User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Clustered Vesicles on the Neck
The Diagnosis: Microcystic Lymphatic Malformation
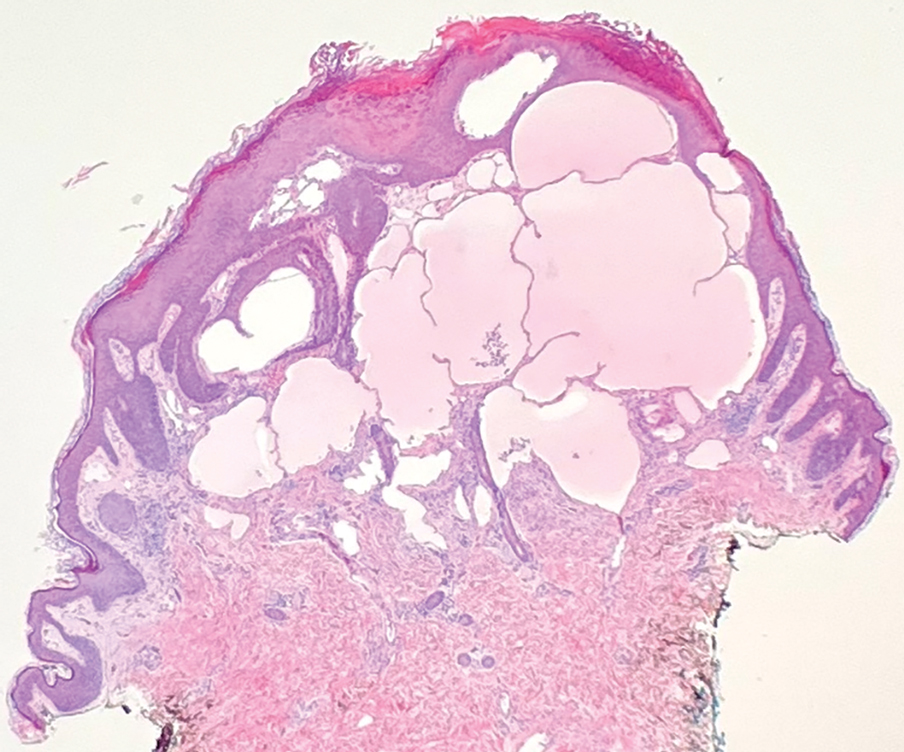
A punch biopsy demonstrated anastomosing fluidfilled spaces within the papillary and reticular dermal layers (Figure), confirming the diagnosis of microcystic lymphatic malformation (LM)(formerly known as lymphangioma circumscriptum), a congenital vascular malformation composed of slow-flow lymphatic channels.1 The patient underwent serial excisions with improvement of the LM, though the treatment course was complicated by hypertrophic scar formation.
The classic clinical presentation of microcystic LM includes a crop of vesicles containing clear or hemorrhagic fluid with associated oozing or bleeding.2 When cutaneous lesions resembling microcystic LM develop in response to lymphatic damage and resulting stasis, such as from prior radiotherapy or surgery, the term lymphangiectasia is used to distinguish this entity from congenital microcystic LM.3
Microcystic LMs are histologically indistinguishable from macrocystic LMs; however, macrocystic LMs typically are clinically evident at birth as ill-defined subcutaneous masses.2,4-6 Dermatitis herpetiformis, a dermatologic manifestation of gluten sensitivity, causes intensely pruritic vesicles in a symmetric distribution on the elbows, knees, and buttocks. Histopathology shows neutrophilic microabscesses in the dermal papillae with subepidermal blistering. Direct immunofluorescence demonstrates the deposition of IgA along the basement membrane with dermal papillae aggregates.6 The underlying dermis also may contain a lymphohistiocytic infiltrate rich in neutrophils. The vesicles of herpes zoster virus are painful and present in a dermatomal distribution. A viral cytopathic effect often is observed in keratinocytes, specifically with multinucleation, molding, and margination of chromatin material. The lesions are accompanied by variable lymphocytic inflammation and epithelial necrosis resulting in intraepidermal blistering.7 Extragenital lichen sclerosus presents as polygonal white papules merging to form plaques and may include hemorrhagic blisters in some instances. Histopathology shows hyperkeratosis, epidermal atrophy with flattened rete ridges, vacuolar interface changes, loss of elastic fibers, and hyalinization of the lamina propria with lymphocytic infiltrate.8
Endothelial cells in LM exhibit activating mutations in the phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha gene, PIK3CA, which may lead to proliferation and overgrowth of the lymphatic vasculature, as well as increased production of cyclic guanosine monophosphate.9,10 Phosphodiesterase 5 (PDE5) is expressed in the perivascular smooth muscle adjacent to lymphatic spaces in LMs but not in the their vasculature. 10 This pattern of PDE5 expression may cause perilesional vasculature to constrict, preventing lymphatic fluid from draining into the veins.11 It is theorized that the PDE5 inhibitor sildenafil leads to relaxation of the vasculature adjacent to LMs, allowing the outflow of the accumulated lymphatic fluid and thus decompression.11-13
Management of LM should not only take into account the depth and location of involvement but also any associated symptoms or complications, such as pruritus, pain, bleeding, or secondary infections. Magnetic resonance imaging (MRI) typically has been considered the gold standard for determining the size and depth of involvement of the malformation.1,3,4 However, ultrasonography with Doppler flow may be considered an initial diagnostic and screening test, as it can distinguish between macrocystic and microcystic components and provide superior images of microcystic lesions, which are below the resolution capacity of MRI.4 Notably, our patient’s LM was undetectable on ultrasonography and was found to be largely superficial in nature on MRI.
Serial excision of the microcystic LM was conducted in our patient, but there currently is no consensus on optimal treatment of LM, and many treatment options are complicated by high recurrence rates or complications.5 Procedural approaches may include excision, cryotherapy, radiotherapy, sclerotherapy, or laser therapy, while pharmacologic approaches may include sildenafil for its inhibition of PDE5 or sirolimus (oral or topical) for its inhibition of mammalian target of rapamycin.5,12-14 Because recurrence is highly likely, patients may require repeat treatments or a combination approach to therapy.1,5 The development of targeted therapies may lead to a shift in management of LMs in the future, as successful use of the PIK3CA inhibitor alpelisib recently has been reported to lead to clinical improvement of PIK3CA-related LMs, including in patients with PIK3CA-related overgrowth syndromes.15
- Garzon MC, Huang JT, Enjolras O, et al. Vascular malformations: part I. J Am Acad Dermatol. 2007;56:353-374. doi:10.1016/j.jaad.2006.05.069
- Alrashdan MS, Hammad HM, Alzumaili BAI, et al. Lymphangioma circumscriptum of the tongue: a case with marked hemorrhagic component. J Cutan Pathol. 2018;45:278-281. doi:10.1111/cup.13101
- Osborne GE, Chinn RJ, Francis ND, et al. Magnetic resonance imaging in the investigation of penile lymphangioma circumscriptum. Br J Dermatol. 2000;143:467-468. doi:10.1046/j.1365-2133.2000.03695.x
- Davies D, Rogers M, Lam A, et al. Localized microcystic lymphatic malformations—ultrasound diagnosis. Pediatr Dermatol. 1999;16: 423-429. doi:10.1046/j.1525-1470.1999.00110.x
- García-Montero P, Del Boz J, Baselga-Torres E, et al. Use of topical rapamycin in the treatment of superficial lymphatic malformations. J Am Acad Dermatol. 2019;80:508-515. doi:10.1016/j.jaad.2018.09.050
- Clarindo MV, Possebon AT, Soligo EM, et al. Dermatitis herpetiformis: pathophysiology, clinical presentation, diagnosis and treatment. An Bras Dermatol. 2014;89:865-875; quiz 876-877. doi:10.1590/abd1806-4841.20142966
- Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): a broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50-58.
- Shiver M, Papasakelariou C, Brown JA, et al. Extragenital bullous lichen sclerosus in a pediatric patient: a case report and literature review. Pediatr Dermatol. 2014;31:383-385. doi:10.1111 /pde.12025
- Blesinger H, Kaulfuß S, Aung T, et al. PIK3CA mutations are specifically localized to lymphatic endothelial cells of lymphatic malformations [published online July 9, 2018]. PLoS One. 2018;13:E0200343. doi:10.1371/journal.pone.0200343
- Green JS, Prok L, Bruckner AL. Expression of phosphodiesterase-5 in lymphatic malformation tissue. JAMA Dermatol. 2014;150:455-456. doi:10.1001/jamadermatol.2013.7002
- Swetman GL, Berk DR, Vasanawala SS, et al. Sildenafil for severe lymphatic malformations. N Engl J Med. 2012;366:384-386. doi:10.1056 /NEJMc1112482
- Tu JH, Tafoya E, Jeng M, et al. Long-term follow-up of lymphatic malformations in children treated with sildenafil. Pediatr Dermatol. 2017;34:559-565. doi:10.1111/pde.13237
- Maruani A, Tavernier E, Boccara O, et al. Sirolimus (rapamycin) for slow-flow malformations in children: the Observational-Phase Randomized Clinical PERFORMUS Trial. JAMA Dermatol. 2021;157:1289-1298. doi:10.1001/jamadermatol.2021.3459
- Delestre F, Venot Q, Bayard C, et al. Alpelisib administration reduced lymphatic malformations in a mouse model and in patients. Sci Transl Med. 2021;13:eabg0809. doi:10.1126/scitranslmed .abg0809
- Garreta Fontelles G, Pardo Pastor J, Grande Moreillo C. Alpelisib to treat CLOVES syndrome, a member of the PIK3CA-related overgrowth syndrome spectrum [published online February 21, 2022]. Br J Clin Pharmacol. 2022;88:3891-3895. doi:10.1111/bcp.15270
The Diagnosis: Microcystic Lymphatic Malformation
A punch biopsy demonstrated anastomosing fluidfilled spaces within the papillary and reticular dermal layers (Figure), confirming the diagnosis of microcystic lymphatic malformation (LM)(formerly known as lymphangioma circumscriptum), a congenital vascular malformation composed of slow-flow lymphatic channels.1 The patient underwent serial excisions with improvement of the LM, though the treatment course was complicated by hypertrophic scar formation.
The classic clinical presentation of microcystic LM includes a crop of vesicles containing clear or hemorrhagic fluid with associated oozing or bleeding.2 When cutaneous lesions resembling microcystic LM develop in response to lymphatic damage and resulting stasis, such as from prior radiotherapy or surgery, the term lymphangiectasia is used to distinguish this entity from congenital microcystic LM.3
Microcystic LMs are histologically indistinguishable from macrocystic LMs; however, macrocystic LMs typically are clinically evident at birth as ill-defined subcutaneous masses.2,4-6 Dermatitis herpetiformis, a dermatologic manifestation of gluten sensitivity, causes intensely pruritic vesicles in a symmetric distribution on the elbows, knees, and buttocks. Histopathology shows neutrophilic microabscesses in the dermal papillae with subepidermal blistering. Direct immunofluorescence demonstrates the deposition of IgA along the basement membrane with dermal papillae aggregates.6 The underlying dermis also may contain a lymphohistiocytic infiltrate rich in neutrophils. The vesicles of herpes zoster virus are painful and present in a dermatomal distribution. A viral cytopathic effect often is observed in keratinocytes, specifically with multinucleation, molding, and margination of chromatin material. The lesions are accompanied by variable lymphocytic inflammation and epithelial necrosis resulting in intraepidermal blistering.7 Extragenital lichen sclerosus presents as polygonal white papules merging to form plaques and may include hemorrhagic blisters in some instances. Histopathology shows hyperkeratosis, epidermal atrophy with flattened rete ridges, vacuolar interface changes, loss of elastic fibers, and hyalinization of the lamina propria with lymphocytic infiltrate.8
Endothelial cells in LM exhibit activating mutations in the phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha gene, PIK3CA, which may lead to proliferation and overgrowth of the lymphatic vasculature, as well as increased production of cyclic guanosine monophosphate.9,10 Phosphodiesterase 5 (PDE5) is expressed in the perivascular smooth muscle adjacent to lymphatic spaces in LMs but not in the their vasculature. 10 This pattern of PDE5 expression may cause perilesional vasculature to constrict, preventing lymphatic fluid from draining into the veins.11 It is theorized that the PDE5 inhibitor sildenafil leads to relaxation of the vasculature adjacent to LMs, allowing the outflow of the accumulated lymphatic fluid and thus decompression.11-13
Management of LM should not only take into account the depth and location of involvement but also any associated symptoms or complications, such as pruritus, pain, bleeding, or secondary infections. Magnetic resonance imaging (MRI) typically has been considered the gold standard for determining the size and depth of involvement of the malformation.1,3,4 However, ultrasonography with Doppler flow may be considered an initial diagnostic and screening test, as it can distinguish between macrocystic and microcystic components and provide superior images of microcystic lesions, which are below the resolution capacity of MRI.4 Notably, our patient’s LM was undetectable on ultrasonography and was found to be largely superficial in nature on MRI.
Serial excision of the microcystic LM was conducted in our patient, but there currently is no consensus on optimal treatment of LM, and many treatment options are complicated by high recurrence rates or complications.5 Procedural approaches may include excision, cryotherapy, radiotherapy, sclerotherapy, or laser therapy, while pharmacologic approaches may include sildenafil for its inhibition of PDE5 or sirolimus (oral or topical) for its inhibition of mammalian target of rapamycin.5,12-14 Because recurrence is highly likely, patients may require repeat treatments or a combination approach to therapy.1,5 The development of targeted therapies may lead to a shift in management of LMs in the future, as successful use of the PIK3CA inhibitor alpelisib recently has been reported to lead to clinical improvement of PIK3CA-related LMs, including in patients with PIK3CA-related overgrowth syndromes.15
The Diagnosis: Microcystic Lymphatic Malformation
A punch biopsy demonstrated anastomosing fluidfilled spaces within the papillary and reticular dermal layers (Figure), confirming the diagnosis of microcystic lymphatic malformation (LM)(formerly known as lymphangioma circumscriptum), a congenital vascular malformation composed of slow-flow lymphatic channels.1 The patient underwent serial excisions with improvement of the LM, though the treatment course was complicated by hypertrophic scar formation.
The classic clinical presentation of microcystic LM includes a crop of vesicles containing clear or hemorrhagic fluid with associated oozing or bleeding.2 When cutaneous lesions resembling microcystic LM develop in response to lymphatic damage and resulting stasis, such as from prior radiotherapy or surgery, the term lymphangiectasia is used to distinguish this entity from congenital microcystic LM.3
Microcystic LMs are histologically indistinguishable from macrocystic LMs; however, macrocystic LMs typically are clinically evident at birth as ill-defined subcutaneous masses.2,4-6 Dermatitis herpetiformis, a dermatologic manifestation of gluten sensitivity, causes intensely pruritic vesicles in a symmetric distribution on the elbows, knees, and buttocks. Histopathology shows neutrophilic microabscesses in the dermal papillae with subepidermal blistering. Direct immunofluorescence demonstrates the deposition of IgA along the basement membrane with dermal papillae aggregates.6 The underlying dermis also may contain a lymphohistiocytic infiltrate rich in neutrophils. The vesicles of herpes zoster virus are painful and present in a dermatomal distribution. A viral cytopathic effect often is observed in keratinocytes, specifically with multinucleation, molding, and margination of chromatin material. The lesions are accompanied by variable lymphocytic inflammation and epithelial necrosis resulting in intraepidermal blistering.7 Extragenital lichen sclerosus presents as polygonal white papules merging to form plaques and may include hemorrhagic blisters in some instances. Histopathology shows hyperkeratosis, epidermal atrophy with flattened rete ridges, vacuolar interface changes, loss of elastic fibers, and hyalinization of the lamina propria with lymphocytic infiltrate.8
Endothelial cells in LM exhibit activating mutations in the phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha gene, PIK3CA, which may lead to proliferation and overgrowth of the lymphatic vasculature, as well as increased production of cyclic guanosine monophosphate.9,10 Phosphodiesterase 5 (PDE5) is expressed in the perivascular smooth muscle adjacent to lymphatic spaces in LMs but not in the their vasculature. 10 This pattern of PDE5 expression may cause perilesional vasculature to constrict, preventing lymphatic fluid from draining into the veins.11 It is theorized that the PDE5 inhibitor sildenafil leads to relaxation of the vasculature adjacent to LMs, allowing the outflow of the accumulated lymphatic fluid and thus decompression.11-13
Management of LM should not only take into account the depth and location of involvement but also any associated symptoms or complications, such as pruritus, pain, bleeding, or secondary infections. Magnetic resonance imaging (MRI) typically has been considered the gold standard for determining the size and depth of involvement of the malformation.1,3,4 However, ultrasonography with Doppler flow may be considered an initial diagnostic and screening test, as it can distinguish between macrocystic and microcystic components and provide superior images of microcystic lesions, which are below the resolution capacity of MRI.4 Notably, our patient’s LM was undetectable on ultrasonography and was found to be largely superficial in nature on MRI.
