User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Wuhan case review: COVID-19 characteristics differ in children vs. adults
Pediatric cases of COVID-19 infection are typically mild, but underlying coinfection may be more common in children than in adults, according to an analysis of clinical, laboratory, and chest CT features of pediatric inpatients in Wuhan, China.

The findings point toward a need for early chest CT with corresponding pathogen detection in children with suspected COVID-19 infection, Wei Xia, MD, of Huazhong University of Science and Technology, Wuhan, China, and colleagues reported in Pediatric Pulmonology.
The most common symptoms in 20 pediatric patients hospitalized between Jan. 23 and Feb. 8, 2020, with COVID-19 infection confirmed by the pharyngeal swab COVID-19 nucleic acid test were fever and cough, which occurred in 60% and 65% of patients, respectively. Coinfection was detected in eight patients (40%), they noted.
Clinical manifestations were similar to those seen in adults, but overall symptoms were relatively mild and overall prognosis was good. Of particular note, 7 of the 20 (35%) patients had a previously diagnosed congenital or acquired diseases, suggesting that children with underlying conditions may be more susceptible, Dr. Xia and colleagues wrote.
Laboratory findings also were notable in that 80% of the children had procalcitonin (PCT) elevations not typically seen in adults with COVID-19. PCT is a marker for bacterial infection and “[this finding] may suggest that routine antibacterial treatment should be considered in pediatric patients,” the investigators wrote.
As for imaging results, chest CT findings in children were similar to those in adults.“The typical manifestations were unilateral or bilateral subpleural ground-glass opacities, and consolidations with surrounding halo signs,” Dr. Xia and associates wrote, adding that consolidations with surrounding halo sign accounted for about half the pediatric cases and should be considered as “typical signs in pediatric patients.”
Pediatric cases were “rather rare” in the early days of the COVID-19 outbreak in Wuhan, where the first cases of infection were reported.
“As a pediatric group is usually susceptible to upper respiratory tract infection, because of their developing immune system, the delayed presence of pediatric patients is confusing,” the investigators wrote, noting that a low detection rate of pharyngeal swab COVID-19 nucleic acid test, distinguishing the virus from other common respiratory tract infectious pathogens in pediatric patients, “is still a problem.”
To better characterize the clinical and imaging features in children versus adults with COVID-19, Dr. Xia and associates reviewed these 20 pediatric cases, including 13 boys and 7 girls with ages ranging from less than 1 month to 14 years, 7 months (median 2 years, 1.5 months). Thirteen had an identified close contact with a COVID-19–diagnosed family member, and all were treated in an isolation ward. A total of 18 children were cured and discharged after an average stay of 13 days, and 2 neonates remained under observation because of positive swab results with negative CT findings. The investigators speculated that the different findings in neonates were perhaps caused by the influence of delivery on sampling or the specific CT manifestations for neonates, adding that more samples are needed for further clarification.
Based on these findings, “the CT imaging of COVID-19 infection should be differentiated with other virus pneumonias such as influenza virus, parainfluenza virus, respiratory syncytial virus, and adenovirus,” they concluded. It also should “be differentiated from bacterial pneumonia, mycoplasma pneumonia, and chlamydia pneumonia ... the density of pneumonia lesions caused by the latter pathogens is relatively higher.”
However, Dr. Xia and colleagues noted that chest CT manifestations of pneumonia caused by different pathogens overlap, and COVID-19 pneumonia “can be superimposed with serious and complex imaging manifestations, so epidemiological and etiological examinations should be combined.”
The investigators concluded that COVID-19 virus pneumonia in children is generally mild, and that the characteristic changes of subpleural ground-glass opacities and consolidations with surrounding halo on chest CT provide an “effective means for follow-up and evaluating the changes of lung lesions.”
“In the case that the positive rate of COVID-19 nucleic acid test from pharyngeal swab samples is not high, the early detection of lesions by CT is conducive to reasonable management and early treatment for pediatric patients. However, the diagnosis of COVID-19 pneumonia by CT imaging alone is not sufficient enough, especially in the case of coinfection with other pathogens,” Dr. Xia and associates wrote. “Therefore, early chest CT screening and timely follow-up, combined with corresponding pathogen detection, is a feasible clinical protocol in children.”
An early study
In a separate retrospective analysis described in a letter to the editor of the New England Journal of Medicine, Weiyong Liu, PhD, of Tongji Hospital of Huazhong University of Science and Technology and colleagues found that the most frequently detected pathogens in 366 children under the age of 16 years hospitalized with respiratory infections in Wuhan during Jan. 7-15, 2020, were influenza A virus (6.3% of cases) and influenza B virus (5.5% of cases), whereas COVID-19 was detected in 1.6% of cases.
The median age of the COVID-19 patients in that series was 3 years (range 1-7 years), and in contrast to the findings of Xia et al., all previously had been “completely healthy.” Common characteristics were high fever and cough in all six patients, and vomiting in four patients. Five had pneumonia as assessed by X-ray, and CTs showed typical viral pneumonia patterns.
One patient was admitted to a pediatric ICU. All patients received antiviral agents, antibiotic agents, and supportive therapies; all recovered after a median hospital stay of 7.5 days (median range, 5-13 days).
In contrast with the findings of Xia et al., the findings of Liu et al. showed COVID-19 caused moderate to severe respiratory illness in children, and that infections in children were occurring early in the epidemic.
Some perspective
In an interview regarding the findings by Xia et al., Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University, and director of pediatric infectious diseases at Boston Medical Center, noted the absence of fever in 40% of cases.
“This is important, as the criteria for testing by public health departments has been high fever, cough, and shortness of breath,” he said. “The absence of fever is not inconsistent with COVID-19 disease.”
Another important point regarding the findings by Xia et al. is that the highest attack rates appear to be in children under 1 year of age, he said, further noting that the finding of concurrent influenza A, influenza B, or respiratory syncytial virus underscores that “concurrent infection can occur, and the presence of another virus in diagnostic tests does not mean that COVID-19 is not causal.”
As for whether the finding of elevated procalcitonin levels in 80% of cases reflects COVID-19 disease or coinfection with bacteria, the answer is unclear. But none of the children in the study were proven to have bacterial disease, he said, adding that “this marker will need to be interpreted with caution in the setting of COVID-19 disease.”
Dr. Xia and colleagues reported having no disclosures. Dr. Liu and associates also reported having no disclosures. The study by Liu et al. was supported by the Ministry of Science and Technology of China, the National Mega Project on Major Infectious Disease Prevention, and the National Key Research and Development Program of China.
SOURCES: Xia W et al. Ped Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718; Liu W et al. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Pediatric cases of COVID-19 infection are typically mild, but underlying coinfection may be more common in children than in adults, according to an analysis of clinical, laboratory, and chest CT features of pediatric inpatients in Wuhan, China.

The findings point toward a need for early chest CT with corresponding pathogen detection in children with suspected COVID-19 infection, Wei Xia, MD, of Huazhong University of Science and Technology, Wuhan, China, and colleagues reported in Pediatric Pulmonology.
The most common symptoms in 20 pediatric patients hospitalized between Jan. 23 and Feb. 8, 2020, with COVID-19 infection confirmed by the pharyngeal swab COVID-19 nucleic acid test were fever and cough, which occurred in 60% and 65% of patients, respectively. Coinfection was detected in eight patients (40%), they noted.
Clinical manifestations were similar to those seen in adults, but overall symptoms were relatively mild and overall prognosis was good. Of particular note, 7 of the 20 (35%) patients had a previously diagnosed congenital or acquired diseases, suggesting that children with underlying conditions may be more susceptible, Dr. Xia and colleagues wrote.
Laboratory findings also were notable in that 80% of the children had procalcitonin (PCT) elevations not typically seen in adults with COVID-19. PCT is a marker for bacterial infection and “[this finding] may suggest that routine antibacterial treatment should be considered in pediatric patients,” the investigators wrote.
As for imaging results, chest CT findings in children were similar to those in adults.“The typical manifestations were unilateral or bilateral subpleural ground-glass opacities, and consolidations with surrounding halo signs,” Dr. Xia and associates wrote, adding that consolidations with surrounding halo sign accounted for about half the pediatric cases and should be considered as “typical signs in pediatric patients.”
Pediatric cases were “rather rare” in the early days of the COVID-19 outbreak in Wuhan, where the first cases of infection were reported.
“As a pediatric group is usually susceptible to upper respiratory tract infection, because of their developing immune system, the delayed presence of pediatric patients is confusing,” the investigators wrote, noting that a low detection rate of pharyngeal swab COVID-19 nucleic acid test, distinguishing the virus from other common respiratory tract infectious pathogens in pediatric patients, “is still a problem.”
To better characterize the clinical and imaging features in children versus adults with COVID-19, Dr. Xia and associates reviewed these 20 pediatric cases, including 13 boys and 7 girls with ages ranging from less than 1 month to 14 years, 7 months (median 2 years, 1.5 months). Thirteen had an identified close contact with a COVID-19–diagnosed family member, and all were treated in an isolation ward. A total of 18 children were cured and discharged after an average stay of 13 days, and 2 neonates remained under observation because of positive swab results with negative CT findings. The investigators speculated that the different findings in neonates were perhaps caused by the influence of delivery on sampling or the specific CT manifestations for neonates, adding that more samples are needed for further clarification.
Based on these findings, “the CT imaging of COVID-19 infection should be differentiated with other virus pneumonias such as influenza virus, parainfluenza virus, respiratory syncytial virus, and adenovirus,” they concluded. It also should “be differentiated from bacterial pneumonia, mycoplasma pneumonia, and chlamydia pneumonia ... the density of pneumonia lesions caused by the latter pathogens is relatively higher.”
However, Dr. Xia and colleagues noted that chest CT manifestations of pneumonia caused by different pathogens overlap, and COVID-19 pneumonia “can be superimposed with serious and complex imaging manifestations, so epidemiological and etiological examinations should be combined.”
The investigators concluded that COVID-19 virus pneumonia in children is generally mild, and that the characteristic changes of subpleural ground-glass opacities and consolidations with surrounding halo on chest CT provide an “effective means for follow-up and evaluating the changes of lung lesions.”
“In the case that the positive rate of COVID-19 nucleic acid test from pharyngeal swab samples is not high, the early detection of lesions by CT is conducive to reasonable management and early treatment for pediatric patients. However, the diagnosis of COVID-19 pneumonia by CT imaging alone is not sufficient enough, especially in the case of coinfection with other pathogens,” Dr. Xia and associates wrote. “Therefore, early chest CT screening and timely follow-up, combined with corresponding pathogen detection, is a feasible clinical protocol in children.”
An early study
In a separate retrospective analysis described in a letter to the editor of the New England Journal of Medicine, Weiyong Liu, PhD, of Tongji Hospital of Huazhong University of Science and Technology and colleagues found that the most frequently detected pathogens in 366 children under the age of 16 years hospitalized with respiratory infections in Wuhan during Jan. 7-15, 2020, were influenza A virus (6.3% of cases) and influenza B virus (5.5% of cases), whereas COVID-19 was detected in 1.6% of cases.
The median age of the COVID-19 patients in that series was 3 years (range 1-7 years), and in contrast to the findings of Xia et al., all previously had been “completely healthy.” Common characteristics were high fever and cough in all six patients, and vomiting in four patients. Five had pneumonia as assessed by X-ray, and CTs showed typical viral pneumonia patterns.
One patient was admitted to a pediatric ICU. All patients received antiviral agents, antibiotic agents, and supportive therapies; all recovered after a median hospital stay of 7.5 days (median range, 5-13 days).
In contrast with the findings of Xia et al., the findings of Liu et al. showed COVID-19 caused moderate to severe respiratory illness in children, and that infections in children were occurring early in the epidemic.
Some perspective
In an interview regarding the findings by Xia et al., Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University, and director of pediatric infectious diseases at Boston Medical Center, noted the absence of fever in 40% of cases.
“This is important, as the criteria for testing by public health departments has been high fever, cough, and shortness of breath,” he said. “The absence of fever is not inconsistent with COVID-19 disease.”
Another important point regarding the findings by Xia et al. is that the highest attack rates appear to be in children under 1 year of age, he said, further noting that the finding of concurrent influenza A, influenza B, or respiratory syncytial virus underscores that “concurrent infection can occur, and the presence of another virus in diagnostic tests does not mean that COVID-19 is not causal.”
As for whether the finding of elevated procalcitonin levels in 80% of cases reflects COVID-19 disease or coinfection with bacteria, the answer is unclear. But none of the children in the study were proven to have bacterial disease, he said, adding that “this marker will need to be interpreted with caution in the setting of COVID-19 disease.”
Dr. Xia and colleagues reported having no disclosures. Dr. Liu and associates also reported having no disclosures. The study by Liu et al. was supported by the Ministry of Science and Technology of China, the National Mega Project on Major Infectious Disease Prevention, and the National Key Research and Development Program of China.
