User login
Liver disease associated with worse COVID-19 outcomes
A growing body of evidence suggests that patients with COVID-19 and preexisting liver disease face increased risks of decompensation and mortality, according to a review of recent literature.
The review aimed to bring together the best approaches for caring for patients with preexisting liver conditions based on recommendations from three major hepatology societies. Findings in included studies could guide clinical decision-making, but a reliable framework for patient management has yet to be established, most likely because of limited research, according to lead author Abdul Mohammed, MD, of Case Western Reserve University, Cleveland, and colleagues.
The relationship between chronic liver diseases and “COVID-19 is not well documented in the literature,” Dr. Mohammed and colleagues wrote in the Journal of Clinical Gastroenterology. “The intricate interplay between immune dysfunction in preexisting liver diseases and the immune dysregulation triggered by the SARS-CoV-2 virus needs further evaluation.”
Such knowledge gaps likely explain the inconsistencies in recommendations between major hepatology societies, including clinical guidance from the American Association for the Study of Liver Disease, the European Association for the Study of the Liver, and the Asian Pacific Association for the Study of the Liver.
Both the literature review and the societal guidance address nonalcoholic fatty liver disease (NAFLD), hepatitis B virus (HBV) infection, autoimmune hepatitis, hepatocellular carcinoma (HCC), cirrhosis, and liver transplantation.
Dr. Mohammed and colleagues first offered an update of the relationship between COVID-19 and liver pathology. While it is clear that SARS-CoV-2 gains hepatic access through binding to ACE2 receptors in bile duct epithelial cells, it remains unclear whether this results in direct hepatic injury or indirect damage from virus-mediated cytokine release. Regardless, more than 90% of patients hospitalized for COVID-19 may develop increased levels of ALT and AST, and these elevations “appear to mirror disease severity,” the investigators wrote.
They noted that severity of COVID-19 appears to correlate with type of preexisting liver disease. For example, one study in the review associated NAFLD with a significantly increased risk of progressive COVID-19 (odds ratio, 6.4; 95% confidence interval, 1.5-31.2), and it also found that patients with NAFLD had longer duration of viral shedding than those without (17 vs. 12 days). Although the AASLD and APASL give no specific recommendations, the EASL recommends prioritizing COVID-19 patients with NAFLD.
Cirrhosis has been associated with a fourfold increased risk of mortality (relative risk, 4.6; 95% CI, 2.6-8.3) According to data from two international self-reporting registries, COVIDHep.net and COVIDCirrhosis.org, likelihood of death appears to move in tandem with Child-Turcotte-Pugh scores. Decompensated cirrhosis appears to predispose patients to having pulmonary complications, but more studies exploring this correlation need to be performed, according to the review authors. One study found that acute-on-chronic liver failure or acute decompensation occurred in 20% of patients who had COVID-19 and cirrhosis. It’s little surprise, then, that both the AASLD and the EASL recommend prioritizing in person evaluation for patients with decompensated cirrhosis.
Chronic HBV infection has also been associated with a higher COVID-19 mortality rate, although Dr. Mohammed and colleagues suggested that “larger studies are needed.” The review notes that the three societies recommend initiating HBV treatment only if there is clinical suspicion of hepatitis flare.
Findings are also cloudy among patients with autoimmune hepatitis and liver transplant recipients; however, the investigators noted that COVID-19 causes tissue damage primarily through cytokine release, and suggested that “immunosuppression can potentially curb this response.” Even so, recommendations from leading hepatology societies allude to a safe middle ground of immunosuppression, albeit with indistinct borders. All three caution against withdrawing immunosuppression, but the societies each describe tailoring regimens in different ways and for different patients, emphasizing continued corticosteroid treatments, according to the review.
Guidance also varies for management of HCC. “Since the tumor doubling time is 4-8 months and current guidelines recommend screening every 6 months, in patients at lower risk for developing HCC, a 2-month delay in ultrasound surveillance has been suggested by the AASLD,” the review authors noted. “In patients with a high risk of developing HCC, 6-month interval screening should be continued.” The AASLD recommends proceeding with treatment with newly diagnosed HCC, the EASL suggests that checkpoint inhibitors should be withheld and locoregional therapies should be postponed, and the APASL calls for a less frequent schedule of tyrosine kinase inhibitors and immunotherapy.
“COVID-19 patients with the preexisting liver disease face a higher risk of decompensation and mortality,” the review authors concluded. “We presented the most up-to-date literature on preexisting liver disease and its interaction with COVID-19.”
While such discrepancies may remain unresolved until further data are available, Wajahat Mehal, MD, PhD, director of the fatty liver disease program at Yale University, New Haven, Conn., suggested that clinicians remain vigilant for nonalcoholic steatohepatitis (NASH), which is common among overweight and obese individuals, an overrepresented group among those hospitalized for COVID-19.
“This is of great significance because patients with various forms of liver disease have a worse outcome with COVID-19,” Dr. Mehal said. “When seeing a patient with COVID-19 it is therefore important to ask if they have underlying liver disease, with attention paid to NASH. This can be approached by seeing if they have any evidence of abnormal liver function tests before the onset of COVID and any evidence of abnormal liver imaging. The Fib-4 test is a good screening tool for the presence of advanced liver fibrosis and a positive result should lead to more specific tests of liver fibrosis status such as fibroscan.”
The investigators reported no conflicts of interest. Dr. Mehal reported having nothing to disclose.
A growing body of evidence suggests that patients with COVID-19 and preexisting liver disease face increased risks of decompensation and mortality, according to a review of recent literature.
The review aimed to bring together the best approaches for caring for patients with preexisting liver conditions based on recommendations from three major hepatology societies. Findings in included studies could guide clinical decision-making, but a reliable framework for patient management has yet to be established, most likely because of limited research, according to lead author Abdul Mohammed, MD, of Case Western Reserve University, Cleveland, and colleagues.
The relationship between chronic liver diseases and “COVID-19 is not well documented in the literature,” Dr. Mohammed and colleagues wrote in the Journal of Clinical Gastroenterology. “The intricate interplay between immune dysfunction in preexisting liver diseases and the immune dysregulation triggered by the SARS-CoV-2 virus needs further evaluation.”
Such knowledge gaps likely explain the inconsistencies in recommendations between major hepatology societies, including clinical guidance from the American Association for the Study of Liver Disease, the European Association for the Study of the Liver, and the Asian Pacific Association for the Study of the Liver.
Both the literature review and the societal guidance address nonalcoholic fatty liver disease (NAFLD), hepatitis B virus (HBV) infection, autoimmune hepatitis, hepatocellular carcinoma (HCC), cirrhosis, and liver transplantation.
Dr. Mohammed and colleagues first offered an update of the relationship between COVID-19 and liver pathology. While it is clear that SARS-CoV-2 gains hepatic access through binding to ACE2 receptors in bile duct epithelial cells, it remains unclear whether this results in direct hepatic injury or indirect damage from virus-mediated cytokine release. Regardless, more than 90% of patients hospitalized for COVID-19 may develop increased levels of ALT and AST, and these elevations “appear to mirror disease severity,” the investigators wrote.
They noted that severity of COVID-19 appears to correlate with type of preexisting liver disease. For example, one study in the review associated NAFLD with a significantly increased risk of progressive COVID-19 (odds ratio, 6.4; 95% confidence interval, 1.5-31.2), and it also found that patients with NAFLD had longer duration of viral shedding than those without (17 vs. 12 days). Although the AASLD and APASL give no specific recommendations, the EASL recommends prioritizing COVID-19 patients with NAFLD.
Cirrhosis has been associated with a fourfold increased risk of mortality (relative risk, 4.6; 95% CI, 2.6-8.3) According to data from two international self-reporting registries, COVIDHep.net and COVIDCirrhosis.org, likelihood of death appears to move in tandem with Child-Turcotte-Pugh scores. Decompensated cirrhosis appears to predispose patients to having pulmonary complications, but more studies exploring this correlation need to be performed, according to the review authors. One study found that acute-on-chronic liver failure or acute decompensation occurred in 20% of patients who had COVID-19 and cirrhosis. It’s little surprise, then, that both the AASLD and the EASL recommend prioritizing in person evaluation for patients with decompensated cirrhosis.
Chronic HBV infection has also been associated with a higher COVID-19 mortality rate, although Dr. Mohammed and colleagues suggested that “larger studies are needed.” The review notes that the three societies recommend initiating HBV treatment only if there is clinical suspicion of hepatitis flare.
Findings are also cloudy among patients with autoimmune hepatitis and liver transplant recipients; however, the investigators noted that COVID-19 causes tissue damage primarily through cytokine release, and suggested that “immunosuppression can potentially curb this response.” Even so, recommendations from leading hepatology societies allude to a safe middle ground of immunosuppression, albeit with indistinct borders. All three caution against withdrawing immunosuppression, but the societies each describe tailoring regimens in different ways and for different patients, emphasizing continued corticosteroid treatments, according to the review.
Guidance also varies for management of HCC. “Since the tumor doubling time is 4-8 months and current guidelines recommend screening every 6 months, in patients at lower risk for developing HCC, a 2-month delay in ultrasound surveillance has been suggested by the AASLD,” the review authors noted. “In patients with a high risk of developing HCC, 6-month interval screening should be continued.” The AASLD recommends proceeding with treatment with newly diagnosed HCC, the EASL suggests that checkpoint inhibitors should be withheld and locoregional therapies should be postponed, and the APASL calls for a less frequent schedule of tyrosine kinase inhibitors and immunotherapy.
“COVID-19 patients with the preexisting liver disease face a higher risk of decompensation and mortality,” the review authors concluded. “We presented the most up-to-date literature on preexisting liver disease and its interaction with COVID-19.”
While such discrepancies may remain unresolved until further data are available, Wajahat Mehal, MD, PhD, director of the fatty liver disease program at Yale University, New Haven, Conn., suggested that clinicians remain vigilant for nonalcoholic steatohepatitis (NASH), which is common among overweight and obese individuals, an overrepresented group among those hospitalized for COVID-19.
“This is of great significance because patients with various forms of liver disease have a worse outcome with COVID-19,” Dr. Mehal said. “When seeing a patient with COVID-19 it is therefore important to ask if they have underlying liver disease, with attention paid to NASH. This can be approached by seeing if they have any evidence of abnormal liver function tests before the onset of COVID and any evidence of abnormal liver imaging. The Fib-4 test is a good screening tool for the presence of advanced liver fibrosis and a positive result should lead to more specific tests of liver fibrosis status such as fibroscan.”
The investigators reported no conflicts of interest. Dr. Mehal reported having nothing to disclose.
A growing body of evidence suggests that patients with COVID-19 and preexisting liver disease face increased risks of decompensation and mortality, according to a review of recent literature.
The review aimed to bring together the best approaches for caring for patients with preexisting liver conditions based on recommendations from three major hepatology societies. Findings in included studies could guide clinical decision-making, but a reliable framework for patient management has yet to be established, most likely because of limited research, according to lead author Abdul Mohammed, MD, of Case Western Reserve University, Cleveland, and colleagues.
The relationship between chronic liver diseases and “COVID-19 is not well documented in the literature,” Dr. Mohammed and colleagues wrote in the Journal of Clinical Gastroenterology. “The intricate interplay between immune dysfunction in preexisting liver diseases and the immune dysregulation triggered by the SARS-CoV-2 virus needs further evaluation.”
Such knowledge gaps likely explain the inconsistencies in recommendations between major hepatology societies, including clinical guidance from the American Association for the Study of Liver Disease, the European Association for the Study of the Liver, and the Asian Pacific Association for the Study of the Liver.
Both the literature review and the societal guidance address nonalcoholic fatty liver disease (NAFLD), hepatitis B virus (HBV) infection, autoimmune hepatitis, hepatocellular carcinoma (HCC), cirrhosis, and liver transplantation.
Dr. Mohammed and colleagues first offered an update of the relationship between COVID-19 and liver pathology. While it is clear that SARS-CoV-2 gains hepatic access through binding to ACE2 receptors in bile duct epithelial cells, it remains unclear whether this results in direct hepatic injury or indirect damage from virus-mediated cytokine release. Regardless, more than 90% of patients hospitalized for COVID-19 may develop increased levels of ALT and AST, and these elevations “appear to mirror disease severity,” the investigators wrote.
They noted that severity of COVID-19 appears to correlate with type of preexisting liver disease. For example, one study in the review associated NAFLD with a significantly increased risk of progressive COVID-19 (odds ratio, 6.4; 95% confidence interval, 1.5-31.2), and it also found that patients with NAFLD had longer duration of viral shedding than those without (17 vs. 12 days). Although the AASLD and APASL give no specific recommendations, the EASL recommends prioritizing COVID-19 patients with NAFLD.
Cirrhosis has been associated with a fourfold increased risk of mortality (relative risk, 4.6; 95% CI, 2.6-8.3) According to data from two international self-reporting registries, COVIDHep.net and COVIDCirrhosis.org, likelihood of death appears to move in tandem with Child-Turcotte-Pugh scores. Decompensated cirrhosis appears to predispose patients to having pulmonary complications, but more studies exploring this correlation need to be performed, according to the review authors. One study found that acute-on-chronic liver failure or acute decompensation occurred in 20% of patients who had COVID-19 and cirrhosis. It’s little surprise, then, that both the AASLD and the EASL recommend prioritizing in person evaluation for patients with decompensated cirrhosis.
Chronic HBV infection has also been associated with a higher COVID-19 mortality rate, although Dr. Mohammed and colleagues suggested that “larger studies are needed.” The review notes that the three societies recommend initiating HBV treatment only if there is clinical suspicion of hepatitis flare.
Findings are also cloudy among patients with autoimmune hepatitis and liver transplant recipients; however, the investigators noted that COVID-19 causes tissue damage primarily through cytokine release, and suggested that “immunosuppression can potentially curb this response.” Even so, recommendations from leading hepatology societies allude to a safe middle ground of immunosuppression, albeit with indistinct borders. All three caution against withdrawing immunosuppression, but the societies each describe tailoring regimens in different ways and for different patients, emphasizing continued corticosteroid treatments, according to the review.
Guidance also varies for management of HCC. “Since the tumor doubling time is 4-8 months and current guidelines recommend screening every 6 months, in patients at lower risk for developing HCC, a 2-month delay in ultrasound surveillance has been suggested by the AASLD,” the review authors noted. “In patients with a high risk of developing HCC, 6-month interval screening should be continued.” The AASLD recommends proceeding with treatment with newly diagnosed HCC, the EASL suggests that checkpoint inhibitors should be withheld and locoregional therapies should be postponed, and the APASL calls for a less frequent schedule of tyrosine kinase inhibitors and immunotherapy.
“COVID-19 patients with the preexisting liver disease face a higher risk of decompensation and mortality,” the review authors concluded. “We presented the most up-to-date literature on preexisting liver disease and its interaction with COVID-19.”
While such discrepancies may remain unresolved until further data are available, Wajahat Mehal, MD, PhD, director of the fatty liver disease program at Yale University, New Haven, Conn., suggested that clinicians remain vigilant for nonalcoholic steatohepatitis (NASH), which is common among overweight and obese individuals, an overrepresented group among those hospitalized for COVID-19.
“This is of great significance because patients with various forms of liver disease have a worse outcome with COVID-19,” Dr. Mehal said. “When seeing a patient with COVID-19 it is therefore important to ask if they have underlying liver disease, with attention paid to NASH. This can be approached by seeing if they have any evidence of abnormal liver function tests before the onset of COVID and any evidence of abnormal liver imaging. The Fib-4 test is a good screening tool for the presence of advanced liver fibrosis and a positive result should lead to more specific tests of liver fibrosis status such as fibroscan.”
The investigators reported no conflicts of interest. Dr. Mehal reported having nothing to disclose.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Endoscopic CRC resection carries recurrence, mortality risks
After endoscopic resection, high-risk T1 colorectal cancer (CRC) may have a tenfold greater risk of recurrence than low-risk disease, based on a meta-analysis involving more than 5,000 patients.
These findings support personalized, histologically based surveillance strategies following endoscopic resection of T1 CRC, reported lead author Hao Dang of Leiden University Medical Center in the Netherlands, and colleagues.
“With the introduction of population-based screening programs, a growing number of early-invasive colorectal cancers (T1 CRCs) are detected and treated with local endoscopic resection,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Success with this approach, however, depends upon accurate risk recurrence data, which have been lacking.
