User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Approval of COVID-19 vaccines will change nature of clinical trials
While stressing the urgent need to vaccinate the whole U.S. population, infectious disease experts and medical ethicists are raising questions about the clinical trials needed to answer important questions about the new COVID-19 vaccines.
In a statement released on Nov. 20, Barbara Alexander, MD, president of the Infectious Diseases Society of America (IDSA) and a professor at Duke University, Durham, N.C., commented on Pfizer and BioNTech’s application to the Food and Drug Administration for an emergency use authorization (EUA) for its COVID-19 vaccine. Besides emphasizing the need for a transparent review of the companies’ trial data prior to the FDA’s granting an EUA, she said, “If emergency use authorization is granted, clinical trials and data collection must continue.”
In an interview, Dr. Alexander said she is convinced that both Pfizer and Moderna, which is also expected to seek an EUA soon, will continue their clinical trials to monitor the long-term safety and efficacy of their vaccines.
“The EUA guidance for COVID vaccine authorization is very clear that clinical trials will move forward,” she said. “Any EUA request would have to include a strategy to ensure that the long-term safety and efficacy of a vaccine could be monitored. I see no evidence that either Pfizer or Moderna is not prepared to follow those regulations.”
Eventually, she added, the drug makers will have to seek full FDA approval to replace an EUA, which as its name signifies, is designed for public health emergencies. “The EUA is a tool to help us get the vaccine into circulation and have it start working as quickly as possible in the current health crisis,” she said. “But once the crisis is over, if the sponsors want to continue to market their vaccines, they have to go forward and get full approval.”
Medical ethicists, however, point out there may be ethical and practical dilemmas involved in continuing or initiating clinical trials once a vaccine has been approved for use even on an emergency basis.
In a commentary in Annals of Internal Medicine, Rafael Dal-Re, MD, PhD, Arthur L. Caplan, PhD, and two other ethicists stipulated that the pandemic requires early licensing and deployment of COVID-19 vaccines. Nevertheless, they noted, additional months of data are required to establish the long-term efficacy and safety of the vaccines. “Moreover, early deployment could interfere with the acquisition of long-term data,” both on these vaccines and on others coming through the pipeline, they wrote.
In countries where an approved vaccine is deployed, the ethicists noted, investigators must inform participants in an ongoing trial about the approved vaccine’s status and ask if they want to continue in the study. If enough participants decline, the trial might have to be terminated early. At that point, researchers may not have sufficient long-term data to identify late-term safety issues, determine how long efficacy lasts, determine whether waning immunity is associated with reduced levels of antibodies, or identify the level of neutralizing antibodies that correlates with immunity.
Moreover, they observed, long-term trials are especially important for vaccines that use mRNA technology, because less is known about them than about traditional kinds of vaccines.
The authors also pointed out that early licensing of any vaccine might make it harder to evaluate vaccines that haven’t yet been approved. “Once a vaccine is licensed, new placebo-controlled RCTs [randomized controlled trials] of other vaccines will not be acceptable ethically, and noninferiority RCTs will be the most likely alternative.
“The goal of noninferiority trials will be to demonstrate that the immune response (that is, neutralizing antibody titers or levels) of the candidate vaccine is not inferior to that of the approved vaccine within a prespecified margin, which the FDA has established as less than 10% for COVID-19 vaccines,” the authors noted.
More data with more study designs
Dial Hewlett Jr., MD, medical director for disease control services, Westchester County Department of Health, White Plains, N.Y., said in an interview that the ethicists raise important issues that have been discussed in other forums, including a recent webinar of the National Academy of Medicine.
“As the authors point out, once you have a vaccine that has been shown to be effective and safe, it’s no longer ethical to enroll people in placebo trials,” he said.
Therefore, he said, Pfizer and Moderna will undoubtedly offer their vaccines to the people in their studies’ placebo groups after the vaccines receive an EUA. Then they will follow everyone who has been vaccinated for 2 years to determine long-term safety. Efficacy will also continue to be measured as an adjunct of safety, he said.
With regard to the difficulty of reconsenting individuals to enter a new clinical trial after a vaccine has been approved, he said, “I’d agree that trying to get all the same participants to come into another study would be a challenge. You can, however, design studies that will allow you to obtain the same information. You will have a large number of people out there who haven’t been vaccinated, and you can do single-arm longitudinal studies and measure a number of things in the individuals who are enrolled in those studies,” he said.
“You can look at the immunologic markers, both antibody and T-cell. You can follow these individuals longitudinally to see if they do develop disease over a period of time. If they do, you can determine what their levels of response were,” he added. “So there are opportunities to design studies that would give you some of the same information, although it would not be in the same population that was in the randomized trials.”
For newer vaccines that have yet to be tested, he said, developers can compare “historical controls” from the trials of approved vaccines, i.e., data from the unvaccinated participants in those studies, with the data from inoculating people with the novel agents. The historical data can be sex- and age-matched, among other things, to individuals in the new trials. Moreover, because the study protocols have been harmonized for all trials under Operation Warp Speed, it doesn’t matter what kind of vaccine they’re testing, he said.
It may be necessary to do additional studies to find out how long immunity lasts after people have been vaccinated, Dr. Hewlett pointed out.
“You may have a different trial design. You don’t need a control arm to determine how long immunity lasts. You’re just comparing the patients who were vaccinated to nothing,” he said. “So you could have a single-arm trial on a group of people who consent to be immunized and followed. You can see what their antibody levels are and other surrogate markers, and you can see when they might develop disease, if they do. You’d need a large sample, but you can do that.”
Dr. Hewlett noted that additional studies will be required to determine whether the new vaccines stop transmission of the coronavirus or just prevent symptoms of COVID-19. Until it’s established that a vaccine halts transmission or the country achieves herd immunity, he said, “we’ll still have to wear masks and take other precautions, because a significant portion of people will still be at risk.”
‘A lot of redundancy’
Dr. Alexander emphasized that any safety or efficacy issues with the first COVID-19 vaccines must be identified before the vaccine is offered to a large portion of the U.S. population.
“While the data from the Pfizer and Moderna trials are said to be favorable, we at IDSA want to make sure that whatever vaccine comes to market is safe,” she said. “Having an unsafe vaccine on the market would be worse than no vaccine, because you’re compromising the public confidence. We have to make sure the public trusts the process and that sufficient data have been evaluated to ensure the vaccine is safe and efficacious.
“I believe the FDA is being very careful and thoughtful in [its] response,” Dr. Alexander said. “They realize how important it is to get a vaccine and save lives. While they’re doing things differently and moving much faster than before, they’re still trying to be thoughtful and reasonable. They don’t seem to be putting people at risk or circumventing the regulatory standards.”
Moreover, she pointed out, the FDA’s Vaccines and Related Biological Products Advisory Committee, which is expected to meet on Dec. 10, will review the trial data before the agency grants an EUA to Pfizer or Moderna. Then the FDA will post the data publicly.
The next step is for the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention to look at the data and decide who in the United States should receive the vaccine first, she pointed out. And both Pfizer and Moderna have shown their data to advisory panels of outside experts.
“There’s a lot of redundancy, and a lot of people are looking at the data,” Dr. Alexander said. “So I don’t think we’re cutting corners to get it out there more quickly.”
A version of this article originally appeared on Medscape.com.
While stressing the urgent need to vaccinate the whole U.S. population, infectious disease experts and medical ethicists are raising questions about the clinical trials needed to answer important questions about the new COVID-19 vaccines.
In a statement released on Nov. 20, Barbara Alexander, MD, president of the Infectious Diseases Society of America (IDSA) and a professor at Duke University, Durham, N.C., commented on Pfizer and BioNTech’s application to the Food and Drug Administration for an emergency use authorization (EUA) for its COVID-19 vaccine. Besides emphasizing the need for a transparent review of the companies’ trial data prior to the FDA’s granting an EUA, she said, “If emergency use authorization is granted, clinical trials and data collection must continue.”
In an interview, Dr. Alexander said she is convinced that both Pfizer and Moderna, which is also expected to seek an EUA soon, will continue their clinical trials to monitor the long-term safety and efficacy of their vaccines.
“The EUA guidance for COVID vaccine authorization is very clear that clinical trials will move forward,” she said. “Any EUA request would have to include a strategy to ensure that the long-term safety and efficacy of a vaccine could be monitored. I see no evidence that either Pfizer or Moderna is not prepared to follow those regulations.”
Eventually, she added, the drug makers will have to seek full FDA approval to replace an EUA, which as its name signifies, is designed for public health emergencies. “The EUA is a tool to help us get the vaccine into circulation and have it start working as quickly as possible in the current health crisis,” she said. “But once the crisis is over, if the sponsors want to continue to market their vaccines, they have to go forward and get full approval.”
Medical ethicists, however, point out there may be ethical and practical dilemmas involved in continuing or initiating clinical trials once a vaccine has been approved for use even on an emergency basis.
In a commentary in Annals of Internal Medicine, Rafael Dal-Re, MD, PhD, Arthur L. Caplan, PhD, and two other ethicists stipulated that the pandemic requires early licensing and deployment of COVID-19 vaccines. Nevertheless, they noted, additional months of data are required to establish the long-term efficacy and safety of the vaccines. “Moreover, early deployment could interfere with the acquisition of long-term data,” both on these vaccines and on others coming through the pipeline, they wrote.
In countries where an approved vaccine is deployed, the ethicists noted, investigators must inform participants in an ongoing trial about the approved vaccine’s status and ask if they want to continue in the study. If enough participants decline, the trial might have to be terminated early. At that point, researchers may not have sufficient long-term data to identify late-term safety issues, determine how long efficacy lasts, determine whether waning immunity is associated with reduced levels of antibodies, or identify the level of neutralizing antibodies that correlates with immunity.
Moreover, they observed, long-term trials are especially important for vaccines that use mRNA technology, because less is known about them than about traditional kinds of vaccines.
The authors also pointed out that early licensing of any vaccine might make it harder to evaluate vaccines that haven’t yet been approved. “Once a vaccine is licensed, new placebo-controlled RCTs [randomized controlled trials] of other vaccines will not be acceptable ethically, and noninferiority RCTs will be the most likely alternative.
“The goal of noninferiority trials will be to demonstrate that the immune response (that is, neutralizing antibody titers or levels) of the candidate vaccine is not inferior to that of the approved vaccine within a prespecified margin, which the FDA has established as less than 10% for COVID-19 vaccines,” the authors noted.
More data with more study designs
Dial Hewlett Jr., MD, medical director for disease control services, Westchester County Department of Health, White Plains, N.Y., said in an interview that the ethicists raise important issues that have been discussed in other forums, including a recent webinar of the National Academy of Medicine.
“As the authors point out, once you have a vaccine that has been shown to be effective and safe, it’s no longer ethical to enroll people in placebo trials,” he said.
Therefore, he said, Pfizer and Moderna will undoubtedly offer their vaccines to the people in their studies’ placebo groups after the vaccines receive an EUA. Then they will follow everyone who has been vaccinated for 2 years to determine long-term safety. Efficacy will also continue to be measured as an adjunct of safety, he said.
With regard to the difficulty of reconsenting individuals to enter a new clinical trial after a vaccine has been approved, he said, “I’d agree that trying to get all the same participants to come into another study would be a challenge. You can, however, design studies that will allow you to obtain the same information. You will have a large number of people out there who haven’t been vaccinated, and you can do single-arm longitudinal studies and measure a number of things in the individuals who are enrolled in those studies,” he said.
“You can look at the immunologic markers, both antibody and T-cell. You can follow these individuals longitudinally to see if they do develop disease over a period of time. If they do, you can determine what their levels of response were,” he added. “So there are opportunities to design studies that would give you some of the same information, although it would not be in the same population that was in the randomized trials.”
For newer vaccines that have yet to be tested, he said, developers can compare “historical controls” from the trials of approved vaccines, i.e., data from the unvaccinated participants in those studies, with the data from inoculating people with the novel agents. The historical data can be sex- and age-matched, among other things, to individuals in the new trials. Moreover, because the study protocols have been harmonized for all trials under Operation Warp Speed, it doesn’t matter what kind of vaccine they’re testing, he said.
It may be necessary to do additional studies to find out how long immunity lasts after people have been vaccinated, Dr. Hewlett pointed out.
“You may have a different trial design. You don’t need a control arm to determine how long immunity lasts. You’re just comparing the patients who were vaccinated to nothing,” he said. “So you could have a single-arm trial on a group of people who consent to be immunized and followed. You can see what their antibody levels are and other surrogate markers, and you can see when they might develop disease, if they do. You’d need a large sample, but you can do that.”
Dr. Hewlett noted that additional studies will be required to determine whether the new vaccines stop transmission of the coronavirus or just prevent symptoms of COVID-19. Until it’s established that a vaccine halts transmission or the country achieves herd immunity, he said, “we’ll still have to wear masks and take other precautions, because a significant portion of people will still be at risk.”
‘A lot of redundancy’
Dr. Alexander emphasized that any safety or efficacy issues with the first COVID-19 vaccines must be identified before the vaccine is offered to a large portion of the U.S. population.
“While the data from the Pfizer and Moderna trials are said to be favorable, we at IDSA want to make sure that whatever vaccine comes to market is safe,” she said. “Having an unsafe vaccine on the market would be worse than no vaccine, because you’re compromising the public confidence. We have to make sure the public trusts the process and that sufficient data have been evaluated to ensure the vaccine is safe and efficacious.
“I believe the FDA is being very careful and thoughtful in [its] response,” Dr. Alexander said. “They realize how important it is to get a vaccine and save lives. While they’re doing things differently and moving much faster than before, they’re still trying to be thoughtful and reasonable. They don’t seem to be putting people at risk or circumventing the regulatory standards.”
Moreover, she pointed out, the FDA’s Vaccines and Related Biological Products Advisory Committee, which is expected to meet on Dec. 10, will review the trial data before the agency grants an EUA to Pfizer or Moderna. Then the FDA will post the data publicly.
The next step is for the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention to look at the data and decide who in the United States should receive the vaccine first, she pointed out. And both Pfizer and Moderna have shown their data to advisory panels of outside experts.
“There’s a lot of redundancy, and a lot of people are looking at the data,” Dr. Alexander said. “So I don’t think we’re cutting corners to get it out there more quickly.”
A version of this article originally appeared on Medscape.com.
While stressing the urgent need to vaccinate the whole U.S. population, infectious disease experts and medical ethicists are raising questions about the clinical trials needed to answer important questions about the new COVID-19 vaccines.
In a statement released on Nov. 20, Barbara Alexander, MD, president of the Infectious Diseases Society of America (IDSA) and a professor at Duke University, Durham, N.C., commented on Pfizer and BioNTech’s application to the Food and Drug Administration for an emergency use authorization (EUA) for its COVID-19 vaccine. Besides emphasizing the need for a transparent review of the companies’ trial data prior to the FDA’s granting an EUA, she said, “If emergency use authorization is granted, clinical trials and data collection must continue.”
In an interview, Dr. Alexander said she is convinced that both Pfizer and Moderna, which is also expected to seek an EUA soon, will continue their clinical trials to monitor the long-term safety and efficacy of their vaccines.
“The EUA guidance for COVID vaccine authorization is very clear that clinical trials will move forward,” she said. “Any EUA request would have to include a strategy to ensure that the long-term safety and efficacy of a vaccine could be monitored. I see no evidence that either Pfizer or Moderna is not prepared to follow those regulations.”
Eventually, she added, the drug makers will have to seek full FDA approval to replace an EUA, which as its name signifies, is designed for public health emergencies. “The EUA is a tool to help us get the vaccine into circulation and have it start working as quickly as possible in the current health crisis,” she said. “But once the crisis is over, if the sponsors want to continue to market their vaccines, they have to go forward and get full approval.”
Medical ethicists, however, point out there may be ethical and practical dilemmas involved in continuing or initiating clinical trials once a vaccine has been approved for use even on an emergency basis.
In a commentary in Annals of Internal Medicine, Rafael Dal-Re, MD, PhD, Arthur L. Caplan, PhD, and two other ethicists stipulated that the pandemic requires early licensing and deployment of COVID-19 vaccines. Nevertheless, they noted, additional months of data are required to establish the long-term efficacy and safety of the vaccines. “Moreover, early deployment could interfere with the acquisition of long-term data,” both on these vaccines and on others coming through the pipeline, they wrote.
In countries where an approved vaccine is deployed, the ethicists noted, investigators must inform participants in an ongoing trial about the approved vaccine’s status and ask if they want to continue in the study. If enough participants decline, the trial might have to be terminated early. At that point, researchers may not have sufficient long-term data to identify late-term safety issues, determine how long efficacy lasts, determine whether waning immunity is associated with reduced levels of antibodies, or identify the level of neutralizing antibodies that correlates with immunity.
Moreover, they observed, long-term trials are especially important for vaccines that use mRNA technology, because less is known about them than about traditional kinds of vaccines.
The authors also pointed out that early licensing of any vaccine might make it harder to evaluate vaccines that haven’t yet been approved. “Once a vaccine is licensed, new placebo-controlled RCTs [randomized controlled trials] of other vaccines will not be acceptable ethically, and noninferiority RCTs will be the most likely alternative.
“The goal of noninferiority trials will be to demonstrate that the immune response (that is, neutralizing antibody titers or levels) of the candidate vaccine is not inferior to that of the approved vaccine within a prespecified margin, which the FDA has established as less than 10% for COVID-19 vaccines,” the authors noted.
More data with more study designs
Dial Hewlett Jr., MD, medical director for disease control services, Westchester County Department of Health, White Plains, N.Y., said in an interview that the ethicists raise important issues that have been discussed in other forums, including a recent webinar of the National Academy of Medicine.
“As the authors point out, once you have a vaccine that has been shown to be effective and safe, it’s no longer ethical to enroll people in placebo trials,” he said.
