User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Like mother, like daughter? Moms pass obesity risk to girls
Girls between 4 and 9 years old were more likely to have high fat mass and a high body mass index if their mothers had excess adiposity – but this relationship was not seen between mothers and sons, or between fathers and sons or daughters, in a new study.
The researchers measured fat mass, lean mass, and BMI in the sons and daughters when they were age 4 (before a phenomenon known as “adiposity rebound”), ages 6-7 (around the adiposity rebound), and ages 8-9 (before or at the onset of puberty).
They also obtained measurements from the mothers and fathers when the offspring were ages 8-9.
The group found “a strong association between the fat mass of mothers and their daughters but not their sons,” Rebecca J. Moon, BM, PhD, and colleagues report.
“It would be important to establish persistence through puberty,” according to the researchers, “but nonetheless, these findings are clinically important, highlighting girls who are born to mothers with high BMI and excess adiposity are at high risk of themselves of becoming overweight/obese or having unfavorable body composition early in childhood.”
The mother-daughter relationship for fat mass appears to be established by age 4 years, note Dr. Moon, of the MRC Lifecourse Epidemiology Centre, University of Southampton (England), and colleagues.
Therefore, “early awareness and intervention is needed in mothers with excess adiposity, and potentially beginning even in the periconception and in utero period.”
Because 97% of the mothers and fathers were White, the findings may not be generalizable to other populations, they caution.
The results, from the Southampton Women’s Survey prospective cohort study, were published online in the Journal of Clinical Endocrinology & Metabolism.
One of the first studies to look at fat mass, not just BMI
Children with overweight or obesity are more likely to have excess weight in adulthood that puts them at risk of developing type 2 diabetes, cardiovascular disease, cancer, and osteoarthritis. Previous research has reported that children with overweight or obesity were more likely to have mothers with adiposity.
However, most prior studies have looked at BMI alone and did not measure fat mass, and it was not known how a father’s obesity might affect offspring or how risk may differ in boy versus girl children.
Researchers analyzed data from a subset of participants in the Southampton Women’s Survey of 3,158 women who were aged 20-34 in 1998-2002 and delivered a liveborn infant.
The current study included 240 mother-father-offspring trios who had data for BMI and dual-energy X-ray absorptiometry (DXA) scans (whole body less head).
Mothers were a mean age of 31 years at delivery and had a median pre-pregnancy BMI of 23.7 kg/m2.
The offspring were 129 boys (54%) and 111 girls.
The offspring had DXA scans at ages 4, 6-7, and 8-9 years, and the mothers and fathers had a DXA scan at the last time point.
At ages 6-7 and ages 8-9, BMI and fat mass of the girls reflected that of their mothers (a significant association).
At age 4, BMI and fat mass of the daughters tended to be associated with that of their mothers, but the 95% confidence interval crossed zero.
There were no significant mother-son, father-son, or father-daughter associations for BMI or fat mass at each of the three studied ages.
The study received funding from the Medical Research Council, the British Heart Foundation, the National Institute for Health and Care Research Southampton Biomedical Research Centre, the NIHR Oxford Biomedical Research Centre, the Seventh Framework Program, the Biotechnology and Biological Sciences Research Council, the Horizon 2020 Framework Program, and the National Institute on Aging. Dr. Moon has reported receiving travel bursaries from Kyowa Kirin unrelated to the current study. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Girls between 4 and 9 years old were more likely to have high fat mass and a high body mass index if their mothers had excess adiposity – but this relationship was not seen between mothers and sons, or between fathers and sons or daughters, in a new study.
The researchers measured fat mass, lean mass, and BMI in the sons and daughters when they were age 4 (before a phenomenon known as “adiposity rebound”), ages 6-7 (around the adiposity rebound), and ages 8-9 (before or at the onset of puberty).
They also obtained measurements from the mothers and fathers when the offspring were ages 8-9.
The group found “a strong association between the fat mass of mothers and their daughters but not their sons,” Rebecca J. Moon, BM, PhD, and colleagues report.
“It would be important to establish persistence through puberty,” according to the researchers, “but nonetheless, these findings are clinically important, highlighting girls who are born to mothers with high BMI and excess adiposity are at high risk of themselves of becoming overweight/obese or having unfavorable body composition early in childhood.”
The mother-daughter relationship for fat mass appears to be established by age 4 years, note Dr. Moon, of the MRC Lifecourse Epidemiology Centre, University of Southampton (England), and colleagues.
Therefore, “early awareness and intervention is needed in mothers with excess adiposity, and potentially beginning even in the periconception and in utero period.”
Because 97% of the mothers and fathers were White, the findings may not be generalizable to other populations, they caution.
The results, from the Southampton Women’s Survey prospective cohort study, were published online in the Journal of Clinical Endocrinology & Metabolism.
One of the first studies to look at fat mass, not just BMI
Children with overweight or obesity are more likely to have excess weight in adulthood that puts them at risk of developing type 2 diabetes, cardiovascular disease, cancer, and osteoarthritis. Previous research has reported that children with overweight or obesity were more likely to have mothers with adiposity.
However, most prior studies have looked at BMI alone and did not measure fat mass, and it was not known how a father’s obesity might affect offspring or how risk may differ in boy versus girl children.
Researchers analyzed data from a subset of participants in the Southampton Women’s Survey of 3,158 women who were aged 20-34 in 1998-2002 and delivered a liveborn infant.
The current study included 240 mother-father-offspring trios who had data for BMI and dual-energy X-ray absorptiometry (DXA) scans (whole body less head).
Mothers were a mean age of 31 years at delivery and had a median pre-pregnancy BMI of 23.7 kg/m2.
The offspring were 129 boys (54%) and 111 girls.
The offspring had DXA scans at ages 4, 6-7, and 8-9 years, and the mothers and fathers had a DXA scan at the last time point.
At ages 6-7 and ages 8-9, BMI and fat mass of the girls reflected that of their mothers (a significant association).
At age 4, BMI and fat mass of the daughters tended to be associated with that of their mothers, but the 95% confidence interval crossed zero.
There were no significant mother-son, father-son, or father-daughter associations for BMI or fat mass at each of the three studied ages.
The study received funding from the Medical Research Council, the British Heart Foundation, the National Institute for Health and Care Research Southampton Biomedical Research Centre, the NIHR Oxford Biomedical Research Centre, the Seventh Framework Program, the Biotechnology and Biological Sciences Research Council, the Horizon 2020 Framework Program, and the National Institute on Aging. Dr. Moon has reported receiving travel bursaries from Kyowa Kirin unrelated to the current study. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Girls between 4 and 9 years old were more likely to have high fat mass and a high body mass index if their mothers had excess adiposity – but this relationship was not seen between mothers and sons, or between fathers and sons or daughters, in a new study.
The researchers measured fat mass, lean mass, and BMI in the sons and daughters when they were age 4 (before a phenomenon known as “adiposity rebound”), ages 6-7 (around the adiposity rebound), and ages 8-9 (before or at the onset of puberty).
They also obtained measurements from the mothers and fathers when the offspring were ages 8-9.
The group found “a strong association between the fat mass of mothers and their daughters but not their sons,” Rebecca J. Moon, BM, PhD, and colleagues report.
“It would be important to establish persistence through puberty,” according to the researchers, “but nonetheless, these findings are clinically important, highlighting girls who are born to mothers with high BMI and excess adiposity are at high risk of themselves of becoming overweight/obese or having unfavorable body composition early in childhood.”
The mother-daughter relationship for fat mass appears to be established by age 4 years, note Dr. Moon, of the MRC Lifecourse Epidemiology Centre, University of Southampton (England), and colleagues.
Therefore, “early awareness and intervention is needed in mothers with excess adiposity, and potentially beginning even in the periconception and in utero period.”
Because 97% of the mothers and fathers were White, the findings may not be generalizable to other populations, they caution.
The results, from the Southampton Women’s Survey prospective cohort study, were published online in the Journal of Clinical Endocrinology & Metabolism.
One of the first studies to look at fat mass, not just BMI
Children with overweight or obesity are more likely to have excess weight in adulthood that puts them at risk of developing type 2 diabetes, cardiovascular disease, cancer, and osteoarthritis. Previous research has reported that children with overweight or obesity were more likely to have mothers with adiposity.
However, most prior studies have looked at BMI alone and did not measure fat mass, and it was not known how a father’s obesity might affect offspring or how risk may differ in boy versus girl children.
Researchers analyzed data from a subset of participants in the Southampton Women’s Survey of 3,158 women who were aged 20-34 in 1998-2002 and delivered a liveborn infant.
The current study included 240 mother-father-offspring trios who had data for BMI and dual-energy X-ray absorptiometry (DXA) scans (whole body less head).
Mothers were a mean age of 31 years at delivery and had a median pre-pregnancy BMI of 23.7 kg/m2.
The offspring were 129 boys (54%) and 111 girls.
The offspring had DXA scans at ages 4, 6-7, and 8-9 years, and the mothers and fathers had a DXA scan at the last time point.
At ages 6-7 and ages 8-9, BMI and fat mass of the girls reflected that of their mothers (a significant association).
At age 4, BMI and fat mass of the daughters tended to be associated with that of their mothers, but the 95% confidence interval crossed zero.
There were no significant mother-son, father-son, or father-daughter associations for BMI or fat mass at each of the three studied ages.
The study received funding from the Medical Research Council, the British Heart Foundation, the National Institute for Health and Care Research Southampton Biomedical Research Centre, the NIHR Oxford Biomedical Research Centre, the Seventh Framework Program, the Biotechnology and Biological Sciences Research Council, the Horizon 2020 Framework Program, and the National Institute on Aging. Dr. Moon has reported receiving travel bursaries from Kyowa Kirin unrelated to the current study. Disclosures for the other authors are listed with the article.
A version of this article originally appeared on Medscape.com.
Living kidney donors should receive money for their costs of donating
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University’s Grossman School of Medicine in New York City.
We try very hard to get organ donation from those who die. That’s a commendable thing to do. I think doctors should always be discussing the opportunity to donate organs upon death, even in primary care settings.
It’s good to find out what people’s attitudes are. Let them learn about organ donation as something they can think about. Let them talk about it with family and friends and partners so that they know their wishes.
However, despite these efforts to encourage organ donation, we still have far fewer organs than we could use to transplant people, many people die on waiting lists because there are no organs to give them, and we’re in a situation where demand for organ transplant is actually increasing.
There is more capacity to do transplants both in the United States and elsewhere, and more people are living longer, so organ failure starts to become more common before, let’s say, terminal illness is really there. Now, we have more people who might benefit from organ transplant in an aging population.
One place to turn to help reduce the shortage of organs is to living donation. At least insofar as kidneys go, kidney donation from living persons has become a prominent source of organs for those who need kidneys – most of whom are surviving on dialysis, by the way, at a very high cost and often with a quality of life that they don’t find particularly easy to accept.
Transplant is far preferred, even though they have to take immunosuppression to keep those organ transplants going, and that has its own risks and side effects. They still get more mobility. They still are able to have a broader diet. They enjoy life far more than they do having to show up for dialysis three times a week for a couple of hours, every week, for every week that they live.
There is an interest in living kidney donation. One battle has been that, well, maybe we could get more kidneys if we just paid people to sell us their kidneys. That has been resisted, and I’ve been resistant to that idea, too, because I worry that it leads to exploitation.
The people who sell their kidneys are poor. They’re often in debt. They feel coerced by their circumstances, so they make a kidney sale. This happens in countries like India, where there are markets underground, and you see that it’s the poorest of the poor who do this, and they don’t really work their way out of debt. They just wind up without a kidney, help relieve their debt a little bit, and pretty soon, because they don’t have a job or an income except that sale of a kidney, they’re not much better off than they were before they started.
Also, people who sell kidneys for money are more likely not to admit to their own health problems, raising risks about the quality of organs. Then, of course, it puts doctors in a position to take out an organ for pay, even though it doesn’t benefit you, so that you can sell it. This raises some questions about whether that’s consistent with medical ethics.
A different idea has emerged. New York State Governor Kathy Hochul just signed legislation that allows living donors to be compensated for legitimate costs. That’s a little different matter. You’re not buying the organ, but you’re saying that if you experience health care problems due to complications from a donation, if you need money for transportation, if you lost money because you did this altruistically and you had to take time off from work and had expenses for a babysitter, restaurants, or other things, the state is going to try to create funds that will compensate you.
That, I think we should agree, is not a bad idea. You’re in a situation there where you don’t want to make people who are heroic, altruistic, and trying to help others by donating a kidney end up financially worse off.
I think there’s a difference between making someone financially whole after the decision to make a kidney available and creating a market where the poorest of the poor come forward to just sell because they see no other choice in terms of how to get rid of debts. I see these situations as not ethically equivalent, so I support efforts to try to compensate people who are our heroes. I don’t think we should ask them to financially suffer.
We’ll watch to see what happens as the New York state law comes into effect. By the way, New York is one of the states that really lags in the supply of organs for transplant, so this measure is particularly important for that state. Many other states should be considering this legislation as well.
It’s one thing to reward, if you will, donors by making sure they don’t suffer financial loss. It’s a very different thing to say, let’s have a free market and we’ll pay whoever it is that’s willing to sell us a kidney to do so. The former seems to me to be humane and just, whereas the latter risks exploitation.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University’s Grossman School of Medicine in New York City.
We try very hard to get organ donation from those who die. That’s a commendable thing to do. I think doctors should always be discussing the opportunity to donate organs upon death, even in primary care settings.
