their diet quality 12 months earlier at baseline, on a scale of 0-100, where 100 is best.
The average weight loss at 12 months was similar in the groups with and without feedback from the app (roughly 3.2% of baseline weight), so the two study arms were combined. The participants had a mean age of 52 years; 80% were women and 87% were White. They had an average body mass index of 33 kg/m2.
Based on the information from the food recall questionnaires, the researchers calculated the patients’ HEI scores at the start and end of the study. The HEI score is a measure of how well a person’s diet adheres to the 2015-2020 Dietary Guidelines for Americans. It is based on an adequate consumption of nine types of foods – total fruits, whole fruits, total vegetables, greens and beans, total protein foods, seafood, and plant proteins (up to 5 points each), and whole grains, dairy, and fatty acids (up to 10 points each) – and reduced consumption of four dietary components – refined grains, sodium, added sugars, and saturated fats (up to 10 points each).
The healthiest diet has an HEI score of 100, and the Healthy People 2020 goal was an HEI score of 74, Dr. Cheng noted.
At 12 months, on average, the participants rated their diet quality at 70.5 points, whereas the researchers calculated that their average HEI score was only 56.
Participants thought they had improved their diet quality by about 20 points, Dr. Cheng reported. “However, the HEI would suggest they’ve improved it by 1.5 points, which is not a lot out of 100.”
“Future studies should examine the effects of helping people close the gap between their perceptions and objective diet quality measurements,” Dr. Cheng said in a press release from the AHA.
The study was funded by the National Heart, Lung, and Blood Institute, a division of the National Institutes of Health. Dr. Cheng and Dr. Laddu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Only 28% of the participants had good agreement – defined as a difference of 6 points or less – between their perceived diet quality and its actual quality based on Healthy Eating Index–2015 (HEI) scores at the end of the 12-month intervention.
Even fewer – only 13% – had good agreement with their perceived and actual improvement in diet quality.
Jessica Cheng, PhD, Harvard School of Public Health, Boston, presented the findings in an oral session at the American Heart Association scientific sessions.
The study suggests that “patients can benefit from concrete advice on aspects of their diet that could most benefit by being changed,” Dr. Cheng said in an interview.
“But once they know what to change, they may need additional advice on how to make and sustain those changes. Providers may direct their patients to resources such as dietitians, medically tailored meals, MyPlate, healthy recipes, etc.,” she advised.
“The findings are not surprising given that dietary recalls are subject to recall bias and depend on the person’s baseline nutrition knowledge or literacy,” Deepika Laddu, PhD, who was not involved with this research, said in an interview.
Misperception of diet intake is common in individuals with overweight or obesity, and one 90-minute session with a dietitian is not enough, according to Dr. Laddu, assistant professor at the University of Illinois at Chicago.
“The Dietary Guidelines for Americans does a really nice job at presenting all of the options,” she said. However, “understanding what a healthy diet pattern is, or how to adopt it, is confusing, due to a lot of ‘noise’, that is, the mixed messaging and unproven health claims, which add to inadequacies in health or nutrition literacy.”
“It is important to recognize that changing dietary practices is behaviorally challenging and complex,” she emphasized.
People who are interested in making dietary changes need to have ongoing conversations with a qualified health care professional, which most often starts with their primary care clinician.
“Given the well-known time constraints during a typical clinical visit, beyond that initial conversation, it is absolutely critical that patients be referred to qualified healthcare professionals such as a registered dietitian, nurse practitioner, health coach/educator or diabetes educator, etc, for ongoing support.”
These providers can assess the patient’s initial diet, perceptions of a healthy diet, and diet goals, and address any gaps in health literacy, to enable the patient to develop long-lasting, realistic, and healthy eating behaviors.
Perceived vs. actual diet quality
Healthy eating is essential for heart and general health and longevity, but it is unclear if people who make lifestyle (diet and physical activity) changes to lose weight have an accurate perception of diet quality.
The researchers analyzed data from the SMARTER trial of 502 adults aged 35-58 living in the greater Pittsburgh area who were trying to lose weight.
Participants received a 90-minute weight loss counseling session addressing behavioral strategies and establishing dietary and physical activity goals. They all received instructions on how to monitor their diet, physical activity, and weight daily, using a smartphone app, a wristband tracker (Fitbit Charge 2), and a smart wireless scale. Half of the participants also received real-time personalized feedback on those behaviors, up to three times a day, via the study app.
The participants replied to two 24-hour dietary recall questionnaires at study entry and two questionnaires at 12 months.
Researchers analyzed data from the 116 participants who provided information about diet quality. At 1 year, they were asked to rate their diet quality, but also rate their diet quality 12 months earlier at baseline, on a scale of 0-100, where 100 is best.
The average weight loss at 12 months was similar in the groups with and without feedback from the app (roughly 3.2% of baseline weight), so the two study arms were combined. The participants had a mean age of 52 years; 80% were women and 87% were White. They had an average body mass index of 33 kg/m2.
Based on the information from the food recall questionnaires, the researchers calculated the patients’ HEI scores at the start and end of the study. The HEI score is a measure of how well a person’s diet adheres to the 2015-2020 Dietary Guidelines for Americans. It is based on an adequate consumption of nine types of foods – total fruits, whole fruits, total vegetables, greens and beans, total protein foods, seafood, and plant proteins (up to 5 points each), and whole grains, dairy, and fatty acids (up to 10 points each) – and reduced consumption of four dietary components – refined grains, sodium, added sugars, and saturated fats (up to 10 points each).
The healthiest diet has an HEI score of 100, and the Healthy People 2020 goal was an HEI score of 74, Dr. Cheng noted.
At 12 months, on average, the participants rated their diet quality at 70.5 points, whereas the researchers calculated that their average HEI score was only 56.
Participants thought they had improved their diet quality by about 20 points, Dr. Cheng reported. “However, the HEI would suggest they’ve improved it by 1.5 points, which is not a lot out of 100.”
“Future studies should examine the effects of helping people close the gap between their perceptions and objective diet quality measurements,” Dr. Cheng said in a press release from the AHA.
The study was funded by the National Heart, Lung, and Blood Institute, a division of the National Institutes of Health. Dr. Cheng and Dr. Laddu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Only 28% of the participants had good agreement – defined as a difference of 6 points or less – between their perceived diet quality and its actual quality based on Healthy Eating Index–2015 (HEI) scores at the end of the 12-month intervention.
Even fewer – only 13% – had good agreement with their perceived and actual improvement in diet quality.
Jessica Cheng, PhD, Harvard School of Public Health, Boston, presented the findings in an oral session at the American Heart Association scientific sessions.
The study suggests that “patients can benefit from concrete advice on aspects of their diet that could most benefit by being changed,” Dr. Cheng said in an interview.
“But once they know what to change, they may need additional advice on how to make and sustain those changes. Providers may direct their patients to resources such as dietitians, medically tailored meals, MyPlate, healthy recipes, etc.,” she advised.
“The findings are not surprising given that dietary recalls are subject to recall bias and depend on the person’s baseline nutrition knowledge or literacy,” Deepika Laddu, PhD, who was not involved with this research, said in an interview.
Misperception of diet intake is common in individuals with overweight or obesity, and one 90-minute session with a dietitian is not enough, according to Dr. Laddu, assistant professor at the University of Illinois at Chicago.
“The Dietary Guidelines for Americans does a really nice job at presenting all of the options,” she said. However, “understanding what a healthy diet pattern is, or how to adopt it, is confusing, due to a lot of ‘noise’, that is, the mixed messaging and unproven health claims, which add to inadequacies in health or nutrition literacy.”
“It is important to recognize that changing dietary practices is behaviorally challenging and complex,” she emphasized.
People who are interested in making dietary changes need to have ongoing conversations with a qualified health care professional, which most often starts with their primary care clinician.
“Given the well-known time constraints during a typical clinical visit, beyond that initial conversation, it is absolutely critical that patients be referred to qualified healthcare professionals such as a registered dietitian, nurse practitioner, health coach/educator or diabetes educator, etc, for ongoing support.”
These providers can assess the patient’s initial diet, perceptions of a healthy diet, and diet goals, and address any gaps in health literacy, to enable the patient to develop long-lasting, realistic, and healthy eating behaviors.
Perceived vs. actual diet quality
Healthy eating is essential for heart and general health and longevity, but it is unclear if people who make lifestyle (diet and physical activity) changes to lose weight have an accurate perception of diet quality.
The researchers analyzed data from the SMARTER trial of 502 adults aged 35-58 living in the greater Pittsburgh area who were trying to lose weight.
Participants received a 90-minute weight loss counseling session addressing behavioral strategies and establishing dietary and physical activity goals. They all received instructions on how to monitor their diet, physical activity, and weight daily, using a smartphone app, a wristband tracker (Fitbit Charge 2), and a smart wireless scale. Half of the participants also received real-time personalized feedback on those behaviors, up to three times a day, via the study app.
The participants replied to two 24-hour dietary recall questionnaires at study entry and two questionnaires at 12 months.
Researchers analyzed data from the 116 participants who provided information about diet quality. At 1 year, they were asked to rate their diet quality, but also rate their diet quality 12 months earlier at baseline, on a scale of 0-100, where 100 is best.
The average weight loss at 12 months was similar in the groups with and without feedback from the app (roughly 3.2% of baseline weight), so the two study arms were combined. The participants had a mean age of 52 years; 80% were women and 87% were White. They had an average body mass index of 33 kg/m2.
Based on the information from the food recall questionnaires, the researchers calculated the patients’ HEI scores at the start and end of the study. The HEI score is a measure of how well a person’s diet adheres to the 2015-2020 Dietary Guidelines for Americans. It is based on an adequate consumption of nine types of foods – total fruits, whole fruits, total vegetables, greens and beans, total protein foods, seafood, and plant proteins (up to 5 points each), and whole grains, dairy, and fatty acids (up to 10 points each) – and reduced consumption of four dietary components – refined grains, sodium, added sugars, and saturated fats (up to 10 points each).
The healthiest diet has an HEI score of 100, and the Healthy People 2020 goal was an HEI score of 74, Dr. Cheng noted.
At 12 months, on average, the participants rated their diet quality at 70.5 points, whereas the researchers calculated that their average HEI score was only 56.
Participants thought they had improved their diet quality by about 20 points, Dr. Cheng reported. “However, the HEI would suggest they’ve improved it by 1.5 points, which is not a lot out of 100.”
“Future studies should examine the effects of helping people close the gap between their perceptions and objective diet quality measurements,” Dr. Cheng said in a press release from the AHA.
The study was funded by the National Heart, Lung, and Blood Institute, a division of the National Institutes of Health. Dr. Cheng and Dr. Laddu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AHA 2022
Mortality after acute stroke worsened by accompanying acute AFib
The study covered in this summary was published on ResearchSquare.com as a preprint and has not yet been peer-reviewed.
Key takeaway
Why this matters
- A comprehensive understanding of the relationship between acute AF and risk for acute ischemic stroke and prognosis will help improve management and treatment of patients with acute ischemic stroke.
Study design
- The retrospective study included patients with acute ischemic stroke within the prior 24 hours; 12-lead electrocardiogram in the emergency department; and hospitalization and treatment at the hospital stroke center.
- The cohort of 706 patients admitted to a single center in Shanghai, China, from December 2019 to December 2021, included 142 with episodes of acute AF and 564 without such episodes.
- Patients with acute ischemic stroke and acute AF – including AF of new onset, paroxysmal, persistent, or permanent with symptoms such as palpitations or dizziness attributed to rapid ventricular rates – were identified.
- Neurological deficits were assessed using the 7-day National Institutes of Health Stroke Scale/Score (NIHSS). Patients with a 7-day NIHSS score of at least 16 were considered to have moderate to severe stroke.
- Associations between acute AF onset and the severity of early neurological deficits were assessed and related to all-cause mortality within 30 days of the stroke.
Key results
- Patients with acute AF were older than those without acute AF (80.3 years vs. 71.0 years; P < .001).
- Baseline NIHSS scores averaged 16.09 for the stroke patients with acute AF and 8.65 for those without acute AF (P < .001).
- Significantly more patients with acute AF than without acute AF had a 7-day NIHSS score of at least 16 (45.1% vs. 14.4%; P < .001).
- More patients with than without acute AF underwent transcatheter thrombectomy (44.4% vs. 24.5%; P < .001) or received thrombolytic therapy (31.6% vs. 19.7%; P = .005).
- Patients aged 73 years or older showed baseline NIHSS score and acute AF as independent risk factors for early neurological deficits in stroke patients admitted to the emergency department.
- Mortality at 30 days was significantly higher in patients with acute AF than in those without acute AF (30.3% vs. 10.1%; P < .001).
- Baseline NIHSS had an adjusted odds ratio for 30-day mortality of 1.18 (95% confidence interval, 1.15-1.22; P < .001).
- Other independent predictors included acute AF (1.87 [95% CI, 1.09-3.19; P = .022]) and age 73 or older (2.00 [95% CI, 1.18-3.37; P = .01]).
Limitations
- The study was retrospective and didn’t have access to some potentially relevant data, such as duration of AF.
- The single-center study with limited generalizability does not necessarily represent the broad population of stroke patients in China or elsewhere.
Disclosures
- This study was supported by the Cardiovascular Multidisciplinary Integrated Research Fund and Construction of Shanghai Municipal Health Commission.
- The authors report no relevant financial relationships.
This is a summary of a preprint research study, “Acute Atrial Fibrillation During Onset of Stroke Indicates Higher Probability of Post-Stroke Death Outcomes,” written by Yongxia Li, from the Shanghai Sixth People’s Hospital, and colleagues, on ResearchSquare.com. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.A version of this article first appeared on Medscape.com.
The study covered in this summary was published on ResearchSquare.com as a preprint and has not yet been peer-reviewed.
Key takeaway
Why this matters
- A comprehensive understanding of the relationship between acute AF and risk for acute ischemic stroke and prognosis will help improve management and treatment of patients with acute ischemic stroke.
Study design
- The retrospective study included patients with acute ischemic stroke within the prior 24 hours; 12-lead electrocardiogram in the emergency department; and hospitalization and treatment at the hospital stroke center.
- The cohort of 706 patients admitted to a single center in Shanghai, China, from December 2019 to December 2021, included 142 with episodes of acute AF and 564 without such episodes.
- Patients with acute ischemic stroke and acute AF – including AF of new onset, paroxysmal, persistent, or permanent with symptoms such as palpitations or dizziness attributed to rapid ventricular rates – were identified.
- Neurological deficits were assessed using the 7-day National Institutes of Health Stroke Scale/Score (NIHSS). Patients with a 7-day NIHSS score of at least 16 were considered to have moderate to severe stroke.
- Associations between acute AF onset and the severity of early neurological deficits were assessed and related to all-cause mortality within 30 days of the stroke.
Key results
- Patients with acute AF were older than those without acute AF (80.3 years vs. 71.0 years; P < .001).
- Baseline NIHSS scores averaged 16.09 for the stroke patients with acute AF and 8.65 for those without acute AF (P < .001).
- Significantly more patients with acute AF than without acute AF had a 7-day NIHSS score of at least 16 (45.1% vs. 14.4%; P < .001).
- More patients with than without acute AF underwent transcatheter thrombectomy (44.4% vs. 24.5%; P < .001) or received thrombolytic therapy (31.6% vs. 19.7%; P = .005).
- Patients aged 73 years or older showed baseline NIHSS score and acute AF as independent risk factors for early neurological deficits in stroke patients admitted to the emergency department.
- Mortality at 30 days was significantly higher in patients with acute AF than in those without acute AF (30.3% vs. 10.1%; P < .001).
- Baseline NIHSS had an adjusted odds ratio for 30-day mortality of 1.18 (95% confidence interval, 1.15-1.22; P < .001).
- Other independent predictors included acute AF (1.87 [95% CI, 1.09-3.19; P = .022]) and age 73 or older (2.00 [95% CI, 1.18-3.37; P = .01]).
Limitations
- The study was retrospective and didn’t have access to some potentially relevant data, such as duration of AF.
- The single-center study with limited generalizability does not necessarily represent the broad population of stroke patients in China or elsewhere.
Disclosures
- This study was supported by the Cardiovascular Multidisciplinary Integrated Research Fund and Construction of Shanghai Municipal Health Commission.
- The authors report no relevant financial relationships.
This is a summary of a preprint research study, “Acute Atrial Fibrillation During Onset of Stroke Indicates Higher Probability of Post-Stroke Death Outcomes,” written by Yongxia Li, from the Shanghai Sixth People’s Hospital, and colleagues, on ResearchSquare.com. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.A version of this article first appeared on Medscape.com.
The study covered in this summary was published on ResearchSquare.com as a preprint and has not yet been peer-reviewed.
Key takeaway
Why this matters
- A comprehensive understanding of the relationship between acute AF and risk for acute ischemic stroke and prognosis will help improve management and treatment of patients with acute ischemic stroke.
Study design
- The retrospective study included patients with acute ischemic stroke within the prior 24 hours; 12-lead electrocardiogram in the emergency department; and hospitalization and treatment at the hospital stroke center.
- The cohort of 706 patients admitted to a single center in Shanghai, China, from December 2019 to December 2021, included 142 with episodes of acute AF and 564 without such episodes.
- Patients with acute ischemic stroke and acute AF – including AF of new onset, paroxysmal, persistent, or permanent with symptoms such as palpitations or dizziness attributed to rapid ventricular rates – were identified.
- Neurological deficits were assessed using the 7-day National Institutes of Health Stroke Scale/Score (NIHSS). Patients with a 7-day NIHSS score of at least 16 were considered to have moderate to severe stroke.
- Associations between acute AF onset and the severity of early neurological deficits were assessed and related to all-cause mortality within 30 days of the stroke.
Key results
- Patients with acute AF were older than those without acute AF (80.3 years vs. 71.0 years; P < .001).
- Baseline NIHSS scores averaged 16.09 for the stroke patients with acute AF and 8.65 for those without acute AF (P < .001).
- Significantly more patients with acute AF than without acute AF had a 7-day NIHSS score of at least 16 (45.1% vs. 14.4%; P < .001).
- More patients with than without acute AF underwent transcatheter thrombectomy (44.4% vs. 24.5%; P < .001) or received thrombolytic therapy (31.6% vs. 19.7%; P = .005).
- Patients aged 73 years or older showed baseline NIHSS score and acute AF as independent risk factors for early neurological deficits in stroke patients admitted to the emergency department.
- Mortality at 30 days was significantly higher in patients with acute AF than in those without acute AF (30.3% vs. 10.1%; P < .001).
- Baseline NIHSS had an adjusted odds ratio for 30-day mortality of 1.18 (95% confidence interval, 1.15-1.22; P < .001).
- Other independent predictors included acute AF (1.87 [95% CI, 1.09-3.19; P = .022]) and age 73 or older (2.00 [95% CI, 1.18-3.37; P = .01]).
Limitations
- The study was retrospective and didn’t have access to some potentially relevant data, such as duration of AF.
- The single-center study with limited generalizability does not necessarily represent the broad population of stroke patients in China or elsewhere.
Disclosures
- This study was supported by the Cardiovascular Multidisciplinary Integrated Research Fund and Construction of Shanghai Municipal Health Commission.
- The authors report no relevant financial relationships.