SOURCES: Xia W et al. Ped Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718; Liu W et al. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
Pediatric cases of COVID-19 infection are typically mild, but underlying coinfection may be more common in children than in adults, according to an analysis of clinical, laboratory, and chest CT features of pediatric inpatients in Wuhan, China.

The findings point toward a need for early chest CT with corresponding pathogen detection in children with suspected COVID-19 infection, Wei Xia, MD, of Huazhong University of Science and Technology, Wuhan, China, and colleagues reported in Pediatric Pulmonology.
The most common symptoms in 20 pediatric patients hospitalized between Jan. 23 and Feb. 8, 2020, with COVID-19 infection confirmed by the pharyngeal swab COVID-19 nucleic acid test were fever and cough, which occurred in 60% and 65% of patients, respectively. Coinfection was detected in eight patients (40%), they noted.
Clinical manifestations were similar to those seen in adults, but overall symptoms were relatively mild and overall prognosis was good. Of particular note, 7 of the 20 (35%) patients had a previously diagnosed congenital or acquired diseases, suggesting that children with underlying conditions may be more susceptible, Dr. Xia and colleagues wrote.
Laboratory findings also were notable in that 80% of the children had procalcitonin (PCT) elevations not typically seen in adults with COVID-19. PCT is a marker for bacterial infection and “[this finding] may suggest that routine antibacterial treatment should be considered in pediatric patients,” the investigators wrote.
As for imaging results, chest CT findings in children were similar to those in adults.“The typical manifestations were unilateral or bilateral subpleural ground-glass opacities, and consolidations with surrounding halo signs,” Dr. Xia and associates wrote, adding that consolidations with surrounding halo sign accounted for about half the pediatric cases and should be considered as “typical signs in pediatric patients.”
Pediatric cases were “rather rare” in the early days of the COVID-19 outbreak in Wuhan, where the first cases of infection were reported.
“As a pediatric group is usually susceptible to upper respiratory tract infection, because of their developing immune system, the delayed presence of pediatric patients is confusing,” the investigators wrote, noting that a low detection rate of pharyngeal swab COVID-19 nucleic acid test, distinguishing the virus from other common respiratory tract infectious pathogens in pediatric patients, “is still a problem.”
To better characterize the clinical and imaging features in children versus adults with COVID-19, Dr. Xia and associates reviewed these 20 pediatric cases, including 13 boys and 7 girls with ages ranging from less than 1 month to 14 years, 7 months (median 2 years, 1.5 months). Thirteen had an identified close contact with a COVID-19–diagnosed family member, and all were treated in an isolation ward. A total of 18 children were cured and discharged after an average stay of 13 days, and 2 neonates remained under observation because of positive swab results with negative CT findings. The investigators speculated that the different findings in neonates were perhaps caused by the influence of delivery on sampling or the specific CT manifestations for neonates, adding that more samples are needed for further clarification.
Based on these findings, “the CT imaging of COVID-19 infection should be differentiated with other virus pneumonias such as influenza virus, parainfluenza virus, respiratory syncytial virus, and adenovirus,” they concluded. It also should “be differentiated from bacterial pneumonia, mycoplasma pneumonia, and chlamydia pneumonia ... the density of pneumonia lesions caused by the latter pathogens is relatively higher.”
However, Dr. Xia and colleagues noted that chest CT manifestations of pneumonia caused by different pathogens overlap, and COVID-19 pneumonia “can be superimposed with serious and complex imaging manifestations, so epidemiological and etiological examinations should be combined.”
The investigators concluded that COVID-19 virus pneumonia in children is generally mild, and that the characteristic changes of subpleural ground-glass opacities and consolidations with surrounding halo on chest CT provide an “effective means for follow-up and evaluating the changes of lung lesions.”
“In the case that the positive rate of COVID-19 nucleic acid test from pharyngeal swab samples is not high, the early detection of lesions by CT is conducive to reasonable management and early treatment for pediatric patients. However, the diagnosis of COVID-19 pneumonia by CT imaging alone is not sufficient enough, especially in the case of coinfection with other pathogens,” Dr. Xia and associates wrote. “Therefore, early chest CT screening and timely follow-up, combined with corresponding pathogen detection, is a feasible clinical protocol in children.”
An early study
In a separate retrospective analysis described in a letter to the editor of the New England Journal of Medicine, Weiyong Liu, PhD, of Tongji Hospital of Huazhong University of Science and Technology and colleagues found that the most frequently detected pathogens in 366 children under the age of 16 years hospitalized with respiratory infections in Wuhan during Jan. 7-15, 2020, were influenza A virus (6.3% of cases) and influenza B virus (5.5% of cases), whereas COVID-19 was detected in 1.6% of cases.
The median age of the COVID-19 patients in that series was 3 years (range 1-7 years), and in contrast to the findings of Xia et al., all previously had been “completely healthy.” Common characteristics were high fever and cough in all six patients, and vomiting in four patients. Five had pneumonia as assessed by X-ray, and CTs showed typical viral pneumonia patterns.
One patient was admitted to a pediatric ICU. All patients received antiviral agents, antibiotic agents, and supportive therapies; all recovered after a median hospital stay of 7.5 days (median range, 5-13 days).
In contrast with the findings of Xia et al., the findings of Liu et al. showed COVID-19 caused moderate to severe respiratory illness in children, and that infections in children were occurring early in the epidemic.
Some perspective
In an interview regarding the findings by Xia et al., Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University, and director of pediatric infectious diseases at Boston Medical Center, noted the absence of fever in 40% of cases.
“This is important, as the criteria for testing by public health departments has been high fever, cough, and shortness of breath,” he said. “The absence of fever is not inconsistent with COVID-19 disease.”
Another important point regarding the findings by Xia et al. is that the highest attack rates appear to be in children under 1 year of age, he said, further noting that the finding of concurrent influenza A, influenza B, or respiratory syncytial virus underscores that “concurrent infection can occur, and the presence of another virus in diagnostic tests does not mean that COVID-19 is not causal.”
As for whether the finding of elevated procalcitonin levels in 80% of cases reflects COVID-19 disease or coinfection with bacteria, the answer is unclear. But none of the children in the study were proven to have bacterial disease, he said, adding that “this marker will need to be interpreted with caution in the setting of COVID-19 disease.”
Dr. Xia and colleagues reported having no disclosures. Dr. Liu and associates also reported having no disclosures. The study by Liu et al. was supported by the Ministry of Science and Technology of China, the National Mega Project on Major Infectious Disease Prevention, and the National Key Research and Development Program of China.
SOURCES: Xia W et al. Ped Pulmonol. 2020 Mar 5. doi: 10.1002/ppul.24718; Liu W et al. N Engl J Med. 2020 Mar 12. doi: 10.1056/NEJMc2003717.
FROM PEDIATRIC PULMONOLOGY
Marijuana allergies on the rise
“Cannabis sativa is a weed and it causes reactions just like any other pollen allergy,” said William Silvers, MD, from the University of Colorado School of Medicine in Aurora.
Silvers’ clinic began to see people with allergic reactions to the plant after the increase in direct exposure that accompanied the legalization of recreational marijuana in Colorado. For people with allergic tendencies, first- and second-hand exposure to C. sativa will increase “classic responses,” such as allergic rhinitis, sneezing, wheezing, itching, and asthma, he told Medscape Medical News.
Smoking the weed, direct exposure to the plant, contact with others who have touched plants, and breathing air in a grow operation “can all cause reactions,” he said. “And the more exposure they had, the greater the reaction, especially those who have allergic tendency,” he said.
The type of exposure to C. sativa is also a factor. Smoking the plant can induce typical allergic responses, the ingestion of hemp seed has been known to induce anaphylaxis, and “working with the plant can lead to dermatitis or contact urticaria,” he explained.
Edibles made with C. sativa have led to overdoses because dosing is difficult to determine. “It takes an hour or so to have an effect, so you don›t have as much control as inhaling it,” Silvers explained.
Stoned Fruit, Stoned Patient
A 2018 case report describes a 24-year-old daily marijuana smoker who experienced anaphylaxis after ingesting hemp seed. He had a history of allergies to stoned fruits, nuts, crustaceans, and aeroallergens. It was his first known exposure to hemp seed.
The patient developed urticaria on his arms after contact with C. sativa leaves and flowers, but had no reaction when smoking marijuana. This case indicates how important mode of exposure is.
“There are only a few cases of anaphylaxis known from ingestion of hemp seed,” Silvers said, “but the ‘stoned fruit, stoned patients’ cross-reactivity looks to be a real thing.”
People allergic to ragweed and sage are more likely than others to have a reaction to cantaloupe and other fruits in the melon family, he explained. There is a common antigen in the C. sativa pollen and in certain foods with cross-reacting proteins, such as tomato, peach, and hazelnut. “We see a pollen and food cross-reactivity via nonspecific lipid transfer proteins.”
A 2017 review of C. sativa allergy points out that few reports of IgE-dependent allergic reactions have been published because of the illegal status of cannabis. However, it is becoming more prevalent as a potential allergen. For example, in Nebraska, C. sativa pollen accounts for 36% of the total pollen count.
People with IgE-mediated cannabis allergy can have a sensitization to the nonspecific lipid transfer protein of C. sativa, Can s 3, which might explain the secondary plant-derived food allergies seen in European patients with a cannabis allergy, according to the review. Can s 3 cross-reacts with various plant homologues.
“This is the sort of information that allergists need to have,” Silvers said.
Stigma Limits Discussion
The fact that federal law prohibits cannabis use in the United States has made research difficult.
A strain distributed by the University of Mississippi can be used for research, “but its potency is very low, at 5% or 7%,” Silvers explained. At medical marijuana dispensaries, the potency of the flower can be as high as 25%, and in other forms, the THC content can be above 80%.
The legal status makes cannabis allergy difficult to diagnose and impossible to treat. Immunotherapy is out of the question. “With federal illegality, we need to stay out of trouble in that regard,” said Silvers, adding that, currently, avoidance is advised.
But research is emerging from Canada, where medicinal and recreational marijuana use is legal.
Stigma around cannabis is still high. “Nobody wants to be seen as a ‘pot doctor’,” said Silvers. But after it became legal in Colorado in 2015, he was asked to give a talk and decided to speak up.
“I have never written a medical prescription for marijuana,” he said, explaining that he is involved with the Center for Bioethics and Humanities at the University of Colorado. “I try to take a societal as well as a medical perspective, looking at the value and concerns for abuse and misuse.”
“As it becomes more available, more legalized, patients are having more reactions,” he said. “Allergists need to get in the game.”
Attitudes need to change. Physicians and allergists need to understand what’s happening in the population “and be open-minded about it so they know what to do,” he added.
Patients Don’t Want to Be Told to Stop
Users of medical marijuana can become dependent, said Ellen Burnham, MD, also from the University of Colorado.
“Patients want a blessing from care providers that it’s okay to use,” she told Medscape Medical News. “We’re in a state where people are really interested in holistic approaches to health, and cannabis is a natural product, but it may exacerbate allergies.”
Some components of cannabis might have bronchodilator properties but there are so many unknowns at this time. “I don’t think allergists should be recommending or condoning cannabis as part of a patient’s therapy,” she said. “It’s not okay for everybody.”
As business flourishes for operators in the cannabis industry and for the legal profession, Burnham said she worries that there isn’t enough protection for workers. “Do workers exposed to plant material on a daily basis have adequate workplace protection,” such as masks and gowns? “There’s a downstream effect that impacts people that nobody has really thought about,” she pointed out.
If the cannabis industry becomes driven by money, with a lobby like the tobacco industry, there will be no way to keep people who are vulnerable from using cannabis.
Is an occasional joint, much like an occasional glass of wine, okay? “We don’t know,” said Burnham. “We just don’t have enough information about it.”
Research is needed to develop medicinal strains of cannabidiol, cannabigerol, and cannabinol, which offer “medicinal and anti-inflammatory relief without the psychologic affects,” Silvers added.
This article first appeared on Medscape.com.
“Cannabis sativa is a weed and it causes reactions just like any other pollen allergy,” said William Silvers, MD, from the University of Colorado School of Medicine in Aurora.
Silvers’ clinic began to see people with allergic reactions to the plant after the increase in direct exposure that accompanied the legalization of recreational marijuana in Colorado. For people with allergic tendencies, first- and second-hand exposure to C. sativa will increase “classic responses,” such as allergic rhinitis, sneezing, wheezing, itching, and asthma, he told Medscape Medical News.
Smoking the weed, direct exposure to the plant, contact with others who have touched plants, and breathing air in a grow operation “can all cause reactions,” he said. “And the more exposure they had, the greater the reaction, especially those who have allergic tendency,” he said.
The type of exposure to C. sativa is also a factor. Smoking the plant can induce typical allergic responses, the ingestion of hemp seed has been known to induce anaphylaxis, and “working with the plant can lead to dermatitis or contact urticaria,” he explained.
Edibles made with C. sativa have led to overdoses because dosing is difficult to determine. “It takes an hour or so to have an effect, so you don›t have as much control as inhaling it,” Silvers explained.
