User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Decreasing the burden of postacute sequelae of SARS-CoV-2 infection: What we know
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
Final rule update – November 2021
The 2,414 page final rule for the CMS Physician Fee Schedule (PFS) was published on November 2, 2021, and contains a number of changes that are important for pulmonary/critical care/ sleep providers. As is typical, the rule does bring some good news, as well as decisions that are seemingly contrary to logic and precedence. Most of the changes will be effective on January 1, 2022, although some will become effective when the inpatient evaluation and management (E/M) changes take effect in 2023. For more information, please see 2021-23972.pdf (federalregister.gov).
The first change to be noted is a decrease in the conversion factor from $34.89 to $33.59. This is due primarily to the expiration of the 3.75% increase that was mandated by the Consolidated Appropriations Act of 2021. On a positive note, CMS did institute a plan to update clinical labor prices over the next 4 years, which will result in an increase in reimbursement for practice expense costs. CMS predicts that the combined impact of these two changes will result in no change in reimbursement for pulmonary or critical care medicine. Unfortunately, CMS did not publish data for sleep medicine.
There will be substantial changes in critical care services beginning next year. The CPT® definition of critical care will continue to be recognized by CMS, and the list of bundled services remains the same. Providers may now report critical care services with E/M visits done on the same day. The E/M visit must precede the critical care service, and it must be documented that the patient did not require critical care services at that time. The critical care visit must also be billed with a –25 modifier. This also applies to multiple practitioners in the same group of the same specialty. Critical care services provided concurrently by multiple practitioners of different specialties may now be billed by each individual practitioner if the services are medically necessary. There was a concern that CMS would not allow billing of critical care services during a surgical global period, but this will be allowed if the critical care services are unrelated to the general surgical procedure performed. There will be a new modifier developed to allow CMS to track this care. If critical care management is transferred from the surgeon to an intensivist, then the latter will append modifier –55 (postoperative management only), as well as the new modifier. Finally, and most importantly, CMS now recognizes the benefit of team-based care and will allow split (or shared) billing of critical care services. Physicians and qualified nonphysician providers (NPP) add their times to determine the level of critical care services. The provider who is responsible for more than half of the critical care time should be the billing provider.
Pulmonary rehabilitation CPT codes 94625 and 94626 were accepted by CMS but the RVU values recommended by the RUC were not. CPT code 94625 received a finalized work RVU of 0.36 and code 94626 received 0.56. On a more positive note, patients hospitalized with COVID-19 who are having persistent symptoms, including respiratory dysfunction, for at least 4 weeks after hospitalization would now qualify for pulmonary rehab services. The current pulmonary rehabilitation HCPCS code G0424 is replaced by the two new CPT codes and should no longer be used after December 31, 2021.
These are but a few of the changes in the final rule that may impact one’s practice. Additional changes may be found in the final rule link 2021-23972.pdf (federalregister.gov) and in future CHEST Physician editions.
The 2,414 page final rule for the CMS Physician Fee Schedule (PFS) was published on November 2, 2021, and contains a number of changes that are important for pulmonary/critical care/ sleep providers. As is typical, the rule does bring some good news, as well as decisions that are seemingly contrary to logic and precedence. Most of the changes will be effective on January 1, 2022, although some will become effective when the inpatient evaluation and management (E/M) changes take effect in 2023. For more information, please see 2021-23972.pdf (federalregister.gov).
The first change to be noted is a decrease in the conversion factor from $34.89 to $33.59. This is due primarily to the expiration of the 3.75% increase that was mandated by the Consolidated Appropriations Act of 2021. On a positive note, CMS did institute a plan to update clinical labor prices over the next 4 years, which will result in an increase in reimbursement for practice expense costs. CMS predicts that the combined impact of these two changes will result in no change in reimbursement for pulmonary or critical care medicine. Unfortunately, CMS did not publish data for sleep medicine.
There will be substantial changes in critical care services beginning next year. The CPT® definition of critical care will continue to be recognized by CMS, and the list of bundled services remains the same. Providers may now report critical care services with E/M visits done on the same day. The E/M visit must precede the critical care service, and it must be documented that the patient did not require critical care services at that time. The critical care visit must also be billed with a –25 modifier. This also applies to multiple practitioners in the same group of the same specialty. Critical care services provided concurrently by multiple practitioners of different specialties may now be billed by each individual practitioner if the services are medically necessary. There was a concern that CMS would not allow billing of critical care services during a surgical global period, but this will be allowed if the critical care services are unrelated to the general surgical procedure performed. There will be a new modifier developed to allow CMS to track this care. If critical care management is transferred from the surgeon to an intensivist, then the latter will append modifier –55 (postoperative management only), as well as the new modifier. Finally, and most importantly, CMS now recognizes the benefit of team-based care and will allow split (or shared) billing of critical care services. Physicians and qualified nonphysician providers (NPP) add their times to determine the level of critical care services. The provider who is responsible for more than half of the critical care time should be the billing provider.
Pulmonary rehabilitation CPT codes 94625 and 94626 were accepted by CMS but the RVU values recommended by the RUC were not. CPT code 94625 received a finalized work RVU of 0.36 and code 94626 received 0.56. On a more positive note, patients hospitalized with COVID-19 who are having persistent symptoms, including respiratory dysfunction, for at least 4 weeks after hospitalization would now qualify for pulmonary rehab services. The current pulmonary rehabilitation HCPCS code G0424 is replaced by the two new CPT codes and should no longer be used after December 31, 2021.
These are but a few of the changes in the final rule that may impact one’s practice. Additional changes may be found in the final rule link 2021-23972.pdf (federalregister.gov) and in future CHEST Physician editions.
The 2,414 page final rule for the CMS Physician Fee Schedule (PFS) was published on November 2, 2021, and contains a number of changes that are important for pulmonary/critical care/ sleep providers. As is typical, the rule does bring some good news, as well as decisions that are seemingly contrary to logic and precedence. Most of the changes will be effective on January 1, 2022, although some will become effective when the inpatient evaluation and management (E/M) changes take effect in 2023. For more information, please see 2021-23972.pdf (federalregister.gov).
The first change to be noted is a decrease in the conversion factor from $34.89 to $33.59. This is due primarily to the expiration of the 3.75% increase that was mandated by the Consolidated Appropriations Act of 2021. On a positive note, CMS did institute a plan to update clinical labor prices over the next 4 years, which will result in an increase in reimbursement for practice expense costs. CMS predicts that the combined impact of these two changes will result in no change in reimbursement for pulmonary or critical care medicine. Unfortunately, CMS did not publish data for sleep medicine.
There will be substantial changes in critical care services beginning next year. The CPT® definition of critical care will continue to be recognized by CMS, and the list of bundled services remains the same. Providers may now report critical care services with E/M visits done on the same day. The E/M visit must precede the critical care service, and it must be documented that the patient did not require critical care services at that time. The critical care visit must also be billed with a –25 modifier. This also applies to multiple practitioners in the same group of the same specialty. Critical care services provided concurrently by multiple practitioners of different specialties may now be billed by each individual practitioner if the services are medically necessary. There was a concern that CMS would not allow billing of critical care services during a surgical global period, but this will be allowed if the critical care services are unrelated to the general surgical procedure performed. There will be a new modifier developed to allow CMS to track this care. If critical care management is transferred from the surgeon to an intensivist, then the latter will append modifier –55 (postoperative management only), as well as the new modifier. Finally, and most importantly, CMS now recognizes the benefit of team-based care and will allow split (or shared) billing of critical care services. Physicians and qualified nonphysician providers (NPP) add their times to determine the level of critical care services. The provider who is responsible for more than half of the critical care time should be the billing provider.
Pulmonary rehabilitation CPT codes 94625 and 94626 were accepted by CMS but the RVU values recommended by the RUC were not. CPT code 94625 received a finalized work RVU of 0.36 and code 94626 received 0.56. On a more positive note, patients hospitalized with COVID-19 who are having persistent symptoms, including respiratory dysfunction, for at least 4 weeks after hospitalization would now qualify for pulmonary rehab services. The current pulmonary rehabilitation HCPCS code G0424 is replaced by the two new CPT codes and should no longer be used after December 31, 2021.
These are but a few of the changes in the final rule that may impact one’s practice. Additional changes may be found in the final rule link 2021-23972.pdf (federalregister.gov) and in future CHEST Physician editions.
CHEST SEEK™ Education enhances learning with interactive discussions
If you’ve ever wondered about the content creation process that goes into exam study material, SEEK is offering you an insider perspective.
Recently added to the SEEK Library, CHEST SEEK™ Peer Review Discussions are behind-the-scenes recordings of the deliberations and debates between SEEK Editorial Board members as they review their draft questions. Each video showcases CHEST authors reviewing and finessing a case-based chest medicine question to prepare for its inclusion in printed SEEK books and the electronic library.
With an opportunity to glean invaluable knowledge from distinguished practitioners in the pulmonary, critical care, and sleep medicine fields, SEEK Peer Review Discussions can be used to help supplement board exam study, advance one’s clinical knowledge, and learn from the peer review process for their own professional development.
“The opportunity to observe how much critical review there is from a scientific content standpoint – and also from a test creation standpoint – is really interesting,” said CHEST SEEK Sleep Editor and President-Elect David Schulman, MD, MPH, FCCP.
“Many of us on SEEK have written for some of the standardized exams that readers will take,” he said. “Somebody can learn how writers come up with wrong answers and think, ‘‘If I can see how this test is constructed, I may have a better chance of doing well on it.’”
SEEK Peer Review Discussions not only offer a more engaging form of education but also provide an opportunity to watch leaders in the field test, challenge, and collaborate with one another.
“The audience gets to see that these big names you see on the page – authors, coauthors, and editors – are just normal people like anybody else,” Dr. Schulman said. “They joke around a little bit, and they push each other a little bit. I think getting to see under the hood of CHEST and seeing what leadership is like is a really valuable experience.”
Through these discussions, CHEST SEEK learners discover the intensity and rigorousness of the conversations with a window into CHEST leaders’ discourse.
The collection of SEEK Peer Review Discussions is part of the new, enhanced CHEST SEEK subscription option, SEEK Library Plus. Available for subscription viewing now are three question videos from the SEEK Pulmonary Medicine Editorial Board and three question videos from the SEEK Sleep Medicine Editorial Board.
Subscribers to SEEK Library Plus also gain access to SEEK Session videos from CHEST Board Review 2021, a print export study pack plus a compilation of favorite questions from SEEK’s 30-year history.
For a sneak peek of the peer review videos and to subscribe to SEEK Library Plus, visit seeklibrary.chestnet.org.
If you’ve ever wondered about the content creation process that goes into exam study material, SEEK is offering you an insider perspective.
Recently added to the SEEK Library, CHEST SEEK™ Peer Review Discussions are behind-the-scenes recordings of the deliberations and debates between SEEK Editorial Board members as they review their draft questions. Each video showcases CHEST authors reviewing and finessing a case-based chest medicine question to prepare for its inclusion in printed SEEK books and the electronic library.