Joseph Feuerstein, MD, of the department of medicine at Harvard Medical School, Boston, and associate clinical chief of gastroenterology at Beth Israel Deaconess Medical Center, Boston, said, “While attempting complete resection of an early cancer with a colonoscopy is appealing, given the very low morbidity associated with it, this technique is only advisable if the risk of recurrence is extremely low when comparing [it] to surgical resection.”
In addition to patient selection, accurate recurrence data could also inform postoperative surveillance.
“To determine the optimal frequency and method of surveillance, it is important to know how often, and at which moments in follow-up local or distant CRC recurrences exactly occur,” wrote Mr. Dang and colleagues. “However, for endoscopically treated T1 CRC patients, the definite answers to these questions have not yet been provided.”
To find answers, Mr. Dang and colleagues conducted a meta-analysis involving 71 studies and 5,167 patients with endoscopically treated T1 CRC. The primary outcome was cumulative incidence and time pattern of CRC recurrence. Data were further characterized by local and/or distant metastasis and CRC-specific mortality.
The pooled cumulative incidence of CRC recurrence was 3.3%, with local and distant recurrences occurring at similar, respective rates of 1.9% and 1.6%. Most recurrences (95.6%) occurred within 72 months of endoscopic resection.
Risk-based recurrence analysis revealed a distinct pattern, with high-risk T1 CRCs recurring at a rate of 7.0% (95% confidence interval, 4.9%-9.9%; I2 = 48.1%), compared with just 0.7% for low-risk tumors (95%-CI, 0.4%-1.2%; I2 = 0%). Mortality data emphasized the clinical importance of this disparity, as the CRC-related mortality rate was 1.7% across the entire population, versus 40.8% among patients with recurrence.
“Our meta-analysis provides quantitative measures of relevant follow-up outcomes, which can form the basis for evidence-based surveillance recommendations for endoscopically treated T1 CRC patients,” the investigators concluded.
According to Dr. Feuerstein, the findings highlight the importance of surveillance after endoscopic resection of CRC while adding clarity to appropriate timing.
“Current guidelines recommend a colonoscopy following a colon cancer diagnosis at 1 year and then 3 years and then every 5 years,” Dr. Feuerstein said. “Adhering to these guidelines would likely identify most cases of recurrence early on within the 72-month window identified in this study.” He noted that “high-risk T1 CRC should probably be monitored more aggressively.”
Anoop Prabhu, MD, of the department of medicine at the University of Michigan Medical Center and director of endoscopy at Ann Arbor Veterans Affairs Medical Center, drew similar conclusions from the findings, noting that “tumor histology appears to be a powerful risk-stratification tool for subsequent surveillance.”
“One of the most important take-home messages from this paper is that, in those patients with low-risk, endoscopically resected colon cancer, surveillance with a colonoscopy in 1 year (as opposed to more intense endoscopic or radiographic surveillance) is likely more than adequate and can save unnecessary testing,” Dr. Prabhu said.
To build upon these findings, Dr. Prabhu suggested that upcoming studies could directly compare different management pathways.
“A potential area for future research would be a cost-effectiveness analysis of competing surveillance strategies after upfront endoscopic resection, with a particular focus on cancer-specific survival,” he said.
The investigators disclosed relationships with Boston Scientific, Cook Medical, and Medtronics. Dr. Feuerstein and Dr. Prabhu reported no relevant conflicts of interest.
Help your patients understand colorectal cancer prevention and screening options by sharing AGA’s patient education from the GI Patient Center: www.gastro.org/CRC.
After endoscopic resection, high-risk T1 colorectal cancer (CRC) may have a tenfold greater risk of recurrence than low-risk disease, based on a meta-analysis involving more than 5,000 patients.
These findings support personalized, histologically based surveillance strategies following endoscopic resection of T1 CRC, reported lead author Hao Dang of Leiden University Medical Center in the Netherlands, and colleagues.
“With the introduction of population-based screening programs, a growing number of early-invasive colorectal cancers (T1 CRCs) are detected and treated with local endoscopic resection,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Success with this approach, however, depends upon accurate risk recurrence data, which have been lacking.
Joseph Feuerstein, MD, of the department of medicine at Harvard Medical School, Boston, and associate clinical chief of gastroenterology at Beth Israel Deaconess Medical Center, Boston, said, “While attempting complete resection of an early cancer with a colonoscopy is appealing, given the very low morbidity associated with it, this technique is only advisable if the risk of recurrence is extremely low when comparing [it] to surgical resection.”
In addition to patient selection, accurate recurrence data could also inform postoperative surveillance.
“To determine the optimal frequency and method of surveillance, it is important to know how often, and at which moments in follow-up local or distant CRC recurrences exactly occur,” wrote Mr. Dang and colleagues. “However, for endoscopically treated T1 CRC patients, the definite answers to these questions have not yet been provided.”
To find answers, Mr. Dang and colleagues conducted a meta-analysis involving 71 studies and 5,167 patients with endoscopically treated T1 CRC. The primary outcome was cumulative incidence and time pattern of CRC recurrence. Data were further characterized by local and/or distant metastasis and CRC-specific mortality.
The pooled cumulative incidence of CRC recurrence was 3.3%, with local and distant recurrences occurring at similar, respective rates of 1.9% and 1.6%. Most recurrences (95.6%) occurred within 72 months of endoscopic resection.
Risk-based recurrence analysis revealed a distinct pattern, with high-risk T1 CRCs recurring at a rate of 7.0% (95% confidence interval, 4.9%-9.9%; I2 = 48.1%), compared with just 0.7% for low-risk tumors (95%-CI, 0.4%-1.2%; I2 = 0%). Mortality data emphasized the clinical importance of this disparity, as the CRC-related mortality rate was 1.7% across the entire population, versus 40.8% among patients with recurrence.
“Our meta-analysis provides quantitative measures of relevant follow-up outcomes, which can form the basis for evidence-based surveillance recommendations for endoscopically treated T1 CRC patients,” the investigators concluded.
According to Dr. Feuerstein, the findings highlight the importance of surveillance after endoscopic resection of CRC while adding clarity to appropriate timing.
“Current guidelines recommend a colonoscopy following a colon cancer diagnosis at 1 year and then 3 years and then every 5 years,” Dr. Feuerstein said. “Adhering to these guidelines would likely identify most cases of recurrence early on within the 72-month window identified in this study.” He noted that “high-risk T1 CRC should probably be monitored more aggressively.”
Anoop Prabhu, MD, of the department of medicine at the University of Michigan Medical Center and director of endoscopy at Ann Arbor Veterans Affairs Medical Center, drew similar conclusions from the findings, noting that “tumor histology appears to be a powerful risk-stratification tool for subsequent surveillance.”
“One of the most important take-home messages from this paper is that, in those patients with low-risk, endoscopically resected colon cancer, surveillance with a colonoscopy in 1 year (as opposed to more intense endoscopic or radiographic surveillance) is likely more than adequate and can save unnecessary testing,” Dr. Prabhu said.
To build upon these findings, Dr. Prabhu suggested that upcoming studies could directly compare different management pathways.
“A potential area for future research would be a cost-effectiveness analysis of competing surveillance strategies after upfront endoscopic resection, with a particular focus on cancer-specific survival,” he said.
The investigators disclosed relationships with Boston Scientific, Cook Medical, and Medtronics. Dr. Feuerstein and Dr. Prabhu reported no relevant conflicts of interest.
Help your patients understand colorectal cancer prevention and screening options by sharing AGA’s patient education from the GI Patient Center: www.gastro.org/CRC.
After endoscopic resection, high-risk T1 colorectal cancer (CRC) may have a tenfold greater risk of recurrence than low-risk disease, based on a meta-analysis involving more than 5,000 patients.
These findings support personalized, histologically based surveillance strategies following endoscopic resection of T1 CRC, reported lead author Hao Dang of Leiden University Medical Center in the Netherlands, and colleagues.
“With the introduction of population-based screening programs, a growing number of early-invasive colorectal cancers (T1 CRCs) are detected and treated with local endoscopic resection,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Success with this approach, however, depends upon accurate risk recurrence data, which have been lacking.
Joseph Feuerstein, MD, of the department of medicine at Harvard Medical School, Boston, and associate clinical chief of gastroenterology at Beth Israel Deaconess Medical Center, Boston, said, “While attempting complete resection of an early cancer with a colonoscopy is appealing, given the very low morbidity associated with it, this technique is only advisable if the risk of recurrence is extremely low when comparing [it] to surgical resection.”
In addition to patient selection, accurate recurrence data could also inform postoperative surveillance.
“To determine the optimal frequency and method of surveillance, it is important to know how often, and at which moments in follow-up local or distant CRC recurrences exactly occur,” wrote Mr. Dang and colleagues. “However, for endoscopically treated T1 CRC patients, the definite answers to these questions have not yet been provided.”
To find answers, Mr. Dang and colleagues conducted a meta-analysis involving 71 studies and 5,167 patients with endoscopically treated T1 CRC. The primary outcome was cumulative incidence and time pattern of CRC recurrence. Data were further characterized by local and/or distant metastasis and CRC-specific mortality.
The pooled cumulative incidence of CRC recurrence was 3.3%, with local and distant recurrences occurring at similar, respective rates of 1.9% and 1.6%. Most recurrences (95.6%) occurred within 72 months of endoscopic resection.
Risk-based recurrence analysis revealed a distinct pattern, with high-risk T1 CRCs recurring at a rate of 7.0% (95% confidence interval, 4.9%-9.9%; I2 = 48.1%), compared with just 0.7% for low-risk tumors (95%-CI, 0.4%-1.2%; I2 = 0%). Mortality data emphasized the clinical importance of this disparity, as the CRC-related mortality rate was 1.7% across the entire population, versus 40.8% among patients with recurrence.
“Our meta-analysis provides quantitative measures of relevant follow-up outcomes, which can form the basis for evidence-based surveillance recommendations for endoscopically treated T1 CRC patients,” the investigators concluded.
According to Dr. Feuerstein, the findings highlight the importance of surveillance after endoscopic resection of CRC while adding clarity to appropriate timing.
“Current guidelines recommend a colonoscopy following a colon cancer diagnosis at 1 year and then 3 years and then every 5 years,” Dr. Feuerstein said. “Adhering to these guidelines would likely identify most cases of recurrence early on within the 72-month window identified in this study.” He noted that “high-risk T1 CRC should probably be monitored more aggressively.”
Anoop Prabhu, MD, of the department of medicine at the University of Michigan Medical Center and director of endoscopy at Ann Arbor Veterans Affairs Medical Center, drew similar conclusions from the findings, noting that “tumor histology appears to be a powerful risk-stratification tool for subsequent surveillance.”
“One of the most important take-home messages from this paper is that, in those patients with low-risk, endoscopically resected colon cancer, surveillance with a colonoscopy in 1 year (as opposed to more intense endoscopic or radiographic surveillance) is likely more than adequate and can save unnecessary testing,” Dr. Prabhu said.
To build upon these findings, Dr. Prabhu suggested that upcoming studies could directly compare different management pathways.
“A potential area for future research would be a cost-effectiveness analysis of competing surveillance strategies after upfront endoscopic resection, with a particular focus on cancer-specific survival,” he said.
The investigators disclosed relationships with Boston Scientific, Cook Medical, and Medtronics. Dr. Feuerstein and Dr. Prabhu reported no relevant conflicts of interest.
Help your patients understand colorectal cancer prevention and screening options by sharing AGA’s patient education from the GI Patient Center: www.gastro.org/CRC.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Endoscopic CRC resection carries recurrence, mortality risks
After endoscopic resection, high-risk T1 colorectal cancer (CRC) may have a tenfold greater risk of recurrence than low-risk disease, based on a meta-analysis involving more than 5,000 patients.
These findings support personalized, histologically based surveillance strategies following endoscopic resection of T1 CRC, reported lead author Hao Dang of Leiden University Medical Center in the Netherlands, and colleagues.
“With the introduction of population-based screening programs, a growing number of early-invasive colorectal cancers (T1 CRCs) are detected and treated with local endoscopic resection,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Success with this approach, however, depends upon accurate risk recurrence data, which have been lacking.
Joseph Feuerstein, MD, of the department of medicine at Harvard Medical School and associate clinical chief of gastroenterology at Beth Israel Deaconess Medical Center, Boston, said, “While attempting complete resection of an early cancer with a colonoscopy is appealing, given the very low morbidity associated with it, this technique is only advisable if the risk of recurrence is extremely low when comparing [it] to surgical resection.”
In addition to patient selection, accurate recurrence data could also inform postoperative surveillance.
“To determine the optimal frequency and method of surveillance, it is important to know how often, and at which moments in follow-up local or distant CRC recurrences exactly occur,” wrote Mr. Dang and colleagues. “However, for endoscopically treated T1 CRC patients, the definite answers to these questions have not yet been provided.”
To find answers, Mr. Dang and colleagues conducted a meta-analysis involving 71 studies and 5,167 patients with endoscopically treated T1 CRC. The primary outcome was cumulative incidence and time pattern of CRC recurrence. Data were further characterized by local and/or distant metastasis and CRC-specific mortality.
The pooled cumulative incidence of CRC recurrence was 3.3%, with local and distant recurrences occurring at similar, respective rates of 1.9% and 1.6%. Most recurrences (95.6%) occurred within 72 months of endoscopic resection.
Risk-based recurrence analysis revealed a distinct pattern, with high-risk T1 CRCs recurring at a rate of 7.0% (95% confidence interval, 4.9%-9.9%; I2 = 48.1%), compared with just 0.7% for low-risk tumors (95%-CI, 0.4%-1.2%; I2 = 0%). Mortality data emphasized the clinical importance of this disparity, as the CRC-related mortality rate was 1.7% across the entire population, versus 40.8% among patients with recurrence.
“Our meta-analysis provides quantitative measures of relevant follow-up outcomes, which can form the basis for evidence-based surveillance recommendations for endoscopically treated T1 CRC patients,” the investigators concluded.
According to Dr. Feuerstein, the findings highlight the importance of surveillance after endoscopic resection of CRC while adding clarity to appropriate timing.
“Current guidelines recommend a colonoscopy following a colon cancer diagnosis at 1 year and then 3 years and then every 5 years,” Dr. Feuerstein said. “Adhering to these guidelines would likely identify most cases of recurrence early on within the 72-month window identified in this study.” He noted that “high-risk T1 CRC should probably be monitored more aggressively.”
Anoop Prabhu, MD, of the department of medicine at the University of Michigan Medical Center and director of endoscopy at Ann Arbor Veterans Affairs Medical Center, drew similar conclusions from the findings, noting that “tumor histology appears to be a powerful risk-stratification tool for subsequent surveillance.”
“One of the most important take-home messages from this paper is that, in those patients with low-risk, endoscopically resected colon cancer, surveillance with a colonoscopy in 1 year (as opposed to more intense endoscopic or radiographic surveillance) is likely more than adequate and can save unnecessary testing,” Dr. Prabhu said.
To build upon these findings, Dr. Prabhu suggested that upcoming studies could directly compare different management pathways.
“A potential area for future research would be a cost-effectiveness analysis of competing surveillance strategies after upfront endoscopic resection, with a particular focus on cancer-specific survival,” he said.
The investigators disclosed relationships with Boston Scientific, Cook Medical, and Medtronics. Dr. Feuerstein and Dr. Prabhu reported no relevant conflicts of interest.
After endoscopic resection, high-risk T1 colorectal cancer (CRC) may have a tenfold greater risk of recurrence than low-risk disease, based on a meta-analysis involving more than 5,000 patients.
These findings support personalized, histologically based surveillance strategies following endoscopic resection of T1 CRC, reported lead author Hao Dang of Leiden University Medical Center in the Netherlands, and colleagues.
“With the introduction of population-based screening programs, a growing number of early-invasive colorectal cancers (T1 CRCs) are detected and treated with local endoscopic resection,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Success with this approach, however, depends upon accurate risk recurrence data, which have been lacking.
Joseph Feuerstein, MD, of the department of medicine at Harvard Medical School and associate clinical chief of gastroenterology at Beth Israel Deaconess Medical Center, Boston, said, “While attempting complete resection of an early cancer with a colonoscopy is appealing, given the very low morbidity associated with it, this technique is only advisable if the risk of recurrence is extremely low when comparing [it] to surgical resection.”
In addition to patient selection, accurate recurrence data could also inform postoperative surveillance.
