User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Out-of-state telehealth visits could help more patients if restrictions eased: Study
About 5% of traditional Medicare patients who had telehealth visits were seen virtually by out-of-state clinicians in the first half of 2021, according to a new study in JAMA Health Forum.
Since then, however, many states have restored restrictions that prevent physicians who are licensed in one state from having telehealth visits with patients unless they’re licensed in the state where the patients live.
This is not fair to many people who live in areas near state borders, the authors argued. For those patients, it is much more convenient to see their primary care physician in a virtual visit from home than to travel to the doctor’s office in another state. This convenience is enjoyed by most patients who reside elsewhere in their state because they’re seeing physicians who are licensed there.
Moreover, the paper said, patients who live in rural areas and in counties with relatively few physicians per capita would also benefit from relaxed telemedicine restrictions.
Using Medicare claims data, the researchers examined the characteristics of out-of-state (OOS) telemedicine visits for the 6 months from January to June 2021. They chose that period for two reasons: by then, health care had stabilized after the chaotic early phase of the pandemic, and in most states, the relaxation of licensing rules for OOS telehealth had not yet lapsed. Earlier periods of time were also used for certain types of comparisons.
Among fee-for-service Medicare beneficiaries, the number of OOS telemedicine visits peaked at 451,086 in April 2020 and slowly fell to 175,545 in June 2021, according to the study. The fraction of OOS telehealth visits among all virtual visits was 4.5% in April 2020 and increased to 5.6% by June 2021.
Staying close to home
Of all beneficiaries with a telemedicine visit in the study period, 33% lived within 15 miles of a state border. That cohort accounted for 57.2% of all OOS telemedicine visits.
The highest rates of OOS telehealth visits were seen in the District of Columbia (38.5%), Wyoming (25.6%), and North Dakota (21.1%). California (1%), Texas (2%), and Massachusetts (2.1%) had the lowest rates.
Though intuitive in retrospect, the correlation of OOS telemedicine use with proximity to state borders was one of the study’s most important findings, lead author Ateev Mehrotra, MD, a professor at Harvard Medical School, Boston, said in an interview. “It makes sense,” he said. “If you’re in D.C. and you need a cardiologist, you don’t think: ‘I’ll stay in D.C.’ No, Maryland is right there, so you might use a Maryland cardiologist. Now you’re out of state, even though that office might be only half a mile away from you.”
Similar dynamics, he noted, are seen in many metropolitan areas that border on other states, such as Cincinnati; Philadelphia; and Portland, Ore.
This finding lines up with another result of the study: The majority of patients who had OOS telemedicine visits had previously seen in person the doctor who conducted the virtual visit.
Across all OOS telemedicine visits in the first half of 2021, the researchers observed a prior in-person visit between March 2019 and the date of the virtual visit with the same patient and the same clinician in 62.8% of those visits. Across all in-state telehealth visits, 75.8% of them were made by patients who had seen the same clinician in person since March 2019. This preponderance of virtual visits to clinicians whom the patients had already seen in person reflects the fact that, during the pandemic, most physicians began conducting telehealth visits with their own patients, Dr. Mehrotra said.
It also lays to rest the concern that some states have had about allowing OOS telemedicine visits to physicians not licensed in those states, he added. “They think that all these docs from far away are going to start taking care of patients they don’t even know. But our study shows that isn’t the case. Most of the time, doctors are seeing a patient who’s switching over from in-person visits to out-of-state telemedicine.”
More specialty care sought
The dominant conditions that patients presented with were the same in OOS telemedicine and within-state virtual visits. However, the use of OOS telemedicine was higher for some types of specialized care.
For example, the rate of OOS telemedicine use, compared with all telemedicine use, was highest for cancer care (9.8%). Drilling down to more specific conditions, the top three in OOS telemedicine visits were assessment of organ transplant (13%); male reproductive cancers, such as prostate cancer (11.3%); and graft-related issues (10.2%).
The specialty trend was also evident in the types of OOS clinicians from whom Medicare patients sought virtual care. The rates of OOS telemedicine use as a percentage of all telemedicine use in particular specialties were highest for uncommon specialties, such as hematology/oncology, rheumatology, urology, medical oncology, and orthopedic surgery (8.5%). There was less use of OOS telemedicine as a percentage of all telemedicine among more common medical specialties (6.4%), mental health specialties (4.4%), and primary care (4.4%).
Despite its relatively low showing in this category, however, behavioral health was the leading condition treated in both within-state and OOS telemedicine visits, accounting for 30.7% and 25.8%, respectively, of those encounters.
States backslide on OOS telehealth
Since the end of the study period, over half of the states have restored some or all of the restrictions on OOS telemedicine that they had lifted during the pandemic.
According to Dr. Mehrotra, 22 states have some kind of regulation in place to allow an OOS clinician to conduct telehealth visits without being licensed in the state. This varies all the way from complete reciprocity with other states’ licenses to “emergency” telemedicine licenses. The other 28 states and Washington, D.C., require an OOS telemedicine practitioner to get a state license.
Various proposals have been floated to ameliorate this situation, the JAMA paper noted. These proposals include an expansion of the Interstate Medical Licensure Compact that the Federation of State Medical Boards organized in 2014. Since the pact became effective in 2014, at least 35 states and the District of Columbia have joined it. Those states have made it simpler for physicians to gain licensure in states other than their original state of licensure. However, Mehrotra said, it’s still not easy, and not many physicians have taken advantage of it.
One new wrinkle has emerged in this policy debate as a result of the Supreme Court decision overturning Roe v. Wade, he noted. Because people are using OOS telemedicine visits to get prescriptions to abort their fetuses, “that has changed the enthusiasm level for it among many states,” he said.
Dr. Mehrotra reported personal fees from the Pew Charitable Trust, Sanofi Pasteur, and Black Opal Ventures outside the submitted work. One coauthor reported receiving grants from Patient-Centered Outcomes Research, National Institute on Aging, Roundtrip, Independence Blue Cross; personal fees or salary from RAND Corporation from Verily Life Sciences; and that the American Telemedicine Association covered a conference fee. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
About 5% of traditional Medicare patients who had telehealth visits were seen virtually by out-of-state clinicians in the first half of 2021, according to a new study in JAMA Health Forum.
Since then, however, many states have restored restrictions that prevent physicians who are licensed in one state from having telehealth visits with patients unless they’re licensed in the state where the patients live.
This is not fair to many people who live in areas near state borders, the authors argued. For those patients, it is much more convenient to see their primary care physician in a virtual visit from home than to travel to the doctor’s office in another state. This convenience is enjoyed by most patients who reside elsewhere in their state because they’re seeing physicians who are licensed there.
Moreover, the paper said, patients who live in rural areas and in counties with relatively few physicians per capita would also benefit from relaxed telemedicine restrictions.
Using Medicare claims data, the researchers examined the characteristics of out-of-state (OOS) telemedicine visits for the 6 months from January to June 2021. They chose that period for two reasons: by then, health care had stabilized after the chaotic early phase of the pandemic, and in most states, the relaxation of licensing rules for OOS telehealth had not yet lapsed. Earlier periods of time were also used for certain types of comparisons.
Among fee-for-service Medicare beneficiaries, the number of OOS telemedicine visits peaked at 451,086 in April 2020 and slowly fell to 175,545 in June 2021, according to the study. The fraction of OOS telehealth visits among all virtual visits was 4.5% in April 2020 and increased to 5.6% by June 2021.
Staying close to home
Of all beneficiaries with a telemedicine visit in the study period, 33% lived within 15 miles of a state border. That cohort accounted for 57.2% of all OOS telemedicine visits.
The highest rates of OOS telehealth visits were seen in the District of Columbia (38.5%), Wyoming (25.6%), and North Dakota (21.1%). California (1%), Texas (2%), and Massachusetts (2.1%) had the lowest rates.
Though intuitive in retrospect, the correlation of OOS telemedicine use with proximity to state borders was one of the study’s most important findings, lead author Ateev Mehrotra, MD, a professor at Harvard Medical School, Boston, said in an interview. “It makes sense,” he said. “If you’re in D.C. and you need a cardiologist, you don’t think: ‘I’ll stay in D.C.’ No, Maryland is right there, so you might use a Maryland cardiologist. Now you’re out of state, even though that office might be only half a mile away from you.”
Similar dynamics, he noted, are seen in many metropolitan areas that border on other states, such as Cincinnati; Philadelphia; and Portland, Ore.
This finding lines up with another result of the study: The majority of patients who had OOS telemedicine visits had previously seen in person the doctor who conducted the virtual visit.
Across all OOS telemedicine visits in the first half of 2021, the researchers observed a prior in-person visit between March 2019 and the date of the virtual visit with the same patient and the same clinician in 62.8% of those visits. Across all in-state telehealth visits, 75.8% of them were made by patients who had seen the same clinician in person since March 2019. This preponderance of virtual visits to clinicians whom the patients had already seen in person reflects the fact that, during the pandemic, most physicians began conducting telehealth visits with their own patients, Dr. Mehrotra said.
It also lays to rest the concern that some states have had about allowing OOS telemedicine visits to physicians not licensed in those states, he added. “They think that all these docs from far away are going to start taking care of patients they don’t even know. But our study shows that isn’t the case. Most of the time, doctors are seeing a patient who’s switching over from in-person visits to out-of-state telemedicine.”
More specialty care sought
The dominant conditions that patients presented with were the same in OOS telemedicine and within-state virtual visits. However, the use of OOS telemedicine was higher for some types of specialized care.
For example, the rate of OOS telemedicine use, compared with all telemedicine use, was highest for cancer care (9.8%). Drilling down to more specific conditions, the top three in OOS telemedicine visits were assessment of organ transplant (13%); male reproductive cancers, such as prostate cancer (11.3%); and graft-related issues (10.2%).
The specialty trend was also evident in the types of OOS clinicians from whom Medicare patients sought virtual care. The rates of OOS telemedicine use as a percentage of all telemedicine use in particular specialties were highest for uncommon specialties, such as hematology/oncology, rheumatology, urology, medical oncology, and orthopedic surgery (8.5%). There was less use of OOS telemedicine as a percentage of all telemedicine among more common medical specialties (6.4%), mental health specialties (4.4%), and primary care (4.4%).
Despite its relatively low showing in this category, however, behavioral health was the leading condition treated in both within-state and OOS telemedicine visits, accounting for 30.7% and 25.8%, respectively, of those encounters.
States backslide on OOS telehealth
Since the end of the study period, over half of the states have restored some or all of the restrictions on OOS telemedicine that they had lifted during the pandemic.
According to Dr. Mehrotra, 22 states have some kind of regulation in place to allow an OOS clinician to conduct telehealth visits without being licensed in the state. This varies all the way from complete reciprocity with other states’ licenses to “emergency” telemedicine licenses. The other 28 states and Washington, D.C., require an OOS telemedicine practitioner to get a state license.
Various proposals have been floated to ameliorate this situation, the JAMA paper noted. These proposals include an expansion of the Interstate Medical Licensure Compact that the Federation of State Medical Boards organized in 2014. Since the pact became effective in 2014, at least 35 states and the District of Columbia have joined it. Those states have made it simpler for physicians to gain licensure in states other than their original state of licensure. However, Mehrotra said, it’s still not easy, and not many physicians have taken advantage of it.
One new wrinkle has emerged in this policy debate as a result of the Supreme Court decision overturning Roe v. Wade, he noted. Because people are using OOS telemedicine visits to get prescriptions to abort their fetuses, “that has changed the enthusiasm level for it among many states,” he said.
Dr. Mehrotra reported personal fees from the Pew Charitable Trust, Sanofi Pasteur, and Black Opal Ventures outside the submitted work. One coauthor reported receiving grants from Patient-Centered Outcomes Research, National Institute on Aging, Roundtrip, Independence Blue Cross; personal fees or salary from RAND Corporation from Verily Life Sciences; and that the American Telemedicine Association covered a conference fee. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
About 5% of traditional Medicare patients who had telehealth visits were seen virtually by out-of-state clinicians in the first half of 2021, according to a new study in JAMA Health Forum.
Since then, however, many states have restored restrictions that prevent physicians who are licensed in one state from having telehealth visits with patients unless they’re licensed in the state where the patients live.
This is not fair to many people who live in areas near state borders, the authors argued. For those patients, it is much more convenient to see their primary care physician in a virtual visit from home than to travel to the doctor’s office in another state. This convenience is enjoyed by most patients who reside elsewhere in their state because they’re seeing physicians who are licensed there.
Moreover, the paper said, patients who live in rural areas and in counties with relatively few physicians per capita would also benefit from relaxed telemedicine restrictions.
Using Medicare claims data, the researchers examined the characteristics of out-of-state (OOS) telemedicine visits for the 6 months from January to June 2021. They chose that period for two reasons: by then, health care had stabilized after the chaotic early phase of the pandemic, and in most states, the relaxation of licensing rules for OOS telehealth had not yet lapsed. Earlier periods of time were also used for certain types of comparisons.
Among fee-for-service Medicare beneficiaries, the number of OOS telemedicine visits peaked at 451,086 in April 2020 and slowly fell to 175,545 in June 2021, according to the study. The fraction of OOS telehealth visits among all virtual visits was 4.5% in April 2020 and increased to 5.6% by June 2021.
Staying close to home
Of all beneficiaries with a telemedicine visit in the study period, 33% lived within 15 miles of a state border. That cohort accounted for 57.2% of all OOS telemedicine visits.
The highest rates of OOS telehealth visits were seen in the District of Columbia (38.5%), Wyoming (25.6%), and North Dakota (21.1%). California (1%), Texas (2%), and Massachusetts (2.1%) had the lowest rates.
Though intuitive in retrospect, the correlation of OOS telemedicine use with proximity to state borders was one of the study’s most important findings, lead author Ateev Mehrotra, MD, a professor at Harvard Medical School, Boston, said in an interview. “It makes sense,” he said. “If you’re in D.C. and you need a cardiologist, you don’t think: ‘I’ll stay in D.C.’ No, Maryland is right there, so you might use a Maryland cardiologist. Now you’re out of state, even though that office might be only half a mile away from you.”
Similar dynamics, he noted, are seen in many metropolitan areas that border on other states, such as Cincinnati; Philadelphia; and Portland, Ore.
This finding lines up with another result of the study: The majority of patients who had OOS telemedicine visits had previously seen in person the doctor who conducted the virtual visit.
Across all OOS telemedicine visits in the first half of 2021, the researchers observed a prior in-person visit between March 2019 and the date of the virtual visit with the same patient and the same clinician in 62.8% of those visits. Across all in-state telehealth visits, 75.8% of them were made by patients who had seen the same clinician in person since March 2019. This preponderance of virtual visits to clinicians whom the patients had already seen in person reflects the fact that, during the pandemic, most physicians began conducting telehealth visits with their own patients, Dr. Mehrotra said.
It also lays to rest the concern that some states have had about allowing OOS telemedicine visits to physicians not licensed in those states, he added. “They think that all these docs from far away are going to start taking care of patients they don’t even know. But our study shows that isn’t the case. Most of the time, doctors are seeing a patient who’s switching over from in-person visits to out-of-state telemedicine.”
More specialty care sought
The dominant conditions that patients presented with were the same in OOS telemedicine and within-state virtual visits. However, the use of OOS telemedicine was higher for some types of specialized care.
For example, the rate of OOS telemedicine use, compared with all telemedicine use, was highest for cancer care (9.8%). Drilling down to more specific conditions, the top three in OOS telemedicine visits were assessment of organ transplant (13%); male reproductive cancers, such as prostate cancer (11.3%); and graft-related issues (10.2%).
The specialty trend was also evident in the types of OOS clinicians from whom Medicare patients sought virtual care. The rates of OOS telemedicine use as a percentage of all telemedicine use in particular specialties were highest for uncommon specialties, such as hematology/oncology, rheumatology, urology, medical oncology, and orthopedic surgery (8.5%). There was less use of OOS telemedicine as a percentage of all telemedicine among more common medical specialties (6.4%), mental health specialties (4.4%), and primary care (4.4%).
Despite its relatively low showing in this category, however, behavioral health was the leading condition treated in both within-state and OOS telemedicine visits, accounting for 30.7% and 25.8%, respectively, of those encounters.
States backslide on OOS telehealth
Since the end of the study period, over half of the states have restored some or all of the restrictions on OOS telemedicine that they had lifted during the pandemic.
According to Dr. Mehrotra, 22 states have some kind of regulation in place to allow an OOS clinician to conduct telehealth visits without being licensed in the state. This varies all the way from complete reciprocity with other states’ licenses to “emergency” telemedicine licenses. The other 28 states and Washington, D.C., require an OOS telemedicine practitioner to get a state license.
Various proposals have been floated to ameliorate this situation, the JAMA paper noted. These proposals include an expansion of the Interstate Medical Licensure Compact that the Federation of State Medical Boards organized in 2014. Since the pact became effective in 2014, at least 35 states and the District of Columbia have joined it. Those states have made it simpler for physicians to gain licensure in states other than their original state of licensure. However, Mehrotra said, it’s still not easy, and not many physicians have taken advantage of it.
One new wrinkle has emerged in this policy debate as a result of the Supreme Court decision overturning Roe v. Wade, he noted. Because people are using OOS telemedicine visits to get prescriptions to abort their fetuses, “that has changed the enthusiasm level for it among many states,” he said.
Dr. Mehrotra reported personal fees from the Pew Charitable Trust, Sanofi Pasteur, and Black Opal Ventures outside the submitted work. One coauthor reported receiving grants from Patient-Centered Outcomes Research, National Institute on Aging, Roundtrip, Independence Blue Cross; personal fees or salary from RAND Corporation from Verily Life Sciences; and that the American Telemedicine Association covered a conference fee. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Despite benefits, extended-interval pembro uptake remains low
In April 2020, the Food and Drug Administration approved extended dosing for standalone pembrolizumab – 400 mg every 6 weeks instead of the standard dosing of 200 mg every 3 weeks. The shift came, in part, to reduce patient health care encounters during the early days of the COVID-19 pandemic, but also because fewer infusions save patients time and out-of-pocket costs and reduce the burden on the health care system.
The FDA deemed this move safe after pharmacologic studies and a small melanoma study found that responses and adverse events were equivalent in comparison with standard dosing.
Given the benefits, one would expect “brisk adoption” of extended-interval dosing, Garth Strohbehn, MD, an oncologist at the VA Medical Center in Ann Arbor, Mich., and colleagues wrote in a recent report in JAMA Oncology.
However, when the team reviewed data on 835 veterans from the Veterans Health Administration who began taking single-agent pembrolizumab between April 1, 2020, and July 1, 2021, only about one-third received extended-interval dosing.
Between April and January 2021, use of extended-interval dosing rose steadily to about 35% of patients but then hovered in that range through August 2021.
Among the patients, age, sex, Charlson comorbidity index, and pembrolizumab indications were well balanced between the standard-dosing and the extended-interval dosing groups.
Notably, Dr. Strohbehn and colleagues also found no difference in time-to-treatment discontinuation between patients receiving extended dosing in comparison with patients receiving standard dosing, which is “a real-world measure of clinical effectiveness,” the team said.
And there was no difference in immune-related side effects between the two regimens, as assessed by incident levothyroxine and prednisone prescriptions.
The real-world near equivalence of extended and standard dosing intervals that was demonstrated in the study is “reassuring” and helps make the case for considering it “as a best practice” for single-agent pembrolizumab, the investigators wrote.
Dr. Strohbehn remained somewhat puzzled by the low uptake of the extended-dosing option.
“I was frankly surprised by the small number of patients who received the extended-interval regimen,” Dr. Strohbehn said in an interview.
“Admittedly, there are patients who would prefer to receive standard-interval therapy, and that preference should of course be accommodated whenever possible, but in my experience, those numbers are small,” at least in the VA system, he noted.
In addition, the authors noted, there is no direct financial incentive for more frequent dosing in the VA system.
It’s possible that low uptake could stem from clinicians’ doubts about switching to an extended-interval dose, given that the FDA’s approval was based largely on a study of 44 patients with melanoma in a single-arm trial.
If that is indeed the case, the new findings – which represent the first health system–level, real-world comparative effectiveness data for standard vs. extended-interval pembrolizumab – should help address these concerns, the team said.
“This observational dataset lends further credence to [the dosing] regimens being clinically equivalent,” said Zachery Reichert, MD, PhD, a urologic oncologist at the University of Michigan, Ann Arbor, who was not involved in the study.
To address the issue, Dr. Strohbehn and his team suggested “clinical guideline promotion to overcome some of the barriers to the adoption of extended-interval pembrolizumab.”
Dr. Riechert suggested further validation of equivalent outcomes for the two regimens, more advocacy to encourage patients to ask about the 6-week option, as well as incentives from insurers to adopt it.
Dr. Strohbehn added that the situation highlights a broader issue in oncology, namely that many drugs “end up on the market with dosing regimens that haven’t necessarily been optimized.”
Across the world, investigators are conducting clinical trials “to identify the minimum dosages, frequencies, and durations patients need in order to achieve their best outcome,” Dr. Strohbehn said. In oncology, much of this effort is being led by Project Optimus, from the FDA’s Oncology Center of Excellence, he said.
The study was funded by the VA National Oncology Program. Dr. Reichert and Dr. Strohbehn have disclosed no relevant financial relationships. One investigator has received grants from Novartis, Bristol-Myers Squibb, Regeneron, and Genentech.
A version of this article first appeared on Medscape.com.
