User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Many physicians live within their means and save, survey shows
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Tiragolumab plus atezolizumab active in PD-L1+ NSCLC
The combination of the anti-TIGIT antibody tiragolumab with the PD-L1 inhibitor atezolizumab was well tolerated and showed preliminary activity in the phase 1b portion of the study, according to investigator Johanna C. Bendell, MD, of Sarah Cannon Research Institute/Tennessee Oncology in Nashville, Tenn.
Objective responses occurred mainly in chemoimmunotherapy-naive, PD-L1-positive tumors. In an expansion cohort of 13 patients with PD-L1-positive non–small cell lung cancer (NSCLC), the confirmed overall response rate was 46%, with several responses demonstrating durability.
Dr. Bendell reported these results at the AACR virtual meeting II.
While several important research questions remain, the results in the lung cancer expansion cohort were encouraging, particularly in patients who were smokers and previous smokers, said invited discussant Michele Teng, PhD, of QIMR Berghofer Medical Research Institute in Brisbane, Australia.
“Although it was [a] small cohort, the data suggest promising duration of response in some of the patients [n = 4] who have been under study for more than 700 days,” Dr. Teng said.
Based on the preliminary safety and activity seen in this study, the combination of tiragolumab and atezolizumab is being evaluated in a randomized, placebo-controlled phase 2 study, and a phase 3 study is recruiting.
Rationale, design, and safety
TIGIT is a novel inhibitory receptor expressed on multiple immune cells, especially CD8-positive T cells and natural killer cells, Dr. Bendell explained. She added that TIGIT is coexpressed with PD-1 on immune cells.
“Using anti-TIGIT antibodies to prevent TIGIT from binding, and cotargeting TIGIT and PD-L1, may restore antitumor response and enhance anti-PD-L1 effect,” Dr. Bendell said.
The phase 1 study Dr. Bendell presented, known as GO30103, was designed to evaluate tiragolumab as a single agent and in combination with atezolizumab in advanced solid tumors.
There were 24 patients in the phase 1a portion of GO30103, which was intended to determine the preliminary safety, tolerability, and recommended phase 2 dose of tiragolumab. There were 49 patients treated with tiragolumab plus atezolizumab in the phase 1b portion, which was intended to provide data on pharmacokinetics as well as preliminary antitumor activity of the combination.
No dose-limiting toxicities were seen in either cohort. The recommended phase 2 dose of tiragolumab was 600 mg every 3 weeks.
Tiragolumab was well tolerated in the phase 1a and 1b portions of the trial, according to Dr. Bendell.
“Immune-related adverse events were seen, but their incidence was not out of proportion to events seen with atezolizumab alone,” she said.
Treatment-related grade 3-4 adverse events occurred in one patient (4%) in the phase 1a portion of the trial and two patients (4%) in the phase 1b portion. There were no grade 5 adverse events related to treatment.
Efficacy and next steps
No objective responses were seen with tiragolumab monotherapy, although several patients did exhibit tumor reduction.
“We were not really expecting much single-agent activity of the anti-TIGIT drug,” Dr. Bendell said. “There’s some preclinical data that suggests that TIGIT may be more important as a single agent in earlier stages of cancer.”
In contrast, the combination of tiragolumab and atezolizumab resulted in several responses, including one in a patient with PD-L1-positive NSCLC who was previously treated with immunotherapy, according to Dr. Bendell.
The 13-patient expansion cohort of patients with PD-L1-positive NSCLC were treated at the recommended phase 2 dose of tiragolumab and atezolizumab. In these chemoimmunotherapy-naive patients, the overall response rate was 46%. Responses occurred in 6 of 13 patients and included 2 complete responses. Four patients had stable disease, so the disease control rate was 85% (11/13).
Based on that expansion cohort, a randomized, phase 2 study called CITYSCAPE was initiated. Results of CITYSCAPE were recently presented as part of the American Society of Clinical Oncology virtual scientific program.
In that study, tiragolumab plus atezolizumab improved the overall response rate and progression-free survival when compared with placebo plus atezolizumab. More substantial improvement was seen in the subgroup of patients with PD-L1 tumor proportion scores of 50% or greater.
The activity and safety of tiragolumab plus atezolizumab will be confirmed in the ongoing SKYSCRAPER-01 trial (NCT04294810), a phase 3 study of first-line treatment in patients with NSCLC and a PD-L1 tumor proportion score of 50% or greater, according to investigators.
The phase 1 study presented by Dr. Bendell was sponsored by Genentech. Dr. Bendell disclosed relationships with Genentech/Roche, Gilead, Five Prime, Lilly, and other companies.
SOURCE: Bendell JC et al. AACR 2020, Abstract CT302.
The combination of the anti-TIGIT antibody tiragolumab with the PD-L1 inhibitor atezolizumab was well tolerated and showed preliminary activity in the phase 1b portion of the study, according to investigator Johanna C. Bendell, MD, of Sarah Cannon Research Institute/Tennessee Oncology in Nashville, Tenn.
Objective responses occurred mainly in chemoimmunotherapy-naive, PD-L1-positive tumors. In an expansion cohort of 13 patients with PD-L1-positive non–small cell lung cancer (NSCLC), the confirmed overall response rate was 46%, with several responses demonstrating durability.
Dr. Bendell reported these results at the AACR virtual meeting II.
While several important research questions remain, the results in the lung cancer expansion cohort were encouraging, particularly in patients who were smokers and previous smokers, said invited discussant Michele Teng, PhD, of QIMR Berghofer Medical Research Institute in Brisbane, Australia.
“Although it was [a] small cohort, the data suggest promising duration of response in some of the patients [n = 4] who have been under study for more than 700 days,” Dr. Teng said.
Based on the preliminary safety and activity seen in this study, the combination of tiragolumab and atezolizumab is being evaluated in a randomized, placebo-controlled phase 2 study, and a phase 3 study is recruiting.
Rationale, design, and safety
TIGIT is a novel inhibitory receptor expressed on multiple immune cells, especially CD8-positive T cells and natural killer cells, Dr. Bendell explained. She added that TIGIT is coexpressed with PD-1 on immune cells.
“Using anti-TIGIT antibodies to prevent TIGIT from binding, and cotargeting TIGIT and PD-L1, may restore antitumor response and enhance anti-PD-L1 effect,” Dr. Bendell said.
The phase 1 study Dr. Bendell presented, known as GO30103, was designed to evaluate tiragolumab as a single agent and in combination with atezolizumab in advanced solid tumors.
There were 24 patients in the phase 1a portion of GO30103, which was intended to determine the preliminary safety, tolerability, and recommended phase 2 dose of tiragolumab. There were 49 patients treated with tiragolumab plus atezolizumab in the phase 1b portion, which was intended to provide data on pharmacokinetics as well as preliminary antitumor activity of the combination.
No dose-limiting toxicities were seen in either cohort. The recommended phase 2 dose of tiragolumab was 600 mg every 3 weeks.
Tiragolumab was well tolerated in the phase 1a and 1b portions of the trial, according to Dr. Bendell.
“Immune-related adverse events were seen, but their incidence was not out of proportion to events seen with atezolizumab alone,” she said.
Treatment-related grade 3-4 adverse events occurred in one patient (4%) in the phase 1a portion of the trial and two patients (4%) in the phase 1b portion. There were no grade 5 adverse events related to treatment.
Efficacy and next steps
No objective responses were seen with tiragolumab monotherapy, although several patients did exhibit tumor reduction.
“We were not really expecting much single-agent activity of the anti-TIGIT drug,” Dr. Bendell said. “There’s some preclinical data that suggests that TIGIT may be more important as a single agent in earlier stages of cancer.”
In contrast, the combination of tiragolumab and atezolizumab resulted in several responses, including one in a patient with PD-L1-positive NSCLC who was previously treated with immunotherapy, according to Dr. Bendell.
The 13-patient expansion cohort of patients with PD-L1-positive NSCLC were treated at the recommended phase 2 dose of tiragolumab and atezolizumab. In these chemoimmunotherapy-naive patients, the overall response rate was 46%. Responses occurred in 6 of 13 patients and included 2 complete responses. Four patients had stable disease, so the disease control rate was 85% (11/13).
Based on that expansion cohort, a randomized, phase 2 study called CITYSCAPE was initiated. Results of CITYSCAPE were recently presented as part of the American Society of Clinical Oncology virtual scientific program.
In that study, tiragolumab plus atezolizumab improved the overall response rate and progression-free survival when compared with placebo plus atezolizumab. More substantial improvement was seen in the subgroup of patients with PD-L1 tumor proportion scores of 50% or greater.
The activity and safety of tiragolumab plus atezolizumab will be confirmed in the ongoing SKYSCRAPER-01 trial (NCT04294810), a phase 3 study of first-line treatment in patients with NSCLC and a PD-L1 tumor proportion score of 50% or greater, according to investigators.
The phase 1 study presented by Dr. Bendell was sponsored by Genentech. Dr. Bendell disclosed relationships with Genentech/Roche, Gilead, Five Prime, Lilly, and other companies.
SOURCE: Bendell JC et al. AACR 2020, Abstract CT302.
