User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Delta variant could drive herd immunity threshold over 80%
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Increases in new COVID cases among children far outpace vaccinations
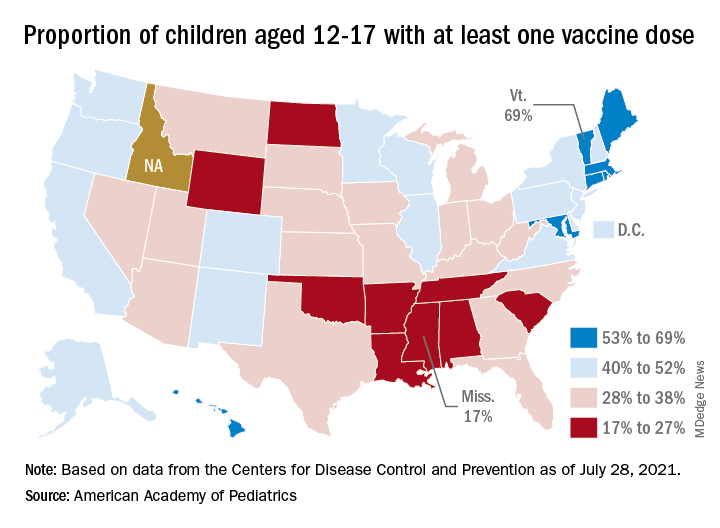
New COVID-19 cases in children soared by almost 86% over the course of just 1 week, while the number of 12- to 17-year-old children who have received at least one dose of vaccine rose by 5.4%, according to two separate sources.
Meanwhile, the increase over the past 2 weeks – from 23,551 new cases for July 16-22 to almost 72,000 – works out to almost 205%, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Children represented 19.0% of the cases reported during the week of July 23-29, and they have made up 14.3% of all cases since the pandemic began, with the total number of cases in children now approaching 4.2 million, the AAP and CHA said in their weekly COVID report. About 22% of the U.S. population is under the age of 18 years.
As of Aug. 2, just over 9.8 million children aged 12-17 years had received at least one dose of the COVID vaccine, which was up by about 500,000, or 5.4%, from a week earlier, based on data from the Centers for Disease Control and Prevention.
Children aged 16-17 have reached a notable milestone on the journey that started with vaccine approval in December: 50.2% have gotten at least one dose and 40.3% are fully vaccinated. Among children aged 12-15 years, the proportion with at least one dose of vaccine is up to 39.5%, compared with 37.1% the previous week, while 29.0% are fully vaccinated (27.8% the week before), the CDC said on its COVID Data Tracker.
The national rates for child vaccination, however, tend to hide the disparities between states. There is a gap between Mississippi (lowest), where just 17% of children aged 12-17 years have gotten at least one dose, and Vermont (highest), which is up to 69%. Vermont also has the highest rate of vaccine completion (60%), while Alabama and Mississippi have the lowest (10%), according to a solo report from the AAP.
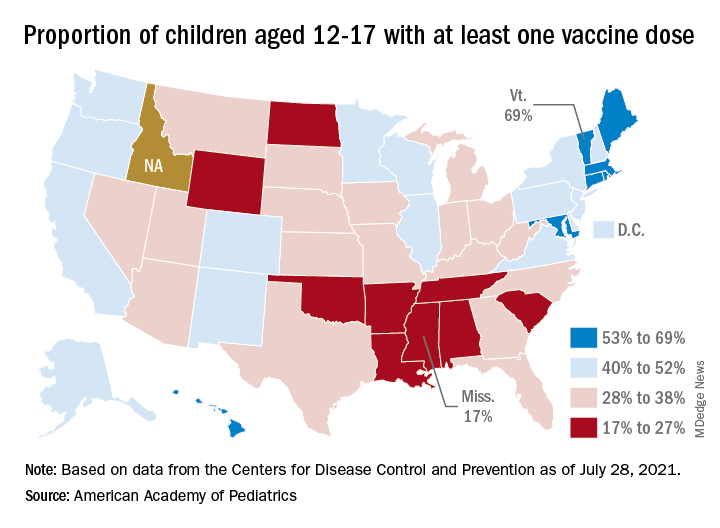
New COVID-19 cases in children soared by almost 86% over the course of just 1 week, while the number of 12- to 17-year-old children who have received at least one dose of vaccine rose by 5.4%, according to two separate sources.
Meanwhile, the increase over the past 2 weeks – from 23,551 new cases for July 16-22 to almost 72,000 – works out to almost 205%, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Children represented 19.0% of the cases reported during the week of July 23-29, and they have made up 14.3% of all cases since the pandemic began, with the total number of cases in children now approaching 4.2 million, the AAP and CHA said in their weekly COVID report. About 22% of the U.S. population is under the age of 18 years.
As of Aug. 2, just over 9.8 million children aged 12-17 years had received at least one dose of the COVID vaccine, which was up by about 500,000, or 5.4%, from a week earlier, based on data from the Centers for Disease Control and Prevention.
Children aged 16-17 have reached a notable milestone on the journey that started with vaccine approval in December: 50.2% have gotten at least one dose and 40.3% are fully vaccinated. Among children aged 12-15 years, the proportion with at least one dose of vaccine is up to 39.5%, compared with 37.1% the previous week, while 29.0% are fully vaccinated (27.8% the week before), the CDC said on its COVID Data Tracker.
The national rates for child vaccination, however, tend to hide the disparities between states. There is a gap between Mississippi (lowest), where just 17% of children aged 12-17 years have gotten at least one dose, and Vermont (highest), which is up to 69%. Vermont also has the highest rate of vaccine completion (60%), while Alabama and Mississippi have the lowest (10%), according to a solo report from the AAP.
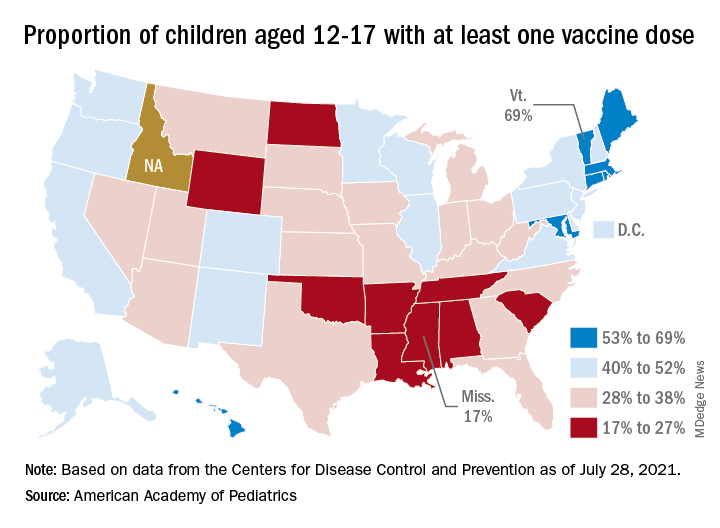
New COVID-19 cases in children soared by almost 86% over the course of just 1 week, while the number of 12- to 17-year-old children who have received at least one dose of vaccine rose by 5.4%, according to two separate sources.