“To determine the optimal frequency and method of surveillance, it is important to know how often, and at which moments in follow-up local or distant CRC recurrences exactly occur,” wrote Mr. Dang and colleagues. “However, for endoscopically treated T1 CRC patients, the definite answers to these questions have not yet been provided.”
To find answers, Mr. Dang and colleagues conducted a meta-analysis involving 71 studies and 5,167 patients with endoscopically treated T1 CRC. The primary outcome was cumulative incidence and time pattern of CRC recurrence. Data were further characterized by local and/or distant metastasis and CRC-specific mortality.
The pooled cumulative incidence of CRC recurrence was 3.3%, with local and distant recurrences occurring at similar, respective rates of 1.9% and 1.6%. Most recurrences (95.6%) occurred within 72 months of endoscopic resection.
Risk-based recurrence analysis revealed a distinct pattern, with high-risk T1 CRCs recurring at a rate of 7.0% (95% confidence interval, 4.9%-9.9%; I2 = 48.1%), compared with just 0.7% for low-risk tumors (95%-CI, 0.4%-1.2%; I2 = 0%). Mortality data emphasized the clinical importance of this disparity, as the CRC-related mortality rate was 1.7% across the entire population, versus 40.8% among patients with recurrence.
“Our meta-analysis provides quantitative measures of relevant follow-up outcomes, which can form the basis for evidence-based surveillance recommendations for endoscopically treated T1 CRC patients,” the investigators concluded.
According to Dr. Feuerstein, the findings highlight the importance of surveillance after endoscopic resection of CRC while adding clarity to appropriate timing.
“Current guidelines recommend a colonoscopy following a colon cancer diagnosis at 1 year and then 3 years and then every 5 years,” Dr. Feuerstein said. “Adhering to these guidelines would likely identify most cases of recurrence early on within the 72-month window identified in this study.” He noted that “high-risk T1 CRC should probably be monitored more aggressively.”
Anoop Prabhu, MD, of the department of medicine at the University of Michigan Medical Center and director of endoscopy at Ann Arbor Veterans Affairs Medical Center, drew similar conclusions from the findings, noting that “tumor histology appears to be a powerful risk-stratification tool for subsequent surveillance.”
“One of the most important take-home messages from this paper is that, in those patients with low-risk, endoscopically resected colon cancer, surveillance with a colonoscopy in 1 year (as opposed to more intense endoscopic or radiographic surveillance) is likely more than adequate and can save unnecessary testing,” Dr. Prabhu said.
To build upon these findings, Dr. Prabhu suggested that upcoming studies could directly compare different management pathways.
“A potential area for future research would be a cost-effectiveness analysis of competing surveillance strategies after upfront endoscopic resection, with a particular focus on cancer-specific survival,” he said.
The investigators disclosed relationships with Boston Scientific, Cook Medical, and Medtronics. Dr. Feuerstein and Dr. Prabhu reported no relevant conflicts of interest.
After endoscopic resection, high-risk T1 colorectal cancer (CRC) may have a tenfold greater risk of recurrence than low-risk disease, based on a meta-analysis involving more than 5,000 patients.
These findings support personalized, histologically based surveillance strategies following endoscopic resection of T1 CRC, reported lead author Hao Dang of Leiden University Medical Center in the Netherlands, and colleagues.
“With the introduction of population-based screening programs, a growing number of early-invasive colorectal cancers (T1 CRCs) are detected and treated with local endoscopic resection,” the investigators wrote in Clinical Gastroenterology and Hepatology.
Success with this approach, however, depends upon accurate risk recurrence data, which have been lacking.
Joseph Feuerstein, MD, of the department of medicine at Harvard Medical School and associate clinical chief of gastroenterology at Beth Israel Deaconess Medical Center, Boston, said, “While attempting complete resection of an early cancer with a colonoscopy is appealing, given the very low morbidity associated with it, this technique is only advisable if the risk of recurrence is extremely low when comparing [it] to surgical resection.”
In addition to patient selection, accurate recurrence data could also inform postoperative surveillance.
“To determine the optimal frequency and method of surveillance, it is important to know how often, and at which moments in follow-up local or distant CRC recurrences exactly occur,” wrote Mr. Dang and colleagues. “However, for endoscopically treated T1 CRC patients, the definite answers to these questions have not yet been provided.”
To find answers, Mr. Dang and colleagues conducted a meta-analysis involving 71 studies and 5,167 patients with endoscopically treated T1 CRC. The primary outcome was cumulative incidence and time pattern of CRC recurrence. Data were further characterized by local and/or distant metastasis and CRC-specific mortality.
The pooled cumulative incidence of CRC recurrence was 3.3%, with local and distant recurrences occurring at similar, respective rates of 1.9% and 1.6%. Most recurrences (95.6%) occurred within 72 months of endoscopic resection.
Risk-based recurrence analysis revealed a distinct pattern, with high-risk T1 CRCs recurring at a rate of 7.0% (95% confidence interval, 4.9%-9.9%; I2 = 48.1%), compared with just 0.7% for low-risk tumors (95%-CI, 0.4%-1.2%; I2 = 0%). Mortality data emphasized the clinical importance of this disparity, as the CRC-related mortality rate was 1.7% across the entire population, versus 40.8% among patients with recurrence.
“Our meta-analysis provides quantitative measures of relevant follow-up outcomes, which can form the basis for evidence-based surveillance recommendations for endoscopically treated T1 CRC patients,” the investigators concluded.
According to Dr. Feuerstein, the findings highlight the importance of surveillance after endoscopic resection of CRC while adding clarity to appropriate timing.
“Current guidelines recommend a colonoscopy following a colon cancer diagnosis at 1 year and then 3 years and then every 5 years,” Dr. Feuerstein said. “Adhering to these guidelines would likely identify most cases of recurrence early on within the 72-month window identified in this study.” He noted that “high-risk T1 CRC should probably be monitored more aggressively.”
Anoop Prabhu, MD, of the department of medicine at the University of Michigan Medical Center and director of endoscopy at Ann Arbor Veterans Affairs Medical Center, drew similar conclusions from the findings, noting that “tumor histology appears to be a powerful risk-stratification tool for subsequent surveillance.”
“One of the most important take-home messages from this paper is that, in those patients with low-risk, endoscopically resected colon cancer, surveillance with a colonoscopy in 1 year (as opposed to more intense endoscopic or radiographic surveillance) is likely more than adequate and can save unnecessary testing,” Dr. Prabhu said.
To build upon these findings, Dr. Prabhu suggested that upcoming studies could directly compare different management pathways.
“A potential area for future research would be a cost-effectiveness analysis of competing surveillance strategies after upfront endoscopic resection, with a particular focus on cancer-specific survival,” he said.
The investigators disclosed relationships with Boston Scientific, Cook Medical, and Medtronics. Dr. Feuerstein and Dr. Prabhu reported no relevant conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
During pandemic, many gastroenterologists report low resilience, insomnia
Almost one-third of gastroenterologists may have low resilient coping skills, a finding linked with clinical insomnia, according to a national survey conducted between May and June of 2020.
The study, which was designed to characterize the psychological health of gastroenterologists during the COVID-19 pandemic, demonstrates how a complex array of factors drives poor psychological health, rather than specific challenges, such as coronavirus exposure risk, reported lead author Eric D. Shah, MD, MBA, of Dartmouth-Hitchcock Health in Lebanon, N.H., and colleagues.
“The COVID-19 pandemic poses unprecedented and unique challenges to gastroenterologists eager to maintain clinical practice, patients’ health, and their own physical/mental well-being,” the investigators wrote in Clinical Gastroenterology and Hepatology.To learn more, Dr. Shah and colleagues conducted a national cross-sectional survey of gastroenterologists in the United States.
Primary outcomes included clinical insomnia (Insomnia Severity Index-7 [ISI-7], general anxiety disorder (General Anxiety Disorder-7 [GAD-7]), and psychological distress (Patient Health Questionnaire-8 [PHQ-8]. The investigators developed additional domains to characterize perceived coronavirus exposure risks, practice-related challenges, and personal challenges. Further assessment determined whether resilient coping skills (Brief Resilient Coping Scale [BRCS]) or well-being (Physician Well-Being Index [PWBI]) were associated with psychological health outcomes.
A total of 153 gastroenterologists from 32 states completed the questionnaire, among whom the mean age and years in practice were 46 years and 13 years, respectively. Almost one-quarter of respondents were female (22.7%).
The survey found that anxiety and depression were uncommon, with respective rates of 7.2% and 8.5%.
In contrast, 30.7% of gastroenterologists reported low resilient coping skills.
“Resilience is defined as the ‘mental processes and behaviors that a person uses to protect themselves from the potential negative effects of stressors,’” the investigators wrote. “Resilient coping skills allow individuals in stressful situations to avoid negative psychological health consequences such as depression and anxiety.”
The study showed that low resilience was associated with clinical insomnia (odds ratio, 3.80; 95% confidence interval, 1.16-12.46), which occurred in more than one-quarter of respondents (25.5%).
Insomnia was also associated with age greater than 60 years, isolation outside the home, and years in practice. After adjusting for sex, age, and resilient coping, univariate analysis showed that insomnia was associated with isolation, female sex, and smaller practice size (fewer than 15 attending physicians).
While most respondents (85%) reported moderate to-high well-being, those who didn’t were significantly more likely to report clinical anxiety, depression, and insomnia (P < .001 for all).
“[W]e found that singular personal challenges, practice-related challenges, and perceived COVID-19–related exposure risks (such as perception of PPE availability) had little association with important psychological health outcomes including depression or anxiety,” wrote Dr. Shah and colleagues.
Instead, the investigators pointed to resilience.
“Physician leaders and other administrators should consider strategies to maintain resilient coping skills among their colleagues such as dedicated resilience training and self-care,” the investigators wrote.
They suggested that multiple stakeholders, including professional societies and policy makers, will be needed to implement such programs, and others. Additional interventions may include ensuring personal protective equipment availability, developing better technology for telemedicine, and supporting small practices that face financial obstacles in canceling elective procedures, the investigators wrote.
Edward L. Barnes, MD, MPH, of the University of North Carolina at Chapel Hill, said that the 30% prevalence rate for low resilient coping skills was the “most striking” finding.
Dr. Barnes went on to suggest that the survey results may actually underplay the current psychological landscape in gastroenterology.
“This study encompassed 2 of the early months of the COVID-19 pandemic (May-June 2020), which makes one wonder whether these same effects would be magnified over an even longer period of assessment,” he said.
Dr. Barnes, who authored an article last year concerning interventions for burnout in young gastroenterologists, offered some practical insight.
“As sleep deprivation has been associated with burnout and medical errors even outside the settings of a global pandemic (Trockel et al. JAMA Netw Open. 2020;3:e2028111), efforts to mitigate sleep deprivation seem key,” he said. “Given that resilience is a skill that can be both learned and improved, focused interventions by health care systems to ensure the presence of resilient coping skills among gastroenterologists could be a critical way to reduce psychological stress, prevent burnout, and improve the overall well-being of health care providers.” Dr. Shah is supported by the AGA Research Foundation’s 2019 AGA-Shire Research Scholar Award in Functional GI and Motility Disorders. He and his fellow investigators, as well as Dr. Barnes, reported no conflicts of interest.
SOURCE: Shah et al. CGH. 2020 Dec 2. doi: 10.1016/j.cgh.2020.11.043.
Almost one-third of gastroenterologists may have low resilient coping skills, a finding linked with clinical insomnia, according to a national survey conducted between May and June of 2020.
The study, which was designed to characterize the psychological health of gastroenterologists during the COVID-19 pandemic, demonstrates how a complex array of factors drives poor psychological health, rather than specific challenges, such as coronavirus exposure risk, reported lead author Eric D. Shah, MD, MBA, of Dartmouth-Hitchcock Health in Lebanon, N.H., and colleagues.
“The COVID-19 pandemic poses unprecedented and unique challenges to gastroenterologists eager to maintain clinical practice, patients’ health, and their own physical/mental well-being,” the investigators wrote in Clinical Gastroenterology and Hepatology.To learn more, Dr. Shah and colleagues conducted a national cross-sectional survey of gastroenterologists in the United States.
Primary outcomes included clinical insomnia (Insomnia Severity Index-7 [ISI-7], general anxiety disorder (General Anxiety Disorder-7 [GAD-7]), and psychological distress (Patient Health Questionnaire-8 [PHQ-8]. The investigators developed additional domains to characterize perceived coronavirus exposure risks, practice-related challenges, and personal challenges. Further assessment determined whether resilient coping skills (Brief Resilient Coping Scale [BRCS]) or well-being (Physician Well-Being Index [PWBI]) were associated with psychological health outcomes.
A total of 153 gastroenterologists from 32 states completed the questionnaire, among whom the mean age and years in practice were 46 years and 13 years, respectively. Almost one-quarter of respondents were female (22.7%).
The survey found that anxiety and depression were uncommon, with respective rates of 7.2% and 8.5%.
In contrast, 30.7% of gastroenterologists reported low resilient coping skills.
“Resilience is defined as the ‘mental processes and behaviors that a person uses to protect themselves from the potential negative effects of stressors,’” the investigators wrote. “Resilient coping skills allow individuals in stressful situations to avoid negative psychological health consequences such as depression and anxiety.”
The study showed that low resilience was associated with clinical insomnia (odds ratio, 3.80; 95% confidence interval, 1.16-12.46), which occurred in more than one-quarter of respondents (25.5%).
Insomnia was also associated with age greater than 60 years, isolation outside the home, and years in practice. After adjusting for sex, age, and resilient coping, univariate analysis showed that insomnia was associated with isolation, female sex, and smaller practice size (fewer than 15 attending physicians).
While most respondents (85%) reported moderate to-high well-being, those who didn’t were significantly more likely to report clinical anxiety, depression, and insomnia (P < .001 for all).
“[W]e found that singular personal challenges, practice-related challenges, and perceived COVID-19–related exposure risks (such as perception of PPE availability) had little association with important psychological health outcomes including depression or anxiety,” wrote Dr. Shah and colleagues.
Instead, the investigators pointed to resilience.
“Physician leaders and other administrators should consider strategies to maintain resilient coping skills among their colleagues such as dedicated resilience training and self-care,” the investigators wrote.
They suggested that multiple stakeholders, including professional societies and policy makers, will be needed to implement such programs, and others. Additional interventions may include ensuring personal protective equipment availability, developing better technology for telemedicine, and supporting small practices that face financial obstacles in canceling elective procedures, the investigators wrote.
Edward L. Barnes, MD, MPH, of the University of North Carolina at Chapel Hill, said that the 30% prevalence rate for low resilient coping skills was the “most striking” finding.
Dr. Barnes went on to suggest that the survey results may actually underplay the current psychological landscape in gastroenterology.
“This study encompassed 2 of the early months of the COVID-19 pandemic (May-June 2020), which makes one wonder whether these same effects would be magnified over an even longer period of assessment,” he said.
Dr. Barnes, who authored an article last year concerning interventions for burnout in young gastroenterologists, offered some practical insight.
“As sleep deprivation has been associated with burnout and medical errors even outside the settings of a global pandemic (Trockel et al. JAMA Netw Open. 2020;3:e2028111), efforts to mitigate sleep deprivation seem key,” he said. “Given that resilience is a skill that can be both learned and improved, focused interventions by health care systems to ensure the presence of resilient coping skills among gastroenterologists could be a critical way to reduce psychological stress, prevent burnout, and improve the overall well-being of health care providers.” Dr. Shah is supported by the AGA Research Foundation’s 2019 AGA-Shire Research Scholar Award in Functional GI and Motility Disorders. He and his fellow investigators, as well as Dr. Barnes, reported no conflicts of interest.
SOURCE: Shah et al. CGH. 2020 Dec 2. doi: 10.1016/j.cgh.2020.11.043.
Almost one-third of gastroenterologists may have low resilient coping skills, a finding linked with clinical insomnia, according to a national survey conducted between May and June of 2020.
The study, which was designed to characterize the psychological health of gastroenterologists during the COVID-19 pandemic, demonstrates how a complex array of factors drives poor psychological health, rather than specific challenges, such as coronavirus exposure risk, reported lead author Eric D. Shah, MD, MBA, of Dartmouth-Hitchcock Health in Lebanon, N.H., and colleagues.