The combination of the anti-TIGIT antibody tiragolumab with the PD-L1 inhibitor atezolizumab was well tolerated and showed preliminary activity in the phase 1b portion of the study, according to investigator Johanna C. Bendell, MD, of Sarah Cannon Research Institute/Tennessee Oncology in Nashville, Tenn.
Objective responses occurred mainly in chemoimmunotherapy-naive, PD-L1-positive tumors. In an expansion cohort of 13 patients with PD-L1-positive non–small cell lung cancer (NSCLC), the confirmed overall response rate was 46%, with several responses demonstrating durability.
Dr. Bendell reported these results at the AACR virtual meeting II.
While several important research questions remain, the results in the lung cancer expansion cohort were encouraging, particularly in patients who were smokers and previous smokers, said invited discussant Michele Teng, PhD, of QIMR Berghofer Medical Research Institute in Brisbane, Australia.
“Although it was [a] small cohort, the data suggest promising duration of response in some of the patients [n = 4] who have been under study for more than 700 days,” Dr. Teng said.
Based on the preliminary safety and activity seen in this study, the combination of tiragolumab and atezolizumab is being evaluated in a randomized, placebo-controlled phase 2 study, and a phase 3 study is recruiting.
Rationale, design, and safety
TIGIT is a novel inhibitory receptor expressed on multiple immune cells, especially CD8-positive T cells and natural killer cells, Dr. Bendell explained. She added that TIGIT is coexpressed with PD-1 on immune cells.
“Using anti-TIGIT antibodies to prevent TIGIT from binding, and cotargeting TIGIT and PD-L1, may restore antitumor response and enhance anti-PD-L1 effect,” Dr. Bendell said.
The phase 1 study Dr. Bendell presented, known as GO30103, was designed to evaluate tiragolumab as a single agent and in combination with atezolizumab in advanced solid tumors.
There were 24 patients in the phase 1a portion of GO30103, which was intended to determine the preliminary safety, tolerability, and recommended phase 2 dose of tiragolumab. There were 49 patients treated with tiragolumab plus atezolizumab in the phase 1b portion, which was intended to provide data on pharmacokinetics as well as preliminary antitumor activity of the combination.
No dose-limiting toxicities were seen in either cohort. The recommended phase 2 dose of tiragolumab was 600 mg every 3 weeks.
Tiragolumab was well tolerated in the phase 1a and 1b portions of the trial, according to Dr. Bendell.
“Immune-related adverse events were seen, but their incidence was not out of proportion to events seen with atezolizumab alone,” she said.
Treatment-related grade 3-4 adverse events occurred in one patient (4%) in the phase 1a portion of the trial and two patients (4%) in the phase 1b portion. There were no grade 5 adverse events related to treatment.
Efficacy and next steps
No objective responses were seen with tiragolumab monotherapy, although several patients did exhibit tumor reduction.
“We were not really expecting much single-agent activity of the anti-TIGIT drug,” Dr. Bendell said. “There’s some preclinical data that suggests that TIGIT may be more important as a single agent in earlier stages of cancer.”
In contrast, the combination of tiragolumab and atezolizumab resulted in several responses, including one in a patient with PD-L1-positive NSCLC who was previously treated with immunotherapy, according to Dr. Bendell.
The 13-patient expansion cohort of patients with PD-L1-positive NSCLC were treated at the recommended phase 2 dose of tiragolumab and atezolizumab. In these chemoimmunotherapy-naive patients, the overall response rate was 46%. Responses occurred in 6 of 13 patients and included 2 complete responses. Four patients had stable disease, so the disease control rate was 85% (11/13).
Based on that expansion cohort, a randomized, phase 2 study called CITYSCAPE was initiated. Results of CITYSCAPE were recently presented as part of the American Society of Clinical Oncology virtual scientific program.
In that study, tiragolumab plus atezolizumab improved the overall response rate and progression-free survival when compared with placebo plus atezolizumab. More substantial improvement was seen in the subgroup of patients with PD-L1 tumor proportion scores of 50% or greater.
The activity and safety of tiragolumab plus atezolizumab will be confirmed in the ongoing SKYSCRAPER-01 trial (NCT04294810), a phase 3 study of first-line treatment in patients with NSCLC and a PD-L1 tumor proportion score of 50% or greater, according to investigators.
The phase 1 study presented by Dr. Bendell was sponsored by Genentech. Dr. Bendell disclosed relationships with Genentech/Roche, Gilead, Five Prime, Lilly, and other companies.
SOURCE: Bendell JC et al. AACR 2020, Abstract CT302.
FROM AACR 2020
Skin patterns of COVID-19 vary widely
according to Christine Ko, MD.
“Things are very fluid,” Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn., said during the virtual annual meeting of the American Academy of Dermatology. “New studies are coming out daily. Due to the need for rapid dissemination, a lot of the studies are case reports, but there are some nice case series. Another caveat for the literature is that a lot of these cases were not necessarily confirmed with testing for SARS-CoV-2, but some were.”
Dr. Ko framed her remarks largely on a case collection survey of images and clinical data from 375 patients in Spain with suspected or confirmed COVID-19 that was published online April 29, 2020, in the British Journal of Dermatology (doi: 10.1111/bjd.19163). Cutaneous manifestations included early vesicular eruptions mainly on the trunk or limbs (9%), maculopapular (47%) to urticarial lesions (19%) mainly on the trunk, and acral areas of erythema sometimes with vesicles or erosion (perniosis-like) (19%) that seemed to be a later manifestation of COVID-19. Retiform purpura or necrosis (6%) was most concerning in terms of skin disease, with an associated with a mortality of 10%.
On histology, the early vesicular eruptions are typically marked by dyskeratotic keratinocytes, Dr. Ko said, while urticarial lesions are characterized by a mixed dermal infiltrate; maculopapular lesions were a broad category. “There are some case reports that show spongiotic dermatitis or parakeratosis with a lymphocytic infiltrate,” she said. “A caveat to keep in mind is that, although these patients may definitely have COVID-19 and be confirmed to have it by testing, hypersensitivity reactions may be due to the multiple medications they’re on.”
Patients can develop a spectrum of lesions that are suggestive of vascular damage or occlusion, Dr. Ko continued. Livedoid lesions may remain static and not eventuate into necrosis or purpura but will self-resolve. Purpuric lesions and acral gangrene have been described, and these lesions correspond to vascular occlusion on biopsy.
A later manifestation are the so-called “COVID toes” with a superficial and deep lymphocytic infiltrate, as published June 1, 2020, in JAAD Case Reports: (doi: 10.1016/j.jdcr.2020.04.011).
“There are patients in the literature that have slightly different pathology, with lymphocytic inflammation as well as occlusion of vessels,” Dr. Ko said. A paper published June 20, 2020, in the British Journal of Dermatology used immunohistochemical staining against the SARS-CoV-2 spike protein, and biopsies of “COVID toes” had positive staining of endothelial cells, supporting the notion that “COVID toes” are a direct manifestation of viral infection (doi: 10.1111/bjd.19327).
“There’s a lot that we still don’t know, and some patterns are going to be outliers,” Dr. Ko concluded. “[As for] determining which skin manifestations are directly from coronavirus infection within the skin, more study is needed and likely time will tell.” She reported having no financial disclosures relevant to her talk.
according to Christine Ko, MD.
“Things are very fluid,” Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn., said during the virtual annual meeting of the American Academy of Dermatology. “New studies are coming out daily. Due to the need for rapid dissemination, a lot of the studies are case reports, but there are some nice case series. Another caveat for the literature is that a lot of these cases were not necessarily confirmed with testing for SARS-CoV-2, but some were.”
Dr. Ko framed her remarks largely on a case collection survey of images and clinical data from 375 patients in Spain with suspected or confirmed COVID-19 that was published online April 29, 2020, in the British Journal of Dermatology (doi: 10.1111/bjd.19163). Cutaneous manifestations included early vesicular eruptions mainly on the trunk or limbs (9%), maculopapular (47%) to urticarial lesions (19%) mainly on the trunk, and acral areas of erythema sometimes with vesicles or erosion (perniosis-like) (19%) that seemed to be a later manifestation of COVID-19. Retiform purpura or necrosis (6%) was most concerning in terms of skin disease, with an associated with a mortality of 10%.
On histology, the early vesicular eruptions are typically marked by dyskeratotic keratinocytes, Dr. Ko said, while urticarial lesions are characterized by a mixed dermal infiltrate; maculopapular lesions were a broad category. “There are some case reports that show spongiotic dermatitis or parakeratosis with a lymphocytic infiltrate,” she said. “A caveat to keep in mind is that, although these patients may definitely have COVID-19 and be confirmed to have it by testing, hypersensitivity reactions may be due to the multiple medications they’re on.”
Patients can develop a spectrum of lesions that are suggestive of vascular damage or occlusion, Dr. Ko continued. Livedoid lesions may remain static and not eventuate into necrosis or purpura but will self-resolve. Purpuric lesions and acral gangrene have been described, and these lesions correspond to vascular occlusion on biopsy.
A later manifestation are the so-called “COVID toes” with a superficial and deep lymphocytic infiltrate, as published June 1, 2020, in JAAD Case Reports: (doi: 10.1016/j.jdcr.2020.04.011).
