User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Five things you should know about ‘free’ at-home COVID tests
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the Coronavirus Aid, Relief and Economic Security, or CARES, Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for polymerase chain reaction tests, COVID treatments and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
1. Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
2. Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare, and Aetna did not respond to requests to discuss this issue.
3. If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41% to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and often avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
4. Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them – at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test – and that is not unheard of – your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has activated a website where Americans can order free tests from a cache of a billion the federal government ordered.
5. Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Ms. Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the Coronavirus Aid, Relief and Economic Security, or CARES, Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for polymerase chain reaction tests, COVID treatments and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
1. Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
2. Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare, and Aetna did not respond to requests to discuss this issue.
3. If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41% to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and often avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
4. Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them – at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test – and that is not unheard of – your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has activated a website where Americans can order free tests from a cache of a billion the federal government ordered.
5. Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Ms. Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the Coronavirus Aid, Relief and Economic Security, or CARES, Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for polymerase chain reaction tests, COVID treatments and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
1. Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
2. Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare, and Aetna did not respond to requests to discuss this issue.
3. If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41% to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and often avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
4. Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them – at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test – and that is not unheard of – your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has activated a website where Americans can order free tests from a cache of a billion the federal government ordered.
5. Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Ms. Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
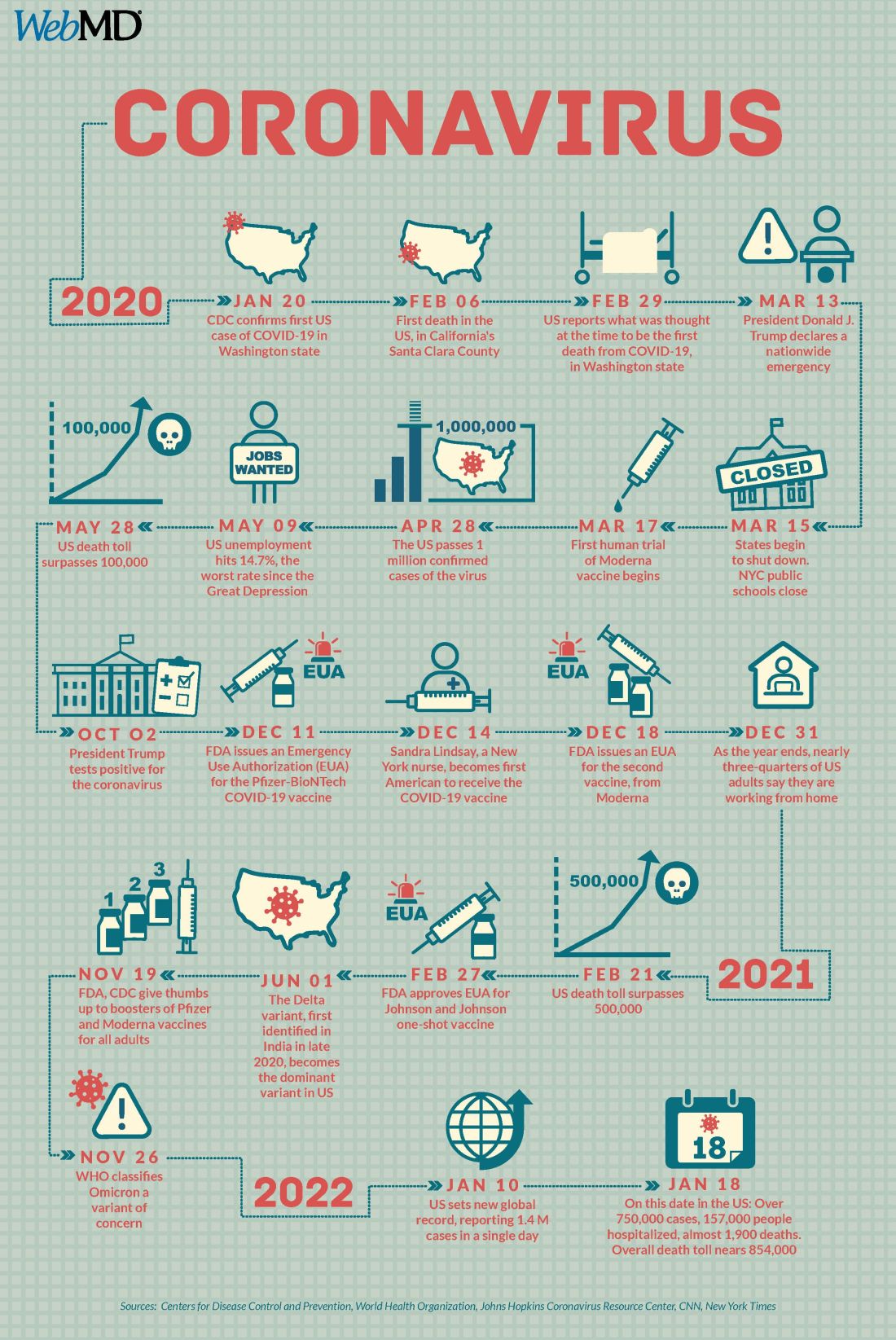
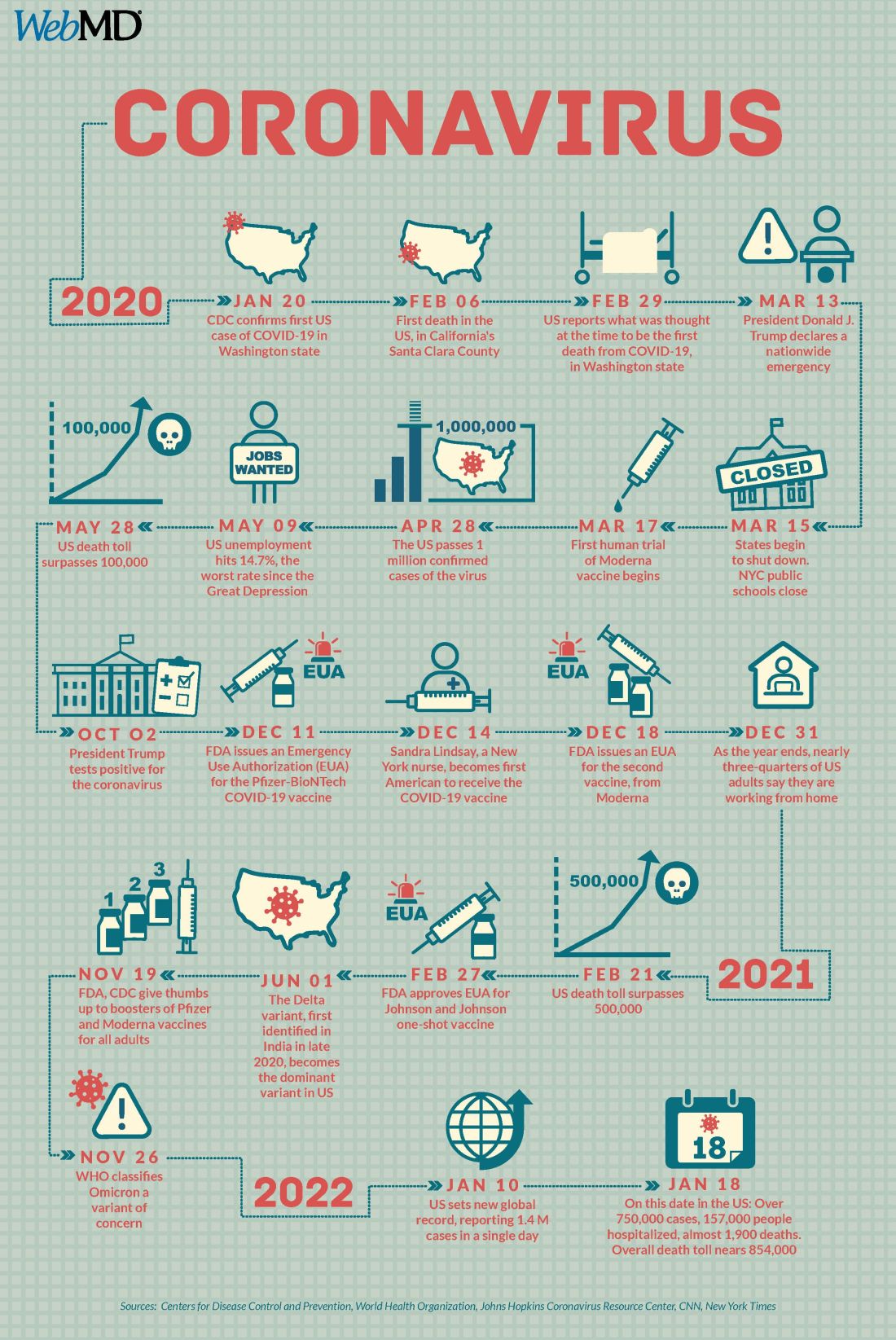
COVID at 2 years: Preparing for a different ‘normal’
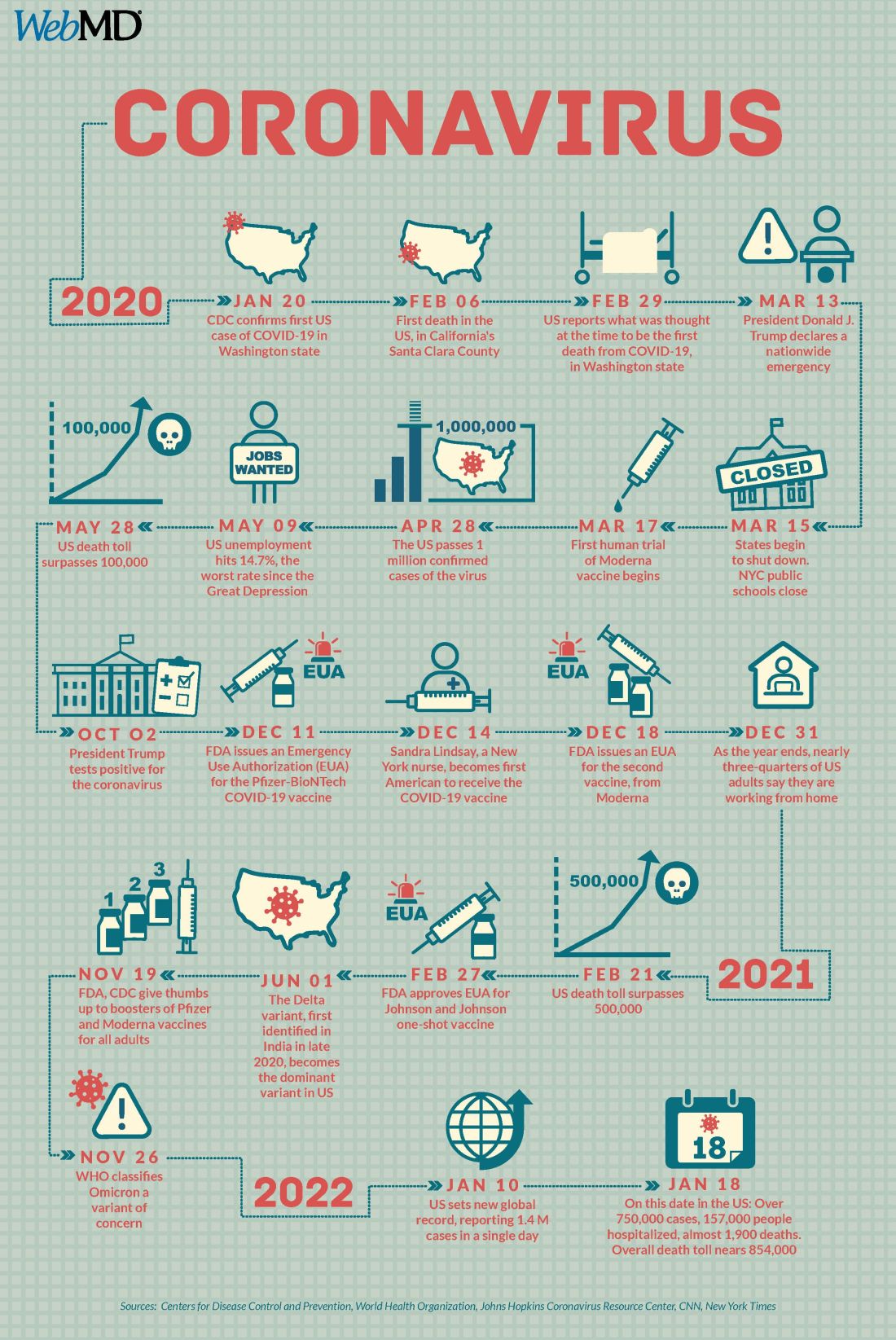
Two years into the COVID-19 pandemic, the United States is still breaking records in hospital overcrowding and new cases.
The United States is logging nearly 800,000 cases a day, hospitals are starting to fray, and deaths have topped 850,000. Schools oscillate from remote to in-person learning, polarizing communities.
The vaccines are lifesaving for many, yet frustration mounts as the numbers of unvaccinated people in this country stays relatively stagnant (63% in the United States are fully vaccinated) and other parts of the world have seen hardly a single dose. Africa has the slowest vaccination rate among continents, with only 14% of the population receiving one shot, according to the New York Times tracker.