“The COVID-19 pandemic poses unprecedented and unique challenges to gastroenterologists eager to maintain clinical practice, patients’ health, and their own physical/mental well-being,” the investigators wrote in Clinical Gastroenterology and Hepatology.To learn more, Dr. Shah and colleagues conducted a national cross-sectional survey of gastroenterologists in the United States.
Primary outcomes included clinical insomnia (Insomnia Severity Index-7 [ISI-7], general anxiety disorder (General Anxiety Disorder-7 [GAD-7]), and psychological distress (Patient Health Questionnaire-8 [PHQ-8]. The investigators developed additional domains to characterize perceived coronavirus exposure risks, practice-related challenges, and personal challenges. Further assessment determined whether resilient coping skills (Brief Resilient Coping Scale [BRCS]) or well-being (Physician Well-Being Index [PWBI]) were associated with psychological health outcomes.
A total of 153 gastroenterologists from 32 states completed the questionnaire, among whom the mean age and years in practice were 46 years and 13 years, respectively. Almost one-quarter of respondents were female (22.7%).
The survey found that anxiety and depression were uncommon, with respective rates of 7.2% and 8.5%.
In contrast, 30.7% of gastroenterologists reported low resilient coping skills.
“Resilience is defined as the ‘mental processes and behaviors that a person uses to protect themselves from the potential negative effects of stressors,’” the investigators wrote. “Resilient coping skills allow individuals in stressful situations to avoid negative psychological health consequences such as depression and anxiety.”
The study showed that low resilience was associated with clinical insomnia (odds ratio, 3.80; 95% confidence interval, 1.16-12.46), which occurred in more than one-quarter of respondents (25.5%).
Insomnia was also associated with age greater than 60 years, isolation outside the home, and years in practice. After adjusting for sex, age, and resilient coping, univariate analysis showed that insomnia was associated with isolation, female sex, and smaller practice size (fewer than 15 attending physicians).
While most respondents (85%) reported moderate to-high well-being, those who didn’t were significantly more likely to report clinical anxiety, depression, and insomnia (P < .001 for all).
“[W]e found that singular personal challenges, practice-related challenges, and perceived COVID-19–related exposure risks (such as perception of PPE availability) had little association with important psychological health outcomes including depression or anxiety,” wrote Dr. Shah and colleagues.
Instead, the investigators pointed to resilience.
“Physician leaders and other administrators should consider strategies to maintain resilient coping skills among their colleagues such as dedicated resilience training and self-care,” the investigators wrote.
They suggested that multiple stakeholders, including professional societies and policy makers, will be needed to implement such programs, and others. Additional interventions may include ensuring personal protective equipment availability, developing better technology for telemedicine, and supporting small practices that face financial obstacles in canceling elective procedures, the investigators wrote.
Edward L. Barnes, MD, MPH, of the University of North Carolina at Chapel Hill, said that the 30% prevalence rate for low resilient coping skills was the “most striking” finding.
Dr. Barnes went on to suggest that the survey results may actually underplay the current psychological landscape in gastroenterology.
“This study encompassed 2 of the early months of the COVID-19 pandemic (May-June 2020), which makes one wonder whether these same effects would be magnified over an even longer period of assessment,” he said.
Dr. Barnes, who authored an article last year concerning interventions for burnout in young gastroenterologists, offered some practical insight.
“As sleep deprivation has been associated with burnout and medical errors even outside the settings of a global pandemic (Trockel et al. JAMA Netw Open. 2020;3:e2028111), efforts to mitigate sleep deprivation seem key,” he said. “Given that resilience is a skill that can be both learned and improved, focused interventions by health care systems to ensure the presence of resilient coping skills among gastroenterologists could be a critical way to reduce psychological stress, prevent burnout, and improve the overall well-being of health care providers.” Dr. Shah is supported by the AGA Research Foundation’s 2019 AGA-Shire Research Scholar Award in Functional GI and Motility Disorders. He and his fellow investigators, as well as Dr. Barnes, reported no conflicts of interest.
SOURCE: Shah et al. CGH. 2020 Dec 2. doi: 10.1016/j.cgh.2020.11.043.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AGA publishes seronegative enteropathy guidance
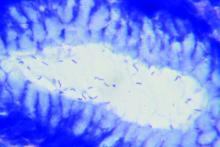
The American Gastroenterological Association has published new guidance for the diagnosis and management of seronegative enteropathies.
Seronegative enteropathies are commonly encountered by gastroenterologists, but accurate diagnosis can be complicated by a wide array of etiologies, misinterpreted histologic findings, suboptimal serology testing, and use of immunosuppressive agents that mask serology findings, reported lead author Maureen M. Leonard, MD, of MassGeneral Hospital for Children in Boston, and colleagues.
“Previous work detailing the prevalence of seronegative celiac disease [CeD], diagnosis of seronegative villous atrophy, and management recommendations for seronegative villous atrophy are available,” the investigators wrote in Gastroenterology. “However, there is limited evidence to guide clinicians regarding the minimal serologic tests necessary, the role of the gluten-free diet in diagnosis and management, and the role of an expert pathologist in evaluating the diagnosis of seronegative enteropathy.”
Patients with seronegative enteropathy tend to a have a poorer prognosis than those with classic CeD and other causes of villous atrophy, the investigators noted, but with an accurate diagnosis, distinct therapies can be highly effective.
After a comprehensive literature review, Dr. Leonard and colleagues reached consensus on eight best practice advice statements.
First, the investigators advised clinicians to review histologic findings with an experienced pathologist specializing in gastroenterology, as an expert can ensure proper duodenal orientation, and possibly link a specific finding with an etiology, such as granulomas with Crohn’s disease, or decreased goblet cells with autoimmune enteropathy. Communications with pathologists should also incorporate medical, travel, and medication history.
“Clinicians should pay particular attention to obtaining a thorough medication history to determine whether a patient is taking an angiotensin II receptor antagonist, such as olmesartan, which has been described as causing enteropathy,” the investigators wrote. “In some cases, this has led patients to be incorrectly diagnosis with refractory CeD. Other medications, including azathioprine and mycophenolate mofetil, among others, also have been reported to cause enteropathy, which resolves with discontinuation of medication.”
According to Dr. Leonard and colleagues, histologic findings suggestive of Crohn’s disease should prompt HLA testing, which requires careful attention to detail.
“It is prudent that the gastroenterologist or CeD specialist review all alleles tested and reported (or obtain the alleles if not reported) by the laboratory because commercial and academic laboratories might not report all possible alleles associated with CeD,” they wrote.
If HLA testing is positive, then the patient should begin empiric treatment with a gluten-free diet, followed by clinical and endoscopic reassessment after 1-3 years.
If HLA testing is negative, then a battery of tests may be needed to detect alternative etiologies, such as giardiasis, small intestinal bacterial overgrowth, HIV, and others.
“In cases where an underlying cause was identified, a follow-up esophagogastroduodenoscopy with biopsy might not be indicated, according to the etiology identified, treatment, and clinical status,” the investigators wrote.
Even with a comprehensive work-up, clinicians may be unable to identify an etiology. This outcome may be relatively common, the investigators suggested, citing a study of 200 cases of seronegative villous atrophy, of which 18% had no identifiable etiology. Yet finding an etiology may ultimately be unnecessary, as 72% of idiopathic cases resolved without intervention within 9 months, suggesting transient villous atrophy.
Still, intervention is needed for clinically unstable patients with idiopathic seronegative villous atrophy. Dr. Leonard and colleagues recommended first-line treatment with budesonide, starting at 9 mg daily. Depending on clinical status and response, subsequent therapies may include azathioprine or prednisone.
The clinical practice update was commissioned and approved by the AGA. The investigators disclosed additional relationships with Takeda Pharmaceuticals, HealthMode, Anokion, and others.
SOURCE: Leonard MM et al. Gastroenterology. 2020 Sep 30. doi: 10.1053/j.gastro.2020.08.061.
The American Gastroenterological Association has published new guidance for the diagnosis and management of seronegative enteropathies.
Seronegative enteropathies are commonly encountered by gastroenterologists, but accurate diagnosis can be complicated by a wide array of etiologies, misinterpreted histologic findings, suboptimal serology testing, and use of immunosuppressive agents that mask serology findings, reported lead author Maureen M. Leonard, MD, of MassGeneral Hospital for Children in Boston, and colleagues.
“Previous work detailing the prevalence of seronegative celiac disease [CeD], diagnosis of seronegative villous atrophy, and management recommendations for seronegative villous atrophy are available,” the investigators wrote in Gastroenterology. “However, there is limited evidence to guide clinicians regarding the minimal serologic tests necessary, the role of the gluten-free diet in diagnosis and management, and the role of an expert pathologist in evaluating the diagnosis of seronegative enteropathy.”
Patients with seronegative enteropathy tend to a have a poorer prognosis than those with classic CeD and other causes of villous atrophy, the investigators noted, but with an accurate diagnosis, distinct therapies can be highly effective.
After a comprehensive literature review, Dr. Leonard and colleagues reached consensus on eight best practice advice statements.
First, the investigators advised clinicians to review histologic findings with an experienced pathologist specializing in gastroenterology, as an expert can ensure proper duodenal orientation, and possibly link a specific finding with an etiology, such as granulomas with Crohn’s disease, or decreased goblet cells with autoimmune enteropathy. Communications with pathologists should also incorporate medical, travel, and medication history.
“Clinicians should pay particular attention to obtaining a thorough medication history to determine whether a patient is taking an angiotensin II receptor antagonist, such as olmesartan, which has been described as causing enteropathy,” the investigators wrote. “In some cases, this has led patients to be incorrectly diagnosis with refractory CeD. Other medications, including azathioprine and mycophenolate mofetil, among others, also have been reported to cause enteropathy, which resolves with discontinuation of medication.”
According to Dr. Leonard and colleagues, histologic findings suggestive of Crohn’s disease should prompt HLA testing, which requires careful attention to detail.
“It is prudent that the gastroenterologist or CeD specialist review all alleles tested and reported (or obtain the alleles if not reported) by the laboratory because commercial and academic laboratories might not report all possible alleles associated with CeD,” they wrote.
If HLA testing is positive, then the patient should begin empiric treatment with a gluten-free diet, followed by clinical and endoscopic reassessment after 1-3 years.
If HLA testing is negative, then a battery of tests may be needed to detect alternative etiologies, such as giardiasis, small intestinal bacterial overgrowth, HIV, and others.
“In cases where an underlying cause was identified, a follow-up esophagogastroduodenoscopy with biopsy might not be indicated, according to the etiology identified, treatment, and clinical status,” the investigators wrote.
Even with a comprehensive work-up, clinicians may be unable to identify an etiology. This outcome may be relatively common, the investigators suggested, citing a study of 200 cases of seronegative villous atrophy, of which 18% had no identifiable etiology. Yet finding an etiology may ultimately be unnecessary, as 72% of idiopathic cases resolved without intervention within 9 months, suggesting transient villous atrophy.
Still, intervention is needed for clinically unstable patients with idiopathic seronegative villous atrophy. Dr. Leonard and colleagues recommended first-line treatment with budesonide, starting at 9 mg daily. Depending on clinical status and response, subsequent therapies may include azathioprine or prednisone.
The clinical practice update was commissioned and approved by the AGA. The investigators disclosed additional relationships with Takeda Pharmaceuticals, HealthMode, Anokion, and others.
SOURCE: Leonard MM et al. Gastroenterology. 2020 Sep 30. doi: 10.1053/j.gastro.2020.08.061.
The American Gastroenterological Association has published new guidance for the diagnosis and management of seronegative enteropathies.
Seronegative enteropathies are commonly encountered by gastroenterologists, but accurate diagnosis can be complicated by a wide array of etiologies, misinterpreted histologic findings, suboptimal serology testing, and use of immunosuppressive agents that mask serology findings, reported lead author Maureen M. Leonard, MD, of MassGeneral Hospital for Children in Boston, and colleagues.
“Previous work detailing the prevalence of seronegative celiac disease [CeD], diagnosis of seronegative villous atrophy, and management recommendations for seronegative villous atrophy are available,” the investigators wrote in Gastroenterology. “However, there is limited evidence to guide clinicians regarding the minimal serologic tests necessary, the role of the gluten-free diet in diagnosis and management, and the role of an expert pathologist in evaluating the diagnosis of seronegative enteropathy.”
Patients with seronegative enteropathy tend to a have a poorer prognosis than those with classic CeD and other causes of villous atrophy, the investigators noted, but with an accurate diagnosis, distinct therapies can be highly effective.
After a comprehensive literature review, Dr. Leonard and colleagues reached consensus on eight best practice advice statements.
First, the investigators advised clinicians to review histologic findings with an experienced pathologist specializing in gastroenterology, as an expert can ensure proper duodenal orientation, and possibly link a specific finding with an etiology, such as granulomas with Crohn’s disease, or decreased goblet cells with autoimmune enteropathy. Communications with pathologists should also incorporate medical, travel, and medication history.
“Clinicians should pay particular attention to obtaining a thorough medication history to determine whether a patient is taking an angiotensin II receptor antagonist, such as olmesartan, which has been described as causing enteropathy,” the investigators wrote. “In some cases, this has led patients to be incorrectly diagnosis with refractory CeD. Other medications, including azathioprine and mycophenolate mofetil, among others, also have been reported to cause enteropathy, which resolves with discontinuation of medication.”
According to Dr. Leonard and colleagues, histologic findings suggestive of Crohn’s disease should prompt HLA testing, which requires careful attention to detail.
“It is prudent that the gastroenterologist or CeD specialist review all alleles tested and reported (or obtain the alleles if not reported) by the laboratory because commercial and academic laboratories might not report all possible alleles associated with CeD,” they wrote.
If HLA testing is positive, then the patient should begin empiric treatment with a gluten-free diet, followed by clinical and endoscopic reassessment after 1-3 years.
If HLA testing is negative, then a battery of tests may be needed to detect alternative etiologies, such as giardiasis, small intestinal bacterial overgrowth, HIV, and others.
“In cases where an underlying cause was identified, a follow-up esophagogastroduodenoscopy with biopsy might not be indicated, according to the etiology identified, treatment, and clinical status,” the investigators wrote.
Even with a comprehensive work-up, clinicians may be unable to identify an etiology. This outcome may be relatively common, the investigators suggested, citing a study of 200 cases of seronegative villous atrophy, of which 18% had no identifiable etiology. Yet finding an etiology may ultimately be unnecessary, as 72% of idiopathic cases resolved without intervention within 9 months, suggesting transient villous atrophy.
Still, intervention is needed for clinically unstable patients with idiopathic seronegative villous atrophy. Dr. Leonard and colleagues recommended first-line treatment with budesonide, starting at 9 mg daily. Depending on clinical status and response, subsequent therapies may include azathioprine or prednisone.
The clinical practice update was commissioned and approved by the AGA. The investigators disclosed additional relationships with Takeda Pharmaceuticals, HealthMode, Anokion, and others.
SOURCE: Leonard MM et al. Gastroenterology. 2020 Sep 30. doi: 10.1053/j.gastro.2020.08.061.
FROM GASTROENTEROLOGY
AGA white paper highlights interventional endoscopic ultrasound
Despite the surgery-sparing potential demonstrated by interventional endoscopic ultrasound (I-EUS), widespread clinical adoption will require more prospective trials, formalized training programs for endoscopists, and greater support from key stakeholders, according to an AGA white paper.
The publication, which was conceived during a session at the 2019 AGA Tech Summit, addresses the current status and future directions of I-EUS, included EUS-guided access, EUS-guided tumor ablation, and endohepatology.
“We hope this white paper guides those interested in adoption of these technologies into clinical practice and serves as a foundation for future research and innovation in the field,” the investigators wrote in Clinical Gastroenterology and Hepatology.
According to senior author senior author Joo Ha Hwang, MD, PhD, of Stanford (Calif.) University, and colleagues, some of the described techniques are not new, but they have yet to be fully realized.
“Some of these techniques initially were reported more than a decade ago,” the investigators wrote, “however, with further device development and refinement in technique there is potential for expanding the application of these techniques and new technologies to a broader group of interventional gastroenterologists.”
For each I-EUS modality, Dr. Hwang and colleagues reviewed available evidence, and if group consensus was reached, offered practical recommendations.
EUS-guided access
“There has been exponential growth in EUS-guided biliary (including gallbladder) access and drainage procedures, as well as entero-enteric anastomotic procedures in recent years,” the investigators wrote. “This change can be attributed to the availability of lumen-apposing metal stents (LAMS).”