“There are patients in the literature that have slightly different pathology, with lymphocytic inflammation as well as occlusion of vessels,” Dr. Ko said. A paper published June 20, 2020, in the British Journal of Dermatology used immunohistochemical staining against the SARS-CoV-2 spike protein, and biopsies of “COVID toes” had positive staining of endothelial cells, supporting the notion that “COVID toes” are a direct manifestation of viral infection (doi: 10.1111/bjd.19327).
“There’s a lot that we still don’t know, and some patterns are going to be outliers,” Dr. Ko concluded. “[As for] determining which skin manifestations are directly from coronavirus infection within the skin, more study is needed and likely time will tell.” She reported having no financial disclosures relevant to her talk.
according to Christine Ko, MD.
“Things are very fluid,” Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn., said during the virtual annual meeting of the American Academy of Dermatology. “New studies are coming out daily. Due to the need for rapid dissemination, a lot of the studies are case reports, but there are some nice case series. Another caveat for the literature is that a lot of these cases were not necessarily confirmed with testing for SARS-CoV-2, but some were.”
Dr. Ko framed her remarks largely on a case collection survey of images and clinical data from 375 patients in Spain with suspected or confirmed COVID-19 that was published online April 29, 2020, in the British Journal of Dermatology (doi: 10.1111/bjd.19163). Cutaneous manifestations included early vesicular eruptions mainly on the trunk or limbs (9%), maculopapular (47%) to urticarial lesions (19%) mainly on the trunk, and acral areas of erythema sometimes with vesicles or erosion (perniosis-like) (19%) that seemed to be a later manifestation of COVID-19. Retiform purpura or necrosis (6%) was most concerning in terms of skin disease, with an associated with a mortality of 10%.
On histology, the early vesicular eruptions are typically marked by dyskeratotic keratinocytes, Dr. Ko said, while urticarial lesions are characterized by a mixed dermal infiltrate; maculopapular lesions were a broad category. “There are some case reports that show spongiotic dermatitis or parakeratosis with a lymphocytic infiltrate,” she said. “A caveat to keep in mind is that, although these patients may definitely have COVID-19 and be confirmed to have it by testing, hypersensitivity reactions may be due to the multiple medications they’re on.”
Patients can develop a spectrum of lesions that are suggestive of vascular damage or occlusion, Dr. Ko continued. Livedoid lesions may remain static and not eventuate into necrosis or purpura but will self-resolve. Purpuric lesions and acral gangrene have been described, and these lesions correspond to vascular occlusion on biopsy.
A later manifestation are the so-called “COVID toes” with a superficial and deep lymphocytic infiltrate, as published June 1, 2020, in JAAD Case Reports: (doi: 10.1016/j.jdcr.2020.04.011).
“There are patients in the literature that have slightly different pathology, with lymphocytic inflammation as well as occlusion of vessels,” Dr. Ko said. A paper published June 20, 2020, in the British Journal of Dermatology used immunohistochemical staining against the SARS-CoV-2 spike protein, and biopsies of “COVID toes” had positive staining of endothelial cells, supporting the notion that “COVID toes” are a direct manifestation of viral infection (doi: 10.1111/bjd.19327).
“There’s a lot that we still don’t know, and some patterns are going to be outliers,” Dr. Ko concluded. “[As for] determining which skin manifestations are directly from coronavirus infection within the skin, more study is needed and likely time will tell.” She reported having no financial disclosures relevant to her talk.
FROM AAD 20
Daily Recap: Transgender patients turn to DIY treatments; ACIP plans priority vaccine groups
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
How racism contributes to the effects of SARS-CoV-2
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
ACIP plans priority groups in advance of COVID-19 vaccine
according to Sarah Mbaeyi, MD, MPH, of the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
“Preparing for vaccination during a pandemic has long been a priority of the CDC and the U.S. government,” said Dr. Mbaeyi. The work group is building on a tiered approach to vaccination that was updated in 2018 after the H1N1 flu pandemic, with occupational and high-risk populations placed in the highest-priority groups, Dr. Mbaeyi said.
There are important differences between COVID-19 and influenza, Dr. Mbaeyi said. “Vaccine prioritization is challenging due to incomplete information on COVID-19 epidemiology and vaccines, including characteristics, timing, and number of doses.”
However, guidance for vaccine prioritization developed after the H1N1 outbreak in 2018 can be adapted for COVID-19.
To help inform ACIP deliberations, the work group reviewed the epidemiology of COVID-19. A large proportion of the population remains susceptible, and prioritizations should be based on data to date and continually refined, she said.
The work group defined the objectives of the COVID-19 vaccine program as follows: “Ensure safety and effectiveness of COVID-19 vaccines; reduce transmission, morbidity, and mortality in the population; help minimize disruption to society and economy, including maintaining health care capacity; and ensure equity in vaccine allocation and distribution.”
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said.
However, vaccines will not be administered until safety and efficacy have been demonstrated, she emphasized. The timing and number of vaccine doses are unknown, and subprioritization may be needed, assuming the vaccine becomes available in incremental quantities over several months.
Next steps for the work group are refinement of priority groups based on ACIP feedback, and assignment of tiers to other groups such as children, pregnant women, and racial/ethnic groups at high risk, Dr. Mbaeyi said.
The goal of the work group is to have a prioritization framework for COVID-19 vaccination to present at the next ACIP meeting.
Committee member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., emphasized that “one of the things we need to know is how is the virus [is] transmitted and who is transmitting,” and that this information will be key to developing strategies for vaccination.
Sarah E. Oliver, MD, an epidemiologist at the National Center for Immunization and Respiratory Diseases, responded that household transmission studies are in progress that will help inform the prioritization process.
Dr. Mbaeyi and Dr. Oliver had no financial conflicts to disclose.
according to Sarah Mbaeyi, MD, MPH, of the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
“Preparing for vaccination during a pandemic has long been a priority of the CDC and the U.S. government,” said Dr. Mbaeyi. The work group is building on a tiered approach to vaccination that was updated in 2018 after the H1N1 flu pandemic, with occupational and high-risk populations placed in the highest-priority groups, Dr. Mbaeyi said.
There are important differences between COVID-19 and influenza, Dr. Mbaeyi said. “Vaccine prioritization is challenging due to incomplete information on COVID-19 epidemiology and vaccines, including characteristics, timing, and number of doses.”
However, guidance for vaccine prioritization developed after the H1N1 outbreak in 2018 can be adapted for COVID-19.
To help inform ACIP deliberations, the work group reviewed the epidemiology of COVID-19. A large proportion of the population remains susceptible, and prioritizations should be based on data to date and continually refined, she said.
The work group defined the objectives of the COVID-19 vaccine program as follows: “Ensure safety and effectiveness of COVID-19 vaccines; reduce transmission, morbidity, and mortality in the population; help minimize disruption to society and economy, including maintaining health care capacity; and ensure equity in vaccine allocation and distribution.”
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said.
However, vaccines will not be administered until safety and efficacy have been demonstrated, she emphasized. The timing and number of vaccine doses are unknown, and subprioritization may be needed, assuming the vaccine becomes available in incremental quantities over several months.
Next steps for the work group are refinement of priority groups based on ACIP feedback, and assignment of tiers to other groups such as children, pregnant women, and racial/ethnic groups at high risk, Dr. Mbaeyi said.
The goal of the work group is to have a prioritization framework for COVID-19 vaccination to present at the next ACIP meeting.
Committee member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., emphasized that “one of the things we need to know is how is the virus [is] transmitted and who is transmitting,” and that this information will be key to developing strategies for vaccination.
Sarah E. Oliver, MD, an epidemiologist at the National Center for Immunization and Respiratory Diseases, responded that household transmission studies are in progress that will help inform the prioritization process.
Dr. Mbaeyi and Dr. Oliver had no financial conflicts to disclose.
according to Sarah Mbaeyi, MD, MPH, of the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
“Preparing for vaccination during a pandemic has long been a priority of the CDC and the U.S. government,” said Dr. Mbaeyi. The work group is building on a tiered approach to vaccination that was updated in 2018 after the H1N1 flu pandemic, with occupational and high-risk populations placed in the highest-priority groups, Dr. Mbaeyi said.
There are important differences between COVID-19 and influenza, Dr. Mbaeyi said. “Vaccine prioritization is challenging due to incomplete information on COVID-19 epidemiology and vaccines, including characteristics, timing, and number of doses.”
However, guidance for vaccine prioritization developed after the H1N1 outbreak in 2018 can be adapted for COVID-19.
To help inform ACIP deliberations, the work group reviewed the epidemiology of COVID-19. A large proportion of the population remains susceptible, and prioritizations should be based on data to date and continually refined, she said.
The work group defined the objectives of the COVID-19 vaccine program as follows: “Ensure safety and effectiveness of COVID-19 vaccines; reduce transmission, morbidity, and mortality in the population; help minimize disruption to society and economy, including maintaining health care capacity; and ensure equity in vaccine allocation and distribution.”
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said.
However, vaccines will not be administered until safety and efficacy have been demonstrated, she emphasized. The timing and number of vaccine doses are unknown, and subprioritization may be needed, assuming the vaccine becomes available in incremental quantities over several months.