Yet
Effective vaccines and treatments that can keep people out of the hospital were developed at an astounding pace, and advances in tracking and testing – in both access and effectiveness – are starting to pay off.
Some experts say it’s possible that the raging Omicron surge will slow by late spring, providing some relief and maybe shifting the pandemic to a slower-burning endemic.
But other experts caution to keep our guard up, saying it’s time to settle into a “new normal” and upend the strategy for fighting COVID-19.
Time to change COVID thinking
Three former members of the Biden-Harris Transition COVID-19 Advisory Board wrote recently in JAMA that COVID-19 has now become one of the many viral respiratory diseases that health care providers and patients will manage each year.
The group of experts from the University of Pennsylvania, University of Minnesota, and New York University write that “many of the measures to reduce transmission of SARS-CoV-2 (for example, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.”
Other experts, including Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, have said it’s been clear since the early days of SARS-CoV-2 that we must learn to live with the virus because it “will be ever present for the remaining history of our species.”
But that doesn’t mean the virus will always have the upper hand. Although the United States has been reaching record numbers of hospitalizations in January, these hospitalizations differ from those of last year – marked by fewer extreme lifesaving measures, fewer deaths, and shorter hospital stays – caused in part by medical and therapeutic advances and in part to the nature of the Omicron variant itself.
One sign of progress, Dr. Adalja said, will be the widespread decoupling of cases from hospitalizations, something that has already happened in countries such as the United Kingdom.
“That’s a reflection of how well they have vaccinated their high-risk population and how poorly we have vaccinated our high-risk population,” he said.
Omicron will bump up natural immunity
Dr. Adalja said though the numbers of unvaccinated in the United States appear to be stuck, Omicron’s sweep will make the difference, leaving behind more natural immunity in the population.
Currently, hospitals are struggling with staffing concerns as a “direct result” of too many unvaccinated people, he said.
Andrew Badley, MD, an infectious diseases specialist at Mayo Clinic in Rochester, Minn., and director of the clinic’s COVID-19 Task Force, said the good news with Omicron is that nearly all people it infects will recover.
Over time, when the body sees foreign antigens repeatedly, the quantity and quality of the antibodies the immune system produces increase and the body becomes better at fighting disease.
So “a large amount of the population will have recovered and have a degree of immunity,” Dr. Badley said.
His optimism is tempered by his belief that “it’s going to get worse before it gets better.”
But Dr. Badley still predicts a turnaround. “We’ll see a downturn in COVID in late spring or early summer,” and well into the second quarter of 2022, “we’ll see a reemergence of control.”
Right now, with Omicron, one infected person is infecting three to five others, he said. The hope is that it will eventually reach one-to-one endemic levels.
As for the threat of new variants, Badley said, “it’s not predictable whether they will be stronger or weaker.”
Masks may be around for years
Many experts predict that masks will continue to be part of the national wardrobe for the foreseeable future.
“We will continue to see new cases for years and years to come. Some will respond to that with masks in public places for a very long time. I personally will do so,” Dr. Badley said.
Two mindsets: Inside/outside the hospital
Emily Landon, MD, an infectious disease doctor and the executive medical director of infection prevention and control at University of Chicago Medicine, told this news organization she views the pandemic from two different vantage points.
As a health care provider, she sees her hospital, like others worldwide, overwhelmed. Supplies of a major weapon to help prevent hospitalization, the monoclonal antibody sotrovimab, are running out. Dr. Landon said she has been calling other hospitals to see if they have supplies and, if so, whether Omicron patients can transfer there.
Bottom line: The things they relied on a month ago to keep people out of the hospital are no longer there, she said.
Meanwhile, “We have more COVID patients than we have ever had,” Dr. Landon said.
Last year, UChicago hit a high of 170 people hospitalized with COVID. This year, so far, the peak was 270.
Dr. Landon said she is frustrated when she leaves that overburdened world inside the hospital for the outside world, where people wear no masks or ineffective face coverings and gather unsafely. Although some of that behavior reflects an intention to flout the advice of medical experts, some is caused in part, she said, by the lack of a clear national health strategy and garbled communication from those in charge of public safety.
Americans are deciding for themselves, on an a la carte basis, whether to wear a mask or get tested or travel, and school districts decide individually when it’s time to go virtual.
“People are exhausted from having to do a risk-benefit analysis for every single activity they, their friends, their kids want to participate in,” she said.
U.S. behind in several areas
Despite our self-image as the global leader in science and medicine, the United States stumbled badly in its response to the pandemic, with grave consequences both at home and abroad, experts say.
In a recent commentary in JAMA, Lawrence Gostin, JD, from Georgetown University, Washington, and Jennifer Nuzzo, DrPH, at Johns Hopkins University, Baltimore, pointed to several critical shortfalls in the nation’s efforts to control the disease.
One such shortfall is public trust.
This news organization reported in June 2021 that a poll of its readers found that 44% said their trust in the CDC had waned during the pandemic, and 33% said their trust in the FDA had eroded as well.
Health care providers who responded to the poll lost trust as well. About half of the doctors and nurses who responded said they disagreed with the FDA’s decision-making during the pandemic. Nearly 60% of doctors and 65% of nurses said they disagreed with the CDC’s overall pandemic guidance.
Lack of trust can make people resist vaccines and efforts to fight the virus, the authors wrote.
“This will become really relevant when we have ample supply of Pfizer’s antiviral medication,” Mr. Gostin, who directs the O’Neill Institute for National and Global Health Law at Georgetown, told this news organization. “The next phase of the pandemic is not to link testing to contact tracing, because we’re way past that, but to link testing to treatment.”
Lack of regional manufacturing of products is also thwarting global progress.
“It is extraordinarily important that our pharmaceutical industry transfer technology in a pandemic,” Mr. Gostin said. “The most glaring failure to do that is the mRNA vaccines. We’ve got this enormously effective vaccine and the two manufacturers – Pfizer and Moderna – are refusing to share the technology with producers in other countries. That keeps coming back to haunt us.”
Another problem: When the vaccines are shared with other countries, they are being delivered close to the date they expire or arriving at a shipyards without warning, so even some of the doses that get delivered are going to waste, Mr. Gostin said.
“It’s one of the greatest moral failures of my lifetime,” he said.
Also a failure is the “jaw-dropping” state of testing 2 years into the pandemic, he said, as people continue to pay high prices for tests or endure long lines.
The U.S. government updated its calculations and ordered 1 billion tests for the general public. The COVIDtests.gov website to order the free tests is now live.
It’s a step in the right direction. Mr. Gostin and Dr. Nuzzo wrote that there is every reason to expect future epidemics that are as serious or more serious than COVID.
“Failure to address clearly observed weaknesses in the COVID-19 response will have preventable adverse health, social, and economic consequences when the next novel outbreak occurs,” they wrote.
A version of this article first appeared on WebMD.com.
Two years into the COVID-19 pandemic, the United States is still breaking records in hospital overcrowding and new cases.
The United States is logging nearly 800,000 cases a day, hospitals are starting to fray, and deaths have topped 850,000. Schools oscillate from remote to in-person learning, polarizing communities.
The vaccines are lifesaving for many, yet frustration mounts as the numbers of unvaccinated people in this country stays relatively stagnant (63% in the United States are fully vaccinated) and other parts of the world have seen hardly a single dose. Africa has the slowest vaccination rate among continents, with only 14% of the population receiving one shot, according to the New York Times tracker.
Yet
Effective vaccines and treatments that can keep people out of the hospital were developed at an astounding pace, and advances in tracking and testing – in both access and effectiveness – are starting to pay off.
Some experts say it’s possible that the raging Omicron surge will slow by late spring, providing some relief and maybe shifting the pandemic to a slower-burning endemic.
But other experts caution to keep our guard up, saying it’s time to settle into a “new normal” and upend the strategy for fighting COVID-19.
Time to change COVID thinking
Three former members of the Biden-Harris Transition COVID-19 Advisory Board wrote recently in JAMA that COVID-19 has now become one of the many viral respiratory diseases that health care providers and patients will manage each year.
The group of experts from the University of Pennsylvania, University of Minnesota, and New York University write that “many of the measures to reduce transmission of SARS-CoV-2 (for example, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.”
Other experts, including Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, have said it’s been clear since the early days of SARS-CoV-2 that we must learn to live with the virus because it “will be ever present for the remaining history of our species.”
But that doesn’t mean the virus will always have the upper hand. Although the United States has been reaching record numbers of hospitalizations in January, these hospitalizations differ from those of last year – marked by fewer extreme lifesaving measures, fewer deaths, and shorter hospital stays – caused in part by medical and therapeutic advances and in part to the nature of the Omicron variant itself.
One sign of progress, Dr. Adalja said, will be the widespread decoupling of cases from hospitalizations, something that has already happened in countries such as the United Kingdom.
“That’s a reflection of how well they have vaccinated their high-risk population and how poorly we have vaccinated our high-risk population,” he said.
Omicron will bump up natural immunity
Dr. Adalja said though the numbers of unvaccinated in the United States appear to be stuck, Omicron’s sweep will make the difference, leaving behind more natural immunity in the population.
Currently, hospitals are struggling with staffing concerns as a “direct result” of too many unvaccinated people, he said.
Andrew Badley, MD, an infectious diseases specialist at Mayo Clinic in Rochester, Minn., and director of the clinic’s COVID-19 Task Force, said the good news with Omicron is that nearly all people it infects will recover.
Over time, when the body sees foreign antigens repeatedly, the quantity and quality of the antibodies the immune system produces increase and the body becomes better at fighting disease.
So “a large amount of the population will have recovered and have a degree of immunity,” Dr. Badley said.
His optimism is tempered by his belief that “it’s going to get worse before it gets better.”
But Dr. Badley still predicts a turnaround. “We’ll see a downturn in COVID in late spring or early summer,” and well into the second quarter of 2022, “we’ll see a reemergence of control.”
Right now, with Omicron, one infected person is infecting three to five others, he said. The hope is that it will eventually reach one-to-one endemic levels.
As for the threat of new variants, Badley said, “it’s not predictable whether they will be stronger or weaker.”
Masks may be around for years
Many experts predict that masks will continue to be part of the national wardrobe for the foreseeable future.
“We will continue to see new cases for years and years to come. Some will respond to that with masks in public places for a very long time. I personally will do so,” Dr. Badley said.
Two mindsets: Inside/outside the hospital
Emily Landon, MD, an infectious disease doctor and the executive medical director of infection prevention and control at University of Chicago Medicine, told this news organization she views the pandemic from two different vantage points.
As a health care provider, she sees her hospital, like others worldwide, overwhelmed. Supplies of a major weapon to help prevent hospitalization, the monoclonal antibody sotrovimab, are running out. Dr. Landon said she has been calling other hospitals to see if they have supplies and, if so, whether Omicron patients can transfer there.
Bottom line: The things they relied on a month ago to keep people out of the hospital are no longer there, she said.
Meanwhile, “We have more COVID patients than we have ever had,” Dr. Landon said.
Last year, UChicago hit a high of 170 people hospitalized with COVID. This year, so far, the peak was 270.
Dr. Landon said she is frustrated when she leaves that overburdened world inside the hospital for the outside world, where people wear no masks or ineffective face coverings and gather unsafely. Although some of that behavior reflects an intention to flout the advice of medical experts, some is caused in part, she said, by the lack of a clear national health strategy and garbled communication from those in charge of public safety.
Americans are deciding for themselves, on an a la carte basis, whether to wear a mask or get tested or travel, and school districts decide individually when it’s time to go virtual.
“People are exhausted from having to do a risk-benefit analysis for every single activity they, their friends, their kids want to participate in,” she said.
U.S. behind in several areas
Despite our self-image as the global leader in science and medicine, the United States stumbled badly in its response to the pandemic, with grave consequences both at home and abroad, experts say.
In a recent commentary in JAMA, Lawrence Gostin, JD, from Georgetown University, Washington, and Jennifer Nuzzo, DrPH, at Johns Hopkins University, Baltimore, pointed to several critical shortfalls in the nation’s efforts to control the disease.
One such shortfall is public trust.
This news organization reported in June 2021 that a poll of its readers found that 44% said their trust in the CDC had waned during the pandemic, and 33% said their trust in the FDA had eroded as well.
Health care providers who responded to the poll lost trust as well. About half of the doctors and nurses who responded said they disagreed with the FDA’s decision-making during the pandemic. Nearly 60% of doctors and 65% of nurses said they disagreed with the CDC’s overall pandemic guidance.
Lack of trust can make people resist vaccines and efforts to fight the virus, the authors wrote.
“This will become really relevant when we have ample supply of Pfizer’s antiviral medication,” Mr. Gostin, who directs the O’Neill Institute for National and Global Health Law at Georgetown, told this news organization. “The next phase of the pandemic is not to link testing to contact tracing, because we’re way past that, but to link testing to treatment.”
Lack of regional manufacturing of products is also thwarting global progress.
