User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
How has the pandemic changed your personal/professional priorities?
COVID-19: Remaining flexible amid the uncertainty
Editor’s Note: With 1 year of the COVID-19 pandemic in the rearview mirror, we decided to check in with the Editorial Advisory Board members of Clinical Psychiatry News about the impact it has had on their practices and lives.
Redefining how to engage
The COVID-19 pandemic has triggered a wave of mental health problems in our population, such as general stress, addiction, weight gain, depression, and social isolation, and these symptoms are exacerbated in mental health patients who are already struggling to cope with personal issues.
When the pandemic lockdown was announced in March 2020, many of my patients became overwhelmed and panicked at the idea of not being able to come to my office for in-person therapy. As an alternative, I started phone call sessions with my clients. These calls forced me to listen extra carefully to patient voice intonations to ascertain their true feelings, since I was unable to view the clients.
Soon thereafter, I transitioned to telemedicine over the Internet, and this visual helped me assess each patient. In addition, my patients became accustomed to telemedicine and embraced it once they saw me and were able to interact with me on the screen.
Although the pandemic disrupted my medical practice, it has redefined the way I can do therapy, as I can practice medicine from a distance. Telemedicine is time efficient for both my patients and me and it provides extreme social distancing, eliminating COVID-19 exposure between doctor and patient.
The pandemic has forced me to be adaptable and to recognize that, if you are open to changing habits, you can find a solution to any situation, including a pandemic.
Richard W. Cohen, MD
Private Practice
Philadelphia
Adjusting to fate
As it became clear in January 2020 that a pandemic was upon us, I made plans and prepared. I needed to remain healthy for my patients and my 102-year-old best friend, Doc.
I purchased PPE and 6 months’ of nonperishable groceries and toilet tissue from a commercial vendor. I made certain that Doc’s caregivers had what they needed to care for him and their families and preached to them, family, patients, and friends the public health guidelines of the day. Also, I needed to remain healthy for my patients who live in a dementia care facility, and I joined other workers there in being careful and proud that our facility remained COVID free.
By March 2020, I left my office, because it was in a building where both residents and staff were becoming ill with COVID. I started audio and video telemedicine as well as standing outside the windows of patients who only read lips and do not use digital technology. Under these new circumstances, patients (and Doc) revealed things about themselves that had remained hidden for decades. There was a sense of urgency and uncertainty.
I also started weekly COVID testing, at first at CVS and then in a public park. Doc, who had had congestive heart failure for 2 years, had celebrated his 103rd birthday in February, and continued to be a source of encouragement and support. We weathered through the spring and summer with him on lockdown in his senior residence. The dementia care facility remained free of COVID.
My plan had been to return to my office in July, however, the facility manager determined that they were not ready to receive my outpatients. I took on a short-term lease for August and was told I could return to my regular office Sept. 1, which I did.
On Aug. 31, 2020, Doc had a middle cerebral artery stroke. He received the clot buster within 40 minutes and was in surgery within 90 minutes. He regained consciousness and lucidity but would always have a left-sided disability. During his third postoperative day he was told that he would never again swallow properly, and he yanked out his nasogastric tube. He had always told me that he would not accept artificial feeding. M. Leslie Felmly, MD, a psychiatrist, died on Sept. 12, 2020, and I buried him beside his family in New Jersey, on Sept. 22, 2020.
After that, I needed routine and normalcy, and therefore, stayed out of work only on the day of Doc’s burial. I took on new patients and continued with my old patients. As the holidays neared I braced myself; for 26 years I had spent Thanksgiving and New Year’s with Doc and Christmas with my family in Texas. None of that was going to happen in 2020. My best female friend and her husband invited me to a socially distanced Thanksgiving meal with the two of them, and I accepted. Christmas and New Year’s I spent alone (I live alone and enjoy my company). Both of those holidays were made special because I spent the eve days at the dementia care facility.
I received my first Pfizer injection on Jan. 6, 2021. One day later, I went to a park to get COVID testing before I returned to the dementia care facility. There, I learned that I was COVID positive, and when I called into the dementia facility, I learned that one resident and several staff members had also tested positive. As I stood in the sunshine outside the testing facility I thought: “So, now what will I do with the rest of my life?”
I began to feel profoundly tired, and over time, developed what felt like a very bad head cold. I had no high temperature or difficulty breathing. Truly, the worst of it was the profound fatigue and the terrorizing fear that I would develop problems breathing. By Jan. 21, I had only symptoms of fatigue, and on the 23rd, I had a negative COVID test. I attributed my course and recovery to my whole-food plant-based diet and routine high-dose vitamin D3 – in spite of my being an overweight, older African American woman. Through it all, I learned to ask for help, and one of my colleagues brought me a thermometer and 2 days of vegan Pho. I learned to be resourceful and ordered myself a fruit basket from Edible Arrangements when I was too fatigued to arrange deliveries by computer. I told Edible Arrangements that I was too weak to cut up a pineapple, and the manager included a cut-up pineapple in the box. I am grateful for the kindness of others.
I returned to work Jan. 25, and for most of each day, I feel better than I have ever felt in my adult life. It is amazing what 2 solid weeks can do for 50 years of arrears of sleep. The overwhelming fatigue was such that I could not not sleep. Thankfully, my remaining fatigue is less and less each day.
On Jan. 27, 2021, I received my second COVID vaccine injection and had no adverse reaction. Then on the 28th, I learned that my male cousin, who was just 6 months younger than I am, died of complications of COVID. Later, I learned that a resident of the dementia care facility had died from the same outbreak that had sickened me.
Since the beginning of the pandemic, I had tried so hard to remain healthy and COVID free and have my family, friends, and patients do the same. I planned, prepared, and executed but fate had other plans in store. Doc and my cousin are gone; I was exposed to COVID in my dementia care facility; and I know what matters for the rest of my life. I will continue to pursue and espouse health for me, my family, my friends, and my patients, and I will endeavor to be the best family member, friend, and physician that I can. To help with this, I remember the wise words of Dr. Felmly, “Your level of frustration will rise directly with your level of expectation” and “Above all else, remain flexible.” Going forward, I am reminded that I am not in charge; I am grateful for so many things; and I will continue to be as flexible as I can be.
Thelissa A. Harris, MD
Private Practice
Hartford, Conn.
Taking time for reflection
One year into the pandemic, I continue to learn to expect the unexpected, anticipate that things may not go as planned, accept that it is not business as usual, appreciate what I have, and focus on what is most important in my life – my family and most especially my children.
Despite the disruptions in our daily lives from the lockdowns, quarantines, and social distancing, my Catholic faith has grown stronger. I am not overly religious, but since the pandemic my children and I have attended online Mass regularly, sometimes in far away churches with different languages. It seems like we listen better now, reflect more on the homilies, and are really more in touch with our spirituality.
Professionally, I have seen the pandemic bring together geriatric psychiatrists from around the globe to tackle issues relevant to the mental health care of older adults. Within the International Psychogeriatric Association, we were spurred into collaborative actions with international colleagues in advocating for human rights of older adults in the context of the pandemic, creating online educational activities, and contributing to the special COVID-19 issue of the International Psychogeriatrics journal.
Maria I. Lapid, MD
Mayo Clinic
Rochester, Minn.
Concentrating on safety
The first year of the pandemic is over. How have my personal and professional goals changed? How has my life changed? Let us start with the latter.
I have been very lucky. I have continued to go into work at my hospital every day, which provides structure and socializing. My hospital has supplied PPE, although, like everywhere else, the rules keep changing.
Masks, face shield, goggles, etc.: I try to loop the mask around my earrings just right so it does not catch and pull the hooks off. I think the goggles make me look cool, like an ant man.
My world has narrowed to work and home. Like all of us, I no longer go to conferences. I do outpatient treatment from my office desk. I see inpatients from 6 feet away, in mask and goggles. The cookies I pass out are now individually wrapped. Takeout instead of restaurants. A new home gym.
I have learned a lot. I now know how to manage psychiatric wards where COVID clusters occur. How to transfer psychiatric patients who convert to COVID positive over to the medicine ward. I faithfully swab my own nose twice a week.
I am constantly saying (very nicely): “Please pull your mask up over your nose.” “Six feet apart, please.”
I saved my surgical masks in case I needed to reuse them. Fortunately, I did not. Now I have three overflowing drawers of masks. Plus, the heavy homemade cloth ones that friends and family sent.
Back to how have my goals changed? Basically they have not. I fix my eyes straight ahead and concentrate on safety. Safety of patients, staff, my family, myself.
And daily add another yellow, or blue, or white, surgical mask to the drawers.
Elspeth Cameron Ritchie, MD, MPH
Washington
Awaiting project’s return
I had been actively involved in community service as the cofounder of The Bold Beauty Project since 2015. We are a Miami-based nonprofit, and we pair women with disabilities with volunteer photographers and create art shows. Our motto: Disability becomes Beauty becomes Art becomes Change.
I have dedicated about half of my time to the project, and it has been incredibly rewarding. It all came to a halt in March 2020, and it has left a real void in my daily schedule and my psyche. I am eagerly awaiting the return of the Bold Beauty Project with a renewed appreciation and enthusiasm. I hope you will check us out boldbeautyproject.com. If you are inspired to get involved, please contact me at [email protected].
Eva Ritvo, MD
Private Practice
Miami Beach, Fla.
COVID-19: Remaining flexible amid the uncertainty
COVID-19: Remaining flexible amid the uncertainty
Editor’s Note: With 1 year of the COVID-19 pandemic in the rearview mirror, we decided to check in with the Editorial Advisory Board members of Clinical Psychiatry News about the impact it has had on their practices and lives.
Redefining how to engage
The COVID-19 pandemic has triggered a wave of mental health problems in our population, such as general stress, addiction, weight gain, depression, and social isolation, and these symptoms are exacerbated in mental health patients who are already struggling to cope with personal issues.
When the pandemic lockdown was announced in March 2020, many of my patients became overwhelmed and panicked at the idea of not being able to come to my office for in-person therapy. As an alternative, I started phone call sessions with my clients. These calls forced me to listen extra carefully to patient voice intonations to ascertain their true feelings, since I was unable to view the clients.
Soon thereafter, I transitioned to telemedicine over the Internet, and this visual helped me assess each patient. In addition, my patients became accustomed to telemedicine and embraced it once they saw me and were able to interact with me on the screen.
Although the pandemic disrupted my medical practice, it has redefined the way I can do therapy, as I can practice medicine from a distance. Telemedicine is time efficient for both my patients and me and it provides extreme social distancing, eliminating COVID-19 exposure between doctor and patient.
The pandemic has forced me to be adaptable and to recognize that, if you are open to changing habits, you can find a solution to any situation, including a pandemic.
Richard W. Cohen, MD
Private Practice
Philadelphia
Adjusting to fate
As it became clear in January 2020 that a pandemic was upon us, I made plans and prepared. I needed to remain healthy for my patients and my 102-year-old best friend, Doc.
I purchased PPE and 6 months’ of nonperishable groceries and toilet tissue from a commercial vendor. I made certain that Doc’s caregivers had what they needed to care for him and their families and preached to them, family, patients, and friends the public health guidelines of the day. Also, I needed to remain healthy for my patients who live in a dementia care facility, and I joined other workers there in being careful and proud that our facility remained COVID free.
By March 2020, I left my office, because it was in a building where both residents and staff were becoming ill with COVID. I started audio and video telemedicine as well as standing outside the windows of patients who only read lips and do not use digital technology. Under these new circumstances, patients (and Doc) revealed things about themselves that had remained hidden for decades. There was a sense of urgency and uncertainty.
I also started weekly COVID testing, at first at CVS and then in a public park. Doc, who had had congestive heart failure for 2 years, had celebrated his 103rd birthday in February, and continued to be a source of encouragement and support. We weathered through the spring and summer with him on lockdown in his senior residence. The dementia care facility remained free of COVID.
My plan had been to return to my office in July, however, the facility manager determined that they were not ready to receive my outpatients. I took on a short-term lease for August and was told I could return to my regular office Sept. 1, which I did.
On Aug. 31, 2020, Doc had a middle cerebral artery stroke. He received the clot buster within 40 minutes and was in surgery within 90 minutes. He regained consciousness and lucidity but would always have a left-sided disability. During his third postoperative day he was told that he would never again swallow properly, and he yanked out his nasogastric tube. He had always told me that he would not accept artificial feeding. M. Leslie Felmly, MD, a psychiatrist, died on Sept. 12, 2020, and I buried him beside his family in New Jersey, on Sept. 22, 2020.
After that, I needed routine and normalcy, and therefore, stayed out of work only on the day of Doc’s burial. I took on new patients and continued with my old patients. As the holidays neared I braced myself; for 26 years I had spent Thanksgiving and New Year’s with Doc and Christmas with my family in Texas. None of that was going to happen in 2020. My best female friend and her husband invited me to a socially distanced Thanksgiving meal with the two of them, and I accepted. Christmas and New Year’s I spent alone (I live alone and enjoy my company). Both of those holidays were made special because I spent the eve days at the dementia care facility.
I received my first Pfizer injection on Jan. 6, 2021. One day later, I went to a park to get COVID testing before I returned to the dementia care facility. There, I learned that I was COVID positive, and when I called into the dementia facility, I learned that one resident and several staff members had also tested positive. As I stood in the sunshine outside the testing facility I thought: “So, now what will I do with the rest of my life?”
I began to feel profoundly tired, and over time, developed what felt like a very bad head cold. I had no high temperature or difficulty breathing. Truly, the worst of it was the profound fatigue and the terrorizing fear that I would develop problems breathing. By Jan. 21, I had only symptoms of fatigue, and on the 23rd, I had a negative COVID test. I attributed my course and recovery to my whole-food plant-based diet and routine high-dose vitamin D3 – in spite of my being an overweight, older African American woman. Through it all, I learned to ask for help, and one of my colleagues brought me a thermometer and 2 days of vegan Pho. I learned to be resourceful and ordered myself a fruit basket from Edible Arrangements when I was too fatigued to arrange deliveries by computer. I told Edible Arrangements that I was too weak to cut up a pineapple, and the manager included a cut-up pineapple in the box. I am grateful for the kindness of others.
I returned to work Jan. 25, and for most of each day, I feel better than I have ever felt in my adult life. It is amazing what 2 solid weeks can do for 50 years of arrears of sleep. The overwhelming fatigue was such that I could not not sleep. Thankfully, my remaining fatigue is less and less each day.