Meanwhile, the increase over the past 2 weeks – from 23,551 new cases for July 16-22 to almost 72,000 – works out to almost 205%, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Children represented 19.0% of the cases reported during the week of July 23-29, and they have made up 14.3% of all cases since the pandemic began, with the total number of cases in children now approaching 4.2 million, the AAP and CHA said in their weekly COVID report. About 22% of the U.S. population is under the age of 18 years.
As of Aug. 2, just over 9.8 million children aged 12-17 years had received at least one dose of the COVID vaccine, which was up by about 500,000, or 5.4%, from a week earlier, based on data from the Centers for Disease Control and Prevention.
Children aged 16-17 have reached a notable milestone on the journey that started with vaccine approval in December: 50.2% have gotten at least one dose and 40.3% are fully vaccinated. Among children aged 12-15 years, the proportion with at least one dose of vaccine is up to 39.5%, compared with 37.1% the previous week, while 29.0% are fully vaccinated (27.8% the week before), the CDC said on its COVID Data Tracker.
The national rates for child vaccination, however, tend to hide the disparities between states. There is a gap between Mississippi (lowest), where just 17% of children aged 12-17 years have gotten at least one dose, and Vermont (highest), which is up to 69%. Vermont also has the highest rate of vaccine completion (60%), while Alabama and Mississippi have the lowest (10%), according to a solo report from the AAP.
COVID-19: Delta variant is raising the stakes
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Empathetic conversations with unvaccinated people desperately needed
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Vaccination alone won’t counter rise of resistant variants: Study
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Indoor masking needed in almost 70% of U.S. counties: CDC data
In announcing new guidance on July 27, the CDC said vaccinated people should wear face masks in indoor public places with “high” or “substantial” community transmission rates of COVID-19.
Data from the CDC shows that designation covers 69.3% of all counties in the United States – 52.2% (1,680 counties) with high community transmission rates and 17.1% (551 counties) with substantial rates.
A county has “high transmission” if it reports 100 or more weekly cases per 100,000 residents or a 10% or higher test positivity rate in the last 7 days, the CDC said. “Substantial transmission” means a county reports 50-99 weekly cases per 100,000 residents or has a positivity rate between 8% and 9.9% in the last 7 days.
About 23% of U.S. counties had moderate rates of community transmission, and 7.67% had low rates.
To find out the transmission rate in your county, go to the CDC COVID data tracker.
Smithsonian requiring masks again
The Smithsonian now requires all visitors over age 2, regardless of vaccination status, to wear face masks indoors and in all museum spaces.
The Smithsonian said in a news release that fully vaccinated visitors won’t have to wear masks at the National Zoo or outdoor gardens for museums.
The new rule goes into effect Aug. 6. It reverses a rule that said fully vaccinated visitors didn’t have to wear masks indoors beginning June 28.
Indoor face masks will be required throughout the District of Columbia beginning July 31., D.C. Mayor Muriel Bowser.
House Republicans protest face mask policy
About 40 maskless Republican members of the U.S. House of Representatives filed onto the Senate floor on July 29 to protest a new rule requiring House members to wear face masks, the Hill reported.
Congress’s attending doctor said in a memo that the 435 members of the House, plus workers, must wear masks indoors, but not the 100 members of the Senate. The Senate is a smaller body and has had better mask compliance than the House.
Rep. Ronny Jackson (R-Tex.), told the Hill that Republicans wanted to show “what it was like on the floor of the Senate versus the floor of the House. Obviously, it’s vastly different.”
Among the group of Republicans who filed onto the Senate floor were Rep. Lauren Boebert of Colorado, Rep. Matt Gaetz and Rep. Byron Donalds of Florida, Rep. Marjorie Taylor Greene of Georgia, Rep. Chip Roy and Rep. Louie Gohmert of Texas, Rep. Madison Cawthorn of North Carolina, Rep. Warren Davidson of Ohio, and Rep. Andy Biggs of Arizona.
A version of this article first appeared on WebMD.com.
In announcing new guidance on July 27, the CDC said vaccinated people should wear face masks in indoor public places with “high” or “substantial” community transmission rates of COVID-19.
Data from the CDC shows that designation covers 69.3% of all counties in the United States – 52.2% (1,680 counties) with high community transmission rates and 17.1% (551 counties) with substantial rates.
A county has “high transmission” if it reports 100 or more weekly cases per 100,000 residents or a 10% or higher test positivity rate in the last 7 days, the CDC said. “Substantial transmission” means a county reports 50-99 weekly cases per 100,000 residents or has a positivity rate between 8% and 9.9% in the last 7 days.
About 23% of U.S. counties had moderate rates of community transmission, and 7.67% had low rates.
To find out the transmission rate in your county, go to the CDC COVID data tracker.
Smithsonian requiring masks again
The Smithsonian now requires all visitors over age 2, regardless of vaccination status, to wear face masks indoors and in all museum spaces.
The Smithsonian said in a news release that fully vaccinated visitors won’t have to wear masks at the National Zoo or outdoor gardens for museums.
The new rule goes into effect Aug. 6. It reverses a rule that said fully vaccinated visitors didn’t have to wear masks indoors beginning June 28.
Indoor face masks will be required throughout the District of Columbia beginning July 31., D.C. Mayor Muriel Bowser.
House Republicans protest face mask policy
About 40 maskless Republican members of the U.S. House of Representatives filed onto the Senate floor on July 29 to protest a new rule requiring House members to wear face masks, the Hill reported.
Congress’s attending doctor said in a memo that the 435 members of the House, plus workers, must wear masks indoors, but not the 100 members of the Senate. The Senate is a smaller body and has had better mask compliance than the House.
Rep. Ronny Jackson (R-Tex.), told the Hill that Republicans wanted to show “what it was like on the floor of the Senate versus the floor of the House. Obviously, it’s vastly different.”
Among the group of Republicans who filed onto the Senate floor were Rep. Lauren Boebert of Colorado, Rep. Matt Gaetz and Rep. Byron Donalds of Florida, Rep. Marjorie Taylor Greene of Georgia, Rep. Chip Roy and Rep. Louie Gohmert of Texas, Rep. Madison Cawthorn of North Carolina, Rep. Warren Davidson of Ohio, and Rep. Andy Biggs of Arizona.
A version of this article first appeared on WebMD.com.
In announcing new guidance on July 27, the CDC said vaccinated people should wear face masks in indoor public places with “high” or “substantial” community transmission rates of COVID-19.
Data from the CDC shows that designation covers 69.3% of all counties in the United States – 52.2% (1,680 counties) with high community transmission rates and 17.1% (551 counties) with substantial rates.
A county has “high transmission” if it reports 100 or more weekly cases per 100,000 residents or a 10% or higher test positivity rate in the last 7 days, the CDC said. “Substantial transmission” means a county reports 50-99 weekly cases per 100,000 residents or has a positivity rate between 8% and 9.9% in the last 7 days.