“It is extraordinarily important that our pharmaceutical industry transfer technology in a pandemic,” Mr. Gostin said. “The most glaring failure to do that is the mRNA vaccines. We’ve got this enormously effective vaccine and the two manufacturers – Pfizer and Moderna – are refusing to share the technology with producers in other countries. That keeps coming back to haunt us.”
Another problem: When the vaccines are shared with other countries, they are being delivered close to the date they expire or arriving at a shipyards without warning, so even some of the doses that get delivered are going to waste, Mr. Gostin said.
“It’s one of the greatest moral failures of my lifetime,” he said.
Also a failure is the “jaw-dropping” state of testing 2 years into the pandemic, he said, as people continue to pay high prices for tests or endure long lines.
The U.S. government updated its calculations and ordered 1 billion tests for the general public. The COVIDtests.gov website to order the free tests is now live.
It’s a step in the right direction. Mr. Gostin and Dr. Nuzzo wrote that there is every reason to expect future epidemics that are as serious or more serious than COVID.
“Failure to address clearly observed weaknesses in the COVID-19 response will have preventable adverse health, social, and economic consequences when the next novel outbreak occurs,” they wrote.
A version of this article first appeared on WebMD.com.
Two years into the COVID-19 pandemic, the United States is still breaking records in hospital overcrowding and new cases.
The United States is logging nearly 800,000 cases a day, hospitals are starting to fray, and deaths have topped 850,000. Schools oscillate from remote to in-person learning, polarizing communities.
The vaccines are lifesaving for many, yet frustration mounts as the numbers of unvaccinated people in this country stays relatively stagnant (63% in the United States are fully vaccinated) and other parts of the world have seen hardly a single dose. Africa has the slowest vaccination rate among continents, with only 14% of the population receiving one shot, according to the New York Times tracker.
Yet
Effective vaccines and treatments that can keep people out of the hospital were developed at an astounding pace, and advances in tracking and testing – in both access and effectiveness – are starting to pay off.
Some experts say it’s possible that the raging Omicron surge will slow by late spring, providing some relief and maybe shifting the pandemic to a slower-burning endemic.
But other experts caution to keep our guard up, saying it’s time to settle into a “new normal” and upend the strategy for fighting COVID-19.
Time to change COVID thinking
Three former members of the Biden-Harris Transition COVID-19 Advisory Board wrote recently in JAMA that COVID-19 has now become one of the many viral respiratory diseases that health care providers and patients will manage each year.
The group of experts from the University of Pennsylvania, University of Minnesota, and New York University write that “many of the measures to reduce transmission of SARS-CoV-2 (for example, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.”
Other experts, including Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore, have said it’s been clear since the early days of SARS-CoV-2 that we must learn to live with the virus because it “will be ever present for the remaining history of our species.”
But that doesn’t mean the virus will always have the upper hand. Although the United States has been reaching record numbers of hospitalizations in January, these hospitalizations differ from those of last year – marked by fewer extreme lifesaving measures, fewer deaths, and shorter hospital stays – caused in part by medical and therapeutic advances and in part to the nature of the Omicron variant itself.
One sign of progress, Dr. Adalja said, will be the widespread decoupling of cases from hospitalizations, something that has already happened in countries such as the United Kingdom.
“That’s a reflection of how well they have vaccinated their high-risk population and how poorly we have vaccinated our high-risk population,” he said.
Omicron will bump up natural immunity
Dr. Adalja said though the numbers of unvaccinated in the United States appear to be stuck, Omicron’s sweep will make the difference, leaving behind more natural immunity in the population.
Currently, hospitals are struggling with staffing concerns as a “direct result” of too many unvaccinated people, he said.
Andrew Badley, MD, an infectious diseases specialist at Mayo Clinic in Rochester, Minn., and director of the clinic’s COVID-19 Task Force, said the good news with Omicron is that nearly all people it infects will recover.
Over time, when the body sees foreign antigens repeatedly, the quantity and quality of the antibodies the immune system produces increase and the body becomes better at fighting disease.
So “a large amount of the population will have recovered and have a degree of immunity,” Dr. Badley said.
His optimism is tempered by his belief that “it’s going to get worse before it gets better.”
But Dr. Badley still predicts a turnaround. “We’ll see a downturn in COVID in late spring or early summer,” and well into the second quarter of 2022, “we’ll see a reemergence of control.”
Right now, with Omicron, one infected person is infecting three to five others, he said. The hope is that it will eventually reach one-to-one endemic levels.
As for the threat of new variants, Badley said, “it’s not predictable whether they will be stronger or weaker.”
Masks may be around for years
Many experts predict that masks will continue to be part of the national wardrobe for the foreseeable future.
“We will continue to see new cases for years and years to come. Some will respond to that with masks in public places for a very long time. I personally will do so,” Dr. Badley said.
Two mindsets: Inside/outside the hospital
Emily Landon, MD, an infectious disease doctor and the executive medical director of infection prevention and control at University of Chicago Medicine, told this news organization she views the pandemic from two different vantage points.
As a health care provider, she sees her hospital, like others worldwide, overwhelmed. Supplies of a major weapon to help prevent hospitalization, the monoclonal antibody sotrovimab, are running out. Dr. Landon said she has been calling other hospitals to see if they have supplies and, if so, whether Omicron patients can transfer there.
Bottom line: The things they relied on a month ago to keep people out of the hospital are no longer there, she said.
Meanwhile, “We have more COVID patients than we have ever had,” Dr. Landon said.
Last year, UChicago hit a high of 170 people hospitalized with COVID. This year, so far, the peak was 270.
Dr. Landon said she is frustrated when she leaves that overburdened world inside the hospital for the outside world, where people wear no masks or ineffective face coverings and gather unsafely. Although some of that behavior reflects an intention to flout the advice of medical experts, some is caused in part, she said, by the lack of a clear national health strategy and garbled communication from those in charge of public safety.
Americans are deciding for themselves, on an a la carte basis, whether to wear a mask or get tested or travel, and school districts decide individually when it’s time to go virtual.
“People are exhausted from having to do a risk-benefit analysis for every single activity they, their friends, their kids want to participate in,” she said.
U.S. behind in several areas
Despite our self-image as the global leader in science and medicine, the United States stumbled badly in its response to the pandemic, with grave consequences both at home and abroad, experts say.
In a recent commentary in JAMA, Lawrence Gostin, JD, from Georgetown University, Washington, and Jennifer Nuzzo, DrPH, at Johns Hopkins University, Baltimore, pointed to several critical shortfalls in the nation’s efforts to control the disease.
One such shortfall is public trust.
This news organization reported in June 2021 that a poll of its readers found that 44% said their trust in the CDC had waned during the pandemic, and 33% said their trust in the FDA had eroded as well.
Health care providers who responded to the poll lost trust as well. About half of the doctors and nurses who responded said they disagreed with the FDA’s decision-making during the pandemic. Nearly 60% of doctors and 65% of nurses said they disagreed with the CDC’s overall pandemic guidance.
Lack of trust can make people resist vaccines and efforts to fight the virus, the authors wrote.
“This will become really relevant when we have ample supply of Pfizer’s antiviral medication,” Mr. Gostin, who directs the O’Neill Institute for National and Global Health Law at Georgetown, told this news organization. “The next phase of the pandemic is not to link testing to contact tracing, because we’re way past that, but to link testing to treatment.”
Lack of regional manufacturing of products is also thwarting global progress.
“It is extraordinarily important that our pharmaceutical industry transfer technology in a pandemic,” Mr. Gostin said. “The most glaring failure to do that is the mRNA vaccines. We’ve got this enormously effective vaccine and the two manufacturers – Pfizer and Moderna – are refusing to share the technology with producers in other countries. That keeps coming back to haunt us.”
Another problem: When the vaccines are shared with other countries, they are being delivered close to the date they expire or arriving at a shipyards without warning, so even some of the doses that get delivered are going to waste, Mr. Gostin said.
“It’s one of the greatest moral failures of my lifetime,” he said.
Also a failure is the “jaw-dropping” state of testing 2 years into the pandemic, he said, as people continue to pay high prices for tests or endure long lines.
The U.S. government updated its calculations and ordered 1 billion tests for the general public. The COVIDtests.gov website to order the free tests is now live.
It’s a step in the right direction. Mr. Gostin and Dr. Nuzzo wrote that there is every reason to expect future epidemics that are as serious or more serious than COVID.
“Failure to address clearly observed weaknesses in the COVID-19 response will have preventable adverse health, social, and economic consequences when the next novel outbreak occurs,” they wrote.
A version of this article first appeared on WebMD.com.
Make America beautiful: Support mask mandates
In space, no one can hear your red blood cells scream
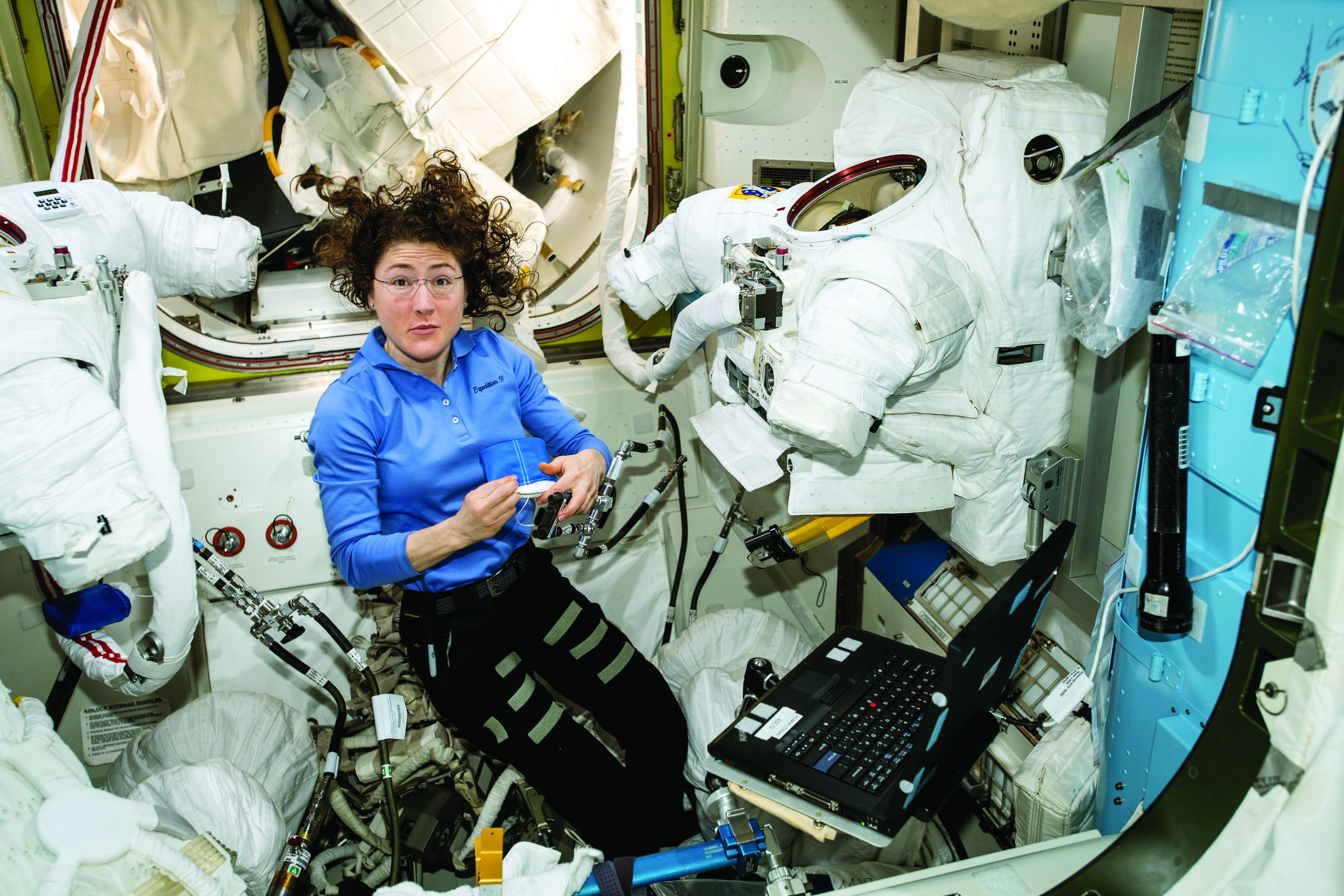
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
Pandemic weighing on physicians’ happiness outside of work: survey
One of the unexpected consequences of the pandemic is that many people are rethinking their priorities and lifestyles, and physicians are no exception.
Pets, prayer, and partners
The pandemic has taken a toll on physicians outside of work as well as on the job. Eight in 10 physicians (82% of men and 80% of women) said they were “somewhat” or “very” happy outside of work before the pandemic. This is almost exactly the same result as in last year’s survey.
However, when asked how happy they are outside of work currently, only 6 in 10 (59%) reported being “somewhat” or “very” happy. While the pandemic has made life difficult for everyone, health care professionals face particular stresses even outside of work. Wayne M. Sotile, PhD, founder of the Center for Physician Resilience, says he has counseled doctors who witnessed COVID-related suffering and death at work, then came home to a partner who didn’t believe that the pandemic was real.
