User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


State of Practice: Management Practice for Thromboprophylaxis in Acutely Ill Medical Patients
In this issue of CHEST Clinical Perspectives, CHEST is undertaking primary research with pulmonologists and intensivists to understand their approach to ordering thromboprophylaxis in acutely ill medical patients for the purpose of reducing risk of VTE. Specifically, this issue focuses on the extent to which management practice has evolved given the introduction of novel anticoagulants. The objectives of this research are to:
- Understand current practice related to ordering thromboprophylaxis, as well as the therapies used with acutely ill medical patients.
- Understand the attitudes toward thromboprophylaxis from a risk and benefit standpoint that underlie decision-making related to deployment of therapy.
- Assess therapeutic, clinical, and administrative factors that impact management choices and the adoption of novel anticoagulants.
- Assess familiarity with and influence of the MAGELLAN study.
- Identify differences in management based on practice tenure and setting (academic vs community-based).
In this issue of CHEST Clinical Perspectives, CHEST is undertaking primary research with pulmonologists and intensivists to understand their approach to ordering thromboprophylaxis in acutely ill medical patients for the purpose of reducing risk of VTE. Specifically, this issue focuses on the extent to which management practice has evolved given the introduction of novel anticoagulants. The objectives of this research are to:
- Understand current practice related to ordering thromboprophylaxis, as well as the therapies used with acutely ill medical patients.
- Understand the attitudes toward thromboprophylaxis from a risk and benefit standpoint that underlie decision-making related to deployment of therapy.
- Assess therapeutic, clinical, and administrative factors that impact management choices and the adoption of novel anticoagulants.
- Assess familiarity with and influence of the MAGELLAN study.
- Identify differences in management based on practice tenure and setting (academic vs community-based).
In this issue of CHEST Clinical Perspectives, CHEST is undertaking primary research with pulmonologists and intensivists to understand their approach to ordering thromboprophylaxis in acutely ill medical patients for the purpose of reducing risk of VTE. Specifically, this issue focuses on the extent to which management practice has evolved given the introduction of novel anticoagulants. The objectives of this research are to:
- Understand current practice related to ordering thromboprophylaxis, as well as the therapies used with acutely ill medical patients.
- Understand the attitudes toward thromboprophylaxis from a risk and benefit standpoint that underlie decision-making related to deployment of therapy.
- Assess therapeutic, clinical, and administrative factors that impact management choices and the adoption of novel anticoagulants.
- Assess familiarity with and influence of the MAGELLAN study.
- Identify differences in management based on practice tenure and setting (academic vs community-based).
Comorbidities increase COVID-19 deaths by factor of 12
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
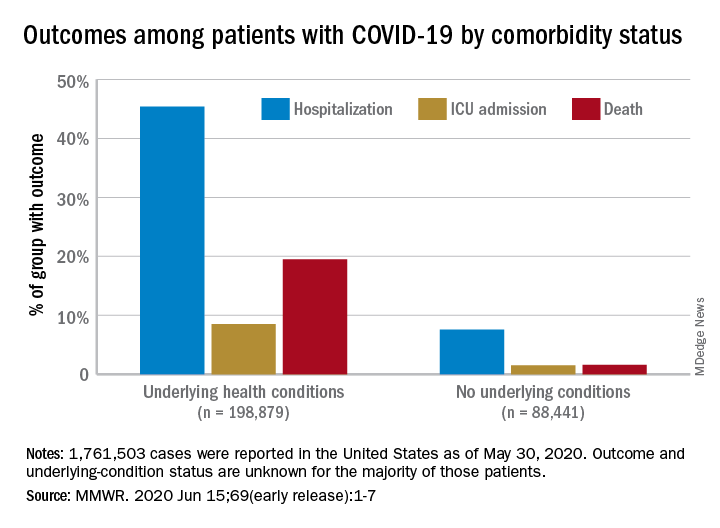
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
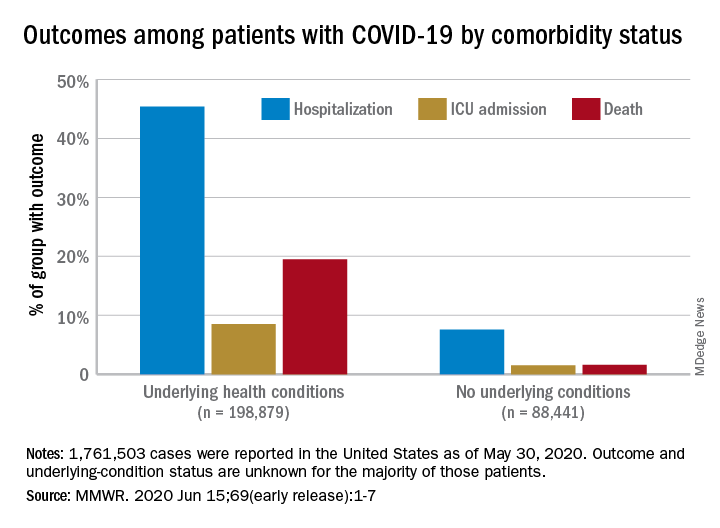
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
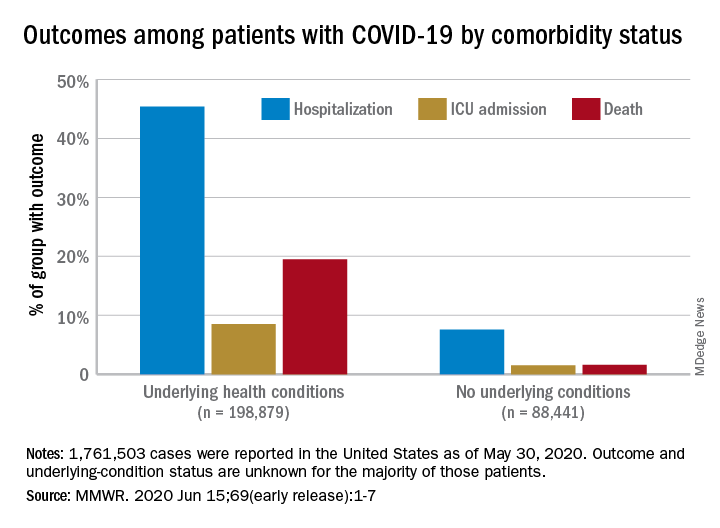
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
FROM MMWR
Lurbinectedin approved for metastatic SCLC
Patients with metastatic small-cell lung cancer (SCLC) whose disease has progressed after or during treatment with platinum-based chemotherapy now have a new option to try — lurbinectedin (Zepzelca, Jazz Pharma/PharmaMar).
The drug was granted accelerated approval by the US Food and Drug Administration (FDA) based on response data. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial, the FDA notes.
“Small-cell lung cancer is a disease with limited treatment options,” said Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals. “While patients may initially respond to traditional chemotherapy, they often experience an aggressive recurrence that is historically resistant to treatment.”