In April 2020, the Food and Drug Administration approved extended dosing for standalone pembrolizumab – 400 mg every 6 weeks instead of the standard dosing of 200 mg every 3 weeks. The shift came, in part, to reduce patient health care encounters during the early days of the COVID-19 pandemic, but also because fewer infusions save patients time and out-of-pocket costs and reduce the burden on the health care system.
The FDA deemed this move safe after pharmacologic studies and a small melanoma study found that responses and adverse events were equivalent in comparison with standard dosing.
Given the benefits, one would expect “brisk adoption” of extended-interval dosing, Garth Strohbehn, MD, an oncologist at the VA Medical Center in Ann Arbor, Mich., and colleagues wrote in a recent report in JAMA Oncology.
However, when the team reviewed data on 835 veterans from the Veterans Health Administration who began taking single-agent pembrolizumab between April 1, 2020, and July 1, 2021, only about one-third received extended-interval dosing.
Between April and January 2021, use of extended-interval dosing rose steadily to about 35% of patients but then hovered in that range through August 2021.
Among the patients, age, sex, Charlson comorbidity index, and pembrolizumab indications were well balanced between the standard-dosing and the extended-interval dosing groups.
Notably, Dr. Strohbehn and colleagues also found no difference in time-to-treatment discontinuation between patients receiving extended dosing in comparison with patients receiving standard dosing, which is “a real-world measure of clinical effectiveness,” the team said.
And there was no difference in immune-related side effects between the two regimens, as assessed by incident levothyroxine and prednisone prescriptions.
The real-world near equivalence of extended and standard dosing intervals that was demonstrated in the study is “reassuring” and helps make the case for considering it “as a best practice” for single-agent pembrolizumab, the investigators wrote.
Dr. Strohbehn remained somewhat puzzled by the low uptake of the extended-dosing option.
“I was frankly surprised by the small number of patients who received the extended-interval regimen,” Dr. Strohbehn said in an interview.
“Admittedly, there are patients who would prefer to receive standard-interval therapy, and that preference should of course be accommodated whenever possible, but in my experience, those numbers are small,” at least in the VA system, he noted.
In addition, the authors noted, there is no direct financial incentive for more frequent dosing in the VA system.
It’s possible that low uptake could stem from clinicians’ doubts about switching to an extended-interval dose, given that the FDA’s approval was based largely on a study of 44 patients with melanoma in a single-arm trial.
If that is indeed the case, the new findings – which represent the first health system–level, real-world comparative effectiveness data for standard vs. extended-interval pembrolizumab – should help address these concerns, the team said.
“This observational dataset lends further credence to [the dosing] regimens being clinically equivalent,” said Zachery Reichert, MD, PhD, a urologic oncologist at the University of Michigan, Ann Arbor, who was not involved in the study.
To address the issue, Dr. Strohbehn and his team suggested “clinical guideline promotion to overcome some of the barriers to the adoption of extended-interval pembrolizumab.”
Dr. Riechert suggested further validation of equivalent outcomes for the two regimens, more advocacy to encourage patients to ask about the 6-week option, as well as incentives from insurers to adopt it.
Dr. Strohbehn added that the situation highlights a broader issue in oncology, namely that many drugs “end up on the market with dosing regimens that haven’t necessarily been optimized.”
Across the world, investigators are conducting clinical trials “to identify the minimum dosages, frequencies, and durations patients need in order to achieve their best outcome,” Dr. Strohbehn said. In oncology, much of this effort is being led by Project Optimus, from the FDA’s Oncology Center of Excellence, he said.
The study was funded by the VA National Oncology Program. Dr. Reichert and Dr. Strohbehn have disclosed no relevant financial relationships. One investigator has received grants from Novartis, Bristol-Myers Squibb, Regeneron, and Genentech.
A version of this article first appeared on Medscape.com.
In April 2020, the Food and Drug Administration approved extended dosing for standalone pembrolizumab – 400 mg every 6 weeks instead of the standard dosing of 200 mg every 3 weeks. The shift came, in part, to reduce patient health care encounters during the early days of the COVID-19 pandemic, but also because fewer infusions save patients time and out-of-pocket costs and reduce the burden on the health care system.
The FDA deemed this move safe after pharmacologic studies and a small melanoma study found that responses and adverse events were equivalent in comparison with standard dosing.
Given the benefits, one would expect “brisk adoption” of extended-interval dosing, Garth Strohbehn, MD, an oncologist at the VA Medical Center in Ann Arbor, Mich., and colleagues wrote in a recent report in JAMA Oncology.
However, when the team reviewed data on 835 veterans from the Veterans Health Administration who began taking single-agent pembrolizumab between April 1, 2020, and July 1, 2021, only about one-third received extended-interval dosing.
Between April and January 2021, use of extended-interval dosing rose steadily to about 35% of patients but then hovered in that range through August 2021.
Among the patients, age, sex, Charlson comorbidity index, and pembrolizumab indications were well balanced between the standard-dosing and the extended-interval dosing groups.
Notably, Dr. Strohbehn and colleagues also found no difference in time-to-treatment discontinuation between patients receiving extended dosing in comparison with patients receiving standard dosing, which is “a real-world measure of clinical effectiveness,” the team said.
And there was no difference in immune-related side effects between the two regimens, as assessed by incident levothyroxine and prednisone prescriptions.
The real-world near equivalence of extended and standard dosing intervals that was demonstrated in the study is “reassuring” and helps make the case for considering it “as a best practice” for single-agent pembrolizumab, the investigators wrote.
Dr. Strohbehn remained somewhat puzzled by the low uptake of the extended-dosing option.
“I was frankly surprised by the small number of patients who received the extended-interval regimen,” Dr. Strohbehn said in an interview.
“Admittedly, there are patients who would prefer to receive standard-interval therapy, and that preference should of course be accommodated whenever possible, but in my experience, those numbers are small,” at least in the VA system, he noted.
In addition, the authors noted, there is no direct financial incentive for more frequent dosing in the VA system.
It’s possible that low uptake could stem from clinicians’ doubts about switching to an extended-interval dose, given that the FDA’s approval was based largely on a study of 44 patients with melanoma in a single-arm trial.
If that is indeed the case, the new findings – which represent the first health system–level, real-world comparative effectiveness data for standard vs. extended-interval pembrolizumab – should help address these concerns, the team said.
“This observational dataset lends further credence to [the dosing] regimens being clinically equivalent,” said Zachery Reichert, MD, PhD, a urologic oncologist at the University of Michigan, Ann Arbor, who was not involved in the study.
To address the issue, Dr. Strohbehn and his team suggested “clinical guideline promotion to overcome some of the barriers to the adoption of extended-interval pembrolizumab.”
Dr. Riechert suggested further validation of equivalent outcomes for the two regimens, more advocacy to encourage patients to ask about the 6-week option, as well as incentives from insurers to adopt it.
Dr. Strohbehn added that the situation highlights a broader issue in oncology, namely that many drugs “end up on the market with dosing regimens that haven’t necessarily been optimized.”
Across the world, investigators are conducting clinical trials “to identify the minimum dosages, frequencies, and durations patients need in order to achieve their best outcome,” Dr. Strohbehn said. In oncology, much of this effort is being led by Project Optimus, from the FDA’s Oncology Center of Excellence, he said.
The study was funded by the VA National Oncology Program. Dr. Reichert and Dr. Strohbehn have disclosed no relevant financial relationships. One investigator has received grants from Novartis, Bristol-Myers Squibb, Regeneron, and Genentech.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
Britain’s hard lessons from handing elder care over to private equity
Domestic and global private equity investors had supercharged the company’s growth, betting that the rising needs of aging Britons would yield big returns.
Within weeks, the Four Seasons brand may be finished.
Christie & Co., a commercial real estate broker, splashed a summer sale across its website that signaled the demise: The last 111 Four Seasons facilities in England, Scotland, and Jersey were on the market. Already sold were its 29 homes in Northern Ireland.
Four Seasons collapsed after years of private equity investors rolling in one after another to buy its business, sell its real estate, and at times wrest multimillion-dollar profits through complex debt schemes – until the last big equity fund, Terra Firma, which in 2012 paid about $1.3 billion for the company, was caught short.
In a country where government health care is a right, the Four Seasons story exemplifies the high-stakes rise – and, ultimately, fall – of private equity investment in health and social services. Hanging over society’s most vulnerable patients, these heavily leveraged deals failed to account for the cost of their care. Private equity firms are known for making a profit on quick-turnaround investments.
“People often say: ‘Why have American investors, as well as professional investors here and in other countries, poured so much into this sector?’ I think they were dazzled by the potential of the demographics,” said Nick Hood, an analyst at Opus Restructuring & Insolvency in London, which advises care homes – the British equivalent of U.S. nursing homes or assisted living facilities. They “saw the baby boomers aging and thought there would be infinite demands.”
What they missed, Mr. Hood said, “was that about half of all the residents in U.K. homes are funded by the government in one way or another. They aren’t private pay – and they’ve got no money.”
Residents as ‘revenue streams’
As in the United States, long-term care homes in Britain serve a mixed market of public- and private-pay residents, and those whose balance sheets rest heavily on government payments are stressed even in better economic times. Andrew Dobbie, a community officer for Unison, a union that represents care home workers, said private equity investors often see homes like Four Seasons as having “two revenue streams, the properties themselves and the residents,” with efficiencies to exploit.
But investors don’t always understand what caregivers do, he said, or that older residents require more time than spreadsheets have calculated. “That’s a problem when you are looking at operating care homes,” Mr. Dobbie said. “Care workers need to have soft skills to work with a vulnerable group of people. It’s not the same skills as stocking shelves in a supermarket.”
A recent study, funded in part by Unison and conducted by University of Surrey researchers, found big changes in the quality of care after private equity investments. More than a dozen staff members, who weren’t identified by name or facility, said companies were “cutting corners” to curb costs because their priority was profit. Staffers said “these changes meant residents sometimes went without the appropriate care, timely medication or sufficient sanitary supplies.”
In August, the House of Commons received a sobering account: The number of adults 65 and older who will need care is speedily rising, estimated to go from 3.5 million in 2018 to 5.2 million in 2038. Yet workers at care homes are among the lowest paid in health care.
“The covid-19 pandemic shone a light on the adult social care sector,” according to the parliamentary report, which noted that “many frustrated and burnt out care workers left” for better-paying jobs. The report’s advice in a year of soaring inflation and energy costs? The government should add “at least £7 billion a year” – more than $8 billion – or risk deterioration of care.
Britain’s care homes are separate from the much-lauded National Health Service, funded by the government. Care homes rely on support from local authorities, akin to counties in the United States. But they have seen a sharp drop in funding from the British government, which cut a third of its payments in the past decade. When the pandemic hit, the differences were apparent: Care home workers were not afforded masks, gloves, or gowns to shield them from the deadly virus.
Years ago, care homes were largely run by families or local entities. In the 1990s, the government promoted privatization, triggering investments and consolidations. Today, private equity firms own three of the country’s five biggest care home providers.
Chris Thomas, a research fellow at the Institute for Public Policy Research, said investors benefited from scant financial oversight. “The accounting practices are horrendously complicated and meant to be complicated,” he said. Local authorities try “to regulate more, but they don’t have the expertise.”
The financial shuffle
At Four Seasons, the speed of change was dizzying. From 2004 to 2017, big money came and went, with revenue at times threaded through multiple offshore vehicles. Among the groups that owned Four Seasons, in part or in its entirety: British private equity firm Alchemy Partners; Allianz Capital Partners, a German private equity firm; Three Delta, an investment fund backed by Qatar; the American hedge fund Monarch Alternative Capital; and Terra Firma, the British private equity group that wallowed in debt demands. H/2 Capital Partners, a hedge fund in Connecticut, was Four Seasons’ main creditor and took over. By 2019, Four Seasons was managed by insolvency experts.
Pressed on whether Four Seasons would exist in any form after the current sale of its property and businesses, MHP Communications, representing the company, said in an email: “It is too early in the process to speculate about the future of the brand.”
Vivek Kotecha, an accountant who has examined the Four Seasons financial shuffle and coauthored the Unison report, said private equity investment – in homes for older residents and, increasingly, in facilities for troubled children – is now part of the financial mainstream. The consulting firm McKinsey in 2022estimated that private markets manage nearly $10 trillion in assets, making them a dominant force in global markets.
“What you find in America with private equity is much the same here,” said Mr. Kotecha, the founder of Trinava Consulting in London. “They are often the same firms, doing the same things.” What was remarkable about Four Seasons was the enormous liability from high-yield bonds that underpinned the deal – one equaling $514 million at 8.75% interest and another for $277 million at 12.75% interest.
Guy Hands, the high-flying British founder of Terra Firma, bought Four Seasons in 2012, soon after losing an epic court battle with Citigroup over the purchase price of the music company EMI Group. Terra Firma acquired the care homes and then a gardening business with more than 100 stores. Neither proved easy, or good, bets. Hands, a Londoner who moved offshore to Guernsey, declined through a representative to discuss Four Seasons.
Mr. Kotecha, however, helped the BBC try to make sense of Four Seasons’ holdings by tracking financial filings. It was “the most complicated spreadsheet I’ve ever seen,” Mr. Kotecha said. “I think there were more subsidiaries involved in Four Seasons’ care homes than there were with General Motors in Europe.”
As Britain’s small homes were swept up in consolidations, some financial practices were dubious. At times, businesses sold the buildings as lease-back deals – not a problem at first – that, after multiple purchases, left operators paying rent with heavy interest that sapped operating budgets. By 2020, some care homes were estimated to be spending as much as 16% of their bed fees on debt payments, according to parliamentary testimony this year.
How could that happen? In part, for-profit providers – backed by private-equity groups and other corporations – had subsidiaries of their parent companies act as lender, setting the rates.
Britain’s elder care was unrecognizable within a generation. By 2022, private-equity companies alone accounted for 55,000 beds, or about 12.6% of the total for-profit care beds for older people in the United Kingdom, according to LaingBuisson, a health care consultancy. LaingBuisson calculated that the average residential care home fee as of February 2022 was about $44,700 a year; the average nursing home fee was $62,275 a year.
From 1980 to 2018, the number of residential care beds provided by local authorities fell 88% – from 141,719 to 17,100, according to the nonprofit Centre for Health and the Public Interest. Independent operators – nonprofits and for-profits – moved in, it said, controlling 243,000 beds by 2018. Nursing homes saw a similar shift: Private providers accounted for 194,100 beds in 2018, compared with 25,500 decades earlier.
Beyond government control
British lawmakers in the winter of 2021-2022 tried – and failed – to bolster financial reporting rules for care homes, including banning the use of government funds to pay off debt.
“I don’t have a problem with offshore companies that make profits if they offer good services. I don’t have a problem with private equity and hedge funds who deliver good returns to their shareholders,” Ros Altmann, a Conservative Party member in the House of Lords and a pension expert, said in a February debate. “I do have a problem if those companies are taking advantage of some of the most vulnerable people in our society without oversight, without controls.”
She cited Four Seasons as an example of how regulators “have no control over the financial models that are used.” Ms. Altmann warned that economic headwinds could worsen matters: “We now have very heavily debt-laden [homes] in an environment where interest rates are heading upward.”
In August, the Bank of England raised borrowing rates. It now forecasts double-digit inflation – as much as 11% – through 2023.
And that leaves care home owner Robert Kilgour pensive about whether government grasps the risks and possibilities that the sector is facing. “It’s a struggle, and it’s becoming more of a struggle,” he said. A global energy crisis is the latest unexpected emergency. Mr. Kilgour said he recently signed electricity contracts, for April 2023, at rates that will rise by 200%. That means an extra $2,400 a day in utility costs for his homes.
Mr. Kilgour founded Four Seasons, opening its first home, in Fife, Scotland, in 1989. His ambition for its growth was modest: “Ten by 2000.” That changed in 1999 when Alchemy swooped in to expand nationally. Mr. Kilgour had left Four Seasons by 2004, turning to other ventures.
Still, he saw opportunity in elder care and opened Renaissance Care, which now operates 16 homes with 750 beds in Scotland. “I missed it,” he said in an interview in London. “It’s people and it’s property, and I like that.”
“People asked me if I had any regrets about selling to private equity. Well, no, the people I dealt with were very fair, very straight. There were no shenanigans,” Mr. Kilgour said, noting that Alchemy made money but invested as well.
Mr. Kilgour said the pandemic motivated him to improve his business. He is spending millions on new LED lighting and boilers, as well as training staffers on digital record-keeping, all to winnow costs. He increased hourly wages by 5%, but employees have suggested other ways to retain staff: shorter shifts and workdays that fit school schedules or allow them to care for their own older relatives.
Debates over whether the government should move back into elder care make little sense to Mr. Kilgour. Britain has had private care for decades, and he doesn’t see that changing. Instead, operators need help balancing private and publicly funded beds “so you have a blended rate for care and some certainty in the business.”
Consolidations are slowing, he said, which might be part of a long-overdue reckoning. “The idea of 200, 300, 400 care homes – that big is good and big is best – those days are gone,” Mr. Kilgour said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Domestic and global private equity investors had supercharged the company’s growth, betting that the rising needs of aging Britons would yield big returns.
Within weeks, the Four Seasons brand may be finished.
Christie & Co., a commercial real estate broker, splashed a summer sale across its website that signaled the demise: The last 111 Four Seasons facilities in England, Scotland, and Jersey were on the market. Already sold were its 29 homes in Northern Ireland.
Four Seasons collapsed after years of private equity investors rolling in one after another to buy its business, sell its real estate, and at times wrest multimillion-dollar profits through complex debt schemes – until the last big equity fund, Terra Firma, which in 2012 paid about $1.3 billion for the company, was caught short.
In a country where government health care is a right, the Four Seasons story exemplifies the high-stakes rise – and, ultimately, fall – of private equity investment in health and social services. Hanging over society’s most vulnerable patients, these heavily leveraged deals failed to account for the cost of their care. Private equity firms are known for making a profit on quick-turnaround investments.
“People often say: ‘Why have American investors, as well as professional investors here and in other countries, poured so much into this sector?’ I think they were dazzled by the potential of the demographics,” said Nick Hood, an analyst at Opus Restructuring & Insolvency in London, which advises care homes – the British equivalent of U.S. nursing homes or assisted living facilities. They “saw the baby boomers aging and thought there would be infinite demands.”
What they missed, Mr. Hood said, “was that about half of all the residents in U.K. homes are funded by the government in one way or another. They aren’t private pay – and they’ve got no money.”
Residents as ‘revenue streams’
As in the United States, long-term care homes in Britain serve a mixed market of public- and private-pay residents, and those whose balance sheets rest heavily on government payments are stressed even in better economic times. Andrew Dobbie, a community officer for Unison, a union that represents care home workers, said private equity investors often see homes like Four Seasons as having “two revenue streams, the properties themselves and the residents,” with efficiencies to exploit.
But investors don’t always understand what caregivers do, he said, or that older residents require more time than spreadsheets have calculated. “That’s a problem when you are looking at operating care homes,” Mr. Dobbie said. “Care workers need to have soft skills to work with a vulnerable group of people. It’s not the same skills as stocking shelves in a supermarket.”
A recent study, funded in part by Unison and conducted by University of Surrey researchers, found big changes in the quality of care after private equity investments. More than a dozen staff members, who weren’t identified by name or facility, said companies were “cutting corners” to curb costs because their priority was profit. Staffers said “these changes meant residents sometimes went without the appropriate care, timely medication or sufficient sanitary supplies.”
In August, the House of Commons received a sobering account: The number of adults 65 and older who will need care is speedily rising, estimated to go from 3.5 million in 2018 to 5.2 million in 2038. Yet workers at care homes are among the lowest paid in health care.
“The covid-19 pandemic shone a light on the adult social care sector,” according to the parliamentary report, which noted that “many frustrated and burnt out care workers left” for better-paying jobs. The report’s advice in a year of soaring inflation and energy costs? The government should add “at least £7 billion a year” – more than $8 billion – or risk deterioration of care.
Britain’s care homes are separate from the much-lauded National Health Service, funded by the government. Care homes rely on support from local authorities, akin to counties in the United States. But they have seen a sharp drop in funding from the British government, which cut a third of its payments in the past decade. When the pandemic hit, the differences were apparent: Care home workers were not afforded masks, gloves, or gowns to shield them from the deadly virus.
Years ago, care homes were largely run by families or local entities. In the 1990s, the government promoted privatization, triggering investments and consolidations. Today, private equity firms own three of the country’s five biggest care home providers.
Chris Thomas, a research fellow at the Institute for Public Policy Research, said investors benefited from scant financial oversight. “The accounting practices are horrendously complicated and meant to be complicated,” he said. Local authorities try “to regulate more, but they don’t have the expertise.”
The financial shuffle
At Four Seasons, the speed of change was dizzying. From 2004 to 2017, big money came and went, with revenue at times threaded through multiple offshore vehicles. Among the groups that owned Four Seasons, in part or in its entirety: British private equity firm Alchemy Partners; Allianz Capital Partners, a German private equity firm; Three Delta, an investment fund backed by Qatar; the American hedge fund Monarch Alternative Capital; and Terra Firma, the British private equity group that wallowed in debt demands. H/2 Capital Partners, a hedge fund in Connecticut, was Four Seasons’ main creditor and took over. By 2019, Four Seasons was managed by insolvency experts.
Pressed on whether Four Seasons would exist in any form after the current sale of its property and businesses, MHP Communications, representing the company, said in an email: “It is too early in the process to speculate about the future of the brand.”
