User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Air pollution tied to stroke risk, subsequent CV events, and death
Results of a UK biobank study show high levels of air pollution were associated with an increased risk of transition from health to a first stroke and subsequent progression to cardiovascular (CV) events and death.
“These results indicate that understanding and reducing the effects of air pollutants on different transition stages in stroke will be beneficial in managing people’s health and preventing the occurrence and progression of stroke,” study investigator Hualiang Lin, PhD, of Sun Yat-sen University School of Public Health, Guangzhou, China, said in a news release.
The study was published online in the journal Neurology.
A way to stop stroke progression?
The researchers assessed air pollution exposure in 318,752 people (mean age, 56) from the UK biobank database. None had a history of stroke or heart disease at the start of the study. Annual concentrations of air pollution near where people lived were estimated through land-use regressions.
During an average follow-up of 12 years, 5,967 people had a stroke, 2,985 developed post-stroke CVD, and 1,020 died.
After adjusting for confounding factors, every 5 µg/m3 increase in exposure to fine particulate matter (PM2.5) was associated with a 24% increase in transition from healthy to first stroke (hazard ratio, 1.24; 95% confidence interval, 1.10-1.40) and a 30% increase in transition from being healthy to dying (HR, 1.30; 95% CI, 1.21-1.40).
PM2.5 is less than 2.5 microns in diameter and includes fly ash from coal combustion. The World Health Organization recommends that annual PM2.5 exposure should not exceed 5 µg/m3.
Those who had a stroke during the study had an average exposure of 10.03 µg/m3 of PM2.5, compared with 9.97 µg/m3 for those who did not have a stroke.
The air pollutants nitrogen oxide and nitrogen dioxide were also associated with an increased risk of stroke and death, but the associations were weaker.
“More research is needed, but it’s possible that decreasing exposure to heavy levels of air pollution could play a role in reducing the progression of stroke,” Dr. Lin said.
“People can reduce their exposure by staying indoors on heavy pollution days, reducing their outdoor exercise, wearing masks to filter out particulate matter, and using air purifiers,” Dr. Lin added.
Public policy implications
Reached for comment, Steffen E. Petersen, MD, MPH, professor of cardiovascular medicine, Barts Health NHS Trust, London, said the study “elegantly confirms the increased risk of stroke due to air pollution in the UK Biobank population study but interestingly suggests that the impact of air pollution may continue to adversely impact cardiovascular health even after the stroke occurred.”
“This is further evidence to inform policymakers to tackle air pollution and get levels below the recommended levels,” Dr. Petersen said.
“On a personal level, everyone, including stroke patients, may wish to consider personal measures to reduce exposure to air pollution, such as avoiding walking along polluted streets and rather take a less polluted route away from the main roads,” Dr. Petersen added.
The study had no targeted funding. Dr. Lin and Dr. Petersen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a UK biobank study show high levels of air pollution were associated with an increased risk of transition from health to a first stroke and subsequent progression to cardiovascular (CV) events and death.
“These results indicate that understanding and reducing the effects of air pollutants on different transition stages in stroke will be beneficial in managing people’s health and preventing the occurrence and progression of stroke,” study investigator Hualiang Lin, PhD, of Sun Yat-sen University School of Public Health, Guangzhou, China, said in a news release.
The study was published online in the journal Neurology.
A way to stop stroke progression?
The researchers assessed air pollution exposure in 318,752 people (mean age, 56) from the UK biobank database. None had a history of stroke or heart disease at the start of the study. Annual concentrations of air pollution near where people lived were estimated through land-use regressions.
During an average follow-up of 12 years, 5,967 people had a stroke, 2,985 developed post-stroke CVD, and 1,020 died.
After adjusting for confounding factors, every 5 µg/m3 increase in exposure to fine particulate matter (PM2.5) was associated with a 24% increase in transition from healthy to first stroke (hazard ratio, 1.24; 95% confidence interval, 1.10-1.40) and a 30% increase in transition from being healthy to dying (HR, 1.30; 95% CI, 1.21-1.40).
PM2.5 is less than 2.5 microns in diameter and includes fly ash from coal combustion. The World Health Organization recommends that annual PM2.5 exposure should not exceed 5 µg/m3.
Those who had a stroke during the study had an average exposure of 10.03 µg/m3 of PM2.5, compared with 9.97 µg/m3 for those who did not have a stroke.
The air pollutants nitrogen oxide and nitrogen dioxide were also associated with an increased risk of stroke and death, but the associations were weaker.
“More research is needed, but it’s possible that decreasing exposure to heavy levels of air pollution could play a role in reducing the progression of stroke,” Dr. Lin said.
“People can reduce their exposure by staying indoors on heavy pollution days, reducing their outdoor exercise, wearing masks to filter out particulate matter, and using air purifiers,” Dr. Lin added.
Public policy implications
Reached for comment, Steffen E. Petersen, MD, MPH, professor of cardiovascular medicine, Barts Health NHS Trust, London, said the study “elegantly confirms the increased risk of stroke due to air pollution in the UK Biobank population study but interestingly suggests that the impact of air pollution may continue to adversely impact cardiovascular health even after the stroke occurred.”
“This is further evidence to inform policymakers to tackle air pollution and get levels below the recommended levels,” Dr. Petersen said.
“On a personal level, everyone, including stroke patients, may wish to consider personal measures to reduce exposure to air pollution, such as avoiding walking along polluted streets and rather take a less polluted route away from the main roads,” Dr. Petersen added.
The study had no targeted funding. Dr. Lin and Dr. Petersen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a UK biobank study show high levels of air pollution were associated with an increased risk of transition from health to a first stroke and subsequent progression to cardiovascular (CV) events and death.
“These results indicate that understanding and reducing the effects of air pollutants on different transition stages in stroke will be beneficial in managing people’s health and preventing the occurrence and progression of stroke,” study investigator Hualiang Lin, PhD, of Sun Yat-sen University School of Public Health, Guangzhou, China, said in a news release.
The study was published online in the journal Neurology.
A way to stop stroke progression?
The researchers assessed air pollution exposure in 318,752 people (mean age, 56) from the UK biobank database. None had a history of stroke or heart disease at the start of the study. Annual concentrations of air pollution near where people lived were estimated through land-use regressions.
During an average follow-up of 12 years, 5,967 people had a stroke, 2,985 developed post-stroke CVD, and 1,020 died.
After adjusting for confounding factors, every 5 µg/m3 increase in exposure to fine particulate matter (PM2.5) was associated with a 24% increase in transition from healthy to first stroke (hazard ratio, 1.24; 95% confidence interval, 1.10-1.40) and a 30% increase in transition from being healthy to dying (HR, 1.30; 95% CI, 1.21-1.40).
PM2.5 is less than 2.5 microns in diameter and includes fly ash from coal combustion. The World Health Organization recommends that annual PM2.5 exposure should not exceed 5 µg/m3.
Those who had a stroke during the study had an average exposure of 10.03 µg/m3 of PM2.5, compared with 9.97 µg/m3 for those who did not have a stroke.
The air pollutants nitrogen oxide and nitrogen dioxide were also associated with an increased risk of stroke and death, but the associations were weaker.
“More research is needed, but it’s possible that decreasing exposure to heavy levels of air pollution could play a role in reducing the progression of stroke,” Dr. Lin said.
“People can reduce their exposure by staying indoors on heavy pollution days, reducing their outdoor exercise, wearing masks to filter out particulate matter, and using air purifiers,” Dr. Lin added.
Public policy implications
Reached for comment, Steffen E. Petersen, MD, MPH, professor of cardiovascular medicine, Barts Health NHS Trust, London, said the study “elegantly confirms the increased risk of stroke due to air pollution in the UK Biobank population study but interestingly suggests that the impact of air pollution may continue to adversely impact cardiovascular health even after the stroke occurred.”