It’s good to find out what people’s attitudes are. Let them learn about organ donation as something they can think about. Let them talk about it with family and friends and partners so that they know their wishes.
However, despite these efforts to encourage organ donation, we still have far fewer organs than we could use to transplant people, many people die on waiting lists because there are no organs to give them, and we’re in a situation where demand for organ transplant is actually increasing.
There is more capacity to do transplants both in the United States and elsewhere, and more people are living longer, so organ failure starts to become more common before, let’s say, terminal illness is really there. Now, we have more people who might benefit from organ transplant in an aging population.
One place to turn to help reduce the shortage of organs is to living donation. At least insofar as kidneys go, kidney donation from living persons has become a prominent source of organs for those who need kidneys – most of whom are surviving on dialysis, by the way, at a very high cost and often with a quality of life that they don’t find particularly easy to accept.
Transplant is far preferred, even though they have to take immunosuppression to keep those organ transplants going, and that has its own risks and side effects. They still get more mobility. They still are able to have a broader diet. They enjoy life far more than they do having to show up for dialysis three times a week for a couple of hours, every week, for every week that they live.
There is an interest in living kidney donation. One battle has been that, well, maybe we could get more kidneys if we just paid people to sell us their kidneys. That has been resisted, and I’ve been resistant to that idea, too, because I worry that it leads to exploitation.
The people who sell their kidneys are poor. They’re often in debt. They feel coerced by their circumstances, so they make a kidney sale. This happens in countries like India, where there are markets underground, and you see that it’s the poorest of the poor who do this, and they don’t really work their way out of debt. They just wind up without a kidney, help relieve their debt a little bit, and pretty soon, because they don’t have a job or an income except that sale of a kidney, they’re not much better off than they were before they started.
Also, people who sell kidneys for money are more likely not to admit to their own health problems, raising risks about the quality of organs. Then, of course, it puts doctors in a position to take out an organ for pay, even though it doesn’t benefit you, so that you can sell it. This raises some questions about whether that’s consistent with medical ethics.
A different idea has emerged. New York State Governor Kathy Hochul just signed legislation that allows living donors to be compensated for legitimate costs. That’s a little different matter. You’re not buying the organ, but you’re saying that if you experience health care problems due to complications from a donation, if you need money for transportation, if you lost money because you did this altruistically and you had to take time off from work and had expenses for a babysitter, restaurants, or other things, the state is going to try to create funds that will compensate you.
That, I think we should agree, is not a bad idea. You’re in a situation there where you don’t want to make people who are heroic, altruistic, and trying to help others by donating a kidney end up financially worse off.
I think there’s a difference between making someone financially whole after the decision to make a kidney available and creating a market where the poorest of the poor come forward to just sell because they see no other choice in terms of how to get rid of debts. I see these situations as not ethically equivalent, so I support efforts to try to compensate people who are our heroes. I don’t think we should ask them to financially suffer.
We’ll watch to see what happens as the New York state law comes into effect. By the way, New York is one of the states that really lags in the supply of organs for transplant, so this measure is particularly important for that state. Many other states should be considering this legislation as well.
It’s one thing to reward, if you will, donors by making sure they don’t suffer financial loss. It’s a very different thing to say, let’s have a free market and we’ll pay whoever it is that’s willing to sell us a kidney to do so. The former seems to me to be humane and just, whereas the latter risks exploitation.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hi. I’m Art Caplan. I’m at the division of medical ethics at New York University’s Grossman School of Medicine in New York City.
We try very hard to get organ donation from those who die. That’s a commendable thing to do. I think doctors should always be discussing the opportunity to donate organs upon death, even in primary care settings.
It’s good to find out what people’s attitudes are. Let them learn about organ donation as something they can think about. Let them talk about it with family and friends and partners so that they know their wishes.
However, despite these efforts to encourage organ donation, we still have far fewer organs than we could use to transplant people, many people die on waiting lists because there are no organs to give them, and we’re in a situation where demand for organ transplant is actually increasing.
There is more capacity to do transplants both in the United States and elsewhere, and more people are living longer, so organ failure starts to become more common before, let’s say, terminal illness is really there. Now, we have more people who might benefit from organ transplant in an aging population.
One place to turn to help reduce the shortage of organs is to living donation. At least insofar as kidneys go, kidney donation from living persons has become a prominent source of organs for those who need kidneys – most of whom are surviving on dialysis, by the way, at a very high cost and often with a quality of life that they don’t find particularly easy to accept.
Transplant is far preferred, even though they have to take immunosuppression to keep those organ transplants going, and that has its own risks and side effects. They still get more mobility. They still are able to have a broader diet. They enjoy life far more than they do having to show up for dialysis three times a week for a couple of hours, every week, for every week that they live.
There is an interest in living kidney donation. One battle has been that, well, maybe we could get more kidneys if we just paid people to sell us their kidneys. That has been resisted, and I’ve been resistant to that idea, too, because I worry that it leads to exploitation.
The people who sell their kidneys are poor. They’re often in debt. They feel coerced by their circumstances, so they make a kidney sale. This happens in countries like India, where there are markets underground, and you see that it’s the poorest of the poor who do this, and they don’t really work their way out of debt. They just wind up without a kidney, help relieve their debt a little bit, and pretty soon, because they don’t have a job or an income except that sale of a kidney, they’re not much better off than they were before they started.
Also, people who sell kidneys for money are more likely not to admit to their own health problems, raising risks about the quality of organs. Then, of course, it puts doctors in a position to take out an organ for pay, even though it doesn’t benefit you, so that you can sell it. This raises some questions about whether that’s consistent with medical ethics.
A different idea has emerged. New York State Governor Kathy Hochul just signed legislation that allows living donors to be compensated for legitimate costs. That’s a little different matter. You’re not buying the organ, but you’re saying that if you experience health care problems due to complications from a donation, if you need money for transportation, if you lost money because you did this altruistically and you had to take time off from work and had expenses for a babysitter, restaurants, or other things, the state is going to try to create funds that will compensate you.
That, I think we should agree, is not a bad idea. You’re in a situation there where you don’t want to make people who are heroic, altruistic, and trying to help others by donating a kidney end up financially worse off.
I think there’s a difference between making someone financially whole after the decision to make a kidney available and creating a market where the poorest of the poor come forward to just sell because they see no other choice in terms of how to get rid of debts. I see these situations as not ethically equivalent, so I support efforts to try to compensate people who are our heroes. I don’t think we should ask them to financially suffer.
We’ll watch to see what happens as the New York state law comes into effect. By the way, New York is one of the states that really lags in the supply of organs for transplant, so this measure is particularly important for that state. Many other states should be considering this legislation as well.
It’s one thing to reward, if you will, donors by making sure they don’t suffer financial loss. It’s a very different thing to say, let’s have a free market and we’ll pay whoever it is that’s willing to sell us a kidney to do so. The former seems to me to be humane and just, whereas the latter risks exploitation.
A version of this article first appeared on Medscape.com.
State medical board chair steps down amid Medicaid fraud accusations
He has stepped down as board chair, and state officials have suspended all Medicaid payments to Dr. Hyatt and his practice, Pinnacle Premier Psychiatry in Rogers, Arkansas.
Dr. Hyatt billed 99.95% of the claims for his patients’ hospital care to Medicaid at the highest severity level, according to an affidavit filed by an investigator with the Medicaid Fraud Control Unit, Arkansas Attorney General’s Office. Other Arkansas psychiatrists billed that same level in only about 39% of claims, the affidavit states.
The possible upcoding alleged in the affidavit was a red flag that prompted the state to temporarily suspend Dr. Hyatt’s Medicaid payments.
Dr. Hyatt has until this Friday to file an appeal. He did not respond to requests from this news organization for comment.
The affidavit pointed to other concerns. For example, a whistleblower who worked at the Northwest Medical Center where Dr. Hyatt admitted patients claimed that Dr. Hyatt was only on the floor a few minutes a day and that he had no contact with patients. A review of hundreds of hours of video by state investigators revealed that Dr. Hyatt did not enter patients’ rooms, nor did he have any contact with patients, according to the affidavit. Dr. Hyatt served as the hospital’s behavioral unit director from 2018 until his contract was abruptly terminated in May 2022, according to the affidavit.
However, Dr. Hyatt claimed to have conducted daily face-to-face evaluation and management with patients, according to the affidavit. In addition, the whistleblower claimed that Dr. Hyatt did not want patients to know his name and instructed staff to cover up his name on patient armbands.
Detaining patients
Dr. Hyatt also faces accusations that he held patients against their will, according to civil lawsuits filed in Washington County, Ark., reports the Arkansas Advocate.
Karla Adrian-Caceres filed suit on Jan. 17. Ms. Adrian-Caceres also named Brooke Green, Northwest Arkansas Hospitals, and 25 unidentified hospital employees as defendants.
According to the complaint, Ms. Adrian-Caceres, an engineering student at the University of Arkansas, arrived at the Northwest Medical Emergency Department after accidentally taking too many Tylenol on Jan. 18, 2022. She was then taken by ambulance to a Northwest psychiatric facility in Springdale, court records show.
According to the complaint, Ms. Adrian-Caceres said that she was given a sedative and asked to sign consent for admission while on the way to Northwest. She said that she “signed some documents without being able to read or understand them at the time.”
When she asked when she could go home, Ms. Adrian-Caceres said, “more than one employee told her there was a minimum stay and that if she asked to leave, they would take her to court where a judge would give her a longer stay because the judge always sides with Dr. Hyatt and Northwest,” according to court documents. Northwest employees stripped Ms. Adrian-Caceres, searched her body, took all of her possessions from her and issued underwear and a uniform, according to the lawsuit.
Ms. Adrian-Caceres’ mother, Katty Caceres, claimed in the lawsuit that she was prohibited from seeing her daughter. Ms. Caceres spoke with five different employees, four of whom had only their first names on their badges. Each of them reportedly said that they could not help, or that the plaintiff “would be in there for some time” and that it was Dr. Hyatt’s decision regarding how long that would be, according to court documents.
Katty Caceres hired a local attorney named Aaron Cash to represent her daughter. On Jan. 20, 2022, Mr. Cash faxed a letter to the hospital demanding her release. When Ms. Caceres arrived to pick up her daughter, she claimed that staff members indicated that the daughter was there voluntarily and refused to release her “at the direction of Dr Hyatt.” During a phone call later that day, the plaintiff told her mother that her status was being changed to an involuntary hold, court documents show.
“At one point she was threatened with the longer time in there if she kept asking to leave,” Mr. Cash told this news organization. In addition, staff members reportedly told Ms. Adrian-Caceres that the “judge always sided with Dr Hyatt” and she “would get way longer there, 30-45 days if [she] went before the judge,” according to Mr. Cash.
Mr. Cash said nine other patients have contacted his firm with similar allegations against Dr. Hyatt.
“We’ve talked to many people that have experienced the same threats,” Mr. Cash said. “When they’re asking to leave, they get these threats, they get coerced … and they’re never taken to court. They’re never given opportunity to talk to a judge or to have a public defender appointed.”
A version of this article first appeared on Medscape.com.
He has stepped down as board chair, and state officials have suspended all Medicaid payments to Dr. Hyatt and his practice, Pinnacle Premier Psychiatry in Rogers, Arkansas.
Dr. Hyatt billed 99.95% of the claims for his patients’ hospital care to Medicaid at the highest severity level, according to an affidavit filed by an investigator with the Medicaid Fraud Control Unit, Arkansas Attorney General’s Office. Other Arkansas psychiatrists billed that same level in only about 39% of claims, the affidavit states.
The possible upcoding alleged in the affidavit was a red flag that prompted the state to temporarily suspend Dr. Hyatt’s Medicaid payments.
Dr. Hyatt has until this Friday to file an appeal. He did not respond to requests from this news organization for comment.
The affidavit pointed to other concerns. For example, a whistleblower who worked at the Northwest Medical Center where Dr. Hyatt admitted patients claimed that Dr. Hyatt was only on the floor a few minutes a day and that he had no contact with patients. A review of hundreds of hours of video by state investigators revealed that Dr. Hyatt did not enter patients’ rooms, nor did he have any contact with patients, according to the affidavit. Dr. Hyatt served as the hospital’s behavioral unit director from 2018 until his contract was abruptly terminated in May 2022, according to the affidavit.
However, Dr. Hyatt claimed to have conducted daily face-to-face evaluation and management with patients, according to the affidavit. In addition, the whistleblower claimed that Dr. Hyatt did not want patients to know his name and instructed staff to cover up his name on patient armbands.
Detaining patients
Dr. Hyatt also faces accusations that he held patients against their will, according to civil lawsuits filed in Washington County, Ark., reports the Arkansas Advocate.
Karla Adrian-Caceres filed suit on Jan. 17. Ms. Adrian-Caceres also named Brooke Green, Northwest Arkansas Hospitals, and 25 unidentified hospital employees as defendants.
According to the complaint, Ms. Adrian-Caceres, an engineering student at the University of Arkansas, arrived at the Northwest Medical Emergency Department after accidentally taking too many Tylenol on Jan. 18, 2022. She was then taken by ambulance to a Northwest psychiatric facility in Springdale, court records show.
According to the complaint, Ms. Adrian-Caceres said that she was given a sedative and asked to sign consent for admission while on the way to Northwest. She said that she “signed some documents without being able to read or understand them at the time.”