“Seeing first-hand the aggressive nature of SCLC and knowing that the large majority of those diagnosed will experience relapse, I am excited to see an effective new treatment demonstrating durable responses,” Jeff Petty, MD, oncology specialist, Wake Forest Baptist Health, Winston-Salem, North Carolina, commented in the company press release. This new drug “is an important and much-needed addition to the treatment landscape for relapsing SCLC,” he added.
Approval based on monotherapy trial
The approval is based on a monotherapy clinical trial in 105 patients, which was published in May in Lancet Oncology, with first author José Trigo, MD, from the Hospital Universitario Virgen de la Victoria in Malaga, Spain.
These were adult patients with both platinum-sensitive and platinum-resistant SCLC who had disease progression after treatment with platinum-based chemotherapy. They were treated at 26 hospitals across six European countries and the US. All patients received lurbinectedin at 3.2 mg/m2 by intravenous infusion over 1 hour. Median follow-up was 17.1 months.
Overall response by investigator assessment was seen in 37 (35.2%) of the 105 patients. The response was greater (at 45%) among the patients with platinum-sensitive disease and smaller (22.2%) among those with platinum-resistant disease.
Lurbinectedin demonstrated a median duration of response of 5.3 months as measured by investigator assessment.
In a post-hoc analysis, among the 37 patients who had an initial objective response, the median overall survival was just over 1 year (12.6 months). It was even longer among patients who had platinum-sensitive disease (15.8 months), although it was shorter in patients with resistant disease (10.9 months).
These data are “particularly encouraging,” comment the authors of an accompanying editorial, led by Oscar Arrieta, MD, from the Thoracic Oncology Unit at the Instituto Nacional de Cancerología in Mexico City, Mexico. These response rates “outperform all previous results achieved with topotecan and other less established treatment schemes including cyclophosphamide, doxorubicin, and vincristine, or platinum re-challenge, in this setting.”
“Lurbinectedin represents an innovative approach to conventional anti-cancer drugs, with an elegant mechanism of action based on the inhibition of transcription-dependent replication stress and genome instability of tumor cells,” the editorialists comment. “The drug binds to specific DNA triplets commonly found in transcription sites and triggers cellular apoptosis.”
“At present, the only evidence-based second-line treatment approved for SCLC is topotecan, a topoisomerase 1 inhibitor with moderate activity in patients with sensitive disease, although its effect is much less evident in patients with resistant SCLC,” they continue.
“Overall, the study by Trigo and colleagues presents novel data for a very challenging disease for which few treatment options exist, and the data on response and survival do seem to outperform data from historical controls,” Arrieta and colleagues write.
The editorialists also note that, in this trial, a few patients had received immunotherapy as part of their first-line treatment, and some of these patients (5 of 8 patients, 68%) had “an outstanding rate of durable response to lurbinectedin.” This raises the possibility of a synergistic effect between immunotherapy and lurbinectedin, as the combination seems to enhance immune memory and impair subsequent tumor growth, they add. Further trials will need to explore sequencing of therapy, they suggest.
A large phase 3 study known as ATLANTIS is currently underway.
The most common grade 3-4 adverse events in the present trial were hematologic abnormalities: anemia (9% of patients), leukopenia (29%), neutropenia (46%), and thrombocytopenia (7%). Serious treatment-related adverse events occurred in 10% of patients, of which neutropenia and febrile neutropenia were the most common (5% each). No treatment-related deaths were reported.
The study was funded by PharmaMar. Trigo and coauthors, and Arrieta and fellow editorialists, all report relationships with pharmaceutical companies, as detailed in the published articles.
This article first appeared on Medscape.com.
Patients with metastatic small-cell lung cancer (SCLC) whose disease has progressed after or during treatment with platinum-based chemotherapy now have a new option to try — lurbinectedin (Zepzelca, Jazz Pharma/PharmaMar).
The drug was granted accelerated approval by the US Food and Drug Administration (FDA) based on response data. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial, the FDA notes.
“Small-cell lung cancer is a disease with limited treatment options,” said Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals. “While patients may initially respond to traditional chemotherapy, they often experience an aggressive recurrence that is historically resistant to treatment.”
“Seeing first-hand the aggressive nature of SCLC and knowing that the large majority of those diagnosed will experience relapse, I am excited to see an effective new treatment demonstrating durable responses,” Jeff Petty, MD, oncology specialist, Wake Forest Baptist Health, Winston-Salem, North Carolina, commented in the company press release. This new drug “is an important and much-needed addition to the treatment landscape for relapsing SCLC,” he added.
Approval based on monotherapy trial
The approval is based on a monotherapy clinical trial in 105 patients, which was published in May in Lancet Oncology, with first author José Trigo, MD, from the Hospital Universitario Virgen de la Victoria in Malaga, Spain.
These were adult patients with both platinum-sensitive and platinum-resistant SCLC who had disease progression after treatment with platinum-based chemotherapy. They were treated at 26 hospitals across six European countries and the US. All patients received lurbinectedin at 3.2 mg/m2 by intravenous infusion over 1 hour. Median follow-up was 17.1 months.
Overall response by investigator assessment was seen in 37 (35.2%) of the 105 patients. The response was greater (at 45%) among the patients with platinum-sensitive disease and smaller (22.2%) among those with platinum-resistant disease.
Lurbinectedin demonstrated a median duration of response of 5.3 months as measured by investigator assessment.
In a post-hoc analysis, among the 37 patients who had an initial objective response, the median overall survival was just over 1 year (12.6 months). It was even longer among patients who had platinum-sensitive disease (15.8 months), although it was shorter in patients with resistant disease (10.9 months).
These data are “particularly encouraging,” comment the authors of an accompanying editorial, led by Oscar Arrieta, MD, from the Thoracic Oncology Unit at the Instituto Nacional de Cancerología in Mexico City, Mexico. These response rates “outperform all previous results achieved with topotecan and other less established treatment schemes including cyclophosphamide, doxorubicin, and vincristine, or platinum re-challenge, in this setting.”
“Lurbinectedin represents an innovative approach to conventional anti-cancer drugs, with an elegant mechanism of action based on the inhibition of transcription-dependent replication stress and genome instability of tumor cells,” the editorialists comment. “The drug binds to specific DNA triplets commonly found in transcription sites and triggers cellular apoptosis.”
“At present, the only evidence-based second-line treatment approved for SCLC is topotecan, a topoisomerase 1 inhibitor with moderate activity in patients with sensitive disease, although its effect is much less evident in patients with resistant SCLC,” they continue.
“Overall, the study by Trigo and colleagues presents novel data for a very challenging disease for which few treatment options exist, and the data on response and survival do seem to outperform data from historical controls,” Arrieta and colleagues write.
The editorialists also note that, in this trial, a few patients had received immunotherapy as part of their first-line treatment, and some of these patients (5 of 8 patients, 68%) had “an outstanding rate of durable response to lurbinectedin.” This raises the possibility of a synergistic effect between immunotherapy and lurbinectedin, as the combination seems to enhance immune memory and impair subsequent tumor growth, they add. Further trials will need to explore sequencing of therapy, they suggest.
A large phase 3 study known as ATLANTIS is currently underway.