“This is further evidence to inform policymakers to tackle air pollution and get levels below the recommended levels,” Dr. Petersen said.
“On a personal level, everyone, including stroke patients, may wish to consider personal measures to reduce exposure to air pollution, such as avoiding walking along polluted streets and rather take a less polluted route away from the main roads,” Dr. Petersen added.
The study had no targeted funding. Dr. Lin and Dr. Petersen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pumping iron improves longevity in older adults
with the strongest effects observed when the two types of exercise are combined, new research shows.
“The novel finding from our study is that weight lifting is independently associated with lower all-cause and CVD-specific mortality, regardless of aerobic activity,” first author Jessica Gorzelitz, PhD, said in an interview.
“What’s less surprising – but consistent and nonetheless noteworthy – is that weight lifting in combination with aerobic exercise provides the lowest...risk for mortality in older adults,” added Dr. Gorzelitz, an assistant professor of health promotion in the department of health and human physiology at the University of Iowa, Iowa City.
Those who undertook weight lifting and aerobic exercise in combination had around a 40% lower risk of death than those who reported no moderate to vigorous aerobic activity or weight lifting. The findings were recently published online in the British Journal of Sports Medicine.
Physical activity guidelines generally recommend regular moderate to vigorous aerobic physical activity, in addition to at least 2 days per week of muscle-strengthening exercise for all major muscle groups for adults to improve health and boost longevity.
However, few observational studies have examined the association between muscle strengthening and mortality, and even fewer have looked specifically at the benefits of weight lifting, Dr. Gorzelitz said.
Benefit of weight lifting stronger in women than men
To investigate, Dr. Gorzelitz and coauthors evaluated data on participants in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial, which, initiated in 1993, and involved adults aged 55-74 at 10 U.S. cancer centers.
Thirteen years into the trial, in 2006, participants completed follow-up questionnaires that included an assessment of weight lifting (not included in a baseline survey).
Among 99,713 participants involved in the current analysis, the mean age at the time of the follow-up questionnaire was 71.3 years. Participants had a mean body mass index of 27.8 kg/m2 and 52.6% were women.
Only about a quarter of adults (23%) reported any weight lifting activity within the previous 12 months, with fewer, at 16%, reporting regular weight lifting of between one and six times per week.
Participants’ physical aerobic activity was also assessed. Physical activity guidelines (2018) recommend at least 150-300 minutes per week of moderate-intensity aerobic physical activity or 75-150 minutes per week of vigorous intensity aerobic activity or an equal combination of the two. Overall, 23.6% of participants reported activity that met the guideline for moderate to vigorous physical activity, and 8% exceeded it.
Over a median follow-up of about 9 years, 28,477 deaths occurred.
Those reporting weight lifting had a 9% lower risk of combined all-cause mortality and CVD mortality, after adjustment for any moderate to vigorous physical activity (each hazard ratio, 0.91).
Adults who met aerobic activity recommendations but did not weight lift had a 32% lower risk of all-cause mortality (HR, 0.68), while those who also reported weight lifting 1-2 times per week in addition to the aerobic activity had as much as a 41% lower risk of death (HR, 0.59), compared with adults reporting no moderate to vigorous aerobic activity or weight lifting.
The benefit of weight lifting in terms of cancer mortality was only observed without adjustment for moderate to vigorous physical activity, and was therefore considered null, which Dr. Gorzelitz said was somewhat surprising. “We will examine this association further because there could still be a signal there,” she said, noting other studies have shown that muscle strengthening activity is associated with lower cancer-specific mortality.
Of note, the benefit of weight lifting appeared stronger in women versus men, Dr. Gorzelitz said.
What are the mechanisms?
Underscoring that the results show only associations and not causation, Dr. Gorzelitz speculated that mechanisms behind a mortality benefit could include known favorable physiological changes of weight lifting.
“If people are weight lifting [to a degree] to reap strength benefits, we generally see improvement in body composition, including reductions in fat and improvements in lean tissue, and we know that those changes are associated with mortality, so it could be that the weight lifting is driving the strength or body composition,” she said.
The full body response involved in weight lifting could also play a key role, she noted.
With weight lifting, “the muscles have to redirect more blood flow, the heart is pumping harder, the lungs breathe more and when the muscles are worked in that fashion, there could be other system-wide adaptations,” she said.
Furthermore, social aspects could play a role, Dr. Gorzelitz observed.
“Unlike muscle strengthening [activities] that can be done in the home setting, weight lifting typically has to be done in recreational facilities or other community centers, and considering that this is an older adult population, that social interaction could be very key for preventing isolation.”
Important limitations include that the study did not determine the nature of the weight lifting, including the duration of the weight lifting sessions or type of weight, which could feasibly range from small hand-held weights to heavier weight lifting.
The study also couldn’t show how long participants had engaged in weight lifting in terms of months or years, hence, the duration needed to see a mortality benefit was not established.
Nevertheless, the study’s finding that the group with the lowest benefits was the one reporting no aerobic or weight lifting exercise underscores the benefits of even small amounts of exercise.
“I think it’s really important to promote the importance of adding muscle strengthening, but also of any physical activity,” Dr. Gorzelitz said. “Start small, but something is better than nothing.”
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
with the strongest effects observed when the two types of exercise are combined, new research shows.
“The novel finding from our study is that weight lifting is independently associated with lower all-cause and CVD-specific mortality, regardless of aerobic activity,” first author Jessica Gorzelitz, PhD, said in an interview.
“What’s less surprising – but consistent and nonetheless noteworthy – is that weight lifting in combination with aerobic exercise provides the lowest...risk for mortality in older adults,” added Dr. Gorzelitz, an assistant professor of health promotion in the department of health and human physiology at the University of Iowa, Iowa City.
Those who undertook weight lifting and aerobic exercise in combination had around a 40% lower risk of death than those who reported no moderate to vigorous aerobic activity or weight lifting. The findings were recently published online in the British Journal of Sports Medicine.
Physical activity guidelines generally recommend regular moderate to vigorous aerobic physical activity, in addition to at least 2 days per week of muscle-strengthening exercise for all major muscle groups for adults to improve health and boost longevity.
However, few observational studies have examined the association between muscle strengthening and mortality, and even fewer have looked specifically at the benefits of weight lifting, Dr. Gorzelitz said.
Benefit of weight lifting stronger in women than men
To investigate, Dr. Gorzelitz and coauthors evaluated data on participants in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial, which, initiated in 1993, and involved adults aged 55-74 at 10 U.S. cancer centers.
Thirteen years into the trial, in 2006, participants completed follow-up questionnaires that included an assessment of weight lifting (not included in a baseline survey).
Among 99,713 participants involved in the current analysis, the mean age at the time of the follow-up questionnaire was 71.3 years. Participants had a mean body mass index of 27.8 kg/m2 and 52.6% were women.
Only about a quarter of adults (23%) reported any weight lifting activity within the previous 12 months, with fewer, at 16%, reporting regular weight lifting of between one and six times per week.
Participants’ physical aerobic activity was also assessed. Physical activity guidelines (2018) recommend at least 150-300 minutes per week of moderate-intensity aerobic physical activity or 75-150 minutes per week of vigorous intensity aerobic activity or an equal combination of the two. Overall, 23.6% of participants reported activity that met the guideline for moderate to vigorous physical activity, and 8% exceeded it.
Over a median follow-up of about 9 years, 28,477 deaths occurred.
Those reporting weight lifting had a 9% lower risk of combined all-cause mortality and CVD mortality, after adjustment for any moderate to vigorous physical activity (each hazard ratio, 0.91).
Adults who met aerobic activity recommendations but did not weight lift had a 32% lower risk of all-cause mortality (HR, 0.68), while those who also reported weight lifting 1-2 times per week in addition to the aerobic activity had as much as a 41% lower risk of death (HR, 0.59), compared with adults reporting no moderate to vigorous aerobic activity or weight lifting.
