User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


The Role of Bronchoscopic Lung Volume Reduction in COPD
Patients with chronic obstructive pulmonary disease (COPD) typically have emphysema, which involves destruction of alveoli and reduction of elasticity leading to airflow obstruction, air trapping, and hyperinflation. Over time, these changes cause low respiratory reserve volume and increased residual volume, which cause dyspnea.
One of the newest treatment options for patients who have advanced COPD with severe emphysema is a minimally invasive procedure called bronchoscopic lung volume reduction (BLVR). Most recently, the FDA approved the use of endobronchial valves for this procedure, which are implanted in the airways of the lungs to reduce air trapping and hyperinflation.
In certain patients, BLVR has been shown to improve lung function, facilitate easier breathing, enhance exercise tolerance, and lead to better quality of life.
In this ReCAP, Dr. Javier Diaz-Mendoza, program director of the Interventional Pulmonology Fellowship at Henry Ford Health System in Detroit, discusses the benefits of BLVR in patients who have advanced COPD with emphysema. He discusses the procedure, patient outcomes, and which patients should be considered for BLVR.
--
Associate Professor of Medicine, Henry Ford Hospital, Wayne State University; Program Director, Interventional Pulmonology Fellowship, Henry Ford Health System, Detroit, MI
Javier Diaz-Mendoza, MD, FCCP, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Ion Intuitive Serve(d) as a speaker or a member of a speakers bureau for: Association of Interventional Pulmonology Program Directors
Patients with chronic obstructive pulmonary disease (COPD) typically have emphysema, which involves destruction of alveoli and reduction of elasticity leading to airflow obstruction, air trapping, and hyperinflation. Over time, these changes cause low respiratory reserve volume and increased residual volume, which cause dyspnea.
One of the newest treatment options for patients who have advanced COPD with severe emphysema is a minimally invasive procedure called bronchoscopic lung volume reduction (BLVR). Most recently, the FDA approved the use of endobronchial valves for this procedure, which are implanted in the airways of the lungs to reduce air trapping and hyperinflation.
In certain patients, BLVR has been shown to improve lung function, facilitate easier breathing, enhance exercise tolerance, and lead to better quality of life.
In this ReCAP, Dr. Javier Diaz-Mendoza, program director of the Interventional Pulmonology Fellowship at Henry Ford Health System in Detroit, discusses the benefits of BLVR in patients who have advanced COPD with emphysema. He discusses the procedure, patient outcomes, and which patients should be considered for BLVR.
--
Associate Professor of Medicine, Henry Ford Hospital, Wayne State University; Program Director, Interventional Pulmonology Fellowship, Henry Ford Health System, Detroit, MI
Javier Diaz-Mendoza, MD, FCCP, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Ion Intuitive Serve(d) as a speaker or a member of a speakers bureau for: Association of Interventional Pulmonology Program Directors
Patients with chronic obstructive pulmonary disease (COPD) typically have emphysema, which involves destruction of alveoli and reduction of elasticity leading to airflow obstruction, air trapping, and hyperinflation. Over time, these changes cause low respiratory reserve volume and increased residual volume, which cause dyspnea.
One of the newest treatment options for patients who have advanced COPD with severe emphysema is a minimally invasive procedure called bronchoscopic lung volume reduction (BLVR). Most recently, the FDA approved the use of endobronchial valves for this procedure, which are implanted in the airways of the lungs to reduce air trapping and hyperinflation.
In certain patients, BLVR has been shown to improve lung function, facilitate easier breathing, enhance exercise tolerance, and lead to better quality of life.
In this ReCAP, Dr. Javier Diaz-Mendoza, program director of the Interventional Pulmonology Fellowship at Henry Ford Health System in Detroit, discusses the benefits of BLVR in patients who have advanced COPD with emphysema. He discusses the procedure, patient outcomes, and which patients should be considered for BLVR.
--
Associate Professor of Medicine, Henry Ford Hospital, Wayne State University; Program Director, Interventional Pulmonology Fellowship, Henry Ford Health System, Detroit, MI
Javier Diaz-Mendoza, MD, FCCP, has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Ion Intuitive Serve(d) as a speaker or a member of a speakers bureau for: Association of Interventional Pulmonology Program Directors

Early cardiac rehab as effective as later start after sternotomy
Cardiac rehabilitation (CR) started 2 weeks after sternotomy for a cardiac procedure was noninferior to usual care, in which CR starts 6 weeks after the procedure, with a greater improvement in 6-minute walk test outcomes, a randomized study suggests.
There was no difference in adverse events between groups, although the researchers pointed out that the study was not powered specifically for safety outcomes.
“Cardiac surgical techniques have evolved significantly over the last 60 years, leading to improved survival and shorter hospital stays,” Gordon McGregor, PhD, University of Warwick, Coventry, England, told this news organization. “However, sternal precautions and rehabilitation guidelines have not changed accordingly. There has never been a guideline based on empirical evidence to support rehabilitation professionals working with cardiac surgery patients after median sternotomy.”
“By adopting a progressive individualized approach,” he added, “cardiac surgery sternotomy patients can start cardiac rehabilitation up to 4 weeks earlier than current guidance, and thus potentially complete their recovery sooner.”
Results of the Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training study were published online in JAMA Cardiology.
In the study, Dr. McGregor and colleagues randomly assigned 158 patients (mean age, 63 years; 84% men) to 8 weeks of 1-hour, twice-weekly supervised CR exercise training starting 2 weeks (early) or 6 weeks (usual care) after sternotomy.
The primary outcome was change in the 6-minute walk test distance from baseline to 10 or 14 weeks after sternotomy, respectively, and 12 months after randomization.
For usual care, training followed British standards: a warm-up with light cardiovascular and mobility exercises; continuous moderate-intensity cardiovascular exercise; a cooldown; functional exercises using resistance machines and free weights; and upper-body exercises designed to prevent sternal and leg wound pain and complications.
There are no specific outpatient CR exercise guidelines for early CR, so study participants followed an individualized exercise program for the first 2-3 weeks after surgery, starting with light mobility and moderate-intensity cardiovascular training when they could do those exercises with minimal discomfort. They then progressed to current British standards, as per usual care.
Forty patients were lost to follow-up, largely because of the pandemic; about half the participants in each group were included in the primary analysis.
Early CR was not inferior to usual care, the authors wrote. The mean change in 6-minute walk distance from baseline to completion of CR was 28 meters greater in the early group than in the usual-care group, and was achieved 4 weeks earlier in the recovery timeline.
Secondary outcomes (functional fitness and quality of life) improved in both groups and between-group differences were not statistically significant, indicating the noninferiority of early CR, the authors noted.
Safety not proven
There were more adverse events in the early group than in the usual-care group (58 vs. 46) and more serious adverse events (18 vs. 14), but fewer deaths (1 vs. 2).
Although there was no between-group difference in the likelihood of having an adverse or serious adverse event, Dr. McGregor acknowledged that the study was “not powered specifically for safety outcomes.” He added that “there is the potential to run a very large multination definitive superiority [randomized, controlled trial] with safety as the primary outcome; however, a very large sample would be required.”
Meanwhile, he said, “we can say with some degree of certainty that early CR was likely as safe as usual-care CR. In the United Kingdom, we work closely with the British Association for Cardiovascular Prevention and Rehabilitation and the Association of Chartered Physiotherapists in Cardiovascular Rehabilitation, who will incorporate our findings in their guidelines and training courses.”
Questions remain
Asked to comment on the study, John Larry, MD, medical director of cardiology and cardiac rehabilitation at the Ohio State University Wexner Medical Center East Hospital, Columbus, said: “For those under time pressure to return to work, [early CR] could be an advantage to allow more rehab time and improved stamina prior to their return-to-work date.”
That said, he noted, “we typically delay any significant upper-body training activities for 8-10 weeks to avoid impact on healing of the sternum. Thus ... starting sooner would limit the amount of time a patient would have to engage in any upper-body resistance training. Many lose upper body strength after surgery, so this is an important part of the recovery/rehab process.”
Matthew Tomey, MD, director of the cardiac intensive care unit, Mount Sinai Morningside, New York, advised “caution” when interpreting the findings, stating that “there was no evident difference in the primary outcome measure of functional capacity by 14 weeks, and the trial was not designed to directly assess impact on either social functioning or economic productivity.”