Previous studies have reported promising success rates with LAMS across a variety of EUS-guided procedures, including biliary drainage (equal to or greater than 85%), gallbladder drainage (90%-98%), and gastrojejunostomy (greater than 90%).
Success with other techniques, however, has been mixed.
While LAMS “have gained popularity in the management of pseudocysts and walled-off necrotic collections,” data regarding superiority over plastic stents have been conflicting, and LAMS may increase risk of bleeding in necrotic cavities, wrote Dr. Hwang and colleagues.
“Placement of coaxial plastic stents through the lumen of LAMS has been advocated to try to minimize the risk of complications related to LAMS,” they added.
According to the white paper, EUS-guided pancreatic interventions remain most challenging; both pancreaticogastrostomy and EUS-guided pancreatic rendezvous are associated with technical failure rates up to 40%, and adverse event rates may be as high as 35%.
“Unlike other EUS-guided drainage and access procedures, there has been limited improvement in technology to make EUS-guided pancreatic access easier or safer,” the investigators noted.
Dr. Hwang and colleagues concluded this discussion of LAMS by calling for randomized prospective trials. They also noted the expense of LAMS, which may cost $4,000-$6,000.
EUS-guided tumor ablation
“Because of the close proximity of the gastrointestinal tract to organs such as the esophagus, liver, and pancreas, EUS would appear to be an ideal tool to provide imaging and potentially ablation of benign and malignant lesions in these locations,” wrote Dr. Hwang and colleagues.
But several challenges may stand in the way, they noted, including insufficient endoscope length and working channel caliber, “the tortuosity of the gastrointestinal lumen” and its location relative to some parts of the liver and pancreas, prohibitive tumor characteristics, and cost. In addition, concerns remain for collateral damage to surrounding organs.
“Further studies evaluating the safety and treatment response to ablation of solid neoplasms is required,” the investigators wrote, noting that this may require further development of noninvasive methods to monitor treated lesions.
EUS-guided liver applications
According to Dr. Hwang and colleagues, a growing body of evidence supports EUS-guided liver biopsy, including a high rate of histologic diagnoses (93.9%), Doppler-based detection of blood flow within the needle track prior to needle removal, ability to perform several needle actuations through a single puncture in the liver capsule, rapid patient recovery, ability to sample both liver lobes, potential for simultaneous endoscopy, and lower overall cost (accounting for complications, recovery time, and nondiagnostic yield).
And biopsies may be the first of many EUS-guided liver procedures to come, the investigators suggested.
“[EUS-guided liver biopsy] likely will be followed by EUS-guided portal pressure gradient measurement and EUS-guided shear wave elastography,” the investigators wrote. “There now is potential for a one-stop-shop diagnosis and staging of liver disease.”
Still, work is needed to facilitate greater clinical adoption of interventional EUS.
“[W]idespread implementation of interventional EUS is likely to require support from gastrointestinal societies and buy-in from other key stakeholders including payors,” wrote Dr. Hwang and colleagues. “Continued work by the gastrointestinal societies and manufacturers in providing training programs, and creating instruments, environments, and policies that motivate endoscopists to adopt new practices, is essential for growing the field of interventional EUS.”
The white paper was resulted from a session focused on interventional EUS a the 2019 ASGA Tech Summit, organized by the AGA Center for GI Innovation and Technology. The investigators disclosed additional relationships with Boston Scientific Corporation, Vyaire Medical, Cook Medical, and others.
SOURCE: DeWitt JM et al. Clin Gastroenterol Hepatol. 2020 Sep 17. doi: 10.1016/j.cgh.2020.09.029.
This story was updated on 12/4/2020.
Despite the surgery-sparing potential demonstrated by interventional endoscopic ultrasound (I-EUS), widespread clinical adoption will require more prospective trials, formalized training programs for endoscopists, and greater support from key stakeholders, according to an AGA white paper.
The publication, which was conceived during a session at the 2019 AGA Tech Summit, addresses the current status and future directions of I-EUS, included EUS-guided access, EUS-guided tumor ablation, and endohepatology.
“We hope this white paper guides those interested in adoption of these technologies into clinical practice and serves as a foundation for future research and innovation in the field,” the investigators wrote in Clinical Gastroenterology and Hepatology.
According to senior author senior author Joo Ha Hwang, MD, PhD, of Stanford (Calif.) University, and colleagues, some of the described techniques are not new, but they have yet to be fully realized.
“Some of these techniques initially were reported more than a decade ago,” the investigators wrote, “however, with further device development and refinement in technique there is potential for expanding the application of these techniques and new technologies to a broader group of interventional gastroenterologists.”
For each I-EUS modality, Dr. Hwang and colleagues reviewed available evidence, and if group consensus was reached, offered practical recommendations.
EUS-guided access
“There has been exponential growth in EUS-guided biliary (including gallbladder) access and drainage procedures, as well as entero-enteric anastomotic procedures in recent years,” the investigators wrote. “This change can be attributed to the availability of lumen-apposing metal stents (LAMS).”
Previous studies have reported promising success rates with LAMS across a variety of EUS-guided procedures, including biliary drainage (equal to or greater than 85%), gallbladder drainage (90%-98%), and gastrojejunostomy (greater than 90%).
Success with other techniques, however, has been mixed.
While LAMS “have gained popularity in the management of pseudocysts and walled-off necrotic collections,” data regarding superiority over plastic stents have been conflicting, and LAMS may increase risk of bleeding in necrotic cavities, wrote Dr. Hwang and colleagues.
“Placement of coaxial plastic stents through the lumen of LAMS has been advocated to try to minimize the risk of complications related to LAMS,” they added.
According to the white paper, EUS-guided pancreatic interventions remain most challenging; both pancreaticogastrostomy and EUS-guided pancreatic rendezvous are associated with technical failure rates up to 40%, and adverse event rates may be as high as 35%.
“Unlike other EUS-guided drainage and access procedures, there has been limited improvement in technology to make EUS-guided pancreatic access easier or safer,” the investigators noted.
Dr. Hwang and colleagues concluded this discussion of LAMS by calling for randomized prospective trials. They also noted the expense of LAMS, which may cost $4,000-$6,000.
EUS-guided tumor ablation
“Because of the close proximity of the gastrointestinal tract to organs such as the esophagus, liver, and pancreas, EUS would appear to be an ideal tool to provide imaging and potentially ablation of benign and malignant lesions in these locations,” wrote Dr. Hwang and colleagues.
But several challenges may stand in the way, they noted, including insufficient endoscope length and working channel caliber, “the tortuosity of the gastrointestinal lumen” and its location relative to some parts of the liver and pancreas, prohibitive tumor characteristics, and cost. In addition, concerns remain for collateral damage to surrounding organs.
“Further studies evaluating the safety and treatment response to ablation of solid neoplasms is required,” the investigators wrote, noting that this may require further development of noninvasive methods to monitor treated lesions.
EUS-guided liver applications
According to Dr. Hwang and colleagues, a growing body of evidence supports EUS-guided liver biopsy, including a high rate of histologic diagnoses (93.9%), Doppler-based detection of blood flow within the needle track prior to needle removal, ability to perform several needle actuations through a single puncture in the liver capsule, rapid patient recovery, ability to sample both liver lobes, potential for simultaneous endoscopy, and lower overall cost (accounting for complications, recovery time, and nondiagnostic yield).
And biopsies may be the first of many EUS-guided liver procedures to come, the investigators suggested.
“[EUS-guided liver biopsy] likely will be followed by EUS-guided portal pressure gradient measurement and EUS-guided shear wave elastography,” the investigators wrote. “There now is potential for a one-stop-shop diagnosis and staging of liver disease.”
Still, work is needed to facilitate greater clinical adoption of interventional EUS.
“[W]idespread implementation of interventional EUS is likely to require support from gastrointestinal societies and buy-in from other key stakeholders including payors,” wrote Dr. Hwang and colleagues. “Continued work by the gastrointestinal societies and manufacturers in providing training programs, and creating instruments, environments, and policies that motivate endoscopists to adopt new practices, is essential for growing the field of interventional EUS.”
The white paper was resulted from a session focused on interventional EUS a the 2019 ASGA Tech Summit, organized by the AGA Center for GI Innovation and Technology. The investigators disclosed additional relationships with Boston Scientific Corporation, Vyaire Medical, Cook Medical, and others.
SOURCE: DeWitt JM et al. Clin Gastroenterol Hepatol. 2020 Sep 17. doi: 10.1016/j.cgh.2020.09.029.
This story was updated on 12/4/2020.
Despite the surgery-sparing potential demonstrated by interventional endoscopic ultrasound (I-EUS), widespread clinical adoption will require more prospective trials, formalized training programs for endoscopists, and greater support from key stakeholders, according to an AGA white paper.
The publication, which was conceived during a session at the 2019 AGA Tech Summit, addresses the current status and future directions of I-EUS, included EUS-guided access, EUS-guided tumor ablation, and endohepatology.
“We hope this white paper guides those interested in adoption of these technologies into clinical practice and serves as a foundation for future research and innovation in the field,” the investigators wrote in Clinical Gastroenterology and Hepatology.
According to senior author senior author Joo Ha Hwang, MD, PhD, of Stanford (Calif.) University, and colleagues, some of the described techniques are not new, but they have yet to be fully realized.
“Some of these techniques initially were reported more than a decade ago,” the investigators wrote, “however, with further device development and refinement in technique there is potential for expanding the application of these techniques and new technologies to a broader group of interventional gastroenterologists.”
For each I-EUS modality, Dr. Hwang and colleagues reviewed available evidence, and if group consensus was reached, offered practical recommendations.
EUS-guided access
“There has been exponential growth in EUS-guided biliary (including gallbladder) access and drainage procedures, as well as entero-enteric anastomotic procedures in recent years,” the investigators wrote. “This change can be attributed to the availability of lumen-apposing metal stents (LAMS).”
Previous studies have reported promising success rates with LAMS across a variety of EUS-guided procedures, including biliary drainage (equal to or greater than 85%), gallbladder drainage (90%-98%), and gastrojejunostomy (greater than 90%).
Success with other techniques, however, has been mixed.
While LAMS “have gained popularity in the management of pseudocysts and walled-off necrotic collections,” data regarding superiority over plastic stents have been conflicting, and LAMS may increase risk of bleeding in necrotic cavities, wrote Dr. Hwang and colleagues.
“Placement of coaxial plastic stents through the lumen of LAMS has been advocated to try to minimize the risk of complications related to LAMS,” they added.
According to the white paper, EUS-guided pancreatic interventions remain most challenging; both pancreaticogastrostomy and EUS-guided pancreatic rendezvous are associated with technical failure rates up to 40%, and adverse event rates may be as high as 35%.
“Unlike other EUS-guided drainage and access procedures, there has been limited improvement in technology to make EUS-guided pancreatic access easier or safer,” the investigators noted.
Dr. Hwang and colleagues concluded this discussion of LAMS by calling for randomized prospective trials. They also noted the expense of LAMS, which may cost $4,000-$6,000.
EUS-guided tumor ablation
“Because of the close proximity of the gastrointestinal tract to organs such as the esophagus, liver, and pancreas, EUS would appear to be an ideal tool to provide imaging and potentially ablation of benign and malignant lesions in these locations,” wrote Dr. Hwang and colleagues.
But several challenges may stand in the way, they noted, including insufficient endoscope length and working channel caliber, “the tortuosity of the gastrointestinal lumen” and its location relative to some parts of the liver and pancreas, prohibitive tumor characteristics, and cost. In addition, concerns remain for collateral damage to surrounding organs.
“Further studies evaluating the safety and treatment response to ablation of solid neoplasms is required,” the investigators wrote, noting that this may require further development of noninvasive methods to monitor treated lesions.
EUS-guided liver applications
According to Dr. Hwang and colleagues, a growing body of evidence supports EUS-guided liver biopsy, including a high rate of histologic diagnoses (93.9%), Doppler-based detection of blood flow within the needle track prior to needle removal, ability to perform several needle actuations through a single puncture in the liver capsule, rapid patient recovery, ability to sample both liver lobes, potential for simultaneous endoscopy, and lower overall cost (accounting for complications, recovery time, and nondiagnostic yield).
And biopsies may be the first of many EUS-guided liver procedures to come, the investigators suggested.
“[EUS-guided liver biopsy] likely will be followed by EUS-guided portal pressure gradient measurement and EUS-guided shear wave elastography,” the investigators wrote. “There now is potential for a one-stop-shop diagnosis and staging of liver disease.”
Still, work is needed to facilitate greater clinical adoption of interventional EUS.
“[W]idespread implementation of interventional EUS is likely to require support from gastrointestinal societies and buy-in from other key stakeholders including payors,” wrote Dr. Hwang and colleagues. “Continued work by the gastrointestinal societies and manufacturers in providing training programs, and creating instruments, environments, and policies that motivate endoscopists to adopt new practices, is essential for growing the field of interventional EUS.”
The white paper was resulted from a session focused on interventional EUS a the 2019 ASGA Tech Summit, organized by the AGA Center for GI Innovation and Technology. The investigators disclosed additional relationships with Boston Scientific Corporation, Vyaire Medical, Cook Medical, and others.
SOURCE: DeWitt JM et al. Clin Gastroenterol Hepatol. 2020 Sep 17. doi: 10.1016/j.cgh.2020.09.029.
This story was updated on 12/4/2020.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AGA publishes recommendations for managing IBD in elderly patients
The American Gastroenterological Association has published a Clinical Practice Update for management of inflammatory bowel disease (IBD) in elderly patients, including 15 best practice advice statements.
According to lead author Ashwin N. Ananthakrishnan, MD, MPH, of Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues, this topic is becoming increasingly relevant, as the population is aging, and prevalence of IBD among elderly is rising approximately 5% per year.
“Up to 15% of IBD in North America and Asia is diagnosed after the age of 60 years,” the investigators wrote in Gastroenterology.
Dr. Ananthakrishnan and colleagues noted that “care of elderly IBD patients poses unique challenges with respect to diagnosis and therapeutic decision-making.”
Challenges include greater frequency of comorbidities, increased risk of infection with anti–tumor necrosis factor therapy, increased risk of lymphoma with thiopurine therapy, greater likelihood of surgical complications, and, for Crohn’s disease, an elevated mortality rate, according to the update.
Another challenge is a lack of data.
“It should be noted that most clinical data to inform these practices are based on observational data or indirect evidence as elderly IBD patients comprise a very small proportion of subjects enrolled in IBD clinical trials or long-term pharmacovigilance initiatives,” the investigators wrote.
With this in mind, the update offers guidance for diagnosis, treatment, and ongoing health maintenance.
Diagnosis
Dr. Ananthakrishnan and colleagues first suggested that clinicians remain vigilant for IBD in elderly people, in consideration of the 15% prevalence rate in this subpopulation.
For elderly individuals with a low probability of IBD, the investigators recommended fecal calprotectin or lactoferrin to determine if endoscopy is needed. For elderly patients with chronic diarrhea or hematochezia, plus moderate to high suspicion of IBD, colorectal neoplasia, or microscopic colitis, they recommended colonoscopy.
Lastly, the expert panel suggested that elderly patients presenting with segmental left-sided colitis and diverticulosis may also have Crohn’s disease or IBD unclassified.
Treatment
The clinical practice update offers 10 best practice statements for treating elderly patients with IBD. There is a recurring emphasis on treatment personalization, which should be informed by patient goals and priorities, risk/presence of severe disease, chronological age, functional status, independence, comorbidities, frailty, and several other age-associated risk factors (e.g., venous thromboembolism).
Concerning specific therapies, the investigators cautioned against systemic corticosteroids for maintenance therapy; instead, nonsystemic corticosteroids (e.g., budesonide) are favored, or possibly early biological therapy if budesonide is not indicated. When selecting a biologic, Dr. Ananthakrishnan and colleagues recommended those associated with a lower risk of malignancy and infection (e.g., ustekinumab or vedolizumab).
The advantages of thiopurine monotherapy being oral, relatively inexpensive compared to biologicals and having a long track record of success in maintenance of remission must be balanced against the need for ongoing serological monitoring, and increased risk of some malignancies.
Finally, the expert panel recommended that all elderly patients receive multidisciplinary care, which may include primary care providers, mental health professionals, nutritionists, and other specialists. It may also be productive to consult with family and caregivers during treatment planning.
Health maintenance
The last two best practice advice statements concern health maintenance.