The benefit of weight lifting in terms of cancer mortality was only observed without adjustment for moderate to vigorous physical activity, and was therefore considered null, which Dr. Gorzelitz said was somewhat surprising. “We will examine this association further because there could still be a signal there,” she said, noting other studies have shown that muscle strengthening activity is associated with lower cancer-specific mortality.
Of note, the benefit of weight lifting appeared stronger in women versus men, Dr. Gorzelitz said.
What are the mechanisms?
Underscoring that the results show only associations and not causation, Dr. Gorzelitz speculated that mechanisms behind a mortality benefit could include known favorable physiological changes of weight lifting.
“If people are weight lifting [to a degree] to reap strength benefits, we generally see improvement in body composition, including reductions in fat and improvements in lean tissue, and we know that those changes are associated with mortality, so it could be that the weight lifting is driving the strength or body composition,” she said.
The full body response involved in weight lifting could also play a key role, she noted.
With weight lifting, “the muscles have to redirect more blood flow, the heart is pumping harder, the lungs breathe more and when the muscles are worked in that fashion, there could be other system-wide adaptations,” she said.
Furthermore, social aspects could play a role, Dr. Gorzelitz observed.
“Unlike muscle strengthening [activities] that can be done in the home setting, weight lifting typically has to be done in recreational facilities or other community centers, and considering that this is an older adult population, that social interaction could be very key for preventing isolation.”
Important limitations include that the study did not determine the nature of the weight lifting, including the duration of the weight lifting sessions or type of weight, which could feasibly range from small hand-held weights to heavier weight lifting.
The study also couldn’t show how long participants had engaged in weight lifting in terms of months or years, hence, the duration needed to see a mortality benefit was not established.
Nevertheless, the study’s finding that the group with the lowest benefits was the one reporting no aerobic or weight lifting exercise underscores the benefits of even small amounts of exercise.
“I think it’s really important to promote the importance of adding muscle strengthening, but also of any physical activity,” Dr. Gorzelitz said. “Start small, but something is better than nothing.”
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
with the strongest effects observed when the two types of exercise are combined, new research shows.
“The novel finding from our study is that weight lifting is independently associated with lower all-cause and CVD-specific mortality, regardless of aerobic activity,” first author Jessica Gorzelitz, PhD, said in an interview.
“What’s less surprising – but consistent and nonetheless noteworthy – is that weight lifting in combination with aerobic exercise provides the lowest...risk for mortality in older adults,” added Dr. Gorzelitz, an assistant professor of health promotion in the department of health and human physiology at the University of Iowa, Iowa City.
Those who undertook weight lifting and aerobic exercise in combination had around a 40% lower risk of death than those who reported no moderate to vigorous aerobic activity or weight lifting. The findings were recently published online in the British Journal of Sports Medicine.
Physical activity guidelines generally recommend regular moderate to vigorous aerobic physical activity, in addition to at least 2 days per week of muscle-strengthening exercise for all major muscle groups for adults to improve health and boost longevity.
However, few observational studies have examined the association between muscle strengthening and mortality, and even fewer have looked specifically at the benefits of weight lifting, Dr. Gorzelitz said.
Benefit of weight lifting stronger in women than men
To investigate, Dr. Gorzelitz and coauthors evaluated data on participants in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial, which, initiated in 1993, and involved adults aged 55-74 at 10 U.S. cancer centers.
Thirteen years into the trial, in 2006, participants completed follow-up questionnaires that included an assessment of weight lifting (not included in a baseline survey).
Among 99,713 participants involved in the current analysis, the mean age at the time of the follow-up questionnaire was 71.3 years. Participants had a mean body mass index of 27.8 kg/m2 and 52.6% were women.
Only about a quarter of adults (23%) reported any weight lifting activity within the previous 12 months, with fewer, at 16%, reporting regular weight lifting of between one and six times per week.
Participants’ physical aerobic activity was also assessed. Physical activity guidelines (2018) recommend at least 150-300 minutes per week of moderate-intensity aerobic physical activity or 75-150 minutes per week of vigorous intensity aerobic activity or an equal combination of the two. Overall, 23.6% of participants reported activity that met the guideline for moderate to vigorous physical activity, and 8% exceeded it.
Over a median follow-up of about 9 years, 28,477 deaths occurred.
Those reporting weight lifting had a 9% lower risk of combined all-cause mortality and CVD mortality, after adjustment for any moderate to vigorous physical activity (each hazard ratio, 0.91).
Adults who met aerobic activity recommendations but did not weight lift had a 32% lower risk of all-cause mortality (HR, 0.68), while those who also reported weight lifting 1-2 times per week in addition to the aerobic activity had as much as a 41% lower risk of death (HR, 0.59), compared with adults reporting no moderate to vigorous aerobic activity or weight lifting.
The benefit of weight lifting in terms of cancer mortality was only observed without adjustment for moderate to vigorous physical activity, and was therefore considered null, which Dr. Gorzelitz said was somewhat surprising. “We will examine this association further because there could still be a signal there,” she said, noting other studies have shown that muscle strengthening activity is associated with lower cancer-specific mortality.
Of note, the benefit of weight lifting appeared stronger in women versus men, Dr. Gorzelitz said.
What are the mechanisms?
Underscoring that the results show only associations and not causation, Dr. Gorzelitz speculated that mechanisms behind a mortality benefit could include known favorable physiological changes of weight lifting.
“If people are weight lifting [to a degree] to reap strength benefits, we generally see improvement in body composition, including reductions in fat and improvements in lean tissue, and we know that those changes are associated with mortality, so it could be that the weight lifting is driving the strength or body composition,” she said.
The full body response involved in weight lifting could also play a key role, she noted.
With weight lifting, “the muscles have to redirect more blood flow, the heart is pumping harder, the lungs breathe more and when the muscles are worked in that fashion, there could be other system-wide adaptations,” she said.
Furthermore, social aspects could play a role, Dr. Gorzelitz observed.
“Unlike muscle strengthening [activities] that can be done in the home setting, weight lifting typically has to be done in recreational facilities or other community centers, and considering that this is an older adult population, that social interaction could be very key for preventing isolation.”
Important limitations include that the study did not determine the nature of the weight lifting, including the duration of the weight lifting sessions or type of weight, which could feasibly range from small hand-held weights to heavier weight lifting.
The study also couldn’t show how long participants had engaged in weight lifting in terms of months or years, hence, the duration needed to see a mortality benefit was not established.
Nevertheless, the study’s finding that the group with the lowest benefits was the one reporting no aerobic or weight lifting exercise underscores the benefits of even small amounts of exercise.
“I think it’s really important to promote the importance of adding muscle strengthening, but also of any physical activity,” Dr. Gorzelitz said. “Start small, but something is better than nothing.”
The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF SPORTS MEDICINE
Physicians speak out: Why they love or hate incentive bonuses
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Three COVID scenarios that could spell trouble for the fall
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nifedipine during labor controls BP in severe preeclampsia
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Long-term antidepressant use tied to an increase in CVD, mortality risk
The investigators drew on 10-year data from the UK Biobank on over 220,000 adults and compared the risk of developing adverse health outcomes among those taking antidepressants with the risk among those who were not taking antidepressants.
After adjusting for preexisting risk factors, they found that 10-year antidepressant use was associated with a twofold higher risk of CHD, an almost-twofold higher risk of CVD as well as CVD mortality, a higher risk of cerebrovascular disease, and more than double the risk of all-cause mortality.
On the other hand, at 10 years, antidepressant use was associated with a 23% lower risk of developing hypertension and a 32% lower risk of diabetes.
The main culprits were mirtazapine, venlafaxine, duloxetine, and trazodone, although SSRIs were also tied to increased risk.