Therefore, he said, Pfizer and Moderna will undoubtedly offer their vaccines to the people in their studies’ placebo groups after the vaccines receive an EUA. Then they will follow everyone who has been vaccinated for 2 years to determine long-term safety. Efficacy will also continue to be measured as an adjunct of safety, he said.
With regard to the difficulty of reconsenting individuals to enter a new clinical trial after a vaccine has been approved, he said, “I’d agree that trying to get all the same participants to come into another study would be a challenge. You can, however, design studies that will allow you to obtain the same information. You will have a large number of people out there who haven’t been vaccinated, and you can do single-arm longitudinal studies and measure a number of things in the individuals who are enrolled in those studies,” he said.
“You can look at the immunologic markers, both antibody and T-cell. You can follow these individuals longitudinally to see if they do develop disease over a period of time. If they do, you can determine what their levels of response were,” he added. “So there are opportunities to design studies that would give you some of the same information, although it would not be in the same population that was in the randomized trials.”
For newer vaccines that have yet to be tested, he said, developers can compare “historical controls” from the trials of approved vaccines, i.e., data from the unvaccinated participants in those studies, with the data from inoculating people with the novel agents. The historical data can be sex- and age-matched, among other things, to individuals in the new trials. Moreover, because the study protocols have been harmonized for all trials under Operation Warp Speed, it doesn’t matter what kind of vaccine they’re testing, he said.
It may be necessary to do additional studies to find out how long immunity lasts after people have been vaccinated, Dr. Hewlett pointed out.
“You may have a different trial design. You don’t need a control arm to determine how long immunity lasts. You’re just comparing the patients who were vaccinated to nothing,” he said. “So you could have a single-arm trial on a group of people who consent to be immunized and followed. You can see what their antibody levels are and other surrogate markers, and you can see when they might develop disease, if they do. You’d need a large sample, but you can do that.”
Dr. Hewlett noted that additional studies will be required to determine whether the new vaccines stop transmission of the coronavirus or just prevent symptoms of COVID-19. Until it’s established that a vaccine halts transmission or the country achieves herd immunity, he said, “we’ll still have to wear masks and take other precautions, because a significant portion of people will still be at risk.”
‘A lot of redundancy’
Dr. Alexander emphasized that any safety or efficacy issues with the first COVID-19 vaccines must be identified before the vaccine is offered to a large portion of the U.S. population.
“While the data from the Pfizer and Moderna trials are said to be favorable, we at IDSA want to make sure that whatever vaccine comes to market is safe,” she said. “Having an unsafe vaccine on the market would be worse than no vaccine, because you’re compromising the public confidence. We have to make sure the public trusts the process and that sufficient data have been evaluated to ensure the vaccine is safe and efficacious.
“I believe the FDA is being very careful and thoughtful in [its] response,” Dr. Alexander said. “They realize how important it is to get a vaccine and save lives. While they’re doing things differently and moving much faster than before, they’re still trying to be thoughtful and reasonable. They don’t seem to be putting people at risk or circumventing the regulatory standards.”
Moreover, she pointed out, the FDA’s Vaccines and Related Biological Products Advisory Committee, which is expected to meet on Dec. 10, will review the trial data before the agency grants an EUA to Pfizer or Moderna. Then the FDA will post the data publicly.
The next step is for the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention to look at the data and decide who in the United States should receive the vaccine first, she pointed out. And both Pfizer and Moderna have shown their data to advisory panels of outside experts.
“There’s a lot of redundancy, and a lot of people are looking at the data,” Dr. Alexander said. “So I don’t think we’re cutting corners to get it out there more quickly.”
A version of this article originally appeared on Medscape.com.
Immune checkpoint inhibitors don’t increase COVID-19 incidence or mortality, studies suggest
Cytokine storm plays a major role in the pathogenesis of COVID-19, according to research published in The Lancet Respiratory Medicine. This has generated concern about using ICIs during the pandemic, given their immunostimulatory activity and the risk of immune-related adverse effects.
However, two retrospective studies suggest ICIs do not increase the risk of developing COVID-19 or dying from the disease.
In a study of 1,545 cancer patients prescribed ICIs and 20,418 matched controls, the incidence of COVID-19 was 1.4% with ICI therapy and 1.0% without it (odds ratio, 1.38; P = .15).
In a case-control study of 50 patients with cancer and COVID-19, 28% of patients who had received ICIs died from COVID-19, compared with 36% of patients who had not received ICIs (OR, 0.36; P = .23).
Vartan Pahalyants and Kevin Tyan, both students in Harvard University’s joint MD/MBA program in Boston, presented these studies at the meeting.
COVID-19 incidence with ICIs
Mr. Pahalyants and colleagues analyzed data from cancer patients treated in the Mass General Brigham health care system. The researchers compared 1,545 patients with at least one ICI prescription between July 1, 2019, and Feb. 29, 2020, with 20,418 matched cancer patients not prescribed ICIs. The team assessed COVID-19 incidence based on positive test results through June 19, 2020, from public health data.
The incidence of COVID-19 was low in both groups – 1.4% in the ICI group and 1.0% in the matched control group (P = .16). Among COVID-19–positive patients, the all-cause death rate was 40.9% in the ICI group and 28.6% in the control group (P = .23).
In multivariate analysis, patients prescribed ICIs did not have a significantly elevated risk for COVID-19 relative to peers not prescribed ICIs (OR, 1.38; P = .15). However, risk was significantly increased for female patients (OR, 1.74; P < .001), those living in a town or county with higher COVID-19 positivity rate (OR, 1.59; P < .001), and those with severe comorbidity (vs. mild or moderate; OR, 9.77; P = .02).
Among COVID-19–positive patients, those prescribed ICIs did not have a significantly elevated risk for all-cause mortality (OR, 1.60; P = .71), but male sex and lower income were associated with an increased risk of death.
“We did not identify an increased risk of [COVID-19] diagnosis among patients prescribed ICIs compared to the controls,” Mr. Pahalyants said. “This information may assist patients and their providers in decision-making around continuation of therapy during this protracted pandemic. However, more research needs to be conducted to determine potential behavioral and testing factors that may have affected COVID-19 diagnosis susceptibility among patients included in the study.”
COVID-19 mortality with ICIs
For their study, Mr. Tyan and colleagues identified 25 cancer patients who had received ICIs in the year before a COVID-19 diagnosis between March 20, 2020, and June 3, 2020, at the Dana-Farber Cancer Institute and Mass General Brigham network. The researchers then matched each patient with a cancer patient having a COVID-19 diagnosis who had not received ICIs during the preceding year.
Overall, 28% of patients who had received ICIs before their COVID-19 diagnosis died from COVID-19, compared with 36% of those who had not received ICIs.
In multivariate analysis, ICI therapy did not predict COVID-19 mortality (OR, 0.36; P = .23). However, the risk of death from COVID-19 increased with age (OR, 1.14; P = .01) and for patients with chronic obstructive pulmonary disease (OR, 12.26; P = .01), and risk was lower for statin users (OR, 0.08; P = .02). Findings were similar in an analysis restricted to hospitalized patients in the ICI group and their matched controls.
Two ICI-treated patients with COVID-19 had persistent immune-related adverse events (hypophysitis in both cases), and one ICI-treated patient developed a new immune-related adverse event (hypothyroidism).
At COVID-19 presentation, relative to counterparts who had not received ICIs, patients who had received ICIs had higher platelet counts (P = .017) and higher D-dimer levels (P = .037). In the context of similar levels of other biomarkers, this finding is “of unclear significance, as all deaths in the cohort were due to respiratory failure as opposed to hypercoagulability,” Mr. Tyan said.
The patients treated with ICIs were more likely to die from COVID-19 if they had elevated troponin levels (P = .01), whereas no such association was seen for those not treated with ICIs.
“We found that ICI therapy is not associated with greater risk for COVID-19 mortality. Our period of follow-up was relatively short, but we did not observe a high incidence of new or persistent immune-related adverse events among our patients taking ICIs,” Mr. Tyan said.
“While larger prospective trials are needed to evaluate long-term safety in the context of COVID-19 infection, our findings support the continuation of ICI therapy during the pandemic as it does not appear to worsen outcomes for cancer patients,” he concluded.
ICI therapy can continue, with precautions
“The question of susceptibility to COVID-19 has been unclear as ICIs do not necessarily cause immunosuppression but certainly result in modulation of a patient’s immune system,” said Deborah Doroshow, MD, PhD, assistant professor at the Tisch Cancer Institute Icahn School of Medicine at Mount Sinai, New York. She was not involved in these studies.
“The findings of the study by Pahalyants and colleagues, which used a very large sample size, appear to convincingly demonstrate that ICI receipt is not associated with an increased susceptibility to COVID-19,” Dr. Doroshow said in an interview.
However, the findings of the study by Tyan and colleagues are more “thought-provoking,” Dr. Doroshow said. She noted that a large study published in Nature Medicine showed previous ICI therapy in cancer patients with COVID-19 increased the risk for hospitalization or severe COVID-19 requiring high-flow oxygen or mechanical ventilation. The new study was much smaller and did not perform statistical comparisons for outcomes such as oxygen requirements.
“I would feel comfortable telling patients that the data suggests that ICI treatment does not increase their risk of COVID-19. However, if they were to be diagnosed with COVID-19, it is unclear whether their previous ICI treatment increases their risk for poor outcomes,” Dr. Doroshow said.
“I would feel comfortable continuing to treat patients with ICIs at this time, but because we know that patients with cancer are generally more likely to develop COVID-19 and have poor outcomes, it is critical that our patients be educated about social distancing and mask wearing to the extent that their living and working situations permit,” she added.
Mr. Pahalyants disclosed no relevant conflicts of interest, and his study did not receive any specific funding. Mr. Tyan disclosed that he is cofounder and chief science officer of Kinnos, and his study did not receive any specific funding. Dr. Doroshow disclosed no relevant conflicts of interest.
SOURCE: Pahalyants V et al. SITC 2020, Abstract 826. Tyan K et al. SITC 2020, Abstract 481.
Cytokine storm plays a major role in the pathogenesis of COVID-19, according to research published in The Lancet Respiratory Medicine. This has generated concern about using ICIs during the pandemic, given their immunostimulatory activity and the risk of immune-related adverse effects.
However, two retrospective studies suggest ICIs do not increase the risk of developing COVID-19 or dying from the disease.
In a study of 1,545 cancer patients prescribed ICIs and 20,418 matched controls, the incidence of COVID-19 was 1.4% with ICI therapy and 1.0% without it (odds ratio, 1.38; P = .15).
In a case-control study of 50 patients with cancer and COVID-19, 28% of patients who had received ICIs died from COVID-19, compared with 36% of patients who had not received ICIs (OR, 0.36; P = .23).
Vartan Pahalyants and Kevin Tyan, both students in Harvard University’s joint MD/MBA program in Boston, presented these studies at the meeting.
COVID-19 incidence with ICIs
Mr. Pahalyants and colleagues analyzed data from cancer patients treated in the Mass General Brigham health care system. The researchers compared 1,545 patients with at least one ICI prescription between July 1, 2019, and Feb. 29, 2020, with 20,418 matched cancer patients not prescribed ICIs. The team assessed COVID-19 incidence based on positive test results through June 19, 2020, from public health data.
The incidence of COVID-19 was low in both groups – 1.4% in the ICI group and 1.0% in the matched control group (P = .16). Among COVID-19–positive patients, the all-cause death rate was 40.9% in the ICI group and 28.6% in the control group (P = .23).
In multivariate analysis, patients prescribed ICIs did not have a significantly elevated risk for COVID-19 relative to peers not prescribed ICIs (OR, 1.38; P = .15). However, risk was significantly increased for female patients (OR, 1.74; P < .001), those living in a town or county with higher COVID-19 positivity rate (OR, 1.59; P < .001), and those with severe comorbidity (vs. mild or moderate; OR, 9.77; P = .02).
Among COVID-19–positive patients, those prescribed ICIs did not have a significantly elevated risk for all-cause mortality (OR, 1.60; P = .71), but male sex and lower income were associated with an increased risk of death.
“We did not identify an increased risk of [COVID-19] diagnosis among patients prescribed ICIs compared to the controls,” Mr. Pahalyants said. “This information may assist patients and their providers in decision-making around continuation of therapy during this protracted pandemic. However, more research needs to be conducted to determine potential behavioral and testing factors that may have affected COVID-19 diagnosis susceptibility among patients included in the study.”
COVID-19 mortality with ICIs
For their study, Mr. Tyan and colleagues identified 25 cancer patients who had received ICIs in the year before a COVID-19 diagnosis between March 20, 2020, and June 3, 2020, at the Dana-Farber Cancer Institute and Mass General Brigham network. The researchers then matched each patient with a cancer patient having a COVID-19 diagnosis who had not received ICIs during the preceding year.
Overall, 28% of patients who had received ICIs before their COVID-19 diagnosis died from COVID-19, compared with 36% of those who had not received ICIs.
In multivariate analysis, ICI therapy did not predict COVID-19 mortality (OR, 0.36; P = .23). However, the risk of death from COVID-19 increased with age (OR, 1.14; P = .01) and for patients with chronic obstructive pulmonary disease (OR, 12.26; P = .01), and risk was lower for statin users (OR, 0.08; P = .02). Findings were similar in an analysis restricted to hospitalized patients in the ICI group and their matched controls.
Two ICI-treated patients with COVID-19 had persistent immune-related adverse events (hypophysitis in both cases), and one ICI-treated patient developed a new immune-related adverse event (hypothyroidism).
At COVID-19 presentation, relative to counterparts who had not received ICIs, patients who had received ICIs had higher platelet counts (P = .017) and higher D-dimer levels (P = .037). In the context of similar levels of other biomarkers, this finding is “of unclear significance, as all deaths in the cohort were due to respiratory failure as opposed to hypercoagulability,” Mr. Tyan said.
The patients treated with ICIs were more likely to die from COVID-19 if they had elevated troponin levels (P = .01), whereas no such association was seen for those not treated with ICIs.
“We found that ICI therapy is not associated with greater risk for COVID-19 mortality. Our period of follow-up was relatively short, but we did not observe a high incidence of new or persistent immune-related adverse events among our patients taking ICIs,” Mr. Tyan said.
“While larger prospective trials are needed to evaluate long-term safety in the context of COVID-19 infection, our findings support the continuation of ICI therapy during the pandemic as it does not appear to worsen outcomes for cancer patients,” he concluded.
ICI therapy can continue, with precautions
“The question of susceptibility to COVID-19 has been unclear as ICIs do not necessarily cause immunosuppression but certainly result in modulation of a patient’s immune system,” said Deborah Doroshow, MD, PhD, assistant professor at the Tisch Cancer Institute Icahn School of Medicine at Mount Sinai, New York. She was not involved in these studies.
“The findings of the study by Pahalyants and colleagues, which used a very large sample size, appear to convincingly demonstrate that ICI receipt is not associated with an increased susceptibility to COVID-19,” Dr. Doroshow said in an interview.
However, the findings of the study by Tyan and colleagues are more “thought-provoking,” Dr. Doroshow said. She noted that a large study published in Nature Medicine showed previous ICI therapy in cancer patients with COVID-19 increased the risk for hospitalization or severe COVID-19 requiring high-flow oxygen or mechanical ventilation. The new study was much smaller and did not perform statistical comparisons for outcomes such as oxygen requirements.
“I would feel comfortable telling patients that the data suggests that ICI treatment does not increase their risk of COVID-19. However, if they were to be diagnosed with COVID-19, it is unclear whether their previous ICI treatment increases their risk for poor outcomes,” Dr. Doroshow said.
“I would feel comfortable continuing to treat patients with ICIs at this time, but because we know that patients with cancer are generally more likely to develop COVID-19 and have poor outcomes, it is critical that our patients be educated about social distancing and mask wearing to the extent that their living and working situations permit,” she added.
Mr. Pahalyants disclosed no relevant conflicts of interest, and his study did not receive any specific funding. Mr. Tyan disclosed that he is cofounder and chief science officer of Kinnos, and his study did not receive any specific funding. Dr. Doroshow disclosed no relevant conflicts of interest.
SOURCE: Pahalyants V et al. SITC 2020, Abstract 826. Tyan K et al. SITC 2020, Abstract 481.
Cytokine storm plays a major role in the pathogenesis of COVID-19, according to research published in The Lancet Respiratory Medicine. This has generated concern about using ICIs during the pandemic, given their immunostimulatory activity and the risk of immune-related adverse effects.
However, two retrospective studies suggest ICIs do not increase the risk of developing COVID-19 or dying from the disease.
In a study of 1,545 cancer patients prescribed ICIs and 20,418 matched controls, the incidence of COVID-19 was 1.4% with ICI therapy and 1.0% without it (odds ratio, 1.38; P = .15).
In a case-control study of 50 patients with cancer and COVID-19, 28% of patients who had received ICIs died from COVID-19, compared with 36% of patients who had not received ICIs (OR, 0.36; P = .23).
Vartan Pahalyants and Kevin Tyan, both students in Harvard University’s joint MD/MBA program in Boston, presented these studies at the meeting.
COVID-19 incidence with ICIs
Mr. Pahalyants and colleagues analyzed data from cancer patients treated in the Mass General Brigham health care system. The researchers compared 1,545 patients with at least one ICI prescription between July 1, 2019, and Feb. 29, 2020, with 20,418 matched cancer patients not prescribed ICIs. The team assessed COVID-19 incidence based on positive test results through June 19, 2020, from public health data.
The incidence of COVID-19 was low in both groups – 1.4% in the ICI group and 1.0% in the matched control group (P = .16). Among COVID-19–positive patients, the all-cause death rate was 40.9% in the ICI group and 28.6% in the control group (P = .23).