On Jan. 27, 2021, I received my second COVID vaccine injection and had no adverse reaction. Then on the 28th, I learned that my male cousin, who was just 6 months younger than I am, died of complications of COVID. Later, I learned that a resident of the dementia care facility had died from the same outbreak that had sickened me.
Since the beginning of the pandemic, I had tried so hard to remain healthy and COVID free and have my family, friends, and patients do the same. I planned, prepared, and executed but fate had other plans in store. Doc and my cousin are gone; I was exposed to COVID in my dementia care facility; and I know what matters for the rest of my life. I will continue to pursue and espouse health for me, my family, my friends, and my patients, and I will endeavor to be the best family member, friend, and physician that I can. To help with this, I remember the wise words of Dr. Felmly, “Your level of frustration will rise directly with your level of expectation” and “Above all else, remain flexible.” Going forward, I am reminded that I am not in charge; I am grateful for so many things; and I will continue to be as flexible as I can be.
Thelissa A. Harris, MD
Private Practice
Hartford, Conn.
Taking time for reflection
One year into the pandemic, I continue to learn to expect the unexpected, anticipate that things may not go as planned, accept that it is not business as usual, appreciate what I have, and focus on what is most important in my life – my family and most especially my children.
Despite the disruptions in our daily lives from the lockdowns, quarantines, and social distancing, my Catholic faith has grown stronger. I am not overly religious, but since the pandemic my children and I have attended online Mass regularly, sometimes in far away churches with different languages. It seems like we listen better now, reflect more on the homilies, and are really more in touch with our spirituality.
Professionally, I have seen the pandemic bring together geriatric psychiatrists from around the globe to tackle issues relevant to the mental health care of older adults. Within the International Psychogeriatric Association, we were spurred into collaborative actions with international colleagues in advocating for human rights of older adults in the context of the pandemic, creating online educational activities, and contributing to the special COVID-19 issue of the International Psychogeriatrics journal.
Maria I. Lapid, MD
Mayo Clinic
Rochester, Minn.
Concentrating on safety
The first year of the pandemic is over. How have my personal and professional goals changed? How has my life changed? Let us start with the latter.
I have been very lucky. I have continued to go into work at my hospital every day, which provides structure and socializing. My hospital has supplied PPE, although, like everywhere else, the rules keep changing.
Masks, face shield, goggles, etc.: I try to loop the mask around my earrings just right so it does not catch and pull the hooks off. I think the goggles make me look cool, like an ant man.
My world has narrowed to work and home. Like all of us, I no longer go to conferences. I do outpatient treatment from my office desk. I see inpatients from 6 feet away, in mask and goggles. The cookies I pass out are now individually wrapped. Takeout instead of restaurants. A new home gym.
I have learned a lot. I now know how to manage psychiatric wards where COVID clusters occur. How to transfer psychiatric patients who convert to COVID positive over to the medicine ward. I faithfully swab my own nose twice a week.
I am constantly saying (very nicely): “Please pull your mask up over your nose.” “Six feet apart, please.”
I saved my surgical masks in case I needed to reuse them. Fortunately, I did not. Now I have three overflowing drawers of masks. Plus, the heavy homemade cloth ones that friends and family sent.
Back to how have my goals changed? Basically they have not. I fix my eyes straight ahead and concentrate on safety. Safety of patients, staff, my family, myself.
And daily add another yellow, or blue, or white, surgical mask to the drawers.
Elspeth Cameron Ritchie, MD, MPH
Washington
Awaiting project’s return
I had been actively involved in community service as the cofounder of The Bold Beauty Project since 2015. We are a Miami-based nonprofit, and we pair women with disabilities with volunteer photographers and create art shows. Our motto: Disability becomes Beauty becomes Art becomes Change.
I have dedicated about half of my time to the project, and it has been incredibly rewarding. It all came to a halt in March 2020, and it has left a real void in my daily schedule and my psyche. I am eagerly awaiting the return of the Bold Beauty Project with a renewed appreciation and enthusiasm. I hope you will check us out boldbeautyproject.com. If you are inspired to get involved, please contact me at [email protected].
Eva Ritvo, MD
Private Practice
Miami Beach, Fla.
Editor’s Note: With 1 year of the COVID-19 pandemic in the rearview mirror, we decided to check in with the Editorial Advisory Board members of Clinical Psychiatry News about the impact it has had on their practices and lives.
Redefining how to engage
The COVID-19 pandemic has triggered a wave of mental health problems in our population, such as general stress, addiction, weight gain, depression, and social isolation, and these symptoms are exacerbated in mental health patients who are already struggling to cope with personal issues.
When the pandemic lockdown was announced in March 2020, many of my patients became overwhelmed and panicked at the idea of not being able to come to my office for in-person therapy. As an alternative, I started phone call sessions with my clients. These calls forced me to listen extra carefully to patient voice intonations to ascertain their true feelings, since I was unable to view the clients.
Soon thereafter, I transitioned to telemedicine over the Internet, and this visual helped me assess each patient. In addition, my patients became accustomed to telemedicine and embraced it once they saw me and were able to interact with me on the screen.
Although the pandemic disrupted my medical practice, it has redefined the way I can do therapy, as I can practice medicine from a distance. Telemedicine is time efficient for both my patients and me and it provides extreme social distancing, eliminating COVID-19 exposure between doctor and patient.
The pandemic has forced me to be adaptable and to recognize that, if you are open to changing habits, you can find a solution to any situation, including a pandemic.
Richard W. Cohen, MD
Private Practice
Philadelphia
Adjusting to fate
As it became clear in January 2020 that a pandemic was upon us, I made plans and prepared. I needed to remain healthy for my patients and my 102-year-old best friend, Doc.
I purchased PPE and 6 months’ of nonperishable groceries and toilet tissue from a commercial vendor. I made certain that Doc’s caregivers had what they needed to care for him and their families and preached to them, family, patients, and friends the public health guidelines of the day. Also, I needed to remain healthy for my patients who live in a dementia care facility, and I joined other workers there in being careful and proud that our facility remained COVID free.
By March 2020, I left my office, because it was in a building where both residents and staff were becoming ill with COVID. I started audio and video telemedicine as well as standing outside the windows of patients who only read lips and do not use digital technology. Under these new circumstances, patients (and Doc) revealed things about themselves that had remained hidden for decades. There was a sense of urgency and uncertainty.
I also started weekly COVID testing, at first at CVS and then in a public park. Doc, who had had congestive heart failure for 2 years, had celebrated his 103rd birthday in February, and continued to be a source of encouragement and support. We weathered through the spring and summer with him on lockdown in his senior residence. The dementia care facility remained free of COVID.
My plan had been to return to my office in July, however, the facility manager determined that they were not ready to receive my outpatients. I took on a short-term lease for August and was told I could return to my regular office Sept. 1, which I did.
On Aug. 31, 2020, Doc had a middle cerebral artery stroke. He received the clot buster within 40 minutes and was in surgery within 90 minutes. He regained consciousness and lucidity but would always have a left-sided disability. During his third postoperative day he was told that he would never again swallow properly, and he yanked out his nasogastric tube. He had always told me that he would not accept artificial feeding. M. Leslie Felmly, MD, a psychiatrist, died on Sept. 12, 2020, and I buried him beside his family in New Jersey, on Sept. 22, 2020.
After that, I needed routine and normalcy, and therefore, stayed out of work only on the day of Doc’s burial. I took on new patients and continued with my old patients. As the holidays neared I braced myself; for 26 years I had spent Thanksgiving and New Year’s with Doc and Christmas with my family in Texas. None of that was going to happen in 2020. My best female friend and her husband invited me to a socially distanced Thanksgiving meal with the two of them, and I accepted. Christmas and New Year’s I spent alone (I live alone and enjoy my company). Both of those holidays were made special because I spent the eve days at the dementia care facility.
I received my first Pfizer injection on Jan. 6, 2021. One day later, I went to a park to get COVID testing before I returned to the dementia care facility. There, I learned that I was COVID positive, and when I called into the dementia facility, I learned that one resident and several staff members had also tested positive. As I stood in the sunshine outside the testing facility I thought: “So, now what will I do with the rest of my life?”
I began to feel profoundly tired, and over time, developed what felt like a very bad head cold. I had no high temperature or difficulty breathing. Truly, the worst of it was the profound fatigue and the terrorizing fear that I would develop problems breathing. By Jan. 21, I had only symptoms of fatigue, and on the 23rd, I had a negative COVID test. I attributed my course and recovery to my whole-food plant-based diet and routine high-dose vitamin D3 – in spite of my being an overweight, older African American woman. Through it all, I learned to ask for help, and one of my colleagues brought me a thermometer and 2 days of vegan Pho. I learned to be resourceful and ordered myself a fruit basket from Edible Arrangements when I was too fatigued to arrange deliveries by computer. I told Edible Arrangements that I was too weak to cut up a pineapple, and the manager included a cut-up pineapple in the box. I am grateful for the kindness of others.
I returned to work Jan. 25, and for most of each day, I feel better than I have ever felt in my adult life. It is amazing what 2 solid weeks can do for 50 years of arrears of sleep. The overwhelming fatigue was such that I could not not sleep. Thankfully, my remaining fatigue is less and less each day.
On Jan. 27, 2021, I received my second COVID vaccine injection and had no adverse reaction. Then on the 28th, I learned that my male cousin, who was just 6 months younger than I am, died of complications of COVID. Later, I learned that a resident of the dementia care facility had died from the same outbreak that had sickened me.
Since the beginning of the pandemic, I had tried so hard to remain healthy and COVID free and have my family, friends, and patients do the same. I planned, prepared, and executed but fate had other plans in store. Doc and my cousin are gone; I was exposed to COVID in my dementia care facility; and I know what matters for the rest of my life. I will continue to pursue and espouse health for me, my family, my friends, and my patients, and I will endeavor to be the best family member, friend, and physician that I can. To help with this, I remember the wise words of Dr. Felmly, “Your level of frustration will rise directly with your level of expectation” and “Above all else, remain flexible.” Going forward, I am reminded that I am not in charge; I am grateful for so many things; and I will continue to be as flexible as I can be.
Thelissa A. Harris, MD
Private Practice
Hartford, Conn.
Taking time for reflection
One year into the pandemic, I continue to learn to expect the unexpected, anticipate that things may not go as planned, accept that it is not business as usual, appreciate what I have, and focus on what is most important in my life – my family and most especially my children.
Despite the disruptions in our daily lives from the lockdowns, quarantines, and social distancing, my Catholic faith has grown stronger. I am not overly religious, but since the pandemic my children and I have attended online Mass regularly, sometimes in far away churches with different languages. It seems like we listen better now, reflect more on the homilies, and are really more in touch with our spirituality.
Professionally, I have seen the pandemic bring together geriatric psychiatrists from around the globe to tackle issues relevant to the mental health care of older adults. Within the International Psychogeriatric Association, we were spurred into collaborative actions with international colleagues in advocating for human rights of older adults in the context of the pandemic, creating online educational activities, and contributing to the special COVID-19 issue of the International Psychogeriatrics journal.
Maria I. Lapid, MD
Mayo Clinic
Rochester, Minn.
Concentrating on safety
The first year of the pandemic is over. How have my personal and professional goals changed? How has my life changed? Let us start with the latter.
I have been very lucky. I have continued to go into work at my hospital every day, which provides structure and socializing. My hospital has supplied PPE, although, like everywhere else, the rules keep changing.
Masks, face shield, goggles, etc.: I try to loop the mask around my earrings just right so it does not catch and pull the hooks off. I think the goggles make me look cool, like an ant man.
My world has narrowed to work and home. Like all of us, I no longer go to conferences. I do outpatient treatment from my office desk. I see inpatients from 6 feet away, in mask and goggles. The cookies I pass out are now individually wrapped. Takeout instead of restaurants. A new home gym.
I have learned a lot. I now know how to manage psychiatric wards where COVID clusters occur. How to transfer psychiatric patients who convert to COVID positive over to the medicine ward. I faithfully swab my own nose twice a week.
I am constantly saying (very nicely): “Please pull your mask up over your nose.” “Six feet apart, please.”
I saved my surgical masks in case I needed to reuse them. Fortunately, I did not. Now I have three overflowing drawers of masks. Plus, the heavy homemade cloth ones that friends and family sent.
Back to how have my goals changed? Basically they have not. I fix my eyes straight ahead and concentrate on safety. Safety of patients, staff, my family, myself.
And daily add another yellow, or blue, or white, surgical mask to the drawers.
Elspeth Cameron Ritchie, MD, MPH
Washington
Awaiting project’s return
I had been actively involved in community service as the cofounder of The Bold Beauty Project since 2015. We are a Miami-based nonprofit, and we pair women with disabilities with volunteer photographers and create art shows. Our motto: Disability becomes Beauty becomes Art becomes Change.
I have dedicated about half of my time to the project, and it has been incredibly rewarding. It all came to a halt in March 2020, and it has left a real void in my daily schedule and my psyche. I am eagerly awaiting the return of the Bold Beauty Project with a renewed appreciation and enthusiasm. I hope you will check us out boldbeautyproject.com. If you are inspired to get involved, please contact me at [email protected].
Eva Ritvo, MD
Private Practice
Miami Beach, Fla.
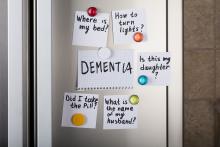
Cannabinoids promising for improving appetite, behavior in dementia
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
Blood pressure meds tied to increased schizophrenia risk
ACE inhibitors may be associated with an increased risk for schizophrenia and may affect psychiatric symptoms, new research suggests.
Investigators found individuals who carry a genetic variant associated with lower levels of the ACE gene and protein have increased liability to schizophrenia, suggesting that drugs that lower ACE levels or activity may do the same.
“Our findings warrant further investigation into the role of ACE in schizophrenia and closer monitoring by clinicians of individuals, especially those with schizophrenia, who may be on medication that lower ACE activity, such as ACE inhibitors,” Sonia Shah, PhD, Institute for Biomedical Sciences, University of Queensland, Brisbane, Australia, said in an interview.
The study was published online March 10, 2021, in JAMA Psychiatry.
Antihypertensives and mental illness
Hypertension is common in patients with psychiatric disorders and observational studies have reported associations between antihypertensive medication and these disorders, although the findings have been mixed.
Dr. Shah and colleagues estimated the potential of different antihypertensive drug classes on schizophrenia, bipolar disorder, and major depressive disorder.
In a two-sample Mendelian randomization study, they evaluated ties between a single-nucleotide variant and drug-target gene expression derived from expression quantitative trait loci data in blood (sample 1) and the SNV disease association from published case-control, genomewide association studies (sample 2).