Next steps for the work group are refinement of priority groups based on ACIP feedback, and assignment of tiers to other groups such as children, pregnant women, and racial/ethnic groups at high risk, Dr. Mbaeyi said.
The goal of the work group is to have a prioritization framework for COVID-19 vaccination to present at the next ACIP meeting.
Committee member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., emphasized that “one of the things we need to know is how is the virus [is] transmitted and who is transmitting,” and that this information will be key to developing strategies for vaccination.
Sarah E. Oliver, MD, an epidemiologist at the National Center for Immunization and Respiratory Diseases, responded that household transmission studies are in progress that will help inform the prioritization process.
Dr. Mbaeyi and Dr. Oliver had no financial conflicts to disclose.
Findings of most heart failure trials reported late or not at all
A large proportion of results from heart failure trials registered with clinicaltrials.gov are published a year or more after completion or not at all, which violates the U.S. FDA Amendments Act (FDAAA), according to a detailed analysis of the interventional and observational trials in this database.
Of the 1,429 heart failure trials identified, 75% of which were randomized interventional studies and the remainder of which were observational, fewer than 20% met the FDAAA 1-year reporting requirement, and 44% have yet to be published at all, reported a team of collaborative investigators led by cardiologists from the Inova Heart and Vascular Institute (IHVI), Falls Church, Va.
“I believe the critical issue is that the FDAAA has thus far never been enforced,” reported Christopher M. O’Connor, MD, a cardiologist and president of IHVI. He was the senior author of the study, reported in the Journal of the American College of Cardiology.
To improve systematic reporting of clinical trials, including negative results, clinicaltrials.gov was created in 2000. In 2007, the FDAAA enacted rules to broaden the requirements for reporting and to make timely reporting of results mandatory.
Ten years later, the FDA was finally authorized to issue a penalty of $10,000 for failure to release results in a timely fashion, a provision of the 2007 amendment but not confirmed at that time, the investigators reported. In the majority of cases, timely reporting was defined as within 12 months of completion of the trial.
The new study shows that reporting of completed trials, timely or otherwise, remains low. Of the 1,243 trials completed after 2007, the proportion meeting the 1-year reporting requirement was just 20%. Although a significant improvement over the 13% reporting in this time frame before 2007, more than 80% of findings are not being released in a timely manner more than 10 years after this was made mandatory.
There are a number of reasons to consider this to be a serious issue, according to Mandeep R. Mehra, MD, of Brigham and Women’s Hospital, Boston. One of the authors of an accompanying editorial regarding this analysis, Dr. Mehra called underreporting “a public health matter because it is an impediment to medical discovery and poses plausible threats to patient safety.”
Among studies registered after 2007, publication rates were higher for trials funded by the National Institutes of Health (71%) relative to industry (49%) or the U.S. Veterans Affairs (45%).
Publication rates were also higher among interventional relative to observational trials (59% vs. 46%) and trials that enrolled more than 1,000 patients relative to those enrolling fewer than 150 (77% vs. 51%), although trial size was not a significant predictor of publication on multivariate analysis. Clinical endpoints, such as death or hospitalization, were also associated with a greater likelihood of publication relative to nonclinical endpoints.
Of the 251 trials terminated before completion, findings were published within 1 year in only 6%. Two years after completion, only 20% were published at all.
Results consistent with the primary hypothesis did not predict timely publication, but only 39% of the studies listed a primary hypothesis. Since 2017, this is another violation of the FDAAA, according to Dr. O’Connor.
The problem is not unique to heart failure trials, according to the authors who cited numerous studies showing low rates of timely publication in other therapeutic areas. Heart failure was selected for evaluation in this study mainly to keep the analysis feasible, although the authors contend this is an area with an urgent need for better treatments.
The problem needs to be fixed, according to Dr. Mehra. In his editorial, he called for rules to be “transitioned to regulations and action taken for underreporting.” Dr. O’Connor agreed.
“A combination of carrots and sticks might be needed to achieve sufficient result sharing,” Dr. O’Connor said. He suggested that stakeholders, such as investigators, sponsors, regulators, and journal editors, should collaborate to address the problem.
So far, the FDA has never levied a fine for lack of reporting or for failure to report in a timely manner. Routine imposition of large fines might not be viable, given the complex reasons that delay or inhibit publication of trial findings, but it would be a large source of revenue.
“According to the FDAAA TrialsTracker, a live tool that tracks FDAAA compliance and promotes trial transparency, the U.S. government could already have imposed more than $2.8 billion in fines for trials due after January 2018,” Dr. O’Connor reported.
The first and senior authors are among those who report financial relationships with pharmaceutical companies.
SOURCE: Psotka MA et al. J Am Coll Cardiol. 2020;75:3151-61.
A large proportion of results from heart failure trials registered with clinicaltrials.gov are published a year or more after completion or not at all, which violates the U.S. FDA Amendments Act (FDAAA), according to a detailed analysis of the interventional and observational trials in this database.
Of the 1,429 heart failure trials identified, 75% of which were randomized interventional studies and the remainder of which were observational, fewer than 20% met the FDAAA 1-year reporting requirement, and 44% have yet to be published at all, reported a team of collaborative investigators led by cardiologists from the Inova Heart and Vascular Institute (IHVI), Falls Church, Va.
“I believe the critical issue is that the FDAAA has thus far never been enforced,” reported Christopher M. O’Connor, MD, a cardiologist and president of IHVI. He was the senior author of the study, reported in the Journal of the American College of Cardiology.
To improve systematic reporting of clinical trials, including negative results, clinicaltrials.gov was created in 2000. In 2007, the FDAAA enacted rules to broaden the requirements for reporting and to make timely reporting of results mandatory.
Ten years later, the FDA was finally authorized to issue a penalty of $10,000 for failure to release results in a timely fashion, a provision of the 2007 amendment but not confirmed at that time, the investigators reported. In the majority of cases, timely reporting was defined as within 12 months of completion of the trial.
The new study shows that reporting of completed trials, timely or otherwise, remains low. Of the 1,243 trials completed after 2007, the proportion meeting the 1-year reporting requirement was just 20%. Although a significant improvement over the 13% reporting in this time frame before 2007, more than 80% of findings are not being released in a timely manner more than 10 years after this was made mandatory.
There are a number of reasons to consider this to be a serious issue, according to Mandeep R. Mehra, MD, of Brigham and Women’s Hospital, Boston. One of the authors of an accompanying editorial regarding this analysis, Dr. Mehra called underreporting “a public health matter because it is an impediment to medical discovery and poses plausible threats to patient safety.”
Among studies registered after 2007, publication rates were higher for trials funded by the National Institutes of Health (71%) relative to industry (49%) or the U.S. Veterans Affairs (45%).
Publication rates were also higher among interventional relative to observational trials (59% vs. 46%) and trials that enrolled more than 1,000 patients relative to those enrolling fewer than 150 (77% vs. 51%), although trial size was not a significant predictor of publication on multivariate analysis. Clinical endpoints, such as death or hospitalization, were also associated with a greater likelihood of publication relative to nonclinical endpoints.
Of the 251 trials terminated before completion, findings were published within 1 year in only 6%. Two years after completion, only 20% were published at all.
Results consistent with the primary hypothesis did not predict timely publication, but only 39% of the studies listed a primary hypothesis. Since 2017, this is another violation of the FDAAA, according to Dr. O’Connor.
The problem is not unique to heart failure trials, according to the authors who cited numerous studies showing low rates of timely publication in other therapeutic areas. Heart failure was selected for evaluation in this study mainly to keep the analysis feasible, although the authors contend this is an area with an urgent need for better treatments.
The problem needs to be fixed, according to Dr. Mehra. In his editorial, he called for rules to be “transitioned to regulations and action taken for underreporting.” Dr. O’Connor agreed.
“A combination of carrots and sticks might be needed to achieve sufficient result sharing,” Dr. O’Connor said. He suggested that stakeholders, such as investigators, sponsors, regulators, and journal editors, should collaborate to address the problem.
So far, the FDA has never levied a fine for lack of reporting or for failure to report in a timely manner. Routine imposition of large fines might not be viable, given the complex reasons that delay or inhibit publication of trial findings, but it would be a large source of revenue.
“According to the FDAAA TrialsTracker, a live tool that tracks FDAAA compliance and promotes trial transparency, the U.S. government could already have imposed more than $2.8 billion in fines for trials due after January 2018,” Dr. O’Connor reported.
The first and senior authors are among those who report financial relationships with pharmaceutical companies.
SOURCE: Psotka MA et al. J Am Coll Cardiol. 2020;75:3151-61.
A large proportion of results from heart failure trials registered with clinicaltrials.gov are published a year or more after completion or not at all, which violates the U.S. FDA Amendments Act (FDAAA), according to a detailed analysis of the interventional and observational trials in this database.
Of the 1,429 heart failure trials identified, 75% of which were randomized interventional studies and the remainder of which were observational, fewer than 20% met the FDAAA 1-year reporting requirement, and 44% have yet to be published at all, reported a team of collaborative investigators led by cardiologists from the Inova Heart and Vascular Institute (IHVI), Falls Church, Va.