In multivariate analysis, patients prescribed ICIs did not have a significantly elevated risk for COVID-19 relative to peers not prescribed ICIs (OR, 1.38; P = .15). However, risk was significantly increased for female patients (OR, 1.74; P < .001), those living in a town or county with higher COVID-19 positivity rate (OR, 1.59; P < .001), and those with severe comorbidity (vs. mild or moderate; OR, 9.77; P = .02).
Among COVID-19–positive patients, those prescribed ICIs did not have a significantly elevated risk for all-cause mortality (OR, 1.60; P = .71), but male sex and lower income were associated with an increased risk of death.
“We did not identify an increased risk of [COVID-19] diagnosis among patients prescribed ICIs compared to the controls,” Mr. Pahalyants said. “This information may assist patients and their providers in decision-making around continuation of therapy during this protracted pandemic. However, more research needs to be conducted to determine potential behavioral and testing factors that may have affected COVID-19 diagnosis susceptibility among patients included in the study.”
COVID-19 mortality with ICIs
For their study, Mr. Tyan and colleagues identified 25 cancer patients who had received ICIs in the year before a COVID-19 diagnosis between March 20, 2020, and June 3, 2020, at the Dana-Farber Cancer Institute and Mass General Brigham network. The researchers then matched each patient with a cancer patient having a COVID-19 diagnosis who had not received ICIs during the preceding year.
Overall, 28% of patients who had received ICIs before their COVID-19 diagnosis died from COVID-19, compared with 36% of those who had not received ICIs.
In multivariate analysis, ICI therapy did not predict COVID-19 mortality (OR, 0.36; P = .23). However, the risk of death from COVID-19 increased with age (OR, 1.14; P = .01) and for patients with chronic obstructive pulmonary disease (OR, 12.26; P = .01), and risk was lower for statin users (OR, 0.08; P = .02). Findings were similar in an analysis restricted to hospitalized patients in the ICI group and their matched controls.
Two ICI-treated patients with COVID-19 had persistent immune-related adverse events (hypophysitis in both cases), and one ICI-treated patient developed a new immune-related adverse event (hypothyroidism).
At COVID-19 presentation, relative to counterparts who had not received ICIs, patients who had received ICIs had higher platelet counts (P = .017) and higher D-dimer levels (P = .037). In the context of similar levels of other biomarkers, this finding is “of unclear significance, as all deaths in the cohort were due to respiratory failure as opposed to hypercoagulability,” Mr. Tyan said.
The patients treated with ICIs were more likely to die from COVID-19 if they had elevated troponin levels (P = .01), whereas no such association was seen for those not treated with ICIs.
“We found that ICI therapy is not associated with greater risk for COVID-19 mortality. Our period of follow-up was relatively short, but we did not observe a high incidence of new or persistent immune-related adverse events among our patients taking ICIs,” Mr. Tyan said.
“While larger prospective trials are needed to evaluate long-term safety in the context of COVID-19 infection, our findings support the continuation of ICI therapy during the pandemic as it does not appear to worsen outcomes for cancer patients,” he concluded.
ICI therapy can continue, with precautions
“The question of susceptibility to COVID-19 has been unclear as ICIs do not necessarily cause immunosuppression but certainly result in modulation of a patient’s immune system,” said Deborah Doroshow, MD, PhD, assistant professor at the Tisch Cancer Institute Icahn School of Medicine at Mount Sinai, New York. She was not involved in these studies.
“The findings of the study by Pahalyants and colleagues, which used a very large sample size, appear to convincingly demonstrate that ICI receipt is not associated with an increased susceptibility to COVID-19,” Dr. Doroshow said in an interview.
However, the findings of the study by Tyan and colleagues are more “thought-provoking,” Dr. Doroshow said. She noted that a large study published in Nature Medicine showed previous ICI therapy in cancer patients with COVID-19 increased the risk for hospitalization or severe COVID-19 requiring high-flow oxygen or mechanical ventilation. The new study was much smaller and did not perform statistical comparisons for outcomes such as oxygen requirements.
“I would feel comfortable telling patients that the data suggests that ICI treatment does not increase their risk of COVID-19. However, if they were to be diagnosed with COVID-19, it is unclear whether their previous ICI treatment increases their risk for poor outcomes,” Dr. Doroshow said.
“I would feel comfortable continuing to treat patients with ICIs at this time, but because we know that patients with cancer are generally more likely to develop COVID-19 and have poor outcomes, it is critical that our patients be educated about social distancing and mask wearing to the extent that their living and working situations permit,” she added.
Mr. Pahalyants disclosed no relevant conflicts of interest, and his study did not receive any specific funding. Mr. Tyan disclosed that he is cofounder and chief science officer of Kinnos, and his study did not receive any specific funding. Dr. Doroshow disclosed no relevant conflicts of interest.
SOURCE: Pahalyants V et al. SITC 2020, Abstract 826. Tyan K et al. SITC 2020, Abstract 481.
FROM SITC 2020
CDC panel delves into priorities for COVID vaccine distribution
On Monday, members of an influential federal panel delved into the challenges ahead in deciding who will get the first doses of COVID-19 vaccines, including questions about which healthcare workers need those initial vaccinations the most.
The Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) did not take any votes or seek to establish formal positions. Instead, the meeting served as a forum for experts to discuss the thorny issues ahead. The US Food and Drug Administration (FDA) could make a decision next month regarding clearance for the first COVID-19 vaccine.
An FDA advisory committee will meet December 10 to review the request for emergency use authorization (EUA) of a COVID-19 vaccine from Pfizer, in partnership with BioNTech. Moderna Inc said on November 16 that it expects to soon ask the FDA for an EUA of its rival COVID vaccine.
ACIP will face a two-part task after the FDA clears COVID-19 vaccines, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. ACIP will need to first decide whether to recommend use of the vaccine and then address the “complicated and difficult” question of which groups should get the initial limited quantities.
“There aren’t any perfect decisions,” she told the ACIP members. “I know this is something that most of you didn’t anticipate doing, making these kinds of huge decisions in the midst of a pandemic.”
There has been considerable public discussion of prioritization of COVID-19 vaccines, including a set of recommendations offered by a special committee created by the National Academies of Sciences, Engineering and Medicine. In addition, CDC staff and members of ACIP outlined what they termed the “four ethical principles” meant to guide these decisions in a November 23 report in the agency’s Morbidity and Mortality Weekly Report. These four principles are to maximize benefits and minimize harms; promote justice; mitigate health inequities; and promote transparency.
But as the issuing of the first EUA nears, it falls to ACIP to move beyond endorsing broad goals. The panel will need to make decisions as to which groups will have to wait for COVID-19 vaccines.
ACIP members on Monday delved into these kinds of more detailed questions, using a proposed three-stage model as a discussion point.
In phase 1a of this model, healthcare workers and residents of long-term care facilities would be the first people to be vaccinated. Phase 1b would include those deemed essential workers, including police officers, firefighters, and those in education, transportation, food, and agriculture sectors. Phase 1c would include adults with high-risk medical conditions and those aged 65 years and older.
ACIP member Grace M. Lee, MD, MPH, of Stanford University, Stanford, California, questioned whether healthcare workers who are not seeing patients in person should wait to get the vaccines. There has been a marked rise in the use of telehealth during the pandemic, which has spared some clinicians from in-person COVID-19 patient visits in their practices.
“Close partnership with our public health colleagues will be critically important to make sure that we are not trying to vaccinate 100% of our healthcare workforce, if some proportion of our workforce can work from home,” Lee said.
ACIP member Pablo Sánchez, MD, of the Research Institute at Nationwide Children’s Hospital in Columbus, Ohio, concurred. Some clinicians, he noted, may have better access to personal protective equipment than others, he said.
“Unfortunately, not all healthcare workers are equal in terms of risk,” Sánchez said. “Within institutions, we’re going to have to prioritize which ones will get” the vaccine.
Clinicians may also make judgments about their own risk and need for early access to COVID-19 vaccinations, Sánchez said.
“I’m 66, and I’d rather give it to somebody much older and sicker than me,” he said.
Broader access
Fairly large populations will essentially be competing for limited doses of the first vaccines to reach the market.
The overlap is significant in the four priority groups put forward by CDC. The CDC staff estimated that about 21 million people would fall into the healthcare personnel category, which includes hospital staff, pharmacists, and those working in long-term care facilities. There are about 87 million people in the essential workers groups. More than 100 million adults in the United States, such as those with diabetes and cancers, fall into the high-risk medical conditions group. Another 53 million people are aged 65 and older.
Department of Health and Human Services Secretary Alex Azar on November 18 said the federal government expects to have about 40 million doses of these two vaccines by the end of December, which is enough to provide the two-dose regimen for about 20 million. If all goes as expected, Pfizer and Moderna will ramp up production.
Moderna has said that it expects by the end of this year to have approximately 20 million doses of its vaccine ready to ship in the United States and that it is on track to manufacture 500 million to 1 billion doses globally in 2021. Pfizer and BioNTech have said they expect to produce globally up to 50 million doses in 2020 and up to 1.3 billion doses by the end of 2021.
At the Monday meeting, several ACIP panelists stressed the need to ensure that essential workers get early doses of vaccines.
In many cases, these workers serve in jobs with significant public interaction and live in poor communities. They put themselves and their families at risk. Many of them lack the resources to take precautions available to those better able to isolate, said ACIP member Beth Bell, MD, MPH, of the University of Washington, Seattle, Washington.
“These essential workers are out there putting themselves at risk to allow the rest of us to socially distance,” she said. “Recognizing that not all of them may want to be vaccinated at this stage, we need to provide them with the opportunity early on in the process.”
In Bell’s view, the initial rollout of COVID-19 vaccines will send an important message about sharing this resource.
“If we’re serious about valuing equity, we need to have that baked in early on in the vaccination program,” she said.
Bell also said she was in favor of including people living in nursing homes in the initial wave of vaccinations. Concerns were raised about the frailty of this population.
“Given the mortality impact on the healthcare system from the number of nursing home residents that have been dying, I think on balance it makes sense to include them in phase 1a,” Bell said.
Other ACIP panelists said missteps with early vaccination of people in nursing homes could undermine faith in the treatments. Because of the ages and medical conditions of people in nursing homes, many of them may die after receiving the COVID-19 vaccine. Such deaths would not be associated with vaccine, but the medical community would not yet have evidence to disprove a connection.
There could be a backlash, with people falsely linking the death of a grandparent to the vaccine.
Fellow ACIP member Robert L. Atmar, MD, Baylor College of Medicine, Houston, Texas, was among those who had raised concerns about including people living in long-term care facilities in phase 1a. He said there are not yet enough data to judge the balance of benefits and harms of vaccination for this population.
The Pfizer and Moderna vaccines are “reactagenic,” meaning people may not feel well in the days after receiving the shots. The symptoms could lead to additional health evaluations of older people in nursing homes as clinicians try to figure out whether the patient’s reactions to the vaccine are caused by some condition or infection, Atmar said.
“Those of us who see these patients in the hospital recognize that there are often medical interventions that are done in the pursuit of a diagnosis, of a change in clinical status, that in and of themselves can lead to harm,” Atmar said.
Clinicians likely will have to encourage their patients of all ages to receive second doses of COVID-19 vaccines, despite the malaise they may provoke.
“We really need to make patients aware that this is not going to be a walk in the park. I mean, they’re going to know they had a vaccine, they’re probably not going to feel wonderful, but they’ve got to come back for that second dose,” said Sandra Adamson Fryhofer, MD, who represented the American Medical Association.
ACIP is expected to meet again to offer specific recommendations on the Pfizer and Moderna vaccines. ACIP’s recommendations trigger reimbursement processes, Azar said at a Tuesday press conference. ACIP’s work will inform decisions made by the federal government and governors about deploying shipments of COVID-19 vaccines, he said.
“At the end of the day, that is a decision, though, of the US government to make, which is where to recommend the prioritization,” Azar said. “It will be our nation’s governors in implementing the distribution plans to tell us” where to ship the vaccine.
This article first appeared on Medscape.com.
On Monday, members of an influential federal panel delved into the challenges ahead in deciding who will get the first doses of COVID-19 vaccines, including questions about which healthcare workers need those initial vaccinations the most.
The Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) did not take any votes or seek to establish formal positions. Instead, the meeting served as a forum for experts to discuss the thorny issues ahead. The US Food and Drug Administration (FDA) could make a decision next month regarding clearance for the first COVID-19 vaccine.
An FDA advisory committee will meet December 10 to review the request for emergency use authorization (EUA) of a COVID-19 vaccine from Pfizer, in partnership with BioNTech. Moderna Inc said on November 16 that it expects to soon ask the FDA for an EUA of its rival COVID vaccine.
ACIP will face a two-part task after the FDA clears COVID-19 vaccines, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. ACIP will need to first decide whether to recommend use of the vaccine and then address the “complicated and difficult” question of which groups should get the initial limited quantities.
“There aren’t any perfect decisions,” she told the ACIP members. “I know this is something that most of you didn’t anticipate doing, making these kinds of huge decisions in the midst of a pandemic.”
There has been considerable public discussion of prioritization of COVID-19 vaccines, including a set of recommendations offered by a special committee created by the National Academies of Sciences, Engineering and Medicine. In addition, CDC staff and members of ACIP outlined what they termed the “four ethical principles” meant to guide these decisions in a November 23 report in the agency’s Morbidity and Mortality Weekly Report. These four principles are to maximize benefits and minimize harms; promote justice; mitigate health inequities; and promote transparency.
But as the issuing of the first EUA nears, it falls to ACIP to move beyond endorsing broad goals. The panel will need to make decisions as to which groups will have to wait for COVID-19 vaccines.
ACIP members on Monday delved into these kinds of more detailed questions, using a proposed three-stage model as a discussion point.
In phase 1a of this model, healthcare workers and residents of long-term care facilities would be the first people to be vaccinated. Phase 1b would include those deemed essential workers, including police officers, firefighters, and those in education, transportation, food, and agriculture sectors. Phase 1c would include adults with high-risk medical conditions and those aged 65 years and older.
ACIP member Grace M. Lee, MD, MPH, of Stanford University, Stanford, California, questioned whether healthcare workers who are not seeing patients in person should wait to get the vaccines. There has been a marked rise in the use of telehealth during the pandemic, which has spared some clinicians from in-person COVID-19 patient visits in their practices.
“Close partnership with our public health colleagues will be critically important to make sure that we are not trying to vaccinate 100% of our healthcare workforce, if some proportion of our workforce can work from home,” Lee said.
ACIP member Pablo Sánchez, MD, of the Research Institute at Nationwide Children’s Hospital in Columbus, Ohio, concurred. Some clinicians, he noted, may have better access to personal protective equipment than others, he said.
“Unfortunately, not all healthcare workers are equal in terms of risk,” Sánchez said. “Within institutions, we’re going to have to prioritize which ones will get” the vaccine.
Clinicians may also make judgments about their own risk and need for early access to COVID-19 vaccinations, Sánchez said.
“I’m 66, and I’d rather give it to somebody much older and sicker than me,” he said.
Broader access
Fairly large populations will essentially be competing for limited doses of the first vaccines to reach the market.
The overlap is significant in the four priority groups put forward by CDC. The CDC staff estimated that about 21 million people would fall into the healthcare personnel category, which includes hospital staff, pharmacists, and those working in long-term care facilities. There are about 87 million people in the essential workers groups. More than 100 million adults in the United States, such as those with diabetes and cancers, fall into the high-risk medical conditions group. Another 53 million people are aged 65 and older.
Department of Health and Human Services Secretary Alex Azar on November 18 said the federal government expects to have about 40 million doses of these two vaccines by the end of December, which is enough to provide the two-dose regimen for about 20 million. If all goes as expected, Pfizer and Moderna will ramp up production.
Moderna has said that it expects by the end of this year to have approximately 20 million doses of its vaccine ready to ship in the United States and that it is on track to manufacture 500 million to 1 billion doses globally in 2021. Pfizer and BioNTech have said they expect to produce globally up to 50 million doses in 2020 and up to 1.3 billion doses by the end of 2021.
At the Monday meeting, several ACIP panelists stressed the need to ensure that essential workers get early doses of vaccines.
In many cases, these workers serve in jobs with significant public interaction and live in poor communities. They put themselves and their families at risk. Many of them lack the resources to take precautions available to those better able to isolate, said ACIP member Beth Bell, MD, MPH, of the University of Washington, Seattle, Washington.
“These essential workers are out there putting themselves at risk to allow the rest of us to socially distance,” she said. “Recognizing that not all of them may want to be vaccinated at this stage, we need to provide them with the opportunity early on in the process.”
In Bell’s view, the initial rollout of COVID-19 vaccines will send an important message about sharing this resource.
“If we’re serious about valuing equity, we need to have that baked in early on in the vaccination program,” she said.
Bell also said she was in favor of including people living in nursing homes in the initial wave of vaccinations. Concerns were raised about the frailty of this population.
“Given the mortality impact on the healthcare system from the number of nursing home residents that have been dying, I think on balance it makes sense to include them in phase 1a,” Bell said.
Other ACIP panelists said missteps with early vaccination of people in nursing homes could undermine faith in the treatments. Because of the ages and medical conditions of people in nursing homes, many of them may die after receiving the COVID-19 vaccine. Such deaths would not be associated with vaccine, but the medical community would not yet have evidence to disprove a connection.
There could be a backlash, with people falsely linking the death of a grandparent to the vaccine.
Fellow ACIP member Robert L. Atmar, MD, Baylor College of Medicine, Houston, Texas, was among those who had raised concerns about including people living in long-term care facilities in phase 1a. He said there are not yet enough data to judge the balance of benefits and harms of vaccination for this population.
The Pfizer and Moderna vaccines are “reactagenic,” meaning people may not feel well in the days after receiving the shots. The symptoms could lead to additional health evaluations of older people in nursing homes as clinicians try to figure out whether the patient’s reactions to the vaccine are caused by some condition or infection, Atmar said.