“I would be interested to [see] more comprehensive data on safety in a larger, more diverse sample of postoperative patients,” he said, “as well as evidence to indicate clear advantage of an earlier start for patient-centered outcomes specifically after cardiac surgery.
“Perhaps the greatest challenges to full realization of the benefits of CR in practice have been gaps in referral and gaps in enrollment,” he added. “It is incumbent upon us as clinicians to counsel our patients and to provide appropriate referrals.”
The study was supported by the Medical and Life Sciences Research Fund and the Jeremy Pilcher Memorial Fund. No conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
Cardiac rehabilitation (CR) started 2 weeks after sternotomy for a cardiac procedure was noninferior to usual care, in which CR starts 6 weeks after the procedure, with a greater improvement in 6-minute walk test outcomes, a randomized study suggests.
There was no difference in adverse events between groups, although the researchers pointed out that the study was not powered specifically for safety outcomes.
“Cardiac surgical techniques have evolved significantly over the last 60 years, leading to improved survival and shorter hospital stays,” Gordon McGregor, PhD, University of Warwick, Coventry, England, told this news organization. “However, sternal precautions and rehabilitation guidelines have not changed accordingly. There has never been a guideline based on empirical evidence to support rehabilitation professionals working with cardiac surgery patients after median sternotomy.”
“By adopting a progressive individualized approach,” he added, “cardiac surgery sternotomy patients can start cardiac rehabilitation up to 4 weeks earlier than current guidance, and thus potentially complete their recovery sooner.”
Results of the Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training study were published online in JAMA Cardiology.
In the study, Dr. McGregor and colleagues randomly assigned 158 patients (mean age, 63 years; 84% men) to 8 weeks of 1-hour, twice-weekly supervised CR exercise training starting 2 weeks (early) or 6 weeks (usual care) after sternotomy.
The primary outcome was change in the 6-minute walk test distance from baseline to 10 or 14 weeks after sternotomy, respectively, and 12 months after randomization.
For usual care, training followed British standards: a warm-up with light cardiovascular and mobility exercises; continuous moderate-intensity cardiovascular exercise; a cooldown; functional exercises using resistance machines and free weights; and upper-body exercises designed to prevent sternal and leg wound pain and complications.
There are no specific outpatient CR exercise guidelines for early CR, so study participants followed an individualized exercise program for the first 2-3 weeks after surgery, starting with light mobility and moderate-intensity cardiovascular training when they could do those exercises with minimal discomfort. They then progressed to current British standards, as per usual care.
Forty patients were lost to follow-up, largely because of the pandemic; about half the participants in each group were included in the primary analysis.
Early CR was not inferior to usual care, the authors wrote. The mean change in 6-minute walk distance from baseline to completion of CR was 28 meters greater in the early group than in the usual-care group, and was achieved 4 weeks earlier in the recovery timeline.
Secondary outcomes (functional fitness and quality of life) improved in both groups and between-group differences were not statistically significant, indicating the noninferiority of early CR, the authors noted.
Safety not proven
There were more adverse events in the early group than in the usual-care group (58 vs. 46) and more serious adverse events (18 vs. 14), but fewer deaths (1 vs. 2).
Although there was no between-group difference in the likelihood of having an adverse or serious adverse event, Dr. McGregor acknowledged that the study was “not powered specifically for safety outcomes.” He added that “there is the potential to run a very large multination definitive superiority [randomized, controlled trial] with safety as the primary outcome; however, a very large sample would be required.”
Meanwhile, he said, “we can say with some degree of certainty that early CR was likely as safe as usual-care CR. In the United Kingdom, we work closely with the British Association for Cardiovascular Prevention and Rehabilitation and the Association of Chartered Physiotherapists in Cardiovascular Rehabilitation, who will incorporate our findings in their guidelines and training courses.”
Questions remain
Asked to comment on the study, John Larry, MD, medical director of cardiology and cardiac rehabilitation at the Ohio State University Wexner Medical Center East Hospital, Columbus, said: “For those under time pressure to return to work, [early CR] could be an advantage to allow more rehab time and improved stamina prior to their return-to-work date.”
That said, he noted, “we typically delay any significant upper-body training activities for 8-10 weeks to avoid impact on healing of the sternum. Thus ... starting sooner would limit the amount of time a patient would have to engage in any upper-body resistance training. Many lose upper body strength after surgery, so this is an important part of the recovery/rehab process.”
Matthew Tomey, MD, director of the cardiac intensive care unit, Mount Sinai Morningside, New York, advised “caution” when interpreting the findings, stating that “there was no evident difference in the primary outcome measure of functional capacity by 14 weeks, and the trial was not designed to directly assess impact on either social functioning or economic productivity.”
“I would be interested to [see] more comprehensive data on safety in a larger, more diverse sample of postoperative patients,” he said, “as well as evidence to indicate clear advantage of an earlier start for patient-centered outcomes specifically after cardiac surgery.
“Perhaps the greatest challenges to full realization of the benefits of CR in practice have been gaps in referral and gaps in enrollment,” he added. “It is incumbent upon us as clinicians to counsel our patients and to provide appropriate referrals.”
The study was supported by the Medical and Life Sciences Research Fund and the Jeremy Pilcher Memorial Fund. No conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
Cardiac rehabilitation (CR) started 2 weeks after sternotomy for a cardiac procedure was noninferior to usual care, in which CR starts 6 weeks after the procedure, with a greater improvement in 6-minute walk test outcomes, a randomized study suggests.
There was no difference in adverse events between groups, although the researchers pointed out that the study was not powered specifically for safety outcomes.
“Cardiac surgical techniques have evolved significantly over the last 60 years, leading to improved survival and shorter hospital stays,” Gordon McGregor, PhD, University of Warwick, Coventry, England, told this news organization. “However, sternal precautions and rehabilitation guidelines have not changed accordingly. There has never been a guideline based on empirical evidence to support rehabilitation professionals working with cardiac surgery patients after median sternotomy.”
“By adopting a progressive individualized approach,” he added, “cardiac surgery sternotomy patients can start cardiac rehabilitation up to 4 weeks earlier than current guidance, and thus potentially complete their recovery sooner.”
Results of the Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training study were published online in JAMA Cardiology.
In the study, Dr. McGregor and colleagues randomly assigned 158 patients (mean age, 63 years; 84% men) to 8 weeks of 1-hour, twice-weekly supervised CR exercise training starting 2 weeks (early) or 6 weeks (usual care) after sternotomy.
The primary outcome was change in the 6-minute walk test distance from baseline to 10 or 14 weeks after sternotomy, respectively, and 12 months after randomization.
For usual care, training followed British standards: a warm-up with light cardiovascular and mobility exercises; continuous moderate-intensity cardiovascular exercise; a cooldown; functional exercises using resistance machines and free weights; and upper-body exercises designed to prevent sternal and leg wound pain and complications.
There are no specific outpatient CR exercise guidelines for early CR, so study participants followed an individualized exercise program for the first 2-3 weeks after surgery, starting with light mobility and moderate-intensity cardiovascular training when they could do those exercises with minimal discomfort. They then progressed to current British standards, as per usual care.
Forty patients were lost to follow-up, largely because of the pandemic; about half the participants in each group were included in the primary analysis.
Early CR was not inferior to usual care, the authors wrote. The mean change in 6-minute walk distance from baseline to completion of CR was 28 meters greater in the early group than in the usual-care group, and was achieved 4 weeks earlier in the recovery timeline.
Secondary outcomes (functional fitness and quality of life) improved in both groups and between-group differences were not statistically significant, indicating the noninferiority of early CR, the authors noted.
Safety not proven
There were more adverse events in the early group than in the usual-care group (58 vs. 46) and more serious adverse events (18 vs. 14), but fewer deaths (1 vs. 2).
Although there was no between-group difference in the likelihood of having an adverse or serious adverse event, Dr. McGregor acknowledged that the study was “not powered specifically for safety outcomes.” He added that “there is the potential to run a very large multination definitive superiority [randomized, controlled trial] with safety as the primary outcome; however, a very large sample would be required.”
