User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Is the presence of enanthem a clue for COVID-19?
Larger studies should explore and confirm this association, the study’s authors and other experts suggested.
Dermatologists are already aware of the connection between enanthem and viral etiology. “As seen with other viral infections, we wondered if COVID-19 could produce enanthem in addition to skin rash exanthem,” one of the study author’s, Juan Jiménez-Cauhe, MD, a dermatologist with Hospital Universitario Ramon y Cajal, Madrid, said in an interview. He and his colleagues summarized their findings in a research letter in JAMA Dermatology.
They examined the oral cavity of 21 COVID-19 patients at a tertiary care hospital who also had a skin rash from March 30 to April 8. They classified enanthems into four categories: petechial, macular, macular with petechiae, or erythematovesicular. Six of the patients presented with oral lesions, all of them located in the palate; in one patient, the enanthem was macular, it was petechial in two patients and was macular with petechiae in three patients. The six patients ranged between the ages of 40 and 69 years; four were women.
Petechial or vesicular patterns are often associated with viral infections. In this particular study, the investigators did not observe vesicular lesions.
On average, mucocutaneous lesions appeared about 12 days after the onset of COVID-19 symptoms. “Interestingly, this latency was shorter in patients with petechial enanthem, compared with those with a macular lesion with petechiae appearance,” the authors wrote.
This shorter time might suggest an association for SARS-CoV-2, said Dr. Jiménez-Cauhe. Strong cough may have also caused petechial lesions on the palate, but it’s unlikely, as they appeared close in time to COVID-19 symptoms. It’s also unlikely that any drugs caused the lesions, as drug rashes can take 2-3 weeks to appear.
This fits in line with other evidence of broader skin manifestations appearing at the same time or after COVID-19, Esther Freeman, MD, said in an interview. Dr. Freeman, director of global health dermatology at Massachusetts General Hospital, Boston, is the principal investigator of the COVID-19 Dermatology Registry, a collaboration of the American Academy of Dermatology and International League of Dermatological Societies.
The study’s small cohort made it difficult to establish a solid association between the oral lesions and SARS-CoV-2. “However, the presence of enanthem in a patient with a skin rash is a useful finding that suggests a viral etiology rather than a drug reaction. This is particularly useful in COVID-19 patients, who were receiving many drugs as part of the treatment,” Dr. Jimenez-Cauhe said. Future studies should assess whether the presence of enanthem and exanthem lead physicians to consider SARS-CoV-2 as possible agents, ruling out infection with a blood or nasopharyngeal test.
This study adds to the growing body of knowledge on cutaneous and mucocutaneous findings associated with SARS-CoV-2 infection, Jules Lipoff, MD, of the department of dermatology, University of Pennsylvania, Philadelphia, said in an interview. “One challenge in evaluating these findings is that these findings are nonspecific, and medication reactions can often cause similar rashes, such as morbilliform eruptions that can be associated with both viruses and medications.”
Enanthems, as the study authors noted, are more specific to viral infections and are less commonly associated with medication reactions. “So, even though this is a small case series with significant limitations, it does add more evidence that COVID-19 is directly responsible for findings in the skin and mucous membranes,” said Dr. Lipoff.
Dr. Freeman noted that the study may also encourage clinicians to look in a patient’s mouth when assessing for SARS-CoV-2. Additional research should examine these data in a larger population.
Several studies by Dr. Freeman, Dr. Lipoff, and others strongly suggest that SARS-CoV-2 has a spectrum of associated dermatologic manifestations. One evaluated perniolike skin lesions (J Am Acad Dermatol. 2020 Aug; 83[2]:486-92). The other was a case series from the COVID-19 registry that examined 716 cases of new-onset dermatologic symptoms in patients from 31 countries with confirmed/suspected SARS-CoV-2 (J Am Acad Dermatol. 2020 Jul 2;S0190-9622[20]32126-5.).
The authors of the report had no disclosures.
SOURCE: Jimenez-Cauhe J et al. JAMA Dermatol. 2020 Jul 15. doi: 10.1001/jamadermatol.2020.2550.
Larger studies should explore and confirm this association, the study’s authors and other experts suggested.
Dermatologists are already aware of the connection between enanthem and viral etiology. “As seen with other viral infections, we wondered if COVID-19 could produce enanthem in addition to skin rash exanthem,” one of the study author’s, Juan Jiménez-Cauhe, MD, a dermatologist with Hospital Universitario Ramon y Cajal, Madrid, said in an interview. He and his colleagues summarized their findings in a research letter in JAMA Dermatology.
They examined the oral cavity of 21 COVID-19 patients at a tertiary care hospital who also had a skin rash from March 30 to April 8. They classified enanthems into four categories: petechial, macular, macular with petechiae, or erythematovesicular. Six of the patients presented with oral lesions, all of them located in the palate; in one patient, the enanthem was macular, it was petechial in two patients and was macular with petechiae in three patients. The six patients ranged between the ages of 40 and 69 years; four were women.
Petechial or vesicular patterns are often associated with viral infections. In this particular study, the investigators did not observe vesicular lesions.
On average, mucocutaneous lesions appeared about 12 days after the onset of COVID-19 symptoms. “Interestingly, this latency was shorter in patients with petechial enanthem, compared with those with a macular lesion with petechiae appearance,” the authors wrote.
This shorter time might suggest an association for SARS-CoV-2, said Dr. Jiménez-Cauhe. Strong cough may have also caused petechial lesions on the palate, but it’s unlikely, as they appeared close in time to COVID-19 symptoms. It’s also unlikely that any drugs caused the lesions, as drug rashes can take 2-3 weeks to appear.
This fits in line with other evidence of broader skin manifestations appearing at the same time or after COVID-19, Esther Freeman, MD, said in an interview. Dr. Freeman, director of global health dermatology at Massachusetts General Hospital, Boston, is the principal investigator of the COVID-19 Dermatology Registry, a collaboration of the American Academy of Dermatology and International League of Dermatological Societies.
The study’s small cohort made it difficult to establish a solid association between the oral lesions and SARS-CoV-2. “However, the presence of enanthem in a patient with a skin rash is a useful finding that suggests a viral etiology rather than a drug reaction. This is particularly useful in COVID-19 patients, who were receiving many drugs as part of the treatment,” Dr. Jimenez-Cauhe said. Future studies should assess whether the presence of enanthem and exanthem lead physicians to consider SARS-CoV-2 as possible agents, ruling out infection with a blood or nasopharyngeal test.
This study adds to the growing body of knowledge on cutaneous and mucocutaneous findings associated with SARS-CoV-2 infection, Jules Lipoff, MD, of the department of dermatology, University of Pennsylvania, Philadelphia, said in an interview. “One challenge in evaluating these findings is that these findings are nonspecific, and medication reactions can often cause similar rashes, such as morbilliform eruptions that can be associated with both viruses and medications.”
Enanthems, as the study authors noted, are more specific to viral infections and are less commonly associated with medication reactions. “So, even though this is a small case series with significant limitations, it does add more evidence that COVID-19 is directly responsible for findings in the skin and mucous membranes,” said Dr. Lipoff.
Dr. Freeman noted that the study may also encourage clinicians to look in a patient’s mouth when assessing for SARS-CoV-2. Additional research should examine these data in a larger population.
Several studies by Dr. Freeman, Dr. Lipoff, and others strongly suggest that SARS-CoV-2 has a spectrum of associated dermatologic manifestations. One evaluated perniolike skin lesions (J Am Acad Dermatol. 2020 Aug; 83[2]:486-92). The other was a case series from the COVID-19 registry that examined 716 cases of new-onset dermatologic symptoms in patients from 31 countries with confirmed/suspected SARS-CoV-2 (J Am Acad Dermatol. 2020 Jul 2;S0190-9622[20]32126-5.).
The authors of the report had no disclosures.
SOURCE: Jimenez-Cauhe J et al. JAMA Dermatol. 2020 Jul 15. doi: 10.1001/jamadermatol.2020.2550.
Larger studies should explore and confirm this association, the study’s authors and other experts suggested.
Dermatologists are already aware of the connection between enanthem and viral etiology. “As seen with other viral infections, we wondered if COVID-19 could produce enanthem in addition to skin rash exanthem,” one of the study author’s, Juan Jiménez-Cauhe, MD, a dermatologist with Hospital Universitario Ramon y Cajal, Madrid, said in an interview. He and his colleagues summarized their findings in a research letter in JAMA Dermatology.
They examined the oral cavity of 21 COVID-19 patients at a tertiary care hospital who also had a skin rash from March 30 to April 8. They classified enanthems into four categories: petechial, macular, macular with petechiae, or erythematovesicular. Six of the patients presented with oral lesions, all of them located in the palate; in one patient, the enanthem was macular, it was petechial in two patients and was macular with petechiae in three patients. The six patients ranged between the ages of 40 and 69 years; four were women.
Petechial or vesicular patterns are often associated with viral infections. In this particular study, the investigators did not observe vesicular lesions.
On average, mucocutaneous lesions appeared about 12 days after the onset of COVID-19 symptoms. “Interestingly, this latency was shorter in patients with petechial enanthem, compared with those with a macular lesion with petechiae appearance,” the authors wrote.
This shorter time might suggest an association for SARS-CoV-2, said Dr. Jiménez-Cauhe. Strong cough may have also caused petechial lesions on the palate, but it’s unlikely, as they appeared close in time to COVID-19 symptoms. It’s also unlikely that any drugs caused the lesions, as drug rashes can take 2-3 weeks to appear.
This fits in line with other evidence of broader skin manifestations appearing at the same time or after COVID-19, Esther Freeman, MD, said in an interview. Dr. Freeman, director of global health dermatology at Massachusetts General Hospital, Boston, is the principal investigator of the COVID-19 Dermatology Registry, a collaboration of the American Academy of Dermatology and International League of Dermatological Societies.
The study’s small cohort made it difficult to establish a solid association between the oral lesions and SARS-CoV-2. “However, the presence of enanthem in a patient with a skin rash is a useful finding that suggests a viral etiology rather than a drug reaction. This is particularly useful in COVID-19 patients, who were receiving many drugs as part of the treatment,” Dr. Jimenez-Cauhe said. Future studies should assess whether the presence of enanthem and exanthem lead physicians to consider SARS-CoV-2 as possible agents, ruling out infection with a blood or nasopharyngeal test.
This study adds to the growing body of knowledge on cutaneous and mucocutaneous findings associated with SARS-CoV-2 infection, Jules Lipoff, MD, of the department of dermatology, University of Pennsylvania, Philadelphia, said in an interview. “One challenge in evaluating these findings is that these findings are nonspecific, and medication reactions can often cause similar rashes, such as morbilliform eruptions that can be associated with both viruses and medications.”
Enanthems, as the study authors noted, are more specific to viral infections and are less commonly associated with medication reactions. “So, even though this is a small case series with significant limitations, it does add more evidence that COVID-19 is directly responsible for findings in the skin and mucous membranes,” said Dr. Lipoff.
Dr. Freeman noted that the study may also encourage clinicians to look in a patient’s mouth when assessing for SARS-CoV-2. Additional research should examine these data in a larger population.
Several studies by Dr. Freeman, Dr. Lipoff, and others strongly suggest that SARS-CoV-2 has a spectrum of associated dermatologic manifestations. One evaluated perniolike skin lesions (J Am Acad Dermatol. 2020 Aug; 83[2]:486-92). The other was a case series from the COVID-19 registry that examined 716 cases of new-onset dermatologic symptoms in patients from 31 countries with confirmed/suspected SARS-CoV-2 (J Am Acad Dermatol. 2020 Jul 2;S0190-9622[20]32126-5.).
The authors of the report had no disclosures.
SOURCE: Jimenez-Cauhe J et al. JAMA Dermatol. 2020 Jul 15. doi: 10.1001/jamadermatol.2020.2550.
FROM JAMA DERMATOLOGY
Internists’ use of ultrasound can reduce radiology referrals
researchers say.
“It’s a safe and very useful tool,” Marco Barchiesi, MD, an internal medicine resident at Luigi Sacco Hospital in Milan, said in an interview. “We had a great reduction in chest x-rays because of the use of ultrasound.”
The finding addresses concerns that ultrasound used in primary care could consume more health care resources or put patients at risk.
Dr. Barchiesi and colleagues published their findings July 20 in the European Journal of Internal Medicine.
Point-of-care ultrasound has become increasingly common as miniaturization of devices has made them more portable. The approach has caught on particularly in emergency departments where quick decisions are of the essence.
Its use in internal medicine has been more controversial, with concerns raised that improperly trained practitioners may miss diagnoses or refer patients for unnecessary tests as a result of uncertainty about their findings.
To measure the effect of point-of-care ultrasound in an internal medicine hospital ward, Dr. Barchiesi and colleagues alternated months when point-of-care ultrasound was allowed with months when it was not allowed, for a total of 4 months each, on an internal medicine unit. They allowed the ultrasound to be used for invasive procedures and excluded patients whose critical condition made point-of-care ultrasound crucial.
The researchers analyzed data on 263 patients in the “on” months when point-of-care ultrasound was used, and 255 in the “off” months when it wasn’t used. The two groups were well balanced in age, sex, comorbidity, and clinical impairment.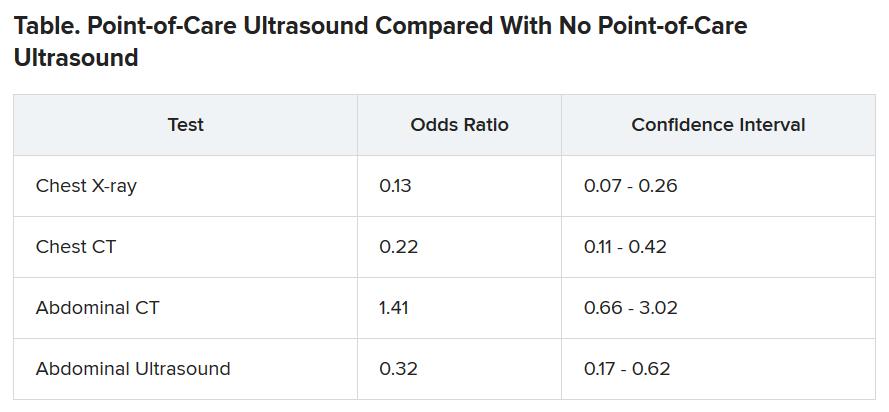
During the on months, the internists ordered 113 diagnostic tests (0.43 per patient). During the off months they ordered 329 tests (1.29 per patient).
The odds of being referred for a chest x-ray were 87% less in the “on” months, compared with the off months, a statistically significant finding (P < .001). The risk for a chest CT scan and abdominal ultrasound were also reduced during the on months, but the risk for an abdominal CT was increased.
Nineteen patients died during the o” months and 10 during the off months, a difference that was not statistically significant (P = .15). The median length of stay in the hospital was almost the same for the two groups: 9 days for the on months and 9 days for the off months. The difference was also not statistically significant (P = .094).
Point-of-care ultrasound is particularly accurate in identifying cardiac abnormalities and pleural fluid and pneumonia, and it can be used effectively for monitoring heart conditions, the researchers wrote. This could explain the reduction in chest x-rays and CT scans.
On the other hand, ultrasound cannot address such questions as staging in an abdominal malignancy, and unexpected findings are more common with abdominal than chest ultrasound. This could explain why the point-of-care ultrasound did not reduce the use of abdominal CT, the researchers speculated.