“Those of us who see these patients in the hospital recognize that there are often medical interventions that are done in the pursuit of a diagnosis, of a change in clinical status, that in and of themselves can lead to harm,” Atmar said.
Clinicians likely will have to encourage their patients of all ages to receive second doses of COVID-19 vaccines, despite the malaise they may provoke.
“We really need to make patients aware that this is not going to be a walk in the park. I mean, they’re going to know they had a vaccine, they’re probably not going to feel wonderful, but they’ve got to come back for that second dose,” said Sandra Adamson Fryhofer, MD, who represented the American Medical Association.
ACIP is expected to meet again to offer specific recommendations on the Pfizer and Moderna vaccines. ACIP’s recommendations trigger reimbursement processes, Azar said at a Tuesday press conference. ACIP’s work will inform decisions made by the federal government and governors about deploying shipments of COVID-19 vaccines, he said.
“At the end of the day, that is a decision, though, of the US government to make, which is where to recommend the prioritization,” Azar said. “It will be our nation’s governors in implementing the distribution plans to tell us” where to ship the vaccine.
This article first appeared on Medscape.com.
On Monday, members of an influential federal panel delved into the challenges ahead in deciding who will get the first doses of COVID-19 vaccines, including questions about which healthcare workers need those initial vaccinations the most.
The Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) did not take any votes or seek to establish formal positions. Instead, the meeting served as a forum for experts to discuss the thorny issues ahead. The US Food and Drug Administration (FDA) could make a decision next month regarding clearance for the first COVID-19 vaccine.
An FDA advisory committee will meet December 10 to review the request for emergency use authorization (EUA) of a COVID-19 vaccine from Pfizer, in partnership with BioNTech. Moderna Inc said on November 16 that it expects to soon ask the FDA for an EUA of its rival COVID vaccine.
ACIP will face a two-part task after the FDA clears COVID-19 vaccines, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. ACIP will need to first decide whether to recommend use of the vaccine and then address the “complicated and difficult” question of which groups should get the initial limited quantities.
“There aren’t any perfect decisions,” she told the ACIP members. “I know this is something that most of you didn’t anticipate doing, making these kinds of huge decisions in the midst of a pandemic.”
There has been considerable public discussion of prioritization of COVID-19 vaccines, including a set of recommendations offered by a special committee created by the National Academies of Sciences, Engineering and Medicine. In addition, CDC staff and members of ACIP outlined what they termed the “four ethical principles” meant to guide these decisions in a November 23 report in the agency’s Morbidity and Mortality Weekly Report. These four principles are to maximize benefits and minimize harms; promote justice; mitigate health inequities; and promote transparency.
But as the issuing of the first EUA nears, it falls to ACIP to move beyond endorsing broad goals. The panel will need to make decisions as to which groups will have to wait for COVID-19 vaccines.
ACIP members on Monday delved into these kinds of more detailed questions, using a proposed three-stage model as a discussion point.
In phase 1a of this model, healthcare workers and residents of long-term care facilities would be the first people to be vaccinated. Phase 1b would include those deemed essential workers, including police officers, firefighters, and those in education, transportation, food, and agriculture sectors. Phase 1c would include adults with high-risk medical conditions and those aged 65 years and older.
ACIP member Grace M. Lee, MD, MPH, of Stanford University, Stanford, California, questioned whether healthcare workers who are not seeing patients in person should wait to get the vaccines. There has been a marked rise in the use of telehealth during the pandemic, which has spared some clinicians from in-person COVID-19 patient visits in their practices.
“Close partnership with our public health colleagues will be critically important to make sure that we are not trying to vaccinate 100% of our healthcare workforce, if some proportion of our workforce can work from home,” Lee said.
ACIP member Pablo Sánchez, MD, of the Research Institute at Nationwide Children’s Hospital in Columbus, Ohio, concurred. Some clinicians, he noted, may have better access to personal protective equipment than others, he said.
“Unfortunately, not all healthcare workers are equal in terms of risk,” Sánchez said. “Within institutions, we’re going to have to prioritize which ones will get” the vaccine.
Clinicians may also make judgments about their own risk and need for early access to COVID-19 vaccinations, Sánchez said.
“I’m 66, and I’d rather give it to somebody much older and sicker than me,” he said.
Broader access
Fairly large populations will essentially be competing for limited doses of the first vaccines to reach the market.
The overlap is significant in the four priority groups put forward by CDC. The CDC staff estimated that about 21 million people would fall into the healthcare personnel category, which includes hospital staff, pharmacists, and those working in long-term care facilities. There are about 87 million people in the essential workers groups. More than 100 million adults in the United States, such as those with diabetes and cancers, fall into the high-risk medical conditions group. Another 53 million people are aged 65 and older.
Department of Health and Human Services Secretary Alex Azar on November 18 said the federal government expects to have about 40 million doses of these two vaccines by the end of December, which is enough to provide the two-dose regimen for about 20 million. If all goes as expected, Pfizer and Moderna will ramp up production.
Moderna has said that it expects by the end of this year to have approximately 20 million doses of its vaccine ready to ship in the United States and that it is on track to manufacture 500 million to 1 billion doses globally in 2021. Pfizer and BioNTech have said they expect to produce globally up to 50 million doses in 2020 and up to 1.3 billion doses by the end of 2021.
At the Monday meeting, several ACIP panelists stressed the need to ensure that essential workers get early doses of vaccines.
In many cases, these workers serve in jobs with significant public interaction and live in poor communities. They put themselves and their families at risk. Many of them lack the resources to take precautions available to those better able to isolate, said ACIP member Beth Bell, MD, MPH, of the University of Washington, Seattle, Washington.
“These essential workers are out there putting themselves at risk to allow the rest of us to socially distance,” she said. “Recognizing that not all of them may want to be vaccinated at this stage, we need to provide them with the opportunity early on in the process.”
In Bell’s view, the initial rollout of COVID-19 vaccines will send an important message about sharing this resource.
“If we’re serious about valuing equity, we need to have that baked in early on in the vaccination program,” she said.
Bell also said she was in favor of including people living in nursing homes in the initial wave of vaccinations. Concerns were raised about the frailty of this population.
“Given the mortality impact on the healthcare system from the number of nursing home residents that have been dying, I think on balance it makes sense to include them in phase 1a,” Bell said.
Other ACIP panelists said missteps with early vaccination of people in nursing homes could undermine faith in the treatments. Because of the ages and medical conditions of people in nursing homes, many of them may die after receiving the COVID-19 vaccine. Such deaths would not be associated with vaccine, but the medical community would not yet have evidence to disprove a connection.
There could be a backlash, with people falsely linking the death of a grandparent to the vaccine.
Fellow ACIP member Robert L. Atmar, MD, Baylor College of Medicine, Houston, Texas, was among those who had raised concerns about including people living in long-term care facilities in phase 1a. He said there are not yet enough data to judge the balance of benefits and harms of vaccination for this population.
The Pfizer and Moderna vaccines are “reactagenic,” meaning people may not feel well in the days after receiving the shots. The symptoms could lead to additional health evaluations of older people in nursing homes as clinicians try to figure out whether the patient’s reactions to the vaccine are caused by some condition or infection, Atmar said.
“Those of us who see these patients in the hospital recognize that there are often medical interventions that are done in the pursuit of a diagnosis, of a change in clinical status, that in and of themselves can lead to harm,” Atmar said.
Clinicians likely will have to encourage their patients of all ages to receive second doses of COVID-19 vaccines, despite the malaise they may provoke.
“We really need to make patients aware that this is not going to be a walk in the park. I mean, they’re going to know they had a vaccine, they’re probably not going to feel wonderful, but they’ve got to come back for that second dose,” said Sandra Adamson Fryhofer, MD, who represented the American Medical Association.
ACIP is expected to meet again to offer specific recommendations on the Pfizer and Moderna vaccines. ACIP’s recommendations trigger reimbursement processes, Azar said at a Tuesday press conference. ACIP’s work will inform decisions made by the federal government and governors about deploying shipments of COVID-19 vaccines, he said.
“At the end of the day, that is a decision, though, of the US government to make, which is where to recommend the prioritization,” Azar said. “It will be our nation’s governors in implementing the distribution plans to tell us” where to ship the vaccine.
This article first appeared on Medscape.com.
FDA expands Xofluza indication to include postexposure flu prophylaxis
The US Food and Drug Administration (FDA) has expanded the indication for the antiviral baloxavir marboxil (Xofluza) to include postexposure prophylaxis of uncomplicated influenza in people aged 12 years and older.
“This expanded indication for Xofluza will provide an important option to help prevent influenza just in time for a flu season that is anticipated to be unlike any other because it will coincide with the coronavirus pandemic,” Debra Birnkrant, MD, director, Division of Antiviral Products, FDA Center for Drug Evaluation and Research, said in a press release.
In addition, Xofluza, which was previously available only in tablet form, is also now available as granules for mixing in water, the FDA said.
The agency first approved baloxavir marboxil in 2018 for the treatment of acute uncomplicated influenza in people aged 12 years or older who have been symptomatic for no more than 48 hours.
A year later, the FDA expanded the indication to include people at high risk of developing influenza-related complications, such as those with asthma, chronic lung disease, diabetes, heart disease, or morbid obesity, as well as adults aged 65 years or older.
The safety and efficacy of Xofluza for influenza postexposure prophylaxis is supported by a randomized, double-blind, controlled trial involving 607 people aged 12 years and older. After exposure to a person with influenza in their household, they received a single dose of Xofluza or placebo.
The primary endpoint was the proportion of individuals who became infected with influenza and presented with fever and at least one respiratory symptom from day 1 to day 10.
Of the 303 people who received Xofluza, 1% of individuals met these criteria, compared with 13% of those who received placebo.
The most common adverse effects of Xofluza include diarrhea, bronchitis, nausea, sinusitis, and headache.
Hypersensitivity, including anaphylaxis, can occur in patients taking Xofluza. The antiviral is contraindicated in people with a known hypersensitivity reaction to Xofluza.
Xofluza should not be coadministered with dairy products, calcium-fortified beverages, laxatives, antacids, or oral supplements containing calcium, iron, magnesium, selenium, aluminium, or zinc.
Full prescribing information is available online.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has expanded the indication for the antiviral baloxavir marboxil (Xofluza) to include postexposure prophylaxis of uncomplicated influenza in people aged 12 years and older.
“This expanded indication for Xofluza will provide an important option to help prevent influenza just in time for a flu season that is anticipated to be unlike any other because it will coincide with the coronavirus pandemic,” Debra Birnkrant, MD, director, Division of Antiviral Products, FDA Center for Drug Evaluation and Research, said in a press release.
In addition, Xofluza, which was previously available only in tablet form, is also now available as granules for mixing in water, the FDA said.
The agency first approved baloxavir marboxil in 2018 for the treatment of acute uncomplicated influenza in people aged 12 years or older who have been symptomatic for no more than 48 hours.
A year later, the FDA expanded the indication to include people at high risk of developing influenza-related complications, such as those with asthma, chronic lung disease, diabetes, heart disease, or morbid obesity, as well as adults aged 65 years or older.
The safety and efficacy of Xofluza for influenza postexposure prophylaxis is supported by a randomized, double-blind, controlled trial involving 607 people aged 12 years and older. After exposure to a person with influenza in their household, they received a single dose of Xofluza or placebo.
The primary endpoint was the proportion of individuals who became infected with influenza and presented with fever and at least one respiratory symptom from day 1 to day 10.
Of the 303 people who received Xofluza, 1% of individuals met these criteria, compared with 13% of those who received placebo.
The most common adverse effects of Xofluza include diarrhea, bronchitis, nausea, sinusitis, and headache.
Hypersensitivity, including anaphylaxis, can occur in patients taking Xofluza. The antiviral is contraindicated in people with a known hypersensitivity reaction to Xofluza.
Xofluza should not be coadministered with dairy products, calcium-fortified beverages, laxatives, antacids, or oral supplements containing calcium, iron, magnesium, selenium, aluminium, or zinc.
Full prescribing information is available online.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has expanded the indication for the antiviral baloxavir marboxil (Xofluza) to include postexposure prophylaxis of uncomplicated influenza in people aged 12 years and older.
“This expanded indication for Xofluza will provide an important option to help prevent influenza just in time for a flu season that is anticipated to be unlike any other because it will coincide with the coronavirus pandemic,” Debra Birnkrant, MD, director, Division of Antiviral Products, FDA Center for Drug Evaluation and Research, said in a press release.
In addition, Xofluza, which was previously available only in tablet form, is also now available as granules for mixing in water, the FDA said.
The agency first approved baloxavir marboxil in 2018 for the treatment of acute uncomplicated influenza in people aged 12 years or older who have been symptomatic for no more than 48 hours.
A year later, the FDA expanded the indication to include people at high risk of developing influenza-related complications, such as those with asthma, chronic lung disease, diabetes, heart disease, or morbid obesity, as well as adults aged 65 years or older.
The safety and efficacy of Xofluza for influenza postexposure prophylaxis is supported by a randomized, double-blind, controlled trial involving 607 people aged 12 years and older. After exposure to a person with influenza in their household, they received a single dose of Xofluza or placebo.
The primary endpoint was the proportion of individuals who became infected with influenza and presented with fever and at least one respiratory symptom from day 1 to day 10.
Of the 303 people who received Xofluza, 1% of individuals met these criteria, compared with 13% of those who received placebo.
The most common adverse effects of Xofluza include diarrhea, bronchitis, nausea, sinusitis, and headache.
Hypersensitivity, including anaphylaxis, can occur in patients taking Xofluza. The antiviral is contraindicated in people with a known hypersensitivity reaction to Xofluza.
Xofluza should not be coadministered with dairy products, calcium-fortified beverages, laxatives, antacids, or oral supplements containing calcium, iron, magnesium, selenium, aluminium, or zinc.
Full prescribing information is available online.
This article first appeared on Medscape.com.
50.6 million tobacco users are not a homogeneous group
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
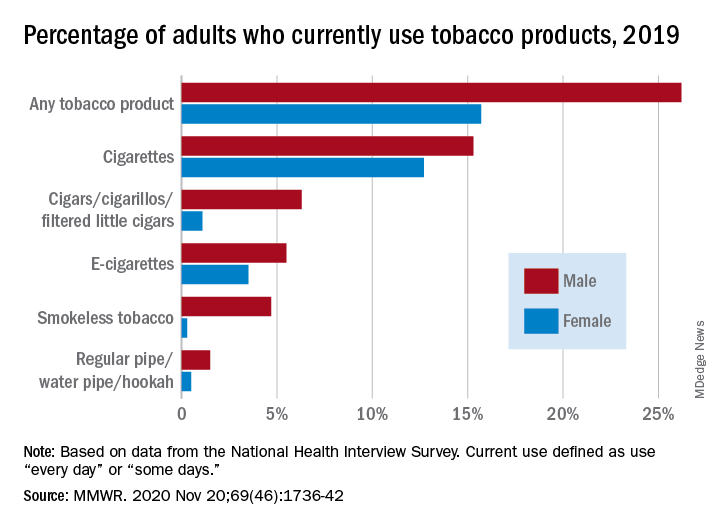
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
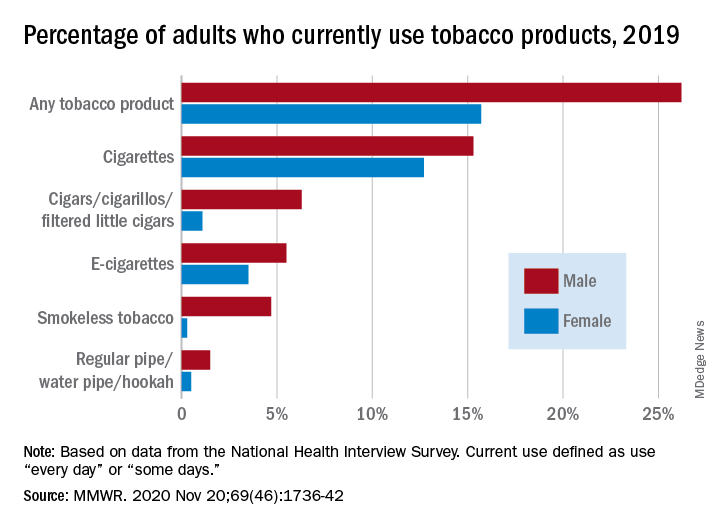
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
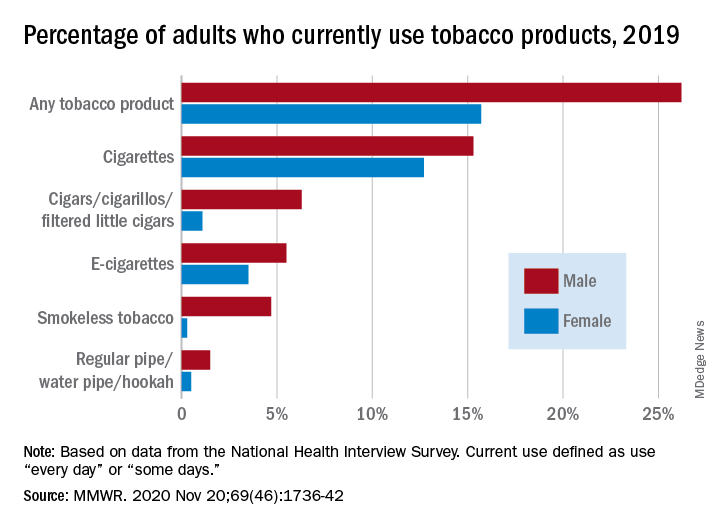
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
FROM MMWR
Liquid oxygen recommended for mobile patients with lung disease
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
Add delirium to checklist of COVID-19 symptoms in seniors
Delirium should be included on checklists of the presenting signs and symptoms of COVID-19, particularly in elderly adults, according to a multicenter study of seniors visiting emergency departments.