When she asked when she could go home, Ms. Adrian-Caceres said, “more than one employee told her there was a minimum stay and that if she asked to leave, they would take her to court where a judge would give her a longer stay because the judge always sides with Dr. Hyatt and Northwest,” according to court documents. Northwest employees stripped Ms. Adrian-Caceres, searched her body, took all of her possessions from her and issued underwear and a uniform, according to the lawsuit.
Ms. Adrian-Caceres’ mother, Katty Caceres, claimed in the lawsuit that she was prohibited from seeing her daughter. Ms. Caceres spoke with five different employees, four of whom had only their first names on their badges. Each of them reportedly said that they could not help, or that the plaintiff “would be in there for some time” and that it was Dr. Hyatt’s decision regarding how long that would be, according to court documents.
Katty Caceres hired a local attorney named Aaron Cash to represent her daughter. On Jan. 20, 2022, Mr. Cash faxed a letter to the hospital demanding her release. When Ms. Caceres arrived to pick up her daughter, she claimed that staff members indicated that the daughter was there voluntarily and refused to release her “at the direction of Dr Hyatt.” During a phone call later that day, the plaintiff told her mother that her status was being changed to an involuntary hold, court documents show.
“At one point she was threatened with the longer time in there if she kept asking to leave,” Mr. Cash told this news organization. In addition, staff members reportedly told Ms. Adrian-Caceres that the “judge always sided with Dr Hyatt” and she “would get way longer there, 30-45 days if [she] went before the judge,” according to Mr. Cash.
Mr. Cash said nine other patients have contacted his firm with similar allegations against Dr. Hyatt.
“We’ve talked to many people that have experienced the same threats,” Mr. Cash said. “When they’re asking to leave, they get these threats, they get coerced … and they’re never taken to court. They’re never given opportunity to talk to a judge or to have a public defender appointed.”
A version of this article first appeared on Medscape.com.
He has stepped down as board chair, and state officials have suspended all Medicaid payments to Dr. Hyatt and his practice, Pinnacle Premier Psychiatry in Rogers, Arkansas.
Dr. Hyatt billed 99.95% of the claims for his patients’ hospital care to Medicaid at the highest severity level, according to an affidavit filed by an investigator with the Medicaid Fraud Control Unit, Arkansas Attorney General’s Office. Other Arkansas psychiatrists billed that same level in only about 39% of claims, the affidavit states.
The possible upcoding alleged in the affidavit was a red flag that prompted the state to temporarily suspend Dr. Hyatt’s Medicaid payments.
Dr. Hyatt has until this Friday to file an appeal. He did not respond to requests from this news organization for comment.
The affidavit pointed to other concerns. For example, a whistleblower who worked at the Northwest Medical Center where Dr. Hyatt admitted patients claimed that Dr. Hyatt was only on the floor a few minutes a day and that he had no contact with patients. A review of hundreds of hours of video by state investigators revealed that Dr. Hyatt did not enter patients’ rooms, nor did he have any contact with patients, according to the affidavit. Dr. Hyatt served as the hospital’s behavioral unit director from 2018 until his contract was abruptly terminated in May 2022, according to the affidavit.
However, Dr. Hyatt claimed to have conducted daily face-to-face evaluation and management with patients, according to the affidavit. In addition, the whistleblower claimed that Dr. Hyatt did not want patients to know his name and instructed staff to cover up his name on patient armbands.
Detaining patients
Dr. Hyatt also faces accusations that he held patients against their will, according to civil lawsuits filed in Washington County, Ark., reports the Arkansas Advocate.
Karla Adrian-Caceres filed suit on Jan. 17. Ms. Adrian-Caceres also named Brooke Green, Northwest Arkansas Hospitals, and 25 unidentified hospital employees as defendants.
According to the complaint, Ms. Adrian-Caceres, an engineering student at the University of Arkansas, arrived at the Northwest Medical Emergency Department after accidentally taking too many Tylenol on Jan. 18, 2022. She was then taken by ambulance to a Northwest psychiatric facility in Springdale, court records show.
According to the complaint, Ms. Adrian-Caceres said that she was given a sedative and asked to sign consent for admission while on the way to Northwest. She said that she “signed some documents without being able to read or understand them at the time.”
When she asked when she could go home, Ms. Adrian-Caceres said, “more than one employee told her there was a minimum stay and that if she asked to leave, they would take her to court where a judge would give her a longer stay because the judge always sides with Dr. Hyatt and Northwest,” according to court documents. Northwest employees stripped Ms. Adrian-Caceres, searched her body, took all of her possessions from her and issued underwear and a uniform, according to the lawsuit.
Ms. Adrian-Caceres’ mother, Katty Caceres, claimed in the lawsuit that she was prohibited from seeing her daughter. Ms. Caceres spoke with five different employees, four of whom had only their first names on their badges. Each of them reportedly said that they could not help, or that the plaintiff “would be in there for some time” and that it was Dr. Hyatt’s decision regarding how long that would be, according to court documents.
Katty Caceres hired a local attorney named Aaron Cash to represent her daughter. On Jan. 20, 2022, Mr. Cash faxed a letter to the hospital demanding her release. When Ms. Caceres arrived to pick up her daughter, she claimed that staff members indicated that the daughter was there voluntarily and refused to release her “at the direction of Dr Hyatt.” During a phone call later that day, the plaintiff told her mother that her status was being changed to an involuntary hold, court documents show.
“At one point she was threatened with the longer time in there if she kept asking to leave,” Mr. Cash told this news organization. In addition, staff members reportedly told Ms. Adrian-Caceres that the “judge always sided with Dr Hyatt” and she “would get way longer there, 30-45 days if [she] went before the judge,” according to Mr. Cash.
Mr. Cash said nine other patients have contacted his firm with similar allegations against Dr. Hyatt.
“We’ve talked to many people that have experienced the same threats,” Mr. Cash said. “When they’re asking to leave, they get these threats, they get coerced … and they’re never taken to court. They’re never given opportunity to talk to a judge or to have a public defender appointed.”
A version of this article first appeared on Medscape.com.
What’s the ‘secret sauce’ to help patients move more?
“Just Do It” is a cute marketing slogan. But let’s face it: Clinically, it doesn’t work well. Most people just don’t exercise. according to recent data from the Centers for Disease Control and Prevention.
Furthermore, when surveyed about aerobic exercise and strength training, only 24.6% meet these weekly recommendations. These low rates of physical activity are alarming, given the immense benefits of exercise in improving mental and physical health and well-being.
Many people know that exercise is good for them but struggle to go workout consistently. I know firsthand how challenging this can be. In addition to being an integrative obesity specialist, I have gone from 0 minutes of physical activity in 2014 to becoming a fitness enthusiast who’s run more than 5,300 miles over 8 years. I know that as doctors and clinicians, we can profoundly influence our patients’ exercise journey.
Here are five tips to help motivate your patients make the change from “I Won’t Do It” to “I’m Doing It.”
Tip 1: ‘[Clinician], heal thyself’
Data don’t lie. Doctors who move more are more likely to counsel patients on exercise. I’ve been the doctor on both sides of the exercise spectrum. At my heaviest weight and lowest physical activity level, I felt hypocritical counseling patients on exercise.
If and when I counseled my patients on exercise, it was very directive and impersonal. When I started running consistently, I went to the opposite end of the spectrum. In my running zeal, it took a while for me to understand that not everyone wants to run dozens of miles a week. Shocking! Some people can’t handle intense workouts. The “I did it so you can too” perspective wasn’t helpful for long-term change in most patients.
What has been beneficial is recalling the obstacles and emotions I had (and still have) with staying consistent with physical activity. When physicians and clinicians move regularly, we’re more equipped to give our patients genuine counseling based on practicality rather than theory.
Now that self-reflection has been addressed, let’s get to patient counseling.
Tip 2: Motivate, don’t berate
Lectures on why patients should exercise are less helpful than asking, “Why aren›t you able to exercise more often?”
Asking open-ended questions is essential in motivational interviewing. Motivational interviewing promotes behavioral change through collaborative conversation.
Instead of telling the patient what to do, motivational interviewing seeks to establish a person’s why and create an effective plan based on their motivation. Asking open-ended questions is also helpful in determining any challenges to regular exercise, rather than calling these challenges “excuses,” which can be counterproductive.
I encourage patients to embrace challenges as opportunities for improvement. If they say: “I can’t find time to work out,” I suggest that they create time to work out by walking 10-15 minutes during lunch or after dinner. The information gleaned from open-ended questions helps set practical SMARTER goals, which we will discuss next.
Tip 3: Set SMARTER goals
After assessing the patient’s motivation and barriers, use this information to transform their desire to change into an actionable plan through a SMARTER goal. SMARTER stands for Specific, Measurable, Attainable, Relevant, Time-Sensitive, Enjoyable, and Rewarding. Practical goals have each of these components. That’s why “Just Do It” or even “Exercise 150 minutes a week” isn’t a clear path for actionable change. SMARTER goals go beyond what to do and help people personalize how to change.
For example, the SMARTER version of “exercise 150 minutes a week” for a busy person who works 50 hours a week may look like this: “My goal is to incorporate 150 minutes of physical activity through 60 minutes of aerobic exercise Monday through Friday (20-minute lunch walks) and 90 minutes of combination resistance training on the weekend (two 45-minute sessions) while listening to my favorite music. To meet my goal, I will reward myself by calling a friend to catch up or buy myself a new workout outfit.”
Exercise prescriptions are another helpful way to empower patients with a realistic exercise strategy. In my practice, I developed my own exercise prescription which focuses on overcoming time barriers to exercise and finding personally enjoyable exercises. To enhance self-directed physical activity, I›ve found it useful to have patients complete part of the “exercise prescription” on their own before or after their visit.
Tip 4: Use accountability tools
Making a SMARTER goal is one thing, but sticking with it takes regular reinforcement. Even with the best plan, once patients leave the office, there are many distractions from their goals. Accountability is the secret sauce to cultivating consistency. Fitness trackers are an affordable form of accountability. Studies show that wearing a fitness tracker can help people get up to 40 minutes of extra walking, compared with people who don’t wear trackers.
Additionally, clinicians can use different ways to offer exercise accountability. For example, more frequent check-ins, individually or in groups, can be helpful. The increase in telehealth has made interval visits easier. Reimbursement and time can limit clinician-level accountability, however. Other options are referring patients to online support groups or programs sponsored by the government or organizations. For years, I coled a Walk With a Doc chapter in Richmond, Va. There are chapters throughout the country.
Tip 5: Prepare and PLAN for setbacks
Breaking news: Most plans don’t go quite as envisioned. Accounting for the potential of setbacks early on helps patients set realistic expectations. As physicians and clinicians, we can help our patients anticipate a few likely obstacles. This may lessen the impact when a setback occurs. Also, it’s helpful to have the patient prepare for a setback with a PLAN for recovering quickly. PLAN stands for Ponder what happened; Learn from it; Adjust the original goal; Now get back on track. Getting back on track as soon as possible is important to keep patients motivated and prevent muscle deconditioning.
Exercise is medicine. Physical inactivity is a leading contributor to many preventable diseases. Although the physical activity statistics are disappointing, improvement is possible. Many systemic changes are needed to increase physical activity on a population level.
While waiting for more extensive changes, we have the power to equip patients with personalized, actionable tools for improving and maintaining physical activity.
We can transform one person at a time through our clinical encounters. Let’s use effective tools to help patients shift from “I Won’t Do It” to “I’m Doing It.”
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness,” was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022. She reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
“Just Do It” is a cute marketing slogan. But let’s face it: Clinically, it doesn’t work well. Most people just don’t exercise. according to recent data from the Centers for Disease Control and Prevention.
Furthermore, when surveyed about aerobic exercise and strength training, only 24.6% meet these weekly recommendations. These low rates of physical activity are alarming, given the immense benefits of exercise in improving mental and physical health and well-being.
Many people know that exercise is good for them but struggle to go workout consistently. I know firsthand how challenging this can be. In addition to being an integrative obesity specialist, I have gone from 0 minutes of physical activity in 2014 to becoming a fitness enthusiast who’s run more than 5,300 miles over 8 years. I know that as doctors and clinicians, we can profoundly influence our patients’ exercise journey.
Here are five tips to help motivate your patients make the change from “I Won’t Do It” to “I’m Doing It.”
Tip 1: ‘[Clinician], heal thyself’
Data don’t lie. Doctors who move more are more likely to counsel patients on exercise. I’ve been the doctor on both sides of the exercise spectrum. At my heaviest weight and lowest physical activity level, I felt hypocritical counseling patients on exercise.
If and when I counseled my patients on exercise, it was very directive and impersonal. When I started running consistently, I went to the opposite end of the spectrum. In my running zeal, it took a while for me to understand that not everyone wants to run dozens of miles a week. Shocking! Some people can’t handle intense workouts. The “I did it so you can too” perspective wasn’t helpful for long-term change in most patients.
What has been beneficial is recalling the obstacles and emotions I had (and still have) with staying consistent with physical activity. When physicians and clinicians move regularly, we’re more equipped to give our patients genuine counseling based on practicality rather than theory.
Now that self-reflection has been addressed, let’s get to patient counseling.
Tip 2: Motivate, don’t berate
Lectures on why patients should exercise are less helpful than asking, “Why aren›t you able to exercise more often?”
Asking open-ended questions is essential in motivational interviewing. Motivational interviewing promotes behavioral change through collaborative conversation.
Instead of telling the patient what to do, motivational interviewing seeks to establish a person’s why and create an effective plan based on their motivation. Asking open-ended questions is also helpful in determining any challenges to regular exercise, rather than calling these challenges “excuses,” which can be counterproductive.