With an opportunity to glean invaluable knowledge from distinguished practitioners in the pulmonary, critical care, and sleep medicine fields, SEEK Peer Review Discussions can be used to help supplement board exam study, advance one’s clinical knowledge, and learn from the peer review process for their own professional development.
“The opportunity to observe how much critical review there is from a scientific content standpoint – and also from a test creation standpoint – is really interesting,” said CHEST SEEK Sleep Editor and President-Elect David Schulman, MD, MPH, FCCP.
“Many of us on SEEK have written for some of the standardized exams that readers will take,” he said. “Somebody can learn how writers come up with wrong answers and think, ‘‘If I can see how this test is constructed, I may have a better chance of doing well on it.’”
SEEK Peer Review Discussions not only offer a more engaging form of education but also provide an opportunity to watch leaders in the field test, challenge, and collaborate with one another.
“The audience gets to see that these big names you see on the page – authors, coauthors, and editors – are just normal people like anybody else,” Dr. Schulman said. “They joke around a little bit, and they push each other a little bit. I think getting to see under the hood of CHEST and seeing what leadership is like is a really valuable experience.”
Through these discussions, CHEST SEEK learners discover the intensity and rigorousness of the conversations with a window into CHEST leaders’ discourse.
The collection of SEEK Peer Review Discussions is part of the new, enhanced CHEST SEEK subscription option, SEEK Library Plus. Available for subscription viewing now are three question videos from the SEEK Pulmonary Medicine Editorial Board and three question videos from the SEEK Sleep Medicine Editorial Board.
Subscribers to SEEK Library Plus also gain access to SEEK Session videos from CHEST Board Review 2021, a print export study pack plus a compilation of favorite questions from SEEK’s 30-year history.
For a sneak peek of the peer review videos and to subscribe to SEEK Library Plus, visit seeklibrary.chestnet.org.
If you’ve ever wondered about the content creation process that goes into exam study material, SEEK is offering you an insider perspective.
Recently added to the SEEK Library, CHEST SEEK™ Peer Review Discussions are behind-the-scenes recordings of the deliberations and debates between SEEK Editorial Board members as they review their draft questions. Each video showcases CHEST authors reviewing and finessing a case-based chest medicine question to prepare for its inclusion in printed SEEK books and the electronic library.
With an opportunity to glean invaluable knowledge from distinguished practitioners in the pulmonary, critical care, and sleep medicine fields, SEEK Peer Review Discussions can be used to help supplement board exam study, advance one’s clinical knowledge, and learn from the peer review process for their own professional development.
“The opportunity to observe how much critical review there is from a scientific content standpoint – and also from a test creation standpoint – is really interesting,” said CHEST SEEK Sleep Editor and President-Elect David Schulman, MD, MPH, FCCP.
“Many of us on SEEK have written for some of the standardized exams that readers will take,” he said. “Somebody can learn how writers come up with wrong answers and think, ‘‘If I can see how this test is constructed, I may have a better chance of doing well on it.’”
SEEK Peer Review Discussions not only offer a more engaging form of education but also provide an opportunity to watch leaders in the field test, challenge, and collaborate with one another.
“The audience gets to see that these big names you see on the page – authors, coauthors, and editors – are just normal people like anybody else,” Dr. Schulman said. “They joke around a little bit, and they push each other a little bit. I think getting to see under the hood of CHEST and seeing what leadership is like is a really valuable experience.”
Through these discussions, CHEST SEEK learners discover the intensity and rigorousness of the conversations with a window into CHEST leaders’ discourse.
The collection of SEEK Peer Review Discussions is part of the new, enhanced CHEST SEEK subscription option, SEEK Library Plus. Available for subscription viewing now are three question videos from the SEEK Pulmonary Medicine Editorial Board and three question videos from the SEEK Sleep Medicine Editorial Board.
Subscribers to SEEK Library Plus also gain access to SEEK Session videos from CHEST Board Review 2021, a print export study pack plus a compilation of favorite questions from SEEK’s 30-year history.
For a sneak peek of the peer review videos and to subscribe to SEEK Library Plus, visit seeklibrary.chestnet.org.
This month in the journal CHEST®
Editor’s picks
Fertility and pregnancy in cystic fibrosis By Dr. M. Shteinberg, et al.Changes in purchases for intensive care medicines during the COVID-19 pandemic: A global time series study By Dr. K. Kim, et al.The impact of obesity in critical illness By Drs. M.R. Anderson and M. Shashaty
Strategies to improve bedside clinical skills teaching By Drs. B. Garibaldi and S.W. RussellAntithrombotic therapy for VTE Disease: Second update of the CHEST guideline and expert panel report – executive summary By Dr. S.M. Stevens, et al.
Editor’s picks
Editor’s picks
Fertility and pregnancy in cystic fibrosis By Dr. M. Shteinberg, et al.Changes in purchases for intensive care medicines during the COVID-19 pandemic: A global time series study By Dr. K. Kim, et al.The impact of obesity in critical illness By Drs. M.R. Anderson and M. Shashaty
Strategies to improve bedside clinical skills teaching By Drs. B. Garibaldi and S.W. RussellAntithrombotic therapy for VTE Disease: Second update of the CHEST guideline and expert panel report – executive summary By Dr. S.M. Stevens, et al.
Fertility and pregnancy in cystic fibrosis By Dr. M. Shteinberg, et al.Changes in purchases for intensive care medicines during the COVID-19 pandemic: A global time series study By Dr. K. Kim, et al.The impact of obesity in critical illness By Drs. M.R. Anderson and M. Shashaty
Strategies to improve bedside clinical skills teaching By Drs. B. Garibaldi and S.W. RussellAntithrombotic therapy for VTE Disease: Second update of the CHEST guideline and expert panel report – executive summary By Dr. S.M. Stevens, et al.
Transitioning from fellow to attending
It’s day 1 of “attendingship,” and I’m back to wearing my white coat after years of being confident enough in myself to think I didn’t need it to look like “the doctor.” Is it okay to park here? Does my clinic have a staff bathroom? Will my log in work? Oh my gosh, how do I place orders?! I remember this feeling – it’s intern year all over again, except there’s no senior resident to rescue me now – here we go!
Starting off
As a new attending, the amount of responsibility can be intimidating and overwhelming. It is important to remember that you are not alone, you have a whole team supporting you whether you are in clinic or the ICU. Be sure to introduce yourself to those who you will be working with, get to know them, their roles, and figure out the best way that you can help each other with the ultimate goal of helping patients. In addition to meeting your own team, it is important to introduce yourself to your new colleagues – especially if you are new to the institution. Drs. Fielder and Sihag suggest putting together an introductory email to those who may be referring to you that includes an overview of what you do and how you can help, as well as your contact information. They also suggest maintaining an open line of communication and keeping the referring provider updated on your mutual patient (Fiedler AG, Sihag S. J Thorac Cardiovasc Surg. 2020 Mar;159[3]:1156-60). While this may sound antiquated, in my experience thus far, my colleagues have greatly appreciated this gesture.
Finding support
Even though you will be surrounded by a plethora of new colleagues, the transition to attending can be lonely – especially if you are moving to a new institution. Be sure to keep in touch with your co-residents, co-fellows, mentors, and, of course, your friends and family. Studies have shown that support mitigates stress and reduces job strain, which can lead to better health outcomes in the long term (Fiedler AG, Sihag S. [above]). Another great source of support for me is my CHEST colleagues. If you have not already, I highly suggest joining the CHEST Network(s) that aligns with your career interests. This is a great way to not only network with those who share the same niche as you but also to explore academic opportunities outside of your institution. Through the CHEST Home Mechanical Ventilation and Sleep NetWorks, I have gained mentors, made friends, and have become more involved in CHEST’s annual meeting, chairing my first session this year.
Staying organized
Adjusting to your new schedule can be just as hard as adjusting to a new role or new institution. After years of moving through the well-oiled, regimented machine that is medical training, there are suddenly no more rotations, no more research blocks, and no more protected time for learning. Dr. Okereke suggests creating a weekly calendar, which blocks time for not only your clinical duties but for studying (as you will be taking boards during your first year), academic endeavors (teaching and/or research), and, most importantly – for fun (Okereke I. J Thorac Cardiovasc Surg. 2020 Mar;159[3]:1161-2). Being cognizant about maintaining work-life balance is key once you become an attending. It is finally time to learn how to take time off, away from all things work, and to not feel guilty about it.
Saying no
This brings me to saying “no.” We are taught to say “yes” to every opportunity throughout our careers and, while that can certainly help us get far, it can also lead to burnout. Once you’re an attending, you’re in it for the long haul, so best to say yes to the things you are most interested in and “spark joy,” as Marie Kondo says, and say no to the things that do not make you happy and are not congruent with your overall goals. Fielder and Sihag (above) note that your division director or chief typically has a vision in mind for you within the department. It is important to communicate with leadership so that everyone is on the same page and the administrative and academic opportunities afforded to you are in alignment with your career goals going forward.
Teaching trainees
To prepare for teaching as an attending, Dr. Greco recommends starting during your own training. She suggests cataloging your study materials and notes for later reference, curating talks throughout your training, and exploring different rounding styles prior to graduation (Greco, A. CHEST Thought Leader Blog. 2021 June). To get more experience in formal speaking, Dr. Shen and colleagues encourage getting involved in resident noon conferences (Shen JZ, Memon AA, Lin C. Stroke. 2019 Sep;50[9]:e250-e252). A benefit of being a critical care attending is that you can gain experience teaching not only with the internal medicine residents but with emergency medicine, anesthesiology, and critical care advanced practice provider residents, as well.
While lecturing is one thing, teaching on service is a whole different ball game. No matter how young, fun, and relatable you think you are, you’re the boss now. You’re the giver of grades and the writer of evaluations. It is important to be self-aware of your influence and be deliberate with the environment you create on rounds and in clinic. Set expectations on day 1 so that everyone understands. Be open with what you are working on. For example, I make daily goals for myself that I share with the team before rounds. Drs. Fielder and Sihag (above) suggest sharing anecdotes from your own time in training that can help both you and your trainees remember that you were just in their shoes. Allowing yourself to be vulnerable creates a safe space in which your learners feel more comfortable doing the same.
Lastly, delegation is key. While many of us have done this since residency, Dr. Shen et al (above) suggest deliberately practicing this during fellowship. If you were the fellow who was able to handle a lot on your own, trust that your own fellows will be able to do that. Delegating to your trainees helps you improve personal and team efficiency, provides fellows with needed autonomy, and allows you to further grow into the role of attending physician.