Stoned Fruit, Stoned Patient
A 2018 case report describes a 24-year-old daily marijuana smoker who experienced anaphylaxis after ingesting hemp seed. He had a history of allergies to stoned fruits, nuts, crustaceans, and aeroallergens. It was his first known exposure to hemp seed.
The patient developed urticaria on his arms after contact with C. sativa leaves and flowers, but had no reaction when smoking marijuana. This case indicates how important mode of exposure is.
“There are only a few cases of anaphylaxis known from ingestion of hemp seed,” Silvers said, “but the ‘stoned fruit, stoned patients’ cross-reactivity looks to be a real thing.”
People allergic to ragweed and sage are more likely than others to have a reaction to cantaloupe and other fruits in the melon family, he explained. There is a common antigen in the C. sativa pollen and in certain foods with cross-reacting proteins, such as tomato, peach, and hazelnut. “We see a pollen and food cross-reactivity via nonspecific lipid transfer proteins.”
A 2017 review of C. sativa allergy points out that few reports of IgE-dependent allergic reactions have been published because of the illegal status of cannabis. However, it is becoming more prevalent as a potential allergen. For example, in Nebraska, C. sativa pollen accounts for 36% of the total pollen count.
People with IgE-mediated cannabis allergy can have a sensitization to the nonspecific lipid transfer protein of C. sativa, Can s 3, which might explain the secondary plant-derived food allergies seen in European patients with a cannabis allergy, according to the review. Can s 3 cross-reacts with various plant homologues.
“This is the sort of information that allergists need to have,” Silvers said.
Stigma Limits Discussion
The fact that federal law prohibits cannabis use in the United States has made research difficult.
A strain distributed by the University of Mississippi can be used for research, “but its potency is very low, at 5% or 7%,” Silvers explained. At medical marijuana dispensaries, the potency of the flower can be as high as 25%, and in other forms, the THC content can be above 80%.
The legal status makes cannabis allergy difficult to diagnose and impossible to treat. Immunotherapy is out of the question. “With federal illegality, we need to stay out of trouble in that regard,” said Silvers, adding that, currently, avoidance is advised.
But research is emerging from Canada, where medicinal and recreational marijuana use is legal.
Stigma around cannabis is still high. “Nobody wants to be seen as a ‘pot doctor’,” said Silvers. But after it became legal in Colorado in 2015, he was asked to give a talk and decided to speak up.
“I have never written a medical prescription for marijuana,” he said, explaining that he is involved with the Center for Bioethics and Humanities at the University of Colorado. “I try to take a societal as well as a medical perspective, looking at the value and concerns for abuse and misuse.”
“As it becomes more available, more legalized, patients are having more reactions,” he said. “Allergists need to get in the game.”
Attitudes need to change. Physicians and allergists need to understand what’s happening in the population “and be open-minded about it so they know what to do,” he added.
Patients Don’t Want to Be Told to Stop
Users of medical marijuana can become dependent, said Ellen Burnham, MD, also from the University of Colorado.
“Patients want a blessing from care providers that it’s okay to use,” she told Medscape Medical News. “We’re in a state where people are really interested in holistic approaches to health, and cannabis is a natural product, but it may exacerbate allergies.”
Some components of cannabis might have bronchodilator properties but there are so many unknowns at this time. “I don’t think allergists should be recommending or condoning cannabis as part of a patient’s therapy,” she said. “It’s not okay for everybody.”
As business flourishes for operators in the cannabis industry and for the legal profession, Burnham said she worries that there isn’t enough protection for workers. “Do workers exposed to plant material on a daily basis have adequate workplace protection,” such as masks and gowns? “There’s a downstream effect that impacts people that nobody has really thought about,” she pointed out.
If the cannabis industry becomes driven by money, with a lobby like the tobacco industry, there will be no way to keep people who are vulnerable from using cannabis.
Is an occasional joint, much like an occasional glass of wine, okay? “We don’t know,” said Burnham. “We just don’t have enough information about it.”
Research is needed to develop medicinal strains of cannabidiol, cannabigerol, and cannabinol, which offer “medicinal and anti-inflammatory relief without the psychologic affects,” Silvers added.
This article first appeared on Medscape.com.
“Cannabis sativa is a weed and it causes reactions just like any other pollen allergy,” said William Silvers, MD, from the University of Colorado School of Medicine in Aurora.
Silvers’ clinic began to see people with allergic reactions to the plant after the increase in direct exposure that accompanied the legalization of recreational marijuana in Colorado. For people with allergic tendencies, first- and second-hand exposure to C. sativa will increase “classic responses,” such as allergic rhinitis, sneezing, wheezing, itching, and asthma, he told Medscape Medical News.
Smoking the weed, direct exposure to the plant, contact with others who have touched plants, and breathing air in a grow operation “can all cause reactions,” he said. “And the more exposure they had, the greater the reaction, especially those who have allergic tendency,” he said.
The type of exposure to C. sativa is also a factor. Smoking the plant can induce typical allergic responses, the ingestion of hemp seed has been known to induce anaphylaxis, and “working with the plant can lead to dermatitis or contact urticaria,” he explained.
Edibles made with C. sativa have led to overdoses because dosing is difficult to determine. “It takes an hour or so to have an effect, so you don›t have as much control as inhaling it,” Silvers explained.
Stoned Fruit, Stoned Patient
A 2018 case report describes a 24-year-old daily marijuana smoker who experienced anaphylaxis after ingesting hemp seed. He had a history of allergies to stoned fruits, nuts, crustaceans, and aeroallergens. It was his first known exposure to hemp seed.
The patient developed urticaria on his arms after contact with C. sativa leaves and flowers, but had no reaction when smoking marijuana. This case indicates how important mode of exposure is.
“There are only a few cases of anaphylaxis known from ingestion of hemp seed,” Silvers said, “but the ‘stoned fruit, stoned patients’ cross-reactivity looks to be a real thing.”
People allergic to ragweed and sage are more likely than others to have a reaction to cantaloupe and other fruits in the melon family, he explained. There is a common antigen in the C. sativa pollen and in certain foods with cross-reacting proteins, such as tomato, peach, and hazelnut. “We see a pollen and food cross-reactivity via nonspecific lipid transfer proteins.”
A 2017 review of C. sativa allergy points out that few reports of IgE-dependent allergic reactions have been published because of the illegal status of cannabis. However, it is becoming more prevalent as a potential allergen. For example, in Nebraska, C. sativa pollen accounts for 36% of the total pollen count.
People with IgE-mediated cannabis allergy can have a sensitization to the nonspecific lipid transfer protein of C. sativa, Can s 3, which might explain the secondary plant-derived food allergies seen in European patients with a cannabis allergy, according to the review. Can s 3 cross-reacts with various plant homologues.
“This is the sort of information that allergists need to have,” Silvers said.
Stigma Limits Discussion
The fact that federal law prohibits cannabis use in the United States has made research difficult.
A strain distributed by the University of Mississippi can be used for research, “but its potency is very low, at 5% or 7%,” Silvers explained. At medical marijuana dispensaries, the potency of the flower can be as high as 25%, and in other forms, the THC content can be above 80%.
The legal status makes cannabis allergy difficult to diagnose and impossible to treat. Immunotherapy is out of the question. “With federal illegality, we need to stay out of trouble in that regard,” said Silvers, adding that, currently, avoidance is advised.
But research is emerging from Canada, where medicinal and recreational marijuana use is legal.
Stigma around cannabis is still high. “Nobody wants to be seen as a ‘pot doctor’,” said Silvers. But after it became legal in Colorado in 2015, he was asked to give a talk and decided to speak up.
“I have never written a medical prescription for marijuana,” he said, explaining that he is involved with the Center for Bioethics and Humanities at the University of Colorado. “I try to take a societal as well as a medical perspective, looking at the value and concerns for abuse and misuse.”
“As it becomes more available, more legalized, patients are having more reactions,” he said. “Allergists need to get in the game.”
Attitudes need to change. Physicians and allergists need to understand what’s happening in the population “and be open-minded about it so they know what to do,” he added.
Patients Don’t Want to Be Told to Stop
Users of medical marijuana can become dependent, said Ellen Burnham, MD, also from the University of Colorado.
“Patients want a blessing from care providers that it’s okay to use,” she told Medscape Medical News. “We’re in a state where people are really interested in holistic approaches to health, and cannabis is a natural product, but it may exacerbate allergies.”
Some components of cannabis might have bronchodilator properties but there are so many unknowns at this time. “I don’t think allergists should be recommending or condoning cannabis as part of a patient’s therapy,” she said. “It’s not okay for everybody.”
As business flourishes for operators in the cannabis industry and for the legal profession, Burnham said she worries that there isn’t enough protection for workers. “Do workers exposed to plant material on a daily basis have adequate workplace protection,” such as masks and gowns? “There’s a downstream effect that impacts people that nobody has really thought about,” she pointed out.
If the cannabis industry becomes driven by money, with a lobby like the tobacco industry, there will be no way to keep people who are vulnerable from using cannabis.
Is an occasional joint, much like an occasional glass of wine, okay? “We don’t know,” said Burnham. “We just don’t have enough information about it.”
Research is needed to develop medicinal strains of cannabidiol, cannabigerol, and cannabinol, which offer “medicinal and anti-inflammatory relief without the psychologic affects,” Silvers added.
This article first appeared on Medscape.com.
Red meat intake linked to increased risk of fatal CHD in men
PHOENIX – Consumption of red meat, particularly the processed form, is linked to a higher risk of developing coronary heart disease in men, results from a large prospective analysis demonstrated.
“The findings of this study are in line with randomized trials showing that the consumption of red meat, as compared with plant-based protein sources, increases LDL cholesterol levels, and with previous studies on red meat and risk of coronary heart disease,” lead study author Laila Al-Shaar, MPH, PhD, said in an interview in advance of the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting.
According to Dr. Al-Shaar, a postdoctoral research fellow in the department of nutrition at the T.H. Chan School of Public Health at Harvard University, Boston, most of the existing studies on red meat and heart disease have examined the impact of increasing consumption of red meat while decreasing consumption of all other foods. For the current study, she and her colleagues used a substitution analysis approach to understand how replacing red meat (total, processed, or unprocessed) with another protein-rich food was associated with the risk of heart disease. “This would potentially provide more specific guidance for healthier alternatives for those planning to cut down their red meat intake,” she said.
She and her colleagues prospectively followed 43,259 men in the Health Professionals Follow-up Study (1986-2012) who had no known history of cancer or cardiovascular disease. Diet was assessed by a standardized and validated food frequency questionnaire that was updated every 4 years. Dr. Al-Shaar and her colleagues used multivariate Cox models to estimate hazard ratios and 95% confidence intervals of CHD risk across categories of red meat consumption. They performed substitution analyses by comparing coefficients in models including alternative foods as continuous variables.
Over roughly 933,000 person-years of follow-up, the researchers documented 4,148 incident CHD cases. Of these, 1,680 were fatal. After multivariate adjustment for dietary and nondietary risk factors, both total and processed red meat intake were associated with a modestly higher risk of CHD (hazard ratio for a one serving/day increment, 1.08; 95% confidence interval, 1.01-1.14 for total red meat; and HR, 1.13; 95% CI, 1.03-1.22 for processed red meat). Substitutions of one serving per day of other foods (including nuts, legumes, soy, whole grains, and low- and high-fat dairy) for one serving per day of total red meat were associated with a 10%-47% lower CHD risk.
Stronger inverse associations were observed between some of these substitutions for red meat and risk of fatal CHD. Substituting nuts lowered the risk of fatal heart disease by 17%, while replacing red meat with whole grains was linked to a 48% reduction in that outcome. Those associations were more pronounced when replacing processed red meat.
“Processed meats and meats in general have been thought to be potentially not favorable in terms of cardiovascular disease and cardiovascular disease risk,” Robert H. Eckel, MD, professor emeritus of medicine at the University of Colorado Anschutz Medical Campus, Aurora, said in an interview. “Now we have increasing data that not only is there a negative cardiovascular disease impact of animal protein, but we see this on all-cause mortality, including cancer.”
Dr. Al-Shaar said that the findings “support current recommendations to limit consumption of red meat and suggest that high-quality plant-based proteins such as nuts, legumes, and soy are good alternatives for individuals planning to have better food choices and healthier eating patterns.”
She acknowledged certain limitations of the study, including its observational design and the fact that it was limited to non-Hispanic white health professionals, “thus limiting the generalizability of its findings to the whole population.”
Dr. Eckel, who is a past president of the American Heart Association, underscored the importance of one’s overall diet in mitigating the risk of developing coronary heart disease. “It’s not simply substituting animal protein with plant protein,” he said. “Fruits and vegetables and whole grains, lean protein from fish – a Mediterranean-style diet – is what the AHA recommends.”
Dr. Al-Shaar reported having no financial disclosures. The study was supported by a T32 training grant from the National Institutes of Health and by other grants from the NIH. The meeting was sponsored by the AHA.
SOURCE: Al-Shaar L et al. Epi/Lifestyle 2020, Abstract P512.