Meanwhile, he said, “we can say with some degree of certainty that early CR was likely as safe as usual-care CR. In the United Kingdom, we work closely with the British Association for Cardiovascular Prevention and Rehabilitation and the Association of Chartered Physiotherapists in Cardiovascular Rehabilitation, who will incorporate our findings in their guidelines and training courses.”
Questions remain
Asked to comment on the study, John Larry, MD, medical director of cardiology and cardiac rehabilitation at the Ohio State University Wexner Medical Center East Hospital, Columbus, said: “For those under time pressure to return to work, [early CR] could be an advantage to allow more rehab time and improved stamina prior to their return-to-work date.”
That said, he noted, “we typically delay any significant upper-body training activities for 8-10 weeks to avoid impact on healing of the sternum. Thus ... starting sooner would limit the amount of time a patient would have to engage in any upper-body resistance training. Many lose upper body strength after surgery, so this is an important part of the recovery/rehab process.”
Matthew Tomey, MD, director of the cardiac intensive care unit, Mount Sinai Morningside, New York, advised “caution” when interpreting the findings, stating that “there was no evident difference in the primary outcome measure of functional capacity by 14 weeks, and the trial was not designed to directly assess impact on either social functioning or economic productivity.”
“I would be interested to [see] more comprehensive data on safety in a larger, more diverse sample of postoperative patients,” he said, “as well as evidence to indicate clear advantage of an earlier start for patient-centered outcomes specifically after cardiac surgery.
“Perhaps the greatest challenges to full realization of the benefits of CR in practice have been gaps in referral and gaps in enrollment,” he added. “It is incumbent upon us as clinicians to counsel our patients and to provide appropriate referrals.”
The study was supported by the Medical and Life Sciences Research Fund and the Jeremy Pilcher Memorial Fund. No conflicts of interest were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY
In the Grand Canyon, norovirus gives new meaning to ‘leave no trace’
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
ACC/AHA issue clinical lexicon for complications of COVID-19
The American College of Cardiology and the American Heart Association have jointly issued a comprehensive set of data standards to help clarify definitions of the cardiovascular (CV) and non-CV complications of COVID-19.
It’s the work of the ACC/AHA Task Force on Clinical Data Standards and has been endorsed by the Heart Failure Society of America and Society for Cardiac Angiography and Interventions.
There is increased importance to understanding the acute and long-term impact of COVID-19 on CV health, the writing group notes. Until now, however, there has not been “clarity or consensus” on definitions of CV conditions related to COVID-19, with different diagnostic terminologies being used for overlapping conditions, such as “myocardial injury,” “myocarditis,” “type Il myocardial infarction,” “stress cardiomyopathy,” and “inflammatory cardiomyopathy,” they point out.
“We, as a research community, did some things right and some things wrong surrounding the COVID pandemic,” Sandeep Das, MD, MPH, vice chair of the writing group, noted in an interview with this news organization.
“The things that we really did right is that everybody responded with enthusiasm, kind of all hands on deck with a massive crisis response, and that was fantastic,” Dr. Das said.
“However, because of the need to hurry, we didn’t structure and organize in the way that we typically would for something that was sort of a slow burn kind of problem rather than an emergency. One of the consequences of that was fragmentation of how things are collected, reported, et cetera, and that leads to confusion,” he added.
The report was published simultaneously June 23 in the Journal of the American College of Cardiology and Circulation: Cardiovascular Quality and Outcomes.
A necessary but not glamorous project
The new data standards for COVID-19 will help standardize definitions and set the framework to capture and better understand how COVID-19 affects CV health.
“It wasn’t exactly a glamorous-type project but, at the same time, it’s super necessary to kind of get everybody on the same page and working together,” Dr. Das said.
Broad agreement on common vocabulary and definitions will help with efforts to pool or compare data from electronic health records, clinical registries, administrative datasets, and other databases, and determine whether these data apply to clinical practice and research endeavors, the writing group says.
They considered data elements relevant to the full range of care provided to COVID-19 patients in all care settings. Among the key items included in the document are:
- Case definitions for confirmed, probable, and suspected acute COVID-19, as well as postacute sequelae of COVID-19.
- Definitions for acute CV complications related to COVID-19, including acute myocardial injury, heart failure, shock, arrhythmia, thromboembolic complications, and .
- Data elements related to COVID-19 vaccination status, comorbidities, and preexisting CV conditions.
- Definitions for postacute CV sequelae of SARS-CoV-2 infection and long-term CV complications of COVID-19.
- Data elements for CV mortality during acute COVID-19.
- Data elements for non-CV complications to help document severity of illness and other competing diagnoses and complications that might affect CV outcomes.
- A list of symptoms and signs related to COVID-19 and CV complications.
- Data elements for diagnostic and therapeutic strategies for COVID-19 and CV conditions.
- A discussion of advanced therapies, including , extracorporeal membrane oxygenation, and end-of-life management strategies.
These data standards will be useful for researchers, registry developers, and clinicians, and they are proposed as a framework for ICD-10 code development of COVID-19–related CV conditions, the writing group says.
The standards are also of “great importance” to patients, clinicians, investigators, scientists, administrators, public health officials, policymakers, and payers, the group says.
Dr. Das said that, although there is no formal plan in place to update the document, he could see sections that might be refined.
“For example, there’s a nice long list of all the various variants, and unfortunately, I suspect that that is going to change and evolve over time,” Dr. Das told this news organization.
“We tried very hard not to include things like specifying specific treatments so we didn’t get proscriptive. We wanted to make it descriptive, so hopefully it will stand the test of time pretty well,” he added.
This research had no commercial funding. The writing group has no relevant disclosures.
A version of this article first appeared on Medscape.com.
The American College of Cardiology and the American Heart Association have jointly issued a comprehensive set of data standards to help clarify definitions of the cardiovascular (CV) and non-CV complications of COVID-19.
It’s the work of the ACC/AHA Task Force on Clinical Data Standards and has been endorsed by the Heart Failure Society of America and Society for Cardiac Angiography and Interventions.
There is increased importance to understanding the acute and long-term impact of COVID-19 on CV health, the writing group notes. Until now, however, there has not been “clarity or consensus” on definitions of CV conditions related to COVID-19, with different diagnostic terminologies being used for overlapping conditions, such as “myocardial injury,” “myocarditis,” “type Il myocardial infarction,” “stress cardiomyopathy,” and “inflammatory cardiomyopathy,” they point out.
“We, as a research community, did some things right and some things wrong surrounding the COVID pandemic,” Sandeep Das, MD, MPH, vice chair of the writing group, noted in an interview with this news organization.
“The things that we really did right is that everybody responded with enthusiasm, kind of all hands on deck with a massive crisis response, and that was fantastic,” Dr. Das said.
“However, because of the need to hurry, we didn’t structure and organize in the way that we typically would for something that was sort of a slow burn kind of problem rather than an emergency. One of the consequences of that was fragmentation of how things are collected, reported, et cetera, and that leads to confusion,” he added.
The report was published simultaneously June 23 in the Journal of the American College of Cardiology and Circulation: Cardiovascular Quality and Outcomes.
A necessary but not glamorous project
The new data standards for COVID-19 will help standardize definitions and set the framework to capture and better understand how COVID-19 affects CV health.
“It wasn’t exactly a glamorous-type project but, at the same time, it’s super necessary to kind of get everybody on the same page and working together,” Dr. Das said.
Broad agreement on common vocabulary and definitions will help with efforts to pool or compare data from electronic health records, clinical registries, administrative datasets, and other databases, and determine whether these data apply to clinical practice and research endeavors, the writing group says.
They considered data elements relevant to the full range of care provided to COVID-19 patients in all care settings. Among the key items included in the document are:
- Case definitions for confirmed, probable, and suspected acute COVID-19, as well as postacute sequelae of COVID-19.
- Definitions for acute CV complications related to COVID-19, including acute myocardial injury, heart failure, shock, arrhythmia, thromboembolic complications, and .
- Data elements related to COVID-19 vaccination status, comorbidities, and preexisting CV conditions.
- Definitions for postacute CV sequelae of SARS-CoV-2 infection and long-term CV complications of COVID-19.
- Data elements for CV mortality during acute COVID-19.
