User login
Color‐coded wristbands: Promoting safety or confusion?
A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

A 62‐year‐old man was transferred from an outside hospital for evaluation of a complicated spinal infection. Like many patients, he had color‐coded wristbands to help identify potential safety hazards (see Fig. 1). The patient, an educated and alert individual, could describe the indications for only 3 of the 5 wristbands, and the transferring hospital supplied no legend. As it turned out, the green band represented a fall risk, the red one a drug allergy alert, and the purple one a tape allergy, whereas the white one was for patient identification. We're still not certain what the yellow one represented, but it was not a Lance Armstrong Livestrong bracelet; such wristbands have been reported to cause confusion in hospitals that have adopted yellow for their do not resuscitate wristbands.1 Although attempts at ensuring patient safety by using color‐coded wristbands are a common practice, the lack of standardization may pose an unknown hazard. Elsewhere in this journal, we present findings from a survey reinforcing the need for standardization around this issue.

- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
- .Wristbands called patient safety risk.St. Petersburg Times 10 Dec2004. p1A.
Identification of Inpatient DNR Status / Sehgal and Wachter
As modern medicine developed the technological capacity to deliver aggressive life‐sustaining interventionsthrough methods such as cardiopulmonary resuscitation (CPR), intensive care units, and mechanical ventilationthe concept of do‐not‐resuscitate (DNR) orders emerged to allow individual patients to choose to forego selected treatments. To encourage patients to articulate these preferences, Congress passed the Patient Self‐Determination Act in 1991, a measure that required health care facilities to discuss advance directives with patients as they enter their system.1 Although the act has had less of an impact on the quality of DNR discussions than originally hoped for,25 its passage was evidence of the importance our society places on patientclinician discussions regarding goals of care. In addition to this legislative push, many organizations and advocacy groups use a variety of marketing campaigns, accreditation standards,6 and standard instruments and tools79 to promote the use of advance directives
Despite all these efforts, fewer than 30% of Americans (54% older than age 65) have completed advance directives.10 Nevertheless, many patientsparticularly those at highest risk for requiring end‐of‐life caredo express preferences regarding resuscitation at the time of hospital admission. In an ideal world, these preferences would be available for all providers to view, respect, and act on.
Unfortunately, research on patient safety and quality has demonstrated wide gaps between ideal and actual practice.1112 In the context of DNR wishes, despite strong efforts to collect patients' preferences, no current regulation provides or mandates a best practice on making these preferences operational. There are also few data that indicate whether patients' preferences are in fact transmitted to providers at the point of care and in an accurate and reliable manner.
Past research on proper identification of DNR orders is limited, with much of the focus on prehospital protocols.1315 Anecdotally, hospitals seem to employ varying strategies to highlight DNR orders using a combination of paper or electronic documentation and color‐coded patient wristbands. There have been several reports of errors involving this issue, including patients receiving CPR despite stated DNR preferences and a patient having CPR withheld because the wrong chart (of another patient with a DNR order) was mistakenly pulled.1617
The patient safety field emphasizes standardization as a key strategy to prevent errors. Because of problems articulating DNR orders (and other important patient‐related information), several hospitals promote the use of color‐coded wristbands to denote preferences for resuscitation. However, without national regulations or standards, the possibility remains that one safety hazard (advance directives on a paper chart distant from a patient's room) may be traded for another hazard (front‐line providers interpreting a color‐coded wristband incorrectly). In addition to the ethical problems inherent in failing to adhere to patients' resuscitation preferences, errors in following advance directives may also create legal liability.18 With all this in mind, we conducted a national survey to determine practice variations in the identification of DNR orders and the use of color‐coded patient wristbands. We hypothesized that there is considerable variation both in identification practices and in the use of color‐coded wristbands across academic medical centers.
METHODS
The project was approved by the University of California, San Francisco Committee on Human Research. We anonymously surveyed nursing executives who are members of the University HealthSystem Consortium (UHC), an alliance of 97 academic medical centers and their affiliated hospitals representing 90% of the nation's nonprofit academic medical centers.19 The nursing executives are senior nursing leaders at participating UHC institutions and members of a dedicated UHC Chief Nursing Officer Council E‐mail listserv. We designed a brief survey and distributed it via their E‐mail listserv using an online commercial survey administration tool.20 Respondents were asked to complete the survey or have one of their colleagues familiar with local DNR identification practices complete it on their behalf. The online tool also provided summary reports and descriptive findings to meet the study objectives. We provided a 1‐month window (during summer 2006) with 1 interval E‐mail reminder to complete the surveys.
RESULTS
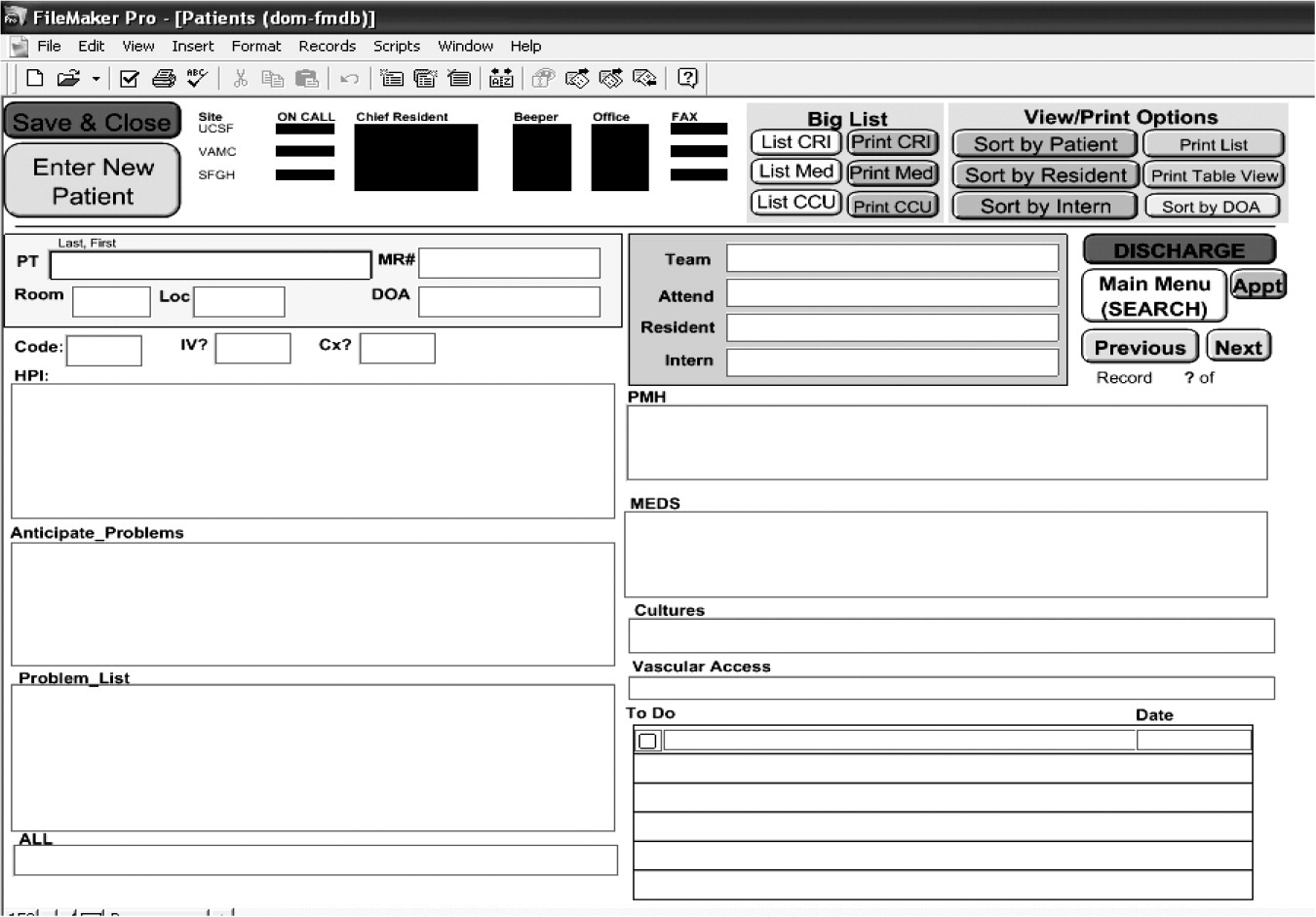
Survey announcements were E‐mailed to 127 nursing executives, 69 of whom completed it (response rate 54%). The respondents represented mostly academic medical centers (87%; another 13% represented affiliated community teaching hospitals), public institutions (89%), and large facilities (60% with more than 400 beds; 40% with 201‐400 beds). More than half the respondents (56%) reported their hospitals use paper chart documentation as the only method of identifying patients with a DNR order, whereas 16% reported their hospitals use only electronic health record (EHR) documentation (Fig. 1). Twenty‐five percent of hospitals (n = 17) use a color‐coded patient wristband in addition to either paper or electronic documentation. Of these 17 hospitals, a total of 8 colors or color schemes were employed to designate DNR status (Table 1).
| Green5 |
| Yellow3 |
| Blue3 |
| White with blue stars versus green stars (full DNR versus limited DNR)1 |
| Red1 |
| Red and white1 |
| Purple1 |
| Gold1 |
| Other (not listed)1 |
The use of color‐coded wristbands was not limited to identification of DNR status. Fifty‐five percent of hospitals (n = 31) use color‐coded wristbands to indicate another piece of patient‐related data such as an allergy, fall risk, or same last name alert (Table 2). In fact, 12 indications were depicted by various colors, with variations in both the color choice for a given indication (eg, allergy wristbands red at one hospital and yellow at another) and across indications (eg, red for allergy at one hospital and red for bleeding risk at another). Nearly 3 of 4 respondents (n = 48) reported being aware of a case at your institution in which confusion about a DNR order led to problems or confusion in patient care. A few respondents shared a brief anecdote of the event, illustrating the spectrum of clinical scenarios that lead to potential confusion (Table 3). Respondents reporting a case of confusion were not more likely to be from an institution that used color‐coded wristbands.
| Indication (n) | Colors used (n) |
|---|---|
| Drug/allergy (22) | Red (16) Yellow (4) White (1) Orange (1) |
| Fall risk (18) | Orange (5) Green (3) (and lime green [1]) Blue (3) Purple (3) Yellow (2) (and fluorescent yellow [1]) |
| Same name alert (7) | Blue (3) Orange (2) Yellow2) |
| Bleeding risk (3) | Red |
| Patient identification (3) | Green Red White |
| Wandering risk (3) | Pink (2) (and hot pink [1]) |
| Contact isolation (2) | Green |
| Latex allergy (2) | Purple |
| No blood draws on this arm (1) | Orange |
| MRSA infection (1) | Green |
| No blood products (1) | Red |
| Sleep apnea (1) | Purple |
| The patient had a DNR order written in the chart but no other identifiers at bedside, so a consult service started CPR while trying to determine code status. |
| Nurse called a code on a patient who was DNR because she failed to see order in chart. |
| Resuscitation efforts took place on a patient with a DNR order because the entire chart did not accompany the patient to a diagnostic testing area. |
| Patient was off the unit for a procedure, and staff in the other department did not know patients code status (DNR) and called a code. |
| Patient transported off nursing unit to radiology and coded. Patient was a DNR, but the order was buried in thinned chart materials. |
| Prior to implementing the wristbands, there were delays in care. Once wristbands were implemented with stars only, there was confusion as to what a blue star meant and what a green star meant (limited versus no resuscitation efforts). |
| We used to place a sticker on the chart. A sticker was left on the chart of a discharged patient when a new patient was admitted. The mistake was caught before an incident occurred. |
When asked whether most (greater than 75%) physicians and nurses could properly identify the color associated with a DNR patient wristband, responses differed by discipline. Eight‐five percent of respondents believed that most nurses at their institutions could correctly report the color for DNR, whereas only 15% believed physicians could do the same. Only 22% of respondents anticipated a change in the current system within the next 2 years; all these changes were a transition from paper to electronic documentation systems.
DISCUSSION
Regardless of whether the DNR documentation occurs in paper or electronic form (and our study demonstrates significant practice variation in the documentation method), the risk that a hospitalized patient may suddenly stop breathing or become pulseless is ever present. When such a patient is discovered, providers race to the bedside and initiate care, but immediately ask, Is the patient a full code? In these often‐chaotic moments, accurate and timely information about DNR status is critical to respecting a patient's preferences and avoiding a potentially devastating error. A number of the anecdotes shared by survey respondents and highlighted in Table 3 reinforce this concern. Many of these scenarios occur in the middle of the night or off a patient's primary unit (ie, at a test or procedure area), increasing the need for quick and easy identification of DNR status.
Our study demonstrates that a logical point‐of‐care solutiona color‐coded DNR patient wristbandmay create its own safety hazards, particularly if the color designations are not known by all providers (including floating and traveling nurses or trainees who rotate at different hospitals) and if the colors being employed represent different indications at a given hospital (see accompanying Images Dx, page 445). We found that approximately 1 in 4 surveyed hospitals depict DNR status by a color‐coded wristband. We also discovered remarkable variation in the colors chosen and the degree to which institutions use color‐coded wristbands to signal a panoply of other patient‐related issues. Human factors research demonstrates that even well‐meaning patient safety solutions may cause harm in new ways if they are poorly implemented or if the interface between the technology and human work patterns is not well appreciated. For example, recent studies illustrate unintended consequences from safety‐driven solutions, such as the implementation of computerized order entry,2122 quality measurement,23 adoption of EHRs,24 and bar code medication administration systems.25 Because standardization is a key mechanism for decreasing the opportunities for error, our findings raise serious concerns about current wristband use.
Interestingly, the lack of standardization and its related risk of failing to recall the conditions associated with color‐coded wristbands are complicated by societal trends. In December 2004 the issue of patient wristbands made headlines in Florida, when hospitals using yellow DNR wristbands (as was the case in 3 hospitals in our sample) reported several near‐misses among patients wearing yellow Lance Armstrong Livestrong bracelets.2627 Given recent estimates that nearly 1 in 5 Americans wears these bracelets to support people living with cancer,28 even safety‐minded journals and national newspapers have highlighted the issue.2930 Most hospitals that continue to use yellow DNR wristbands now either remove or cover Livestrong bracelets at the time of hospital admission. Furthermore, many other self‐help organizations now issue wristbands in a variety of colors as well, creating a potential hazard for any person wearing one in the hospital. Although patients do not mind wearing color‐coded wristbands,31 they might feel differently if they knew the potential for confusion.
After these anecdotal reports of identification mistakes surfaced, several states, most notably Arizona and Pennsylvania, launched initiatives to address the problem.3233 Arizona, after discovering 8 colors being used in the state, developed plans for a purple DNR color‐coded wristband. The choice of purple, and the careful decision to avoid blue, occurred because many hospitals call their resuscitative efforts a code blue, creating yet another potential source of confusion if a blue wristband is associated with a DNR order. The Pennsylvania Patient Safety Authority also found tremendous color variations in patient wristbands used in a statewide survey. Both states ultimately promoted standardized colors and indications and provided tool kits and implementation manuals.3233
Although statewide initiatives represent a step forward, we believe that a national standard for color‐coded wristbands would improve patient safety. Precedents for this call to action exist. For many years, anecdotal information circulated about the errors caused by ambiguous use of abbreviations, such as qd instead of daily or U instead of units. Individual hospitals often banned or limited the use of such abbreviations, but no standard list of high‐risk abbreviations guided practice or required adherence, and cross‐hospital variation undoubtedly led to confusion. In 2004 the Joint Commission created a uniform list of high‐risk abbreviations as part of their National Patient Safety Goals, which instantly ended the debate about which abbreviations to ban and mandated compliance with the safety practice.34 A national group of stakeholders should similarly be convened to develop a list of colors and associated conditions that should be widely disseminated and enforced by the Joint Commission or a similar body. The statewide efforts by Arizona and Pennsylvania are instructive in this regard. Despite being guided by the goal of standardization, these 2 states chose different colors for DNR identification (interestingly, Pennsylvania chose blue for DNR, perhaps for the same reason that Arizona avoided itcode blue), further supporting the need for national guidelines (Table 4).
| Indication | Color (PA) | Color (AZ) |
|---|---|---|
| DNR | Blue | Purple |
| Allergy | Red | Red |
| Fall risk | Yellow | Yellow |
| Latex allergy | Green | |
| Restricted extremity | Pink | |
| Preregistration in emergency room | Yellow | |
| Admission and identification | Clear |
Our study represents the first national sample of DNR identification practices. Although it targeted academic health centers and affiliated institutions, we believe that these practice variations likely exist in all health care settings. Our study limitations included reliance on self‐reported institutional practices rather than direct review of existing policies and limited information about the surveyed population, making it impossible to compare respondents and nonrespondents. However, we have no reason to believe that these groups differed sufficiently to influence the study's main findings.
In the future, better technology may ultimately replace color‐coded wristbands. For instance, the time may come when wireless technologies seamlessly linked to the electronic health record will alert providers to a patient's DNR status when entering the patient's room. However, for today, point‐of‐care solutions using color‐coded wristbands remain a reasonable solution. Creating a nationally enforced standardized methodology, understandable and memorable to providers and free of stigma to patients (eg, a black wristband for DNR or writing DNR on a wristband) should be a patient safety priority. Because simplification is another key characteristic of safe systems, it seems prudent to aim for a national system that involves a maximum of 3‐4 colors.
CONCLUSIONS
Patients and families dedicate tremendous energy to making decisions about their advance directives, and discussions of these issues often create considerable angst and sadness. Health care providers are trained to elicit and advocate for such directives so they can act with patients' wishes in mind. Despite the high stakes, all these efforts can be undermined when the system for making providers aware of a patient's DNR status is flawed. Our data confirm the tremendous variability in the systems used to indicate DNR status (and other types of indications), variability that may place patients at risk from catastrophic errors. Following the lead of a few states, we call for a national mandate to standardize the identification of DNR orders and to make the colors of wristbands for a small set of indications uniform in every hospital across the country.
Acknowledgements
We thank Mark Keroack, MD, MPH, and Cathy Krsek, RN, MSN, MBA, from the University HealthSystem Consortium for their contributions to the survey and assistance with administration. We also thank members of the UHC Chief Nursing Council for participating in the survey study.
As modern medicine developed the technological capacity to deliver aggressive life‐sustaining interventionsthrough methods such as cardiopulmonary resuscitation (CPR), intensive care units, and mechanical ventilationthe concept of do‐not‐resuscitate (DNR) orders emerged to allow individual patients to choose to forego selected treatments. To encourage patients to articulate these preferences, Congress passed the Patient Self‐Determination Act in 1991, a measure that required health care facilities to discuss advance directives with patients as they enter their system.1 Although the act has had less of an impact on the quality of DNR discussions than originally hoped for,25 its passage was evidence of the importance our society places on patientclinician discussions regarding goals of care. In addition to this legislative push, many organizations and advocacy groups use a variety of marketing campaigns, accreditation standards,6 and standard instruments and tools79 to promote the use of advance directives
Despite all these efforts, fewer than 30% of Americans (54% older than age 65) have completed advance directives.10 Nevertheless, many patientsparticularly those at highest risk for requiring end‐of‐life caredo express preferences regarding resuscitation at the time of hospital admission. In an ideal world, these preferences would be available for all providers to view, respect, and act on.
Unfortunately, research on patient safety and quality has demonstrated wide gaps between ideal and actual practice.1112 In the context of DNR wishes, despite strong efforts to collect patients' preferences, no current regulation provides or mandates a best practice on making these preferences operational. There are also few data that indicate whether patients' preferences are in fact transmitted to providers at the point of care and in an accurate and reliable manner.
Past research on proper identification of DNR orders is limited, with much of the focus on prehospital protocols.1315 Anecdotally, hospitals seem to employ varying strategies to highlight DNR orders using a combination of paper or electronic documentation and color‐coded patient wristbands. There have been several reports of errors involving this issue, including patients receiving CPR despite stated DNR preferences and a patient having CPR withheld because the wrong chart (of another patient with a DNR order) was mistakenly pulled.1617
The patient safety field emphasizes standardization as a key strategy to prevent errors. Because of problems articulating DNR orders (and other important patient‐related information), several hospitals promote the use of color‐coded wristbands to denote preferences for resuscitation. However, without national regulations or standards, the possibility remains that one safety hazard (advance directives on a paper chart distant from a patient's room) may be traded for another hazard (front‐line providers interpreting a color‐coded wristband incorrectly). In addition to the ethical problems inherent in failing to adhere to patients' resuscitation preferences, errors in following advance directives may also create legal liability.18 With all this in mind, we conducted a national survey to determine practice variations in the identification of DNR orders and the use of color‐coded patient wristbands. We hypothesized that there is considerable variation both in identification practices and in the use of color‐coded wristbands across academic medical centers.
METHODS
The project was approved by the University of California, San Francisco Committee on Human Research. We anonymously surveyed nursing executives who are members of the University HealthSystem Consortium (UHC), an alliance of 97 academic medical centers and their affiliated hospitals representing 90% of the nation's nonprofit academic medical centers.19 The nursing executives are senior nursing leaders at participating UHC institutions and members of a dedicated UHC Chief Nursing Officer Council E‐mail listserv. We designed a brief survey and distributed it via their E‐mail listserv using an online commercial survey administration tool.20 Respondents were asked to complete the survey or have one of their colleagues familiar with local DNR identification practices complete it on their behalf. The online tool also provided summary reports and descriptive findings to meet the study objectives. We provided a 1‐month window (during summer 2006) with 1 interval E‐mail reminder to complete the surveys.
RESULTS
Survey announcements were E‐mailed to 127 nursing executives, 69 of whom completed it (response rate 54%). The respondents represented mostly academic medical centers (87%; another 13% represented affiliated community teaching hospitals), public institutions (89%), and large facilities (60% with more than 400 beds; 40% with 201‐400 beds). More than half the respondents (56%) reported their hospitals use paper chart documentation as the only method of identifying patients with a DNR order, whereas 16% reported their hospitals use only electronic health record (EHR) documentation (Fig. 1). Twenty‐five percent of hospitals (n = 17) use a color‐coded patient wristband in addition to either paper or electronic documentation. Of these 17 hospitals, a total of 8 colors or color schemes were employed to designate DNR status (Table 1).
| Green5 |
| Yellow3 |
| Blue3 |
| White with blue stars versus green stars (full DNR versus limited DNR)1 |
| Red1 |
| Red and white1 |
| Purple1 |
| Gold1 |
| Other (not listed)1 |
The use of color‐coded wristbands was not limited to identification of DNR status. Fifty‐five percent of hospitals (n = 31) use color‐coded wristbands to indicate another piece of patient‐related data such as an allergy, fall risk, or same last name alert (Table 2). In fact, 12 indications were depicted by various colors, with variations in both the color choice for a given indication (eg, allergy wristbands red at one hospital and yellow at another) and across indications (eg, red for allergy at one hospital and red for bleeding risk at another). Nearly 3 of 4 respondents (n = 48) reported being aware of a case at your institution in which confusion about a DNR order led to problems or confusion in patient care. A few respondents shared a brief anecdote of the event, illustrating the spectrum of clinical scenarios that lead to potential confusion (Table 3). Respondents reporting a case of confusion were not more likely to be from an institution that used color‐coded wristbands.
| Indication (n) | Colors used (n) |
|---|---|
| Drug/allergy (22) | Red (16) Yellow (4) White (1) Orange (1) |
| Fall risk (18) | Orange (5) Green (3) (and lime green [1]) Blue (3) Purple (3) Yellow (2) (and fluorescent yellow [1]) |
| Same name alert (7) | Blue (3) Orange (2) Yellow2) |
| Bleeding risk (3) | Red |
| Patient identification (3) | Green Red White |
| Wandering risk (3) | Pink (2) (and hot pink [1]) |
| Contact isolation (2) | Green |
| Latex allergy (2) | Purple |
| No blood draws on this arm (1) | Orange |
| MRSA infection (1) | Green |
| No blood products (1) | Red |
| Sleep apnea (1) | Purple |
| The patient had a DNR order written in the chart but no other identifiers at bedside, so a consult service started CPR while trying to determine code status. |
| Nurse called a code on a patient who was DNR because she failed to see order in chart. |
| Resuscitation efforts took place on a patient with a DNR order because the entire chart did not accompany the patient to a diagnostic testing area. |
| Patient was off the unit for a procedure, and staff in the other department did not know patients code status (DNR) and called a code. |
| Patient transported off nursing unit to radiology and coded. Patient was a DNR, but the order was buried in thinned chart materials. |
| Prior to implementing the wristbands, there were delays in care. Once wristbands were implemented with stars only, there was confusion as to what a blue star meant and what a green star meant (limited versus no resuscitation efforts). |
| We used to place a sticker on the chart. A sticker was left on the chart of a discharged patient when a new patient was admitted. The mistake was caught before an incident occurred. |
When asked whether most (greater than 75%) physicians and nurses could properly identify the color associated with a DNR patient wristband, responses differed by discipline. Eight‐five percent of respondents believed that most nurses at their institutions could correctly report the color for DNR, whereas only 15% believed physicians could do the same. Only 22% of respondents anticipated a change in the current system within the next 2 years; all these changes were a transition from paper to electronic documentation systems.
DISCUSSION
Regardless of whether the DNR documentation occurs in paper or electronic form (and our study demonstrates significant practice variation in the documentation method), the risk that a hospitalized patient may suddenly stop breathing or become pulseless is ever present. When such a patient is discovered, providers race to the bedside and initiate care, but immediately ask, Is the patient a full code? In these often‐chaotic moments, accurate and timely information about DNR status is critical to respecting a patient's preferences and avoiding a potentially devastating error. A number of the anecdotes shared by survey respondents and highlighted in Table 3 reinforce this concern. Many of these scenarios occur in the middle of the night or off a patient's primary unit (ie, at a test or procedure area), increasing the need for quick and easy identification of DNR status.