Vivek Kotecha, an accountant who has examined the Four Seasons financial shuffle and coauthored the Unison report, said private equity investment – in homes for older residents and, increasingly, in facilities for troubled children – is now part of the financial mainstream. The consulting firm McKinsey in 2022estimated that private markets manage nearly $10 trillion in assets, making them a dominant force in global markets.
“What you find in America with private equity is much the same here,” said Mr. Kotecha, the founder of Trinava Consulting in London. “They are often the same firms, doing the same things.” What was remarkable about Four Seasons was the enormous liability from high-yield bonds that underpinned the deal – one equaling $514 million at 8.75% interest and another for $277 million at 12.75% interest.
Guy Hands, the high-flying British founder of Terra Firma, bought Four Seasons in 2012, soon after losing an epic court battle with Citigroup over the purchase price of the music company EMI Group. Terra Firma acquired the care homes and then a gardening business with more than 100 stores. Neither proved easy, or good, bets. Hands, a Londoner who moved offshore to Guernsey, declined through a representative to discuss Four Seasons.
Mr. Kotecha, however, helped the BBC try to make sense of Four Seasons’ holdings by tracking financial filings. It was “the most complicated spreadsheet I’ve ever seen,” Mr. Kotecha said. “I think there were more subsidiaries involved in Four Seasons’ care homes than there were with General Motors in Europe.”
As Britain’s small homes were swept up in consolidations, some financial practices were dubious. At times, businesses sold the buildings as lease-back deals – not a problem at first – that, after multiple purchases, left operators paying rent with heavy interest that sapped operating budgets. By 2020, some care homes were estimated to be spending as much as 16% of their bed fees on debt payments, according to parliamentary testimony this year.
How could that happen? In part, for-profit providers – backed by private-equity groups and other corporations – had subsidiaries of their parent companies act as lender, setting the rates.
Britain’s elder care was unrecognizable within a generation. By 2022, private-equity companies alone accounted for 55,000 beds, or about 12.6% of the total for-profit care beds for older people in the United Kingdom, according to LaingBuisson, a health care consultancy. LaingBuisson calculated that the average residential care home fee as of February 2022 was about $44,700 a year; the average nursing home fee was $62,275 a year.
From 1980 to 2018, the number of residential care beds provided by local authorities fell 88% – from 141,719 to 17,100, according to the nonprofit Centre for Health and the Public Interest. Independent operators – nonprofits and for-profits – moved in, it said, controlling 243,000 beds by 2018. Nursing homes saw a similar shift: Private providers accounted for 194,100 beds in 2018, compared with 25,500 decades earlier.
Beyond government control
British lawmakers in the winter of 2021-2022 tried – and failed – to bolster financial reporting rules for care homes, including banning the use of government funds to pay off debt.
“I don’t have a problem with offshore companies that make profits if they offer good services. I don’t have a problem with private equity and hedge funds who deliver good returns to their shareholders,” Ros Altmann, a Conservative Party member in the House of Lords and a pension expert, said in a February debate. “I do have a problem if those companies are taking advantage of some of the most vulnerable people in our society without oversight, without controls.”
She cited Four Seasons as an example of how regulators “have no control over the financial models that are used.” Ms. Altmann warned that economic headwinds could worsen matters: “We now have very heavily debt-laden [homes] in an environment where interest rates are heading upward.”
In August, the Bank of England raised borrowing rates. It now forecasts double-digit inflation – as much as 11% – through 2023.
And that leaves care home owner Robert Kilgour pensive about whether government grasps the risks and possibilities that the sector is facing. “It’s a struggle, and it’s becoming more of a struggle,” he said. A global energy crisis is the latest unexpected emergency. Mr. Kilgour said he recently signed electricity contracts, for April 2023, at rates that will rise by 200%. That means an extra $2,400 a day in utility costs for his homes.
Mr. Kilgour founded Four Seasons, opening its first home, in Fife, Scotland, in 1989. His ambition for its growth was modest: “Ten by 2000.” That changed in 1999 when Alchemy swooped in to expand nationally. Mr. Kilgour had left Four Seasons by 2004, turning to other ventures.
Still, he saw opportunity in elder care and opened Renaissance Care, which now operates 16 homes with 750 beds in Scotland. “I missed it,” he said in an interview in London. “It’s people and it’s property, and I like that.”
“People asked me if I had any regrets about selling to private equity. Well, no, the people I dealt with were very fair, very straight. There were no shenanigans,” Mr. Kilgour said, noting that Alchemy made money but invested as well.
Mr. Kilgour said the pandemic motivated him to improve his business. He is spending millions on new LED lighting and boilers, as well as training staffers on digital record-keeping, all to winnow costs. He increased hourly wages by 5%, but employees have suggested other ways to retain staff: shorter shifts and workdays that fit school schedules or allow them to care for their own older relatives.
Debates over whether the government should move back into elder care make little sense to Mr. Kilgour. Britain has had private care for decades, and he doesn’t see that changing. Instead, operators need help balancing private and publicly funded beds “so you have a blended rate for care and some certainty in the business.”
Consolidations are slowing, he said, which might be part of a long-overdue reckoning. “The idea of 200, 300, 400 care homes – that big is good and big is best – those days are gone,” Mr. Kilgour said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Domestic and global private equity investors had supercharged the company’s growth, betting that the rising needs of aging Britons would yield big returns.
Within weeks, the Four Seasons brand may be finished.
Christie & Co., a commercial real estate broker, splashed a summer sale across its website that signaled the demise: The last 111 Four Seasons facilities in England, Scotland, and Jersey were on the market. Already sold were its 29 homes in Northern Ireland.
Four Seasons collapsed after years of private equity investors rolling in one after another to buy its business, sell its real estate, and at times wrest multimillion-dollar profits through complex debt schemes – until the last big equity fund, Terra Firma, which in 2012 paid about $1.3 billion for the company, was caught short.
In a country where government health care is a right, the Four Seasons story exemplifies the high-stakes rise – and, ultimately, fall – of private equity investment in health and social services. Hanging over society’s most vulnerable patients, these heavily leveraged deals failed to account for the cost of their care. Private equity firms are known for making a profit on quick-turnaround investments.
“People often say: ‘Why have American investors, as well as professional investors here and in other countries, poured so much into this sector?’ I think they were dazzled by the potential of the demographics,” said Nick Hood, an analyst at Opus Restructuring & Insolvency in London, which advises care homes – the British equivalent of U.S. nursing homes or assisted living facilities. They “saw the baby boomers aging and thought there would be infinite demands.”
What they missed, Mr. Hood said, “was that about half of all the residents in U.K. homes are funded by the government in one way or another. They aren’t private pay – and they’ve got no money.”
Residents as ‘revenue streams’
As in the United States, long-term care homes in Britain serve a mixed market of public- and private-pay residents, and those whose balance sheets rest heavily on government payments are stressed even in better economic times. Andrew Dobbie, a community officer for Unison, a union that represents care home workers, said private equity investors often see homes like Four Seasons as having “two revenue streams, the properties themselves and the residents,” with efficiencies to exploit.
But investors don’t always understand what caregivers do, he said, or that older residents require more time than spreadsheets have calculated. “That’s a problem when you are looking at operating care homes,” Mr. Dobbie said. “Care workers need to have soft skills to work with a vulnerable group of people. It’s not the same skills as stocking shelves in a supermarket.”
A recent study, funded in part by Unison and conducted by University of Surrey researchers, found big changes in the quality of care after private equity investments. More than a dozen staff members, who weren’t identified by name or facility, said companies were “cutting corners” to curb costs because their priority was profit. Staffers said “these changes meant residents sometimes went without the appropriate care, timely medication or sufficient sanitary supplies.”
In August, the House of Commons received a sobering account: The number of adults 65 and older who will need care is speedily rising, estimated to go from 3.5 million in 2018 to 5.2 million in 2038. Yet workers at care homes are among the lowest paid in health care.
“The covid-19 pandemic shone a light on the adult social care sector,” according to the parliamentary report, which noted that “many frustrated and burnt out care workers left” for better-paying jobs. The report’s advice in a year of soaring inflation and energy costs? The government should add “at least £7 billion a year” – more than $8 billion – or risk deterioration of care.
Britain’s care homes are separate from the much-lauded National Health Service, funded by the government. Care homes rely on support from local authorities, akin to counties in the United States. But they have seen a sharp drop in funding from the British government, which cut a third of its payments in the past decade. When the pandemic hit, the differences were apparent: Care home workers were not afforded masks, gloves, or gowns to shield them from the deadly virus.
Years ago, care homes were largely run by families or local entities. In the 1990s, the government promoted privatization, triggering investments and consolidations. Today, private equity firms own three of the country’s five biggest care home providers.
Chris Thomas, a research fellow at the Institute for Public Policy Research, said investors benefited from scant financial oversight. “The accounting practices are horrendously complicated and meant to be complicated,” he said. Local authorities try “to regulate more, but they don’t have the expertise.”
The financial shuffle
At Four Seasons, the speed of change was dizzying. From 2004 to 2017, big money came and went, with revenue at times threaded through multiple offshore vehicles. Among the groups that owned Four Seasons, in part or in its entirety: British private equity firm Alchemy Partners; Allianz Capital Partners, a German private equity firm; Three Delta, an investment fund backed by Qatar; the American hedge fund Monarch Alternative Capital; and Terra Firma, the British private equity group that wallowed in debt demands. H/2 Capital Partners, a hedge fund in Connecticut, was Four Seasons’ main creditor and took over. By 2019, Four Seasons was managed by insolvency experts.
Pressed on whether Four Seasons would exist in any form after the current sale of its property and businesses, MHP Communications, representing the company, said in an email: “It is too early in the process to speculate about the future of the brand.”
Vivek Kotecha, an accountant who has examined the Four Seasons financial shuffle and coauthored the Unison report, said private equity investment – in homes for older residents and, increasingly, in facilities for troubled children – is now part of the financial mainstream. The consulting firm McKinsey in 2022estimated that private markets manage nearly $10 trillion in assets, making them a dominant force in global markets.
“What you find in America with private equity is much the same here,” said Mr. Kotecha, the founder of Trinava Consulting in London. “They are often the same firms, doing the same things.” What was remarkable about Four Seasons was the enormous liability from high-yield bonds that underpinned the deal – one equaling $514 million at 8.75% interest and another for $277 million at 12.75% interest.
Guy Hands, the high-flying British founder of Terra Firma, bought Four Seasons in 2012, soon after losing an epic court battle with Citigroup over the purchase price of the music company EMI Group. Terra Firma acquired the care homes and then a gardening business with more than 100 stores. Neither proved easy, or good, bets. Hands, a Londoner who moved offshore to Guernsey, declined through a representative to discuss Four Seasons.
Mr. Kotecha, however, helped the BBC try to make sense of Four Seasons’ holdings by tracking financial filings. It was “the most complicated spreadsheet I’ve ever seen,” Mr. Kotecha said. “I think there were more subsidiaries involved in Four Seasons’ care homes than there were with General Motors in Europe.”
As Britain’s small homes were swept up in consolidations, some financial practices were dubious. At times, businesses sold the buildings as lease-back deals – not a problem at first – that, after multiple purchases, left operators paying rent with heavy interest that sapped operating budgets. By 2020, some care homes were estimated to be spending as much as 16% of their bed fees on debt payments, according to parliamentary testimony this year.
How could that happen? In part, for-profit providers – backed by private-equity groups and other corporations – had subsidiaries of their parent companies act as lender, setting the rates.
Britain’s elder care was unrecognizable within a generation. By 2022, private-equity companies alone accounted for 55,000 beds, or about 12.6% of the total for-profit care beds for older people in the United Kingdom, according to LaingBuisson, a health care consultancy. LaingBuisson calculated that the average residential care home fee as of February 2022 was about $44,700 a year; the average nursing home fee was $62,275 a year.
From 1980 to 2018, the number of residential care beds provided by local authorities fell 88% – from 141,719 to 17,100, according to the nonprofit Centre for Health and the Public Interest. Independent operators – nonprofits and for-profits – moved in, it said, controlling 243,000 beds by 2018. Nursing homes saw a similar shift: Private providers accounted for 194,100 beds in 2018, compared with 25,500 decades earlier.
Beyond government control
British lawmakers in the winter of 2021-2022 tried – and failed – to bolster financial reporting rules for care homes, including banning the use of government funds to pay off debt.
“I don’t have a problem with offshore companies that make profits if they offer good services. I don’t have a problem with private equity and hedge funds who deliver good returns to their shareholders,” Ros Altmann, a Conservative Party member in the House of Lords and a pension expert, said in a February debate. “I do have a problem if those companies are taking advantage of some of the most vulnerable people in our society without oversight, without controls.”
She cited Four Seasons as an example of how regulators “have no control over the financial models that are used.” Ms. Altmann warned that economic headwinds could worsen matters: “We now have very heavily debt-laden [homes] in an environment where interest rates are heading upward.”
In August, the Bank of England raised borrowing rates. It now forecasts double-digit inflation – as much as 11% – through 2023.
And that leaves care home owner Robert Kilgour pensive about whether government grasps the risks and possibilities that the sector is facing. “It’s a struggle, and it’s becoming more of a struggle,” he said. A global energy crisis is the latest unexpected emergency. Mr. Kilgour said he recently signed electricity contracts, for April 2023, at rates that will rise by 200%. That means an extra $2,400 a day in utility costs for his homes.
Mr. Kilgour founded Four Seasons, opening its first home, in Fife, Scotland, in 1989. His ambition for its growth was modest: “Ten by 2000.” That changed in 1999 when Alchemy swooped in to expand nationally. Mr. Kilgour had left Four Seasons by 2004, turning to other ventures.
Still, he saw opportunity in elder care and opened Renaissance Care, which now operates 16 homes with 750 beds in Scotland. “I missed it,” he said in an interview in London. “It’s people and it’s property, and I like that.”
“People asked me if I had any regrets about selling to private equity. Well, no, the people I dealt with were very fair, very straight. There were no shenanigans,” Mr. Kilgour said, noting that Alchemy made money but invested as well.
Mr. Kilgour said the pandemic motivated him to improve his business. He is spending millions on new LED lighting and boilers, as well as training staffers on digital record-keeping, all to winnow costs. He increased hourly wages by 5%, but employees have suggested other ways to retain staff: shorter shifts and workdays that fit school schedules or allow them to care for their own older relatives.
Debates over whether the government should move back into elder care make little sense to Mr. Kilgour. Britain has had private care for decades, and he doesn’t see that changing. Instead, operators need help balancing private and publicly funded beds “so you have a blended rate for care and some certainty in the business.”
Consolidations are slowing, he said, which might be part of a long-overdue reckoning. “The idea of 200, 300, 400 care homes – that big is good and big is best – those days are gone,” Mr. Kilgour said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Newer 3D lung models starting to remake research
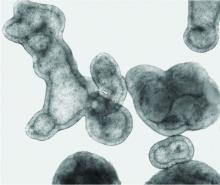
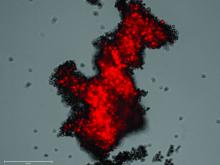
Pulmonologist-scientist Veena B. Antony, MD, professor of medicine at the University of Alabama in Birmingham, grows “pulmospheres” in her lab. The tiny spheres, about 1 mL in diameter, contain cells representing all of the cell types in a lung struck with pulmonary fibrosis.
They are a three-dimensional model of idiopathic pulmonary fibrosis (IPF) that can be used to study the behavior of invasive myofibroblasts and to predict in vivo responsiveness to antifibrotic drugs;
“The utility is extensive, including looking at the impact of early-life exposures on mid-life lung disease. We can ask all kinds of questions and answer them much faster, and with more accuracy, than with any 2D model,” said Dr. Antony, also professor of environmental health sciences and director of UAB’s program for environmental and translational medicine.
“The future of 3D modeling of the lung will happen step by step ... but we’re right at the edge of a prime explosion of information coming from these models, in all kinds of lung diseases,” she said.
Two-dimensional model systems – mainly monolayer cell cultures where cells adhere to and grow on a plate – cannot approximate the variety of cell types and architecture found in tissue, nor can they recapitulate cell-cell communication, biochemical cues, and other factors that are key to lung development and the pathogenesis of disease.
Dr. Antony’s pulmospheres resemble what have come to be known as organoids – 3D tissue cultures emanating from induced pluripotent stem cells (iPSC) or adult stem cells, in which multiple cell types self-organize, usually while suspended in natural or synthetic extracellular matrix (with or without a scaffold of some kind).
Lung-on-a-chip
In lung-on-a-chip (LOC) models, multiple cell types are seeded into miniature chambers, or “chips,” that contain networks of microfabricated channels designed to deliver and remove fluids, chemical cues, oxygen, and biomechanical forces. LOCs and other organs-on-chips – also called tissues-on-chips – can be continuously perfused and are highly structured and precisely controlled.
It’s the organs-on-chip model – or potential fusions of the organoid and organs-on-chip models – that will likely impact drug development. Almost 9 out of 10 investigational drugs fail in clinical trials – approximately 60% because of lack of efficacy and 30% because of toxicity. More reliable and predictive preclinical investigation is key, said Danilo A. Tagle, PhD, director of the Office of Special Initiatives in the National Center for Advancing Translational Sciences, of the National Institutes of Health.
“We have so many candidate drugs that go through preclinical safety testing, and that do relatively well in animal studies of efficacy, but then fail in clinical trials,” Dr. Tagle said. “We need better preclinical models.”
In its 10 years of life, the Tissue Chip for Drug Screening Program led by the NCATS – and funded by the NIH and Defense Advanced Research Projects Agency – has shown that organs-on-chips can be used to model disease and to predict both the safety and efficacy of clinical compounds, he said.
Lung organoids
Dr. Antony’s pulmospheres emanate not from stem cells but from primary tissue obtained from diseased lung. “We reconstitute the lung cells in single-cell suspensions, and then we allow them to come back together to form lung tissue,” she said. The pulmospheres take about 3 days to grow.
In a study published 5 years ago of pulmospheres of 20 patients with IPF and 9 control subjects, Dr. Antony and colleagues quantitated invasiveness and found “remarkable” differences in the invasiveness of IPF pulmospheres following exposure to the Food and Drug Administration–approved antifibrotic drugs nintedanib and pirfenidone. Some pulmospheres responded to one or the other drug, some to both, and two to neither – findings that Dr. Antony said offer hope for the goals of personalizing therapy and assessing new drugs.
Moreover, clinical disease progression correlated with invasiveness of the pulmospheres, showing that the organoid-like structures “do give us a model that [reflects] what’s happening in the clinical setting,” she said. (Lung tissue for the study was obtained via video-assisted thoracic surgery biopsy of IPF patients and from failed donor lung explants, but bronchoscopic forceps biopsies have become a useful method for obtaining tissue.)
The pulmospheres are not yet in clinical use, Dr. Antony said, but her lab is testing other fibrosis modifiers and continuing to use the model as a research tool.
One state to the east, at Vanderbilt University, Nashville, Tenn., Amanda Linkous, PhD, grows “branching lung organoids” and brain organoids to study the biology of small cell lung cancer (SCLC).
“We want to understand how [SCLC] cells change in the primary organ site, compared with metastatic sites like the brain. ... Are different transcription factors expressed [for instance] depending on where the tumor is growing?” said Dr. Linkous, scientific center manager of the National Cancer Institute’s Center for Systems Biology of SCLC at Vanderbilt. “Then we hope to start drug screening within the next year.”
Her lung organoids take shape from either human embryonic stem cells or iPSCs. Within commercially available media, the cells mature through several stages of differentiation, forming definitive endoderm, anterior foregut endoderm, and then circular lung bud structures – the latter of which are then placed into droplets of Matrigel, an extracellular matrix gel.
“In the Matrigel droplets, the lung bud cells will develop proximal and distal-like branching structures that express things like EPCAM, MUC1, SOX2, SOX9, and NKX2.1 – key markers that you should see in a more mature lung microenvironment,” she said. Tumor cells from established SCLC cell lines will then easily invade the branching lung organoid.
Dr. Linkous said she has found her organoid models highly reproducible and values their long-lasting nature – especially for future drug screening. “We can keep organoids going for months at a time,” said Dr. Linkous, a research associate professor in Vanderbilt’s department of biochemistry.
Like Dr. Antony, she envisions personalizing treatment in the future. “SCLC is a very heterogeneous tumor with many different cell types, so what works for one patient may not work well at all for another patient,” she said.
As recently as 5 years ago, “many in the cancer field would have been resistant to moving away from mouse models,” Dr. Linkous noted. “But preclinical studies in mice often don’t pan out in the clinic ... so we’re moving toward a human microenvironment to study human disease.”
The greatest challenge, Dr. Linkous and Dr. Antony said, lies in integrating both vascular blood flow and air into these models. “We just don’t have that combination as of yet,” Dr. Antony said.
LOC models
One of the first LOC models – and a galvanizing event for organs-on-chips more broadly – was a 1- to 2-cm–long model of the alveolar-capillary interface developed at the Wyss Institute for Biologically Inspired Engineering at Harvard Medical School, Boston.
Microchannels ran alongside a porous membrane coated with extracellular matrix, with alveolar cells seeded on one side and lung endothelial cells on the other side. When a vacuum was applied rhythmically to the channels, the cell-lined membrane stretched and relaxed, mimicking breathing movements.
Lead investigator Dongeun (Dan) Huh, PhD, then a postdoctoral student working with Donald E. Ingber, MD, PhD, founding director of the institute, ran tests showing that the model could reproduce organ-level responses to bacteria and inflammatory cytokines, as well as to silica nanoparticles. The widely cited paper was published in 2010 (Science. 2010;328[5986]:1662-8), and was followed by another study published in 2012 (Sci Transl Med. 2012;4[159]:159ra147) that used the LOC device to reproduce drug toxicity–induced pulmonary edema. “Here we were demonstrating for the first time that we could use the lung-on-chip to model human lung disease,” said Dr. Huh, who started his own lab at the University of Pennsylvania, Philadelphia, in 2013.