Serial excision of the microcystic LM was conducted in our patient, but there currently is no consensus on optimal treatment of LM, and many treatment options are complicated by high recurrence rates or complications.5 Procedural approaches may include excision, cryotherapy, radiotherapy, sclerotherapy, or laser therapy, while pharmacologic approaches may include sildenafil for its inhibition of PDE5 or sirolimus (oral or topical) for its inhibition of mammalian target of rapamycin.5,12-14 Because recurrence is highly likely, patients may require repeat treatments or a combination approach to therapy.1,5 The development of targeted therapies may lead to a shift in management of LMs in the future, as successful use of the PIK3CA inhibitor alpelisib recently has been reported to lead to clinical improvement of PIK3CA-related LMs, including in patients with PIK3CA-related overgrowth syndromes.15
- Garzon MC, Huang JT, Enjolras O, et al. Vascular malformations: part I. J Am Acad Dermatol. 2007;56:353-374. doi:10.1016/j.jaad.2006.05.069
- Alrashdan MS, Hammad HM, Alzumaili BAI, et al. Lymphangioma circumscriptum of the tongue: a case with marked hemorrhagic component. J Cutan Pathol. 2018;45:278-281. doi:10.1111/cup.13101
- Osborne GE, Chinn RJ, Francis ND, et al. Magnetic resonance imaging in the investigation of penile lymphangioma circumscriptum. Br J Dermatol. 2000;143:467-468. doi:10.1046/j.1365-2133.2000.03695.x
- Davies D, Rogers M, Lam A, et al. Localized microcystic lymphatic malformations—ultrasound diagnosis. Pediatr Dermatol. 1999;16: 423-429. doi:10.1046/j.1525-1470.1999.00110.x
- García-Montero P, Del Boz J, Baselga-Torres E, et al. Use of topical rapamycin in the treatment of superficial lymphatic malformations. J Am Acad Dermatol. 2019;80:508-515. doi:10.1016/j.jaad.2018.09.050
- Clarindo MV, Possebon AT, Soligo EM, et al. Dermatitis herpetiformis: pathophysiology, clinical presentation, diagnosis and treatment. An Bras Dermatol. 2014;89:865-875; quiz 876-877. doi:10.1590/abd1806-4841.20142966
- Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): a broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50-58.
- Shiver M, Papasakelariou C, Brown JA, et al. Extragenital bullous lichen sclerosus in a pediatric patient: a case report and literature review. Pediatr Dermatol. 2014;31:383-385. doi:10.1111 /pde.12025
- Blesinger H, Kaulfuß S, Aung T, et al. PIK3CA mutations are specifically localized to lymphatic endothelial cells of lymphatic malformations [published online July 9, 2018]. PLoS One. 2018;13:E0200343. doi:10.1371/journal.pone.0200343
- Green JS, Prok L, Bruckner AL. Expression of phosphodiesterase-5 in lymphatic malformation tissue. JAMA Dermatol. 2014;150:455-456. doi:10.1001/jamadermatol.2013.7002
- Swetman GL, Berk DR, Vasanawala SS, et al. Sildenafil for severe lymphatic malformations. N Engl J Med. 2012;366:384-386. doi:10.1056 /NEJMc1112482
- Tu JH, Tafoya E, Jeng M, et al. Long-term follow-up of lymphatic malformations in children treated with sildenafil. Pediatr Dermatol. 2017;34:559-565. doi:10.1111/pde.13237
- Maruani A, Tavernier E, Boccara O, et al. Sirolimus (rapamycin) for slow-flow malformations in children: the Observational-Phase Randomized Clinical PERFORMUS Trial. JAMA Dermatol. 2021;157:1289-1298. doi:10.1001/jamadermatol.2021.3459
- Delestre F, Venot Q, Bayard C, et al. Alpelisib administration reduced lymphatic malformations in a mouse model and in patients. Sci Transl Med. 2021;13:eabg0809. doi:10.1126/scitranslmed .abg0809
- Garreta Fontelles G, Pardo Pastor J, Grande Moreillo C. Alpelisib to treat CLOVES syndrome, a member of the PIK3CA-related overgrowth syndrome spectrum [published online February 21, 2022]. Br J Clin Pharmacol. 2022;88:3891-3895. doi:10.1111/bcp.15270
- Garzon MC, Huang JT, Enjolras O, et al. Vascular malformations: part I. J Am Acad Dermatol. 2007;56:353-374. doi:10.1016/j.jaad.2006.05.069
- Alrashdan MS, Hammad HM, Alzumaili BAI, et al. Lymphangioma circumscriptum of the tongue: a case with marked hemorrhagic component. J Cutan Pathol. 2018;45:278-281. doi:10.1111/cup.13101
- Osborne GE, Chinn RJ, Francis ND, et al. Magnetic resonance imaging in the investigation of penile lymphangioma circumscriptum. Br J Dermatol. 2000;143:467-468. doi:10.1046/j.1365-2133.2000.03695.x
- Davies D, Rogers M, Lam A, et al. Localized microcystic lymphatic malformations—ultrasound diagnosis. Pediatr Dermatol. 1999;16: 423-429. doi:10.1046/j.1525-1470.1999.00110.x
- García-Montero P, Del Boz J, Baselga-Torres E, et al. Use of topical rapamycin in the treatment of superficial lymphatic malformations. J Am Acad Dermatol. 2019;80:508-515. doi:10.1016/j.jaad.2018.09.050
- Clarindo MV, Possebon AT, Soligo EM, et al. Dermatitis herpetiformis: pathophysiology, clinical presentation, diagnosis and treatment. An Bras Dermatol. 2014;89:865-875; quiz 876-877. doi:10.1590/abd1806-4841.20142966
- Leinweber B, Kerl H, Cerroni L. Histopathologic features of cutaneous herpes virus infections (herpes simplex, herpes varicella/zoster): a broad spectrum of presentations with common pseudolymphomatous aspects. Am J Surg Pathol. 2006;30:50-58.
- Shiver M, Papasakelariou C, Brown JA, et al. Extragenital bullous lichen sclerosus in a pediatric patient: a case report and literature review. Pediatr Dermatol. 2014;31:383-385. doi:10.1111 /pde.12025
- Blesinger H, Kaulfuß S, Aung T, et al. PIK3CA mutations are specifically localized to lymphatic endothelial cells of lymphatic malformations [published online July 9, 2018]. PLoS One. 2018;13:E0200343. doi:10.1371/journal.pone.0200343
- Green JS, Prok L, Bruckner AL. Expression of phosphodiesterase-5 in lymphatic malformation tissue. JAMA Dermatol. 2014;150:455-456. doi:10.1001/jamadermatol.2013.7002
- Swetman GL, Berk DR, Vasanawala SS, et al. Sildenafil for severe lymphatic malformations. N Engl J Med. 2012;366:384-386. doi:10.1056 /NEJMc1112482
- Tu JH, Tafoya E, Jeng M, et al. Long-term follow-up of lymphatic malformations in children treated with sildenafil. Pediatr Dermatol. 2017;34:559-565. doi:10.1111/pde.13237
- Maruani A, Tavernier E, Boccara O, et al. Sirolimus (rapamycin) for slow-flow malformations in children: the Observational-Phase Randomized Clinical PERFORMUS Trial. JAMA Dermatol. 2021;157:1289-1298. doi:10.1001/jamadermatol.2021.3459
- Delestre F, Venot Q, Bayard C, et al. Alpelisib administration reduced lymphatic malformations in a mouse model and in patients. Sci Transl Med. 2021;13:eabg0809. doi:10.1126/scitranslmed .abg0809
- Garreta Fontelles G, Pardo Pastor J, Grande Moreillo C. Alpelisib to treat CLOVES syndrome, a member of the PIK3CA-related overgrowth syndrome spectrum [published online February 21, 2022]. Br J Clin Pharmacol. 2022;88:3891-3895. doi:10.1111/bcp.15270
A 6-year-old girl presented to the dermatology clinic with a rash on the right side of the neck that was noted at birth as a small raised lesion but slowly increased over time in size and number of lesions. She reported pruritus and irritation, particularly when rubbed or scratched. There was no family history of similar skin abnormalities. Her medical history was notable for a left-sided cholesteatoma on tympanomastoidectomy. Physical examination revealed clustered vesicles on the right side of the neck with underlying erythema. The vesicles contained mostly clear fluid with a few focal areas of hemorrhagic fluid. Ultrasonography was unremarkable, and magnetic resonance imaging revealed superficial T2 hyperintense nonenhancing cutaneous and subcutaneous lesions overlying the right lateral neck with minimal extension into the superficial right supraclavicular soft tissues.

Endoscopic sinus surgery for chronic rhinosinusitis has no impact on comorbid asthma
Endoscopic sinus surgery (ESS) has no significant impact on asthma symptoms for patients with chronic rhinosinusitis up to a year after the procedure, a study of 64 patients shows.
, Anyull Dayanna Bohórquez Caballero said in a presentation at the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) 2023 annual meeting.
The study “offers a unique approach to explore the effects of endoscopic sinus surgery in a real-world context, with valuable insights that differ from previous research,” Dr. Bohórquez Caballero, an international medical graduate and research fellow of the Mayo Clinic, Jacksonville, Fla., said in an interview.
Under the leadership of senior author Angela Donaldson, MD, Dr. Bohórquez Caballero and colleagues at the Mayo Clinic in Jacksonville analyzed data from 185 adults with both asthma and chronic rhinosinusitis who underwent ESS at the clinic between 2013 and 2023. Asthma severity was evaluated up to 3 months before and 1 year after surgery. Patients’ asthma severity was classified as mild, moderate, or severe on the basis of current Global Initiative for Asthma guidelines using medication requirements.
The final study population included 64 patients; 42 of these (66.7%) had chronic rhinosinusitis with nasal polyps. Outcomes included differences in asthma severity, asthma medication doses, and the number of medications.
Overall, there was no significant difference in measures of mild, moderate, or severe asthma before and after ESS in a McNemar paired test (P values: .130, .999, and .288, respectively). Similarly, no difference was found before and after ESS in terms of total inhaled corticosteroid dose (P = .999), number of medications prescribed (P = .157), or control of the disease (P = .078).
The findings were limited by the relatively small number of patients. The study is the first known to assess the real-world impact of ESS on asthma severity, said Bohórquez Caballero.
Expected reduction in asthma severity not seen
Past studies have suggested that ESS improves parameters such as pulmonary function test results or sinonasal outcomes, Dr. Bohórquez Caballero told this news organization. “Our findings indicate that ESS does not significantly impact asthma severity or trends in treatment, including the number and/or dose of medications, in everyday practice.
Our study also identified crucial opportunities to reinforce interdisciplinary follow-up after ESS,” she noted, and it provides a comprehensive depiction of the outcomes experienced by patients with chronic rhinosinusitis and asthma who undergo ESS.
“We were expecting a reduction in severity or a decrease in the dose of inhaled corticosteroid therapies, and we expected to see a translation from previous evidence into clinical practice; however, we did not,” said Dr. Bohórquez Caballero.
“The take-home message is that while there is a strong correlation between CRS and asthma, it does not appear that ESS alone improves real-world treatment based on asthma severity,” she said. “However, our findings have shown that patients may experience a longer period without the need for a reliever medication in the early postoperative period.”
Looking ahead, “We want to explore what happens 5 or 6 months after sinus surgery that would explain the sudden need for a reliever medication,” she added. “Future studies are warranted to investigate the long-term effects of ESS on asthma severity as it relates to modifications of asthma regimens.”
Data important for patient discussions
The current study is important because of the frequency of comorbid asthma among patients with chronic rhinosinusitis, Megan Durr, MD, of the University of California, San Francisco, said in an interview.
“When we are considering functional endoscopy sinus surgery with patients, we are often asked if the surgery will impact the severity of their asthma symptoms,” said Dr. Durr, who served as a moderator for the session in which the study was presented.
“I am surprised the study did not see any difference in asthma severity after sinus surgery, as we often talk to patients about the unified airway that refers to the shared epidemiologic and pathophysiologic relationship between the upper and lower airways,” she told this news organization.
“This study will allow us to have a more informed evidenced-based discussion with patients and their primary care providers and/or pulmonologists” about what to expect for asthma outcomes following surgery, she said.
The study received no outside funding. Dr. Durr has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Endoscopic sinus surgery (ESS) has no significant impact on asthma symptoms for patients with chronic rhinosinusitis up to a year after the procedure, a study of 64 patients shows.
, Anyull Dayanna Bohórquez Caballero said in a presentation at the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) 2023 annual meeting.
The study “offers a unique approach to explore the effects of endoscopic sinus surgery in a real-world context, with valuable insights that differ from previous research,” Dr. Bohórquez Caballero, an international medical graduate and research fellow of the Mayo Clinic, Jacksonville, Fla., said in an interview.
Under the leadership of senior author Angela Donaldson, MD, Dr. Bohórquez Caballero and colleagues at the Mayo Clinic in Jacksonville analyzed data from 185 adults with both asthma and chronic rhinosinusitis who underwent ESS at the clinic between 2013 and 2023. Asthma severity was evaluated up to 3 months before and 1 year after surgery. Patients’ asthma severity was classified as mild, moderate, or severe on the basis of current Global Initiative for Asthma guidelines using medication requirements.
The final study population included 64 patients; 42 of these (66.7%) had chronic rhinosinusitis with nasal polyps. Outcomes included differences in asthma severity, asthma medication doses, and the number of medications.
Overall, there was no significant difference in measures of mild, moderate, or severe asthma before and after ESS in a McNemar paired test (P values: .130, .999, and .288, respectively). Similarly, no difference was found before and after ESS in terms of total inhaled corticosteroid dose (P = .999), number of medications prescribed (P = .157), or control of the disease (P = .078).
The findings were limited by the relatively small number of patients. The study is the first known to assess the real-world impact of ESS on asthma severity, said Bohórquez Caballero.
Expected reduction in asthma severity not seen
Past studies have suggested that ESS improves parameters such as pulmonary function test results or sinonasal outcomes, Dr. Bohórquez Caballero told this news organization. “Our findings indicate that ESS does not significantly impact asthma severity or trends in treatment, including the number and/or dose of medications, in everyday practice.