- Data elements for non-CV complications to help document severity of illness and other competing diagnoses and complications that might affect CV outcomes.
- A list of symptoms and signs related to COVID-19 and CV complications.
- Data elements for diagnostic and therapeutic strategies for COVID-19 and CV conditions.
- A discussion of advanced therapies, including , extracorporeal membrane oxygenation, and end-of-life management strategies.
These data standards will be useful for researchers, registry developers, and clinicians, and they are proposed as a framework for ICD-10 code development of COVID-19–related CV conditions, the writing group says.
The standards are also of “great importance” to patients, clinicians, investigators, scientists, administrators, public health officials, policymakers, and payers, the group says.
Dr. Das said that, although there is no formal plan in place to update the document, he could see sections that might be refined.
“For example, there’s a nice long list of all the various variants, and unfortunately, I suspect that that is going to change and evolve over time,” Dr. Das told this news organization.
“We tried very hard not to include things like specifying specific treatments so we didn’t get proscriptive. We wanted to make it descriptive, so hopefully it will stand the test of time pretty well,” he added.
This research had no commercial funding. The writing group has no relevant disclosures.
A version of this article first appeared on Medscape.com.
The American College of Cardiology and the American Heart Association have jointly issued a comprehensive set of data standards to help clarify definitions of the cardiovascular (CV) and non-CV complications of COVID-19.
It’s the work of the ACC/AHA Task Force on Clinical Data Standards and has been endorsed by the Heart Failure Society of America and Society for Cardiac Angiography and Interventions.
There is increased importance to understanding the acute and long-term impact of COVID-19 on CV health, the writing group notes. Until now, however, there has not been “clarity or consensus” on definitions of CV conditions related to COVID-19, with different diagnostic terminologies being used for overlapping conditions, such as “myocardial injury,” “myocarditis,” “type Il myocardial infarction,” “stress cardiomyopathy,” and “inflammatory cardiomyopathy,” they point out.
“We, as a research community, did some things right and some things wrong surrounding the COVID pandemic,” Sandeep Das, MD, MPH, vice chair of the writing group, noted in an interview with this news organization.
“The things that we really did right is that everybody responded with enthusiasm, kind of all hands on deck with a massive crisis response, and that was fantastic,” Dr. Das said.
“However, because of the need to hurry, we didn’t structure and organize in the way that we typically would for something that was sort of a slow burn kind of problem rather than an emergency. One of the consequences of that was fragmentation of how things are collected, reported, et cetera, and that leads to confusion,” he added.
The report was published simultaneously June 23 in the Journal of the American College of Cardiology and Circulation: Cardiovascular Quality and Outcomes.
A necessary but not glamorous project
The new data standards for COVID-19 will help standardize definitions and set the framework to capture and better understand how COVID-19 affects CV health.
“It wasn’t exactly a glamorous-type project but, at the same time, it’s super necessary to kind of get everybody on the same page and working together,” Dr. Das said.
Broad agreement on common vocabulary and definitions will help with efforts to pool or compare data from electronic health records, clinical registries, administrative datasets, and other databases, and determine whether these data apply to clinical practice and research endeavors, the writing group says.
They considered data elements relevant to the full range of care provided to COVID-19 patients in all care settings. Among the key items included in the document are:
- Case definitions for confirmed, probable, and suspected acute COVID-19, as well as postacute sequelae of COVID-19.
- Definitions for acute CV complications related to COVID-19, including acute myocardial injury, heart failure, shock, arrhythmia, thromboembolic complications, and .
- Data elements related to COVID-19 vaccination status, comorbidities, and preexisting CV conditions.
- Definitions for postacute CV sequelae of SARS-CoV-2 infection and long-term CV complications of COVID-19.
- Data elements for CV mortality during acute COVID-19.
- Data elements for non-CV complications to help document severity of illness and other competing diagnoses and complications that might affect CV outcomes.
- A list of symptoms and signs related to COVID-19 and CV complications.
- Data elements for diagnostic and therapeutic strategies for COVID-19 and CV conditions.
- A discussion of advanced therapies, including , extracorporeal membrane oxygenation, and end-of-life management strategies.
These data standards will be useful for researchers, registry developers, and clinicians, and they are proposed as a framework for ICD-10 code development of COVID-19–related CV conditions, the writing group says.
The standards are also of “great importance” to patients, clinicians, investigators, scientists, administrators, public health officials, policymakers, and payers, the group says.
Dr. Das said that, although there is no formal plan in place to update the document, he could see sections that might be refined.
“For example, there’s a nice long list of all the various variants, and unfortunately, I suspect that that is going to change and evolve over time,” Dr. Das told this news organization.
“We tried very hard not to include things like specifying specific treatments so we didn’t get proscriptive. We wanted to make it descriptive, so hopefully it will stand the test of time pretty well,” he added.
This research had no commercial funding. The writing group has no relevant disclosures.
A version of this article first appeared on Medscape.com.
More evidence the flu vaccine may guard against Alzheimer’s
In a large propensity-matched cohort of older adults, those who had received at least one influenza inoculation were 40% less likely than unvaccinated peers to develop AD over the course of 4 years.
“Influenza infection can cause serious health complications, particularly in adults 65 and older. Our study’s findings – that vaccination against the flu virus may also reduce the risk of Alzheimer’s dementia for at least a few years – adds to the already compelling reasons get the flu vaccine annually,” Avram Bukhbinder, MD, of the University of Texas, Houston, said in an interview.
The new findings support earlier work by the same researchers that also suggested a protective effect of flu vaccination on dementia risk.
The latest study was published online in the Journal of Alzheimer’s Disease.
40% lower risk
Prior studies have found a lower risk of dementia of any etiology following influenza vaccination in selected populations, including veterans and patients with serious chronic health conditions.
However, the effect of influenza vaccination on AD risk in a general cohort of older U.S. adults has not been characterized.
Dr. Bukhbinder and colleagues used claims data to create a propensity-matched cohort of 935,887 influenza-vaccinated adults and a like number of unvaccinated adults aged 65 and older.
The median age of the persons in the matched sample was 73.7 years, and 57% were women. All were free of dementia during the 6-year look-back study period.
During median follow-up of 46 months, 47,889 (5.1%) flu-vaccinated adults and 79,630 (8.5%) unvaccinated adults developed AD.
The risk of AD was 40% lower in the vaccinated group (relative risk, 0.60; 95% confidence interval, 0.59-0.61). The absolute risk reduction was 0.034 (95% CI, 0.033-0.035), corresponding to a number needed to treat of 29.4.
Mechanism unclear
“Our study does not address the mechanism(s) underlying the apparent effect of influenza vaccination on Alzheimer’s risk, but we look forward to future research investigating this important question,” Dr. Bukhbinder said.
“One possible mechanism is that, by helping to prevent or mitigate infection with the flu virus and the systemic inflammation that follows such an infection, the flu vaccine helps to decrease the systemic inflammation that may have otherwise occurred,” he explained.
It’s also possible that influenza vaccination may trigger non–influenza-specific changes in the immune system that help to reduce the damage caused by AD pathology, including amyloid plaques and neurofibrillary tangles, he said.
“For example, the influenza vaccine may alter the brain’s immune cells such that they are better at clearing Alzheimer’s pathologies, an effect that has been seen in mice, or it may reprogram these immune cells to respond to Alzheimer’s pathologies in ways that are less likely to damage nearby healthy brain cells, or it may do both,” Dr. Bukhbinder noted.
Alzheimer’s expert weighs in
Heather M. Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said this study “suggests that flu vaccination may be valuable for maintaining cognition and memory as we age. This is even more relevant today in the COVID-19 environment.
“It is too early to tell if getting flu vaccine, on its own, can reduce risk of Alzheimer’s. More research is needed to understand the biological mechanisms behind the results in this study,” Dr. Snyder said in an interview.
“For example, it is possible that people who are getting vaccinated also take better care of their health in other ways, and these things add up to lower risk of Alzheimer’s and other dementias,” she noted.
“It is also possible that there are issues related to unequal access and/or vaccine hesitancy and how this may influence the study population and the research results,” Dr. Snyder said.