The analyses included 40,675 patients with schizophrenia and 64,643 controls; 20,352 with bipolar disorder and 31,358 controls; and 135,458 with major depressive disorder and 344,901 controls.
The major finding was that a one standard deviation–lower expression of the ACE gene in blood was associated with lower systolic blood pressure of 4.0 mm Hg (95% confidence interval, 2.7-5.3), but also an increased risk of schizophrenia (odds ratio, 1.75; 95% CI, 1.28-2.38).
Could ACE inhibitors worsen symptoms or trigger episodes?
In their article, the researchers noted that, in most patients, onset of schizophrenia occurs in late adolescence or early adult life, ruling out ACE inhibitor treatment as a potential causal factor for most cases.
“However, if lower ACE levels play a causal role for schizophrenia risk, it would be reasonable to hypothesize that further lowering of ACE activity in existing patients could worsen symptoms or trigger a new episode,” they wrote.
Dr. Shah emphasized that evidence from genetic analyses alone is “not sufficient to justify changes in prescription guidelines.”
“Patients should not stop taking these medications if they are effective at controlling their blood pressure and they don’t suffer any adverse effects. But it would be reasonable to encourage greater pharmacovigilance,” she said in an interview.
“One way in which we are hoping to follow up these findings,” said Dr. Shah, “is to access electronic health record data for millions of individuals to investigate if there is evidence of increased rates of psychotic episodes in individuals who use ACE inhibitors, compared to other classes of blood pressure–lowering medication.”
Caution warranted
Reached for comment, Timothy Sullivan, MD, chair of psychiatry and behavioral sciences at Staten Island University Hospital in New York, noted that this is an “extremely complicated” study and urged caution in interpreting the results.
“Since most people develop schizophrenia earlier in life, before they usually develop problems with blood pressure, it’s not so much that these drugs might cause schizophrenia,” Dr. Sullivan said.
“But because of their effects on this particular gene, there’s a possibility that they might worsen symptoms or in somebody with borderline risk might cause them to develop symptoms later in life. This may apply to a relatively small number of people who develop symptoms of schizophrenia in their 40s and beyond,” he added.
That’s where “pharmacovigilance” comes into play, Dr. Sullivan said. “In other words, that they otherwise wouldn’t experience?”
Support for the study was provided by the National Health and Medical Research Council (Australia) and U.S. National Institute for Mental Health. Dr. Shah and Dr. Sullivan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ACE inhibitors may be associated with an increased risk for schizophrenia and may affect psychiatric symptoms, new research suggests.
Investigators found individuals who carry a genetic variant associated with lower levels of the ACE gene and protein have increased liability to schizophrenia, suggesting that drugs that lower ACE levels or activity may do the same.
“Our findings warrant further investigation into the role of ACE in schizophrenia and closer monitoring by clinicians of individuals, especially those with schizophrenia, who may be on medication that lower ACE activity, such as ACE inhibitors,” Sonia Shah, PhD, Institute for Biomedical Sciences, University of Queensland, Brisbane, Australia, said in an interview.
The study was published online March 10, 2021, in JAMA Psychiatry.
Antihypertensives and mental illness
Hypertension is common in patients with psychiatric disorders and observational studies have reported associations between antihypertensive medication and these disorders, although the findings have been mixed.
Dr. Shah and colleagues estimated the potential of different antihypertensive drug classes on schizophrenia, bipolar disorder, and major depressive disorder.
In a two-sample Mendelian randomization study, they evaluated ties between a single-nucleotide variant and drug-target gene expression derived from expression quantitative trait loci data in blood (sample 1) and the SNV disease association from published case-control, genomewide association studies (sample 2).
The analyses included 40,675 patients with schizophrenia and 64,643 controls; 20,352 with bipolar disorder and 31,358 controls; and 135,458 with major depressive disorder and 344,901 controls.
The major finding was that a one standard deviation–lower expression of the ACE gene in blood was associated with lower systolic blood pressure of 4.0 mm Hg (95% confidence interval, 2.7-5.3), but also an increased risk of schizophrenia (odds ratio, 1.75; 95% CI, 1.28-2.38).
Could ACE inhibitors worsen symptoms or trigger episodes?
In their article, the researchers noted that, in most patients, onset of schizophrenia occurs in late adolescence or early adult life, ruling out ACE inhibitor treatment as a potential causal factor for most cases.
“However, if lower ACE levels play a causal role for schizophrenia risk, it would be reasonable to hypothesize that further lowering of ACE activity in existing patients could worsen symptoms or trigger a new episode,” they wrote.
Dr. Shah emphasized that evidence from genetic analyses alone is “not sufficient to justify changes in prescription guidelines.”
“Patients should not stop taking these medications if they are effective at controlling their blood pressure and they don’t suffer any adverse effects. But it would be reasonable to encourage greater pharmacovigilance,” she said in an interview.
“One way in which we are hoping to follow up these findings,” said Dr. Shah, “is to access electronic health record data for millions of individuals to investigate if there is evidence of increased rates of psychotic episodes in individuals who use ACE inhibitors, compared to other classes of blood pressure–lowering medication.”
Caution warranted
Reached for comment, Timothy Sullivan, MD, chair of psychiatry and behavioral sciences at Staten Island University Hospital in New York, noted that this is an “extremely complicated” study and urged caution in interpreting the results.
“Since most people develop schizophrenia earlier in life, before they usually develop problems with blood pressure, it’s not so much that these drugs might cause schizophrenia,” Dr. Sullivan said.
“But because of their effects on this particular gene, there’s a possibility that they might worsen symptoms or in somebody with borderline risk might cause them to develop symptoms later in life. This may apply to a relatively small number of people who develop symptoms of schizophrenia in their 40s and beyond,” he added.
That’s where “pharmacovigilance” comes into play, Dr. Sullivan said. “In other words, that they otherwise wouldn’t experience?”
Support for the study was provided by the National Health and Medical Research Council (Australia) and U.S. National Institute for Mental Health. Dr. Shah and Dr. Sullivan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ACE inhibitors may be associated with an increased risk for schizophrenia and may affect psychiatric symptoms, new research suggests.
Investigators found individuals who carry a genetic variant associated with lower levels of the ACE gene and protein have increased liability to schizophrenia, suggesting that drugs that lower ACE levels or activity may do the same.
“Our findings warrant further investigation into the role of ACE in schizophrenia and closer monitoring by clinicians of individuals, especially those with schizophrenia, who may be on medication that lower ACE activity, such as ACE inhibitors,” Sonia Shah, PhD, Institute for Biomedical Sciences, University of Queensland, Brisbane, Australia, said in an interview.
The study was published online March 10, 2021, in JAMA Psychiatry.
Antihypertensives and mental illness
Hypertension is common in patients with psychiatric disorders and observational studies have reported associations between antihypertensive medication and these disorders, although the findings have been mixed.
Dr. Shah and colleagues estimated the potential of different antihypertensive drug classes on schizophrenia, bipolar disorder, and major depressive disorder.
In a two-sample Mendelian randomization study, they evaluated ties between a single-nucleotide variant and drug-target gene expression derived from expression quantitative trait loci data in blood (sample 1) and the SNV disease association from published case-control, genomewide association studies (sample 2).
The analyses included 40,675 patients with schizophrenia and 64,643 controls; 20,352 with bipolar disorder and 31,358 controls; and 135,458 with major depressive disorder and 344,901 controls.
The major finding was that a one standard deviation–lower expression of the ACE gene in blood was associated with lower systolic blood pressure of 4.0 mm Hg (95% confidence interval, 2.7-5.3), but also an increased risk of schizophrenia (odds ratio, 1.75; 95% CI, 1.28-2.38).
Could ACE inhibitors worsen symptoms or trigger episodes?
In their article, the researchers noted that, in most patients, onset of schizophrenia occurs in late adolescence or early adult life, ruling out ACE inhibitor treatment as a potential causal factor for most cases.
“However, if lower ACE levels play a causal role for schizophrenia risk, it would be reasonable to hypothesize that further lowering of ACE activity in existing patients could worsen symptoms or trigger a new episode,” they wrote.
Dr. Shah emphasized that evidence from genetic analyses alone is “not sufficient to justify changes in prescription guidelines.”
“Patients should not stop taking these medications if they are effective at controlling their blood pressure and they don’t suffer any adverse effects. But it would be reasonable to encourage greater pharmacovigilance,” she said in an interview.
“One way in which we are hoping to follow up these findings,” said Dr. Shah, “is to access electronic health record data for millions of individuals to investigate if there is evidence of increased rates of psychotic episodes in individuals who use ACE inhibitors, compared to other classes of blood pressure–lowering medication.”
Caution warranted
Reached for comment, Timothy Sullivan, MD, chair of psychiatry and behavioral sciences at Staten Island University Hospital in New York, noted that this is an “extremely complicated” study and urged caution in interpreting the results.
“Since most people develop schizophrenia earlier in life, before they usually develop problems with blood pressure, it’s not so much that these drugs might cause schizophrenia,” Dr. Sullivan said.
“But because of their effects on this particular gene, there’s a possibility that they might worsen symptoms or in somebody with borderline risk might cause them to develop symptoms later in life. This may apply to a relatively small number of people who develop symptoms of schizophrenia in their 40s and beyond,” he added.
That’s where “pharmacovigilance” comes into play, Dr. Sullivan said. “In other words, that they otherwise wouldn’t experience?”
Support for the study was provided by the National Health and Medical Research Council (Australia) and U.S. National Institute for Mental Health. Dr. Shah and Dr. Sullivan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Update: U.S. regulators question AstraZeneca vaccine trial data
Federal regulators on March 23 said they were “concerned” that drug maker AstraZeneca included “outdated information” in its announcement the previous day that the company’s COVID-19 vaccine was effective.
The federal Data and Safety Monitoring Board shared those concerns with the company as well as with the National Institute of Allergy and Infectious Diseases, and the U.S. Biomedical Advanced Research and Development Authority, according to a statement from NIAID issued early March 23.
“We urge the company to work with the DSMB to review the efficacy data and ensure the most accurate, up-to-date efficacy data be made public as quickly as possible,” the agency said.
The NIAID statement does not say what data may have been outdated or how it may have changed the results. The company said March 22 it plans to see U.S. authorization for the vaccine in April.
The statement from NIAID comes a day after AstraZeneca said the interim results of their phase III U.S. study found it was 79% effective against symptomatic COVID-19, 80% effective in people 65 years and older, and 100% effective against severe or critical disease and hospitalization.
Company officials and clinical trial investigators on March 22 also addressed the recent concerns about blood clots, how well the vaccine will perform against variants, and provided a timeline for seeking regulatory approval.
“There are many countries in Europe and throughout the world that have already authorized this. The fact that a United States-run study has confirmed the efficacy and safety of this vaccine, I think is an important contribution to global health in general,” Anthony Fauci, MD, chief medical advisor to President Joe Biden, said during a White House press briefing March 22.
Andy Slavitt, White House senior advisor for the COVID-19 Response Team, had a more tempered reaction.
“It’s important to remind everyone we cannot and will not get ahead of the FDA,” he said. “While we would certainly call today’s news encouraging, it’s the kind of thing we like to see, we have a rigorous process that will come once an EUA is submitted and that will give us more information.”
With 30 million doses at the ready, the company plans to file for FDA emergency use authorization “within weeks,” Menelas Pangalos, executive vice president of biopharmaceuticals research and development at AstraZeneca, said during a media briefing March 22.
Risk of thrombosis addressed
Regarding highly publicized reports of problems with blood clots from the AstraZeneca vaccine, the World Health Organization found the vaccine creates no greater risks, as did the European Medicines Agency
“We’ve had absolute confidence in the efficacy of the vaccine. Seeing this data now I hope gives others increased confidence that this is a very safe and effective vaccine,” Mr. Pangalos said.
“We’re glad this is being investigated really thoroughly,” Magda Sobieszczyk, MD, an infectious disease specialist at Columbia University In New York City, said. “It’s incredibly reassuring that the regulatory agencies have looked at the data thoroughly and there is no enhanced signal above what is seen in the population.”
“There were no concerning signals noted in the U.S. data,” she added.
Regarding the risk of blood clots, “These data are therefore timely in further addressing any safety concerns that could undermine vaccine uptake.” Andrew Garrett, PhD, executive vice president of scientific operations at ICON Clinical Research, agreed.
The vaccine was well-tolerated, the company reported, with no serious adverse events. Temporary pain and tenderness at the injection site, mild-to-moderate headaches, fatigue, chills, fever, muscle aches. and malaise were among the reported reactions.
The phase III interim results show 141 cases of symptomatic COVID-19 in the study of 32,449 adults. “We don’t have the whole breakdown yet . . . these are the high-level results we just got this week,” Mr. Pangalos said. Further information on rates of mild to moderate COVID-19 illness between groups is not yet available, for example.
The company explained that participants were randomly assigned to vaccine or placebo, with twice as many receiving the actual vaccine.
The trial is ongoing, so the FDA will receive information on more than the 141 COVID-19 symptomatic cases when the company submits a full primary analysis to the agency, Mr. Pangalos said.
In the phase III study, patients received two doses 4 weeks apart.
Beyond the U.S. study, the company has additional information, including real-world data from the United Kingdom, that it intends to submit to the FDA. Part of this evidence suggests increased efficacy when a second dose is administered at 3 months
‘Robust’ findings
“This is a large study, so these results can be expected to be robust. They could be expected to be even more so if there were more cases to compare between the groups, but 141 is still a substantial number of cases,” said Peter English, MD, of Horsham, United Kingdom, who is immediate past chair of the British Medical Association Public Health Medicine Committee.
Experts welcomed the 80% efficacy in people 65 and older in particular. “Importantly, the trial provides further support for efficacy in the elderly where previous clinical trial data, other than immunologic data, had been lacking,” Dr. Garrett said.
“It is clear this vaccine has very good efficacy. Remember that 60% was, prior to any trials being started, regarded as a good target,” said Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene & Tropical Medicine. “This efficacy does not show a notable decline at older ages. This was expected and the speculation that it was ineffective or quasi-ineffective at older ages was totally unjustified.
“This is good news for the global community and one hopes that any political statements around this good news are avoided,” he added.
Efficacy against variants?
Regarding virus variants, Mr. Pangalos noted the study was conducted when several variants of concern were in circulation.
“What I can say is given this study was conducted much later in terms of timing, it’s very encouraging that we’ve got such high efficacy numbers when undoubtedly there are variants of concern in circulation in this study,” Mr. Pangalos said.