Overall, 28% of the 817 older adults who presented to the emergency department and were diagnosed with COVID-19 had delirium, according to a study published online November 19 in JAMA Network Open. Moreover, 16% of these patients had delirium that was not accompanied by typical symptoms or signs of SARS-CoV-2 infection.
Among patients with delirium, there was a greater probability of admission to the intensive care unit compared with patients who presented without delirium (adjusted relative risk [aRR], 1.67; 95% CI, 1.30 – 2.15), as well as a greater probability of death (aRR, 1.24; 95% CI, 1.00 – 1.55).
“These findings suggest the clinical importance of including delirium on checklists of presenting signs and symptoms of COVID-19 that guide screening, testing, and evaluation,” write Maura Kennedy, MD, MPH, and colleagues.
“I was absolutely seeing cases of delirium where there were no other symptoms of COVID-19, but we didn’t have lot of data on the frequency of this,” explained Kennedy, an emergency department physician at Massachusetts General Hospital and an assistant professor of emergency medicine at Harvard Medical School, Boston.
“And the rate was somewhat surprising compared with that seen in non-COVID studies of delirium, but then our study population was more at risk, coming from long-term care facilities and having prior stroke or dementia,” she said. The most common form of delirium was hypoactive sleepiness and nonresponsiveness, although hyperactivity and agitation were also seen.
Kennedy thinks the addition of delirium as a common presenting symptom to diagnostic checklists would prevent some cases from being missed and allow earlier identification and management of COVID-19 patients at high risk for poor outcomes. “We certainly don’t want to send them back undiagnosed to a long-term care facility or promote transmission within the hospital,” she told Medscape Medical News.
That step has already been implemented in some US centers. “Delirium is something we’ve been looking at since the early summer,” said geriatrician Angela Catic, MD, an assistant professor at Baylor College of Medicine’s Huffington Center on Aging and the Michael E. DeBakey VA Medical Center, Houston, Texas.
“If we see delirium, we’re looking for COVID-19,” said Catic, who was not involved in the study.
In Catic’s experience, it is “not at all atypical” to see patients whose only symptom of COVID-19 is delirium. As with other infections and diseases, “the aging brain is incredibly vulnerable,” she said.
According to William W. Hung, MD, MPH, an assistant professor of geriatrics and palliative medicine at the Icahn School of Medicine at Mount Sinai, New York City, delirium is “generally a common sign of something seriously wrong” in older adults. “In the case of COVID-19, low oxygenation caused by the infection may play a role,” he told Medscape Medical News. Although he agreed that delirium should be included in the differential diagnosis of COVID-19, how frequently it is the only symptom at presentation would need to be determined in a considerably larger population, he said.
Joining the company of those observing this COVID-19 manifestation is Christopher R. Carpenter, MD, a professor of emergency medicine at Washington University in St. Louis, St. Louis, Missouri. He was not a participant in the current study.
“I have absolutely seen and documented delirium as the presenting complaint in older adult patients who were ultimately diagnosed with SARS-CoV-2, and since March, I contemplate SARS-CoV-2 each time I identify delirium,” Carpenter told Medscape Medical News. “Honestly, I ― and most of my colleagues ― are considering SARS-CoV-2 for a range of symptoms and complaints these days, because of the odd presentations we’ve all encountered.”
Study details
For the study, Kennedy and colleagues enrolled consecutive adults aged 65 years and older who were diagnosed with active COVID-19 and who presented to emergency departments at seven centers in Massachusetts, Maine, Connecticut, Michigan, and North Carolina on or after March 13, 2020. Active infection with SARS-CoV-2 was determined on the basis of results of nasal swab polymerase chain reaction tests (99% of cases) or the appearance and distribution of ground-glass opacities on chest radiography or CT (1%).
Of the 817 patients enrolled, 386 (47%) were men, 493 (62%) were White, 215 (27%) were Black, and 54 (7%) were Hispanic or Latinx. The mean age of patients was 77.7 years (standard deviation, 8.2). Their age placed them at risk for chronic comorbidities and cognitive problems; indeed, 15% had at least four chronic conditions, and 30% had existing cognitive impairment.
The authors note that among the 226 patients (28%) who had delirium at presentation, 60 (27%) had experienced delirium for a duration of 2 to 7 days.
Additionally, of the 226 patients who exhibited delirium as a primary symptom, 84 (37%) showed no typical COVID-19 symptoms or signs, such as cough, fever, or shortness of breath.
The presence of delirium did not correlate with any of the typical COVID-19 symptoms in particular; Kennedy noted that only 56% of patients in the cohort had a fever at presentation.
Delirium at presentation was significantly associated with a median hospital stay of more than 8 days (aRR, 1.14; 95% CI, .97 – 1.35) and a greater risk for discharge to a rehabilitation facility (aRR, 1.55; 95% CI, 1.07 – 2.26). Factors associated with delirium included age older than 75 years, residence in a nursing home or assisted-living facility, previous use of psychoactive medications, vision impairment, hearing impairment, stroke, and Parkinson’s disease.
Kennedy noted that the rate of delirium observed in this study is much higher than that generally reported in emergency department studies conducted before the COVID-19 pandemic. In those studies, the delirium rate ranged from 7% to 20%. The associated risk factors, however, are comparable.
“Mounting evidence supports the high occurrence of delirium and other neuropsychiatric manifestations with COVID-19, with previously reported rates of 22% to 33% among hospitalized patients,” Kennedy and associates write.
In Carpenter’s opinion, the development of incident delirium while receiving care in the emergency department, as opposed to delirium at the time of presentation, has been exacerbated by the no-visitor policies mandated by the pandemic, which have prevented visits even from personal caregivers of patients with moderate to severe dementia. “Although healthcare systems need to be cognizant of the risk of spread to uninfected caregivers, there’s a risk-benefit balance that must be found, because having one caregiver at the bedside can prevent delirium in cognitively impaired patients,” said Carpenter, who was not involved in the current study.
Among the barriers to improving the situation, Carpenter cited the lack of routine delirium screening and the absence of high-quality evidence to support emergency department interventions to mitigate delirium.
“Layer those challenges on top of COVID-19’s rapidly evolving diagnostic landscape, frequent atypical presentations, and asymptomatic carriers across all age groups and the negative impact of delirium is magnified,” Carpenter said.
Once elderly patients are hospitalized, Kennedy recommends the nonpharmacologic guidelines of the Hospital Elder Life Program for reducing delirium risk. Recommendations include the providing of adequate sleep, hydration, and nutrition, as well as function restoration, precipitant avoidance, and reorientation.
The study was supported in part by the National Institute on Aging and the Massachusetts Medical School. The authors, Carpenter, Hung, and Catic have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Delirium should be included on checklists of the presenting signs and symptoms of COVID-19, particularly in elderly adults, according to a multicenter study of seniors visiting emergency departments.
Overall, 28% of the 817 older adults who presented to the emergency department and were diagnosed with COVID-19 had delirium, according to a study published online November 19 in JAMA Network Open. Moreover, 16% of these patients had delirium that was not accompanied by typical symptoms or signs of SARS-CoV-2 infection.
Among patients with delirium, there was a greater probability of admission to the intensive care unit compared with patients who presented without delirium (adjusted relative risk [aRR], 1.67; 95% CI, 1.30 – 2.15), as well as a greater probability of death (aRR, 1.24; 95% CI, 1.00 – 1.55).
“These findings suggest the clinical importance of including delirium on checklists of presenting signs and symptoms of COVID-19 that guide screening, testing, and evaluation,” write Maura Kennedy, MD, MPH, and colleagues.
“I was absolutely seeing cases of delirium where there were no other symptoms of COVID-19, but we didn’t have lot of data on the frequency of this,” explained Kennedy, an emergency department physician at Massachusetts General Hospital and an assistant professor of emergency medicine at Harvard Medical School, Boston.
“And the rate was somewhat surprising compared with that seen in non-COVID studies of delirium, but then our study population was more at risk, coming from long-term care facilities and having prior stroke or dementia,” she said. The most common form of delirium was hypoactive sleepiness and nonresponsiveness, although hyperactivity and agitation were also seen.
Kennedy thinks the addition of delirium as a common presenting symptom to diagnostic checklists would prevent some cases from being missed and allow earlier identification and management of COVID-19 patients at high risk for poor outcomes. “We certainly don’t want to send them back undiagnosed to a long-term care facility or promote transmission within the hospital,” she told Medscape Medical News.
That step has already been implemented in some US centers. “Delirium is something we’ve been looking at since the early summer,” said geriatrician Angela Catic, MD, an assistant professor at Baylor College of Medicine’s Huffington Center on Aging and the Michael E. DeBakey VA Medical Center, Houston, Texas.
“If we see delirium, we’re looking for COVID-19,” said Catic, who was not involved in the study.
In Catic’s experience, it is “not at all atypical” to see patients whose only symptom of COVID-19 is delirium. As with other infections and diseases, “the aging brain is incredibly vulnerable,” she said.
According to William W. Hung, MD, MPH, an assistant professor of geriatrics and palliative medicine at the Icahn School of Medicine at Mount Sinai, New York City, delirium is “generally a common sign of something seriously wrong” in older adults. “In the case of COVID-19, low oxygenation caused by the infection may play a role,” he told Medscape Medical News. Although he agreed that delirium should be included in the differential diagnosis of COVID-19, how frequently it is the only symptom at presentation would need to be determined in a considerably larger population, he said.
Joining the company of those observing this COVID-19 manifestation is Christopher R. Carpenter, MD, a professor of emergency medicine at Washington University in St. Louis, St. Louis, Missouri. He was not a participant in the current study.
“I have absolutely seen and documented delirium as the presenting complaint in older adult patients who were ultimately diagnosed with SARS-CoV-2, and since March, I contemplate SARS-CoV-2 each time I identify delirium,” Carpenter told Medscape Medical News. “Honestly, I ― and most of my colleagues ― are considering SARS-CoV-2 for a range of symptoms and complaints these days, because of the odd presentations we’ve all encountered.”
Study details
For the study, Kennedy and colleagues enrolled consecutive adults aged 65 years and older who were diagnosed with active COVID-19 and who presented to emergency departments at seven centers in Massachusetts, Maine, Connecticut, Michigan, and North Carolina on or after March 13, 2020. Active infection with SARS-CoV-2 was determined on the basis of results of nasal swab polymerase chain reaction tests (99% of cases) or the appearance and distribution of ground-glass opacities on chest radiography or CT (1%).
Of the 817 patients enrolled, 386 (47%) were men, 493 (62%) were White, 215 (27%) were Black, and 54 (7%) were Hispanic or Latinx. The mean age of patients was 77.7 years (standard deviation, 8.2). Their age placed them at risk for chronic comorbidities and cognitive problems; indeed, 15% had at least four chronic conditions, and 30% had existing cognitive impairment.
The authors note that among the 226 patients (28%) who had delirium at presentation, 60 (27%) had experienced delirium for a duration of 2 to 7 days.
Additionally, of the 226 patients who exhibited delirium as a primary symptom, 84 (37%) showed no typical COVID-19 symptoms or signs, such as cough, fever, or shortness of breath.
The presence of delirium did not correlate with any of the typical COVID-19 symptoms in particular; Kennedy noted that only 56% of patients in the cohort had a fever at presentation.
Delirium at presentation was significantly associated with a median hospital stay of more than 8 days (aRR, 1.14; 95% CI, .97 – 1.35) and a greater risk for discharge to a rehabilitation facility (aRR, 1.55; 95% CI, 1.07 – 2.26). Factors associated with delirium included age older than 75 years, residence in a nursing home or assisted-living facility, previous use of psychoactive medications, vision impairment, hearing impairment, stroke, and Parkinson’s disease.
Kennedy noted that the rate of delirium observed in this study is much higher than that generally reported in emergency department studies conducted before the COVID-19 pandemic. In those studies, the delirium rate ranged from 7% to 20%. The associated risk factors, however, are comparable.
“Mounting evidence supports the high occurrence of delirium and other neuropsychiatric manifestations with COVID-19, with previously reported rates of 22% to 33% among hospitalized patients,” Kennedy and associates write.
In Carpenter’s opinion, the development of incident delirium while receiving care in the emergency department, as opposed to delirium at the time of presentation, has been exacerbated by the no-visitor policies mandated by the pandemic, which have prevented visits even from personal caregivers of patients with moderate to severe dementia. “Although healthcare systems need to be cognizant of the risk of spread to uninfected caregivers, there’s a risk-benefit balance that must be found, because having one caregiver at the bedside can prevent delirium in cognitively impaired patients,” said Carpenter, who was not involved in the current study.
Among the barriers to improving the situation, Carpenter cited the lack of routine delirium screening and the absence of high-quality evidence to support emergency department interventions to mitigate delirium.
“Layer those challenges on top of COVID-19’s rapidly evolving diagnostic landscape, frequent atypical presentations, and asymptomatic carriers across all age groups and the negative impact of delirium is magnified,” Carpenter said.
Once elderly patients are hospitalized, Kennedy recommends the nonpharmacologic guidelines of the Hospital Elder Life Program for reducing delirium risk. Recommendations include the providing of adequate sleep, hydration, and nutrition, as well as function restoration, precipitant avoidance, and reorientation.
The study was supported in part by the National Institute on Aging and the Massachusetts Medical School. The authors, Carpenter, Hung, and Catic have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Delirium should be included on checklists of the presenting signs and symptoms of COVID-19, particularly in elderly adults, according to a multicenter study of seniors visiting emergency departments.
Overall, 28% of the 817 older adults who presented to the emergency department and were diagnosed with COVID-19 had delirium, according to a study published online November 19 in JAMA Network Open. Moreover, 16% of these patients had delirium that was not accompanied by typical symptoms or signs of SARS-CoV-2 infection.
Among patients with delirium, there was a greater probability of admission to the intensive care unit compared with patients who presented without delirium (adjusted relative risk [aRR], 1.67; 95% CI, 1.30 – 2.15), as well as a greater probability of death (aRR, 1.24; 95% CI, 1.00 – 1.55).
“These findings suggest the clinical importance of including delirium on checklists of presenting signs and symptoms of COVID-19 that guide screening, testing, and evaluation,” write Maura Kennedy, MD, MPH, and colleagues.
“I was absolutely seeing cases of delirium where there were no other symptoms of COVID-19, but we didn’t have lot of data on the frequency of this,” explained Kennedy, an emergency department physician at Massachusetts General Hospital and an assistant professor of emergency medicine at Harvard Medical School, Boston.
“And the rate was somewhat surprising compared with that seen in non-COVID studies of delirium, but then our study population was more at risk, coming from long-term care facilities and having prior stroke or dementia,” she said. The most common form of delirium was hypoactive sleepiness and nonresponsiveness, although hyperactivity and agitation were also seen.
Kennedy thinks the addition of delirium as a common presenting symptom to diagnostic checklists would prevent some cases from being missed and allow earlier identification and management of COVID-19 patients at high risk for poor outcomes. “We certainly don’t want to send them back undiagnosed to a long-term care facility or promote transmission within the hospital,” she told Medscape Medical News.
That step has already been implemented in some US centers. “Delirium is something we’ve been looking at since the early summer,” said geriatrician Angela Catic, MD, an assistant professor at Baylor College of Medicine’s Huffington Center on Aging and the Michael E. DeBakey VA Medical Center, Houston, Texas.
“If we see delirium, we’re looking for COVID-19,” said Catic, who was not involved in the study.
In Catic’s experience, it is “not at all atypical” to see patients whose only symptom of COVID-19 is delirium. As with other infections and diseases, “the aging brain is incredibly vulnerable,” she said.
According to William W. Hung, MD, MPH, an assistant professor of geriatrics and palliative medicine at the Icahn School of Medicine at Mount Sinai, New York City, delirium is “generally a common sign of something seriously wrong” in older adults. “In the case of COVID-19, low oxygenation caused by the infection may play a role,” he told Medscape Medical News. Although he agreed that delirium should be included in the differential diagnosis of COVID-19, how frequently it is the only symptom at presentation would need to be determined in a considerably larger population, he said.
Joining the company of those observing this COVID-19 manifestation is Christopher R. Carpenter, MD, a professor of emergency medicine at Washington University in St. Louis, St. Louis, Missouri. He was not a participant in the current study.
“I have absolutely seen and documented delirium as the presenting complaint in older adult patients who were ultimately diagnosed with SARS-CoV-2, and since March, I contemplate SARS-CoV-2 each time I identify delirium,” Carpenter told Medscape Medical News. “Honestly, I ― and most of my colleagues ― are considering SARS-CoV-2 for a range of symptoms and complaints these days, because of the odd presentations we’ve all encountered.”
Study details
For the study, Kennedy and colleagues enrolled consecutive adults aged 65 years and older who were diagnosed with active COVID-19 and who presented to emergency departments at seven centers in Massachusetts, Maine, Connecticut, Michigan, and North Carolina on or after March 13, 2020. Active infection with SARS-CoV-2 was determined on the basis of results of nasal swab polymerase chain reaction tests (99% of cases) or the appearance and distribution of ground-glass opacities on chest radiography or CT (1%).
Of the 817 patients enrolled, 386 (47%) were men, 493 (62%) were White, 215 (27%) were Black, and 54 (7%) were Hispanic or Latinx. The mean age of patients was 77.7 years (standard deviation, 8.2). Their age placed them at risk for chronic comorbidities and cognitive problems; indeed, 15% had at least four chronic conditions, and 30% had existing cognitive impairment.
The authors note that among the 226 patients (28%) who had delirium at presentation, 60 (27%) had experienced delirium for a duration of 2 to 7 days.
Additionally, of the 226 patients who exhibited delirium as a primary symptom, 84 (37%) showed no typical COVID-19 symptoms or signs, such as cough, fever, or shortness of breath.