Conclusion
While you may be nervous starting out, trust that you have been well trained and have the clinical knowledge and skills you need to do your job – you are ready. Get to know the staff you will be working with, your colleagues, and keep in touch with your co-trainees and mentors who have helped you along the way. Make daily goals for yourself, and make time to read and reflect so that you can continue to learn and grow. Most of all, make time for yourself, your friends, and your family, because after years of supporting you through all of your hard work, you’ve finally made it – congrats!
Dr. Greer is Assistant Professor of Medicine, Emory University Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, Atlanta, GA.
It’s day 1 of “attendingship,” and I’m back to wearing my white coat after years of being confident enough in myself to think I didn’t need it to look like “the doctor.” Is it okay to park here? Does my clinic have a staff bathroom? Will my log in work? Oh my gosh, how do I place orders?! I remember this feeling – it’s intern year all over again, except there’s no senior resident to rescue me now – here we go!
Starting off
As a new attending, the amount of responsibility can be intimidating and overwhelming. It is important to remember that you are not alone, you have a whole team supporting you whether you are in clinic or the ICU. Be sure to introduce yourself to those who you will be working with, get to know them, their roles, and figure out the best way that you can help each other with the ultimate goal of helping patients. In addition to meeting your own team, it is important to introduce yourself to your new colleagues – especially if you are new to the institution. Drs. Fielder and Sihag suggest putting together an introductory email to those who may be referring to you that includes an overview of what you do and how you can help, as well as your contact information. They also suggest maintaining an open line of communication and keeping the referring provider updated on your mutual patient (Fiedler AG, Sihag S. J Thorac Cardiovasc Surg. 2020 Mar;159[3]:1156-60). While this may sound antiquated, in my experience thus far, my colleagues have greatly appreciated this gesture.
Finding support
Even though you will be surrounded by a plethora of new colleagues, the transition to attending can be lonely – especially if you are moving to a new institution. Be sure to keep in touch with your co-residents, co-fellows, mentors, and, of course, your friends and family. Studies have shown that support mitigates stress and reduces job strain, which can lead to better health outcomes in the long term (Fiedler AG, Sihag S. [above]). Another great source of support for me is my CHEST colleagues. If you have not already, I highly suggest joining the CHEST Network(s) that aligns with your career interests. This is a great way to not only network with those who share the same niche as you but also to explore academic opportunities outside of your institution. Through the CHEST Home Mechanical Ventilation and Sleep NetWorks, I have gained mentors, made friends, and have become more involved in CHEST’s annual meeting, chairing my first session this year.
Staying organized
Adjusting to your new schedule can be just as hard as adjusting to a new role or new institution. After years of moving through the well-oiled, regimented machine that is medical training, there are suddenly no more rotations, no more research blocks, and no more protected time for learning. Dr. Okereke suggests creating a weekly calendar, which blocks time for not only your clinical duties but for studying (as you will be taking boards during your first year), academic endeavors (teaching and/or research), and, most importantly – for fun (Okereke I. J Thorac Cardiovasc Surg. 2020 Mar;159[3]:1161-2). Being cognizant about maintaining work-life balance is key once you become an attending. It is finally time to learn how to take time off, away from all things work, and to not feel guilty about it.
Saying no
This brings me to saying “no.” We are taught to say “yes” to every opportunity throughout our careers and, while that can certainly help us get far, it can also lead to burnout. Once you’re an attending, you’re in it for the long haul, so best to say yes to the things you are most interested in and “spark joy,” as Marie Kondo says, and say no to the things that do not make you happy and are not congruent with your overall goals. Fielder and Sihag (above) note that your division director or chief typically has a vision in mind for you within the department. It is important to communicate with leadership so that everyone is on the same page and the administrative and academic opportunities afforded to you are in alignment with your career goals going forward.
Teaching trainees
To prepare for teaching as an attending, Dr. Greco recommends starting during your own training. She suggests cataloging your study materials and notes for later reference, curating talks throughout your training, and exploring different rounding styles prior to graduation (Greco, A. CHEST Thought Leader Blog. 2021 June). To get more experience in formal speaking, Dr. Shen and colleagues encourage getting involved in resident noon conferences (Shen JZ, Memon AA, Lin C. Stroke. 2019 Sep;50[9]:e250-e252). A benefit of being a critical care attending is that you can gain experience teaching not only with the internal medicine residents but with emergency medicine, anesthesiology, and critical care advanced practice provider residents, as well.
While lecturing is one thing, teaching on service is a whole different ball game. No matter how young, fun, and relatable you think you are, you’re the boss now. You’re the giver of grades and the writer of evaluations. It is important to be self-aware of your influence and be deliberate with the environment you create on rounds and in clinic. Set expectations on day 1 so that everyone understands. Be open with what you are working on. For example, I make daily goals for myself that I share with the team before rounds. Drs. Fielder and Sihag (above) suggest sharing anecdotes from your own time in training that can help both you and your trainees remember that you were just in their shoes. Allowing yourself to be vulnerable creates a safe space in which your learners feel more comfortable doing the same.
Lastly, delegation is key. While many of us have done this since residency, Dr. Shen et al (above) suggest deliberately practicing this during fellowship. If you were the fellow who was able to handle a lot on your own, trust that your own fellows will be able to do that. Delegating to your trainees helps you improve personal and team efficiency, provides fellows with needed autonomy, and allows you to further grow into the role of attending physician.
Conclusion
While you may be nervous starting out, trust that you have been well trained and have the clinical knowledge and skills you need to do your job – you are ready. Get to know the staff you will be working with, your colleagues, and keep in touch with your co-trainees and mentors who have helped you along the way. Make daily goals for yourself, and make time to read and reflect so that you can continue to learn and grow. Most of all, make time for yourself, your friends, and your family, because after years of supporting you through all of your hard work, you’ve finally made it – congrats!
Dr. Greer is Assistant Professor of Medicine, Emory University Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, Atlanta, GA.
It’s day 1 of “attendingship,” and I’m back to wearing my white coat after years of being confident enough in myself to think I didn’t need it to look like “the doctor.” Is it okay to park here? Does my clinic have a staff bathroom? Will my log in work? Oh my gosh, how do I place orders?! I remember this feeling – it’s intern year all over again, except there’s no senior resident to rescue me now – here we go!
Starting off
As a new attending, the amount of responsibility can be intimidating and overwhelming. It is important to remember that you are not alone, you have a whole team supporting you whether you are in clinic or the ICU. Be sure to introduce yourself to those who you will be working with, get to know them, their roles, and figure out the best way that you can help each other with the ultimate goal of helping patients. In addition to meeting your own team, it is important to introduce yourself to your new colleagues – especially if you are new to the institution. Drs. Fielder and Sihag suggest putting together an introductory email to those who may be referring to you that includes an overview of what you do and how you can help, as well as your contact information. They also suggest maintaining an open line of communication and keeping the referring provider updated on your mutual patient (Fiedler AG, Sihag S. J Thorac Cardiovasc Surg. 2020 Mar;159[3]:1156-60). While this may sound antiquated, in my experience thus far, my colleagues have greatly appreciated this gesture.
Finding support
Even though you will be surrounded by a plethora of new colleagues, the transition to attending can be lonely – especially if you are moving to a new institution. Be sure to keep in touch with your co-residents, co-fellows, mentors, and, of course, your friends and family. Studies have shown that support mitigates stress and reduces job strain, which can lead to better health outcomes in the long term (Fiedler AG, Sihag S. [above]). Another great source of support for me is my CHEST colleagues. If you have not already, I highly suggest joining the CHEST Network(s) that aligns with your career interests. This is a great way to not only network with those who share the same niche as you but also to explore academic opportunities outside of your institution. Through the CHEST Home Mechanical Ventilation and Sleep NetWorks, I have gained mentors, made friends, and have become more involved in CHEST’s annual meeting, chairing my first session this year.
Staying organized
Adjusting to your new schedule can be just as hard as adjusting to a new role or new institution. After years of moving through the well-oiled, regimented machine that is medical training, there are suddenly no more rotations, no more research blocks, and no more protected time for learning. Dr. Okereke suggests creating a weekly calendar, which blocks time for not only your clinical duties but for studying (as you will be taking boards during your first year), academic endeavors (teaching and/or research), and, most importantly – for fun (Okereke I. J Thorac Cardiovasc Surg. 2020 Mar;159[3]:1161-2). Being cognizant about maintaining work-life balance is key once you become an attending. It is finally time to learn how to take time off, away from all things work, and to not feel guilty about it.
Saying no
This brings me to saying “no.” We are taught to say “yes” to every opportunity throughout our careers and, while that can certainly help us get far, it can also lead to burnout. Once you’re an attending, you’re in it for the long haul, so best to say yes to the things you are most interested in and “spark joy,” as Marie Kondo says, and say no to the things that do not make you happy and are not congruent with your overall goals. Fielder and Sihag (above) note that your division director or chief typically has a vision in mind for you within the department. It is important to communicate with leadership so that everyone is on the same page and the administrative and academic opportunities afforded to you are in alignment with your career goals going forward.
Teaching trainees
To prepare for teaching as an attending, Dr. Greco recommends starting during your own training. She suggests cataloging your study materials and notes for later reference, curating talks throughout your training, and exploring different rounding styles prior to graduation (Greco, A. CHEST Thought Leader Blog. 2021 June). To get more experience in formal speaking, Dr. Shen and colleagues encourage getting involved in resident noon conferences (Shen JZ, Memon AA, Lin C. Stroke. 2019 Sep;50[9]:e250-e252). A benefit of being a critical care attending is that you can gain experience teaching not only with the internal medicine residents but with emergency medicine, anesthesiology, and critical care advanced practice provider residents, as well.
While lecturing is one thing, teaching on service is a whole different ball game. No matter how young, fun, and relatable you think you are, you’re the boss now. You’re the giver of grades and the writer of evaluations. It is important to be self-aware of your influence and be deliberate with the environment you create on rounds and in clinic. Set expectations on day 1 so that everyone understands. Be open with what you are working on. For example, I make daily goals for myself that I share with the team before rounds. Drs. Fielder and Sihag (above) suggest sharing anecdotes from your own time in training that can help both you and your trainees remember that you were just in their shoes. Allowing yourself to be vulnerable creates a safe space in which your learners feel more comfortable doing the same.
Lastly, delegation is key. While many of us have done this since residency, Dr. Shen et al (above) suggest deliberately practicing this during fellowship. If you were the fellow who was able to handle a lot on your own, trust that your own fellows will be able to do that. Delegating to your trainees helps you improve personal and team efficiency, provides fellows with needed autonomy, and allows you to further grow into the role of attending physician.
Conclusion
While you may be nervous starting out, trust that you have been well trained and have the clinical knowledge and skills you need to do your job – you are ready. Get to know the staff you will be working with, your colleagues, and keep in touch with your co-trainees and mentors who have helped you along the way. Make daily goals for yourself, and make time to read and reflect so that you can continue to learn and grow. Most of all, make time for yourself, your friends, and your family, because after years of supporting you through all of your hard work, you’ve finally made it – congrats!