Still, physicians reported that spending time with people they love and engaging in favorite activities helps them stay happy. “Spending time with pets” and “religious practice/prayer” were frequent “other” responses to the question, “What do you do to maintain happiness and mental health?” Seven in 10 physicians reported having some kind of religious or spiritual beliefs.
The majority of physicians (83%) are either married or living with a partner, with male physicians edging out their female peers (89% vs. 75%). Among married physicians, 8 in 10 physicians reported that their union is “good” or “very good.” The pandemic may have helped in this respect. Dr. Sotile says he’s heard physicians say that they’ve connected more with their families in the past 18 months. Specialists with the highest rates of happy marriages were otolaryngologists and immunologists (both 91%), followed closely by dermatologists, rheumatologists, and nephrologists (all 90%).
Among physicians balancing a medical career and parenthood, female physicians reported feeling conflicted more often than males (48% vs. 29%). Nicole A. Sparks, MD, an ob.gyn. and a health and lifestyle blogger, cites not being there for her kids as a source of stress. She notes that her two young children notice when she’s not there to help with homework, read bedtime stories, or make their dinner. “Mom guilt can definitely set in if I have to miss important events,” she says.
Work-life balance is an important, if elusive, goal for physicians, and not just females. Sixty percent of female doctors and 53% of male doctors said they would be willing to take a cut in pay if it meant more free time and a better work-life balance. Many doctors do manage to get away from work occasionally, with one-fifth of all physicians taking 5 or more weeks of vacation each year.
Seeking a ‘balanced life’
Alexis Polles, MD, medical director for the Professionals Resource Network, points out the importance of taking time for personal health and wellness. “When we work with professionals who have problems with mental health or substance abuse, they often don’t have a balanced life,” she says. “They are usually in a workaholic mindset and disregard their own needs.”
Few physicians seem to prioritize self-care, with a third indicating they “always” or “most of the time” spend enough time on their own health and wellness. But of those who do, males (38%) are more likely than females (27%) to spend enough time on their own health and wellness. Dr. Polles adds that exercising after a shift can help physicians better make the transition from professional to personal life. Though they did not report when they exercised, about a third of physicians reported doing so four or more times per week. Controlling weight is an issue as well, with 49% of male and 55% of female physicians saying they are currently trying to lose weight.
Of physicians who drink alcohol, about a third have three or more drinks per week. (The CDC defines “heavy drinking” as consuming 15 drinks or more per week for men and eight drinks or more per week for women.)
Of those surveyed, 92% say they do not regularly use cannabidiol or cannabis, and a mere 4% of respondents said they would use at least one of these substances if they were to become legal in their state.
A version of this article first appeared on Medscape.com.
One of the unexpected consequences of the pandemic is that many people are rethinking their priorities and lifestyles, and physicians are no exception.
Pets, prayer, and partners
The pandemic has taken a toll on physicians outside of work as well as on the job. Eight in 10 physicians (82% of men and 80% of women) said they were “somewhat” or “very” happy outside of work before the pandemic. This is almost exactly the same result as in last year’s survey.
However, when asked how happy they are outside of work currently, only 6 in 10 (59%) reported being “somewhat” or “very” happy. While the pandemic has made life difficult for everyone, health care professionals face particular stresses even outside of work. Wayne M. Sotile, PhD, founder of the Center for Physician Resilience, says he has counseled doctors who witnessed COVID-related suffering and death at work, then came home to a partner who didn’t believe that the pandemic was real.
Still, physicians reported that spending time with people they love and engaging in favorite activities helps them stay happy. “Spending time with pets” and “religious practice/prayer” were frequent “other” responses to the question, “What do you do to maintain happiness and mental health?” Seven in 10 physicians reported having some kind of religious or spiritual beliefs.
The majority of physicians (83%) are either married or living with a partner, with male physicians edging out their female peers (89% vs. 75%). Among married physicians, 8 in 10 physicians reported that their union is “good” or “very good.” The pandemic may have helped in this respect. Dr. Sotile says he’s heard physicians say that they’ve connected more with their families in the past 18 months. Specialists with the highest rates of happy marriages were otolaryngologists and immunologists (both 91%), followed closely by dermatologists, rheumatologists, and nephrologists (all 90%).
Among physicians balancing a medical career and parenthood, female physicians reported feeling conflicted more often than males (48% vs. 29%). Nicole A. Sparks, MD, an ob.gyn. and a health and lifestyle blogger, cites not being there for her kids as a source of stress. She notes that her two young children notice when she’s not there to help with homework, read bedtime stories, or make their dinner. “Mom guilt can definitely set in if I have to miss important events,” she says.
Work-life balance is an important, if elusive, goal for physicians, and not just females. Sixty percent of female doctors and 53% of male doctors said they would be willing to take a cut in pay if it meant more free time and a better work-life balance. Many doctors do manage to get away from work occasionally, with one-fifth of all physicians taking 5 or more weeks of vacation each year.
Seeking a ‘balanced life’
Alexis Polles, MD, medical director for the Professionals Resource Network, points out the importance of taking time for personal health and wellness. “When we work with professionals who have problems with mental health or substance abuse, they often don’t have a balanced life,” she says. “They are usually in a workaholic mindset and disregard their own needs.”
Few physicians seem to prioritize self-care, with a third indicating they “always” or “most of the time” spend enough time on their own health and wellness. But of those who do, males (38%) are more likely than females (27%) to spend enough time on their own health and wellness. Dr. Polles adds that exercising after a shift can help physicians better make the transition from professional to personal life. Though they did not report when they exercised, about a third of physicians reported doing so four or more times per week. Controlling weight is an issue as well, with 49% of male and 55% of female physicians saying they are currently trying to lose weight.
Of physicians who drink alcohol, about a third have three or more drinks per week. (The CDC defines “heavy drinking” as consuming 15 drinks or more per week for men and eight drinks or more per week for women.)
Of those surveyed, 92% say they do not regularly use cannabidiol or cannabis, and a mere 4% of respondents said they would use at least one of these substances if they were to become legal in their state.
A version of this article first appeared on Medscape.com.
One of the unexpected consequences of the pandemic is that many people are rethinking their priorities and lifestyles, and physicians are no exception.
Pets, prayer, and partners
The pandemic has taken a toll on physicians outside of work as well as on the job. Eight in 10 physicians (82% of men and 80% of women) said they were “somewhat” or “very” happy outside of work before the pandemic. This is almost exactly the same result as in last year’s survey.
However, when asked how happy they are outside of work currently, only 6 in 10 (59%) reported being “somewhat” or “very” happy. While the pandemic has made life difficult for everyone, health care professionals face particular stresses even outside of work. Wayne M. Sotile, PhD, founder of the Center for Physician Resilience, says he has counseled doctors who witnessed COVID-related suffering and death at work, then came home to a partner who didn’t believe that the pandemic was real.
Still, physicians reported that spending time with people they love and engaging in favorite activities helps them stay happy. “Spending time with pets” and “religious practice/prayer” were frequent “other” responses to the question, “What do you do to maintain happiness and mental health?” Seven in 10 physicians reported having some kind of religious or spiritual beliefs.
The majority of physicians (83%) are either married or living with a partner, with male physicians edging out their female peers (89% vs. 75%). Among married physicians, 8 in 10 physicians reported that their union is “good” or “very good.” The pandemic may have helped in this respect. Dr. Sotile says he’s heard physicians say that they’ve connected more with their families in the past 18 months. Specialists with the highest rates of happy marriages were otolaryngologists and immunologists (both 91%), followed closely by dermatologists, rheumatologists, and nephrologists (all 90%).
Among physicians balancing a medical career and parenthood, female physicians reported feeling conflicted more often than males (48% vs. 29%). Nicole A. Sparks, MD, an ob.gyn. and a health and lifestyle blogger, cites not being there for her kids as a source of stress. She notes that her two young children notice when she’s not there to help with homework, read bedtime stories, or make their dinner. “Mom guilt can definitely set in if I have to miss important events,” she says.
Work-life balance is an important, if elusive, goal for physicians, and not just females. Sixty percent of female doctors and 53% of male doctors said they would be willing to take a cut in pay if it meant more free time and a better work-life balance. Many doctors do manage to get away from work occasionally, with one-fifth of all physicians taking 5 or more weeks of vacation each year.
Seeking a ‘balanced life’
Alexis Polles, MD, medical director for the Professionals Resource Network, points out the importance of taking time for personal health and wellness. “When we work with professionals who have problems with mental health or substance abuse, they often don’t have a balanced life,” she says. “They are usually in a workaholic mindset and disregard their own needs.”
Few physicians seem to prioritize self-care, with a third indicating they “always” or “most of the time” spend enough time on their own health and wellness. But of those who do, males (38%) are more likely than females (27%) to spend enough time on their own health and wellness. Dr. Polles adds that exercising after a shift can help physicians better make the transition from professional to personal life. Though they did not report when they exercised, about a third of physicians reported doing so four or more times per week. Controlling weight is an issue as well, with 49% of male and 55% of female physicians saying they are currently trying to lose weight.
Of physicians who drink alcohol, about a third have three or more drinks per week. (The CDC defines “heavy drinking” as consuming 15 drinks or more per week for men and eight drinks or more per week for women.)
Of those surveyed, 92% say they do not regularly use cannabidiol or cannabis, and a mere 4% of respondents said they would use at least one of these substances if they were to become legal in their state.
A version of this article first appeared on Medscape.com.
Severe outcomes increased in youth hospitalized after positive COVID-19 test
Approximately 3% of youth who tested positive for COVID-19 in an emergency department setting had severe outcomes after 2 weeks, but this risk was 0.5% among those not admitted to the hospital, based on data from more than 3,000 individuals aged 18 and younger.
In the early stages of the COVID-19 pandemic, youth younger than 18 years accounted for fewer than 5% of reported cases, but now account for approximately 25% of positive cases, wrote Anna L. Funk, PhD, of the University of Calgary, Alberta, Canada, and colleagues.
However, the risk of severe outcomes of youth with COVID-19 remains poorly understood and data from large studies are lacking, they noted.
In a prospective cohort study published in JAMA Network Open, the researchers reviewed data from 3,221 children and adolescents who were tested for COVID-19 at one of 41 emergency departments in 10 countries including Argentina, Australia, Canada, Costa Rica, Italy, New Zealand, Paraguay, Singapore, Spain, and the United States between March 2020 and June 2021. Positive infections were confirmed by polymerase chain reaction (PCR) testing. At 14 days’ follow-up after a positive test, 735 patients (22.8%), were hospitalized, 107 (3.3%) had severe outcomes, and 4 (0.12%) had died. Severe outcomes were significantly more likely in children aged 5-10 years and 10-18 years vs. less than 1 year (odds ratios, 1.60 and 2.39, respectively), and in children with a self-reported chronic illness (OR, 2.34) or a prior episode of pneumonia (OR, 3.15).
Severe outcomes were more likely in patients who presented with symptoms that started 4-7 days before seeking care, compared with those whose symptoms started 0-3 days before seeking care (OR, 2.22).
The researchers also reviewed data from a subgroup of 2,510 individuals who were discharged home from the ED after initial testing. At 14 days’ follow-up, 50 of these patients (2.0%) were hospitalized and 12 (0.5%) had severe outcomes. In addition, the researchers found that the risk of severe outcomes among hospitalized COVID-19–positive youth was nearly four times higher, compared with hospitalized youth who tested negative for COVID-19 (risk difference, 3.9%).
Previous retrospective studies of severe outcomes in children and adolescents with COVID-19 have yielded varying results, in part because of the variation in study populations, the researchers noted in their discussion of the findings. “Our study population provides a risk estimate for youths brought for ED care.” Therefore, “Our lower estimate of severe disease likely reflects our stringent definition, which required the occurrence of complications or specific invasive interventions,” they said.
The study limitations included the potential overestimation of the risk of severe outcomes because patients were recruited in the ED, the researchers noted. Other limitations included variation in regional case definitions, screening criteria, and testing capacity among different sites and time periods. “Thus, 5% of our SARS-CoV-2–positive participants were asymptomatic – most of whom were tested as they were positive contacts of known cases or as part of routine screening procedures,” they said. The findings also are not generalizable to all community EDs and did not account for variants, they added.
However, the results were strengthened by the ability to compare outcomes for children with positive tests to similar children with negative tests, and add to the literature showing an increased risk of severe outcomes for those hospitalized with positive tests, the researchers concluded.
Data may inform clinical decisions
“The data [in the current study] are concerning for severe outcomes for children even prior to the Omicron strain,” said Margaret Thew, DNP, FP-BC, of Children’s Wisconsin-Milwaukee Hospital, in an interview. “Presently, the number of children infected with the Omicron strain is much higher and hospitalizations among children are at their highest since COVID-19 began,” she said. “For medical providers caring for this population, the study sheds light on pediatric patients who may be at higher risk of severe illness when they become infected with COVID-19,” she added.
