User login
In epilepsy, brain-responsive stimulation passes long-term tests
Two new long-term studies, one an extension trial and the other an analysis of real-world experience, show that Both studies showed that the benefit from the devices increased over time.
That accruing benefit may be because of improved protocols as clinicians gain experience with the device or because of network remodeling that occurs over time as seizures are controlled. “I think it’s both,” said Martha Morrell, MD, a clinical professor of neurology at Stanford (Calif.) University and chief medical officer at NeuroPace, the company that has marketed the device since it gained FDA approval in 2013.
In both studies, the slope of improvement over time was similar, but the real-world study showed greater improvement at the beginning of treatment. “I think the slopes represent physiological changes, but the fact that [the real-world study] starts with better outcomes is, I think, directly attributable to learning. When the long-term study was started in 2004, this had never been done before, and we had to make a highly educated guess about what we should do, and the initial stimulatory parameters were programmed in a way that’s very similar to what was used for movement disorders,” Dr. Morrell said in an interview.
The long-term treatment study appeared online July 20 in the journal Neurology, while the real-world analysis was published July 13 in Epilepsia.
An alternative option
Medications can effectively treat some seizures, but 30%-40% of patients must turn to other options for control. Surgery can sometimes be curative, but is not suitable for some patients. Other stimulation devices include vagus nerve stimulation (VNS), which sends pulses from a chest implant to the vagus nerve, reducing epileptic attacks through an unknown mechanism. Deep brain stimulation (DBS) places electrodes that deliver stimulation to the anterior nucleus of the thalamus, which can spread initially localized seizures.
The RNS device consists of a neurostimulator implanted cranially and connected to leads that are placed based on the individual patient’s seizure focus or foci. It also continuously monitors brain activity and delivers stimulation only when its signal suggests the beginning of a seizure.
That capacity for recording is a key benefit because the information can be stored and analyzed, according to Vikram Rao, MD, PhD, a coinvestigator in the real-world trial and an associate professor and the epilepsy division chief at the University of California, San Francisco, which was one of the trial centers. “You know more precisely than we previously did how many seizures a patient is having. Many of our patients are not able to quantify their seizures with perfect accuracy, so we’re better quantifying their seizure burden,” Dr. Rao said in an interview.
The ability to monitor patients can also improve clinical management. Dr. Morrell recounted an elderly patient who for many years has driven 5 hours for appointments. Recently she was able to review his data from the RNS System remotely. She determined that he was doing fine and, after a telephone consultation, told him he didn’t need to come in for a scheduled visit.
Real-world analysis
In the real-world analysis, researchers led by Babak Razavi, PhD, and Casey Halpern, MD, at Stanford University conducted a chart review of 150 patients at eight centers who underwent treatment with the RNS system between 2013 and 2018. All patients were followed at least 1 year, with a mean of 2.3 years. Patients had a median of 7.7 disabling seizures per month. The mean value was 52 and the numbers ranged from 0.1 to 3,000. A total of 60% had abnormal brain MRI findings.
At 1 year, subjects achieved a mean 67% decrease in seizure frequency (interquartile range, 50%-94%). At 2 years, that grew to 77%; at 3 or more years, 84%. There was no significant difference in seizure reduction at 1 year according to age, age at epilepsy onset, duration of epilepsy, location of seizure foci, presence of brain MRI abnormalities, prior intracranial monitoring, prior epilepsy surgery, or prior VNS treatment. When patients who underwent a resection at the time of RNS placement were excluded, the results were similar. There were no significant differences in outcome by center.
A total of 11.3% of patients experienced a device-related serious adverse event, and 4% developed infections. The rate of infection was not significantly different between patients who had the neurostimulator and leads implanted alone (3.0%) and patients who had intracranial EEG diagnostic monitoring (ICM) electrodes removed at the same time (6.1%; P = .38).
Although about one-third of the patients who started the long-term study dropped out before completion, most were because the participants moved away from treatment centers, according to Dr. Morrell, and other evidence points squarely to patient satisfaction. “At the end of the battery’s longevity, the neurostimulator needs to be replaced. It’s an outpatient, 45-minute procedure. Over 90% of patients chose to have it replaced. It’s not the answer for everybody, but the substantial majority of patients choose to continue,” she said.
Extension trial
The open-label extension trial, led by Dileep Nair, MD, of the Cleveland Clinic Foundation and Dr. Morrell, followed 230 of the 256 patients who participated in 2-year phase 3 study or feasibility studies, extending device usage to 9 years. A total of 162 completed follow-up (mean, 7.5 years). The median reduction of seizure frequency was 58% at the end of year 3, and 75% by year 9 (P < .0001; Wilcoxon signed rank). Although patient population enrichment could have explained this observation, other analyses confirmed that the improvement was real.
Nearly 75% had at least a 50% reduction in seizure frequency; 35% had a 90% or greater reduction in seizure frequency. Some patients (18.4%) had at least a full year with no seizures, and 62% who had a 1-year seizure-free period experienced no seizures at the latest follow-up. Overall, 21% had no seizures in the last 6 months of follow-up.
For those with a seizure-free period of more than 1 year, the average duration was 3.2 years (range, 1.04-9.6 years). There was no difference in response among patients based on previous antiseizure medication use or previous epilepsy surgery, VNS treatment, or intracranial monitoring, and there were no differences by patient age at enrollment, age of seizure onset, brain imaging abnormality, seizure onset locality, or number of foci.
The researchers noted improvement in overall Quality of Life in Epilepsy Inventory–89 scores at 1 year (mean, +3.2; P < .0001), which continued through year 9 (mean, +1.9; P < .05). Improvements were also seen in epilepsy targeted (mean, +4.5; P < .001) and cognitive domains (mean, +2.5; P = .005). Risk of infection was 4.1% per procedure, and 12.1% of subjects overall experienced a serious device-related implant infection. Of 35 infections, 16 led to device removal.
The extension study was funded by NeuroPace. NeuroPace supported data entry and institutional review board submission for the real-world trial. Dr. Morrell owns stock and is an employee of NeuroPace. Dr Rao has received support from and/or consulted for NeuroPace.
SOURCE: Nair DR et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010154. Razavi B et al. Epilepsia. 2020 Jul 13. doi: 10.1111/epi.16593.
Two new long-term studies, one an extension trial and the other an analysis of real-world experience, show that Both studies showed that the benefit from the devices increased over time.
That accruing benefit may be because of improved protocols as clinicians gain experience with the device or because of network remodeling that occurs over time as seizures are controlled. “I think it’s both,” said Martha Morrell, MD, a clinical professor of neurology at Stanford (Calif.) University and chief medical officer at NeuroPace, the company that has marketed the device since it gained FDA approval in 2013.
In both studies, the slope of improvement over time was similar, but the real-world study showed greater improvement at the beginning of treatment. “I think the slopes represent physiological changes, but the fact that [the real-world study] starts with better outcomes is, I think, directly attributable to learning. When the long-term study was started in 2004, this had never been done before, and we had to make a highly educated guess about what we should do, and the initial stimulatory parameters were programmed in a way that’s very similar to what was used for movement disorders,” Dr. Morrell said in an interview.
The long-term treatment study appeared online July 20 in the journal Neurology, while the real-world analysis was published July 13 in Epilepsia.
An alternative option
Medications can effectively treat some seizures, but 30%-40% of patients must turn to other options for control. Surgery can sometimes be curative, but is not suitable for some patients. Other stimulation devices include vagus nerve stimulation (VNS), which sends pulses from a chest implant to the vagus nerve, reducing epileptic attacks through an unknown mechanism. Deep brain stimulation (DBS) places electrodes that deliver stimulation to the anterior nucleus of the thalamus, which can spread initially localized seizures.
The RNS device consists of a neurostimulator implanted cranially and connected to leads that are placed based on the individual patient’s seizure focus or foci. It also continuously monitors brain activity and delivers stimulation only when its signal suggests the beginning of a seizure.
That capacity for recording is a key benefit because the information can be stored and analyzed, according to Vikram Rao, MD, PhD, a coinvestigator in the real-world trial and an associate professor and the epilepsy division chief at the University of California, San Francisco, which was one of the trial centers. “You know more precisely than we previously did how many seizures a patient is having. Many of our patients are not able to quantify their seizures with perfect accuracy, so we’re better quantifying their seizure burden,” Dr. Rao said in an interview.
The ability to monitor patients can also improve clinical management. Dr. Morrell recounted an elderly patient who for many years has driven 5 hours for appointments. Recently she was able to review his data from the RNS System remotely. She determined that he was doing fine and, after a telephone consultation, told him he didn’t need to come in for a scheduled visit.
Real-world analysis
In the real-world analysis, researchers led by Babak Razavi, PhD, and Casey Halpern, MD, at Stanford University conducted a chart review of 150 patients at eight centers who underwent treatment with the RNS system between 2013 and 2018. All patients were followed at least 1 year, with a mean of 2.3 years. Patients had a median of 7.7 disabling seizures per month. The mean value was 52 and the numbers ranged from 0.1 to 3,000. A total of 60% had abnormal brain MRI findings.
At 1 year, subjects achieved a mean 67% decrease in seizure frequency (interquartile range, 50%-94%). At 2 years, that grew to 77%; at 3 or more years, 84%. There was no significant difference in seizure reduction at 1 year according to age, age at epilepsy onset, duration of epilepsy, location of seizure foci, presence of brain MRI abnormalities, prior intracranial monitoring, prior epilepsy surgery, or prior VNS treatment. When patients who underwent a resection at the time of RNS placement were excluded, the results were similar. There were no significant differences in outcome by center.
A total of 11.3% of patients experienced a device-related serious adverse event, and 4% developed infections. The rate of infection was not significantly different between patients who had the neurostimulator and leads implanted alone (3.0%) and patients who had intracranial EEG diagnostic monitoring (ICM) electrodes removed at the same time (6.1%; P = .38).
Although about one-third of the patients who started the long-term study dropped out before completion, most were because the participants moved away from treatment centers, according to Dr. Morrell, and other evidence points squarely to patient satisfaction. “At the end of the battery’s longevity, the neurostimulator needs to be replaced. It’s an outpatient, 45-minute procedure. Over 90% of patients chose to have it replaced. It’s not the answer for everybody, but the substantial majority of patients choose to continue,” she said.
Extension trial
The open-label extension trial, led by Dileep Nair, MD, of the Cleveland Clinic Foundation and Dr. Morrell, followed 230 of the 256 patients who participated in 2-year phase 3 study or feasibility studies, extending device usage to 9 years. A total of 162 completed follow-up (mean, 7.5 years). The median reduction of seizure frequency was 58% at the end of year 3, and 75% by year 9 (P < .0001; Wilcoxon signed rank). Although patient population enrichment could have explained this observation, other analyses confirmed that the improvement was real.
Nearly 75% had at least a 50% reduction in seizure frequency; 35% had a 90% or greater reduction in seizure frequency. Some patients (18.4%) had at least a full year with no seizures, and 62% who had a 1-year seizure-free period experienced no seizures at the latest follow-up. Overall, 21% had no seizures in the last 6 months of follow-up.
For those with a seizure-free period of more than 1 year, the average duration was 3.2 years (range, 1.04-9.6 years). There was no difference in response among patients based on previous antiseizure medication use or previous epilepsy surgery, VNS treatment, or intracranial monitoring, and there were no differences by patient age at enrollment, age of seizure onset, brain imaging abnormality, seizure onset locality, or number of foci.
The researchers noted improvement in overall Quality of Life in Epilepsy Inventory–89 scores at 1 year (mean, +3.2; P < .0001), which continued through year 9 (mean, +1.9; P < .05). Improvements were also seen in epilepsy targeted (mean, +4.5; P < .001) and cognitive domains (mean, +2.5; P = .005). Risk of infection was 4.1% per procedure, and 12.1% of subjects overall experienced a serious device-related implant infection. Of 35 infections, 16 led to device removal.
The extension study was funded by NeuroPace. NeuroPace supported data entry and institutional review board submission for the real-world trial. Dr. Morrell owns stock and is an employee of NeuroPace. Dr Rao has received support from and/or consulted for NeuroPace.
SOURCE: Nair DR et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010154. Razavi B et al. Epilepsia. 2020 Jul 13. doi: 10.1111/epi.16593.
Two new long-term studies, one an extension trial and the other an analysis of real-world experience, show that Both studies showed that the benefit from the devices increased over time.
That accruing benefit may be because of improved protocols as clinicians gain experience with the device or because of network remodeling that occurs over time as seizures are controlled. “I think it’s both,” said Martha Morrell, MD, a clinical professor of neurology at Stanford (Calif.) University and chief medical officer at NeuroPace, the company that has marketed the device since it gained FDA approval in 2013.
In both studies, the slope of improvement over time was similar, but the real-world study showed greater improvement at the beginning of treatment. “I think the slopes represent physiological changes, but the fact that [the real-world study] starts with better outcomes is, I think, directly attributable to learning. When the long-term study was started in 2004, this had never been done before, and we had to make a highly educated guess about what we should do, and the initial stimulatory parameters were programmed in a way that’s very similar to what was used for movement disorders,” Dr. Morrell said in an interview.
The long-term treatment study appeared online July 20 in the journal Neurology, while the real-world analysis was published July 13 in Epilepsia.
An alternative option
Medications can effectively treat some seizures, but 30%-40% of patients must turn to other options for control. Surgery can sometimes be curative, but is not suitable for some patients. Other stimulation devices include vagus nerve stimulation (VNS), which sends pulses from a chest implant to the vagus nerve, reducing epileptic attacks through an unknown mechanism. Deep brain stimulation (DBS) places electrodes that deliver stimulation to the anterior nucleus of the thalamus, which can spread initially localized seizures.
The RNS device consists of a neurostimulator implanted cranially and connected to leads that are placed based on the individual patient’s seizure focus or foci. It also continuously monitors brain activity and delivers stimulation only when its signal suggests the beginning of a seizure.
That capacity for recording is a key benefit because the information can be stored and analyzed, according to Vikram Rao, MD, PhD, a coinvestigator in the real-world trial and an associate professor and the epilepsy division chief at the University of California, San Francisco, which was one of the trial centers. “You know more precisely than we previously did how many seizures a patient is having. Many of our patients are not able to quantify their seizures with perfect accuracy, so we’re better quantifying their seizure burden,” Dr. Rao said in an interview.
The ability to monitor patients can also improve clinical management. Dr. Morrell recounted an elderly patient who for many years has driven 5 hours for appointments. Recently she was able to review his data from the RNS System remotely. She determined that he was doing fine and, after a telephone consultation, told him he didn’t need to come in for a scheduled visit.
Real-world analysis
In the real-world analysis, researchers led by Babak Razavi, PhD, and Casey Halpern, MD, at Stanford University conducted a chart review of 150 patients at eight centers who underwent treatment with the RNS system between 2013 and 2018. All patients were followed at least 1 year, with a mean of 2.3 years. Patients had a median of 7.7 disabling seizures per month. The mean value was 52 and the numbers ranged from 0.1 to 3,000. A total of 60% had abnormal brain MRI findings.
At 1 year, subjects achieved a mean 67% decrease in seizure frequency (interquartile range, 50%-94%). At 2 years, that grew to 77%; at 3 or more years, 84%. There was no significant difference in seizure reduction at 1 year according to age, age at epilepsy onset, duration of epilepsy, location of seizure foci, presence of brain MRI abnormalities, prior intracranial monitoring, prior epilepsy surgery, or prior VNS treatment. When patients who underwent a resection at the time of RNS placement were excluded, the results were similar. There were no significant differences in outcome by center.
A total of 11.3% of patients experienced a device-related serious adverse event, and 4% developed infections. The rate of infection was not significantly different between patients who had the neurostimulator and leads implanted alone (3.0%) and patients who had intracranial EEG diagnostic monitoring (ICM) electrodes removed at the same time (6.1%; P = .38).
Although about one-third of the patients who started the long-term study dropped out before completion, most were because the participants moved away from treatment centers, according to Dr. Morrell, and other evidence points squarely to patient satisfaction. “At the end of the battery’s longevity, the neurostimulator needs to be replaced. It’s an outpatient, 45-minute procedure. Over 90% of patients chose to have it replaced. It’s not the answer for everybody, but the substantial majority of patients choose to continue,” she said.
Extension trial
The open-label extension trial, led by Dileep Nair, MD, of the Cleveland Clinic Foundation and Dr. Morrell, followed 230 of the 256 patients who participated in 2-year phase 3 study or feasibility studies, extending device usage to 9 years. A total of 162 completed follow-up (mean, 7.5 years). The median reduction of seizure frequency was 58% at the end of year 3, and 75% by year 9 (P < .0001; Wilcoxon signed rank). Although patient population enrichment could have explained this observation, other analyses confirmed that the improvement was real.
Nearly 75% had at least a 50% reduction in seizure frequency; 35% had a 90% or greater reduction in seizure frequency. Some patients (18.4%) had at least a full year with no seizures, and 62% who had a 1-year seizure-free period experienced no seizures at the latest follow-up. Overall, 21% had no seizures in the last 6 months of follow-up.
For those with a seizure-free period of more than 1 year, the average duration was 3.2 years (range, 1.04-9.6 years). There was no difference in response among patients based on previous antiseizure medication use or previous epilepsy surgery, VNS treatment, or intracranial monitoring, and there were no differences by patient age at enrollment, age of seizure onset, brain imaging abnormality, seizure onset locality, or number of foci.
The researchers noted improvement in overall Quality of Life in Epilepsy Inventory–89 scores at 1 year (mean, +3.2; P < .0001), which continued through year 9 (mean, +1.9; P < .05). Improvements were also seen in epilepsy targeted (mean, +4.5; P < .001) and cognitive domains (mean, +2.5; P = .005). Risk of infection was 4.1% per procedure, and 12.1% of subjects overall experienced a serious device-related implant infection. Of 35 infections, 16 led to device removal.
The extension study was funded by NeuroPace. NeuroPace supported data entry and institutional review board submission for the real-world trial. Dr. Morrell owns stock and is an employee of NeuroPace. Dr Rao has received support from and/or consulted for NeuroPace.
SOURCE: Nair DR et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010154. Razavi B et al. Epilepsia. 2020 Jul 13. doi: 10.1111/epi.16593.