This is a summary of a preprint research study, “Acute Atrial Fibrillation During Onset of Stroke Indicates Higher Probability of Post-Stroke Death Outcomes,” written by Yongxia Li, from the Shanghai Sixth People’s Hospital, and colleagues, on ResearchSquare.com. This study has not yet been peer reviewed. The full text of the study can be found on ResearchSquare.com.A version of this article first appeared on Medscape.com.
Major life stressors ‘strongly predictive’ of long COVID symptoms
new research suggests.
Major life stressors in the year after hospital discharge for COVID-19 are “strongly predictive of a lot of the important outcomes that people may face after COVID,” lead investigator Jennifer A. Frontera, MD, a professor in the department of neurology at New York University Langone Health, said in an interview.
These outcomes include depression, brain fog, fatigue, trouble sleeping, and other long COVID symptoms.
The findings were published online in the Journal of the Neurological Sciences.
Major stressful events common
Dr. Frontera and the NYU Neurology COVID-19 study team evaluated 451 adults who survived a COVID hospital stay. Of these, 383 completed a 6-month follow-up, 242 completed a 12-month follow-up, and 174 completed follow-up at both time points.
Within 1 year of discharge, 77 (17%) patients died and 51% suffered a major stressful life event.
In multivariable analyses, major life stressors – including financial insecurity, food insecurity, death of a close contact, and new disability – were strong independent predictors of disability, trouble with activities of daily living, depression, fatigue, sleep problems, and prolonged post-acute COVID symptoms. The adjusted odds ratios for these outcomes ranged from 2.5 to 20.8.
The research also confirmed the contribution of traditional risk factors for long COVID symptoms, as shown in past studies. These include older age, poor pre-COVID functional status, and more severe initial COVID-19 infection.
Long-term sequelae of COVID are increasingly recognized as major public health issues.
It has been estimated that roughly 16 million U.S. adults aged 18-65 years ave long COVID, with the often debilitating symptoms keeping up to 4 million out of work.
Holistic approach
Dr. Frontera said it’s important to realize that “sleep, fatigue, anxiety, depression, even cognition are so interwoven with each other that anything that impacts any one of them could have repercussions on the other.”
She added that it “certainly makes sense that there is an interplay or even a bidirectional relationship between the stressors that people face and how well they can recover after COVID.”
Therapies that lessen the trauma of the most stress-inducing life events need to be a central part of treatment for long COVID, with more research needed to validate the best approaches, Dr. Frontera said.
She also noted that social services or case management resources may be able to help address at least some of the stressors that individuals are under – and it is important to refer them to these resources. Referral to mental health services is also important.
“I think it’s really important to take a holistic approach and try to deal with whatever the problem may be,” said Dr. Frontera.
“I’m a neurologist, but as part of my evaluation, I really need to address if there are life stressors or mental health issues that may be impacting this person’s function,” she added.
The study had no commercial funding. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Major life stressors in the year after hospital discharge for COVID-19 are “strongly predictive of a lot of the important outcomes that people may face after COVID,” lead investigator Jennifer A. Frontera, MD, a professor in the department of neurology at New York University Langone Health, said in an interview.
These outcomes include depression, brain fog, fatigue, trouble sleeping, and other long COVID symptoms.
The findings were published online in the Journal of the Neurological Sciences.
Major stressful events common
Dr. Frontera and the NYU Neurology COVID-19 study team evaluated 451 adults who survived a COVID hospital stay. Of these, 383 completed a 6-month follow-up, 242 completed a 12-month follow-up, and 174 completed follow-up at both time points.
Within 1 year of discharge, 77 (17%) patients died and 51% suffered a major stressful life event.
In multivariable analyses, major life stressors – including financial insecurity, food insecurity, death of a close contact, and new disability – were strong independent predictors of disability, trouble with activities of daily living, depression, fatigue, sleep problems, and prolonged post-acute COVID symptoms. The adjusted odds ratios for these outcomes ranged from 2.5 to 20.8.
The research also confirmed the contribution of traditional risk factors for long COVID symptoms, as shown in past studies. These include older age, poor pre-COVID functional status, and more severe initial COVID-19 infection.
Long-term sequelae of COVID are increasingly recognized as major public health issues.
It has been estimated that roughly 16 million U.S. adults aged 18-65 years ave long COVID, with the often debilitating symptoms keeping up to 4 million out of work.
Holistic approach
Dr. Frontera said it’s important to realize that “sleep, fatigue, anxiety, depression, even cognition are so interwoven with each other that anything that impacts any one of them could have repercussions on the other.”
She added that it “certainly makes sense that there is an interplay or even a bidirectional relationship between the stressors that people face and how well they can recover after COVID.”
Therapies that lessen the trauma of the most stress-inducing life events need to be a central part of treatment for long COVID, with more research needed to validate the best approaches, Dr. Frontera said.
She also noted that social services or case management resources may be able to help address at least some of the stressors that individuals are under – and it is important to refer them to these resources. Referral to mental health services is also important.
“I think it’s really important to take a holistic approach and try to deal with whatever the problem may be,” said Dr. Frontera.
“I’m a neurologist, but as part of my evaluation, I really need to address if there are life stressors or mental health issues that may be impacting this person’s function,” she added.
The study had no commercial funding. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Major life stressors in the year after hospital discharge for COVID-19 are “strongly predictive of a lot of the important outcomes that people may face after COVID,” lead investigator Jennifer A. Frontera, MD, a professor in the department of neurology at New York University Langone Health, said in an interview.
These outcomes include depression, brain fog, fatigue, trouble sleeping, and other long COVID symptoms.
The findings were published online in the Journal of the Neurological Sciences.
Major stressful events common
Dr. Frontera and the NYU Neurology COVID-19 study team evaluated 451 adults who survived a COVID hospital stay. Of these, 383 completed a 6-month follow-up, 242 completed a 12-month follow-up, and 174 completed follow-up at both time points.
Within 1 year of discharge, 77 (17%) patients died and 51% suffered a major stressful life event.
In multivariable analyses, major life stressors – including financial insecurity, food insecurity, death of a close contact, and new disability – were strong independent predictors of disability, trouble with activities of daily living, depression, fatigue, sleep problems, and prolonged post-acute COVID symptoms. The adjusted odds ratios for these outcomes ranged from 2.5 to 20.8.
The research also confirmed the contribution of traditional risk factors for long COVID symptoms, as shown in past studies. These include older age, poor pre-COVID functional status, and more severe initial COVID-19 infection.
Long-term sequelae of COVID are increasingly recognized as major public health issues.
It has been estimated that roughly 16 million U.S. adults aged 18-65 years ave long COVID, with the often debilitating symptoms keeping up to 4 million out of work.
Holistic approach
Dr. Frontera said it’s important to realize that “sleep, fatigue, anxiety, depression, even cognition are so interwoven with each other that anything that impacts any one of them could have repercussions on the other.”
She added that it “certainly makes sense that there is an interplay or even a bidirectional relationship between the stressors that people face and how well they can recover after COVID.”
Therapies that lessen the trauma of the most stress-inducing life events need to be a central part of treatment for long COVID, with more research needed to validate the best approaches, Dr. Frontera said.
She also noted that social services or case management resources may be able to help address at least some of the stressors that individuals are under – and it is important to refer them to these resources. Referral to mental health services is also important.
“I think it’s really important to take a holistic approach and try to deal with whatever the problem may be,” said Dr. Frontera.
“I’m a neurologist, but as part of my evaluation, I really need to address if there are life stressors or mental health issues that may be impacting this person’s function,” she added.
The study had no commercial funding. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE NEUROLOGICAL SCIENCES
Why your professional persona may be considered unprofessional
On one of the first days of medical school, Adaira Landry, MD, applied her favorite dark shade of lipstick and headed to her orientation. She was eager to learn about program expectations and connect with fellow aspiring physicians. But when Dr. Landry got there, one of her brand-new peers turned to her and asked, “Why do you wear your lipstick like an angry Black woman?”
“Imagine hearing that,” Dr. Landry, now an emergency medical physician in Boston, says. “It was so hurtful.”
So, what is a “standard-issue doctor” expected to look like? Physicians manage their appearances in myriad ways: through clothes, accessories, hair style, makeup; through a social media presence or lack thereof; in the rhythms and nuances of their interactions with patients and colleagues. These things add up to a professional “persona” – the Latin word for “mask,” or the face on display for the world to see.
While the health care field itself is diversifying, its guidelines for professionalism appear slower to change, often excluding or frowning upon expressions of individual personality or identity.
“Medicine is run primarily by men. It’s an objective truth,” Dr. Landry says. “Currently and historically, the standard of professionalism, especially in the physical sense, was set by them. As we increase diversity and welcome people bringing their authentic self to work, the prior definitions of professionalism are obviously in need of change.”
Split social media personalities
In August 2020, the Journal of Vascular Surgery published a study on the “prevalence of unprofessional social media content among young vascular surgeons.” The content that was deemed “unprofessional” included opinions on political issues like abortion and gun control. Photos of physicians holding alcoholic drinks or wearing “inappropriate/offensive attire,” including underwear, “provocative Halloween costumes,” and “bikinis/swimwear” were also censured. Six men and one woman worked on the study, and three of the male researchers took on the task of seeking out the “unprofessional” photos on social media. The resulting paper was reviewed by an all-male editorial board.
The study sparked immediate backlash and prompted hundreds of health care professionals to post photos of themselves in bathing suits with the hashtag “#medbikini.” The journal then retracted the study and issued an apology on Twitter, recognizing “errors in the design of the study with regards to conscious and unconscious bias.”
The researchers’ original definition of professionalism suggests that physicians should manage their personae even outside of work hours. “I think medicine in general is a very conservative and hierarchical field of study and of work, to say the least,” says Sarah Fraser, MD, a family medicine physician in Nova Scotia, Canada. “There’s this view that we have to have completely separate personal and professional lives, like church and state.”
The #medbikini controversy inspired Dr. Fraser to write an op-ed for the British Medical Journal blog about the flaws of requiring physicians to keep their personal and professional selves separate. The piece referenced Robert Louis Stevenson’s 1886 Gothic novella “The Strange Case of Dr. Jekyll and Mr. Hyde,” in which the respected scientist Dr. Jekyll creates an alter ego so he can express his evil urges without experiencing guilt, punishment, or loss of livelihood. Dr. Fraser likened this story to the pressure physicians feel to shrink or split themselves to squeeze into a narrow definition of professionalism.
But Dr. Landry points out that some elements of expression seen as unprofessional cannot be entirely separated from a physician’s fundamental identity. “For Black women, our daily behaviors and forms of expression that are deemed ‘unprofessional’ are much more subtle than being able to wear a bikini on social media,” she says. “The way we wear our hair, the tone of our voice, the color of our lipstick, the way we wear scrub caps are parts of us that are called into question.”
Keeping up appearances
The stereotype of what a doctor should look like starts to shape physicians’ professional personae in medical school. When Jennifer Caputo-Seidler, MD, started medical school in 2008, the dress code requirements for male students were simple: pants, a button-down shirt, a tie. But then there were the rules for women: Hair should be tied back. Minimal makeup. No flashy jewelry. Nothing without sleeves. Neutral colors. High necklines. Low hemlines. “The message I got was that we need to dress like the men in order to be taken seriously and to be seen as professional,” says Dr. Caputo-Seidler, now an assistant professor of medicine at the University of South Florida, Tampa, “and so that’s what I did.”
A 2018 analysis of 78 “draw-a-scientist” studies found that children have overwhelmingly associated scientific fields with men for the last 50 years. Overall, children drew 73% of scientists as men. The drawings grew more gender diverse over time, but even as more women entered scientific fields, both boys and girls continued to draw significantly more male than female scientists.
Not everyone at Dr. Caputo-Seidler’s medical school adhered to the environment’s gendered expectations. One resident she worked with often wore voluminous hairstyles, lipstick, and high heels. Dr. Caputo-Seidler overheard her peers as they gossiped behind the resident’s back, ridiculing the way she looked.
“She was good at her job,” Dr. Caputo-Seidler says. “She knew her patients. She had things down. She was, by all measures, very competent. But when people saw her dressing outside the norm and being forward with her femininity, there was definitely a lot of chatter about it.”
While expectations for a conservative appearance may disproportionately affect women, and particularly women of color, they also affect men who deviate from the norm. “As an LGBTQ+ person working as a ‘professional,’ I have countless stories and moments where I had my professionalism questioned,” Blair Peters, MD, a plastic surgeon and assistant professor at Oregon Health & Science University, Portland, wrote on Twitter. “Why is it ‘unprofessional’ to have colored hair? Why is it ‘unprofessional’ to have a visible tattoo? Why is it ‘unprofessional’ to wear bright colors and patterns?”
Dr. Fraser remembers a fellow medical student who had full-sleeve tattoos on both of his arms. A preceptor made a comment about it to Dr. Fraser, and then instructed the student to cover up his tattoos. “I think that there are scenarios when having tattoos or having different-colored hair or expressing your individual personality could help you even better bond with your patients,” Dr. Fraser says, “especially if you’re, for example, working with youth.”
Unmasking health care
Beyond the facets of dress codes and social media posts, the issue of professional personae speaks to the deeper issue of inclusion in medicine. As the field grows increasingly diverse, health care institutions and those they serve may need to expand their definitions of professionalism to include more truthful expressions of who contemporary health care professionals are as people.
Dr. Fraser suggests that the benefits of physicians embracing self-expression – rather than assimilating to an outdated model of professionalism – extend beyond the individual.
“Whether it comes to what you choose to wear to the clinic on a day-to-day basis, or what you choose to share on a social media account, as long as it’s not harming others, then I think that it’s a positive thing to be able to be yourself and express yourself,” she says. “I feel like doctors are expected to have a different personality when we’re at the clinic, and usually it’s more conservative or objective or aloof. But I think that by being open about who we are, we’ll actually help build a trusting relationship with both patients and society.”
A version of this article first appeared on Medscape.com.
On one of the first days of medical school, Adaira Landry, MD, applied her favorite dark shade of lipstick and headed to her orientation. She was eager to learn about program expectations and connect with fellow aspiring physicians. But when Dr. Landry got there, one of her brand-new peers turned to her and asked, “Why do you wear your lipstick like an angry Black woman?”
“Imagine hearing that,” Dr. Landry, now an emergency medical physician in Boston, says. “It was so hurtful.”
So, what is a “standard-issue doctor” expected to look like? Physicians manage their appearances in myriad ways: through clothes, accessories, hair style, makeup; through a social media presence or lack thereof; in the rhythms and nuances of their interactions with patients and colleagues. These things add up to a professional “persona” – the Latin word for “mask,” or the face on display for the world to see.
While the health care field itself is diversifying, its guidelines for professionalism appear slower to change, often excluding or frowning upon expressions of individual personality or identity.
“Medicine is run primarily by men. It’s an objective truth,” Dr. Landry says. “Currently and historically, the standard of professionalism, especially in the physical sense, was set by them. As we increase diversity and welcome people bringing their authentic self to work, the prior definitions of professionalism are obviously in need of change.”
Split social media personalities
In August 2020, the Journal of Vascular Surgery published a study on the “prevalence of unprofessional social media content among young vascular surgeons.” The content that was deemed “unprofessional” included opinions on political issues like abortion and gun control. Photos of physicians holding alcoholic drinks or wearing “inappropriate/offensive attire,” including underwear, “provocative Halloween costumes,” and “bikinis/swimwear” were also censured. Six men and one woman worked on the study, and three of the male researchers took on the task of seeking out the “unprofessional” photos on social media. The resulting paper was reviewed by an all-male editorial board.
The study sparked immediate backlash and prompted hundreds of health care professionals to post photos of themselves in bathing suits with the hashtag “#medbikini.” The journal then retracted the study and issued an apology on Twitter, recognizing “errors in the design of the study with regards to conscious and unconscious bias.”
The researchers’ original definition of professionalism suggests that physicians should manage their personae even outside of work hours. “I think medicine in general is a very conservative and hierarchical field of study and of work, to say the least,” says Sarah Fraser, MD, a family medicine physician in Nova Scotia, Canada. “There’s this view that we have to have completely separate personal and professional lives, like church and state.”
The #medbikini controversy inspired Dr. Fraser to write an op-ed for the British Medical Journal blog about the flaws of requiring physicians to keep their personal and professional selves separate. The piece referenced Robert Louis Stevenson’s 1886 Gothic novella “The Strange Case of Dr. Jekyll and Mr. Hyde,” in which the respected scientist Dr. Jekyll creates an alter ego so he can express his evil urges without experiencing guilt, punishment, or loss of livelihood. Dr. Fraser likened this story to the pressure physicians feel to shrink or split themselves to squeeze into a narrow definition of professionalism.
But Dr. Landry points out that some elements of expression seen as unprofessional cannot be entirely separated from a physician’s fundamental identity. “For Black women, our daily behaviors and forms of expression that are deemed ‘unprofessional’ are much more subtle than being able to wear a bikini on social media,” she says. “The way we wear our hair, the tone of our voice, the color of our lipstick, the way we wear scrub caps are parts of us that are called into question.”
Keeping up appearances
The stereotype of what a doctor should look like starts to shape physicians’ professional personae in medical school. When Jennifer Caputo-Seidler, MD, started medical school in 2008, the dress code requirements for male students were simple: pants, a button-down shirt, a tie. But then there were the rules for women: Hair should be tied back. Minimal makeup. No flashy jewelry. Nothing without sleeves. Neutral colors. High necklines. Low hemlines. “The message I got was that we need to dress like the men in order to be taken seriously and to be seen as professional,” says Dr. Caputo-Seidler, now an assistant professor of medicine at the University of South Florida, Tampa, “and so that’s what I did.”
A 2018 analysis of 78 “draw-a-scientist” studies found that children have overwhelmingly associated scientific fields with men for the last 50 years. Overall, children drew 73% of scientists as men. The drawings grew more gender diverse over time, but even as more women entered scientific fields, both boys and girls continued to draw significantly more male than female scientists.
Not everyone at Dr. Caputo-Seidler’s medical school adhered to the environment’s gendered expectations. One resident she worked with often wore voluminous hairstyles, lipstick, and high heels. Dr. Caputo-Seidler overheard her peers as they gossiped behind the resident’s back, ridiculing the way she looked.
“She was good at her job,” Dr. Caputo-Seidler says. “She knew her patients. She had things down. She was, by all measures, very competent. But when people saw her dressing outside the norm and being forward with her femininity, there was definitely a lot of chatter about it.”
While expectations for a conservative appearance may disproportionately affect women, and particularly women of color, they also affect men who deviate from the norm. “As an LGBTQ+ person working as a ‘professional,’ I have countless stories and moments where I had my professionalism questioned,” Blair Peters, MD, a plastic surgeon and assistant professor at Oregon Health & Science University, Portland, wrote on Twitter. “Why is it ‘unprofessional’ to have colored hair? Why is it ‘unprofessional’ to have a visible tattoo? Why is it ‘unprofessional’ to wear bright colors and patterns?”
Dr. Fraser remembers a fellow medical student who had full-sleeve tattoos on both of his arms. A preceptor made a comment about it to Dr. Fraser, and then instructed the student to cover up his tattoos. “I think that there are scenarios when having tattoos or having different-colored hair or expressing your individual personality could help you even better bond with your patients,” Dr. Fraser says, “especially if you’re, for example, working with youth.”