“I was surprised by how high the number of pediatric patients hospitalized (22%) and the percentage (3%) with severe disease were during this time,” given that the timeline for these data preceded the spread of the Omicron strain, said Ms. Thew. “The risk of prior pneumonia was quite surprising. I do not recall seeing prior pneumonia as a risk factor for more severe COVID-19 with children or adults,” she added.
The take-home messaging for clinicians caring for children and adolescents is the added knowledge of the risk factors for severe outcomes from COVID-19, including the 10-18 age range, chronic illness, prior pneumonia, and longer symptom duration before seeking care in the ED, Ms. Thew emphasized.
However, additional research is needed on the impact of the new strains of COVID-19 on pediatric and adolescent hospitalizations, Ms. Thew said. Research also is needed on the other illnesses that have resulted from COVID-19, including illness requiring antibiotic use or medical interventions or treatments, and on the risk of combined COVID-19 and influenza viruses, she noted.
The study was supported by the Canadian Institutes of Health Research, Alberta Innovates, the Alberta Health Services University of Calgary Clinical Research Fund, the Alberta Children’s Hospital Research Institute, the COVID-19 Research Accelerator Funding Track (CRAFT) Program at the University of California, Davis, and the Cincinnati Children’s Hospital Medical Center Division of Emergency Medicine Small Grants Program. Lead author Dr. Funk was supported by the University of Calgary Eyes-High Post-Doctoral Research Fund, but had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
Approximately 3% of youth who tested positive for COVID-19 in an emergency department setting had severe outcomes after 2 weeks, but this risk was 0.5% among those not admitted to the hospital, based on data from more than 3,000 individuals aged 18 and younger.
In the early stages of the COVID-19 pandemic, youth younger than 18 years accounted for fewer than 5% of reported cases, but now account for approximately 25% of positive cases, wrote Anna L. Funk, PhD, of the University of Calgary, Alberta, Canada, and colleagues.
However, the risk of severe outcomes of youth with COVID-19 remains poorly understood and data from large studies are lacking, they noted.
In a prospective cohort study published in JAMA Network Open, the researchers reviewed data from 3,221 children and adolescents who were tested for COVID-19 at one of 41 emergency departments in 10 countries including Argentina, Australia, Canada, Costa Rica, Italy, New Zealand, Paraguay, Singapore, Spain, and the United States between March 2020 and June 2021. Positive infections were confirmed by polymerase chain reaction (PCR) testing. At 14 days’ follow-up after a positive test, 735 patients (22.8%), were hospitalized, 107 (3.3%) had severe outcomes, and 4 (0.12%) had died. Severe outcomes were significantly more likely in children aged 5-10 years and 10-18 years vs. less than 1 year (odds ratios, 1.60 and 2.39, respectively), and in children with a self-reported chronic illness (OR, 2.34) or a prior episode of pneumonia (OR, 3.15).
Severe outcomes were more likely in patients who presented with symptoms that started 4-7 days before seeking care, compared with those whose symptoms started 0-3 days before seeking care (OR, 2.22).
The researchers also reviewed data from a subgroup of 2,510 individuals who were discharged home from the ED after initial testing. At 14 days’ follow-up, 50 of these patients (2.0%) were hospitalized and 12 (0.5%) had severe outcomes. In addition, the researchers found that the risk of severe outcomes among hospitalized COVID-19–positive youth was nearly four times higher, compared with hospitalized youth who tested negative for COVID-19 (risk difference, 3.9%).
Previous retrospective studies of severe outcomes in children and adolescents with COVID-19 have yielded varying results, in part because of the variation in study populations, the researchers noted in their discussion of the findings. “Our study population provides a risk estimate for youths brought for ED care.” Therefore, “Our lower estimate of severe disease likely reflects our stringent definition, which required the occurrence of complications or specific invasive interventions,” they said.
The study limitations included the potential overestimation of the risk of severe outcomes because patients were recruited in the ED, the researchers noted. Other limitations included variation in regional case definitions, screening criteria, and testing capacity among different sites and time periods. “Thus, 5% of our SARS-CoV-2–positive participants were asymptomatic – most of whom were tested as they were positive contacts of known cases or as part of routine screening procedures,” they said. The findings also are not generalizable to all community EDs and did not account for variants, they added.
However, the results were strengthened by the ability to compare outcomes for children with positive tests to similar children with negative tests, and add to the literature showing an increased risk of severe outcomes for those hospitalized with positive tests, the researchers concluded.
Data may inform clinical decisions
“The data [in the current study] are concerning for severe outcomes for children even prior to the Omicron strain,” said Margaret Thew, DNP, FP-BC, of Children’s Wisconsin-Milwaukee Hospital, in an interview. “Presently, the number of children infected with the Omicron strain is much higher and hospitalizations among children are at their highest since COVID-19 began,” she said. “For medical providers caring for this population, the study sheds light on pediatric patients who may be at higher risk of severe illness when they become infected with COVID-19,” she added.
“I was surprised by how high the number of pediatric patients hospitalized (22%) and the percentage (3%) with severe disease were during this time,” given that the timeline for these data preceded the spread of the Omicron strain, said Ms. Thew. “The risk of prior pneumonia was quite surprising. I do not recall seeing prior pneumonia as a risk factor for more severe COVID-19 with children or adults,” she added.
The take-home messaging for clinicians caring for children and adolescents is the added knowledge of the risk factors for severe outcomes from COVID-19, including the 10-18 age range, chronic illness, prior pneumonia, and longer symptom duration before seeking care in the ED, Ms. Thew emphasized.
However, additional research is needed on the impact of the new strains of COVID-19 on pediatric and adolescent hospitalizations, Ms. Thew said. Research also is needed on the other illnesses that have resulted from COVID-19, including illness requiring antibiotic use or medical interventions or treatments, and on the risk of combined COVID-19 and influenza viruses, she noted.
The study was supported by the Canadian Institutes of Health Research, Alberta Innovates, the Alberta Health Services University of Calgary Clinical Research Fund, the Alberta Children’s Hospital Research Institute, the COVID-19 Research Accelerator Funding Track (CRAFT) Program at the University of California, Davis, and the Cincinnati Children’s Hospital Medical Center Division of Emergency Medicine Small Grants Program. Lead author Dr. Funk was supported by the University of Calgary Eyes-High Post-Doctoral Research Fund, but had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
Approximately 3% of youth who tested positive for COVID-19 in an emergency department setting had severe outcomes after 2 weeks, but this risk was 0.5% among those not admitted to the hospital, based on data from more than 3,000 individuals aged 18 and younger.
In the early stages of the COVID-19 pandemic, youth younger than 18 years accounted for fewer than 5% of reported cases, but now account for approximately 25% of positive cases, wrote Anna L. Funk, PhD, of the University of Calgary, Alberta, Canada, and colleagues.
However, the risk of severe outcomes of youth with COVID-19 remains poorly understood and data from large studies are lacking, they noted.
In a prospective cohort study published in JAMA Network Open, the researchers reviewed data from 3,221 children and adolescents who were tested for COVID-19 at one of 41 emergency departments in 10 countries including Argentina, Australia, Canada, Costa Rica, Italy, New Zealand, Paraguay, Singapore, Spain, and the United States between March 2020 and June 2021. Positive infections were confirmed by polymerase chain reaction (PCR) testing. At 14 days’ follow-up after a positive test, 735 patients (22.8%), were hospitalized, 107 (3.3%) had severe outcomes, and 4 (0.12%) had died. Severe outcomes were significantly more likely in children aged 5-10 years and 10-18 years vs. less than 1 year (odds ratios, 1.60 and 2.39, respectively), and in children with a self-reported chronic illness (OR, 2.34) or a prior episode of pneumonia (OR, 3.15).
Severe outcomes were more likely in patients who presented with symptoms that started 4-7 days before seeking care, compared with those whose symptoms started 0-3 days before seeking care (OR, 2.22).
The researchers also reviewed data from a subgroup of 2,510 individuals who were discharged home from the ED after initial testing. At 14 days’ follow-up, 50 of these patients (2.0%) were hospitalized and 12 (0.5%) had severe outcomes. In addition, the researchers found that the risk of severe outcomes among hospitalized COVID-19–positive youth was nearly four times higher, compared with hospitalized youth who tested negative for COVID-19 (risk difference, 3.9%).
Previous retrospective studies of severe outcomes in children and adolescents with COVID-19 have yielded varying results, in part because of the variation in study populations, the researchers noted in their discussion of the findings. “Our study population provides a risk estimate for youths brought for ED care.” Therefore, “Our lower estimate of severe disease likely reflects our stringent definition, which required the occurrence of complications or specific invasive interventions,” they said.
The study limitations included the potential overestimation of the risk of severe outcomes because patients were recruited in the ED, the researchers noted. Other limitations included variation in regional case definitions, screening criteria, and testing capacity among different sites and time periods. “Thus, 5% of our SARS-CoV-2–positive participants were asymptomatic – most of whom were tested as they were positive contacts of known cases or as part of routine screening procedures,” they said. The findings also are not generalizable to all community EDs and did not account for variants, they added.
However, the results were strengthened by the ability to compare outcomes for children with positive tests to similar children with negative tests, and add to the literature showing an increased risk of severe outcomes for those hospitalized with positive tests, the researchers concluded.
Data may inform clinical decisions
“The data [in the current study] are concerning for severe outcomes for children even prior to the Omicron strain,” said Margaret Thew, DNP, FP-BC, of Children’s Wisconsin-Milwaukee Hospital, in an interview. “Presently, the number of children infected with the Omicron strain is much higher and hospitalizations among children are at their highest since COVID-19 began,” she said. “For medical providers caring for this population, the study sheds light on pediatric patients who may be at higher risk of severe illness when they become infected with COVID-19,” she added.
“I was surprised by how high the number of pediatric patients hospitalized (22%) and the percentage (3%) with severe disease were during this time,” given that the timeline for these data preceded the spread of the Omicron strain, said Ms. Thew. “The risk of prior pneumonia was quite surprising. I do not recall seeing prior pneumonia as a risk factor for more severe COVID-19 with children or adults,” she added.
The take-home messaging for clinicians caring for children and adolescents is the added knowledge of the risk factors for severe outcomes from COVID-19, including the 10-18 age range, chronic illness, prior pneumonia, and longer symptom duration before seeking care in the ED, Ms. Thew emphasized.
However, additional research is needed on the impact of the new strains of COVID-19 on pediatric and adolescent hospitalizations, Ms. Thew said. Research also is needed on the other illnesses that have resulted from COVID-19, including illness requiring antibiotic use or medical interventions or treatments, and on the risk of combined COVID-19 and influenza viruses, she noted.
The study was supported by the Canadian Institutes of Health Research, Alberta Innovates, the Alberta Health Services University of Calgary Clinical Research Fund, the Alberta Children’s Hospital Research Institute, the COVID-19 Research Accelerator Funding Track (CRAFT) Program at the University of California, Davis, and the Cincinnati Children’s Hospital Medical Center Division of Emergency Medicine Small Grants Program. Lead author Dr. Funk was supported by the University of Calgary Eyes-High Post-Doctoral Research Fund, but had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
FROM JAMA NETWORK OPEN
CVS Caremark formulary change freezes out apixaban
Patients looking to refill a prescription for apixaban (Eliquis) through CVS Caremark may be in for a surprise following its decision to exclude the direct oral anticoagulant (DOAC) from its formulary starting Jan. 1.
The move leaves just one DOAC, rivaroxaban (Xarelto), on CVS’ commercial formulary and is being assailed as the latest example of “nonmedical switching” used by health insurers to control costs.
In a letter to CVS Caremark backed by 14 provider and patient organizations, the nonprofit Partnership to Advance Cardiovascular Health (PACH) calls on the pharmacy chain to reverse its “dangerously disruptive” decision to force stable patients at high risk of cardiovascular events to switch anticoagulation, without an apparent option to be grandfathered into the new plan.
PACH president Dharmesh Patel, MD, Stern Cardiovascular Center, Memphis, called the formulary change “reckless and irresponsible, especially because the decision is not based in science and evidence, but on budgets. Patients and their health care providers, not insurance companies, need to be trusted to determine what medication is best,” he said in a statement.
Craig Beavers, PharmD, vice president of Baptist Health Paducah, Kentucky, said that, as chair of the American College of Cardiology’s Cardiovascular Team Section, he and other organizations have met with CVS Caremark medical leadership to advocate for patients and to understand the company’s perspective.
“The underlying driver is cost,” he told this news organization.
Current guidelines recommend DOACs in general for a variety of indications, including to reduce the risk of stroke and embolism in nonvalvular atrial fibrillation and to prevent deep vein thrombosis, but there are select instances where a particular DOAC might be more appropriate, he observed.
“Apixaban may be better for a patient with a history of GI bleeding because there’s less GI bleeding, but the guidelines don’t necessarily spell those things out,” Dr. Beavers said. “That’s where the clinician should advocate for their patient and, unfortunately, they are making their decision strictly based off the guidelines.”