The study had no specific funding. Dr. Bukhbinder and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large propensity-matched cohort of older adults, those who had received at least one influenza inoculation were 40% less likely than unvaccinated peers to develop AD over the course of 4 years.
“Influenza infection can cause serious health complications, particularly in adults 65 and older. Our study’s findings – that vaccination against the flu virus may also reduce the risk of Alzheimer’s dementia for at least a few years – adds to the already compelling reasons get the flu vaccine annually,” Avram Bukhbinder, MD, of the University of Texas, Houston, said in an interview.
The new findings support earlier work by the same researchers that also suggested a protective effect of flu vaccination on dementia risk.
The latest study was published online in the Journal of Alzheimer’s Disease.
40% lower risk
Prior studies have found a lower risk of dementia of any etiology following influenza vaccination in selected populations, including veterans and patients with serious chronic health conditions.
However, the effect of influenza vaccination on AD risk in a general cohort of older U.S. adults has not been characterized.
Dr. Bukhbinder and colleagues used claims data to create a propensity-matched cohort of 935,887 influenza-vaccinated adults and a like number of unvaccinated adults aged 65 and older.
The median age of the persons in the matched sample was 73.7 years, and 57% were women. All were free of dementia during the 6-year look-back study period.
During median follow-up of 46 months, 47,889 (5.1%) flu-vaccinated adults and 79,630 (8.5%) unvaccinated adults developed AD.
The risk of AD was 40% lower in the vaccinated group (relative risk, 0.60; 95% confidence interval, 0.59-0.61). The absolute risk reduction was 0.034 (95% CI, 0.033-0.035), corresponding to a number needed to treat of 29.4.
Mechanism unclear
“Our study does not address the mechanism(s) underlying the apparent effect of influenza vaccination on Alzheimer’s risk, but we look forward to future research investigating this important question,” Dr. Bukhbinder said.
“One possible mechanism is that, by helping to prevent or mitigate infection with the flu virus and the systemic inflammation that follows such an infection, the flu vaccine helps to decrease the systemic inflammation that may have otherwise occurred,” he explained.
It’s also possible that influenza vaccination may trigger non–influenza-specific changes in the immune system that help to reduce the damage caused by AD pathology, including amyloid plaques and neurofibrillary tangles, he said.
“For example, the influenza vaccine may alter the brain’s immune cells such that they are better at clearing Alzheimer’s pathologies, an effect that has been seen in mice, or it may reprogram these immune cells to respond to Alzheimer’s pathologies in ways that are less likely to damage nearby healthy brain cells, or it may do both,” Dr. Bukhbinder noted.
Alzheimer’s expert weighs in
Heather M. Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said this study “suggests that flu vaccination may be valuable for maintaining cognition and memory as we age. This is even more relevant today in the COVID-19 environment.
“It is too early to tell if getting flu vaccine, on its own, can reduce risk of Alzheimer’s. More research is needed to understand the biological mechanisms behind the results in this study,” Dr. Snyder said in an interview.
“For example, it is possible that people who are getting vaccinated also take better care of their health in other ways, and these things add up to lower risk of Alzheimer’s and other dementias,” she noted.
“It is also possible that there are issues related to unequal access and/or vaccine hesitancy and how this may influence the study population and the research results,” Dr. Snyder said.
The study had no specific funding. Dr. Bukhbinder and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large propensity-matched cohort of older adults, those who had received at least one influenza inoculation were 40% less likely than unvaccinated peers to develop AD over the course of 4 years.
“Influenza infection can cause serious health complications, particularly in adults 65 and older. Our study’s findings – that vaccination against the flu virus may also reduce the risk of Alzheimer’s dementia for at least a few years – adds to the already compelling reasons get the flu vaccine annually,” Avram Bukhbinder, MD, of the University of Texas, Houston, said in an interview.
The new findings support earlier work by the same researchers that also suggested a protective effect of flu vaccination on dementia risk.
The latest study was published online in the Journal of Alzheimer’s Disease.
40% lower risk
Prior studies have found a lower risk of dementia of any etiology following influenza vaccination in selected populations, including veterans and patients with serious chronic health conditions.
However, the effect of influenza vaccination on AD risk in a general cohort of older U.S. adults has not been characterized.
Dr. Bukhbinder and colleagues used claims data to create a propensity-matched cohort of 935,887 influenza-vaccinated adults and a like number of unvaccinated adults aged 65 and older.
The median age of the persons in the matched sample was 73.7 years, and 57% were women. All were free of dementia during the 6-year look-back study period.
During median follow-up of 46 months, 47,889 (5.1%) flu-vaccinated adults and 79,630 (8.5%) unvaccinated adults developed AD.
The risk of AD was 40% lower in the vaccinated group (relative risk, 0.60; 95% confidence interval, 0.59-0.61). The absolute risk reduction was 0.034 (95% CI, 0.033-0.035), corresponding to a number needed to treat of 29.4.
Mechanism unclear
“Our study does not address the mechanism(s) underlying the apparent effect of influenza vaccination on Alzheimer’s risk, but we look forward to future research investigating this important question,” Dr. Bukhbinder said.
“One possible mechanism is that, by helping to prevent or mitigate infection with the flu virus and the systemic inflammation that follows such an infection, the flu vaccine helps to decrease the systemic inflammation that may have otherwise occurred,” he explained.
It’s also possible that influenza vaccination may trigger non–influenza-specific changes in the immune system that help to reduce the damage caused by AD pathology, including amyloid plaques and neurofibrillary tangles, he said.
“For example, the influenza vaccine may alter the brain’s immune cells such that they are better at clearing Alzheimer’s pathologies, an effect that has been seen in mice, or it may reprogram these immune cells to respond to Alzheimer’s pathologies in ways that are less likely to damage nearby healthy brain cells, or it may do both,” Dr. Bukhbinder noted.
Alzheimer’s expert weighs in
Heather M. Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said this study “suggests that flu vaccination may be valuable for maintaining cognition and memory as we age. This is even more relevant today in the COVID-19 environment.
“It is too early to tell if getting flu vaccine, on its own, can reduce risk of Alzheimer’s. More research is needed to understand the biological mechanisms behind the results in this study,” Dr. Snyder said in an interview.
“For example, it is possible that people who are getting vaccinated also take better care of their health in other ways, and these things add up to lower risk of Alzheimer’s and other dementias,” she noted.
“It is also possible that there are issues related to unequal access and/or vaccine hesitancy and how this may influence the study population and the research results,” Dr. Snyder said.
The study had no specific funding. Dr. Bukhbinder and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ALZHEIMER’S DISEASE
COVID-19 tied to increased risk for Alzheimer’s disease and Parkinson’s disease
a new study suggests. However, the research also showed there was no excess risk of these neurologic disorders following COVID than other respiratory infections such as influenza or community-acquired bacterial pneumonia.
Considering these results, study investigator Pardis Zarifkar, MD, department of neurology, Rigshospitalet, Copenhagen University Hospital, urged doctors to “keep an eye on” COVID patients and use “a critical mindset” if these patients present with neurologic issues.
“They should consider whether the patient’s condition is something new or if there were already signs and symptoms before they had COVID-19,” she said.
The findings were presented at the 2022 congress of the European Academy of Neurology and published online in Frontiers in Neurology.
‘Surprising’ increased risk
Previous research shows more than 80% of patients hospitalized with COVID-19 have neurologic symptoms including anosmia, dysgeusia, headache, dizziness, memory and concentration difficulties, fatigue, and irritability.
However, it’s unclear whether COVID-19 affects the risk for specific neurologic diseases and if so, whether this association differs from other respiratory infections.
From electronic health records covering about half the Danish population, researchers identified adults who were tested for COVID-19 or diagnosed with community-acquired bacterial pneumonia from February 2020 to November 2021. They also flagged individuals with influenza in the corresponding prepandemic period (February 2018–November 2019).
Dr. Zarifkar noted influenza A or B and community-acquired bacterial pneumonia are two of the most common respiratory tract infections.
The investigators tracked neurologic diseases up to 12 months after a positive test. They looked at two neurodegenerative diseases, Alzheimer’s disease and Parkinson’s disease, as well as cerebrovascular disorders including ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage.