Our study demonstrates that a logical point‐of‐care solutiona color‐coded DNR patient wristbandmay create its own safety hazards, particularly if the color designations are not known by all providers (including floating and traveling nurses or trainees who rotate at different hospitals) and if the colors being employed represent different indications at a given hospital (see accompanying Images Dx, page 445). We found that approximately 1 in 4 surveyed hospitals depict DNR status by a color‐coded wristband. We also discovered remarkable variation in the colors chosen and the degree to which institutions use color‐coded wristbands to signal a panoply of other patient‐related issues. Human factors research demonstrates that even well‐meaning patient safety solutions may cause harm in new ways if they are poorly implemented or if the interface between the technology and human work patterns is not well appreciated. For example, recent studies illustrate unintended consequences from safety‐driven solutions, such as the implementation of computerized order entry,2122 quality measurement,23 adoption of EHRs,24 and bar code medication administration systems.25 Because standardization is a key mechanism for decreasing the opportunities for error, our findings raise serious concerns about current wristband use.
Interestingly, the lack of standardization and its related risk of failing to recall the conditions associated with color‐coded wristbands are complicated by societal trends. In December 2004 the issue of patient wristbands made headlines in Florida, when hospitals using yellow DNR wristbands (as was the case in 3 hospitals in our sample) reported several near‐misses among patients wearing yellow Lance Armstrong Livestrong bracelets.2627 Given recent estimates that nearly 1 in 5 Americans wears these bracelets to support people living with cancer,28 even safety‐minded journals and national newspapers have highlighted the issue.2930 Most hospitals that continue to use yellow DNR wristbands now either remove or cover Livestrong bracelets at the time of hospital admission. Furthermore, many other self‐help organizations now issue wristbands in a variety of colors as well, creating a potential hazard for any person wearing one in the hospital. Although patients do not mind wearing color‐coded wristbands,31 they might feel differently if they knew the potential for confusion.
After these anecdotal reports of identification mistakes surfaced, several states, most notably Arizona and Pennsylvania, launched initiatives to address the problem.3233 Arizona, after discovering 8 colors being used in the state, developed plans for a purple DNR color‐coded wristband. The choice of purple, and the careful decision to avoid blue, occurred because many hospitals call their resuscitative efforts a code blue, creating yet another potential source of confusion if a blue wristband is associated with a DNR order. The Pennsylvania Patient Safety Authority also found tremendous color variations in patient wristbands used in a statewide survey. Both states ultimately promoted standardized colors and indications and provided tool kits and implementation manuals.3233
Although statewide initiatives represent a step forward, we believe that a national standard for color‐coded wristbands would improve patient safety. Precedents for this call to action exist. For many years, anecdotal information circulated about the errors caused by ambiguous use of abbreviations, such as qd instead of daily or U instead of units. Individual hospitals often banned or limited the use of such abbreviations, but no standard list of high‐risk abbreviations guided practice or required adherence, and cross‐hospital variation undoubtedly led to confusion. In 2004 the Joint Commission created a uniform list of high‐risk abbreviations as part of their National Patient Safety Goals, which instantly ended the debate about which abbreviations to ban and mandated compliance with the safety practice.34 A national group of stakeholders should similarly be convened to develop a list of colors and associated conditions that should be widely disseminated and enforced by the Joint Commission or a similar body. The statewide efforts by Arizona and Pennsylvania are instructive in this regard. Despite being guided by the goal of standardization, these 2 states chose different colors for DNR identification (interestingly, Pennsylvania chose blue for DNR, perhaps for the same reason that Arizona avoided itcode blue), further supporting the need for national guidelines (Table 4).
| Indication | Color (PA) | Color (AZ) |
|---|---|---|
| DNR | Blue | Purple |
| Allergy | Red | Red |
| Fall risk | Yellow | Yellow |
| Latex allergy | Green | |
| Restricted extremity | Pink | |
| Preregistration in emergency room | Yellow | |
| Admission and identification | Clear |
Our study represents the first national sample of DNR identification practices. Although it targeted academic health centers and affiliated institutions, we believe that these practice variations likely exist in all health care settings. Our study limitations included reliance on self‐reported institutional practices rather than direct review of existing policies and limited information about the surveyed population, making it impossible to compare respondents and nonrespondents. However, we have no reason to believe that these groups differed sufficiently to influence the study's main findings.
In the future, better technology may ultimately replace color‐coded wristbands. For instance, the time may come when wireless technologies seamlessly linked to the electronic health record will alert providers to a patient's DNR status when entering the patient's room. However, for today, point‐of‐care solutions using color‐coded wristbands remain a reasonable solution. Creating a nationally enforced standardized methodology, understandable and memorable to providers and free of stigma to patients (eg, a black wristband for DNR or writing DNR on a wristband) should be a patient safety priority. Because simplification is another key characteristic of safe systems, it seems prudent to aim for a national system that involves a maximum of 3‐4 colors.
CONCLUSIONS
Patients and families dedicate tremendous energy to making decisions about their advance directives, and discussions of these issues often create considerable angst and sadness. Health care providers are trained to elicit and advocate for such directives so they can act with patients' wishes in mind. Despite the high stakes, all these efforts can be undermined when the system for making providers aware of a patient's DNR status is flawed. Our data confirm the tremendous variability in the systems used to indicate DNR status (and other types of indications), variability that may place patients at risk from catastrophic errors. Following the lead of a few states, we call for a national mandate to standardize the identification of DNR orders and to make the colors of wristbands for a small set of indications uniform in every hospital across the country.
Acknowledgements
We thank Mark Keroack, MD, MPH, and Cathy Krsek, RN, MSN, MBA, from the University HealthSystem Consortium for their contributions to the survey and assistance with administration. We also thank members of the UHC Chief Nursing Council for participating in the survey study.
As modern medicine developed the technological capacity to deliver aggressive life‐sustaining interventionsthrough methods such as cardiopulmonary resuscitation (CPR), intensive care units, and mechanical ventilationthe concept of do‐not‐resuscitate (DNR) orders emerged to allow individual patients to choose to forego selected treatments. To encourage patients to articulate these preferences, Congress passed the Patient Self‐Determination Act in 1991, a measure that required health care facilities to discuss advance directives with patients as they enter their system.1 Although the act has had less of an impact on the quality of DNR discussions than originally hoped for,25 its passage was evidence of the importance our society places on patientclinician discussions regarding goals of care. In addition to this legislative push, many organizations and advocacy groups use a variety of marketing campaigns, accreditation standards,6 and standard instruments and tools79 to promote the use of advance directives
Despite all these efforts, fewer than 30% of Americans (54% older than age 65) have completed advance directives.10 Nevertheless, many patientsparticularly those at highest risk for requiring end‐of‐life caredo express preferences regarding resuscitation at the time of hospital admission. In an ideal world, these preferences would be available for all providers to view, respect, and act on.
Unfortunately, research on patient safety and quality has demonstrated wide gaps between ideal and actual practice.1112 In the context of DNR wishes, despite strong efforts to collect patients' preferences, no current regulation provides or mandates a best practice on making these preferences operational. There are also few data that indicate whether patients' preferences are in fact transmitted to providers at the point of care and in an accurate and reliable manner.
Past research on proper identification of DNR orders is limited, with much of the focus on prehospital protocols.1315 Anecdotally, hospitals seem to employ varying strategies to highlight DNR orders using a combination of paper or electronic documentation and color‐coded patient wristbands. There have been several reports of errors involving this issue, including patients receiving CPR despite stated DNR preferences and a patient having CPR withheld because the wrong chart (of another patient with a DNR order) was mistakenly pulled.1617
The patient safety field emphasizes standardization as a key strategy to prevent errors. Because of problems articulating DNR orders (and other important patient‐related information), several hospitals promote the use of color‐coded wristbands to denote preferences for resuscitation. However, without national regulations or standards, the possibility remains that one safety hazard (advance directives on a paper chart distant from a patient's room) may be traded for another hazard (front‐line providers interpreting a color‐coded wristband incorrectly). In addition to the ethical problems inherent in failing to adhere to patients' resuscitation preferences, errors in following advance directives may also create legal liability.18 With all this in mind, we conducted a national survey to determine practice variations in the identification of DNR orders and the use of color‐coded patient wristbands. We hypothesized that there is considerable variation both in identification practices and in the use of color‐coded wristbands across academic medical centers.
METHODS
The project was approved by the University of California, San Francisco Committee on Human Research. We anonymously surveyed nursing executives who are members of the University HealthSystem Consortium (UHC), an alliance of 97 academic medical centers and their affiliated hospitals representing 90% of the nation's nonprofit academic medical centers.19 The nursing executives are senior nursing leaders at participating UHC institutions and members of a dedicated UHC Chief Nursing Officer Council E‐mail listserv. We designed a brief survey and distributed it via their E‐mail listserv using an online commercial survey administration tool.20 Respondents were asked to complete the survey or have one of their colleagues familiar with local DNR identification practices complete it on their behalf. The online tool also provided summary reports and descriptive findings to meet the study objectives. We provided a 1‐month window (during summer 2006) with 1 interval E‐mail reminder to complete the surveys.
RESULTS
Survey announcements were E‐mailed to 127 nursing executives, 69 of whom completed it (response rate 54%). The respondents represented mostly academic medical centers (87%; another 13% represented affiliated community teaching hospitals), public institutions (89%), and large facilities (60% with more than 400 beds; 40% with 201‐400 beds). More than half the respondents (56%) reported their hospitals use paper chart documentation as the only method of identifying patients with a DNR order, whereas 16% reported their hospitals use only electronic health record (EHR) documentation (Fig. 1). Twenty‐five percent of hospitals (n = 17) use a color‐coded patient wristband in addition to either paper or electronic documentation. Of these 17 hospitals, a total of 8 colors or color schemes were employed to designate DNR status (Table 1).
| Green5 |
| Yellow3 |
| Blue3 |
| White with blue stars versus green stars (full DNR versus limited DNR)1 |
| Red1 |
| Red and white1 |
| Purple1 |
| Gold1 |
| Other (not listed)1 |
The use of color‐coded wristbands was not limited to identification of DNR status. Fifty‐five percent of hospitals (n = 31) use color‐coded wristbands to indicate another piece of patient‐related data such as an allergy, fall risk, or same last name alert (Table 2). In fact, 12 indications were depicted by various colors, with variations in both the color choice for a given indication (eg, allergy wristbands red at one hospital and yellow at another) and across indications (eg, red for allergy at one hospital and red for bleeding risk at another). Nearly 3 of 4 respondents (n = 48) reported being aware of a case at your institution in which confusion about a DNR order led to problems or confusion in patient care. A few respondents shared a brief anecdote of the event, illustrating the spectrum of clinical scenarios that lead to potential confusion (Table 3). Respondents reporting a case of confusion were not more likely to be from an institution that used color‐coded wristbands.
| Indication (n) | Colors used (n) |
|---|---|
| Drug/allergy (22) | Red (16) Yellow (4) White (1) Orange (1) |
| Fall risk (18) | Orange (5) Green (3) (and lime green [1]) Blue (3) Purple (3) Yellow (2) (and fluorescent yellow [1]) |
| Same name alert (7) | Blue (3) Orange (2) Yellow2) |
| Bleeding risk (3) | Red |
| Patient identification (3) | Green Red White |
| Wandering risk (3) | Pink (2) (and hot pink [1]) |
| Contact isolation (2) | Green |
| Latex allergy (2) | Purple |
| No blood draws on this arm (1) | Orange |
| MRSA infection (1) | Green |
| No blood products (1) | Red |
| Sleep apnea (1) | Purple |
| The patient had a DNR order written in the chart but no other identifiers at bedside, so a consult service started CPR while trying to determine code status. |
| Nurse called a code on a patient who was DNR because she failed to see order in chart. |
| Resuscitation efforts took place on a patient with a DNR order because the entire chart did not accompany the patient to a diagnostic testing area. |
| Patient was off the unit for a procedure, and staff in the other department did not know patients code status (DNR) and called a code. |
| Patient transported off nursing unit to radiology and coded. Patient was a DNR, but the order was buried in thinned chart materials. |
| Prior to implementing the wristbands, there were delays in care. Once wristbands were implemented with stars only, there was confusion as to what a blue star meant and what a green star meant (limited versus no resuscitation efforts). |
| We used to place a sticker on the chart. A sticker was left on the chart of a discharged patient when a new patient was admitted. The mistake was caught before an incident occurred. |
When asked whether most (greater than 75%) physicians and nurses could properly identify the color associated with a DNR patient wristband, responses differed by discipline. Eight‐five percent of respondents believed that most nurses at their institutions could correctly report the color for DNR, whereas only 15% believed physicians could do the same. Only 22% of respondents anticipated a change in the current system within the next 2 years; all these changes were a transition from paper to electronic documentation systems.
DISCUSSION
Regardless of whether the DNR documentation occurs in paper or electronic form (and our study demonstrates significant practice variation in the documentation method), the risk that a hospitalized patient may suddenly stop breathing or become pulseless is ever present. When such a patient is discovered, providers race to the bedside and initiate care, but immediately ask, Is the patient a full code? In these often‐chaotic moments, accurate and timely information about DNR status is critical to respecting a patient's preferences and avoiding a potentially devastating error. A number of the anecdotes shared by survey respondents and highlighted in Table 3 reinforce this concern. Many of these scenarios occur in the middle of the night or off a patient's primary unit (ie, at a test or procedure area), increasing the need for quick and easy identification of DNR status.
Our study demonstrates that a logical point‐of‐care solutiona color‐coded DNR patient wristbandmay create its own safety hazards, particularly if the color designations are not known by all providers (including floating and traveling nurses or trainees who rotate at different hospitals) and if the colors being employed represent different indications at a given hospital (see accompanying Images Dx, page 445). We found that approximately 1 in 4 surveyed hospitals depict DNR status by a color‐coded wristband. We also discovered remarkable variation in the colors chosen and the degree to which institutions use color‐coded wristbands to signal a panoply of other patient‐related issues. Human factors research demonstrates that even well‐meaning patient safety solutions may cause harm in new ways if they are poorly implemented or if the interface between the technology and human work patterns is not well appreciated. For example, recent studies illustrate unintended consequences from safety‐driven solutions, such as the implementation of computerized order entry,2122 quality measurement,23 adoption of EHRs,24 and bar code medication administration systems.25 Because standardization is a key mechanism for decreasing the opportunities for error, our findings raise serious concerns about current wristband use.
Interestingly, the lack of standardization and its related risk of failing to recall the conditions associated with color‐coded wristbands are complicated by societal trends. In December 2004 the issue of patient wristbands made headlines in Florida, when hospitals using yellow DNR wristbands (as was the case in 3 hospitals in our sample) reported several near‐misses among patients wearing yellow Lance Armstrong Livestrong bracelets.2627 Given recent estimates that nearly 1 in 5 Americans wears these bracelets to support people living with cancer,28 even safety‐minded journals and national newspapers have highlighted the issue.2930 Most hospitals that continue to use yellow DNR wristbands now either remove or cover Livestrong bracelets at the time of hospital admission. Furthermore, many other self‐help organizations now issue wristbands in a variety of colors as well, creating a potential hazard for any person wearing one in the hospital. Although patients do not mind wearing color‐coded wristbands,31 they might feel differently if they knew the potential for confusion.
After these anecdotal reports of identification mistakes surfaced, several states, most notably Arizona and Pennsylvania, launched initiatives to address the problem.3233 Arizona, after discovering 8 colors being used in the state, developed plans for a purple DNR color‐coded wristband. The choice of purple, and the careful decision to avoid blue, occurred because many hospitals call their resuscitative efforts a code blue, creating yet another potential source of confusion if a blue wristband is associated with a DNR order. The Pennsylvania Patient Safety Authority also found tremendous color variations in patient wristbands used in a statewide survey. Both states ultimately promoted standardized colors and indications and provided tool kits and implementation manuals.3233
Although statewide initiatives represent a step forward, we believe that a national standard for color‐coded wristbands would improve patient safety. Precedents for this call to action exist. For many years, anecdotal information circulated about the errors caused by ambiguous use of abbreviations, such as qd instead of daily or U instead of units. Individual hospitals often banned or limited the use of such abbreviations, but no standard list of high‐risk abbreviations guided practice or required adherence, and cross‐hospital variation undoubtedly led to confusion. In 2004 the Joint Commission created a uniform list of high‐risk abbreviations as part of their National Patient Safety Goals, which instantly ended the debate about which abbreviations to ban and mandated compliance with the safety practice.34 A national group of stakeholders should similarly be convened to develop a list of colors and associated conditions that should be widely disseminated and enforced by the Joint Commission or a similar body. The statewide efforts by Arizona and Pennsylvania are instructive in this regard. Despite being guided by the goal of standardization, these 2 states chose different colors for DNR identification (interestingly, Pennsylvania chose blue for DNR, perhaps for the same reason that Arizona avoided itcode blue), further supporting the need for national guidelines (Table 4).
| Indication | Color (PA) | Color (AZ) |
|---|---|---|
| DNR | Blue | Purple |
| Allergy | Red | Red |
| Fall risk | Yellow | Yellow |
| Latex allergy | Green | |
| Restricted extremity | Pink | |
| Preregistration in emergency room | Yellow | |
| Admission and identification | Clear |
Our study represents the first national sample of DNR identification practices. Although it targeted academic health centers and affiliated institutions, we believe that these practice variations likely exist in all health care settings. Our study limitations included reliance on self‐reported institutional practices rather than direct review of existing policies and limited information about the surveyed population, making it impossible to compare respondents and nonrespondents. However, we have no reason to believe that these groups differed sufficiently to influence the study's main findings.
In the future, better technology may ultimately replace color‐coded wristbands. For instance, the time may come when wireless technologies seamlessly linked to the electronic health record will alert providers to a patient's DNR status when entering the patient's room. However, for today, point‐of‐care solutions using color‐coded wristbands remain a reasonable solution. Creating a nationally enforced standardized methodology, understandable and memorable to providers and free of stigma to patients (eg, a black wristband for DNR or writing DNR on a wristband) should be a patient safety priority. Because simplification is another key characteristic of safe systems, it seems prudent to aim for a national system that involves a maximum of 3‐4 colors.
CONCLUSIONS
Patients and families dedicate tremendous energy to making decisions about their advance directives, and discussions of these issues often create considerable angst and sadness. Health care providers are trained to elicit and advocate for such directives so they can act with patients' wishes in mind. Despite the high stakes, all these efforts can be undermined when the system for making providers aware of a patient's DNR status is flawed. Our data confirm the tremendous variability in the systems used to indicate DNR status (and other types of indications), variability that may place patients at risk from catastrophic errors. Following the lead of a few states, we call for a national mandate to standardize the identification of DNR orders and to make the colors of wristbands for a small set of indications uniform in every hospital across the country.
Acknowledgements
We thank Mark Keroack, MD, MPH, and Cathy Krsek, RN, MSN, MBA, from the University HealthSystem Consortium for their contributions to the survey and assistance with administration. We also thank members of the UHC Chief Nursing Council for participating in the survey study.
Copyright © 2007 Society of Hospital Medicine
Penetrating Point
Soon after they form, most new medical fields begin agitating for a special certification, something that says, We're here, and we're different. As I've noted previously in the Journal of Hospital Medicine, the field of hospital medicine resisted this impulse in its early years, fearing that any special designation or certification would actually harm the field's growth and status.1 The concern was that managed‐care organizationsconvinced by the evidence that hospitalists improve efficiency and might improve quality2would react to any new hospitalist sheepskin by mandating that anyone providing hospital care to its covered patients have one. The backlash from primary care physicians locked out of the hospital by such a mandate would have been swift and ultimately damaging to hospitalists. In addition to these political considerations, the early field of hospital medicine lacked the academic credibility and scientific underpinning needed for specialty designation.3
Times have changed. There are now more than 15,000 hospitalists in the United States, and nearly half of American hospitals have hospitalists on their medical staffs. In many markets, including my own, hospitalists care for most internal medicine inpatients, as well as significant numbers of pediatric and surgical patients. The field has achieved academic legitimacy, with this journal, several textbooks, large and flourishing groups in every academic medical center, and several residency tracks and fellowship programs.4, 5 The Society of Hospital Medicine (SHM) has grown to more than 6000 members, become a widely respected and dynamic member of the community of professional societies, and published its core competencies.6
With this as a background, in 2004 SHM asked the American Board of Internal Medicine (ABIM) to consider a program of certification for hospitalists. As a past SHM president and now a member of the ABIM Board of Directors, I am privileged to have a bird's‐eye view of the process. In this article, I reflect on some of the key issues it raises.
THE NUTS AND BOLTS OF BOARD CERTIFICATION
Since the first board (ophthalmology) was formed in 1917, 24 specialty boards have emerged, all under the umbrella of the American Board of Medical Specialties (ABMS).7 Because no one type of physician can do it all, certifying boards have had to struggle not only with how to assess competency in existing disciplines, but with the dynamic and often controversial questions raised when new fields emerge. In the past few decades, certifying boards have grappled with specialties formed around new procedures (such as cardiac electrophysiology), discrete populations (geriatrics, palliative care), complex diseases (HIV medicine), and sites of care (intensive care medicine, emergency medicine). It is this latter category that now includes hospital medicine.
In the past, it was relatively simple for a physician to obtain board certification. Residency or fellowship training was believed to confer on its graduates the presumption of competence and professionalismthe program director's attestation served as the graduate's Good Housekeeping seal of approval. Passing the board exam was the final step, ensuring that newly minted graduates had the requisite knowledge and judgment to practice in their fields.
Remarkably, for the first half century of the specialty boards, all certifications lasted for a physician's professional lifetime. Beginning with the 1969 decision of the American Board of Family Practice to limit the validity of its certificates to 7 years, all ABMS member boards now time limit their certifications, usually to 7‐10 years.7 Of course, in an environment of rapidly changing medical knowledge and new procedures, periodiceven continuousdemonstration of competence is increasingly expected by the public.
For ABIM, the mechanism to promote lifelong learning and demonstrate ongoing competence in the face of a rapidly changing environment is known as maintenance of certification (MOC).8 Through MOC, board‐certified internists demonstrate their ongoing clinical expertise and judgment, their involvement in lifelong learning and quality improvement activities, and their professionalism. Because MOC involves no new training requirements and includes an assessment of a physician's actual practice, it provides a potential mechanism, heretofore untapped, of demonstrating a unique professional focus that emerges after the completion of formal training.
HOSPITALIST CERTIFICATION AND THE MOC PROCESS
As ABIM considered a separate certification pathway for hospital medicine, it faced a conundrum. The vast majority of hospitalists are general internists (most of the rest are generalists in family medicine or pediatrics) who entered hospital medicine at the completion of their internal medicine training or after a period of primary care practice. Job opportunities for hospitalists are plentiful, andexcept for additional training in quality improvement, systems leadership, care transitions, palliative care, and communication9there is little clinical rationale to prolong internal medicine training for hospitalists (some individuals may opt for fellowships to enhance their leadership skills or to launch a research career,5 but few would argue for mandatory additional clinical training in hospital medicine at this time).
So, in the absence of formal training, how could the ABIM (or other boards) recognize the focused practice of hospitalists? This question must be framed within a broader challenge: Is it possible and appropriate for certifying boards to recognize expertise and focus that is accrued not through formal training, but through actual practice experience and accompanying self‐directed learning?
In 2006, the ABIM took up this question, producing a report (New and Emerging Disciplines in Internal Medicine II [NEDIM II]) that delineated several criteria to guide whether a new field merited focused recognition through MOC (Table 1). Judging by these criteria, hospital medicine appears to be a suitable first candidate for recognition of focused practice through MOC.
|
PRELIMINARY THOUGHTS ON FOCUSED RECOGNITION IN HOSPITAL MEDICINE
The ABIM has endorsed the concept of recognition of focused practice in hospital medicine and charged a subcommittee (that I chair) with working out the details. It would be premature to describe the committee's deliberations in detail (particularly because the final plan needs to be approved by both the ABIM and the ABMS), but the following are some key issues being discussed.
First, demonstration of focused practice requires some minimum volume of hospitalized patients. In the absence of hard data defining a threshold number of cases for hospitalists, we are likely to endorse a number that has face validity and that reliably separates self‐identified hospitalists from nonhospitalist generalists. As with all volume requirements, we will struggle over how to handle academic physicians, physician‐administrators, and physician‐researchers who limit their overall clinical practice but who spend most of their clinical time in hospital medicine and the bulk of their nonclinical time trying to improve hospital care.
The requirements to demonstrate performance in practice and lifelong learning may be more straightforward. As with all such MOC requirements, the ABIM is increasingly looking to use real practice data, trying to harmonize its data requirements with those of other organizations such as insurers, Medicare, the Joint Commission, or for pay‐for‐performance initiatives. Despite the operational challenges, this effort is vital: for MOC (including focused recognition) to be highly valued by patients, purchasers, and diplomates, it will increasingly need to measure not only what physicians know, but also what they do.
Finally, there is the test. It is likely that a secure exam for MOC with Recognition of Focused Practice in Hospital Medicine will involve core content in internal medicine (information that every internist should know), augmented by substantial and challenging content in hospital medicine. Because it will be vital that a competent hospitalist understand key elements of outpatient practice, the exam will not be stripped of ambulatory content but will likely have fewer questions on topics that hospitalists are unlikely to confront (osteoporosis, cancer screening).
ONGOING ISSUES
As hospital medicine continues its explosive growth, it is important to develop ways to make board certification relevant to hospitalists. The ABIM believes that modifying the MOC process to recognize physicians who have focused their practice and achieved special expertise in hospital medicine is a good way to launch this effort. Ultimately, this process is likely to evolve, particularly if separate training pathways for hospital medicine emerge. For now, the development of Recognition of Focused Practice in Hospital Medicine will further legitimize the new field, provide ABIM with insights into how to recognize physicians who have advanced through practice‐based learning rather than through training, and help to guide other certifying boards (particularly family medicine and pediatrics) considering hospitalist certification. In the end, the process will need to be user‐friendly for and satisfying to diplomates, flexible enough to allow for career transitions (both toward and away from hospital medicine), and sufficiently rigorous to be credible to all stakeholders, particularly patients.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- ,.The hospitalist movement 5 years later.JAMA2002;287:487–94.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,.Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- .Recertification in the United States.BMJ.1999;319:1183–1185.