Since then, “as a field we’ve come a long way in modeling the complexity of human lung tissues ... with more advanced devices that can be used to mimic different parts of the lung and different processes, like immune responses in asthma and viral infections,” said Dr. Huh, “and with several studies using primary human cells taken from lung disease patients.”
Among Dr. Huh’s latest devices, built with NIH funding, is an asthma-on-a-chip device. Lung cells isolated from asthma patients are grown in a microfabricated device to create multilayered airway tissue, with airspace, that contains a fully differentiated epithelium and a vascularized stroma. “We can compress the entire engineered area of asthmatic human tissue in a lateral direction to mimic bronchoconstriction that happens during an asthma attack,” he said.
A paper soon to be published will describe how “abnormal pathophysiologic compressive forces due to bronchoconstriction in asthmatic lungs can make the lungs fibrotic, and how those mechanical forces also can induce increased vascularity,” said Dr. Huh, associate professor in the university’s department of bioengineering. “The increased vascular density can also change the phenotype of blood vessels in asthmatic airways.”
Dr. Huh also has an $8.3 million contract with the government’s Biomedical Advanced Research and Development Authority to study how chlorine gas damages lung tissues and identify biomarkers of chlorine gas–induced lung injury, with the goal of developing therapeutics.
Dr. Ingber and associates have developed a device modeling cystic fibrosis (CF). The chip is lined with primary human CF bronchial epithelial cells grown under an air-liquid interface and interfaced with primary lung microvascular endothelium that are exposed to fluid flow.
The chip reproduced, “with high fidelity, many of the structural, biochemical, and pathophysiological features of the human CF lung airway and its response to pathogens and circulating immune cells in vitro,” Dr. Ingber and colleagues reported (J Cyst Fibros. 2022;21:605-15).
Government investment in tissue chips
Efforts to commercialize organs-on-chip platforms and translate them for nonengineers have also picked in recent years. Several companies in the United States (including Emulate, a Wyss start-up) and in Europe now offer microengineered lung tissue models that can be used for research and drug testing. And some large pharmaceutical companies, said Dr. Tagle, have begun integrating tissue chip technology into their drug development programs.
The FDA, meanwhile, “has come to embrace the technology and see its promise,” Dr. Tagle said. An FDA pilot program announced in 2021 – called ISTAND (Innovative Science and Technology Approaches for New Drugs) – allows for tissue chip data to be submitted, as standalone data, for some drug applications.
The first 5 years of the government’s Tissue Chip for Drug Screening Program focused on safety and toxicity, and it “was successful in that model organ systems were able to capture the human response that [had been missed in] animal models,” he said.
For example, when a liver-tissue model was used to test several compounds that had passed animal testing for toxicity/safety but then failed in human clinical trials – killing some of the participants – the model showed a 100% sensitivity and a 87% specificity in predicting the human response, said Dr. Tagle, who recently coauthored a review on the future of organs-on-chips (Nature Reviews I Drug Discovery. 2021;20:345-61).
The second 5 years of the program, currently winding down, have focused on efficacy – the ability of organs-on-chip models to recreate the pathophysiology of chronic obstructive pulmonary disease, influenza, and other diseases, so that potential drugs can be assessed. In 2020, with extra support from the Coronavirus Aid, Relief, and Economic Security Act, NCATS funded academic labs to use organs-on-chip technology to evaluate SARS-CoV-2 and potential therapeutics.
Dr. Ingbar was one of the grantees. His team screened a number of FDA-approved drugs for potential repurposing using a bronchial-airway-on-a-chip and compared results with 2D model systems (Nat Biomed Eng. 2021;5:815-29). Amodiaquine inhibited infection in the 3D model and is now in phase 2 COVID trials. Several other drugs showed effectiveness in a 2D model but not in the chip.
Now, in a next phase of study at NCATS, coined Clinical Trials on a Chip, the center has awarded $35.5 million for investigators to test candidate therapies, often in parallel to ongoing clinical trials. The hope is that organs-on-chips can improve clinical trial design, from enrollment criteria and patient stratification to endpoints and the use of biomarkers. And in his lab, Dr. Huh is now engineering a shift to “organoids-on-a-chip” that combines the best features of each approach. “The idea,” he said, “is to grow organoids, and maintain the organoids in the microengineered systems where we can control their environment better ... and apply cues to allow them to develop into even more realistic tissues.”
Drs. Antony, Linkous, and Tagle reported no relevant disclosures. Dr. Huh is a co-founder of Vivodyne Inc, and owns shares in Vivodyne Inc. and Emulate Inc.
Pulmonologist-scientist Veena B. Antony, MD, professor of medicine at the University of Alabama in Birmingham, grows “pulmospheres” in her lab. The tiny spheres, about 1 mL in diameter, contain cells representing all of the cell types in a lung struck with pulmonary fibrosis.
They are a three-dimensional model of idiopathic pulmonary fibrosis (IPF) that can be used to study the behavior of invasive myofibroblasts and to predict in vivo responsiveness to antifibrotic drugs;
“The utility is extensive, including looking at the impact of early-life exposures on mid-life lung disease. We can ask all kinds of questions and answer them much faster, and with more accuracy, than with any 2D model,” said Dr. Antony, also professor of environmental health sciences and director of UAB’s program for environmental and translational medicine.
“The future of 3D modeling of the lung will happen step by step ... but we’re right at the edge of a prime explosion of information coming from these models, in all kinds of lung diseases,” she said.
Two-dimensional model systems – mainly monolayer cell cultures where cells adhere to and grow on a plate – cannot approximate the variety of cell types and architecture found in tissue, nor can they recapitulate cell-cell communication, biochemical cues, and other factors that are key to lung development and the pathogenesis of disease.
Dr. Antony’s pulmospheres resemble what have come to be known as organoids – 3D tissue cultures emanating from induced pluripotent stem cells (iPSC) or adult stem cells, in which multiple cell types self-organize, usually while suspended in natural or synthetic extracellular matrix (with or without a scaffold of some kind).
Lung-on-a-chip
In lung-on-a-chip (LOC) models, multiple cell types are seeded into miniature chambers, or “chips,” that contain networks of microfabricated channels designed to deliver and remove fluids, chemical cues, oxygen, and biomechanical forces. LOCs and other organs-on-chips – also called tissues-on-chips – can be continuously perfused and are highly structured and precisely controlled.
It’s the organs-on-chip model – or potential fusions of the organoid and organs-on-chip models – that will likely impact drug development. Almost 9 out of 10 investigational drugs fail in clinical trials – approximately 60% because of lack of efficacy and 30% because of toxicity. More reliable and predictive preclinical investigation is key, said Danilo A. Tagle, PhD, director of the Office of Special Initiatives in the National Center for Advancing Translational Sciences, of the National Institutes of Health.
“We have so many candidate drugs that go through preclinical safety testing, and that do relatively well in animal studies of efficacy, but then fail in clinical trials,” Dr. Tagle said. “We need better preclinical models.”
In its 10 years of life, the Tissue Chip for Drug Screening Program led by the NCATS – and funded by the NIH and Defense Advanced Research Projects Agency – has shown that organs-on-chips can be used to model disease and to predict both the safety and efficacy of clinical compounds, he said.
Lung organoids
Dr. Antony’s pulmospheres emanate not from stem cells but from primary tissue obtained from diseased lung. “We reconstitute the lung cells in single-cell suspensions, and then we allow them to come back together to form lung tissue,” she said. The pulmospheres take about 3 days to grow.
In a study published 5 years ago of pulmospheres of 20 patients with IPF and 9 control subjects, Dr. Antony and colleagues quantitated invasiveness and found “remarkable” differences in the invasiveness of IPF pulmospheres following exposure to the Food and Drug Administration–approved antifibrotic drugs nintedanib and pirfenidone. Some pulmospheres responded to one or the other drug, some to both, and two to neither – findings that Dr. Antony said offer hope for the goals of personalizing therapy and assessing new drugs.
Moreover, clinical disease progression correlated with invasiveness of the pulmospheres, showing that the organoid-like structures “do give us a model that [reflects] what’s happening in the clinical setting,” she said. (Lung tissue for the study was obtained via video-assisted thoracic surgery biopsy of IPF patients and from failed donor lung explants, but bronchoscopic forceps biopsies have become a useful method for obtaining tissue.)
The pulmospheres are not yet in clinical use, Dr. Antony said, but her lab is testing other fibrosis modifiers and continuing to use the model as a research tool.
One state to the east, at Vanderbilt University, Nashville, Tenn., Amanda Linkous, PhD, grows “branching lung organoids” and brain organoids to study the biology of small cell lung cancer (SCLC).
“We want to understand how [SCLC] cells change in the primary organ site, compared with metastatic sites like the brain. ... Are different transcription factors expressed [for instance] depending on where the tumor is growing?” said Dr. Linkous, scientific center manager of the National Cancer Institute’s Center for Systems Biology of SCLC at Vanderbilt. “Then we hope to start drug screening within the next year.”
Her lung organoids take shape from either human embryonic stem cells or iPSCs. Within commercially available media, the cells mature through several stages of differentiation, forming definitive endoderm, anterior foregut endoderm, and then circular lung bud structures – the latter of which are then placed into droplets of Matrigel, an extracellular matrix gel.
“In the Matrigel droplets, the lung bud cells will develop proximal and distal-like branching structures that express things like EPCAM, MUC1, SOX2, SOX9, and NKX2.1 – key markers that you should see in a more mature lung microenvironment,” she said. Tumor cells from established SCLC cell lines will then easily invade the branching lung organoid.
Dr. Linkous said she has found her organoid models highly reproducible and values their long-lasting nature – especially for future drug screening. “We can keep organoids going for months at a time,” said Dr. Linkous, a research associate professor in Vanderbilt’s department of biochemistry.
Like Dr. Antony, she envisions personalizing treatment in the future. “SCLC is a very heterogeneous tumor with many different cell types, so what works for one patient may not work well at all for another patient,” she said.
As recently as 5 years ago, “many in the cancer field would have been resistant to moving away from mouse models,” Dr. Linkous noted. “But preclinical studies in mice often don’t pan out in the clinic ... so we’re moving toward a human microenvironment to study human disease.”
The greatest challenge, Dr. Linkous and Dr. Antony said, lies in integrating both vascular blood flow and air into these models. “We just don’t have that combination as of yet,” Dr. Antony said.
LOC models
One of the first LOC models – and a galvanizing event for organs-on-chips more broadly – was a 1- to 2-cm–long model of the alveolar-capillary interface developed at the Wyss Institute for Biologically Inspired Engineering at Harvard Medical School, Boston.
Microchannels ran alongside a porous membrane coated with extracellular matrix, with alveolar cells seeded on one side and lung endothelial cells on the other side. When a vacuum was applied rhythmically to the channels, the cell-lined membrane stretched and relaxed, mimicking breathing movements.
Lead investigator Dongeun (Dan) Huh, PhD, then a postdoctoral student working with Donald E. Ingber, MD, PhD, founding director of the institute, ran tests showing that the model could reproduce organ-level responses to bacteria and inflammatory cytokines, as well as to silica nanoparticles. The widely cited paper was published in 2010 (Science. 2010;328[5986]:1662-8), and was followed by another study published in 2012 (Sci Transl Med. 2012;4[159]:159ra147) that used the LOC device to reproduce drug toxicity–induced pulmonary edema. “Here we were demonstrating for the first time that we could use the lung-on-chip to model human lung disease,” said Dr. Huh, who started his own lab at the University of Pennsylvania, Philadelphia, in 2013.
Since then, “as a field we’ve come a long way in modeling the complexity of human lung tissues ... with more advanced devices that can be used to mimic different parts of the lung and different processes, like immune responses in asthma and viral infections,” said Dr. Huh, “and with several studies using primary human cells taken from lung disease patients.”
Among Dr. Huh’s latest devices, built with NIH funding, is an asthma-on-a-chip device. Lung cells isolated from asthma patients are grown in a microfabricated device to create multilayered airway tissue, with airspace, that contains a fully differentiated epithelium and a vascularized stroma. “We can compress the entire engineered area of asthmatic human tissue in a lateral direction to mimic bronchoconstriction that happens during an asthma attack,” he said.
A paper soon to be published will describe how “abnormal pathophysiologic compressive forces due to bronchoconstriction in asthmatic lungs can make the lungs fibrotic, and how those mechanical forces also can induce increased vascularity,” said Dr. Huh, associate professor in the university’s department of bioengineering. “The increased vascular density can also change the phenotype of blood vessels in asthmatic airways.”
Dr. Huh also has an $8.3 million contract with the government’s Biomedical Advanced Research and Development Authority to study how chlorine gas damages lung tissues and identify biomarkers of chlorine gas–induced lung injury, with the goal of developing therapeutics.
Dr. Ingber and associates have developed a device modeling cystic fibrosis (CF). The chip is lined with primary human CF bronchial epithelial cells grown under an air-liquid interface and interfaced with primary lung microvascular endothelium that are exposed to fluid flow.
The chip reproduced, “with high fidelity, many of the structural, biochemical, and pathophysiological features of the human CF lung airway and its response to pathogens and circulating immune cells in vitro,” Dr. Ingber and colleagues reported (J Cyst Fibros. 2022;21:605-15).
Government investment in tissue chips
Efforts to commercialize organs-on-chip platforms and translate them for nonengineers have also picked in recent years. Several companies in the United States (including Emulate, a Wyss start-up) and in Europe now offer microengineered lung tissue models that can be used for research and drug testing. And some large pharmaceutical companies, said Dr. Tagle, have begun integrating tissue chip technology into their drug development programs.
The FDA, meanwhile, “has come to embrace the technology and see its promise,” Dr. Tagle said. An FDA pilot program announced in 2021 – called ISTAND (Innovative Science and Technology Approaches for New Drugs) – allows for tissue chip data to be submitted, as standalone data, for some drug applications.
The first 5 years of the government’s Tissue Chip for Drug Screening Program focused on safety and toxicity, and it “was successful in that model organ systems were able to capture the human response that [had been missed in] animal models,” he said.
For example, when a liver-tissue model was used to test several compounds that had passed animal testing for toxicity/safety but then failed in human clinical trials – killing some of the participants – the model showed a 100% sensitivity and a 87% specificity in predicting the human response, said Dr. Tagle, who recently coauthored a review on the future of organs-on-chips (Nature Reviews I Drug Discovery. 2021;20:345-61).
The second 5 years of the program, currently winding down, have focused on efficacy – the ability of organs-on-chip models to recreate the pathophysiology of chronic obstructive pulmonary disease, influenza, and other diseases, so that potential drugs can be assessed. In 2020, with extra support from the Coronavirus Aid, Relief, and Economic Security Act, NCATS funded academic labs to use organs-on-chip technology to evaluate SARS-CoV-2 and potential therapeutics.
Dr. Ingbar was one of the grantees. His team screened a number of FDA-approved drugs for potential repurposing using a bronchial-airway-on-a-chip and compared results with 2D model systems (Nat Biomed Eng. 2021;5:815-29). Amodiaquine inhibited infection in the 3D model and is now in phase 2 COVID trials. Several other drugs showed effectiveness in a 2D model but not in the chip.
Now, in a next phase of study at NCATS, coined Clinical Trials on a Chip, the center has awarded $35.5 million for investigators to test candidate therapies, often in parallel to ongoing clinical trials. The hope is that organs-on-chips can improve clinical trial design, from enrollment criteria and patient stratification to endpoints and the use of biomarkers. And in his lab, Dr. Huh is now engineering a shift to “organoids-on-a-chip” that combines the best features of each approach. “The idea,” he said, “is to grow organoids, and maintain the organoids in the microengineered systems where we can control their environment better ... and apply cues to allow them to develop into even more realistic tissues.”
Drs. Antony, Linkous, and Tagle reported no relevant disclosures. Dr. Huh is a co-founder of Vivodyne Inc, and owns shares in Vivodyne Inc. and Emulate Inc.
Pulmonologist-scientist Veena B. Antony, MD, professor of medicine at the University of Alabama in Birmingham, grows “pulmospheres” in her lab. The tiny spheres, about 1 mL in diameter, contain cells representing all of the cell types in a lung struck with pulmonary fibrosis.
They are a three-dimensional model of idiopathic pulmonary fibrosis (IPF) that can be used to study the behavior of invasive myofibroblasts and to predict in vivo responsiveness to antifibrotic drugs;
“The utility is extensive, including looking at the impact of early-life exposures on mid-life lung disease. We can ask all kinds of questions and answer them much faster, and with more accuracy, than with any 2D model,” said Dr. Antony, also professor of environmental health sciences and director of UAB’s program for environmental and translational medicine.
“The future of 3D modeling of the lung will happen step by step ... but we’re right at the edge of a prime explosion of information coming from these models, in all kinds of lung diseases,” she said.
Two-dimensional model systems – mainly monolayer cell cultures where cells adhere to and grow on a plate – cannot approximate the variety of cell types and architecture found in tissue, nor can they recapitulate cell-cell communication, biochemical cues, and other factors that are key to lung development and the pathogenesis of disease.
Dr. Antony’s pulmospheres resemble what have come to be known as organoids – 3D tissue cultures emanating from induced pluripotent stem cells (iPSC) or adult stem cells, in which multiple cell types self-organize, usually while suspended in natural or synthetic extracellular matrix (with or without a scaffold of some kind).
Lung-on-a-chip
In lung-on-a-chip (LOC) models, multiple cell types are seeded into miniature chambers, or “chips,” that contain networks of microfabricated channels designed to deliver and remove fluids, chemical cues, oxygen, and biomechanical forces. LOCs and other organs-on-chips – also called tissues-on-chips – can be continuously perfused and are highly structured and precisely controlled.
It’s the organs-on-chip model – or potential fusions of the organoid and organs-on-chip models – that will likely impact drug development. Almost 9 out of 10 investigational drugs fail in clinical trials – approximately 60% because of lack of efficacy and 30% because of toxicity. More reliable and predictive preclinical investigation is key, said Danilo A. Tagle, PhD, director of the Office of Special Initiatives in the National Center for Advancing Translational Sciences, of the National Institutes of Health.
“We have so many candidate drugs that go through preclinical safety testing, and that do relatively well in animal studies of efficacy, but then fail in clinical trials,” Dr. Tagle said. “We need better preclinical models.”
In its 10 years of life, the Tissue Chip for Drug Screening Program led by the NCATS – and funded by the NIH and Defense Advanced Research Projects Agency – has shown that organs-on-chips can be used to model disease and to predict both the safety and efficacy of clinical compounds, he said.
Lung organoids
Dr. Antony’s pulmospheres emanate not from stem cells but from primary tissue obtained from diseased lung. “We reconstitute the lung cells in single-cell suspensions, and then we allow them to come back together to form lung tissue,” she said. The pulmospheres take about 3 days to grow.
In a study published 5 years ago of pulmospheres of 20 patients with IPF and 9 control subjects, Dr. Antony and colleagues quantitated invasiveness and found “remarkable” differences in the invasiveness of IPF pulmospheres following exposure to the Food and Drug Administration–approved antifibrotic drugs nintedanib and pirfenidone. Some pulmospheres responded to one or the other drug, some to both, and two to neither – findings that Dr. Antony said offer hope for the goals of personalizing therapy and assessing new drugs.
Moreover, clinical disease progression correlated with invasiveness of the pulmospheres, showing that the organoid-like structures “do give us a model that [reflects] what’s happening in the clinical setting,” she said. (Lung tissue for the study was obtained via video-assisted thoracic surgery biopsy of IPF patients and from failed donor lung explants, but bronchoscopic forceps biopsies have become a useful method for obtaining tissue.)
The pulmospheres are not yet in clinical use, Dr. Antony said, but her lab is testing other fibrosis modifiers and continuing to use the model as a research tool.
One state to the east, at Vanderbilt University, Nashville, Tenn., Amanda Linkous, PhD, grows “branching lung organoids” and brain organoids to study the biology of small cell lung cancer (SCLC).
“We want to understand how [SCLC] cells change in the primary organ site, compared with metastatic sites like the brain. ... Are different transcription factors expressed [for instance] depending on where the tumor is growing?” said Dr. Linkous, scientific center manager of the National Cancer Institute’s Center for Systems Biology of SCLC at Vanderbilt. “Then we hope to start drug screening within the next year.”
Her lung organoids take shape from either human embryonic stem cells or iPSCs. Within commercially available media, the cells mature through several stages of differentiation, forming definitive endoderm, anterior foregut endoderm, and then circular lung bud structures – the latter of which are then placed into droplets of Matrigel, an extracellular matrix gel.
“In the Matrigel droplets, the lung bud cells will develop proximal and distal-like branching structures that express things like EPCAM, MUC1, SOX2, SOX9, and NKX2.1 – key markers that you should see in a more mature lung microenvironment,” she said. Tumor cells from established SCLC cell lines will then easily invade the branching lung organoid.
Dr. Linkous said she has found her organoid models highly reproducible and values their long-lasting nature – especially for future drug screening. “We can keep organoids going for months at a time,” said Dr. Linkous, a research associate professor in Vanderbilt’s department of biochemistry.
Like Dr. Antony, she envisions personalizing treatment in the future. “SCLC is a very heterogeneous tumor with many different cell types, so what works for one patient may not work well at all for another patient,” she said.