PHOENIX – Consumption of red meat, particularly the processed form, is linked to a higher risk of developing coronary heart disease in men, results from a large prospective analysis demonstrated.
“The findings of this study are in line with randomized trials showing that the consumption of red meat, as compared with plant-based protein sources, increases LDL cholesterol levels, and with previous studies on red meat and risk of coronary heart disease,” lead study author Laila Al-Shaar, MPH, PhD, said in an interview in advance of the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting.
According to Dr. Al-Shaar, a postdoctoral research fellow in the department of nutrition at the T.H. Chan School of Public Health at Harvard University, Boston, most of the existing studies on red meat and heart disease have examined the impact of increasing consumption of red meat while decreasing consumption of all other foods. For the current study, she and her colleagues used a substitution analysis approach to understand how replacing red meat (total, processed, or unprocessed) with another protein-rich food was associated with the risk of heart disease. “This would potentially provide more specific guidance for healthier alternatives for those planning to cut down their red meat intake,” she said.
She and her colleagues prospectively followed 43,259 men in the Health Professionals Follow-up Study (1986-2012) who had no known history of cancer or cardiovascular disease. Diet was assessed by a standardized and validated food frequency questionnaire that was updated every 4 years. Dr. Al-Shaar and her colleagues used multivariate Cox models to estimate hazard ratios and 95% confidence intervals of CHD risk across categories of red meat consumption. They performed substitution analyses by comparing coefficients in models including alternative foods as continuous variables.
Over roughly 933,000 person-years of follow-up, the researchers documented 4,148 incident CHD cases. Of these, 1,680 were fatal. After multivariate adjustment for dietary and nondietary risk factors, both total and processed red meat intake were associated with a modestly higher risk of CHD (hazard ratio for a one serving/day increment, 1.08; 95% confidence interval, 1.01-1.14 for total red meat; and HR, 1.13; 95% CI, 1.03-1.22 for processed red meat). Substitutions of one serving per day of other foods (including nuts, legumes, soy, whole grains, and low- and high-fat dairy) for one serving per day of total red meat were associated with a 10%-47% lower CHD risk.
Stronger inverse associations were observed between some of these substitutions for red meat and risk of fatal CHD. Substituting nuts lowered the risk of fatal heart disease by 17%, while replacing red meat with whole grains was linked to a 48% reduction in that outcome. Those associations were more pronounced when replacing processed red meat.
“Processed meats and meats in general have been thought to be potentially not favorable in terms of cardiovascular disease and cardiovascular disease risk,” Robert H. Eckel, MD, professor emeritus of medicine at the University of Colorado Anschutz Medical Campus, Aurora, said in an interview. “Now we have increasing data that not only is there a negative cardiovascular disease impact of animal protein, but we see this on all-cause mortality, including cancer.”
Dr. Al-Shaar said that the findings “support current recommendations to limit consumption of red meat and suggest that high-quality plant-based proteins such as nuts, legumes, and soy are good alternatives for individuals planning to have better food choices and healthier eating patterns.”
She acknowledged certain limitations of the study, including its observational design and the fact that it was limited to non-Hispanic white health professionals, “thus limiting the generalizability of its findings to the whole population.”
Dr. Eckel, who is a past president of the American Heart Association, underscored the importance of one’s overall diet in mitigating the risk of developing coronary heart disease. “It’s not simply substituting animal protein with plant protein,” he said. “Fruits and vegetables and whole grains, lean protein from fish – a Mediterranean-style diet – is what the AHA recommends.”
Dr. Al-Shaar reported having no financial disclosures. The study was supported by a T32 training grant from the National Institutes of Health and by other grants from the NIH. The meeting was sponsored by the AHA.
SOURCE: Al-Shaar L et al. Epi/Lifestyle 2020, Abstract P512.
PHOENIX – Consumption of red meat, particularly the processed form, is linked to a higher risk of developing coronary heart disease in men, results from a large prospective analysis demonstrated.
“The findings of this study are in line with randomized trials showing that the consumption of red meat, as compared with plant-based protein sources, increases LDL cholesterol levels, and with previous studies on red meat and risk of coronary heart disease,” lead study author Laila Al-Shaar, MPH, PhD, said in an interview in advance of the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting.
According to Dr. Al-Shaar, a postdoctoral research fellow in the department of nutrition at the T.H. Chan School of Public Health at Harvard University, Boston, most of the existing studies on red meat and heart disease have examined the impact of increasing consumption of red meat while decreasing consumption of all other foods. For the current study, she and her colleagues used a substitution analysis approach to understand how replacing red meat (total, processed, or unprocessed) with another protein-rich food was associated with the risk of heart disease. “This would potentially provide more specific guidance for healthier alternatives for those planning to cut down their red meat intake,” she said.
She and her colleagues prospectively followed 43,259 men in the Health Professionals Follow-up Study (1986-2012) who had no known history of cancer or cardiovascular disease. Diet was assessed by a standardized and validated food frequency questionnaire that was updated every 4 years. Dr. Al-Shaar and her colleagues used multivariate Cox models to estimate hazard ratios and 95% confidence intervals of CHD risk across categories of red meat consumption. They performed substitution analyses by comparing coefficients in models including alternative foods as continuous variables.
Over roughly 933,000 person-years of follow-up, the researchers documented 4,148 incident CHD cases. Of these, 1,680 were fatal. After multivariate adjustment for dietary and nondietary risk factors, both total and processed red meat intake were associated with a modestly higher risk of CHD (hazard ratio for a one serving/day increment, 1.08; 95% confidence interval, 1.01-1.14 for total red meat; and HR, 1.13; 95% CI, 1.03-1.22 for processed red meat). Substitutions of one serving per day of other foods (including nuts, legumes, soy, whole grains, and low- and high-fat dairy) for one serving per day of total red meat were associated with a 10%-47% lower CHD risk.
Stronger inverse associations were observed between some of these substitutions for red meat and risk of fatal CHD. Substituting nuts lowered the risk of fatal heart disease by 17%, while replacing red meat with whole grains was linked to a 48% reduction in that outcome. Those associations were more pronounced when replacing processed red meat.
“Processed meats and meats in general have been thought to be potentially not favorable in terms of cardiovascular disease and cardiovascular disease risk,” Robert H. Eckel, MD, professor emeritus of medicine at the University of Colorado Anschutz Medical Campus, Aurora, said in an interview. “Now we have increasing data that not only is there a negative cardiovascular disease impact of animal protein, but we see this on all-cause mortality, including cancer.”
Dr. Al-Shaar said that the findings “support current recommendations to limit consumption of red meat and suggest that high-quality plant-based proteins such as nuts, legumes, and soy are good alternatives for individuals planning to have better food choices and healthier eating patterns.”
She acknowledged certain limitations of the study, including its observational design and the fact that it was limited to non-Hispanic white health professionals, “thus limiting the generalizability of its findings to the whole population.”
Dr. Eckel, who is a past president of the American Heart Association, underscored the importance of one’s overall diet in mitigating the risk of developing coronary heart disease. “It’s not simply substituting animal protein with plant protein,” he said. “Fruits and vegetables and whole grains, lean protein from fish – a Mediterranean-style diet – is what the AHA recommends.”
Dr. Al-Shaar reported having no financial disclosures. The study was supported by a T32 training grant from the National Institutes of Health and by other grants from the NIH. The meeting was sponsored by the AHA.
SOURCE: Al-Shaar L et al. Epi/Lifestyle 2020, Abstract P512.
REPORTING FROM EPI/LIFESTYLE 2020
Health professionals fight against COVID-19 myths and misinformation
Misinformation about the COVID-19 travels faster than the virus and complicates the job of doctors who are treating those infected and responding to concerns of their other patients.
An array of myths springing up around this disease can be found on the Internet. The main themes appear to be false narratives about the origin of the virus, the size of the outbreak in the United States and in other countries, the availability of cures and treatments, and ways to prevent infection. Widespread misinformation hampers public health efforts to control the disease outbreak, confuses the public, and requires medical professionals to spend time refuting myths and re-educating patients.
A group of infectious disease experts became so alarmed by the misinformation trend they published a statement in The Lancet decrying the spread of false statements being circulated by some media outlets. “The rapid, open, and transparent sharing of data on this outbreak is now being threatened by rumours and misinformation ... Conspiracy theories do nothing but create fear, rumours, and prejudice that jeopardise our global collaboration in the fight against this virus,” wrote Charles H. Calisher, PhD, of Colorado State University, Fort Collins, and colleagues.
What can physicians do to counter misinformation?
Pulmonologist and critical care physician Cedric “Jamie” Rutland, MD, who practices in Riverside, Calif., sees misinformation about the novel coronavirus every day at home and on the job. His patients worry that everyone who gets infected will die or end up in the ICU. His neighbors ask him to pilfer surgical masks to protect them from the false notion that Chinese people in their community posed some kind of COVID-19 risk.
As he pondered how to counter myths with facts, Dr. Rutland turned to an unusual resource: His 7-year-old daughter Amelia. He explained to her how COVID-19 works and found that she could easily understand the basics. Now, Dr. Rutland draws upon the lessons from chats with his daughter as he explains COVID-19 to his patient audience on his YouTube channel “Medicine Deconstructed.” Simplicity, but not too much simplicity, is key, he said. Dr. Rutland uses a visual aid – a rough drawing of a virus – and shows how inflammation and antibodies enter the picture after infection. “I just teach them that if you’re a healthy person, this is how the body works, and this is what the immune system will do,” he said. “For the most part, you can calm people down when you make time for education.”
What are best practices? In a series of interviews, specialists emphasized the importance of fact-finding, wide-ranging communication, and – perhaps most difficult of all – humility.
Dr. Rutland emphasizes thoughtful communication based on facts and humility when communicating to patients about this potential health risk. “A lot of people finish medical school and think, ‘Everyone should trust me because I’m the pulmonologist or the GI doc.’ That’s not how it works. You still have to earn people’s trust,” he said.
Make sure all staff get reliable information
Hospitals are scrambling to keep staff safe with up-to-date directives and debunk false narratives about the virus. Keeping all hospital staff informed with verified and authoritative facts about the coronavirus is a key objective of the Massachusetts General Hospital’s Center for Disaster Medicine. The Center’s coronavirus educational materials are distributed to all staffers from physicians to janitors. “These provide information that they need to understand the risks and keep themselves safe,” said Eileen Searle, PhD, the Biothreats Clinical Operations program manager in the CDM.
According to Dr. Searle, the hospital keeps a continually updated COVID-19 Frequently Asked Questions document in its internal computer system. All employees can access it, she said, and it’s updated to include questions as they come up.
Even valets and front-desk volunteers are encouraged to read the FAQ, she said, since “they’re the first people that family and patients are interacting with.” The document “gives them reassurance about delivering messages,” she said.
Use patience with your patients
Dr. Rutland urges colleagues to take the time to listen to patients and educate them. “Reduce the gap between you and them,” said Dr. Rutland, who treats patients in Orange and Riverside counties. “Take off your white coat, sit down, and talk to the person about their concerns.”
Boston cardiologist Haider Warraich, MD, of Brigham and Women’s Hospital, Boston, said it’s important to “put medical information into a greater human context.” For example, he has told patients that he’s still taking his daughter to school despite COVID-19 risks. “I take the information I provide and apply it to my own life,” he said.
The Washington State Department of Health offers this advice to physicians to counter false information and stigma: “Stay updated and informed on COVID-19 to avoid miscommunication or inaccurate information. Talk openly about the harm of stigma. View people directly impacted by stigma as people first. Be conscious of your language. Acknowledge access and language barriers.”
Speak out on social media – but don’t fight
Should medical professionals speak out about COVID-19 misinformation via social media? It’s an individual decision, Dr. Warraich said, “but my sense is that it’s never been more important for physicians to be part of the fray and help quell the epidemic of misinformation that almost always follows any type of medial calamity.”
Dr. Rutland, vice president and founding member of the Association for Healthcare Social Media, cautioned that effective communication via social media requires care. Avoid confrontation, he advised. “Don’t call people stupid or say things like, ‘I went to medical school and I’m smarter than you.’ ”
Instead, he said, “it’s important to just state the facts: These are the people who are dying, these are the people who are getting infected.”
And, he added, remember to push the most important message of all: Wash your hands!
Public health organizations fight the ‘infodemic’
In a trend that hearkens back to the days of snake oil cures for all maladies, advertisements for fake treatments are popping up on the Internet and on other media.
Facebook and Amazon have acted to remove these ads but these messages continue to flood social media such as Twitter, WhatsApp, and other sites. Discussion groups on platforms such as Reddit continue to pump out misinformation about COVID-19. Conspiracy theories that link the virus to espionage and bioweapons are making the rounds on the Internet and talk radio. Wrong information about the effectiveness of non-N95 face masks to protect wearers against infection is widespread, leading to shortages for medical personnel and price gouging. Pernicious rumors about the effectiveness of substances such a vinegar, silver, garlic, lemon juice, and even vodka to disinfect hands and surfaces abound on the Internet. An especially dangerous stream of misinformation stigmatizes ethnic groups and individuals as sources of the infection.