About 23% of U.S. counties had moderate rates of community transmission, and 7.67% had low rates.
To find out the transmission rate in your county, go to the CDC COVID data tracker.
Smithsonian requiring masks again
The Smithsonian now requires all visitors over age 2, regardless of vaccination status, to wear face masks indoors and in all museum spaces.
The Smithsonian said in a news release that fully vaccinated visitors won’t have to wear masks at the National Zoo or outdoor gardens for museums.
The new rule goes into effect Aug. 6. It reverses a rule that said fully vaccinated visitors didn’t have to wear masks indoors beginning June 28.
Indoor face masks will be required throughout the District of Columbia beginning July 31., D.C. Mayor Muriel Bowser.
House Republicans protest face mask policy
About 40 maskless Republican members of the U.S. House of Representatives filed onto the Senate floor on July 29 to protest a new rule requiring House members to wear face masks, the Hill reported.
Congress’s attending doctor said in a memo that the 435 members of the House, plus workers, must wear masks indoors, but not the 100 members of the Senate. The Senate is a smaller body and has had better mask compliance than the House.
Rep. Ronny Jackson (R-Tex.), told the Hill that Republicans wanted to show “what it was like on the floor of the Senate versus the floor of the House. Obviously, it’s vastly different.”
Among the group of Republicans who filed onto the Senate floor were Rep. Lauren Boebert of Colorado, Rep. Matt Gaetz and Rep. Byron Donalds of Florida, Rep. Marjorie Taylor Greene of Georgia, Rep. Chip Roy and Rep. Louie Gohmert of Texas, Rep. Madison Cawthorn of North Carolina, Rep. Warren Davidson of Ohio, and Rep. Andy Biggs of Arizona.
A version of this article first appeared on WebMD.com.
‘War has changed’: CDC says Delta as contagious as chicken pox
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
Internal Centers for Disease Control and Prevention documents support the high transmission rate of the Delta variant and put the risk in easier to understand terms.
In addition, the agency released a new study that shows that breakthrough infections in the vaccinated make people about as contagious as those who are unvaccinated. The new report, published July 30 in Morbidity and Mortality Weekly Report (MMWR), also reveals that the Delta variant likely causes more severe COVID-19 illness.
Given these recent findings, the internal CDC slide show advises that the agency should “acknowledge the war has changed.”
A ‘pivotal discovery’
CDC Director Rochelle Walensky, MD, MPH, said in a statement that the MMWR report demonstrates “that [D]elta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people.
“High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with [D]elta can transmit the virus,” she added. “This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation.”
The investigators analyzed 469 COVID-19 cases reported in Massachusetts residents July 3 through 17, 2021. The infections were associated with an outbreak following multiple events and large gatherings in Provincetown in that state’s easternmost Barnstable County, also known as Cape Cod.
Notably, 346 infections, or 74%, of the cases occurred in fully vaccinated individuals. This group had a median age of 42, and 87% were male. Also, 79% of the breakthrough infections were symptomatic.
Researchers also identified the Delta variant in 90% of 133 specimens collected for analysis. Furthermore, viral loads were about the same between samples taken from people who were fully vaccinated and those who were not.
Four of the five people hospitalized were fully vaccinated. No deaths were reported.
The publication of these results was highly anticipated following the CDC’s updated mask recommendations on July 27.
Outside the scope of the MMWR report is the total number of cases associated with the outbreak, including visitors from outside Massachusetts, which now approach 900 infections, NBC Boston reported.
‘Very sobering’ data
“The new information from the CDC around the [D]elta variant is very sobering,” David Hirschwerk, MD, infectious disease specialist at Northwell Health in New Hyde Park, N.Y., said in an interview.
“The CDC is trying to convey and present this uncertain situation clearly to the public based on new, accumulated data,” he said. For example, given the evidence for higher contagiousness of the Delta variant, Dr. Hirschwerk added, “there will be situations where vaccinated people get infected, because the amount of the virus overwhelms the immune protection.
“What is new that is concerning is that people who are vaccinated still have the potential to transmit the virus to the same degree,” he said.
The MMWR study “helps us better understand the question related to whether or not a person who has completed a COVID-19 series can spread the infection,” agreed Michelle Barron, MD, a professor in the division of infectious disease at the University of Colorado, Aurora.
“The message is that, because the [D]elta variant is much more contagious than the original strain, unvaccinated persons need to get vaccinated because it is nearly impossible to avoid the virus indefinitely,” Michael Lin, MD, MPH, infectious diseases specialist and epidemiologist at Rush University Medical Center, Chicago, said when asked to comment.
The new data highlight “that vaccinated persons, if they become sick, should still seek COVID-19 testing and should still isolate, as they are likely contagious,” Dr. Lin added.
More contagious than other infections
The internal CDC slide presentation also puts the new transmission risk in simple terms. Saying that the Delta variant is about as contagious as chicken pox, for example, immediately brings back vivid memories for some of staying indoors and away from friends during childhood or teenage outbreaks.
“A lot of people will remember getting chicken pox and then having their siblings get it shortly thereafter,” Dr. Barron said. “The only key thing to note is that this does not mean that the COVID-19 [D]elta variant mechanism of spread is the same as chicken pox and Ebola. The primary means of spread of COVID-19, even the Delta variant, is via droplets.”
This also means each person infected with the Delta variant could infect an average of eight or nine others.
In contrast, the original strain of the SARS-CoV-2 virus was about as infectious as the common cold. In other words, someone was likely to infect about two other people on average.
In addition to the cold, the CDC notes that the Delta variant is now more contagious than Ebola, the seasonal flu, or small pox.
These Delta variant comparisons are one tangible way of explaining why the CDC on July 27 recommended a return to masking in schools and other indoor spaces for people – vaccinated and unvaccinated – in about 70% of the counties across the United States.
In comparing the Delta variant with other infections, “I think the CDC is trying to help people understand a little bit better the situation we now face since the information is so new. We are in a very different position now than just a few weeks ago, and it is hard for people to accept this,” Dr. Hirschwerk said.
The Delta variant is so different that the CDC considers it almost acting like a new virus altogether.
The CDC’s internal documents were first released by The Washington Post on July 29. The slides cite communication challenges for the agency to continue promoting vaccination while also acknowledging that breakthrough cases are occurring and therefore the fully vaccinated, in some instances, are likely infecting others.
Moving back to science talk, the CDC used the recent outbreak in Barnstable County as an example. The cycle threshold, or Ct values, a measure of viral load, were about the same between 80 vaccinated people linked to the outbreak who had a mean Ct value of 21.9, compared with 65 other unvaccinated people with a Ct of 21.5.
Many experts are quick to note that vaccination remains essential, in part because a vaccinated person also walks around with a much lower risk for severe outcomes, hospitalization, and death. In the internal slide show, the CDC points out that vaccination reduces the risk for infection threefold.