They acknowledged that the patients in their sample had an average age of 81 years, raising questions about how well their data could be applied to a younger population. And they noted that they used point-of-care ultrasound frequently, so they were particularly adept with it. “We use it almost every day in our clinical practice,” said Dr. Barchiesi.
Those factors may have played a key role in the success of point-of-care ultrasound in this study, said Michael Wagner, MD, an assistant professor of medicine at the University of South Carolina, Greenville, who has helped colleagues incorporate ultrasound into their practices.
Elderly patients often present with multiple comorbidities and atypical signs and symptoms, he said. “Sometimes they can be very confusing as to the underlying clinical picture. Ultrasound is being used frequently to better assess these complicated patients.”
Dr. Wagner said extensive training is required to use point-of-care ultrasound accurately.
Dr. Barchiesi also acknowledged that the devices used in this study were large portable machines, not the simpler and less expensive hand-held versions that are also available for similar purposes.
Point-of-care ultrasound is a promising innovation, said Thomas Melgar, MD, a professor of medicine at Western Michigan University, Kalamazoo. “The advantage is that the exam is being done by someone who knows the patient and specifically what they’re looking for. It’s done at the bedside so you don’t have to move the patient.”
The study could help address opposition to internal medicine residents being trained in the technique, he said, adding that “I think it’s very exciting.”
The study was partially supported by Philips, which provided the ultrasound devices. Dr. Barchiesi, Dr. Melgar, and Dr. Wagner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
researchers say.
“It’s a safe and very useful tool,” Marco Barchiesi, MD, an internal medicine resident at Luigi Sacco Hospital in Milan, said in an interview. “We had a great reduction in chest x-rays because of the use of ultrasound.”
The finding addresses concerns that ultrasound used in primary care could consume more health care resources or put patients at risk.
Dr. Barchiesi and colleagues published their findings July 20 in the European Journal of Internal Medicine.
Point-of-care ultrasound has become increasingly common as miniaturization of devices has made them more portable. The approach has caught on particularly in emergency departments where quick decisions are of the essence.
Its use in internal medicine has been more controversial, with concerns raised that improperly trained practitioners may miss diagnoses or refer patients for unnecessary tests as a result of uncertainty about their findings.
To measure the effect of point-of-care ultrasound in an internal medicine hospital ward, Dr. Barchiesi and colleagues alternated months when point-of-care ultrasound was allowed with months when it was not allowed, for a total of 4 months each, on an internal medicine unit. They allowed the ultrasound to be used for invasive procedures and excluded patients whose critical condition made point-of-care ultrasound crucial.
The researchers analyzed data on 263 patients in the “on” months when point-of-care ultrasound was used, and 255 in the “off” months when it wasn’t used. The two groups were well balanced in age, sex, comorbidity, and clinical impairment.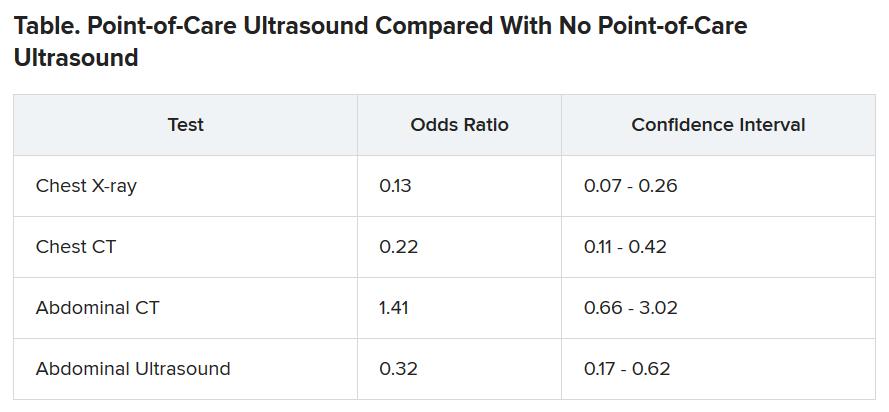
During the on months, the internists ordered 113 diagnostic tests (0.43 per patient). During the off months they ordered 329 tests (1.29 per patient).
The odds of being referred for a chest x-ray were 87% less in the “on” months, compared with the off months, a statistically significant finding (P < .001). The risk for a chest CT scan and abdominal ultrasound were also reduced during the on months, but the risk for an abdominal CT was increased.
Nineteen patients died during the o” months and 10 during the off months, a difference that was not statistically significant (P = .15). The median length of stay in the hospital was almost the same for the two groups: 9 days for the on months and 9 days for the off months. The difference was also not statistically significant (P = .094).
Point-of-care ultrasound is particularly accurate in identifying cardiac abnormalities and pleural fluid and pneumonia, and it can be used effectively for monitoring heart conditions, the researchers wrote. This could explain the reduction in chest x-rays and CT scans.
On the other hand, ultrasound cannot address such questions as staging in an abdominal malignancy, and unexpected findings are more common with abdominal than chest ultrasound. This could explain why the point-of-care ultrasound did not reduce the use of abdominal CT, the researchers speculated.
They acknowledged that the patients in their sample had an average age of 81 years, raising questions about how well their data could be applied to a younger population. And they noted that they used point-of-care ultrasound frequently, so they were particularly adept with it. “We use it almost every day in our clinical practice,” said Dr. Barchiesi.
Those factors may have played a key role in the success of point-of-care ultrasound in this study, said Michael Wagner, MD, an assistant professor of medicine at the University of South Carolina, Greenville, who has helped colleagues incorporate ultrasound into their practices.
Elderly patients often present with multiple comorbidities and atypical signs and symptoms, he said. “Sometimes they can be very confusing as to the underlying clinical picture. Ultrasound is being used frequently to better assess these complicated patients.”
Dr. Wagner said extensive training is required to use point-of-care ultrasound accurately.
Dr. Barchiesi also acknowledged that the devices used in this study were large portable machines, not the simpler and less expensive hand-held versions that are also available for similar purposes.
Point-of-care ultrasound is a promising innovation, said Thomas Melgar, MD, a professor of medicine at Western Michigan University, Kalamazoo. “The advantage is that the exam is being done by someone who knows the patient and specifically what they’re looking for. It’s done at the bedside so you don’t have to move the patient.”
The study could help address opposition to internal medicine residents being trained in the technique, he said, adding that “I think it’s very exciting.”
The study was partially supported by Philips, which provided the ultrasound devices. Dr. Barchiesi, Dr. Melgar, and Dr. Wagner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
researchers say.
“It’s a safe and very useful tool,” Marco Barchiesi, MD, an internal medicine resident at Luigi Sacco Hospital in Milan, said in an interview. “We had a great reduction in chest x-rays because of the use of ultrasound.”
The finding addresses concerns that ultrasound used in primary care could consume more health care resources or put patients at risk.
Dr. Barchiesi and colleagues published their findings July 20 in the European Journal of Internal Medicine.
Point-of-care ultrasound has become increasingly common as miniaturization of devices has made them more portable. The approach has caught on particularly in emergency departments where quick decisions are of the essence.
Its use in internal medicine has been more controversial, with concerns raised that improperly trained practitioners may miss diagnoses or refer patients for unnecessary tests as a result of uncertainty about their findings.
To measure the effect of point-of-care ultrasound in an internal medicine hospital ward, Dr. Barchiesi and colleagues alternated months when point-of-care ultrasound was allowed with months when it was not allowed, for a total of 4 months each, on an internal medicine unit. They allowed the ultrasound to be used for invasive procedures and excluded patients whose critical condition made point-of-care ultrasound crucial.
The researchers analyzed data on 263 patients in the “on” months when point-of-care ultrasound was used, and 255 in the “off” months when it wasn’t used. The two groups were well balanced in age, sex, comorbidity, and clinical impairment.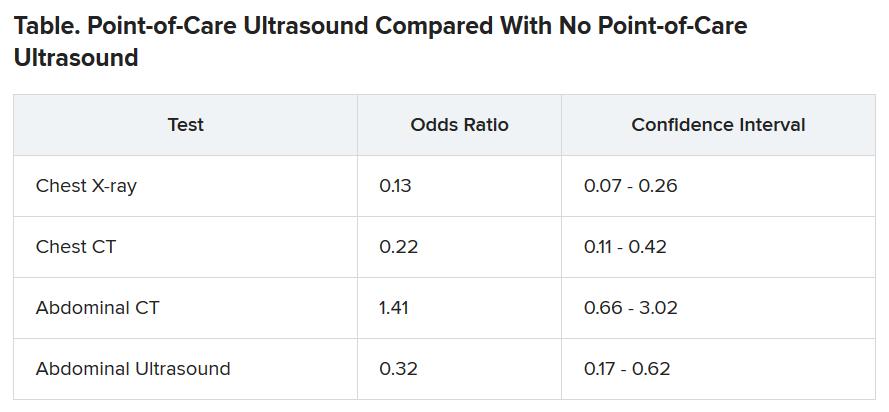
During the on months, the internists ordered 113 diagnostic tests (0.43 per patient). During the off months they ordered 329 tests (1.29 per patient).
The odds of being referred for a chest x-ray were 87% less in the “on” months, compared with the off months, a statistically significant finding (P < .001). The risk for a chest CT scan and abdominal ultrasound were also reduced during the on months, but the risk for an abdominal CT was increased.
Nineteen patients died during the o” months and 10 during the off months, a difference that was not statistically significant (P = .15). The median length of stay in the hospital was almost the same for the two groups: 9 days for the on months and 9 days for the off months. The difference was also not statistically significant (P = .094).
Point-of-care ultrasound is particularly accurate in identifying cardiac abnormalities and pleural fluid and pneumonia, and it can be used effectively for monitoring heart conditions, the researchers wrote. This could explain the reduction in chest x-rays and CT scans.
On the other hand, ultrasound cannot address such questions as staging in an abdominal malignancy, and unexpected findings are more common with abdominal than chest ultrasound. This could explain why the point-of-care ultrasound did not reduce the use of abdominal CT, the researchers speculated.
They acknowledged that the patients in their sample had an average age of 81 years, raising questions about how well their data could be applied to a younger population. And they noted that they used point-of-care ultrasound frequently, so they were particularly adept with it. “We use it almost every day in our clinical practice,” said Dr. Barchiesi.
Those factors may have played a key role in the success of point-of-care ultrasound in this study, said Michael Wagner, MD, an assistant professor of medicine at the University of South Carolina, Greenville, who has helped colleagues incorporate ultrasound into their practices.
Elderly patients often present with multiple comorbidities and atypical signs and symptoms, he said. “Sometimes they can be very confusing as to the underlying clinical picture. Ultrasound is being used frequently to better assess these complicated patients.”
Dr. Wagner said extensive training is required to use point-of-care ultrasound accurately.
Dr. Barchiesi also acknowledged that the devices used in this study were large portable machines, not the simpler and less expensive hand-held versions that are also available for similar purposes.
Point-of-care ultrasound is a promising innovation, said Thomas Melgar, MD, a professor of medicine at Western Michigan University, Kalamazoo. “The advantage is that the exam is being done by someone who knows the patient and specifically what they’re looking for. It’s done at the bedside so you don’t have to move the patient.”
The study could help address opposition to internal medicine residents being trained in the technique, he said, adding that “I think it’s very exciting.”
The study was partially supported by Philips, which provided the ultrasound devices. Dr. Barchiesi, Dr. Melgar, and Dr. Wagner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Ob.gyns. struggle to keep pace with changing COVID-19 knowledge
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
In early April, Maura Quinlan, MD, was working nights on the labor and delivery unit at Northwestern Medicine Prentice Women’s Hospital in Chicago. At the time, hospital policy was to test only patients with known COVID-19 symptoms for SARS-CoV-2. Women in labor wore N95 masks, but only while pushing – and practitioners didn’t always don proper protection in time.
Babies came and families rejoiced. But Dr. Quinlan looks back on those weeks with a degree of horror. “We were laboring a bunch of patients that probably had COVID,” she said, and they were doing so without proper protection.
She’s probably right. According to one study in the New England Journal of Medicine, 13.7% of 211 women who came into the labor and delivery unit at one New York City hospital between March 22 and April 2 were asymptomatic but infected, potentially putting staff and doctors at risk.
Dr. Quinlan already knew she and her fellow ob.gyns. had been walking a thin line and, upon seeing that research, her heart sank. In the middle of a pandemic, they had been racing to keep up with the reality of delivering babies. But despite their efforts to protect both practitioners and patients, some aspects slipped through the cracks. Today, every laboring patient admitted to Northwestern is now tested for the novel coronavirus.
Across the country, hospital labor and delivery wards have been working to find a careful and informed balance among multiple competing interests: the safety of their health care workers, the health of tiny and vulnerable new humans, and the stability of a birthing mother. Each hospital has been making the best decisions it can based on available data. The result is a patchwork of policies, but all of them center around rapid testing and appropriate protection.
Shifting recommendations
One case study of women in a New York City hospital during the height of the city’s surge found that, of seven confirmed COVID-19–positive patients, two were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. The women’s care prior to their positive diagnosis had exposed multiple health care workers, all of whom lacked appropriate personal protective equipment (PPE), the study authors wrote. “Further, five of seven confirmed COVID-19–positive women were afebrile on initial screen, and four did not first report a cough. In some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.”
As studies like this pour in, societies continue to update their recommendations accordingly. The latest guidance from the American College of Obstetricians and Gynecologists came on July 1. The group suggests testing all labor and delivery patients, particularly in high-prevalence areas. If tests are in short supply, it recommends prioritizing testing pregnant women with suspected COVID-19 and those who develop symptoms during admission.
At Northwestern, the hospital requests patients stay home and quarantine for the weeks leading up to their delivery date. Then, they rapidly test every patient who comes in for delivery and aim to have results available within a few hours.
The hospital’s 30-room labor and delivery wing remains reserved for patients who test negative. Those with positive COVID-19 results are sent to a 6-bed COVID labor and delivery unit elsewhere in the hospital. “We were lucky we had the space to do that, because smaller community hospitals wouldn’t have a separate unused unit where they could put these women,” Dr. Quinlan said.
In the COVID unit, women deliver without a support person – no partner, doula, or family member can join. Doctors and nurses wear full PPE and work only in that ward. And because some research shows that pregnant women who are asymptomatic or presymptomatic may develop symptoms quickly after starting labor with no measurable illness, Dr. Quinlan must decide on a case-by-case basis what to do, if anything at all.
Delaying an induction could allow the infection to resolve or it could result in her patient moving from presymptomatic disease to full-blown pneumonia. Accelerating labor could bring on symptoms or it could allow a mother to deliver safely and get out of the hospital as quickly as possible. “There is an advantage to having the baby now if you feel okay – even if it’s alone – and getting home,” Dr. Quinlan said.
The hospital also tests the partners of women who are COVID-19 positive. Those with negative results can take the newborn home and try to maintain distance until the mother is no longer symptomatic.
In different parts of the country, hospitals have developed different approaches. Southern California is experiencing its own surge, but at the Ronald Reagan University of California, Los Angeles, Medical Center there still haven’t been enough COVID-19 patients to warrant a separate labor and delivery unit.
At UCLA, staff swab patients when they enter the labor and delivery ward — those who test positive have specific room designations. For both COVID-19–positive patients and women who progress faster than test results can be returned, the goals are the same, said Rashmi Rao, MD, an ob.gyn. at UCLA: Deliver in the safest way possible for both mother and baby.