The presence of delirium did not correlate with any of the typical COVID-19 symptoms in particular; Kennedy noted that only 56% of patients in the cohort had a fever at presentation.
Delirium at presentation was significantly associated with a median hospital stay of more than 8 days (aRR, 1.14; 95% CI, .97 – 1.35) and a greater risk for discharge to a rehabilitation facility (aRR, 1.55; 95% CI, 1.07 – 2.26). Factors associated with delirium included age older than 75 years, residence in a nursing home or assisted-living facility, previous use of psychoactive medications, vision impairment, hearing impairment, stroke, and Parkinson’s disease.
Kennedy noted that the rate of delirium observed in this study is much higher than that generally reported in emergency department studies conducted before the COVID-19 pandemic. In those studies, the delirium rate ranged from 7% to 20%. The associated risk factors, however, are comparable.
“Mounting evidence supports the high occurrence of delirium and other neuropsychiatric manifestations with COVID-19, with previously reported rates of 22% to 33% among hospitalized patients,” Kennedy and associates write.
In Carpenter’s opinion, the development of incident delirium while receiving care in the emergency department, as opposed to delirium at the time of presentation, has been exacerbated by the no-visitor policies mandated by the pandemic, which have prevented visits even from personal caregivers of patients with moderate to severe dementia. “Although healthcare systems need to be cognizant of the risk of spread to uninfected caregivers, there’s a risk-benefit balance that must be found, because having one caregiver at the bedside can prevent delirium in cognitively impaired patients,” said Carpenter, who was not involved in the current study.
Among the barriers to improving the situation, Carpenter cited the lack of routine delirium screening and the absence of high-quality evidence to support emergency department interventions to mitigate delirium.
“Layer those challenges on top of COVID-19’s rapidly evolving diagnostic landscape, frequent atypical presentations, and asymptomatic carriers across all age groups and the negative impact of delirium is magnified,” Carpenter said.
Once elderly patients are hospitalized, Kennedy recommends the nonpharmacologic guidelines of the Hospital Elder Life Program for reducing delirium risk. Recommendations include the providing of adequate sleep, hydration, and nutrition, as well as function restoration, precipitant avoidance, and reorientation.
The study was supported in part by the National Institute on Aging and the Massachusetts Medical School. The authors, Carpenter, Hung, and Catic have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
COVID-19 cases in children continue to set records
As far as the pandemic is concerned, it seems like a pretty small thing. A difference of just 0.3%. Children now represent 11.8% of all COVID-19 cases that have occurred since the beginning of the pandemic, compared with 11.5% 1 week ago, according to the American Academy of Pediatrics and the Children’s Hospital Association.

Hiding behind that 0.3%, however, is a much larger number: 144,145. That is the number of new child cases that occurred during the week that ended Nov. 19, and it’s the highest weekly figure yet, eclipsing the previous high of 111,946 from the week of Nov. 12, the AAP and the CHA said in their latest COVID-19 report. For the week ending Nov. 19, children represented 14.1% of all new cases, up from 14.0% the week before.
In the United States, more than 1.18 million children have been infected by the coronavirus since the beginning of the pandemic, with the total among all ages topping 10 million in 49 states (New York is not providing age distribution), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP/CHA data show. That works out to 11.8% of all cases.
The overall rate of child COVID-19 cases is now up to 1,573 per 100,000 children nationally, with considerable variation seen among the states. The lowest rates can be found in Vermont (344 per 100,000), Maine (452), and Hawaii (675), and the highest in North Dakota (5,589), South Dakota (3,993), and Wisconsin (3,727), the AAP and CHA said in the report.
Comparisons between states are somewhat problematic, though, because “each state makes different decisions about how to report the age distribution of COVID-19 cases, and as a result the age range for reported cases varies by state. … It is not possible to standardize more detailed age ranges for children based on what is publicly available from the states at this time,” the two organizations noted.
Five more COVID-19–related deaths in children were reported during the week of Nov. 19, bringing the count to 138 and holding at just 0.06% of the total for all ages, based on data from 43 states and New York City. Children’s share of hospitalizations increased slightly in the last week, rising from 1.7% to 1.8% in the 24 states (and NYC) that are reporting such data. The total number of child hospitalizations in those jurisdictions is just over 6,700, the AAP and CHA said.
As far as the pandemic is concerned, it seems like a pretty small thing. A difference of just 0.3%. Children now represent 11.8% of all COVID-19 cases that have occurred since the beginning of the pandemic, compared with 11.5% 1 week ago, according to the American Academy of Pediatrics and the Children’s Hospital Association.

Hiding behind that 0.3%, however, is a much larger number: 144,145. That is the number of new child cases that occurred during the week that ended Nov. 19, and it’s the highest weekly figure yet, eclipsing the previous high of 111,946 from the week of Nov. 12, the AAP and the CHA said in their latest COVID-19 report. For the week ending Nov. 19, children represented 14.1% of all new cases, up from 14.0% the week before.
In the United States, more than 1.18 million children have been infected by the coronavirus since the beginning of the pandemic, with the total among all ages topping 10 million in 49 states (New York is not providing age distribution), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP/CHA data show. That works out to 11.8% of all cases.
The overall rate of child COVID-19 cases is now up to 1,573 per 100,000 children nationally, with considerable variation seen among the states. The lowest rates can be found in Vermont (344 per 100,000), Maine (452), and Hawaii (675), and the highest in North Dakota (5,589), South Dakota (3,993), and Wisconsin (3,727), the AAP and CHA said in the report.
Comparisons between states are somewhat problematic, though, because “each state makes different decisions about how to report the age distribution of COVID-19 cases, and as a result the age range for reported cases varies by state. … It is not possible to standardize more detailed age ranges for children based on what is publicly available from the states at this time,” the two organizations noted.
Five more COVID-19–related deaths in children were reported during the week of Nov. 19, bringing the count to 138 and holding at just 0.06% of the total for all ages, based on data from 43 states and New York City. Children’s share of hospitalizations increased slightly in the last week, rising from 1.7% to 1.8% in the 24 states (and NYC) that are reporting such data. The total number of child hospitalizations in those jurisdictions is just over 6,700, the AAP and CHA said.
As far as the pandemic is concerned, it seems like a pretty small thing. A difference of just 0.3%. Children now represent 11.8% of all COVID-19 cases that have occurred since the beginning of the pandemic, compared with 11.5% 1 week ago, according to the American Academy of Pediatrics and the Children’s Hospital Association.

Hiding behind that 0.3%, however, is a much larger number: 144,145. That is the number of new child cases that occurred during the week that ended Nov. 19, and it’s the highest weekly figure yet, eclipsing the previous high of 111,946 from the week of Nov. 12, the AAP and the CHA said in their latest COVID-19 report. For the week ending Nov. 19, children represented 14.1% of all new cases, up from 14.0% the week before.
In the United States, more than 1.18 million children have been infected by the coronavirus since the beginning of the pandemic, with the total among all ages topping 10 million in 49 states (New York is not providing age distribution), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP/CHA data show. That works out to 11.8% of all cases.
The overall rate of child COVID-19 cases is now up to 1,573 per 100,000 children nationally, with considerable variation seen among the states. The lowest rates can be found in Vermont (344 per 100,000), Maine (452), and Hawaii (675), and the highest in North Dakota (5,589), South Dakota (3,993), and Wisconsin (3,727), the AAP and CHA said in the report.
Comparisons between states are somewhat problematic, though, because “each state makes different decisions about how to report the age distribution of COVID-19 cases, and as a result the age range for reported cases varies by state. … It is not possible to standardize more detailed age ranges for children based on what is publicly available from the states at this time,” the two organizations noted.
Five more COVID-19–related deaths in children were reported during the week of Nov. 19, bringing the count to 138 and holding at just 0.06% of the total for all ages, based on data from 43 states and New York City. Children’s share of hospitalizations increased slightly in the last week, rising from 1.7% to 1.8% in the 24 states (and NYC) that are reporting such data. The total number of child hospitalizations in those jurisdictions is just over 6,700, the AAP and CHA said.
Rationale for baricitinib’s use in COVID-19 patients demonstrated
It should not be surprising that the RA drug baricitinib (Olumiant), a Janus kinase (JAK) 1/2 inhibitor, might be beneficial in controlling the cytokine storm of hyperinflammation that can follow severe SARS-CoV-2 infections and lead to lung damage and acute respiratory distress syndrome – the leading cause of death from the virus.
But to demonstrate within a matter of months, at least preliminarily, that baricitinib reduces mortality and morbidity in hospitalized patients with COVID-19 pneumonia required a widely cross-disciplinary international team of researchers from 10 countries working at breakneck speed, said Justin Stebbing, PhD, the principal investigator of a new baricitinib study published Nov. 13 in Science Advances. “We went from modeling and mechanistic investigations to clinical tests in a number of settings and laboratory analysis in record time.”
The international team of 50 researchers included medical specialists in rheumatology, virology, geriatrics, oncology, and general medicine, along with experts in molecular and cellular biology, bioinformatics, statistics and trial design, computer modeling, pathology, genetics, and super-resolution microscopy, Dr. Stebbing, professor of cancer medicine and medical oncology at Imperial College, London, said in an interview.
Artificial intelligence, provided by the London-based firm BenevolentAI, was used to sift through a huge repository of structured medical information to identify drugs that might block the SARS-CoV-2 infection process. It predicted that baricitinib would be a promising candidate to inhibit inflammation and reduce viral load in COVID-19. Previous reports by Dr. Stebbing and colleagues (here and here) describe this AI-mediated testing, which was validated by the new study.
The researchers also used three-dimensional miniature human liver organoids in vitro and super-resolution microscopy to perform further lab investigations, which showed that baricitinib reversed expression of the SARS-CoV-2 receptor ACE2 triggered by type I interferons. Baricitinib inhibited the significant increase in ACE2 expression caused by interferon alpha-2, and thus cytokine-mediated inflammation, and also reduced infectivity, Dr. Stebbing said. “Our study of baricitinib shows that it has both antiviral and anticytokine effects and appears to be safe.”
71% mortality reduction
The team found a 71% reduction in mortality for a group of 83 hospitalized patients with COVID-19 pneumonia in Italy and Spain – early epicenters of the pandemic – who received baricitinib along with standard care, compared with propensity-matched groups that received only standard care. At that time, between mid-March and mid-April, standard COVID-19 care included antibiotics, glucocorticoids, hydroxychloroquine, low-molecular-weight heparin, and the antiretroviral combination lopinavir/ritonavir.
In the Spanish and Italian cohorts, baricitinib was generally well tolerated, although not without side effects, including bacterial infections and increases in liver enzyme levels, which may not have been related to baricitinib. Patients showed reductions in inflammation within days of starting treatment. “We did not observe thrombotic or vascular events in our cohorts, but most of the patients were receiving low molecular weight heparin,” he said.
The fact that baricitinib is approved by the Food and Drug Administration, is already well studied for safety, can be taken conveniently as a once-daily oral tablet, and is less expensive than many other antiviral treatments all make it an good target for further study, including randomized, controlled trials that are already underway, Dr. Stebbing noted. His study cohort also included elderly patients (median age, 81 years) who are the most likely to experience severe disease or death from COVID-19.
The National Library of Medicine’s clinicaltrials.gov registry of federally funded clinical studies lists 15 current research initiatives involving baricitinib and COVID-19. Dr. Stebbing suggested that data generated so far are helping to guide ongoing studies on dose and duration of treatment – in other words, who it works for, when to give it, and at what dose it should be taken and for how long.
Manufacturer Eli Lilly, which markets baricitinib in 2-mg or 4-mg tablets, announced in October that initial data are starting to emerge from 1,000-plus patients enrolled in ACTT-2 (the Adaptive COVID-19 Treatment Trial 2). ACTT-2 compared patients on the broad-spectrum intravenous antiviral drug remdesivir (Veklury) with those receiving remdesivir in combination with baricitinib. Based on ACTT-2 results that suggested a reduced time to recovery and improved clinical outcomes for the combination group, the FDA issued an emergency-use authorization on Nov. 19 for the combination of baricitinib and remdesivir for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized adults and pediatric patients aged 2 years or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Interrupting the cytokine outbreak
Baricitinib has the potential to reduce or interrupt the passage of SARS-CoV-2 into cells, and thus to inhibit the JAK1- and JAK2-mediated cytokine outbreak, researcher Heinz-Josef Lenz, MD, professor of medicine and preventive medicine at the University of Southern California’s Norris Comprehensive Cancer Center in Los Angeles, said in a comment. Baricitinib was also identified, using BenevolentAI’s proprietary, artificial intelligence-derived knowledge graph, as a numb-associated kinase inhibitor, with high affinity for AP2-associated protein kinase 1, an important endocytosis regulator.
Early clinical data suggest a potent biologic effect of baricitinib 2 mg or 4 mg daily on circulating interleukin-6 levels and other inflammatory markers, including C-reactive protein. Dr. Lenz said the evidence for advantageous action of baricitinib on viral endocytosis and excessive cytokine release constitutes the rationale for using it in combination with other antivirals such as remdesivir in patients with moderate to severe COVID-19 illness.
“Although baricitinib may display antiviral activity on its own, its anti-inflammatory effects could hypothetically delay viral clearance,” Dr. Lenz added. “The data from Stebbing et al. confirm the dual actions of baricitinib, demonstrating its ability to inhibit viral entry into primary human hepatocyte spheroids and the reduction in inflammatory markers in COVID-19 patients.”
Other JAK inhibitors were not advanced as promising candidates for the research team’s attention by its artificial intelligence search, Dr. Stebbing noted. “The history of the pandemic has taught us the importance of well-designed observational studies as well as randomized, controlled trials. When it comes to COVID, pyrite looks much like gold, as failed studies of four antivirals have shown.”
Although the current translational research study did not use a placebo group, it is an important next step toward future randomized, controlled trials. “What’s great about this study is its high degree of collaboration, done with real urgency,” he added. “It’s harder to produce a paper that crosses multiple boundaries, like this one does, than a single-focused piece of work. But we wanted to link all of these threads together.”
The study was supported by the Imperial Biomedical Research Centre and Experimental Cancer Medicine Centre, the National Institute for Health Research, and the U.K. National Health Service’s Accelerated Access Collaborative. Dr. Stebbing has served on scientific advisory boards for Eli Lilly and other companies. Dr. Lenz had no relevant disclosures to report.
SOURCE: Stebbing J et al. Sci Adv. 2020 Nov 13. doi: 10.1126/sciadv.abe4724.
It should not be surprising that the RA drug baricitinib (Olumiant), a Janus kinase (JAK) 1/2 inhibitor, might be beneficial in controlling the cytokine storm of hyperinflammation that can follow severe SARS-CoV-2 infections and lead to lung damage and acute respiratory distress syndrome – the leading cause of death from the virus.
But to demonstrate within a matter of months, at least preliminarily, that baricitinib reduces mortality and morbidity in hospitalized patients with COVID-19 pneumonia required a widely cross-disciplinary international team of researchers from 10 countries working at breakneck speed, said Justin Stebbing, PhD, the principal investigator of a new baricitinib study published Nov. 13 in Science Advances. “We went from modeling and mechanistic investigations to clinical tests in a number of settings and laboratory analysis in record time.”
The international team of 50 researchers included medical specialists in rheumatology, virology, geriatrics, oncology, and general medicine, along with experts in molecular and cellular biology, bioinformatics, statistics and trial design, computer modeling, pathology, genetics, and super-resolution microscopy, Dr. Stebbing, professor of cancer medicine and medical oncology at Imperial College, London, said in an interview.
Artificial intelligence, provided by the London-based firm BenevolentAI, was used to sift through a huge repository of structured medical information to identify drugs that might block the SARS-CoV-2 infection process. It predicted that baricitinib would be a promising candidate to inhibit inflammation and reduce viral load in COVID-19. Previous reports by Dr. Stebbing and colleagues (here and here) describe this AI-mediated testing, which was validated by the new study.
The researchers also used three-dimensional miniature human liver organoids in vitro and super-resolution microscopy to perform further lab investigations, which showed that baricitinib reversed expression of the SARS-CoV-2 receptor ACE2 triggered by type I interferons. Baricitinib inhibited the significant increase in ACE2 expression caused by interferon alpha-2, and thus cytokine-mediated inflammation, and also reduced infectivity, Dr. Stebbing said. “Our study of baricitinib shows that it has both antiviral and anticytokine effects and appears to be safe.”
71% mortality reduction
The team found a 71% reduction in mortality for a group of 83 hospitalized patients with COVID-19 pneumonia in Italy and Spain – early epicenters of the pandemic – who received baricitinib along with standard care, compared with propensity-matched groups that received only standard care. At that time, between mid-March and mid-April, standard COVID-19 care included antibiotics, glucocorticoids, hydroxychloroquine, low-molecular-weight heparin, and the antiretroviral combination lopinavir/ritonavir.
In the Spanish and Italian cohorts, baricitinib was generally well tolerated, although not without side effects, including bacterial infections and increases in liver enzyme levels, which may not have been related to baricitinib. Patients showed reductions in inflammation within days of starting treatment. “We did not observe thrombotic or vascular events in our cohorts, but most of the patients were receiving low molecular weight heparin,” he said.
The fact that baricitinib is approved by the Food and Drug Administration, is already well studied for safety, can be taken conveniently as a once-daily oral tablet, and is less expensive than many other antiviral treatments all make it an good target for further study, including randomized, controlled trials that are already underway, Dr. Stebbing noted. His study cohort also included elderly patients (median age, 81 years) who are the most likely to experience severe disease or death from COVID-19.
The National Library of Medicine’s clinicaltrials.gov registry of federally funded clinical studies lists 15 current research initiatives involving baricitinib and COVID-19. Dr. Stebbing suggested that data generated so far are helping to guide ongoing studies on dose and duration of treatment – in other words, who it works for, when to give it, and at what dose it should be taken and for how long.