I encourage patients to embrace challenges as opportunities for improvement. If they say: “I can’t find time to work out,” I suggest that they create time to work out by walking 10-15 minutes during lunch or after dinner. The information gleaned from open-ended questions helps set practical SMARTER goals, which we will discuss next.
Tip 3: Set SMARTER goals
After assessing the patient’s motivation and barriers, use this information to transform their desire to change into an actionable plan through a SMARTER goal. SMARTER stands for Specific, Measurable, Attainable, Relevant, Time-Sensitive, Enjoyable, and Rewarding. Practical goals have each of these components. That’s why “Just Do It” or even “Exercise 150 minutes a week” isn’t a clear path for actionable change. SMARTER goals go beyond what to do and help people personalize how to change.
For example, the SMARTER version of “exercise 150 minutes a week” for a busy person who works 50 hours a week may look like this: “My goal is to incorporate 150 minutes of physical activity through 60 minutes of aerobic exercise Monday through Friday (20-minute lunch walks) and 90 minutes of combination resistance training on the weekend (two 45-minute sessions) while listening to my favorite music. To meet my goal, I will reward myself by calling a friend to catch up or buy myself a new workout outfit.”
Exercise prescriptions are another helpful way to empower patients with a realistic exercise strategy. In my practice, I developed my own exercise prescription which focuses on overcoming time barriers to exercise and finding personally enjoyable exercises. To enhance self-directed physical activity, I›ve found it useful to have patients complete part of the “exercise prescription” on their own before or after their visit.
Tip 4: Use accountability tools
Making a SMARTER goal is one thing, but sticking with it takes regular reinforcement. Even with the best plan, once patients leave the office, there are many distractions from their goals. Accountability is the secret sauce to cultivating consistency. Fitness trackers are an affordable form of accountability. Studies show that wearing a fitness tracker can help people get up to 40 minutes of extra walking, compared with people who don’t wear trackers.
Additionally, clinicians can use different ways to offer exercise accountability. For example, more frequent check-ins, individually or in groups, can be helpful. The increase in telehealth has made interval visits easier. Reimbursement and time can limit clinician-level accountability, however. Other options are referring patients to online support groups or programs sponsored by the government or organizations. For years, I coled a Walk With a Doc chapter in Richmond, Va. There are chapters throughout the country.
Tip 5: Prepare and PLAN for setbacks
Breaking news: Most plans don’t go quite as envisioned. Accounting for the potential of setbacks early on helps patients set realistic expectations. As physicians and clinicians, we can help our patients anticipate a few likely obstacles. This may lessen the impact when a setback occurs. Also, it’s helpful to have the patient prepare for a setback with a PLAN for recovering quickly. PLAN stands for Ponder what happened; Learn from it; Adjust the original goal; Now get back on track. Getting back on track as soon as possible is important to keep patients motivated and prevent muscle deconditioning.
Exercise is medicine. Physical inactivity is a leading contributor to many preventable diseases. Although the physical activity statistics are disappointing, improvement is possible. Many systemic changes are needed to increase physical activity on a population level.
While waiting for more extensive changes, we have the power to equip patients with personalized, actionable tools for improving and maintaining physical activity.
We can transform one person at a time through our clinical encounters. Let’s use effective tools to help patients shift from “I Won’t Do It” to “I’m Doing It.”
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness,” was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022. She reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
“Just Do It” is a cute marketing slogan. But let’s face it: Clinically, it doesn’t work well. Most people just don’t exercise. according to recent data from the Centers for Disease Control and Prevention.
Furthermore, when surveyed about aerobic exercise and strength training, only 24.6% meet these weekly recommendations. These low rates of physical activity are alarming, given the immense benefits of exercise in improving mental and physical health and well-being.
Many people know that exercise is good for them but struggle to go workout consistently. I know firsthand how challenging this can be. In addition to being an integrative obesity specialist, I have gone from 0 minutes of physical activity in 2014 to becoming a fitness enthusiast who’s run more than 5,300 miles over 8 years. I know that as doctors and clinicians, we can profoundly influence our patients’ exercise journey.
Here are five tips to help motivate your patients make the change from “I Won’t Do It” to “I’m Doing It.”
Tip 1: ‘[Clinician], heal thyself’
Data don’t lie. Doctors who move more are more likely to counsel patients on exercise. I’ve been the doctor on both sides of the exercise spectrum. At my heaviest weight and lowest physical activity level, I felt hypocritical counseling patients on exercise.
If and when I counseled my patients on exercise, it was very directive and impersonal. When I started running consistently, I went to the opposite end of the spectrum. In my running zeal, it took a while for me to understand that not everyone wants to run dozens of miles a week. Shocking! Some people can’t handle intense workouts. The “I did it so you can too” perspective wasn’t helpful for long-term change in most patients.
What has been beneficial is recalling the obstacles and emotions I had (and still have) with staying consistent with physical activity. When physicians and clinicians move regularly, we’re more equipped to give our patients genuine counseling based on practicality rather than theory.
Now that self-reflection has been addressed, let’s get to patient counseling.
Tip 2: Motivate, don’t berate
Lectures on why patients should exercise are less helpful than asking, “Why aren›t you able to exercise more often?”
Asking open-ended questions is essential in motivational interviewing. Motivational interviewing promotes behavioral change through collaborative conversation.
Instead of telling the patient what to do, motivational interviewing seeks to establish a person’s why and create an effective plan based on their motivation. Asking open-ended questions is also helpful in determining any challenges to regular exercise, rather than calling these challenges “excuses,” which can be counterproductive.
I encourage patients to embrace challenges as opportunities for improvement. If they say: “I can’t find time to work out,” I suggest that they create time to work out by walking 10-15 minutes during lunch or after dinner. The information gleaned from open-ended questions helps set practical SMARTER goals, which we will discuss next.
Tip 3: Set SMARTER goals
After assessing the patient’s motivation and barriers, use this information to transform their desire to change into an actionable plan through a SMARTER goal. SMARTER stands for Specific, Measurable, Attainable, Relevant, Time-Sensitive, Enjoyable, and Rewarding. Practical goals have each of these components. That’s why “Just Do It” or even “Exercise 150 minutes a week” isn’t a clear path for actionable change. SMARTER goals go beyond what to do and help people personalize how to change.
For example, the SMARTER version of “exercise 150 minutes a week” for a busy person who works 50 hours a week may look like this: “My goal is to incorporate 150 minutes of physical activity through 60 minutes of aerobic exercise Monday through Friday (20-minute lunch walks) and 90 minutes of combination resistance training on the weekend (two 45-minute sessions) while listening to my favorite music. To meet my goal, I will reward myself by calling a friend to catch up or buy myself a new workout outfit.”
Exercise prescriptions are another helpful way to empower patients with a realistic exercise strategy. In my practice, I developed my own exercise prescription which focuses on overcoming time barriers to exercise and finding personally enjoyable exercises. To enhance self-directed physical activity, I›ve found it useful to have patients complete part of the “exercise prescription” on their own before or after their visit.
Tip 4: Use accountability tools
Making a SMARTER goal is one thing, but sticking with it takes regular reinforcement. Even with the best plan, once patients leave the office, there are many distractions from their goals. Accountability is the secret sauce to cultivating consistency. Fitness trackers are an affordable form of accountability. Studies show that wearing a fitness tracker can help people get up to 40 minutes of extra walking, compared with people who don’t wear trackers.
Additionally, clinicians can use different ways to offer exercise accountability. For example, more frequent check-ins, individually or in groups, can be helpful. The increase in telehealth has made interval visits easier. Reimbursement and time can limit clinician-level accountability, however. Other options are referring patients to online support groups or programs sponsored by the government or organizations. For years, I coled a Walk With a Doc chapter in Richmond, Va. There are chapters throughout the country.
Tip 5: Prepare and PLAN for setbacks
Breaking news: Most plans don’t go quite as envisioned. Accounting for the potential of setbacks early on helps patients set realistic expectations. As physicians and clinicians, we can help our patients anticipate a few likely obstacles. This may lessen the impact when a setback occurs. Also, it’s helpful to have the patient prepare for a setback with a PLAN for recovering quickly. PLAN stands for Ponder what happened; Learn from it; Adjust the original goal; Now get back on track. Getting back on track as soon as possible is important to keep patients motivated and prevent muscle deconditioning.
Exercise is medicine. Physical inactivity is a leading contributor to many preventable diseases. Although the physical activity statistics are disappointing, improvement is possible. Many systemic changes are needed to increase physical activity on a population level.
While waiting for more extensive changes, we have the power to equip patients with personalized, actionable tools for improving and maintaining physical activity.
We can transform one person at a time through our clinical encounters. Let’s use effective tools to help patients shift from “I Won’t Do It” to “I’m Doing It.”
Sylvia Gonsahn-Bollie, MD, DipABOM, is an integrative obesity specialist focused on individualized solutions for emotional and biological overeating. Her bestselling book, “Embrace You: Your Guide to Transforming Weight Loss Misconceptions Into Lifelong Wellness,” was Healthline.com’s Best Overall Weight Loss Book of 2022 and one of Livestrong.com’s 8 Best Weight-Loss Books to Read in 2022. She reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
California picks generic drug company Civica to produce low-cost insulin
Gov. Gavin Newsom on March 18 announced the selection of Utah-based generic drug manufacturer Civica to produce low-cost insulin for California, an unprecedented move that makes good on his promise to put state government in direct competition with the brand-name drug companies that dominate the market.
“People should not be forced to go into debt to get lifesaving prescriptions,” Gov. Newsom said. “Californians will have access to some of the most inexpensive insulin available, helping them save thousands of dollars each year.”
The contract, with an initial cost of $50 million that Gov. Newsom and his fellow Democratic lawmakers approved last year, calls for Civica to manufacture state-branded insulin and make the lifesaving drug available to any Californian who needs it, regardless of insurance coverage, by mail order and at local pharmacies. But insulin is just the beginning. Gov. Newsom said the state will also look to produce the opioid overdose reversal drug naloxone.
Allan Coukell, Civica’s senior vice president of public policy, said in an interview that the nonprofit drugmaker is also in talks with the Newsom administration to potentially produce other generic medications, but he declined to elaborate, saying the company is focused on making cheap insulin widely available first.
“We are very excited about this partnership with the state of California,” Mr. Coukell said. “We’re not looking to have 100% of the market, but we do want 100% of people to have access to fair insulin prices.”
As insulin costs for consumers have soared, Democratic lawmakers and activists have called on the industry to rein in prices. Just weeks after President Joe Biden attacked Big Pharma for jacking up insulin prices, the three drugmakers that control the insulin market – Eli Lilly, Novo Nordisk, and Sanofi – announced they would slash the list prices of some products.
Gov. Newsom, who has previously accused the pharmaceutical industry of gouging Californians with “sky-high prices,” argued that the launch of the state’s generic drug label, CalRx, will add competition and apply pressure on the industry. Administration officials declined to say when California’s insulin products would be available, but experts say it could be as soon as 2025. Mr. Coukell said the state-branded medication will still require approval from the Food and Drug Administration, which can take roughly 10 months.
The Pharmaceutical Research and Manufacturers of America, which lobbies on behalf of brand-name companies, blasted California’s move. Reid Porter, senior director of state public affairs for PhRMA, said Gov. Newsom just “wants to score political points.”
“If the governor wants to impact what patients pay for insulins and other medicines meaningfully, he should expand his focus to others in the system that often make patients pay more than they do for medicines,” Mr. Porter said, blaming pharmaceutical go-between companies, known as pharmacy benefit managers, that negotiate with manufacturers on behalf of insurers for rebates and discounts on drugs.
The Pharmaceutical Care Management Association, which represents pharmacy benefit managers argued in turn that it’s pharmaceutical companies that are to blame for high prices.
Drug pricing experts, however, say pharmacy benefit managers and drugmakers share the blame.
Gov. Newsom administration officials say that inflated insulin costs force some to pay as much as $300 per vial or $500 for a box of injectable pens, and that too many Californians with diabetes skip or ration their medication. Doing so can lead to blindness, amputations, and life-threatening conditions such as heart disease and kidney failure. Nearly 10% of California adults have diabetes.
Civica is developing three types of generic insulin, known as a biosimilar, which will be available both in vials and in injectable pens. They are expected to be interchangeable with brand-name products including Lantus, Humalog, and NovoLog. Mr. Coukell said the company would make the drug available for no more than $30 a vial, or $55 for five injectable pens.
Gov. Newsom said the state’s insulin will save many patients $2,000-$4,000 a year, though critical questions about how California would get the products into the hands of consumers remain unanswered, including how it would persuade pharmacies, insurers, and retailers to distribute the drugs.
In 2022, Gov. Newsom also secured $50 million in seed money to build a facility to manufacture insulin; Mr. Coukell said Civica is exploring building a plant in California.
California’s move, though never previously tried by a state government, could be blunted by recent industry decisions to lower insulin prices. In March, Lilly, Novo Nordisk, and Sanofi vowed to cut prices, with Lilly offering a vial at $25 per month, Novo Nordisk promising major reductions that would bring the price of a particular generic vial to $48, and Sanofi pegging one vial at $64.
The governor’s office said it will cost the state $30 per vial to manufacture and distribute insulin and it will be sold at that price. Doing so, the administration argued, “will prevent the egregious cost-shifting that happens in traditional pharmaceutical price games.”
Drug pricing experts said generic production in California could further lower costs for insulin, and benefit people with high-deductible health insurance plans or no insurance.