Unmasking health care
Beyond the facets of dress codes and social media posts, the issue of professional personae speaks to the deeper issue of inclusion in medicine. As the field grows increasingly diverse, health care institutions and those they serve may need to expand their definitions of professionalism to include more truthful expressions of who contemporary health care professionals are as people.
Dr. Fraser suggests that the benefits of physicians embracing self-expression – rather than assimilating to an outdated model of professionalism – extend beyond the individual.
“Whether it comes to what you choose to wear to the clinic on a day-to-day basis, or what you choose to share on a social media account, as long as it’s not harming others, then I think that it’s a positive thing to be able to be yourself and express yourself,” she says. “I feel like doctors are expected to have a different personality when we’re at the clinic, and usually it’s more conservative or objective or aloof. But I think that by being open about who we are, we’ll actually help build a trusting relationship with both patients and society.”
A version of this article first appeared on Medscape.com.
On one of the first days of medical school, Adaira Landry, MD, applied her favorite dark shade of lipstick and headed to her orientation. She was eager to learn about program expectations and connect with fellow aspiring physicians. But when Dr. Landry got there, one of her brand-new peers turned to her and asked, “Why do you wear your lipstick like an angry Black woman?”
“Imagine hearing that,” Dr. Landry, now an emergency medical physician in Boston, says. “It was so hurtful.”
So, what is a “standard-issue doctor” expected to look like? Physicians manage their appearances in myriad ways: through clothes, accessories, hair style, makeup; through a social media presence or lack thereof; in the rhythms and nuances of their interactions with patients and colleagues. These things add up to a professional “persona” – the Latin word for “mask,” or the face on display for the world to see.
While the health care field itself is diversifying, its guidelines for professionalism appear slower to change, often excluding or frowning upon expressions of individual personality or identity.
“Medicine is run primarily by men. It’s an objective truth,” Dr. Landry says. “Currently and historically, the standard of professionalism, especially in the physical sense, was set by them. As we increase diversity and welcome people bringing their authentic self to work, the prior definitions of professionalism are obviously in need of change.”
Split social media personalities
In August 2020, the Journal of Vascular Surgery published a study on the “prevalence of unprofessional social media content among young vascular surgeons.” The content that was deemed “unprofessional” included opinions on political issues like abortion and gun control. Photos of physicians holding alcoholic drinks or wearing “inappropriate/offensive attire,” including underwear, “provocative Halloween costumes,” and “bikinis/swimwear” were also censured. Six men and one woman worked on the study, and three of the male researchers took on the task of seeking out the “unprofessional” photos on social media. The resulting paper was reviewed by an all-male editorial board.
The study sparked immediate backlash and prompted hundreds of health care professionals to post photos of themselves in bathing suits with the hashtag “#medbikini.” The journal then retracted the study and issued an apology on Twitter, recognizing “errors in the design of the study with regards to conscious and unconscious bias.”
The researchers’ original definition of professionalism suggests that physicians should manage their personae even outside of work hours. “I think medicine in general is a very conservative and hierarchical field of study and of work, to say the least,” says Sarah Fraser, MD, a family medicine physician in Nova Scotia, Canada. “There’s this view that we have to have completely separate personal and professional lives, like church and state.”
The #medbikini controversy inspired Dr. Fraser to write an op-ed for the British Medical Journal blog about the flaws of requiring physicians to keep their personal and professional selves separate. The piece referenced Robert Louis Stevenson’s 1886 Gothic novella “The Strange Case of Dr. Jekyll and Mr. Hyde,” in which the respected scientist Dr. Jekyll creates an alter ego so he can express his evil urges without experiencing guilt, punishment, or loss of livelihood. Dr. Fraser likened this story to the pressure physicians feel to shrink or split themselves to squeeze into a narrow definition of professionalism.
But Dr. Landry points out that some elements of expression seen as unprofessional cannot be entirely separated from a physician’s fundamental identity. “For Black women, our daily behaviors and forms of expression that are deemed ‘unprofessional’ are much more subtle than being able to wear a bikini on social media,” she says. “The way we wear our hair, the tone of our voice, the color of our lipstick, the way we wear scrub caps are parts of us that are called into question.”
Keeping up appearances
The stereotype of what a doctor should look like starts to shape physicians’ professional personae in medical school. When Jennifer Caputo-Seidler, MD, started medical school in 2008, the dress code requirements for male students were simple: pants, a button-down shirt, a tie. But then there were the rules for women: Hair should be tied back. Minimal makeup. No flashy jewelry. Nothing without sleeves. Neutral colors. High necklines. Low hemlines. “The message I got was that we need to dress like the men in order to be taken seriously and to be seen as professional,” says Dr. Caputo-Seidler, now an assistant professor of medicine at the University of South Florida, Tampa, “and so that’s what I did.”
A 2018 analysis of 78 “draw-a-scientist” studies found that children have overwhelmingly associated scientific fields with men for the last 50 years. Overall, children drew 73% of scientists as men. The drawings grew more gender diverse over time, but even as more women entered scientific fields, both boys and girls continued to draw significantly more male than female scientists.
Not everyone at Dr. Caputo-Seidler’s medical school adhered to the environment’s gendered expectations. One resident she worked with often wore voluminous hairstyles, lipstick, and high heels. Dr. Caputo-Seidler overheard her peers as they gossiped behind the resident’s back, ridiculing the way she looked.
“She was good at her job,” Dr. Caputo-Seidler says. “She knew her patients. She had things down. She was, by all measures, very competent. But when people saw her dressing outside the norm and being forward with her femininity, there was definitely a lot of chatter about it.”
While expectations for a conservative appearance may disproportionately affect women, and particularly women of color, they also affect men who deviate from the norm. “As an LGBTQ+ person working as a ‘professional,’ I have countless stories and moments where I had my professionalism questioned,” Blair Peters, MD, a plastic surgeon and assistant professor at Oregon Health & Science University, Portland, wrote on Twitter. “Why is it ‘unprofessional’ to have colored hair? Why is it ‘unprofessional’ to have a visible tattoo? Why is it ‘unprofessional’ to wear bright colors and patterns?”
Dr. Fraser remembers a fellow medical student who had full-sleeve tattoos on both of his arms. A preceptor made a comment about it to Dr. Fraser, and then instructed the student to cover up his tattoos. “I think that there are scenarios when having tattoos or having different-colored hair or expressing your individual personality could help you even better bond with your patients,” Dr. Fraser says, “especially if you’re, for example, working with youth.”
Unmasking health care
Beyond the facets of dress codes and social media posts, the issue of professional personae speaks to the deeper issue of inclusion in medicine. As the field grows increasingly diverse, health care institutions and those they serve may need to expand their definitions of professionalism to include more truthful expressions of who contemporary health care professionals are as people.
Dr. Fraser suggests that the benefits of physicians embracing self-expression – rather than assimilating to an outdated model of professionalism – extend beyond the individual.
“Whether it comes to what you choose to wear to the clinic on a day-to-day basis, or what you choose to share on a social media account, as long as it’s not harming others, then I think that it’s a positive thing to be able to be yourself and express yourself,” she says. “I feel like doctors are expected to have a different personality when we’re at the clinic, and usually it’s more conservative or objective or aloof. But I think that by being open about who we are, we’ll actually help build a trusting relationship with both patients and society.”
A version of this article first appeared on Medscape.com.
IRONMAN galvanizes case for IV iron repletion in heart failure
CHICAGO – Another major study appears to back the use of intravenous iron repletion in patients with heart failure (HF) and iron deficiency, strengthening largely consistent evidence, researchers say, that the treatment may improve symptoms and prevent some HF-related hospital admissions.
To be sure, the IRONMAN trial, which compared intravenous iron versus usual care in such patients – most with reduced ejection fraction and not hospitalized – failed to show a benefit for its primary endpoint. The 18% reduction in risk for HF hospitalization or cardiovascular (CV) death seen in the trial, however encouraging, can only be called a trend (P = .07).
But the intervention showed signs of benefit for some secondary endpoints, including quality of life scores, and hinted at such an effect on HF hospitalization. Risk for the latter endpoint dropped 20% (P = .085) over a median follow-up of 2.7 years.
The findings “build upon the other data we have that correcting iron deficiency can help improve well-being, and particularly reduce the risk of hospitalization, in a broad range of [HF] patients,” said Paul Kalra, MD, of the University of Glasgow and Portsmouth (England) Hospitals University NHS Trust.
The tested regimen “was well tolerated with no safety concerns” and offers “reassurance about the long-term safety” of the intravenous iron it used, ferric derisomaltose (MonoFerric), in patients with HF, Dr. Kalra said at a media briefing on the trial.
The remarks preceded his formal presentation of IRONMAN at the American Heart Association scientific sessions. Dr. Kalra is also lead author on the trial’s publication in The Lancet.
IRONMAN strengthens the base of evidence supporting intravenous iron in HF with iron deficiency, especially chronic HF in outpatients, Dr. Kalra and others said. It also supports efficacy for a form of intravenous iron not previously tested in a major HF trial.
Still, “the totality of data are now supporting intravenous iron per se,” regardless of the iron agent used, said Dr. Kalra. But ferric derisomaltose may have dosing advantages, he observed, “and we’ve now got these long-term safety data.”
The strongest prior support for intravenous iron in HF came from hospitalized patients who received it as ferric carboxymaltose (Ferinject) and were followed only 12 months. That was in the AFFIRM-AHF trial, published 2 years ago, which also missed its primary endpoint – the same one used in IRONMAN. Some outcomes in the two trials were similar.
The risk for HF hospitalization or CV death for intravenous iron therapy, compared with usual care, in AFFIRM-AHF fell 21% (P = .059), missing significance but apparently driven by a 26% drop in risk for HF readmissions (P = .013). But neither that trial nor IRONMAN suggested a benefit for CV mortality on its own.
The COVID effect
In IRONMAN, Dr. Kalra said, usual care could include oral iron supplementation, which 17% of patients in the control group received. That could potentially have kept the intravenous iron group from making a better showing for the primary endpoint, he proposed.
And some iron doses and other treatments were missed by a substantial number of patients in both groups who entered the trial after the United Kingdom’s national lockdown in response to the COVID-19 pandemic, he observed. “Patients were not able to come into hospitals for research visits, or in fact when they were able, may not have wanted to.”
So, the group conducted a “prespecified” sensitivity analysis that excluded the 9% of patients enrolled by the end of March 2020, about the time of the first lockdown, and followed the remainder for another 6 months.
In that analysis, risk for HF hospitalization or CV death declined 24% in the intravenous iron group, a marginal but significant result (P = .047) that was dominated by an improvement in HF hospitalizations.
Effects on guidelines
The intravenous iron recommendations in the European HF guidelines refer only to ferric carboxymaltose without mentioning other forms, such as ferric derisomaltose, “but this is now a class effect given the similarities between AFFIRM-AHF and IRONMAN,” said Gregory D. Lewis, MD, Mass General Brigham, Boston, invited discussant for Dr. Kalra’s presentation at the AHA session.
“In the United States, we relegate IV iron to improvement in functional capacity as a comorbidity of heart failure. Perhaps this role will expand,” added Dr. Lewis, who is medical director of his center’s heart transplant program.
He also wondered aloud whether the purported clinical benefits of intravenous iron in HF patients with iron deficiency, not as yet supported by a significant primary-endpoint showing in one of the major trials, currently justify expansion of its use in practice.
“With the benefits of IV iron on exercise capacity and quality of life, and the safety of administering high doses of IV iron,” potentially reducing HF polypharmacy, he noted, “should we be considering IV iron more commonly for utilization in our patients even if we find that heart failure hospitalizations and mortality are only modestly improved?”
IRONMAN “asked whether there’s benefit to IV iron in the longer term,” Kiran Musunuru, MD, PhD, MPH, University of Pennsylvania,Philadelphia, observed at the media briefing. As the trial was reported, “that does in fact, seem to be the case,” said Dr. Musunuru, who was not involved in IRONMAN.
Therefore, he said, “this study reinforces the message that we should be routinely monitoring our heart failure patients for iron deficiency and supplementing them as needed.”
A commentary linked to the IRONMAN publication agreed. The trial “increases the evidence base for the treatment of iron deficiency with intravenous iron supplementation,” wrote the editorialists, led by Theresa A. McDonagh, MD, King’s College Hospital and School of Cardiovascular Sciences, London.
Patients with acute or chronic HF, iron deficiency, and reduced or mildly reduced ejection fractions “should be offered treatment with intravenous iron to reduce their risk of hospital admission for heart failure,” they concluded.
Mostly reduced-EF outpatients
The open-label, blinded-endpoint IRONMAN trial, conducted at 70 centers in the United Kingdom, entered adults with HF, ejection fractions 45% or lower within the previous 2 years, and iron deficiency defined as transferrin saturation less than 20% or serum ferritin levels below 100 mcg/L, the report states. They were either hospitalized for HF, had such a hospitalization within the past 6 months, or were outpatients with elevated natriuretic peptide levels; the third category accounted for two thirds of the trial population.
Of the 1,137 randomized patients, 569 were assigned to receive intravenous ferric derisomaltose at weight- and hemoglobin-adjusted dosages; 568 went to the usual-care group.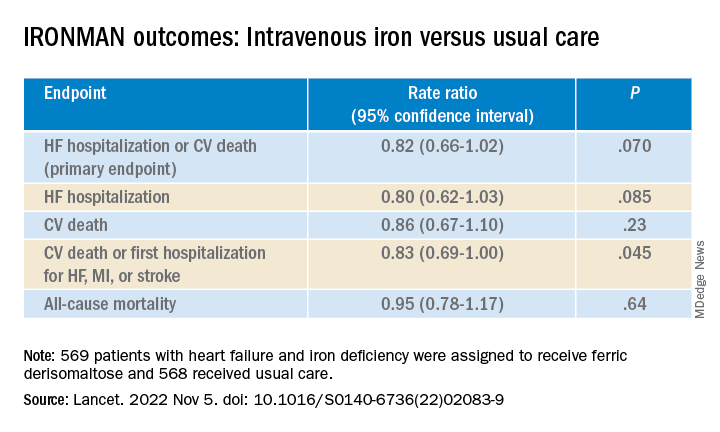
Those receiving intravenous iron visited the trial clinic 4 weeks later and then every 4 months. At those visits, they received a round of ferric derisomaltose if their ferritin levels were below 100 mcg/L, or 400 mcg/L or lower if transferrin saturation was below 25%, the published report states.
Mean scores on the Minnesota Living with Heart Failure Questionnaire improved by a marginally significant 3.33 points (P = .050) at 4 months in the intravenous iron group. The gain receded to a nonsignificant 2.57 points by 20 months (P = .23).
In COVID-related sensitivity analysis, the intravenous iron group showed a significant benefit for the primary endpoint and a trend for improved HF hospitalizations.
- HF hospitalization or CV death: RR, 0.76 (95% confidence interval, 0.58-1.00; P = .047)
- HF hospitalization: RR 0.76 (95% CI, 0.56-1.03; P = .077)
Fewer patients in the intravenous iron group experienced serious cardiac adverse events, 36% compared with 43% in for those on usual care, P = .016.
The recently updated European Society of Cardiology guidelines for HF made it a class 1 recommendation to assess iron status in every patient, Kalra observed. “It doesn›t specify how frequently, but I think we should be thinking about every 4-6 months.”
Dr. Kalra disclosed receiving research grants from Pharmacosmos; and consulting or lecturing for Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Pfizer, Pharmacosmos, Servier, and Vifor Pharma. Dr. Musunuru disclosed significant ownership interest in Verve Therapeutics and Variant Bio. Dr. Lewis disclosed relationships with NXT, American Regent, and RIVUS; and receiving research grants from Cytokinetics and Amgen.
A version of this article first appeared on Medscape.com.
CHICAGO – Another major study appears to back the use of intravenous iron repletion in patients with heart failure (HF) and iron deficiency, strengthening largely consistent evidence, researchers say, that the treatment may improve symptoms and prevent some HF-related hospital admissions.
To be sure, the IRONMAN trial, which compared intravenous iron versus usual care in such patients – most with reduced ejection fraction and not hospitalized – failed to show a benefit for its primary endpoint. The 18% reduction in risk for HF hospitalization or cardiovascular (CV) death seen in the trial, however encouraging, can only be called a trend (P = .07).
But the intervention showed signs of benefit for some secondary endpoints, including quality of life scores, and hinted at such an effect on HF hospitalization. Risk for the latter endpoint dropped 20% (P = .085) over a median follow-up of 2.7 years.
The findings “build upon the other data we have that correcting iron deficiency can help improve well-being, and particularly reduce the risk of hospitalization, in a broad range of [HF] patients,” said Paul Kalra, MD, of the University of Glasgow and Portsmouth (England) Hospitals University NHS Trust.
The tested regimen “was well tolerated with no safety concerns” and offers “reassurance about the long-term safety” of the intravenous iron it used, ferric derisomaltose (MonoFerric), in patients with HF, Dr. Kalra said at a media briefing on the trial.
The remarks preceded his formal presentation of IRONMAN at the American Heart Association scientific sessions. Dr. Kalra is also lead author on the trial’s publication in The Lancet.
IRONMAN strengthens the base of evidence supporting intravenous iron in HF with iron deficiency, especially chronic HF in outpatients, Dr. Kalra and others said. It also supports efficacy for a form of intravenous iron not previously tested in a major HF trial.
Still, “the totality of data are now supporting intravenous iron per se,” regardless of the iron agent used, said Dr. Kalra. But ferric derisomaltose may have dosing advantages, he observed, “and we’ve now got these long-term safety data.”
The strongest prior support for intravenous iron in HF came from hospitalized patients who received it as ferric carboxymaltose (Ferinject) and were followed only 12 months. That was in the AFFIRM-AHF trial, published 2 years ago, which also missed its primary endpoint – the same one used in IRONMAN. Some outcomes in the two trials were similar.
The risk for HF hospitalization or CV death for intravenous iron therapy, compared with usual care, in AFFIRM-AHF fell 21% (P = .059), missing significance but apparently driven by a 26% drop in risk for HF readmissions (P = .013). But neither that trial nor IRONMAN suggested a benefit for CV mortality on its own.
The COVID effect
In IRONMAN, Dr. Kalra said, usual care could include oral iron supplementation, which 17% of patients in the control group received. That could potentially have kept the intravenous iron group from making a better showing for the primary endpoint, he proposed.
And some iron doses and other treatments were missed by a substantial number of patients in both groups who entered the trial after the United Kingdom’s national lockdown in response to the COVID-19 pandemic, he observed. “Patients were not able to come into hospitals for research visits, or in fact when they were able, may not have wanted to.”
So, the group conducted a “prespecified” sensitivity analysis that excluded the 9% of patients enrolled by the end of March 2020, about the time of the first lockdown, and followed the remainder for another 6 months.
In that analysis, risk for HF hospitalization or CV death declined 24% in the intravenous iron group, a marginal but significant result (P = .047) that was dominated by an improvement in HF hospitalizations.
Effects on guidelines
The intravenous iron recommendations in the European HF guidelines refer only to ferric carboxymaltose without mentioning other forms, such as ferric derisomaltose, “but this is now a class effect given the similarities between AFFIRM-AHF and IRONMAN,” said Gregory D. Lewis, MD, Mass General Brigham, Boston, invited discussant for Dr. Kalra’s presentation at the AHA session.