“Our message for clinicians is that prescribing of antidepressants in the long term may not be harm free [and] we hope that this study will help doctors and patients have more informed conversations when they weigh up the potential risks and benefits of treatments for depression,” study investigator Narinder Bansal, MD, honorary research fellow, Centre for Academic Health and Centre for Academic Primary Care, University of Bristol (England), said in a news release.
“Regardless of whether the drugs are the underlying cause of these problems, our findings emphasize the importance of proactive cardiovascular monitoring and prevention in patients who have depression and are on antidepressants, given that both have been associated with higher risks,” she added.
The study was published online in the British Journal of Psychiatry Open.
Monitoring of CVD risk ‘critical’
Antidepressants are among the most widely prescribed drugs; 70 million prescriptions were dispensed in 2018 alone, representing a doubling of prescriptions for these agents in a decade, the investigators noted. “This striking rise in prescribing is attributed to long-term treatment rather than an increased incidence of depression.”
Most trials that have assessed antidepressant efficacy have been “poorly suited to examining adverse outcomes.” One reason for this is that many of the trials are short-term studies. Since depression is “strongly associated” with CVD risk factors, “careful assessment of the long-term cardiometabolic effects of antidepressant treatment is critical.”
Moreover, information about “a wide range of prospectively measured confounders ... is needed to provide robust estimates of the risks associated with long-term antidepressant use,” the authors noted.
The researchers examined the association between antidepressant use and four cardiometabolic morbidity outcomes – diabetes, hypertension, cerebrovascular disease, and CHD. In addition, they assessed two mortality outcomes – CVD mortality and all-cause mortality. Participants were divided into cohorts on the basis of outcome of interest.
The dataset contains detailed information on socioeconomic status, demographics, anthropometric, behavioral, and biochemical risk factors, disability, and health status and is linked to datasets of primary care records and deaths.
The study included 222,121 participants whose data had been linked to primary care records during 2018 (median age of participants, 56-57 years). About half were women, and 96% were of White ethnicity.
Participants were excluded if they had been prescribed antidepressants 12 months or less before baseline, if they had previously been diagnosed for the outcome of interest, if they had been previously prescribed psychotropic drugs, if they used cardiometabolic drugs at baseline, or if they had undergone treatment with antidepressant polytherapy.
Potential confounders included age, gender, body mass index, waist/hip ratio, smoking and alcohol intake status, physical activity, parental history of outcome, biochemical and hematologic biomarkers, socioeconomic status, and long-term illness, disability, or infirmity.
Mechanism unclear
By the end of the 5- and 10-year follow-up periods, an average of 8% and 6% of participants in each cohort, respectively, had been prescribed an antidepressant. SSRIs constituted the most commonly prescribed class (80%-82%), and citalopram was the most commonly prescribed SSRI (46%-47%). Mirtazapine was the most frequently prescribed non-SSRI antidepressant (44%-46%).
At 5 years, any antidepressant use was associated with an increased risk for diabetes, CHD, and all-cause mortality, but the findings were attenuated after further adjustment for confounders. In fact, SSRIs were associated with a reduced risk of diabetes at 5 years (hazard ratio, 0.64; 95% confidence interval, 0.49-0.83).
At 10 years, SSRIs were associated with an increased risk of cerebrovascular disease, CVD mortality, and all-cause mortality; non-SSRIs were associated with an increased risk of CHD, CVD, and all-cause mortality.
On the other hand, SSRIs were associated with a decrease in risk of diabetes and hypertension at 10 years (HR, 0.68; 95% CI, 0.53-0.87; and HR, 0.77; 95% CI, 0.66-0.89, respectively).
“While we have taken into account a wide range of pre-existing risk factors for cardiovascular disease, including those that are linked to depression such as excess weight, smoking, and low physical activity, it is difficult to fully control for the effects of depression in this kind of study, partly because there is considerable variability in the recording of depression severity in primary care,” said Dr. Bansal.
“This is important because many people taking antidepressants such as mirtazapine, venlafaxine, duloxetine and trazodone may have a more severe depression. This makes it difficult to fully separate the effects of the depression from the effects of medication,” she said.
Further research “is needed to assess whether the associations we have seen are genuinely due to the drugs; and, if so, why this might be,” she added.
Strengths, limitations
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology and head of the mood disorders psychopharmacology unit at the University of Toronto,, discussed the strengths and weaknesses of the study.
The UK Biobank is a “well-described, well-phenotyped dataset of good quality,” said Dr. McIntyre, chairperson and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study. Another strength is the “impressive number of variables the database contains, which enabled the authors to go much deeper into the topics.”
A “significant limitation” is the confounding that is inherent to the disorder itself – “people with depression have a much higher intrinsic risk of CVD, [cerebrovascular disease], and cardiovascular mortality,” Dr. McIntyre noted.
The researchers did not adjust for trauma or childhood maltreatment, “which are the biggest risk factors for both depression and CVD; and drug and alcohol misuse were also not accounted for.”
Additionally, “to determine whether something is an association or potentially causative, it must satisfy the Bradford-Hill criteria,” said Dr. McIntyre. “Since we’re moving more toward using these big databases and because we depend on them to give us long-term perspectives, we would want to see coherent, compelling Bradford-Hill criteria regarding causation. If you don’t have any, that’s fine too, but then it’s important to make clear that there is no clear causative line, just an association.”
The research was funded by the National Institute of Health Research School for Primary Care Research and was supported by the NI Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol. Dr. McIntyre has received research grant support from CI/GACD/National Natural Science Foundation of China and the Milken Institute and speaker/consultation fees from numerous companies. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
The investigators drew on 10-year data from the UK Biobank on over 220,000 adults and compared the risk of developing adverse health outcomes among those taking antidepressants with the risk among those who were not taking antidepressants.
After adjusting for preexisting risk factors, they found that 10-year antidepressant use was associated with a twofold higher risk of CHD, an almost-twofold higher risk of CVD as well as CVD mortality, a higher risk of cerebrovascular disease, and more than double the risk of all-cause mortality.
On the other hand, at 10 years, antidepressant use was associated with a 23% lower risk of developing hypertension and a 32% lower risk of diabetes.
The main culprits were mirtazapine, venlafaxine, duloxetine, and trazodone, although SSRIs were also tied to increased risk.
“Our message for clinicians is that prescribing of antidepressants in the long term may not be harm free [and] we hope that this study will help doctors and patients have more informed conversations when they weigh up the potential risks and benefits of treatments for depression,” study investigator Narinder Bansal, MD, honorary research fellow, Centre for Academic Health and Centre for Academic Primary Care, University of Bristol (England), said in a news release.
“Regardless of whether the drugs are the underlying cause of these problems, our findings emphasize the importance of proactive cardiovascular monitoring and prevention in patients who have depression and are on antidepressants, given that both have been associated with higher risks,” she added.
The study was published online in the British Journal of Psychiatry Open.
Monitoring of CVD risk ‘critical’
Antidepressants are among the most widely prescribed drugs; 70 million prescriptions were dispensed in 2018 alone, representing a doubling of prescriptions for these agents in a decade, the investigators noted. “This striking rise in prescribing is attributed to long-term treatment rather than an increased incidence of depression.”
Most trials that have assessed antidepressant efficacy have been “poorly suited to examining adverse outcomes.” One reason for this is that many of the trials are short-term studies. Since depression is “strongly associated” with CVD risk factors, “careful assessment of the long-term cardiometabolic effects of antidepressant treatment is critical.”
Moreover, information about “a wide range of prospectively measured confounders ... is needed to provide robust estimates of the risks associated with long-term antidepressant use,” the authors noted.
The researchers examined the association between antidepressant use and four cardiometabolic morbidity outcomes – diabetes, hypertension, cerebrovascular disease, and CHD. In addition, they assessed two mortality outcomes – CVD mortality and all-cause mortality. Participants were divided into cohorts on the basis of outcome of interest.