- ,.Professional standards in the USA: overview and new developments.Clin Med.2006;6:363–367.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
Soon after they form, most new medical fields begin agitating for a special certification, something that says, We're here, and we're different. As I've noted previously in the Journal of Hospital Medicine, the field of hospital medicine resisted this impulse in its early years, fearing that any special designation or certification would actually harm the field's growth and status.1 The concern was that managed‐care organizationsconvinced by the evidence that hospitalists improve efficiency and might improve quality2would react to any new hospitalist sheepskin by mandating that anyone providing hospital care to its covered patients have one. The backlash from primary care physicians locked out of the hospital by such a mandate would have been swift and ultimately damaging to hospitalists. In addition to these political considerations, the early field of hospital medicine lacked the academic credibility and scientific underpinning needed for specialty designation.3
Times have changed. There are now more than 15,000 hospitalists in the United States, and nearly half of American hospitals have hospitalists on their medical staffs. In many markets, including my own, hospitalists care for most internal medicine inpatients, as well as significant numbers of pediatric and surgical patients. The field has achieved academic legitimacy, with this journal, several textbooks, large and flourishing groups in every academic medical center, and several residency tracks and fellowship programs.4, 5 The Society of Hospital Medicine (SHM) has grown to more than 6000 members, become a widely respected and dynamic member of the community of professional societies, and published its core competencies.6
With this as a background, in 2004 SHM asked the American Board of Internal Medicine (ABIM) to consider a program of certification for hospitalists. As a past SHM president and now a member of the ABIM Board of Directors, I am privileged to have a bird's‐eye view of the process. In this article, I reflect on some of the key issues it raises.
THE NUTS AND BOLTS OF BOARD CERTIFICATION
Since the first board (ophthalmology) was formed in 1917, 24 specialty boards have emerged, all under the umbrella of the American Board of Medical Specialties (ABMS).7 Because no one type of physician can do it all, certifying boards have had to struggle not only with how to assess competency in existing disciplines, but with the dynamic and often controversial questions raised when new fields emerge. In the past few decades, certifying boards have grappled with specialties formed around new procedures (such as cardiac electrophysiology), discrete populations (geriatrics, palliative care), complex diseases (HIV medicine), and sites of care (intensive care medicine, emergency medicine). It is this latter category that now includes hospital medicine.
In the past, it was relatively simple for a physician to obtain board certification. Residency or fellowship training was believed to confer on its graduates the presumption of competence and professionalismthe program director's attestation served as the graduate's Good Housekeeping seal of approval. Passing the board exam was the final step, ensuring that newly minted graduates had the requisite knowledge and judgment to practice in their fields.
Remarkably, for the first half century of the specialty boards, all certifications lasted for a physician's professional lifetime. Beginning with the 1969 decision of the American Board of Family Practice to limit the validity of its certificates to 7 years, all ABMS member boards now time limit their certifications, usually to 7‐10 years.7 Of course, in an environment of rapidly changing medical knowledge and new procedures, periodiceven continuousdemonstration of competence is increasingly expected by the public.
For ABIM, the mechanism to promote lifelong learning and demonstrate ongoing competence in the face of a rapidly changing environment is known as maintenance of certification (MOC).8 Through MOC, board‐certified internists demonstrate their ongoing clinical expertise and judgment, their involvement in lifelong learning and quality improvement activities, and their professionalism. Because MOC involves no new training requirements and includes an assessment of a physician's actual practice, it provides a potential mechanism, heretofore untapped, of demonstrating a unique professional focus that emerges after the completion of formal training.
HOSPITALIST CERTIFICATION AND THE MOC PROCESS
As ABIM considered a separate certification pathway for hospital medicine, it faced a conundrum. The vast majority of hospitalists are general internists (most of the rest are generalists in family medicine or pediatrics) who entered hospital medicine at the completion of their internal medicine training or after a period of primary care practice. Job opportunities for hospitalists are plentiful, andexcept for additional training in quality improvement, systems leadership, care transitions, palliative care, and communication9there is little clinical rationale to prolong internal medicine training for hospitalists (some individuals may opt for fellowships to enhance their leadership skills or to launch a research career,5 but few would argue for mandatory additional clinical training in hospital medicine at this time).
So, in the absence of formal training, how could the ABIM (or other boards) recognize the focused practice of hospitalists? This question must be framed within a broader challenge: Is it possible and appropriate for certifying boards to recognize expertise and focus that is accrued not through formal training, but through actual practice experience and accompanying self‐directed learning?
In 2006, the ABIM took up this question, producing a report (New and Emerging Disciplines in Internal Medicine II [NEDIM II]) that delineated several criteria to guide whether a new field merited focused recognition through MOC (Table 1). Judging by these criteria, hospital medicine appears to be a suitable first candidate for recognition of focused practice through MOC.
|
PRELIMINARY THOUGHTS ON FOCUSED RECOGNITION IN HOSPITAL MEDICINE
The ABIM has endorsed the concept of recognition of focused practice in hospital medicine and charged a subcommittee (that I chair) with working out the details. It would be premature to describe the committee's deliberations in detail (particularly because the final plan needs to be approved by both the ABIM and the ABMS), but the following are some key issues being discussed.
First, demonstration of focused practice requires some minimum volume of hospitalized patients. In the absence of hard data defining a threshold number of cases for hospitalists, we are likely to endorse a number that has face validity and that reliably separates self‐identified hospitalists from nonhospitalist generalists. As with all volume requirements, we will struggle over how to handle academic physicians, physician‐administrators, and physician‐researchers who limit their overall clinical practice but who spend most of their clinical time in hospital medicine and the bulk of their nonclinical time trying to improve hospital care.
The requirements to demonstrate performance in practice and lifelong learning may be more straightforward. As with all such MOC requirements, the ABIM is increasingly looking to use real practice data, trying to harmonize its data requirements with those of other organizations such as insurers, Medicare, the Joint Commission, or for pay‐for‐performance initiatives. Despite the operational challenges, this effort is vital: for MOC (including focused recognition) to be highly valued by patients, purchasers, and diplomates, it will increasingly need to measure not only what physicians know, but also what they do.
Finally, there is the test. It is likely that a secure exam for MOC with Recognition of Focused Practice in Hospital Medicine will involve core content in internal medicine (information that every internist should know), augmented by substantial and challenging content in hospital medicine. Because it will be vital that a competent hospitalist understand key elements of outpatient practice, the exam will not be stripped of ambulatory content but will likely have fewer questions on topics that hospitalists are unlikely to confront (osteoporosis, cancer screening).
ONGOING ISSUES
As hospital medicine continues its explosive growth, it is important to develop ways to make board certification relevant to hospitalists. The ABIM believes that modifying the MOC process to recognize physicians who have focused their practice and achieved special expertise in hospital medicine is a good way to launch this effort. Ultimately, this process is likely to evolve, particularly if separate training pathways for hospital medicine emerge. For now, the development of Recognition of Focused Practice in Hospital Medicine will further legitimize the new field, provide ABIM with insights into how to recognize physicians who have advanced through practice‐based learning rather than through training, and help to guide other certifying boards (particularly family medicine and pediatrics) considering hospitalist certification. In the end, the process will need to be user‐friendly for and satisfying to diplomates, flexible enough to allow for career transitions (both toward and away from hospital medicine), and sufficiently rigorous to be credible to all stakeholders, particularly patients.
Soon after they form, most new medical fields begin agitating for a special certification, something that says, We're here, and we're different. As I've noted previously in the Journal of Hospital Medicine, the field of hospital medicine resisted this impulse in its early years, fearing that any special designation or certification would actually harm the field's growth and status.1 The concern was that managed‐care organizationsconvinced by the evidence that hospitalists improve efficiency and might improve quality2would react to any new hospitalist sheepskin by mandating that anyone providing hospital care to its covered patients have one. The backlash from primary care physicians locked out of the hospital by such a mandate would have been swift and ultimately damaging to hospitalists. In addition to these political considerations, the early field of hospital medicine lacked the academic credibility and scientific underpinning needed for specialty designation.3
Times have changed. There are now more than 15,000 hospitalists in the United States, and nearly half of American hospitals have hospitalists on their medical staffs. In many markets, including my own, hospitalists care for most internal medicine inpatients, as well as significant numbers of pediatric and surgical patients. The field has achieved academic legitimacy, with this journal, several textbooks, large and flourishing groups in every academic medical center, and several residency tracks and fellowship programs.4, 5 The Society of Hospital Medicine (SHM) has grown to more than 6000 members, become a widely respected and dynamic member of the community of professional societies, and published its core competencies.6
With this as a background, in 2004 SHM asked the American Board of Internal Medicine (ABIM) to consider a program of certification for hospitalists. As a past SHM president and now a member of the ABIM Board of Directors, I am privileged to have a bird's‐eye view of the process. In this article, I reflect on some of the key issues it raises.
THE NUTS AND BOLTS OF BOARD CERTIFICATION
Since the first board (ophthalmology) was formed in 1917, 24 specialty boards have emerged, all under the umbrella of the American Board of Medical Specialties (ABMS).7 Because no one type of physician can do it all, certifying boards have had to struggle not only with how to assess competency in existing disciplines, but with the dynamic and often controversial questions raised when new fields emerge. In the past few decades, certifying boards have grappled with specialties formed around new procedures (such as cardiac electrophysiology), discrete populations (geriatrics, palliative care), complex diseases (HIV medicine), and sites of care (intensive care medicine, emergency medicine). It is this latter category that now includes hospital medicine.
In the past, it was relatively simple for a physician to obtain board certification. Residency or fellowship training was believed to confer on its graduates the presumption of competence and professionalismthe program director's attestation served as the graduate's Good Housekeeping seal of approval. Passing the board exam was the final step, ensuring that newly minted graduates had the requisite knowledge and judgment to practice in their fields.
Remarkably, for the first half century of the specialty boards, all certifications lasted for a physician's professional lifetime. Beginning with the 1969 decision of the American Board of Family Practice to limit the validity of its certificates to 7 years, all ABMS member boards now time limit their certifications, usually to 7‐10 years.7 Of course, in an environment of rapidly changing medical knowledge and new procedures, periodiceven continuousdemonstration of competence is increasingly expected by the public.
For ABIM, the mechanism to promote lifelong learning and demonstrate ongoing competence in the face of a rapidly changing environment is known as maintenance of certification (MOC).8 Through MOC, board‐certified internists demonstrate their ongoing clinical expertise and judgment, their involvement in lifelong learning and quality improvement activities, and their professionalism. Because MOC involves no new training requirements and includes an assessment of a physician's actual practice, it provides a potential mechanism, heretofore untapped, of demonstrating a unique professional focus that emerges after the completion of formal training.
HOSPITALIST CERTIFICATION AND THE MOC PROCESS
As ABIM considered a separate certification pathway for hospital medicine, it faced a conundrum. The vast majority of hospitalists are general internists (most of the rest are generalists in family medicine or pediatrics) who entered hospital medicine at the completion of their internal medicine training or after a period of primary care practice. Job opportunities for hospitalists are plentiful, andexcept for additional training in quality improvement, systems leadership, care transitions, palliative care, and communication9there is little clinical rationale to prolong internal medicine training for hospitalists (some individuals may opt for fellowships to enhance their leadership skills or to launch a research career,5 but few would argue for mandatory additional clinical training in hospital medicine at this time).
So, in the absence of formal training, how could the ABIM (or other boards) recognize the focused practice of hospitalists? This question must be framed within a broader challenge: Is it possible and appropriate for certifying boards to recognize expertise and focus that is accrued not through formal training, but through actual practice experience and accompanying self‐directed learning?
In 2006, the ABIM took up this question, producing a report (New and Emerging Disciplines in Internal Medicine II [NEDIM II]) that delineated several criteria to guide whether a new field merited focused recognition through MOC (Table 1). Judging by these criteria, hospital medicine appears to be a suitable first candidate for recognition of focused practice through MOC.
|
PRELIMINARY THOUGHTS ON FOCUSED RECOGNITION IN HOSPITAL MEDICINE
The ABIM has endorsed the concept of recognition of focused practice in hospital medicine and charged a subcommittee (that I chair) with working out the details. It would be premature to describe the committee's deliberations in detail (particularly because the final plan needs to be approved by both the ABIM and the ABMS), but the following are some key issues being discussed.
First, demonstration of focused practice requires some minimum volume of hospitalized patients. In the absence of hard data defining a threshold number of cases for hospitalists, we are likely to endorse a number that has face validity and that reliably separates self‐identified hospitalists from nonhospitalist generalists. As with all volume requirements, we will struggle over how to handle academic physicians, physician‐administrators, and physician‐researchers who limit their overall clinical practice but who spend most of their clinical time in hospital medicine and the bulk of their nonclinical time trying to improve hospital care.
The requirements to demonstrate performance in practice and lifelong learning may be more straightforward. As with all such MOC requirements, the ABIM is increasingly looking to use real practice data, trying to harmonize its data requirements with those of other organizations such as insurers, Medicare, the Joint Commission, or for pay‐for‐performance initiatives. Despite the operational challenges, this effort is vital: for MOC (including focused recognition) to be highly valued by patients, purchasers, and diplomates, it will increasingly need to measure not only what physicians know, but also what they do.
Finally, there is the test. It is likely that a secure exam for MOC with Recognition of Focused Practice in Hospital Medicine will involve core content in internal medicine (information that every internist should know), augmented by substantial and challenging content in hospital medicine. Because it will be vital that a competent hospitalist understand key elements of outpatient practice, the exam will not be stripped of ambulatory content but will likely have fewer questions on topics that hospitalists are unlikely to confront (osteoporosis, cancer screening).
ONGOING ISSUES
As hospital medicine continues its explosive growth, it is important to develop ways to make board certification relevant to hospitalists. The ABIM believes that modifying the MOC process to recognize physicians who have focused their practice and achieved special expertise in hospital medicine is a good way to launch this effort. Ultimately, this process is likely to evolve, particularly if separate training pathways for hospital medicine emerge. For now, the development of Recognition of Focused Practice in Hospital Medicine will further legitimize the new field, provide ABIM with insights into how to recognize physicians who have advanced through practice‐based learning rather than through training, and help to guide other certifying boards (particularly family medicine and pediatrics) considering hospitalist certification. In the end, the process will need to be user‐friendly for and satisfying to diplomates, flexible enough to allow for career transitions (both toward and away from hospital medicine), and sufficiently rigorous to be credible to all stakeholders, particularly patients.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- ,.The hospitalist movement 5 years later.JAMA2002;287:487–94.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,.Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- .Recertification in the United States.BMJ.1999;319:1183–1185.
- ,.Professional standards in the USA: overview and new developments.Clin Med.2006;6:363–367.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1:248–252.
- ,.The hospitalist movement 5 years later.JAMA2002;287:487–94.
- .The hospitalist: a new medical specialty?Ann Intern Med.1999;130:373–375.
- ,.Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- ,,,.Hospital medicine fellowships: works in progress.Am J Med.2006;119:72.e1–e7.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1:48–56.
- .Recertification in the United States.BMJ.1999;319:1183–1185.
- ,.Professional standards in the USA: overview and new developments.Clin Med.2006;6:363–367.
- ,,,.Hospitalists' perceptions of their residency training needs: results of a national survey.Am J Med.2001;111:247–254.
Strategies for a Safe and Effective Resident Sign‐Out
Modern‐day continuity of patient care in teaching hospitals, once remarkably high because of a cadre of sleep‐deprived residents, is now peppered with breaks, each accompanied by the transfer of patient care responsibility from one resident to another; a process often referred to as a handoff. Such transitions have long been a part of medical practice but have recently received increased attention because of restrictions in the duty hours of house staff. In July 2003 the Accreditation Council for Graduate Medical Education (ACGME) mandated reduced duty hours for all trainees in hopes of improving resident education and well‐being and patient safety.1 In fact, some studies have shown improved resident well‐being2 and fewer medical errors with reductions in duty hours,3, 4 but the growing consensus about the negative consequences of resident fatigue on patient safety has been accompanied by parallel concerns about the potential for information loss with each break in the continuity of care.5, 6
Although the tradeoff of increased discontinuity of care for fewer hours worked is sometimes characterized as an unintended consequence of duty hour regulations, it is in fact predictable and essential. As individuals work fewer hours, discontinuity must necessarily increase (assuming 24‐hour coverage).7 The extent to which this occurs may vary, but the link is consistent. At the University of California, San Francisco (UCSF), for example, we found that compliance with new duty hour requirements for internal medicine resulted in an average of 15 handoffs per patient during a 5‐day hospitalization. Each individual intern was involved in more than 300 handoffs in an average month‐long rotation, an increase of 40% since system changes were introduced to decrease duty hours. We found similar increases at Brigham and Women's Hospital (BWH) and the University of Chicago. Because U.S. teaching hospitals care for more than 6 million patients each year,8 the impact of these handoffs on the quality and efficiency of care is tremendous.
Discontinuity of care is currently managed by sign‐out, or the transfer of patient information from one physician to another. Recognizing the importance of information transfer at these vulnerable transition times for patients, the Joint Commission on Accreditation of Hospital Organizations (JCAHO) issued the 2006 National Patient Safety Goal 2E: Implement a standardized approach to hand off communications, including an opportunity to ask and respond to questions.9 Hospitals have little data to draw on to determine how to comply with this mandate and even less data to guide them in how to achieve its intended goals of improving communication and thus patient safety.
In an effort to better understand sign‐outs and ways to improve this process for house staff on in‐patient services, we reviewed data from the fields of aviation, communications, systems engineering, and human factors research, and we also searched the medical literature using key words pass‐off, handoff, sign‐out, duty hours, work hours, and discontinuity of care and MeSH headings Continuity of Patient Care Internship and Residency/*organization & administration, Personnel Staffing and Scheduling/*organization & administration, and Quality of Health Care. We also searched the websites of the Agency of Healthcare Quality and Research and the National Patient Safety Foundation. On the basis of these reviews, our experiences as hospitalist medical educators organizing resident sign‐out efforts at the University of California, San Francisco, the University of Chicago, and Brigham and Women's Hospital, and our efforts leading national training sessions on sign‐outs at the Society of General Internal Medicine (2004 and 2005), the Society of Hospital Medicine (2004), and the Association of Program Directors in Internal Medicine (2005, 2006), we propose a set of best practices regarding the content and process of sign‐out in an effort to improve communication between residents caring for hospitalized patients, assist programs in building safe and effective sign‐out systems, and improve the quality of patient care.
Effects of Discontinuity on Patient Safety
Research on the effects of discontinuity of care, although limited, suggests it has a negative impact on patient safety. In a study that investigated the institution of code 405 (the regulation that reduced duty hours in New York State), researchers found that the presumed increase in discontinuity with decreased duty hours resulted in delayed test ordering and an increased number of hospital complications.10 Another study found that the number of potentially preventable adverse events doubled when patients were under the care of a physician from a nonprimary team (eg, the cross‐covering intern).11 Studies have also linked resident discontinuity with longer length of stay, increased laboratory testing, and increased medication errors.12, 13
Managing Discontinuity: Sign‐Out as the Means of Information Transfer
In theory, more effective sign‐out systems should mitigate the potential for patient harm, but there is little in the literature describing current effective sign‐out practices or the best ways to design and implement such systems in the health care field. Examining information transfer mechanisms used in fields outside health care can assist in developing these systems.
Information Transfer in Other Industries
Although there is a paucity of data on sign‐out in the medical literature, information transfer has been the subject of substantial research in other industries in which safety depends on effective communication.
Aviation, for example, created systems and processes to improve handoff communication in response to accidents linked to failures in information transfer. One example, the 1977 collision of 2 747s on an airport runway in Tenerife, the Canary Islands, occurred after a garbled transmission from an air traffic controller to the cockpit of one of the aircraft. It was determined that a culture of adherence to a steep hierarchy prevented subordinates from questioning the captain's mistaken certainty that a runway was clear,14 an erroneous belief that was the basis for his decision to continue the aircraft on its course, resulting in its collision with the other airplane.
Subsequently, commercial aviation designed systems that standardized and formalized the process of information transfer and improved teamwork and coordination. These interventions were developed on the basis of detailed observations of cockpit interactions, reviews of communication errors, and focus groups.15 Because of these efforts, today's pilots use standardized checklists to transfer information content, communicate at designated times in specific undistracted environments, and use standard language and read‐backs to enhance understanding.16 The result has been a remarkable decrease in the risk of aviation crashes, one that most experts attribute in large part to these efforts to improve communication.17
Observation of how communication occurs in other high‐risk industries has informed the arena of effective information transfer. For example, direct observation of information transfer at NASA, in nuclear power plants, and in the railway industry identified specific strategies for effective handoffs/sign‐outs such as standardizing the information transferred, ensuring information is up to date, limiting interruptions, and having a structured face‐to‐face verbal interchange.18
Other strategies noted to be effective in diminishing errors are the use of a standardized phonetic alphabet to ensure that information is correctly heard and understood4 and having interactive verbal communication occur at a whiteboard.19
Information Transfer in Health Care
Those in the discipline of nursing have vast experience in the transfer of patient care information. The sign‐out process employed by nurses includes face‐to‐face discussions, typed information, and, most commonly, taped verbal communication.20 Interestingly, this process has not been subject to detailed scrutiny, and there is little information in the literature about best practices in sign‐out. Most articles in the literature on nursing handoffs are ethnographic descriptions of patient care responsibilities,21 on the basis of which, the authors advocate standardization of the information to be transferred, formalization of the channel used to communicate, and attention to increasing a culture of professionalism during sign‐out in order to improve efficiency.20, 22
There is little in the literature on transfer of care among physicians. Improvements in sign‐out have been suggested as part of broad strategies, such as increased training and information technology support,4, 7, 23, 24 and specific strategies have been offered such as managing barriers to communication, including specific types of data when transferring care,25 and involving nurses and senior physicians in sign‐outs.26 Specific outcomes data in this area have focused primarily on the use of computerized systems to improve information transfer. For example, the use of a computerized sign‐out system at Brigham and Women's Hospital (BWH), linked to the hospital's information system to ensure up‐to‐date information on patient demographics, medications, and laboratory values, has resulted in fewer errors,27 as have other similar systems.28 At the University of Washington, use of a similarly linked computerized sign‐out system resulted in fewer patients being missed on rounds and improvement in the quality of sign‐out and continuity of care according to resident self‐reports.29 Unfortunately, fewer than 10% of hospitals have such integrated hospitalwide information systems to support the sign‐out function.30
It has been noted that verbal communication, in concert with advances in technological communication, is important in information transfer in health care,18, 31 especially in emergent or urgent conditions.32 For example, eliminating the phoned‐in report from the lab to the ER and replacing it with delivery by an electronic reporting system lacking verbal communicationresulted in 45% of emergent lab results going unchecked.32 Structured verbal communication tools have been efficacious in improving information transfer outside the formal sign‐outfor example, read‐backs, which reduced errors in the reporting of critical laboratory values,33 and the SBAR (situation, background, assessment, recommendation) tool (designed to frame the transfer of critical information), which improved physician and nurse patient care information transfer in the in‐patient setting of the Kaiser Permanente health system.34
In focus groups and in response to formal and informal surveys, residents at our 3 sites suggested inclusion of the following information, provided in writing and orally, to improve sign‐outs: up‐to‐date administrative information (eg, room number, primary care physician); patient's recent cognitive or cardiopulmonary status; problems the patient had already experienced and treatments previously tried, both successfully and unsuccessfully; patient's code status and discussions on level of care; test results or consultation recommendations that were likely to come back while covering the patient and what to do with the results; and relevant psychosocial information (eg, complex family dynamics).35
The Current Practice of Sign‐Out
In examining sign‐outs at our 3 institutions, we found them to be unstructured and unstandardized. From discussion with faculty participating in national workshops on sign‐out, we found that most sign‐outs are conducted by interns, usually with little or no formal training. Templates, checklists, or other methods to standardize the content of the information transferred were rarely used.