Dr. Greer is Assistant Professor of Medicine, Emory University Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine, Atlanta, GA.
FDA authorizes Pfizer boosters for 16- and 17-year-olds
, clearing the way for millions of teenagers to get a third dose of vaccine starting 6 months after their second dose.
The FDA said it was basing its emergency authorization of boosters for 16- and 17-year-olds on data from 200 individuals who were 18-55 years of age when they received a booster dose. They are requiring Pfizer to collect data on safety in postauthorization studies.
“The FDA has determined that the benefits of a single booster dose of the Pfizer-BioNTech COVID-19 Vaccine or Comirnaty outweigh the risks of myocarditis and pericarditis in individuals 16 and 17 years of age to provide continued protection against COVID-19 and the associated serious consequences that can occur including hospitalization and death,” the agency said in a news release.
Israel has been giving booster doses of Pfizer’s vaccine to everyone 12 and up since late August. Data from that country show that myocarditis cases continue to be very rare, even in younger age groups, and are mild and temporary.
The authorization comes as the effectiveness of the current vaccines against the new Omicron variant has become a point of intense scientific inquiry.
Early studies suggest that booster doses may be necessary to keep Omicron at bay, at least until new variant-specific vaccines are ready next spring.
Current evidence suggests that the protection of the vaccines is holding up well against severe disease and death, at least with Delta and early iterations of the virus.
How well they will do against Omicron, and how severe Omicron infections may be for different age groups, remain open questions.
On Dec. 8, the World Health Organization urged countries not to wait for all the science to come in, but to act now to contain any potential threat.
The first pieces of evidence on Omicron suggest that it is highly contagious, perhaps even more than Delta, though early reports suggest symptoms caused by this version of the new coronavirus may be less severe than in previous waves. Experts have cautioned that the true severity of Omicron infections isn’t yet known, since the first cases have been detected in younger people, who tend to have milder COVID-19 symptoms than those of adults and seniors.
“Vaccination and getting a booster when eligible, along with other preventive measures like masking and avoiding large crowds and poorly ventilated spaces, remain our most effective methods for fighting COVID-19,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release. “As people gather indoors with family and friends for the holidays, we can’t let up on all the preventive public health measures that we have been taking during the pandemic. With both the Delta and Omicron variants continuing to spread, vaccination remains the best protection against COVID-19.”
In mid-November, the FDA authorized boosters of the Pfizer vaccine for all individuals 18 and older, but the agency held off on expanding the use of boosters for younger age groups, partly because they have the highest risk of myocarditis, a very rare side effect.
Myocarditis cases seem to be temporary, with patients making a full recovery, though they need to be monitored in the hospital. The risk of myocarditis with a COVID-19 infection is many times higher than it is from a vaccine.
There have been little data to support the need for boosters in this age group, because children and teens tend to experience milder COVID-19 disease, though they are still at risk for post–COVID-19 complications such as long COVID and a delayed reaction to the virus called Post Acute Sequelae of SARS-CoV2 Infection among Children, or PAS-C.
All that changed with the arrival of Omicron.
A version of this article first appeared on WebMD.com.
, clearing the way for millions of teenagers to get a third dose of vaccine starting 6 months after their second dose.
The FDA said it was basing its emergency authorization of boosters for 16- and 17-year-olds on data from 200 individuals who were 18-55 years of age when they received a booster dose. They are requiring Pfizer to collect data on safety in postauthorization studies.
“The FDA has determined that the benefits of a single booster dose of the Pfizer-BioNTech COVID-19 Vaccine or Comirnaty outweigh the risks of myocarditis and pericarditis in individuals 16 and 17 years of age to provide continued protection against COVID-19 and the associated serious consequences that can occur including hospitalization and death,” the agency said in a news release.
Israel has been giving booster doses of Pfizer’s vaccine to everyone 12 and up since late August. Data from that country show that myocarditis cases continue to be very rare, even in younger age groups, and are mild and temporary.
The authorization comes as the effectiveness of the current vaccines against the new Omicron variant has become a point of intense scientific inquiry.
Early studies suggest that booster doses may be necessary to keep Omicron at bay, at least until new variant-specific vaccines are ready next spring.
Current evidence suggests that the protection of the vaccines is holding up well against severe disease and death, at least with Delta and early iterations of the virus.
How well they will do against Omicron, and how severe Omicron infections may be for different age groups, remain open questions.
On Dec. 8, the World Health Organization urged countries not to wait for all the science to come in, but to act now to contain any potential threat.
The first pieces of evidence on Omicron suggest that it is highly contagious, perhaps even more than Delta, though early reports suggest symptoms caused by this version of the new coronavirus may be less severe than in previous waves. Experts have cautioned that the true severity of Omicron infections isn’t yet known, since the first cases have been detected in younger people, who tend to have milder COVID-19 symptoms than those of adults and seniors.
“Vaccination and getting a booster when eligible, along with other preventive measures like masking and avoiding large crowds and poorly ventilated spaces, remain our most effective methods for fighting COVID-19,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release. “As people gather indoors with family and friends for the holidays, we can’t let up on all the preventive public health measures that we have been taking during the pandemic. With both the Delta and Omicron variants continuing to spread, vaccination remains the best protection against COVID-19.”
In mid-November, the FDA authorized boosters of the Pfizer vaccine for all individuals 18 and older, but the agency held off on expanding the use of boosters for younger age groups, partly because they have the highest risk of myocarditis, a very rare side effect.
Myocarditis cases seem to be temporary, with patients making a full recovery, though they need to be monitored in the hospital. The risk of myocarditis with a COVID-19 infection is many times higher than it is from a vaccine.
There have been little data to support the need for boosters in this age group, because children and teens tend to experience milder COVID-19 disease, though they are still at risk for post–COVID-19 complications such as long COVID and a delayed reaction to the virus called Post Acute Sequelae of SARS-CoV2 Infection among Children, or PAS-C.
All that changed with the arrival of Omicron.
A version of this article first appeared on WebMD.com.
, clearing the way for millions of teenagers to get a third dose of vaccine starting 6 months after their second dose.
The FDA said it was basing its emergency authorization of boosters for 16- and 17-year-olds on data from 200 individuals who were 18-55 years of age when they received a booster dose. They are requiring Pfizer to collect data on safety in postauthorization studies.
“The FDA has determined that the benefits of a single booster dose of the Pfizer-BioNTech COVID-19 Vaccine or Comirnaty outweigh the risks of myocarditis and pericarditis in individuals 16 and 17 years of age to provide continued protection against COVID-19 and the associated serious consequences that can occur including hospitalization and death,” the agency said in a news release.
Israel has been giving booster doses of Pfizer’s vaccine to everyone 12 and up since late August. Data from that country show that myocarditis cases continue to be very rare, even in younger age groups, and are mild and temporary.
The authorization comes as the effectiveness of the current vaccines against the new Omicron variant has become a point of intense scientific inquiry.
Early studies suggest that booster doses may be necessary to keep Omicron at bay, at least until new variant-specific vaccines are ready next spring.
Current evidence suggests that the protection of the vaccines is holding up well against severe disease and death, at least with Delta and early iterations of the virus.
How well they will do against Omicron, and how severe Omicron infections may be for different age groups, remain open questions.
On Dec. 8, the World Health Organization urged countries not to wait for all the science to come in, but to act now to contain any potential threat.
The first pieces of evidence on Omicron suggest that it is highly contagious, perhaps even more than Delta, though early reports suggest symptoms caused by this version of the new coronavirus may be less severe than in previous waves. Experts have cautioned that the true severity of Omicron infections isn’t yet known, since the first cases have been detected in younger people, who tend to have milder COVID-19 symptoms than those of adults and seniors.
“Vaccination and getting a booster when eligible, along with other preventive measures like masking and avoiding large crowds and poorly ventilated spaces, remain our most effective methods for fighting COVID-19,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release. “As people gather indoors with family and friends for the holidays, we can’t let up on all the preventive public health measures that we have been taking during the pandemic. With both the Delta and Omicron variants continuing to spread, vaccination remains the best protection against COVID-19.”
In mid-November, the FDA authorized boosters of the Pfizer vaccine for all individuals 18 and older, but the agency held off on expanding the use of boosters for younger age groups, partly because they have the highest risk of myocarditis, a very rare side effect.
Myocarditis cases seem to be temporary, with patients making a full recovery, though they need to be monitored in the hospital. The risk of myocarditis with a COVID-19 infection is many times higher than it is from a vaccine.
There have been little data to support the need for boosters in this age group, because children and teens tend to experience milder COVID-19 disease, though they are still at risk for post–COVID-19 complications such as long COVID and a delayed reaction to the virus called Post Acute Sequelae of SARS-CoV2 Infection among Children, or PAS-C.
All that changed with the arrival of Omicron.
A version of this article first appeared on WebMD.com.
Medical board stops warning docs against giving false COVID information
Under pressure from Republican state lawmakers, t
The board’s 7-3 vote on December 7 to delete the statement followed repeated threats by a powerful state House Republican to dissolve the board and appoint all new members if it did not immediately take it down.
The Tennessee board’s statement was a verbatim restatement of a warning to physicians issued by the Federation of State Medical Boards in July. The federation cited a “dramatic increase” in dissemination of misinformation and disinformation about the COVID-19 vaccine by physicians. It said that’s dangerous because physicians enjoy a high degree of public credibility.
Across the country, state medical licensing boards and state and national medical associations and specialty boards are struggling with how to respond to scientifically baseless public statements about COVID-19 by some physicians, which they say are increasing public confusion, political conflict, and preventable illnesses and deaths.
There have been only a small number of disciplinary actions by medical boards against physicians for spreading false COVID-19 information. Critics say the boards have been weak in responding to these dangerous violations of medical standards. As an example, they cite the State Medical Board of Ohio’s September renewal of the medical license of Sherri Tenpenny, DO, who had previously testified before Ohio lawmakers that COVID-19 vaccines magnetize their recipients and “interface” with cell phone towers.
“I’m not satisfied with what medical boards have done, and we are ramping up our efforts to press the boards to hold these physicians accountable,” said Nick Sawyer, MD, an emergency physician in Sacramento, Calif., who heads a group of healthcare professionals called No License for Disinformation.
Still, Tennessee board members insisted that the board’s policy of disciplining physicians who disseminate false information about COVID-19 vaccinations remains in effect, because state law empowers the board to take action against doctors whose unprofessional behavior endangers the public.
“COVID misinformation and disinformation has caused undue loss of life and jobs and other incalculable loss in our society,” said Melanie Blake, MD, MBA, a Chattanooga internist who’s president of the board. “Physicians have a responsibility to uphold their oath and put forward consensus-driven medical principles.”
But state Rep. John Ragan, the Republican co-chairman of the Joint Government Operations Committee, told the Tennessean newspaper that deleting the statement from the board’s website was equivalent to rescinding the policy. Ragan, who identifies himself as a business consultant and retired Air Force pilot, did not respond to a request for comment for this article.