The most common grade 3-4 adverse events in the present trial were hematologic abnormalities: anemia (9% of patients), leukopenia (29%), neutropenia (46%), and thrombocytopenia (7%). Serious treatment-related adverse events occurred in 10% of patients, of which neutropenia and febrile neutropenia were the most common (5% each). No treatment-related deaths were reported.
The study was funded by PharmaMar. Trigo and coauthors, and Arrieta and fellow editorialists, all report relationships with pharmaceutical companies, as detailed in the published articles.
This article first appeared on Medscape.com.
Patients with metastatic small-cell lung cancer (SCLC) whose disease has progressed after or during treatment with platinum-based chemotherapy now have a new option to try — lurbinectedin (Zepzelca, Jazz Pharma/PharmaMar).
The drug was granted accelerated approval by the US Food and Drug Administration (FDA) based on response data. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial, the FDA notes.
“Small-cell lung cancer is a disease with limited treatment options,” said Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals. “While patients may initially respond to traditional chemotherapy, they often experience an aggressive recurrence that is historically resistant to treatment.”
“Seeing first-hand the aggressive nature of SCLC and knowing that the large majority of those diagnosed will experience relapse, I am excited to see an effective new treatment demonstrating durable responses,” Jeff Petty, MD, oncology specialist, Wake Forest Baptist Health, Winston-Salem, North Carolina, commented in the company press release. This new drug “is an important and much-needed addition to the treatment landscape for relapsing SCLC,” he added.
Approval based on monotherapy trial
The approval is based on a monotherapy clinical trial in 105 patients, which was published in May in Lancet Oncology, with first author José Trigo, MD, from the Hospital Universitario Virgen de la Victoria in Malaga, Spain.
These were adult patients with both platinum-sensitive and platinum-resistant SCLC who had disease progression after treatment with platinum-based chemotherapy. They were treated at 26 hospitals across six European countries and the US. All patients received lurbinectedin at 3.2 mg/m2 by intravenous infusion over 1 hour. Median follow-up was 17.1 months.
Overall response by investigator assessment was seen in 37 (35.2%) of the 105 patients. The response was greater (at 45%) among the patients with platinum-sensitive disease and smaller (22.2%) among those with platinum-resistant disease.
Lurbinectedin demonstrated a median duration of response of 5.3 months as measured by investigator assessment.
In a post-hoc analysis, among the 37 patients who had an initial objective response, the median overall survival was just over 1 year (12.6 months). It was even longer among patients who had platinum-sensitive disease (15.8 months), although it was shorter in patients with resistant disease (10.9 months).
These data are “particularly encouraging,” comment the authors of an accompanying editorial, led by Oscar Arrieta, MD, from the Thoracic Oncology Unit at the Instituto Nacional de Cancerología in Mexico City, Mexico. These response rates “outperform all previous results achieved with topotecan and other less established treatment schemes including cyclophosphamide, doxorubicin, and vincristine, or platinum re-challenge, in this setting.”
“Lurbinectedin represents an innovative approach to conventional anti-cancer drugs, with an elegant mechanism of action based on the inhibition of transcription-dependent replication stress and genome instability of tumor cells,” the editorialists comment. “The drug binds to specific DNA triplets commonly found in transcription sites and triggers cellular apoptosis.”
“At present, the only evidence-based second-line treatment approved for SCLC is topotecan, a topoisomerase 1 inhibitor with moderate activity in patients with sensitive disease, although its effect is much less evident in patients with resistant SCLC,” they continue.
“Overall, the study by Trigo and colleagues presents novel data for a very challenging disease for which few treatment options exist, and the data on response and survival do seem to outperform data from historical controls,” Arrieta and colleagues write.
The editorialists also note that, in this trial, a few patients had received immunotherapy as part of their first-line treatment, and some of these patients (5 of 8 patients, 68%) had “an outstanding rate of durable response to lurbinectedin.” This raises the possibility of a synergistic effect between immunotherapy and lurbinectedin, as the combination seems to enhance immune memory and impair subsequent tumor growth, they add. Further trials will need to explore sequencing of therapy, they suggest.
A large phase 3 study known as ATLANTIS is currently underway.
The most common grade 3-4 adverse events in the present trial were hematologic abnormalities: anemia (9% of patients), leukopenia (29%), neutropenia (46%), and thrombocytopenia (7%). Serious treatment-related adverse events occurred in 10% of patients, of which neutropenia and febrile neutropenia were the most common (5% each). No treatment-related deaths were reported.
The study was funded by PharmaMar. Trigo and coauthors, and Arrieta and fellow editorialists, all report relationships with pharmaceutical companies, as detailed in the published articles.
This article first appeared on Medscape.com.
Health experts link rise in Arizona COVID cases to end of stay-at-home order
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Survey: 26% of parents hesitant about influenza vaccine
according to a nationally representative survey.
Influenza vaccination hesitancy may be driven by concerns about vaccine effectiveness, researchers wrote in Pediatrics. These findings “underscore the importance of better communicating to providers and parents the effectiveness of influenza vaccines in reducing severity and morbidity from influenza, even in years when the vaccine has relatively low effectiveness,” noted Allison Kempe, MD, MPH, professor of pediatrics and director of the Adult and Child Consortium for Health Outcomes Research and Delivery Science at the University of Colorado at Denver, Aurora, and colleagues.
The World Health Organization considers vaccine hesitancy a leading threat to global health, but national data about vaccine hesitancy in the United States are limited. To assess hesitancy about routine childhood and influenza vaccinations and related factors, Dr. Kempe and colleagues surveyed more than 2,000 parents in February 2019.
The investigators used an online panel to survey a nationally representative sample of families with children aged between 6 months and 18 years. Parents completed a modified version of the Vaccine Hesitancy Scale, which measures confidence in and concerns about vaccines. Parents with an average score greater than 3 on the scale were considered hesitant.
Factors associated with vaccine hesitancy
Of 4,445 parents sampled, 2,176 completed the survey and 2,052 were eligible respondents. For routine childhood vaccines, the average score on the modified Vaccine Hesitancy Scale was 2 and the percentage of hesitant parents was 6%. For influenza vaccine, the average score was 2 and the percentage of hesitant parents was 26%.
Among hesitant parents, 68% had deferred or refused routine childhood vaccination, compared with 9% of nonhesitant parents (risk ratio, 8.0). For the influenza vaccine, 70% of hesitant parents had deferred or refused influenza vaccination for their child versus 10% of nonhesitant parents (RR, 7.0). Parents were more likely to strongly agree that routine childhood vaccines are effective, compared with the influenza vaccine (70% vs. 26%). “Hesitancy about influenza vaccination is largely driven by concerns about low vaccine effectiveness,” Dr. Kempe and associates wrote.
Although concern about serious side effects was the factor most associated with hesitancy, the percentage of parents who were strongly (12%) or somewhat (27%) concerned about serious side effects was the same for routine childhood vaccines and influenza vaccines. Other factors associated with hesitancy for both routine childhood vaccines and influenza vaccines included lower educational level and household income less than 400% of the federal poverty level.