We also noted that the vehicle for written sign‐out is highly variable. At UCSF, different residency training programs used a variety of modalities for written sign‐outs, including index cards, Excel spreadsheets, Word documents, and loose sheets of paper. Recently, the UCSF Department of Medicine designed a simple database (on Filemaker Pro) that allows members of the house staff to update their sign‐out information, share it with other house staff and nurses, and access it at locations throughout the hospital (Fig. 1). Although this database is not yet linked to the hospital information system (planned for 2006), anecdotally resident satisfaction with sign‐out has vastly improved since its implementation. The cost of design and implementation was approximately $10,000. At the University of Chicago, interns used Microsoft Word to create sign‐out sheets containing patient summaries to transfer information. However, during structured interviews, 95% of the interns reported that these sheets were frequently lost or misplaced.7 Although medicine residents at BWH use a computerized system to produce sign‐out sheets, this system did not guarantee complete and structured information. For example, a survey at BWH found that 56% of cross‐covering residents said that when paged about a patient overnight, the relevant information needed to care for that patient was present less than half the time; and 27% of residents reported being paged more than 3 times in the previous 2 weeks about a test result or consultant recommendation that they did not know was pending.36
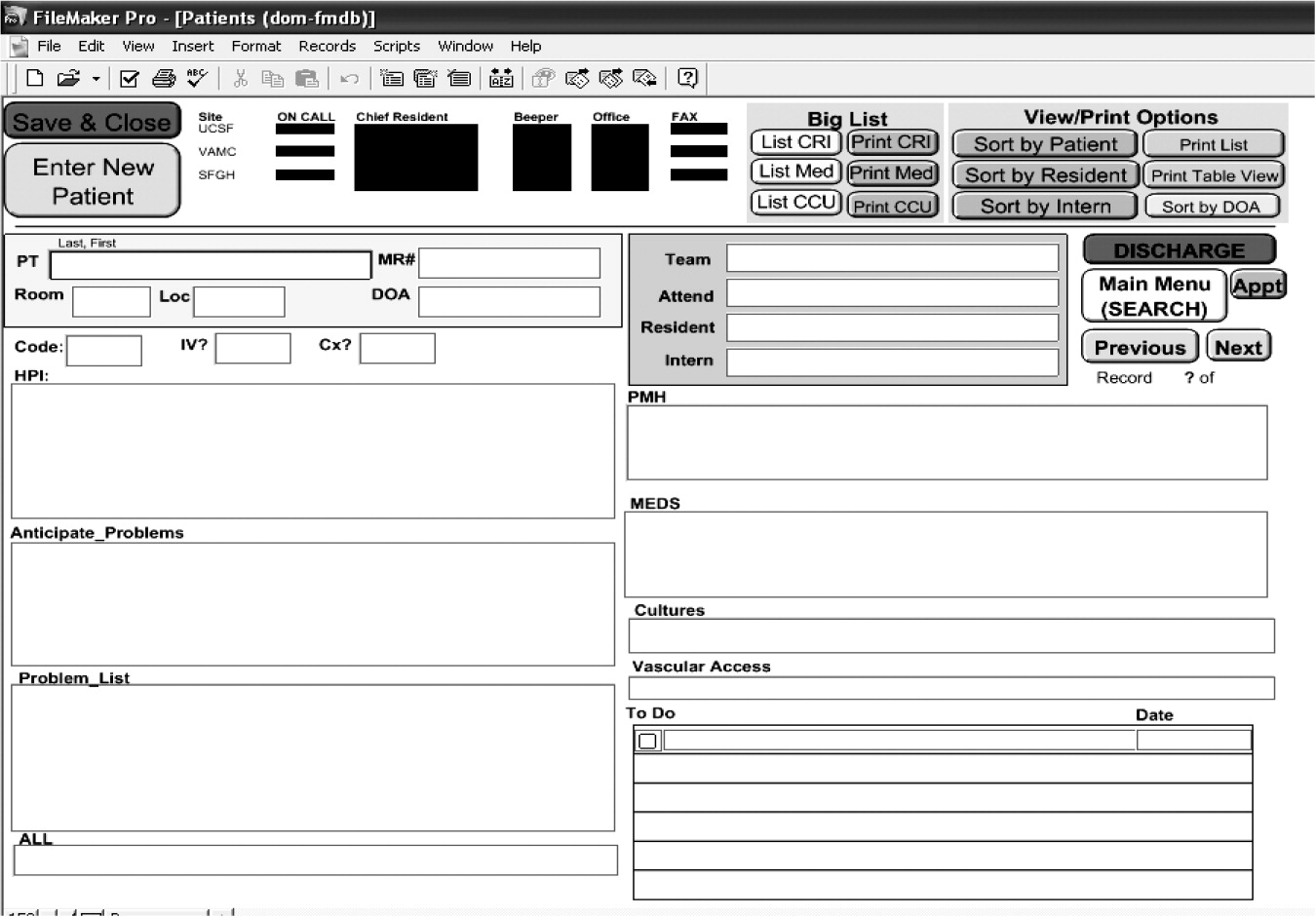
The process of sign‐out also varied across disciplines and institutions. From our experiences at our sites and at the sites of faculty nationally, we found limited standardization about whether sign‐out was verbal, the data transmitted, and the setting in which it was transmitted. In fact, at UCSF most residents signed out verbally on the fly, wherever and whenever they could find the cross‐coverage intern. At BWH, only 37% of residents said that sign‐out occurred in a quiet place most of the time, and only 52% signed out on every patient both orally and in writing.36 At the University of Chicago, the sign‐out process was characterized by outright failures in communication because of omission of needed information (ie, medications, active or anticipated medical problems, etc.) or by failure‐prone communication (ie, lack of face‐to‐face communication, illegible writing). These failures often led to uncertainty in making patient care decisions, potentially resulting in inefficient or suboptimal care.35
Strategies for Safe and Effective Sign‐Out
Given the current landscape of variability in sign‐outs, the recognition that information lost during sign‐out may result in harm to patients, and evidence of improvements in information transfer in areas outside health care, we aimed to develop mechanisms to improve the sign‐out process for residents working in a hospital setting. These strategies are based on our review of the existing literature supplemented by our experiences at our 3 institutions.
Content of Sign‐Out
The elements of content necessary for safe and effective sign‐out can be divided into 5 broad categories (Table 1), contained in the mnemonic ANTICipate: Administrative information, New clinical information, specific Tasks to be performed, assessment of severity of Illness, and Contingency plans or anticipated problems (Table 1, Fig. 2).
| ✓ Administrative data |
| □ Patient name, age, sex |
| □ Medical record number |
| □ Room number |
| □ Admission date |
| □ Primary inpatient medical team, primary care physician |
| □ Family contact information |
| ✓ New information (clinical update) |
| □ Chief complaint, brief HPI, and diagnosis (or differential diagnosis) |
| □ Updated list of medications with doses, updated allergies |
| □ Updated, brief assessment by system/problem, with dates |
| □ Current baseline status (eg, mental status, cardiopulmonary, vital signs, especially if abnormal but stable) |
| □ Recent procedures and significant events |
| ✓ Tasks (what needs to be done) |
| □ Specific, using if‐then statements |
| □ Prepare cross‐coverage (eg, patient consent for blood transfusion) |
| □ Alert to incoming information (eg, study results, consultant recommendations), and what action, if any, needs to be taken during the cross‐coverage |
| ✓ Illness |
| □ Is the patient sick? |
| ✓ Contingency planning/Code status |
| □ What may go wrong and what to do about it |
| □ What has or has not worked before (eg, responds to 40 mg IV furosemide) |
| □ Difficult family or psychosocial situations |
| □ Code status, especially recent changes or family discussions |
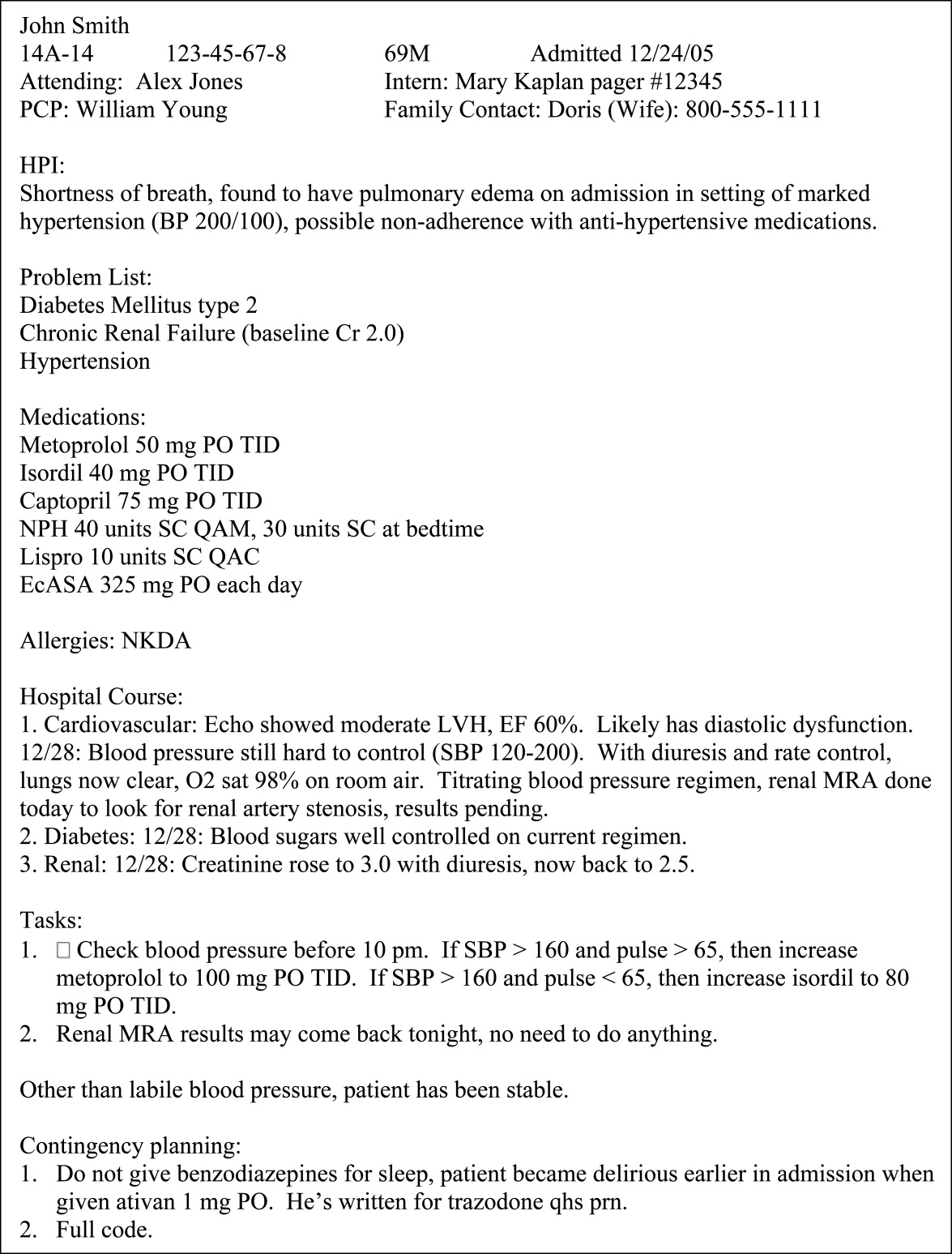
Several general points about this list should be noted. First, the sign‐out content is not meant to replace the chart. The information included reflects the goal of a sign‐out, namely, to provide enough information to allow for a safe transition in patient care. Information we believe is not essential to the sign‐out includes: a complete history and physical exam from the day of admission, a list of tasks already completed, and data necessary only to complete a discharge summary.
Sign‐out must be also be a closed loopthe process of signing in is as important as the process of signing out. This usually entails members of the primary team obtaining information from the cross‐covering physician when they resume care of the patient. The information conveyed in this case is different and includes details on events during cross‐coverage such as: 1) time called to assess patient; 2) reason for call; 3) a brief assessment of the patient, including vital signs; 4) actions taken, for example, medications given and tests ordered; and 5) rationale for those actions. Some of this information may also be included in the chart as an event note (see Fig. 3).
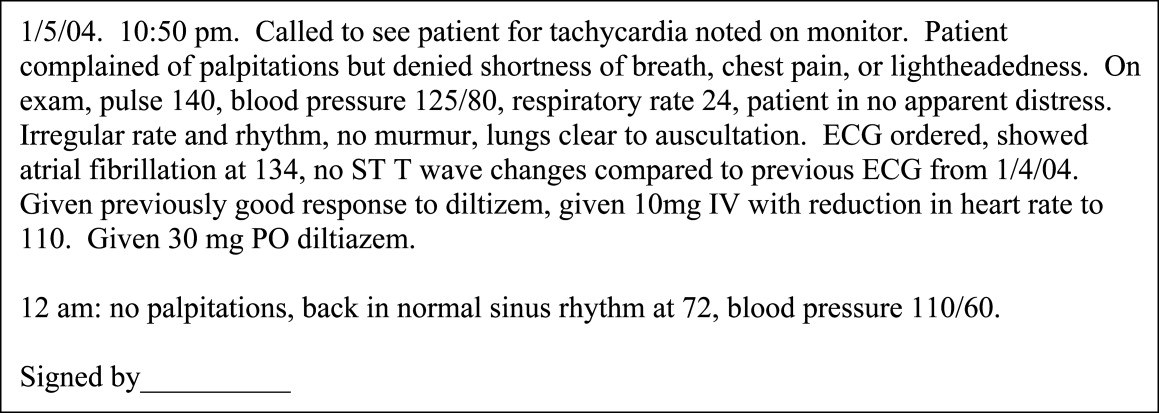
The Vehicle for Sign‐Out
We recommend a computer‐assisted vehicle for patient information transfer. Ideally, this would be linked to the hospital information system to ensure accurate and up‐to‐date information Easy access to the computerized sign‐out is essential (eg, using a hospitalwide computer system, shared hard drive service, intranet, or PDA linked to the computer system), and it should be customizable for the varied needs of different services and departments. The system should have templates to standardize the content of sign‐out, contain robust backup systems, and be HIPAA compliant (ie, restrict access to required health care personnel). However, the perfect should not be the enemy of the good: systems that do not meet these criteria may still help to protect patients by providing legible, predictable, and accessible information.
Sign‐Out Processes
Verbal communication.
Although electronic solutions can facilitate the standardization of written content, face‐to‐face verbal communication adds additional value.19 We recommend that each patient be reviewed separately. Identification of each patient verbally ensures that those engaged in the sign‐out are discussing the same patient. Reiterating the major medical problems gives a snapshot of the patient and frames the sign‐out. The to‐do list, the list of tasks that the cross‐cover resident needs to complete during cross coverage, should be specific and articulated as if, then statements (eg, if the urine output is less than 1 L, then give 40 mg of IV furosemide). The receiver of sign‐out should read back to the person giving the sign‐out each item on the to‐do list (eg, So, I should check the ins and outs at about 10:00 pm, and give 40 of furosemide if the patient is not 1 L negative, right?).
Anticipated problems should also be verbally communicated to promote a dialogue. Points that cannot be adequately transferred in the written sign‐out are particularly important to transmit verbally. Examples include previous code discussions, unusual responses to treatment, and psychosocial and family issues. When delivering verbal sign‐out, it is important to consider the a priori knowledge of the recipient. How much knowledge about a patient is already shared between the outgoing and incoming physicians and the level of experience of the physicians may affect the extent to which information needs be transmitted.37 For instance, 2 experienced physicians who already have been working to cover the same patient will likely have an abbreviated discussion, in contrast to the lengthier sign‐out necessary if the outgoing and incoming physicians are interns, and the incoming intern has no prior knowledge of the patient. Similarly, it is likely the level of detail transmitted will need to be greater during a permanent transfer of patient care (ie, at the end of a resident's rotation) than during a brief, temporary transition (eg, overnight coverage).
The challenges of a busy inpatient service may preclude a complete verbal sign‐out for all patients; we contend, though, it is best to use these practices to the extent possible, especially for patients with treatment plans in flux, those whose status is tenuous, and those who have anticipated changes in status during cross‐coverage. One tool that may be effectively used in signing out such patients is the SBAR tool, according to which a brief description of the situation is given, followed by the background and the physician's specific assessment and complete recommendation.38 For example, a resident signing out might begin by stating, I have 18 patients to sign‐out to you. I'm going to describe 6 active patients in detail. Twelve others are fairly stable, and I will give you basic information about them, and the details are in the written sign‐out. One patient has a plan in flux. The situation is Mr. S. is having trouble breathing, the background is that he has both CHF and COPD, my assessment is that this is more cardiac than pulmonary, and I recommend that you see him first and discuss with the cardiology consultant. Using the tools described here (Table 2), a sign‐out of 15 patients of variable acuity could be verbally signed out in less than 10 minutes.
| ✓ WHO should participate in the sign‐out process? |
| □ Outgoing clinician primarily responsible for patient's care |
| □ Oncoming clinician who will be primarily responsible for patient's care (avoid passing this task to someone else, even if busy) |
| □ Consider supervision by experienced clinicians if early in training |
| ✓ WHAT content needs to be verbally communicated? |
| Use situation briefing model, or SBAR, technique: |
| □ SituationIdentify each patient (name, age, sex, chief complaint) and briefly state any major problems (active and those that may become active during cross‐coverage). |
| □ Backgroundpertinent information relevant to current care (eg, recent vitals and/or baseline exam, labs, test results, etc). |
| □ Assessmentworking diagnosis, response to treatment, anticipated problems during cross‐coverage including anything not adequately described using written form (eg, complex family discussions). |
| □ Recommendationto‐do lists and if/then recommendations. |
| ✓ WHERE should sign‐out occur? |
| □ Designated room or place for sign‐out (eg, avoid patient areas because of HIPPA requirements) |
| □ Proper lighting |
| □ Avoid excessive noise (eg, high‐traffic areas) |
| □ Minimize disruptions (eg, hand over pagers) |
| □ Ensure systems support for sign‐out (eg, computers, printer, paper, etc.) |
| ✓ WHEN is the optimal time for sign‐out? |
| □ Designated time when both parties can be present and pay attention (eg, beware of clinic, other obligations) |
| □ Have enough time for interactive questions at the end (eg, avoid rush at the end of the shift) |
| ✓ HOW should verbal communication be performed? |
| □ Face to face, allowing for questions |
| □ Verbalize data in the same order for each patient at each sign‐out |
| □ Read back all to‐do items |
| □ Adjust length and depth of review according to baseline knowledge of parties involved and type of transition in care |
The Environment and setting.
To improve the setting of sign‐out, we recommend: a designated space that is well lit, quiet, and respects patient confidentiality and a designated time when sign‐out will occur. To limit known distractions and interruptions39, 40 in the hospital, we also recommend the outgoing physician hand off his or her pager to someone else during sign‐out. Also key to an environment conducive to information transfer is ensuring adequate computer support for electronic sign‐out and access to updated clinical information.
Organizational culture and institutional leadership.
The way residents transfer patient care information reflects the culture of the institution. Changing the culture to one in which interactive questioning is valued regardless of position in the hierarchy has been shown to reduce errors in aviation.41 Educating residents on the impact of sign‐outs on patient care is a first step toward improving the culture of sign‐out. Resident commitment to the new sign‐out can be gained by engaging residents in development of the process itself. To cement these changes into the culture, practitioners at all levels should be aware of and support the new system. The role of an institution's leaders in achieving these changes cannot be overlooked. Leaders will need to be creative in order to support sign‐out as described within the obvious constraints of money, time, personnel, and space. Gaining institutional buy‐in can start with heightening the awareness of leaders of the issues surrounding sign‐out, including patient safety, resident efficiency, and the financial impact of discontinuity. Ongoing evaluation of efforts to improve sign‐out is also crucial and can be accomplished with surveys, focus groups, and direct observation. Feeding back the positive impact of the changes to all involved stakeholders will promote confidence in the new systems and pride in their efforts.
CONCLUSIONS
Sign‐outs are a part of the current landscape of academic medical centers as well as hospitals at large. Interns, residents, and consulting fellows, not to mention nurses, physical therapists, and nutritionists, transfer patient care information at each transition point. There are few resources that can assist these caregivers in identifying and implementing the most effective ways to transfer patient care information. Hospitals and other care facilities are now mandated to develop standards and systems to improve sign‐out. On the basis of the limited literature to date and our own experiences, we have proposed standards and best practices to assist hospitals, training programs, and institutional leaders in designing safe and usable sign‐out systems. Effective implementation of the standards must include appropriate allocation of resources, individualization to meet specific needs of each program or institution, intensive training, and ongoing evaluation. Future research should focus on developing valid surrogate measures of continuity of care, conducting rigorous trials to determine the elements of sign‐out that lead to the best patient outcomes, and studying the most effective ways of implementing these improvements. By improving the content and process of sign‐out, we can meet the challenges of the new health care landscape while putting patient safety at the forefront.
- ,,.New requirements for resident duty hours.JAMA.2002;288:1112–1114.
- ,,,,.Effects of limited work hours on surgical training.J Am Coll Surg.2002;195:531–538.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351:1829–1837.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- .A precarious exchange.N Engl J Med.2004;351:1822–1824.
- .Awake and informed.N Engl J Med.2004;351:1884.
- . Fumbled handoff: missed communication between teams. Cases and Commentary: Hospital Medicine, Morbidity 269:374–378.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121:866–872.
- ,,,.Post‐call transfer of resident responsibility: its effect on patient care.J Gen Intern Med.1990;5:501–505.
- ,,,.Effect of a change in house staff work schedule on resource utilization and patient care.Arch Intern Med.1991;151:2065–2070.
- ,.Internal Bleeding: the Truth behind America's Terrifying Epidemic of Medical Mistakes.New York City:Rugged Land, LLC;2004:448.
- ,,.Crew resource management and its applications in medicine. In:Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment Number 43, AHRQ Publication 01‐E058.Rockville, MD:Agency for Healthcare Research and Quality;2001.
- ,,.System safety and threat and error management: the line operations safety audit (LOSA). In:Jensen RS, ed. Proceedings of the Eleventh International Symposium on Aviation Psychology.Columbus, OH:Ohio State University;2001:1–6.
- ,,.Translating teamwork behaviours from aviation to healthcare: development of behavioural markers for neonatal resuscitation.Qual Saf Health Care.2004;13(Suppl 1):i57–i64.
- ,,,.Handoff strategies in settings with high consequences for failure: lessons for healthcare operations.Intl J Qual Health Care.2004;16:125–132.
- . Available at: http://www.agilemodeling.com/essays/communication.htm. Accessed December 15,2005.
- .Ensuring continuing care: styles and efficiency of the handover process.Aust J Adv Nurs.1998;16:23–27.
- ,.The handover: uncovering the hidden practices of nurses.Intensive Crit Care Nurs.2000;16:373–383.
- .The patient handover: a study of its form, function and efficiency.Nurs Stand.1995;9(52):33–36.
- ,.Residents' suggestions for reducing errors in teaching hospitals.N Engl J Med.2003;348:851–855.
- ,.Is 80 the cost of saving lives? Reduced duty hours, errors, and cost.J Gen Intern Med.2005;20:969–970.
- ,,,.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- British Medical Association.Safe Handover: Safe Patients: Guidance on Clinical Handover for Clinicians and Managers.London:British Medical Association, Junior Doctors Committee;2004.
- ,,,,.Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998;24(2):77–87.
- ,,,.Organizing the transfer of patient care information: the development of a computerized resident sign‐out system.Surgery.2004;136:5–13.
- ,,,,.A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- ,,,.Computerized physician order entry in U.S. hospitals: results of a 2002 survey.J Am Med Inform Assoc.2004;11:95–99.
- ,,,,,.The impact of verbal communication on physician prescribing patterns in hospitalized patients with diabetes.Diabetes Educ.2003;29:827–836.
- ,.Use of computer terminals on wards to access emergency test results: a retrospective audit.Br Med J.2001;322:1101–1103.
- ,,,,,.Improving patient safety by repeating (read‐back) telephone reports of critical information.Am J Clin Pathol.2004;121:801–803.
- ,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13(Suppl 1):i85–i90.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14:401–407.
- ,,.Intern curriculum: the impact of a focused training program on the process and content of signout out patients. Harvard Medical School Education Day, Boston, MA;2004.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7:277–286.
- SBAR technique for communication: a situational briefing model. Available at: http://www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm. Accessed December2005.
- ,,,,.Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco.Acad Med.2006;81:76–81.
- ,.Communication behaviours in a hospital setting: an observational study.Br Med J.1998;316:673–676.
- ,,.Communication failures: an insidious contributor to medical mishapsAcad Med.2004;79(2):186–194.
Modern‐day continuity of patient care in teaching hospitals, once remarkably high because of a cadre of sleep‐deprived residents, is now peppered with breaks, each accompanied by the transfer of patient care responsibility from one resident to another; a process often referred to as a handoff. Such transitions have long been a part of medical practice but have recently received increased attention because of restrictions in the duty hours of house staff. In July 2003 the Accreditation Council for Graduate Medical Education (ACGME) mandated reduced duty hours for all trainees in hopes of improving resident education and well‐being and patient safety.1 In fact, some studies have shown improved resident well‐being2 and fewer medical errors with reductions in duty hours,3, 4 but the growing consensus about the negative consequences of resident fatigue on patient safety has been accompanied by parallel concerns about the potential for information loss with each break in the continuity of care.5, 6
Although the tradeoff of increased discontinuity of care for fewer hours worked is sometimes characterized as an unintended consequence of duty hour regulations, it is in fact predictable and essential. As individuals work fewer hours, discontinuity must necessarily increase (assuming 24‐hour coverage).7 The extent to which this occurs may vary, but the link is consistent. At the University of California, San Francisco (UCSF), for example, we found that compliance with new duty hour requirements for internal medicine resulted in an average of 15 handoffs per patient during a 5‐day hospitalization. Each individual intern was involved in more than 300 handoffs in an average month‐long rotation, an increase of 40% since system changes were introduced to decrease duty hours. We found similar increases at Brigham and Women's Hospital (BWH) and the University of Chicago. Because U.S. teaching hospitals care for more than 6 million patients each year,8 the impact of these handoffs on the quality and efficiency of care is tremendous.
Discontinuity of care is currently managed by sign‐out, or the transfer of patient information from one physician to another. Recognizing the importance of information transfer at these vulnerable transition times for patients, the Joint Commission on Accreditation of Hospital Organizations (JCAHO) issued the 2006 National Patient Safety Goal 2E: Implement a standardized approach to hand off communications, including an opportunity to ask and respond to questions.9 Hospitals have little data to draw on to determine how to comply with this mandate and even less data to guide them in how to achieve its intended goals of improving communication and thus patient safety.
In an effort to better understand sign‐outs and ways to improve this process for house staff on in‐patient services, we reviewed data from the fields of aviation, communications, systems engineering, and human factors research, and we also searched the medical literature using key words pass‐off, handoff, sign‐out, duty hours, work hours, and discontinuity of care and MeSH headings Continuity of Patient Care Internship and Residency/*organization & administration, Personnel Staffing and Scheduling/*organization & administration, and Quality of Health Care. We also searched the websites of the Agency of Healthcare Quality and Research and the National Patient Safety Foundation. On the basis of these reviews, our experiences as hospitalist medical educators organizing resident sign‐out efforts at the University of California, San Francisco, the University of Chicago, and Brigham and Women's Hospital, and our efforts leading national training sessions on sign‐outs at the Society of General Internal Medicine (2004 and 2005), the Society of Hospital Medicine (2004), and the Association of Program Directors in Internal Medicine (2005, 2006), we propose a set of best practices regarding the content and process of sign‐out in an effort to improve communication between residents caring for hospitalized patients, assist programs in building safe and effective sign‐out systems, and improve the quality of patient care.
Effects of Discontinuity on Patient Safety
Research on the effects of discontinuity of care, although limited, suggests it has a negative impact on patient safety. In a study that investigated the institution of code 405 (the regulation that reduced duty hours in New York State), researchers found that the presumed increase in discontinuity with decreased duty hours resulted in delayed test ordering and an increased number of hospital complications.10 Another study found that the number of potentially preventable adverse events doubled when patients were under the care of a physician from a nonprimary team (eg, the cross‐covering intern).11 Studies have also linked resident discontinuity with longer length of stay, increased laboratory testing, and increased medication errors.12, 13
Managing Discontinuity: Sign‐Out as the Means of Information Transfer
In theory, more effective sign‐out systems should mitigate the potential for patient harm, but there is little in the literature describing current effective sign‐out practices or the best ways to design and implement such systems in the health care field. Examining information transfer mechanisms used in fields outside health care can assist in developing these systems.
Information Transfer in Other Industries
Although there is a paucity of data on sign‐out in the medical literature, information transfer has been the subject of substantial research in other industries in which safety depends on effective communication.