“In the United States, we relegate IV iron to improvement in functional capacity as a comorbidity of heart failure. Perhaps this role will expand,” added Dr. Lewis, who is medical director of his center’s heart transplant program.
He also wondered aloud whether the purported clinical benefits of intravenous iron in HF patients with iron deficiency, not as yet supported by a significant primary-endpoint showing in one of the major trials, currently justify expansion of its use in practice.
“With the benefits of IV iron on exercise capacity and quality of life, and the safety of administering high doses of IV iron,” potentially reducing HF polypharmacy, he noted, “should we be considering IV iron more commonly for utilization in our patients even if we find that heart failure hospitalizations and mortality are only modestly improved?”
IRONMAN “asked whether there’s benefit to IV iron in the longer term,” Kiran Musunuru, MD, PhD, MPH, University of Pennsylvania,Philadelphia, observed at the media briefing. As the trial was reported, “that does in fact, seem to be the case,” said Dr. Musunuru, who was not involved in IRONMAN.
Therefore, he said, “this study reinforces the message that we should be routinely monitoring our heart failure patients for iron deficiency and supplementing them as needed.”
A commentary linked to the IRONMAN publication agreed. The trial “increases the evidence base for the treatment of iron deficiency with intravenous iron supplementation,” wrote the editorialists, led by Theresa A. McDonagh, MD, King’s College Hospital and School of Cardiovascular Sciences, London.
Patients with acute or chronic HF, iron deficiency, and reduced or mildly reduced ejection fractions “should be offered treatment with intravenous iron to reduce their risk of hospital admission for heart failure,” they concluded.
Mostly reduced-EF outpatients
The open-label, blinded-endpoint IRONMAN trial, conducted at 70 centers in the United Kingdom, entered adults with HF, ejection fractions 45% or lower within the previous 2 years, and iron deficiency defined as transferrin saturation less than 20% or serum ferritin levels below 100 mcg/L, the report states. They were either hospitalized for HF, had such a hospitalization within the past 6 months, or were outpatients with elevated natriuretic peptide levels; the third category accounted for two thirds of the trial population.
Of the 1,137 randomized patients, 569 were assigned to receive intravenous ferric derisomaltose at weight- and hemoglobin-adjusted dosages; 568 went to the usual-care group.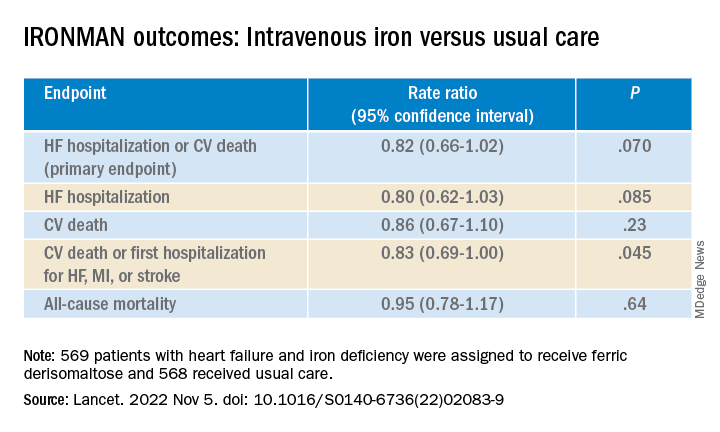
Those receiving intravenous iron visited the trial clinic 4 weeks later and then every 4 months. At those visits, they received a round of ferric derisomaltose if their ferritin levels were below 100 mcg/L, or 400 mcg/L or lower if transferrin saturation was below 25%, the published report states.
Mean scores on the Minnesota Living with Heart Failure Questionnaire improved by a marginally significant 3.33 points (P = .050) at 4 months in the intravenous iron group. The gain receded to a nonsignificant 2.57 points by 20 months (P = .23).
In COVID-related sensitivity analysis, the intravenous iron group showed a significant benefit for the primary endpoint and a trend for improved HF hospitalizations.
- HF hospitalization or CV death: RR, 0.76 (95% confidence interval, 0.58-1.00; P = .047)
- HF hospitalization: RR 0.76 (95% CI, 0.56-1.03; P = .077)
Fewer patients in the intravenous iron group experienced serious cardiac adverse events, 36% compared with 43% in for those on usual care, P = .016.
The recently updated European Society of Cardiology guidelines for HF made it a class 1 recommendation to assess iron status in every patient, Kalra observed. “It doesn›t specify how frequently, but I think we should be thinking about every 4-6 months.”
Dr. Kalra disclosed receiving research grants from Pharmacosmos; and consulting or lecturing for Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Pfizer, Pharmacosmos, Servier, and Vifor Pharma. Dr. Musunuru disclosed significant ownership interest in Verve Therapeutics and Variant Bio. Dr. Lewis disclosed relationships with NXT, American Regent, and RIVUS; and receiving research grants from Cytokinetics and Amgen.
A version of this article first appeared on Medscape.com.
CHICAGO – Another major study appears to back the use of intravenous iron repletion in patients with heart failure (HF) and iron deficiency, strengthening largely consistent evidence, researchers say, that the treatment may improve symptoms and prevent some HF-related hospital admissions.
To be sure, the IRONMAN trial, which compared intravenous iron versus usual care in such patients – most with reduced ejection fraction and not hospitalized – failed to show a benefit for its primary endpoint. The 18% reduction in risk for HF hospitalization or cardiovascular (CV) death seen in the trial, however encouraging, can only be called a trend (P = .07).
But the intervention showed signs of benefit for some secondary endpoints, including quality of life scores, and hinted at such an effect on HF hospitalization. Risk for the latter endpoint dropped 20% (P = .085) over a median follow-up of 2.7 years.
The findings “build upon the other data we have that correcting iron deficiency can help improve well-being, and particularly reduce the risk of hospitalization, in a broad range of [HF] patients,” said Paul Kalra, MD, of the University of Glasgow and Portsmouth (England) Hospitals University NHS Trust.
The tested regimen “was well tolerated with no safety concerns” and offers “reassurance about the long-term safety” of the intravenous iron it used, ferric derisomaltose (MonoFerric), in patients with HF, Dr. Kalra said at a media briefing on the trial.
The remarks preceded his formal presentation of IRONMAN at the American Heart Association scientific sessions. Dr. Kalra is also lead author on the trial’s publication in The Lancet.
IRONMAN strengthens the base of evidence supporting intravenous iron in HF with iron deficiency, especially chronic HF in outpatients, Dr. Kalra and others said. It also supports efficacy for a form of intravenous iron not previously tested in a major HF trial.
Still, “the totality of data are now supporting intravenous iron per se,” regardless of the iron agent used, said Dr. Kalra. But ferric derisomaltose may have dosing advantages, he observed, “and we’ve now got these long-term safety data.”
The strongest prior support for intravenous iron in HF came from hospitalized patients who received it as ferric carboxymaltose (Ferinject) and were followed only 12 months. That was in the AFFIRM-AHF trial, published 2 years ago, which also missed its primary endpoint – the same one used in IRONMAN. Some outcomes in the two trials were similar.
The risk for HF hospitalization or CV death for intravenous iron therapy, compared with usual care, in AFFIRM-AHF fell 21% (P = .059), missing significance but apparently driven by a 26% drop in risk for HF readmissions (P = .013). But neither that trial nor IRONMAN suggested a benefit for CV mortality on its own.
The COVID effect
In IRONMAN, Dr. Kalra said, usual care could include oral iron supplementation, which 17% of patients in the control group received. That could potentially have kept the intravenous iron group from making a better showing for the primary endpoint, he proposed.
And some iron doses and other treatments were missed by a substantial number of patients in both groups who entered the trial after the United Kingdom’s national lockdown in response to the COVID-19 pandemic, he observed. “Patients were not able to come into hospitals for research visits, or in fact when they were able, may not have wanted to.”
So, the group conducted a “prespecified” sensitivity analysis that excluded the 9% of patients enrolled by the end of March 2020, about the time of the first lockdown, and followed the remainder for another 6 months.
In that analysis, risk for HF hospitalization or CV death declined 24% in the intravenous iron group, a marginal but significant result (P = .047) that was dominated by an improvement in HF hospitalizations.
Effects on guidelines
The intravenous iron recommendations in the European HF guidelines refer only to ferric carboxymaltose without mentioning other forms, such as ferric derisomaltose, “but this is now a class effect given the similarities between AFFIRM-AHF and IRONMAN,” said Gregory D. Lewis, MD, Mass General Brigham, Boston, invited discussant for Dr. Kalra’s presentation at the AHA session.
“In the United States, we relegate IV iron to improvement in functional capacity as a comorbidity of heart failure. Perhaps this role will expand,” added Dr. Lewis, who is medical director of his center’s heart transplant program.
He also wondered aloud whether the purported clinical benefits of intravenous iron in HF patients with iron deficiency, not as yet supported by a significant primary-endpoint showing in one of the major trials, currently justify expansion of its use in practice.
“With the benefits of IV iron on exercise capacity and quality of life, and the safety of administering high doses of IV iron,” potentially reducing HF polypharmacy, he noted, “should we be considering IV iron more commonly for utilization in our patients even if we find that heart failure hospitalizations and mortality are only modestly improved?”
IRONMAN “asked whether there’s benefit to IV iron in the longer term,” Kiran Musunuru, MD, PhD, MPH, University of Pennsylvania,Philadelphia, observed at the media briefing. As the trial was reported, “that does in fact, seem to be the case,” said Dr. Musunuru, who was not involved in IRONMAN.
Therefore, he said, “this study reinforces the message that we should be routinely monitoring our heart failure patients for iron deficiency and supplementing them as needed.”
A commentary linked to the IRONMAN publication agreed. The trial “increases the evidence base for the treatment of iron deficiency with intravenous iron supplementation,” wrote the editorialists, led by Theresa A. McDonagh, MD, King’s College Hospital and School of Cardiovascular Sciences, London.
Patients with acute or chronic HF, iron deficiency, and reduced or mildly reduced ejection fractions “should be offered treatment with intravenous iron to reduce their risk of hospital admission for heart failure,” they concluded.
Mostly reduced-EF outpatients
The open-label, blinded-endpoint IRONMAN trial, conducted at 70 centers in the United Kingdom, entered adults with HF, ejection fractions 45% or lower within the previous 2 years, and iron deficiency defined as transferrin saturation less than 20% or serum ferritin levels below 100 mcg/L, the report states. They were either hospitalized for HF, had such a hospitalization within the past 6 months, or were outpatients with elevated natriuretic peptide levels; the third category accounted for two thirds of the trial population.
Of the 1,137 randomized patients, 569 were assigned to receive intravenous ferric derisomaltose at weight- and hemoglobin-adjusted dosages; 568 went to the usual-care group.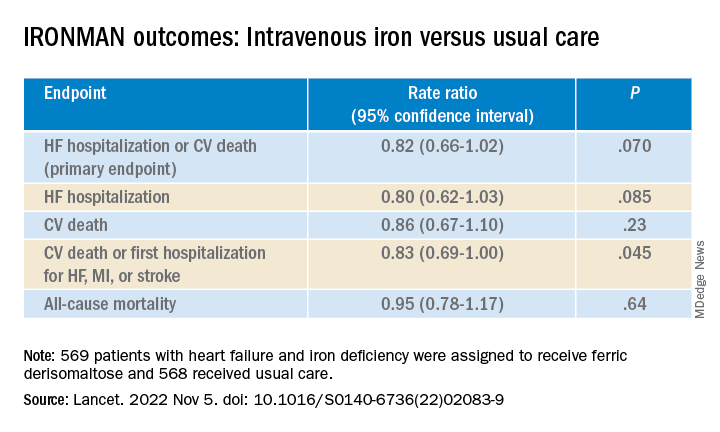
Those receiving intravenous iron visited the trial clinic 4 weeks later and then every 4 months. At those visits, they received a round of ferric derisomaltose if their ferritin levels were below 100 mcg/L, or 400 mcg/L or lower if transferrin saturation was below 25%, the published report states.
Mean scores on the Minnesota Living with Heart Failure Questionnaire improved by a marginally significant 3.33 points (P = .050) at 4 months in the intravenous iron group. The gain receded to a nonsignificant 2.57 points by 20 months (P = .23).
In COVID-related sensitivity analysis, the intravenous iron group showed a significant benefit for the primary endpoint and a trend for improved HF hospitalizations.
- HF hospitalization or CV death: RR, 0.76 (95% confidence interval, 0.58-1.00; P = .047)
- HF hospitalization: RR 0.76 (95% CI, 0.56-1.03; P = .077)
Fewer patients in the intravenous iron group experienced serious cardiac adverse events, 36% compared with 43% in for those on usual care, P = .016.
The recently updated European Society of Cardiology guidelines for HF made it a class 1 recommendation to assess iron status in every patient, Kalra observed. “It doesn›t specify how frequently, but I think we should be thinking about every 4-6 months.”
Dr. Kalra disclosed receiving research grants from Pharmacosmos; and consulting or lecturing for Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Pfizer, Pharmacosmos, Servier, and Vifor Pharma. Dr. Musunuru disclosed significant ownership interest in Verve Therapeutics and Variant Bio. Dr. Lewis disclosed relationships with NXT, American Regent, and RIVUS; and receiving research grants from Cytokinetics and Amgen.
A version of this article first appeared on Medscape.com.
AT AHA 2022
Be aware, mindfulness training can lower systolic BP: MB-BP
CHICAGO – It’s been said that one can observe a lot just by watching. Turning such observation inward, new evidence suggests, might lead to blood pressure (BP) reductions that approach what’s possible from an antihypertensive agent.
Systolic BP fell over 6 months by almost 6 mm Hg, on average, in people with elevated BP who participated in an 8-week mindful awareness program as part of a randomized trial that included a usual-care control group.
The program taught established mindfulness-training techniques aimed at modifying behaviors regarding diet, exercise, and other controllable influences on the success of antihypertensive therapy.
Participants in the program, called Mindfulness-Based Blood Pressure Reduction (MB-BP), also the name of the single-center study, “showed potentially clinically relevant reductions in systolic blood pressure,” said principal investigator Eric B. Loucks, PhD, Brown University, Providence, R.I.
The phase 2 trial has some limitations, he observed, including on generalizability. For example, it entered about 200 mostly White, college-educated adults from one metropolitan area.
But if these findings are replicated in further studies, “preferably by other research groups, in a larger and broader population, and with longer follow-up,” Dr. Loucks said, the MB-BP intervention could become “an appealing approach to help control blood pressure.”
Dr. Loucks made the comments at a press conference prior to his formal presentation of MB-BP Nov. 6 at American Heart Association (AHA) Scientific Sessions 2022, held in Chicago and virtually.
Mindfulness-based interventions for elevated BP have not been widely studied, “so this is exactly what we need: a well-done trial with a control group to show that it actually works,” Amit Khera, MD, not connected with MB-BP, told this news organization.
The trial is “really important for proof of concept, but it had only 200 people. You need a larger one, and you need longer-term data,” agreed Dr. Khera, who directs the preventive cardiology program at the University of Texas Southwestern Medical Center, in Dallas. “Six months is good, but we want to see if it’s durable.”
Rhian M. Touyz, MBBCh, also not part of MB-BP, agreed that the nearly 6 mm Hg mean systolic BP reduction among program participants is clinically relevant. “I think in the context of global risk and reduction of target organ damage and cardiovascular events, it is significant in terms of events at a population level,” Dr. Touyz, McGill University Health Centre, Montreal, told this news organization.
Many patients on antihypertensive therapy that’s falling short resist the addition of another such agent, she observed, and instead might show further BP reduction from mindfulness training. The intervention probably also “would benefit health in general.” Mindfulness-based approaches could therefore be useful additions to treatment protocols for elevated BP, Dr. Touyz said.
How the training works
The MB-BP program used validated mindfulness-based stress-management techniques, adapted to address elevated BP, that included “personalized feedback and education about hypertension risk factors, mindful awareness training of participants’ relationships with hypertension risk factors, and support for behavior change,” Dr. Loucks and colleagues reported.
Participants were trained in mindfulness skills that included “self-awareness and emotion regulation,” Dr. Loucks said, which they then could apply to their “relationships with the things that we know influence blood pressure, like physical activity, diet, antihypertensive medication adherence, or alcohol consumption.”
One goal is to promote greater “attention control,” he said, “so that there’s some self-awareness that arises in terms of how we feel the next day, after a lot of alcohol consumption, for example, or lack of physical activity.” The process can provide insights that inspire patients to modify behaviors and risk factors that elevate BP, Dr. Loucks explained.
Effects on medication use
Systolic BP responses led some program participants to be managed on fewer or reduced dosages of antihypertensive meds, he told this news organization. Physicians seen outside of the trial could adjust their prescriptions, intensifying or pulling back on meds depending on their assessments of the patient. Any prescription changes would be documented by the researchers at the patient’s next class or trial-clinic visit.
The group that did the training, Dr. Loucks said, was 33% less likely to increase and 30% more likely to decrease their use of BP-lowering medications compared with the control group.
Elevated BP is so common and undertreated that “there is a need for every possible level of intervention, starting from the population level to the individual and everything else in between,” nephrologist Janani Rangaswami, MD, George Washington University, Washington, said at the press conference.
Therefore, “this mindfulness-based approach, in addition to standard of care with pharmacotherapy, is a really welcome addition to the hypertension literature,” said Dr. Rangaswami, who directs her center’s cardiorenal program. The systolic BP reduction seen in the intervention group, she agreed, was “clinically important and meaningful.”
Blinded assessments
The trial entered 201 patients with systolic and diastolic BP greater than 120 mm Hg and 80 mm Hg, respectively; 58.7% were women, 81% were White, and 73% were college-educated, Dr. Loucks reported.
The 100 assigned to the “enhanced usual care” control group received educational materials on controlling high BP. They and the 101 who followed the mindfulness-based program were given and trained on a home BP-monitoring device. They were then followed for the primary endpoint of change in systolic BP at 6 months.
Data management and outcomes assessments were conducted by trialists not involved in the training intervention who were blinded to randomization assignment.
In a prespecified unadjusted analysis by intention-to-treat, systolic BP in the intervention group dropped by a mean of 5.9 mm Hg (P < .001) compared with baseline and 4.5 mm Hg (P = .045), compared with the control group.
A post hoc analysis adjusted for sex and baseline BP showed an average 4.3 mm Hg reduction (P = .056) in those following the MB-BP program, compared with controls.
There were no observed significant effects on diastolic BP.
The study offered clues to how engagement in the MB-BP program might promote reductions in systolic BP, Dr. Loucks observed. For example, it may have led to increased activity levels, reduced sodium intake, and other dietary improvements.
Indeed, program participants averaged about 351 minutes less sedentary time (P = .02) and showed a 0.32-point improvement in Dietary Approaches to Stop Hypertension scores (P = .08), compared with the control group, Dr. Loucks reported. Other modifiable risk factors for elevated BP that could have responded to the mindfulness-based training, he proposed, include obesity, alcohol intake, and reaction to stress.
Dr. Loucks reports that he developed the MB-BP training and was a program instructor but did not receive related financial compensation; he had no other disclosures. Dr. Khera, Dr. Touyz, and Dr. Rangaswami had no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – It’s been said that one can observe a lot just by watching. Turning such observation inward, new evidence suggests, might lead to blood pressure (BP) reductions that approach what’s possible from an antihypertensive agent.