As recently as 5 years ago, “many in the cancer field would have been resistant to moving away from mouse models,” Dr. Linkous noted. “But preclinical studies in mice often don’t pan out in the clinic ... so we’re moving toward a human microenvironment to study human disease.”
The greatest challenge, Dr. Linkous and Dr. Antony said, lies in integrating both vascular blood flow and air into these models. “We just don’t have that combination as of yet,” Dr. Antony said.
LOC models
One of the first LOC models – and a galvanizing event for organs-on-chips more broadly – was a 1- to 2-cm–long model of the alveolar-capillary interface developed at the Wyss Institute for Biologically Inspired Engineering at Harvard Medical School, Boston.
Microchannels ran alongside a porous membrane coated with extracellular matrix, with alveolar cells seeded on one side and lung endothelial cells on the other side. When a vacuum was applied rhythmically to the channels, the cell-lined membrane stretched and relaxed, mimicking breathing movements.
Lead investigator Dongeun (Dan) Huh, PhD, then a postdoctoral student working with Donald E. Ingber, MD, PhD, founding director of the institute, ran tests showing that the model could reproduce organ-level responses to bacteria and inflammatory cytokines, as well as to silica nanoparticles. The widely cited paper was published in 2010 (Science. 2010;328[5986]:1662-8), and was followed by another study published in 2012 (Sci Transl Med. 2012;4[159]:159ra147) that used the LOC device to reproduce drug toxicity–induced pulmonary edema. “Here we were demonstrating for the first time that we could use the lung-on-chip to model human lung disease,” said Dr. Huh, who started his own lab at the University of Pennsylvania, Philadelphia, in 2013.
Since then, “as a field we’ve come a long way in modeling the complexity of human lung tissues ... with more advanced devices that can be used to mimic different parts of the lung and different processes, like immune responses in asthma and viral infections,” said Dr. Huh, “and with several studies using primary human cells taken from lung disease patients.”
Among Dr. Huh’s latest devices, built with NIH funding, is an asthma-on-a-chip device. Lung cells isolated from asthma patients are grown in a microfabricated device to create multilayered airway tissue, with airspace, that contains a fully differentiated epithelium and a vascularized stroma. “We can compress the entire engineered area of asthmatic human tissue in a lateral direction to mimic bronchoconstriction that happens during an asthma attack,” he said.
A paper soon to be published will describe how “abnormal pathophysiologic compressive forces due to bronchoconstriction in asthmatic lungs can make the lungs fibrotic, and how those mechanical forces also can induce increased vascularity,” said Dr. Huh, associate professor in the university’s department of bioengineering. “The increased vascular density can also change the phenotype of blood vessels in asthmatic airways.”
Dr. Huh also has an $8.3 million contract with the government’s Biomedical Advanced Research and Development Authority to study how chlorine gas damages lung tissues and identify biomarkers of chlorine gas–induced lung injury, with the goal of developing therapeutics.
Dr. Ingber and associates have developed a device modeling cystic fibrosis (CF). The chip is lined with primary human CF bronchial epithelial cells grown under an air-liquid interface and interfaced with primary lung microvascular endothelium that are exposed to fluid flow.
The chip reproduced, “with high fidelity, many of the structural, biochemical, and pathophysiological features of the human CF lung airway and its response to pathogens and circulating immune cells in vitro,” Dr. Ingber and colleagues reported (J Cyst Fibros. 2022;21:605-15).
Government investment in tissue chips
Efforts to commercialize organs-on-chip platforms and translate them for nonengineers have also picked in recent years. Several companies in the United States (including Emulate, a Wyss start-up) and in Europe now offer microengineered lung tissue models that can be used for research and drug testing. And some large pharmaceutical companies, said Dr. Tagle, have begun integrating tissue chip technology into their drug development programs.
The FDA, meanwhile, “has come to embrace the technology and see its promise,” Dr. Tagle said. An FDA pilot program announced in 2021 – called ISTAND (Innovative Science and Technology Approaches for New Drugs) – allows for tissue chip data to be submitted, as standalone data, for some drug applications.
The first 5 years of the government’s Tissue Chip for Drug Screening Program focused on safety and toxicity, and it “was successful in that model organ systems were able to capture the human response that [had been missed in] animal models,” he said.
For example, when a liver-tissue model was used to test several compounds that had passed animal testing for toxicity/safety but then failed in human clinical trials – killing some of the participants – the model showed a 100% sensitivity and a 87% specificity in predicting the human response, said Dr. Tagle, who recently coauthored a review on the future of organs-on-chips (Nature Reviews I Drug Discovery. 2021;20:345-61).
The second 5 years of the program, currently winding down, have focused on efficacy – the ability of organs-on-chip models to recreate the pathophysiology of chronic obstructive pulmonary disease, influenza, and other diseases, so that potential drugs can be assessed. In 2020, with extra support from the Coronavirus Aid, Relief, and Economic Security Act, NCATS funded academic labs to use organs-on-chip technology to evaluate SARS-CoV-2 and potential therapeutics.
Dr. Ingbar was one of the grantees. His team screened a number of FDA-approved drugs for potential repurposing using a bronchial-airway-on-a-chip and compared results with 2D model systems (Nat Biomed Eng. 2021;5:815-29). Amodiaquine inhibited infection in the 3D model and is now in phase 2 COVID trials. Several other drugs showed effectiveness in a 2D model but not in the chip.
Now, in a next phase of study at NCATS, coined Clinical Trials on a Chip, the center has awarded $35.5 million for investigators to test candidate therapies, often in parallel to ongoing clinical trials. The hope is that organs-on-chips can improve clinical trial design, from enrollment criteria and patient stratification to endpoints and the use of biomarkers. And in his lab, Dr. Huh is now engineering a shift to “organoids-on-a-chip” that combines the best features of each approach. “The idea,” he said, “is to grow organoids, and maintain the organoids in the microengineered systems where we can control their environment better ... and apply cues to allow them to develop into even more realistic tissues.”
Drs. Antony, Linkous, and Tagle reported no relevant disclosures. Dr. Huh is a co-founder of Vivodyne Inc, and owns shares in Vivodyne Inc. and Emulate Inc.
Increasing primary care doctors’ knowledge of IPF could speed up diagnoses, suggests white paper
The nonspecific nature of the symptoms of idiopathic pulmonary fibrosis (IPF) especially in early stages, and the relative rarity of IPF compared with other conditions that have similar symptoms, may contribute to a delay in diagnosis in the primary care setting, wrote Daniel F. Dilling, MD, of Loyola University Chicago, Maywood, Ill., and colleagues in Chest: Clinical Perspectives (Dilling et al. State of Practice: Factors Driving Diagnostic Delays in Idiopathic Pulmonary Fibrosis. Chest. 2022).
“We have learned over and over again through research, and also through talking with our own patients with IPF, that there is often a long lag between the first signs of the disease and a diagnosis of IPF,” corresponding author Dr. Dilling said in an interview.
“Even some pulmonary specialists can be uncertain about how to approach the diagnosis when a CT scan or other test first suggests the possibility; this can cost a patient precious time, as being on drug therapy earlier can result in preservation of lung function,” he said. “By sounding the alarm bell with this paper, we hope to promote awareness and education/training within the primary care community as well as the pulmonary community, and also to make all of them aware of the possibility of referral to specialty ILD [interstitial lung disease] centers when desired and possible,” he added.
The researchers conducted a pair of online surveys to inform the development of improving education on IPF among primary care providers.
In the white paper, which can be accessed online, the authors reported results of the surveys. One included 100 general pulmonologists and the other included 306 primary care physicians (156 practiced family physicians and 150 practiced general internal medicine). The data were collected between April 11, 2022, and May 16, 2022. Participants were asked to respond to a patient case scenario of a 55-year-old woman with nonspecific symptoms such as shortness of breath on moderate exertion, cough, exhaustion, and trouble sleeping.
The PCPs were most likely to evaluate the patient for a cardiac condition (46%), 25% would evaluate for chronic obstructive pulmonary disease (COPD), and 23% for asthma. More than half (58%) ranked progressive fibrosing ILD as one of their bottom two diagnoses.
A total of 87% of PCPs said they would begin a diagnostic workup to evaluate symptoms if the patient had no preexisting respiratory disease, compared with 61% for patients with a respiratory diagnosis.
Although 93% of PCPs cited a chest x-ray as part of the initial patient workup, fewer than half said they would order an echocardiogram, spirometry, or pulmonary function test (PFT), and 11% said they would include diffusion capacity testing in the initial workup.
In addition, PCPs were less likely to ask patients about issues that might prompt an IPF diagnosis, such as exposures to agents through work, hobbies, the environment, or comorbidities.
In the pulmonology survey, more than 75% of respondents cited patient history, high-resolution tomography scan, serologic testing, and review for autoimmune disease symptoms as first steps in a diagnostic response to patients with suspected IPF.
Differences between PCPs’ and pulmonolgists’ responses
Both PCPs and pulmonologists responded to several questions to assess knowledge and opinion gaps related to IPF. Overall, pulmonologists were more likely than PCPs to cite both imaging and testing issues and waiting 6-8 weeks after symptom onset before imaging as contributing factors to diagnostic delays.
PCPs more often expressed beliefs that delayed diagnosis had little impact on a patient with IPF, and that the treatments may be worse than the disease.
Dr. Dilling said he was not surprised by the survey findings, as similar clues about the underdiagnosis of IPF have surfaced in prior studies.
“We need to get the word out to primary care physicians, to pulmonary physicians, and even to the public, that idiopathic pulmonary fibrosis and other forms of interstitial lung disease are out there and prevalent, and that making the right diagnosis in a timely way can lead to better outcomes for patients,” he said.
The take-home message for primary care is to think outside the COPD box, said Dr. Dilling. “Just because someone has shortness of breath or cough and used to smoke does not automatically mean that they have COPD,” he emphasized. “Listen carefully for crackles (rales) on exam. Get spirometry or PFTs before you secure the diagnosis of COPD, or else you will be missing all of your cases of pulmonary fibrosis; think of pulmonary fibrosis and use imaging to help guide your diagnosis,” he said.
The authors suggested several education goals for PCPs, including establishing the importance of early evaluation, outlining the correct approach to a patient workup, encouraging prompt referral, and empowering PCPs as part of the team approach to IPF patients’ care. For pulmonologists, only 11% of those surveyed said they were aware of the latest developments in antifibrotic research, and education efforts might include information about drug pipelines and clinical trials, as well as technology.
Looking ahead, “We need to better understand how to find the pulmonary fibrosis in the community,” Dr. Dilling said. This understanding may come in part from greater education and awareness, he noted. However, eventually there may be ways to enhance the reading of PFTs and of CT scans through artificial intelligence technologies that would not only prompt clinicians to recognize what they are seeing, but would prompt them to refer and send the patient on the correct diagnostic path as soon as possible, he added.
Key message: Include ILD in differential diagnosis of patients with shortness of breath and/or cough
Advances in diagnostics and therapies for interstitial lung disease can take time to be absorbed and adopted, and patients with ILD and pulmonologists caring for ILD, specifically IPF, continue to report delays in diagnosis and therapy, said Krishna Thavarajah, MD, a pulmonologist at Henry Ford Hospital, Detroit, Mich., in an interview.
The current study findings of the time to diagnosis and the approach to patient workups echo her own clinical experience, Dr. Thavarajah said. “There is a delay in IPF diagnosis as physicians look to more common diagnoses, such as cardiac disease or chronic obstructive pulmonary disease, prior to pursuit of additional workup, and the attitude toward treatment has, in some ways, lagged behind advances in therapy, including timing and feasibility of therapy for IPF,” she said.
The key message for primary care physicians is to include ILD in the differential diagnosis of patients with shortness of breath and/or cough, especially if the initial cardiac and pulmonary test (meaning at least a chest x-ray and pulmonary function tests, including a diffusion capacity) are not pointing to an alternative cause within 3 months of presentation, Dr. Thavarajah said.
Once IPF is diagnosed, primary care clinicians should know that there are FDA-approved therapies that improve survival, said Dr. Thavarajah. “There are identifiable and treatable comorbid conditions,” she added. “The statement of ‘time lost is lung lost’ sums up the care of an IPF patient; partnerships between primary care clinicians, pulmonologists, and referral centers can provide the patient multiple levels of support with quality-of-life interventions, treatments, and also clinical trials, delivered by a team of providers,” she said.
In the wake of the current study, more research is needed with outcome studies regarding educational interventions targeting primary care and pulmonologists on appropriate workup, timing of workup, and current therapy for IPF patients, she added.
The white paper received no outside funding. The authors and Dr. Thavarajah had no financial conflicts to disclose.
The nonspecific nature of the symptoms of idiopathic pulmonary fibrosis (IPF) especially in early stages, and the relative rarity of IPF compared with other conditions that have similar symptoms, may contribute to a delay in diagnosis in the primary care setting, wrote Daniel F. Dilling, MD, of Loyola University Chicago, Maywood, Ill., and colleagues in Chest: Clinical Perspectives (Dilling et al. State of Practice: Factors Driving Diagnostic Delays in Idiopathic Pulmonary Fibrosis. Chest. 2022).
“We have learned over and over again through research, and also through talking with our own patients with IPF, that there is often a long lag between the first signs of the disease and a diagnosis of IPF,” corresponding author Dr. Dilling said in an interview.
“Even some pulmonary specialists can be uncertain about how to approach the diagnosis when a CT scan or other test first suggests the possibility; this can cost a patient precious time, as being on drug therapy earlier can result in preservation of lung function,” he said. “By sounding the alarm bell with this paper, we hope to promote awareness and education/training within the primary care community as well as the pulmonary community, and also to make all of them aware of the possibility of referral to specialty ILD [interstitial lung disease] centers when desired and possible,” he added.
The researchers conducted a pair of online surveys to inform the development of improving education on IPF among primary care providers.
In the white paper, which can be accessed online, the authors reported results of the surveys. One included 100 general pulmonologists and the other included 306 primary care physicians (156 practiced family physicians and 150 practiced general internal medicine). The data were collected between April 11, 2022, and May 16, 2022. Participants were asked to respond to a patient case scenario of a 55-year-old woman with nonspecific symptoms such as shortness of breath on moderate exertion, cough, exhaustion, and trouble sleeping.
The PCPs were most likely to evaluate the patient for a cardiac condition (46%), 25% would evaluate for chronic obstructive pulmonary disease (COPD), and 23% for asthma. More than half (58%) ranked progressive fibrosing ILD as one of their bottom two diagnoses.
A total of 87% of PCPs said they would begin a diagnostic workup to evaluate symptoms if the patient had no preexisting respiratory disease, compared with 61% for patients with a respiratory diagnosis.
Although 93% of PCPs cited a chest x-ray as part of the initial patient workup, fewer than half said they would order an echocardiogram, spirometry, or pulmonary function test (PFT), and 11% said they would include diffusion capacity testing in the initial workup.
In addition, PCPs were less likely to ask patients about issues that might prompt an IPF diagnosis, such as exposures to agents through work, hobbies, the environment, or comorbidities.
In the pulmonology survey, more than 75% of respondents cited patient history, high-resolution tomography scan, serologic testing, and review for autoimmune disease symptoms as first steps in a diagnostic response to patients with suspected IPF.
Differences between PCPs’ and pulmonolgists’ responses
Both PCPs and pulmonologists responded to several questions to assess knowledge and opinion gaps related to IPF. Overall, pulmonologists were more likely than PCPs to cite both imaging and testing issues and waiting 6-8 weeks after symptom onset before imaging as contributing factors to diagnostic delays.
PCPs more often expressed beliefs that delayed diagnosis had little impact on a patient with IPF, and that the treatments may be worse than the disease.
Dr. Dilling said he was not surprised by the survey findings, as similar clues about the underdiagnosis of IPF have surfaced in prior studies.
“We need to get the word out to primary care physicians, to pulmonary physicians, and even to the public, that idiopathic pulmonary fibrosis and other forms of interstitial lung disease are out there and prevalent, and that making the right diagnosis in a timely way can lead to better outcomes for patients,” he said.
The take-home message for primary care is to think outside the COPD box, said Dr. Dilling. “Just because someone has shortness of breath or cough and used to smoke does not automatically mean that they have COPD,” he emphasized. “Listen carefully for crackles (rales) on exam. Get spirometry or PFTs before you secure the diagnosis of COPD, or else you will be missing all of your cases of pulmonary fibrosis; think of pulmonary fibrosis and use imaging to help guide your diagnosis,” he said.
The authors suggested several education goals for PCPs, including establishing the importance of early evaluation, outlining the correct approach to a patient workup, encouraging prompt referral, and empowering PCPs as part of the team approach to IPF patients’ care. For pulmonologists, only 11% of those surveyed said they were aware of the latest developments in antifibrotic research, and education efforts might include information about drug pipelines and clinical trials, as well as technology.
Looking ahead, “We need to better understand how to find the pulmonary fibrosis in the community,” Dr. Dilling said. This understanding may come in part from greater education and awareness, he noted. However, eventually there may be ways to enhance the reading of PFTs and of CT scans through artificial intelligence technologies that would not only prompt clinicians to recognize what they are seeing, but would prompt them to refer and send the patient on the correct diagnostic path as soon as possible, he added.
Key message: Include ILD in differential diagnosis of patients with shortness of breath and/or cough
Advances in diagnostics and therapies for interstitial lung disease can take time to be absorbed and adopted, and patients with ILD and pulmonologists caring for ILD, specifically IPF, continue to report delays in diagnosis and therapy, said Krishna Thavarajah, MD, a pulmonologist at Henry Ford Hospital, Detroit, Mich., in an interview.
The current study findings of the time to diagnosis and the approach to patient workups echo her own clinical experience, Dr. Thavarajah said. “There is a delay in IPF diagnosis as physicians look to more common diagnoses, such as cardiac disease or chronic obstructive pulmonary disease, prior to pursuit of additional workup, and the attitude toward treatment has, in some ways, lagged behind advances in therapy, including timing and feasibility of therapy for IPF,” she said.
The key message for primary care physicians is to include ILD in the differential diagnosis of patients with shortness of breath and/or cough, especially if the initial cardiac and pulmonary test (meaning at least a chest x-ray and pulmonary function tests, including a diffusion capacity) are not pointing to an alternative cause within 3 months of presentation, Dr. Thavarajah said.
Once IPF is diagnosed, primary care clinicians should know that there are FDA-approved therapies that improve survival, said Dr. Thavarajah. “There are identifiable and treatable comorbid conditions,” she added. “The statement of ‘time lost is lung lost’ sums up the care of an IPF patient; partnerships between primary care clinicians, pulmonologists, and referral centers can provide the patient multiple levels of support with quality-of-life interventions, treatments, and also clinical trials, delivered by a team of providers,” she said.
In the wake of the current study, more research is needed with outcome studies regarding educational interventions targeting primary care and pulmonologists on appropriate workup, timing of workup, and current therapy for IPF patients, she added.
The white paper received no outside funding. The authors and Dr. Thavarajah had no financial conflicts to disclose.
The nonspecific nature of the symptoms of idiopathic pulmonary fibrosis (IPF) especially in early stages, and the relative rarity of IPF compared with other conditions that have similar symptoms, may contribute to a delay in diagnosis in the primary care setting, wrote Daniel F. Dilling, MD, of Loyola University Chicago, Maywood, Ill., and colleagues in Chest: Clinical Perspectives (Dilling et al. State of Practice: Factors Driving Diagnostic Delays in Idiopathic Pulmonary Fibrosis. Chest. 2022).
“We have learned over and over again through research, and also through talking with our own patients with IPF, that there is often a long lag between the first signs of the disease and a diagnosis of IPF,” corresponding author Dr. Dilling said in an interview.
“Even some pulmonary specialists can be uncertain about how to approach the diagnosis when a CT scan or other test first suggests the possibility; this can cost a patient precious time, as being on drug therapy earlier can result in preservation of lung function,” he said. “By sounding the alarm bell with this paper, we hope to promote awareness and education/training within the primary care community as well as the pulmonary community, and also to make all of them aware of the possibility of referral to specialty ILD [interstitial lung disease] centers when desired and possible,” he added.
The researchers conducted a pair of online surveys to inform the development of improving education on IPF among primary care providers.
In the white paper, which can be accessed online, the authors reported results of the surveys. One included 100 general pulmonologists and the other included 306 primary care physicians (156 practiced family physicians and 150 practiced general internal medicine). The data were collected between April 11, 2022, and May 16, 2022. Participants were asked to respond to a patient case scenario of a 55-year-old woman with nonspecific symptoms such as shortness of breath on moderate exertion, cough, exhaustion, and trouble sleeping.
The PCPs were most likely to evaluate the patient for a cardiac condition (46%), 25% would evaluate for chronic obstructive pulmonary disease (COPD), and 23% for asthma. More than half (58%) ranked progressive fibrosing ILD as one of their bottom two diagnoses.
A total of 87% of PCPs said they would begin a diagnostic workup to evaluate symptoms if the patient had no preexisting respiratory disease, compared with 61% for patients with a respiratory diagnosis.
Although 93% of PCPs cited a chest x-ray as part of the initial patient workup, fewer than half said they would order an echocardiogram, spirometry, or pulmonary function test (PFT), and 11% said they would include diffusion capacity testing in the initial workup.
In addition, PCPs were less likely to ask patients about issues that might prompt an IPF diagnosis, such as exposures to agents through work, hobbies, the environment, or comorbidities.