“I believe the critical issue is that the FDAAA has thus far never been enforced,” reported Christopher M. O’Connor, MD, a cardiologist and president of IHVI. He was the senior author of the study, reported in the Journal of the American College of Cardiology.
To improve systematic reporting of clinical trials, including negative results, clinicaltrials.gov was created in 2000. In 2007, the FDAAA enacted rules to broaden the requirements for reporting and to make timely reporting of results mandatory.
Ten years later, the FDA was finally authorized to issue a penalty of $10,000 for failure to release results in a timely fashion, a provision of the 2007 amendment but not confirmed at that time, the investigators reported. In the majority of cases, timely reporting was defined as within 12 months of completion of the trial.
The new study shows that reporting of completed trials, timely or otherwise, remains low. Of the 1,243 trials completed after 2007, the proportion meeting the 1-year reporting requirement was just 20%. Although a significant improvement over the 13% reporting in this time frame before 2007, more than 80% of findings are not being released in a timely manner more than 10 years after this was made mandatory.
There are a number of reasons to consider this to be a serious issue, according to Mandeep R. Mehra, MD, of Brigham and Women’s Hospital, Boston. One of the authors of an accompanying editorial regarding this analysis, Dr. Mehra called underreporting “a public health matter because it is an impediment to medical discovery and poses plausible threats to patient safety.”
Among studies registered after 2007, publication rates were higher for trials funded by the National Institutes of Health (71%) relative to industry (49%) or the U.S. Veterans Affairs (45%).
Publication rates were also higher among interventional relative to observational trials (59% vs. 46%) and trials that enrolled more than 1,000 patients relative to those enrolling fewer than 150 (77% vs. 51%), although trial size was not a significant predictor of publication on multivariate analysis. Clinical endpoints, such as death or hospitalization, were also associated with a greater likelihood of publication relative to nonclinical endpoints.
Of the 251 trials terminated before completion, findings were published within 1 year in only 6%. Two years after completion, only 20% were published at all.
Results consistent with the primary hypothesis did not predict timely publication, but only 39% of the studies listed a primary hypothesis. Since 2017, this is another violation of the FDAAA, according to Dr. O’Connor.
The problem is not unique to heart failure trials, according to the authors who cited numerous studies showing low rates of timely publication in other therapeutic areas. Heart failure was selected for evaluation in this study mainly to keep the analysis feasible, although the authors contend this is an area with an urgent need for better treatments.
The problem needs to be fixed, according to Dr. Mehra. In his editorial, he called for rules to be “transitioned to regulations and action taken for underreporting.” Dr. O’Connor agreed.
“A combination of carrots and sticks might be needed to achieve sufficient result sharing,” Dr. O’Connor said. He suggested that stakeholders, such as investigators, sponsors, regulators, and journal editors, should collaborate to address the problem.
So far, the FDA has never levied a fine for lack of reporting or for failure to report in a timely manner. Routine imposition of large fines might not be viable, given the complex reasons that delay or inhibit publication of trial findings, but it would be a large source of revenue.
“According to the FDAAA TrialsTracker, a live tool that tracks FDAAA compliance and promotes trial transparency, the U.S. government could already have imposed more than $2.8 billion in fines for trials due after January 2018,” Dr. O’Connor reported.
The first and senior authors are among those who report financial relationships with pharmaceutical companies.
SOURCE: Psotka MA et al. J Am Coll Cardiol. 2020;75:3151-61.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Treatments linked to death in COVID patients with thoracic cancers
Prior treatment with steroids, anticoagulants, chemotherapy alone, or chemotherapy plus immunotherapy were all associated with an increased risk of death, but prior treatment with tyrosine kinase inhibitors or immunotherapy alone were not.
At the same time, there were no COVID-19–directed treatments that seemed to affect the risk of death.
“When we look at therapies administered to treat COVID-19 … including anticoagulation, antibiotics, antivirals, hydroxychloroquine, we found that no particular therapy was associated with increased chance of recovery from COVID-19,” said Leora Horn, MD, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Dr. Horn presented these findings as part of the American Society of Clinical Oncology virtual scientific program.
About TERAVOLT
The TERAVOLT registry is the brainchild of Marina Garassino, MD, of the National Cancer Institute of Milan. On March 15, Dr. Garassino emailed colleagues around the world with the idea of starting the registry. Within 5 days, the final protocol was approved, and the first patient was entered onto TERAVOLT.
In creating a registry, Dr. Garassino and colleagues wanted to “determine the demographic factors, comorbidities, cancer characteristics, and therapies that place patients with thoracic malignancies who develop COVID-19 most at risk for hospitalization and death,” Dr. Horn said.
Other goals of the registry are “to understand the clinical course of patients with thoracic malignancies who are infected by SARS-CoV-2, to provide practitioners with real-time data on therapeutic strategies that may impact survival, [and] to evaluate the long-term impact on cancer outcomes related to care adjustments and delays in patients with thoracic malignancies,” she added.
Dr. Garassino presented the first analysis of TERAVOLT data at the AACR virtual meeting I in April. Results were recently published in The Lancet Oncology as well. That analysis included 200 patients, 98% of whom were from Europe, and the median follow-up was 15 days.
Baseline characteristics and outcomes
Dr. Horn’s updated analysis included 400 patients with a median follow-up of 33 days from COVID-19 diagnosis. The data encompassed patients from North and South America, Europe, Africa, Asia, and Australia.
Of the 400 patients, 169 had recovered, 141 had died, and 118 were still in the hospital at the time of analysis. In all, 334 patients (78.3%) required a hospital admission, and 33 (8.3%) were admitted to the ICU. The median length of hospitalization was 10 days.
Across the three outcome groups (recovered, died, ongoing), the median age was 67-70 years. Most patients had non–small cell lung cancer (74.5%-81.9%), and most had stage IV disease (61.4%-76.8%).
A majority of patients were male (63.3%-70.2%), and most were current or former smokers (77.5%-86.9%). The median body mass index was 24-25 kg/m2, and 35%-46.4% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0.
Most patients (82.2%-90.7%) had COVID-19 diagnosed via real-time polymerase chain reaction, although some patients were diagnosed via clinical findings alone (3.1%-5%).
“[R]egardless of outcome, the most common presenting symptom was fever, cough, or dyspnea,” Dr. Horn noted.
As for complications of COVID-19, 71% of patients who died had pneumonitis/pneumonia, 49.6% had acute respiratory distress syndrome, 14.9% had multiorgan failure, 12.1% had sepsis, and 5.7% had coagulopathy.
Among recovered patients, 59% had pneumonitis/pneumonia, 4.1% had acute respiratory distress syndrome, 3% had coagulopathy, 0.6% had sepsis, and none had multiorgan failure.
Patients who recovered were more likely to have no comorbidities at baseline, and 31.2% of patients who died had at least one comorbidity. The most frequent comorbidities were hypertension, chronic obstructive pulmonary disease, vascular disease, diabetes, and renal insufficiencies.
Prior treatments and COVID therapy
Among patients who died, 33.4% were on ACE inhibitors or angiotensin II receptor blockers, 27% were on anticoagulants, and 23.4% were on steroids (the equivalent of at least 10 mg of prednisone per day) at the time of COVID-19 diagnosis.
Among recovered patients, 20.7% were on ACE inhibitors or angiotensin II receptor blockers, 18.3% were on anticoagulants, and 14.2% were on steroids at the time of COVID-19 diagnosis.
“When we look at cancer therapy in the last 3 months, we can see that, regardless of outcome, the majority of patients had either not been treated or were on first-line therapy at the time of their COVID-19 diagnosis,” Dr. Horn noted.
Among patients who died, 46.8% had received chemotherapy, 22% had received immunotherapy, 12.8% had received targeted therapy, and 9.2% had received radiotherapy.
Among recovered patients, 33.7% had received chemotherapy, 26.6% had received immunotherapy, 19.5% had received targeted therapy, and 14.2% had received radiotherapy.
COVID-19–directed treatments included anticoagulation, antibiotics, antivirals, antifungals, steroids, interleukin-6 inhibitors, and hydroxychloroquine. Use of these therapies was similar among patients who recovered and patients who died.
Factors associated with death
In all, 79.4% of deaths were attributed to COVID-19, 10.6% were attributed to cancer, 8.5% were attributed to cancer and COVID-19, and 1.4% of deaths had an unknown cause.
In a univariate analysis, baseline characteristics associated with an increased risk of death were age of 65 years or older (P = .0033), one or more comorbidity (P = .0351), and ECOG performance status of 1 (P < .0001). Therapies associated with an increased risk of death in a univariate analysis included steroids (P = .0186), anticoagulation (P = .0562), and either chemotherapy alone or chemotherapy plus immunotherapy (P = .0256).
In a multivariate analysis, age over 65 years (P = .018), ECOG performance status of 1 (P < .001), prior use of steroids (P = .052), and receipt of chemotherapy alone or in combination with immunotherapy (P = .025) were all associated with an increased risk of death.
“There is no impact of gender [sex], body mass index, smoking status, stage, or type of cancer on risk of death,” Dr. Horn said. “Therapy administered to treat COVID-19 is not significantly associated with outcome.”