All women, positive or negative, must wear masks during labor – as much as they can tolerate, at least. For patients who are only mildly ill or asymptomatic, the only difference is that everyone wears protective gear. But if a patient’s oxygen levels dip, or her baby is in distress, the team moves more quickly to a cesarean delivery than they’d do with a healthy patient.
Just as hospital policies have been evolving, rules for visitors have been constantly changing too. Initially, UCLA allowed a support person to be present during delivery but had to leave immediately following. Now, each new mother is allowed one visitor for the duration of their stay. And the hospital suggests that patients who are COVID-19 positive recover in separate rooms from their babies and encourages them to maintain distance from their infants, except when breastfeeding.
“We respect and understand that this is a joyous occasion and we’re trying to keep families together as much as possible,” Dr. Rao said.
Care conundrums
How hospitals protect their smallest charges keeps changing too. Reports have been circulating about newborns being taken away from COVID-19-positive mothers, especially in marginalized communities. The stories have led many to worry they’d be forcibly separated from their babies. Most hospitals, however, leave it up to the woman and her doctors to decide how much separation is needed. “After delivery, it depends on how someone is feeling,” Dr. Rao said.
The American Academy of Pediatrics recommends that mothers who are COVID-19–positive pump breast milk and have a healthy caregiver use that milk, or formula, to bottle-feed the baby, with the new mother remaining 6 feet away from the child as much as she can. If that’s not possible, she should wear gloves and a mask while breastfeeding until she has been naturally afebrile for 72 hours and at least 1 week removed from the first appearance of her symptoms.
“It’s tragically hard,” said Dr. Quinlan, to keep a COVID-19–positive mother even 6 feet away from her newborn baby. “If a mother declines separation, we ask the acting pediatric team to discuss the theoretical risks and paucity of data.”
Until recently, research indicated that SARS-CoV-2 wasn’t being transmitted through the uterus from mothers to their babies. And despite a recent case study reporting transplacental transmission between a mother and her fetus in France, researchers still say that the risk of transference is low. To ensure newborn risk remains as low as possible, UCLA’s policy is to swab the baby when he/she is 24 hours old and keep watch for signs of infection: increased lethargy, difficulty waking, or gastrointestinal symptoms like vomiting.
Transmission via breast milk has also, to date, proven relatively unlikely. One study in The Lancet detected the novel coronavirus in breast milk, although it’s not clear that the virus can be passed on in the fluid, says Christina Chambers, PhD, a professor of pediatrics at the University of California, San Diego. Dr. Chambers is studying breast milk to see if the virus or antibodies to it are present. She is also investigating how infection with SARS-CoV-2 impacts women at different times in pregnancy, something that’s still an open question.
“[In] pregnant women with a deteriorating infection, the decisions are the same you would make with any delivery: Save the mom and save the baby,” Dr. Chambers said. “Beyond that, I am encouraged to see that pregnant women are prioritized to being tested,” something that will help researchers understand prevalence of disease in order to better understand whether some symptoms are more dangerous than others.
The situation is evolving so quickly that hospitals and providers are simply trying to stay abreast of the flood of new research. In the absence of definitive answers, they are using the information available and adjusting on the fly. “We are cautiously waiting for more data,” said Dr. Rao. “With the information we have we are doing the best we can to keep our patients safe. And we’re just going to keep at it.”
A version of this article originally appeared on Medscape.com.
OSHA in the COVID-19 era
As more and more reopened medical practices ramp up toward normal activity, the safety of patients and health care workers alike remains paramount. As always,
Most of the modified guidelines are already familiar: wear masks (and other personal protective equipment as necessary); maintain social distancing; have hand cleaner, soap, and water readily available; and sanitize between patient examinations.
It is also important to remember that COVID-19 is now a reportable disease; check with your local health authorities as to where and how. Also remember that, if you decide to screen employees and/or patients for fevers and other symptoms of COVID-19, those data are subject to HIPAA rules and must be kept confidential.
Now might be a good time to confirm that you remain in compliance with both the new and old regulations. Even if you hold regular safety meetings – which often is not the case – it is always a good idea to occasionally conduct a comprehensive review, which could save you a lot in fines.
So get your OSHA logs out, and walk through your office. Start by making sure you have an official OSHA poster, which enumerates employee rights and explains how to file complaints. Every office must have one posted in plain site, and is what an OSHA inspector will look for first. They are available for free at OSHA’s website or you can order one by calling 800-321-OSHA.
How long have you had your written exposure control plan for blood-borne pathogens? This plan should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, as well as your implementation of universal precautions. It should be updated annually to reflect changes in technology – and new threats, such as COVID-19.
Review your list of hazardous substances, which all employees have a right to know about. OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are classified as “hazardous.” Also remember that you’re probably using new disinfectants, which may need to be added to your list. For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
It is not necessary to adopt every new safety device as it comes on the market, but you should document which ones you are using and which ones you decide not to use – and why. For example, if you and your employees decide against buying a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it is worth, you still should document how you made that decision and why you believe that your current protocol is as good or better.
All at-risk employees should be provided with hepatitis B vaccine at no cost to them. And after any exposure to dangerous pathogens – which now include COVID-19 – you also must provide and pay for appropriate medical treatment and follow-up.
Another important consideration in your review: Electrical devices and their power sources in the office. All electrically powered equipment – medical or clerical – must operate safely and should all be examined. It is particularly important to check how wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Medical and dental offices are not required to keep an injury and illness log under federal OSHA regulations, which other businesses must. However, your state may have a requirement that supersedes the federal law so you should check with your state, or with your local OSHA office, regarding any such requirements.
It is important to take OSHA regulations seriously because failure to comply with them can result in stiff penalties running into many thousands of dollars.
To be certain you are complying with all the rules, you can call your local OSHA office and request an inspection. This is the easiest and cheapest way because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they discover.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
As more and more reopened medical practices ramp up toward normal activity, the safety of patients and health care workers alike remains paramount. As always,
Most of the modified guidelines are already familiar: wear masks (and other personal protective equipment as necessary); maintain social distancing; have hand cleaner, soap, and water readily available; and sanitize between patient examinations.
It is also important to remember that COVID-19 is now a reportable disease; check with your local health authorities as to where and how. Also remember that, if you decide to screen employees and/or patients for fevers and other symptoms of COVID-19, those data are subject to HIPAA rules and must be kept confidential.
Now might be a good time to confirm that you remain in compliance with both the new and old regulations. Even if you hold regular safety meetings – which often is not the case – it is always a good idea to occasionally conduct a comprehensive review, which could save you a lot in fines.
So get your OSHA logs out, and walk through your office. Start by making sure you have an official OSHA poster, which enumerates employee rights and explains how to file complaints. Every office must have one posted in plain site, and is what an OSHA inspector will look for first. They are available for free at OSHA’s website or you can order one by calling 800-321-OSHA.
How long have you had your written exposure control plan for blood-borne pathogens? This plan should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, as well as your implementation of universal precautions. It should be updated annually to reflect changes in technology – and new threats, such as COVID-19.
Review your list of hazardous substances, which all employees have a right to know about. OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are classified as “hazardous.” Also remember that you’re probably using new disinfectants, which may need to be added to your list. For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
It is not necessary to adopt every new safety device as it comes on the market, but you should document which ones you are using and which ones you decide not to use – and why. For example, if you and your employees decide against buying a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it is worth, you still should document how you made that decision and why you believe that your current protocol is as good or better.
All at-risk employees should be provided with hepatitis B vaccine at no cost to them. And after any exposure to dangerous pathogens – which now include COVID-19 – you also must provide and pay for appropriate medical treatment and follow-up.
Another important consideration in your review: Electrical devices and their power sources in the office. All electrically powered equipment – medical or clerical – must operate safely and should all be examined. It is particularly important to check how wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Medical and dental offices are not required to keep an injury and illness log under federal OSHA regulations, which other businesses must. However, your state may have a requirement that supersedes the federal law so you should check with your state, or with your local OSHA office, regarding any such requirements.
It is important to take OSHA regulations seriously because failure to comply with them can result in stiff penalties running into many thousands of dollars.
To be certain you are complying with all the rules, you can call your local OSHA office and request an inspection. This is the easiest and cheapest way because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they discover.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
As more and more reopened medical practices ramp up toward normal activity, the safety of patients and health care workers alike remains paramount. As always,
Most of the modified guidelines are already familiar: wear masks (and other personal protective equipment as necessary); maintain social distancing; have hand cleaner, soap, and water readily available; and sanitize between patient examinations.
It is also important to remember that COVID-19 is now a reportable disease; check with your local health authorities as to where and how. Also remember that, if you decide to screen employees and/or patients for fevers and other symptoms of COVID-19, those data are subject to HIPAA rules and must be kept confidential.
Now might be a good time to confirm that you remain in compliance with both the new and old regulations. Even if you hold regular safety meetings – which often is not the case – it is always a good idea to occasionally conduct a comprehensive review, which could save you a lot in fines.
So get your OSHA logs out, and walk through your office. Start by making sure you have an official OSHA poster, which enumerates employee rights and explains how to file complaints. Every office must have one posted in plain site, and is what an OSHA inspector will look for first. They are available for free at OSHA’s website or you can order one by calling 800-321-OSHA.
How long have you had your written exposure control plan for blood-borne pathogens? This plan should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, as well as your implementation of universal precautions. It should be updated annually to reflect changes in technology – and new threats, such as COVID-19.
Review your list of hazardous substances, which all employees have a right to know about. OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are classified as “hazardous.” Also remember that you’re probably using new disinfectants, which may need to be added to your list. For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
It is not necessary to adopt every new safety device as it comes on the market, but you should document which ones you are using and which ones you decide not to use – and why. For example, if you and your employees decide against buying a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it is worth, you still should document how you made that decision and why you believe that your current protocol is as good or better.
All at-risk employees should be provided with hepatitis B vaccine at no cost to them. And after any exposure to dangerous pathogens – which now include COVID-19 – you also must provide and pay for appropriate medical treatment and follow-up.
Another important consideration in your review: Electrical devices and their power sources in the office. All electrically powered equipment – medical or clerical – must operate safely and should all be examined. It is particularly important to check how wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it and that circuit breakers are present and functioning.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Medical and dental offices are not required to keep an injury and illness log under federal OSHA regulations, which other businesses must. However, your state may have a requirement that supersedes the federal law so you should check with your state, or with your local OSHA office, regarding any such requirements.
It is important to take OSHA regulations seriously because failure to comply with them can result in stiff penalties running into many thousands of dollars.
To be certain you are complying with all the rules, you can call your local OSHA office and request an inspection. This is the easiest and cheapest way because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they discover.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Heavy toll from ongoing cancer referral delays
Delays in cancer referrals caused by the COVID-19 pandemic and the ensuing shutdown in cancer services will lead to thousands of additional deaths and tens of thousands of life-years lost, suggest two new modeling studies from the United Kingdom.
Clearing the backlog in cancer diagnoses will require a coordinated effort from the government and the National Health Service (NHS), say the authors, inasmuch as services were already running at “full capacity” before the pandemic.
Both studies were published in The Lancet Oncology on July 20.
When the UK-wide lockdown to combat the COVID-19 pandemic was implemented on March 23, cancer screening and routine outpatient referrals in the NHS were suspended, and treatment of cancer patients either halted or slowed down.
Moreover, because of physical distancing measures, which are expected to continue for up to a year, urgent 3-week referrals for suspected cancer cases have fallen by as much as 80%.
To estimate the potential impact on cancer deaths, Ajay Aggarwal, MD, from the London School of Hygiene and Tropical Medicine, United Kingdom, and colleagues conducted a population-based modeling study.
They collected data on 32,583 patients with breast cancer, 24,975 with colorectal cancer, 6744 with esophageal cancer, and 29,305 with lung cancer. Patients were diagnosed between 2010 and 2012 and were followed to 2015.
The investigators used that data to estimate the impact of diagnostic delays resulting from 12 months of physical distancing.
For breast cancer, this would lead to a 7.9%-9.6% increase in the number of cancer deaths within 5 years after diagnosis, or to 281-344 additional deaths.
For colorectal cancer, there would be a 15.3%-16.7% increase in mortality over 5 years, or an additional 1,445-1,563 deaths.
For lung cancer, there would a 4.8%-5.3% increase in mortality, or an additional 1235-1372 deaths.
For esophageal cancer, the mortality increase over 5 years would be 5.8%-6.0%, leading to 330-342 additional deaths.
Across the four tumor types, 59,204-63,229 life-years would be lost because of physical distancing compared to the prepandemic era.
Resources need to be increased
These additional deaths are not inevitable, the researchers suggest.
To prevent the increase in colorectal cancer deaths, for example, Aggarwal said, “It is vital that more resources are made urgently available for endoscopy and colonoscopy services, which are managing significant backlogs currently.
“Whilst currently attention is being focused on diagnostic pathways where cancer is suspected, the issue is that a significant number of cancers are diagnosed in patients awaiting investigation for symptoms not considered related to be cancer,” he added in a statement.
“Therefore we need a whole system approach to avoid the predicted excess deaths.”
Coauthor Bernard Rachet, PhD, also from the London School of Hygiene and Tropical Medicine, added that “to absorb the cancer patient backlog, the healthcare community also needs to establish clear criteria to prioritise patients on clinical grounds, in order to maintain equitability in care delivery.”
It will not be easy “to pin down the exact number of additional cancer deaths we expect to see over the coming years, but studies like this help us to understand the devastating long-term effect a pandemic like COVID-19 will have on the lives of thousands of cancer patients,” commented Michelle Mitchell, chief executive of Cancer Research UK.
Underlining the “enormous backlog” of cancer care that has built up during the pandemic, she said: “Diagnosing and treating people swiftly is vital to give people with cancer the greatest chances of survival.
“The government must work closely with the NHS to ensure it has sufficient staff and equipment to clear the backlog while giving patients the care that they need, quickly and safely,” Mitchell added.
Increasing resources will not be easy. In an accompanying editorial, William Hamilton, MD, PhD, University of Exeter, United Kingdom, warns that many NHS imaging departments, for example, were “working at full capacity before the COVID-19 pandemic.”
Consequently, they “might not be able to meet the increase in demand” resulting from the backlog in patients, especially as “the need to keep patients separate and to clean equipment has reduced their efficiency.
“The UK has had a long-term shortage of diagnostic capacity, although this shortage is not simply of equipment, but also of personnel, which is not so easily improved,” he cautions.
Another study, similar estimates
For the second study, Clare Turnbull, PhD, Institute of Cancer Research, London, and colleagues obtained age- and stage-stratified 10-year cancer survival estimates for patients in England diagnosed with 20 common tumor types between 2008 and 2017.
They also gathered data on cancer diagnoses made via urgent 2-week referrals between 2013 and 2016. They estimate that 6,281 patients were diagnosed with cancer of stages I-III per month.
Of those, 1,691 (27%) would die within 10 years of their diagnosis, they found.
They then calculated that delays in 2-week referrals during a 3-month lockdown would lead to an average delay in presentation of 2 months per patient.
A resulting 25% backlog in referrals would lead to 181 additional lives and 3,316 life-years lost. With a 75% backlog in referrals, an additional 276 lives and 5,075 life-years would be lost.