“It also highlights why we believe that against severe disease, our vaccine will be effective against all variants of concern,” he added.
Once the company submits its EUA to the FDA, the company is ready to immediately distribute 30 million doses of the vaccine and expects to ship 50 million total within the first month, Ruud Dobber, PhD, AstraZeneca executive vice president and president of the AZ Biopharmaceuticals Business Unit, said during the briefing.
The vaccine can be stored at 2 to 8 degrees Celsius for at least 6 months. Like other COVID-19 vaccines already authorized for emergency use, the duration of protection with the AstraZeneca product remains unknown.
This article was updated March 23, 2021.
A version of this article first appeared on WebMD.com.
Federal regulators on March 23 said they were “concerned” that drug maker AstraZeneca included “outdated information” in its announcement the previous day that the company’s COVID-19 vaccine was effective.
The federal Data and Safety Monitoring Board shared those concerns with the company as well as with the National Institute of Allergy and Infectious Diseases, and the U.S. Biomedical Advanced Research and Development Authority, according to a statement from NIAID issued early March 23.
“We urge the company to work with the DSMB to review the efficacy data and ensure the most accurate, up-to-date efficacy data be made public as quickly as possible,” the agency said.
The NIAID statement does not say what data may have been outdated or how it may have changed the results. The company said March 22 it plans to see U.S. authorization for the vaccine in April.
The statement from NIAID comes a day after AstraZeneca said the interim results of their phase III U.S. study found it was 79% effective against symptomatic COVID-19, 80% effective in people 65 years and older, and 100% effective against severe or critical disease and hospitalization.
Company officials and clinical trial investigators on March 22 also addressed the recent concerns about blood clots, how well the vaccine will perform against variants, and provided a timeline for seeking regulatory approval.
“There are many countries in Europe and throughout the world that have already authorized this. The fact that a United States-run study has confirmed the efficacy and safety of this vaccine, I think is an important contribution to global health in general,” Anthony Fauci, MD, chief medical advisor to President Joe Biden, said during a White House press briefing March 22.
Andy Slavitt, White House senior advisor for the COVID-19 Response Team, had a more tempered reaction.
“It’s important to remind everyone we cannot and will not get ahead of the FDA,” he said. “While we would certainly call today’s news encouraging, it’s the kind of thing we like to see, we have a rigorous process that will come once an EUA is submitted and that will give us more information.”
With 30 million doses at the ready, the company plans to file for FDA emergency use authorization “within weeks,” Menelas Pangalos, executive vice president of biopharmaceuticals research and development at AstraZeneca, said during a media briefing March 22.
Risk of thrombosis addressed
Regarding highly publicized reports of problems with blood clots from the AstraZeneca vaccine, the World Health Organization found the vaccine creates no greater risks, as did the European Medicines Agency
“We’ve had absolute confidence in the efficacy of the vaccine. Seeing this data now I hope gives others increased confidence that this is a very safe and effective vaccine,” Mr. Pangalos said.
“We’re glad this is being investigated really thoroughly,” Magda Sobieszczyk, MD, an infectious disease specialist at Columbia University In New York City, said. “It’s incredibly reassuring that the regulatory agencies have looked at the data thoroughly and there is no enhanced signal above what is seen in the population.”
“There were no concerning signals noted in the U.S. data,” she added.
Regarding the risk of blood clots, “These data are therefore timely in further addressing any safety concerns that could undermine vaccine uptake.” Andrew Garrett, PhD, executive vice president of scientific operations at ICON Clinical Research, agreed.
The vaccine was well-tolerated, the company reported, with no serious adverse events. Temporary pain and tenderness at the injection site, mild-to-moderate headaches, fatigue, chills, fever, muscle aches. and malaise were among the reported reactions.
The phase III interim results show 141 cases of symptomatic COVID-19 in the study of 32,449 adults. “We don’t have the whole breakdown yet . . . these are the high-level results we just got this week,” Mr. Pangalos said. Further information on rates of mild to moderate COVID-19 illness between groups is not yet available, for example.
The company explained that participants were randomly assigned to vaccine or placebo, with twice as many receiving the actual vaccine.
The trial is ongoing, so the FDA will receive information on more than the 141 COVID-19 symptomatic cases when the company submits a full primary analysis to the agency, Mr. Pangalos said.
In the phase III study, patients received two doses 4 weeks apart.
Beyond the U.S. study, the company has additional information, including real-world data from the United Kingdom, that it intends to submit to the FDA. Part of this evidence suggests increased efficacy when a second dose is administered at 3 months
‘Robust’ findings
“This is a large study, so these results can be expected to be robust. They could be expected to be even more so if there were more cases to compare between the groups, but 141 is still a substantial number of cases,” said Peter English, MD, of Horsham, United Kingdom, who is immediate past chair of the British Medical Association Public Health Medicine Committee.
Experts welcomed the 80% efficacy in people 65 and older in particular. “Importantly, the trial provides further support for efficacy in the elderly where previous clinical trial data, other than immunologic data, had been lacking,” Dr. Garrett said.
“It is clear this vaccine has very good efficacy. Remember that 60% was, prior to any trials being started, regarded as a good target,” said Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene & Tropical Medicine. “This efficacy does not show a notable decline at older ages. This was expected and the speculation that it was ineffective or quasi-ineffective at older ages was totally unjustified.
“This is good news for the global community and one hopes that any political statements around this good news are avoided,” he added.
Efficacy against variants?
Regarding virus variants, Mr. Pangalos noted the study was conducted when several variants of concern were in circulation.
“What I can say is given this study was conducted much later in terms of timing, it’s very encouraging that we’ve got such high efficacy numbers when undoubtedly there are variants of concern in circulation in this study,” Mr. Pangalos said.
“It also highlights why we believe that against severe disease, our vaccine will be effective against all variants of concern,” he added.
Once the company submits its EUA to the FDA, the company is ready to immediately distribute 30 million doses of the vaccine and expects to ship 50 million total within the first month, Ruud Dobber, PhD, AstraZeneca executive vice president and president of the AZ Biopharmaceuticals Business Unit, said during the briefing.
The vaccine can be stored at 2 to 8 degrees Celsius for at least 6 months. Like other COVID-19 vaccines already authorized for emergency use, the duration of protection with the AstraZeneca product remains unknown.
This article was updated March 23, 2021.
A version of this article first appeared on WebMD.com.
Federal regulators on March 23 said they were “concerned” that drug maker AstraZeneca included “outdated information” in its announcement the previous day that the company’s COVID-19 vaccine was effective.
The federal Data and Safety Monitoring Board shared those concerns with the company as well as with the National Institute of Allergy and Infectious Diseases, and the U.S. Biomedical Advanced Research and Development Authority, according to a statement from NIAID issued early March 23.
“We urge the company to work with the DSMB to review the efficacy data and ensure the most accurate, up-to-date efficacy data be made public as quickly as possible,” the agency said.
The NIAID statement does not say what data may have been outdated or how it may have changed the results. The company said March 22 it plans to see U.S. authorization for the vaccine in April.
The statement from NIAID comes a day after AstraZeneca said the interim results of their phase III U.S. study found it was 79% effective against symptomatic COVID-19, 80% effective in people 65 years and older, and 100% effective against severe or critical disease and hospitalization.
Company officials and clinical trial investigators on March 22 also addressed the recent concerns about blood clots, how well the vaccine will perform against variants, and provided a timeline for seeking regulatory approval.
“There are many countries in Europe and throughout the world that have already authorized this. The fact that a United States-run study has confirmed the efficacy and safety of this vaccine, I think is an important contribution to global health in general,” Anthony Fauci, MD, chief medical advisor to President Joe Biden, said during a White House press briefing March 22.
Andy Slavitt, White House senior advisor for the COVID-19 Response Team, had a more tempered reaction.
“It’s important to remind everyone we cannot and will not get ahead of the FDA,” he said. “While we would certainly call today’s news encouraging, it’s the kind of thing we like to see, we have a rigorous process that will come once an EUA is submitted and that will give us more information.”
With 30 million doses at the ready, the company plans to file for FDA emergency use authorization “within weeks,” Menelas Pangalos, executive vice president of biopharmaceuticals research and development at AstraZeneca, said during a media briefing March 22.
Risk of thrombosis addressed
Regarding highly publicized reports of problems with blood clots from the AstraZeneca vaccine, the World Health Organization found the vaccine creates no greater risks, as did the European Medicines Agency
“We’ve had absolute confidence in the efficacy of the vaccine. Seeing this data now I hope gives others increased confidence that this is a very safe and effective vaccine,” Mr. Pangalos said.
“We’re glad this is being investigated really thoroughly,” Magda Sobieszczyk, MD, an infectious disease specialist at Columbia University In New York City, said. “It’s incredibly reassuring that the regulatory agencies have looked at the data thoroughly and there is no enhanced signal above what is seen in the population.”
“There were no concerning signals noted in the U.S. data,” she added.
Regarding the risk of blood clots, “These data are therefore timely in further addressing any safety concerns that could undermine vaccine uptake.” Andrew Garrett, PhD, executive vice president of scientific operations at ICON Clinical Research, agreed.
The vaccine was well-tolerated, the company reported, with no serious adverse events. Temporary pain and tenderness at the injection site, mild-to-moderate headaches, fatigue, chills, fever, muscle aches. and malaise were among the reported reactions.
The phase III interim results show 141 cases of symptomatic COVID-19 in the study of 32,449 adults. “We don’t have the whole breakdown yet . . . these are the high-level results we just got this week,” Mr. Pangalos said. Further information on rates of mild to moderate COVID-19 illness between groups is not yet available, for example.
The company explained that participants were randomly assigned to vaccine or placebo, with twice as many receiving the actual vaccine.
The trial is ongoing, so the FDA will receive information on more than the 141 COVID-19 symptomatic cases when the company submits a full primary analysis to the agency, Mr. Pangalos said.
In the phase III study, patients received two doses 4 weeks apart.
Beyond the U.S. study, the company has additional information, including real-world data from the United Kingdom, that it intends to submit to the FDA. Part of this evidence suggests increased efficacy when a second dose is administered at 3 months
‘Robust’ findings
“This is a large study, so these results can be expected to be robust. They could be expected to be even more so if there were more cases to compare between the groups, but 141 is still a substantial number of cases,” said Peter English, MD, of Horsham, United Kingdom, who is immediate past chair of the British Medical Association Public Health Medicine Committee.
Experts welcomed the 80% efficacy in people 65 and older in particular. “Importantly, the trial provides further support for efficacy in the elderly where previous clinical trial data, other than immunologic data, had been lacking,” Dr. Garrett said.
“It is clear this vaccine has very good efficacy. Remember that 60% was, prior to any trials being started, regarded as a good target,” said Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene & Tropical Medicine. “This efficacy does not show a notable decline at older ages. This was expected and the speculation that it was ineffective or quasi-ineffective at older ages was totally unjustified.
“This is good news for the global community and one hopes that any political statements around this good news are avoided,” he added.
Efficacy against variants?
Regarding virus variants, Mr. Pangalos noted the study was conducted when several variants of concern were in circulation.
“What I can say is given this study was conducted much later in terms of timing, it’s very encouraging that we’ve got such high efficacy numbers when undoubtedly there are variants of concern in circulation in this study,” Mr. Pangalos said.
“It also highlights why we believe that against severe disease, our vaccine will be effective against all variants of concern,” he added.
Once the company submits its EUA to the FDA, the company is ready to immediately distribute 30 million doses of the vaccine and expects to ship 50 million total within the first month, Ruud Dobber, PhD, AstraZeneca executive vice president and president of the AZ Biopharmaceuticals Business Unit, said during the briefing.
The vaccine can be stored at 2 to 8 degrees Celsius for at least 6 months. Like other COVID-19 vaccines already authorized for emergency use, the duration of protection with the AstraZeneca product remains unknown.
This article was updated March 23, 2021.
A version of this article first appeared on WebMD.com.
Match Day 2021: Psychiatry continues strong growth
In a record year for the Match, psychiatry residencies filled 99.8% of their available positions in 2021, which were up 2.6% over last year, according to the National Resident Matching Program.
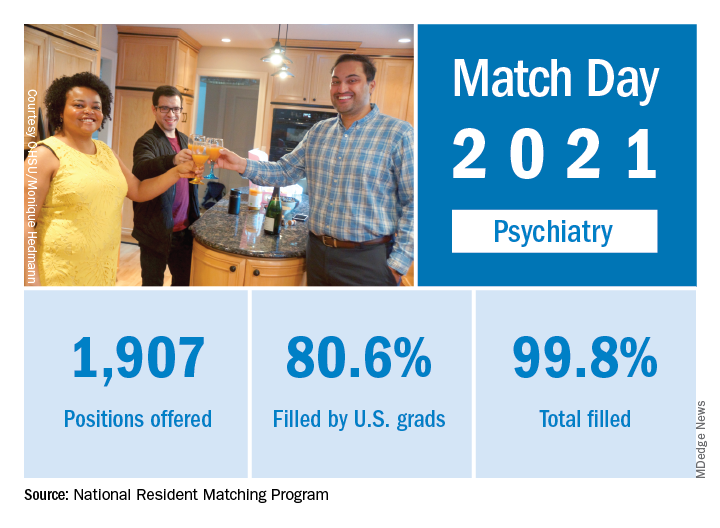
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, which was up from 94.6% the year before.
Psychiatry offered 1,907 positions in this year’s Match, up by 2.6% over 2020, and filled 1,904, for a 1-year increase of 3.6% and a fill rate of 99.8%. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in psychiatry residencies has increased by 412 (27.6%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Psychiatry also increased its share of all available residency positions from 5.1% in 2018 to 5.4% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, psychiatry residencies filled 99.8% of their available positions in 2021, which were up 2.6% over last year, according to the National Resident Matching Program.
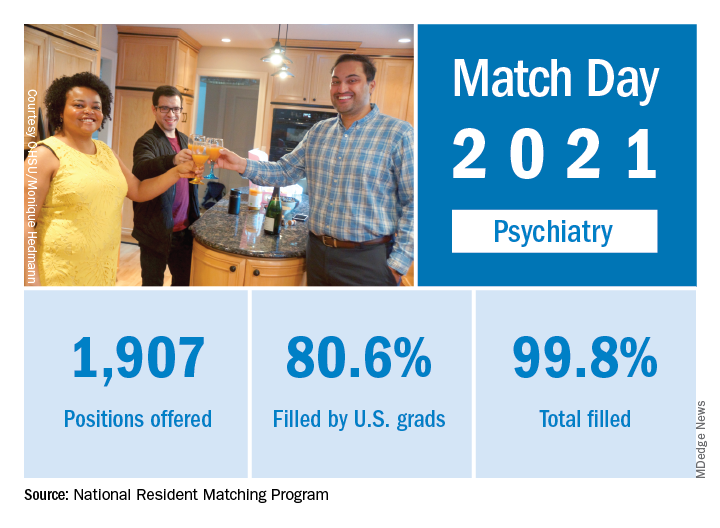
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, which was up from 94.6% the year before.