“Even with this high amount of virus, [the Delta variant] did not necessarily make the vaccinated individuals as sick,” Dr. Barron said.
In her statement, Dr. Walensky credited collaboration with the Commonwealth of Massachusetts Department of Public Health and the CDC for the new data. She also thanked the residents of Barnstable County for participating in interviews done by contact tracers and their willingness to get tested and adhere to safety protocols after learning of their exposure.
Next moves by CDC?
The agency notes that next steps include consideration of prevention measures such as vaccine mandates for healthcare professionals to protect vulnerable populations, universal masking for source control and prevention, and reconsidering other community mitigation strategies.
Asked if this potential policy is appropriate and feasible, Dr. Lin said, “Yes, I believe that every person working in health care should be vaccinated for COVID-19, and it is feasible.”
Dr. Barron agreed as well. “We as health care providers choose to work in health care, and we should be doing everything feasible to ensure that we are protecting our patients and keeping our coworkers safe.”
“Whether you are a health care professional or not, I would urge everyone to get the COVID-19 vaccine, especially as cases across the country continue to rise,” Dr. Hirschwerk said. “Unequivocally vaccines protect you from the virus.”
A version of this article first appeared on Medscape.com.
COVID brings evolutionary virologists out of the shadows, into the fight
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
It has been a strange, exhausting year for many evolutionary virologists.
“Scientists are not used to having attention and are not used to being in the press and are not used to being attacked on Twitter,” Martha Nelson, PhD, a staff scientist who studies viral evolution at the National Institutes of Health, said in an interview.
Over the past year and a half, the theory of evolution has been thrust into the spotlight – more now than ever, perhaps, as the world is stalked by the Delta variant and fears arise of a mutation that’s even worse.
The origins of SARS-CoV-2 and the rise of the Delta variant have been debated, and vaccine efficacy and the possible need for booster shots have been speculated upon. In all these instances, consciously or not, there is engagement with the field of evolutionary virology.
It has been central to deepening the understanding of the ongoing pandemic, even as SARS-CoV-2 has exposed gaps in what we understand about how viruses behave and evolve.
Evolutionary virology experts believe that, after the pandemic, their expertise and tools could be applied to and integrated with clinical medicine to improve outcomes and understanding of disease.
“From our perspective, evolutionary biology has been a side dish and something that hasn’t been integrated into the core practice of medicine,” said Dr. Nelson. “I’m really curious to see how that changes over time.”
Pandemic evolution
Novel pathogens, antibiotic-resistant bacteria, and cancer cells are all products of ongoing evolution. “Just like cellular organisms, viruses have genomes, and all genomes evolve,” Eugene Koonin, PhD, evolutionary genomics group leader at the NIH, said in an interview.
Compared with cellular organisms, viruses evolve quite fast, he said.
A study published in the Proceedings of the National Academy of Sciences exemplifies evolutionary virology in action. In the study, Dr. Koonin and fellow researchers analyzed more than 300,000 genome sequences of SARS-CoV-2 variants that were publicly available as of January 2021 and mapped all the mutations in each sequence.
The researchers identified a small subset of mutations that arose independently more than once and that likely aided viral adaptation, said Nash Rochman, PhD, a research fellow at the NIH and coauthor of the PNAS study.
Many of these mutations were concentrated in two areas of the genome – the receptor binding domain of the spike protein, and a region of the nucleocapsid protein – and were often grouped together, possibly creating greater advantages for the virus than would have occurred individually, he said.
The researchers also found that, from the beginning of the pandemic, the SARS-CoV-2 genome has been evolving and diversifying in different regions around the world, allowing for the rise of new lineages and, possibly, even new species, Dr. Koonin said.
During the pandemic, researchers have used evolutionary virology tools to tackle many other questions. For example, Dr. Nelson tracked the spread of SARS-CoV-2 across Europe and North America. In a study that is currently undergoing peer review, the investigators found recently vaccinated individuals, who are only partially immune, are at the highest risk for incubating antibody-resistant variants.
C. Brandon Ogbunu, PhD, an evolutionary geneticist at Yale University, New Haven, Conn., whose work is focused on disease evolution, studied whether SARS-CoV-2 would evolve to become more transmissible, and if so, would it also become more or less virulent. His lab also investigated the transmission and spread of the virus.
“I think the last year, on one end, has been this opportunity to apply concepts and perspectives that we’ve been developing for the last several decades,” Dr. Ogbunu said in an interview. “At the same time, this pandemic has also been this wake-up call for many of us with regards to revealing the things we do not understand about the ways viruses infect, spread, and how evolution works within viruses.”
He emphasizes the need for evolutionary biology to partner with other fields – including information theory and biophysics – to help unlock viral mysteries: “We need to think very, very carefully about the way those fields intersect.”
Dr. Nelson also pointed to the need for better, more centralized data gathering in the United States.
The sheer volume of information scientists have collected about SARS-CoV-2 will aid in the study of virus evolution for years to come, said Dr. Koonin.
Evolution in medicine
Evolutionary virology and related research can be applied to medicine outside of the context of a global pandemic. “The principles and technical portions of evolutionary virology are very applicable to other diseases, including cancer,” Dr. Koonin said.
Viruses, bacteria, and cancer cells are all evolving systems. Viruses and bacteria are constantly evolving to thwart drugs and vaccines. How physicians and health care professionals practice medicine shapes the selection pressures driving how these pathogens evolve, Dr. Nelson said.
The rise of antibiotic-resistant bacteria is a particularly relevant example of how evolution affects the way physicians treat patients. Having an evolutionary perspective can help inform how to treat patients most effectively, both for individual patients as well as for broader public health, she said.
“For a long time, there’s been a lot of interest in pathogen evolution that hasn’t translated so much into clinical practice,” said Dr. Nelson. “There’s been kind of a gulf between the research side of evolutionary virology and pathogen emergence and actual practice of medicine.”
As genomic sequencing has become faster and cheaper, that gulf has started to narrow, she said. As this technology continues to prove itself by, for example, tracking the evolution of one virus in real time, Dr. Nelson hopes there will be a positive snowball effect, leading to more attention, investment, and improvements in genomic data and that its use in epidemiology and medicine will expand going forward.
Bringing viral evolution studies more into medicine will require a mindset shift, Dr. Ogbunu said. Clinical practice is, by design, very focused on the individual patient. Evolutionary biology, on the other hand, deals with populations and probabilities.
Being able to engage with evolutionary biology would help physicians better understand disease and explain it to their patients, he said.
To start, Dr. Nelson recommended requiring at least one course in evolutionary biology or evolutionary medicine in medical school and crafting continuing education in this area for physicians. (Presentations at conferences could be one way to do this.)
Dr. Nelson also recommended deeper engagement and collaboration between physicians who collect samples from patients and evolutionary biologists who analyze genetic data. This would improve the quality of the data, the analysis, and the eventual findings that could be relevant to patients and clinical practice.