First, the investigators recommended that elderly patients with IBD adhere to vaccination schedules, including herpes zoster, pneumococcus, and influenza vaccines, ideally, before starting immunosuppression.
Second, Dr. Ananthakrishnan and colleagues advised that cessation of colorectal cancer surveillance may be considered in elderly patients with IBD; however, this decision should take into account a variety of factors, including comorbidities, age, life expectancy, likelihood of endoscopic resection, and surgical candidacy.
The review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. The investigators disclosed relationships with Gilead, Sun Pharma, Kyn Therapeutics, and others.
SOURCE: Ananthakrishnan AN et al. Gastroenterology. 2020 Sep 30. doi: 10.1053/j.gastro.2020.08.060.
This story was updated on 12/4/2020.
The American Gastroenterological Association has published a Clinical Practice Update for management of inflammatory bowel disease (IBD) in elderly patients, including 15 best practice advice statements.
According to lead author Ashwin N. Ananthakrishnan, MD, MPH, of Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues, this topic is becoming increasingly relevant, as the population is aging, and prevalence of IBD among elderly is rising approximately 5% per year.
“Up to 15% of IBD in North America and Asia is diagnosed after the age of 60 years,” the investigators wrote in Gastroenterology.
Dr. Ananthakrishnan and colleagues noted that “care of elderly IBD patients poses unique challenges with respect to diagnosis and therapeutic decision-making.”
Challenges include greater frequency of comorbidities, increased risk of infection with anti–tumor necrosis factor therapy, increased risk of lymphoma with thiopurine therapy, greater likelihood of surgical complications, and, for Crohn’s disease, an elevated mortality rate, according to the update.
Another challenge is a lack of data.
“It should be noted that most clinical data to inform these practices are based on observational data or indirect evidence as elderly IBD patients comprise a very small proportion of subjects enrolled in IBD clinical trials or long-term pharmacovigilance initiatives,” the investigators wrote.
With this in mind, the update offers guidance for diagnosis, treatment, and ongoing health maintenance.
Diagnosis
Dr. Ananthakrishnan and colleagues first suggested that clinicians remain vigilant for IBD in elderly people, in consideration of the 15% prevalence rate in this subpopulation.
For elderly individuals with a low probability of IBD, the investigators recommended fecal calprotectin or lactoferrin to determine if endoscopy is needed. For elderly patients with chronic diarrhea or hematochezia, plus moderate to high suspicion of IBD, colorectal neoplasia, or microscopic colitis, they recommended colonoscopy.
Lastly, the expert panel suggested that elderly patients presenting with segmental left-sided colitis and diverticulosis may also have Crohn’s disease or IBD unclassified.
Treatment
The clinical practice update offers 10 best practice statements for treating elderly patients with IBD. There is a recurring emphasis on treatment personalization, which should be informed by patient goals and priorities, risk/presence of severe disease, chronological age, functional status, independence, comorbidities, frailty, and several other age-associated risk factors (e.g., venous thromboembolism).
Concerning specific therapies, the investigators cautioned against systemic corticosteroids for maintenance therapy; instead, nonsystemic corticosteroids (e.g., budesonide) are favored, or possibly early biological therapy if budesonide is not indicated. When selecting a biologic, Dr. Ananthakrishnan and colleagues recommended those associated with a lower risk of malignancy and infection (e.g., ustekinumab or vedolizumab).
The advantages of thiopurine monotherapy being oral, relatively inexpensive compared to biologicals and having a long track record of success in maintenance of remission must be balanced against the need for ongoing serological monitoring, and increased risk of some malignancies.
Finally, the expert panel recommended that all elderly patients receive multidisciplinary care, which may include primary care providers, mental health professionals, nutritionists, and other specialists. It may also be productive to consult with family and caregivers during treatment planning.
Health maintenance
The last two best practice advice statements concern health maintenance.
First, the investigators recommended that elderly patients with IBD adhere to vaccination schedules, including herpes zoster, pneumococcus, and influenza vaccines, ideally, before starting immunosuppression.
Second, Dr. Ananthakrishnan and colleagues advised that cessation of colorectal cancer surveillance may be considered in elderly patients with IBD; however, this decision should take into account a variety of factors, including comorbidities, age, life expectancy, likelihood of endoscopic resection, and surgical candidacy.
The review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. The investigators disclosed relationships with Gilead, Sun Pharma, Kyn Therapeutics, and others.
SOURCE: Ananthakrishnan AN et al. Gastroenterology. 2020 Sep 30. doi: 10.1053/j.gastro.2020.08.060.
This story was updated on 12/4/2020.
The American Gastroenterological Association has published a Clinical Practice Update for management of inflammatory bowel disease (IBD) in elderly patients, including 15 best practice advice statements.
According to lead author Ashwin N. Ananthakrishnan, MD, MPH, of Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues, this topic is becoming increasingly relevant, as the population is aging, and prevalence of IBD among elderly is rising approximately 5% per year.
“Up to 15% of IBD in North America and Asia is diagnosed after the age of 60 years,” the investigators wrote in Gastroenterology.
Dr. Ananthakrishnan and colleagues noted that “care of elderly IBD patients poses unique challenges with respect to diagnosis and therapeutic decision-making.”
Challenges include greater frequency of comorbidities, increased risk of infection with anti–tumor necrosis factor therapy, increased risk of lymphoma with thiopurine therapy, greater likelihood of surgical complications, and, for Crohn’s disease, an elevated mortality rate, according to the update.
Another challenge is a lack of data.
“It should be noted that most clinical data to inform these practices are based on observational data or indirect evidence as elderly IBD patients comprise a very small proportion of subjects enrolled in IBD clinical trials or long-term pharmacovigilance initiatives,” the investigators wrote.
With this in mind, the update offers guidance for diagnosis, treatment, and ongoing health maintenance.
Diagnosis
Dr. Ananthakrishnan and colleagues first suggested that clinicians remain vigilant for IBD in elderly people, in consideration of the 15% prevalence rate in this subpopulation.
For elderly individuals with a low probability of IBD, the investigators recommended fecal calprotectin or lactoferrin to determine if endoscopy is needed. For elderly patients with chronic diarrhea or hematochezia, plus moderate to high suspicion of IBD, colorectal neoplasia, or microscopic colitis, they recommended colonoscopy.
Lastly, the expert panel suggested that elderly patients presenting with segmental left-sided colitis and diverticulosis may also have Crohn’s disease or IBD unclassified.
Treatment
The clinical practice update offers 10 best practice statements for treating elderly patients with IBD. There is a recurring emphasis on treatment personalization, which should be informed by patient goals and priorities, risk/presence of severe disease, chronological age, functional status, independence, comorbidities, frailty, and several other age-associated risk factors (e.g., venous thromboembolism).
Concerning specific therapies, the investigators cautioned against systemic corticosteroids for maintenance therapy; instead, nonsystemic corticosteroids (e.g., budesonide) are favored, or possibly early biological therapy if budesonide is not indicated. When selecting a biologic, Dr. Ananthakrishnan and colleagues recommended those associated with a lower risk of malignancy and infection (e.g., ustekinumab or vedolizumab).
The advantages of thiopurine monotherapy being oral, relatively inexpensive compared to biologicals and having a long track record of success in maintenance of remission must be balanced against the need for ongoing serological monitoring, and increased risk of some malignancies.
Finally, the expert panel recommended that all elderly patients receive multidisciplinary care, which may include primary care providers, mental health professionals, nutritionists, and other specialists. It may also be productive to consult with family and caregivers during treatment planning.
Health maintenance
The last two best practice advice statements concern health maintenance.
First, the investigators recommended that elderly patients with IBD adhere to vaccination schedules, including herpes zoster, pneumococcus, and influenza vaccines, ideally, before starting immunosuppression.
Second, Dr. Ananthakrishnan and colleagues advised that cessation of colorectal cancer surveillance may be considered in elderly patients with IBD; however, this decision should take into account a variety of factors, including comorbidities, age, life expectancy, likelihood of endoscopic resection, and surgical candidacy.
The review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. The investigators disclosed relationships with Gilead, Sun Pharma, Kyn Therapeutics, and others.
SOURCE: Ananthakrishnan AN et al. Gastroenterology. 2020 Sep 30. doi: 10.1053/j.gastro.2020.08.060.
This story was updated on 12/4/2020.
FROM GASTROENTEROLOGY
One-third of critical illness survivors emerge from ICU with functional deterioration
More patients are surviving critical illnesses requiring ICU care but many emerge with physical debility that may or may not eventually resolve.
Over the past decade, functional status deterioration after critical illness has become more common and of greater magnitude, despite concurrent efforts to reduce post–intensive care syndrome, based on a retrospective analysis of more than 100,000 patients.
Almost one-third of patients who survived nonsurgical ICU admission had evidence of functional status decline, reported lead author Nicholas E. Ingraham, MD, of the University of Minnesota, Minneapolis, and colleagues.
“Increasing capacity and decreasing mortality have created an evolving and diverse population of ICU survivors,” the investigators wrote in Critical Care Medicine. “Today’s survivors of critical illness are increasingly burdened by extensive physical and psychological comorbidities, often resulting in reduced quality of life.”
To determine trends in post–intensive care syndrome from 2008 to 2016, Dr. Ingraham and colleagues analyzed data from the Cerner Acute Physiology and Chronic Health Evaluation outcomes database, a national prospective cohort. Out of 202,786 adult patients admitted to the ICU, 129,917 were eligible for the study. Patients were excluded because of surgical admission, death, lack of functional status documentation, or inadequate hospital size or duration of participation. The final dataset had a median age of 63 years, with a slight predominance of male patients (54.0%). Most patients (80.9%) were White.
The primary outcome was defined as presence or absence of functional status deterioration, based on functional status at admission versus time of discharge. The secondary outcome was magnitude of deterioration over time.
The analysis, which controlled for age and severity of illness, revealed concerning trends for both outcomes.
Across the entire cohort 38,116 patients (29.3%) had functional status deterioration, with a 15% increase in prevalence over the course of the decade that spanned all disease categories (prevalence rate ratio, 1.15; 95% confidence interval, 1.13-1.17; P < .001). The magnitude of functional status decline also increased by 4% (odds ratio, 1.04; P < .001), with all but nonsurgical trauma patients showing greater deterioration over time.
“However, despite the decreasing magnitude of functional status deterioration in nonsurgical trauma, many admission diagnoses in this category remain in the top quartile of higher risk for functional status deterioration,” the investigators noted.
Functional status decline was most common among patients with head and polytrauma (OR, 3.39), followed closely by chest and spine trauma (OR, 3.38), and spine trauma (OR, 3.19). The top quartile of categories for prevalence of deterioration included nonsurgical trauma, neurologic, pulmonary, and gastrointestinal diseases.
Functional status decline was least common among patients diagnosed with diabetic ketoacidosis (OR, 0.27) or asthma (OR, 0.35).
“We believe our study provides important information that can be used in beginning to identify patients at high risk of functional status decline,” the investigators concluded. “Improving the identification of these patients and targeting appropriate interventions to mitigate this decline will be important directions for future studies in this area.”
According to David L. Bowton, MD, FCCP, professor emeritus, section on critical care, Wake Forest Baptist Health, Winston-Salem, N.C., the findings show just how common functional decline is after critical illness, and may actually underestimate prevalence.
“Because the authors employed a course evaluation tool employing only three categories of ability/disability and abstracted the level of disability from the medical record, they likely underestimated the frequency of clinically important, though not detected, disability at the time of hospital discharge,” Dr. Bowton said. “The study did not address cognitive impairment which can be detected in half of patients at 3 months following critical illness, and which significantly affects patients’ quality of life (Am J Respir Crit Care Med. 2020;202[2]:193-201).”
Dr. Bowton suggested that evidence-based methods of preventing post–intensive care syndrome are limited.
“Current efforts to improve post-ICU functional and cognitive outcomes suffer from the lack of proven effective interventions (Crit Care Med. 2019;47[11]:1607-18),” he said. “Observational data indicates that compliance with the ABCDEF bundle decreases the duration and incidence of delirium, ICU length of stay, duration of mechanical ventilation, and mortality (Crit Care Med. 2019;47[1]:3-14). However, the implications of these improvements on postdischarge functional outcomes are unknown as area the relative importance of individual elements of the bundle. Early mobility and patient and family diaries appear to improve functional status at discharge and postdischarge anxiety and depression, though the evidence supporting this is thin.”
Appropriate intervention may be especially challenging during the COVID-19 pandemic, he added.
“The impact of COVID on ICU staffing adequacy and stress is significant and the impact on quality bundle compliance and the availability of support services is currently not clear, but likely to be detrimental, especially to support services such as physical therapy that are already commonly understaffed,” Dr. Bowton said.
The study was supported by grants from the University of Minnesota’s Critical Care Research and Programmatic Development Program; the National Heart, Lung, and Blood Institute; and the University of Minnesota Clinical and Translational Science via the National Center for Advancing Translational Sciences. The investigators reported financial relationships with no other relevant organizations. Dr. Bowton reported no conflicts of interest.
SOURCE: Ingraham NE et al. Crit Care Med. 2020 Nov. doi: 10.1097/CCM.0000000000004524.
More patients are surviving critical illnesses requiring ICU care but many emerge with physical debility that may or may not eventually resolve.
Over the past decade, functional status deterioration after critical illness has become more common and of greater magnitude, despite concurrent efforts to reduce post–intensive care syndrome, based on a retrospective analysis of more than 100,000 patients.
Almost one-third of patients who survived nonsurgical ICU admission had evidence of functional status decline, reported lead author Nicholas E. Ingraham, MD, of the University of Minnesota, Minneapolis, and colleagues.
“Increasing capacity and decreasing mortality have created an evolving and diverse population of ICU survivors,” the investigators wrote in Critical Care Medicine. “Today’s survivors of critical illness are increasingly burdened by extensive physical and psychological comorbidities, often resulting in reduced quality of life.”
To determine trends in post–intensive care syndrome from 2008 to 2016, Dr. Ingraham and colleagues analyzed data from the Cerner Acute Physiology and Chronic Health Evaluation outcomes database, a national prospective cohort. Out of 202,786 adult patients admitted to the ICU, 129,917 were eligible for the study. Patients were excluded because of surgical admission, death, lack of functional status documentation, or inadequate hospital size or duration of participation. The final dataset had a median age of 63 years, with a slight predominance of male patients (54.0%). Most patients (80.9%) were White.
The primary outcome was defined as presence or absence of functional status deterioration, based on functional status at admission versus time of discharge. The secondary outcome was magnitude of deterioration over time.
The analysis, which controlled for age and severity of illness, revealed concerning trends for both outcomes.
Across the entire cohort 38,116 patients (29.3%) had functional status deterioration, with a 15% increase in prevalence over the course of the decade that spanned all disease categories (prevalence rate ratio, 1.15; 95% confidence interval, 1.13-1.17; P < .001). The magnitude of functional status decline also increased by 4% (odds ratio, 1.04; P < .001), with all but nonsurgical trauma patients showing greater deterioration over time.
“However, despite the decreasing magnitude of functional status deterioration in nonsurgical trauma, many admission diagnoses in this category remain in the top quartile of higher risk for functional status deterioration,” the investigators noted.
Functional status decline was most common among patients with head and polytrauma (OR, 3.39), followed closely by chest and spine trauma (OR, 3.38), and spine trauma (OR, 3.19). The top quartile of categories for prevalence of deterioration included nonsurgical trauma, neurologic, pulmonary, and gastrointestinal diseases.
Functional status decline was least common among patients diagnosed with diabetic ketoacidosis (OR, 0.27) or asthma (OR, 0.35).
“We believe our study provides important information that can be used in beginning to identify patients at high risk of functional status decline,” the investigators concluded. “Improving the identification of these patients and targeting appropriate interventions to mitigate this decline will be important directions for future studies in this area.”
According to David L. Bowton, MD, FCCP, professor emeritus, section on critical care, Wake Forest Baptist Health, Winston-Salem, N.C., the findings show just how common functional decline is after critical illness, and may actually underestimate prevalence.
“Because the authors employed a course evaluation tool employing only three categories of ability/disability and abstracted the level of disability from the medical record, they likely underestimated the frequency of clinically important, though not detected, disability at the time of hospital discharge,” Dr. Bowton said. “The study did not address cognitive impairment which can be detected in half of patients at 3 months following critical illness, and which significantly affects patients’ quality of life (Am J Respir Crit Care Med. 2020;202[2]:193-201).”