Psychiatry offered 1,907 positions in this year’s Match, up by 2.6% over 2020, and filled 1,904, for a 1-year increase of 3.6% and a fill rate of 99.8%. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in psychiatry residencies has increased by 412 (27.6%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Psychiatry also increased its share of all available residency positions from 5.1% in 2018 to 5.4% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, psychiatry residencies filled 99.8% of their available positions in 2021, which were up 2.6% over last year, according to the National Resident Matching Program.
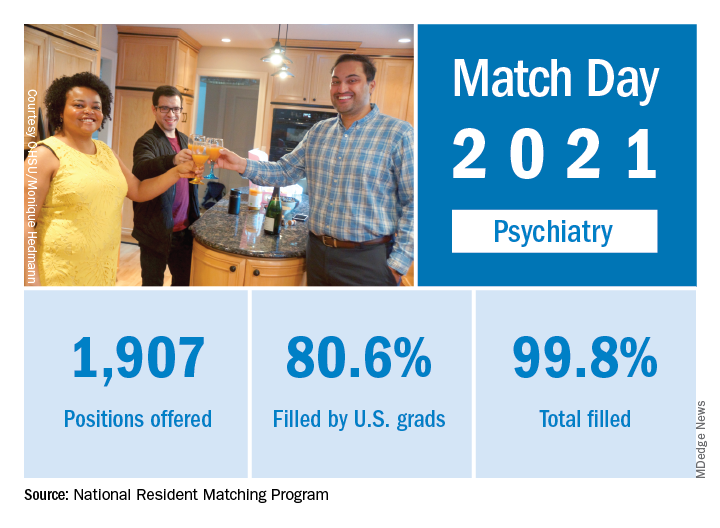
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, which was up from 94.6% the year before.
Psychiatry offered 1,907 positions in this year’s Match, up by 2.6% over 2020, and filled 1,904, for a 1-year increase of 3.6% and a fill rate of 99.8%. The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
The number of positions offered in psychiatry residencies has increased by 412 (27.6%) since 2017, and such growth over time may “be a predictor of future physician workforce supply,” the NRMP suggested. Psychiatry also increased its share of all available residency positions from 5.1% in 2018 to 5.4% in 2021.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
How to talk to patients reluctant to get a COVID-19 vaccine
Family physician Mitchell A. Kaminski, MD, MBA, was still awash in feelings of joy and relief at recently being vaccinated against COVID-19 when a patient’s comments stopped him cold. The patient, a middle-aged man with several comorbidities had just declined the pneumonia vaccine – and he added, without prompting, that he wouldn’t be getting the COVID vaccine either. This patient had heard getting vaccinated could kill him.
Dr. Kaminski countered with medical facts, including that the very rare side effects hadn’t killed anyone in the United States but COVID was killing thousands of people every day. “Well then, I’ll just risk getting COVID,” Dr. Kaminski recalled the patient saying. Conversation over.
That experience caused Dr. Kaminski, who is program director for population health at Thomas Jefferson University, Philadelphia, to rethink the way he talks to patients who are uncertain or skeptical about getting a COVID-19 vaccine. Now, if he saw that patient who seemed fearful of dying from a vaccination, Dr. Kaminski said he would be more curious.
Instead of outright contradicting the beliefs of a patient who is reluctant to get vaccinated, Dr. Kaminski now gently asks about the reasons for their discomfort and offers information about the vaccines. But mostly, he listens.
Conversations between physicians and patients about the risks that come with getting a COVID-19 vaccine are becoming more common in general as eligibility for immunizations expands.
About 80% of Americans say that they are most likely to turn to doctors, nurses and other health professionals for help in deciding whether to get the COVID vaccine, according to research by the Kaiser Family Foundation.
Getting beyond the distrust
While patients often feel a strong connection with their health providers, distrust in the medical establishment still exists, especially among some populations. The Kaiser Family Foundation reported that a third of Black respondents are taking a “wait-and-see” approach, while 23% said they will get it only if it’s required – or not at all.
Distrust persists from historical racist events in medicine, such as the infamous Tuskegee experiments in which treatment was withheld from Black men with syphilis. But physicians shouldn’t assume that all Black patients have the same reasons for vaccine hesitancy, said Krys Foster, MD, MPH, a family physician at Thomas Jefferson University.
“In my experience caring for patients who are uncertain or have concerns about receiving the vaccine, I’ve learned that many are just seeking more information, or even my approval to say that it is safe to proceed given their medical history,” she said.
Sources such as the COVID Racial Data Tracker have found that Black Americans have a higher COVID death rate than other racial or ethnic groups, making vaccination even more vital. Yet fear of the vaccine could be triggered by misinformation that can be found in various places online, Dr. Foster said.
To encourage people to get vaccinated and dispel false information, Dr. Foster takes time to discuss how safe it is to get a COVID-19 vaccine and the vaccines’ side effects, then quickly pivots to discussing how to get vaccinated.
It can be difficult for some people to find appointments or access testing sites. The failure to get the vaccine shouldn’t automatically be attributed to “hesitancy,” she said. “The onus is on the medical community to help fix the health injustices inflicted on communities of color by providing equitable information and access and stop placing blame on them for having the ‘wrong’ vaccine attitude.”
Give your testimonial
Jamie Loehr, MD, of Cayuga Family Medicine in Ithaca, N.Y., said he has always had a higher-than-average number of patients who refused or delayed their children’s vaccines. He does not kick them out of his practice but politely continues to educate them about the vaccines.
When patients ask Dr. Loehr if he trusts the vaccine, he responds with confidence: “I not only believe in it, I got it and I recommend it to anyone who can possibly get it.”
He was surprised recently when a mother who has expressed reluctance to vaccinate her young children came for a checkup and told him she had already received a COVID vaccine. “She made the decision on her own that this was important enough that she wanted to get it,” he said.
Health care worker hesitancy
Some health care workers’ unease about being at the front of the line for vaccines may be another source of vaccine hesitancy among members of the general population that physicians need to address. In a survey of almost 3,500 health care workers conducted in October and November 2020 and published in January 2021 in Vaccines, only about a third (36%) said they would get the vaccine as soon as it became available. By mid- to late-February, 54% of health care workers reported having been vaccinated and another 10% planned to get the vaccine as soon as possible, according to the Kaiser Family Foundation COVID-19 Vaccine Monitor.
Resolving doubts about the vaccines requires a thoughtful approach toward health care colleagues, said Eileen Barrett, MD, MPH, an internist and hospitalist who was a coauthor of the Vaccines paper and who serves on the editorial advisory board of Internal Medicine News. “We should meet people where they are and do our best to hear their concerns, listening thoughtfully without condescension. Validate how important their role is in endorsing vaccination and also validate asking questions.”
There’s power in the strong personal testimonial of physicians and other health care workers – not just to influence patients, but as a model for fellow health professionals, as well, noted Dr. Barrett, who cares for COVID-19 patients and is associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
‘Do it for your loved ones’
The Reagan-Udall Foundation, a nonprofit organization created by Congress to support the Food and Drug Administration, tested some messaging with focus groups. Participants responded favorably to this statement about why the vaccines were developed so quickly: “Vaccine development moved faster than normal because everyone’s making it their highest priority.”
People did not feel motivated to get the vaccine out of a sense of civic duty, said Susan Winckler, RPh, Esq, who is CEO of the foundation. But they did think the following was a good reason to get vaccinated: “By getting a vaccine, I could protect my children, my parents, and other loved ones.”
Physicians also can work with community influencers, such as faith leaders, to build confidence in vaccines. That’s part of the strategy of Roll Up Your Sleeves, a campaign spearheaded by agilon health, a company that partners with physician practices to develop value-based care for Medicare Advantage patients.
For example, Wilmington Health in North Carolina answered questions about the vaccines in Facebook Live events and created a Spanish-language video to boost vaccine confidence in the Latinx community. Additionally, PriMED Physicians in Dayton, Ohio, reached out to Black churches to provide a vaccine-awareness video and a PriMED doctor participated in a webinar sponsored by the Nigerian Women Cultural Organization to help dispel myths about COVID-19 and the vaccines.
“This is a way to deepen our relationship with our patients,” said Ben Kornitzer, MD, chief medical officer of agilon. “It’s helping to walk them through this door where on one side is the pandemic and social isolation and on the other side is a return to their life and loved ones.”
The messages provided by primary care physicians can be powerful and affirming, said Ms. Winckler.
“The path forward is to make a space for people to ask questions,” she continued, noting that the Reagan-Udall Foundation provides charts that show how the timeline for vaccine development was compressed without skipping any steps.
Strategies and background information on how to reinforce confidence in COVID-19 vaccines are also available on a page of the Centers for Disease Control and Prevention’s website.
None of the experts interviewed reported any relevant conflicts of interest. The Reagan-Udall Foundation has received sponsorships from Johnson & Johnson and AstraZeneca and has had a safety surveillance contract with Pfizer.
Family physician Mitchell A. Kaminski, MD, MBA, was still awash in feelings of joy and relief at recently being vaccinated against COVID-19 when a patient’s comments stopped him cold. The patient, a middle-aged man with several comorbidities had just declined the pneumonia vaccine – and he added, without prompting, that he wouldn’t be getting the COVID vaccine either. This patient had heard getting vaccinated could kill him.
Dr. Kaminski countered with medical facts, including that the very rare side effects hadn’t killed anyone in the United States but COVID was killing thousands of people every day. “Well then, I’ll just risk getting COVID,” Dr. Kaminski recalled the patient saying. Conversation over.
That experience caused Dr. Kaminski, who is program director for population health at Thomas Jefferson University, Philadelphia, to rethink the way he talks to patients who are uncertain or skeptical about getting a COVID-19 vaccine. Now, if he saw that patient who seemed fearful of dying from a vaccination, Dr. Kaminski said he would be more curious.
Instead of outright contradicting the beliefs of a patient who is reluctant to get vaccinated, Dr. Kaminski now gently asks about the reasons for their discomfort and offers information about the vaccines. But mostly, he listens.
Conversations between physicians and patients about the risks that come with getting a COVID-19 vaccine are becoming more common in general as eligibility for immunizations expands.
About 80% of Americans say that they are most likely to turn to doctors, nurses and other health professionals for help in deciding whether to get the COVID vaccine, according to research by the Kaiser Family Foundation.
Getting beyond the distrust
While patients often feel a strong connection with their health providers, distrust in the medical establishment still exists, especially among some populations. The Kaiser Family Foundation reported that a third of Black respondents are taking a “wait-and-see” approach, while 23% said they will get it only if it’s required – or not at all.
Distrust persists from historical racist events in medicine, such as the infamous Tuskegee experiments in which treatment was withheld from Black men with syphilis. But physicians shouldn’t assume that all Black patients have the same reasons for vaccine hesitancy, said Krys Foster, MD, MPH, a family physician at Thomas Jefferson University.
“In my experience caring for patients who are uncertain or have concerns about receiving the vaccine, I’ve learned that many are just seeking more information, or even my approval to say that it is safe to proceed given their medical history,” she said.
Sources such as the COVID Racial Data Tracker have found that Black Americans have a higher COVID death rate than other racial or ethnic groups, making vaccination even more vital. Yet fear of the vaccine could be triggered by misinformation that can be found in various places online, Dr. Foster said.
To encourage people to get vaccinated and dispel false information, Dr. Foster takes time to discuss how safe it is to get a COVID-19 vaccine and the vaccines’ side effects, then quickly pivots to discussing how to get vaccinated.
It can be difficult for some people to find appointments or access testing sites. The failure to get the vaccine shouldn’t automatically be attributed to “hesitancy,” she said. “The onus is on the medical community to help fix the health injustices inflicted on communities of color by providing equitable information and access and stop placing blame on them for having the ‘wrong’ vaccine attitude.”
Give your testimonial
Jamie Loehr, MD, of Cayuga Family Medicine in Ithaca, N.Y., said he has always had a higher-than-average number of patients who refused or delayed their children’s vaccines. He does not kick them out of his practice but politely continues to educate them about the vaccines.
When patients ask Dr. Loehr if he trusts the vaccine, he responds with confidence: “I not only believe in it, I got it and I recommend it to anyone who can possibly get it.”
He was surprised recently when a mother who has expressed reluctance to vaccinate her young children came for a checkup and told him she had already received a COVID vaccine. “She made the decision on her own that this was important enough that she wanted to get it,” he said.
Health care worker hesitancy
Some health care workers’ unease about being at the front of the line for vaccines may be another source of vaccine hesitancy among members of the general population that physicians need to address. In a survey of almost 3,500 health care workers conducted in October and November 2020 and published in January 2021 in Vaccines, only about a third (36%) said they would get the vaccine as soon as it became available. By mid- to late-February, 54% of health care workers reported having been vaccinated and another 10% planned to get the vaccine as soon as possible, according to the Kaiser Family Foundation COVID-19 Vaccine Monitor.
Resolving doubts about the vaccines requires a thoughtful approach toward health care colleagues, said Eileen Barrett, MD, MPH, an internist and hospitalist who was a coauthor of the Vaccines paper and who serves on the editorial advisory board of Internal Medicine News. “We should meet people where they are and do our best to hear their concerns, listening thoughtfully without condescension. Validate how important their role is in endorsing vaccination and also validate asking questions.”
There’s power in the strong personal testimonial of physicians and other health care workers – not just to influence patients, but as a model for fellow health professionals, as well, noted Dr. Barrett, who cares for COVID-19 patients and is associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
‘Do it for your loved ones’
The Reagan-Udall Foundation, a nonprofit organization created by Congress to support the Food and Drug Administration, tested some messaging with focus groups. Participants responded favorably to this statement about why the vaccines were developed so quickly: “Vaccine development moved faster than normal because everyone’s making it their highest priority.”
People did not feel motivated to get the vaccine out of a sense of civic duty, said Susan Winckler, RPh, Esq, who is CEO of the foundation. But they did think the following was a good reason to get vaccinated: “By getting a vaccine, I could protect my children, my parents, and other loved ones.”