Manufacturer Eli Lilly, which markets baricitinib in 2-mg or 4-mg tablets, announced in October that initial data are starting to emerge from 1,000-plus patients enrolled in ACTT-2 (the Adaptive COVID-19 Treatment Trial 2). ACTT-2 compared patients on the broad-spectrum intravenous antiviral drug remdesivir (Veklury) with those receiving remdesivir in combination with baricitinib. Based on ACTT-2 results that suggested a reduced time to recovery and improved clinical outcomes for the combination group, the FDA issued an emergency-use authorization on Nov. 19 for the combination of baricitinib and remdesivir for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized adults and pediatric patients aged 2 years or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Interrupting the cytokine outbreak
Baricitinib has the potential to reduce or interrupt the passage of SARS-CoV-2 into cells, and thus to inhibit the JAK1- and JAK2-mediated cytokine outbreak, researcher Heinz-Josef Lenz, MD, professor of medicine and preventive medicine at the University of Southern California’s Norris Comprehensive Cancer Center in Los Angeles, said in a comment. Baricitinib was also identified, using BenevolentAI’s proprietary, artificial intelligence-derived knowledge graph, as a numb-associated kinase inhibitor, with high affinity for AP2-associated protein kinase 1, an important endocytosis regulator.
Early clinical data suggest a potent biologic effect of baricitinib 2 mg or 4 mg daily on circulating interleukin-6 levels and other inflammatory markers, including C-reactive protein. Dr. Lenz said the evidence for advantageous action of baricitinib on viral endocytosis and excessive cytokine release constitutes the rationale for using it in combination with other antivirals such as remdesivir in patients with moderate to severe COVID-19 illness.
“Although baricitinib may display antiviral activity on its own, its anti-inflammatory effects could hypothetically delay viral clearance,” Dr. Lenz added. “The data from Stebbing et al. confirm the dual actions of baricitinib, demonstrating its ability to inhibit viral entry into primary human hepatocyte spheroids and the reduction in inflammatory markers in COVID-19 patients.”
Other JAK inhibitors were not advanced as promising candidates for the research team’s attention by its artificial intelligence search, Dr. Stebbing noted. “The history of the pandemic has taught us the importance of well-designed observational studies as well as randomized, controlled trials. When it comes to COVID, pyrite looks much like gold, as failed studies of four antivirals have shown.”
Although the current translational research study did not use a placebo group, it is an important next step toward future randomized, controlled trials. “What’s great about this study is its high degree of collaboration, done with real urgency,” he added. “It’s harder to produce a paper that crosses multiple boundaries, like this one does, than a single-focused piece of work. But we wanted to link all of these threads together.”
The study was supported by the Imperial Biomedical Research Centre and Experimental Cancer Medicine Centre, the National Institute for Health Research, and the U.K. National Health Service’s Accelerated Access Collaborative. Dr. Stebbing has served on scientific advisory boards for Eli Lilly and other companies. Dr. Lenz had no relevant disclosures to report.
SOURCE: Stebbing J et al. Sci Adv. 2020 Nov 13. doi: 10.1126/sciadv.abe4724.
It should not be surprising that the RA drug baricitinib (Olumiant), a Janus kinase (JAK) 1/2 inhibitor, might be beneficial in controlling the cytokine storm of hyperinflammation that can follow severe SARS-CoV-2 infections and lead to lung damage and acute respiratory distress syndrome – the leading cause of death from the virus.
But to demonstrate within a matter of months, at least preliminarily, that baricitinib reduces mortality and morbidity in hospitalized patients with COVID-19 pneumonia required a widely cross-disciplinary international team of researchers from 10 countries working at breakneck speed, said Justin Stebbing, PhD, the principal investigator of a new baricitinib study published Nov. 13 in Science Advances. “We went from modeling and mechanistic investigations to clinical tests in a number of settings and laboratory analysis in record time.”
The international team of 50 researchers included medical specialists in rheumatology, virology, geriatrics, oncology, and general medicine, along with experts in molecular and cellular biology, bioinformatics, statistics and trial design, computer modeling, pathology, genetics, and super-resolution microscopy, Dr. Stebbing, professor of cancer medicine and medical oncology at Imperial College, London, said in an interview.
Artificial intelligence, provided by the London-based firm BenevolentAI, was used to sift through a huge repository of structured medical information to identify drugs that might block the SARS-CoV-2 infection process. It predicted that baricitinib would be a promising candidate to inhibit inflammation and reduce viral load in COVID-19. Previous reports by Dr. Stebbing and colleagues (here and here) describe this AI-mediated testing, which was validated by the new study.
The researchers also used three-dimensional miniature human liver organoids in vitro and super-resolution microscopy to perform further lab investigations, which showed that baricitinib reversed expression of the SARS-CoV-2 receptor ACE2 triggered by type I interferons. Baricitinib inhibited the significant increase in ACE2 expression caused by interferon alpha-2, and thus cytokine-mediated inflammation, and also reduced infectivity, Dr. Stebbing said. “Our study of baricitinib shows that it has both antiviral and anticytokine effects and appears to be safe.”
71% mortality reduction
The team found a 71% reduction in mortality for a group of 83 hospitalized patients with COVID-19 pneumonia in Italy and Spain – early epicenters of the pandemic – who received baricitinib along with standard care, compared with propensity-matched groups that received only standard care. At that time, between mid-March and mid-April, standard COVID-19 care included antibiotics, glucocorticoids, hydroxychloroquine, low-molecular-weight heparin, and the antiretroviral combination lopinavir/ritonavir.
In the Spanish and Italian cohorts, baricitinib was generally well tolerated, although not without side effects, including bacterial infections and increases in liver enzyme levels, which may not have been related to baricitinib. Patients showed reductions in inflammation within days of starting treatment. “We did not observe thrombotic or vascular events in our cohorts, but most of the patients were receiving low molecular weight heparin,” he said.
The fact that baricitinib is approved by the Food and Drug Administration, is already well studied for safety, can be taken conveniently as a once-daily oral tablet, and is less expensive than many other antiviral treatments all make it an good target for further study, including randomized, controlled trials that are already underway, Dr. Stebbing noted. His study cohort also included elderly patients (median age, 81 years) who are the most likely to experience severe disease or death from COVID-19.
The National Library of Medicine’s clinicaltrials.gov registry of federally funded clinical studies lists 15 current research initiatives involving baricitinib and COVID-19. Dr. Stebbing suggested that data generated so far are helping to guide ongoing studies on dose and duration of treatment – in other words, who it works for, when to give it, and at what dose it should be taken and for how long.
Manufacturer Eli Lilly, which markets baricitinib in 2-mg or 4-mg tablets, announced in October that initial data are starting to emerge from 1,000-plus patients enrolled in ACTT-2 (the Adaptive COVID-19 Treatment Trial 2). ACTT-2 compared patients on the broad-spectrum intravenous antiviral drug remdesivir (Veklury) with those receiving remdesivir in combination with baricitinib. Based on ACTT-2 results that suggested a reduced time to recovery and improved clinical outcomes for the combination group, the FDA issued an emergency-use authorization on Nov. 19 for the combination of baricitinib and remdesivir for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized adults and pediatric patients aged 2 years or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Interrupting the cytokine outbreak
Baricitinib has the potential to reduce or interrupt the passage of SARS-CoV-2 into cells, and thus to inhibit the JAK1- and JAK2-mediated cytokine outbreak, researcher Heinz-Josef Lenz, MD, professor of medicine and preventive medicine at the University of Southern California’s Norris Comprehensive Cancer Center in Los Angeles, said in a comment. Baricitinib was also identified, using BenevolentAI’s proprietary, artificial intelligence-derived knowledge graph, as a numb-associated kinase inhibitor, with high affinity for AP2-associated protein kinase 1, an important endocytosis regulator.
Early clinical data suggest a potent biologic effect of baricitinib 2 mg or 4 mg daily on circulating interleukin-6 levels and other inflammatory markers, including C-reactive protein. Dr. Lenz said the evidence for advantageous action of baricitinib on viral endocytosis and excessive cytokine release constitutes the rationale for using it in combination with other antivirals such as remdesivir in patients with moderate to severe COVID-19 illness.
“Although baricitinib may display antiviral activity on its own, its anti-inflammatory effects could hypothetically delay viral clearance,” Dr. Lenz added. “The data from Stebbing et al. confirm the dual actions of baricitinib, demonstrating its ability to inhibit viral entry into primary human hepatocyte spheroids and the reduction in inflammatory markers in COVID-19 patients.”
Other JAK inhibitors were not advanced as promising candidates for the research team’s attention by its artificial intelligence search, Dr. Stebbing noted. “The history of the pandemic has taught us the importance of well-designed observational studies as well as randomized, controlled trials. When it comes to COVID, pyrite looks much like gold, as failed studies of four antivirals have shown.”
Although the current translational research study did not use a placebo group, it is an important next step toward future randomized, controlled trials. “What’s great about this study is its high degree of collaboration, done with real urgency,” he added. “It’s harder to produce a paper that crosses multiple boundaries, like this one does, than a single-focused piece of work. But we wanted to link all of these threads together.”
The study was supported by the Imperial Biomedical Research Centre and Experimental Cancer Medicine Centre, the National Institute for Health Research, and the U.K. National Health Service’s Accelerated Access Collaborative. Dr. Stebbing has served on scientific advisory boards for Eli Lilly and other companies. Dr. Lenz had no relevant disclosures to report.
SOURCE: Stebbing J et al. Sci Adv. 2020 Nov 13. doi: 10.1126/sciadv.abe4724.
FROM SCIENCE ADVANCES
IDSA updates COVID guidelines for antibodies, antivirals, other drugs
An infectious disease expert panel cautions against routine use of bamlanivimab (Eli Lilly) and notes that remdesivir (Veklury) can shorten the clinical course of COVID-19 – which could be critical “as hospitals fill up” across the United States.
The group also said the monoclonal antibodies approved for emergency use by the Food and Drug Administration and still in development hold promise, although more clinical trial data are needed.
These and other recommendations appear in updated guidelines from the Infectious Diseases Society of America, released Nov. 18 and Nov. 22.
A conditional ‘no’ on routine bamlanivimab
“The guideline panel gave a conditional recommendation against the routine use of bamlanivimab,” Adarsh Bhimraj, MD, cochair of the IDSA COVID-19 Treatment and Management Guidelines Expert Panel, said.
On Nov. 10, the FDA issued an emergency-use authorization (EUA) for bamlanivimab for use in ambulatory patients with mild to moderate COVID-19.
“We did have a remark that it may be used in patients who have increased risk of severe COVID-19, as it is outlined in the FDA emergency-use authorization issued last week,” he said. He added that use should follow an informed discussion between provider and patient, one in which “the patient puts a very high value on the uncertain benefits and a low value on uncertain adverse events.”
The panel’s rationale was based in part on interim analysis of the phase 2 BLAZE-1 trial, which found 1.6% of people randomly assigned to bamlanivimab had an emergency department visit or hospitalization compared with 6.3% of those receiving a placebo.
“We thought the estimate was too fragile because the number in each arm was very low. Even a small change in these numbers could make the difference nonsignificant,” said Bhimraj, head of the neurologic infectious diseases section in the department of infectious diseases at the Cleveland (Ohio) Clinic.
Awaiting more data on antibody combination
On November 21, the FDA granted an EUA to the casirivimab and imbdevimab monoclonal antibody combination (Regeneron), indicated to treated mild to moderate COVID-19.
“Surprisingly, the preliminary results released in the EUA look a lot like bamlanivimab,” Dr. Bhimraj said.
Unlike bamlanivimab, for which trial details were published, the panel does not yet have the totality of data on casirivimab and imbdevimab, and therefore is not yet making a recommendation. “We want to be cautious as a guideline panel. We are anxiously awaiting the full publication,” he added.
“I do think these monoclonal antibodies show potential for benefit, but as Dr. Bhimraj said, it’s very difficult with the relatively small numbers we’re talking about,” said Rajesh T. Gandhi, MD, cochair of the IDSA COVID-19 Treatment and Management Guidelines Expert Panel.
Remaining questions include the degree of efficacy these antibody therapies will have, as well as which patients are most likely to benefit, added Dr. Gandhi, who is also a professor of medicine at Harvard Medical School and director of HIV Clinical Services and Education at Massachusetts General Hospital, both in Boston.
Furthermore, although there appear to be adequate supplies of remdesivir and dexamethasone, for example, availability and distribution of monoclonal antibodies could present logistic challenges. Prioritizing which high-risk patients receive this therapy and ensuring equity and access to communities most affected by COVID-19, including minority and low socioeconomic populations, need to be addressed, Dr. Gandhi said.
Remdesivir recommended to shorten hospital stays
The panel’s recommendations regarding the use of remdesivir “has largely remained the same,” Dr. Gandhi said. Evidence indicates recovery is faster with remdesivir at 10 days vs 15 days in people taking a placebo.
In the ACTT-1 trial, for example, participants in the treatment group recovered in a median 10 days versus 15 days in the placebo group.
Therefore, the IDSA panel continues to recommend remdesivir treatment for hospitalized patients with COVID-19.
“As hospitals around the United States fill up, the IDSA panel believes the effect of remdesivir on speeding up recovery could be an important benefit, and that is why we continue to suggest its use,” Dr. Gandhi said.
When asked about the World Health Organization–sponsored trial that showed no benefit in terms of mortality, he replied, “Remdesivir is not a home run – we need better drugs.”
A recommendation against lopinavir and ritonavir
In contrast, the panel recommends against use of the lopinavir/ritonavir protease inhibitor combination therapy, based in part on data from a preprint of the Solidarity study.
The open-label Solidarity trial in 30 countries, sponsored by WHO, assessed hydroxychloroquine, interferon, lopinavir/ritonavir, and remdesivir in people hospitalized with COVID-19.
None of these drugs showed an effect on mortality, Dr. Gandhi said. “Better medicines that improve survival are clearly needed.”
Dexamethasone remains the only agent demonstrated to reduce mortality in people hospitalized with COVID-19, he added.
Tocilizumab not for routine use
After critical review of the studies that have emerged since the last IDSA recommendation regarding tocilizumab (Actemra) in September, “the panel still stood with the recommendation against routine use of tocilizumab in hospitalized patients with COVID-19,” Dr. Bhimraj said.
The guidance is based on trials including COVACTA and EMPACTA. Treatment with tocilizumab was not associated with significant differences in mortality. In these and other studies, “we did not really find a significant difference, and that was the reason for the conditional recommendation against routine use of tocilizumab in hospitalized patients,” Dr. Bhimraj said.
Also, although the trials were blinded, “we know treatment with tocilizumab can cause a reduction in C-reactive protein levels,” which could indicate to researchers which participants were receiving active treatment versus placebo, he said.
Jury still out on baricitinib, remdesivir combination
The FDA granted an EUA to the combination of remdesivir and baricitinib (Olumiant) on Nov. 19. However, the IDSA panel is reserving its recommendation on this therapeutic combination until more data emerge.
“We still don’t have complete results of the ACTT-2 study, and the information we do have is what is available in the EUA,” Dr. Bhimraj said. The panel expects to issue guidance once the totality of data become available.
Unanswered questions include why investigators chose a 4-mg dose of baricitinib – twice the 2-mg dose commonly used for treating rheumatoid arthritis – and how many patients in the trial also were treated with steroids.
Dr. Gandhi agreed that the proportion of patients taking a steroid is “really an important consideration.” He added that dexamethasone has become standard of care because it reduces mortality, as well as the number of people requiring oxygen. He said it will be important to know how the baricitinib/remdesivir combination compares with dexamethasone.
“You don’t want to give a drug with less certain benefit over a drug for which there is more certain benefit,” Dr. Gandhi said.
Future possibilities
“The monoclonal antibodies are important to continue studying, particularly in combinations,” Dr. Gandhi said. Researchers are investigating formulations other than IV infusion to make therapy more convenient. For example, a subcutaneous injection like insulin would make administration at home more of a possibility.
Investigators are also looking at oral antiviral therapy, inhaled antivirals, and the promise of using interferon therapy. Dr. Gandhi added there is also “a lot of work around medications to reduce the excess inflammation that drives very severe COVID-19.”
‘Exciting news’ on AstraZeneca vaccine
Although not part of the IDSA guidelines, “we saw the news from AstraZeneca this morning, which is exciting,” Dr. Gandhi said during a media briefing.
Unlike the Pfizer and Moderna messenger RNA vaccines, which use the genetic material of the virus to make the virus proteins that elicit an immune response, the AstraZeneca/Oxford University vaccine uses a viral vector to carry the SARS-CoV-2 protein, to which the body produces an immune response.
“I’m thrilled that several different vaccines are showing important effects at rates higher than the FDA benchmark of 50%, and these are well exceeding that,” Dr. Gandhi said.
“One interesting thing from the [AstraZeneca] press release is they show asymptomatic infection being reduced,” he added. “That is critical because we know a lot of transmission of SARS-CoV-2 comes from asymptomatic people.”
Reasons for optimism
In response to a question about whether the experts feel more optimistic about COVID-19, Dr. Bhimraj said he is cautiously optimistic. “We have made tremendous progress in therapeutic agents, and in how the world has come together in the middle of a catastrophe to collaborate, setting our differences apart, to do trials. That is commendable.”
Dr. Gandhi said he felt more optimistic than he did in the spring. He pointed out that physicians and researchers know a lot more about potential blood clotting complications, how to support patients through severe COVID-19 and keep them off a ventilator whenever possible, and how to provide dexamethasone to reduce the risk of death.
Those benefits are in hospitalized patients, however, and “we need ways to prevent people from getting into the hospital, and that is why we are looking at the monoclonal antibodies,” Dr. Gandhi said. “If borne out in larger trials, that will be a major advance.”