Systolic BP fell over 6 months by almost 6 mm Hg, on average, in people with elevated BP who participated in an 8-week mindful awareness program as part of a randomized trial that included a usual-care control group.
The program taught established mindfulness-training techniques aimed at modifying behaviors regarding diet, exercise, and other controllable influences on the success of antihypertensive therapy.
Participants in the program, called Mindfulness-Based Blood Pressure Reduction (MB-BP), also the name of the single-center study, “showed potentially clinically relevant reductions in systolic blood pressure,” said principal investigator Eric B. Loucks, PhD, Brown University, Providence, R.I.
The phase 2 trial has some limitations, he observed, including on generalizability. For example, it entered about 200 mostly White, college-educated adults from one metropolitan area.
But if these findings are replicated in further studies, “preferably by other research groups, in a larger and broader population, and with longer follow-up,” Dr. Loucks said, the MB-BP intervention could become “an appealing approach to help control blood pressure.”
Dr. Loucks made the comments at a press conference prior to his formal presentation of MB-BP Nov. 6 at American Heart Association (AHA) Scientific Sessions 2022, held in Chicago and virtually.
Mindfulness-based interventions for elevated BP have not been widely studied, “so this is exactly what we need: a well-done trial with a control group to show that it actually works,” Amit Khera, MD, not connected with MB-BP, told this news organization.
The trial is “really important for proof of concept, but it had only 200 people. You need a larger one, and you need longer-term data,” agreed Dr. Khera, who directs the preventive cardiology program at the University of Texas Southwestern Medical Center, in Dallas. “Six months is good, but we want to see if it’s durable.”
Rhian M. Touyz, MBBCh, also not part of MB-BP, agreed that the nearly 6 mm Hg mean systolic BP reduction among program participants is clinically relevant. “I think in the context of global risk and reduction of target organ damage and cardiovascular events, it is significant in terms of events at a population level,” Dr. Touyz, McGill University Health Centre, Montreal, told this news organization.
Many patients on antihypertensive therapy that’s falling short resist the addition of another such agent, she observed, and instead might show further BP reduction from mindfulness training. The intervention probably also “would benefit health in general.” Mindfulness-based approaches could therefore be useful additions to treatment protocols for elevated BP, Dr. Touyz said.
How the training works
The MB-BP program used validated mindfulness-based stress-management techniques, adapted to address elevated BP, that included “personalized feedback and education about hypertension risk factors, mindful awareness training of participants’ relationships with hypertension risk factors, and support for behavior change,” Dr. Loucks and colleagues reported.
Participants were trained in mindfulness skills that included “self-awareness and emotion regulation,” Dr. Loucks said, which they then could apply to their “relationships with the things that we know influence blood pressure, like physical activity, diet, antihypertensive medication adherence, or alcohol consumption.”
One goal is to promote greater “attention control,” he said, “so that there’s some self-awareness that arises in terms of how we feel the next day, after a lot of alcohol consumption, for example, or lack of physical activity.” The process can provide insights that inspire patients to modify behaviors and risk factors that elevate BP, Dr. Loucks explained.
Effects on medication use
Systolic BP responses led some program participants to be managed on fewer or reduced dosages of antihypertensive meds, he told this news organization. Physicians seen outside of the trial could adjust their prescriptions, intensifying or pulling back on meds depending on their assessments of the patient. Any prescription changes would be documented by the researchers at the patient’s next class or trial-clinic visit.
The group that did the training, Dr. Loucks said, was 33% less likely to increase and 30% more likely to decrease their use of BP-lowering medications compared with the control group.
Elevated BP is so common and undertreated that “there is a need for every possible level of intervention, starting from the population level to the individual and everything else in between,” nephrologist Janani Rangaswami, MD, George Washington University, Washington, said at the press conference.
Therefore, “this mindfulness-based approach, in addition to standard of care with pharmacotherapy, is a really welcome addition to the hypertension literature,” said Dr. Rangaswami, who directs her center’s cardiorenal program. The systolic BP reduction seen in the intervention group, she agreed, was “clinically important and meaningful.”
Blinded assessments
The trial entered 201 patients with systolic and diastolic BP greater than 120 mm Hg and 80 mm Hg, respectively; 58.7% were women, 81% were White, and 73% were college-educated, Dr. Loucks reported.
The 100 assigned to the “enhanced usual care” control group received educational materials on controlling high BP. They and the 101 who followed the mindfulness-based program were given and trained on a home BP-monitoring device. They were then followed for the primary endpoint of change in systolic BP at 6 months.
Data management and outcomes assessments were conducted by trialists not involved in the training intervention who were blinded to randomization assignment.
In a prespecified unadjusted analysis by intention-to-treat, systolic BP in the intervention group dropped by a mean of 5.9 mm Hg (P < .001) compared with baseline and 4.5 mm Hg (P = .045), compared with the control group.
A post hoc analysis adjusted for sex and baseline BP showed an average 4.3 mm Hg reduction (P = .056) in those following the MB-BP program, compared with controls.
There were no observed significant effects on diastolic BP.
The study offered clues to how engagement in the MB-BP program might promote reductions in systolic BP, Dr. Loucks observed. For example, it may have led to increased activity levels, reduced sodium intake, and other dietary improvements.
Indeed, program participants averaged about 351 minutes less sedentary time (P = .02) and showed a 0.32-point improvement in Dietary Approaches to Stop Hypertension scores (P = .08), compared with the control group, Dr. Loucks reported. Other modifiable risk factors for elevated BP that could have responded to the mindfulness-based training, he proposed, include obesity, alcohol intake, and reaction to stress.
Dr. Loucks reports that he developed the MB-BP training and was a program instructor but did not receive related financial compensation; he had no other disclosures. Dr. Khera, Dr. Touyz, and Dr. Rangaswami had no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – It’s been said that one can observe a lot just by watching. Turning such observation inward, new evidence suggests, might lead to blood pressure (BP) reductions that approach what’s possible from an antihypertensive agent.
Systolic BP fell over 6 months by almost 6 mm Hg, on average, in people with elevated BP who participated in an 8-week mindful awareness program as part of a randomized trial that included a usual-care control group.
The program taught established mindfulness-training techniques aimed at modifying behaviors regarding diet, exercise, and other controllable influences on the success of antihypertensive therapy.
Participants in the program, called Mindfulness-Based Blood Pressure Reduction (MB-BP), also the name of the single-center study, “showed potentially clinically relevant reductions in systolic blood pressure,” said principal investigator Eric B. Loucks, PhD, Brown University, Providence, R.I.
The phase 2 trial has some limitations, he observed, including on generalizability. For example, it entered about 200 mostly White, college-educated adults from one metropolitan area.
But if these findings are replicated in further studies, “preferably by other research groups, in a larger and broader population, and with longer follow-up,” Dr. Loucks said, the MB-BP intervention could become “an appealing approach to help control blood pressure.”
Dr. Loucks made the comments at a press conference prior to his formal presentation of MB-BP Nov. 6 at American Heart Association (AHA) Scientific Sessions 2022, held in Chicago and virtually.
Mindfulness-based interventions for elevated BP have not been widely studied, “so this is exactly what we need: a well-done trial with a control group to show that it actually works,” Amit Khera, MD, not connected with MB-BP, told this news organization.
The trial is “really important for proof of concept, but it had only 200 people. You need a larger one, and you need longer-term data,” agreed Dr. Khera, who directs the preventive cardiology program at the University of Texas Southwestern Medical Center, in Dallas. “Six months is good, but we want to see if it’s durable.”
Rhian M. Touyz, MBBCh, also not part of MB-BP, agreed that the nearly 6 mm Hg mean systolic BP reduction among program participants is clinically relevant. “I think in the context of global risk and reduction of target organ damage and cardiovascular events, it is significant in terms of events at a population level,” Dr. Touyz, McGill University Health Centre, Montreal, told this news organization.
Many patients on antihypertensive therapy that’s falling short resist the addition of another such agent, she observed, and instead might show further BP reduction from mindfulness training. The intervention probably also “would benefit health in general.” Mindfulness-based approaches could therefore be useful additions to treatment protocols for elevated BP, Dr. Touyz said.
How the training works
The MB-BP program used validated mindfulness-based stress-management techniques, adapted to address elevated BP, that included “personalized feedback and education about hypertension risk factors, mindful awareness training of participants’ relationships with hypertension risk factors, and support for behavior change,” Dr. Loucks and colleagues reported.
Participants were trained in mindfulness skills that included “self-awareness and emotion regulation,” Dr. Loucks said, which they then could apply to their “relationships with the things that we know influence blood pressure, like physical activity, diet, antihypertensive medication adherence, or alcohol consumption.”
One goal is to promote greater “attention control,” he said, “so that there’s some self-awareness that arises in terms of how we feel the next day, after a lot of alcohol consumption, for example, or lack of physical activity.” The process can provide insights that inspire patients to modify behaviors and risk factors that elevate BP, Dr. Loucks explained.
Effects on medication use
Systolic BP responses led some program participants to be managed on fewer or reduced dosages of antihypertensive meds, he told this news organization. Physicians seen outside of the trial could adjust their prescriptions, intensifying or pulling back on meds depending on their assessments of the patient. Any prescription changes would be documented by the researchers at the patient’s next class or trial-clinic visit.
The group that did the training, Dr. Loucks said, was 33% less likely to increase and 30% more likely to decrease their use of BP-lowering medications compared with the control group.
Elevated BP is so common and undertreated that “there is a need for every possible level of intervention, starting from the population level to the individual and everything else in between,” nephrologist Janani Rangaswami, MD, George Washington University, Washington, said at the press conference.
Therefore, “this mindfulness-based approach, in addition to standard of care with pharmacotherapy, is a really welcome addition to the hypertension literature,” said Dr. Rangaswami, who directs her center’s cardiorenal program. The systolic BP reduction seen in the intervention group, she agreed, was “clinically important and meaningful.”
Blinded assessments
The trial entered 201 patients with systolic and diastolic BP greater than 120 mm Hg and 80 mm Hg, respectively; 58.7% were women, 81% were White, and 73% were college-educated, Dr. Loucks reported.
The 100 assigned to the “enhanced usual care” control group received educational materials on controlling high BP. They and the 101 who followed the mindfulness-based program were given and trained on a home BP-monitoring device. They were then followed for the primary endpoint of change in systolic BP at 6 months.
Data management and outcomes assessments were conducted by trialists not involved in the training intervention who were blinded to randomization assignment.
In a prespecified unadjusted analysis by intention-to-treat, systolic BP in the intervention group dropped by a mean of 5.9 mm Hg (P < .001) compared with baseline and 4.5 mm Hg (P = .045), compared with the control group.
A post hoc analysis adjusted for sex and baseline BP showed an average 4.3 mm Hg reduction (P = .056) in those following the MB-BP program, compared with controls.
There were no observed significant effects on diastolic BP.
The study offered clues to how engagement in the MB-BP program might promote reductions in systolic BP, Dr. Loucks observed. For example, it may have led to increased activity levels, reduced sodium intake, and other dietary improvements.
Indeed, program participants averaged about 351 minutes less sedentary time (P = .02) and showed a 0.32-point improvement in Dietary Approaches to Stop Hypertension scores (P = .08), compared with the control group, Dr. Loucks reported. Other modifiable risk factors for elevated BP that could have responded to the mindfulness-based training, he proposed, include obesity, alcohol intake, and reaction to stress.
Dr. Loucks reports that he developed the MB-BP training and was a program instructor but did not receive related financial compensation; he had no other disclosures. Dr. Khera, Dr. Touyz, and Dr. Rangaswami had no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AHA 2022
Night lights in the city link to increased risk of diabetes
Higher levels of exposure to outdoor artificial light at night are significantly linked with markers of diabetes and impaired glucose homeostasis, in a new national, cross-sectional study from China.
The results showed a 7% significant increase in diabetes prevalence per quintile exposure to artificial light at night (prevalence ratio, 1.07), report Ruizhi Zheng, PhD, of the Shanghai (China) Jiaotong University School of Medicine, and colleagues. People living in areas with the most exposure to light at night had a 28% higher prevalence of diabetes than those living in places with the lowest exposure (PR, 1.28), the researchers found.
The study was published online in Diabetologia.
Previous animal studies have shown that exposure to light at night may interfere with circadian rhythms and affect glucose homeostasis, the study team note. Other research has demonstrated that chronic exposure to moderate indoor light during sleep elevated the prevalence of diabetes in older adults, compared with those sleeping in a dim setting, the authors add.
“Our findings contribute to the growing literature suggesting that artificial light at night is detrimental to health and demonstrate that artificial light at night may be a potential novel risk factor for diabetes,” they write.
“Considering the coexistence of the diabetes epidemic and the widespread influence of light pollution at night, the positive associations indicate an urgent need for countries and governments to develop effective prevention and intervention policies and to protect people from the adverse health effects of light pollution at night,” the study authors stress.
Gareth Nye, PhD, senior lecturer at the University of Chester, England, agreed that prior research has found an association between metabolic conditions, such as diabetes, and artificial light at night, with most theories as to the cause focusing on the body’s natural circadian cycle.
He said that internal clocks regulate a variety of bodily processes, such as metabolism and hormone synthesis. They also affect sleep patterns by interfering with synthesis of the hormone melatonin, which is essential for sound sleep, Dr. Nye told the UK Science Media Centre.
However, he stressed that much more research is needed before any link can be considered definitive.
Outdoor night light exposure linked to fasting glucose, A1c
The Chinese researchers set out to approximate the relationships between diabetes prevalence and glucose homeostasis with chronic exposure to outdoor light at night.
They assessed 98,658 participants from the China Noncommunicable Disease Surveillance Study across 162 sites. The mean age of participants was 42.7 years. Female participants comprised 49.2% of the study cohort.
Diabetes was defined based on American Diabetes Association criteria. Satellite data were used to determine exposure to outdoor light at night in 2010. The associations between light exposure at night and indicators of glucose homeostasis were investigated.
Prevalence ratios were calculated and adjusted for sex, age, smoking status, education, body mass index, physical activity, household income, family history of diabetes, rural/urban areas, drinking status, and use of lipid-lowering prescription drugs (primarily statins) or antihypertensives.
The findings showed exposure levels to outdoor light at night were positively linked with 2-hour and fasting glucose concentrations, A1c, and insulin resistance (measured using homeostatic model assessment [HOMA]), but negatively related to β-cell function (measured using HOMA).
More research needed
“We advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to light at night,” the researchers conclude.
Dr. Nye agreed.
“One issue with this study is that the areas with the highest outdoor artificial light levels are likely to be those in urban areas and bigger cities. It has been known for a long time now that living in an urbanized area increases your risk of obesity through increased access to high-fat and convenience food, less physical activity levels due to transport links, and less social activities. The authors also state this and the fact participants tended to be older,” he noted.
Large datasets are used in this investigation, however, which generally increases the reliability of the data, he observed.
But it is also “unclear as to whether the population here was selected for this study or was retrospectively analyzed, which poses reliability issues, as does the selection of the representative sample, as it is not discussed,” he noted.
Ultimately, there is no confirmed evidence of the link, and until further work is done to directly link light exposure and diabetes in humans, “the link will remain an association only,” he concluded.
A version of this article first appeared on Medscape.com.
Higher levels of exposure to outdoor artificial light at night are significantly linked with markers of diabetes and impaired glucose homeostasis, in a new national, cross-sectional study from China.
The results showed a 7% significant increase in diabetes prevalence per quintile exposure to artificial light at night (prevalence ratio, 1.07), report Ruizhi Zheng, PhD, of the Shanghai (China) Jiaotong University School of Medicine, and colleagues. People living in areas with the most exposure to light at night had a 28% higher prevalence of diabetes than those living in places with the lowest exposure (PR, 1.28), the researchers found.
The study was published online in Diabetologia.
Previous animal studies have shown that exposure to light at night may interfere with circadian rhythms and affect glucose homeostasis, the study team note. Other research has demonstrated that chronic exposure to moderate indoor light during sleep elevated the prevalence of diabetes in older adults, compared with those sleeping in a dim setting, the authors add.
“Our findings contribute to the growing literature suggesting that artificial light at night is detrimental to health and demonstrate that artificial light at night may be a potential novel risk factor for diabetes,” they write.
“Considering the coexistence of the diabetes epidemic and the widespread influence of light pollution at night, the positive associations indicate an urgent need for countries and governments to develop effective prevention and intervention policies and to protect people from the adverse health effects of light pollution at night,” the study authors stress.
Gareth Nye, PhD, senior lecturer at the University of Chester, England, agreed that prior research has found an association between metabolic conditions, such as diabetes, and artificial light at night, with most theories as to the cause focusing on the body’s natural circadian cycle.
He said that internal clocks regulate a variety of bodily processes, such as metabolism and hormone synthesis. They also affect sleep patterns by interfering with synthesis of the hormone melatonin, which is essential for sound sleep, Dr. Nye told the UK Science Media Centre.
However, he stressed that much more research is needed before any link can be considered definitive.
Outdoor night light exposure linked to fasting glucose, A1c
The Chinese researchers set out to approximate the relationships between diabetes prevalence and glucose homeostasis with chronic exposure to outdoor light at night.
They assessed 98,658 participants from the China Noncommunicable Disease Surveillance Study across 162 sites. The mean age of participants was 42.7 years. Female participants comprised 49.2% of the study cohort.
Diabetes was defined based on American Diabetes Association criteria. Satellite data were used to determine exposure to outdoor light at night in 2010. The associations between light exposure at night and indicators of glucose homeostasis were investigated.
Prevalence ratios were calculated and adjusted for sex, age, smoking status, education, body mass index, physical activity, household income, family history of diabetes, rural/urban areas, drinking status, and use of lipid-lowering prescription drugs (primarily statins) or antihypertensives.
The findings showed exposure levels to outdoor light at night were positively linked with 2-hour and fasting glucose concentrations, A1c, and insulin resistance (measured using homeostatic model assessment [HOMA]), but negatively related to β-cell function (measured using HOMA).
More research needed
“We advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to light at night,” the researchers conclude.
Dr. Nye agreed.
“One issue with this study is that the areas with the highest outdoor artificial light levels are likely to be those in urban areas and bigger cities. It has been known for a long time now that living in an urbanized area increases your risk of obesity through increased access to high-fat and convenience food, less physical activity levels due to transport links, and less social activities. The authors also state this and the fact participants tended to be older,” he noted.
Large datasets are used in this investigation, however, which generally increases the reliability of the data, he observed.
But it is also “unclear as to whether the population here was selected for this study or was retrospectively analyzed, which poses reliability issues, as does the selection of the representative sample, as it is not discussed,” he noted.
Ultimately, there is no confirmed evidence of the link, and until further work is done to directly link light exposure and diabetes in humans, “the link will remain an association only,” he concluded.
A version of this article first appeared on Medscape.com.
Higher levels of exposure to outdoor artificial light at night are significantly linked with markers of diabetes and impaired glucose homeostasis, in a new national, cross-sectional study from China.
The results showed a 7% significant increase in diabetes prevalence per quintile exposure to artificial light at night (prevalence ratio, 1.07), report Ruizhi Zheng, PhD, of the Shanghai (China) Jiaotong University School of Medicine, and colleagues. People living in areas with the most exposure to light at night had a 28% higher prevalence of diabetes than those living in places with the lowest exposure (PR, 1.28), the researchers found.
The study was published online in Diabetologia.