Physicians also can work with community influencers, such as faith leaders, to build confidence in vaccines. That’s part of the strategy of Roll Up Your Sleeves, a campaign spearheaded by agilon health, a company that partners with physician practices to develop value-based care for Medicare Advantage patients.
For example, Wilmington Health in North Carolina answered questions about the vaccines in Facebook Live events and created a Spanish-language video to boost vaccine confidence in the Latinx community. Additionally, PriMED Physicians in Dayton, Ohio, reached out to Black churches to provide a vaccine-awareness video and a PriMED doctor participated in a webinar sponsored by the Nigerian Women Cultural Organization to help dispel myths about COVID-19 and the vaccines.
“This is a way to deepen our relationship with our patients,” said Ben Kornitzer, MD, chief medical officer of agilon. “It’s helping to walk them through this door where on one side is the pandemic and social isolation and on the other side is a return to their life and loved ones.”
The messages provided by primary care physicians can be powerful and affirming, said Ms. Winckler.
“The path forward is to make a space for people to ask questions,” she continued, noting that the Reagan-Udall Foundation provides charts that show how the timeline for vaccine development was compressed without skipping any steps.
Strategies and background information on how to reinforce confidence in COVID-19 vaccines are also available on a page of the Centers for Disease Control and Prevention’s website.
None of the experts interviewed reported any relevant conflicts of interest. The Reagan-Udall Foundation has received sponsorships from Johnson & Johnson and AstraZeneca and has had a safety surveillance contract with Pfizer.
Family physician Mitchell A. Kaminski, MD, MBA, was still awash in feelings of joy and relief at recently being vaccinated against COVID-19 when a patient’s comments stopped him cold. The patient, a middle-aged man with several comorbidities had just declined the pneumonia vaccine – and he added, without prompting, that he wouldn’t be getting the COVID vaccine either. This patient had heard getting vaccinated could kill him.
Dr. Kaminski countered with medical facts, including that the very rare side effects hadn’t killed anyone in the United States but COVID was killing thousands of people every day. “Well then, I’ll just risk getting COVID,” Dr. Kaminski recalled the patient saying. Conversation over.
That experience caused Dr. Kaminski, who is program director for population health at Thomas Jefferson University, Philadelphia, to rethink the way he talks to patients who are uncertain or skeptical about getting a COVID-19 vaccine. Now, if he saw that patient who seemed fearful of dying from a vaccination, Dr. Kaminski said he would be more curious.
Instead of outright contradicting the beliefs of a patient who is reluctant to get vaccinated, Dr. Kaminski now gently asks about the reasons for their discomfort and offers information about the vaccines. But mostly, he listens.
Conversations between physicians and patients about the risks that come with getting a COVID-19 vaccine are becoming more common in general as eligibility for immunizations expands.
About 80% of Americans say that they are most likely to turn to doctors, nurses and other health professionals for help in deciding whether to get the COVID vaccine, according to research by the Kaiser Family Foundation.
Getting beyond the distrust
While patients often feel a strong connection with their health providers, distrust in the medical establishment still exists, especially among some populations. The Kaiser Family Foundation reported that a third of Black respondents are taking a “wait-and-see” approach, while 23% said they will get it only if it’s required – or not at all.
Distrust persists from historical racist events in medicine, such as the infamous Tuskegee experiments in which treatment was withheld from Black men with syphilis. But physicians shouldn’t assume that all Black patients have the same reasons for vaccine hesitancy, said Krys Foster, MD, MPH, a family physician at Thomas Jefferson University.
“In my experience caring for patients who are uncertain or have concerns about receiving the vaccine, I’ve learned that many are just seeking more information, or even my approval to say that it is safe to proceed given their medical history,” she said.
Sources such as the COVID Racial Data Tracker have found that Black Americans have a higher COVID death rate than other racial or ethnic groups, making vaccination even more vital. Yet fear of the vaccine could be triggered by misinformation that can be found in various places online, Dr. Foster said.
To encourage people to get vaccinated and dispel false information, Dr. Foster takes time to discuss how safe it is to get a COVID-19 vaccine and the vaccines’ side effects, then quickly pivots to discussing how to get vaccinated.
It can be difficult for some people to find appointments or access testing sites. The failure to get the vaccine shouldn’t automatically be attributed to “hesitancy,” she said. “The onus is on the medical community to help fix the health injustices inflicted on communities of color by providing equitable information and access and stop placing blame on them for having the ‘wrong’ vaccine attitude.”
Give your testimonial
Jamie Loehr, MD, of Cayuga Family Medicine in Ithaca, N.Y., said he has always had a higher-than-average number of patients who refused or delayed their children’s vaccines. He does not kick them out of his practice but politely continues to educate them about the vaccines.
When patients ask Dr. Loehr if he trusts the vaccine, he responds with confidence: “I not only believe in it, I got it and I recommend it to anyone who can possibly get it.”
He was surprised recently when a mother who has expressed reluctance to vaccinate her young children came for a checkup and told him she had already received a COVID vaccine. “She made the decision on her own that this was important enough that she wanted to get it,” he said.
Health care worker hesitancy
Some health care workers’ unease about being at the front of the line for vaccines may be another source of vaccine hesitancy among members of the general population that physicians need to address. In a survey of almost 3,500 health care workers conducted in October and November 2020 and published in January 2021 in Vaccines, only about a third (36%) said they would get the vaccine as soon as it became available. By mid- to late-February, 54% of health care workers reported having been vaccinated and another 10% planned to get the vaccine as soon as possible, according to the Kaiser Family Foundation COVID-19 Vaccine Monitor.
Resolving doubts about the vaccines requires a thoughtful approach toward health care colleagues, said Eileen Barrett, MD, MPH, an internist and hospitalist who was a coauthor of the Vaccines paper and who serves on the editorial advisory board of Internal Medicine News. “We should meet people where they are and do our best to hear their concerns, listening thoughtfully without condescension. Validate how important their role is in endorsing vaccination and also validate asking questions.”
There’s power in the strong personal testimonial of physicians and other health care workers – not just to influence patients, but as a model for fellow health professionals, as well, noted Dr. Barrett, who cares for COVID-19 patients and is associate professor in the division of hospital medicine, department of internal medicine, at the University of New Mexico, Albuquerque.
‘Do it for your loved ones’
The Reagan-Udall Foundation, a nonprofit organization created by Congress to support the Food and Drug Administration, tested some messaging with focus groups. Participants responded favorably to this statement about why the vaccines were developed so quickly: “Vaccine development moved faster than normal because everyone’s making it their highest priority.”
People did not feel motivated to get the vaccine out of a sense of civic duty, said Susan Winckler, RPh, Esq, who is CEO of the foundation. But they did think the following was a good reason to get vaccinated: “By getting a vaccine, I could protect my children, my parents, and other loved ones.”
Physicians also can work with community influencers, such as faith leaders, to build confidence in vaccines. That’s part of the strategy of Roll Up Your Sleeves, a campaign spearheaded by agilon health, a company that partners with physician practices to develop value-based care for Medicare Advantage patients.
For example, Wilmington Health in North Carolina answered questions about the vaccines in Facebook Live events and created a Spanish-language video to boost vaccine confidence in the Latinx community. Additionally, PriMED Physicians in Dayton, Ohio, reached out to Black churches to provide a vaccine-awareness video and a PriMED doctor participated in a webinar sponsored by the Nigerian Women Cultural Organization to help dispel myths about COVID-19 and the vaccines.
“This is a way to deepen our relationship with our patients,” said Ben Kornitzer, MD, chief medical officer of agilon. “It’s helping to walk them through this door where on one side is the pandemic and social isolation and on the other side is a return to their life and loved ones.”
The messages provided by primary care physicians can be powerful and affirming, said Ms. Winckler.
“The path forward is to make a space for people to ask questions,” she continued, noting that the Reagan-Udall Foundation provides charts that show how the timeline for vaccine development was compressed without skipping any steps.
Strategies and background information on how to reinforce confidence in COVID-19 vaccines are also available on a page of the Centers for Disease Control and Prevention’s website.
None of the experts interviewed reported any relevant conflicts of interest. The Reagan-Udall Foundation has received sponsorships from Johnson & Johnson and AstraZeneca and has had a safety surveillance contract with Pfizer.
New data on worldwide mental health impact of COVID-19
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
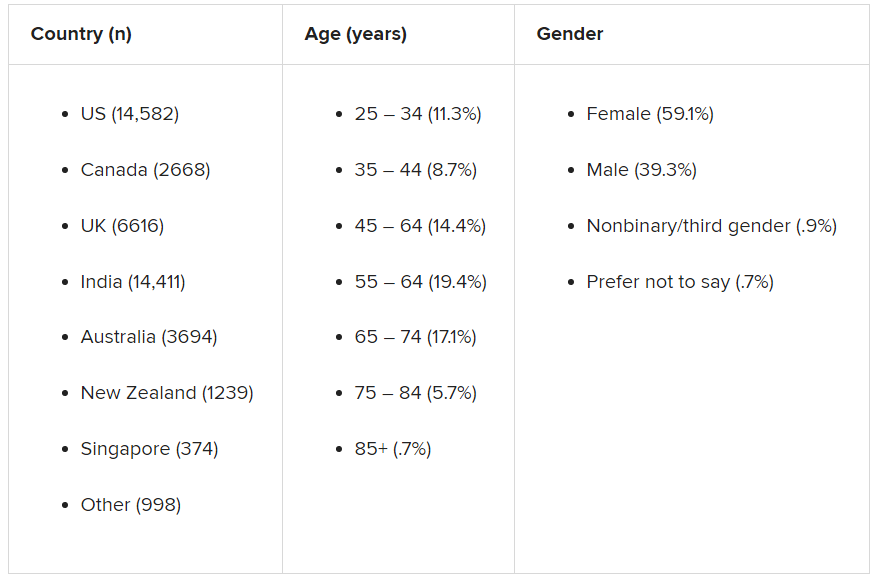
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
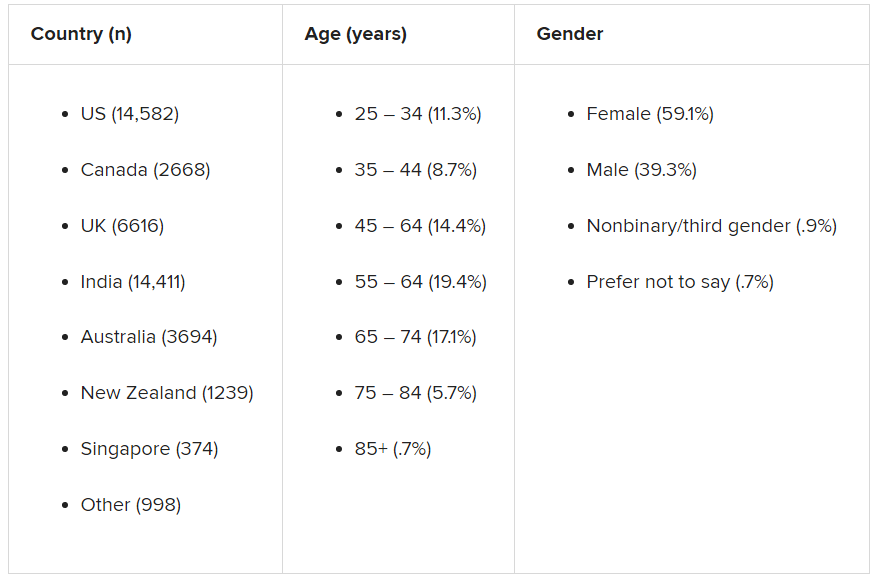
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new survey that assessed the mental health impact of COVID-19 across the globe shows high rates of trauma and clinical mood disorders related to the pandemic.
The survey, carried out by Sapien Labs, was conducted in eight English-speaking countries and included 49,000 adults. It showed that 57% of respondents experienced some COVID-19–related adversity or trauma.
Roughly one-quarter showed clinical signs of or were at risk for a mood disorder, and 40% described themselves as “succeeding or thriving.”
Those who reported the poorest mental health were young adults and individuals who experienced financial adversity or were unable to receive care for other medical conditions. Nonbinary gender and not getting enough sleep, exercise, or face-to-face socialization also increased the risk for poorer mental well-being.
“The data suggest that there will be long-term fallout from the pandemic on the mental health front,” Tara Thiagarajan, PhD, Sapien Labs founder and chief scientist, said in a press release.
Novel initiative
Dr. Thiagarajan said in an interview that she was running a company that provided microloans to 30,000 villages in India. The company included a research group the goal of which was to understand what predicts success in an individual and in a particular ecosystem, she said – “Why did some villages succeed and others didn’t?”
Dr. Thiagarajan and associates thought that “something big is happening in our life circumstances that causes changes in our brain and felt that we need to understand what they are and how they affect humanity. This was the impetus for founding Sapien Labs. “
The survey, which is part of the company’s Mental Health Million project, is an ongoing research initiative that makes data freely available to other researchers.
The investigators developed a “free and anonymous assessment tool,” the Mental Health Quotient (MHQ), which “encompasses a comprehensive view of our emotional, social, and cognitive function and capability,” said Dr. Thiagarajan.
The MHQ consists of 47 “elements of mental well-being.” Respondents’ MHQ scores ranged from –100 to +200. Negative scores indicate poorer mental well-being. Respondents were categorized as clinical, at risk, enduring, managing, succeeding, and thriving.
MHQ scores were computed for six “broad dimensions” of mental health: Core cognition, complex cognition, mood and outlook, drive and motivation, social self, and mind-body connection.
Participants were recruited through advertising on Google and Facebook in eight English-speaking countries – Canada, the United States, the United Kingdom, South Africa, Singapore, Australia, New Zealand, and India. The researchers collected demographic information, including age, education, and gender.
First step
The assessment was completed by 48,808 respondents between April 8 and Dec. 31, 2020.