The study included 43,262 individuals with a positive COVID test without a history of influenza A/B in the past year and 876,356 without a positive COVID test. It also included 1,474 individuals with community-acquired pneumonia without a history of COVID and 8,102 with influenza A or B.
“We wanted to investigate whether COVID-19 is really that much worse than all these other common respiratory infections that we have had for ages and see every single year,” said Dr. Zarifkar.
After 12 months, the relative risk for Alzheimer’s disease was 3.4 (95% confidence interval, 2.3-5.1) in the COVID-positive group versus the COVID-negative group. The risks were greater among inpatients versus outpatients.
These results were rather unexpected, said Dr. Zarifkar. “I would have expected a small increase, but the extent of the increase was quite surprising.”
However, there was no difference when comparing the COVID-19 group with the influenza or bacterial pneumonia groups, which Dr. Zarifkar said was “very reassuring.”
The findings were similar for Parkinson’s disease, where there was a 2.2-fold increased risk of a Parkinson’s disease diagnosis within the first 12 months in COVID-positive individuals, compared with COVID-negative people (RR, 2.2; 95% CI, 1.5-3.4). Again, there was no excess risk, compared with influenza or bacterial pneumonia.
Potential mechanisms
Dr. Zarifkar believes a “constellation” of factors may explain higher risks of these diagnoses in COVID patients. Part of it could be a result of neuroinflammation, which can lead to a toxic accumulation of beta amyloid in Alzheimer’s disease and alpha-synuclein in Parkinson’s disease.
“It can accelerate a neurodegenerative disease already in the making,” she said. But perhaps the biggest driver of differences between the groups is the “scientific focus” on COVID patients. “In Denmark, almost everyone who has had COVID-19, especially severe COVID-19, is offered some sort of cognitive testing, and if you hand out MoCAs [Montreal Cognitive Assessments] which is the cognitive test we use, to almost everyone you’re meeting, you’re going to catch these disorders earlier than you might have otherwise.”
As for cerebrovascular disorders, the study showed an increased risk of ischemic stroke in COVID-positive versus COVID-negative subjects at 12 months (RR, 2.87; 95% confidence interval, 2.2-3.2).
The relatively strong inflammatory response associated with COVID-19, which may create a hypercoagulable state, may help explain the increased ischemic stroke risk in COVID patients, said Dr. Zarifkar.
The study did not show an increased risk for subarachnoid hemorrhage in COVID-positive, compared with COVID-negative, subjects but did reveal an increased risk of intracerebral hemorrhage after 12 months (RR, 4.8; 95% CI, 1.8-12.9).
This could be explained by COVID-positive subjects having a higher risk for ischemic stroke and receiving thrombolysis that may increase risk for bleeding in the brain. However, an analysis accounting for medication use found differences in thrombolysis rates didn’t change the result, said Dr. Zarifkar.
It’s also possible that extracorporeal membrane oxygenation and mechanical ventilation – interventions more frequently used in COVID-19 patients – may increase the risk for bleeding in brain, she added.
The researchers did not find an increased risk for multiple sclerosis, myasthenia gravis, Guillain-Barré syndrome, or narcolepsy in COVID patients. However, Dr. Zarifkar noted that it can take years to detect an association with autoimmune disorders.
The investigators did not stratify risk by disease severity, although this would be an important step, she said. “The threshold of being admitted to the hospital with COVID-19 has been much lower than for influenza or bacterial pneumonia where you’re typically quite ill before you’re admitted, so this might actually dilute the findings and underestimate our findings.”
A national, registry-based study that includes the entire Danish population and additional information on vaccination status, virus variants, socioeconomic status, and comorbidities is needed, said Dr. Zarifkar.
The study was supported by Lundbeck Foundation and Novo Nordisk. Dr. Zarifkar reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new study suggests. However, the research also showed there was no excess risk of these neurologic disorders following COVID than other respiratory infections such as influenza or community-acquired bacterial pneumonia.
Considering these results, study investigator Pardis Zarifkar, MD, department of neurology, Rigshospitalet, Copenhagen University Hospital, urged doctors to “keep an eye on” COVID patients and use “a critical mindset” if these patients present with neurologic issues.
“They should consider whether the patient’s condition is something new or if there were already signs and symptoms before they had COVID-19,” she said.
The findings were presented at the 2022 congress of the European Academy of Neurology and published online in Frontiers in Neurology.
‘Surprising’ increased risk
Previous research shows more than 80% of patients hospitalized with COVID-19 have neurologic symptoms including anosmia, dysgeusia, headache, dizziness, memory and concentration difficulties, fatigue, and irritability.
However, it’s unclear whether COVID-19 affects the risk for specific neurologic diseases and if so, whether this association differs from other respiratory infections.
From electronic health records covering about half the Danish population, researchers identified adults who were tested for COVID-19 or diagnosed with community-acquired bacterial pneumonia from February 2020 to November 2021. They also flagged individuals with influenza in the corresponding prepandemic period (February 2018–November 2019).
Dr. Zarifkar noted influenza A or B and community-acquired bacterial pneumonia are two of the most common respiratory tract infections.
The investigators tracked neurologic diseases up to 12 months after a positive test. They looked at two neurodegenerative diseases, Alzheimer’s disease and Parkinson’s disease, as well as cerebrovascular disorders including ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage.
The study included 43,262 individuals with a positive COVID test without a history of influenza A/B in the past year and 876,356 without a positive COVID test. It also included 1,474 individuals with community-acquired pneumonia without a history of COVID and 8,102 with influenza A or B.
“We wanted to investigate whether COVID-19 is really that much worse than all these other common respiratory infections that we have had for ages and see every single year,” said Dr. Zarifkar.
After 12 months, the relative risk for Alzheimer’s disease was 3.4 (95% confidence interval, 2.3-5.1) in the COVID-positive group versus the COVID-negative group. The risks were greater among inpatients versus outpatients.
These results were rather unexpected, said Dr. Zarifkar. “I would have expected a small increase, but the extent of the increase was quite surprising.”
However, there was no difference when comparing the COVID-19 group with the influenza or bacterial pneumonia groups, which Dr. Zarifkar said was “very reassuring.”
The findings were similar for Parkinson’s disease, where there was a 2.2-fold increased risk of a Parkinson’s disease diagnosis within the first 12 months in COVID-positive individuals, compared with COVID-negative people (RR, 2.2; 95% CI, 1.5-3.4). Again, there was no excess risk, compared with influenza or bacterial pneumonia.
Potential mechanisms
Dr. Zarifkar believes a “constellation” of factors may explain higher risks of these diagnoses in COVID patients. Part of it could be a result of neuroinflammation, which can lead to a toxic accumulation of beta amyloid in Alzheimer’s disease and alpha-synuclein in Parkinson’s disease.
“It can accelerate a neurodegenerative disease already in the making,” she said. But perhaps the biggest driver of differences between the groups is the “scientific focus” on COVID patients. “In Denmark, almost everyone who has had COVID-19, especially severe COVID-19, is offered some sort of cognitive testing, and if you hand out MoCAs [Montreal Cognitive Assessments] which is the cognitive test we use, to almost everyone you’re meeting, you’re going to catch these disorders earlier than you might have otherwise.”
As for cerebrovascular disorders, the study showed an increased risk of ischemic stroke in COVID-positive versus COVID-negative subjects at 12 months (RR, 2.87; 95% confidence interval, 2.2-3.2).
The relatively strong inflammatory response associated with COVID-19, which may create a hypercoagulable state, may help explain the increased ischemic stroke risk in COVID patients, said Dr. Zarifkar.
The study did not show an increased risk for subarachnoid hemorrhage in COVID-positive, compared with COVID-negative, subjects but did reveal an increased risk of intracerebral hemorrhage after 12 months (RR, 4.8; 95% CI, 1.8-12.9).
This could be explained by COVID-positive subjects having a higher risk for ischemic stroke and receiving thrombolysis that may increase risk for bleeding in the brain. However, an analysis accounting for medication use found differences in thrombolysis rates didn’t change the result, said Dr. Zarifkar.
It’s also possible that extracorporeal membrane oxygenation and mechanical ventilation – interventions more frequently used in COVID-19 patients – may increase the risk for bleeding in brain, she added.