Our study also identified crucial opportunities to reinforce interdisciplinary follow-up after ESS,” she noted, and it provides a comprehensive depiction of the outcomes experienced by patients with chronic rhinosinusitis and asthma who undergo ESS.
“We were expecting a reduction in severity or a decrease in the dose of inhaled corticosteroid therapies, and we expected to see a translation from previous evidence into clinical practice; however, we did not,” said Dr. Bohórquez Caballero.
“The take-home message is that while there is a strong correlation between CRS and asthma, it does not appear that ESS alone improves real-world treatment based on asthma severity,” she said. “However, our findings have shown that patients may experience a longer period without the need for a reliever medication in the early postoperative period.”
Looking ahead, “We want to explore what happens 5 or 6 months after sinus surgery that would explain the sudden need for a reliever medication,” she added. “Future studies are warranted to investigate the long-term effects of ESS on asthma severity as it relates to modifications of asthma regimens.”
Data important for patient discussions
The current study is important because of the frequency of comorbid asthma among patients with chronic rhinosinusitis, Megan Durr, MD, of the University of California, San Francisco, said in an interview.
“When we are considering functional endoscopy sinus surgery with patients, we are often asked if the surgery will impact the severity of their asthma symptoms,” said Dr. Durr, who served as a moderator for the session in which the study was presented.
“I am surprised the study did not see any difference in asthma severity after sinus surgery, as we often talk to patients about the unified airway that refers to the shared epidemiologic and pathophysiologic relationship between the upper and lower airways,” she told this news organization.
“This study will allow us to have a more informed evidenced-based discussion with patients and their primary care providers and/or pulmonologists” about what to expect for asthma outcomes following surgery, she said.
The study received no outside funding. Dr. Durr has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Endoscopic sinus surgery (ESS) has no significant impact on asthma symptoms for patients with chronic rhinosinusitis up to a year after the procedure, a study of 64 patients shows.
, Anyull Dayanna Bohórquez Caballero said in a presentation at the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) 2023 annual meeting.
The study “offers a unique approach to explore the effects of endoscopic sinus surgery in a real-world context, with valuable insights that differ from previous research,” Dr. Bohórquez Caballero, an international medical graduate and research fellow of the Mayo Clinic, Jacksonville, Fla., said in an interview.
Under the leadership of senior author Angela Donaldson, MD, Dr. Bohórquez Caballero and colleagues at the Mayo Clinic in Jacksonville analyzed data from 185 adults with both asthma and chronic rhinosinusitis who underwent ESS at the clinic between 2013 and 2023. Asthma severity was evaluated up to 3 months before and 1 year after surgery. Patients’ asthma severity was classified as mild, moderate, or severe on the basis of current Global Initiative for Asthma guidelines using medication requirements.
The final study population included 64 patients; 42 of these (66.7%) had chronic rhinosinusitis with nasal polyps. Outcomes included differences in asthma severity, asthma medication doses, and the number of medications.
Overall, there was no significant difference in measures of mild, moderate, or severe asthma before and after ESS in a McNemar paired test (P values: .130, .999, and .288, respectively). Similarly, no difference was found before and after ESS in terms of total inhaled corticosteroid dose (P = .999), number of medications prescribed (P = .157), or control of the disease (P = .078).
The findings were limited by the relatively small number of patients. The study is the first known to assess the real-world impact of ESS on asthma severity, said Bohórquez Caballero.
Expected reduction in asthma severity not seen
Past studies have suggested that ESS improves parameters such as pulmonary function test results or sinonasal outcomes, Dr. Bohórquez Caballero told this news organization. “Our findings indicate that ESS does not significantly impact asthma severity or trends in treatment, including the number and/or dose of medications, in everyday practice.
Our study also identified crucial opportunities to reinforce interdisciplinary follow-up after ESS,” she noted, and it provides a comprehensive depiction of the outcomes experienced by patients with chronic rhinosinusitis and asthma who undergo ESS.
“We were expecting a reduction in severity or a decrease in the dose of inhaled corticosteroid therapies, and we expected to see a translation from previous evidence into clinical practice; however, we did not,” said Dr. Bohórquez Caballero.
“The take-home message is that while there is a strong correlation between CRS and asthma, it does not appear that ESS alone improves real-world treatment based on asthma severity,” she said. “However, our findings have shown that patients may experience a longer period without the need for a reliever medication in the early postoperative period.”
Looking ahead, “We want to explore what happens 5 or 6 months after sinus surgery that would explain the sudden need for a reliever medication,” she added. “Future studies are warranted to investigate the long-term effects of ESS on asthma severity as it relates to modifications of asthma regimens.”
Data important for patient discussions
The current study is important because of the frequency of comorbid asthma among patients with chronic rhinosinusitis, Megan Durr, MD, of the University of California, San Francisco, said in an interview.
“When we are considering functional endoscopy sinus surgery with patients, we are often asked if the surgery will impact the severity of their asthma symptoms,” said Dr. Durr, who served as a moderator for the session in which the study was presented.
“I am surprised the study did not see any difference in asthma severity after sinus surgery, as we often talk to patients about the unified airway that refers to the shared epidemiologic and pathophysiologic relationship between the upper and lower airways,” she told this news organization.
“This study will allow us to have a more informed evidenced-based discussion with patients and their primary care providers and/or pulmonologists” about what to expect for asthma outcomes following surgery, she said.
The study received no outside funding. Dr. Durr has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAO-HNSF 2023
Systematic review spotlights the use of nutraceuticals for acne
.
“While many topical and systemic prescription options are available for the treatment of acne, some patients may be interested in natural and complementary therapies as either an adjunctive or an alternative to prescription medications,” researchers led by John S. Barbieri, MD, MBA, of the department of dermatology at Brigham and Women’s Hospital, Boston, wrote in their study, which was published online in JAMA Dermatology. The researchers defined nutraceuticals as products derived from food sources that provide both nutritional and medicinal benefits, such as vitamins, dietary supplements, and herbal products. “Although patients may be interested in nutraceuticals as a potential treatment option for acne, there is uncertainty regarding the efficacy and safety of these products,” they wrote.
For the systematic review, they searched the PubMed, Embase, Cochrane Central Register of Controlled Trials, and Web of Science databases from inception through January 30, 2023, to identify randomized clinical trials that evaluated oral nutraceutical interventions such as vitamins and minerals, botanical extracts, prebiotics, and probiotics in individuals with acne. They extracted clinician-reported outcomes, patient-reported outcomes, and adverse events from the included studies, and used the Cochrane Risk of Bias checklist tool to assess the quality of evidence in randomized clinical trials. Based on this tool, they used Agency for Healthcare Research and Quality standards to categorize the articles as good, fair, or poor quality.
The search yielded 42 unique studies with 3,346 participants. Of these 42 studies, 27 were considered poor quality, 11 were considered fair quality, and 4 were considered good quality. The good-quality studies separately evaluated four interventions: vitamin D, green tea extract, probiotics, and cheongsangbangpoong-tang, an herbal formula approved for use in acne by the Korea Food and Drug Administration.
The 11 fair-quality studies suggested potential effectiveness for pantothenic acid (vitamin B5), the fatty acids omega-3 (eicosapentaenoic acid [EPA] and/or docosahexaenoic acid [DHA]) and omega-6 (gamma-linoleic acid), and probiotics.
Zinc was the most studied nutraceutical identified in the review, but “there was substantial heterogeneity in the results, with only slightly greater than one-half of studies finding zinc to be efficacious,” the authors noted. “Studies using higher doses more often found zinc to be efficacious,” they said, adding that zinc “had the highest rate of adverse effect reporting of any nutraceuticals assessed in this review.”
Dr. Barbieri and colleagues acknowledged limitations of their analysis, including the fact that few of the nutraceuticals considered to have good or fair evidence for their use were evaluated in more than one study. “In addition, some studies had inconsistent results depending on the outcome measure assessed,” they wrote. “For instance, although green tea extract led to statistically significant improvements in lesion counts, it did not result in statistically significant improvements in quality of life, suggesting the observed lesion count differences may not be clinically meaningful to patients.”
And while probiotics had the most studies supporting their efficacy, they were generally of very small sample size.
Asked to comment on the study, Jonette Keri, MD, PhD, a dermatologist who directs the Acne and Rosacea Treatment Center at the University of Miami, who was not involved with the study, said that while the review was exhaustive, more research is needed to better determine the efficacy and side effects of the products studied. “The real strength of this wonderful review is now we have all of this information in one place, and this will serve as a great patient care resource,” she told this news organization.
Dr. Barbieri reported personal fees from Dexcel Pharma for consulting outside the submitted work. Dr. Keri disclosed that she is a consultant for L’Oréal.
.
“While many topical and systemic prescription options are available for the treatment of acne, some patients may be interested in natural and complementary therapies as either an adjunctive or an alternative to prescription medications,” researchers led by John S. Barbieri, MD, MBA, of the department of dermatology at Brigham and Women’s Hospital, Boston, wrote in their study, which was published online in JAMA Dermatology. The researchers defined nutraceuticals as products derived from food sources that provide both nutritional and medicinal benefits, such as vitamins, dietary supplements, and herbal products. “Although patients may be interested in nutraceuticals as a potential treatment option for acne, there is uncertainty regarding the efficacy and safety of these products,” they wrote.
For the systematic review, they searched the PubMed, Embase, Cochrane Central Register of Controlled Trials, and Web of Science databases from inception through January 30, 2023, to identify randomized clinical trials that evaluated oral nutraceutical interventions such as vitamins and minerals, botanical extracts, prebiotics, and probiotics in individuals with acne. They extracted clinician-reported outcomes, patient-reported outcomes, and adverse events from the included studies, and used the Cochrane Risk of Bias checklist tool to assess the quality of evidence in randomized clinical trials. Based on this tool, they used Agency for Healthcare Research and Quality standards to categorize the articles as good, fair, or poor quality.
The search yielded 42 unique studies with 3,346 participants. Of these 42 studies, 27 were considered poor quality, 11 were considered fair quality, and 4 were considered good quality. The good-quality studies separately evaluated four interventions: vitamin D, green tea extract, probiotics, and cheongsangbangpoong-tang, an herbal formula approved for use in acne by the Korea Food and Drug Administration.
The 11 fair-quality studies suggested potential effectiveness for pantothenic acid (vitamin B5), the fatty acids omega-3 (eicosapentaenoic acid [EPA] and/or docosahexaenoic acid [DHA]) and omega-6 (gamma-linoleic acid), and probiotics.
Zinc was the most studied nutraceutical identified in the review, but “there was substantial heterogeneity in the results, with only slightly greater than one-half of studies finding zinc to be efficacious,” the authors noted. “Studies using higher doses more often found zinc to be efficacious,” they said, adding that zinc “had the highest rate of adverse effect reporting of any nutraceuticals assessed in this review.”
Dr. Barbieri and colleagues acknowledged limitations of their analysis, including the fact that few of the nutraceuticals considered to have good or fair evidence for their use were evaluated in more than one study. “In addition, some studies had inconsistent results depending on the outcome measure assessed,” they wrote. “For instance, although green tea extract led to statistically significant improvements in lesion counts, it did not result in statistically significant improvements in quality of life, suggesting the observed lesion count differences may not be clinically meaningful to patients.”
And while probiotics had the most studies supporting their efficacy, they were generally of very small sample size.
Asked to comment on the study, Jonette Keri, MD, PhD, a dermatologist who directs the Acne and Rosacea Treatment Center at the University of Miami, who was not involved with the study, said that while the review was exhaustive, more research is needed to better determine the efficacy and side effects of the products studied. “The real strength of this wonderful review is now we have all of this information in one place, and this will serve as a great patient care resource,” she told this news organization.
Dr. Barbieri reported personal fees from Dexcel Pharma for consulting outside the submitted work. Dr. Keri disclosed that she is a consultant for L’Oréal.
.
“While many topical and systemic prescription options are available for the treatment of acne, some patients may be interested in natural and complementary therapies as either an adjunctive or an alternative to prescription medications,” researchers led by John S. Barbieri, MD, MBA, of the department of dermatology at Brigham and Women’s Hospital, Boston, wrote in their study, which was published online in JAMA Dermatology. The researchers defined nutraceuticals as products derived from food sources that provide both nutritional and medicinal benefits, such as vitamins, dietary supplements, and herbal products. “Although patients may be interested in nutraceuticals as a potential treatment option for acne, there is uncertainty regarding the efficacy and safety of these products,” they wrote.
For the systematic review, they searched the PubMed, Embase, Cochrane Central Register of Controlled Trials, and Web of Science databases from inception through January 30, 2023, to identify randomized clinical trials that evaluated oral nutraceutical interventions such as vitamins and minerals, botanical extracts, prebiotics, and probiotics in individuals with acne. They extracted clinician-reported outcomes, patient-reported outcomes, and adverse events from the included studies, and used the Cochrane Risk of Bias checklist tool to assess the quality of evidence in randomized clinical trials. Based on this tool, they used Agency for Healthcare Research and Quality standards to categorize the articles as good, fair, or poor quality.
The search yielded 42 unique studies with 3,346 participants. Of these 42 studies, 27 were considered poor quality, 11 were considered fair quality, and 4 were considered good quality. The good-quality studies separately evaluated four interventions: vitamin D, green tea extract, probiotics, and cheongsangbangpoong-tang, an herbal formula approved for use in acne by the Korea Food and Drug Administration.
The 11 fair-quality studies suggested potential effectiveness for pantothenic acid (vitamin B5), the fatty acids omega-3 (eicosapentaenoic acid [EPA] and/or docosahexaenoic acid [DHA]) and omega-6 (gamma-linoleic acid), and probiotics.
Zinc was the most studied nutraceutical identified in the review, but “there was substantial heterogeneity in the results, with only slightly greater than one-half of studies finding zinc to be efficacious,” the authors noted. “Studies using higher doses more often found zinc to be efficacious,” they said, adding that zinc “had the highest rate of adverse effect reporting of any nutraceuticals assessed in this review.”
Dr. Barbieri and colleagues acknowledged limitations of their analysis, including the fact that few of the nutraceuticals considered to have good or fair evidence for their use were evaluated in more than one study. “In addition, some studies had inconsistent results depending on the outcome measure assessed,” they wrote. “For instance, although green tea extract led to statistically significant improvements in lesion counts, it did not result in statistically significant improvements in quality of life, suggesting the observed lesion count differences may not be clinically meaningful to patients.”
And while probiotics had the most studies supporting their efficacy, they were generally of very small sample size.
Asked to comment on the study, Jonette Keri, MD, PhD, a dermatologist who directs the Acne and Rosacea Treatment Center at the University of Miami, who was not involved with the study, said that while the review was exhaustive, more research is needed to better determine the efficacy and side effects of the products studied. “The real strength of this wonderful review is now we have all of this information in one place, and this will serve as a great patient care resource,” she told this news organization.
Dr. Barbieri reported personal fees from Dexcel Pharma for consulting outside the submitted work. Dr. Keri disclosed that she is a consultant for L’Oréal.
FROM JAMA DERMATOLOGY
mRNA vaccine cuts COVID-related Guillain-Barré risk
TOPLINE:
, according to a new study that also showed receipt of the Pfizer-BioNTech mRNA vaccine reduced GSB risk by 59%.
METHODOLOGY:
- The nested-case control study analyzed data from the largest healthcare provider in Israel for 3.2 million patients aged 16 years and older, with no history of GBS.
- GBS cases (n = 76) were identified based on hospital discharge data from January 2021 to June 2022.
- For every GBS case, investigators chose 10 controls at random, matched for age, gender, and follow-up duration (n = 760).
- Investigators examined the association between GBS and SARS-CoV-2 infection, established through documentation of prior positive SARS-CoV-2 test (PCR or antigen), and any COVID-19 vaccine administration.