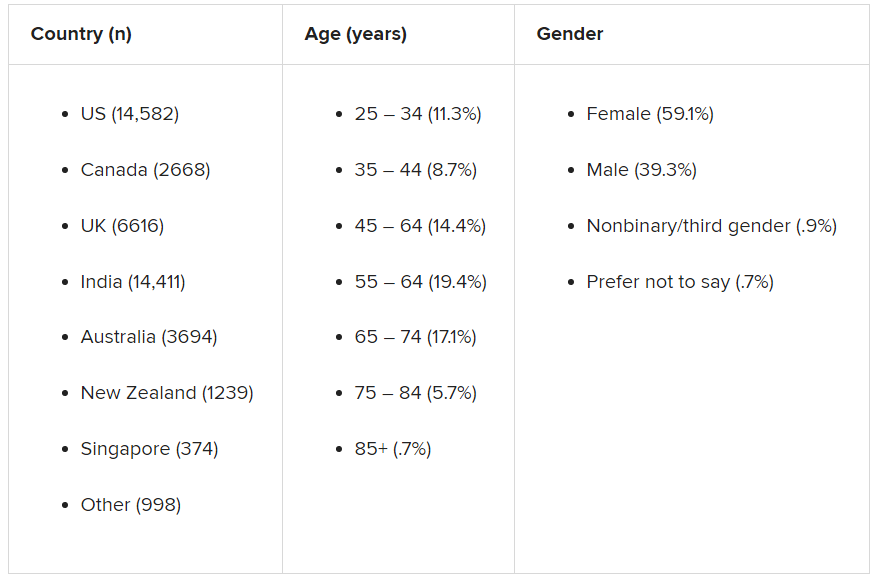
A smaller sample of 2,000 people from the same countries who were polled by the investigators in 2019 was used as a comparator.
Taken together, the overall mental well-being score for 2020 was 8% lower than the score obtained in 2019 from the same countries, and the percentage of respondents who fell into the “clinical” category increased from 14% in 2009 to 26% in 2020.
Residents of Singapore had the highest MHQ score, followed by residents of the United States. At the other extreme, respondents from the United Kingdom and South Africa had the poorest MHQ scores.
“It is important to keep in mind that the English-speaking, Internet-enabled populace is not necessarily representative of each country as a whole,” the authors noted.
Youth hardest hit
whose average MHQ score was 29% lower than those aged at least 65 years.
Worldwide, 70% of respondents aged at least 65 years fell into the categories of “succeeding” or “thriving,” compared with just 17% of those aged 18-24 years.
“We saw a massive trend of diminishing mental well-being in younger individuals, suggesting that some societal force is at play that we need to get to the bottom of,” said Dr. Thiagarajan.
“Young people are still learning how to calibrate themselves in the world, and with age comes maturity, leading to a difference in emotional resilience,” she said.
Highest risk group
Mental well-being was poorest among nonbinary/third-gender respondents. Among those persons, more than 50% were classified as being at clinical risk, in comparison with males and females combined, and their MHQ scores were about 47 points lower.
Nonbinary individuals “are universally doing very poorly, relative to males or females,” said Dr. Thiagarajan. “This is a demographic at very high risk with a lot of suicidal thoughts.”
Respondents who had insufficient sleep, who lacked social interaction, and whose level of exercise was insufficient had lower MHQ scores of an “unexpected magnitude,” compared with their counterparts who had sufficient sleep, more social interaction, and more exercise (a discrepancy of 82, 66, and 46 points, respectively).
Only 3.9% of respondents reported having had COVID-19; 0.7% reported having had a severe case. Yet 57% of respondents reported that the pandemic had had negative consequences with regard to their health or their finances or social situation.
Those who were unable to get care for their other health conditions because of the pandemic (2% of all respondents) reported the worst mental well-being, followed by those who struggled for basic necessities (1.4%).
Reduced household income was associated with a 4% lower score but affected a higher percentage of people (17%). Social isolation was associated with a score of about 20 less. Higher rates of lifetime traumas and adversities were likewise associated with lower scores for mental well-being.
Creative, generous approach
Commenting on the survey results, Ken Duckworth, MD, clinical professor at Harvard Medical School, Boston, and chief medical officer of the National Alliance of Mental Illness, noted that the findings were similar to findings from studies in the United States, which showed disproportionately higher rates of mental health problems in younger individuals. Dr. Duckworth was not involved with the survey.
“The idea that this is an international phenomenon and the broad-stroke finding that younger people are suffering across nations is compelling and important for policymakers to look at,” he said.
Dr. Duckworth noted that although the findings are not “representative” of entire populations in a given country, the report is a “first step in a long journey.”
He described the report as “extremely brilliant, creative, and generous, allowing any academician to get access to the data.”
He saw it “less as a definitive report and more as a directionally informative survey that will yield great fruit over time.”
In a comment, Joshua Morganstein, MD, chair of the American Psychiatric Association’s Committee on the Psychiatric Dimensions of Disaster, said: “One of the important things a document like this highlights is the importance of understanding more where risk [for mental health disorders] is concentrated and what things have occurred or might occur that can buffer against that risk or protect us from it. We see that each nation has similar but also different challenges.”
Dr. Thiagarajan is the founder and chief scientist of Sapien Labs. Her coauthors are employees of Sapien Labs. Dr. Duckworth and Dr. Morganstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Tips to share with patients feeling vaccine FOMO
COVID-19 has filled our lives with so many challenges, and now we are faced with a new one. For some of our patients, getting a vaccine appointment feels a lot like winning the lottery.
At first, it might have been easy to be joyful for others’ good fortune, but after weeks and now months of seeing others get vaccinated, patience can wear thin. It also creates an imbalance when one member of a “bubble” is vaccinated and others aren’t. It can be painful to be the one who continues to miss out on activities as those around resume pleasures such as seeing friends, dining out, shopping, and traveling.
So many of our patients are feeling worn down from the chronic stress and are not in the best shape to deal with another issue: the fear of missing out. Yet,
Here are some tips to share with patients who are feeling vaccine envy.
- Acknowledge your feelings. Sure, you want to be happy for those getting vaccinated but it does hurt to be left behind. These feelings are real and deserve space. Share them with a trusted friend or therapist. It is indeed quite upsetting to have to wait. In the United States, we are used to having speedy access to medical care. It is unfortunate that so many have to wait for such an important intervention. You have a right to be upset.
- Express your concern to the family member or friend who is vaccinated. Discuss how it could affect your relationship and activities.
- Focus on what you can control. Double down on efforts to not catch or spread COVID. Vaccines are only one very modern way out of the pandemic. Stick to the basics so you feel a sense of control over your health destiny.
- Take advantage of the remaining days or weeks of quarantine. What did you want to accomplish during your time of limited activity? Did you always want to play the piano? These last slower days or weeks might be a great time to try (over Zoom of course). Have you put off cleaning your closet and organizing your drawers? There is nothing like a deadline to kick us into gear.
- Take your best guess for when you will be vaccinated and start to plan. Start to make those plans for late summer and fall.
- Keep things in perspective. We are ALL so fortunate that several vaccines were developed so quickly. Even if the wait is a few more weeks, an end is in sight. One year ago, we had no idea what lay ahead and the uncertainty caused so much anxiety. Now we can feel hopeful that more “normal days” will be returning soon in a predictable time frame.
- Focus on the herd. By now we know that “we are all in this together.” Although we aren’t leaving at the exact same time, mere months will separate us. The more our friends and family get vaccinated, the safer we all are.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018).
COVID-19 has filled our lives with so many challenges, and now we are faced with a new one. For some of our patients, getting a vaccine appointment feels a lot like winning the lottery.
At first, it might have been easy to be joyful for others’ good fortune, but after weeks and now months of seeing others get vaccinated, patience can wear thin. It also creates an imbalance when one member of a “bubble” is vaccinated and others aren’t. It can be painful to be the one who continues to miss out on activities as those around resume pleasures such as seeing friends, dining out, shopping, and traveling.
So many of our patients are feeling worn down from the chronic stress and are not in the best shape to deal with another issue: the fear of missing out. Yet,
Here are some tips to share with patients who are feeling vaccine envy.
- Acknowledge your feelings. Sure, you want to be happy for those getting vaccinated but it does hurt to be left behind. These feelings are real and deserve space. Share them with a trusted friend or therapist. It is indeed quite upsetting to have to wait. In the United States, we are used to having speedy access to medical care. It is unfortunate that so many have to wait for such an important intervention. You have a right to be upset.
- Express your concern to the family member or friend who is vaccinated. Discuss how it could affect your relationship and activities.
- Focus on what you can control. Double down on efforts to not catch or spread COVID. Vaccines are only one very modern way out of the pandemic. Stick to the basics so you feel a sense of control over your health destiny.
- Take advantage of the remaining days or weeks of quarantine. What did you want to accomplish during your time of limited activity? Did you always want to play the piano? These last slower days or weeks might be a great time to try (over Zoom of course). Have you put off cleaning your closet and organizing your drawers? There is nothing like a deadline to kick us into gear.
- Take your best guess for when you will be vaccinated and start to plan. Start to make those plans for late summer and fall.
- Keep things in perspective. We are ALL so fortunate that several vaccines were developed so quickly. Even if the wait is a few more weeks, an end is in sight. One year ago, we had no idea what lay ahead and the uncertainty caused so much anxiety. Now we can feel hopeful that more “normal days” will be returning soon in a predictable time frame.
- Focus on the herd. By now we know that “we are all in this together.” Although we aren’t leaving at the exact same time, mere months will separate us. The more our friends and family get vaccinated, the safer we all are.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018).
COVID-19 has filled our lives with so many challenges, and now we are faced with a new one. For some of our patients, getting a vaccine appointment feels a lot like winning the lottery.
At first, it might have been easy to be joyful for others’ good fortune, but after weeks and now months of seeing others get vaccinated, patience can wear thin. It also creates an imbalance when one member of a “bubble” is vaccinated and others aren’t. It can be painful to be the one who continues to miss out on activities as those around resume pleasures such as seeing friends, dining out, shopping, and traveling.
So many of our patients are feeling worn down from the chronic stress and are not in the best shape to deal with another issue: the fear of missing out. Yet,
Here are some tips to share with patients who are feeling vaccine envy.
- Acknowledge your feelings. Sure, you want to be happy for those getting vaccinated but it does hurt to be left behind. These feelings are real and deserve space. Share them with a trusted friend or therapist. It is indeed quite upsetting to have to wait. In the United States, we are used to having speedy access to medical care. It is unfortunate that so many have to wait for such an important intervention. You have a right to be upset.
- Express your concern to the family member or friend who is vaccinated. Discuss how it could affect your relationship and activities.
- Focus on what you can control. Double down on efforts to not catch or spread COVID. Vaccines are only one very modern way out of the pandemic. Stick to the basics so you feel a sense of control over your health destiny.
- Take advantage of the remaining days or weeks of quarantine. What did you want to accomplish during your time of limited activity? Did you always want to play the piano? These last slower days or weeks might be a great time to try (over Zoom of course). Have you put off cleaning your closet and organizing your drawers? There is nothing like a deadline to kick us into gear.
- Take your best guess for when you will be vaccinated and start to plan. Start to make those plans for late summer and fall.
- Keep things in perspective. We are ALL so fortunate that several vaccines were developed so quickly. Even if the wait is a few more weeks, an end is in sight. One year ago, we had no idea what lay ahead and the uncertainty caused so much anxiety. Now we can feel hopeful that more “normal days” will be returning soon in a predictable time frame.
- Focus on the herd. By now we know that “we are all in this together.” Although we aren’t leaving at the exact same time, mere months will separate us. The more our friends and family get vaccinated, the safer we all are.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018).
Dr. Richard W. Cohen joins CPN’s Editorial Advisory Board
Clinical Psychiatry News is pleased to announce the addition of Richard W. Cohen, MD, to its Editorial Advisory Board.
Dr. Cohen is a board-certified psychiatrist. For the last 25 years, he has been in full-time private practice in Center City Philadelphia, where he treats patients with depression, anxiety disorders, relationship problems using psychoanalytically oriented psychotherapy, cognitive-behavioral therapy, and medication management. Dr. Cohen has a special interest in sports psychology – improving the mental toughness and performance of junior, collegiate, and pro athletes.
He graduated from medical school at Temple University, Philadelphia, where he had a wonderful experience assisting the late behaviorist Joseph Wolpe, MD, in agoraphobia research.
Dr. Cohen was chief resident at Albert Einstein Medical Center in New York, and at one point held a trifaculty appointment at Thomas Jefferson University Hospital, Philadelphia, in psychiatry, family medicine, and otolaryngology. At Jefferson, Dr. Cohen codirector of the alcohol and substance abuse education program. He also edited a textbook entitled “What a Student Should Know,” which integrated issues of alcoholism into all subjects in the medical school curriculum.
He has lectured extensively both locally and nationwide at tennis academies helping players improve their overall accomplishments. In addition, Dr. Cohen has appeared on various television shows discussing addictions, relationship issues, and sports psychiatry. Furthermore, he has published numerous articles on these topics.
Dr. Cohen was the fifth-ranked high school tennis player in the United States and he has been ranked No. 1 in both the Middle States and the country in various junior and senior age divisions. He was the captain of the University of Pennsylvania Ivy League Championship tennis team and played No. 1 on Penn’s National Intercollegiate Championship squash team. Dr. Cohen has garnered 17 National Tennis Championship Gold Balls over the years. In 2012, Dr. Cohen was inducted into the Philadelphia Jewish Sports Hall of Fame.
He lives in Philadelphia with his wife, Nancy, and they have two adult children, Josh and Julia, who are world-class tennis players.
Clinical Psychiatry News is pleased to announce the addition of Richard W. Cohen, MD, to its Editorial Advisory Board.
Dr. Cohen is a board-certified psychiatrist. For the last 25 years, he has been in full-time private practice in Center City Philadelphia, where he treats patients with depression, anxiety disorders, relationship problems using psychoanalytically oriented psychotherapy, cognitive-behavioral therapy, and medication management. Dr. Cohen has a special interest in sports psychology – improving the mental toughness and performance of junior, collegiate, and pro athletes.
He graduated from medical school at Temple University, Philadelphia, where he had a wonderful experience assisting the late behaviorist Joseph Wolpe, MD, in agoraphobia research.
Dr. Cohen was chief resident at Albert Einstein Medical Center in New York, and at one point held a trifaculty appointment at Thomas Jefferson University Hospital, Philadelphia, in psychiatry, family medicine, and otolaryngology. At Jefferson, Dr. Cohen codirector of the alcohol and substance abuse education program. He also edited a textbook entitled “What a Student Should Know,” which integrated issues of alcoholism into all subjects in the medical school curriculum.
He has lectured extensively both locally and nationwide at tennis academies helping players improve their overall accomplishments. In addition, Dr. Cohen has appeared on various television shows discussing addictions, relationship issues, and sports psychiatry. Furthermore, he has published numerous articles on these topics.