The team says that additional diagnostic delays spread over 3-8 months after the lockdown could increase the impact of a 25% backlog in referrals to 401 additional lives and 14,873 life-years lost.
For a 75% backlog in referrals, the additional lives lost would rise to 1,231, and the number of life-years lost would reach 22,635.
“Substantial additional deaths from diagnostic delays on top of those expected from delays in presentation – because many people are simply too afraid to visit their GP or hospital – are likely, especially if rapid provision of additional capacity, including technical provision and increased staffing, is not forthcoming,” Turnbull commented in a statement.
The study by Aggarwal and colleagues was funded by the U.K. Research and Innovation Economic and Social Research Council. Several of the researchers were supported by Cancer Research UK and Breast Cancer Now. Turnbull reports receiving support from the Movember Foundation.
This article first appeared on Medscape.com.
Delays in cancer referrals caused by the COVID-19 pandemic and the ensuing shutdown in cancer services will lead to thousands of additional deaths and tens of thousands of life-years lost, suggest two new modeling studies from the United Kingdom.
Clearing the backlog in cancer diagnoses will require a coordinated effort from the government and the National Health Service (NHS), say the authors, inasmuch as services were already running at “full capacity” before the pandemic.
Both studies were published in The Lancet Oncology on July 20.
When the UK-wide lockdown to combat the COVID-19 pandemic was implemented on March 23, cancer screening and routine outpatient referrals in the NHS were suspended, and treatment of cancer patients either halted or slowed down.
Moreover, because of physical distancing measures, which are expected to continue for up to a year, urgent 3-week referrals for suspected cancer cases have fallen by as much as 80%.
To estimate the potential impact on cancer deaths, Ajay Aggarwal, MD, from the London School of Hygiene and Tropical Medicine, United Kingdom, and colleagues conducted a population-based modeling study.
They collected data on 32,583 patients with breast cancer, 24,975 with colorectal cancer, 6744 with esophageal cancer, and 29,305 with lung cancer. Patients were diagnosed between 2010 and 2012 and were followed to 2015.
The investigators used that data to estimate the impact of diagnostic delays resulting from 12 months of physical distancing.
For breast cancer, this would lead to a 7.9%-9.6% increase in the number of cancer deaths within 5 years after diagnosis, or to 281-344 additional deaths.
For colorectal cancer, there would be a 15.3%-16.7% increase in mortality over 5 years, or an additional 1,445-1,563 deaths.
For lung cancer, there would a 4.8%-5.3% increase in mortality, or an additional 1235-1372 deaths.
For esophageal cancer, the mortality increase over 5 years would be 5.8%-6.0%, leading to 330-342 additional deaths.
Across the four tumor types, 59,204-63,229 life-years would be lost because of physical distancing compared to the prepandemic era.
Resources need to be increased
These additional deaths are not inevitable, the researchers suggest.
To prevent the increase in colorectal cancer deaths, for example, Aggarwal said, “It is vital that more resources are made urgently available for endoscopy and colonoscopy services, which are managing significant backlogs currently.
“Whilst currently attention is being focused on diagnostic pathways where cancer is suspected, the issue is that a significant number of cancers are diagnosed in patients awaiting investigation for symptoms not considered related to be cancer,” he added in a statement.
“Therefore we need a whole system approach to avoid the predicted excess deaths.”
Coauthor Bernard Rachet, PhD, also from the London School of Hygiene and Tropical Medicine, added that “to absorb the cancer patient backlog, the healthcare community also needs to establish clear criteria to prioritise patients on clinical grounds, in order to maintain equitability in care delivery.”
It will not be easy “to pin down the exact number of additional cancer deaths we expect to see over the coming years, but studies like this help us to understand the devastating long-term effect a pandemic like COVID-19 will have on the lives of thousands of cancer patients,” commented Michelle Mitchell, chief executive of Cancer Research UK.
Underlining the “enormous backlog” of cancer care that has built up during the pandemic, she said: “Diagnosing and treating people swiftly is vital to give people with cancer the greatest chances of survival.
“The government must work closely with the NHS to ensure it has sufficient staff and equipment to clear the backlog while giving patients the care that they need, quickly and safely,” Mitchell added.
Increasing resources will not be easy. In an accompanying editorial, William Hamilton, MD, PhD, University of Exeter, United Kingdom, warns that many NHS imaging departments, for example, were “working at full capacity before the COVID-19 pandemic.”
Consequently, they “might not be able to meet the increase in demand” resulting from the backlog in patients, especially as “the need to keep patients separate and to clean equipment has reduced their efficiency.
“The UK has had a long-term shortage of diagnostic capacity, although this shortage is not simply of equipment, but also of personnel, which is not so easily improved,” he cautions.
Another study, similar estimates
For the second study, Clare Turnbull, PhD, Institute of Cancer Research, London, and colleagues obtained age- and stage-stratified 10-year cancer survival estimates for patients in England diagnosed with 20 common tumor types between 2008 and 2017.
They also gathered data on cancer diagnoses made via urgent 2-week referrals between 2013 and 2016. They estimate that 6,281 patients were diagnosed with cancer of stages I-III per month.
Of those, 1,691 (27%) would die within 10 years of their diagnosis, they found.
They then calculated that delays in 2-week referrals during a 3-month lockdown would lead to an average delay in presentation of 2 months per patient.
A resulting 25% backlog in referrals would lead to 181 additional lives and 3,316 life-years lost. With a 75% backlog in referrals, an additional 276 lives and 5,075 life-years would be lost.
The team says that additional diagnostic delays spread over 3-8 months after the lockdown could increase the impact of a 25% backlog in referrals to 401 additional lives and 14,873 life-years lost.
For a 75% backlog in referrals, the additional lives lost would rise to 1,231, and the number of life-years lost would reach 22,635.
“Substantial additional deaths from diagnostic delays on top of those expected from delays in presentation – because many people are simply too afraid to visit their GP or hospital – are likely, especially if rapid provision of additional capacity, including technical provision and increased staffing, is not forthcoming,” Turnbull commented in a statement.
The study by Aggarwal and colleagues was funded by the U.K. Research and Innovation Economic and Social Research Council. Several of the researchers were supported by Cancer Research UK and Breast Cancer Now. Turnbull reports receiving support from the Movember Foundation.
This article first appeared on Medscape.com.
Delays in cancer referrals caused by the COVID-19 pandemic and the ensuing shutdown in cancer services will lead to thousands of additional deaths and tens of thousands of life-years lost, suggest two new modeling studies from the United Kingdom.
Clearing the backlog in cancer diagnoses will require a coordinated effort from the government and the National Health Service (NHS), say the authors, inasmuch as services were already running at “full capacity” before the pandemic.
Both studies were published in The Lancet Oncology on July 20.
When the UK-wide lockdown to combat the COVID-19 pandemic was implemented on March 23, cancer screening and routine outpatient referrals in the NHS were suspended, and treatment of cancer patients either halted or slowed down.
Moreover, because of physical distancing measures, which are expected to continue for up to a year, urgent 3-week referrals for suspected cancer cases have fallen by as much as 80%.
To estimate the potential impact on cancer deaths, Ajay Aggarwal, MD, from the London School of Hygiene and Tropical Medicine, United Kingdom, and colleagues conducted a population-based modeling study.
They collected data on 32,583 patients with breast cancer, 24,975 with colorectal cancer, 6744 with esophageal cancer, and 29,305 with lung cancer. Patients were diagnosed between 2010 and 2012 and were followed to 2015.
The investigators used that data to estimate the impact of diagnostic delays resulting from 12 months of physical distancing.
For breast cancer, this would lead to a 7.9%-9.6% increase in the number of cancer deaths within 5 years after diagnosis, or to 281-344 additional deaths.
For colorectal cancer, there would be a 15.3%-16.7% increase in mortality over 5 years, or an additional 1,445-1,563 deaths.
For lung cancer, there would a 4.8%-5.3% increase in mortality, or an additional 1235-1372 deaths.
For esophageal cancer, the mortality increase over 5 years would be 5.8%-6.0%, leading to 330-342 additional deaths.
Across the four tumor types, 59,204-63,229 life-years would be lost because of physical distancing compared to the prepandemic era.
Resources need to be increased
These additional deaths are not inevitable, the researchers suggest.
To prevent the increase in colorectal cancer deaths, for example, Aggarwal said, “It is vital that more resources are made urgently available for endoscopy and colonoscopy services, which are managing significant backlogs currently.
“Whilst currently attention is being focused on diagnostic pathways where cancer is suspected, the issue is that a significant number of cancers are diagnosed in patients awaiting investigation for symptoms not considered related to be cancer,” he added in a statement.
“Therefore we need a whole system approach to avoid the predicted excess deaths.”
Coauthor Bernard Rachet, PhD, also from the London School of Hygiene and Tropical Medicine, added that “to absorb the cancer patient backlog, the healthcare community also needs to establish clear criteria to prioritise patients on clinical grounds, in order to maintain equitability in care delivery.”
It will not be easy “to pin down the exact number of additional cancer deaths we expect to see over the coming years, but studies like this help us to understand the devastating long-term effect a pandemic like COVID-19 will have on the lives of thousands of cancer patients,” commented Michelle Mitchell, chief executive of Cancer Research UK.
Underlining the “enormous backlog” of cancer care that has built up during the pandemic, she said: “Diagnosing and treating people swiftly is vital to give people with cancer the greatest chances of survival.
“The government must work closely with the NHS to ensure it has sufficient staff and equipment to clear the backlog while giving patients the care that they need, quickly and safely,” Mitchell added.
Increasing resources will not be easy. In an accompanying editorial, William Hamilton, MD, PhD, University of Exeter, United Kingdom, warns that many NHS imaging departments, for example, were “working at full capacity before the COVID-19 pandemic.”
Consequently, they “might not be able to meet the increase in demand” resulting from the backlog in patients, especially as “the need to keep patients separate and to clean equipment has reduced their efficiency.
“The UK has had a long-term shortage of diagnostic capacity, although this shortage is not simply of equipment, but also of personnel, which is not so easily improved,” he cautions.
Another study, similar estimates
For the second study, Clare Turnbull, PhD, Institute of Cancer Research, London, and colleagues obtained age- and stage-stratified 10-year cancer survival estimates for patients in England diagnosed with 20 common tumor types between 2008 and 2017.
They also gathered data on cancer diagnoses made via urgent 2-week referrals between 2013 and 2016. They estimate that 6,281 patients were diagnosed with cancer of stages I-III per month.
Of those, 1,691 (27%) would die within 10 years of their diagnosis, they found.
They then calculated that delays in 2-week referrals during a 3-month lockdown would lead to an average delay in presentation of 2 months per patient.
A resulting 25% backlog in referrals would lead to 181 additional lives and 3,316 life-years lost. With a 75% backlog in referrals, an additional 276 lives and 5,075 life-years would be lost.
The team says that additional diagnostic delays spread over 3-8 months after the lockdown could increase the impact of a 25% backlog in referrals to 401 additional lives and 14,873 life-years lost.
For a 75% backlog in referrals, the additional lives lost would rise to 1,231, and the number of life-years lost would reach 22,635.
“Substantial additional deaths from diagnostic delays on top of those expected from delays in presentation – because many people are simply too afraid to visit their GP or hospital – are likely, especially if rapid provision of additional capacity, including technical provision and increased staffing, is not forthcoming,” Turnbull commented in a statement.
The study by Aggarwal and colleagues was funded by the U.K. Research and Innovation Economic and Social Research Council. Several of the researchers were supported by Cancer Research UK and Breast Cancer Now. Turnbull reports receiving support from the Movember Foundation.
This article first appeared on Medscape.com.
Acute EVALI remains a diagnosis of exclusion
according to a synthesis of current information presented at the virtual Pediatric Hospital Medicine.
Respiratory symptoms, including cough, chest pain, and shortness of breath are common but so are constitutive symptoms, including fever, sore throat, muscle aches, nausea and vomiting, said Yamini Kuchipudi, MD, a staff physician at Cincinnati Children’s Hospital, during the session at the virtual meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
If EVALI is not considered across this broad array of symptoms, of which respiratory complaints might not be the most prominent at the time of presentation, the diagnosis might be delayed, Dr. Kuchipudi warned during the virtual meeting.
Teenagers and young adults are the most common users of e-cigarettes and vaping devices. In these patients or in any individual suspected of having EVALI, Dr. Kuchipudi recommended posing questions about vaping relatively early in the work-up “in a confidential and nonjudgmental way.”
Eliciting a truthful history will be particularly important, because the risk of EVALI appears to be largely related to vaping with tetrahydrocannabinol (THC)-containing products rather than with nicotine alone. Although the exact cause of EVALI is not yet completely clear, this condition is now strongly associated with additives to the THC, according to Issa Hanna, MD, of the department of pediatrics at the University of Florida, Jacksonville.
“E-liquid contains products like hydrocarbons, vitamin E acetate, and heavy metals that appear to damage the alveolar epithelium by direct cellular inflammation,” Dr. Hanna explained.
These products are not only found in THC processed for vaping but also for dabbing, a related but different form of inhalation that involves vaporization of highly concentrated THC waxes or resins. Dr. Hanna suggested that the decline in reported cases of EVALI, which has followed the peak incidence in September 2019, is likely to be related to a decline in THC additives as well as greater caution among users.
E-cigarettes were introduced in 2007, according to Dr. Hanna, but EVALI was not widely recognized until cases began accruing early in 2019. By June 2019, the growing number of case reports had attracted the attention of the media as well as public health officials, intensifying the effort to isolate the risks and causes.
Consistent with greater use of e-cigarettes and vaping among younger individuals, nearly 80% of the 2,807 patients hospitalized for EVALI in the United States by February of this year occurred in individuals aged less than 35 years, according to data released by the Centers for Disease Control and Prevention. The median age was less than 25 years. Of these hospitalizations, 68 deaths (2.5%) in 29 states and Washington, D.C., were attributed to EVALI.
Because of the nonspecific symptoms and lack of a definitive diagnostic test, EVALI is considered a diagnosis of exclusion, according to Abigail Musial, MD, who is completing a fellowship in hospital medicine at Cincinnati Children’s. She presented a case in which a patient suspected of EVALI went home after symptoms abated on steroids.
“Less than 24 hours later, she returned to the ED with tachypnea and hypoxemia,” Dr. Musial recounted. Although a chest x-ray at the initial evaluation showed lung opacities, a repeat chest x-ray when she returned to the ED showed bilateral worsening of these opacities and persistent elevation of inflammatory markers.
“She was started on steroids and also on antibiotics,” Dr. Musial said. “She was weaned quickly from oxygen once the steroids were started and was discharged on hospital day 3.”
For patients suspected of EVALI, COVID-19 testing should be part of the work-up, according to Dr. Kuchipudi. She also recommended an x-ray or CT scan of the lung as well as an evaluation of inflammatory markers.
Dr. Kuchipudi said that more invasive studies than lung function tests, such as bronchoalveolar lavage or lung biopsy, might be considered when severe symptoms make aggressive diagnostic studies attractive.
Steroids and antibiotics typically lead to control of acute symptoms, but patients should be clinically stable for 24-48 hours prior to hospital discharge, according to Dr. Kuchipudi. Follow-up after discharge should include lung function tests and imaging 2-4 weeks later to confirm resolution of abnormalities.