Requests to speak with medical officers at CVS Caremark went unanswered, but its executive director of communications, Christina Peaslee, told this news organization that the formulary decision “maintains clinically appropriate, cost-effective prescription coverage” for its clients and members.
“Both the American Heart Association/American College of Cardiology/Heart Rhythm Society and 2021 CHEST guidelines recommend DOACs over warfarin for treatment of various cardiology conditions such as atrial fibrillation, but neither list a specific agent as preferred – showing that consensus clinical guidelines do not favor one over the other,” she said in an email. “Further, Xarelto has more FDA-approved indications than Eliquis (e.g., Xarelto is approved for a reduction in risk of major CV events in patients with CAD or PAD) in addition to all the same FDA indications as Eliquis.”
Ms. Peaslee pointed out that all formulary changes are evaluated by an external medical expert specializing in the disease state, followed by review and approval by an independent national Pharmacy & Therapeutics Committee.
The decision to exclude apixaban is also limited to a “subset of commercial drug lists,” she said, although specifics on which plans and the number of affected patients were not forthcoming.
The choice of DOAC is a timely question in cardiology, with recent studies suggesting an advantage for apixaban over rivaroxaban in reducing the risk of recurrent venous thromboembolism, as well as reducing the risk of major ischemic or hemorrhagic events in atrial fibrillation.
Ms. Peaslee said CVS Caremark closely monitors medical literature for relevant clinical trial data and that most clients allow reasonable formulary exceptions when justified. “This formulary exceptions process has been successfully used for changes of this type and allows patients to get a medication that is safe and effective, as determined by their prescriber.”
The company will also continue to provide “robust, personalized outreach to the small number of members who will need to switch to an alternative medication,” she added.
Dr. Beavers said negotiations with CVS are still in the early stages, but, in the meantime, the ACC is providing health care providers with tools, such as drug copay cards and electronic prior authorizations, to help ensure patients don’t have gaps in coverage.
In a Jan. 14 news release addressing the formulary change, ACC notes that a patient’s pharmacy can also request a one-time override when trying to fill a nonpreferred DOAC in January to buy time if switching medications with their clinician or requesting a formulary exception.
During discussions with CVS Caremark, it says the ACC and the American Society of Hematology “underscored the negative impacts of this decision on patients currently taking one of the nonpreferred DOACs and on those who have previously tried rivaroxaban and changed medications.”
The groups also highlighted difficulties with other prior authorization programs in terms of the need for dedicated staff and time away from direct patient care.
“The ACC and ASH will continue discussions with CVS Caremark regarding the burden on clinicians and the effect of the formulary decision on patient access,” the release says.
In its letter to CVS, PACH argues that the apixaban exclusion will disproportionately affect historically disadvantaged patients, leaving those who can least afford the change with limited options. Notably, no generic is available for either apixaban or rivaroxaban.
The group also highlights a 2019 national poll, in which nearly 40% of patients who had their medication switched were so frustrated that they stopped their medication altogether.
PACH has an online petition against nonmedical switching, which at press time had garnered 2,126 signatures.
One signee, Jan Griffin, who survived bilateral pulmonary embolisms, writes that she has been on Eliquis [apixaban] successfully since her hospital discharge. “Now, as of midnight, Caremark apparently knows better than my hematologist as to what blood thinner is better for me and will no longer cover my Eliquis prescription. This is criminal, immoral, and unethical. #StopTheSwitch.”
A version of this article first appeared on Medscape.com.
Patients looking to refill a prescription for apixaban (Eliquis) through CVS Caremark may be in for a surprise following its decision to exclude the direct oral anticoagulant (DOAC) from its formulary starting Jan. 1.
The move leaves just one DOAC, rivaroxaban (Xarelto), on CVS’ commercial formulary and is being assailed as the latest example of “nonmedical switching” used by health insurers to control costs.
In a letter to CVS Caremark backed by 14 provider and patient organizations, the nonprofit Partnership to Advance Cardiovascular Health (PACH) calls on the pharmacy chain to reverse its “dangerously disruptive” decision to force stable patients at high risk of cardiovascular events to switch anticoagulation, without an apparent option to be grandfathered into the new plan.
PACH president Dharmesh Patel, MD, Stern Cardiovascular Center, Memphis, called the formulary change “reckless and irresponsible, especially because the decision is not based in science and evidence, but on budgets. Patients and their health care providers, not insurance companies, need to be trusted to determine what medication is best,” he said in a statement.
Craig Beavers, PharmD, vice president of Baptist Health Paducah, Kentucky, said that, as chair of the American College of Cardiology’s Cardiovascular Team Section, he and other organizations have met with CVS Caremark medical leadership to advocate for patients and to understand the company’s perspective.
“The underlying driver is cost,” he told this news organization.
Current guidelines recommend DOACs in general for a variety of indications, including to reduce the risk of stroke and embolism in nonvalvular atrial fibrillation and to prevent deep vein thrombosis, but there are select instances where a particular DOAC might be more appropriate, he observed.
“Apixaban may be better for a patient with a history of GI bleeding because there’s less GI bleeding, but the guidelines don’t necessarily spell those things out,” Dr. Beavers said. “That’s where the clinician should advocate for their patient and, unfortunately, they are making their decision strictly based off the guidelines.”
Requests to speak with medical officers at CVS Caremark went unanswered, but its executive director of communications, Christina Peaslee, told this news organization that the formulary decision “maintains clinically appropriate, cost-effective prescription coverage” for its clients and members.
“Both the American Heart Association/American College of Cardiology/Heart Rhythm Society and 2021 CHEST guidelines recommend DOACs over warfarin for treatment of various cardiology conditions such as atrial fibrillation, but neither list a specific agent as preferred – showing that consensus clinical guidelines do not favor one over the other,” she said in an email. “Further, Xarelto has more FDA-approved indications than Eliquis (e.g., Xarelto is approved for a reduction in risk of major CV events in patients with CAD or PAD) in addition to all the same FDA indications as Eliquis.”
Ms. Peaslee pointed out that all formulary changes are evaluated by an external medical expert specializing in the disease state, followed by review and approval by an independent national Pharmacy & Therapeutics Committee.
The decision to exclude apixaban is also limited to a “subset of commercial drug lists,” she said, although specifics on which plans and the number of affected patients were not forthcoming.
The choice of DOAC is a timely question in cardiology, with recent studies suggesting an advantage for apixaban over rivaroxaban in reducing the risk of recurrent venous thromboembolism, as well as reducing the risk of major ischemic or hemorrhagic events in atrial fibrillation.
Ms. Peaslee said CVS Caremark closely monitors medical literature for relevant clinical trial data and that most clients allow reasonable formulary exceptions when justified. “This formulary exceptions process has been successfully used for changes of this type and allows patients to get a medication that is safe and effective, as determined by their prescriber.”
The company will also continue to provide “robust, personalized outreach to the small number of members who will need to switch to an alternative medication,” she added.
Dr. Beavers said negotiations with CVS are still in the early stages, but, in the meantime, the ACC is providing health care providers with tools, such as drug copay cards and electronic prior authorizations, to help ensure patients don’t have gaps in coverage.
In a Jan. 14 news release addressing the formulary change, ACC notes that a patient’s pharmacy can also request a one-time override when trying to fill a nonpreferred DOAC in January to buy time if switching medications with their clinician or requesting a formulary exception.
During discussions with CVS Caremark, it says the ACC and the American Society of Hematology “underscored the negative impacts of this decision on patients currently taking one of the nonpreferred DOACs and on those who have previously tried rivaroxaban and changed medications.”
The groups also highlighted difficulties with other prior authorization programs in terms of the need for dedicated staff and time away from direct patient care.
“The ACC and ASH will continue discussions with CVS Caremark regarding the burden on clinicians and the effect of the formulary decision on patient access,” the release says.
In its letter to CVS, PACH argues that the apixaban exclusion will disproportionately affect historically disadvantaged patients, leaving those who can least afford the change with limited options. Notably, no generic is available for either apixaban or rivaroxaban.
The group also highlights a 2019 national poll, in which nearly 40% of patients who had their medication switched were so frustrated that they stopped their medication altogether.
PACH has an online petition against nonmedical switching, which at press time had garnered 2,126 signatures.
One signee, Jan Griffin, who survived bilateral pulmonary embolisms, writes that she has been on Eliquis [apixaban] successfully since her hospital discharge. “Now, as of midnight, Caremark apparently knows better than my hematologist as to what blood thinner is better for me and will no longer cover my Eliquis prescription. This is criminal, immoral, and unethical. #StopTheSwitch.”
A version of this article first appeared on Medscape.com.
Patients looking to refill a prescription for apixaban (Eliquis) through CVS Caremark may be in for a surprise following its decision to exclude the direct oral anticoagulant (DOAC) from its formulary starting Jan. 1.
The move leaves just one DOAC, rivaroxaban (Xarelto), on CVS’ commercial formulary and is being assailed as the latest example of “nonmedical switching” used by health insurers to control costs.
In a letter to CVS Caremark backed by 14 provider and patient organizations, the nonprofit Partnership to Advance Cardiovascular Health (PACH) calls on the pharmacy chain to reverse its “dangerously disruptive” decision to force stable patients at high risk of cardiovascular events to switch anticoagulation, without an apparent option to be grandfathered into the new plan.
PACH president Dharmesh Patel, MD, Stern Cardiovascular Center, Memphis, called the formulary change “reckless and irresponsible, especially because the decision is not based in science and evidence, but on budgets. Patients and their health care providers, not insurance companies, need to be trusted to determine what medication is best,” he said in a statement.
Craig Beavers, PharmD, vice president of Baptist Health Paducah, Kentucky, said that, as chair of the American College of Cardiology’s Cardiovascular Team Section, he and other organizations have met with CVS Caremark medical leadership to advocate for patients and to understand the company’s perspective.
“The underlying driver is cost,” he told this news organization.
Current guidelines recommend DOACs in general for a variety of indications, including to reduce the risk of stroke and embolism in nonvalvular atrial fibrillation and to prevent deep vein thrombosis, but there are select instances where a particular DOAC might be more appropriate, he observed.
“Apixaban may be better for a patient with a history of GI bleeding because there’s less GI bleeding, but the guidelines don’t necessarily spell those things out,” Dr. Beavers said. “That’s where the clinician should advocate for their patient and, unfortunately, they are making their decision strictly based off the guidelines.”
Requests to speak with medical officers at CVS Caremark went unanswered, but its executive director of communications, Christina Peaslee, told this news organization that the formulary decision “maintains clinically appropriate, cost-effective prescription coverage” for its clients and members.
“Both the American Heart Association/American College of Cardiology/Heart Rhythm Society and 2021 CHEST guidelines recommend DOACs over warfarin for treatment of various cardiology conditions such as atrial fibrillation, but neither list a specific agent as preferred – showing that consensus clinical guidelines do not favor one over the other,” she said in an email. “Further, Xarelto has more FDA-approved indications than Eliquis (e.g., Xarelto is approved for a reduction in risk of major CV events in patients with CAD or PAD) in addition to all the same FDA indications as Eliquis.”
Ms. Peaslee pointed out that all formulary changes are evaluated by an external medical expert specializing in the disease state, followed by review and approval by an independent national Pharmacy & Therapeutics Committee.
The decision to exclude apixaban is also limited to a “subset of commercial drug lists,” she said, although specifics on which plans and the number of affected patients were not forthcoming.
The choice of DOAC is a timely question in cardiology, with recent studies suggesting an advantage for apixaban over rivaroxaban in reducing the risk of recurrent venous thromboembolism, as well as reducing the risk of major ischemic or hemorrhagic events in atrial fibrillation.
Ms. Peaslee said CVS Caremark closely monitors medical literature for relevant clinical trial data and that most clients allow reasonable formulary exceptions when justified. “This formulary exceptions process has been successfully used for changes of this type and allows patients to get a medication that is safe and effective, as determined by their prescriber.”
The company will also continue to provide “robust, personalized outreach to the small number of members who will need to switch to an alternative medication,” she added.
Dr. Beavers said negotiations with CVS are still in the early stages, but, in the meantime, the ACC is providing health care providers with tools, such as drug copay cards and electronic prior authorizations, to help ensure patients don’t have gaps in coverage.
In a Jan. 14 news release addressing the formulary change, ACC notes that a patient’s pharmacy can also request a one-time override when trying to fill a nonpreferred DOAC in January to buy time if switching medications with their clinician or requesting a formulary exception.
During discussions with CVS Caremark, it says the ACC and the American Society of Hematology “underscored the negative impacts of this decision on patients currently taking one of the nonpreferred DOACs and on those who have previously tried rivaroxaban and changed medications.”
The groups also highlighted difficulties with other prior authorization programs in terms of the need for dedicated staff and time away from direct patient care.
“The ACC and ASH will continue discussions with CVS Caremark regarding the burden on clinicians and the effect of the formulary decision on patient access,” the release says.
In its letter to CVS, PACH argues that the apixaban exclusion will disproportionately affect historically disadvantaged patients, leaving those who can least afford the change with limited options. Notably, no generic is available for either apixaban or rivaroxaban.