TAKEAWAY:
- Among those diagnosed with GBS, 8 were exposed to SARS-CoV-2 infection only, 7 were exposed to COVID-19 vaccination only, and 1 patient was exposed to both SARS-CoV-2 infection and COVID-19 vaccination in the prior 6 weeks, leaving 60 GBS patients without exposure to either infection or vaccination.
- All COVID-19 vaccine doses administered in GBS cases within 6 weeks of the index date, and all but two doses administered in controls in the same timeframe, were Pfizer-BioNTech vaccines.
- Compared with people without GBS, those with the condition were more than six times as likely to have had SARS-CoV-2 infection within 6 weeks of GBS diagnosis (adjusted odds ratio, 6.30; 95% confidence interval, 2.55-15.56).
- People who received the COVID-19 vaccine were 59% less likely to develop GBS than those who did not get the vaccine (aOR, 0.41; 95% CI, 0.17-0.96).
IN PRACTICE:
“While Guillain-Barré is extremely rare, people should be aware that having a COVID infection can increase their risk of developing the disorder, and receiving an mRNA vaccine can decrease their risk,” study author Anat Arbel, MD, of Lady Davis Carmel Medical Center and the Technion-Israel Institute of Technology, Haifa, Israel, said in a press release.
SOURCE:
In addition to Dr. Arbel, the other lead author is Haya Bishara, MD, of Lady Davis Carmel Medical Center. The research was published online in the journal Neurology.
LIMITATIONS:
There is a possibility of misclassification of SARS-CoV-2 infection, which could lead to an overestimation of the magnitude of association between infection and GBS. The diagnosis of GBS relied solely on ICD-9 coding, which has been shown in prior studies to contain errors.
DISCLOSURES:
The study was unfunded. Dr. Bishara and Dr. Arbel report no relevant financial relationships. One co-author, Eitan Auriel, MD, has received lecturer fees from Novo Nordisk, Pfizer, Boehringer Ingelheim, and Medison.
A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a new study that also showed receipt of the Pfizer-BioNTech mRNA vaccine reduced GSB risk by 59%.
METHODOLOGY:
- The nested-case control study analyzed data from the largest healthcare provider in Israel for 3.2 million patients aged 16 years and older, with no history of GBS.
- GBS cases (n = 76) were identified based on hospital discharge data from January 2021 to June 2022.
- For every GBS case, investigators chose 10 controls at random, matched for age, gender, and follow-up duration (n = 760).
- Investigators examined the association between GBS and SARS-CoV-2 infection, established through documentation of prior positive SARS-CoV-2 test (PCR or antigen), and any COVID-19 vaccine administration.
TAKEAWAY:
- Among those diagnosed with GBS, 8 were exposed to SARS-CoV-2 infection only, 7 were exposed to COVID-19 vaccination only, and 1 patient was exposed to both SARS-CoV-2 infection and COVID-19 vaccination in the prior 6 weeks, leaving 60 GBS patients without exposure to either infection or vaccination.
- All COVID-19 vaccine doses administered in GBS cases within 6 weeks of the index date, and all but two doses administered in controls in the same timeframe, were Pfizer-BioNTech vaccines.
- Compared with people without GBS, those with the condition were more than six times as likely to have had SARS-CoV-2 infection within 6 weeks of GBS diagnosis (adjusted odds ratio, 6.30; 95% confidence interval, 2.55-15.56).
- People who received the COVID-19 vaccine were 59% less likely to develop GBS than those who did not get the vaccine (aOR, 0.41; 95% CI, 0.17-0.96).
IN PRACTICE:
“While Guillain-Barré is extremely rare, people should be aware that having a COVID infection can increase their risk of developing the disorder, and receiving an mRNA vaccine can decrease their risk,” study author Anat Arbel, MD, of Lady Davis Carmel Medical Center and the Technion-Israel Institute of Technology, Haifa, Israel, said in a press release.
SOURCE:
In addition to Dr. Arbel, the other lead author is Haya Bishara, MD, of Lady Davis Carmel Medical Center. The research was published online in the journal Neurology.
LIMITATIONS:
There is a possibility of misclassification of SARS-CoV-2 infection, which could lead to an overestimation of the magnitude of association between infection and GBS. The diagnosis of GBS relied solely on ICD-9 coding, which has been shown in prior studies to contain errors.
DISCLOSURES:
The study was unfunded. Dr. Bishara and Dr. Arbel report no relevant financial relationships. One co-author, Eitan Auriel, MD, has received lecturer fees from Novo Nordisk, Pfizer, Boehringer Ingelheim, and Medison.
A version of this article first appeared on Medscape.com.
TOPLINE:
, according to a new study that also showed receipt of the Pfizer-BioNTech mRNA vaccine reduced GSB risk by 59%.
METHODOLOGY:
- The nested-case control study analyzed data from the largest healthcare provider in Israel for 3.2 million patients aged 16 years and older, with no history of GBS.
- GBS cases (n = 76) were identified based on hospital discharge data from January 2021 to June 2022.
- For every GBS case, investigators chose 10 controls at random, matched for age, gender, and follow-up duration (n = 760).
- Investigators examined the association between GBS and SARS-CoV-2 infection, established through documentation of prior positive SARS-CoV-2 test (PCR or antigen), and any COVID-19 vaccine administration.
TAKEAWAY:
- Among those diagnosed with GBS, 8 were exposed to SARS-CoV-2 infection only, 7 were exposed to COVID-19 vaccination only, and 1 patient was exposed to both SARS-CoV-2 infection and COVID-19 vaccination in the prior 6 weeks, leaving 60 GBS patients without exposure to either infection or vaccination.
- All COVID-19 vaccine doses administered in GBS cases within 6 weeks of the index date, and all but two doses administered in controls in the same timeframe, were Pfizer-BioNTech vaccines.
- Compared with people without GBS, those with the condition were more than six times as likely to have had SARS-CoV-2 infection within 6 weeks of GBS diagnosis (adjusted odds ratio, 6.30; 95% confidence interval, 2.55-15.56).
- People who received the COVID-19 vaccine were 59% less likely to develop GBS than those who did not get the vaccine (aOR, 0.41; 95% CI, 0.17-0.96).
IN PRACTICE:
“While Guillain-Barré is extremely rare, people should be aware that having a COVID infection can increase their risk of developing the disorder, and receiving an mRNA vaccine can decrease their risk,” study author Anat Arbel, MD, of Lady Davis Carmel Medical Center and the Technion-Israel Institute of Technology, Haifa, Israel, said in a press release.
SOURCE:
In addition to Dr. Arbel, the other lead author is Haya Bishara, MD, of Lady Davis Carmel Medical Center. The research was published online in the journal Neurology.
LIMITATIONS:
There is a possibility of misclassification of SARS-CoV-2 infection, which could lead to an overestimation of the magnitude of association between infection and GBS. The diagnosis of GBS relied solely on ICD-9 coding, which has been shown in prior studies to contain errors.
DISCLOSURES:
The study was unfunded. Dr. Bishara and Dr. Arbel report no relevant financial relationships. One co-author, Eitan Auriel, MD, has received lecturer fees from Novo Nordisk, Pfizer, Boehringer Ingelheim, and Medison.
A version of this article first appeared on Medscape.com.
Higher weight loss on tirzepatide links to seven factors
TOPLINE:
Among the 3,188 people with type 2 diabetes who were adherent to their tirzepatide (Mounjaro, Lilly) regimen in four pivotal trials of the agent, a quarter achieved at least a 15% cut from their baseline body weight after 40-42 weeks of treatment, and researchers found seven baseline variables that were significantly linked with a higher incidence of this level of weight loss.
say the authors.
METHODOLOGY:
- Investigators conducted a post hoc analysis of data collected from a total of 3,188 people with type 2 diabetes who had been adherent to their assigned tirzepatide regimen for 40-42 weeks in any one of four pivotal trials of the agent.
- The researchers aimed to identify predictors of a reduction in body weight of at least 15% with tirzepatide treatment at any of the three tested doses – 5 mg, 10 mg, or 15 mg – which were administered by subcutaneous injection once a week.
- All four trials that provided data prohibited concurrent therapy that would promote weight loss, and the people included in the analysis did not receive any rescue medications for controlling glycemia.
- The primary efficacy measure in all four studies was the ability of tirzepatide to improve glycemic control (measured by A1c level), compared with placebo, semaglutide (Ozempic) 1 mg SC once weekly, insulin degludec (Tresiba, Novo Nordisk), or insulin glargine (Basaglar, Lilly).
TAKEAWAY:
- Among the 3,188 people who remained adherent to their tirzepatide regimen for 40-42 weeks, 792 (25%) experienced a weight reduction of at least 15% from baseline.
- Multivariate analysis of baseline covariates showed that these seven factors were significantly linked with greater than or equal to 15% weight loss: higher tirzepatide dose, being female, being of White or Asian race, being of younger age, undergoing treatment with metformin, having better glycemic control (based on lower A1c and lower fasting serum glucose), and having lower non–high-density lipoprotein cholesterol level.
- During follow-up, achievement of at least a 15% cut in baseline body weight was significantly associated with greater reductions in A1c, fasting serum glucose level, waist circumference, blood pressure, serum triglyceride level, and serum level of the liver enzyme alanine transaminase.
IN PRACTICE:
“These findings may provide valuable information to clinicians and people with type 2 diabetes regarding the likelihood of achieving substantial body weight reduction with tirzepatide and also help to signal likely improvements to be seen in a range of cardiometabolic risk parameters with tirzepatide-induced weight loss,” the authors concluded in their report.
SOURCE:
The study was largely run by researchers who are employees of Lilly, the company that markets tirzepatide (Mounjaro). It was published in Diabetes Care.
LIMITATIONS:
- The analysis was post hoc.
- The follow-up was limited.
- The analysis focused entirely on baseline parameters as potential predictors of weight loss magnitude.
DISCLOSURES:
The study was funded by Eli Lilly, the company that markets tirzepatide (Mounjaro) and that sponsored the SURPASS trials. Six authors are employees of Lilly, one is a contractor for Lilly, and the two remaining authors have had financial relationships with Lilly and with several other companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Among the 3,188 people with type 2 diabetes who were adherent to their tirzepatide (Mounjaro, Lilly) regimen in four pivotal trials of the agent, a quarter achieved at least a 15% cut from their baseline body weight after 40-42 weeks of treatment, and researchers found seven baseline variables that were significantly linked with a higher incidence of this level of weight loss.
say the authors.
METHODOLOGY:
- Investigators conducted a post hoc analysis of data collected from a total of 3,188 people with type 2 diabetes who had been adherent to their assigned tirzepatide regimen for 40-42 weeks in any one of four pivotal trials of the agent.
- The researchers aimed to identify predictors of a reduction in body weight of at least 15% with tirzepatide treatment at any of the three tested doses – 5 mg, 10 mg, or 15 mg – which were administered by subcutaneous injection once a week.
- All four trials that provided data prohibited concurrent therapy that would promote weight loss, and the people included in the analysis did not receive any rescue medications for controlling glycemia.
- The primary efficacy measure in all four studies was the ability of tirzepatide to improve glycemic control (measured by A1c level), compared with placebo, semaglutide (Ozempic) 1 mg SC once weekly, insulin degludec (Tresiba, Novo Nordisk), or insulin glargine (Basaglar, Lilly).
TAKEAWAY:
- Among the 3,188 people who remained adherent to their tirzepatide regimen for 40-42 weeks, 792 (25%) experienced a weight reduction of at least 15% from baseline.
- Multivariate analysis of baseline covariates showed that these seven factors were significantly linked with greater than or equal to 15% weight loss: higher tirzepatide dose, being female, being of White or Asian race, being of younger age, undergoing treatment with metformin, having better glycemic control (based on lower A1c and lower fasting serum glucose), and having lower non–high-density lipoprotein cholesterol level.
- During follow-up, achievement of at least a 15% cut in baseline body weight was significantly associated with greater reductions in A1c, fasting serum glucose level, waist circumference, blood pressure, serum triglyceride level, and serum level of the liver enzyme alanine transaminase.
IN PRACTICE:
“These findings may provide valuable information to clinicians and people with type 2 diabetes regarding the likelihood of achieving substantial body weight reduction with tirzepatide and also help to signal likely improvements to be seen in a range of cardiometabolic risk parameters with tirzepatide-induced weight loss,” the authors concluded in their report.
SOURCE:
The study was largely run by researchers who are employees of Lilly, the company that markets tirzepatide (Mounjaro). It was published in Diabetes Care.
LIMITATIONS:
- The analysis was post hoc.
- The follow-up was limited.
- The analysis focused entirely on baseline parameters as potential predictors of weight loss magnitude.
DISCLOSURES:
The study was funded by Eli Lilly, the company that markets tirzepatide (Mounjaro) and that sponsored the SURPASS trials. Six authors are employees of Lilly, one is a contractor for Lilly, and the two remaining authors have had financial relationships with Lilly and with several other companies.
A version of this article first appeared on Medscape.com.
TOPLINE:
Among the 3,188 people with type 2 diabetes who were adherent to their tirzepatide (Mounjaro, Lilly) regimen in four pivotal trials of the agent, a quarter achieved at least a 15% cut from their baseline body weight after 40-42 weeks of treatment, and researchers found seven baseline variables that were significantly linked with a higher incidence of this level of weight loss.
say the authors.
METHODOLOGY:
- Investigators conducted a post hoc analysis of data collected from a total of 3,188 people with type 2 diabetes who had been adherent to their assigned tirzepatide regimen for 40-42 weeks in any one of four pivotal trials of the agent.
- The researchers aimed to identify predictors of a reduction in body weight of at least 15% with tirzepatide treatment at any of the three tested doses – 5 mg, 10 mg, or 15 mg – which were administered by subcutaneous injection once a week.
- All four trials that provided data prohibited concurrent therapy that would promote weight loss, and the people included in the analysis did not receive any rescue medications for controlling glycemia.
- The primary efficacy measure in all four studies was the ability of tirzepatide to improve glycemic control (measured by A1c level), compared with placebo, semaglutide (Ozempic) 1 mg SC once weekly, insulin degludec (Tresiba, Novo Nordisk), or insulin glargine (Basaglar, Lilly).
TAKEAWAY:
- Among the 3,188 people who remained adherent to their tirzepatide regimen for 40-42 weeks, 792 (25%) experienced a weight reduction of at least 15% from baseline.
- Multivariate analysis of baseline covariates showed that these seven factors were significantly linked with greater than or equal to 15% weight loss: higher tirzepatide dose, being female, being of White or Asian race, being of younger age, undergoing treatment with metformin, having better glycemic control (based on lower A1c and lower fasting serum glucose), and having lower non–high-density lipoprotein cholesterol level.
- During follow-up, achievement of at least a 15% cut in baseline body weight was significantly associated with greater reductions in A1c, fasting serum glucose level, waist circumference, blood pressure, serum triglyceride level, and serum level of the liver enzyme alanine transaminase.
IN PRACTICE:
“These findings may provide valuable information to clinicians and people with type 2 diabetes regarding the likelihood of achieving substantial body weight reduction with tirzepatide and also help to signal likely improvements to be seen in a range of cardiometabolic risk parameters with tirzepatide-induced weight loss,” the authors concluded in their report.
SOURCE:
The study was largely run by researchers who are employees of Lilly, the company that markets tirzepatide (Mounjaro). It was published in Diabetes Care.
LIMITATIONS:
- The analysis was post hoc.
- The follow-up was limited.
- The analysis focused entirely on baseline parameters as potential predictors of weight loss magnitude.