Dr. Kuchipudi stressed the opportunity that an episode of EVALI provides to induce patients to give up nicotine and vaping entirely. Such strategies, such as a nicotine patch, deserve consideration, but she also cautioned that e-cigarettes for smoking cessation should not be recommended to EVALI patients.
The speakers reported no potential conflicts of interest relevant to this study.
according to a synthesis of current information presented at the virtual Pediatric Hospital Medicine.
Respiratory symptoms, including cough, chest pain, and shortness of breath are common but so are constitutive symptoms, including fever, sore throat, muscle aches, nausea and vomiting, said Yamini Kuchipudi, MD, a staff physician at Cincinnati Children’s Hospital, during the session at the virtual meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
If EVALI is not considered across this broad array of symptoms, of which respiratory complaints might not be the most prominent at the time of presentation, the diagnosis might be delayed, Dr. Kuchipudi warned during the virtual meeting.
Teenagers and young adults are the most common users of e-cigarettes and vaping devices. In these patients or in any individual suspected of having EVALI, Dr. Kuchipudi recommended posing questions about vaping relatively early in the work-up “in a confidential and nonjudgmental way.”
Eliciting a truthful history will be particularly important, because the risk of EVALI appears to be largely related to vaping with tetrahydrocannabinol (THC)-containing products rather than with nicotine alone. Although the exact cause of EVALI is not yet completely clear, this condition is now strongly associated with additives to the THC, according to Issa Hanna, MD, of the department of pediatrics at the University of Florida, Jacksonville.
“E-liquid contains products like hydrocarbons, vitamin E acetate, and heavy metals that appear to damage the alveolar epithelium by direct cellular inflammation,” Dr. Hanna explained.
These products are not only found in THC processed for vaping but also for dabbing, a related but different form of inhalation that involves vaporization of highly concentrated THC waxes or resins. Dr. Hanna suggested that the decline in reported cases of EVALI, which has followed the peak incidence in September 2019, is likely to be related to a decline in THC additives as well as greater caution among users.
E-cigarettes were introduced in 2007, according to Dr. Hanna, but EVALI was not widely recognized until cases began accruing early in 2019. By June 2019, the growing number of case reports had attracted the attention of the media as well as public health officials, intensifying the effort to isolate the risks and causes.
Consistent with greater use of e-cigarettes and vaping among younger individuals, nearly 80% of the 2,807 patients hospitalized for EVALI in the United States by February of this year occurred in individuals aged less than 35 years, according to data released by the Centers for Disease Control and Prevention. The median age was less than 25 years. Of these hospitalizations, 68 deaths (2.5%) in 29 states and Washington, D.C., were attributed to EVALI.
Because of the nonspecific symptoms and lack of a definitive diagnostic test, EVALI is considered a diagnosis of exclusion, according to Abigail Musial, MD, who is completing a fellowship in hospital medicine at Cincinnati Children’s. She presented a case in which a patient suspected of EVALI went home after symptoms abated on steroids.
“Less than 24 hours later, she returned to the ED with tachypnea and hypoxemia,” Dr. Musial recounted. Although a chest x-ray at the initial evaluation showed lung opacities, a repeat chest x-ray when she returned to the ED showed bilateral worsening of these opacities and persistent elevation of inflammatory markers.
“She was started on steroids and also on antibiotics,” Dr. Musial said. “She was weaned quickly from oxygen once the steroids were started and was discharged on hospital day 3.”
For patients suspected of EVALI, COVID-19 testing should be part of the work-up, according to Dr. Kuchipudi. She also recommended an x-ray or CT scan of the lung as well as an evaluation of inflammatory markers.
Dr. Kuchipudi said that more invasive studies than lung function tests, such as bronchoalveolar lavage or lung biopsy, might be considered when severe symptoms make aggressive diagnostic studies attractive.
Steroids and antibiotics typically lead to control of acute symptoms, but patients should be clinically stable for 24-48 hours prior to hospital discharge, according to Dr. Kuchipudi. Follow-up after discharge should include lung function tests and imaging 2-4 weeks later to confirm resolution of abnormalities.
Dr. Kuchipudi stressed the opportunity that an episode of EVALI provides to induce patients to give up nicotine and vaping entirely. Such strategies, such as a nicotine patch, deserve consideration, but she also cautioned that e-cigarettes for smoking cessation should not be recommended to EVALI patients.
The speakers reported no potential conflicts of interest relevant to this study.
according to a synthesis of current information presented at the virtual Pediatric Hospital Medicine.
Respiratory symptoms, including cough, chest pain, and shortness of breath are common but so are constitutive symptoms, including fever, sore throat, muscle aches, nausea and vomiting, said Yamini Kuchipudi, MD, a staff physician at Cincinnati Children’s Hospital, during the session at the virtual meeting, sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
If EVALI is not considered across this broad array of symptoms, of which respiratory complaints might not be the most prominent at the time of presentation, the diagnosis might be delayed, Dr. Kuchipudi warned during the virtual meeting.
Teenagers and young adults are the most common users of e-cigarettes and vaping devices. In these patients or in any individual suspected of having EVALI, Dr. Kuchipudi recommended posing questions about vaping relatively early in the work-up “in a confidential and nonjudgmental way.”
Eliciting a truthful history will be particularly important, because the risk of EVALI appears to be largely related to vaping with tetrahydrocannabinol (THC)-containing products rather than with nicotine alone. Although the exact cause of EVALI is not yet completely clear, this condition is now strongly associated with additives to the THC, according to Issa Hanna, MD, of the department of pediatrics at the University of Florida, Jacksonville.
“E-liquid contains products like hydrocarbons, vitamin E acetate, and heavy metals that appear to damage the alveolar epithelium by direct cellular inflammation,” Dr. Hanna explained.
These products are not only found in THC processed for vaping but also for dabbing, a related but different form of inhalation that involves vaporization of highly concentrated THC waxes or resins. Dr. Hanna suggested that the decline in reported cases of EVALI, which has followed the peak incidence in September 2019, is likely to be related to a decline in THC additives as well as greater caution among users.
E-cigarettes were introduced in 2007, according to Dr. Hanna, but EVALI was not widely recognized until cases began accruing early in 2019. By June 2019, the growing number of case reports had attracted the attention of the media as well as public health officials, intensifying the effort to isolate the risks and causes.
Consistent with greater use of e-cigarettes and vaping among younger individuals, nearly 80% of the 2,807 patients hospitalized for EVALI in the United States by February of this year occurred in individuals aged less than 35 years, according to data released by the Centers for Disease Control and Prevention. The median age was less than 25 years. Of these hospitalizations, 68 deaths (2.5%) in 29 states and Washington, D.C., were attributed to EVALI.
Because of the nonspecific symptoms and lack of a definitive diagnostic test, EVALI is considered a diagnosis of exclusion, according to Abigail Musial, MD, who is completing a fellowship in hospital medicine at Cincinnati Children’s. She presented a case in which a patient suspected of EVALI went home after symptoms abated on steroids.
“Less than 24 hours later, she returned to the ED with tachypnea and hypoxemia,” Dr. Musial recounted. Although a chest x-ray at the initial evaluation showed lung opacities, a repeat chest x-ray when she returned to the ED showed bilateral worsening of these opacities and persistent elevation of inflammatory markers.
“She was started on steroids and also on antibiotics,” Dr. Musial said. “She was weaned quickly from oxygen once the steroids were started and was discharged on hospital day 3.”
For patients suspected of EVALI, COVID-19 testing should be part of the work-up, according to Dr. Kuchipudi. She also recommended an x-ray or CT scan of the lung as well as an evaluation of inflammatory markers.
Dr. Kuchipudi said that more invasive studies than lung function tests, such as bronchoalveolar lavage or lung biopsy, might be considered when severe symptoms make aggressive diagnostic studies attractive.
Steroids and antibiotics typically lead to control of acute symptoms, but patients should be clinically stable for 24-48 hours prior to hospital discharge, according to Dr. Kuchipudi. Follow-up after discharge should include lung function tests and imaging 2-4 weeks later to confirm resolution of abnormalities.
Dr. Kuchipudi stressed the opportunity that an episode of EVALI provides to induce patients to give up nicotine and vaping entirely. Such strategies, such as a nicotine patch, deserve consideration, but she also cautioned that e-cigarettes for smoking cessation should not be recommended to EVALI patients.
The speakers reported no potential conflicts of interest relevant to this study.
FROM PHM20
New oral anticoagulants drive ACC consensus on bleeding
Patients on oral anticoagulants who experience a bleeding event may be able to discontinue therapy if certain circumstances apply, according to updated guidance from the American College of Cardiology.
The emergence of direct-acting oral anticoagulants (DOACs) to prevent venous thromboembolism and the introduction of new reversal strategies for factor Xa inhibitors prompted the creation of an Expert Consensus Decision Pathway to update the version from 2017, according to the ACC. Expert consensus decision pathways (ECDPs) are a component of the solution sets issued by the ACC to “address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care.”
In an ECDP published in the Journal of the American College of Cardiology, the writing committee members developed treatment algorithms for managing bleeding in patients on DOACs and vitamin K antagonists (VKAs).
Bleeding was classified as major or nonmajor, with major defined as “bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion of at least 2 units of packed red blood cells [RBCs]), or results in a hemoglobin drop greater than 2 g/dL. All other types of bleeding were classified as nonmajor.
The document includes a graphic algorithm for assessing bleed severity and managing major versus nonmajor bleeding, and a separate graphic describes considerations for reversal and use of hemostatic agents according to whether the patient is taking a VKA (warfarin and other coumarins), a direct thrombin inhibitor (dabigatran), the factor Xa inhibitors apixaban and rivaroxaban, or the factor Xa inhibitors betrixaban and edoxaban.
Another algorithm outlines whether to discontinue, delay, or restart anticoagulation. Considerations for restarting anticoagulation include whether the patient is pregnant, awaiting an invasive procedure, not able to receive medication by mouth, has a high risk of rebleeding, or is being bridged back to a vitamin K antagonist with high thrombotic risk.
In most cases of GI bleeding, for example, current data support restarting oral anticoagulants once hemostasis is achieved, but patients who experience intracranial hemorrhage should delay restarting any anticoagulation for at least 4 weeks if they are without high thrombotic risk, according to the document.
The report also recommends clinician-patient discussion before resuming anticoagulation, ideally with time allowed for patients to develop questions. Discussions should include the signs of bleeding, assessment of risk for a thromboembolic event, and the benefits of anticoagulation.
“The proliferation of oral anticoagulants (warfarin and DOACs) and growing indications for their use prompted the need for guidance on the management of these drugs,” said Gordon F. Tomaselli, MD, chair of the writing committee, in an interview. “This document provides guidance on management at the time of a bleeding complication. This includes acute management, starting and stopping drugs, and use of reversal agents,” he said. “This of course will be a dynamic document as the list of these drugs and their antidotes expand,” he noted.
“The biggest change from the previous guidelines are twofold: an update on laboratory assessment to monitor drug levels and use of reversal agents,” while the acute management strategies have otherwise remained similar to previous documents, said Dr. Tomaselli.
Dr. Tomaselli said that he was not surprised by the biological aspects of recent research while developing the statement. However, “the extent of the use of multiple anticoagulants and antiplatelet agents was a bit surprising and complicates therapy with each of the agents,” he noted.
The way the pathways are presented may make them challenging to follow in clinical practice, said Dr. Tomaselli. “The pathways are described linearly and in practice often many things have to happen at once,” he said. “The other main issue may be limitations in the availability of some of the newer reversal agents,” he added.
“The complication of bleeding is difficult to avoid,” said Dr. Tomaselli, and for future research, “the focus needs to continue to refine the indications for anticoagulation and appropriate use with other drugs that predispose to bleeding. We also need better methods and testing to monitor drugs levels and the effect on coagulation,” he said.
In accordance with the ACC Solution Set Oversight Committee, the writing committee members, including Dr. Tomaselli, had no relevant relationships with industry to disclose.
SOURCE: Tomaselli GF et al. J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.053.
Patients on oral anticoagulants who experience a bleeding event may be able to discontinue therapy if certain circumstances apply, according to updated guidance from the American College of Cardiology.
The emergence of direct-acting oral anticoagulants (DOACs) to prevent venous thromboembolism and the introduction of new reversal strategies for factor Xa inhibitors prompted the creation of an Expert Consensus Decision Pathway to update the version from 2017, according to the ACC. Expert consensus decision pathways (ECDPs) are a component of the solution sets issued by the ACC to “address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care.”
In an ECDP published in the Journal of the American College of Cardiology, the writing committee members developed treatment algorithms for managing bleeding in patients on DOACs and vitamin K antagonists (VKAs).
Bleeding was classified as major or nonmajor, with major defined as “bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion of at least 2 units of packed red blood cells [RBCs]), or results in a hemoglobin drop greater than 2 g/dL. All other types of bleeding were classified as nonmajor.
The document includes a graphic algorithm for assessing bleed severity and managing major versus nonmajor bleeding, and a separate graphic describes considerations for reversal and use of hemostatic agents according to whether the patient is taking a VKA (warfarin and other coumarins), a direct thrombin inhibitor (dabigatran), the factor Xa inhibitors apixaban and rivaroxaban, or the factor Xa inhibitors betrixaban and edoxaban.
Another algorithm outlines whether to discontinue, delay, or restart anticoagulation. Considerations for restarting anticoagulation include whether the patient is pregnant, awaiting an invasive procedure, not able to receive medication by mouth, has a high risk of rebleeding, or is being bridged back to a vitamin K antagonist with high thrombotic risk.
In most cases of GI bleeding, for example, current data support restarting oral anticoagulants once hemostasis is achieved, but patients who experience intracranial hemorrhage should delay restarting any anticoagulation for at least 4 weeks if they are without high thrombotic risk, according to the document.
The report also recommends clinician-patient discussion before resuming anticoagulation, ideally with time allowed for patients to develop questions. Discussions should include the signs of bleeding, assessment of risk for a thromboembolic event, and the benefits of anticoagulation.
“The proliferation of oral anticoagulants (warfarin and DOACs) and growing indications for their use prompted the need for guidance on the management of these drugs,” said Gordon F. Tomaselli, MD, chair of the writing committee, in an interview. “This document provides guidance on management at the time of a bleeding complication. This includes acute management, starting and stopping drugs, and use of reversal agents,” he said. “This of course will be a dynamic document as the list of these drugs and their antidotes expand,” he noted.
“The biggest change from the previous guidelines are twofold: an update on laboratory assessment to monitor drug levels and use of reversal agents,” while the acute management strategies have otherwise remained similar to previous documents, said Dr. Tomaselli.
Dr. Tomaselli said that he was not surprised by the biological aspects of recent research while developing the statement. However, “the extent of the use of multiple anticoagulants and antiplatelet agents was a bit surprising and complicates therapy with each of the agents,” he noted.
The way the pathways are presented may make them challenging to follow in clinical practice, said Dr. Tomaselli. “The pathways are described linearly and in practice often many things have to happen at once,” he said. “The other main issue may be limitations in the availability of some of the newer reversal agents,” he added.
“The complication of bleeding is difficult to avoid,” said Dr. Tomaselli, and for future research, “the focus needs to continue to refine the indications for anticoagulation and appropriate use with other drugs that predispose to bleeding. We also need better methods and testing to monitor drugs levels and the effect on coagulation,” he said.
In accordance with the ACC Solution Set Oversight Committee, the writing committee members, including Dr. Tomaselli, had no relevant relationships with industry to disclose.