The researchers did not find an increased risk for multiple sclerosis, myasthenia gravis, Guillain-Barré syndrome, or narcolepsy in COVID patients. However, Dr. Zarifkar noted that it can take years to detect an association with autoimmune disorders.
The investigators did not stratify risk by disease severity, although this would be an important step, she said. “The threshold of being admitted to the hospital with COVID-19 has been much lower than for influenza or bacterial pneumonia where you’re typically quite ill before you’re admitted, so this might actually dilute the findings and underestimate our findings.”
A national, registry-based study that includes the entire Danish population and additional information on vaccination status, virus variants, socioeconomic status, and comorbidities is needed, said Dr. Zarifkar.
The study was supported by Lundbeck Foundation and Novo Nordisk. Dr. Zarifkar reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new study suggests. However, the research also showed there was no excess risk of these neurologic disorders following COVID than other respiratory infections such as influenza or community-acquired bacterial pneumonia.
Considering these results, study investigator Pardis Zarifkar, MD, department of neurology, Rigshospitalet, Copenhagen University Hospital, urged doctors to “keep an eye on” COVID patients and use “a critical mindset” if these patients present with neurologic issues.
“They should consider whether the patient’s condition is something new or if there were already signs and symptoms before they had COVID-19,” she said.
The findings were presented at the 2022 congress of the European Academy of Neurology and published online in Frontiers in Neurology.
‘Surprising’ increased risk
Previous research shows more than 80% of patients hospitalized with COVID-19 have neurologic symptoms including anosmia, dysgeusia, headache, dizziness, memory and concentration difficulties, fatigue, and irritability.
However, it’s unclear whether COVID-19 affects the risk for specific neurologic diseases and if so, whether this association differs from other respiratory infections.
From electronic health records covering about half the Danish population, researchers identified adults who were tested for COVID-19 or diagnosed with community-acquired bacterial pneumonia from February 2020 to November 2021. They also flagged individuals with influenza in the corresponding prepandemic period (February 2018–November 2019).
Dr. Zarifkar noted influenza A or B and community-acquired bacterial pneumonia are two of the most common respiratory tract infections.
The investigators tracked neurologic diseases up to 12 months after a positive test. They looked at two neurodegenerative diseases, Alzheimer’s disease and Parkinson’s disease, as well as cerebrovascular disorders including ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage.
The study included 43,262 individuals with a positive COVID test without a history of influenza A/B in the past year and 876,356 without a positive COVID test. It also included 1,474 individuals with community-acquired pneumonia without a history of COVID and 8,102 with influenza A or B.
“We wanted to investigate whether COVID-19 is really that much worse than all these other common respiratory infections that we have had for ages and see every single year,” said Dr. Zarifkar.
After 12 months, the relative risk for Alzheimer’s disease was 3.4 (95% confidence interval, 2.3-5.1) in the COVID-positive group versus the COVID-negative group. The risks were greater among inpatients versus outpatients.
These results were rather unexpected, said Dr. Zarifkar. “I would have expected a small increase, but the extent of the increase was quite surprising.”
However, there was no difference when comparing the COVID-19 group with the influenza or bacterial pneumonia groups, which Dr. Zarifkar said was “very reassuring.”
The findings were similar for Parkinson’s disease, where there was a 2.2-fold increased risk of a Parkinson’s disease diagnosis within the first 12 months in COVID-positive individuals, compared with COVID-negative people (RR, 2.2; 95% CI, 1.5-3.4). Again, there was no excess risk, compared with influenza or bacterial pneumonia.
Potential mechanisms
Dr. Zarifkar believes a “constellation” of factors may explain higher risks of these diagnoses in COVID patients. Part of it could be a result of neuroinflammation, which can lead to a toxic accumulation of beta amyloid in Alzheimer’s disease and alpha-synuclein in Parkinson’s disease.
“It can accelerate a neurodegenerative disease already in the making,” she said. But perhaps the biggest driver of differences between the groups is the “scientific focus” on COVID patients. “In Denmark, almost everyone who has had COVID-19, especially severe COVID-19, is offered some sort of cognitive testing, and if you hand out MoCAs [Montreal Cognitive Assessments] which is the cognitive test we use, to almost everyone you’re meeting, you’re going to catch these disorders earlier than you might have otherwise.”
As for cerebrovascular disorders, the study showed an increased risk of ischemic stroke in COVID-positive versus COVID-negative subjects at 12 months (RR, 2.87; 95% confidence interval, 2.2-3.2).
The relatively strong inflammatory response associated with COVID-19, which may create a hypercoagulable state, may help explain the increased ischemic stroke risk in COVID patients, said Dr. Zarifkar.
The study did not show an increased risk for subarachnoid hemorrhage in COVID-positive, compared with COVID-negative, subjects but did reveal an increased risk of intracerebral hemorrhage after 12 months (RR, 4.8; 95% CI, 1.8-12.9).
This could be explained by COVID-positive subjects having a higher risk for ischemic stroke and receiving thrombolysis that may increase risk for bleeding in the brain. However, an analysis accounting for medication use found differences in thrombolysis rates didn’t change the result, said Dr. Zarifkar.
It’s also possible that extracorporeal membrane oxygenation and mechanical ventilation – interventions more frequently used in COVID-19 patients – may increase the risk for bleeding in brain, she added.
The researchers did not find an increased risk for multiple sclerosis, myasthenia gravis, Guillain-Barré syndrome, or narcolepsy in COVID patients. However, Dr. Zarifkar noted that it can take years to detect an association with autoimmune disorders.
The investigators did not stratify risk by disease severity, although this would be an important step, she said. “The threshold of being admitted to the hospital with COVID-19 has been much lower than for influenza or bacterial pneumonia where you’re typically quite ill before you’re admitted, so this might actually dilute the findings and underestimate our findings.”
A national, registry-based study that includes the entire Danish population and additional information on vaccination status, virus variants, socioeconomic status, and comorbidities is needed, said Dr. Zarifkar.
The study was supported by Lundbeck Foundation and Novo Nordisk. Dr. Zarifkar reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN NEUROLOGY
FDA Class I recall: Batteries for CARESCAPE 2860 Ventilator
A total of 1,533 complaints allege that the batteries are draining much faster than expected, prompting manufacturer GE Healthcare to initiate the recall. There have been no injuries, and no deaths associated with the use of this device, according to an FDA corrected announcement.
Health care personnel and those patients who receive breathing support with these ventilators should be cautious about using CARESCAPE battery products moving forward, the agency said.
This type of ventilator is primarily powered by plugging into a wall outlet, but it has the capability to operate on backup batteries. These batteries are not solely for emergency situations such as power outages, but are also for routine situations such as transporting a patient within the hospital. GE Healthcare supplies these backup batteries with the ventilator, and sells replacements when they run out.
However, if the ventilator loses power because of battery malfunction, the patient may lose access to oxygen, leading to hypoxia, which can lead to brain injury and death. Therefore, if these batteries drain quicker than anticipated, it may put the patient at risk.
To prevent this danger, GE Healthcare recommends customers perform a battery performance test after they see this notice and every 3 months following. Consumers should take extra precaution and make sure their batteries are charged following a long period of inactivity. If the device is inactive for a while, the company says users should keep it plugged in to avoid draining the battery. Batteries should be replaced at a minimum of every 3 years.
When these devices are still plugged into the wall, they’re safe to use, according to the FDA. But when using the backup power source, clinicians should make sure to have alternative routes for breathing support on hand, such as with a bag-valve mask system.
There are 4,222 of these possibly defective batteries currently on the market. They were distributed from April 2, 2019, through April 18 of this year, when GE Healthcare stopped distributing these products and began the recall process. Any issues with these products should be reported to the FDA’s MedWatch database or by sending a medical device notification acknowledgment response to GE at the email address listed at the bottom of the recall announcement.
A version of this article first appeared on Medscape.com.
This article was updated 7/6/22.
A total of 1,533 complaints allege that the batteries are draining much faster than expected, prompting manufacturer GE Healthcare to initiate the recall. There have been no injuries, and no deaths associated with the use of this device, according to an FDA corrected announcement.
Health care personnel and those patients who receive breathing support with these ventilators should be cautious about using CARESCAPE battery products moving forward, the agency said.