Aviation, for example, created systems and processes to improve handoff communication in response to accidents linked to failures in information transfer. One example, the 1977 collision of 2 747s on an airport runway in Tenerife, the Canary Islands, occurred after a garbled transmission from an air traffic controller to the cockpit of one of the aircraft. It was determined that a culture of adherence to a steep hierarchy prevented subordinates from questioning the captain's mistaken certainty that a runway was clear,14 an erroneous belief that was the basis for his decision to continue the aircraft on its course, resulting in its collision with the other airplane.
Subsequently, commercial aviation designed systems that standardized and formalized the process of information transfer and improved teamwork and coordination. These interventions were developed on the basis of detailed observations of cockpit interactions, reviews of communication errors, and focus groups.15 Because of these efforts, today's pilots use standardized checklists to transfer information content, communicate at designated times in specific undistracted environments, and use standard language and read‐backs to enhance understanding.16 The result has been a remarkable decrease in the risk of aviation crashes, one that most experts attribute in large part to these efforts to improve communication.17
Observation of how communication occurs in other high‐risk industries has informed the arena of effective information transfer. For example, direct observation of information transfer at NASA, in nuclear power plants, and in the railway industry identified specific strategies for effective handoffs/sign‐outs such as standardizing the information transferred, ensuring information is up to date, limiting interruptions, and having a structured face‐to‐face verbal interchange.18
Other strategies noted to be effective in diminishing errors are the use of a standardized phonetic alphabet to ensure that information is correctly heard and understood4 and having interactive verbal communication occur at a whiteboard.19
Information Transfer in Health Care
Those in the discipline of nursing have vast experience in the transfer of patient care information. The sign‐out process employed by nurses includes face‐to‐face discussions, typed information, and, most commonly, taped verbal communication.20 Interestingly, this process has not been subject to detailed scrutiny, and there is little information in the literature about best practices in sign‐out. Most articles in the literature on nursing handoffs are ethnographic descriptions of patient care responsibilities,21 on the basis of which, the authors advocate standardization of the information to be transferred, formalization of the channel used to communicate, and attention to increasing a culture of professionalism during sign‐out in order to improve efficiency.20, 22
There is little in the literature on transfer of care among physicians. Improvements in sign‐out have been suggested as part of broad strategies, such as increased training and information technology support,4, 7, 23, 24 and specific strategies have been offered such as managing barriers to communication, including specific types of data when transferring care,25 and involving nurses and senior physicians in sign‐outs.26 Specific outcomes data in this area have focused primarily on the use of computerized systems to improve information transfer. For example, the use of a computerized sign‐out system at Brigham and Women's Hospital (BWH), linked to the hospital's information system to ensure up‐to‐date information on patient demographics, medications, and laboratory values, has resulted in fewer errors,27 as have other similar systems.28 At the University of Washington, use of a similarly linked computerized sign‐out system resulted in fewer patients being missed on rounds and improvement in the quality of sign‐out and continuity of care according to resident self‐reports.29 Unfortunately, fewer than 10% of hospitals have such integrated hospitalwide information systems to support the sign‐out function.30
It has been noted that verbal communication, in concert with advances in technological communication, is important in information transfer in health care,18, 31 especially in emergent or urgent conditions.32 For example, eliminating the phoned‐in report from the lab to the ER and replacing it with delivery by an electronic reporting system lacking verbal communicationresulted in 45% of emergent lab results going unchecked.32 Structured verbal communication tools have been efficacious in improving information transfer outside the formal sign‐outfor example, read‐backs, which reduced errors in the reporting of critical laboratory values,33 and the SBAR (situation, background, assessment, recommendation) tool (designed to frame the transfer of critical information), which improved physician and nurse patient care information transfer in the in‐patient setting of the Kaiser Permanente health system.34
In focus groups and in response to formal and informal surveys, residents at our 3 sites suggested inclusion of the following information, provided in writing and orally, to improve sign‐outs: up‐to‐date administrative information (eg, room number, primary care physician); patient's recent cognitive or cardiopulmonary status; problems the patient had already experienced and treatments previously tried, both successfully and unsuccessfully; patient's code status and discussions on level of care; test results or consultation recommendations that were likely to come back while covering the patient and what to do with the results; and relevant psychosocial information (eg, complex family dynamics).35
The Current Practice of Sign‐Out
In examining sign‐outs at our 3 institutions, we found them to be unstructured and unstandardized. From discussion with faculty participating in national workshops on sign‐out, we found that most sign‐outs are conducted by interns, usually with little or no formal training. Templates, checklists, or other methods to standardize the content of the information transferred were rarely used.
We also noted that the vehicle for written sign‐out is highly variable. At UCSF, different residency training programs used a variety of modalities for written sign‐outs, including index cards, Excel spreadsheets, Word documents, and loose sheets of paper. Recently, the UCSF Department of Medicine designed a simple database (on Filemaker Pro) that allows members of the house staff to update their sign‐out information, share it with other house staff and nurses, and access it at locations throughout the hospital (Fig. 1). Although this database is not yet linked to the hospital information system (planned for 2006), anecdotally resident satisfaction with sign‐out has vastly improved since its implementation. The cost of design and implementation was approximately $10,000. At the University of Chicago, interns used Microsoft Word to create sign‐out sheets containing patient summaries to transfer information. However, during structured interviews, 95% of the interns reported that these sheets were frequently lost or misplaced.7 Although medicine residents at BWH use a computerized system to produce sign‐out sheets, this system did not guarantee complete and structured information. For example, a survey at BWH found that 56% of cross‐covering residents said that when paged about a patient overnight, the relevant information needed to care for that patient was present less than half the time; and 27% of residents reported being paged more than 3 times in the previous 2 weeks about a test result or consultant recommendation that they did not know was pending.36
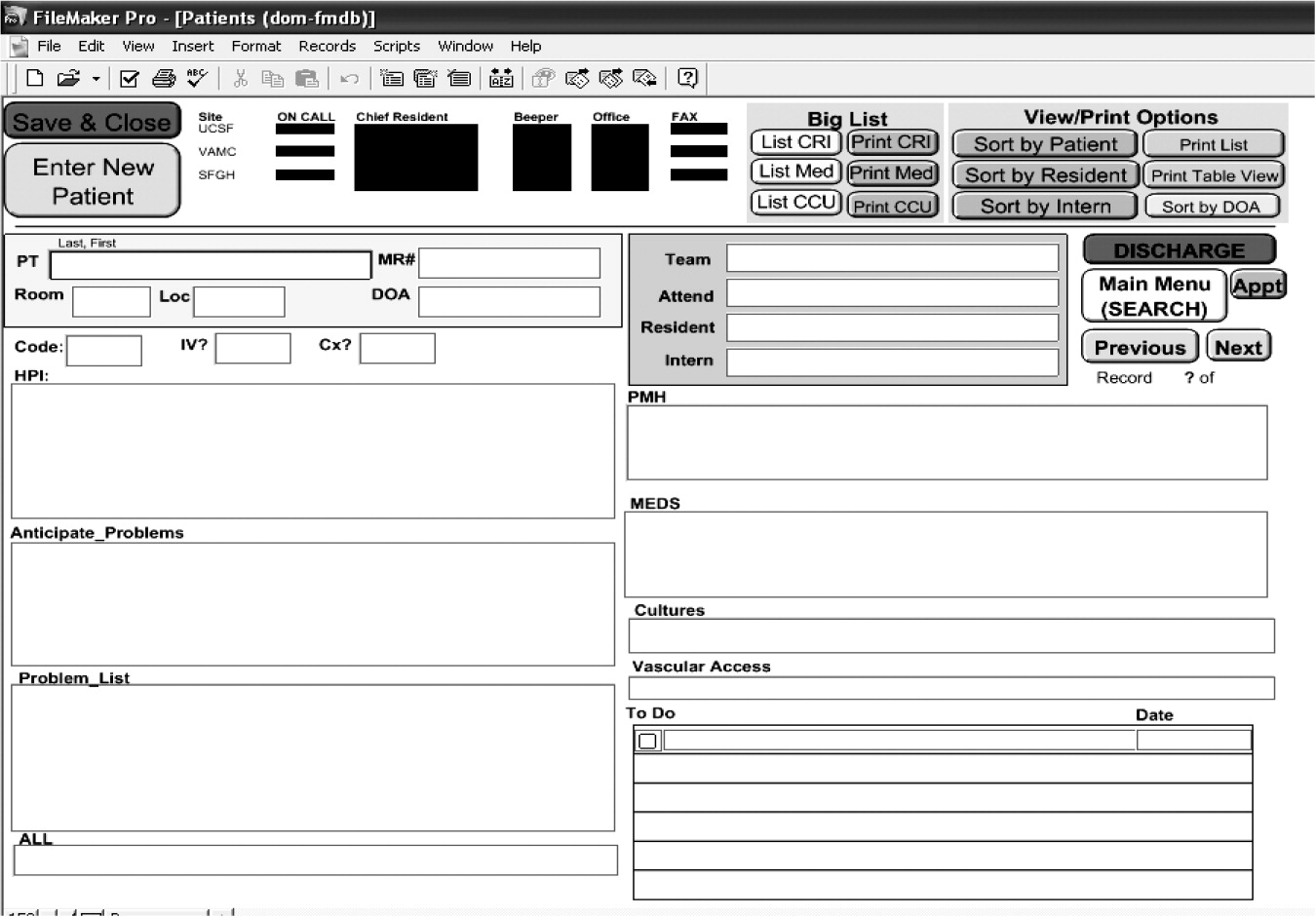
The process of sign‐out also varied across disciplines and institutions. From our experiences at our sites and at the sites of faculty nationally, we found limited standardization about whether sign‐out was verbal, the data transmitted, and the setting in which it was transmitted. In fact, at UCSF most residents signed out verbally on the fly, wherever and whenever they could find the cross‐coverage intern. At BWH, only 37% of residents said that sign‐out occurred in a quiet place most of the time, and only 52% signed out on every patient both orally and in writing.36 At the University of Chicago, the sign‐out process was characterized by outright failures in communication because of omission of needed information (ie, medications, active or anticipated medical problems, etc.) or by failure‐prone communication (ie, lack of face‐to‐face communication, illegible writing). These failures often led to uncertainty in making patient care decisions, potentially resulting in inefficient or suboptimal care.35
Strategies for Safe and Effective Sign‐Out
Given the current landscape of variability in sign‐outs, the recognition that information lost during sign‐out may result in harm to patients, and evidence of improvements in information transfer in areas outside health care, we aimed to develop mechanisms to improve the sign‐out process for residents working in a hospital setting. These strategies are based on our review of the existing literature supplemented by our experiences at our 3 institutions.
Content of Sign‐Out
The elements of content necessary for safe and effective sign‐out can be divided into 5 broad categories (Table 1), contained in the mnemonic ANTICipate: Administrative information, New clinical information, specific Tasks to be performed, assessment of severity of Illness, and Contingency plans or anticipated problems (Table 1, Fig. 2).
| ✓ Administrative data |
| □ Patient name, age, sex |
| □ Medical record number |
| □ Room number |
| □ Admission date |
| □ Primary inpatient medical team, primary care physician |
| □ Family contact information |
| ✓ New information (clinical update) |
| □ Chief complaint, brief HPI, and diagnosis (or differential diagnosis) |
| □ Updated list of medications with doses, updated allergies |
| □ Updated, brief assessment by system/problem, with dates |
| □ Current baseline status (eg, mental status, cardiopulmonary, vital signs, especially if abnormal but stable) |
| □ Recent procedures and significant events |
| ✓ Tasks (what needs to be done) |
| □ Specific, using if‐then statements |
| □ Prepare cross‐coverage (eg, patient consent for blood transfusion) |
| □ Alert to incoming information (eg, study results, consultant recommendations), and what action, if any, needs to be taken during the cross‐coverage |
| ✓ Illness |
| □ Is the patient sick? |
| ✓ Contingency planning/Code status |
| □ What may go wrong and what to do about it |
| □ What has or has not worked before (eg, responds to 40 mg IV furosemide) |
| □ Difficult family or psychosocial situations |
| □ Code status, especially recent changes or family discussions |
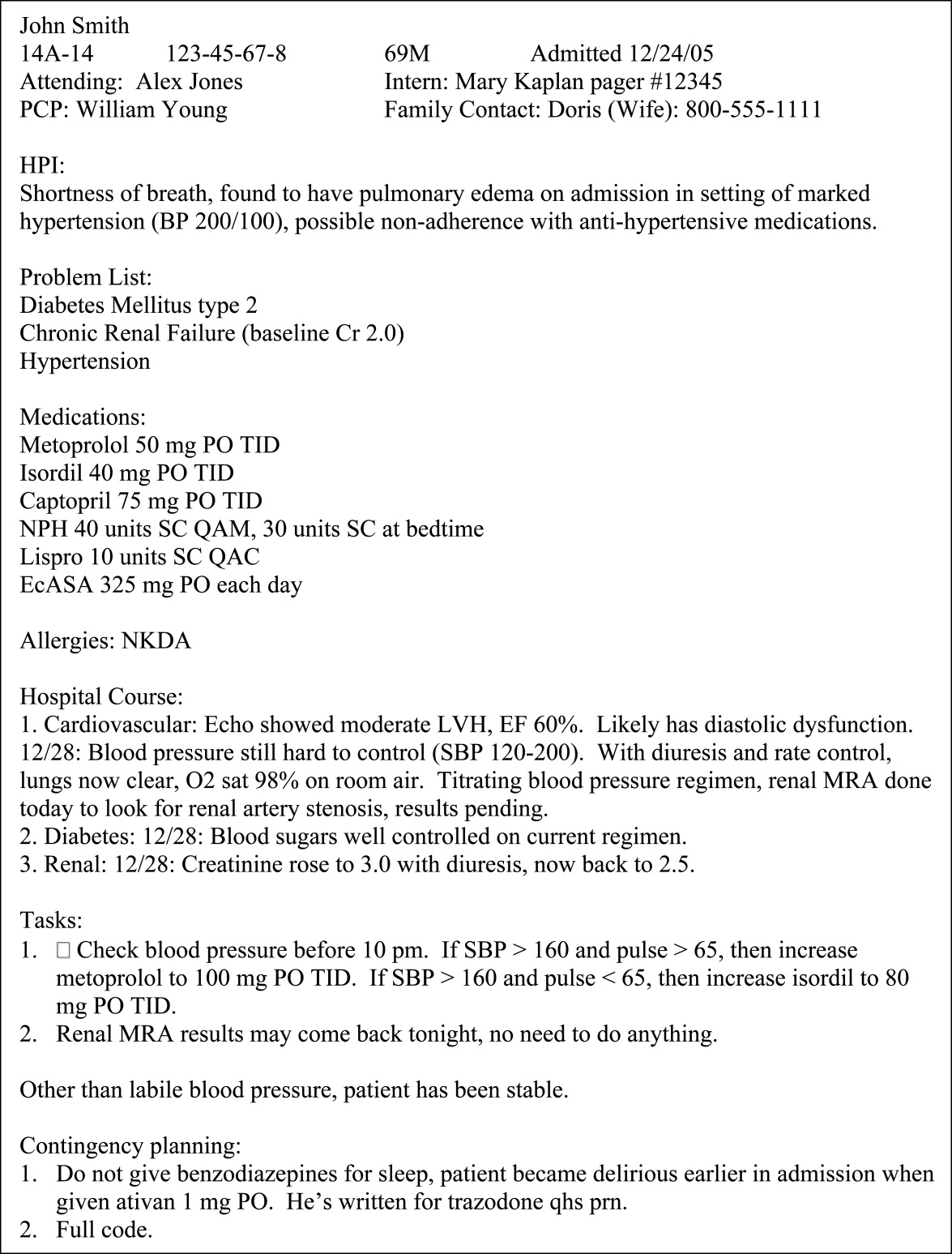
Several general points about this list should be noted. First, the sign‐out content is not meant to replace the chart. The information included reflects the goal of a sign‐out, namely, to provide enough information to allow for a safe transition in patient care. Information we believe is not essential to the sign‐out includes: a complete history and physical exam from the day of admission, a list of tasks already completed, and data necessary only to complete a discharge summary.
Sign‐out must be also be a closed loopthe process of signing in is as important as the process of signing out. This usually entails members of the primary team obtaining information from the cross‐covering physician when they resume care of the patient. The information conveyed in this case is different and includes details on events during cross‐coverage such as: 1) time called to assess patient; 2) reason for call; 3) a brief assessment of the patient, including vital signs; 4) actions taken, for example, medications given and tests ordered; and 5) rationale for those actions. Some of this information may also be included in the chart as an event note (see Fig. 3).
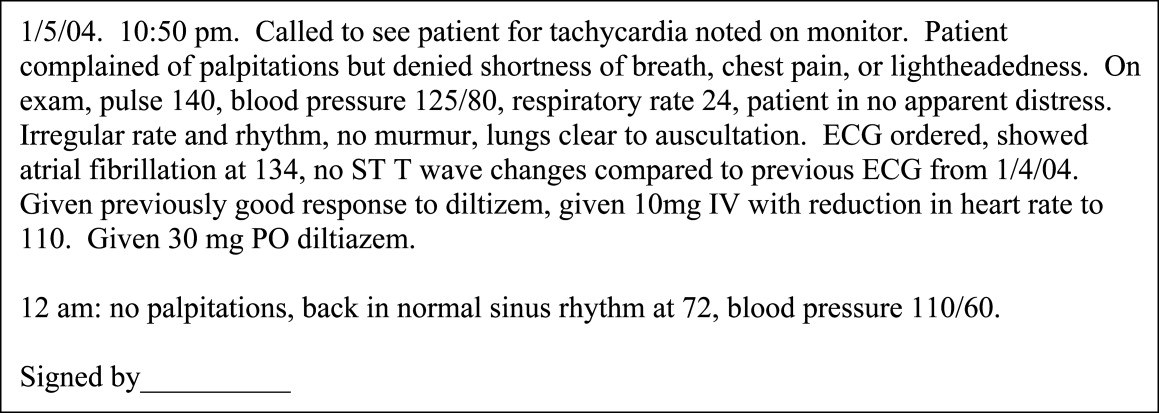
The Vehicle for Sign‐Out
We recommend a computer‐assisted vehicle for patient information transfer. Ideally, this would be linked to the hospital information system to ensure accurate and up‐to‐date information Easy access to the computerized sign‐out is essential (eg, using a hospitalwide computer system, shared hard drive service, intranet, or PDA linked to the computer system), and it should be customizable for the varied needs of different services and departments. The system should have templates to standardize the content of sign‐out, contain robust backup systems, and be HIPAA compliant (ie, restrict access to required health care personnel). However, the perfect should not be the enemy of the good: systems that do not meet these criteria may still help to protect patients by providing legible, predictable, and accessible information.
Sign‐Out Processes
Verbal communication.
Although electronic solutions can facilitate the standardization of written content, face‐to‐face verbal communication adds additional value.19 We recommend that each patient be reviewed separately. Identification of each patient verbally ensures that those engaged in the sign‐out are discussing the same patient. Reiterating the major medical problems gives a snapshot of the patient and frames the sign‐out. The to‐do list, the list of tasks that the cross‐cover resident needs to complete during cross coverage, should be specific and articulated as if, then statements (eg, if the urine output is less than 1 L, then give 40 mg of IV furosemide). The receiver of sign‐out should read back to the person giving the sign‐out each item on the to‐do list (eg, So, I should check the ins and outs at about 10:00 pm, and give 40 of furosemide if the patient is not 1 L negative, right?).
Anticipated problems should also be verbally communicated to promote a dialogue. Points that cannot be adequately transferred in the written sign‐out are particularly important to transmit verbally. Examples include previous code discussions, unusual responses to treatment, and psychosocial and family issues. When delivering verbal sign‐out, it is important to consider the a priori knowledge of the recipient. How much knowledge about a patient is already shared between the outgoing and incoming physicians and the level of experience of the physicians may affect the extent to which information needs be transmitted.37 For instance, 2 experienced physicians who already have been working to cover the same patient will likely have an abbreviated discussion, in contrast to the lengthier sign‐out necessary if the outgoing and incoming physicians are interns, and the incoming intern has no prior knowledge of the patient. Similarly, it is likely the level of detail transmitted will need to be greater during a permanent transfer of patient care (ie, at the end of a resident's rotation) than during a brief, temporary transition (eg, overnight coverage).
The challenges of a busy inpatient service may preclude a complete verbal sign‐out for all patients; we contend, though, it is best to use these practices to the extent possible, especially for patients with treatment plans in flux, those whose status is tenuous, and those who have anticipated changes in status during cross‐coverage. One tool that may be effectively used in signing out such patients is the SBAR tool, according to which a brief description of the situation is given, followed by the background and the physician's specific assessment and complete recommendation.38 For example, a resident signing out might begin by stating, I have 18 patients to sign‐out to you. I'm going to describe 6 active patients in detail. Twelve others are fairly stable, and I will give you basic information about them, and the details are in the written sign‐out. One patient has a plan in flux. The situation is Mr. S. is having trouble breathing, the background is that he has both CHF and COPD, my assessment is that this is more cardiac than pulmonary, and I recommend that you see him first and discuss with the cardiology consultant. Using the tools described here (Table 2), a sign‐out of 15 patients of variable acuity could be verbally signed out in less than 10 minutes.
| ✓ WHO should participate in the sign‐out process? |
| □ Outgoing clinician primarily responsible for patient's care |
| □ Oncoming clinician who will be primarily responsible for patient's care (avoid passing this task to someone else, even if busy) |
| □ Consider supervision by experienced clinicians if early in training |
| ✓ WHAT content needs to be verbally communicated? |
| Use situation briefing model, or SBAR, technique: |
| □ SituationIdentify each patient (name, age, sex, chief complaint) and briefly state any major problems (active and those that may become active during cross‐coverage). |
| □ Backgroundpertinent information relevant to current care (eg, recent vitals and/or baseline exam, labs, test results, etc). |
| □ Assessmentworking diagnosis, response to treatment, anticipated problems during cross‐coverage including anything not adequately described using written form (eg, complex family discussions). |
| □ Recommendationto‐do lists and if/then recommendations. |
| ✓ WHERE should sign‐out occur? |
| □ Designated room or place for sign‐out (eg, avoid patient areas because of HIPPA requirements) |
| □ Proper lighting |
| □ Avoid excessive noise (eg, high‐traffic areas) |
| □ Minimize disruptions (eg, hand over pagers) |
| □ Ensure systems support for sign‐out (eg, computers, printer, paper, etc.) |
| ✓ WHEN is the optimal time for sign‐out? |
| □ Designated time when both parties can be present and pay attention (eg, beware of clinic, other obligations) |
| □ Have enough time for interactive questions at the end (eg, avoid rush at the end of the shift) |
| ✓ HOW should verbal communication be performed? |
| □ Face to face, allowing for questions |
| □ Verbalize data in the same order for each patient at each sign‐out |
| □ Read back all to‐do items |
| □ Adjust length and depth of review according to baseline knowledge of parties involved and type of transition in care |
The Environment and setting.
To improve the setting of sign‐out, we recommend: a designated space that is well lit, quiet, and respects patient confidentiality and a designated time when sign‐out will occur. To limit known distractions and interruptions39, 40 in the hospital, we also recommend the outgoing physician hand off his or her pager to someone else during sign‐out. Also key to an environment conducive to information transfer is ensuring adequate computer support for electronic sign‐out and access to updated clinical information.
Organizational culture and institutional leadership.
The way residents transfer patient care information reflects the culture of the institution. Changing the culture to one in which interactive questioning is valued regardless of position in the hierarchy has been shown to reduce errors in aviation.41 Educating residents on the impact of sign‐outs on patient care is a first step toward improving the culture of sign‐out. Resident commitment to the new sign‐out can be gained by engaging residents in development of the process itself. To cement these changes into the culture, practitioners at all levels should be aware of and support the new system. The role of an institution's leaders in achieving these changes cannot be overlooked. Leaders will need to be creative in order to support sign‐out as described within the obvious constraints of money, time, personnel, and space. Gaining institutional buy‐in can start with heightening the awareness of leaders of the issues surrounding sign‐out, including patient safety, resident efficiency, and the financial impact of discontinuity. Ongoing evaluation of efforts to improve sign‐out is also crucial and can be accomplished with surveys, focus groups, and direct observation. Feeding back the positive impact of the changes to all involved stakeholders will promote confidence in the new systems and pride in their efforts.
CONCLUSIONS
Sign‐outs are a part of the current landscape of academic medical centers as well as hospitals at large. Interns, residents, and consulting fellows, not to mention nurses, physical therapists, and nutritionists, transfer patient care information at each transition point. There are few resources that can assist these caregivers in identifying and implementing the most effective ways to transfer patient care information. Hospitals and other care facilities are now mandated to develop standards and systems to improve sign‐out. On the basis of the limited literature to date and our own experiences, we have proposed standards and best practices to assist hospitals, training programs, and institutional leaders in designing safe and usable sign‐out systems. Effective implementation of the standards must include appropriate allocation of resources, individualization to meet specific needs of each program or institution, intensive training, and ongoing evaluation. Future research should focus on developing valid surrogate measures of continuity of care, conducting rigorous trials to determine the elements of sign‐out that lead to the best patient outcomes, and studying the most effective ways of implementing these improvements. By improving the content and process of sign‐out, we can meet the challenges of the new health care landscape while putting patient safety at the forefront.
Modern‐day continuity of patient care in teaching hospitals, once remarkably high because of a cadre of sleep‐deprived residents, is now peppered with breaks, each accompanied by the transfer of patient care responsibility from one resident to another; a process often referred to as a handoff. Such transitions have long been a part of medical practice but have recently received increased attention because of restrictions in the duty hours of house staff. In July 2003 the Accreditation Council for Graduate Medical Education (ACGME) mandated reduced duty hours for all trainees in hopes of improving resident education and well‐being and patient safety.1 In fact, some studies have shown improved resident well‐being2 and fewer medical errors with reductions in duty hours,3, 4 but the growing consensus about the negative consequences of resident fatigue on patient safety has been accompanied by parallel concerns about the potential for information loss with each break in the continuity of care.5, 6
Although the tradeoff of increased discontinuity of care for fewer hours worked is sometimes characterized as an unintended consequence of duty hour regulations, it is in fact predictable and essential. As individuals work fewer hours, discontinuity must necessarily increase (assuming 24‐hour coverage).7 The extent to which this occurs may vary, but the link is consistent. At the University of California, San Francisco (UCSF), for example, we found that compliance with new duty hour requirements for internal medicine resulted in an average of 15 handoffs per patient during a 5‐day hospitalization. Each individual intern was involved in more than 300 handoffs in an average month‐long rotation, an increase of 40% since system changes were introduced to decrease duty hours. We found similar increases at Brigham and Women's Hospital (BWH) and the University of Chicago. Because U.S. teaching hospitals care for more than 6 million patients each year,8 the impact of these handoffs on the quality and efficiency of care is tremendous.