The survey data may be subject to reporting bias based on social desirability, the authors noted. In addition, the exclusion of infants younger than 6 months may have resulted in an underestimate of hesitancy.
“Although influenza vaccine could be included as a ‘routine’ vaccine, in that it is recommended yearly, we hypothesized that parents view it differently from other childhood vaccines because each year it needs to be given again, its content and effectiveness vary, and it addresses a disease that is often perceived as minor, compared with other childhood diseases,” Dr. Kempe and colleagues wrote. Interventions to counter hesitancy have “a surprising lack of evidence,” and “more work needs to be done to develop methods that are practical and effective for convincing vaccine-hesitant parents to vaccinate.”
Logical next step
“From the pragmatic standpoint of improving immunization rates and disease control, determining the correct evidence-based messaging to counter these perceptions is the next logical step,” Annabelle de St. Maurice, MD, MPH, an assistant professor of pediatrics in the division of infectious diseases at University of California, Los Angeles, and Kathryn Edwards, MD, a professor of pediatrics and director of the vaccine research program at Vanderbilt University, Nashville, wrote in an accompanying editorial.
“Communications should be focused on the burden of influenza in children, rebranding influenza vaccine as a ‘routine’ childhood immunization, reassurance on influenza vaccine safety, and discussion of the efficacy of influenza vaccine in preventing severe disease,” they wrote. “Even in the years when there is a poor match, the vaccine is impactful.”
The research was supported by the National Institutes of Health. Two study authors disclosed financial ties to Sanofi Pasteur, with one also disclosing financial ties to Merck, for work related to vaccinations. The remaining investigators had no relevant financial disclosures. Dr. de St. Maurice indicated that she had no relevant financial disclosures. Dr. Edwards disclosed grants from the Centers for Disease Control and Prevention and the NIH; consulting for Merck, Bionet, and IBM; and serving on data safety and monitoring boards for Sanofi, X4 Pharmaceuticals, Seqirus, Moderna, and Pfizer.
SOURCE: Kempe A et al. Pediatrics. 2020 Jun 15. doi: 10.1542/peds.2019-3852.
according to a nationally representative survey.
Influenza vaccination hesitancy may be driven by concerns about vaccine effectiveness, researchers wrote in Pediatrics. These findings “underscore the importance of better communicating to providers and parents the effectiveness of influenza vaccines in reducing severity and morbidity from influenza, even in years when the vaccine has relatively low effectiveness,” noted Allison Kempe, MD, MPH, professor of pediatrics and director of the Adult and Child Consortium for Health Outcomes Research and Delivery Science at the University of Colorado at Denver, Aurora, and colleagues.
The World Health Organization considers vaccine hesitancy a leading threat to global health, but national data about vaccine hesitancy in the United States are limited. To assess hesitancy about routine childhood and influenza vaccinations and related factors, Dr. Kempe and colleagues surveyed more than 2,000 parents in February 2019.
The investigators used an online panel to survey a nationally representative sample of families with children aged between 6 months and 18 years. Parents completed a modified version of the Vaccine Hesitancy Scale, which measures confidence in and concerns about vaccines. Parents with an average score greater than 3 on the scale were considered hesitant.
Factors associated with vaccine hesitancy
Of 4,445 parents sampled, 2,176 completed the survey and 2,052 were eligible respondents. For routine childhood vaccines, the average score on the modified Vaccine Hesitancy Scale was 2 and the percentage of hesitant parents was 6%. For influenza vaccine, the average score was 2 and the percentage of hesitant parents was 26%.
Among hesitant parents, 68% had deferred or refused routine childhood vaccination, compared with 9% of nonhesitant parents (risk ratio, 8.0). For the influenza vaccine, 70% of hesitant parents had deferred or refused influenza vaccination for their child versus 10% of nonhesitant parents (RR, 7.0). Parents were more likely to strongly agree that routine childhood vaccines are effective, compared with the influenza vaccine (70% vs. 26%). “Hesitancy about influenza vaccination is largely driven by concerns about low vaccine effectiveness,” Dr. Kempe and associates wrote.
Although concern about serious side effects was the factor most associated with hesitancy, the percentage of parents who were strongly (12%) or somewhat (27%) concerned about serious side effects was the same for routine childhood vaccines and influenza vaccines. Other factors associated with hesitancy for both routine childhood vaccines and influenza vaccines included lower educational level and household income less than 400% of the federal poverty level.
The survey data may be subject to reporting bias based on social desirability, the authors noted. In addition, the exclusion of infants younger than 6 months may have resulted in an underestimate of hesitancy.
“Although influenza vaccine could be included as a ‘routine’ vaccine, in that it is recommended yearly, we hypothesized that parents view it differently from other childhood vaccines because each year it needs to be given again, its content and effectiveness vary, and it addresses a disease that is often perceived as minor, compared with other childhood diseases,” Dr. Kempe and colleagues wrote. Interventions to counter hesitancy have “a surprising lack of evidence,” and “more work needs to be done to develop methods that are practical and effective for convincing vaccine-hesitant parents to vaccinate.”
Logical next step
“From the pragmatic standpoint of improving immunization rates and disease control, determining the correct evidence-based messaging to counter these perceptions is the next logical step,” Annabelle de St. Maurice, MD, MPH, an assistant professor of pediatrics in the division of infectious diseases at University of California, Los Angeles, and Kathryn Edwards, MD, a professor of pediatrics and director of the vaccine research program at Vanderbilt University, Nashville, wrote in an accompanying editorial.
“Communications should be focused on the burden of influenza in children, rebranding influenza vaccine as a ‘routine’ childhood immunization, reassurance on influenza vaccine safety, and discussion of the efficacy of influenza vaccine in preventing severe disease,” they wrote. “Even in the years when there is a poor match, the vaccine is impactful.”
The research was supported by the National Institutes of Health. Two study authors disclosed financial ties to Sanofi Pasteur, with one also disclosing financial ties to Merck, for work related to vaccinations. The remaining investigators had no relevant financial disclosures. Dr. de St. Maurice indicated that she had no relevant financial disclosures. Dr. Edwards disclosed grants from the Centers for Disease Control and Prevention and the NIH; consulting for Merck, Bionet, and IBM; and serving on data safety and monitoring boards for Sanofi, X4 Pharmaceuticals, Seqirus, Moderna, and Pfizer.
SOURCE: Kempe A et al. Pediatrics. 2020 Jun 15. doi: 10.1542/peds.2019-3852.
according to a nationally representative survey.
Influenza vaccination hesitancy may be driven by concerns about vaccine effectiveness, researchers wrote in Pediatrics. These findings “underscore the importance of better communicating to providers and parents the effectiveness of influenza vaccines in reducing severity and morbidity from influenza, even in years when the vaccine has relatively low effectiveness,” noted Allison Kempe, MD, MPH, professor of pediatrics and director of the Adult and Child Consortium for Health Outcomes Research and Delivery Science at the University of Colorado at Denver, Aurora, and colleagues.