“This is an extraordinary move in the pharmaceutical industry, not just for insulin but potentially for all kinds of drugs,” said Robin Feldman, a professor at the University of California, San Francisco. “It’s a very difficult industry to disrupt, but California is poised to do just that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Gov. Gavin Newsom on March 18 announced the selection of Utah-based generic drug manufacturer Civica to produce low-cost insulin for California, an unprecedented move that makes good on his promise to put state government in direct competition with the brand-name drug companies that dominate the market.
“People should not be forced to go into debt to get lifesaving prescriptions,” Gov. Newsom said. “Californians will have access to some of the most inexpensive insulin available, helping them save thousands of dollars each year.”
The contract, with an initial cost of $50 million that Gov. Newsom and his fellow Democratic lawmakers approved last year, calls for Civica to manufacture state-branded insulin and make the lifesaving drug available to any Californian who needs it, regardless of insurance coverage, by mail order and at local pharmacies. But insulin is just the beginning. Gov. Newsom said the state will also look to produce the opioid overdose reversal drug naloxone.
Allan Coukell, Civica’s senior vice president of public policy, said in an interview that the nonprofit drugmaker is also in talks with the Newsom administration to potentially produce other generic medications, but he declined to elaborate, saying the company is focused on making cheap insulin widely available first.
“We are very excited about this partnership with the state of California,” Mr. Coukell said. “We’re not looking to have 100% of the market, but we do want 100% of people to have access to fair insulin prices.”
As insulin costs for consumers have soared, Democratic lawmakers and activists have called on the industry to rein in prices. Just weeks after President Joe Biden attacked Big Pharma for jacking up insulin prices, the three drugmakers that control the insulin market – Eli Lilly, Novo Nordisk, and Sanofi – announced they would slash the list prices of some products.
Gov. Newsom, who has previously accused the pharmaceutical industry of gouging Californians with “sky-high prices,” argued that the launch of the state’s generic drug label, CalRx, will add competition and apply pressure on the industry. Administration officials declined to say when California’s insulin products would be available, but experts say it could be as soon as 2025. Mr. Coukell said the state-branded medication will still require approval from the Food and Drug Administration, which can take roughly 10 months.
The Pharmaceutical Research and Manufacturers of America, which lobbies on behalf of brand-name companies, blasted California’s move. Reid Porter, senior director of state public affairs for PhRMA, said Gov. Newsom just “wants to score political points.”
“If the governor wants to impact what patients pay for insulins and other medicines meaningfully, he should expand his focus to others in the system that often make patients pay more than they do for medicines,” Mr. Porter said, blaming pharmaceutical go-between companies, known as pharmacy benefit managers, that negotiate with manufacturers on behalf of insurers for rebates and discounts on drugs.
The Pharmaceutical Care Management Association, which represents pharmacy benefit managers argued in turn that it’s pharmaceutical companies that are to blame for high prices.
Drug pricing experts, however, say pharmacy benefit managers and drugmakers share the blame.
Gov. Newsom administration officials say that inflated insulin costs force some to pay as much as $300 per vial or $500 for a box of injectable pens, and that too many Californians with diabetes skip or ration their medication. Doing so can lead to blindness, amputations, and life-threatening conditions such as heart disease and kidney failure. Nearly 10% of California adults have diabetes.
Civica is developing three types of generic insulin, known as a biosimilar, which will be available both in vials and in injectable pens. They are expected to be interchangeable with brand-name products including Lantus, Humalog, and NovoLog. Mr. Coukell said the company would make the drug available for no more than $30 a vial, or $55 for five injectable pens.
Gov. Newsom said the state’s insulin will save many patients $2,000-$4,000 a year, though critical questions about how California would get the products into the hands of consumers remain unanswered, including how it would persuade pharmacies, insurers, and retailers to distribute the drugs.
In 2022, Gov. Newsom also secured $50 million in seed money to build a facility to manufacture insulin; Mr. Coukell said Civica is exploring building a plant in California.
California’s move, though never previously tried by a state government, could be blunted by recent industry decisions to lower insulin prices. In March, Lilly, Novo Nordisk, and Sanofi vowed to cut prices, with Lilly offering a vial at $25 per month, Novo Nordisk promising major reductions that would bring the price of a particular generic vial to $48, and Sanofi pegging one vial at $64.
The governor’s office said it will cost the state $30 per vial to manufacture and distribute insulin and it will be sold at that price. Doing so, the administration argued, “will prevent the egregious cost-shifting that happens in traditional pharmaceutical price games.”
Drug pricing experts said generic production in California could further lower costs for insulin, and benefit people with high-deductible health insurance plans or no insurance.
“This is an extraordinary move in the pharmaceutical industry, not just for insulin but potentially for all kinds of drugs,” said Robin Feldman, a professor at the University of California, San Francisco. “It’s a very difficult industry to disrupt, but California is poised to do just that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Gov. Gavin Newsom on March 18 announced the selection of Utah-based generic drug manufacturer Civica to produce low-cost insulin for California, an unprecedented move that makes good on his promise to put state government in direct competition with the brand-name drug companies that dominate the market.
“People should not be forced to go into debt to get lifesaving prescriptions,” Gov. Newsom said. “Californians will have access to some of the most inexpensive insulin available, helping them save thousands of dollars each year.”
The contract, with an initial cost of $50 million that Gov. Newsom and his fellow Democratic lawmakers approved last year, calls for Civica to manufacture state-branded insulin and make the lifesaving drug available to any Californian who needs it, regardless of insurance coverage, by mail order and at local pharmacies. But insulin is just the beginning. Gov. Newsom said the state will also look to produce the opioid overdose reversal drug naloxone.
Allan Coukell, Civica’s senior vice president of public policy, said in an interview that the nonprofit drugmaker is also in talks with the Newsom administration to potentially produce other generic medications, but he declined to elaborate, saying the company is focused on making cheap insulin widely available first.
“We are very excited about this partnership with the state of California,” Mr. Coukell said. “We’re not looking to have 100% of the market, but we do want 100% of people to have access to fair insulin prices.”
As insulin costs for consumers have soared, Democratic lawmakers and activists have called on the industry to rein in prices. Just weeks after President Joe Biden attacked Big Pharma for jacking up insulin prices, the three drugmakers that control the insulin market – Eli Lilly, Novo Nordisk, and Sanofi – announced they would slash the list prices of some products.
Gov. Newsom, who has previously accused the pharmaceutical industry of gouging Californians with “sky-high prices,” argued that the launch of the state’s generic drug label, CalRx, will add competition and apply pressure on the industry. Administration officials declined to say when California’s insulin products would be available, but experts say it could be as soon as 2025. Mr. Coukell said the state-branded medication will still require approval from the Food and Drug Administration, which can take roughly 10 months.
The Pharmaceutical Research and Manufacturers of America, which lobbies on behalf of brand-name companies, blasted California’s move. Reid Porter, senior director of state public affairs for PhRMA, said Gov. Newsom just “wants to score political points.”
“If the governor wants to impact what patients pay for insulins and other medicines meaningfully, he should expand his focus to others in the system that often make patients pay more than they do for medicines,” Mr. Porter said, blaming pharmaceutical go-between companies, known as pharmacy benefit managers, that negotiate with manufacturers on behalf of insurers for rebates and discounts on drugs.
The Pharmaceutical Care Management Association, which represents pharmacy benefit managers argued in turn that it’s pharmaceutical companies that are to blame for high prices.
Drug pricing experts, however, say pharmacy benefit managers and drugmakers share the blame.
Gov. Newsom administration officials say that inflated insulin costs force some to pay as much as $300 per vial or $500 for a box of injectable pens, and that too many Californians with diabetes skip or ration their medication. Doing so can lead to blindness, amputations, and life-threatening conditions such as heart disease and kidney failure. Nearly 10% of California adults have diabetes.
Civica is developing three types of generic insulin, known as a biosimilar, which will be available both in vials and in injectable pens. They are expected to be interchangeable with brand-name products including Lantus, Humalog, and NovoLog. Mr. Coukell said the company would make the drug available for no more than $30 a vial, or $55 for five injectable pens.
Gov. Newsom said the state’s insulin will save many patients $2,000-$4,000 a year, though critical questions about how California would get the products into the hands of consumers remain unanswered, including how it would persuade pharmacies, insurers, and retailers to distribute the drugs.
In 2022, Gov. Newsom also secured $50 million in seed money to build a facility to manufacture insulin; Mr. Coukell said Civica is exploring building a plant in California.
California’s move, though never previously tried by a state government, could be blunted by recent industry decisions to lower insulin prices. In March, Lilly, Novo Nordisk, and Sanofi vowed to cut prices, with Lilly offering a vial at $25 per month, Novo Nordisk promising major reductions that would bring the price of a particular generic vial to $48, and Sanofi pegging one vial at $64.
The governor’s office said it will cost the state $30 per vial to manufacture and distribute insulin and it will be sold at that price. Doing so, the administration argued, “will prevent the egregious cost-shifting that happens in traditional pharmaceutical price games.”
Drug pricing experts said generic production in California could further lower costs for insulin, and benefit people with high-deductible health insurance plans or no insurance.
“This is an extraordinary move in the pharmaceutical industry, not just for insulin but potentially for all kinds of drugs,” said Robin Feldman, a professor at the University of California, San Francisco. “It’s a very difficult industry to disrupt, but California is poised to do just that.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Mediterranean diet linked to 24% reduction in CVD risk in women
The Mediterranean diet appears to be associated with a lower incidence of cardiovascular disease (CVD) and mortality in women, new observational data suggest.
Those who had a higher adherence to a Mediterranean diet had a 24% lower risk for cardiovascular disease and 23% lower risk for death.
“A healthy diet is a huge factor in preventing heart disease. However, current guidelines on preventing heart disease lack sex-specific recommendations,” said senior author Sarah Zaman, MBBS, PhD, an associate professor of medicine and principal research fellow at the University of Sydney’s Westmead Applied Research Centre.
“Historically, research trials and studies have had predominantly male participants or lacked sex-specific analysis,” she said. “Our results will pave the way to bridge this gap and also highlight the need for more research to ensure health guidelines and policies include diverse perspectives.”
The study was published online in the journal Heart.
Analyzing cardiovascular outcomes
Dr. Zaman and colleagues conducted a systematic review and meta-analysis of 16 studies published between 2006 and 2021 that reported a Mediterranean diet score and included either all women or had stratified outcomes by sex. They excluded studies that referred to only certain components of the Mediterranean diet or combined it with other lifestyle-related factors.
The studies, which were mainly conducted in the United States and Europe, included 722,495 adult women without previous clinical or subclinical CVD, with a median follow-up of 12.5 years.
Higher Mediterranean diet adherence was defined as the highest category reporting the highest range of Mediterranean diet scores, and lower adherence was defined as the lowest category reporting lowest scores. Incident CVD included coronary heart disease, myocardial infarction, stroke, heart failure, cardiovascular death, major adverse cardiovascular events, major adverse cardiac cerebrovascular events, and patient-reported CVD.
Overall, higher adherence to a Mediterranean diet was associated with lower CVD incidence (hazard ratio, 0.76; 95% confidence interval, 0.72-0.81), total mortality (HR, 0.77; 95% CI, 0.74-0.80), and coronary heart disease (HR, 0.75; 95% CI, 0.65-0.87).
Stroke incidence was also lower among women who adhered to the Mediterranean diet, although it wasn’t considered statistically significant (HR, 0.87; 95% CI, 0.76-1.01).
Additional analyses found similar reductions in risk across women of different ethnicities. Higher Mediterranean diet adherence was associated with lower CVD incidence for both women of European descent (HR, 0.76; 95% CI, 0.59-0.98) and women of non-European descent – Asian, Native Hawaiian, and African American – (HR, 0.79; 95% CI, 0.72-0.87).
The results didn’t materially change in sensitivity analyses, the authors note. Excluding one study at a time, the pooled HRs for the highest versus the lowest Mediterranean diet adherence ranged from 0.76 (95% CI, 0.72-0.80) to 0.83 (95% CI, 0.70-0.98) for incident CVD and from 0.77 (95% CI, 0.75-0.80) to 0.77 (95% CI, 0.74-0.81) for total mortality among women.
At the same time, the authors pointed to several limitations, including the observational nature of all of the studies, the reliance on self-reported food frequency questionnaires, and heterogeneity in the adjustments for influential factors across the studies.
Additional considerations
Dr. Zaman and colleagues called for more sex-specific research in cardiology, including risk factors related to premature menopause, preeclampsia, gestational diabetes, and autoimmune diseases such as systemic lupus.
Future studies should also explore the underlying mechanisms that may explain the links between the Mediterranean diet, cardiovascular disease, and death, the authors write. For instance, the diet may reduce inflammation and cardiovascular risk factors through antioxidant and beneficial gut microbiome pathways. Other components of the diet – such as polyphenols, nitrates, omega-3 fatty acids, higher fiber intake, and reduced glycemic load – may also play a role.
“It was striking to see how strong the long-term cardioprotective properties of a Mediterranean-type dietary pattern were,” said Samia Mora, MD, MHS, a professor of medicine at Harvard Medical School and director of the Center for Lipid Metabolomics at Brigham and Women’s Hospital.
Dr. Mora, who wasn’t involved with this study, has researched potential mechanisms related to the Mediterranean diet, cardiovascular events, and diabetes in women. She and colleagues have found that women with high adherence to the diet are more likely to have lower inflammation, insulin resistance, body mass index, and blood pressure, as well as improved lipid and metabolic profiles.