Dr. Bowton suggested that evidence-based methods of preventing post–intensive care syndrome are limited.
“Current efforts to improve post-ICU functional and cognitive outcomes suffer from the lack of proven effective interventions (Crit Care Med. 2019;47[11]:1607-18),” he said. “Observational data indicates that compliance with the ABCDEF bundle decreases the duration and incidence of delirium, ICU length of stay, duration of mechanical ventilation, and mortality (Crit Care Med. 2019;47[1]:3-14). However, the implications of these improvements on postdischarge functional outcomes are unknown as area the relative importance of individual elements of the bundle. Early mobility and patient and family diaries appear to improve functional status at discharge and postdischarge anxiety and depression, though the evidence supporting this is thin.”
Appropriate intervention may be especially challenging during the COVID-19 pandemic, he added.
“The impact of COVID on ICU staffing adequacy and stress is significant and the impact on quality bundle compliance and the availability of support services is currently not clear, but likely to be detrimental, especially to support services such as physical therapy that are already commonly understaffed,” Dr. Bowton said.
The study was supported by grants from the University of Minnesota’s Critical Care Research and Programmatic Development Program; the National Heart, Lung, and Blood Institute; and the University of Minnesota Clinical and Translational Science via the National Center for Advancing Translational Sciences. The investigators reported financial relationships with no other relevant organizations. Dr. Bowton reported no conflicts of interest.
SOURCE: Ingraham NE et al. Crit Care Med. 2020 Nov. doi: 10.1097/CCM.0000000000004524.
More patients are surviving critical illnesses requiring ICU care but many emerge with physical debility that may or may not eventually resolve.
Over the past decade, functional status deterioration after critical illness has become more common and of greater magnitude, despite concurrent efforts to reduce post–intensive care syndrome, based on a retrospective analysis of more than 100,000 patients.
Almost one-third of patients who survived nonsurgical ICU admission had evidence of functional status decline, reported lead author Nicholas E. Ingraham, MD, of the University of Minnesota, Minneapolis, and colleagues.
“Increasing capacity and decreasing mortality have created an evolving and diverse population of ICU survivors,” the investigators wrote in Critical Care Medicine. “Today’s survivors of critical illness are increasingly burdened by extensive physical and psychological comorbidities, often resulting in reduced quality of life.”
To determine trends in post–intensive care syndrome from 2008 to 2016, Dr. Ingraham and colleagues analyzed data from the Cerner Acute Physiology and Chronic Health Evaluation outcomes database, a national prospective cohort. Out of 202,786 adult patients admitted to the ICU, 129,917 were eligible for the study. Patients were excluded because of surgical admission, death, lack of functional status documentation, or inadequate hospital size or duration of participation. The final dataset had a median age of 63 years, with a slight predominance of male patients (54.0%). Most patients (80.9%) were White.
The primary outcome was defined as presence or absence of functional status deterioration, based on functional status at admission versus time of discharge. The secondary outcome was magnitude of deterioration over time.
The analysis, which controlled for age and severity of illness, revealed concerning trends for both outcomes.
Across the entire cohort 38,116 patients (29.3%) had functional status deterioration, with a 15% increase in prevalence over the course of the decade that spanned all disease categories (prevalence rate ratio, 1.15; 95% confidence interval, 1.13-1.17; P < .001). The magnitude of functional status decline also increased by 4% (odds ratio, 1.04; P < .001), with all but nonsurgical trauma patients showing greater deterioration over time.
“However, despite the decreasing magnitude of functional status deterioration in nonsurgical trauma, many admission diagnoses in this category remain in the top quartile of higher risk for functional status deterioration,” the investigators noted.
Functional status decline was most common among patients with head and polytrauma (OR, 3.39), followed closely by chest and spine trauma (OR, 3.38), and spine trauma (OR, 3.19). The top quartile of categories for prevalence of deterioration included nonsurgical trauma, neurologic, pulmonary, and gastrointestinal diseases.
Functional status decline was least common among patients diagnosed with diabetic ketoacidosis (OR, 0.27) or asthma (OR, 0.35).
“We believe our study provides important information that can be used in beginning to identify patients at high risk of functional status decline,” the investigators concluded. “Improving the identification of these patients and targeting appropriate interventions to mitigate this decline will be important directions for future studies in this area.”
According to David L. Bowton, MD, FCCP, professor emeritus, section on critical care, Wake Forest Baptist Health, Winston-Salem, N.C., the findings show just how common functional decline is after critical illness, and may actually underestimate prevalence.
“Because the authors employed a course evaluation tool employing only three categories of ability/disability and abstracted the level of disability from the medical record, they likely underestimated the frequency of clinically important, though not detected, disability at the time of hospital discharge,” Dr. Bowton said. “The study did not address cognitive impairment which can be detected in half of patients at 3 months following critical illness, and which significantly affects patients’ quality of life (Am J Respir Crit Care Med. 2020;202[2]:193-201).”
Dr. Bowton suggested that evidence-based methods of preventing post–intensive care syndrome are limited.
“Current efforts to improve post-ICU functional and cognitive outcomes suffer from the lack of proven effective interventions (Crit Care Med. 2019;47[11]:1607-18),” he said. “Observational data indicates that compliance with the ABCDEF bundle decreases the duration and incidence of delirium, ICU length of stay, duration of mechanical ventilation, and mortality (Crit Care Med. 2019;47[1]:3-14). However, the implications of these improvements on postdischarge functional outcomes are unknown as area the relative importance of individual elements of the bundle. Early mobility and patient and family diaries appear to improve functional status at discharge and postdischarge anxiety and depression, though the evidence supporting this is thin.”
Appropriate intervention may be especially challenging during the COVID-19 pandemic, he added.
“The impact of COVID on ICU staffing adequacy and stress is significant and the impact on quality bundle compliance and the availability of support services is currently not clear, but likely to be detrimental, especially to support services such as physical therapy that are already commonly understaffed,” Dr. Bowton said.
The study was supported by grants from the University of Minnesota’s Critical Care Research and Programmatic Development Program; the National Heart, Lung, and Blood Institute; and the University of Minnesota Clinical and Translational Science via the National Center for Advancing Translational Sciences. The investigators reported financial relationships with no other relevant organizations. Dr. Bowton reported no conflicts of interest.
SOURCE: Ingraham NE et al. Crit Care Med. 2020 Nov. doi: 10.1097/CCM.0000000000004524.
FROM CRITICAL CARE MEDICINE
Black patients less likely to receive H. pylori eradication testing
Black patients may be significantly less likely to receive eradication testing after treatment for Helicobacter pylori infection than patients of other races/ethnic groups, based on a retrospective analysis of more than 1,700 individuals.
This disparity may exacerbate the already increased burden of H. pylori infection and gastric cancer among Black individuals, according to principal author David A. Leiman, MD, MSHP, of Duke University Medical Center in Durham, N.C.
“H. pylori infection disproportionately affects racial/ethnic minorities and those of lower socioeconomic status,” Dr. Leiman, coauthor Julius Wilder, MD, PhD, of Duke University in Durham, and colleagues wrote in their abstract presented at the annual meeting of the American College of Gastroenterology. “ACG guidelines recommend treatment for H. pylori infection followed by confirmation of cure. Adherence to these recommendations varies and its impact on practice patterns is unclear. This study characterizes the management of H. pylori infection and predictors of guideline adherence.”
The investigators analyzed electronic medical records from 1,711 patients diagnosed with H. pylori infection through the Duke University Health System between June 2016 and June 2018, most often (71%) via serum antibody test. Approximately two-thirds of those diagnosed were non-White (66%) and female (63%). Out of 1,711 patients, 622 (36%) underwent eradication testing, of whom 559 (90%) were cured.
Despite publication of the ACG H. pylori guideline midway through the study (February 2017), testing rates dropped significantly from 43.1% in 2016 to 35.9% in 2017, and finally 25.5% in 2018 (P < .0001).
“These findings are consistent with other work that has shown low rates of testing to confirm cure in patients treated for H. pylori,” Dr. Leiman said. “There remains a disappointingly low number of patients who are tested for cure.”
Across the entire study period, patients were significantly more likely to undergo eradication testing if they were treated in the gastroenterology department (52.4%), compared with rates ranging from 33% to 34.6% for internal medicine, family medicine, and other departments (P < .001).
Across all departments, Black patients underwent eradication testing significantly less often than patients of other races/ethnicities, at a rate of 30.5% versus 32.2% for White patients, 35.1% for Asian patients, and 36.7% for patients who were of other backgrounds (P < .001). Compared with White patients, Black patients were 38% less likely to undergo eradication testing (odds ratio, 0.62; 95% confidence interval, 0.48-0.79).
Dr. Leiman noted that these findings contrast with a study by Dr. Shria Kumar and colleagues from earlier this year, which found no racial disparity in eradication testing within a Veterans Health Affairs cohort.
“Black patients are significantly less likely to undergo testing for eradication than [patients of other races/ethnicities],” Dr. Leiman said. “More work is needed to understand the mechanisms driving this disparity.” He suggested a number of possible contributing factors, including provider knowledge gaps, fragmented care, and social determinants of health.
“It is clear that a greater emphasis on characterizing and addressing the social determinants of health, including poverty, education, and location, are needed,” Dr. Leiman said. “Although health systems are not solely responsible for the known and ongoing observations of disparities in care, interventions must be identified and implemented to mitigate these issues.” Such interventions would likely require broad participation, he said, including policy makers, health systems, and individual practitioners.
“We plan to perform a prospective mixed methods study to contextualize which social determinants are associated with a decreased likelihood of receiving appropriate eradication testing by exploring barriers at patient, practitioner, and health-system levels,” Dr. Leiman said. “Ultimately, we aim to leverage these findings to develop an evidence-based intervention to circumnavigate those identified barriers, thereby eliminating the observed disparities in H. pylori care.”
According to Gregory L. Hall, MD, of Northeast Ohio Medical University, Rootstown, and Case Western Reserve University, Cleveland, and codirector of the Partnership for Urban Health Research, Atlanta, the higher rate of H. pylori infection in Black individuals may stem partly from genetic factors.
“Studies have shown that African Americans with a higher proportion of African ancestry have higher rates of H. pylori, suggesting a genetic component to this increased risk,” he said.
Still, Dr. Hall, who is the author of the book Patient-Centered Clinical Care for African Americans, went on to emphasize appropriate H. pylori management and recognition of racial disparities in medicine.
“The ability to test for, treat, and confirm eradication of H. pylori infections represents a great opportunity to improve quality of life through decreased gastritis, gastric ulcers, and gastric cancer,” he said. “[The present findings] show yet another disparity in our clinical care of African Americans that needs increased awareness among providers to these communities.”
Rotonya Carr, MD, of the Hospital of the University of Pennsylvania, Philadelphia, and lead author of a recent publication addressing racism and health disparities in gastroenterology, said the findings of the present study add weight to a known equity gap.
“These data are concerning in view of the twofold higher prevalence of H. pylori seropositivity and twofold higher incidence of gastric cancer in Black patients, compared with White patients,” Dr. Carr said. “These and other data support a comprehensive approach to reduce GI disparities that includes targeted education of both GI specialists and referring providers.”
According to Dr. Leiman, individual practitioners may work toward more equitable outcomes through a comprehensive clinical approach, regardless of patient race or ethnicity.
“Clinicians should consider H. pylori therapy an episode of care that spans diagnosis, treatment, and confirmation of cure,” he said. “Closing the loop in that episode by ensuring eradication is vital to conforming with best practices, and to reduce patients’ long-term risks.”The investigators disclosed relationships with Exact Sciences, Guardant Health, and Phathom Pharmaceuticals. Dr. Hall and Dr. Carr reported no relevant conflicts of interest.
SOURCE: Reichstein J et al. ACG 2020. Abstract S1332.
Black patients may be significantly less likely to receive eradication testing after treatment for Helicobacter pylori infection than patients of other races/ethnic groups, based on a retrospective analysis of more than 1,700 individuals.
This disparity may exacerbate the already increased burden of H. pylori infection and gastric cancer among Black individuals, according to principal author David A. Leiman, MD, MSHP, of Duke University Medical Center in Durham, N.C.
“H. pylori infection disproportionately affects racial/ethnic minorities and those of lower socioeconomic status,” Dr. Leiman, coauthor Julius Wilder, MD, PhD, of Duke University in Durham, and colleagues wrote in their abstract presented at the annual meeting of the American College of Gastroenterology. “ACG guidelines recommend treatment for H. pylori infection followed by confirmation of cure. Adherence to these recommendations varies and its impact on practice patterns is unclear. This study characterizes the management of H. pylori infection and predictors of guideline adherence.”
The investigators analyzed electronic medical records from 1,711 patients diagnosed with H. pylori infection through the Duke University Health System between June 2016 and June 2018, most often (71%) via serum antibody test. Approximately two-thirds of those diagnosed were non-White (66%) and female (63%). Out of 1,711 patients, 622 (36%) underwent eradication testing, of whom 559 (90%) were cured.
Despite publication of the ACG H. pylori guideline midway through the study (February 2017), testing rates dropped significantly from 43.1% in 2016 to 35.9% in 2017, and finally 25.5% in 2018 (P < .0001).
“These findings are consistent with other work that has shown low rates of testing to confirm cure in patients treated for H. pylori,” Dr. Leiman said. “There remains a disappointingly low number of patients who are tested for cure.”
Across the entire study period, patients were significantly more likely to undergo eradication testing if they were treated in the gastroenterology department (52.4%), compared with rates ranging from 33% to 34.6% for internal medicine, family medicine, and other departments (P < .001).
Across all departments, Black patients underwent eradication testing significantly less often than patients of other races/ethnicities, at a rate of 30.5% versus 32.2% for White patients, 35.1% for Asian patients, and 36.7% for patients who were of other backgrounds (P < .001). Compared with White patients, Black patients were 38% less likely to undergo eradication testing (odds ratio, 0.62; 95% confidence interval, 0.48-0.79).
Dr. Leiman noted that these findings contrast with a study by Dr. Shria Kumar and colleagues from earlier this year, which found no racial disparity in eradication testing within a Veterans Health Affairs cohort.
“Black patients are significantly less likely to undergo testing for eradication than [patients of other races/ethnicities],” Dr. Leiman said. “More work is needed to understand the mechanisms driving this disparity.” He suggested a number of possible contributing factors, including provider knowledge gaps, fragmented care, and social determinants of health.
“It is clear that a greater emphasis on characterizing and addressing the social determinants of health, including poverty, education, and location, are needed,” Dr. Leiman said. “Although health systems are not solely responsible for the known and ongoing observations of disparities in care, interventions must be identified and implemented to mitigate these issues.” Such interventions would likely require broad participation, he said, including policy makers, health systems, and individual practitioners.
“We plan to perform a prospective mixed methods study to contextualize which social determinants are associated with a decreased likelihood of receiving appropriate eradication testing by exploring barriers at patient, practitioner, and health-system levels,” Dr. Leiman said. “Ultimately, we aim to leverage these findings to develop an evidence-based intervention to circumnavigate those identified barriers, thereby eliminating the observed disparities in H. pylori care.”
According to Gregory L. Hall, MD, of Northeast Ohio Medical University, Rootstown, and Case Western Reserve University, Cleveland, and codirector of the Partnership for Urban Health Research, Atlanta, the higher rate of H. pylori infection in Black individuals may stem partly from genetic factors.
“Studies have shown that African Americans with a higher proportion of African ancestry have higher rates of H. pylori, suggesting a genetic component to this increased risk,” he said.
Still, Dr. Hall, who is the author of the book Patient-Centered Clinical Care for African Americans, went on to emphasize appropriate H. pylori management and recognition of racial disparities in medicine.
“The ability to test for, treat, and confirm eradication of H. pylori infections represents a great opportunity to improve quality of life through decreased gastritis, gastric ulcers, and gastric cancer,” he said. “[The present findings] show yet another disparity in our clinical care of African Americans that needs increased awareness among providers to these communities.”
Rotonya Carr, MD, of the Hospital of the University of Pennsylvania, Philadelphia, and lead author of a recent publication addressing racism and health disparities in gastroenterology, said the findings of the present study add weight to a known equity gap.
“These data are concerning in view of the twofold higher prevalence of H. pylori seropositivity and twofold higher incidence of gastric cancer in Black patients, compared with White patients,” Dr. Carr said. “These and other data support a comprehensive approach to reduce GI disparities that includes targeted education of both GI specialists and referring providers.”