Discontinuity of care is currently managed by sign‐out, or the transfer of patient information from one physician to another. Recognizing the importance of information transfer at these vulnerable transition times for patients, the Joint Commission on Accreditation of Hospital Organizations (JCAHO) issued the 2006 National Patient Safety Goal 2E: Implement a standardized approach to hand off communications, including an opportunity to ask and respond to questions.9 Hospitals have little data to draw on to determine how to comply with this mandate and even less data to guide them in how to achieve its intended goals of improving communication and thus patient safety.
In an effort to better understand sign‐outs and ways to improve this process for house staff on in‐patient services, we reviewed data from the fields of aviation, communications, systems engineering, and human factors research, and we also searched the medical literature using key words pass‐off, handoff, sign‐out, duty hours, work hours, and discontinuity of care and MeSH headings Continuity of Patient Care Internship and Residency/*organization & administration, Personnel Staffing and Scheduling/*organization & administration, and Quality of Health Care. We also searched the websites of the Agency of Healthcare Quality and Research and the National Patient Safety Foundation. On the basis of these reviews, our experiences as hospitalist medical educators organizing resident sign‐out efforts at the University of California, San Francisco, the University of Chicago, and Brigham and Women's Hospital, and our efforts leading national training sessions on sign‐outs at the Society of General Internal Medicine (2004 and 2005), the Society of Hospital Medicine (2004), and the Association of Program Directors in Internal Medicine (2005, 2006), we propose a set of best practices regarding the content and process of sign‐out in an effort to improve communication between residents caring for hospitalized patients, assist programs in building safe and effective sign‐out systems, and improve the quality of patient care.
Effects of Discontinuity on Patient Safety
Research on the effects of discontinuity of care, although limited, suggests it has a negative impact on patient safety. In a study that investigated the institution of code 405 (the regulation that reduced duty hours in New York State), researchers found that the presumed increase in discontinuity with decreased duty hours resulted in delayed test ordering and an increased number of hospital complications.10 Another study found that the number of potentially preventable adverse events doubled when patients were under the care of a physician from a nonprimary team (eg, the cross‐covering intern).11 Studies have also linked resident discontinuity with longer length of stay, increased laboratory testing, and increased medication errors.12, 13
Managing Discontinuity: Sign‐Out as the Means of Information Transfer
In theory, more effective sign‐out systems should mitigate the potential for patient harm, but there is little in the literature describing current effective sign‐out practices or the best ways to design and implement such systems in the health care field. Examining information transfer mechanisms used in fields outside health care can assist in developing these systems.
Information Transfer in Other Industries
Although there is a paucity of data on sign‐out in the medical literature, information transfer has been the subject of substantial research in other industries in which safety depends on effective communication.
Aviation, for example, created systems and processes to improve handoff communication in response to accidents linked to failures in information transfer. One example, the 1977 collision of 2 747s on an airport runway in Tenerife, the Canary Islands, occurred after a garbled transmission from an air traffic controller to the cockpit of one of the aircraft. It was determined that a culture of adherence to a steep hierarchy prevented subordinates from questioning the captain's mistaken certainty that a runway was clear,14 an erroneous belief that was the basis for his decision to continue the aircraft on its course, resulting in its collision with the other airplane.
Subsequently, commercial aviation designed systems that standardized and formalized the process of information transfer and improved teamwork and coordination. These interventions were developed on the basis of detailed observations of cockpit interactions, reviews of communication errors, and focus groups.15 Because of these efforts, today's pilots use standardized checklists to transfer information content, communicate at designated times in specific undistracted environments, and use standard language and read‐backs to enhance understanding.16 The result has been a remarkable decrease in the risk of aviation crashes, one that most experts attribute in large part to these efforts to improve communication.17
Observation of how communication occurs in other high‐risk industries has informed the arena of effective information transfer. For example, direct observation of information transfer at NASA, in nuclear power plants, and in the railway industry identified specific strategies for effective handoffs/sign‐outs such as standardizing the information transferred, ensuring information is up to date, limiting interruptions, and having a structured face‐to‐face verbal interchange.18
Other strategies noted to be effective in diminishing errors are the use of a standardized phonetic alphabet to ensure that information is correctly heard and understood4 and having interactive verbal communication occur at a whiteboard.19
Information Transfer in Health Care
Those in the discipline of nursing have vast experience in the transfer of patient care information. The sign‐out process employed by nurses includes face‐to‐face discussions, typed information, and, most commonly, taped verbal communication.20 Interestingly, this process has not been subject to detailed scrutiny, and there is little information in the literature about best practices in sign‐out. Most articles in the literature on nursing handoffs are ethnographic descriptions of patient care responsibilities,21 on the basis of which, the authors advocate standardization of the information to be transferred, formalization of the channel used to communicate, and attention to increasing a culture of professionalism during sign‐out in order to improve efficiency.20, 22
There is little in the literature on transfer of care among physicians. Improvements in sign‐out have been suggested as part of broad strategies, such as increased training and information technology support,4, 7, 23, 24 and specific strategies have been offered such as managing barriers to communication, including specific types of data when transferring care,25 and involving nurses and senior physicians in sign‐outs.26 Specific outcomes data in this area have focused primarily on the use of computerized systems to improve information transfer. For example, the use of a computerized sign‐out system at Brigham and Women's Hospital (BWH), linked to the hospital's information system to ensure up‐to‐date information on patient demographics, medications, and laboratory values, has resulted in fewer errors,27 as have other similar systems.28 At the University of Washington, use of a similarly linked computerized sign‐out system resulted in fewer patients being missed on rounds and improvement in the quality of sign‐out and continuity of care according to resident self‐reports.29 Unfortunately, fewer than 10% of hospitals have such integrated hospitalwide information systems to support the sign‐out function.30
It has been noted that verbal communication, in concert with advances in technological communication, is important in information transfer in health care,18, 31 especially in emergent or urgent conditions.32 For example, eliminating the phoned‐in report from the lab to the ER and replacing it with delivery by an electronic reporting system lacking verbal communicationresulted in 45% of emergent lab results going unchecked.32 Structured verbal communication tools have been efficacious in improving information transfer outside the formal sign‐outfor example, read‐backs, which reduced errors in the reporting of critical laboratory values,33 and the SBAR (situation, background, assessment, recommendation) tool (designed to frame the transfer of critical information), which improved physician and nurse patient care information transfer in the in‐patient setting of the Kaiser Permanente health system.34
In focus groups and in response to formal and informal surveys, residents at our 3 sites suggested inclusion of the following information, provided in writing and orally, to improve sign‐outs: up‐to‐date administrative information (eg, room number, primary care physician); patient's recent cognitive or cardiopulmonary status; problems the patient had already experienced and treatments previously tried, both successfully and unsuccessfully; patient's code status and discussions on level of care; test results or consultation recommendations that were likely to come back while covering the patient and what to do with the results; and relevant psychosocial information (eg, complex family dynamics).35
The Current Practice of Sign‐Out
In examining sign‐outs at our 3 institutions, we found them to be unstructured and unstandardized. From discussion with faculty participating in national workshops on sign‐out, we found that most sign‐outs are conducted by interns, usually with little or no formal training. Templates, checklists, or other methods to standardize the content of the information transferred were rarely used.
We also noted that the vehicle for written sign‐out is highly variable. At UCSF, different residency training programs used a variety of modalities for written sign‐outs, including index cards, Excel spreadsheets, Word documents, and loose sheets of paper. Recently, the UCSF Department of Medicine designed a simple database (on Filemaker Pro) that allows members of the house staff to update their sign‐out information, share it with other house staff and nurses, and access it at locations throughout the hospital (Fig. 1). Although this database is not yet linked to the hospital information system (planned for 2006), anecdotally resident satisfaction with sign‐out has vastly improved since its implementation. The cost of design and implementation was approximately $10,000. At the University of Chicago, interns used Microsoft Word to create sign‐out sheets containing patient summaries to transfer information. However, during structured interviews, 95% of the interns reported that these sheets were frequently lost or misplaced.7 Although medicine residents at BWH use a computerized system to produce sign‐out sheets, this system did not guarantee complete and structured information. For example, a survey at BWH found that 56% of cross‐covering residents said that when paged about a patient overnight, the relevant information needed to care for that patient was present less than half the time; and 27% of residents reported being paged more than 3 times in the previous 2 weeks about a test result or consultant recommendation that they did not know was pending.36
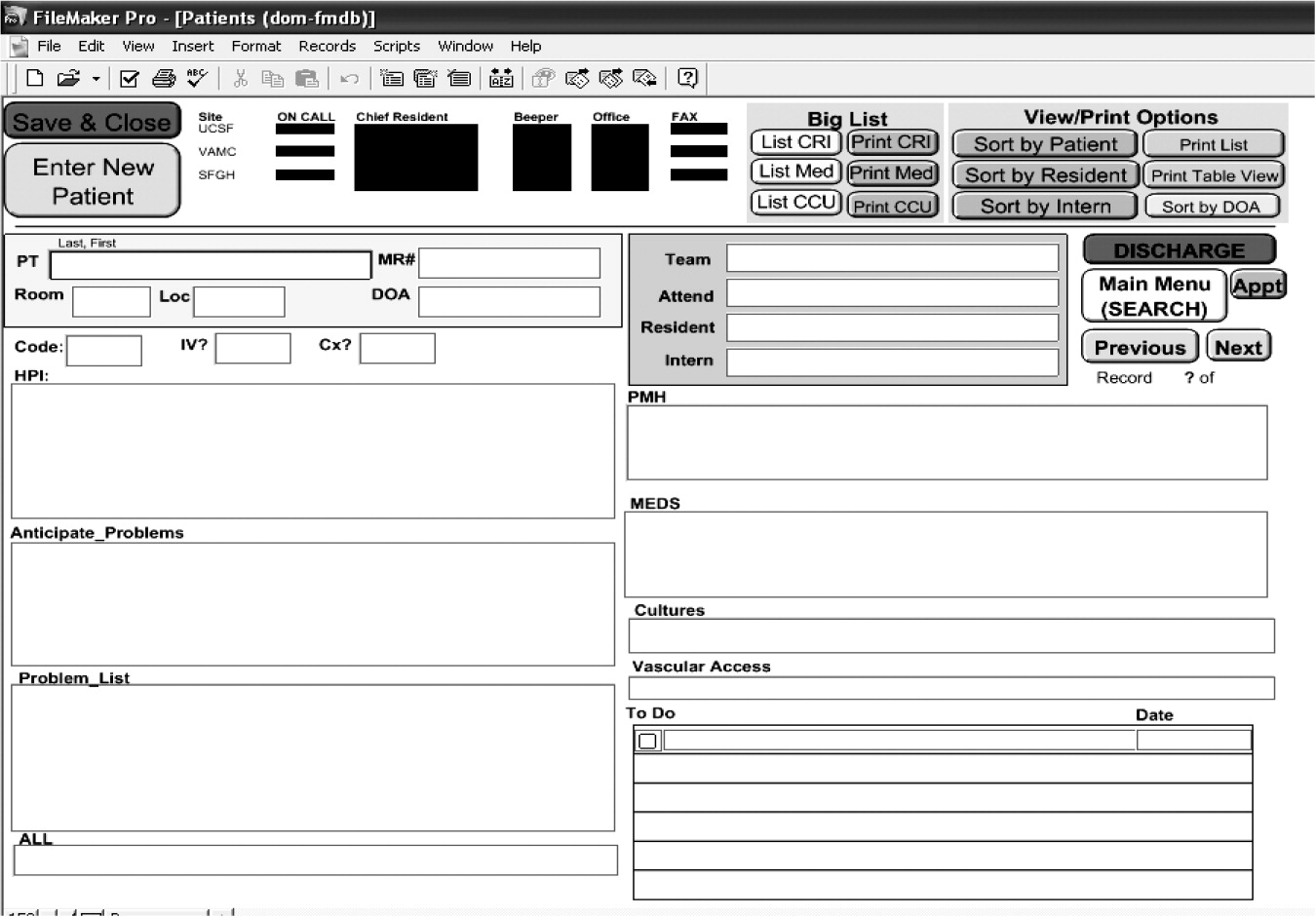
The process of sign‐out also varied across disciplines and institutions. From our experiences at our sites and at the sites of faculty nationally, we found limited standardization about whether sign‐out was verbal, the data transmitted, and the setting in which it was transmitted. In fact, at UCSF most residents signed out verbally on the fly, wherever and whenever they could find the cross‐coverage intern. At BWH, only 37% of residents said that sign‐out occurred in a quiet place most of the time, and only 52% signed out on every patient both orally and in writing.36 At the University of Chicago, the sign‐out process was characterized by outright failures in communication because of omission of needed information (ie, medications, active or anticipated medical problems, etc.) or by failure‐prone communication (ie, lack of face‐to‐face communication, illegible writing). These failures often led to uncertainty in making patient care decisions, potentially resulting in inefficient or suboptimal care.35
Strategies for Safe and Effective Sign‐Out
Given the current landscape of variability in sign‐outs, the recognition that information lost during sign‐out may result in harm to patients, and evidence of improvements in information transfer in areas outside health care, we aimed to develop mechanisms to improve the sign‐out process for residents working in a hospital setting. These strategies are based on our review of the existing literature supplemented by our experiences at our 3 institutions.
Content of Sign‐Out
The elements of content necessary for safe and effective sign‐out can be divided into 5 broad categories (Table 1), contained in the mnemonic ANTICipate: Administrative information, New clinical information, specific Tasks to be performed, assessment of severity of Illness, and Contingency plans or anticipated problems (Table 1, Fig. 2).
| ✓ Administrative data |
| □ Patient name, age, sex |
| □ Medical record number |
| □ Room number |
| □ Admission date |
| □ Primary inpatient medical team, primary care physician |
| □ Family contact information |
| ✓ New information (clinical update) |
| □ Chief complaint, brief HPI, and diagnosis (or differential diagnosis) |
| □ Updated list of medications with doses, updated allergies |
| □ Updated, brief assessment by system/problem, with dates |
| □ Current baseline status (eg, mental status, cardiopulmonary, vital signs, especially if abnormal but stable) |
| □ Recent procedures and significant events |
| ✓ Tasks (what needs to be done) |
| □ Specific, using if‐then statements |
| □ Prepare cross‐coverage (eg, patient consent for blood transfusion) |
| □ Alert to incoming information (eg, study results, consultant recommendations), and what action, if any, needs to be taken during the cross‐coverage |
| ✓ Illness |
| □ Is the patient sick? |
| ✓ Contingency planning/Code status |
| □ What may go wrong and what to do about it |
| □ What has or has not worked before (eg, responds to 40 mg IV furosemide) |
| □ Difficult family or psychosocial situations |
| □ Code status, especially recent changes or family discussions |
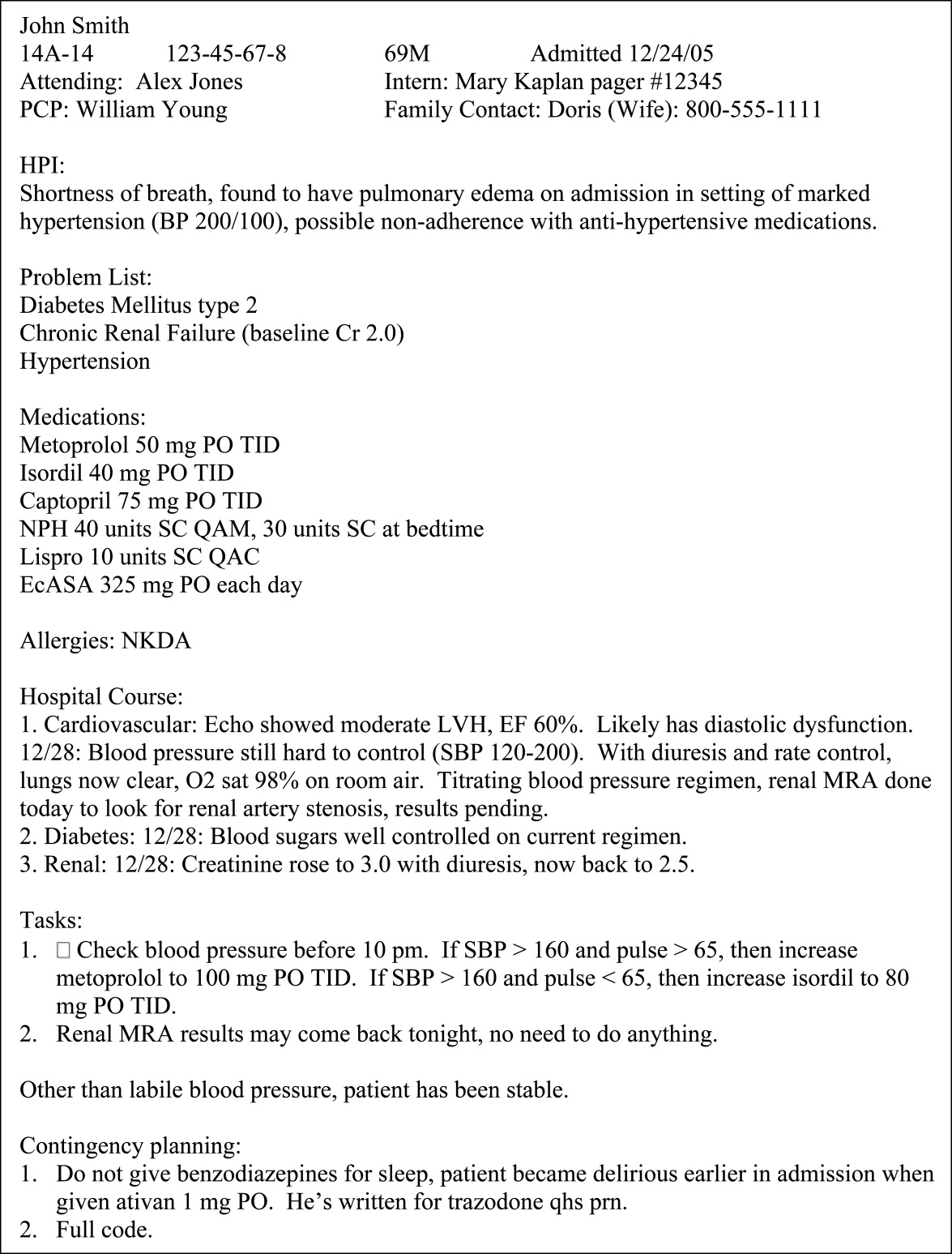
Several general points about this list should be noted. First, the sign‐out content is not meant to replace the chart. The information included reflects the goal of a sign‐out, namely, to provide enough information to allow for a safe transition in patient care. Information we believe is not essential to the sign‐out includes: a complete history and physical exam from the day of admission, a list of tasks already completed, and data necessary only to complete a discharge summary.
Sign‐out must be also be a closed loopthe process of signing in is as important as the process of signing out. This usually entails members of the primary team obtaining information from the cross‐covering physician when they resume care of the patient. The information conveyed in this case is different and includes details on events during cross‐coverage such as: 1) time called to assess patient; 2) reason for call; 3) a brief assessment of the patient, including vital signs; 4) actions taken, for example, medications given and tests ordered; and 5) rationale for those actions. Some of this information may also be included in the chart as an event note (see Fig. 3).
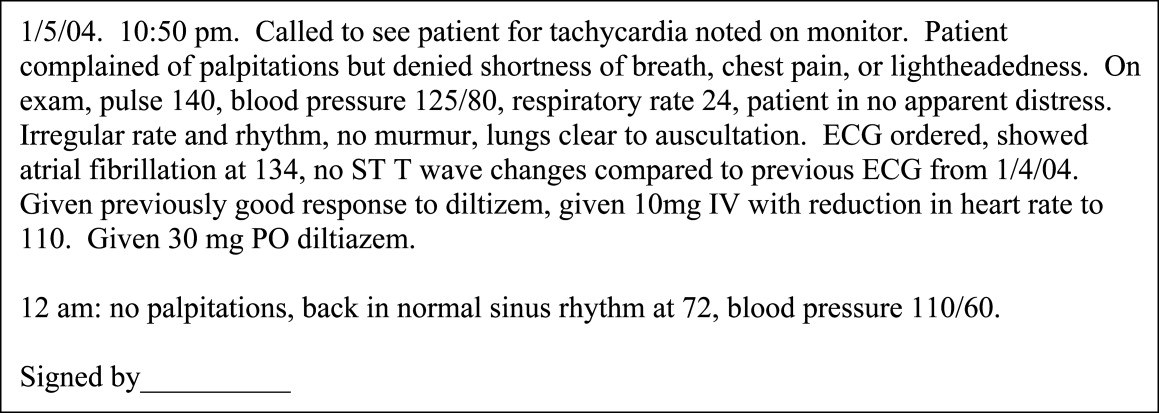
The Vehicle for Sign‐Out
We recommend a computer‐assisted vehicle for patient information transfer. Ideally, this would be linked to the hospital information system to ensure accurate and up‐to‐date information Easy access to the computerized sign‐out is essential (eg, using a hospitalwide computer system, shared hard drive service, intranet, or PDA linked to the computer system), and it should be customizable for the varied needs of different services and departments. The system should have templates to standardize the content of sign‐out, contain robust backup systems, and be HIPAA compliant (ie, restrict access to required health care personnel). However, the perfect should not be the enemy of the good: systems that do not meet these criteria may still help to protect patients by providing legible, predictable, and accessible information.
Sign‐Out Processes
Verbal communication.
Although electronic solutions can facilitate the standardization of written content, face‐to‐face verbal communication adds additional value.19 We recommend that each patient be reviewed separately. Identification of each patient verbally ensures that those engaged in the sign‐out are discussing the same patient. Reiterating the major medical problems gives a snapshot of the patient and frames the sign‐out. The to‐do list, the list of tasks that the cross‐cover resident needs to complete during cross coverage, should be specific and articulated as if, then statements (eg, if the urine output is less than 1 L, then give 40 mg of IV furosemide). The receiver of sign‐out should read back to the person giving the sign‐out each item on the to‐do list (eg, So, I should check the ins and outs at about 10:00 pm, and give 40 of furosemide if the patient is not 1 L negative, right?).
Anticipated problems should also be verbally communicated to promote a dialogue. Points that cannot be adequately transferred in the written sign‐out are particularly important to transmit verbally. Examples include previous code discussions, unusual responses to treatment, and psychosocial and family issues. When delivering verbal sign‐out, it is important to consider the a priori knowledge of the recipient. How much knowledge about a patient is already shared between the outgoing and incoming physicians and the level of experience of the physicians may affect the extent to which information needs be transmitted.37 For instance, 2 experienced physicians who already have been working to cover the same patient will likely have an abbreviated discussion, in contrast to the lengthier sign‐out necessary if the outgoing and incoming physicians are interns, and the incoming intern has no prior knowledge of the patient. Similarly, it is likely the level of detail transmitted will need to be greater during a permanent transfer of patient care (ie, at the end of a resident's rotation) than during a brief, temporary transition (eg, overnight coverage).
The challenges of a busy inpatient service may preclude a complete verbal sign‐out for all patients; we contend, though, it is best to use these practices to the extent possible, especially for patients with treatment plans in flux, those whose status is tenuous, and those who have anticipated changes in status during cross‐coverage. One tool that may be effectively used in signing out such patients is the SBAR tool, according to which a brief description of the situation is given, followed by the background and the physician's specific assessment and complete recommendation.38 For example, a resident signing out might begin by stating, I have 18 patients to sign‐out to you. I'm going to describe 6 active patients in detail. Twelve others are fairly stable, and I will give you basic information about them, and the details are in the written sign‐out. One patient has a plan in flux. The situation is Mr. S. is having trouble breathing, the background is that he has both CHF and COPD, my assessment is that this is more cardiac than pulmonary, and I recommend that you see him first and discuss with the cardiology consultant. Using the tools described here (Table 2), a sign‐out of 15 patients of variable acuity could be verbally signed out in less than 10 minutes.
| ✓ WHO should participate in the sign‐out process? |
| □ Outgoing clinician primarily responsible for patient's care |
| □ Oncoming clinician who will be primarily responsible for patient's care (avoid passing this task to someone else, even if busy) |
| □ Consider supervision by experienced clinicians if early in training |
| ✓ WHAT content needs to be verbally communicated? |
| Use situation briefing model, or SBAR, technique: |
| □ SituationIdentify each patient (name, age, sex, chief complaint) and briefly state any major problems (active and those that may become active during cross‐coverage). |
| □ Backgroundpertinent information relevant to current care (eg, recent vitals and/or baseline exam, labs, test results, etc). |
| □ Assessmentworking diagnosis, response to treatment, anticipated problems during cross‐coverage including anything not adequately described using written form (eg, complex family discussions). |
| □ Recommendationto‐do lists and if/then recommendations. |
| ✓ WHERE should sign‐out occur? |
| □ Designated room or place for sign‐out (eg, avoid patient areas because of HIPPA requirements) |
| □ Proper lighting |
| □ Avoid excessive noise (eg, high‐traffic areas) |
| □ Minimize disruptions (eg, hand over pagers) |
| □ Ensure systems support for sign‐out (eg, computers, printer, paper, etc.) |
| ✓ WHEN is the optimal time for sign‐out? |
| □ Designated time when both parties can be present and pay attention (eg, beware of clinic, other obligations) |
| □ Have enough time for interactive questions at the end (eg, avoid rush at the end of the shift) |
| ✓ HOW should verbal communication be performed? |
| □ Face to face, allowing for questions |
| □ Verbalize data in the same order for each patient at each sign‐out |
| □ Read back all to‐do items |
| □ Adjust length and depth of review according to baseline knowledge of parties involved and type of transition in care |
The Environment and setting.