“This could represent an opportunity to intervene earlier and more intensively on improving inflammation, insulin resistance, and cardiometabolic health through evidence-based dietary approaches such as the Mediterranean diet,” she said. “As health care providers, we should promote the healthy dietary attributes of the Mediterranean diet, especially as many of our patients in the U.S. are less familiar with the Mediterranean diet and how to incorporate its components into daily food intake.”
The study did not receive any funding. Dr. Zaman was supported by a Heart Foundation Future Leader Fellowship. The authors declared no conflicts of interest. Dr. Mora reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Mediterranean diet appears to be associated with a lower incidence of cardiovascular disease (CVD) and mortality in women, new observational data suggest.
Those who had a higher adherence to a Mediterranean diet had a 24% lower risk for cardiovascular disease and 23% lower risk for death.
“A healthy diet is a huge factor in preventing heart disease. However, current guidelines on preventing heart disease lack sex-specific recommendations,” said senior author Sarah Zaman, MBBS, PhD, an associate professor of medicine and principal research fellow at the University of Sydney’s Westmead Applied Research Centre.
“Historically, research trials and studies have had predominantly male participants or lacked sex-specific analysis,” she said. “Our results will pave the way to bridge this gap and also highlight the need for more research to ensure health guidelines and policies include diverse perspectives.”
The study was published online in the journal Heart.
Analyzing cardiovascular outcomes
Dr. Zaman and colleagues conducted a systematic review and meta-analysis of 16 studies published between 2006 and 2021 that reported a Mediterranean diet score and included either all women or had stratified outcomes by sex. They excluded studies that referred to only certain components of the Mediterranean diet or combined it with other lifestyle-related factors.
The studies, which were mainly conducted in the United States and Europe, included 722,495 adult women without previous clinical or subclinical CVD, with a median follow-up of 12.5 years.
Higher Mediterranean diet adherence was defined as the highest category reporting the highest range of Mediterranean diet scores, and lower adherence was defined as the lowest category reporting lowest scores. Incident CVD included coronary heart disease, myocardial infarction, stroke, heart failure, cardiovascular death, major adverse cardiovascular events, major adverse cardiac cerebrovascular events, and patient-reported CVD.
Overall, higher adherence to a Mediterranean diet was associated with lower CVD incidence (hazard ratio, 0.76; 95% confidence interval, 0.72-0.81), total mortality (HR, 0.77; 95% CI, 0.74-0.80), and coronary heart disease (HR, 0.75; 95% CI, 0.65-0.87).
Stroke incidence was also lower among women who adhered to the Mediterranean diet, although it wasn’t considered statistically significant (HR, 0.87; 95% CI, 0.76-1.01).
Additional analyses found similar reductions in risk across women of different ethnicities. Higher Mediterranean diet adherence was associated with lower CVD incidence for both women of European descent (HR, 0.76; 95% CI, 0.59-0.98) and women of non-European descent – Asian, Native Hawaiian, and African American – (HR, 0.79; 95% CI, 0.72-0.87).
The results didn’t materially change in sensitivity analyses, the authors note. Excluding one study at a time, the pooled HRs for the highest versus the lowest Mediterranean diet adherence ranged from 0.76 (95% CI, 0.72-0.80) to 0.83 (95% CI, 0.70-0.98) for incident CVD and from 0.77 (95% CI, 0.75-0.80) to 0.77 (95% CI, 0.74-0.81) for total mortality among women.
At the same time, the authors pointed to several limitations, including the observational nature of all of the studies, the reliance on self-reported food frequency questionnaires, and heterogeneity in the adjustments for influential factors across the studies.
Additional considerations
Dr. Zaman and colleagues called for more sex-specific research in cardiology, including risk factors related to premature menopause, preeclampsia, gestational diabetes, and autoimmune diseases such as systemic lupus.
Future studies should also explore the underlying mechanisms that may explain the links between the Mediterranean diet, cardiovascular disease, and death, the authors write. For instance, the diet may reduce inflammation and cardiovascular risk factors through antioxidant and beneficial gut microbiome pathways. Other components of the diet – such as polyphenols, nitrates, omega-3 fatty acids, higher fiber intake, and reduced glycemic load – may also play a role.
“It was striking to see how strong the long-term cardioprotective properties of a Mediterranean-type dietary pattern were,” said Samia Mora, MD, MHS, a professor of medicine at Harvard Medical School and director of the Center for Lipid Metabolomics at Brigham and Women’s Hospital.
Dr. Mora, who wasn’t involved with this study, has researched potential mechanisms related to the Mediterranean diet, cardiovascular events, and diabetes in women. She and colleagues have found that women with high adherence to the diet are more likely to have lower inflammation, insulin resistance, body mass index, and blood pressure, as well as improved lipid and metabolic profiles.
“This could represent an opportunity to intervene earlier and more intensively on improving inflammation, insulin resistance, and cardiometabolic health through evidence-based dietary approaches such as the Mediterranean diet,” she said. “As health care providers, we should promote the healthy dietary attributes of the Mediterranean diet, especially as many of our patients in the U.S. are less familiar with the Mediterranean diet and how to incorporate its components into daily food intake.”
The study did not receive any funding. Dr. Zaman was supported by a Heart Foundation Future Leader Fellowship. The authors declared no conflicts of interest. Dr. Mora reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Mediterranean diet appears to be associated with a lower incidence of cardiovascular disease (CVD) and mortality in women, new observational data suggest.
Those who had a higher adherence to a Mediterranean diet had a 24% lower risk for cardiovascular disease and 23% lower risk for death.
“A healthy diet is a huge factor in preventing heart disease. However, current guidelines on preventing heart disease lack sex-specific recommendations,” said senior author Sarah Zaman, MBBS, PhD, an associate professor of medicine and principal research fellow at the University of Sydney’s Westmead Applied Research Centre.
“Historically, research trials and studies have had predominantly male participants or lacked sex-specific analysis,” she said. “Our results will pave the way to bridge this gap and also highlight the need for more research to ensure health guidelines and policies include diverse perspectives.”
The study was published online in the journal Heart.
Analyzing cardiovascular outcomes
Dr. Zaman and colleagues conducted a systematic review and meta-analysis of 16 studies published between 2006 and 2021 that reported a Mediterranean diet score and included either all women or had stratified outcomes by sex. They excluded studies that referred to only certain components of the Mediterranean diet or combined it with other lifestyle-related factors.
The studies, which were mainly conducted in the United States and Europe, included 722,495 adult women without previous clinical or subclinical CVD, with a median follow-up of 12.5 years.
Higher Mediterranean diet adherence was defined as the highest category reporting the highest range of Mediterranean diet scores, and lower adherence was defined as the lowest category reporting lowest scores. Incident CVD included coronary heart disease, myocardial infarction, stroke, heart failure, cardiovascular death, major adverse cardiovascular events, major adverse cardiac cerebrovascular events, and patient-reported CVD.
Overall, higher adherence to a Mediterranean diet was associated with lower CVD incidence (hazard ratio, 0.76; 95% confidence interval, 0.72-0.81), total mortality (HR, 0.77; 95% CI, 0.74-0.80), and coronary heart disease (HR, 0.75; 95% CI, 0.65-0.87).
Stroke incidence was also lower among women who adhered to the Mediterranean diet, although it wasn’t considered statistically significant (HR, 0.87; 95% CI, 0.76-1.01).
Additional analyses found similar reductions in risk across women of different ethnicities. Higher Mediterranean diet adherence was associated with lower CVD incidence for both women of European descent (HR, 0.76; 95% CI, 0.59-0.98) and women of non-European descent – Asian, Native Hawaiian, and African American – (HR, 0.79; 95% CI, 0.72-0.87).
The results didn’t materially change in sensitivity analyses, the authors note. Excluding one study at a time, the pooled HRs for the highest versus the lowest Mediterranean diet adherence ranged from 0.76 (95% CI, 0.72-0.80) to 0.83 (95% CI, 0.70-0.98) for incident CVD and from 0.77 (95% CI, 0.75-0.80) to 0.77 (95% CI, 0.74-0.81) for total mortality among women.
At the same time, the authors pointed to several limitations, including the observational nature of all of the studies, the reliance on self-reported food frequency questionnaires, and heterogeneity in the adjustments for influential factors across the studies.
Additional considerations
Dr. Zaman and colleagues called for more sex-specific research in cardiology, including risk factors related to premature menopause, preeclampsia, gestational diabetes, and autoimmune diseases such as systemic lupus.
Future studies should also explore the underlying mechanisms that may explain the links between the Mediterranean diet, cardiovascular disease, and death, the authors write. For instance, the diet may reduce inflammation and cardiovascular risk factors through antioxidant and beneficial gut microbiome pathways. Other components of the diet – such as polyphenols, nitrates, omega-3 fatty acids, higher fiber intake, and reduced glycemic load – may also play a role.
“It was striking to see how strong the long-term cardioprotective properties of a Mediterranean-type dietary pattern were,” said Samia Mora, MD, MHS, a professor of medicine at Harvard Medical School and director of the Center for Lipid Metabolomics at Brigham and Women’s Hospital.
Dr. Mora, who wasn’t involved with this study, has researched potential mechanisms related to the Mediterranean diet, cardiovascular events, and diabetes in women. She and colleagues have found that women with high adherence to the diet are more likely to have lower inflammation, insulin resistance, body mass index, and blood pressure, as well as improved lipid and metabolic profiles.
“This could represent an opportunity to intervene earlier and more intensively on improving inflammation, insulin resistance, and cardiometabolic health through evidence-based dietary approaches such as the Mediterranean diet,” she said. “As health care providers, we should promote the healthy dietary attributes of the Mediterranean diet, especially as many of our patients in the U.S. are less familiar with the Mediterranean diet and how to incorporate its components into daily food intake.”
The study did not receive any funding. Dr. Zaman was supported by a Heart Foundation Future Leader Fellowship. The authors declared no conflicts of interest. Dr. Mora reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Holy smoke: Air pollution link to bone damage confirmed
Air pollution appears to contribute independently to bone damage in postmenopausal women, new data suggest.
The findings come from a new analysis of data from the Women’s Health Initiative (WHI) and location-specific air particulate information from the U.S. Environmental Protection Agency.
“Our findings confirm that poor air quality may be a risk factor for bone loss, independent of socioeconomic or demographic factors, and expands previous findings to postmenopausal women. Indeed, to our knowledge, this is the first study of the impact of criteria air pollutants on bone health in postmenopausal women,” Diddier Prada, MD, PhD, Columbia University, New York, and colleagues wrote.
The results are also the first to show that “nitrogen oxides contribute the most to bone damage and that the lumbar spine is one of the most susceptible sites,” they added.
Public health policies should aim to reduce air pollution in general, they wrote, and reducing nitrogen oxides, in particular, will reduce bone damage in postmenopausal women, prevent bone fractures, and reduce the health cost burden associated with osteoporosis in this population.
The findings were recently published in eClinicalMedicine.
Asked to comment, Giovanni Adami, MD, PhD, said in an interview that the study “adds to the body of literature on air pollution and bone health. The study confirms and provides further evidence linking air pollution exposure and osteoporosis.”
Dr. Adami, of the University of Verona (Italy), who also studies this topic, said that these new findings align with those from his group and others.
“The scientific literature in the field is clearly pointing toward a negative effect of chronic pollution exposure on bone health.”
He pointed to one study from his group that found chronic exposure to ultrafine particulate matter is associated with low BMD, and consequently, bone fragility, and another study that showed acute exposure to high levels of pollutants could actually cause fractures.
As for what might be done clinically, Dr. Adami said: “It is difficult to extrapolate direct and immediate recommendations for patients.
“However, it might be acceptable to say that patients at risk of osteoporosis, such as older women or those with prior bone fractures, should avoid chronic exposure to air pollution, perhaps using masks when walking in traffic or using air filters for indoor ventilation.”
Dr. Adami also said that this evidence so far might spur the future inclusion of chronic exposure to air pollution in fracture risk assessment tools, although this isn’t likely to come about in the near future.
Particulates linked to whole-body, hip, lumbar, and femoral neck BMD
The prospective observational study included 9,041 WHI participants seen over 32,663 visits who were an average of 63 years old at baseline. More than 70% were White, and just under half were college graduates.
With geocoded address data used to estimate particulate matter concentrations, mean levels of particulate matter of 10 mcm or less, nitrogen oxide nitrogen dioxide, and sulfur dioxide over 1, 3, and 5 years were all negatively associated with whole-body, total hip, femoral neck, and lumbar spine BMD.
In the multivariate analysis, the highest correlations were found between nitrogen oxide and nitrogen dioxide. For example, lumbar spine BMD decreased by 0.026 g/cm2 per year per 10% increase in 3-year mean nitrogen dioxide concentration.
“Our findings show that both particulate matter and gases may adversely impact BMD and that nitrogen oxides may play a critical role in bone damage and osteoporosis risk,” Dr. Prada and colleagues wrote.
Dr. Adami added: “We need more data to understand the precise magnitude of effect of air pollution on fractures, which might depend on levels of exposure but also on genetics and lifestyle.”
The study was funded by the National Institutes of Health. The authors reported no relevant financial relationships. Dr. Adami reported receiving fees from Amgen, Eli Lilly, UCB, Fresenius Kabi, Galapagos, and Theramex.
A version of this article originally appeared on Medscape.com.
Air pollution appears to contribute independently to bone damage in postmenopausal women, new data suggest.