The World Health Organization identified early in the COVID-19 outbreak the global wave of misinformation about the virus and dubbed the problem the “infodemic.” The WHO “Q & A” page on COVID-19 is updated frequently and addresses myths and rumors currently circulating.
According to the WHO website, the agency has reached out to social media players such as Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, and Weibo, the microblogging site in China. WHO has worked with these sites to curb the “infodemic” of misinformation and has used these sites for public education outreach on COVID-19. “Myth busting” infographics posted on a WHO web page are also reposted on major social media sites.
The CDC has followed with its own “frequently asked questions” page to address questions and rumors. State health agencies have put up COVID-19 pages to address public concerns and offer advice on prevention. The Maryland Department of Health web page directly addresses dangerous misinformation: “Do not stigmatize people of any specific ethnicities or racial background. Viruses do not target people from specific populations, ethnicities or racial backgrounds. Stay informed and seek information from reliable, official sources. Be wary of myths, rumors and misinformation circulating online and elsewhere. Health information shared through social media is frequently inaccurate, unless coming from an official, reliable source such as the CDC, MDH or local health departments.”
The Washington State Department of Health has taken a more assertive stance on stigma. The COVID-19 web page recommends to the public: “Show compassion and support for individuals and communities more closely impacted. Avoid stigmatizing people who are in quarantine. They are making the right choice for their communities. Do not make assumptions about someone’s health status based on their ethnicity, race or national origin.”
Misinformation about the COVID-19 travels faster than the virus and complicates the job of doctors who are treating those infected and responding to concerns of their other patients.
An array of myths springing up around this disease can be found on the Internet. The main themes appear to be false narratives about the origin of the virus, the size of the outbreak in the United States and in other countries, the availability of cures and treatments, and ways to prevent infection. Widespread misinformation hampers public health efforts to control the disease outbreak, confuses the public, and requires medical professionals to spend time refuting myths and re-educating patients.
A group of infectious disease experts became so alarmed by the misinformation trend they published a statement in The Lancet decrying the spread of false statements being circulated by some media outlets. “The rapid, open, and transparent sharing of data on this outbreak is now being threatened by rumours and misinformation ... Conspiracy theories do nothing but create fear, rumours, and prejudice that jeopardise our global collaboration in the fight against this virus,” wrote Charles H. Calisher, PhD, of Colorado State University, Fort Collins, and colleagues.
What can physicians do to counter misinformation?
Pulmonologist and critical care physician Cedric “Jamie” Rutland, MD, who practices in Riverside, Calif., sees misinformation about the novel coronavirus every day at home and on the job. His patients worry that everyone who gets infected will die or end up in the ICU. His neighbors ask him to pilfer surgical masks to protect them from the false notion that Chinese people in their community posed some kind of COVID-19 risk.
As he pondered how to counter myths with facts, Dr. Rutland turned to an unusual resource: His 7-year-old daughter Amelia. He explained to her how COVID-19 works and found that she could easily understand the basics. Now, Dr. Rutland draws upon the lessons from chats with his daughter as he explains COVID-19 to his patient audience on his YouTube channel “Medicine Deconstructed.” Simplicity, but not too much simplicity, is key, he said. Dr. Rutland uses a visual aid – a rough drawing of a virus – and shows how inflammation and antibodies enter the picture after infection. “I just teach them that if you’re a healthy person, this is how the body works, and this is what the immune system will do,” he said. “For the most part, you can calm people down when you make time for education.”
What are best practices? In a series of interviews, specialists emphasized the importance of fact-finding, wide-ranging communication, and – perhaps most difficult of all – humility.
Dr. Rutland emphasizes thoughtful communication based on facts and humility when communicating to patients about this potential health risk. “A lot of people finish medical school and think, ‘Everyone should trust me because I’m the pulmonologist or the GI doc.’ That’s not how it works. You still have to earn people’s trust,” he said.
Make sure all staff get reliable information
Hospitals are scrambling to keep staff safe with up-to-date directives and debunk false narratives about the virus. Keeping all hospital staff informed with verified and authoritative facts about the coronavirus is a key objective of the Massachusetts General Hospital’s Center for Disaster Medicine. The Center’s coronavirus educational materials are distributed to all staffers from physicians to janitors. “These provide information that they need to understand the risks and keep themselves safe,” said Eileen Searle, PhD, the Biothreats Clinical Operations program manager in the CDM.
According to Dr. Searle, the hospital keeps a continually updated COVID-19 Frequently Asked Questions document in its internal computer system. All employees can access it, she said, and it’s updated to include questions as they come up.
Even valets and front-desk volunteers are encouraged to read the FAQ, she said, since “they’re the first people that family and patients are interacting with.” The document “gives them reassurance about delivering messages,” she said.
Use patience with your patients
Dr. Rutland urges colleagues to take the time to listen to patients and educate them. “Reduce the gap between you and them,” said Dr. Rutland, who treats patients in Orange and Riverside counties. “Take off your white coat, sit down, and talk to the person about their concerns.”
Boston cardiologist Haider Warraich, MD, of Brigham and Women’s Hospital, Boston, said it’s important to “put medical information into a greater human context.” For example, he has told patients that he’s still taking his daughter to school despite COVID-19 risks. “I take the information I provide and apply it to my own life,” he said.
The Washington State Department of Health offers this advice to physicians to counter false information and stigma: “Stay updated and informed on COVID-19 to avoid miscommunication or inaccurate information. Talk openly about the harm of stigma. View people directly impacted by stigma as people first. Be conscious of your language. Acknowledge access and language barriers.”
Speak out on social media – but don’t fight
Should medical professionals speak out about COVID-19 misinformation via social media? It’s an individual decision, Dr. Warraich said, “but my sense is that it’s never been more important for physicians to be part of the fray and help quell the epidemic of misinformation that almost always follows any type of medial calamity.”
Dr. Rutland, vice president and founding member of the Association for Healthcare Social Media, cautioned that effective communication via social media requires care. Avoid confrontation, he advised. “Don’t call people stupid or say things like, ‘I went to medical school and I’m smarter than you.’ ”
Instead, he said, “it’s important to just state the facts: These are the people who are dying, these are the people who are getting infected.”
And, he added, remember to push the most important message of all: Wash your hands!
Public health organizations fight the ‘infodemic’
In a trend that hearkens back to the days of snake oil cures for all maladies, advertisements for fake treatments are popping up on the Internet and on other media.
Facebook and Amazon have acted to remove these ads but these messages continue to flood social media such as Twitter, WhatsApp, and other sites. Discussion groups on platforms such as Reddit continue to pump out misinformation about COVID-19. Conspiracy theories that link the virus to espionage and bioweapons are making the rounds on the Internet and talk radio. Wrong information about the effectiveness of non-N95 face masks to protect wearers against infection is widespread, leading to shortages for medical personnel and price gouging. Pernicious rumors about the effectiveness of substances such a vinegar, silver, garlic, lemon juice, and even vodka to disinfect hands and surfaces abound on the Internet. An especially dangerous stream of misinformation stigmatizes ethnic groups and individuals as sources of the infection.
The World Health Organization identified early in the COVID-19 outbreak the global wave of misinformation about the virus and dubbed the problem the “infodemic.” The WHO “Q & A” page on COVID-19 is updated frequently and addresses myths and rumors currently circulating.
According to the WHO website, the agency has reached out to social media players such as Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, and Weibo, the microblogging site in China. WHO has worked with these sites to curb the “infodemic” of misinformation and has used these sites for public education outreach on COVID-19. “Myth busting” infographics posted on a WHO web page are also reposted on major social media sites.
The CDC has followed with its own “frequently asked questions” page to address questions and rumors. State health agencies have put up COVID-19 pages to address public concerns and offer advice on prevention. The Maryland Department of Health web page directly addresses dangerous misinformation: “Do not stigmatize people of any specific ethnicities or racial background. Viruses do not target people from specific populations, ethnicities or racial backgrounds. Stay informed and seek information from reliable, official sources. Be wary of myths, rumors and misinformation circulating online and elsewhere. Health information shared through social media is frequently inaccurate, unless coming from an official, reliable source such as the CDC, MDH or local health departments.”
The Washington State Department of Health has taken a more assertive stance on stigma. The COVID-19 web page recommends to the public: “Show compassion and support for individuals and communities more closely impacted. Avoid stigmatizing people who are in quarantine. They are making the right choice for their communities. Do not make assumptions about someone’s health status based on their ethnicity, race or national origin.”
Misinformation about the COVID-19 travels faster than the virus and complicates the job of doctors who are treating those infected and responding to concerns of their other patients.
An array of myths springing up around this disease can be found on the Internet. The main themes appear to be false narratives about the origin of the virus, the size of the outbreak in the United States and in other countries, the availability of cures and treatments, and ways to prevent infection. Widespread misinformation hampers public health efforts to control the disease outbreak, confuses the public, and requires medical professionals to spend time refuting myths and re-educating patients.
A group of infectious disease experts became so alarmed by the misinformation trend they published a statement in The Lancet decrying the spread of false statements being circulated by some media outlets. “The rapid, open, and transparent sharing of data on this outbreak is now being threatened by rumours and misinformation ... Conspiracy theories do nothing but create fear, rumours, and prejudice that jeopardise our global collaboration in the fight against this virus,” wrote Charles H. Calisher, PhD, of Colorado State University, Fort Collins, and colleagues.
What can physicians do to counter misinformation?
Pulmonologist and critical care physician Cedric “Jamie” Rutland, MD, who practices in Riverside, Calif., sees misinformation about the novel coronavirus every day at home and on the job. His patients worry that everyone who gets infected will die or end up in the ICU. His neighbors ask him to pilfer surgical masks to protect them from the false notion that Chinese people in their community posed some kind of COVID-19 risk.
As he pondered how to counter myths with facts, Dr. Rutland turned to an unusual resource: His 7-year-old daughter Amelia. He explained to her how COVID-19 works and found that she could easily understand the basics. Now, Dr. Rutland draws upon the lessons from chats with his daughter as he explains COVID-19 to his patient audience on his YouTube channel “Medicine Deconstructed.” Simplicity, but not too much simplicity, is key, he said. Dr. Rutland uses a visual aid – a rough drawing of a virus – and shows how inflammation and antibodies enter the picture after infection. “I just teach them that if you’re a healthy person, this is how the body works, and this is what the immune system will do,” he said. “For the most part, you can calm people down when you make time for education.”
What are best practices? In a series of interviews, specialists emphasized the importance of fact-finding, wide-ranging communication, and – perhaps most difficult of all – humility.
Dr. Rutland emphasizes thoughtful communication based on facts and humility when communicating to patients about this potential health risk. “A lot of people finish medical school and think, ‘Everyone should trust me because I’m the pulmonologist or the GI doc.’ That’s not how it works. You still have to earn people’s trust,” he said.
Make sure all staff get reliable information
Hospitals are scrambling to keep staff safe with up-to-date directives and debunk false narratives about the virus. Keeping all hospital staff informed with verified and authoritative facts about the coronavirus is a key objective of the Massachusetts General Hospital’s Center for Disaster Medicine. The Center’s coronavirus educational materials are distributed to all staffers from physicians to janitors. “These provide information that they need to understand the risks and keep themselves safe,” said Eileen Searle, PhD, the Biothreats Clinical Operations program manager in the CDM.
According to Dr. Searle, the hospital keeps a continually updated COVID-19 Frequently Asked Questions document in its internal computer system. All employees can access it, she said, and it’s updated to include questions as they come up.
Even valets and front-desk volunteers are encouraged to read the FAQ, she said, since “they’re the first people that family and patients are interacting with.” The document “gives them reassurance about delivering messages,” she said.
Use patience with your patients
Dr. Rutland urges colleagues to take the time to listen to patients and educate them. “Reduce the gap between you and them,” said Dr. Rutland, who treats patients in Orange and Riverside counties. “Take off your white coat, sit down, and talk to the person about their concerns.”
Boston cardiologist Haider Warraich, MD, of Brigham and Women’s Hospital, Boston, said it’s important to “put medical information into a greater human context.” For example, he has told patients that he’s still taking his daughter to school despite COVID-19 risks. “I take the information I provide and apply it to my own life,” he said.
The Washington State Department of Health offers this advice to physicians to counter false information and stigma: “Stay updated and informed on COVID-19 to avoid miscommunication or inaccurate information. Talk openly about the harm of stigma. View people directly impacted by stigma as people first. Be conscious of your language. Acknowledge access and language barriers.”
Speak out on social media – but don’t fight
Should medical professionals speak out about COVID-19 misinformation via social media? It’s an individual decision, Dr. Warraich said, “but my sense is that it’s never been more important for physicians to be part of the fray and help quell the epidemic of misinformation that almost always follows any type of medial calamity.”
Dr. Rutland, vice president and founding member of the Association for Healthcare Social Media, cautioned that effective communication via social media requires care. Avoid confrontation, he advised. “Don’t call people stupid or say things like, ‘I went to medical school and I’m smarter than you.’ ”
Instead, he said, “it’s important to just state the facts: These are the people who are dying, these are the people who are getting infected.”