Still, “my first and inevitable reaction is I would so much rather prefer to exist in relative obscurity,” said Dr. Koonin, noting that the tragedy of the pandemic outweighs the advancements in the field.
Although there’s no going back to prepandemic times, there is an enormous opportunity in the aftermath of COVID to increase dialogue between physicians and evolutionary virologists to improve medical practice as well as public health.
Dr. Nelson summed it up: “Everything we uncover about these pathogens may help us prevent something like this again.”
A version of this article first appeared on Medscape.com.
Doctors’ offices may be hot spot for transmission of respiratory infections
Prior research has examined the issue of hospital-acquired infections. A 2014 study published in the New England Journal of Medicine, for example, found that 4% of hospitalized patients acquired a health care–associated infection during their stay. Furthermore, the Centers for Disease Control and Prevention estimates that, on any given day, one in 31 hospital patients has at least one health care–associated infection. However, researchers for the new study, published in Health Affairs, said evidence about the risk of acquiring respiratory viral infections in medical office settings is limited.
“Hospital-acquired infections has been a problem for a while,” study author Hannah Neprash, PhD, of the department of health policy and management at the University of Minnesota School of Public Health, Minneapolis, said in an interview. “However, there’s never been a similar study of whether a similar phenomenon happens in physician offices. This is especially relevant now when we’re dealing with respiratory infections.”
Methods and results
For the new study, Dr. Neprash and her colleagues analyzed deidentified billing and scheduling data from 2016-2017 for 105,462,600 outpatient visits that occurred at 6,709 office-based primary care practices. They used the World Health Organization case definition for influenzalike illness “to capture cases in which the physician may suspect this illness even if a specific diagnosis code was not present.” Their control conditions included exposure to urinary tract infections and back pain.
Doctor visits were considered unexposed if they were scheduled to start at least 90 minutes before the first influenzalike illness visit of the day. They were considered exposed if they were scheduled to start at the same time or after the first influenzalike illness visit of the day at that practice.
Researchers quantified whether exposed patients were more likely to return with a similar illness in the next 2 weeks, compared with nonexposed patients seen earlier in the day
They found that 2.7 patients per 1,000 returned within 2 weeks with an influenzalike illness.
Patients were more likely to return with influenzalike illness if their visit occurred after an influenzalike illness visit versus before, the researchers said.
The authors of the paper said their new research highlights the importance of infection control in health care settings, including outpatient offices.
Where did the exposure occur?
Diego Hijano, MD, MSc, pediatric infectious disease specialist at St. Jude’s Children’s Research Hospital, Memphis, Tenn., said he was not surprised by the findings, but noted that it’s hard to say if the exposure to influenzalike illnesses happened in the office or in the community.
“If you start to see individuals with influenza in your office it’s because [there’s influenza] in the community,” Dr. Hijano explained. “So that means that you will have more patients coming in with influenza.”
To reduce the transmission of infections, Dr. Neprash suggested that doctors’ offices follow the CDC guidelines for indoor conduct, which include masking, washing hands, and “taking appropriate infection control measures.”
So potentially masking within offices is a way to minimize transmission between whatever people are there to be seen when it’s contagious, Dr. Neprash said.
“Telehealth really took off in 2020 and it’s unclear what the state of telehealth will be going forward. [These findings] suggest that there’s a patient safety argument for continuing to enable primary care physicians to provide visits either by phone or by video,” he added.
Dr. Hijano thinks it would be helpful for doctors to separate patients with respiratory illnesses from those without respiratory illnesses.
Driver of transmissions
Dr. Neprash suggested that another driver of these transmissions could be doctors not washing their hands, which is a “notorious issue,” and Dr. Hijano agreed with that statement.
“We did know that the hands of physicians and nurses and care providers are the main driver of infections in the health care setting,” Dr. Hijano explained. “I mean, washing your hands properly between encounters is the single best way that any given health care provider can prevent the spread of infections.”
“We have a unique opportunity with COVID-19 to change how these clinics are operating now,” Dr. Hijano said. “Many clinics are actually asking patients to call ahead of time if you have symptoms of a respiratory illness that could be contagious, and those who are not are still mandating the use of mask and physical distance in the waiting areas and limiting the amount of number of patients in any given hour. So I think that those are really big practices that would kind of make an impact in respiratory illness in terms of decreasing transmission in clinics.”
The authors, who had no conflicts of interest said their hope is that their study will help inform policy for reopening outpatient care settings. Dr. Hijano, who was not involved in the study also had no conflicts.
Prior research has examined the issue of hospital-acquired infections. A 2014 study published in the New England Journal of Medicine, for example, found that 4% of hospitalized patients acquired a health care–associated infection during their stay. Furthermore, the Centers for Disease Control and Prevention estimates that, on any given day, one in 31 hospital patients has at least one health care–associated infection. However, researchers for the new study, published in Health Affairs, said evidence about the risk of acquiring respiratory viral infections in medical office settings is limited.
“Hospital-acquired infections has been a problem for a while,” study author Hannah Neprash, PhD, of the department of health policy and management at the University of Minnesota School of Public Health, Minneapolis, said in an interview. “However, there’s never been a similar study of whether a similar phenomenon happens in physician offices. This is especially relevant now when we’re dealing with respiratory infections.”
Methods and results
For the new study, Dr. Neprash and her colleagues analyzed deidentified billing and scheduling data from 2016-2017 for 105,462,600 outpatient visits that occurred at 6,709 office-based primary care practices. They used the World Health Organization case definition for influenzalike illness “to capture cases in which the physician may suspect this illness even if a specific diagnosis code was not present.” Their control conditions included exposure to urinary tract infections and back pain.
Doctor visits were considered unexposed if they were scheduled to start at least 90 minutes before the first influenzalike illness visit of the day. They were considered exposed if they were scheduled to start at the same time or after the first influenzalike illness visit of the day at that practice.
Researchers quantified whether exposed patients were more likely to return with a similar illness in the next 2 weeks, compared with nonexposed patients seen earlier in the day
They found that 2.7 patients per 1,000 returned within 2 weeks with an influenzalike illness.
Patients were more likely to return with influenzalike illness if their visit occurred after an influenzalike illness visit versus before, the researchers said.
The authors of the paper said their new research highlights the importance of infection control in health care settings, including outpatient offices.
Where did the exposure occur?
Diego Hijano, MD, MSc, pediatric infectious disease specialist at St. Jude’s Children’s Research Hospital, Memphis, Tenn., said he was not surprised by the findings, but noted that it’s hard to say if the exposure to influenzalike illnesses happened in the office or in the community.
“If you start to see individuals with influenza in your office it’s because [there’s influenza] in the community,” Dr. Hijano explained. “So that means that you will have more patients coming in with influenza.”
To reduce the transmission of infections, Dr. Neprash suggested that doctors’ offices follow the CDC guidelines for indoor conduct, which include masking, washing hands, and “taking appropriate infection control measures.”
So potentially masking within offices is a way to minimize transmission between whatever people are there to be seen when it’s contagious, Dr. Neprash said.