The dataset contains detailed information on socioeconomic status, demographics, anthropometric, behavioral, and biochemical risk factors, disability, and health status and is linked to datasets of primary care records and deaths.
The study included 222,121 participants whose data had been linked to primary care records during 2018 (median age of participants, 56-57 years). About half were women, and 96% were of White ethnicity.
Participants were excluded if they had been prescribed antidepressants 12 months or less before baseline, if they had previously been diagnosed for the outcome of interest, if they had been previously prescribed psychotropic drugs, if they used cardiometabolic drugs at baseline, or if they had undergone treatment with antidepressant polytherapy.
Potential confounders included age, gender, body mass index, waist/hip ratio, smoking and alcohol intake status, physical activity, parental history of outcome, biochemical and hematologic biomarkers, socioeconomic status, and long-term illness, disability, or infirmity.
Mechanism unclear
By the end of the 5- and 10-year follow-up periods, an average of 8% and 6% of participants in each cohort, respectively, had been prescribed an antidepressant. SSRIs constituted the most commonly prescribed class (80%-82%), and citalopram was the most commonly prescribed SSRI (46%-47%). Mirtazapine was the most frequently prescribed non-SSRI antidepressant (44%-46%).
At 5 years, any antidepressant use was associated with an increased risk for diabetes, CHD, and all-cause mortality, but the findings were attenuated after further adjustment for confounders. In fact, SSRIs were associated with a reduced risk of diabetes at 5 years (hazard ratio, 0.64; 95% confidence interval, 0.49-0.83).
At 10 years, SSRIs were associated with an increased risk of cerebrovascular disease, CVD mortality, and all-cause mortality; non-SSRIs were associated with an increased risk of CHD, CVD, and all-cause mortality.
On the other hand, SSRIs were associated with a decrease in risk of diabetes and hypertension at 10 years (HR, 0.68; 95% CI, 0.53-0.87; and HR, 0.77; 95% CI, 0.66-0.89, respectively).
“While we have taken into account a wide range of pre-existing risk factors for cardiovascular disease, including those that are linked to depression such as excess weight, smoking, and low physical activity, it is difficult to fully control for the effects of depression in this kind of study, partly because there is considerable variability in the recording of depression severity in primary care,” said Dr. Bansal.
“This is important because many people taking antidepressants such as mirtazapine, venlafaxine, duloxetine and trazodone may have a more severe depression. This makes it difficult to fully separate the effects of the depression from the effects of medication,” she said.
Further research “is needed to assess whether the associations we have seen are genuinely due to the drugs; and, if so, why this might be,” she added.
Strengths, limitations
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology and head of the mood disorders psychopharmacology unit at the University of Toronto,, discussed the strengths and weaknesses of the study.
The UK Biobank is a “well-described, well-phenotyped dataset of good quality,” said Dr. McIntyre, chairperson and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study. Another strength is the “impressive number of variables the database contains, which enabled the authors to go much deeper into the topics.”
A “significant limitation” is the confounding that is inherent to the disorder itself – “people with depression have a much higher intrinsic risk of CVD, [cerebrovascular disease], and cardiovascular mortality,” Dr. McIntyre noted.
The researchers did not adjust for trauma or childhood maltreatment, “which are the biggest risk factors for both depression and CVD; and drug and alcohol misuse were also not accounted for.”
Additionally, “to determine whether something is an association or potentially causative, it must satisfy the Bradford-Hill criteria,” said Dr. McIntyre. “Since we’re moving more toward using these big databases and because we depend on them to give us long-term perspectives, we would want to see coherent, compelling Bradford-Hill criteria regarding causation. If you don’t have any, that’s fine too, but then it’s important to make clear that there is no clear causative line, just an association.”
The research was funded by the National Institute of Health Research School for Primary Care Research and was supported by the NI Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol. Dr. McIntyre has received research grant support from CI/GACD/National Natural Science Foundation of China and the Milken Institute and speaker/consultation fees from numerous companies. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
The investigators drew on 10-year data from the UK Biobank on over 220,000 adults and compared the risk of developing adverse health outcomes among those taking antidepressants with the risk among those who were not taking antidepressants.
After adjusting for preexisting risk factors, they found that 10-year antidepressant use was associated with a twofold higher risk of CHD, an almost-twofold higher risk of CVD as well as CVD mortality, a higher risk of cerebrovascular disease, and more than double the risk of all-cause mortality.
On the other hand, at 10 years, antidepressant use was associated with a 23% lower risk of developing hypertension and a 32% lower risk of diabetes.
The main culprits were mirtazapine, venlafaxine, duloxetine, and trazodone, although SSRIs were also tied to increased risk.
“Our message for clinicians is that prescribing of antidepressants in the long term may not be harm free [and] we hope that this study will help doctors and patients have more informed conversations when they weigh up the potential risks and benefits of treatments for depression,” study investigator Narinder Bansal, MD, honorary research fellow, Centre for Academic Health and Centre for Academic Primary Care, University of Bristol (England), said in a news release.
“Regardless of whether the drugs are the underlying cause of these problems, our findings emphasize the importance of proactive cardiovascular monitoring and prevention in patients who have depression and are on antidepressants, given that both have been associated with higher risks,” she added.
The study was published online in the British Journal of Psychiatry Open.
Monitoring of CVD risk ‘critical’
Antidepressants are among the most widely prescribed drugs; 70 million prescriptions were dispensed in 2018 alone, representing a doubling of prescriptions for these agents in a decade, the investigators noted. “This striking rise in prescribing is attributed to long-term treatment rather than an increased incidence of depression.”
Most trials that have assessed antidepressant efficacy have been “poorly suited to examining adverse outcomes.” One reason for this is that many of the trials are short-term studies. Since depression is “strongly associated” with CVD risk factors, “careful assessment of the long-term cardiometabolic effects of antidepressant treatment is critical.”
Moreover, information about “a wide range of prospectively measured confounders ... is needed to provide robust estimates of the risks associated with long-term antidepressant use,” the authors noted.
The researchers examined the association between antidepressant use and four cardiometabolic morbidity outcomes – diabetes, hypertension, cerebrovascular disease, and CHD. In addition, they assessed two mortality outcomes – CVD mortality and all-cause mortality. Participants were divided into cohorts on the basis of outcome of interest.
The dataset contains detailed information on socioeconomic status, demographics, anthropometric, behavioral, and biochemical risk factors, disability, and health status and is linked to datasets of primary care records and deaths.
The study included 222,121 participants whose data had been linked to primary care records during 2018 (median age of participants, 56-57 years). About half were women, and 96% were of White ethnicity.
Participants were excluded if they had been prescribed antidepressants 12 months or less before baseline, if they had previously been diagnosed for the outcome of interest, if they had been previously prescribed psychotropic drugs, if they used cardiometabolic drugs at baseline, or if they had undergone treatment with antidepressant polytherapy.
Potential confounders included age, gender, body mass index, waist/hip ratio, smoking and alcohol intake status, physical activity, parental history of outcome, biochemical and hematologic biomarkers, socioeconomic status, and long-term illness, disability, or infirmity.
Mechanism unclear
By the end of the 5- and 10-year follow-up periods, an average of 8% and 6% of participants in each cohort, respectively, had been prescribed an antidepressant. SSRIs constituted the most commonly prescribed class (80%-82%), and citalopram was the most commonly prescribed SSRI (46%-47%). Mirtazapine was the most frequently prescribed non-SSRI antidepressant (44%-46%).
At 5 years, any antidepressant use was associated with an increased risk for diabetes, CHD, and all-cause mortality, but the findings were attenuated after further adjustment for confounders. In fact, SSRIs were associated with a reduced risk of diabetes at 5 years (hazard ratio, 0.64; 95% confidence interval, 0.49-0.83).