The findings come from a new analysis of data from the Women’s Health Initiative (WHI) and location-specific air particulate information from the U.S. Environmental Protection Agency.
“Our findings confirm that poor air quality may be a risk factor for bone loss, independent of socioeconomic or demographic factors, and expands previous findings to postmenopausal women. Indeed, to our knowledge, this is the first study of the impact of criteria air pollutants on bone health in postmenopausal women,” Diddier Prada, MD, PhD, Columbia University, New York, and colleagues wrote.
The results are also the first to show that “nitrogen oxides contribute the most to bone damage and that the lumbar spine is one of the most susceptible sites,” they added.
Public health policies should aim to reduce air pollution in general, they wrote, and reducing nitrogen oxides, in particular, will reduce bone damage in postmenopausal women, prevent bone fractures, and reduce the health cost burden associated with osteoporosis in this population.
The findings were recently published in eClinicalMedicine.
Asked to comment, Giovanni Adami, MD, PhD, said in an interview that the study “adds to the body of literature on air pollution and bone health. The study confirms and provides further evidence linking air pollution exposure and osteoporosis.”
Dr. Adami, of the University of Verona (Italy), who also studies this topic, said that these new findings align with those from his group and others.
“The scientific literature in the field is clearly pointing toward a negative effect of chronic pollution exposure on bone health.”
He pointed to one study from his group that found chronic exposure to ultrafine particulate matter is associated with low BMD, and consequently, bone fragility, and another study that showed acute exposure to high levels of pollutants could actually cause fractures.
As for what might be done clinically, Dr. Adami said: “It is difficult to extrapolate direct and immediate recommendations for patients.
“However, it might be acceptable to say that patients at risk of osteoporosis, such as older women or those with prior bone fractures, should avoid chronic exposure to air pollution, perhaps using masks when walking in traffic or using air filters for indoor ventilation.”
Dr. Adami also said that this evidence so far might spur the future inclusion of chronic exposure to air pollution in fracture risk assessment tools, although this isn’t likely to come about in the near future.
Particulates linked to whole-body, hip, lumbar, and femoral neck BMD
The prospective observational study included 9,041 WHI participants seen over 32,663 visits who were an average of 63 years old at baseline. More than 70% were White, and just under half were college graduates.
With geocoded address data used to estimate particulate matter concentrations, mean levels of particulate matter of 10 mcm or less, nitrogen oxide nitrogen dioxide, and sulfur dioxide over 1, 3, and 5 years were all negatively associated with whole-body, total hip, femoral neck, and lumbar spine BMD.
In the multivariate analysis, the highest correlations were found between nitrogen oxide and nitrogen dioxide. For example, lumbar spine BMD decreased by 0.026 g/cm2 per year per 10% increase in 3-year mean nitrogen dioxide concentration.
“Our findings show that both particulate matter and gases may adversely impact BMD and that nitrogen oxides may play a critical role in bone damage and osteoporosis risk,” Dr. Prada and colleagues wrote.
Dr. Adami added: “We need more data to understand the precise magnitude of effect of air pollution on fractures, which might depend on levels of exposure but also on genetics and lifestyle.”
The study was funded by the National Institutes of Health. The authors reported no relevant financial relationships. Dr. Adami reported receiving fees from Amgen, Eli Lilly, UCB, Fresenius Kabi, Galapagos, and Theramex.
A version of this article originally appeared on Medscape.com.
Air pollution appears to contribute independently to bone damage in postmenopausal women, new data suggest.
The findings come from a new analysis of data from the Women’s Health Initiative (WHI) and location-specific air particulate information from the U.S. Environmental Protection Agency.
“Our findings confirm that poor air quality may be a risk factor for bone loss, independent of socioeconomic or demographic factors, and expands previous findings to postmenopausal women. Indeed, to our knowledge, this is the first study of the impact of criteria air pollutants on bone health in postmenopausal women,” Diddier Prada, MD, PhD, Columbia University, New York, and colleagues wrote.
The results are also the first to show that “nitrogen oxides contribute the most to bone damage and that the lumbar spine is one of the most susceptible sites,” they added.
Public health policies should aim to reduce air pollution in general, they wrote, and reducing nitrogen oxides, in particular, will reduce bone damage in postmenopausal women, prevent bone fractures, and reduce the health cost burden associated with osteoporosis in this population.
The findings were recently published in eClinicalMedicine.
Asked to comment, Giovanni Adami, MD, PhD, said in an interview that the study “adds to the body of literature on air pollution and bone health. The study confirms and provides further evidence linking air pollution exposure and osteoporosis.”
Dr. Adami, of the University of Verona (Italy), who also studies this topic, said that these new findings align with those from his group and others.
“The scientific literature in the field is clearly pointing toward a negative effect of chronic pollution exposure on bone health.”
He pointed to one study from his group that found chronic exposure to ultrafine particulate matter is associated with low BMD, and consequently, bone fragility, and another study that showed acute exposure to high levels of pollutants could actually cause fractures.
As for what might be done clinically, Dr. Adami said: “It is difficult to extrapolate direct and immediate recommendations for patients.
“However, it might be acceptable to say that patients at risk of osteoporosis, such as older women or those with prior bone fractures, should avoid chronic exposure to air pollution, perhaps using masks when walking in traffic or using air filters for indoor ventilation.”
Dr. Adami also said that this evidence so far might spur the future inclusion of chronic exposure to air pollution in fracture risk assessment tools, although this isn’t likely to come about in the near future.
Particulates linked to whole-body, hip, lumbar, and femoral neck BMD
The prospective observational study included 9,041 WHI participants seen over 32,663 visits who were an average of 63 years old at baseline. More than 70% were White, and just under half were college graduates.
With geocoded address data used to estimate particulate matter concentrations, mean levels of particulate matter of 10 mcm or less, nitrogen oxide nitrogen dioxide, and sulfur dioxide over 1, 3, and 5 years were all negatively associated with whole-body, total hip, femoral neck, and lumbar spine BMD.
In the multivariate analysis, the highest correlations were found between nitrogen oxide and nitrogen dioxide. For example, lumbar spine BMD decreased by 0.026 g/cm2 per year per 10% increase in 3-year mean nitrogen dioxide concentration.
“Our findings show that both particulate matter and gases may adversely impact BMD and that nitrogen oxides may play a critical role in bone damage and osteoporosis risk,” Dr. Prada and colleagues wrote.
Dr. Adami added: “We need more data to understand the precise magnitude of effect of air pollution on fractures, which might depend on levels of exposure but also on genetics and lifestyle.”
The study was funded by the National Institutes of Health. The authors reported no relevant financial relationships. Dr. Adami reported receiving fees from Amgen, Eli Lilly, UCB, Fresenius Kabi, Galapagos, and Theramex.
A version of this article originally appeared on Medscape.com.
FROM ECLINICALMEDICINE
Match Day: Record number of residencies offered
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
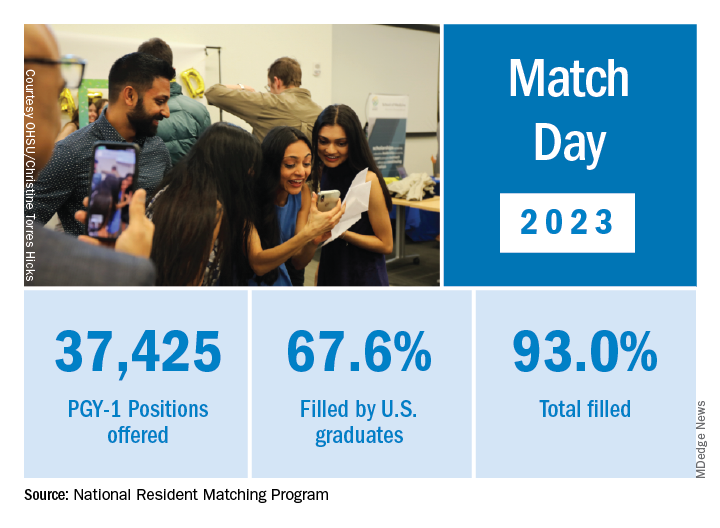
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
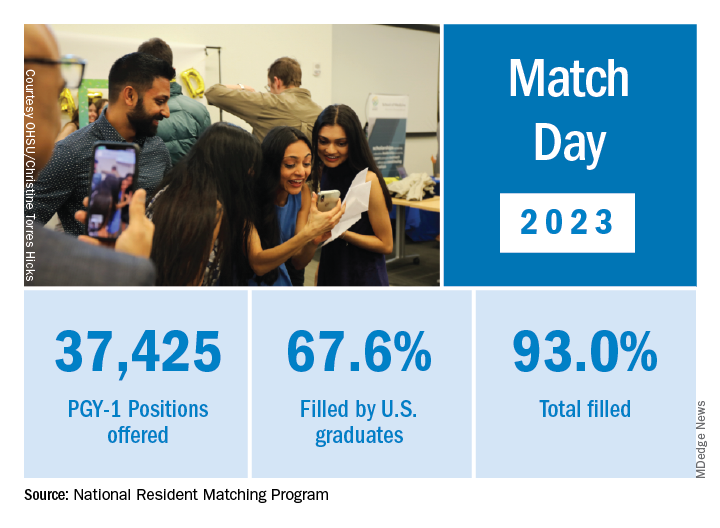
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
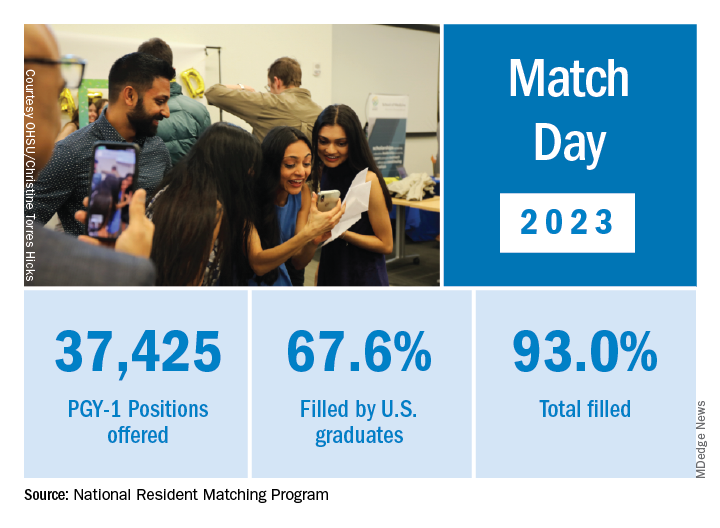
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Increased cancer in military pilots and ground crew: Pentagon
“Military aircrew and ground crew were overall more likely to be diagnosed with cancer, but less likely to die from cancer compared to the U.S. population,” the report concludes.
The study involved 156,050 aircrew and 737,891 ground crew. Participants were followed between 1992 and 2017. Both groups were predominantly male and non-Hispanic.
Data on cancer incidence and mortality for these two groups were compared with data from groups of similar age in the general population through use of the Surveillance, Epidemiology, and End Results (SEER) Database of the National Cancer Institute.
For aircrew, the study found an 87% higher rate of melanoma, a 39% higher rate of thyroid cancer, a 16% higher rate of prostate cancer, and a 24% higher rate of cancer for all sites combined.
A higher rate of melanoma and prostate cancer among aircrew has been reported previously, but the increased rate of thyroid cancer is a new finding, the authors note.
The uptick in melanoma has also been reported in studies of civilian pilots and cabin crew. It has been attributed to exposure to hazardous ultraviolet and cosmic radiation.
For ground crew members, the analysis found a 19% higher rate of cancers of the brain and nervous system, a 15% higher rate of thyroid cancer, a 9% higher rate of melanoma and of kidney and renal pelvis cancers, and a 3% higher rate of cancer for all sites combined.
There is little to compare these findings with: This is the first time that cancer risk has been evaluated in such a large population of military ground crew.
Lower rates of cancer mortality
In contrast to the increase in cancer incidence, the report found a decrease in cancer mortality.
When compared with a demographically similar U.S. population, the mortality rate among aircrew was 56% lower for all cancer sites; for ground crew, the mortality rate was 35% lower.
However, the report authors emphasize that “it is important to note that the military study population was relatively young.”
The median age at the end of follow-up for the cancer incidence analysis was 41 years for aircrew and 26 years for ground crew. The median age at the end of follow-up for the cancer mortality analysis was 48 years for aircrew and 41 years for ground crew.
“Results may have differed if additional older former Service members had been included in the study, since cancer risk and mortality rates increase with age,” the authors comment.
Other studies have found an increase in deaths from melanoma as well as an increase in the incidence of melanoma. A meta-analysis published in 2019 in the British Journal of Dermatology found that airline pilots and cabin crew have about twice the risk of melanoma and other skin cancers than the general population. Pilots are also more likely to die from melanoma.
Further study underway
The findings on military air and ground crew come from phase 1 of a study that was required by Congress in the 2021 defense bill. Because the investigators found an increase in the incidence of cancer, phase 2 of the study is now necessary.
The report authors explain that phase 2 will consist of identifying the carcinogenic toxicants or hazardous materials associated with military flight operations; identifying operating environments that could be associated with increased amounts of ionizing and nonionizing radiation; identifying specific duties, dates of service, and types of aircraft flown that could have increased the risk for cancer; identifying duty locations associated with a higher incidence of cancers; identifying potential exposures through military service that are not related to aviation; and determining the appropriate age to begin screening military aircrew and ground crew for cancers.
A version of this article first appeared on Medscape.com.