Blake acknowledged that removing the statement from the board’s website has the potential to confuse Tennessee physicians. And the pressure from GOP lawmakers, who overwhelmingly control the Tennessee legislature, could discourage investigations and disciplinary actions against physicians who allegedly spread COVID-19 misinformation, she added. “It’s hard for me to answer whether this puts a chill on us,” she said.
In September, the Tennessee board, besides approving the general statement that physicians who spread COVID-19 disinformation could face licensure action, also directed the State Department of Health to prioritize investigations of physicians who spread outrageous claims. The board cited statements such as the vaccines are poisonous, cause infertility, contain microchips, or magnetize the body.
In response, the Tennessee General Assembly passed a bill in late October prohibiting the board from implementing any disciplinary process regarding the prescribing of “medication for COVID-19” without review and approval by Ragan’s committee. It’s not clear whether that language covers vaccines.
Last summer, in a similar move, Ragan threatened to dissolve the State Department of Health because its top vaccination official wrote a letter to medical providers explaining that state law allowed them to give COVID-19 vaccinations to minors older than 14 without parental consent. That official, Michelle Fiscus, MD, was fired in July.
Republican Sen. Richard Briggs, MD, a cardiothoracic surgeon who voted against the October legislation affecting COVID-related disciplinary actions, criticized his GOP colleagues’ interference in the medical board’s licensure decisions. “The mission of the board is to protect the health and safety of Tennessee citizens, and this was in complete conflict with that mission,” he said.
The Federation of State Medical Boards similarly condemned the Tennessee lawmakers’ moves. “The FSMB strongly opposes restricting a board’s authority to evaluate the standard of care and assess potential risk for patient harm,” a spokesman said. “Any interference, politically motivated or otherwise, is unhelpful and dangerous.”
But Arthur Caplan, PhD, a professor of bioethics at NYU School of Medicine, doubts that state medical boards are up to the task of policing disinformation spread by physicians. That’s because they ultimately are under the control of elected state officials, who may force the boards to base policy on ideology rather than science.
He said medical board members in Florida and another GOP-controlled state have told him they do not want to pursue disciplinary actions against physicians for COVID-19 misinformation for fear of political backlash.
Michele Heisler, MD, medical director of Physicians for Human Rights, agreed that the Tennessee situation highlights the looming political threat to the independence of state medical boards. She urged other medical organizations, particularly medical specialty boards, to step in.
“As a profession, we need to take a stance against this,” said Heisler, who’s a professor of internal medicine and public health at the University of Michigan. “Our credibility as physicians is at stake.”
A version of this article first appeared on Medscape.com.
Under pressure from Republican state lawmakers, t
The board’s 7-3 vote on December 7 to delete the statement followed repeated threats by a powerful state House Republican to dissolve the board and appoint all new members if it did not immediately take it down.
The Tennessee board’s statement was a verbatim restatement of a warning to physicians issued by the Federation of State Medical Boards in July. The federation cited a “dramatic increase” in dissemination of misinformation and disinformation about the COVID-19 vaccine by physicians. It said that’s dangerous because physicians enjoy a high degree of public credibility.
Across the country, state medical licensing boards and state and national medical associations and specialty boards are struggling with how to respond to scientifically baseless public statements about COVID-19 by some physicians, which they say are increasing public confusion, political conflict, and preventable illnesses and deaths.
There have been only a small number of disciplinary actions by medical boards against physicians for spreading false COVID-19 information. Critics say the boards have been weak in responding to these dangerous violations of medical standards. As an example, they cite the State Medical Board of Ohio’s September renewal of the medical license of Sherri Tenpenny, DO, who had previously testified before Ohio lawmakers that COVID-19 vaccines magnetize their recipients and “interface” with cell phone towers.
“I’m not satisfied with what medical boards have done, and we are ramping up our efforts to press the boards to hold these physicians accountable,” said Nick Sawyer, MD, an emergency physician in Sacramento, Calif., who heads a group of healthcare professionals called No License for Disinformation.
Still, Tennessee board members insisted that the board’s policy of disciplining physicians who disseminate false information about COVID-19 vaccinations remains in effect, because state law empowers the board to take action against doctors whose unprofessional behavior endangers the public.
“COVID misinformation and disinformation has caused undue loss of life and jobs and other incalculable loss in our society,” said Melanie Blake, MD, MBA, a Chattanooga internist who’s president of the board. “Physicians have a responsibility to uphold their oath and put forward consensus-driven medical principles.”
But state Rep. John Ragan, the Republican co-chairman of the Joint Government Operations Committee, told the Tennessean newspaper that deleting the statement from the board’s website was equivalent to rescinding the policy. Ragan, who identifies himself as a business consultant and retired Air Force pilot, did not respond to a request for comment for this article.
Blake acknowledged that removing the statement from the board’s website has the potential to confuse Tennessee physicians. And the pressure from GOP lawmakers, who overwhelmingly control the Tennessee legislature, could discourage investigations and disciplinary actions against physicians who allegedly spread COVID-19 misinformation, she added. “It’s hard for me to answer whether this puts a chill on us,” she said.
In September, the Tennessee board, besides approving the general statement that physicians who spread COVID-19 disinformation could face licensure action, also directed the State Department of Health to prioritize investigations of physicians who spread outrageous claims. The board cited statements such as the vaccines are poisonous, cause infertility, contain microchips, or magnetize the body.
In response, the Tennessee General Assembly passed a bill in late October prohibiting the board from implementing any disciplinary process regarding the prescribing of “medication for COVID-19” without review and approval by Ragan’s committee. It’s not clear whether that language covers vaccines.
Last summer, in a similar move, Ragan threatened to dissolve the State Department of Health because its top vaccination official wrote a letter to medical providers explaining that state law allowed them to give COVID-19 vaccinations to minors older than 14 without parental consent. That official, Michelle Fiscus, MD, was fired in July.
Republican Sen. Richard Briggs, MD, a cardiothoracic surgeon who voted against the October legislation affecting COVID-related disciplinary actions, criticized his GOP colleagues’ interference in the medical board’s licensure decisions. “The mission of the board is to protect the health and safety of Tennessee citizens, and this was in complete conflict with that mission,” he said.
The Federation of State Medical Boards similarly condemned the Tennessee lawmakers’ moves. “The FSMB strongly opposes restricting a board’s authority to evaluate the standard of care and assess potential risk for patient harm,” a spokesman said. “Any interference, politically motivated or otherwise, is unhelpful and dangerous.”
But Arthur Caplan, PhD, a professor of bioethics at NYU School of Medicine, doubts that state medical boards are up to the task of policing disinformation spread by physicians. That’s because they ultimately are under the control of elected state officials, who may force the boards to base policy on ideology rather than science.
He said medical board members in Florida and another GOP-controlled state have told him they do not want to pursue disciplinary actions against physicians for COVID-19 misinformation for fear of political backlash.
Michele Heisler, MD, medical director of Physicians for Human Rights, agreed that the Tennessee situation highlights the looming political threat to the independence of state medical boards. She urged other medical organizations, particularly medical specialty boards, to step in.
“As a profession, we need to take a stance against this,” said Heisler, who’s a professor of internal medicine and public health at the University of Michigan. “Our credibility as physicians is at stake.”
A version of this article first appeared on Medscape.com.
Under pressure from Republican state lawmakers, t
The board’s 7-3 vote on December 7 to delete the statement followed repeated threats by a powerful state House Republican to dissolve the board and appoint all new members if it did not immediately take it down.
The Tennessee board’s statement was a verbatim restatement of a warning to physicians issued by the Federation of State Medical Boards in July. The federation cited a “dramatic increase” in dissemination of misinformation and disinformation about the COVID-19 vaccine by physicians. It said that’s dangerous because physicians enjoy a high degree of public credibility.
Across the country, state medical licensing boards and state and national medical associations and specialty boards are struggling with how to respond to scientifically baseless public statements about COVID-19 by some physicians, which they say are increasing public confusion, political conflict, and preventable illnesses and deaths.
There have been only a small number of disciplinary actions by medical boards against physicians for spreading false COVID-19 information. Critics say the boards have been weak in responding to these dangerous violations of medical standards. As an example, they cite the State Medical Board of Ohio’s September renewal of the medical license of Sherri Tenpenny, DO, who had previously testified before Ohio lawmakers that COVID-19 vaccines magnetize their recipients and “interface” with cell phone towers.
“I’m not satisfied with what medical boards have done, and we are ramping up our efforts to press the boards to hold these physicians accountable,” said Nick Sawyer, MD, an emergency physician in Sacramento, Calif., who heads a group of healthcare professionals called No License for Disinformation.
Still, Tennessee board members insisted that the board’s policy of disciplining physicians who disseminate false information about COVID-19 vaccinations remains in effect, because state law empowers the board to take action against doctors whose unprofessional behavior endangers the public.
“COVID misinformation and disinformation has caused undue loss of life and jobs and other incalculable loss in our society,” said Melanie Blake, MD, MBA, a Chattanooga internist who’s president of the board. “Physicians have a responsibility to uphold their oath and put forward consensus-driven medical principles.”
But state Rep. John Ragan, the Republican co-chairman of the Joint Government Operations Committee, told the Tennessean newspaper that deleting the statement from the board’s website was equivalent to rescinding the policy. Ragan, who identifies himself as a business consultant and retired Air Force pilot, did not respond to a request for comment for this article.
Blake acknowledged that removing the statement from the board’s website has the potential to confuse Tennessee physicians. And the pressure from GOP lawmakers, who overwhelmingly control the Tennessee legislature, could discourage investigations and disciplinary actions against physicians who allegedly spread COVID-19 misinformation, she added. “It’s hard for me to answer whether this puts a chill on us,” she said.
In September, the Tennessee board, besides approving the general statement that physicians who spread COVID-19 disinformation could face licensure action, also directed the State Department of Health to prioritize investigations of physicians who spread outrageous claims. The board cited statements such as the vaccines are poisonous, cause infertility, contain microchips, or magnetize the body.
In response, the Tennessee General Assembly passed a bill in late October prohibiting the board from implementing any disciplinary process regarding the prescribing of “medication for COVID-19” without review and approval by Ragan’s committee. It’s not clear whether that language covers vaccines.
Last summer, in a similar move, Ragan threatened to dissolve the State Department of Health because its top vaccination official wrote a letter to medical providers explaining that state law allowed them to give COVID-19 vaccinations to minors older than 14 without parental consent. That official, Michelle Fiscus, MD, was fired in July.
Republican Sen. Richard Briggs, MD, a cardiothoracic surgeon who voted against the October legislation affecting COVID-related disciplinary actions, criticized his GOP colleagues’ interference in the medical board’s licensure decisions. “The mission of the board is to protect the health and safety of Tennessee citizens, and this was in complete conflict with that mission,” he said.