FROM EPILEPSIA AND FROM NEUROLOGY
OK to treat many cancer patients despite pandemic, says ESMO
Not all are highly vulnerable to COVID-19
Another important recommendation is to stop labeling all patients with cancer as being vulnerable to infection with the virus as it can lead to inappropriate care with potential negative outcomes.
“Although it was reasonable to adopt over-protective measures for our patients at the outbreak of a novel infective disease which was not previously observed in humans, we now need to step away from the assumption that all cancer patients are vulnerable to COVID-19,” said first author of the consensus article Giuseppe Curigliano, MD, PhD, of the European Institute of Oncology, Milan, Italy, in a statement. “The implications have been important because for some patients treatment was delayed or interrupted over the last few months, and I believe that we will see the impact of this over-precautionary approach in the...future.”
The recommendations were issued by the European Society of Medical Oncology (ESMO) to help guide physicians in “optimizing the pathway to cancer care” as well as to improve outcomes during the pandemic. The recommendations were published online July 31 in Annals of Oncology.
Studies have found that patients with cancer face a higher risk of serious complications and death if they develop COVID-19. Data from the COVID-19 and Cancer Consortium registry, for example, showed that patients with progressing cancer and COVID-19 infection had a fivefold increase in the risk of 30-day mortality compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer.
But while this may be true for some patients, Curigliano and colleagues emphasize that individuals with cancer are not a heterogeneous group and that the term “cancer” itself represents myriad different diseases. The European experts note that current evidence suggests many patients with solid tumors are not more vulnerable to serious complications than the general population.
Thus, cancer prognoses vary considerably, and addressing all patients with cancer as being “COVID-19-vulnerable is probably neither reasonable nor informative,” say the authors.
Dramatic changes were initiated in cancer management for all cancer types, nevertheless, and although these changes seemed reasonable in an acute pandemic situation, note the authors, they were made in the absence of strong supportive evidence. Attempts to define the individualized risk for a given patient, taking into account their primary tumor subtype, stage, age, and gender, have been limited.
“Based on current evidence, only patients who are elderly, with multiple comorbidities, and receiving chemotherapy are vulnerable to the infection,” explained Curigliano.
However, on a positive note, a recently published prospective cohort study looked at approximately 800 patients with cancer – who had symptomatic COVID-19 – in the United Kingdom. The analysis showed no association at all between the risk for death and receiving chemotherapy or immunotherapy, points out Medscape commentator David Kerr, MD, of the University of Oxford, UK, in a recent commentary.
Key recommendations
An international consortium was established by ESMO, and the interdisciplinary expert panel consisted of 64 experts and one voting patient advocate. They agreed on 28 statements that can be used to help with many of the current clinical and technical areas of uncertainty that range from diagnosis to treatment decisions.
The following are several of the key recommendations:
- Patients with cancer who face the highest risk of severe COVID-19 are characterized by active and progressive cancer, advanced age, poor performance status, smoking status, comorbidities, and possibly type of cancer.
- Telehealth and digital health can be excellent tools for some types of care such as primary care triage and counseling, but meeting in person may be more effective for situations that include delivery of key cancer-related information and for patients with complex cancer needs.
- Prior to hospital admission, patients with cancer should be tested for COVID-19, if feasible, and if they are considered at high risk, regardless of symptoms or chest radiological findings.
- Patients with cancer and COVID-19 have a higher risk of thromboembolic events, and prophylaxis using low molecular weight or novel oral anticoagulants is recommended.
- Immune checkpoint inhibitors should not be withheld or delayed when there is a significant survival benefit, but use should be postponed in patients who test positive for COVID-19 until they recover.
- Use of high-dose steroids in patients with cancer infected with COVID-19 could potentially increase the risk of mortality, and a switch should be made to another immunosuppressant, if possible.
- The decision to use tyrosine kinase inhibitors (TKIs) of the PI3K/AKT/mTOR or RAS/RAF/MEK axis is complex, as they interfere with critical pathways involved in innate or adaptive immune responses. Stopping or withholding therapy depends on the risk-benefit balance, and the magnitude of benefit from the TKI needs to be considered.
The authors conclude that “ultimately, this set of statements will serve as a dynamic knowledge repository that will be better informed by accumulating data on SARS-CoV-2 biology, COVID-19 pandemic characteristics, on the risk of cancer patients for COVID-19 and its modulating factors, and finally, on optimal cancer care in the presence of the virus.”
No funding was reported for the current study. Several authors have disclosed relationships with industry, which are listed in the article.
This article first appeared on Medscape.com.
Not all are highly vulnerable to COVID-19
Not all are highly vulnerable to COVID-19
Another important recommendation is to stop labeling all patients with cancer as being vulnerable to infection with the virus as it can lead to inappropriate care with potential negative outcomes.
“Although it was reasonable to adopt over-protective measures for our patients at the outbreak of a novel infective disease which was not previously observed in humans, we now need to step away from the assumption that all cancer patients are vulnerable to COVID-19,” said first author of the consensus article Giuseppe Curigliano, MD, PhD, of the European Institute of Oncology, Milan, Italy, in a statement. “The implications have been important because for some patients treatment was delayed or interrupted over the last few months, and I believe that we will see the impact of this over-precautionary approach in the...future.”
The recommendations were issued by the European Society of Medical Oncology (ESMO) to help guide physicians in “optimizing the pathway to cancer care” as well as to improve outcomes during the pandemic. The recommendations were published online July 31 in Annals of Oncology.
Studies have found that patients with cancer face a higher risk of serious complications and death if they develop COVID-19. Data from the COVID-19 and Cancer Consortium registry, for example, showed that patients with progressing cancer and COVID-19 infection had a fivefold increase in the risk of 30-day mortality compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer.
But while this may be true for some patients, Curigliano and colleagues emphasize that individuals with cancer are not a heterogeneous group and that the term “cancer” itself represents myriad different diseases. The European experts note that current evidence suggests many patients with solid tumors are not more vulnerable to serious complications than the general population.
Thus, cancer prognoses vary considerably, and addressing all patients with cancer as being “COVID-19-vulnerable is probably neither reasonable nor informative,” say the authors.
Dramatic changes were initiated in cancer management for all cancer types, nevertheless, and although these changes seemed reasonable in an acute pandemic situation, note the authors, they were made in the absence of strong supportive evidence. Attempts to define the individualized risk for a given patient, taking into account their primary tumor subtype, stage, age, and gender, have been limited.
“Based on current evidence, only patients who are elderly, with multiple comorbidities, and receiving chemotherapy are vulnerable to the infection,” explained Curigliano.
However, on a positive note, a recently published prospective cohort study looked at approximately 800 patients with cancer – who had symptomatic COVID-19 – in the United Kingdom. The analysis showed no association at all between the risk for death and receiving chemotherapy or immunotherapy, points out Medscape commentator David Kerr, MD, of the University of Oxford, UK, in a recent commentary.
Key recommendations
An international consortium was established by ESMO, and the interdisciplinary expert panel consisted of 64 experts and one voting patient advocate. They agreed on 28 statements that can be used to help with many of the current clinical and technical areas of uncertainty that range from diagnosis to treatment decisions.
The following are several of the key recommendations:
- Patients with cancer who face the highest risk of severe COVID-19 are characterized by active and progressive cancer, advanced age, poor performance status, smoking status, comorbidities, and possibly type of cancer.
- Telehealth and digital health can be excellent tools for some types of care such as primary care triage and counseling, but meeting in person may be more effective for situations that include delivery of key cancer-related information and for patients with complex cancer needs.
- Prior to hospital admission, patients with cancer should be tested for COVID-19, if feasible, and if they are considered at high risk, regardless of symptoms or chest radiological findings.
- Patients with cancer and COVID-19 have a higher risk of thromboembolic events, and prophylaxis using low molecular weight or novel oral anticoagulants is recommended.
- Immune checkpoint inhibitors should not be withheld or delayed when there is a significant survival benefit, but use should be postponed in patients who test positive for COVID-19 until they recover.
- Use of high-dose steroids in patients with cancer infected with COVID-19 could potentially increase the risk of mortality, and a switch should be made to another immunosuppressant, if possible.
- The decision to use tyrosine kinase inhibitors (TKIs) of the PI3K/AKT/mTOR or RAS/RAF/MEK axis is complex, as they interfere with critical pathways involved in innate or adaptive immune responses. Stopping or withholding therapy depends on the risk-benefit balance, and the magnitude of benefit from the TKI needs to be considered.
The authors conclude that “ultimately, this set of statements will serve as a dynamic knowledge repository that will be better informed by accumulating data on SARS-CoV-2 biology, COVID-19 pandemic characteristics, on the risk of cancer patients for COVID-19 and its modulating factors, and finally, on optimal cancer care in the presence of the virus.”
No funding was reported for the current study. Several authors have disclosed relationships with industry, which are listed in the article.
This article first appeared on Medscape.com.
Another important recommendation is to stop labeling all patients with cancer as being vulnerable to infection with the virus as it can lead to inappropriate care with potential negative outcomes.
“Although it was reasonable to adopt over-protective measures for our patients at the outbreak of a novel infective disease which was not previously observed in humans, we now need to step away from the assumption that all cancer patients are vulnerable to COVID-19,” said first author of the consensus article Giuseppe Curigliano, MD, PhD, of the European Institute of Oncology, Milan, Italy, in a statement. “The implications have been important because for some patients treatment was delayed or interrupted over the last few months, and I believe that we will see the impact of this over-precautionary approach in the...future.”
The recommendations were issued by the European Society of Medical Oncology (ESMO) to help guide physicians in “optimizing the pathway to cancer care” as well as to improve outcomes during the pandemic. The recommendations were published online July 31 in Annals of Oncology.
Studies have found that patients with cancer face a higher risk of serious complications and death if they develop COVID-19. Data from the COVID-19 and Cancer Consortium registry, for example, showed that patients with progressing cancer and COVID-19 infection had a fivefold increase in the risk of 30-day mortality compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer.
But while this may be true for some patients, Curigliano and colleagues emphasize that individuals with cancer are not a heterogeneous group and that the term “cancer” itself represents myriad different diseases. The European experts note that current evidence suggests many patients with solid tumors are not more vulnerable to serious complications than the general population.
Thus, cancer prognoses vary considerably, and addressing all patients with cancer as being “COVID-19-vulnerable is probably neither reasonable nor informative,” say the authors.
Dramatic changes were initiated in cancer management for all cancer types, nevertheless, and although these changes seemed reasonable in an acute pandemic situation, note the authors, they were made in the absence of strong supportive evidence. Attempts to define the individualized risk for a given patient, taking into account their primary tumor subtype, stage, age, and gender, have been limited.
“Based on current evidence, only patients who are elderly, with multiple comorbidities, and receiving chemotherapy are vulnerable to the infection,” explained Curigliano.
However, on a positive note, a recently published prospective cohort study looked at approximately 800 patients with cancer – who had symptomatic COVID-19 – in the United Kingdom. The analysis showed no association at all between the risk for death and receiving chemotherapy or immunotherapy, points out Medscape commentator David Kerr, MD, of the University of Oxford, UK, in a recent commentary.
Key recommendations
An international consortium was established by ESMO, and the interdisciplinary expert panel consisted of 64 experts and one voting patient advocate. They agreed on 28 statements that can be used to help with many of the current clinical and technical areas of uncertainty that range from diagnosis to treatment decisions.
The following are several of the key recommendations:
- Patients with cancer who face the highest risk of severe COVID-19 are characterized by active and progressive cancer, advanced age, poor performance status, smoking status, comorbidities, and possibly type of cancer.
- Telehealth and digital health can be excellent tools for some types of care such as primary care triage and counseling, but meeting in person may be more effective for situations that include delivery of key cancer-related information and for patients with complex cancer needs.
- Prior to hospital admission, patients with cancer should be tested for COVID-19, if feasible, and if they are considered at high risk, regardless of symptoms or chest radiological findings.
- Patients with cancer and COVID-19 have a higher risk of thromboembolic events, and prophylaxis using low molecular weight or novel oral anticoagulants is recommended.
- Immune checkpoint inhibitors should not be withheld or delayed when there is a significant survival benefit, but use should be postponed in patients who test positive for COVID-19 until they recover.
- Use of high-dose steroids in patients with cancer infected with COVID-19 could potentially increase the risk of mortality, and a switch should be made to another immunosuppressant, if possible.
- The decision to use tyrosine kinase inhibitors (TKIs) of the PI3K/AKT/mTOR or RAS/RAF/MEK axis is complex, as they interfere with critical pathways involved in innate or adaptive immune responses. Stopping or withholding therapy depends on the risk-benefit balance, and the magnitude of benefit from the TKI needs to be considered.
The authors conclude that “ultimately, this set of statements will serve as a dynamic knowledge repository that will be better informed by accumulating data on SARS-CoV-2 biology, COVID-19 pandemic characteristics, on the risk of cancer patients for COVID-19 and its modulating factors, and finally, on optimal cancer care in the presence of the virus.”
No funding was reported for the current study. Several authors have disclosed relationships with industry, which are listed in the article.
This article first appeared on Medscape.com.
Postmenopausal use of estrogen alone lowers breast cancer cases, deaths
A new follow-up study of menopausal hormone therapy found that prior use of conjugated equine estrogen (CEE) decreased both breast cancer incidence and mortality, while prior use of CEE plus medroxyprogesterone acetate (MPA) was associated with an increase in incidence.
“Prior use of CEE alone is, to our knowledge, the first pharmacologic intervention demonstrated to be associated with a statistically significantly reduction in deaths from breast cancer,” wrote Rowan T. Chlebowski, MD, PhD, of the Lundquist Institute for Biomedical Innovation in Torrance, Calif., and his coauthors. The study was published July 28 in JAMA.
To further investigate the outcomes of the Women’s Health Initiative in regard to hormone therapy and breast cancer risk, the researchers analyzed the long-term follow-up of two randomized trials that included 27,347 postmenopausal women with no prior breast cancer and negative mammograms at baseline. Their mean (SD) age was 63.4 (7.2) years. Enrollment took place from 1993 to 1998; participants were contacted for follow-up every 6 months through 2005 and annually from then on. Mortality data were gathered from follow-up and the National Death Index.
The first trial included 16,608 women with a uterus. Among these women, 8,506 received 0.625 mg/day of CEE plus 2.5 mg/day of MPA, and 8,102 received placebo. The second trial included 10,739 women who’d gotten a hysterectomy, 5,310 of whom received 0.625 mg/day of CEE alone and 5,429 of whom received placebo. The first trial ended in 2002 after a median intervention period of 5.6 years, and the second trial ended in 2004 after a period of 7.2 years.
An analysis in 2015 found that CEE alone was associated with lower risk of breast cancer and CEE plus MPA was associated with increased risk.
The current analysis confirmed that, after a median of 20.3 years of follow-up, and with mortality data now available for more than 98% of participants, CEE alone was associated with fewer cases of breast cancer (238 cases, annualized rate 0.30%), compared with placebo (296 cases, annualized rate 0.37%; hazard ratio 0.78; 95% confidence interval, 0.65-0.93; P = .005).
Furthermore, CEE alone was also associated with lower mortality (30 deaths, annualized mortality rate 0.031%), compared with placebo (46 deaths, annualized mortality rate 0.046%; HR 0.60; 95% CI, 0.37-0.97; P = .04).
By comparison, CEE plus MPA was linked with more cases of breast cancer (584 cases, annualized rate 0.45%) than placebo (447 cases, annualized rate 0.36%; HR 1.28; 95% CI, 1.13-1.45; P < .001). In regard to mortality, there was no statistically significant difference between CEE plus MPA (71 deaths, annualized mortality rate 0.045%) and placebo (53 deaths, annualized mortality rate 0.035%; HR 1.35; 95% CI, 0.94-1.95; P = .11).
“The big thing to think about is estrogen alone reducing breast cancer mortality by 40%,” said Dr. Chlebowski in an interview. “None of the other interventions, including tamoxifen, had any change on mortality. This should change the way we look at breast cancer prevention, though we might have to be a little creative about it. I think you have to be a little away from menopause for it to reduce breast cancer. But we wanted to start that debate.
“On the other hand,” he said, “a woman takes estrogen plus progestin and when you look at that curve, it’s staying about 25% increased. You take it for 5.6 years and the increase continues through 20 years, so you’re maybe buying a lifetime of increase in breast cancer by taking estrogen plus progestin for 5 years.”
He also highlighted the comprehensiveness of the mortality data, noting that “when you hook up to the National Death Index, they find 98% of all deaths in the United States. That’s really remarkable; you retain the whole power of the randomization. It means our data, between the death index and our follow-up of participants, is essentially complete.”
Use of hormone therapy, and decoding the outcomes, remains ‘complex’
Decades after the data were gathered from the Women’s Health Initiative clinical trials, they continue to assist researchers and patients alike, wrote Christina A. Minami, MD, of Brigham and Women’s Hospital in Boston and Rachel A. Freedman, MD, of the Dana-Farber Cancer Institute in Boston, in an accompanying editorial.
That said, in regard to the findings of this latest analysis, “many questions still remain on whether (and how) a hormone therapy intervention that occurred many years earlier may continue to affect breast cancer risk and mortality at 20 years,” they wrote. They noted that it’s “impossible” to isolate how exposure to certain therapies can impact long-term outcomes, and that a high percentage of patients who discontinued the drugs during each trial muddy the waters even further.
“Decisions to initiate these medications remain complex,” they added, emphasizing that breast cancer risk is just one of many factors that physicians must consider when considering hormone therapy for their patients.
Dr. Chlebowski and his coauthors acknowledged their study’s limitations, including the use of very specifically administered and formulated dosages making their findings “not necessarily generalizable to other preparations.” In addition, they noted the significant percentage of patients – 54% with CEE alone and 42% with CEE plus MPA – who discontinued drug usage during their respective trials.
The Women’s Health Initiative is supported by the National Institutes of Health and the Department of Health and Human Services. The authors reported numerous potential conflicts of interest, including receiving personal fees and grants from various government organizations, foundations, and pharmaceutical companies. The editorial’s authors reported no conflicts of interest.
SOURCE: Chlebowski RT et al. JAMA. 2020 Jul 28. doi: 10.1001/jama.2020.9482.