Dr. Cohen was the fifth-ranked high school tennis player in the United States and he has been ranked No. 1 in both the Middle States and the country in various junior and senior age divisions. He was the captain of the University of Pennsylvania Ivy League Championship tennis team and played No. 1 on Penn’s National Intercollegiate Championship squash team. Dr. Cohen has garnered 17 National Tennis Championship Gold Balls over the years. In 2012, Dr. Cohen was inducted into the Philadelphia Jewish Sports Hall of Fame.
He lives in Philadelphia with his wife, Nancy, and they have two adult children, Josh and Julia, who are world-class tennis players.
Clinical Psychiatry News is pleased to announce the addition of Richard W. Cohen, MD, to its Editorial Advisory Board.
Dr. Cohen is a board-certified psychiatrist. For the last 25 years, he has been in full-time private practice in Center City Philadelphia, where he treats patients with depression, anxiety disorders, relationship problems using psychoanalytically oriented psychotherapy, cognitive-behavioral therapy, and medication management. Dr. Cohen has a special interest in sports psychology – improving the mental toughness and performance of junior, collegiate, and pro athletes.
He graduated from medical school at Temple University, Philadelphia, where he had a wonderful experience assisting the late behaviorist Joseph Wolpe, MD, in agoraphobia research.
Dr. Cohen was chief resident at Albert Einstein Medical Center in New York, and at one point held a trifaculty appointment at Thomas Jefferson University Hospital, Philadelphia, in psychiatry, family medicine, and otolaryngology. At Jefferson, Dr. Cohen codirector of the alcohol and substance abuse education program. He also edited a textbook entitled “What a Student Should Know,” which integrated issues of alcoholism into all subjects in the medical school curriculum.
He has lectured extensively both locally and nationwide at tennis academies helping players improve their overall accomplishments. In addition, Dr. Cohen has appeared on various television shows discussing addictions, relationship issues, and sports psychiatry. Furthermore, he has published numerous articles on these topics.
Dr. Cohen was the fifth-ranked high school tennis player in the United States and he has been ranked No. 1 in both the Middle States and the country in various junior and senior age divisions. He was the captain of the University of Pennsylvania Ivy League Championship tennis team and played No. 1 on Penn’s National Intercollegiate Championship squash team. Dr. Cohen has garnered 17 National Tennis Championship Gold Balls over the years. In 2012, Dr. Cohen was inducted into the Philadelphia Jewish Sports Hall of Fame.
He lives in Philadelphia with his wife, Nancy, and they have two adult children, Josh and Julia, who are world-class tennis players.
1 in 3 on levothyroxine take meds that interfere with thyroid tests
, potentially compromising treatment decisions, new research shows.
“We know from previous studies that thyroid hormone use is common in older adults and that there are a multitude of medications that can interfere with thyroid function tests in different ways,” senior author Maria Papaleontiou, MD, told Medscape Medical News.
“However, to our knowledge, the extent of concurrent use of thyroid hormone and interfering medications in older adults, age 65 years and older, has not been previously explored,” added Dr. Papaleontiou, of the Division of Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor.
The findings were presented as a poster during virtual ENDO 2021, the Endocrine Society’s annual meeting.
Commenting on the study, Thanh Duc Hoang, DO, an endocrinologist with the Walter Reed National Military Medical Center, in Bethesda, Md., said: “It is important for clinicians to be aware of various interactions and interferences of medications affecting the accuracy of thyroid function tests.”
“If patients are not able to discontinue the medications shortly before the bloodwork, the clinicians may consider ordering different thyroid tests or assays that avoid the interferences,” he told Medscape Medical News.
32% of patients taking meds that could interfere with tests
In evaluating data on 538,137 patients treated with thyroid hormones from the Corporate Data Warehouse of the Veterans Health Administration, spanning 2004-2017, first author Rachel Beeson, MD, and colleagues with the University of Michigan found most patients in the study were men (96.5%), White (77.1%), and had two or more comorbidities (62.6%).
Of this total, 170,261 (31.6%) patients treated with thyroid hormones, over a median follow-up of 56 months, were taking at least one drug that could potentially interfere with thyroid function tests.
Among the drugs with potential thyroid test interference, about 28% of patients were taking prednisone or prednisolone, 8% were taking amiodarone, and 1.42% were taking phenytoin. Other reported drugs that could potentially interfere included carbamazepine (0.91%), phenobarbital (0.15%), lithium (0.40%), and tamoxifen (0.11%).
Multivariate analysis showed that characteristics associated with those most likely to have concurrent medication use included non-Whites (OR, 1.18 vs Whites), Hispanic ethnicity (OR 1.11 vs non-Hispanic), female sex (OR 1.12 vs males), and presence of comorbidities (eg, Charlson-Deyo comorbidity score ≥ 2, OR, 2.47 vs score of 0).
Meanwhile, older patients age 85 years and over had a lower likelihood of concurrent medications interfering with thyroid tests (OR, 0.47 vs age 65-74 years).
The findings are concerning given the wide use of levothyroxine to treat hypothyroidism, which is the most widely prescribed drug in the United States.
“Our findings not only highlight the complexity of thyroid hormone management in older adults in the context of polypharmacy and multimorbidity, but they also draw attention to vulnerable groups for this practice, which included female patients, non-Whites, patients of Hispanic ethnicity, and patients with comorbidities,” Dr. Papaleontiou said.
Nature of interference possibilities varies
Medications or supplements can interfere with thyroid function tests in a variety of ways, she explained. “Some medications could lead to a decrease in the absorption of levothyroxine, others may affect how well the pill dissolves.”
In addition, certain medications can affect the circulation of thyroid hormone in the blood and how it binds with proteins, or they can lead to decreasing thyroid hormone levels due to a variety of interactions.
And in contrast, “What is even more challenging is that some medications or supplements may appear to affect thyroid function based on lab tests when in reality they don’t actually affect thyroid function and may lead to dose adjustments unnecessarily,” Dr. Papaleontiou noted.
Recommendations to counter interference
Current recommendations to try to counter the effects of polypharmacy on thyroid treatment include advising patients to take thyroid hormones on an empty stomach at least 30-60 minutes prior to eating for optimal absorption.
If the patient is taking medications known to interfere with absorption of thyroid hormones, the recommendation is to space those out by at least 4 hours.
“The big challenge in older adults is that many of them do experience polypharmacy, being at risk for multiple drug-drug interactions,” Dr. Papaleontiou said.
“Physicians and patients should be vigilant and communicate closely every time there is initiation of a new medication or supplement to consider whether there may be interference.”
The authors have reported no relevant financial relationships. Dr. Hoang has reported being a speaker for Acella Pharmaceuticals.
A version of this article first appeared on Medscape.com.
, potentially compromising treatment decisions, new research shows.
“We know from previous studies that thyroid hormone use is common in older adults and that there are a multitude of medications that can interfere with thyroid function tests in different ways,” senior author Maria Papaleontiou, MD, told Medscape Medical News.
“However, to our knowledge, the extent of concurrent use of thyroid hormone and interfering medications in older adults, age 65 years and older, has not been previously explored,” added Dr. Papaleontiou, of the Division of Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor.
The findings were presented as a poster during virtual ENDO 2021, the Endocrine Society’s annual meeting.
Commenting on the study, Thanh Duc Hoang, DO, an endocrinologist with the Walter Reed National Military Medical Center, in Bethesda, Md., said: “It is important for clinicians to be aware of various interactions and interferences of medications affecting the accuracy of thyroid function tests.”
“If patients are not able to discontinue the medications shortly before the bloodwork, the clinicians may consider ordering different thyroid tests or assays that avoid the interferences,” he told Medscape Medical News.
32% of patients taking meds that could interfere with tests
In evaluating data on 538,137 patients treated with thyroid hormones from the Corporate Data Warehouse of the Veterans Health Administration, spanning 2004-2017, first author Rachel Beeson, MD, and colleagues with the University of Michigan found most patients in the study were men (96.5%), White (77.1%), and had two or more comorbidities (62.6%).
Of this total, 170,261 (31.6%) patients treated with thyroid hormones, over a median follow-up of 56 months, were taking at least one drug that could potentially interfere with thyroid function tests.
Among the drugs with potential thyroid test interference, about 28% of patients were taking prednisone or prednisolone, 8% were taking amiodarone, and 1.42% were taking phenytoin. Other reported drugs that could potentially interfere included carbamazepine (0.91%), phenobarbital (0.15%), lithium (0.40%), and tamoxifen (0.11%).
Multivariate analysis showed that characteristics associated with those most likely to have concurrent medication use included non-Whites (OR, 1.18 vs Whites), Hispanic ethnicity (OR 1.11 vs non-Hispanic), female sex (OR 1.12 vs males), and presence of comorbidities (eg, Charlson-Deyo comorbidity score ≥ 2, OR, 2.47 vs score of 0).
Meanwhile, older patients age 85 years and over had a lower likelihood of concurrent medications interfering with thyroid tests (OR, 0.47 vs age 65-74 years).
The findings are concerning given the wide use of levothyroxine to treat hypothyroidism, which is the most widely prescribed drug in the United States.
“Our findings not only highlight the complexity of thyroid hormone management in older adults in the context of polypharmacy and multimorbidity, but they also draw attention to vulnerable groups for this practice, which included female patients, non-Whites, patients of Hispanic ethnicity, and patients with comorbidities,” Dr. Papaleontiou said.
Nature of interference possibilities varies
Medications or supplements can interfere with thyroid function tests in a variety of ways, she explained. “Some medications could lead to a decrease in the absorption of levothyroxine, others may affect how well the pill dissolves.”
In addition, certain medications can affect the circulation of thyroid hormone in the blood and how it binds with proteins, or they can lead to decreasing thyroid hormone levels due to a variety of interactions.
And in contrast, “What is even more challenging is that some medications or supplements may appear to affect thyroid function based on lab tests when in reality they don’t actually affect thyroid function and may lead to dose adjustments unnecessarily,” Dr. Papaleontiou noted.
Recommendations to counter interference
Current recommendations to try to counter the effects of polypharmacy on thyroid treatment include advising patients to take thyroid hormones on an empty stomach at least 30-60 minutes prior to eating for optimal absorption.
If the patient is taking medications known to interfere with absorption of thyroid hormones, the recommendation is to space those out by at least 4 hours.
“The big challenge in older adults is that many of them do experience polypharmacy, being at risk for multiple drug-drug interactions,” Dr. Papaleontiou said.
“Physicians and patients should be vigilant and communicate closely every time there is initiation of a new medication or supplement to consider whether there may be interference.”
The authors have reported no relevant financial relationships. Dr. Hoang has reported being a speaker for Acella Pharmaceuticals.
A version of this article first appeared on Medscape.com.
, potentially compromising treatment decisions, new research shows.
“We know from previous studies that thyroid hormone use is common in older adults and that there are a multitude of medications that can interfere with thyroid function tests in different ways,” senior author Maria Papaleontiou, MD, told Medscape Medical News.
“However, to our knowledge, the extent of concurrent use of thyroid hormone and interfering medications in older adults, age 65 years and older, has not been previously explored,” added Dr. Papaleontiou, of the Division of Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor.
The findings were presented as a poster during virtual ENDO 2021, the Endocrine Society’s annual meeting.
Commenting on the study, Thanh Duc Hoang, DO, an endocrinologist with the Walter Reed National Military Medical Center, in Bethesda, Md., said: “It is important for clinicians to be aware of various interactions and interferences of medications affecting the accuracy of thyroid function tests.”
“If patients are not able to discontinue the medications shortly before the bloodwork, the clinicians may consider ordering different thyroid tests or assays that avoid the interferences,” he told Medscape Medical News.
32% of patients taking meds that could interfere with tests
In evaluating data on 538,137 patients treated with thyroid hormones from the Corporate Data Warehouse of the Veterans Health Administration, spanning 2004-2017, first author Rachel Beeson, MD, and colleagues with the University of Michigan found most patients in the study were men (96.5%), White (77.1%), and had two or more comorbidities (62.6%).
Of this total, 170,261 (31.6%) patients treated with thyroid hormones, over a median follow-up of 56 months, were taking at least one drug that could potentially interfere with thyroid function tests.
Among the drugs with potential thyroid test interference, about 28% of patients were taking prednisone or prednisolone, 8% were taking amiodarone, and 1.42% were taking phenytoin. Other reported drugs that could potentially interfere included carbamazepine (0.91%), phenobarbital (0.15%), lithium (0.40%), and tamoxifen (0.11%).
Multivariate analysis showed that characteristics associated with those most likely to have concurrent medication use included non-Whites (OR, 1.18 vs Whites), Hispanic ethnicity (OR 1.11 vs non-Hispanic), female sex (OR 1.12 vs males), and presence of comorbidities (eg, Charlson-Deyo comorbidity score ≥ 2, OR, 2.47 vs score of 0).
Meanwhile, older patients age 85 years and over had a lower likelihood of concurrent medications interfering with thyroid tests (OR, 0.47 vs age 65-74 years).
The findings are concerning given the wide use of levothyroxine to treat hypothyroidism, which is the most widely prescribed drug in the United States.
“Our findings not only highlight the complexity of thyroid hormone management in older adults in the context of polypharmacy and multimorbidity, but they also draw attention to vulnerable groups for this practice, which included female patients, non-Whites, patients of Hispanic ethnicity, and patients with comorbidities,” Dr. Papaleontiou said.
Nature of interference possibilities varies
Medications or supplements can interfere with thyroid function tests in a variety of ways, she explained. “Some medications could lead to a decrease in the absorption of levothyroxine, others may affect how well the pill dissolves.”
In addition, certain medications can affect the circulation of thyroid hormone in the blood and how it binds with proteins, or they can lead to decreasing thyroid hormone levels due to a variety of interactions.
And in contrast, “What is even more challenging is that some medications or supplements may appear to affect thyroid function based on lab tests when in reality they don’t actually affect thyroid function and may lead to dose adjustments unnecessarily,” Dr. Papaleontiou noted.
Recommendations to counter interference
Current recommendations to try to counter the effects of polypharmacy on thyroid treatment include advising patients to take thyroid hormones on an empty stomach at least 30-60 minutes prior to eating for optimal absorption.
If the patient is taking medications known to interfere with absorption of thyroid hormones, the recommendation is to space those out by at least 4 hours.
“The big challenge in older adults is that many of them do experience polypharmacy, being at risk for multiple drug-drug interactions,” Dr. Papaleontiou said.
“Physicians and patients should be vigilant and communicate closely every time there is initiation of a new medication or supplement to consider whether there may be interference.”
The authors have reported no relevant financial relationships. Dr. Hoang has reported being a speaker for Acella Pharmaceuticals.
A version of this article first appeared on Medscape.com.