At 10 years, SSRIs were associated with an increased risk of cerebrovascular disease, CVD mortality, and all-cause mortality; non-SSRIs were associated with an increased risk of CHD, CVD, and all-cause mortality.
On the other hand, SSRIs were associated with a decrease in risk of diabetes and hypertension at 10 years (HR, 0.68; 95% CI, 0.53-0.87; and HR, 0.77; 95% CI, 0.66-0.89, respectively).
“While we have taken into account a wide range of pre-existing risk factors for cardiovascular disease, including those that are linked to depression such as excess weight, smoking, and low physical activity, it is difficult to fully control for the effects of depression in this kind of study, partly because there is considerable variability in the recording of depression severity in primary care,” said Dr. Bansal.
“This is important because many people taking antidepressants such as mirtazapine, venlafaxine, duloxetine and trazodone may have a more severe depression. This makes it difficult to fully separate the effects of the depression from the effects of medication,” she said.
Further research “is needed to assess whether the associations we have seen are genuinely due to the drugs; and, if so, why this might be,” she added.
Strengths, limitations
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology and head of the mood disorders psychopharmacology unit at the University of Toronto,, discussed the strengths and weaknesses of the study.
The UK Biobank is a “well-described, well-phenotyped dataset of good quality,” said Dr. McIntyre, chairperson and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study. Another strength is the “impressive number of variables the database contains, which enabled the authors to go much deeper into the topics.”
A “significant limitation” is the confounding that is inherent to the disorder itself – “people with depression have a much higher intrinsic risk of CVD, [cerebrovascular disease], and cardiovascular mortality,” Dr. McIntyre noted.
The researchers did not adjust for trauma or childhood maltreatment, “which are the biggest risk factors for both depression and CVD; and drug and alcohol misuse were also not accounted for.”
Additionally, “to determine whether something is an association or potentially causative, it must satisfy the Bradford-Hill criteria,” said Dr. McIntyre. “Since we’re moving more toward using these big databases and because we depend on them to give us long-term perspectives, we would want to see coherent, compelling Bradford-Hill criteria regarding causation. If you don’t have any, that’s fine too, but then it’s important to make clear that there is no clear causative line, just an association.”
The research was funded by the National Institute of Health Research School for Primary Care Research and was supported by the NI Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol. Dr. McIntyre has received research grant support from CI/GACD/National Natural Science Foundation of China and the Milken Institute and speaker/consultation fees from numerous companies. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF PSYCHIATRY OPEN
Too old to practice medicine?
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Eating earlier offers health benefits, studies say
New research suggests there may be better times during the day for eating and fasting.
Eating earlier in the day may help you lose weight, and eating meals within a 10-hour window could improve blood sugar and cholesterol levels, according to two new studies published in Cell Metabolism.
“You have this internal biological clock that makes you better at doing different things at different times of the day,” Courtney Peterson, PhD, an associate professor of nutrition sciences at the University of Alabama at Birmingham, told NBC News. Dr. Peterson wasn’t involved with the studies.
“It seems like the best time for your metabolism, in most people, is the mid to late morning,” she said.
In one study, researchers found that eating later in the day made people hungrier during a 24-hour period, as compared with eating the same meals earlier in the day. Combined, the changes may increase the risk for obesity, the study authors found.
In another study, among firefighters as shift workers, researchers found that eating meals within a 10-hour window decreased the size of bad cholesterol particles, which could reduce risk factors for heart disease. The 10-hour eating window also improved blood pressure and blood sugar levels among those with health conditions such as diabetes, high blood pressure, and high cholesterol.
The two new studies confirm findings from previous studies that indicate humans may have an ideal eating window based on the body’s circadian rhythms, which regulate sleep and wake cycles and can affect appetite, metabolism, and blood sugar levels.
In the firefighter study, for instance, the 10-hour window appears to be a “sweet spot” for the body, the authors found. More severe restrictions, as found with many intermittent fasting diets, could be difficult for the body to maintain.
“When we think about 6 or 8 hours, you might see a benefit, but people might not stick to it for a long time,” Satchidananda Panda, PhD, one of the study authors and a professor at the Salk Institute, La Jolla, Calif., told NBC News.
The new studies had small sample sizes, though they offer insight for future research. In the first study, 16 people who were overweight or obese tried two eating plans for 24-hour periods. Some of them began eating an hour after their natural wake-up time, and others waited to begin eating until about 5 hours after waking up. They ate the same meals with the same calories and nutrients.
The researchers measured their hormone levels and found that eating later decreased the levels of leptin, which helps people to feel full. Eating later also doubled the odds that people felt hungry throughout the day. Those in the study who ate later in the day also had more cravings for starchy or salty foods, as well as meat and dairy, which are energy-dense foods.
The research team also found changes in fat tissue, which could lead to a higher chance of building up new fat cells and a lower chance of burning fat. Late eaters burned about 60 fewer calories than early eaters during the day.
“Your body processes calories differently when you eat late in the day. It tips the scale in favor of weight gain and fat gain,” Dr. Peterson said. “From this study, we can get pretty clear recommendations that people shouldn’t skip breakfast.”
The second study followed 137 firefighters in San Diego who ate a Mediterranean diet with fish, vegetables, fruit, and olive oil for 12 weeks. Among those, 70 firefighters ate during a 10-hour window, and the rest ate during a longer window, generally about 13 hours. They logged their meals in an app and wore devices to track blood sugar levels.
In the 10-hour group, most firefighters ate between 8 a.m. or 9 a.m. and 6 p.m. or 7 p.m. The time-restricted eating appeared to be linked with health benefits, such as less harmful cholesterol buildup and reduced heart disease.
Among firefighters with risk factors for heart disease, such as high blood pressure and high blood sugar, the time-restricted eating decreased their blood pressure and blood sugar levels.
The restricted window appears to allow the body to break down toxins and get rid of sodium and other things that can drive up blood pressure and blood sugar, the authors wrote.
During periods of fasting, “organs get some rest from digesting food so they can divert their energy toward repairing cells,” Dr. Panda said.
A version of this article first appeared on WebMD.com.
New research suggests there may be better times during the day for eating and fasting.
Eating earlier in the day may help you lose weight, and eating meals within a 10-hour window could improve blood sugar and cholesterol levels, according to two new studies published in Cell Metabolism.
“You have this internal biological clock that makes you better at doing different things at different times of the day,” Courtney Peterson, PhD, an associate professor of nutrition sciences at the University of Alabama at Birmingham, told NBC News. Dr. Peterson wasn’t involved with the studies.
“It seems like the best time for your metabolism, in most people, is the mid to late morning,” she said.
In one study, researchers found that eating later in the day made people hungrier during a 24-hour period, as compared with eating the same meals earlier in the day. Combined, the changes may increase the risk for obesity, the study authors found.
In another study, among firefighters as shift workers, researchers found that eating meals within a 10-hour window decreased the size of bad cholesterol particles, which could reduce risk factors for heart disease. The 10-hour eating window also improved blood pressure and blood sugar levels among those with health conditions such as diabetes, high blood pressure, and high cholesterol.
The two new studies confirm findings from previous studies that indicate humans may have an ideal eating window based on the body’s circadian rhythms, which regulate sleep and wake cycles and can affect appetite, metabolism, and blood sugar levels.
In the firefighter study, for instance, the 10-hour window appears to be a “sweet spot” for the body, the authors found. More severe restrictions, as found with many intermittent fasting diets, could be difficult for the body to maintain.
“When we think about 6 or 8 hours, you might see a benefit, but people might not stick to it for a long time,” Satchidananda Panda, PhD, one of the study authors and a professor at the Salk Institute, La Jolla, Calif., told NBC News.