A new follow-up study of menopausal hormone therapy found that prior use of conjugated equine estrogen (CEE) decreased both breast cancer incidence and mortality, while prior use of CEE plus medroxyprogesterone acetate (MPA) was associated with an increase in incidence.
“Prior use of CEE alone is, to our knowledge, the first pharmacologic intervention demonstrated to be associated with a statistically significantly reduction in deaths from breast cancer,” wrote Rowan T. Chlebowski, MD, PhD, of the Lundquist Institute for Biomedical Innovation in Torrance, Calif., and his coauthors. The study was published July 28 in JAMA.
To further investigate the outcomes of the Women’s Health Initiative in regard to hormone therapy and breast cancer risk, the researchers analyzed the long-term follow-up of two randomized trials that included 27,347 postmenopausal women with no prior breast cancer and negative mammograms at baseline. Their mean (SD) age was 63.4 (7.2) years. Enrollment took place from 1993 to 1998; participants were contacted for follow-up every 6 months through 2005 and annually from then on. Mortality data were gathered from follow-up and the National Death Index.
The first trial included 16,608 women with a uterus. Among these women, 8,506 received 0.625 mg/day of CEE plus 2.5 mg/day of MPA, and 8,102 received placebo. The second trial included 10,739 women who’d gotten a hysterectomy, 5,310 of whom received 0.625 mg/day of CEE alone and 5,429 of whom received placebo. The first trial ended in 2002 after a median intervention period of 5.6 years, and the second trial ended in 2004 after a period of 7.2 years.
An analysis in 2015 found that CEE alone was associated with lower risk of breast cancer and CEE plus MPA was associated with increased risk.
The current analysis confirmed that, after a median of 20.3 years of follow-up, and with mortality data now available for more than 98% of participants, CEE alone was associated with fewer cases of breast cancer (238 cases, annualized rate 0.30%), compared with placebo (296 cases, annualized rate 0.37%; hazard ratio 0.78; 95% confidence interval, 0.65-0.93; P = .005).
Furthermore, CEE alone was also associated with lower mortality (30 deaths, annualized mortality rate 0.031%), compared with placebo (46 deaths, annualized mortality rate 0.046%; HR 0.60; 95% CI, 0.37-0.97; P = .04).
By comparison, CEE plus MPA was linked with more cases of breast cancer (584 cases, annualized rate 0.45%) than placebo (447 cases, annualized rate 0.36%; HR 1.28; 95% CI, 1.13-1.45; P < .001). In regard to mortality, there was no statistically significant difference between CEE plus MPA (71 deaths, annualized mortality rate 0.045%) and placebo (53 deaths, annualized mortality rate 0.035%; HR 1.35; 95% CI, 0.94-1.95; P = .11).
“The big thing to think about is estrogen alone reducing breast cancer mortality by 40%,” said Dr. Chlebowski in an interview. “None of the other interventions, including tamoxifen, had any change on mortality. This should change the way we look at breast cancer prevention, though we might have to be a little creative about it. I think you have to be a little away from menopause for it to reduce breast cancer. But we wanted to start that debate.
“On the other hand,” he said, “a woman takes estrogen plus progestin and when you look at that curve, it’s staying about 25% increased. You take it for 5.6 years and the increase continues through 20 years, so you’re maybe buying a lifetime of increase in breast cancer by taking estrogen plus progestin for 5 years.”
He also highlighted the comprehensiveness of the mortality data, noting that “when you hook up to the National Death Index, they find 98% of all deaths in the United States. That’s really remarkable; you retain the whole power of the randomization. It means our data, between the death index and our follow-up of participants, is essentially complete.”
Use of hormone therapy, and decoding the outcomes, remains ‘complex’
Decades after the data were gathered from the Women’s Health Initiative clinical trials, they continue to assist researchers and patients alike, wrote Christina A. Minami, MD, of Brigham and Women’s Hospital in Boston and Rachel A. Freedman, MD, of the Dana-Farber Cancer Institute in Boston, in an accompanying editorial.
That said, in regard to the findings of this latest analysis, “many questions still remain on whether (and how) a hormone therapy intervention that occurred many years earlier may continue to affect breast cancer risk and mortality at 20 years,” they wrote. They noted that it’s “impossible” to isolate how exposure to certain therapies can impact long-term outcomes, and that a high percentage of patients who discontinued the drugs during each trial muddy the waters even further.
“Decisions to initiate these medications remain complex,” they added, emphasizing that breast cancer risk is just one of many factors that physicians must consider when considering hormone therapy for their patients.
Dr. Chlebowski and his coauthors acknowledged their study’s limitations, including the use of very specifically administered and formulated dosages making their findings “not necessarily generalizable to other preparations.” In addition, they noted the significant percentage of patients – 54% with CEE alone and 42% with CEE plus MPA – who discontinued drug usage during their respective trials.
The Women’s Health Initiative is supported by the National Institutes of Health and the Department of Health and Human Services. The authors reported numerous potential conflicts of interest, including receiving personal fees and grants from various government organizations, foundations, and pharmaceutical companies. The editorial’s authors reported no conflicts of interest.
SOURCE: Chlebowski RT et al. JAMA. 2020 Jul 28. doi: 10.1001/jama.2020.9482.
A new follow-up study of menopausal hormone therapy found that prior use of conjugated equine estrogen (CEE) decreased both breast cancer incidence and mortality, while prior use of CEE plus medroxyprogesterone acetate (MPA) was associated with an increase in incidence.
“Prior use of CEE alone is, to our knowledge, the first pharmacologic intervention demonstrated to be associated with a statistically significantly reduction in deaths from breast cancer,” wrote Rowan T. Chlebowski, MD, PhD, of the Lundquist Institute for Biomedical Innovation in Torrance, Calif., and his coauthors. The study was published July 28 in JAMA.
To further investigate the outcomes of the Women’s Health Initiative in regard to hormone therapy and breast cancer risk, the researchers analyzed the long-term follow-up of two randomized trials that included 27,347 postmenopausal women with no prior breast cancer and negative mammograms at baseline. Their mean (SD) age was 63.4 (7.2) years. Enrollment took place from 1993 to 1998; participants were contacted for follow-up every 6 months through 2005 and annually from then on. Mortality data were gathered from follow-up and the National Death Index.
The first trial included 16,608 women with a uterus. Among these women, 8,506 received 0.625 mg/day of CEE plus 2.5 mg/day of MPA, and 8,102 received placebo. The second trial included 10,739 women who’d gotten a hysterectomy, 5,310 of whom received 0.625 mg/day of CEE alone and 5,429 of whom received placebo. The first trial ended in 2002 after a median intervention period of 5.6 years, and the second trial ended in 2004 after a period of 7.2 years.
An analysis in 2015 found that CEE alone was associated with lower risk of breast cancer and CEE plus MPA was associated with increased risk.
The current analysis confirmed that, after a median of 20.3 years of follow-up, and with mortality data now available for more than 98% of participants, CEE alone was associated with fewer cases of breast cancer (238 cases, annualized rate 0.30%), compared with placebo (296 cases, annualized rate 0.37%; hazard ratio 0.78; 95% confidence interval, 0.65-0.93; P = .005).
Furthermore, CEE alone was also associated with lower mortality (30 deaths, annualized mortality rate 0.031%), compared with placebo (46 deaths, annualized mortality rate 0.046%; HR 0.60; 95% CI, 0.37-0.97; P = .04).
By comparison, CEE plus MPA was linked with more cases of breast cancer (584 cases, annualized rate 0.45%) than placebo (447 cases, annualized rate 0.36%; HR 1.28; 95% CI, 1.13-1.45; P < .001). In regard to mortality, there was no statistically significant difference between CEE plus MPA (71 deaths, annualized mortality rate 0.045%) and placebo (53 deaths, annualized mortality rate 0.035%; HR 1.35; 95% CI, 0.94-1.95; P = .11).
“The big thing to think about is estrogen alone reducing breast cancer mortality by 40%,” said Dr. Chlebowski in an interview. “None of the other interventions, including tamoxifen, had any change on mortality. This should change the way we look at breast cancer prevention, though we might have to be a little creative about it. I think you have to be a little away from menopause for it to reduce breast cancer. But we wanted to start that debate.
“On the other hand,” he said, “a woman takes estrogen plus progestin and when you look at that curve, it’s staying about 25% increased. You take it for 5.6 years and the increase continues through 20 years, so you’re maybe buying a lifetime of increase in breast cancer by taking estrogen plus progestin for 5 years.”
He also highlighted the comprehensiveness of the mortality data, noting that “when you hook up to the National Death Index, they find 98% of all deaths in the United States. That’s really remarkable; you retain the whole power of the randomization. It means our data, between the death index and our follow-up of participants, is essentially complete.”
Use of hormone therapy, and decoding the outcomes, remains ‘complex’
Decades after the data were gathered from the Women’s Health Initiative clinical trials, they continue to assist researchers and patients alike, wrote Christina A. Minami, MD, of Brigham and Women’s Hospital in Boston and Rachel A. Freedman, MD, of the Dana-Farber Cancer Institute in Boston, in an accompanying editorial.
That said, in regard to the findings of this latest analysis, “many questions still remain on whether (and how) a hormone therapy intervention that occurred many years earlier may continue to affect breast cancer risk and mortality at 20 years,” they wrote. They noted that it’s “impossible” to isolate how exposure to certain therapies can impact long-term outcomes, and that a high percentage of patients who discontinued the drugs during each trial muddy the waters even further.
“Decisions to initiate these medications remain complex,” they added, emphasizing that breast cancer risk is just one of many factors that physicians must consider when considering hormone therapy for their patients.
Dr. Chlebowski and his coauthors acknowledged their study’s limitations, including the use of very specifically administered and formulated dosages making their findings “not necessarily generalizable to other preparations.” In addition, they noted the significant percentage of patients – 54% with CEE alone and 42% with CEE plus MPA – who discontinued drug usage during their respective trials.
The Women’s Health Initiative is supported by the National Institutes of Health and the Department of Health and Human Services. The authors reported numerous potential conflicts of interest, including receiving personal fees and grants from various government organizations, foundations, and pharmaceutical companies. The editorial’s authors reported no conflicts of interest.
SOURCE: Chlebowski RT et al. JAMA. 2020 Jul 28. doi: 10.1001/jama.2020.9482.
FROM JAMA
CCC19, other registries help define COVID/cancer landscape
Initial results from the CCC19 registry were reported as part of the American Society of Clinical Oncology (ASCO) virtual scientific program and published in The Lancet (Lancet. 2020 Jun 20;395[10241]:1907-18).
The latest data were presented at the AACR virtual meeting: COVID-19 and Cancer by Brian I. Rini, MD, of Vanderbilt University, Nashville, Tenn. They were simultaneously published in Cancer Discovery (Cancer Discov. 2020 Jul 22;CD-20-0941).
The CCC19 registry was launched in March by a few institutions as part of “a grassroots idea ... to collect granular data regarding cancer patients and their outcomes with COVID,” Dr. Rini said.
Within a few months of its inception, the registry had partnered with more than 100 institutions worldwide and accrued data from more than 2,000 patients.
The reports in The Lancet and at ASCO included outcomes for the first 928 patients and showed a 13% mortality rate as well as a fivefold increase in the risk of 30-day mortality among patients with COVID-19 and progressing cancer.
The data also showed an increased mortality risk among older patients, men, former smokers, those with poor performance status, those with multiple comorbidities, and those treated with hydroxychloroquine and azithromycin.
The latest data
The CCC19 registry has grown to include 114 sites worldwide, including major comprehensive cancer centers and community sites. As of June 26, there were 2,749 patients enrolled.
Since the last data were reported, the mortality rate increased from 13% to 16% (versus 5% globally). In addition, the increased mortality risk among non-Hispanic black patients and patients with hematologic malignancies reached statistical significance, Dr. Rini said. He noted that the increase in mortality rate was largely attributable to improved follow-up.
Mechanical ventilation was required in 12% of patients, ICU admission was required in 16%, oxygen was required in 45%, and hospitalization was required in 60%. The composite outcome of death, severe illness requiring hospitalization, ICU admission, or mechanical ventilation was reached in 29% of patients, Dr. Rini said.
Mortality rates across cancer types ranged from 3% to 26%, with thyroid and breast cancer patients having the lowest rates (3% and 8%, respectively), and with lymphoma and lung cancer patients having the highest (22% and 26%, respectively), Dr. Rini said.
He noted that the TERAVOLT registry, a COVID-19 registry for patients with thoracic cancers, also showed a very high mortality rate in this subgroup of patients.
Results from TERAVOLT were reported at the AACR virtual meeting I, presented at ASCO, and published in The Lancet (Lancet Oncol. 2020 Jul;21[7]:914-22). The most recent results showed a mortality rate of nearly 36% and reinforce the high mortality rate seen in lung cancer patients in CCC19, Dr. Rini said.
Increased mortality risk
After adjustment for several demographic and disease characteristics, the updated CCC19 data showed a significantly increased risk of mortality among:
- Older patients (adjusted odds ratio [aOR] per decade of age, 1.52).
- Men (aOR, 1.43).
- Current or former smokers vs. never smokers (aOR, 1.28).
- Patients with Eastern Cooperative Oncology Group performance scores of 1 vs. 0 (aOR of 1.80) or 2 vs. 0 (aOR, 4.22).
- Stable cancer vs. remission (aOR, 1.47).
- Progressive cancer vs. remission (aOR, 2.96).
- Non-Hispanic Black vs. White patients (aOR, 1.56).
- Hematologic malignancies vs. solid tumors (aOR, 1.80).
“Importantly, there were some factors that did not reach statistical significance,” Dr. Rini said. These include obesity (aOR, 1.23), recent surgery (aOR, 1.05), receipt of cytotoxic chemotherapy vs. no chemotherapy (aOR, 1.14), and receipt of noncytotoxic chemotherapy vs. no chemotherapy (aOR, 0.75).
“I think this provides some reassurance that cancer care can and should continue for these patients,” Dr. Rini said.
He noted, however, that in TERAVOLT, chemotherapy with or without other treatment was a risk factor for mortality in lung cancer patients when compared with no chemotherapy (OR, 1.71) and when compared with immunotherapy or targeted therapy (OR, 1.64).
NCCAPS and other registries
Dr. Rini discussed a number of registries looking at outcomes in COVID-19 patients with cancer, and he said the findings to date appear to confirm a higher mortality rate among cancer patients, particularly those with lung cancer.
Several factors are emerging that appear to be related to risk, including both cancer-related and non–cancer-related factors, he added.
The ongoing prospective National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS) “will provide much needed longitudinal data and, importantly, biospecimen collection in a large cohort of patients who have active cancer and are receiving treatment, said Dr. Rini, who is the study’s protocol chair. NCCAPS is a natural history study in that population, he said.
The planned accrual is about 2,000 patients who will be followed for up to 2 years for data collection, imaging scans, and research specimens.
The use of specimens is “a unique and special part of this study,” Dr. Rini said, explaining that the specimens will be used to look for development of antibodies over time, to describe the trajectory of cytokine abnormalities – especially in patients with more acute inpatient courses – to perform DNA-based genome-wide association studies, and to assess coagulation parameters.
NCCAPS is activated at 546 sties, 10 patients were enrolled as of June 21, and rapid accrual is expected over the next several months, he said.
Gypsyamber D’Souza, PhD, session moderator and an infectious disease epidemiologist at Johns Hopkins University in Baltimore, acknowledged the challenge that registry administrators face when trying to balance the need to get data out against the desire to ask the right questions and to have the right comparison groups, stratification, and analyses, especially amid a crisis like the COVID-19 pandemic.
Dr. Rini said it has indeed been a bit of a struggle with CCC19 to determine what information should be published and when, and what constitutes an important update.
“It’s been a learning experience, and frankly, I think we’re still learning,” he said. “This has been such a unique time in terms of a rush to get data out, balanced against making sure that there’s quality data and that you’re actually answering important questions.”
In fact, a number of ongoing registries “should start to produce great data [that will be presented] at upcoming big conferences,” Dr. Rini said. He added that those data “will help piece together different important aspects of this and different hypotheses, and hopefully complement the clinical data that’s starting to come out.”
The CCC19 registry is sponsored by Vanderbilt-Ingram Cancer Center. Dr. Rini disclosed relationships with Pfizer, Merck, Genentech/Roche, Aveo, AstraZeneca, Bristol Myers Squibb, Exelixis, Synthorx, Peloton, Compugen, Corvus, Surface Oncology, 3DMedicines, Aravive, Alkermes, Arrowhead, and PTC Therapeutics. Dr. D’Souza did not disclose any conflicts.
SOURCE: Rini BI. AACR: COVID-19 and Cancer. Abstract IA26.
Initial results from the CCC19 registry were reported as part of the American Society of Clinical Oncology (ASCO) virtual scientific program and published in The Lancet (Lancet. 2020 Jun 20;395[10241]:1907-18).
The latest data were presented at the AACR virtual meeting: COVID-19 and Cancer by Brian I. Rini, MD, of Vanderbilt University, Nashville, Tenn. They were simultaneously published in Cancer Discovery (Cancer Discov. 2020 Jul 22;CD-20-0941).
The CCC19 registry was launched in March by a few institutions as part of “a grassroots idea ... to collect granular data regarding cancer patients and their outcomes with COVID,” Dr. Rini said.
Within a few months of its inception, the registry had partnered with more than 100 institutions worldwide and accrued data from more than 2,000 patients.
The reports in The Lancet and at ASCO included outcomes for the first 928 patients and showed a 13% mortality rate as well as a fivefold increase in the risk of 30-day mortality among patients with COVID-19 and progressing cancer.
The data also showed an increased mortality risk among older patients, men, former smokers, those with poor performance status, those with multiple comorbidities, and those treated with hydroxychloroquine and azithromycin.
The latest data
The CCC19 registry has grown to include 114 sites worldwide, including major comprehensive cancer centers and community sites. As of June 26, there were 2,749 patients enrolled.
Since the last data were reported, the mortality rate increased from 13% to 16% (versus 5% globally). In addition, the increased mortality risk among non-Hispanic black patients and patients with hematologic malignancies reached statistical significance, Dr. Rini said. He noted that the increase in mortality rate was largely attributable to improved follow-up.