“Telehealth really took off in 2020 and it’s unclear what the state of telehealth will be going forward. [These findings] suggest that there’s a patient safety argument for continuing to enable primary care physicians to provide visits either by phone or by video,” he added.
Dr. Hijano thinks it would be helpful for doctors to separate patients with respiratory illnesses from those without respiratory illnesses.
Driver of transmissions
Dr. Neprash suggested that another driver of these transmissions could be doctors not washing their hands, which is a “notorious issue,” and Dr. Hijano agreed with that statement.
“We did know that the hands of physicians and nurses and care providers are the main driver of infections in the health care setting,” Dr. Hijano explained. “I mean, washing your hands properly between encounters is the single best way that any given health care provider can prevent the spread of infections.”
“We have a unique opportunity with COVID-19 to change how these clinics are operating now,” Dr. Hijano said. “Many clinics are actually asking patients to call ahead of time if you have symptoms of a respiratory illness that could be contagious, and those who are not are still mandating the use of mask and physical distance in the waiting areas and limiting the amount of number of patients in any given hour. So I think that those are really big practices that would kind of make an impact in respiratory illness in terms of decreasing transmission in clinics.”
The authors, who had no conflicts of interest said their hope is that their study will help inform policy for reopening outpatient care settings. Dr. Hijano, who was not involved in the study also had no conflicts.
Prior research has examined the issue of hospital-acquired infections. A 2014 study published in the New England Journal of Medicine, for example, found that 4% of hospitalized patients acquired a health care–associated infection during their stay. Furthermore, the Centers for Disease Control and Prevention estimates that, on any given day, one in 31 hospital patients has at least one health care–associated infection. However, researchers for the new study, published in Health Affairs, said evidence about the risk of acquiring respiratory viral infections in medical office settings is limited.
“Hospital-acquired infections has been a problem for a while,” study author Hannah Neprash, PhD, of the department of health policy and management at the University of Minnesota School of Public Health, Minneapolis, said in an interview. “However, there’s never been a similar study of whether a similar phenomenon happens in physician offices. This is especially relevant now when we’re dealing with respiratory infections.”
Methods and results
For the new study, Dr. Neprash and her colleagues analyzed deidentified billing and scheduling data from 2016-2017 for 105,462,600 outpatient visits that occurred at 6,709 office-based primary care practices. They used the World Health Organization case definition for influenzalike illness “to capture cases in which the physician may suspect this illness even if a specific diagnosis code was not present.” Their control conditions included exposure to urinary tract infections and back pain.
Doctor visits were considered unexposed if they were scheduled to start at least 90 minutes before the first influenzalike illness visit of the day. They were considered exposed if they were scheduled to start at the same time or after the first influenzalike illness visit of the day at that practice.
Researchers quantified whether exposed patients were more likely to return with a similar illness in the next 2 weeks, compared with nonexposed patients seen earlier in the day
They found that 2.7 patients per 1,000 returned within 2 weeks with an influenzalike illness.
Patients were more likely to return with influenzalike illness if their visit occurred after an influenzalike illness visit versus before, the researchers said.
The authors of the paper said their new research highlights the importance of infection control in health care settings, including outpatient offices.
Where did the exposure occur?
Diego Hijano, MD, MSc, pediatric infectious disease specialist at St. Jude’s Children’s Research Hospital, Memphis, Tenn., said he was not surprised by the findings, but noted that it’s hard to say if the exposure to influenzalike illnesses happened in the office or in the community.
“If you start to see individuals with influenza in your office it’s because [there’s influenza] in the community,” Dr. Hijano explained. “So that means that you will have more patients coming in with influenza.”
To reduce the transmission of infections, Dr. Neprash suggested that doctors’ offices follow the CDC guidelines for indoor conduct, which include masking, washing hands, and “taking appropriate infection control measures.”
So potentially masking within offices is a way to minimize transmission between whatever people are there to be seen when it’s contagious, Dr. Neprash said.
“Telehealth really took off in 2020 and it’s unclear what the state of telehealth will be going forward. [These findings] suggest that there’s a patient safety argument for continuing to enable primary care physicians to provide visits either by phone or by video,” he added.
Dr. Hijano thinks it would be helpful for doctors to separate patients with respiratory illnesses from those without respiratory illnesses.
Driver of transmissions
Dr. Neprash suggested that another driver of these transmissions could be doctors not washing their hands, which is a “notorious issue,” and Dr. Hijano agreed with that statement.
“We did know that the hands of physicians and nurses and care providers are the main driver of infections in the health care setting,” Dr. Hijano explained. “I mean, washing your hands properly between encounters is the single best way that any given health care provider can prevent the spread of infections.”
“We have a unique opportunity with COVID-19 to change how these clinics are operating now,” Dr. Hijano said. “Many clinics are actually asking patients to call ahead of time if you have symptoms of a respiratory illness that could be contagious, and those who are not are still mandating the use of mask and physical distance in the waiting areas and limiting the amount of number of patients in any given hour. So I think that those are really big practices that would kind of make an impact in respiratory illness in terms of decreasing transmission in clinics.”
The authors, who had no conflicts of interest said their hope is that their study will help inform policy for reopening outpatient care settings. Dr. Hijano, who was not involved in the study also had no conflicts.
FROM HEALTH AFFAIRS
CDC to show vaccinated people infected with Delta remain contagious
and infect others, the New York Times reported on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the New York Times said. The bottom line is that the CDC data shows people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on Jul 29 that the CDC’s updated mask guidance followed an outbreak on Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
A version of this article first appeared on Medscape.com.
and infect others, the New York Times reported on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the New York Times said. The bottom line is that the CDC data shows people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on Jul 29 that the CDC’s updated mask guidance followed an outbreak on Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
A version of this article first appeared on Medscape.com.
and infect others, the New York Times reported on July 29.
The revelation is one reason the agency reversed course this week and said fully vaccinated people should go back to wearing masks in many cases.
The new findings also are a reversal from what scientists had believed to be true about other variants of the virus, the New York Times said. The bottom line is that the CDC data shows people with so-called breakthrough cases of the Delta variant may be just as contagious as unvaccinated people, even if they do not show symptoms.
ABC News reported earlier on Jul 29 that the CDC’s updated mask guidance followed an outbreak on Cape Cod, where crowds gathered for the Fourth of July.
As of July 29, 882 people were tied to the outbreak centered in Provincetown, Mass. Of those who live in Massachusetts, 74% were unvaccinated. ABC said the majority were showing symptoms of COVID-19.
A version of this article first appeared on Medscape.com.
Short sleep is linked to future dementia
, according to a new analysis of data from the Whitehall II cohort study.
Previous work had identified links between short sleep duration and dementia risk, but few studies examined sleep habits long before onset of dementia. Those that did produced inconsistent results, according to Séverine Sabia, PhD, who is a research associate at Inserm (France) and the University College London.