In the pulmonology survey, more than 75% of respondents cited patient history, high-resolution tomography scan, serologic testing, and review for autoimmune disease symptoms as first steps in a diagnostic response to patients with suspected IPF.
Differences between PCPs’ and pulmonolgists’ responses
Both PCPs and pulmonologists responded to several questions to assess knowledge and opinion gaps related to IPF. Overall, pulmonologists were more likely than PCPs to cite both imaging and testing issues and waiting 6-8 weeks after symptom onset before imaging as contributing factors to diagnostic delays.
PCPs more often expressed beliefs that delayed diagnosis had little impact on a patient with IPF, and that the treatments may be worse than the disease.
Dr. Dilling said he was not surprised by the survey findings, as similar clues about the underdiagnosis of IPF have surfaced in prior studies.
“We need to get the word out to primary care physicians, to pulmonary physicians, and even to the public, that idiopathic pulmonary fibrosis and other forms of interstitial lung disease are out there and prevalent, and that making the right diagnosis in a timely way can lead to better outcomes for patients,” he said.
The take-home message for primary care is to think outside the COPD box, said Dr. Dilling. “Just because someone has shortness of breath or cough and used to smoke does not automatically mean that they have COPD,” he emphasized. “Listen carefully for crackles (rales) on exam. Get spirometry or PFTs before you secure the diagnosis of COPD, or else you will be missing all of your cases of pulmonary fibrosis; think of pulmonary fibrosis and use imaging to help guide your diagnosis,” he said.
The authors suggested several education goals for PCPs, including establishing the importance of early evaluation, outlining the correct approach to a patient workup, encouraging prompt referral, and empowering PCPs as part of the team approach to IPF patients’ care. For pulmonologists, only 11% of those surveyed said they were aware of the latest developments in antifibrotic research, and education efforts might include information about drug pipelines and clinical trials, as well as technology.
Looking ahead, “We need to better understand how to find the pulmonary fibrosis in the community,” Dr. Dilling said. This understanding may come in part from greater education and awareness, he noted. However, eventually there may be ways to enhance the reading of PFTs and of CT scans through artificial intelligence technologies that would not only prompt clinicians to recognize what they are seeing, but would prompt them to refer and send the patient on the correct diagnostic path as soon as possible, he added.
Key message: Include ILD in differential diagnosis of patients with shortness of breath and/or cough
Advances in diagnostics and therapies for interstitial lung disease can take time to be absorbed and adopted, and patients with ILD and pulmonologists caring for ILD, specifically IPF, continue to report delays in diagnosis and therapy, said Krishna Thavarajah, MD, a pulmonologist at Henry Ford Hospital, Detroit, Mich., in an interview.
The current study findings of the time to diagnosis and the approach to patient workups echo her own clinical experience, Dr. Thavarajah said. “There is a delay in IPF diagnosis as physicians look to more common diagnoses, such as cardiac disease or chronic obstructive pulmonary disease, prior to pursuit of additional workup, and the attitude toward treatment has, in some ways, lagged behind advances in therapy, including timing and feasibility of therapy for IPF,” she said.
The key message for primary care physicians is to include ILD in the differential diagnosis of patients with shortness of breath and/or cough, especially if the initial cardiac and pulmonary test (meaning at least a chest x-ray and pulmonary function tests, including a diffusion capacity) are not pointing to an alternative cause within 3 months of presentation, Dr. Thavarajah said.
Once IPF is diagnosed, primary care clinicians should know that there are FDA-approved therapies that improve survival, said Dr. Thavarajah. “There are identifiable and treatable comorbid conditions,” she added. “The statement of ‘time lost is lung lost’ sums up the care of an IPF patient; partnerships between primary care clinicians, pulmonologists, and referral centers can provide the patient multiple levels of support with quality-of-life interventions, treatments, and also clinical trials, delivered by a team of providers,” she said.
In the wake of the current study, more research is needed with outcome studies regarding educational interventions targeting primary care and pulmonologists on appropriate workup, timing of workup, and current therapy for IPF patients, she added.
The white paper received no outside funding. The authors and Dr. Thavarajah had no financial conflicts to disclose.
FROM CHEST CLINICAL PERSPECTIVES
What we know about long COVID so far
Long COVID: The name says it all. It’s an illness that, for many people, has not yet stopped.
Eric Roach became ill with COVID-19 in November 2020, and he’s still sick. “I have brain fog, memory loss,” says the 67-year-old Navy veteran from Spearfish, S.D. “The fatigue has just been insane.”
Long COVID, more formally known as post-acute sequelae of COVID (PASC), is the lay term to describe when people start to recover, or seem to recover, from a bout of COVID-19 but then continue to suffer from symptoms. For some, it’s gone on for 2 years or longer. While the governments of the United Statesand several other countries formally recognize the existence of long COVID, the National Institutes of Health (NIH) has yet to formally define it. There’s no approved treatment, and the causes are not understood.
Here’s what is known: and it is affecting enough people to cause concern for employers, health insurers, and governments.
First, the many symptoms
According to the Centers for Disease Control and Prvention, long COVID symptoms may include:
- Tiredness or fatigue that interferes with daily life.
- Symptoms that get worse after physical or mental effort.
- Fever.
- Difficulty breathing or shortness of breath.
- Cough.
- Chest pain.
- Heart palpitations.
- Difficulty thinking or concentrating (sometimes referred to as “brain fog”).
- Headache.
- Sleep problems.
- Dizziness when standing.
- Pins-and-needles feelings.
- Change in smell or taste.
- Depression or anxiety.
- Diarrhea.
- Stomach pain.
- Joint or muscle pain.
- Rash.
- Changes in menstrual cycles.
“People with post-COVID conditions may develop or continue to have symptoms that are hard to explain and manage,” the CDC says on its website. “Clinical evaluations and results of routine blood tests, chest x-rays, and electrocardiograms may be normal. The symptoms are similar to those reported by people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and other poorly understood chronic illnesses that may occur after other infections.”
Doctors may not fully appreciate the subtle nature of some of the symptoms.
“People with these unexplained symptoms may be misunderstood by their health care providers, which can result in a long time for them to get a diagnosis and receive appropriate care or treatment,” the CDC says.
Health professionals should recognize that long COVID can be disabling, the U.S. Department of Health and Human Services says. “Long COVID can substantially limit a major life activity,” HHS says in civil rights guidance. One possible example: “A person with long COVID who has lung damage that causes shortness of breath, fatigue, and related effects is substantially limited in respiratory function, among other major life activities,” the HHS notes.
How many people are affected?
This has been difficult to judge because not everyone who has had COVID-19 gets tested for it and there are no formal diagnostic criteria yet for long COVID. The CDC estimates that 19% of patients in the United States who have ever had COVID-19 have long COVID symptoms.
Some estimates go higher. A University of Oxford study in September 2021 found more than a third of patients had symptoms of long COVID between 3 months and 6 months after a COVID-19 diagnosis. As many as 55% of COVID-19 patients in one Chinese study had one or more lingering symptoms 2 years later, Lixue Huang, MD, of the China-Japan Friendship Hospital in Beijing, and colleagues reported in the journal Lancet Respiratory Medicine in May.
According to the CDC, age is a factor. “Older adults are less likely to have long COVID than younger adults. Nearly three times as many adults ages 50-59 currently have long COVID than those age 80 and older,” the CDC says. Women and racial and ethnic minorities are more likely to be affected.
Many people are experiencing neurological effects, such as the so-called brain fog, according to Ziyad Al-Aly, MD, of Washington University and the VA St. Louis Health Care System, and colleagues, whose report was published in Nature Medicine in September. They estimated that 6.6 million Americans have brain impairments associated with COVID infection.
“Some of the neurologic disorders reported here are serious chronic conditions that will impact some people for a lifetime,” they wrote. “Given the colossal scale of the pandemic, and even though the absolute numbers reported in this work are small, these may translate into a large number of affected individuals around the world – and this will likely contribute to a rise in the burden of neurologic diseases.”
Causes
It’s not clear what the underlying causes are, but most research points to a combination of factors. Suspects include ongoing inflammation, tiny blood clots, and reactivation of latent viruses. In May, Brent Palmer, PhD, of the University of Colorado, Denver, and colleagues found people with long COVID had persistent activation of T-cells that were specific for SARS-CoV-2.
COVID-19 itself can damage organs, and long COVID might be caused by ongoing damage. In August, Alexandros Rovas, MD, of University Hospital Munster in Germany, and colleagues found patients with long COVID had evidence of damage to their capillaries. “Whether, to what extent, and when the observed damage might be reversible remains unclear,” they wrote in the journal Angiogenesis.
People with long COVID have immune responses to other viruses, such as Epstein-Barr – evidence that COVID-19 might reactivate latent viruses. “Our data suggest the involvement of persistent antigen, reactivation of latent herpesviruses, and chronic inflammation,” immunobiologist Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., and colleagues wrote in a study posted in August that had not yet been peer-reviewed for publication.
This might be causing an autoimmune response. “The infection may cause the immune system to start making autoantibodies that attack a person’s own organs and tissues,” the NIH says.
There could be other factors. A study by Harvard researchers found that people who felt stressed, depressed, or lonely before catching COVID-19 were more likely to develop long COVID afterward. “Distress was more strongly associated with developing long COVID than physical health risk factors such as obesity, asthma, and hypertension,” Siwen Wang, MD, a research fellow with Harvard University’s T.H. Chan School of Public Health, Boston, said in a statement. Plus, nearly 44% of those in the study developed COVID-19 infections after having been assessed for stress, Dr. Wang and colleagues reported in the journal JAMA Psychiatry.
Vaccine protection
There’s evidence that vaccination protects against long COVID, both by preventing infection in the first place, but also even for people who have breakthrough infections.
A meta-analysis covering studies involving 17 million people found evidence vaccination might reduce the severity of COVID-19 or might help the body clear any lingering virus after an infection.
“Overall, vaccination was associated with reduced risks or odds of long COVID, with preliminary evidence suggesting that two doses are more effective than one dose,” wrote Cesar Fernandez de las Penas, PhD, of King Juan Carlos University in Madrid, and colleagues. Their report is in The Lancet’s eClinicalMedicine.
A team in Milan found that unvaccinated people in their study were nearly three times as likely to have serious symptoms for longer than 4 weeks compared to vaccinated volunteers. According to their report in JAMA, Elena Azzolini, MD, PhD, assistant professor at Humanitas Research Hospital, and colleagues found two or three doses of vaccine reduced the risk of hospitalization from COVID to 16% or 17% compared to 42% for the unvaccinated.
Treatments
With no diagnostic criteria and no understanding of the causes, it’s hard for doctors to determine treatments.
Most experts dealing with long COVID, even those at the specialty centers that have been set up at hospitals and health systems in the United States, recommend that patients start with their primary care doctors before moving on to specialists.
“The mainstay of management is supportive, holistic care, symptom control, and detection of treatable complications,” Trish Greenhalgh, MD, professor of primary care health sciences at the University of Oxford, England, and colleagues wrote in the journal The BMJ in September. “Patients with long COVID greatly value input from their primary care clinician. Generalist clinicians can help patients considerably by hearing the patient’s story and validating their experience … (and) making the diagnosis of long COVID (which does not have to be by exclusion) and excluding alternative diagnoses.”
Evidence is building that long COVID closely resembles other postviral conditions – something that can provide clues for treatment. For example, several studies indicate that exercise doesn’t help most patients.
But there are approaches that can work. Treatments may include pulmonary rehabilitation; autonomic conditioning therapy, which includes breathing therapy; and cognitive rehabilitation to relieve brain fog. Doctors are also trying the antidepressant amitriptyline to help with sleep disturbances and headaches; the antiseizure medication gabapentin to help with pain, numbness, and other neurological symptoms; and drugs to relieve low blood pressure in patients experiencing postural orthostatic tachycardia syndrome (POTS).
The NIH is sponsoring studies that have recruited just over 8,200 adults. And more than two dozen researchers from Harvard; Stanford; the University of California, San Francisco; the J. Craig Venter Institute; Johns Hopkins University; the University of Pennsylvania; Mount Sinai Hospitals; Cardiff University; and Yale announced in September they were forming the Long COVID Research Initiative to speed up studies.
The group, with funding from private enterprise, plans to conduct tissue biopsy, imaging studies, and autopsies and will search for potential biomarkers in the blood of patients.
A version of this article first appeared on WebMD.com.
Long COVID: The name says it all. It’s an illness that, for many people, has not yet stopped.
Eric Roach became ill with COVID-19 in November 2020, and he’s still sick. “I have brain fog, memory loss,” says the 67-year-old Navy veteran from Spearfish, S.D. “The fatigue has just been insane.”
Long COVID, more formally known as post-acute sequelae of COVID (PASC), is the lay term to describe when people start to recover, or seem to recover, from a bout of COVID-19 but then continue to suffer from symptoms. For some, it’s gone on for 2 years or longer. While the governments of the United Statesand several other countries formally recognize the existence of long COVID, the National Institutes of Health (NIH) has yet to formally define it. There’s no approved treatment, and the causes are not understood.
Here’s what is known: and it is affecting enough people to cause concern for employers, health insurers, and governments.
First, the many symptoms
According to the Centers for Disease Control and Prvention, long COVID symptoms may include:
- Tiredness or fatigue that interferes with daily life.
- Symptoms that get worse after physical or mental effort.
- Fever.
- Difficulty breathing or shortness of breath.
- Cough.
- Chest pain.
- Heart palpitations.
- Difficulty thinking or concentrating (sometimes referred to as “brain fog”).
- Headache.
- Sleep problems.
- Dizziness when standing.
- Pins-and-needles feelings.
- Change in smell or taste.
- Depression or anxiety.
- Diarrhea.
- Stomach pain.
- Joint or muscle pain.
- Rash.
- Changes in menstrual cycles.
“People with post-COVID conditions may develop or continue to have symptoms that are hard to explain and manage,” the CDC says on its website. “Clinical evaluations and results of routine blood tests, chest x-rays, and electrocardiograms may be normal. The symptoms are similar to those reported by people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and other poorly understood chronic illnesses that may occur after other infections.”
Doctors may not fully appreciate the subtle nature of some of the symptoms.
“People with these unexplained symptoms may be misunderstood by their health care providers, which can result in a long time for them to get a diagnosis and receive appropriate care or treatment,” the CDC says.
Health professionals should recognize that long COVID can be disabling, the U.S. Department of Health and Human Services says. “Long COVID can substantially limit a major life activity,” HHS says in civil rights guidance. One possible example: “A person with long COVID who has lung damage that causes shortness of breath, fatigue, and related effects is substantially limited in respiratory function, among other major life activities,” the HHS notes.
How many people are affected?
This has been difficult to judge because not everyone who has had COVID-19 gets tested for it and there are no formal diagnostic criteria yet for long COVID. The CDC estimates that 19% of patients in the United States who have ever had COVID-19 have long COVID symptoms.
Some estimates go higher. A University of Oxford study in September 2021 found more than a third of patients had symptoms of long COVID between 3 months and 6 months after a COVID-19 diagnosis. As many as 55% of COVID-19 patients in one Chinese study had one or more lingering symptoms 2 years later, Lixue Huang, MD, of the China-Japan Friendship Hospital in Beijing, and colleagues reported in the journal Lancet Respiratory Medicine in May.
According to the CDC, age is a factor. “Older adults are less likely to have long COVID than younger adults. Nearly three times as many adults ages 50-59 currently have long COVID than those age 80 and older,” the CDC says. Women and racial and ethnic minorities are more likely to be affected.
Many people are experiencing neurological effects, such as the so-called brain fog, according to Ziyad Al-Aly, MD, of Washington University and the VA St. Louis Health Care System, and colleagues, whose report was published in Nature Medicine in September. They estimated that 6.6 million Americans have brain impairments associated with COVID infection.
“Some of the neurologic disorders reported here are serious chronic conditions that will impact some people for a lifetime,” they wrote. “Given the colossal scale of the pandemic, and even though the absolute numbers reported in this work are small, these may translate into a large number of affected individuals around the world – and this will likely contribute to a rise in the burden of neurologic diseases.”
Causes
It’s not clear what the underlying causes are, but most research points to a combination of factors. Suspects include ongoing inflammation, tiny blood clots, and reactivation of latent viruses. In May, Brent Palmer, PhD, of the University of Colorado, Denver, and colleagues found people with long COVID had persistent activation of T-cells that were specific for SARS-CoV-2.
COVID-19 itself can damage organs, and long COVID might be caused by ongoing damage. In August, Alexandros Rovas, MD, of University Hospital Munster in Germany, and colleagues found patients with long COVID had evidence of damage to their capillaries. “Whether, to what extent, and when the observed damage might be reversible remains unclear,” they wrote in the journal Angiogenesis.
People with long COVID have immune responses to other viruses, such as Epstein-Barr – evidence that COVID-19 might reactivate latent viruses. “Our data suggest the involvement of persistent antigen, reactivation of latent herpesviruses, and chronic inflammation,” immunobiologist Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., and colleagues wrote in a study posted in August that had not yet been peer-reviewed for publication.
This might be causing an autoimmune response. “The infection may cause the immune system to start making autoantibodies that attack a person’s own organs and tissues,” the NIH says.
There could be other factors. A study by Harvard researchers found that people who felt stressed, depressed, or lonely before catching COVID-19 were more likely to develop long COVID afterward. “Distress was more strongly associated with developing long COVID than physical health risk factors such as obesity, asthma, and hypertension,” Siwen Wang, MD, a research fellow with Harvard University’s T.H. Chan School of Public Health, Boston, said in a statement. Plus, nearly 44% of those in the study developed COVID-19 infections after having been assessed for stress, Dr. Wang and colleagues reported in the journal JAMA Psychiatry.
Vaccine protection
There’s evidence that vaccination protects against long COVID, both by preventing infection in the first place, but also even for people who have breakthrough infections.
A meta-analysis covering studies involving 17 million people found evidence vaccination might reduce the severity of COVID-19 or might help the body clear any lingering virus after an infection.
“Overall, vaccination was associated with reduced risks or odds of long COVID, with preliminary evidence suggesting that two doses are more effective than one dose,” wrote Cesar Fernandez de las Penas, PhD, of King Juan Carlos University in Madrid, and colleagues. Their report is in The Lancet’s eClinicalMedicine.
A team in Milan found that unvaccinated people in their study were nearly three times as likely to have serious symptoms for longer than 4 weeks compared to vaccinated volunteers. According to their report in JAMA, Elena Azzolini, MD, PhD, assistant professor at Humanitas Research Hospital, and colleagues found two or three doses of vaccine reduced the risk of hospitalization from COVID to 16% or 17% compared to 42% for the unvaccinated.
Treatments
With no diagnostic criteria and no understanding of the causes, it’s hard for doctors to determine treatments.
Most experts dealing with long COVID, even those at the specialty centers that have been set up at hospitals and health systems in the United States, recommend that patients start with their primary care doctors before moving on to specialists.
“The mainstay of management is supportive, holistic care, symptom control, and detection of treatable complications,” Trish Greenhalgh, MD, professor of primary care health sciences at the University of Oxford, England, and colleagues wrote in the journal The BMJ in September. “Patients with long COVID greatly value input from their primary care clinician. Generalist clinicians can help patients considerably by hearing the patient’s story and validating their experience … (and) making the diagnosis of long COVID (which does not have to be by exclusion) and excluding alternative diagnoses.”
Evidence is building that long COVID closely resembles other postviral conditions – something that can provide clues for treatment. For example, several studies indicate that exercise doesn’t help most patients.
But there are approaches that can work. Treatments may include pulmonary rehabilitation; autonomic conditioning therapy, which includes breathing therapy; and cognitive rehabilitation to relieve brain fog. Doctors are also trying the antidepressant amitriptyline to help with sleep disturbances and headaches; the antiseizure medication gabapentin to help with pain, numbness, and other neurological symptoms; and drugs to relieve low blood pressure in patients experiencing postural orthostatic tachycardia syndrome (POTS).
The NIH is sponsoring studies that have recruited just over 8,200 adults. And more than two dozen researchers from Harvard; Stanford; the University of California, San Francisco; the J. Craig Venter Institute; Johns Hopkins University; the University of Pennsylvania; Mount Sinai Hospitals; Cardiff University; and Yale announced in September they were forming the Long COVID Research Initiative to speed up studies.
The group, with funding from private enterprise, plans to conduct tissue biopsy, imaging studies, and autopsies and will search for potential biomarkers in the blood of patients.
A version of this article first appeared on WebMD.com.
Long COVID: The name says it all. It’s an illness that, for many people, has not yet stopped.
Eric Roach became ill with COVID-19 in November 2020, and he’s still sick. “I have brain fog, memory loss,” says the 67-year-old Navy veteran from Spearfish, S.D. “The fatigue has just been insane.”
Long COVID, more formally known as post-acute sequelae of COVID (PASC), is the lay term to describe when people start to recover, or seem to recover, from a bout of COVID-19 but then continue to suffer from symptoms. For some, it’s gone on for 2 years or longer. While the governments of the United Statesand several other countries formally recognize the existence of long COVID, the National Institutes of Health (NIH) has yet to formally define it. There’s no approved treatment, and the causes are not understood.
Here’s what is known: and it is affecting enough people to cause concern for employers, health insurers, and governments.
First, the many symptoms
According to the Centers for Disease Control and Prvention, long COVID symptoms may include:
- Tiredness or fatigue that interferes with daily life.
- Symptoms that get worse after physical or mental effort.
- Fever.
- Difficulty breathing or shortness of breath.
- Cough.
- Chest pain.
- Heart palpitations.
- Difficulty thinking or concentrating (sometimes referred to as “brain fog”).