Mechanical ventilation was required in 12% of patients, ICU admission was required in 16%, oxygen was required in 45%, and hospitalization was required in 60%. The composite outcome of death, severe illness requiring hospitalization, ICU admission, or mechanical ventilation was reached in 29% of patients, Dr. Rini said.
Mortality rates across cancer types ranged from 3% to 26%, with thyroid and breast cancer patients having the lowest rates (3% and 8%, respectively), and with lymphoma and lung cancer patients having the highest (22% and 26%, respectively), Dr. Rini said.
He noted that the TERAVOLT registry, a COVID-19 registry for patients with thoracic cancers, also showed a very high mortality rate in this subgroup of patients.
Results from TERAVOLT were reported at the AACR virtual meeting I, presented at ASCO, and published in The Lancet (Lancet Oncol. 2020 Jul;21[7]:914-22). The most recent results showed a mortality rate of nearly 36% and reinforce the high mortality rate seen in lung cancer patients in CCC19, Dr. Rini said.
Increased mortality risk
After adjustment for several demographic and disease characteristics, the updated CCC19 data showed a significantly increased risk of mortality among:
- Older patients (adjusted odds ratio [aOR] per decade of age, 1.52).
- Men (aOR, 1.43).
- Current or former smokers vs. never smokers (aOR, 1.28).
- Patients with Eastern Cooperative Oncology Group performance scores of 1 vs. 0 (aOR of 1.80) or 2 vs. 0 (aOR, 4.22).
- Stable cancer vs. remission (aOR, 1.47).
- Progressive cancer vs. remission (aOR, 2.96).
- Non-Hispanic Black vs. White patients (aOR, 1.56).
- Hematologic malignancies vs. solid tumors (aOR, 1.80).
“Importantly, there were some factors that did not reach statistical significance,” Dr. Rini said. These include obesity (aOR, 1.23), recent surgery (aOR, 1.05), receipt of cytotoxic chemotherapy vs. no chemotherapy (aOR, 1.14), and receipt of noncytotoxic chemotherapy vs. no chemotherapy (aOR, 0.75).
“I think this provides some reassurance that cancer care can and should continue for these patients,” Dr. Rini said.
He noted, however, that in TERAVOLT, chemotherapy with or without other treatment was a risk factor for mortality in lung cancer patients when compared with no chemotherapy (OR, 1.71) and when compared with immunotherapy or targeted therapy (OR, 1.64).
NCCAPS and other registries
Dr. Rini discussed a number of registries looking at outcomes in COVID-19 patients with cancer, and he said the findings to date appear to confirm a higher mortality rate among cancer patients, particularly those with lung cancer.
Several factors are emerging that appear to be related to risk, including both cancer-related and non–cancer-related factors, he added.
The ongoing prospective National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS) “will provide much needed longitudinal data and, importantly, biospecimen collection in a large cohort of patients who have active cancer and are receiving treatment, said Dr. Rini, who is the study’s protocol chair. NCCAPS is a natural history study in that population, he said.
The planned accrual is about 2,000 patients who will be followed for up to 2 years for data collection, imaging scans, and research specimens.
The use of specimens is “a unique and special part of this study,” Dr. Rini said, explaining that the specimens will be used to look for development of antibodies over time, to describe the trajectory of cytokine abnormalities – especially in patients with more acute inpatient courses – to perform DNA-based genome-wide association studies, and to assess coagulation parameters.
NCCAPS is activated at 546 sties, 10 patients were enrolled as of June 21, and rapid accrual is expected over the next several months, he said.
Gypsyamber D’Souza, PhD, session moderator and an infectious disease epidemiologist at Johns Hopkins University in Baltimore, acknowledged the challenge that registry administrators face when trying to balance the need to get data out against the desire to ask the right questions and to have the right comparison groups, stratification, and analyses, especially amid a crisis like the COVID-19 pandemic.
Dr. Rini said it has indeed been a bit of a struggle with CCC19 to determine what information should be published and when, and what constitutes an important update.
“It’s been a learning experience, and frankly, I think we’re still learning,” he said. “This has been such a unique time in terms of a rush to get data out, balanced against making sure that there’s quality data and that you’re actually answering important questions.”
In fact, a number of ongoing registries “should start to produce great data [that will be presented] at upcoming big conferences,” Dr. Rini said. He added that those data “will help piece together different important aspects of this and different hypotheses, and hopefully complement the clinical data that’s starting to come out.”
The CCC19 registry is sponsored by Vanderbilt-Ingram Cancer Center. Dr. Rini disclosed relationships with Pfizer, Merck, Genentech/Roche, Aveo, AstraZeneca, Bristol Myers Squibb, Exelixis, Synthorx, Peloton, Compugen, Corvus, Surface Oncology, 3DMedicines, Aravive, Alkermes, Arrowhead, and PTC Therapeutics. Dr. D’Souza did not disclose any conflicts.
SOURCE: Rini BI. AACR: COVID-19 and Cancer. Abstract IA26.
Initial results from the CCC19 registry were reported as part of the American Society of Clinical Oncology (ASCO) virtual scientific program and published in The Lancet (Lancet. 2020 Jun 20;395[10241]:1907-18).
The latest data were presented at the AACR virtual meeting: COVID-19 and Cancer by Brian I. Rini, MD, of Vanderbilt University, Nashville, Tenn. They were simultaneously published in Cancer Discovery (Cancer Discov. 2020 Jul 22;CD-20-0941).
The CCC19 registry was launched in March by a few institutions as part of “a grassroots idea ... to collect granular data regarding cancer patients and their outcomes with COVID,” Dr. Rini said.
Within a few months of its inception, the registry had partnered with more than 100 institutions worldwide and accrued data from more than 2,000 patients.
The reports in The Lancet and at ASCO included outcomes for the first 928 patients and showed a 13% mortality rate as well as a fivefold increase in the risk of 30-day mortality among patients with COVID-19 and progressing cancer.
The data also showed an increased mortality risk among older patients, men, former smokers, those with poor performance status, those with multiple comorbidities, and those treated with hydroxychloroquine and azithromycin.
The latest data
The CCC19 registry has grown to include 114 sites worldwide, including major comprehensive cancer centers and community sites. As of June 26, there were 2,749 patients enrolled.
Since the last data were reported, the mortality rate increased from 13% to 16% (versus 5% globally). In addition, the increased mortality risk among non-Hispanic black patients and patients with hematologic malignancies reached statistical significance, Dr. Rini said. He noted that the increase in mortality rate was largely attributable to improved follow-up.
Mechanical ventilation was required in 12% of patients, ICU admission was required in 16%, oxygen was required in 45%, and hospitalization was required in 60%. The composite outcome of death, severe illness requiring hospitalization, ICU admission, or mechanical ventilation was reached in 29% of patients, Dr. Rini said.
Mortality rates across cancer types ranged from 3% to 26%, with thyroid and breast cancer patients having the lowest rates (3% and 8%, respectively), and with lymphoma and lung cancer patients having the highest (22% and 26%, respectively), Dr. Rini said.
He noted that the TERAVOLT registry, a COVID-19 registry for patients with thoracic cancers, also showed a very high mortality rate in this subgroup of patients.
Results from TERAVOLT were reported at the AACR virtual meeting I, presented at ASCO, and published in The Lancet (Lancet Oncol. 2020 Jul;21[7]:914-22). The most recent results showed a mortality rate of nearly 36% and reinforce the high mortality rate seen in lung cancer patients in CCC19, Dr. Rini said.
Increased mortality risk
After adjustment for several demographic and disease characteristics, the updated CCC19 data showed a significantly increased risk of mortality among:
- Older patients (adjusted odds ratio [aOR] per decade of age, 1.52).
- Men (aOR, 1.43).
- Current or former smokers vs. never smokers (aOR, 1.28).
- Patients with Eastern Cooperative Oncology Group performance scores of 1 vs. 0 (aOR of 1.80) or 2 vs. 0 (aOR, 4.22).
- Stable cancer vs. remission (aOR, 1.47).
- Progressive cancer vs. remission (aOR, 2.96).
- Non-Hispanic Black vs. White patients (aOR, 1.56).
- Hematologic malignancies vs. solid tumors (aOR, 1.80).
“Importantly, there were some factors that did not reach statistical significance,” Dr. Rini said. These include obesity (aOR, 1.23), recent surgery (aOR, 1.05), receipt of cytotoxic chemotherapy vs. no chemotherapy (aOR, 1.14), and receipt of noncytotoxic chemotherapy vs. no chemotherapy (aOR, 0.75).
“I think this provides some reassurance that cancer care can and should continue for these patients,” Dr. Rini said.
He noted, however, that in TERAVOLT, chemotherapy with or without other treatment was a risk factor for mortality in lung cancer patients when compared with no chemotherapy (OR, 1.71) and when compared with immunotherapy or targeted therapy (OR, 1.64).
NCCAPS and other registries
Dr. Rini discussed a number of registries looking at outcomes in COVID-19 patients with cancer, and he said the findings to date appear to confirm a higher mortality rate among cancer patients, particularly those with lung cancer.
Several factors are emerging that appear to be related to risk, including both cancer-related and non–cancer-related factors, he added.
The ongoing prospective National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS) “will provide much needed longitudinal data and, importantly, biospecimen collection in a large cohort of patients who have active cancer and are receiving treatment, said Dr. Rini, who is the study’s protocol chair. NCCAPS is a natural history study in that population, he said.
The planned accrual is about 2,000 patients who will be followed for up to 2 years for data collection, imaging scans, and research specimens.
The use of specimens is “a unique and special part of this study,” Dr. Rini said, explaining that the specimens will be used to look for development of antibodies over time, to describe the trajectory of cytokine abnormalities – especially in patients with more acute inpatient courses – to perform DNA-based genome-wide association studies, and to assess coagulation parameters.
NCCAPS is activated at 546 sties, 10 patients were enrolled as of June 21, and rapid accrual is expected over the next several months, he said.
Gypsyamber D’Souza, PhD, session moderator and an infectious disease epidemiologist at Johns Hopkins University in Baltimore, acknowledged the challenge that registry administrators face when trying to balance the need to get data out against the desire to ask the right questions and to have the right comparison groups, stratification, and analyses, especially amid a crisis like the COVID-19 pandemic.
Dr. Rini said it has indeed been a bit of a struggle with CCC19 to determine what information should be published and when, and what constitutes an important update.
“It’s been a learning experience, and frankly, I think we’re still learning,” he said. “This has been such a unique time in terms of a rush to get data out, balanced against making sure that there’s quality data and that you’re actually answering important questions.”
In fact, a number of ongoing registries “should start to produce great data [that will be presented] at upcoming big conferences,” Dr. Rini said. He added that those data “will help piece together different important aspects of this and different hypotheses, and hopefully complement the clinical data that’s starting to come out.”
The CCC19 registry is sponsored by Vanderbilt-Ingram Cancer Center. Dr. Rini disclosed relationships with Pfizer, Merck, Genentech/Roche, Aveo, AstraZeneca, Bristol Myers Squibb, Exelixis, Synthorx, Peloton, Compugen, Corvus, Surface Oncology, 3DMedicines, Aravive, Alkermes, Arrowhead, and PTC Therapeutics. Dr. D’Souza did not disclose any conflicts.
SOURCE: Rini BI. AACR: COVID-19 and Cancer. Abstract IA26.
FROM AACR: COVID-19 and CANCER
Genetic differences by ancestry shouldn’t impact efficacy of prostate cancer therapies
, according to an analysis published in Clinical Cancer Research.
“[N]o significant differences were seen in clinically actionable DNA repair genes, MSI-high [microsatellite instability–high] status, and tumor mutation burden, suggesting that current therapeutic strategies may be equally beneficial in both populations,” wrote study author Yusuke Koga, of the Boston University, and colleagues.
“Since these findings suggest that the frequency of targetable genetic alterations is similar in patients of predominantly African versus European ancestry, offering comprehensive genomic profiling and biomarker-based therapies to all patients, including African American patients, is a critical component of promoting equity in the management of metastatic prostate cancer,” said Atish D. Choudhury, MD, PhD, of the Dana-Farber Cancer Institute in Boston, who was not involved in this study.
Mr. Koga and colleagues noted that, when compared with European-American men, African American men have a higher incidence of prostate cancer, present with more advanced disease at an earlier age, and have increased mortality. These differences persist even after adjustment for socioeconomic covariates. That raises the question of the role of genetics.
“There is emerging evidence that, across some clinical trials and equal-access health systems, outcomes between AFR [African-American] men and European-American men with prostate cancer are similar,” the investigators wrote. “Although these data suggest that disparities can be ameliorated, there is limited knowledge of the genomic alterations that differ between groups and that could impact clinical outcomes.”
Study details and results
To get a handle on the issue, the investigators performed a meta-analysis of tumors from 250 African American men and 611 European-American men to compare the frequencies of somatic alterations across datasets from the Cancer Genome Atlas, the African Ancestry prostate cancer cohort, and the Memorial Sloan Kettering–Integrated Mutation Profiling of Actionable Cancer Targets panel.
The team also compared prostate cancer sequencing data from a commercial platform, the Foundation Medicine assay, from 436 African-American men and 3,018 European-American men.
In the meta-analysis, mutations in ZFHX3 and focal deletions in ETV3 were more common in tumors from African American men than in tumors from European-American men. Both genes are putative prostate cancer tumor suppressors, the investigators noted.
TP53 mutations, meanwhile, were associated with increasing Gleason scores in both groups, suggesting “that if TP53 mutations are found in low-grade disease, they may potentially indicate a more aggressive clinical trajectory,” the investigators wrote.
In the analysis with the commercial assay, MYC amplifications were more frequent in African American men with metastatic disease, raising “the possibility that MYC amplifications may also contribute to high-risk disease in this population,” the team wrote.
Deletions in PTEN and rearrangements in TMPRSS2-ERG were less frequent in tumors from African American men, but KMT2D truncations and CCND1 amplifications were more frequent.
“Higher expression of CCND1 has been implicated with perineural invasion in prostate cancer, an aggressive histological feature in prostate cancer. Truncating mutations in KMT2D have been reported in both localized and metastatic prostate cancer patients with unclear clinical significance,” the investigators noted.
“The genomic differences seen in genes such as MYC, ZFHX3, PTEN, and TMPRSS2-ERG suggest that different pathways of carcinogenesis may be active in AFR [African American] men, which could lead to further disparities if targeted therapies for some of these alterations become available,” the team wrote.
They noted that the meta-analysis was limited by the fact that some cohorts lacked matched tumors from European-American men, which limited the investigators’ ability to control for differences in region, clinical setting, or sequencing assay. Furthermore, age, tumor stage, and Gleason grade were unavailable in the cohort analyzed with the commercial assay.
This research was funded by the Department of Defense, the National Cancer Institute, and the Prostate Cancer Foundation. Two authors are employees of Foundation Medicine.
SOURCE: Koga Y et al. Clin Cancer Res. 2020 Jul 10. doi: 10.1158/1078-0432.CCR-19-4112.
, according to an analysis published in Clinical Cancer Research.
“[N]o significant differences were seen in clinically actionable DNA repair genes, MSI-high [microsatellite instability–high] status, and tumor mutation burden, suggesting that current therapeutic strategies may be equally beneficial in both populations,” wrote study author Yusuke Koga, of the Boston University, and colleagues.
“Since these findings suggest that the frequency of targetable genetic alterations is similar in patients of predominantly African versus European ancestry, offering comprehensive genomic profiling and biomarker-based therapies to all patients, including African American patients, is a critical component of promoting equity in the management of metastatic prostate cancer,” said Atish D. Choudhury, MD, PhD, of the Dana-Farber Cancer Institute in Boston, who was not involved in this study.
Mr. Koga and colleagues noted that, when compared with European-American men, African American men have a higher incidence of prostate cancer, present with more advanced disease at an earlier age, and have increased mortality. These differences persist even after adjustment for socioeconomic covariates. That raises the question of the role of genetics.
“There is emerging evidence that, across some clinical trials and equal-access health systems, outcomes between AFR [African-American] men and European-American men with prostate cancer are similar,” the investigators wrote. “Although these data suggest that disparities can be ameliorated, there is limited knowledge of the genomic alterations that differ between groups and that could impact clinical outcomes.”
Study details and results
To get a handle on the issue, the investigators performed a meta-analysis of tumors from 250 African American men and 611 European-American men to compare the frequencies of somatic alterations across datasets from the Cancer Genome Atlas, the African Ancestry prostate cancer cohort, and the Memorial Sloan Kettering–Integrated Mutation Profiling of Actionable Cancer Targets panel.
The team also compared prostate cancer sequencing data from a commercial platform, the Foundation Medicine assay, from 436 African-American men and 3,018 European-American men.
In the meta-analysis, mutations in ZFHX3 and focal deletions in ETV3 were more common in tumors from African American men than in tumors from European-American men. Both genes are putative prostate cancer tumor suppressors, the investigators noted.
TP53 mutations, meanwhile, were associated with increasing Gleason scores in both groups, suggesting “that if TP53 mutations are found in low-grade disease, they may potentially indicate a more aggressive clinical trajectory,” the investigators wrote.
In the analysis with the commercial assay, MYC amplifications were more frequent in African American men with metastatic disease, raising “the possibility that MYC amplifications may also contribute to high-risk disease in this population,” the team wrote.
Deletions in PTEN and rearrangements in TMPRSS2-ERG were less frequent in tumors from African American men, but KMT2D truncations and CCND1 amplifications were more frequent.
“Higher expression of CCND1 has been implicated with perineural invasion in prostate cancer, an aggressive histological feature in prostate cancer. Truncating mutations in KMT2D have been reported in both localized and metastatic prostate cancer patients with unclear clinical significance,” the investigators noted.
“The genomic differences seen in genes such as MYC, ZFHX3, PTEN, and TMPRSS2-ERG suggest that different pathways of carcinogenesis may be active in AFR [African American] men, which could lead to further disparities if targeted therapies for some of these alterations become available,” the team wrote.
They noted that the meta-analysis was limited by the fact that some cohorts lacked matched tumors from European-American men, which limited the investigators’ ability to control for differences in region, clinical setting, or sequencing assay. Furthermore, age, tumor stage, and Gleason grade were unavailable in the cohort analyzed with the commercial assay.
This research was funded by the Department of Defense, the National Cancer Institute, and the Prostate Cancer Foundation. Two authors are employees of Foundation Medicine.