DISCLOSURES:
The study was funded by Eli Lilly, the company that markets tirzepatide (Mounjaro) and that sponsored the SURPASS trials. Six authors are employees of Lilly, one is a contractor for Lilly, and the two remaining authors have had financial relationships with Lilly and with several other companies.
A version of this article first appeared on Medscape.com.
Adolescents with atopic dermatitis more likely to have experienced bullying, study finds
TOPLINE:
METHODOLOGY:
- Adolescents with AD have reported appearance-based bullying.
- To evaluate the association between AD and the prevalence and frequency of bullying, researchers analyzed cross-sectional data from adult caregivers of U.S. adolescents aged 12-17 years who participated in the 2021 National Health Interview Survey.
- Logistic regression and ordinal logistic regression were used to compare the prevalence of experiencing one or more bullying encounters during the previous 12 months and the frequency of bullying between adolescents with and those without AD.
TAKEAWAY:
- A total of 3,207 adolescents were included in the analysis. The mean age of the participants was 14.5 years, and 11.9% currently had AD. The prevalence of experiencing bullying was significantly higher among adolescents with AD, compared with those without AD (33.2% vs. 19%; P < .001), as was the prevalence of cyberbullying (9.1% vs. 5.8%; P = .04).
- Following adjustment for demographics and atopic comorbidities, adolescents with AD were at increased odds of bullying, compared with their peers without AD (adjusted odds ratio, 1.99; 95% confidence interval, 1.45-2.73).
- Following adjustment for demographics, adolescents with AD were also at increased odds of cyberbullying, compared with their peers without AD (AOR, 1.65; 95% CI, 1.04-2.62), but no association was observed following adjustment for atopic comorbidities (AOR, 1.27; 95% CI, 0.82-1.96).
- Following ordinal logistic regression that was adjusted for demographics and atopic comorbidities, adolescents with AD were at greater odds of being bullied at a higher frequency, compared with their peers without AD (AOR, 1.97; 95% CI, 1.44-2.68).
IN PRACTICE:
“Larger, future studies using clinical AD diagnoses and adolescent self-report can advance understanding of bullying and AD,” the researchers wrote. “Clinicians, families, and schools should address and monitor bullying among adolescents.”
SOURCE:
Howa Yeung, MD, of the department of dermatology at Emory University School of Medicine, Atlanta, led the research. The study was published online in JAMA Dermatology.
LIMITATIONS:
Limitations include the study’s cross-sectional design. In addition, the investigators could not directly attribute bullying to skin-specific findings, and it was a caregiver report.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One of the authors, Joy Wan, MD, received grants from Pfizer and personal fees from Janssen and Sun Pharmaceuticals outside of the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Adolescents with AD have reported appearance-based bullying.
- To evaluate the association between AD and the prevalence and frequency of bullying, researchers analyzed cross-sectional data from adult caregivers of U.S. adolescents aged 12-17 years who participated in the 2021 National Health Interview Survey.
- Logistic regression and ordinal logistic regression were used to compare the prevalence of experiencing one or more bullying encounters during the previous 12 months and the frequency of bullying between adolescents with and those without AD.
TAKEAWAY:
- A total of 3,207 adolescents were included in the analysis. The mean age of the participants was 14.5 years, and 11.9% currently had AD. The prevalence of experiencing bullying was significantly higher among adolescents with AD, compared with those without AD (33.2% vs. 19%; P < .001), as was the prevalence of cyberbullying (9.1% vs. 5.8%; P = .04).
- Following adjustment for demographics and atopic comorbidities, adolescents with AD were at increased odds of bullying, compared with their peers without AD (adjusted odds ratio, 1.99; 95% confidence interval, 1.45-2.73).
- Following adjustment for demographics, adolescents with AD were also at increased odds of cyberbullying, compared with their peers without AD (AOR, 1.65; 95% CI, 1.04-2.62), but no association was observed following adjustment for atopic comorbidities (AOR, 1.27; 95% CI, 0.82-1.96).
- Following ordinal logistic regression that was adjusted for demographics and atopic comorbidities, adolescents with AD were at greater odds of being bullied at a higher frequency, compared with their peers without AD (AOR, 1.97; 95% CI, 1.44-2.68).
IN PRACTICE:
“Larger, future studies using clinical AD diagnoses and adolescent self-report can advance understanding of bullying and AD,” the researchers wrote. “Clinicians, families, and schools should address and monitor bullying among adolescents.”
SOURCE:
Howa Yeung, MD, of the department of dermatology at Emory University School of Medicine, Atlanta, led the research. The study was published online in JAMA Dermatology.
LIMITATIONS:
Limitations include the study’s cross-sectional design. In addition, the investigators could not directly attribute bullying to skin-specific findings, and it was a caregiver report.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One of the authors, Joy Wan, MD, received grants from Pfizer and personal fees from Janssen and Sun Pharmaceuticals outside of the submitted work.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Adolescents with AD have reported appearance-based bullying.
- To evaluate the association between AD and the prevalence and frequency of bullying, researchers analyzed cross-sectional data from adult caregivers of U.S. adolescents aged 12-17 years who participated in the 2021 National Health Interview Survey.
- Logistic regression and ordinal logistic regression were used to compare the prevalence of experiencing one or more bullying encounters during the previous 12 months and the frequency of bullying between adolescents with and those without AD.
TAKEAWAY:
- A total of 3,207 adolescents were included in the analysis. The mean age of the participants was 14.5 years, and 11.9% currently had AD. The prevalence of experiencing bullying was significantly higher among adolescents with AD, compared with those without AD (33.2% vs. 19%; P < .001), as was the prevalence of cyberbullying (9.1% vs. 5.8%; P = .04).
- Following adjustment for demographics and atopic comorbidities, adolescents with AD were at increased odds of bullying, compared with their peers without AD (adjusted odds ratio, 1.99; 95% confidence interval, 1.45-2.73).
- Following adjustment for demographics, adolescents with AD were also at increased odds of cyberbullying, compared with their peers without AD (AOR, 1.65; 95% CI, 1.04-2.62), but no association was observed following adjustment for atopic comorbidities (AOR, 1.27; 95% CI, 0.82-1.96).
- Following ordinal logistic regression that was adjusted for demographics and atopic comorbidities, adolescents with AD were at greater odds of being bullied at a higher frequency, compared with their peers without AD (AOR, 1.97; 95% CI, 1.44-2.68).
IN PRACTICE:
“Larger, future studies using clinical AD diagnoses and adolescent self-report can advance understanding of bullying and AD,” the researchers wrote. “Clinicians, families, and schools should address and monitor bullying among adolescents.”
SOURCE:
Howa Yeung, MD, of the department of dermatology at Emory University School of Medicine, Atlanta, led the research. The study was published online in JAMA Dermatology.
LIMITATIONS:
Limitations include the study’s cross-sectional design. In addition, the investigators could not directly attribute bullying to skin-specific findings, and it was a caregiver report.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One of the authors, Joy Wan, MD, received grants from Pfizer and personal fees from Janssen and Sun Pharmaceuticals outside of the submitted work.
A version of this article first appeared on Medscape.com.
Heart rate variability: Are we ignoring a harbinger of health?
A very long time ago, when I ran clinical labs, one of the most ordered tests was the “sed rate” (aka ESR, the erythrocyte sedimentation rate). Easy, quick, and low cost, with high sensitivity but very low specificity. If the sed rate was normal, the patient probably did not have an infectious or inflammatory disease. If it was elevated, they probably did, but no telling what. Later, the C-reactive protein (CRP) test came into common use. Same general inferences: If the CRP was low, the patient was unlikely to have an inflammatory process; if high, they were sick, but we didn’t know what with.
Could the heart rate variability (HRV) score come to be thought of similarly? Much as the sed rate and CRP are sensitivity indicators of infectious or inflammatory diseases, might the HRV score be a sensitivity indicator for nervous system (central and autonomic) and cardiovascular (especially heart rhythm) malfunctions?
A substantial and relatively old body of heart rhythm literature ties HRV alterations to posttraumatic stress disorder, physician occupational stress, sleep disorders, depression, autonomic nervous system derangements, various cardiac arrhythmias, fatigue, overexertion, medications, and age itself.
More than 100 million Americans are now believed to use smartwatches or personal fitness monitors. Some 30%-40% of these devices measure HRV. So what? Credible research about this huge mass of accumulating data from “wearables” is lacking.
What is HRV?
HRV is the variation in time between each heartbeat, in milliseconds. HRV is influenced by the autonomic nervous system, perhaps reflecting sympathetic-parasympathetic balance. Some devices measure HRV 24/7. My Fitbit Inspire 2 reports only nighttime measures during 3 hours of sustained sleep. Most trackers report averages; some calculate the root mean squares; others calculate standard deviations. All fitness trackers warn not to use the data for medical purposes.
Normal values (reference ranges) for HRV begin at an average of 100 msec in the first decade of life and decline by approximately 10 msec per decade lived. At age 30-40, the average is 70 msec; age 60-70, it’s 40 msec; and at age 90-100, it’s 10 msec.
As a long-time lab guy, I used to teach proper use of lab tests. Fitness trackers are “lab tests” of a sort. We taught never to do a lab test unless you know what you are going to do with the result, no matter what it is. We also taught “never do anything just because you can.” Curiosity, we know, is a frequent driver of lab test ordering.
That underlying philosophy gives me a hard time when it comes to wearables. I have been enamored of watching my step count, active zone minutes, resting heart rate, active heart rate, various sleep scores, and breathing rate (and, of course, a manually entered early morning daily body weight) for several years. I even check my “readiness score” (a calculation using resting heart rate, recent sleep, recent active zone minutes, and perhaps HRV) each morning and adjust my behaviors accordingly.
Why monitor HRV?
But what should we do with HRV scores? Ignore them? Try to understand them, perhaps as a screening tool? Or monitor HRV for consistency or change? “Monitoring” is a proper and common use of lab tests.
Some say we should improve the HRV score by managing stress, getting regular exercise, eating a healthy diet, getting enough sleep, and not smoking or consuming excess alcohol. Duh! I do all of that anyway.
The claims that HRV is a “simple but powerful tool that can be used to track overall health and well-being” might turn out to be true. Proper study and sharing of data will enable that determination.
To advance understanding, I offer an n-of-1, a real-world personal anecdote about HRV.
I did not request the HRV function on my Fitbit Inspire 2. It simply appeared, and I ignored it for some time.
A year or two ago, I started noticing my HRV score every morning. Initially, I did not like to see my “low” score, until I learned that the reference range was dramatically affected by age and I was in my late 80s at the time. The vast majority of my HRV readings were in the range of 17 msec to 27 msec.
Last week, I was administered the new Moderna COVID-19 Spikevax vaccine and the old folks’ influenza vaccine simultaneously. In my case, side effects from each vaccine have been modest in the past, but I never previously had both administered at the same time. My immune response was, shall we say, robust. Chills, muscle aches, headache, fatigue, deltoid swelling, fitful sleep, and increased resting heart rate.
My nightly average HRV had been running between 17 msec and 35 msec for many months. WHOA! After the shots, my overnight HRV score plummeted from 24 msec to 10 msec, my lowest ever. Instant worry. The next day, it rebounded to 28 msec, and it has been in the high teens or low 20s since then.
Off to PubMed. A recent study of HRV on the second and 10th days after administering the Pfizer mRNA vaccine to 75 healthy volunteers found that the HRV on day 2 was dramatically lower than prevaccination levels and by day 10, it had returned to prevaccination levels. Some comfort there.
Another review article has reported a rapid fall and rapid rebound of HRV after COVID-19 vaccination. A 2010 report demonstrated a significant but not dramatic short-term lowering of HRV after influenza A vaccination and correlated it with CRP changes.
Some believe that the decline in HRV after vaccination reflects an increased immune response and sympathetic nervous activity.
I don’t plan to receive my flu and COVID vaccines on the same day again.
So, I went back to review what happened to my HRV when I had COVID in 2023. My HRV was 14 msec and 12 msec on the first 2 days of symptoms, and then returned to the 20 msec range.
I received the RSV vaccine this year without adverse effects, and my HRV scores were 29 msec, 33 msec, and 32 msec on the first 3 days after vaccination. Finally, after receiving a pneumococcal vaccine in 2023, I had no adverse effects, and my HRV scores on the 5 days after vaccination were indeterminate: 19 msec, 14 msec, 18 msec, 13 msec, and 17 msec.
Of course, correlation is not causation. Cause and effect remain undetermined. But I find these observations interesting for a potentially useful screening test.
George D. Lundberg, MD, is the Editor in Chief of Cancer Commons.
A version of this article first appeared on Medscape.com.
A very long time ago, when I ran clinical labs, one of the most ordered tests was the “sed rate” (aka ESR, the erythrocyte sedimentation rate). Easy, quick, and low cost, with high sensitivity but very low specificity. If the sed rate was normal, the patient probably did not have an infectious or inflammatory disease. If it was elevated, they probably did, but no telling what. Later, the C-reactive protein (CRP) test came into common use. Same general inferences: If the CRP was low, the patient was unlikely to have an inflammatory process; if high, they were sick, but we didn’t know what with.
Could the heart rate variability (HRV) score come to be thought of similarly? Much as the sed rate and CRP are sensitivity indicators of infectious or inflammatory diseases, might the HRV score be a sensitivity indicator for nervous system (central and autonomic) and cardiovascular (especially heart rhythm) malfunctions?
A substantial and relatively old body of heart rhythm literature ties HRV alterations to posttraumatic stress disorder, physician occupational stress, sleep disorders, depression, autonomic nervous system derangements, various cardiac arrhythmias, fatigue, overexertion, medications, and age itself.
More than 100 million Americans are now believed to use smartwatches or personal fitness monitors. Some 30%-40% of these devices measure HRV. So what? Credible research about this huge mass of accumulating data from “wearables” is lacking.
What is HRV?
HRV is the variation in time between each heartbeat, in milliseconds. HRV is influenced by the autonomic nervous system, perhaps reflecting sympathetic-parasympathetic balance. Some devices measure HRV 24/7. My Fitbit Inspire 2 reports only nighttime measures during 3 hours of sustained sleep. Most trackers report averages; some calculate the root mean squares; others calculate standard deviations. All fitness trackers warn not to use the data for medical purposes.
Normal values (reference ranges) for HRV begin at an average of 100 msec in the first decade of life and decline by approximately 10 msec per decade lived. At age 30-40, the average is 70 msec; age 60-70, it’s 40 msec; and at age 90-100, it’s 10 msec.
As a long-time lab guy, I used to teach proper use of lab tests. Fitness trackers are “lab tests” of a sort. We taught never to do a lab test unless you know what you are going to do with the result, no matter what it is. We also taught “never do anything just because you can.” Curiosity, we know, is a frequent driver of lab test ordering.
That underlying philosophy gives me a hard time when it comes to wearables. I have been enamored of watching my step count, active zone minutes, resting heart rate, active heart rate, various sleep scores, and breathing rate (and, of course, a manually entered early morning daily body weight) for several years. I even check my “readiness score” (a calculation using resting heart rate, recent sleep, recent active zone minutes, and perhaps HRV) each morning and adjust my behaviors accordingly.
Why monitor HRV?
But what should we do with HRV scores? Ignore them? Try to understand them, perhaps as a screening tool? Or monitor HRV for consistency or change? “Monitoring” is a proper and common use of lab tests.
Some say we should improve the HRV score by managing stress, getting regular exercise, eating a healthy diet, getting enough sleep, and not smoking or consuming excess alcohol. Duh! I do all of that anyway.
The claims that HRV is a “simple but powerful tool that can be used to track overall health and well-being” might turn out to be true. Proper study and sharing of data will enable that determination.
To advance understanding, I offer an n-of-1, a real-world personal anecdote about HRV.