“We need to keep our focus on prevention and go back to our idea of flattening the curve. That is critical so our health care systems do not get overwhelmed during this massive surge we are in,” Dr. Gandhi said. “So masking and social distancing are just as important as they always have been.”
Dr. Bhimraj disclosed no relevant financial relationships. Dr. Gandhi has no disclosures for the past 12 months; in the past 3 years, he has served on scientific advisory boards for Gilead and Merck.
This article first appeared on Medscape.com.
An infectious disease expert panel cautions against routine use of bamlanivimab (Eli Lilly) and notes that remdesivir (Veklury) can shorten the clinical course of COVID-19 – which could be critical “as hospitals fill up” across the United States.
The group also said the monoclonal antibodies approved for emergency use by the Food and Drug Administration and still in development hold promise, although more clinical trial data are needed.
These and other recommendations appear in updated guidelines from the Infectious Diseases Society of America, released Nov. 18 and Nov. 22.
A conditional ‘no’ on routine bamlanivimab
“The guideline panel gave a conditional recommendation against the routine use of bamlanivimab,” Adarsh Bhimraj, MD, cochair of the IDSA COVID-19 Treatment and Management Guidelines Expert Panel, said.
On Nov. 10, the FDA issued an emergency-use authorization (EUA) for bamlanivimab for use in ambulatory patients with mild to moderate COVID-19.
“We did have a remark that it may be used in patients who have increased risk of severe COVID-19, as it is outlined in the FDA emergency-use authorization issued last week,” he said. He added that use should follow an informed discussion between provider and patient, one in which “the patient puts a very high value on the uncertain benefits and a low value on uncertain adverse events.”
The panel’s rationale was based in part on interim analysis of the phase 2 BLAZE-1 trial, which found 1.6% of people randomly assigned to bamlanivimab had an emergency department visit or hospitalization compared with 6.3% of those receiving a placebo.
“We thought the estimate was too fragile because the number in each arm was very low. Even a small change in these numbers could make the difference nonsignificant,” said Bhimraj, head of the neurologic infectious diseases section in the department of infectious diseases at the Cleveland (Ohio) Clinic.
Awaiting more data on antibody combination
On November 21, the FDA granted an EUA to the casirivimab and imbdevimab monoclonal antibody combination (Regeneron), indicated to treated mild to moderate COVID-19.
“Surprisingly, the preliminary results released in the EUA look a lot like bamlanivimab,” Dr. Bhimraj said.
Unlike bamlanivimab, for which trial details were published, the panel does not yet have the totality of data on casirivimab and imbdevimab, and therefore is not yet making a recommendation. “We want to be cautious as a guideline panel. We are anxiously awaiting the full publication,” he added.
“I do think these monoclonal antibodies show potential for benefit, but as Dr. Bhimraj said, it’s very difficult with the relatively small numbers we’re talking about,” said Rajesh T. Gandhi, MD, cochair of the IDSA COVID-19 Treatment and Management Guidelines Expert Panel.
Remaining questions include the degree of efficacy these antibody therapies will have, as well as which patients are most likely to benefit, added Dr. Gandhi, who is also a professor of medicine at Harvard Medical School and director of HIV Clinical Services and Education at Massachusetts General Hospital, both in Boston.
Furthermore, although there appear to be adequate supplies of remdesivir and dexamethasone, for example, availability and distribution of monoclonal antibodies could present logistic challenges. Prioritizing which high-risk patients receive this therapy and ensuring equity and access to communities most affected by COVID-19, including minority and low socioeconomic populations, need to be addressed, Dr. Gandhi said.
Remdesivir recommended to shorten hospital stays
The panel’s recommendations regarding the use of remdesivir “has largely remained the same,” Dr. Gandhi said. Evidence indicates recovery is faster with remdesivir at 10 days vs 15 days in people taking a placebo.
In the ACTT-1 trial, for example, participants in the treatment group recovered in a median 10 days versus 15 days in the placebo group.
Therefore, the IDSA panel continues to recommend remdesivir treatment for hospitalized patients with COVID-19.
“As hospitals around the United States fill up, the IDSA panel believes the effect of remdesivir on speeding up recovery could be an important benefit, and that is why we continue to suggest its use,” Dr. Gandhi said.
When asked about the World Health Organization–sponsored trial that showed no benefit in terms of mortality, he replied, “Remdesivir is not a home run – we need better drugs.”
A recommendation against lopinavir and ritonavir
In contrast, the panel recommends against use of the lopinavir/ritonavir protease inhibitor combination therapy, based in part on data from a preprint of the Solidarity study.
The open-label Solidarity trial in 30 countries, sponsored by WHO, assessed hydroxychloroquine, interferon, lopinavir/ritonavir, and remdesivir in people hospitalized with COVID-19.
None of these drugs showed an effect on mortality, Dr. Gandhi said. “Better medicines that improve survival are clearly needed.”
Dexamethasone remains the only agent demonstrated to reduce mortality in people hospitalized with COVID-19, he added.
Tocilizumab not for routine use
After critical review of the studies that have emerged since the last IDSA recommendation regarding tocilizumab (Actemra) in September, “the panel still stood with the recommendation against routine use of tocilizumab in hospitalized patients with COVID-19,” Dr. Bhimraj said.
The guidance is based on trials including COVACTA and EMPACTA. Treatment with tocilizumab was not associated with significant differences in mortality. In these and other studies, “we did not really find a significant difference, and that was the reason for the conditional recommendation against routine use of tocilizumab in hospitalized patients,” Dr. Bhimraj said.
Also, although the trials were blinded, “we know treatment with tocilizumab can cause a reduction in C-reactive protein levels,” which could indicate to researchers which participants were receiving active treatment versus placebo, he said.
Jury still out on baricitinib, remdesivir combination
The FDA granted an EUA to the combination of remdesivir and baricitinib (Olumiant) on Nov. 19. However, the IDSA panel is reserving its recommendation on this therapeutic combination until more data emerge.
“We still don’t have complete results of the ACTT-2 study, and the information we do have is what is available in the EUA,” Dr. Bhimraj said. The panel expects to issue guidance once the totality of data become available.
Unanswered questions include why investigators chose a 4-mg dose of baricitinib – twice the 2-mg dose commonly used for treating rheumatoid arthritis – and how many patients in the trial also were treated with steroids.
Dr. Gandhi agreed that the proportion of patients taking a steroid is “really an important consideration.” He added that dexamethasone has become standard of care because it reduces mortality, as well as the number of people requiring oxygen. He said it will be important to know how the baricitinib/remdesivir combination compares with dexamethasone.
“You don’t want to give a drug with less certain benefit over a drug for which there is more certain benefit,” Dr. Gandhi said.
Future possibilities
“The monoclonal antibodies are important to continue studying, particularly in combinations,” Dr. Gandhi said. Researchers are investigating formulations other than IV infusion to make therapy more convenient. For example, a subcutaneous injection like insulin would make administration at home more of a possibility.
Investigators are also looking at oral antiviral therapy, inhaled antivirals, and the promise of using interferon therapy. Dr. Gandhi added there is also “a lot of work around medications to reduce the excess inflammation that drives very severe COVID-19.”
‘Exciting news’ on AstraZeneca vaccine
Although not part of the IDSA guidelines, “we saw the news from AstraZeneca this morning, which is exciting,” Dr. Gandhi said during a media briefing.
Unlike the Pfizer and Moderna messenger RNA vaccines, which use the genetic material of the virus to make the virus proteins that elicit an immune response, the AstraZeneca/Oxford University vaccine uses a viral vector to carry the SARS-CoV-2 protein, to which the body produces an immune response.
“I’m thrilled that several different vaccines are showing important effects at rates higher than the FDA benchmark of 50%, and these are well exceeding that,” Dr. Gandhi said.
“One interesting thing from the [AstraZeneca] press release is they show asymptomatic infection being reduced,” he added. “That is critical because we know a lot of transmission of SARS-CoV-2 comes from asymptomatic people.”
Reasons for optimism
In response to a question about whether the experts feel more optimistic about COVID-19, Dr. Bhimraj said he is cautiously optimistic. “We have made tremendous progress in therapeutic agents, and in how the world has come together in the middle of a catastrophe to collaborate, setting our differences apart, to do trials. That is commendable.”
Dr. Gandhi said he felt more optimistic than he did in the spring. He pointed out that physicians and researchers know a lot more about potential blood clotting complications, how to support patients through severe COVID-19 and keep them off a ventilator whenever possible, and how to provide dexamethasone to reduce the risk of death.
Those benefits are in hospitalized patients, however, and “we need ways to prevent people from getting into the hospital, and that is why we are looking at the monoclonal antibodies,” Dr. Gandhi said. “If borne out in larger trials, that will be a major advance.”
“We need to keep our focus on prevention and go back to our idea of flattening the curve. That is critical so our health care systems do not get overwhelmed during this massive surge we are in,” Dr. Gandhi said. “So masking and social distancing are just as important as they always have been.”
Dr. Bhimraj disclosed no relevant financial relationships. Dr. Gandhi has no disclosures for the past 12 months; in the past 3 years, he has served on scientific advisory boards for Gilead and Merck.
This article first appeared on Medscape.com.
An infectious disease expert panel cautions against routine use of bamlanivimab (Eli Lilly) and notes that remdesivir (Veklury) can shorten the clinical course of COVID-19 – which could be critical “as hospitals fill up” across the United States.
The group also said the monoclonal antibodies approved for emergency use by the Food and Drug Administration and still in development hold promise, although more clinical trial data are needed.
These and other recommendations appear in updated guidelines from the Infectious Diseases Society of America, released Nov. 18 and Nov. 22.
A conditional ‘no’ on routine bamlanivimab
“The guideline panel gave a conditional recommendation against the routine use of bamlanivimab,” Adarsh Bhimraj, MD, cochair of the IDSA COVID-19 Treatment and Management Guidelines Expert Panel, said.
On Nov. 10, the FDA issued an emergency-use authorization (EUA) for bamlanivimab for use in ambulatory patients with mild to moderate COVID-19.
“We did have a remark that it may be used in patients who have increased risk of severe COVID-19, as it is outlined in the FDA emergency-use authorization issued last week,” he said. He added that use should follow an informed discussion between provider and patient, one in which “the patient puts a very high value on the uncertain benefits and a low value on uncertain adverse events.”
The panel’s rationale was based in part on interim analysis of the phase 2 BLAZE-1 trial, which found 1.6% of people randomly assigned to bamlanivimab had an emergency department visit or hospitalization compared with 6.3% of those receiving a placebo.
“We thought the estimate was too fragile because the number in each arm was very low. Even a small change in these numbers could make the difference nonsignificant,” said Bhimraj, head of the neurologic infectious diseases section in the department of infectious diseases at the Cleveland (Ohio) Clinic.
Awaiting more data on antibody combination
On November 21, the FDA granted an EUA to the casirivimab and imbdevimab monoclonal antibody combination (Regeneron), indicated to treated mild to moderate COVID-19.
“Surprisingly, the preliminary results released in the EUA look a lot like bamlanivimab,” Dr. Bhimraj said.
Unlike bamlanivimab, for which trial details were published, the panel does not yet have the totality of data on casirivimab and imbdevimab, and therefore is not yet making a recommendation. “We want to be cautious as a guideline panel. We are anxiously awaiting the full publication,” he added.
“I do think these monoclonal antibodies show potential for benefit, but as Dr. Bhimraj said, it’s very difficult with the relatively small numbers we’re talking about,” said Rajesh T. Gandhi, MD, cochair of the IDSA COVID-19 Treatment and Management Guidelines Expert Panel.
Remaining questions include the degree of efficacy these antibody therapies will have, as well as which patients are most likely to benefit, added Dr. Gandhi, who is also a professor of medicine at Harvard Medical School and director of HIV Clinical Services and Education at Massachusetts General Hospital, both in Boston.
Furthermore, although there appear to be adequate supplies of remdesivir and dexamethasone, for example, availability and distribution of monoclonal antibodies could present logistic challenges. Prioritizing which high-risk patients receive this therapy and ensuring equity and access to communities most affected by COVID-19, including minority and low socioeconomic populations, need to be addressed, Dr. Gandhi said.
Remdesivir recommended to shorten hospital stays
The panel’s recommendations regarding the use of remdesivir “has largely remained the same,” Dr. Gandhi said. Evidence indicates recovery is faster with remdesivir at 10 days vs 15 days in people taking a placebo.
In the ACTT-1 trial, for example, participants in the treatment group recovered in a median 10 days versus 15 days in the placebo group.
Therefore, the IDSA panel continues to recommend remdesivir treatment for hospitalized patients with COVID-19.
“As hospitals around the United States fill up, the IDSA panel believes the effect of remdesivir on speeding up recovery could be an important benefit, and that is why we continue to suggest its use,” Dr. Gandhi said.
When asked about the World Health Organization–sponsored trial that showed no benefit in terms of mortality, he replied, “Remdesivir is not a home run – we need better drugs.”
A recommendation against lopinavir and ritonavir
In contrast, the panel recommends against use of the lopinavir/ritonavir protease inhibitor combination therapy, based in part on data from a preprint of the Solidarity study.
The open-label Solidarity trial in 30 countries, sponsored by WHO, assessed hydroxychloroquine, interferon, lopinavir/ritonavir, and remdesivir in people hospitalized with COVID-19.
None of these drugs showed an effect on mortality, Dr. Gandhi said. “Better medicines that improve survival are clearly needed.”
Dexamethasone remains the only agent demonstrated to reduce mortality in people hospitalized with COVID-19, he added.
Tocilizumab not for routine use
After critical review of the studies that have emerged since the last IDSA recommendation regarding tocilizumab (Actemra) in September, “the panel still stood with the recommendation against routine use of tocilizumab in hospitalized patients with COVID-19,” Dr. Bhimraj said.
The guidance is based on trials including COVACTA and EMPACTA. Treatment with tocilizumab was not associated with significant differences in mortality. In these and other studies, “we did not really find a significant difference, and that was the reason for the conditional recommendation against routine use of tocilizumab in hospitalized patients,” Dr. Bhimraj said.
Also, although the trials were blinded, “we know treatment with tocilizumab can cause a reduction in C-reactive protein levels,” which could indicate to researchers which participants were receiving active treatment versus placebo, he said.
Jury still out on baricitinib, remdesivir combination
The FDA granted an EUA to the combination of remdesivir and baricitinib (Olumiant) on Nov. 19. However, the IDSA panel is reserving its recommendation on this therapeutic combination until more data emerge.
“We still don’t have complete results of the ACTT-2 study, and the information we do have is what is available in the EUA,” Dr. Bhimraj said. The panel expects to issue guidance once the totality of data become available.
Unanswered questions include why investigators chose a 4-mg dose of baricitinib – twice the 2-mg dose commonly used for treating rheumatoid arthritis – and how many patients in the trial also were treated with steroids.
Dr. Gandhi agreed that the proportion of patients taking a steroid is “really an important consideration.” He added that dexamethasone has become standard of care because it reduces mortality, as well as the number of people requiring oxygen. He said it will be important to know how the baricitinib/remdesivir combination compares with dexamethasone.
“You don’t want to give a drug with less certain benefit over a drug for which there is more certain benefit,” Dr. Gandhi said.
Future possibilities
“The monoclonal antibodies are important to continue studying, particularly in combinations,” Dr. Gandhi said. Researchers are investigating formulations other than IV infusion to make therapy more convenient. For example, a subcutaneous injection like insulin would make administration at home more of a possibility.
Investigators are also looking at oral antiviral therapy, inhaled antivirals, and the promise of using interferon therapy. Dr. Gandhi added there is also “a lot of work around medications to reduce the excess inflammation that drives very severe COVID-19.”
‘Exciting news’ on AstraZeneca vaccine
Although not part of the IDSA guidelines, “we saw the news from AstraZeneca this morning, which is exciting,” Dr. Gandhi said during a media briefing.
Unlike the Pfizer and Moderna messenger RNA vaccines, which use the genetic material of the virus to make the virus proteins that elicit an immune response, the AstraZeneca/Oxford University vaccine uses a viral vector to carry the SARS-CoV-2 protein, to which the body produces an immune response.
“I’m thrilled that several different vaccines are showing important effects at rates higher than the FDA benchmark of 50%, and these are well exceeding that,” Dr. Gandhi said.
“One interesting thing from the [AstraZeneca] press release is they show asymptomatic infection being reduced,” he added. “That is critical because we know a lot of transmission of SARS-CoV-2 comes from asymptomatic people.”
Reasons for optimism
In response to a question about whether the experts feel more optimistic about COVID-19, Dr. Bhimraj said he is cautiously optimistic. “We have made tremendous progress in therapeutic agents, and in how the world has come together in the middle of a catastrophe to collaborate, setting our differences apart, to do trials. That is commendable.”
Dr. Gandhi said he felt more optimistic than he did in the spring. He pointed out that physicians and researchers know a lot more about potential blood clotting complications, how to support patients through severe COVID-19 and keep them off a ventilator whenever possible, and how to provide dexamethasone to reduce the risk of death.
Those benefits are in hospitalized patients, however, and “we need ways to prevent people from getting into the hospital, and that is why we are looking at the monoclonal antibodies,” Dr. Gandhi said. “If borne out in larger trials, that will be a major advance.”
“We need to keep our focus on prevention and go back to our idea of flattening the curve. That is critical so our health care systems do not get overwhelmed during this massive surge we are in,” Dr. Gandhi said. “So masking and social distancing are just as important as they always have been.”
Dr. Bhimraj disclosed no relevant financial relationships. Dr. Gandhi has no disclosures for the past 12 months; in the past 3 years, he has served on scientific advisory boards for Gilead and Merck.
This article first appeared on Medscape.com.