SOURCE: Koga Y et al. Clin Cancer Res. 2020 Jul 10. doi: 10.1158/1078-0432.CCR-19-4112.
, according to an analysis published in Clinical Cancer Research.
“[N]o significant differences were seen in clinically actionable DNA repair genes, MSI-high [microsatellite instability–high] status, and tumor mutation burden, suggesting that current therapeutic strategies may be equally beneficial in both populations,” wrote study author Yusuke Koga, of the Boston University, and colleagues.
“Since these findings suggest that the frequency of targetable genetic alterations is similar in patients of predominantly African versus European ancestry, offering comprehensive genomic profiling and biomarker-based therapies to all patients, including African American patients, is a critical component of promoting equity in the management of metastatic prostate cancer,” said Atish D. Choudhury, MD, PhD, of the Dana-Farber Cancer Institute in Boston, who was not involved in this study.
Mr. Koga and colleagues noted that, when compared with European-American men, African American men have a higher incidence of prostate cancer, present with more advanced disease at an earlier age, and have increased mortality. These differences persist even after adjustment for socioeconomic covariates. That raises the question of the role of genetics.
“There is emerging evidence that, across some clinical trials and equal-access health systems, outcomes between AFR [African-American] men and European-American men with prostate cancer are similar,” the investigators wrote. “Although these data suggest that disparities can be ameliorated, there is limited knowledge of the genomic alterations that differ between groups and that could impact clinical outcomes.”
Study details and results
To get a handle on the issue, the investigators performed a meta-analysis of tumors from 250 African American men and 611 European-American men to compare the frequencies of somatic alterations across datasets from the Cancer Genome Atlas, the African Ancestry prostate cancer cohort, and the Memorial Sloan Kettering–Integrated Mutation Profiling of Actionable Cancer Targets panel.
The team also compared prostate cancer sequencing data from a commercial platform, the Foundation Medicine assay, from 436 African-American men and 3,018 European-American men.
In the meta-analysis, mutations in ZFHX3 and focal deletions in ETV3 were more common in tumors from African American men than in tumors from European-American men. Both genes are putative prostate cancer tumor suppressors, the investigators noted.
TP53 mutations, meanwhile, were associated with increasing Gleason scores in both groups, suggesting “that if TP53 mutations are found in low-grade disease, they may potentially indicate a more aggressive clinical trajectory,” the investigators wrote.
In the analysis with the commercial assay, MYC amplifications were more frequent in African American men with metastatic disease, raising “the possibility that MYC amplifications may also contribute to high-risk disease in this population,” the team wrote.
Deletions in PTEN and rearrangements in TMPRSS2-ERG were less frequent in tumors from African American men, but KMT2D truncations and CCND1 amplifications were more frequent.
“Higher expression of CCND1 has been implicated with perineural invasion in prostate cancer, an aggressive histological feature in prostate cancer. Truncating mutations in KMT2D have been reported in both localized and metastatic prostate cancer patients with unclear clinical significance,” the investigators noted.
“The genomic differences seen in genes such as MYC, ZFHX3, PTEN, and TMPRSS2-ERG suggest that different pathways of carcinogenesis may be active in AFR [African American] men, which could lead to further disparities if targeted therapies for some of these alterations become available,” the team wrote.
They noted that the meta-analysis was limited by the fact that some cohorts lacked matched tumors from European-American men, which limited the investigators’ ability to control for differences in region, clinical setting, or sequencing assay. Furthermore, age, tumor stage, and Gleason grade were unavailable in the cohort analyzed with the commercial assay.
This research was funded by the Department of Defense, the National Cancer Institute, and the Prostate Cancer Foundation. Two authors are employees of Foundation Medicine.
SOURCE: Koga Y et al. Clin Cancer Res. 2020 Jul 10. doi: 10.1158/1078-0432.CCR-19-4112.
FROM CLINICAL CANCER RESEARCH
Ticagrelor/aspirin combo: Fewer repeat strokes and deaths, but more bleeds
, new data show. However, severe bleeding was more common in the ticagrelor/aspirin group than in the aspirin-only group.
“We found that ticagrelor plus aspirin reduced the risk of stroke or death, compared to aspirin alone in patients presenting acutely with stroke or TIA,” reported lead author S. Claiborne Johnston, MD, PhD, dean and vice president for medical affairs, Dell Medical School, the University of Texas, Austin.
Although the combination also increased the risk for major hemorrhage, that increase was small and would not overwhelm the benefit, he said.
The study was published online July 16 in The New England Journal of Medicine.
Attractive properties
“Lots of patients have stroke in the days to weeks after first presenting with a stroke or TIA,” said Dr. Johnston, who is also the Frank and Charmaine Denius Distinguished Dean’s Chair at Dell Medical School. “Aspirin has been the standard of care but is only partially effective. Clopidogrel plus aspirin is another option that has recently been proven, [but] ticagrelor has attractive properties as an antiplatelet agent and works synergistically with aspirin,” he added.
Ticagrelor is a direct-acting antiplatelet agent that does not depend on metabolic activation and that “reversibly binds” and inhibits the P2Y12 receptor on platelets. Previous research has evaluated clopidogrel and aspirin for the secondary prevention of ischemic stroke or TIA. In an earlier trial, ticagrelor was no better than aspirin in preventing these subsequent events. However, the investigators noted that the combination of the two drugs has not been well studied.
The randomized, placebo-controlled, double-blind trial involved 11,016 patients at 414 sites in 28 countries. Patients who had experienced mild to moderate acute noncardioembolic ischemic stroke (mean age, 65 years; 39% women; roughly 54% White) were randomly assigned to receive either ticagrelor plus aspirin (n = 5,523) or aspirin alone (n = 5,493) for 30 days. Of these patients, 91% had sustained a stroke, and 9% had sustained a TIA.
Thirty days was chosen as the treatment period because the risk for subsequent stroke tends to occur mainly in the first month after an acute ischemic stroke or TIA. The primary outcome was “a composite of stroke or death in a time-to-first-event analysis from randomization to 30 days of follow-up.” For the study, “stroke” encompassed ischemic, hemorrhagic, or stroke of undetermined type, and “death” included deaths of all causes. Secondary outcomes included first subsequent ischemic stroke and disability (defined as a score of >1 on the Rankin Scale).
Almost all patients (99.5%) were taking aspirin during the treatment period, and most were also taking an antihypertensive and a statin (74% and 83%, respectively).
Patients in the ticagrelor/aspirin group had fewer primary-outcome events in comparison with those in the aspirin-only group (303 patients [5.5%] vs. 362 patients [6.6%]; hazard ratio, 0.83; 95% confidence interval, 0.71-0.96; P = 0.02). Incidence of subsequent ischemic stroke were similarly lower in the ticagrelor/aspirin group in comparison with the aspirin-only group (276 patients [5.0%] vs. 345 patients [6.3%]; HR, 0.79; 95% CI, 0.68-0.93; P = .004).
On the other hand, there was no significant difference between the groups in the incidence of overall disability (23.8% of the patients in the ticagrelor/aspirin group and in 24.1% of the patients in the aspirin group; odds ratio, 0.98; 95% CI, 0.89-1.07; P = .61).
There were differences between the groups in severe bleeding, which occurred in 28 patients (0.5%) in the ticagrelor/aspirin group and in seven patients (0.15) in the ticagrelor group (HR, 3.99; 95% CI, 1.74-9.14; P = .001). Moreover, more patients in the ticagrelor/aspirin group experienced a composite of intracranial hemorrhage or fatal bleeding compared with the aspirin-only group (0.4% vs 0.1%). Fatal bleeding occurred in 0.2% of patients in the ticagrelor/aspirin group versus 0.1% of patients in the aspirin group. More patients in the ticagrelor-aspirin group permanently discontinued the treatment because of bleeding than in the aspirin-only group (2.8% vs. 0.6%).
“The benefit from treatment with ticagrelor/aspirin, as compared with aspirin alone, would be expected to result in a number needed to treat of 92 to prevent one primary outcome event, and a number needed to harm of 263 for severe bleeding,” the authors noted.
Risks versus benefits
Commenting on the study, Konark Malhotra, MD, a vascular neurologist at Allegheny Health Network, Pittsburgh, noted that ticagrelor is an antiplatelet medication “that adds to the armamentarium of stroke neurologists for the treatment of mild acute ischemic or high-risk TIA patients.” Dr. Malhotra, who was not involved with the study, added that the “combined use of ticagrelor and aspirin is effective in the reduction of ischemic events, however, at the expense of increased risk of bleeding events.”
In an accompanying editorial, Peter Rothwell, MD, PhD, of the Wolfson Center for Prevention of Stroke and Dementia, Nuffield Department of Clinical Neurosciences at the University of Oxford (England) who was not involved with the study, suggested that the “bleeding risk associated with ticagrelor and aspirin might exceed the benefit among lower-risk patients who make up the majority in practice, and so the results should not be overgeneralized.” Moreover, “regardless of which combination of antiplatelet therapy is favored for the high-risk minority, all patients should receive aspirin immediately after TIA, unless aspirin is contraindicated.”
He noted that “too many patients are sent home from emergency departments without this simple treatment that substantially reduces the risk and severity of early recurrent stroke.”
The study was supported by AstraZeneca. Dr. Johnston has received a grant from AstraZeneca and nonfinancial support from SANOFI. Dr. Rothwell has received personal fees from Bayer and BMS. Dr. Malhotra has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, new data show. However, severe bleeding was more common in the ticagrelor/aspirin group than in the aspirin-only group.
“We found that ticagrelor plus aspirin reduced the risk of stroke or death, compared to aspirin alone in patients presenting acutely with stroke or TIA,” reported lead author S. Claiborne Johnston, MD, PhD, dean and vice president for medical affairs, Dell Medical School, the University of Texas, Austin.
Although the combination also increased the risk for major hemorrhage, that increase was small and would not overwhelm the benefit, he said.
The study was published online July 16 in The New England Journal of Medicine.
Attractive properties
“Lots of patients have stroke in the days to weeks after first presenting with a stroke or TIA,” said Dr. Johnston, who is also the Frank and Charmaine Denius Distinguished Dean’s Chair at Dell Medical School. “Aspirin has been the standard of care but is only partially effective. Clopidogrel plus aspirin is another option that has recently been proven, [but] ticagrelor has attractive properties as an antiplatelet agent and works synergistically with aspirin,” he added.
Ticagrelor is a direct-acting antiplatelet agent that does not depend on metabolic activation and that “reversibly binds” and inhibits the P2Y12 receptor on platelets. Previous research has evaluated clopidogrel and aspirin for the secondary prevention of ischemic stroke or TIA. In an earlier trial, ticagrelor was no better than aspirin in preventing these subsequent events. However, the investigators noted that the combination of the two drugs has not been well studied.
The randomized, placebo-controlled, double-blind trial involved 11,016 patients at 414 sites in 28 countries. Patients who had experienced mild to moderate acute noncardioembolic ischemic stroke (mean age, 65 years; 39% women; roughly 54% White) were randomly assigned to receive either ticagrelor plus aspirin (n = 5,523) or aspirin alone (n = 5,493) for 30 days. Of these patients, 91% had sustained a stroke, and 9% had sustained a TIA.
Thirty days was chosen as the treatment period because the risk for subsequent stroke tends to occur mainly in the first month after an acute ischemic stroke or TIA. The primary outcome was “a composite of stroke or death in a time-to-first-event analysis from randomization to 30 days of follow-up.” For the study, “stroke” encompassed ischemic, hemorrhagic, or stroke of undetermined type, and “death” included deaths of all causes. Secondary outcomes included first subsequent ischemic stroke and disability (defined as a score of >1 on the Rankin Scale).
Almost all patients (99.5%) were taking aspirin during the treatment period, and most were also taking an antihypertensive and a statin (74% and 83%, respectively).
Patients in the ticagrelor/aspirin group had fewer primary-outcome events in comparison with those in the aspirin-only group (303 patients [5.5%] vs. 362 patients [6.6%]; hazard ratio, 0.83; 95% confidence interval, 0.71-0.96; P = 0.02). Incidence of subsequent ischemic stroke were similarly lower in the ticagrelor/aspirin group in comparison with the aspirin-only group (276 patients [5.0%] vs. 345 patients [6.3%]; HR, 0.79; 95% CI, 0.68-0.93; P = .004).
On the other hand, there was no significant difference between the groups in the incidence of overall disability (23.8% of the patients in the ticagrelor/aspirin group and in 24.1% of the patients in the aspirin group; odds ratio, 0.98; 95% CI, 0.89-1.07; P = .61).
There were differences between the groups in severe bleeding, which occurred in 28 patients (0.5%) in the ticagrelor/aspirin group and in seven patients (0.15) in the ticagrelor group (HR, 3.99; 95% CI, 1.74-9.14; P = .001). Moreover, more patients in the ticagrelor/aspirin group experienced a composite of intracranial hemorrhage or fatal bleeding compared with the aspirin-only group (0.4% vs 0.1%). Fatal bleeding occurred in 0.2% of patients in the ticagrelor/aspirin group versus 0.1% of patients in the aspirin group. More patients in the ticagrelor-aspirin group permanently discontinued the treatment because of bleeding than in the aspirin-only group (2.8% vs. 0.6%).
“The benefit from treatment with ticagrelor/aspirin, as compared with aspirin alone, would be expected to result in a number needed to treat of 92 to prevent one primary outcome event, and a number needed to harm of 263 for severe bleeding,” the authors noted.
Risks versus benefits
Commenting on the study, Konark Malhotra, MD, a vascular neurologist at Allegheny Health Network, Pittsburgh, noted that ticagrelor is an antiplatelet medication “that adds to the armamentarium of stroke neurologists for the treatment of mild acute ischemic or high-risk TIA patients.” Dr. Malhotra, who was not involved with the study, added that the “combined use of ticagrelor and aspirin is effective in the reduction of ischemic events, however, at the expense of increased risk of bleeding events.”
In an accompanying editorial, Peter Rothwell, MD, PhD, of the Wolfson Center for Prevention of Stroke and Dementia, Nuffield Department of Clinical Neurosciences at the University of Oxford (England) who was not involved with the study, suggested that the “bleeding risk associated with ticagrelor and aspirin might exceed the benefit among lower-risk patients who make up the majority in practice, and so the results should not be overgeneralized.” Moreover, “regardless of which combination of antiplatelet therapy is favored for the high-risk minority, all patients should receive aspirin immediately after TIA, unless aspirin is contraindicated.”
He noted that “too many patients are sent home from emergency departments without this simple treatment that substantially reduces the risk and severity of early recurrent stroke.”
The study was supported by AstraZeneca. Dr. Johnston has received a grant from AstraZeneca and nonfinancial support from SANOFI. Dr. Rothwell has received personal fees from Bayer and BMS. Dr. Malhotra has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, new data show. However, severe bleeding was more common in the ticagrelor/aspirin group than in the aspirin-only group.
“We found that ticagrelor plus aspirin reduced the risk of stroke or death, compared to aspirin alone in patients presenting acutely with stroke or TIA,” reported lead author S. Claiborne Johnston, MD, PhD, dean and vice president for medical affairs, Dell Medical School, the University of Texas, Austin.
Although the combination also increased the risk for major hemorrhage, that increase was small and would not overwhelm the benefit, he said.
The study was published online July 16 in The New England Journal of Medicine.
Attractive properties
“Lots of patients have stroke in the days to weeks after first presenting with a stroke or TIA,” said Dr. Johnston, who is also the Frank and Charmaine Denius Distinguished Dean’s Chair at Dell Medical School. “Aspirin has been the standard of care but is only partially effective. Clopidogrel plus aspirin is another option that has recently been proven, [but] ticagrelor has attractive properties as an antiplatelet agent and works synergistically with aspirin,” he added.
Ticagrelor is a direct-acting antiplatelet agent that does not depend on metabolic activation and that “reversibly binds” and inhibits the P2Y12 receptor on platelets. Previous research has evaluated clopidogrel and aspirin for the secondary prevention of ischemic stroke or TIA. In an earlier trial, ticagrelor was no better than aspirin in preventing these subsequent events. However, the investigators noted that the combination of the two drugs has not been well studied.
The randomized, placebo-controlled, double-blind trial involved 11,016 patients at 414 sites in 28 countries. Patients who had experienced mild to moderate acute noncardioembolic ischemic stroke (mean age, 65 years; 39% women; roughly 54% White) were randomly assigned to receive either ticagrelor plus aspirin (n = 5,523) or aspirin alone (n = 5,493) for 30 days. Of these patients, 91% had sustained a stroke, and 9% had sustained a TIA.
Thirty days was chosen as the treatment period because the risk for subsequent stroke tends to occur mainly in the first month after an acute ischemic stroke or TIA. The primary outcome was “a composite of stroke or death in a time-to-first-event analysis from randomization to 30 days of follow-up.” For the study, “stroke” encompassed ischemic, hemorrhagic, or stroke of undetermined type, and “death” included deaths of all causes. Secondary outcomes included first subsequent ischemic stroke and disability (defined as a score of >1 on the Rankin Scale).
Almost all patients (99.5%) were taking aspirin during the treatment period, and most were also taking an antihypertensive and a statin (74% and 83%, respectively).
Patients in the ticagrelor/aspirin group had fewer primary-outcome events in comparison with those in the aspirin-only group (303 patients [5.5%] vs. 362 patients [6.6%]; hazard ratio, 0.83; 95% confidence interval, 0.71-0.96; P = 0.02). Incidence of subsequent ischemic stroke were similarly lower in the ticagrelor/aspirin group in comparison with the aspirin-only group (276 patients [5.0%] vs. 345 patients [6.3%]; HR, 0.79; 95% CI, 0.68-0.93; P = .004).
On the other hand, there was no significant difference between the groups in the incidence of overall disability (23.8% of the patients in the ticagrelor/aspirin group and in 24.1% of the patients in the aspirin group; odds ratio, 0.98; 95% CI, 0.89-1.07; P = .61).