Previous animal studies have shown that exposure to light at night may interfere with circadian rhythms and affect glucose homeostasis, the study team note. Other research has demonstrated that chronic exposure to moderate indoor light during sleep elevated the prevalence of diabetes in older adults, compared with those sleeping in a dim setting, the authors add.
“Our findings contribute to the growing literature suggesting that artificial light at night is detrimental to health and demonstrate that artificial light at night may be a potential novel risk factor for diabetes,” they write.
“Considering the coexistence of the diabetes epidemic and the widespread influence of light pollution at night, the positive associations indicate an urgent need for countries and governments to develop effective prevention and intervention policies and to protect people from the adverse health effects of light pollution at night,” the study authors stress.
Gareth Nye, PhD, senior lecturer at the University of Chester, England, agreed that prior research has found an association between metabolic conditions, such as diabetes, and artificial light at night, with most theories as to the cause focusing on the body’s natural circadian cycle.
He said that internal clocks regulate a variety of bodily processes, such as metabolism and hormone synthesis. They also affect sleep patterns by interfering with synthesis of the hormone melatonin, which is essential for sound sleep, Dr. Nye told the UK Science Media Centre.
However, he stressed that much more research is needed before any link can be considered definitive.
Outdoor night light exposure linked to fasting glucose, A1c
The Chinese researchers set out to approximate the relationships between diabetes prevalence and glucose homeostasis with chronic exposure to outdoor light at night.
They assessed 98,658 participants from the China Noncommunicable Disease Surveillance Study across 162 sites. The mean age of participants was 42.7 years. Female participants comprised 49.2% of the study cohort.
Diabetes was defined based on American Diabetes Association criteria. Satellite data were used to determine exposure to outdoor light at night in 2010. The associations between light exposure at night and indicators of glucose homeostasis were investigated.
Prevalence ratios were calculated and adjusted for sex, age, smoking status, education, body mass index, physical activity, household income, family history of diabetes, rural/urban areas, drinking status, and use of lipid-lowering prescription drugs (primarily statins) or antihypertensives.
The findings showed exposure levels to outdoor light at night were positively linked with 2-hour and fasting glucose concentrations, A1c, and insulin resistance (measured using homeostatic model assessment [HOMA]), but negatively related to β-cell function (measured using HOMA).
More research needed
“We advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to light at night,” the researchers conclude.
Dr. Nye agreed.
“One issue with this study is that the areas with the highest outdoor artificial light levels are likely to be those in urban areas and bigger cities. It has been known for a long time now that living in an urbanized area increases your risk of obesity through increased access to high-fat and convenience food, less physical activity levels due to transport links, and less social activities. The authors also state this and the fact participants tended to be older,” he noted.
Large datasets are used in this investigation, however, which generally increases the reliability of the data, he observed.
But it is also “unclear as to whether the population here was selected for this study or was retrospectively analyzed, which poses reliability issues, as does the selection of the representative sample, as it is not discussed,” he noted.
Ultimately, there is no confirmed evidence of the link, and until further work is done to directly link light exposure and diabetes in humans, “the link will remain an association only,” he concluded.
A version of this article first appeared on Medscape.com.
Hypertension linked to risk of severe COVID
U.K. researchers have established that hypertension is associated with a 22% greater risk of severe COVID-19, with the odds of severe COVID-19 unaffected by medication type.
Hypertension “appears to be one of the commonest comorbidities in COVID-19 patients”, explained the authors of a new study, published in PLOS ONE. The authors highlighted that previous research had shown that hypertension was more prevalent in severe and fatal cases compared with all cases of COVID-19.
They pointed out, however, that whether hypertensive individuals have a higher risk of severe COVID-19, compared with nonhypertensives, and whether the absolute level of systolic blood pressure or the type of antihypertensive medication is related to this risk, remained “unclear.”
To try to answer these questions, the research team, led by University of Cambridge researchers, analyzed data from 16,134 individuals who tested positive for COVID-19 (mean age 65.3 years, 47% male, 90% white), 40% were diagnosed with essential hypertension at the analysis baseline – 22% of whom had developed severe COVID-19.
Systolic blood pressure (SBP) was categorized by 10–mm Hg ranges, starting from < 120 mm Hg up to 180+ mm Hg, with the reference category defined as 120-129 mm Hg, based on data from the SPRINT study, which demonstrated that intensive SBP lowering to below 120 mm Hg, as compared with the traditional threshold of 140 mm Hg, was beneficial. Diastolic blood pressure was categorized by 10–mm Hg ranges, starting from < 60 mm Hg up to 100+ mm Hg with 80-90 mm Hg being the reference category.
In their analyses the researchers adjusted for age, sex, body mass index, ethnicity, smoking status, diabetes status, socioeconomic status, and inflammation (C-reactive protein [CRP]), as these were proposed as potential confounders. To assess the direct effect of hypertension on COVID-19, they also adjusted for intermediate variables, including cardiovascular comorbidities and stroke, on the causal pathway between hypertension and severe COVID-19.
Majority of effect of hypertension on severe COVID-19 was direct
The unadjusted odds ratio of the association between hypertension and severe COVID-19 was 2.33 (95% confidence interval, 2.16-2.51), the authors emphasized. They found that, after adjusting for all confounding variables, hypertension was associated with 22% higher odds of severe COVID-19 (OR, 1.22; 95% CI, 1.12-1.33), compared with normotension.
Individuals with severe COVID-19 were marginally older, more likely to be male, and more deprived, the authors said. “They were also more likely to be hypertensive, compared with individuals without severe COVID-19, and a greater proportion of individuals with severe COVID-19 had cardiovascular comorbidities.”
The majority of the effect of hypertension on development of severe COVID-19 was “direct,” they said. However, a modest proportion of the effect was mediated via cardiovascular comorbidities such as peripheral vascular disease, MI, coronary heart disease, arrhythmias, and stroke. Of note, those with a history of stroke had a 47% higher risk of severe COVID-19 and those with a history of other cardiovascular comorbidities had a 30% higher risk of severe COVID-19, the authors commented.
J-shaped relationship
Of the total of 6,517 (40%) individuals who had a diagnosis of essential hypertension at baseline, 67% were treated (41% with monotherapy, 59% with combination therapy), and 33% were untreated.
There were similar numbers of severe COVID-19 in each medication group: ACE inhibitors, 34%; angiotensin receptor blockers (ARBs), 36%; and “other” medications 34%.
In hypertensive individuals receiving antihypertensive medications, there was a “J-shaped relationship” between the level of blood pressure and risk of severe COVID-19 when using a systolic blood pressure level of 120-129 mm Hg as a reference – 150-159 mm Hg versus 120-129 mm Hg (OR 1.91; 95% CI, 1.44-2.53), > 180+ mm Hg versus 120-129 mm Hg (OR 1.93; 95% CI, 1.06-3.51).
The authors commented that there was no evidence of a higher risk of severe COVID-19 until systolic blood pressure “exceeded 150 mm Hg.”
They said it was an interesting finding that “very well-controlled” systolic blood pressure < 120 mm Hg was associated with a 40% (OR, 1.40; 95% CI, 1.11-1.78) greater odds of severe COVID-19. “This may be due to reverse causality, where low systolic blood pressure levels may indicate poorer health, such that the occurrence of severe COVID-19 may be related to underlying disease rather than the level of SBP per se,” they suggested.
The J-shaped association observed remained after multiple adjustments, including presence of known cardiovascular comorbidities, which suggested a possible “real effect” of low SBP on severe COVID-19, “at least in treated hypertensive individuals.”
Their analyses also identified that, compared with a “normal” diastolic blood pressure (80-90 mm Hg), having a diastolic blood pressure higher than 90 mm Hg was associated with higher odds of severe COVID-19.
The association between hypertension and COVID-19 was “amplified” if the individuals were treated and their BP remained uncontrolled, the authors pointed out.
There did not appear to be any difference in the risk of severe COVID-19 between individuals taking ACE inhibitors and those taking ARBs or other antihypertensive medications, the authors said.
Better understanding of underlying mechanisms needed
Individuals with hypertension who tested positive for COVID-19 had “over twice” the risk of developing severe COVID-19, compared with nonhypertensive individuals, the authors said.
They highlighted that their findings also suggest that there are “further effects” influencing the severity of COVID-19 beyond a “dichotomous” diagnosis of hypertension.
“Individuals with a higher-than-target systolic blood pressure may be less healthy, less active, suffering more severe hypertension, or have developed drug-resistant hypertension, all suggesting that the effects of hypertension have already had detrimental physiological effects on the cardiovascular system, which in turn may offer some explanation for the higher risk of severe COVID-19 with uncontrolled SBP,” they explained.
“Hypertension is an important risk factor for COVID-19,” reiterated the authors, who emphasized that a better understanding of the underlying mechanisms driving this increased risk is warranted in case of “more severe strains or other viruses” in the future.
The authors have declared no competing interests.
A version of this article first appeared on Medscape UK.
U.K. researchers have established that hypertension is associated with a 22% greater risk of severe COVID-19, with the odds of severe COVID-19 unaffected by medication type.
Hypertension “appears to be one of the commonest comorbidities in COVID-19 patients”, explained the authors of a new study, published in PLOS ONE. The authors highlighted that previous research had shown that hypertension was more prevalent in severe and fatal cases compared with all cases of COVID-19.
They pointed out, however, that whether hypertensive individuals have a higher risk of severe COVID-19, compared with nonhypertensives, and whether the absolute level of systolic blood pressure or the type of antihypertensive medication is related to this risk, remained “unclear.”
To try to answer these questions, the research team, led by University of Cambridge researchers, analyzed data from 16,134 individuals who tested positive for COVID-19 (mean age 65.3 years, 47% male, 90% white), 40% were diagnosed with essential hypertension at the analysis baseline – 22% of whom had developed severe COVID-19.
Systolic blood pressure (SBP) was categorized by 10–mm Hg ranges, starting from < 120 mm Hg up to 180+ mm Hg, with the reference category defined as 120-129 mm Hg, based on data from the SPRINT study, which demonstrated that intensive SBP lowering to below 120 mm Hg, as compared with the traditional threshold of 140 mm Hg, was beneficial. Diastolic blood pressure was categorized by 10–mm Hg ranges, starting from < 60 mm Hg up to 100+ mm Hg with 80-90 mm Hg being the reference category.
In their analyses the researchers adjusted for age, sex, body mass index, ethnicity, smoking status, diabetes status, socioeconomic status, and inflammation (C-reactive protein [CRP]), as these were proposed as potential confounders. To assess the direct effect of hypertension on COVID-19, they also adjusted for intermediate variables, including cardiovascular comorbidities and stroke, on the causal pathway between hypertension and severe COVID-19.
Majority of effect of hypertension on severe COVID-19 was direct
The unadjusted odds ratio of the association between hypertension and severe COVID-19 was 2.33 (95% confidence interval, 2.16-2.51), the authors emphasized. They found that, after adjusting for all confounding variables, hypertension was associated with 22% higher odds of severe COVID-19 (OR, 1.22; 95% CI, 1.12-1.33), compared with normotension.
Individuals with severe COVID-19 were marginally older, more likely to be male, and more deprived, the authors said. “They were also more likely to be hypertensive, compared with individuals without severe COVID-19, and a greater proportion of individuals with severe COVID-19 had cardiovascular comorbidities.”
The majority of the effect of hypertension on development of severe COVID-19 was “direct,” they said. However, a modest proportion of the effect was mediated via cardiovascular comorbidities such as peripheral vascular disease, MI, coronary heart disease, arrhythmias, and stroke. Of note, those with a history of stroke had a 47% higher risk of severe COVID-19 and those with a history of other cardiovascular comorbidities had a 30% higher risk of severe COVID-19, the authors commented.
J-shaped relationship
Of the total of 6,517 (40%) individuals who had a diagnosis of essential hypertension at baseline, 67% were treated (41% with monotherapy, 59% with combination therapy), and 33% were untreated.
There were similar numbers of severe COVID-19 in each medication group: ACE inhibitors, 34%; angiotensin receptor blockers (ARBs), 36%; and “other” medications 34%.
In hypertensive individuals receiving antihypertensive medications, there was a “J-shaped relationship” between the level of blood pressure and risk of severe COVID-19 when using a systolic blood pressure level of 120-129 mm Hg as a reference – 150-159 mm Hg versus 120-129 mm Hg (OR 1.91; 95% CI, 1.44-2.53), > 180+ mm Hg versus 120-129 mm Hg (OR 1.93; 95% CI, 1.06-3.51).
The authors commented that there was no evidence of a higher risk of severe COVID-19 until systolic blood pressure “exceeded 150 mm Hg.”
They said it was an interesting finding that “very well-controlled” systolic blood pressure < 120 mm Hg was associated with a 40% (OR, 1.40; 95% CI, 1.11-1.78) greater odds of severe COVID-19. “This may be due to reverse causality, where low systolic blood pressure levels may indicate poorer health, such that the occurrence of severe COVID-19 may be related to underlying disease rather than the level of SBP per se,” they suggested.
The J-shaped association observed remained after multiple adjustments, including presence of known cardiovascular comorbidities, which suggested a possible “real effect” of low SBP on severe COVID-19, “at least in treated hypertensive individuals.”
Their analyses also identified that, compared with a “normal” diastolic blood pressure (80-90 mm Hg), having a diastolic blood pressure higher than 90 mm Hg was associated with higher odds of severe COVID-19.
The association between hypertension and COVID-19 was “amplified” if the individuals were treated and their BP remained uncontrolled, the authors pointed out.
There did not appear to be any difference in the risk of severe COVID-19 between individuals taking ACE inhibitors and those taking ARBs or other antihypertensive medications, the authors said.
Better understanding of underlying mechanisms needed
Individuals with hypertension who tested positive for COVID-19 had “over twice” the risk of developing severe COVID-19, compared with nonhypertensive individuals, the authors said.
They highlighted that their findings also suggest that there are “further effects” influencing the severity of COVID-19 beyond a “dichotomous” diagnosis of hypertension.
“Individuals with a higher-than-target systolic blood pressure may be less healthy, less active, suffering more severe hypertension, or have developed drug-resistant hypertension, all suggesting that the effects of hypertension have already had detrimental physiological effects on the cardiovascular system, which in turn may offer some explanation for the higher risk of severe COVID-19 with uncontrolled SBP,” they explained.
“Hypertension is an important risk factor for COVID-19,” reiterated the authors, who emphasized that a better understanding of the underlying mechanisms driving this increased risk is warranted in case of “more severe strains or other viruses” in the future.
The authors have declared no competing interests.
A version of this article first appeared on Medscape UK.
U.K. researchers have established that hypertension is associated with a 22% greater risk of severe COVID-19, with the odds of severe COVID-19 unaffected by medication type.
Hypertension “appears to be one of the commonest comorbidities in COVID-19 patients”, explained the authors of a new study, published in PLOS ONE. The authors highlighted that previous research had shown that hypertension was more prevalent in severe and fatal cases compared with all cases of COVID-19.
They pointed out, however, that whether hypertensive individuals have a higher risk of severe COVID-19, compared with nonhypertensives, and whether the absolute level of systolic blood pressure or the type of antihypertensive medication is related to this risk, remained “unclear.”
To try to answer these questions, the research team, led by University of Cambridge researchers, analyzed data from 16,134 individuals who tested positive for COVID-19 (mean age 65.3 years, 47% male, 90% white), 40% were diagnosed with essential hypertension at the analysis baseline – 22% of whom had developed severe COVID-19.
Systolic blood pressure (SBP) was categorized by 10–mm Hg ranges, starting from < 120 mm Hg up to 180+ mm Hg, with the reference category defined as 120-129 mm Hg, based on data from the SPRINT study, which demonstrated that intensive SBP lowering to below 120 mm Hg, as compared with the traditional threshold of 140 mm Hg, was beneficial. Diastolic blood pressure was categorized by 10–mm Hg ranges, starting from < 60 mm Hg up to 100+ mm Hg with 80-90 mm Hg being the reference category.
In their analyses the researchers adjusted for age, sex, body mass index, ethnicity, smoking status, diabetes status, socioeconomic status, and inflammation (C-reactive protein [CRP]), as these were proposed as potential confounders. To assess the direct effect of hypertension on COVID-19, they also adjusted for intermediate variables, including cardiovascular comorbidities and stroke, on the causal pathway between hypertension and severe COVID-19.
Majority of effect of hypertension on severe COVID-19 was direct
The unadjusted odds ratio of the association between hypertension and severe COVID-19 was 2.33 (95% confidence interval, 2.16-2.51), the authors emphasized. They found that, after adjusting for all confounding variables, hypertension was associated with 22% higher odds of severe COVID-19 (OR, 1.22; 95% CI, 1.12-1.33), compared with normotension.
Individuals with severe COVID-19 were marginally older, more likely to be male, and more deprived, the authors said. “They were also more likely to be hypertensive, compared with individuals without severe COVID-19, and a greater proportion of individuals with severe COVID-19 had cardiovascular comorbidities.”
The majority of the effect of hypertension on development of severe COVID-19 was “direct,” they said. However, a modest proportion of the effect was mediated via cardiovascular comorbidities such as peripheral vascular disease, MI, coronary heart disease, arrhythmias, and stroke. Of note, those with a history of stroke had a 47% higher risk of severe COVID-19 and those with a history of other cardiovascular comorbidities had a 30% higher risk of severe COVID-19, the authors commented.
J-shaped relationship
Of the total of 6,517 (40%) individuals who had a diagnosis of essential hypertension at baseline, 67% were treated (41% with monotherapy, 59% with combination therapy), and 33% were untreated.
There were similar numbers of severe COVID-19 in each medication group: ACE inhibitors, 34%; angiotensin receptor blockers (ARBs), 36%; and “other” medications 34%.
In hypertensive individuals receiving antihypertensive medications, there was a “J-shaped relationship” between the level of blood pressure and risk of severe COVID-19 when using a systolic blood pressure level of 120-129 mm Hg as a reference – 150-159 mm Hg versus 120-129 mm Hg (OR 1.91; 95% CI, 1.44-2.53), > 180+ mm Hg versus 120-129 mm Hg (OR 1.93; 95% CI, 1.06-3.51).
The authors commented that there was no evidence of a higher risk of severe COVID-19 until systolic blood pressure “exceeded 150 mm Hg.”
They said it was an interesting finding that “very well-controlled” systolic blood pressure < 120 mm Hg was associated with a 40% (OR, 1.40; 95% CI, 1.11-1.78) greater odds of severe COVID-19. “This may be due to reverse causality, where low systolic blood pressure levels may indicate poorer health, such that the occurrence of severe COVID-19 may be related to underlying disease rather than the level of SBP per se,” they suggested.
The J-shaped association observed remained after multiple adjustments, including presence of known cardiovascular comorbidities, which suggested a possible “real effect” of low SBP on severe COVID-19, “at least in treated hypertensive individuals.”
Their analyses also identified that, compared with a “normal” diastolic blood pressure (80-90 mm Hg), having a diastolic blood pressure higher than 90 mm Hg was associated with higher odds of severe COVID-19.
The association between hypertension and COVID-19 was “amplified” if the individuals were treated and their BP remained uncontrolled, the authors pointed out.
There did not appear to be any difference in the risk of severe COVID-19 between individuals taking ACE inhibitors and those taking ARBs or other antihypertensive medications, the authors said.