The World Health Organization considers vaccine hesitancy a leading threat to global health, but national data about vaccine hesitancy in the United States are limited. To assess hesitancy about routine childhood and influenza vaccinations and related factors, Dr. Kempe and colleagues surveyed more than 2,000 parents in February 2019.
The investigators used an online panel to survey a nationally representative sample of families with children aged between 6 months and 18 years. Parents completed a modified version of the Vaccine Hesitancy Scale, which measures confidence in and concerns about vaccines. Parents with an average score greater than 3 on the scale were considered hesitant.
Factors associated with vaccine hesitancy
Of 4,445 parents sampled, 2,176 completed the survey and 2,052 were eligible respondents. For routine childhood vaccines, the average score on the modified Vaccine Hesitancy Scale was 2 and the percentage of hesitant parents was 6%. For influenza vaccine, the average score was 2 and the percentage of hesitant parents was 26%.
Among hesitant parents, 68% had deferred or refused routine childhood vaccination, compared with 9% of nonhesitant parents (risk ratio, 8.0). For the influenza vaccine, 70% of hesitant parents had deferred or refused influenza vaccination for their child versus 10% of nonhesitant parents (RR, 7.0). Parents were more likely to strongly agree that routine childhood vaccines are effective, compared with the influenza vaccine (70% vs. 26%). “Hesitancy about influenza vaccination is largely driven by concerns about low vaccine effectiveness,” Dr. Kempe and associates wrote.
Although concern about serious side effects was the factor most associated with hesitancy, the percentage of parents who were strongly (12%) or somewhat (27%) concerned about serious side effects was the same for routine childhood vaccines and influenza vaccines. Other factors associated with hesitancy for both routine childhood vaccines and influenza vaccines included lower educational level and household income less than 400% of the federal poverty level.
The survey data may be subject to reporting bias based on social desirability, the authors noted. In addition, the exclusion of infants younger than 6 months may have resulted in an underestimate of hesitancy.
“Although influenza vaccine could be included as a ‘routine’ vaccine, in that it is recommended yearly, we hypothesized that parents view it differently from other childhood vaccines because each year it needs to be given again, its content and effectiveness vary, and it addresses a disease that is often perceived as minor, compared with other childhood diseases,” Dr. Kempe and colleagues wrote. Interventions to counter hesitancy have “a surprising lack of evidence,” and “more work needs to be done to develop methods that are practical and effective for convincing vaccine-hesitant parents to vaccinate.”
Logical next step
“From the pragmatic standpoint of improving immunization rates and disease control, determining the correct evidence-based messaging to counter these perceptions is the next logical step,” Annabelle de St. Maurice, MD, MPH, an assistant professor of pediatrics in the division of infectious diseases at University of California, Los Angeles, and Kathryn Edwards, MD, a professor of pediatrics and director of the vaccine research program at Vanderbilt University, Nashville, wrote in an accompanying editorial.
“Communications should be focused on the burden of influenza in children, rebranding influenza vaccine as a ‘routine’ childhood immunization, reassurance on influenza vaccine safety, and discussion of the efficacy of influenza vaccine in preventing severe disease,” they wrote. “Even in the years when there is a poor match, the vaccine is impactful.”
The research was supported by the National Institutes of Health. Two study authors disclosed financial ties to Sanofi Pasteur, with one also disclosing financial ties to Merck, for work related to vaccinations. The remaining investigators had no relevant financial disclosures. Dr. de St. Maurice indicated that she had no relevant financial disclosures. Dr. Edwards disclosed grants from the Centers for Disease Control and Prevention and the NIH; consulting for Merck, Bionet, and IBM; and serving on data safety and monitoring boards for Sanofi, X4 Pharmaceuticals, Seqirus, Moderna, and Pfizer.
SOURCE: Kempe A et al. Pediatrics. 2020 Jun 15. doi: 10.1542/peds.2019-3852.
FROM PEDIATRICS
FDA revokes emergency use of hydroxychloroquine
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
Perfect storm of SARS-CoV-2 during flu season
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
Learning the ICU
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Smart phones boosted compliance for cardiac device data transmission
A phone, an app, and the next generation of implanted cardiac device data signaling produced an unprecedented level of data transmission compliance in a single-arm, multicenter, pilot study with 245 patients, adding momentum to the expanding penetration of personal smart devices into cardiac electrophysiology.
During 12-month follow-up, the 245 patients who received either a medically indicated pacemaker or cardiac resynchronization therapy (CRT)–pacemaker equipped with Bluetooth remote transmission capability had successful data transfer to their clinicians for 95% of their scheduled data uploads while using a personal phone or tablet as the link between their heart implant and the Internet. This rate significantly surpassed the transmission-success rates tallied by traditional, bedside transmitters in historical control groups, Khaldoun G. Tarakji, MD, said at the annual scientific sessions of the Heart Rhythm Society, held online because of COVID-19.
A related analysis by Dr. Tarakji and colleagues of 811 patients from real-world practice who received similar implanted cardiac devices with the same remote-transmission capability showed a 93% rate of successful data transfers via smart devices.
In contrast, historical performance showed a 77% success rate in matched patients drawn from a pool of more than 69,000 people in routine care who had received a pacemaker or CRT-pacemaker that automatically transmitted to a bedside monitor. Historical transmission success among matched patients from a pool of more than 128,000 routine-care patients with similar implants who used a wand to interrogate their implants before the attached monitor transmitted their data had a 56% rate of successful transmissions.
Cardiac device signals that flow directly into a patient’s phone or pad and then relay automatically via an app to the clinic “are clearly much easier,” than the methods now used, observed Dr. Tarakji, a cardiac electrophysiologist at the Cleveland Clinic. “It is truly as seamless as possible. Patients don’t really need to do anything,” he said during a press briefing. The key is that most patients tend to keep their smart devices, especially their phones, near them all the time, which minimizes the chance that the implanted cardiac device might try to file a report when the patient is not positioned near the device that’s facilitating transmission. When patients use conventional, bedside transmitters they can forget to bring them on trips, while many fewer fail to take their phone. Another advantage is that the link between a phone and a cardiac implant can be started in the clinic once the patient downloads an app. Bedside units need home setup, and “some patients never even get theirs out of the box,” Dr. Tarakji lamented.
Another feature of handheld device transmissions that run off an app is that the app can display clinical metrics, activity, device performance, and transmission history, as well as educational information. All of these features can enhance patient engagement with their implanted device, their arrhythmia, and their health status. Bedside units often give patients little feedback, and they don’t display clinical data. “The real challenge for clinicians is what data you let patients see. That’s complicated,” Dr. Tarakji said.
“This study was designed to see whether the technology works. The next step is to study how it affects risk-factor modification” or other outcomes. “There are many opportunities” to explore with this new data transmission and processing capability, he concluded.
The BlueSync Field Evaluation study enrolled patients at 20 centers in the United States, France, Italy, and the United Kingdom during 2018, and the 245 patients who received a BlueSync device and were included in the analysis sent at least one of their scheduled data transmissions during their 12 months of follow-up. Participants were eligible if they were willing to use their own smart phone or pad that could interact with their cardiac implant, and included both first-time implant recipients as well as some patients who received replacement units.