There were differences between the groups in severe bleeding, which occurred in 28 patients (0.5%) in the ticagrelor/aspirin group and in seven patients (0.15) in the ticagrelor group (HR, 3.99; 95% CI, 1.74-9.14; P = .001). Moreover, more patients in the ticagrelor/aspirin group experienced a composite of intracranial hemorrhage or fatal bleeding compared with the aspirin-only group (0.4% vs 0.1%). Fatal bleeding occurred in 0.2% of patients in the ticagrelor/aspirin group versus 0.1% of patients in the aspirin group. More patients in the ticagrelor-aspirin group permanently discontinued the treatment because of bleeding than in the aspirin-only group (2.8% vs. 0.6%).
“The benefit from treatment with ticagrelor/aspirin, as compared with aspirin alone, would be expected to result in a number needed to treat of 92 to prevent one primary outcome event, and a number needed to harm of 263 for severe bleeding,” the authors noted.
Risks versus benefits
Commenting on the study, Konark Malhotra, MD, a vascular neurologist at Allegheny Health Network, Pittsburgh, noted that ticagrelor is an antiplatelet medication “that adds to the armamentarium of stroke neurologists for the treatment of mild acute ischemic or high-risk TIA patients.” Dr. Malhotra, who was not involved with the study, added that the “combined use of ticagrelor and aspirin is effective in the reduction of ischemic events, however, at the expense of increased risk of bleeding events.”
In an accompanying editorial, Peter Rothwell, MD, PhD, of the Wolfson Center for Prevention of Stroke and Dementia, Nuffield Department of Clinical Neurosciences at the University of Oxford (England) who was not involved with the study, suggested that the “bleeding risk associated with ticagrelor and aspirin might exceed the benefit among lower-risk patients who make up the majority in practice, and so the results should not be overgeneralized.” Moreover, “regardless of which combination of antiplatelet therapy is favored for the high-risk minority, all patients should receive aspirin immediately after TIA, unless aspirin is contraindicated.”
He noted that “too many patients are sent home from emergency departments without this simple treatment that substantially reduces the risk and severity of early recurrent stroke.”
The study was supported by AstraZeneca. Dr. Johnston has received a grant from AstraZeneca and nonfinancial support from SANOFI. Dr. Rothwell has received personal fees from Bayer and BMS. Dr. Malhotra has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
From New England Journal of Medicine
‘Knowledge is power’: Knowing BRCA1/2 status tied to survival
The study, conducted among Ashkenazi Jewish women in Israel, showed that among women who knew their carrier status before they developed breast cancer, diagnoses were made at an earlier disease stage and 5-year survival was improved compared to women who learned their carrier status only after their disease had been diagnosed.
The study was published online on July 9 in JAMA Oncology.
“I don’t want to belittle the complexities of knowing that you’re a carrier. But I think these results really show that knowledge is power,” first author Ephrat Levy-Lahad, MD, director of the medical genetics unit at Shaare Zedek Medical Center in Jerusalem, Israel, told Medscape Medical News.
Carrying a BRCA1/2 pathogenic mutation is associated with a 70% to 80% lifetime risk for breast cancer and about a 10% to 50% lifetime risk for ovarian cancer, depending on the specific mutation. Only about 10% of carriers will not develop either cancer during their lifetime.
The study provides support for genetic screening for pathogenic BRCA1/2 mutations, especially in high-risk populations, according to Levy-Lahad.
“For me, the results are part of a bigger picture.... I think we should be moving towards general population screening, certainly in high-risk populations like Ashkenazi Jews,” she said.
In Israel, that decision has already been made: a new policy, introduced in January 2020, offers testing for common BRCA1/2 mutations for all Ashkenazi Jewish women.
However, women in other countries may also benefit from testing, she argues. About half of BRCA1/2 carriers in a general population like that of the United States do not have a family history that would indicate a need for testing. That means many women who carry these mutations may not be taking advantage of recommended surveillance and prevention measures, she said.
But screening for BRCA1/2 mutations becomes more complicated when applied to more general populations, she acknowledged.
About 2.5% of women of Ashkenazi Jewish descent carry pathogenic mutations for BRCA1/2, compared to 0.5% in the general White population.
Also, screening in the Ashkenazi Jewish population is probably simpler than in the general population. Just three mutations are definitely known to cause disease and need to be tested for among Ashkenazi Jews. Screening in a larger population would require full sequencing of the gene. That increases the likelihood of finding variants of unknown significance (VUSs), which muddies the water. Knowledge is incomplete about whether some of these VUSs increase cancer risk, and physicians do not always know how to manage them in women who test positive.
Moreover, Israel has a national health system. Screening in a country without universal health insurance such as the United States raises questions about whether follow-up would be covered by insurance carriers for women who test positive.
Mehmet Copur, MD, an oncologist at Morrison Cancer Center in Hastings, Nebraska, questions how general population screening could be done in “real life.”
“These findings should be taken into consideration in the context of the patient population who would agree to genetic testing, who would agree to comply with the recommended guidelines for risk reduction, and who would have insurance coverage or resources to comply with the recommendations,” Copur told Medscape Medical News.
“If BRCA-positive patients did not or could not follow these recommendations, the results would different,” he added.
The most crucial component of screening for these mutations is genetic counselors, who are in short supply in the United States, according to Copur.
Another issue is that of cost. Genetic counseling is not always covered by insurance, especially for individuals who do not have a family history of BRCA-related cancers. Genetic testing is not cheap, and the costs of monitoring women who test positive could be prohibitive, especially in a healthcare system burdened by COVID-19.
“Whether our current healthcare system could bear the cost of such a change is up for debate. The screening itself may be feasible, but offering lifelong surveillance to every woman identified with mutations could present huge capacity issues,” Copur said. “Maybe in the future, the healthcare system can be ready for such an undertaking, but I don’t think we are there yet.”
Although she acknowledges the differences in risk between Ashkenazi Jews and the general population, Levy-Lahad thinks not having screening is like “throwing the baby out with the bath water.”
“Maybe we’re not ready for total general population screening, but I think we have to start thinking along those lines,” she said. “We have this incredible tool for cancer prevention, and we should really be using it, certainly in populations like Ashkenazi Jews.”
Researchers conducted a retrospective analysis that included 105 women diagnosed with breast cancer at Shaare Zedek Medical Center in Jerusalem between 2005 and 2016. Forty-two women knew they were carriers before their breast cancer diagnosis, and 63 learned of their carrier status only after diagnosis. Of the participants, 83% were Ashkenazi Jews. For both prediagnosis and postdiagnosis groups, the age at diagnosis was the same (50.4 years). For both groups, distributions of pathogenic mutations were similar. There were no significant differences in hormone receptor or ERBB2 status.
Among women who knew they were carriers before diagnosis, 80.9% (34/42) were diagnosed either with ductal carcinoma in situ or stage 1 disease. Only 9.5% (4/42) of these women were diagnosed with disease of stage 2 or higher.
In comparison, among women who learned their carrier status after diagnosis, 30% (19/63) had early-stage disease at diagnosis, and 52.4% (33/63) were diagnosed at stage 2 or higher (P < .001).
Compared to women who knew their carrier status before diagnosis, women who found out after diagnosis had 12 times higher odds of being diagnosed with disease of advanced clinical stage (P = .001) and eight times higher odds of being diagnosed with disease of advanced pathologic stage (P = .002).
A sentinel node biopsy was sufficient in 85.7% (36/42) of women who knew their carrier status before diagnosis; 7.2% (3/42) of these women needed a full lymph node dissection. In contrast, 3.2% (2/63) of women who learned their carrier status after diagnosis underwent sentinel node biopsy, and 34.9% (25/105) needed a full lymph node dissection (P < .001).
Among women who knew their carrier status before diagnosis, 54.8% (23/42) did not need chemotherapy at all, and none needed neoadjuvant chemotherapy. Only 4.8% (3/63) of women who learned their mutation status after diagnosis were able to forgo chemotherapy (P < .001); 22.2% (14/63) needed neoadjuvant therapy (P = .001).
These findings appeared to translate into better outcomes. Overall 5-year survival was significantly higher among women who knew their carrier status before diagnosis compared to women who found out afterward (94% [SE 4%] vs 78% [SE 5%]; P = .03). Only two of 42 women (4.8%) in the prediagnosis group died, compared to 16 of 63 (25.4%) in the postdiagnosis group.
Analyses that controlled for year at diagnosis showed that women who learned their carrier status before diagnosis had significantly lower risk for overall mortality compared with those who found out after diagnosis (hazard ratio [HR], 0.20; 95% CI, 0.04 – 0.93; P = .04). However, these results lost significance when controlled for age, socioeconomic index, family history, and gene variant (HR, 0.16; 95% CI, 0.02 – 1.4; P = .10).
Higher socioeconomic status (HR, 0.76; 95% CI, 0.6 – 0.97; P = .03), gene variant (BRCA2 vs BRCA1: HR, 0.15; 95% CI, 0.03 – 0.75; P = .02), and age at diagnosis (HR, 1.047; 95% CI, 1.003 – 1.093; P = .04) were all associated with overall mortality.
“I can’t infer causation, but we suspect that the reason for these results is the difference in follow-up,” Levy-Lahad said.
Most of the women (95.2%, 40/42) who knew their carrier status before diagnosis received their follow-up at the medical center’s high-risk carrier clinic. Twenty-seven of 42 (64.3%) of these women were diagnosed with breast MRI. By contrast, only 1.6% (1/63) of women who found out their carrier status after diagnosis were diagnosed with breast MRI. Breast MRI is not routinely used for breast cancer screening but can be more sensitive than mammography for detecting breast cancer.
The study was funded by the Breast Cancer Research Foundation and by a gift from Ellie and David Werber to ShaareZedek Medical Center.
Levy-Lahad received grants from the Breast Cancer Research Foundation and from the Israel Cancer Association during the conduct of the study and personal fees from AstraZeneca outside the submitted work. Copur has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The study, conducted among Ashkenazi Jewish women in Israel, showed that among women who knew their carrier status before they developed breast cancer, diagnoses were made at an earlier disease stage and 5-year survival was improved compared to women who learned their carrier status only after their disease had been diagnosed.
The study was published online on July 9 in JAMA Oncology.
“I don’t want to belittle the complexities of knowing that you’re a carrier. But I think these results really show that knowledge is power,” first author Ephrat Levy-Lahad, MD, director of the medical genetics unit at Shaare Zedek Medical Center in Jerusalem, Israel, told Medscape Medical News.
Carrying a BRCA1/2 pathogenic mutation is associated with a 70% to 80% lifetime risk for breast cancer and about a 10% to 50% lifetime risk for ovarian cancer, depending on the specific mutation. Only about 10% of carriers will not develop either cancer during their lifetime.
The study provides support for genetic screening for pathogenic BRCA1/2 mutations, especially in high-risk populations, according to Levy-Lahad.
“For me, the results are part of a bigger picture.... I think we should be moving towards general population screening, certainly in high-risk populations like Ashkenazi Jews,” she said.
In Israel, that decision has already been made: a new policy, introduced in January 2020, offers testing for common BRCA1/2 mutations for all Ashkenazi Jewish women.
However, women in other countries may also benefit from testing, she argues. About half of BRCA1/2 carriers in a general population like that of the United States do not have a family history that would indicate a need for testing. That means many women who carry these mutations may not be taking advantage of recommended surveillance and prevention measures, she said.
But screening for BRCA1/2 mutations becomes more complicated when applied to more general populations, she acknowledged.
About 2.5% of women of Ashkenazi Jewish descent carry pathogenic mutations for BRCA1/2, compared to 0.5% in the general White population.
Also, screening in the Ashkenazi Jewish population is probably simpler than in the general population. Just three mutations are definitely known to cause disease and need to be tested for among Ashkenazi Jews. Screening in a larger population would require full sequencing of the gene. That increases the likelihood of finding variants of unknown significance (VUSs), which muddies the water. Knowledge is incomplete about whether some of these VUSs increase cancer risk, and physicians do not always know how to manage them in women who test positive.
Moreover, Israel has a national health system. Screening in a country without universal health insurance such as the United States raises questions about whether follow-up would be covered by insurance carriers for women who test positive.
Mehmet Copur, MD, an oncologist at Morrison Cancer Center in Hastings, Nebraska, questions how general population screening could be done in “real life.”
“These findings should be taken into consideration in the context of the patient population who would agree to genetic testing, who would agree to comply with the recommended guidelines for risk reduction, and who would have insurance coverage or resources to comply with the recommendations,” Copur told Medscape Medical News.
“If BRCA-positive patients did not or could not follow these recommendations, the results would different,” he added.
The most crucial component of screening for these mutations is genetic counselors, who are in short supply in the United States, according to Copur.
Another issue is that of cost. Genetic counseling is not always covered by insurance, especially for individuals who do not have a family history of BRCA-related cancers. Genetic testing is not cheap, and the costs of monitoring women who test positive could be prohibitive, especially in a healthcare system burdened by COVID-19.
“Whether our current healthcare system could bear the cost of such a change is up for debate. The screening itself may be feasible, but offering lifelong surveillance to every woman identified with mutations could present huge capacity issues,” Copur said. “Maybe in the future, the healthcare system can be ready for such an undertaking, but I don’t think we are there yet.”
Although she acknowledges the differences in risk between Ashkenazi Jews and the general population, Levy-Lahad thinks not having screening is like “throwing the baby out with the bath water.”
“Maybe we’re not ready for total general population screening, but I think we have to start thinking along those lines,” she said. “We have this incredible tool for cancer prevention, and we should really be using it, certainly in populations like Ashkenazi Jews.”
Researchers conducted a retrospective analysis that included 105 women diagnosed with breast cancer at Shaare Zedek Medical Center in Jerusalem between 2005 and 2016. Forty-two women knew they were carriers before their breast cancer diagnosis, and 63 learned of their carrier status only after diagnosis. Of the participants, 83% were Ashkenazi Jews. For both prediagnosis and postdiagnosis groups, the age at diagnosis was the same (50.4 years). For both groups, distributions of pathogenic mutations were similar. There were no significant differences in hormone receptor or ERBB2 status.
Among women who knew they were carriers before diagnosis, 80.9% (34/42) were diagnosed either with ductal carcinoma in situ or stage 1 disease. Only 9.5% (4/42) of these women were diagnosed with disease of stage 2 or higher.
In comparison, among women who learned their carrier status after diagnosis, 30% (19/63) had early-stage disease at diagnosis, and 52.4% (33/63) were diagnosed at stage 2 or higher (P < .001).
Compared to women who knew their carrier status before diagnosis, women who found out after diagnosis had 12 times higher odds of being diagnosed with disease of advanced clinical stage (P = .001) and eight times higher odds of being diagnosed with disease of advanced pathologic stage (P = .002).
A sentinel node biopsy was sufficient in 85.7% (36/42) of women who knew their carrier status before diagnosis; 7.2% (3/42) of these women needed a full lymph node dissection. In contrast, 3.2% (2/63) of women who learned their carrier status after diagnosis underwent sentinel node biopsy, and 34.9% (25/105) needed a full lymph node dissection (P < .001).
Among women who knew their carrier status before diagnosis, 54.8% (23/42) did not need chemotherapy at all, and none needed neoadjuvant chemotherapy. Only 4.8% (3/63) of women who learned their mutation status after diagnosis were able to forgo chemotherapy (P < .001); 22.2% (14/63) needed neoadjuvant therapy (P = .001).
These findings appeared to translate into better outcomes. Overall 5-year survival was significantly higher among women who knew their carrier status before diagnosis compared to women who found out afterward (94% [SE 4%] vs 78% [SE 5%]; P = .03). Only two of 42 women (4.8%) in the prediagnosis group died, compared to 16 of 63 (25.4%) in the postdiagnosis group.
Analyses that controlled for year at diagnosis showed that women who learned their carrier status before diagnosis had significantly lower risk for overall mortality compared with those who found out after diagnosis (hazard ratio [HR], 0.20; 95% CI, 0.04 – 0.93; P = .04). However, these results lost significance when controlled for age, socioeconomic index, family history, and gene variant (HR, 0.16; 95% CI, 0.02 – 1.4; P = .10).
Higher socioeconomic status (HR, 0.76; 95% CI, 0.6 – 0.97; P = .03), gene variant (BRCA2 vs BRCA1: HR, 0.15; 95% CI, 0.03 – 0.75; P = .02), and age at diagnosis (HR, 1.047; 95% CI, 1.003 – 1.093; P = .04) were all associated with overall mortality.
“I can’t infer causation, but we suspect that the reason for these results is the difference in follow-up,” Levy-Lahad said.
Most of the women (95.2%, 40/42) who knew their carrier status before diagnosis received their follow-up at the medical center’s high-risk carrier clinic. Twenty-seven of 42 (64.3%) of these women were diagnosed with breast MRI. By contrast, only 1.6% (1/63) of women who found out their carrier status after diagnosis were diagnosed with breast MRI. Breast MRI is not routinely used for breast cancer screening but can be more sensitive than mammography for detecting breast cancer.
The study was funded by the Breast Cancer Research Foundation and by a gift from Ellie and David Werber to ShaareZedek Medical Center.
Levy-Lahad received grants from the Breast Cancer Research Foundation and from the Israel Cancer Association during the conduct of the study and personal fees from AstraZeneca outside the submitted work. Copur has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The study, conducted among Ashkenazi Jewish women in Israel, showed that among women who knew their carrier status before they developed breast cancer, diagnoses were made at an earlier disease stage and 5-year survival was improved compared to women who learned their carrier status only after their disease had been diagnosed.
The study was published online on July 9 in JAMA Oncology.
“I don’t want to belittle the complexities of knowing that you’re a carrier. But I think these results really show that knowledge is power,” first author Ephrat Levy-Lahad, MD, director of the medical genetics unit at Shaare Zedek Medical Center in Jerusalem, Israel, told Medscape Medical News.
Carrying a BRCA1/2 pathogenic mutation is associated with a 70% to 80% lifetime risk for breast cancer and about a 10% to 50% lifetime risk for ovarian cancer, depending on the specific mutation. Only about 10% of carriers will not develop either cancer during their lifetime.
The study provides support for genetic screening for pathogenic BRCA1/2 mutations, especially in high-risk populations, according to Levy-Lahad.
“For me, the results are part of a bigger picture.... I think we should be moving towards general population screening, certainly in high-risk populations like Ashkenazi Jews,” she said.
In Israel, that decision has already been made: a new policy, introduced in January 2020, offers testing for common BRCA1/2 mutations for all Ashkenazi Jewish women.