SOURCE: Tomaselli GF et al. J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.053.
Patients on oral anticoagulants who experience a bleeding event may be able to discontinue therapy if certain circumstances apply, according to updated guidance from the American College of Cardiology.
The emergence of direct-acting oral anticoagulants (DOACs) to prevent venous thromboembolism and the introduction of new reversal strategies for factor Xa inhibitors prompted the creation of an Expert Consensus Decision Pathway to update the version from 2017, according to the ACC. Expert consensus decision pathways (ECDPs) are a component of the solution sets issued by the ACC to “address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care.”
In an ECDP published in the Journal of the American College of Cardiology, the writing committee members developed treatment algorithms for managing bleeding in patients on DOACs and vitamin K antagonists (VKAs).
Bleeding was classified as major or nonmajor, with major defined as “bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion of at least 2 units of packed red blood cells [RBCs]), or results in a hemoglobin drop greater than 2 g/dL. All other types of bleeding were classified as nonmajor.
The document includes a graphic algorithm for assessing bleed severity and managing major versus nonmajor bleeding, and a separate graphic describes considerations for reversal and use of hemostatic agents according to whether the patient is taking a VKA (warfarin and other coumarins), a direct thrombin inhibitor (dabigatran), the factor Xa inhibitors apixaban and rivaroxaban, or the factor Xa inhibitors betrixaban and edoxaban.
Another algorithm outlines whether to discontinue, delay, or restart anticoagulation. Considerations for restarting anticoagulation include whether the patient is pregnant, awaiting an invasive procedure, not able to receive medication by mouth, has a high risk of rebleeding, or is being bridged back to a vitamin K antagonist with high thrombotic risk.
In most cases of GI bleeding, for example, current data support restarting oral anticoagulants once hemostasis is achieved, but patients who experience intracranial hemorrhage should delay restarting any anticoagulation for at least 4 weeks if they are without high thrombotic risk, according to the document.
The report also recommends clinician-patient discussion before resuming anticoagulation, ideally with time allowed for patients to develop questions. Discussions should include the signs of bleeding, assessment of risk for a thromboembolic event, and the benefits of anticoagulation.
“The proliferation of oral anticoagulants (warfarin and DOACs) and growing indications for their use prompted the need for guidance on the management of these drugs,” said Gordon F. Tomaselli, MD, chair of the writing committee, in an interview. “This document provides guidance on management at the time of a bleeding complication. This includes acute management, starting and stopping drugs, and use of reversal agents,” he said. “This of course will be a dynamic document as the list of these drugs and their antidotes expand,” he noted.
“The biggest change from the previous guidelines are twofold: an update on laboratory assessment to monitor drug levels and use of reversal agents,” while the acute management strategies have otherwise remained similar to previous documents, said Dr. Tomaselli.
Dr. Tomaselli said that he was not surprised by the biological aspects of recent research while developing the statement. However, “the extent of the use of multiple anticoagulants and antiplatelet agents was a bit surprising and complicates therapy with each of the agents,” he noted.
The way the pathways are presented may make them challenging to follow in clinical practice, said Dr. Tomaselli. “The pathways are described linearly and in practice often many things have to happen at once,” he said. “The other main issue may be limitations in the availability of some of the newer reversal agents,” he added.
“The complication of bleeding is difficult to avoid,” said Dr. Tomaselli, and for future research, “the focus needs to continue to refine the indications for anticoagulation and appropriate use with other drugs that predispose to bleeding. We also need better methods and testing to monitor drugs levels and the effect on coagulation,” he said.
In accordance with the ACC Solution Set Oversight Committee, the writing committee members, including Dr. Tomaselli, had no relevant relationships with industry to disclose.
SOURCE: Tomaselli GF et al. J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.053.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Medics with ‘long COVID’ call for clinical recognition
Thousands of coronavirus patients risk going without treatment and support for debilitating symptoms lasting months because of a lack of awareness of ‘long COVID’, according to a group formed by clinicians with extended serious after-effects of the virus.
Many members of the 100-strong Facebook group UK doctors: COVID “Long tail” have been unable to work for weeks after failing to recover from an episode of COVID-19. They warn of the need for clinical recognition of “long COVID,” along with systems to log symptoms and manage patients in the community. Without this, there could be major consequences for return to work across all professions, as well as implications for disease prevention.
‘Weird symptoms’
Three of the group: Dr Amali Lokugamage, consultant obstetrician at the Whittington Hospital; Dr Sharon Taylor, child psychiatrist at St Mary’s Hospital London, and Dr Clare Rayner, a retired occupational health physician and lecturer at the University of Manchester, have highlighted their concerns in The BMJ and on social media groups. They say colleagues are observing a range of symptoms of long COVID in their practices.
These include cardiac, gut and respiratory symptoms, skin manifestations, neurological and psychiatric symptoms, severe fatigue, and relapsing fevers, sometimes continuing for more than 16 weeks, and which they say go well beyond definitions of chronic fatigue. The authors are also aware of a pattern of symptom clusters recurring every third or fourth day, which in some cases are so severe that people are having to take extended periods of sick leave.
Writing in The BMJ the authors say: “Concerns have been raised about the lack of awareness among NHS doctors, nurses, paramedics, and other healthcare professionals with regard to the prolonged, varied, and weird symptoms [of COVID-19].”
Speaking to Medscape News UK, Dr. Clare Rayner said: “We see a huge need that is not being met, because these cases are just not being seen in hospital. All the attention has been on the acute illness.”
She pointed to the urgent need for government planning for a surge in people requiring support to return to work following long-term COVID-19 symptoms. According to occupational health research, only 10-40% of people who take 6 weeks off work return to work, dropping to 5%-10% after an absence of 6 months.
In her own case, she is recovering after 4 months of illness, including a hospital admission with gut symptoms and dehydration, and 2 weeks of social service home support. She has experienced a range of relapsing and remitting symptoms, which she describes as ‘bizarre and coming in phases’.
Stimulating recovery
The recently-announced NHS portal for COVID-19 patients has been welcomed by the authors as an opportunity for long-standing symptoms to reach the medical and Government radar. But Dr Taylor believes it should have been set up from the start with input from patients with symptoms, to make sure that any support provided reflects the nature of the problems experienced.
In her case, as a previously regular gym attender with a resting heart rate in the 50s, she has now been diagnosed as having multi-organ disease affecting her heart, spleen, lung, and autonomic system. She has fluid on the lungs and heart, and suffers from continuous chest pain and oxygen desaturation when lying down. She has not been able to work since she contracted COVID-19 in March.
“COVID patients with the chronic form of the disease need to be involved in research right from the start to ensure the right questions are asked - not just those who have had acute disease,” she insists to Medscape News UK. “We need to gather evidence, to inform the development of a multi-disciplinary approach and a range of rehabilitation options depending on the organs involved.
“The focus needs to be on stimulating recovery and preventing development of chronic problems. We still don’t know if those with chronic COVID disease are infectious, how long their prolonged cardio-respiratory and neurological complications will last, and crucially whether treatment will reduce the duration of their problems. The worry is that left unattended, these patients may develop irreversible damage leading to chronic illness.”
General practice
GPs have been at the forefront of management of the long-standing consequences of COVID-19. In its recent report General practice in the post-COVID world, the Royal College of General Practitioners highlights the need for urgent government planning and funding to prepare general practice services for facilitating the recovery of local communities.
The report calls on the four governments of the UK each to produce a comprehensive plan to support GPs in managing the longer-term effects of COVID-19 in the community, including costed proposals for additional funding for general practice; workforce solutions; reductions in regulatory burdens and ‘red tape’; a systematic approach for identifying patients most likely to need primary care support, and proposals for how health inequalities will be minimized to ensure all patients have access to the necessary post-COVID-19 care.
RCGP Chair Professor Martin Marshall said: “COVID-19 will leave a lingering and difficult legacy and it is GPs working with patients in their communities who will be picking up the pieces.”
One issue is the lack of a reliable estimate of the prevalence of post viral symptoms for other viruses, let alone for COVID-19. Even a 1% chance of long-term problems amongst survivors would suggest 2500 with a need for extra support, but experience with post-viral syndrome generally suggests the prevalence may be more like 3%.
The BMA has been carrying out tracker surveys of its own members at 2-week intervals since March. The most recent, involving more than 5000 doctors, indicated that around 30% of doctors who believed they’d had COVID-19 were still experiencing physical symptoms they thought were caused by the virus, 21% had taken sick leave, and a further 9% had taken annual leave to deal with ongoing symptoms.
Dr David Strain, chair of the BMA medical academic staff committee and clinical senior lecturer at the University of Exeter Medical School, has a particular interest in the after-effects of COVID-19. He said it was becoming evident that the virus was leaving a lasting legacy with a significant number of people, even younger ones.
He told Medscape News UK: “Once COVID-19 enters the nervous system, the lasting symptoms on people can range from a mild loss of sense of smell or taste, to more severe symptoms such as difficulties in concentration. A small number have also been left with chronic fatigue syndrome, which is poorly understood, and can be difficult to treat. This does not appear to be dependent on the initial severity of COVID-19 symptoms.
“Currently, it is impossible to predict the prevalence of longer-lasting effects. A full assessment of COVID-19’s impact will only be possible once people return to work on a regular basis and the effect on their physical health becomes evident. Of the doctors in the BMA survey who had experienced COVID-19, 15% took sick leave beyond their acute illness, and another 6% used annual leave allowance to extend their recovery time.
“Clearly, more research will be needed into the long-term consequences of COVID-19 and the future treatments needed to deal with them.”
Further research
The National Institute for Health Research (NIHR) has called for applications for research to enhance understanding and management of the health and social care consequences of the global COVID-19 pandemic beyond the acute phase, with a particular focus on ‘health outcomes, public health, social care and health service delivery and to mitigate the impact of subsequent phases and aftermath’.
The authors of The BMJ article stress the wide-ranging nature of ‘long COVID’ symptoms and warn of the dangers of treating them for research purposes under the banner of chronic fatigue. They say: “These wide-ranging, unusual, and potentially very serious symptoms can be anxiety-provoking, particularly secondary to a virus that has only been known to the world for 8 months and which we have barely begun to understand. However, it is dismissive solely to attribute such symptoms to anxiety in the thousands of patients like ourselves who have attended hospital or general practice with chronic COVID-19.”
This article first appeared on Medscape.com.
Thousands of coronavirus patients risk going without treatment and support for debilitating symptoms lasting months because of a lack of awareness of ‘long COVID’, according to a group formed by clinicians with extended serious after-effects of the virus.
Many members of the 100-strong Facebook group UK doctors: COVID “Long tail” have been unable to work for weeks after failing to recover from an episode of COVID-19. They warn of the need for clinical recognition of “long COVID,” along with systems to log symptoms and manage patients in the community. Without this, there could be major consequences for return to work across all professions, as well as implications for disease prevention.
‘Weird symptoms’
Three of the group: Dr Amali Lokugamage, consultant obstetrician at the Whittington Hospital; Dr Sharon Taylor, child psychiatrist at St Mary’s Hospital London, and Dr Clare Rayner, a retired occupational health physician and lecturer at the University of Manchester, have highlighted their concerns in The BMJ and on social media groups. They say colleagues are observing a range of symptoms of long COVID in their practices.
These include cardiac, gut and respiratory symptoms, skin manifestations, neurological and psychiatric symptoms, severe fatigue, and relapsing fevers, sometimes continuing for more than 16 weeks, and which they say go well beyond definitions of chronic fatigue. The authors are also aware of a pattern of symptom clusters recurring every third or fourth day, which in some cases are so severe that people are having to take extended periods of sick leave.
Writing in The BMJ the authors say: “Concerns have been raised about the lack of awareness among NHS doctors, nurses, paramedics, and other healthcare professionals with regard to the prolonged, varied, and weird symptoms [of COVID-19].”
Speaking to Medscape News UK, Dr. Clare Rayner said: “We see a huge need that is not being met, because these cases are just not being seen in hospital. All the attention has been on the acute illness.”
She pointed to the urgent need for government planning for a surge in people requiring support to return to work following long-term COVID-19 symptoms. According to occupational health research, only 10-40% of people who take 6 weeks off work return to work, dropping to 5%-10% after an absence of 6 months.
In her own case, she is recovering after 4 months of illness, including a hospital admission with gut symptoms and dehydration, and 2 weeks of social service home support. She has experienced a range of relapsing and remitting symptoms, which she describes as ‘bizarre and coming in phases’.
Stimulating recovery
The recently-announced NHS portal for COVID-19 patients has been welcomed by the authors as an opportunity for long-standing symptoms to reach the medical and Government radar. But Dr Taylor believes it should have been set up from the start with input from patients with symptoms, to make sure that any support provided reflects the nature of the problems experienced.
In her case, as a previously regular gym attender with a resting heart rate in the 50s, she has now been diagnosed as having multi-organ disease affecting her heart, spleen, lung, and autonomic system. She has fluid on the lungs and heart, and suffers from continuous chest pain and oxygen desaturation when lying down. She has not been able to work since she contracted COVID-19 in March.
“COVID patients with the chronic form of the disease need to be involved in research right from the start to ensure the right questions are asked - not just those who have had acute disease,” she insists to Medscape News UK. “We need to gather evidence, to inform the development of a multi-disciplinary approach and a range of rehabilitation options depending on the organs involved.
“The focus needs to be on stimulating recovery and preventing development of chronic problems. We still don’t know if those with chronic COVID disease are infectious, how long their prolonged cardio-respiratory and neurological complications will last, and crucially whether treatment will reduce the duration of their problems. The worry is that left unattended, these patients may develop irreversible damage leading to chronic illness.”
General practice
GPs have been at the forefront of management of the long-standing consequences of COVID-19. In its recent report General practice in the post-COVID world, the Royal College of General Practitioners highlights the need for urgent government planning and funding to prepare general practice services for facilitating the recovery of local communities.
The report calls on the four governments of the UK each to produce a comprehensive plan to support GPs in managing the longer-term effects of COVID-19 in the community, including costed proposals for additional funding for general practice; workforce solutions; reductions in regulatory burdens and ‘red tape’; a systematic approach for identifying patients most likely to need primary care support, and proposals for how health inequalities will be minimized to ensure all patients have access to the necessary post-COVID-19 care.
RCGP Chair Professor Martin Marshall said: “COVID-19 will leave a lingering and difficult legacy and it is GPs working with patients in their communities who will be picking up the pieces.”
One issue is the lack of a reliable estimate of the prevalence of post viral symptoms for other viruses, let alone for COVID-19. Even a 1% chance of long-term problems amongst survivors would suggest 2500 with a need for extra support, but experience with post-viral syndrome generally suggests the prevalence may be more like 3%.
The BMA has been carrying out tracker surveys of its own members at 2-week intervals since March. The most recent, involving more than 5000 doctors, indicated that around 30% of doctors who believed they’d had COVID-19 were still experiencing physical symptoms they thought were caused by the virus, 21% had taken sick leave, and a further 9% had taken annual leave to deal with ongoing symptoms.
Dr David Strain, chair of the BMA medical academic staff committee and clinical senior lecturer at the University of Exeter Medical School, has a particular interest in the after-effects of COVID-19. He said it was becoming evident that the virus was leaving a lasting legacy with a significant number of people, even younger ones.