Personal device–based data transmission from cardiac implants “will no doubt change the way we manage patients,” commented Nassir F. Marrouche, MD, a cardiac electrophysiologist and professor of medicine at Tulane University in New Orleans, and a designated discussant for the report. “Every implanted cardiac device should be able to connect with a phone, which can improve adoption and adherence,” he said.
But the study has several limitations for interpreting the implications of the findings, starting with its limited size and single-arm design, noted a second discussant, Roderick Tung, MD, director of cardiac electrophysiology at the University of Chicago. Another issue is the generalizability of the findings, which are likely biased by involving only patients who own a smart phone or tablet and may be more likely to transmit their data regardless of the means. And comparing transmission success in a prospective study with rates that occurred during real-world, routine practice could have a Hawthorne effect bias, where people under study behave differently than they do in everyday life. But that effect may be mitigated by confirmatory findings from a real-world group that also used smart-device transmission included in the report. Despite these caveats, it’s valuable to develop new ways of improving data collection from cardiac devices, Dr. Tung said.
The BlueSync Field Evaluation study was sponsored by Medtronic, the company that markets Bluetooth-enabled cardiac devices. Dr. Tarakji has been a consultant to Medtronic, and also to AliveCor, Boston Scientific, and Johnson & Johnson. Dr. Marrouche has been a consultant to Medtronic as well as to Biosense Webster, Biotronik, Cardiac Design, and Preventice, and he has received research funding from Abbott, Biosense Webster, Boston Scientific, and GE Healthcare. Dr. Tung has been a speaker on behalf of Abbott, Boston Scientific, and Biosense Webster.
SOURCE: Tarakji KG. Heart Rhythm 2020, Abstract D-LBCT04-01.
A phone, an app, and the next generation of implanted cardiac device data signaling produced an unprecedented level of data transmission compliance in a single-arm, multicenter, pilot study with 245 patients, adding momentum to the expanding penetration of personal smart devices into cardiac electrophysiology.
During 12-month follow-up, the 245 patients who received either a medically indicated pacemaker or cardiac resynchronization therapy (CRT)–pacemaker equipped with Bluetooth remote transmission capability had successful data transfer to their clinicians for 95% of their scheduled data uploads while using a personal phone or tablet as the link between their heart implant and the Internet. This rate significantly surpassed the transmission-success rates tallied by traditional, bedside transmitters in historical control groups, Khaldoun G. Tarakji, MD, said at the annual scientific sessions of the Heart Rhythm Society, held online because of COVID-19.
A related analysis by Dr. Tarakji and colleagues of 811 patients from real-world practice who received similar implanted cardiac devices with the same remote-transmission capability showed a 93% rate of successful data transfers via smart devices.
In contrast, historical performance showed a 77% success rate in matched patients drawn from a pool of more than 69,000 people in routine care who had received a pacemaker or CRT-pacemaker that automatically transmitted to a bedside monitor. Historical transmission success among matched patients from a pool of more than 128,000 routine-care patients with similar implants who used a wand to interrogate their implants before the attached monitor transmitted their data had a 56% rate of successful transmissions.
Cardiac device signals that flow directly into a patient’s phone or pad and then relay automatically via an app to the clinic “are clearly much easier,” than the methods now used, observed Dr. Tarakji, a cardiac electrophysiologist at the Cleveland Clinic. “It is truly as seamless as possible. Patients don’t really need to do anything,” he said during a press briefing. The key is that most patients tend to keep their smart devices, especially their phones, near them all the time, which minimizes the chance that the implanted cardiac device might try to file a report when the patient is not positioned near the device that’s facilitating transmission. When patients use conventional, bedside transmitters they can forget to bring them on trips, while many fewer fail to take their phone. Another advantage is that the link between a phone and a cardiac implant can be started in the clinic once the patient downloads an app. Bedside units need home setup, and “some patients never even get theirs out of the box,” Dr. Tarakji lamented.
Another feature of handheld device transmissions that run off an app is that the app can display clinical metrics, activity, device performance, and transmission history, as well as educational information. All of these features can enhance patient engagement with their implanted device, their arrhythmia, and their health status. Bedside units often give patients little feedback, and they don’t display clinical data. “The real challenge for clinicians is what data you let patients see. That’s complicated,” Dr. Tarakji said.
“This study was designed to see whether the technology works. The next step is to study how it affects risk-factor modification” or other outcomes. “There are many opportunities” to explore with this new data transmission and processing capability, he concluded.
The BlueSync Field Evaluation study enrolled patients at 20 centers in the United States, France, Italy, and the United Kingdom during 2018, and the 245 patients who received a BlueSync device and were included in the analysis sent at least one of their scheduled data transmissions during their 12 months of follow-up. Participants were eligible if they were willing to use their own smart phone or pad that could interact with their cardiac implant, and included both first-time implant recipients as well as some patients who received replacement units.
Personal device–based data transmission from cardiac implants “will no doubt change the way we manage patients,” commented Nassir F. Marrouche, MD, a cardiac electrophysiologist and professor of medicine at Tulane University in New Orleans, and a designated discussant for the report. “Every implanted cardiac device should be able to connect with a phone, which can improve adoption and adherence,” he said.
But the study has several limitations for interpreting the implications of the findings, starting with its limited size and single-arm design, noted a second discussant, Roderick Tung, MD, director of cardiac electrophysiology at the University of Chicago. Another issue is the generalizability of the findings, which are likely biased by involving only patients who own a smart phone or tablet and may be more likely to transmit their data regardless of the means. And comparing transmission success in a prospective study with rates that occurred during real-world, routine practice could have a Hawthorne effect bias, where people under study behave differently than they do in everyday life. But that effect may be mitigated by confirmatory findings from a real-world group that also used smart-device transmission included in the report. Despite these caveats, it’s valuable to develop new ways of improving data collection from cardiac devices, Dr. Tung said.
The BlueSync Field Evaluation study was sponsored by Medtronic, the company that markets Bluetooth-enabled cardiac devices. Dr. Tarakji has been a consultant to Medtronic, and also to AliveCor, Boston Scientific, and Johnson & Johnson. Dr. Marrouche has been a consultant to Medtronic as well as to Biosense Webster, Biotronik, Cardiac Design, and Preventice, and he has received research funding from Abbott, Biosense Webster, Boston Scientific, and GE Healthcare. Dr. Tung has been a speaker on behalf of Abbott, Boston Scientific, and Biosense Webster.
SOURCE: Tarakji KG. Heart Rhythm 2020, Abstract D-LBCT04-01.
A phone, an app, and the next generation of implanted cardiac device data signaling produced an unprecedented level of data transmission compliance in a single-arm, multicenter, pilot study with 245 patients, adding momentum to the expanding penetration of personal smart devices into cardiac electrophysiology.
During 12-month follow-up, the 245 patients who received either a medically indicated pacemaker or cardiac resynchronization therapy (CRT)–pacemaker equipped with Bluetooth remote transmission capability had successful data transfer to their clinicians for 95% of their scheduled data uploads while using a personal phone or tablet as the link between their heart implant and the Internet. This rate significantly surpassed the transmission-success rates tallied by traditional, bedside transmitters in historical control groups, Khaldoun G. Tarakji, MD, said at the annual scientific sessions of the Heart Rhythm Society, held online because of COVID-19.