The group also highlights a 2019 national poll, in which nearly 40% of patients who had their medication switched were so frustrated that they stopped their medication altogether.
PACH has an online petition against nonmedical switching, which at press time had garnered 2,126 signatures.
One signee, Jan Griffin, who survived bilateral pulmonary embolisms, writes that she has been on Eliquis [apixaban] successfully since her hospital discharge. “Now, as of midnight, Caremark apparently knows better than my hematologist as to what blood thinner is better for me and will no longer cover my Eliquis prescription. This is criminal, immoral, and unethical. #StopTheSwitch.”
A version of this article first appeared on Medscape.com.
Pediatric community-acquired pneumonia: 5 days of antibiotics better than 10 days
The evidence is in: and had the added benefit of a lower risk of inducing antibiotic resistance, according to the randomized, controlled SCOUT-CAP trial.
“Several studies have shown shorter antibiotic courses to be non-inferior to the standard treatment strategy, but in our study, we show that a shortened 5-day course of therapy was superior to standard therapy because the short course achieved similar outcomes with fewer days of antibiotics,” Derek Williams, MD, MPH, Vanderbilt University Medical Center, Nashville, Tenn., said in an email.
“These data are immediately applicable to frontline clinicians, and we hope this study will shift the paradigm towards more judicious treatment approaches for childhood pneumonia, resulting in care that is safer and more effective,” he added.
The study was published online Jan. 18 in JAMA Pediatrics.
Uncomplicated CAP
The study enrolled children aged 6 months to 71 months diagnosed with uncomplicated CAP who demonstrated early clinical improvement in response to 5 days of antibiotic treatment. Participants were prescribed either amoxicillin, amoxicillin and clavulanate, or cefdinir according to standard of care and were randomized on day 6 to another 5 days of their initially prescribed antibiotic course or to placebo.
“Those assessed on day 6 were eligible only if they had not yet received a dose of antibiotic therapy on that day,” the authors write. The primary endpoint was end-of-treatment response, adjusted for the duration of antibiotic risk as assessed by RADAR. As the authors explain, RADAR is a composite endpoint that ranks each child’s clinical response, resolution of symptoms, and antibiotic-associated adverse effects (AEs) in an ordinal desirability of outcome ranking, or DOOR.
“There were no differences between strategies in the DOOR or in its individual components,” Dr. Williams and colleagues point out. A total of 380 children took part in the study. The mean age of participants was 35.7 months, and half were male.
Over 90% of children randomized to active therapy were prescribed amoxicillin. “Fewer than 10% of children in either strategy had an inadequate clinical response,” the authors report.
However, the 5-day antibiotic strategy had a 69% (95% CI, 63%-75%) probability of children achieving a more desirable RADAR outcome compared with the standard, 10-day course, as assessed either on days 6 to 10 at outcome assessment visit one (OAV1) or at OAV2 on days 19 to 25.
There were also no significant differences between the two groups in the percentage of participants with persistent symptoms at either assessment point, they note. At assessment visit one, 40% of children assigned to the short-course strategy and 37% of children assigned to the 10-day strategy reported an antibiotic-related AE, most of which were mild.
Resistome analysis
Some 171 children were included in a resistome analysis in which throat swabs were collected between study days 19 and 25 to quantify antibiotic resistance genes in oropharyngeal flora. The total number of resistance genes per prokaryotic cell (RGPC) was significantly lower in children treated with antibiotics for 5 days compared with children who were treated for 10 days.
Specifically, the median number of total RGPC was 1.17 (95% CI, 0.35-2.43) for the short-course strategy and 1.33 (95% CI, 0.46-11.08) for the standard-course strategy (P = .01). Similarly, the median number of β-lactamase RGPC was 0.55 (0.18-1.24) for the short-course strategy and 0.60 (0.21-2.45) for the standard-course strategy (P = .03).
“Providing the shortest duration of antibiotics necessary to effectively treat an infection is a central tenet of antimicrobial stewardship and a convenient and cost-effective strategy for caregivers,” the authors observe. For example, reducing treatment from 10 to 5 days for outpatient CAP could reduce the number of days spent on antibiotics by up to 7.5 million days in the U.S. each year.
“If we can safely reduce antibiotic exposure, we can minimize antibiotic side effects while also helping to slow antibiotic resistance,” Dr. Williams pointed out.
Fewer days of having to give their child repeated doses of antibiotics is also more convenient for families, he added.
Asked to comment on the study, David Greenberg, MD, professor of pediatrics and infectious diseases, Ben Gurion University of the Negev, Israel, explained that the length of antibiotic therapy as recommended by various guidelines is more or less arbitrary, some infections being excepted.
“There have been no studies evaluating the recommendation for a 100-day treatment course, and it’s kind of a joke because if you look at the treatment of just about any infection, it’s either for 7 days or 14 days or even 20 days because it’s easy to calculate – it’s not that anybody proved that treatment of whatever infection it is should last this long,” he told this news organization.
Moreover, adherence to a shorter antibiotic course is much better than it is to a longer course. If, for example, physicians tell a mother to take two bottles of antibiotics for a treatment course of 10 days, she’ll finish the first bottle which is good for 5 days and, because the child is fine, “she forgets about the second bottle,” Dr. Greenberg said.
In one of the first studies to compare a short versus long course of antibiotic therapy in uncomplicated CAP in young children, Dr. Greenberg and colleagues initially compared a 3-day course of high-dose amoxicillin to a 10-day course of the same treatment, but the 3-day course was associated with an unacceptable failure rate. (At the time, the World Health Organization was recommending a 3-day course of antibiotics for the treatment of uncomplicated CAP in children.)
They stopped the study and then initiated a second study in which they compared a 5-day course of the same antibiotic to a 10-day course and found the 5-day course was comparable to the 10-day course in terms of clinical cure rates. As a result of his study, Dr. Greenberg has long since prescribed a 5-day course of antibiotics for his own patients.
“Five days is good,” he affirmed. “And if patients start a 10-day course of an antibiotic for, say, a urinary tract infection and a subsequent culture comes back negative, they don’t have to finish the antibiotics either.” Dr. Greenberg said.
Dr. Williams said he has no financial ties to industry. Dr. Greenberg said he has served as a consultant for Pfizer, Merck, Johnson & Johnson, and AstraZeneca. He is also a founder of the company Beyond Air.
A version of this article first appeared on Medscape.com.
The evidence is in: and had the added benefit of a lower risk of inducing antibiotic resistance, according to the randomized, controlled SCOUT-CAP trial.
“Several studies have shown shorter antibiotic courses to be non-inferior to the standard treatment strategy, but in our study, we show that a shortened 5-day course of therapy was superior to standard therapy because the short course achieved similar outcomes with fewer days of antibiotics,” Derek Williams, MD, MPH, Vanderbilt University Medical Center, Nashville, Tenn., said in an email.
“These data are immediately applicable to frontline clinicians, and we hope this study will shift the paradigm towards more judicious treatment approaches for childhood pneumonia, resulting in care that is safer and more effective,” he added.
The study was published online Jan. 18 in JAMA Pediatrics.
Uncomplicated CAP
The study enrolled children aged 6 months to 71 months diagnosed with uncomplicated CAP who demonstrated early clinical improvement in response to 5 days of antibiotic treatment. Participants were prescribed either amoxicillin, amoxicillin and clavulanate, or cefdinir according to standard of care and were randomized on day 6 to another 5 days of their initially prescribed antibiotic course or to placebo.
“Those assessed on day 6 were eligible only if they had not yet received a dose of antibiotic therapy on that day,” the authors write. The primary endpoint was end-of-treatment response, adjusted for the duration of antibiotic risk as assessed by RADAR. As the authors explain, RADAR is a composite endpoint that ranks each child’s clinical response, resolution of symptoms, and antibiotic-associated adverse effects (AEs) in an ordinal desirability of outcome ranking, or DOOR.
“There were no differences between strategies in the DOOR or in its individual components,” Dr. Williams and colleagues point out. A total of 380 children took part in the study. The mean age of participants was 35.7 months, and half were male.
Over 90% of children randomized to active therapy were prescribed amoxicillin. “Fewer than 10% of children in either strategy had an inadequate clinical response,” the authors report.
However, the 5-day antibiotic strategy had a 69% (95% CI, 63%-75%) probability of children achieving a more desirable RADAR outcome compared with the standard, 10-day course, as assessed either on days 6 to 10 at outcome assessment visit one (OAV1) or at OAV2 on days 19 to 25.
There were also no significant differences between the two groups in the percentage of participants with persistent symptoms at either assessment point, they note. At assessment visit one, 40% of children assigned to the short-course strategy and 37% of children assigned to the 10-day strategy reported an antibiotic-related AE, most of which were mild.
Resistome analysis
Some 171 children were included in a resistome analysis in which throat swabs were collected between study days 19 and 25 to quantify antibiotic resistance genes in oropharyngeal flora. The total number of resistance genes per prokaryotic cell (RGPC) was significantly lower in children treated with antibiotics for 5 days compared with children who were treated for 10 days.
Specifically, the median number of total RGPC was 1.17 (95% CI, 0.35-2.43) for the short-course strategy and 1.33 (95% CI, 0.46-11.08) for the standard-course strategy (P = .01). Similarly, the median number of β-lactamase RGPC was 0.55 (0.18-1.24) for the short-course strategy and 0.60 (0.21-2.45) for the standard-course strategy (P = .03).
“Providing the shortest duration of antibiotics necessary to effectively treat an infection is a central tenet of antimicrobial stewardship and a convenient and cost-effective strategy for caregivers,” the authors observe. For example, reducing treatment from 10 to 5 days for outpatient CAP could reduce the number of days spent on antibiotics by up to 7.5 million days in the U.S. each year.
“If we can safely reduce antibiotic exposure, we can minimize antibiotic side effects while also helping to slow antibiotic resistance,” Dr. Williams pointed out.
Fewer days of having to give their child repeated doses of antibiotics is also more convenient for families, he added.
Asked to comment on the study, David Greenberg, MD, professor of pediatrics and infectious diseases, Ben Gurion University of the Negev, Israel, explained that the length of antibiotic therapy as recommended by various guidelines is more or less arbitrary, some infections being excepted.
“There have been no studies evaluating the recommendation for a 100-day treatment course, and it’s kind of a joke because if you look at the treatment of just about any infection, it’s either for 7 days or 14 days or even 20 days because it’s easy to calculate – it’s not that anybody proved that treatment of whatever infection it is should last this long,” he told this news organization.
Moreover, adherence to a shorter antibiotic course is much better than it is to a longer course. If, for example, physicians tell a mother to take two bottles of antibiotics for a treatment course of 10 days, she’ll finish the first bottle which is good for 5 days and, because the child is fine, “she forgets about the second bottle,” Dr. Greenberg said.
In one of the first studies to compare a short versus long course of antibiotic therapy in uncomplicated CAP in young children, Dr. Greenberg and colleagues initially compared a 3-day course of high-dose amoxicillin to a 10-day course of the same treatment, but the 3-day course was associated with an unacceptable failure rate. (At the time, the World Health Organization was recommending a 3-day course of antibiotics for the treatment of uncomplicated CAP in children.)
They stopped the study and then initiated a second study in which they compared a 5-day course of the same antibiotic to a 10-day course and found the 5-day course was comparable to the 10-day course in terms of clinical cure rates. As a result of his study, Dr. Greenberg has long since prescribed a 5-day course of antibiotics for his own patients.
“Five days is good,” he affirmed. “And if patients start a 10-day course of an antibiotic for, say, a urinary tract infection and a subsequent culture comes back negative, they don’t have to finish the antibiotics either.” Dr. Greenberg said.
Dr. Williams said he has no financial ties to industry. Dr. Greenberg said he has served as a consultant for Pfizer, Merck, Johnson & Johnson, and AstraZeneca. He is also a founder of the company Beyond Air.
A version of this article first appeared on Medscape.com.
The evidence is in: and had the added benefit of a lower risk of inducing antibiotic resistance, according to the randomized, controlled SCOUT-CAP trial.
“Several studies have shown shorter antibiotic courses to be non-inferior to the standard treatment strategy, but in our study, we show that a shortened 5-day course of therapy was superior to standard therapy because the short course achieved similar outcomes with fewer days of antibiotics,” Derek Williams, MD, MPH, Vanderbilt University Medical Center, Nashville, Tenn., said in an email.
“These data are immediately applicable to frontline clinicians, and we hope this study will shift the paradigm towards more judicious treatment approaches for childhood pneumonia, resulting in care that is safer and more effective,” he added.
The study was published online Jan. 18 in JAMA Pediatrics.
Uncomplicated CAP
The study enrolled children aged 6 months to 71 months diagnosed with uncomplicated CAP who demonstrated early clinical improvement in response to 5 days of antibiotic treatment. Participants were prescribed either amoxicillin, amoxicillin and clavulanate, or cefdinir according to standard of care and were randomized on day 6 to another 5 days of their initially prescribed antibiotic course or to placebo.