He told Medscape News UK: “Once COVID-19 enters the nervous system, the lasting symptoms on people can range from a mild loss of sense of smell or taste, to more severe symptoms such as difficulties in concentration. A small number have also been left with chronic fatigue syndrome, which is poorly understood, and can be difficult to treat. This does not appear to be dependent on the initial severity of COVID-19 symptoms.
“Currently, it is impossible to predict the prevalence of longer-lasting effects. A full assessment of COVID-19’s impact will only be possible once people return to work on a regular basis and the effect on their physical health becomes evident. Of the doctors in the BMA survey who had experienced COVID-19, 15% took sick leave beyond their acute illness, and another 6% used annual leave allowance to extend their recovery time.
“Clearly, more research will be needed into the long-term consequences of COVID-19 and the future treatments needed to deal with them.”
Further research
The National Institute for Health Research (NIHR) has called for applications for research to enhance understanding and management of the health and social care consequences of the global COVID-19 pandemic beyond the acute phase, with a particular focus on ‘health outcomes, public health, social care and health service delivery and to mitigate the impact of subsequent phases and aftermath’.
The authors of The BMJ article stress the wide-ranging nature of ‘long COVID’ symptoms and warn of the dangers of treating them for research purposes under the banner of chronic fatigue. They say: “These wide-ranging, unusual, and potentially very serious symptoms can be anxiety-provoking, particularly secondary to a virus that has only been known to the world for 8 months and which we have barely begun to understand. However, it is dismissive solely to attribute such symptoms to anxiety in the thousands of patients like ourselves who have attended hospital or general practice with chronic COVID-19.”
This article first appeared on Medscape.com.
Thousands of coronavirus patients risk going without treatment and support for debilitating symptoms lasting months because of a lack of awareness of ‘long COVID’, according to a group formed by clinicians with extended serious after-effects of the virus.
Many members of the 100-strong Facebook group UK doctors: COVID “Long tail” have been unable to work for weeks after failing to recover from an episode of COVID-19. They warn of the need for clinical recognition of “long COVID,” along with systems to log symptoms and manage patients in the community. Without this, there could be major consequences for return to work across all professions, as well as implications for disease prevention.
‘Weird symptoms’
Three of the group: Dr Amali Lokugamage, consultant obstetrician at the Whittington Hospital; Dr Sharon Taylor, child psychiatrist at St Mary’s Hospital London, and Dr Clare Rayner, a retired occupational health physician and lecturer at the University of Manchester, have highlighted their concerns in The BMJ and on social media groups. They say colleagues are observing a range of symptoms of long COVID in their practices.
These include cardiac, gut and respiratory symptoms, skin manifestations, neurological and psychiatric symptoms, severe fatigue, and relapsing fevers, sometimes continuing for more than 16 weeks, and which they say go well beyond definitions of chronic fatigue. The authors are also aware of a pattern of symptom clusters recurring every third or fourth day, which in some cases are so severe that people are having to take extended periods of sick leave.
Writing in The BMJ the authors say: “Concerns have been raised about the lack of awareness among NHS doctors, nurses, paramedics, and other healthcare professionals with regard to the prolonged, varied, and weird symptoms [of COVID-19].”
Speaking to Medscape News UK, Dr. Clare Rayner said: “We see a huge need that is not being met, because these cases are just not being seen in hospital. All the attention has been on the acute illness.”
She pointed to the urgent need for government planning for a surge in people requiring support to return to work following long-term COVID-19 symptoms. According to occupational health research, only 10-40% of people who take 6 weeks off work return to work, dropping to 5%-10% after an absence of 6 months.
In her own case, she is recovering after 4 months of illness, including a hospital admission with gut symptoms and dehydration, and 2 weeks of social service home support. She has experienced a range of relapsing and remitting symptoms, which she describes as ‘bizarre and coming in phases’.
Stimulating recovery
The recently-announced NHS portal for COVID-19 patients has been welcomed by the authors as an opportunity for long-standing symptoms to reach the medical and Government radar. But Dr Taylor believes it should have been set up from the start with input from patients with symptoms, to make sure that any support provided reflects the nature of the problems experienced.
In her case, as a previously regular gym attender with a resting heart rate in the 50s, she has now been diagnosed as having multi-organ disease affecting her heart, spleen, lung, and autonomic system. She has fluid on the lungs and heart, and suffers from continuous chest pain and oxygen desaturation when lying down. She has not been able to work since she contracted COVID-19 in March.
“COVID patients with the chronic form of the disease need to be involved in research right from the start to ensure the right questions are asked - not just those who have had acute disease,” she insists to Medscape News UK. “We need to gather evidence, to inform the development of a multi-disciplinary approach and a range of rehabilitation options depending on the organs involved.
“The focus needs to be on stimulating recovery and preventing development of chronic problems. We still don’t know if those with chronic COVID disease are infectious, how long their prolonged cardio-respiratory and neurological complications will last, and crucially whether treatment will reduce the duration of their problems. The worry is that left unattended, these patients may develop irreversible damage leading to chronic illness.”
General practice
GPs have been at the forefront of management of the long-standing consequences of COVID-19. In its recent report General practice in the post-COVID world, the Royal College of General Practitioners highlights the need for urgent government planning and funding to prepare general practice services for facilitating the recovery of local communities.
The report calls on the four governments of the UK each to produce a comprehensive plan to support GPs in managing the longer-term effects of COVID-19 in the community, including costed proposals for additional funding for general practice; workforce solutions; reductions in regulatory burdens and ‘red tape’; a systematic approach for identifying patients most likely to need primary care support, and proposals for how health inequalities will be minimized to ensure all patients have access to the necessary post-COVID-19 care.
RCGP Chair Professor Martin Marshall said: “COVID-19 will leave a lingering and difficult legacy and it is GPs working with patients in their communities who will be picking up the pieces.”
One issue is the lack of a reliable estimate of the prevalence of post viral symptoms for other viruses, let alone for COVID-19. Even a 1% chance of long-term problems amongst survivors would suggest 2500 with a need for extra support, but experience with post-viral syndrome generally suggests the prevalence may be more like 3%.
The BMA has been carrying out tracker surveys of its own members at 2-week intervals since March. The most recent, involving more than 5000 doctors, indicated that around 30% of doctors who believed they’d had COVID-19 were still experiencing physical symptoms they thought were caused by the virus, 21% had taken sick leave, and a further 9% had taken annual leave to deal with ongoing symptoms.
Dr David Strain, chair of the BMA medical academic staff committee and clinical senior lecturer at the University of Exeter Medical School, has a particular interest in the after-effects of COVID-19. He said it was becoming evident that the virus was leaving a lasting legacy with a significant number of people, even younger ones.
He told Medscape News UK: “Once COVID-19 enters the nervous system, the lasting symptoms on people can range from a mild loss of sense of smell or taste, to more severe symptoms such as difficulties in concentration. A small number have also been left with chronic fatigue syndrome, which is poorly understood, and can be difficult to treat. This does not appear to be dependent on the initial severity of COVID-19 symptoms.
“Currently, it is impossible to predict the prevalence of longer-lasting effects. A full assessment of COVID-19’s impact will only be possible once people return to work on a regular basis and the effect on their physical health becomes evident. Of the doctors in the BMA survey who had experienced COVID-19, 15% took sick leave beyond their acute illness, and another 6% used annual leave allowance to extend their recovery time.
“Clearly, more research will be needed into the long-term consequences of COVID-19 and the future treatments needed to deal with them.”
Further research
The National Institute for Health Research (NIHR) has called for applications for research to enhance understanding and management of the health and social care consequences of the global COVID-19 pandemic beyond the acute phase, with a particular focus on ‘health outcomes, public health, social care and health service delivery and to mitigate the impact of subsequent phases and aftermath’.
The authors of The BMJ article stress the wide-ranging nature of ‘long COVID’ symptoms and warn of the dangers of treating them for research purposes under the banner of chronic fatigue. They say: “These wide-ranging, unusual, and potentially very serious symptoms can be anxiety-provoking, particularly secondary to a virus that has only been known to the world for 8 months and which we have barely begun to understand. However, it is dismissive solely to attribute such symptoms to anxiety in the thousands of patients like ourselves who have attended hospital or general practice with chronic COVID-19.”
This article first appeared on Medscape.com.
Work-life balance dwarfs pay in female doctors’ top concerns
who responded to a new Medscape survey, far outpacing concerns about pay.
A psychiatrist who responded to the survey commented, “I’ve been trying to use all my vacation to spend time with my spouse. I’m always apologizing for being late, not being able to go to an event due to my work schedule, and missing out on life with my husband.”
Nearly two thirds (64%) said the balance was their top concern whereas 43% put pay at the top.
Medscape surveyed more than 3,000 women physicians about how they deal with parenthood, work pressures, and relationships in Women Physicians 2020: The Issues They Care About.
Almost all are making personal trade-offs
An overwhelming percentage (94%) said they have had to make personal trade-offs for work obligations.
“Women are more likely to make work compromises to benefit their families,” a cardiologist responded. “I won’t/can’t take a position that would disrupt my husband’s community ties, my children’s schooling, and relationships with family.”
More than one-third of women (36%) said that being a woman had a negative or very negative impact on their compensation. Only 4% said their gender had a positive or very positive impact on pay and 59% said gender had no effect.
The Medscape Physician Compensation Report 2020 showed male specialists made 31% more than their female counterparts and male primary care physicians earned 25% more.
Some factors may help explain some of the difference, but others remain unclear.
Poor negotiating skills have long been cited as a reason women get paid less; in this survey 39% said they were unskilled or very unskilled in salary negotiations, compared with 28% who said they were skilled or very skilled in those talks.
Katie Donovan, founder of Equal Pay Negotiations, reports that only 30% of women negotiate pay at all, compared with 46% of men.
Additionally, women tend to gravitate in specialties that don’t pay as well.
They are poorly represented in some of the highest-paying specialties: orthopedics (9%), urology (12%), and cardiology (14%).
“Society’s view of women as caretaker is powerful,” a radiologist commented. “Women feel like they need to choose specialties where they can work part-time or flexible time in order to be the primary caretaker at home.”
Confidence high in leadership abilities
The survey asked women about their confidence in taking a leadership role, and 90% answered that they were confident about taking such a role. However, only half said they had a leadership or supervisory role.
According to the American Medical Association, women make up 3% of healthcare chief medical officers, 6% of department chairs, and 9% of division leaders.
Asked whether women have experienced gender inequity in the workplace, respondents were almost evenly split, but hospital-based physicians at 61% were more likely to report inequity than were 42% of office-based physicians.
A family physician responded, “I have experienced gender inequality more from administrators than from my male colleagues. I think it’s coming from corporate more than from medical professionals.”
In this survey, 3% said their male colleagues were unsupportive of gender equality in the workplace.
The survey responses indicate most women physicians who have children are also conflicted as parents regarding their careers. Almost two-thirds (64%) said they were always or often conflicted with these dueling priorities; only 8% said they sometimes or rarely are.
Those conflicts start even before having children. More than half in this survey (52%) said their career influenced the number of children they have.
A family physician said, “I delayed starting a family because of my career. That affected my fertility and made it hard to complete [in-vitro fertilization].”
Family responsibilities meet stigma
Half of the respondents said women physicians are stigmatized for taking a full maternity leave (6 weeks or longer). An even higher percentage (65%) said women are stigmatized for taking more flexible or fewer hours to accommodate family responsibilities.
A 2019 survey of 844 physician mothers found that physicians who took maternity leave received lower peer evaluation scores, lost potential income, and reported experiencing discrimination. One-quarter of the participants (25.8%) reported experiencing discrimination related to breastfeeding or breast milk pumping upon their return to work.
Burnout at work puts stress on primary relationships, 63% of respondents said, although 24% said it did not strain those relationships. Thirteen percent of women gave the response “not applicable.”
“I try to be present when I’m home, but to be honest, I don’t deal with it very well,” a family physician commented.
A version of this article originally appeared on Medscape.com.
who responded to a new Medscape survey, far outpacing concerns about pay.
A psychiatrist who responded to the survey commented, “I’ve been trying to use all my vacation to spend time with my spouse. I’m always apologizing for being late, not being able to go to an event due to my work schedule, and missing out on life with my husband.”
Nearly two thirds (64%) said the balance was their top concern whereas 43% put pay at the top.
Medscape surveyed more than 3,000 women physicians about how they deal with parenthood, work pressures, and relationships in Women Physicians 2020: The Issues They Care About.
Almost all are making personal trade-offs
An overwhelming percentage (94%) said they have had to make personal trade-offs for work obligations.
“Women are more likely to make work compromises to benefit their families,” a cardiologist responded. “I won’t/can’t take a position that would disrupt my husband’s community ties, my children’s schooling, and relationships with family.”
More than one-third of women (36%) said that being a woman had a negative or very negative impact on their compensation. Only 4% said their gender had a positive or very positive impact on pay and 59% said gender had no effect.
The Medscape Physician Compensation Report 2020 showed male specialists made 31% more than their female counterparts and male primary care physicians earned 25% more.
Some factors may help explain some of the difference, but others remain unclear.
Poor negotiating skills have long been cited as a reason women get paid less; in this survey 39% said they were unskilled or very unskilled in salary negotiations, compared with 28% who said they were skilled or very skilled in those talks.
Katie Donovan, founder of Equal Pay Negotiations, reports that only 30% of women negotiate pay at all, compared with 46% of men.
Additionally, women tend to gravitate in specialties that don’t pay as well.
They are poorly represented in some of the highest-paying specialties: orthopedics (9%), urology (12%), and cardiology (14%).
“Society’s view of women as caretaker is powerful,” a radiologist commented. “Women feel like they need to choose specialties where they can work part-time or flexible time in order to be the primary caretaker at home.”
Confidence high in leadership abilities
The survey asked women about their confidence in taking a leadership role, and 90% answered that they were confident about taking such a role. However, only half said they had a leadership or supervisory role.
According to the American Medical Association, women make up 3% of healthcare chief medical officers, 6% of department chairs, and 9% of division leaders.
Asked whether women have experienced gender inequity in the workplace, respondents were almost evenly split, but hospital-based physicians at 61% were more likely to report inequity than were 42% of office-based physicians.
A family physician responded, “I have experienced gender inequality more from administrators than from my male colleagues. I think it’s coming from corporate more than from medical professionals.”
In this survey, 3% said their male colleagues were unsupportive of gender equality in the workplace.
The survey responses indicate most women physicians who have children are also conflicted as parents regarding their careers. Almost two-thirds (64%) said they were always or often conflicted with these dueling priorities; only 8% said they sometimes or rarely are.
Those conflicts start even before having children. More than half in this survey (52%) said their career influenced the number of children they have.
A family physician said, “I delayed starting a family because of my career. That affected my fertility and made it hard to complete [in-vitro fertilization].”
Family responsibilities meet stigma
Half of the respondents said women physicians are stigmatized for taking a full maternity leave (6 weeks or longer). An even higher percentage (65%) said women are stigmatized for taking more flexible or fewer hours to accommodate family responsibilities.
A 2019 survey of 844 physician mothers found that physicians who took maternity leave received lower peer evaluation scores, lost potential income, and reported experiencing discrimination. One-quarter of the participants (25.8%) reported experiencing discrimination related to breastfeeding or breast milk pumping upon their return to work.
Burnout at work puts stress on primary relationships, 63% of respondents said, although 24% said it did not strain those relationships. Thirteen percent of women gave the response “not applicable.”