A related analysis by Dr. Tarakji and colleagues of 811 patients from real-world practice who received similar implanted cardiac devices with the same remote-transmission capability showed a 93% rate of successful data transfers via smart devices.
In contrast, historical performance showed a 77% success rate in matched patients drawn from a pool of more than 69,000 people in routine care who had received a pacemaker or CRT-pacemaker that automatically transmitted to a bedside monitor. Historical transmission success among matched patients from a pool of more than 128,000 routine-care patients with similar implants who used a wand to interrogate their implants before the attached monitor transmitted their data had a 56% rate of successful transmissions.
Cardiac device signals that flow directly into a patient’s phone or pad and then relay automatically via an app to the clinic “are clearly much easier,” than the methods now used, observed Dr. Tarakji, a cardiac electrophysiologist at the Cleveland Clinic. “It is truly as seamless as possible. Patients don’t really need to do anything,” he said during a press briefing. The key is that most patients tend to keep their smart devices, especially their phones, near them all the time, which minimizes the chance that the implanted cardiac device might try to file a report when the patient is not positioned near the device that’s facilitating transmission. When patients use conventional, bedside transmitters they can forget to bring them on trips, while many fewer fail to take their phone. Another advantage is that the link between a phone and a cardiac implant can be started in the clinic once the patient downloads an app. Bedside units need home setup, and “some patients never even get theirs out of the box,” Dr. Tarakji lamented.
Another feature of handheld device transmissions that run off an app is that the app can display clinical metrics, activity, device performance, and transmission history, as well as educational information. All of these features can enhance patient engagement with their implanted device, their arrhythmia, and their health status. Bedside units often give patients little feedback, and they don’t display clinical data. “The real challenge for clinicians is what data you let patients see. That’s complicated,” Dr. Tarakji said.
“This study was designed to see whether the technology works. The next step is to study how it affects risk-factor modification” or other outcomes. “There are many opportunities” to explore with this new data transmission and processing capability, he concluded.
The BlueSync Field Evaluation study enrolled patients at 20 centers in the United States, France, Italy, and the United Kingdom during 2018, and the 245 patients who received a BlueSync device and were included in the analysis sent at least one of their scheduled data transmissions during their 12 months of follow-up. Participants were eligible if they were willing to use their own smart phone or pad that could interact with their cardiac implant, and included both first-time implant recipients as well as some patients who received replacement units.
Personal device–based data transmission from cardiac implants “will no doubt change the way we manage patients,” commented Nassir F. Marrouche, MD, a cardiac electrophysiologist and professor of medicine at Tulane University in New Orleans, and a designated discussant for the report. “Every implanted cardiac device should be able to connect with a phone, which can improve adoption and adherence,” he said.
But the study has several limitations for interpreting the implications of the findings, starting with its limited size and single-arm design, noted a second discussant, Roderick Tung, MD, director of cardiac electrophysiology at the University of Chicago. Another issue is the generalizability of the findings, which are likely biased by involving only patients who own a smart phone or tablet and may be more likely to transmit their data regardless of the means. And comparing transmission success in a prospective study with rates that occurred during real-world, routine practice could have a Hawthorne effect bias, where people under study behave differently than they do in everyday life. But that effect may be mitigated by confirmatory findings from a real-world group that also used smart-device transmission included in the report. Despite these caveats, it’s valuable to develop new ways of improving data collection from cardiac devices, Dr. Tung said.
The BlueSync Field Evaluation study was sponsored by Medtronic, the company that markets Bluetooth-enabled cardiac devices. Dr. Tarakji has been a consultant to Medtronic, and also to AliveCor, Boston Scientific, and Johnson & Johnson. Dr. Marrouche has been a consultant to Medtronic as well as to Biosense Webster, Biotronik, Cardiac Design, and Preventice, and he has received research funding from Abbott, Biosense Webster, Boston Scientific, and GE Healthcare. Dr. Tung has been a speaker on behalf of Abbott, Boston Scientific, and Biosense Webster.
SOURCE: Tarakji KG. Heart Rhythm 2020, Abstract D-LBCT04-01.
FROM HEART RHYTHM 2020
Seropositivity in RA linked with doubled pneumonia incidence
from a single U.S. medical system.
“Patients with seropositive RA, particularly RF [rheumatoid factor]-positive RA, had increased risk for pneumonia throughout the RA disease course that was not explained by measured confounders, including smoking status, multimorbidity, medications, and [erythrocyte sedimentation rate] level,” Jeffrey A. Sparks, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“There has been much interest about the relationship between lung inflammation and the generation of RF and CCP [cyclic citrullinated protein] prior to the onset of RA. We hypothesized that patients with seropositive RA might have subclinical lung injury that could predispose them to pneumonia after clinical RA onset,” Dr. Sparks said in an interview. “Pneumonia is one of the most common serious infections in both patients with RA and the general population, and it causes serious morbidity and mortality.”
The doubled relative risk for pneumonia seen in the findings “translates into a clinically meaningful finding when considering the high rate and the many patients at risk since RA is relatively common,” said Dr. Sparks, a rheumatologist at Brigham and Women’s Hospital in Boston.
“Patients with RF-positive RA who present with symptoms concerning for pneumonia should be evaluated carefully for this and for other possible pulmonary manifestations of RA. Vaccination for pneumonia should be strongly considered for patients with RA who are on disease-modifying antirheumatic drugs, and we hope that our report encourages clinicians and patients” to undertake vaccination, he said.
His study used a database of more than 60,000 patients diagnosed with RA as of November 2013 in the records of a large Boston-area medical system that includes physicians affiliated with Brigham and Women’s Hospital and Massachusetts General Hospital. The researchers applied a validated algorithm for calculating a patient’s probability of having RA, and at the level of 97% probability they narrowed the cohort down to just under 10,000 patients. Additional winnowing because of missing data or a history of pneumonia yielded a study group of 4,110, which included 3,279 (80%) who were seropositive for either or both CCP and RF, and 831 (20%) who were seronegative. During a median follow-up of 7.8 years and total follow-up of more than 32,000 patient-years, the overall pneumonia incidence was 5.8%, with a 2.8% rate among the seronegatives and a 6.6% rate among seropositives. After adjustment for age, sex, glucocorticoid use, disease-modifying antirheumatic drug use, and several other possible confounders, the researchers calculated a 99% relative increased rate of pneumonia among all seropositive patients, compared with the seronegatives.
Further analysis looked at pneumonia incidence rates among patients positive only for CCP antibody, positive only for RF antibody, or both, compared with seronegative patients. This showed that CCP seropositivity had no statistically significant link with incident pneumonia, while RF seropositivity linked with a statistically significant, roughly twofold higher rate. Only 6% of all seropositive patients were positive only for CCP antibody, 59% were positive specifically for RF antibody, and 35% for both.