The Federation of State Medical Boards similarly condemned the Tennessee lawmakers’ moves. “The FSMB strongly opposes restricting a board’s authority to evaluate the standard of care and assess potential risk for patient harm,” a spokesman said. “Any interference, politically motivated or otherwise, is unhelpful and dangerous.”
But Arthur Caplan, PhD, a professor of bioethics at NYU School of Medicine, doubts that state medical boards are up to the task of policing disinformation spread by physicians. That’s because they ultimately are under the control of elected state officials, who may force the boards to base policy on ideology rather than science.
He said medical board members in Florida and another GOP-controlled state have told him they do not want to pursue disciplinary actions against physicians for COVID-19 misinformation for fear of political backlash.
Michele Heisler, MD, medical director of Physicians for Human Rights, agreed that the Tennessee situation highlights the looming political threat to the independence of state medical boards. She urged other medical organizations, particularly medical specialty boards, to step in.
“As a profession, we need to take a stance against this,” said Heisler, who’s a professor of internal medicine and public health at the University of Michigan. “Our credibility as physicians is at stake.”
A version of this article first appeared on Medscape.com.
AMA, hospital group sue federal government over surprise billing law
which tilts toward using prevailing rates paid for services.
The American Hospital Association and American Medical Association said they will ask the U.S. District Court for the District of Columbia to try to prevent implementation of certain provisions of new federal rules on surprise bills. This court is often a venue for fights over federal rules. Also joining the suit are Nevada-based Renown Health, UMass Memorial Health, and two physicians based in North Carolina, AHA and AMA said.
Federal agencies, including the Department of Health & Human Services, in September had unveiled the rule on surprise medical bills that will take effect Jan. 1.
Under this rule, a key benchmark for payment disputes would be the qualifying payment amount (QPA), which is pegged to median contracted rates. In the dispute-resolution process outlined in the rule, there is a presumption that the QPA is the appropriate out-of-network rate.
The rule allows for exceptions in which the independent mediating organization handling the payment dispute resolution has “credible information” as to why the QPA is materially different from the appropriate out-of-network rate.
In the view of the federal agencies that issued the rule, this approach “encourages predictable outcomes,” which likely would reduce the number of disputes that go through the resolution process while also “providing equitable and clear standards” for cases to appropriately deviate from QPA. HHS was joined in issuing the rule by the Treasury and Labor Departments and the Office of Personnel Management.
AMA and AHA disagree with their view, seeing this approach as a boon for insurers at the expense of physicians and hospitals.
In a press release, they said the rule’s approach to surprise billing would “all but ensure that hospitals, physicians, and other providers will routinely be undercompensated by commercial insurers, and patients will have fewer choices for access to in-network services.”
The rule is part of the implementation of a federal law passed in December 2020, known as the No Surprises Act. In their statement, AHA and AMA said their legal challenge would not prevent “core patient protections’’ of that law from moving forward.
“No patient should fear receiving a surprise medical bill,” Rick Pollack, AHA president and chief executive, said in the statement. “That is why hospitals and health systems supported the No Surprises Act to protect patients and keep them out of the middle of disputes between providers and insurers. Congress carefully crafted the law with a balanced, patient-friendly approach and it should be implemented as intended.”
AMA President Gerald E. Harmon, MD, added the approach used in the rule on surprise billing could create “an unsustainable situation for physicians.”
“Our legal challenge urges regulators to ensure there is a fair and meaningful process to resolve disputes between health care providers and insurance companies,” Dr. Harmon said.
AHA and AMA included with their statement a link to a November letter from more than 150 members of Congress, who also objected to the approach taken in designing the independent dispute-resolution (IDR) process.
“This directive establishes a de facto benchmark rate, making the median in-network rate the default factor considered in the IDR process. This approach is contrary to statute and could incentivize insurance companies to set artificially low payment rates, which would narrow provider networks and jeopardize patient access to care – the exact opposite of the goal of the law,” wrote the members of Congress, including Rep. Raul Ruiz, MD, a California Democrat, and Rep. Larry Bucshon, MD, an Indiana Republican.
A version of this article first appeared on Medscape.com.
which tilts toward using prevailing rates paid for services.
The American Hospital Association and American Medical Association said they will ask the U.S. District Court for the District of Columbia to try to prevent implementation of certain provisions of new federal rules on surprise bills. This court is often a venue for fights over federal rules. Also joining the suit are Nevada-based Renown Health, UMass Memorial Health, and two physicians based in North Carolina, AHA and AMA said.
Federal agencies, including the Department of Health & Human Services, in September had unveiled the rule on surprise medical bills that will take effect Jan. 1.
Under this rule, a key benchmark for payment disputes would be the qualifying payment amount (QPA), which is pegged to median contracted rates. In the dispute-resolution process outlined in the rule, there is a presumption that the QPA is the appropriate out-of-network rate.
The rule allows for exceptions in which the independent mediating organization handling the payment dispute resolution has “credible information” as to why the QPA is materially different from the appropriate out-of-network rate.
In the view of the federal agencies that issued the rule, this approach “encourages predictable outcomes,” which likely would reduce the number of disputes that go through the resolution process while also “providing equitable and clear standards” for cases to appropriately deviate from QPA. HHS was joined in issuing the rule by the Treasury and Labor Departments and the Office of Personnel Management.
AMA and AHA disagree with their view, seeing this approach as a boon for insurers at the expense of physicians and hospitals.
In a press release, they said the rule’s approach to surprise billing would “all but ensure that hospitals, physicians, and other providers will routinely be undercompensated by commercial insurers, and patients will have fewer choices for access to in-network services.”
The rule is part of the implementation of a federal law passed in December 2020, known as the No Surprises Act. In their statement, AHA and AMA said their legal challenge would not prevent “core patient protections’’ of that law from moving forward.
“No patient should fear receiving a surprise medical bill,” Rick Pollack, AHA president and chief executive, said in the statement. “That is why hospitals and health systems supported the No Surprises Act to protect patients and keep them out of the middle of disputes between providers and insurers. Congress carefully crafted the law with a balanced, patient-friendly approach and it should be implemented as intended.”
AMA President Gerald E. Harmon, MD, added the approach used in the rule on surprise billing could create “an unsustainable situation for physicians.”
“Our legal challenge urges regulators to ensure there is a fair and meaningful process to resolve disputes between health care providers and insurance companies,” Dr. Harmon said.
AHA and AMA included with their statement a link to a November letter from more than 150 members of Congress, who also objected to the approach taken in designing the independent dispute-resolution (IDR) process.
“This directive establishes a de facto benchmark rate, making the median in-network rate the default factor considered in the IDR process. This approach is contrary to statute and could incentivize insurance companies to set artificially low payment rates, which would narrow provider networks and jeopardize patient access to care – the exact opposite of the goal of the law,” wrote the members of Congress, including Rep. Raul Ruiz, MD, a California Democrat, and Rep. Larry Bucshon, MD, an Indiana Republican.
A version of this article first appeared on Medscape.com.
which tilts toward using prevailing rates paid for services.
The American Hospital Association and American Medical Association said they will ask the U.S. District Court for the District of Columbia to try to prevent implementation of certain provisions of new federal rules on surprise bills. This court is often a venue for fights over federal rules. Also joining the suit are Nevada-based Renown Health, UMass Memorial Health, and two physicians based in North Carolina, AHA and AMA said.
Federal agencies, including the Department of Health & Human Services, in September had unveiled the rule on surprise medical bills that will take effect Jan. 1.
Under this rule, a key benchmark for payment disputes would be the qualifying payment amount (QPA), which is pegged to median contracted rates. In the dispute-resolution process outlined in the rule, there is a presumption that the QPA is the appropriate out-of-network rate.
The rule allows for exceptions in which the independent mediating organization handling the payment dispute resolution has “credible information” as to why the QPA is materially different from the appropriate out-of-network rate.
In the view of the federal agencies that issued the rule, this approach “encourages predictable outcomes,” which likely would reduce the number of disputes that go through the resolution process while also “providing equitable and clear standards” for cases to appropriately deviate from QPA. HHS was joined in issuing the rule by the Treasury and Labor Departments and the Office of Personnel Management.
AMA and AHA disagree with their view, seeing this approach as a boon for insurers at the expense of physicians and hospitals.
In a press release, they said the rule’s approach to surprise billing would “all but ensure that hospitals, physicians, and other providers will routinely be undercompensated by commercial insurers, and patients will have fewer choices for access to in-network services.”
The rule is part of the implementation of a federal law passed in December 2020, known as the No Surprises Act. In their statement, AHA and AMA said their legal challenge would not prevent “core patient protections’’ of that law from moving forward.
“No patient should fear receiving a surprise medical bill,” Rick Pollack, AHA president and chief executive, said in the statement. “That is why hospitals and health systems supported the No Surprises Act to protect patients and keep them out of the middle of disputes between providers and insurers. Congress carefully crafted the law with a balanced, patient-friendly approach and it should be implemented as intended.”
AMA President Gerald E. Harmon, MD, added the approach used in the rule on surprise billing could create “an unsustainable situation for physicians.”
“Our legal challenge urges regulators to ensure there is a fair and meaningful process to resolve disputes between health care providers and insurance companies,” Dr. Harmon said.
AHA and AMA included with their statement a link to a November letter from more than 150 members of Congress, who also objected to the approach taken in designing the independent dispute-resolution (IDR) process.
“This directive establishes a de facto benchmark rate, making the median in-network rate the default factor considered in the IDR process. This approach is contrary to statute and could incentivize insurance companies to set artificially low payment rates, which would narrow provider networks and jeopardize patient access to care – the exact opposite of the goal of the law,” wrote the members of Congress, including Rep. Raul Ruiz, MD, a California Democrat, and Rep. Larry Bucshon, MD, an Indiana Republican.
A version of this article first appeared on Medscape.com.
Risk for severe COVID-19 and death plummets with Pfizer booster
Both studies were completed before the advent of the Omicron variant.
In one study that included data on more than 4 million patients, led by Yinon M. Bar-On, MSc, of the Weizmann Institute of Science in Rehovot, Israel, the rate of confirmed SARS-CoV-2 infection was lower in the booster group than in the nonbooster group by a factor of about 10.
This was true across all five age groups studied (range among the groups [starting with age 16], 9.0-17.2).
The risk for severe COVID-19 in the primary analysis decreased in the booster group by a factor of 17.9 (95% confidence interval, 15.1-21.2), among those aged 60 years or older. Risk for severe illness in those ages 40-59 was lower by a factor of 21.7 (95% CI, 10.6-44.2).
Among the 60 and older age group, risk for death was also reduced by a factor of 14.7 (95% CI, 10.0-21.4).
Researchers analyzed data for the period from July 30 to Oct. 10, 2021, from the Israel Ministry of Health database on 4.69 million people at least 16 years old who had received two Pfizer doses at least 5 months earlier.
In the main analysis, the researchers compared the rates of confirmed COVID-19, severe disease, and death among those who had gotten a booster at least 12 days earlier with the rates in a nonbooster group.