I did not request the HRV function on my Fitbit Inspire 2. It simply appeared, and I ignored it for some time.
A year or two ago, I started noticing my HRV score every morning. Initially, I did not like to see my “low” score, until I learned that the reference range was dramatically affected by age and I was in my late 80s at the time. The vast majority of my HRV readings were in the range of 17 msec to 27 msec.
Last week, I was administered the new Moderna COVID-19 Spikevax vaccine and the old folks’ influenza vaccine simultaneously. In my case, side effects from each vaccine have been modest in the past, but I never previously had both administered at the same time. My immune response was, shall we say, robust. Chills, muscle aches, headache, fatigue, deltoid swelling, fitful sleep, and increased resting heart rate.
My nightly average HRV had been running between 17 msec and 35 msec for many months. WHOA! After the shots, my overnight HRV score plummeted from 24 msec to 10 msec, my lowest ever. Instant worry. The next day, it rebounded to 28 msec, and it has been in the high teens or low 20s since then.
Off to PubMed. A recent study of HRV on the second and 10th days after administering the Pfizer mRNA vaccine to 75 healthy volunteers found that the HRV on day 2 was dramatically lower than prevaccination levels and by day 10, it had returned to prevaccination levels. Some comfort there.
Another review article has reported a rapid fall and rapid rebound of HRV after COVID-19 vaccination. A 2010 report demonstrated a significant but not dramatic short-term lowering of HRV after influenza A vaccination and correlated it with CRP changes.
Some believe that the decline in HRV after vaccination reflects an increased immune response and sympathetic nervous activity.
I don’t plan to receive my flu and COVID vaccines on the same day again.
So, I went back to review what happened to my HRV when I had COVID in 2023. My HRV was 14 msec and 12 msec on the first 2 days of symptoms, and then returned to the 20 msec range.
I received the RSV vaccine this year without adverse effects, and my HRV scores were 29 msec, 33 msec, and 32 msec on the first 3 days after vaccination. Finally, after receiving a pneumococcal vaccine in 2023, I had no adverse effects, and my HRV scores on the 5 days after vaccination were indeterminate: 19 msec, 14 msec, 18 msec, 13 msec, and 17 msec.
Of course, correlation is not causation. Cause and effect remain undetermined. But I find these observations interesting for a potentially useful screening test.
George D. Lundberg, MD, is the Editor in Chief of Cancer Commons.
A version of this article first appeared on Medscape.com.
A very long time ago, when I ran clinical labs, one of the most ordered tests was the “sed rate” (aka ESR, the erythrocyte sedimentation rate). Easy, quick, and low cost, with high sensitivity but very low specificity. If the sed rate was normal, the patient probably did not have an infectious or inflammatory disease. If it was elevated, they probably did, but no telling what. Later, the C-reactive protein (CRP) test came into common use. Same general inferences: If the CRP was low, the patient was unlikely to have an inflammatory process; if high, they were sick, but we didn’t know what with.
Could the heart rate variability (HRV) score come to be thought of similarly? Much as the sed rate and CRP are sensitivity indicators of infectious or inflammatory diseases, might the HRV score be a sensitivity indicator for nervous system (central and autonomic) and cardiovascular (especially heart rhythm) malfunctions?
A substantial and relatively old body of heart rhythm literature ties HRV alterations to posttraumatic stress disorder, physician occupational stress, sleep disorders, depression, autonomic nervous system derangements, various cardiac arrhythmias, fatigue, overexertion, medications, and age itself.
More than 100 million Americans are now believed to use smartwatches or personal fitness monitors. Some 30%-40% of these devices measure HRV. So what? Credible research about this huge mass of accumulating data from “wearables” is lacking.
What is HRV?
HRV is the variation in time between each heartbeat, in milliseconds. HRV is influenced by the autonomic nervous system, perhaps reflecting sympathetic-parasympathetic balance. Some devices measure HRV 24/7. My Fitbit Inspire 2 reports only nighttime measures during 3 hours of sustained sleep. Most trackers report averages; some calculate the root mean squares; others calculate standard deviations. All fitness trackers warn not to use the data for medical purposes.
Normal values (reference ranges) for HRV begin at an average of 100 msec in the first decade of life and decline by approximately 10 msec per decade lived. At age 30-40, the average is 70 msec; age 60-70, it’s 40 msec; and at age 90-100, it’s 10 msec.
As a long-time lab guy, I used to teach proper use of lab tests. Fitness trackers are “lab tests” of a sort. We taught never to do a lab test unless you know what you are going to do with the result, no matter what it is. We also taught “never do anything just because you can.” Curiosity, we know, is a frequent driver of lab test ordering.
That underlying philosophy gives me a hard time when it comes to wearables. I have been enamored of watching my step count, active zone minutes, resting heart rate, active heart rate, various sleep scores, and breathing rate (and, of course, a manually entered early morning daily body weight) for several years. I even check my “readiness score” (a calculation using resting heart rate, recent sleep, recent active zone minutes, and perhaps HRV) each morning and adjust my behaviors accordingly.
Why monitor HRV?
But what should we do with HRV scores? Ignore them? Try to understand them, perhaps as a screening tool? Or monitor HRV for consistency or change? “Monitoring” is a proper and common use of lab tests.
Some say we should improve the HRV score by managing stress, getting regular exercise, eating a healthy diet, getting enough sleep, and not smoking or consuming excess alcohol. Duh! I do all of that anyway.
The claims that HRV is a “simple but powerful tool that can be used to track overall health and well-being” might turn out to be true. Proper study and sharing of data will enable that determination.
To advance understanding, I offer an n-of-1, a real-world personal anecdote about HRV.
I did not request the HRV function on my Fitbit Inspire 2. It simply appeared, and I ignored it for some time.
A year or two ago, I started noticing my HRV score every morning. Initially, I did not like to see my “low” score, until I learned that the reference range was dramatically affected by age and I was in my late 80s at the time. The vast majority of my HRV readings were in the range of 17 msec to 27 msec.
Last week, I was administered the new Moderna COVID-19 Spikevax vaccine and the old folks’ influenza vaccine simultaneously. In my case, side effects from each vaccine have been modest in the past, but I never previously had both administered at the same time. My immune response was, shall we say, robust. Chills, muscle aches, headache, fatigue, deltoid swelling, fitful sleep, and increased resting heart rate.
My nightly average HRV had been running between 17 msec and 35 msec for many months. WHOA! After the shots, my overnight HRV score plummeted from 24 msec to 10 msec, my lowest ever. Instant worry. The next day, it rebounded to 28 msec, and it has been in the high teens or low 20s since then.
Off to PubMed. A recent study of HRV on the second and 10th days after administering the Pfizer mRNA vaccine to 75 healthy volunteers found that the HRV on day 2 was dramatically lower than prevaccination levels and by day 10, it had returned to prevaccination levels. Some comfort there.
Another review article has reported a rapid fall and rapid rebound of HRV after COVID-19 vaccination. A 2010 report demonstrated a significant but not dramatic short-term lowering of HRV after influenza A vaccination and correlated it with CRP changes.
Some believe that the decline in HRV after vaccination reflects an increased immune response and sympathetic nervous activity.
I don’t plan to receive my flu and COVID vaccines on the same day again.
So, I went back to review what happened to my HRV when I had COVID in 2023. My HRV was 14 msec and 12 msec on the first 2 days of symptoms, and then returned to the 20 msec range.
I received the RSV vaccine this year without adverse effects, and my HRV scores were 29 msec, 33 msec, and 32 msec on the first 3 days after vaccination. Finally, after receiving a pneumococcal vaccine in 2023, I had no adverse effects, and my HRV scores on the 5 days after vaccination were indeterminate: 19 msec, 14 msec, 18 msec, 13 msec, and 17 msec.
Of course, correlation is not causation. Cause and effect remain undetermined. But I find these observations interesting for a potentially useful screening test.
George D. Lundberg, MD, is the Editor in Chief of Cancer Commons.
A version of this article first appeared on Medscape.com.
Upper respiratory infections: Viral testing in primary care
It’s upper respiratory infection (URI) season. The following is a clinical scenario drawn from my own practice. I’ll tell you what I plan to do, but I’m most interested in crowdsourcing a response from all of you to collectively determine best practice. So please answer the polling questions and contribute your thoughts in the comments, whether you agree or disagree with me.
The patient
The patient is a 69-year-old woman with a 3-day history of cough, nasal congestion, malaise, tactile fever, and poor appetite. She has no sick contacts. She denies dyspnea, presyncope, and chest pain. She has tried guaifenesin and ibuprofen for her symptoms, which helped a little.
She is up to date on immunizations, including four doses of COVID-19 vaccine and the influenza vaccine, which she received 2 months ago.
The patient has a history of heart failure with reduced ejection fraction, coronary artery disease, hypertension, chronic kidney disease stage 3aA2, obesity, and osteoarthritis. Current medications include atorvastatin, losartan, metoprolol, and aspirin.
Her weight is stable at 212 lb, and her vital signs today are:
- Temperature: 37.5° C
- Pulse: 60 beats/min
- Blood pressure: 150/88 mm Hg
- Respiration rate: 14 breaths/min
- SpO2: 93% on room air
What information is most critical before deciding on management?
Your peers chose:
- The patient’s history of viral URIs
14%
- Whether her cough is productive and the color of the sputum
38%
- How well this season’s flu vaccine matches circulating influenza viruses
8%
- Local epidemiology of major viral pathogens (e.g., SARS-CoV-2, influenza, RSV)
40%
Dr. Vega’s take
To provide the best care for our patients when they are threatened with multiple viral upper respiratory pathogens, it is imperative that clinicians have some idea regarding the epidemiology of viral infections, with as much local data as possible. This knowledge will help direct appropriate testing and treatment.
Modern viral molecular testing platforms are highly accurate, but they are not infallible. Small flaws in specificity and sensitivity of testing are magnified when community viral circulation is low. In a U.K. study conducted during a period of low COVID-19 prevalence, the positive predictive value of reverse-transcriptase polymerase chain reaction (RT-PCR) testing was just 16%. Although the negative predictive value was much higher, the false-positive rate of testing was still 0.5%. The authors of the study describe important potential consequences of false-positive results, such as being temporarily removed from an organ transplant list and unnecessary contact tracing.
Testing and treatment
Your county public health department maintains a website describing local activity of SARS-CoV-2 and influenza. Both viruses are in heavy circulation now.
What is the next best step in this patient’s management?
Your peers chose:
- Treat empirically with ritonavir-boosted nirmatrelvir
7%
- Treat empirically with oseltamivir or baloxavir
14%
- Perform lab-based multiplex RT-PCR testing and wait to treat on the basis of results
34%
- Perform rapid nucleic acid amplification testing (NAAT) and treat on the basis of results
45%
Every practice has different resources and should use the best means available to treat patients. Ideally, this patient would undergo rapid NAAT with results available within 30 minutes. Test results will help guide not only treatment decisions but also infection-control measures.
The Infectious Diseases Society of America has provided updates for testing for URIs since the onset of the COVID-19 pandemic. Both laboratory-based and point-of-care rapid NAATs are recommended for testing. Rapid NAATs have been demonstrated to have a sensitivity of 96% and specificity of 100% in the detection of SARS-CoV-2. Obviously, they also offer a highly efficient means to make treatment and isolation decisions.
There are multiple platforms for molecular testing available. Laboratory-based platforms can test for dozens of potential pathogens, including bacteria. Rapid NAATs often have the ability to test for SARS-CoV-2, influenza, and respiratory syncytial virus (RSV). This functionality is important, because these infections generally are difficult to discriminate on the basis of clinical information alone.
The IDSA clearly recognizes the challenges of trying to manage cases of URI. For example, they state that testing of the anterior nares (AN) or oropharynx (OP) is acceptable, even though testing from the nasopharynx offers increased sensitivity. However, testing at the AN/OP allows for patient self-collection of samples, which is also recommended as an option by the IDSA. In an analysis of six cohort studies, the pooled sensitivity of patient-collected nasopharyngeal samples from the AN/OP was 88%, whereas the respective value for samples taken by health care providers was 95%.
The U.S. Centers for Disease Control and Prevention also provides recommendations for the management of patients with acute upper respiratory illness. Patients who are sick enough to be hospitalized should be tested at least for SARS-CoV-2 and influenza using molecular assays. Outpatients should be tested for SARS-CoV-2 with either molecular or antigen testing, and influenza testing should be offered if the findings will change decisions regarding treatment or isolation. Practically speaking, the recommendations for influenza testing mean that most individuals should be tested, including patients at high risk for complications of influenza and those who might have exposure to individuals at high risk.
Treatment of COVID-19 should only be provided in cases of a positive test within 5 days of symptom onset. However, clinicians may treat patients with anti-influenza medications presumptively if test results are not immediately available and the patient has worsening symptoms or is in a group at high risk for complications.
What are some of the challenges that you have faced during the COVID-19 pandemic regarding the management of patients with acute URIs? What have you found in terms of solutions, and where do gaps in quality of care persist? Please add your comments. I will review and circle back with a response. Thank you!
A version of this article first appeared on Medscape.com.
It’s upper respiratory infection (URI) season. The following is a clinical scenario drawn from my own practice. I’ll tell you what I plan to do, but I’m most interested in crowdsourcing a response from all of you to collectively determine best practice. So please answer the polling questions and contribute your thoughts in the comments, whether you agree or disagree with me.
The patient
The patient is a 69-year-old woman with a 3-day history of cough, nasal congestion, malaise, tactile fever, and poor appetite. She has no sick contacts. She denies dyspnea, presyncope, and chest pain. She has tried guaifenesin and ibuprofen for her symptoms, which helped a little.
She is up to date on immunizations, including four doses of COVID-19 vaccine and the influenza vaccine, which she received 2 months ago.
The patient has a history of heart failure with reduced ejection fraction, coronary artery disease, hypertension, chronic kidney disease stage 3aA2, obesity, and osteoarthritis. Current medications include atorvastatin, losartan, metoprolol, and aspirin.
Her weight is stable at 212 lb, and her vital signs today are:
- Temperature: 37.5° C
- Pulse: 60 beats/min
- Blood pressure: 150/88 mm Hg
- Respiration rate: 14 breaths/min
- SpO2: 93% on room air
What information is most critical before deciding on management?
Your peers chose:
- The patient’s history of viral URIs
14%
- Whether her cough is productive and the color of the sputum
38%
- How well this season’s flu vaccine matches circulating influenza viruses
8%
- Local epidemiology of major viral pathogens (e.g., SARS-CoV-2, influenza, RSV)
40%
Dr. Vega’s take
To provide the best care for our patients when they are threatened with multiple viral upper respiratory pathogens, it is imperative that clinicians have some idea regarding the epidemiology of viral infections, with as much local data as possible. This knowledge will help direct appropriate testing and treatment.
Modern viral molecular testing platforms are highly accurate, but they are not infallible. Small flaws in specificity and sensitivity of testing are magnified when community viral circulation is low. In a U.K. study conducted during a period of low COVID-19 prevalence, the positive predictive value of reverse-transcriptase polymerase chain reaction (RT-PCR) testing was just 16%. Although the negative predictive value was much higher, the false-positive rate of testing was still 0.5%. The authors of the study describe important potential consequences of false-positive results, such as being temporarily removed from an organ transplant list and unnecessary contact tracing.
Testing and treatment
Your county public health department maintains a website describing local activity of SARS-CoV-2 and influenza. Both viruses are in heavy circulation now.
What is the next best step in this patient’s management?