The data Dr. Sparks presented did not include information on pneumonia type, the timing of the pneumonia, compared with the onset of RA, disease activity, or smoking intensity.
“We anticipated that both RF positive and CCP positive would each be associated with pneumonia, so it was somewhat surprising that we only detected this for RF,” Dr. Sparks said. But he added that, because the number of patients with only CCP positivity was relatively so small, “it is still possible that CCP [antibody] could also increase pneumonia risk.”
The study had no commercial funding. Dr. Sparks had no disclosures.
SOURCE: Sparks JA et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:73, Abstract OP0111.
from a single U.S. medical system.
“Patients with seropositive RA, particularly RF [rheumatoid factor]-positive RA, had increased risk for pneumonia throughout the RA disease course that was not explained by measured confounders, including smoking status, multimorbidity, medications, and [erythrocyte sedimentation rate] level,” Jeffrey A. Sparks, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“There has been much interest about the relationship between lung inflammation and the generation of RF and CCP [cyclic citrullinated protein] prior to the onset of RA. We hypothesized that patients with seropositive RA might have subclinical lung injury that could predispose them to pneumonia after clinical RA onset,” Dr. Sparks said in an interview. “Pneumonia is one of the most common serious infections in both patients with RA and the general population, and it causes serious morbidity and mortality.”
The doubled relative risk for pneumonia seen in the findings “translates into a clinically meaningful finding when considering the high rate and the many patients at risk since RA is relatively common,” said Dr. Sparks, a rheumatologist at Brigham and Women’s Hospital in Boston.
“Patients with RF-positive RA who present with symptoms concerning for pneumonia should be evaluated carefully for this and for other possible pulmonary manifestations of RA. Vaccination for pneumonia should be strongly considered for patients with RA who are on disease-modifying antirheumatic drugs, and we hope that our report encourages clinicians and patients” to undertake vaccination, he said.
His study used a database of more than 60,000 patients diagnosed with RA as of November 2013 in the records of a large Boston-area medical system that includes physicians affiliated with Brigham and Women’s Hospital and Massachusetts General Hospital. The researchers applied a validated algorithm for calculating a patient’s probability of having RA, and at the level of 97% probability they narrowed the cohort down to just under 10,000 patients. Additional winnowing because of missing data or a history of pneumonia yielded a study group of 4,110, which included 3,279 (80%) who were seropositive for either or both CCP and RF, and 831 (20%) who were seronegative. During a median follow-up of 7.8 years and total follow-up of more than 32,000 patient-years, the overall pneumonia incidence was 5.8%, with a 2.8% rate among the seronegatives and a 6.6% rate among seropositives. After adjustment for age, sex, glucocorticoid use, disease-modifying antirheumatic drug use, and several other possible confounders, the researchers calculated a 99% relative increased rate of pneumonia among all seropositive patients, compared with the seronegatives.
Further analysis looked at pneumonia incidence rates among patients positive only for CCP antibody, positive only for RF antibody, or both, compared with seronegative patients. This showed that CCP seropositivity had no statistically significant link with incident pneumonia, while RF seropositivity linked with a statistically significant, roughly twofold higher rate. Only 6% of all seropositive patients were positive only for CCP antibody, 59% were positive specifically for RF antibody, and 35% for both.
The data Dr. Sparks presented did not include information on pneumonia type, the timing of the pneumonia, compared with the onset of RA, disease activity, or smoking intensity.
“We anticipated that both RF positive and CCP positive would each be associated with pneumonia, so it was somewhat surprising that we only detected this for RF,” Dr. Sparks said. But he added that, because the number of patients with only CCP positivity was relatively so small, “it is still possible that CCP [antibody] could also increase pneumonia risk.”
The study had no commercial funding. Dr. Sparks had no disclosures.
SOURCE: Sparks JA et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:73, Abstract OP0111.
from a single U.S. medical system.
“Patients with seropositive RA, particularly RF [rheumatoid factor]-positive RA, had increased risk for pneumonia throughout the RA disease course that was not explained by measured confounders, including smoking status, multimorbidity, medications, and [erythrocyte sedimentation rate] level,” Jeffrey A. Sparks, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
“There has been much interest about the relationship between lung inflammation and the generation of RF and CCP [cyclic citrullinated protein] prior to the onset of RA. We hypothesized that patients with seropositive RA might have subclinical lung injury that could predispose them to pneumonia after clinical RA onset,” Dr. Sparks said in an interview. “Pneumonia is one of the most common serious infections in both patients with RA and the general population, and it causes serious morbidity and mortality.”
The doubled relative risk for pneumonia seen in the findings “translates into a clinically meaningful finding when considering the high rate and the many patients at risk since RA is relatively common,” said Dr. Sparks, a rheumatologist at Brigham and Women’s Hospital in Boston.
“Patients with RF-positive RA who present with symptoms concerning for pneumonia should be evaluated carefully for this and for other possible pulmonary manifestations of RA. Vaccination for pneumonia should be strongly considered for patients with RA who are on disease-modifying antirheumatic drugs, and we hope that our report encourages clinicians and patients” to undertake vaccination, he said.
His study used a database of more than 60,000 patients diagnosed with RA as of November 2013 in the records of a large Boston-area medical system that includes physicians affiliated with Brigham and Women’s Hospital and Massachusetts General Hospital. The researchers applied a validated algorithm for calculating a patient’s probability of having RA, and at the level of 97% probability they narrowed the cohort down to just under 10,000 patients. Additional winnowing because of missing data or a history of pneumonia yielded a study group of 4,110, which included 3,279 (80%) who were seropositive for either or both CCP and RF, and 831 (20%) who were seronegative. During a median follow-up of 7.8 years and total follow-up of more than 32,000 patient-years, the overall pneumonia incidence was 5.8%, with a 2.8% rate among the seronegatives and a 6.6% rate among seropositives. After adjustment for age, sex, glucocorticoid use, disease-modifying antirheumatic drug use, and several other possible confounders, the researchers calculated a 99% relative increased rate of pneumonia among all seropositive patients, compared with the seronegatives.
Further analysis looked at pneumonia incidence rates among patients positive only for CCP antibody, positive only for RF antibody, or both, compared with seronegative patients. This showed that CCP seropositivity had no statistically significant link with incident pneumonia, while RF seropositivity linked with a statistically significant, roughly twofold higher rate. Only 6% of all seropositive patients were positive only for CCP antibody, 59% were positive specifically for RF antibody, and 35% for both.
The data Dr. Sparks presented did not include information on pneumonia type, the timing of the pneumonia, compared with the onset of RA, disease activity, or smoking intensity.
“We anticipated that both RF positive and CCP positive would each be associated with pneumonia, so it was somewhat surprising that we only detected this for RF,” Dr. Sparks said. But he added that, because the number of patients with only CCP positivity was relatively so small, “it is still possible that CCP [antibody] could also increase pneumonia risk.”
The study had no commercial funding. Dr. Sparks had no disclosures.
SOURCE: Sparks JA et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:73, Abstract OP0111.
FROM THE EULAR 2020 E-CONGRESS