“Military aircrew and ground crew were overall more likely to be diagnosed with cancer, but less likely to die from cancer compared to the U.S. population,” the report concludes.
The study involved 156,050 aircrew and 737,891 ground crew. Participants were followed between 1992 and 2017. Both groups were predominantly male and non-Hispanic.
Data on cancer incidence and mortality for these two groups were compared with data from groups of similar age in the general population through use of the Surveillance, Epidemiology, and End Results (SEER) Database of the National Cancer Institute.
For aircrew, the study found an 87% higher rate of melanoma, a 39% higher rate of thyroid cancer, a 16% higher rate of prostate cancer, and a 24% higher rate of cancer for all sites combined.
A higher rate of melanoma and prostate cancer among aircrew has been reported previously, but the increased rate of thyroid cancer is a new finding, the authors note.
The uptick in melanoma has also been reported in studies of civilian pilots and cabin crew. It has been attributed to exposure to hazardous ultraviolet and cosmic radiation.
For ground crew members, the analysis found a 19% higher rate of cancers of the brain and nervous system, a 15% higher rate of thyroid cancer, a 9% higher rate of melanoma and of kidney and renal pelvis cancers, and a 3% higher rate of cancer for all sites combined.
There is little to compare these findings with: This is the first time that cancer risk has been evaluated in such a large population of military ground crew.
Lower rates of cancer mortality
In contrast to the increase in cancer incidence, the report found a decrease in cancer mortality.
When compared with a demographically similar U.S. population, the mortality rate among aircrew was 56% lower for all cancer sites; for ground crew, the mortality rate was 35% lower.
However, the report authors emphasize that “it is important to note that the military study population was relatively young.”
The median age at the end of follow-up for the cancer incidence analysis was 41 years for aircrew and 26 years for ground crew. The median age at the end of follow-up for the cancer mortality analysis was 48 years for aircrew and 41 years for ground crew.
“Results may have differed if additional older former Service members had been included in the study, since cancer risk and mortality rates increase with age,” the authors comment.
Other studies have found an increase in deaths from melanoma as well as an increase in the incidence of melanoma. A meta-analysis published in 2019 in the British Journal of Dermatology found that airline pilots and cabin crew have about twice the risk of melanoma and other skin cancers than the general population. Pilots are also more likely to die from melanoma.
Further study underway
The findings on military air and ground crew come from phase 1 of a study that was required by Congress in the 2021 defense bill. Because the investigators found an increase in the incidence of cancer, phase 2 of the study is now necessary.
The report authors explain that phase 2 will consist of identifying the carcinogenic toxicants or hazardous materials associated with military flight operations; identifying operating environments that could be associated with increased amounts of ionizing and nonionizing radiation; identifying specific duties, dates of service, and types of aircraft flown that could have increased the risk for cancer; identifying duty locations associated with a higher incidence of cancers; identifying potential exposures through military service that are not related to aviation; and determining the appropriate age to begin screening military aircrew and ground crew for cancers.
A version of this article first appeared on Medscape.com.
“Military aircrew and ground crew were overall more likely to be diagnosed with cancer, but less likely to die from cancer compared to the U.S. population,” the report concludes.
The study involved 156,050 aircrew and 737,891 ground crew. Participants were followed between 1992 and 2017. Both groups were predominantly male and non-Hispanic.
Data on cancer incidence and mortality for these two groups were compared with data from groups of similar age in the general population through use of the Surveillance, Epidemiology, and End Results (SEER) Database of the National Cancer Institute.
For aircrew, the study found an 87% higher rate of melanoma, a 39% higher rate of thyroid cancer, a 16% higher rate of prostate cancer, and a 24% higher rate of cancer for all sites combined.
A higher rate of melanoma and prostate cancer among aircrew has been reported previously, but the increased rate of thyroid cancer is a new finding, the authors note.
The uptick in melanoma has also been reported in studies of civilian pilots and cabin crew. It has been attributed to exposure to hazardous ultraviolet and cosmic radiation.
For ground crew members, the analysis found a 19% higher rate of cancers of the brain and nervous system, a 15% higher rate of thyroid cancer, a 9% higher rate of melanoma and of kidney and renal pelvis cancers, and a 3% higher rate of cancer for all sites combined.
There is little to compare these findings with: This is the first time that cancer risk has been evaluated in such a large population of military ground crew.
Lower rates of cancer mortality
In contrast to the increase in cancer incidence, the report found a decrease in cancer mortality.
When compared with a demographically similar U.S. population, the mortality rate among aircrew was 56% lower for all cancer sites; for ground crew, the mortality rate was 35% lower.
However, the report authors emphasize that “it is important to note that the military study population was relatively young.”
The median age at the end of follow-up for the cancer incidence analysis was 41 years for aircrew and 26 years for ground crew. The median age at the end of follow-up for the cancer mortality analysis was 48 years for aircrew and 41 years for ground crew.
“Results may have differed if additional older former Service members had been included in the study, since cancer risk and mortality rates increase with age,” the authors comment.
Other studies have found an increase in deaths from melanoma as well as an increase in the incidence of melanoma. A meta-analysis published in 2019 in the British Journal of Dermatology found that airline pilots and cabin crew have about twice the risk of melanoma and other skin cancers than the general population. Pilots are also more likely to die from melanoma.
Further study underway
The findings on military air and ground crew come from phase 1 of a study that was required by Congress in the 2021 defense bill. Because the investigators found an increase in the incidence of cancer, phase 2 of the study is now necessary.
The report authors explain that phase 2 will consist of identifying the carcinogenic toxicants or hazardous materials associated with military flight operations; identifying operating environments that could be associated with increased amounts of ionizing and nonionizing radiation; identifying specific duties, dates of service, and types of aircraft flown that could have increased the risk for cancer; identifying duty locations associated with a higher incidence of cancers; identifying potential exposures through military service that are not related to aviation; and determining the appropriate age to begin screening military aircrew and ground crew for cancers.
A version of this article first appeared on Medscape.com.
How to become wise
The only true wisdom is in knowing you know nothing. – Socrates
At what age is one supposed to be wise? I feel like I’m falling behind. I’ve crossed the middle of life and can check the prerequisite experiences: Joy, tragedy, love, adventure, love again. I lived a jetsetter life with an overnight bag always packed. I’ve sported the “Dad AF” tee with a fully loaded dad-pack. I’ve seen the 50 states and had my picture wrapped on a city bus (super-weird when you pull up next to one). Yet, when a moment arrives to pop in pithy advice for a resident or drop a few reassuring lines for a grieving friend, I’m often unable to find the words. If life were a video game, I’ve not earned the wisdom level yet.
Who are the wise men and women in your life? It’s difficult to list them. This is because it’s a complex attribute and hard to explain. It’s also because the wise who walk among us are rare. Wise is more than being brilliant at bullous diseases or knowing how to sleep train a baby. Nor is wise the buddy who purchased $1,000 of Bitcoin in 2010 (although stay close with him, he probably owns a jet). Neither content experts nor lucky friends rise to the appellation. Both experience and empathy.
The ancients considered wisdom to be one of the vital virtues. It was personified in high-profile gods like Apollo and Athena. It’s rare and important enough to be seen as spiritual. It features heavily in the Bible, the Bhagavad Gita, the Meditations of Marcus Aurelius. In some cultures the wise are called elders or sages. In all cultures they are helpful, respected, sought after, appreciated. We need more wise people in this game of life. I want to be one. But there’s no Coursera for it.
To become wise you have to pass through many levels, put in a lot of reps, suffer through many sleepless nights. Like the third molar, also known as the wisdom tooth, it takes years. You also have to emerge stronger and smarter through those experiences. FDR would not have become one of the wisest presidents in history had it not been for his trials, and victories, over polio. Osler missed Cushing syndrome multiple times before he got it right. It seems you have to go to the mountain, like Batman, and fight a few battles to realize your full wisdom potential.
You must also reflect on your experiences and hone your insight. The management sage Peter Drucker would write what he expected to happen after a decision. Then he’d return to it to hone his intuition and judgment.
Lastly, you have to use your powers for good. Using insight to win your NCAA bracket pool isn’t wisdom. Helping a friend whose marriage is falling apart or colleague whose patient is suing them or a resident whose excision hit an arteriole surely is.
I’ve got a ways to go before anyone puts me on their wise friend list. I’m working on it though. Perhaps you will too – we are desperately short-staffed in this area. For now, I can start with writing better condolences.
“Who maintains that it is not a heavy blow? But it is part of being human.” – Seneca
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
The only true wisdom is in knowing you know nothing. – Socrates
At what age is one supposed to be wise? I feel like I’m falling behind. I’ve crossed the middle of life and can check the prerequisite experiences: Joy, tragedy, love, adventure, love again. I lived a jetsetter life with an overnight bag always packed. I’ve sported the “Dad AF” tee with a fully loaded dad-pack. I’ve seen the 50 states and had my picture wrapped on a city bus (super-weird when you pull up next to one). Yet, when a moment arrives to pop in pithy advice for a resident or drop a few reassuring lines for a grieving friend, I’m often unable to find the words. If life were a video game, I’ve not earned the wisdom level yet.
Who are the wise men and women in your life? It’s difficult to list them. This is because it’s a complex attribute and hard to explain. It’s also because the wise who walk among us are rare. Wise is more than being brilliant at bullous diseases or knowing how to sleep train a baby. Nor is wise the buddy who purchased $1,000 of Bitcoin in 2010 (although stay close with him, he probably owns a jet). Neither content experts nor lucky friends rise to the appellation. Both experience and empathy.
The ancients considered wisdom to be one of the vital virtues. It was personified in high-profile gods like Apollo and Athena. It’s rare and important enough to be seen as spiritual. It features heavily in the Bible, the Bhagavad Gita, the Meditations of Marcus Aurelius. In some cultures the wise are called elders or sages. In all cultures they are helpful, respected, sought after, appreciated. We need more wise people in this game of life. I want to be one. But there’s no Coursera for it.
To become wise you have to pass through many levels, put in a lot of reps, suffer through many sleepless nights. Like the third molar, also known as the wisdom tooth, it takes years. You also have to emerge stronger and smarter through those experiences. FDR would not have become one of the wisest presidents in history had it not been for his trials, and victories, over polio. Osler missed Cushing syndrome multiple times before he got it right. It seems you have to go to the mountain, like Batman, and fight a few battles to realize your full wisdom potential.
You must also reflect on your experiences and hone your insight. The management sage Peter Drucker would write what he expected to happen after a decision. Then he’d return to it to hone his intuition and judgment.
Lastly, you have to use your powers for good. Using insight to win your NCAA bracket pool isn’t wisdom. Helping a friend whose marriage is falling apart or colleague whose patient is suing them or a resident whose excision hit an arteriole surely is.
I’ve got a ways to go before anyone puts me on their wise friend list. I’m working on it though. Perhaps you will too – we are desperately short-staffed in this area. For now, I can start with writing better condolences.
“Who maintains that it is not a heavy blow? But it is part of being human.” – Seneca
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
The only true wisdom is in knowing you know nothing. – Socrates
At what age is one supposed to be wise? I feel like I’m falling behind. I’ve crossed the middle of life and can check the prerequisite experiences: Joy, tragedy, love, adventure, love again. I lived a jetsetter life with an overnight bag always packed. I’ve sported the “Dad AF” tee with a fully loaded dad-pack. I’ve seen the 50 states and had my picture wrapped on a city bus (super-weird when you pull up next to one). Yet, when a moment arrives to pop in pithy advice for a resident or drop a few reassuring lines for a grieving friend, I’m often unable to find the words. If life were a video game, I’ve not earned the wisdom level yet.
Who are the wise men and women in your life? It’s difficult to list them. This is because it’s a complex attribute and hard to explain. It’s also because the wise who walk among us are rare. Wise is more than being brilliant at bullous diseases or knowing how to sleep train a baby. Nor is wise the buddy who purchased $1,000 of Bitcoin in 2010 (although stay close with him, he probably owns a jet). Neither content experts nor lucky friends rise to the appellation. Both experience and empathy.
The ancients considered wisdom to be one of the vital virtues. It was personified in high-profile gods like Apollo and Athena. It’s rare and important enough to be seen as spiritual. It features heavily in the Bible, the Bhagavad Gita, the Meditations of Marcus Aurelius. In some cultures the wise are called elders or sages. In all cultures they are helpful, respected, sought after, appreciated. We need more wise people in this game of life. I want to be one. But there’s no Coursera for it.
To become wise you have to pass through many levels, put in a lot of reps, suffer through many sleepless nights. Like the third molar, also known as the wisdom tooth, it takes years. You also have to emerge stronger and smarter through those experiences. FDR would not have become one of the wisest presidents in history had it not been for his trials, and victories, over polio. Osler missed Cushing syndrome multiple times before he got it right. It seems you have to go to the mountain, like Batman, and fight a few battles to realize your full wisdom potential.
You must also reflect on your experiences and hone your insight. The management sage Peter Drucker would write what he expected to happen after a decision. Then he’d return to it to hone his intuition and judgment.
Lastly, you have to use your powers for good. Using insight to win your NCAA bracket pool isn’t wisdom. Helping a friend whose marriage is falling apart or colleague whose patient is suing them or a resident whose excision hit an arteriole surely is.
I’ve got a ways to go before anyone puts me on their wise friend list. I’m working on it though. Perhaps you will too – we are desperately short-staffed in this area. For now, I can start with writing better condolences.
“Who maintains that it is not a heavy blow? But it is part of being human.” – Seneca
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].