“I try to be present when I’m home, but to be honest, I don’t deal with it very well,” a family physician commented.
A version of this article originally appeared on Medscape.com.
who responded to a new Medscape survey, far outpacing concerns about pay.
A psychiatrist who responded to the survey commented, “I’ve been trying to use all my vacation to spend time with my spouse. I’m always apologizing for being late, not being able to go to an event due to my work schedule, and missing out on life with my husband.”
Nearly two thirds (64%) said the balance was their top concern whereas 43% put pay at the top.
Medscape surveyed more than 3,000 women physicians about how they deal with parenthood, work pressures, and relationships in Women Physicians 2020: The Issues They Care About.
Almost all are making personal trade-offs
An overwhelming percentage (94%) said they have had to make personal trade-offs for work obligations.
“Women are more likely to make work compromises to benefit their families,” a cardiologist responded. “I won’t/can’t take a position that would disrupt my husband’s community ties, my children’s schooling, and relationships with family.”
More than one-third of women (36%) said that being a woman had a negative or very negative impact on their compensation. Only 4% said their gender had a positive or very positive impact on pay and 59% said gender had no effect.
The Medscape Physician Compensation Report 2020 showed male specialists made 31% more than their female counterparts and male primary care physicians earned 25% more.
Some factors may help explain some of the difference, but others remain unclear.
Poor negotiating skills have long been cited as a reason women get paid less; in this survey 39% said they were unskilled or very unskilled in salary negotiations, compared with 28% who said they were skilled or very skilled in those talks.
Katie Donovan, founder of Equal Pay Negotiations, reports that only 30% of women negotiate pay at all, compared with 46% of men.
Additionally, women tend to gravitate in specialties that don’t pay as well.
They are poorly represented in some of the highest-paying specialties: orthopedics (9%), urology (12%), and cardiology (14%).
“Society’s view of women as caretaker is powerful,” a radiologist commented. “Women feel like they need to choose specialties where they can work part-time or flexible time in order to be the primary caretaker at home.”
Confidence high in leadership abilities
The survey asked women about their confidence in taking a leadership role, and 90% answered that they were confident about taking such a role. However, only half said they had a leadership or supervisory role.
According to the American Medical Association, women make up 3% of healthcare chief medical officers, 6% of department chairs, and 9% of division leaders.
Asked whether women have experienced gender inequity in the workplace, respondents were almost evenly split, but hospital-based physicians at 61% were more likely to report inequity than were 42% of office-based physicians.
A family physician responded, “I have experienced gender inequality more from administrators than from my male colleagues. I think it’s coming from corporate more than from medical professionals.”
In this survey, 3% said their male colleagues were unsupportive of gender equality in the workplace.
The survey responses indicate most women physicians who have children are also conflicted as parents regarding their careers. Almost two-thirds (64%) said they were always or often conflicted with these dueling priorities; only 8% said they sometimes or rarely are.
Those conflicts start even before having children. More than half in this survey (52%) said their career influenced the number of children they have.
A family physician said, “I delayed starting a family because of my career. That affected my fertility and made it hard to complete [in-vitro fertilization].”
Family responsibilities meet stigma
Half of the respondents said women physicians are stigmatized for taking a full maternity leave (6 weeks or longer). An even higher percentage (65%) said women are stigmatized for taking more flexible or fewer hours to accommodate family responsibilities.
A 2019 survey of 844 physician mothers found that physicians who took maternity leave received lower peer evaluation scores, lost potential income, and reported experiencing discrimination. One-quarter of the participants (25.8%) reported experiencing discrimination related to breastfeeding or breast milk pumping upon their return to work.
Burnout at work puts stress on primary relationships, 63% of respondents said, although 24% said it did not strain those relationships. Thirteen percent of women gave the response “not applicable.”
“I try to be present when I’m home, but to be honest, I don’t deal with it very well,” a family physician commented.
A version of this article originally appeared on Medscape.com.
Sewage as our salvation: Tracking COVID-19
“The sewer is the conscience of the city. Everything there converges and confronts everything else. In that livid spot there are shades, but there are no longer any secrets.” Victor Hugo – “Les Miserables”
To get a sense of the prevalence of COVID-19 in a community you need to test hundreds to thousands of people. This is difficult, resource intensive, and requires cooperation for testing among people both with and without symptoms.
In various locations from China to medieval London, there have been attempts to utilize human excrement for the betterment of mankind, from employing it as fertilizer to processing it to make gunpowder. Such attempts did not always work as planned. The use of sewage for fertilizer in Europe and the United States in the 1840s and 1850s led to the spread of waterborne diseases, including cholera and typhoid. As the importance of sanitary elimination of human waste became ever clearer, ideas and technology for our modern system of sewage management evolved. We have since advanced a great deal, so that all industrialized nations now have a well-developed system for clean water entry, as well as sewage treatment and disposal. Nonetheless, there remains a nagging question of whether human waste could be used for something productive.1
In the early 2000s, SCIM was developed as a technique to assess population-level human health and disease. In SCIM, untreated sewage is tested for a chemical of interest which reflects a health parameter for a community. Chemicals of interest and usage rates can be calculated for substances as varied as opioids, tobacco, pesticides, and even nonnutritive sweeteners. For instance, relative opioid use can be calculated over time for a given “sewershed” or sewage catchment area. The calculation of community-wide exposure to substances as a means of getting real-time data on shifts of usage without having to collect and collate data from thousands of individuals has been termed wastewater-based epidemiology.
We use urine and stool testing in so many other areas, such as urinalysis, urine drug testing, urine Legionella antigen testing, and stool testing for common pathogens. What a rich source of information is present in the combination of urine and stool that collectively make up sewage! With the average volume of urine per adult being approximately 1 liter daily (and with urine calculated to be approximately 1% of wastewater), accurate analytic techniques can estimate per capita exposure to different substances. Applications of wastewater-based epidemiology have included tracking community prevalence of enteric viral infections, opioid and tobacco use, and many other indicators of health and disease.2
Given the enormous work in the field over the last 2 decades and that SARS-CoV-2 RNA has been detected in feces of both symptomatic and asymptomatic patients, it was only a short conceptual step for those familiar with sewage epidemiology to consider adapting it to assess the prevalence of COVID-19 in a community.
An elegant study collected untreated sewage from southeast Queensland, Australia. The sewage was processed, concentrated, and then tested with reverse transcriptase polymerase chain reaction analysis for SARS-CoV-2 RNA. The number of RNA copies was then entered into an equation that included the population served by the sewage encatchment area, as well as the measured liters of wastewater and grams of feces per day. This provided an estimate of the number of persons infected in the community, and the researchers were able to show reasonable agreement between the numbers estimated by sewage analysis and that found in traditional clinical testing.3,4
The promise of wastewater-based epidemiology is large. Early research indicates that quantification of viral particles in sewage can be accurately assessed and correlated with the prevalence of the infection in the community. Such levels can then be used to track infection rates of COVID-19 over time, as well as to compare the relative rates in different communities.
Our sewage may hold the answer to accurately and easily tracking COVID-19, and ultimately help us gain a better hold on this disease.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. History of water supply and sanitation. Wikipedia, https://en.wikipedia.org/wiki/History_of_water_supply_and_sanitation.
2. Daughton C. Monitoring wastewater for assessing community health: Sewage Chemical-Information Mining (SCIM). Sci Total Environ. 2017 Nov 29. doi: 10.1016/j.scitotenv.2017.11.102.
3. Ahmed W et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ. 2020 Apr 18. doi: doi.org/10.1016/j.scitotenv.2020.138764.
4. Daughton C. The international imperative to rapidly and inexpensively monitor community-wide COVID-19 infection status and trends. Sci Total Environ. 2020 Mar 23. doi: 10.1016/j.scitotenv.2020.138149.
“The sewer is the conscience of the city. Everything there converges and confronts everything else. In that livid spot there are shades, but there are no longer any secrets.” Victor Hugo – “Les Miserables”
To get a sense of the prevalence of COVID-19 in a community you need to test hundreds to thousands of people. This is difficult, resource intensive, and requires cooperation for testing among people both with and without symptoms.
In various locations from China to medieval London, there have been attempts to utilize human excrement for the betterment of mankind, from employing it as fertilizer to processing it to make gunpowder. Such attempts did not always work as planned. The use of sewage for fertilizer in Europe and the United States in the 1840s and 1850s led to the spread of waterborne diseases, including cholera and typhoid. As the importance of sanitary elimination of human waste became ever clearer, ideas and technology for our modern system of sewage management evolved. We have since advanced a great deal, so that all industrialized nations now have a well-developed system for clean water entry, as well as sewage treatment and disposal. Nonetheless, there remains a nagging question of whether human waste could be used for something productive.1
In the early 2000s, SCIM was developed as a technique to assess population-level human health and disease. In SCIM, untreated sewage is tested for a chemical of interest which reflects a health parameter for a community. Chemicals of interest and usage rates can be calculated for substances as varied as opioids, tobacco, pesticides, and even nonnutritive sweeteners. For instance, relative opioid use can be calculated over time for a given “sewershed” or sewage catchment area. The calculation of community-wide exposure to substances as a means of getting real-time data on shifts of usage without having to collect and collate data from thousands of individuals has been termed wastewater-based epidemiology.
We use urine and stool testing in so many other areas, such as urinalysis, urine drug testing, urine Legionella antigen testing, and stool testing for common pathogens. What a rich source of information is present in the combination of urine and stool that collectively make up sewage! With the average volume of urine per adult being approximately 1 liter daily (and with urine calculated to be approximately 1% of wastewater), accurate analytic techniques can estimate per capita exposure to different substances. Applications of wastewater-based epidemiology have included tracking community prevalence of enteric viral infections, opioid and tobacco use, and many other indicators of health and disease.2
Given the enormous work in the field over the last 2 decades and that SARS-CoV-2 RNA has been detected in feces of both symptomatic and asymptomatic patients, it was only a short conceptual step for those familiar with sewage epidemiology to consider adapting it to assess the prevalence of COVID-19 in a community.
An elegant study collected untreated sewage from southeast Queensland, Australia. The sewage was processed, concentrated, and then tested with reverse transcriptase polymerase chain reaction analysis for SARS-CoV-2 RNA. The number of RNA copies was then entered into an equation that included the population served by the sewage encatchment area, as well as the measured liters of wastewater and grams of feces per day. This provided an estimate of the number of persons infected in the community, and the researchers were able to show reasonable agreement between the numbers estimated by sewage analysis and that found in traditional clinical testing.3,4
The promise of wastewater-based epidemiology is large. Early research indicates that quantification of viral particles in sewage can be accurately assessed and correlated with the prevalence of the infection in the community. Such levels can then be used to track infection rates of COVID-19 over time, as well as to compare the relative rates in different communities.
Our sewage may hold the answer to accurately and easily tracking COVID-19, and ultimately help us gain a better hold on this disease.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. History of water supply and sanitation. Wikipedia, https://en.wikipedia.org/wiki/History_of_water_supply_and_sanitation.
2. Daughton C. Monitoring wastewater for assessing community health: Sewage Chemical-Information Mining (SCIM). Sci Total Environ. 2017 Nov 29. doi: 10.1016/j.scitotenv.2017.11.102.
3. Ahmed W et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ. 2020 Apr 18. doi: doi.org/10.1016/j.scitotenv.2020.138764.
4. Daughton C. The international imperative to rapidly and inexpensively monitor community-wide COVID-19 infection status and trends. Sci Total Environ. 2020 Mar 23. doi: 10.1016/j.scitotenv.2020.138149.
“The sewer is the conscience of the city. Everything there converges and confronts everything else. In that livid spot there are shades, but there are no longer any secrets.” Victor Hugo – “Les Miserables”
To get a sense of the prevalence of COVID-19 in a community you need to test hundreds to thousands of people. This is difficult, resource intensive, and requires cooperation for testing among people both with and without symptoms.
In various locations from China to medieval London, there have been attempts to utilize human excrement for the betterment of mankind, from employing it as fertilizer to processing it to make gunpowder. Such attempts did not always work as planned. The use of sewage for fertilizer in Europe and the United States in the 1840s and 1850s led to the spread of waterborne diseases, including cholera and typhoid. As the importance of sanitary elimination of human waste became ever clearer, ideas and technology for our modern system of sewage management evolved. We have since advanced a great deal, so that all industrialized nations now have a well-developed system for clean water entry, as well as sewage treatment and disposal. Nonetheless, there remains a nagging question of whether human waste could be used for something productive.1
In the early 2000s, SCIM was developed as a technique to assess population-level human health and disease. In SCIM, untreated sewage is tested for a chemical of interest which reflects a health parameter for a community. Chemicals of interest and usage rates can be calculated for substances as varied as opioids, tobacco, pesticides, and even nonnutritive sweeteners. For instance, relative opioid use can be calculated over time for a given “sewershed” or sewage catchment area. The calculation of community-wide exposure to substances as a means of getting real-time data on shifts of usage without having to collect and collate data from thousands of individuals has been termed wastewater-based epidemiology.
We use urine and stool testing in so many other areas, such as urinalysis, urine drug testing, urine Legionella antigen testing, and stool testing for common pathogens. What a rich source of information is present in the combination of urine and stool that collectively make up sewage! With the average volume of urine per adult being approximately 1 liter daily (and with urine calculated to be approximately 1% of wastewater), accurate analytic techniques can estimate per capita exposure to different substances. Applications of wastewater-based epidemiology have included tracking community prevalence of enteric viral infections, opioid and tobacco use, and many other indicators of health and disease.2
Given the enormous work in the field over the last 2 decades and that SARS-CoV-2 RNA has been detected in feces of both symptomatic and asymptomatic patients, it was only a short conceptual step for those familiar with sewage epidemiology to consider adapting it to assess the prevalence of COVID-19 in a community.
An elegant study collected untreated sewage from southeast Queensland, Australia. The sewage was processed, concentrated, and then tested with reverse transcriptase polymerase chain reaction analysis for SARS-CoV-2 RNA. The number of RNA copies was then entered into an equation that included the population served by the sewage encatchment area, as well as the measured liters of wastewater and grams of feces per day. This provided an estimate of the number of persons infected in the community, and the researchers were able to show reasonable agreement between the numbers estimated by sewage analysis and that found in traditional clinical testing.3,4
The promise of wastewater-based epidemiology is large. Early research indicates that quantification of viral particles in sewage can be accurately assessed and correlated with the prevalence of the infection in the community. Such levels can then be used to track infection rates of COVID-19 over time, as well as to compare the relative rates in different communities.
Our sewage may hold the answer to accurately and easily tracking COVID-19, and ultimately help us gain a better hold on this disease.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
References
1. History of water supply and sanitation. Wikipedia, https://en.wikipedia.org/wiki/History_of_water_supply_and_sanitation.
2. Daughton C. Monitoring wastewater for assessing community health: Sewage Chemical-Information Mining (SCIM). Sci Total Environ. 2017 Nov 29. doi: 10.1016/j.scitotenv.2017.11.102.
3. Ahmed W et al. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci Total Environ. 2020 Apr 18. doi: doi.org/10.1016/j.scitotenv.2020.138764.
4. Daughton C. The international imperative to rapidly and inexpensively monitor community-wide COVID-19 infection status and trends. Sci Total Environ. 2020 Mar 23. doi: 10.1016/j.scitotenv.2020.138149.