- Headache.
- Sleep problems.
- Dizziness when standing.
- Pins-and-needles feelings.
- Change in smell or taste.
- Depression or anxiety.
- Diarrhea.
- Stomach pain.
- Joint or muscle pain.
- Rash.
- Changes in menstrual cycles.
“People with post-COVID conditions may develop or continue to have symptoms that are hard to explain and manage,” the CDC says on its website. “Clinical evaluations and results of routine blood tests, chest x-rays, and electrocardiograms may be normal. The symptoms are similar to those reported by people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and other poorly understood chronic illnesses that may occur after other infections.”
Doctors may not fully appreciate the subtle nature of some of the symptoms.
“People with these unexplained symptoms may be misunderstood by their health care providers, which can result in a long time for them to get a diagnosis and receive appropriate care or treatment,” the CDC says.
Health professionals should recognize that long COVID can be disabling, the U.S. Department of Health and Human Services says. “Long COVID can substantially limit a major life activity,” HHS says in civil rights guidance. One possible example: “A person with long COVID who has lung damage that causes shortness of breath, fatigue, and related effects is substantially limited in respiratory function, among other major life activities,” the HHS notes.
How many people are affected?
This has been difficult to judge because not everyone who has had COVID-19 gets tested for it and there are no formal diagnostic criteria yet for long COVID. The CDC estimates that 19% of patients in the United States who have ever had COVID-19 have long COVID symptoms.
Some estimates go higher. A University of Oxford study in September 2021 found more than a third of patients had symptoms of long COVID between 3 months and 6 months after a COVID-19 diagnosis. As many as 55% of COVID-19 patients in one Chinese study had one or more lingering symptoms 2 years later, Lixue Huang, MD, of the China-Japan Friendship Hospital in Beijing, and colleagues reported in the journal Lancet Respiratory Medicine in May.
According to the CDC, age is a factor. “Older adults are less likely to have long COVID than younger adults. Nearly three times as many adults ages 50-59 currently have long COVID than those age 80 and older,” the CDC says. Women and racial and ethnic minorities are more likely to be affected.
Many people are experiencing neurological effects, such as the so-called brain fog, according to Ziyad Al-Aly, MD, of Washington University and the VA St. Louis Health Care System, and colleagues, whose report was published in Nature Medicine in September. They estimated that 6.6 million Americans have brain impairments associated with COVID infection.
“Some of the neurologic disorders reported here are serious chronic conditions that will impact some people for a lifetime,” they wrote. “Given the colossal scale of the pandemic, and even though the absolute numbers reported in this work are small, these may translate into a large number of affected individuals around the world – and this will likely contribute to a rise in the burden of neurologic diseases.”
Causes
It’s not clear what the underlying causes are, but most research points to a combination of factors. Suspects include ongoing inflammation, tiny blood clots, and reactivation of latent viruses. In May, Brent Palmer, PhD, of the University of Colorado, Denver, and colleagues found people with long COVID had persistent activation of T-cells that were specific for SARS-CoV-2.
COVID-19 itself can damage organs, and long COVID might be caused by ongoing damage. In August, Alexandros Rovas, MD, of University Hospital Munster in Germany, and colleagues found patients with long COVID had evidence of damage to their capillaries. “Whether, to what extent, and when the observed damage might be reversible remains unclear,” they wrote in the journal Angiogenesis.
People with long COVID have immune responses to other viruses, such as Epstein-Barr – evidence that COVID-19 might reactivate latent viruses. “Our data suggest the involvement of persistent antigen, reactivation of latent herpesviruses, and chronic inflammation,” immunobiologist Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., and colleagues wrote in a study posted in August that had not yet been peer-reviewed for publication.
This might be causing an autoimmune response. “The infection may cause the immune system to start making autoantibodies that attack a person’s own organs and tissues,” the NIH says.
There could be other factors. A study by Harvard researchers found that people who felt stressed, depressed, or lonely before catching COVID-19 were more likely to develop long COVID afterward. “Distress was more strongly associated with developing long COVID than physical health risk factors such as obesity, asthma, and hypertension,” Siwen Wang, MD, a research fellow with Harvard University’s T.H. Chan School of Public Health, Boston, said in a statement. Plus, nearly 44% of those in the study developed COVID-19 infections after having been assessed for stress, Dr. Wang and colleagues reported in the journal JAMA Psychiatry.
Vaccine protection
There’s evidence that vaccination protects against long COVID, both by preventing infection in the first place, but also even for people who have breakthrough infections.
A meta-analysis covering studies involving 17 million people found evidence vaccination might reduce the severity of COVID-19 or might help the body clear any lingering virus after an infection.
“Overall, vaccination was associated with reduced risks or odds of long COVID, with preliminary evidence suggesting that two doses are more effective than one dose,” wrote Cesar Fernandez de las Penas, PhD, of King Juan Carlos University in Madrid, and colleagues. Their report is in The Lancet’s eClinicalMedicine.
A team in Milan found that unvaccinated people in their study were nearly three times as likely to have serious symptoms for longer than 4 weeks compared to vaccinated volunteers. According to their report in JAMA, Elena Azzolini, MD, PhD, assistant professor at Humanitas Research Hospital, and colleagues found two or three doses of vaccine reduced the risk of hospitalization from COVID to 16% or 17% compared to 42% for the unvaccinated.
Treatments
With no diagnostic criteria and no understanding of the causes, it’s hard for doctors to determine treatments.
Most experts dealing with long COVID, even those at the specialty centers that have been set up at hospitals and health systems in the United States, recommend that patients start with their primary care doctors before moving on to specialists.
“The mainstay of management is supportive, holistic care, symptom control, and detection of treatable complications,” Trish Greenhalgh, MD, professor of primary care health sciences at the University of Oxford, England, and colleagues wrote in the journal The BMJ in September. “Patients with long COVID greatly value input from their primary care clinician. Generalist clinicians can help patients considerably by hearing the patient’s story and validating their experience … (and) making the diagnosis of long COVID (which does not have to be by exclusion) and excluding alternative diagnoses.”
Evidence is building that long COVID closely resembles other postviral conditions – something that can provide clues for treatment. For example, several studies indicate that exercise doesn’t help most patients.
But there are approaches that can work. Treatments may include pulmonary rehabilitation; autonomic conditioning therapy, which includes breathing therapy; and cognitive rehabilitation to relieve brain fog. Doctors are also trying the antidepressant amitriptyline to help with sleep disturbances and headaches; the antiseizure medication gabapentin to help with pain, numbness, and other neurological symptoms; and drugs to relieve low blood pressure in patients experiencing postural orthostatic tachycardia syndrome (POTS).
The NIH is sponsoring studies that have recruited just over 8,200 adults. And more than two dozen researchers from Harvard; Stanford; the University of California, San Francisco; the J. Craig Venter Institute; Johns Hopkins University; the University of Pennsylvania; Mount Sinai Hospitals; Cardiff University; and Yale announced in September they were forming the Long COVID Research Initiative to speed up studies.
The group, with funding from private enterprise, plans to conduct tissue biopsy, imaging studies, and autopsies and will search for potential biomarkers in the blood of patients.
A version of this article first appeared on WebMD.com.
Children and COVID: September slowdown continues
New COVID-19 cases and hospital admissions in children continue to decline, while the slow pace of vaccinations has not deterred manufacturers from seeking new emergency authorizations.
Since reaching a post-Omicron peak of 112,000 in late May, the number of weekly cases has fluctuated, with no stretch of increases or decreases lasting more than 4 weeks or the weekly count rising above 97,000 or falling lower than the current 55,000, according to state-level data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
New admissions with confirmed COVID for children aged 0-17 years, which did not follow that pattern and instead continued to rise through the spring and early summer, have been largely decreasing in recent weeks and had fallen to 0.27 per 100,000 population as of Sept. 21 after peaking at 0.46 per 100,000 in late July, the Centers for Disease Control and Prevention reported. A similar decline has been seen for emergency department visits since late August.
The biggest vaccination news of the week came from Moderna and Pfizer and BioNTech, which are each seeking emergency authorization from the Food and Drug Administration for bivalent vaccine boosters that target both the original COVID strain and the BA.4 and BA.5 strains of Omicron.
“Pfizer’s booster would be for children 5 to 11 who have completed a primary vaccination series [and] Moderna’s updated boosters would be for children ages 6 to 17 who have completed a primary vaccination series,” WebMD said.
Although almost 61% of children aged 12-17 years are already fully vaccinated, that is not the case among those aged 5-11, of whom only 31.4% have completed the initial vaccine regimen. Since becoming eligible in June, just 1.9% of children under 5 years of age have been fully vaccinated and 6.3% have received at least one dose, the CDC said on its COVID Data Tracker. The latest data put the already boosted child populations at 28.8% for 12- to 17-year-olds and 14.8% in those aged 5-11.
About 51,000 children under age 5 years received their initial COVID vaccination during the week of Sept. 15-21, and the trend for that measure is one of gradual decline since July. Among the older children that same week, there were 28,000 initial vaccinations in the 5- to 11-year-olds and 18,000 for those aged 12-17, and activity in both age groups has largely stagnated since the spring, according to a separate AAP report based on CDC data.
New COVID-19 cases and hospital admissions in children continue to decline, while the slow pace of vaccinations has not deterred manufacturers from seeking new emergency authorizations.
Since reaching a post-Omicron peak of 112,000 in late May, the number of weekly cases has fluctuated, with no stretch of increases or decreases lasting more than 4 weeks or the weekly count rising above 97,000 or falling lower than the current 55,000, according to state-level data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
New admissions with confirmed COVID for children aged 0-17 years, which did not follow that pattern and instead continued to rise through the spring and early summer, have been largely decreasing in recent weeks and had fallen to 0.27 per 100,000 population as of Sept. 21 after peaking at 0.46 per 100,000 in late July, the Centers for Disease Control and Prevention reported. A similar decline has been seen for emergency department visits since late August.
The biggest vaccination news of the week came from Moderna and Pfizer and BioNTech, which are each seeking emergency authorization from the Food and Drug Administration for bivalent vaccine boosters that target both the original COVID strain and the BA.4 and BA.5 strains of Omicron.
“Pfizer’s booster would be for children 5 to 11 who have completed a primary vaccination series [and] Moderna’s updated boosters would be for children ages 6 to 17 who have completed a primary vaccination series,” WebMD said.
Although almost 61% of children aged 12-17 years are already fully vaccinated, that is not the case among those aged 5-11, of whom only 31.4% have completed the initial vaccine regimen. Since becoming eligible in June, just 1.9% of children under 5 years of age have been fully vaccinated and 6.3% have received at least one dose, the CDC said on its COVID Data Tracker. The latest data put the already boosted child populations at 28.8% for 12- to 17-year-olds and 14.8% in those aged 5-11.
About 51,000 children under age 5 years received their initial COVID vaccination during the week of Sept. 15-21, and the trend for that measure is one of gradual decline since July. Among the older children that same week, there were 28,000 initial vaccinations in the 5- to 11-year-olds and 18,000 for those aged 12-17, and activity in both age groups has largely stagnated since the spring, according to a separate AAP report based on CDC data.
New COVID-19 cases and hospital admissions in children continue to decline, while the slow pace of vaccinations has not deterred manufacturers from seeking new emergency authorizations.
Since reaching a post-Omicron peak of 112,000 in late May, the number of weekly cases has fluctuated, with no stretch of increases or decreases lasting more than 4 weeks or the weekly count rising above 97,000 or falling lower than the current 55,000, according to state-level data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
New admissions with confirmed COVID for children aged 0-17 years, which did not follow that pattern and instead continued to rise through the spring and early summer, have been largely decreasing in recent weeks and had fallen to 0.27 per 100,000 population as of Sept. 21 after peaking at 0.46 per 100,000 in late July, the Centers for Disease Control and Prevention reported. A similar decline has been seen for emergency department visits since late August.
The biggest vaccination news of the week came from Moderna and Pfizer and BioNTech, which are each seeking emergency authorization from the Food and Drug Administration for bivalent vaccine boosters that target both the original COVID strain and the BA.4 and BA.5 strains of Omicron.
“Pfizer’s booster would be for children 5 to 11 who have completed a primary vaccination series [and] Moderna’s updated boosters would be for children ages 6 to 17 who have completed a primary vaccination series,” WebMD said.
Although almost 61% of children aged 12-17 years are already fully vaccinated, that is not the case among those aged 5-11, of whom only 31.4% have completed the initial vaccine regimen. Since becoming eligible in June, just 1.9% of children under 5 years of age have been fully vaccinated and 6.3% have received at least one dose, the CDC said on its COVID Data Tracker. The latest data put the already boosted child populations at 28.8% for 12- to 17-year-olds and 14.8% in those aged 5-11.
About 51,000 children under age 5 years received their initial COVID vaccination during the week of Sept. 15-21, and the trend for that measure is one of gradual decline since July. Among the older children that same week, there were 28,000 initial vaccinations in the 5- to 11-year-olds and 18,000 for those aged 12-17, and activity in both age groups has largely stagnated since the spring, according to a separate AAP report based on CDC data.
Uncontrolled BP linked to one-third of ED visits for CVD
A look at the top cardiovascular disease (CVD) diagnoses in U.S. emergency departments (EDs) suggests that many heart-related emergencies are due to poorly controlled high blood pressure.
In a study of more than 20 million ED visits, about one-third of CVD-related ED visits in the United States were for hypertension-related conditions.
Overall, 13% of ED visits, representing more than 2.7 million individuals, were for essential hypertension.
The fact that these visits rarely led to an inpatient admission (< 3%) or death (< 0.1%) suggests they were “mostly related to the management of hypertension,” lead author Mamas A. Mamas, MD, Keele University, Staffordshire, England, said in a news release.
The study was published online in the Journal of the American Heart Association.
Nationwide sample
The researchers studied more than 20.6 million ED encounters in adults with a primary CVD diagnosis using data from the Nationwide Emergency Department Sample between 2016 and 2018.
In the sample, 49% were women, and the median age was 67 years. Men had poorer overall baseline cardiometabolic profiles, but women had higher rates of obesity, hypertension, and cerebrovascular disease. The majority had Medicare or Medicaid insurance.
In women, essential hypertension was the most common reason for an ED visit (16%), followed by hypertensive heart or kidney disease (14%) and atrial fibrillation (AF)/flutter (10%).
In men, the top three reasons were hypertensive heart or kidney disease (15%), essential hypertension (11%), and acute myocardial infarction (AMI, 11%).
On presentation, women were significantly more likely to have essential hypertension, hypertensive crisis, AF/flutter, supraventricular tachycardia, pulmonary embolism, or ischemic stroke, while men were more likely to have AMI, or cardiac arrest.
“Previous studies have shown sex differences in patterns of CVD among hospitalized patients,” Dr. Mamas noted. “However, examining CVD encounters in the ED provides a more complete picture of the cardiovascular healthcare needs of men and women, as it captures encounters prior to hospitalization.”
He noted that previous studies of CVD emergency visits are limited to suspected MI visits. “Therefore, this analysis of 15 CVD conditions helps to better understand the full spectrum of acute CVD needs, including sex disparities in hospitalization and risk of death,” Dr. Mamas said.
Sex differences in outcomes
The study found that outcomes from the emergency CVD visits were slightly different for men and women.
Overall, women were less likely than were men to die (3.3% vs. 4.3%) or be hospitalized (49.1% vs. 52.3%) after an ED visit for CVD. The difference may be due to women’s generally lower-risk diagnoses, Dr. Mamas said, but there could be an underestimation of deaths in women.
In logistic regression models adjusted for baseline covariates, women with intracranial hemorrhage (ICH) had a higher risk of being admitted to hospital or dying compared with men with ICH.
Men were more likely to die if they presented with hypertensive heart or kidney disease, AF/flutter, AMI or cardiac arrest, the researchers found.
“We did not track deaths outside of the hospital setting,” Dr. Mamas pointed out. Given past evidence that women are more likely to be inappropriately discharged from the ED, and strong evidence for the systemic undertreatment of women, further study is warranted to track outcomes beyond the ED visit,” he added.
The researchers called for further research into understanding the underlying factors driving the differences in CVD patterns and outcomes between men and women.
Reached for comment, Maryann McLaughlin, MD, a cardiologist at Mount Sinai Hospital, New York, said: “Hypertension is a silent killer” and this study “reiterates that people need to get their blood pressure checked more regularly.
“In the very least, if they do present to the hospital as not feeling well or whatever it is, and they are identified as having high blood pressure, that’s an important opportunity to really teach them about hypertension and have them follow-up with it,” Dr. McLaughlin told this news organization.
The study was supported by Health Data Research UK. Dr. Keele and Dr. McLaughlin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A look at the top cardiovascular disease (CVD) diagnoses in U.S. emergency departments (EDs) suggests that many heart-related emergencies are due to poorly controlled high blood pressure.
In a study of more than 20 million ED visits, about one-third of CVD-related ED visits in the United States were for hypertension-related conditions.
Overall, 13% of ED visits, representing more than 2.7 million individuals, were for essential hypertension.
The fact that these visits rarely led to an inpatient admission (< 3%) or death (< 0.1%) suggests they were “mostly related to the management of hypertension,” lead author Mamas A. Mamas, MD, Keele University, Staffordshire, England, said in a news release.
The study was published online in the Journal of the American Heart Association.
Nationwide sample
The researchers studied more than 20.6 million ED encounters in adults with a primary CVD diagnosis using data from the Nationwide Emergency Department Sample between 2016 and 2018.
In the sample, 49% were women, and the median age was 67 years. Men had poorer overall baseline cardiometabolic profiles, but women had higher rates of obesity, hypertension, and cerebrovascular disease. The majority had Medicare or Medicaid insurance.
In women, essential hypertension was the most common reason for an ED visit (16%), followed by hypertensive heart or kidney disease (14%) and atrial fibrillation (AF)/flutter (10%).
In men, the top three reasons were hypertensive heart or kidney disease (15%), essential hypertension (11%), and acute myocardial infarction (AMI, 11%).
On presentation, women were significantly more likely to have essential hypertension, hypertensive crisis, AF/flutter, supraventricular tachycardia, pulmonary embolism, or ischemic stroke, while men were more likely to have AMI, or cardiac arrest.
“Previous studies have shown sex differences in patterns of CVD among hospitalized patients,” Dr. Mamas noted. “However, examining CVD encounters in the ED provides a more complete picture of the cardiovascular healthcare needs of men and women, as it captures encounters prior to hospitalization.”
He noted that previous studies of CVD emergency visits are limited to suspected MI visits. “Therefore, this analysis of 15 CVD conditions helps to better understand the full spectrum of acute CVD needs, including sex disparities in hospitalization and risk of death,” Dr. Mamas said.
Sex differences in outcomes
The study found that outcomes from the emergency CVD visits were slightly different for men and women.
Overall, women were less likely than were men to die (3.3% vs. 4.3%) or be hospitalized (49.1% vs. 52.3%) after an ED visit for CVD. The difference may be due to women’s generally lower-risk diagnoses, Dr. Mamas said, but there could be an underestimation of deaths in women.
In logistic regression models adjusted for baseline covariates, women with intracranial hemorrhage (ICH) had a higher risk of being admitted to hospital or dying compared with men with ICH.
Men were more likely to die if they presented with hypertensive heart or kidney disease, AF/flutter, AMI or cardiac arrest, the researchers found.
“We did not track deaths outside of the hospital setting,” Dr. Mamas pointed out. Given past evidence that women are more likely to be inappropriately discharged from the ED, and strong evidence for the systemic undertreatment of women, further study is warranted to track outcomes beyond the ED visit,” he added.
The researchers called for further research into understanding the underlying factors driving the differences in CVD patterns and outcomes between men and women.
Reached for comment, Maryann McLaughlin, MD, a cardiologist at Mount Sinai Hospital, New York, said: “Hypertension is a silent killer” and this study “reiterates that people need to get their blood pressure checked more regularly.
“In the very least, if they do present to the hospital as not feeling well or whatever it is, and they are identified as having high blood pressure, that’s an important opportunity to really teach them about hypertension and have them follow-up with it,” Dr. McLaughlin told this news organization.
The study was supported by Health Data Research UK. Dr. Keele and Dr. McLaughlin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A look at the top cardiovascular disease (CVD) diagnoses in U.S. emergency departments (EDs) suggests that many heart-related emergencies are due to poorly controlled high blood pressure.
In a study of more than 20 million ED visits, about one-third of CVD-related ED visits in the United States were for hypertension-related conditions.
Overall, 13% of ED visits, representing more than 2.7 million individuals, were for essential hypertension.
The fact that these visits rarely led to an inpatient admission (< 3%) or death (< 0.1%) suggests they were “mostly related to the management of hypertension,” lead author Mamas A. Mamas, MD, Keele University, Staffordshire, England, said in a news release.
The study was published online in the Journal of the American Heart Association.
Nationwide sample
The researchers studied more than 20.6 million ED encounters in adults with a primary CVD diagnosis using data from the Nationwide Emergency Department Sample between 2016 and 2018.
In the sample, 49% were women, and the median age was 67 years. Men had poorer overall baseline cardiometabolic profiles, but women had higher rates of obesity, hypertension, and cerebrovascular disease. The majority had Medicare or Medicaid insurance.
In women, essential hypertension was the most common reason for an ED visit (16%), followed by hypertensive heart or kidney disease (14%) and atrial fibrillation (AF)/flutter (10%).
In men, the top three reasons were hypertensive heart or kidney disease (15%), essential hypertension (11%), and acute myocardial infarction (AMI, 11%).