Better understanding of underlying mechanisms needed
Individuals with hypertension who tested positive for COVID-19 had “over twice” the risk of developing severe COVID-19, compared with nonhypertensive individuals, the authors said.
They highlighted that their findings also suggest that there are “further effects” influencing the severity of COVID-19 beyond a “dichotomous” diagnosis of hypertension.
“Individuals with a higher-than-target systolic blood pressure may be less healthy, less active, suffering more severe hypertension, or have developed drug-resistant hypertension, all suggesting that the effects of hypertension have already had detrimental physiological effects on the cardiovascular system, which in turn may offer some explanation for the higher risk of severe COVID-19 with uncontrolled SBP,” they explained.
“Hypertension is an important risk factor for COVID-19,” reiterated the authors, who emphasized that a better understanding of the underlying mechanisms driving this increased risk is warranted in case of “more severe strains or other viruses” in the future.
The authors have declared no competing interests.
A version of this article first appeared on Medscape UK.
FROM PLOS ONE
Staving off holiday weight gain
Five pounds of weight gain during the holidays is a disproven myth that pops up annually like holiday lights. But before you do a happy dance and pile that extra whipped cream on your pie, you should know two things. One, people do gain weight during the holidays. Two, the extra pounds tend to stick around because most people never lose their holiday weight. Over time, these extra pounds can lead to obesity and weight-related conditions such as diabetes and hypertension.
Let’s be clear. Your weight is one of many markers of your wellness and metabolic health. However, weight changes can indicate that your health is off balance. Holiday weight gain often comes from indulging in increased rich foods, less physical activity, higher stress levels, and sleep disruption.
Optimizing lifestyle factors and trying to lose weight is challenging any time of the year. However, the holiday bustle makes losing weight during this time even more challenging for most people. But maintaining your weight and overall wellness is manageable with three simple shifts in mindset, mindful eating, and meal strategy. Let’s discuss each.
Mindset
From personal and professional experience, I see two primary attitudes regarding holiday eating. They are either “I’ll wait till January to go on a diet” or “I’m on a diet, so I can’t eat anything I like during the holidays.” Both attitude extremes prevent enjoyable and healthy eating during the holidays because they place the focus on food. With both mindsets, food is in control, which leaves you feeling out of control. Rather than having an “all or none” mindset during the holidays, I encourage you to ask yourself:
- “What matters most to me during the holidays?” In a recent survey, 72% of Americans said they look forward to during the holidays. Although food often accompanies family celebrations, it’s the time with family that matters most. Choose to savor sweet time spent with loved ones instead of stuffing yourself with excess sugary sweets.
- “How can I enjoy myself without food or alcoholic beverages?” So often, we eat or drink certain foods out of habit. Shift your mindset from “we always do this” to “what could we do instead?” Asking this question may be the doorway to creating new, non–food-centered traditions.
- “How can I have the foods I love during the holidays and still meet my weight and wellness goals?” This question helps you create opportunities instead of depriving yourself. Rather than depriving yourself, you could cut back on snacking or reduce your sugar intake elsewhere. Or add an extra workout session or stress reduction practice during the holidays.
Mindful eating
The purpose of mindful eating isn’t weight loss. Some studies suggest it may help maintain weight. More importantly, mindfulness can improve your relationship with food and promote wellness. Traditional tips for mindful eating include doing the following as you eat: Being present in the moment, not judging your food, slowing down, and savoring the taste of your food. During the holidays, asking additional questions may enhance mindful eating. For instance:
- “Am I eating to avoid uncomfortable emotions?” The holidays can trigger emotions such as grief, sadness, and anxiety. Also, preexisting can worsen. Decadent foods become a quick fix leading to more emotional eating during this season. Addressing these emotions can help you avoid overeating during the holidays. For mental health resources, visit the
- “What food or drink do I most enjoy during the holidays?” Trying to resist your favorite holiday treats can be an exhausting test of “willpower.” Eventually, and psychological reasons, and you “cheat” on your plan to not eat holiday treats. To prevent this painful battle of treat versus cheat, plan to eat your “indulgence food” in moderation. Savor the foods you enjoy. Then cut out the rest of the food you don’t like or feel you must eat because “Aunty Sarah will feel bad.”
Meal strategy
Many holiday treats and parties are unavoidable unless you plan to hide in a cave for the next few weeks. Rather than torturing yourself nibbling on celery and sipping on sparkling water during your holiday event, create a strategy. For 8 years, I’ve been on my weight loss and wellness journey. I have a holiday strategy that helps my patients, clients, and me maintain our weight and wellness during the holidays. One critical part of the strategy is to anticipate indulgence events. Specifically, look at all the planned holiday events and choose three indulgence events. The rest of the time, do your best to stay on your plan. Knowing your indulgence events to look forward to gives you a sense of control over when you indulge. On non-indulgent days, think, “I can eat it but choose not to” instead of the limiting thought, “I can’t eat that.” Choice is a powerful tool. Once at an indulgence event, I focus on mindful eating and enjoying people around me, which cuts down on overeating just because “I can.”
This holiday season is a reunion time for many people, after enduring long separations from family and friends due to the pandemic. Relishing time with loved ones should be your focus during the holidays – not eating yourself into worse health or worrying about dieting. Even if you choose not to make all the shifts in mindset, mindful eating, and meal strategy mentioned, choosing even one change to focus on can help you both enjoy the holidays and have increased control over your weight and wellness. Whatever you do, may you and your loved ones have a safe, healthy, and enjoyable holiday season.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist who specializes in individualized solutions for emotional and biological overeating. She is CEO and lead physician at Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed having no relevant financial relationships. A version of this article first appeared on Medscape.com.
Five pounds of weight gain during the holidays is a disproven myth that pops up annually like holiday lights. But before you do a happy dance and pile that extra whipped cream on your pie, you should know two things. One, people do gain weight during the holidays. Two, the extra pounds tend to stick around because most people never lose their holiday weight. Over time, these extra pounds can lead to obesity and weight-related conditions such as diabetes and hypertension.
Let’s be clear. Your weight is one of many markers of your wellness and metabolic health. However, weight changes can indicate that your health is off balance. Holiday weight gain often comes from indulging in increased rich foods, less physical activity, higher stress levels, and sleep disruption.
Optimizing lifestyle factors and trying to lose weight is challenging any time of the year. However, the holiday bustle makes losing weight during this time even more challenging for most people. But maintaining your weight and overall wellness is manageable with three simple shifts in mindset, mindful eating, and meal strategy. Let’s discuss each.
Mindset
From personal and professional experience, I see two primary attitudes regarding holiday eating. They are either “I’ll wait till January to go on a diet” or “I’m on a diet, so I can’t eat anything I like during the holidays.” Both attitude extremes prevent enjoyable and healthy eating during the holidays because they place the focus on food. With both mindsets, food is in control, which leaves you feeling out of control. Rather than having an “all or none” mindset during the holidays, I encourage you to ask yourself:
- “What matters most to me during the holidays?” In a recent survey, 72% of Americans said they look forward to during the holidays. Although food often accompanies family celebrations, it’s the time with family that matters most. Choose to savor sweet time spent with loved ones instead of stuffing yourself with excess sugary sweets.
- “How can I enjoy myself without food or alcoholic beverages?” So often, we eat or drink certain foods out of habit. Shift your mindset from “we always do this” to “what could we do instead?” Asking this question may be the doorway to creating new, non–food-centered traditions.
- “How can I have the foods I love during the holidays and still meet my weight and wellness goals?” This question helps you create opportunities instead of depriving yourself. Rather than depriving yourself, you could cut back on snacking or reduce your sugar intake elsewhere. Or add an extra workout session or stress reduction practice during the holidays.
Mindful eating
The purpose of mindful eating isn’t weight loss. Some studies suggest it may help maintain weight. More importantly, mindfulness can improve your relationship with food and promote wellness. Traditional tips for mindful eating include doing the following as you eat: Being present in the moment, not judging your food, slowing down, and savoring the taste of your food. During the holidays, asking additional questions may enhance mindful eating. For instance:
- “Am I eating to avoid uncomfortable emotions?” The holidays can trigger emotions such as grief, sadness, and anxiety. Also, preexisting can worsen. Decadent foods become a quick fix leading to more emotional eating during this season. Addressing these emotions can help you avoid overeating during the holidays. For mental health resources, visit the
- “What food or drink do I most enjoy during the holidays?” Trying to resist your favorite holiday treats can be an exhausting test of “willpower.” Eventually, and psychological reasons, and you “cheat” on your plan to not eat holiday treats. To prevent this painful battle of treat versus cheat, plan to eat your “indulgence food” in moderation. Savor the foods you enjoy. Then cut out the rest of the food you don’t like or feel you must eat because “Aunty Sarah will feel bad.”
Meal strategy
Many holiday treats and parties are unavoidable unless you plan to hide in a cave for the next few weeks. Rather than torturing yourself nibbling on celery and sipping on sparkling water during your holiday event, create a strategy. For 8 years, I’ve been on my weight loss and wellness journey. I have a holiday strategy that helps my patients, clients, and me maintain our weight and wellness during the holidays. One critical part of the strategy is to anticipate indulgence events. Specifically, look at all the planned holiday events and choose three indulgence events. The rest of the time, do your best to stay on your plan. Knowing your indulgence events to look forward to gives you a sense of control over when you indulge. On non-indulgent days, think, “I can eat it but choose not to” instead of the limiting thought, “I can’t eat that.” Choice is a powerful tool. Once at an indulgence event, I focus on mindful eating and enjoying people around me, which cuts down on overeating just because “I can.”
This holiday season is a reunion time for many people, after enduring long separations from family and friends due to the pandemic. Relishing time with loved ones should be your focus during the holidays – not eating yourself into worse health or worrying about dieting. Even if you choose not to make all the shifts in mindset, mindful eating, and meal strategy mentioned, choosing even one change to focus on can help you both enjoy the holidays and have increased control over your weight and wellness. Whatever you do, may you and your loved ones have a safe, healthy, and enjoyable holiday season.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist who specializes in individualized solutions for emotional and biological overeating. She is CEO and lead physician at Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed having no relevant financial relationships. A version of this article first appeared on Medscape.com.
Five pounds of weight gain during the holidays is a disproven myth that pops up annually like holiday lights. But before you do a happy dance and pile that extra whipped cream on your pie, you should know two things. One, people do gain weight during the holidays. Two, the extra pounds tend to stick around because most people never lose their holiday weight. Over time, these extra pounds can lead to obesity and weight-related conditions such as diabetes and hypertension.
Let’s be clear. Your weight is one of many markers of your wellness and metabolic health. However, weight changes can indicate that your health is off balance. Holiday weight gain often comes from indulging in increased rich foods, less physical activity, higher stress levels, and sleep disruption.
Optimizing lifestyle factors and trying to lose weight is challenging any time of the year. However, the holiday bustle makes losing weight during this time even more challenging for most people. But maintaining your weight and overall wellness is manageable with three simple shifts in mindset, mindful eating, and meal strategy. Let’s discuss each.
Mindset
From personal and professional experience, I see two primary attitudes regarding holiday eating. They are either “I’ll wait till January to go on a diet” or “I’m on a diet, so I can’t eat anything I like during the holidays.” Both attitude extremes prevent enjoyable and healthy eating during the holidays because they place the focus on food. With both mindsets, food is in control, which leaves you feeling out of control. Rather than having an “all or none” mindset during the holidays, I encourage you to ask yourself:
- “What matters most to me during the holidays?” In a recent survey, 72% of Americans said they look forward to during the holidays. Although food often accompanies family celebrations, it’s the time with family that matters most. Choose to savor sweet time spent with loved ones instead of stuffing yourself with excess sugary sweets.
- “How can I enjoy myself without food or alcoholic beverages?” So often, we eat or drink certain foods out of habit. Shift your mindset from “we always do this” to “what could we do instead?” Asking this question may be the doorway to creating new, non–food-centered traditions.
- “How can I have the foods I love during the holidays and still meet my weight and wellness goals?” This question helps you create opportunities instead of depriving yourself. Rather than depriving yourself, you could cut back on snacking or reduce your sugar intake elsewhere. Or add an extra workout session or stress reduction practice during the holidays.
Mindful eating
The purpose of mindful eating isn’t weight loss. Some studies suggest it may help maintain weight. More importantly, mindfulness can improve your relationship with food and promote wellness. Traditional tips for mindful eating include doing the following as you eat: Being present in the moment, not judging your food, slowing down, and savoring the taste of your food. During the holidays, asking additional questions may enhance mindful eating. For instance:
- “Am I eating to avoid uncomfortable emotions?” The holidays can trigger emotions such as grief, sadness, and anxiety. Also, preexisting can worsen. Decadent foods become a quick fix leading to more emotional eating during this season. Addressing these emotions can help you avoid overeating during the holidays. For mental health resources, visit the
- “What food or drink do I most enjoy during the holidays?” Trying to resist your favorite holiday treats can be an exhausting test of “willpower.” Eventually, and psychological reasons, and you “cheat” on your plan to not eat holiday treats. To prevent this painful battle of treat versus cheat, plan to eat your “indulgence food” in moderation. Savor the foods you enjoy. Then cut out the rest of the food you don’t like or feel you must eat because “Aunty Sarah will feel bad.”
Meal strategy
Many holiday treats and parties are unavoidable unless you plan to hide in a cave for the next few weeks. Rather than torturing yourself nibbling on celery and sipping on sparkling water during your holiday event, create a strategy. For 8 years, I’ve been on my weight loss and wellness journey. I have a holiday strategy that helps my patients, clients, and me maintain our weight and wellness during the holidays. One critical part of the strategy is to anticipate indulgence events. Specifically, look at all the planned holiday events and choose three indulgence events. The rest of the time, do your best to stay on your plan. Knowing your indulgence events to look forward to gives you a sense of control over when you indulge. On non-indulgent days, think, “I can eat it but choose not to” instead of the limiting thought, “I can’t eat that.” Choice is a powerful tool. Once at an indulgence event, I focus on mindful eating and enjoying people around me, which cuts down on overeating just because “I can.”
This holiday season is a reunion time for many people, after enduring long separations from family and friends due to the pandemic. Relishing time with loved ones should be your focus during the holidays – not eating yourself into worse health or worrying about dieting. Even if you choose not to make all the shifts in mindset, mindful eating, and meal strategy mentioned, choosing even one change to focus on can help you both enjoy the holidays and have increased control over your weight and wellness. Whatever you do, may you and your loved ones have a safe, healthy, and enjoyable holiday season.
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist who specializes in individualized solutions for emotional and biological overeating. She is CEO and lead physician at Embrace You Weight and Wellness, Telehealth & Virtual Counseling. She has disclosed having no relevant financial relationships. A version of this article first appeared on Medscape.com.
Medical school culinary medicine programs grow despite limited funding
The way he sees it, the stakes couldn’t be higher. He believes doctors need to see food as medicine to be able to stem the tide of chronic disease.
About 6 in 10 adults in the United States live with chronic diseases, according to the Centers for Disease Control and Prevention, costing $4.1 trillion in annual health care costs. Adult obesity rates are rising, as are obesity-related conditions such as heart disease, stroke, type 2 diabetes, and certain types of cancer.
To turn the tide, Dr. Marvasti created a culinary medicine program in 2020 in collaboration with the University of Arizona Cooperative Extension and local chefs.
Dr. Marvasti, who is board certified in family medicine, graduated from the University of Arizona, Phoenix, where he serves as the director of the medical school’s Culinary Medicine Program.
The program offers an elective course for third- and fourth-year medical students, which introduces the evidence-based field of culinary medicine. Dr Marvasti’s goal is for the course to teach students how to use this science and the joy of cooking to improve long-term health outcomes for their patients.
As part of Dr. Marvasti’s program, students learn cooking fundamentals through chef demonstrations and hands-on practice – to teach students how food can be used to prevent and treat many chronic diseases.
One of the dishes students learn to make includes a quinoa salad made with cucumber, onion, bell peppers, corn, cherry tomatoes, beans, garlic, olive oil, and lemon juice. Another recipe includes a healthier take on dessert: Dark chocolate mousse made with three large, ripe avocados, dark chocolate powder, three tablespoons of agave or maple, coconut cream, nondairy milk, salt, and vanilla. Dr. Marvasti and his team are set to build out the existing program to develop additional resources for medically underserved and rural communities in Arizona, according to a statement from the university. These plans will be funded by a $750,000 grant from Novo Nordisk.
“We’re going to develop an open education curriculum to share, so it’s open access to everyone,” said Dr. Marvasti, who is also director of Public Health, Prevention and Health Promotion and an associate professor at the university. “It can be adaptable at the undergraduate, graduate, and postgraduate level.”
Dr. Marvasti and his colleagues at the University of Arizona aren’t alone. In fact, culinary medicine programs are sprouting some serious legs.
Culinary medicine programs catch on
Jaclyn Albin, MD, CCMS, an associate professor in the departments of internal medicine and pediatrics at UT Southwestern Medical Center, Dallas, conducted a scoping review of the literature on culinary medicine programs for medical students.* Her purpose was to learn how the programs were structured and how they assessed student knowledge and attitudes regarding nutrition counseling for patients.
Dr. Albin and her colleagues performed an initial literature search between June 1 and Aug. 1, 2020, of papers published between Jan. 1, 2012, and Aug. 1, 2020 – excluding some newer programs such as the one at the University of Arizona. The results of their research were published in Academic Medicine.
Ultimately, the authors identified and examined 34 programs offering medical student–focused culinary medicine courses.
Program instructors typically included a team of physicians, dietitians, chefs, and other professionals, the study found.
Most program participants exclusively taught medical students, though the training years of participants varied among programs, and they included first-, second-, third-, and fourth-year students. Some programs allowed students from outside their respective medical school to participate in the trainings.
As for the formats of the program, most included cohorts of 10-20 students attending multiple 2- to 3-hour sessions over the course of several months. The University of Alabama at Birmingham offers one of the longest courses, which spans 4-5 months, according to the paper. In contrast, the University of Rochester (N.Y.) program offers only a 1-day lab divided into four sessions, with each session lasting about 2 hours.
The culinary medicine programs’ course sessions tended to include a 10- to 30-minute didactic session involving videos, research articles, culinary theories, and other lectures, a 60- to 90-minute hands-on cooking session, and a 30-minute discussion around nutrition, culture, and patient care.
Most programs used pre- and post-program surveys to evaluate outcomes, though results varied between programs, according to the study. While each program evaluation had different metrics, the surveys generally revealed students felt more confident discussing dietary interventions with patients and in their own cooking skills following completion.
Course correction
Most of those programs are unfunded or minimally funded, Dr. Albin said.
Her own program, which is immensely popular with medical students, is one she teaches on a volunteer basis.
“I do this for free, in the evenings, because I believe in it,” she said.
Medical school education real estate is limited, so convincing medical schools to add something to the curriculum is difficult, Dr. Albin noted.
But it’s worth it, she said, because nutrition is the underpinning of so many diseases.
“Food is the top risk factor for early death in the U.S.,” Dr. Albin said. “I like to say that five times in a row. People have not digested it.”
During her culinary medicine courses, she also asks her medical students: “Who is comfortable in the kitchen?” Some sheepishly raise their hands, she said. Some don’t. Many don’t know anything about cooking.
Then she teaches students about healthy food and how to make it. As part of her program, medical students are given a pantry starter kit with olive oil and a variety of spices to take home and use.