The authors wrote: “Booster vaccination programs may provide a way to control transmission without costly social-distancing measures and quarantines. Our findings provide evidence for the short-term effectiveness of the booster dose against the currently dominant Delta variant in persons 16 years of age or older.”
Death risk down by 90%
A second study, led by Ronen Arbel, PhD, with the community medical services division, Clalit Health Services (CHS), Tel Aviv, which included more than 800,000 participants, also found mortality risk was greatly reduced among those who received the booster compared with those who didn’t get the booster.
Participants aged 50 years or older who received a booster at least 5 months after a second Pfizer dose had 90% lower mortality risk because of COVID-19 than participants who did not get the booster.
The adjusted hazard ratio for death as a result of COVID-19 in the booster group, as compared with the nonbooster group, was 0.10 (95% CI, 0.07-0.14; P < .001). Of the 843,208 eligible participants, 758,118 (90%) received the booster during the 54-day study period.
The study included all CHS members who were aged 50 years or older on the study start date and had received two Pfizer doses at least 5 months earlier. CHS covers about 52% of the Israeli population and is the largest of four health care organizations in Israel that provide mandatory health care.
The authors noted that, although the study period was only 54 days (Aug. 6–Sept. 29), during that time “the incidence of COVID-19 in Israel was one of the highest in the world.”
The authors of both original articles pointed out that the studies are limited by short time periods and that longer-term studies are needed to see how the booster shots stand up to known and future variants, such as Omicron.
None of the authors involved in both studies reported relevant financial relationships.
A version of this article first appeared on Medscape.com.
Both studies were completed before the advent of the Omicron variant.
In one study that included data on more than 4 million patients, led by Yinon M. Bar-On, MSc, of the Weizmann Institute of Science in Rehovot, Israel, the rate of confirmed SARS-CoV-2 infection was lower in the booster group than in the nonbooster group by a factor of about 10.
This was true across all five age groups studied (range among the groups [starting with age 16], 9.0-17.2).
The risk for severe COVID-19 in the primary analysis decreased in the booster group by a factor of 17.9 (95% confidence interval, 15.1-21.2), among those aged 60 years or older. Risk for severe illness in those ages 40-59 was lower by a factor of 21.7 (95% CI, 10.6-44.2).
Among the 60 and older age group, risk for death was also reduced by a factor of 14.7 (95% CI, 10.0-21.4).
Researchers analyzed data for the period from July 30 to Oct. 10, 2021, from the Israel Ministry of Health database on 4.69 million people at least 16 years old who had received two Pfizer doses at least 5 months earlier.
In the main analysis, the researchers compared the rates of confirmed COVID-19, severe disease, and death among those who had gotten a booster at least 12 days earlier with the rates in a nonbooster group.
The authors wrote: “Booster vaccination programs may provide a way to control transmission without costly social-distancing measures and quarantines. Our findings provide evidence for the short-term effectiveness of the booster dose against the currently dominant Delta variant in persons 16 years of age or older.”
Death risk down by 90%
A second study, led by Ronen Arbel, PhD, with the community medical services division, Clalit Health Services (CHS), Tel Aviv, which included more than 800,000 participants, also found mortality risk was greatly reduced among those who received the booster compared with those who didn’t get the booster.
Participants aged 50 years or older who received a booster at least 5 months after a second Pfizer dose had 90% lower mortality risk because of COVID-19 than participants who did not get the booster.
The adjusted hazard ratio for death as a result of COVID-19 in the booster group, as compared with the nonbooster group, was 0.10 (95% CI, 0.07-0.14; P < .001). Of the 843,208 eligible participants, 758,118 (90%) received the booster during the 54-day study period.
The study included all CHS members who were aged 50 years or older on the study start date and had received two Pfizer doses at least 5 months earlier. CHS covers about 52% of the Israeli population and is the largest of four health care organizations in Israel that provide mandatory health care.
The authors noted that, although the study period was only 54 days (Aug. 6–Sept. 29), during that time “the incidence of COVID-19 in Israel was one of the highest in the world.”
The authors of both original articles pointed out that the studies are limited by short time periods and that longer-term studies are needed to see how the booster shots stand up to known and future variants, such as Omicron.
None of the authors involved in both studies reported relevant financial relationships.
A version of this article first appeared on Medscape.com.
Both studies were completed before the advent of the Omicron variant.
In one study that included data on more than 4 million patients, led by Yinon M. Bar-On, MSc, of the Weizmann Institute of Science in Rehovot, Israel, the rate of confirmed SARS-CoV-2 infection was lower in the booster group than in the nonbooster group by a factor of about 10.
This was true across all five age groups studied (range among the groups [starting with age 16], 9.0-17.2).
The risk for severe COVID-19 in the primary analysis decreased in the booster group by a factor of 17.9 (95% confidence interval, 15.1-21.2), among those aged 60 years or older. Risk for severe illness in those ages 40-59 was lower by a factor of 21.7 (95% CI, 10.6-44.2).
Among the 60 and older age group, risk for death was also reduced by a factor of 14.7 (95% CI, 10.0-21.4).
Researchers analyzed data for the period from July 30 to Oct. 10, 2021, from the Israel Ministry of Health database on 4.69 million people at least 16 years old who had received two Pfizer doses at least 5 months earlier.
In the main analysis, the researchers compared the rates of confirmed COVID-19, severe disease, and death among those who had gotten a booster at least 12 days earlier with the rates in a nonbooster group.
The authors wrote: “Booster vaccination programs may provide a way to control transmission without costly social-distancing measures and quarantines. Our findings provide evidence for the short-term effectiveness of the booster dose against the currently dominant Delta variant in persons 16 years of age or older.”
Death risk down by 90%
A second study, led by Ronen Arbel, PhD, with the community medical services division, Clalit Health Services (CHS), Tel Aviv, which included more than 800,000 participants, also found mortality risk was greatly reduced among those who received the booster compared with those who didn’t get the booster.
Participants aged 50 years or older who received a booster at least 5 months after a second Pfizer dose had 90% lower mortality risk because of COVID-19 than participants who did not get the booster.
The adjusted hazard ratio for death as a result of COVID-19 in the booster group, as compared with the nonbooster group, was 0.10 (95% CI, 0.07-0.14; P < .001). Of the 843,208 eligible participants, 758,118 (90%) received the booster during the 54-day study period.
The study included all CHS members who were aged 50 years or older on the study start date and had received two Pfizer doses at least 5 months earlier. CHS covers about 52% of the Israeli population and is the largest of four health care organizations in Israel that provide mandatory health care.
The authors noted that, although the study period was only 54 days (Aug. 6–Sept. 29), during that time “the incidence of COVID-19 in Israel was one of the highest in the world.”
The authors of both original articles pointed out that the studies are limited by short time periods and that longer-term studies are needed to see how the booster shots stand up to known and future variants, such as Omicron.
None of the authors involved in both studies reported relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Spam filter failure: Selling physician emails equals big $$
Despite the best efforts of my institution’s spam filter, I’ve realized that I spend at least 4 minutes every day of the week removing junk email from my in basket: EMR vendors, predatory journals trying to lure me into paying their outrageous publication fees, people who want to help me with my billing software (evidently that .edu extension hasn’t clicked for them yet), headhunters trying to fill specialty positions in other states, market researchers offering a gift card for 40 minutes filling out a survey.
If you do the math, 4 minutes daily is 1,460 minutes per year. That’s an entire day of my life lost each year to this useless nonsense, which I never agreed to receive in the first place. Now multiply that by the 22 million health care workers in the United States, or even just by the 985,000 licensed physicians in this country. Then factor in the $638 per hour in gross revenue generated by the average primary care physician, as a conservative, well-documented value.
By my reckoning, these bozos owe the United States alone over $15 billion in lost GDP each year.
So why don’t we shut it down!? The CAN-SPAM Act of 2003 attempted to at least mitigate the problem. It applies only to commercial entities (I know, I’d love to report some political groups, too). To avoid violating the law and risking fines of up to $16,000 per individual email, senders must:
- Not use misleading header info (including domain name and email address)
- Not use deceptive subject lines
- Clearly label the email as an ad
- Give an actual physical address of the sender
- Tell recipients how to opt out of future emails
- Honor opt-out requests within 10 business days
- Monitor the activities of any subcontractor sending email on their behalf
I can say with certainty that much of the trash in my inbox violates at least one of these. But that doesn’t matter if there is not an efficient way to report the violators and ensure that they’ll be tracked down. Hard enough if they live here, impossible if the email is routed from overseas, as much of it clearly is.
If you receive email in violation of the act, experts recommend that you write down the email address and the business name of the sender, fill out a complaint form on the Federal Trade Commission website, or send an email to [email protected], then send an email to your Internet service provider’s abuse desk. If you’re not working within a big institution like mine that has hot and cold running IT personnel that operate their own abuse prevention office, the address you’ll need is likely abuse@domain_name or postmaster@domain_name. Just hitting the spam button at the top of your browser/email software may do the trick. There’s more good advice at the FTC’s consumer spam page.
The answer came, ironically, to my email inbox in the form of one of those emails that did indeed violate the law.
I rolled my eyes and started into my reporting subroutine but then stopped cold. Just 1 second. If this person is selling lists of email addresses of conference attendees, somebody within the conference structure must be providing them. How is that legal? I have never agreed, in registering for a medical conference, to allow them to share my email address with anyone. To think that they are making money from that is extremely galling.
Vermont, at least, has enacted a law requiring companies that traffic in such email lists to register with the state. Although it has been in effect for 2 years, the jury is out regarding its efficacy. Our European counterparts are protected by the General Data Protection Regulation, which specifies that commercial email can be sent only to individuals who have explicitly opted into such mailings, and that purchased email lists are not compliant with the requirement.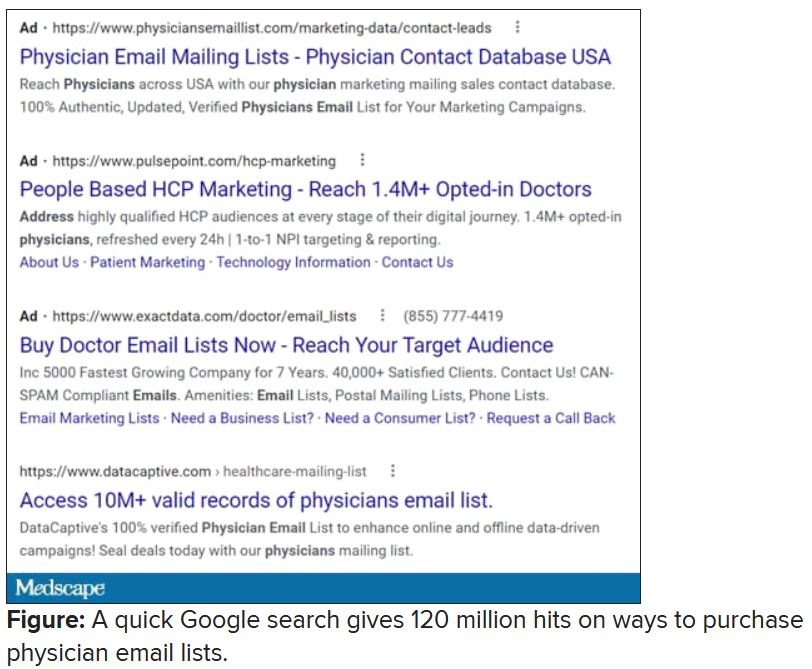
Anybody have the inside scoop on this? Can we demand that our professional societies safeguard their attendee databases so this won’t happen? If they won’t, why am I paying big money to attend their conferences, only for them to make even more money at my expense?