According to Dr. Leiman, individual practitioners may work toward more equitable outcomes through a comprehensive clinical approach, regardless of patient race or ethnicity.
“Clinicians should consider H. pylori therapy an episode of care that spans diagnosis, treatment, and confirmation of cure,” he said. “Closing the loop in that episode by ensuring eradication is vital to conforming with best practices, and to reduce patients’ long-term risks.”The investigators disclosed relationships with Exact Sciences, Guardant Health, and Phathom Pharmaceuticals. Dr. Hall and Dr. Carr reported no relevant conflicts of interest.
SOURCE: Reichstein J et al. ACG 2020. Abstract S1332.
Black patients may be significantly less likely to receive eradication testing after treatment for Helicobacter pylori infection than patients of other races/ethnic groups, based on a retrospective analysis of more than 1,700 individuals.
This disparity may exacerbate the already increased burden of H. pylori infection and gastric cancer among Black individuals, according to principal author David A. Leiman, MD, MSHP, of Duke University Medical Center in Durham, N.C.
“H. pylori infection disproportionately affects racial/ethnic minorities and those of lower socioeconomic status,” Dr. Leiman, coauthor Julius Wilder, MD, PhD, of Duke University in Durham, and colleagues wrote in their abstract presented at the annual meeting of the American College of Gastroenterology. “ACG guidelines recommend treatment for H. pylori infection followed by confirmation of cure. Adherence to these recommendations varies and its impact on practice patterns is unclear. This study characterizes the management of H. pylori infection and predictors of guideline adherence.”
The investigators analyzed electronic medical records from 1,711 patients diagnosed with H. pylori infection through the Duke University Health System between June 2016 and June 2018, most often (71%) via serum antibody test. Approximately two-thirds of those diagnosed were non-White (66%) and female (63%). Out of 1,711 patients, 622 (36%) underwent eradication testing, of whom 559 (90%) were cured.
Despite publication of the ACG H. pylori guideline midway through the study (February 2017), testing rates dropped significantly from 43.1% in 2016 to 35.9% in 2017, and finally 25.5% in 2018 (P < .0001).
“These findings are consistent with other work that has shown low rates of testing to confirm cure in patients treated for H. pylori,” Dr. Leiman said. “There remains a disappointingly low number of patients who are tested for cure.”
Across the entire study period, patients were significantly more likely to undergo eradication testing if they were treated in the gastroenterology department (52.4%), compared with rates ranging from 33% to 34.6% for internal medicine, family medicine, and other departments (P < .001).
Across all departments, Black patients underwent eradication testing significantly less often than patients of other races/ethnicities, at a rate of 30.5% versus 32.2% for White patients, 35.1% for Asian patients, and 36.7% for patients who were of other backgrounds (P < .001). Compared with White patients, Black patients were 38% less likely to undergo eradication testing (odds ratio, 0.62; 95% confidence interval, 0.48-0.79).
Dr. Leiman noted that these findings contrast with a study by Dr. Shria Kumar and colleagues from earlier this year, which found no racial disparity in eradication testing within a Veterans Health Affairs cohort.
“Black patients are significantly less likely to undergo testing for eradication than [patients of other races/ethnicities],” Dr. Leiman said. “More work is needed to understand the mechanisms driving this disparity.” He suggested a number of possible contributing factors, including provider knowledge gaps, fragmented care, and social determinants of health.
“It is clear that a greater emphasis on characterizing and addressing the social determinants of health, including poverty, education, and location, are needed,” Dr. Leiman said. “Although health systems are not solely responsible for the known and ongoing observations of disparities in care, interventions must be identified and implemented to mitigate these issues.” Such interventions would likely require broad participation, he said, including policy makers, health systems, and individual practitioners.
“We plan to perform a prospective mixed methods study to contextualize which social determinants are associated with a decreased likelihood of receiving appropriate eradication testing by exploring barriers at patient, practitioner, and health-system levels,” Dr. Leiman said. “Ultimately, we aim to leverage these findings to develop an evidence-based intervention to circumnavigate those identified barriers, thereby eliminating the observed disparities in H. pylori care.”
According to Gregory L. Hall, MD, of Northeast Ohio Medical University, Rootstown, and Case Western Reserve University, Cleveland, and codirector of the Partnership for Urban Health Research, Atlanta, the higher rate of H. pylori infection in Black individuals may stem partly from genetic factors.
“Studies have shown that African Americans with a higher proportion of African ancestry have higher rates of H. pylori, suggesting a genetic component to this increased risk,” he said.
Still, Dr. Hall, who is the author of the book Patient-Centered Clinical Care for African Americans, went on to emphasize appropriate H. pylori management and recognition of racial disparities in medicine.
“The ability to test for, treat, and confirm eradication of H. pylori infections represents a great opportunity to improve quality of life through decreased gastritis, gastric ulcers, and gastric cancer,” he said. “[The present findings] show yet another disparity in our clinical care of African Americans that needs increased awareness among providers to these communities.”
Rotonya Carr, MD, of the Hospital of the University of Pennsylvania, Philadelphia, and lead author of a recent publication addressing racism and health disparities in gastroenterology, said the findings of the present study add weight to a known equity gap.
“These data are concerning in view of the twofold higher prevalence of H. pylori seropositivity and twofold higher incidence of gastric cancer in Black patients, compared with White patients,” Dr. Carr said. “These and other data support a comprehensive approach to reduce GI disparities that includes targeted education of both GI specialists and referring providers.”
According to Dr. Leiman, individual practitioners may work toward more equitable outcomes through a comprehensive clinical approach, regardless of patient race or ethnicity.
“Clinicians should consider H. pylori therapy an episode of care that spans diagnosis, treatment, and confirmation of cure,” he said. “Closing the loop in that episode by ensuring eradication is vital to conforming with best practices, and to reduce patients’ long-term risks.”The investigators disclosed relationships with Exact Sciences, Guardant Health, and Phathom Pharmaceuticals. Dr. Hall and Dr. Carr reported no relevant conflicts of interest.
SOURCE: Reichstein J et al. ACG 2020. Abstract S1332.
FROM ACG 2020
Cirrhosis, Child-Pugh score predict ERCP complications
Cirrhosis may increase the risk of complications from endoscopic retrograde cholangiopancreatography (ERCP), according to a retrospective study involving almost 700 patients.
The study also showed that Child-Pugh class was a better predictor of risk than Model for End-Stage Liver Disease (MELD) score, reported lead author Michelle Bernshteyn, MD, a third-year internal medicine resident at State University of New York, Syracuse , and colleagues.
“There remains a scarcity in the literature regarding complications and adverse effects after ERCP in cirrhotic patients, particularly those incorporating Child-Pugh class and MELD score or type of intervention as predictors,” Dr. Bernshteyn said during a virtual presentation at the American College of Gastroenterology annual meeting. “Furthermore, literature review demonstrates inconsistency among results.”
To gain clarity, Dr. Bernshteyn and colleagues reviewed electronic medical records from 692 patients who underwent ERCP, of whom 174 had cirrhosis and 518 did not. For all patients, the investigators analyzed demographics, comorbidities, indications for ERCP, type of sedation, type of intervention, and complications within a 30-day period. Complications included bleeding, pancreatitis, cholangitis, perforation, mortality caused by ERCP, and mortality from other causes. Patients with cirrhosis were further analyzed based on etiology of cirrhosis, Child-Pugh class, and MELD score.
The analysis revealed that complications were significantly more common in patients with cirrhosis than in those without cirrhosis (21.30% vs. 13.51%; P = .015). No specific complications were significantly more common in patients with cirrhosis than in those without cirrhosis.
In patients with cirrhosis, 41.18% of Child-Pugh class C patients had complications, compared with 15.15% of class B patients and 19.30% of class A patients (P = .010). In contrast, MELD scores were not significantly associated with adverse events.
Further analysis showed that, in patients without cirrhosis, diagnostic-only ERCP and underlying chronic obstructive pulmonary disease were associated with high rates of complications (P = .039 and P = .003, respectively). In patients with cirrhosis, underlying chronic obstructive pulmonary disease and hypertension predicted adverse events (P = .009 and P = .003, respectively).
“The results of our study reaffirm that liver cirrhosis has an impact on the occurrence of complications during ERCP,” Dr. Bernshteyn said. “Child-Pugh class seems to be more reliable as compared to MELD score in predicting complications of ERCP in cirrhosis patients,” she added. “However, we are also aware that Child-Pugh and MELD scores are complementary to each other while evaluating outcomes of any surgery in patients with cirrhosis.”
In 2017, Udayakumar Navaneethan, MD, a gastroenterologist at AdventHealth Orlando’s Center for Interventional Endoscopy, and an assistant professor at the University of Central Florida, Orlando, and colleagues published a national database study concerning the safety of ERCP in patients with liver cirrhosis.
“[The present] study is important as it highlights the fact that ERCP is associated with significant complications in cirrhotic patients compared to those without cirrhosis,” Dr. Navaneethan said when asked to comment. “Also, Child-Pugh score appeared to be more reliable than MELD score in predicting complications of ERCP in cirrhotic patients.”
He went on to explain relevance for practicing clinicians. “The clinical implications of the study are that a detailed risk-benefit discussion needs to be done with patients with liver cirrhosis, particularly with advanced liver disease Child-Pugh class C, irrespective of the etiology,” Dr. Navaneethan said. “ERCP should be performed when there is clear evidence that the benefits outweigh the risks.” The investigators and Dr. Navaneethan reported no conflicts of interest.
SOURCE: Bernshteyn M et al. ACG 2020, Abstract S0982.
Cirrhosis may increase the risk of complications from endoscopic retrograde cholangiopancreatography (ERCP), according to a retrospective study involving almost 700 patients.
The study also showed that Child-Pugh class was a better predictor of risk than Model for End-Stage Liver Disease (MELD) score, reported lead author Michelle Bernshteyn, MD, a third-year internal medicine resident at State University of New York, Syracuse , and colleagues.
“There remains a scarcity in the literature regarding complications and adverse effects after ERCP in cirrhotic patients, particularly those incorporating Child-Pugh class and MELD score or type of intervention as predictors,” Dr. Bernshteyn said during a virtual presentation at the American College of Gastroenterology annual meeting. “Furthermore, literature review demonstrates inconsistency among results.”
To gain clarity, Dr. Bernshteyn and colleagues reviewed electronic medical records from 692 patients who underwent ERCP, of whom 174 had cirrhosis and 518 did not. For all patients, the investigators analyzed demographics, comorbidities, indications for ERCP, type of sedation, type of intervention, and complications within a 30-day period. Complications included bleeding, pancreatitis, cholangitis, perforation, mortality caused by ERCP, and mortality from other causes. Patients with cirrhosis were further analyzed based on etiology of cirrhosis, Child-Pugh class, and MELD score.
The analysis revealed that complications were significantly more common in patients with cirrhosis than in those without cirrhosis (21.30% vs. 13.51%; P = .015). No specific complications were significantly more common in patients with cirrhosis than in those without cirrhosis.
In patients with cirrhosis, 41.18% of Child-Pugh class C patients had complications, compared with 15.15% of class B patients and 19.30% of class A patients (P = .010). In contrast, MELD scores were not significantly associated with adverse events.
Further analysis showed that, in patients without cirrhosis, diagnostic-only ERCP and underlying chronic obstructive pulmonary disease were associated with high rates of complications (P = .039 and P = .003, respectively). In patients with cirrhosis, underlying chronic obstructive pulmonary disease and hypertension predicted adverse events (P = .009 and P = .003, respectively).
“The results of our study reaffirm that liver cirrhosis has an impact on the occurrence of complications during ERCP,” Dr. Bernshteyn said. “Child-Pugh class seems to be more reliable as compared to MELD score in predicting complications of ERCP in cirrhosis patients,” she added. “However, we are also aware that Child-Pugh and MELD scores are complementary to each other while evaluating outcomes of any surgery in patients with cirrhosis.”
In 2017, Udayakumar Navaneethan, MD, a gastroenterologist at AdventHealth Orlando’s Center for Interventional Endoscopy, and an assistant professor at the University of Central Florida, Orlando, and colleagues published a national database study concerning the safety of ERCP in patients with liver cirrhosis.
“[The present] study is important as it highlights the fact that ERCP is associated with significant complications in cirrhotic patients compared to those without cirrhosis,” Dr. Navaneethan said when asked to comment. “Also, Child-Pugh score appeared to be more reliable than MELD score in predicting complications of ERCP in cirrhotic patients.”
He went on to explain relevance for practicing clinicians. “The clinical implications of the study are that a detailed risk-benefit discussion needs to be done with patients with liver cirrhosis, particularly with advanced liver disease Child-Pugh class C, irrespective of the etiology,” Dr. Navaneethan said. “ERCP should be performed when there is clear evidence that the benefits outweigh the risks.” The investigators and Dr. Navaneethan reported no conflicts of interest.
SOURCE: Bernshteyn M et al. ACG 2020, Abstract S0982.
Cirrhosis may increase the risk of complications from endoscopic retrograde cholangiopancreatography (ERCP), according to a retrospective study involving almost 700 patients.
The study also showed that Child-Pugh class was a better predictor of risk than Model for End-Stage Liver Disease (MELD) score, reported lead author Michelle Bernshteyn, MD, a third-year internal medicine resident at State University of New York, Syracuse , and colleagues.
“There remains a scarcity in the literature regarding complications and adverse effects after ERCP in cirrhotic patients, particularly those incorporating Child-Pugh class and MELD score or type of intervention as predictors,” Dr. Bernshteyn said during a virtual presentation at the American College of Gastroenterology annual meeting. “Furthermore, literature review demonstrates inconsistency among results.”
To gain clarity, Dr. Bernshteyn and colleagues reviewed electronic medical records from 692 patients who underwent ERCP, of whom 174 had cirrhosis and 518 did not. For all patients, the investigators analyzed demographics, comorbidities, indications for ERCP, type of sedation, type of intervention, and complications within a 30-day period. Complications included bleeding, pancreatitis, cholangitis, perforation, mortality caused by ERCP, and mortality from other causes. Patients with cirrhosis were further analyzed based on etiology of cirrhosis, Child-Pugh class, and MELD score.
The analysis revealed that complications were significantly more common in patients with cirrhosis than in those without cirrhosis (21.30% vs. 13.51%; P = .015). No specific complications were significantly more common in patients with cirrhosis than in those without cirrhosis.
In patients with cirrhosis, 41.18% of Child-Pugh class C patients had complications, compared with 15.15% of class B patients and 19.30% of class A patients (P = .010). In contrast, MELD scores were not significantly associated with adverse events.
Further analysis showed that, in patients without cirrhosis, diagnostic-only ERCP and underlying chronic obstructive pulmonary disease were associated with high rates of complications (P = .039 and P = .003, respectively). In patients with cirrhosis, underlying chronic obstructive pulmonary disease and hypertension predicted adverse events (P = .009 and P = .003, respectively).
“The results of our study reaffirm that liver cirrhosis has an impact on the occurrence of complications during ERCP,” Dr. Bernshteyn said. “Child-Pugh class seems to be more reliable as compared to MELD score in predicting complications of ERCP in cirrhosis patients,” she added. “However, we are also aware that Child-Pugh and MELD scores are complementary to each other while evaluating outcomes of any surgery in patients with cirrhosis.”
In 2017, Udayakumar Navaneethan, MD, a gastroenterologist at AdventHealth Orlando’s Center for Interventional Endoscopy, and an assistant professor at the University of Central Florida, Orlando, and colleagues published a national database study concerning the safety of ERCP in patients with liver cirrhosis.
“[The present] study is important as it highlights the fact that ERCP is associated with significant complications in cirrhotic patients compared to those without cirrhosis,” Dr. Navaneethan said when asked to comment. “Also, Child-Pugh score appeared to be more reliable than MELD score in predicting complications of ERCP in cirrhotic patients.”
He went on to explain relevance for practicing clinicians. “The clinical implications of the study are that a detailed risk-benefit discussion needs to be done with patients with liver cirrhosis, particularly with advanced liver disease Child-Pugh class C, irrespective of the etiology,” Dr. Navaneethan said. “ERCP should be performed when there is clear evidence that the benefits outweigh the risks.” The investigators and Dr. Navaneethan reported no conflicts of interest.
SOURCE: Bernshteyn M et al. ACG 2020, Abstract S0982.
FROM ACG 2020