Some recipes Dr. Albin teaches includes mango chili shrimp salad with lime vinaigrette, eggplant sliders, yellow vegetable curry, and strawberry banana chia pudding.
“If you figure out how to do it for your own busy, everyday life, you are now empowered to tell someone else about it,” she said.
A dietitian’s involvement
Milette Siler, RD, LD, CCMS, works with Dr. Albin to educate medical students and patients about food as medicine. A significant chunk of her job involves teaching future doctors what dietitians do.
When the class starts, many students don’t know two of the five basic things dietitians do, Ms. Siler said. By the end of the class, all students know what a dietitian does.
That’s important as students go on to become doctors.
“For us to remove barriers to care, we have to acknowledge most patients’ entry into health care is their physician,” she said. “The dietitian is often a referral. Doctors need to know enough to do no harm.”
Clinicians are often siloed, she said, and the key to better serving patients is partnership, transparency, and relationships. “I think everybody is at a point where everyone is saying what we’re doing isn’t working,” she said. “The American public deserves better, physicians deserve better, and clinicians deserve better.”
Popular with students
While the old guard has been slow to embrace the shift, her students have helped drive the growth of the culinary medicine field, Dr. Albin said.
“They are not settling for the inadequacy that somehow the rest of us did,” she continued. “I’m so hopeful for the future of the health system. We have a generation of people who will not stand for neglecting the most vital elements.”

Lyndon Bui, a second-year medical student at the University of Arizona, Phoenix, is an example of one of these people.
As a member of a culinary medicine interest group on campus, he said, he has learned a lot about the importance of diet for long-term health. This has given him confidence to talk about food and nutrition.
His group does cooking demos at the Phoenix Farmers Market using food from various local vendors. They usually make a salad from local greens and cook seasonal veggies in a stir fry, he said.
They’ve previously made salad with microgreens – young seedlings of edible vegetables and herbs – and pomegranate seeds with a honey mustard vinaigrette, eggplant or cucumber, and hummus on pita bread, as well as almond butter and honey sandwiches, according to the university.
The group also talks with people in the community, answers questions, and learns about community needs.
Mr. Bui’s participation in this group has helped him cultivate a passion for community outreach that he wants to incorporate into his career.
“I feel like I have the knowledge to provide better advice to patients,” he said. “Knowing all these things about food, I feel more comfortable talking about it and more inclined to refer to a dietitian when maybe I wouldn’t have before.”
Family physician applauds culinary medicine programs
When Angie Neison, MD, CCMS, went to medical school, she was surprised there wasn’t more education on nutrition.
In fact, on average, physicians receive less than 20 hours of nutrition education, according to the University of Arizona.
Now 15 years into her career as a family physician, Dr. Neison says nutrition is a huge part of her practice. She spends time working to bust myths about nutrition for her patients – including that healthy food is boring and bland, that making it is time consuming, and that healthy food is expensive. She also spends time teaching aspects of culinary medicine to her colleagues – many of whom are well into their careers – so they can better serve their patients.
It’s worth it to spend time learning about nutrition, she said, whether that’s as a medical student in a culinary medicine program or a practicing physician taking additional courses.
Nutrition education in medical school hasn’t been a priority, she said, maybe because there is so much to learn, or maybe because there is no money to be made in prevention.
“If doctors learn it, they are able to better guide patients,” she said.
Correction, 11/29/22: An earlier version of this article misstated Dr. Albin's institution.
The way he sees it, the stakes couldn’t be higher. He believes doctors need to see food as medicine to be able to stem the tide of chronic disease.
About 6 in 10 adults in the United States live with chronic diseases, according to the Centers for Disease Control and Prevention, costing $4.1 trillion in annual health care costs. Adult obesity rates are rising, as are obesity-related conditions such as heart disease, stroke, type 2 diabetes, and certain types of cancer.
To turn the tide, Dr. Marvasti created a culinary medicine program in 2020 in collaboration with the University of Arizona Cooperative Extension and local chefs.
Dr. Marvasti, who is board certified in family medicine, graduated from the University of Arizona, Phoenix, where he serves as the director of the medical school’s Culinary Medicine Program.
The program offers an elective course for third- and fourth-year medical students, which introduces the evidence-based field of culinary medicine. Dr Marvasti’s goal is for the course to teach students how to use this science and the joy of cooking to improve long-term health outcomes for their patients.
As part of Dr. Marvasti’s program, students learn cooking fundamentals through chef demonstrations and hands-on practice – to teach students how food can be used to prevent and treat many chronic diseases.
One of the dishes students learn to make includes a quinoa salad made with cucumber, onion, bell peppers, corn, cherry tomatoes, beans, garlic, olive oil, and lemon juice. Another recipe includes a healthier take on dessert: Dark chocolate mousse made with three large, ripe avocados, dark chocolate powder, three tablespoons of agave or maple, coconut cream, nondairy milk, salt, and vanilla. Dr. Marvasti and his team are set to build out the existing program to develop additional resources for medically underserved and rural communities in Arizona, according to a statement from the university. These plans will be funded by a $750,000 grant from Novo Nordisk.
“We’re going to develop an open education curriculum to share, so it’s open access to everyone,” said Dr. Marvasti, who is also director of Public Health, Prevention and Health Promotion and an associate professor at the university. “It can be adaptable at the undergraduate, graduate, and postgraduate level.”
Dr. Marvasti and his colleagues at the University of Arizona aren’t alone. In fact, culinary medicine programs are sprouting some serious legs.
Culinary medicine programs catch on
Jaclyn Albin, MD, CCMS, an associate professor in the departments of internal medicine and pediatrics at UT Southwestern Medical Center, Dallas, conducted a scoping review of the literature on culinary medicine programs for medical students.* Her purpose was to learn how the programs were structured and how they assessed student knowledge and attitudes regarding nutrition counseling for patients.
Dr. Albin and her colleagues performed an initial literature search between June 1 and Aug. 1, 2020, of papers published between Jan. 1, 2012, and Aug. 1, 2020 – excluding some newer programs such as the one at the University of Arizona. The results of their research were published in Academic Medicine.
Ultimately, the authors identified and examined 34 programs offering medical student–focused culinary medicine courses.
Program instructors typically included a team of physicians, dietitians, chefs, and other professionals, the study found.
Most program participants exclusively taught medical students, though the training years of participants varied among programs, and they included first-, second-, third-, and fourth-year students. Some programs allowed students from outside their respective medical school to participate in the trainings.
As for the formats of the program, most included cohorts of 10-20 students attending multiple 2- to 3-hour sessions over the course of several months. The University of Alabama at Birmingham offers one of the longest courses, which spans 4-5 months, according to the paper. In contrast, the University of Rochester (N.Y.) program offers only a 1-day lab divided into four sessions, with each session lasting about 2 hours.
The culinary medicine programs’ course sessions tended to include a 10- to 30-minute didactic session involving videos, research articles, culinary theories, and other lectures, a 60- to 90-minute hands-on cooking session, and a 30-minute discussion around nutrition, culture, and patient care.
Most programs used pre- and post-program surveys to evaluate outcomes, though results varied between programs, according to the study. While each program evaluation had different metrics, the surveys generally revealed students felt more confident discussing dietary interventions with patients and in their own cooking skills following completion.
Course correction
Most of those programs are unfunded or minimally funded, Dr. Albin said.
Her own program, which is immensely popular with medical students, is one she teaches on a volunteer basis.
“I do this for free, in the evenings, because I believe in it,” she said.
Medical school education real estate is limited, so convincing medical schools to add something to the curriculum is difficult, Dr. Albin noted.
But it’s worth it, she said, because nutrition is the underpinning of so many diseases.
“Food is the top risk factor for early death in the U.S.,” Dr. Albin said. “I like to say that five times in a row. People have not digested it.”
During her culinary medicine courses, she also asks her medical students: “Who is comfortable in the kitchen?” Some sheepishly raise their hands, she said. Some don’t. Many don’t know anything about cooking.
Then she teaches students about healthy food and how to make it. As part of her program, medical students are given a pantry starter kit with olive oil and a variety of spices to take home and use.
Some recipes Dr. Albin teaches includes mango chili shrimp salad with lime vinaigrette, eggplant sliders, yellow vegetable curry, and strawberry banana chia pudding.
“If you figure out how to do it for your own busy, everyday life, you are now empowered to tell someone else about it,” she said.
A dietitian’s involvement
Milette Siler, RD, LD, CCMS, works with Dr. Albin to educate medical students and patients about food as medicine. A significant chunk of her job involves teaching future doctors what dietitians do.
When the class starts, many students don’t know two of the five basic things dietitians do, Ms. Siler said. By the end of the class, all students know what a dietitian does.
That’s important as students go on to become doctors.
“For us to remove barriers to care, we have to acknowledge most patients’ entry into health care is their physician,” she said. “The dietitian is often a referral. Doctors need to know enough to do no harm.”
Clinicians are often siloed, she said, and the key to better serving patients is partnership, transparency, and relationships. “I think everybody is at a point where everyone is saying what we’re doing isn’t working,” she said. “The American public deserves better, physicians deserve better, and clinicians deserve better.”
Popular with students
While the old guard has been slow to embrace the shift, her students have helped drive the growth of the culinary medicine field, Dr. Albin said.
“They are not settling for the inadequacy that somehow the rest of us did,” she continued. “I’m so hopeful for the future of the health system. We have a generation of people who will not stand for neglecting the most vital elements.”

Lyndon Bui, a second-year medical student at the University of Arizona, Phoenix, is an example of one of these people.
As a member of a culinary medicine interest group on campus, he said, he has learned a lot about the importance of diet for long-term health. This has given him confidence to talk about food and nutrition.
His group does cooking demos at the Phoenix Farmers Market using food from various local vendors. They usually make a salad from local greens and cook seasonal veggies in a stir fry, he said.
They’ve previously made salad with microgreens – young seedlings of edible vegetables and herbs – and pomegranate seeds with a honey mustard vinaigrette, eggplant or cucumber, and hummus on pita bread, as well as almond butter and honey sandwiches, according to the university.
The group also talks with people in the community, answers questions, and learns about community needs.
Mr. Bui’s participation in this group has helped him cultivate a passion for community outreach that he wants to incorporate into his career.
“I feel like I have the knowledge to provide better advice to patients,” he said. “Knowing all these things about food, I feel more comfortable talking about it and more inclined to refer to a dietitian when maybe I wouldn’t have before.”
Family physician applauds culinary medicine programs
When Angie Neison, MD, CCMS, went to medical school, she was surprised there wasn’t more education on nutrition.
In fact, on average, physicians receive less than 20 hours of nutrition education, according to the University of Arizona.
Now 15 years into her career as a family physician, Dr. Neison says nutrition is a huge part of her practice. She spends time working to bust myths about nutrition for her patients – including that healthy food is boring and bland, that making it is time consuming, and that healthy food is expensive. She also spends time teaching aspects of culinary medicine to her colleagues – many of whom are well into their careers – so they can better serve their patients.
It’s worth it to spend time learning about nutrition, she said, whether that’s as a medical student in a culinary medicine program or a practicing physician taking additional courses.
Nutrition education in medical school hasn’t been a priority, she said, maybe because there is so much to learn, or maybe because there is no money to be made in prevention.
“If doctors learn it, they are able to better guide patients,” she said.
Correction, 11/29/22: An earlier version of this article misstated Dr. Albin's institution.
The way he sees it, the stakes couldn’t be higher. He believes doctors need to see food as medicine to be able to stem the tide of chronic disease.
About 6 in 10 adults in the United States live with chronic diseases, according to the Centers for Disease Control and Prevention, costing $4.1 trillion in annual health care costs. Adult obesity rates are rising, as are obesity-related conditions such as heart disease, stroke, type 2 diabetes, and certain types of cancer.
To turn the tide, Dr. Marvasti created a culinary medicine program in 2020 in collaboration with the University of Arizona Cooperative Extension and local chefs.
Dr. Marvasti, who is board certified in family medicine, graduated from the University of Arizona, Phoenix, where he serves as the director of the medical school’s Culinary Medicine Program.
The program offers an elective course for third- and fourth-year medical students, which introduces the evidence-based field of culinary medicine. Dr Marvasti’s goal is for the course to teach students how to use this science and the joy of cooking to improve long-term health outcomes for their patients.
As part of Dr. Marvasti’s program, students learn cooking fundamentals through chef demonstrations and hands-on practice – to teach students how food can be used to prevent and treat many chronic diseases.
One of the dishes students learn to make includes a quinoa salad made with cucumber, onion, bell peppers, corn, cherry tomatoes, beans, garlic, olive oil, and lemon juice. Another recipe includes a healthier take on dessert: Dark chocolate mousse made with three large, ripe avocados, dark chocolate powder, three tablespoons of agave or maple, coconut cream, nondairy milk, salt, and vanilla. Dr. Marvasti and his team are set to build out the existing program to develop additional resources for medically underserved and rural communities in Arizona, according to a statement from the university. These plans will be funded by a $750,000 grant from Novo Nordisk.
“We’re going to develop an open education curriculum to share, so it’s open access to everyone,” said Dr. Marvasti, who is also director of Public Health, Prevention and Health Promotion and an associate professor at the university. “It can be adaptable at the undergraduate, graduate, and postgraduate level.”
Dr. Marvasti and his colleagues at the University of Arizona aren’t alone. In fact, culinary medicine programs are sprouting some serious legs.
Culinary medicine programs catch on
Jaclyn Albin, MD, CCMS, an associate professor in the departments of internal medicine and pediatrics at UT Southwestern Medical Center, Dallas, conducted a scoping review of the literature on culinary medicine programs for medical students.* Her purpose was to learn how the programs were structured and how they assessed student knowledge and attitudes regarding nutrition counseling for patients.
Dr. Albin and her colleagues performed an initial literature search between June 1 and Aug. 1, 2020, of papers published between Jan. 1, 2012, and Aug. 1, 2020 – excluding some newer programs such as the one at the University of Arizona. The results of their research were published in Academic Medicine.
Ultimately, the authors identified and examined 34 programs offering medical student–focused culinary medicine courses.
Program instructors typically included a team of physicians, dietitians, chefs, and other professionals, the study found.
Most program participants exclusively taught medical students, though the training years of participants varied among programs, and they included first-, second-, third-, and fourth-year students. Some programs allowed students from outside their respective medical school to participate in the trainings.
As for the formats of the program, most included cohorts of 10-20 students attending multiple 2- to 3-hour sessions over the course of several months. The University of Alabama at Birmingham offers one of the longest courses, which spans 4-5 months, according to the paper. In contrast, the University of Rochester (N.Y.) program offers only a 1-day lab divided into four sessions, with each session lasting about 2 hours.
The culinary medicine programs’ course sessions tended to include a 10- to 30-minute didactic session involving videos, research articles, culinary theories, and other lectures, a 60- to 90-minute hands-on cooking session, and a 30-minute discussion around nutrition, culture, and patient care.
Most programs used pre- and post-program surveys to evaluate outcomes, though results varied between programs, according to the study. While each program evaluation had different metrics, the surveys generally revealed students felt more confident discussing dietary interventions with patients and in their own cooking skills following completion.
Course correction
Most of those programs are unfunded or minimally funded, Dr. Albin said.
Her own program, which is immensely popular with medical students, is one she teaches on a volunteer basis.
“I do this for free, in the evenings, because I believe in it,” she said.
Medical school education real estate is limited, so convincing medical schools to add something to the curriculum is difficult, Dr. Albin noted.
But it’s worth it, she said, because nutrition is the underpinning of so many diseases.
“Food is the top risk factor for early death in the U.S.,” Dr. Albin said. “I like to say that five times in a row. People have not digested it.”
During her culinary medicine courses, she also asks her medical students: “Who is comfortable in the kitchen?” Some sheepishly raise their hands, she said. Some don’t. Many don’t know anything about cooking.
Then she teaches students about healthy food and how to make it. As part of her program, medical students are given a pantry starter kit with olive oil and a variety of spices to take home and use.
Some recipes Dr. Albin teaches includes mango chili shrimp salad with lime vinaigrette, eggplant sliders, yellow vegetable curry, and strawberry banana chia pudding.
“If you figure out how to do it for your own busy, everyday life, you are now empowered to tell someone else about it,” she said.
A dietitian’s involvement
Milette Siler, RD, LD, CCMS, works with Dr. Albin to educate medical students and patients about food as medicine. A significant chunk of her job involves teaching future doctors what dietitians do.
When the class starts, many students don’t know two of the five basic things dietitians do, Ms. Siler said. By the end of the class, all students know what a dietitian does.
That’s important as students go on to become doctors.
“For us to remove barriers to care, we have to acknowledge most patients’ entry into health care is their physician,” she said. “The dietitian is often a referral. Doctors need to know enough to do no harm.”
Clinicians are often siloed, she said, and the key to better serving patients is partnership, transparency, and relationships. “I think everybody is at a point where everyone is saying what we’re doing isn’t working,” she said. “The American public deserves better, physicians deserve better, and clinicians deserve better.”
Popular with students
While the old guard has been slow to embrace the shift, her students have helped drive the growth of the culinary medicine field, Dr. Albin said.
“They are not settling for the inadequacy that somehow the rest of us did,” she continued. “I’m so hopeful for the future of the health system. We have a generation of people who will not stand for neglecting the most vital elements.”

Lyndon Bui, a second-year medical student at the University of Arizona, Phoenix, is an example of one of these people.
As a member of a culinary medicine interest group on campus, he said, he has learned a lot about the importance of diet for long-term health. This has given him confidence to talk about food and nutrition.
His group does cooking demos at the Phoenix Farmers Market using food from various local vendors. They usually make a salad from local greens and cook seasonal veggies in a stir fry, he said.
They’ve previously made salad with microgreens – young seedlings of edible vegetables and herbs – and pomegranate seeds with a honey mustard vinaigrette, eggplant or cucumber, and hummus on pita bread, as well as almond butter and honey sandwiches, according to the university.
The group also talks with people in the community, answers questions, and learns about community needs.
Mr. Bui’s participation in this group has helped him cultivate a passion for community outreach that he wants to incorporate into his career.
“I feel like I have the knowledge to provide better advice to patients,” he said. “Knowing all these things about food, I feel more comfortable talking about it and more inclined to refer to a dietitian when maybe I wouldn’t have before.”
Family physician applauds culinary medicine programs
When Angie Neison, MD, CCMS, went to medical school, she was surprised there wasn’t more education on nutrition.
In fact, on average, physicians receive less than 20 hours of nutrition education, according to the University of Arizona.
Now 15 years into her career as a family physician, Dr. Neison says nutrition is a huge part of her practice. She spends time working to bust myths about nutrition for her patients – including that healthy food is boring and bland, that making it is time consuming, and that healthy food is expensive. She also spends time teaching aspects of culinary medicine to her colleagues – many of whom are well into their careers – so they can better serve their patients.
It’s worth it to spend time learning about nutrition, she said, whether that’s as a medical student in a culinary medicine program or a practicing physician taking additional courses.
Nutrition education in medical school hasn’t been a priority, she said, maybe because there is so much to learn, or maybe because there is no money to be made in prevention.
“If doctors learn it, they are able to better guide patients,” she said.
Correction, 11/29/22: An earlier version of this article misstated Dr. Albin's institution.
FROM ACADEMIC MEDICINE