And, he added, remember to push the most important message of all: Wash your hands!
Public health organizations fight the ‘infodemic’
In a trend that hearkens back to the days of snake oil cures for all maladies, advertisements for fake treatments are popping up on the Internet and on other media.
Facebook and Amazon have acted to remove these ads but these messages continue to flood social media such as Twitter, WhatsApp, and other sites. Discussion groups on platforms such as Reddit continue to pump out misinformation about COVID-19. Conspiracy theories that link the virus to espionage and bioweapons are making the rounds on the Internet and talk radio. Wrong information about the effectiveness of non-N95 face masks to protect wearers against infection is widespread, leading to shortages for medical personnel and price gouging. Pernicious rumors about the effectiveness of substances such a vinegar, silver, garlic, lemon juice, and even vodka to disinfect hands and surfaces abound on the Internet. An especially dangerous stream of misinformation stigmatizes ethnic groups and individuals as sources of the infection.
The World Health Organization identified early in the COVID-19 outbreak the global wave of misinformation about the virus and dubbed the problem the “infodemic.” The WHO “Q & A” page on COVID-19 is updated frequently and addresses myths and rumors currently circulating.
According to the WHO website, the agency has reached out to social media players such as Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, and Weibo, the microblogging site in China. WHO has worked with these sites to curb the “infodemic” of misinformation and has used these sites for public education outreach on COVID-19. “Myth busting” infographics posted on a WHO web page are also reposted on major social media sites.
The CDC has followed with its own “frequently asked questions” page to address questions and rumors. State health agencies have put up COVID-19 pages to address public concerns and offer advice on prevention. The Maryland Department of Health web page directly addresses dangerous misinformation: “Do not stigmatize people of any specific ethnicities or racial background. Viruses do not target people from specific populations, ethnicities or racial backgrounds. Stay informed and seek information from reliable, official sources. Be wary of myths, rumors and misinformation circulating online and elsewhere. Health information shared through social media is frequently inaccurate, unless coming from an official, reliable source such as the CDC, MDH or local health departments.”
The Washington State Department of Health has taken a more assertive stance on stigma. The COVID-19 web page recommends to the public: “Show compassion and support for individuals and communities more closely impacted. Avoid stigmatizing people who are in quarantine. They are making the right choice for their communities. Do not make assumptions about someone’s health status based on their ethnicity, race or national origin.”
Early GI symptoms in COVID-19 may indicate fecal transmission
Fecal-oral transmission may be part of the COVID-19 clinical picture, according to two reports published in Gastroenterology. The researchers find that RNA and proteins from SARS-CoV-2, the viral cause of COVID-19, are shed in feces early in infection and persist after respiratory symptoms abate.
But the discovery is preliminary. “There is evidence of the virus in stool, but not evidence of infectious virus,” David A. Johnson, MD, professor of medicine and chief of gastroenterology at the Eastern Virginia School of Medicine in Norfolk, told Medscape Medical News.
The findings are not entirely unexpected. Both of the coronaviruses behind SARS and MERS are shed in stool, Jinyang Gu, MD, from Shanghai Jiao Tong University School of Medicine in Shanghai, China, and colleagues, note in one of the newly published articles.
In addition, as COVID-19 spread beyond China, clinicians began noticing initial mild gastrointestinal (GI) symptoms in some patients, including diarrhea, nausea, vomiting, and abdominal pain, preceding the hallmark fever, dry cough, and dyspnea. The first patient diagnosed in the United States with COVID-19 reported having 2 days of nausea and vomiting, with viral RNA detected in fecal and respiratory specimens, according to an earlier report.
Gu and colleagues warn that initial investigations would likely have not considered cases that manifested initially only as mild gastrointestinal symptoms.
Although early reports indicated that only about 10% of people with COVID-19 have GI symptoms, it isn’t known whether some infected individuals have only GI symptoms, Johnson said.
The GI manifestations are consistent with the distribution of ACE2 receptors, which serve as entry points for SARS-CoV-2, as well as SARS-CoV-1, which causes SARS. The receptors are most abundant in the cell membranes of lung AT2 cells, as well as in enterocytes in the ileum and colon.
“Altogether, many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” Gu and colleagues conclude.
But Johnson cautions, “gastroenterologists are not the ones managing diagnosis of COVID-19. It is diagnosed as a respiratory illness, but we are seeing concomitant gastrointestinal shedding in stool and saliva, and GI symptoms.”
Samples From 73 Patients Studied
In the second article published, Fei Xiao, MD, of Sun Yat-sen University in Guangdong Province, China, and colleagues report detecting viral RNA in samples from the mouths, noses, throats, urine, and feces of 73 patients hospitalized during the first 2 weeks of February.
Of the 73 hospitalized patients, 39 (53.24%; 25 males and 14 females) had viral RNA in their feces, present from 1 to 12 days. Seventeen (23.29%) of the patients continued to have viral RNA in their stool after respiratory symptoms had improved.
One patient underwent endoscopy. There was no evidence of damage to the GI epithelium, but the clinicians detected slightly elevated levels of lymphocytes and plasma cells.
The researcher used laser scanning confocal microscopy to analyze samples taken during the endoscopy. They found evidence of both ACE2 receptors and viral nucleocapsid proteins in the gastric, duodenal, and rectal glandular epithelial cells.
Finding evidence of SARS-CoV-2 throughout the GI system, if not direct infectivity, suggests a fecal-oral route of transmission, the researchers conclude. “Our immunofluorescent data showed that ACE2 protein, a cell receptor for SARS-CoV-2, is abundantly expressed in the glandular cells of gastric, duodenal and rectal epithelia, supporting the entry of SARS-CoV-2 into the host cells.”
Detection of viral RNA at different time points in infection, they write, suggests that the virions are continually secreted and therefore likely infectious, which is under investigation. “Prevention of fecal-oral transmission should be taken into consideration to control the spread of the virus,” they write.
Current recommendations do not require that patients’ fecal samples be tested before being considered noninfectious. However, given their findings and evidence from other studies, Xiao and colleagues recommend that real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) testing of fecal samples be added to current protocols.
Johnson offers practical suggestions based on the “potty hygiene” suggestions he gives to patients dealing with fecal shedding in Clostridioides difficile infection.
“To combat the microaerosolization of C. diff spores, I have patients do a complete bacteriocidal washing out of the toilet bowl, as well as clean surface areas and especially toothbrushes.” Keeping the bowl closed when not in use is important too in preventing “fecal-oral transmission of remnants” of toilet contents, he adds.
The new papers add to other reports suggesting that virus-bearing droplets may reach people in various ways, Johnson said. “Maybe the virus isn’t only spread by a cough or a sneeze.”
The researchers and commentator have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Fecal-oral transmission may be part of the COVID-19 clinical picture, according to two reports published in Gastroenterology. The researchers find that RNA and proteins from SARS-CoV-2, the viral cause of COVID-19, are shed in feces early in infection and persist after respiratory symptoms abate.
But the discovery is preliminary. “There is evidence of the virus in stool, but not evidence of infectious virus,” David A. Johnson, MD, professor of medicine and chief of gastroenterology at the Eastern Virginia School of Medicine in Norfolk, told Medscape Medical News.
The findings are not entirely unexpected. Both of the coronaviruses behind SARS and MERS are shed in stool, Jinyang Gu, MD, from Shanghai Jiao Tong University School of Medicine in Shanghai, China, and colleagues, note in one of the newly published articles.
In addition, as COVID-19 spread beyond China, clinicians began noticing initial mild gastrointestinal (GI) symptoms in some patients, including diarrhea, nausea, vomiting, and abdominal pain, preceding the hallmark fever, dry cough, and dyspnea. The first patient diagnosed in the United States with COVID-19 reported having 2 days of nausea and vomiting, with viral RNA detected in fecal and respiratory specimens, according to an earlier report.
Gu and colleagues warn that initial investigations would likely have not considered cases that manifested initially only as mild gastrointestinal symptoms.
Although early reports indicated that only about 10% of people with COVID-19 have GI symptoms, it isn’t known whether some infected individuals have only GI symptoms, Johnson said.
The GI manifestations are consistent with the distribution of ACE2 receptors, which serve as entry points for SARS-CoV-2, as well as SARS-CoV-1, which causes SARS. The receptors are most abundant in the cell membranes of lung AT2 cells, as well as in enterocytes in the ileum and colon.
“Altogether, many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” Gu and colleagues conclude.
But Johnson cautions, “gastroenterologists are not the ones managing diagnosis of COVID-19. It is diagnosed as a respiratory illness, but we are seeing concomitant gastrointestinal shedding in stool and saliva, and GI symptoms.”
Samples From 73 Patients Studied
In the second article published, Fei Xiao, MD, of Sun Yat-sen University in Guangdong Province, China, and colleagues report detecting viral RNA in samples from the mouths, noses, throats, urine, and feces of 73 patients hospitalized during the first 2 weeks of February.
Of the 73 hospitalized patients, 39 (53.24%; 25 males and 14 females) had viral RNA in their feces, present from 1 to 12 days. Seventeen (23.29%) of the patients continued to have viral RNA in their stool after respiratory symptoms had improved.
One patient underwent endoscopy. There was no evidence of damage to the GI epithelium, but the clinicians detected slightly elevated levels of lymphocytes and plasma cells.
The researcher used laser scanning confocal microscopy to analyze samples taken during the endoscopy. They found evidence of both ACE2 receptors and viral nucleocapsid proteins in the gastric, duodenal, and rectal glandular epithelial cells.
Finding evidence of SARS-CoV-2 throughout the GI system, if not direct infectivity, suggests a fecal-oral route of transmission, the researchers conclude. “Our immunofluorescent data showed that ACE2 protein, a cell receptor for SARS-CoV-2, is abundantly expressed in the glandular cells of gastric, duodenal and rectal epithelia, supporting the entry of SARS-CoV-2 into the host cells.”
Detection of viral RNA at different time points in infection, they write, suggests that the virions are continually secreted and therefore likely infectious, which is under investigation. “Prevention of fecal-oral transmission should be taken into consideration to control the spread of the virus,” they write.
Current recommendations do not require that patients’ fecal samples be tested before being considered noninfectious. However, given their findings and evidence from other studies, Xiao and colleagues recommend that real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) testing of fecal samples be added to current protocols.
Johnson offers practical suggestions based on the “potty hygiene” suggestions he gives to patients dealing with fecal shedding in Clostridioides difficile infection.
“To combat the microaerosolization of C. diff spores, I have patients do a complete bacteriocidal washing out of the toilet bowl, as well as clean surface areas and especially toothbrushes.” Keeping the bowl closed when not in use is important too in preventing “fecal-oral transmission of remnants” of toilet contents, he adds.
The new papers add to other reports suggesting that virus-bearing droplets may reach people in various ways, Johnson said. “Maybe the virus isn’t only spread by a cough or a sneeze.”
The researchers and commentator have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Fecal-oral transmission may be part of the COVID-19 clinical picture, according to two reports published in Gastroenterology. The researchers find that RNA and proteins from SARS-CoV-2, the viral cause of COVID-19, are shed in feces early in infection and persist after respiratory symptoms abate.
But the discovery is preliminary. “There is evidence of the virus in stool, but not evidence of infectious virus,” David A. Johnson, MD, professor of medicine and chief of gastroenterology at the Eastern Virginia School of Medicine in Norfolk, told Medscape Medical News.
The findings are not entirely unexpected. Both of the coronaviruses behind SARS and MERS are shed in stool, Jinyang Gu, MD, from Shanghai Jiao Tong University School of Medicine in Shanghai, China, and colleagues, note in one of the newly published articles.
In addition, as COVID-19 spread beyond China, clinicians began noticing initial mild gastrointestinal (GI) symptoms in some patients, including diarrhea, nausea, vomiting, and abdominal pain, preceding the hallmark fever, dry cough, and dyspnea. The first patient diagnosed in the United States with COVID-19 reported having 2 days of nausea and vomiting, with viral RNA detected in fecal and respiratory specimens, according to an earlier report.
Gu and colleagues warn that initial investigations would likely have not considered cases that manifested initially only as mild gastrointestinal symptoms.
Although early reports indicated that only about 10% of people with COVID-19 have GI symptoms, it isn’t known whether some infected individuals have only GI symptoms, Johnson said.
The GI manifestations are consistent with the distribution of ACE2 receptors, which serve as entry points for SARS-CoV-2, as well as SARS-CoV-1, which causes SARS. The receptors are most abundant in the cell membranes of lung AT2 cells, as well as in enterocytes in the ileum and colon.
“Altogether, many efforts should be made to be alert on the initial digestive symptoms of COVID-19 for early detection, early diagnosis, early isolation and early intervention,” Gu and colleagues conclude.
But Johnson cautions, “gastroenterologists are not the ones managing diagnosis of COVID-19. It is diagnosed as a respiratory illness, but we are seeing concomitant gastrointestinal shedding in stool and saliva, and GI symptoms.”