To improve the setting of sign‐out, we recommend: a designated space that is well lit, quiet, and respects patient confidentiality and a designated time when sign‐out will occur. To limit known distractions and interruptions39, 40 in the hospital, we also recommend the outgoing physician hand off his or her pager to someone else during sign‐out. Also key to an environment conducive to information transfer is ensuring adequate computer support for electronic sign‐out and access to updated clinical information.
Organizational culture and institutional leadership.
The way residents transfer patient care information reflects the culture of the institution. Changing the culture to one in which interactive questioning is valued regardless of position in the hierarchy has been shown to reduce errors in aviation.41 Educating residents on the impact of sign‐outs on patient care is a first step toward improving the culture of sign‐out. Resident commitment to the new sign‐out can be gained by engaging residents in development of the process itself. To cement these changes into the culture, practitioners at all levels should be aware of and support the new system. The role of an institution's leaders in achieving these changes cannot be overlooked. Leaders will need to be creative in order to support sign‐out as described within the obvious constraints of money, time, personnel, and space. Gaining institutional buy‐in can start with heightening the awareness of leaders of the issues surrounding sign‐out, including patient safety, resident efficiency, and the financial impact of discontinuity. Ongoing evaluation of efforts to improve sign‐out is also crucial and can be accomplished with surveys, focus groups, and direct observation. Feeding back the positive impact of the changes to all involved stakeholders will promote confidence in the new systems and pride in their efforts.
CONCLUSIONS
Sign‐outs are a part of the current landscape of academic medical centers as well as hospitals at large. Interns, residents, and consulting fellows, not to mention nurses, physical therapists, and nutritionists, transfer patient care information at each transition point. There are few resources that can assist these caregivers in identifying and implementing the most effective ways to transfer patient care information. Hospitals and other care facilities are now mandated to develop standards and systems to improve sign‐out. On the basis of the limited literature to date and our own experiences, we have proposed standards and best practices to assist hospitals, training programs, and institutional leaders in designing safe and usable sign‐out systems. Effective implementation of the standards must include appropriate allocation of resources, individualization to meet specific needs of each program or institution, intensive training, and ongoing evaluation. Future research should focus on developing valid surrogate measures of continuity of care, conducting rigorous trials to determine the elements of sign‐out that lead to the best patient outcomes, and studying the most effective ways of implementing these improvements. By improving the content and process of sign‐out, we can meet the challenges of the new health care landscape while putting patient safety at the forefront.
- ,,.New requirements for resident duty hours.JAMA.2002;288:1112–1114.
- ,,,,.Effects of limited work hours on surgical training.J Am Coll Surg.2002;195:531–538.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351:1829–1837.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- .A precarious exchange.N Engl J Med.2004;351:1822–1824.
- .Awake and informed.N Engl J Med.2004;351:1884.
- . Fumbled handoff: missed communication between teams. Cases and Commentary: Hospital Medicine, Morbidity 269:374–378.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121:866–872.
- ,,,.Post‐call transfer of resident responsibility: its effect on patient care.J Gen Intern Med.1990;5:501–505.
- ,,,.Effect of a change in house staff work schedule on resource utilization and patient care.Arch Intern Med.1991;151:2065–2070.
- ,.Internal Bleeding: the Truth behind America's Terrifying Epidemic of Medical Mistakes.New York City:Rugged Land, LLC;2004:448.
- ,,.Crew resource management and its applications in medicine. In:Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment Number 43, AHRQ Publication 01‐E058.Rockville, MD:Agency for Healthcare Research and Quality;2001.
- ,,.System safety and threat and error management: the line operations safety audit (LOSA). In:Jensen RS, ed. Proceedings of the Eleventh International Symposium on Aviation Psychology.Columbus, OH:Ohio State University;2001:1–6.
- ,,.Translating teamwork behaviours from aviation to healthcare: development of behavioural markers for neonatal resuscitation.Qual Saf Health Care.2004;13(Suppl 1):i57–i64.
- ,,,.Handoff strategies in settings with high consequences for failure: lessons for healthcare operations.Intl J Qual Health Care.2004;16:125–132.
- . Available at: http://www.agilemodeling.com/essays/communication.htm. Accessed December 15,2005.
- .Ensuring continuing care: styles and efficiency of the handover process.Aust J Adv Nurs.1998;16:23–27.
- ,.The handover: uncovering the hidden practices of nurses.Intensive Crit Care Nurs.2000;16:373–383.
- .The patient handover: a study of its form, function and efficiency.Nurs Stand.1995;9(52):33–36.
- ,.Residents' suggestions for reducing errors in teaching hospitals.N Engl J Med.2003;348:851–855.
- ,.Is 80 the cost of saving lives? Reduced duty hours, errors, and cost.J Gen Intern Med.2005;20:969–970.
- ,,,.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- British Medical Association.Safe Handover: Safe Patients: Guidance on Clinical Handover for Clinicians and Managers.London:British Medical Association, Junior Doctors Committee;2004.
- ,,,,.Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998;24(2):77–87.
- ,,,.Organizing the transfer of patient care information: the development of a computerized resident sign‐out system.Surgery.2004;136:5–13.
- ,,,,.A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- ,,,.Computerized physician order entry in U.S. hospitals: results of a 2002 survey.J Am Med Inform Assoc.2004;11:95–99.
- ,,,,,.The impact of verbal communication on physician prescribing patterns in hospitalized patients with diabetes.Diabetes Educ.2003;29:827–836.
- ,.Use of computer terminals on wards to access emergency test results: a retrospective audit.Br Med J.2001;322:1101–1103.
- ,,,,,.Improving patient safety by repeating (read‐back) telephone reports of critical information.Am J Clin Pathol.2004;121:801–803.
- ,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13(Suppl 1):i85–i90.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14:401–407.
- ,,.Intern curriculum: the impact of a focused training program on the process and content of signout out patients. Harvard Medical School Education Day, Boston, MA;2004.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7:277–286.
- SBAR technique for communication: a situational briefing model. Available at: http://www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm. Accessed December2005.
- ,,,,.Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco.Acad Med.2006;81:76–81.
- ,.Communication behaviours in a hospital setting: an observational study.Br Med J.1998;316:673–676.
- ,,.Communication failures: an insidious contributor to medical mishapsAcad Med.2004;79(2):186–194.
- ,,.New requirements for resident duty hours.JAMA.2002;288:1112–1114.
- ,,,,.Effects of limited work hours on surgical training.J Am Coll Surg.2002;195:531–538.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351:1829–1837.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- .A precarious exchange.N Engl J Med.2004;351:1822–1824.
- .Awake and informed.N Engl J Med.2004;351:1884.
- . Fumbled handoff: missed communication between teams. Cases and Commentary: Hospital Medicine, Morbidity 269:374–378.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121:866–872.
- ,,,.Post‐call transfer of resident responsibility: its effect on patient care.J Gen Intern Med.1990;5:501–505.
- ,,,.Effect of a change in house staff work schedule on resource utilization and patient care.Arch Intern Med.1991;151:2065–2070.
- ,.Internal Bleeding: the Truth behind America's Terrifying Epidemic of Medical Mistakes.New York City:Rugged Land, LLC;2004:448.
- ,,.Crew resource management and its applications in medicine. In:Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment Number 43, AHRQ Publication 01‐E058.Rockville, MD:Agency for Healthcare Research and Quality;2001.
- ,,.System safety and threat and error management: the line operations safety audit (LOSA). In:Jensen RS, ed. Proceedings of the Eleventh International Symposium on Aviation Psychology.Columbus, OH:Ohio State University;2001:1–6.
- ,,.Translating teamwork behaviours from aviation to healthcare: development of behavioural markers for neonatal resuscitation.Qual Saf Health Care.2004;13(Suppl 1):i57–i64.
- ,,,.Handoff strategies in settings with high consequences for failure: lessons for healthcare operations.Intl J Qual Health Care.2004;16:125–132.
- . Available at: http://www.agilemodeling.com/essays/communication.htm. Accessed December 15,2005.
- .Ensuring continuing care: styles and efficiency of the handover process.Aust J Adv Nurs.1998;16:23–27.
- ,.The handover: uncovering the hidden practices of nurses.Intensive Crit Care Nurs.2000;16:373–383.
- .The patient handover: a study of its form, function and efficiency.Nurs Stand.1995;9(52):33–36.
- ,.Residents' suggestions for reducing errors in teaching hospitals.N Engl J Med.2003;348:851–855.
- ,.Is 80 the cost of saving lives? Reduced duty hours, errors, and cost.J Gen Intern Med.2005;20:969–970.
- ,,,.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- British Medical Association.Safe Handover: Safe Patients: Guidance on Clinical Handover for Clinicians and Managers.London:British Medical Association, Junior Doctors Committee;2004.
- ,,,,.Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998;24(2):77–87.
- ,,,.Organizing the transfer of patient care information: the development of a computerized resident sign‐out system.Surgery.2004;136:5–13.
- ,,,,.A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- ,,,.Computerized physician order entry in U.S. hospitals: results of a 2002 survey.J Am Med Inform Assoc.2004;11:95–99.
- ,,,,,.The impact of verbal communication on physician prescribing patterns in hospitalized patients with diabetes.Diabetes Educ.2003;29:827–836.
- ,.Use of computer terminals on wards to access emergency test results: a retrospective audit.Br Med J.2001;322:1101–1103.
- ,,,,,.Improving patient safety by repeating (read‐back) telephone reports of critical information.Am J Clin Pathol.2004;121:801–803.
- ,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13(Suppl 1):i85–i90.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14:401–407.
- ,,.Intern curriculum: the impact of a focused training program on the process and content of signout out patients. Harvard Medical School Education Day, Boston, MA;2004.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7:277–286.
- SBAR technique for communication: a situational briefing model. Available at: http://www.ihi.org/IHI/Topics/PatientSafety/SafetyGeneral/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.htm. Accessed December2005.
- ,,,,.Impact of reduced duty hours on residents' educational satisfaction at the University of California, San Francisco.Acad Med.2006;81:76–81.
- ,.Communication behaviours in a hospital setting: an observational study.Br Med J.1998;316:673–676.
- ,,.Communication failures: an insidious contributor to medical mishapsAcad Med.2004;79(2):186–194.
Reflections on Hospitalist Movement
Most people believe the term hospitalist first appeared in the literature in the August 15, 1996, issue of the New England Journal of Medicine (NEJM). That issue carried an article that Lee Goldman and I wrote titled The Emerging Role of Hospitalists in the American Health Care System.1 But the term was actually coined about a year earlier, in an article I wrote for our University of California, San Francisco (UCSF), residents' newsletter, the Medical Residents' Progress Note (MRPN), circulation about 180. In that article, I mused about a new model of care in which separate physicians assumed the role of caring for inpatients in place of patients' primary care doctors. Several peopleboth residents and facultyapproached me soon after the MRPN article was published and said, I read your articleyou should really buff it up and send it to a real journal. (By the way, when you publish a scholarly article, people generally say, I saw your article, rather than I read your article). This prompting led me to polish up the piece, with Lee Goldman's able assistance, and send it to the NEJM.
Although people often introduce me today as the guy who invented hospitalists (to which I typically respond, yeah, just like Al Gore invented the Internet), I did no such thingI merely kept my eyes and ears open, spotted the trend early, and gave it a name that stuck. In the mid‐1990s, the California market was being besieged by managed care, which was seeking new ways to cut hospital utilization and costs. In 1994, the huge Kaiser Permanente system decided to reorganize its hospital care around a cadre of hospital‐based specialists (HBSs), essentially dichotomizing the roles of inpatient and outpatient physicians. (Interestingly, Kaiser's main motivations were to improve outpatient satisfaction by assuring constant availability of primary care physicians and to create a vehicle to promote inpatient quality improvement activities, not necessarily to improve inpatient efficiency.) Around the same time, I read reports in throwaway magazines about Park Nicollet in Minneapolis and the Scripps Clinic in La Jolla, California, doing the same thing. Then one day I heard that a talented young UCSF faculty member was leaving our VA system to take a job as the inpatient manager at a local community teaching hospital. A few weeks later, I took him out to lunchI was intrigued by this new role and wanted to better understand it. As he described it to me over sandwiches, it made all the sense in the world, and the seeds of the MRPNand later NEJMarticle was planted.
I have always had an abiding interest in the notion of valuea fundamental belief that our system is inexorably becoming one in which health care choices and competition will be based on demonstrable quality, safety, the patient's experience, and cost rather than on tradition, impression, and proximity. As I began thinking about hospital care, it seemed likely this new modeldichotomizing the roles of inpatient and outpatient doctors such that the former could be constantly available and become an expert in inpatient clinical care and hospital microsystemswould provide more value than the traditional structure, both in community settings (replacing the single primary care doctor managing both inpatients and outpatients) and the academic setting (replacing the traditional one‐month‐a‐year ward attending).
At the time I was thinking all this through, a new chairman of our department of medicine arrived from Harvard. Lee Goldman, who virtually invented the field of clinical epidemiology, came to UCSF with a powerful vision that matched mineto transform training and clinical care to improve both value and education. Lee had been a resident at UCSF 20 years earlier and returned in 1995 to an inpatient service whose structure and culture had barely changed over a generation. Lee (who, to my great chagrin, recently left UCSF to become Columbia's medical school dean, and who does not have the term good enough in his vocabulary) sat down with me and articulated his vision for a new type of academic inpatient model, led by faculty who cared for inpatients and taught trainees hospital medicine for a living. This was entirely in sync with my thoughts, and so we set out to build it.
Reaction to both the New England Journal of Medicine article and our vision for an academic hospitalist service was swift and negative. One letter to the NEJM said it all:
Patients ill enough to be in the hospital are those who need their regular physicians the most. This is especially true if the patients have incurable diseases, in the context of which the usual buzzwords of efficiency and outcomes have little meaning. It is sad, but the most important part of medicine, the relationship between the doctor and the patient, is being forgotten. It is especially sad that physicians are beginning to think like MBAs.2
Our response to this and the other letters emphasized the need for evidence:
Our description of the emerging role of hospitalists is based not on an assertion that the hospitalist model is the only way to provide in‐hospital care, but rather on irrefutable evidence that both teaching and non‐teaching hospitals are adopting the model. We do not believe the debate about hospitalists is served by anecdotal claims about greater satisfaction among patients and providers. We recommend that the shape of our health care system be guided by measuring clinical outcomes, costs, and satisfaction rather than by following passion or tradition.3
My father, a retired businessman living in Florida, brought the controversy to an even finer point a year later. I met this guy playing tennis today, he told me on the phone one day. And he's heard of you! I listened for the heartwarming sounds of fatherly pride, but none were forthcoming. He hates you, he added.
Our attempts to build an academic hospitalist program generated other concerns. Many faculty enjoyed serving as ward attendings and worried about being kicked off the wards (although many privately told me that they knew their time was up and were grateful for a way to exit with dignity.) One world‐famous faculty member bolted out of his seat during the Q&A period after my medical grand rounds at his institution in 1997. How will the house staff learn anything if we don't allow them to learn from their mistakes? he huffed. (I told him that I was flying cross‐country the next day, and I'll be really pissed off if my pilot is there to learn from his mistakes.) Our residents also worried terribly about losing their autonomy, having these bright young attendings breathing down our backs. Everyone worried about where the resources to pay for the program would come from.
At UCSF, our strategy was to reassure everyone that we would be measuring the impact of the new model in terms of cost, quality, patient satisfaction, and education. By making clear that the results of this research would guide further change (and that we were willing to end the experiment if it turned out negatively), the faculty and house staff largely suspended their disbelief for the first year. That study4 would demonstrate impressive cost savings with no adverse impact on quality and patient satisfaction and a hint of improved resident satisfaction (later proven more conclusively5), allowing us to expand the program over time and to make the argument for ongoing medical center support of the new model.
Just as Lee Goldman's arrival at UCSF in 1995 was a remarkable and crucial bit of serendipity, my partnership with Dr. Win Whitcomb and Dr. John Nelson was every bit as important for the growth of the movement nationally. John, at that time a young internist in Gainesville, Florida, had been practicing as a hospitalist (though it wasn't called that) since completing his internal medicine residency in the later 1980s. He had hooked up with Win, another young internist who had left a private practice job to begin a hospital‐based practice at Mercy Medical Center in Springfield, Massachusetts. Together the two of them had begun to network with the handful of physicians around the country who were practicing in this new model. But they needed a larger megaphone, both to let other hospitalists know about each other, and to make hospitals and systems more aware of this new model of care.
John tells the story of pulling the August 15, 1996, issue of the NEJM out of his mailbox, seeing my article, and literally running into to his house to tell his wife that his practice had finally been discovered. John's thoughtful exuberance is one of the reasons for the growth of our field, and he did something that is uniquely Johncalling the author of an article that piqued his interest to discuss its contents, something he'd been doing for years. At that point, Lee Goldman was an internationally known leader in internal medicine; as chair of a major academic department, he had several layers of administrative assistants running interference when he received cold calls. I, on the other hand, ran a sleepy medical service and had little to do other than to answer calls and to respond to this new thing called e‐mail. John didn't know that; in his experience, first authors of articles in major journals were nearly always too busy to answer calls from country docs like him. So he tried Lee Goldman first but failed to get through. Win, on the other hand, decided to call me and had no problem getting through immediately. We hit it off like we'd been buddies for decades, sharing our instinctive recognition that that we were at the cutting edge of a new specialty. In what, in retrospect, seems like an extraordinary amount of hubris, we essentially divided up the world, asking the question: what does an emerging specialty need in order to be successful? I'm reminded of one of my favorite parts of the brilliant dialogue by Mel Brooks and Carl Reiner, The 2000 Year Old Man. Brooks, playing the title part, describes his relationship with Joan of Arc (What a cutie, he gushes) to Reiner (playing the interviewer), and how Joan's mission got in the way of their ardor. She used to say to me, Ive got to save France,' says the 2000 Year Old Man. I said, Look, Ive got to wash up, you save France, I'll see you later' That was usWin and John agreed to focus on building a new professional society and on networking with community‐based hospitalists, while I emphasized the academic side of things: organizing meetings, developing training programs, publishing a textbook, and launching a research agenda.
The first national gathering of hospitalists was astonishing. In the spring of 1997, I hosted what I thought would be a small hospital medicine CME meeting at a Holiday Inn in San Francisco in a seedy part of town. I expected about 50 people to attend and was shocked to see 3 times that (plus several homeless people who wandered into the sessions). Most remarkably, at the end of day 1, following 8 hours of clinical lectures, Win, John, and I asked the attendees if anybody wanted to stay a while and discuss the possibility of forming a new society. To our amazement, virtually everybody stayedmore than 100 people! Would anybody be willing to contribute some money to get this started? asked John, expecting nothing. And people began passing $20 bills up to the front of the room. That was the moment we knew we were onto something very bigthe atmosphere was electric, the enthusiasm easily palpable.
We initially called the new society the National Association of Inpatient Physicians (NAIP), as the name hospitalist was still very controversial, and many thought it would not have legsthe term inpatient physician was believed to be more inclusive. NAIP rapidly reached a crucial turning point. Our few hundred dollars in dues collections and ad revenues lived in Win's shoebox in Massachusetts (and later in a checking account opened by Ron Angus in Texas), and Win, John, and I were keeping databases of hospitalists on our computers and the backs of napkins. It was clear we needed to either create a full‐fledged infrastructure or partner with an organization that could help us. I approached Hal Sox, now the editor of the Annals of Internal Medicine but at that time president of the American College of Physicians (and an old fellowship mentor of mine), about the possibility of NAIP establishing a formal relationship with the ACP. Hal was reluctant at first, noting many ACP members were pretty strongly against the idea of hospitalists. In one of many acts of brinksmanship, I told him we would need to look for other partners if ACP did not get over its ambivalence and embrace our new field. To his credit and to the credit particularly of Dr. Walt McDonald, ACP's executive director at the time, both recognized the potential growth of this new field and worked through the internal politics to offer us an affiliation. However, we found their initial offerto become the Section on Hospital Medicine within the ACPunattractive. Wanting to be a full‐fledged independent organization that enjoyed a relationship with the College, we proposed a relationship that would link us and allow ACP to support our infrastructure, but that allowed us to retain independent decision making, governance, and budget. John, in his charming Southern drawl, described our position to an early gathering of about 100 hospitalists at a NAIP meeting in San Diego. Their offer would have them up here, and we'd be down there, he said, his hands depicting an obvious hierarchy, with us on the bottom. But we insisted on being equal partners, he said, with his hands on the same plane. I turned to Win, sitting next to me in the audience, and whispered something like, Yeah, equalexcept for the small fact that they have 120,000 members and we have 87. Nevertheless, they agreed, and our relationship has been incredibly positive for hospitalists, and I believe for the ACP as well.
The rest, as they say, is history. The society, renamed the Society of Hospital Medicine in April 2003, has thrived under the leadership of a strong series of boards, a wonderful staff, and a charismatic and highly effective CEO, Dr. Larry Wellikson. We successfully navigated the many early challenges and took advantage of key opportunities. In this regard, I consider our 3 most important decisions and actions to be: 1) creating a body of research that demonstrated, in an evidence‐based way, that the theoretical promise of the field was real6 (it was this research that led hospitals to embrace the field more vigorously and that justified the crucial support that most hospitals provide their hospitalist programs); 2) vigorously pushing back against managed care‐based hospitalist models that had begun to force primary care physicians to hand their patients off to hospitalists against their will (NAIP's first policy pronouncement was to come out strongly against such mandatory models, which seemed counterintuitive to some but which markedly decreased our vulnerability to being tagged as a cost‐cutting vehicle of managed care); and 3) linking ourselves as strongly as possible with the growing quality and safety movements. When the IOM reports on medical errors7 and later quality8 were published, we immediately saw in the new agendas a tremendous opportunity to brand hospitalists as indispensable leaders of quality and safety in hospitalsanother key rationale for hospitalists' value proposition and another reason for hospitals and policymakers to support the young field.
Looking back at the 1996 New England Journal of Medicine article, I am struck by both the number of things I got right (even a blind squirrel) and the number that I did not anticipate or got wrong. Lee and I thought that many hospitalists would be subspecialists who would focus on hospital medicine for only part of their work. This was true early on, but the field has evolved to be more of a generalist endeavor (although recently there have emerged laborists, neurology hospitalists, and even surgical hospitalists). I probably could have anticipated the growth of the field in pediatrics, but it certainly was not on my radar screen until years later.9 I did not count on the work hours of house staff being regulated; even if I had, I'm not sure I would have fully recognized how the need to create nonteaching services would turbo‐charge the growth of the hospitalist field in teaching hospitals. The one mild disappointment: I anticipated stronger evidence by now of the field's salutary impact on safety and quality. The effort to study and hopefully demonstrate such improvements should be a major focus for the next 510 years. Finally, although I thought the field would grow rapidly, I did not anticipate that a decade later there would be 15,000 hospitalists nationally or 24 in my group at UCSF. I also did not guess that an April 2006 Medline search of hospitalist would find 561 articles or that a Google search of hospitalist would yield 689,000 entries (hell, there was no Google to search in 1996!).
As I reflect back on the last decade, I am humbled by the remarkable work I have seen from hospitalists around the country and grateful for the wonderful friendships I have enjoyed with my colleagues in our new field. I am even more convinced of the fundamental accuracy of my underlying premise: the U.S. health care system will increasingly embrace models, strategies, and providers who can demonstrably improve the value of care. I have no doubt thatcollectivelyAmerican hospitalists have saved tens of thousands of lives, prevented tens of thousands of errors, orchestrated tens of thousands of good deaths, comforted tens of thousands of families, and saved billions of dollars. It is an ongoing legacy that gives me considerable pride and joy.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517. http://content.nejm.org/cgi/content/full/335/7/514
- .The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,.The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,,,,.Reorganizing an academic medical service: Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,,,.Effects of hospitalist attendings on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- .The hospitalist movement 5 years later.J Am Med Assoc2002;282:487–494.
- ,,.To Err Is Human: Building a Safer Health System.Washington, DC:Committee on Quality of Health Care in America, Institute of Medicine.National Academy Press;2000.
- Committee on Quality of Health Care in America, IOM.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–77.
Most people believe the term hospitalist first appeared in the literature in the August 15, 1996, issue of the New England Journal of Medicine (NEJM). That issue carried an article that Lee Goldman and I wrote titled The Emerging Role of Hospitalists in the American Health Care System.1 But the term was actually coined about a year earlier, in an article I wrote for our University of California, San Francisco (UCSF), residents' newsletter, the Medical Residents' Progress Note (MRPN), circulation about 180. In that article, I mused about a new model of care in which separate physicians assumed the role of caring for inpatients in place of patients' primary care doctors. Several peopleboth residents and facultyapproached me soon after the MRPN article was published and said, I read your articleyou should really buff it up and send it to a real journal. (By the way, when you publish a scholarly article, people generally say, I saw your article, rather than I read your article). This prompting led me to polish up the piece, with Lee Goldman's able assistance, and send it to the NEJM.
Although people often introduce me today as the guy who invented hospitalists (to which I typically respond, yeah, just like Al Gore invented the Internet), I did no such thingI merely kept my eyes and ears open, spotted the trend early, and gave it a name that stuck. In the mid‐1990s, the California market was being besieged by managed care, which was seeking new ways to cut hospital utilization and costs. In 1994, the huge Kaiser Permanente system decided to reorganize its hospital care around a cadre of hospital‐based specialists (HBSs), essentially dichotomizing the roles of inpatient and outpatient physicians. (Interestingly, Kaiser's main motivations were to improve outpatient satisfaction by assuring constant availability of primary care physicians and to create a vehicle to promote inpatient quality improvement activities, not necessarily to improve inpatient efficiency.) Around the same time, I read reports in throwaway magazines about Park Nicollet in Minneapolis and the Scripps Clinic in La Jolla, California, doing the same thing. Then one day I heard that a talented young UCSF faculty member was leaving our VA system to take a job as the inpatient manager at a local community teaching hospital. A few weeks later, I took him out to lunchI was intrigued by this new role and wanted to better understand it. As he described it to me over sandwiches, it made all the sense in the world, and the seeds of the MRPNand later NEJMarticle was planted.