“One potential reason for these inconstancies is the large range of ages of the study populations, and the small number of participants within each sleep duration group. The novelty of our study is to examine this association among almost 8,000 participants with a follow-up of 30 years, using repeated measures of sleep duration starting in midlife to consider sleep duration at specific ages,” Dr. Sabia said in an interview. She presented the research at the 2021 Alzheimer’s Association International Conference.
Those previous studies found a U-shaped association between sleep duration and dementia risk, with lowest risk associated with 7-8 hours of sleep, but greater risk for shorter and longer durations. However, because the studies had follow-up periods shorter than 10 years, they are at greater risk of reverse causation bias. Longer follow-up studies tended to have small sample sizes or to focus on older adults.
The longer follow-up in the current study makes for a more compelling case, said Claire Sexton, DPhil, director of Scientific Programs & Outreach for the Alzheimer’s Association. Observations of short or long sleep closer to the onset of symptoms could just be a warning sign of dementia. “But looking at age 50, age 60 ... if you’re seeing those relationships, then it’s less likely that it is just purely prodromal,” said Dr. Sexton. But it still doesn’t necessarily confirm causation. “It could also be a risk factor,” Dr. Sexton added.
Multifactorial risk
Dr. Sabia also noted that the magnitude of risk was similar to that seen with smoking or obesity, and many factors play a role in dementia risk. “Even if the risk of dementia was 30% higher in those with persistent short sleep duration, in absolute terms, the percentage of those with persistent short duration who developed dementia was 8%, and 6% in those with persistent sleep duration of 7 hours. Dementia is a multifactorial disease, which means that several factors are likely to influence its onset. Sleep duration is one of them, but if a person has poor sleep and does not manage to increase it, there are other important prevention measures. It is important to keep a healthy lifestyle and cardiometabolic measures in the normal range. All together it is likely to be beneficial for brain health in later life,” she said.
Dr. Sexton agreed. “With sleep we’re still trying to tease apart what aspect of sleep is important. Is it the sleep duration? Is it the quality of sleep? Is it certain sleep stages?” she said.
Regardless of sleep’s potential influence on dementia risk, both Dr. Sexton and Dr. Sabia noted the importance of sleep for general health. “These types of problems are very prevalent, so it’s good for people to be aware of them. And then if they notice any problems with their sleep, or any changes, to go and see their health care provider, and to be discussing them, and then to be investigating the cause, and to see whether changes in sleep hygiene and treatments for insomnia could address these sleep problems,” said Dr. Sexton.
Decades of data
During the Whitehall II study, researchers assessed average sleep duration (“How many hours of sleep do you have on an average weeknight?”) six times over 30 years of follow-up. Dr. Sabia’s group extracted self-reported sleep duration data at ages 50, 60, and 70. Short sleep duration was defined as fewer than 5 hours, or 6 hours. Normal sleep duration was defined as 7 hours. Long duration was defined as 8 hours or more.
A questioner during the Q&A period noted that this grouping is a little unusual. Many studies define 7-8 hours as normal. Dr. Sabia answered that they were unable to examine periods of 9 hours or more due to the nature of the data, and the lowest associated risk was found at 7 hours.
The researchers analyzed data from 7,959 participants (33.0% women). At age 50, compared with 7 hours of sleep, 6 or few hours of sleep was associated with a higher risk of dementia over the ensuing 25 years of follow-up (hazard ratio [HR], 1.22; 95% confidence interval [CI], 1.01-1.48). The same was true at age 60 (15 years of follow-up HR, 1.37; 95% CI, 1.10-1.72). There was a trend at age 70 (8 years follow-up; HR, 1.24; 95% CI, 0.98-1.57). For 8 or more hours of sleep, there were trends toward increased risk at age 50 (HR, 1.25; 95% CI, 0.98-1.60). Long sleep at age 60 and 70 was associated with heightened risk, but the confidence intervals were well outside statistical significance.
Twenty percent of participants had persistent short sleep over the course of follow-up, 37% had persistent normal sleep, and 7% had persistent long sleep. Seven percent of participants experienced a change from normal sleep to short sleep, 16% had a change from short sleep to normal sleep, and 13% had a change from normal sleep to long sleep.
Persistent short sleep between age 50 and 70 was associated with a 30% increased risk of dementia (HR, 1.30; 95% CI, 1.00-1.69). There were no statistically significant associations between dementia risk and any of the changing sleep pattern groups.
Dr. Sabia and Dr. Sexton have no relevant financial disclosures.
, according to a new analysis of data from the Whitehall II cohort study.
Previous work had identified links between short sleep duration and dementia risk, but few studies examined sleep habits long before onset of dementia. Those that did produced inconsistent results, according to Séverine Sabia, PhD, who is a research associate at Inserm (France) and the University College London.
“One potential reason for these inconstancies is the large range of ages of the study populations, and the small number of participants within each sleep duration group. The novelty of our study is to examine this association among almost 8,000 participants with a follow-up of 30 years, using repeated measures of sleep duration starting in midlife to consider sleep duration at specific ages,” Dr. Sabia said in an interview. She presented the research at the 2021 Alzheimer’s Association International Conference.
Those previous studies found a U-shaped association between sleep duration and dementia risk, with lowest risk associated with 7-8 hours of sleep, but greater risk for shorter and longer durations. However, because the studies had follow-up periods shorter than 10 years, they are at greater risk of reverse causation bias. Longer follow-up studies tended to have small sample sizes or to focus on older adults.
The longer follow-up in the current study makes for a more compelling case, said Claire Sexton, DPhil, director of Scientific Programs & Outreach for the Alzheimer’s Association. Observations of short or long sleep closer to the onset of symptoms could just be a warning sign of dementia. “But looking at age 50, age 60 ... if you’re seeing those relationships, then it’s less likely that it is just purely prodromal,” said Dr. Sexton. But it still doesn’t necessarily confirm causation. “It could also be a risk factor,” Dr. Sexton added.
Multifactorial risk
Dr. Sabia also noted that the magnitude of risk was similar to that seen with smoking or obesity, and many factors play a role in dementia risk. “Even if the risk of dementia was 30% higher in those with persistent short sleep duration, in absolute terms, the percentage of those with persistent short duration who developed dementia was 8%, and 6% in those with persistent sleep duration of 7 hours. Dementia is a multifactorial disease, which means that several factors are likely to influence its onset. Sleep duration is one of them, but if a person has poor sleep and does not manage to increase it, there are other important prevention measures. It is important to keep a healthy lifestyle and cardiometabolic measures in the normal range. All together it is likely to be beneficial for brain health in later life,” she said.
Dr. Sexton agreed. “With sleep we’re still trying to tease apart what aspect of sleep is important. Is it the sleep duration? Is it the quality of sleep? Is it certain sleep stages?” she said.