Samples From 73 Patients Studied
In the second article published, Fei Xiao, MD, of Sun Yat-sen University in Guangdong Province, China, and colleagues report detecting viral RNA in samples from the mouths, noses, throats, urine, and feces of 73 patients hospitalized during the first 2 weeks of February.
Of the 73 hospitalized patients, 39 (53.24%; 25 males and 14 females) had viral RNA in their feces, present from 1 to 12 days. Seventeen (23.29%) of the patients continued to have viral RNA in their stool after respiratory symptoms had improved.
One patient underwent endoscopy. There was no evidence of damage to the GI epithelium, but the clinicians detected slightly elevated levels of lymphocytes and plasma cells.
The researcher used laser scanning confocal microscopy to analyze samples taken during the endoscopy. They found evidence of both ACE2 receptors and viral nucleocapsid proteins in the gastric, duodenal, and rectal glandular epithelial cells.
Finding evidence of SARS-CoV-2 throughout the GI system, if not direct infectivity, suggests a fecal-oral route of transmission, the researchers conclude. “Our immunofluorescent data showed that ACE2 protein, a cell receptor for SARS-CoV-2, is abundantly expressed in the glandular cells of gastric, duodenal and rectal epithelia, supporting the entry of SARS-CoV-2 into the host cells.”
Detection of viral RNA at different time points in infection, they write, suggests that the virions are continually secreted and therefore likely infectious, which is under investigation. “Prevention of fecal-oral transmission should be taken into consideration to control the spread of the virus,” they write.
Current recommendations do not require that patients’ fecal samples be tested before being considered noninfectious. However, given their findings and evidence from other studies, Xiao and colleagues recommend that real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) testing of fecal samples be added to current protocols.
Johnson offers practical suggestions based on the “potty hygiene” suggestions he gives to patients dealing with fecal shedding in Clostridioides difficile infection.
“To combat the microaerosolization of C. diff spores, I have patients do a complete bacteriocidal washing out of the toilet bowl, as well as clean surface areas and especially toothbrushes.” Keeping the bowl closed when not in use is important too in preventing “fecal-oral transmission of remnants” of toilet contents, he adds.
The new papers add to other reports suggesting that virus-bearing droplets may reach people in various ways, Johnson said. “Maybe the virus isn’t only spread by a cough or a sneeze.”
The researchers and commentator have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Risk factors for death from COVID-19 identified in Wuhan patients
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
Patients who did not survive hospitalization for COVID-19 in Wuhan were more likely to be older, have comorbidities, and elevated D-dimer, according to the first study to examine risk factors associated with death among adults hospitalized with COVID-19. “Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes, and the prolonged use of noninvasive ventilation were important factors in the deaths of these patients,” coauthor Zhibo Liu said in a news release. Abnormal blood clotting was part of the clinical picture too.
Fei Zhou, MD, from the Chinese Academy of Medical Sciences, and colleagues conducted a retrospective, observational, multicenter cohort study of 191 patients, 137 of whom were discharged and 54 of whom died in the hospital.
The study, published online today in The Lancet, included all adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31 of this year. Severely ill patients in the province were transferred to these hospitals until February 1.
The researchers compared demographic, clinical, treatment, and laboratory data from electronic medical records between survivors and those who succumbed to the disease. The analysis also tested serial samples for viral RNA. Overall, 91 (48%) of the 191 patients had comorbidity. Most common was hypertension (30%), followed by diabetes (19%) and coronary heart disease (8%).
The odds of dying in the hospital increased with age (odds ratio 1.10; 95% confidence interval, 1.03-1.17; per year increase in age), higher Sequential Organ Failure Assessment (SOFA) score (5.65, 2.61-12.23; P < .0001), and D-dimer level exceeding 1 mcg/L on admission. The SOFA was previously called the “sepsis-related organ failure assessment score” and assesses rate of organ failure in intensive care units. Elevated D-dimer indicates increased risk of abnormal blood clotting, such as deep vein thrombosis.
Nonsurvivors compared with survivors had higher frequencies of respiratory failure (98% vs 36%), sepsis (100%, vs 42%), and secondary infections (50% vs 1%).
The average age of survivors was 52 years compared to 69 for those who died. Liu cited weakening of the immune system and increased inflammation, which damages organs and also promotes viral replication, as explanations for the age effect.
From the time of initial symptoms, median time to discharge from the hospital was 22 days. Average time to death was 18.5 days.
Fever persisted for a median of 12 days among all patients, and cough persisted for a median 19 days; 45% of the survivors were still coughing on discharge. In survivors, shortness of breath improved after 13 days, but persisted until death in the others.
Viral shedding persisted for a median duration of 20 days in survivors, ranging from 8 to 37. The virus (SARS-CoV-2) was detectable in nonsurvivors until death. Antiviral treatment did not curtail viral shedding.
But the viral shedding data come with a caveat. “The extended viral shedding noted in our study has important implications for guiding decisions around isolation precautions and antiviral treatment in patients with confirmed COVID-19 infection. However, we need to be clear that viral shedding time should not be confused with other self-isolation guidance for people who may have been exposed to COVID-19 but do not have symptoms, as this guidance is based on the incubation time of the virus,” explained colead author Bin Cao.
“Older age, elevated D-dimer levels, and high SOFA score could help clinicians to identify at an early stage those patients with COVID-19 who have poor prognosis. Prolonged viral shedding provides the rationale for a strategy of isolation of infected patients and optimal antiviral interventions in the future,” the researchers conclude.
A limitation in interpreting the findings of the study is that hospitalized patients do not represent the entire infected population. The researchers caution that “the number of deaths does not reflect the true mortality of COVID-19.” They also note that they did not have enough genetic material to accurately assess duration of viral shedding.
This article first appeared on Medscape.com.
WHO declares COVID-19 outbreak a pandemic
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
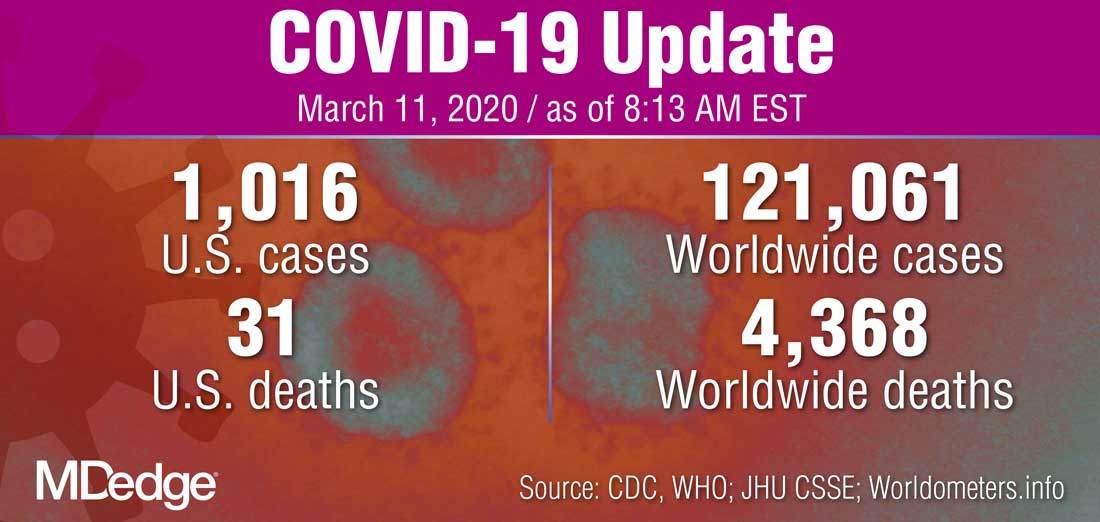
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
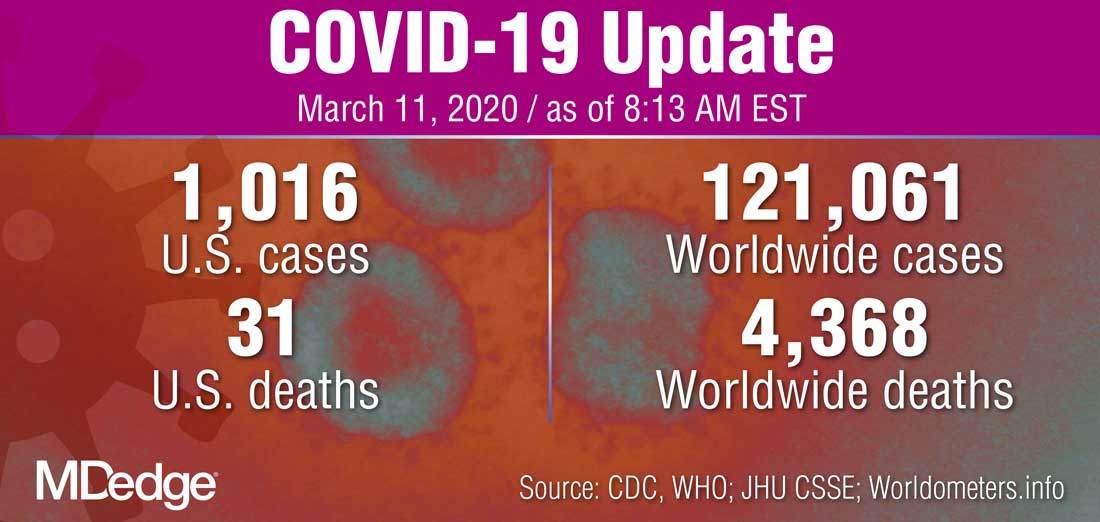
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
The World Health Organization has formally declared the COVID-19 outbreak a pandemic.
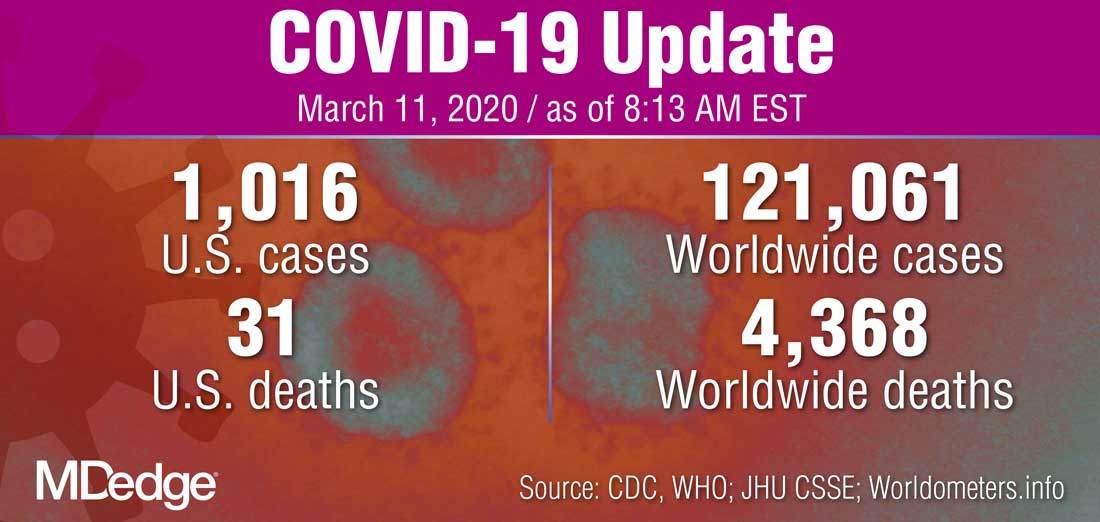
“WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction,” WHO Director-General Tedros Adhanom Ghebreyesus said during a March 11 press briefing. “We therefore made the assessment that COVID-19 can be characterized as a pandemic.”
He noted that this is the first time a coronavirus has been seen as a pandemic.
The Director-General cautioned that just looking at the number of countries affected, 114 countries, “does not tell the full story. ... We cannot say this loudly enough, or clearly enough, or often enough: All countries can still change the course of this pandemic.”
He reiterated the need for a whole-of-government and a whole-of-society approach to dealing with this, including taking precautions such as isolating, testing, and treating every case and tracing every contact, as well as readying hospitals and health care professionals.
“Let’s look out for each other, because we need each other,” he said.
FDA broadens nintedanib interstitial lung disease indication
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
A new indication for the tyrosine kinase inhibitor nintedanib approved by the Food and Drug Administration on March 9, 2020, broadened the drug’s targeted population to include patients with chronic fibrosing interstitial lung diseases with a progressive phenotype.
This new group of patients eligible for nintedanib treatment extends the drug’s labeling beyond patients with idiopathic pulmonary fibrosis (IPF) or interstitial lung disease (ILD) associated with systemic sclerosis or scleroderma, and may come close to doubling the total number of eligible patients.
The new, expanded indication “helps to fulfill an unmet treatment need, as patients with these life-threatening lung diseases have not had an approved medication until now,” said Banu Karimi-Shah, MD, acting deputy director of the division of pulmonary, allergy, and rheumatology products in the FDA’s Center for Drug Evaluation and Research, in a written agency statement that announced the new indication.