I have always had an abiding interest in the notion of valuea fundamental belief that our system is inexorably becoming one in which health care choices and competition will be based on demonstrable quality, safety, the patient's experience, and cost rather than on tradition, impression, and proximity. As I began thinking about hospital care, it seemed likely this new modeldichotomizing the roles of inpatient and outpatient doctors such that the former could be constantly available and become an expert in inpatient clinical care and hospital microsystemswould provide more value than the traditional structure, both in community settings (replacing the single primary care doctor managing both inpatients and outpatients) and the academic setting (replacing the traditional one‐month‐a‐year ward attending).
At the time I was thinking all this through, a new chairman of our department of medicine arrived from Harvard. Lee Goldman, who virtually invented the field of clinical epidemiology, came to UCSF with a powerful vision that matched mineto transform training and clinical care to improve both value and education. Lee had been a resident at UCSF 20 years earlier and returned in 1995 to an inpatient service whose structure and culture had barely changed over a generation. Lee (who, to my great chagrin, recently left UCSF to become Columbia's medical school dean, and who does not have the term good enough in his vocabulary) sat down with me and articulated his vision for a new type of academic inpatient model, led by faculty who cared for inpatients and taught trainees hospital medicine for a living. This was entirely in sync with my thoughts, and so we set out to build it.
Reaction to both the New England Journal of Medicine article and our vision for an academic hospitalist service was swift and negative. One letter to the NEJM said it all:
Patients ill enough to be in the hospital are those who need their regular physicians the most. This is especially true if the patients have incurable diseases, in the context of which the usual buzzwords of efficiency and outcomes have little meaning. It is sad, but the most important part of medicine, the relationship between the doctor and the patient, is being forgotten. It is especially sad that physicians are beginning to think like MBAs.2
Our response to this and the other letters emphasized the need for evidence:
Our description of the emerging role of hospitalists is based not on an assertion that the hospitalist model is the only way to provide in‐hospital care, but rather on irrefutable evidence that both teaching and non‐teaching hospitals are adopting the model. We do not believe the debate about hospitalists is served by anecdotal claims about greater satisfaction among patients and providers. We recommend that the shape of our health care system be guided by measuring clinical outcomes, costs, and satisfaction rather than by following passion or tradition.3
My father, a retired businessman living in Florida, brought the controversy to an even finer point a year later. I met this guy playing tennis today, he told me on the phone one day. And he's heard of you! I listened for the heartwarming sounds of fatherly pride, but none were forthcoming. He hates you, he added.
Our attempts to build an academic hospitalist program generated other concerns. Many faculty enjoyed serving as ward attendings and worried about being kicked off the wards (although many privately told me that they knew their time was up and were grateful for a way to exit with dignity.) One world‐famous faculty member bolted out of his seat during the Q&A period after my medical grand rounds at his institution in 1997. How will the house staff learn anything if we don't allow them to learn from their mistakes? he huffed. (I told him that I was flying cross‐country the next day, and I'll be really pissed off if my pilot is there to learn from his mistakes.) Our residents also worried terribly about losing their autonomy, having these bright young attendings breathing down our backs. Everyone worried about where the resources to pay for the program would come from.
At UCSF, our strategy was to reassure everyone that we would be measuring the impact of the new model in terms of cost, quality, patient satisfaction, and education. By making clear that the results of this research would guide further change (and that we were willing to end the experiment if it turned out negatively), the faculty and house staff largely suspended their disbelief for the first year. That study4 would demonstrate impressive cost savings with no adverse impact on quality and patient satisfaction and a hint of improved resident satisfaction (later proven more conclusively5), allowing us to expand the program over time and to make the argument for ongoing medical center support of the new model.
Just as Lee Goldman's arrival at UCSF in 1995 was a remarkable and crucial bit of serendipity, my partnership with Dr. Win Whitcomb and Dr. John Nelson was every bit as important for the growth of the movement nationally. John, at that time a young internist in Gainesville, Florida, had been practicing as a hospitalist (though it wasn't called that) since completing his internal medicine residency in the later 1980s. He had hooked up with Win, another young internist who had left a private practice job to begin a hospital‐based practice at Mercy Medical Center in Springfield, Massachusetts. Together the two of them had begun to network with the handful of physicians around the country who were practicing in this new model. But they needed a larger megaphone, both to let other hospitalists know about each other, and to make hospitals and systems more aware of this new model of care.
John tells the story of pulling the August 15, 1996, issue of the NEJM out of his mailbox, seeing my article, and literally running into to his house to tell his wife that his practice had finally been discovered. John's thoughtful exuberance is one of the reasons for the growth of our field, and he did something that is uniquely Johncalling the author of an article that piqued his interest to discuss its contents, something he'd been doing for years. At that point, Lee Goldman was an internationally known leader in internal medicine; as chair of a major academic department, he had several layers of administrative assistants running interference when he received cold calls. I, on the other hand, ran a sleepy medical service and had little to do other than to answer calls and to respond to this new thing called e‐mail. John didn't know that; in his experience, first authors of articles in major journals were nearly always too busy to answer calls from country docs like him. So he tried Lee Goldman first but failed to get through. Win, on the other hand, decided to call me and had no problem getting through immediately. We hit it off like we'd been buddies for decades, sharing our instinctive recognition that that we were at the cutting edge of a new specialty. In what, in retrospect, seems like an extraordinary amount of hubris, we essentially divided up the world, asking the question: what does an emerging specialty need in order to be successful? I'm reminded of one of my favorite parts of the brilliant dialogue by Mel Brooks and Carl Reiner, The 2000 Year Old Man. Brooks, playing the title part, describes his relationship with Joan of Arc (What a cutie, he gushes) to Reiner (playing the interviewer), and how Joan's mission got in the way of their ardor. She used to say to me, Ive got to save France,' says the 2000 Year Old Man. I said, Look, Ive got to wash up, you save France, I'll see you later' That was usWin and John agreed to focus on building a new professional society and on networking with community‐based hospitalists, while I emphasized the academic side of things: organizing meetings, developing training programs, publishing a textbook, and launching a research agenda.
The first national gathering of hospitalists was astonishing. In the spring of 1997, I hosted what I thought would be a small hospital medicine CME meeting at a Holiday Inn in San Francisco in a seedy part of town. I expected about 50 people to attend and was shocked to see 3 times that (plus several homeless people who wandered into the sessions). Most remarkably, at the end of day 1, following 8 hours of clinical lectures, Win, John, and I asked the attendees if anybody wanted to stay a while and discuss the possibility of forming a new society. To our amazement, virtually everybody stayedmore than 100 people! Would anybody be willing to contribute some money to get this started? asked John, expecting nothing. And people began passing $20 bills up to the front of the room. That was the moment we knew we were onto something very bigthe atmosphere was electric, the enthusiasm easily palpable.
We initially called the new society the National Association of Inpatient Physicians (NAIP), as the name hospitalist was still very controversial, and many thought it would not have legsthe term inpatient physician was believed to be more inclusive. NAIP rapidly reached a crucial turning point. Our few hundred dollars in dues collections and ad revenues lived in Win's shoebox in Massachusetts (and later in a checking account opened by Ron Angus in Texas), and Win, John, and I were keeping databases of hospitalists on our computers and the backs of napkins. It was clear we needed to either create a full‐fledged infrastructure or partner with an organization that could help us. I approached Hal Sox, now the editor of the Annals of Internal Medicine but at that time president of the American College of Physicians (and an old fellowship mentor of mine), about the possibility of NAIP establishing a formal relationship with the ACP. Hal was reluctant at first, noting many ACP members were pretty strongly against the idea of hospitalists. In one of many acts of brinksmanship, I told him we would need to look for other partners if ACP did not get over its ambivalence and embrace our new field. To his credit and to the credit particularly of Dr. Walt McDonald, ACP's executive director at the time, both recognized the potential growth of this new field and worked through the internal politics to offer us an affiliation. However, we found their initial offerto become the Section on Hospital Medicine within the ACPunattractive. Wanting to be a full‐fledged independent organization that enjoyed a relationship with the College, we proposed a relationship that would link us and allow ACP to support our infrastructure, but that allowed us to retain independent decision making, governance, and budget. John, in his charming Southern drawl, described our position to an early gathering of about 100 hospitalists at a NAIP meeting in San Diego. Their offer would have them up here, and we'd be down there, he said, his hands depicting an obvious hierarchy, with us on the bottom. But we insisted on being equal partners, he said, with his hands on the same plane. I turned to Win, sitting next to me in the audience, and whispered something like, Yeah, equalexcept for the small fact that they have 120,000 members and we have 87. Nevertheless, they agreed, and our relationship has been incredibly positive for hospitalists, and I believe for the ACP as well.
The rest, as they say, is history. The society, renamed the Society of Hospital Medicine in April 2003, has thrived under the leadership of a strong series of boards, a wonderful staff, and a charismatic and highly effective CEO, Dr. Larry Wellikson. We successfully navigated the many early challenges and took advantage of key opportunities. In this regard, I consider our 3 most important decisions and actions to be: 1) creating a body of research that demonstrated, in an evidence‐based way, that the theoretical promise of the field was real6 (it was this research that led hospitals to embrace the field more vigorously and that justified the crucial support that most hospitals provide their hospitalist programs); 2) vigorously pushing back against managed care‐based hospitalist models that had begun to force primary care physicians to hand their patients off to hospitalists against their will (NAIP's first policy pronouncement was to come out strongly against such mandatory models, which seemed counterintuitive to some but which markedly decreased our vulnerability to being tagged as a cost‐cutting vehicle of managed care); and 3) linking ourselves as strongly as possible with the growing quality and safety movements. When the IOM reports on medical errors7 and later quality8 were published, we immediately saw in the new agendas a tremendous opportunity to brand hospitalists as indispensable leaders of quality and safety in hospitalsanother key rationale for hospitalists' value proposition and another reason for hospitals and policymakers to support the young field.
Looking back at the 1996 New England Journal of Medicine article, I am struck by both the number of things I got right (even a blind squirrel) and the number that I did not anticipate or got wrong. Lee and I thought that many hospitalists would be subspecialists who would focus on hospital medicine for only part of their work. This was true early on, but the field has evolved to be more of a generalist endeavor (although recently there have emerged laborists, neurology hospitalists, and even surgical hospitalists). I probably could have anticipated the growth of the field in pediatrics, but it certainly was not on my radar screen until years later.9 I did not count on the work hours of house staff being regulated; even if I had, I'm not sure I would have fully recognized how the need to create nonteaching services would turbo‐charge the growth of the hospitalist field in teaching hospitals. The one mild disappointment: I anticipated stronger evidence by now of the field's salutary impact on safety and quality. The effort to study and hopefully demonstrate such improvements should be a major focus for the next 510 years. Finally, although I thought the field would grow rapidly, I did not anticipate that a decade later there would be 15,000 hospitalists nationally or 24 in my group at UCSF. I also did not guess that an April 2006 Medline search of hospitalist would find 561 articles or that a Google search of hospitalist would yield 689,000 entries (hell, there was no Google to search in 1996!).
As I reflect back on the last decade, I am humbled by the remarkable work I have seen from hospitalists around the country and grateful for the wonderful friendships I have enjoyed with my colleagues in our new field. I am even more convinced of the fundamental accuracy of my underlying premise: the U.S. health care system will increasingly embrace models, strategies, and providers who can demonstrably improve the value of care. I have no doubt thatcollectivelyAmerican hospitalists have saved tens of thousands of lives, prevented tens of thousands of errors, orchestrated tens of thousands of good deaths, comforted tens of thousands of families, and saved billions of dollars. It is an ongoing legacy that gives me considerable pride and joy.
Most people believe the term hospitalist first appeared in the literature in the August 15, 1996, issue of the New England Journal of Medicine (NEJM). That issue carried an article that Lee Goldman and I wrote titled The Emerging Role of Hospitalists in the American Health Care System.1 But the term was actually coined about a year earlier, in an article I wrote for our University of California, San Francisco (UCSF), residents' newsletter, the Medical Residents' Progress Note (MRPN), circulation about 180. In that article, I mused about a new model of care in which separate physicians assumed the role of caring for inpatients in place of patients' primary care doctors. Several peopleboth residents and facultyapproached me soon after the MRPN article was published and said, I read your articleyou should really buff it up and send it to a real journal. (By the way, when you publish a scholarly article, people generally say, I saw your article, rather than I read your article). This prompting led me to polish up the piece, with Lee Goldman's able assistance, and send it to the NEJM.
Although people often introduce me today as the guy who invented hospitalists (to which I typically respond, yeah, just like Al Gore invented the Internet), I did no such thingI merely kept my eyes and ears open, spotted the trend early, and gave it a name that stuck. In the mid‐1990s, the California market was being besieged by managed care, which was seeking new ways to cut hospital utilization and costs. In 1994, the huge Kaiser Permanente system decided to reorganize its hospital care around a cadre of hospital‐based specialists (HBSs), essentially dichotomizing the roles of inpatient and outpatient physicians. (Interestingly, Kaiser's main motivations were to improve outpatient satisfaction by assuring constant availability of primary care physicians and to create a vehicle to promote inpatient quality improvement activities, not necessarily to improve inpatient efficiency.) Around the same time, I read reports in throwaway magazines about Park Nicollet in Minneapolis and the Scripps Clinic in La Jolla, California, doing the same thing. Then one day I heard that a talented young UCSF faculty member was leaving our VA system to take a job as the inpatient manager at a local community teaching hospital. A few weeks later, I took him out to lunchI was intrigued by this new role and wanted to better understand it. As he described it to me over sandwiches, it made all the sense in the world, and the seeds of the MRPNand later NEJMarticle was planted.
I have always had an abiding interest in the notion of valuea fundamental belief that our system is inexorably becoming one in which health care choices and competition will be based on demonstrable quality, safety, the patient's experience, and cost rather than on tradition, impression, and proximity. As I began thinking about hospital care, it seemed likely this new modeldichotomizing the roles of inpatient and outpatient doctors such that the former could be constantly available and become an expert in inpatient clinical care and hospital microsystemswould provide more value than the traditional structure, both in community settings (replacing the single primary care doctor managing both inpatients and outpatients) and the academic setting (replacing the traditional one‐month‐a‐year ward attending).
At the time I was thinking all this through, a new chairman of our department of medicine arrived from Harvard. Lee Goldman, who virtually invented the field of clinical epidemiology, came to UCSF with a powerful vision that matched mineto transform training and clinical care to improve both value and education. Lee had been a resident at UCSF 20 years earlier and returned in 1995 to an inpatient service whose structure and culture had barely changed over a generation. Lee (who, to my great chagrin, recently left UCSF to become Columbia's medical school dean, and who does not have the term good enough in his vocabulary) sat down with me and articulated his vision for a new type of academic inpatient model, led by faculty who cared for inpatients and taught trainees hospital medicine for a living. This was entirely in sync with my thoughts, and so we set out to build it.
Reaction to both the New England Journal of Medicine article and our vision for an academic hospitalist service was swift and negative. One letter to the NEJM said it all:
Patients ill enough to be in the hospital are those who need their regular physicians the most. This is especially true if the patients have incurable diseases, in the context of which the usual buzzwords of efficiency and outcomes have little meaning. It is sad, but the most important part of medicine, the relationship between the doctor and the patient, is being forgotten. It is especially sad that physicians are beginning to think like MBAs.2
Our response to this and the other letters emphasized the need for evidence:
Our description of the emerging role of hospitalists is based not on an assertion that the hospitalist model is the only way to provide in‐hospital care, but rather on irrefutable evidence that both teaching and non‐teaching hospitals are adopting the model. We do not believe the debate about hospitalists is served by anecdotal claims about greater satisfaction among patients and providers. We recommend that the shape of our health care system be guided by measuring clinical outcomes, costs, and satisfaction rather than by following passion or tradition.3
My father, a retired businessman living in Florida, brought the controversy to an even finer point a year later. I met this guy playing tennis today, he told me on the phone one day. And he's heard of you! I listened for the heartwarming sounds of fatherly pride, but none were forthcoming. He hates you, he added.
Our attempts to build an academic hospitalist program generated other concerns. Many faculty enjoyed serving as ward attendings and worried about being kicked off the wards (although many privately told me that they knew their time was up and were grateful for a way to exit with dignity.) One world‐famous faculty member bolted out of his seat during the Q&A period after my medical grand rounds at his institution in 1997. How will the house staff learn anything if we don't allow them to learn from their mistakes? he huffed. (I told him that I was flying cross‐country the next day, and I'll be really pissed off if my pilot is there to learn from his mistakes.) Our residents also worried terribly about losing their autonomy, having these bright young attendings breathing down our backs. Everyone worried about where the resources to pay for the program would come from.
At UCSF, our strategy was to reassure everyone that we would be measuring the impact of the new model in terms of cost, quality, patient satisfaction, and education. By making clear that the results of this research would guide further change (and that we were willing to end the experiment if it turned out negatively), the faculty and house staff largely suspended their disbelief for the first year. That study4 would demonstrate impressive cost savings with no adverse impact on quality and patient satisfaction and a hint of improved resident satisfaction (later proven more conclusively5), allowing us to expand the program over time and to make the argument for ongoing medical center support of the new model.
Just as Lee Goldman's arrival at UCSF in 1995 was a remarkable and crucial bit of serendipity, my partnership with Dr. Win Whitcomb and Dr. John Nelson was every bit as important for the growth of the movement nationally. John, at that time a young internist in Gainesville, Florida, had been practicing as a hospitalist (though it wasn't called that) since completing his internal medicine residency in the later 1980s. He had hooked up with Win, another young internist who had left a private practice job to begin a hospital‐based practice at Mercy Medical Center in Springfield, Massachusetts. Together the two of them had begun to network with the handful of physicians around the country who were practicing in this new model. But they needed a larger megaphone, both to let other hospitalists know about each other, and to make hospitals and systems more aware of this new model of care.
John tells the story of pulling the August 15, 1996, issue of the NEJM out of his mailbox, seeing my article, and literally running into to his house to tell his wife that his practice had finally been discovered. John's thoughtful exuberance is one of the reasons for the growth of our field, and he did something that is uniquely Johncalling the author of an article that piqued his interest to discuss its contents, something he'd been doing for years. At that point, Lee Goldman was an internationally known leader in internal medicine; as chair of a major academic department, he had several layers of administrative assistants running interference when he received cold calls. I, on the other hand, ran a sleepy medical service and had little to do other than to answer calls and to respond to this new thing called e‐mail. John didn't know that; in his experience, first authors of articles in major journals were nearly always too busy to answer calls from country docs like him. So he tried Lee Goldman first but failed to get through. Win, on the other hand, decided to call me and had no problem getting through immediately. We hit it off like we'd been buddies for decades, sharing our instinctive recognition that that we were at the cutting edge of a new specialty. In what, in retrospect, seems like an extraordinary amount of hubris, we essentially divided up the world, asking the question: what does an emerging specialty need in order to be successful? I'm reminded of one of my favorite parts of the brilliant dialogue by Mel Brooks and Carl Reiner, The 2000 Year Old Man. Brooks, playing the title part, describes his relationship with Joan of Arc (What a cutie, he gushes) to Reiner (playing the interviewer), and how Joan's mission got in the way of their ardor. She used to say to me, Ive got to save France,' says the 2000 Year Old Man. I said, Look, Ive got to wash up, you save France, I'll see you later' That was usWin and John agreed to focus on building a new professional society and on networking with community‐based hospitalists, while I emphasized the academic side of things: organizing meetings, developing training programs, publishing a textbook, and launching a research agenda.
The first national gathering of hospitalists was astonishing. In the spring of 1997, I hosted what I thought would be a small hospital medicine CME meeting at a Holiday Inn in San Francisco in a seedy part of town. I expected about 50 people to attend and was shocked to see 3 times that (plus several homeless people who wandered into the sessions). Most remarkably, at the end of day 1, following 8 hours of clinical lectures, Win, John, and I asked the attendees if anybody wanted to stay a while and discuss the possibility of forming a new society. To our amazement, virtually everybody stayedmore than 100 people! Would anybody be willing to contribute some money to get this started? asked John, expecting nothing. And people began passing $20 bills up to the front of the room. That was the moment we knew we were onto something very bigthe atmosphere was electric, the enthusiasm easily palpable.
We initially called the new society the National Association of Inpatient Physicians (NAIP), as the name hospitalist was still very controversial, and many thought it would not have legsthe term inpatient physician was believed to be more inclusive. NAIP rapidly reached a crucial turning point. Our few hundred dollars in dues collections and ad revenues lived in Win's shoebox in Massachusetts (and later in a checking account opened by Ron Angus in Texas), and Win, John, and I were keeping databases of hospitalists on our computers and the backs of napkins. It was clear we needed to either create a full‐fledged infrastructure or partner with an organization that could help us. I approached Hal Sox, now the editor of the Annals of Internal Medicine but at that time president of the American College of Physicians (and an old fellowship mentor of mine), about the possibility of NAIP establishing a formal relationship with the ACP. Hal was reluctant at first, noting many ACP members were pretty strongly against the idea of hospitalists. In one of many acts of brinksmanship, I told him we would need to look for other partners if ACP did not get over its ambivalence and embrace our new field. To his credit and to the credit particularly of Dr. Walt McDonald, ACP's executive director at the time, both recognized the potential growth of this new field and worked through the internal politics to offer us an affiliation. However, we found their initial offerto become the Section on Hospital Medicine within the ACPunattractive. Wanting to be a full‐fledged independent organization that enjoyed a relationship with the College, we proposed a relationship that would link us and allow ACP to support our infrastructure, but that allowed us to retain independent decision making, governance, and budget. John, in his charming Southern drawl, described our position to an early gathering of about 100 hospitalists at a NAIP meeting in San Diego. Their offer would have them up here, and we'd be down there, he said, his hands depicting an obvious hierarchy, with us on the bottom. But we insisted on being equal partners, he said, with his hands on the same plane. I turned to Win, sitting next to me in the audience, and whispered something like, Yeah, equalexcept for the small fact that they have 120,000 members and we have 87. Nevertheless, they agreed, and our relationship has been incredibly positive for hospitalists, and I believe for the ACP as well.
The rest, as they say, is history. The society, renamed the Society of Hospital Medicine in April 2003, has thrived under the leadership of a strong series of boards, a wonderful staff, and a charismatic and highly effective CEO, Dr. Larry Wellikson. We successfully navigated the many early challenges and took advantage of key opportunities. In this regard, I consider our 3 most important decisions and actions to be: 1) creating a body of research that demonstrated, in an evidence‐based way, that the theoretical promise of the field was real6 (it was this research that led hospitals to embrace the field more vigorously and that justified the crucial support that most hospitals provide their hospitalist programs); 2) vigorously pushing back against managed care‐based hospitalist models that had begun to force primary care physicians to hand their patients off to hospitalists against their will (NAIP's first policy pronouncement was to come out strongly against such mandatory models, which seemed counterintuitive to some but which markedly decreased our vulnerability to being tagged as a cost‐cutting vehicle of managed care); and 3) linking ourselves as strongly as possible with the growing quality and safety movements. When the IOM reports on medical errors7 and later quality8 were published, we immediately saw in the new agendas a tremendous opportunity to brand hospitalists as indispensable leaders of quality and safety in hospitalsanother key rationale for hospitalists' value proposition and another reason for hospitals and policymakers to support the young field.
Looking back at the 1996 New England Journal of Medicine article, I am struck by both the number of things I got right (even a blind squirrel) and the number that I did not anticipate or got wrong. Lee and I thought that many hospitalists would be subspecialists who would focus on hospital medicine for only part of their work. This was true early on, but the field has evolved to be more of a generalist endeavor (although recently there have emerged laborists, neurology hospitalists, and even surgical hospitalists). I probably could have anticipated the growth of the field in pediatrics, but it certainly was not on my radar screen until years later.9 I did not count on the work hours of house staff being regulated; even if I had, I'm not sure I would have fully recognized how the need to create nonteaching services would turbo‐charge the growth of the hospitalist field in teaching hospitals. The one mild disappointment: I anticipated stronger evidence by now of the field's salutary impact on safety and quality. The effort to study and hopefully demonstrate such improvements should be a major focus for the next 510 years. Finally, although I thought the field would grow rapidly, I did not anticipate that a decade later there would be 15,000 hospitalists nationally or 24 in my group at UCSF. I also did not guess that an April 2006 Medline search of hospitalist would find 561 articles or that a Google search of hospitalist would yield 689,000 entries (hell, there was no Google to search in 1996!).
As I reflect back on the last decade, I am humbled by the remarkable work I have seen from hospitalists around the country and grateful for the wonderful friendships I have enjoyed with my colleagues in our new field. I am even more convinced of the fundamental accuracy of my underlying premise: the U.S. health care system will increasingly embrace models, strategies, and providers who can demonstrably improve the value of care. I have no doubt thatcollectivelyAmerican hospitalists have saved tens of thousands of lives, prevented tens of thousands of errors, orchestrated tens of thousands of good deaths, comforted tens of thousands of families, and saved billions of dollars. It is an ongoing legacy that gives me considerable pride and joy.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517. http://content.nejm.org/cgi/content/full/335/7/514
- .The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,.The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,,,,.Reorganizing an academic medical service: Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,,,.Effects of hospitalist attendings on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- .The hospitalist movement 5 years later.J Am Med Assoc2002;282:487–494.
- ,,.To Err Is Human: Building a Safer Health System.Washington, DC:Committee on Quality of Health Care in America, Institute of Medicine.National Academy Press;2000.
- Committee on Quality of Health Care in America, IOM.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–77.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517. http://content.nejm.org/cgi/content/full/335/7/514
- .The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,.The role of “hospitalists” in the health care system.N Engl J Med.1996;336:444–446.
- ,,,,.Reorganizing an academic medical service: Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- ,,,,.Effects of hospitalist attendings on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- .The hospitalist movement 5 years later.J Am Med Assoc2002;282:487–494.
- ,,.To Err Is Human: Building a Safer Health System.Washington, DC:Committee on Quality of Health Care in America, Institute of Medicine.National Academy Press;2000.
- Committee on Quality of Health Care in America, IOM.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,.The hospitalist movement and its implications for the care of hospitalized children.Pediatrics.1999;103:473–77.