“The impact of COVID-19 infection on cancer management and outcomes must be evaluated,” she added. “Data collection is ongoing, with additional analysis and studies planned to look at patient and provider perception of COVID-19 and the impact it has had on cancer care.”
Strengths and limitations
There are several limitations to findings from the TERAVOLT registry, according to invited discussant Giuseppe Curigliano, MD, PhD, of the University of Milan.
He said the results are limited by the differences in triage decisions between European and other centers, the fact that most patients in TERAVOLT were hospitalized, the high proportion of patients with stage IV non–small cell lung cancer, and methods of data collection and analysis.
“There is no real-time data capture, no auditing, no standardized outcome definitions, and CRFs [case report forms] had a lot of limitations,” Dr. Curigliano said. “We have multiple biases, including selection bias, recall bias, confounding by indication, and changes in practice or disease evolution.”
Dr. Curigliano noted, however, that TERAVOLT is the largest real-world dataset of patients with COVID-19 and thoracic malignancies.
Furthermore, results from TERAVOLT correspond to results from the CCC-19 registry. Data from both registries suggest that older age, the presence of comorbidities, higher ECOG performances status, and chemotherapy alone or in combination with other therapies are associated with increased mortality among patients with cancer and COVID-19.
The TERAVOLT registry is funded, in part, by the International Association for the Study of Lung Cancer. Dr. Horn disclosed relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, and other pharmaceutical companies. Dr. Curigliano disclosed relationships with AstraZeneca, Boehringer Ingelheim, Ellipses Pharma, and other pharmaceutical companies.
SOURCE: Horn L et al. ASCO 2020, Abstract LBA111.
Prior treatment with steroids, anticoagulants, chemotherapy alone, or chemotherapy plus immunotherapy were all associated with an increased risk of death, but prior treatment with tyrosine kinase inhibitors or immunotherapy alone were not.
At the same time, there were no COVID-19–directed treatments that seemed to affect the risk of death.
“When we look at therapies administered to treat COVID-19 … including anticoagulation, antibiotics, antivirals, hydroxychloroquine, we found that no particular therapy was associated with increased chance of recovery from COVID-19,” said Leora Horn, MD, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Dr. Horn presented these findings as part of the American Society of Clinical Oncology virtual scientific program.
About TERAVOLT
The TERAVOLT registry is the brainchild of Marina Garassino, MD, of the National Cancer Institute of Milan. On March 15, Dr. Garassino emailed colleagues around the world with the idea of starting the registry. Within 5 days, the final protocol was approved, and the first patient was entered onto TERAVOLT.
In creating a registry, Dr. Garassino and colleagues wanted to “determine the demographic factors, comorbidities, cancer characteristics, and therapies that place patients with thoracic malignancies who develop COVID-19 most at risk for hospitalization and death,” Dr. Horn said.
Other goals of the registry are “to understand the clinical course of patients with thoracic malignancies who are infected by SARS-CoV-2, to provide practitioners with real-time data on therapeutic strategies that may impact survival, [and] to evaluate the long-term impact on cancer outcomes related to care adjustments and delays in patients with thoracic malignancies,” she added.
Dr. Garassino presented the first analysis of TERAVOLT data at the AACR virtual meeting I in April. Results were recently published in The Lancet Oncology as well. That analysis included 200 patients, 98% of whom were from Europe, and the median follow-up was 15 days.
Baseline characteristics and outcomes
Dr. Horn’s updated analysis included 400 patients with a median follow-up of 33 days from COVID-19 diagnosis. The data encompassed patients from North and South America, Europe, Africa, Asia, and Australia.
Of the 400 patients, 169 had recovered, 141 had died, and 118 were still in the hospital at the time of analysis. In all, 334 patients (78.3%) required a hospital admission, and 33 (8.3%) were admitted to the ICU. The median length of hospitalization was 10 days.
Across the three outcome groups (recovered, died, ongoing), the median age was 67-70 years. Most patients had non–small cell lung cancer (74.5%-81.9%), and most had stage IV disease (61.4%-76.8%).
A majority of patients were male (63.3%-70.2%), and most were current or former smokers (77.5%-86.9%). The median body mass index was 24-25 kg/m2, and 35%-46.4% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0.
Most patients (82.2%-90.7%) had COVID-19 diagnosed via real-time polymerase chain reaction, although some patients were diagnosed via clinical findings alone (3.1%-5%).
“[R]egardless of outcome, the most common presenting symptom was fever, cough, or dyspnea,” Dr. Horn noted.
As for complications of COVID-19, 71% of patients who died had pneumonitis/pneumonia, 49.6% had acute respiratory distress syndrome, 14.9% had multiorgan failure, 12.1% had sepsis, and 5.7% had coagulopathy.
Among recovered patients, 59% had pneumonitis/pneumonia, 4.1% had acute respiratory distress syndrome, 3% had coagulopathy, 0.6% had sepsis, and none had multiorgan failure.
Patients who recovered were more likely to have no comorbidities at baseline, and 31.2% of patients who died had at least one comorbidity. The most frequent comorbidities were hypertension, chronic obstructive pulmonary disease, vascular disease, diabetes, and renal insufficiencies.
Prior treatments and COVID therapy
Among patients who died, 33.4% were on ACE inhibitors or angiotensin II receptor blockers, 27% were on anticoagulants, and 23.4% were on steroids (the equivalent of at least 10 mg of prednisone per day) at the time of COVID-19 diagnosis.
Among recovered patients, 20.7% were on ACE inhibitors or angiotensin II receptor blockers, 18.3% were on anticoagulants, and 14.2% were on steroids at the time of COVID-19 diagnosis.
“When we look at cancer therapy in the last 3 months, we can see that, regardless of outcome, the majority of patients had either not been treated or were on first-line therapy at the time of their COVID-19 diagnosis,” Dr. Horn noted.
Among patients who died, 46.8% had received chemotherapy, 22% had received immunotherapy, 12.8% had received targeted therapy, and 9.2% had received radiotherapy.
Among recovered patients, 33.7% had received chemotherapy, 26.6% had received immunotherapy, 19.5% had received targeted therapy, and 14.2% had received radiotherapy.
COVID-19–directed treatments included anticoagulation, antibiotics, antivirals, antifungals, steroids, interleukin-6 inhibitors, and hydroxychloroquine. Use of these therapies was similar among patients who recovered and patients who died.
Factors associated with death
In all, 79.4% of deaths were attributed to COVID-19, 10.6% were attributed to cancer, 8.5% were attributed to cancer and COVID-19, and 1.4% of deaths had an unknown cause.
In a univariate analysis, baseline characteristics associated with an increased risk of death were age of 65 years or older (P = .0033), one or more comorbidity (P = .0351), and ECOG performance status of 1 (P < .0001). Therapies associated with an increased risk of death in a univariate analysis included steroids (P = .0186), anticoagulation (P = .0562), and either chemotherapy alone or chemotherapy plus immunotherapy (P = .0256).
In a multivariate analysis, age over 65 years (P = .018), ECOG performance status of 1 (P < .001), prior use of steroids (P = .052), and receipt of chemotherapy alone or in combination with immunotherapy (P = .025) were all associated with an increased risk of death.
“There is no impact of gender [sex], body mass index, smoking status, stage, or type of cancer on risk of death,” Dr. Horn said. “Therapy administered to treat COVID-19 is not significantly associated with outcome.”
“The impact of COVID-19 infection on cancer management and outcomes must be evaluated,” she added. “Data collection is ongoing, with additional analysis and studies planned to look at patient and provider perception of COVID-19 and the impact it has had on cancer care.”
Strengths and limitations
There are several limitations to findings from the TERAVOLT registry, according to invited discussant Giuseppe Curigliano, MD, PhD, of the University of Milan.
He said the results are limited by the differences in triage decisions between European and other centers, the fact that most patients in TERAVOLT were hospitalized, the high proportion of patients with stage IV non–small cell lung cancer, and methods of data collection and analysis.
“There is no real-time data capture, no auditing, no standardized outcome definitions, and CRFs [case report forms] had a lot of limitations,” Dr. Curigliano said. “We have multiple biases, including selection bias, recall bias, confounding by indication, and changes in practice or disease evolution.”
Dr. Curigliano noted, however, that TERAVOLT is the largest real-world dataset of patients with COVID-19 and thoracic malignancies.
Furthermore, results from TERAVOLT correspond to results from the CCC-19 registry. Data from both registries suggest that older age, the presence of comorbidities, higher ECOG performances status, and chemotherapy alone or in combination with other therapies are associated with increased mortality among patients with cancer and COVID-19.
The TERAVOLT registry is funded, in part, by the International Association for the Study of Lung Cancer. Dr. Horn disclosed relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, and other pharmaceutical companies. Dr. Curigliano disclosed relationships with AstraZeneca, Boehringer Ingelheim, Ellipses Pharma, and other pharmaceutical companies.
SOURCE: Horn L et al. ASCO 2020, Abstract LBA111.