This type of ventilator is primarily powered by plugging into a wall outlet, but it has the capability to operate on backup batteries. These batteries are not solely for emergency situations such as power outages, but are also for routine situations such as transporting a patient within the hospital. GE Healthcare supplies these backup batteries with the ventilator, and sells replacements when they run out.
However, if the ventilator loses power because of battery malfunction, the patient may lose access to oxygen, leading to hypoxia, which can lead to brain injury and death. Therefore, if these batteries drain quicker than anticipated, it may put the patient at risk.
To prevent this danger, GE Healthcare recommends customers perform a battery performance test after they see this notice and every 3 months following. Consumers should take extra precaution and make sure their batteries are charged following a long period of inactivity. If the device is inactive for a while, the company says users should keep it plugged in to avoid draining the battery. Batteries should be replaced at a minimum of every 3 years.
When these devices are still plugged into the wall, they’re safe to use, according to the FDA. But when using the backup power source, clinicians should make sure to have alternative routes for breathing support on hand, such as with a bag-valve mask system.
There are 4,222 of these possibly defective batteries currently on the market. They were distributed from April 2, 2019, through April 18 of this year, when GE Healthcare stopped distributing these products and began the recall process. Any issues with these products should be reported to the FDA’s MedWatch database or by sending a medical device notification acknowledgment response to GE at the email address listed at the bottom of the recall announcement.
A version of this article first appeared on Medscape.com.
This article was updated 7/6/22.
A total of 1,533 complaints allege that the batteries are draining much faster than expected, prompting manufacturer GE Healthcare to initiate the recall. There have been no injuries, and no deaths associated with the use of this device, according to an FDA corrected announcement.
Health care personnel and those patients who receive breathing support with these ventilators should be cautious about using CARESCAPE battery products moving forward, the agency said.
This type of ventilator is primarily powered by plugging into a wall outlet, but it has the capability to operate on backup batteries. These batteries are not solely for emergency situations such as power outages, but are also for routine situations such as transporting a patient within the hospital. GE Healthcare supplies these backup batteries with the ventilator, and sells replacements when they run out.
However, if the ventilator loses power because of battery malfunction, the patient may lose access to oxygen, leading to hypoxia, which can lead to brain injury and death. Therefore, if these batteries drain quicker than anticipated, it may put the patient at risk.
To prevent this danger, GE Healthcare recommends customers perform a battery performance test after they see this notice and every 3 months following. Consumers should take extra precaution and make sure their batteries are charged following a long period of inactivity. If the device is inactive for a while, the company says users should keep it plugged in to avoid draining the battery. Batteries should be replaced at a minimum of every 3 years.
When these devices are still plugged into the wall, they’re safe to use, according to the FDA. But when using the backup power source, clinicians should make sure to have alternative routes for breathing support on hand, such as with a bag-valve mask system.
There are 4,222 of these possibly defective batteries currently on the market. They were distributed from April 2, 2019, through April 18 of this year, when GE Healthcare stopped distributing these products and began the recall process. Any issues with these products should be reported to the FDA’s MedWatch database or by sending a medical device notification acknowledgment response to GE at the email address listed at the bottom of the recall announcement.
A version of this article first appeared on Medscape.com.
This article was updated 7/6/22.
Race drives disparities in life expectancy across states
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
FROM ANNALS OF INTERNAL MEDICINE
Cardiologists concerned for patient safety after abortion ruling
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Children and COVID: Vaccination off to slow start for the newly eligible
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.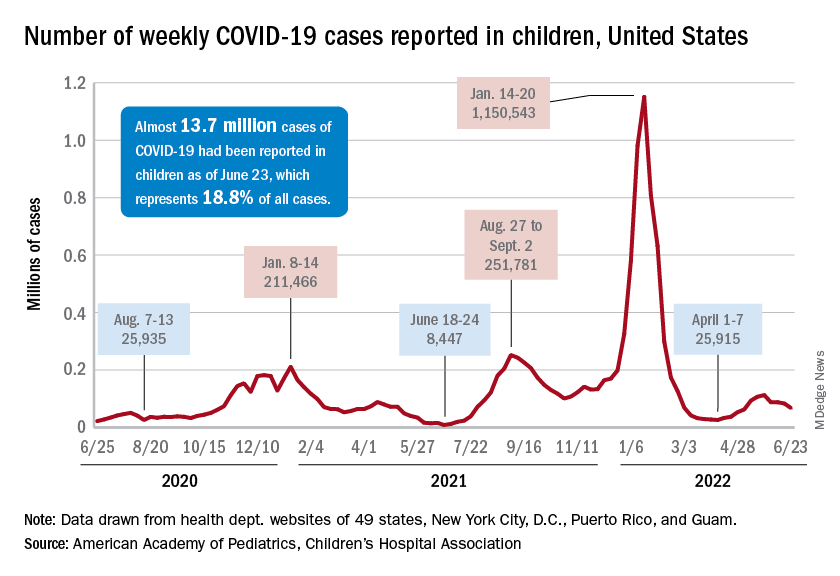
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.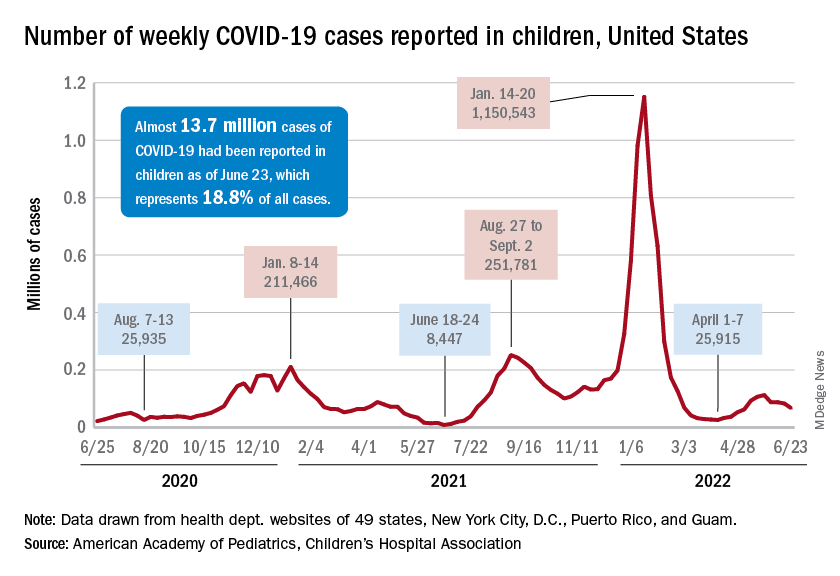
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.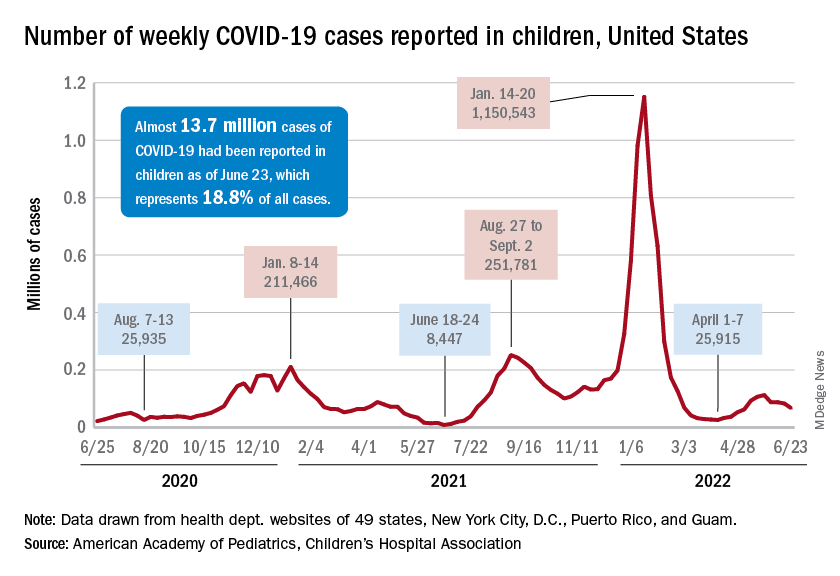
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.