The new studies had small sample sizes, though they offer insight for future research. In the first study, 16 people who were overweight or obese tried two eating plans for 24-hour periods. Some of them began eating an hour after their natural wake-up time, and others waited to begin eating until about 5 hours after waking up. They ate the same meals with the same calories and nutrients.
The researchers measured their hormone levels and found that eating later decreased the levels of leptin, which helps people to feel full. Eating later also doubled the odds that people felt hungry throughout the day. Those in the study who ate later in the day also had more cravings for starchy or salty foods, as well as meat and dairy, which are energy-dense foods.
The research team also found changes in fat tissue, which could lead to a higher chance of building up new fat cells and a lower chance of burning fat. Late eaters burned about 60 fewer calories than early eaters during the day.
“Your body processes calories differently when you eat late in the day. It tips the scale in favor of weight gain and fat gain,” Dr. Peterson said. “From this study, we can get pretty clear recommendations that people shouldn’t skip breakfast.”
The second study followed 137 firefighters in San Diego who ate a Mediterranean diet with fish, vegetables, fruit, and olive oil for 12 weeks. Among those, 70 firefighters ate during a 10-hour window, and the rest ate during a longer window, generally about 13 hours. They logged their meals in an app and wore devices to track blood sugar levels.
In the 10-hour group, most firefighters ate between 8 a.m. or 9 a.m. and 6 p.m. or 7 p.m. The time-restricted eating appeared to be linked with health benefits, such as less harmful cholesterol buildup and reduced heart disease.
Among firefighters with risk factors for heart disease, such as high blood pressure and high blood sugar, the time-restricted eating decreased their blood pressure and blood sugar levels.
The restricted window appears to allow the body to break down toxins and get rid of sodium and other things that can drive up blood pressure and blood sugar, the authors wrote.
During periods of fasting, “organs get some rest from digesting food so they can divert their energy toward repairing cells,” Dr. Panda said.
A version of this article first appeared on WebMD.com.
New research suggests there may be better times during the day for eating and fasting.
Eating earlier in the day may help you lose weight, and eating meals within a 10-hour window could improve blood sugar and cholesterol levels, according to two new studies published in Cell Metabolism.
“You have this internal biological clock that makes you better at doing different things at different times of the day,” Courtney Peterson, PhD, an associate professor of nutrition sciences at the University of Alabama at Birmingham, told NBC News. Dr. Peterson wasn’t involved with the studies.
“It seems like the best time for your metabolism, in most people, is the mid to late morning,” she said.
In one study, researchers found that eating later in the day made people hungrier during a 24-hour period, as compared with eating the same meals earlier in the day. Combined, the changes may increase the risk for obesity, the study authors found.
In another study, among firefighters as shift workers, researchers found that eating meals within a 10-hour window decreased the size of bad cholesterol particles, which could reduce risk factors for heart disease. The 10-hour eating window also improved blood pressure and blood sugar levels among those with health conditions such as diabetes, high blood pressure, and high cholesterol.
The two new studies confirm findings from previous studies that indicate humans may have an ideal eating window based on the body’s circadian rhythms, which regulate sleep and wake cycles and can affect appetite, metabolism, and blood sugar levels.
In the firefighter study, for instance, the 10-hour window appears to be a “sweet spot” for the body, the authors found. More severe restrictions, as found with many intermittent fasting diets, could be difficult for the body to maintain.
“When we think about 6 or 8 hours, you might see a benefit, but people might not stick to it for a long time,” Satchidananda Panda, PhD, one of the study authors and a professor at the Salk Institute, La Jolla, Calif., told NBC News.
The new studies had small sample sizes, though they offer insight for future research. In the first study, 16 people who were overweight or obese tried two eating plans for 24-hour periods. Some of them began eating an hour after their natural wake-up time, and others waited to begin eating until about 5 hours after waking up. They ate the same meals with the same calories and nutrients.
The researchers measured their hormone levels and found that eating later decreased the levels of leptin, which helps people to feel full. Eating later also doubled the odds that people felt hungry throughout the day. Those in the study who ate later in the day also had more cravings for starchy or salty foods, as well as meat and dairy, which are energy-dense foods.
The research team also found changes in fat tissue, which could lead to a higher chance of building up new fat cells and a lower chance of burning fat. Late eaters burned about 60 fewer calories than early eaters during the day.
“Your body processes calories differently when you eat late in the day. It tips the scale in favor of weight gain and fat gain,” Dr. Peterson said. “From this study, we can get pretty clear recommendations that people shouldn’t skip breakfast.”
The second study followed 137 firefighters in San Diego who ate a Mediterranean diet with fish, vegetables, fruit, and olive oil for 12 weeks. Among those, 70 firefighters ate during a 10-hour window, and the rest ate during a longer window, generally about 13 hours. They logged their meals in an app and wore devices to track blood sugar levels.
In the 10-hour group, most firefighters ate between 8 a.m. or 9 a.m. and 6 p.m. or 7 p.m. The time-restricted eating appeared to be linked with health benefits, such as less harmful cholesterol buildup and reduced heart disease.
Among firefighters with risk factors for heart disease, such as high blood pressure and high blood sugar, the time-restricted eating decreased their blood pressure and blood sugar levels.
The restricted window appears to allow the body to break down toxins and get rid of sodium and other things that can drive up blood pressure and blood sugar, the authors wrote.
During periods of fasting, “organs get some rest from digesting food so they can divert their energy toward repairing cells,” Dr. Panda said.
A version of this article first appeared on WebMD.com.
FROM CELL METABOLISM
Is another COVID-19 booster really needed?
Many countries around the globe are starting to roll out another booster of the COVID-19 vaccine but, with public interest waning and a sense of normalcy firmly installed in our minds, this may prove an ill-fated effort, unless authorities can provide a coherent answer to the question “Is another jab really needed?” (The short answer is a firm “yes,” of course.)
In what we could call the “chronic” phase of the pandemic, most countries have now settled for a certain number of daily cases and a (relatively low) number of complications and deaths. It’s the vaccines that have afforded us this peace of mind, lest we forget. But they are different to other vaccines that we are more familiar with, such as the MMR that we get as kids and then forget about for the rest of our lives. As good as the different COVID-19 vaccines are, they never came with the promise of generating lifelong antibodies. We knew early on that the immunity they provide slowly wanes with time. That doesn’t mean that those who have their vaccination records up to date (which included a booster probably earlier in 2022) are suddenly exposed. Data suggest that although people several months past their last booster would now be more prone to getting reinfected, the protection against severe disease still hangs around 85%. In other words, their chances of ending up in the hospital are low.
Why worry, then, about further boosting the immune system? The same studies show that an additional jab would increase this percentage up to 99%. Is this roughly 10% improvement really worth another worldwide vaccination campaign? Well, this is a numbers game, after all. The current form of the virus is extremely infectious, and the Northern Hemisphere is heading toward the cold months of the year, which we have seen in past years increases COVID-19 contagions, as you would expect from any airborne virus. Thus, it’s easy to expect a new peak in the number of cases, especially considering that we are not going to apply any of the usual restrictions to prevent this. In these conditions, extending the safety net to a further 10% of the population would substantially reduce the total number of victims. It seems like a good investment of resources.
We can be more surgical about it and direct this new vaccination campaign to the population most likely to end up in the hospital. People with concomitant pathologies are at the top of the list, but it’s also an age issue. On the basis of different studies of the most common ages of admission, the cutoff point for the booster varies from country to country, with the lowest being 50 and in other cases hovering around 65 years of age. Given the safety of these vaccines, if we can afford it, the wider we cast the net, the better, but at least we should make every effort to fully vaccinate the higher age brackets.
The final question is which vaccine to give. There are confounding studies about the importance of switching to Omicron-specific jabs, which are finally available. Although this seems like a good idea, since Omicron infections elicit a more effective range of antibodies and new variants seem to better escape our defenses, recent studies suggest that there actually may not be so much difference with the old formula.