“Those assessed on day 6 were eligible only if they had not yet received a dose of antibiotic therapy on that day,” the authors write. The primary endpoint was end-of-treatment response, adjusted for the duration of antibiotic risk as assessed by RADAR. As the authors explain, RADAR is a composite endpoint that ranks each child’s clinical response, resolution of symptoms, and antibiotic-associated adverse effects (AEs) in an ordinal desirability of outcome ranking, or DOOR.
“There were no differences between strategies in the DOOR or in its individual components,” Dr. Williams and colleagues point out. A total of 380 children took part in the study. The mean age of participants was 35.7 months, and half were male.
Over 90% of children randomized to active therapy were prescribed amoxicillin. “Fewer than 10% of children in either strategy had an inadequate clinical response,” the authors report.
However, the 5-day antibiotic strategy had a 69% (95% CI, 63%-75%) probability of children achieving a more desirable RADAR outcome compared with the standard, 10-day course, as assessed either on days 6 to 10 at outcome assessment visit one (OAV1) or at OAV2 on days 19 to 25.
There were also no significant differences between the two groups in the percentage of participants with persistent symptoms at either assessment point, they note. At assessment visit one, 40% of children assigned to the short-course strategy and 37% of children assigned to the 10-day strategy reported an antibiotic-related AE, most of which were mild.
Resistome analysis
Some 171 children were included in a resistome analysis in which throat swabs were collected between study days 19 and 25 to quantify antibiotic resistance genes in oropharyngeal flora. The total number of resistance genes per prokaryotic cell (RGPC) was significantly lower in children treated with antibiotics for 5 days compared with children who were treated for 10 days.
Specifically, the median number of total RGPC was 1.17 (95% CI, 0.35-2.43) for the short-course strategy and 1.33 (95% CI, 0.46-11.08) for the standard-course strategy (P = .01). Similarly, the median number of β-lactamase RGPC was 0.55 (0.18-1.24) for the short-course strategy and 0.60 (0.21-2.45) for the standard-course strategy (P = .03).
“Providing the shortest duration of antibiotics necessary to effectively treat an infection is a central tenet of antimicrobial stewardship and a convenient and cost-effective strategy for caregivers,” the authors observe. For example, reducing treatment from 10 to 5 days for outpatient CAP could reduce the number of days spent on antibiotics by up to 7.5 million days in the U.S. each year.
“If we can safely reduce antibiotic exposure, we can minimize antibiotic side effects while also helping to slow antibiotic resistance,” Dr. Williams pointed out.
Fewer days of having to give their child repeated doses of antibiotics is also more convenient for families, he added.
Asked to comment on the study, David Greenberg, MD, professor of pediatrics and infectious diseases, Ben Gurion University of the Negev, Israel, explained that the length of antibiotic therapy as recommended by various guidelines is more or less arbitrary, some infections being excepted.
“There have been no studies evaluating the recommendation for a 100-day treatment course, and it’s kind of a joke because if you look at the treatment of just about any infection, it’s either for 7 days or 14 days or even 20 days because it’s easy to calculate – it’s not that anybody proved that treatment of whatever infection it is should last this long,” he told this news organization.
Moreover, adherence to a shorter antibiotic course is much better than it is to a longer course. If, for example, physicians tell a mother to take two bottles of antibiotics for a treatment course of 10 days, she’ll finish the first bottle which is good for 5 days and, because the child is fine, “she forgets about the second bottle,” Dr. Greenberg said.
In one of the first studies to compare a short versus long course of antibiotic therapy in uncomplicated CAP in young children, Dr. Greenberg and colleagues initially compared a 3-day course of high-dose amoxicillin to a 10-day course of the same treatment, but the 3-day course was associated with an unacceptable failure rate. (At the time, the World Health Organization was recommending a 3-day course of antibiotics for the treatment of uncomplicated CAP in children.)
They stopped the study and then initiated a second study in which they compared a 5-day course of the same antibiotic to a 10-day course and found the 5-day course was comparable to the 10-day course in terms of clinical cure rates. As a result of his study, Dr. Greenberg has long since prescribed a 5-day course of antibiotics for his own patients.
“Five days is good,” he affirmed. “And if patients start a 10-day course of an antibiotic for, say, a urinary tract infection and a subsequent culture comes back negative, they don’t have to finish the antibiotics either.” Dr. Greenberg said.
Dr. Williams said he has no financial ties to industry. Dr. Greenberg said he has served as a consultant for Pfizer, Merck, Johnson & Johnson, and AstraZeneca. He is also a founder of the company Beyond Air.
A version of this article first appeared on Medscape.com.
Study finds genetic factor for COVID smell and taste loss
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
FROM NATURE GENETICS
Fourth vaccine shot less effective against Omicron, Israeli study says
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
Children and COVID: U.S. sees almost 1 million new cases
Another record week for COVID-19 brought almost 1 million new cases to the children of the United States, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
The pre-Omicron high for new cases in a week – 252,000 during the Delta surge of the late summer and early fall – has been surpassed each of the last 3 weeks and now stands at 981,000 (Jan. 7-13), according to the AAP/CHA weekly COVID-19 report. Over the 3-week stretch from Dec. 17 to Jan. 13, weekly cases increased by 394%.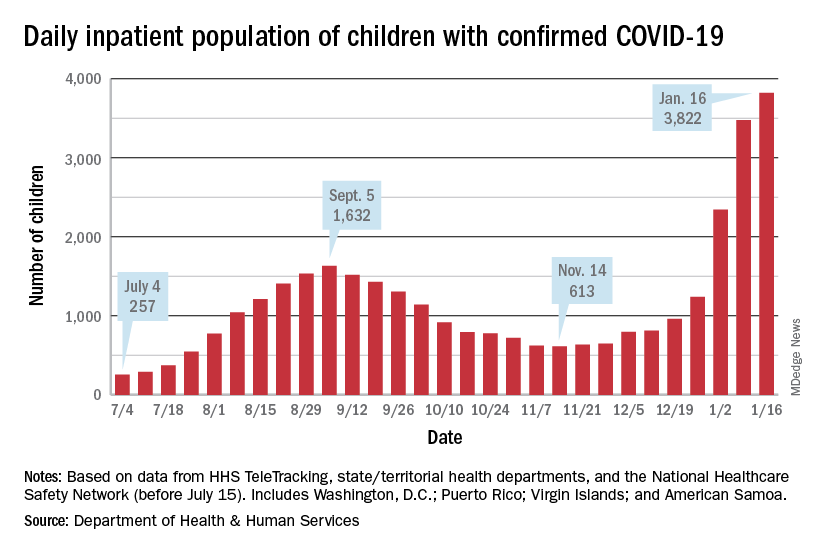
Hospitalizations also climbed to new heights, as daily admissions reached 1.23 per 100,000 children on Jan. 14, an increase of 547% since Nov. 30, when the rate was 0.19 per 100,000. Before Omicron, the highest rate for children was 0.47 per 100,000, based on data from the Centers for Disease Control and Prevention.
The inpatient population count, meanwhile, has followed suit. On Jan. 16, there were 3,822 children hospitalized in pediatric inpatient beds with laboratory-confirmed COVID-19, which is 523% higher than the 613 children who were hospitalized on Nov. 14, according to the Department of Health & Human Services. In the last week, though, the population was up by just 10%.
The one thing that has not surged in the last few weeks is vaccination. Among children aged 5-11 years, the weekly count of those who have received at least one dose dropped by 34% over the last 5 weeks, falling from 527,000 for Dec.11-17 to 347,000 during Jan. 8-14, the CDC said on the COVID Data Tracker, which also noted that just 18.4% of this age group is fully vaccinated.
The situation was reversed in children aged 12-15, who were up by 36% over that same time, but their numbers were much smaller: 78,000 for the week of Dec. 11-17 and 106,000 for Jan. 8-14. Those aged 16-17 were up by just 4% over that 5-week span, the CDC data show.
Over the course of the entire pandemic, almost 9.5 million cases of COVID-19 in children have been reported, and children represent 17.8% of all cases reported in 49 states (excluding New York but including New York City), the District of Columbia, Puerto Rico, and Guam, the AAP and CHA said in their report.
Three states (Alabama, Nebraska, and Texas) stopped public reporting over the summer, but many states count individuals up to age 19 as children, and others (South Carolina, Tennessee, and West Virginia) go up to age 20, the AAP and CHA noted. The CDC, by comparison, puts the number of cases for those aged 0-17 at 8.3 million, but that estimate is based on only 51 million of the nearly 67 million U.S. cases as of Jan. 18.
Another record week for COVID-19 brought almost 1 million new cases to the children of the United States, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
The pre-Omicron high for new cases in a week – 252,000 during the Delta surge of the late summer and early fall – has been surpassed each of the last 3 weeks and now stands at 981,000 (Jan. 7-13), according to the AAP/CHA weekly COVID-19 report. Over the 3-week stretch from Dec. 17 to Jan. 13, weekly cases increased by 394%.
Hospitalizations also climbed to new heights, as daily admissions reached 1.23 per 100,000 children on Jan. 14, an increase of 547% since Nov. 30, when the rate was 0.19 per 100,000. Before Omicron, the highest rate for children was 0.47 per 100,000, based on data from the Centers for Disease Control and Prevention.
The inpatient population count, meanwhile, has followed suit. On Jan. 16, there were 3,822 children hospitalized in pediatric inpatient beds with laboratory-confirmed COVID-19, which is 523% higher than the 613 children who were hospitalized on Nov. 14, according to the Department of Health & Human Services. In the last week, though, the population was up by just 10%.
The one thing that has not surged in the last few weeks is vaccination. Among children aged 5-11 years, the weekly count of those who have received at least one dose dropped by 34% over the last 5 weeks, falling from 527,000 for Dec.11-17 to 347,000 during Jan. 8-14, the CDC said on the COVID Data Tracker, which also noted that just 18.4% of this age group is fully vaccinated.
The situation was reversed in children aged 12-15, who were up by 36% over that same time, but their numbers were much smaller: 78,000 for the week of Dec. 11-17 and 106,000 for Jan. 8-14. Those aged 16-17 were up by just 4% over that 5-week span, the CDC data show.
Over the course of the entire pandemic, almost 9.5 million cases of COVID-19 in children have been reported, and children represent 17.8% of all cases reported in 49 states (excluding New York but including New York City), the District of Columbia, Puerto Rico, and Guam, the AAP and CHA said in their report.
Three states (Alabama, Nebraska, and Texas) stopped public reporting over the summer, but many states count individuals up to age 19 as children, and others (South Carolina, Tennessee, and West Virginia) go up to age 20, the AAP and CHA noted. The CDC, by comparison, puts the number of cases for those aged 0-17 at 8.3 million, but that estimate is based on only 51 million of the nearly 67 million U.S. cases as of Jan. 18.
Another record week for COVID-19 brought almost 1 million new cases to the children of the United States, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
The pre-Omicron high for new cases in a week – 252,000 during the Delta surge of the late summer and early fall – has been surpassed each of the last 3 weeks and now stands at 981,000 (Jan. 7-13), according to the AAP/CHA weekly COVID-19 report. Over the 3-week stretch from Dec. 17 to Jan. 13, weekly cases increased by 394%.
Hospitalizations also climbed to new heights, as daily admissions reached 1.23 per 100,000 children on Jan. 14, an increase of 547% since Nov. 30, when the rate was 0.19 per 100,000. Before Omicron, the highest rate for children was 0.47 per 100,000, based on data from the Centers for Disease Control and Prevention.
The inpatient population count, meanwhile, has followed suit. On Jan. 16, there were 3,822 children hospitalized in pediatric inpatient beds with laboratory-confirmed COVID-19, which is 523% higher than the 613 children who were hospitalized on Nov. 14, according to the Department of Health & Human Services. In the last week, though, the population was up by just 10%.
The one thing that has not surged in the last few weeks is vaccination. Among children aged 5-11 years, the weekly count of those who have received at least one dose dropped by 34% over the last 5 weeks, falling from 527,000 for Dec.11-17 to 347,000 during Jan. 8-14, the CDC said on the COVID Data Tracker, which also noted that just 18.4% of this age group is fully vaccinated.
The situation was reversed in children aged 12-15, who were up by 36% over that same time, but their numbers were much smaller: 78,000 for the week of Dec. 11-17 and 106,000 for Jan. 8-14. Those aged 16-17 were up by just 4% over that 5-week span, the CDC data show.
Over the course of the entire pandemic, almost 9.5 million cases of COVID-19 in children have been reported, and children represent 17.8% of all cases reported in 49 states (excluding New York but including New York City), the District of Columbia, Puerto Rico, and Guam, the AAP and CHA said in their report.
Three states (Alabama, Nebraska, and Texas) stopped public reporting over the summer, but many states count individuals up to age 19 as children, and others (South Carolina, Tennessee, and West Virginia) go up to age 20, the AAP and CHA noted. The CDC, by comparison, puts the number of cases for those aged 0-17 at 8.3 million, but that estimate is based on only 51 million of the nearly 67 million U.S. cases as of Jan. 18.