Regardless of sleep’s potential influence on dementia risk, both Dr. Sexton and Dr. Sabia noted the importance of sleep for general health. “These types of problems are very prevalent, so it’s good for people to be aware of them. And then if they notice any problems with their sleep, or any changes, to go and see their health care provider, and to be discussing them, and then to be investigating the cause, and to see whether changes in sleep hygiene and treatments for insomnia could address these sleep problems,” said Dr. Sexton.
Decades of data
During the Whitehall II study, researchers assessed average sleep duration (“How many hours of sleep do you have on an average weeknight?”) six times over 30 years of follow-up. Dr. Sabia’s group extracted self-reported sleep duration data at ages 50, 60, and 70. Short sleep duration was defined as fewer than 5 hours, or 6 hours. Normal sleep duration was defined as 7 hours. Long duration was defined as 8 hours or more.
A questioner during the Q&A period noted that this grouping is a little unusual. Many studies define 7-8 hours as normal. Dr. Sabia answered that they were unable to examine periods of 9 hours or more due to the nature of the data, and the lowest associated risk was found at 7 hours.
The researchers analyzed data from 7,959 participants (33.0% women). At age 50, compared with 7 hours of sleep, 6 or few hours of sleep was associated with a higher risk of dementia over the ensuing 25 years of follow-up (hazard ratio [HR], 1.22; 95% confidence interval [CI], 1.01-1.48). The same was true at age 60 (15 years of follow-up HR, 1.37; 95% CI, 1.10-1.72). There was a trend at age 70 (8 years follow-up; HR, 1.24; 95% CI, 0.98-1.57). For 8 or more hours of sleep, there were trends toward increased risk at age 50 (HR, 1.25; 95% CI, 0.98-1.60). Long sleep at age 60 and 70 was associated with heightened risk, but the confidence intervals were well outside statistical significance.
Twenty percent of participants had persistent short sleep over the course of follow-up, 37% had persistent normal sleep, and 7% had persistent long sleep. Seven percent of participants experienced a change from normal sleep to short sleep, 16% had a change from short sleep to normal sleep, and 13% had a change from normal sleep to long sleep.
Persistent short sleep between age 50 and 70 was associated with a 30% increased risk of dementia (HR, 1.30; 95% CI, 1.00-1.69). There were no statistically significant associations between dementia risk and any of the changing sleep pattern groups.
Dr. Sabia and Dr. Sexton have no relevant financial disclosures.
, according to a new analysis of data from the Whitehall II cohort study.
Previous work had identified links between short sleep duration and dementia risk, but few studies examined sleep habits long before onset of dementia. Those that did produced inconsistent results, according to Séverine Sabia, PhD, who is a research associate at Inserm (France) and the University College London.
“One potential reason for these inconstancies is the large range of ages of the study populations, and the small number of participants within each sleep duration group. The novelty of our study is to examine this association among almost 8,000 participants with a follow-up of 30 years, using repeated measures of sleep duration starting in midlife to consider sleep duration at specific ages,” Dr. Sabia said in an interview. She presented the research at the 2021 Alzheimer’s Association International Conference.
Those previous studies found a U-shaped association between sleep duration and dementia risk, with lowest risk associated with 7-8 hours of sleep, but greater risk for shorter and longer durations. However, because the studies had follow-up periods shorter than 10 years, they are at greater risk of reverse causation bias. Longer follow-up studies tended to have small sample sizes or to focus on older adults.
The longer follow-up in the current study makes for a more compelling case, said Claire Sexton, DPhil, director of Scientific Programs & Outreach for the Alzheimer’s Association. Observations of short or long sleep closer to the onset of symptoms could just be a warning sign of dementia. “But looking at age 50, age 60 ... if you’re seeing those relationships, then it’s less likely that it is just purely prodromal,” said Dr. Sexton. But it still doesn’t necessarily confirm causation. “It could also be a risk factor,” Dr. Sexton added.
Multifactorial risk
Dr. Sabia also noted that the magnitude of risk was similar to that seen with smoking or obesity, and many factors play a role in dementia risk. “Even if the risk of dementia was 30% higher in those with persistent short sleep duration, in absolute terms, the percentage of those with persistent short duration who developed dementia was 8%, and 6% in those with persistent sleep duration of 7 hours. Dementia is a multifactorial disease, which means that several factors are likely to influence its onset. Sleep duration is one of them, but if a person has poor sleep and does not manage to increase it, there are other important prevention measures. It is important to keep a healthy lifestyle and cardiometabolic measures in the normal range. All together it is likely to be beneficial for brain health in later life,” she said.
Dr. Sexton agreed. “With sleep we’re still trying to tease apart what aspect of sleep is important. Is it the sleep duration? Is it the quality of sleep? Is it certain sleep stages?” she said.
Regardless of sleep’s potential influence on dementia risk, both Dr. Sexton and Dr. Sabia noted the importance of sleep for general health. “These types of problems are very prevalent, so it’s good for people to be aware of them. And then if they notice any problems with their sleep, or any changes, to go and see their health care provider, and to be discussing them, and then to be investigating the cause, and to see whether changes in sleep hygiene and treatments for insomnia could address these sleep problems,” said Dr. Sexton.
Decades of data
During the Whitehall II study, researchers assessed average sleep duration (“How many hours of sleep do you have on an average weeknight?”) six times over 30 years of follow-up. Dr. Sabia’s group extracted self-reported sleep duration data at ages 50, 60, and 70. Short sleep duration was defined as fewer than 5 hours, or 6 hours. Normal sleep duration was defined as 7 hours. Long duration was defined as 8 hours or more.
A questioner during the Q&A period noted that this grouping is a little unusual. Many studies define 7-8 hours as normal. Dr. Sabia answered that they were unable to examine periods of 9 hours or more due to the nature of the data, and the lowest associated risk was found at 7 hours.
The researchers analyzed data from 7,959 participants (33.0% women). At age 50, compared with 7 hours of sleep, 6 or few hours of sleep was associated with a higher risk of dementia over the ensuing 25 years of follow-up (hazard ratio [HR], 1.22; 95% confidence interval [CI], 1.01-1.48). The same was true at age 60 (15 years of follow-up HR, 1.37; 95% CI, 1.10-1.72). There was a trend at age 70 (8 years follow-up; HR, 1.24; 95% CI, 0.98-1.57). For 8 or more hours of sleep, there were trends toward increased risk at age 50 (HR, 1.25; 95% CI, 0.98-1.60). Long sleep at age 60 and 70 was associated with heightened risk, but the confidence intervals were well outside statistical significance.
Twenty percent of participants had persistent short sleep over the course of follow-up, 37% had persistent normal sleep, and 7% had persistent long sleep. Seven percent of participants experienced a change from normal sleep to short sleep, 16% had a change from short sleep to normal sleep, and 13% had a change from normal sleep to long sleep.
Persistent short sleep between age 50 and 70 was associated with a 30% increased risk of dementia (HR, 1.30; 95% CI, 1.00-1.69). There were no statistically significant associations between dementia risk and any of the changing sleep pattern groups.
Dr. Sabia and Dr. Sexton have no relevant financial disclosures.
FROM AAIC 2021