The conclusion? This regimen of yearly boosters for some may be the scenario for the upcoming years, similar to what we already do for the flu, so we should get used to it.
Dr. Macip is associate professor, department of molecular and cellular biology, University of Leicester (England). He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Many countries around the globe are starting to roll out another booster of the COVID-19 vaccine but, with public interest waning and a sense of normalcy firmly installed in our minds, this may prove an ill-fated effort, unless authorities can provide a coherent answer to the question “Is another jab really needed?” (The short answer is a firm “yes,” of course.)
In what we could call the “chronic” phase of the pandemic, most countries have now settled for a certain number of daily cases and a (relatively low) number of complications and deaths. It’s the vaccines that have afforded us this peace of mind, lest we forget. But they are different to other vaccines that we are more familiar with, such as the MMR that we get as kids and then forget about for the rest of our lives. As good as the different COVID-19 vaccines are, they never came with the promise of generating lifelong antibodies. We knew early on that the immunity they provide slowly wanes with time. That doesn’t mean that those who have their vaccination records up to date (which included a booster probably earlier in 2022) are suddenly exposed. Data suggest that although people several months past their last booster would now be more prone to getting reinfected, the protection against severe disease still hangs around 85%. In other words, their chances of ending up in the hospital are low.
Why worry, then, about further boosting the immune system? The same studies show that an additional jab would increase this percentage up to 99%. Is this roughly 10% improvement really worth another worldwide vaccination campaign? Well, this is a numbers game, after all. The current form of the virus is extremely infectious, and the Northern Hemisphere is heading toward the cold months of the year, which we have seen in past years increases COVID-19 contagions, as you would expect from any airborne virus. Thus, it’s easy to expect a new peak in the number of cases, especially considering that we are not going to apply any of the usual restrictions to prevent this. In these conditions, extending the safety net to a further 10% of the population would substantially reduce the total number of victims. It seems like a good investment of resources.
We can be more surgical about it and direct this new vaccination campaign to the population most likely to end up in the hospital. People with concomitant pathologies are at the top of the list, but it’s also an age issue. On the basis of different studies of the most common ages of admission, the cutoff point for the booster varies from country to country, with the lowest being 50 and in other cases hovering around 65 years of age. Given the safety of these vaccines, if we can afford it, the wider we cast the net, the better, but at least we should make every effort to fully vaccinate the higher age brackets.
The final question is which vaccine to give. There are confounding studies about the importance of switching to Omicron-specific jabs, which are finally available. Although this seems like a good idea, since Omicron infections elicit a more effective range of antibodies and new variants seem to better escape our defenses, recent studies suggest that there actually may not be so much difference with the old formula.
The conclusion? This regimen of yearly boosters for some may be the scenario for the upcoming years, similar to what we already do for the flu, so we should get used to it.
Dr. Macip is associate professor, department of molecular and cellular biology, University of Leicester (England). He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Many countries around the globe are starting to roll out another booster of the COVID-19 vaccine but, with public interest waning and a sense of normalcy firmly installed in our minds, this may prove an ill-fated effort, unless authorities can provide a coherent answer to the question “Is another jab really needed?” (The short answer is a firm “yes,” of course.)
In what we could call the “chronic” phase of the pandemic, most countries have now settled for a certain number of daily cases and a (relatively low) number of complications and deaths. It’s the vaccines that have afforded us this peace of mind, lest we forget. But they are different to other vaccines that we are more familiar with, such as the MMR that we get as kids and then forget about for the rest of our lives. As good as the different COVID-19 vaccines are, they never came with the promise of generating lifelong antibodies. We knew early on that the immunity they provide slowly wanes with time. That doesn’t mean that those who have their vaccination records up to date (which included a booster probably earlier in 2022) are suddenly exposed. Data suggest that although people several months past their last booster would now be more prone to getting reinfected, the protection against severe disease still hangs around 85%. In other words, their chances of ending up in the hospital are low.
Why worry, then, about further boosting the immune system? The same studies show that an additional jab would increase this percentage up to 99%. Is this roughly 10% improvement really worth another worldwide vaccination campaign? Well, this is a numbers game, after all. The current form of the virus is extremely infectious, and the Northern Hemisphere is heading toward the cold months of the year, which we have seen in past years increases COVID-19 contagions, as you would expect from any airborne virus. Thus, it’s easy to expect a new peak in the number of cases, especially considering that we are not going to apply any of the usual restrictions to prevent this. In these conditions, extending the safety net to a further 10% of the population would substantially reduce the total number of victims. It seems like a good investment of resources.
We can be more surgical about it and direct this new vaccination campaign to the population most likely to end up in the hospital. People with concomitant pathologies are at the top of the list, but it’s also an age issue. On the basis of different studies of the most common ages of admission, the cutoff point for the booster varies from country to country, with the lowest being 50 and in other cases hovering around 65 years of age. Given the safety of these vaccines, if we can afford it, the wider we cast the net, the better, but at least we should make every effort to fully vaccinate the higher age brackets.
The final question is which vaccine to give. There are confounding studies about the importance of switching to Omicron-specific jabs, which are finally available. Although this seems like a good idea, since Omicron infections elicit a more effective range of antibodies and new variants seem to better escape our defenses, recent studies suggest that there actually may not be so much difference with the old formula.
The conclusion? This regimen of yearly boosters for some may be the scenario for the upcoming years, similar to what we already do for the flu, so we should get used to it.
Dr. Macip is associate professor, department of molecular and cellular biology, University of Leicester (England). He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Salt pills for patients with acute decompensated heart failure?
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.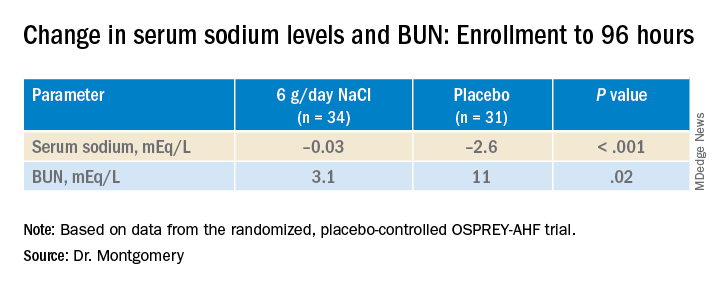
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.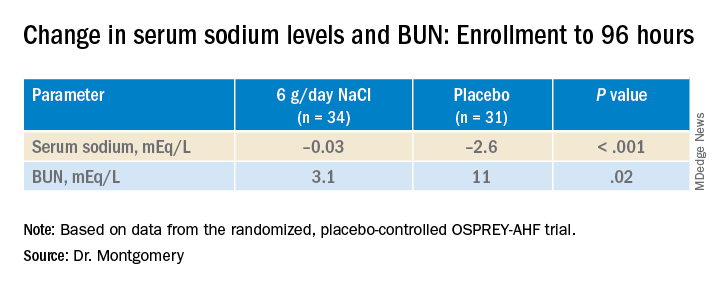
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.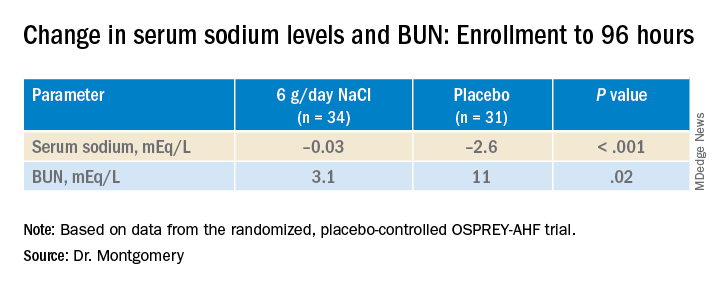
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HFSA 2022