Prior treatment with steroids, anticoagulants, chemotherapy alone, or chemotherapy plus immunotherapy were all associated with an increased risk of death, but prior treatment with tyrosine kinase inhibitors or immunotherapy alone were not.
At the same time, there were no COVID-19–directed treatments that seemed to affect the risk of death.
“When we look at therapies administered to treat COVID-19 … including anticoagulation, antibiotics, antivirals, hydroxychloroquine, we found that no particular therapy was associated with increased chance of recovery from COVID-19,” said Leora Horn, MD, of Vanderbilt-Ingram Cancer Center in Nashville, Tenn.
Dr. Horn presented these findings as part of the American Society of Clinical Oncology virtual scientific program.
About TERAVOLT
The TERAVOLT registry is the brainchild of Marina Garassino, MD, of the National Cancer Institute of Milan. On March 15, Dr. Garassino emailed colleagues around the world with the idea of starting the registry. Within 5 days, the final protocol was approved, and the first patient was entered onto TERAVOLT.
In creating a registry, Dr. Garassino and colleagues wanted to “determine the demographic factors, comorbidities, cancer characteristics, and therapies that place patients with thoracic malignancies who develop COVID-19 most at risk for hospitalization and death,” Dr. Horn said.
Other goals of the registry are “to understand the clinical course of patients with thoracic malignancies who are infected by SARS-CoV-2, to provide practitioners with real-time data on therapeutic strategies that may impact survival, [and] to evaluate the long-term impact on cancer outcomes related to care adjustments and delays in patients with thoracic malignancies,” she added.
Dr. Garassino presented the first analysis of TERAVOLT data at the AACR virtual meeting I in April. Results were recently published in The Lancet Oncology as well. That analysis included 200 patients, 98% of whom were from Europe, and the median follow-up was 15 days.
Baseline characteristics and outcomes
Dr. Horn’s updated analysis included 400 patients with a median follow-up of 33 days from COVID-19 diagnosis. The data encompassed patients from North and South America, Europe, Africa, Asia, and Australia.
Of the 400 patients, 169 had recovered, 141 had died, and 118 were still in the hospital at the time of analysis. In all, 334 patients (78.3%) required a hospital admission, and 33 (8.3%) were admitted to the ICU. The median length of hospitalization was 10 days.
Across the three outcome groups (recovered, died, ongoing), the median age was 67-70 years. Most patients had non–small cell lung cancer (74.5%-81.9%), and most had stage IV disease (61.4%-76.8%).
A majority of patients were male (63.3%-70.2%), and most were current or former smokers (77.5%-86.9%). The median body mass index was 24-25 kg/m2, and 35%-46.4% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0.
Most patients (82.2%-90.7%) had COVID-19 diagnosed via real-time polymerase chain reaction, although some patients were diagnosed via clinical findings alone (3.1%-5%).
“[R]egardless of outcome, the most common presenting symptom was fever, cough, or dyspnea,” Dr. Horn noted.
As for complications of COVID-19, 71% of patients who died had pneumonitis/pneumonia, 49.6% had acute respiratory distress syndrome, 14.9% had multiorgan failure, 12.1% had sepsis, and 5.7% had coagulopathy.
Among recovered patients, 59% had pneumonitis/pneumonia, 4.1% had acute respiratory distress syndrome, 3% had coagulopathy, 0.6% had sepsis, and none had multiorgan failure.
Patients who recovered were more likely to have no comorbidities at baseline, and 31.2% of patients who died had at least one comorbidity. The most frequent comorbidities were hypertension, chronic obstructive pulmonary disease, vascular disease, diabetes, and renal insufficiencies.
Prior treatments and COVID therapy
Among patients who died, 33.4% were on ACE inhibitors or angiotensin II receptor blockers, 27% were on anticoagulants, and 23.4% were on steroids (the equivalent of at least 10 mg of prednisone per day) at the time of COVID-19 diagnosis.
Among recovered patients, 20.7% were on ACE inhibitors or angiotensin II receptor blockers, 18.3% were on anticoagulants, and 14.2% were on steroids at the time of COVID-19 diagnosis.
“When we look at cancer therapy in the last 3 months, we can see that, regardless of outcome, the majority of patients had either not been treated or were on first-line therapy at the time of their COVID-19 diagnosis,” Dr. Horn noted.
Among patients who died, 46.8% had received chemotherapy, 22% had received immunotherapy, 12.8% had received targeted therapy, and 9.2% had received radiotherapy.
Among recovered patients, 33.7% had received chemotherapy, 26.6% had received immunotherapy, 19.5% had received targeted therapy, and 14.2% had received radiotherapy.
COVID-19–directed treatments included anticoagulation, antibiotics, antivirals, antifungals, steroids, interleukin-6 inhibitors, and hydroxychloroquine. Use of these therapies was similar among patients who recovered and patients who died.
Factors associated with death
In all, 79.4% of deaths were attributed to COVID-19, 10.6% were attributed to cancer, 8.5% were attributed to cancer and COVID-19, and 1.4% of deaths had an unknown cause.
In a univariate analysis, baseline characteristics associated with an increased risk of death were age of 65 years or older (P = .0033), one or more comorbidity (P = .0351), and ECOG performance status of 1 (P < .0001). Therapies associated with an increased risk of death in a univariate analysis included steroids (P = .0186), anticoagulation (P = .0562), and either chemotherapy alone or chemotherapy plus immunotherapy (P = .0256).
In a multivariate analysis, age over 65 years (P = .018), ECOG performance status of 1 (P < .001), prior use of steroids (P = .052), and receipt of chemotherapy alone or in combination with immunotherapy (P = .025) were all associated with an increased risk of death.
“There is no impact of gender [sex], body mass index, smoking status, stage, or type of cancer on risk of death,” Dr. Horn said. “Therapy administered to treat COVID-19 is not significantly associated with outcome.”
“The impact of COVID-19 infection on cancer management and outcomes must be evaluated,” she added. “Data collection is ongoing, with additional analysis and studies planned to look at patient and provider perception of COVID-19 and the impact it has had on cancer care.”
Strengths and limitations
There are several limitations to findings from the TERAVOLT registry, according to invited discussant Giuseppe Curigliano, MD, PhD, of the University of Milan.
He said the results are limited by the differences in triage decisions between European and other centers, the fact that most patients in TERAVOLT were hospitalized, the high proportion of patients with stage IV non–small cell lung cancer, and methods of data collection and analysis.
“There is no real-time data capture, no auditing, no standardized outcome definitions, and CRFs [case report forms] had a lot of limitations,” Dr. Curigliano said. “We have multiple biases, including selection bias, recall bias, confounding by indication, and changes in practice or disease evolution.”
Dr. Curigliano noted, however, that TERAVOLT is the largest real-world dataset of patients with COVID-19 and thoracic malignancies.
Furthermore, results from TERAVOLT correspond to results from the CCC-19 registry. Data from both registries suggest that older age, the presence of comorbidities, higher ECOG performances status, and chemotherapy alone or in combination with other therapies are associated with increased mortality among patients with cancer and COVID-19.
The TERAVOLT registry is funded, in part, by the International Association for the Study of Lung Cancer. Dr. Horn disclosed relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, and other pharmaceutical companies. Dr. Curigliano disclosed relationships with AstraZeneca, Boehringer Ingelheim, Ellipses Pharma, and other pharmaceutical companies.
SOURCE: Horn L et al. ASCO 2020, Abstract LBA111.
FROM ASCO 2020
Black women at highest risk for asthma
Women are much more likely than men to have asthma, and , according to the Centers for Disease Control and Prevention.
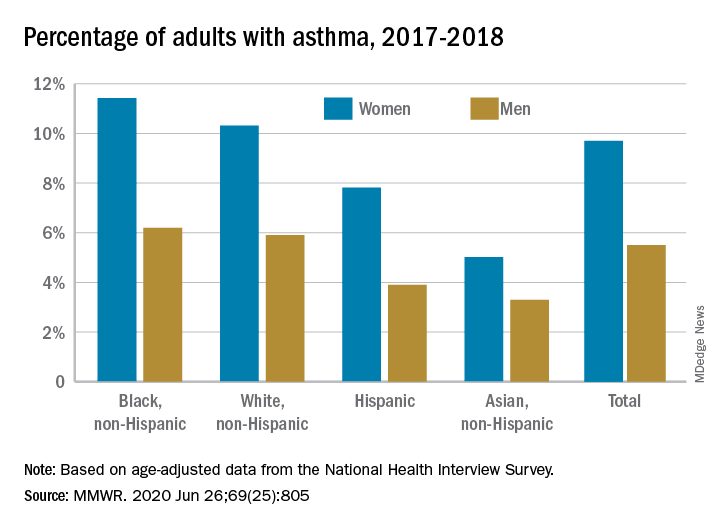
Among all women aged 18 years and older, 9.7% reported that they currently had asthma in 2017-2018, compared with 5.5% of men, based on age-adjusted data from the National Health Interview Survey.
The proportion of black, non-Hispanic women with asthma, however, was even higher, at 11.4%. White non-Hispanic women were next at 10.3%, followed by Hispanic (7.8%) and Asian (5.0%) women, the CDC reported June 26 in the Morbidity and Mortality Weekly Report.