On presentation, women were significantly more likely to have essential hypertension, hypertensive crisis, AF/flutter, supraventricular tachycardia, pulmonary embolism, or ischemic stroke, while men were more likely to have AMI, or cardiac arrest.
“Previous studies have shown sex differences in patterns of CVD among hospitalized patients,” Dr. Mamas noted. “However, examining CVD encounters in the ED provides a more complete picture of the cardiovascular healthcare needs of men and women, as it captures encounters prior to hospitalization.”
He noted that previous studies of CVD emergency visits are limited to suspected MI visits. “Therefore, this analysis of 15 CVD conditions helps to better understand the full spectrum of acute CVD needs, including sex disparities in hospitalization and risk of death,” Dr. Mamas said.
Sex differences in outcomes
The study found that outcomes from the emergency CVD visits were slightly different for men and women.
Overall, women were less likely than were men to die (3.3% vs. 4.3%) or be hospitalized (49.1% vs. 52.3%) after an ED visit for CVD. The difference may be due to women’s generally lower-risk diagnoses, Dr. Mamas said, but there could be an underestimation of deaths in women.
In logistic regression models adjusted for baseline covariates, women with intracranial hemorrhage (ICH) had a higher risk of being admitted to hospital or dying compared with men with ICH.
Men were more likely to die if they presented with hypertensive heart or kidney disease, AF/flutter, AMI or cardiac arrest, the researchers found.
“We did not track deaths outside of the hospital setting,” Dr. Mamas pointed out. Given past evidence that women are more likely to be inappropriately discharged from the ED, and strong evidence for the systemic undertreatment of women, further study is warranted to track outcomes beyond the ED visit,” he added.
The researchers called for further research into understanding the underlying factors driving the differences in CVD patterns and outcomes between men and women.
Reached for comment, Maryann McLaughlin, MD, a cardiologist at Mount Sinai Hospital, New York, said: “Hypertension is a silent killer” and this study “reiterates that people need to get their blood pressure checked more regularly.
“In the very least, if they do present to the hospital as not feeling well or whatever it is, and they are identified as having high blood pressure, that’s an important opportunity to really teach them about hypertension and have them follow-up with it,” Dr. McLaughlin told this news organization.
The study was supported by Health Data Research UK. Dr. Keele and Dr. McLaughlin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Experts issue health warning about giving melatonin to children
The American Academy of Sleep Medicine has issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
“While melatonin can be useful in treating certain sleep-wake disorders, like jet lag, there is much less evidence it can help healthy children or adults fall asleep faster,” Muhammad Adeel Rishi, MD, MBBS, vice chair of the AASM public safety committee, said in a news release.
Spike in poisoning calls
Research previously published in JAMA suggests that the use of melatonin has increased over the past 2 decades among people of all ages.
With this increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related emergency department visits for children.
Federal data show that the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021.
More than 4,000 of the reported ingestions led to a hospital stay, and 287 children required intensive care.
The AASM notes that next to multivitamins, melatonin is the second most popular “natural” product parents give to their children.
Melatonin is widely available over the counter. It’s marketed as a sleep aid, but there is little evidence that taking it as a supplement is effective in treating insomnia in healthy children, the AASM cautions.
Because it is regulated by the U.S. Food and Drug Administration as a dietary supplement, melatonin receives less oversight. Research shows that the melatonin content in supplements can vary widely, the AASM points out.
In one study, amounts of melatonin ranged from less than one-half to more than four times the amounts stated on the labels. The greatest variability in melatonin content was in chewable tablets, which are most likely to be used for children.
“The availability of melatonin as gummies or chewable tablets makes it more tempting to give to children and more likely for them to overdose,” said Dr. Rishi, a pulmonology, sleep medicine, and critical care specialist at Indiana University Health Physicians, Indianapolis.
“Parents should talk directly with their child’s health care professional before giving their children melatonin products,” he added.
Keep out of reach
The AASM advises that melatonin be managed as any other medication and that it be kept out of reach of children.
Before giving melatonin or any supplement to their children, parents should discuss this decision with a pediatric health care professional.
If use of melatonin is warranted, health care professionals can recommend the appropriate dose and timing in addressing the sleep problem, and they can ensure that the melatonin product that is being used has a USP verified mark.
“Instead of turning to melatonin, parents should encourage children to develop good sleep habits, like setting a regular bedtime and wake time, having a bedtime routine, and limiting screen time as bedtime approaches,” Dr. Rishi said.
A version of this article first appeared on Medscape.com.
The American Academy of Sleep Medicine has issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
“While melatonin can be useful in treating certain sleep-wake disorders, like jet lag, there is much less evidence it can help healthy children or adults fall asleep faster,” Muhammad Adeel Rishi, MD, MBBS, vice chair of the AASM public safety committee, said in a news release.
Spike in poisoning calls
Research previously published in JAMA suggests that the use of melatonin has increased over the past 2 decades among people of all ages.
With this increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related emergency department visits for children.
Federal data show that the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021.
More than 4,000 of the reported ingestions led to a hospital stay, and 287 children required intensive care.
The AASM notes that next to multivitamins, melatonin is the second most popular “natural” product parents give to their children.
Melatonin is widely available over the counter. It’s marketed as a sleep aid, but there is little evidence that taking it as a supplement is effective in treating insomnia in healthy children, the AASM cautions.
Because it is regulated by the U.S. Food and Drug Administration as a dietary supplement, melatonin receives less oversight. Research shows that the melatonin content in supplements can vary widely, the AASM points out.
In one study, amounts of melatonin ranged from less than one-half to more than four times the amounts stated on the labels. The greatest variability in melatonin content was in chewable tablets, which are most likely to be used for children.
“The availability of melatonin as gummies or chewable tablets makes it more tempting to give to children and more likely for them to overdose,” said Dr. Rishi, a pulmonology, sleep medicine, and critical care specialist at Indiana University Health Physicians, Indianapolis.
“Parents should talk directly with their child’s health care professional before giving their children melatonin products,” he added.
Keep out of reach
The AASM advises that melatonin be managed as any other medication and that it be kept out of reach of children.
Before giving melatonin or any supplement to their children, parents should discuss this decision with a pediatric health care professional.
If use of melatonin is warranted, health care professionals can recommend the appropriate dose and timing in addressing the sleep problem, and they can ensure that the melatonin product that is being used has a USP verified mark.
“Instead of turning to melatonin, parents should encourage children to develop good sleep habits, like setting a regular bedtime and wake time, having a bedtime routine, and limiting screen time as bedtime approaches,” Dr. Rishi said.
A version of this article first appeared on Medscape.com.
The American Academy of Sleep Medicine has issued a health advisory encouraging parents to talk to a health care professional before giving melatonin or any supplement to children.
“While melatonin can be useful in treating certain sleep-wake disorders, like jet lag, there is much less evidence it can help healthy children or adults fall asleep faster,” Muhammad Adeel Rishi, MD, MBBS, vice chair of the AASM public safety committee, said in a news release.
Spike in poisoning calls
Research previously published in JAMA suggests that the use of melatonin has increased over the past 2 decades among people of all ages.
With this increased use has come a spike in reports of melatonin overdose, calls to poison control centers, and related emergency department visits for children.
Federal data show that the number of U.S. children who unintentionally ingested melatonin supplements jumped 530% from 2012 to 2021.
More than 4,000 of the reported ingestions led to a hospital stay, and 287 children required intensive care.
The AASM notes that next to multivitamins, melatonin is the second most popular “natural” product parents give to their children.
Melatonin is widely available over the counter. It’s marketed as a sleep aid, but there is little evidence that taking it as a supplement is effective in treating insomnia in healthy children, the AASM cautions.
Because it is regulated by the U.S. Food and Drug Administration as a dietary supplement, melatonin receives less oversight. Research shows that the melatonin content in supplements can vary widely, the AASM points out.
In one study, amounts of melatonin ranged from less than one-half to more than four times the amounts stated on the labels. The greatest variability in melatonin content was in chewable tablets, which are most likely to be used for children.
“The availability of melatonin as gummies or chewable tablets makes it more tempting to give to children and more likely for them to overdose,” said Dr. Rishi, a pulmonology, sleep medicine, and critical care specialist at Indiana University Health Physicians, Indianapolis.
“Parents should talk directly with their child’s health care professional before giving their children melatonin products,” he added.
Keep out of reach
The AASM advises that melatonin be managed as any other medication and that it be kept out of reach of children.
Before giving melatonin or any supplement to their children, parents should discuss this decision with a pediatric health care professional.
If use of melatonin is warranted, health care professionals can recommend the appropriate dose and timing in addressing the sleep problem, and they can ensure that the melatonin product that is being used has a USP verified mark.
“Instead of turning to melatonin, parents should encourage children to develop good sleep habits, like setting a regular bedtime and wake time, having a bedtime routine, and limiting screen time as bedtime approaches,” Dr. Rishi said.
A version of this article first appeared on Medscape.com.
Weight gain linked to cancer survival in men and women
Cancer cachexia is a syndrome of weight loss that frequently occurs during cancer treatment. Consequences can include skeletal muscle loss, fatigue, functional impairment, worse quality of life, and worse survival. On the other hand, weight gain during cancer treatment has been tied to better survival.
Few studies have examined the relationship between weight gain and outcomes by sex.
“The finding that weight gain occurred in subsets of males and females is a new observation. The fact that weight gain occurs in cancer patients during anticancer treatment could confound results of clinical [trials] evaluating novel anticachexia treatments. Simultaneously studying longitudinal body weights and serum and cellular biomarkers in cancer patients might provide insights into mechanisms involved in cachexia. Increased understanding of mechanisms driving cachexia could lead to new therapeutic strategies,” said study coauthor Philip Bonomi, MD, who is an oncologist at Rush Medical College, Chicago.
“This data, although it appears to be very basic, is critically important, especially as we consider our novel interventions in the treatment of cancer cachexia,” said Eric Roeland, MD, during his presentation of the study at the annual meeting of European Society for Medical Oncology. Dr. Roeland is a medical oncologist at Oregon Health & Science University, Portland.
Dr. Roeland is also the lead author of cancer cachexia guidelines published by the American Society of Clinical Oncology in 2020. The guidelines suggest that dietary counseling can be offered to patients, but warns against routine use of enteral feeding tubes and parenteral nutrition. Although no specific drug can be recommended for cancer cachexia, progesterone analogs and corticosteroids used over the short term (weeks) can be used on a trial base to improve appetite and weight gain. While not approved in the United States, anamorelin was approved in 2020 in Japan for cancer cachexia in NSCLC, gastric cancer, pancreatic cancer, and colorectal cancer.
The new study should raise awareness of the importance of adverse effects of cancer treatments, said Karin Jordan, MD, University Hospital Heidelberg (Germany). She served as a discussant following the presentation. “As a medical oncologist, we focus a bit too much on the benefits of antineoplastic therapy, both on cure and on the survival benefit. But what is also very, very important to do is a balanced oncology treatment to focus on the risks of oncology therapies,” she said.
The study is limited by its retrospective nature and potential for bias. “The hypothesis that weight gain leads to improved survival is not really proven as it likewise may be the other way around,” Dr. Jordan said.
However, in oncology research, a phenomenon called the “obesity paradox” is increasingly catching the interest of investigators. Observational studies have shown that overweight patients with certain cancers (specifically, colorectal, endometrial and lung cancer). actually have improved overall survival as compared with normal-weight patients.
Details from the new study
The researchers pooled data 1,030 patients who participated in three phase 3 clinical trials conducted between 2005 and 2011. The patients all received platinum-based chemotherapy as part of control arms. 304 were female and 726 were male. The median age was 62. 16.7% were Asian, the mean body mass index was 24.6 kg/m2, 88.5% had stage 4 disease, 36.9% had adenocarcinoma, and 86.3% were current or former smokers.
Males and females had similar magnitudes and rate of weight gain over the course of treatment. Any weight gain was associated with improved overall survival in both males (12.7 vs. 8.0 months; hazard ratio, 0.60; P < .001) and females (16.2 vs. 10.1 months; HR, 0.65; P = .0028). Patients who had a weight gain of 2.5% of body weight or more saw an improvement in overall survival in both males (14.0 vs. 8.2 months; HR, 0.57; P < .001) and females (16.7 vs. 11.3 months; HR, 0.61; P = .0041).
Patients with a weight gain of 5% or more was associated with improved survival in males (13.6 vs. 8.9 months; HR, 0.62; P = .0001), but there was no statistically significant association in females (16.7 vs. 12.6 months; HR, 0.69; P = .1107).
Regardless of weight-gain status, males had lower survival rates than females. All of the associations were independent of smoking status.
The study was funded by Pfizer. Dr. Bonomi has received honoraria from Pfizer and Helsinn for participation in scientific advisory boards. Dr. Jordan has consulted for Amgen, Hexal, Riemser, Helsinn, Voluntis, Pfizer, and BD Solution. She has received research funding from Deutsche Krebshilfe. She has received honoraria from MSD, Merck, Amgen, Hexal, Riemser, Helsinn, Voluntis, Pfizer, Pomme-med, PharmaMar, arttemoi, OnkoUpdate, Stemline, and Roche.
Cancer cachexia is a syndrome of weight loss that frequently occurs during cancer treatment. Consequences can include skeletal muscle loss, fatigue, functional impairment, worse quality of life, and worse survival. On the other hand, weight gain during cancer treatment has been tied to better survival.
Few studies have examined the relationship between weight gain and outcomes by sex.
“The finding that weight gain occurred in subsets of males and females is a new observation. The fact that weight gain occurs in cancer patients during anticancer treatment could confound results of clinical [trials] evaluating novel anticachexia treatments. Simultaneously studying longitudinal body weights and serum and cellular biomarkers in cancer patients might provide insights into mechanisms involved in cachexia. Increased understanding of mechanisms driving cachexia could lead to new therapeutic strategies,” said study coauthor Philip Bonomi, MD, who is an oncologist at Rush Medical College, Chicago.
“This data, although it appears to be very basic, is critically important, especially as we consider our novel interventions in the treatment of cancer cachexia,” said Eric Roeland, MD, during his presentation of the study at the annual meeting of European Society for Medical Oncology. Dr. Roeland is a medical oncologist at Oregon Health & Science University, Portland.
Dr. Roeland is also the lead author of cancer cachexia guidelines published by the American Society of Clinical Oncology in 2020. The guidelines suggest that dietary counseling can be offered to patients, but warns against routine use of enteral feeding tubes and parenteral nutrition. Although no specific drug can be recommended for cancer cachexia, progesterone analogs and corticosteroids used over the short term (weeks) can be used on a trial base to improve appetite and weight gain. While not approved in the United States, anamorelin was approved in 2020 in Japan for cancer cachexia in NSCLC, gastric cancer, pancreatic cancer, and colorectal cancer.
The new study should raise awareness of the importance of adverse effects of cancer treatments, said Karin Jordan, MD, University Hospital Heidelberg (Germany). She served as a discussant following the presentation. “As a medical oncologist, we focus a bit too much on the benefits of antineoplastic therapy, both on cure and on the survival benefit. But what is also very, very important to do is a balanced oncology treatment to focus on the risks of oncology therapies,” she said.
The study is limited by its retrospective nature and potential for bias. “The hypothesis that weight gain leads to improved survival is not really proven as it likewise may be the other way around,” Dr. Jordan said.
However, in oncology research, a phenomenon called the “obesity paradox” is increasingly catching the interest of investigators. Observational studies have shown that overweight patients with certain cancers (specifically, colorectal, endometrial and lung cancer). actually have improved overall survival as compared with normal-weight patients.
Details from the new study
The researchers pooled data 1,030 patients who participated in three phase 3 clinical trials conducted between 2005 and 2011. The patients all received platinum-based chemotherapy as part of control arms. 304 were female and 726 were male. The median age was 62. 16.7% were Asian, the mean body mass index was 24.6 kg/m2, 88.5% had stage 4 disease, 36.9% had adenocarcinoma, and 86.3% were current or former smokers.
Males and females had similar magnitudes and rate of weight gain over the course of treatment. Any weight gain was associated with improved overall survival in both males (12.7 vs. 8.0 months; hazard ratio, 0.60; P < .001) and females (16.2 vs. 10.1 months; HR, 0.65; P = .0028). Patients who had a weight gain of 2.5% of body weight or more saw an improvement in overall survival in both males (14.0 vs. 8.2 months; HR, 0.57; P < .001) and females (16.7 vs. 11.3 months; HR, 0.61; P = .0041).
Patients with a weight gain of 5% or more was associated with improved survival in males (13.6 vs. 8.9 months; HR, 0.62; P = .0001), but there was no statistically significant association in females (16.7 vs. 12.6 months; HR, 0.69; P = .1107).
Regardless of weight-gain status, males had lower survival rates than females. All of the associations were independent of smoking status.
The study was funded by Pfizer. Dr. Bonomi has received honoraria from Pfizer and Helsinn for participation in scientific advisory boards. Dr. Jordan has consulted for Amgen, Hexal, Riemser, Helsinn, Voluntis, Pfizer, and BD Solution. She has received research funding from Deutsche Krebshilfe. She has received honoraria from MSD, Merck, Amgen, Hexal, Riemser, Helsinn, Voluntis, Pfizer, Pomme-med, PharmaMar, arttemoi, OnkoUpdate, Stemline, and Roche.
Cancer cachexia is a syndrome of weight loss that frequently occurs during cancer treatment. Consequences can include skeletal muscle loss, fatigue, functional impairment, worse quality of life, and worse survival. On the other hand, weight gain during cancer treatment has been tied to better survival.
Few studies have examined the relationship between weight gain and outcomes by sex.
“The finding that weight gain occurred in subsets of males and females is a new observation. The fact that weight gain occurs in cancer patients during anticancer treatment could confound results of clinical [trials] evaluating novel anticachexia treatments. Simultaneously studying longitudinal body weights and serum and cellular biomarkers in cancer patients might provide insights into mechanisms involved in cachexia. Increased understanding of mechanisms driving cachexia could lead to new therapeutic strategies,” said study coauthor Philip Bonomi, MD, who is an oncologist at Rush Medical College, Chicago.
“This data, although it appears to be very basic, is critically important, especially as we consider our novel interventions in the treatment of cancer cachexia,” said Eric Roeland, MD, during his presentation of the study at the annual meeting of European Society for Medical Oncology. Dr. Roeland is a medical oncologist at Oregon Health & Science University, Portland.
Dr. Roeland is also the lead author of cancer cachexia guidelines published by the American Society of Clinical Oncology in 2020. The guidelines suggest that dietary counseling can be offered to patients, but warns against routine use of enteral feeding tubes and parenteral nutrition. Although no specific drug can be recommended for cancer cachexia, progesterone analogs and corticosteroids used over the short term (weeks) can be used on a trial base to improve appetite and weight gain. While not approved in the United States, anamorelin was approved in 2020 in Japan for cancer cachexia in NSCLC, gastric cancer, pancreatic cancer, and colorectal cancer.
The new study should raise awareness of the importance of adverse effects of cancer treatments, said Karin Jordan, MD, University Hospital Heidelberg (Germany). She served as a discussant following the presentation. “As a medical oncologist, we focus a bit too much on the benefits of antineoplastic therapy, both on cure and on the survival benefit. But what is also very, very important to do is a balanced oncology treatment to focus on the risks of oncology therapies,” she said.
The study is limited by its retrospective nature and potential for bias. “The hypothesis that weight gain leads to improved survival is not really proven as it likewise may be the other way around,” Dr. Jordan said.
However, in oncology research, a phenomenon called the “obesity paradox” is increasingly catching the interest of investigators. Observational studies have shown that overweight patients with certain cancers (specifically, colorectal, endometrial and lung cancer). actually have improved overall survival as compared with normal-weight patients.
Details from the new study
The researchers pooled data 1,030 patients who participated in three phase 3 clinical trials conducted between 2005 and 2011. The patients all received platinum-based chemotherapy as part of control arms. 304 were female and 726 were male. The median age was 62. 16.7% were Asian, the mean body mass index was 24.6 kg/m2, 88.5% had stage 4 disease, 36.9% had adenocarcinoma, and 86.3% were current or former smokers.
Males and females had similar magnitudes and rate of weight gain over the course of treatment. Any weight gain was associated with improved overall survival in both males (12.7 vs. 8.0 months; hazard ratio, 0.60; P < .001) and females (16.2 vs. 10.1 months; HR, 0.65; P = .0028). Patients who had a weight gain of 2.5% of body weight or more saw an improvement in overall survival in both males (14.0 vs. 8.2 months; HR, 0.57; P < .001) and females (16.7 vs. 11.3 months; HR, 0.61; P = .0041).
Patients with a weight gain of 5% or more was associated with improved survival in males (13.6 vs. 8.9 months; HR, 0.62; P = .0001), but there was no statistically significant association in females (16.7 vs. 12.6 months; HR, 0.69; P = .1107).
Regardless of weight-gain status, males had lower survival rates than females. All of the associations were independent of smoking status.
The study was funded by Pfizer. Dr. Bonomi has received honoraria from Pfizer and Helsinn for participation in scientific advisory boards. Dr. Jordan has consulted for Amgen, Hexal, Riemser, Helsinn, Voluntis, Pfizer, and BD Solution. She has received research funding from Deutsche Krebshilfe. She has received honoraria from MSD, Merck, Amgen, Hexal, Riemser, Helsinn, Voluntis, Pfizer, Pomme-med, PharmaMar, arttemoi, OnkoUpdate, Stemline, and Roche.
FROM ESMO CONGRESS 2022