Your peers chose:
- Treat empirically with ritonavir-boosted nirmatrelvir
7%
- Treat empirically with oseltamivir or baloxavir
14%
- Perform lab-based multiplex RT-PCR testing and wait to treat on the basis of results
34%
- Perform rapid nucleic acid amplification testing (NAAT) and treat on the basis of results
45%
Every practice has different resources and should use the best means available to treat patients. Ideally, this patient would undergo rapid NAAT with results available within 30 minutes. Test results will help guide not only treatment decisions but also infection-control measures.
The Infectious Diseases Society of America has provided updates for testing for URIs since the onset of the COVID-19 pandemic. Both laboratory-based and point-of-care rapid NAATs are recommended for testing. Rapid NAATs have been demonstrated to have a sensitivity of 96% and specificity of 100% in the detection of SARS-CoV-2. Obviously, they also offer a highly efficient means to make treatment and isolation decisions.
There are multiple platforms for molecular testing available. Laboratory-based platforms can test for dozens of potential pathogens, including bacteria. Rapid NAATs often have the ability to test for SARS-CoV-2, influenza, and respiratory syncytial virus (RSV). This functionality is important, because these infections generally are difficult to discriminate on the basis of clinical information alone.
The IDSA clearly recognizes the challenges of trying to manage cases of URI. For example, they state that testing of the anterior nares (AN) or oropharynx (OP) is acceptable, even though testing from the nasopharynx offers increased sensitivity. However, testing at the AN/OP allows for patient self-collection of samples, which is also recommended as an option by the IDSA. In an analysis of six cohort studies, the pooled sensitivity of patient-collected nasopharyngeal samples from the AN/OP was 88%, whereas the respective value for samples taken by health care providers was 95%.
The U.S. Centers for Disease Control and Prevention also provides recommendations for the management of patients with acute upper respiratory illness. Patients who are sick enough to be hospitalized should be tested at least for SARS-CoV-2 and influenza using molecular assays. Outpatients should be tested for SARS-CoV-2 with either molecular or antigen testing, and influenza testing should be offered if the findings will change decisions regarding treatment or isolation. Practically speaking, the recommendations for influenza testing mean that most individuals should be tested, including patients at high risk for complications of influenza and those who might have exposure to individuals at high risk.
Treatment of COVID-19 should only be provided in cases of a positive test within 5 days of symptom onset. However, clinicians may treat patients with anti-influenza medications presumptively if test results are not immediately available and the patient has worsening symptoms or is in a group at high risk for complications.
What are some of the challenges that you have faced during the COVID-19 pandemic regarding the management of patients with acute URIs? What have you found in terms of solutions, and where do gaps in quality of care persist? Please add your comments. I will review and circle back with a response. Thank you!
A version of this article first appeared on Medscape.com.
It’s upper respiratory infection (URI) season. The following is a clinical scenario drawn from my own practice. I’ll tell you what I plan to do, but I’m most interested in crowdsourcing a response from all of you to collectively determine best practice. So please answer the polling questions and contribute your thoughts in the comments, whether you agree or disagree with me.
The patient
The patient is a 69-year-old woman with a 3-day history of cough, nasal congestion, malaise, tactile fever, and poor appetite. She has no sick contacts. She denies dyspnea, presyncope, and chest pain. She has tried guaifenesin and ibuprofen for her symptoms, which helped a little.
She is up to date on immunizations, including four doses of COVID-19 vaccine and the influenza vaccine, which she received 2 months ago.
The patient has a history of heart failure with reduced ejection fraction, coronary artery disease, hypertension, chronic kidney disease stage 3aA2, obesity, and osteoarthritis. Current medications include atorvastatin, losartan, metoprolol, and aspirin.
Her weight is stable at 212 lb, and her vital signs today are:
- Temperature: 37.5° C
- Pulse: 60 beats/min
- Blood pressure: 150/88 mm Hg
- Respiration rate: 14 breaths/min
- SpO2: 93% on room air
What information is most critical before deciding on management?
Your peers chose:
- The patient’s history of viral URIs
14%
- Whether her cough is productive and the color of the sputum
38%
- How well this season’s flu vaccine matches circulating influenza viruses
8%
- Local epidemiology of major viral pathogens (e.g., SARS-CoV-2, influenza, RSV)
40%
Dr. Vega’s take
To provide the best care for our patients when they are threatened with multiple viral upper respiratory pathogens, it is imperative that clinicians have some idea regarding the epidemiology of viral infections, with as much local data as possible. This knowledge will help direct appropriate testing and treatment.
Modern viral molecular testing platforms are highly accurate, but they are not infallible. Small flaws in specificity and sensitivity of testing are magnified when community viral circulation is low. In a U.K. study conducted during a period of low COVID-19 prevalence, the positive predictive value of reverse-transcriptase polymerase chain reaction (RT-PCR) testing was just 16%. Although the negative predictive value was much higher, the false-positive rate of testing was still 0.5%. The authors of the study describe important potential consequences of false-positive results, such as being temporarily removed from an organ transplant list and unnecessary contact tracing.
Testing and treatment
Your county public health department maintains a website describing local activity of SARS-CoV-2 and influenza. Both viruses are in heavy circulation now.
What is the next best step in this patient’s management?
Your peers chose:
- Treat empirically with ritonavir-boosted nirmatrelvir
7%
- Treat empirically with oseltamivir or baloxavir
14%
- Perform lab-based multiplex RT-PCR testing and wait to treat on the basis of results
34%
- Perform rapid nucleic acid amplification testing (NAAT) and treat on the basis of results
45%
Every practice has different resources and should use the best means available to treat patients. Ideally, this patient would undergo rapid NAAT with results available within 30 minutes. Test results will help guide not only treatment decisions but also infection-control measures.
The Infectious Diseases Society of America has provided updates for testing for URIs since the onset of the COVID-19 pandemic. Both laboratory-based and point-of-care rapid NAATs are recommended for testing. Rapid NAATs have been demonstrated to have a sensitivity of 96% and specificity of 100% in the detection of SARS-CoV-2. Obviously, they also offer a highly efficient means to make treatment and isolation decisions.
There are multiple platforms for molecular testing available. Laboratory-based platforms can test for dozens of potential pathogens, including bacteria. Rapid NAATs often have the ability to test for SARS-CoV-2, influenza, and respiratory syncytial virus (RSV). This functionality is important, because these infections generally are difficult to discriminate on the basis of clinical information alone.
The IDSA clearly recognizes the challenges of trying to manage cases of URI. For example, they state that testing of the anterior nares (AN) or oropharynx (OP) is acceptable, even though testing from the nasopharynx offers increased sensitivity. However, testing at the AN/OP allows for patient self-collection of samples, which is also recommended as an option by the IDSA. In an analysis of six cohort studies, the pooled sensitivity of patient-collected nasopharyngeal samples from the AN/OP was 88%, whereas the respective value for samples taken by health care providers was 95%.
The U.S. Centers for Disease Control and Prevention also provides recommendations for the management of patients with acute upper respiratory illness. Patients who are sick enough to be hospitalized should be tested at least for SARS-CoV-2 and influenza using molecular assays. Outpatients should be tested for SARS-CoV-2 with either molecular or antigen testing, and influenza testing should be offered if the findings will change decisions regarding treatment or isolation. Practically speaking, the recommendations for influenza testing mean that most individuals should be tested, including patients at high risk for complications of influenza and those who might have exposure to individuals at high risk.
Treatment of COVID-19 should only be provided in cases of a positive test within 5 days of symptom onset. However, clinicians may treat patients with anti-influenza medications presumptively if test results are not immediately available and the patient has worsening symptoms or is in a group at high risk for complications.
What are some of the challenges that you have faced during the COVID-19 pandemic regarding the management of patients with acute URIs? What have you found in terms of solutions, and where do gaps in quality of care persist? Please add your comments. I will review and circle back with a response. Thank you!
A version of this article first appeared on Medscape.com.
Orthostatic hypotension no deterrent to hypertension treatment
TOPLINE:
Intensive antihypertensive treatment provides the same benefit with regard to cardiovascular disease (CVD) and all-cause mortality regardless of the presence or absence of orthostatic or standing hypotension, new research shows.
METHODOLOGY:
- In response to ongoing concern about the benefits of intensive versus standard blood pressure treatment for adults with orthostatic hypotension (OH), researchers conducted a meta-analysis of individual patient data from nine randomized clinical trials to see whether the benefit of antihypertensive treatment was diminished for patients who had OH at baseline. Benefit was defined as a reduction in nonfatal CVD events and all-cause mortality.
- The included trials assessed BP pharmacologic treatment (more intensive BP goal or active agent) and had data on OH.
TAKEAWAY:
- The nine trials included 29,235 participants (mean age, 69 years; 48% women) who were followed for a median of 4 years; 9% had OH and 5% had standing hypotension at baseline.
- Having OH at baseline was significantly associated with the composite of CVD or all-cause mortality (hazard ratio, 1.14; 95% confidence interval, 1.04-1.26) and with all-cause mortality (HR, 1.24; 95% CI, 1.09-1.41). The same was true for baseline standing hypotension (composite outcome: HR, 1.39; 95% CI, 1.24-1.57; all-cause mortality: HR, 1.38; 95% CI, 1.14-1.66).
- More intensive BP treatment or active therapy significantly and similarly lowered risk of CVD or all-cause mortality among adults who did not have OH at baseline (HR, 0.81; 95% CI, 0.76-0.86) as well as those with OH at baseline (HR, 0.83; 95% CI, 0.70-1.00).
- More intensive BP treatment or active therapy also significantly lowered risk of CVD or all-cause mortality among those without baseline standing hypotension (HR, 0.80; 95% CI, 0.75-0.85) and nonsignificantly lowered the risk among those with baseline standing hypotension (HR, 0.94; 95% CI, 0.75-1.18).
IN PRACTICE:
“These findings suggest that orthostatic hypotension alone (that is, without symptoms) and standing hypotension measured prior to intensification of BP treatment should not deter adoption of more intensive BP treatment in adults with hypertension,” the authors conclude.
The findings should “reassure clinicians that patients with OH (and perhaps standing hypotension) will derive the full expected benefits from antihypertensive therapy,” add the authors of an accompanying editorial. “This also applies to patients treated to lower BP goals, albeit with less certainty.”
SOURCE:
The study, with first author Stephen Juraschek, MD, PhD, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, and the accompanying editorial were published online in JAMA.
LIMITATIONS:
In the hypertension trials that were included in the analysis, the study populations differed, as did BP measurement procedures, interventions, duration, and CVD outcome ascertainment processes and definitions. Some trials excluded adults with low standing systolic BP, limiting the number of participants with standing hypotension. OH was determined on the basis of a seated-to-standing protocol; supine-to-standing protocols are more sensitive and may not be interchangeable. Medications used in the trials may not reflect current medicine practice, or the trials may not have included agents thought to be more likely to affect OH and falls.
DISCLOSURES:
The study had no specific funding. Dr. Juraschek has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Intensive antihypertensive treatment provides the same benefit with regard to cardiovascular disease (CVD) and all-cause mortality regardless of the presence or absence of orthostatic or standing hypotension, new research shows.
METHODOLOGY:
- In response to ongoing concern about the benefits of intensive versus standard blood pressure treatment for adults with orthostatic hypotension (OH), researchers conducted a meta-analysis of individual patient data from nine randomized clinical trials to see whether the benefit of antihypertensive treatment was diminished for patients who had OH at baseline. Benefit was defined as a reduction in nonfatal CVD events and all-cause mortality.
- The included trials assessed BP pharmacologic treatment (more intensive BP goal or active agent) and had data on OH.
TAKEAWAY:
- The nine trials included 29,235 participants (mean age, 69 years; 48% women) who were followed for a median of 4 years; 9% had OH and 5% had standing hypotension at baseline.
- Having OH at baseline was significantly associated with the composite of CVD or all-cause mortality (hazard ratio, 1.14; 95% confidence interval, 1.04-1.26) and with all-cause mortality (HR, 1.24; 95% CI, 1.09-1.41). The same was true for baseline standing hypotension (composite outcome: HR, 1.39; 95% CI, 1.24-1.57; all-cause mortality: HR, 1.38; 95% CI, 1.14-1.66).
- More intensive BP treatment or active therapy significantly and similarly lowered risk of CVD or all-cause mortality among adults who did not have OH at baseline (HR, 0.81; 95% CI, 0.76-0.86) as well as those with OH at baseline (HR, 0.83; 95% CI, 0.70-1.00).
- More intensive BP treatment or active therapy also significantly lowered risk of CVD or all-cause mortality among those without baseline standing hypotension (HR, 0.80; 95% CI, 0.75-0.85) and nonsignificantly lowered the risk among those with baseline standing hypotension (HR, 0.94; 95% CI, 0.75-1.18).
IN PRACTICE:
“These findings suggest that orthostatic hypotension alone (that is, without symptoms) and standing hypotension measured prior to intensification of BP treatment should not deter adoption of more intensive BP treatment in adults with hypertension,” the authors conclude.
The findings should “reassure clinicians that patients with OH (and perhaps standing hypotension) will derive the full expected benefits from antihypertensive therapy,” add the authors of an accompanying editorial. “This also applies to patients treated to lower BP goals, albeit with less certainty.”
SOURCE:
The study, with first author Stephen Juraschek, MD, PhD, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, and the accompanying editorial were published online in JAMA.
LIMITATIONS:
In the hypertension trials that were included in the analysis, the study populations differed, as did BP measurement procedures, interventions, duration, and CVD outcome ascertainment processes and definitions. Some trials excluded adults with low standing systolic BP, limiting the number of participants with standing hypotension. OH was determined on the basis of a seated-to-standing protocol; supine-to-standing protocols are more sensitive and may not be interchangeable. Medications used in the trials may not reflect current medicine practice, or the trials may not have included agents thought to be more likely to affect OH and falls.
DISCLOSURES:
The study had no specific funding. Dr. Juraschek has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Intensive antihypertensive treatment provides the same benefit with regard to cardiovascular disease (CVD) and all-cause mortality regardless of the presence or absence of orthostatic or standing hypotension, new research shows.
METHODOLOGY:
- In response to ongoing concern about the benefits of intensive versus standard blood pressure treatment for adults with orthostatic hypotension (OH), researchers conducted a meta-analysis of individual patient data from nine randomized clinical trials to see whether the benefit of antihypertensive treatment was diminished for patients who had OH at baseline. Benefit was defined as a reduction in nonfatal CVD events and all-cause mortality.
- The included trials assessed BP pharmacologic treatment (more intensive BP goal or active agent) and had data on OH.
TAKEAWAY:
- The nine trials included 29,235 participants (mean age, 69 years; 48% women) who were followed for a median of 4 years; 9% had OH and 5% had standing hypotension at baseline.
- Having OH at baseline was significantly associated with the composite of CVD or all-cause mortality (hazard ratio, 1.14; 95% confidence interval, 1.04-1.26) and with all-cause mortality (HR, 1.24; 95% CI, 1.09-1.41). The same was true for baseline standing hypotension (composite outcome: HR, 1.39; 95% CI, 1.24-1.57; all-cause mortality: HR, 1.38; 95% CI, 1.14-1.66).
- More intensive BP treatment or active therapy significantly and similarly lowered risk of CVD or all-cause mortality among adults who did not have OH at baseline (HR, 0.81; 95% CI, 0.76-0.86) as well as those with OH at baseline (HR, 0.83; 95% CI, 0.70-1.00).
- More intensive BP treatment or active therapy also significantly lowered risk of CVD or all-cause mortality among those without baseline standing hypotension (HR, 0.80; 95% CI, 0.75-0.85) and nonsignificantly lowered the risk among those with baseline standing hypotension (HR, 0.94; 95% CI, 0.75-1.18).