However, women in other countries may also benefit from testing, she argues. About half of BRCA1/2 carriers in a general population like that of the United States do not have a family history that would indicate a need for testing. That means many women who carry these mutations may not be taking advantage of recommended surveillance and prevention measures, she said.
But screening for BRCA1/2 mutations becomes more complicated when applied to more general populations, she acknowledged.
About 2.5% of women of Ashkenazi Jewish descent carry pathogenic mutations for BRCA1/2, compared to 0.5% in the general White population.
Also, screening in the Ashkenazi Jewish population is probably simpler than in the general population. Just three mutations are definitely known to cause disease and need to be tested for among Ashkenazi Jews. Screening in a larger population would require full sequencing of the gene. That increases the likelihood of finding variants of unknown significance (VUSs), which muddies the water. Knowledge is incomplete about whether some of these VUSs increase cancer risk, and physicians do not always know how to manage them in women who test positive.
Moreover, Israel has a national health system. Screening in a country without universal health insurance such as the United States raises questions about whether follow-up would be covered by insurance carriers for women who test positive.
Mehmet Copur, MD, an oncologist at Morrison Cancer Center in Hastings, Nebraska, questions how general population screening could be done in “real life.”
“These findings should be taken into consideration in the context of the patient population who would agree to genetic testing, who would agree to comply with the recommended guidelines for risk reduction, and who would have insurance coverage or resources to comply with the recommendations,” Copur told Medscape Medical News.
“If BRCA-positive patients did not or could not follow these recommendations, the results would different,” he added.
The most crucial component of screening for these mutations is genetic counselors, who are in short supply in the United States, according to Copur.
Another issue is that of cost. Genetic counseling is not always covered by insurance, especially for individuals who do not have a family history of BRCA-related cancers. Genetic testing is not cheap, and the costs of monitoring women who test positive could be prohibitive, especially in a healthcare system burdened by COVID-19.
“Whether our current healthcare system could bear the cost of such a change is up for debate. The screening itself may be feasible, but offering lifelong surveillance to every woman identified with mutations could present huge capacity issues,” Copur said. “Maybe in the future, the healthcare system can be ready for such an undertaking, but I don’t think we are there yet.”
Although she acknowledges the differences in risk between Ashkenazi Jews and the general population, Levy-Lahad thinks not having screening is like “throwing the baby out with the bath water.”
“Maybe we’re not ready for total general population screening, but I think we have to start thinking along those lines,” she said. “We have this incredible tool for cancer prevention, and we should really be using it, certainly in populations like Ashkenazi Jews.”
Researchers conducted a retrospective analysis that included 105 women diagnosed with breast cancer at Shaare Zedek Medical Center in Jerusalem between 2005 and 2016. Forty-two women knew they were carriers before their breast cancer diagnosis, and 63 learned of their carrier status only after diagnosis. Of the participants, 83% were Ashkenazi Jews. For both prediagnosis and postdiagnosis groups, the age at diagnosis was the same (50.4 years). For both groups, distributions of pathogenic mutations were similar. There were no significant differences in hormone receptor or ERBB2 status.
Among women who knew they were carriers before diagnosis, 80.9% (34/42) were diagnosed either with ductal carcinoma in situ or stage 1 disease. Only 9.5% (4/42) of these women were diagnosed with disease of stage 2 or higher.
In comparison, among women who learned their carrier status after diagnosis, 30% (19/63) had early-stage disease at diagnosis, and 52.4% (33/63) were diagnosed at stage 2 or higher (P < .001).
Compared to women who knew their carrier status before diagnosis, women who found out after diagnosis had 12 times higher odds of being diagnosed with disease of advanced clinical stage (P = .001) and eight times higher odds of being diagnosed with disease of advanced pathologic stage (P = .002).
A sentinel node biopsy was sufficient in 85.7% (36/42) of women who knew their carrier status before diagnosis; 7.2% (3/42) of these women needed a full lymph node dissection. In contrast, 3.2% (2/63) of women who learned their carrier status after diagnosis underwent sentinel node biopsy, and 34.9% (25/105) needed a full lymph node dissection (P < .001).
Among women who knew their carrier status before diagnosis, 54.8% (23/42) did not need chemotherapy at all, and none needed neoadjuvant chemotherapy. Only 4.8% (3/63) of women who learned their mutation status after diagnosis were able to forgo chemotherapy (P < .001); 22.2% (14/63) needed neoadjuvant therapy (P = .001).
These findings appeared to translate into better outcomes. Overall 5-year survival was significantly higher among women who knew their carrier status before diagnosis compared to women who found out afterward (94% [SE 4%] vs 78% [SE 5%]; P = .03). Only two of 42 women (4.8%) in the prediagnosis group died, compared to 16 of 63 (25.4%) in the postdiagnosis group.
Analyses that controlled for year at diagnosis showed that women who learned their carrier status before diagnosis had significantly lower risk for overall mortality compared with those who found out after diagnosis (hazard ratio [HR], 0.20; 95% CI, 0.04 – 0.93; P = .04). However, these results lost significance when controlled for age, socioeconomic index, family history, and gene variant (HR, 0.16; 95% CI, 0.02 – 1.4; P = .10).
Higher socioeconomic status (HR, 0.76; 95% CI, 0.6 – 0.97; P = .03), gene variant (BRCA2 vs BRCA1: HR, 0.15; 95% CI, 0.03 – 0.75; P = .02), and age at diagnosis (HR, 1.047; 95% CI, 1.003 – 1.093; P = .04) were all associated with overall mortality.
“I can’t infer causation, but we suspect that the reason for these results is the difference in follow-up,” Levy-Lahad said.
Most of the women (95.2%, 40/42) who knew their carrier status before diagnosis received their follow-up at the medical center’s high-risk carrier clinic. Twenty-seven of 42 (64.3%) of these women were diagnosed with breast MRI. By contrast, only 1.6% (1/63) of women who found out their carrier status after diagnosis were diagnosed with breast MRI. Breast MRI is not routinely used for breast cancer screening but can be more sensitive than mammography for detecting breast cancer.
The study was funded by the Breast Cancer Research Foundation and by a gift from Ellie and David Werber to ShaareZedek Medical Center.
Levy-Lahad received grants from the Breast Cancer Research Foundation and from the Israel Cancer Association during the conduct of the study and personal fees from AstraZeneca outside the submitted work. Copur has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Early screening may halve breast cancer mortality in childhood cancer survivors
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
FROM ANNALS OF INTERNAL MEDICINE
Cardiovascular risk factors tied to midlife cognitive decline
new research shows. The findings suggest that the relationship between CVRFs and cognition becomes evident much earlier than previously realized. Investigators found that individuals who smoked were 65% more likely to have accelerated cognitive decline, those with hypertension were 87% more likely, and individuals with diabetes had nearly a 200% increased risk.
“What is new here is that almost no one has looked at cardiovascular risk factors in such a young age [mean, 50 years] and cognitive change in middle age from 50 to 55 or so. Almost all other studies have looked at mid- or late-life cardiovascular risk factors and late-life cognition or dementia,” said study investigator Kristine Yaffe, MD.
The research was published online July 15 in Neurology.
New insight
Previous research has shown a strong association between CVRFs and a greater risk for cognitive decline and dementia in late life, but the investigators note that data about the influence of CVRFs on cognition in midlife are “sparse.” Longitudinal studies have also shown that several cognitive domains – particularly processing speed and executive function – may start to decline in midlife, but whether CVRFs, many of which also emerge in midlife, contribute to these changes is unclear.
To assess the effect of CVRFs on cognitive changes in midlife, the investigators analyzed data from the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a multicenter longitudinal study designed to measure risk factors for coronary artery disease in a large cohort of Black and White men and women.
The analysis was based on data from 2,675 participants who underwent CVRF assessment and cognitive testing at baseline and 5 years later. At baseline, participants’ mean age was 50.2 years. Approximately 57% of participants were women, 55% were White, and the mean number of years of education was 15. At study outset, 43% (n = 1,133) of participants were considered obese, 31% (n = 826) had hypertension, 15% (n = 701) were current smokers, 11% (n = 290) had diabetes, and 9% (n = 248) had high cholesterol.
Cognition was assessed using the Digit Symbol Substitution Test, which measures processing speed and executive function; the Stroop Test, which measures executive function; and the Rey Auditory Verbal Learning Test, which measures verbal memory.
Dose-dependent effect
Overall results showed that, for 5% of participants, cognitive decline was accelerated at 5 years. In unadjusted models, the odds of developing accelerated cognitive decline over 5 years was associated with hypertension (7.5% vs. 4.3%; odds ratio, 1.79, 95% confidence interval, 1.27-2.52), diabetes (10.3% vs. 4.7%; OR, 2.33; 95% CI, 1.53-3.56), and smoking (7.7% current smokers vs. 4.3% never smokers; OR, 1.87; 95% CI, 1.21-2.90). After adjusting for age, sex, and race, the associations remained significant.
The researchers found no significant effect of high cholesterol (6.9% vs. 5.2%; OR, 1.35; 95% CI, 0.80-2.28) or obesity (6.1% vs. 4.8%; OR, 1.29; 95% CI, 0.92-1.82) on accelerated cognitive decline.
Compared with participants with no CVRFs, the likelihood of accelerated cognitive decline was higher for individuals with one or two risk factors (OR, 1.94; 95% CI, 1.16-3.25) and was higher still for those with three or more risk factors (OR, 3.51; 95% CI, 2.05-6.00).
The fact that there was no association between midlife cognitive decline and obesity or high cholesterol did not come as a surprise, said Dr. Yaffe. “Most studies have not shown a consistent finding with high cholesterol and later-life cognition, so it is not surprising we did not see one in midlife, when there is not as much cognitive change.”
The study’s results, said Dr. Yaffe, provide physicians with another good reason to help patients address CVRFs and to work with them to lower blood pressure, stop smoking, reduce diabetes incidence, or control diabetes.
Dr. Yaffe said she and her colleagues plan further research into CVRFs and accelerated cognitive decline. “We want to know if this earlier cognitive decline [in midlife] is connected to greater decline later in life. We also want to know if improving these risk factors in midlife might prevent or slow dementia later.”
More to explore
Commenting on the findings, Michelle M. Mielke, PhD, professor of epidemiology and neurology at Mayo Clinic, Rochester, Minn., said one of the study’s main implications “is that the prevention and treatment of midlife hypertension and diabetes and smoking cessation directly impacts shorter-term changes in cognition.”
She added that the study also provides a foundation for answering further questions about the effects of CVRFs on cognition in midlife. For example, questions about sex differences remain unanswered. Men develop CVRFs earlier than women, but the investigators did not provide the prevalence of cardiovascular risk factors by sex.
“It was also not reported whether a specific midlife cardiovascular risk factor was more strongly associated with accelerated cognitive decline for women or for men,” she said. In addition, the mean age of the population at baseline is the approximate age of the onset of menopause, after which cardiovascular risk factors increase among women.
“Additional research is needed to understand the emergence of cardiovascular risk factors pre- versus post menopause on subsequent cognition and also consider the use of menopausal hormone therapy,” said Dr. Mielke.
“Another future research avenue is to further understand the impact of antihypertensive and diabetes medications,” she continued. “For example, in the current study, it was not clear how many [participants] with hypertension were treated versus untreated and whether this impacted subsequent cognition. Similarly, it is not known whether specific antihypertensives are more beneficial for cognition in midlife.”
CARDIA is supported by the National Heart, Lung, and Blood Institute; the University of Alabama at Birmingham; Northwestern University, Chicago; the University of Minnesota; and the Kaiser Foundation Research Institute. Dr. Yaffe serves on data safety monitoring boards for Eli Lilly and studies sponsored by the National Institute on Aging. She is a board member of Alector and is a member of the Beeson Scientific Advisory Board and the Global Council on Brain Health. Dr. Mielke has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research shows. The findings suggest that the relationship between CVRFs and cognition becomes evident much earlier than previously realized. Investigators found that individuals who smoked were 65% more likely to have accelerated cognitive decline, those with hypertension were 87% more likely, and individuals with diabetes had nearly a 200% increased risk.
“What is new here is that almost no one has looked at cardiovascular risk factors in such a young age [mean, 50 years] and cognitive change in middle age from 50 to 55 or so. Almost all other studies have looked at mid- or late-life cardiovascular risk factors and late-life cognition or dementia,” said study investigator Kristine Yaffe, MD.
The research was published online July 15 in Neurology.
New insight
Previous research has shown a strong association between CVRFs and a greater risk for cognitive decline and dementia in late life, but the investigators note that data about the influence of CVRFs on cognition in midlife are “sparse.” Longitudinal studies have also shown that several cognitive domains – particularly processing speed and executive function – may start to decline in midlife, but whether CVRFs, many of which also emerge in midlife, contribute to these changes is unclear.
To assess the effect of CVRFs on cognitive changes in midlife, the investigators analyzed data from the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a multicenter longitudinal study designed to measure risk factors for coronary artery disease in a large cohort of Black and White men and women.
The analysis was based on data from 2,675 participants who underwent CVRF assessment and cognitive testing at baseline and 5 years later. At baseline, participants’ mean age was 50.2 years. Approximately 57% of participants were women, 55% were White, and the mean number of years of education was 15. At study outset, 43% (n = 1,133) of participants were considered obese, 31% (n = 826) had hypertension, 15% (n = 701) were current smokers, 11% (n = 290) had diabetes, and 9% (n = 248) had high cholesterol.
Cognition was assessed using the Digit Symbol Substitution Test, which measures processing speed and executive function; the Stroop Test, which measures executive function; and the Rey Auditory Verbal Learning Test, which measures verbal memory.
Dose-dependent effect
Overall results showed that, for 5% of participants, cognitive decline was accelerated at 5 years. In unadjusted models, the odds of developing accelerated cognitive decline over 5 years was associated with hypertension (7.5% vs. 4.3%; odds ratio, 1.79, 95% confidence interval, 1.27-2.52), diabetes (10.3% vs. 4.7%; OR, 2.33; 95% CI, 1.53-3.56), and smoking (7.7% current smokers vs. 4.3% never smokers; OR, 1.87; 95% CI, 1.21-2.90). After adjusting for age, sex, and race, the associations remained significant.
The researchers found no significant effect of high cholesterol (6.9% vs. 5.2%; OR, 1.35; 95% CI, 0.80-2.28) or obesity (6.1% vs. 4.8%; OR, 1.29; 95% CI, 0.92-1.82) on accelerated cognitive decline.
Compared with participants with no CVRFs, the likelihood of accelerated cognitive decline was higher for individuals with one or two risk factors (OR, 1.94; 95% CI, 1.16-3.25) and was higher still for those with three or more risk factors (OR, 3.51; 95% CI, 2.05-6.00).
The fact that there was no association between midlife cognitive decline and obesity or high cholesterol did not come as a surprise, said Dr. Yaffe. “Most studies have not shown a consistent finding with high cholesterol and later-life cognition, so it is not surprising we did not see one in midlife, when there is not as much cognitive change.”
The study’s results, said Dr. Yaffe, provide physicians with another good reason to help patients address CVRFs and to work with them to lower blood pressure, stop smoking, reduce diabetes incidence, or control diabetes.
Dr. Yaffe said she and her colleagues plan further research into CVRFs and accelerated cognitive decline. “We want to know if this earlier cognitive decline [in midlife] is connected to greater decline later in life. We also want to know if improving these risk factors in midlife might prevent or slow dementia later.”
More to explore
Commenting on the findings, Michelle M. Mielke, PhD, professor of epidemiology and neurology at Mayo Clinic, Rochester, Minn., said one of the study’s main implications “is that the prevention and treatment of midlife hypertension and diabetes and smoking cessation directly impacts shorter-term changes in cognition.”
She added that the study also provides a foundation for answering further questions about the effects of CVRFs on cognition in midlife. For example, questions about sex differences remain unanswered. Men develop CVRFs earlier than women, but the investigators did not provide the prevalence of cardiovascular risk factors by sex.
“It was also not reported whether a specific midlife cardiovascular risk factor was more strongly associated with accelerated cognitive decline for women or for men,” she said. In addition, the mean age of the population at baseline is the approximate age of the onset of menopause, after which cardiovascular risk factors increase among women.
“Additional research is needed to understand the emergence of cardiovascular risk factors pre- versus post menopause on subsequent cognition and also consider the use of menopausal hormone therapy,” said Dr. Mielke.
“Another future research avenue is to further understand the impact of antihypertensive and diabetes medications,” she continued. “For example, in the current study, it was not clear how many [participants] with hypertension were treated versus untreated and whether this impacted subsequent cognition. Similarly, it is not known whether specific antihypertensives are more beneficial for cognition in midlife.”
CARDIA is supported by the National Heart, Lung, and Blood Institute; the University of Alabama at Birmingham; Northwestern University, Chicago; the University of Minnesota; and the Kaiser Foundation Research Institute. Dr. Yaffe serves on data safety monitoring boards for Eli Lilly and studies sponsored by the National Institute on Aging. She is a board member of Alector and is a member of the Beeson Scientific Advisory Board and the Global Council on Brain Health. Dr. Mielke has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research shows. The findings suggest that the relationship between CVRFs and cognition becomes evident much earlier than previously realized. Investigators found that individuals who smoked were 65% more likely to have accelerated cognitive decline, those with hypertension were 87% more likely, and individuals with diabetes had nearly a 200% increased risk.
“What is new here is that almost no one has looked at cardiovascular risk factors in such a young age [mean, 50 years] and cognitive change in middle age from 50 to 55 or so. Almost all other studies have looked at mid- or late-life cardiovascular risk factors and late-life cognition or dementia,” said study investigator Kristine Yaffe, MD.
The research was published online July 15 in Neurology.
New insight
Previous research has shown a strong association between CVRFs and a greater risk for cognitive decline and dementia in late life, but the investigators note that data about the influence of CVRFs on cognition in midlife are “sparse.” Longitudinal studies have also shown that several cognitive domains – particularly processing speed and executive function – may start to decline in midlife, but whether CVRFs, many of which also emerge in midlife, contribute to these changes is unclear.
To assess the effect of CVRFs on cognitive changes in midlife, the investigators analyzed data from the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a multicenter longitudinal study designed to measure risk factors for coronary artery disease in a large cohort of Black and White men and women.