The same pattern held for men: 6.2% of black men had asthma in 2017-2018, compared with 5.9% of whites, 3.9% of Hispanics, and 3.3% of Asian men, the CDC said.
SOURCE: MMWR. 2020 Jun 26;69(25):805.
Women are much more likely than men to have asthma, and , according to the Centers for Disease Control and Prevention.
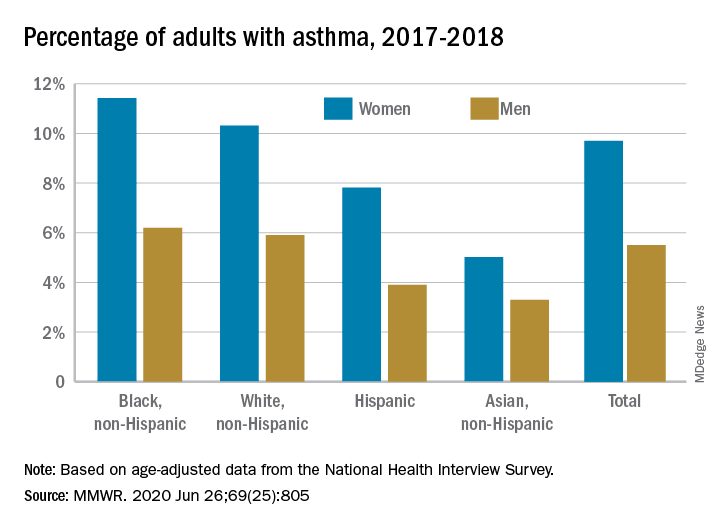
Among all women aged 18 years and older, 9.7% reported that they currently had asthma in 2017-2018, compared with 5.5% of men, based on age-adjusted data from the National Health Interview Survey.
The proportion of black, non-Hispanic women with asthma, however, was even higher, at 11.4%. White non-Hispanic women were next at 10.3%, followed by Hispanic (7.8%) and Asian (5.0%) women, the CDC reported June 26 in the Morbidity and Mortality Weekly Report.
The same pattern held for men: 6.2% of black men had asthma in 2017-2018, compared with 5.9% of whites, 3.9% of Hispanics, and 3.3% of Asian men, the CDC said.
SOURCE: MMWR. 2020 Jun 26;69(25):805.
Women are much more likely than men to have asthma, and , according to the Centers for Disease Control and Prevention.
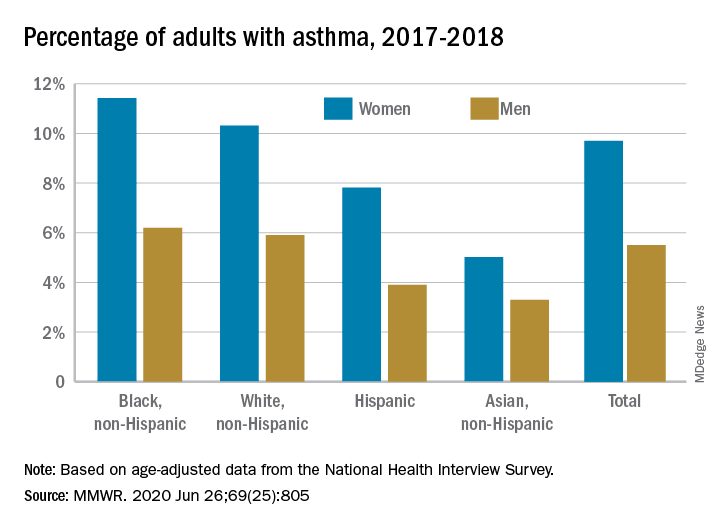
Among all women aged 18 years and older, 9.7% reported that they currently had asthma in 2017-2018, compared with 5.5% of men, based on age-adjusted data from the National Health Interview Survey.
The proportion of black, non-Hispanic women with asthma, however, was even higher, at 11.4%. White non-Hispanic women were next at 10.3%, followed by Hispanic (7.8%) and Asian (5.0%) women, the CDC reported June 26 in the Morbidity and Mortality Weekly Report.
The same pattern held for men: 6.2% of black men had asthma in 2017-2018, compared with 5.9% of whites, 3.9% of Hispanics, and 3.3% of Asian men, the CDC said.
SOURCE: MMWR. 2020 Jun 26;69(25):805.
FROM MMWR
Daily Recap: Higher risk of severe COVID-19 seen in pregnancy, primary care practices at risk
Here are the stories our MDedge editors across specialties think you need to know about today:
Pregnant women at higher risk for severe COVID-19
Pregnant women may be at increased risk for severe COVID-19 illness, according to a report published online June 26 in Morbidity and Mortality Weekly Report.
Among reproductive-aged women (15-44 years) infected with SARS-CoV-2, pregnancy was associated with a greater likelihood of hospitalization, admission to the intensive care unit (ICU), and mechanical ventilation, but not death. Pregnant women were 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to need mechanical ventilation, after adjustment for age, underlying conditions, and race/ethnicity.
CDC researchers said that preventing COVID-19 infection in pregnant women should be a priority and any potential barriers to compliance with preventive measures need to be removed.
“During pregnancy, women experience immunologic and physiologic changes that could increase their risk for more severe illness from respiratory infections,” they wrote. Read more.
Going out of business: Primary care practices at risk
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. In an interview with Kenny Lin, MD, MPH, a family physician, Dr. Frieden discussed the future of primary care.
Here is a sample of Dr. Frieden’s observations:
“When I’ve looked around the United States, I’ve been extremely concerned about both the risk that primary care practitioners are subjected to in their everyday practice and the economic risk that we could lose many of our primary care practices around the country. It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.” Read more.
Surge in out-of-hospital cardiac arrests
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests that placed a huge burden on first responders, according to a new analysis.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
Read more.
Fenfluramine approved for Dravet syndrome
The U.S. Food and Drug Administration has approved fenfluramine (Fintepla, Zogenix) oral solution, a Schedule IV controlled substance, for the treatment of seizures associated with Dravet syndrome in children age 2 years and older.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy.
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Pregnant women at higher risk for severe COVID-19
Pregnant women may be at increased risk for severe COVID-19 illness, according to a report published online June 26 in Morbidity and Mortality Weekly Report.
Among reproductive-aged women (15-44 years) infected with SARS-CoV-2, pregnancy was associated with a greater likelihood of hospitalization, admission to the intensive care unit (ICU), and mechanical ventilation, but not death. Pregnant women were 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to need mechanical ventilation, after adjustment for age, underlying conditions, and race/ethnicity.
CDC researchers said that preventing COVID-19 infection in pregnant women should be a priority and any potential barriers to compliance with preventive measures need to be removed.
“During pregnancy, women experience immunologic and physiologic changes that could increase their risk for more severe illness from respiratory infections,” they wrote. Read more.
Going out of business: Primary care practices at risk
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. In an interview with Kenny Lin, MD, MPH, a family physician, Dr. Frieden discussed the future of primary care.
Here is a sample of Dr. Frieden’s observations:
“When I’ve looked around the United States, I’ve been extremely concerned about both the risk that primary care practitioners are subjected to in their everyday practice and the economic risk that we could lose many of our primary care practices around the country. It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.” Read more.
Surge in out-of-hospital cardiac arrests
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests that placed a huge burden on first responders, according to a new analysis.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
Read more.
Fenfluramine approved for Dravet syndrome
The U.S. Food and Drug Administration has approved fenfluramine (Fintepla, Zogenix) oral solution, a Schedule IV controlled substance, for the treatment of seizures associated with Dravet syndrome in children age 2 years and older.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy.
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Pregnant women at higher risk for severe COVID-19
Pregnant women may be at increased risk for severe COVID-19 illness, according to a report published online June 26 in Morbidity and Mortality Weekly Report.
Among reproductive-aged women (15-44 years) infected with SARS-CoV-2, pregnancy was associated with a greater likelihood of hospitalization, admission to the intensive care unit (ICU), and mechanical ventilation, but not death. Pregnant women were 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to need mechanical ventilation, after adjustment for age, underlying conditions, and race/ethnicity.
CDC researchers said that preventing COVID-19 infection in pregnant women should be a priority and any potential barriers to compliance with preventive measures need to be removed.
“During pregnancy, women experience immunologic and physiologic changes that could increase their risk for more severe illness from respiratory infections,” they wrote. Read more.
Going out of business: Primary care practices at risk
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. In an interview with Kenny Lin, MD, MPH, a family physician, Dr. Frieden discussed the future of primary care.
Here is a sample of Dr. Frieden’s observations:
“When I’ve looked around the United States, I’ve been extremely concerned about both the risk that primary care practitioners are subjected to in their everyday practice and the economic risk that we could lose many of our primary care practices around the country. It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.” Read more.
Surge in out-of-hospital cardiac arrests
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests that placed a huge burden on first responders, according to a new analysis.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
Read more.
Fenfluramine approved for Dravet syndrome
The U.S. Food and Drug Administration has approved fenfluramine (Fintepla, Zogenix) oral solution, a Schedule IV controlled substance, for the treatment of seizures associated with Dravet syndrome in children age 2 years and older.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy.
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.