IN PRACTICE:
“These findings suggest that orthostatic hypotension alone (that is, without symptoms) and standing hypotension measured prior to intensification of BP treatment should not deter adoption of more intensive BP treatment in adults with hypertension,” the authors conclude.
The findings should “reassure clinicians that patients with OH (and perhaps standing hypotension) will derive the full expected benefits from antihypertensive therapy,” add the authors of an accompanying editorial. “This also applies to patients treated to lower BP goals, albeit with less certainty.”
SOURCE:
The study, with first author Stephen Juraschek, MD, PhD, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, and the accompanying editorial were published online in JAMA.
LIMITATIONS:
In the hypertension trials that were included in the analysis, the study populations differed, as did BP measurement procedures, interventions, duration, and CVD outcome ascertainment processes and definitions. Some trials excluded adults with low standing systolic BP, limiting the number of participants with standing hypotension. OH was determined on the basis of a seated-to-standing protocol; supine-to-standing protocols are more sensitive and may not be interchangeable. Medications used in the trials may not reflect current medicine practice, or the trials may not have included agents thought to be more likely to affect OH and falls.
DISCLOSURES:
The study had no specific funding. Dr. Juraschek has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Massive databases unleash discovery, but not so much in the U.S.
Which conditions are caused by infection? Though it may seem like an amateur concern in the era of advanced microscopy, some culprits evade conventional methods of detection. Large medical databases hold the power to unlock answers.
A recent study from Sweden and Denmark meticulously traced the lives and medical histories of nearly one million men and women in those countries who had received blood transfusions over nearly five decades. Some of these patients later experienced brain bleeds. The inescapable question: Could a virus found in some donor blood have caused the hemorrhages?
Traditionally, brain bleeds have been thought to strike at random. But the new study, published in JAMA, points toward an infection that causes or, at the very least, is linked to the condition. The researchers used a large databank to make the discovery. 
“As health data becomes more available and easier to analyze, we’ll see all kinds of cases like this,” said Jingcheng Zhao, MD, of the clinical epidemiology division of Sweden’s Karolinska Institutet in Solna and lead author of the study.
Scientists say the field of medical research is on the cusp of a revolution as immense health databases guide discovery and improve clinical care.
“If you can aggregate data, you have the statistical power to identify associations,” said David R. Crosslin, PhD, professor in the division of biomedical informatics and genomics at Tulane University in New Orleans. “It opens up the world for understanding diseases.”
With access to the large database, Dr. Zhao and his team found that some blood donors later experienced brain bleeds. And it turned out that the recipients of blood from those same donors carried the highest risk of experiencing a brain bleed later in life. Meanwhile, patients whose donors remained bleed-free had the lowest risk.
Not so fast in the United States
In Nordic countries, all hospitals, clinics, and pharmacies report data on diagnoses and health care visits to the government, tracking that began with paper and pen in the 1960s. But the United States health care system is too fragmented to replicate such efforts, with several brands of electronic medical records operating across different systems. Data sharing across institutions is minimal.
Most comparable health data in the United States comes from reimbursement information collected by the Centers for Medicare & Medicaid Services on government-sponsored insurance programs.
“We would need all the health care systems in the country to operate within the same IT system or use the same data model,” said Euan Ashley, MD, PhD, professor of genomics at Stanford (Calif.) University. “It’s an exciting prospect. But I think [the United States] is one of the last countries where it’ll happen.”
States, meanwhile, collect health data on specific areas like sexually transmitted infection cases and rates. Other states have registries, like the Connecticut Tumor Registry, which was established in 1941 and is the oldest population-based cancer registry in the world.
But all of these efforts are ad hoc, and no equivalent exists for heart disease and other conditions.
Health data companies have recently entered the U.S. data industry mainly through partnerships with health systems and insurance companies, using deidentified information from patient charts.
The large databases have yielded important findings that randomized clinical trials simply cannot, according to Dr. Ashley.
For instance, a study found that a heavily-lauded immunotherapy treatment did not provide meaningful outcomes for patients aged 75 years or older, but it did for younger patients.
This sort of analysis might enable clinicians to administer treatments based on how effective they are for patients with particular demographics, according to Cary Gross, MD, professor at Yale University in New Haven, Conn.
“From a bedside standpoint, these large databases can identify who benefits from what,” Dr. Gross said. “Precision medicine is not just about genetic tailoring.” These large datasets also provide insight into genetic and environmental variables that contribute to disease.
For instance, the UK Biobank has more than 500,000 participants paired with their medical records and scans of their body and brain. Researchers perform cognitive tests on participants and extract DNA from blood samples over their lifetime, allowing examination of interactions between risk factors.
A similar but much smaller-scale effort underway in the United States, called the All of Us Research Program, has enrolled more than 650,000 people, less than one-third the size of the UK Biobank by relative populations. The goal of the program is to provide insights into prevention and treatment of chronic disease among a diverse set of at least one million participants. The database includes information on sexual orientation, which is a fairly new datapoint collected by researchers in an effort to study health outcomes and inequities among the LGBTQ+ community.
Dr. Crosslin and his colleagues are writing a grant proposal to use the All of Us database to identify genetic risks for preeclampsia. People with certain genetic profiles may be predisposed to the life-threatening condition, and researchers may discover that lifestyle changes could decrease risk, Dr. Crosslin said.
Changes in the United States
The COVID-19 pandemic exposed the lack of centralized data in the United States because a majority of research on the virus has been conducted abroad in countries with national health care systems and these large databases.
The U.S. gap spurred a group of researchers to create the National Institutes of Health–funded National COVID Cohort Collaborative (N3C), a project that gathers medical records from millions of patients across health systems and provides access to research teams investigating a wide spectrum of topics, such as optimal timing for ventilator use.
But until government or private health systems develop a way to share and regulate health data ethically and efficiently, significant limits will persist on what large-scale databases can do, Dr. Gross said.
“At the federal level, we need to ensure this health information is made available for public health researchers so we don’t create these private fiefdoms of data,” Dr. Gross said. “Things have to be transparent. I think our country needs to take a step back and think about what we’re doing with our health data and how we can make sure it’s being managed ethically.”
A version of this article first appeared on Medscape.com.
Which conditions are caused by infection? Though it may seem like an amateur concern in the era of advanced microscopy, some culprits evade conventional methods of detection. Large medical databases hold the power to unlock answers.
A recent study from Sweden and Denmark meticulously traced the lives and medical histories of nearly one million men and women in those countries who had received blood transfusions over nearly five decades. Some of these patients later experienced brain bleeds. The inescapable question: Could a virus found in some donor blood have caused the hemorrhages?
Traditionally, brain bleeds have been thought to strike at random. But the new study, published in JAMA, points toward an infection that causes or, at the very least, is linked to the condition. The researchers used a large databank to make the discovery. 
“As health data becomes more available and easier to analyze, we’ll see all kinds of cases like this,” said Jingcheng Zhao, MD, of the clinical epidemiology division of Sweden’s Karolinska Institutet in Solna and lead author of the study.
Scientists say the field of medical research is on the cusp of a revolution as immense health databases guide discovery and improve clinical care.
“If you can aggregate data, you have the statistical power to identify associations,” said David R. Crosslin, PhD, professor in the division of biomedical informatics and genomics at Tulane University in New Orleans. “It opens up the world for understanding diseases.”
With access to the large database, Dr. Zhao and his team found that some blood donors later experienced brain bleeds. And it turned out that the recipients of blood from those same donors carried the highest risk of experiencing a brain bleed later in life. Meanwhile, patients whose donors remained bleed-free had the lowest risk.
Not so fast in the United States
In Nordic countries, all hospitals, clinics, and pharmacies report data on diagnoses and health care visits to the government, tracking that began with paper and pen in the 1960s. But the United States health care system is too fragmented to replicate such efforts, with several brands of electronic medical records operating across different systems. Data sharing across institutions is minimal.
Most comparable health data in the United States comes from reimbursement information collected by the Centers for Medicare & Medicaid Services on government-sponsored insurance programs.
“We would need all the health care systems in the country to operate within the same IT system or use the same data model,” said Euan Ashley, MD, PhD, professor of genomics at Stanford (Calif.) University. “It’s an exciting prospect. But I think [the United States] is one of the last countries where it’ll happen.”
States, meanwhile, collect health data on specific areas like sexually transmitted infection cases and rates. Other states have registries, like the Connecticut Tumor Registry, which was established in 1941 and is the oldest population-based cancer registry in the world.
But all of these efforts are ad hoc, and no equivalent exists for heart disease and other conditions.
Health data companies have recently entered the U.S. data industry mainly through partnerships with health systems and insurance companies, using deidentified information from patient charts.
The large databases have yielded important findings that randomized clinical trials simply cannot, according to Dr. Ashley.
For instance, a study found that a heavily-lauded immunotherapy treatment did not provide meaningful outcomes for patients aged 75 years or older, but it did for younger patients.
This sort of analysis might enable clinicians to administer treatments based on how effective they are for patients with particular demographics, according to Cary Gross, MD, professor at Yale University in New Haven, Conn.
“From a bedside standpoint, these large databases can identify who benefits from what,” Dr. Gross said. “Precision medicine is not just about genetic tailoring.” These large datasets also provide insight into genetic and environmental variables that contribute to disease.
For instance, the UK Biobank has more than 500,000 participants paired with their medical records and scans of their body and brain. Researchers perform cognitive tests on participants and extract DNA from blood samples over their lifetime, allowing examination of interactions between risk factors.
A similar but much smaller-scale effort underway in the United States, called the All of Us Research Program, has enrolled more than 650,000 people, less than one-third the size of the UK Biobank by relative populations. The goal of the program is to provide insights into prevention and treatment of chronic disease among a diverse set of at least one million participants. The database includes information on sexual orientation, which is a fairly new datapoint collected by researchers in an effort to study health outcomes and inequities among the LGBTQ+ community.
Dr. Crosslin and his colleagues are writing a grant proposal to use the All of Us database to identify genetic risks for preeclampsia. People with certain genetic profiles may be predisposed to the life-threatening condition, and researchers may discover that lifestyle changes could decrease risk, Dr. Crosslin said.
Changes in the United States
The COVID-19 pandemic exposed the lack of centralized data in the United States because a majority of research on the virus has been conducted abroad in countries with national health care systems and these large databases.
The U.S. gap spurred a group of researchers to create the National Institutes of Health–funded National COVID Cohort Collaborative (N3C), a project that gathers medical records from millions of patients across health systems and provides access to research teams investigating a wide spectrum of topics, such as optimal timing for ventilator use.
But until government or private health systems develop a way to share and regulate health data ethically and efficiently, significant limits will persist on what large-scale databases can do, Dr. Gross said.
“At the federal level, we need to ensure this health information is made available for public health researchers so we don’t create these private fiefdoms of data,” Dr. Gross said. “Things have to be transparent. I think our country needs to take a step back and think about what we’re doing with our health data and how we can make sure it’s being managed ethically.”
A version of this article first appeared on Medscape.com.
Which conditions are caused by infection? Though it may seem like an amateur concern in the era of advanced microscopy, some culprits evade conventional methods of detection. Large medical databases hold the power to unlock answers.
A recent study from Sweden and Denmark meticulously traced the lives and medical histories of nearly one million men and women in those countries who had received blood transfusions over nearly five decades. Some of these patients later experienced brain bleeds. The inescapable question: Could a virus found in some donor blood have caused the hemorrhages?
Traditionally, brain bleeds have been thought to strike at random. But the new study, published in JAMA, points toward an infection that causes or, at the very least, is linked to the condition. The researchers used a large databank to make the discovery. 
“As health data becomes more available and easier to analyze, we’ll see all kinds of cases like this,” said Jingcheng Zhao, MD, of the clinical epidemiology division of Sweden’s Karolinska Institutet in Solna and lead author of the study.
Scientists say the field of medical research is on the cusp of a revolution as immense health databases guide discovery and improve clinical care.
“If you can aggregate data, you have the statistical power to identify associations,” said David R. Crosslin, PhD, professor in the division of biomedical informatics and genomics at Tulane University in New Orleans. “It opens up the world for understanding diseases.”
With access to the large database, Dr. Zhao and his team found that some blood donors later experienced brain bleeds. And it turned out that the recipients of blood from those same donors carried the highest risk of experiencing a brain bleed later in life. Meanwhile, patients whose donors remained bleed-free had the lowest risk.
Not so fast in the United States
In Nordic countries, all hospitals, clinics, and pharmacies report data on diagnoses and health care visits to the government, tracking that began with paper and pen in the 1960s. But the United States health care system is too fragmented to replicate such efforts, with several brands of electronic medical records operating across different systems. Data sharing across institutions is minimal.
Most comparable health data in the United States comes from reimbursement information collected by the Centers for Medicare & Medicaid Services on government-sponsored insurance programs.
“We would need all the health care systems in the country to operate within the same IT system or use the same data model,” said Euan Ashley, MD, PhD, professor of genomics at Stanford (Calif.) University. “It’s an exciting prospect. But I think [the United States] is one of the last countries where it’ll happen.”
States, meanwhile, collect health data on specific areas like sexually transmitted infection cases and rates. Other states have registries, like the Connecticut Tumor Registry, which was established in 1941 and is the oldest population-based cancer registry in the world.
But all of these efforts are ad hoc, and no equivalent exists for heart disease and other conditions.
Health data companies have recently entered the U.S. data industry mainly through partnerships with health systems and insurance companies, using deidentified information from patient charts.
The large databases have yielded important findings that randomized clinical trials simply cannot, according to Dr. Ashley.
For instance, a study found that a heavily-lauded immunotherapy treatment did not provide meaningful outcomes for patients aged 75 years or older, but it did for younger patients.
This sort of analysis might enable clinicians to administer treatments based on how effective they are for patients with particular demographics, according to Cary Gross, MD, professor at Yale University in New Haven, Conn.
“From a bedside standpoint, these large databases can identify who benefits from what,” Dr. Gross said. “Precision medicine is not just about genetic tailoring.” These large datasets also provide insight into genetic and environmental variables that contribute to disease.
For instance, the UK Biobank has more than 500,000 participants paired with their medical records and scans of their body and brain. Researchers perform cognitive tests on participants and extract DNA from blood samples over their lifetime, allowing examination of interactions between risk factors.
A similar but much smaller-scale effort underway in the United States, called the All of Us Research Program, has enrolled more than 650,000 people, less than one-third the size of the UK Biobank by relative populations. The goal of the program is to provide insights into prevention and treatment of chronic disease among a diverse set of at least one million participants. The database includes information on sexual orientation, which is a fairly new datapoint collected by researchers in an effort to study health outcomes and inequities among the LGBTQ+ community.
Dr. Crosslin and his colleagues are writing a grant proposal to use the All of Us database to identify genetic risks for preeclampsia. People with certain genetic profiles may be predisposed to the life-threatening condition, and researchers may discover that lifestyle changes could decrease risk, Dr. Crosslin said.
Changes in the United States
The COVID-19 pandemic exposed the lack of centralized data in the United States because a majority of research on the virus has been conducted abroad in countries with national health care systems and these large databases.
The U.S. gap spurred a group of researchers to create the National Institutes of Health–funded National COVID Cohort Collaborative (N3C), a project that gathers medical records from millions of patients across health systems and provides access to research teams investigating a wide spectrum of topics, such as optimal timing for ventilator use.
But until government or private health systems develop a way to share and regulate health data ethically and efficiently, significant limits will persist on what large-scale databases can do, Dr. Gross said.
“At the federal level, we need to ensure this health information is made available for public health researchers so we don’t create these private fiefdoms of data,” Dr. Gross said. “Things have to be transparent. I think our country needs to take a step back and think about what we’re doing with our health data and how we can make sure it’s being managed ethically.”
A version of this article first appeared on Medscape.com.