The FDA first approved nintedanib (Ofev) for treating IPF in October 2014, and then granted a second indication in September 2019 for ILD associated with systemic sclerosis or scleroderma.
A recent assessment of 1,285 Canadian patients diagnosed with fibrotic ILD and entered into a national registry (CARE-PF) showed that IPF was the associated diagnosis for 25% of patients, and that the majority of patients had other primary diagnoses such as connective tissue disease ILD in 33% of enrolled patients, unclassifiable ILD in 22%, chronic sensitivity pneumonitis in about 8%, sarcoidosis in 3%, as well as other types (BMC Pulm Med. 2019 Nov 27. doi: 10.1186/s12890-019-0986-4).
It remains unclear right now what percentage of patients with fibrotic ILD have the progressive form that would make them eligible for nintedanib treatment under the new indication, but it’s probably about another quarter of the entire ILD population, or roughly similar to the number of patients with an IPF etiology who are already eligible to get the drug, commented Martin Kolb, MD, a professor of respirology at McMaster University, Hamilton, Ont., and a coinvestigator on the CARE-PF registry. A goal of the registry, which has now enrolled nearly 3,700 ILD patients, is to track them serially to get a better handle on the prevalence of progressive disease. The percentage of patients with ILD associated with systemic sclerosis or scleroderma is “relatively small,” compared with these other two patients subgroups, Dr. Kolb said in an interview.
The evidence base for treating patients with progressive ILD is “really strong,” he noted, and comes primarily from a major trial reported last year – the INBUILD study – that randomized 663 patients to treatment with either nintedanib or placebo and showed that nintedanib treatment significantly cut the rate of decline in forced vital capacity during 1 year of treatment (New Engl J Med. 2019 Oct 31;381[18]:1718-27). The patients entered the study as referrals from routine practice with documented ILD with progressive fibrosis that was not responsive to treatment with steroids or other immunosuppressive drugs, and reflects real-world, community practice, Dr. Kolb said.
“Conceptually, it makes so much sense” to treat the patients enrolled in INBUILD, the same patients who fit the new indication, with an agent like nintedanib that slows fibrosis progression, and in some patients may bring progression to a virtual halt, said Dr. Kolb, a coinvestigator on the INBUILD study. Future treatment of these patients will likely involve coupling an antifibrotic drug like nintedanib with an anti-inflammatory agent, although combined treatment of this type needs more study, he noted. In the more than 5 years since nintedanib came onto the U.S. market, it has been used on more than 10,000 patients and has generated no new safety concerns beyond those first included in the drug’s label.
The INBUILD study was sponsored by Boehringer Ingelheim, the company that markets nintedanib. Dr. Kolb has been a consultant to, received honoraria from, and received research funding from Boehringer Ingelheim. He has also received consulting fees or honoraria from Genoa, Gilead, GlaxoSmithKline, Indalo, Prometic, Roche, and Third Pole, and he has received research funding from Actelion, Alkermes, Gilead, GlaxoSmithKline, Pharmaxis, Prometic, RespiVert, and Roche.
Young women with insomnia at higher risk for car accidents
and reported daytime sleepiness represent a subpopulation at specific risk, according to an analysis of a 5-year population sample. The new research was published online in Sleep and led by Charles Morin, PhD, of Laval University, Quebec City.
The risks of daytime sleepiness and MVA are generally thought of in the context of obstructive sleep apnea (OSA) or men, but the results of the new work suggest that insomnia should not be overlooked, according to Krishna Sundar, MD, clinical professor of pulmonary, critical care, and sleep medicine, and medical director of the Sleep-Wake Center, at the University of Utah, Salt Lake City.
“The notion has been that it may keep them more hypervigilant and less prone to motor vehicle accidents because they are less able to fall asleep even if they want to during the daytime, as compared to other conditions like sleep apnea where there is a higher tendency to doze off,” Dr. Sundar said in an interview.
It should also be remembered that patients aren’t always completely reliable when it comes to self-assessment, according to Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta. “Most people with insomnia won’t say they are sleepy in the daytime, but when you objectively look, you do see an element of daytime sleepiness even if it’s not perceived that well by insomnia patients,” said Dr. Seay.
The heightened risks in young women with insomnia is notable, according to Dr. Sundar. Insomnia is more common in women, and they may also be more susceptible to unintended consequences of sleep medications because they metabolize them more slowly. “Especially for younger women, if they are insomniac and on prescription medicines, and if they have excess daytime sleepiness, this [risk of MVA] needs to be factored in,” said Dr. Sundar.
Insomnia is a condition that waxes and wanes over time, and can vary in its presentation across age groups, which is why the authors chose to conduct a prospective longitudinal study in a Canadian sample. They recruited 3,413 adults with insomnia (median age, 49.0 years; range, 18-96; 61.5% female). After 5 years, the retention rate was 68.7%.
After filling out baseline information, participants were asked every 6 months about MVAs and what role they believed daytime consequences of insomnia played if an accident occurred. Prescription and over-the-counter medication use were also self-reported.
In the first 2 years of the study, 8.2% of women aged 18-29 reported MVAs, which was the highest of any demographic (range, 2.3%-4.3%). By the third year, the frequency in this group overlapped that of men in the same age group, and both remained higher than older age groups.
Participants judged that insomnia consequences played a role in 39.4% of reported MVA. In 17.2% of accidents, participants said insomnia consequences contributed at least 50% of the cause.
MVA risk was associated individually with presence of insomnia symptoms (hazard ratio [HR], 1.20; 95% confidence interval, 1.00-1.45) and daytime fatigue (HR, 1.21; 95% CI, 1.01-1.47), but there were only trends toward associations with sleeping fewer than 6 hours (P = .16) and excessive daytime sleepiness (P = .06). MVAs were associated with reported past-year use of prescribed sleep medications (HR, 1.50; 95% CI, 1.17-1.91) and reported use of OTC medications (HR, 1.42; 95% CI, 1.02-1.98).
In women aged 18-29, MVAs were associated with insomnia symptoms (HR, 1.83; 95% CI, 1.13-2.98) and excessive daytime sleepiness (HR, 2.42; 95% CI, 1.11-5.24).
The study was limited by its reliance on self-reporting and lack of data on specific medications used.
The study was funded by the Canadian Institutes of Health.
SOURCE: Morin C et al. Sleep. 2020 Feb 29. DOI: 10.1093/sleep/zsaa032.
and reported daytime sleepiness represent a subpopulation at specific risk, according to an analysis of a 5-year population sample. The new research was published online in Sleep and led by Charles Morin, PhD, of Laval University, Quebec City.
The risks of daytime sleepiness and MVA are generally thought of in the context of obstructive sleep apnea (OSA) or men, but the results of the new work suggest that insomnia should not be overlooked, according to Krishna Sundar, MD, clinical professor of pulmonary, critical care, and sleep medicine, and medical director of the Sleep-Wake Center, at the University of Utah, Salt Lake City.
“The notion has been that it may keep them more hypervigilant and less prone to motor vehicle accidents because they are less able to fall asleep even if they want to during the daytime, as compared to other conditions like sleep apnea where there is a higher tendency to doze off,” Dr. Sundar said in an interview.
It should also be remembered that patients aren’t always completely reliable when it comes to self-assessment, according to Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta. “Most people with insomnia won’t say they are sleepy in the daytime, but when you objectively look, you do see an element of daytime sleepiness even if it’s not perceived that well by insomnia patients,” said Dr. Seay.
The heightened risks in young women with insomnia is notable, according to Dr. Sundar. Insomnia is more common in women, and they may also be more susceptible to unintended consequences of sleep medications because they metabolize them more slowly. “Especially for younger women, if they are insomniac and on prescription medicines, and if they have excess daytime sleepiness, this [risk of MVA] needs to be factored in,” said Dr. Sundar.
Insomnia is a condition that waxes and wanes over time, and can vary in its presentation across age groups, which is why the authors chose to conduct a prospective longitudinal study in a Canadian sample. They recruited 3,413 adults with insomnia (median age, 49.0 years; range, 18-96; 61.5% female). After 5 years, the retention rate was 68.7%.
After filling out baseline information, participants were asked every 6 months about MVAs and what role they believed daytime consequences of insomnia played if an accident occurred. Prescription and over-the-counter medication use were also self-reported.
In the first 2 years of the study, 8.2% of women aged 18-29 reported MVAs, which was the highest of any demographic (range, 2.3%-4.3%). By the third year, the frequency in this group overlapped that of men in the same age group, and both remained higher than older age groups.
Participants judged that insomnia consequences played a role in 39.4% of reported MVA. In 17.2% of accidents, participants said insomnia consequences contributed at least 50% of the cause.
MVA risk was associated individually with presence of insomnia symptoms (hazard ratio [HR], 1.20; 95% confidence interval, 1.00-1.45) and daytime fatigue (HR, 1.21; 95% CI, 1.01-1.47), but there were only trends toward associations with sleeping fewer than 6 hours (P = .16) and excessive daytime sleepiness (P = .06). MVAs were associated with reported past-year use of prescribed sleep medications (HR, 1.50; 95% CI, 1.17-1.91) and reported use of OTC medications (HR, 1.42; 95% CI, 1.02-1.98).
In women aged 18-29, MVAs were associated with insomnia symptoms (HR, 1.83; 95% CI, 1.13-2.98) and excessive daytime sleepiness (HR, 2.42; 95% CI, 1.11-5.24).
The study was limited by its reliance on self-reporting and lack of data on specific medications used.
The study was funded by the Canadian Institutes of Health.
SOURCE: Morin C et al. Sleep. 2020 Feb 29. DOI: 10.1093/sleep/zsaa032.
and reported daytime sleepiness represent a subpopulation at specific risk, according to an analysis of a 5-year population sample. The new research was published online in Sleep and led by Charles Morin, PhD, of Laval University, Quebec City.
The risks of daytime sleepiness and MVA are generally thought of in the context of obstructive sleep apnea (OSA) or men, but the results of the new work suggest that insomnia should not be overlooked, according to Krishna Sundar, MD, clinical professor of pulmonary, critical care, and sleep medicine, and medical director of the Sleep-Wake Center, at the University of Utah, Salt Lake City.
“The notion has been that it may keep them more hypervigilant and less prone to motor vehicle accidents because they are less able to fall asleep even if they want to during the daytime, as compared to other conditions like sleep apnea where there is a higher tendency to doze off,” Dr. Sundar said in an interview.
It should also be remembered that patients aren’t always completely reliable when it comes to self-assessment, according to Brandon M. Seay, MD, a pediatric pulmonologist and sleep specialist at Children’s Healthcare of Atlanta. “Most people with insomnia won’t say they are sleepy in the daytime, but when you objectively look, you do see an element of daytime sleepiness even if it’s not perceived that well by insomnia patients,” said Dr. Seay.
The heightened risks in young women with insomnia is notable, according to Dr. Sundar. Insomnia is more common in women, and they may also be more susceptible to unintended consequences of sleep medications because they metabolize them more slowly. “Especially for younger women, if they are insomniac and on prescription medicines, and if they have excess daytime sleepiness, this [risk of MVA] needs to be factored in,” said Dr. Sundar.
Insomnia is a condition that waxes and wanes over time, and can vary in its presentation across age groups, which is why the authors chose to conduct a prospective longitudinal study in a Canadian sample. They recruited 3,413 adults with insomnia (median age, 49.0 years; range, 18-96; 61.5% female). After 5 years, the retention rate was 68.7%.
After filling out baseline information, participants were asked every 6 months about MVAs and what role they believed daytime consequences of insomnia played if an accident occurred. Prescription and over-the-counter medication use were also self-reported.
In the first 2 years of the study, 8.2% of women aged 18-29 reported MVAs, which was the highest of any demographic (range, 2.3%-4.3%). By the third year, the frequency in this group overlapped that of men in the same age group, and both remained higher than older age groups.
Participants judged that insomnia consequences played a role in 39.4% of reported MVA. In 17.2% of accidents, participants said insomnia consequences contributed at least 50% of the cause.
MVA risk was associated individually with presence of insomnia symptoms (hazard ratio [HR], 1.20; 95% confidence interval, 1.00-1.45) and daytime fatigue (HR, 1.21; 95% CI, 1.01-1.47), but there were only trends toward associations with sleeping fewer than 6 hours (P = .16) and excessive daytime sleepiness (P = .06). MVAs were associated with reported past-year use of prescribed sleep medications (HR, 1.50; 95% CI, 1.17-1.91) and reported use of OTC medications (HR, 1.42; 95% CI, 1.02-1.98).
In women aged 18-29, MVAs were associated with insomnia symptoms (HR, 1.83; 95% CI, 1.13-2.98) and excessive daytime sleepiness (HR, 2.42; 95% CI, 1.11-5.24).
The study was limited by its reliance on self-reporting and lack of data on specific medications used.
The study was funded by the Canadian Institutes of Health.
SOURCE: Morin C et al. Sleep. 2020 Feb 29. DOI: 10.1093/sleep/zsaa032.
FROM SLEEP
Managing children’s fear, anxiety in the age of COVID-19
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.