Dr. Hitchcock is assistant professor, department of radiation oncology, at the University of Florida, Gainesville. She reported receiving research grant money from Merck. A version of this article first appeared on Medscape.com.
Despite the best efforts of my institution’s spam filter, I’ve realized that I spend at least 4 minutes every day of the week removing junk email from my in basket: EMR vendors, predatory journals trying to lure me into paying their outrageous publication fees, people who want to help me with my billing software (evidently that .edu extension hasn’t clicked for them yet), headhunters trying to fill specialty positions in other states, market researchers offering a gift card for 40 minutes filling out a survey.
If you do the math, 4 minutes daily is 1,460 minutes per year. That’s an entire day of my life lost each year to this useless nonsense, which I never agreed to receive in the first place. Now multiply that by the 22 million health care workers in the United States, or even just by the 985,000 licensed physicians in this country. Then factor in the $638 per hour in gross revenue generated by the average primary care physician, as a conservative, well-documented value.
By my reckoning, these bozos owe the United States alone over $15 billion in lost GDP each year.
So why don’t we shut it down!? The CAN-SPAM Act of 2003 attempted to at least mitigate the problem. It applies only to commercial entities (I know, I’d love to report some political groups, too). To avoid violating the law and risking fines of up to $16,000 per individual email, senders must:
- Not use misleading header info (including domain name and email address)
- Not use deceptive subject lines
- Clearly label the email as an ad
- Give an actual physical address of the sender
- Tell recipients how to opt out of future emails
- Honor opt-out requests within 10 business days
- Monitor the activities of any subcontractor sending email on their behalf
I can say with certainty that much of the trash in my inbox violates at least one of these. But that doesn’t matter if there is not an efficient way to report the violators and ensure that they’ll be tracked down. Hard enough if they live here, impossible if the email is routed from overseas, as much of it clearly is.
If you receive email in violation of the act, experts recommend that you write down the email address and the business name of the sender, fill out a complaint form on the Federal Trade Commission website, or send an email to [email protected], then send an email to your Internet service provider’s abuse desk. If you’re not working within a big institution like mine that has hot and cold running IT personnel that operate their own abuse prevention office, the address you’ll need is likely abuse@domain_name or postmaster@domain_name. Just hitting the spam button at the top of your browser/email software may do the trick. There’s more good advice at the FTC’s consumer spam page.
The answer came, ironically, to my email inbox in the form of one of those emails that did indeed violate the law.
I rolled my eyes and started into my reporting subroutine but then stopped cold. Just 1 second. If this person is selling lists of email addresses of conference attendees, somebody within the conference structure must be providing them. How is that legal? I have never agreed, in registering for a medical conference, to allow them to share my email address with anyone. To think that they are making money from that is extremely galling.
Vermont, at least, has enacted a law requiring companies that traffic in such email lists to register with the state. Although it has been in effect for 2 years, the jury is out regarding its efficacy. Our European counterparts are protected by the General Data Protection Regulation, which specifies that commercial email can be sent only to individuals who have explicitly opted into such mailings, and that purchased email lists are not compliant with the requirement.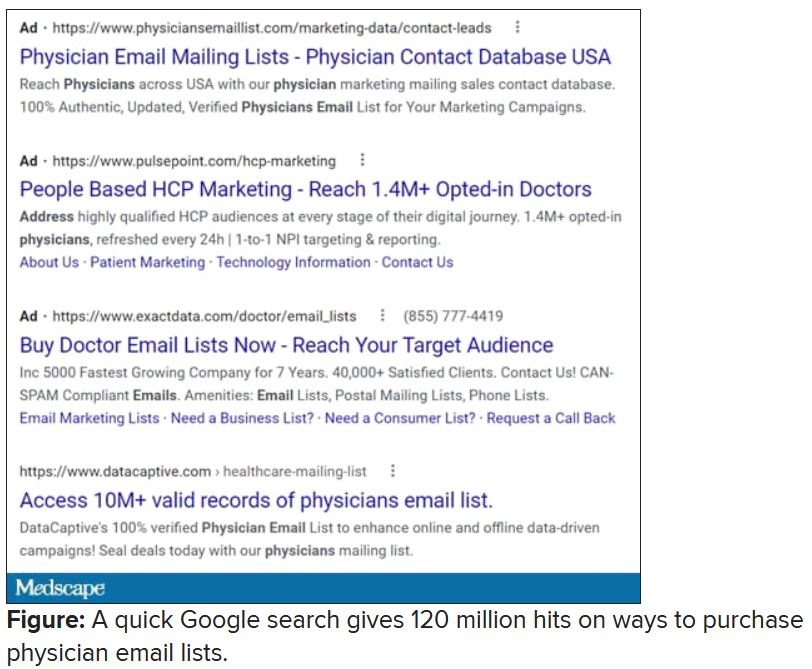
Anybody have the inside scoop on this? Can we demand that our professional societies safeguard their attendee databases so this won’t happen? If they won’t, why am I paying big money to attend their conferences, only for them to make even more money at my expense?
Dr. Hitchcock is assistant professor, department of radiation oncology, at the University of Florida, Gainesville. She reported receiving research grant money from Merck. A version of this article first appeared on Medscape.com.
Despite the best efforts of my institution’s spam filter, I’ve realized that I spend at least 4 minutes every day of the week removing junk email from my in basket: EMR vendors, predatory journals trying to lure me into paying their outrageous publication fees, people who want to help me with my billing software (evidently that .edu extension hasn’t clicked for them yet), headhunters trying to fill specialty positions in other states, market researchers offering a gift card for 40 minutes filling out a survey.
If you do the math, 4 minutes daily is 1,460 minutes per year. That’s an entire day of my life lost each year to this useless nonsense, which I never agreed to receive in the first place. Now multiply that by the 22 million health care workers in the United States, or even just by the 985,000 licensed physicians in this country. Then factor in the $638 per hour in gross revenue generated by the average primary care physician, as a conservative, well-documented value.
By my reckoning, these bozos owe the United States alone over $15 billion in lost GDP each year.
So why don’t we shut it down!? The CAN-SPAM Act of 2003 attempted to at least mitigate the problem. It applies only to commercial entities (I know, I’d love to report some political groups, too). To avoid violating the law and risking fines of up to $16,000 per individual email, senders must:
- Not use misleading header info (including domain name and email address)
- Not use deceptive subject lines
- Clearly label the email as an ad
- Give an actual physical address of the sender
- Tell recipients how to opt out of future emails
- Honor opt-out requests within 10 business days
- Monitor the activities of any subcontractor sending email on their behalf
I can say with certainty that much of the trash in my inbox violates at least one of these. But that doesn’t matter if there is not an efficient way to report the violators and ensure that they’ll be tracked down. Hard enough if they live here, impossible if the email is routed from overseas, as much of it clearly is.
If you receive email in violation of the act, experts recommend that you write down the email address and the business name of the sender, fill out a complaint form on the Federal Trade Commission website, or send an email to [email protected], then send an email to your Internet service provider’s abuse desk. If you’re not working within a big institution like mine that has hot and cold running IT personnel that operate their own abuse prevention office, the address you’ll need is likely abuse@domain_name or postmaster@domain_name. Just hitting the spam button at the top of your browser/email software may do the trick. There’s more good advice at the FTC’s consumer spam page.
The answer came, ironically, to my email inbox in the form of one of those emails that did indeed violate the law.
I rolled my eyes and started into my reporting subroutine but then stopped cold. Just 1 second. If this person is selling lists of email addresses of conference attendees, somebody within the conference structure must be providing them. How is that legal? I have never agreed, in registering for a medical conference, to allow them to share my email address with anyone. To think that they are making money from that is extremely galling.
Vermont, at least, has enacted a law requiring companies that traffic in such email lists to register with the state. Although it has been in effect for 2 years, the jury is out regarding its efficacy. Our European counterparts are protected by the General Data Protection Regulation, which specifies that commercial email can be sent only to individuals who have explicitly opted into such mailings, and that purchased email lists are not compliant with the requirement.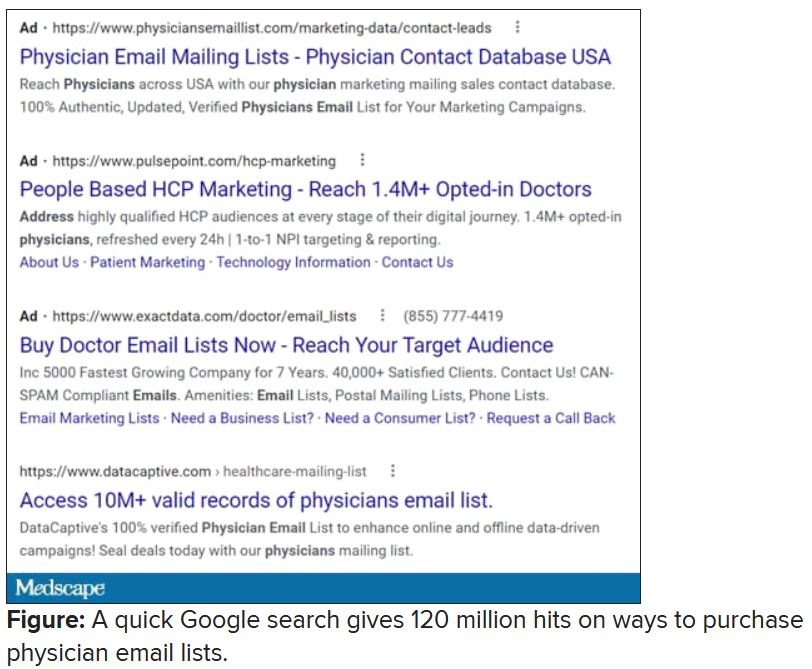
Anybody have the inside scoop on this? Can we demand that our professional societies safeguard their attendee databases so this won’t happen? If they won’t, why am I paying big money to attend their conferences, only for them to make even more money at my expense?
Dr. Hitchcock is assistant professor, department of radiation oncology, at the University of Florida, Gainesville. She reported receiving research grant money from Merck. A version of this article first appeared on Medscape.com.