The analysis was based on data from 2,675 participants who underwent CVRF assessment and cognitive testing at baseline and 5 years later. At baseline, participants’ mean age was 50.2 years. Approximately 57% of participants were women, 55% were White, and the mean number of years of education was 15. At study outset, 43% (n = 1,133) of participants were considered obese, 31% (n = 826) had hypertension, 15% (n = 701) were current smokers, 11% (n = 290) had diabetes, and 9% (n = 248) had high cholesterol.
Cognition was assessed using the Digit Symbol Substitution Test, which measures processing speed and executive function; the Stroop Test, which measures executive function; and the Rey Auditory Verbal Learning Test, which measures verbal memory.
Dose-dependent effect
Overall results showed that, for 5% of participants, cognitive decline was accelerated at 5 years. In unadjusted models, the odds of developing accelerated cognitive decline over 5 years was associated with hypertension (7.5% vs. 4.3%; odds ratio, 1.79, 95% confidence interval, 1.27-2.52), diabetes (10.3% vs. 4.7%; OR, 2.33; 95% CI, 1.53-3.56), and smoking (7.7% current smokers vs. 4.3% never smokers; OR, 1.87; 95% CI, 1.21-2.90). After adjusting for age, sex, and race, the associations remained significant.
The researchers found no significant effect of high cholesterol (6.9% vs. 5.2%; OR, 1.35; 95% CI, 0.80-2.28) or obesity (6.1% vs. 4.8%; OR, 1.29; 95% CI, 0.92-1.82) on accelerated cognitive decline.
Compared with participants with no CVRFs, the likelihood of accelerated cognitive decline was higher for individuals with one or two risk factors (OR, 1.94; 95% CI, 1.16-3.25) and was higher still for those with three or more risk factors (OR, 3.51; 95% CI, 2.05-6.00).
The fact that there was no association between midlife cognitive decline and obesity or high cholesterol did not come as a surprise, said Dr. Yaffe. “Most studies have not shown a consistent finding with high cholesterol and later-life cognition, so it is not surprising we did not see one in midlife, when there is not as much cognitive change.”
The study’s results, said Dr. Yaffe, provide physicians with another good reason to help patients address CVRFs and to work with them to lower blood pressure, stop smoking, reduce diabetes incidence, or control diabetes.
Dr. Yaffe said she and her colleagues plan further research into CVRFs and accelerated cognitive decline. “We want to know if this earlier cognitive decline [in midlife] is connected to greater decline later in life. We also want to know if improving these risk factors in midlife might prevent or slow dementia later.”
More to explore
Commenting on the findings, Michelle M. Mielke, PhD, professor of epidemiology and neurology at Mayo Clinic, Rochester, Minn., said one of the study’s main implications “is that the prevention and treatment of midlife hypertension and diabetes and smoking cessation directly impacts shorter-term changes in cognition.”
She added that the study also provides a foundation for answering further questions about the effects of CVRFs on cognition in midlife. For example, questions about sex differences remain unanswered. Men develop CVRFs earlier than women, but the investigators did not provide the prevalence of cardiovascular risk factors by sex.
“It was also not reported whether a specific midlife cardiovascular risk factor was more strongly associated with accelerated cognitive decline for women or for men,” she said. In addition, the mean age of the population at baseline is the approximate age of the onset of menopause, after which cardiovascular risk factors increase among women.
“Additional research is needed to understand the emergence of cardiovascular risk factors pre- versus post menopause on subsequent cognition and also consider the use of menopausal hormone therapy,” said Dr. Mielke.
“Another future research avenue is to further understand the impact of antihypertensive and diabetes medications,” she continued. “For example, in the current study, it was not clear how many [participants] with hypertension were treated versus untreated and whether this impacted subsequent cognition. Similarly, it is not known whether specific antihypertensives are more beneficial for cognition in midlife.”
CARDIA is supported by the National Heart, Lung, and Blood Institute; the University of Alabama at Birmingham; Northwestern University, Chicago; the University of Minnesota; and the Kaiser Foundation Research Institute. Dr. Yaffe serves on data safety monitoring boards for Eli Lilly and studies sponsored by the National Institute on Aging. She is a board member of Alector and is a member of the Beeson Scientific Advisory Board and the Global Council on Brain Health. Dr. Mielke has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Early data support further study of ivosidenib in mIDH1 glioma
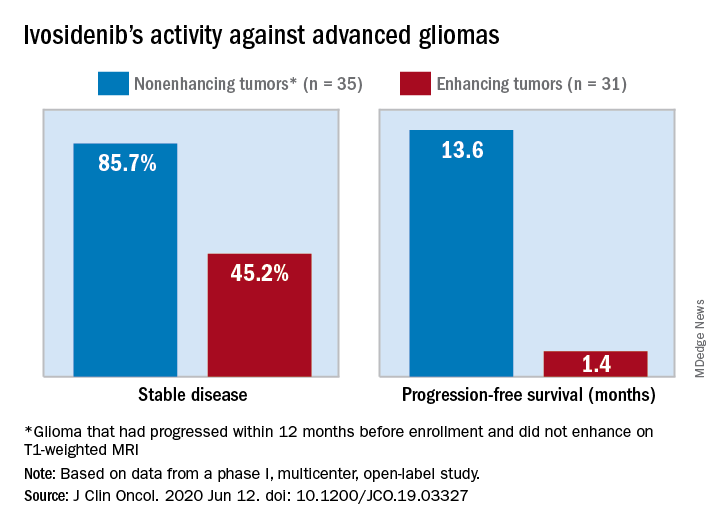
The median progression-free survival was 13.6 months for patients with nonenhancing tumors and 1.4 months for patients with enhancing tumors in a study of 66 adults with mIDH1 advanced glioma.
“On the basis of these data, additional clinical development of mIDH inhibitors for mIDH low-grade gliomas is warranted,” Ingo Mellinghoff, MD, of Memorial Sloan Kettering Cancer Center in New York, and colleagues wrote in the Journal of Clinical Oncology.
“This is not a home run but is of interest to the community,” said Lawrence Recht, MD, of Stanford (Calif.) University, who was not involved in this study. “Other companies are also developing agents like this.”
Considering that the ivosidenib study “is uncontrolled, one cannot say for sure that this wasn’t just the natural history of the disease,” Dr. Recht continued. “This type of tumor can behave very indolently, and patients can survive years without treatment, so this is rather a short interval to make a long-time statement. I think the authors are a bit overenthusiastic.”
The authors tested ivosidenib in 66 adults with mIDH1 glioma – 35 with nonenhancing glioma and 31 with enhancing glioma. Tumors had recurred after, or did not respond to, initial surgery, radiation, or chemotherapy.
The patients’ median age was 41 years (range, 21-71 years), and 25 patients (37.9%) were women. The most common tumor type at screening was oligodendroglioma in 23 patients (34.8%).
Patients received ivosidenib at doses ranging from 100 mg twice a day to 900 mg once a day. A total of 50 patients received the phase 2 recommended dose – 500 mg once a day. There were no dose-limiting toxicities, and there was no maximum-tolerated dose.
Adverse events of grade 3 or higher occurred in 19.7% of patients and included headache, seizure, hyperglycemia, neutropenia, and hypophosphatemia. Grade 3 or higher treatment-related adverse events occurred in two patients.
A total of 30 patients with nonenhancing tumors (85.7%) and 14 with enhancing tumors (45.2%) had a best response of stable disease. There was one partial response in a nonenhancing patient on 500 mg/day. The rest of the subjects had a best response of progressive disease.
The median treatment duration was 18.4 months among patients with nonenhancing tumors and 1.9 months among those with enhancing tumors. Discontinuation was caused byo progression in all but one case.
Among patients with measurable disease, tumor measurements decreased from baseline in 22 nonenhancing tumors (66.7%) and in 9 enhancing tumors (33.3%).
“Despite the heterogeneous patient population in our trial, the nonrandomized design, and the lack of central pathology review, the data from our trial suggest that ivosidenib has greater activity against nonenhancing gliomas than against enhancing gliomas,” the investigators wrote. “This finding may seem surprising because the absence of contrast enhancement is typically associated with impaired drug delivery.
“We hypothesize that ivosidenib may be more effective in nonenhancing gliomas because these tumors represent an earlier disease stage with fewer genetic alterations, reminiscent of the greater antitumor activity of the BCR-ABL inhibitor imatinib in earlier stages of chronic myeloid leukemia,” the investigators wrote.
The team also noted that the median progression-free survival for patients with nonenhancing gliomas in the current study “compares favorably to that reported for temozolomide” in advanced mIDH1 low-grade glioma, which was approximately 7 months.
This research was funded by Agios Pharmaceuticals, the company developing ivosidenib. Dr. Mellinghoff receives travel compensation from and is an adviser to the company. Several other investigators are employees. Dr. Recht disclosed no conflicts of interest.
SOURCE: Mellinghoff I et al. J Clin Oncol. 2020 Jun 12. doi: 10.1200/JCO.19.03327
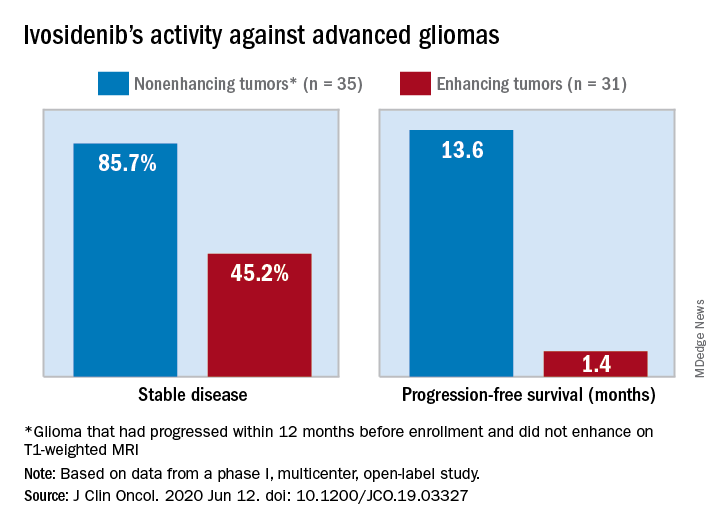
The median progression-free survival was 13.6 months for patients with nonenhancing tumors and 1.4 months for patients with enhancing tumors in a study of 66 adults with mIDH1 advanced glioma.
“On the basis of these data, additional clinical development of mIDH inhibitors for mIDH low-grade gliomas is warranted,” Ingo Mellinghoff, MD, of Memorial Sloan Kettering Cancer Center in New York, and colleagues wrote in the Journal of Clinical Oncology.
“This is not a home run but is of interest to the community,” said Lawrence Recht, MD, of Stanford (Calif.) University, who was not involved in this study. “Other companies are also developing agents like this.”
Considering that the ivosidenib study “is uncontrolled, one cannot say for sure that this wasn’t just the natural history of the disease,” Dr. Recht continued. “This type of tumor can behave very indolently, and patients can survive years without treatment, so this is rather a short interval to make a long-time statement. I think the authors are a bit overenthusiastic.”
The authors tested ivosidenib in 66 adults with mIDH1 glioma – 35 with nonenhancing glioma and 31 with enhancing glioma. Tumors had recurred after, or did not respond to, initial surgery, radiation, or chemotherapy.
The patients’ median age was 41 years (range, 21-71 years), and 25 patients (37.9%) were women. The most common tumor type at screening was oligodendroglioma in 23 patients (34.8%).
Patients received ivosidenib at doses ranging from 100 mg twice a day to 900 mg once a day. A total of 50 patients received the phase 2 recommended dose – 500 mg once a day. There were no dose-limiting toxicities, and there was no maximum-tolerated dose.
Adverse events of grade 3 or higher occurred in 19.7% of patients and included headache, seizure, hyperglycemia, neutropenia, and hypophosphatemia. Grade 3 or higher treatment-related adverse events occurred in two patients.
A total of 30 patients with nonenhancing tumors (85.7%) and 14 with enhancing tumors (45.2%) had a best response of stable disease. There was one partial response in a nonenhancing patient on 500 mg/day. The rest of the subjects had a best response of progressive disease.
The median treatment duration was 18.4 months among patients with nonenhancing tumors and 1.9 months among those with enhancing tumors. Discontinuation was caused byo progression in all but one case.
Among patients with measurable disease, tumor measurements decreased from baseline in 22 nonenhancing tumors (66.7%) and in 9 enhancing tumors (33.3%).
“Despite the heterogeneous patient population in our trial, the nonrandomized design, and the lack of central pathology review, the data from our trial suggest that ivosidenib has greater activity against nonenhancing gliomas than against enhancing gliomas,” the investigators wrote. “This finding may seem surprising because the absence of contrast enhancement is typically associated with impaired drug delivery.
“We hypothesize that ivosidenib may be more effective in nonenhancing gliomas because these tumors represent an earlier disease stage with fewer genetic alterations, reminiscent of the greater antitumor activity of the BCR-ABL inhibitor imatinib in earlier stages of chronic myeloid leukemia,” the investigators wrote.
The team also noted that the median progression-free survival for patients with nonenhancing gliomas in the current study “compares favorably to that reported for temozolomide” in advanced mIDH1 low-grade glioma, which was approximately 7 months.
This research was funded by Agios Pharmaceuticals, the company developing ivosidenib. Dr. Mellinghoff receives travel compensation from and is an adviser to the company. Several other investigators are employees. Dr. Recht disclosed no conflicts of interest.
SOURCE: Mellinghoff I et al. J Clin Oncol. 2020 Jun 12. doi: 10.1200/JCO.19.03327
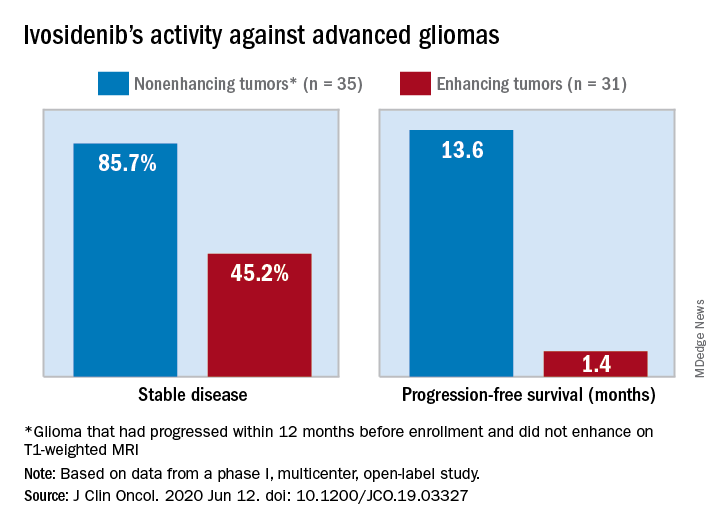
The median progression-free survival was 13.6 months for patients with nonenhancing tumors and 1.4 months for patients with enhancing tumors in a study of 66 adults with mIDH1 advanced glioma.
“On the basis of these data, additional clinical development of mIDH inhibitors for mIDH low-grade gliomas is warranted,” Ingo Mellinghoff, MD, of Memorial Sloan Kettering Cancer Center in New York, and colleagues wrote in the Journal of Clinical Oncology.
“This is not a home run but is of interest to the community,” said Lawrence Recht, MD, of Stanford (Calif.) University, who was not involved in this study. “Other companies are also developing agents like this.”
Considering that the ivosidenib study “is uncontrolled, one cannot say for sure that this wasn’t just the natural history of the disease,” Dr. Recht continued. “This type of tumor can behave very indolently, and patients can survive years without treatment, so this is rather a short interval to make a long-time statement. I think the authors are a bit overenthusiastic.”
The authors tested ivosidenib in 66 adults with mIDH1 glioma – 35 with nonenhancing glioma and 31 with enhancing glioma. Tumors had recurred after, or did not respond to, initial surgery, radiation, or chemotherapy.
The patients’ median age was 41 years (range, 21-71 years), and 25 patients (37.9%) were women. The most common tumor type at screening was oligodendroglioma in 23 patients (34.8%).
Patients received ivosidenib at doses ranging from 100 mg twice a day to 900 mg once a day. A total of 50 patients received the phase 2 recommended dose – 500 mg once a day. There were no dose-limiting toxicities, and there was no maximum-tolerated dose.
Adverse events of grade 3 or higher occurred in 19.7% of patients and included headache, seizure, hyperglycemia, neutropenia, and hypophosphatemia. Grade 3 or higher treatment-related adverse events occurred in two patients.
A total of 30 patients with nonenhancing tumors (85.7%) and 14 with enhancing tumors (45.2%) had a best response of stable disease. There was one partial response in a nonenhancing patient on 500 mg/day. The rest of the subjects had a best response of progressive disease.
The median treatment duration was 18.4 months among patients with nonenhancing tumors and 1.9 months among those with enhancing tumors. Discontinuation was caused byo progression in all but one case.
Among patients with measurable disease, tumor measurements decreased from baseline in 22 nonenhancing tumors (66.7%) and in 9 enhancing tumors (33.3%).
“Despite the heterogeneous patient population in our trial, the nonrandomized design, and the lack of central pathology review, the data from our trial suggest that ivosidenib has greater activity against nonenhancing gliomas than against enhancing gliomas,” the investigators wrote. “This finding may seem surprising because the absence of contrast enhancement is typically associated with impaired drug delivery.
“We hypothesize that ivosidenib may be more effective in nonenhancing gliomas because these tumors represent an earlier disease stage with fewer genetic alterations, reminiscent of the greater antitumor activity of the BCR-ABL inhibitor imatinib in earlier stages of chronic myeloid leukemia,” the investigators wrote.
The team also noted that the median progression-free survival for patients with nonenhancing gliomas in the current study “compares favorably to that reported for temozolomide” in advanced mIDH1 low-grade glioma, which was approximately 7 months.
This research was funded by Agios Pharmaceuticals, the company developing ivosidenib. Dr. Mellinghoff receives travel compensation from and is an adviser to the company. Several other investigators are employees. Dr. Recht disclosed no conflicts of interest.
SOURCE: Mellinghoff I et al. J Clin Oncol. 2020 Jun 12. doi: 10.1200/JCO.19.03327
FROM THE JOURNAL OF CLINICAL ONCOLOGY



